User login
Reported penicillin allergies hike inpatient costs
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
FROM JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY: IN PRACTICE
Key clinical point: Inpatient costs were $1,145 – $4,254 higher for those reporting penicillin allergy.
Major finding: Though most studies addressed inpatient admissions, outpatient costs were also significantly higher.
Study details: Systematic review and meta-analysis of 30 articles addressing reported penicillin allergy.
Disclosures: The study was sponsored by ALK.
Source: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
REPROVE: Ceftazidime-avibactam noninferior to meropenem for nosocomial pneumonia
Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia including ventilator-associated pneumonia from gram-negative organisms, results from the REPROVE trial demonstrated.
Nosocomial or hospital-acquired pneumonia is a common hospital-acquired infection associated with increased cost and mortality. Further, nosocomial pneumonia is associated with gram-negative pathogens such as Pseudomonas aeruginosa and Enterobacteriaceae that may carry extended-spectrum beta-lactamases and carbapenemase, thereby limiting the treatment options. However, ceftazidime-avibactam has both antipseudomonal and extended beta-lactamase coverage for multidrug-resistant gram-negative infections, and may provide an alternative to meropenem.
Antoni Torres, MD, of the University of Barcelona and his colleagues sought to compare the safety and efficacy of ceftazidime-avibactam to meropenem in patients with nosocomial and ventilator-associated pneumonia. The REPROVE study was a phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries. Patients were randomly assigned 1:1 to receive either ceftazidime-avibactam (500-2,000 mg every 8 hours) or meropenem (1,000 mg every 8 hours) with adjustment as needed for renal function.
Participants included in the study were 18-90 years of age with nosocomial pneumonia as evidenced by pneumonia 48 hours or more after admission or within 7 days after discharge from an inpatient facility. Patients with ventilator-associated pneumonia had lung infection within 48 hours of intubation and mechanical ventilation. Sputum culture and gram stains were obtained within 48 hours before randomization, and patients were excluded for evidence of gram-positive–only pathogens or those not expected to respond to meropenem or ceftazidime-avibactam.
The study involved a safety population (808 patients), a clinically modified intention-to-treat population (726), and a clinically evaluable population (527). The intention-to-treat population demonstrated a predominance of Klebsiella pneumoniae (37%), and Pseudomonas aeruginosa (30%); 28% of the intention-to-treat population were identified as not susceptible to ceftazidime.
Overall, the clinically modified intention-to-treat group demonstrated a clinical cure rate of 68.8% (245/356) in the ceftazidime-avibactam and 73.0% (270/370) for the meropenem group (difference, –4.2%; 95% confidence interval, –10.8 to 2.5). The evaluable population demonstrated a clinical cure rate of 77.4% (199/257) in the ceftazidime-avibactam group and 78.1% (211/270) in the meropenem group (–0.7%; 95% CI, –7.9 to 6.4).
The all-cause mortality rate was similar between groups at the test-of-cure date and at day 28. The clinically modified intention-to-treat population demonstrated a mortality of 8.1% vs. 6.8% at the test-of-cure date and 8.4% vs. 7.3% at day 28 for ceftazidime-avibactam and meropenem, respectively.
Adverse events were noted in 75% vs. 74% of patients in the ceftazidime-avibactam groups and meropenem groups, respectively. Most adverse events were rated as mild to moderate and deemed likely unrelated to the treatment.
However, serious adverse events occurred in 19% (n = 75) in the ceftazidime-avibactam group and 13% (n = 54) in the meropenem group. Four serious adverse events were thought to be possibly related to the study drug ceftazidime-avibactam and included diarrhea, acute coronary syndrome, subacute hepatic failure, and abnormal liver function test results. The authors noted the adverse events in the trial were consistent and detected no new safety concerns for ceftazidime-avibactam.
Limitations of the study included an inability to establish the optimal duration of treatment for nosocomial pneumonia treated with meropenem or ceftazidime-avibactam.
“Our results show noninferiority for the treatment of nosocomial pneumonia caused by ceftazidime-nonsusceptible or ceftazidime-susceptible gram-negative aerobic pathogens,” the authors concluded.
The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
SOURCE: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia including ventilator-associated pneumonia from gram-negative organisms, results from the REPROVE trial demonstrated.
Nosocomial or hospital-acquired pneumonia is a common hospital-acquired infection associated with increased cost and mortality. Further, nosocomial pneumonia is associated with gram-negative pathogens such as Pseudomonas aeruginosa and Enterobacteriaceae that may carry extended-spectrum beta-lactamases and carbapenemase, thereby limiting the treatment options. However, ceftazidime-avibactam has both antipseudomonal and extended beta-lactamase coverage for multidrug-resistant gram-negative infections, and may provide an alternative to meropenem.
Antoni Torres, MD, of the University of Barcelona and his colleagues sought to compare the safety and efficacy of ceftazidime-avibactam to meropenem in patients with nosocomial and ventilator-associated pneumonia. The REPROVE study was a phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries. Patients were randomly assigned 1:1 to receive either ceftazidime-avibactam (500-2,000 mg every 8 hours) or meropenem (1,000 mg every 8 hours) with adjustment as needed for renal function.
Participants included in the study were 18-90 years of age with nosocomial pneumonia as evidenced by pneumonia 48 hours or more after admission or within 7 days after discharge from an inpatient facility. Patients with ventilator-associated pneumonia had lung infection within 48 hours of intubation and mechanical ventilation. Sputum culture and gram stains were obtained within 48 hours before randomization, and patients were excluded for evidence of gram-positive–only pathogens or those not expected to respond to meropenem or ceftazidime-avibactam.
The study involved a safety population (808 patients), a clinically modified intention-to-treat population (726), and a clinically evaluable population (527). The intention-to-treat population demonstrated a predominance of Klebsiella pneumoniae (37%), and Pseudomonas aeruginosa (30%); 28% of the intention-to-treat population were identified as not susceptible to ceftazidime.
Overall, the clinically modified intention-to-treat group demonstrated a clinical cure rate of 68.8% (245/356) in the ceftazidime-avibactam and 73.0% (270/370) for the meropenem group (difference, –4.2%; 95% confidence interval, –10.8 to 2.5). The evaluable population demonstrated a clinical cure rate of 77.4% (199/257) in the ceftazidime-avibactam group and 78.1% (211/270) in the meropenem group (–0.7%; 95% CI, –7.9 to 6.4).
The all-cause mortality rate was similar between groups at the test-of-cure date and at day 28. The clinically modified intention-to-treat population demonstrated a mortality of 8.1% vs. 6.8% at the test-of-cure date and 8.4% vs. 7.3% at day 28 for ceftazidime-avibactam and meropenem, respectively.
Adverse events were noted in 75% vs. 74% of patients in the ceftazidime-avibactam groups and meropenem groups, respectively. Most adverse events were rated as mild to moderate and deemed likely unrelated to the treatment.
However, serious adverse events occurred in 19% (n = 75) in the ceftazidime-avibactam group and 13% (n = 54) in the meropenem group. Four serious adverse events were thought to be possibly related to the study drug ceftazidime-avibactam and included diarrhea, acute coronary syndrome, subacute hepatic failure, and abnormal liver function test results. The authors noted the adverse events in the trial were consistent and detected no new safety concerns for ceftazidime-avibactam.
Limitations of the study included an inability to establish the optimal duration of treatment for nosocomial pneumonia treated with meropenem or ceftazidime-avibactam.
“Our results show noninferiority for the treatment of nosocomial pneumonia caused by ceftazidime-nonsusceptible or ceftazidime-susceptible gram-negative aerobic pathogens,” the authors concluded.
The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
SOURCE: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia including ventilator-associated pneumonia from gram-negative organisms, results from the REPROVE trial demonstrated.
Nosocomial or hospital-acquired pneumonia is a common hospital-acquired infection associated with increased cost and mortality. Further, nosocomial pneumonia is associated with gram-negative pathogens such as Pseudomonas aeruginosa and Enterobacteriaceae that may carry extended-spectrum beta-lactamases and carbapenemase, thereby limiting the treatment options. However, ceftazidime-avibactam has both antipseudomonal and extended beta-lactamase coverage for multidrug-resistant gram-negative infections, and may provide an alternative to meropenem.
Antoni Torres, MD, of the University of Barcelona and his colleagues sought to compare the safety and efficacy of ceftazidime-avibactam to meropenem in patients with nosocomial and ventilator-associated pneumonia. The REPROVE study was a phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries. Patients were randomly assigned 1:1 to receive either ceftazidime-avibactam (500-2,000 mg every 8 hours) or meropenem (1,000 mg every 8 hours) with adjustment as needed for renal function.
Participants included in the study were 18-90 years of age with nosocomial pneumonia as evidenced by pneumonia 48 hours or more after admission or within 7 days after discharge from an inpatient facility. Patients with ventilator-associated pneumonia had lung infection within 48 hours of intubation and mechanical ventilation. Sputum culture and gram stains were obtained within 48 hours before randomization, and patients were excluded for evidence of gram-positive–only pathogens or those not expected to respond to meropenem or ceftazidime-avibactam.
The study involved a safety population (808 patients), a clinically modified intention-to-treat population (726), and a clinically evaluable population (527). The intention-to-treat population demonstrated a predominance of Klebsiella pneumoniae (37%), and Pseudomonas aeruginosa (30%); 28% of the intention-to-treat population were identified as not susceptible to ceftazidime.
Overall, the clinically modified intention-to-treat group demonstrated a clinical cure rate of 68.8% (245/356) in the ceftazidime-avibactam and 73.0% (270/370) for the meropenem group (difference, –4.2%; 95% confidence interval, –10.8 to 2.5). The evaluable population demonstrated a clinical cure rate of 77.4% (199/257) in the ceftazidime-avibactam group and 78.1% (211/270) in the meropenem group (–0.7%; 95% CI, –7.9 to 6.4).
The all-cause mortality rate was similar between groups at the test-of-cure date and at day 28. The clinically modified intention-to-treat population demonstrated a mortality of 8.1% vs. 6.8% at the test-of-cure date and 8.4% vs. 7.3% at day 28 for ceftazidime-avibactam and meropenem, respectively.
Adverse events were noted in 75% vs. 74% of patients in the ceftazidime-avibactam groups and meropenem groups, respectively. Most adverse events were rated as mild to moderate and deemed likely unrelated to the treatment.
However, serious adverse events occurred in 19% (n = 75) in the ceftazidime-avibactam group and 13% (n = 54) in the meropenem group. Four serious adverse events were thought to be possibly related to the study drug ceftazidime-avibactam and included diarrhea, acute coronary syndrome, subacute hepatic failure, and abnormal liver function test results. The authors noted the adverse events in the trial were consistent and detected no new safety concerns for ceftazidime-avibactam.
Limitations of the study included an inability to establish the optimal duration of treatment for nosocomial pneumonia treated with meropenem or ceftazidime-avibactam.
“Our results show noninferiority for the treatment of nosocomial pneumonia caused by ceftazidime-nonsusceptible or ceftazidime-susceptible gram-negative aerobic pathogens,” the authors concluded.
The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
SOURCE: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
FROM THE LANCET INFECTIOUS DISEASES
Key clinical point: Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia.
Major finding: The clinically modified intention-to-treat group demonstrated clinical cure rates of 69% and 73% in the ceftazidime-avibactam vs. the meropenem group, respectively.
Data source: A phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries.
Disclosures: The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
Source: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
Paring the risk of antibiotic resistance
One unintended consequence of the increased attention to early sepsis identification and intervention can be unnecessary or excessive antibiotic use. Overuse of broad-spectrum antibiotics, in turn, can fuel the emergence of life-threatening infections such as antibiotic-resistant Clostridium difficile, a scourge in many hospitals.
For a sepsis quality improvement (QI) initiative at the University of Utah, Salt Lake City, the hospitalist coleaders took several precautions to lessen the risk of antibiotic overuse. Kencee K. Graves, MD, said she and her colleague Devin J. Horton, MD, designed the hospital’s order sets in collaboration with an infectious disease specialist and pharmacist so they could avoid overly broad antibiotics whenever possible. The project also included an educational effort to get pharmacists in the habit of prompting medical providers to initiate antibiotic de-escalation at 48 hours. The hospital had an antibiotic stewardship program that likely helped as well, she said. As a result of their precautions, the team found no significant difference in the amount of broad-spectrum antibiotics doled out before and after their QI pilot project.
Infection control and antimicrobial specialists also can help; they can monitor an area’s resistance profile, create a antibiogram and reevaluate sepsis pathways and order sets to adjust the recommended antibiotics as the resistance profile changes. “I think we still have a long ways to go,” said Andy Odden, MD, SFHM, patient safety officer in the department of medicine at Washington University in St. Louis. “The initial risk of mortality is so much more dramatic than the long-term risks of developing antimicrobial resistors that unless you have the antimicrobial stewardship people with a seat at the table, that voice can get drowned out very easily.”
The antimicrobial stewardship program at University of Pennsylvania, Philadelphia, has received a boost from technology. The program offers initial guidance on which broad-spectrum antibiotics to consider depending on the suspected source of the sepsis-linked infection. Software by Jackson, Wyo.–based biotech company Teqqa also synthesizes the university hospital’s resistance data based on blood, urine, and sputum cultures. “It can predict the antibiotic sensitivity of a given bug growing out of a given culture on a given unit,” said Craig A. Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine at the university.
The bigger issue, Dr. Umscheid said, is when and how to de-escalate antibiotic treatment. “If somebody is feeling better in 48 hours or 72 hours and no cultures have grown back, they have no more fever, and their white counts have normalized, do you start pulling off the antibiotics slowly and, if so, how do you do that?” Several trials are examining such questions, including a multicenter collaboration called DETOURS (De-Escalating Empiric Treatment: Opting-Out of Rx for Selected Patients With Suspected Sepsis). One of the trial’s chief aims is to set up a new opt-out protocol for acute care patients in the wards.
One unintended consequence of the increased attention to early sepsis identification and intervention can be unnecessary or excessive antibiotic use. Overuse of broad-spectrum antibiotics, in turn, can fuel the emergence of life-threatening infections such as antibiotic-resistant Clostridium difficile, a scourge in many hospitals.
For a sepsis quality improvement (QI) initiative at the University of Utah, Salt Lake City, the hospitalist coleaders took several precautions to lessen the risk of antibiotic overuse. Kencee K. Graves, MD, said she and her colleague Devin J. Horton, MD, designed the hospital’s order sets in collaboration with an infectious disease specialist and pharmacist so they could avoid overly broad antibiotics whenever possible. The project also included an educational effort to get pharmacists in the habit of prompting medical providers to initiate antibiotic de-escalation at 48 hours. The hospital had an antibiotic stewardship program that likely helped as well, she said. As a result of their precautions, the team found no significant difference in the amount of broad-spectrum antibiotics doled out before and after their QI pilot project.
Infection control and antimicrobial specialists also can help; they can monitor an area’s resistance profile, create a antibiogram and reevaluate sepsis pathways and order sets to adjust the recommended antibiotics as the resistance profile changes. “I think we still have a long ways to go,” said Andy Odden, MD, SFHM, patient safety officer in the department of medicine at Washington University in St. Louis. “The initial risk of mortality is so much more dramatic than the long-term risks of developing antimicrobial resistors that unless you have the antimicrobial stewardship people with a seat at the table, that voice can get drowned out very easily.”
The antimicrobial stewardship program at University of Pennsylvania, Philadelphia, has received a boost from technology. The program offers initial guidance on which broad-spectrum antibiotics to consider depending on the suspected source of the sepsis-linked infection. Software by Jackson, Wyo.–based biotech company Teqqa also synthesizes the university hospital’s resistance data based on blood, urine, and sputum cultures. “It can predict the antibiotic sensitivity of a given bug growing out of a given culture on a given unit,” said Craig A. Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine at the university.
The bigger issue, Dr. Umscheid said, is when and how to de-escalate antibiotic treatment. “If somebody is feeling better in 48 hours or 72 hours and no cultures have grown back, they have no more fever, and their white counts have normalized, do you start pulling off the antibiotics slowly and, if so, how do you do that?” Several trials are examining such questions, including a multicenter collaboration called DETOURS (De-Escalating Empiric Treatment: Opting-Out of Rx for Selected Patients With Suspected Sepsis). One of the trial’s chief aims is to set up a new opt-out protocol for acute care patients in the wards.
One unintended consequence of the increased attention to early sepsis identification and intervention can be unnecessary or excessive antibiotic use. Overuse of broad-spectrum antibiotics, in turn, can fuel the emergence of life-threatening infections such as antibiotic-resistant Clostridium difficile, a scourge in many hospitals.
For a sepsis quality improvement (QI) initiative at the University of Utah, Salt Lake City, the hospitalist coleaders took several precautions to lessen the risk of antibiotic overuse. Kencee K. Graves, MD, said she and her colleague Devin J. Horton, MD, designed the hospital’s order sets in collaboration with an infectious disease specialist and pharmacist so they could avoid overly broad antibiotics whenever possible. The project also included an educational effort to get pharmacists in the habit of prompting medical providers to initiate antibiotic de-escalation at 48 hours. The hospital had an antibiotic stewardship program that likely helped as well, she said. As a result of their precautions, the team found no significant difference in the amount of broad-spectrum antibiotics doled out before and after their QI pilot project.
Infection control and antimicrobial specialists also can help; they can monitor an area’s resistance profile, create a antibiogram and reevaluate sepsis pathways and order sets to adjust the recommended antibiotics as the resistance profile changes. “I think we still have a long ways to go,” said Andy Odden, MD, SFHM, patient safety officer in the department of medicine at Washington University in St. Louis. “The initial risk of mortality is so much more dramatic than the long-term risks of developing antimicrobial resistors that unless you have the antimicrobial stewardship people with a seat at the table, that voice can get drowned out very easily.”
The antimicrobial stewardship program at University of Pennsylvania, Philadelphia, has received a boost from technology. The program offers initial guidance on which broad-spectrum antibiotics to consider depending on the suspected source of the sepsis-linked infection. Software by Jackson, Wyo.–based biotech company Teqqa also synthesizes the university hospital’s resistance data based on blood, urine, and sputum cultures. “It can predict the antibiotic sensitivity of a given bug growing out of a given culture on a given unit,” said Craig A. Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine at the university.
The bigger issue, Dr. Umscheid said, is when and how to de-escalate antibiotic treatment. “If somebody is feeling better in 48 hours or 72 hours and no cultures have grown back, they have no more fever, and their white counts have normalized, do you start pulling off the antibiotics slowly and, if so, how do you do that?” Several trials are examining such questions, including a multicenter collaboration called DETOURS (De-Escalating Empiric Treatment: Opting-Out of Rx for Selected Patients With Suspected Sepsis). One of the trial’s chief aims is to set up a new opt-out protocol for acute care patients in the wards.
Psychiatric issues common among hepatitis C inpatients
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
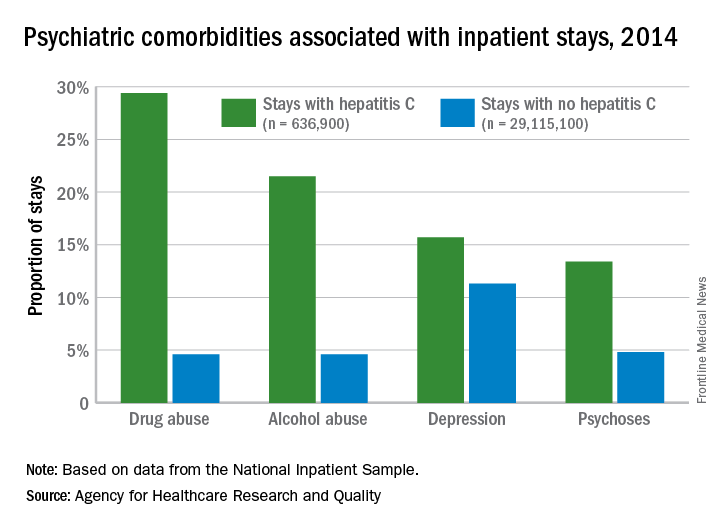
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
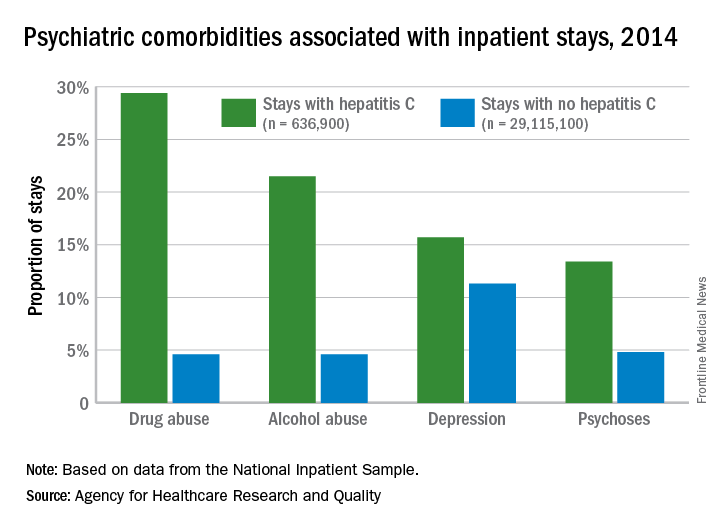
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
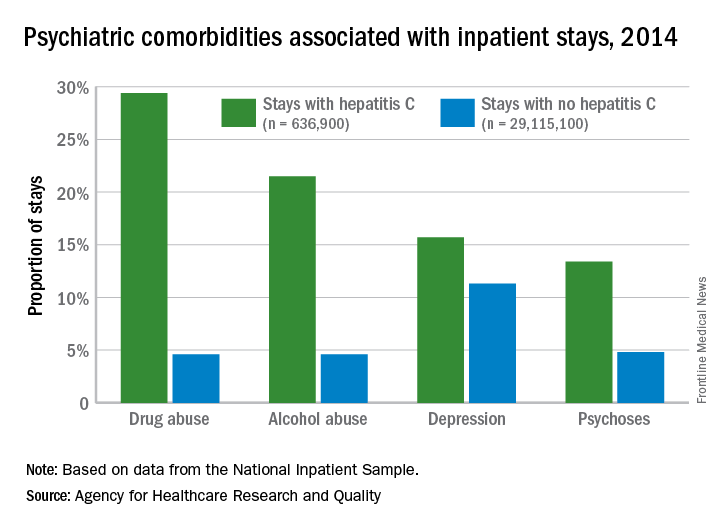
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Drug combo indicated for bacterial pneumonia
(Avycaz) to include hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) in adults.
Specifically, the approved indication is for infections caused by certain Gram-negative bacteria – some of which are increasingly resistant to available antibiotics – including, Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, Pseudomonas aeruginosa, and Haemophilus influenzae.
There have not been new treatment options for HABP/VABP caused by Gram-negative bacteria in more than 15 years, according to Allergan, the drug’s manufacturer.
This is the third approved indication for ceftazidime/avibactam; the other two indications are for complicated intra-abdominal infections (in combination with metronidazole) and for complicated urinary tract infections.
(Avycaz) to include hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) in adults.
Specifically, the approved indication is for infections caused by certain Gram-negative bacteria – some of which are increasingly resistant to available antibiotics – including, Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, Pseudomonas aeruginosa, and Haemophilus influenzae.
There have not been new treatment options for HABP/VABP caused by Gram-negative bacteria in more than 15 years, according to Allergan, the drug’s manufacturer.
This is the third approved indication for ceftazidime/avibactam; the other two indications are for complicated intra-abdominal infections (in combination with metronidazole) and for complicated urinary tract infections.
(Avycaz) to include hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) in adults.
Specifically, the approved indication is for infections caused by certain Gram-negative bacteria – some of which are increasingly resistant to available antibiotics – including, Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, Pseudomonas aeruginosa, and Haemophilus influenzae.
There have not been new treatment options for HABP/VABP caused by Gram-negative bacteria in more than 15 years, according to Allergan, the drug’s manufacturer.
This is the third approved indication for ceftazidime/avibactam; the other two indications are for complicated intra-abdominal infections (in combination with metronidazole) and for complicated urinary tract infections.
Hospitals filling as flu season worsens
Through the last full week of January, the cumulative “hospitalization rate is the highest we’ve seen,” acting Centers for Disease Control and Prevention director Anne Schuchat, MD, said. For the current season so far, the hospitalization rate stands at 51.4 per 100,000 population, putting it on pace to top the total of 710,000 flu-related admissions that occurred during the 2014-2015 season, she said in a weekly briefing Feb. 2.
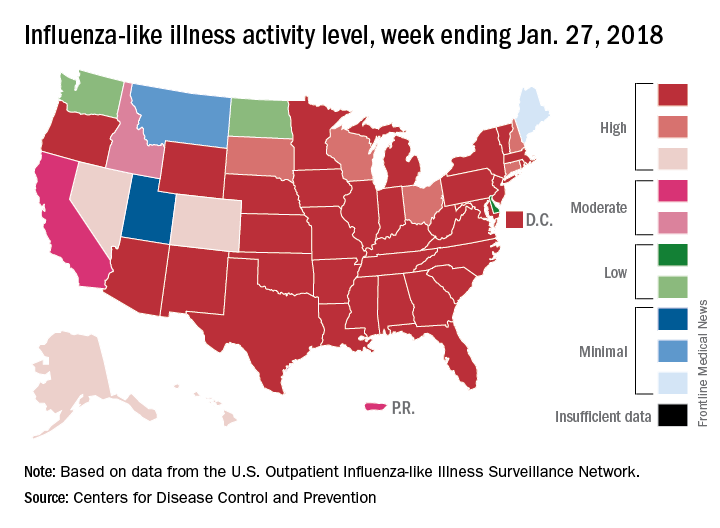
Flu-related pediatric deaths also took a big jump for the week as another 16 were reported, which brings the total for the season to 53. Of the children who have died so far, only 20% were vaccinated, said Dan Jernigan, MD, MPH, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta. He also noted that half of the children who have been hospitalized did not had an underlying condition.
The one bit of good news for the week was that activity in the West seems to be easing up, Dr. Schuchat said. The geographic spread of ILI was reported as widespread in 48 states, which is down from 49 the previous week because Oregon dropped off the list. To go along with that, the ILI activity level in California has dropped 2 weeks in a row and now stands at level 7, the CDC data show.
Through the last full week of January, the cumulative “hospitalization rate is the highest we’ve seen,” acting Centers for Disease Control and Prevention director Anne Schuchat, MD, said. For the current season so far, the hospitalization rate stands at 51.4 per 100,000 population, putting it on pace to top the total of 710,000 flu-related admissions that occurred during the 2014-2015 season, she said in a weekly briefing Feb. 2.
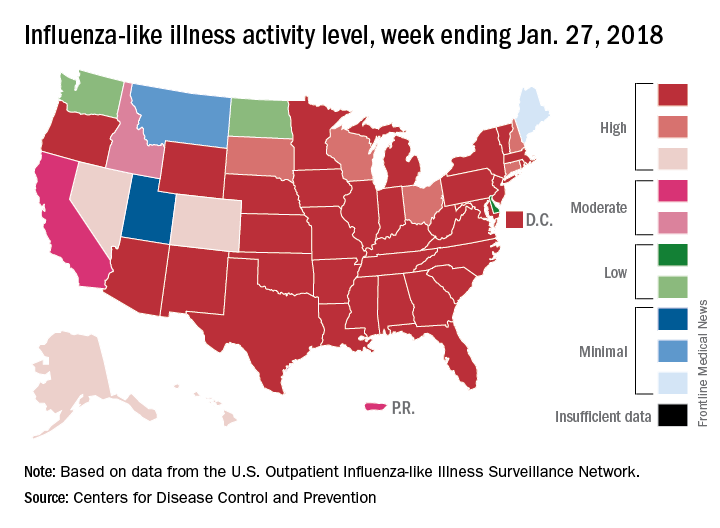
Flu-related pediatric deaths also took a big jump for the week as another 16 were reported, which brings the total for the season to 53. Of the children who have died so far, only 20% were vaccinated, said Dan Jernigan, MD, MPH, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta. He also noted that half of the children who have been hospitalized did not had an underlying condition.
The one bit of good news for the week was that activity in the West seems to be easing up, Dr. Schuchat said. The geographic spread of ILI was reported as widespread in 48 states, which is down from 49 the previous week because Oregon dropped off the list. To go along with that, the ILI activity level in California has dropped 2 weeks in a row and now stands at level 7, the CDC data show.
Through the last full week of January, the cumulative “hospitalization rate is the highest we’ve seen,” acting Centers for Disease Control and Prevention director Anne Schuchat, MD, said. For the current season so far, the hospitalization rate stands at 51.4 per 100,000 population, putting it on pace to top the total of 710,000 flu-related admissions that occurred during the 2014-2015 season, she said in a weekly briefing Feb. 2.
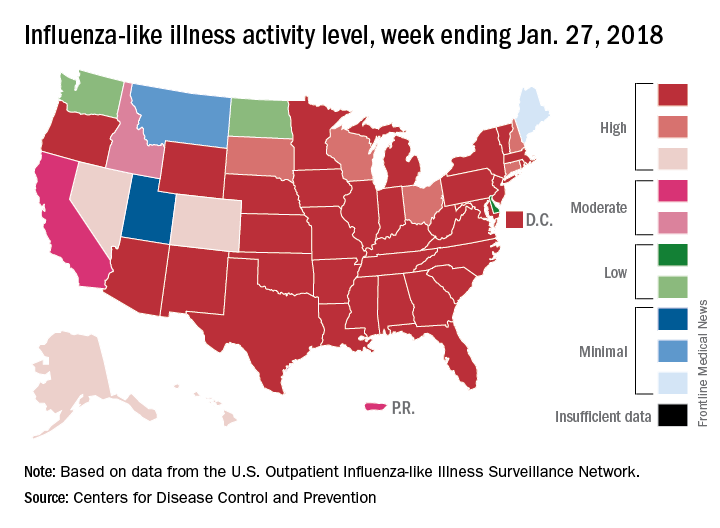
Flu-related pediatric deaths also took a big jump for the week as another 16 were reported, which brings the total for the season to 53. Of the children who have died so far, only 20% were vaccinated, said Dan Jernigan, MD, MPH, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta. He also noted that half of the children who have been hospitalized did not had an underlying condition.
The one bit of good news for the week was that activity in the West seems to be easing up, Dr. Schuchat said. The geographic spread of ILI was reported as widespread in 48 states, which is down from 49 the previous week because Oregon dropped off the list. To go along with that, the ILI activity level in California has dropped 2 weeks in a row and now stands at level 7, the CDC data show.
Preventing sepsis alert fatigue
If they’re too infrequent, alerts can delay sepsis identification and treatment. If they’re too abundant, the alerts can overwhelm providers. Finding the sweet spot for sepsis alerts, QI leaders say, can require time, technology, patience – and sometimes trial and error.
University Hospital in Salt Lake City wanted to broaden its sepsis recognition system to ensure that decompensating patients were seen and resuscitated quickly, regardless of the cause. Another hospital offered a lesson in what not to do when a staff member cautioned that a sepsis alert system based on SIRS alone had been a “total disaster” and left providers fuming. One report suggested that nearly half of all ward patients meet SIRS criteria at some point during their hospitalization, and that using the criteria for sepsis screening in hospital wards is both “time consuming and impractical.”1
Instead, University Hospital tweaked its MEWS or Modified Early Warning System, based on consultations with hospitalists, ICU physicians, and other providers about the appropriate thresholds for vital signs. “It’s kind of like asking someone, ‘Well, when are you really scared of the heart rate and when are you sort of scared and when are you not scared at all?’ ” said project coleader Devin J. Horton, MD, an academic hospitalist.
The team also analyzed the number of alerts per week per unit and their sensitivity and specificity in detecting sepsis. As junior faculty members, Dr. Horton and his collaborator, academic hospitalist Kencee K. Graves, MD, were mindful to avoid angering other doctors over being alerted too often. For their MEWS scoring system, they sacrificed a bit of sensitivity to ensure that the number of alerts remained manageable.
Before going live with its own new alert system, Middlesex Hospital in Middletown, Conn., had a subgroup spend several weeks testing the system in silent mode and tweaking different parameters such as respiratory rate and heart rate to reduce the potential for too many alerts. “If you look at each and every alert, then you can identify how to make your adjustment so that it’s not overly sensitive,” said Terri Savino, MSN, RN, CPHQ, the hospital’s manager of patient experience and service excellence.
A sepsis task force also shared data showing the hospital’s significant reductions in sepsis mortality, total hospital mortality, and sepsis length of stay. “Medical staff were willing to accept the frequency and high sensitivity of the alert because the data demonstrated that it was making a difference in the lives of our patients,” said David M. Cosentino, MD, the hospital’s chief medical information officer.
Other alert systems’ mixed performances have yielded important lessons. At the University of Pennsylvania, Philadelphia, one prototype detected clinically deteriorating patients and sent an alert to the nurse, physician, and a rapid response team. Alerted providers converged on the patient’s bedside within 30 minutes and decided whether to elevate the level of care. Craig Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine, said the system was associated with a suggestion of reduced mortality.2 But it was noisy and less helpful than it could have been, he said, because it didn’t separate out declining patients already known to the team from those who were still unrecognized.
Tools to predict which patients may develop severe sepsis or septic shock have worked even less well, he said. One triggered an alarm before patients showed signs of clinical deterioration. “The team didn’t know what to do with that prediction,” Dr. Umscheid said. As a result, the alert didn’t improve mortality or discharges to home. “If you’re making this prediction too early and providers don’t know what to do with the information, it’s not going to change care or affect patient outcomes,” he said. “It’s just going to frustrate providers.”
References
1. Churpek MM et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015 Oct 15;192(8):958-64.
2. Umscheid CA et al. Development, implementation, and impact of an automated early warning and response system for sepsis. J Hosp Med. 2015 Jan;10: 26-31.
If they’re too infrequent, alerts can delay sepsis identification and treatment. If they’re too abundant, the alerts can overwhelm providers. Finding the sweet spot for sepsis alerts, QI leaders say, can require time, technology, patience – and sometimes trial and error.
University Hospital in Salt Lake City wanted to broaden its sepsis recognition system to ensure that decompensating patients were seen and resuscitated quickly, regardless of the cause. Another hospital offered a lesson in what not to do when a staff member cautioned that a sepsis alert system based on SIRS alone had been a “total disaster” and left providers fuming. One report suggested that nearly half of all ward patients meet SIRS criteria at some point during their hospitalization, and that using the criteria for sepsis screening in hospital wards is both “time consuming and impractical.”1
Instead, University Hospital tweaked its MEWS or Modified Early Warning System, based on consultations with hospitalists, ICU physicians, and other providers about the appropriate thresholds for vital signs. “It’s kind of like asking someone, ‘Well, when are you really scared of the heart rate and when are you sort of scared and when are you not scared at all?’ ” said project coleader Devin J. Horton, MD, an academic hospitalist.
The team also analyzed the number of alerts per week per unit and their sensitivity and specificity in detecting sepsis. As junior faculty members, Dr. Horton and his collaborator, academic hospitalist Kencee K. Graves, MD, were mindful to avoid angering other doctors over being alerted too often. For their MEWS scoring system, they sacrificed a bit of sensitivity to ensure that the number of alerts remained manageable.
Before going live with its own new alert system, Middlesex Hospital in Middletown, Conn., had a subgroup spend several weeks testing the system in silent mode and tweaking different parameters such as respiratory rate and heart rate to reduce the potential for too many alerts. “If you look at each and every alert, then you can identify how to make your adjustment so that it’s not overly sensitive,” said Terri Savino, MSN, RN, CPHQ, the hospital’s manager of patient experience and service excellence.
A sepsis task force also shared data showing the hospital’s significant reductions in sepsis mortality, total hospital mortality, and sepsis length of stay. “Medical staff were willing to accept the frequency and high sensitivity of the alert because the data demonstrated that it was making a difference in the lives of our patients,” said David M. Cosentino, MD, the hospital’s chief medical information officer.
Other alert systems’ mixed performances have yielded important lessons. At the University of Pennsylvania, Philadelphia, one prototype detected clinically deteriorating patients and sent an alert to the nurse, physician, and a rapid response team. Alerted providers converged on the patient’s bedside within 30 minutes and decided whether to elevate the level of care. Craig Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine, said the system was associated with a suggestion of reduced mortality.2 But it was noisy and less helpful than it could have been, he said, because it didn’t separate out declining patients already known to the team from those who were still unrecognized.
Tools to predict which patients may develop severe sepsis or septic shock have worked even less well, he said. One triggered an alarm before patients showed signs of clinical deterioration. “The team didn’t know what to do with that prediction,” Dr. Umscheid said. As a result, the alert didn’t improve mortality or discharges to home. “If you’re making this prediction too early and providers don’t know what to do with the information, it’s not going to change care or affect patient outcomes,” he said. “It’s just going to frustrate providers.”
References
1. Churpek MM et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015 Oct 15;192(8):958-64.
2. Umscheid CA et al. Development, implementation, and impact of an automated early warning and response system for sepsis. J Hosp Med. 2015 Jan;10: 26-31.
If they’re too infrequent, alerts can delay sepsis identification and treatment. If they’re too abundant, the alerts can overwhelm providers. Finding the sweet spot for sepsis alerts, QI leaders say, can require time, technology, patience – and sometimes trial and error.
University Hospital in Salt Lake City wanted to broaden its sepsis recognition system to ensure that decompensating patients were seen and resuscitated quickly, regardless of the cause. Another hospital offered a lesson in what not to do when a staff member cautioned that a sepsis alert system based on SIRS alone had been a “total disaster” and left providers fuming. One report suggested that nearly half of all ward patients meet SIRS criteria at some point during their hospitalization, and that using the criteria for sepsis screening in hospital wards is both “time consuming and impractical.”1
Instead, University Hospital tweaked its MEWS or Modified Early Warning System, based on consultations with hospitalists, ICU physicians, and other providers about the appropriate thresholds for vital signs. “It’s kind of like asking someone, ‘Well, when are you really scared of the heart rate and when are you sort of scared and when are you not scared at all?’ ” said project coleader Devin J. Horton, MD, an academic hospitalist.
The team also analyzed the number of alerts per week per unit and their sensitivity and specificity in detecting sepsis. As junior faculty members, Dr. Horton and his collaborator, academic hospitalist Kencee K. Graves, MD, were mindful to avoid angering other doctors over being alerted too often. For their MEWS scoring system, they sacrificed a bit of sensitivity to ensure that the number of alerts remained manageable.
Before going live with its own new alert system, Middlesex Hospital in Middletown, Conn., had a subgroup spend several weeks testing the system in silent mode and tweaking different parameters such as respiratory rate and heart rate to reduce the potential for too many alerts. “If you look at each and every alert, then you can identify how to make your adjustment so that it’s not overly sensitive,” said Terri Savino, MSN, RN, CPHQ, the hospital’s manager of patient experience and service excellence.
A sepsis task force also shared data showing the hospital’s significant reductions in sepsis mortality, total hospital mortality, and sepsis length of stay. “Medical staff were willing to accept the frequency and high sensitivity of the alert because the data demonstrated that it was making a difference in the lives of our patients,” said David M. Cosentino, MD, the hospital’s chief medical information officer.
Other alert systems’ mixed performances have yielded important lessons. At the University of Pennsylvania, Philadelphia, one prototype detected clinically deteriorating patients and sent an alert to the nurse, physician, and a rapid response team. Alerted providers converged on the patient’s bedside within 30 minutes and decided whether to elevate the level of care. Craig Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine, said the system was associated with a suggestion of reduced mortality.2 But it was noisy and less helpful than it could have been, he said, because it didn’t separate out declining patients already known to the team from those who were still unrecognized.
Tools to predict which patients may develop severe sepsis or septic shock have worked even less well, he said. One triggered an alarm before patients showed signs of clinical deterioration. “The team didn’t know what to do with that prediction,” Dr. Umscheid said. As a result, the alert didn’t improve mortality or discharges to home. “If you’re making this prediction too early and providers don’t know what to do with the information, it’s not going to change care or affect patient outcomes,” he said. “It’s just going to frustrate providers.”
References
1. Churpek MM et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015 Oct 15;192(8):958-64.
2. Umscheid CA et al. Development, implementation, and impact of an automated early warning and response system for sepsis. J Hosp Med. 2015 Jan;10: 26-31.
Controversy surrounds calf vein thrombosis treatment
CHICAGO – The use of therapeutic-dose anticoagulation in hospitalized patients with calf vein thrombosis significantly reduces the risk of venous thromboembolic complications, compared with lower-dose prophylactic anticoagulation or surveillance alone, Heron E. Rodriguez, MD, said at a symposium on vascular surgery sponsored by Northwestern University.
Moreover, placement of an inferior vena cava filter in patients with calf vein thrombosis when anticoagulation is contraindicated accomplishes nothing beneficial and had a 10% complication rate in a large retrospective single-center study, added Dr. Rodriguez of Northwestern University, Chicago.
Deep vein thrombosis (DVT) remains a significant source of morbidity and mortality despite worldwide awareness of the problem.
“Specifically, calf vein thrombosis [CVT] is very common, and we know that in some series up to 30% of patients end up propagating proximally if they’re not treated, and a good number of them develop chronic venous insufficiency, with long-term consequences,” he noted.
“Unfortunately there is no consensus regarding treatment. The guidelines are very vague. For example, there is no mention [in current American College of Chest Physicians guidelines] of how to manage muscular vein thrombosis and much ambiguity on how to treat calf vein thrombosis,” he continued.
Dr. Rodriguez cited as an indication of the lack of consensus on management of CVT a single-institution survey by other investigators of the practices of physicians in various specialties. Forty-nine percent of respondents indicated they anticoagulate patients with CVT; 51% don’t. Of those who did, 62% prescribed low-molecular-weight heparin and 11% intravenous heparin. Fifty-eight percent of physicians who anticoagulated did so for 3 months, 30% for 6. And 46% of physicians used an inferior vena cava (IVC) filter when anticoagulation was contraindicated (Vascular. 2014 Apr;22[2]:93-7).
That rate of IVC placement “seemed really high” given the paucity of supporting evidence for safety and efficacy of filter placement in the setting of CVT, so Dr. Rodriguez and coinvestigators decided to conduct a retrospective review of practices at Northwestern Memorial Hospital. He explained the study hypothesis: “Our thinking was that these kinds of thrombi are associated with low risk of propagation and pulmonary embolism, and they can and should be managed conservatively.”
Of 647 patients with isolated thrombosis of the anterior and posterior tibial, soleal, peroneal, or gastrocnemius veins, 44% received an IVC filter, and the rest got medical treatment alone. Of the 362 patients managed medically, 49% received therapeutic anticoagulation, 12% got low-dose prophylactic anticoagulation, and 39% underwent surveillance without anticoagulation.
The primary outcome was the incidence of venous thromboembolic complications – that is, propagation of DVT or pulmonary embolism. The incidence was 35% in the surveillance-only group, 30% with prophylactic anticoagulation, and 10% in patients who got therapeutic anticoagulation.
Of note, the rate of the most feared complication, pulmonary embolism, was low and similar in the filter recipients and medically managed group: 2.5% in the IVC group, 3.3% with medical management.
“Distal vein thromboses have low rates of pulmonary embolism, regardless of whether or not they are so-called protected with a filter. On the other hand, a filter was associated with a 10% rate of complications. I have to make clear that these were radiographic abnormalities – tilting, migration, caval perforation – that didn’t have clinical consequences, but we were very aggressive in removing the IVC filters, and I’m guessing if they’d been left inside they would create problems in the long term,” Dr. Rodriguez said.
An important point about this study is that these were all sick patients, and most were hospitalized. The filter recipients and medical groups differed in key ways. For example, 49% of the filter patients had a malignancy, and 56% had a baseline history of venous thromboembolic events, compared with 26% and 16%, respectively, of the medical group. For that reason, the investigators performed propensity score matching and came up with 157 closely matched patient pairs. The outcomes remained unchanged.
Of course, this was a retrospective study, with its inherent limitations, but Dr. Rodriguez characterized the published randomized trials on management of CVT as “small and limited.” The most frequently quoted study is the double-blind multicenter CACTUS trial, which randomized 252 outpatients with symptomatic CVT to 6 weeks of low-molecular-weight heparin or placebo and found no difference in the rates of proximal extension of venous thromboembolic events (Lancet Haematol. 2016 Dec;3[12]:e556-62). But these were all low-risk patients. Prior DVT or malignancy were exclusion criteria, so this was a very different population than treated at Northwestern.
Based upon the results of the retrospective study at Northwestern, which have been published (J Vasc Surg Venous Lymphat Disord. 2017 Jan;5[1]:25-32), the vascular surgery service has developed a management algorithm for DVT management based upon the lesion site. If a patient is unable to undergo anticoagulation, venous duplex ultrasound is repeated at 1 week. If the imaging shows propagation into the popliteal vein and anticoagulation remains contraindicated, only then is placement of an IVC filter warranted.
Dr. Rodriguez reported serving as a paid speaker for Abbott, Endologix, and W.L. Gore.
CHICAGO – The use of therapeutic-dose anticoagulation in hospitalized patients with calf vein thrombosis significantly reduces the risk of venous thromboembolic complications, compared with lower-dose prophylactic anticoagulation or surveillance alone, Heron E. Rodriguez, MD, said at a symposium on vascular surgery sponsored by Northwestern University.
Moreover, placement of an inferior vena cava filter in patients with calf vein thrombosis when anticoagulation is contraindicated accomplishes nothing beneficial and had a 10% complication rate in a large retrospective single-center study, added Dr. Rodriguez of Northwestern University, Chicago.
Deep vein thrombosis (DVT) remains a significant source of morbidity and mortality despite worldwide awareness of the problem.
“Specifically, calf vein thrombosis [CVT] is very common, and we know that in some series up to 30% of patients end up propagating proximally if they’re not treated, and a good number of them develop chronic venous insufficiency, with long-term consequences,” he noted.
“Unfortunately there is no consensus regarding treatment. The guidelines are very vague. For example, there is no mention [in current American College of Chest Physicians guidelines] of how to manage muscular vein thrombosis and much ambiguity on how to treat calf vein thrombosis,” he continued.
Dr. Rodriguez cited as an indication of the lack of consensus on management of CVT a single-institution survey by other investigators of the practices of physicians in various specialties. Forty-nine percent of respondents indicated they anticoagulate patients with CVT; 51% don’t. Of those who did, 62% prescribed low-molecular-weight heparin and 11% intravenous heparin. Fifty-eight percent of physicians who anticoagulated did so for 3 months, 30% for 6. And 46% of physicians used an inferior vena cava (IVC) filter when anticoagulation was contraindicated (Vascular. 2014 Apr;22[2]:93-7).
That rate of IVC placement “seemed really high” given the paucity of supporting evidence for safety and efficacy of filter placement in the setting of CVT, so Dr. Rodriguez and coinvestigators decided to conduct a retrospective review of practices at Northwestern Memorial Hospital. He explained the study hypothesis: “Our thinking was that these kinds of thrombi are associated with low risk of propagation and pulmonary embolism, and they can and should be managed conservatively.”
Of 647 patients with isolated thrombosis of the anterior and posterior tibial, soleal, peroneal, or gastrocnemius veins, 44% received an IVC filter, and the rest got medical treatment alone. Of the 362 patients managed medically, 49% received therapeutic anticoagulation, 12% got low-dose prophylactic anticoagulation, and 39% underwent surveillance without anticoagulation.
The primary outcome was the incidence of venous thromboembolic complications – that is, propagation of DVT or pulmonary embolism. The incidence was 35% in the surveillance-only group, 30% with prophylactic anticoagulation, and 10% in patients who got therapeutic anticoagulation.
Of note, the rate of the most feared complication, pulmonary embolism, was low and similar in the filter recipients and medically managed group: 2.5% in the IVC group, 3.3% with medical management.
“Distal vein thromboses have low rates of pulmonary embolism, regardless of whether or not they are so-called protected with a filter. On the other hand, a filter was associated with a 10% rate of complications. I have to make clear that these were radiographic abnormalities – tilting, migration, caval perforation – that didn’t have clinical consequences, but we were very aggressive in removing the IVC filters, and I’m guessing if they’d been left inside they would create problems in the long term,” Dr. Rodriguez said.
An important point about this study is that these were all sick patients, and most were hospitalized. The filter recipients and medical groups differed in key ways. For example, 49% of the filter patients had a malignancy, and 56% had a baseline history of venous thromboembolic events, compared with 26% and 16%, respectively, of the medical group. For that reason, the investigators performed propensity score matching and came up with 157 closely matched patient pairs. The outcomes remained unchanged.
Of course, this was a retrospective study, with its inherent limitations, but Dr. Rodriguez characterized the published randomized trials on management of CVT as “small and limited.” The most frequently quoted study is the double-blind multicenter CACTUS trial, which randomized 252 outpatients with symptomatic CVT to 6 weeks of low-molecular-weight heparin or placebo and found no difference in the rates of proximal extension of venous thromboembolic events (Lancet Haematol. 2016 Dec;3[12]:e556-62). But these were all low-risk patients. Prior DVT or malignancy were exclusion criteria, so this was a very different population than treated at Northwestern.
Based upon the results of the retrospective study at Northwestern, which have been published (J Vasc Surg Venous Lymphat Disord. 2017 Jan;5[1]:25-32), the vascular surgery service has developed a management algorithm for DVT management based upon the lesion site. If a patient is unable to undergo anticoagulation, venous duplex ultrasound is repeated at 1 week. If the imaging shows propagation into the popliteal vein and anticoagulation remains contraindicated, only then is placement of an IVC filter warranted.
Dr. Rodriguez reported serving as a paid speaker for Abbott, Endologix, and W.L. Gore.
CHICAGO – The use of therapeutic-dose anticoagulation in hospitalized patients with calf vein thrombosis significantly reduces the risk of venous thromboembolic complications, compared with lower-dose prophylactic anticoagulation or surveillance alone, Heron E. Rodriguez, MD, said at a symposium on vascular surgery sponsored by Northwestern University.
Moreover, placement of an inferior vena cava filter in patients with calf vein thrombosis when anticoagulation is contraindicated accomplishes nothing beneficial and had a 10% complication rate in a large retrospective single-center study, added Dr. Rodriguez of Northwestern University, Chicago.
Deep vein thrombosis (DVT) remains a significant source of morbidity and mortality despite worldwide awareness of the problem.
“Specifically, calf vein thrombosis [CVT] is very common, and we know that in some series up to 30% of patients end up propagating proximally if they’re not treated, and a good number of them develop chronic venous insufficiency, with long-term consequences,” he noted.
“Unfortunately there is no consensus regarding treatment. The guidelines are very vague. For example, there is no mention [in current American College of Chest Physicians guidelines] of how to manage muscular vein thrombosis and much ambiguity on how to treat calf vein thrombosis,” he continued.
Dr. Rodriguez cited as an indication of the lack of consensus on management of CVT a single-institution survey by other investigators of the practices of physicians in various specialties. Forty-nine percent of respondents indicated they anticoagulate patients with CVT; 51% don’t. Of those who did, 62% prescribed low-molecular-weight heparin and 11% intravenous heparin. Fifty-eight percent of physicians who anticoagulated did so for 3 months, 30% for 6. And 46% of physicians used an inferior vena cava (IVC) filter when anticoagulation was contraindicated (Vascular. 2014 Apr;22[2]:93-7).
That rate of IVC placement “seemed really high” given the paucity of supporting evidence for safety and efficacy of filter placement in the setting of CVT, so Dr. Rodriguez and coinvestigators decided to conduct a retrospective review of practices at Northwestern Memorial Hospital. He explained the study hypothesis: “Our thinking was that these kinds of thrombi are associated with low risk of propagation and pulmonary embolism, and they can and should be managed conservatively.”
Of 647 patients with isolated thrombosis of the anterior and posterior tibial, soleal, peroneal, or gastrocnemius veins, 44% received an IVC filter, and the rest got medical treatment alone. Of the 362 patients managed medically, 49% received therapeutic anticoagulation, 12% got low-dose prophylactic anticoagulation, and 39% underwent surveillance without anticoagulation.
The primary outcome was the incidence of venous thromboembolic complications – that is, propagation of DVT or pulmonary embolism. The incidence was 35% in the surveillance-only group, 30% with prophylactic anticoagulation, and 10% in patients who got therapeutic anticoagulation.
Of note, the rate of the most feared complication, pulmonary embolism, was low and similar in the filter recipients and medically managed group: 2.5% in the IVC group, 3.3% with medical management.
“Distal vein thromboses have low rates of pulmonary embolism, regardless of whether or not they are so-called protected with a filter. On the other hand, a filter was associated with a 10% rate of complications. I have to make clear that these were radiographic abnormalities – tilting, migration, caval perforation – that didn’t have clinical consequences, but we were very aggressive in removing the IVC filters, and I’m guessing if they’d been left inside they would create problems in the long term,” Dr. Rodriguez said.
An important point about this study is that these were all sick patients, and most were hospitalized. The filter recipients and medical groups differed in key ways. For example, 49% of the filter patients had a malignancy, and 56% had a baseline history of venous thromboembolic events, compared with 26% and 16%, respectively, of the medical group. For that reason, the investigators performed propensity score matching and came up with 157 closely matched patient pairs. The outcomes remained unchanged.
Of course, this was a retrospective study, with its inherent limitations, but Dr. Rodriguez characterized the published randomized trials on management of CVT as “small and limited.” The most frequently quoted study is the double-blind multicenter CACTUS trial, which randomized 252 outpatients with symptomatic CVT to 6 weeks of low-molecular-weight heparin or placebo and found no difference in the rates of proximal extension of venous thromboembolic events (Lancet Haematol. 2016 Dec;3[12]:e556-62). But these were all low-risk patients. Prior DVT or malignancy were exclusion criteria, so this was a very different population than treated at Northwestern.
Based upon the results of the retrospective study at Northwestern, which have been published (J Vasc Surg Venous Lymphat Disord. 2017 Jan;5[1]:25-32), the vascular surgery service has developed a management algorithm for DVT management based upon the lesion site. If a patient is unable to undergo anticoagulation, venous duplex ultrasound is repeated at 1 week. If the imaging shows propagation into the popliteal vein and anticoagulation remains contraindicated, only then is placement of an IVC filter warranted.
Dr. Rodriguez reported serving as a paid speaker for Abbott, Endologix, and W.L. Gore.
EXPERT ANALYSIS FROM NORTHWESTERN VASCULAR SYMPOSIUM
Multidisciplinary care improves surgical outcomes for elderly patients
and were able to leave the hospital after a shorter stay, according to findings from a case-control study of nearly 400 patients.
Data from previous studies suggest that preoperative assessment by geriatric experts can improve outcomes for the elderly, who are more likely than are younger patients to develop preventable postoperative complications, and “this evidence supports the formulation of a different approach to preoperative assessment and postoperative care for this population,” wrote Shelley R. McDonald, DO, of Duke University, Durham, N.C., and colleagues.
The intervention, known as the Perioperative Optimization of Senior Health (POSH), was described as “a quality improvement initiative with prospective data collection.” Patients in a geriatrics clinic within an academic center were selected for the study if they were at high risk for complications linked to elective abdominal surgery. High risk was defined as older than 85 years of age, or older than 65 years of age with conditions including cognitive impairment, recent weight loss, multiple comorbidities, and polypharmacy (JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513).
The POSH intervention patients received preoperative evaluation from a team including a geriatrician, geriatric resource nurse, social worker, program administrator, and nurse practitioner from the preoperative anesthesia testing clinic. Patients and families were advised on risk management and care optimization involving cognition, comorbidities, medications, mobility, functional status, nutrition, hydration, pain, and advanced care planning.
Patients in the POSH group were on average older, had more comorbidities, and were more likely to be smokers. But despite these disadvantaging characteristics, they still had better outcomes in several important variables than did those in the control group.
The POSH group had significantly shorter hospital stays, compared with controls (4 days vs. 6 days), and significantly lower all-cause readmission rates at both 7 days (2.8% vs. 9.9%) and 30 days (7.8% vs. 18.3%). The significance persisted whether the surgeries were laparoscopic or open.
The overall complication rate was lower in the POSH group, compared with the controls, but fell short of statistical significance (44.8% vs. 58.7%, P = .01). However, rates of specific complications were significantly lower in the POSH group, compared with controls, including postoperative cardiogenic or hypovolemic shock (2.2% vs. 8.4%), bleeding, either during or after surgery (6.1% vs. 15.4%), and postoperative ileus (4.9% vs. 20.3%).
“Delirium was identified in POSH patients at higher rates than in the control group, which is not unexpected because higher postoperative delirium rates are known to be identified with increased screening,” the researchers noted. “Collaborative care allows for increasing the recognition of geriatric syndromes like delirium, more focus on symptom management, and proactively anticipating complications,” they said.
The study results were limited by several factors including a long enrollment period for the POSH patients, and potential changes in surgical protocols, the researchers said. However, the findings support the need for further research and more refined analysis to identify the most beneficial aspects of care, and to support better clinical decision making about the timing of interventions and the type of patient who could benefit, they noted.
The researchers had no financial conflicts to disclose. The John A. Hartford Foundation Center of Excellence National Program Award provided salary and database support.
SOURCE: McDonald S et al. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513.
and were able to leave the hospital after a shorter stay, according to findings from a case-control study of nearly 400 patients.
Data from previous studies suggest that preoperative assessment by geriatric experts can improve outcomes for the elderly, who are more likely than are younger patients to develop preventable postoperative complications, and “this evidence supports the formulation of a different approach to preoperative assessment and postoperative care for this population,” wrote Shelley R. McDonald, DO, of Duke University, Durham, N.C., and colleagues.
The intervention, known as the Perioperative Optimization of Senior Health (POSH), was described as “a quality improvement initiative with prospective data collection.” Patients in a geriatrics clinic within an academic center were selected for the study if they were at high risk for complications linked to elective abdominal surgery. High risk was defined as older than 85 years of age, or older than 65 years of age with conditions including cognitive impairment, recent weight loss, multiple comorbidities, and polypharmacy (JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513).
The POSH intervention patients received preoperative evaluation from a team including a geriatrician, geriatric resource nurse, social worker, program administrator, and nurse practitioner from the preoperative anesthesia testing clinic. Patients and families were advised on risk management and care optimization involving cognition, comorbidities, medications, mobility, functional status, nutrition, hydration, pain, and advanced care planning.
Patients in the POSH group were on average older, had more comorbidities, and were more likely to be smokers. But despite these disadvantaging characteristics, they still had better outcomes in several important variables than did those in the control group.
The POSH group had significantly shorter hospital stays, compared with controls (4 days vs. 6 days), and significantly lower all-cause readmission rates at both 7 days (2.8% vs. 9.9%) and 30 days (7.8% vs. 18.3%). The significance persisted whether the surgeries were laparoscopic or open.
The overall complication rate was lower in the POSH group, compared with the controls, but fell short of statistical significance (44.8% vs. 58.7%, P = .01). However, rates of specific complications were significantly lower in the POSH group, compared with controls, including postoperative cardiogenic or hypovolemic shock (2.2% vs. 8.4%), bleeding, either during or after surgery (6.1% vs. 15.4%), and postoperative ileus (4.9% vs. 20.3%).
“Delirium was identified in POSH patients at higher rates than in the control group, which is not unexpected because higher postoperative delirium rates are known to be identified with increased screening,” the researchers noted. “Collaborative care allows for increasing the recognition of geriatric syndromes like delirium, more focus on symptom management, and proactively anticipating complications,” they said.
The study results were limited by several factors including a long enrollment period for the POSH patients, and potential changes in surgical protocols, the researchers said. However, the findings support the need for further research and more refined analysis to identify the most beneficial aspects of care, and to support better clinical decision making about the timing of interventions and the type of patient who could benefit, they noted.
The researchers had no financial conflicts to disclose. The John A. Hartford Foundation Center of Excellence National Program Award provided salary and database support.
SOURCE: McDonald S et al. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513.
and were able to leave the hospital after a shorter stay, according to findings from a case-control study of nearly 400 patients.
Data from previous studies suggest that preoperative assessment by geriatric experts can improve outcomes for the elderly, who are more likely than are younger patients to develop preventable postoperative complications, and “this evidence supports the formulation of a different approach to preoperative assessment and postoperative care for this population,” wrote Shelley R. McDonald, DO, of Duke University, Durham, N.C., and colleagues.
The intervention, known as the Perioperative Optimization of Senior Health (POSH), was described as “a quality improvement initiative with prospective data collection.” Patients in a geriatrics clinic within an academic center were selected for the study if they were at high risk for complications linked to elective abdominal surgery. High risk was defined as older than 85 years of age, or older than 65 years of age with conditions including cognitive impairment, recent weight loss, multiple comorbidities, and polypharmacy (JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513).
The POSH intervention patients received preoperative evaluation from a team including a geriatrician, geriatric resource nurse, social worker, program administrator, and nurse practitioner from the preoperative anesthesia testing clinic. Patients and families were advised on risk management and care optimization involving cognition, comorbidities, medications, mobility, functional status, nutrition, hydration, pain, and advanced care planning.
Patients in the POSH group were on average older, had more comorbidities, and were more likely to be smokers. But despite these disadvantaging characteristics, they still had better outcomes in several important variables than did those in the control group.
The POSH group had significantly shorter hospital stays, compared with controls (4 days vs. 6 days), and significantly lower all-cause readmission rates at both 7 days (2.8% vs. 9.9%) and 30 days (7.8% vs. 18.3%). The significance persisted whether the surgeries were laparoscopic or open.
The overall complication rate was lower in the POSH group, compared with the controls, but fell short of statistical significance (44.8% vs. 58.7%, P = .01). However, rates of specific complications were significantly lower in the POSH group, compared with controls, including postoperative cardiogenic or hypovolemic shock (2.2% vs. 8.4%), bleeding, either during or after surgery (6.1% vs. 15.4%), and postoperative ileus (4.9% vs. 20.3%).
“Delirium was identified in POSH patients at higher rates than in the control group, which is not unexpected because higher postoperative delirium rates are known to be identified with increased screening,” the researchers noted. “Collaborative care allows for increasing the recognition of geriatric syndromes like delirium, more focus on symptom management, and proactively anticipating complications,” they said.
The study results were limited by several factors including a long enrollment period for the POSH patients, and potential changes in surgical protocols, the researchers said. However, the findings support the need for further research and more refined analysis to identify the most beneficial aspects of care, and to support better clinical decision making about the timing of interventions and the type of patient who could benefit, they noted.
The researchers had no financial conflicts to disclose. The John A. Hartford Foundation Center of Excellence National Program Award provided salary and database support.
SOURCE: McDonald S et al. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513.
FROM JAMA SURGERY
Key clinical point: A preoperative surgical intervention improved outcomes and shortened hospital stays for seniors.
Major finding: The POSH group had significantly shorter hospital stays compared with controls (4 days vs. 6 days).
Study details: The data come from a study of 183 surgery patients and 143 controls.
Disclosures: The researchers had no financial conflicts to disclose.
Source: McDonald S JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513
Short takes
Pacing in syncope for select patients only
The 2017 ACC/AHA/HRD guideline for syncope evaluation and management concludes that the evidence does not yet support the use of pacing for reflex-mediated except among those with both recurrent vasovagal syncope and asystole documented by implantable loop recorder.
Citation: Varosy P et al. Pacing as a treatment for reflex-mediated (vasovagal, situational, or carotid sinus hypersensitivity) syncope: A systematic review for the 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. J Am Coll Cardiol. 2017 Aug 1;20(5):664-79.
Postoperative opioids often underutilized
Between 67% and 92% of patients report postoperative opioid oversupply, defined as filled but unused opioid prescriptions or unfilled opioid prescriptions. Half of the filled prescriptions were unused, with the majority reporting that the narcotics were not stored in locked containers.
Citation: Bicket MC et al. Prescription opioid analgesics commonly unused after surgery: A systematic review. JAMA Surg. 2017 Aug 2. doi: 10.1001/jamasurg.2017.0831
5-hour protocol for contrast allergy safe and effective
Observational study showing a 5-hour IV steroid protocol was noninferior to a traditional 13-hour oral premedication regimen in patients at high risk for IV contrast reactions.
Citation: Mervak BM et al. Intravenous corticosteroid premedication administered 5 hours before CT, compared with a traditional 13-hour oral regimen. Radiology. 2017 Nov;285(2):425-33.
Poor food intake and chills predict true bacteremia in hospitalized patients
Observational study showing that poor food consumption had a sensitivity of 93.7% and shaking chills a specificity of 95.1% in diagnosing true bacteremia based on blood culture results.
Citation: Komatsu T et al. A simple algorithm for predicting bacteremia using food consumption and shaking chills: a prospective observational study. J Hosp Med. 2017 Jul;12(7),510-5.
Lower readmission rates do not lead to increased postdischarge mortality at 30 days
Post–Affordable Care Act reductions in 30-day hospital risk-adjusted readmission rates for heart failure, acute MI, and pneumonia among Medicare beneficiaries did not increase but were weakly associated with decreased 30-day post–hospital discharge risk-adjusted mortality.
Citation: Dharmarajan K et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017Jul 18;318(3):270-8.
Pacing in syncope for select patients only
The 2017 ACC/AHA/HRD guideline for syncope evaluation and management concludes that the evidence does not yet support the use of pacing for reflex-mediated except among those with both recurrent vasovagal syncope and asystole documented by implantable loop recorder.
Citation: Varosy P et al. Pacing as a treatment for reflex-mediated (vasovagal, situational, or carotid sinus hypersensitivity) syncope: A systematic review for the 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. J Am Coll Cardiol. 2017 Aug 1;20(5):664-79.
Postoperative opioids often underutilized
Between 67% and 92% of patients report postoperative opioid oversupply, defined as filled but unused opioid prescriptions or unfilled opioid prescriptions. Half of the filled prescriptions were unused, with the majority reporting that the narcotics were not stored in locked containers.
Citation: Bicket MC et al. Prescription opioid analgesics commonly unused after surgery: A systematic review. JAMA Surg. 2017 Aug 2. doi: 10.1001/jamasurg.2017.0831
5-hour protocol for contrast allergy safe and effective
Observational study showing a 5-hour IV steroid protocol was noninferior to a traditional 13-hour oral premedication regimen in patients at high risk for IV contrast reactions.
Citation: Mervak BM et al. Intravenous corticosteroid premedication administered 5 hours before CT, compared with a traditional 13-hour oral regimen. Radiology. 2017 Nov;285(2):425-33.
Poor food intake and chills predict true bacteremia in hospitalized patients
Observational study showing that poor food consumption had a sensitivity of 93.7% and shaking chills a specificity of 95.1% in diagnosing true bacteremia based on blood culture results.
Citation: Komatsu T et al. A simple algorithm for predicting bacteremia using food consumption and shaking chills: a prospective observational study. J Hosp Med. 2017 Jul;12(7),510-5.
Lower readmission rates do not lead to increased postdischarge mortality at 30 days
Post–Affordable Care Act reductions in 30-day hospital risk-adjusted readmission rates for heart failure, acute MI, and pneumonia among Medicare beneficiaries did not increase but were weakly associated with decreased 30-day post–hospital discharge risk-adjusted mortality.
Citation: Dharmarajan K et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017Jul 18;318(3):270-8.
Pacing in syncope for select patients only
The 2017 ACC/AHA/HRD guideline for syncope evaluation and management concludes that the evidence does not yet support the use of pacing for reflex-mediated except among those with both recurrent vasovagal syncope and asystole documented by implantable loop recorder.
Citation: Varosy P et al. Pacing as a treatment for reflex-mediated (vasovagal, situational, or carotid sinus hypersensitivity) syncope: A systematic review for the 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. J Am Coll Cardiol. 2017 Aug 1;20(5):664-79.
Postoperative opioids often underutilized
Between 67% and 92% of patients report postoperative opioid oversupply, defined as filled but unused opioid prescriptions or unfilled opioid prescriptions. Half of the filled prescriptions were unused, with the majority reporting that the narcotics were not stored in locked containers.
Citation: Bicket MC et al. Prescription opioid analgesics commonly unused after surgery: A systematic review. JAMA Surg. 2017 Aug 2. doi: 10.1001/jamasurg.2017.0831
5-hour protocol for contrast allergy safe and effective
Observational study showing a 5-hour IV steroid protocol was noninferior to a traditional 13-hour oral premedication regimen in patients at high risk for IV contrast reactions.
Citation: Mervak BM et al. Intravenous corticosteroid premedication administered 5 hours before CT, compared with a traditional 13-hour oral regimen. Radiology. 2017 Nov;285(2):425-33.
Poor food intake and chills predict true bacteremia in hospitalized patients
Observational study showing that poor food consumption had a sensitivity of 93.7% and shaking chills a specificity of 95.1% in diagnosing true bacteremia based on blood culture results.
Citation: Komatsu T et al. A simple algorithm for predicting bacteremia using food consumption and shaking chills: a prospective observational study. J Hosp Med. 2017 Jul;12(7),510-5.
Lower readmission rates do not lead to increased postdischarge mortality at 30 days
Post–Affordable Care Act reductions in 30-day hospital risk-adjusted readmission rates for heart failure, acute MI, and pneumonia among Medicare beneficiaries did not increase but were weakly associated with decreased 30-day post–hospital discharge risk-adjusted mortality.
Citation: Dharmarajan K et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017Jul 18;318(3):270-8.