User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'medstat-accordion-set article-series')]
Medical licensing questions continue to violate ADA
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
FROM JAMA
BEAT-LUPUS: Belimumab after rituximab delays severe flares
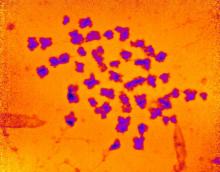
Using belimumab after rituximab to treat patients with systemic lupus erythematosus (SLE) refractory to conventional therapy not only significantly decreased levels of serum IgG anti-dsDNA antibody levels but also prolonged the time before severe flares of disease occurred in the phase 2b BEAT-LUPUS (Belimumab after B cell depletion in SLE) study.
The trial’s primary outcome of serum IgG anti-dsDNA antibody levels showed a decline from a geometric mean of 162 IU/mL at baseline to 69 IU/mL at 24 weeks and 47 IU/mL at 1 year in patients treated with belimumab (Benlysta) after rituximab (Rituxan and biosimilars). These reductions were significantly lower than the values seen in the placebo after rituximab arm (a respective 121 IU/mL, 99 IU/mL, and 103 IU/mL; P < .001).
Just 3 patients who received belimumab versus 10 who received placebo after rituximab experienced a severe BILAG (British Isles Lupus Assessment Group) index A flare by the end of the study at 52 weeks. The hazard ratio (HR) for the flare reduction was 0.27 (P = .03), indicating a 73% reduction.
The use of belimumab rather than a placebo also led to a small reduction in total serum IgG, and significantly suppressed B-cell repopulation (P = .03).
These results need confirming in a larger, phase 3 trial, the trial’s principal investigator, Michael Ehrenstein, PhD, said at the annual European Congress of Rheumatology. They are “clearly encouraging” and “support the hypothesis that BAFF [B-cell–activating factor] can drive flares after rituximab,” he said.
Although B-cell depletion with rituximab is recommended by national and international guidelines to treat some patients with SLE who are refractory to conventional therapy, its use is not licensed.
“Certainly, rituximab is a controversial drug in lupus,” Dr. Ehrenstein, a consultant rheumatologist based at University College London, said in an interview. Although there is real-world evidence from registries and open-label studies suggesting that it is widely used and effective in some patients, the randomized, controlled trials conducted with rituximab about 10 years ago failed to meet their primary endpoints.
“A lot has been written about why that was, but probably the biggest reason was the high dose of steroids in both groups,” Dr. Ehrenstein said. To try to avoid muddying the waters of the BEAT-LUPUS trial findings, the maximum dose of prednisolone allowed to be used as background therapy was 20 mg/day. The trial’s investigators were also encouraged to reduce the baseline steroid dose to at least 50% by the trial’s 6-month halfway point.
“We tried to reflect what was going on in the U.K.,” Dr. Ehrenstein said, noting that the inspiration for the trial was a patient who had received sequential rituximab treatment. Although she got better with each cycle of rituximab, when her disease flared it would be worse than the time before, with increasingly higher anti-dsDNA levels recorded. The reason for this seemed to be because of increasing BAFF levels, and so the hypothesis was that if rituximab was associated with increased BAFF levels, then co-targeting BAFF with belimumab should be able to prevent those flares from happening.
The BEAT-LUPUS trial has been a huge collaborative effort and was conducted across 16 U.K. centers. From initial funding to the data analysis, it has taken 6 years to complete and was made possible by a unique partnership between Versus Arthritis, University College London Hospitals Biomedical Research Center, the National Institute for Health Research UK Musculoskeletal Translational Research Collaboration, and GlaxoSmithKline (GSK). GSK provided belimumab free of charge, as well as additional funding, but had no role in the design of the study and will not have any role going forward.
From an initial 172 patients assessed for eligibility, 52 patients were finally enrolled into the trial and received rituximab as two infusions given 2 weeks apart. Patients were then randomized in a double-blind manner to receive either belimumab (n = 26) or placebo (n = 26) 4-8 weeks after their first dose of rituximab. The intention-to-treat population consisted of 43 patients.
The use of belimumab after rituximab did not increase the risk for infection – serious or otherwise – or adverse effects, Dr. Ehrenstein reported. Serious adverse events were reported in six (23%) patients in each arm, and serious infections were seen in two (8%) of the belimumab- and four (15%) of the placebo-treated patients.
“I think the take-home message is that it seems that belimumab can reduce the number of severe flares that occur after rituximab therapy,” Dr. Ehrenstein said. “It’s promising, but not definitive,” he added. The next step is of course to publish these data and to perform a phase 3 trial.
In the discussion time following the presentation, session moderator Xavier Mariette, MD, PhD, of Bicêtre Hospital, Paris-Saclay University, asked why not give belimumab first before rituximab if using belimumab afterward works?
“Our strategy was driven by the observation that BAFF levels surged after rituximab, and therefore it’s logical to give the belimumab to block that BAFF surge,” he answered.
“Certainly, there are ideas that belimumab releases mature B cells into the circulation and rituximab can target that,” he added. That strategy is under investigation in the BLISS-BELIEVE trial, which should also report by the end of this year. It’s a much larger, phase 3 trial, involving nearly 300 patients and is sponsored by GSK.
“Clearly, this is a combination treatment [but] whether you give one before the other is uncertain,” Dr. Ehrenstein observed.
Another member of the viewing audience asked whether it would have been a fairer comparison if another dose of rituximab had been given to patients at week 24 instead of no treatment. Dr. Ehrenstein noted that it was a “good point” to make, but the investigators mainly wanted to answer whether giving belimumab after rituximab would target BAFF and thereby drop serum anti-dsDNA antibody levels. He said that a full trial of rituximab for patients with SLE, perhaps adding this extra dose, needs to be conducted.
Dr. Ehrenstein disclosed receiving research funding and educational grants from GSK and participating in advisory panels for the company.
Using belimumab after rituximab to treat patients with systemic lupus erythematosus (SLE) refractory to conventional therapy not only significantly decreased levels of serum IgG anti-dsDNA antibody levels but also prolonged the time before severe flares of disease occurred in the phase 2b BEAT-LUPUS (Belimumab after B cell depletion in SLE) study.
The trial’s primary outcome of serum IgG anti-dsDNA antibody levels showed a decline from a geometric mean of 162 IU/mL at baseline to 69 IU/mL at 24 weeks and 47 IU/mL at 1 year in patients treated with belimumab (Benlysta) after rituximab (Rituxan and biosimilars). These reductions were significantly lower than the values seen in the placebo after rituximab arm (a respective 121 IU/mL, 99 IU/mL, and 103 IU/mL; P < .001).
Just 3 patients who received belimumab versus 10 who received placebo after rituximab experienced a severe BILAG (British Isles Lupus Assessment Group) index A flare by the end of the study at 52 weeks. The hazard ratio (HR) for the flare reduction was 0.27 (P = .03), indicating a 73% reduction.
The use of belimumab rather than a placebo also led to a small reduction in total serum IgG, and significantly suppressed B-cell repopulation (P = .03).
These results need confirming in a larger, phase 3 trial, the trial’s principal investigator, Michael Ehrenstein, PhD, said at the annual European Congress of Rheumatology. They are “clearly encouraging” and “support the hypothesis that BAFF [B-cell–activating factor] can drive flares after rituximab,” he said.
Although B-cell depletion with rituximab is recommended by national and international guidelines to treat some patients with SLE who are refractory to conventional therapy, its use is not licensed.
“Certainly, rituximab is a controversial drug in lupus,” Dr. Ehrenstein, a consultant rheumatologist based at University College London, said in an interview. Although there is real-world evidence from registries and open-label studies suggesting that it is widely used and effective in some patients, the randomized, controlled trials conducted with rituximab about 10 years ago failed to meet their primary endpoints.
“A lot has been written about why that was, but probably the biggest reason was the high dose of steroids in both groups,” Dr. Ehrenstein said. To try to avoid muddying the waters of the BEAT-LUPUS trial findings, the maximum dose of prednisolone allowed to be used as background therapy was 20 mg/day. The trial’s investigators were also encouraged to reduce the baseline steroid dose to at least 50% by the trial’s 6-month halfway point.
“We tried to reflect what was going on in the U.K.,” Dr. Ehrenstein said, noting that the inspiration for the trial was a patient who had received sequential rituximab treatment. Although she got better with each cycle of rituximab, when her disease flared it would be worse than the time before, with increasingly higher anti-dsDNA levels recorded. The reason for this seemed to be because of increasing BAFF levels, and so the hypothesis was that if rituximab was associated with increased BAFF levels, then co-targeting BAFF with belimumab should be able to prevent those flares from happening.
The BEAT-LUPUS trial has been a huge collaborative effort and was conducted across 16 U.K. centers. From initial funding to the data analysis, it has taken 6 years to complete and was made possible by a unique partnership between Versus Arthritis, University College London Hospitals Biomedical Research Center, the National Institute for Health Research UK Musculoskeletal Translational Research Collaboration, and GlaxoSmithKline (GSK). GSK provided belimumab free of charge, as well as additional funding, but had no role in the design of the study and will not have any role going forward.
From an initial 172 patients assessed for eligibility, 52 patients were finally enrolled into the trial and received rituximab as two infusions given 2 weeks apart. Patients were then randomized in a double-blind manner to receive either belimumab (n = 26) or placebo (n = 26) 4-8 weeks after their first dose of rituximab. The intention-to-treat population consisted of 43 patients.
The use of belimumab after rituximab did not increase the risk for infection – serious or otherwise – or adverse effects, Dr. Ehrenstein reported. Serious adverse events were reported in six (23%) patients in each arm, and serious infections were seen in two (8%) of the belimumab- and four (15%) of the placebo-treated patients.
“I think the take-home message is that it seems that belimumab can reduce the number of severe flares that occur after rituximab therapy,” Dr. Ehrenstein said. “It’s promising, but not definitive,” he added. The next step is of course to publish these data and to perform a phase 3 trial.
In the discussion time following the presentation, session moderator Xavier Mariette, MD, PhD, of Bicêtre Hospital, Paris-Saclay University, asked why not give belimumab first before rituximab if using belimumab afterward works?
“Our strategy was driven by the observation that BAFF levels surged after rituximab, and therefore it’s logical to give the belimumab to block that BAFF surge,” he answered.
“Certainly, there are ideas that belimumab releases mature B cells into the circulation and rituximab can target that,” he added. That strategy is under investigation in the BLISS-BELIEVE trial, which should also report by the end of this year. It’s a much larger, phase 3 trial, involving nearly 300 patients and is sponsored by GSK.
“Clearly, this is a combination treatment [but] whether you give one before the other is uncertain,” Dr. Ehrenstein observed.
Another member of the viewing audience asked whether it would have been a fairer comparison if another dose of rituximab had been given to patients at week 24 instead of no treatment. Dr. Ehrenstein noted that it was a “good point” to make, but the investigators mainly wanted to answer whether giving belimumab after rituximab would target BAFF and thereby drop serum anti-dsDNA antibody levels. He said that a full trial of rituximab for patients with SLE, perhaps adding this extra dose, needs to be conducted.
Dr. Ehrenstein disclosed receiving research funding and educational grants from GSK and participating in advisory panels for the company.
Using belimumab after rituximab to treat patients with systemic lupus erythematosus (SLE) refractory to conventional therapy not only significantly decreased levels of serum IgG anti-dsDNA antibody levels but also prolonged the time before severe flares of disease occurred in the phase 2b BEAT-LUPUS (Belimumab after B cell depletion in SLE) study.
The trial’s primary outcome of serum IgG anti-dsDNA antibody levels showed a decline from a geometric mean of 162 IU/mL at baseline to 69 IU/mL at 24 weeks and 47 IU/mL at 1 year in patients treated with belimumab (Benlysta) after rituximab (Rituxan and biosimilars). These reductions were significantly lower than the values seen in the placebo after rituximab arm (a respective 121 IU/mL, 99 IU/mL, and 103 IU/mL; P < .001).
Just 3 patients who received belimumab versus 10 who received placebo after rituximab experienced a severe BILAG (British Isles Lupus Assessment Group) index A flare by the end of the study at 52 weeks. The hazard ratio (HR) for the flare reduction was 0.27 (P = .03), indicating a 73% reduction.
The use of belimumab rather than a placebo also led to a small reduction in total serum IgG, and significantly suppressed B-cell repopulation (P = .03).
These results need confirming in a larger, phase 3 trial, the trial’s principal investigator, Michael Ehrenstein, PhD, said at the annual European Congress of Rheumatology. They are “clearly encouraging” and “support the hypothesis that BAFF [B-cell–activating factor] can drive flares after rituximab,” he said.
Although B-cell depletion with rituximab is recommended by national and international guidelines to treat some patients with SLE who are refractory to conventional therapy, its use is not licensed.
“Certainly, rituximab is a controversial drug in lupus,” Dr. Ehrenstein, a consultant rheumatologist based at University College London, said in an interview. Although there is real-world evidence from registries and open-label studies suggesting that it is widely used and effective in some patients, the randomized, controlled trials conducted with rituximab about 10 years ago failed to meet their primary endpoints.
“A lot has been written about why that was, but probably the biggest reason was the high dose of steroids in both groups,” Dr. Ehrenstein said. To try to avoid muddying the waters of the BEAT-LUPUS trial findings, the maximum dose of prednisolone allowed to be used as background therapy was 20 mg/day. The trial’s investigators were also encouraged to reduce the baseline steroid dose to at least 50% by the trial’s 6-month halfway point.
“We tried to reflect what was going on in the U.K.,” Dr. Ehrenstein said, noting that the inspiration for the trial was a patient who had received sequential rituximab treatment. Although she got better with each cycle of rituximab, when her disease flared it would be worse than the time before, with increasingly higher anti-dsDNA levels recorded. The reason for this seemed to be because of increasing BAFF levels, and so the hypothesis was that if rituximab was associated with increased BAFF levels, then co-targeting BAFF with belimumab should be able to prevent those flares from happening.
The BEAT-LUPUS trial has been a huge collaborative effort and was conducted across 16 U.K. centers. From initial funding to the data analysis, it has taken 6 years to complete and was made possible by a unique partnership between Versus Arthritis, University College London Hospitals Biomedical Research Center, the National Institute for Health Research UK Musculoskeletal Translational Research Collaboration, and GlaxoSmithKline (GSK). GSK provided belimumab free of charge, as well as additional funding, but had no role in the design of the study and will not have any role going forward.
From an initial 172 patients assessed for eligibility, 52 patients were finally enrolled into the trial and received rituximab as two infusions given 2 weeks apart. Patients were then randomized in a double-blind manner to receive either belimumab (n = 26) or placebo (n = 26) 4-8 weeks after their first dose of rituximab. The intention-to-treat population consisted of 43 patients.
The use of belimumab after rituximab did not increase the risk for infection – serious or otherwise – or adverse effects, Dr. Ehrenstein reported. Serious adverse events were reported in six (23%) patients in each arm, and serious infections were seen in two (8%) of the belimumab- and four (15%) of the placebo-treated patients.
“I think the take-home message is that it seems that belimumab can reduce the number of severe flares that occur after rituximab therapy,” Dr. Ehrenstein said. “It’s promising, but not definitive,” he added. The next step is of course to publish these data and to perform a phase 3 trial.
In the discussion time following the presentation, session moderator Xavier Mariette, MD, PhD, of Bicêtre Hospital, Paris-Saclay University, asked why not give belimumab first before rituximab if using belimumab afterward works?
“Our strategy was driven by the observation that BAFF levels surged after rituximab, and therefore it’s logical to give the belimumab to block that BAFF surge,” he answered.
“Certainly, there are ideas that belimumab releases mature B cells into the circulation and rituximab can target that,” he added. That strategy is under investigation in the BLISS-BELIEVE trial, which should also report by the end of this year. It’s a much larger, phase 3 trial, involving nearly 300 patients and is sponsored by GSK.
“Clearly, this is a combination treatment [but] whether you give one before the other is uncertain,” Dr. Ehrenstein observed.
Another member of the viewing audience asked whether it would have been a fairer comparison if another dose of rituximab had been given to patients at week 24 instead of no treatment. Dr. Ehrenstein noted that it was a “good point” to make, but the investigators mainly wanted to answer whether giving belimumab after rituximab would target BAFF and thereby drop serum anti-dsDNA antibody levels. He said that a full trial of rituximab for patients with SLE, perhaps adding this extra dose, needs to be conducted.
Dr. Ehrenstein disclosed receiving research funding and educational grants from GSK and participating in advisory panels for the company.
FROM THE EULAR 2021 CONGRESS
EULAR COVID-19 recommendations set for update
The European Alliance of Associations for Rheumatology has started the process of updating their recommendations on how to manage patients with rheumatic and musculoskeletal diseases (RMDs) in the context of the SARS-CoV-2 pandemic.
So far, the first part of the systematic literature review has been performed and the conclusions that have been drawn appear to back up the recommendations that have already been made. It’s “hard to say” if there will need to be changes, said Robert B.M. Landewé, MD, PhD, at the annual European Congress of Rheumatology, as the next phase will be for the task force members to meet and discuss the implications of the literature research.“I think there will only be minor modifications and a few novel recommendations, but that is personal opinion,” speculated Dr. Landewé, who is professor of rheumatology at the Amsterdam Medical Center, University of Amsterdam.
The recommendations, which were developed a little over a year ago and published in Annals of the Rheumatic Diseases, set out provisional guidance covering four themes: infection prevention, managing patients when social distancing measures are in effect, managing patients with RMDs who develop COVID-19, and the prevention of infections other than SARS-CoV-2.
Emphasis on quality of evidence
According to EULAR’s standard operating procedures “updates should only be done if the evolving evidence mandates to do so,” and be based on “rational arguments,” Dr. Landewé said. “The last year was a bit unprecedented in that regard as we didn’t have those rational arguments before we designed our first set of recommendations and, as you can expect, that is totally due to the character of the pandemic.”
So much has been published on COVID-19 since then it was time to reappraise the situation. The task force behind the recommendations met in January 2021 to discuss the results of the literature search that was centered around five main research questions.
- Do patients with RMDs face more risk of contracting SARS-CoV-2 than the general population?
- If patients contract the virus, do they have a worse prognosis?
- Are antirheumatic medications associated with a worse outcome in people with RMDs?
- Should patients continue their antirheumatic medications?
- What evidence informs the use of vaccination against SARS-CoV-2 in patients with RMDs?
The latter research question is pending discussion since there were no studies to review at the time as the various vaccines had only just started to be widely available.
“We put a lot of emphasis on the quality of evidence,” Dr. Landewé said. In addition to making sure that patients did indeed have COVID-19 and checking that hospitalization and death records were caused by the disease, the task force team also looked to see if there was a control group being used. An extensive risk of bias assessment was undertaken, the results of which are pending.
Of 6,665 records identified during the literature search, just 113 full-text articles were assessed for eligibility. Of those, 60% were rejected as they did not pass the quality assessment, leaving 49 articles for consideration. The majority of these looked at the incidence of COVID-19, with others focusing on risk factors or both.
Literature search findings on main research questions
Dr. Landewé observed that the task force concluded that “current literature provides no evidence that patients with RMDs face more risk of contracting SARS-CoV-2 than individuals without RMDs.” They also concluded that patients with RMDs who do contract COVID-19 do not have a worse prognosis either, even though there have been a few studies suggesting a higher rate of hospitalization.
Both findings are reassuring as they fit with the existing recommendation to follow the same preventive and control measures in patients with RMDs as for the general population, but the task force is yet to determine if that recommendation should be amended.
There did not appear to be any hard evidence of any unique demographic feature or comorbidity that puts people with RMDs at more risk for severe COVID-19 than the general population. Think older age, male gender, high bodyweight, cardiovascular disease, diabetes, and chronic lung disease, Dr. Landewé said.
He noted, however, that there were some single-center reports suggesting that moderate or high levels of disease activity could put people with RMDs at greater risk for COVID-related death, “which is an intriguing finding in the context of discontinuing antirheumatic medication.” That is likely something the task force will be discussing when they decide how to update their recommendations.
The type of RMD may also be important, but again only single-center evidence to show that there might be an increased hospitalization risk in patients with autoinflammatory disease or risk for severe COVID-19 in those with certain connective tissue diseases. “These associations were not consistently found in other studies,” so it’s an open question how the task force decides to incorporate this into the updated guidance.
As for antirheumatic medications, conclusions from the literature review suggest that there doesn’t appear to be an increased or decreased risk for severe COVID-19 among users of NSAIDs or antimalarials.
That’s not the case for glucocorticoids. There appears to be an increased risk for hospitalization and COVID-19–related death, notably among those using higher (>10 mg) daily doses. “This is, so to say, the elephant in the room,” Dr. Landewé said. The current recommendation states that chronic users of glucocorticoids should continue their treatment. “The reports of additional risk could be due to glucocorticoids or to biases such as confounding by indication. So, the conclusion that we draw [is] not completely clear.”
In response to a question, he clarified this a little further: “We think ‘glucocorticoid use’ is a determinant of worse health, as is the case in many RMDs. Be aware that finding a positive association between [glucocorticoid] use and bad outcome does not mean that if you reduce [glucocorticoids], your patient will have a better outcome.”
The jury is also out on rituximab, which has been reported to increase the risk of severe COVID-19 and COVID-related death in two studies. There are also equivocal data on whether not using disease-modifying antirheumatic drugs increases the risk for these worse outcomes.
Asked about the absence of a recommendation on the use of the interleukin-6 inhibitor tocilizumab, Dr. Landewé responded: “We are caught up by evolving evidence. That is a generic problem in a dynamic field of COVID-19, I am afraid. What you recommend today is sometimes ‘old history’ tomorrow.”
Dr. Landewé had no relevant disclosures to make.
The European Alliance of Associations for Rheumatology has started the process of updating their recommendations on how to manage patients with rheumatic and musculoskeletal diseases (RMDs) in the context of the SARS-CoV-2 pandemic.
So far, the first part of the systematic literature review has been performed and the conclusions that have been drawn appear to back up the recommendations that have already been made. It’s “hard to say” if there will need to be changes, said Robert B.M. Landewé, MD, PhD, at the annual European Congress of Rheumatology, as the next phase will be for the task force members to meet and discuss the implications of the literature research.“I think there will only be minor modifications and a few novel recommendations, but that is personal opinion,” speculated Dr. Landewé, who is professor of rheumatology at the Amsterdam Medical Center, University of Amsterdam.
The recommendations, which were developed a little over a year ago and published in Annals of the Rheumatic Diseases, set out provisional guidance covering four themes: infection prevention, managing patients when social distancing measures are in effect, managing patients with RMDs who develop COVID-19, and the prevention of infections other than SARS-CoV-2.
Emphasis on quality of evidence
According to EULAR’s standard operating procedures “updates should only be done if the evolving evidence mandates to do so,” and be based on “rational arguments,” Dr. Landewé said. “The last year was a bit unprecedented in that regard as we didn’t have those rational arguments before we designed our first set of recommendations and, as you can expect, that is totally due to the character of the pandemic.”
So much has been published on COVID-19 since then it was time to reappraise the situation. The task force behind the recommendations met in January 2021 to discuss the results of the literature search that was centered around five main research questions.
- Do patients with RMDs face more risk of contracting SARS-CoV-2 than the general population?
- If patients contract the virus, do they have a worse prognosis?
- Are antirheumatic medications associated with a worse outcome in people with RMDs?
- Should patients continue their antirheumatic medications?
- What evidence informs the use of vaccination against SARS-CoV-2 in patients with RMDs?
The latter research question is pending discussion since there were no studies to review at the time as the various vaccines had only just started to be widely available.
“We put a lot of emphasis on the quality of evidence,” Dr. Landewé said. In addition to making sure that patients did indeed have COVID-19 and checking that hospitalization and death records were caused by the disease, the task force team also looked to see if there was a control group being used. An extensive risk of bias assessment was undertaken, the results of which are pending.
Of 6,665 records identified during the literature search, just 113 full-text articles were assessed for eligibility. Of those, 60% were rejected as they did not pass the quality assessment, leaving 49 articles for consideration. The majority of these looked at the incidence of COVID-19, with others focusing on risk factors or both.
Literature search findings on main research questions
Dr. Landewé observed that the task force concluded that “current literature provides no evidence that patients with RMDs face more risk of contracting SARS-CoV-2 than individuals without RMDs.” They also concluded that patients with RMDs who do contract COVID-19 do not have a worse prognosis either, even though there have been a few studies suggesting a higher rate of hospitalization.
Both findings are reassuring as they fit with the existing recommendation to follow the same preventive and control measures in patients with RMDs as for the general population, but the task force is yet to determine if that recommendation should be amended.
There did not appear to be any hard evidence of any unique demographic feature or comorbidity that puts people with RMDs at more risk for severe COVID-19 than the general population. Think older age, male gender, high bodyweight, cardiovascular disease, diabetes, and chronic lung disease, Dr. Landewé said.
He noted, however, that there were some single-center reports suggesting that moderate or high levels of disease activity could put people with RMDs at greater risk for COVID-related death, “which is an intriguing finding in the context of discontinuing antirheumatic medication.” That is likely something the task force will be discussing when they decide how to update their recommendations.
The type of RMD may also be important, but again only single-center evidence to show that there might be an increased hospitalization risk in patients with autoinflammatory disease or risk for severe COVID-19 in those with certain connective tissue diseases. “These associations were not consistently found in other studies,” so it’s an open question how the task force decides to incorporate this into the updated guidance.
As for antirheumatic medications, conclusions from the literature review suggest that there doesn’t appear to be an increased or decreased risk for severe COVID-19 among users of NSAIDs or antimalarials.
That’s not the case for glucocorticoids. There appears to be an increased risk for hospitalization and COVID-19–related death, notably among those using higher (>10 mg) daily doses. “This is, so to say, the elephant in the room,” Dr. Landewé said. The current recommendation states that chronic users of glucocorticoids should continue their treatment. “The reports of additional risk could be due to glucocorticoids or to biases such as confounding by indication. So, the conclusion that we draw [is] not completely clear.”
In response to a question, he clarified this a little further: “We think ‘glucocorticoid use’ is a determinant of worse health, as is the case in many RMDs. Be aware that finding a positive association between [glucocorticoid] use and bad outcome does not mean that if you reduce [glucocorticoids], your patient will have a better outcome.”
The jury is also out on rituximab, which has been reported to increase the risk of severe COVID-19 and COVID-related death in two studies. There are also equivocal data on whether not using disease-modifying antirheumatic drugs increases the risk for these worse outcomes.
Asked about the absence of a recommendation on the use of the interleukin-6 inhibitor tocilizumab, Dr. Landewé responded: “We are caught up by evolving evidence. That is a generic problem in a dynamic field of COVID-19, I am afraid. What you recommend today is sometimes ‘old history’ tomorrow.”
Dr. Landewé had no relevant disclosures to make.
The European Alliance of Associations for Rheumatology has started the process of updating their recommendations on how to manage patients with rheumatic and musculoskeletal diseases (RMDs) in the context of the SARS-CoV-2 pandemic.
So far, the first part of the systematic literature review has been performed and the conclusions that have been drawn appear to back up the recommendations that have already been made. It’s “hard to say” if there will need to be changes, said Robert B.M. Landewé, MD, PhD, at the annual European Congress of Rheumatology, as the next phase will be for the task force members to meet and discuss the implications of the literature research.“I think there will only be minor modifications and a few novel recommendations, but that is personal opinion,” speculated Dr. Landewé, who is professor of rheumatology at the Amsterdam Medical Center, University of Amsterdam.
The recommendations, which were developed a little over a year ago and published in Annals of the Rheumatic Diseases, set out provisional guidance covering four themes: infection prevention, managing patients when social distancing measures are in effect, managing patients with RMDs who develop COVID-19, and the prevention of infections other than SARS-CoV-2.
Emphasis on quality of evidence
According to EULAR’s standard operating procedures “updates should only be done if the evolving evidence mandates to do so,” and be based on “rational arguments,” Dr. Landewé said. “The last year was a bit unprecedented in that regard as we didn’t have those rational arguments before we designed our first set of recommendations and, as you can expect, that is totally due to the character of the pandemic.”
So much has been published on COVID-19 since then it was time to reappraise the situation. The task force behind the recommendations met in January 2021 to discuss the results of the literature search that was centered around five main research questions.
- Do patients with RMDs face more risk of contracting SARS-CoV-2 than the general population?
- If patients contract the virus, do they have a worse prognosis?
- Are antirheumatic medications associated with a worse outcome in people with RMDs?
- Should patients continue their antirheumatic medications?
- What evidence informs the use of vaccination against SARS-CoV-2 in patients with RMDs?
The latter research question is pending discussion since there were no studies to review at the time as the various vaccines had only just started to be widely available.
“We put a lot of emphasis on the quality of evidence,” Dr. Landewé said. In addition to making sure that patients did indeed have COVID-19 and checking that hospitalization and death records were caused by the disease, the task force team also looked to see if there was a control group being used. An extensive risk of bias assessment was undertaken, the results of which are pending.
Of 6,665 records identified during the literature search, just 113 full-text articles were assessed for eligibility. Of those, 60% were rejected as they did not pass the quality assessment, leaving 49 articles for consideration. The majority of these looked at the incidence of COVID-19, with others focusing on risk factors or both.
Literature search findings on main research questions
Dr. Landewé observed that the task force concluded that “current literature provides no evidence that patients with RMDs face more risk of contracting SARS-CoV-2 than individuals without RMDs.” They also concluded that patients with RMDs who do contract COVID-19 do not have a worse prognosis either, even though there have been a few studies suggesting a higher rate of hospitalization.
Both findings are reassuring as they fit with the existing recommendation to follow the same preventive and control measures in patients with RMDs as for the general population, but the task force is yet to determine if that recommendation should be amended.
There did not appear to be any hard evidence of any unique demographic feature or comorbidity that puts people with RMDs at more risk for severe COVID-19 than the general population. Think older age, male gender, high bodyweight, cardiovascular disease, diabetes, and chronic lung disease, Dr. Landewé said.
He noted, however, that there were some single-center reports suggesting that moderate or high levels of disease activity could put people with RMDs at greater risk for COVID-related death, “which is an intriguing finding in the context of discontinuing antirheumatic medication.” That is likely something the task force will be discussing when they decide how to update their recommendations.
The type of RMD may also be important, but again only single-center evidence to show that there might be an increased hospitalization risk in patients with autoinflammatory disease or risk for severe COVID-19 in those with certain connective tissue diseases. “These associations were not consistently found in other studies,” so it’s an open question how the task force decides to incorporate this into the updated guidance.
As for antirheumatic medications, conclusions from the literature review suggest that there doesn’t appear to be an increased or decreased risk for severe COVID-19 among users of NSAIDs or antimalarials.
That’s not the case for glucocorticoids. There appears to be an increased risk for hospitalization and COVID-19–related death, notably among those using higher (>10 mg) daily doses. “This is, so to say, the elephant in the room,” Dr. Landewé said. The current recommendation states that chronic users of glucocorticoids should continue their treatment. “The reports of additional risk could be due to glucocorticoids or to biases such as confounding by indication. So, the conclusion that we draw [is] not completely clear.”
In response to a question, he clarified this a little further: “We think ‘glucocorticoid use’ is a determinant of worse health, as is the case in many RMDs. Be aware that finding a positive association between [glucocorticoid] use and bad outcome does not mean that if you reduce [glucocorticoids], your patient will have a better outcome.”
The jury is also out on rituximab, which has been reported to increase the risk of severe COVID-19 and COVID-related death in two studies. There are also equivocal data on whether not using disease-modifying antirheumatic drugs increases the risk for these worse outcomes.
Asked about the absence of a recommendation on the use of the interleukin-6 inhibitor tocilizumab, Dr. Landewé responded: “We are caught up by evolving evidence. That is a generic problem in a dynamic field of COVID-19, I am afraid. What you recommend today is sometimes ‘old history’ tomorrow.”
Dr. Landewé had no relevant disclosures to make.
FROM THE EULAR 2021 CONGRESS
Intravenous immunoglobulin controls dermatomyositis in phase 3 trial
Nearly 50% achieve moderate improvement or better
The first multinational, phase 3, placebo-controlled trial conducted with intravenous immunoglobulin therapy (IVIg) for dermatomyositis has confirmed significant efficacy and acceptable safety, according to data presented at the opening plenary abstract session of the annual European Congress of Rheumatology.
At the week 16 evaluation of the trial, called ProDERM, the response rates were 78.7% and 43.8% (P = .0008) for active therapy and placebo, respectively, reported Rohit Aggarwal, MD, medical director of the Arthritis and Autoimmunity Center at the University of Pittsburgh.
ProDERM is a “much-awaited study,” according to session moderator Hendrik Schulze-Koops, MD, PhD, of the division of rheumatology and clinical immunology at Ludwig Maximilian University of Munich (Germany). He was not involved in the study.
“We all have been doing what we have been doing,” Dr. Schulze-Koops said, referring to the use of IVIg for the control of dermatomyositis, “but we had no evidence for support.”
This statement could apply not only to IVIg, which has long been listed among treatment options by the Myositis Association despite the absence of controlled studies, but also to most immunosuppressive therapies and other options used for this challenging disease.
The proprietary IVIg employed in this study, Octagam 10%, has been approved in the United States for the treatment of chronic immune thrombocytopenic purpura. Its manufacturer, Octagam, plans to file a supplemental new drug application with the Food and Drug Administration for the treatment of dermatomyositis. The agent is already approved for dermatomyositis by the European Medicines Agency, according to Dr. Aggarwal.
Multiple response criteria favor IVIg
In the trial, 95 patients with dermatomyositis were randomized to 2 g/kg of IVIg (Octagam 10%) or placebo administered every 4 weeks. In a subsequent open-label extension study in which patients on placebo were switched to active therapy, the same every-4-week treatment schedule was used. The patients’ mean age was 53; 75% were women, and 92% were White.
The primary endpoint was at least minimal improvement on 2016 ACR/EULAR (American College of Rheumatology/European Alliance of Associations for Rheumatology) myositis response criteria, defined as a 20-point or greater gain in the Total Improvement Score (TIS) and no clinical worsening at two consecutive visits. But IVIg also provided a large relative benefit over placebo using more rigorous definitions of improvement. For moderate improvement, defined as at least a 40-point TIS improvement, there was a 45.2% relative advantage for IVIg over placebo (68.1% vs. 22.9%; P < .0001). For major improvement, defined as at least a 60-point TIS improvement, the relative advantage was 23.6% (31.9% vs. 8.3%; P < .0062).
At 16 weeks, the mean TIS score was more than twice as high in those receiving IVIg than in those randomized to placebo (48.4 vs. 21.6). At that point, an open-label extension was initiated. Those in the IVIg group were permitted to remain on therapy for an additional 24 weeks if they had not worsened in the blinded phase.
The mean TIS score in the IVIg group continued to rise during the extension phase. By 12 weeks in this phase, it reached 54.0. Over the same period, mean TIS scores climbed steeply among the placebo-treated patients who had switched to active therapy, reaching 44.4.
At the end of 24 weeks of the extension trial, when patients initiated on IVIg had been on active therapy for 40 weeks, the mean TIS score advantage of starting on IVIg rather than placebo was relatively modest (55.4 vs. 51.1).
Benefit is significant for skin and muscle
Changes in the two major components of dermatomyositis were tracked individually. For skin symptoms, patients were evaluated with the Cutaneous Dermatomyositis Disease Areas and Severity Index (CDASI). For muscle involvement, symptoms were evaluated with the 8-item Manual Muscle Testing (MMT-8) tool.
“The effects of IVIg on the muscle and the skin were both highly statistically significant,” Dr. Aggarwal reported. He said the CDASI score was reduced by almost half at the end of 16 weeks among those treated with IVIg relative to those treated with placebo. Improvement in MMT-8 scores were also clinically as well as statistically significant.
The IVIg therapy was well tolerated. The most common adverse effects in this study, like those reported with IVIg when used to treat other diseases, were headache, pyrexia, and nausea, but Dr. Aggarwal reported that these were generally mild.
Serious adverse events, particularly thromboembolism, did occur over the course of the study, but the rate of events was only slightly higher in the group receiving active therapy (5.8% vs. 4.2%).
Patients who entered the study were permitted to remain on most immunosuppressive therapies, such as methotrexate, mycophenolate, tacrolimus, and glucocorticoids. Dr. Aggarwal said that the majority of patients were taking a glucocorticoid and at least one nonglucocorticoid immunosuppressant.
Effect on associated conditions is planned
The data from this trial have not yet been analyzed for the impact of IVIg on conditions that occur frequently in association with dermatomyositis, such as interstitial lung disease (ILD) and dysphagia, but Dr. Aggarwal reported that there are plans to do so. Although severe ILD was a trial exclusion, the presence of mild to moderate ILD and dysphagia were evaluated at baseline, so the impact of treatment can be assessed.
There are also plans to evaluate how the presence or absence of myositis-specific antibodies, which were also evaluated at baseline, affected response to IVIg.
Dr. Aggarwal has financial relationships with more than 15 pharmaceutical companies, including Octapharma, which provided financial support for this trial. Dr. Schulze-Koops reported no relevant potential conflicts of interest.
Nearly 50% achieve moderate improvement or better
Nearly 50% achieve moderate improvement or better
The first multinational, phase 3, placebo-controlled trial conducted with intravenous immunoglobulin therapy (IVIg) for dermatomyositis has confirmed significant efficacy and acceptable safety, according to data presented at the opening plenary abstract session of the annual European Congress of Rheumatology.
At the week 16 evaluation of the trial, called ProDERM, the response rates were 78.7% and 43.8% (P = .0008) for active therapy and placebo, respectively, reported Rohit Aggarwal, MD, medical director of the Arthritis and Autoimmunity Center at the University of Pittsburgh.
ProDERM is a “much-awaited study,” according to session moderator Hendrik Schulze-Koops, MD, PhD, of the division of rheumatology and clinical immunology at Ludwig Maximilian University of Munich (Germany). He was not involved in the study.
“We all have been doing what we have been doing,” Dr. Schulze-Koops said, referring to the use of IVIg for the control of dermatomyositis, “but we had no evidence for support.”
This statement could apply not only to IVIg, which has long been listed among treatment options by the Myositis Association despite the absence of controlled studies, but also to most immunosuppressive therapies and other options used for this challenging disease.
The proprietary IVIg employed in this study, Octagam 10%, has been approved in the United States for the treatment of chronic immune thrombocytopenic purpura. Its manufacturer, Octagam, plans to file a supplemental new drug application with the Food and Drug Administration for the treatment of dermatomyositis. The agent is already approved for dermatomyositis by the European Medicines Agency, according to Dr. Aggarwal.
Multiple response criteria favor IVIg
In the trial, 95 patients with dermatomyositis were randomized to 2 g/kg of IVIg (Octagam 10%) or placebo administered every 4 weeks. In a subsequent open-label extension study in which patients on placebo were switched to active therapy, the same every-4-week treatment schedule was used. The patients’ mean age was 53; 75% were women, and 92% were White.
The primary endpoint was at least minimal improvement on 2016 ACR/EULAR (American College of Rheumatology/European Alliance of Associations for Rheumatology) myositis response criteria, defined as a 20-point or greater gain in the Total Improvement Score (TIS) and no clinical worsening at two consecutive visits. But IVIg also provided a large relative benefit over placebo using more rigorous definitions of improvement. For moderate improvement, defined as at least a 40-point TIS improvement, there was a 45.2% relative advantage for IVIg over placebo (68.1% vs. 22.9%; P < .0001). For major improvement, defined as at least a 60-point TIS improvement, the relative advantage was 23.6% (31.9% vs. 8.3%; P < .0062).
At 16 weeks, the mean TIS score was more than twice as high in those receiving IVIg than in those randomized to placebo (48.4 vs. 21.6). At that point, an open-label extension was initiated. Those in the IVIg group were permitted to remain on therapy for an additional 24 weeks if they had not worsened in the blinded phase.
The mean TIS score in the IVIg group continued to rise during the extension phase. By 12 weeks in this phase, it reached 54.0. Over the same period, mean TIS scores climbed steeply among the placebo-treated patients who had switched to active therapy, reaching 44.4.
At the end of 24 weeks of the extension trial, when patients initiated on IVIg had been on active therapy for 40 weeks, the mean TIS score advantage of starting on IVIg rather than placebo was relatively modest (55.4 vs. 51.1).
Benefit is significant for skin and muscle
Changes in the two major components of dermatomyositis were tracked individually. For skin symptoms, patients were evaluated with the Cutaneous Dermatomyositis Disease Areas and Severity Index (CDASI). For muscle involvement, symptoms were evaluated with the 8-item Manual Muscle Testing (MMT-8) tool.
“The effects of IVIg on the muscle and the skin were both highly statistically significant,” Dr. Aggarwal reported. He said the CDASI score was reduced by almost half at the end of 16 weeks among those treated with IVIg relative to those treated with placebo. Improvement in MMT-8 scores were also clinically as well as statistically significant.
The IVIg therapy was well tolerated. The most common adverse effects in this study, like those reported with IVIg when used to treat other diseases, were headache, pyrexia, and nausea, but Dr. Aggarwal reported that these were generally mild.
Serious adverse events, particularly thromboembolism, did occur over the course of the study, but the rate of events was only slightly higher in the group receiving active therapy (5.8% vs. 4.2%).
Patients who entered the study were permitted to remain on most immunosuppressive therapies, such as methotrexate, mycophenolate, tacrolimus, and glucocorticoids. Dr. Aggarwal said that the majority of patients were taking a glucocorticoid and at least one nonglucocorticoid immunosuppressant.
Effect on associated conditions is planned
The data from this trial have not yet been analyzed for the impact of IVIg on conditions that occur frequently in association with dermatomyositis, such as interstitial lung disease (ILD) and dysphagia, but Dr. Aggarwal reported that there are plans to do so. Although severe ILD was a trial exclusion, the presence of mild to moderate ILD and dysphagia were evaluated at baseline, so the impact of treatment can be assessed.
There are also plans to evaluate how the presence or absence of myositis-specific antibodies, which were also evaluated at baseline, affected response to IVIg.
Dr. Aggarwal has financial relationships with more than 15 pharmaceutical companies, including Octapharma, which provided financial support for this trial. Dr. Schulze-Koops reported no relevant potential conflicts of interest.
The first multinational, phase 3, placebo-controlled trial conducted with intravenous immunoglobulin therapy (IVIg) for dermatomyositis has confirmed significant efficacy and acceptable safety, according to data presented at the opening plenary abstract session of the annual European Congress of Rheumatology.
At the week 16 evaluation of the trial, called ProDERM, the response rates were 78.7% and 43.8% (P = .0008) for active therapy and placebo, respectively, reported Rohit Aggarwal, MD, medical director of the Arthritis and Autoimmunity Center at the University of Pittsburgh.
ProDERM is a “much-awaited study,” according to session moderator Hendrik Schulze-Koops, MD, PhD, of the division of rheumatology and clinical immunology at Ludwig Maximilian University of Munich (Germany). He was not involved in the study.
“We all have been doing what we have been doing,” Dr. Schulze-Koops said, referring to the use of IVIg for the control of dermatomyositis, “but we had no evidence for support.”
This statement could apply not only to IVIg, which has long been listed among treatment options by the Myositis Association despite the absence of controlled studies, but also to most immunosuppressive therapies and other options used for this challenging disease.
The proprietary IVIg employed in this study, Octagam 10%, has been approved in the United States for the treatment of chronic immune thrombocytopenic purpura. Its manufacturer, Octagam, plans to file a supplemental new drug application with the Food and Drug Administration for the treatment of dermatomyositis. The agent is already approved for dermatomyositis by the European Medicines Agency, according to Dr. Aggarwal.
Multiple response criteria favor IVIg
In the trial, 95 patients with dermatomyositis were randomized to 2 g/kg of IVIg (Octagam 10%) or placebo administered every 4 weeks. In a subsequent open-label extension study in which patients on placebo were switched to active therapy, the same every-4-week treatment schedule was used. The patients’ mean age was 53; 75% were women, and 92% were White.
The primary endpoint was at least minimal improvement on 2016 ACR/EULAR (American College of Rheumatology/European Alliance of Associations for Rheumatology) myositis response criteria, defined as a 20-point or greater gain in the Total Improvement Score (TIS) and no clinical worsening at two consecutive visits. But IVIg also provided a large relative benefit over placebo using more rigorous definitions of improvement. For moderate improvement, defined as at least a 40-point TIS improvement, there was a 45.2% relative advantage for IVIg over placebo (68.1% vs. 22.9%; P < .0001). For major improvement, defined as at least a 60-point TIS improvement, the relative advantage was 23.6% (31.9% vs. 8.3%; P < .0062).
At 16 weeks, the mean TIS score was more than twice as high in those receiving IVIg than in those randomized to placebo (48.4 vs. 21.6). At that point, an open-label extension was initiated. Those in the IVIg group were permitted to remain on therapy for an additional 24 weeks if they had not worsened in the blinded phase.
The mean TIS score in the IVIg group continued to rise during the extension phase. By 12 weeks in this phase, it reached 54.0. Over the same period, mean TIS scores climbed steeply among the placebo-treated patients who had switched to active therapy, reaching 44.4.
At the end of 24 weeks of the extension trial, when patients initiated on IVIg had been on active therapy for 40 weeks, the mean TIS score advantage of starting on IVIg rather than placebo was relatively modest (55.4 vs. 51.1).
Benefit is significant for skin and muscle
Changes in the two major components of dermatomyositis were tracked individually. For skin symptoms, patients were evaluated with the Cutaneous Dermatomyositis Disease Areas and Severity Index (CDASI). For muscle involvement, symptoms were evaluated with the 8-item Manual Muscle Testing (MMT-8) tool.
“The effects of IVIg on the muscle and the skin were both highly statistically significant,” Dr. Aggarwal reported. He said the CDASI score was reduced by almost half at the end of 16 weeks among those treated with IVIg relative to those treated with placebo. Improvement in MMT-8 scores were also clinically as well as statistically significant.
The IVIg therapy was well tolerated. The most common adverse effects in this study, like those reported with IVIg when used to treat other diseases, were headache, pyrexia, and nausea, but Dr. Aggarwal reported that these were generally mild.
Serious adverse events, particularly thromboembolism, did occur over the course of the study, but the rate of events was only slightly higher in the group receiving active therapy (5.8% vs. 4.2%).
Patients who entered the study were permitted to remain on most immunosuppressive therapies, such as methotrexate, mycophenolate, tacrolimus, and glucocorticoids. Dr. Aggarwal said that the majority of patients were taking a glucocorticoid and at least one nonglucocorticoid immunosuppressant.
Effect on associated conditions is planned
The data from this trial have not yet been analyzed for the impact of IVIg on conditions that occur frequently in association with dermatomyositis, such as interstitial lung disease (ILD) and dysphagia, but Dr. Aggarwal reported that there are plans to do so. Although severe ILD was a trial exclusion, the presence of mild to moderate ILD and dysphagia were evaluated at baseline, so the impact of treatment can be assessed.
There are also plans to evaluate how the presence or absence of myositis-specific antibodies, which were also evaluated at baseline, affected response to IVIg.
Dr. Aggarwal has financial relationships with more than 15 pharmaceutical companies, including Octapharma, which provided financial support for this trial. Dr. Schulze-Koops reported no relevant potential conflicts of interest.
FROM THE EULAR 2021 CONGRESS
FDA approves secukinumab in psoriasis patients age six and older
The who are candidates for systemic therapy or phototherapy. The expanded indication marks the first time the drug has been available for a pediatric population in the United States.
Children with plaque psoriasis are often undertreated because of fear of side effects of therapies, according to Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco. “Now, more and more medicines are being tested for safety and efficacy in children, and we no longer have to rely on adult studies to inform treatment choices for children,” Dr. Cordoro told this news organization.
The FDA approval of secukinumab for children aged 6 and older with moderate to severe psoriasis “is a welcome addition to the therapeutic toolbox for pediatric psoriasis,” she said. “We’ve entered an era where severe pediatric psoriasis has become a condition that can be adequately controlled with minimal risk and with the convenience of intermittent injections. This has changed the playing field for these children and their families completely. Given the potential short- and long-term negative impact of chronic inflammation on the body of a growing child, we now have approved treatments that can safely offset the risks of undertreated severe psoriasis on the functional and psychological health of the child.”
The approved pediatric dosing for secukinumab is 75 mg or 150 mg depending on the child’s weight at the time of dosing, and it is administered by subcutaneous injection every 4 weeks after an initial loading regimen. According to a press release from Novartis, the FDA approval came on the heels of two phase 3 studies that evaluated the use of secukinumab in children aged 6 to younger than 18 years with plaque psoriasis. The first was a 52-week, randomized, double-blind, placebo- and active-controlled study which included 162 children 6 years of age and older with severe plaque psoriasis. The doses evaluated were 75 mg for children who weighed less than 50 kg and 150 mg for those 50 kg or greater.
At week 12, the Psoriasis Area Severity Index (PASI)-75 response was 55% among children in the 75-mg dosing group vs. 10% in the placebo group and 86% in the 150-mg dosing group vs. 19% in the placebo group.
Meanwhile, the Investigator’s Global Assessment modified 2011 (IGA) “clear” response was achieved in 32% of children in the 75-mg dosing group vs. 5% in the placebo group and in 81% of children in the 150-mg dosing group vs. 5% in the placebo group. An IGA “almost clear” skin response was achieved in 81% of children in the 75-mg dosing group vs. 5% in the placebo group.
The second phase 3 study was a randomized open-label, 208-week trial of 84 subjects 6 years of age and older with moderate to severe plaque psoriasis. According to the Novartis press release, the safety profile reported in both trials was consistent with the safety profile reported in adult plaque psoriasis trials and no new safety signals were observed. The updated prescribing information for secukinumab can be found here.
“When considering treatment with a systemic agent such as a biologic, it is important to consider objective measures of severity, such as extent of disease and involvement of joints but also subjective indicators of severity such as impact beyond the skin on psychological well-being,” Dr. Cordoro said in the interview. “Kids with psoriasis in visible locations may socially isolate themselves due to embarrassment or bullying. Therefore, the impact of moderate to severe psoriasis not only on overall health but on self-esteem and identity formation can be significant, and therefore adequately treating children of all ages to prevent the downstream negative consequences of childhood psoriasis is critical.”
Dr. Cordoro reported having no financial disclosures.
The who are candidates for systemic therapy or phototherapy. The expanded indication marks the first time the drug has been available for a pediatric population in the United States.
Children with plaque psoriasis are often undertreated because of fear of side effects of therapies, according to Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco. “Now, more and more medicines are being tested for safety and efficacy in children, and we no longer have to rely on adult studies to inform treatment choices for children,” Dr. Cordoro told this news organization.
The FDA approval of secukinumab for children aged 6 and older with moderate to severe psoriasis “is a welcome addition to the therapeutic toolbox for pediatric psoriasis,” she said. “We’ve entered an era where severe pediatric psoriasis has become a condition that can be adequately controlled with minimal risk and with the convenience of intermittent injections. This has changed the playing field for these children and their families completely. Given the potential short- and long-term negative impact of chronic inflammation on the body of a growing child, we now have approved treatments that can safely offset the risks of undertreated severe psoriasis on the functional and psychological health of the child.”
The approved pediatric dosing for secukinumab is 75 mg or 150 mg depending on the child’s weight at the time of dosing, and it is administered by subcutaneous injection every 4 weeks after an initial loading regimen. According to a press release from Novartis, the FDA approval came on the heels of two phase 3 studies that evaluated the use of secukinumab in children aged 6 to younger than 18 years with plaque psoriasis. The first was a 52-week, randomized, double-blind, placebo- and active-controlled study which included 162 children 6 years of age and older with severe plaque psoriasis. The doses evaluated were 75 mg for children who weighed less than 50 kg and 150 mg for those 50 kg or greater.
At week 12, the Psoriasis Area Severity Index (PASI)-75 response was 55% among children in the 75-mg dosing group vs. 10% in the placebo group and 86% in the 150-mg dosing group vs. 19% in the placebo group.
Meanwhile, the Investigator’s Global Assessment modified 2011 (IGA) “clear” response was achieved in 32% of children in the 75-mg dosing group vs. 5% in the placebo group and in 81% of children in the 150-mg dosing group vs. 5% in the placebo group. An IGA “almost clear” skin response was achieved in 81% of children in the 75-mg dosing group vs. 5% in the placebo group.
The second phase 3 study was a randomized open-label, 208-week trial of 84 subjects 6 years of age and older with moderate to severe plaque psoriasis. According to the Novartis press release, the safety profile reported in both trials was consistent with the safety profile reported in adult plaque psoriasis trials and no new safety signals were observed. The updated prescribing information for secukinumab can be found here.
“When considering treatment with a systemic agent such as a biologic, it is important to consider objective measures of severity, such as extent of disease and involvement of joints but also subjective indicators of severity such as impact beyond the skin on psychological well-being,” Dr. Cordoro said in the interview. “Kids with psoriasis in visible locations may socially isolate themselves due to embarrassment or bullying. Therefore, the impact of moderate to severe psoriasis not only on overall health but on self-esteem and identity formation can be significant, and therefore adequately treating children of all ages to prevent the downstream negative consequences of childhood psoriasis is critical.”
Dr. Cordoro reported having no financial disclosures.
The who are candidates for systemic therapy or phototherapy. The expanded indication marks the first time the drug has been available for a pediatric population in the United States.
Children with plaque psoriasis are often undertreated because of fear of side effects of therapies, according to Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco. “Now, more and more medicines are being tested for safety and efficacy in children, and we no longer have to rely on adult studies to inform treatment choices for children,” Dr. Cordoro told this news organization.
The FDA approval of secukinumab for children aged 6 and older with moderate to severe psoriasis “is a welcome addition to the therapeutic toolbox for pediatric psoriasis,” she said. “We’ve entered an era where severe pediatric psoriasis has become a condition that can be adequately controlled with minimal risk and with the convenience of intermittent injections. This has changed the playing field for these children and their families completely. Given the potential short- and long-term negative impact of chronic inflammation on the body of a growing child, we now have approved treatments that can safely offset the risks of undertreated severe psoriasis on the functional and psychological health of the child.”
The approved pediatric dosing for secukinumab is 75 mg or 150 mg depending on the child’s weight at the time of dosing, and it is administered by subcutaneous injection every 4 weeks after an initial loading regimen. According to a press release from Novartis, the FDA approval came on the heels of two phase 3 studies that evaluated the use of secukinumab in children aged 6 to younger than 18 years with plaque psoriasis. The first was a 52-week, randomized, double-blind, placebo- and active-controlled study which included 162 children 6 years of age and older with severe plaque psoriasis. The doses evaluated were 75 mg for children who weighed less than 50 kg and 150 mg for those 50 kg or greater.
At week 12, the Psoriasis Area Severity Index (PASI)-75 response was 55% among children in the 75-mg dosing group vs. 10% in the placebo group and 86% in the 150-mg dosing group vs. 19% in the placebo group.
Meanwhile, the Investigator’s Global Assessment modified 2011 (IGA) “clear” response was achieved in 32% of children in the 75-mg dosing group vs. 5% in the placebo group and in 81% of children in the 150-mg dosing group vs. 5% in the placebo group. An IGA “almost clear” skin response was achieved in 81% of children in the 75-mg dosing group vs. 5% in the placebo group.
The second phase 3 study was a randomized open-label, 208-week trial of 84 subjects 6 years of age and older with moderate to severe plaque psoriasis. According to the Novartis press release, the safety profile reported in both trials was consistent with the safety profile reported in adult plaque psoriasis trials and no new safety signals were observed. The updated prescribing information for secukinumab can be found here.
“When considering treatment with a systemic agent such as a biologic, it is important to consider objective measures of severity, such as extent of disease and involvement of joints but also subjective indicators of severity such as impact beyond the skin on psychological well-being,” Dr. Cordoro said in the interview. “Kids with psoriasis in visible locations may socially isolate themselves due to embarrassment or bullying. Therefore, the impact of moderate to severe psoriasis not only on overall health but on self-esteem and identity formation can be significant, and therefore adequately treating children of all ages to prevent the downstream negative consequences of childhood psoriasis is critical.”
Dr. Cordoro reported having no financial disclosures.
Noses can be electronic, and toilets can be smart
Cancer loses … by a nose
Since the human nose is unpredictable at best, we’ve learned to rely on animals for our detailed nozzle needs. But researchers have found the next best thing to man’s best friend to accurately identify cancers.
A team at the University of Pennsylvania has developed an electronic olfaction, or “e-nose,” that has a 95% accuracy rate in distinguishing benign and malignant pancreatic and ovarian cancer cells from a single blood sample. How?
The e-nose system is equipped with nanosensors that are able to detect the volatile organic compounds (VOCs) emitted by cells in a blood sample. Not only does this create an opportunity for an easier, noninvasive screening practice, but it’s fast. The e-nose can distinguish VOCs from healthy to cancerous blood cells in 20 minutes or less and is just as effective in picking up on early- and late-stage cancers.
The investigators hope that this innovative technology can pave the way for similar devices with other uses. Thanks to the e-nose, a handheld device is in development that may be able to sniff out the signature odor of people with COVID-19.
That’s one smart schnoz.
Do you think this is a (food) game?
Dieting and eating healthy is tough, even during the best of times, and it has not been the best of times. With all respect to Charles Dickens, it’s been the worst of times, full stop. Millions of people have spent the past year sitting around their homes doing nothing, and it’s only natural that many would let their discipline slide.
Naturally, the solution to unhealthy eating habits is to sit down and play with your phone. No, that’s not the joke, the Food Trainer app, available on all cellular devices near you, is designed to encourage healthy eating by turning it into a game of sorts. When users open the app, they’re presented with images of food, and they’re trained to tap on images of healthy food and pass on images of unhealthy ones. The process takes less than 5 minutes.
It sounds really simple, but in a study of more than 1,000 people, consumption of junk food fell by 1 point on an 8-point scale (ranging from four times per day to zero to one time per month), participants lost about half a kilogram (a little over one pound), and more healthy food was eaten. Those who used the app more regularly, along the lines of 10 times per month or more, saw greater benefits.
The authors did acknowledge that those who used the app more may have been more motivated to lose weight anyway, which perhaps limits the overall benefit, but reviews on Google Play were overall quite positive, and if there’s one great truth in this world, it’s that Internet reviewers are almost impossible to please. So perhaps this app is worth looking into if you’re like the LOTME staff and you’re up at the top end of that 8-point scale. What, pizza is delicious, who wouldn’t eat it four times a day? And you can also get it from your phone!
It’s time for a little mass kickin’
The universe, scientists tell us, is a big place. Really big. Chromosomes, scientists tell us, are small. Really small. But despite this very fundamental difference, the universe and chromosomes share a deep, dark secret: unexplained mass.
This being a medical publication, we’ll start with chromosomes. A group of researchers measured their mass with x-rays for the first time and found that “the 46 chromosomes in each of our cells weigh 242 picograms (trillionths of a gram). This is heavier than we would expect, and, if replicated, points to unexplained excess mass in chromosomes,” Ian K. Robinson, PhD, said in a written statement.
We’re not just talking about a bit of a beer belly here. “The chromosomes were about 20 times heavier than the DNA they contained,” according to the investigators.
Now to the universe. Here’s what CERN, the European Council for Nuclear Research, has to say about the mass of the universe: “Galaxies in our universe … are rotating with such speed that the gravity generated by their observable matter could not possibly hold them together. … which leads scientists to believe that something we cannot see is at work. They think something we have yet to detect directly is giving these galaxies extra mass.”
But wait, there’s more! “The matter we know and that makes up all stars and galaxies only accounts for 5% of the content of the universe!”
So chromosomes are about 20 times heavier than the DNA they contain, and the universe is about 20 times heavier than the matter that can be seen. Interesting.
We are, of course, happy to share this news with our readers, but there is one catch: Don’t tell Neil deGrasse Tyson. He’ll want to reclassify our genetic solar system into 45 chromosomes and one dwarf chromosome.
A photo finish for the Smart Toilet
We know that poop can tell us a lot about our health, but new research by scientists at Duke University is really on a roll. Their Smart Toilet has been created to help people keep an eye on their bowel health. The device takes pictures of poop after it is flushed and can tell whether the consistency is loose, bloody, or normal.
The Smart Toilet can really help people with issues such as irritable bowel syndrome and inflammatory bowel disease by helping them, and their doctors, keep tabs on their poop. “Typically, gastroenterologists have to rely on patient self-reported information about their stool to help determine the cause of their gastrointestinal health issues, which can be very unreliable,” study lead author Deborah Fisher said.
Not many people look too closely at their poop before it’s flushed, so the fecal photos can make a big difference. The Smart Toilet is installed into the pipes of a toilet and does its thing when the toilet is flushed, so there doesn’t seem to be much work on the patient’s end. Other than the, um, you know, usual work from the patient’s end.
Cancer loses … by a nose
Since the human nose is unpredictable at best, we’ve learned to rely on animals for our detailed nozzle needs. But researchers have found the next best thing to man’s best friend to accurately identify cancers.
A team at the University of Pennsylvania has developed an electronic olfaction, or “e-nose,” that has a 95% accuracy rate in distinguishing benign and malignant pancreatic and ovarian cancer cells from a single blood sample. How?
The e-nose system is equipped with nanosensors that are able to detect the volatile organic compounds (VOCs) emitted by cells in a blood sample. Not only does this create an opportunity for an easier, noninvasive screening practice, but it’s fast. The e-nose can distinguish VOCs from healthy to cancerous blood cells in 20 minutes or less and is just as effective in picking up on early- and late-stage cancers.
The investigators hope that this innovative technology can pave the way for similar devices with other uses. Thanks to the e-nose, a handheld device is in development that may be able to sniff out the signature odor of people with COVID-19.
That’s one smart schnoz.
Do you think this is a (food) game?
Dieting and eating healthy is tough, even during the best of times, and it has not been the best of times. With all respect to Charles Dickens, it’s been the worst of times, full stop. Millions of people have spent the past year sitting around their homes doing nothing, and it’s only natural that many would let their discipline slide.
Naturally, the solution to unhealthy eating habits is to sit down and play with your phone. No, that’s not the joke, the Food Trainer app, available on all cellular devices near you, is designed to encourage healthy eating by turning it into a game of sorts. When users open the app, they’re presented with images of food, and they’re trained to tap on images of healthy food and pass on images of unhealthy ones. The process takes less than 5 minutes.
It sounds really simple, but in a study of more than 1,000 people, consumption of junk food fell by 1 point on an 8-point scale (ranging from four times per day to zero to one time per month), participants lost about half a kilogram (a little over one pound), and more healthy food was eaten. Those who used the app more regularly, along the lines of 10 times per month or more, saw greater benefits.
The authors did acknowledge that those who used the app more may have been more motivated to lose weight anyway, which perhaps limits the overall benefit, but reviews on Google Play were overall quite positive, and if there’s one great truth in this world, it’s that Internet reviewers are almost impossible to please. So perhaps this app is worth looking into if you’re like the LOTME staff and you’re up at the top end of that 8-point scale. What, pizza is delicious, who wouldn’t eat it four times a day? And you can also get it from your phone!
It’s time for a little mass kickin’
The universe, scientists tell us, is a big place. Really big. Chromosomes, scientists tell us, are small. Really small. But despite this very fundamental difference, the universe and chromosomes share a deep, dark secret: unexplained mass.
This being a medical publication, we’ll start with chromosomes. A group of researchers measured their mass with x-rays for the first time and found that “the 46 chromosomes in each of our cells weigh 242 picograms (trillionths of a gram). This is heavier than we would expect, and, if replicated, points to unexplained excess mass in chromosomes,” Ian K. Robinson, PhD, said in a written statement.
We’re not just talking about a bit of a beer belly here. “The chromosomes were about 20 times heavier than the DNA they contained,” according to the investigators.
Now to the universe. Here’s what CERN, the European Council for Nuclear Research, has to say about the mass of the universe: “Galaxies in our universe … are rotating with such speed that the gravity generated by their observable matter could not possibly hold them together. … which leads scientists to believe that something we cannot see is at work. They think something we have yet to detect directly is giving these galaxies extra mass.”
But wait, there’s more! “The matter we know and that makes up all stars and galaxies only accounts for 5% of the content of the universe!”
So chromosomes are about 20 times heavier than the DNA they contain, and the universe is about 20 times heavier than the matter that can be seen. Interesting.
We are, of course, happy to share this news with our readers, but there is one catch: Don’t tell Neil deGrasse Tyson. He’ll want to reclassify our genetic solar system into 45 chromosomes and one dwarf chromosome.
A photo finish for the Smart Toilet
We know that poop can tell us a lot about our health, but new research by scientists at Duke University is really on a roll. Their Smart Toilet has been created to help people keep an eye on their bowel health. The device takes pictures of poop after it is flushed and can tell whether the consistency is loose, bloody, or normal.
The Smart Toilet can really help people with issues such as irritable bowel syndrome and inflammatory bowel disease by helping them, and their doctors, keep tabs on their poop. “Typically, gastroenterologists have to rely on patient self-reported information about their stool to help determine the cause of their gastrointestinal health issues, which can be very unreliable,” study lead author Deborah Fisher said.
Not many people look too closely at their poop before it’s flushed, so the fecal photos can make a big difference. The Smart Toilet is installed into the pipes of a toilet and does its thing when the toilet is flushed, so there doesn’t seem to be much work on the patient’s end. Other than the, um, you know, usual work from the patient’s end.
Cancer loses … by a nose
Since the human nose is unpredictable at best, we’ve learned to rely on animals for our detailed nozzle needs. But researchers have found the next best thing to man’s best friend to accurately identify cancers.
A team at the University of Pennsylvania has developed an electronic olfaction, or “e-nose,” that has a 95% accuracy rate in distinguishing benign and malignant pancreatic and ovarian cancer cells from a single blood sample. How?
The e-nose system is equipped with nanosensors that are able to detect the volatile organic compounds (VOCs) emitted by cells in a blood sample. Not only does this create an opportunity for an easier, noninvasive screening practice, but it’s fast. The e-nose can distinguish VOCs from healthy to cancerous blood cells in 20 minutes or less and is just as effective in picking up on early- and late-stage cancers.
The investigators hope that this innovative technology can pave the way for similar devices with other uses. Thanks to the e-nose, a handheld device is in development that may be able to sniff out the signature odor of people with COVID-19.
That’s one smart schnoz.
Do you think this is a (food) game?
Dieting and eating healthy is tough, even during the best of times, and it has not been the best of times. With all respect to Charles Dickens, it’s been the worst of times, full stop. Millions of people have spent the past year sitting around their homes doing nothing, and it’s only natural that many would let their discipline slide.
Naturally, the solution to unhealthy eating habits is to sit down and play with your phone. No, that’s not the joke, the Food Trainer app, available on all cellular devices near you, is designed to encourage healthy eating by turning it into a game of sorts. When users open the app, they’re presented with images of food, and they’re trained to tap on images of healthy food and pass on images of unhealthy ones. The process takes less than 5 minutes.
It sounds really simple, but in a study of more than 1,000 people, consumption of junk food fell by 1 point on an 8-point scale (ranging from four times per day to zero to one time per month), participants lost about half a kilogram (a little over one pound), and more healthy food was eaten. Those who used the app more regularly, along the lines of 10 times per month or more, saw greater benefits.
The authors did acknowledge that those who used the app more may have been more motivated to lose weight anyway, which perhaps limits the overall benefit, but reviews on Google Play were overall quite positive, and if there’s one great truth in this world, it’s that Internet reviewers are almost impossible to please. So perhaps this app is worth looking into if you’re like the LOTME staff and you’re up at the top end of that 8-point scale. What, pizza is delicious, who wouldn’t eat it four times a day? And you can also get it from your phone!
It’s time for a little mass kickin’
The universe, scientists tell us, is a big place. Really big. Chromosomes, scientists tell us, are small. Really small. But despite this very fundamental difference, the universe and chromosomes share a deep, dark secret: unexplained mass.
This being a medical publication, we’ll start with chromosomes. A group of researchers measured their mass with x-rays for the first time and found that “the 46 chromosomes in each of our cells weigh 242 picograms (trillionths of a gram). This is heavier than we would expect, and, if replicated, points to unexplained excess mass in chromosomes,” Ian K. Robinson, PhD, said in a written statement.
We’re not just talking about a bit of a beer belly here. “The chromosomes were about 20 times heavier than the DNA they contained,” according to the investigators.
Now to the universe. Here’s what CERN, the European Council for Nuclear Research, has to say about the mass of the universe: “Galaxies in our universe … are rotating with such speed that the gravity generated by their observable matter could not possibly hold them together. … which leads scientists to believe that something we cannot see is at work. They think something we have yet to detect directly is giving these galaxies extra mass.”
But wait, there’s more! “The matter we know and that makes up all stars and galaxies only accounts for 5% of the content of the universe!”
So chromosomes are about 20 times heavier than the DNA they contain, and the universe is about 20 times heavier than the matter that can be seen. Interesting.
We are, of course, happy to share this news with our readers, but there is one catch: Don’t tell Neil deGrasse Tyson. He’ll want to reclassify our genetic solar system into 45 chromosomes and one dwarf chromosome.
A photo finish for the Smart Toilet
We know that poop can tell us a lot about our health, but new research by scientists at Duke University is really on a roll. Their Smart Toilet has been created to help people keep an eye on their bowel health. The device takes pictures of poop after it is flushed and can tell whether the consistency is loose, bloody, or normal.
The Smart Toilet can really help people with issues such as irritable bowel syndrome and inflammatory bowel disease by helping them, and their doctors, keep tabs on their poop. “Typically, gastroenterologists have to rely on patient self-reported information about their stool to help determine the cause of their gastrointestinal health issues, which can be very unreliable,” study lead author Deborah Fisher said.
Not many people look too closely at their poop before it’s flushed, so the fecal photos can make a big difference. The Smart Toilet is installed into the pipes of a toilet and does its thing when the toilet is flushed, so there doesn’t seem to be much work on the patient’s end. Other than the, um, you know, usual work from the patient’s end.
Subclinical myocarditis found in some athletes post COVID
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
DOJ charges 14 with COVID-19–related fraud nearing $150M
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
Lower glucocorticoid dose proves effective for new-onset ANCA-associated vasculitis
A reduced dose of prednisolone plus rituximab was as effective as a conventionally high dose in treating patients with newly diagnosed antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, according to a new Japanese study, along with significantly fewer adverse events as well.
“To our knowledge, this is the first trial in ANCA-associated vasculitis showing that a lower glucocorticoid dose may reduce serious adverse events,” wrote Shunsuke Furuta, MD, PhD, of the department of allergy and clinical immunology at Chiba (Japan) University Hospital, and colleagues. The study was published June 1, 2021, in JAMA.
To determine the most effective and safe dose of glucocorticoids for treating this specific subset of patients with vasculitis, the researchers launched an open-label noninferiority clinical trial at 21 hospitals in Japan. A group of 140 patients with new-onset ANCA-associated vasculitis (AAV) without severe glomerulonephritis or alveolar hemorrhage were enrolled and split evenly into two treatment subgroups: reduced-dose prednisolone (0.5 mg/kg per day) plus four doses of rituximab (375 mg/m2 per week) or high-dose prednisolone (1 mg/kg per day) plus rituximab. The median age for all enrolled patients was 73, and approximately 58% were women.
Of the 140 original patients, 134 (95.7%) completed the trial. After 6 months, 49 participants in the reduced-dose group (71%) and 45 in the high-dose group (69.2%) achieved remission, as assessed via the Birmingham Vasculitis Activity Score. The difference between the two groups – 1.8 percentage points (one-sided 97.5% confidence interval, –13.7 to infinity) – met the prespecified margin of –20 percentage points for noninferiority (P = .003 for noninferiority). Relapse within 6 months occurred in three participants in the reduced-dose group and zero in the high-dose group, frequencies that the researchers identified as not statistically different (difference, 4.3%; 95% CI, –0.5% to 9.3%; P = .24).
Serious adverse events occurred less frequently in the reduced-dose group (21 events in 13 patients, 18.8%), compared with the high-dose group (41 events in 24 patients, 36.9%), as did serious infections in the reduced-dose group (7 events in 5 patients, 7.2%) versus the high-dose group (20 events in 13 patients, 20%). Two patients died in the reduced-dose group and three died in the high-dose group; those frequencies were noted as not statistically different (difference, –1.7%; 95% CI, –4.7% to 8.2%; P = .67). Causes of death included subarachnoid hemorrhage in a 58-year-old in the reduced-dose group, along with a case of sepsis in an 80-year-old and two gastrointestinal bleedings in a 75-year-old and an 85-year-old in the high-dose group.
End-stage kidney disease (ESKD) occurred in one patient in the high-dose group and none in the reduced-dose group. Cumulative survival rates at 6 months were not significantly different between the reduced-dose (97.1%) and the high-dose (95.3%) groups (95% CI, –4.7% to 8.2%; P = .58).
Less glucocorticoids makes sense for subset of patients with milder vasculitis
“We always worry about how much steroids we’re giving our patients,” said Anisha B. Dua, MD, an associate professor of rheumatology at Northwestern University, Chicago. “And it’s not a shock to find out that we can use less. That’s been the theme of many studies across vasculitities that have been coming out: ‘Maybe we are using too much steroids.’ It’s really important to have actual data supporting that, though, so clinicians can feel more confident and figure out what population it applies to.”
She added that, because the study focused on patients with milder disease, it’s no surprise that remission was achieved with a lesser dose.
“I see a lot of vasculitis patients, and this gives me more confidence in a subset of them – new ANCA vasculitis, MPO positive, not very severe disease – to get away with using less steroids up front,” she said.
To apply these findings more broadly across vasculitis patients, Dr. Dua stressed the need for a follow-up study, preferably a randomized, controlled trial, with an expanded population and a longer duration.
“There were 3 relapses in the low-dose group and zero in the high-dose group in the first 6 months,” she said. “I’d be interested to know when those happened and also, over time, whether the low-dose regiment up front impacts the rate of relapse in the long term.”
The authors acknowledged the study’s limitations, including the necessity of an open-label trial because of the inevitable visible effects of high-dose glucocorticoid on patients. They also addressed the potential subjectivity of the Birmingham Vasculitis Activity Score, though they added that “other endpoints, including death, ESKD, and serious adverse events, were objective.” Finally, they acknowledged that their study was nationwide but not international, with disease phenotypes that were typical of Japanese patients with AAV. That said, “previous studies have shown that treatment responses are similar between Japan and other countries,” they wrote.
The study was funded by an intramural competitive grant from Chiba University Hospital. The authors reported numerous potential conflicts of interest, including receiving grant support, lecture fees, and personal fees from various pharmaceutical companies.
A reduced dose of prednisolone plus rituximab was as effective as a conventionally high dose in treating patients with newly diagnosed antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, according to a new Japanese study, along with significantly fewer adverse events as well.
“To our knowledge, this is the first trial in ANCA-associated vasculitis showing that a lower glucocorticoid dose may reduce serious adverse events,” wrote Shunsuke Furuta, MD, PhD, of the department of allergy and clinical immunology at Chiba (Japan) University Hospital, and colleagues. The study was published June 1, 2021, in JAMA.
To determine the most effective and safe dose of glucocorticoids for treating this specific subset of patients with vasculitis, the researchers launched an open-label noninferiority clinical trial at 21 hospitals in Japan. A group of 140 patients with new-onset ANCA-associated vasculitis (AAV) without severe glomerulonephritis or alveolar hemorrhage were enrolled and split evenly into two treatment subgroups: reduced-dose prednisolone (0.5 mg/kg per day) plus four doses of rituximab (375 mg/m2 per week) or high-dose prednisolone (1 mg/kg per day) plus rituximab. The median age for all enrolled patients was 73, and approximately 58% were women.
Of the 140 original patients, 134 (95.7%) completed the trial. After 6 months, 49 participants in the reduced-dose group (71%) and 45 in the high-dose group (69.2%) achieved remission, as assessed via the Birmingham Vasculitis Activity Score. The difference between the two groups – 1.8 percentage points (one-sided 97.5% confidence interval, –13.7 to infinity) – met the prespecified margin of –20 percentage points for noninferiority (P = .003 for noninferiority). Relapse within 6 months occurred in three participants in the reduced-dose group and zero in the high-dose group, frequencies that the researchers identified as not statistically different (difference, 4.3%; 95% CI, –0.5% to 9.3%; P = .24).
Serious adverse events occurred less frequently in the reduced-dose group (21 events in 13 patients, 18.8%), compared with the high-dose group (41 events in 24 patients, 36.9%), as did serious infections in the reduced-dose group (7 events in 5 patients, 7.2%) versus the high-dose group (20 events in 13 patients, 20%). Two patients died in the reduced-dose group and three died in the high-dose group; those frequencies were noted as not statistically different (difference, –1.7%; 95% CI, –4.7% to 8.2%; P = .67). Causes of death included subarachnoid hemorrhage in a 58-year-old in the reduced-dose group, along with a case of sepsis in an 80-year-old and two gastrointestinal bleedings in a 75-year-old and an 85-year-old in the high-dose group.
End-stage kidney disease (ESKD) occurred in one patient in the high-dose group and none in the reduced-dose group. Cumulative survival rates at 6 months were not significantly different between the reduced-dose (97.1%) and the high-dose (95.3%) groups (95% CI, –4.7% to 8.2%; P = .58).
Less glucocorticoids makes sense for subset of patients with milder vasculitis
“We always worry about how much steroids we’re giving our patients,” said Anisha B. Dua, MD, an associate professor of rheumatology at Northwestern University, Chicago. “And it’s not a shock to find out that we can use less. That’s been the theme of many studies across vasculitities that have been coming out: ‘Maybe we are using too much steroids.’ It’s really important to have actual data supporting that, though, so clinicians can feel more confident and figure out what population it applies to.”
She added that, because the study focused on patients with milder disease, it’s no surprise that remission was achieved with a lesser dose.
“I see a lot of vasculitis patients, and this gives me more confidence in a subset of them – new ANCA vasculitis, MPO positive, not very severe disease – to get away with using less steroids up front,” she said.
To apply these findings more broadly across vasculitis patients, Dr. Dua stressed the need for a follow-up study, preferably a randomized, controlled trial, with an expanded population and a longer duration.
“There were 3 relapses in the low-dose group and zero in the high-dose group in the first 6 months,” she said. “I’d be interested to know when those happened and also, over time, whether the low-dose regiment up front impacts the rate of relapse in the long term.”
The authors acknowledged the study’s limitations, including the necessity of an open-label trial because of the inevitable visible effects of high-dose glucocorticoid on patients. They also addressed the potential subjectivity of the Birmingham Vasculitis Activity Score, though they added that “other endpoints, including death, ESKD, and serious adverse events, were objective.” Finally, they acknowledged that their study was nationwide but not international, with disease phenotypes that were typical of Japanese patients with AAV. That said, “previous studies have shown that treatment responses are similar between Japan and other countries,” they wrote.
The study was funded by an intramural competitive grant from Chiba University Hospital. The authors reported numerous potential conflicts of interest, including receiving grant support, lecture fees, and personal fees from various pharmaceutical companies.
A reduced dose of prednisolone plus rituximab was as effective as a conventionally high dose in treating patients with newly diagnosed antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, according to a new Japanese study, along with significantly fewer adverse events as well.
“To our knowledge, this is the first trial in ANCA-associated vasculitis showing that a lower glucocorticoid dose may reduce serious adverse events,” wrote Shunsuke Furuta, MD, PhD, of the department of allergy and clinical immunology at Chiba (Japan) University Hospital, and colleagues. The study was published June 1, 2021, in JAMA.
To determine the most effective and safe dose of glucocorticoids for treating this specific subset of patients with vasculitis, the researchers launched an open-label noninferiority clinical trial at 21 hospitals in Japan. A group of 140 patients with new-onset ANCA-associated vasculitis (AAV) without severe glomerulonephritis or alveolar hemorrhage were enrolled and split evenly into two treatment subgroups: reduced-dose prednisolone (0.5 mg/kg per day) plus four doses of rituximab (375 mg/m2 per week) or high-dose prednisolone (1 mg/kg per day) plus rituximab. The median age for all enrolled patients was 73, and approximately 58% were women.
Of the 140 original patients, 134 (95.7%) completed the trial. After 6 months, 49 participants in the reduced-dose group (71%) and 45 in the high-dose group (69.2%) achieved remission, as assessed via the Birmingham Vasculitis Activity Score. The difference between the two groups – 1.8 percentage points (one-sided 97.5% confidence interval, –13.7 to infinity) – met the prespecified margin of –20 percentage points for noninferiority (P = .003 for noninferiority). Relapse within 6 months occurred in three participants in the reduced-dose group and zero in the high-dose group, frequencies that the researchers identified as not statistically different (difference, 4.3%; 95% CI, –0.5% to 9.3%; P = .24).
Serious adverse events occurred less frequently in the reduced-dose group (21 events in 13 patients, 18.8%), compared with the high-dose group (41 events in 24 patients, 36.9%), as did serious infections in the reduced-dose group (7 events in 5 patients, 7.2%) versus the high-dose group (20 events in 13 patients, 20%). Two patients died in the reduced-dose group and three died in the high-dose group; those frequencies were noted as not statistically different (difference, –1.7%; 95% CI, –4.7% to 8.2%; P = .67). Causes of death included subarachnoid hemorrhage in a 58-year-old in the reduced-dose group, along with a case of sepsis in an 80-year-old and two gastrointestinal bleedings in a 75-year-old and an 85-year-old in the high-dose group.
End-stage kidney disease (ESKD) occurred in one patient in the high-dose group and none in the reduced-dose group. Cumulative survival rates at 6 months were not significantly different between the reduced-dose (97.1%) and the high-dose (95.3%) groups (95% CI, –4.7% to 8.2%; P = .58).
Less glucocorticoids makes sense for subset of patients with milder vasculitis
“We always worry about how much steroids we’re giving our patients,” said Anisha B. Dua, MD, an associate professor of rheumatology at Northwestern University, Chicago. “And it’s not a shock to find out that we can use less. That’s been the theme of many studies across vasculitities that have been coming out: ‘Maybe we are using too much steroids.’ It’s really important to have actual data supporting that, though, so clinicians can feel more confident and figure out what population it applies to.”
She added that, because the study focused on patients with milder disease, it’s no surprise that remission was achieved with a lesser dose.
“I see a lot of vasculitis patients, and this gives me more confidence in a subset of them – new ANCA vasculitis, MPO positive, not very severe disease – to get away with using less steroids up front,” she said.
To apply these findings more broadly across vasculitis patients, Dr. Dua stressed the need for a follow-up study, preferably a randomized, controlled trial, with an expanded population and a longer duration.
“There were 3 relapses in the low-dose group and zero in the high-dose group in the first 6 months,” she said. “I’d be interested to know when those happened and also, over time, whether the low-dose regiment up front impacts the rate of relapse in the long term.”
The authors acknowledged the study’s limitations, including the necessity of an open-label trial because of the inevitable visible effects of high-dose glucocorticoid on patients. They also addressed the potential subjectivity of the Birmingham Vasculitis Activity Score, though they added that “other endpoints, including death, ESKD, and serious adverse events, were objective.” Finally, they acknowledged that their study was nationwide but not international, with disease phenotypes that were typical of Japanese patients with AAV. That said, “previous studies have shown that treatment responses are similar between Japan and other countries,” they wrote.
The study was funded by an intramural competitive grant from Chiba University Hospital. The authors reported numerous potential conflicts of interest, including receiving grant support, lecture fees, and personal fees from various pharmaceutical companies.
FROM JAMA
Bill seeks to streamline prior authorization in Medicare Advantage plans
A group of bipartisan lawmakers intends to compel insurers to streamline prior authorization processes for Medicare Advantage plans, including a bid to end the use of faxes and develop systems that can allow for real-time decisions.
Rep. Suzan DelBene (D-Wash.); Rep. Mike Kelly (R-Pa.); Rep. Ami Bera, MD (D-Calif.); and Rep. Larry Bucshon, MD, (R-Ind.) on May 13 introduced a bill that would task federal officials with refining standards regarding prior authorization for Medicare Advantage. Titled the Improving Seniors’ Timely Access to Care Act of 2021, the bill would direct the Department of Health & Human Services to create rules intended to make prior authorization more transparent and speedy for the insurer-run Medicare plans. Known as Medicare Advantage, these plans cover about 24.1 million people of the 62 million enrolled in the giant federal health program, according to the nonprofit Kaiser Family Foundation.
These revamped prior authorization systems could not rely on faxes nor could they employ proprietary payer portals that did not meet HHS’ standards, says the text of the bill released by Rep. DelBene. Insurers would also have to report to the Centers for Medicare & Medicaid Services about the extent of their use of prior authorization and the rate of approvals or denials. The bill seeks to encourage plans to adopt prior authorization programs that adhere to evidence-based medical guidelines in consultation with physicians.
There were several reasons for focusing on Medicare Advantage plans, although prior authorization concerns extend more broadly in the U.S. health care system, said Susan Bailey, MD, president of the American Medical Association.
There’s an ample body of research about issues seen in the Medicare Advantage plans. Dr. Bailey also said that, in her experience, Medicare Advantage plans have had some of the most restrictive policies. And, by starting with Medicare Advantage, there’s a potential for a ripple effect in the industry, easing this issue when physicians work with other insurers as well.
“When Medicare adopts a policy whether it be a payment policy or a coverage policy, private insurers typically follow along,” she said.
Strong support among health care groups
There’s strong support for streamlining prior authorization both in the medical community and in Congress.
The bill has the support of about 70 health care organizations, including the AMA and the American Academy of Family Physicians, according to its sponsors. As of May 17, the bill had attracted the backing of 97 members of the House of Representatives, roughly evenly split among Democrats and Republicans.
Rep. DelBene’s previous version of this bill, the Improving Seniors’ Timely Access to Care Act of 2019, attracted 143 Democratic cosponsors and 137 Republican ones, or more than half of the members of the House. This bill was not completed during the previous session of Congress (January 2019–January 2021) because of the more urgent needs of pandemic response, said Rep. Bucshon, who practiced cardiothoracic surgery before joining Congress.
“It wasn’t quite on the radar as much as it might have been if we didn’t have COVID,” Rep. Bucshon said.
Rep. Bucshon added that he expects strong Senate support for a companion measure of the House bill, which could make the difference for efforts to pass it this year.
Insurers have become more aggressive over time in denying payments through prior authorization systems for services that physicians say their patients need, according to Rep. Bucshon. There may be some “bad actors” in medicine who would order unnecessary procedures, Rep. Bucshon allowed, but in most cases, the cumbersome prior authorization processes only put a hurdle for patients seeking needed treatments, he said.
“The premise is that it controls health care costs but actually what it does is it helps insurance company’s bottom line,” Rep. Bucshon said.
In a prepared statement, former Pennsylvania representative Allyson Y. Schwartz, now CEO of the Better Medicare Alliance, said her group had spoken with sponsors of this legislation and appreciates “their receptiveness to feedback in this process.”
“Prior authorization ensures beneficiaries receive clinically appropriate care and reduces exposures to duplicative and unnecessary services,” Ms. Schwartz said. “We share an interest in ensuring prior authorization works as smoothly and effectively as possible for beneficiaries while protecting its essential function of facilitating safe, evidenced-based care.”
The Better Medicare Alliance said its funders include UnitedHealth, Humana, and CVS Health/Aetna, which run Advantage plans. The group also lists as its partners many medical organizations.
“Rationing care by hassling”
Like Rep. Bucshon, Dr. Bailey sees a different motivation in insurers’ persistence in keeping the prior authorization process cumbersome.
Phone calls and faxes remain the key methods for handling prior authorization for medical services, according to the results of a survey done by the AMA in December. Phone calls were always or often required for prior authorization for medical services (59%), with faxes the second-most common approach (46%), followed by health plans’ online portals (39%), electronic health records and practice management systems (29%), and email or U.S. mail (26%), according to the AMA’s report on the survey.
“It seems like every step in the process is designed to make the patient less likely to get the therapy that the doctor thinks that the patient needs,” Dr. Bailey said. “It’s almost like rationing care by hassling the patient and the physician.”
The findings of an investigation by HHS’ internal watchdog unit appear to support Dr. Bailey’s view, showing that insurer-run Medicare plans had a pattern of often walking back their initial rejections.
In 2018, the Office of the Inspector General for HHS reported that Medicare Advantage organizations (MAOs) overturned 75% of their own denials during 2014-16. In addition, independent reviewers within the appeals process overturned additional denials in favor of patients and clinicians, OIG said.
“The high number of overturned denials raises concerns that some Medicare Advantage beneficiaries and providers were initially denied services and payments that should have been provided,” the OIG said in the report. “This is especially concerning because beneficiaries and providers rarely used the appeals process, which is designed to ensure access to care and payment.”
During 2014-2016, patients and clinicians appealed only 1% of denials to the first level of appeal, OIG said. In the report, the watchdog group noted that CMS audits had highlighted “widespread and persistent MAO performance problems related to denials of care and payment.” In 2015, for example, CMS cited 56% of audited contracts for making inappropriate denials.
Dr. Bailey also said in an interview that she routinely encounters problems with prior authorization in her own practice as an allergist and immunologist in Fort Worth, Tex.
In late May, for example, a Medicare Advantage plan made a patient whose chronic asthma had been stable for years change to a new inhaler that resulted in him developing a yeast infection in his mouth, Dr. Bailey said.
“We treated the yeast infection, made some changes in the way he uses his inhaler, so hopefully he would tolerate it better,” Dr. Bailey said. “He had a reaction to the medication to treat the yeast infection and ended up in the hospital. How is that helping anyone? It certainly hasn’t helped my patient.”
Dr. Bailey said insurers have also asked to seek prior authorization to prescribe medications that have been generic for years and have used the process to challenge her on cases of what seem to be common sense in medical practice. This included a bid to have Dr. Bailey prescribe a medication in pill form for a 6-month-old baby who had no teeth.
“Every doctor has got absurd stories like that, but unfortunately, every doctor is going to have tragic stories where prior authorization has resulted in death and harm to the patients,” Dr. Bailey said.
Some physicians leave it to the patient to try to overcome insurers’ decisions on prior authorization, seeing this task as falling outside of their duties, Dr. Bailey said.
“I don’t do that. I fight. I spend a lot of time fighting. I don’t like to lose. I don’t like my patients to lose, so I will go to the mat for them,” Dr. Bailey said. “But I’m blessed to be in a specialty where I’ve got loads more control over my schedule than many other specialties do.”
A version of this article first appeared on Medscape.com.
A group of bipartisan lawmakers intends to compel insurers to streamline prior authorization processes for Medicare Advantage plans, including a bid to end the use of faxes and develop systems that can allow for real-time decisions.
Rep. Suzan DelBene (D-Wash.); Rep. Mike Kelly (R-Pa.); Rep. Ami Bera, MD (D-Calif.); and Rep. Larry Bucshon, MD, (R-Ind.) on May 13 introduced a bill that would task federal officials with refining standards regarding prior authorization for Medicare Advantage. Titled the Improving Seniors’ Timely Access to Care Act of 2021, the bill would direct the Department of Health & Human Services to create rules intended to make prior authorization more transparent and speedy for the insurer-run Medicare plans. Known as Medicare Advantage, these plans cover about 24.1 million people of the 62 million enrolled in the giant federal health program, according to the nonprofit Kaiser Family Foundation.
These revamped prior authorization systems could not rely on faxes nor could they employ proprietary payer portals that did not meet HHS’ standards, says the text of the bill released by Rep. DelBene. Insurers would also have to report to the Centers for Medicare & Medicaid Services about the extent of their use of prior authorization and the rate of approvals or denials. The bill seeks to encourage plans to adopt prior authorization programs that adhere to evidence-based medical guidelines in consultation with physicians.
There were several reasons for focusing on Medicare Advantage plans, although prior authorization concerns extend more broadly in the U.S. health care system, said Susan Bailey, MD, president of the American Medical Association.
There’s an ample body of research about issues seen in the Medicare Advantage plans. Dr. Bailey also said that, in her experience, Medicare Advantage plans have had some of the most restrictive policies. And, by starting with Medicare Advantage, there’s a potential for a ripple effect in the industry, easing this issue when physicians work with other insurers as well.
“When Medicare adopts a policy whether it be a payment policy or a coverage policy, private insurers typically follow along,” she said.
Strong support among health care groups
There’s strong support for streamlining prior authorization both in the medical community and in Congress.
The bill has the support of about 70 health care organizations, including the AMA and the American Academy of Family Physicians, according to its sponsors. As of May 17, the bill had attracted the backing of 97 members of the House of Representatives, roughly evenly split among Democrats and Republicans.
Rep. DelBene’s previous version of this bill, the Improving Seniors’ Timely Access to Care Act of 2019, attracted 143 Democratic cosponsors and 137 Republican ones, or more than half of the members of the House. This bill was not completed during the previous session of Congress (January 2019–January 2021) because of the more urgent needs of pandemic response, said Rep. Bucshon, who practiced cardiothoracic surgery before joining Congress.
“It wasn’t quite on the radar as much as it might have been if we didn’t have COVID,” Rep. Bucshon said.
Rep. Bucshon added that he expects strong Senate support for a companion measure of the House bill, which could make the difference for efforts to pass it this year.
Insurers have become more aggressive over time in denying payments through prior authorization systems for services that physicians say their patients need, according to Rep. Bucshon. There may be some “bad actors” in medicine who would order unnecessary procedures, Rep. Bucshon allowed, but in most cases, the cumbersome prior authorization processes only put a hurdle for patients seeking needed treatments, he said.
“The premise is that it controls health care costs but actually what it does is it helps insurance company’s bottom line,” Rep. Bucshon said.
In a prepared statement, former Pennsylvania representative Allyson Y. Schwartz, now CEO of the Better Medicare Alliance, said her group had spoken with sponsors of this legislation and appreciates “their receptiveness to feedback in this process.”
“Prior authorization ensures beneficiaries receive clinically appropriate care and reduces exposures to duplicative and unnecessary services,” Ms. Schwartz said. “We share an interest in ensuring prior authorization works as smoothly and effectively as possible for beneficiaries while protecting its essential function of facilitating safe, evidenced-based care.”
The Better Medicare Alliance said its funders include UnitedHealth, Humana, and CVS Health/Aetna, which run Advantage plans. The group also lists as its partners many medical organizations.
“Rationing care by hassling”
Like Rep. Bucshon, Dr. Bailey sees a different motivation in insurers’ persistence in keeping the prior authorization process cumbersome.
Phone calls and faxes remain the key methods for handling prior authorization for medical services, according to the results of a survey done by the AMA in December. Phone calls were always or often required for prior authorization for medical services (59%), with faxes the second-most common approach (46%), followed by health plans’ online portals (39%), electronic health records and practice management systems (29%), and email or U.S. mail (26%), according to the AMA’s report on the survey.
“It seems like every step in the process is designed to make the patient less likely to get the therapy that the doctor thinks that the patient needs,” Dr. Bailey said. “It’s almost like rationing care by hassling the patient and the physician.”
The findings of an investigation by HHS’ internal watchdog unit appear to support Dr. Bailey’s view, showing that insurer-run Medicare plans had a pattern of often walking back their initial rejections.
In 2018, the Office of the Inspector General for HHS reported that Medicare Advantage organizations (MAOs) overturned 75% of their own denials during 2014-16. In addition, independent reviewers within the appeals process overturned additional denials in favor of patients and clinicians, OIG said.
“The high number of overturned denials raises concerns that some Medicare Advantage beneficiaries and providers were initially denied services and payments that should have been provided,” the OIG said in the report. “This is especially concerning because beneficiaries and providers rarely used the appeals process, which is designed to ensure access to care and payment.”
During 2014-2016, patients and clinicians appealed only 1% of denials to the first level of appeal, OIG said. In the report, the watchdog group noted that CMS audits had highlighted “widespread and persistent MAO performance problems related to denials of care and payment.” In 2015, for example, CMS cited 56% of audited contracts for making inappropriate denials.
Dr. Bailey also said in an interview that she routinely encounters problems with prior authorization in her own practice as an allergist and immunologist in Fort Worth, Tex.
In late May, for example, a Medicare Advantage plan made a patient whose chronic asthma had been stable for years change to a new inhaler that resulted in him developing a yeast infection in his mouth, Dr. Bailey said.
“We treated the yeast infection, made some changes in the way he uses his inhaler, so hopefully he would tolerate it better,” Dr. Bailey said. “He had a reaction to the medication to treat the yeast infection and ended up in the hospital. How is that helping anyone? It certainly hasn’t helped my patient.”
Dr. Bailey said insurers have also asked to seek prior authorization to prescribe medications that have been generic for years and have used the process to challenge her on cases of what seem to be common sense in medical practice. This included a bid to have Dr. Bailey prescribe a medication in pill form for a 6-month-old baby who had no teeth.
“Every doctor has got absurd stories like that, but unfortunately, every doctor is going to have tragic stories where prior authorization has resulted in death and harm to the patients,” Dr. Bailey said.
Some physicians leave it to the patient to try to overcome insurers’ decisions on prior authorization, seeing this task as falling outside of their duties, Dr. Bailey said.
“I don’t do that. I fight. I spend a lot of time fighting. I don’t like to lose. I don’t like my patients to lose, so I will go to the mat for them,” Dr. Bailey said. “But I’m blessed to be in a specialty where I’ve got loads more control over my schedule than many other specialties do.”
A version of this article first appeared on Medscape.com.
A group of bipartisan lawmakers intends to compel insurers to streamline prior authorization processes for Medicare Advantage plans, including a bid to end the use of faxes and develop systems that can allow for real-time decisions.
Rep. Suzan DelBene (D-Wash.); Rep. Mike Kelly (R-Pa.); Rep. Ami Bera, MD (D-Calif.); and Rep. Larry Bucshon, MD, (R-Ind.) on May 13 introduced a bill that would task federal officials with refining standards regarding prior authorization for Medicare Advantage. Titled the Improving Seniors’ Timely Access to Care Act of 2021, the bill would direct the Department of Health & Human Services to create rules intended to make prior authorization more transparent and speedy for the insurer-run Medicare plans. Known as Medicare Advantage, these plans cover about 24.1 million people of the 62 million enrolled in the giant federal health program, according to the nonprofit Kaiser Family Foundation.
These revamped prior authorization systems could not rely on faxes nor could they employ proprietary payer portals that did not meet HHS’ standards, says the text of the bill released by Rep. DelBene. Insurers would also have to report to the Centers for Medicare & Medicaid Services about the extent of their use of prior authorization and the rate of approvals or denials. The bill seeks to encourage plans to adopt prior authorization programs that adhere to evidence-based medical guidelines in consultation with physicians.
There were several reasons for focusing on Medicare Advantage plans, although prior authorization concerns extend more broadly in the U.S. health care system, said Susan Bailey, MD, president of the American Medical Association.
There’s an ample body of research about issues seen in the Medicare Advantage plans. Dr. Bailey also said that, in her experience, Medicare Advantage plans have had some of the most restrictive policies. And, by starting with Medicare Advantage, there’s a potential for a ripple effect in the industry, easing this issue when physicians work with other insurers as well.
“When Medicare adopts a policy whether it be a payment policy or a coverage policy, private insurers typically follow along,” she said.
Strong support among health care groups
There’s strong support for streamlining prior authorization both in the medical community and in Congress.
The bill has the support of about 70 health care organizations, including the AMA and the American Academy of Family Physicians, according to its sponsors. As of May 17, the bill had attracted the backing of 97 members of the House of Representatives, roughly evenly split among Democrats and Republicans.
Rep. DelBene’s previous version of this bill, the Improving Seniors’ Timely Access to Care Act of 2019, attracted 143 Democratic cosponsors and 137 Republican ones, or more than half of the members of the House. This bill was not completed during the previous session of Congress (January 2019–January 2021) because of the more urgent needs of pandemic response, said Rep. Bucshon, who practiced cardiothoracic surgery before joining Congress.
“It wasn’t quite on the radar as much as it might have been if we didn’t have COVID,” Rep. Bucshon said.
Rep. Bucshon added that he expects strong Senate support for a companion measure of the House bill, which could make the difference for efforts to pass it this year.
Insurers have become more aggressive over time in denying payments through prior authorization systems for services that physicians say their patients need, according to Rep. Bucshon. There may be some “bad actors” in medicine who would order unnecessary procedures, Rep. Bucshon allowed, but in most cases, the cumbersome prior authorization processes only put a hurdle for patients seeking needed treatments, he said.
“The premise is that it controls health care costs but actually what it does is it helps insurance company’s bottom line,” Rep. Bucshon said.
In a prepared statement, former Pennsylvania representative Allyson Y. Schwartz, now CEO of the Better Medicare Alliance, said her group had spoken with sponsors of this legislation and appreciates “their receptiveness to feedback in this process.”
“Prior authorization ensures beneficiaries receive clinically appropriate care and reduces exposures to duplicative and unnecessary services,” Ms. Schwartz said. “We share an interest in ensuring prior authorization works as smoothly and effectively as possible for beneficiaries while protecting its essential function of facilitating safe, evidenced-based care.”
The Better Medicare Alliance said its funders include UnitedHealth, Humana, and CVS Health/Aetna, which run Advantage plans. The group also lists as its partners many medical organizations.
“Rationing care by hassling”
Like Rep. Bucshon, Dr. Bailey sees a different motivation in insurers’ persistence in keeping the prior authorization process cumbersome.
Phone calls and faxes remain the key methods for handling prior authorization for medical services, according to the results of a survey done by the AMA in December. Phone calls were always or often required for prior authorization for medical services (59%), with faxes the second-most common approach (46%), followed by health plans’ online portals (39%), electronic health records and practice management systems (29%), and email or U.S. mail (26%), according to the AMA’s report on the survey.
“It seems like every step in the process is designed to make the patient less likely to get the therapy that the doctor thinks that the patient needs,” Dr. Bailey said. “It’s almost like rationing care by hassling the patient and the physician.”
The findings of an investigation by HHS’ internal watchdog unit appear to support Dr. Bailey’s view, showing that insurer-run Medicare plans had a pattern of often walking back their initial rejections.
In 2018, the Office of the Inspector General for HHS reported that Medicare Advantage organizations (MAOs) overturned 75% of their own denials during 2014-16. In addition, independent reviewers within the appeals process overturned additional denials in favor of patients and clinicians, OIG said.
“The high number of overturned denials raises concerns that some Medicare Advantage beneficiaries and providers were initially denied services and payments that should have been provided,” the OIG said in the report. “This is especially concerning because beneficiaries and providers rarely used the appeals process, which is designed to ensure access to care and payment.”
During 2014-2016, patients and clinicians appealed only 1% of denials to the first level of appeal, OIG said. In the report, the watchdog group noted that CMS audits had highlighted “widespread and persistent MAO performance problems related to denials of care and payment.” In 2015, for example, CMS cited 56% of audited contracts for making inappropriate denials.
Dr. Bailey also said in an interview that she routinely encounters problems with prior authorization in her own practice as an allergist and immunologist in Fort Worth, Tex.
In late May, for example, a Medicare Advantage plan made a patient whose chronic asthma had been stable for years change to a new inhaler that resulted in him developing a yeast infection in his mouth, Dr. Bailey said.
“We treated the yeast infection, made some changes in the way he uses his inhaler, so hopefully he would tolerate it better,” Dr. Bailey said. “He had a reaction to the medication to treat the yeast infection and ended up in the hospital. How is that helping anyone? It certainly hasn’t helped my patient.”
Dr. Bailey said insurers have also asked to seek prior authorization to prescribe medications that have been generic for years and have used the process to challenge her on cases of what seem to be common sense in medical practice. This included a bid to have Dr. Bailey prescribe a medication in pill form for a 6-month-old baby who had no teeth.
“Every doctor has got absurd stories like that, but unfortunately, every doctor is going to have tragic stories where prior authorization has resulted in death and harm to the patients,” Dr. Bailey said.
Some physicians leave it to the patient to try to overcome insurers’ decisions on prior authorization, seeing this task as falling outside of their duties, Dr. Bailey said.
“I don’t do that. I fight. I spend a lot of time fighting. I don’t like to lose. I don’t like my patients to lose, so I will go to the mat for them,” Dr. Bailey said. “But I’m blessed to be in a specialty where I’ve got loads more control over my schedule than many other specialties do.”
A version of this article first appeared on Medscape.com.