User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Immune dysregulation may drive long-term postpartum depression
Postpartum depression, anxiety, and posttraumatic stress disorder that persist 2-3 years after birth are associated with a dysregulated immune system that is characterized by increased inflammatory signaling, according to investigators.
These findings suggest that mental health screening for women who have given birth should continue beyond the first year post partum, reported lead author Jennifer M. Nicoloro-SantaBarbara, PhD, of Brigham and Women’s Hospital, Harvard Medical School, Boston, and colleagues.
“Delayed postpartum depression, also known as late-onset postpartum depression, can affect women up to 18 months after delivery,” the investigators wrote in the American Journal of Reproductive Immunology. “It can appear even later in some women, depending on the hormonal changes that occur after having a baby (for example, timing of weaning). However, the majority of research on maternal mental health focuses on the first year post birth, leaving a gap in research beyond 12 months post partum.”
To address this gap, the investigators enrolled 33 women who were 2-3 years post partum. Participants completed self-guided questionnaires on PTSD, depression, and anxiety, and provided blood samples for gene expression analysis.
Sixteen of the 33 women had clinically significant mood disturbances. and significantly reduced activation of genes associated with viral response.
“The results provide preliminary evidence of a mechanism (e.g., immune dysregulation) that might be contributing to mood disorders and bring us closer to the goal of identifying targetable biomarkers for mood disorders,” Dr. Nicoloro-SantaBarbara said in a written comment. “This work highlights the need for standardized and continual depression and anxiety screening in ob.gyn. and primary care settings that extends beyond the 6-week maternal visit and possibly beyond the first postpartum year.”
Findings draw skepticism
“The authors argue that mothers need to be screened for depression/anxiety longer than the first year post partum, and this is true, but it has nothing to do with their findings,” said Jennifer L. Payne, MD, an expert in reproductive psychiatry at the University of Virginia, Charlottesville.
In a written comment, she explained that the cross-sectional design makes it impossible to know whether the mood disturbances were linked with delivery at all.
“It is unclear if the depression/anxiety symptoms began after delivery or not,” Dr. Payne said. “In addition, it is unclear if the findings are causative or a result of depression/anxiety symptoms (the authors admit this in the limitations section). It is likely that the findings are not specific or even related to having delivered a child, but rather reflect a more general process related to depression/anxiety outside of the postpartum time period.”
Only prospective studies can answer these questions, she said.
Dr. Nicoloro-SantaBarbara agreed that further research is needed.
“Our findings are exciting, but still need to be replicated in larger samples with diverse women in order to make sure they generalize,” she said. “More work is needed to understand why inflammation plays a role in postpartum mental illness for some women and not others.”
The study was supported by a Cedars-Sinai Precision Health Grant, the Cousins Center for Psychoneuroimmunology, University of California, Los Angeles, and the National Institute of Mental Health. The investigators and Dr. Payne disclosed no relevant conflicts of interest.
Postpartum depression, anxiety, and posttraumatic stress disorder that persist 2-3 years after birth are associated with a dysregulated immune system that is characterized by increased inflammatory signaling, according to investigators.
These findings suggest that mental health screening for women who have given birth should continue beyond the first year post partum, reported lead author Jennifer M. Nicoloro-SantaBarbara, PhD, of Brigham and Women’s Hospital, Harvard Medical School, Boston, and colleagues.
“Delayed postpartum depression, also known as late-onset postpartum depression, can affect women up to 18 months after delivery,” the investigators wrote in the American Journal of Reproductive Immunology. “It can appear even later in some women, depending on the hormonal changes that occur after having a baby (for example, timing of weaning). However, the majority of research on maternal mental health focuses on the first year post birth, leaving a gap in research beyond 12 months post partum.”
To address this gap, the investigators enrolled 33 women who were 2-3 years post partum. Participants completed self-guided questionnaires on PTSD, depression, and anxiety, and provided blood samples for gene expression analysis.
Sixteen of the 33 women had clinically significant mood disturbances. and significantly reduced activation of genes associated with viral response.
“The results provide preliminary evidence of a mechanism (e.g., immune dysregulation) that might be contributing to mood disorders and bring us closer to the goal of identifying targetable biomarkers for mood disorders,” Dr. Nicoloro-SantaBarbara said in a written comment. “This work highlights the need for standardized and continual depression and anxiety screening in ob.gyn. and primary care settings that extends beyond the 6-week maternal visit and possibly beyond the first postpartum year.”
Findings draw skepticism
“The authors argue that mothers need to be screened for depression/anxiety longer than the first year post partum, and this is true, but it has nothing to do with their findings,” said Jennifer L. Payne, MD, an expert in reproductive psychiatry at the University of Virginia, Charlottesville.
In a written comment, she explained that the cross-sectional design makes it impossible to know whether the mood disturbances were linked with delivery at all.
“It is unclear if the depression/anxiety symptoms began after delivery or not,” Dr. Payne said. “In addition, it is unclear if the findings are causative or a result of depression/anxiety symptoms (the authors admit this in the limitations section). It is likely that the findings are not specific or even related to having delivered a child, but rather reflect a more general process related to depression/anxiety outside of the postpartum time period.”
Only prospective studies can answer these questions, she said.
Dr. Nicoloro-SantaBarbara agreed that further research is needed.
“Our findings are exciting, but still need to be replicated in larger samples with diverse women in order to make sure they generalize,” she said. “More work is needed to understand why inflammation plays a role in postpartum mental illness for some women and not others.”
The study was supported by a Cedars-Sinai Precision Health Grant, the Cousins Center for Psychoneuroimmunology, University of California, Los Angeles, and the National Institute of Mental Health. The investigators and Dr. Payne disclosed no relevant conflicts of interest.
Postpartum depression, anxiety, and posttraumatic stress disorder that persist 2-3 years after birth are associated with a dysregulated immune system that is characterized by increased inflammatory signaling, according to investigators.
These findings suggest that mental health screening for women who have given birth should continue beyond the first year post partum, reported lead author Jennifer M. Nicoloro-SantaBarbara, PhD, of Brigham and Women’s Hospital, Harvard Medical School, Boston, and colleagues.
“Delayed postpartum depression, also known as late-onset postpartum depression, can affect women up to 18 months after delivery,” the investigators wrote in the American Journal of Reproductive Immunology. “It can appear even later in some women, depending on the hormonal changes that occur after having a baby (for example, timing of weaning). However, the majority of research on maternal mental health focuses on the first year post birth, leaving a gap in research beyond 12 months post partum.”
To address this gap, the investigators enrolled 33 women who were 2-3 years post partum. Participants completed self-guided questionnaires on PTSD, depression, and anxiety, and provided blood samples for gene expression analysis.
Sixteen of the 33 women had clinically significant mood disturbances. and significantly reduced activation of genes associated with viral response.
“The results provide preliminary evidence of a mechanism (e.g., immune dysregulation) that might be contributing to mood disorders and bring us closer to the goal of identifying targetable biomarkers for mood disorders,” Dr. Nicoloro-SantaBarbara said in a written comment. “This work highlights the need for standardized and continual depression and anxiety screening in ob.gyn. and primary care settings that extends beyond the 6-week maternal visit and possibly beyond the first postpartum year.”
Findings draw skepticism
“The authors argue that mothers need to be screened for depression/anxiety longer than the first year post partum, and this is true, but it has nothing to do with their findings,” said Jennifer L. Payne, MD, an expert in reproductive psychiatry at the University of Virginia, Charlottesville.
In a written comment, she explained that the cross-sectional design makes it impossible to know whether the mood disturbances were linked with delivery at all.
“It is unclear if the depression/anxiety symptoms began after delivery or not,” Dr. Payne said. “In addition, it is unclear if the findings are causative or a result of depression/anxiety symptoms (the authors admit this in the limitations section). It is likely that the findings are not specific or even related to having delivered a child, but rather reflect a more general process related to depression/anxiety outside of the postpartum time period.”
Only prospective studies can answer these questions, she said.
Dr. Nicoloro-SantaBarbara agreed that further research is needed.
“Our findings are exciting, but still need to be replicated in larger samples with diverse women in order to make sure they generalize,” she said. “More work is needed to understand why inflammation plays a role in postpartum mental illness for some women and not others.”
The study was supported by a Cedars-Sinai Precision Health Grant, the Cousins Center for Psychoneuroimmunology, University of California, Los Angeles, and the National Institute of Mental Health. The investigators and Dr. Payne disclosed no relevant conflicts of interest.
FROM THE AMERICAN JOURNAL OF REPRODUCTIVE IMMUNOLOGY
SSRI tied to improved cognition in comorbid depression, dementia
The results of the 12-week open-label, single-group study are positive, study investigator Michael Cronquist Christensen, MPA, DrPH, a director with the Lundbeck pharmaceutical company, told this news organization before presenting the results in a poster at the 15th Clinical Trials on Alzheimer’s Disease conference.
“The study confirms earlier findings of improvement in both depressive symptoms and cognitive performance with vortioxetine in patients with depression and dementia and adds to this research that these clinical effects also extend to improvement in health-related quality of life and patients’ daily functioning,” Dr. Christensen said.
“It also demonstrates that patients with depression and comorbid dementia can be safely treated with 20 mg vortioxetine – starting dose of 5 mg for the first week and up-titration to 10 mg at day 8,” he added.
However, he reported that Lundbeck doesn’t plan to seek approval from the U.S. Food and Drug Administration for a new indication. Vortioxetine received FDA approval in 2013 to treat MDD, but 3 years later the agency rejected an expansion of its indication to include cognitive dysfunction.
“Vortioxetine is approved for MDD, but the product can be used in patients with MDD who have other diseases, including other mental illnesses,” Dr. Christensen said.
Potential neurotransmission modulator
Vortioxetine is a selective serotonin reuptake inhibitor and serotonin receptor modulator. According to Dr. Christensen, evidence suggests the drug’s receptor targets “have the potential to modulate neurotransmitter systems that are essential for regulation of cognitive function.”
The researchers recruited 83 individuals aged 55-85 with recurrent MDD that had started before the age of 55. All had MDD episodes within the previous 6 months and comorbid dementia for at least 6 months.
Of the participants, 65.9% were female. In addition, 42.7% had Alzheimer’s disease, 26.8% had mixed-type dementia, and the rest had other types of dementia.
The daily oral dose of vortioxetine started at 5 mg for up to week 1 and then was increased to 10 mg. It was then increased to 20 mg or decreased to 5 mg “based on investigator judgment and patient response.” The average daily dose was 12.3 mg.
In regard to the primary outcome, at week 12 (n = 70), scores on the Montgomery-Åsberg Depression Rating Scale (MADRS) fell by a mean of –12.4 (.78, P < .0001), which researchers deemed to be a significant reduction in severe symptoms.
“A significant and clinically meaningful effect was observed from week 1,” the researchers reported.
“As a basis for comparison, we typically see an improvement around 13-14 points during 8 weeks of antidepressant treatment in adults with MDD who do not have dementia,” Dr. Christensen added.
More than a third of patients (35.7%) saw a reduction in MADRS score by more than 50% at week 12, and 17.2% were considered to have reached MDD depression remission, defined as a MADRS score at or under 10.
For secondary outcomes, the total Digit Symbol Substitution test score grew by 0.65 (standardized effect size) by week 12, showing significant improvement (P < .0001). In addition, participants improved on some other cognitive measures, and Dr. Christensen noted that “significant improvement was also observed in the patients’ health-related quality of life and daily functioning.”
A third of patients had drug-related treatment-emergent adverse events.
Vortioxetine is one of the most expensive antidepressants: It has a list price of $444 a month, and no generic version is currently available.
Small trial, open-label design
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, said the study “reflects a valuable aspect of treatment research because of the close connection between depression and dementia. Depression is a known risk factor for dementia, including Alzheimer’s disease, and those who have dementia may experience depression.”
She cautioned, however, that the trial was small and had an open-label design instead of the “gold standard” of a double-blinded trial with a control group.
The study was funded by Lundbeck, where Dr. Christensen is an employee. Another author is a Lundbeck employee, and a third author reported various disclosures. Dr. Sexton reported no disclosures.
A version of this article first appeared on Medscape.com.
The results of the 12-week open-label, single-group study are positive, study investigator Michael Cronquist Christensen, MPA, DrPH, a director with the Lundbeck pharmaceutical company, told this news organization before presenting the results in a poster at the 15th Clinical Trials on Alzheimer’s Disease conference.
“The study confirms earlier findings of improvement in both depressive symptoms and cognitive performance with vortioxetine in patients with depression and dementia and adds to this research that these clinical effects also extend to improvement in health-related quality of life and patients’ daily functioning,” Dr. Christensen said.
“It also demonstrates that patients with depression and comorbid dementia can be safely treated with 20 mg vortioxetine – starting dose of 5 mg for the first week and up-titration to 10 mg at day 8,” he added.
However, he reported that Lundbeck doesn’t plan to seek approval from the U.S. Food and Drug Administration for a new indication. Vortioxetine received FDA approval in 2013 to treat MDD, but 3 years later the agency rejected an expansion of its indication to include cognitive dysfunction.
“Vortioxetine is approved for MDD, but the product can be used in patients with MDD who have other diseases, including other mental illnesses,” Dr. Christensen said.
Potential neurotransmission modulator
Vortioxetine is a selective serotonin reuptake inhibitor and serotonin receptor modulator. According to Dr. Christensen, evidence suggests the drug’s receptor targets “have the potential to modulate neurotransmitter systems that are essential for regulation of cognitive function.”
The researchers recruited 83 individuals aged 55-85 with recurrent MDD that had started before the age of 55. All had MDD episodes within the previous 6 months and comorbid dementia for at least 6 months.
Of the participants, 65.9% were female. In addition, 42.7% had Alzheimer’s disease, 26.8% had mixed-type dementia, and the rest had other types of dementia.
The daily oral dose of vortioxetine started at 5 mg for up to week 1 and then was increased to 10 mg. It was then increased to 20 mg or decreased to 5 mg “based on investigator judgment and patient response.” The average daily dose was 12.3 mg.
In regard to the primary outcome, at week 12 (n = 70), scores on the Montgomery-Åsberg Depression Rating Scale (MADRS) fell by a mean of –12.4 (.78, P < .0001), which researchers deemed to be a significant reduction in severe symptoms.
“A significant and clinically meaningful effect was observed from week 1,” the researchers reported.
“As a basis for comparison, we typically see an improvement around 13-14 points during 8 weeks of antidepressant treatment in adults with MDD who do not have dementia,” Dr. Christensen added.
More than a third of patients (35.7%) saw a reduction in MADRS score by more than 50% at week 12, and 17.2% were considered to have reached MDD depression remission, defined as a MADRS score at or under 10.
For secondary outcomes, the total Digit Symbol Substitution test score grew by 0.65 (standardized effect size) by week 12, showing significant improvement (P < .0001). In addition, participants improved on some other cognitive measures, and Dr. Christensen noted that “significant improvement was also observed in the patients’ health-related quality of life and daily functioning.”
A third of patients had drug-related treatment-emergent adverse events.
Vortioxetine is one of the most expensive antidepressants: It has a list price of $444 a month, and no generic version is currently available.
Small trial, open-label design
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, said the study “reflects a valuable aspect of treatment research because of the close connection between depression and dementia. Depression is a known risk factor for dementia, including Alzheimer’s disease, and those who have dementia may experience depression.”
She cautioned, however, that the trial was small and had an open-label design instead of the “gold standard” of a double-blinded trial with a control group.
The study was funded by Lundbeck, where Dr. Christensen is an employee. Another author is a Lundbeck employee, and a third author reported various disclosures. Dr. Sexton reported no disclosures.
A version of this article first appeared on Medscape.com.
The results of the 12-week open-label, single-group study are positive, study investigator Michael Cronquist Christensen, MPA, DrPH, a director with the Lundbeck pharmaceutical company, told this news organization before presenting the results in a poster at the 15th Clinical Trials on Alzheimer’s Disease conference.
“The study confirms earlier findings of improvement in both depressive symptoms and cognitive performance with vortioxetine in patients with depression and dementia and adds to this research that these clinical effects also extend to improvement in health-related quality of life and patients’ daily functioning,” Dr. Christensen said.
“It also demonstrates that patients with depression and comorbid dementia can be safely treated with 20 mg vortioxetine – starting dose of 5 mg for the first week and up-titration to 10 mg at day 8,” he added.
However, he reported that Lundbeck doesn’t plan to seek approval from the U.S. Food and Drug Administration for a new indication. Vortioxetine received FDA approval in 2013 to treat MDD, but 3 years later the agency rejected an expansion of its indication to include cognitive dysfunction.
“Vortioxetine is approved for MDD, but the product can be used in patients with MDD who have other diseases, including other mental illnesses,” Dr. Christensen said.
Potential neurotransmission modulator
Vortioxetine is a selective serotonin reuptake inhibitor and serotonin receptor modulator. According to Dr. Christensen, evidence suggests the drug’s receptor targets “have the potential to modulate neurotransmitter systems that are essential for regulation of cognitive function.”
The researchers recruited 83 individuals aged 55-85 with recurrent MDD that had started before the age of 55. All had MDD episodes within the previous 6 months and comorbid dementia for at least 6 months.
Of the participants, 65.9% were female. In addition, 42.7% had Alzheimer’s disease, 26.8% had mixed-type dementia, and the rest had other types of dementia.
The daily oral dose of vortioxetine started at 5 mg for up to week 1 and then was increased to 10 mg. It was then increased to 20 mg or decreased to 5 mg “based on investigator judgment and patient response.” The average daily dose was 12.3 mg.
In regard to the primary outcome, at week 12 (n = 70), scores on the Montgomery-Åsberg Depression Rating Scale (MADRS) fell by a mean of –12.4 (.78, P < .0001), which researchers deemed to be a significant reduction in severe symptoms.
“A significant and clinically meaningful effect was observed from week 1,” the researchers reported.
“As a basis for comparison, we typically see an improvement around 13-14 points during 8 weeks of antidepressant treatment in adults with MDD who do not have dementia,” Dr. Christensen added.
More than a third of patients (35.7%) saw a reduction in MADRS score by more than 50% at week 12, and 17.2% were considered to have reached MDD depression remission, defined as a MADRS score at or under 10.
For secondary outcomes, the total Digit Symbol Substitution test score grew by 0.65 (standardized effect size) by week 12, showing significant improvement (P < .0001). In addition, participants improved on some other cognitive measures, and Dr. Christensen noted that “significant improvement was also observed in the patients’ health-related quality of life and daily functioning.”
A third of patients had drug-related treatment-emergent adverse events.
Vortioxetine is one of the most expensive antidepressants: It has a list price of $444 a month, and no generic version is currently available.
Small trial, open-label design
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, said the study “reflects a valuable aspect of treatment research because of the close connection between depression and dementia. Depression is a known risk factor for dementia, including Alzheimer’s disease, and those who have dementia may experience depression.”
She cautioned, however, that the trial was small and had an open-label design instead of the “gold standard” of a double-blinded trial with a control group.
The study was funded by Lundbeck, where Dr. Christensen is an employee. Another author is a Lundbeck employee, and a third author reported various disclosures. Dr. Sexton reported no disclosures.
A version of this article first appeared on Medscape.com.
FROM CTAD 2022
Let people take illegal drugs under medical supervision?
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m the director of the division of medical ethics at New York University.
One is up in Washington Heights in Manhattan; the other, I believe, is over in Harlem.
These two centers will supervise people taking drugs. They have available all of the anti-overdose medications, such as Narcan. If you overdose, they will help you and try to counsel you to get off drugs, but they don’t insist that you do so. You can go there, even if you’re an addict, and continue to take drugs under supervision. This is called a risk-reduction strategy.
Some people note that there are over 100 centers like this worldwide. They’re in Canada, Switzerland, and many other countries, and they seem to work. “Working” means more people seem to come off drugs slowly – not huge numbers, but some – than if you don’t do something like this, and death rates from overdose go way down.
By the way, having these centers in place has other benefits. They save money because when someone overdoses out in the community, you have to pay all the costs of the ambulances and emergency rooms, and there are risks to the first responders due to fentanyl or other things. There are fewer syringes littering parks and public places where people shoot up. You have everything controlled when they come into a center, so that’s less burden on the community.
It turns out that you have less crime because people just aren’t out there harming or robbing other people to get money to get their next fix. The drugs are provided for them. Crime rates in neighborhoods around the world where these centers operate seem to dip. There are many positives.
There are also some negatives. People say it shouldn’t be the job of the state to keep people addicted. It’s just not the right role. Everything should be aimed at getting people off drugs, maybe including criminal penalties if that’s what it takes to get them to stop using.
My own view is that hasn’t worked. Implementing tough prison sentences in trying to fight the war on drugs just doesn’t seem to work. We had 100,000 deaths last year from drug overdoses. That number has been climbing. We all know that we’ve got a terrible epidemic of deaths due to drug overdose.
It seems to me that these centers that are involved in risk reduction are a better option for now, until we figure out some interventions that can cut the desire or the drive to use drugs, or antidotes that are effective for months or years, to prevent people from getting high no matter what drugs they take.
I’m going to come out and say that I think the New York experiment has worked. I think it has saved upward of 600 lives, they estimate, in the past year that would have been overdoses. I think costwise, it’s effective. [Reductions in] related damages and injuries from syringes being scattered around, and robbery, and so forth, are all to the good. There are even a few people coming off drugs due to counseling, which is a better outcome than we get when they’re just out in the streets.
I think other cities want to try this. I know Philadelphia does. I know New York wants to expand its program. The federal government isn’t sure, but I think the time has come to try an expansion. I think we’ve got something that – although far from perfect and I wish we had other tools – may be the best we’ve got. In the war on drugs, little victories ought to be reinforced.
Dr. Caplan disclosed that he has served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position), and is a contributing author and adviser for Medscape. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m the director of the division of medical ethics at New York University.
One is up in Washington Heights in Manhattan; the other, I believe, is over in Harlem.
These two centers will supervise people taking drugs. They have available all of the anti-overdose medications, such as Narcan. If you overdose, they will help you and try to counsel you to get off drugs, but they don’t insist that you do so. You can go there, even if you’re an addict, and continue to take drugs under supervision. This is called a risk-reduction strategy.
Some people note that there are over 100 centers like this worldwide. They’re in Canada, Switzerland, and many other countries, and they seem to work. “Working” means more people seem to come off drugs slowly – not huge numbers, but some – than if you don’t do something like this, and death rates from overdose go way down.
By the way, having these centers in place has other benefits. They save money because when someone overdoses out in the community, you have to pay all the costs of the ambulances and emergency rooms, and there are risks to the first responders due to fentanyl or other things. There are fewer syringes littering parks and public places where people shoot up. You have everything controlled when they come into a center, so that’s less burden on the community.
It turns out that you have less crime because people just aren’t out there harming or robbing other people to get money to get their next fix. The drugs are provided for them. Crime rates in neighborhoods around the world where these centers operate seem to dip. There are many positives.
There are also some negatives. People say it shouldn’t be the job of the state to keep people addicted. It’s just not the right role. Everything should be aimed at getting people off drugs, maybe including criminal penalties if that’s what it takes to get them to stop using.
My own view is that hasn’t worked. Implementing tough prison sentences in trying to fight the war on drugs just doesn’t seem to work. We had 100,000 deaths last year from drug overdoses. That number has been climbing. We all know that we’ve got a terrible epidemic of deaths due to drug overdose.
It seems to me that these centers that are involved in risk reduction are a better option for now, until we figure out some interventions that can cut the desire or the drive to use drugs, or antidotes that are effective for months or years, to prevent people from getting high no matter what drugs they take.
I’m going to come out and say that I think the New York experiment has worked. I think it has saved upward of 600 lives, they estimate, in the past year that would have been overdoses. I think costwise, it’s effective. [Reductions in] related damages and injuries from syringes being scattered around, and robbery, and so forth, are all to the good. There are even a few people coming off drugs due to counseling, which is a better outcome than we get when they’re just out in the streets.
I think other cities want to try this. I know Philadelphia does. I know New York wants to expand its program. The federal government isn’t sure, but I think the time has come to try an expansion. I think we’ve got something that – although far from perfect and I wish we had other tools – may be the best we’ve got. In the war on drugs, little victories ought to be reinforced.
Dr. Caplan disclosed that he has served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position), and is a contributing author and adviser for Medscape. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m the director of the division of medical ethics at New York University.
One is up in Washington Heights in Manhattan; the other, I believe, is over in Harlem.
These two centers will supervise people taking drugs. They have available all of the anti-overdose medications, such as Narcan. If you overdose, they will help you and try to counsel you to get off drugs, but they don’t insist that you do so. You can go there, even if you’re an addict, and continue to take drugs under supervision. This is called a risk-reduction strategy.
Some people note that there are over 100 centers like this worldwide. They’re in Canada, Switzerland, and many other countries, and they seem to work. “Working” means more people seem to come off drugs slowly – not huge numbers, but some – than if you don’t do something like this, and death rates from overdose go way down.
By the way, having these centers in place has other benefits. They save money because when someone overdoses out in the community, you have to pay all the costs of the ambulances and emergency rooms, and there are risks to the first responders due to fentanyl or other things. There are fewer syringes littering parks and public places where people shoot up. You have everything controlled when they come into a center, so that’s less burden on the community.
It turns out that you have less crime because people just aren’t out there harming or robbing other people to get money to get their next fix. The drugs are provided for them. Crime rates in neighborhoods around the world where these centers operate seem to dip. There are many positives.
There are also some negatives. People say it shouldn’t be the job of the state to keep people addicted. It’s just not the right role. Everything should be aimed at getting people off drugs, maybe including criminal penalties if that’s what it takes to get them to stop using.
My own view is that hasn’t worked. Implementing tough prison sentences in trying to fight the war on drugs just doesn’t seem to work. We had 100,000 deaths last year from drug overdoses. That number has been climbing. We all know that we’ve got a terrible epidemic of deaths due to drug overdose.
It seems to me that these centers that are involved in risk reduction are a better option for now, until we figure out some interventions that can cut the desire or the drive to use drugs, or antidotes that are effective for months or years, to prevent people from getting high no matter what drugs they take.
I’m going to come out and say that I think the New York experiment has worked. I think it has saved upward of 600 lives, they estimate, in the past year that would have been overdoses. I think costwise, it’s effective. [Reductions in] related damages and injuries from syringes being scattered around, and robbery, and so forth, are all to the good. There are even a few people coming off drugs due to counseling, which is a better outcome than we get when they’re just out in the streets.
I think other cities want to try this. I know Philadelphia does. I know New York wants to expand its program. The federal government isn’t sure, but I think the time has come to try an expansion. I think we’ve got something that – although far from perfect and I wish we had other tools – may be the best we’ve got. In the war on drugs, little victories ought to be reinforced.
Dr. Caplan disclosed that he has served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position), and is a contributing author and adviser for Medscape. A version of this article first appeared on Medscape.com.
Why doctors are losing trust in patients; what should be done?
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University.
I want to talk about a paper that my colleagues in my division just published in Health Affairs.
As they pointed out, there’s a large amount of literature about what makes patients trust their doctor. There are many studies that show that, although patients sometimes have become more critical of the medical profession, in general they still try to trust their individual physician. Nurses remain in fairly high esteem among those who are getting hospital care.
What isn’t studied, as this paper properly points out, is, what can the doctor and the nurse do to trust the patient? How can that be assessed? Isn’t that just as important as saying that patients have to trust their doctors to do and comply with what they’re told?
What if doctors are afraid of violence? What if doctors are fearful that they can’t trust patients to listen, pay attention, or do what they’re being told? What if they think that patients are coming in with all kinds of disinformation, false information, or things they pick up on the Internet, so that even though you try your best to get across accurate and complete information about what to do about infectious diseases, taking care of a kid with strep throat, or whatever it might be, you’re thinking, Can I trust this patient to do what it is that I want them to do?
One particular problem that’s causing distrust is that more and more patients are showing stress and dependence on drugs and alcohol. That doesn’t make them less trustworthy per se, but it means they can’t regulate their own behavior as well.
That obviously has to be something that the physician or the nurse is thinking about. Is this person going to be able to contain anger? Is this person going to be able to handle bad news? Is this person going to deal with me when I tell them that some of the things they believe to be true about what’s good for their health care are false?
I think we have to really start to push administrators and people in positions of power to teach doctors and nurses how to defuse situations and how to make people more comfortable when they come in and the doctor suspects that they might be under the influence, impaired, or angry because of things they’ve seen on social media, whatever those might be – including concerns about racism, bigotry, and bias, which some patients are bringing into the clinic and the hospital setting.
We need more training. We’ve got to address this as a serious issue. What can we do to defuse situations where the doctor or the nurse rightly thinks that they can’t control or they can’t trust what the patient is thinking or how the patient might behave?
It’s also the case that I think we need more backup and quick access to security so that people feel safe and comfortable in providing care. We have to make sure that if you need someone to restrain a patient or to get somebody out of a situation, that they can get there quickly and respond rapidly, and that they know what to do to deescalate a situation.
It’s sad to say, but security in today’s health care world has to be something that we really test and check – not because we’re worried, as many places are, about a shooter entering the premises, which is its own bit of concern – but I’m just talking about when the doctor or the nurse says that this patient might be acting up, could get violent, or is someone I can’t trust.
My coauthors are basically saying that it’s not a one-way street. Yes, we have to figure out ways to make sure that our patients can trust what we say. Trust is absolutely the lubricant that makes health care flow. If patients don’t trust their doctors, they’re not going to do what they say. They’re not going to get their prescriptions filled. They’re not going to be compliant. They’re not going to try to lose weight or control their diabetes.
It also goes the other way. The doctor or the nurse has to trust the patient. They have to believe that they’re safe. They have to believe that the patient is capable of controlling themselves. They have to believe that the patient is capable of listening and hearing what they’re saying, and that they’re competent to follow up on instructions, including to come back if that’s what’s required.
Everybody has to feel secure in the environment in which they’re working. Security, sadly, has to be a priority if we’re going to have a health care workforce that really feels safe and comfortable dealing with a patient population that is increasingly aggressive and perhaps not as trustworthy.
That’s not news I like to read when my colleagues write it up, but it’s important and we have to take it seriously.
Dr. Caplan disclosed that he has served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position), and is a contributing author and adviser for Medscape. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University.
I want to talk about a paper that my colleagues in my division just published in Health Affairs.
As they pointed out, there’s a large amount of literature about what makes patients trust their doctor. There are many studies that show that, although patients sometimes have become more critical of the medical profession, in general they still try to trust their individual physician. Nurses remain in fairly high esteem among those who are getting hospital care.
What isn’t studied, as this paper properly points out, is, what can the doctor and the nurse do to trust the patient? How can that be assessed? Isn’t that just as important as saying that patients have to trust their doctors to do and comply with what they’re told?
What if doctors are afraid of violence? What if doctors are fearful that they can’t trust patients to listen, pay attention, or do what they’re being told? What if they think that patients are coming in with all kinds of disinformation, false information, or things they pick up on the Internet, so that even though you try your best to get across accurate and complete information about what to do about infectious diseases, taking care of a kid with strep throat, or whatever it might be, you’re thinking, Can I trust this patient to do what it is that I want them to do?
One particular problem that’s causing distrust is that more and more patients are showing stress and dependence on drugs and alcohol. That doesn’t make them less trustworthy per se, but it means they can’t regulate their own behavior as well.
That obviously has to be something that the physician or the nurse is thinking about. Is this person going to be able to contain anger? Is this person going to be able to handle bad news? Is this person going to deal with me when I tell them that some of the things they believe to be true about what’s good for their health care are false?
I think we have to really start to push administrators and people in positions of power to teach doctors and nurses how to defuse situations and how to make people more comfortable when they come in and the doctor suspects that they might be under the influence, impaired, or angry because of things they’ve seen on social media, whatever those might be – including concerns about racism, bigotry, and bias, which some patients are bringing into the clinic and the hospital setting.
We need more training. We’ve got to address this as a serious issue. What can we do to defuse situations where the doctor or the nurse rightly thinks that they can’t control or they can’t trust what the patient is thinking or how the patient might behave?
It’s also the case that I think we need more backup and quick access to security so that people feel safe and comfortable in providing care. We have to make sure that if you need someone to restrain a patient or to get somebody out of a situation, that they can get there quickly and respond rapidly, and that they know what to do to deescalate a situation.
It’s sad to say, but security in today’s health care world has to be something that we really test and check – not because we’re worried, as many places are, about a shooter entering the premises, which is its own bit of concern – but I’m just talking about when the doctor or the nurse says that this patient might be acting up, could get violent, or is someone I can’t trust.
My coauthors are basically saying that it’s not a one-way street. Yes, we have to figure out ways to make sure that our patients can trust what we say. Trust is absolutely the lubricant that makes health care flow. If patients don’t trust their doctors, they’re not going to do what they say. They’re not going to get their prescriptions filled. They’re not going to be compliant. They’re not going to try to lose weight or control their diabetes.
It also goes the other way. The doctor or the nurse has to trust the patient. They have to believe that they’re safe. They have to believe that the patient is capable of controlling themselves. They have to believe that the patient is capable of listening and hearing what they’re saying, and that they’re competent to follow up on instructions, including to come back if that’s what’s required.
Everybody has to feel secure in the environment in which they’re working. Security, sadly, has to be a priority if we’re going to have a health care workforce that really feels safe and comfortable dealing with a patient population that is increasingly aggressive and perhaps not as trustworthy.
That’s not news I like to read when my colleagues write it up, but it’s important and we have to take it seriously.
Dr. Caplan disclosed that he has served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position), and is a contributing author and adviser for Medscape. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University.
I want to talk about a paper that my colleagues in my division just published in Health Affairs.
As they pointed out, there’s a large amount of literature about what makes patients trust their doctor. There are many studies that show that, although patients sometimes have become more critical of the medical profession, in general they still try to trust their individual physician. Nurses remain in fairly high esteem among those who are getting hospital care.
What isn’t studied, as this paper properly points out, is, what can the doctor and the nurse do to trust the patient? How can that be assessed? Isn’t that just as important as saying that patients have to trust their doctors to do and comply with what they’re told?
What if doctors are afraid of violence? What if doctors are fearful that they can’t trust patients to listen, pay attention, or do what they’re being told? What if they think that patients are coming in with all kinds of disinformation, false information, or things they pick up on the Internet, so that even though you try your best to get across accurate and complete information about what to do about infectious diseases, taking care of a kid with strep throat, or whatever it might be, you’re thinking, Can I trust this patient to do what it is that I want them to do?
One particular problem that’s causing distrust is that more and more patients are showing stress and dependence on drugs and alcohol. That doesn’t make them less trustworthy per se, but it means they can’t regulate their own behavior as well.
That obviously has to be something that the physician or the nurse is thinking about. Is this person going to be able to contain anger? Is this person going to be able to handle bad news? Is this person going to deal with me when I tell them that some of the things they believe to be true about what’s good for their health care are false?
I think we have to really start to push administrators and people in positions of power to teach doctors and nurses how to defuse situations and how to make people more comfortable when they come in and the doctor suspects that they might be under the influence, impaired, or angry because of things they’ve seen on social media, whatever those might be – including concerns about racism, bigotry, and bias, which some patients are bringing into the clinic and the hospital setting.
We need more training. We’ve got to address this as a serious issue. What can we do to defuse situations where the doctor or the nurse rightly thinks that they can’t control or they can’t trust what the patient is thinking or how the patient might behave?
It’s also the case that I think we need more backup and quick access to security so that people feel safe and comfortable in providing care. We have to make sure that if you need someone to restrain a patient or to get somebody out of a situation, that they can get there quickly and respond rapidly, and that they know what to do to deescalate a situation.
It’s sad to say, but security in today’s health care world has to be something that we really test and check – not because we’re worried, as many places are, about a shooter entering the premises, which is its own bit of concern – but I’m just talking about when the doctor or the nurse says that this patient might be acting up, could get violent, or is someone I can’t trust.
My coauthors are basically saying that it’s not a one-way street. Yes, we have to figure out ways to make sure that our patients can trust what we say. Trust is absolutely the lubricant that makes health care flow. If patients don’t trust their doctors, they’re not going to do what they say. They’re not going to get their prescriptions filled. They’re not going to be compliant. They’re not going to try to lose weight or control their diabetes.
It also goes the other way. The doctor or the nurse has to trust the patient. They have to believe that they’re safe. They have to believe that the patient is capable of controlling themselves. They have to believe that the patient is capable of listening and hearing what they’re saying, and that they’re competent to follow up on instructions, including to come back if that’s what’s required.
Everybody has to feel secure in the environment in which they’re working. Security, sadly, has to be a priority if we’re going to have a health care workforce that really feels safe and comfortable dealing with a patient population that is increasingly aggressive and perhaps not as trustworthy.
That’s not news I like to read when my colleagues write it up, but it’s important and we have to take it seriously.
Dr. Caplan disclosed that he has served as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position), and is a contributing author and adviser for Medscape. A version of this article first appeared on Medscape.com.
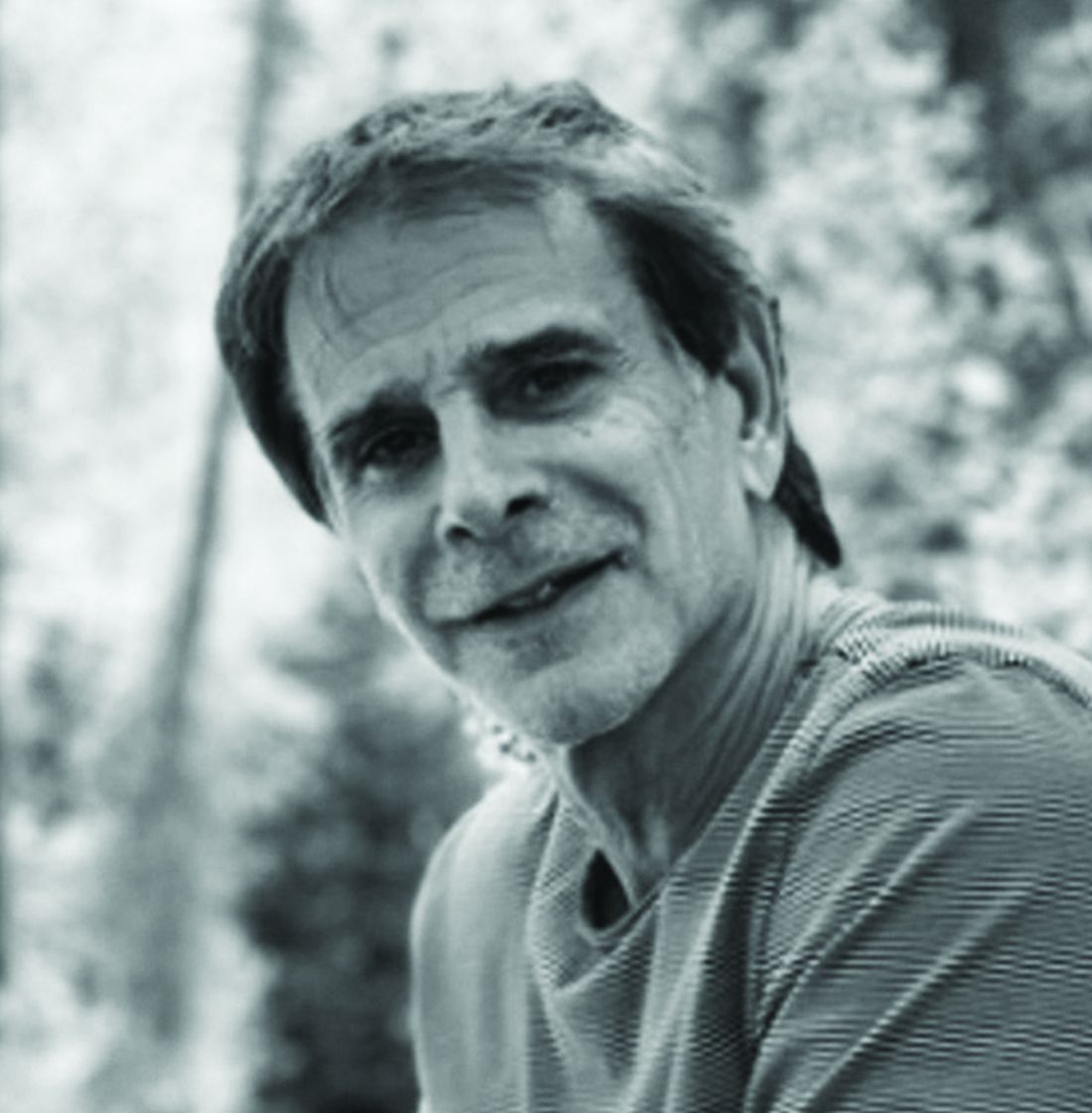
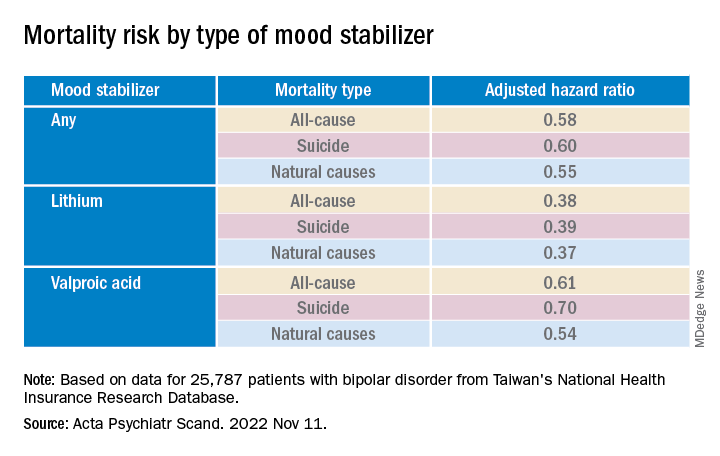
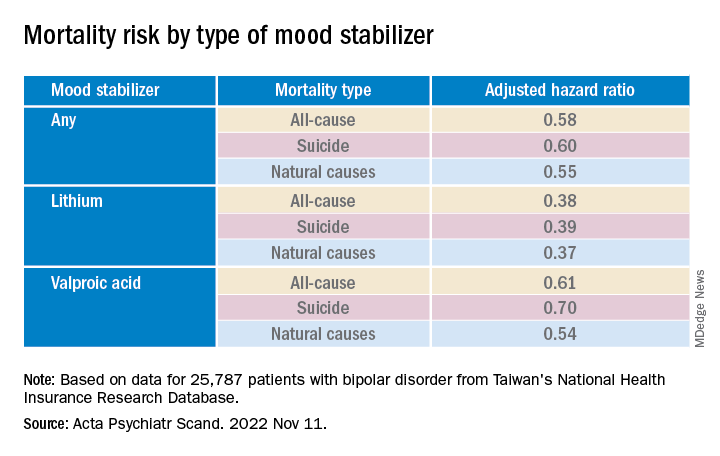
Mood stabilizers, particularly lithium, potential lifesavers in bipolar disorder
Investigators led by Pao-Huan Chen, MD, of the department of psychiatry, Taipei Medical University Hospital, Taiwan, evaluated the association between the use of mood stabilizers and the risks for all-cause mortality, suicide, and natural mortality in more than 25,000 patients with BD and found that those with BD had higher mortality.
However, they also found that patients with BD had a significantly decreased adjusted 5-year risk of dying from any cause, suicide, and natural causes. Lithium was associated with the largest risk reduction compared with the other mood stabilizers.
“The present findings highlight the potential role of mood stabilizers, particularly lithium, in reducing mortality among patients with bipolar disorder,” the authors write.
“The findings of this study could inform future clinical and mechanistic research evaluating the multifaceted effects of mood stabilizers, particularly lithium, on the psychological and physiological statuses of patients with bipolar disorder,” they add.
The study was published online in Acta Psychiatrica Scandinavica.
Research gap
Patients with BD have an elevated risk for multiple comorbidities in addition to mood symptoms and neurocognitive dysfunction, with previous research suggesting a mortality rate due to suicide and natural causes that is at least twice as high as that of the general population, the authors write.
Lithium, in particular, has been associated with decreased risk for all-cause mortality and suicide in patients with BD, but findings regarding anticonvulsant mood stabilizers have been “inconsistent.”
To fill this research gap, the researchers evaluated 16 years of data from Taiwan’s National Health Insurance Research Database, which includes information about more than 23 million residents of Taiwan. The current study, which encompassed 25,787 patients with BD, looked at data from the 5-year period after index hospitalization.
The researchers hypothesized that mood stabilizers “would decrease the risk of mortality” among patients with BD and that “different mood stabilizers would exhibit different associations with mortality, owing to their varying effects on mood symptoms and physiological function.”
Covariates included sex, age, employment status, comorbidities, and concomitant drugs.
Of the patients with BD, 4,000 died within the 5-year period. Suicide and natural causes accounted for 19.0% and 73.7% of these deaths, respectively.
Cardioprotective effects?
The standardized mortality ratios (SMRs) – the ratios of observed mortality in the BD cohort to the number of expected deaths in the general population – were 5.26 for all causes (95% confidence interval, 5.10-5.43), 26.02 for suicide (95% CI, 24.20-27.93), and 4.68 for natural causes (95% CI, 4.51-4.85).
The cumulative mortality rate was higher among men vs. women, a difference that was even larger among patients who had died from any cause or natural causes (crude hazard ratios, .60 and .52, respectively; both Ps < .001).
The suicide risk peaked between ages 45 and 65 years, whereas the risks for all-cause and natural mortality increased with age and were highest in those older than 65 years.
Patients who had died from any cause or from natural causes had a higher risk for physical and psychiatric comorbidities, whereas those who had died by suicide had a higher risk for primarily psychiatric comorbidities.
Mood stabilizers were associated with decreased risks for all-cause mortality and natural mortality, with lithium and valproic acid tied to the lowest risk for all three mortality types (all Ps < .001).
Lamotrigine and carbamazepine were “not significantly associated with any type of mortality,” the authors report.
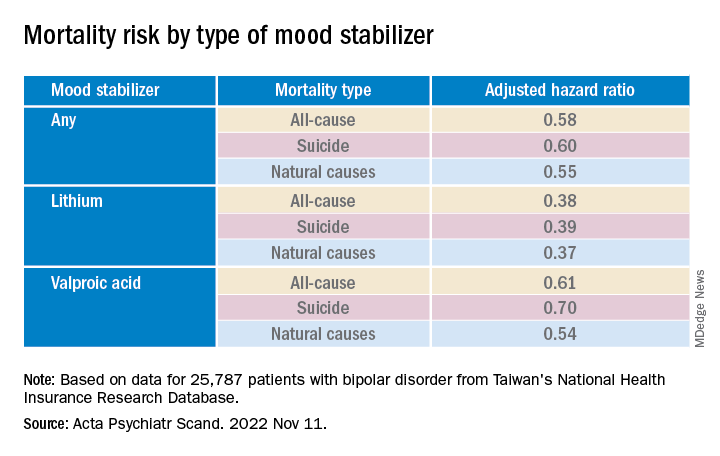
Longer duration of lithium use and a higher cumulative dose of lithium were both associated with lower risks for all three types of mortality (all Ps < .001).
Valproic acid was associated with dose-dependent decreases in all-cause and natural mortality risks.
The findings suggest that mood stabilizers “may improve not only psychosocial outcomes but also the physical health of patients with BD,” the investigators note.
The association between mood stabilizer use and reduced natural mortality risk “may be attributable to the potential benefits of psychiatric care” but may also “have resulted from the direct effects of mood stabilizers on physiological functions,” they add.
Some research suggests lithium treatment may reduce the risk for cardiovascular disease in patients with BD. Mechanistic studies have also pointed to potential cardioprotective effects from valproic acid.
The authors note several study limitations. Focusing on hospitalized patients “may have led to selection bias and overestimated mortality risk.” Moreover, the analyses were “based on the prescription, not the consumption, of mood stabilizers” and information regarding adherence was unavailable.
The absence of a protective mechanism of lamotrigine and carbamazepine may be attributable to “bias toward the relatively poor treatment responses” of these agents, neither of which is used as a first-line medication to treat BD in Taiwan. Patients taking these agents “may not receive medical care at a level equal to those taking lithium, who tend to receive closer surveillance, owing to the narrow therapeutic index.”
First-line treatment
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the data “add to a growing confluence of data from observational studies indicating that lithium especially is capable of reducing all-cause mortality, suicide mortality, and natural mortality.”
Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study, agreed with the authors that lamotrigine is “not a very popular drug in Taiwan, therefore we may not have sufficient assay sensitivity to document the effect.”
But lamotrigine “does have recurrence prevention effects in BD, especially bipolar depression, and it would be expected that it would reduce suicide potentially especially in such a large sample.”
The study’s take-home message “is that the extant evidence now indicates that lithium should be a first-line treatment in persons who live with BD who are experiencing suicidal ideation and/or behavior and these data should inform algorithms of treatment selection and sequencing in clinical practice guidelines,” said Dr. McIntyre.
This research was supported by grants from the Ministry of Science and Technology in Taiwan and Taipei City Hospital. The authors declared no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China, and the Milken Institute; and speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe Pharma, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators led by Pao-Huan Chen, MD, of the department of psychiatry, Taipei Medical University Hospital, Taiwan, evaluated the association between the use of mood stabilizers and the risks for all-cause mortality, suicide, and natural mortality in more than 25,000 patients with BD and found that those with BD had higher mortality.
However, they also found that patients with BD had a significantly decreased adjusted 5-year risk of dying from any cause, suicide, and natural causes. Lithium was associated with the largest risk reduction compared with the other mood stabilizers.
“The present findings highlight the potential role of mood stabilizers, particularly lithium, in reducing mortality among patients with bipolar disorder,” the authors write.
“The findings of this study could inform future clinical and mechanistic research evaluating the multifaceted effects of mood stabilizers, particularly lithium, on the psychological and physiological statuses of patients with bipolar disorder,” they add.
The study was published online in Acta Psychiatrica Scandinavica.
Research gap
Patients with BD have an elevated risk for multiple comorbidities in addition to mood symptoms and neurocognitive dysfunction, with previous research suggesting a mortality rate due to suicide and natural causes that is at least twice as high as that of the general population, the authors write.
Lithium, in particular, has been associated with decreased risk for all-cause mortality and suicide in patients with BD, but findings regarding anticonvulsant mood stabilizers have been “inconsistent.”
To fill this research gap, the researchers evaluated 16 years of data from Taiwan’s National Health Insurance Research Database, which includes information about more than 23 million residents of Taiwan. The current study, which encompassed 25,787 patients with BD, looked at data from the 5-year period after index hospitalization.
The researchers hypothesized that mood stabilizers “would decrease the risk of mortality” among patients with BD and that “different mood stabilizers would exhibit different associations with mortality, owing to their varying effects on mood symptoms and physiological function.”
Covariates included sex, age, employment status, comorbidities, and concomitant drugs.
Of the patients with BD, 4,000 died within the 5-year period. Suicide and natural causes accounted for 19.0% and 73.7% of these deaths, respectively.
Cardioprotective effects?
The standardized mortality ratios (SMRs) – the ratios of observed mortality in the BD cohort to the number of expected deaths in the general population – were 5.26 for all causes (95% confidence interval, 5.10-5.43), 26.02 for suicide (95% CI, 24.20-27.93), and 4.68 for natural causes (95% CI, 4.51-4.85).
The cumulative mortality rate was higher among men vs. women, a difference that was even larger among patients who had died from any cause or natural causes (crude hazard ratios, .60 and .52, respectively; both Ps < .001).
The suicide risk peaked between ages 45 and 65 years, whereas the risks for all-cause and natural mortality increased with age and were highest in those older than 65 years.
Patients who had died from any cause or from natural causes had a higher risk for physical and psychiatric comorbidities, whereas those who had died by suicide had a higher risk for primarily psychiatric comorbidities.
Mood stabilizers were associated with decreased risks for all-cause mortality and natural mortality, with lithium and valproic acid tied to the lowest risk for all three mortality types (all Ps < .001).
Lamotrigine and carbamazepine were “not significantly associated with any type of mortality,” the authors report.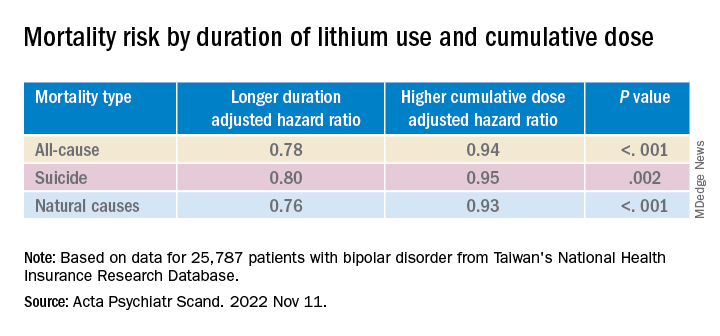
Longer duration of lithium use and a higher cumulative dose of lithium were both associated with lower risks for all three types of mortality (all Ps < .001).
Valproic acid was associated with dose-dependent decreases in all-cause and natural mortality risks.
The findings suggest that mood stabilizers “may improve not only psychosocial outcomes but also the physical health of patients with BD,” the investigators note.
The association between mood stabilizer use and reduced natural mortality risk “may be attributable to the potential benefits of psychiatric care” but may also “have resulted from the direct effects of mood stabilizers on physiological functions,” they add.
Some research suggests lithium treatment may reduce the risk for cardiovascular disease in patients with BD. Mechanistic studies have also pointed to potential cardioprotective effects from valproic acid.
The authors note several study limitations. Focusing on hospitalized patients “may have led to selection bias and overestimated mortality risk.” Moreover, the analyses were “based on the prescription, not the consumption, of mood stabilizers” and information regarding adherence was unavailable.
The absence of a protective mechanism of lamotrigine and carbamazepine may be attributable to “bias toward the relatively poor treatment responses” of these agents, neither of which is used as a first-line medication to treat BD in Taiwan. Patients taking these agents “may not receive medical care at a level equal to those taking lithium, who tend to receive closer surveillance, owing to the narrow therapeutic index.”
First-line treatment
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the data “add to a growing confluence of data from observational studies indicating that lithium especially is capable of reducing all-cause mortality, suicide mortality, and natural mortality.”
Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study, agreed with the authors that lamotrigine is “not a very popular drug in Taiwan, therefore we may not have sufficient assay sensitivity to document the effect.”
But lamotrigine “does have recurrence prevention effects in BD, especially bipolar depression, and it would be expected that it would reduce suicide potentially especially in such a large sample.”
The study’s take-home message “is that the extant evidence now indicates that lithium should be a first-line treatment in persons who live with BD who are experiencing suicidal ideation and/or behavior and these data should inform algorithms of treatment selection and sequencing in clinical practice guidelines,” said Dr. McIntyre.
This research was supported by grants from the Ministry of Science and Technology in Taiwan and Taipei City Hospital. The authors declared no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China, and the Milken Institute; and speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe Pharma, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators led by Pao-Huan Chen, MD, of the department of psychiatry, Taipei Medical University Hospital, Taiwan, evaluated the association between the use of mood stabilizers and the risks for all-cause mortality, suicide, and natural mortality in more than 25,000 patients with BD and found that those with BD had higher mortality.
However, they also found that patients with BD had a significantly decreased adjusted 5-year risk of dying from any cause, suicide, and natural causes. Lithium was associated with the largest risk reduction compared with the other mood stabilizers.
“The present findings highlight the potential role of mood stabilizers, particularly lithium, in reducing mortality among patients with bipolar disorder,” the authors write.
“The findings of this study could inform future clinical and mechanistic research evaluating the multifaceted effects of mood stabilizers, particularly lithium, on the psychological and physiological statuses of patients with bipolar disorder,” they add.
The study was published online in Acta Psychiatrica Scandinavica.
Research gap
Patients with BD have an elevated risk for multiple comorbidities in addition to mood symptoms and neurocognitive dysfunction, with previous research suggesting a mortality rate due to suicide and natural causes that is at least twice as high as that of the general population, the authors write.
Lithium, in particular, has been associated with decreased risk for all-cause mortality and suicide in patients with BD, but findings regarding anticonvulsant mood stabilizers have been “inconsistent.”
To fill this research gap, the researchers evaluated 16 years of data from Taiwan’s National Health Insurance Research Database, which includes information about more than 23 million residents of Taiwan. The current study, which encompassed 25,787 patients with BD, looked at data from the 5-year period after index hospitalization.
The researchers hypothesized that mood stabilizers “would decrease the risk of mortality” among patients with BD and that “different mood stabilizers would exhibit different associations with mortality, owing to their varying effects on mood symptoms and physiological function.”
Covariates included sex, age, employment status, comorbidities, and concomitant drugs.
Of the patients with BD, 4,000 died within the 5-year period. Suicide and natural causes accounted for 19.0% and 73.7% of these deaths, respectively.
Cardioprotective effects?
The standardized mortality ratios (SMRs) – the ratios of observed mortality in the BD cohort to the number of expected deaths in the general population – were 5.26 for all causes (95% confidence interval, 5.10-5.43), 26.02 for suicide (95% CI, 24.20-27.93), and 4.68 for natural causes (95% CI, 4.51-4.85).
The cumulative mortality rate was higher among men vs. women, a difference that was even larger among patients who had died from any cause or natural causes (crude hazard ratios, .60 and .52, respectively; both Ps < .001).
The suicide risk peaked between ages 45 and 65 years, whereas the risks for all-cause and natural mortality increased with age and were highest in those older than 65 years.
Patients who had died from any cause or from natural causes had a higher risk for physical and psychiatric comorbidities, whereas those who had died by suicide had a higher risk for primarily psychiatric comorbidities.
Mood stabilizers were associated with decreased risks for all-cause mortality and natural mortality, with lithium and valproic acid tied to the lowest risk for all three mortality types (all Ps < .001).
Lamotrigine and carbamazepine were “not significantly associated with any type of mortality,” the authors report.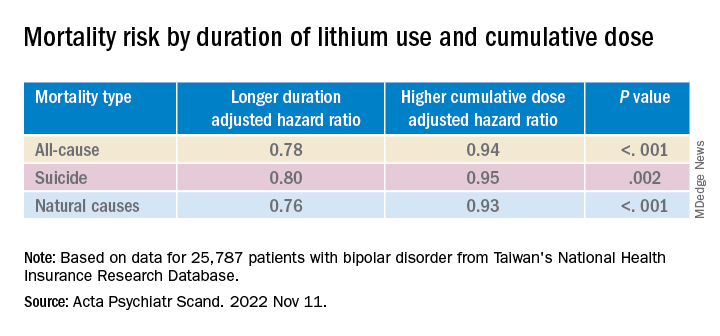
Longer duration of lithium use and a higher cumulative dose of lithium were both associated with lower risks for all three types of mortality (all Ps < .001).
Valproic acid was associated with dose-dependent decreases in all-cause and natural mortality risks.
The findings suggest that mood stabilizers “may improve not only psychosocial outcomes but also the physical health of patients with BD,” the investigators note.
The association between mood stabilizer use and reduced natural mortality risk “may be attributable to the potential benefits of psychiatric care” but may also “have resulted from the direct effects of mood stabilizers on physiological functions,” they add.
Some research suggests lithium treatment may reduce the risk for cardiovascular disease in patients with BD. Mechanistic studies have also pointed to potential cardioprotective effects from valproic acid.
The authors note several study limitations. Focusing on hospitalized patients “may have led to selection bias and overestimated mortality risk.” Moreover, the analyses were “based on the prescription, not the consumption, of mood stabilizers” and information regarding adherence was unavailable.
The absence of a protective mechanism of lamotrigine and carbamazepine may be attributable to “bias toward the relatively poor treatment responses” of these agents, neither of which is used as a first-line medication to treat BD in Taiwan. Patients taking these agents “may not receive medical care at a level equal to those taking lithium, who tend to receive closer surveillance, owing to the narrow therapeutic index.”
First-line treatment
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the data “add to a growing confluence of data from observational studies indicating that lithium especially is capable of reducing all-cause mortality, suicide mortality, and natural mortality.”
Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study, agreed with the authors that lamotrigine is “not a very popular drug in Taiwan, therefore we may not have sufficient assay sensitivity to document the effect.”
But lamotrigine “does have recurrence prevention effects in BD, especially bipolar depression, and it would be expected that it would reduce suicide potentially especially in such a large sample.”
The study’s take-home message “is that the extant evidence now indicates that lithium should be a first-line treatment in persons who live with BD who are experiencing suicidal ideation and/or behavior and these data should inform algorithms of treatment selection and sequencing in clinical practice guidelines,” said Dr. McIntyre.
This research was supported by grants from the Ministry of Science and Technology in Taiwan and Taipei City Hospital. The authors declared no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China, and the Milken Institute; and speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe Pharma, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
FROM ACTA PSYCHIATRICA SCANDINAVICA
Digital treatment may help relieve PTSD, panic disorder
The 28-day home-based treatment, known as the capnometry guided respiratory intervention (CGRI), uses an app-based feedback protocol to normalize respiration and increase patients’ ability to cope with symptoms of stress, anxiety, and panic by providing real time breath-to-breath feedback of respiratory rate and carbon dioxide (CO2) levels via a nasal cannula.
Results from the large real-world study showed that over 65% of patients with PD and over 72% of those with PTSD responded to the treatment. In addition, almost 75% of participants adhered to the study protocol, with low dropout rates.
“The brief duration of treatment, high adherence rates, and clinical benefit suggests that CGRI provides an important addition to treatment options for PD and PTSD,” the investigators write.
The study was published online in Frontiers in Digital Health.
‘New kid on the block’
The “respiratory dysregulation hypothesis” links CO2 sensitivity to panic attacks and PD, and similar reactivity has been identified in PTSD, but a “common limitation of psychotherapeutic and pharmacologic approaches to PD and PTSD is that neither address the role of respiratory physiology and breathing style,” the investigators note.
The most widely studied treatment for PTSD is trauma-focused psychotherapy, in which the patient reviews and revisits the trauma, but it has a high dropout rate, study investigator Michael Telch, PhD, director of the Laboratory for the Study of Anxiety Disorders, University of Texas, Austin, told this news organization.
He described CGRI for PTSD as a “relatively new kid on the block, so to speak.” The intervention was cleared by the U.S. Food and Drug Administration for treatment of PD and PTSD in 2013 and 2018, respectively, and is currently available through the Veterans Administration for veterans with PTSD. It is also covered by some commercial insurance plans.
“The underlying assumption [of CGRI] is that a person can learn to develop skills for controlling some of their physiological reactions that are triggered as a result of trauma,” said Dr. Telch.
The device uses a biofeedback approach to give patients “greater control over their physiological reactions, such as hyperventilation and increased respiration rate, and the focus is on providing a sense of mastery,” he said.
Participants with PTSD were assigned to a health coach. The device was delivered to the patient’s home, and patients met with the trained coach weekly and could check in between visits via text or e-mail. Twice-daily sessions were recommended.
“The coach gets feedback about what’s happening with the patient’s respiration and end-tidal CO2 levels [etCO2] and instructs participants how to keep their respiration rate and etCO2 at a more normal level,” said Dr. Telch.
The CGRI “teaches a specific breathing style via a system providing real-time feedback of respiratory rate (RR) and exhaled carbon dioxide levels facilitated by data capture,” the authors note.
Sense of mastery
Of the 1,569 participants, 1,395 had PD and 174 had PTSD (mean age, 39.2 [standard deviation, 13.9] years and 40.9 [SD, 14.9] years, respectively; 76% and 73% female, respectively). Those with PD completed the Panic Disorder Severity Scale (PDSS) and those with PTSD completed the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5), before and after the intervention.
The treatment response rate for PD was defined as a 40% or greater reduction in PDSS total scores, whereas treatment response rate for PTSD was defined as a 10-point or greater reduction in PCL-5 scores.
At baseline, patients were classified either as normocapnic or hypocapnic (etCO2 ≥ 37 or < 37, respectively), with 65% classified as normocapnic and 35% classified as hypocapnic.
Among patients with PD, there was a 50.2% mean pre- to posttreatment reduction in total PDSS scores (P < .001; d = 1.31), with a treatment response rate of 65.3% of patients.
Among patients with PTSD, there was a 41.1% pre- to posttreatment reduction in total PCL-5 scores (P < .001; d = 1.16), with a treatment response rate of 72.4%.
When investigators analyzed the response at the individual level, they found that 55.7% of patients with PD and 53.5% of those with PTSD were classified as treatment responders. This determination was based on a two-pronged approach that first calculated the Reliable Change Index (RCI) for each participant, and, in participants showing statistically reliable improvement, whether the posttreatment score was closer to the distribution of scores for patients without or with the given disorder.
“Patients with both normal and below-normal baseline exhaled CO2 levels experienced comparable benefit,” the authors report.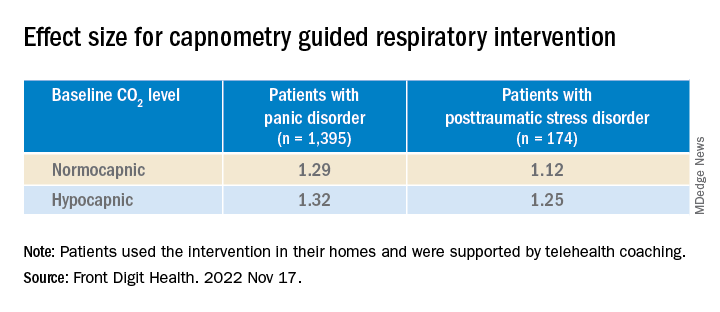
There were high levels of adherence across the full treatment period in both the PD and the PTSD groups (74.8% and 74.9%, respectively), with low dropout rates (10% and 11%, respectively).
“Not every single patient who undergoes any treatment has a perfect response, but the response rates to this treatment have, surprisingly, been quite positive and there have been no negative side effects,” Dr. Telch remarked.
He noted that one of the effects of PTSD is that the “patient has negative beliefs about their ability to control the world. ‘I can’t control my reactions. At any time, I could have a flashback.’ Helping the patient to develop any sense of mastery over some of their reactions can spill over and give them a greater sense of mastery and control, which can have a positive effect in reducing PTSD symptoms.”
‘A viable alternative’
Commenting on the research, Charles Marmar, MD, chair and Peter H. Schub Professor of Psychiatry, department of psychiatry, New York University, said that the study has some limitations, probably the most significant of which is that most participants had normal baseline CO2 levels.
“The treatment is fundamentally designed for people who hyperventilate and blow off too much CO2 so they can breathe in a more calm, relaxed way, but most people in the trial had normal CO2 to begin with,” said Dr. Marmar, who was not involved with the study.
“It’s likely that the major benefits were the relaxation from doing the breathing exercises rather than the change in CO2 levels,” he speculated.
The treatment is “probably a good thing for those patients who actually have abnormal CO2 levels. This treatment could be used in precision medicine, where you tailor treatments to those who actually need them rather than giving the same treatment to everyone,” he said.
“For patients who don’t respond to trauma-focused therapy or it’s too aversive for them to undergo, this new intervention provides a viable alternative,” Dr. Telch added.
The study was internally funded by Freespira. Dr. Telch is a scientific advisor at Freespira and receives compensation by way of stock options. The other authors’ disclosures are listed on the original paper. Dr. Marmar has declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The 28-day home-based treatment, known as the capnometry guided respiratory intervention (CGRI), uses an app-based feedback protocol to normalize respiration and increase patients’ ability to cope with symptoms of stress, anxiety, and panic by providing real time breath-to-breath feedback of respiratory rate and carbon dioxide (CO2) levels via a nasal cannula.
Results from the large real-world study showed that over 65% of patients with PD and over 72% of those with PTSD responded to the treatment. In addition, almost 75% of participants adhered to the study protocol, with low dropout rates.
“The brief duration of treatment, high adherence rates, and clinical benefit suggests that CGRI provides an important addition to treatment options for PD and PTSD,” the investigators write.
The study was published online in Frontiers in Digital Health.
‘New kid on the block’
The “respiratory dysregulation hypothesis” links CO2 sensitivity to panic attacks and PD, and similar reactivity has been identified in PTSD, but a “common limitation of psychotherapeutic and pharmacologic approaches to PD and PTSD is that neither address the role of respiratory physiology and breathing style,” the investigators note.
The most widely studied treatment for PTSD is trauma-focused psychotherapy, in which the patient reviews and revisits the trauma, but it has a high dropout rate, study investigator Michael Telch, PhD, director of the Laboratory for the Study of Anxiety Disorders, University of Texas, Austin, told this news organization.
He described CGRI for PTSD as a “relatively new kid on the block, so to speak.” The intervention was cleared by the U.S. Food and Drug Administration for treatment of PD and PTSD in 2013 and 2018, respectively, and is currently available through the Veterans Administration for veterans with PTSD. It is also covered by some commercial insurance plans.
“The underlying assumption [of CGRI] is that a person can learn to develop skills for controlling some of their physiological reactions that are triggered as a result of trauma,” said Dr. Telch.
The device uses a biofeedback approach to give patients “greater control over their physiological reactions, such as hyperventilation and increased respiration rate, and the focus is on providing a sense of mastery,” he said.
Participants with PTSD were assigned to a health coach. The device was delivered to the patient’s home, and patients met with the trained coach weekly and could check in between visits via text or e-mail. Twice-daily sessions were recommended.
“The coach gets feedback about what’s happening with the patient’s respiration and end-tidal CO2 levels [etCO2] and instructs participants how to keep their respiration rate and etCO2 at a more normal level,” said Dr. Telch.
The CGRI “teaches a specific breathing style via a system providing real-time feedback of respiratory rate (RR) and exhaled carbon dioxide levels facilitated by data capture,” the authors note.
Sense of mastery
Of the 1,569 participants, 1,395 had PD and 174 had PTSD (mean age, 39.2 [standard deviation, 13.9] years and 40.9 [SD, 14.9] years, respectively; 76% and 73% female, respectively). Those with PD completed the Panic Disorder Severity Scale (PDSS) and those with PTSD completed the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5), before and after the intervention.
The treatment response rate for PD was defined as a 40% or greater reduction in PDSS total scores, whereas treatment response rate for PTSD was defined as a 10-point or greater reduction in PCL-5 scores.
At baseline, patients were classified either as normocapnic or hypocapnic (etCO2 ≥ 37 or < 37, respectively), with 65% classified as normocapnic and 35% classified as hypocapnic.
Among patients with PD, there was a 50.2% mean pre- to posttreatment reduction in total PDSS scores (P < .001; d = 1.31), with a treatment response rate of 65.3% of patients.
Among patients with PTSD, there was a 41.1% pre- to posttreatment reduction in total PCL-5 scores (P < .001; d = 1.16), with a treatment response rate of 72.4%.
When investigators analyzed the response at the individual level, they found that 55.7% of patients with PD and 53.5% of those with PTSD were classified as treatment responders. This determination was based on a two-pronged approach that first calculated the Reliable Change Index (RCI) for each participant, and, in participants showing statistically reliable improvement, whether the posttreatment score was closer to the distribution of scores for patients without or with the given disorder.
“Patients with both normal and below-normal baseline exhaled CO2 levels experienced comparable benefit,” the authors report.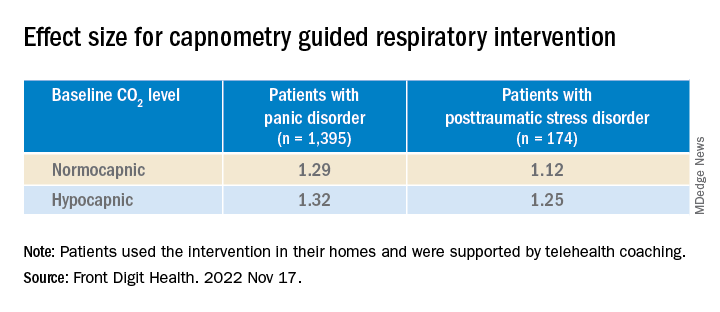
There were high levels of adherence across the full treatment period in both the PD and the PTSD groups (74.8% and 74.9%, respectively), with low dropout rates (10% and 11%, respectively).
“Not every single patient who undergoes any treatment has a perfect response, but the response rates to this treatment have, surprisingly, been quite positive and there have been no negative side effects,” Dr. Telch remarked.
He noted that one of the effects of PTSD is that the “patient has negative beliefs about their ability to control the world. ‘I can’t control my reactions. At any time, I could have a flashback.’ Helping the patient to develop any sense of mastery over some of their reactions can spill over and give them a greater sense of mastery and control, which can have a positive effect in reducing PTSD symptoms.”
‘A viable alternative’
Commenting on the research, Charles Marmar, MD, chair and Peter H. Schub Professor of Psychiatry, department of psychiatry, New York University, said that the study has some limitations, probably the most significant of which is that most participants had normal baseline CO2 levels.
“The treatment is fundamentally designed for people who hyperventilate and blow off too much CO2 so they can breathe in a more calm, relaxed way, but most people in the trial had normal CO2 to begin with,” said Dr. Marmar, who was not involved with the study.
“It’s likely that the major benefits were the relaxation from doing the breathing exercises rather than the change in CO2 levels,” he speculated.
The treatment is “probably a good thing for those patients who actually have abnormal CO2 levels. This treatment could be used in precision medicine, where you tailor treatments to those who actually need them rather than giving the same treatment to everyone,” he said.
“For patients who don’t respond to trauma-focused therapy or it’s too aversive for them to undergo, this new intervention provides a viable alternative,” Dr. Telch added.
The study was internally funded by Freespira. Dr. Telch is a scientific advisor at Freespira and receives compensation by way of stock options. The other authors’ disclosures are listed on the original paper. Dr. Marmar has declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The 28-day home-based treatment, known as the capnometry guided respiratory intervention (CGRI), uses an app-based feedback protocol to normalize respiration and increase patients’ ability to cope with symptoms of stress, anxiety, and panic by providing real time breath-to-breath feedback of respiratory rate and carbon dioxide (CO2) levels via a nasal cannula.
Results from the large real-world study showed that over 65% of patients with PD and over 72% of those with PTSD responded to the treatment. In addition, almost 75% of participants adhered to the study protocol, with low dropout rates.
“The brief duration of treatment, high adherence rates, and clinical benefit suggests that CGRI provides an important addition to treatment options for PD and PTSD,” the investigators write.
The study was published online in Frontiers in Digital Health.
‘New kid on the block’
The “respiratory dysregulation hypothesis” links CO2 sensitivity to panic attacks and PD, and similar reactivity has been identified in PTSD, but a “common limitation of psychotherapeutic and pharmacologic approaches to PD and PTSD is that neither address the role of respiratory physiology and breathing style,” the investigators note.
The most widely studied treatment for PTSD is trauma-focused psychotherapy, in which the patient reviews and revisits the trauma, but it has a high dropout rate, study investigator Michael Telch, PhD, director of the Laboratory for the Study of Anxiety Disorders, University of Texas, Austin, told this news organization.
He described CGRI for PTSD as a “relatively new kid on the block, so to speak.” The intervention was cleared by the U.S. Food and Drug Administration for treatment of PD and PTSD in 2013 and 2018, respectively, and is currently available through the Veterans Administration for veterans with PTSD. It is also covered by some commercial insurance plans.
“The underlying assumption [of CGRI] is that a person can learn to develop skills for controlling some of their physiological reactions that are triggered as a result of trauma,” said Dr. Telch.
The device uses a biofeedback approach to give patients “greater control over their physiological reactions, such as hyperventilation and increased respiration rate, and the focus is on providing a sense of mastery,” he said.
Participants with PTSD were assigned to a health coach. The device was delivered to the patient’s home, and patients met with the trained coach weekly and could check in between visits via text or e-mail. Twice-daily sessions were recommended.
“The coach gets feedback about what’s happening with the patient’s respiration and end-tidal CO2 levels [etCO2] and instructs participants how to keep their respiration rate and etCO2 at a more normal level,” said Dr. Telch.
The CGRI “teaches a specific breathing style via a system providing real-time feedback of respiratory rate (RR) and exhaled carbon dioxide levels facilitated by data capture,” the authors note.
Sense of mastery
Of the 1,569 participants, 1,395 had PD and 174 had PTSD (mean age, 39.2 [standard deviation, 13.9] years and 40.9 [SD, 14.9] years, respectively; 76% and 73% female, respectively). Those with PD completed the Panic Disorder Severity Scale (PDSS) and those with PTSD completed the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5), before and after the intervention.
The treatment response rate for PD was defined as a 40% or greater reduction in PDSS total scores, whereas treatment response rate for PTSD was defined as a 10-point or greater reduction in PCL-5 scores.
At baseline, patients were classified either as normocapnic or hypocapnic (etCO2 ≥ 37 or < 37, respectively), with 65% classified as normocapnic and 35% classified as hypocapnic.
Among patients with PD, there was a 50.2% mean pre- to posttreatment reduction in total PDSS scores (P < .001; d = 1.31), with a treatment response rate of 65.3% of patients.
Among patients with PTSD, there was a 41.1% pre- to posttreatment reduction in total PCL-5 scores (P < .001; d = 1.16), with a treatment response rate of 72.4%.
When investigators analyzed the response at the individual level, they found that 55.7% of patients with PD and 53.5% of those with PTSD were classified as treatment responders. This determination was based on a two-pronged approach that first calculated the Reliable Change Index (RCI) for each participant, and, in participants showing statistically reliable improvement, whether the posttreatment score was closer to the distribution of scores for patients without or with the given disorder.
“Patients with both normal and below-normal baseline exhaled CO2 levels experienced comparable benefit,” the authors report.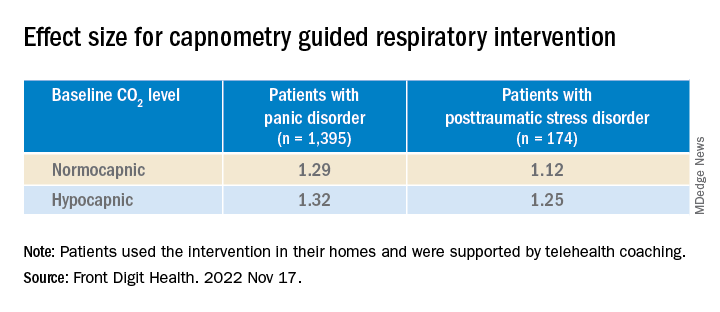
There were high levels of adherence across the full treatment period in both the PD and the PTSD groups (74.8% and 74.9%, respectively), with low dropout rates (10% and 11%, respectively).
“Not every single patient who undergoes any treatment has a perfect response, but the response rates to this treatment have, surprisingly, been quite positive and there have been no negative side effects,” Dr. Telch remarked.
He noted that one of the effects of PTSD is that the “patient has negative beliefs about their ability to control the world. ‘I can’t control my reactions. At any time, I could have a flashback.’ Helping the patient to develop any sense of mastery over some of their reactions can spill over and give them a greater sense of mastery and control, which can have a positive effect in reducing PTSD symptoms.”
‘A viable alternative’
Commenting on the research, Charles Marmar, MD, chair and Peter H. Schub Professor of Psychiatry, department of psychiatry, New York University, said that the study has some limitations, probably the most significant of which is that most participants had normal baseline CO2 levels.
“The treatment is fundamentally designed for people who hyperventilate and blow off too much CO2 so they can breathe in a more calm, relaxed way, but most people in the trial had normal CO2 to begin with,” said Dr. Marmar, who was not involved with the study.
“It’s likely that the major benefits were the relaxation from doing the breathing exercises rather than the change in CO2 levels,” he speculated.
The treatment is “probably a good thing for those patients who actually have abnormal CO2 levels. This treatment could be used in precision medicine, where you tailor treatments to those who actually need them rather than giving the same treatment to everyone,” he said.
“For patients who don’t respond to trauma-focused therapy or it’s too aversive for them to undergo, this new intervention provides a viable alternative,” Dr. Telch added.
The study was internally funded by Freespira. Dr. Telch is a scientific advisor at Freespira and receives compensation by way of stock options. The other authors’ disclosures are listed on the original paper. Dr. Marmar has declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN DIGITAL HEALTH
How your voice could reveal hidden disease
: First during puberty, as the vocal cords thicken and the voice box migrates down the throat. Then a second time as aging causes structural changes that may weaken the voice.
But for some of us, there’s another voice shift, when a disease begins or when our mental health declines.
This is why more doctors are looking into voice as a biomarker – something that tells you that a disease is present.
Vital signs like blood pressure or heart rate “can give a general idea of how sick we are. But they’re not specific to certain diseases,” says Yael Bensoussan, MD, director of the University of South Florida, Tampa’s Health Voice Center and the coprincipal investigator for the National Institutes of Health’s Voice as a Biomarker of Health project.
“We’re learning that there are patterns” in voice changes that can indicate a range of conditions, including diseases of the nervous system and mental illnesses, she says.
Speaking is complicated, involving everything from the lungs and voice box to the mouth and brain. “A breakdown in any of those parts can affect the voice,” says Maria Powell, PhD, an assistant professor of otolaryngology (the study of diseases of the ear and throat) at Vanderbilt University, Nashville, Tenn., who is working on the NIH project.
You or those around you may not notice the changes. But researchers say voice analysis as a standard part of patient care – akin to blood pressure checks or cholesterol tests – could help identify those who need medical attention earlier.
Often, all it takes is a smartphone – “something that’s cheap, off-the-shelf, and that everyone can use,” says Ariana Anderson, PhD, director of the University of California, Los Angeles, Laboratory of Computational Neuropsychology.
“You can provide voice data in your pajamas, on your couch,” says Frank Rudzicz, PhD, a computer scientist for the NIH project. “It doesn’t require very complicated or expensive equipment, and it doesn’t require a lot of expertise to obtain.” Plus, multiple samples can be collected over time, giving a more accurate picture of health than a single snapshot from, say, a cognitive test.
Over the next 4 years, the Voice as a Biomarker team will receive nearly $18 million to gather a massive amount of voice data. The goal is 20,000-30,000 samples, along with health data about each person being studied. The result will be a sprawling database scientists can use to develop algorithms linking health conditions to the way we speak.
For the first 2 years, new data will be collected exclusively via universities and high-volume clinics to control quality and accuracy. Eventually, people will be invited to submit their own voice recordings, creating a crowdsourced dataset. “Google, Alexa, Amazon – they have access to tons of voice data,” says Dr. Bensoussan. “But it’s not usable in a clinical way, because they don’t have the health information.”
Dr. Bensoussan and her colleagues hope to fill that void with advance voice screening apps, which could prove especially valuable in remote communities that lack access to specialists or as a tool for telemedicine. Down the line, wearable devices with voice analysis could alert people with chronic conditions when they need to see a doctor.
“The watch says, ‘I’ve analyzed your breathing and coughing, and today, you’re really not doing well. You should go to the hospital,’ ” says Dr. Bensoussan, envisioning a wearable for patients with COPD. “It could tell people early that things are declining.”
Artificial intelligence may be better than a brain at pinpointing the right disease. For example, slurred speech could indicate Parkinson’s, a stroke, or ALS, among other things.
“We can hold approximately seven pieces of information in our head at one time,” says Dr. Rudzicz. “It’s really hard for us to get a holistic picture using dozens or hundreds of variables at once.” But a computer can consider a whole range of vocal markers at the same time, piecing them together for a more accurate assessment.
“The goal is not to outperform a ... clinician,” says Dr. Bensoussan. Yet the potential is unmistakably there: In a recent study of patients with cancer of the larynx, an automated voice analysis tool more accurately flagged the disease than laryngologists did.
“Algorithms have a larger training base,” says Dr. Anderson, who developed an app called ChatterBaby that analyzes infant cries. “We have a million samples at our disposal to train our algorithms. I don’t know if I’ve heard a million different babies crying in my life.”
So which health conditions show the most promise for voice analysis? The Voice as a Biomarker project will focus on five categories.
Voice disorders (cancers of the larynx, vocal fold paralysis, benign lesions on the larynx)
Obviously, vocal changes are a hallmark of these conditions, which cause things like breathiness or “roughness,” a type of vocal irregularity. Hoarseness that lasts at least 2 weeks is often one of the earliest signs of laryngeal cancer. Yet it can take months – one study found 16 weeks was the average – for patients to see a doctor after noticing the changes. Even then, laryngologists still misdiagnosed some cases of cancer when relying on vocal cues alone.
Now imagine a different scenario: The patient speaks into a smartphone app. An algorithm compares the vocal sample with the voices of laryngeal cancer patients. The app spits out the estimated odds of laryngeal cancer, helping providers decide whether to offer the patient specialist care.
Or consider spasmodic dysphonia, a neurological voice disorder that triggers spasms in the muscles of the voice box, causing a strained or breathy voice. Doctors who lack experience with vocal disorders may miss the condition. This is why diagnosis takes an average of nearly 4.5 years, according to a study in the Journal of Voice, and may include everything from allergy testing to psychiatric evaluation, says Dr. Powell. Artificial intelligence technology trained to recognize the disorder could help eliminate such unnecessary testing.
Neurological and neurodegenerative disorders (Alzheimer’s, Parkinson’s, stroke, ALS)
For Alzheimer’s and Parkinson’s, “one of the first changes that’s notable is voice,” usually appearing before a formal diagnosis, says Anais Rameau, MD, an assistant professor of laryngology at Weill Cornell Medicine, New York, and another member of the NIH project. Parkinson’s may soften the voice or make it sound monotone, while Alzheimer’s disease may change the content of speech, leading to an uptick in “umms” and a preference for pronouns over nouns.
With Parkinson’s, vocal changes can occur decades before movement is affected. If doctors could detect the disease at this stage, before tremor emerged, they might be able to flag patients for early intervention, says Max Little, PhD, project director for the Parkinson’s Voice Initiative. “That is the ‘holy grail’ for finding an eventual cure.”
Again, the smartphone shows potential. In a 2022 Australian study, an AI-powered app was able to identify people with Parkinson’s based on brief voice recordings, although the sample size was small. On a larger scale, the Parkinson’s Voice Initiative collected some 17,000 samples from people across the world. “The aim was to remotely detect those with the condition using a telephone call,” says Dr. Little. It did so with about 65% accuracy. “While this is not accurate enough for clinical use, it shows the potential of the idea,” he says.
Dr. Rudzicz worked on the team behind Winterlight, an iPad app that analyzes 550 features of speech to detect dementia and Alzheimer’s (as well as mental illness). “We deployed it in long-term care facilities,” he says, identifying patients who need further review of their mental skills. Stroke is another area of interest, because slurred speech is a highly subjective measure, says Dr. Anderson. AI technology could provide a more objective evaluation.
Mood and psychiatric disorders (depression, schizophrenia, bipolar disorders)
No established biomarkers exist for diagnosing depression. Yet if you’re feeling down, there’s a good chance your friends can tell – even over the phone.
“We carry a lot of our mood in our voice,” says Dr. Powell. Bipolar disorder can also alter voice, making it louder and faster during manic periods, then slower and quieter during depressive bouts. The catatonic stage of schizophrenia often comes with “a very monotone, robotic voice,” says Dr. Anderson. “These are all something an algorithm can measure.”
Apps are already being used – often in research settings – to monitor voices during phone calls, analyzing rate, rhythm, volume, and pitch, to predict mood changes. For example, the PRIORI project at the University of Michigan is working on a smartphone app to identify mood changes in people with bipolar disorder, especially shifts that could increase suicide risk.
The content of speech may also offer clues. In a University of California, Los Angeles, study published in the journal PLoS One, people with mental illnesses answered computer-programmed questions (like “How have you been over the past few days?”) over the phone. An app analyzed their word choices, paying attention to how they changed over time. The researchers found that AI analysis of mood aligned well with doctors’ assessments and that some people in the study actually felt more comfortable talking to a computer.
Respiratory disorders (pneumonia, COPD)
Beyond talking, respiratory sounds like gasping or coughing may point to specific conditions. “Emphysema cough is different, COPD cough is different,” says Dr. Bensoussan. Researchers are trying to find out if COVID-19 has a distinct cough.
Breathing sounds can also serve as signposts. “There are different sounds when we can’t breathe,” says Dr. Bensoussan. One is called stridor, a high-pitched wheezing often resulting from a blocked airway. “I see tons of people [with stridor] misdiagnosed for years – they’ve been told they have asthma, but they don’t,” says Dr. Bensoussan. AI analysis of these sounds could help doctors more quickly identify respiratory disorders.
Pediatric voice and speech disorders (speech and language delays, autism)
Babies who later have autism cry differently as early as 6 months of age, which means an app like ChatterBaby could help flag children for early intervention, says Dr. Anderson. Autism is linked to several other diagnoses, such as epilepsy and sleep disorders. So analyzing an infant’s cry could prompt pediatricians to screen for a range of conditions.
ChatterBaby has been “incredibly accurate” in identifying when babies are in pain, says Dr. Anderson, because pain increases muscle tension, resulting in a louder, more energetic cry. The next goal: “We’re collecting voices from babies around the world,” she says, and then tracking those children for 7 years, looking to see if early vocal signs could predict developmental disorders. Vocal samples from young children could serve a similar purpose.
And that’s only the beginning
Eventually, AI technology may pick up disease-related voice changes that we can’t even hear. In a new Mayo Clinic study, certain vocal features detectable by AI – but not by the human ear – were linked to a three-fold increase in the likelihood of having plaque buildup in the arteries.
“Voice is a huge spectrum of vibrations,” explains study author Amir Lerman, MD. “We hear a very narrow range.”
The researchers aren’t sure why heart disease alters voice, but the autonomic nervous system may play a role, because it regulates the voice box as well as blood pressure and heart rate. Dr. Lerman says other conditions, like diseases of the nerves and gut, may similarly alter the voice. Beyond patient screening, this discovery could help doctors adjust medication doses remotely, in line with these inaudible vocal signals.
“Hopefully, in the next few years, this is going to come to practice,” says Dr. Lerman.
Still, in the face of that hope, privacy concerns remain. Voice is an identifier that’s protected by the federal Health Insurance Portability and Accountability Act, which requires privacy of personal health information. That is a major reason why no large voice databases exist yet, says Dr. Bensoussan. (This makes collecting samples from children especially challenging.) Perhaps more concerning is the potential for diagnosing disease based on voice alone. “You could use that tool on anyone, including officials like the president,” says Dr. Rameau.
But the primary hurdle is the ethical sourcing of data to ensure a diversity of vocal samples. For the Voice as a Biomarker project, the researchers will establish voice quotas for different races and ethnicities, ensuring algorithms can accurately analyze a range of accents. Data from people with speech impediments will also be gathered.
Despite these challenges, researchers are optimistic. “Vocal analysis is going to be a great equalizer and improve health outcomes,” predicts Dr. Anderson. “I’m really happy that we are beginning to understand the strength of the voice.”
A version of this article first appeared on WebMD.com.
: First during puberty, as the vocal cords thicken and the voice box migrates down the throat. Then a second time as aging causes structural changes that may weaken the voice.
But for some of us, there’s another voice shift, when a disease begins or when our mental health declines.
This is why more doctors are looking into voice as a biomarker – something that tells you that a disease is present.
Vital signs like blood pressure or heart rate “can give a general idea of how sick we are. But they’re not specific to certain diseases,” says Yael Bensoussan, MD, director of the University of South Florida, Tampa’s Health Voice Center and the coprincipal investigator for the National Institutes of Health’s Voice as a Biomarker of Health project.
“We’re learning that there are patterns” in voice changes that can indicate a range of conditions, including diseases of the nervous system and mental illnesses, she says.
Speaking is complicated, involving everything from the lungs and voice box to the mouth and brain. “A breakdown in any of those parts can affect the voice,” says Maria Powell, PhD, an assistant professor of otolaryngology (the study of diseases of the ear and throat) at Vanderbilt University, Nashville, Tenn., who is working on the NIH project.
You or those around you may not notice the changes. But researchers say voice analysis as a standard part of patient care – akin to blood pressure checks or cholesterol tests – could help identify those who need medical attention earlier.
Often, all it takes is a smartphone – “something that’s cheap, off-the-shelf, and that everyone can use,” says Ariana Anderson, PhD, director of the University of California, Los Angeles, Laboratory of Computational Neuropsychology.
“You can provide voice data in your pajamas, on your couch,” says Frank Rudzicz, PhD, a computer scientist for the NIH project. “It doesn’t require very complicated or expensive equipment, and it doesn’t require a lot of expertise to obtain.” Plus, multiple samples can be collected over time, giving a more accurate picture of health than a single snapshot from, say, a cognitive test.
Over the next 4 years, the Voice as a Biomarker team will receive nearly $18 million to gather a massive amount of voice data. The goal is 20,000-30,000 samples, along with health data about each person being studied. The result will be a sprawling database scientists can use to develop algorithms linking health conditions to the way we speak.
For the first 2 years, new data will be collected exclusively via universities and high-volume clinics to control quality and accuracy. Eventually, people will be invited to submit their own voice recordings, creating a crowdsourced dataset. “Google, Alexa, Amazon – they have access to tons of voice data,” says Dr. Bensoussan. “But it’s not usable in a clinical way, because they don’t have the health information.”
Dr. Bensoussan and her colleagues hope to fill that void with advance voice screening apps, which could prove especially valuable in remote communities that lack access to specialists or as a tool for telemedicine. Down the line, wearable devices with voice analysis could alert people with chronic conditions when they need to see a doctor.
“The watch says, ‘I’ve analyzed your breathing and coughing, and today, you’re really not doing well. You should go to the hospital,’ ” says Dr. Bensoussan, envisioning a wearable for patients with COPD. “It could tell people early that things are declining.”
Artificial intelligence may be better than a brain at pinpointing the right disease. For example, slurred speech could indicate Parkinson’s, a stroke, or ALS, among other things.
“We can hold approximately seven pieces of information in our head at one time,” says Dr. Rudzicz. “It’s really hard for us to get a holistic picture using dozens or hundreds of variables at once.” But a computer can consider a whole range of vocal markers at the same time, piecing them together for a more accurate assessment.
“The goal is not to outperform a ... clinician,” says Dr. Bensoussan. Yet the potential is unmistakably there: In a recent study of patients with cancer of the larynx, an automated voice analysis tool more accurately flagged the disease than laryngologists did.
“Algorithms have a larger training base,” says Dr. Anderson, who developed an app called ChatterBaby that analyzes infant cries. “We have a million samples at our disposal to train our algorithms. I don’t know if I’ve heard a million different babies crying in my life.”
So which health conditions show the most promise for voice analysis? The Voice as a Biomarker project will focus on five categories.
Voice disorders (cancers of the larynx, vocal fold paralysis, benign lesions on the larynx)
Obviously, vocal changes are a hallmark of these conditions, which cause things like breathiness or “roughness,” a type of vocal irregularity. Hoarseness that lasts at least 2 weeks is often one of the earliest signs of laryngeal cancer. Yet it can take months – one study found 16 weeks was the average – for patients to see a doctor after noticing the changes. Even then, laryngologists still misdiagnosed some cases of cancer when relying on vocal cues alone.
Now imagine a different scenario: The patient speaks into a smartphone app. An algorithm compares the vocal sample with the voices of laryngeal cancer patients. The app spits out the estimated odds of laryngeal cancer, helping providers decide whether to offer the patient specialist care.
Or consider spasmodic dysphonia, a neurological voice disorder that triggers spasms in the muscles of the voice box, causing a strained or breathy voice. Doctors who lack experience with vocal disorders may miss the condition. This is why diagnosis takes an average of nearly 4.5 years, according to a study in the Journal of Voice, and may include everything from allergy testing to psychiatric evaluation, says Dr. Powell. Artificial intelligence technology trained to recognize the disorder could help eliminate such unnecessary testing.
Neurological and neurodegenerative disorders (Alzheimer’s, Parkinson’s, stroke, ALS)
For Alzheimer’s and Parkinson’s, “one of the first changes that’s notable is voice,” usually appearing before a formal diagnosis, says Anais Rameau, MD, an assistant professor of laryngology at Weill Cornell Medicine, New York, and another member of the NIH project. Parkinson’s may soften the voice or make it sound monotone, while Alzheimer’s disease may change the content of speech, leading to an uptick in “umms” and a preference for pronouns over nouns.
With Parkinson’s, vocal changes can occur decades before movement is affected. If doctors could detect the disease at this stage, before tremor emerged, they might be able to flag patients for early intervention, says Max Little, PhD, project director for the Parkinson’s Voice Initiative. “That is the ‘holy grail’ for finding an eventual cure.”
Again, the smartphone shows potential. In a 2022 Australian study, an AI-powered app was able to identify people with Parkinson’s based on brief voice recordings, although the sample size was small. On a larger scale, the Parkinson’s Voice Initiative collected some 17,000 samples from people across the world. “The aim was to remotely detect those with the condition using a telephone call,” says Dr. Little. It did so with about 65% accuracy. “While this is not accurate enough for clinical use, it shows the potential of the idea,” he says.
Dr. Rudzicz worked on the team behind Winterlight, an iPad app that analyzes 550 features of speech to detect dementia and Alzheimer’s (as well as mental illness). “We deployed it in long-term care facilities,” he says, identifying patients who need further review of their mental skills. Stroke is another area of interest, because slurred speech is a highly subjective measure, says Dr. Anderson. AI technology could provide a more objective evaluation.
Mood and psychiatric disorders (depression, schizophrenia, bipolar disorders)
No established biomarkers exist for diagnosing depression. Yet if you’re feeling down, there’s a good chance your friends can tell – even over the phone.
“We carry a lot of our mood in our voice,” says Dr. Powell. Bipolar disorder can also alter voice, making it louder and faster during manic periods, then slower and quieter during depressive bouts. The catatonic stage of schizophrenia often comes with “a very monotone, robotic voice,” says Dr. Anderson. “These are all something an algorithm can measure.”
Apps are already being used – often in research settings – to monitor voices during phone calls, analyzing rate, rhythm, volume, and pitch, to predict mood changes. For example, the PRIORI project at the University of Michigan is working on a smartphone app to identify mood changes in people with bipolar disorder, especially shifts that could increase suicide risk.
The content of speech may also offer clues. In a University of California, Los Angeles, study published in the journal PLoS One, people with mental illnesses answered computer-programmed questions (like “How have you been over the past few days?”) over the phone. An app analyzed their word choices, paying attention to how they changed over time. The researchers found that AI analysis of mood aligned well with doctors’ assessments and that some people in the study actually felt more comfortable talking to a computer.
Respiratory disorders (pneumonia, COPD)
Beyond talking, respiratory sounds like gasping or coughing may point to specific conditions. “Emphysema cough is different, COPD cough is different,” says Dr. Bensoussan. Researchers are trying to find out if COVID-19 has a distinct cough.
Breathing sounds can also serve as signposts. “There are different sounds when we can’t breathe,” says Dr. Bensoussan. One is called stridor, a high-pitched wheezing often resulting from a blocked airway. “I see tons of people [with stridor] misdiagnosed for years – they’ve been told they have asthma, but they don’t,” says Dr. Bensoussan. AI analysis of these sounds could help doctors more quickly identify respiratory disorders.
Pediatric voice and speech disorders (speech and language delays, autism)
Babies who later have autism cry differently as early as 6 months of age, which means an app like ChatterBaby could help flag children for early intervention, says Dr. Anderson. Autism is linked to several other diagnoses, such as epilepsy and sleep disorders. So analyzing an infant’s cry could prompt pediatricians to screen for a range of conditions.
ChatterBaby has been “incredibly accurate” in identifying when babies are in pain, says Dr. Anderson, because pain increases muscle tension, resulting in a louder, more energetic cry. The next goal: “We’re collecting voices from babies around the world,” she says, and then tracking those children for 7 years, looking to see if early vocal signs could predict developmental disorders. Vocal samples from young children could serve a similar purpose.
And that’s only the beginning
Eventually, AI technology may pick up disease-related voice changes that we can’t even hear. In a new Mayo Clinic study, certain vocal features detectable by AI – but not by the human ear – were linked to a three-fold increase in the likelihood of having plaque buildup in the arteries.
“Voice is a huge spectrum of vibrations,” explains study author Amir Lerman, MD. “We hear a very narrow range.”
The researchers aren’t sure why heart disease alters voice, but the autonomic nervous system may play a role, because it regulates the voice box as well as blood pressure and heart rate. Dr. Lerman says other conditions, like diseases of the nerves and gut, may similarly alter the voice. Beyond patient screening, this discovery could help doctors adjust medication doses remotely, in line with these inaudible vocal signals.
“Hopefully, in the next few years, this is going to come to practice,” says Dr. Lerman.
Still, in the face of that hope, privacy concerns remain. Voice is an identifier that’s protected by the federal Health Insurance Portability and Accountability Act, which requires privacy of personal health information. That is a major reason why no large voice databases exist yet, says Dr. Bensoussan. (This makes collecting samples from children especially challenging.) Perhaps more concerning is the potential for diagnosing disease based on voice alone. “You could use that tool on anyone, including officials like the president,” says Dr. Rameau.
But the primary hurdle is the ethical sourcing of data to ensure a diversity of vocal samples. For the Voice as a Biomarker project, the researchers will establish voice quotas for different races and ethnicities, ensuring algorithms can accurately analyze a range of accents. Data from people with speech impediments will also be gathered.
Despite these challenges, researchers are optimistic. “Vocal analysis is going to be a great equalizer and improve health outcomes,” predicts Dr. Anderson. “I’m really happy that we are beginning to understand the strength of the voice.”
A version of this article first appeared on WebMD.com.
: First during puberty, as the vocal cords thicken and the voice box migrates down the throat. Then a second time as aging causes structural changes that may weaken the voice.
But for some of us, there’s another voice shift, when a disease begins or when our mental health declines.
This is why more doctors are looking into voice as a biomarker – something that tells you that a disease is present.
Vital signs like blood pressure or heart rate “can give a general idea of how sick we are. But they’re not specific to certain diseases,” says Yael Bensoussan, MD, director of the University of South Florida, Tampa’s Health Voice Center and the coprincipal investigator for the National Institutes of Health’s Voice as a Biomarker of Health project.
“We’re learning that there are patterns” in voice changes that can indicate a range of conditions, including diseases of the nervous system and mental illnesses, she says.
Speaking is complicated, involving everything from the lungs and voice box to the mouth and brain. “A breakdown in any of those parts can affect the voice,” says Maria Powell, PhD, an assistant professor of otolaryngology (the study of diseases of the ear and throat) at Vanderbilt University, Nashville, Tenn., who is working on the NIH project.
You or those around you may not notice the changes. But researchers say voice analysis as a standard part of patient care – akin to blood pressure checks or cholesterol tests – could help identify those who need medical attention earlier.
Often, all it takes is a smartphone – “something that’s cheap, off-the-shelf, and that everyone can use,” says Ariana Anderson, PhD, director of the University of California, Los Angeles, Laboratory of Computational Neuropsychology.
“You can provide voice data in your pajamas, on your couch,” says Frank Rudzicz, PhD, a computer scientist for the NIH project. “It doesn’t require very complicated or expensive equipment, and it doesn’t require a lot of expertise to obtain.” Plus, multiple samples can be collected over time, giving a more accurate picture of health than a single snapshot from, say, a cognitive test.
Over the next 4 years, the Voice as a Biomarker team will receive nearly $18 million to gather a massive amount of voice data. The goal is 20,000-30,000 samples, along with health data about each person being studied. The result will be a sprawling database scientists can use to develop algorithms linking health conditions to the way we speak.
For the first 2 years, new data will be collected exclusively via universities and high-volume clinics to control quality and accuracy. Eventually, people will be invited to submit their own voice recordings, creating a crowdsourced dataset. “Google, Alexa, Amazon – they have access to tons of voice data,” says Dr. Bensoussan. “But it’s not usable in a clinical way, because they don’t have the health information.”
Dr. Bensoussan and her colleagues hope to fill that void with advance voice screening apps, which could prove especially valuable in remote communities that lack access to specialists or as a tool for telemedicine. Down the line, wearable devices with voice analysis could alert people with chronic conditions when they need to see a doctor.
“The watch says, ‘I’ve analyzed your breathing and coughing, and today, you’re really not doing well. You should go to the hospital,’ ” says Dr. Bensoussan, envisioning a wearable for patients with COPD. “It could tell people early that things are declining.”
Artificial intelligence may be better than a brain at pinpointing the right disease. For example, slurred speech could indicate Parkinson’s, a stroke, or ALS, among other things.
“We can hold approximately seven pieces of information in our head at one time,” says Dr. Rudzicz. “It’s really hard for us to get a holistic picture using dozens or hundreds of variables at once.” But a computer can consider a whole range of vocal markers at the same time, piecing them together for a more accurate assessment.
“The goal is not to outperform a ... clinician,” says Dr. Bensoussan. Yet the potential is unmistakably there: In a recent study of patients with cancer of the larynx, an automated voice analysis tool more accurately flagged the disease than laryngologists did.
“Algorithms have a larger training base,” says Dr. Anderson, who developed an app called ChatterBaby that analyzes infant cries. “We have a million samples at our disposal to train our algorithms. I don’t know if I’ve heard a million different babies crying in my life.”
So which health conditions show the most promise for voice analysis? The Voice as a Biomarker project will focus on five categories.
Voice disorders (cancers of the larynx, vocal fold paralysis, benign lesions on the larynx)
Obviously, vocal changes are a hallmark of these conditions, which cause things like breathiness or “roughness,” a type of vocal irregularity. Hoarseness that lasts at least 2 weeks is often one of the earliest signs of laryngeal cancer. Yet it can take months – one study found 16 weeks was the average – for patients to see a doctor after noticing the changes. Even then, laryngologists still misdiagnosed some cases of cancer when relying on vocal cues alone.
Now imagine a different scenario: The patient speaks into a smartphone app. An algorithm compares the vocal sample with the voices of laryngeal cancer patients. The app spits out the estimated odds of laryngeal cancer, helping providers decide whether to offer the patient specialist care.
Or consider spasmodic dysphonia, a neurological voice disorder that triggers spasms in the muscles of the voice box, causing a strained or breathy voice. Doctors who lack experience with vocal disorders may miss the condition. This is why diagnosis takes an average of nearly 4.5 years, according to a study in the Journal of Voice, and may include everything from allergy testing to psychiatric evaluation, says Dr. Powell. Artificial intelligence technology trained to recognize the disorder could help eliminate such unnecessary testing.
Neurological and neurodegenerative disorders (Alzheimer’s, Parkinson’s, stroke, ALS)
For Alzheimer’s and Parkinson’s, “one of the first changes that’s notable is voice,” usually appearing before a formal diagnosis, says Anais Rameau, MD, an assistant professor of laryngology at Weill Cornell Medicine, New York, and another member of the NIH project. Parkinson’s may soften the voice or make it sound monotone, while Alzheimer’s disease may change the content of speech, leading to an uptick in “umms” and a preference for pronouns over nouns.
With Parkinson’s, vocal changes can occur decades before movement is affected. If doctors could detect the disease at this stage, before tremor emerged, they might be able to flag patients for early intervention, says Max Little, PhD, project director for the Parkinson’s Voice Initiative. “That is the ‘holy grail’ for finding an eventual cure.”
Again, the smartphone shows potential. In a 2022 Australian study, an AI-powered app was able to identify people with Parkinson’s based on brief voice recordings, although the sample size was small. On a larger scale, the Parkinson’s Voice Initiative collected some 17,000 samples from people across the world. “The aim was to remotely detect those with the condition using a telephone call,” says Dr. Little. It did so with about 65% accuracy. “While this is not accurate enough for clinical use, it shows the potential of the idea,” he says.
Dr. Rudzicz worked on the team behind Winterlight, an iPad app that analyzes 550 features of speech to detect dementia and Alzheimer’s (as well as mental illness). “We deployed it in long-term care facilities,” he says, identifying patients who need further review of their mental skills. Stroke is another area of interest, because slurred speech is a highly subjective measure, says Dr. Anderson. AI technology could provide a more objective evaluation.
Mood and psychiatric disorders (depression, schizophrenia, bipolar disorders)
No established biomarkers exist for diagnosing depression. Yet if you’re feeling down, there’s a good chance your friends can tell – even over the phone.
“We carry a lot of our mood in our voice,” says Dr. Powell. Bipolar disorder can also alter voice, making it louder and faster during manic periods, then slower and quieter during depressive bouts. The catatonic stage of schizophrenia often comes with “a very monotone, robotic voice,” says Dr. Anderson. “These are all something an algorithm can measure.”
Apps are already being used – often in research settings – to monitor voices during phone calls, analyzing rate, rhythm, volume, and pitch, to predict mood changes. For example, the PRIORI project at the University of Michigan is working on a smartphone app to identify mood changes in people with bipolar disorder, especially shifts that could increase suicide risk.
The content of speech may also offer clues. In a University of California, Los Angeles, study published in the journal PLoS One, people with mental illnesses answered computer-programmed questions (like “How have you been over the past few days?”) over the phone. An app analyzed their word choices, paying attention to how they changed over time. The researchers found that AI analysis of mood aligned well with doctors’ assessments and that some people in the study actually felt more comfortable talking to a computer.
Respiratory disorders (pneumonia, COPD)
Beyond talking, respiratory sounds like gasping or coughing may point to specific conditions. “Emphysema cough is different, COPD cough is different,” says Dr. Bensoussan. Researchers are trying to find out if COVID-19 has a distinct cough.
Breathing sounds can also serve as signposts. “There are different sounds when we can’t breathe,” says Dr. Bensoussan. One is called stridor, a high-pitched wheezing often resulting from a blocked airway. “I see tons of people [with stridor] misdiagnosed for years – they’ve been told they have asthma, but they don’t,” says Dr. Bensoussan. AI analysis of these sounds could help doctors more quickly identify respiratory disorders.
Pediatric voice and speech disorders (speech and language delays, autism)
Babies who later have autism cry differently as early as 6 months of age, which means an app like ChatterBaby could help flag children for early intervention, says Dr. Anderson. Autism is linked to several other diagnoses, such as epilepsy and sleep disorders. So analyzing an infant’s cry could prompt pediatricians to screen for a range of conditions.
ChatterBaby has been “incredibly accurate” in identifying when babies are in pain, says Dr. Anderson, because pain increases muscle tension, resulting in a louder, more energetic cry. The next goal: “We’re collecting voices from babies around the world,” she says, and then tracking those children for 7 years, looking to see if early vocal signs could predict developmental disorders. Vocal samples from young children could serve a similar purpose.
And that’s only the beginning
Eventually, AI technology may pick up disease-related voice changes that we can’t even hear. In a new Mayo Clinic study, certain vocal features detectable by AI – but not by the human ear – were linked to a three-fold increase in the likelihood of having plaque buildup in the arteries.
“Voice is a huge spectrum of vibrations,” explains study author Amir Lerman, MD. “We hear a very narrow range.”
The researchers aren’t sure why heart disease alters voice, but the autonomic nervous system may play a role, because it regulates the voice box as well as blood pressure and heart rate. Dr. Lerman says other conditions, like diseases of the nerves and gut, may similarly alter the voice. Beyond patient screening, this discovery could help doctors adjust medication doses remotely, in line with these inaudible vocal signals.
“Hopefully, in the next few years, this is going to come to practice,” says Dr. Lerman.
Still, in the face of that hope, privacy concerns remain. Voice is an identifier that’s protected by the federal Health Insurance Portability and Accountability Act, which requires privacy of personal health information. That is a major reason why no large voice databases exist yet, says Dr. Bensoussan. (This makes collecting samples from children especially challenging.) Perhaps more concerning is the potential for diagnosing disease based on voice alone. “You could use that tool on anyone, including officials like the president,” says Dr. Rameau.
But the primary hurdle is the ethical sourcing of data to ensure a diversity of vocal samples. For the Voice as a Biomarker project, the researchers will establish voice quotas for different races and ethnicities, ensuring algorithms can accurately analyze a range of accents. Data from people with speech impediments will also be gathered.
Despite these challenges, researchers are optimistic. “Vocal analysis is going to be a great equalizer and improve health outcomes,” predicts Dr. Anderson. “I’m really happy that we are beginning to understand the strength of the voice.”
A version of this article first appeared on WebMD.com.
No, you can’t see a different doctor: We need zero tolerance of patient bias
It was 1970. I was in my second year of medical school. I can remember the hurt and embarrassment as if it were yesterday.
Coming from the Deep South, I was very familiar with racial bias, but I did not expect it at that level and in that environment. From that point on, I was anxious at each patient encounter, concerned that this might happen again. And it did several times during my residency and fellowship.
The Occupational Safety and Health Administration defines workplace violence as “any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site. It ranges from threats and verbal abuse to physical assaults.”
There is considerable media focus on incidents of physical violence against health care workers, but when patients, their families, or visitors openly display bias and request a different doctor, nurse, or technician for nonmedical reasons, the impact is profound. This is extremely hurtful to a professional who has worked long and hard to acquire skills and expertise. And, while speech may not constitute violence in the strictest sense of the word, there is growing evidence that it can be physically harmful through its effect on the nervous system, even if no physical contact is involved.
Incidents of bias occur regularly and are clearly on the rise. In most cases the request for a different health care worker is granted to honor the rights of the patient. The healthcare worker is left alone and emotionally wounded; the healthcare institutions are complicit.
This bias is mostly racial but can also be based on religion, sexual orientation, age, disability, body size, accent, or gender.
An entire issue of the American Medical Association Journal of Ethics was devoted to this topic. From recognizing that there are limits to what clinicians should be expected to tolerate when patients’ preferences express unjust bias, the issue also explored where those limits should be placed, why, and who is obliged to enforce them.
The newly adopted Mass General Patient Code of Conduct is evidence that health care systems are beginning to recognize this problem and that such behavior will not be tolerated.
But having a zero-tolerance policy is not enough. We must have procedures in place to discourage and mitigate the impact of patient bias.
A clear definition of what constitutes a bias incident is essential. All team members must be made aware of the procedures for reporting such incidents and the chain of command for escalation. Reporting should be encouraged, and resources must be made available to impacted team members. Surveillance, monitoring, and review are also essential as is clarification on when patient preferences should be honored.
The Mayo Clinic 5 Step Plan is an excellent example of a protocol to deal with patient bias against health care workers and is based on a thoughtful analysis of what constitutes an unreasonable request for a different clinician. I’m pleased to report that my health care system (Inova Health) is developing a similar protocol.
The health care setting should be a bias-free zone for both patients and health care workers. I have been a strong advocate of patients’ rights and worked hard to guard against bias and eliminate disparities in care, but health care workers have rights as well.
We should expect to be treated with respect.
The views expressed by the author are those of the author alone and do not represent the views of the Inova Health System. Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
It was 1970. I was in my second year of medical school. I can remember the hurt and embarrassment as if it were yesterday.
Coming from the Deep South, I was very familiar with racial bias, but I did not expect it at that level and in that environment. From that point on, I was anxious at each patient encounter, concerned that this might happen again. And it did several times during my residency and fellowship.
The Occupational Safety and Health Administration defines workplace violence as “any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site. It ranges from threats and verbal abuse to physical assaults.”
There is considerable media focus on incidents of physical violence against health care workers, but when patients, their families, or visitors openly display bias and request a different doctor, nurse, or technician for nonmedical reasons, the impact is profound. This is extremely hurtful to a professional who has worked long and hard to acquire skills and expertise. And, while speech may not constitute violence in the strictest sense of the word, there is growing evidence that it can be physically harmful through its effect on the nervous system, even if no physical contact is involved.
Incidents of bias occur regularly and are clearly on the rise. In most cases the request for a different health care worker is granted to honor the rights of the patient. The healthcare worker is left alone and emotionally wounded; the healthcare institutions are complicit.
This bias is mostly racial but can also be based on religion, sexual orientation, age, disability, body size, accent, or gender.
An entire issue of the American Medical Association Journal of Ethics was devoted to this topic. From recognizing that there are limits to what clinicians should be expected to tolerate when patients’ preferences express unjust bias, the issue also explored where those limits should be placed, why, and who is obliged to enforce them.
The newly adopted Mass General Patient Code of Conduct is evidence that health care systems are beginning to recognize this problem and that such behavior will not be tolerated.
But having a zero-tolerance policy is not enough. We must have procedures in place to discourage and mitigate the impact of patient bias.
A clear definition of what constitutes a bias incident is essential. All team members must be made aware of the procedures for reporting such incidents and the chain of command for escalation. Reporting should be encouraged, and resources must be made available to impacted team members. Surveillance, monitoring, and review are also essential as is clarification on when patient preferences should be honored.
The Mayo Clinic 5 Step Plan is an excellent example of a protocol to deal with patient bias against health care workers and is based on a thoughtful analysis of what constitutes an unreasonable request for a different clinician. I’m pleased to report that my health care system (Inova Health) is developing a similar protocol.
The health care setting should be a bias-free zone for both patients and health care workers. I have been a strong advocate of patients’ rights and worked hard to guard against bias and eliminate disparities in care, but health care workers have rights as well.
We should expect to be treated with respect.
The views expressed by the author are those of the author alone and do not represent the views of the Inova Health System. Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
It was 1970. I was in my second year of medical school. I can remember the hurt and embarrassment as if it were yesterday.
Coming from the Deep South, I was very familiar with racial bias, but I did not expect it at that level and in that environment. From that point on, I was anxious at each patient encounter, concerned that this might happen again. And it did several times during my residency and fellowship.
The Occupational Safety and Health Administration defines workplace violence as “any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site. It ranges from threats and verbal abuse to physical assaults.”
There is considerable media focus on incidents of physical violence against health care workers, but when patients, their families, or visitors openly display bias and request a different doctor, nurse, or technician for nonmedical reasons, the impact is profound. This is extremely hurtful to a professional who has worked long and hard to acquire skills and expertise. And, while speech may not constitute violence in the strictest sense of the word, there is growing evidence that it can be physically harmful through its effect on the nervous system, even if no physical contact is involved.
Incidents of bias occur regularly and are clearly on the rise. In most cases the request for a different health care worker is granted to honor the rights of the patient. The healthcare worker is left alone and emotionally wounded; the healthcare institutions are complicit.
This bias is mostly racial but can also be based on religion, sexual orientation, age, disability, body size, accent, or gender.
An entire issue of the American Medical Association Journal of Ethics was devoted to this topic. From recognizing that there are limits to what clinicians should be expected to tolerate when patients’ preferences express unjust bias, the issue also explored where those limits should be placed, why, and who is obliged to enforce them.
The newly adopted Mass General Patient Code of Conduct is evidence that health care systems are beginning to recognize this problem and that such behavior will not be tolerated.
But having a zero-tolerance policy is not enough. We must have procedures in place to discourage and mitigate the impact of patient bias.
A clear definition of what constitutes a bias incident is essential. All team members must be made aware of the procedures for reporting such incidents and the chain of command for escalation. Reporting should be encouraged, and resources must be made available to impacted team members. Surveillance, monitoring, and review are also essential as is clarification on when patient preferences should be honored.
The Mayo Clinic 5 Step Plan is an excellent example of a protocol to deal with patient bias against health care workers and is based on a thoughtful analysis of what constitutes an unreasonable request for a different clinician. I’m pleased to report that my health care system (Inova Health) is developing a similar protocol.
The health care setting should be a bias-free zone for both patients and health care workers. I have been a strong advocate of patients’ rights and worked hard to guard against bias and eliminate disparities in care, but health care workers have rights as well.
We should expect to be treated with respect.
The views expressed by the author are those of the author alone and do not represent the views of the Inova Health System. Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
States cracking down harder on docs who sexually abuse patients
It’s the latest example of states taking doctor sexual misconduct more seriously after longstanding criticism that medical boards have been too lenient.
The law, which takes effect in January 2023, requires the state’s medical board to permanently revoke these doctors’ licenses instead of allowing them to petition the board for reinstatement after 3 years.
“Physician licenses should not be reinstated after egregious sexual misconduct with patients. The doctor-patient relationship has to remain sacrosanct and trusted,” said Peter Yellowlees, MD, a professor of psychiatry at the University of California, Davis.
Although the vast majority of the nation’s estimated 1 million doctors don’t sexually abuse patients, the problem is a national one.
The Federation of State Medical Boards defines sexual misconduct as the exploitation of the physician-patient relationship in a sexual way. The exploitation may be verbal or physical and can occur in person or virtually.
The FSMB conducted a 2-year review of how medical boards handled cases of sexual misconduct, issuing a report in 2020 that contained 38 recommended actions.
Four states in addition to California have enacted laws that incorporate some FSMB recommendations. These include revoking doctors’ licenses after a single egregious act of sexual misconduct (including sexual assault), regardless of whether the physician was charged or convicted; increased reporting by hospitals and doctors of sexual misconduct; and training of physicians to recognize and report sexual misconduct.
The four state laws are:
- Georgia’s HB 458. It was signed into law in May 2021, and it authorizes the medical board to revoke or suspend a license if a physician is found guilty of sexually assaulting a patient in a criminal case. Doctors are required to report other doctors who have sexually abused patients and to take continuing medical education (CME) units on sexual misconduct.
- Florida’s SB 1934. This legislation was signed into law in June 2021, and it bars physicians charged with serious crimes such as sexual assault, sexual misconduct against patients, or possession of child pornography from seeing patients until those charges are resolved by the legal system.
- West Virginia’s SB 603. Signed into law in March 2022 it prohibits the medical board from issuing a license to a physician who engaged in sexual activity or misconduct with a patient whose license was revoked in another state or was involved in other violations.
- Tennessee HB 1045. It was signed into law in May 2021, and authorizes the medical board, upon learning of an indictment against a physician for a controlled substance violation or sexual offense, to immediately suspend the doctor’s ability to prescribe controlled substances until the doctor’s case is resolved.
A published study identified a total of 1,721 reports of physician sexual misconduct that were submitted to the National Practitioner Data Bank between 2000 and 2019. The annual incidence of sexual misconduct reports averaged 10.8 per 100,000 U.S. physician licensees, said the researchers.
In a groundbreaking 2016 investigation, the Atlanta Journal-Constitution reviewed thousands of documents and found more than 2,400 doctors whose sexual misconduct cases clearly involved patients since 1999.
Physician sexual misconduct is likely underreported
The actual incidence of physician-patient sexual misconduct is likely higher as a result of underreporting, according to the researchers.
Because a substantial power differential exists between patients and their physicians, the researchers noted, it follows that patient victims, like other sexual assault victims, may be unwilling or unable to report the incident in question.
Many violations involving physician sexual misconduct of patients never came to the attention of state regulators, according to the Journal-Constitution investigation. Reporting showed that hospitals, clinics, and fellow doctors fail to report sexual misconduct to regulators, despite laws in most states requiring them to do so.
Media investigations highlight medical board shortcomings
Public pressure on the California Medical Board increased after the Los Angeles Times investigated what happened to doctors who surrendered or had their licenses revoked after being reported for sexual abuse with patients. The Times revealed in 2021 that the board reinstated 10 of 17 doctors who petitioned for reinstatement.
They include Esmail Nadjmabadi, MD, of Bakersfield, Calif., who had sexually abused six female patients, including one in her mid-teens. The Times reported that, in 2009, he pleaded no contest to a criminal charge that he sexually exploited two or more women and surrendered his medical license the following year.
Five years later, Dr. Nadjmabadi petitioned the medical board to be reinstated and the board approved his request.
The California board has also reinstated several doctors who underwent sex offender rehabilitation. Board members rely heavily on a doctor’s evidence of rehabilitation, usually with the testimony of therapists hired by the doctor, and no input from the patients who were harmed, according to the Times’ investigation.
High-profile sexual misconduct or abuse cases involving Larry Nassar, MD, and Robert Anderson, MD, in Michigan; Richard Strauss, MD, in Ohio; and Ricardo Cruciani, MD, in New York, added to the mounting criticism that medical boards were too lenient in their handling of complaints of sexual misconduct.
Another state tackles sexual misconduct
Ohio’s medical board created an administrative rule stating that licensed physicians have a legal and ethical duty to report colleagues for sexual misconduct with patients and to complete a 1-hour CME training. Failure to report sexual misconduct complaints can lead to a doctor being permanently stripped of his license.
This happened to Robert S. Geiger, MD, in 2016 after not reporting his colleague James Bressi, MD, to the medical board after receiving complaints that Dr. Bressi was sexually abusing female patients at their pain clinic.
Dr. Bressi was convicted of sexual misconduct with a patient, stripped of his medical license, and sentenced to 59 days in prison.
“I think all of these reforms are a step in the right direction and will help to deter doctors from committing sexual misconduct to some extent,” said California activist Marian Hollingsworth, cofounder of the Patient Safety League.
But there’s room for improvement, she said, since “most states fall short in not requiring medical boards to notify law enforcement when they get a complaint of doctor sexual misconduct so the public can be aware of it.”
A version of this article first appeared on Medscape.com.
It’s the latest example of states taking doctor sexual misconduct more seriously after longstanding criticism that medical boards have been too lenient.
The law, which takes effect in January 2023, requires the state’s medical board to permanently revoke these doctors’ licenses instead of allowing them to petition the board for reinstatement after 3 years.
“Physician licenses should not be reinstated after egregious sexual misconduct with patients. The doctor-patient relationship has to remain sacrosanct and trusted,” said Peter Yellowlees, MD, a professor of psychiatry at the University of California, Davis.
Although the vast majority of the nation’s estimated 1 million doctors don’t sexually abuse patients, the problem is a national one.
The Federation of State Medical Boards defines sexual misconduct as the exploitation of the physician-patient relationship in a sexual way. The exploitation may be verbal or physical and can occur in person or virtually.
The FSMB conducted a 2-year review of how medical boards handled cases of sexual misconduct, issuing a report in 2020 that contained 38 recommended actions.
Four states in addition to California have enacted laws that incorporate some FSMB recommendations. These include revoking doctors’ licenses after a single egregious act of sexual misconduct (including sexual assault), regardless of whether the physician was charged or convicted; increased reporting by hospitals and doctors of sexual misconduct; and training of physicians to recognize and report sexual misconduct.
The four state laws are:
- Georgia’s HB 458. It was signed into law in May 2021, and it authorizes the medical board to revoke or suspend a license if a physician is found guilty of sexually assaulting a patient in a criminal case. Doctors are required to report other doctors who have sexually abused patients and to take continuing medical education (CME) units on sexual misconduct.
- Florida’s SB 1934. This legislation was signed into law in June 2021, and it bars physicians charged with serious crimes such as sexual assault, sexual misconduct against patients, or possession of child pornography from seeing patients until those charges are resolved by the legal system.
- West Virginia’s SB 603. Signed into law in March 2022 it prohibits the medical board from issuing a license to a physician who engaged in sexual activity or misconduct with a patient whose license was revoked in another state or was involved in other violations.
- Tennessee HB 1045. It was signed into law in May 2021, and authorizes the medical board, upon learning of an indictment against a physician for a controlled substance violation or sexual offense, to immediately suspend the doctor’s ability to prescribe controlled substances until the doctor’s case is resolved.
A published study identified a total of 1,721 reports of physician sexual misconduct that were submitted to the National Practitioner Data Bank between 2000 and 2019. The annual incidence of sexual misconduct reports averaged 10.8 per 100,000 U.S. physician licensees, said the researchers.
In a groundbreaking 2016 investigation, the Atlanta Journal-Constitution reviewed thousands of documents and found more than 2,400 doctors whose sexual misconduct cases clearly involved patients since 1999.
Physician sexual misconduct is likely underreported
The actual incidence of physician-patient sexual misconduct is likely higher as a result of underreporting, according to the researchers.
Because a substantial power differential exists between patients and their physicians, the researchers noted, it follows that patient victims, like other sexual assault victims, may be unwilling or unable to report the incident in question.
Many violations involving physician sexual misconduct of patients never came to the attention of state regulators, according to the Journal-Constitution investigation. Reporting showed that hospitals, clinics, and fellow doctors fail to report sexual misconduct to regulators, despite laws in most states requiring them to do so.
Media investigations highlight medical board shortcomings
Public pressure on the California Medical Board increased after the Los Angeles Times investigated what happened to doctors who surrendered or had their licenses revoked after being reported for sexual abuse with patients. The Times revealed in 2021 that the board reinstated 10 of 17 doctors who petitioned for reinstatement.
They include Esmail Nadjmabadi, MD, of Bakersfield, Calif., who had sexually abused six female patients, including one in her mid-teens. The Times reported that, in 2009, he pleaded no contest to a criminal charge that he sexually exploited two or more women and surrendered his medical license the following year.
Five years later, Dr. Nadjmabadi petitioned the medical board to be reinstated and the board approved his request.
The California board has also reinstated several doctors who underwent sex offender rehabilitation. Board members rely heavily on a doctor’s evidence of rehabilitation, usually with the testimony of therapists hired by the doctor, and no input from the patients who were harmed, according to the Times’ investigation.
High-profile sexual misconduct or abuse cases involving Larry Nassar, MD, and Robert Anderson, MD, in Michigan; Richard Strauss, MD, in Ohio; and Ricardo Cruciani, MD, in New York, added to the mounting criticism that medical boards were too lenient in their handling of complaints of sexual misconduct.
Another state tackles sexual misconduct
Ohio’s medical board created an administrative rule stating that licensed physicians have a legal and ethical duty to report colleagues for sexual misconduct with patients and to complete a 1-hour CME training. Failure to report sexual misconduct complaints can lead to a doctor being permanently stripped of his license.
This happened to Robert S. Geiger, MD, in 2016 after not reporting his colleague James Bressi, MD, to the medical board after receiving complaints that Dr. Bressi was sexually abusing female patients at their pain clinic.
Dr. Bressi was convicted of sexual misconduct with a patient, stripped of his medical license, and sentenced to 59 days in prison.
“I think all of these reforms are a step in the right direction and will help to deter doctors from committing sexual misconduct to some extent,” said California activist Marian Hollingsworth, cofounder of the Patient Safety League.
But there’s room for improvement, she said, since “most states fall short in not requiring medical boards to notify law enforcement when they get a complaint of doctor sexual misconduct so the public can be aware of it.”
A version of this article first appeared on Medscape.com.
It’s the latest example of states taking doctor sexual misconduct more seriously after longstanding criticism that medical boards have been too lenient.
The law, which takes effect in January 2023, requires the state’s medical board to permanently revoke these doctors’ licenses instead of allowing them to petition the board for reinstatement after 3 years.
“Physician licenses should not be reinstated after egregious sexual misconduct with patients. The doctor-patient relationship has to remain sacrosanct and trusted,” said Peter Yellowlees, MD, a professor of psychiatry at the University of California, Davis.
Although the vast majority of the nation’s estimated 1 million doctors don’t sexually abuse patients, the problem is a national one.
The Federation of State Medical Boards defines sexual misconduct as the exploitation of the physician-patient relationship in a sexual way. The exploitation may be verbal or physical and can occur in person or virtually.
The FSMB conducted a 2-year review of how medical boards handled cases of sexual misconduct, issuing a report in 2020 that contained 38 recommended actions.
Four states in addition to California have enacted laws that incorporate some FSMB recommendations. These include revoking doctors’ licenses after a single egregious act of sexual misconduct (including sexual assault), regardless of whether the physician was charged or convicted; increased reporting by hospitals and doctors of sexual misconduct; and training of physicians to recognize and report sexual misconduct.
The four state laws are:
- Georgia’s HB 458. It was signed into law in May 2021, and it authorizes the medical board to revoke or suspend a license if a physician is found guilty of sexually assaulting a patient in a criminal case. Doctors are required to report other doctors who have sexually abused patients and to take continuing medical education (CME) units on sexual misconduct.
- Florida’s SB 1934. This legislation was signed into law in June 2021, and it bars physicians charged with serious crimes such as sexual assault, sexual misconduct against patients, or possession of child pornography from seeing patients until those charges are resolved by the legal system.
- West Virginia’s SB 603. Signed into law in March 2022 it prohibits the medical board from issuing a license to a physician who engaged in sexual activity or misconduct with a patient whose license was revoked in another state or was involved in other violations.
- Tennessee HB 1045. It was signed into law in May 2021, and authorizes the medical board, upon learning of an indictment against a physician for a controlled substance violation or sexual offense, to immediately suspend the doctor’s ability to prescribe controlled substances until the doctor’s case is resolved.
A published study identified a total of 1,721 reports of physician sexual misconduct that were submitted to the National Practitioner Data Bank between 2000 and 2019. The annual incidence of sexual misconduct reports averaged 10.8 per 100,000 U.S. physician licensees, said the researchers.
In a groundbreaking 2016 investigation, the Atlanta Journal-Constitution reviewed thousands of documents and found more than 2,400 doctors whose sexual misconduct cases clearly involved patients since 1999.
Physician sexual misconduct is likely underreported
The actual incidence of physician-patient sexual misconduct is likely higher as a result of underreporting, according to the researchers.
Because a substantial power differential exists between patients and their physicians, the researchers noted, it follows that patient victims, like other sexual assault victims, may be unwilling or unable to report the incident in question.
Many violations involving physician sexual misconduct of patients never came to the attention of state regulators, according to the Journal-Constitution investigation. Reporting showed that hospitals, clinics, and fellow doctors fail to report sexual misconduct to regulators, despite laws in most states requiring them to do so.
Media investigations highlight medical board shortcomings
Public pressure on the California Medical Board increased after the Los Angeles Times investigated what happened to doctors who surrendered or had their licenses revoked after being reported for sexual abuse with patients. The Times revealed in 2021 that the board reinstated 10 of 17 doctors who petitioned for reinstatement.
They include Esmail Nadjmabadi, MD, of Bakersfield, Calif., who had sexually abused six female patients, including one in her mid-teens. The Times reported that, in 2009, he pleaded no contest to a criminal charge that he sexually exploited two or more women and surrendered his medical license the following year.
Five years later, Dr. Nadjmabadi petitioned the medical board to be reinstated and the board approved his request.
The California board has also reinstated several doctors who underwent sex offender rehabilitation. Board members rely heavily on a doctor’s evidence of rehabilitation, usually with the testimony of therapists hired by the doctor, and no input from the patients who were harmed, according to the Times’ investigation.
High-profile sexual misconduct or abuse cases involving Larry Nassar, MD, and Robert Anderson, MD, in Michigan; Richard Strauss, MD, in Ohio; and Ricardo Cruciani, MD, in New York, added to the mounting criticism that medical boards were too lenient in their handling of complaints of sexual misconduct.
Another state tackles sexual misconduct
Ohio’s medical board created an administrative rule stating that licensed physicians have a legal and ethical duty to report colleagues for sexual misconduct with patients and to complete a 1-hour CME training. Failure to report sexual misconduct complaints can lead to a doctor being permanently stripped of his license.
This happened to Robert S. Geiger, MD, in 2016 after not reporting his colleague James Bressi, MD, to the medical board after receiving complaints that Dr. Bressi was sexually abusing female patients at their pain clinic.
Dr. Bressi was convicted of sexual misconduct with a patient, stripped of his medical license, and sentenced to 59 days in prison.
“I think all of these reforms are a step in the right direction and will help to deter doctors from committing sexual misconduct to some extent,” said California activist Marian Hollingsworth, cofounder of the Patient Safety League.
But there’s room for improvement, she said, since “most states fall short in not requiring medical boards to notify law enforcement when they get a complaint of doctor sexual misconduct so the public can be aware of it.”
A version of this article first appeared on Medscape.com.
Poison centers fielding more calls about teen cannabis use
Poison control centers in the United States now receive more calls about adolescents abusing cannabis than alcohol or any other substance, according to a new study.
Many helpline calls about cannabis involve edible products, the researchers noted.
Over-the-counter medications – especially dextromethorphan-containing cough and cold medications and oral antihistamines, such as Benadryl – are other commonly abused substances.
But cannabis recently started topping the list.
“Since 2018, the most reported misused/abused substance involved exposure to marijuana,” according to the study, which was published online in Clinical Toxicology.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health & Science University, Portland, and colleagues analyzed calls to United States poison control centers between 2000 and 2020. They focused on 338,000 calls about intentional substance abuse or misuse, including for the purpose of getting high, in individuals aged 6-18 years.
The calls were made to 55 certified helplines for health professionals, public health agencies, and members of the public seeking guidance about exposures to various substances.
Cannabis vs. alcohol
In 2000, alcohol was the substance involved in the largest number of cases (1,318, or 9.8% of all calls). Between 2000 and 2013, cases of alcohol abuse exceeded the number of cannabis cases each year.
But that changed in 2014, when cannabis overtook alcohol.
Over the 20-year study period, calls about exposure to cannabis increased 245%, from 510 in 2000 to 1,761 in 2020.
Edibles played a key role.
“Edible marijuana preparations accounted for the highest increase in call rates, compared with all other forms of marijuana,” the researchers reported.
Edible products are “often marketed in ways that are attractive to young people, and they are considered more discrete and convenient,” Dr. Hughes said. But they can have “unpredictable” effects.
“Compared to smoking cannabis, which typically results in an immediate high, intoxication from edible forms usually takes several hours, which may lead some individuals to consume greater amounts and experience unexpected and unpredictable highs,” she said.
For example, prior research has shown that edible cannabis consumption may lead to more acute psychiatric symptoms and cardiovascular events than does inhaled cannabis.
Trends in alcohol use may have held relatively steady, despite some minor declines in the poison center data, Dr. Hughes said.
“Anecdotally, there hasn’t been an obvious notable reduction in alcohol cases in the emergency department,” she said. “However, I wouldn’t expect a huge change given our data only found a slow mild decline in alcohol cases over the study period.”
The increase in cannabis-related calls coincides with more states legalizing or decriminalizing the drug for medical or recreational purposes. Currently, 21 states have approved recreational cannabis for adults who are at least 21 years old.
What are the risks?
Parents typically call a poison center about cannabis exposure after they see or suspect that their child has ingested loose cannabis leaves or edibles containing the substance, Dr. Hughes said.
“The poison center provides guidance to parents about whether or not their child can be watched at home or requires referral to a health care facility,” she said. “While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products.”
Intentional misuse or abuse tends to occur in older children and teens.
Nonprescription drugs have a high potential for abuse because they are legal and may be perceived as safe, Dr. Hughes said.
If a child has a history of misusing or abusing substances or if a parent is worried that their child is at high risk for this behavior, they should consider securing medicines in a lock box, she advised.
That applies to cannabis too.
“I would recommend that parents also consider locking up their cannabis products,” she said.
The National Poison Data System relies on voluntary reporting, and the data are not expected to represent the actual number of intentional misuse and abuse exposures, the researchers noted.
Poison control centers in the United States are available for consultation about patients with known or suspected cannabis ingestion or other suspected poisonings (1-800-222-1222).
The researchers had no disclosures.
A version of this article first appeared on Medscape.com.
Poison control centers in the United States now receive more calls about adolescents abusing cannabis than alcohol or any other substance, according to a new study.
Many helpline calls about cannabis involve edible products, the researchers noted.
Over-the-counter medications – especially dextromethorphan-containing cough and cold medications and oral antihistamines, such as Benadryl – are other commonly abused substances.
But cannabis recently started topping the list.
“Since 2018, the most reported misused/abused substance involved exposure to marijuana,” according to the study, which was published online in Clinical Toxicology.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health & Science University, Portland, and colleagues analyzed calls to United States poison control centers between 2000 and 2020. They focused on 338,000 calls about intentional substance abuse or misuse, including for the purpose of getting high, in individuals aged 6-18 years.
The calls were made to 55 certified helplines for health professionals, public health agencies, and members of the public seeking guidance about exposures to various substances.
Cannabis vs. alcohol
In 2000, alcohol was the substance involved in the largest number of cases (1,318, or 9.8% of all calls). Between 2000 and 2013, cases of alcohol abuse exceeded the number of cannabis cases each year.
But that changed in 2014, when cannabis overtook alcohol.
Over the 20-year study period, calls about exposure to cannabis increased 245%, from 510 in 2000 to 1,761 in 2020.
Edibles played a key role.
“Edible marijuana preparations accounted for the highest increase in call rates, compared with all other forms of marijuana,” the researchers reported.
Edible products are “often marketed in ways that are attractive to young people, and they are considered more discrete and convenient,” Dr. Hughes said. But they can have “unpredictable” effects.
“Compared to smoking cannabis, which typically results in an immediate high, intoxication from edible forms usually takes several hours, which may lead some individuals to consume greater amounts and experience unexpected and unpredictable highs,” she said.
For example, prior research has shown that edible cannabis consumption may lead to more acute psychiatric symptoms and cardiovascular events than does inhaled cannabis.
Trends in alcohol use may have held relatively steady, despite some minor declines in the poison center data, Dr. Hughes said.
“Anecdotally, there hasn’t been an obvious notable reduction in alcohol cases in the emergency department,” she said. “However, I wouldn’t expect a huge change given our data only found a slow mild decline in alcohol cases over the study period.”
The increase in cannabis-related calls coincides with more states legalizing or decriminalizing the drug for medical or recreational purposes. Currently, 21 states have approved recreational cannabis for adults who are at least 21 years old.
What are the risks?
Parents typically call a poison center about cannabis exposure after they see or suspect that their child has ingested loose cannabis leaves or edibles containing the substance, Dr. Hughes said.
“The poison center provides guidance to parents about whether or not their child can be watched at home or requires referral to a health care facility,” she said. “While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products.”
Intentional misuse or abuse tends to occur in older children and teens.
Nonprescription drugs have a high potential for abuse because they are legal and may be perceived as safe, Dr. Hughes said.
If a child has a history of misusing or abusing substances or if a parent is worried that their child is at high risk for this behavior, they should consider securing medicines in a lock box, she advised.
That applies to cannabis too.
“I would recommend that parents also consider locking up their cannabis products,” she said.
The National Poison Data System relies on voluntary reporting, and the data are not expected to represent the actual number of intentional misuse and abuse exposures, the researchers noted.
Poison control centers in the United States are available for consultation about patients with known or suspected cannabis ingestion or other suspected poisonings (1-800-222-1222).
The researchers had no disclosures.
A version of this article first appeared on Medscape.com.
Poison control centers in the United States now receive more calls about adolescents abusing cannabis than alcohol or any other substance, according to a new study.
Many helpline calls about cannabis involve edible products, the researchers noted.
Over-the-counter medications – especially dextromethorphan-containing cough and cold medications and oral antihistamines, such as Benadryl – are other commonly abused substances.
But cannabis recently started topping the list.
“Since 2018, the most reported misused/abused substance involved exposure to marijuana,” according to the study, which was published online in Clinical Toxicology.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health & Science University, Portland, and colleagues analyzed calls to United States poison control centers between 2000 and 2020. They focused on 338,000 calls about intentional substance abuse or misuse, including for the purpose of getting high, in individuals aged 6-18 years.
The calls were made to 55 certified helplines for health professionals, public health agencies, and members of the public seeking guidance about exposures to various substances.
Cannabis vs. alcohol
In 2000, alcohol was the substance involved in the largest number of cases (1,318, or 9.8% of all calls). Between 2000 and 2013, cases of alcohol abuse exceeded the number of cannabis cases each year.
But that changed in 2014, when cannabis overtook alcohol.
Over the 20-year study period, calls about exposure to cannabis increased 245%, from 510 in 2000 to 1,761 in 2020.
Edibles played a key role.
“Edible marijuana preparations accounted for the highest increase in call rates, compared with all other forms of marijuana,” the researchers reported.
Edible products are “often marketed in ways that are attractive to young people, and they are considered more discrete and convenient,” Dr. Hughes said. But they can have “unpredictable” effects.
“Compared to smoking cannabis, which typically results in an immediate high, intoxication from edible forms usually takes several hours, which may lead some individuals to consume greater amounts and experience unexpected and unpredictable highs,” she said.
For example, prior research has shown that edible cannabis consumption may lead to more acute psychiatric symptoms and cardiovascular events than does inhaled cannabis.
Trends in alcohol use may have held relatively steady, despite some minor declines in the poison center data, Dr. Hughes said.
“Anecdotally, there hasn’t been an obvious notable reduction in alcohol cases in the emergency department,” she said. “However, I wouldn’t expect a huge change given our data only found a slow mild decline in alcohol cases over the study period.”
The increase in cannabis-related calls coincides with more states legalizing or decriminalizing the drug for medical or recreational purposes. Currently, 21 states have approved recreational cannabis for adults who are at least 21 years old.
What are the risks?
Parents typically call a poison center about cannabis exposure after they see or suspect that their child has ingested loose cannabis leaves or edibles containing the substance, Dr. Hughes said.
“The poison center provides guidance to parents about whether or not their child can be watched at home or requires referral to a health care facility,” she said. “While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products.”
Intentional misuse or abuse tends to occur in older children and teens.
Nonprescription drugs have a high potential for abuse because they are legal and may be perceived as safe, Dr. Hughes said.
If a child has a history of misusing or abusing substances or if a parent is worried that their child is at high risk for this behavior, they should consider securing medicines in a lock box, she advised.
That applies to cannabis too.
“I would recommend that parents also consider locking up their cannabis products,” she said.
The National Poison Data System relies on voluntary reporting, and the data are not expected to represent the actual number of intentional misuse and abuse exposures, the researchers noted.
Poison control centers in the United States are available for consultation about patients with known or suspected cannabis ingestion or other suspected poisonings (1-800-222-1222).
The researchers had no disclosures.
A version of this article first appeared on Medscape.com.