User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
‘Defending Jacob’ and defending psychiatry
The 2012 crime fiction novel, “Defending Jacob,” by William Landay was dramatized into a miniseries created by Mark Bomback that premiered on April 24, 2020, on Apple TV+ (and for those resisting a subscription, “The Morning Show” and “Defending Jacob” are both worth it). Both the “Defending Jacob” novel and the miniseries have themes that are of interest to psychiatry, especially to child and forensic psychiatrists, and both the literary and TV versions are excellent, albeit disturbing, diversions from the current pandemic.
(Spoiler alert!) The story is set in the affluent town of Newton, Mass., where crime is generally low and homicides extremely infrequent. Protagonist Andy Barber, a 51-year-old Jewish assistant district attorney, is played by a younger Chris Evans in the miniseries. His wife, Laurie Gold Barber, a 51-year-old Jewish former schoolteacher and stay-at-home mom, is played by a younger Michelle Dockery of Downton Abbey fame. In the miniseries, her character is actively working as a teacher and social activist for children. Other differences between the novel and the miniseries will be pointed out when relevant, but the overall narrative is similar. Both stories are cleverly told through Andy Barber speaking in retrospect as he is being questioned in front of a grand jury for a potential indictment.
When 14-year-old Ben Rifkin is found stabbed to death in Cold Spring Park before school one morning, Andy Barber initially takes the case despite his boss’s reservations that there may be a conflict because Andy’s son Jacob is a student in Ben’s class at school. As the title suggests, it soon becomes clear that Jacob may have had something to do with the murder. At that point, Andy is taken off the case and it is given to a junior colleague, Neal Logiudice, who demonstrates both admiration and contempt for his former mentor, perhaps because of underlying jealousy and insecurity. Neal Logiudice becomes the DA questioning Andy Barber.
Prior to Jacob’s formal accusation of murder, the Barbers appear to be fiercely loyal and unable to fully see and understand their son. The difficulty with objectivity and the reasons why family member physicians should never treat family members – and why family member attorneys should never represent loved ones – is abundantly clear in this story. When Andy receives an anonymous tip that Jacob’s childhood best friend, Derek Yoo, posted on Facebook, “Jake, everyone knows you did it. You have a knife. I’ve seen it,’ ” Andy then looks through Jacob’s drawers and finds a folding knife in one of his T-shirts. In the chapter aptly titled “Denial,” Andy, an experienced prosecutor, does not turn the knife over as evidence, but instead disposes of it – believing Jacob that he did not take the knife to school the day his classmate was stabbed.
After Jacob is indicted, Andy Barber confesses to his wife, Laurie, that his estranged father who left when he was 6 is actually in prison convicted of murdering and raping a woman. In the novel, his grandfather and great-grandfather are also convicted felons. Laurie reveals this family history to Jacob’s attorney, and the attorney subsequently refers the family to a forensic psychologist. In the novel, she is a large Jewish woman; in the miniseries she is played by a very thin Poorna Jagannathan (who incidentally has portrayed a therapist in the television series “Sorry for your Loss,” and a doctor in “The Act,” “Better Call Saul,” “NCIS: Los Angeles,” “House of Cards,” “The Game,” “Law and Order: Criminal Intent,” “Rescue Me,” “Jonny Zero,” “An Actor Prepares,” “The Circle,” “Thanks for Sharing,” and “Montclair.”) Although the goal of the defense was a finding of “not guilty,” a psychiatric defense was going to be used as a last resort if necessary.
Laurie had already googled and learned of “the murder gene,” which was further explained by the forensic psychologist as a mutation called:
“MAOA Knockout. It has been argued in court as a trigger for violence before, but the argument was too simplistic, and it was rejected. Our understanding of the gene-environment interplay has improved since then – the science is getting better and very quickly – and we may have better testimony now. The second mutation is located in what’s called the serotonin transporter gene. The official name for the gene is SLC6A4. It’s located on chromosome 17. It encodes a protein that facilitates the activity of the serotonin transporter system, which is what enables the reuptake of serotonin from the synapse back into the neuron.”1
She further explains that there have been many studies on the “nurture” side of the nature/nurture question and that, with new developments in DNA studies, it is now becoming possible to study the “nature” side.
“Defending Jacob” explores the nature/nurture issue, as well as issues with forensic testimony in court and the criminal justice system in general. The issue of repressing feelings and hiding secrets and then having to confront both in a brutal manner is another theme addressed in the story. Andy tried to hide and forget that his father was in prison and the criminal history in his family, but he was forced to face this and his feelings about it when confronted with his own son being accused of murder. Of note, he does not seek help from a therapist despite these life-altering events. (Humongous spoiler alert:) The story that began with a murder of an unrelated child may end with a family murder, one that would be well described and could be understood by psychiatrists using the categories of motives initially described by Phillip Resnick, MD.2
Once again, and unfortunately, as we have pointed out in other media reviews, the portrayal of psychiatric/psychological themes is problematic. Using a psychologist to explain the science of DNA and not a psychiatrist is an interesting choice. Diagnosing a 14-year-old with personality disorders also contributes to misunderstanding and stigma. In addition, no timely attempt is made to refer the accused Jacob for mental health treatment. The stigmatization of psychiatry in the media was addressed by the World Psychiatric Association task force guidance on how to combat stigmatization of psychiatry and psychiatrists,3 including breaking down negative views of psychiatrists and psychiatry in the general public, among medical students, other health professionals, and patients and relatives. The task force made recommendations for national psychiatric societies and for individual practitioners to help reduce stigma of the profession of psychiatry. We would argue that speaking to the media, including fiction authors, to help educate about mental health is an important role for psychiatrists. It would lead to more realistic portrayals in film and books.
Overall, “Defending Jacob” is a compelling story in both the novel and the miniseries. Despite some problems with how it depicts mental health issues, both are engaging and contain thoughtful, extremely well-written themes of interest to many clinical and forensic psychiatrists.
References
1. Landay W. Defending Jacob, a novel. New York: Delacorte Press, 2012.
2. Friedman SH. Family Murder: Pathologies of Love and Hate. Washington: American Psychiatric Association Publishing, 2019.
3. Sartorius N et al. World Psychiatry. 2010 Oct;9(3):131-44.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and on the faculty at Weill Cornell Medical Center. Dr. Hatters Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Association Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law and was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association.
The 2012 crime fiction novel, “Defending Jacob,” by William Landay was dramatized into a miniseries created by Mark Bomback that premiered on April 24, 2020, on Apple TV+ (and for those resisting a subscription, “The Morning Show” and “Defending Jacob” are both worth it). Both the “Defending Jacob” novel and the miniseries have themes that are of interest to psychiatry, especially to child and forensic psychiatrists, and both the literary and TV versions are excellent, albeit disturbing, diversions from the current pandemic.
(Spoiler alert!) The story is set in the affluent town of Newton, Mass., where crime is generally low and homicides extremely infrequent. Protagonist Andy Barber, a 51-year-old Jewish assistant district attorney, is played by a younger Chris Evans in the miniseries. His wife, Laurie Gold Barber, a 51-year-old Jewish former schoolteacher and stay-at-home mom, is played by a younger Michelle Dockery of Downton Abbey fame. In the miniseries, her character is actively working as a teacher and social activist for children. Other differences between the novel and the miniseries will be pointed out when relevant, but the overall narrative is similar. Both stories are cleverly told through Andy Barber speaking in retrospect as he is being questioned in front of a grand jury for a potential indictment.
When 14-year-old Ben Rifkin is found stabbed to death in Cold Spring Park before school one morning, Andy Barber initially takes the case despite his boss’s reservations that there may be a conflict because Andy’s son Jacob is a student in Ben’s class at school. As the title suggests, it soon becomes clear that Jacob may have had something to do with the murder. At that point, Andy is taken off the case and it is given to a junior colleague, Neal Logiudice, who demonstrates both admiration and contempt for his former mentor, perhaps because of underlying jealousy and insecurity. Neal Logiudice becomes the DA questioning Andy Barber.
Prior to Jacob’s formal accusation of murder, the Barbers appear to be fiercely loyal and unable to fully see and understand their son. The difficulty with objectivity and the reasons why family member physicians should never treat family members – and why family member attorneys should never represent loved ones – is abundantly clear in this story. When Andy receives an anonymous tip that Jacob’s childhood best friend, Derek Yoo, posted on Facebook, “Jake, everyone knows you did it. You have a knife. I’ve seen it,’ ” Andy then looks through Jacob’s drawers and finds a folding knife in one of his T-shirts. In the chapter aptly titled “Denial,” Andy, an experienced prosecutor, does not turn the knife over as evidence, but instead disposes of it – believing Jacob that he did not take the knife to school the day his classmate was stabbed.
After Jacob is indicted, Andy Barber confesses to his wife, Laurie, that his estranged father who left when he was 6 is actually in prison convicted of murdering and raping a woman. In the novel, his grandfather and great-grandfather are also convicted felons. Laurie reveals this family history to Jacob’s attorney, and the attorney subsequently refers the family to a forensic psychologist. In the novel, she is a large Jewish woman; in the miniseries she is played by a very thin Poorna Jagannathan (who incidentally has portrayed a therapist in the television series “Sorry for your Loss,” and a doctor in “The Act,” “Better Call Saul,” “NCIS: Los Angeles,” “House of Cards,” “The Game,” “Law and Order: Criminal Intent,” “Rescue Me,” “Jonny Zero,” “An Actor Prepares,” “The Circle,” “Thanks for Sharing,” and “Montclair.”) Although the goal of the defense was a finding of “not guilty,” a psychiatric defense was going to be used as a last resort if necessary.
Laurie had already googled and learned of “the murder gene,” which was further explained by the forensic psychologist as a mutation called:
“MAOA Knockout. It has been argued in court as a trigger for violence before, but the argument was too simplistic, and it was rejected. Our understanding of the gene-environment interplay has improved since then – the science is getting better and very quickly – and we may have better testimony now. The second mutation is located in what’s called the serotonin transporter gene. The official name for the gene is SLC6A4. It’s located on chromosome 17. It encodes a protein that facilitates the activity of the serotonin transporter system, which is what enables the reuptake of serotonin from the synapse back into the neuron.”1
She further explains that there have been many studies on the “nurture” side of the nature/nurture question and that, with new developments in DNA studies, it is now becoming possible to study the “nature” side.
“Defending Jacob” explores the nature/nurture issue, as well as issues with forensic testimony in court and the criminal justice system in general. The issue of repressing feelings and hiding secrets and then having to confront both in a brutal manner is another theme addressed in the story. Andy tried to hide and forget that his father was in prison and the criminal history in his family, but he was forced to face this and his feelings about it when confronted with his own son being accused of murder. Of note, he does not seek help from a therapist despite these life-altering events. (Humongous spoiler alert:) The story that began with a murder of an unrelated child may end with a family murder, one that would be well described and could be understood by psychiatrists using the categories of motives initially described by Phillip Resnick, MD.2
Once again, and unfortunately, as we have pointed out in other media reviews, the portrayal of psychiatric/psychological themes is problematic. Using a psychologist to explain the science of DNA and not a psychiatrist is an interesting choice. Diagnosing a 14-year-old with personality disorders also contributes to misunderstanding and stigma. In addition, no timely attempt is made to refer the accused Jacob for mental health treatment. The stigmatization of psychiatry in the media was addressed by the World Psychiatric Association task force guidance on how to combat stigmatization of psychiatry and psychiatrists,3 including breaking down negative views of psychiatrists and psychiatry in the general public, among medical students, other health professionals, and patients and relatives. The task force made recommendations for national psychiatric societies and for individual practitioners to help reduce stigma of the profession of psychiatry. We would argue that speaking to the media, including fiction authors, to help educate about mental health is an important role for psychiatrists. It would lead to more realistic portrayals in film and books.
Overall, “Defending Jacob” is a compelling story in both the novel and the miniseries. Despite some problems with how it depicts mental health issues, both are engaging and contain thoughtful, extremely well-written themes of interest to many clinical and forensic psychiatrists.
References
1. Landay W. Defending Jacob, a novel. New York: Delacorte Press, 2012.
2. Friedman SH. Family Murder: Pathologies of Love and Hate. Washington: American Psychiatric Association Publishing, 2019.
3. Sartorius N et al. World Psychiatry. 2010 Oct;9(3):131-44.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and on the faculty at Weill Cornell Medical Center. Dr. Hatters Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Association Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law and was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association.
The 2012 crime fiction novel, “Defending Jacob,” by William Landay was dramatized into a miniseries created by Mark Bomback that premiered on April 24, 2020, on Apple TV+ (and for those resisting a subscription, “The Morning Show” and “Defending Jacob” are both worth it). Both the “Defending Jacob” novel and the miniseries have themes that are of interest to psychiatry, especially to child and forensic psychiatrists, and both the literary and TV versions are excellent, albeit disturbing, diversions from the current pandemic.
(Spoiler alert!) The story is set in the affluent town of Newton, Mass., where crime is generally low and homicides extremely infrequent. Protagonist Andy Barber, a 51-year-old Jewish assistant district attorney, is played by a younger Chris Evans in the miniseries. His wife, Laurie Gold Barber, a 51-year-old Jewish former schoolteacher and stay-at-home mom, is played by a younger Michelle Dockery of Downton Abbey fame. In the miniseries, her character is actively working as a teacher and social activist for children. Other differences between the novel and the miniseries will be pointed out when relevant, but the overall narrative is similar. Both stories are cleverly told through Andy Barber speaking in retrospect as he is being questioned in front of a grand jury for a potential indictment.
When 14-year-old Ben Rifkin is found stabbed to death in Cold Spring Park before school one morning, Andy Barber initially takes the case despite his boss’s reservations that there may be a conflict because Andy’s son Jacob is a student in Ben’s class at school. As the title suggests, it soon becomes clear that Jacob may have had something to do with the murder. At that point, Andy is taken off the case and it is given to a junior colleague, Neal Logiudice, who demonstrates both admiration and contempt for his former mentor, perhaps because of underlying jealousy and insecurity. Neal Logiudice becomes the DA questioning Andy Barber.
Prior to Jacob’s formal accusation of murder, the Barbers appear to be fiercely loyal and unable to fully see and understand their son. The difficulty with objectivity and the reasons why family member physicians should never treat family members – and why family member attorneys should never represent loved ones – is abundantly clear in this story. When Andy receives an anonymous tip that Jacob’s childhood best friend, Derek Yoo, posted on Facebook, “Jake, everyone knows you did it. You have a knife. I’ve seen it,’ ” Andy then looks through Jacob’s drawers and finds a folding knife in one of his T-shirts. In the chapter aptly titled “Denial,” Andy, an experienced prosecutor, does not turn the knife over as evidence, but instead disposes of it – believing Jacob that he did not take the knife to school the day his classmate was stabbed.
After Jacob is indicted, Andy Barber confesses to his wife, Laurie, that his estranged father who left when he was 6 is actually in prison convicted of murdering and raping a woman. In the novel, his grandfather and great-grandfather are also convicted felons. Laurie reveals this family history to Jacob’s attorney, and the attorney subsequently refers the family to a forensic psychologist. In the novel, she is a large Jewish woman; in the miniseries she is played by a very thin Poorna Jagannathan (who incidentally has portrayed a therapist in the television series “Sorry for your Loss,” and a doctor in “The Act,” “Better Call Saul,” “NCIS: Los Angeles,” “House of Cards,” “The Game,” “Law and Order: Criminal Intent,” “Rescue Me,” “Jonny Zero,” “An Actor Prepares,” “The Circle,” “Thanks for Sharing,” and “Montclair.”) Although the goal of the defense was a finding of “not guilty,” a psychiatric defense was going to be used as a last resort if necessary.
Laurie had already googled and learned of “the murder gene,” which was further explained by the forensic psychologist as a mutation called:
“MAOA Knockout. It has been argued in court as a trigger for violence before, but the argument was too simplistic, and it was rejected. Our understanding of the gene-environment interplay has improved since then – the science is getting better and very quickly – and we may have better testimony now. The second mutation is located in what’s called the serotonin transporter gene. The official name for the gene is SLC6A4. It’s located on chromosome 17. It encodes a protein that facilitates the activity of the serotonin transporter system, which is what enables the reuptake of serotonin from the synapse back into the neuron.”1
She further explains that there have been many studies on the “nurture” side of the nature/nurture question and that, with new developments in DNA studies, it is now becoming possible to study the “nature” side.
“Defending Jacob” explores the nature/nurture issue, as well as issues with forensic testimony in court and the criminal justice system in general. The issue of repressing feelings and hiding secrets and then having to confront both in a brutal manner is another theme addressed in the story. Andy tried to hide and forget that his father was in prison and the criminal history in his family, but he was forced to face this and his feelings about it when confronted with his own son being accused of murder. Of note, he does not seek help from a therapist despite these life-altering events. (Humongous spoiler alert:) The story that began with a murder of an unrelated child may end with a family murder, one that would be well described and could be understood by psychiatrists using the categories of motives initially described by Phillip Resnick, MD.2
Once again, and unfortunately, as we have pointed out in other media reviews, the portrayal of psychiatric/psychological themes is problematic. Using a psychologist to explain the science of DNA and not a psychiatrist is an interesting choice. Diagnosing a 14-year-old with personality disorders also contributes to misunderstanding and stigma. In addition, no timely attempt is made to refer the accused Jacob for mental health treatment. The stigmatization of psychiatry in the media was addressed by the World Psychiatric Association task force guidance on how to combat stigmatization of psychiatry and psychiatrists,3 including breaking down negative views of psychiatrists and psychiatry in the general public, among medical students, other health professionals, and patients and relatives. The task force made recommendations for national psychiatric societies and for individual practitioners to help reduce stigma of the profession of psychiatry. We would argue that speaking to the media, including fiction authors, to help educate about mental health is an important role for psychiatrists. It would lead to more realistic portrayals in film and books.
Overall, “Defending Jacob” is a compelling story in both the novel and the miniseries. Despite some problems with how it depicts mental health issues, both are engaging and contain thoughtful, extremely well-written themes of interest to many clinical and forensic psychiatrists.
References
1. Landay W. Defending Jacob, a novel. New York: Delacorte Press, 2012.
2. Friedman SH. Family Murder: Pathologies of Love and Hate. Washington: American Psychiatric Association Publishing, 2019.
3. Sartorius N et al. World Psychiatry. 2010 Oct;9(3):131-44.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and on the faculty at Weill Cornell Medical Center. Dr. Hatters Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Association Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law and was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association.
Lenalidomide may be an answer for refractory cutaneous lupus
Cutaneous lupus erythematosus (CLE) is present in 25% of patients with systemic lupus at the time of diagnosis, but it can also occur in up to 85% of cases at some point in their disease course, Eveline Y. Wu, MD, said during the virtual annual meeting of the Society for Pediatric Dermatology.
“CLE can also occur without any systemic disease,” said Dr. Wu, associate professor of pediatrics at the University of North Carolina at Chapel Hill. “It’s been shown that the risk of developing systemic lupus differs according to the type of skin involvement, meaning that cutaneous lupus can be classified into acute, subacute, chronic, and intermittent forms.”
Malar rash is the prototypical acute cutaneous lesion and is associated with active systemic lupus erythematosus (SLE) and anti–double stranded DNA antibody positivity, while discoid lupus erythematosus is the most common chronic lesion. “A small percentage of patients with discoid lupus can develop systemic lupus, particularly when the lesions are more disseminated,” said Dr. Wu, who specializes in pediatric rheumatology as well as allergy and immunology.
In the American College of Rheumatology’s 1997 classification system, mucocutaneous manifestations constitute 4 out of the 11 criteria that clinicians use to make a diagnosis of SLE: malar rash, discoid-lupus rash, photosensitivity, and oral or nasal mucocutaneous ulcerations. Dr. Wu recommends performing an oral exam on suspect cases, “because the oral ulcers that we see in systemic lupus tend to be painless, so oftentimes patients don’t realize they have them.”
Five other organ-specific manifestations of SLE include nonerosive arthritis, nephritis, encephalopathy, pleuritis or pericarditis, and cytopenia. The two other criteria are positive immunoserology and a positive antinuclear antibody test. “If you have any individuals present with one of these [mucocutaneous manifestations criteria], you want to think about getting a CBC to look for cytopenia or a urinalysis to look for evidence of nephritis, and potentially some additional blood studies, depending on your level of suspicion for systemic lupus,” Dr. Wu said.
Other rarer CLE manifestations include lupus pernio or chilblains, lupus panniculitis, livedo reticularis, bullous LE, urticarial vasculitis, neutrophilic dermatoses, and alopecia.
Common treatments for cutaneous manifestations associated pediatric SLE include hydroxychloroquine, low dose corticosteroids, topical steroids, methotrexate, and leflunomide. Other options for increasing severity of systemic disease include lenalidomide/thalidomide, azathioprine, calcineurin inhibitors, belimumab (Benlysta), high-dose corticosteroids, mycophenolate mofetil (CellCept), rituximab (Rituxan), and cyclophosphamide. Cutaneous manifestations of pediatric SLE can often be refractory to treatments.
In 2017, Dr. Wu and associates published a retrospective chart review of 10 adolescents who received lenalidomide for refractory CLE. One of the subjects was a 21-year-old male with a significant malar rash despite being on hydroxychloroquine, azathioprine, and prednisone 40 mg daily. “One month after being on lenalidomide he had a pretty impressive response,” Dr. Wu said. “It’s not quite clear how lenalidomide works in cutaneous lupus. Currently it’s only approved for use in myelodysplastic syndromes, multiple myeloma, as well as certain lymphomas. It’s thought to modulate different parts of the immune system, which collectively result in the cytotoxicity against tumor cells.”
Lenalidomide is supplied in capsule sizes ranging from 2.5 mg to 25 mg and is given once daily. “For a smaller child, I would think about starting 5 mg once a day,” Dr. Wu said. “For an adult-sized adolescent, you could start at 10 mg once a day and then titrate up based on response. Side effects that you need to worry about are cytopenia and GI symptoms. The venous and arterial thromboembolism risk has been seen in patients with multiple myeloma, and it is unclear if this risk is applicable to all indications.” Use of the medication requires enrollment into a safety monitoring program.
She reported having no financial disclosures.
Cutaneous lupus erythematosus (CLE) is present in 25% of patients with systemic lupus at the time of diagnosis, but it can also occur in up to 85% of cases at some point in their disease course, Eveline Y. Wu, MD, said during the virtual annual meeting of the Society for Pediatric Dermatology.
“CLE can also occur without any systemic disease,” said Dr. Wu, associate professor of pediatrics at the University of North Carolina at Chapel Hill. “It’s been shown that the risk of developing systemic lupus differs according to the type of skin involvement, meaning that cutaneous lupus can be classified into acute, subacute, chronic, and intermittent forms.”
Malar rash is the prototypical acute cutaneous lesion and is associated with active systemic lupus erythematosus (SLE) and anti–double stranded DNA antibody positivity, while discoid lupus erythematosus is the most common chronic lesion. “A small percentage of patients with discoid lupus can develop systemic lupus, particularly when the lesions are more disseminated,” said Dr. Wu, who specializes in pediatric rheumatology as well as allergy and immunology.
In the American College of Rheumatology’s 1997 classification system, mucocutaneous manifestations constitute 4 out of the 11 criteria that clinicians use to make a diagnosis of SLE: malar rash, discoid-lupus rash, photosensitivity, and oral or nasal mucocutaneous ulcerations. Dr. Wu recommends performing an oral exam on suspect cases, “because the oral ulcers that we see in systemic lupus tend to be painless, so oftentimes patients don’t realize they have them.”
Five other organ-specific manifestations of SLE include nonerosive arthritis, nephritis, encephalopathy, pleuritis or pericarditis, and cytopenia. The two other criteria are positive immunoserology and a positive antinuclear antibody test. “If you have any individuals present with one of these [mucocutaneous manifestations criteria], you want to think about getting a CBC to look for cytopenia or a urinalysis to look for evidence of nephritis, and potentially some additional blood studies, depending on your level of suspicion for systemic lupus,” Dr. Wu said.
Other rarer CLE manifestations include lupus pernio or chilblains, lupus panniculitis, livedo reticularis, bullous LE, urticarial vasculitis, neutrophilic dermatoses, and alopecia.
Common treatments for cutaneous manifestations associated pediatric SLE include hydroxychloroquine, low dose corticosteroids, topical steroids, methotrexate, and leflunomide. Other options for increasing severity of systemic disease include lenalidomide/thalidomide, azathioprine, calcineurin inhibitors, belimumab (Benlysta), high-dose corticosteroids, mycophenolate mofetil (CellCept), rituximab (Rituxan), and cyclophosphamide. Cutaneous manifestations of pediatric SLE can often be refractory to treatments.
In 2017, Dr. Wu and associates published a retrospective chart review of 10 adolescents who received lenalidomide for refractory CLE. One of the subjects was a 21-year-old male with a significant malar rash despite being on hydroxychloroquine, azathioprine, and prednisone 40 mg daily. “One month after being on lenalidomide he had a pretty impressive response,” Dr. Wu said. “It’s not quite clear how lenalidomide works in cutaneous lupus. Currently it’s only approved for use in myelodysplastic syndromes, multiple myeloma, as well as certain lymphomas. It’s thought to modulate different parts of the immune system, which collectively result in the cytotoxicity against tumor cells.”
Lenalidomide is supplied in capsule sizes ranging from 2.5 mg to 25 mg and is given once daily. “For a smaller child, I would think about starting 5 mg once a day,” Dr. Wu said. “For an adult-sized adolescent, you could start at 10 mg once a day and then titrate up based on response. Side effects that you need to worry about are cytopenia and GI symptoms. The venous and arterial thromboembolism risk has been seen in patients with multiple myeloma, and it is unclear if this risk is applicable to all indications.” Use of the medication requires enrollment into a safety monitoring program.
She reported having no financial disclosures.
Cutaneous lupus erythematosus (CLE) is present in 25% of patients with systemic lupus at the time of diagnosis, but it can also occur in up to 85% of cases at some point in their disease course, Eveline Y. Wu, MD, said during the virtual annual meeting of the Society for Pediatric Dermatology.
“CLE can also occur without any systemic disease,” said Dr. Wu, associate professor of pediatrics at the University of North Carolina at Chapel Hill. “It’s been shown that the risk of developing systemic lupus differs according to the type of skin involvement, meaning that cutaneous lupus can be classified into acute, subacute, chronic, and intermittent forms.”
Malar rash is the prototypical acute cutaneous lesion and is associated with active systemic lupus erythematosus (SLE) and anti–double stranded DNA antibody positivity, while discoid lupus erythematosus is the most common chronic lesion. “A small percentage of patients with discoid lupus can develop systemic lupus, particularly when the lesions are more disseminated,” said Dr. Wu, who specializes in pediatric rheumatology as well as allergy and immunology.
In the American College of Rheumatology’s 1997 classification system, mucocutaneous manifestations constitute 4 out of the 11 criteria that clinicians use to make a diagnosis of SLE: malar rash, discoid-lupus rash, photosensitivity, and oral or nasal mucocutaneous ulcerations. Dr. Wu recommends performing an oral exam on suspect cases, “because the oral ulcers that we see in systemic lupus tend to be painless, so oftentimes patients don’t realize they have them.”
Five other organ-specific manifestations of SLE include nonerosive arthritis, nephritis, encephalopathy, pleuritis or pericarditis, and cytopenia. The two other criteria are positive immunoserology and a positive antinuclear antibody test. “If you have any individuals present with one of these [mucocutaneous manifestations criteria], you want to think about getting a CBC to look for cytopenia or a urinalysis to look for evidence of nephritis, and potentially some additional blood studies, depending on your level of suspicion for systemic lupus,” Dr. Wu said.
Other rarer CLE manifestations include lupus pernio or chilblains, lupus panniculitis, livedo reticularis, bullous LE, urticarial vasculitis, neutrophilic dermatoses, and alopecia.
Common treatments for cutaneous manifestations associated pediatric SLE include hydroxychloroquine, low dose corticosteroids, topical steroids, methotrexate, and leflunomide. Other options for increasing severity of systemic disease include lenalidomide/thalidomide, azathioprine, calcineurin inhibitors, belimumab (Benlysta), high-dose corticosteroids, mycophenolate mofetil (CellCept), rituximab (Rituxan), and cyclophosphamide. Cutaneous manifestations of pediatric SLE can often be refractory to treatments.
In 2017, Dr. Wu and associates published a retrospective chart review of 10 adolescents who received lenalidomide for refractory CLE. One of the subjects was a 21-year-old male with a significant malar rash despite being on hydroxychloroquine, azathioprine, and prednisone 40 mg daily. “One month after being on lenalidomide he had a pretty impressive response,” Dr. Wu said. “It’s not quite clear how lenalidomide works in cutaneous lupus. Currently it’s only approved for use in myelodysplastic syndromes, multiple myeloma, as well as certain lymphomas. It’s thought to modulate different parts of the immune system, which collectively result in the cytotoxicity against tumor cells.”
Lenalidomide is supplied in capsule sizes ranging from 2.5 mg to 25 mg and is given once daily. “For a smaller child, I would think about starting 5 mg once a day,” Dr. Wu said. “For an adult-sized adolescent, you could start at 10 mg once a day and then titrate up based on response. Side effects that you need to worry about are cytopenia and GI symptoms. The venous and arterial thromboembolism risk has been seen in patients with multiple myeloma, and it is unclear if this risk is applicable to all indications.” Use of the medication requires enrollment into a safety monitoring program.
She reported having no financial disclosures.
FROM SPD 2020
Rapid drop of antibodies seen in those with mild COVID-19
The research was conducted by F. Javier Ibarrondo, PhD, and colleagues and was published online on July 21 in a letter to the editor of the New England Journal of Medicine. Ibarrondo is associate researcher at the University of California, Los Angeles. (The original letter incorrectly calculated the half-life at 73 days.)
Coauthor Otto Yang, MD, professor of medicine in the division of infectious diseases at UCLA, told Medscape Medical News that the rapidity in the antibody drop at 5 weeks “is striking compared to other infections.”
The phenomenon has been suspected and has been observed before but had not been quantified.
“Our paper is the first to put firm numbers on the dropping of antibodies after early infection,” he said.
The researchers evaluated 34 people (average age, 43 years) who had recovered from mild COVID-19 and had referred themselves to UCLA for observational research.
Previous report also found a quick fade
As Medscape Medical News reported, a previous study from China that was published in Nature Medicine also found that the antibodies fade quickly.
Interpreting the meaning of the current research comes with a few caveats, Dr. Yang said.
“One is that we don’t know for sure that antibodies are what protect people from getting infected,” he said. Although it’s a reasonable assumption, he said, that’s not always the case.
Another caveat is that even if antibodies do protect, the tests being used to measure them – including the test that was used in this study – may not measure them the right way, and it is not yet known how many antibodies are needed for protection, he explained.
The UCLA researchers used an enzyme-linked immunosorbent assay to detect anti–SARS-CoV-2 spike receptor–binding domain immunoglobulin G concentrations.
“No reason for anybody to be getting an antibody test medically”
The study provides further proof that “[t]here’s no reason for anybody to be getting an antibody test medically right now,” Dr. Yang said.
Additionally, “FDA-approved tests are not approved for quantitative measures, only qualitative,” he continued. He noted that the findings may have implications with respect to herd immunity.
“Herd immunity depends on a lot of people having immunity to the infection all at the same time. If infection is followed by only brief protection from infection, the natural infection is not going to reach herd immunity,” he explained.
Buddy Creech, MD, MPH, associate professor of pediatrics and director of the Vanderbilt Vaccine Research Program in Nashville, Tenn., pointed out that antibodies “are just part of the story.”
“When we make an immune response to any germ,” he said, “we not only make an immune response for the time being but for the future. The next time we’re exposed, we can call into action B cells and T cells who have been there and done that.”
So even though the antibodies fade over time, other arms of the immune system are being trained for future action, he said.
Herd immunity does not require that populations have a huge level of antibodies that remains forever, he explained.
“It requires that in general, we’re not going to get infected as easily, and we’re not going to have disease as easily, and we’re not going to transmit the virus for as long,” he said.
Dr. Creech said he and others researching COVID-19 find that studies that show that antibodies fade quickly provide more proof “that this coronavirus is going to be here to stay unless we can take care of it through very effective treatments to take it from potentially fatal disease to one that is nothing more than a cold” or until a vaccine is developed.
He noted there are four other coronaviruses in widespread circulation every year that “amount to about 25% of the common cold.”
This study may help narrow the window as to when convalescent plasma – plasma that is taken from people who have recovered from COVID-19 and that is used to help people who are acutely ill with the disease – will be most effective, Dr. Creech explained. He said the results suggest that it is important that plasma be collected within the first couple of months after recovery so as to capture the most antibodies.
This study is important as another snapshot “so we understand the differences between severe and mild disease, so we can study it over time, so we have all the tools we need as we start these pivotal vaccine studies to make sure we’re making the right immune response for the right duration of time so we can put an end to this pandemic,” Dr. Creech concluded.
The study was supported by grants from the AIDS Healthcare Foundation, the Doris Duke Charitable Foundation, the National Institutes of Health, the James B. Pendleton Charitable Trust, and the McCarthy Family Foundation. A coauthor reports receiving grants from Gilead outside the submitted work. Dr. Creech has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The research was conducted by F. Javier Ibarrondo, PhD, and colleagues and was published online on July 21 in a letter to the editor of the New England Journal of Medicine. Ibarrondo is associate researcher at the University of California, Los Angeles. (The original letter incorrectly calculated the half-life at 73 days.)
Coauthor Otto Yang, MD, professor of medicine in the division of infectious diseases at UCLA, told Medscape Medical News that the rapidity in the antibody drop at 5 weeks “is striking compared to other infections.”
The phenomenon has been suspected and has been observed before but had not been quantified.
“Our paper is the first to put firm numbers on the dropping of antibodies after early infection,” he said.
The researchers evaluated 34 people (average age, 43 years) who had recovered from mild COVID-19 and had referred themselves to UCLA for observational research.
Previous report also found a quick fade
As Medscape Medical News reported, a previous study from China that was published in Nature Medicine also found that the antibodies fade quickly.
Interpreting the meaning of the current research comes with a few caveats, Dr. Yang said.
“One is that we don’t know for sure that antibodies are what protect people from getting infected,” he said. Although it’s a reasonable assumption, he said, that’s not always the case.
Another caveat is that even if antibodies do protect, the tests being used to measure them – including the test that was used in this study – may not measure them the right way, and it is not yet known how many antibodies are needed for protection, he explained.
The UCLA researchers used an enzyme-linked immunosorbent assay to detect anti–SARS-CoV-2 spike receptor–binding domain immunoglobulin G concentrations.
“No reason for anybody to be getting an antibody test medically”
The study provides further proof that “[t]here’s no reason for anybody to be getting an antibody test medically right now,” Dr. Yang said.
Additionally, “FDA-approved tests are not approved for quantitative measures, only qualitative,” he continued. He noted that the findings may have implications with respect to herd immunity.
“Herd immunity depends on a lot of people having immunity to the infection all at the same time. If infection is followed by only brief protection from infection, the natural infection is not going to reach herd immunity,” he explained.
Buddy Creech, MD, MPH, associate professor of pediatrics and director of the Vanderbilt Vaccine Research Program in Nashville, Tenn., pointed out that antibodies “are just part of the story.”
“When we make an immune response to any germ,” he said, “we not only make an immune response for the time being but for the future. The next time we’re exposed, we can call into action B cells and T cells who have been there and done that.”
So even though the antibodies fade over time, other arms of the immune system are being trained for future action, he said.
Herd immunity does not require that populations have a huge level of antibodies that remains forever, he explained.
“It requires that in general, we’re not going to get infected as easily, and we’re not going to have disease as easily, and we’re not going to transmit the virus for as long,” he said.
Dr. Creech said he and others researching COVID-19 find that studies that show that antibodies fade quickly provide more proof “that this coronavirus is going to be here to stay unless we can take care of it through very effective treatments to take it from potentially fatal disease to one that is nothing more than a cold” or until a vaccine is developed.
He noted there are four other coronaviruses in widespread circulation every year that “amount to about 25% of the common cold.”
This study may help narrow the window as to when convalescent plasma – plasma that is taken from people who have recovered from COVID-19 and that is used to help people who are acutely ill with the disease – will be most effective, Dr. Creech explained. He said the results suggest that it is important that plasma be collected within the first couple of months after recovery so as to capture the most antibodies.
This study is important as another snapshot “so we understand the differences between severe and mild disease, so we can study it over time, so we have all the tools we need as we start these pivotal vaccine studies to make sure we’re making the right immune response for the right duration of time so we can put an end to this pandemic,” Dr. Creech concluded.
The study was supported by grants from the AIDS Healthcare Foundation, the Doris Duke Charitable Foundation, the National Institutes of Health, the James B. Pendleton Charitable Trust, and the McCarthy Family Foundation. A coauthor reports receiving grants from Gilead outside the submitted work. Dr. Creech has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The research was conducted by F. Javier Ibarrondo, PhD, and colleagues and was published online on July 21 in a letter to the editor of the New England Journal of Medicine. Ibarrondo is associate researcher at the University of California, Los Angeles. (The original letter incorrectly calculated the half-life at 73 days.)
Coauthor Otto Yang, MD, professor of medicine in the division of infectious diseases at UCLA, told Medscape Medical News that the rapidity in the antibody drop at 5 weeks “is striking compared to other infections.”
The phenomenon has been suspected and has been observed before but had not been quantified.
“Our paper is the first to put firm numbers on the dropping of antibodies after early infection,” he said.
The researchers evaluated 34 people (average age, 43 years) who had recovered from mild COVID-19 and had referred themselves to UCLA for observational research.
Previous report also found a quick fade
As Medscape Medical News reported, a previous study from China that was published in Nature Medicine also found that the antibodies fade quickly.
Interpreting the meaning of the current research comes with a few caveats, Dr. Yang said.
“One is that we don’t know for sure that antibodies are what protect people from getting infected,” he said. Although it’s a reasonable assumption, he said, that’s not always the case.
Another caveat is that even if antibodies do protect, the tests being used to measure them – including the test that was used in this study – may not measure them the right way, and it is not yet known how many antibodies are needed for protection, he explained.
The UCLA researchers used an enzyme-linked immunosorbent assay to detect anti–SARS-CoV-2 spike receptor–binding domain immunoglobulin G concentrations.
“No reason for anybody to be getting an antibody test medically”
The study provides further proof that “[t]here’s no reason for anybody to be getting an antibody test medically right now,” Dr. Yang said.
Additionally, “FDA-approved tests are not approved for quantitative measures, only qualitative,” he continued. He noted that the findings may have implications with respect to herd immunity.
“Herd immunity depends on a lot of people having immunity to the infection all at the same time. If infection is followed by only brief protection from infection, the natural infection is not going to reach herd immunity,” he explained.
Buddy Creech, MD, MPH, associate professor of pediatrics and director of the Vanderbilt Vaccine Research Program in Nashville, Tenn., pointed out that antibodies “are just part of the story.”
“When we make an immune response to any germ,” he said, “we not only make an immune response for the time being but for the future. The next time we’re exposed, we can call into action B cells and T cells who have been there and done that.”
So even though the antibodies fade over time, other arms of the immune system are being trained for future action, he said.
Herd immunity does not require that populations have a huge level of antibodies that remains forever, he explained.
“It requires that in general, we’re not going to get infected as easily, and we’re not going to have disease as easily, and we’re not going to transmit the virus for as long,” he said.
Dr. Creech said he and others researching COVID-19 find that studies that show that antibodies fade quickly provide more proof “that this coronavirus is going to be here to stay unless we can take care of it through very effective treatments to take it from potentially fatal disease to one that is nothing more than a cold” or until a vaccine is developed.
He noted there are four other coronaviruses in widespread circulation every year that “amount to about 25% of the common cold.”
This study may help narrow the window as to when convalescent plasma – plasma that is taken from people who have recovered from COVID-19 and that is used to help people who are acutely ill with the disease – will be most effective, Dr. Creech explained. He said the results suggest that it is important that plasma be collected within the first couple of months after recovery so as to capture the most antibodies.
This study is important as another snapshot “so we understand the differences between severe and mild disease, so we can study it over time, so we have all the tools we need as we start these pivotal vaccine studies to make sure we’re making the right immune response for the right duration of time so we can put an end to this pandemic,” Dr. Creech concluded.
The study was supported by grants from the AIDS Healthcare Foundation, the Doris Duke Charitable Foundation, the National Institutes of Health, the James B. Pendleton Charitable Trust, and the McCarthy Family Foundation. A coauthor reports receiving grants from Gilead outside the submitted work. Dr. Creech has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Is the presence of enanthem a clue for COVID-19?
Larger studies should explore and confirm this association, the study’s authors and other experts suggested.
Dermatologists are already aware of the connection between enanthem and viral etiology. “As seen with other viral infections, we wondered if COVID-19 could produce enanthem in addition to skin rash exanthem,” one of the study author’s, Juan Jiménez-Cauhe, MD, a dermatologist with Hospital Universitario Ramon y Cajal, Madrid, said in an interview. He and his colleagues summarized their findings in a research letter in JAMA Dermatology.
They examined the oral cavity of 21 COVID-19 patients at a tertiary care hospital who also had a skin rash from March 30 to April 8. They classified enanthems into four categories: petechial, macular, macular with petechiae, or erythematovesicular. Six of the patients presented with oral lesions, all of them located in the palate; in one patient, the enanthem was macular, it was petechial in two patients and was macular with petechiae in three patients. The six patients ranged between the ages of 40 and 69 years; four were women.
Petechial or vesicular patterns are often associated with viral infections. In this particular study, the investigators did not observe vesicular lesions.
On average, mucocutaneous lesions appeared about 12 days after the onset of COVID-19 symptoms. “Interestingly, this latency was shorter in patients with petechial enanthem, compared with those with a macular lesion with petechiae appearance,” the authors wrote.
This shorter time might suggest an association for SARS-CoV-2, said Dr. Jiménez-Cauhe. Strong cough may have also caused petechial lesions on the palate, but it’s unlikely, as they appeared close in time to COVID-19 symptoms. It’s also unlikely that any drugs caused the lesions, as drug rashes can take 2-3 weeks to appear.
This fits in line with other evidence of broader skin manifestations appearing at the same time or after COVID-19, Esther Freeman, MD, said in an interview. Dr. Freeman, director of global health dermatology at Massachusetts General Hospital, Boston, is the principal investigator of the COVID-19 Dermatology Registry, a collaboration of the American Academy of Dermatology and International League of Dermatological Societies.
The study’s small cohort made it difficult to establish a solid association between the oral lesions and SARS-CoV-2. “However, the presence of enanthem in a patient with a skin rash is a useful finding that suggests a viral etiology rather than a drug reaction. This is particularly useful in COVID-19 patients, who were receiving many drugs as part of the treatment,” Dr. Jimenez-Cauhe said. Future studies should assess whether the presence of enanthem and exanthem lead physicians to consider SARS-CoV-2 as possible agents, ruling out infection with a blood or nasopharyngeal test.
This study adds to the growing body of knowledge on cutaneous and mucocutaneous findings associated with SARS-CoV-2 infection, Jules Lipoff, MD, of the department of dermatology, University of Pennsylvania, Philadelphia, said in an interview. “One challenge in evaluating these findings is that these findings are nonspecific, and medication reactions can often cause similar rashes, such as morbilliform eruptions that can be associated with both viruses and medications.”
Enanthems, as the study authors noted, are more specific to viral infections and are less commonly associated with medication reactions. “So, even though this is a small case series with significant limitations, it does add more evidence that COVID-19 is directly responsible for findings in the skin and mucous membranes,” said Dr. Lipoff.
Dr. Freeman noted that the study may also encourage clinicians to look in a patient’s mouth when assessing for SARS-CoV-2. Additional research should examine these data in a larger population.
Several studies by Dr. Freeman, Dr. Lipoff, and others strongly suggest that SARS-CoV-2 has a spectrum of associated dermatologic manifestations. One evaluated perniolike skin lesions (J Am Acad Dermatol. 2020 Aug; 83[2]:486-92). The other was a case series from the COVID-19 registry that examined 716 cases of new-onset dermatologic symptoms in patients from 31 countries with confirmed/suspected SARS-CoV-2 (J Am Acad Dermatol. 2020 Jul 2;S0190-9622[20]32126-5.).
The authors of the report had no disclosures.
SOURCE: Jimenez-Cauhe J et al. JAMA Dermatol. 2020 Jul 15. doi: 10.1001/jamadermatol.2020.2550.
Larger studies should explore and confirm this association, the study’s authors and other experts suggested.
Dermatologists are already aware of the connection between enanthem and viral etiology. “As seen with other viral infections, we wondered if COVID-19 could produce enanthem in addition to skin rash exanthem,” one of the study author’s, Juan Jiménez-Cauhe, MD, a dermatologist with Hospital Universitario Ramon y Cajal, Madrid, said in an interview. He and his colleagues summarized their findings in a research letter in JAMA Dermatology.
They examined the oral cavity of 21 COVID-19 patients at a tertiary care hospital who also had a skin rash from March 30 to April 8. They classified enanthems into four categories: petechial, macular, macular with petechiae, or erythematovesicular. Six of the patients presented with oral lesions, all of them located in the palate; in one patient, the enanthem was macular, it was petechial in two patients and was macular with petechiae in three patients. The six patients ranged between the ages of 40 and 69 years; four were women.
Petechial or vesicular patterns are often associated with viral infections. In this particular study, the investigators did not observe vesicular lesions.
On average, mucocutaneous lesions appeared about 12 days after the onset of COVID-19 symptoms. “Interestingly, this latency was shorter in patients with petechial enanthem, compared with those with a macular lesion with petechiae appearance,” the authors wrote.
This shorter time might suggest an association for SARS-CoV-2, said Dr. Jiménez-Cauhe. Strong cough may have also caused petechial lesions on the palate, but it’s unlikely, as they appeared close in time to COVID-19 symptoms. It’s also unlikely that any drugs caused the lesions, as drug rashes can take 2-3 weeks to appear.
This fits in line with other evidence of broader skin manifestations appearing at the same time or after COVID-19, Esther Freeman, MD, said in an interview. Dr. Freeman, director of global health dermatology at Massachusetts General Hospital, Boston, is the principal investigator of the COVID-19 Dermatology Registry, a collaboration of the American Academy of Dermatology and International League of Dermatological Societies.
The study’s small cohort made it difficult to establish a solid association between the oral lesions and SARS-CoV-2. “However, the presence of enanthem in a patient with a skin rash is a useful finding that suggests a viral etiology rather than a drug reaction. This is particularly useful in COVID-19 patients, who were receiving many drugs as part of the treatment,” Dr. Jimenez-Cauhe said. Future studies should assess whether the presence of enanthem and exanthem lead physicians to consider SARS-CoV-2 as possible agents, ruling out infection with a blood or nasopharyngeal test.
This study adds to the growing body of knowledge on cutaneous and mucocutaneous findings associated with SARS-CoV-2 infection, Jules Lipoff, MD, of the department of dermatology, University of Pennsylvania, Philadelphia, said in an interview. “One challenge in evaluating these findings is that these findings are nonspecific, and medication reactions can often cause similar rashes, such as morbilliform eruptions that can be associated with both viruses and medications.”
Enanthems, as the study authors noted, are more specific to viral infections and are less commonly associated with medication reactions. “So, even though this is a small case series with significant limitations, it does add more evidence that COVID-19 is directly responsible for findings in the skin and mucous membranes,” said Dr. Lipoff.
Dr. Freeman noted that the study may also encourage clinicians to look in a patient’s mouth when assessing for SARS-CoV-2. Additional research should examine these data in a larger population.
Several studies by Dr. Freeman, Dr. Lipoff, and others strongly suggest that SARS-CoV-2 has a spectrum of associated dermatologic manifestations. One evaluated perniolike skin lesions (J Am Acad Dermatol. 2020 Aug; 83[2]:486-92). The other was a case series from the COVID-19 registry that examined 716 cases of new-onset dermatologic symptoms in patients from 31 countries with confirmed/suspected SARS-CoV-2 (J Am Acad Dermatol. 2020 Jul 2;S0190-9622[20]32126-5.).
The authors of the report had no disclosures.
SOURCE: Jimenez-Cauhe J et al. JAMA Dermatol. 2020 Jul 15. doi: 10.1001/jamadermatol.2020.2550.
Larger studies should explore and confirm this association, the study’s authors and other experts suggested.
Dermatologists are already aware of the connection between enanthem and viral etiology. “As seen with other viral infections, we wondered if COVID-19 could produce enanthem in addition to skin rash exanthem,” one of the study author’s, Juan Jiménez-Cauhe, MD, a dermatologist with Hospital Universitario Ramon y Cajal, Madrid, said in an interview. He and his colleagues summarized their findings in a research letter in JAMA Dermatology.
They examined the oral cavity of 21 COVID-19 patients at a tertiary care hospital who also had a skin rash from March 30 to April 8. They classified enanthems into four categories: petechial, macular, macular with petechiae, or erythematovesicular. Six of the patients presented with oral lesions, all of them located in the palate; in one patient, the enanthem was macular, it was petechial in two patients and was macular with petechiae in three patients. The six patients ranged between the ages of 40 and 69 years; four were women.
Petechial or vesicular patterns are often associated with viral infections. In this particular study, the investigators did not observe vesicular lesions.
On average, mucocutaneous lesions appeared about 12 days after the onset of COVID-19 symptoms. “Interestingly, this latency was shorter in patients with petechial enanthem, compared with those with a macular lesion with petechiae appearance,” the authors wrote.
This shorter time might suggest an association for SARS-CoV-2, said Dr. Jiménez-Cauhe. Strong cough may have also caused petechial lesions on the palate, but it’s unlikely, as they appeared close in time to COVID-19 symptoms. It’s also unlikely that any drugs caused the lesions, as drug rashes can take 2-3 weeks to appear.
This fits in line with other evidence of broader skin manifestations appearing at the same time or after COVID-19, Esther Freeman, MD, said in an interview. Dr. Freeman, director of global health dermatology at Massachusetts General Hospital, Boston, is the principal investigator of the COVID-19 Dermatology Registry, a collaboration of the American Academy of Dermatology and International League of Dermatological Societies.
The study’s small cohort made it difficult to establish a solid association between the oral lesions and SARS-CoV-2. “However, the presence of enanthem in a patient with a skin rash is a useful finding that suggests a viral etiology rather than a drug reaction. This is particularly useful in COVID-19 patients, who were receiving many drugs as part of the treatment,” Dr. Jimenez-Cauhe said. Future studies should assess whether the presence of enanthem and exanthem lead physicians to consider SARS-CoV-2 as possible agents, ruling out infection with a blood or nasopharyngeal test.
This study adds to the growing body of knowledge on cutaneous and mucocutaneous findings associated with SARS-CoV-2 infection, Jules Lipoff, MD, of the department of dermatology, University of Pennsylvania, Philadelphia, said in an interview. “One challenge in evaluating these findings is that these findings are nonspecific, and medication reactions can often cause similar rashes, such as morbilliform eruptions that can be associated with both viruses and medications.”
Enanthems, as the study authors noted, are more specific to viral infections and are less commonly associated with medication reactions. “So, even though this is a small case series with significant limitations, it does add more evidence that COVID-19 is directly responsible for findings in the skin and mucous membranes,” said Dr. Lipoff.
Dr. Freeman noted that the study may also encourage clinicians to look in a patient’s mouth when assessing for SARS-CoV-2. Additional research should examine these data in a larger population.
Several studies by Dr. Freeman, Dr. Lipoff, and others strongly suggest that SARS-CoV-2 has a spectrum of associated dermatologic manifestations. One evaluated perniolike skin lesions (J Am Acad Dermatol. 2020 Aug; 83[2]:486-92). The other was a case series from the COVID-19 registry that examined 716 cases of new-onset dermatologic symptoms in patients from 31 countries with confirmed/suspected SARS-CoV-2 (J Am Acad Dermatol. 2020 Jul 2;S0190-9622[20]32126-5.).
The authors of the report had no disclosures.
SOURCE: Jimenez-Cauhe J et al. JAMA Dermatol. 2020 Jul 15. doi: 10.1001/jamadermatol.2020.2550.
FROM JAMA DERMATOLOGY
Levonorgestrel IUDs offer safe, effective care for disabled adolescents
for menstrual management and contraception, based on data from a retrospective study of 159 patients.
“Desire for menstrual management or suppression is common in young women with special needs, including complex medical conditions and physical, intellectual, and developmental disabilities,” and many of these patients require estrogen-free options because of comorbidities, medication interactions, or decreased mobility, wrote Beth I. Schwartz, MD, and colleagues at Cincinnati Children’s Hospital Medical Center. Dr. Schwartz currently is of Thomas Jefferson University, Philadelphia.
In a study published in Pediatrics, the researchers identified 159 nulliparous patients aged 22 years and younger with physical, intellectual, or developmental disabilities who received levonorgestrel IUDs at a tertiary care children’s hospital between July 1, 2004, and June 30, 2014.
A total of 185 levonorgestrel IUDs were placed. The patients ranged in age from 9 to 22 years with a mean age of 16 years; 4% had ever been sexually active.
Overall, the IUD continuation rate was 95% after 1 year and 73% after 5 years. Most of the IUDs (96%) were inserted in the operating room.
Device malposition and expulsion accounted for a 5% rate of complications. Of the five expulsions, four were completely expelled from the uterus, and a fifth was partial and identified on ultrasound. No cases of pelvic inflammatory disease, pregnancy, or uterine perforation were reported, and the amenorrhea rate was approximately 60%.
Unique concerns regarding the use of IUDs in the disabled population include the appropriateness of IUDs as a first strategy for menstrual management or contraception, as well as potential distress related to bleeding and cramping that patients might find hard to articulate, the researchers said. However, the high continuation rate and low reports of side effects in the study suggests that the devices were well tolerated, and the data show that complications were minimal and manageable, they said.
The study findings were limited primarily by the retrospective design, “which involved loss of patients to follow-up, missing data, and reliance on adequate documentation,” Dr. Schwartz and associates noted. However, the study is the largest to date on levonorgestrel IUD use in young people with disabilities, and provides needed data on the safety and benefits of IUDs for menstrual management and contraception in this population, they said. Prospective studies are needed to assess continuation, outcomes, and long-term satisfaction with IUDs.
“However, these data are promising and should be used to allow more accurate counseling of adolescents with special needs and their families,” and it should be considered as an option for them, Dr. Schwartz and colleagues concluded.
“Clinicians should recognize that adolescents with disabilities have a range of decision-making capacities,” Cynthia Robbins, MD, and Mary A. Ott, MD, of Indiana University, Indianapolis, wrote in an accompanying editorial. Adolescents with disabilities may be left out of reproductive health discussions even if they are able, and the decisions are made by parents and caregivers.
For adolescents with mild disability, a shared decision-making approach is appropriate, in which providers and adolescents discuss reproductive health, with parent involvement as needed; “the adolescent is supported by the provider to express their preferences,” the editorialists wrote.
For those with more significant disability, they advised supported decision-making, in which the adolescent identifies a parent, family member, or caregiver as a trusted adult. “This supportive adult helps the adolescent communicate their goals and understand the decision and assists the provider in communication with the adolescent,” they said. For adolescents with a profound disability, the risks of placement and use of IUDs “should be thought of in a similar manner as other procedures that are routinely done to improve quality of life.”
“As clinicians, it is up to us to highlight these adolescents’ abilities to exercise their rights to sexual and reproductive health,” Dr. Robbins and Dr. Ott conclude.
The study was supported by a Bayer Healthcare Investigator-Initiated Research grant for women’s health to Dr. Schwartz and coauthor Lesley L. Breech, MD. The researchers had no other financial conflicts to disclose.
Dr. Ott disclosed providing expert consultation to Bayer, and that her spouse is employed Eli Lilly. Dr. Robbins had no relevant financial conflicts to disclose. They received no external funding for their editorial.
SOURCE: Schwartz BI et al. Pediatrics. 2020 Jul 23. doi: 10.1542/peds.2020-0016. Robbins C and Ott MA. Pediatrics. 2020 Jul 23. doi: 10.1542/peds.2020-006296.
for menstrual management and contraception, based on data from a retrospective study of 159 patients.
“Desire for menstrual management or suppression is common in young women with special needs, including complex medical conditions and physical, intellectual, and developmental disabilities,” and many of these patients require estrogen-free options because of comorbidities, medication interactions, or decreased mobility, wrote Beth I. Schwartz, MD, and colleagues at Cincinnati Children’s Hospital Medical Center. Dr. Schwartz currently is of Thomas Jefferson University, Philadelphia.
In a study published in Pediatrics, the researchers identified 159 nulliparous patients aged 22 years and younger with physical, intellectual, or developmental disabilities who received levonorgestrel IUDs at a tertiary care children’s hospital between July 1, 2004, and June 30, 2014.
A total of 185 levonorgestrel IUDs were placed. The patients ranged in age from 9 to 22 years with a mean age of 16 years; 4% had ever been sexually active.
Overall, the IUD continuation rate was 95% after 1 year and 73% after 5 years. Most of the IUDs (96%) were inserted in the operating room.
Device malposition and expulsion accounted for a 5% rate of complications. Of the five expulsions, four were completely expelled from the uterus, and a fifth was partial and identified on ultrasound. No cases of pelvic inflammatory disease, pregnancy, or uterine perforation were reported, and the amenorrhea rate was approximately 60%.
Unique concerns regarding the use of IUDs in the disabled population include the appropriateness of IUDs as a first strategy for menstrual management or contraception, as well as potential distress related to bleeding and cramping that patients might find hard to articulate, the researchers said. However, the high continuation rate and low reports of side effects in the study suggests that the devices were well tolerated, and the data show that complications were minimal and manageable, they said.
The study findings were limited primarily by the retrospective design, “which involved loss of patients to follow-up, missing data, and reliance on adequate documentation,” Dr. Schwartz and associates noted. However, the study is the largest to date on levonorgestrel IUD use in young people with disabilities, and provides needed data on the safety and benefits of IUDs for menstrual management and contraception in this population, they said. Prospective studies are needed to assess continuation, outcomes, and long-term satisfaction with IUDs.
“However, these data are promising and should be used to allow more accurate counseling of adolescents with special needs and their families,” and it should be considered as an option for them, Dr. Schwartz and colleagues concluded.
“Clinicians should recognize that adolescents with disabilities have a range of decision-making capacities,” Cynthia Robbins, MD, and Mary A. Ott, MD, of Indiana University, Indianapolis, wrote in an accompanying editorial. Adolescents with disabilities may be left out of reproductive health discussions even if they are able, and the decisions are made by parents and caregivers.
For adolescents with mild disability, a shared decision-making approach is appropriate, in which providers and adolescents discuss reproductive health, with parent involvement as needed; “the adolescent is supported by the provider to express their preferences,” the editorialists wrote.
For those with more significant disability, they advised supported decision-making, in which the adolescent identifies a parent, family member, or caregiver as a trusted adult. “This supportive adult helps the adolescent communicate their goals and understand the decision and assists the provider in communication with the adolescent,” they said. For adolescents with a profound disability, the risks of placement and use of IUDs “should be thought of in a similar manner as other procedures that are routinely done to improve quality of life.”
“As clinicians, it is up to us to highlight these adolescents’ abilities to exercise their rights to sexual and reproductive health,” Dr. Robbins and Dr. Ott conclude.
The study was supported by a Bayer Healthcare Investigator-Initiated Research grant for women’s health to Dr. Schwartz and coauthor Lesley L. Breech, MD. The researchers had no other financial conflicts to disclose.
Dr. Ott disclosed providing expert consultation to Bayer, and that her spouse is employed Eli Lilly. Dr. Robbins had no relevant financial conflicts to disclose. They received no external funding for their editorial.
SOURCE: Schwartz BI et al. Pediatrics. 2020 Jul 23. doi: 10.1542/peds.2020-0016. Robbins C and Ott MA. Pediatrics. 2020 Jul 23. doi: 10.1542/peds.2020-006296.
for menstrual management and contraception, based on data from a retrospective study of 159 patients.
“Desire for menstrual management or suppression is common in young women with special needs, including complex medical conditions and physical, intellectual, and developmental disabilities,” and many of these patients require estrogen-free options because of comorbidities, medication interactions, or decreased mobility, wrote Beth I. Schwartz, MD, and colleagues at Cincinnati Children’s Hospital Medical Center. Dr. Schwartz currently is of Thomas Jefferson University, Philadelphia.
In a study published in Pediatrics, the researchers identified 159 nulliparous patients aged 22 years and younger with physical, intellectual, or developmental disabilities who received levonorgestrel IUDs at a tertiary care children’s hospital between July 1, 2004, and June 30, 2014.
A total of 185 levonorgestrel IUDs were placed. The patients ranged in age from 9 to 22 years with a mean age of 16 years; 4% had ever been sexually active.
Overall, the IUD continuation rate was 95% after 1 year and 73% after 5 years. Most of the IUDs (96%) were inserted in the operating room.
Device malposition and expulsion accounted for a 5% rate of complications. Of the five expulsions, four were completely expelled from the uterus, and a fifth was partial and identified on ultrasound. No cases of pelvic inflammatory disease, pregnancy, or uterine perforation were reported, and the amenorrhea rate was approximately 60%.
Unique concerns regarding the use of IUDs in the disabled population include the appropriateness of IUDs as a first strategy for menstrual management or contraception, as well as potential distress related to bleeding and cramping that patients might find hard to articulate, the researchers said. However, the high continuation rate and low reports of side effects in the study suggests that the devices were well tolerated, and the data show that complications were minimal and manageable, they said.
The study findings were limited primarily by the retrospective design, “which involved loss of patients to follow-up, missing data, and reliance on adequate documentation,” Dr. Schwartz and associates noted. However, the study is the largest to date on levonorgestrel IUD use in young people with disabilities, and provides needed data on the safety and benefits of IUDs for menstrual management and contraception in this population, they said. Prospective studies are needed to assess continuation, outcomes, and long-term satisfaction with IUDs.
“However, these data are promising and should be used to allow more accurate counseling of adolescents with special needs and their families,” and it should be considered as an option for them, Dr. Schwartz and colleagues concluded.
“Clinicians should recognize that adolescents with disabilities have a range of decision-making capacities,” Cynthia Robbins, MD, and Mary A. Ott, MD, of Indiana University, Indianapolis, wrote in an accompanying editorial. Adolescents with disabilities may be left out of reproductive health discussions even if they are able, and the decisions are made by parents and caregivers.
For adolescents with mild disability, a shared decision-making approach is appropriate, in which providers and adolescents discuss reproductive health, with parent involvement as needed; “the adolescent is supported by the provider to express their preferences,” the editorialists wrote.
For those with more significant disability, they advised supported decision-making, in which the adolescent identifies a parent, family member, or caregiver as a trusted adult. “This supportive adult helps the adolescent communicate their goals and understand the decision and assists the provider in communication with the adolescent,” they said. For adolescents with a profound disability, the risks of placement and use of IUDs “should be thought of in a similar manner as other procedures that are routinely done to improve quality of life.”
“As clinicians, it is up to us to highlight these adolescents’ abilities to exercise their rights to sexual and reproductive health,” Dr. Robbins and Dr. Ott conclude.
The study was supported by a Bayer Healthcare Investigator-Initiated Research grant for women’s health to Dr. Schwartz and coauthor Lesley L. Breech, MD. The researchers had no other financial conflicts to disclose.
Dr. Ott disclosed providing expert consultation to Bayer, and that her spouse is employed Eli Lilly. Dr. Robbins had no relevant financial conflicts to disclose. They received no external funding for their editorial.
SOURCE: Schwartz BI et al. Pediatrics. 2020 Jul 23. doi: 10.1542/peds.2020-0016. Robbins C and Ott MA. Pediatrics. 2020 Jul 23. doi: 10.1542/peds.2020-006296.
FROM PEDIATRICS
Patch testing in children: An evolving science
“Time needs to be allocated for a patch test consultation, placement, removal, and reading,” she said at the virtual annual meeting of the Society for Pediatric Dermatology. “You will need more time in the day that you’re reading the patch test for patient education. However, your staff will need more time on the front end of the patch test process for application. Also, if they are customizing patch tests, they’ll need time to make the patch tests along with access to a refrigerator and plenty of counter space.”
Other factors to consider are the site of service, your payer mix, and if you need to complete prior authorizations for patch testing.
Dr. Martin, associate professor of dermatology and child health at the University of Missouri–Columbia, said that the diagnosis of allergic contact dermatitis (ACD) crosses her mind when she sees a patient with new dermatitis, especially in an older child; if the dermatitis is patterned or regional; if there’s exacerbation of an underlying, previously stable skin disease; or if it’s a pattern known to be associated with systemic contact dermatitis. “In fact, 13%-25% of healthy, asymptomatic kids have allergen sensitization,” she said. “If you take that a step further and look at kids who are suspected of having allergic contact dermatitis, 25%-96% have allergen sensitization. Still, that doesn’t mean that those tests are relevant to the dermatitis that’s going on. If you take kids who are referred to tertiary centers for patch testing, about half will have relevant patch test results.”
Pediatric ACD differs from adult ACD in three ways, Dr. Martin said. First, children have a different clinical morphology and distribution on presentation, compared with adults. “In adults, the most common clinical presentation is hand dermatitis, while kids more often present with a scattered generalized morphology of dermatitis,” she said. “This occurs in about one-third of children with ACD. Their patterns of allergen exposure are also different. For the most part, adults are in control of their own environments and what is placed on their skin, whereas kids are not. When thinking about what you might need to patch test a child to if you’re considering ACD, it’s important to think about not only what the parent or caregiver puts directly on the child’s skin but also any connubial or consort allergen exposure – the most common ones coming from the caregivers themselves, such as fragrance or hair dyes that are transferred to a young child.”
The third factor that differs between pediatric and adult ACD is the allergen source. Dr. Martin noted that children and adults use different personal care products, wear different types of clothing, and spend different amounts of time in play versus work. “Children have many more hobbies in general that are unfortunately lost as many of us age,” she said. That means “thinking through the child’s entire day and how the seasons differ for them, such as what sports they’re in and what protective equipment may be involved with where their dermatitis is, or what musical instruments they play.”
Applying the T.R.U.E. patch test panel or a customized patch test panel to young children poses certain challenges, considering their limited body surface area and propensity to squirm. Dr. Martin often employs distraction techniques when placing patches on young patients, including the use of bubbles, music, movies, and games. “The goal is always to get as much of the patches on the back or the flanks as possible,” she said. “If you need additional space you can use the upper outer arms, the abdomen, or the anterior lateral thighs. Another thing to consider is how to set up your week for pediatric patch testing. There’s a standardized process for adults where we place the patches on day 0, read them on day 2, with removal of the patches at that time, and then perform a delayed read between day 4-7.”
The process is similar for postpubescent children, despite the lack of clear guidelines in the medical literature. “There is much controversy and different practices between different pediatric patch test centers,” Dr. Martin said. “There is more consensus between the older kids and the prepubescent group ages 6-12. Most clinicians will still do a similar placement on day 0 with removal and initial read on day 2, with a delayed read on day 4-7. However, some groups will remove patches at 24 hours, especially in those with atopic dermatitis (AD) or a generalized dermatitis, to reduce irritant reactions. Others will also use half-strength concentrations of allergens.”
The most controversy lies with children younger than 6 years, she said. For those aged 3-6 years, who do not have AD, most practices use a standardized pediatric tray with a 24- to 48-hour contact time. However, patch testing can be “very challenging” for children who are under 3 years of age, and children with AD who are under 6 years, “so there needs to be a very high degree of suspicion for ACD and very careful selection of the allergens and contact time that is used in those particular cases,” she noted.
The most common allergens in children are nickel, fragrance mix I, cobalt, balsam of Peru, neomycin, and bacitracin, which largely match the common allergens seen in adults. However, allergens more common in children, compared with adults, include gold, propylene glycol, 2-Bromo-2-nitropropane-1,3-diol, and cocamidopropyl betaine. “If the child presents with a regional dermatitis or a patterned dermatitis, sometimes you can hone in on your suspected allergens and only test for a few,” Dr. Martin said. “In a child with eyelid dermatitis, you’re going to worry more about cocamidopropyl betaine in their shampoos and cleansers. Also, a metal allergen could be transferred from their hands from toys or coins, specifically nickel and cobalt. They also may have different sports gear such as goggles that may be affecting their eyelid dermatitis, which you would not necessarily see in an adult.”
Periorificial contact dermatitis can also differ in presentation between children and adults. “In kids, think about musical instruments, flavored lip balms, gum, and pacifiers,” she said. “For ACD on the buttocks and posterior thighs, think about toilet seat allergens, especially those in the potty training ages, and the nickel bolts on school chairs.”
In 2018, Dr. Martin and her colleagues on the Pediatric Contact Dermatitis Workgroup published a pediatric baseline patch test series as a way to expand on the T.R.U.E. test (Dermatitis. 2018;29[4]:206-12). “It’s nice to have this panel available as a baseline screening tool when you’re unsure of possible triggers of the dermatitis but you still have high suspicion of allergic dermatitis,” Dr. Martin said. “This also is helpful for patients who present with generalized dermatitis. It’s still not perfect. We are collecting prospective data to fine-tune this baseline series.”
She reported having no financial disclosures.
“Time needs to be allocated for a patch test consultation, placement, removal, and reading,” she said at the virtual annual meeting of the Society for Pediatric Dermatology. “You will need more time in the day that you’re reading the patch test for patient education. However, your staff will need more time on the front end of the patch test process for application. Also, if they are customizing patch tests, they’ll need time to make the patch tests along with access to a refrigerator and plenty of counter space.”
Other factors to consider are the site of service, your payer mix, and if you need to complete prior authorizations for patch testing.
Dr. Martin, associate professor of dermatology and child health at the University of Missouri–Columbia, said that the diagnosis of allergic contact dermatitis (ACD) crosses her mind when she sees a patient with new dermatitis, especially in an older child; if the dermatitis is patterned or regional; if there’s exacerbation of an underlying, previously stable skin disease; or if it’s a pattern known to be associated with systemic contact dermatitis. “In fact, 13%-25% of healthy, asymptomatic kids have allergen sensitization,” she said. “If you take that a step further and look at kids who are suspected of having allergic contact dermatitis, 25%-96% have allergen sensitization. Still, that doesn’t mean that those tests are relevant to the dermatitis that’s going on. If you take kids who are referred to tertiary centers for patch testing, about half will have relevant patch test results.”
Pediatric ACD differs from adult ACD in three ways, Dr. Martin said. First, children have a different clinical morphology and distribution on presentation, compared with adults. “In adults, the most common clinical presentation is hand dermatitis, while kids more often present with a scattered generalized morphology of dermatitis,” she said. “This occurs in about one-third of children with ACD. Their patterns of allergen exposure are also different. For the most part, adults are in control of their own environments and what is placed on their skin, whereas kids are not. When thinking about what you might need to patch test a child to if you’re considering ACD, it’s important to think about not only what the parent or caregiver puts directly on the child’s skin but also any connubial or consort allergen exposure – the most common ones coming from the caregivers themselves, such as fragrance or hair dyes that are transferred to a young child.”
The third factor that differs between pediatric and adult ACD is the allergen source. Dr. Martin noted that children and adults use different personal care products, wear different types of clothing, and spend different amounts of time in play versus work. “Children have many more hobbies in general that are unfortunately lost as many of us age,” she said. That means “thinking through the child’s entire day and how the seasons differ for them, such as what sports they’re in and what protective equipment may be involved with where their dermatitis is, or what musical instruments they play.”
Applying the T.R.U.E. patch test panel or a customized patch test panel to young children poses certain challenges, considering their limited body surface area and propensity to squirm. Dr. Martin often employs distraction techniques when placing patches on young patients, including the use of bubbles, music, movies, and games. “The goal is always to get as much of the patches on the back or the flanks as possible,” she said. “If you need additional space you can use the upper outer arms, the abdomen, or the anterior lateral thighs. Another thing to consider is how to set up your week for pediatric patch testing. There’s a standardized process for adults where we place the patches on day 0, read them on day 2, with removal of the patches at that time, and then perform a delayed read between day 4-7.”
The process is similar for postpubescent children, despite the lack of clear guidelines in the medical literature. “There is much controversy and different practices between different pediatric patch test centers,” Dr. Martin said. “There is more consensus between the older kids and the prepubescent group ages 6-12. Most clinicians will still do a similar placement on day 0 with removal and initial read on day 2, with a delayed read on day 4-7. However, some groups will remove patches at 24 hours, especially in those with atopic dermatitis (AD) or a generalized dermatitis, to reduce irritant reactions. Others will also use half-strength concentrations of allergens.”
The most controversy lies with children younger than 6 years, she said. For those aged 3-6 years, who do not have AD, most practices use a standardized pediatric tray with a 24- to 48-hour contact time. However, patch testing can be “very challenging” for children who are under 3 years of age, and children with AD who are under 6 years, “so there needs to be a very high degree of suspicion for ACD and very careful selection of the allergens and contact time that is used in those particular cases,” she noted.
The most common allergens in children are nickel, fragrance mix I, cobalt, balsam of Peru, neomycin, and bacitracin, which largely match the common allergens seen in adults. However, allergens more common in children, compared with adults, include gold, propylene glycol, 2-Bromo-2-nitropropane-1,3-diol, and cocamidopropyl betaine. “If the child presents with a regional dermatitis or a patterned dermatitis, sometimes you can hone in on your suspected allergens and only test for a few,” Dr. Martin said. “In a child with eyelid dermatitis, you’re going to worry more about cocamidopropyl betaine in their shampoos and cleansers. Also, a metal allergen could be transferred from their hands from toys or coins, specifically nickel and cobalt. They also may have different sports gear such as goggles that may be affecting their eyelid dermatitis, which you would not necessarily see in an adult.”
Periorificial contact dermatitis can also differ in presentation between children and adults. “In kids, think about musical instruments, flavored lip balms, gum, and pacifiers,” she said. “For ACD on the buttocks and posterior thighs, think about toilet seat allergens, especially those in the potty training ages, and the nickel bolts on school chairs.”
In 2018, Dr. Martin and her colleagues on the Pediatric Contact Dermatitis Workgroup published a pediatric baseline patch test series as a way to expand on the T.R.U.E. test (Dermatitis. 2018;29[4]:206-12). “It’s nice to have this panel available as a baseline screening tool when you’re unsure of possible triggers of the dermatitis but you still have high suspicion of allergic dermatitis,” Dr. Martin said. “This also is helpful for patients who present with generalized dermatitis. It’s still not perfect. We are collecting prospective data to fine-tune this baseline series.”
She reported having no financial disclosures.
“Time needs to be allocated for a patch test consultation, placement, removal, and reading,” she said at the virtual annual meeting of the Society for Pediatric Dermatology. “You will need more time in the day that you’re reading the patch test for patient education. However, your staff will need more time on the front end of the patch test process for application. Also, if they are customizing patch tests, they’ll need time to make the patch tests along with access to a refrigerator and plenty of counter space.”
Other factors to consider are the site of service, your payer mix, and if you need to complete prior authorizations for patch testing.
Dr. Martin, associate professor of dermatology and child health at the University of Missouri–Columbia, said that the diagnosis of allergic contact dermatitis (ACD) crosses her mind when she sees a patient with new dermatitis, especially in an older child; if the dermatitis is patterned or regional; if there’s exacerbation of an underlying, previously stable skin disease; or if it’s a pattern known to be associated with systemic contact dermatitis. “In fact, 13%-25% of healthy, asymptomatic kids have allergen sensitization,” she said. “If you take that a step further and look at kids who are suspected of having allergic contact dermatitis, 25%-96% have allergen sensitization. Still, that doesn’t mean that those tests are relevant to the dermatitis that’s going on. If you take kids who are referred to tertiary centers for patch testing, about half will have relevant patch test results.”
Pediatric ACD differs from adult ACD in three ways, Dr. Martin said. First, children have a different clinical morphology and distribution on presentation, compared with adults. “In adults, the most common clinical presentation is hand dermatitis, while kids more often present with a scattered generalized morphology of dermatitis,” she said. “This occurs in about one-third of children with ACD. Their patterns of allergen exposure are also different. For the most part, adults are in control of their own environments and what is placed on their skin, whereas kids are not. When thinking about what you might need to patch test a child to if you’re considering ACD, it’s important to think about not only what the parent or caregiver puts directly on the child’s skin but also any connubial or consort allergen exposure – the most common ones coming from the caregivers themselves, such as fragrance or hair dyes that are transferred to a young child.”
The third factor that differs between pediatric and adult ACD is the allergen source. Dr. Martin noted that children and adults use different personal care products, wear different types of clothing, and spend different amounts of time in play versus work. “Children have many more hobbies in general that are unfortunately lost as many of us age,” she said. That means “thinking through the child’s entire day and how the seasons differ for them, such as what sports they’re in and what protective equipment may be involved with where their dermatitis is, or what musical instruments they play.”
Applying the T.R.U.E. patch test panel or a customized patch test panel to young children poses certain challenges, considering their limited body surface area and propensity to squirm. Dr. Martin often employs distraction techniques when placing patches on young patients, including the use of bubbles, music, movies, and games. “The goal is always to get as much of the patches on the back or the flanks as possible,” she said. “If you need additional space you can use the upper outer arms, the abdomen, or the anterior lateral thighs. Another thing to consider is how to set up your week for pediatric patch testing. There’s a standardized process for adults where we place the patches on day 0, read them on day 2, with removal of the patches at that time, and then perform a delayed read between day 4-7.”
The process is similar for postpubescent children, despite the lack of clear guidelines in the medical literature. “There is much controversy and different practices between different pediatric patch test centers,” Dr. Martin said. “There is more consensus between the older kids and the prepubescent group ages 6-12. Most clinicians will still do a similar placement on day 0 with removal and initial read on day 2, with a delayed read on day 4-7. However, some groups will remove patches at 24 hours, especially in those with atopic dermatitis (AD) or a generalized dermatitis, to reduce irritant reactions. Others will also use half-strength concentrations of allergens.”
The most controversy lies with children younger than 6 years, she said. For those aged 3-6 years, who do not have AD, most practices use a standardized pediatric tray with a 24- to 48-hour contact time. However, patch testing can be “very challenging” for children who are under 3 years of age, and children with AD who are under 6 years, “so there needs to be a very high degree of suspicion for ACD and very careful selection of the allergens and contact time that is used in those particular cases,” she noted.
The most common allergens in children are nickel, fragrance mix I, cobalt, balsam of Peru, neomycin, and bacitracin, which largely match the common allergens seen in adults. However, allergens more common in children, compared with adults, include gold, propylene glycol, 2-Bromo-2-nitropropane-1,3-diol, and cocamidopropyl betaine. “If the child presents with a regional dermatitis or a patterned dermatitis, sometimes you can hone in on your suspected allergens and only test for a few,” Dr. Martin said. “In a child with eyelid dermatitis, you’re going to worry more about cocamidopropyl betaine in their shampoos and cleansers. Also, a metal allergen could be transferred from their hands from toys or coins, specifically nickel and cobalt. They also may have different sports gear such as goggles that may be affecting their eyelid dermatitis, which you would not necessarily see in an adult.”
Periorificial contact dermatitis can also differ in presentation between children and adults. “In kids, think about musical instruments, flavored lip balms, gum, and pacifiers,” she said. “For ACD on the buttocks and posterior thighs, think about toilet seat allergens, especially those in the potty training ages, and the nickel bolts on school chairs.”
In 2018, Dr. Martin and her colleagues on the Pediatric Contact Dermatitis Workgroup published a pediatric baseline patch test series as a way to expand on the T.R.U.E. test (Dermatitis. 2018;29[4]:206-12). “It’s nice to have this panel available as a baseline screening tool when you’re unsure of possible triggers of the dermatitis but you still have high suspicion of allergic dermatitis,” Dr. Martin said. “This also is helpful for patients who present with generalized dermatitis. It’s still not perfect. We are collecting prospective data to fine-tune this baseline series.”
She reported having no financial disclosures.
FROM SPD 2020
Internists’ use of ultrasound can reduce radiology referrals
researchers say.
“It’s a safe and very useful tool,” Marco Barchiesi, MD, an internal medicine resident at Luigi Sacco Hospital in Milan, said in an interview. “We had a great reduction in chest x-rays because of the use of ultrasound.”
The finding addresses concerns that ultrasound used in primary care could consume more health care resources or put patients at risk.
Dr. Barchiesi and colleagues published their findings July 20 in the European Journal of Internal Medicine.
Point-of-care ultrasound has become increasingly common as miniaturization of devices has made them more portable. The approach has caught on particularly in emergency departments where quick decisions are of the essence.
Its use in internal medicine has been more controversial, with concerns raised that improperly trained practitioners may miss diagnoses or refer patients for unnecessary tests as a result of uncertainty about their findings.
To measure the effect of point-of-care ultrasound in an internal medicine hospital ward, Dr. Barchiesi and colleagues alternated months when point-of-care ultrasound was allowed with months when it was not allowed, for a total of 4 months each, on an internal medicine unit. They allowed the ultrasound to be used for invasive procedures and excluded patients whose critical condition made point-of-care ultrasound crucial.
The researchers analyzed data on 263 patients in the “on” months when point-of-care ultrasound was used, and 255 in the “off” months when it wasn’t used. The two groups were well balanced in age, sex, comorbidity, and clinical impairment.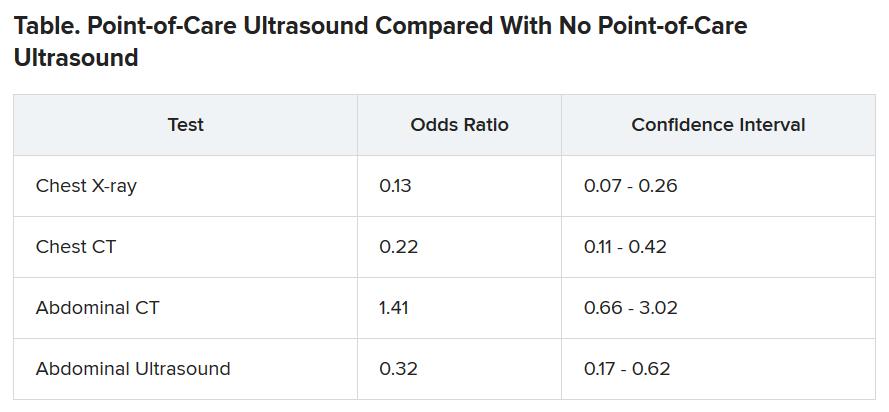
During the on months, the internists ordered 113 diagnostic tests (0.43 per patient). During the off months they ordered 329 tests (1.29 per patient).
The odds of being referred for a chest x-ray were 87% less in the “on” months, compared with the off months, a statistically significant finding (P < .001). The risk for a chest CT scan and abdominal ultrasound were also reduced during the on months, but the risk for an abdominal CT was increased.
Nineteen patients died during the o” months and 10 during the off months, a difference that was not statistically significant (P = .15). The median length of stay in the hospital was almost the same for the two groups: 9 days for the on months and 9 days for the off months. The difference was also not statistically significant (P = .094).
Point-of-care ultrasound is particularly accurate in identifying cardiac abnormalities and pleural fluid and pneumonia, and it can be used effectively for monitoring heart conditions, the researchers wrote. This could explain the reduction in chest x-rays and CT scans.
On the other hand, ultrasound cannot address such questions as staging in an abdominal malignancy, and unexpected findings are more common with abdominal than chest ultrasound. This could explain why the point-of-care ultrasound did not reduce the use of abdominal CT, the researchers speculated.
They acknowledged that the patients in their sample had an average age of 81 years, raising questions about how well their data could be applied to a younger population. And they noted that they used point-of-care ultrasound frequently, so they were particularly adept with it. “We use it almost every day in our clinical practice,” said Dr. Barchiesi.
Those factors may have played a key role in the success of point-of-care ultrasound in this study, said Michael Wagner, MD, an assistant professor of medicine at the University of South Carolina, Greenville, who has helped colleagues incorporate ultrasound into their practices.
Elderly patients often present with multiple comorbidities and atypical signs and symptoms, he said. “Sometimes they can be very confusing as to the underlying clinical picture. Ultrasound is being used frequently to better assess these complicated patients.”
Dr. Wagner said extensive training is required to use point-of-care ultrasound accurately.
Dr. Barchiesi also acknowledged that the devices used in this study were large portable machines, not the simpler and less expensive hand-held versions that are also available for similar purposes.
Point-of-care ultrasound is a promising innovation, said Thomas Melgar, MD, a professor of medicine at Western Michigan University, Kalamazoo. “The advantage is that the exam is being done by someone who knows the patient and specifically what they’re looking for. It’s done at the bedside so you don’t have to move the patient.”
The study could help address opposition to internal medicine residents being trained in the technique, he said, adding that “I think it’s very exciting.”
The study was partially supported by Philips, which provided the ultrasound devices. Dr. Barchiesi, Dr. Melgar, and Dr. Wagner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
researchers say.
“It’s a safe and very useful tool,” Marco Barchiesi, MD, an internal medicine resident at Luigi Sacco Hospital in Milan, said in an interview. “We had a great reduction in chest x-rays because of the use of ultrasound.”
The finding addresses concerns that ultrasound used in primary care could consume more health care resources or put patients at risk.
Dr. Barchiesi and colleagues published their findings July 20 in the European Journal of Internal Medicine.
Point-of-care ultrasound has become increasingly common as miniaturization of devices has made them more portable. The approach has caught on particularly in emergency departments where quick decisions are of the essence.
Its use in internal medicine has been more controversial, with concerns raised that improperly trained practitioners may miss diagnoses or refer patients for unnecessary tests as a result of uncertainty about their findings.
To measure the effect of point-of-care ultrasound in an internal medicine hospital ward, Dr. Barchiesi and colleagues alternated months when point-of-care ultrasound was allowed with months when it was not allowed, for a total of 4 months each, on an internal medicine unit. They allowed the ultrasound to be used for invasive procedures and excluded patients whose critical condition made point-of-care ultrasound crucial.
The researchers analyzed data on 263 patients in the “on” months when point-of-care ultrasound was used, and 255 in the “off” months when it wasn’t used. The two groups were well balanced in age, sex, comorbidity, and clinical impairment.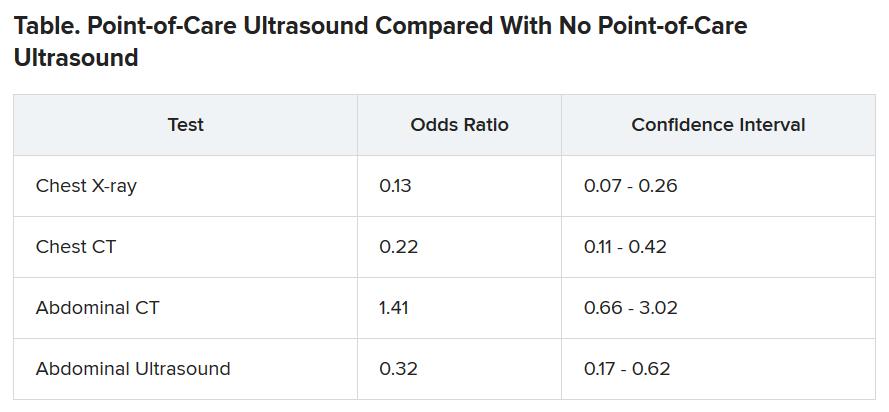
During the on months, the internists ordered 113 diagnostic tests (0.43 per patient). During the off months they ordered 329 tests (1.29 per patient).
The odds of being referred for a chest x-ray were 87% less in the “on” months, compared with the off months, a statistically significant finding (P < .001). The risk for a chest CT scan and abdominal ultrasound were also reduced during the on months, but the risk for an abdominal CT was increased.
Nineteen patients died during the o” months and 10 during the off months, a difference that was not statistically significant (P = .15). The median length of stay in the hospital was almost the same for the two groups: 9 days for the on months and 9 days for the off months. The difference was also not statistically significant (P = .094).
Point-of-care ultrasound is particularly accurate in identifying cardiac abnormalities and pleural fluid and pneumonia, and it can be used effectively for monitoring heart conditions, the researchers wrote. This could explain the reduction in chest x-rays and CT scans.
On the other hand, ultrasound cannot address such questions as staging in an abdominal malignancy, and unexpected findings are more common with abdominal than chest ultrasound. This could explain why the point-of-care ultrasound did not reduce the use of abdominal CT, the researchers speculated.
They acknowledged that the patients in their sample had an average age of 81 years, raising questions about how well their data could be applied to a younger population. And they noted that they used point-of-care ultrasound frequently, so they were particularly adept with it. “We use it almost every day in our clinical practice,” said Dr. Barchiesi.
Those factors may have played a key role in the success of point-of-care ultrasound in this study, said Michael Wagner, MD, an assistant professor of medicine at the University of South Carolina, Greenville, who has helped colleagues incorporate ultrasound into their practices.
Elderly patients often present with multiple comorbidities and atypical signs and symptoms, he said. “Sometimes they can be very confusing as to the underlying clinical picture. Ultrasound is being used frequently to better assess these complicated patients.”
Dr. Wagner said extensive training is required to use point-of-care ultrasound accurately.
Dr. Barchiesi also acknowledged that the devices used in this study were large portable machines, not the simpler and less expensive hand-held versions that are also available for similar purposes.
Point-of-care ultrasound is a promising innovation, said Thomas Melgar, MD, a professor of medicine at Western Michigan University, Kalamazoo. “The advantage is that the exam is being done by someone who knows the patient and specifically what they’re looking for. It’s done at the bedside so you don’t have to move the patient.”
The study could help address opposition to internal medicine residents being trained in the technique, he said, adding that “I think it’s very exciting.”
The study was partially supported by Philips, which provided the ultrasound devices. Dr. Barchiesi, Dr. Melgar, and Dr. Wagner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
researchers say.
“It’s a safe and very useful tool,” Marco Barchiesi, MD, an internal medicine resident at Luigi Sacco Hospital in Milan, said in an interview. “We had a great reduction in chest x-rays because of the use of ultrasound.”
The finding addresses concerns that ultrasound used in primary care could consume more health care resources or put patients at risk.
Dr. Barchiesi and colleagues published their findings July 20 in the European Journal of Internal Medicine.
Point-of-care ultrasound has become increasingly common as miniaturization of devices has made them more portable. The approach has caught on particularly in emergency departments where quick decisions are of the essence.
Its use in internal medicine has been more controversial, with concerns raised that improperly trained practitioners may miss diagnoses or refer patients for unnecessary tests as a result of uncertainty about their findings.
To measure the effect of point-of-care ultrasound in an internal medicine hospital ward, Dr. Barchiesi and colleagues alternated months when point-of-care ultrasound was allowed with months when it was not allowed, for a total of 4 months each, on an internal medicine unit. They allowed the ultrasound to be used for invasive procedures and excluded patients whose critical condition made point-of-care ultrasound crucial.
The researchers analyzed data on 263 patients in the “on” months when point-of-care ultrasound was used, and 255 in the “off” months when it wasn’t used. The two groups were well balanced in age, sex, comorbidity, and clinical impairment.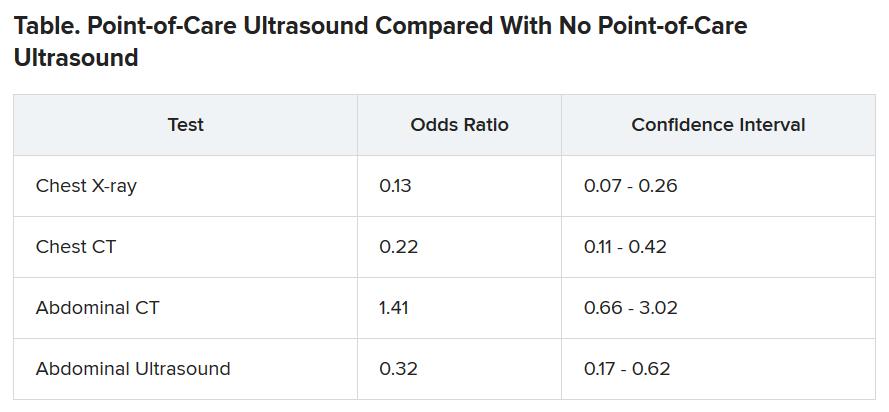
During the on months, the internists ordered 113 diagnostic tests (0.43 per patient). During the off months they ordered 329 tests (1.29 per patient).
The odds of being referred for a chest x-ray were 87% less in the “on” months, compared with the off months, a statistically significant finding (P < .001). The risk for a chest CT scan and abdominal ultrasound were also reduced during the on months, but the risk for an abdominal CT was increased.
Nineteen patients died during the o” months and 10 during the off months, a difference that was not statistically significant (P = .15). The median length of stay in the hospital was almost the same for the two groups: 9 days for the on months and 9 days for the off months. The difference was also not statistically significant (P = .094).
Point-of-care ultrasound is particularly accurate in identifying cardiac abnormalities and pleural fluid and pneumonia, and it can be used effectively for monitoring heart conditions, the researchers wrote. This could explain the reduction in chest x-rays and CT scans.
On the other hand, ultrasound cannot address such questions as staging in an abdominal malignancy, and unexpected findings are more common with abdominal than chest ultrasound. This could explain why the point-of-care ultrasound did not reduce the use of abdominal CT, the researchers speculated.
They acknowledged that the patients in their sample had an average age of 81 years, raising questions about how well their data could be applied to a younger population. And they noted that they used point-of-care ultrasound frequently, so they were particularly adept with it. “We use it almost every day in our clinical practice,” said Dr. Barchiesi.
Those factors may have played a key role in the success of point-of-care ultrasound in this study, said Michael Wagner, MD, an assistant professor of medicine at the University of South Carolina, Greenville, who has helped colleagues incorporate ultrasound into their practices.
Elderly patients often present with multiple comorbidities and atypical signs and symptoms, he said. “Sometimes they can be very confusing as to the underlying clinical picture. Ultrasound is being used frequently to better assess these complicated patients.”
Dr. Wagner said extensive training is required to use point-of-care ultrasound accurately.
Dr. Barchiesi also acknowledged that the devices used in this study were large portable machines, not the simpler and less expensive hand-held versions that are also available for similar purposes.
Point-of-care ultrasound is a promising innovation, said Thomas Melgar, MD, a professor of medicine at Western Michigan University, Kalamazoo. “The advantage is that the exam is being done by someone who knows the patient and specifically what they’re looking for. It’s done at the bedside so you don’t have to move the patient.”
The study could help address opposition to internal medicine residents being trained in the technique, he said, adding that “I think it’s very exciting.”
The study was partially supported by Philips, which provided the ultrasound devices. Dr. Barchiesi, Dr. Melgar, and Dr. Wagner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Ob.gyns. struggle to keep pace with changing COVID-19 knowledge
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
OSHA in the COVID-19 era
As more and more reopened medical practices ramp up toward normal activity, the safety of patients and health care workers alike remains paramount. As always,
Most of the modified guidelines are already familiar: wear masks (and other personal protective equipment as necessary); maintain social distancing; have hand cleaner, soap, and water readily available; and sanitize between patient examinations.
It is also important to remember that COVID-19 is now a reportable disease; check with your local health authorities as to where and how. Also remember that, if you decide to screen employees and/or patients for fevers and other symptoms of COVID-19, those data are subject to HIPAA rules and must be kept confidential.
Now might be a good time to confirm that you remain in compliance with both the new and old regulations. Even if you hold regular safety meetings – which often is not the case – it is always a good idea to occasionally conduct a comprehensive review, which could save you a lot in fines.
So get your OSHA logs out, and walk through your office. Start by making sure you have an official OSHA poster, which enumerates employee rights and explains how to file complaints. Every office must have one posted in plain site, and is what an OSHA inspector will look for first. They are available for free at OSHA’s website or you can order one by calling 800-321-OSHA.
How long have you had your written exposure control plan for blood-borne pathogens? This plan should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, as well as your implementation of universal precautions. It should be updated annually to reflect changes in technology – and new threats, such as COVID-19.
Review your list of hazardous substances, which all employees have a right to know about. OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are classified as “hazardous.” Also remember that you’re probably using new disinfectants, which may need to be added to your list. For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
It is not necessary to adopt every new safety device as it comes on the market, but you should document which ones you are using and which ones you decide not to use – and why. For example, if you and your employees decide against buying a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it is worth, you still should document how you made that decision and why you believe that your current protocol is as good or better.
All at-risk employees should be provided with hepatitis B vaccine at no cost to them. And after any exposure to dangerous pathogens – which now include COVID-19 – you also must provide and pay for appropriate medical treatment and follow-up.
Another important consideration in your review: Electrical devices and their power sources in the office. All electrically powered equipment – medical or clerical – must operate safely and should all be examined. It is particularly important to check how wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Medical and dental offices are not required to keep an injury and illness log under federal OSHA regulations, which other businesses must. However, your state may have a requirement that supersedes the federal law so you should check with your state, or with your local OSHA office, regarding any such requirements.
It is important to take OSHA regulations seriously because failure to comply with them can result in stiff penalties running into many thousands of dollars.
To be certain you are complying with all the rules, you can call your local OSHA office and request an inspection. This is the easiest and cheapest way because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they discover.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
As more and more reopened medical practices ramp up toward normal activity, the safety of patients and health care workers alike remains paramount. As always,
Most of the modified guidelines are already familiar: wear masks (and other personal protective equipment as necessary); maintain social distancing; have hand cleaner, soap, and water readily available; and sanitize between patient examinations.
It is also important to remember that COVID-19 is now a reportable disease; check with your local health authorities as to where and how. Also remember that, if you decide to screen employees and/or patients for fevers and other symptoms of COVID-19, those data are subject to HIPAA rules and must be kept confidential.
Now might be a good time to confirm that you remain in compliance with both the new and old regulations. Even if you hold regular safety meetings – which often is not the case – it is always a good idea to occasionally conduct a comprehensive review, which could save you a lot in fines.
So get your OSHA logs out, and walk through your office. Start by making sure you have an official OSHA poster, which enumerates employee rights and explains how to file complaints. Every office must have one posted in plain site, and is what an OSHA inspector will look for first. They are available for free at OSHA’s website or you can order one by calling 800-321-OSHA.
How long have you had your written exposure control plan for blood-borne pathogens? This plan should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, as well as your implementation of universal precautions. It should be updated annually to reflect changes in technology – and new threats, such as COVID-19.
Review your list of hazardous substances, which all employees have a right to know about. OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are classified as “hazardous.” Also remember that you’re probably using new disinfectants, which may need to be added to your list. For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
It is not necessary to adopt every new safety device as it comes on the market, but you should document which ones you are using and which ones you decide not to use – and why. For example, if you and your employees decide against buying a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it is worth, you still should document how you made that decision and why you believe that your current protocol is as good or better.
All at-risk employees should be provided with hepatitis B vaccine at no cost to them. And after any exposure to dangerous pathogens – which now include COVID-19 – you also must provide and pay for appropriate medical treatment and follow-up.
Another important consideration in your review: Electrical devices and their power sources in the office. All electrically powered equipment – medical or clerical – must operate safely and should all be examined. It is particularly important to check how wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Medical and dental offices are not required to keep an injury and illness log under federal OSHA regulations, which other businesses must. However, your state may have a requirement that supersedes the federal law so you should check with your state, or with your local OSHA office, regarding any such requirements.
It is important to take OSHA regulations seriously because failure to comply with them can result in stiff penalties running into many thousands of dollars.
To be certain you are complying with all the rules, you can call your local OSHA office and request an inspection. This is the easiest and cheapest way because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they discover.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
As more and more reopened medical practices ramp up toward normal activity, the safety of patients and health care workers alike remains paramount. As always,
Most of the modified guidelines are already familiar: wear masks (and other personal protective equipment as necessary); maintain social distancing; have hand cleaner, soap, and water readily available; and sanitize between patient examinations.
It is also important to remember that COVID-19 is now a reportable disease; check with your local health authorities as to where and how. Also remember that, if you decide to screen employees and/or patients for fevers and other symptoms of COVID-19, those data are subject to HIPAA rules and must be kept confidential.
Now might be a good time to confirm that you remain in compliance with both the new and old regulations. Even if you hold regular safety meetings – which often is not the case – it is always a good idea to occasionally conduct a comprehensive review, which could save you a lot in fines.
So get your OSHA logs out, and walk through your office. Start by making sure you have an official OSHA poster, which enumerates employee rights and explains how to file complaints. Every office must have one posted in plain site, and is what an OSHA inspector will look for first. They are available for free at OSHA’s website or you can order one by calling 800-321-OSHA.
How long have you had your written exposure control plan for blood-borne pathogens? This plan should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, as well as your implementation of universal precautions. It should be updated annually to reflect changes in technology – and new threats, such as COVID-19.
Review your list of hazardous substances, which all employees have a right to know about. OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are classified as “hazardous.” Also remember that you’re probably using new disinfectants, which may need to be added to your list. For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
It is not necessary to adopt every new safety device as it comes on the market, but you should document which ones you are using and which ones you decide not to use – and why. For example, if you and your employees decide against buying a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it is worth, you still should document how you made that decision and why you believe that your current protocol is as good or better.
All at-risk employees should be provided with hepatitis B vaccine at no cost to them. And after any exposure to dangerous pathogens – which now include COVID-19 – you also must provide and pay for appropriate medical treatment and follow-up.
Another important consideration in your review: Electrical devices and their power sources in the office. All electrically powered equipment – medical or clerical – must operate safely and should all be examined. It is particularly important to check how wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Medical and dental offices are not required to keep an injury and illness log under federal OSHA regulations, which other businesses must. However, your state may have a requirement that supersedes the federal law so you should check with your state, or with your local OSHA office, regarding any such requirements.
It is important to take OSHA regulations seriously because failure to comply with them can result in stiff penalties running into many thousands of dollars.
To be certain you are complying with all the rules, you can call your local OSHA office and request an inspection. This is the easiest and cheapest way because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they discover.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Survey: Most FPs live at or below their means
a Medscape survey has found.
According to the Medscape Family Physician Debt and Net Worth Report 2020, almost half of FPs (46%) reported having that amount as their net worth, compared with the 18% of gastroenterologists and 19% of urologists who fell into that category.
And whereas 19% of orthopedists reported at least $5 million in net worth, only 3% of FPs did.
A third are paying off student loans
FPs were also more likely, along with physical medicine and rehabilitation physicians, at 34%, to report that they are continuing to pay off student loans. Conversely, 14% of gastroenterologists and 15% of nephrologists and rheumatologists said they were still paying off the loans.
Student loan debt was third on the list for FPs. Two-thirds of FPs were paying off a mortgage, and 41% had car loan payments.
Overall, FPs appear to manage their finances well and are living within their means. Only 6% of FPs said they live above their means, whereas 51% said they live at their means, and 42% said they live below that threshold.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., said in an interview he recommends saving 20% of gross salary each year.
The survey was completed before Feb. 11 and before the financial effects of the COVID-19 pandemic could be known. The report is based on responses from more than 17,000 physicians across 30 specialties.
A lower level of net worth among FPs corresponds with their being close to the bottom among physicians in compensation. They made $234,000 on average, according to the report. By contrast, orthopedists made more than twice as much, at $511,000.
Smaller homes, less mortgage debt
FPs were among the least likely to indicate that they had a home of more than 5,000 square feet. That was true for only 6% of FPs; it was true for 22% of plastic surgeons and orthopedists. Most (61%) lived in dwellings of 3,000 square feet or less.
At the same time, FPs reported smaller mortgages than many of their colleagues.
Nearly half (49%) of FPs have mortgages of $300,000 or less; 26% have no mortgage at all. That figure was much higher than the 37% of physicians overall who had mortgages of $300,000 or less, although almost the same percentage had no mortgage at all.
Most had no financial loss in the past year
In further good news, most FPs (70%) said they did not experience a financial loss in the past year. Of those who did experience a loss, the top reasons were problems with their practice, such as reimbursement changes or changes in practice situations, or bad investments.
FPs socked away more into tax-deferred than taxable accounts, the survey showed.
More than half (54%) of FPs put at least $1,000 into tax-deferred accounts, such as college savings or retirement accounts, although 14% said they do not regularly contribute to such accounts.
Fewer (29%) contributed at least $1,000 to a taxable account.
As for who pays the day-to-day bills in households, 56% of FPs said they pool resources with a spouse or partner and pay bills from a common fund. Only 4% split the bills equally, no matter the income difference. One in four said they do not have joint finances with a spouse or partner.
FPs were divided as to whether they are currently working with a financial planner (38%) or had not worked with one (37%); the remainder said they had met with or used one in the past.
A version of this article originally appeared on Medscape.com.
a Medscape survey has found.
According to the Medscape Family Physician Debt and Net Worth Report 2020, almost half of FPs (46%) reported having that amount as their net worth, compared with the 18% of gastroenterologists and 19% of urologists who fell into that category.
And whereas 19% of orthopedists reported at least $5 million in net worth, only 3% of FPs did.
A third are paying off student loans
FPs were also more likely, along with physical medicine and rehabilitation physicians, at 34%, to report that they are continuing to pay off student loans. Conversely, 14% of gastroenterologists and 15% of nephrologists and rheumatologists said they were still paying off the loans.
Student loan debt was third on the list for FPs. Two-thirds of FPs were paying off a mortgage, and 41% had car loan payments.
Overall, FPs appear to manage their finances well and are living within their means. Only 6% of FPs said they live above their means, whereas 51% said they live at their means, and 42% said they live below that threshold.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., said in an interview he recommends saving 20% of gross salary each year.
The survey was completed before Feb. 11 and before the financial effects of the COVID-19 pandemic could be known. The report is based on responses from more than 17,000 physicians across 30 specialties.
A lower level of net worth among FPs corresponds with their being close to the bottom among physicians in compensation. They made $234,000 on average, according to the report. By contrast, orthopedists made more than twice as much, at $511,000.
Smaller homes, less mortgage debt
FPs were among the least likely to indicate that they had a home of more than 5,000 square feet. That was true for only 6% of FPs; it was true for 22% of plastic surgeons and orthopedists. Most (61%) lived in dwellings of 3,000 square feet or less.
At the same time, FPs reported smaller mortgages than many of their colleagues.
Nearly half (49%) of FPs have mortgages of $300,000 or less; 26% have no mortgage at all. That figure was much higher than the 37% of physicians overall who had mortgages of $300,000 or less, although almost the same percentage had no mortgage at all.
Most had no financial loss in the past year
In further good news, most FPs (70%) said they did not experience a financial loss in the past year. Of those who did experience a loss, the top reasons were problems with their practice, such as reimbursement changes or changes in practice situations, or bad investments.
FPs socked away more into tax-deferred than taxable accounts, the survey showed.
More than half (54%) of FPs put at least $1,000 into tax-deferred accounts, such as college savings or retirement accounts, although 14% said they do not regularly contribute to such accounts.
Fewer (29%) contributed at least $1,000 to a taxable account.
As for who pays the day-to-day bills in households, 56% of FPs said they pool resources with a spouse or partner and pay bills from a common fund. Only 4% split the bills equally, no matter the income difference. One in four said they do not have joint finances with a spouse or partner.
FPs were divided as to whether they are currently working with a financial planner (38%) or had not worked with one (37%); the remainder said they had met with or used one in the past.
A version of this article originally appeared on Medscape.com.
a Medscape survey has found.
According to the Medscape Family Physician Debt and Net Worth Report 2020, almost half of FPs (46%) reported having that amount as their net worth, compared with the 18% of gastroenterologists and 19% of urologists who fell into that category.
And whereas 19% of orthopedists reported at least $5 million in net worth, only 3% of FPs did.
A third are paying off student loans
FPs were also more likely, along with physical medicine and rehabilitation physicians, at 34%, to report that they are continuing to pay off student loans. Conversely, 14% of gastroenterologists and 15% of nephrologists and rheumatologists said they were still paying off the loans.
Student loan debt was third on the list for FPs. Two-thirds of FPs were paying off a mortgage, and 41% had car loan payments.
Overall, FPs appear to manage their finances well and are living within their means. Only 6% of FPs said they live above their means, whereas 51% said they live at their means, and 42% said they live below that threshold.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., said in an interview he recommends saving 20% of gross salary each year.
The survey was completed before Feb. 11 and before the financial effects of the COVID-19 pandemic could be known. The report is based on responses from more than 17,000 physicians across 30 specialties.
A lower level of net worth among FPs corresponds with their being close to the bottom among physicians in compensation. They made $234,000 on average, according to the report. By contrast, orthopedists made more than twice as much, at $511,000.
Smaller homes, less mortgage debt
FPs were among the least likely to indicate that they had a home of more than 5,000 square feet. That was true for only 6% of FPs; it was true for 22% of plastic surgeons and orthopedists. Most (61%) lived in dwellings of 3,000 square feet or less.
At the same time, FPs reported smaller mortgages than many of their colleagues.
Nearly half (49%) of FPs have mortgages of $300,000 or less; 26% have no mortgage at all. That figure was much higher than the 37% of physicians overall who had mortgages of $300,000 or less, although almost the same percentage had no mortgage at all.
Most had no financial loss in the past year
In further good news, most FPs (70%) said they did not experience a financial loss in the past year. Of those who did experience a loss, the top reasons were problems with their practice, such as reimbursement changes or changes in practice situations, or bad investments.
FPs socked away more into tax-deferred than taxable accounts, the survey showed.
More than half (54%) of FPs put at least $1,000 into tax-deferred accounts, such as college savings or retirement accounts, although 14% said they do not regularly contribute to such accounts.
Fewer (29%) contributed at least $1,000 to a taxable account.
As for who pays the day-to-day bills in households, 56% of FPs said they pool resources with a spouse or partner and pay bills from a common fund. Only 4% split the bills equally, no matter the income difference. One in four said they do not have joint finances with a spouse or partner.
FPs were divided as to whether they are currently working with a financial planner (38%) or had not worked with one (37%); the remainder said they had met with or used one in the past.
A version of this article originally appeared on Medscape.com.












