User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Children and COVID: Cases drop again, admission rate up slightly
The decline in new cases of child COVID-19 in the last week continued at about the same, somewhat slower pace as the week before, but admissions have moved upward slightly, according to the most recent data.
which, in turn, was 5.2% lower than a week earlier, according to the American Academy of Pediatrics and the Children’s Hospital Association, which have been collecting COVID-related data from state and territorial health departments since the early stages of the pandemic. New case declines in previous weeks had ranged from 9.3% to 46%.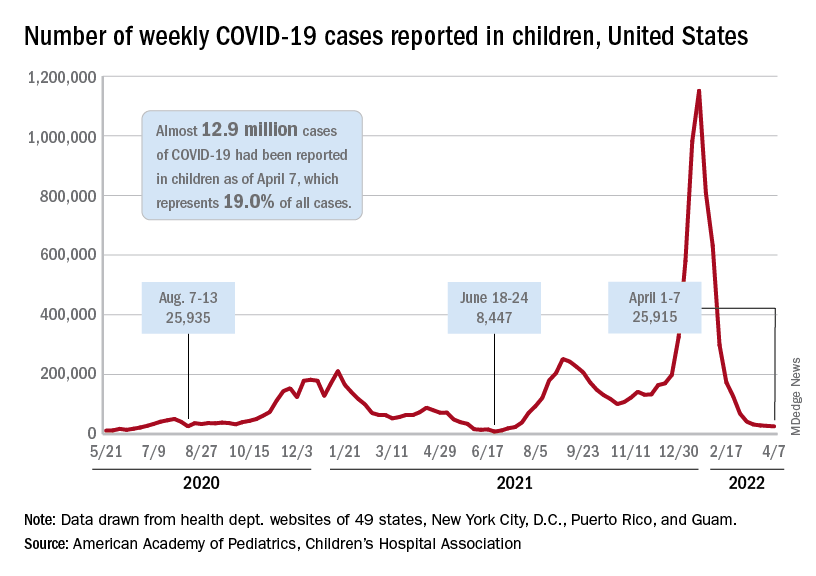
The nearly 26,000 cases reported during the first week of April represent a fall of 97.7% from the peak of the Omicron surge in mid-January, when weekly cases hit 1.15 million, and they represent the lowest weekly count since mid-July of 2021. Cumulative cases in children now number close to 12.9 million over the course of the pandemic, which is 19.0% of cases among all ages, the AAP and CHA said in their weekly COVID report.
Data on new-case rates from the Centers for Disease Control and Prevention show the same continued decline, but the CDC acknowledges the possibility of reporting delays in recent weeks. The numbers for the latest week, April 3-9, maintain the larger overall decline, but there have been a couple of small, temporary increases over the last month, the CDC reported on its COVID Data Tracker.
Daily new admissions of children aged 0-17 years with confirmed COVID were right around 0.14 per 100,000 population for April 3-9, compared with 0.13 per 100,000 during the week ending April 2, the CDC said, with reporting delays making it possible that the 0.14 figure could be revised upward in the near future. The highest admission rate, 1.25 children per 100,000 population, occurred on Jan. 15 and 16.
The latest on vaccination
New vaccinations slipped a bit in the last week, with the drop slightly larger among those aged 12-17 years – from 47,000 for the week of March 24-30 to 43,000 during March 31 to April 6 – than in children aged 5-11, who went from 70,000 initial doses to 69,000 over the same 2-week period, the AAP said in its weekly report on vaccination trends.
Among the states, Vermont has fully vaccinated more children aged 5-11 (58%) than any other state, while Hawaii is the leader in fully vaccinated 12- to 17-year-olds at 86%. The lowest comparable figures for both groups can be found in Alabama, where 10% of children aged 5-11 are fully vaccinated and 34% of those aged 12-17 have received both doses of the Pfizer-BioNTech vaccine, the AAP said.
National figures show equally large COVID vaccination gaps between the two age groups. As of April 11, 68% of all children aged 12-17 years had received at least one dose, compared with 34.6% of those aged 5-11, and 58.5% of the older group was fully vaccinated, versus 28.0% of the 5- to 11-year-olds, the CDC reported.
The decline in new cases of child COVID-19 in the last week continued at about the same, somewhat slower pace as the week before, but admissions have moved upward slightly, according to the most recent data.
which, in turn, was 5.2% lower than a week earlier, according to the American Academy of Pediatrics and the Children’s Hospital Association, which have been collecting COVID-related data from state and territorial health departments since the early stages of the pandemic. New case declines in previous weeks had ranged from 9.3% to 46%.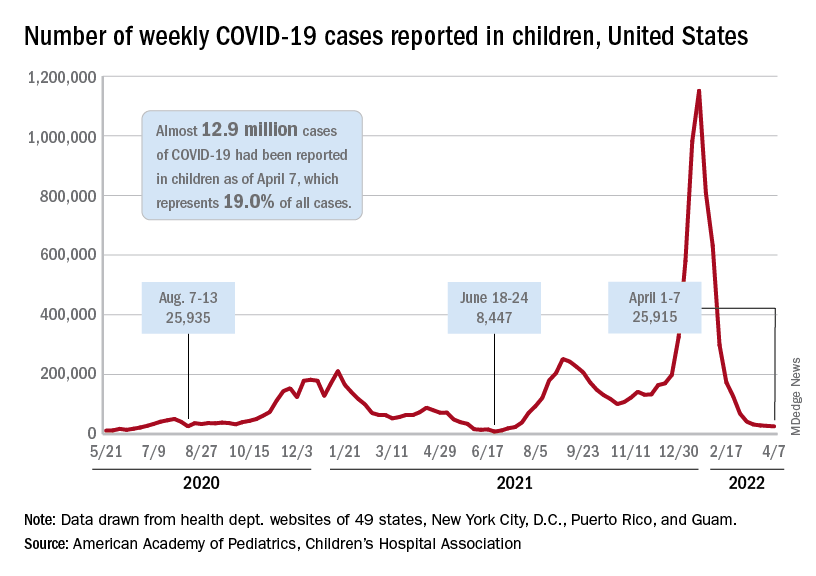
The nearly 26,000 cases reported during the first week of April represent a fall of 97.7% from the peak of the Omicron surge in mid-January, when weekly cases hit 1.15 million, and they represent the lowest weekly count since mid-July of 2021. Cumulative cases in children now number close to 12.9 million over the course of the pandemic, which is 19.0% of cases among all ages, the AAP and CHA said in their weekly COVID report.
Data on new-case rates from the Centers for Disease Control and Prevention show the same continued decline, but the CDC acknowledges the possibility of reporting delays in recent weeks. The numbers for the latest week, April 3-9, maintain the larger overall decline, but there have been a couple of small, temporary increases over the last month, the CDC reported on its COVID Data Tracker.
Daily new admissions of children aged 0-17 years with confirmed COVID were right around 0.14 per 100,000 population for April 3-9, compared with 0.13 per 100,000 during the week ending April 2, the CDC said, with reporting delays making it possible that the 0.14 figure could be revised upward in the near future. The highest admission rate, 1.25 children per 100,000 population, occurred on Jan. 15 and 16.
The latest on vaccination
New vaccinations slipped a bit in the last week, with the drop slightly larger among those aged 12-17 years – from 47,000 for the week of March 24-30 to 43,000 during March 31 to April 6 – than in children aged 5-11, who went from 70,000 initial doses to 69,000 over the same 2-week period, the AAP said in its weekly report on vaccination trends.
Among the states, Vermont has fully vaccinated more children aged 5-11 (58%) than any other state, while Hawaii is the leader in fully vaccinated 12- to 17-year-olds at 86%. The lowest comparable figures for both groups can be found in Alabama, where 10% of children aged 5-11 are fully vaccinated and 34% of those aged 12-17 have received both doses of the Pfizer-BioNTech vaccine, the AAP said.
National figures show equally large COVID vaccination gaps between the two age groups. As of April 11, 68% of all children aged 12-17 years had received at least one dose, compared with 34.6% of those aged 5-11, and 58.5% of the older group was fully vaccinated, versus 28.0% of the 5- to 11-year-olds, the CDC reported.
The decline in new cases of child COVID-19 in the last week continued at about the same, somewhat slower pace as the week before, but admissions have moved upward slightly, according to the most recent data.
which, in turn, was 5.2% lower than a week earlier, according to the American Academy of Pediatrics and the Children’s Hospital Association, which have been collecting COVID-related data from state and territorial health departments since the early stages of the pandemic. New case declines in previous weeks had ranged from 9.3% to 46%.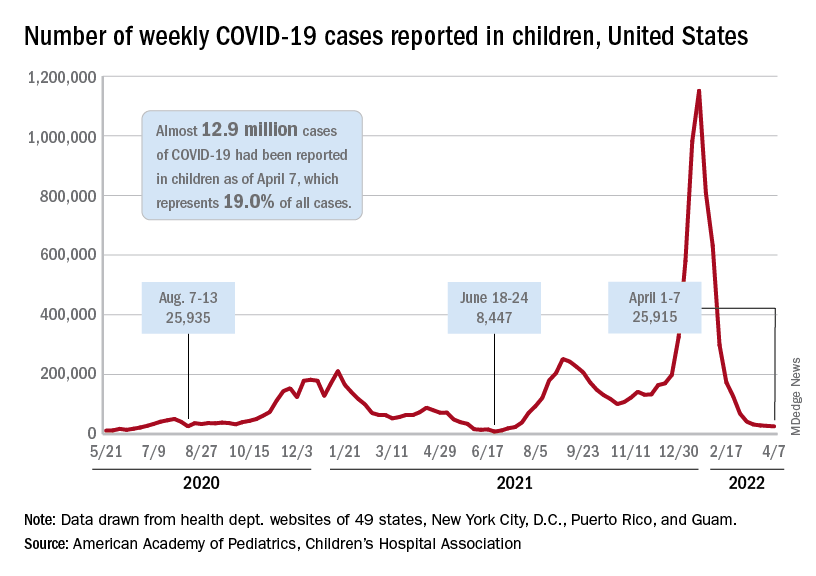
The nearly 26,000 cases reported during the first week of April represent a fall of 97.7% from the peak of the Omicron surge in mid-January, when weekly cases hit 1.15 million, and they represent the lowest weekly count since mid-July of 2021. Cumulative cases in children now number close to 12.9 million over the course of the pandemic, which is 19.0% of cases among all ages, the AAP and CHA said in their weekly COVID report.
Data on new-case rates from the Centers for Disease Control and Prevention show the same continued decline, but the CDC acknowledges the possibility of reporting delays in recent weeks. The numbers for the latest week, April 3-9, maintain the larger overall decline, but there have been a couple of small, temporary increases over the last month, the CDC reported on its COVID Data Tracker.
Daily new admissions of children aged 0-17 years with confirmed COVID were right around 0.14 per 100,000 population for April 3-9, compared with 0.13 per 100,000 during the week ending April 2, the CDC said, with reporting delays making it possible that the 0.14 figure could be revised upward in the near future. The highest admission rate, 1.25 children per 100,000 population, occurred on Jan. 15 and 16.
The latest on vaccination
New vaccinations slipped a bit in the last week, with the drop slightly larger among those aged 12-17 years – from 47,000 for the week of March 24-30 to 43,000 during March 31 to April 6 – than in children aged 5-11, who went from 70,000 initial doses to 69,000 over the same 2-week period, the AAP said in its weekly report on vaccination trends.
Among the states, Vermont has fully vaccinated more children aged 5-11 (58%) than any other state, while Hawaii is the leader in fully vaccinated 12- to 17-year-olds at 86%. The lowest comparable figures for both groups can be found in Alabama, where 10% of children aged 5-11 are fully vaccinated and 34% of those aged 12-17 have received both doses of the Pfizer-BioNTech vaccine, the AAP said.
National figures show equally large COVID vaccination gaps between the two age groups. As of April 11, 68% of all children aged 12-17 years had received at least one dose, compared with 34.6% of those aged 5-11, and 58.5% of the older group was fully vaccinated, versus 28.0% of the 5- to 11-year-olds, the CDC reported.
Adolescent overdose deaths nearly doubled in 2020 and spiked again in 2021
The number of overdose deaths in adolescents nearly doubled in 2020 from the year before and increased substantially again in 2021 after nearly a decade of fairly stable rates, according to data published in a JAMA research letter.
Most of the deaths involved fentanyl, the researchers found.
Joseph Friedman, MPH, of the Center for Social Medicine and Humanities at the University of California, Los Angeles, led the study, which analyzed adolescent (14-18 years old) overdose deaths in the United States from 2010 to June 2021 in light of increasing contamination in the supply of illicit drugs.
The researchers found there were 518 deaths among adolescents (2.40 per 100,000 population) in 2010, and the rates remained stable through 2019 with 492 deaths (2.36 per 100,000).
In 2020, however, deaths spiked to 954 (4.57 per 100 000), increasing by 94.3%, compared with 2019. In 2021, they increased another 20%.
The rise in fentanyl-involved deaths was particularly striking. Fentanyl-involved deaths increased from 253 (1.21 per 100,000) in 2019 to 680 (3.26 per 100,000) in 2020. The numbers through June 2021 were annualized for 2021 and calculations predicted 884 deaths (4.23 per 100,000) for the year.
Numbers point to fentanyl potency
In 2021, more than three-fourths (77.14%) of adolescent overdose deaths involved fentanyl, compared with 13.26% for benzodiazepines, 9.77% for methamphetamine, 7.33% for cocaine, 5.76% for prescription opioids, and 2.27% for heroin.
American Indian and Alaska Native adolescents had the highest overdose rate in 2021 (n = 24; 11.79 per 100,000), followed by Latinx adolescents (n = 354; 6.98 per 100,000).
“These adolescent trends fit a wider pattern of increasing racial and ethnic inequalities in overdose that deserve further investigation and intervention efforts,” the authors wrote.
Pandemic’s role unclear
The spikes in adolescent overdoses overlap the COVID-19 pandemic, but Dr. Friedman said in an interview the pandemic “may or may not have been a big factor. “
The authors wrote that drug use had generally been stable among adolescents between 2010 and 2020. The number of 10th graders reporting any illicit drug use was 30.2% in 2010 and 30.4% in 2020.
“So it’s not that more teens are using drugs. It’s just that drug use is becoming more dangerous due to the spread of counterfeit pills containing fentanyls,” Dr. Friedman said.
The authors noted that “the illicit drug supply has increasingly become contaminated with illicitly manufactured fentanyls and other synthetic opioid and benzodiazepine analogues.”
Mr. Friedman said the pandemic may have accelerated the spread of more dangerous forms of drugs as supply chains were disrupted.
Benjamin Brady, DrPH, an assistant professor at the University of Arizona, Tucson, who also has an appointment in the university’s Comprehensive Pain and Addiction Center, said in an interview the numbers that Dr. Friedman and colleagues present represent “worst fears coming true.”
He said he and his colleagues in the field “were anticipating a rise in overdose deaths for the next 5-10 years because of the way the supply-and-demand environment exists in the U.S.”
Dr. Brady explained that restricting access to prescription opioids has had an unfortunate side effect in decreasing access to a safer supply of drugs.
“Without having solutions that would reduce demand at the same rate, supply of the safer form of the drug has been reduced; that has pushed people toward heroin and street drugs and from 2016 on those have been adulterated with fentanyl,” he said.
He said the United States, compared with other developed nations, has been slower to embrace longer-term harm-reduction strategies and to improve access to treatment and care.
COVID likely also has exacerbated the problem in terms of isolation and reduction in quality of life that has adolescents seeking to fill that void with drugs, Dr. Brady said. They may be completely unaware that the drugs they are seeking are commonly cut with counterfeit fentanyl.
“Fentanyl can be up to 50 times stronger than heroin,” he noted. “Even just a little bit of fentanyl dramatically changes the risk profile on an overdose.”
Increasing rates of mental health concerns among adolescents over decades also contribute to drug-seeking trends, Dr. Brady noted.
Overdose increases in the overall population were smaller
In the overall population, the percentage increases were not nearly as large in 2020 and 2021 as they were for adolescents.
Rates of overdose deaths in the overall population increased steadily from 2010 and reached 70,630 in 2019. In 2020, the deaths increased to 91,799 (an increase of 29.48% from 2019) and increased 11.48% in 2021.
The researchers analyzed numbers from the Centers for Disease Control and Prevention WONDER (Wide-Ranging Online Data for Epidemiologic Research) database, which has records of all U.S. deaths for which drug overdose was listed as the underlying cause.
The authors and Dr. Brady report no relevant financial relationships.
The number of overdose deaths in adolescents nearly doubled in 2020 from the year before and increased substantially again in 2021 after nearly a decade of fairly stable rates, according to data published in a JAMA research letter.
Most of the deaths involved fentanyl, the researchers found.
Joseph Friedman, MPH, of the Center for Social Medicine and Humanities at the University of California, Los Angeles, led the study, which analyzed adolescent (14-18 years old) overdose deaths in the United States from 2010 to June 2021 in light of increasing contamination in the supply of illicit drugs.
The researchers found there were 518 deaths among adolescents (2.40 per 100,000 population) in 2010, and the rates remained stable through 2019 with 492 deaths (2.36 per 100,000).
In 2020, however, deaths spiked to 954 (4.57 per 100 000), increasing by 94.3%, compared with 2019. In 2021, they increased another 20%.
The rise in fentanyl-involved deaths was particularly striking. Fentanyl-involved deaths increased from 253 (1.21 per 100,000) in 2019 to 680 (3.26 per 100,000) in 2020. The numbers through June 2021 were annualized for 2021 and calculations predicted 884 deaths (4.23 per 100,000) for the year.
Numbers point to fentanyl potency
In 2021, more than three-fourths (77.14%) of adolescent overdose deaths involved fentanyl, compared with 13.26% for benzodiazepines, 9.77% for methamphetamine, 7.33% for cocaine, 5.76% for prescription opioids, and 2.27% for heroin.
American Indian and Alaska Native adolescents had the highest overdose rate in 2021 (n = 24; 11.79 per 100,000), followed by Latinx adolescents (n = 354; 6.98 per 100,000).
“These adolescent trends fit a wider pattern of increasing racial and ethnic inequalities in overdose that deserve further investigation and intervention efforts,” the authors wrote.
Pandemic’s role unclear
The spikes in adolescent overdoses overlap the COVID-19 pandemic, but Dr. Friedman said in an interview the pandemic “may or may not have been a big factor. “
The authors wrote that drug use had generally been stable among adolescents between 2010 and 2020. The number of 10th graders reporting any illicit drug use was 30.2% in 2010 and 30.4% in 2020.
“So it’s not that more teens are using drugs. It’s just that drug use is becoming more dangerous due to the spread of counterfeit pills containing fentanyls,” Dr. Friedman said.
The authors noted that “the illicit drug supply has increasingly become contaminated with illicitly manufactured fentanyls and other synthetic opioid and benzodiazepine analogues.”
Mr. Friedman said the pandemic may have accelerated the spread of more dangerous forms of drugs as supply chains were disrupted.
Benjamin Brady, DrPH, an assistant professor at the University of Arizona, Tucson, who also has an appointment in the university’s Comprehensive Pain and Addiction Center, said in an interview the numbers that Dr. Friedman and colleagues present represent “worst fears coming true.”
He said he and his colleagues in the field “were anticipating a rise in overdose deaths for the next 5-10 years because of the way the supply-and-demand environment exists in the U.S.”
Dr. Brady explained that restricting access to prescription opioids has had an unfortunate side effect in decreasing access to a safer supply of drugs.
“Without having solutions that would reduce demand at the same rate, supply of the safer form of the drug has been reduced; that has pushed people toward heroin and street drugs and from 2016 on those have been adulterated with fentanyl,” he said.
He said the United States, compared with other developed nations, has been slower to embrace longer-term harm-reduction strategies and to improve access to treatment and care.
COVID likely also has exacerbated the problem in terms of isolation and reduction in quality of life that has adolescents seeking to fill that void with drugs, Dr. Brady said. They may be completely unaware that the drugs they are seeking are commonly cut with counterfeit fentanyl.
“Fentanyl can be up to 50 times stronger than heroin,” he noted. “Even just a little bit of fentanyl dramatically changes the risk profile on an overdose.”
Increasing rates of mental health concerns among adolescents over decades also contribute to drug-seeking trends, Dr. Brady noted.
Overdose increases in the overall population were smaller
In the overall population, the percentage increases were not nearly as large in 2020 and 2021 as they were for adolescents.
Rates of overdose deaths in the overall population increased steadily from 2010 and reached 70,630 in 2019. In 2020, the deaths increased to 91,799 (an increase of 29.48% from 2019) and increased 11.48% in 2021.
The researchers analyzed numbers from the Centers for Disease Control and Prevention WONDER (Wide-Ranging Online Data for Epidemiologic Research) database, which has records of all U.S. deaths for which drug overdose was listed as the underlying cause.
The authors and Dr. Brady report no relevant financial relationships.
The number of overdose deaths in adolescents nearly doubled in 2020 from the year before and increased substantially again in 2021 after nearly a decade of fairly stable rates, according to data published in a JAMA research letter.
Most of the deaths involved fentanyl, the researchers found.
Joseph Friedman, MPH, of the Center for Social Medicine and Humanities at the University of California, Los Angeles, led the study, which analyzed adolescent (14-18 years old) overdose deaths in the United States from 2010 to June 2021 in light of increasing contamination in the supply of illicit drugs.
The researchers found there were 518 deaths among adolescents (2.40 per 100,000 population) in 2010, and the rates remained stable through 2019 with 492 deaths (2.36 per 100,000).
In 2020, however, deaths spiked to 954 (4.57 per 100 000), increasing by 94.3%, compared with 2019. In 2021, they increased another 20%.
The rise in fentanyl-involved deaths was particularly striking. Fentanyl-involved deaths increased from 253 (1.21 per 100,000) in 2019 to 680 (3.26 per 100,000) in 2020. The numbers through June 2021 were annualized for 2021 and calculations predicted 884 deaths (4.23 per 100,000) for the year.
Numbers point to fentanyl potency
In 2021, more than three-fourths (77.14%) of adolescent overdose deaths involved fentanyl, compared with 13.26% for benzodiazepines, 9.77% for methamphetamine, 7.33% for cocaine, 5.76% for prescription opioids, and 2.27% for heroin.
American Indian and Alaska Native adolescents had the highest overdose rate in 2021 (n = 24; 11.79 per 100,000), followed by Latinx adolescents (n = 354; 6.98 per 100,000).
“These adolescent trends fit a wider pattern of increasing racial and ethnic inequalities in overdose that deserve further investigation and intervention efforts,” the authors wrote.
Pandemic’s role unclear
The spikes in adolescent overdoses overlap the COVID-19 pandemic, but Dr. Friedman said in an interview the pandemic “may or may not have been a big factor. “
The authors wrote that drug use had generally been stable among adolescents between 2010 and 2020. The number of 10th graders reporting any illicit drug use was 30.2% in 2010 and 30.4% in 2020.
“So it’s not that more teens are using drugs. It’s just that drug use is becoming more dangerous due to the spread of counterfeit pills containing fentanyls,” Dr. Friedman said.
The authors noted that “the illicit drug supply has increasingly become contaminated with illicitly manufactured fentanyls and other synthetic opioid and benzodiazepine analogues.”
Mr. Friedman said the pandemic may have accelerated the spread of more dangerous forms of drugs as supply chains were disrupted.
Benjamin Brady, DrPH, an assistant professor at the University of Arizona, Tucson, who also has an appointment in the university’s Comprehensive Pain and Addiction Center, said in an interview the numbers that Dr. Friedman and colleagues present represent “worst fears coming true.”
He said he and his colleagues in the field “were anticipating a rise in overdose deaths for the next 5-10 years because of the way the supply-and-demand environment exists in the U.S.”
Dr. Brady explained that restricting access to prescription opioids has had an unfortunate side effect in decreasing access to a safer supply of drugs.
“Without having solutions that would reduce demand at the same rate, supply of the safer form of the drug has been reduced; that has pushed people toward heroin and street drugs and from 2016 on those have been adulterated with fentanyl,” he said.
He said the United States, compared with other developed nations, has been slower to embrace longer-term harm-reduction strategies and to improve access to treatment and care.
COVID likely also has exacerbated the problem in terms of isolation and reduction in quality of life that has adolescents seeking to fill that void with drugs, Dr. Brady said. They may be completely unaware that the drugs they are seeking are commonly cut with counterfeit fentanyl.
“Fentanyl can be up to 50 times stronger than heroin,” he noted. “Even just a little bit of fentanyl dramatically changes the risk profile on an overdose.”
Increasing rates of mental health concerns among adolescents over decades also contribute to drug-seeking trends, Dr. Brady noted.
Overdose increases in the overall population were smaller
In the overall population, the percentage increases were not nearly as large in 2020 and 2021 as they were for adolescents.
Rates of overdose deaths in the overall population increased steadily from 2010 and reached 70,630 in 2019. In 2020, the deaths increased to 91,799 (an increase of 29.48% from 2019) and increased 11.48% in 2021.
The researchers analyzed numbers from the Centers for Disease Control and Prevention WONDER (Wide-Ranging Online Data for Epidemiologic Research) database, which has records of all U.S. deaths for which drug overdose was listed as the underlying cause.
The authors and Dr. Brady report no relevant financial relationships.
FROM JAMA
Commentary: Adolescents are undertested for STIs
Despite current guidelines permitting opt-out STI screening and the ability in most states to treat adolescents 13 years old and older for STIs without parental notification, STI testing rates remain low. The articles about the 2019 survey raise several concerns.
Screening was more common with certain known risky behaviors, so risk-based screening seems prevalent. Of note, one recently reported factor increasing risky behaviors, but not noted above, is homelessness, suggesting it also be a trigger for STI screening (Child Youth Services Rev. 2022;139. doi: 10.1016/j.childyouth.2022.106538). But won’t risk-based screening inevitably lead to undertesting/treating? Are adolescents comfortable/willing to answer even the most carefully crafted, gentle, and simple questions about risky behaviors?
Because STIs are so frequent in adolescents (many asymptomatic), is risk-based screening/testing adequate for common STIs? Could urine-based screening for gonorrhea and chlamydia be useful in any adolescent who has been sexually active or uses the ED for routine care? Syphilis seems different. Screening requires a blood draw and is more difficult to implement, so risk-based testing seems okay. Also, the CDC recommends risk-based screening for syphilis.
Chief complaints at adolescent visits are usually not STI-related, unless symptomatic or visible, e.g., genital warts or herpes. So STI screening (even opt-out) will lengthen visits, perhaps a lot, over what was scheduled – even if only to explain negative results. Multiple visits with screening in the same morning could wreck patient flow. Maybe this doesn’t influence decisions to screen/test, but reexamining our approach can maximize appropriate STI screening/testing.
STIs run in packs, so if you detect one, expand testing to include the others.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Despite current guidelines permitting opt-out STI screening and the ability in most states to treat adolescents 13 years old and older for STIs without parental notification, STI testing rates remain low. The articles about the 2019 survey raise several concerns.
Screening was more common with certain known risky behaviors, so risk-based screening seems prevalent. Of note, one recently reported factor increasing risky behaviors, but not noted above, is homelessness, suggesting it also be a trigger for STI screening (Child Youth Services Rev. 2022;139. doi: 10.1016/j.childyouth.2022.106538). But won’t risk-based screening inevitably lead to undertesting/treating? Are adolescents comfortable/willing to answer even the most carefully crafted, gentle, and simple questions about risky behaviors?
Because STIs are so frequent in adolescents (many asymptomatic), is risk-based screening/testing adequate for common STIs? Could urine-based screening for gonorrhea and chlamydia be useful in any adolescent who has been sexually active or uses the ED for routine care? Syphilis seems different. Screening requires a blood draw and is more difficult to implement, so risk-based testing seems okay. Also, the CDC recommends risk-based screening for syphilis.
Chief complaints at adolescent visits are usually not STI-related, unless symptomatic or visible, e.g., genital warts or herpes. So STI screening (even opt-out) will lengthen visits, perhaps a lot, over what was scheduled – even if only to explain negative results. Multiple visits with screening in the same morning could wreck patient flow. Maybe this doesn’t influence decisions to screen/test, but reexamining our approach can maximize appropriate STI screening/testing.
STIs run in packs, so if you detect one, expand testing to include the others.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Despite current guidelines permitting opt-out STI screening and the ability in most states to treat adolescents 13 years old and older for STIs without parental notification, STI testing rates remain low. The articles about the 2019 survey raise several concerns.
Screening was more common with certain known risky behaviors, so risk-based screening seems prevalent. Of note, one recently reported factor increasing risky behaviors, but not noted above, is homelessness, suggesting it also be a trigger for STI screening (Child Youth Services Rev. 2022;139. doi: 10.1016/j.childyouth.2022.106538). But won’t risk-based screening inevitably lead to undertesting/treating? Are adolescents comfortable/willing to answer even the most carefully crafted, gentle, and simple questions about risky behaviors?
Because STIs are so frequent in adolescents (many asymptomatic), is risk-based screening/testing adequate for common STIs? Could urine-based screening for gonorrhea and chlamydia be useful in any adolescent who has been sexually active or uses the ED for routine care? Syphilis seems different. Screening requires a blood draw and is more difficult to implement, so risk-based testing seems okay. Also, the CDC recommends risk-based screening for syphilis.
Chief complaints at adolescent visits are usually not STI-related, unless symptomatic or visible, e.g., genital warts or herpes. So STI screening (even opt-out) will lengthen visits, perhaps a lot, over what was scheduled – even if only to explain negative results. Multiple visits with screening in the same morning could wreck patient flow. Maybe this doesn’t influence decisions to screen/test, but reexamining our approach can maximize appropriate STI screening/testing.
STIs run in packs, so if you detect one, expand testing to include the others.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
What can be new about developmental milestones?
The American Academy of Pediatrics, with funding from the Centers for Disease Control and Prevention, studied the CDC’s “Learn the Signs. Act Early” developmental surveillance milestones for children 0-5 years to update the milestones based on published studies. The goal was to improve this tool for developmental surveillance and use by the public. Developmental surveillance is not just observing a child at a check-up but rather “is a longitudinal process that involves eliciting concerns, taking a developmental history based on milestone attainment, observing milestones and other behaviors, examining the child, and applying clinical judgment during health supervision visits (HSVs).”1
While the milestones we were trained on were a good start and highlighted the developmental progression central to pediatrics, they were not based on norms or cut scores indicating significant developmental risk unless taught from a validated tool. The CDC was concerned that their public handouts and apps were based on median ages (middle number of the entire range) of attainment not the mode (most common) or even average ages. That means that about half of all typically developing children would “not have attained” that skill at the age noted, potentially evoking unnecessary concern for parents and a “wait-and-see” message from a knowledgeable provider who realized the statistical meaning and the broad range of normal. Another potential problem with using milestones set at the median age is that parents, especially those with several children or experienced friends, may see the provider as an alarmist when they have seen great variation in children who later were normal. This reaction can dampen provider willingness to discuss development or even to screen with validated tools. We have learned the hard way from COVID-19 that it is difficult to convey concepts of risk effectively both balancing fear and stimulating action.
The AAP experts reviewed the English literature for data-based milestones, finding 34 articles, 10 of which had an opinion for at least one milestone. If this sounds like a very small number, you are correct. You may not realize that almost all screening and diagnostic tools have been based on data collected by Gesell in 1928!2 While most of health care has changed since then, which milestones are measured in infants has not.
The biggest change from this review was deciding to use as milestones skills reported for 75% of children at each age of typical HSVs, adding ones for 15 and 30 months. The implication is that children not attaining these milestones are all at risk and deserving of more careful history, examination, and administration of a validated screening tool; not true when based on median data. Of the 94 existing CDC milestones retained after the review, one-third were moved to a different age with 21 of 31 assigned to an older age. Domains of functioning for the milestones were consolidated into social emotional, cognitive, language/communication, and motor, to help parents learn to distinguish these areas, and, although many milestones reflect several domains, each was included only once to reduce confusion.
Psychosocial assessment is recommended by the AAP and Bright Futures at every HSV but the fewest milestones with normative data were identified for this domain, often self-help rather than social engagement or emotion regulation skills. The cross-cultural study cited for many of the new milestones was reassuring overall in that the median ages for 67%-88% of milestones in most domains were equivalent across the four countries sampled, but only 22% of self-help skills were equivalent.3 This should remind us that parenting has more influence over psychosocial skills than other domains. Psychosocial and behavioral functioning, especially emotional regulation, also deserve “surveillance” as they have enormous impact on life outcomes but need to be measured and supported differently. Routine use of validated tools such as the Early Childhood Screening Assessment or the Ages & Stages Questionnaires: Social-Emotional for these domains are also needed.
Normal variations in temperament and patterns of attachment can affect many milestones including courage for walking, exploration, social engagement, and prosocial behaviors or self-control for social situations, attention, range of affect, and cooperation. All of these skills are among the 42 total (14 new) social-emotional milestones for 0- to 5-year-olds. Variations in these functions are at the root of the most common “challenging behaviors” in our studies in primary care. They are also the most vulnerable to suboptimal parent-child relationships, adverse childhood experiences, and social determinants of health.
As primary care providers, we not only need to detect children at risk for developmental problems but also promote and celebrate developmental progress. I hope that changing the threshold for concern to 75% will allow for a more positive review with the family (as fewer will be flagged as at risk) and chance to congratulate parents on all that is going well. But I also hope the change will not make us overlook parenting challenges, often from the psychosocial milestones most amenable to our guidance and support.
Early identification is mainly important to obtain the early intervention shown to improve outcomes. However, less than 25% of children with delays or disabilities receive early intervention before age 3 and most with emotional, behavioral, and developmental conditions, other than autism spectrum disorder, not before age 5. Since early intervention services are freely available in all states, we also need to do better at getting children to this care.
Let’s reconsider the process of developmental surveillance in this light of delayed referral: “Eliciting concerns” is key as parents have been shown to be usually correct in their worries. Listening to how they express the concerns can help you connect their specific issues when discussing reasons for referral. While most parent “recall of past milestones” is not accurate, current milestones reported are; thus, the need to have the new more accurate norms for all ages for comparison. When we make observations of a child’s abilities and behaviors ourselves we may not only pick up on issues missed by the parent, but will be more convincing in conveying the need for referral when indicated. When we “examine” the child we can use our professional skills to determine the very important risk factor of the quality of how a skill is performed, not just that it is. The recommended “use of validated screening tools” when the new milestones are not met give us an objective tool to share with parents, more confidence in when referral is warranted, which we will convey to parents (and perhaps skeptical relatives), and baseline documentation from which we can “track” referrals, progress, and, hopefully, better outcomes.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
References
1. Zubler JM et al. Pediatrics. 2022;149(3):e2021052138.
2. Gessell A et al. Macmillan: New York, 1928.
3. Ertem IO et al. Lancet Glob Health. 2018 Mar;6(3):e279-91.
The American Academy of Pediatrics, with funding from the Centers for Disease Control and Prevention, studied the CDC’s “Learn the Signs. Act Early” developmental surveillance milestones for children 0-5 years to update the milestones based on published studies. The goal was to improve this tool for developmental surveillance and use by the public. Developmental surveillance is not just observing a child at a check-up but rather “is a longitudinal process that involves eliciting concerns, taking a developmental history based on milestone attainment, observing milestones and other behaviors, examining the child, and applying clinical judgment during health supervision visits (HSVs).”1
While the milestones we were trained on were a good start and highlighted the developmental progression central to pediatrics, they were not based on norms or cut scores indicating significant developmental risk unless taught from a validated tool. The CDC was concerned that their public handouts and apps were based on median ages (middle number of the entire range) of attainment not the mode (most common) or even average ages. That means that about half of all typically developing children would “not have attained” that skill at the age noted, potentially evoking unnecessary concern for parents and a “wait-and-see” message from a knowledgeable provider who realized the statistical meaning and the broad range of normal. Another potential problem with using milestones set at the median age is that parents, especially those with several children or experienced friends, may see the provider as an alarmist when they have seen great variation in children who later were normal. This reaction can dampen provider willingness to discuss development or even to screen with validated tools. We have learned the hard way from COVID-19 that it is difficult to convey concepts of risk effectively both balancing fear and stimulating action.
The AAP experts reviewed the English literature for data-based milestones, finding 34 articles, 10 of which had an opinion for at least one milestone. If this sounds like a very small number, you are correct. You may not realize that almost all screening and diagnostic tools have been based on data collected by Gesell in 1928!2 While most of health care has changed since then, which milestones are measured in infants has not.
The biggest change from this review was deciding to use as milestones skills reported for 75% of children at each age of typical HSVs, adding ones for 15 and 30 months. The implication is that children not attaining these milestones are all at risk and deserving of more careful history, examination, and administration of a validated screening tool; not true when based on median data. Of the 94 existing CDC milestones retained after the review, one-third were moved to a different age with 21 of 31 assigned to an older age. Domains of functioning for the milestones were consolidated into social emotional, cognitive, language/communication, and motor, to help parents learn to distinguish these areas, and, although many milestones reflect several domains, each was included only once to reduce confusion.
Psychosocial assessment is recommended by the AAP and Bright Futures at every HSV but the fewest milestones with normative data were identified for this domain, often self-help rather than social engagement or emotion regulation skills. The cross-cultural study cited for many of the new milestones was reassuring overall in that the median ages for 67%-88% of milestones in most domains were equivalent across the four countries sampled, but only 22% of self-help skills were equivalent.3 This should remind us that parenting has more influence over psychosocial skills than other domains. Psychosocial and behavioral functioning, especially emotional regulation, also deserve “surveillance” as they have enormous impact on life outcomes but need to be measured and supported differently. Routine use of validated tools such as the Early Childhood Screening Assessment or the Ages & Stages Questionnaires: Social-Emotional for these domains are also needed.
Normal variations in temperament and patterns of attachment can affect many milestones including courage for walking, exploration, social engagement, and prosocial behaviors or self-control for social situations, attention, range of affect, and cooperation. All of these skills are among the 42 total (14 new) social-emotional milestones for 0- to 5-year-olds. Variations in these functions are at the root of the most common “challenging behaviors” in our studies in primary care. They are also the most vulnerable to suboptimal parent-child relationships, adverse childhood experiences, and social determinants of health.
As primary care providers, we not only need to detect children at risk for developmental problems but also promote and celebrate developmental progress. I hope that changing the threshold for concern to 75% will allow for a more positive review with the family (as fewer will be flagged as at risk) and chance to congratulate parents on all that is going well. But I also hope the change will not make us overlook parenting challenges, often from the psychosocial milestones most amenable to our guidance and support.
Early identification is mainly important to obtain the early intervention shown to improve outcomes. However, less than 25% of children with delays or disabilities receive early intervention before age 3 and most with emotional, behavioral, and developmental conditions, other than autism spectrum disorder, not before age 5. Since early intervention services are freely available in all states, we also need to do better at getting children to this care.
Let’s reconsider the process of developmental surveillance in this light of delayed referral: “Eliciting concerns” is key as parents have been shown to be usually correct in their worries. Listening to how they express the concerns can help you connect their specific issues when discussing reasons for referral. While most parent “recall of past milestones” is not accurate, current milestones reported are; thus, the need to have the new more accurate norms for all ages for comparison. When we make observations of a child’s abilities and behaviors ourselves we may not only pick up on issues missed by the parent, but will be more convincing in conveying the need for referral when indicated. When we “examine” the child we can use our professional skills to determine the very important risk factor of the quality of how a skill is performed, not just that it is. The recommended “use of validated screening tools” when the new milestones are not met give us an objective tool to share with parents, more confidence in when referral is warranted, which we will convey to parents (and perhaps skeptical relatives), and baseline documentation from which we can “track” referrals, progress, and, hopefully, better outcomes.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
References
1. Zubler JM et al. Pediatrics. 2022;149(3):e2021052138.
2. Gessell A et al. Macmillan: New York, 1928.
3. Ertem IO et al. Lancet Glob Health. 2018 Mar;6(3):e279-91.
The American Academy of Pediatrics, with funding from the Centers for Disease Control and Prevention, studied the CDC’s “Learn the Signs. Act Early” developmental surveillance milestones for children 0-5 years to update the milestones based on published studies. The goal was to improve this tool for developmental surveillance and use by the public. Developmental surveillance is not just observing a child at a check-up but rather “is a longitudinal process that involves eliciting concerns, taking a developmental history based on milestone attainment, observing milestones and other behaviors, examining the child, and applying clinical judgment during health supervision visits (HSVs).”1
While the milestones we were trained on were a good start and highlighted the developmental progression central to pediatrics, they were not based on norms or cut scores indicating significant developmental risk unless taught from a validated tool. The CDC was concerned that their public handouts and apps were based on median ages (middle number of the entire range) of attainment not the mode (most common) or even average ages. That means that about half of all typically developing children would “not have attained” that skill at the age noted, potentially evoking unnecessary concern for parents and a “wait-and-see” message from a knowledgeable provider who realized the statistical meaning and the broad range of normal. Another potential problem with using milestones set at the median age is that parents, especially those with several children or experienced friends, may see the provider as an alarmist when they have seen great variation in children who later were normal. This reaction can dampen provider willingness to discuss development or even to screen with validated tools. We have learned the hard way from COVID-19 that it is difficult to convey concepts of risk effectively both balancing fear and stimulating action.
The AAP experts reviewed the English literature for data-based milestones, finding 34 articles, 10 of which had an opinion for at least one milestone. If this sounds like a very small number, you are correct. You may not realize that almost all screening and diagnostic tools have been based on data collected by Gesell in 1928!2 While most of health care has changed since then, which milestones are measured in infants has not.
The biggest change from this review was deciding to use as milestones skills reported for 75% of children at each age of typical HSVs, adding ones for 15 and 30 months. The implication is that children not attaining these milestones are all at risk and deserving of more careful history, examination, and administration of a validated screening tool; not true when based on median data. Of the 94 existing CDC milestones retained after the review, one-third were moved to a different age with 21 of 31 assigned to an older age. Domains of functioning for the milestones were consolidated into social emotional, cognitive, language/communication, and motor, to help parents learn to distinguish these areas, and, although many milestones reflect several domains, each was included only once to reduce confusion.
Psychosocial assessment is recommended by the AAP and Bright Futures at every HSV but the fewest milestones with normative data were identified for this domain, often self-help rather than social engagement or emotion regulation skills. The cross-cultural study cited for many of the new milestones was reassuring overall in that the median ages for 67%-88% of milestones in most domains were equivalent across the four countries sampled, but only 22% of self-help skills were equivalent.3 This should remind us that parenting has more influence over psychosocial skills than other domains. Psychosocial and behavioral functioning, especially emotional regulation, also deserve “surveillance” as they have enormous impact on life outcomes but need to be measured and supported differently. Routine use of validated tools such as the Early Childhood Screening Assessment or the Ages & Stages Questionnaires: Social-Emotional for these domains are also needed.
Normal variations in temperament and patterns of attachment can affect many milestones including courage for walking, exploration, social engagement, and prosocial behaviors or self-control for social situations, attention, range of affect, and cooperation. All of these skills are among the 42 total (14 new) social-emotional milestones for 0- to 5-year-olds. Variations in these functions are at the root of the most common “challenging behaviors” in our studies in primary care. They are also the most vulnerable to suboptimal parent-child relationships, adverse childhood experiences, and social determinants of health.
As primary care providers, we not only need to detect children at risk for developmental problems but also promote and celebrate developmental progress. I hope that changing the threshold for concern to 75% will allow for a more positive review with the family (as fewer will be flagged as at risk) and chance to congratulate parents on all that is going well. But I also hope the change will not make us overlook parenting challenges, often from the psychosocial milestones most amenable to our guidance and support.
Early identification is mainly important to obtain the early intervention shown to improve outcomes. However, less than 25% of children with delays or disabilities receive early intervention before age 3 and most with emotional, behavioral, and developmental conditions, other than autism spectrum disorder, not before age 5. Since early intervention services are freely available in all states, we also need to do better at getting children to this care.
Let’s reconsider the process of developmental surveillance in this light of delayed referral: “Eliciting concerns” is key as parents have been shown to be usually correct in their worries. Listening to how they express the concerns can help you connect their specific issues when discussing reasons for referral. While most parent “recall of past milestones” is not accurate, current milestones reported are; thus, the need to have the new more accurate norms for all ages for comparison. When we make observations of a child’s abilities and behaviors ourselves we may not only pick up on issues missed by the parent, but will be more convincing in conveying the need for referral when indicated. When we “examine” the child we can use our professional skills to determine the very important risk factor of the quality of how a skill is performed, not just that it is. The recommended “use of validated screening tools” when the new milestones are not met give us an objective tool to share with parents, more confidence in when referral is warranted, which we will convey to parents (and perhaps skeptical relatives), and baseline documentation from which we can “track” referrals, progress, and, hopefully, better outcomes.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
References
1. Zubler JM et al. Pediatrics. 2022;149(3):e2021052138.
2. Gessell A et al. Macmillan: New York, 1928.
3. Ertem IO et al. Lancet Glob Health. 2018 Mar;6(3):e279-91.
COVID cases rising in about half of states
About half the states have reported increases in COVID cases fueled by the Omicron subvariant, Axios reported. Alaska, Vermont, and Rhode Island had the highest increases, with more than 20 new cases per 100,000 people.
Nationally, the statistics are encouraging, with the 7-day average of daily cases around 26,000 on April 6, down from around 41,000 on March 6, according to the Centers for Disease Control and Prevention. The number of deaths has dropped to an average of around 600 a day, down 34% from 2 weeks ago.
National health officials have said some spots would have a lot of COVID cases.
“Looking across the country, we see that 95% of counties are reporting low COVID-19 community levels, which represent over 97% of the U.S. population,” CDC Director Rochelle Walensky, MD, said April 5 at a White House news briefing.
“If we look more closely at the local level, we find a handful of counties where we are seeing increases in both cases and markers of more severe disease, like hospitalizations and in-patient bed capacity, which have resulted in an increased COVID-19 community level in some areas.”
Meanwhile, the Commonwealth Fund issued a report April 8 saying the U.S. vaccine program had prevented an estimated 2.2 million deaths and 17 million hospitalizations.
If the vaccine program didn’t exist, the United States would have had another 66 million COVID infections and spent about $900 billion more on health care, the foundation said.
The United States has reported about 982,000 COVID-related deaths so far with about 80 million COVID cases, according to the CDC.
“Our findings highlight the profound and ongoing impact of the vaccination program in reducing infections, hospitalizations, and deaths,” the Commonwealth Fund said.
“Investing in vaccination programs also has produced substantial cost savings – approximately the size of one-fifth of annual national health expenditures – by dramatically reducing the amount spent on COVID-19 hospitalizations.”
A version of this article first appeared on WebMD.com.
About half the states have reported increases in COVID cases fueled by the Omicron subvariant, Axios reported. Alaska, Vermont, and Rhode Island had the highest increases, with more than 20 new cases per 100,000 people.
Nationally, the statistics are encouraging, with the 7-day average of daily cases around 26,000 on April 6, down from around 41,000 on March 6, according to the Centers for Disease Control and Prevention. The number of deaths has dropped to an average of around 600 a day, down 34% from 2 weeks ago.
National health officials have said some spots would have a lot of COVID cases.
“Looking across the country, we see that 95% of counties are reporting low COVID-19 community levels, which represent over 97% of the U.S. population,” CDC Director Rochelle Walensky, MD, said April 5 at a White House news briefing.
“If we look more closely at the local level, we find a handful of counties where we are seeing increases in both cases and markers of more severe disease, like hospitalizations and in-patient bed capacity, which have resulted in an increased COVID-19 community level in some areas.”
Meanwhile, the Commonwealth Fund issued a report April 8 saying the U.S. vaccine program had prevented an estimated 2.2 million deaths and 17 million hospitalizations.
If the vaccine program didn’t exist, the United States would have had another 66 million COVID infections and spent about $900 billion more on health care, the foundation said.
The United States has reported about 982,000 COVID-related deaths so far with about 80 million COVID cases, according to the CDC.
“Our findings highlight the profound and ongoing impact of the vaccination program in reducing infections, hospitalizations, and deaths,” the Commonwealth Fund said.
“Investing in vaccination programs also has produced substantial cost savings – approximately the size of one-fifth of annual national health expenditures – by dramatically reducing the amount spent on COVID-19 hospitalizations.”
A version of this article first appeared on WebMD.com.
About half the states have reported increases in COVID cases fueled by the Omicron subvariant, Axios reported. Alaska, Vermont, and Rhode Island had the highest increases, with more than 20 new cases per 100,000 people.
Nationally, the statistics are encouraging, with the 7-day average of daily cases around 26,000 on April 6, down from around 41,000 on March 6, according to the Centers for Disease Control and Prevention. The number of deaths has dropped to an average of around 600 a day, down 34% from 2 weeks ago.
National health officials have said some spots would have a lot of COVID cases.
“Looking across the country, we see that 95% of counties are reporting low COVID-19 community levels, which represent over 97% of the U.S. population,” CDC Director Rochelle Walensky, MD, said April 5 at a White House news briefing.
“If we look more closely at the local level, we find a handful of counties where we are seeing increases in both cases and markers of more severe disease, like hospitalizations and in-patient bed capacity, which have resulted in an increased COVID-19 community level in some areas.”
Meanwhile, the Commonwealth Fund issued a report April 8 saying the U.S. vaccine program had prevented an estimated 2.2 million deaths and 17 million hospitalizations.
If the vaccine program didn’t exist, the United States would have had another 66 million COVID infections and spent about $900 billion more on health care, the foundation said.
The United States has reported about 982,000 COVID-related deaths so far with about 80 million COVID cases, according to the CDC.
“Our findings highlight the profound and ongoing impact of the vaccination program in reducing infections, hospitalizations, and deaths,” the Commonwealth Fund said.
“Investing in vaccination programs also has produced substantial cost savings – approximately the size of one-fifth of annual national health expenditures – by dramatically reducing the amount spent on COVID-19 hospitalizations.”
A version of this article first appeared on WebMD.com.
Adolescents are undertested for STIs
Approximately 20% of sexually active high schoolers reported testing for a sexually transmitted infection in the previous year, based on data from 2,501 respondents to the 2019 national Youth Risk Behavior Survey.
Data suggest that half of all new STIs in the United States occur in youth aged 15-24 years, and that 25% of sexually active young women in the United States have an STI, wrote Nicole Liddon, PhD, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
Although organizations including the American Academy of Pediatrics and the U.S. Preventive Services Task Force recommend varying degrees of routine STI screening for adolescents, data on the prevalence of testing in this population are limited, the researchers said.
However, the addition in 2019 of a question on STI testing to the national Youth Risk Behavior Survey (YRBS) provided an opportunity to assess prevalence of STI testing, identify potential barriers, and increase screening rates, they wrote.
In a study published in Pediatrics, the researchers reviewed data from the 2019 national YRBS, an anonymous survey administered biannually to public and private high school students across the United States.
The study population included 2,501 individuals who reported sexual activity with at least one person during the 3 months prior to the survey.
Overall, 20.4% of the respondents reported being tested for an STI in the previous year, including significantly more females than males (26.1% vs. 13.7%).
The prevalence of testing among females was not significantly different according to race/ethnicity, sexual identity, or the sex of sexual contacts, but the prevalence increased with age; 12.6%, 22.8%, 28.5%, and 36.9% for females aged 15 years and younger, 16 years, 17 years, and 18 years, respectively.
Among males, no significant differences in STI testing were noted according to race/ethnicity, age, sexual identity, or sex of sexual contacts.
The researchers also analyzed prevalence of STI tested based on sexual behaviors. Among female students, the prevalence of STI testing was higher among those who reported the following behaviors, compared with those who did not: nonuse of condoms at last sexual intercourse (34.1% vs. 18.2%), substance use at last sexual intercourse (32.0% vs. 24.7%), and having four or more lifetime sex partners (31.9% vs. 24.7%).
Among male students, the prevalence of STI testing was higher among those who reported the following behaviors, compared with those who did not: sex before age 13 years (27.1% vs. 12.1%), having two or more recent sex partners (22.4% vs. 10.4%), having four or more lifetime sex partners (22.3% vs. 9.5%), and substance use at last sexual intercourse (19.2% vs. 12.1%).
The low prevalence of STI testing in teens has become more urgent in the wake of the coronavirus pandemic, the researchers wrote. “These prevalence estimates were derived before the possible profound impacts of the pandemic on adolescent sexual behavior and access to and use of health care services.”
Current guidelines allow health care providers the options for opt-out STI screening as a strategy to improve screening rates and testing; however, this option does not eliminate the need for conversations with adolescent patients about sexual activity, they emphasized.
The study findings were limited by several other factors including the inability to directly assess adherence to screening recommendations specifically, the inability to determine whether low testing rates resulted from limited access to health care or missed screening opportunities at visits, and the inclusion only of high school students but not out-of-school youth who may have more limited access to testing.
However, the results highlight the need to improve STI testing services for adolescents, and to address barriers at the individual and clinic level, they said. The addition of a question about past-year STI testing to the 2019 and future YRBS survey will promote ongoing monitoring of efforts to increase testing rates.
Teen sexual health goes beyond testing
The current study shows that routine testing for STIs according to published guidelines is low, Cynthia Holland-Hall, MD, and Andrea E. Bonny, MD, of Nationwide Children’s Hospital and Ohio State University, both in Columbus, wrote in an accompanying editorial.
Notably, sexually active females and males who had sex with male partners, two groups for whom annual testing is specifically recommended by multiple organizations, had testing rates of less than 30%, they said. The authors highlighted the study’s lack of information on which specific barriers, such as lack of access to the health care system, lack of knowledge, and fear of disclosure, contributed to overall low rates of testing.
However, STI testing is only one element of sexual and reproductive health care. Although opt-out testing may improve detection rates, the editorialists emphasized the need for patient-provider conversations about sex, citing recent studies showing that adolescents who spent some time alone with providers were more likely to receive sexual and reproductive health (SRH) services in the past year.
“Resources such as confidentiality policies, checklists, and written screening tools may facilitate SRH discussions,” Dr. Holland-Hall and Dr. Bonny said. “With a little practice, respect, and intention, a caring provider can take the awkward out of discussing sexual health but must not opt out of the conversation.”
Privacy and time issues exacerbate low testing rates
The current study is especially important at this time because many adolescents have likely missed well visits, and therefore important STI screens, because of disruptions caused by the COVID-19 pandemic, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
“I was surprised that the rate of screening was only one in five,” said Dr. Kinsella. “I knew it would be suboptimal, but not that low.”
According to Dr. Kinsella, there are two major barriers to increasing STI testing in adolescents in primary care. One barrier is that insurance companies will often state on the bill what the testing was for, which will lead to an uncomfortable conversation at a later date for the adolescent and parent when the bill arrives in the mail. A second barrier is when to test during a visit,. “If we obtain urine samples on all adolescents and many of them are not sexually active, we are wasting a lot of time in the short visit to obtain urine,” she explained. “If testing is scheduled for the end of the visit, they often leave without providing a urine sample.”
Overall, the study is an important reminder to general pediatricians about STI testing for sexually active teens, she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Approximately 20% of sexually active high schoolers reported testing for a sexually transmitted infection in the previous year, based on data from 2,501 respondents to the 2019 national Youth Risk Behavior Survey.
Data suggest that half of all new STIs in the United States occur in youth aged 15-24 years, and that 25% of sexually active young women in the United States have an STI, wrote Nicole Liddon, PhD, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
Although organizations including the American Academy of Pediatrics and the U.S. Preventive Services Task Force recommend varying degrees of routine STI screening for adolescents, data on the prevalence of testing in this population are limited, the researchers said.
However, the addition in 2019 of a question on STI testing to the national Youth Risk Behavior Survey (YRBS) provided an opportunity to assess prevalence of STI testing, identify potential barriers, and increase screening rates, they wrote.
In a study published in Pediatrics, the researchers reviewed data from the 2019 national YRBS, an anonymous survey administered biannually to public and private high school students across the United States.
The study population included 2,501 individuals who reported sexual activity with at least one person during the 3 months prior to the survey.
Overall, 20.4% of the respondents reported being tested for an STI in the previous year, including significantly more females than males (26.1% vs. 13.7%).
The prevalence of testing among females was not significantly different according to race/ethnicity, sexual identity, or the sex of sexual contacts, but the prevalence increased with age; 12.6%, 22.8%, 28.5%, and 36.9% for females aged 15 years and younger, 16 years, 17 years, and 18 years, respectively.
Among males, no significant differences in STI testing were noted according to race/ethnicity, age, sexual identity, or sex of sexual contacts.
The researchers also analyzed prevalence of STI tested based on sexual behaviors. Among female students, the prevalence of STI testing was higher among those who reported the following behaviors, compared with those who did not: nonuse of condoms at last sexual intercourse (34.1% vs. 18.2%), substance use at last sexual intercourse (32.0% vs. 24.7%), and having four or more lifetime sex partners (31.9% vs. 24.7%).
Among male students, the prevalence of STI testing was higher among those who reported the following behaviors, compared with those who did not: sex before age 13 years (27.1% vs. 12.1%), having two or more recent sex partners (22.4% vs. 10.4%), having four or more lifetime sex partners (22.3% vs. 9.5%), and substance use at last sexual intercourse (19.2% vs. 12.1%).
The low prevalence of STI testing in teens has become more urgent in the wake of the coronavirus pandemic, the researchers wrote. “These prevalence estimates were derived before the possible profound impacts of the pandemic on adolescent sexual behavior and access to and use of health care services.”
Current guidelines allow health care providers the options for opt-out STI screening as a strategy to improve screening rates and testing; however, this option does not eliminate the need for conversations with adolescent patients about sexual activity, they emphasized.
The study findings were limited by several other factors including the inability to directly assess adherence to screening recommendations specifically, the inability to determine whether low testing rates resulted from limited access to health care or missed screening opportunities at visits, and the inclusion only of high school students but not out-of-school youth who may have more limited access to testing.
However, the results highlight the need to improve STI testing services for adolescents, and to address barriers at the individual and clinic level, they said. The addition of a question about past-year STI testing to the 2019 and future YRBS survey will promote ongoing monitoring of efforts to increase testing rates.
Teen sexual health goes beyond testing
The current study shows that routine testing for STIs according to published guidelines is low, Cynthia Holland-Hall, MD, and Andrea E. Bonny, MD, of Nationwide Children’s Hospital and Ohio State University, both in Columbus, wrote in an accompanying editorial.
Notably, sexually active females and males who had sex with male partners, two groups for whom annual testing is specifically recommended by multiple organizations, had testing rates of less than 30%, they said. The authors highlighted the study’s lack of information on which specific barriers, such as lack of access to the health care system, lack of knowledge, and fear of disclosure, contributed to overall low rates of testing.
However, STI testing is only one element of sexual and reproductive health care. Although opt-out testing may improve detection rates, the editorialists emphasized the need for patient-provider conversations about sex, citing recent studies showing that adolescents who spent some time alone with providers were more likely to receive sexual and reproductive health (SRH) services in the past year.
“Resources such as confidentiality policies, checklists, and written screening tools may facilitate SRH discussions,” Dr. Holland-Hall and Dr. Bonny said. “With a little practice, respect, and intention, a caring provider can take the awkward out of discussing sexual health but must not opt out of the conversation.”
Privacy and time issues exacerbate low testing rates
The current study is especially important at this time because many adolescents have likely missed well visits, and therefore important STI screens, because of disruptions caused by the COVID-19 pandemic, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
“I was surprised that the rate of screening was only one in five,” said Dr. Kinsella. “I knew it would be suboptimal, but not that low.”
According to Dr. Kinsella, there are two major barriers to increasing STI testing in adolescents in primary care. One barrier is that insurance companies will often state on the bill what the testing was for, which will lead to an uncomfortable conversation at a later date for the adolescent and parent when the bill arrives in the mail. A second barrier is when to test during a visit,. “If we obtain urine samples on all adolescents and many of them are not sexually active, we are wasting a lot of time in the short visit to obtain urine,” she explained. “If testing is scheduled for the end of the visit, they often leave without providing a urine sample.”
Overall, the study is an important reminder to general pediatricians about STI testing for sexually active teens, she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Approximately 20% of sexually active high schoolers reported testing for a sexually transmitted infection in the previous year, based on data from 2,501 respondents to the 2019 national Youth Risk Behavior Survey.
Data suggest that half of all new STIs in the United States occur in youth aged 15-24 years, and that 25% of sexually active young women in the United States have an STI, wrote Nicole Liddon, PhD, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
Although organizations including the American Academy of Pediatrics and the U.S. Preventive Services Task Force recommend varying degrees of routine STI screening for adolescents, data on the prevalence of testing in this population are limited, the researchers said.
However, the addition in 2019 of a question on STI testing to the national Youth Risk Behavior Survey (YRBS) provided an opportunity to assess prevalence of STI testing, identify potential barriers, and increase screening rates, they wrote.
In a study published in Pediatrics, the researchers reviewed data from the 2019 national YRBS, an anonymous survey administered biannually to public and private high school students across the United States.
The study population included 2,501 individuals who reported sexual activity with at least one person during the 3 months prior to the survey.
Overall, 20.4% of the respondents reported being tested for an STI in the previous year, including significantly more females than males (26.1% vs. 13.7%).
The prevalence of testing among females was not significantly different according to race/ethnicity, sexual identity, or the sex of sexual contacts, but the prevalence increased with age; 12.6%, 22.8%, 28.5%, and 36.9% for females aged 15 years and younger, 16 years, 17 years, and 18 years, respectively.
Among males, no significant differences in STI testing were noted according to race/ethnicity, age, sexual identity, or sex of sexual contacts.
The researchers also analyzed prevalence of STI tested based on sexual behaviors. Among female students, the prevalence of STI testing was higher among those who reported the following behaviors, compared with those who did not: nonuse of condoms at last sexual intercourse (34.1% vs. 18.2%), substance use at last sexual intercourse (32.0% vs. 24.7%), and having four or more lifetime sex partners (31.9% vs. 24.7%).
Among male students, the prevalence of STI testing was higher among those who reported the following behaviors, compared with those who did not: sex before age 13 years (27.1% vs. 12.1%), having two or more recent sex partners (22.4% vs. 10.4%), having four or more lifetime sex partners (22.3% vs. 9.5%), and substance use at last sexual intercourse (19.2% vs. 12.1%).
The low prevalence of STI testing in teens has become more urgent in the wake of the coronavirus pandemic, the researchers wrote. “These prevalence estimates were derived before the possible profound impacts of the pandemic on adolescent sexual behavior and access to and use of health care services.”
Current guidelines allow health care providers the options for opt-out STI screening as a strategy to improve screening rates and testing; however, this option does not eliminate the need for conversations with adolescent patients about sexual activity, they emphasized.
The study findings were limited by several other factors including the inability to directly assess adherence to screening recommendations specifically, the inability to determine whether low testing rates resulted from limited access to health care or missed screening opportunities at visits, and the inclusion only of high school students but not out-of-school youth who may have more limited access to testing.
However, the results highlight the need to improve STI testing services for adolescents, and to address barriers at the individual and clinic level, they said. The addition of a question about past-year STI testing to the 2019 and future YRBS survey will promote ongoing monitoring of efforts to increase testing rates.
Teen sexual health goes beyond testing
The current study shows that routine testing for STIs according to published guidelines is low, Cynthia Holland-Hall, MD, and Andrea E. Bonny, MD, of Nationwide Children’s Hospital and Ohio State University, both in Columbus, wrote in an accompanying editorial.
Notably, sexually active females and males who had sex with male partners, two groups for whom annual testing is specifically recommended by multiple organizations, had testing rates of less than 30%, they said. The authors highlighted the study’s lack of information on which specific barriers, such as lack of access to the health care system, lack of knowledge, and fear of disclosure, contributed to overall low rates of testing.
However, STI testing is only one element of sexual and reproductive health care. Although opt-out testing may improve detection rates, the editorialists emphasized the need for patient-provider conversations about sex, citing recent studies showing that adolescents who spent some time alone with providers were more likely to receive sexual and reproductive health (SRH) services in the past year.
“Resources such as confidentiality policies, checklists, and written screening tools may facilitate SRH discussions,” Dr. Holland-Hall and Dr. Bonny said. “With a little practice, respect, and intention, a caring provider can take the awkward out of discussing sexual health but must not opt out of the conversation.”
Privacy and time issues exacerbate low testing rates
The current study is especially important at this time because many adolescents have likely missed well visits, and therefore important STI screens, because of disruptions caused by the COVID-19 pandemic, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
“I was surprised that the rate of screening was only one in five,” said Dr. Kinsella. “I knew it would be suboptimal, but not that low.”
According to Dr. Kinsella, there are two major barriers to increasing STI testing in adolescents in primary care. One barrier is that insurance companies will often state on the bill what the testing was for, which will lead to an uncomfortable conversation at a later date for the adolescent and parent when the bill arrives in the mail. A second barrier is when to test during a visit,. “If we obtain urine samples on all adolescents and many of them are not sexually active, we are wasting a lot of time in the short visit to obtain urine,” she explained. “If testing is scheduled for the end of the visit, they often leave without providing a urine sample.”
Overall, the study is an important reminder to general pediatricians about STI testing for sexually active teens, she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM PEDIATRICS
Rapper sings about living with sickle cell disease
MANCHESTER, ENGLAND – A London-based rapper known for his gospel-inspired music has now given a voice to patients with sickle cell disease. He is using one of his music videos to raise awareness and educate health care professionals about living with the condition.
One important aim of the video, he says, is to help educate health care professionals, some of whom have not come across this condition, he explained at a session during the annual meeting of the British Society for Haematology, held recently in Manchester, England.
“It’s kind of frustrating to feel like your safe space, when you’re in front of doctors and nurses and paramedics who are supposed to know what it is and react with treatment, [and they] don’t know what it is,” Mr. Gaspar said.
He recalled an occasion in which he was experiencing a crisis, and his wife called for an ambulance. The paramedics arrived and his wife asked them for “gas and air and morphine, and they were, like, no, we don’t want to give that to him.” She tried to explain that he has sickle cell disease, but the paramedics had not heard of the condition and were suspicious that the request for morphine was a sign of drug addiction.
Mr. Gaspar expressed his frustration over “constantly having to prove that you have something serious enough to need the treatment you are asking for.”
At the meeting, Mr. Gaspar was talking on the stage with hematologist Dr. Stephen Hibbs from Barts Health NHS Trust, London.
Mr. Gaspar explained that it took years before he eventually reached “a point where I understood that it’s something that affects me and affects many other people, and I didn’t want to hide it any more.”
Sickle cell disease, which occurs primarily in people of Afro-Caribbean background, is a taboo subject in his community, Mr. Gaspar elaborated in an interview.
The condition has been associated with a great deal of stigma, with young sufferers traditionally seen as “demonically possessed,” he commented.
“So there was always a shameful aspect around it when it came to African families speaking about it, especially back in Africa.”
But after his parents came to the United Kingdom, he was able to “do his research and understand that it’s just genetics.”
This knowledge, Mr. Gaspar said, “takes away the spiritual aspect” and allows people to “have the conversation about sickle cell with potential partners” and ask them to find out their genotype, which in turn helps to “break down the barriers and the stigma.”
Mr. Gaspar emphasizes that there is much more work still to do.
In the video, he appeals to the Black community to make blood donations.
He said that something that “haunts” him is that currently, only 1% of Black people in the United Kingdom give blood, “so I really want the song to move my community to take a step forward and make that difference.”
He has been in contact with NHS Blood and Transplant, which provides blood and transplantation service to the National Health Service. They “really liked” the song, Mr. Gaspar said, and helped him get access to a hospital ward in University College Hospital, London, for the video.
“I really wanted to make a video that made people uncomfortable when watching it,” he said. It shows him hospitalized for pain and breathlessness and recalling having to use a Zimmer frame at the age of 25.
“This is a side of sickle cell that normally people don’t know,” he said.
Since releasing the song and the video, Mr. Gaspar says he has been contacted by many fellow patients. They have told him that he is now their “voice”; when they are asked how the condition affects them, “they can show someone the Hidden Pain video and say: This is how it feels.”
Clinicians have also approached him, asking if they can show his video to illustrate to patients and their families how having the condition may affect their lives.
Preventable deaths
At the meeting, Dr. Hibbs highlighted the 2021 report No One’s Listening, which was issued by the Sickle Cell Society following an inquiry into avoidable deaths and failures of care for sickle cell patients.
The inquiry, published by an All-Party Parliamentary group, found “serious care failings” in acute services and evidence of attitudes underpinned by racism. There was evidence of substandard care for sickle cell patients who were admitted to general wards or to hospital accident and emergency departments, as well as low awareness of the condition among health care professionals.
The report noted that the care failings have led to patient deaths, some which could have been prevented, and that there have been many “near misses.”
Many patients with sickle cell disease said they are “not being listened to” or are not being understood, especially during that vulnerable period when they are “in a crisis.”
Mr. Gaspar said that the report, and also the deaths, really struck a chord with him and many in his community. “We felt like that was us. ... We’ve all been in that same position where we’ve been misunderstood and not heard by nurses, doctors, or paramedics.”
He emphasized the need for awareness of the condition and the need for timely treatment. Just 3 weeks ago, Mr. Gaspar attended the funeral of one of his friends who is in the Hidden Pain video, a fellow sickle cell disease patient, who died at 30 years of age.
Ignorance about the condition ‘all too common’
The lack of awareness about sickle cell disease, even among health care professionals, is “all too common,” says Dr. Subarna Chakravorty, consultant pediatric hematologist, King’s College Hospital, London.
Even in London, where there is a large Black community and the teaching hospitals have world-class expertise, patients with sickle cell disease are “still facing a lot of problems with knowledge” among health care professionals, she said in an interview.
“Often people are having to speak for their own condition; which is fine, except that sometimes they are not believed,” she commented.
“On the one hand, you rely on the patient to provide information about their disease, and then when you receive it, you don’t do anything about it. So [they’re] between a rock and a hard place.”
Why are sickle cell patients treated in this way?
For Dr. Chakravorty, there is “a lot to be said about racism and disparities” in treating patients “as morphine-seekers, opiate addicts, even in children.”
“So we really need to improve the knowledge and perceptions among nonspecialist staff,” she said, “and even among specialists.”
Mr. Gaspar aims to help with this effort and hopes that his song and video will be useful to health care professionals. Sickle cell disease “needs to be spoken about,” and more doctors and nurses need to “know what it is,” he said.
He said it is a relief to encounter health care professionals who are knowledgeable about his condition. There have been times when he has been “having a crisis at home, calling the ambulance, and the paramedic comes and says: ‘Mr. Gaspar, you have sickle cell...we believe that you usually have gas and air and morphine, is that correct?’”
“That gives me a sense of peace, to know that I don’t have to fight my case or convince someone I have sickle cell, and I need to start treatment. They already know.”
No relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
MANCHESTER, ENGLAND – A London-based rapper known for his gospel-inspired music has now given a voice to patients with sickle cell disease. He is using one of his music videos to raise awareness and educate health care professionals about living with the condition.
One important aim of the video, he says, is to help educate health care professionals, some of whom have not come across this condition, he explained at a session during the annual meeting of the British Society for Haematology, held recently in Manchester, England.
“It’s kind of frustrating to feel like your safe space, when you’re in front of doctors and nurses and paramedics who are supposed to know what it is and react with treatment, [and they] don’t know what it is,” Mr. Gaspar said.
He recalled an occasion in which he was experiencing a crisis, and his wife called for an ambulance. The paramedics arrived and his wife asked them for “gas and air and morphine, and they were, like, no, we don’t want to give that to him.” She tried to explain that he has sickle cell disease, but the paramedics had not heard of the condition and were suspicious that the request for morphine was a sign of drug addiction.
Mr. Gaspar expressed his frustration over “constantly having to prove that you have something serious enough to need the treatment you are asking for.”
At the meeting, Mr. Gaspar was talking on the stage with hematologist Dr. Stephen Hibbs from Barts Health NHS Trust, London.
Mr. Gaspar explained that it took years before he eventually reached “a point where I understood that it’s something that affects me and affects many other people, and I didn’t want to hide it any more.”
Sickle cell disease, which occurs primarily in people of Afro-Caribbean background, is a taboo subject in his community, Mr. Gaspar elaborated in an interview.
The condition has been associated with a great deal of stigma, with young sufferers traditionally seen as “demonically possessed,” he commented.
“So there was always a shameful aspect around it when it came to African families speaking about it, especially back in Africa.”
But after his parents came to the United Kingdom, he was able to “do his research and understand that it’s just genetics.”
This knowledge, Mr. Gaspar said, “takes away the spiritual aspect” and allows people to “have the conversation about sickle cell with potential partners” and ask them to find out their genotype, which in turn helps to “break down the barriers and the stigma.”
Mr. Gaspar emphasizes that there is much more work still to do.
In the video, he appeals to the Black community to make blood donations.
He said that something that “haunts” him is that currently, only 1% of Black people in the United Kingdom give blood, “so I really want the song to move my community to take a step forward and make that difference.”
He has been in contact with NHS Blood and Transplant, which provides blood and transplantation service to the National Health Service. They “really liked” the song, Mr. Gaspar said, and helped him get access to a hospital ward in University College Hospital, London, for the video.
“I really wanted to make a video that made people uncomfortable when watching it,” he said. It shows him hospitalized for pain and breathlessness and recalling having to use a Zimmer frame at the age of 25.
“This is a side of sickle cell that normally people don’t know,” he said.
Since releasing the song and the video, Mr. Gaspar says he has been contacted by many fellow patients. They have told him that he is now their “voice”; when they are asked how the condition affects them, “they can show someone the Hidden Pain video and say: This is how it feels.”
Clinicians have also approached him, asking if they can show his video to illustrate to patients and their families how having the condition may affect their lives.
Preventable deaths
At the meeting, Dr. Hibbs highlighted the 2021 report No One’s Listening, which was issued by the Sickle Cell Society following an inquiry into avoidable deaths and failures of care for sickle cell patients.
The inquiry, published by an All-Party Parliamentary group, found “serious care failings” in acute services and evidence of attitudes underpinned by racism. There was evidence of substandard care for sickle cell patients who were admitted to general wards or to hospital accident and emergency departments, as well as low awareness of the condition among health care professionals.
The report noted that the care failings have led to patient deaths, some which could have been prevented, and that there have been many “near misses.”
Many patients with sickle cell disease said they are “not being listened to” or are not being understood, especially during that vulnerable period when they are “in a crisis.”
Mr. Gaspar said that the report, and also the deaths, really struck a chord with him and many in his community. “We felt like that was us. ... We’ve all been in that same position where we’ve been misunderstood and not heard by nurses, doctors, or paramedics.”
He emphasized the need for awareness of the condition and the need for timely treatment. Just 3 weeks ago, Mr. Gaspar attended the funeral of one of his friends who is in the Hidden Pain video, a fellow sickle cell disease patient, who died at 30 years of age.
Ignorance about the condition ‘all too common’
The lack of awareness about sickle cell disease, even among health care professionals, is “all too common,” says Dr. Subarna Chakravorty, consultant pediatric hematologist, King’s College Hospital, London.
Even in London, where there is a large Black community and the teaching hospitals have world-class expertise, patients with sickle cell disease are “still facing a lot of problems with knowledge” among health care professionals, she said in an interview.
“Often people are having to speak for their own condition; which is fine, except that sometimes they are not believed,” she commented.
“On the one hand, you rely on the patient to provide information about their disease, and then when you receive it, you don’t do anything about it. So [they’re] between a rock and a hard place.”
Why are sickle cell patients treated in this way?
For Dr. Chakravorty, there is “a lot to be said about racism and disparities” in treating patients “as morphine-seekers, opiate addicts, even in children.”
“So we really need to improve the knowledge and perceptions among nonspecialist staff,” she said, “and even among specialists.”
Mr. Gaspar aims to help with this effort and hopes that his song and video will be useful to health care professionals. Sickle cell disease “needs to be spoken about,” and more doctors and nurses need to “know what it is,” he said.
He said it is a relief to encounter health care professionals who are knowledgeable about his condition. There have been times when he has been “having a crisis at home, calling the ambulance, and the paramedic comes and says: ‘Mr. Gaspar, you have sickle cell...we believe that you usually have gas and air and morphine, is that correct?’”
“That gives me a sense of peace, to know that I don’t have to fight my case or convince someone I have sickle cell, and I need to start treatment. They already know.”
No relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
MANCHESTER, ENGLAND – A London-based rapper known for his gospel-inspired music has now given a voice to patients with sickle cell disease. He is using one of his music videos to raise awareness and educate health care professionals about living with the condition.
One important aim of the video, he says, is to help educate health care professionals, some of whom have not come across this condition, he explained at a session during the annual meeting of the British Society for Haematology, held recently in Manchester, England.
“It’s kind of frustrating to feel like your safe space, when you’re in front of doctors and nurses and paramedics who are supposed to know what it is and react with treatment, [and they] don’t know what it is,” Mr. Gaspar said.
He recalled an occasion in which he was experiencing a crisis, and his wife called for an ambulance. The paramedics arrived and his wife asked them for “gas and air and morphine, and they were, like, no, we don’t want to give that to him.” She tried to explain that he has sickle cell disease, but the paramedics had not heard of the condition and were suspicious that the request for morphine was a sign of drug addiction.
Mr. Gaspar expressed his frustration over “constantly having to prove that you have something serious enough to need the treatment you are asking for.”
At the meeting, Mr. Gaspar was talking on the stage with hematologist Dr. Stephen Hibbs from Barts Health NHS Trust, London.
Mr. Gaspar explained that it took years before he eventually reached “a point where I understood that it’s something that affects me and affects many other people, and I didn’t want to hide it any more.”
Sickle cell disease, which occurs primarily in people of Afro-Caribbean background, is a taboo subject in his community, Mr. Gaspar elaborated in an interview.
The condition has been associated with a great deal of stigma, with young sufferers traditionally seen as “demonically possessed,” he commented.
“So there was always a shameful aspect around it when it came to African families speaking about it, especially back in Africa.”
But after his parents came to the United Kingdom, he was able to “do his research and understand that it’s just genetics.”
This knowledge, Mr. Gaspar said, “takes away the spiritual aspect” and allows people to “have the conversation about sickle cell with potential partners” and ask them to find out their genotype, which in turn helps to “break down the barriers and the stigma.”
Mr. Gaspar emphasizes that there is much more work still to do.
In the video, he appeals to the Black community to make blood donations.
He said that something that “haunts” him is that currently, only 1% of Black people in the United Kingdom give blood, “so I really want the song to move my community to take a step forward and make that difference.”
He has been in contact with NHS Blood and Transplant, which provides blood and transplantation service to the National Health Service. They “really liked” the song, Mr. Gaspar said, and helped him get access to a hospital ward in University College Hospital, London, for the video.
“I really wanted to make a video that made people uncomfortable when watching it,” he said. It shows him hospitalized for pain and breathlessness and recalling having to use a Zimmer frame at the age of 25.
“This is a side of sickle cell that normally people don’t know,” he said.
Since releasing the song and the video, Mr. Gaspar says he has been contacted by many fellow patients. They have told him that he is now their “voice”; when they are asked how the condition affects them, “they can show someone the Hidden Pain video and say: This is how it feels.”
Clinicians have also approached him, asking if they can show his video to illustrate to patients and their families how having the condition may affect their lives.
Preventable deaths
At the meeting, Dr. Hibbs highlighted the 2021 report No One’s Listening, which was issued by the Sickle Cell Society following an inquiry into avoidable deaths and failures of care for sickle cell patients.
The inquiry, published by an All-Party Parliamentary group, found “serious care failings” in acute services and evidence of attitudes underpinned by racism. There was evidence of substandard care for sickle cell patients who were admitted to general wards or to hospital accident and emergency departments, as well as low awareness of the condition among health care professionals.
The report noted that the care failings have led to patient deaths, some which could have been prevented, and that there have been many “near misses.”
Many patients with sickle cell disease said they are “not being listened to” or are not being understood, especially during that vulnerable period when they are “in a crisis.”
Mr. Gaspar said that the report, and also the deaths, really struck a chord with him and many in his community. “We felt like that was us. ... We’ve all been in that same position where we’ve been misunderstood and not heard by nurses, doctors, or paramedics.”
He emphasized the need for awareness of the condition and the need for timely treatment. Just 3 weeks ago, Mr. Gaspar attended the funeral of one of his friends who is in the Hidden Pain video, a fellow sickle cell disease patient, who died at 30 years of age.
Ignorance about the condition ‘all too common’
The lack of awareness about sickle cell disease, even among health care professionals, is “all too common,” says Dr. Subarna Chakravorty, consultant pediatric hematologist, King’s College Hospital, London.
Even in London, where there is a large Black community and the teaching hospitals have world-class expertise, patients with sickle cell disease are “still facing a lot of problems with knowledge” among health care professionals, she said in an interview.
“Often people are having to speak for their own condition; which is fine, except that sometimes they are not believed,” she commented.
“On the one hand, you rely on the patient to provide information about their disease, and then when you receive it, you don’t do anything about it. So [they’re] between a rock and a hard place.”
Why are sickle cell patients treated in this way?
For Dr. Chakravorty, there is “a lot to be said about racism and disparities” in treating patients “as morphine-seekers, opiate addicts, even in children.”
“So we really need to improve the knowledge and perceptions among nonspecialist staff,” she said, “and even among specialists.”
Mr. Gaspar aims to help with this effort and hopes that his song and video will be useful to health care professionals. Sickle cell disease “needs to be spoken about,” and more doctors and nurses need to “know what it is,” he said.
He said it is a relief to encounter health care professionals who are knowledgeable about his condition. There have been times when he has been “having a crisis at home, calling the ambulance, and the paramedic comes and says: ‘Mr. Gaspar, you have sickle cell...we believe that you usually have gas and air and morphine, is that correct?’”
“That gives me a sense of peace, to know that I don’t have to fight my case or convince someone I have sickle cell, and I need to start treatment. They already know.”
No relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
Transgender youth: Bringing evidence to the political debates
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
Study: Physical fitness in children linked with concentration, quality of life
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
FROM THE JOURNAL OF CLINICAL MEDICINE
Hospitalists and PCPs crave greater communication
Hospitalists and PCPs want more dialogue while patients are in the hospital in order to coordinate and personalize care, according to data collected at Beth Israel Deaconess Medical Center, Boston. The results were presented at the annual meeting of the Society of General Internal Medicine.
“I think a major takeaway is that both hospitalists and primary care doctors agree that it’s important for primary care doctors to be involved in a patient’s hospitalization. They both identified a value that PCPs can bring to the table,” coresearcher Kristen Flint, MD, a primary care resident, told this news organization.
A majority in both camps reported that communication with the other party occurred in less than 25% of cases, whereas ideally it would happen half of the time. Dr. Flint noted that communication tools differ among hospitals, limiting the applicability of the findings.
The research team surveyed 39 hospitalists and 28 PCPs employed by the medical center during the first half of 2021. They also interviewed six hospitalists as they admitted and discharged patients.
The hospitalist movement, which took hold in response to cost and efficiency demands of managed care, led to the start of inpatient specialists, thereby reducing the need for PCPs to commute between their offices and the hospital to care for patients in both settings.
Primary care involvement is important during hospitalization
In the Beth Israel Deaconess survey, four out of five hospitalists and three-quarters of PCPs agreed that primary care involvement is still important during hospitalization, most critically during discharge and admission. Hospitalists reported that PCPs provide valuable data about a patient’s medical status, social supports, mental health, and goals for care. They also said having such data helps to boost patient trust and improve the quality of inpatient care.
“Most projects around communication between inpatient and outpatient doctors have really focused on the time of discharge,” when clinicians identify what care a patient will need after they leave the hospital, Dr. Flint said. “But we found that both sides felt increased communication at time of admission would also be beneficial.”
The biggest barrier for PCPs, cited by 82% of respondents, was lack of time. Hospitalists’ top impediment was being unable to find contact information for the other party, which was cited by 79% of these survey participants.
Hospitalists operate ‘in a very stressful environment’
The Beth Israel Deaconess research “documents what has largely been suspected,” said primary care general internist Allan Goroll, MD.
Dr. Goroll, a professor of medicine at Harvard Medical School, Boston, said in an interview that hospitalists operate “in a very stressful environment.”
“They [hospitalists] appreciate accurate information about a patient’s recent medical history, test results, and responses to treatment as well as a briefing on patient values and preferences, family dynamics, and priorities for the admission. It makes for a safer, more personalized, and more efficient hospital admission,” said Dr. Goroll, who was not involved in the research.
In a 2015 article in the New England Journal of Medicine, Dr. Goroll and Daniel Hunt, MD, director of hospital medicine at Emory University, Atlanta, proposed a collaborative model in which PCPs visit hospitalized patients and serve as consultants to inpatient staff. Dr. Goroll said Massachusetts General Hospital in Boston, where he practices, initiated a study of that approach, but it was interrupted by the pandemic.
“As limited time is the most often cited barrier to communication, future interventions such as asynchronous forms of communication between the two groups should be considered,” the researchers wrote in the NEJM perspective.
To narrow the gap, Beth Israel Deaconess will study converting an admission notification letter sent to PCPs into a two-way communication tool in which PCPs can insert patient information, Dr. Flint said.
Dr. Flint and Dr. Goroll have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hospitalists and PCPs want more dialogue while patients are in the hospital in order to coordinate and personalize care, according to data collected at Beth Israel Deaconess Medical Center, Boston. The results were presented at the annual meeting of the Society of General Internal Medicine.
“I think a major takeaway is that both hospitalists and primary care doctors agree that it’s important for primary care doctors to be involved in a patient’s hospitalization. They both identified a value that PCPs can bring to the table,” coresearcher Kristen Flint, MD, a primary care resident, told this news organization.
A majority in both camps reported that communication with the other party occurred in less than 25% of cases, whereas ideally it would happen half of the time. Dr. Flint noted that communication tools differ among hospitals, limiting the applicability of the findings.
The research team surveyed 39 hospitalists and 28 PCPs employed by the medical center during the first half of 2021. They also interviewed six hospitalists as they admitted and discharged patients.
The hospitalist movement, which took hold in response to cost and efficiency demands of managed care, led to the start of inpatient specialists, thereby reducing the need for PCPs to commute between their offices and the hospital to care for patients in both settings.
Primary care involvement is important during hospitalization
In the Beth Israel Deaconess survey, four out of five hospitalists and three-quarters of PCPs agreed that primary care involvement is still important during hospitalization, most critically during discharge and admission. Hospitalists reported that PCPs provide valuable data about a patient’s medical status, social supports, mental health, and goals for care. They also said having such data helps to boost patient trust and improve the quality of inpatient care.
“Most projects around communication between inpatient and outpatient doctors have really focused on the time of discharge,” when clinicians identify what care a patient will need after they leave the hospital, Dr. Flint said. “But we found that both sides felt increased communication at time of admission would also be beneficial.”
The biggest barrier for PCPs, cited by 82% of respondents, was lack of time. Hospitalists’ top impediment was being unable to find contact information for the other party, which was cited by 79% of these survey participants.
Hospitalists operate ‘in a very stressful environment’
The Beth Israel Deaconess research “documents what has largely been suspected,” said primary care general internist Allan Goroll, MD.
Dr. Goroll, a professor of medicine at Harvard Medical School, Boston, said in an interview that hospitalists operate “in a very stressful environment.”
“They [hospitalists] appreciate accurate information about a patient’s recent medical history, test results, and responses to treatment as well as a briefing on patient values and preferences, family dynamics, and priorities for the admission. It makes for a safer, more personalized, and more efficient hospital admission,” said Dr. Goroll, who was not involved in the research.
In a 2015 article in the New England Journal of Medicine, Dr. Goroll and Daniel Hunt, MD, director of hospital medicine at Emory University, Atlanta, proposed a collaborative model in which PCPs visit hospitalized patients and serve as consultants to inpatient staff. Dr. Goroll said Massachusetts General Hospital in Boston, where he practices, initiated a study of that approach, but it was interrupted by the pandemic.
“As limited time is the most often cited barrier to communication, future interventions such as asynchronous forms of communication between the two groups should be considered,” the researchers wrote in the NEJM perspective.
To narrow the gap, Beth Israel Deaconess will study converting an admission notification letter sent to PCPs into a two-way communication tool in which PCPs can insert patient information, Dr. Flint said.
Dr. Flint and Dr. Goroll have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hospitalists and PCPs want more dialogue while patients are in the hospital in order to coordinate and personalize care, according to data collected at Beth Israel Deaconess Medical Center, Boston. The results were presented at the annual meeting of the Society of General Internal Medicine.
“I think a major takeaway is that both hospitalists and primary care doctors agree that it’s important for primary care doctors to be involved in a patient’s hospitalization. They both identified a value that PCPs can bring to the table,” coresearcher Kristen Flint, MD, a primary care resident, told this news organization.
A majority in both camps reported that communication with the other party occurred in less than 25% of cases, whereas ideally it would happen half of the time. Dr. Flint noted that communication tools differ among hospitals, limiting the applicability of the findings.
The research team surveyed 39 hospitalists and 28 PCPs employed by the medical center during the first half of 2021. They also interviewed six hospitalists as they admitted and discharged patients.
The hospitalist movement, which took hold in response to cost and efficiency demands of managed care, led to the start of inpatient specialists, thereby reducing the need for PCPs to commute between their offices and the hospital to care for patients in both settings.
Primary care involvement is important during hospitalization
In the Beth Israel Deaconess survey, four out of five hospitalists and three-quarters of PCPs agreed that primary care involvement is still important during hospitalization, most critically during discharge and admission. Hospitalists reported that PCPs provide valuable data about a patient’s medical status, social supports, mental health, and goals for care. They also said having such data helps to boost patient trust and improve the quality of inpatient care.
“Most projects around communication between inpatient and outpatient doctors have really focused on the time of discharge,” when clinicians identify what care a patient will need after they leave the hospital, Dr. Flint said. “But we found that both sides felt increased communication at time of admission would also be beneficial.”
The biggest barrier for PCPs, cited by 82% of respondents, was lack of time. Hospitalists’ top impediment was being unable to find contact information for the other party, which was cited by 79% of these survey participants.
Hospitalists operate ‘in a very stressful environment’
The Beth Israel Deaconess research “documents what has largely been suspected,” said primary care general internist Allan Goroll, MD.
Dr. Goroll, a professor of medicine at Harvard Medical School, Boston, said in an interview that hospitalists operate “in a very stressful environment.”
“They [hospitalists] appreciate accurate information about a patient’s recent medical history, test results, and responses to treatment as well as a briefing on patient values and preferences, family dynamics, and priorities for the admission. It makes for a safer, more personalized, and more efficient hospital admission,” said Dr. Goroll, who was not involved in the research.
In a 2015 article in the New England Journal of Medicine, Dr. Goroll and Daniel Hunt, MD, director of hospital medicine at Emory University, Atlanta, proposed a collaborative model in which PCPs visit hospitalized patients and serve as consultants to inpatient staff. Dr. Goroll said Massachusetts General Hospital in Boston, where he practices, initiated a study of that approach, but it was interrupted by the pandemic.
“As limited time is the most often cited barrier to communication, future interventions such as asynchronous forms of communication between the two groups should be considered,” the researchers wrote in the NEJM perspective.
To narrow the gap, Beth Israel Deaconess will study converting an admission notification letter sent to PCPs into a two-way communication tool in which PCPs can insert patient information, Dr. Flint said.
Dr. Flint and Dr. Goroll have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SGIM 2022



