User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Supreme Court appears ready to overturn Roe
to the news outlet Politico.
The draft opinion, written by Justice Samuel Alito, outlines ways a presumed majority of the nine justices believes the 1973 ruling in Roe v. Wade was incorrect. If signed by a majority of the court, the ruling would eliminate the protections for abortion rights that Roe provided and give the 50 states the power to legislate abortion.
“We hold that Roe and Casey must be overruled,” Justice Alito writes in the draft. “It is time to heed the Constitution and return the issue of abortion to the people’s elected representatives.”
While a final ruling was not expected from the court until June, the leaked draft – a nearly unprecedented breach of the court’s internal workings – gives a strong signal of the court’s five most conservative members’ decisions. During oral arguments in the case in December, conservative justices appeared prepared to undo at least part of the country’s abortion protections.
President Joe Biden said his administration was already preparing for a potential ruling that struck down federal abortion protections.
The White House, he said in a statement, is working on a “response to the continued attack on abortion and reproductive rights, under a variety of possible outcomes in the cases pending before the Supreme Court. We will be ready when any ruling is issued.”
But if the draft opinion becomes final, he said the fight will move to the states.
“It will fall on our nation’s elected officials at all levels of government to protect a woman’s right to choose,” he said. “And it will fall on voters to elect pro-choice officials this November.”
With more pro-abortion rights members of Congress, it would be possible to pass federal legislation protecting abortion rights, “which I will work to pass and sign into law.”
Should the Alito draft become law, its first impact would be to allow a Mississippi law that bans abortions after 15 weeks to take effect.
But quickly after that, abortions would become illegal in many states. Several conservative-leaning states, mostly in the South and Midwest, have already passed laws severely restricting abortions well beyond what Roe allowed. Should Roe be overturned then, those laws would take effect without the threat of lengthy lawsuits or rulings from lower-court judges who have blocked them.
Nearly half of the states, mostly in the Northeast and West, would likely allow abortion to continue in some way. In fact, several states, including Colorado and Vermont, have already passed laws granting the right to an abortion into state law.
The leaked draft, however, is still a draft, meaning it remains possible Roe survives. Anthony Kreis, PhD, a professor of law at Georgia State University, says that could have been the point of whoever leaked the draft.
“It suggests to me that whoever leaked it knew that public outrage was the last resort to stopping the court from overturning Roe v. Wade and letting states ban all abortions,” Dr. Kreis said. “The danger that abortions won’t be legal in most of the country is very real.”
A version of this article first appeared on WebMD.com.
This article was updated 5/3/22.
to the news outlet Politico.
The draft opinion, written by Justice Samuel Alito, outlines ways a presumed majority of the nine justices believes the 1973 ruling in Roe v. Wade was incorrect. If signed by a majority of the court, the ruling would eliminate the protections for abortion rights that Roe provided and give the 50 states the power to legislate abortion.
“We hold that Roe and Casey must be overruled,” Justice Alito writes in the draft. “It is time to heed the Constitution and return the issue of abortion to the people’s elected representatives.”
While a final ruling was not expected from the court until June, the leaked draft – a nearly unprecedented breach of the court’s internal workings – gives a strong signal of the court’s five most conservative members’ decisions. During oral arguments in the case in December, conservative justices appeared prepared to undo at least part of the country’s abortion protections.
President Joe Biden said his administration was already preparing for a potential ruling that struck down federal abortion protections.
The White House, he said in a statement, is working on a “response to the continued attack on abortion and reproductive rights, under a variety of possible outcomes in the cases pending before the Supreme Court. We will be ready when any ruling is issued.”
But if the draft opinion becomes final, he said the fight will move to the states.
“It will fall on our nation’s elected officials at all levels of government to protect a woman’s right to choose,” he said. “And it will fall on voters to elect pro-choice officials this November.”
With more pro-abortion rights members of Congress, it would be possible to pass federal legislation protecting abortion rights, “which I will work to pass and sign into law.”
Should the Alito draft become law, its first impact would be to allow a Mississippi law that bans abortions after 15 weeks to take effect.
But quickly after that, abortions would become illegal in many states. Several conservative-leaning states, mostly in the South and Midwest, have already passed laws severely restricting abortions well beyond what Roe allowed. Should Roe be overturned then, those laws would take effect without the threat of lengthy lawsuits or rulings from lower-court judges who have blocked them.
Nearly half of the states, mostly in the Northeast and West, would likely allow abortion to continue in some way. In fact, several states, including Colorado and Vermont, have already passed laws granting the right to an abortion into state law.
The leaked draft, however, is still a draft, meaning it remains possible Roe survives. Anthony Kreis, PhD, a professor of law at Georgia State University, says that could have been the point of whoever leaked the draft.
“It suggests to me that whoever leaked it knew that public outrage was the last resort to stopping the court from overturning Roe v. Wade and letting states ban all abortions,” Dr. Kreis said. “The danger that abortions won’t be legal in most of the country is very real.”
A version of this article first appeared on WebMD.com.
This article was updated 5/3/22.
to the news outlet Politico.
The draft opinion, written by Justice Samuel Alito, outlines ways a presumed majority of the nine justices believes the 1973 ruling in Roe v. Wade was incorrect. If signed by a majority of the court, the ruling would eliminate the protections for abortion rights that Roe provided and give the 50 states the power to legislate abortion.
“We hold that Roe and Casey must be overruled,” Justice Alito writes in the draft. “It is time to heed the Constitution and return the issue of abortion to the people’s elected representatives.”
While a final ruling was not expected from the court until June, the leaked draft – a nearly unprecedented breach of the court’s internal workings – gives a strong signal of the court’s five most conservative members’ decisions. During oral arguments in the case in December, conservative justices appeared prepared to undo at least part of the country’s abortion protections.
President Joe Biden said his administration was already preparing for a potential ruling that struck down federal abortion protections.
The White House, he said in a statement, is working on a “response to the continued attack on abortion and reproductive rights, under a variety of possible outcomes in the cases pending before the Supreme Court. We will be ready when any ruling is issued.”
But if the draft opinion becomes final, he said the fight will move to the states.
“It will fall on our nation’s elected officials at all levels of government to protect a woman’s right to choose,” he said. “And it will fall on voters to elect pro-choice officials this November.”
With more pro-abortion rights members of Congress, it would be possible to pass federal legislation protecting abortion rights, “which I will work to pass and sign into law.”
Should the Alito draft become law, its first impact would be to allow a Mississippi law that bans abortions after 15 weeks to take effect.
But quickly after that, abortions would become illegal in many states. Several conservative-leaning states, mostly in the South and Midwest, have already passed laws severely restricting abortions well beyond what Roe allowed. Should Roe be overturned then, those laws would take effect without the threat of lengthy lawsuits or rulings from lower-court judges who have blocked them.
Nearly half of the states, mostly in the Northeast and West, would likely allow abortion to continue in some way. In fact, several states, including Colorado and Vermont, have already passed laws granting the right to an abortion into state law.
The leaked draft, however, is still a draft, meaning it remains possible Roe survives. Anthony Kreis, PhD, a professor of law at Georgia State University, says that could have been the point of whoever leaked the draft.
“It suggests to me that whoever leaked it knew that public outrage was the last resort to stopping the court from overturning Roe v. Wade and letting states ban all abortions,” Dr. Kreis said. “The danger that abortions won’t be legal in most of the country is very real.”
A version of this article first appeared on WebMD.com.
This article was updated 5/3/22.
Commentary: WHO, UNICEF warn about increased risk of measles outbreaks
The newly released global estimate is now 25 million children (2 million more than in 2020) missing scheduled vaccines. This continues to bode badly for multiple vaccine-preventable infections, but maybe the most for measles in 2022.
Specifically for measles vaccine, global two-dose coverage was only 71%. Coverage was less than 50% in 8 countries: Chad, Guinea, Samoa, North Korea, Central African Republic, Somalia, Angola, and South Sudan. These eight areas seem ripe for outbreaks this year and indeed Somalia is having an outbreak.
Overall, worldwide measles cases increased 79% in early 2022, compared with 2021. The top 10 countries for measles cases from November 2021 to April 2022, per the World Health Organization, include Nigeria, India, Soma Ethiopia, Pakistan, DR Congo, Afghanistan, Liberia, Cameroon, and Ivory Coast.
In the United States, we have been lucky so far with only 55 cases since the start of 2021. However, MMR two-dose coverage has dropped since the pandemic’s start. The list of U.S. areas with the lowest overall two-dose MMR coverage as of 2021 were D.C. (78.9%), Houston (93.7%), Idaho (86.5%), Wisconsin (87.2%), Maryland (87.6%), Georgia (88.5%), Kentucky (88.9%), Ohio (89.6%), and Minnesota (89.8%). Only 14 states had rates over the targeted 95% rate needed for community (herd) immunity against measles (MMWR Morb Mortal Wkly Rep. 2022;71:561-8).
Two bits of good news are that there seems to be some catch-up occurring in vaccine uptake overall (including MMR) and we now have two MMR suppliers in the United States since GlaxoSmithKline’s MMR was recently approved by the Food and Drug Administration for persons over 1 year of age. Let’s all redouble our efforts at adding to the catch-up efforts.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
The newly released global estimate is now 25 million children (2 million more than in 2020) missing scheduled vaccines. This continues to bode badly for multiple vaccine-preventable infections, but maybe the most for measles in 2022.
Specifically for measles vaccine, global two-dose coverage was only 71%. Coverage was less than 50% in 8 countries: Chad, Guinea, Samoa, North Korea, Central African Republic, Somalia, Angola, and South Sudan. These eight areas seem ripe for outbreaks this year and indeed Somalia is having an outbreak.
Overall, worldwide measles cases increased 79% in early 2022, compared with 2021. The top 10 countries for measles cases from November 2021 to April 2022, per the World Health Organization, include Nigeria, India, Soma Ethiopia, Pakistan, DR Congo, Afghanistan, Liberia, Cameroon, and Ivory Coast.
In the United States, we have been lucky so far with only 55 cases since the start of 2021. However, MMR two-dose coverage has dropped since the pandemic’s start. The list of U.S. areas with the lowest overall two-dose MMR coverage as of 2021 were D.C. (78.9%), Houston (93.7%), Idaho (86.5%), Wisconsin (87.2%), Maryland (87.6%), Georgia (88.5%), Kentucky (88.9%), Ohio (89.6%), and Minnesota (89.8%). Only 14 states had rates over the targeted 95% rate needed for community (herd) immunity against measles (MMWR Morb Mortal Wkly Rep. 2022;71:561-8).
Two bits of good news are that there seems to be some catch-up occurring in vaccine uptake overall (including MMR) and we now have two MMR suppliers in the United States since GlaxoSmithKline’s MMR was recently approved by the Food and Drug Administration for persons over 1 year of age. Let’s all redouble our efforts at adding to the catch-up efforts.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
The newly released global estimate is now 25 million children (2 million more than in 2020) missing scheduled vaccines. This continues to bode badly for multiple vaccine-preventable infections, but maybe the most for measles in 2022.
Specifically for measles vaccine, global two-dose coverage was only 71%. Coverage was less than 50% in 8 countries: Chad, Guinea, Samoa, North Korea, Central African Republic, Somalia, Angola, and South Sudan. These eight areas seem ripe for outbreaks this year and indeed Somalia is having an outbreak.
Overall, worldwide measles cases increased 79% in early 2022, compared with 2021. The top 10 countries for measles cases from November 2021 to April 2022, per the World Health Organization, include Nigeria, India, Soma Ethiopia, Pakistan, DR Congo, Afghanistan, Liberia, Cameroon, and Ivory Coast.
In the United States, we have been lucky so far with only 55 cases since the start of 2021. However, MMR two-dose coverage has dropped since the pandemic’s start. The list of U.S. areas with the lowest overall two-dose MMR coverage as of 2021 were D.C. (78.9%), Houston (93.7%), Idaho (86.5%), Wisconsin (87.2%), Maryland (87.6%), Georgia (88.5%), Kentucky (88.9%), Ohio (89.6%), and Minnesota (89.8%). Only 14 states had rates over the targeted 95% rate needed for community (herd) immunity against measles (MMWR Morb Mortal Wkly Rep. 2022;71:561-8).
Two bits of good news are that there seems to be some catch-up occurring in vaccine uptake overall (including MMR) and we now have two MMR suppliers in the United States since GlaxoSmithKline’s MMR was recently approved by the Food and Drug Administration for persons over 1 year of age. Let’s all redouble our efforts at adding to the catch-up efforts.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Cases of hepatitis of unknown origin in children raise alarm
After several cases of acute hepatitis of unknown origin in children in the United Kingdom were reported, further cases have now been reported in France (two cases), Denmark, Ireland, the Netherlands, and Spain. More than 80 cases have been reported overall, raising fears of an epidemic, according to a press release from the European Centre for Disease Prevention and Control (ECDC).
Furthermore, nine cases have allegedly been reported since last autumn in Alabama in the United States. These cases have mainly been in children aged 1-6 years.
Investigations are ongoing in all these countries, particularly as the “exact causes of these cases of acute hepatitis remain unknown.” Nevertheless, the team working on these cases in the United Kingdom believes that, based on clinical and epidemiologic data, the cause is probably infectious in origin.
Coordinated by the ECDC, European medical societies such as the European Association for the Study of the Liver and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) are working together to promote information sharing, according to the European agency.
Potential infectious agent
For context, on April 5, the United Kingdom reported about 10 cases of acute hepatitis of unknown origin in children younger than 10 in Scotland with no underlying conditions. Seven days later, the UK reported that 61 additional cases were under investigation in England, Wales, and Northern Ireland, the majority of which were in children aged 2-5 years.
The cases in the United Kingdom presented with severe acute hepatitis, with increased liver enzyme levels (aspartate aminotransferase [AST] and alanine aminotransferase [ALT] levels above 500 IU/L), and most presented with jaundice. Some reported gastrointestinal symptoms such as abdominal pain, diarrhea, and vomiting in the previous weeks.
The majority had no fever.
Although no deaths had been reported at press time, some cases needed to be seen by a liver specialist in the hospital, and others had to undergo transplantation (six transplants in Europe and two in the United States).
Initial hypotheses have focused on a potential infectious agent or exposure to a toxin. No link to COVID-19 vaccination has been established.
Which type of hepatitis?
The ECDC reports that laboratory tests have ruled out the possibility of attributing the cases to type A, B, C, D, and E viral hepatitis. Of the 13 cases in Scotland, 3 tested positive for SARS-CoV-2, 5 were negative, and 2 had contracted COVID-19 over the course of the last 3 months.
One positive test for adenovirus was found in 5 of the 13 Scottish cases, out of the 11 that were tested. All the cases reported in the United States tested positive for an adenovirus, five of which were for adenovirus type 41, which is responsible for inflammation of the bowel. Investigations are ongoing to assess any possible involvement of this virus in other cases. It should be noted that adenoviruses can cause hepatitis in children, but generally only in those who are immunosuppressed.
The pandemic could be another possible explanation, Nancy Reau, MD, head of the hepatology department at Rush University, Chicago, told this news organization. “The possibility that these cases are linked to COVID still exists,” she said. Some cases in the United Kingdom tested positive for COVID-19; none of these children had received the COVID-19 vaccine.
“COVID has been regularly seen to raise liver markers. It has also been shown to affect organs other than the lungs,” she stated. “It could be the case that, as it evolves, this virus has the potential to cause hepatitis in children.”
A version of this article first appeared on Medscape.com.
After several cases of acute hepatitis of unknown origin in children in the United Kingdom were reported, further cases have now been reported in France (two cases), Denmark, Ireland, the Netherlands, and Spain. More than 80 cases have been reported overall, raising fears of an epidemic, according to a press release from the European Centre for Disease Prevention and Control (ECDC).
Furthermore, nine cases have allegedly been reported since last autumn in Alabama in the United States. These cases have mainly been in children aged 1-6 years.
Investigations are ongoing in all these countries, particularly as the “exact causes of these cases of acute hepatitis remain unknown.” Nevertheless, the team working on these cases in the United Kingdom believes that, based on clinical and epidemiologic data, the cause is probably infectious in origin.
Coordinated by the ECDC, European medical societies such as the European Association for the Study of the Liver and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) are working together to promote information sharing, according to the European agency.
Potential infectious agent
For context, on April 5, the United Kingdom reported about 10 cases of acute hepatitis of unknown origin in children younger than 10 in Scotland with no underlying conditions. Seven days later, the UK reported that 61 additional cases were under investigation in England, Wales, and Northern Ireland, the majority of which were in children aged 2-5 years.
The cases in the United Kingdom presented with severe acute hepatitis, with increased liver enzyme levels (aspartate aminotransferase [AST] and alanine aminotransferase [ALT] levels above 500 IU/L), and most presented with jaundice. Some reported gastrointestinal symptoms such as abdominal pain, diarrhea, and vomiting in the previous weeks.
The majority had no fever.
Although no deaths had been reported at press time, some cases needed to be seen by a liver specialist in the hospital, and others had to undergo transplantation (six transplants in Europe and two in the United States).
Initial hypotheses have focused on a potential infectious agent or exposure to a toxin. No link to COVID-19 vaccination has been established.
Which type of hepatitis?
The ECDC reports that laboratory tests have ruled out the possibility of attributing the cases to type A, B, C, D, and E viral hepatitis. Of the 13 cases in Scotland, 3 tested positive for SARS-CoV-2, 5 were negative, and 2 had contracted COVID-19 over the course of the last 3 months.
One positive test for adenovirus was found in 5 of the 13 Scottish cases, out of the 11 that were tested. All the cases reported in the United States tested positive for an adenovirus, five of which were for adenovirus type 41, which is responsible for inflammation of the bowel. Investigations are ongoing to assess any possible involvement of this virus in other cases. It should be noted that adenoviruses can cause hepatitis in children, but generally only in those who are immunosuppressed.
The pandemic could be another possible explanation, Nancy Reau, MD, head of the hepatology department at Rush University, Chicago, told this news organization. “The possibility that these cases are linked to COVID still exists,” she said. Some cases in the United Kingdom tested positive for COVID-19; none of these children had received the COVID-19 vaccine.
“COVID has been regularly seen to raise liver markers. It has also been shown to affect organs other than the lungs,” she stated. “It could be the case that, as it evolves, this virus has the potential to cause hepatitis in children.”
A version of this article first appeared on Medscape.com.
After several cases of acute hepatitis of unknown origin in children in the United Kingdom were reported, further cases have now been reported in France (two cases), Denmark, Ireland, the Netherlands, and Spain. More than 80 cases have been reported overall, raising fears of an epidemic, according to a press release from the European Centre for Disease Prevention and Control (ECDC).
Furthermore, nine cases have allegedly been reported since last autumn in Alabama in the United States. These cases have mainly been in children aged 1-6 years.
Investigations are ongoing in all these countries, particularly as the “exact causes of these cases of acute hepatitis remain unknown.” Nevertheless, the team working on these cases in the United Kingdom believes that, based on clinical and epidemiologic data, the cause is probably infectious in origin.
Coordinated by the ECDC, European medical societies such as the European Association for the Study of the Liver and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) are working together to promote information sharing, according to the European agency.
Potential infectious agent
For context, on April 5, the United Kingdom reported about 10 cases of acute hepatitis of unknown origin in children younger than 10 in Scotland with no underlying conditions. Seven days later, the UK reported that 61 additional cases were under investigation in England, Wales, and Northern Ireland, the majority of which were in children aged 2-5 years.
The cases in the United Kingdom presented with severe acute hepatitis, with increased liver enzyme levels (aspartate aminotransferase [AST] and alanine aminotransferase [ALT] levels above 500 IU/L), and most presented with jaundice. Some reported gastrointestinal symptoms such as abdominal pain, diarrhea, and vomiting in the previous weeks.
The majority had no fever.
Although no deaths had been reported at press time, some cases needed to be seen by a liver specialist in the hospital, and others had to undergo transplantation (six transplants in Europe and two in the United States).
Initial hypotheses have focused on a potential infectious agent or exposure to a toxin. No link to COVID-19 vaccination has been established.
Which type of hepatitis?
The ECDC reports that laboratory tests have ruled out the possibility of attributing the cases to type A, B, C, D, and E viral hepatitis. Of the 13 cases in Scotland, 3 tested positive for SARS-CoV-2, 5 were negative, and 2 had contracted COVID-19 over the course of the last 3 months.
One positive test for adenovirus was found in 5 of the 13 Scottish cases, out of the 11 that were tested. All the cases reported in the United States tested positive for an adenovirus, five of which were for adenovirus type 41, which is responsible for inflammation of the bowel. Investigations are ongoing to assess any possible involvement of this virus in other cases. It should be noted that adenoviruses can cause hepatitis in children, but generally only in those who are immunosuppressed.
The pandemic could be another possible explanation, Nancy Reau, MD, head of the hepatology department at Rush University, Chicago, told this news organization. “The possibility that these cases are linked to COVID still exists,” she said. Some cases in the United Kingdom tested positive for COVID-19; none of these children had received the COVID-19 vaccine.
“COVID has been regularly seen to raise liver markers. It has also been shown to affect organs other than the lungs,” she stated. “It could be the case that, as it evolves, this virus has the potential to cause hepatitis in children.”
A version of this article first appeared on Medscape.com.
Vegetarian diet as good for children, with slight risk of underweight
With more families placing their children on vegetarian diets, the results from a Canadian longitudinal cohort study are reassuring: It found no clinically meaningful differences in height, growth, or biochemical measures of nutrition in young children on vegetarian and nonvegetarian diets.
While z scores (the standard deviation above or below the mean) were similar in both dietary groups, there was a weak association between a vegetarian diet and lower mean z height, as well as slightly higher odds of underweight.
No significant associations were identified between vegetarian and nonvegetarian diets for child z body mass index (BMI), serum ferritin, 25(OH)D, and serum lipids, according to Jonathon L. Maguire, MD. MSc, of St. Michael’s Hospital Pediatric Clinic in Toronto.
Moreover, the magnitude of the height and vegetarian diet association was small at just 0.3 cm for a 3-year-old child and unlikely to be clinically meaningful, Dr. Maguire and colleagues wrote online in Pediatrics.
In a secondary study outcome, cow’s milk consumption was associated with higher serum lipid levels for both diets. Serum lipids were similar among those who did or did not consume a vegetarian diet and consumed the recommended 2 cups of cow’s milk per day.
“The vast majority of children with vegetarian diets have similar growth and nutrition as children without vegetarian diets,” said Dr. Maguire, who is also a professor of pediatrics and nutritional sciences at the University of Toronto, in an interview. “But, I think we should be mindful to carefully plan vegetarian diets for children [who are] underweight.”
The study conclusion was based on 8,907 children, 6 months to 8 years of age, including 248 vegetarian and 25 vegan children, at baseline. They were part of theTARGet Kids! practice-based research network in Toronto.
The mean age of children at baseline was 2.2 years (standard deviation, 1.5), and 52.4% were male. Participants were followed for an average of 2.8 years (SD, 1.7).
Those with a vegetarian diet had longer breastfeeding duration: 12.6 months (SD, 9.5) versus 10.0 months (SD, 7.0). They were also more likely to be of Asian ethnicity: 33.8% versus 19.0%. Otherwise, children with and without a vegetarian diet were similar at baseline.
In study outcomes, vegetarian children had higher odds of underweight: body mass index z score less than –2 (odds ratio 1.87; 95% confidence interval, 1.19-2.96, P = .007), while no association with overweight or obesity was found.
In a secondary outcome, cow’s milk consumption was associated with higher levels of non–high-density lipoprotein cholesterol (P = .03), total cholesterol (P = .04), and low-density lipoprotein cholesterol (P = .02) in young children on a vegetarian diet. Levels were similar in children with and without a vegetarian diet who consumed the recommended 2 cups of cow’s milk per day.
Previous studies have found that vegetarian children have normal growth and development but tend to be leaner than their omnivore peers.
As for the potential effect of following a fully vegan diet on these nutritional measures, Dr. Maguire said, “Unfortunately, there were not enough children with vegan diets to make meaningful conclusions.”
Would results likely be similar in older children who have more independence and engage more with their peers?“ I don’t know, but we will be following these children for many years to come through the TARGet Kids! research network, Dr. Maguire said.
Studies such as this are timely as plant-based eating becomes more widespread in the United States. The 2007-2010 National Health and Nutrition Examination Surveys found that 2.1% of American adults followed a vegetarian diet, and that figure appears to have increased, with 5% of American adults self-identifying as vegetarian in a 2019 Gallup poll.
Offering her perspective on the Canadian study but not involved in it, Stephanie Di Figlia-Peck, MS, RDN, agreed the results indicate that “a vegetarian diet is not a negative thing for growth and development.” She is a lead registered dietitian in the division of adolescent medicine at Cohen Children’s Medical Center in New Hyde Park, N.Y. She noted, however, that the study looked only at very young children on average.
She stressed that vegetarian regimens require family commitment and agreed on the need for planning. “For these diets to work, a lot has to go into it. But if they’re carefully planned, there is adequate protein and micro- and macronutrients and there’s a nonnegative effect on growth and development.”
The study results mirror what she sees in clinical practice, with vegetarian children tending to weigh less. “Some obese and overweight children will adopt vegetarian diets to lose weight,” Ms. Di Figlia-Peck said.
And perseverance has rewards. “When people follow a vegetarian diet, they tend to have lower blood pressure and cholesterol. A plant-based diet can favorably impact diseases for an entire lifetime.”
This study was supported by the Canadian Institutes of Health Research and the St. Michael’s Hospital and SickKids Hospital foundations. Dr. Maguire received an unrestricted research grant for a previous investigator-initiated study from Dairy Farmers of Canada, and D drops provided nonfinancial support (vitamin D supplements) for a previous investigator-initiated study on vitamin D and respiratory tract infections. Coauthor David Jenkins, MD, PhD, DSc, reported research support from multiple private-sector and nonprivate organizations; several of his family members are involved in the promotion of vegetarian diets. Ms. Di Figlia-Peck had no competing interests to declare.
With more families placing their children on vegetarian diets, the results from a Canadian longitudinal cohort study are reassuring: It found no clinically meaningful differences in height, growth, or biochemical measures of nutrition in young children on vegetarian and nonvegetarian diets.
While z scores (the standard deviation above or below the mean) were similar in both dietary groups, there was a weak association between a vegetarian diet and lower mean z height, as well as slightly higher odds of underweight.
No significant associations were identified between vegetarian and nonvegetarian diets for child z body mass index (BMI), serum ferritin, 25(OH)D, and serum lipids, according to Jonathon L. Maguire, MD. MSc, of St. Michael’s Hospital Pediatric Clinic in Toronto.
Moreover, the magnitude of the height and vegetarian diet association was small at just 0.3 cm for a 3-year-old child and unlikely to be clinically meaningful, Dr. Maguire and colleagues wrote online in Pediatrics.
In a secondary study outcome, cow’s milk consumption was associated with higher serum lipid levels for both diets. Serum lipids were similar among those who did or did not consume a vegetarian diet and consumed the recommended 2 cups of cow’s milk per day.
“The vast majority of children with vegetarian diets have similar growth and nutrition as children without vegetarian diets,” said Dr. Maguire, who is also a professor of pediatrics and nutritional sciences at the University of Toronto, in an interview. “But, I think we should be mindful to carefully plan vegetarian diets for children [who are] underweight.”
The study conclusion was based on 8,907 children, 6 months to 8 years of age, including 248 vegetarian and 25 vegan children, at baseline. They were part of theTARGet Kids! practice-based research network in Toronto.
The mean age of children at baseline was 2.2 years (standard deviation, 1.5), and 52.4% were male. Participants were followed for an average of 2.8 years (SD, 1.7).
Those with a vegetarian diet had longer breastfeeding duration: 12.6 months (SD, 9.5) versus 10.0 months (SD, 7.0). They were also more likely to be of Asian ethnicity: 33.8% versus 19.0%. Otherwise, children with and without a vegetarian diet were similar at baseline.
In study outcomes, vegetarian children had higher odds of underweight: body mass index z score less than –2 (odds ratio 1.87; 95% confidence interval, 1.19-2.96, P = .007), while no association with overweight or obesity was found.
In a secondary outcome, cow’s milk consumption was associated with higher levels of non–high-density lipoprotein cholesterol (P = .03), total cholesterol (P = .04), and low-density lipoprotein cholesterol (P = .02) in young children on a vegetarian diet. Levels were similar in children with and without a vegetarian diet who consumed the recommended 2 cups of cow’s milk per day.
Previous studies have found that vegetarian children have normal growth and development but tend to be leaner than their omnivore peers.
As for the potential effect of following a fully vegan diet on these nutritional measures, Dr. Maguire said, “Unfortunately, there were not enough children with vegan diets to make meaningful conclusions.”
Would results likely be similar in older children who have more independence and engage more with their peers?“ I don’t know, but we will be following these children for many years to come through the TARGet Kids! research network, Dr. Maguire said.
Studies such as this are timely as plant-based eating becomes more widespread in the United States. The 2007-2010 National Health and Nutrition Examination Surveys found that 2.1% of American adults followed a vegetarian diet, and that figure appears to have increased, with 5% of American adults self-identifying as vegetarian in a 2019 Gallup poll.
Offering her perspective on the Canadian study but not involved in it, Stephanie Di Figlia-Peck, MS, RDN, agreed the results indicate that “a vegetarian diet is not a negative thing for growth and development.” She is a lead registered dietitian in the division of adolescent medicine at Cohen Children’s Medical Center in New Hyde Park, N.Y. She noted, however, that the study looked only at very young children on average.
She stressed that vegetarian regimens require family commitment and agreed on the need for planning. “For these diets to work, a lot has to go into it. But if they’re carefully planned, there is adequate protein and micro- and macronutrients and there’s a nonnegative effect on growth and development.”
The study results mirror what she sees in clinical practice, with vegetarian children tending to weigh less. “Some obese and overweight children will adopt vegetarian diets to lose weight,” Ms. Di Figlia-Peck said.
And perseverance has rewards. “When people follow a vegetarian diet, they tend to have lower blood pressure and cholesterol. A plant-based diet can favorably impact diseases for an entire lifetime.”
This study was supported by the Canadian Institutes of Health Research and the St. Michael’s Hospital and SickKids Hospital foundations. Dr. Maguire received an unrestricted research grant for a previous investigator-initiated study from Dairy Farmers of Canada, and D drops provided nonfinancial support (vitamin D supplements) for a previous investigator-initiated study on vitamin D and respiratory tract infections. Coauthor David Jenkins, MD, PhD, DSc, reported research support from multiple private-sector and nonprivate organizations; several of his family members are involved in the promotion of vegetarian diets. Ms. Di Figlia-Peck had no competing interests to declare.
With more families placing their children on vegetarian diets, the results from a Canadian longitudinal cohort study are reassuring: It found no clinically meaningful differences in height, growth, or biochemical measures of nutrition in young children on vegetarian and nonvegetarian diets.
While z scores (the standard deviation above or below the mean) were similar in both dietary groups, there was a weak association between a vegetarian diet and lower mean z height, as well as slightly higher odds of underweight.
No significant associations were identified between vegetarian and nonvegetarian diets for child z body mass index (BMI), serum ferritin, 25(OH)D, and serum lipids, according to Jonathon L. Maguire, MD. MSc, of St. Michael’s Hospital Pediatric Clinic in Toronto.
Moreover, the magnitude of the height and vegetarian diet association was small at just 0.3 cm for a 3-year-old child and unlikely to be clinically meaningful, Dr. Maguire and colleagues wrote online in Pediatrics.
In a secondary study outcome, cow’s milk consumption was associated with higher serum lipid levels for both diets. Serum lipids were similar among those who did or did not consume a vegetarian diet and consumed the recommended 2 cups of cow’s milk per day.
“The vast majority of children with vegetarian diets have similar growth and nutrition as children without vegetarian diets,” said Dr. Maguire, who is also a professor of pediatrics and nutritional sciences at the University of Toronto, in an interview. “But, I think we should be mindful to carefully plan vegetarian diets for children [who are] underweight.”
The study conclusion was based on 8,907 children, 6 months to 8 years of age, including 248 vegetarian and 25 vegan children, at baseline. They were part of theTARGet Kids! practice-based research network in Toronto.
The mean age of children at baseline was 2.2 years (standard deviation, 1.5), and 52.4% were male. Participants were followed for an average of 2.8 years (SD, 1.7).
Those with a vegetarian diet had longer breastfeeding duration: 12.6 months (SD, 9.5) versus 10.0 months (SD, 7.0). They were also more likely to be of Asian ethnicity: 33.8% versus 19.0%. Otherwise, children with and without a vegetarian diet were similar at baseline.
In study outcomes, vegetarian children had higher odds of underweight: body mass index z score less than –2 (odds ratio 1.87; 95% confidence interval, 1.19-2.96, P = .007), while no association with overweight or obesity was found.
In a secondary outcome, cow’s milk consumption was associated with higher levels of non–high-density lipoprotein cholesterol (P = .03), total cholesterol (P = .04), and low-density lipoprotein cholesterol (P = .02) in young children on a vegetarian diet. Levels were similar in children with and without a vegetarian diet who consumed the recommended 2 cups of cow’s milk per day.
Previous studies have found that vegetarian children have normal growth and development but tend to be leaner than their omnivore peers.
As for the potential effect of following a fully vegan diet on these nutritional measures, Dr. Maguire said, “Unfortunately, there were not enough children with vegan diets to make meaningful conclusions.”
Would results likely be similar in older children who have more independence and engage more with their peers?“ I don’t know, but we will be following these children for many years to come through the TARGet Kids! research network, Dr. Maguire said.
Studies such as this are timely as plant-based eating becomes more widespread in the United States. The 2007-2010 National Health and Nutrition Examination Surveys found that 2.1% of American adults followed a vegetarian diet, and that figure appears to have increased, with 5% of American adults self-identifying as vegetarian in a 2019 Gallup poll.
Offering her perspective on the Canadian study but not involved in it, Stephanie Di Figlia-Peck, MS, RDN, agreed the results indicate that “a vegetarian diet is not a negative thing for growth and development.” She is a lead registered dietitian in the division of adolescent medicine at Cohen Children’s Medical Center in New Hyde Park, N.Y. She noted, however, that the study looked only at very young children on average.
She stressed that vegetarian regimens require family commitment and agreed on the need for planning. “For these diets to work, a lot has to go into it. But if they’re carefully planned, there is adequate protein and micro- and macronutrients and there’s a nonnegative effect on growth and development.”
The study results mirror what she sees in clinical practice, with vegetarian children tending to weigh less. “Some obese and overweight children will adopt vegetarian diets to lose weight,” Ms. Di Figlia-Peck said.
And perseverance has rewards. “When people follow a vegetarian diet, they tend to have lower blood pressure and cholesterol. A plant-based diet can favorably impact diseases for an entire lifetime.”
This study was supported by the Canadian Institutes of Health Research and the St. Michael’s Hospital and SickKids Hospital foundations. Dr. Maguire received an unrestricted research grant for a previous investigator-initiated study from Dairy Farmers of Canada, and D drops provided nonfinancial support (vitamin D supplements) for a previous investigator-initiated study on vitamin D and respiratory tract infections. Coauthor David Jenkins, MD, PhD, DSc, reported research support from multiple private-sector and nonprivate organizations; several of his family members are involved in the promotion of vegetarian diets. Ms. Di Figlia-Peck had no competing interests to declare.
FROM PEDIATRICS
Commentary: Antibiotics use and vaccine antibody levels
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Antibiotics use and vaccine antibody levels
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).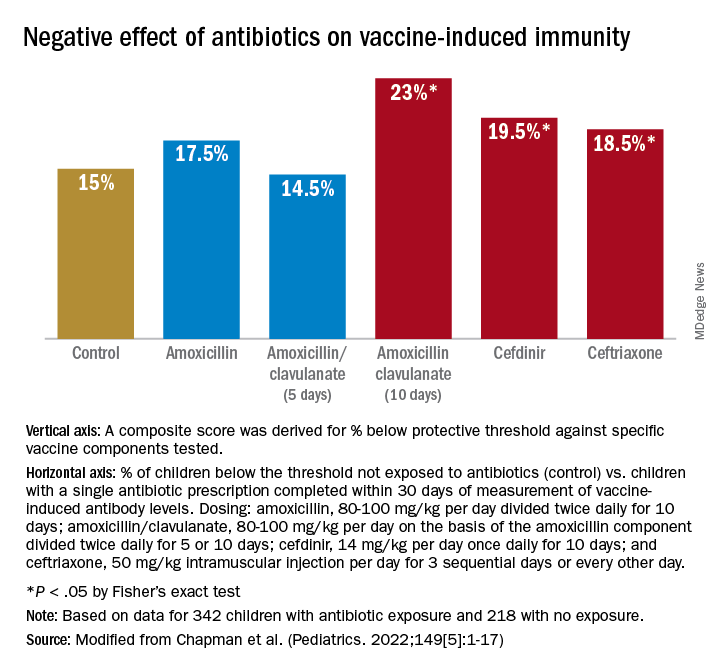
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).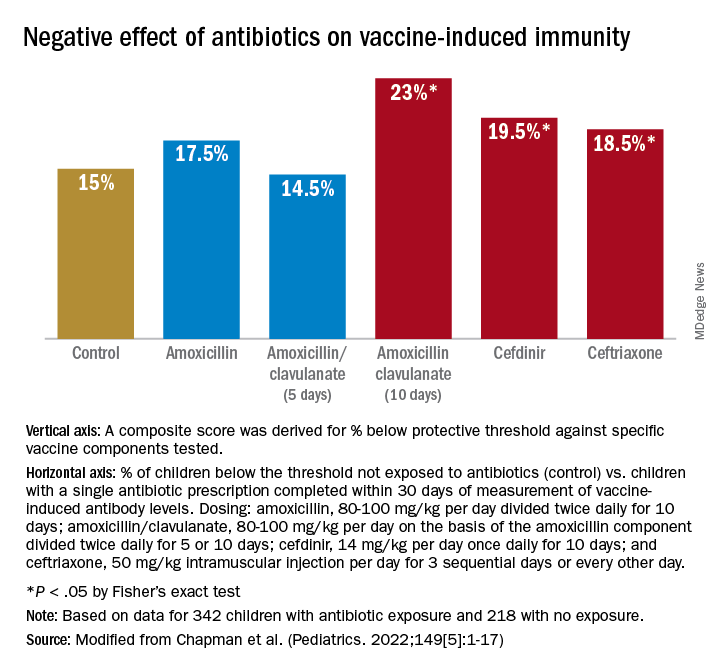
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).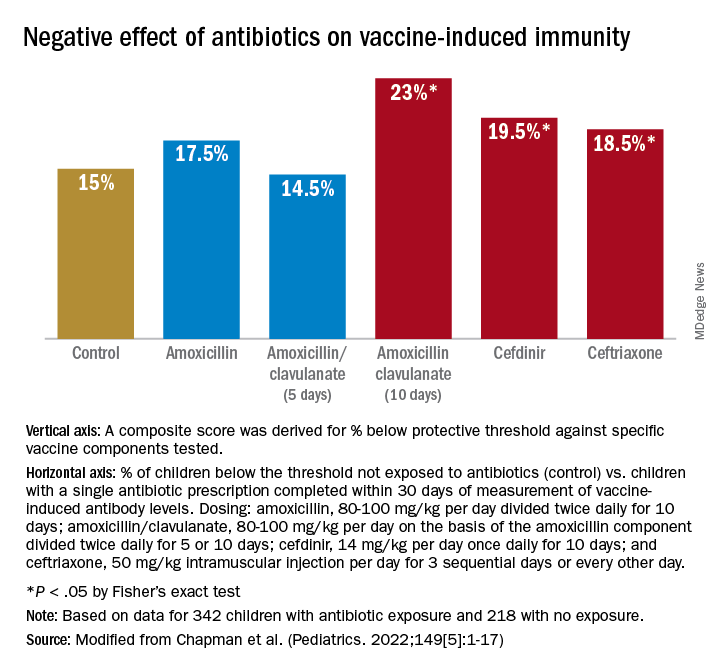
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
How to communicate effectively with patients when tension is high
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
AT INTERNAL MEDICINE 2022
Homelessness seems to have greater link to death than common diseases, says physician
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
REPORTING FROM INTERNAL MEDICINE 2022
Screening for anxiety in young children
On April 12, 2022, the U.S. Preventive Services Task Force released the draft of a recommendation statement titled Screening for Anxiety in Children and Adolescents. Based on their observation that 7.8% of children and adolescents have a current anxiety disorder and their analysis of the magnitude of the net benefit, the Task Force plans on recommending that children ages 8-18 years be screened for the condition. However, the group could not find evidence to support screening for children 7 years and younger.
Over more than 4 decades of general pediatric practice, it became obvious to me that anxiety was driving a high percentage of my office visits. Most often in young children it was parental anxiety that was prompting the phone call or office visit. In older childhood and adolescence it was patient anxiety that began to play a larger role.
Over the last 2 decades the level of anxiety in all age groups has seemed to increase. How large a role the events of Sept. 11, 2001, and other terrorist attacks were playing in this phenomenon is unclear to me. However, I suspect they were significant. More recently the pandemic and the failure of both political parties to forge a working arrangement have fueled even more anxiety in many demographic segments. It may be safe to say that everyone is anxious to one degree or another.
Broad-based anxiety in the general population and the incidence of anxiety disorders severe enough to disrupt a child’s life are certainly two different kettles of fish. However, the factors that have raised the level of anxiety across all age groups certainly hasn’t made things any easier for the child who has inherited or developed an anxiety disorder.
Glancing at the 600-page evidence synthesis that accompanies the task force’s report it is clear that they have taken their challenge seriously. However, I wonder whether looking at the 7-and-under age group with a different lens might have resulted in the inclusion of younger children in their recommendation.
I understand that to support their recommendations the U.S. Preventive Services Task Forces must rely on data from peer-reviewed studies that have looked at quantifiable outcomes. However, I suspect the task force would agree that its recommendations shouldn’t prevent the rest of us from using our own observations and intuition when deciding whether to selectively screen our younger patients for anxiety disorders.
Although it may not generate a measurable data point, providing the parents of a 5-year-old whose troubling behavior is in part the result of an anxiety disorder is invaluable. Do we need to screen all 5-year-olds? The task force says probably not given the current state of our knowledge and I agree. But, the fact that almost 8% of the pediatric population carries the diagnosis and my anecdotal observations suggest that as pediatricians we should be learning more about anxiety disorders and their wide variety of presentations. Then we should selectively screen more of our patients. In fact, I suspect we might help our patients and ourselves by questioning more parents about their own mental health histories even before we have any inkling that their child has a problem. While the degree to which anxiety disorders are inheritable and the exact mechanism is far from clear, I think this history might be a valuable piece of information to learn as early as the prenatal get-acquainted visit. A simple question to a new or expecting parent about what worries them most about becoming a parent would be a good opener. Your reassurance that you expect parents to be worried and welcome hearing about their concerns should be a step in building a strong foundation for a family-provider relationship.
Anxiety happens and unfortunately so do anxiety disorders. We need to be doing a better job of acknowledging and responding to these two realities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
*This column was updated on 5/4/2022.
On April 12, 2022, the U.S. Preventive Services Task Force released the draft of a recommendation statement titled Screening for Anxiety in Children and Adolescents. Based on their observation that 7.8% of children and adolescents have a current anxiety disorder and their analysis of the magnitude of the net benefit, the Task Force plans on recommending that children ages 8-18 years be screened for the condition. However, the group could not find evidence to support screening for children 7 years and younger.
Over more than 4 decades of general pediatric practice, it became obvious to me that anxiety was driving a high percentage of my office visits. Most often in young children it was parental anxiety that was prompting the phone call or office visit. In older childhood and adolescence it was patient anxiety that began to play a larger role.
Over the last 2 decades the level of anxiety in all age groups has seemed to increase. How large a role the events of Sept. 11, 2001, and other terrorist attacks were playing in this phenomenon is unclear to me. However, I suspect they were significant. More recently the pandemic and the failure of both political parties to forge a working arrangement have fueled even more anxiety in many demographic segments. It may be safe to say that everyone is anxious to one degree or another.
Broad-based anxiety in the general population and the incidence of anxiety disorders severe enough to disrupt a child’s life are certainly two different kettles of fish. However, the factors that have raised the level of anxiety across all age groups certainly hasn’t made things any easier for the child who has inherited or developed an anxiety disorder.
Glancing at the 600-page evidence synthesis that accompanies the task force’s report it is clear that they have taken their challenge seriously. However, I wonder whether looking at the 7-and-under age group with a different lens might have resulted in the inclusion of younger children in their recommendation.
I understand that to support their recommendations the U.S. Preventive Services Task Forces must rely on data from peer-reviewed studies that have looked at quantifiable outcomes. However, I suspect the task force would agree that its recommendations shouldn’t prevent the rest of us from using our own observations and intuition when deciding whether to selectively screen our younger patients for anxiety disorders.
Although it may not generate a measurable data point, providing the parents of a 5-year-old whose troubling behavior is in part the result of an anxiety disorder is invaluable. Do we need to screen all 5-year-olds? The task force says probably not given the current state of our knowledge and I agree. But, the fact that almost 8% of the pediatric population carries the diagnosis and my anecdotal observations suggest that as pediatricians we should be learning more about anxiety disorders and their wide variety of presentations. Then we should selectively screen more of our patients. In fact, I suspect we might help our patients and ourselves by questioning more parents about their own mental health histories even before we have any inkling that their child has a problem. While the degree to which anxiety disorders are inheritable and the exact mechanism is far from clear, I think this history might be a valuable piece of information to learn as early as the prenatal get-acquainted visit. A simple question to a new or expecting parent about what worries them most about becoming a parent would be a good opener. Your reassurance that you expect parents to be worried and welcome hearing about their concerns should be a step in building a strong foundation for a family-provider relationship.
Anxiety happens and unfortunately so do anxiety disorders. We need to be doing a better job of acknowledging and responding to these two realities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
*This column was updated on 5/4/2022.
On April 12, 2022, the U.S. Preventive Services Task Force released the draft of a recommendation statement titled Screening for Anxiety in Children and Adolescents. Based on their observation that 7.8% of children and adolescents have a current anxiety disorder and their analysis of the magnitude of the net benefit, the Task Force plans on recommending that children ages 8-18 years be screened for the condition. However, the group could not find evidence to support screening for children 7 years and younger.
Over more than 4 decades of general pediatric practice, it became obvious to me that anxiety was driving a high percentage of my office visits. Most often in young children it was parental anxiety that was prompting the phone call or office visit. In older childhood and adolescence it was patient anxiety that began to play a larger role.
Over the last 2 decades the level of anxiety in all age groups has seemed to increase. How large a role the events of Sept. 11, 2001, and other terrorist attacks were playing in this phenomenon is unclear to me. However, I suspect they were significant. More recently the pandemic and the failure of both political parties to forge a working arrangement have fueled even more anxiety in many demographic segments. It may be safe to say that everyone is anxious to one degree or another.
Broad-based anxiety in the general population and the incidence of anxiety disorders severe enough to disrupt a child’s life are certainly two different kettles of fish. However, the factors that have raised the level of anxiety across all age groups certainly hasn’t made things any easier for the child who has inherited or developed an anxiety disorder.
Glancing at the 600-page evidence synthesis that accompanies the task force’s report it is clear that they have taken their challenge seriously. However, I wonder whether looking at the 7-and-under age group with a different lens might have resulted in the inclusion of younger children in their recommendation.
I understand that to support their recommendations the U.S. Preventive Services Task Forces must rely on data from peer-reviewed studies that have looked at quantifiable outcomes. However, I suspect the task force would agree that its recommendations shouldn’t prevent the rest of us from using our own observations and intuition when deciding whether to selectively screen our younger patients for anxiety disorders.
Although it may not generate a measurable data point, providing the parents of a 5-year-old whose troubling behavior is in part the result of an anxiety disorder is invaluable. Do we need to screen all 5-year-olds? The task force says probably not given the current state of our knowledge and I agree. But, the fact that almost 8% of the pediatric population carries the diagnosis and my anecdotal observations suggest that as pediatricians we should be learning more about anxiety disorders and their wide variety of presentations. Then we should selectively screen more of our patients. In fact, I suspect we might help our patients and ourselves by questioning more parents about their own mental health histories even before we have any inkling that their child has a problem. While the degree to which anxiety disorders are inheritable and the exact mechanism is far from clear, I think this history might be a valuable piece of information to learn as early as the prenatal get-acquainted visit. A simple question to a new or expecting parent about what worries them most about becoming a parent would be a good opener. Your reassurance that you expect parents to be worried and welcome hearing about their concerns should be a step in building a strong foundation for a family-provider relationship.
Anxiety happens and unfortunately so do anxiety disorders. We need to be doing a better job of acknowledging and responding to these two realities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
*This column was updated on 5/4/2022.
Smartphone diagnosis in infant seizures could be highly effective
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.










