User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Corticosteroid bursts may increase risk of sepsis, GI bleeding in children
The adverse events are rare, and the risk attenuates in subsequent months, the analysis shows. Still, the study “provides evidence that corticosteroid bursts are not innocuous but may pose potentially serious health risks,” study author Tsung-Chieh Yao, MD, PhD, and colleagues said. “Clinicians prescribing corticosteroid bursts to children need to weigh the benefits against the risks of severe adverse events.”
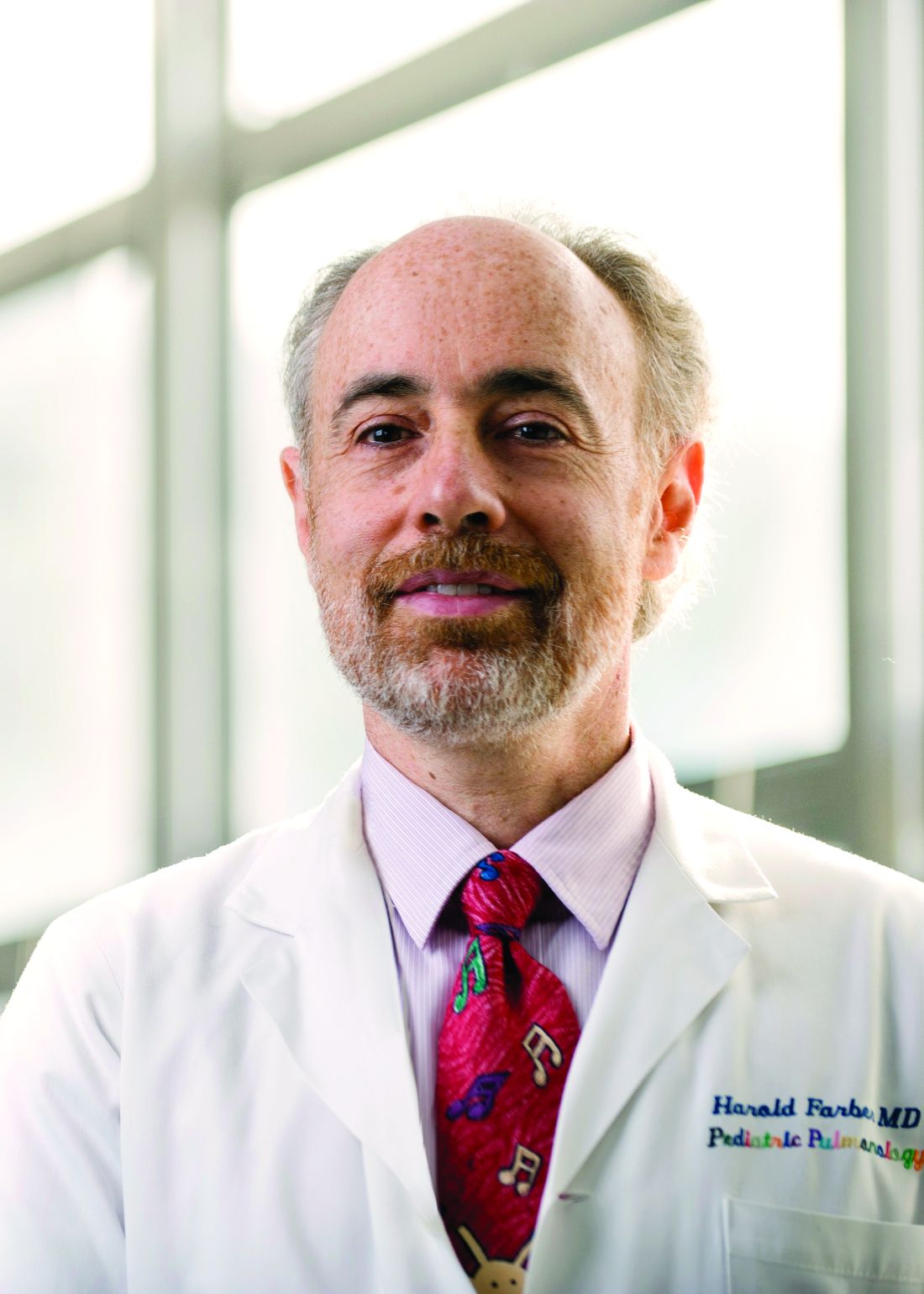
The study, which was published online in JAMA Pediatrics, indicates that oral corticosteroids are “not a benign medication, which is something that we should have all along known,” commented Harold J. Farber, MD, MSPH, professor of pediatrics at Baylor College of Medicine and a pediatric pulmonologist at Texas Children’s Hospital, both in Houston.
While oral corticosteroids may be important for the treatment of asthma, inflammatory bowel disease, and rheumatoid arthritis, they often are overprescribed – a phenomenon that Dr. Farber and collaborators saw when they analyzed data from children with public health insurance in Texas.
The medication is “not uncommonly used for minor asthma exacerbations or minor respiratory symptoms, which do not require oral steroids,” said Dr. Farber, who was not involved with the study. “What this study tells us is to save it for when they are really needed,” such as to treat a severe asthma exacerbation.
Despite the risk of adverse events, oral corticosteroids remain an important medication, and clinicians should aim to strike “the right balance,” Dr. Farber said.
Prior research has shown that the long-term use of oral corticosteroids is associated with adverse events such as infections, glaucoma, hyperglycemia, cardiovascular diseases, and osteoporosis. In addition, data indicate that corticosteroid bursts are associated with GI bleeding and sepsis in adults. But few studies have looked at the risk of corticosteroid bursts in children, the researchers said.
To evaluate associations of corticosteroid bursts – defined as the use of oral corticosteroids for 14 days or less – with GI bleeding, sepsis, pneumonia, and glaucoma in children, Dr. Yao and colleagues analyzed data from the National Health Insurance Research Database in Taiwan between 2013 and 2017. Dr. Yao is affiliated with the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan City, Taiwan.
Of more than 4.5 million children in the database, 42% received at least one corticosteroid burst, typically for acute respiratory tract infections and allergic diseases. The researchers focused on 1,064,587 children who received a single corticosteroid burst, and compared the incidence of adverse events before and after treatment using a self-controlled case series design. “Corticosteroid bursts were significantly associated with a 1.4- to 2.2-fold increase of GI bleeding, sepsis, and pneumonia, but not glaucoma, within the first month after initiation of corticosteroid therapy,” the investigators reported.
Incidence rate ratios in the 5-30 days after starting corticosteroid bursts were 1.41 for GI bleeding, 2.02 for sepsis, 2.19 for pneumonia, and 0.98 for glaucoma, compared with a pretreatment reference period.
The incidence rate per 1,000 person-years for GI bleeding was 2.48 with corticosteroid bursts, compared with 1.88 without corticosteroids. For sepsis, the rates with and without corticosteroids were 0.37 and 0.34, respectively. And for pneumonia, the rates were 25.74 versus 16.39.
Further research is needed to assess the validity of these findings, the authors noted. Because many children receive corticosteroid bursts worldwide, however, the “findings call for a careful reevaluation regarding the prudent use” of this treatment.
The study was supported by grants from the National Health Research Institutes; Ministry of Science and Technology of Taiwan; National Cheng Kung University, Tainan, Taiwan; Chang Gung Medical Foundation; and the National Institutes of Health. A coauthor disclosed grants from GlaxoSmithKline outside of the study.
The adverse events are rare, and the risk attenuates in subsequent months, the analysis shows. Still, the study “provides evidence that corticosteroid bursts are not innocuous but may pose potentially serious health risks,” study author Tsung-Chieh Yao, MD, PhD, and colleagues said. “Clinicians prescribing corticosteroid bursts to children need to weigh the benefits against the risks of severe adverse events.”
The study, which was published online in JAMA Pediatrics, indicates that oral corticosteroids are “not a benign medication, which is something that we should have all along known,” commented Harold J. Farber, MD, MSPH, professor of pediatrics at Baylor College of Medicine and a pediatric pulmonologist at Texas Children’s Hospital, both in Houston.
While oral corticosteroids may be important for the treatment of asthma, inflammatory bowel disease, and rheumatoid arthritis, they often are overprescribed – a phenomenon that Dr. Farber and collaborators saw when they analyzed data from children with public health insurance in Texas.
The medication is “not uncommonly used for minor asthma exacerbations or minor respiratory symptoms, which do not require oral steroids,” said Dr. Farber, who was not involved with the study. “What this study tells us is to save it for when they are really needed,” such as to treat a severe asthma exacerbation.
Despite the risk of adverse events, oral corticosteroids remain an important medication, and clinicians should aim to strike “the right balance,” Dr. Farber said.
Prior research has shown that the long-term use of oral corticosteroids is associated with adverse events such as infections, glaucoma, hyperglycemia, cardiovascular diseases, and osteoporosis. In addition, data indicate that corticosteroid bursts are associated with GI bleeding and sepsis in adults. But few studies have looked at the risk of corticosteroid bursts in children, the researchers said.
To evaluate associations of corticosteroid bursts – defined as the use of oral corticosteroids for 14 days or less – with GI bleeding, sepsis, pneumonia, and glaucoma in children, Dr. Yao and colleagues analyzed data from the National Health Insurance Research Database in Taiwan between 2013 and 2017. Dr. Yao is affiliated with the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan City, Taiwan.
Of more than 4.5 million children in the database, 42% received at least one corticosteroid burst, typically for acute respiratory tract infections and allergic diseases. The researchers focused on 1,064,587 children who received a single corticosteroid burst, and compared the incidence of adverse events before and after treatment using a self-controlled case series design. “Corticosteroid bursts were significantly associated with a 1.4- to 2.2-fold increase of GI bleeding, sepsis, and pneumonia, but not glaucoma, within the first month after initiation of corticosteroid therapy,” the investigators reported.
Incidence rate ratios in the 5-30 days after starting corticosteroid bursts were 1.41 for GI bleeding, 2.02 for sepsis, 2.19 for pneumonia, and 0.98 for glaucoma, compared with a pretreatment reference period.
The incidence rate per 1,000 person-years for GI bleeding was 2.48 with corticosteroid bursts, compared with 1.88 without corticosteroids. For sepsis, the rates with and without corticosteroids were 0.37 and 0.34, respectively. And for pneumonia, the rates were 25.74 versus 16.39.
Further research is needed to assess the validity of these findings, the authors noted. Because many children receive corticosteroid bursts worldwide, however, the “findings call for a careful reevaluation regarding the prudent use” of this treatment.
The study was supported by grants from the National Health Research Institutes; Ministry of Science and Technology of Taiwan; National Cheng Kung University, Tainan, Taiwan; Chang Gung Medical Foundation; and the National Institutes of Health. A coauthor disclosed grants from GlaxoSmithKline outside of the study.
The adverse events are rare, and the risk attenuates in subsequent months, the analysis shows. Still, the study “provides evidence that corticosteroid bursts are not innocuous but may pose potentially serious health risks,” study author Tsung-Chieh Yao, MD, PhD, and colleagues said. “Clinicians prescribing corticosteroid bursts to children need to weigh the benefits against the risks of severe adverse events.”
The study, which was published online in JAMA Pediatrics, indicates that oral corticosteroids are “not a benign medication, which is something that we should have all along known,” commented Harold J. Farber, MD, MSPH, professor of pediatrics at Baylor College of Medicine and a pediatric pulmonologist at Texas Children’s Hospital, both in Houston.
While oral corticosteroids may be important for the treatment of asthma, inflammatory bowel disease, and rheumatoid arthritis, they often are overprescribed – a phenomenon that Dr. Farber and collaborators saw when they analyzed data from children with public health insurance in Texas.
The medication is “not uncommonly used for minor asthma exacerbations or minor respiratory symptoms, which do not require oral steroids,” said Dr. Farber, who was not involved with the study. “What this study tells us is to save it for when they are really needed,” such as to treat a severe asthma exacerbation.
Despite the risk of adverse events, oral corticosteroids remain an important medication, and clinicians should aim to strike “the right balance,” Dr. Farber said.
Prior research has shown that the long-term use of oral corticosteroids is associated with adverse events such as infections, glaucoma, hyperglycemia, cardiovascular diseases, and osteoporosis. In addition, data indicate that corticosteroid bursts are associated with GI bleeding and sepsis in adults. But few studies have looked at the risk of corticosteroid bursts in children, the researchers said.
To evaluate associations of corticosteroid bursts – defined as the use of oral corticosteroids for 14 days or less – with GI bleeding, sepsis, pneumonia, and glaucoma in children, Dr. Yao and colleagues analyzed data from the National Health Insurance Research Database in Taiwan between 2013 and 2017. Dr. Yao is affiliated with the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan City, Taiwan.
Of more than 4.5 million children in the database, 42% received at least one corticosteroid burst, typically for acute respiratory tract infections and allergic diseases. The researchers focused on 1,064,587 children who received a single corticosteroid burst, and compared the incidence of adverse events before and after treatment using a self-controlled case series design. “Corticosteroid bursts were significantly associated with a 1.4- to 2.2-fold increase of GI bleeding, sepsis, and pneumonia, but not glaucoma, within the first month after initiation of corticosteroid therapy,” the investigators reported.
Incidence rate ratios in the 5-30 days after starting corticosteroid bursts were 1.41 for GI bleeding, 2.02 for sepsis, 2.19 for pneumonia, and 0.98 for glaucoma, compared with a pretreatment reference period.
The incidence rate per 1,000 person-years for GI bleeding was 2.48 with corticosteroid bursts, compared with 1.88 without corticosteroids. For sepsis, the rates with and without corticosteroids were 0.37 and 0.34, respectively. And for pneumonia, the rates were 25.74 versus 16.39.
Further research is needed to assess the validity of these findings, the authors noted. Because many children receive corticosteroid bursts worldwide, however, the “findings call for a careful reevaluation regarding the prudent use” of this treatment.
The study was supported by grants from the National Health Research Institutes; Ministry of Science and Technology of Taiwan; National Cheng Kung University, Tainan, Taiwan; Chang Gung Medical Foundation; and the National Institutes of Health. A coauthor disclosed grants from GlaxoSmithKline outside of the study.
FROM JAMA PEDIATRICS
AHA guidance on blood clots linked to COVID-19 vaccine
A newly released report is offering guidance concerning rare conditions associated with COVID-19 as well as vaccines against the virus.
The report was released April 29, 2021, by the American Heart Association/American Stroke Association Stroke Council Leadership in answer to the decision April 23 by the Centers for Disease Control and Prevention and the Food and Drug Administration to lift an earlier “pause” in administration of the Johnson & Johnson (Janssen) vaccine.
That pause had been put in place after reports were received of a possible association between the J&J vaccine and cerebral venous sinus thrombosis (CVST) and thrombosis-thrombocytopenia syndrome (TTS, blood clots plus low blood platelets). CVST and TTS were also linked to patients in Europe and Canada who received the AstraZeneca COVID-19 vaccine.
However, the new report noted that these conditions are very rare.
“The risk of CVST due to infection with COVID-19 is 8-10 times higher than the risk of CVST after receiving a COVID-19 vaccine,” lead author Karen L. Furie, MD, chair of the department of neurology at Brown University, Providence, R.I., said in a press release.
“The public can be reassured by the CDC’s and FDA’s investigation and these statistics – the likelihood of developing CVST after a COVID-19 vaccine is extremely low,” said Dr. Furie, adding that the authors “urge all adults to receive any of the approved COVID-19 vaccines.”
The new guidance, which was published online April 29, 2021, in Stroke, discusses signs and symptoms of CVST and TTS, as well as vaccine-induced immune thrombotic thrombocytopenia (VITT). It also recommends best options for treating these conditions.
Assessing 81 million patients
In their analysis, the investigators assessed a database of 59 health care organizations and 81 million patients, 98% of whom were in the United States.
Of almost 514,000 patients diagnosed with COVID-19 between January 2020 and March 2021, 20 also received a diagnosis of CVST.
Among about 490,000 adults who received either the Pfizer or Moderna vaccines, there were no diagnosed cases of thrombocytopenia.
Dr. Furie reiterated that CVST blood clots “are very rare adverse events,” but recommended that any patient in the ED with a suspected clot should be screened immediately to determine if they received a COVID vaccine during the previous few weeks.
For those who have recently received the COVID-19 vaccine, a suspected clot should be treated with nonheparin anticoagulants, Dr. Furie said.
“No heparin products in any dose should be given for suspected CVST, TTS, or VITT. With the right treatment, most patients can have a full recovery,” she added. The report includes additional, detailed treatment recommendations if one of these conditions are suspected.
Rare events
The authors noted that cases of TTS/VITT occurred up to 2.5 weeks after receiving the J&J vaccine in the United States and up to 3.5 weeks after receiving the AstraZeneca vaccine in Europe.
An April 23 report from the CDC and FDA noted that, out of almost 7 million adults who received the J&J vaccine, the agencies investigated only 15 reported cases of TTS.
An April 7 report from the European Medicines Agency noted that, out of more than 25 million people who received the AstraZeneca vaccine in the European Union, it found 62 cases of CVST.
A statement put out by the American Heart Association/American Stroke Association urges “everyone to receive a COVID-19 vaccine” as soon as possible.
“We are confident the benefits of vaccination far exceed the very small, rare risks,” the organizations said. “The risks of vaccination are also far smaller than the risk of COVID-19 and its potentially fatal consequences.”
A version of this article first appeared on Medscape.com.
A newly released report is offering guidance concerning rare conditions associated with COVID-19 as well as vaccines against the virus.
The report was released April 29, 2021, by the American Heart Association/American Stroke Association Stroke Council Leadership in answer to the decision April 23 by the Centers for Disease Control and Prevention and the Food and Drug Administration to lift an earlier “pause” in administration of the Johnson & Johnson (Janssen) vaccine.
That pause had been put in place after reports were received of a possible association between the J&J vaccine and cerebral venous sinus thrombosis (CVST) and thrombosis-thrombocytopenia syndrome (TTS, blood clots plus low blood platelets). CVST and TTS were also linked to patients in Europe and Canada who received the AstraZeneca COVID-19 vaccine.
However, the new report noted that these conditions are very rare.
“The risk of CVST due to infection with COVID-19 is 8-10 times higher than the risk of CVST after receiving a COVID-19 vaccine,” lead author Karen L. Furie, MD, chair of the department of neurology at Brown University, Providence, R.I., said in a press release.
“The public can be reassured by the CDC’s and FDA’s investigation and these statistics – the likelihood of developing CVST after a COVID-19 vaccine is extremely low,” said Dr. Furie, adding that the authors “urge all adults to receive any of the approved COVID-19 vaccines.”
The new guidance, which was published online April 29, 2021, in Stroke, discusses signs and symptoms of CVST and TTS, as well as vaccine-induced immune thrombotic thrombocytopenia (VITT). It also recommends best options for treating these conditions.
Assessing 81 million patients
In their analysis, the investigators assessed a database of 59 health care organizations and 81 million patients, 98% of whom were in the United States.
Of almost 514,000 patients diagnosed with COVID-19 between January 2020 and March 2021, 20 also received a diagnosis of CVST.
Among about 490,000 adults who received either the Pfizer or Moderna vaccines, there were no diagnosed cases of thrombocytopenia.
Dr. Furie reiterated that CVST blood clots “are very rare adverse events,” but recommended that any patient in the ED with a suspected clot should be screened immediately to determine if they received a COVID vaccine during the previous few weeks.
For those who have recently received the COVID-19 vaccine, a suspected clot should be treated with nonheparin anticoagulants, Dr. Furie said.
“No heparin products in any dose should be given for suspected CVST, TTS, or VITT. With the right treatment, most patients can have a full recovery,” she added. The report includes additional, detailed treatment recommendations if one of these conditions are suspected.
Rare events
The authors noted that cases of TTS/VITT occurred up to 2.5 weeks after receiving the J&J vaccine in the United States and up to 3.5 weeks after receiving the AstraZeneca vaccine in Europe.
An April 23 report from the CDC and FDA noted that, out of almost 7 million adults who received the J&J vaccine, the agencies investigated only 15 reported cases of TTS.
An April 7 report from the European Medicines Agency noted that, out of more than 25 million people who received the AstraZeneca vaccine in the European Union, it found 62 cases of CVST.
A statement put out by the American Heart Association/American Stroke Association urges “everyone to receive a COVID-19 vaccine” as soon as possible.
“We are confident the benefits of vaccination far exceed the very small, rare risks,” the organizations said. “The risks of vaccination are also far smaller than the risk of COVID-19 and its potentially fatal consequences.”
A version of this article first appeared on Medscape.com.
A newly released report is offering guidance concerning rare conditions associated with COVID-19 as well as vaccines against the virus.
The report was released April 29, 2021, by the American Heart Association/American Stroke Association Stroke Council Leadership in answer to the decision April 23 by the Centers for Disease Control and Prevention and the Food and Drug Administration to lift an earlier “pause” in administration of the Johnson & Johnson (Janssen) vaccine.
That pause had been put in place after reports were received of a possible association between the J&J vaccine and cerebral venous sinus thrombosis (CVST) and thrombosis-thrombocytopenia syndrome (TTS, blood clots plus low blood platelets). CVST and TTS were also linked to patients in Europe and Canada who received the AstraZeneca COVID-19 vaccine.
However, the new report noted that these conditions are very rare.
“The risk of CVST due to infection with COVID-19 is 8-10 times higher than the risk of CVST after receiving a COVID-19 vaccine,” lead author Karen L. Furie, MD, chair of the department of neurology at Brown University, Providence, R.I., said in a press release.
“The public can be reassured by the CDC’s and FDA’s investigation and these statistics – the likelihood of developing CVST after a COVID-19 vaccine is extremely low,” said Dr. Furie, adding that the authors “urge all adults to receive any of the approved COVID-19 vaccines.”
The new guidance, which was published online April 29, 2021, in Stroke, discusses signs and symptoms of CVST and TTS, as well as vaccine-induced immune thrombotic thrombocytopenia (VITT). It also recommends best options for treating these conditions.
Assessing 81 million patients
In their analysis, the investigators assessed a database of 59 health care organizations and 81 million patients, 98% of whom were in the United States.
Of almost 514,000 patients diagnosed with COVID-19 between January 2020 and March 2021, 20 also received a diagnosis of CVST.
Among about 490,000 adults who received either the Pfizer or Moderna vaccines, there were no diagnosed cases of thrombocytopenia.
Dr. Furie reiterated that CVST blood clots “are very rare adverse events,” but recommended that any patient in the ED with a suspected clot should be screened immediately to determine if they received a COVID vaccine during the previous few weeks.
For those who have recently received the COVID-19 vaccine, a suspected clot should be treated with nonheparin anticoagulants, Dr. Furie said.
“No heparin products in any dose should be given for suspected CVST, TTS, or VITT. With the right treatment, most patients can have a full recovery,” she added. The report includes additional, detailed treatment recommendations if one of these conditions are suspected.
Rare events
The authors noted that cases of TTS/VITT occurred up to 2.5 weeks after receiving the J&J vaccine in the United States and up to 3.5 weeks after receiving the AstraZeneca vaccine in Europe.
An April 23 report from the CDC and FDA noted that, out of almost 7 million adults who received the J&J vaccine, the agencies investigated only 15 reported cases of TTS.
An April 7 report from the European Medicines Agency noted that, out of more than 25 million people who received the AstraZeneca vaccine in the European Union, it found 62 cases of CVST.
A statement put out by the American Heart Association/American Stroke Association urges “everyone to receive a COVID-19 vaccine” as soon as possible.
“We are confident the benefits of vaccination far exceed the very small, rare risks,” the organizations said. “The risks of vaccination are also far smaller than the risk of COVID-19 and its potentially fatal consequences.”
A version of this article first appeared on Medscape.com.
Marijuana vaping more common among Hispanic teens
Hispanic adolescents were more likely to use e-cigarettes to vape marijuana than were their Black and White counterparts in 2020, according to a recent study conducted by the Centers for Disease Control and Prevention and published in JAMA Pediatrics.
Researchers found that 25.6% of Hispanic students reported vaping marijuana, compared to 19.4% of Black students and 18.2% of White students. The study, which is an analysis of 2017, 2018, and 2020 results from the National Youth Tobacco Survey, also revealed that increases in this recreational practice occurred among all racial and ethnic groups within those 3 years, with Hispanic students having the largest percent increase, 11.6%, followed by Black students at 8.8% and White students at 7.4%.
“The initial motivation [to do this study] was to gain a better understanding of the prevalence of use of marijuana in e-cigarettes among youth, particularly given the context of the 2019 outbreak of e-cigarette, or vaping, product use–associated lung injury (EVALI),” study author Christina Vaughan Watson, DrPH, health scientist at the CDC’s National Center for Chronic Disease Prevention and Health Promotion, said in an interview.
The findings could help clinicians and physicians understand demographic variations among marijuana vapers and help inform targeted interventions for specific populations.
“Understanding demographic variations among those who are using marijuana in e-cigarettes can help inform evidenced-based interventions that may resonate with specific populations,” Dr. Watson explained.
Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, who was not involved in the study, said in an interview that the findings were “eye opening” and revealed a pattern she hasn’t seen before in her adolescent clinic.
“I would have thought African-American or non-Hispanic Blacks would’ve been a higher group of use, because when we screen kids that’s what we tend to get from the population we see here,” Ms. Thew said.
Ms. Thew said the findings also had made her reconsider her clinic’s approach to screening adolescents for marijuana use as well as address possible language barriers.
“We are probably missing access to some of the kids that we may need to seek out,” she explained. “I also thought it sends a good message that we need to direct some of our education probably a little differently, especially if it’s a Hispanic population and English may not be the primary language.”
Dr. Watson said more research is needed to assess why differences in marijuana use in e-cigarettes exist among youth.
Marijuana use in e-cigarettes has become increasingly popular among U.S. teens, with one in five students in grades 10 and 12 reporting vaping marijuana within the past year in a 2019 study conducted by the National Institute on Drug Abuse.
Dr. Watson and colleagues also found statistically significant increases in vaping marijuana, with 19.5% of students reporting smoking marijuana via e-cigarettes in 2020, compared to 11.1% of them vaping the drug in 2017. They believe the rise in marijuana vaping among youth may be attributed to states increasingly legalizing adult marijuana sales, which could impact ease of access and social acceptance.
Ms. Thew believes the rise in marijuana vaping among youth can be attributed to the legalization of marijuana, which may send “a message to adolescents that it must be safe for them to use,” as well as the increasing popularity of e-cigarettes.
In fact, as of April 2021, marijuana is legal for adults in 16 states and the District of Columbia. Meanwhile, medical marijuana is legal in 36 states, according to the National Conference of State Legislatures.
“I mean, there’s just definitely been a lot more use of [e-cigarettes]. Vaping and things like that definitely took off between 2019 and 2020,” Ms. Thew explained. “And I think marijuana use in itself is going up tremendously, I think more kids who would have used alcohol in the past use weed.”
Although public attitudes toward marijuana have relaxed, previous studies have linked it to memory dysfunction, as well as long-term cognitive effects that can interfere with perception of time and motor function. However, studies also have shown that cannabis use can combat age-related cognitive decline and help with pain reduction.
However, when it comes to adolescents, Dr. Watson and colleagues said e-cigarette use among youth and young adults is unsafe, regardless of the substances used in these products, including marijuana. Furthermore, they said marijuana use can lead to higher risks of more problematic use later in life, adding that evidence-based strategies to reduce marijuana use in e-cigarettes are important for protecting young people.
The study author and experts disclosed no relevant financial relationships.
Hispanic adolescents were more likely to use e-cigarettes to vape marijuana than were their Black and White counterparts in 2020, according to a recent study conducted by the Centers for Disease Control and Prevention and published in JAMA Pediatrics.
Researchers found that 25.6% of Hispanic students reported vaping marijuana, compared to 19.4% of Black students and 18.2% of White students. The study, which is an analysis of 2017, 2018, and 2020 results from the National Youth Tobacco Survey, also revealed that increases in this recreational practice occurred among all racial and ethnic groups within those 3 years, with Hispanic students having the largest percent increase, 11.6%, followed by Black students at 8.8% and White students at 7.4%.
“The initial motivation [to do this study] was to gain a better understanding of the prevalence of use of marijuana in e-cigarettes among youth, particularly given the context of the 2019 outbreak of e-cigarette, or vaping, product use–associated lung injury (EVALI),” study author Christina Vaughan Watson, DrPH, health scientist at the CDC’s National Center for Chronic Disease Prevention and Health Promotion, said in an interview.
The findings could help clinicians and physicians understand demographic variations among marijuana vapers and help inform targeted interventions for specific populations.
“Understanding demographic variations among those who are using marijuana in e-cigarettes can help inform evidenced-based interventions that may resonate with specific populations,” Dr. Watson explained.
Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, who was not involved in the study, said in an interview that the findings were “eye opening” and revealed a pattern she hasn’t seen before in her adolescent clinic.
“I would have thought African-American or non-Hispanic Blacks would’ve been a higher group of use, because when we screen kids that’s what we tend to get from the population we see here,” Ms. Thew said.
Ms. Thew said the findings also had made her reconsider her clinic’s approach to screening adolescents for marijuana use as well as address possible language barriers.
“We are probably missing access to some of the kids that we may need to seek out,” she explained. “I also thought it sends a good message that we need to direct some of our education probably a little differently, especially if it’s a Hispanic population and English may not be the primary language.”
Dr. Watson said more research is needed to assess why differences in marijuana use in e-cigarettes exist among youth.
Marijuana use in e-cigarettes has become increasingly popular among U.S. teens, with one in five students in grades 10 and 12 reporting vaping marijuana within the past year in a 2019 study conducted by the National Institute on Drug Abuse.
Dr. Watson and colleagues also found statistically significant increases in vaping marijuana, with 19.5% of students reporting smoking marijuana via e-cigarettes in 2020, compared to 11.1% of them vaping the drug in 2017. They believe the rise in marijuana vaping among youth may be attributed to states increasingly legalizing adult marijuana sales, which could impact ease of access and social acceptance.
Ms. Thew believes the rise in marijuana vaping among youth can be attributed to the legalization of marijuana, which may send “a message to adolescents that it must be safe for them to use,” as well as the increasing popularity of e-cigarettes.
In fact, as of April 2021, marijuana is legal for adults in 16 states and the District of Columbia. Meanwhile, medical marijuana is legal in 36 states, according to the National Conference of State Legislatures.
“I mean, there’s just definitely been a lot more use of [e-cigarettes]. Vaping and things like that definitely took off between 2019 and 2020,” Ms. Thew explained. “And I think marijuana use in itself is going up tremendously, I think more kids who would have used alcohol in the past use weed.”
Although public attitudes toward marijuana have relaxed, previous studies have linked it to memory dysfunction, as well as long-term cognitive effects that can interfere with perception of time and motor function. However, studies also have shown that cannabis use can combat age-related cognitive decline and help with pain reduction.
However, when it comes to adolescents, Dr. Watson and colleagues said e-cigarette use among youth and young adults is unsafe, regardless of the substances used in these products, including marijuana. Furthermore, they said marijuana use can lead to higher risks of more problematic use later in life, adding that evidence-based strategies to reduce marijuana use in e-cigarettes are important for protecting young people.
The study author and experts disclosed no relevant financial relationships.
Hispanic adolescents were more likely to use e-cigarettes to vape marijuana than were their Black and White counterparts in 2020, according to a recent study conducted by the Centers for Disease Control and Prevention and published in JAMA Pediatrics.
Researchers found that 25.6% of Hispanic students reported vaping marijuana, compared to 19.4% of Black students and 18.2% of White students. The study, which is an analysis of 2017, 2018, and 2020 results from the National Youth Tobacco Survey, also revealed that increases in this recreational practice occurred among all racial and ethnic groups within those 3 years, with Hispanic students having the largest percent increase, 11.6%, followed by Black students at 8.8% and White students at 7.4%.
“The initial motivation [to do this study] was to gain a better understanding of the prevalence of use of marijuana in e-cigarettes among youth, particularly given the context of the 2019 outbreak of e-cigarette, or vaping, product use–associated lung injury (EVALI),” study author Christina Vaughan Watson, DrPH, health scientist at the CDC’s National Center for Chronic Disease Prevention and Health Promotion, said in an interview.
The findings could help clinicians and physicians understand demographic variations among marijuana vapers and help inform targeted interventions for specific populations.
“Understanding demographic variations among those who are using marijuana in e-cigarettes can help inform evidenced-based interventions that may resonate with specific populations,” Dr. Watson explained.
Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, who was not involved in the study, said in an interview that the findings were “eye opening” and revealed a pattern she hasn’t seen before in her adolescent clinic.
“I would have thought African-American or non-Hispanic Blacks would’ve been a higher group of use, because when we screen kids that’s what we tend to get from the population we see here,” Ms. Thew said.
Ms. Thew said the findings also had made her reconsider her clinic’s approach to screening adolescents for marijuana use as well as address possible language barriers.
“We are probably missing access to some of the kids that we may need to seek out,” she explained. “I also thought it sends a good message that we need to direct some of our education probably a little differently, especially if it’s a Hispanic population and English may not be the primary language.”
Dr. Watson said more research is needed to assess why differences in marijuana use in e-cigarettes exist among youth.
Marijuana use in e-cigarettes has become increasingly popular among U.S. teens, with one in five students in grades 10 and 12 reporting vaping marijuana within the past year in a 2019 study conducted by the National Institute on Drug Abuse.
Dr. Watson and colleagues also found statistically significant increases in vaping marijuana, with 19.5% of students reporting smoking marijuana via e-cigarettes in 2020, compared to 11.1% of them vaping the drug in 2017. They believe the rise in marijuana vaping among youth may be attributed to states increasingly legalizing adult marijuana sales, which could impact ease of access and social acceptance.
Ms. Thew believes the rise in marijuana vaping among youth can be attributed to the legalization of marijuana, which may send “a message to adolescents that it must be safe for them to use,” as well as the increasing popularity of e-cigarettes.
In fact, as of April 2021, marijuana is legal for adults in 16 states and the District of Columbia. Meanwhile, medical marijuana is legal in 36 states, according to the National Conference of State Legislatures.
“I mean, there’s just definitely been a lot more use of [e-cigarettes]. Vaping and things like that definitely took off between 2019 and 2020,” Ms. Thew explained. “And I think marijuana use in itself is going up tremendously, I think more kids who would have used alcohol in the past use weed.”
Although public attitudes toward marijuana have relaxed, previous studies have linked it to memory dysfunction, as well as long-term cognitive effects that can interfere with perception of time and motor function. However, studies also have shown that cannabis use can combat age-related cognitive decline and help with pain reduction.
However, when it comes to adolescents, Dr. Watson and colleagues said e-cigarette use among youth and young adults is unsafe, regardless of the substances used in these products, including marijuana. Furthermore, they said marijuana use can lead to higher risks of more problematic use later in life, adding that evidence-based strategies to reduce marijuana use in e-cigarettes are important for protecting young people.
The study author and experts disclosed no relevant financial relationships.
Study calls for sex-specific concussion management in adolescent soccer players
A large study of adolescent soccer players in Michigan revealed key differences in concussion injury metrics among males and females, underscoring a need to develop sex-specific approaches to managing injury in the sport.
Sport-related concussion (SRC) is a specific concern in young female athletes, study authors Abigail C. Bretzin, PhD, and colleagues noted in their paper, which appears in JAMA Network Open. Previous surveillance studies on SRC at the high school and college level have reported higher rates of injury risk and longer recovery outcomes in female soccer athletes. Taking a deeper dive into these trends, the investigators explored whether sex-associated differences existed in SRC, addressing the mechanics, management, and recovery from SRC.
“This is an area that is remarkably underresearched,” William Stewart, MBChB, PhD, the study’s corresponding author, said in an interview. Prior studies of males and females have shown that female axons are thinner, with fewer microtubules or internal scaffolding than male axons. This potentially increases risk of shear injury in females. Limited research has also cited differences in concussion risk across the menstrual cycle in female athletes.
Reporting system targets four injury areas
The investigators conducted a high school injury surveillance project in 43,741 male and 39,637 female soccer athletes participating in the Michigan High School Athletic Association (MHSAA) Head Injury Reporting System. The study included students from 9th to 12th grade, spanning from the beginning of academic year 2016-2017 to the end of academic year 2018-2019. Since 2015, the state has mandated high schools to submit data to MHSAA.
MHSAA captures data on four categories: person-to-person contact, person-to-object contact, person-to-playing surface contact, or uncertain about cause of the event. Study outcomes included details regarding injury mechanism, immediate management, and return-to-play time for each documented SRC.
Investigators reported notable differences among male and female players. Documented SRC risk was 1.88 times higher among adolescent girls than boys across all academic years (RR, 1.88; 95% CI, 1.69-2.09; P < .001). They also cited inconsistencies in distribution of injury mechanisms among the sexes. Females were most likely to suffer injury from equipment contact such as heading a ball (41.9%), whereas male players commonly sustained SRC from contact with another player (48.4%). The authors suggested that “female soccer athletes have lower neck strength and girth, compared with male athletes, with these variables inversely associated with linear and rotational head acceleration after soccer ball heading.”
Boys had greater odds of immediate removal from play and but also returned to the sport 2 days sooner than girls. “The possibility exists, therefore, that this longer recovery time might, in part, be reflective of our observed differences in immediate care, in particular removal from play,” the authors wrote. Immediate removal from play was also more common in cases where an athletic trainer played a part in evaluating players for SRC.
Eliminating the one-size-fits-all approach
Current concussion management is based on a “one-size-fits-all” model, said Dr. Stewart. Male and female athletes are treated following a common concussion management protocol, covering concussion detection through to rehabilitation. “This model of management is based on research that is almost exclusively in male athletes.”
What the study showed is this one-size-fits-all approach may be flawed, letting down female athletes. “We should be pursuing more research in sex differences in concussion and, importantly, putting these into practice in sex-specific concussion management protocols,” he suggested.
Future studies should also look at the effects of athletic trainer employment on SRC metrics. “Although this was a large, statewide epidemiological study of reported SRC in adolescent soccer athletes, inclusive of high schools with and without access to athletic trainers, the Head Injury Reporting System did not include information on the whether there were athletic trainer services available at each school, including specific athletic training services for soccer,” wrote the investigators, in citing the study’s limitations.
Girls report symptoms more often
“The researchers are to be commended for taking a prospective approach to address this common observation in high school sports,” said Keith J. Loud, MD, MSc, FAAP, a sports pediatrician at Children’s Hospital at Dartmouth-Hitchcock in Manchester, N.H. The results are “entirely believable,” said Dr. Loud, who was not affiliated with the study. “We have long postulated differences in neurophysiology, neck strength, style of play, and tendency to report as explanations for the observation that girls in high school soccer are diagnosed with more concussions than boys.”
The findings suggest that boys play more aggressively, but sustain fewer concussions, he added. Girls in the meantime, are more likely to speak up about their injury.
“Concussion diagnosis still relies to a large degree on the athlete to report symptoms, which is one of our hypotheses as to why girls seem to sustain more concussions – they report symptoms more often. That could also be why they have a prolonged recovery,” offered Dr. Loud. A main limitation of this study is it can’t overcome this reporting bias.
Dr. Loud was also concerned that girls were less likely to be removed from game play, even though they apparently sustained more concussions. “Perhaps that is because their injuries are less obvious on the field, and they are diagnosed when reported after the games.”
Dr. Stewart reported receiving grants from The Football Association and National Health Service Research Scotland during the study. He also served as a nonremunerated member of the Fédération Internationale de Football Association Independent Football Concussion Advisory Group and the Football Association Expert Panel on Concussion and Head Injury in Football. None of the other authors had disclosures.
A large study of adolescent soccer players in Michigan revealed key differences in concussion injury metrics among males and females, underscoring a need to develop sex-specific approaches to managing injury in the sport.
Sport-related concussion (SRC) is a specific concern in young female athletes, study authors Abigail C. Bretzin, PhD, and colleagues noted in their paper, which appears in JAMA Network Open. Previous surveillance studies on SRC at the high school and college level have reported higher rates of injury risk and longer recovery outcomes in female soccer athletes. Taking a deeper dive into these trends, the investigators explored whether sex-associated differences existed in SRC, addressing the mechanics, management, and recovery from SRC.
“This is an area that is remarkably underresearched,” William Stewart, MBChB, PhD, the study’s corresponding author, said in an interview. Prior studies of males and females have shown that female axons are thinner, with fewer microtubules or internal scaffolding than male axons. This potentially increases risk of shear injury in females. Limited research has also cited differences in concussion risk across the menstrual cycle in female athletes.
Reporting system targets four injury areas
The investigators conducted a high school injury surveillance project in 43,741 male and 39,637 female soccer athletes participating in the Michigan High School Athletic Association (MHSAA) Head Injury Reporting System. The study included students from 9th to 12th grade, spanning from the beginning of academic year 2016-2017 to the end of academic year 2018-2019. Since 2015, the state has mandated high schools to submit data to MHSAA.
MHSAA captures data on four categories: person-to-person contact, person-to-object contact, person-to-playing surface contact, or uncertain about cause of the event. Study outcomes included details regarding injury mechanism, immediate management, and return-to-play time for each documented SRC.
Investigators reported notable differences among male and female players. Documented SRC risk was 1.88 times higher among adolescent girls than boys across all academic years (RR, 1.88; 95% CI, 1.69-2.09; P < .001). They also cited inconsistencies in distribution of injury mechanisms among the sexes. Females were most likely to suffer injury from equipment contact such as heading a ball (41.9%), whereas male players commonly sustained SRC from contact with another player (48.4%). The authors suggested that “female soccer athletes have lower neck strength and girth, compared with male athletes, with these variables inversely associated with linear and rotational head acceleration after soccer ball heading.”
Boys had greater odds of immediate removal from play and but also returned to the sport 2 days sooner than girls. “The possibility exists, therefore, that this longer recovery time might, in part, be reflective of our observed differences in immediate care, in particular removal from play,” the authors wrote. Immediate removal from play was also more common in cases where an athletic trainer played a part in evaluating players for SRC.
Eliminating the one-size-fits-all approach
Current concussion management is based on a “one-size-fits-all” model, said Dr. Stewart. Male and female athletes are treated following a common concussion management protocol, covering concussion detection through to rehabilitation. “This model of management is based on research that is almost exclusively in male athletes.”
What the study showed is this one-size-fits-all approach may be flawed, letting down female athletes. “We should be pursuing more research in sex differences in concussion and, importantly, putting these into practice in sex-specific concussion management protocols,” he suggested.
Future studies should also look at the effects of athletic trainer employment on SRC metrics. “Although this was a large, statewide epidemiological study of reported SRC in adolescent soccer athletes, inclusive of high schools with and without access to athletic trainers, the Head Injury Reporting System did not include information on the whether there were athletic trainer services available at each school, including specific athletic training services for soccer,” wrote the investigators, in citing the study’s limitations.
Girls report symptoms more often
“The researchers are to be commended for taking a prospective approach to address this common observation in high school sports,” said Keith J. Loud, MD, MSc, FAAP, a sports pediatrician at Children’s Hospital at Dartmouth-Hitchcock in Manchester, N.H. The results are “entirely believable,” said Dr. Loud, who was not affiliated with the study. “We have long postulated differences in neurophysiology, neck strength, style of play, and tendency to report as explanations for the observation that girls in high school soccer are diagnosed with more concussions than boys.”
The findings suggest that boys play more aggressively, but sustain fewer concussions, he added. Girls in the meantime, are more likely to speak up about their injury.
“Concussion diagnosis still relies to a large degree on the athlete to report symptoms, which is one of our hypotheses as to why girls seem to sustain more concussions – they report symptoms more often. That could also be why they have a prolonged recovery,” offered Dr. Loud. A main limitation of this study is it can’t overcome this reporting bias.
Dr. Loud was also concerned that girls were less likely to be removed from game play, even though they apparently sustained more concussions. “Perhaps that is because their injuries are less obvious on the field, and they are diagnosed when reported after the games.”
Dr. Stewart reported receiving grants from The Football Association and National Health Service Research Scotland during the study. He also served as a nonremunerated member of the Fédération Internationale de Football Association Independent Football Concussion Advisory Group and the Football Association Expert Panel on Concussion and Head Injury in Football. None of the other authors had disclosures.
A large study of adolescent soccer players in Michigan revealed key differences in concussion injury metrics among males and females, underscoring a need to develop sex-specific approaches to managing injury in the sport.
Sport-related concussion (SRC) is a specific concern in young female athletes, study authors Abigail C. Bretzin, PhD, and colleagues noted in their paper, which appears in JAMA Network Open. Previous surveillance studies on SRC at the high school and college level have reported higher rates of injury risk and longer recovery outcomes in female soccer athletes. Taking a deeper dive into these trends, the investigators explored whether sex-associated differences existed in SRC, addressing the mechanics, management, and recovery from SRC.
“This is an area that is remarkably underresearched,” William Stewart, MBChB, PhD, the study’s corresponding author, said in an interview. Prior studies of males and females have shown that female axons are thinner, with fewer microtubules or internal scaffolding than male axons. This potentially increases risk of shear injury in females. Limited research has also cited differences in concussion risk across the menstrual cycle in female athletes.
Reporting system targets four injury areas
The investigators conducted a high school injury surveillance project in 43,741 male and 39,637 female soccer athletes participating in the Michigan High School Athletic Association (MHSAA) Head Injury Reporting System. The study included students from 9th to 12th grade, spanning from the beginning of academic year 2016-2017 to the end of academic year 2018-2019. Since 2015, the state has mandated high schools to submit data to MHSAA.
MHSAA captures data on four categories: person-to-person contact, person-to-object contact, person-to-playing surface contact, or uncertain about cause of the event. Study outcomes included details regarding injury mechanism, immediate management, and return-to-play time for each documented SRC.
Investigators reported notable differences among male and female players. Documented SRC risk was 1.88 times higher among adolescent girls than boys across all academic years (RR, 1.88; 95% CI, 1.69-2.09; P < .001). They also cited inconsistencies in distribution of injury mechanisms among the sexes. Females were most likely to suffer injury from equipment contact such as heading a ball (41.9%), whereas male players commonly sustained SRC from contact with another player (48.4%). The authors suggested that “female soccer athletes have lower neck strength and girth, compared with male athletes, with these variables inversely associated with linear and rotational head acceleration after soccer ball heading.”
Boys had greater odds of immediate removal from play and but also returned to the sport 2 days sooner than girls. “The possibility exists, therefore, that this longer recovery time might, in part, be reflective of our observed differences in immediate care, in particular removal from play,” the authors wrote. Immediate removal from play was also more common in cases where an athletic trainer played a part in evaluating players for SRC.
Eliminating the one-size-fits-all approach
Current concussion management is based on a “one-size-fits-all” model, said Dr. Stewart. Male and female athletes are treated following a common concussion management protocol, covering concussion detection through to rehabilitation. “This model of management is based on research that is almost exclusively in male athletes.”
What the study showed is this one-size-fits-all approach may be flawed, letting down female athletes. “We should be pursuing more research in sex differences in concussion and, importantly, putting these into practice in sex-specific concussion management protocols,” he suggested.
Future studies should also look at the effects of athletic trainer employment on SRC metrics. “Although this was a large, statewide epidemiological study of reported SRC in adolescent soccer athletes, inclusive of high schools with and without access to athletic trainers, the Head Injury Reporting System did not include information on the whether there were athletic trainer services available at each school, including specific athletic training services for soccer,” wrote the investigators, in citing the study’s limitations.
Girls report symptoms more often
“The researchers are to be commended for taking a prospective approach to address this common observation in high school sports,” said Keith J. Loud, MD, MSc, FAAP, a sports pediatrician at Children’s Hospital at Dartmouth-Hitchcock in Manchester, N.H. The results are “entirely believable,” said Dr. Loud, who was not affiliated with the study. “We have long postulated differences in neurophysiology, neck strength, style of play, and tendency to report as explanations for the observation that girls in high school soccer are diagnosed with more concussions than boys.”
The findings suggest that boys play more aggressively, but sustain fewer concussions, he added. Girls in the meantime, are more likely to speak up about their injury.
“Concussion diagnosis still relies to a large degree on the athlete to report symptoms, which is one of our hypotheses as to why girls seem to sustain more concussions – they report symptoms more often. That could also be why they have a prolonged recovery,” offered Dr. Loud. A main limitation of this study is it can’t overcome this reporting bias.
Dr. Loud was also concerned that girls were less likely to be removed from game play, even though they apparently sustained more concussions. “Perhaps that is because their injuries are less obvious on the field, and they are diagnosed when reported after the games.”
Dr. Stewart reported receiving grants from The Football Association and National Health Service Research Scotland during the study. He also served as a nonremunerated member of the Fédération Internationale de Football Association Independent Football Concussion Advisory Group and the Football Association Expert Panel on Concussion and Head Injury in Football. None of the other authors had disclosures.
FROM JAMA NETWORK OPEN
Challenges persist in adolescents with rheumatic disease transitioning to adult care
The inadequacies and challenges of transitioning pediatric rheumatology patients to adult care were highlighted in several research studies shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
“Not surprisingly, these studies demonstrate that transition challenges remain pervasive,” Rebecca Sadun, MD, PhD, who was not involved in any of the research, said in an interview. Nevertheless, she pointed out that one of the studies showed that eight of nine sites participating in one of the studies had at least developed a formal transition policy, and three were able to fully integrate that policy into their health care system despite the ongoing pandemic.
In that study, Joyce Chang, MD, of the Children’s Hospital of Philadelphia and colleagues used structured interviews and then quantitative research to explore processes for transition polices across nine rheumatology sites. Aside from the three that had already implemented their policies, three others were preparing implementation. The other three withdrew because of COVID-19. None of the sites had reached sustainment phase. Six of the sites had access to a social work network, and two sites had fewer than four providers.
The authors found that a higher level of change efficacy or change commitment using the Organizational Readiness for Implementing Change framework did not correspond with reaching implementation.
“The first sites to reach implementation had access to [information technology] support and involved nursing, though this was not sufficient or necessary,” the authors wrote. They noted the need for strategies to reduce the burden of data collection to improve the resilience of implementation efforts against health care system stress.
Who more often transitions to adult care?
Effective transition policies can help reduce the likelihood of young patients falling through the cracks as they grow from adolescence into young adulthood, especially those at highest risk for losing continuity of care.
“Young adults who are both medically and socially complex are at highest risk,” said Dr. Sadun, an assistant professor of adult and pediatric rheumatology at Duke University, Durham, N.C. “This is especially true for patients with systemic illnesses, patients requiring biologic medications, and patients with custody, transportation, and financial barriers.”
Research led by Emily A. Smitherman, MD, an assistant professor of pediatric rheumatology at Children’s of Alabama in Birmingham, looked more closely at who is and is not transitioning their care. The researchers analyzed retrospective data from the CARRA Registry, including the Long-Term Follow-Up Call Registry, through December 2019. Among 1,311 patients with inactive status, 537 of these patients had juvenile idiopathic arthritis and were aged at least 18 years. Only 186 of those patients, however, had data in the Long-Term Follow-Up Registry. Patients who were Black or had lower income were less likely to have data in the Long-Term Follow-Up Registry.
Just over half the patients in the long-term registry had transferred their care to an adult rheumatologist, and 83% overall were under the care of any physician. Patients who transferred their care were significantly more likely to have private insurance (87% vs. 70%; P = .009) and were more likely to be full-time students (74% vs. 58%; P = .036).
The researchers found no association between patients’ disease status at their last CARRA Registry visit and a successful transition to adult care. However, those who had transferred care to an adult rheumatologist tended to have a higher median level of pain (4 vs. 2 on a scale of 0-10) and more disease activity (3 vs. 1 on 0-10 scale) than did those who had not transferred care (P = .022 and P = .011, respectively). A higher proportion of those who transferred care had also experienced morning stiffness over the past week (49% vs. 30%; P = .015).
How young adults prefer to learn transition skills
The third study aimed to better understand the experience and preferences of young adults themselves as they transitioned from pediatric to adult care. Kristine Carandang, PhD, a postdoctoral scholar at the University of California, San Diego, and colleagues first conducted focus groups with 39 adolescents and young adults, ages 16-28 years, who had rheumatic conditions. Using the qualitative data from the focus groups, they designed a survey to capture quantitative data on young patients’ experiences.
“What we’re always trying to work on is, how do we bring that youth voice more clearly into the research literature?” Courtney K. Wells, PhD, MSW, an assistant professor of social work at the University of Wisconsin–River Falls, said in an interview. She noted that both she and Dr. Carandang were patients with rheumatic diseases, so they had lived and grown up with disease themselves and then become researchers.
“We have the information that’s in the literature, but then we also both work with youth in a couple different ways, and what we hear from youth is what we heard in our paper, but it isn’t all represented in the literature,” Dr. Wells said. That disconnect is why they also included two young adults as coauthors in the study.
“As much as we appreciate the model of the six components [of health care transition], we recognize that the youth voice isn’t represented very well,” Dr. Wells said. “The way it’s written is more for doctors and policy makers and targeted for the health care system rather than the young people themselves.”
Their research bore that out. Among 137 survey respondents, aged 18-28 years, the vast majority (89%) were women and most (75%) were White. Half the patients (50%) had a diagnosis of lupus.
“For 9 out of 11 self-management and self-advocacy skills examined, there was a significant difference between how adolescent and young adult patients experienced learning self- management skills versus how they would have preferred to learn the skills,” the researchers concluded. “Overall, adolescent and young adult patients most frequently learned about transition skills from their parents. Most participants would have preferred to learn these skills from their rheumatology team.”
For example, 46.7% of the respondents learned how to communicate their medical history from their parents, but 48.5% would have preferred to learn that from their rheumatology team. Only a quarter (24.8%) had learned that skill from their health care team.
“For most of these skills, they were getting that information from their parents, which is concerning because their parents don’t necessarily have information that is accurate,” Dr. Wells said. “Their parents managed their health care, and they taught them to do it the way they were doing it.”
Just over one-third of respondents said they learned from their parents how to track their symptoms so they could answer the rheumatologists’ questions. Only one in five respondents (20.4%) had learned this skill from their rheumatology team, but 41.2% would have preferred hearing it from their health care team, compared with 22.1% who preferred learning it from their parents.
Nearly half the respondents reported learning from their parents how to advocate for themselves when dissatisfied with their care or symptoms (49.6%) and how to talk to the office staff to make appointments, fill out paperwork, and access health records (47.4%). Just over half (51.5%) would have preferred to learn about office communication from their health care team. Preferences on self-advocacy were split between learning from parents (36.8%) and learning from their health care team (31.6%).
An opportunity for other organizations to support transition
The researchers noted that education did not necessarily need to come only from rheumatologists. Other health care professionals, including nurses and social workers, could help young patients develop skills as well.
“They said they’re also open to talking to other people, but they want their rheumatologist to lead the whole process,” Dr. Wells said. While reimbursement gaps may have presented a barrier in the past, Dr. Wells said that current billing codes have removed that obstacle, allowing physicians to bill for discussing transition skills and care.
“Largely, it’s a time issue,” Dr. Wells said. “Rheumatologists are going to tell patients first about their disease, ask how their medication is working and how their health is. Then, if we have time, we’ll cover the transition pieces, and what it boils down to is that they just don’t have time.”
The respondents indicated an interest in technology that can help their education and transition, such as patient portals, telehealth, and smartphone apps.
While 66.4% of respondents said they would attend an in-person health care appointment to learn skills for transitioning to adult care, 74.5% would attend a telehealth appointment, and 77.2% would complete a structured program within a patient portal.
Dr. Wells said she doesn’t see many of the health care system pressures easing up to allow rheumatologists more time for transition care, but she sees an opportunity for organizations, such as the Arthritis Foundation or Lupus Foundation of America, to step in and help.
“It is a matter of being creative and that, ultimately, is the barrier: Whose job is it to make it happen?” she said. “That’s where some other groups are going to need to be advocates.”
Another notable set of findings from this research was the need for young patients’ access to mental health and sexual/reproductive health services. Just over two-thirds of respondents preferred to discuss these topics with their rheumatology team, but only 59.1% felt comfortable starting the conversation about mental health, and only 47.4% felt comfortable broaching the topic of reproductive/sexual health. Even more patients preferred discussing use of drugs and alcohol with their health care team (71.5%), but more patients also felt comfortable initiating that discussion (72.2%).
“It may be that somebody who’s trained to address those issues, especially the mental health piece, may be more appropriate to have that role, and that’s part of the transition, too, these other larger life issues,” Dr. Wells said. “One of the benefits of going to an adult rheumatologist is that they are the most knowledgeable and prepared to help you with those topics.”
None of the individuals quoted in this story had any disclosures to report.
The inadequacies and challenges of transitioning pediatric rheumatology patients to adult care were highlighted in several research studies shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
“Not surprisingly, these studies demonstrate that transition challenges remain pervasive,” Rebecca Sadun, MD, PhD, who was not involved in any of the research, said in an interview. Nevertheless, she pointed out that one of the studies showed that eight of nine sites participating in one of the studies had at least developed a formal transition policy, and three were able to fully integrate that policy into their health care system despite the ongoing pandemic.
In that study, Joyce Chang, MD, of the Children’s Hospital of Philadelphia and colleagues used structured interviews and then quantitative research to explore processes for transition polices across nine rheumatology sites. Aside from the three that had already implemented their policies, three others were preparing implementation. The other three withdrew because of COVID-19. None of the sites had reached sustainment phase. Six of the sites had access to a social work network, and two sites had fewer than four providers.
The authors found that a higher level of change efficacy or change commitment using the Organizational Readiness for Implementing Change framework did not correspond with reaching implementation.
“The first sites to reach implementation had access to [information technology] support and involved nursing, though this was not sufficient or necessary,” the authors wrote. They noted the need for strategies to reduce the burden of data collection to improve the resilience of implementation efforts against health care system stress.
Who more often transitions to adult care?
Effective transition policies can help reduce the likelihood of young patients falling through the cracks as they grow from adolescence into young adulthood, especially those at highest risk for losing continuity of care.
“Young adults who are both medically and socially complex are at highest risk,” said Dr. Sadun, an assistant professor of adult and pediatric rheumatology at Duke University, Durham, N.C. “This is especially true for patients with systemic illnesses, patients requiring biologic medications, and patients with custody, transportation, and financial barriers.”
Research led by Emily A. Smitherman, MD, an assistant professor of pediatric rheumatology at Children’s of Alabama in Birmingham, looked more closely at who is and is not transitioning their care. The researchers analyzed retrospective data from the CARRA Registry, including the Long-Term Follow-Up Call Registry, through December 2019. Among 1,311 patients with inactive status, 537 of these patients had juvenile idiopathic arthritis and were aged at least 18 years. Only 186 of those patients, however, had data in the Long-Term Follow-Up Registry. Patients who were Black or had lower income were less likely to have data in the Long-Term Follow-Up Registry.
Just over half the patients in the long-term registry had transferred their care to an adult rheumatologist, and 83% overall were under the care of any physician. Patients who transferred their care were significantly more likely to have private insurance (87% vs. 70%; P = .009) and were more likely to be full-time students (74% vs. 58%; P = .036).
The researchers found no association between patients’ disease status at their last CARRA Registry visit and a successful transition to adult care. However, those who had transferred care to an adult rheumatologist tended to have a higher median level of pain (4 vs. 2 on a scale of 0-10) and more disease activity (3 vs. 1 on 0-10 scale) than did those who had not transferred care (P = .022 and P = .011, respectively). A higher proportion of those who transferred care had also experienced morning stiffness over the past week (49% vs. 30%; P = .015).
How young adults prefer to learn transition skills
The third study aimed to better understand the experience and preferences of young adults themselves as they transitioned from pediatric to adult care. Kristine Carandang, PhD, a postdoctoral scholar at the University of California, San Diego, and colleagues first conducted focus groups with 39 adolescents and young adults, ages 16-28 years, who had rheumatic conditions. Using the qualitative data from the focus groups, they designed a survey to capture quantitative data on young patients’ experiences.
“What we’re always trying to work on is, how do we bring that youth voice more clearly into the research literature?” Courtney K. Wells, PhD, MSW, an assistant professor of social work at the University of Wisconsin–River Falls, said in an interview. She noted that both she and Dr. Carandang were patients with rheumatic diseases, so they had lived and grown up with disease themselves and then become researchers.
“We have the information that’s in the literature, but then we also both work with youth in a couple different ways, and what we hear from youth is what we heard in our paper, but it isn’t all represented in the literature,” Dr. Wells said. That disconnect is why they also included two young adults as coauthors in the study.
“As much as we appreciate the model of the six components [of health care transition], we recognize that the youth voice isn’t represented very well,” Dr. Wells said. “The way it’s written is more for doctors and policy makers and targeted for the health care system rather than the young people themselves.”
Their research bore that out. Among 137 survey respondents, aged 18-28 years, the vast majority (89%) were women and most (75%) were White. Half the patients (50%) had a diagnosis of lupus.
“For 9 out of 11 self-management and self-advocacy skills examined, there was a significant difference between how adolescent and young adult patients experienced learning self- management skills versus how they would have preferred to learn the skills,” the researchers concluded. “Overall, adolescent and young adult patients most frequently learned about transition skills from their parents. Most participants would have preferred to learn these skills from their rheumatology team.”
For example, 46.7% of the respondents learned how to communicate their medical history from their parents, but 48.5% would have preferred to learn that from their rheumatology team. Only a quarter (24.8%) had learned that skill from their health care team.
“For most of these skills, they were getting that information from their parents, which is concerning because their parents don’t necessarily have information that is accurate,” Dr. Wells said. “Their parents managed their health care, and they taught them to do it the way they were doing it.”
Just over one-third of respondents said they learned from their parents how to track their symptoms so they could answer the rheumatologists’ questions. Only one in five respondents (20.4%) had learned this skill from their rheumatology team, but 41.2% would have preferred hearing it from their health care team, compared with 22.1% who preferred learning it from their parents.
Nearly half the respondents reported learning from their parents how to advocate for themselves when dissatisfied with their care or symptoms (49.6%) and how to talk to the office staff to make appointments, fill out paperwork, and access health records (47.4%). Just over half (51.5%) would have preferred to learn about office communication from their health care team. Preferences on self-advocacy were split between learning from parents (36.8%) and learning from their health care team (31.6%).
An opportunity for other organizations to support transition
The researchers noted that education did not necessarily need to come only from rheumatologists. Other health care professionals, including nurses and social workers, could help young patients develop skills as well.
“They said they’re also open to talking to other people, but they want their rheumatologist to lead the whole process,” Dr. Wells said. While reimbursement gaps may have presented a barrier in the past, Dr. Wells said that current billing codes have removed that obstacle, allowing physicians to bill for discussing transition skills and care.
“Largely, it’s a time issue,” Dr. Wells said. “Rheumatologists are going to tell patients first about their disease, ask how their medication is working and how their health is. Then, if we have time, we’ll cover the transition pieces, and what it boils down to is that they just don’t have time.”
The respondents indicated an interest in technology that can help their education and transition, such as patient portals, telehealth, and smartphone apps.
While 66.4% of respondents said they would attend an in-person health care appointment to learn skills for transitioning to adult care, 74.5% would attend a telehealth appointment, and 77.2% would complete a structured program within a patient portal.
Dr. Wells said she doesn’t see many of the health care system pressures easing up to allow rheumatologists more time for transition care, but she sees an opportunity for organizations, such as the Arthritis Foundation or Lupus Foundation of America, to step in and help.
“It is a matter of being creative and that, ultimately, is the barrier: Whose job is it to make it happen?” she said. “That’s where some other groups are going to need to be advocates.”
Another notable set of findings from this research was the need for young patients’ access to mental health and sexual/reproductive health services. Just over two-thirds of respondents preferred to discuss these topics with their rheumatology team, but only 59.1% felt comfortable starting the conversation about mental health, and only 47.4% felt comfortable broaching the topic of reproductive/sexual health. Even more patients preferred discussing use of drugs and alcohol with their health care team (71.5%), but more patients also felt comfortable initiating that discussion (72.2%).
“It may be that somebody who’s trained to address those issues, especially the mental health piece, may be more appropriate to have that role, and that’s part of the transition, too, these other larger life issues,” Dr. Wells said. “One of the benefits of going to an adult rheumatologist is that they are the most knowledgeable and prepared to help you with those topics.”
None of the individuals quoted in this story had any disclosures to report.
The inadequacies and challenges of transitioning pediatric rheumatology patients to adult care were highlighted in several research studies shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
“Not surprisingly, these studies demonstrate that transition challenges remain pervasive,” Rebecca Sadun, MD, PhD, who was not involved in any of the research, said in an interview. Nevertheless, she pointed out that one of the studies showed that eight of nine sites participating in one of the studies had at least developed a formal transition policy, and three were able to fully integrate that policy into their health care system despite the ongoing pandemic.
In that study, Joyce Chang, MD, of the Children’s Hospital of Philadelphia and colleagues used structured interviews and then quantitative research to explore processes for transition polices across nine rheumatology sites. Aside from the three that had already implemented their policies, three others were preparing implementation. The other three withdrew because of COVID-19. None of the sites had reached sustainment phase. Six of the sites had access to a social work network, and two sites had fewer than four providers.
The authors found that a higher level of change efficacy or change commitment using the Organizational Readiness for Implementing Change framework did not correspond with reaching implementation.
“The first sites to reach implementation had access to [information technology] support and involved nursing, though this was not sufficient or necessary,” the authors wrote. They noted the need for strategies to reduce the burden of data collection to improve the resilience of implementation efforts against health care system stress.
Who more often transitions to adult care?
Effective transition policies can help reduce the likelihood of young patients falling through the cracks as they grow from adolescence into young adulthood, especially those at highest risk for losing continuity of care.
“Young adults who are both medically and socially complex are at highest risk,” said Dr. Sadun, an assistant professor of adult and pediatric rheumatology at Duke University, Durham, N.C. “This is especially true for patients with systemic illnesses, patients requiring biologic medications, and patients with custody, transportation, and financial barriers.”
Research led by Emily A. Smitherman, MD, an assistant professor of pediatric rheumatology at Children’s of Alabama in Birmingham, looked more closely at who is and is not transitioning their care. The researchers analyzed retrospective data from the CARRA Registry, including the Long-Term Follow-Up Call Registry, through December 2019. Among 1,311 patients with inactive status, 537 of these patients had juvenile idiopathic arthritis and were aged at least 18 years. Only 186 of those patients, however, had data in the Long-Term Follow-Up Registry. Patients who were Black or had lower income were less likely to have data in the Long-Term Follow-Up Registry.
Just over half the patients in the long-term registry had transferred their care to an adult rheumatologist, and 83% overall were under the care of any physician. Patients who transferred their care were significantly more likely to have private insurance (87% vs. 70%; P = .009) and were more likely to be full-time students (74% vs. 58%; P = .036).
The researchers found no association between patients’ disease status at their last CARRA Registry visit and a successful transition to adult care. However, those who had transferred care to an adult rheumatologist tended to have a higher median level of pain (4 vs. 2 on a scale of 0-10) and more disease activity (3 vs. 1 on 0-10 scale) than did those who had not transferred care (P = .022 and P = .011, respectively). A higher proportion of those who transferred care had also experienced morning stiffness over the past week (49% vs. 30%; P = .015).
How young adults prefer to learn transition skills
The third study aimed to better understand the experience and preferences of young adults themselves as they transitioned from pediatric to adult care. Kristine Carandang, PhD, a postdoctoral scholar at the University of California, San Diego, and colleagues first conducted focus groups with 39 adolescents and young adults, ages 16-28 years, who had rheumatic conditions. Using the qualitative data from the focus groups, they designed a survey to capture quantitative data on young patients’ experiences.
“What we’re always trying to work on is, how do we bring that youth voice more clearly into the research literature?” Courtney K. Wells, PhD, MSW, an assistant professor of social work at the University of Wisconsin–River Falls, said in an interview. She noted that both she and Dr. Carandang were patients with rheumatic diseases, so they had lived and grown up with disease themselves and then become researchers.
“We have the information that’s in the literature, but then we also both work with youth in a couple different ways, and what we hear from youth is what we heard in our paper, but it isn’t all represented in the literature,” Dr. Wells said. That disconnect is why they also included two young adults as coauthors in the study.
“As much as we appreciate the model of the six components [of health care transition], we recognize that the youth voice isn’t represented very well,” Dr. Wells said. “The way it’s written is more for doctors and policy makers and targeted for the health care system rather than the young people themselves.”
Their research bore that out. Among 137 survey respondents, aged 18-28 years, the vast majority (89%) were women and most (75%) were White. Half the patients (50%) had a diagnosis of lupus.
“For 9 out of 11 self-management and self-advocacy skills examined, there was a significant difference between how adolescent and young adult patients experienced learning self- management skills versus how they would have preferred to learn the skills,” the researchers concluded. “Overall, adolescent and young adult patients most frequently learned about transition skills from their parents. Most participants would have preferred to learn these skills from their rheumatology team.”
For example, 46.7% of the respondents learned how to communicate their medical history from their parents, but 48.5% would have preferred to learn that from their rheumatology team. Only a quarter (24.8%) had learned that skill from their health care team.
“For most of these skills, they were getting that information from their parents, which is concerning because their parents don’t necessarily have information that is accurate,” Dr. Wells said. “Their parents managed their health care, and they taught them to do it the way they were doing it.”
Just over one-third of respondents said they learned from their parents how to track their symptoms so they could answer the rheumatologists’ questions. Only one in five respondents (20.4%) had learned this skill from their rheumatology team, but 41.2% would have preferred hearing it from their health care team, compared with 22.1% who preferred learning it from their parents.
Nearly half the respondents reported learning from their parents how to advocate for themselves when dissatisfied with their care or symptoms (49.6%) and how to talk to the office staff to make appointments, fill out paperwork, and access health records (47.4%). Just over half (51.5%) would have preferred to learn about office communication from their health care team. Preferences on self-advocacy were split between learning from parents (36.8%) and learning from their health care team (31.6%).
An opportunity for other organizations to support transition
The researchers noted that education did not necessarily need to come only from rheumatologists. Other health care professionals, including nurses and social workers, could help young patients develop skills as well.
“They said they’re also open to talking to other people, but they want their rheumatologist to lead the whole process,” Dr. Wells said. While reimbursement gaps may have presented a barrier in the past, Dr. Wells said that current billing codes have removed that obstacle, allowing physicians to bill for discussing transition skills and care.
“Largely, it’s a time issue,” Dr. Wells said. “Rheumatologists are going to tell patients first about their disease, ask how their medication is working and how their health is. Then, if we have time, we’ll cover the transition pieces, and what it boils down to is that they just don’t have time.”
The respondents indicated an interest in technology that can help their education and transition, such as patient portals, telehealth, and smartphone apps.
While 66.4% of respondents said they would attend an in-person health care appointment to learn skills for transitioning to adult care, 74.5% would attend a telehealth appointment, and 77.2% would complete a structured program within a patient portal.
Dr. Wells said she doesn’t see many of the health care system pressures easing up to allow rheumatologists more time for transition care, but she sees an opportunity for organizations, such as the Arthritis Foundation or Lupus Foundation of America, to step in and help.
“It is a matter of being creative and that, ultimately, is the barrier: Whose job is it to make it happen?” she said. “That’s where some other groups are going to need to be advocates.”
Another notable set of findings from this research was the need for young patients’ access to mental health and sexual/reproductive health services. Just over two-thirds of respondents preferred to discuss these topics with their rheumatology team, but only 59.1% felt comfortable starting the conversation about mental health, and only 47.4% felt comfortable broaching the topic of reproductive/sexual health. Even more patients preferred discussing use of drugs and alcohol with their health care team (71.5%), but more patients also felt comfortable initiating that discussion (72.2%).
“It may be that somebody who’s trained to address those issues, especially the mental health piece, may be more appropriate to have that role, and that’s part of the transition, too, these other larger life issues,” Dr. Wells said. “One of the benefits of going to an adult rheumatologist is that they are the most knowledgeable and prepared to help you with those topics.”
None of the individuals quoted in this story had any disclosures to report.
FROM CARRA 2021
FDA moves to ban menthol in cigarettes
The Food and Drug Administration said that within a year it will ban menthol in cigarettes and ban all flavors including menthol in cigars.
Menthol makes it easier to start smoking, and also enhances the effects of nicotine, making it more addictive and harder to quit, the FDA said in announcing its actions on Thursday.
Nineteen organizations – including the American Academy of Pediatrics, American Cancer Society, American College of Chest Physicians, American Medical Association, American Heart Association, and the National Medical Association – have pushed the FDA to ban menthol for years. The agency banned all flavors in cigarettes in 2009 but did not take any action against menthol. In 2013, the groups filed a petition demanding that the FDA ban menthol, too. The agency responded months later with a notice that it would start the process.
But it never took any action. Action on Smoking and Health and the African American Tobacco Control Leadership Council, later joined by the AMA and the NMA, sued in 2020 to compel the agency to do something. Now it has finally agreed to act.
The African American Tobacco Control Leadership Council welcomed the move but said the fight is not over and encouraged tobacco control activists to fight to ban menthol tobacco products at the local, state and federal level. “We know that this rule-making process could take years and we know that the tobacco industry will continue to do everything in their power to derail any attempt to remove their deadly products from the market,” Phillip Gardiner, MD, council cochair, said in a statement.
The AMA is urging the FDA to quickly implement the ban and remove the products “without further delay,” AMA President Susan R. Bailey, MD, said in a statement.
“FDA’s long-awaited decision to take action to eliminate menthol flavoring in cigarettes and all flavors in cigars ends a decades-long deference to the tobacco industry, which has repeatedly demonstrated its willingness to profit from products that result in death,” Lisa Lacasse, president of the American Cancer Society Cancer Action Network, said in her own statement.
Ms. Lacasse said banning menthol will help eliminate health disparities. She said 86% of Black people who smoke use menthol cigarettes, compared with 46% of Hispanic people who smoke, 39% of Asian people who smoke, and 29% of White people who smoke. “FDA’s actions today send a clear message that Big Tobacco’s strategy to profit off addicting Black communities will no longer be tolerated,” she said.
Not all groups are on board, however. The American Civil Liberties Union and several other organizations wrote to the country’s top health officials urging them to reconsider.
“Such a ban will trigger criminal penalties which will disproportionately impact people of color, as well as prioritize criminalization over public health and harm reduction,” the letter says. “A ban will also lead to unconstitutional policing and other negative interactions with local law enforcement.”
The letter calls the proposed ban “well intentioned,” but said any effort to reduce death and disease from tobacco “must avoid solutions that will create yet another reason for armed police to engage citizens on the street based on pretext or conduct that does not pose a threat to public safety.”
Instead of a ban, the organizations said, policy makers should consider increased education for adults and minors, stop-smoking programs, and increased funding for health centers in communities of color.
The Biden administration, however, pressed the point that banning menthol will bring many positives. Acting FDA Commissioner Janet Woodcock, MD said in a statement that banning menthol “will help significantly reduce youth initiation, increase the chances of smoking cessation among current smokers, and address health disparities experienced by communities of color, low-income populations, and LGBTQ-plus individuals, all of whom are far more likely to use these tobacco products.”
The FDA cited data showing that, in the first year or so after a ban goes into effect, an additional 923,000 smokers would quit, including 230,000 African Americans. Another study suggests that 633,000 deaths would be averted, including 237,000 Black Americans.
Dr. Woodcock added that, “armed with strong scientific evidence, and with full support from the [Biden] administration, we believe these actions will launch us on a trajectory toward ending tobacco-related disease and death in the U.S.”
The FDA estimates that 18.6 million Americans who are current smokers use menthol cigarettes, with a disproportionately high number being Black people. Menthol cigarette use among Black and Hispanic youth increased from 2011 to 2018, but declined for non-Hispanic White youth.
Flavored mass-produced cigars and cigarillos are disproportionately popular among youth, especially non-Hispanic Black high school students, who in 2020 reported past 30-day cigar smoking at levels twice as high as their White counterparts, said the FDA. Three-quarters of 12- to 17-year-olds reported they smoke cigars because they like the flavors. In 2020, more young people tried a cigar every day than tried a cigarette, reports the agency.
“This long-overdue decision will protect future generations of young people from nicotine addiction, especially Black children and communities, which have disproportionately suffered from menthol tobacco use due to targeted efforts from the tobacco industry,” Lee Savio Beers, MD, president of the American Academy of Pediatrics, said in a statement.
The FDA’s announcement “is only a first step that must be followed with urgent, comprehensive action to remove these flavored products from the market,” he said.
A version of this article first appeared on WebMD.com.
The Food and Drug Administration said that within a year it will ban menthol in cigarettes and ban all flavors including menthol in cigars.
Menthol makes it easier to start smoking, and also enhances the effects of nicotine, making it more addictive and harder to quit, the FDA said in announcing its actions on Thursday.
Nineteen organizations – including the American Academy of Pediatrics, American Cancer Society, American College of Chest Physicians, American Medical Association, American Heart Association, and the National Medical Association – have pushed the FDA to ban menthol for years. The agency banned all flavors in cigarettes in 2009 but did not take any action against menthol. In 2013, the groups filed a petition demanding that the FDA ban menthol, too. The agency responded months later with a notice that it would start the process.
But it never took any action. Action on Smoking and Health and the African American Tobacco Control Leadership Council, later joined by the AMA and the NMA, sued in 2020 to compel the agency to do something. Now it has finally agreed to act.
The African American Tobacco Control Leadership Council welcomed the move but said the fight is not over and encouraged tobacco control activists to fight to ban menthol tobacco products at the local, state and federal level. “We know that this rule-making process could take years and we know that the tobacco industry will continue to do everything in their power to derail any attempt to remove their deadly products from the market,” Phillip Gardiner, MD, council cochair, said in a statement.
The AMA is urging the FDA to quickly implement the ban and remove the products “without further delay,” AMA President Susan R. Bailey, MD, said in a statement.
“FDA’s long-awaited decision to take action to eliminate menthol flavoring in cigarettes and all flavors in cigars ends a decades-long deference to the tobacco industry, which has repeatedly demonstrated its willingness to profit from products that result in death,” Lisa Lacasse, president of the American Cancer Society Cancer Action Network, said in her own statement.
Ms. Lacasse said banning menthol will help eliminate health disparities. She said 86% of Black people who smoke use menthol cigarettes, compared with 46% of Hispanic people who smoke, 39% of Asian people who smoke, and 29% of White people who smoke. “FDA’s actions today send a clear message that Big Tobacco’s strategy to profit off addicting Black communities will no longer be tolerated,” she said.
Not all groups are on board, however. The American Civil Liberties Union and several other organizations wrote to the country’s top health officials urging them to reconsider.
“Such a ban will trigger criminal penalties which will disproportionately impact people of color, as well as prioritize criminalization over public health and harm reduction,” the letter says. “A ban will also lead to unconstitutional policing and other negative interactions with local law enforcement.”
The letter calls the proposed ban “well intentioned,” but said any effort to reduce death and disease from tobacco “must avoid solutions that will create yet another reason for armed police to engage citizens on the street based on pretext or conduct that does not pose a threat to public safety.”
Instead of a ban, the organizations said, policy makers should consider increased education for adults and minors, stop-smoking programs, and increased funding for health centers in communities of color.
The Biden administration, however, pressed the point that banning menthol will bring many positives. Acting FDA Commissioner Janet Woodcock, MD said in a statement that banning menthol “will help significantly reduce youth initiation, increase the chances of smoking cessation among current smokers, and address health disparities experienced by communities of color, low-income populations, and LGBTQ-plus individuals, all of whom are far more likely to use these tobacco products.”
The FDA cited data showing that, in the first year or so after a ban goes into effect, an additional 923,000 smokers would quit, including 230,000 African Americans. Another study suggests that 633,000 deaths would be averted, including 237,000 Black Americans.
Dr. Woodcock added that, “armed with strong scientific evidence, and with full support from the [Biden] administration, we believe these actions will launch us on a trajectory toward ending tobacco-related disease and death in the U.S.”
The FDA estimates that 18.6 million Americans who are current smokers use menthol cigarettes, with a disproportionately high number being Black people. Menthol cigarette use among Black and Hispanic youth increased from 2011 to 2018, but declined for non-Hispanic White youth.
Flavored mass-produced cigars and cigarillos are disproportionately popular among youth, especially non-Hispanic Black high school students, who in 2020 reported past 30-day cigar smoking at levels twice as high as their White counterparts, said the FDA. Three-quarters of 12- to 17-year-olds reported they smoke cigars because they like the flavors. In 2020, more young people tried a cigar every day than tried a cigarette, reports the agency.
“This long-overdue decision will protect future generations of young people from nicotine addiction, especially Black children and communities, which have disproportionately suffered from menthol tobacco use due to targeted efforts from the tobacco industry,” Lee Savio Beers, MD, president of the American Academy of Pediatrics, said in a statement.
The FDA’s announcement “is only a first step that must be followed with urgent, comprehensive action to remove these flavored products from the market,” he said.
A version of this article first appeared on WebMD.com.
The Food and Drug Administration said that within a year it will ban menthol in cigarettes and ban all flavors including menthol in cigars.
Menthol makes it easier to start smoking, and also enhances the effects of nicotine, making it more addictive and harder to quit, the FDA said in announcing its actions on Thursday.
Nineteen organizations – including the American Academy of Pediatrics, American Cancer Society, American College of Chest Physicians, American Medical Association, American Heart Association, and the National Medical Association – have pushed the FDA to ban menthol for years. The agency banned all flavors in cigarettes in 2009 but did not take any action against menthol. In 2013, the groups filed a petition demanding that the FDA ban menthol, too. The agency responded months later with a notice that it would start the process.
But it never took any action. Action on Smoking and Health and the African American Tobacco Control Leadership Council, later joined by the AMA and the NMA, sued in 2020 to compel the agency to do something. Now it has finally agreed to act.
The African American Tobacco Control Leadership Council welcomed the move but said the fight is not over and encouraged tobacco control activists to fight to ban menthol tobacco products at the local, state and federal level. “We know that this rule-making process could take years and we know that the tobacco industry will continue to do everything in their power to derail any attempt to remove their deadly products from the market,” Phillip Gardiner, MD, council cochair, said in a statement.
The AMA is urging the FDA to quickly implement the ban and remove the products “without further delay,” AMA President Susan R. Bailey, MD, said in a statement.
“FDA’s long-awaited decision to take action to eliminate menthol flavoring in cigarettes and all flavors in cigars ends a decades-long deference to the tobacco industry, which has repeatedly demonstrated its willingness to profit from products that result in death,” Lisa Lacasse, president of the American Cancer Society Cancer Action Network, said in her own statement.
Ms. Lacasse said banning menthol will help eliminate health disparities. She said 86% of Black people who smoke use menthol cigarettes, compared with 46% of Hispanic people who smoke, 39% of Asian people who smoke, and 29% of White people who smoke. “FDA’s actions today send a clear message that Big Tobacco’s strategy to profit off addicting Black communities will no longer be tolerated,” she said.
Not all groups are on board, however. The American Civil Liberties Union and several other organizations wrote to the country’s top health officials urging them to reconsider.
“Such a ban will trigger criminal penalties which will disproportionately impact people of color, as well as prioritize criminalization over public health and harm reduction,” the letter says. “A ban will also lead to unconstitutional policing and other negative interactions with local law enforcement.”
The letter calls the proposed ban “well intentioned,” but said any effort to reduce death and disease from tobacco “must avoid solutions that will create yet another reason for armed police to engage citizens on the street based on pretext or conduct that does not pose a threat to public safety.”
Instead of a ban, the organizations said, policy makers should consider increased education for adults and minors, stop-smoking programs, and increased funding for health centers in communities of color.
The Biden administration, however, pressed the point that banning menthol will bring many positives. Acting FDA Commissioner Janet Woodcock, MD said in a statement that banning menthol “will help significantly reduce youth initiation, increase the chances of smoking cessation among current smokers, and address health disparities experienced by communities of color, low-income populations, and LGBTQ-plus individuals, all of whom are far more likely to use these tobacco products.”
The FDA cited data showing that, in the first year or so after a ban goes into effect, an additional 923,000 smokers would quit, including 230,000 African Americans. Another study suggests that 633,000 deaths would be averted, including 237,000 Black Americans.
Dr. Woodcock added that, “armed with strong scientific evidence, and with full support from the [Biden] administration, we believe these actions will launch us on a trajectory toward ending tobacco-related disease and death in the U.S.”
The FDA estimates that 18.6 million Americans who are current smokers use menthol cigarettes, with a disproportionately high number being Black people. Menthol cigarette use among Black and Hispanic youth increased from 2011 to 2018, but declined for non-Hispanic White youth.
Flavored mass-produced cigars and cigarillos are disproportionately popular among youth, especially non-Hispanic Black high school students, who in 2020 reported past 30-day cigar smoking at levels twice as high as their White counterparts, said the FDA. Three-quarters of 12- to 17-year-olds reported they smoke cigars because they like the flavors. In 2020, more young people tried a cigar every day than tried a cigarette, reports the agency.
“This long-overdue decision will protect future generations of young people from nicotine addiction, especially Black children and communities, which have disproportionately suffered from menthol tobacco use due to targeted efforts from the tobacco industry,” Lee Savio Beers, MD, president of the American Academy of Pediatrics, said in a statement.
The FDA’s announcement “is only a first step that must be followed with urgent, comprehensive action to remove these flavored products from the market,” he said.
A version of this article first appeared on WebMD.com.
CDC guidelines coming on long COVID
The Centers for Disease Control and Prevention is finalizing new guidelines to help clinicians diagnose and manage long COVID, or postacute sequelae of SARS-CoV-2 infection.
In a day-long congressional hearing on April 28, John Brooks, MD, a medical epidemiologist at the CDC’s division of HIV/AIDS prevention, testified that the guidelines were going through the clearance process at the agency, but would be forthcoming.
“They should be coming out very shortly,” Dr. Brooks said.
The guidelines, which were developed in collaboration with newly established long-COVID clinics and patient advocacy groups, will “illustrate how to diagnose and begin to pull together what we know about management,” of the complex condition, he said.
For many doctors and patients who are struggling to understand symptoms that persist for months after the initial viral infection, the guidelines can’t come soon enough.
National Institutes of Health Director Francis Collins, MD, PhD, who also testified at the hearing, estimated that as many as 3 million people could be left with chronic health problems after even mild COVID infections.
“I can’t overstate how serious this issue is for the health of our nation,” he said.
Dr. Collins said his estimate was based on studies showing that roughly 10% of people who get COVID could be affected by this and whose “long-term course is uncertain,” he said. So far, more than 32 million Americans are known to have been infected with the new coronavirus.
“We need to make sure we put our arms around them and bring answers and care to them,” said Rep. Anna Eshoo (D-Calif.), chairwoman of the Subcommittee on Health.
Jennifer Possick, MD, who directs the post-COVID recovery program at Yale New Haven (Conn.) Hospital, testified that the tidal wave of patients she and her colleagues were seeing was overwhelming.
“We are a well-resourced program at an academic medical center, but we are swamped by the need in our community. This year, we have seen more patients with post COVID-19 conditions in our clinic alone than we have new cases of asthma and COPD combined,” she said. “The magnitude of the challenge is daunting.”
Dr. Possick estimated that there are “over 60” clinics in the United States that have started to treat long-COVID patients, but said they are grassroots efforts and all very different from each other.
“Whoever had the resources, had the time, [and] was able to take the initiative and forge to the relationships because most of them are multidisciplinary, did so,” she said.
Patients testify
Several representatives shared moving personal stories of loved ones or staffers who remained ill months after a COVID diagnosis.
Rep. Ann Kuster, from New Hampshire, talked about her 34-year-old niece, a member of the U.S. Ski Team, who had COVID just over a year ago and “continues to struggle with everything, even the simplest activities of daily living” she said. “She has to choose between taking a shower or making dinner. I’m so proud of her for hanging in there.”
Long-COVID patients invited to testify by the subcommittee described months of disability that left them with soaring medical bills and no ability to work to pay them.
“I am now a poor, Black, disabled woman, living with long COVID,” said Chimere Smith, who said she had been a school teacher in Baltimore. “Saying it aloud makes it no more easy to accept.”
She said COVID had affected her ability to think clearly and caused debilitating fatigue, which prevented her from working. She said she lost her vision for almost 5 months because doctors misdiagnosed a cataract caused by long COVID as dry eye.
“If I did not have a loving family, I [would] be speaking to you today [from] my car, the only property I now own.”
Ms. Smith said that long-COVID clinics, which are mostly housed within academic medical centers, were not going to be accessible for all long-haulers, who are disproportionately women of color. She has started a clinic, based out of her church, to help other patients from her community.
“No one wants to hear that long COVID has decimated my life or the lives of other black women in less than a year,” Ms. Smith said. “We’ve just been waiting and hoping for compassionate doctors and politicians who would acknowledge us.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention is finalizing new guidelines to help clinicians diagnose and manage long COVID, or postacute sequelae of SARS-CoV-2 infection.
In a day-long congressional hearing on April 28, John Brooks, MD, a medical epidemiologist at the CDC’s division of HIV/AIDS prevention, testified that the guidelines were going through the clearance process at the agency, but would be forthcoming.
“They should be coming out very shortly,” Dr. Brooks said.
The guidelines, which were developed in collaboration with newly established long-COVID clinics and patient advocacy groups, will “illustrate how to diagnose and begin to pull together what we know about management,” of the complex condition, he said.
For many doctors and patients who are struggling to understand symptoms that persist for months after the initial viral infection, the guidelines can’t come soon enough.
National Institutes of Health Director Francis Collins, MD, PhD, who also testified at the hearing, estimated that as many as 3 million people could be left with chronic health problems after even mild COVID infections.
“I can’t overstate how serious this issue is for the health of our nation,” he said.
Dr. Collins said his estimate was based on studies showing that roughly 10% of people who get COVID could be affected by this and whose “long-term course is uncertain,” he said. So far, more than 32 million Americans are known to have been infected with the new coronavirus.
“We need to make sure we put our arms around them and bring answers and care to them,” said Rep. Anna Eshoo (D-Calif.), chairwoman of the Subcommittee on Health.
Jennifer Possick, MD, who directs the post-COVID recovery program at Yale New Haven (Conn.) Hospital, testified that the tidal wave of patients she and her colleagues were seeing was overwhelming.
“We are a well-resourced program at an academic medical center, but we are swamped by the need in our community. This year, we have seen more patients with post COVID-19 conditions in our clinic alone than we have new cases of asthma and COPD combined,” she said. “The magnitude of the challenge is daunting.”
Dr. Possick estimated that there are “over 60” clinics in the United States that have started to treat long-COVID patients, but said they are grassroots efforts and all very different from each other.
“Whoever had the resources, had the time, [and] was able to take the initiative and forge to the relationships because most of them are multidisciplinary, did so,” she said.
Patients testify
Several representatives shared moving personal stories of loved ones or staffers who remained ill months after a COVID diagnosis.
Rep. Ann Kuster, from New Hampshire, talked about her 34-year-old niece, a member of the U.S. Ski Team, who had COVID just over a year ago and “continues to struggle with everything, even the simplest activities of daily living” she said. “She has to choose between taking a shower or making dinner. I’m so proud of her for hanging in there.”
Long-COVID patients invited to testify by the subcommittee described months of disability that left them with soaring medical bills and no ability to work to pay them.
“I am now a poor, Black, disabled woman, living with long COVID,” said Chimere Smith, who said she had been a school teacher in Baltimore. “Saying it aloud makes it no more easy to accept.”
She said COVID had affected her ability to think clearly and caused debilitating fatigue, which prevented her from working. She said she lost her vision for almost 5 months because doctors misdiagnosed a cataract caused by long COVID as dry eye.
“If I did not have a loving family, I [would] be speaking to you today [from] my car, the only property I now own.”
Ms. Smith said that long-COVID clinics, which are mostly housed within academic medical centers, were not going to be accessible for all long-haulers, who are disproportionately women of color. She has started a clinic, based out of her church, to help other patients from her community.
“No one wants to hear that long COVID has decimated my life or the lives of other black women in less than a year,” Ms. Smith said. “We’ve just been waiting and hoping for compassionate doctors and politicians who would acknowledge us.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention is finalizing new guidelines to help clinicians diagnose and manage long COVID, or postacute sequelae of SARS-CoV-2 infection.
In a day-long congressional hearing on April 28, John Brooks, MD, a medical epidemiologist at the CDC’s division of HIV/AIDS prevention, testified that the guidelines were going through the clearance process at the agency, but would be forthcoming.
“They should be coming out very shortly,” Dr. Brooks said.
The guidelines, which were developed in collaboration with newly established long-COVID clinics and patient advocacy groups, will “illustrate how to diagnose and begin to pull together what we know about management,” of the complex condition, he said.
For many doctors and patients who are struggling to understand symptoms that persist for months after the initial viral infection, the guidelines can’t come soon enough.
National Institutes of Health Director Francis Collins, MD, PhD, who also testified at the hearing, estimated that as many as 3 million people could be left with chronic health problems after even mild COVID infections.
“I can’t overstate how serious this issue is for the health of our nation,” he said.
Dr. Collins said his estimate was based on studies showing that roughly 10% of people who get COVID could be affected by this and whose “long-term course is uncertain,” he said. So far, more than 32 million Americans are known to have been infected with the new coronavirus.
“We need to make sure we put our arms around them and bring answers and care to them,” said Rep. Anna Eshoo (D-Calif.), chairwoman of the Subcommittee on Health.
Jennifer Possick, MD, who directs the post-COVID recovery program at Yale New Haven (Conn.) Hospital, testified that the tidal wave of patients she and her colleagues were seeing was overwhelming.
“We are a well-resourced program at an academic medical center, but we are swamped by the need in our community. This year, we have seen more patients with post COVID-19 conditions in our clinic alone than we have new cases of asthma and COPD combined,” she said. “The magnitude of the challenge is daunting.”
Dr. Possick estimated that there are “over 60” clinics in the United States that have started to treat long-COVID patients, but said they are grassroots efforts and all very different from each other.
“Whoever had the resources, had the time, [and] was able to take the initiative and forge to the relationships because most of them are multidisciplinary, did so,” she said.
Patients testify
Several representatives shared moving personal stories of loved ones or staffers who remained ill months after a COVID diagnosis.
Rep. Ann Kuster, from New Hampshire, talked about her 34-year-old niece, a member of the U.S. Ski Team, who had COVID just over a year ago and “continues to struggle with everything, even the simplest activities of daily living” she said. “She has to choose between taking a shower or making dinner. I’m so proud of her for hanging in there.”
Long-COVID patients invited to testify by the subcommittee described months of disability that left them with soaring medical bills and no ability to work to pay them.
“I am now a poor, Black, disabled woman, living with long COVID,” said Chimere Smith, who said she had been a school teacher in Baltimore. “Saying it aloud makes it no more easy to accept.”
She said COVID had affected her ability to think clearly and caused debilitating fatigue, which prevented her from working. She said she lost her vision for almost 5 months because doctors misdiagnosed a cataract caused by long COVID as dry eye.
“If I did not have a loving family, I [would] be speaking to you today [from] my car, the only property I now own.”
Ms. Smith said that long-COVID clinics, which are mostly housed within academic medical centers, were not going to be accessible for all long-haulers, who are disproportionately women of color. She has started a clinic, based out of her church, to help other patients from her community.
“No one wants to hear that long COVID has decimated my life or the lives of other black women in less than a year,” Ms. Smith said. “We’ve just been waiting and hoping for compassionate doctors and politicians who would acknowledge us.”
A version of this article first appeared on Medscape.com.
TNF inhibitors linked to threefold increased risk of psoriasis in JIA patients
Children with juvenile idiopathic arthritis (JIA) have nearly triple the risk of developing psoriasis after they begin therapy with tumor necrosis factor (TNF) inhibitors, according to preliminary research shared at the annual meeting of the Childhood Arthritis and Rheumatology Research Alliance (CARRA).
Previous retrospective research at the Children’s Hospital of Philadelphia had found similar results, so the goal of this study was to look at prospectively collected data from the CARRA registry that represented a broader patient population than that of a single institution, lead author Yongdong (Dan) Zhao, MD, PhD, assistant professor of rheumatology at the University of Washington, Seattle, and pediatric rheumatologist at Seattle Children’s Hospital, said in an interview.
“The take-home message is that we confirmed this finding, and everyone who prescribed this should be aware [of the risk] and also make the family aware because often the family just thinks this is eczema and they self-manage without reporting it to the physician,” Dr. Zhao said. He advised that physicians look for evidence of psoriasis at visits and, depending on the severity, be prepared with a management plan if needed.
The researchers analyzed data from patients with JIA enrolled in the CARRA registry during June 2015–January 2020. They excluded patients with a diagnosis of inflammatory bowel disease, psoriasis at or before their JIA diagnosis, or missing data regarding the timing of psoriasis diagnosis or starting TNF inhibitors.
Among 8,222 children (29% of whom were male), just over half (54%) had ever used TNF inhibitors. Most of the patients (76%) were White, and their average age at the time of JIA diagnosis was 7 years. Compared to those with no exposure to the drugs, patients who had ever been prescribed a TNF inhibitor were three times more likely to receive a diagnosis of psoriasis afterward (unadjusted hazard ratio [HR] = 3.01; P < .01). The risk dropped only slightly (HR = 2.93; P < .01) after adjustment for gender, race, family history of psoriasis, initial International League of Associations for Rheumatology classification category, and ever having taken methotrexate.
Overall median follow-up time for the cohort was 46.7 months. The overall incidence of psoriasis in the cohort was 5.28 cases per 1,000 person-years, which split into 3.24 cases for those never exposed to TNF inhibitors and 8.49 for those ever exposed. The incidence was similar (8.31 cases per 1,000 person-years) after only the first course of TNF inhibitors.
The risk appeared greatest for adalimumab, with an incidence of 12.2 cases per 1,000 person-years after a first course in TNF inhibitor-naive patients, compared to etanercept (6.31 cases) and infliximab (9.04 cases), which did not reach statistical significance. Incidence for cumulative exposure was greater for adalimumab: 13.17 cases per 1,000 person-years, compared to 5.19 cases for etanercept and 8.77 cases for infliximab.
TNF inhibitors are first-line biologic treatment for JIA and have a longer track record for safety and effectiveness than that of newer drugs, Dr. Zhao said. They’re also commonly used for children with psoriasis, said Pamela Weiss, MD, associate professor of pediatrics and epidemiology, at the University of Pennsylvania, Philadelphia, and clinical research director of rheumatology at Children’s Hospital of Philadelphia. She was not involved in the study.
“TNF inhibitors are an incredibly useful class of medications for children with arthritis, including psoriatic arthritis,” Dr. Weiss said in an interview. “I don’t think these findings impact the risk-benefit profile of TNF inhibitors as paradoxical psoriasis is a known side effect of the medication and something most of us already counsel our families and patients about before starting a TNF inhibitor medication.”
Dr. Zhao likewise did not think the findings changed these drugs’ benefit-risk profile as long as people are aware of it. If the psoriasis is mild, he said, it’s often possible to continue the TNF inhibitor therapy along with a topical medication for the psoriasis, “but if it’s really severe, or by patient preference, you may have to switch to a different TNF inhibitor or stop it,” he said. Occasionally, he has added an additional biologic to treat the psoriasis because the underlying JIA disease in the patient couldn’t be controlled without the TNF inhibitor.
Dr. Weiss similarly said that management will depend on the severity and on shared decision-making between the physician, patient, and family.
“If it’s a small area, it can often be managed with topical corticosteroids,” Dr. Weiss said. “If it involves a large area of the body or severely affects the scalp, then stopping the TNF inhibitor therapy and starting another therapy that targets a different pathway might be considered.”
The research was funded by CARRA. Dr. Zhao has received research funding from Bristol-Myers Squibb and has consulted for Novartis. Dr. Weiss has received consulting fees from Pfizer and Lilly.
Children with juvenile idiopathic arthritis (JIA) have nearly triple the risk of developing psoriasis after they begin therapy with tumor necrosis factor (TNF) inhibitors, according to preliminary research shared at the annual meeting of the Childhood Arthritis and Rheumatology Research Alliance (CARRA).
Previous retrospective research at the Children’s Hospital of Philadelphia had found similar results, so the goal of this study was to look at prospectively collected data from the CARRA registry that represented a broader patient population than that of a single institution, lead author Yongdong (Dan) Zhao, MD, PhD, assistant professor of rheumatology at the University of Washington, Seattle, and pediatric rheumatologist at Seattle Children’s Hospital, said in an interview.
“The take-home message is that we confirmed this finding, and everyone who prescribed this should be aware [of the risk] and also make the family aware because often the family just thinks this is eczema and they self-manage without reporting it to the physician,” Dr. Zhao said. He advised that physicians look for evidence of psoriasis at visits and, depending on the severity, be prepared with a management plan if needed.
The researchers analyzed data from patients with JIA enrolled in the CARRA registry during June 2015–January 2020. They excluded patients with a diagnosis of inflammatory bowel disease, psoriasis at or before their JIA diagnosis, or missing data regarding the timing of psoriasis diagnosis or starting TNF inhibitors.
Among 8,222 children (29% of whom were male), just over half (54%) had ever used TNF inhibitors. Most of the patients (76%) were White, and their average age at the time of JIA diagnosis was 7 years. Compared to those with no exposure to the drugs, patients who had ever been prescribed a TNF inhibitor were three times more likely to receive a diagnosis of psoriasis afterward (unadjusted hazard ratio [HR] = 3.01; P < .01). The risk dropped only slightly (HR = 2.93; P < .01) after adjustment for gender, race, family history of psoriasis, initial International League of Associations for Rheumatology classification category, and ever having taken methotrexate.
Overall median follow-up time for the cohort was 46.7 months. The overall incidence of psoriasis in the cohort was 5.28 cases per 1,000 person-years, which split into 3.24 cases for those never exposed to TNF inhibitors and 8.49 for those ever exposed. The incidence was similar (8.31 cases per 1,000 person-years) after only the first course of TNF inhibitors.
The risk appeared greatest for adalimumab, with an incidence of 12.2 cases per 1,000 person-years after a first course in TNF inhibitor-naive patients, compared to etanercept (6.31 cases) and infliximab (9.04 cases), which did not reach statistical significance. Incidence for cumulative exposure was greater for adalimumab: 13.17 cases per 1,000 person-years, compared to 5.19 cases for etanercept and 8.77 cases for infliximab.
TNF inhibitors are first-line biologic treatment for JIA and have a longer track record for safety and effectiveness than that of newer drugs, Dr. Zhao said. They’re also commonly used for children with psoriasis, said Pamela Weiss, MD, associate professor of pediatrics and epidemiology, at the University of Pennsylvania, Philadelphia, and clinical research director of rheumatology at Children’s Hospital of Philadelphia. She was not involved in the study.
“TNF inhibitors are an incredibly useful class of medications for children with arthritis, including psoriatic arthritis,” Dr. Weiss said in an interview. “I don’t think these findings impact the risk-benefit profile of TNF inhibitors as paradoxical psoriasis is a known side effect of the medication and something most of us already counsel our families and patients about before starting a TNF inhibitor medication.”
Dr. Zhao likewise did not think the findings changed these drugs’ benefit-risk profile as long as people are aware of it. If the psoriasis is mild, he said, it’s often possible to continue the TNF inhibitor therapy along with a topical medication for the psoriasis, “but if it’s really severe, or by patient preference, you may have to switch to a different TNF inhibitor or stop it,” he said. Occasionally, he has added an additional biologic to treat the psoriasis because the underlying JIA disease in the patient couldn’t be controlled without the TNF inhibitor.
Dr. Weiss similarly said that management will depend on the severity and on shared decision-making between the physician, patient, and family.
“If it’s a small area, it can often be managed with topical corticosteroids,” Dr. Weiss said. “If it involves a large area of the body or severely affects the scalp, then stopping the TNF inhibitor therapy and starting another therapy that targets a different pathway might be considered.”
The research was funded by CARRA. Dr. Zhao has received research funding from Bristol-Myers Squibb and has consulted for Novartis. Dr. Weiss has received consulting fees from Pfizer and Lilly.
Children with juvenile idiopathic arthritis (JIA) have nearly triple the risk of developing psoriasis after they begin therapy with tumor necrosis factor (TNF) inhibitors, according to preliminary research shared at the annual meeting of the Childhood Arthritis and Rheumatology Research Alliance (CARRA).
Previous retrospective research at the Children’s Hospital of Philadelphia had found similar results, so the goal of this study was to look at prospectively collected data from the CARRA registry that represented a broader patient population than that of a single institution, lead author Yongdong (Dan) Zhao, MD, PhD, assistant professor of rheumatology at the University of Washington, Seattle, and pediatric rheumatologist at Seattle Children’s Hospital, said in an interview.
“The take-home message is that we confirmed this finding, and everyone who prescribed this should be aware [of the risk] and also make the family aware because often the family just thinks this is eczema and they self-manage without reporting it to the physician,” Dr. Zhao said. He advised that physicians look for evidence of psoriasis at visits and, depending on the severity, be prepared with a management plan if needed.
The researchers analyzed data from patients with JIA enrolled in the CARRA registry during June 2015–January 2020. They excluded patients with a diagnosis of inflammatory bowel disease, psoriasis at or before their JIA diagnosis, or missing data regarding the timing of psoriasis diagnosis or starting TNF inhibitors.
Among 8,222 children (29% of whom were male), just over half (54%) had ever used TNF inhibitors. Most of the patients (76%) were White, and their average age at the time of JIA diagnosis was 7 years. Compared to those with no exposure to the drugs, patients who had ever been prescribed a TNF inhibitor were three times more likely to receive a diagnosis of psoriasis afterward (unadjusted hazard ratio [HR] = 3.01; P < .01). The risk dropped only slightly (HR = 2.93; P < .01) after adjustment for gender, race, family history of psoriasis, initial International League of Associations for Rheumatology classification category, and ever having taken methotrexate.
Overall median follow-up time for the cohort was 46.7 months. The overall incidence of psoriasis in the cohort was 5.28 cases per 1,000 person-years, which split into 3.24 cases for those never exposed to TNF inhibitors and 8.49 for those ever exposed. The incidence was similar (8.31 cases per 1,000 person-years) after only the first course of TNF inhibitors.
The risk appeared greatest for adalimumab, with an incidence of 12.2 cases per 1,000 person-years after a first course in TNF inhibitor-naive patients, compared to etanercept (6.31 cases) and infliximab (9.04 cases), which did not reach statistical significance. Incidence for cumulative exposure was greater for adalimumab: 13.17 cases per 1,000 person-years, compared to 5.19 cases for etanercept and 8.77 cases for infliximab.
TNF inhibitors are first-line biologic treatment for JIA and have a longer track record for safety and effectiveness than that of newer drugs, Dr. Zhao said. They’re also commonly used for children with psoriasis, said Pamela Weiss, MD, associate professor of pediatrics and epidemiology, at the University of Pennsylvania, Philadelphia, and clinical research director of rheumatology at Children’s Hospital of Philadelphia. She was not involved in the study.
“TNF inhibitors are an incredibly useful class of medications for children with arthritis, including psoriatic arthritis,” Dr. Weiss said in an interview. “I don’t think these findings impact the risk-benefit profile of TNF inhibitors as paradoxical psoriasis is a known side effect of the medication and something most of us already counsel our families and patients about before starting a TNF inhibitor medication.”
Dr. Zhao likewise did not think the findings changed these drugs’ benefit-risk profile as long as people are aware of it. If the psoriasis is mild, he said, it’s often possible to continue the TNF inhibitor therapy along with a topical medication for the psoriasis, “but if it’s really severe, or by patient preference, you may have to switch to a different TNF inhibitor or stop it,” he said. Occasionally, he has added an additional biologic to treat the psoriasis because the underlying JIA disease in the patient couldn’t be controlled without the TNF inhibitor.
Dr. Weiss similarly said that management will depend on the severity and on shared decision-making between the physician, patient, and family.
“If it’s a small area, it can often be managed with topical corticosteroids,” Dr. Weiss said. “If it involves a large area of the body or severely affects the scalp, then stopping the TNF inhibitor therapy and starting another therapy that targets a different pathway might be considered.”
The research was funded by CARRA. Dr. Zhao has received research funding from Bristol-Myers Squibb and has consulted for Novartis. Dr. Weiss has received consulting fees from Pfizer and Lilly.
FROM CARRA 2021
Pfizer developing pill to treat COVID-19 symptoms
“If all goes well, and we implement the same speed that we are, and if regulators do the same, and they are, I hope that (it will be available) by the end of the year,” Dr. Bourla said on CNBC’s Squawk Box.
So far, the only antiviral drug authorized for use with COVID-19 is remdesivir, which is produced by Gilead Sciences and must be administered by injection in a health care setting.
An oral drug like the one Pfizer is developing could be taken at home and might keep people out of the hospital.
“Particular attention is on the oral because it provides several advantages,” Dr. Bourla said. “One of them is that you don’t need to go to the hospital to get the treatment, which is the case with all the injectables so far. You could get it at home, and that could be a game-changer.”
The drug might be effective against the emerging variants, he said. Pfizer is also working on an injectable antiviral drug.
Pfizer, with its European partner BioNTech, developed the first coronavirus vaccine authorized for use in the United States and Europe. The Pfizer pill under development would not be a vaccine to protect people from the virus but a drug to treat people who catch the virus.
The company announced in late March that it was starting clinical trials on the oral drug.
In a news release, the company said the oral drug would work by blocking protease, a critical enzyme that the virus needs to replicate. Protease inhibitors are used in medicines to treat HIV and hepatitis C.
A coronavirus vaccine that could be taken as a pill may enter clinical trials in the second quarter of 2021. The oral vaccine is being developed by Oravax Medical, a new joint venture of the Israeli-American company Oramed and the Indian company Premas Biotech. So far, all coronavirus vaccines are injectable.
A version of this article first appeared on WebMD.com.
“If all goes well, and we implement the same speed that we are, and if regulators do the same, and they are, I hope that (it will be available) by the end of the year,” Dr. Bourla said on CNBC’s Squawk Box.
So far, the only antiviral drug authorized for use with COVID-19 is remdesivir, which is produced by Gilead Sciences and must be administered by injection in a health care setting.
An oral drug like the one Pfizer is developing could be taken at home and might keep people out of the hospital.
“Particular attention is on the oral because it provides several advantages,” Dr. Bourla said. “One of them is that you don’t need to go to the hospital to get the treatment, which is the case with all the injectables so far. You could get it at home, and that could be a game-changer.”
The drug might be effective against the emerging variants, he said. Pfizer is also working on an injectable antiviral drug.
Pfizer, with its European partner BioNTech, developed the first coronavirus vaccine authorized for use in the United States and Europe. The Pfizer pill under development would not be a vaccine to protect people from the virus but a drug to treat people who catch the virus.
The company announced in late March that it was starting clinical trials on the oral drug.
In a news release, the company said the oral drug would work by blocking protease, a critical enzyme that the virus needs to replicate. Protease inhibitors are used in medicines to treat HIV and hepatitis C.
A coronavirus vaccine that could be taken as a pill may enter clinical trials in the second quarter of 2021. The oral vaccine is being developed by Oravax Medical, a new joint venture of the Israeli-American company Oramed and the Indian company Premas Biotech. So far, all coronavirus vaccines are injectable.
A version of this article first appeared on WebMD.com.
“If all goes well, and we implement the same speed that we are, and if regulators do the same, and they are, I hope that (it will be available) by the end of the year,” Dr. Bourla said on CNBC’s Squawk Box.
So far, the only antiviral drug authorized for use with COVID-19 is remdesivir, which is produced by Gilead Sciences and must be administered by injection in a health care setting.
An oral drug like the one Pfizer is developing could be taken at home and might keep people out of the hospital.
“Particular attention is on the oral because it provides several advantages,” Dr. Bourla said. “One of them is that you don’t need to go to the hospital to get the treatment, which is the case with all the injectables so far. You could get it at home, and that could be a game-changer.”
The drug might be effective against the emerging variants, he said. Pfizer is also working on an injectable antiviral drug.
Pfizer, with its European partner BioNTech, developed the first coronavirus vaccine authorized for use in the United States and Europe. The Pfizer pill under development would not be a vaccine to protect people from the virus but a drug to treat people who catch the virus.
The company announced in late March that it was starting clinical trials on the oral drug.
In a news release, the company said the oral drug would work by blocking protease, a critical enzyme that the virus needs to replicate. Protease inhibitors are used in medicines to treat HIV and hepatitis C.
A coronavirus vaccine that could be taken as a pill may enter clinical trials in the second quarter of 2021. The oral vaccine is being developed by Oravax Medical, a new joint venture of the Israeli-American company Oramed and the Indian company Premas Biotech. So far, all coronavirus vaccines are injectable.
A version of this article first appeared on WebMD.com.
Psoriasis associated with an increased risk of COVID-19 in real-world study
in patients, compared with those on topical therapy, a new study finds.
“Our study results suggest that psoriasis is an independent risk factor for COVID-19 illness,” study coauthor Jeffrey Liu, a medical student at the University of Southern California, Los Angeles, said in an interview after he presented the findings at the American Academy of Dermatology Virtual Meeting Experience. “And our findings are consistent with the hypothesis that certain systemic agents may confer a protective effect against COVID-19 illness.”
Mr. Liu and coinvestigators used a Symphony Health dataset to analyze the health records of 167,027 U.S. patients diagnosed with psoriasis and a control group of 1,002,162 patients. The participants, all at least 20 years old, had been treated for psoriasis or psoriatic arthritis from May 2019 through Jan. 1, 2020, and were tracked until Nov. 11, 2020.
The ages and races of peoples in the two groups were roughly similar. Overall, 55% were women and 75% were White, and their average age was 58 years. Type 2 diabetes was more common in the psoriasis group than the control group (23% vs. 16%), as was obesity (27% vs. 15%). Of the patients with psoriasis, 60% were on topical treatments, 19% were on oral therapies, and 22% were on biologic therapy, with only a few taking both oral and biologic therapies.
After adjustment for age and gender, patients with psoriasis were 33% more likely than the control group to develop COVID-19 (adjusted incidence rate ratio, 1.33; 95% confidence interval, 1.23-1.38; P < .0001).
In a separate analysis, the gap persisted after adjustment for demographics and comorbidities: Patients with psoriasis had a higher rate of COVID-19 infection vs. controls (adjusted odds ratio, 1.18; 95% CI, 1.13-1.23; P < .0001). Among all patients, non-White race, older age, and comorbidities were all linked to higher risk of COVID-19 (all P < .0001).
Psoriasis might make patients more vulnerable to COVID-19 because the presence of up-regulated genes in psoriatic skin “may lead to systemic hyperinflammation and sensitization of patients with psoriasis to proinflammatory cytokine storm,” Mr. Liu said. This, in turn, may trigger more severe symptomatic disease that requires medical treatment, he said.
Reduced risk, compared with topical therapies
After adjustment for age and gender, those treated with TNF-alpha inhibitors, methotrexate, and apremilast (Otezla) all had statistically lower risks of COVID-19 vs. those on topical therapy (aIRR, 0.82; 95% CI, 0.69-0.95; P < .0029 for TNF-alpha inhibitors; aIRR, 0.75; 95% CI, 0.67-0.86; P < .0001 for methotrexate; and aIRR, 0.69; 95% CI, 0.55-0.85; P < .0006 for apremilast).
Reduced risk held true for those in the separate analysis after adjustment for comorbidities and demographics (respectively, aOR, 0.87; 95% CI, 0.77-1.00; P < .0469; aOR, 0.81; 95% CI, 0.71-0.92; P < .0011; and aOR, 0.70; 95% CI, 0.57-0.87; P < .0014).
Apremilast and methotrexate may boost protection against COVID-19 by inhibiting the body’s production of cytokines, Mr. Liu said.
One message of the study is that “dermatologists should not be scared of prescribing biologics or oral therapies for psoriasis,” the study’s lead author Jashin J. Wu, MD, of the Dermatology Research and Education Foundation in Irvine, Calif., said in an interview.
However, the results on the effects of systemic therapies were not all positive. Interleukin (IL)–17 inhibitors were an outlier: After adjustment for age and gender, patients treated with this class of drugs were 36% more likely to develop COVID-19 than those on oral agents (aIRR, 1.36; 95% CI, 1.13-1.63; P < .0009).
Among patients on biologics, those taking IL-17 inhibitors had the highest risk of COVID-19, Mr. Liu said. “The risk was higher in this class regardless of reference group – general population, the topical cohort, and the oral cohort,” he said. “This may relate to the observation that this biologic class exerts more broad immunosuppressive effects on antiviral host immunity. Notably, large meta-estimates of pivotal trials have observed increased risk of respiratory tract infections for patients on IL-17 inhibitors.”
In an interview, Erica Dommasch, MD, MPH, of the department of dermatology at Beth Israel Deaconess Medical Center, Boston, cautioned that “the data from this study is very hard to interpret.”
It’s likely that some patients with psoriasis on systemic medications “may have been the most careful about limiting exposures,” she said. “Thus, it’s hard to account for behavioral changes in individuals that may have led to the decreased incidence in psoriasis in patients on systemic agents versus topical therapy alone.”
Patients with psoriasis may also be tested more often for COVID-19, and unmeasured comorbidities like chronic kidney disease may play a role too, she said. Still, she added, “it’s reassuring that the authors did not find an increased rate of COVID among psoriasis patients on systemic agents versus topicals alone.” And she agreed with Dr. Wu about the importance of treating psoriasis with therapy beyond topical treatments during the pandemic: “Providers should feel comfortable prescribing systemic medications to psoriasis patients when otherwise appropriate.”
As for the next steps, Dr. Wu said, “we will be exploring more about the prognosis of COVID-19 infection in psoriasis patients. In addition, we will be exploring the relationship of COVID-19 infection with other inflammatory skin diseases, such as atopic dermatitis.”
No study funding is reported. Dr. Wu discloses investigator, consultant, or speaker relationships with AbbVie, Almirall, Amgen, Arcutis, Aristea Therapeutics, Boehringer Ingelheim, Bristol-Myers Squibb, Dermavant, Dr. Reddy’s Laboratories, Eli Lilly, Galderma, Janssen, LEO Pharma, Mindera, Novartis, Regeneron, Sanofi Genzyme, Solius, Sun Pharmaceutical, UCB, Valeant Pharmaceuticals North America, and Zerigo Health. Mr. Liu and Dr. Dommasch have no disclosures.
in patients, compared with those on topical therapy, a new study finds.
“Our study results suggest that psoriasis is an independent risk factor for COVID-19 illness,” study coauthor Jeffrey Liu, a medical student at the University of Southern California, Los Angeles, said in an interview after he presented the findings at the American Academy of Dermatology Virtual Meeting Experience. “And our findings are consistent with the hypothesis that certain systemic agents may confer a protective effect against COVID-19 illness.”
Mr. Liu and coinvestigators used a Symphony Health dataset to analyze the health records of 167,027 U.S. patients diagnosed with psoriasis and a control group of 1,002,162 patients. The participants, all at least 20 years old, had been treated for psoriasis or psoriatic arthritis from May 2019 through Jan. 1, 2020, and were tracked until Nov. 11, 2020.
The ages and races of peoples in the two groups were roughly similar. Overall, 55% were women and 75% were White, and their average age was 58 years. Type 2 diabetes was more common in the psoriasis group than the control group (23% vs. 16%), as was obesity (27% vs. 15%). Of the patients with psoriasis, 60% were on topical treatments, 19% were on oral therapies, and 22% were on biologic therapy, with only a few taking both oral and biologic therapies.
After adjustment for age and gender, patients with psoriasis were 33% more likely than the control group to develop COVID-19 (adjusted incidence rate ratio, 1.33; 95% confidence interval, 1.23-1.38; P < .0001).
In a separate analysis, the gap persisted after adjustment for demographics and comorbidities: Patients with psoriasis had a higher rate of COVID-19 infection vs. controls (adjusted odds ratio, 1.18; 95% CI, 1.13-1.23; P < .0001). Among all patients, non-White race, older age, and comorbidities were all linked to higher risk of COVID-19 (all P < .0001).
Psoriasis might make patients more vulnerable to COVID-19 because the presence of up-regulated genes in psoriatic skin “may lead to systemic hyperinflammation and sensitization of patients with psoriasis to proinflammatory cytokine storm,” Mr. Liu said. This, in turn, may trigger more severe symptomatic disease that requires medical treatment, he said.
Reduced risk, compared with topical therapies
After adjustment for age and gender, those treated with TNF-alpha inhibitors, methotrexate, and apremilast (Otezla) all had statistically lower risks of COVID-19 vs. those on topical therapy (aIRR, 0.82; 95% CI, 0.69-0.95; P < .0029 for TNF-alpha inhibitors; aIRR, 0.75; 95% CI, 0.67-0.86; P < .0001 for methotrexate; and aIRR, 0.69; 95% CI, 0.55-0.85; P < .0006 for apremilast).
Reduced risk held true for those in the separate analysis after adjustment for comorbidities and demographics (respectively, aOR, 0.87; 95% CI, 0.77-1.00; P < .0469; aOR, 0.81; 95% CI, 0.71-0.92; P < .0011; and aOR, 0.70; 95% CI, 0.57-0.87; P < .0014).
Apremilast and methotrexate may boost protection against COVID-19 by inhibiting the body’s production of cytokines, Mr. Liu said.
One message of the study is that “dermatologists should not be scared of prescribing biologics or oral therapies for psoriasis,” the study’s lead author Jashin J. Wu, MD, of the Dermatology Research and Education Foundation in Irvine, Calif., said in an interview.
However, the results on the effects of systemic therapies were not all positive. Interleukin (IL)–17 inhibitors were an outlier: After adjustment for age and gender, patients treated with this class of drugs were 36% more likely to develop COVID-19 than those on oral agents (aIRR, 1.36; 95% CI, 1.13-1.63; P < .0009).
Among patients on biologics, those taking IL-17 inhibitors had the highest risk of COVID-19, Mr. Liu said. “The risk was higher in this class regardless of reference group – general population, the topical cohort, and the oral cohort,” he said. “This may relate to the observation that this biologic class exerts more broad immunosuppressive effects on antiviral host immunity. Notably, large meta-estimates of pivotal trials have observed increased risk of respiratory tract infections for patients on IL-17 inhibitors.”
In an interview, Erica Dommasch, MD, MPH, of the department of dermatology at Beth Israel Deaconess Medical Center, Boston, cautioned that “the data from this study is very hard to interpret.”
It’s likely that some patients with psoriasis on systemic medications “may have been the most careful about limiting exposures,” she said. “Thus, it’s hard to account for behavioral changes in individuals that may have led to the decreased incidence in psoriasis in patients on systemic agents versus topical therapy alone.”
Patients with psoriasis may also be tested more often for COVID-19, and unmeasured comorbidities like chronic kidney disease may play a role too, she said. Still, she added, “it’s reassuring that the authors did not find an increased rate of COVID among psoriasis patients on systemic agents versus topicals alone.” And she agreed with Dr. Wu about the importance of treating psoriasis with therapy beyond topical treatments during the pandemic: “Providers should feel comfortable prescribing systemic medications to psoriasis patients when otherwise appropriate.”
As for the next steps, Dr. Wu said, “we will be exploring more about the prognosis of COVID-19 infection in psoriasis patients. In addition, we will be exploring the relationship of COVID-19 infection with other inflammatory skin diseases, such as atopic dermatitis.”
No study funding is reported. Dr. Wu discloses investigator, consultant, or speaker relationships with AbbVie, Almirall, Amgen, Arcutis, Aristea Therapeutics, Boehringer Ingelheim, Bristol-Myers Squibb, Dermavant, Dr. Reddy’s Laboratories, Eli Lilly, Galderma, Janssen, LEO Pharma, Mindera, Novartis, Regeneron, Sanofi Genzyme, Solius, Sun Pharmaceutical, UCB, Valeant Pharmaceuticals North America, and Zerigo Health. Mr. Liu and Dr. Dommasch have no disclosures.
in patients, compared with those on topical therapy, a new study finds.
“Our study results suggest that psoriasis is an independent risk factor for COVID-19 illness,” study coauthor Jeffrey Liu, a medical student at the University of Southern California, Los Angeles, said in an interview after he presented the findings at the American Academy of Dermatology Virtual Meeting Experience. “And our findings are consistent with the hypothesis that certain systemic agents may confer a protective effect against COVID-19 illness.”
Mr. Liu and coinvestigators used a Symphony Health dataset to analyze the health records of 167,027 U.S. patients diagnosed with psoriasis and a control group of 1,002,162 patients. The participants, all at least 20 years old, had been treated for psoriasis or psoriatic arthritis from May 2019 through Jan. 1, 2020, and were tracked until Nov. 11, 2020.
The ages and races of peoples in the two groups were roughly similar. Overall, 55% were women and 75% were White, and their average age was 58 years. Type 2 diabetes was more common in the psoriasis group than the control group (23% vs. 16%), as was obesity (27% vs. 15%). Of the patients with psoriasis, 60% were on topical treatments, 19% were on oral therapies, and 22% were on biologic therapy, with only a few taking both oral and biologic therapies.
After adjustment for age and gender, patients with psoriasis were 33% more likely than the control group to develop COVID-19 (adjusted incidence rate ratio, 1.33; 95% confidence interval, 1.23-1.38; P < .0001).
In a separate analysis, the gap persisted after adjustment for demographics and comorbidities: Patients with psoriasis had a higher rate of COVID-19 infection vs. controls (adjusted odds ratio, 1.18; 95% CI, 1.13-1.23; P < .0001). Among all patients, non-White race, older age, and comorbidities were all linked to higher risk of COVID-19 (all P < .0001).
Psoriasis might make patients more vulnerable to COVID-19 because the presence of up-regulated genes in psoriatic skin “may lead to systemic hyperinflammation and sensitization of patients with psoriasis to proinflammatory cytokine storm,” Mr. Liu said. This, in turn, may trigger more severe symptomatic disease that requires medical treatment, he said.
Reduced risk, compared with topical therapies
After adjustment for age and gender, those treated with TNF-alpha inhibitors, methotrexate, and apremilast (Otezla) all had statistically lower risks of COVID-19 vs. those on topical therapy (aIRR, 0.82; 95% CI, 0.69-0.95; P < .0029 for TNF-alpha inhibitors; aIRR, 0.75; 95% CI, 0.67-0.86; P < .0001 for methotrexate; and aIRR, 0.69; 95% CI, 0.55-0.85; P < .0006 for apremilast).
Reduced risk held true for those in the separate analysis after adjustment for comorbidities and demographics (respectively, aOR, 0.87; 95% CI, 0.77-1.00; P < .0469; aOR, 0.81; 95% CI, 0.71-0.92; P < .0011; and aOR, 0.70; 95% CI, 0.57-0.87; P < .0014).
Apremilast and methotrexate may boost protection against COVID-19 by inhibiting the body’s production of cytokines, Mr. Liu said.
One message of the study is that “dermatologists should not be scared of prescribing biologics or oral therapies for psoriasis,” the study’s lead author Jashin J. Wu, MD, of the Dermatology Research and Education Foundation in Irvine, Calif., said in an interview.
However, the results on the effects of systemic therapies were not all positive. Interleukin (IL)–17 inhibitors were an outlier: After adjustment for age and gender, patients treated with this class of drugs were 36% more likely to develop COVID-19 than those on oral agents (aIRR, 1.36; 95% CI, 1.13-1.63; P < .0009).
Among patients on biologics, those taking IL-17 inhibitors had the highest risk of COVID-19, Mr. Liu said. “The risk was higher in this class regardless of reference group – general population, the topical cohort, and the oral cohort,” he said. “This may relate to the observation that this biologic class exerts more broad immunosuppressive effects on antiviral host immunity. Notably, large meta-estimates of pivotal trials have observed increased risk of respiratory tract infections for patients on IL-17 inhibitors.”
In an interview, Erica Dommasch, MD, MPH, of the department of dermatology at Beth Israel Deaconess Medical Center, Boston, cautioned that “the data from this study is very hard to interpret.”
It’s likely that some patients with psoriasis on systemic medications “may have been the most careful about limiting exposures,” she said. “Thus, it’s hard to account for behavioral changes in individuals that may have led to the decreased incidence in psoriasis in patients on systemic agents versus topical therapy alone.”
Patients with psoriasis may also be tested more often for COVID-19, and unmeasured comorbidities like chronic kidney disease may play a role too, she said. Still, she added, “it’s reassuring that the authors did not find an increased rate of COVID among psoriasis patients on systemic agents versus topicals alone.” And she agreed with Dr. Wu about the importance of treating psoriasis with therapy beyond topical treatments during the pandemic: “Providers should feel comfortable prescribing systemic medications to psoriasis patients when otherwise appropriate.”
As for the next steps, Dr. Wu said, “we will be exploring more about the prognosis of COVID-19 infection in psoriasis patients. In addition, we will be exploring the relationship of COVID-19 infection with other inflammatory skin diseases, such as atopic dermatitis.”
No study funding is reported. Dr. Wu discloses investigator, consultant, or speaker relationships with AbbVie, Almirall, Amgen, Arcutis, Aristea Therapeutics, Boehringer Ingelheim, Bristol-Myers Squibb, Dermavant, Dr. Reddy’s Laboratories, Eli Lilly, Galderma, Janssen, LEO Pharma, Mindera, Novartis, Regeneron, Sanofi Genzyme, Solius, Sun Pharmaceutical, UCB, Valeant Pharmaceuticals North America, and Zerigo Health. Mr. Liu and Dr. Dommasch have no disclosures.
FROM AAD VMX 2021