User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Mouse embryo experiment could teach us about miscarriages
Miscarriages are a devastating, if natural, occurrence. Nearly 1 million pregnant people in the United States experience a miscarriage every year, according to the National Advocates for Pregnant Women. New research could lend insight into the causes of some types of early pregnancy loss and maybe one day help prevent miscarriages.
In the bioengineering breakthrough, scientists created a mouse embryo in a lab without using sperm or eggs. The experimental embryo, called a model, was grown out of stem cells and developed further than any earlier experiments, with a beating heart and the foundation of a brain within a yolk sac, according to the researchers.
The experiment, while conducted with mouse stem cells, could help explain why some human pregnancies fail. Miscarriages occur in up to 15% of pregnancies confirmed by doctors, according to some studies, and also for many pregnant people before they even knew of the pregnancy. This experiment gives researchers a glimpse of a critical developmental stage for the first time.
“We are building mouse embryo models, but they have exactly the same principle as real human embryos,” says lead researcher Magdalena Zernicka-Goetz, PhD, professor in mammalian development and stem cell biology at Cambridge (England) University. “That’s why they tell us about real pregnancy.”
With the new mouse models, the researchers can study implantation, the stage when embryos embed themselves in the mother’s body – a stage that’s often difficult for embryos to survive. The same process happens in mouse embryos, which develop very similarly to human embryos at this early stage of life.
Six years ago, researchers from the University of Cambridge and the California Institute of Technology set out to create models that would allow them to study fetal development in three-dimensional form but without the need for human embryos.
“We are trying to understand the major principles of time and space that have to be fulfilled” to form a successful pregnancy, Dr. Zernicka-Goetz explains. “If those principles are not fulfilled, the pregnancies are terminated, even before women know they’re pregnant.”
There are limits on using human embryos for research, and previous experiments have tended to replicate only one aspect of development. That led to two-dimensional experiments: flat cells on the bottom of a petri dish that lack the structural organization of real tissue.
The new models are three-dimensional with beating hearts and the yolk sacs in which embryos feed and grow. The models even progressed to forming the beginning of a brain – a research first.
The scientists used the foundational cellular “building blocks” called stem cells and managed to get the cells to communicate along a timeline that mimicked natural development, simulating those developmental stages, says Dr. Zernicka-Goetz. Those “building blocks” are actually three types of stem cells: pluripotent stem cells that build body tissue, and two other types of stem cells that build the placenta and the amniotic sac.
Completing the experiment required the right quantity of each stem cell type. The researchers also needed to understand how those cells exchange information before they can begin to grow. The researchers were able to “decipher the code” of how the cells talk to each other, Dr. Zernicka-Goetz says.
Initially, the three types of stem cells combine, almost like a soup, but when the timing is right, they have to recognize each other and sort themselves. Next, each stem cell type must start building a different structure necessary for fetal development. Dr. Zernicka-Goetz thinks of this construction as the architecture of human tissue.
With the new technique, researchers can continue investigating the implantation stage and beyond. And they did – tweaking the experiment to create a genetically flawed embryo on purpose.
Dr. Zernicka-Goetz and her team eliminated a certain gene known to regulate how cells establish their own identities. Doing so resulted in the same brain development flaws as in human embryos, providing “a proof of concept” that the experimental models can be used to study other genetic mysteries, she says.
Scientists are still in the dark about what some genes do, as well as the point when they become critical to brain development.
“Many genes have very early roles in specifying, for example, the position of the head and also how our brain will function,” Dr. Zernicka-Goetz says. “We can now use this model system to assess the function of those genes.”
A version of this article first appeared on WebMD.com.
Miscarriages are a devastating, if natural, occurrence. Nearly 1 million pregnant people in the United States experience a miscarriage every year, according to the National Advocates for Pregnant Women. New research could lend insight into the causes of some types of early pregnancy loss and maybe one day help prevent miscarriages.
In the bioengineering breakthrough, scientists created a mouse embryo in a lab without using sperm or eggs. The experimental embryo, called a model, was grown out of stem cells and developed further than any earlier experiments, with a beating heart and the foundation of a brain within a yolk sac, according to the researchers.
The experiment, while conducted with mouse stem cells, could help explain why some human pregnancies fail. Miscarriages occur in up to 15% of pregnancies confirmed by doctors, according to some studies, and also for many pregnant people before they even knew of the pregnancy. This experiment gives researchers a glimpse of a critical developmental stage for the first time.
“We are building mouse embryo models, but they have exactly the same principle as real human embryos,” says lead researcher Magdalena Zernicka-Goetz, PhD, professor in mammalian development and stem cell biology at Cambridge (England) University. “That’s why they tell us about real pregnancy.”
With the new mouse models, the researchers can study implantation, the stage when embryos embed themselves in the mother’s body – a stage that’s often difficult for embryos to survive. The same process happens in mouse embryos, which develop very similarly to human embryos at this early stage of life.
Six years ago, researchers from the University of Cambridge and the California Institute of Technology set out to create models that would allow them to study fetal development in three-dimensional form but without the need for human embryos.
“We are trying to understand the major principles of time and space that have to be fulfilled” to form a successful pregnancy, Dr. Zernicka-Goetz explains. “If those principles are not fulfilled, the pregnancies are terminated, even before women know they’re pregnant.”
There are limits on using human embryos for research, and previous experiments have tended to replicate only one aspect of development. That led to two-dimensional experiments: flat cells on the bottom of a petri dish that lack the structural organization of real tissue.
The new models are three-dimensional with beating hearts and the yolk sacs in which embryos feed and grow. The models even progressed to forming the beginning of a brain – a research first.
The scientists used the foundational cellular “building blocks” called stem cells and managed to get the cells to communicate along a timeline that mimicked natural development, simulating those developmental stages, says Dr. Zernicka-Goetz. Those “building blocks” are actually three types of stem cells: pluripotent stem cells that build body tissue, and two other types of stem cells that build the placenta and the amniotic sac.
Completing the experiment required the right quantity of each stem cell type. The researchers also needed to understand how those cells exchange information before they can begin to grow. The researchers were able to “decipher the code” of how the cells talk to each other, Dr. Zernicka-Goetz says.
Initially, the three types of stem cells combine, almost like a soup, but when the timing is right, they have to recognize each other and sort themselves. Next, each stem cell type must start building a different structure necessary for fetal development. Dr. Zernicka-Goetz thinks of this construction as the architecture of human tissue.
With the new technique, researchers can continue investigating the implantation stage and beyond. And they did – tweaking the experiment to create a genetically flawed embryo on purpose.
Dr. Zernicka-Goetz and her team eliminated a certain gene known to regulate how cells establish their own identities. Doing so resulted in the same brain development flaws as in human embryos, providing “a proof of concept” that the experimental models can be used to study other genetic mysteries, she says.
Scientists are still in the dark about what some genes do, as well as the point when they become critical to brain development.
“Many genes have very early roles in specifying, for example, the position of the head and also how our brain will function,” Dr. Zernicka-Goetz says. “We can now use this model system to assess the function of those genes.”
A version of this article first appeared on WebMD.com.
Miscarriages are a devastating, if natural, occurrence. Nearly 1 million pregnant people in the United States experience a miscarriage every year, according to the National Advocates for Pregnant Women. New research could lend insight into the causes of some types of early pregnancy loss and maybe one day help prevent miscarriages.
In the bioengineering breakthrough, scientists created a mouse embryo in a lab without using sperm or eggs. The experimental embryo, called a model, was grown out of stem cells and developed further than any earlier experiments, with a beating heart and the foundation of a brain within a yolk sac, according to the researchers.
The experiment, while conducted with mouse stem cells, could help explain why some human pregnancies fail. Miscarriages occur in up to 15% of pregnancies confirmed by doctors, according to some studies, and also for many pregnant people before they even knew of the pregnancy. This experiment gives researchers a glimpse of a critical developmental stage for the first time.
“We are building mouse embryo models, but they have exactly the same principle as real human embryos,” says lead researcher Magdalena Zernicka-Goetz, PhD, professor in mammalian development and stem cell biology at Cambridge (England) University. “That’s why they tell us about real pregnancy.”
With the new mouse models, the researchers can study implantation, the stage when embryos embed themselves in the mother’s body – a stage that’s often difficult for embryos to survive. The same process happens in mouse embryos, which develop very similarly to human embryos at this early stage of life.
Six years ago, researchers from the University of Cambridge and the California Institute of Technology set out to create models that would allow them to study fetal development in three-dimensional form but without the need for human embryos.
“We are trying to understand the major principles of time and space that have to be fulfilled” to form a successful pregnancy, Dr. Zernicka-Goetz explains. “If those principles are not fulfilled, the pregnancies are terminated, even before women know they’re pregnant.”
There are limits on using human embryos for research, and previous experiments have tended to replicate only one aspect of development. That led to two-dimensional experiments: flat cells on the bottom of a petri dish that lack the structural organization of real tissue.
The new models are three-dimensional with beating hearts and the yolk sacs in which embryos feed and grow. The models even progressed to forming the beginning of a brain – a research first.
The scientists used the foundational cellular “building blocks” called stem cells and managed to get the cells to communicate along a timeline that mimicked natural development, simulating those developmental stages, says Dr. Zernicka-Goetz. Those “building blocks” are actually three types of stem cells: pluripotent stem cells that build body tissue, and two other types of stem cells that build the placenta and the amniotic sac.
Completing the experiment required the right quantity of each stem cell type. The researchers also needed to understand how those cells exchange information before they can begin to grow. The researchers were able to “decipher the code” of how the cells talk to each other, Dr. Zernicka-Goetz says.
Initially, the three types of stem cells combine, almost like a soup, but when the timing is right, they have to recognize each other and sort themselves. Next, each stem cell type must start building a different structure necessary for fetal development. Dr. Zernicka-Goetz thinks of this construction as the architecture of human tissue.
With the new technique, researchers can continue investigating the implantation stage and beyond. And they did – tweaking the experiment to create a genetically flawed embryo on purpose.
Dr. Zernicka-Goetz and her team eliminated a certain gene known to regulate how cells establish their own identities. Doing so resulted in the same brain development flaws as in human embryos, providing “a proof of concept” that the experimental models can be used to study other genetic mysteries, she says.
Scientists are still in the dark about what some genes do, as well as the point when they become critical to brain development.
“Many genes have very early roles in specifying, for example, the position of the head and also how our brain will function,” Dr. Zernicka-Goetz says. “We can now use this model system to assess the function of those genes.”
A version of this article first appeared on WebMD.com.
Med groups urge feds to protect physicians from anti-trans violence
Several leading medical groups on Oct. 3 called on U.S. Attorney General Merrick Garland to investigate and prosecute those responsible for a recent spate of threats and attacks against hospitals and physicians who are providing gender-affirming care.
In an Oct. 3 letter, the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the Children’s Hospital Association detailed the risk posed by these threats to physicians, patients, and the federally protected right to health care.
The letter comes during a campaign of intimidation and misinformation that has disrupted gender-related care in Seattle, Akron, Ohio, Nashville, Tenn., and Boston in the past few weeks. Hospitals across the country and their ambulatory sites have been forced to substantially increase protection, and “some providers have needed 24/7 security,” according to the letter.
Not only do the threats bully physicians providing gender-affirming care and the patients who receive that care, but “they have also disrupted many other services to families seeking care,” the letter claims.
According to STAT, many hospitals that provide gender-affirming care have responded to the threats by removing information about the treatment from their websites.
At one hospital, a new mother was separated from her preterm infant because the facility’s neonatal intensive care unit was locked down as the result of a bomb threat. (It’s not clear whether that incident is the same as a similar threat that led to the arrest of a 37-year-old Massachusetts woman, who is facing criminal charges in the episode.)
“The attacks are rooted in an intentional campaign of disinformation” by high-profile social media users, according to the letter. The medical organizations have also called on major tech companies, including TikTok, Twitter, and Meta, to do more to prevent the coordination of disinformation campaigns and violence against health care providers and patients.
“We now urge your office to take swift action to investigate and prosecute all organizations, individuals, and entities responsible,” the letter states.
“We cannot stand by as threats of violence against our members and their patients proliferate with little consequence. We call on the Department of Justice to investigate these attacks and social media platforms to reduce the spread of the misinformation enabling them,” AAP President Moira Szilagyi, MD, PhD, FAAP, said in a press release.
In addition to physical threats at their workplace, providers face threats on their personal social media accounts and harassment via phone and email. The letter notes that these unchecked attacks are coming after health care workers spent 3 years working on the front lines of a pandemic.
“Individuals in all workplaces have the right to a safe environment, out of harm’s way and free of intimidation or reprisal,” AMA President Jack Resneck Jr, MD, said in a statement. “The AMA will continue to work with federal, state, and local law enforcement officials to develop and implement strategies that protect hard-working, law-abiding physicians and other health care workers from senseless acts of violence, abuse, and intimidation.”
A version of this article first appeared on Medscape.com.
Several leading medical groups on Oct. 3 called on U.S. Attorney General Merrick Garland to investigate and prosecute those responsible for a recent spate of threats and attacks against hospitals and physicians who are providing gender-affirming care.
In an Oct. 3 letter, the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the Children’s Hospital Association detailed the risk posed by these threats to physicians, patients, and the federally protected right to health care.
The letter comes during a campaign of intimidation and misinformation that has disrupted gender-related care in Seattle, Akron, Ohio, Nashville, Tenn., and Boston in the past few weeks. Hospitals across the country and their ambulatory sites have been forced to substantially increase protection, and “some providers have needed 24/7 security,” according to the letter.
Not only do the threats bully physicians providing gender-affirming care and the patients who receive that care, but “they have also disrupted many other services to families seeking care,” the letter claims.
According to STAT, many hospitals that provide gender-affirming care have responded to the threats by removing information about the treatment from their websites.
At one hospital, a new mother was separated from her preterm infant because the facility’s neonatal intensive care unit was locked down as the result of a bomb threat. (It’s not clear whether that incident is the same as a similar threat that led to the arrest of a 37-year-old Massachusetts woman, who is facing criminal charges in the episode.)
“The attacks are rooted in an intentional campaign of disinformation” by high-profile social media users, according to the letter. The medical organizations have also called on major tech companies, including TikTok, Twitter, and Meta, to do more to prevent the coordination of disinformation campaigns and violence against health care providers and patients.
“We now urge your office to take swift action to investigate and prosecute all organizations, individuals, and entities responsible,” the letter states.
“We cannot stand by as threats of violence against our members and their patients proliferate with little consequence. We call on the Department of Justice to investigate these attacks and social media platforms to reduce the spread of the misinformation enabling them,” AAP President Moira Szilagyi, MD, PhD, FAAP, said in a press release.
In addition to physical threats at their workplace, providers face threats on their personal social media accounts and harassment via phone and email. The letter notes that these unchecked attacks are coming after health care workers spent 3 years working on the front lines of a pandemic.
“Individuals in all workplaces have the right to a safe environment, out of harm’s way and free of intimidation or reprisal,” AMA President Jack Resneck Jr, MD, said in a statement. “The AMA will continue to work with federal, state, and local law enforcement officials to develop and implement strategies that protect hard-working, law-abiding physicians and other health care workers from senseless acts of violence, abuse, and intimidation.”
A version of this article first appeared on Medscape.com.
Several leading medical groups on Oct. 3 called on U.S. Attorney General Merrick Garland to investigate and prosecute those responsible for a recent spate of threats and attacks against hospitals and physicians who are providing gender-affirming care.
In an Oct. 3 letter, the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the Children’s Hospital Association detailed the risk posed by these threats to physicians, patients, and the federally protected right to health care.
The letter comes during a campaign of intimidation and misinformation that has disrupted gender-related care in Seattle, Akron, Ohio, Nashville, Tenn., and Boston in the past few weeks. Hospitals across the country and their ambulatory sites have been forced to substantially increase protection, and “some providers have needed 24/7 security,” according to the letter.
Not only do the threats bully physicians providing gender-affirming care and the patients who receive that care, but “they have also disrupted many other services to families seeking care,” the letter claims.
According to STAT, many hospitals that provide gender-affirming care have responded to the threats by removing information about the treatment from their websites.
At one hospital, a new mother was separated from her preterm infant because the facility’s neonatal intensive care unit was locked down as the result of a bomb threat. (It’s not clear whether that incident is the same as a similar threat that led to the arrest of a 37-year-old Massachusetts woman, who is facing criminal charges in the episode.)
“The attacks are rooted in an intentional campaign of disinformation” by high-profile social media users, according to the letter. The medical organizations have also called on major tech companies, including TikTok, Twitter, and Meta, to do more to prevent the coordination of disinformation campaigns and violence against health care providers and patients.
“We now urge your office to take swift action to investigate and prosecute all organizations, individuals, and entities responsible,” the letter states.
“We cannot stand by as threats of violence against our members and their patients proliferate with little consequence. We call on the Department of Justice to investigate these attacks and social media platforms to reduce the spread of the misinformation enabling them,” AAP President Moira Szilagyi, MD, PhD, FAAP, said in a press release.
In addition to physical threats at their workplace, providers face threats on their personal social media accounts and harassment via phone and email. The letter notes that these unchecked attacks are coming after health care workers spent 3 years working on the front lines of a pandemic.
“Individuals in all workplaces have the right to a safe environment, out of harm’s way and free of intimidation or reprisal,” AMA President Jack Resneck Jr, MD, said in a statement. “The AMA will continue to work with federal, state, and local law enforcement officials to develop and implement strategies that protect hard-working, law-abiding physicians and other health care workers from senseless acts of violence, abuse, and intimidation.”
A version of this article first appeared on Medscape.com.
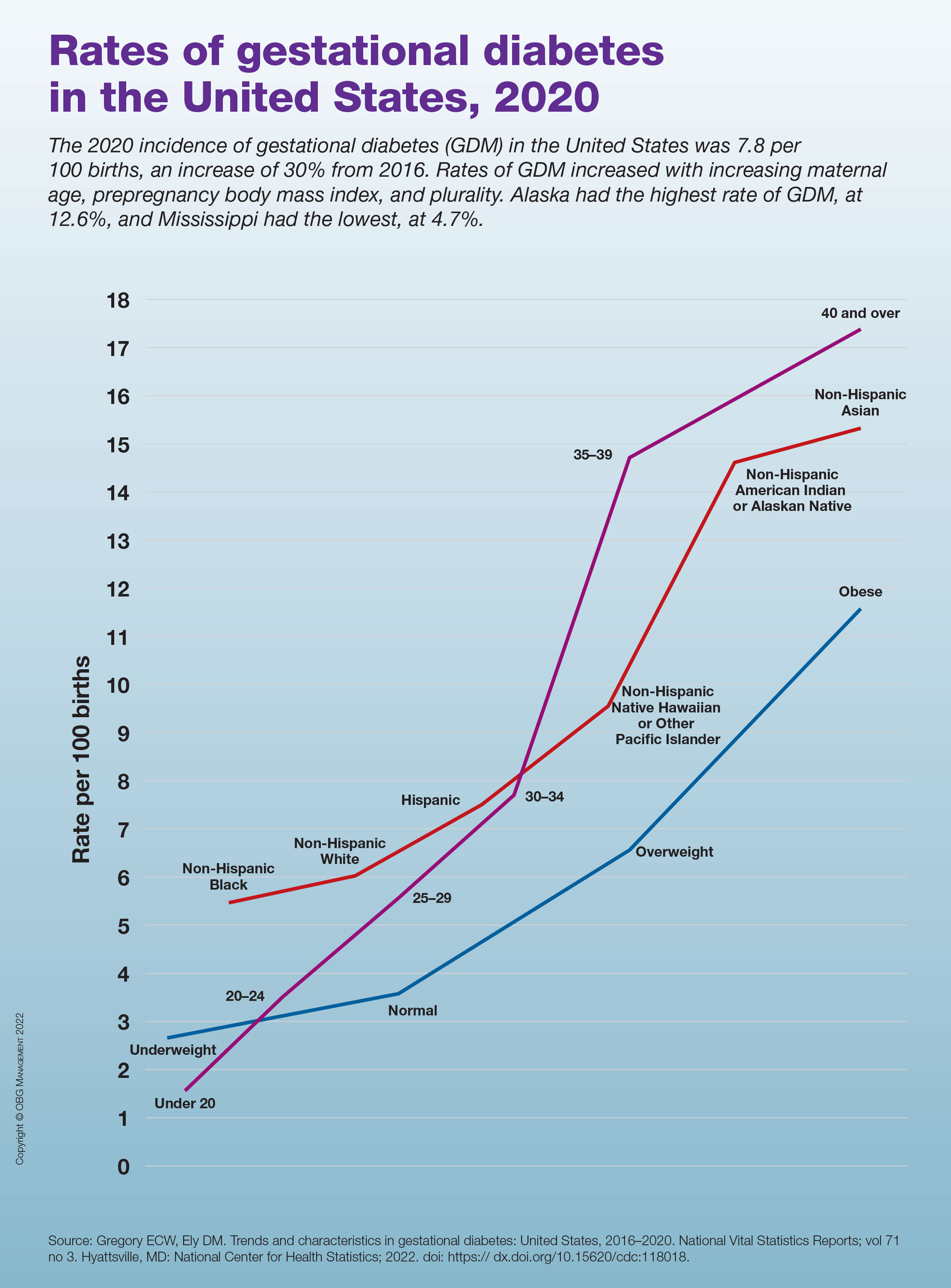
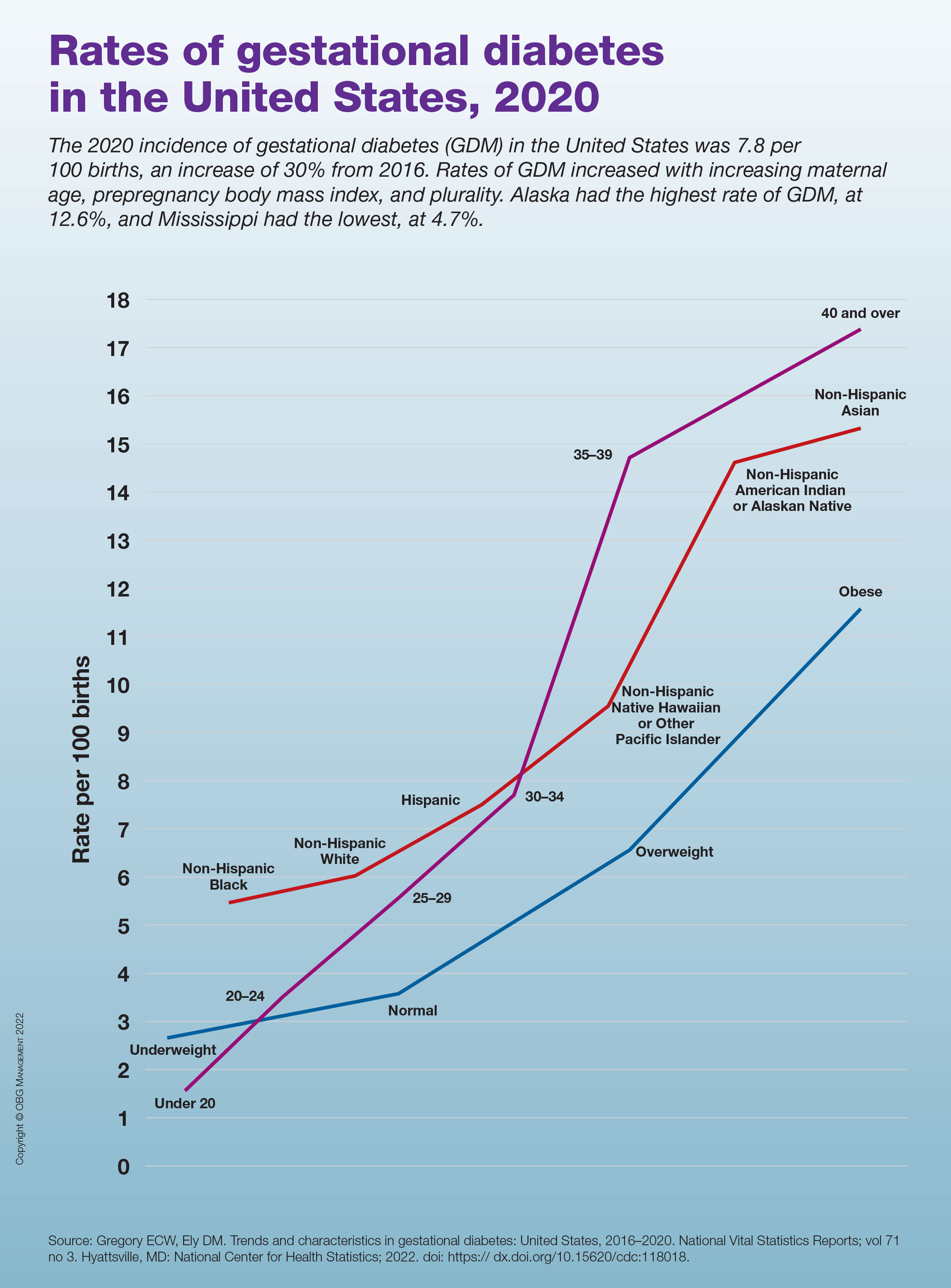
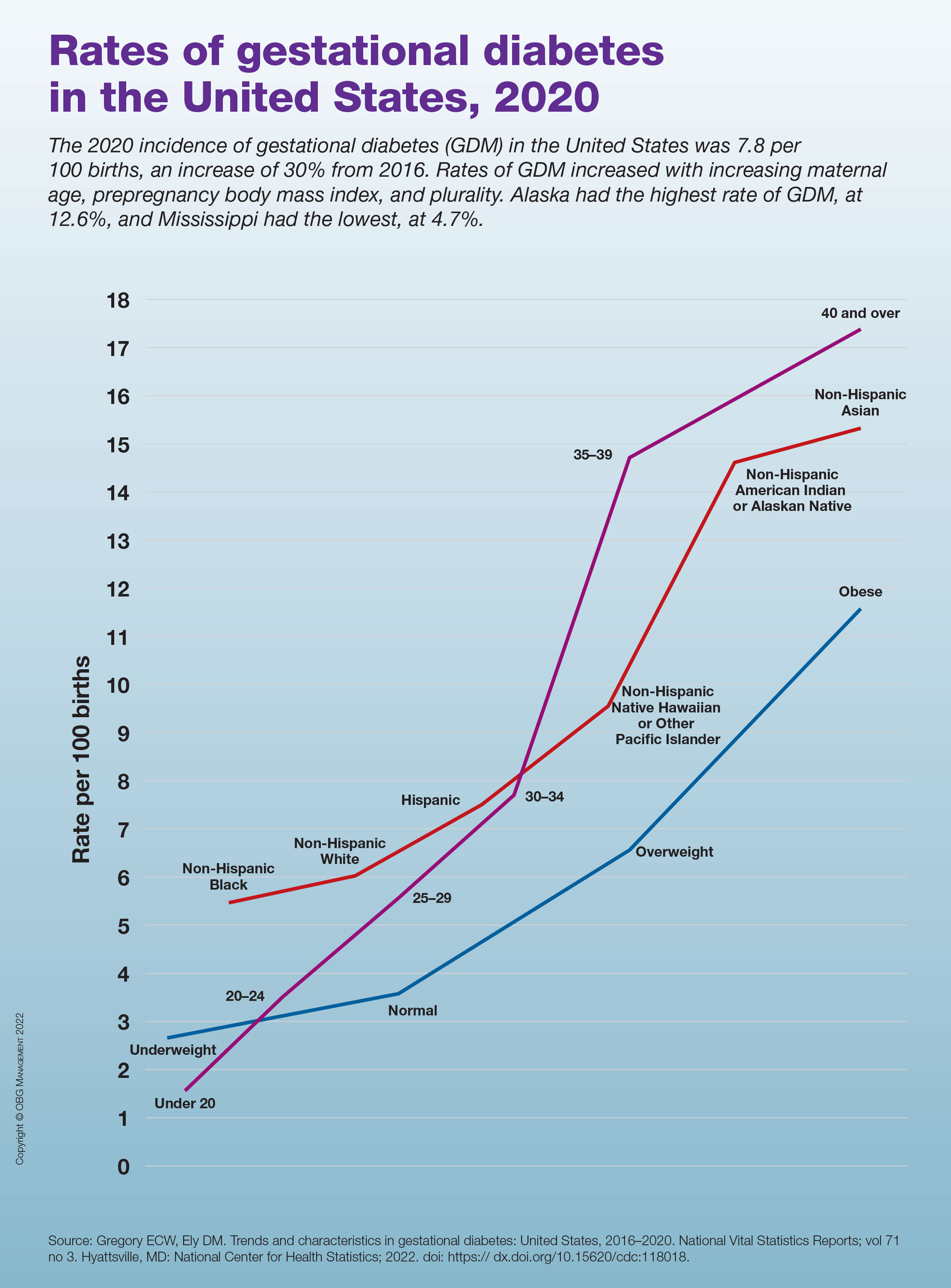
Rates of gestational diabetes in the United States, 2020
Folic acid tied to a reduction in suicide attempts
new research suggests.
After adjusting for multiple factors, results from a large pharmaco-epidemiological study showed taking folic acid was associated with a 44% reduction in suicide events.
“These results are really putting folic acid squarely on the map as a potential for large-scale, population-level prevention,” lead author Robert D. Gibbons, PhD, professor of biostatistics, Center for Health Statistics, University of Chicago, said in an interview.
“Folic acid is safe, inexpensive, and generally available, and if future randomized controlled trials show this association is beyond a shadow of a doubt causal, we have a new tool in the arsenal,” Dr. Gibbons said.
Having such a tool would be extremely important given that suicide is such a significant public health crisis worldwide, he added.
The findings were published online in JAMA Psychiatry.
Previous research ‘fairly thin’
Folate, the naturally occurring form of B9, is essential for neurogenesis, nucleotide synthesis, and methylation of homocysteine. Past research has suggested that taking folate can prevent neural tube and heart defects in the fetus during pregnancy – and may prevent strokes and reduce age-related hearing loss in adults.
In psychiatry, the role of folate has been recognized for more than a decade. It may enhance the effects of antidepressants; and folate deficiency can predict poorer response to SSRIs.
This has led to recommendations for folate augmentation in patients with low or normal levels at the start of depression treatment.
Although previous research has shown a link between folic acid and suicidality, the findings have been “fairly thin,” with studies being “generally small, and many are case series,” Dr. Gibbons said.
The current study follows an earlier analysis that used a novel statistical methodology for generating drug safety signals that was developed by Dr. Gibbons and colleagues. That study compared rates of suicide attempts before and after initiation of 922 drugs with at least 3,000 prescriptions.
Its results showed 10 drugs were associated with increased risk after exposure, with the strongest associations for alprazolam, butalbital, hydrocodone, and combination codeine/promethazine. In addition, 44 drugs were associated with decreased risk, many of which were antidepressants and antipsychotics.
“One of the most interesting findings in terms of the decreased risk was for folic acid,” said Dr. Gibbons.
He and his colleagues initially thought this was because of women taking folic acid during pregnancy. But when restricting the analysis to men, they found the same effect.
Their next step was to carry out the current large-scale pharmaco-epidemiological study.
Prescriptions for pain
The researchers used a health claims database that included 164 million enrollees. The study cohort was comprised of 866,586 adults with private health insurance (81.3% women; 10.4% aged 60 years and older) who filled a folic acid prescription between 2012 and 2017.
More than half of the folic acid prescriptions were associated with pain disorders. About 48% were for a single agent at a dosage of 1 mg/d, which is the upper tolerable limit for adults – including in pregnancy and lactation.
Other single-agent daily dosages ranging from 0.4 mg to 5 mg accounted for 0.11% of prescriptions. The remainder were multivitamins.
The participants were followed for 24 months. The within-person analysis compared suicide attempts or self-harm events resulting in an outpatient visit or inpatient admission during periods of folic acid treatment versus during periods without treatment.
During the study period, the overall suicidal event rate was 133 per 100,000 population, which is one-fourth the national rate reported by the National Institutes of Health of 600 per 100,000.
After adjusting for age, sex, diagnoses related to suicidal behavior and folic acid deficiency, history of folate-reducing medications, and history of suicidal events, the estimated hazard ratio for suicide events when taking folic acid was 0.56 (95% confidence interal, 0.48-0.65) – which indicates a 44% reduction in suicide events.
“This is a very large decrease and is extremely significant and exciting,” Dr. Gibbons said.
He noted the decrease in suicidal events may have been even greater considering the study captured only prescription folic acid, and participants may also have also taken over-the-counter products.
“The 44% reduction in suicide attempts may actually be an underestimate,” said Dr. Gibbons.
Age and sex did not moderate the association between folic acid and suicide attempts, and a similar association was found in women of childbearing age.
Provocative results?
The investigators also assessed a negative control group of 236,610 individuals using cyanocobalamin during the study period. Cyanocobalamin is a form of vitamin B12 that is essential for metabolism, blood cell synthesis, and the nervous system. It does not contain folic acid and is commonly used to treat anemia.
Results showed no association between cyanocobalamin and suicidal events in the adjusted analysis (HR, 1.01; 95% CI, 0.80-1.27) or unadjusted analysis (HR, 1.02; 95% CI, 0.80-1.28).
Dr. Gibbons noted this result boosts the argument that the association between folic acid and reduced suicidal attempts “isn’t just about health-seeking behavior like taking vitamin supplements.”
Another sensitivity analysis showed every additional month of treatment was associated with a 5% reduction in the suicidal event rate.
“This means the longer you take folic acid, the greater the benefit, which is what you would expect to see if there was a real association between a treatment and an outcome,” said Dr. Gibbons.
The new results “are so provocative that they really mandate the need for a well-controlled randomized controlled trial of folic acid and suicide events,” possibly in a high-risk population such as veterans, he noted.
Such a study could use longitudinal assessments of suicidal events, such as the validated Computerized Adaptive Test Suicide Scale, he added. This continuous scale of suicidality ranges from subclinical, signifying helplessness, hopelessness, and loss of pleasure, to suicide attempts and completion.
As for study limitations, the investigators noted that this study was observational, so there could be selection effects. And using claims data likely underrepresented the number of suicidal events because of incomplete reporting. As the researchers pointed out, the rate of suicidal events in this study was much lower than the national rate.
Other limitations cited were that the association between folic acid and suicidal events may be explained by healthy user bias; and although the investigators conducted a sensitivity analysis in women of childbearing age, they did not have data on women actively planning for a pregnancy.
‘Impressive, encouraging’
In a comment, Shirley Yen, PhD, associate professor of psychology, Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, described the new findings as “quite impressive” and “extremely encouraging.”
However, she noted “it’s too premature” to suggest widespread use of folic acid in patients with depressive symptoms.
Dr. Yen, who has researched suicide risks previously, was not involved with the current study.
She did agree with the investigators that the results call for “more robustly controlled studies. These could include double-blind, randomized, controlled trials that could “more formally assess” all folic acid usage as opposed to prescriptions only, Dr. Yen said.
The study was funded by the NIH, the Agency for Healthcare Research and Quality, and the Center of Excellence for Suicide Prevention. Dr. Gibbons reported serving as an expert witness in cases for the Department of Justice; receiving expert witness fees from Merck, GlaxoSmithKline, Pfizer, and Wyeth; and having founded Adaptive Testing Technologies, which distributes the Computerized Adaptive Test Suicide Scale. Dr. Yen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
After adjusting for multiple factors, results from a large pharmaco-epidemiological study showed taking folic acid was associated with a 44% reduction in suicide events.
“These results are really putting folic acid squarely on the map as a potential for large-scale, population-level prevention,” lead author Robert D. Gibbons, PhD, professor of biostatistics, Center for Health Statistics, University of Chicago, said in an interview.
“Folic acid is safe, inexpensive, and generally available, and if future randomized controlled trials show this association is beyond a shadow of a doubt causal, we have a new tool in the arsenal,” Dr. Gibbons said.
Having such a tool would be extremely important given that suicide is such a significant public health crisis worldwide, he added.
The findings were published online in JAMA Psychiatry.
Previous research ‘fairly thin’
Folate, the naturally occurring form of B9, is essential for neurogenesis, nucleotide synthesis, and methylation of homocysteine. Past research has suggested that taking folate can prevent neural tube and heart defects in the fetus during pregnancy – and may prevent strokes and reduce age-related hearing loss in adults.
In psychiatry, the role of folate has been recognized for more than a decade. It may enhance the effects of antidepressants; and folate deficiency can predict poorer response to SSRIs.
This has led to recommendations for folate augmentation in patients with low or normal levels at the start of depression treatment.
Although previous research has shown a link between folic acid and suicidality, the findings have been “fairly thin,” with studies being “generally small, and many are case series,” Dr. Gibbons said.
The current study follows an earlier analysis that used a novel statistical methodology for generating drug safety signals that was developed by Dr. Gibbons and colleagues. That study compared rates of suicide attempts before and after initiation of 922 drugs with at least 3,000 prescriptions.
Its results showed 10 drugs were associated with increased risk after exposure, with the strongest associations for alprazolam, butalbital, hydrocodone, and combination codeine/promethazine. In addition, 44 drugs were associated with decreased risk, many of which were antidepressants and antipsychotics.
“One of the most interesting findings in terms of the decreased risk was for folic acid,” said Dr. Gibbons.
He and his colleagues initially thought this was because of women taking folic acid during pregnancy. But when restricting the analysis to men, they found the same effect.
Their next step was to carry out the current large-scale pharmaco-epidemiological study.
Prescriptions for pain
The researchers used a health claims database that included 164 million enrollees. The study cohort was comprised of 866,586 adults with private health insurance (81.3% women; 10.4% aged 60 years and older) who filled a folic acid prescription between 2012 and 2017.
More than half of the folic acid prescriptions were associated with pain disorders. About 48% were for a single agent at a dosage of 1 mg/d, which is the upper tolerable limit for adults – including in pregnancy and lactation.
Other single-agent daily dosages ranging from 0.4 mg to 5 mg accounted for 0.11% of prescriptions. The remainder were multivitamins.
The participants were followed for 24 months. The within-person analysis compared suicide attempts or self-harm events resulting in an outpatient visit or inpatient admission during periods of folic acid treatment versus during periods without treatment.
During the study period, the overall suicidal event rate was 133 per 100,000 population, which is one-fourth the national rate reported by the National Institutes of Health of 600 per 100,000.
After adjusting for age, sex, diagnoses related to suicidal behavior and folic acid deficiency, history of folate-reducing medications, and history of suicidal events, the estimated hazard ratio for suicide events when taking folic acid was 0.56 (95% confidence interal, 0.48-0.65) – which indicates a 44% reduction in suicide events.
“This is a very large decrease and is extremely significant and exciting,” Dr. Gibbons said.
He noted the decrease in suicidal events may have been even greater considering the study captured only prescription folic acid, and participants may also have also taken over-the-counter products.
“The 44% reduction in suicide attempts may actually be an underestimate,” said Dr. Gibbons.
Age and sex did not moderate the association between folic acid and suicide attempts, and a similar association was found in women of childbearing age.
Provocative results?
The investigators also assessed a negative control group of 236,610 individuals using cyanocobalamin during the study period. Cyanocobalamin is a form of vitamin B12 that is essential for metabolism, blood cell synthesis, and the nervous system. It does not contain folic acid and is commonly used to treat anemia.
Results showed no association between cyanocobalamin and suicidal events in the adjusted analysis (HR, 1.01; 95% CI, 0.80-1.27) or unadjusted analysis (HR, 1.02; 95% CI, 0.80-1.28).
Dr. Gibbons noted this result boosts the argument that the association between folic acid and reduced suicidal attempts “isn’t just about health-seeking behavior like taking vitamin supplements.”
Another sensitivity analysis showed every additional month of treatment was associated with a 5% reduction in the suicidal event rate.
“This means the longer you take folic acid, the greater the benefit, which is what you would expect to see if there was a real association between a treatment and an outcome,” said Dr. Gibbons.
The new results “are so provocative that they really mandate the need for a well-controlled randomized controlled trial of folic acid and suicide events,” possibly in a high-risk population such as veterans, he noted.
Such a study could use longitudinal assessments of suicidal events, such as the validated Computerized Adaptive Test Suicide Scale, he added. This continuous scale of suicidality ranges from subclinical, signifying helplessness, hopelessness, and loss of pleasure, to suicide attempts and completion.
As for study limitations, the investigators noted that this study was observational, so there could be selection effects. And using claims data likely underrepresented the number of suicidal events because of incomplete reporting. As the researchers pointed out, the rate of suicidal events in this study was much lower than the national rate.
Other limitations cited were that the association between folic acid and suicidal events may be explained by healthy user bias; and although the investigators conducted a sensitivity analysis in women of childbearing age, they did not have data on women actively planning for a pregnancy.
‘Impressive, encouraging’
In a comment, Shirley Yen, PhD, associate professor of psychology, Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, described the new findings as “quite impressive” and “extremely encouraging.”
However, she noted “it’s too premature” to suggest widespread use of folic acid in patients with depressive symptoms.
Dr. Yen, who has researched suicide risks previously, was not involved with the current study.
She did agree with the investigators that the results call for “more robustly controlled studies. These could include double-blind, randomized, controlled trials that could “more formally assess” all folic acid usage as opposed to prescriptions only, Dr. Yen said.
The study was funded by the NIH, the Agency for Healthcare Research and Quality, and the Center of Excellence for Suicide Prevention. Dr. Gibbons reported serving as an expert witness in cases for the Department of Justice; receiving expert witness fees from Merck, GlaxoSmithKline, Pfizer, and Wyeth; and having founded Adaptive Testing Technologies, which distributes the Computerized Adaptive Test Suicide Scale. Dr. Yen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
After adjusting for multiple factors, results from a large pharmaco-epidemiological study showed taking folic acid was associated with a 44% reduction in suicide events.
“These results are really putting folic acid squarely on the map as a potential for large-scale, population-level prevention,” lead author Robert D. Gibbons, PhD, professor of biostatistics, Center for Health Statistics, University of Chicago, said in an interview.
“Folic acid is safe, inexpensive, and generally available, and if future randomized controlled trials show this association is beyond a shadow of a doubt causal, we have a new tool in the arsenal,” Dr. Gibbons said.
Having such a tool would be extremely important given that suicide is such a significant public health crisis worldwide, he added.
The findings were published online in JAMA Psychiatry.
Previous research ‘fairly thin’
Folate, the naturally occurring form of B9, is essential for neurogenesis, nucleotide synthesis, and methylation of homocysteine. Past research has suggested that taking folate can prevent neural tube and heart defects in the fetus during pregnancy – and may prevent strokes and reduce age-related hearing loss in adults.
In psychiatry, the role of folate has been recognized for more than a decade. It may enhance the effects of antidepressants; and folate deficiency can predict poorer response to SSRIs.
This has led to recommendations for folate augmentation in patients with low or normal levels at the start of depression treatment.
Although previous research has shown a link between folic acid and suicidality, the findings have been “fairly thin,” with studies being “generally small, and many are case series,” Dr. Gibbons said.
The current study follows an earlier analysis that used a novel statistical methodology for generating drug safety signals that was developed by Dr. Gibbons and colleagues. That study compared rates of suicide attempts before and after initiation of 922 drugs with at least 3,000 prescriptions.
Its results showed 10 drugs were associated with increased risk after exposure, with the strongest associations for alprazolam, butalbital, hydrocodone, and combination codeine/promethazine. In addition, 44 drugs were associated with decreased risk, many of which were antidepressants and antipsychotics.
“One of the most interesting findings in terms of the decreased risk was for folic acid,” said Dr. Gibbons.
He and his colleagues initially thought this was because of women taking folic acid during pregnancy. But when restricting the analysis to men, they found the same effect.
Their next step was to carry out the current large-scale pharmaco-epidemiological study.
Prescriptions for pain
The researchers used a health claims database that included 164 million enrollees. The study cohort was comprised of 866,586 adults with private health insurance (81.3% women; 10.4% aged 60 years and older) who filled a folic acid prescription between 2012 and 2017.
More than half of the folic acid prescriptions were associated with pain disorders. About 48% were for a single agent at a dosage of 1 mg/d, which is the upper tolerable limit for adults – including in pregnancy and lactation.
Other single-agent daily dosages ranging from 0.4 mg to 5 mg accounted for 0.11% of prescriptions. The remainder were multivitamins.
The participants were followed for 24 months. The within-person analysis compared suicide attempts or self-harm events resulting in an outpatient visit or inpatient admission during periods of folic acid treatment versus during periods without treatment.
During the study period, the overall suicidal event rate was 133 per 100,000 population, which is one-fourth the national rate reported by the National Institutes of Health of 600 per 100,000.
After adjusting for age, sex, diagnoses related to suicidal behavior and folic acid deficiency, history of folate-reducing medications, and history of suicidal events, the estimated hazard ratio for suicide events when taking folic acid was 0.56 (95% confidence interal, 0.48-0.65) – which indicates a 44% reduction in suicide events.
“This is a very large decrease and is extremely significant and exciting,” Dr. Gibbons said.
He noted the decrease in suicidal events may have been even greater considering the study captured only prescription folic acid, and participants may also have also taken over-the-counter products.
“The 44% reduction in suicide attempts may actually be an underestimate,” said Dr. Gibbons.
Age and sex did not moderate the association between folic acid and suicide attempts, and a similar association was found in women of childbearing age.
Provocative results?
The investigators also assessed a negative control group of 236,610 individuals using cyanocobalamin during the study period. Cyanocobalamin is a form of vitamin B12 that is essential for metabolism, blood cell synthesis, and the nervous system. It does not contain folic acid and is commonly used to treat anemia.
Results showed no association between cyanocobalamin and suicidal events in the adjusted analysis (HR, 1.01; 95% CI, 0.80-1.27) or unadjusted analysis (HR, 1.02; 95% CI, 0.80-1.28).
Dr. Gibbons noted this result boosts the argument that the association between folic acid and reduced suicidal attempts “isn’t just about health-seeking behavior like taking vitamin supplements.”
Another sensitivity analysis showed every additional month of treatment was associated with a 5% reduction in the suicidal event rate.
“This means the longer you take folic acid, the greater the benefit, which is what you would expect to see if there was a real association between a treatment and an outcome,” said Dr. Gibbons.
The new results “are so provocative that they really mandate the need for a well-controlled randomized controlled trial of folic acid and suicide events,” possibly in a high-risk population such as veterans, he noted.
Such a study could use longitudinal assessments of suicidal events, such as the validated Computerized Adaptive Test Suicide Scale, he added. This continuous scale of suicidality ranges from subclinical, signifying helplessness, hopelessness, and loss of pleasure, to suicide attempts and completion.
As for study limitations, the investigators noted that this study was observational, so there could be selection effects. And using claims data likely underrepresented the number of suicidal events because of incomplete reporting. As the researchers pointed out, the rate of suicidal events in this study was much lower than the national rate.
Other limitations cited were that the association between folic acid and suicidal events may be explained by healthy user bias; and although the investigators conducted a sensitivity analysis in women of childbearing age, they did not have data on women actively planning for a pregnancy.
‘Impressive, encouraging’
In a comment, Shirley Yen, PhD, associate professor of psychology, Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, described the new findings as “quite impressive” and “extremely encouraging.”
However, she noted “it’s too premature” to suggest widespread use of folic acid in patients with depressive symptoms.
Dr. Yen, who has researched suicide risks previously, was not involved with the current study.
She did agree with the investigators that the results call for “more robustly controlled studies. These could include double-blind, randomized, controlled trials that could “more formally assess” all folic acid usage as opposed to prescriptions only, Dr. Yen said.
The study was funded by the NIH, the Agency for Healthcare Research and Quality, and the Center of Excellence for Suicide Prevention. Dr. Gibbons reported serving as an expert witness in cases for the Department of Justice; receiving expert witness fees from Merck, GlaxoSmithKline, Pfizer, and Wyeth; and having founded Adaptive Testing Technologies, which distributes the Computerized Adaptive Test Suicide Scale. Dr. Yen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Physician bias may prevent quality care for patients with disabilities
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
High-dose folic acid during pregnancy tied to cancer risk in children
new data from a Scandinavian registry of more than 3 million pregnancies suggests.
The increased risk for cancer did not change after considering other factors that could explain the risk, such as use of antiseizure medication (ASM).
There was no increased risk for cancer in children of mothers without epilepsy who used high-dose folic acid.
The results of this study “should be considered when the risks and benefits of folic acid supplements for women with epilepsy are discussed and before decisions about optimal dose recommendations are made,” the authors write.
“Although we believe that the association between prescription fills for high-dose folic acid and cancer in children born to mothers with epilepsy is robust, it is important to underline that these are the findings of one study only,” first author Håkon Magne Vegrim, MD, with University of Bergen (Norway) told this news organization.
The study was published online in JAMA Neurology.
Risks and benefits
Women with epilepsy are advised to take high doses of folic acid before and during pregnancy owing to the risk for congenital malformations associated with ASM. Whether high-dose folic acid is associated with increases in the risk for childhood cancer is unknown.
To investigate, the researchers analyzed registry data from Denmark, Norway, and Sweden for 3.3 million children followed to a median age of 7.3 years.
Among the 27,784 children born to mothers with epilepsy, 5,934 (21.4%) were exposed to high-dose folic acid (mean dose, 4.3 mg), with a cancer incidence rate of 42.5 per 100,000 person-years in 18 exposed cancer cases compared with 18.4 per 100,000 person-years in 29 unexposed cancer cases – yielding an adjusted hazard ratio of 2.7 (95% confidence interval, 1.2-6.3).
The absolute risk with exposure was 1.5% (95% CI, 0.5%-3.5%) in children of mothers with epilepsy compared with 0.6% (95% CI, 0.3%-1.1%) in children of mothers with epilepsy who were not exposed high-dose folic acid.
Prenatal exposure to high-dose folic acid was not associated with an increased risk for cancer in children of mothers without epilepsy.
In children of mothers without epilepsy, 46,646 (1.4%) were exposed to high-dose folic acid (mean dose, 2.9 mg). There were 69 exposed and 4,927 unexposed cancer cases and an aHR for cancer of 1.1 (95% CI, 0.9-1.4) and absolute risk for cancer of 0.4% (95% CI, 0.3%-0.5%).
There was no association between any specific ASM and childhood cancer.
“Removing mothers with any prescription fills for carbamazepine and valproate was not associated with the point estimate. Hence, these two ASMs were not important effect modifiers for the cancer association,” the investigators note in their study.
They also note that the most common childhood cancer types in children among mothers with epilepsy who took high-dose folic acid did not differ from the distribution in the general population.
“We need to get more knowledge about the potential mechanisms behind high-dose folic acid and childhood cancer, and it is important to identify the optimal dose to balance risks and benefits – and whether folic acid supplementation should be more individualized, based on factors like the serum level of folate and what type of antiseizure medication that is being used,” said Dr. Vegrim.
Practice changing?
Weighing in on the study, Elizabeth E. Gerard, MD, director of the Women with Epilepsy Program and associate professor of neurology at Northwestern University in Chicago, said, “There are known benefits of folic acid supplementation during pregnancy including a decreased risk of neural tube defects in the general population and improved neurodevelopmental outcomes in children born to mothers with and without epilepsy.”
“However, despite some expert guidelines recommending high-dose folic acid supplementation, there is a lack of certainty surrounding the ‘just right’ dose for patients with epilepsy who may become pregnant,” said Dr. Gerard, who wasn’t involved in the study.
Dr. Gerard, a member of the American Epilepsy Society, noted that other epidemiologic studies of folic acid supplementation and cancer have had “contradictory results, thus further research on this association will be needed. Additionally, differences in maternal/fetal folate metabolism and blood levels may be an important factor to study in the future.
“That said, this study definitely should cause us to pause and reevaluate the common practice of high-dose folic acid supplementation for patients with epilepsy who are considering pregnancy,” said Dr. Gerard.
The study was supported by the NordForsk Nordic Program on Health and Welfare. Dr. Vegrim and Dr. Gerard report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new data from a Scandinavian registry of more than 3 million pregnancies suggests.
The increased risk for cancer did not change after considering other factors that could explain the risk, such as use of antiseizure medication (ASM).
There was no increased risk for cancer in children of mothers without epilepsy who used high-dose folic acid.
The results of this study “should be considered when the risks and benefits of folic acid supplements for women with epilepsy are discussed and before decisions about optimal dose recommendations are made,” the authors write.
“Although we believe that the association between prescription fills for high-dose folic acid and cancer in children born to mothers with epilepsy is robust, it is important to underline that these are the findings of one study only,” first author Håkon Magne Vegrim, MD, with University of Bergen (Norway) told this news organization.
The study was published online in JAMA Neurology.
Risks and benefits
Women with epilepsy are advised to take high doses of folic acid before and during pregnancy owing to the risk for congenital malformations associated with ASM. Whether high-dose folic acid is associated with increases in the risk for childhood cancer is unknown.
To investigate, the researchers analyzed registry data from Denmark, Norway, and Sweden for 3.3 million children followed to a median age of 7.3 years.
Among the 27,784 children born to mothers with epilepsy, 5,934 (21.4%) were exposed to high-dose folic acid (mean dose, 4.3 mg), with a cancer incidence rate of 42.5 per 100,000 person-years in 18 exposed cancer cases compared with 18.4 per 100,000 person-years in 29 unexposed cancer cases – yielding an adjusted hazard ratio of 2.7 (95% confidence interval, 1.2-6.3).
The absolute risk with exposure was 1.5% (95% CI, 0.5%-3.5%) in children of mothers with epilepsy compared with 0.6% (95% CI, 0.3%-1.1%) in children of mothers with epilepsy who were not exposed high-dose folic acid.
Prenatal exposure to high-dose folic acid was not associated with an increased risk for cancer in children of mothers without epilepsy.
In children of mothers without epilepsy, 46,646 (1.4%) were exposed to high-dose folic acid (mean dose, 2.9 mg). There were 69 exposed and 4,927 unexposed cancer cases and an aHR for cancer of 1.1 (95% CI, 0.9-1.4) and absolute risk for cancer of 0.4% (95% CI, 0.3%-0.5%).
There was no association between any specific ASM and childhood cancer.
“Removing mothers with any prescription fills for carbamazepine and valproate was not associated with the point estimate. Hence, these two ASMs were not important effect modifiers for the cancer association,” the investigators note in their study.
They also note that the most common childhood cancer types in children among mothers with epilepsy who took high-dose folic acid did not differ from the distribution in the general population.
“We need to get more knowledge about the potential mechanisms behind high-dose folic acid and childhood cancer, and it is important to identify the optimal dose to balance risks and benefits – and whether folic acid supplementation should be more individualized, based on factors like the serum level of folate and what type of antiseizure medication that is being used,” said Dr. Vegrim.
Practice changing?
Weighing in on the study, Elizabeth E. Gerard, MD, director of the Women with Epilepsy Program and associate professor of neurology at Northwestern University in Chicago, said, “There are known benefits of folic acid supplementation during pregnancy including a decreased risk of neural tube defects in the general population and improved neurodevelopmental outcomes in children born to mothers with and without epilepsy.”
“However, despite some expert guidelines recommending high-dose folic acid supplementation, there is a lack of certainty surrounding the ‘just right’ dose for patients with epilepsy who may become pregnant,” said Dr. Gerard, who wasn’t involved in the study.
Dr. Gerard, a member of the American Epilepsy Society, noted that other epidemiologic studies of folic acid supplementation and cancer have had “contradictory results, thus further research on this association will be needed. Additionally, differences in maternal/fetal folate metabolism and blood levels may be an important factor to study in the future.
“That said, this study definitely should cause us to pause and reevaluate the common practice of high-dose folic acid supplementation for patients with epilepsy who are considering pregnancy,” said Dr. Gerard.
The study was supported by the NordForsk Nordic Program on Health and Welfare. Dr. Vegrim and Dr. Gerard report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new data from a Scandinavian registry of more than 3 million pregnancies suggests.
The increased risk for cancer did not change after considering other factors that could explain the risk, such as use of antiseizure medication (ASM).
There was no increased risk for cancer in children of mothers without epilepsy who used high-dose folic acid.
The results of this study “should be considered when the risks and benefits of folic acid supplements for women with epilepsy are discussed and before decisions about optimal dose recommendations are made,” the authors write.
“Although we believe that the association between prescription fills for high-dose folic acid and cancer in children born to mothers with epilepsy is robust, it is important to underline that these are the findings of one study only,” first author Håkon Magne Vegrim, MD, with University of Bergen (Norway) told this news organization.
The study was published online in JAMA Neurology.
Risks and benefits
Women with epilepsy are advised to take high doses of folic acid before and during pregnancy owing to the risk for congenital malformations associated with ASM. Whether high-dose folic acid is associated with increases in the risk for childhood cancer is unknown.
To investigate, the researchers analyzed registry data from Denmark, Norway, and Sweden for 3.3 million children followed to a median age of 7.3 years.
Among the 27,784 children born to mothers with epilepsy, 5,934 (21.4%) were exposed to high-dose folic acid (mean dose, 4.3 mg), with a cancer incidence rate of 42.5 per 100,000 person-years in 18 exposed cancer cases compared with 18.4 per 100,000 person-years in 29 unexposed cancer cases – yielding an adjusted hazard ratio of 2.7 (95% confidence interval, 1.2-6.3).
The absolute risk with exposure was 1.5% (95% CI, 0.5%-3.5%) in children of mothers with epilepsy compared with 0.6% (95% CI, 0.3%-1.1%) in children of mothers with epilepsy who were not exposed high-dose folic acid.
Prenatal exposure to high-dose folic acid was not associated with an increased risk for cancer in children of mothers without epilepsy.
In children of mothers without epilepsy, 46,646 (1.4%) were exposed to high-dose folic acid (mean dose, 2.9 mg). There were 69 exposed and 4,927 unexposed cancer cases and an aHR for cancer of 1.1 (95% CI, 0.9-1.4) and absolute risk for cancer of 0.4% (95% CI, 0.3%-0.5%).
There was no association between any specific ASM and childhood cancer.
“Removing mothers with any prescription fills for carbamazepine and valproate was not associated with the point estimate. Hence, these two ASMs were not important effect modifiers for the cancer association,” the investigators note in their study.
They also note that the most common childhood cancer types in children among mothers with epilepsy who took high-dose folic acid did not differ from the distribution in the general population.
“We need to get more knowledge about the potential mechanisms behind high-dose folic acid and childhood cancer, and it is important to identify the optimal dose to balance risks and benefits – and whether folic acid supplementation should be more individualized, based on factors like the serum level of folate and what type of antiseizure medication that is being used,” said Dr. Vegrim.
Practice changing?
Weighing in on the study, Elizabeth E. Gerard, MD, director of the Women with Epilepsy Program and associate professor of neurology at Northwestern University in Chicago, said, “There are known benefits of folic acid supplementation during pregnancy including a decreased risk of neural tube defects in the general population and improved neurodevelopmental outcomes in children born to mothers with and without epilepsy.”
“However, despite some expert guidelines recommending high-dose folic acid supplementation, there is a lack of certainty surrounding the ‘just right’ dose for patients with epilepsy who may become pregnant,” said Dr. Gerard, who wasn’t involved in the study.
Dr. Gerard, a member of the American Epilepsy Society, noted that other epidemiologic studies of folic acid supplementation and cancer have had “contradictory results, thus further research on this association will be needed. Additionally, differences in maternal/fetal folate metabolism and blood levels may be an important factor to study in the future.
“That said, this study definitely should cause us to pause and reevaluate the common practice of high-dose folic acid supplementation for patients with epilepsy who are considering pregnancy,” said Dr. Gerard.
The study was supported by the NordForsk Nordic Program on Health and Welfare. Dr. Vegrim and Dr. Gerard report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
Top pregnancy apps for your patients
Pregnancy apps are more popular as patients use the internet to seek information about pregnancy and childbirth.1 Research has shown that over 50% of pregnant patients download apps focused on pregnancy, with an average of 3 being tried.2 This is especially true during the COVID-19 pandemic, when patients seek information but may want to minimize clinical exposures. Other research has shown that women primarily use apps to monitor fetal development and to obtain information on nutrition and antenatal care.3
We identified apps and rated their contents and features.4 To identify the apps, we performed a Google search to mimic what a patient may do. We scored the identified apps based on what has been shown to make apps successful, as well as desired functions of the most commonly used apps. The quality of the applications was relatively varied, with many of the apps (60%) not having comprehensive information for every stage of pregnancy and no app attaining a perfect score. However, the top 3 apps had near perfect scores of 15/16 and 14/16, missing points only for having advertisements and requiring an internet connection.
The table details these top 3 recommended pregnancy apps, along with a detailed shortened version of the APPLICATIONS scoring system, APPLI (App comprehensiveness, Price, Platform, Literature Used, Other special features). We hope this column will help you feel comfortable in helping patients use pregnancy apps, should they ask for recommendations.
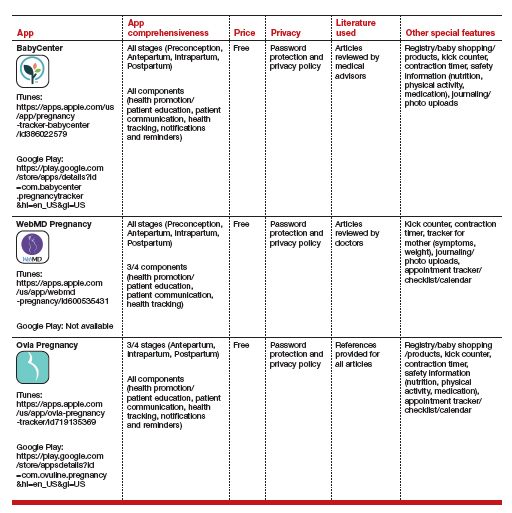
1. Romano AM. A changing landscape: implications of pregnant women’s internet use for childbirth educators. J Perinat Educ. 2007;16:18-24. doi: 10.1624/105812407X244903.
2. Jayaseelan R, Pichandy C, Rushandramani D. Usage of smartphone apps by women on their maternal life. J Mass Communicat Journalism. 2015;29:05:158-164. doi: 10.4172/2165-7912.1000267.
3. Wang N, Deng Z, Wen LM, et al. Understanding the use of smartphone apps for health information among pregnant Chinese women: mixed methods study. JMIR mHealth uHealth. 2019;18:7:e12631. doi: 10.2196/12631.
4. Frid G, Bogaert K, Chen KT. Mobile health apps for pregnant women: systematic search, evaluation, and analysis of features. J Med Internet Res. 2021;18:23:e25667. doi: 10.2196/25667.
Pregnancy apps are more popular as patients use the internet to seek information about pregnancy and childbirth.1 Research has shown that over 50% of pregnant patients download apps focused on pregnancy, with an average of 3 being tried.2 This is especially true during the COVID-19 pandemic, when patients seek information but may want to minimize clinical exposures. Other research has shown that women primarily use apps to monitor fetal development and to obtain information on nutrition and antenatal care.3
We identified apps and rated their contents and features.4 To identify the apps, we performed a Google search to mimic what a patient may do. We scored the identified apps based on what has been shown to make apps successful, as well as desired functions of the most commonly used apps. The quality of the applications was relatively varied, with many of the apps (60%) not having comprehensive information for every stage of pregnancy and no app attaining a perfect score. However, the top 3 apps had near perfect scores of 15/16 and 14/16, missing points only for having advertisements and requiring an internet connection.
The table details these top 3 recommended pregnancy apps, along with a detailed shortened version of the APPLICATIONS scoring system, APPLI (App comprehensiveness, Price, Platform, Literature Used, Other special features). We hope this column will help you feel comfortable in helping patients use pregnancy apps, should they ask for recommendations.
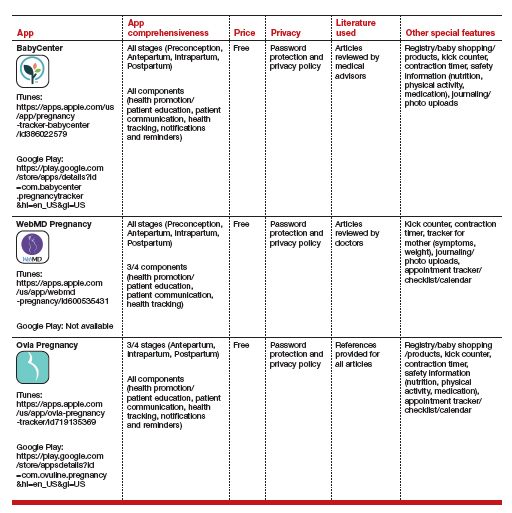
Pregnancy apps are more popular as patients use the internet to seek information about pregnancy and childbirth.1 Research has shown that over 50% of pregnant patients download apps focused on pregnancy, with an average of 3 being tried.2 This is especially true during the COVID-19 pandemic, when patients seek information but may want to minimize clinical exposures. Other research has shown that women primarily use apps to monitor fetal development and to obtain information on nutrition and antenatal care.3
We identified apps and rated their contents and features.4 To identify the apps, we performed a Google search to mimic what a patient may do. We scored the identified apps based on what has been shown to make apps successful, as well as desired functions of the most commonly used apps. The quality of the applications was relatively varied, with many of the apps (60%) not having comprehensive information for every stage of pregnancy and no app attaining a perfect score. However, the top 3 apps had near perfect scores of 15/16 and 14/16, missing points only for having advertisements and requiring an internet connection.
The table details these top 3 recommended pregnancy apps, along with a detailed shortened version of the APPLICATIONS scoring system, APPLI (App comprehensiveness, Price, Platform, Literature Used, Other special features). We hope this column will help you feel comfortable in helping patients use pregnancy apps, should they ask for recommendations.
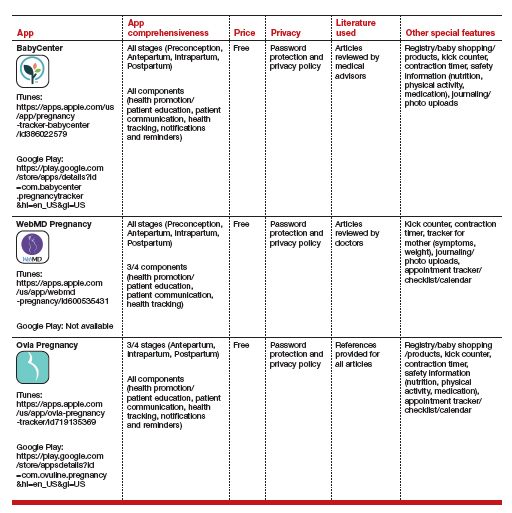
1. Romano AM. A changing landscape: implications of pregnant women’s internet use for childbirth educators. J Perinat Educ. 2007;16:18-24. doi: 10.1624/105812407X244903.
2. Jayaseelan R, Pichandy C, Rushandramani D. Usage of smartphone apps by women on their maternal life. J Mass Communicat Journalism. 2015;29:05:158-164. doi: 10.4172/2165-7912.1000267.
3. Wang N, Deng Z, Wen LM, et al. Understanding the use of smartphone apps for health information among pregnant Chinese women: mixed methods study. JMIR mHealth uHealth. 2019;18:7:e12631. doi: 10.2196/12631.
4. Frid G, Bogaert K, Chen KT. Mobile health apps for pregnant women: systematic search, evaluation, and analysis of features. J Med Internet Res. 2021;18:23:e25667. doi: 10.2196/25667.
1. Romano AM. A changing landscape: implications of pregnant women’s internet use for childbirth educators. J Perinat Educ. 2007;16:18-24. doi: 10.1624/105812407X244903.
2. Jayaseelan R, Pichandy C, Rushandramani D. Usage of smartphone apps by women on their maternal life. J Mass Communicat Journalism. 2015;29:05:158-164. doi: 10.4172/2165-7912.1000267.
3. Wang N, Deng Z, Wen LM, et al. Understanding the use of smartphone apps for health information among pregnant Chinese women: mixed methods study. JMIR mHealth uHealth. 2019;18:7:e12631. doi: 10.2196/12631.
4. Frid G, Bogaert K, Chen KT. Mobile health apps for pregnant women: systematic search, evaluation, and analysis of features. J Med Internet Res. 2021;18:23:e25667. doi: 10.2196/25667.
Models stratify hysterectomy risk with benign conditions
New models can help predict whether women having a hysterectomy for benign conditions are likely to have major complications, according to researchers.
The models, which use routinely collected data, are meant to aid surgeons in counseling women before surgery and help guide shared decision-making. The tools may lead to referrals for centers with greater surgical experience or may result in seeking nonsurgical treatment options, the researchers indicate.
The tools are not applicable to patients having hysterectomy for malignant disease.
Findings of the study, led by Krupa Madhvani, MD, of Barts and the London School of Medicine and Dentistry in London, are published online in the Canadian Medical Association Journal.
Calculators complement surgeons’ intuition
“Our aim was to generate prediction models that can be used in conjunction with a surgeon’s intuition to enhance preoperative patient counseling and match the advances made in the technical aspects of surgery,” the authors write.
“Internal–external cross-validation and external validation showed moderate discrimination,” they note.
The study included 68,599 patients who had laparoscopic hysterectomies and 125,971 patients who had an abdominal hysterectomy, all English National Health System patients between 2011 and 2018.
Among their findings were that major complications occurred in 4.4% of laparoscopic and 4.9% of abdominal hysterectomies. Major complications in this study included ureteric, gastrointestinal, and vascular injury and wound complications.
Adhesions biggest predictors of complications
Adhesions were most predictive of complications – with double the odds – in both models (laparoscopic: odds ratio, 1.92; 95% confidence interval, 1.73-2.13; abdominal: OR, 2.46; 95% CI, 2.27-2.66). That finding was consistent with previous literature.
“Adhesions should be suspected if there is a previous history of laparotomy, cesarean section, pelvic infection, or endometriosis, and can be reliably diagnosed preoperatively using ultrasonography,” the authors write. “As the global rate of cesarean sections continues to rise, this will undoubtedly remain a key determinant of major complications.”
Other factors that best predicted complications included adenomyosis in the laparoscopic model, and Asian ethnicity and diabetes in the abdominal model. Diabetes was not a predictive factor for complications in laparoscopic hysterectomy as it was in a previous study.
Obesity was not a significant predictor of major complications for either form of hysterectomy.
Factors protective against major complications included younger age and diagnosed menstrual disorders or benign adnexal mass (both models) and diagnosis of fibroids in the abdominal model.
Models miss surgeon experience
Jon Ivar Einarsson MD, PhD, MPH, founder of the division of minimally invasive gynecologic surgery at Brigham and Women’s Hospital, Boston, said it’s good to have these models to estimate risk as “there’s possibly a tendency to underestimate the risk by the surgeon.”
However, he told this publication that, though these models are based on a very large data set, the models are missing some key variables – often a problem with database studies – that are more indicative of complications. The most important factor missing, he said, is surgeon experience.
“We’ve shown in our publications that there’s a correlation between that and the risk of complications,“ Dr. Einarsson said.
Among other variables missing, he noted, are some that the authors list when acknowledging the limitations: severity of endometriosis and severity of adhesions.
He said his team wouldn’t use such models because they rely on their own data for gauging risk. He encourages other surgeons to track their own data and outcomes as well.
“I think the external validity here is nonexistent because we’re dealing with a different patient population in a different country with different surgeons [who] have various degrees of expertise,” Dr. Einarsson said.
“But if surgeons have not collected their own data, then this could be useful,” he said.
Links to online calculators
The online calculator can be found at www.evidencio.com (laparoscopic, www.evidencio.com/models/show/2551; abdominal, www.evidencio.com/models/show/2552).
The large, national multi-institutional database helps with generalizability of findings, the authors write. Additionally, patients had a unique identifier number so if patients were admitted to a different hospital after surgery, they were not lost to follow-up.
Limitations, in addition to those mentioned, include gaps in detailed clinical information, such as exact body mass index, and location, type, and size of leiomyoma, the authors write.
“Further research should focus on improving the discriminatory ability of these tools by including factors other than patient characteristics, including surgeon volume, as this has been shown to reduce complications,” they write.
Dr. Madhvani has received article-processing fees from Elly Charity (East London International Women’s Health Charity). No other competing interests were declared. Dr. Einarsson reports no relevant financial relationships. The acquisition of the data was funded by the British Society for Gynaecological Endoscopy. They were not involved in the study design, analysis, interpretation of data, the writing of the report, or the decision to submit the article for publication. Coauthor Khalid Khan, MD is a distinguished investigator funded by the Beatriz Galindo Program grant given to the University of Granada by the Ministry of Science, Innovation, and Universities of the Government of Spain.
New models can help predict whether women having a hysterectomy for benign conditions are likely to have major complications, according to researchers.
The models, which use routinely collected data, are meant to aid surgeons in counseling women before surgery and help guide shared decision-making. The tools may lead to referrals for centers with greater surgical experience or may result in seeking nonsurgical treatment options, the researchers indicate.
The tools are not applicable to patients having hysterectomy for malignant disease.
Findings of the study, led by Krupa Madhvani, MD, of Barts and the London School of Medicine and Dentistry in London, are published online in the Canadian Medical Association Journal.
Calculators complement surgeons’ intuition
“Our aim was to generate prediction models that can be used in conjunction with a surgeon’s intuition to enhance preoperative patient counseling and match the advances made in the technical aspects of surgery,” the authors write.
“Internal–external cross-validation and external validation showed moderate discrimination,” they note.
The study included 68,599 patients who had laparoscopic hysterectomies and 125,971 patients who had an abdominal hysterectomy, all English National Health System patients between 2011 and 2018.
Among their findings were that major complications occurred in 4.4% of laparoscopic and 4.9% of abdominal hysterectomies. Major complications in this study included ureteric, gastrointestinal, and vascular injury and wound complications.
Adhesions biggest predictors of complications
Adhesions were most predictive of complications – with double the odds – in both models (laparoscopic: odds ratio, 1.92; 95% confidence interval, 1.73-2.13; abdominal: OR, 2.46; 95% CI, 2.27-2.66). That finding was consistent with previous literature.
“Adhesions should be suspected if there is a previous history of laparotomy, cesarean section, pelvic infection, or endometriosis, and can be reliably diagnosed preoperatively using ultrasonography,” the authors write. “As the global rate of cesarean sections continues to rise, this will undoubtedly remain a key determinant of major complications.”
Other factors that best predicted complications included adenomyosis in the laparoscopic model, and Asian ethnicity and diabetes in the abdominal model. Diabetes was not a predictive factor for complications in laparoscopic hysterectomy as it was in a previous study.
Obesity was not a significant predictor of major complications for either form of hysterectomy.
Factors protective against major complications included younger age and diagnosed menstrual disorders or benign adnexal mass (both models) and diagnosis of fibroids in the abdominal model.
Models miss surgeon experience
Jon Ivar Einarsson MD, PhD, MPH, founder of the division of minimally invasive gynecologic surgery at Brigham and Women’s Hospital, Boston, said it’s good to have these models to estimate risk as “there’s possibly a tendency to underestimate the risk by the surgeon.”
However, he told this publication that, though these models are based on a very large data set, the models are missing some key variables – often a problem with database studies – that are more indicative of complications. The most important factor missing, he said, is surgeon experience.
“We’ve shown in our publications that there’s a correlation between that and the risk of complications,“ Dr. Einarsson said.
Among other variables missing, he noted, are some that the authors list when acknowledging the limitations: severity of endometriosis and severity of adhesions.
He said his team wouldn’t use such models because they rely on their own data for gauging risk. He encourages other surgeons to track their own data and outcomes as well.
“I think the external validity here is nonexistent because we’re dealing with a different patient population in a different country with different surgeons [who] have various degrees of expertise,” Dr. Einarsson said.
“But if surgeons have not collected their own data, then this could be useful,” he said.
Links to online calculators
The online calculator can be found at www.evidencio.com (laparoscopic, www.evidencio.com/models/show/2551; abdominal, www.evidencio.com/models/show/2552).
The large, national multi-institutional database helps with generalizability of findings, the authors write. Additionally, patients had a unique identifier number so if patients were admitted to a different hospital after surgery, they were not lost to follow-up.
Limitations, in addition to those mentioned, include gaps in detailed clinical information, such as exact body mass index, and location, type, and size of leiomyoma, the authors write.
“Further research should focus on improving the discriminatory ability of these tools by including factors other than patient characteristics, including surgeon volume, as this has been shown to reduce complications,” they write.
Dr. Madhvani has received article-processing fees from Elly Charity (East London International Women’s Health Charity). No other competing interests were declared. Dr. Einarsson reports no relevant financial relationships. The acquisition of the data was funded by the British Society for Gynaecological Endoscopy. They were not involved in the study design, analysis, interpretation of data, the writing of the report, or the decision to submit the article for publication. Coauthor Khalid Khan, MD is a distinguished investigator funded by the Beatriz Galindo Program grant given to the University of Granada by the Ministry of Science, Innovation, and Universities of the Government of Spain.
New models can help predict whether women having a hysterectomy for benign conditions are likely to have major complications, according to researchers.
The models, which use routinely collected data, are meant to aid surgeons in counseling women before surgery and help guide shared decision-making. The tools may lead to referrals for centers with greater surgical experience or may result in seeking nonsurgical treatment options, the researchers indicate.
The tools are not applicable to patients having hysterectomy for malignant disease.
Findings of the study, led by Krupa Madhvani, MD, of Barts and the London School of Medicine and Dentistry in London, are published online in the Canadian Medical Association Journal.
Calculators complement surgeons’ intuition
“Our aim was to generate prediction models that can be used in conjunction with a surgeon’s intuition to enhance preoperative patient counseling and match the advances made in the technical aspects of surgery,” the authors write.
“Internal–external cross-validation and external validation showed moderate discrimination,” they note.
The study included 68,599 patients who had laparoscopic hysterectomies and 125,971 patients who had an abdominal hysterectomy, all English National Health System patients between 2011 and 2018.
Among their findings were that major complications occurred in 4.4% of laparoscopic and 4.9% of abdominal hysterectomies. Major complications in this study included ureteric, gastrointestinal, and vascular injury and wound complications.
Adhesions biggest predictors of complications
Adhesions were most predictive of complications – with double the odds – in both models (laparoscopic: odds ratio, 1.92; 95% confidence interval, 1.73-2.13; abdominal: OR, 2.46; 95% CI, 2.27-2.66). That finding was consistent with previous literature.
“Adhesions should be suspected if there is a previous history of laparotomy, cesarean section, pelvic infection, or endometriosis, and can be reliably diagnosed preoperatively using ultrasonography,” the authors write. “As the global rate of cesarean sections continues to rise, this will undoubtedly remain a key determinant of major complications.”
Other factors that best predicted complications included adenomyosis in the laparoscopic model, and Asian ethnicity and diabetes in the abdominal model. Diabetes was not a predictive factor for complications in laparoscopic hysterectomy as it was in a previous study.
Obesity was not a significant predictor of major complications for either form of hysterectomy.
Factors protective against major complications included younger age and diagnosed menstrual disorders or benign adnexal mass (both models) and diagnosis of fibroids in the abdominal model.
Models miss surgeon experience
Jon Ivar Einarsson MD, PhD, MPH, founder of the division of minimally invasive gynecologic surgery at Brigham and Women’s Hospital, Boston, said it’s good to have these models to estimate risk as “there’s possibly a tendency to underestimate the risk by the surgeon.”
However, he told this publication that, though these models are based on a very large data set, the models are missing some key variables – often a problem with database studies – that are more indicative of complications. The most important factor missing, he said, is surgeon experience.
“We’ve shown in our publications that there’s a correlation between that and the risk of complications,“ Dr. Einarsson said.
Among other variables missing, he noted, are some that the authors list when acknowledging the limitations: severity of endometriosis and severity of adhesions.
He said his team wouldn’t use such models because they rely on their own data for gauging risk. He encourages other surgeons to track their own data and outcomes as well.
“I think the external validity here is nonexistent because we’re dealing with a different patient population in a different country with different surgeons [who] have various degrees of expertise,” Dr. Einarsson said.
“But if surgeons have not collected their own data, then this could be useful,” he said.
Links to online calculators
The online calculator can be found at www.evidencio.com (laparoscopic, www.evidencio.com/models/show/2551; abdominal, www.evidencio.com/models/show/2552).
The large, national multi-institutional database helps with generalizability of findings, the authors write. Additionally, patients had a unique identifier number so if patients were admitted to a different hospital after surgery, they were not lost to follow-up.
Limitations, in addition to those mentioned, include gaps in detailed clinical information, such as exact body mass index, and location, type, and size of leiomyoma, the authors write.
“Further research should focus on improving the discriminatory ability of these tools by including factors other than patient characteristics, including surgeon volume, as this has been shown to reduce complications,” they write.
Dr. Madhvani has received article-processing fees from Elly Charity (East London International Women’s Health Charity). No other competing interests were declared. Dr. Einarsson reports no relevant financial relationships. The acquisition of the data was funded by the British Society for Gynaecological Endoscopy. They were not involved in the study design, analysis, interpretation of data, the writing of the report, or the decision to submit the article for publication. Coauthor Khalid Khan, MD is a distinguished investigator funded by the Beatriz Galindo Program grant given to the University of Granada by the Ministry of Science, Innovation, and Universities of the Government of Spain.
FROM CANADIAN MEDICAL ASSOCIATION JOURNAL
Cost paramount when choosing metastatic breast cancer treatment
While efficacy and quality of life outcomes are similar across commonly used treatments for endocrine-refractory or triple-negative metastatic breast cancer, the costs of these agents vary widely, a recent analysis reveals.
Notably, the authors found that
Given “razor thin” differences in outcomes, cost should become a major consideration, the researchers concluded.
“As a society, we urgently need more strategies to reduce cancer drug costs without compromising outcomes, and our analysis provides quantifiable evidence to help providers choose lower priced, but equally effective sequences of drugs,” first author Stephanie B. Wheeler, PhD, from the University of North Carolina at Chapel Hill, explained in a press release.
Although the drugs Dr. Wheeler and colleagues studied are reimbursed in the metastatic breast cancer setting, “the optimal sequencing of them has been unclear, which has led to considerable variation in physician preference and practice,” Dr. Wheeler said.
In the study, published in the Journal of Clinical Oncology, Dr. Wheeler and colleagues estimated the cost-effectiveness of different therapeutic options from the first- to third-line setting for this patient population.
The researchers used three dynamic microsimulation computer models to predict how hypothetical sets of 10,000 patients with specific types of metastatic breast cancer would respond to various therapy types and sequences. The cohorts were grouped according to prior chemotherapy exposure: cohort 1 had no taxane or anthracycline exposure, cohort 2 had taxane and anthracycline exposure, and cohort 3 had taxane exposure but was anthracycline naive.
On the basis of feedback from oncologists, the investigators focused on different agents in the three cohorts: paclitaxel, capecitabine, or pegylated liposomal doxorubicin for cohort 1; eribulin, capecitabine, or carboplatin for cohort 2; and pegylated liposomal doxorubicin, capecitabine, or eribulin for cohort 3.
Overall, the models showed “nearly indistinguishable differences” in quality of life. In fact, the “razor-thin incremental differences in quality-adjusted survival” across the treatment sequences often amounted to differences of only a few days or weeks, the authors noted, adding that, even in the most extreme of cases, 3 weeks separated the best and worst options for quality-adjusted life-years.
But the models did show considerable differences in costs.
The authors found that, for cohort 1, treatment with paclitaxel followed by capecitabine and then pegylated liposomal doxorubicin corresponded to the highest expected quality-adjusted life-year gain and the lowest costs – $686 per month versus the highest cost option of $1,765.
For cohort 2, treatment with carboplatin followed by capecitabine and then eribulin corresponded to the highest expected quality-adjusted life-year gain and lowest costs.
For cohort 3, treatment sequences beginning with capecitabine or pegylated liposomal doxorubicin followed by eribulin was most cost effective.
Notably, the authors found that eribulin – the most expensive treatment with a high expected adverse event burden – performed particularly poorly in the two cohorts in which it was evaluated, “suggesting it should be used last in a sequence, on the basis of cost-effectiveness alone.”
In other words, “more spending on cancer care does not necessarily confer greater health benefits,” said Dr. Wheeler, also a professor of health policy.
“I hope our study will help expand the framework that we use to make these decisions from one where we just think about the biologic action of the drug to one where we also consider the bigger picture of what the treatment experience is like for the patient, including their financial burden, investment of time, and side effects,” study coauthor Katherine E. Reeder-Hayes, MD, section chief of breast oncology at UNC, said in the press release.
The results demonstrate that therapeutic decisions in the endocrine-refractory or triple-negative metastatic setting “may prioritize costs without affecting clinical outcomes” and highlight the direct impact that a “high-quality, transparent, and accessible economic analysis” can have on patient care, Scott D. Ramsey, MD, PhD, of Fred Hutchinson Cancer Research Center, Seattle, and colleagues wrote in an accompanying editorial.
Following the treatment sequences outlined in this study would “reduce patient financial burden and save our health system hundreds of millions of dollars annually,” the editorialists wrote.
As for next steps, Dr. Wheeler and colleagues have developed a financial navigation program to help patients manage their out-of-pocket cancer care costs and are currently scaling up the intervention in nine rural and nonrural oncology practices across North Carolina.
The study was supported by the Center for Disease Control and Prevention through the Prevention Research Centers Program. Dr. Wheeler has received research funding and payment for travel, accommodations, and expenses from Pfizer. Dr. Ramsey has had consulting or advisory roles and has received research funding and/or payment for travel, accommodations, and expenses from Bayer, Genentech, AstraZeneca, Merck, GRAIL, Seattle Genetics, Biovica, and/or Flatiron Health. Because of their editorial roles at the journal, the Journal of Clinical Oncology recused Dr. Wheeler and Dr. Ramsey from having any role in the peer review of their respective manuscripts.
A version of this article first appeared on Medscape.com.
While efficacy and quality of life outcomes are similar across commonly used treatments for endocrine-refractory or triple-negative metastatic breast cancer, the costs of these agents vary widely, a recent analysis reveals.
Notably, the authors found that
Given “razor thin” differences in outcomes, cost should become a major consideration, the researchers concluded.
“As a society, we urgently need more strategies to reduce cancer drug costs without compromising outcomes, and our analysis provides quantifiable evidence to help providers choose lower priced, but equally effective sequences of drugs,” first author Stephanie B. Wheeler, PhD, from the University of North Carolina at Chapel Hill, explained in a press release.
Although the drugs Dr. Wheeler and colleagues studied are reimbursed in the metastatic breast cancer setting, “the optimal sequencing of them has been unclear, which has led to considerable variation in physician preference and practice,” Dr. Wheeler said.
In the study, published in the Journal of Clinical Oncology, Dr. Wheeler and colleagues estimated the cost-effectiveness of different therapeutic options from the first- to third-line setting for this patient population.
The researchers used three dynamic microsimulation computer models to predict how hypothetical sets of 10,000 patients with specific types of metastatic breast cancer would respond to various therapy types and sequences. The cohorts were grouped according to prior chemotherapy exposure: cohort 1 had no taxane or anthracycline exposure, cohort 2 had taxane and anthracycline exposure, and cohort 3 had taxane exposure but was anthracycline naive.
On the basis of feedback from oncologists, the investigators focused on different agents in the three cohorts: paclitaxel, capecitabine, or pegylated liposomal doxorubicin for cohort 1; eribulin, capecitabine, or carboplatin for cohort 2; and pegylated liposomal doxorubicin, capecitabine, or eribulin for cohort 3.
Overall, the models showed “nearly indistinguishable differences” in quality of life. In fact, the “razor-thin incremental differences in quality-adjusted survival” across the treatment sequences often amounted to differences of only a few days or weeks, the authors noted, adding that, even in the most extreme of cases, 3 weeks separated the best and worst options for quality-adjusted life-years.
But the models did show considerable differences in costs.
The authors found that, for cohort 1, treatment with paclitaxel followed by capecitabine and then pegylated liposomal doxorubicin corresponded to the highest expected quality-adjusted life-year gain and the lowest costs – $686 per month versus the highest cost option of $1,765.
For cohort 2, treatment with carboplatin followed by capecitabine and then eribulin corresponded to the highest expected quality-adjusted life-year gain and lowest costs.
For cohort 3, treatment sequences beginning with capecitabine or pegylated liposomal doxorubicin followed by eribulin was most cost effective.
Notably, the authors found that eribulin – the most expensive treatment with a high expected adverse event burden – performed particularly poorly in the two cohorts in which it was evaluated, “suggesting it should be used last in a sequence, on the basis of cost-effectiveness alone.”
In other words, “more spending on cancer care does not necessarily confer greater health benefits,” said Dr. Wheeler, also a professor of health policy.
“I hope our study will help expand the framework that we use to make these decisions from one where we just think about the biologic action of the drug to one where we also consider the bigger picture of what the treatment experience is like for the patient, including their financial burden, investment of time, and side effects,” study coauthor Katherine E. Reeder-Hayes, MD, section chief of breast oncology at UNC, said in the press release.
The results demonstrate that therapeutic decisions in the endocrine-refractory or triple-negative metastatic setting “may prioritize costs without affecting clinical outcomes” and highlight the direct impact that a “high-quality, transparent, and accessible economic analysis” can have on patient care, Scott D. Ramsey, MD, PhD, of Fred Hutchinson Cancer Research Center, Seattle, and colleagues wrote in an accompanying editorial.
Following the treatment sequences outlined in this study would “reduce patient financial burden and save our health system hundreds of millions of dollars annually,” the editorialists wrote.
As for next steps, Dr. Wheeler and colleagues have developed a financial navigation program to help patients manage their out-of-pocket cancer care costs and are currently scaling up the intervention in nine rural and nonrural oncology practices across North Carolina.
The study was supported by the Center for Disease Control and Prevention through the Prevention Research Centers Program. Dr. Wheeler has received research funding and payment for travel, accommodations, and expenses from Pfizer. Dr. Ramsey has had consulting or advisory roles and has received research funding and/or payment for travel, accommodations, and expenses from Bayer, Genentech, AstraZeneca, Merck, GRAIL, Seattle Genetics, Biovica, and/or Flatiron Health. Because of their editorial roles at the journal, the Journal of Clinical Oncology recused Dr. Wheeler and Dr. Ramsey from having any role in the peer review of their respective manuscripts.
A version of this article first appeared on Medscape.com.
While efficacy and quality of life outcomes are similar across commonly used treatments for endocrine-refractory or triple-negative metastatic breast cancer, the costs of these agents vary widely, a recent analysis reveals.
Notably, the authors found that
Given “razor thin” differences in outcomes, cost should become a major consideration, the researchers concluded.
“As a society, we urgently need more strategies to reduce cancer drug costs without compromising outcomes, and our analysis provides quantifiable evidence to help providers choose lower priced, but equally effective sequences of drugs,” first author Stephanie B. Wheeler, PhD, from the University of North Carolina at Chapel Hill, explained in a press release.
Although the drugs Dr. Wheeler and colleagues studied are reimbursed in the metastatic breast cancer setting, “the optimal sequencing of them has been unclear, which has led to considerable variation in physician preference and practice,” Dr. Wheeler said.
In the study, published in the Journal of Clinical Oncology, Dr. Wheeler and colleagues estimated the cost-effectiveness of different therapeutic options from the first- to third-line setting for this patient population.
The researchers used three dynamic microsimulation computer models to predict how hypothetical sets of 10,000 patients with specific types of metastatic breast cancer would respond to various therapy types and sequences. The cohorts were grouped according to prior chemotherapy exposure: cohort 1 had no taxane or anthracycline exposure, cohort 2 had taxane and anthracycline exposure, and cohort 3 had taxane exposure but was anthracycline naive.
On the basis of feedback from oncologists, the investigators focused on different agents in the three cohorts: paclitaxel, capecitabine, or pegylated liposomal doxorubicin for cohort 1; eribulin, capecitabine, or carboplatin for cohort 2; and pegylated liposomal doxorubicin, capecitabine, or eribulin for cohort 3.
Overall, the models showed “nearly indistinguishable differences” in quality of life. In fact, the “razor-thin incremental differences in quality-adjusted survival” across the treatment sequences often amounted to differences of only a few days or weeks, the authors noted, adding that, even in the most extreme of cases, 3 weeks separated the best and worst options for quality-adjusted life-years.
But the models did show considerable differences in costs.
The authors found that, for cohort 1, treatment with paclitaxel followed by capecitabine and then pegylated liposomal doxorubicin corresponded to the highest expected quality-adjusted life-year gain and the lowest costs – $686 per month versus the highest cost option of $1,765.
For cohort 2, treatment with carboplatin followed by capecitabine and then eribulin corresponded to the highest expected quality-adjusted life-year gain and lowest costs.
For cohort 3, treatment sequences beginning with capecitabine or pegylated liposomal doxorubicin followed by eribulin was most cost effective.
Notably, the authors found that eribulin – the most expensive treatment with a high expected adverse event burden – performed particularly poorly in the two cohorts in which it was evaluated, “suggesting it should be used last in a sequence, on the basis of cost-effectiveness alone.”
In other words, “more spending on cancer care does not necessarily confer greater health benefits,” said Dr. Wheeler, also a professor of health policy.
“I hope our study will help expand the framework that we use to make these decisions from one where we just think about the biologic action of the drug to one where we also consider the bigger picture of what the treatment experience is like for the patient, including their financial burden, investment of time, and side effects,” study coauthor Katherine E. Reeder-Hayes, MD, section chief of breast oncology at UNC, said in the press release.
The results demonstrate that therapeutic decisions in the endocrine-refractory or triple-negative metastatic setting “may prioritize costs without affecting clinical outcomes” and highlight the direct impact that a “high-quality, transparent, and accessible economic analysis” can have on patient care, Scott D. Ramsey, MD, PhD, of Fred Hutchinson Cancer Research Center, Seattle, and colleagues wrote in an accompanying editorial.
Following the treatment sequences outlined in this study would “reduce patient financial burden and save our health system hundreds of millions of dollars annually,” the editorialists wrote.
As for next steps, Dr. Wheeler and colleagues have developed a financial navigation program to help patients manage their out-of-pocket cancer care costs and are currently scaling up the intervention in nine rural and nonrural oncology practices across North Carolina.
The study was supported by the Center for Disease Control and Prevention through the Prevention Research Centers Program. Dr. Wheeler has received research funding and payment for travel, accommodations, and expenses from Pfizer. Dr. Ramsey has had consulting or advisory roles and has received research funding and/or payment for travel, accommodations, and expenses from Bayer, Genentech, AstraZeneca, Merck, GRAIL, Seattle Genetics, Biovica, and/or Flatiron Health. Because of their editorial roles at the journal, the Journal of Clinical Oncology recused Dr. Wheeler and Dr. Ramsey from having any role in the peer review of their respective manuscripts.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
USPSTF: Screen at-risk, nonpregnant people for syphilis
People at increased risk for syphilis – including asymptomatic, nonpregnant adolescents and adults who have ever been sexually active and are at high risk for the disease – should be screened for it, according to a reaffirmation by the United States Preventive Services Task Force of its 2016 recommendation of syphilis screening for people at increased risk for infection.
“Using a reaffirmation process, the authors, led by Carol M. Mangione, MD, MSPH, of the University of California, Los Angeles, wrote in JAMA.
Reported cases in the United States of primary and secondary syphilis – a sexually transmitted infection caused by the bacterium Treponema pallidum that can damage the brain, nerves, eyes, and cardiovascular system if left untreated – increased from a low of 2.1 cases per 100,000 people in 2000 and 2001 to 11.9 cases per 100,000 in 2019, the authors reported. In 2019, men accounted for 83% of all primary and secondary syphilis cases, and men who have sex with men (MSM) accounted for 57% of all primary and secondary syphilis cases in men. Screening and follow-up treatment can cure syphilis and prevent complications.
To help them evaluate the effectiveness and safety of screening, the USPSTF authors reviewed the literature and visually displayed key questions and linkages to interventions and outcomes, Michelle L. Henninger, PhD, Sarah I. Bean, MPH, and Jennifer S. Lin, MD, MCR, of the Kaiser Permanente Evidence-based Practice Center in Portland, Ore., noted in a related evidence report of the post-2016 recommendation data.
Reaffirming its 2016 recommendation, the USPSTF now advises clinicians to:
Assess risk:
- Clinicians should know how common syphilis is in their community and assess their patient’s individual risk.
- Risk for syphilis is higher in MSM, people with HIV infection or other STIs, and those who use illicit drugs or have a history of incarceration, sex work, or military service.
Screen and confirm by testing:
- Traditional screening algorithm: Start with a nontreponemal test such as Venereal Disease Research Laborator or rapid plasma reagin. If positive, confirm result with a treponemal antibody detection test, such as T. pallidum particle agglutination.
- Reverse sequence algorithm: Screen with an initial automated treponemal test such as enzyme-linked or chemiluminescence immunoassay. If positive, confirm result with a nontreponemal test.
Consider screening interval:
- Evidence on optimal screening intervals is limited for the general population, but MSM and people with HIV may benefit from screening yearly or every 3-6 months if they remain at high risk.
The authors acknowledged that primary and secondary syphilis rates are higher in Blacks, Hispanics, Native Americans/Alaska Native, and Native Hawaiians/Pacific Islanders, and that the disparities are primarily driven by social determinants of health including differences in income, education, and access to coverage and care.
They added that differences in sexual networks also play a role in disparities and that sexually active people in communities with higher STI rates may be more likely to become infected.
More testing, treatment, and research are needed
Four experts welcomed the reaffirmation.
“It is important and necessary that the task force has chosen to reaffirm their syphilis screening recommendations, given the continued increase in sexually transmitted infections in the U.S. since the 2016 published recommendations,” Judith A. O’Donnell, MD, director of the department of infection prevention and control at Penn Presbyterian Medical Center in Philadelphia, said in an interview.
“Awareness of the ongoing incidence, understanding of the importance of screening in interrupting transmission, and getting people diagnosed and treated before serious complications are key,” she added.
Heidi Gullettt, MD, MPH, associate director of the Center for Community Health Integration at Case Western Reserve University, Cleveland, said: “The reaffirmation document authors demonstrated a comprehensive review of high-quality studies and epidemiologic data.
“Primary care clinicians rely on USPSTF recommendations to help prioritize evidence-based prevention in practice, so this reaffirmation is a critical step to remind us of the importance of regularly assessing risk and screening with a readily available screening test in the office,” she added.
Testing during office visits is not easy, Dr. Gullettt said, because of competing priorities, stigma associated with STIs, and testing and treatment costs.
“Under the Affordable Care Act, USPSTF screening recommendations are supposed to be covered without cost sharing by patients. This should be the case for syphilis screening,” Dr. Gullett pointed out. “Patients are often reluctant to do screening because of cost.”
Michael Anthony Moody, MD, director of the Collaborative Influenza Vaccine Innovation Center at Duke University, Durham, N.C., said that the true incidence and prevalence of syphilis is unknown.
“The more we test, the more accurate our data will be,” he said. “Syphilis can hide in plain sight, has symptoms that mimic many other diseases, and is usually not diagnosed. Reaffirming that testing for syphilis is important reminds providers that this is a key test for their patient’s health.”
Aniruddha Hazra, MD, medical director of the University of Chicago Medicine Sexual Wellness Clinic, noted that the United States is in a syphilis epidemic.
“Screening asymptomatic people at risk for syphilis is important, but without comprehensive education and training of primary care providers on how to address STIs and sexual health, these recommendations fall flat,” he said.
In an accompanying editorial, Susan Tuddenham, MD, MPH; and Khalil G. Ghanem, MD, PhD, of Johns Hopkins University, Baltimore, urged that funding to develop novel syphilis diagnostics be prioritized, “just as there has been for development of syphilis vaccines, which are still many years from becoming a reality.”
“Relying on emerging biomedical prevention interventions that hold promise, such as doxycycline postexposure prophylaxis, without concomitant robust screening strategies will not lead to syphilis control. Failure to modernize screening strategies for syphilis will also mean failure to control this infection,” they cautioned.
The authors of the recommendation statement and the evidence report, as well as Dr. O’Donnell, Dr. Gullettt, Dr. Moody, and Dr. Hazra, who were not involved in the study, reported no relevant financial relationships. Dr. Tuddenham reported financial relationships with the pharmaceutical and publishing industries. Dr. Ghanem reported financial relationships with the publishing industry. The research was federally funded.
A version of this article first appeared on Medscape.com.
People at increased risk for syphilis – including asymptomatic, nonpregnant adolescents and adults who have ever been sexually active and are at high risk for the disease – should be screened for it, according to a reaffirmation by the United States Preventive Services Task Force of its 2016 recommendation of syphilis screening for people at increased risk for infection.
“Using a reaffirmation process, the authors, led by Carol M. Mangione, MD, MSPH, of the University of California, Los Angeles, wrote in JAMA.
Reported cases in the United States of primary and secondary syphilis – a sexually transmitted infection caused by the bacterium Treponema pallidum that can damage the brain, nerves, eyes, and cardiovascular system if left untreated – increased from a low of 2.1 cases per 100,000 people in 2000 and 2001 to 11.9 cases per 100,000 in 2019, the authors reported. In 2019, men accounted for 83% of all primary and secondary syphilis cases, and men who have sex with men (MSM) accounted for 57% of all primary and secondary syphilis cases in men. Screening and follow-up treatment can cure syphilis and prevent complications.
To help them evaluate the effectiveness and safety of screening, the USPSTF authors reviewed the literature and visually displayed key questions and linkages to interventions and outcomes, Michelle L. Henninger, PhD, Sarah I. Bean, MPH, and Jennifer S. Lin, MD, MCR, of the Kaiser Permanente Evidence-based Practice Center in Portland, Ore., noted in a related evidence report of the post-2016 recommendation data.
Reaffirming its 2016 recommendation, the USPSTF now advises clinicians to:
Assess risk:
- Clinicians should know how common syphilis is in their community and assess their patient’s individual risk.
- Risk for syphilis is higher in MSM, people with HIV infection or other STIs, and those who use illicit drugs or have a history of incarceration, sex work, or military service.
Screen and confirm by testing:
- Traditional screening algorithm: Start with a nontreponemal test such as Venereal Disease Research Laborator or rapid plasma reagin. If positive, confirm result with a treponemal antibody detection test, such as T. pallidum particle agglutination.
- Reverse sequence algorithm: Screen with an initial automated treponemal test such as enzyme-linked or chemiluminescence immunoassay. If positive, confirm result with a nontreponemal test.
Consider screening interval:
- Evidence on optimal screening intervals is limited for the general population, but MSM and people with HIV may benefit from screening yearly or every 3-6 months if they remain at high risk.
The authors acknowledged that primary and secondary syphilis rates are higher in Blacks, Hispanics, Native Americans/Alaska Native, and Native Hawaiians/Pacific Islanders, and that the disparities are primarily driven by social determinants of health including differences in income, education, and access to coverage and care.
They added that differences in sexual networks also play a role in disparities and that sexually active people in communities with higher STI rates may be more likely to become infected.
More testing, treatment, and research are needed
Four experts welcomed the reaffirmation.
“It is important and necessary that the task force has chosen to reaffirm their syphilis screening recommendations, given the continued increase in sexually transmitted infections in the U.S. since the 2016 published recommendations,” Judith A. O’Donnell, MD, director of the department of infection prevention and control at Penn Presbyterian Medical Center in Philadelphia, said in an interview.
“Awareness of the ongoing incidence, understanding of the importance of screening in interrupting transmission, and getting people diagnosed and treated before serious complications are key,” she added.
Heidi Gullettt, MD, MPH, associate director of the Center for Community Health Integration at Case Western Reserve University, Cleveland, said: “The reaffirmation document authors demonstrated a comprehensive review of high-quality studies and epidemiologic data.
“Primary care clinicians rely on USPSTF recommendations to help prioritize evidence-based prevention in practice, so this reaffirmation is a critical step to remind us of the importance of regularly assessing risk and screening with a readily available screening test in the office,” she added.
Testing during office visits is not easy, Dr. Gullettt said, because of competing priorities, stigma associated with STIs, and testing and treatment costs.
“Under the Affordable Care Act, USPSTF screening recommendations are supposed to be covered without cost sharing by patients. This should be the case for syphilis screening,” Dr. Gullett pointed out. “Patients are often reluctant to do screening because of cost.”
Michael Anthony Moody, MD, director of the Collaborative Influenza Vaccine Innovation Center at Duke University, Durham, N.C., said that the true incidence and prevalence of syphilis is unknown.
“The more we test, the more accurate our data will be,” he said. “Syphilis can hide in plain sight, has symptoms that mimic many other diseases, and is usually not diagnosed. Reaffirming that testing for syphilis is important reminds providers that this is a key test for their patient’s health.”
Aniruddha Hazra, MD, medical director of the University of Chicago Medicine Sexual Wellness Clinic, noted that the United States is in a syphilis epidemic.
“Screening asymptomatic people at risk for syphilis is important, but without comprehensive education and training of primary care providers on how to address STIs and sexual health, these recommendations fall flat,” he said.
In an accompanying editorial, Susan Tuddenham, MD, MPH; and Khalil G. Ghanem, MD, PhD, of Johns Hopkins University, Baltimore, urged that funding to develop novel syphilis diagnostics be prioritized, “just as there has been for development of syphilis vaccines, which are still many years from becoming a reality.”
“Relying on emerging biomedical prevention interventions that hold promise, such as doxycycline postexposure prophylaxis, without concomitant robust screening strategies will not lead to syphilis control. Failure to modernize screening strategies for syphilis will also mean failure to control this infection,” they cautioned.
The authors of the recommendation statement and the evidence report, as well as Dr. O’Donnell, Dr. Gullettt, Dr. Moody, and Dr. Hazra, who were not involved in the study, reported no relevant financial relationships. Dr. Tuddenham reported financial relationships with the pharmaceutical and publishing industries. Dr. Ghanem reported financial relationships with the publishing industry. The research was federally funded.
A version of this article first appeared on Medscape.com.
People at increased risk for syphilis – including asymptomatic, nonpregnant adolescents and adults who have ever been sexually active and are at high risk for the disease – should be screened for it, according to a reaffirmation by the United States Preventive Services Task Force of its 2016 recommendation of syphilis screening for people at increased risk for infection.
“Using a reaffirmation process, the authors, led by Carol M. Mangione, MD, MSPH, of the University of California, Los Angeles, wrote in JAMA.
Reported cases in the United States of primary and secondary syphilis – a sexually transmitted infection caused by the bacterium Treponema pallidum that can damage the brain, nerves, eyes, and cardiovascular system if left untreated – increased from a low of 2.1 cases per 100,000 people in 2000 and 2001 to 11.9 cases per 100,000 in 2019, the authors reported. In 2019, men accounted for 83% of all primary and secondary syphilis cases, and men who have sex with men (MSM) accounted for 57% of all primary and secondary syphilis cases in men. Screening and follow-up treatment can cure syphilis and prevent complications.
To help them evaluate the effectiveness and safety of screening, the USPSTF authors reviewed the literature and visually displayed key questions and linkages to interventions and outcomes, Michelle L. Henninger, PhD, Sarah I. Bean, MPH, and Jennifer S. Lin, MD, MCR, of the Kaiser Permanente Evidence-based Practice Center in Portland, Ore., noted in a related evidence report of the post-2016 recommendation data.
Reaffirming its 2016 recommendation, the USPSTF now advises clinicians to:
Assess risk:
- Clinicians should know how common syphilis is in their community and assess their patient’s individual risk.
- Risk for syphilis is higher in MSM, people with HIV infection or other STIs, and those who use illicit drugs or have a history of incarceration, sex work, or military service.
Screen and confirm by testing:
- Traditional screening algorithm: Start with a nontreponemal test such as Venereal Disease Research Laborator or rapid plasma reagin. If positive, confirm result with a treponemal antibody detection test, such as T. pallidum particle agglutination.
- Reverse sequence algorithm: Screen with an initial automated treponemal test such as enzyme-linked or chemiluminescence immunoassay. If positive, confirm result with a nontreponemal test.
Consider screening interval:
- Evidence on optimal screening intervals is limited for the general population, but MSM and people with HIV may benefit from screening yearly or every 3-6 months if they remain at high risk.
The authors acknowledged that primary and secondary syphilis rates are higher in Blacks, Hispanics, Native Americans/Alaska Native, and Native Hawaiians/Pacific Islanders, and that the disparities are primarily driven by social determinants of health including differences in income, education, and access to coverage and care.
They added that differences in sexual networks also play a role in disparities and that sexually active people in communities with higher STI rates may be more likely to become infected.
More testing, treatment, and research are needed
Four experts welcomed the reaffirmation.
“It is important and necessary that the task force has chosen to reaffirm their syphilis screening recommendations, given the continued increase in sexually transmitted infections in the U.S. since the 2016 published recommendations,” Judith A. O’Donnell, MD, director of the department of infection prevention and control at Penn Presbyterian Medical Center in Philadelphia, said in an interview.
“Awareness of the ongoing incidence, understanding of the importance of screening in interrupting transmission, and getting people diagnosed and treated before serious complications are key,” she added.
Heidi Gullettt, MD, MPH, associate director of the Center for Community Health Integration at Case Western Reserve University, Cleveland, said: “The reaffirmation document authors demonstrated a comprehensive review of high-quality studies and epidemiologic data.
“Primary care clinicians rely on USPSTF recommendations to help prioritize evidence-based prevention in practice, so this reaffirmation is a critical step to remind us of the importance of regularly assessing risk and screening with a readily available screening test in the office,” she added.
Testing during office visits is not easy, Dr. Gullettt said, because of competing priorities, stigma associated with STIs, and testing and treatment costs.
“Under the Affordable Care Act, USPSTF screening recommendations are supposed to be covered without cost sharing by patients. This should be the case for syphilis screening,” Dr. Gullett pointed out. “Patients are often reluctant to do screening because of cost.”
Michael Anthony Moody, MD, director of the Collaborative Influenza Vaccine Innovation Center at Duke University, Durham, N.C., said that the true incidence and prevalence of syphilis is unknown.
“The more we test, the more accurate our data will be,” he said. “Syphilis can hide in plain sight, has symptoms that mimic many other diseases, and is usually not diagnosed. Reaffirming that testing for syphilis is important reminds providers that this is a key test for their patient’s health.”
Aniruddha Hazra, MD, medical director of the University of Chicago Medicine Sexual Wellness Clinic, noted that the United States is in a syphilis epidemic.
“Screening asymptomatic people at risk for syphilis is important, but without comprehensive education and training of primary care providers on how to address STIs and sexual health, these recommendations fall flat,” he said.
In an accompanying editorial, Susan Tuddenham, MD, MPH; and Khalil G. Ghanem, MD, PhD, of Johns Hopkins University, Baltimore, urged that funding to develop novel syphilis diagnostics be prioritized, “just as there has been for development of syphilis vaccines, which are still many years from becoming a reality.”
“Relying on emerging biomedical prevention interventions that hold promise, such as doxycycline postexposure prophylaxis, without concomitant robust screening strategies will not lead to syphilis control. Failure to modernize screening strategies for syphilis will also mean failure to control this infection,” they cautioned.
The authors of the recommendation statement and the evidence report, as well as Dr. O’Donnell, Dr. Gullettt, Dr. Moody, and Dr. Hazra, who were not involved in the study, reported no relevant financial relationships. Dr. Tuddenham reported financial relationships with the pharmaceutical and publishing industries. Dr. Ghanem reported financial relationships with the publishing industry. The research was federally funded.
A version of this article first appeared on Medscape.com.
FROM JAMA





