User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Immunodeficiencies tied to psychiatric disorders in offspring
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.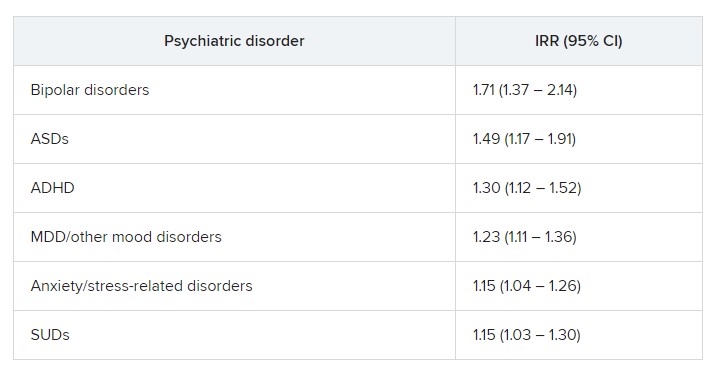
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.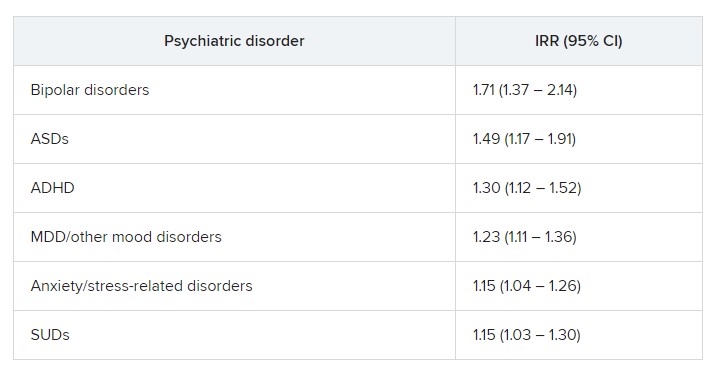
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.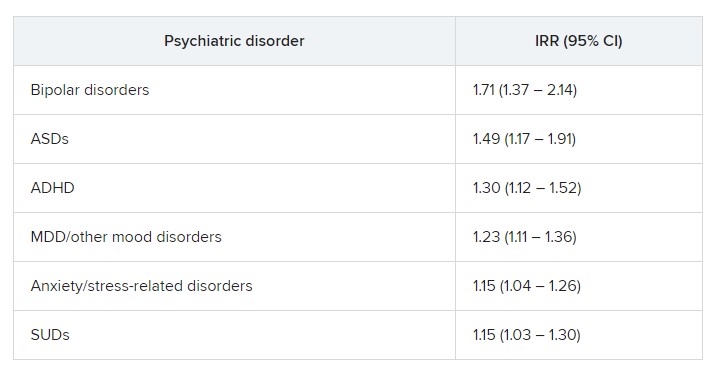
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Breast cancer exacts high financial toll worldwide
but in low- and middle-income countries as well, a meta-analysis found.
Although the rate of financial toxicity was much higher in low- and middle-income countries – affecting 79% of patients – more than 35% of patients in high-income countries also incurred financial hardship, the study team found.
The findings highlight the need for policies to offset the burden of direct and indirect costs for breast cancer care and improve the financial health of vulnerable patients, said the study authors, led by Kavitha Ranganathan, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston.
The study was published online in JAMA Network Open.
The most expensive malignancy?
Patients with breast cancer may be particularly burdened by costs of care, with one study showing substantially higher out-of-pocket costs for patients with breast cancer than colorectal, lung, and prostate cancer combined.
A Lancet Oncology Commission report revealed that breast cancer was the most expensive cancer in the United States in 2010, accounting for $16.5 billion, or 13% of all cancer-related spending. A separate analysis found that individual direct medical costs of breast cancer care can reach $100,000.
In high-income countries, the financial burden of breast cancer care may be the result of novel and costly cancer therapeutics and interventions, overuse of services, increased willingness to pay, and varying insurance coverage. In low- and middle-income countries, women may experience delayed diagnosis because of limited access to screening and high-quality diagnostic services, leading to more later-stage diagnoses requiring more extensive treatments. Lower baseline income, limited insurance coverage, and greater distance to treatment centers may also be factors.
“Establishing the global extent of financial toxicity and comparing the economic burden of disease in different populations is imperative to help policy makers prioritize funding of breast cancer care infrastructure,” Dr. Ranganathan and colleagues write.
In their meta-analysis of 18 studies – 14 from high-income countries and 4 from low – published from 2008 to 2021, the authors found that the definition of financial toxicity varied widely across studies.
For example, some used specific numerical criteria for defining financial toxicity, such as medical cost exceeding 40% of household capacity to pay or potential income or out-of-pocket costs exceeding 30% of annual household income.
Others used patient-reported outcome measures instruments evaluating subjective statements of financial difficulty, such as an affirmative answer to having financial difficulty or trouble paying medical bills, or paying more for medical care than is affordable.
In other studies, financial toxicity was defined according to a patient’s report of specific, objective financial consequences of care, including losing income or a job; having to borrow money or go into debt; having trouble paying for food, rent, or transportation; or having to forgo any type of medical care because of cost.
In their analysis, the pooled rate of financial toxicity among patients with breast cancer was 35.3% in high-income countries and 78.8% in low/middle-income countries, both demonstrating high heterogeneity or variability (P for heterogeneity < .001). In contrast, typical financial toxicity rates across all health conditions in low-income countries ranged from 6% to 12%, the investigators noted.
One study assessing quality of life measures in Egypt found that 47.5% of patients were food insecure, 66% needed financial assistance, 34% used savings to pay for treatment, and 41.2% lacked savings altogether.
Burden reduction
Given the high rates of financial toxicity associated with breast cancer, what strategies might reduce this cost burden?
When exploring potential factors associated with financial toxicity, the researchers found no clear association between financial toxicity and race, employment status, and age, and could draw no firm conclusions about the impact of comorbidities and urban vs. rural place of residence. In addition, cancer stage and treatments were “extremely” heterogeneous across studies and the authors found no clear association between either factor and financial toxicity.
But the authors noted that the highest-priority patients are typically those who have low education, have low socioeconomic status, lack health insurance, and live in low-resource areas.
To reduce financial toxicity and improve outcomes among patients with breast cancer, the study team recommended four potential strategies:
- Use targeted educational campaigns to raise awareness about the signs and symptoms of breast cancer and the importance of early diagnosis and treatment.
- Expand health care coverage to minimize direct medical out-of-pocket costs.
- Develop programs to assist with direct nonmedical and indirect costs, such as transportation to and lodging near treatment centers and childcare.
- Improve screening, referral, and treatment infrastructure for breast cancer care.
The researchers also noted that their data highlight the value of universal health care coverage as a policy strategy, with evidence of lower financial toxicity rates in countries with universal health coverage.
Support for the study was provided in part by the National Cancer Institute, United Nations Institute for Training and Research and the Global Surgery Foundation, Harvard Global Health Institute, Connors Center for Women’s Health and Gender Biology, the Center for Surgery and Public Health, and the National Endowment for Plastic Surgery. Dr. Ranganathan reports no relevant financial relationships. Several coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
but in low- and middle-income countries as well, a meta-analysis found.
Although the rate of financial toxicity was much higher in low- and middle-income countries – affecting 79% of patients – more than 35% of patients in high-income countries also incurred financial hardship, the study team found.
The findings highlight the need for policies to offset the burden of direct and indirect costs for breast cancer care and improve the financial health of vulnerable patients, said the study authors, led by Kavitha Ranganathan, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston.
The study was published online in JAMA Network Open.
The most expensive malignancy?
Patients with breast cancer may be particularly burdened by costs of care, with one study showing substantially higher out-of-pocket costs for patients with breast cancer than colorectal, lung, and prostate cancer combined.
A Lancet Oncology Commission report revealed that breast cancer was the most expensive cancer in the United States in 2010, accounting for $16.5 billion, or 13% of all cancer-related spending. A separate analysis found that individual direct medical costs of breast cancer care can reach $100,000.
In high-income countries, the financial burden of breast cancer care may be the result of novel and costly cancer therapeutics and interventions, overuse of services, increased willingness to pay, and varying insurance coverage. In low- and middle-income countries, women may experience delayed diagnosis because of limited access to screening and high-quality diagnostic services, leading to more later-stage diagnoses requiring more extensive treatments. Lower baseline income, limited insurance coverage, and greater distance to treatment centers may also be factors.
“Establishing the global extent of financial toxicity and comparing the economic burden of disease in different populations is imperative to help policy makers prioritize funding of breast cancer care infrastructure,” Dr. Ranganathan and colleagues write.
In their meta-analysis of 18 studies – 14 from high-income countries and 4 from low – published from 2008 to 2021, the authors found that the definition of financial toxicity varied widely across studies.
For example, some used specific numerical criteria for defining financial toxicity, such as medical cost exceeding 40% of household capacity to pay or potential income or out-of-pocket costs exceeding 30% of annual household income.
Others used patient-reported outcome measures instruments evaluating subjective statements of financial difficulty, such as an affirmative answer to having financial difficulty or trouble paying medical bills, or paying more for medical care than is affordable.
In other studies, financial toxicity was defined according to a patient’s report of specific, objective financial consequences of care, including losing income or a job; having to borrow money or go into debt; having trouble paying for food, rent, or transportation; or having to forgo any type of medical care because of cost.
In their analysis, the pooled rate of financial toxicity among patients with breast cancer was 35.3% in high-income countries and 78.8% in low/middle-income countries, both demonstrating high heterogeneity or variability (P for heterogeneity < .001). In contrast, typical financial toxicity rates across all health conditions in low-income countries ranged from 6% to 12%, the investigators noted.
One study assessing quality of life measures in Egypt found that 47.5% of patients were food insecure, 66% needed financial assistance, 34% used savings to pay for treatment, and 41.2% lacked savings altogether.
Burden reduction
Given the high rates of financial toxicity associated with breast cancer, what strategies might reduce this cost burden?
When exploring potential factors associated with financial toxicity, the researchers found no clear association between financial toxicity and race, employment status, and age, and could draw no firm conclusions about the impact of comorbidities and urban vs. rural place of residence. In addition, cancer stage and treatments were “extremely” heterogeneous across studies and the authors found no clear association between either factor and financial toxicity.
But the authors noted that the highest-priority patients are typically those who have low education, have low socioeconomic status, lack health insurance, and live in low-resource areas.
To reduce financial toxicity and improve outcomes among patients with breast cancer, the study team recommended four potential strategies:
- Use targeted educational campaigns to raise awareness about the signs and symptoms of breast cancer and the importance of early diagnosis and treatment.
- Expand health care coverage to minimize direct medical out-of-pocket costs.
- Develop programs to assist with direct nonmedical and indirect costs, such as transportation to and lodging near treatment centers and childcare.
- Improve screening, referral, and treatment infrastructure for breast cancer care.
The researchers also noted that their data highlight the value of universal health care coverage as a policy strategy, with evidence of lower financial toxicity rates in countries with universal health coverage.
Support for the study was provided in part by the National Cancer Institute, United Nations Institute for Training and Research and the Global Surgery Foundation, Harvard Global Health Institute, Connors Center for Women’s Health and Gender Biology, the Center for Surgery and Public Health, and the National Endowment for Plastic Surgery. Dr. Ranganathan reports no relevant financial relationships. Several coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
but in low- and middle-income countries as well, a meta-analysis found.
Although the rate of financial toxicity was much higher in low- and middle-income countries – affecting 79% of patients – more than 35% of patients in high-income countries also incurred financial hardship, the study team found.
The findings highlight the need for policies to offset the burden of direct and indirect costs for breast cancer care and improve the financial health of vulnerable patients, said the study authors, led by Kavitha Ranganathan, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston.
The study was published online in JAMA Network Open.
The most expensive malignancy?
Patients with breast cancer may be particularly burdened by costs of care, with one study showing substantially higher out-of-pocket costs for patients with breast cancer than colorectal, lung, and prostate cancer combined.
A Lancet Oncology Commission report revealed that breast cancer was the most expensive cancer in the United States in 2010, accounting for $16.5 billion, or 13% of all cancer-related spending. A separate analysis found that individual direct medical costs of breast cancer care can reach $100,000.
In high-income countries, the financial burden of breast cancer care may be the result of novel and costly cancer therapeutics and interventions, overuse of services, increased willingness to pay, and varying insurance coverage. In low- and middle-income countries, women may experience delayed diagnosis because of limited access to screening and high-quality diagnostic services, leading to more later-stage diagnoses requiring more extensive treatments. Lower baseline income, limited insurance coverage, and greater distance to treatment centers may also be factors.
“Establishing the global extent of financial toxicity and comparing the economic burden of disease in different populations is imperative to help policy makers prioritize funding of breast cancer care infrastructure,” Dr. Ranganathan and colleagues write.
In their meta-analysis of 18 studies – 14 from high-income countries and 4 from low – published from 2008 to 2021, the authors found that the definition of financial toxicity varied widely across studies.
For example, some used specific numerical criteria for defining financial toxicity, such as medical cost exceeding 40% of household capacity to pay or potential income or out-of-pocket costs exceeding 30% of annual household income.
Others used patient-reported outcome measures instruments evaluating subjective statements of financial difficulty, such as an affirmative answer to having financial difficulty or trouble paying medical bills, or paying more for medical care than is affordable.
In other studies, financial toxicity was defined according to a patient’s report of specific, objective financial consequences of care, including losing income or a job; having to borrow money or go into debt; having trouble paying for food, rent, or transportation; or having to forgo any type of medical care because of cost.
In their analysis, the pooled rate of financial toxicity among patients with breast cancer was 35.3% in high-income countries and 78.8% in low/middle-income countries, both demonstrating high heterogeneity or variability (P for heterogeneity < .001). In contrast, typical financial toxicity rates across all health conditions in low-income countries ranged from 6% to 12%, the investigators noted.
One study assessing quality of life measures in Egypt found that 47.5% of patients were food insecure, 66% needed financial assistance, 34% used savings to pay for treatment, and 41.2% lacked savings altogether.
Burden reduction
Given the high rates of financial toxicity associated with breast cancer, what strategies might reduce this cost burden?
When exploring potential factors associated with financial toxicity, the researchers found no clear association between financial toxicity and race, employment status, and age, and could draw no firm conclusions about the impact of comorbidities and urban vs. rural place of residence. In addition, cancer stage and treatments were “extremely” heterogeneous across studies and the authors found no clear association between either factor and financial toxicity.
But the authors noted that the highest-priority patients are typically those who have low education, have low socioeconomic status, lack health insurance, and live in low-resource areas.
To reduce financial toxicity and improve outcomes among patients with breast cancer, the study team recommended four potential strategies:
- Use targeted educational campaigns to raise awareness about the signs and symptoms of breast cancer and the importance of early diagnosis and treatment.
- Expand health care coverage to minimize direct medical out-of-pocket costs.
- Develop programs to assist with direct nonmedical and indirect costs, such as transportation to and lodging near treatment centers and childcare.
- Improve screening, referral, and treatment infrastructure for breast cancer care.
The researchers also noted that their data highlight the value of universal health care coverage as a policy strategy, with evidence of lower financial toxicity rates in countries with universal health coverage.
Support for the study was provided in part by the National Cancer Institute, United Nations Institute for Training and Research and the Global Surgery Foundation, Harvard Global Health Institute, Connors Center for Women’s Health and Gender Biology, the Center for Surgery and Public Health, and the National Endowment for Plastic Surgery. Dr. Ranganathan reports no relevant financial relationships. Several coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Medicare ‘offers’ cancer patient a choice: Less life or more debt
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
Obstetric violence: How it’s defined and how we face it
In a recent, tragic case, a newborn died from being crushed by its mother, who fell asleep from the fatigue of numerous hours of labor. The case has brought the issue of obstetric violence (OV) to the attention of the Italian media. OV is defined as neglect, physical abuse, or disrespect during childbirth, according to the World Health Organization. The WHO outlined fundamental actions to be taken at various levels for its prevention, especially by health care systems, in a 2014 position paper.
Gender-based abuse
Considered a form of gender-based abuse, OV was first described in Latin America in the early 2000s. It is widespread and is increasing in European countries.
From the scientific literature on the subject, OV seems to be strongly associated with a lack of communication between health care personnel and pregnant women. It appears to have more to do with authoritarian and paternalistic behavior than actual real-life medical issues. Actively involving women in decision-making regarding childbirth and postpartum care seems to reduce the incidence of OV. Pregnant women who are more involved appear to trust health care professionals more and are therefore less likely to report disrespectful and abusive behavior.
Estimates of the prevalence of OV vary, depending on the country, the childbirth facility, and its definition. In Italy, inspired by the web campaign “#Bastatacere: le madri hanno voce [#EnoughSilence: mothers have a voice],” in 2017, the Obstetric Violence Database (OVO) investigated perceptions of having been a victim of OV in a representative sample of Italian women aged 18-54 years who had at least one child.
In 2017, just over 20% of the women interviewed considered themselves victims of OV; 33% felt they had not received adequate care; and around 35% reported serious problems concerning privacy or trust. Following the treatment received, approximately 15% of the women decided not to return to the same health care facility, and 6% did not want to proceed with further pregnancies.
At the time of publication, the results sparked a debate among relevant medical associations (the Association of Obstetricians and Gynecologists of Italian Hospitals, the Italian Society of Gynecology and Obstetrics, and the Association of Italian University Gynecologists), which immediately recognized the importance of the topic and accepted an invitation for further discussion on physician-patient relationships. They expressed reservations concerning the methodologies used by the OVO for data collection, especially regarding the representativeness of the sample.
Lack of communication
“In general, women who claim to have suffered from obstetric violence do not do so because they have been denied an aspect of care but because they have had an overall experience that, for whatever reason, did not conform with their expectations,” said Irene Cetin, MD, PhD, professor of obstetrics and gynecology at the University of Milan and director of the obstetrics and gynecology unit of the Buzzi Hospital in Milan. “Following the OVO’s exposé, the Italian Society of Gynecology and Obstetrics also conducted a large-scale study throughout Italy on all women who had given birth within a 3-month period. That investigation painted a very different picture. It wasn’t the case that no instances of obstetric violence were found, but the results were more contained. This is a very delicate subject, given that every report that we receive in hospital is always valued and looked into in detail, and women come to speak to us about errors and things that were missed.”
She added, “Experience leads me to say that complaints about what happens in the delivery room are extremely rare. What we hear more of, but still not often, are problems experienced during days spent in hospital immediately after childbirth.” There are never enough resources, which is the reason behind most problems. “The real hardships are found in the wards,” continued Dr. Cetin, “where the midwife-to-bed ratio is one or two to 30, and therefore this is where it is more difficult to feel like you’re being listened to. With COVID-19, the situation has gotten even worse, even though in my hospital we have always guaranteed, not without struggle, the presence of the partner in the delivery room.”
Only relatively recently have women’s partners been allowed into the hospital. In addition, a number of services, such as having the right beds and giving the correct explanations and information on how to establish a relationship with the child, are now being offered. These steps are necessary to guarantee what is referred to as a “humanizing birth,” a process in which the woman is at the center of the experience and is the main protagonist of the birth.
Lack of resources
This trend also is observed at the systemic level, where there is a lack of organization and resources. Few staff members are in the ward, even fewer specialists are in the psychological field, and contact is almost nonexistent after discharge from many hospitals and in many regions across Italy. There are, however, some positive aspects and hope for the future. “Just think,” said Dr. Cetin, “of how degree courses in obstetrics have changed over time, with a large part of teaching and training now being centered around the emotional aspects of birth.” From the gynecologist’s side, “most of the problems have been inherited from the past,” said Dr. Cetin. “Let’s not forget that we have only recently been giving birth in hospital. The so-called medicalization of childbirth has been responsible for a decline in the death rate and morbidity rate of pregnant women, but initially, there was little interest or care in how women felt in this situation, including with regard to physical pain. Since the 1970s, with Leboyer from France and Miraglia from Italy [promoters of so-called sweet birth], a path was cleared for a different line of thought. For this reason, I believe that the situation will improve over time.
“To continuously improve physician-patient communication,” concluded Dr. Cetin, “it would perhaps be appropriate to make sure that, even in the preparatory phase, women are well aware of possible complications and of the necessary and rapid emergency procedures that must be implemented by health care personnel. This way, a trusting relationship could be maintained, and the perception of having suffered abuse due to not being involved in strictly medical decisions could be stemmed.”
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
In a recent, tragic case, a newborn died from being crushed by its mother, who fell asleep from the fatigue of numerous hours of labor. The case has brought the issue of obstetric violence (OV) to the attention of the Italian media. OV is defined as neglect, physical abuse, or disrespect during childbirth, according to the World Health Organization. The WHO outlined fundamental actions to be taken at various levels for its prevention, especially by health care systems, in a 2014 position paper.
Gender-based abuse
Considered a form of gender-based abuse, OV was first described in Latin America in the early 2000s. It is widespread and is increasing in European countries.
From the scientific literature on the subject, OV seems to be strongly associated with a lack of communication between health care personnel and pregnant women. It appears to have more to do with authoritarian and paternalistic behavior than actual real-life medical issues. Actively involving women in decision-making regarding childbirth and postpartum care seems to reduce the incidence of OV. Pregnant women who are more involved appear to trust health care professionals more and are therefore less likely to report disrespectful and abusive behavior.
Estimates of the prevalence of OV vary, depending on the country, the childbirth facility, and its definition. In Italy, inspired by the web campaign “#Bastatacere: le madri hanno voce [#EnoughSilence: mothers have a voice],” in 2017, the Obstetric Violence Database (OVO) investigated perceptions of having been a victim of OV in a representative sample of Italian women aged 18-54 years who had at least one child.
In 2017, just over 20% of the women interviewed considered themselves victims of OV; 33% felt they had not received adequate care; and around 35% reported serious problems concerning privacy or trust. Following the treatment received, approximately 15% of the women decided not to return to the same health care facility, and 6% did not want to proceed with further pregnancies.
At the time of publication, the results sparked a debate among relevant medical associations (the Association of Obstetricians and Gynecologists of Italian Hospitals, the Italian Society of Gynecology and Obstetrics, and the Association of Italian University Gynecologists), which immediately recognized the importance of the topic and accepted an invitation for further discussion on physician-patient relationships. They expressed reservations concerning the methodologies used by the OVO for data collection, especially regarding the representativeness of the sample.
Lack of communication
“In general, women who claim to have suffered from obstetric violence do not do so because they have been denied an aspect of care but because they have had an overall experience that, for whatever reason, did not conform with their expectations,” said Irene Cetin, MD, PhD, professor of obstetrics and gynecology at the University of Milan and director of the obstetrics and gynecology unit of the Buzzi Hospital in Milan. “Following the OVO’s exposé, the Italian Society of Gynecology and Obstetrics also conducted a large-scale study throughout Italy on all women who had given birth within a 3-month period. That investigation painted a very different picture. It wasn’t the case that no instances of obstetric violence were found, but the results were more contained. This is a very delicate subject, given that every report that we receive in hospital is always valued and looked into in detail, and women come to speak to us about errors and things that were missed.”
She added, “Experience leads me to say that complaints about what happens in the delivery room are extremely rare. What we hear more of, but still not often, are problems experienced during days spent in hospital immediately after childbirth.” There are never enough resources, which is the reason behind most problems. “The real hardships are found in the wards,” continued Dr. Cetin, “where the midwife-to-bed ratio is one or two to 30, and therefore this is where it is more difficult to feel like you’re being listened to. With COVID-19, the situation has gotten even worse, even though in my hospital we have always guaranteed, not without struggle, the presence of the partner in the delivery room.”
Only relatively recently have women’s partners been allowed into the hospital. In addition, a number of services, such as having the right beds and giving the correct explanations and information on how to establish a relationship with the child, are now being offered. These steps are necessary to guarantee what is referred to as a “humanizing birth,” a process in which the woman is at the center of the experience and is the main protagonist of the birth.
Lack of resources
This trend also is observed at the systemic level, where there is a lack of organization and resources. Few staff members are in the ward, even fewer specialists are in the psychological field, and contact is almost nonexistent after discharge from many hospitals and in many regions across Italy. There are, however, some positive aspects and hope for the future. “Just think,” said Dr. Cetin, “of how degree courses in obstetrics have changed over time, with a large part of teaching and training now being centered around the emotional aspects of birth.” From the gynecologist’s side, “most of the problems have been inherited from the past,” said Dr. Cetin. “Let’s not forget that we have only recently been giving birth in hospital. The so-called medicalization of childbirth has been responsible for a decline in the death rate and morbidity rate of pregnant women, but initially, there was little interest or care in how women felt in this situation, including with regard to physical pain. Since the 1970s, with Leboyer from France and Miraglia from Italy [promoters of so-called sweet birth], a path was cleared for a different line of thought. For this reason, I believe that the situation will improve over time.
“To continuously improve physician-patient communication,” concluded Dr. Cetin, “it would perhaps be appropriate to make sure that, even in the preparatory phase, women are well aware of possible complications and of the necessary and rapid emergency procedures that must be implemented by health care personnel. This way, a trusting relationship could be maintained, and the perception of having suffered abuse due to not being involved in strictly medical decisions could be stemmed.”
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
In a recent, tragic case, a newborn died from being crushed by its mother, who fell asleep from the fatigue of numerous hours of labor. The case has brought the issue of obstetric violence (OV) to the attention of the Italian media. OV is defined as neglect, physical abuse, or disrespect during childbirth, according to the World Health Organization. The WHO outlined fundamental actions to be taken at various levels for its prevention, especially by health care systems, in a 2014 position paper.
Gender-based abuse
Considered a form of gender-based abuse, OV was first described in Latin America in the early 2000s. It is widespread and is increasing in European countries.
From the scientific literature on the subject, OV seems to be strongly associated with a lack of communication between health care personnel and pregnant women. It appears to have more to do with authoritarian and paternalistic behavior than actual real-life medical issues. Actively involving women in decision-making regarding childbirth and postpartum care seems to reduce the incidence of OV. Pregnant women who are more involved appear to trust health care professionals more and are therefore less likely to report disrespectful and abusive behavior.
Estimates of the prevalence of OV vary, depending on the country, the childbirth facility, and its definition. In Italy, inspired by the web campaign “#Bastatacere: le madri hanno voce [#EnoughSilence: mothers have a voice],” in 2017, the Obstetric Violence Database (OVO) investigated perceptions of having been a victim of OV in a representative sample of Italian women aged 18-54 years who had at least one child.
In 2017, just over 20% of the women interviewed considered themselves victims of OV; 33% felt they had not received adequate care; and around 35% reported serious problems concerning privacy or trust. Following the treatment received, approximately 15% of the women decided not to return to the same health care facility, and 6% did not want to proceed with further pregnancies.
At the time of publication, the results sparked a debate among relevant medical associations (the Association of Obstetricians and Gynecologists of Italian Hospitals, the Italian Society of Gynecology and Obstetrics, and the Association of Italian University Gynecologists), which immediately recognized the importance of the topic and accepted an invitation for further discussion on physician-patient relationships. They expressed reservations concerning the methodologies used by the OVO for data collection, especially regarding the representativeness of the sample.
Lack of communication
“In general, women who claim to have suffered from obstetric violence do not do so because they have been denied an aspect of care but because they have had an overall experience that, for whatever reason, did not conform with their expectations,” said Irene Cetin, MD, PhD, professor of obstetrics and gynecology at the University of Milan and director of the obstetrics and gynecology unit of the Buzzi Hospital in Milan. “Following the OVO’s exposé, the Italian Society of Gynecology and Obstetrics also conducted a large-scale study throughout Italy on all women who had given birth within a 3-month period. That investigation painted a very different picture. It wasn’t the case that no instances of obstetric violence were found, but the results were more contained. This is a very delicate subject, given that every report that we receive in hospital is always valued and looked into in detail, and women come to speak to us about errors and things that were missed.”
She added, “Experience leads me to say that complaints about what happens in the delivery room are extremely rare. What we hear more of, but still not often, are problems experienced during days spent in hospital immediately after childbirth.” There are never enough resources, which is the reason behind most problems. “The real hardships are found in the wards,” continued Dr. Cetin, “where the midwife-to-bed ratio is one or two to 30, and therefore this is where it is more difficult to feel like you’re being listened to. With COVID-19, the situation has gotten even worse, even though in my hospital we have always guaranteed, not without struggle, the presence of the partner in the delivery room.”
Only relatively recently have women’s partners been allowed into the hospital. In addition, a number of services, such as having the right beds and giving the correct explanations and information on how to establish a relationship with the child, are now being offered. These steps are necessary to guarantee what is referred to as a “humanizing birth,” a process in which the woman is at the center of the experience and is the main protagonist of the birth.
Lack of resources
This trend also is observed at the systemic level, where there is a lack of organization and resources. Few staff members are in the ward, even fewer specialists are in the psychological field, and contact is almost nonexistent after discharge from many hospitals and in many regions across Italy. There are, however, some positive aspects and hope for the future. “Just think,” said Dr. Cetin, “of how degree courses in obstetrics have changed over time, with a large part of teaching and training now being centered around the emotional aspects of birth.” From the gynecologist’s side, “most of the problems have been inherited from the past,” said Dr. Cetin. “Let’s not forget that we have only recently been giving birth in hospital. The so-called medicalization of childbirth has been responsible for a decline in the death rate and morbidity rate of pregnant women, but initially, there was little interest or care in how women felt in this situation, including with regard to physical pain. Since the 1970s, with Leboyer from France and Miraglia from Italy [promoters of so-called sweet birth], a path was cleared for a different line of thought. For this reason, I believe that the situation will improve over time.
“To continuously improve physician-patient communication,” concluded Dr. Cetin, “it would perhaps be appropriate to make sure that, even in the preparatory phase, women are well aware of possible complications and of the necessary and rapid emergency procedures that must be implemented by health care personnel. This way, a trusting relationship could be maintained, and the perception of having suffered abuse due to not being involved in strictly medical decisions could be stemmed.”
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
Genomic clues to poor outcomes in young breast cancer patients
and offer clues about molecular targets for future trials.
Compared with older women with early stage HR-positive breast cancer, women under 40 years of age had significantly higher frequencies of certain mutations, such as GATA3, as well as genomic features associated with a poor prognosis. Notably, the researchers found that women with such poor prognostic features vs. those with none had a significantly worse 8-year distant recurrence-free interval and overall survival.
“We have demonstrated age-related differences in genomic profiles with enrichment of genomic features associated with poor prognosis in these younger premenopausal women compared with older premenopausal and postmenopausal women,” the authors wrote in the study, published in the Annals of Oncology. Importantly, the genomic features highlight “the potential for age-focused treatment strategies.”
Charis Eng, MD, PhD, of the Cleveland Clinic Genomic Medicine Institute, Ohio, noted that the findings are promising but need further validation.
“With time and the appropriate clinical trials in place, I envision that these findings will enable the personalized genomics-driven management of these cancers – not only treatment, but also toward prevention,” said Dr. Eng, who was not involved in the study.
Young premenopausal women, particularly those with HR-positive, luminal breast cancer, are known to have significantly higher recurrence rates and worse survival, compared with older women, but the reasons have remained unclear.
Although previous studies have identified key gene expression signatures linked to worse outcomes in younger patients with breast cancer, there are limited data on this younger patient population, especially by breast cancer subtype. Given that breast cancer treatment strategies are often similar across age groups, such evidence gaps could represent missed opportunities for developing more targeted treatment strategies for this high-risk population of young women.
To further investigate the cancer-specific genetic profiles in younger women, Sherene Loi, MD, PhD, of the Peter MacCallum Cancer Centre, University of Melbourne, and colleagues turned to data from the pivotal, multicenter Suppression of Ovarian Function Trial (SOFT).
Using next-generation sequencing, Dr. Loi and colleagues evaluated HR-positive, HER2-negative tumors among a subset of 1,276 premenopausal women who were diagnosed with early stage breast cancer. The study employed deep-targeted sequencing for most patients (n = 1,258) as well as whole-exome sequencing in a matched case-control subsample of young women with a median age of 38 years (n = 82).
Compared with women aged 40 and older, those under 40 years of age (n = 359) had significantly higher frequencies of mutations in GATA3 (19% vs. 16%) and copy number-amplifications (47% vs. 26%).
Younger women also had significantly higher features suggestive of homologous recombination deficiency (27% vs. 21% in older women), and a higher proportion of PIK3CA mutations with concurrent copy number-amplifications (23% vs. 11%, respectively), all considered to be poor prognostic features.
In addition, younger women had significantly lower frequencies of certain mutations, including PIK3CA (32% vs. 47%), CDH1 (3% vs. 9%), and MAP3K1 (7% vs. 12%), compared with older women.
Overall, 46% of women had poor prognostic features. These poor prognostic features were observed in 72% of patients under age 35, compared with 54% aged 35-39, and 40% of those 40 and over.
Compared with women without those features, women with poor prognostic features had a lower 8-year distant recurrence-free interval of 84% vs. 94% (hazard ratio, 1.85), and worse 8-year overall survival of 88% vs. 96%, respectively (HR, 2.20). Notably, younger women under age 40 had the poorest outcomes, with an 8-year distant recurrence-free interval rate of 74% vs. 85% in older women, and an 8-year overall survival of 80% vs. 93%, respectively.
How might these results inform potential therapeutics?
Drugs targeting the homologous recombination deficiency pathway are well established, and up to 36% of very young patients in the study showed genomic features of homologous recombination deficiency, the authors noted.
In addition, Dr. Eng explained, there are other Food and Drug Administration–approved treatments that can target the copy number amplified, PIK3CA-mutated tumors, including therapies that target PIK3CA itself, or proteins downstream of it. However, use of such therapies would need “to be tested experimentally, especially since pathway inhibition sometimes may result in rebound signaling to promote tumor growth,” Dr. Eng said.
An important caveat is that patients with germline BRCA1 or BRCA2 mutations may be underrepresented in the SOFT clinical trial, as the trial excluded patients who already had bilateral oophorectomy or planned to within 5 years, the authors noted.
Nevertheless, Dr. Loi said that the study is important because “there are no other datasets as large or with this long follow-up for very young women with breast cancer.”
Furthermore, “the SOFT clinical trial was practice-changing, so using the tumor samples associated with this study is more impactful than smaller cohorts with no outcome data or institutional retrospective cohorts,” she said.
Dr. Eng agreed that the study’s size is an important attribute, allowing the authors to “identify differences that would have been missed in a smaller and more heterogeneous series.”
She added that future research should also include ancestry and racial diversity.
“While young women have higher occurrences of aggressive breast cancers, mortality is twice as likely in young Black women, compared to young White women,” Dr. Eng said.
The study received funding from a Susan G. Komen for the Cure Promise Grant, the National Health and Research Council of Australia, the Breast Cancer Research Foundation, and the National Breast Cancer Foundation of Australia, and support from the family of Judy Eisman in Australia. Dr. Loi and Dr. Eng report no relevant financial disclosures.
A version of this article originally appeared on Medscape.com.
and offer clues about molecular targets for future trials.
Compared with older women with early stage HR-positive breast cancer, women under 40 years of age had significantly higher frequencies of certain mutations, such as GATA3, as well as genomic features associated with a poor prognosis. Notably, the researchers found that women with such poor prognostic features vs. those with none had a significantly worse 8-year distant recurrence-free interval and overall survival.
“We have demonstrated age-related differences in genomic profiles with enrichment of genomic features associated with poor prognosis in these younger premenopausal women compared with older premenopausal and postmenopausal women,” the authors wrote in the study, published in the Annals of Oncology. Importantly, the genomic features highlight “the potential for age-focused treatment strategies.”
Charis Eng, MD, PhD, of the Cleveland Clinic Genomic Medicine Institute, Ohio, noted that the findings are promising but need further validation.
“With time and the appropriate clinical trials in place, I envision that these findings will enable the personalized genomics-driven management of these cancers – not only treatment, but also toward prevention,” said Dr. Eng, who was not involved in the study.
Young premenopausal women, particularly those with HR-positive, luminal breast cancer, are known to have significantly higher recurrence rates and worse survival, compared with older women, but the reasons have remained unclear.
Although previous studies have identified key gene expression signatures linked to worse outcomes in younger patients with breast cancer, there are limited data on this younger patient population, especially by breast cancer subtype. Given that breast cancer treatment strategies are often similar across age groups, such evidence gaps could represent missed opportunities for developing more targeted treatment strategies for this high-risk population of young women.
To further investigate the cancer-specific genetic profiles in younger women, Sherene Loi, MD, PhD, of the Peter MacCallum Cancer Centre, University of Melbourne, and colleagues turned to data from the pivotal, multicenter Suppression of Ovarian Function Trial (SOFT).
Using next-generation sequencing, Dr. Loi and colleagues evaluated HR-positive, HER2-negative tumors among a subset of 1,276 premenopausal women who were diagnosed with early stage breast cancer. The study employed deep-targeted sequencing for most patients (n = 1,258) as well as whole-exome sequencing in a matched case-control subsample of young women with a median age of 38 years (n = 82).
Compared with women aged 40 and older, those under 40 years of age (n = 359) had significantly higher frequencies of mutations in GATA3 (19% vs. 16%) and copy number-amplifications (47% vs. 26%).
Younger women also had significantly higher features suggestive of homologous recombination deficiency (27% vs. 21% in older women), and a higher proportion of PIK3CA mutations with concurrent copy number-amplifications (23% vs. 11%, respectively), all considered to be poor prognostic features.
In addition, younger women had significantly lower frequencies of certain mutations, including PIK3CA (32% vs. 47%), CDH1 (3% vs. 9%), and MAP3K1 (7% vs. 12%), compared with older women.
Overall, 46% of women had poor prognostic features. These poor prognostic features were observed in 72% of patients under age 35, compared with 54% aged 35-39, and 40% of those 40 and over.
Compared with women without those features, women with poor prognostic features had a lower 8-year distant recurrence-free interval of 84% vs. 94% (hazard ratio, 1.85), and worse 8-year overall survival of 88% vs. 96%, respectively (HR, 2.20). Notably, younger women under age 40 had the poorest outcomes, with an 8-year distant recurrence-free interval rate of 74% vs. 85% in older women, and an 8-year overall survival of 80% vs. 93%, respectively.
How might these results inform potential therapeutics?
Drugs targeting the homologous recombination deficiency pathway are well established, and up to 36% of very young patients in the study showed genomic features of homologous recombination deficiency, the authors noted.
In addition, Dr. Eng explained, there are other Food and Drug Administration–approved treatments that can target the copy number amplified, PIK3CA-mutated tumors, including therapies that target PIK3CA itself, or proteins downstream of it. However, use of such therapies would need “to be tested experimentally, especially since pathway inhibition sometimes may result in rebound signaling to promote tumor growth,” Dr. Eng said.
An important caveat is that patients with germline BRCA1 or BRCA2 mutations may be underrepresented in the SOFT clinical trial, as the trial excluded patients who already had bilateral oophorectomy or planned to within 5 years, the authors noted.
Nevertheless, Dr. Loi said that the study is important because “there are no other datasets as large or with this long follow-up for very young women with breast cancer.”
Furthermore, “the SOFT clinical trial was practice-changing, so using the tumor samples associated with this study is more impactful than smaller cohorts with no outcome data or institutional retrospective cohorts,” she said.
Dr. Eng agreed that the study’s size is an important attribute, allowing the authors to “identify differences that would have been missed in a smaller and more heterogeneous series.”
She added that future research should also include ancestry and racial diversity.
“While young women have higher occurrences of aggressive breast cancers, mortality is twice as likely in young Black women, compared to young White women,” Dr. Eng said.
The study received funding from a Susan G. Komen for the Cure Promise Grant, the National Health and Research Council of Australia, the Breast Cancer Research Foundation, and the National Breast Cancer Foundation of Australia, and support from the family of Judy Eisman in Australia. Dr. Loi and Dr. Eng report no relevant financial disclosures.
A version of this article originally appeared on Medscape.com.
and offer clues about molecular targets for future trials.
Compared with older women with early stage HR-positive breast cancer, women under 40 years of age had significantly higher frequencies of certain mutations, such as GATA3, as well as genomic features associated with a poor prognosis. Notably, the researchers found that women with such poor prognostic features vs. those with none had a significantly worse 8-year distant recurrence-free interval and overall survival.
“We have demonstrated age-related differences in genomic profiles with enrichment of genomic features associated with poor prognosis in these younger premenopausal women compared with older premenopausal and postmenopausal women,” the authors wrote in the study, published in the Annals of Oncology. Importantly, the genomic features highlight “the potential for age-focused treatment strategies.”
Charis Eng, MD, PhD, of the Cleveland Clinic Genomic Medicine Institute, Ohio, noted that the findings are promising but need further validation.
“With time and the appropriate clinical trials in place, I envision that these findings will enable the personalized genomics-driven management of these cancers – not only treatment, but also toward prevention,” said Dr. Eng, who was not involved in the study.
Young premenopausal women, particularly those with HR-positive, luminal breast cancer, are known to have significantly higher recurrence rates and worse survival, compared with older women, but the reasons have remained unclear.
Although previous studies have identified key gene expression signatures linked to worse outcomes in younger patients with breast cancer, there are limited data on this younger patient population, especially by breast cancer subtype. Given that breast cancer treatment strategies are often similar across age groups, such evidence gaps could represent missed opportunities for developing more targeted treatment strategies for this high-risk population of young women.
To further investigate the cancer-specific genetic profiles in younger women, Sherene Loi, MD, PhD, of the Peter MacCallum Cancer Centre, University of Melbourne, and colleagues turned to data from the pivotal, multicenter Suppression of Ovarian Function Trial (SOFT).
Using next-generation sequencing, Dr. Loi and colleagues evaluated HR-positive, HER2-negative tumors among a subset of 1,276 premenopausal women who were diagnosed with early stage breast cancer. The study employed deep-targeted sequencing for most patients (n = 1,258) as well as whole-exome sequencing in a matched case-control subsample of young women with a median age of 38 years (n = 82).
Compared with women aged 40 and older, those under 40 years of age (n = 359) had significantly higher frequencies of mutations in GATA3 (19% vs. 16%) and copy number-amplifications (47% vs. 26%).
Younger women also had significantly higher features suggestive of homologous recombination deficiency (27% vs. 21% in older women), and a higher proportion of PIK3CA mutations with concurrent copy number-amplifications (23% vs. 11%, respectively), all considered to be poor prognostic features.
In addition, younger women had significantly lower frequencies of certain mutations, including PIK3CA (32% vs. 47%), CDH1 (3% vs. 9%), and MAP3K1 (7% vs. 12%), compared with older women.
Overall, 46% of women had poor prognostic features. These poor prognostic features were observed in 72% of patients under age 35, compared with 54% aged 35-39, and 40% of those 40 and over.
Compared with women without those features, women with poor prognostic features had a lower 8-year distant recurrence-free interval of 84% vs. 94% (hazard ratio, 1.85), and worse 8-year overall survival of 88% vs. 96%, respectively (HR, 2.20). Notably, younger women under age 40 had the poorest outcomes, with an 8-year distant recurrence-free interval rate of 74% vs. 85% in older women, and an 8-year overall survival of 80% vs. 93%, respectively.
How might these results inform potential therapeutics?
Drugs targeting the homologous recombination deficiency pathway are well established, and up to 36% of very young patients in the study showed genomic features of homologous recombination deficiency, the authors noted.
In addition, Dr. Eng explained, there are other Food and Drug Administration–approved treatments that can target the copy number amplified, PIK3CA-mutated tumors, including therapies that target PIK3CA itself, or proteins downstream of it. However, use of such therapies would need “to be tested experimentally, especially since pathway inhibition sometimes may result in rebound signaling to promote tumor growth,” Dr. Eng said.
An important caveat is that patients with germline BRCA1 or BRCA2 mutations may be underrepresented in the SOFT clinical trial, as the trial excluded patients who already had bilateral oophorectomy or planned to within 5 years, the authors noted.
Nevertheless, Dr. Loi said that the study is important because “there are no other datasets as large or with this long follow-up for very young women with breast cancer.”
Furthermore, “the SOFT clinical trial was practice-changing, so using the tumor samples associated with this study is more impactful than smaller cohorts with no outcome data or institutional retrospective cohorts,” she said.
Dr. Eng agreed that the study’s size is an important attribute, allowing the authors to “identify differences that would have been missed in a smaller and more heterogeneous series.”
She added that future research should also include ancestry and racial diversity.
“While young women have higher occurrences of aggressive breast cancers, mortality is twice as likely in young Black women, compared to young White women,” Dr. Eng said.
The study received funding from a Susan G. Komen for the Cure Promise Grant, the National Health and Research Council of Australia, the Breast Cancer Research Foundation, and the National Breast Cancer Foundation of Australia, and support from the family of Judy Eisman in Australia. Dr. Loi and Dr. Eng report no relevant financial disclosures.
A version of this article originally appeared on Medscape.com.
FROM ANNALS OF ONCOLOGY
Saying goodbye: How to transition teens to adult medical care
However, many clinicians feel insufficiently prepared to provide comprehensive transition services. This can result in the actual handoff or transfer into adult care being abrupt, incomplete, or outright unsuccessful. By following the recommended best practices of transitions, providers of pediatric care can ensure that this challenging goodbye prepares everyone for the next steps ahead.
Using a structured transition process
In 2011, a health care transition clinical report based on expert opinion and practice consensus and endorsed by the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians – Society of Internal Medicine was released. This report provided a decision-making algorithm for “practice-based implementation of transition for all youth beginning in early adolescence.”
The Got Transition organization, funded by the Maternal Child Health Bureau and Health Resources and Services Administration, provides web-based information and materials for health care providers and families to establish a smooth and successful transition. At the center of these recommendations are the Six Core Elements of Health Care Transition – the essential components of a structured transition process: 1) transition policy/guide; 2) tracking and monitoring; 3) readiness; 4) planning; 5) transfer of care, and 6) transition completion.
This transition process should start early in adolescence, preferably by age 12-14 years, to give adequate time to progress successfully through these elements and improve the likelihood of a smooth, final transfer into the care of an adult clinician.
Preparing your patients for transfer
Despite the availability of these recommendations, national surveys show that the overwhelming majority of adolescents with and without special health care needs report not receiving transition services. Lack of time, resources, interest, and patients being lost to care during adolescence all contribute to this deficit in care. Without transition preparation, the actual handoff or transfer to adult care can be difficult for adolescents, caregivers, and clinicians alike. Adolescents and caregivers may feel a sense of abandonment or have inadequate health knowledge/literacy, pediatric clinicians may fear that the patient is not ready for the expected independence, and adult clinicians face numerous challenges integrating these young patients into their practice.
A structured transition process can help the family and clinicians know what to expect during the transfer of care. Pediatric clinicians can gradually move from a pediatric model of care, in which the caregiver is the center of communication, to an adult model, putting the patient at the center. By encouraging the adolescent to be the direct communicator, the pediatric clinician can promote independence and assess health knowledge, allowing for education where gaps exist.
Assisting the patient in identifying and even meeting the adult clinician well ahead of the final transfer date can also make the process less daunting for the adolescent.
Adult clinicians should consider allowing more time for the first visit with a new young adult patient and welcome caregiver input early in the transfer process, particularly for patients with a chronic disease. By engaging patients and families in an intentional, gradual transition process with an expected outcome, all those involved will be more prepared for the final handoff.
Utilizing transition tools and engaging the adolescent
Numerous tools can assist in the preparation for transfer to adult care. These include transition summaries and emergency plans, which contain essential information such as current medical problems, allergies, medications, prior procedures and treatments, and sick day plans. Such tools can also be built into electronic medical records for easy modification and updating. They can be used as methods to engage and teach adolescents about their disease history and current regimen and can contain essential components for information handoff at the time of transfer to adult care. If the patient carries a rare diagnosis, or one that has historically been associated with lower survival to adulthood, these transfer documents can also include summary information about disease states and contact information for pediatric specialty clinicians.
Adolescent engagement in their health care during the time of transition can also be prompted through the use of patient portals within an electronic health record. Such portals put health information directly at the adolescent’s fingertips, provide them with an outlet for communication with their clinicians, and give reminders regarding health maintenance.
Completing the transfer: The final handoff
The best and most recommended means of relaying information at the time of transfer to adult care is a direct, verbal handoff between clinicians. This direct handoff has several goals:
(1) To ensure the patient has scheduled or attended the first appointment with the adult clinician
(2) To ensure record transfer has occurred successfully
(3) To answer any questions the receiving clinician may have about prior or ongoing care.
(4) To offer the adult clinician ongoing access to the pediatric clinician as an “expert” resource for additional questions.
By remaining available as a resource, the pediatric clinician can alleviate concerns for both the patient and caregiver as well as the receiving adult clinician.
As valuable as verbal handoffs can be, they are not always possible due to patients not having selected an adult clinician prior to leaving the pediatric clinician, an inability to reach the receiving clinician, and/or time limitations. Many of these barriers can be alleviated by early discussions of transitions of care as well as utilization of structured documentation tools as noted above.
It is also recommended that the pediatric clinician follows up with the patient and/or caregiver several months after the transfer is complete. This allows for the adolescent and/or the caregiver to reflect on the transition process and provide feedback to the pediatric clinicians and their practice for ongoing process improvement.
Reflection as a pediatrician
Ideally, all transition steps occur for the adolescent; in our opinion, a crucial component is to prepare the adolescent patient for the change from a pediatric to adult model of care, in which they are independent in their health communication and decision-making. By engaging adolescents to understand their health, how to maintain it, and when to seek care, we empower them to advocate for their own health as young adults. With appropriate health knowledge and literacy, adolescents are more likely to actively engage with their health care providers and make healthy lifestyle choices. So though saying goodbye may still be difficult, it can be done with the confidence that the patients will continue to get the care they need as they transition into adulthood.
Dr. Kim is assistant clinical professor, department of pediatrics, University of California, San Diego. Dr. Mennito is associate professor of pediatrics and internal medicine, Medical University of South Carolina, Charleston, S.C. Dr. Kim and Dr. Mennito have disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
However, many clinicians feel insufficiently prepared to provide comprehensive transition services. This can result in the actual handoff or transfer into adult care being abrupt, incomplete, or outright unsuccessful. By following the recommended best practices of transitions, providers of pediatric care can ensure that this challenging goodbye prepares everyone for the next steps ahead.
Using a structured transition process
In 2011, a health care transition clinical report based on expert opinion and practice consensus and endorsed by the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians – Society of Internal Medicine was released. This report provided a decision-making algorithm for “practice-based implementation of transition for all youth beginning in early adolescence.”
The Got Transition organization, funded by the Maternal Child Health Bureau and Health Resources and Services Administration, provides web-based information and materials for health care providers and families to establish a smooth and successful transition. At the center of these recommendations are the Six Core Elements of Health Care Transition – the essential components of a structured transition process: 1) transition policy/guide; 2) tracking and monitoring; 3) readiness; 4) planning; 5) transfer of care, and 6) transition completion.
This transition process should start early in adolescence, preferably by age 12-14 years, to give adequate time to progress successfully through these elements and improve the likelihood of a smooth, final transfer into the care of an adult clinician.
Preparing your patients for transfer
Despite the availability of these recommendations, national surveys show that the overwhelming majority of adolescents with and without special health care needs report not receiving transition services. Lack of time, resources, interest, and patients being lost to care during adolescence all contribute to this deficit in care. Without transition preparation, the actual handoff or transfer to adult care can be difficult for adolescents, caregivers, and clinicians alike. Adolescents and caregivers may feel a sense of abandonment or have inadequate health knowledge/literacy, pediatric clinicians may fear that the patient is not ready for the expected independence, and adult clinicians face numerous challenges integrating these young patients into their practice.
A structured transition process can help the family and clinicians know what to expect during the transfer of care. Pediatric clinicians can gradually move from a pediatric model of care, in which the caregiver is the center of communication, to an adult model, putting the patient at the center. By encouraging the adolescent to be the direct communicator, the pediatric clinician can promote independence and assess health knowledge, allowing for education where gaps exist.
Assisting the patient in identifying and even meeting the adult clinician well ahead of the final transfer date can also make the process less daunting for the adolescent.
Adult clinicians should consider allowing more time for the first visit with a new young adult patient and welcome caregiver input early in the transfer process, particularly for patients with a chronic disease. By engaging patients and families in an intentional, gradual transition process with an expected outcome, all those involved will be more prepared for the final handoff.
Utilizing transition tools and engaging the adolescent
Numerous tools can assist in the preparation for transfer to adult care. These include transition summaries and emergency plans, which contain essential information such as current medical problems, allergies, medications, prior procedures and treatments, and sick day plans. Such tools can also be built into electronic medical records for easy modification and updating. They can be used as methods to engage and teach adolescents about their disease history and current regimen and can contain essential components for information handoff at the time of transfer to adult care. If the patient carries a rare diagnosis, or one that has historically been associated with lower survival to adulthood, these transfer documents can also include summary information about disease states and contact information for pediatric specialty clinicians.
Adolescent engagement in their health care during the time of transition can also be prompted through the use of patient portals within an electronic health record. Such portals put health information directly at the adolescent’s fingertips, provide them with an outlet for communication with their clinicians, and give reminders regarding health maintenance.
Completing the transfer: The final handoff
The best and most recommended means of relaying information at the time of transfer to adult care is a direct, verbal handoff between clinicians. This direct handoff has several goals:
(1) To ensure the patient has scheduled or attended the first appointment with the adult clinician
(2) To ensure record transfer has occurred successfully
(3) To answer any questions the receiving clinician may have about prior or ongoing care.
(4) To offer the adult clinician ongoing access to the pediatric clinician as an “expert” resource for additional questions.
By remaining available as a resource, the pediatric clinician can alleviate concerns for both the patient and caregiver as well as the receiving adult clinician.
As valuable as verbal handoffs can be, they are not always possible due to patients not having selected an adult clinician prior to leaving the pediatric clinician, an inability to reach the receiving clinician, and/or time limitations. Many of these barriers can be alleviated by early discussions of transitions of care as well as utilization of structured documentation tools as noted above.
It is also recommended that the pediatric clinician follows up with the patient and/or caregiver several months after the transfer is complete. This allows for the adolescent and/or the caregiver to reflect on the transition process and provide feedback to the pediatric clinicians and their practice for ongoing process improvement.
Reflection as a pediatrician
Ideally, all transition steps occur for the adolescent; in our opinion, a crucial component is to prepare the adolescent patient for the change from a pediatric to adult model of care, in which they are independent in their health communication and decision-making. By engaging adolescents to understand their health, how to maintain it, and when to seek care, we empower them to advocate for their own health as young adults. With appropriate health knowledge and literacy, adolescents are more likely to actively engage with their health care providers and make healthy lifestyle choices. So though saying goodbye may still be difficult, it can be done with the confidence that the patients will continue to get the care they need as they transition into adulthood.
Dr. Kim is assistant clinical professor, department of pediatrics, University of California, San Diego. Dr. Mennito is associate professor of pediatrics and internal medicine, Medical University of South Carolina, Charleston, S.C. Dr. Kim and Dr. Mennito have disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
However, many clinicians feel insufficiently prepared to provide comprehensive transition services. This can result in the actual handoff or transfer into adult care being abrupt, incomplete, or outright unsuccessful. By following the recommended best practices of transitions, providers of pediatric care can ensure that this challenging goodbye prepares everyone for the next steps ahead.
Using a structured transition process
In 2011, a health care transition clinical report based on expert opinion and practice consensus and endorsed by the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians – Society of Internal Medicine was released. This report provided a decision-making algorithm for “practice-based implementation of transition for all youth beginning in early adolescence.”
The Got Transition organization, funded by the Maternal Child Health Bureau and Health Resources and Services Administration, provides web-based information and materials for health care providers and families to establish a smooth and successful transition. At the center of these recommendations are the Six Core Elements of Health Care Transition – the essential components of a structured transition process: 1) transition policy/guide; 2) tracking and monitoring; 3) readiness; 4) planning; 5) transfer of care, and 6) transition completion.
This transition process should start early in adolescence, preferably by age 12-14 years, to give adequate time to progress successfully through these elements and improve the likelihood of a smooth, final transfer into the care of an adult clinician.
Preparing your patients for transfer
Despite the availability of these recommendations, national surveys show that the overwhelming majority of adolescents with and without special health care needs report not receiving transition services. Lack of time, resources, interest, and patients being lost to care during adolescence all contribute to this deficit in care. Without transition preparation, the actual handoff or transfer to adult care can be difficult for adolescents, caregivers, and clinicians alike. Adolescents and caregivers may feel a sense of abandonment or have inadequate health knowledge/literacy, pediatric clinicians may fear that the patient is not ready for the expected independence, and adult clinicians face numerous challenges integrating these young patients into their practice.
A structured transition process can help the family and clinicians know what to expect during the transfer of care. Pediatric clinicians can gradually move from a pediatric model of care, in which the caregiver is the center of communication, to an adult model, putting the patient at the center. By encouraging the adolescent to be the direct communicator, the pediatric clinician can promote independence and assess health knowledge, allowing for education where gaps exist.
Assisting the patient in identifying and even meeting the adult clinician well ahead of the final transfer date can also make the process less daunting for the adolescent.
Adult clinicians should consider allowing more time for the first visit with a new young adult patient and welcome caregiver input early in the transfer process, particularly for patients with a chronic disease. By engaging patients and families in an intentional, gradual transition process with an expected outcome, all those involved will be more prepared for the final handoff.
Utilizing transition tools and engaging the adolescent
Numerous tools can assist in the preparation for transfer to adult care. These include transition summaries and emergency plans, which contain essential information such as current medical problems, allergies, medications, prior procedures and treatments, and sick day plans. Such tools can also be built into electronic medical records for easy modification and updating. They can be used as methods to engage and teach adolescents about their disease history and current regimen and can contain essential components for information handoff at the time of transfer to adult care. If the patient carries a rare diagnosis, or one that has historically been associated with lower survival to adulthood, these transfer documents can also include summary information about disease states and contact information for pediatric specialty clinicians.
Adolescent engagement in their health care during the time of transition can also be prompted through the use of patient portals within an electronic health record. Such portals put health information directly at the adolescent’s fingertips, provide them with an outlet for communication with their clinicians, and give reminders regarding health maintenance.
Completing the transfer: The final handoff
The best and most recommended means of relaying information at the time of transfer to adult care is a direct, verbal handoff between clinicians. This direct handoff has several goals:
(1) To ensure the patient has scheduled or attended the first appointment with the adult clinician
(2) To ensure record transfer has occurred successfully
(3) To answer any questions the receiving clinician may have about prior or ongoing care.
(4) To offer the adult clinician ongoing access to the pediatric clinician as an “expert” resource for additional questions.
By remaining available as a resource, the pediatric clinician can alleviate concerns for both the patient and caregiver as well as the receiving adult clinician.
As valuable as verbal handoffs can be, they are not always possible due to patients not having selected an adult clinician prior to leaving the pediatric clinician, an inability to reach the receiving clinician, and/or time limitations. Many of these barriers can be alleviated by early discussions of transitions of care as well as utilization of structured documentation tools as noted above.
It is also recommended that the pediatric clinician follows up with the patient and/or caregiver several months after the transfer is complete. This allows for the adolescent and/or the caregiver to reflect on the transition process and provide feedback to the pediatric clinicians and their practice for ongoing process improvement.
Reflection as a pediatrician
Ideally, all transition steps occur for the adolescent; in our opinion, a crucial component is to prepare the adolescent patient for the change from a pediatric to adult model of care, in which they are independent in their health communication and decision-making. By engaging adolescents to understand their health, how to maintain it, and when to seek care, we empower them to advocate for their own health as young adults. With appropriate health knowledge and literacy, adolescents are more likely to actively engage with their health care providers and make healthy lifestyle choices. So though saying goodbye may still be difficult, it can be done with the confidence that the patients will continue to get the care they need as they transition into adulthood.
Dr. Kim is assistant clinical professor, department of pediatrics, University of California, San Diego. Dr. Mennito is associate professor of pediatrics and internal medicine, Medical University of South Carolina, Charleston, S.C. Dr. Kim and Dr. Mennito have disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
Physicians don’t feel safe with some patients: Here’s how to reduce the danger
“I talked to him about whether he was okay seeing me and he said yes,” Dr. Cheng said. “But I remained vigilant and conscious of what the patient was doing the whole time so he couldn’t take advantage of the situation.”
Dr. Cheng never turned his back to the patient and even backed out of the exam room. That encounter passed without incident. However, a urologist Dr. Cheng knew from residency wasn’t so fortunate. Ronald Gilbert, MD, of Newport Beach, Calif., was shot and killed by a patient in his office. The patient blamed him for complications following prostate surgery 25 years earlier.
In 2022, a gunman in Tulsa, Okla., blamed his physician for pain from a recent back surgery and shot and killed him, another physician, and two others in a medical building before taking his own life.
Nearly 9 in 10 physicians reported in a recent Medscape poll that they had experienced one or more violent or potentially violent incidents in the past year. The most common patient behaviors were verbal abuse, getting angry and leaving, and behaving erratically.
About one in three respondents said that the patients threatened to harm them, and about one in five said that the patients became violent.
Experts say that many factors contribute to this potentially lethal situation: Health care services have become more impersonal, patients experience longer wait times, some abuse prescription drugs, mental health services are lacking, and security is poor or nonexistent at some health care facilities.
Violence against hospital workers has become so common that a bill was introduced in 2022 in Congress to better protect them. The Safety From Violence for Healthcare Employees Act includes stiffer penalties for acts involving the use of a dangerous weapon or committed during a public emergency and would also provide $25 million in grants to hospitals for programs aimed at reducing violent incidents in health care settings, including de-escalation training. The American Hospital Association and American College of Emergency Physicians support the bill, which is now before the House Judiciary Subcommittee on Crime, Terrorism, and Homeland Security.
The worst day of their lives
“You have people who already are having the worst day of their lives and feeling on edge. If they already have a short fuse or substance abuse issues, that can translate into agitation, violence, or aggression,” said Scott Zeller, MD, vice president of acute psychiatry at Vituity, a physician-owned multispecialty group that operates in several states.
Health care workers in psychiatric and substance abuse hospitals were 10 times more likely to experience nonfatal injuries by others in 2018 than were health care workers in ambulatory settings, according to an April 2020 Bureau of Labor Statistics report. In addition, health care workers were five times more likely to suffer a workplace violence injury than were workers overall in 2018.
Psychiatrists who responded to the poll were the specialists most likely to report that they encountered violent patients and potentially violent patients. “Historically, inpatient psychiatry, which requires more acute care and monitoring, is considered the most dangerous profession outside of the police,” said Dr. Zeller.
Emergency physicians have reported an uptick in violence from patients; 85% said in a survey by ACEP in 2022 that they believed the rate of violence in emergency departments has increased over the past 5 years, whereas 45% indicated that it has greatly increased.
Some doctors have been threatened with violence or actually killed by family members. Alex Skog, MD, president-elect of ACEP’s Oregon chapter, told HealthCare Dive that “a patient’s family member with a gun holster on his hip threatened to kill me and kill my entire family after I told his father that he needed to be admitted because he had coronavirus.”
“I’ve been scared for my safety as well as the safety of my family,” Dr. Skog said. “That was just not something that we were seeing 3, 4, or 5 years ago.”
Many patients are already upset by the time they see doctors, according to the poll.
“The most common reason patients are upset is that they’re already in a lot of pain, which can be expressed as anger, hostility, or aggression. They’re very anxious and afraid of what’s happening and may be thinking about the worst-case scenario – that a bump or lump is cancer,” Dr. Zeller said.
Patients may also get upset if they disagree with their doctors’ diagnosis or treatment plan or the doctor refuses to prescribe them the drugs or tests they want.
“One doctor commented recently: ‘After over 30 years in this business, I can say patients are worse now than at any point in my career. Entitled, demanding, obnoxious. Any denial is met with outrage and indignity, whether it’s an opioid request or a demand for MRI of something because they ‘want to know.’ ”
An orthopedic surgeon in Indiana lost his life after he refused to prescribe opioids to a patient. Her angry husband shot and killed the doctor in the parking lot only 2 hours after confronting him in his office.
Decreased physician-patient trust
“When doctors experience something frightening, they become more apprehensive in the future. There’s no doubt that after the first violent experience, they think of things differently,” said Dr. Zeller.
More than half of the doctors who reported experiencing at least one violent or potentially violent incident in the poll said they trusted patients less.
This diminished trust can negatively impact the physician-patient relationship, said the authors of a recent Health Affairs article.
“The more patients harm their health care providers, intentionally or unintentionally, the more difficult it will be for those providers to trust them, leading to yet another unfortunate pattern: physicians pulling back on some of the behaviors thought to be most trust-building, for example, talking about their personal lives, building rapport, displaying compassion, or giving out their personal cell phone numbers,” the article stated.
What doctors can do
Most doctors who experienced a violent or potentially violent incident said they had tried to defuse the situation and that they succeeded at least some of the time, the poll results show.
One of the best ways to defuse a situation is to be empathetic and show the person that you’re on their side and not the enemy, said Dr. Cheng,.
“Rather than making general statements like ‘I understand that you’re upset,’ it’s better to be specific about the reason the person is upset. For example: ‘I understand that you’re upset that the pharmacy didn’t fill your prescription’ or ‘I understand how you’re feeling about Doctor So-and-so, who didn’t treat you right,’ ” Dr. Cheng stated.
Dr. Zeller urged physicians to talk to patients about why they’re upset and how they can help them. That approach worked with a patient who was having a psychotic episode.
“I told the staff, who wanted to forcibly restrain him and inject him with medication, that I would talk to him. I asked the patient, who was screaming ‘ya ya ya ya,’ whether he would take his medication if I gave it to him and he said yes. When he was calm, he explained that he was screaming to stop the voices telling him to kill his parents. He then got the help he needed,” said Dr. Zeller.
Dr. Cheng was trained in de-escalation techniques as an Orange County reserve deputy sheriff. He and Dr. Zeller recommended that physicians and staff receive training in how to spot potentially violent behavior and defuse these situations before they escalate.
Dr. Cheng suggests looking at the person’s body language for signs of increasing agitation or tension, such as clenched fists, tense posture, tight jaw, or fidgeting that may be accompanied by shouting and/or verbal abuse.
Physicians also need to consider where they are physically in relation to patients they see. “You don’t want to be too close to the patient or stand in front of them, which can be seen as confrontational. Instead, stand or sit off to the side, and never block the door if the patient’s upset,” said Dr. Cheng.
He recommended that physician practices prepare for violent incidents by developing detailed plans, including how and when to escape, how to protect patients, and how to cooperate with law enforcement.
“If a violent incident is inescapable, physicians and staff must be ready to fight back with whatever tools they have available, which may include fire extinguishers, chairs, or scalpels,” said Dr. Cheng.
A version of this article originally appeared on Medscape.com.
“I talked to him about whether he was okay seeing me and he said yes,” Dr. Cheng said. “But I remained vigilant and conscious of what the patient was doing the whole time so he couldn’t take advantage of the situation.”
Dr. Cheng never turned his back to the patient and even backed out of the exam room. That encounter passed without incident. However, a urologist Dr. Cheng knew from residency wasn’t so fortunate. Ronald Gilbert, MD, of Newport Beach, Calif., was shot and killed by a patient in his office. The patient blamed him for complications following prostate surgery 25 years earlier.
In 2022, a gunman in Tulsa, Okla., blamed his physician for pain from a recent back surgery and shot and killed him, another physician, and two others in a medical building before taking his own life.
Nearly 9 in 10 physicians reported in a recent Medscape poll that they had experienced one or more violent or potentially violent incidents in the past year. The most common patient behaviors were verbal abuse, getting angry and leaving, and behaving erratically.
About one in three respondents said that the patients threatened to harm them, and about one in five said that the patients became violent.
Experts say that many factors contribute to this potentially lethal situation: Health care services have become more impersonal, patients experience longer wait times, some abuse prescription drugs, mental health services are lacking, and security is poor or nonexistent at some health care facilities.
Violence against hospital workers has become so common that a bill was introduced in 2022 in Congress to better protect them. The Safety From Violence for Healthcare Employees Act includes stiffer penalties for acts involving the use of a dangerous weapon or committed during a public emergency and would also provide $25 million in grants to hospitals for programs aimed at reducing violent incidents in health care settings, including de-escalation training. The American Hospital Association and American College of Emergency Physicians support the bill, which is now before the House Judiciary Subcommittee on Crime, Terrorism, and Homeland Security.
The worst day of their lives
“You have people who already are having the worst day of their lives and feeling on edge. If they already have a short fuse or substance abuse issues, that can translate into agitation, violence, or aggression,” said Scott Zeller, MD, vice president of acute psychiatry at Vituity, a physician-owned multispecialty group that operates in several states.
Health care workers in psychiatric and substance abuse hospitals were 10 times more likely to experience nonfatal injuries by others in 2018 than were health care workers in ambulatory settings, according to an April 2020 Bureau of Labor Statistics report. In addition, health care workers were five times more likely to suffer a workplace violence injury than were workers overall in 2018.
Psychiatrists who responded to the poll were the specialists most likely to report that they encountered violent patients and potentially violent patients. “Historically, inpatient psychiatry, which requires more acute care and monitoring, is considered the most dangerous profession outside of the police,” said Dr. Zeller.
Emergency physicians have reported an uptick in violence from patients; 85% said in a survey by ACEP in 2022 that they believed the rate of violence in emergency departments has increased over the past 5 years, whereas 45% indicated that it has greatly increased.
Some doctors have been threatened with violence or actually killed by family members. Alex Skog, MD, president-elect of ACEP’s Oregon chapter, told HealthCare Dive that “a patient’s family member with a gun holster on his hip threatened to kill me and kill my entire family after I told his father that he needed to be admitted because he had coronavirus.”
“I’ve been scared for my safety as well as the safety of my family,” Dr. Skog said. “That was just not something that we were seeing 3, 4, or 5 years ago.”
Many patients are already upset by the time they see doctors, according to the poll.
“The most common reason patients are upset is that they’re already in a lot of pain, which can be expressed as anger, hostility, or aggression. They’re very anxious and afraid of what’s happening and may be thinking about the worst-case scenario – that a bump or lump is cancer,” Dr. Zeller said.
Patients may also get upset if they disagree with their doctors’ diagnosis or treatment plan or the doctor refuses to prescribe them the drugs or tests they want.
“One doctor commented recently: ‘After over 30 years in this business, I can say patients are worse now than at any point in my career. Entitled, demanding, obnoxious. Any denial is met with outrage and indignity, whether it’s an opioid request or a demand for MRI of something because they ‘want to know.’ ”
An orthopedic surgeon in Indiana lost his life after he refused to prescribe opioids to a patient. Her angry husband shot and killed the doctor in the parking lot only 2 hours after confronting him in his office.
Decreased physician-patient trust
“When doctors experience something frightening, they become more apprehensive in the future. There’s no doubt that after the first violent experience, they think of things differently,” said Dr. Zeller.
More than half of the doctors who reported experiencing at least one violent or potentially violent incident in the poll said they trusted patients less.
This diminished trust can negatively impact the physician-patient relationship, said the authors of a recent Health Affairs article.
“The more patients harm their health care providers, intentionally or unintentionally, the more difficult it will be for those providers to trust them, leading to yet another unfortunate pattern: physicians pulling back on some of the behaviors thought to be most trust-building, for example, talking about their personal lives, building rapport, displaying compassion, or giving out their personal cell phone numbers,” the article stated.
What doctors can do
Most doctors who experienced a violent or potentially violent incident said they had tried to defuse the situation and that they succeeded at least some of the time, the poll results show.
One of the best ways to defuse a situation is to be empathetic and show the person that you’re on their side and not the enemy, said Dr. Cheng,.
“Rather than making general statements like ‘I understand that you’re upset,’ it’s better to be specific about the reason the person is upset. For example: ‘I understand that you’re upset that the pharmacy didn’t fill your prescription’ or ‘I understand how you’re feeling about Doctor So-and-so, who didn’t treat you right,’ ” Dr. Cheng stated.
Dr. Zeller urged physicians to talk to patients about why they’re upset and how they can help them. That approach worked with a patient who was having a psychotic episode.
“I told the staff, who wanted to forcibly restrain him and inject him with medication, that I would talk to him. I asked the patient, who was screaming ‘ya ya ya ya,’ whether he would take his medication if I gave it to him and he said yes. When he was calm, he explained that he was screaming to stop the voices telling him to kill his parents. He then got the help he needed,” said Dr. Zeller.
Dr. Cheng was trained in de-escalation techniques as an Orange County reserve deputy sheriff. He and Dr. Zeller recommended that physicians and staff receive training in how to spot potentially violent behavior and defuse these situations before they escalate.
Dr. Cheng suggests looking at the person’s body language for signs of increasing agitation or tension, such as clenched fists, tense posture, tight jaw, or fidgeting that may be accompanied by shouting and/or verbal abuse.
Physicians also need to consider where they are physically in relation to patients they see. “You don’t want to be too close to the patient or stand in front of them, which can be seen as confrontational. Instead, stand or sit off to the side, and never block the door if the patient’s upset,” said Dr. Cheng.
He recommended that physician practices prepare for violent incidents by developing detailed plans, including how and when to escape, how to protect patients, and how to cooperate with law enforcement.
“If a violent incident is inescapable, physicians and staff must be ready to fight back with whatever tools they have available, which may include fire extinguishers, chairs, or scalpels,” said Dr. Cheng.
A version of this article originally appeared on Medscape.com.
“I talked to him about whether he was okay seeing me and he said yes,” Dr. Cheng said. “But I remained vigilant and conscious of what the patient was doing the whole time so he couldn’t take advantage of the situation.”
Dr. Cheng never turned his back to the patient and even backed out of the exam room. That encounter passed without incident. However, a urologist Dr. Cheng knew from residency wasn’t so fortunate. Ronald Gilbert, MD, of Newport Beach, Calif., was shot and killed by a patient in his office. The patient blamed him for complications following prostate surgery 25 years earlier.
In 2022, a gunman in Tulsa, Okla., blamed his physician for pain from a recent back surgery and shot and killed him, another physician, and two others in a medical building before taking his own life.
Nearly 9 in 10 physicians reported in a recent Medscape poll that they had experienced one or more violent or potentially violent incidents in the past year. The most common patient behaviors were verbal abuse, getting angry and leaving, and behaving erratically.
About one in three respondents said that the patients threatened to harm them, and about one in five said that the patients became violent.
Experts say that many factors contribute to this potentially lethal situation: Health care services have become more impersonal, patients experience longer wait times, some abuse prescription drugs, mental health services are lacking, and security is poor or nonexistent at some health care facilities.
Violence against hospital workers has become so common that a bill was introduced in 2022 in Congress to better protect them. The Safety From Violence for Healthcare Employees Act includes stiffer penalties for acts involving the use of a dangerous weapon or committed during a public emergency and would also provide $25 million in grants to hospitals for programs aimed at reducing violent incidents in health care settings, including de-escalation training. The American Hospital Association and American College of Emergency Physicians support the bill, which is now before the House Judiciary Subcommittee on Crime, Terrorism, and Homeland Security.
The worst day of their lives
“You have people who already are having the worst day of their lives and feeling on edge. If they already have a short fuse or substance abuse issues, that can translate into agitation, violence, or aggression,” said Scott Zeller, MD, vice president of acute psychiatry at Vituity, a physician-owned multispecialty group that operates in several states.
Health care workers in psychiatric and substance abuse hospitals were 10 times more likely to experience nonfatal injuries by others in 2018 than were health care workers in ambulatory settings, according to an April 2020 Bureau of Labor Statistics report. In addition, health care workers were five times more likely to suffer a workplace violence injury than were workers overall in 2018.
Psychiatrists who responded to the poll were the specialists most likely to report that they encountered violent patients and potentially violent patients. “Historically, inpatient psychiatry, which requires more acute care and monitoring, is considered the most dangerous profession outside of the police,” said Dr. Zeller.
Emergency physicians have reported an uptick in violence from patients; 85% said in a survey by ACEP in 2022 that they believed the rate of violence in emergency departments has increased over the past 5 years, whereas 45% indicated that it has greatly increased.
Some doctors have been threatened with violence or actually killed by family members. Alex Skog, MD, president-elect of ACEP’s Oregon chapter, told HealthCare Dive that “a patient’s family member with a gun holster on his hip threatened to kill me and kill my entire family after I told his father that he needed to be admitted because he had coronavirus.”
“I’ve been scared for my safety as well as the safety of my family,” Dr. Skog said. “That was just not something that we were seeing 3, 4, or 5 years ago.”
Many patients are already upset by the time they see doctors, according to the poll.
“The most common reason patients are upset is that they’re already in a lot of pain, which can be expressed as anger, hostility, or aggression. They’re very anxious and afraid of what’s happening and may be thinking about the worst-case scenario – that a bump or lump is cancer,” Dr. Zeller said.
Patients may also get upset if they disagree with their doctors’ diagnosis or treatment plan or the doctor refuses to prescribe them the drugs or tests they want.
“One doctor commented recently: ‘After over 30 years in this business, I can say patients are worse now than at any point in my career. Entitled, demanding, obnoxious. Any denial is met with outrage and indignity, whether it’s an opioid request or a demand for MRI of something because they ‘want to know.’ ”
An orthopedic surgeon in Indiana lost his life after he refused to prescribe opioids to a patient. Her angry husband shot and killed the doctor in the parking lot only 2 hours after confronting him in his office.
Decreased physician-patient trust
“When doctors experience something frightening, they become more apprehensive in the future. There’s no doubt that after the first violent experience, they think of things differently,” said Dr. Zeller.
More than half of the doctors who reported experiencing at least one violent or potentially violent incident in the poll said they trusted patients less.
This diminished trust can negatively impact the physician-patient relationship, said the authors of a recent Health Affairs article.
“The more patients harm their health care providers, intentionally or unintentionally, the more difficult it will be for those providers to trust them, leading to yet another unfortunate pattern: physicians pulling back on some of the behaviors thought to be most trust-building, for example, talking about their personal lives, building rapport, displaying compassion, or giving out their personal cell phone numbers,” the article stated.
What doctors can do
Most doctors who experienced a violent or potentially violent incident said they had tried to defuse the situation and that they succeeded at least some of the time, the poll results show.
One of the best ways to defuse a situation is to be empathetic and show the person that you’re on their side and not the enemy, said Dr. Cheng,.
“Rather than making general statements like ‘I understand that you’re upset,’ it’s better to be specific about the reason the person is upset. For example: ‘I understand that you’re upset that the pharmacy didn’t fill your prescription’ or ‘I understand how you’re feeling about Doctor So-and-so, who didn’t treat you right,’ ” Dr. Cheng stated.
Dr. Zeller urged physicians to talk to patients about why they’re upset and how they can help them. That approach worked with a patient who was having a psychotic episode.
“I told the staff, who wanted to forcibly restrain him and inject him with medication, that I would talk to him. I asked the patient, who was screaming ‘ya ya ya ya,’ whether he would take his medication if I gave it to him and he said yes. When he was calm, he explained that he was screaming to stop the voices telling him to kill his parents. He then got the help he needed,” said Dr. Zeller.
Dr. Cheng was trained in de-escalation techniques as an Orange County reserve deputy sheriff. He and Dr. Zeller recommended that physicians and staff receive training in how to spot potentially violent behavior and defuse these situations before they escalate.
Dr. Cheng suggests looking at the person’s body language for signs of increasing agitation or tension, such as clenched fists, tense posture, tight jaw, or fidgeting that may be accompanied by shouting and/or verbal abuse.
Physicians also need to consider where they are physically in relation to patients they see. “You don’t want to be too close to the patient or stand in front of them, which can be seen as confrontational. Instead, stand or sit off to the side, and never block the door if the patient’s upset,” said Dr. Cheng.
He recommended that physician practices prepare for violent incidents by developing detailed plans, including how and when to escape, how to protect patients, and how to cooperate with law enforcement.
“If a violent incident is inescapable, physicians and staff must be ready to fight back with whatever tools they have available, which may include fire extinguishers, chairs, or scalpels,” said Dr. Cheng.
A version of this article originally appeared on Medscape.com.
Don’t keep your patients waiting
Recently, the results of a survey of consumers regarding their health care experiences were reported by Carta Healthcare. As you might expect, I’ve written about punctuality before, but this is such a ubiquitous problem that it bears repeating. Here are some suggestions:
Start on time. That seems obvious, but I’m always amazed at the number of doctors who admit to running late who also admit that they start late. If you’re in the hole before you even start, you can seldom dig yourself out. Sometimes an on-time start is the solution to the entire problem! If you doubt me, try it.
Book realistically. Everyone works at a different pace. Determine the number of patients you can comfortably see in an hour, and book only that number. If you want to see more patients, the solution is working longer hours or hiring physicians or physician extenders (or both), not overloading your schedule.
Time-stamp each chart. Pay attention to patient arrival times if your EHR records them, and step up your pace if you start to fall behind. If your EHR does not record arrival times or you are still using paper records, buy a time clock and have your receptionist time-stamp the “encounter form” that goes to the back with the patient. One glance at the stamp will tell you exactly how long that patient has been waiting.
Schedule all surgeries. If you haven’t scheduled the time necessary for a surgical procedure, don’t do it. It’s frequently tempting to “squeeze in” an excision, often because you feel guilty that the patient has already had to wait for you. But every unscheduled surgery puts you that much further behind. And hurrying through a procedure increases the risk of mistakes. Tell the patient that surgery requires extra time and it can’t be rushed, so you will have to schedule that time.
Work-ins come last, not first. Patients with urgent problems should be seen after scheduled patients. That may seem counterintuitive; receptionists often assume it’s better to squeeze them in early, while you’re still running on time. But doing that guarantees you will run late, and it isn’t fair to patients who have appointments and expect to be seen promptly.
Work-ins, on the other hand, expect a wait because they have no appointment. We tell them, “Our schedule is full today; but if you come at the end of hours, the doctor will see you. But you may have a wait.” Far from complaining, they invariably thank us for seeing them.
Seize the list. You know the list I mean. “Number 16: My right big toe itches. Number 17: I think I feel something on my back. Number 18: This weird chartreuse thing on my arm ...” One long list can leave an entire half-day schedule in shambles.
When a list is produced, the best option is to take it and read it yourself. Identify the most important two or three problems, and address them. For the rest, I will say, “This group of problems deserves a visit of its own, and we will schedule that visit.”
Ask if you can place the list (or a photocopy) in the patient’s chart. (It is, after all, important clinical information.) All of these problems are important to the patient and should be addressed – but on your schedule, not the patient’s.
Avoid interruptions. Especially phone calls. Unless it’s an emergency or an immediate family member, my receptionists say, “I’m sorry, the doctor is with patients. May I take a message?” Everyone – even other physicians – understands. But be sure to return those calls promptly.
Pharmaceutical reps should not be allowed to interrupt you, either. Have them make an appointment, just like everybody else.
There will be times, of course, when you run late. But these should be the exception rather than the rule. By streamlining your procedures and avoiding the pitfalls mentioned, you can give nearly every patient all the time he or she deserves without keeping the next patient waiting.
Incidentally, other common patient complaints in that survey were the following:
- Couldn’t schedule an appointment within a week.
- Spent too little time with me.
- Didn’t provide test results promptly.
- Didn’t respond to my phone calls promptly.
Now would be an excellent opportunity to identify and address any of those problems as well.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently, the results of a survey of consumers regarding their health care experiences were reported by Carta Healthcare. As you might expect, I’ve written about punctuality before, but this is such a ubiquitous problem that it bears repeating. Here are some suggestions:
Start on time. That seems obvious, but I’m always amazed at the number of doctors who admit to running late who also admit that they start late. If you’re in the hole before you even start, you can seldom dig yourself out. Sometimes an on-time start is the solution to the entire problem! If you doubt me, try it.
Book realistically. Everyone works at a different pace. Determine the number of patients you can comfortably see in an hour, and book only that number. If you want to see more patients, the solution is working longer hours or hiring physicians or physician extenders (or both), not overloading your schedule.
Time-stamp each chart. Pay attention to patient arrival times if your EHR records them, and step up your pace if you start to fall behind. If your EHR does not record arrival times or you are still using paper records, buy a time clock and have your receptionist time-stamp the “encounter form” that goes to the back with the patient. One glance at the stamp will tell you exactly how long that patient has been waiting.
Schedule all surgeries. If you haven’t scheduled the time necessary for a surgical procedure, don’t do it. It’s frequently tempting to “squeeze in” an excision, often because you feel guilty that the patient has already had to wait for you. But every unscheduled surgery puts you that much further behind. And hurrying through a procedure increases the risk of mistakes. Tell the patient that surgery requires extra time and it can’t be rushed, so you will have to schedule that time.
Work-ins come last, not first. Patients with urgent problems should be seen after scheduled patients. That may seem counterintuitive; receptionists often assume it’s better to squeeze them in early, while you’re still running on time. But doing that guarantees you will run late, and it isn’t fair to patients who have appointments and expect to be seen promptly.
Work-ins, on the other hand, expect a wait because they have no appointment. We tell them, “Our schedule is full today; but if you come at the end of hours, the doctor will see you. But you may have a wait.” Far from complaining, they invariably thank us for seeing them.
Seize the list. You know the list I mean. “Number 16: My right big toe itches. Number 17: I think I feel something on my back. Number 18: This weird chartreuse thing on my arm ...” One long list can leave an entire half-day schedule in shambles.
When a list is produced, the best option is to take it and read it yourself. Identify the most important two or three problems, and address them. For the rest, I will say, “This group of problems deserves a visit of its own, and we will schedule that visit.”
Ask if you can place the list (or a photocopy) in the patient’s chart. (It is, after all, important clinical information.) All of these problems are important to the patient and should be addressed – but on your schedule, not the patient’s.
Avoid interruptions. Especially phone calls. Unless it’s an emergency or an immediate family member, my receptionists say, “I’m sorry, the doctor is with patients. May I take a message?” Everyone – even other physicians – understands. But be sure to return those calls promptly.
Pharmaceutical reps should not be allowed to interrupt you, either. Have them make an appointment, just like everybody else.
There will be times, of course, when you run late. But these should be the exception rather than the rule. By streamlining your procedures and avoiding the pitfalls mentioned, you can give nearly every patient all the time he or she deserves without keeping the next patient waiting.
Incidentally, other common patient complaints in that survey were the following:
- Couldn’t schedule an appointment within a week.
- Spent too little time with me.
- Didn’t provide test results promptly.
- Didn’t respond to my phone calls promptly.
Now would be an excellent opportunity to identify and address any of those problems as well.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently, the results of a survey of consumers regarding their health care experiences were reported by Carta Healthcare. As you might expect, I’ve written about punctuality before, but this is such a ubiquitous problem that it bears repeating. Here are some suggestions:
Start on time. That seems obvious, but I’m always amazed at the number of doctors who admit to running late who also admit that they start late. If you’re in the hole before you even start, you can seldom dig yourself out. Sometimes an on-time start is the solution to the entire problem! If you doubt me, try it.
Book realistically. Everyone works at a different pace. Determine the number of patients you can comfortably see in an hour, and book only that number. If you want to see more patients, the solution is working longer hours or hiring physicians or physician extenders (or both), not overloading your schedule.
Time-stamp each chart. Pay attention to patient arrival times if your EHR records them, and step up your pace if you start to fall behind. If your EHR does not record arrival times or you are still using paper records, buy a time clock and have your receptionist time-stamp the “encounter form” that goes to the back with the patient. One glance at the stamp will tell you exactly how long that patient has been waiting.
Schedule all surgeries. If you haven’t scheduled the time necessary for a surgical procedure, don’t do it. It’s frequently tempting to “squeeze in” an excision, often because you feel guilty that the patient has already had to wait for you. But every unscheduled surgery puts you that much further behind. And hurrying through a procedure increases the risk of mistakes. Tell the patient that surgery requires extra time and it can’t be rushed, so you will have to schedule that time.
Work-ins come last, not first. Patients with urgent problems should be seen after scheduled patients. That may seem counterintuitive; receptionists often assume it’s better to squeeze them in early, while you’re still running on time. But doing that guarantees you will run late, and it isn’t fair to patients who have appointments and expect to be seen promptly.
Work-ins, on the other hand, expect a wait because they have no appointment. We tell them, “Our schedule is full today; but if you come at the end of hours, the doctor will see you. But you may have a wait.” Far from complaining, they invariably thank us for seeing them.
Seize the list. You know the list I mean. “Number 16: My right big toe itches. Number 17: I think I feel something on my back. Number 18: This weird chartreuse thing on my arm ...” One long list can leave an entire half-day schedule in shambles.
When a list is produced, the best option is to take it and read it yourself. Identify the most important two or three problems, and address them. For the rest, I will say, “This group of problems deserves a visit of its own, and we will schedule that visit.”
Ask if you can place the list (or a photocopy) in the patient’s chart. (It is, after all, important clinical information.) All of these problems are important to the patient and should be addressed – but on your schedule, not the patient’s.
Avoid interruptions. Especially phone calls. Unless it’s an emergency or an immediate family member, my receptionists say, “I’m sorry, the doctor is with patients. May I take a message?” Everyone – even other physicians – understands. But be sure to return those calls promptly.
Pharmaceutical reps should not be allowed to interrupt you, either. Have them make an appointment, just like everybody else.
There will be times, of course, when you run late. But these should be the exception rather than the rule. By streamlining your procedures and avoiding the pitfalls mentioned, you can give nearly every patient all the time he or she deserves without keeping the next patient waiting.
Incidentally, other common patient complaints in that survey were the following:
- Couldn’t schedule an appointment within a week.
- Spent too little time with me.
- Didn’t provide test results promptly.
- Didn’t respond to my phone calls promptly.
Now would be an excellent opportunity to identify and address any of those problems as well.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Money can buy health but it may not be affordable
It is said that “Money cannot buy happiness.” But ask anyone who does not have it and you will find that money can buy security and freedom from many fears and aggravations. There are no guarantees, but the odds are better with resources than without them. Nations with higher per capita gross domestic product have longer life expectancies, have more freedom, and offer more opportunities for the favored subsets of their populations. The adage is that a rising tide lifts all boats.
It is also said that “Money cannot buy health.” That is also a half lie. Again, there is no guarantee that money can cure what ails you. But over the past 4 decades, modern medical care has added on average 3 years to the average American’s life expectancy. These gains in life expectancy came at a steep cost. The United States has been paying a luxurious, premium price for health care compared with similarly developed nations. When I started my career studying health economics 40 years ago, U.S. health care had increased from 6% of the gross domestic product, was passing 9%, and per my professors, appeared headed for 12% – at which point the predictions were that the sky would start falling. Costs continued to rise and for the past decade about 17% of the U.S. GDP has been going to health care before the pandemic blip.
U.S. life expectancy in the past 150 years nearly doubled. This was primarily due to public health measures rather than the small contributions of medical care for individuals. Life expectancy has mostly risen by reducing infant mortality and childhood mortality. The civil engineers who figured out how to get clean running water into cities and sewage out without the two intermingling have saved far more lives than all the doctors graduating from the medical schools. Better nutrition, better sanitation, vaccines, and, to a smaller extent, antibiotics, have all contributed worthy but lesser effects.
When it comes to individual behavior rather than public health measures, the biggest effect comes from advice physicians have been doling out for decades: Stop smoking, exercise, wear your seatbelt, and do not drink and drive. Over the past generation, medical technology added an incremental improvement to the life span (life expectancy once you attain age 60). This has occurred in cardiovascular health by treating high blood pressure, reducing stroke risk, and lowering hemoglobin A1c. Those measures added about 3 years to life span before the obesity epidemic, the opioid epidemic, and the COVID pandemic wiped out the gains. In round numbers, the price for those 3 extra years of life was about the earnings of working an extra 1-2 years in a lifetime. To share those benefits with everyone, the working stiff has to postpone retirement and work an extra 3 years.
Most recently, modern medicine has produced some very expensive therapies that can add months or years to the lives of people with certain diseases. These therapies may involve over $100,000 worth of marginally beneficial medication that statistically adds a few months to the lives of people with certain varieties of prostate, lung, and breast cancers. Similarly, treatments for chronic disease such as AIDS and cystic fibrosis may involve ongoing medication costs of $10,000 or $20,000 or more per year every year for a lifetime. There are even more extreme examples on the horizon. CAR T-cells and Aduhelm [aducanumab] have the potential to break the Medicare bank. Kaftrio [ivacaftor/tezacaftor/elexacaftor], for cystic fibrosis, is being offered only to wealthier countries.
Medical expenses are hard to analyze because the cited “cost” of many of these medications is like a manufacturer’s suggested retail price that few are actually paying. I am a highly educated consumer, and a physician, but various policies at insurance companies and at national chain pharmacies make it impossible for me to comparison shop for lower prices on my personal medicines. It is not just medications. Over the past 15 years, I have noticed that the “cost” charged for routine lab tests I get have also increased to be 300%-900% higher than what the lab ultimately gets paid by my insurance. It is a farce, and I am chagrined to have been a part of the medical system (managed care organizations, pharmacies, hospitals, and government) that concocted this Frankenstein’s monster of health care payments.
Communicating these issues to a polarized public will require leadership. It will also require better speech writing than the distorted story President Biden used to discuss insulin prices during the State of the Union address. The expensive insulin analogues in common use for diabetes are not the same insulin that was discovered a century ago. The newer medications do provide extra benefits. Assigning a fair value to those benefits is the real issue.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
It is said that “Money cannot buy happiness.” But ask anyone who does not have it and you will find that money can buy security and freedom from many fears and aggravations. There are no guarantees, but the odds are better with resources than without them. Nations with higher per capita gross domestic product have longer life expectancies, have more freedom, and offer more opportunities for the favored subsets of their populations. The adage is that a rising tide lifts all boats.
It is also said that “Money cannot buy health.” That is also a half lie. Again, there is no guarantee that money can cure what ails you. But over the past 4 decades, modern medical care has added on average 3 years to the average American’s life expectancy. These gains in life expectancy came at a steep cost. The United States has been paying a luxurious, premium price for health care compared with similarly developed nations. When I started my career studying health economics 40 years ago, U.S. health care had increased from 6% of the gross domestic product, was passing 9%, and per my professors, appeared headed for 12% – at which point the predictions were that the sky would start falling. Costs continued to rise and for the past decade about 17% of the U.S. GDP has been going to health care before the pandemic blip.
U.S. life expectancy in the past 150 years nearly doubled. This was primarily due to public health measures rather than the small contributions of medical care for individuals. Life expectancy has mostly risen by reducing infant mortality and childhood mortality. The civil engineers who figured out how to get clean running water into cities and sewage out without the two intermingling have saved far more lives than all the doctors graduating from the medical schools. Better nutrition, better sanitation, vaccines, and, to a smaller extent, antibiotics, have all contributed worthy but lesser effects.
When it comes to individual behavior rather than public health measures, the biggest effect comes from advice physicians have been doling out for decades: Stop smoking, exercise, wear your seatbelt, and do not drink and drive. Over the past generation, medical technology added an incremental improvement to the life span (life expectancy once you attain age 60). This has occurred in cardiovascular health by treating high blood pressure, reducing stroke risk, and lowering hemoglobin A1c. Those measures added about 3 years to life span before the obesity epidemic, the opioid epidemic, and the COVID pandemic wiped out the gains. In round numbers, the price for those 3 extra years of life was about the earnings of working an extra 1-2 years in a lifetime. To share those benefits with everyone, the working stiff has to postpone retirement and work an extra 3 years.
Most recently, modern medicine has produced some very expensive therapies that can add months or years to the lives of people with certain diseases. These therapies may involve over $100,000 worth of marginally beneficial medication that statistically adds a few months to the lives of people with certain varieties of prostate, lung, and breast cancers. Similarly, treatments for chronic disease such as AIDS and cystic fibrosis may involve ongoing medication costs of $10,000 or $20,000 or more per year every year for a lifetime. There are even more extreme examples on the horizon. CAR T-cells and Aduhelm [aducanumab] have the potential to break the Medicare bank. Kaftrio [ivacaftor/tezacaftor/elexacaftor], for cystic fibrosis, is being offered only to wealthier countries.
Medical expenses are hard to analyze because the cited “cost” of many of these medications is like a manufacturer’s suggested retail price that few are actually paying. I am a highly educated consumer, and a physician, but various policies at insurance companies and at national chain pharmacies make it impossible for me to comparison shop for lower prices on my personal medicines. It is not just medications. Over the past 15 years, I have noticed that the “cost” charged for routine lab tests I get have also increased to be 300%-900% higher than what the lab ultimately gets paid by my insurance. It is a farce, and I am chagrined to have been a part of the medical system (managed care organizations, pharmacies, hospitals, and government) that concocted this Frankenstein’s monster of health care payments.
Communicating these issues to a polarized public will require leadership. It will also require better speech writing than the distorted story President Biden used to discuss insulin prices during the State of the Union address. The expensive insulin analogues in common use for diabetes are not the same insulin that was discovered a century ago. The newer medications do provide extra benefits. Assigning a fair value to those benefits is the real issue.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
It is said that “Money cannot buy happiness.” But ask anyone who does not have it and you will find that money can buy security and freedom from many fears and aggravations. There are no guarantees, but the odds are better with resources than without them. Nations with higher per capita gross domestic product have longer life expectancies, have more freedom, and offer more opportunities for the favored subsets of their populations. The adage is that a rising tide lifts all boats.
It is also said that “Money cannot buy health.” That is also a half lie. Again, there is no guarantee that money can cure what ails you. But over the past 4 decades, modern medical care has added on average 3 years to the average American’s life expectancy. These gains in life expectancy came at a steep cost. The United States has been paying a luxurious, premium price for health care compared with similarly developed nations. When I started my career studying health economics 40 years ago, U.S. health care had increased from 6% of the gross domestic product, was passing 9%, and per my professors, appeared headed for 12% – at which point the predictions were that the sky would start falling. Costs continued to rise and for the past decade about 17% of the U.S. GDP has been going to health care before the pandemic blip.
U.S. life expectancy in the past 150 years nearly doubled. This was primarily due to public health measures rather than the small contributions of medical care for individuals. Life expectancy has mostly risen by reducing infant mortality and childhood mortality. The civil engineers who figured out how to get clean running water into cities and sewage out without the two intermingling have saved far more lives than all the doctors graduating from the medical schools. Better nutrition, better sanitation, vaccines, and, to a smaller extent, antibiotics, have all contributed worthy but lesser effects.
When it comes to individual behavior rather than public health measures, the biggest effect comes from advice physicians have been doling out for decades: Stop smoking, exercise, wear your seatbelt, and do not drink and drive. Over the past generation, medical technology added an incremental improvement to the life span (life expectancy once you attain age 60). This has occurred in cardiovascular health by treating high blood pressure, reducing stroke risk, and lowering hemoglobin A1c. Those measures added about 3 years to life span before the obesity epidemic, the opioid epidemic, and the COVID pandemic wiped out the gains. In round numbers, the price for those 3 extra years of life was about the earnings of working an extra 1-2 years in a lifetime. To share those benefits with everyone, the working stiff has to postpone retirement and work an extra 3 years.
Most recently, modern medicine has produced some very expensive therapies that can add months or years to the lives of people with certain diseases. These therapies may involve over $100,000 worth of marginally beneficial medication that statistically adds a few months to the lives of people with certain varieties of prostate, lung, and breast cancers. Similarly, treatments for chronic disease such as AIDS and cystic fibrosis may involve ongoing medication costs of $10,000 or $20,000 or more per year every year for a lifetime. There are even more extreme examples on the horizon. CAR T-cells and Aduhelm [aducanumab] have the potential to break the Medicare bank. Kaftrio [ivacaftor/tezacaftor/elexacaftor], for cystic fibrosis, is being offered only to wealthier countries.
Medical expenses are hard to analyze because the cited “cost” of many of these medications is like a manufacturer’s suggested retail price that few are actually paying. I am a highly educated consumer, and a physician, but various policies at insurance companies and at national chain pharmacies make it impossible for me to comparison shop for lower prices on my personal medicines. It is not just medications. Over the past 15 years, I have noticed that the “cost” charged for routine lab tests I get have also increased to be 300%-900% higher than what the lab ultimately gets paid by my insurance. It is a farce, and I am chagrined to have been a part of the medical system (managed care organizations, pharmacies, hospitals, and government) that concocted this Frankenstein’s monster of health care payments.
Communicating these issues to a polarized public will require leadership. It will also require better speech writing than the distorted story President Biden used to discuss insulin prices during the State of the Union address. The expensive insulin analogues in common use for diabetes are not the same insulin that was discovered a century ago. The newer medications do provide extra benefits. Assigning a fair value to those benefits is the real issue.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Expelled from high school, Alister Martin became a Harvard doc
It’s not often that a high school brawl with gang members sets you down a path to becoming a Harvard-trained doctor. But that’s exactly how Alister Martin’s life unfolded.
In retrospect, he should have seen the whole thing coming. That night at the party, his best friend was attacked by a gang member from a nearby high school. Martin was not in a gang but he jumped into the fray to defend his friend.
“I wanted to save the day, but that’s not what happened,” he says. “There were just too many of them.”
When his mother rushed to the hospital, he was so bruised and bloody that she couldn’t recognize him at first. Ever since he was a baby, she had done her best to shield him from the neighborhood where gang violence was a regular disruption. But it hadn’t worked.
“My high school had a zero-tolerance policy for gang violence,” Martin says, “so even though I wasn’t in a gang, I was kicked out.”
Now expelled from high school, his mother wanted him out of town, fearing gang retaliation, or that Martin might seek vengeance on the boy who had brutally beaten him. So, the biology teacher and single mom who worked numerous jobs to keep them afloat, came up with a plan to get him far away from any temptations.
Martin had loved tennis since middle school, when his 8th-grade math teacher, Billie Weise, also a tennis pro, got him a job as a court sweeper at an upscale tennis club nearby. He knew nothing then about tennis but would come to fall in love with the sport. To get her son out of town, Martin’s mother took out loans for $30,000 and sent him to a Florida tennis training camp.
After 6 months of training, Martin, who earned a GED degree while attending the camp, was offered a scholarship to play tennis at Rutgers University in New Brunswick, N.J. The transition to college was tough, however. He was nervous and felt out of place. “I could have died that first day. It became so obvious how poorly my high school education had prepared me for this.”
But the unease he felt was also motivating in a way. Worried about failure, “he locked himself in a room with another student and they studied day and night,” recalls Kamal Khan, director of the office for diversity and academic success at Rutgers. “I’ve never seen anything like it.”
And Martin displayed other attributes that would draw others to him – and later prove important in his career as a doctor. His ability to display empathy and interact with students and teachers separated him from his peers, Mr. Khan says. “There’re a lot of really smart students out there,” he says, “but not many who understand people like Martin.”
After graduating, he decided to pursue his dream of becoming a doctor. He’d wanted to be a doctor since he was 10 years old after his mom was diagnosed with metastatic breast cancer. He remembers overhearing a conversation she was having with a family friend about where he would go if she died.
“That’s when I knew it was serious,” he says.
Doctors saved her life, and it’s something he’ll never forget. But it wasn’t until his time at Rutgers that he finally had the confidence to think he could succeed in medical school.
Martin went on to attend Harvard Medical School and Harvard Kennedy School of Government as well as serving as chief resident at Brigham and Women’s Hospital. He was also a fellow at the White House in the Office of the Vice President and today, he’s an assistant professor at Harvard Medical School in Boston..
He is most at home in the emergency room at Massachusetts General Hospital, where he works as an emergency medical specialist. For him, the ER is the first line of defense for meeting the community’s health needs. Growing up in Neptune, the ER “was where poor folks got their care,” he says. His mom worked two jobs and when she got off work at 8 p.m. there was no pediatrician open. “When I was sick as a kid we always went to the emergency room,” he says.
While at Harvard, he also pursued a degree from the Kennedy School of Government, because of the huge role he feels that politics play in our health care system and especially in bringing care to impoverished communities. And since then he’s taken numerous steps to bridge the gap.
Addiction, for example, became an important issue for Martin, ever since a patient he encountered in his first week as an internist. She was a mom of two who had recently gotten surgery because she broke her ankle falling down the stairs at her child’s daycare, he says. Prescribed oxycodone, she feared she was becoming addicted and needed help. But at the time, there was nothing the ER could do.
“I remember that look in her eyes when we had to turn her away,” he says.
Martin has worked to change protocol at his hospital and others throughout the nation so they can be better set up to treat opioid addiction. He’s the founder of GetWaivered, an organization that trains doctors throughout the country to use evidence-based medicine to manage opioid addiction. In the U.S. doctors need what’s called a DEA X waiver to be able to prescribe buprenorphine to opioid-addicted patients. That means that currently only about 1% of all emergency room doctors nationwide have the waiver and without it, it’s impossible to help patients when they need it the most.
Shuhan He, MD, an internist with Martin at Massachusetts General Hospital who also works on the GetWaivered program, says Martin has a particular trait that helps him be successful.
“He’s a doer and when he sees a problem, he’s gonna try and fix it.”
A version of this article first appeared on Medscape.com.
It’s not often that a high school brawl with gang members sets you down a path to becoming a Harvard-trained doctor. But that’s exactly how Alister Martin’s life unfolded.
In retrospect, he should have seen the whole thing coming. That night at the party, his best friend was attacked by a gang member from a nearby high school. Martin was not in a gang but he jumped into the fray to defend his friend.
“I wanted to save the day, but that’s not what happened,” he says. “There were just too many of them.”
When his mother rushed to the hospital, he was so bruised and bloody that she couldn’t recognize him at first. Ever since he was a baby, she had done her best to shield him from the neighborhood where gang violence was a regular disruption. But it hadn’t worked.
“My high school had a zero-tolerance policy for gang violence,” Martin says, “so even though I wasn’t in a gang, I was kicked out.”
Now expelled from high school, his mother wanted him out of town, fearing gang retaliation, or that Martin might seek vengeance on the boy who had brutally beaten him. So, the biology teacher and single mom who worked numerous jobs to keep them afloat, came up with a plan to get him far away from any temptations.
Martin had loved tennis since middle school, when his 8th-grade math teacher, Billie Weise, also a tennis pro, got him a job as a court sweeper at an upscale tennis club nearby. He knew nothing then about tennis but would come to fall in love with the sport. To get her son out of town, Martin’s mother took out loans for $30,000 and sent him to a Florida tennis training camp.
After 6 months of training, Martin, who earned a GED degree while attending the camp, was offered a scholarship to play tennis at Rutgers University in New Brunswick, N.J. The transition to college was tough, however. He was nervous and felt out of place. “I could have died that first day. It became so obvious how poorly my high school education had prepared me for this.”
But the unease he felt was also motivating in a way. Worried about failure, “he locked himself in a room with another student and they studied day and night,” recalls Kamal Khan, director of the office for diversity and academic success at Rutgers. “I’ve never seen anything like it.”
And Martin displayed other attributes that would draw others to him – and later prove important in his career as a doctor. His ability to display empathy and interact with students and teachers separated him from his peers, Mr. Khan says. “There’re a lot of really smart students out there,” he says, “but not many who understand people like Martin.”
After graduating, he decided to pursue his dream of becoming a doctor. He’d wanted to be a doctor since he was 10 years old after his mom was diagnosed with metastatic breast cancer. He remembers overhearing a conversation she was having with a family friend about where he would go if she died.
“That’s when I knew it was serious,” he says.
Doctors saved her life, and it’s something he’ll never forget. But it wasn’t until his time at Rutgers that he finally had the confidence to think he could succeed in medical school.
Martin went on to attend Harvard Medical School and Harvard Kennedy School of Government as well as serving as chief resident at Brigham and Women’s Hospital. He was also a fellow at the White House in the Office of the Vice President and today, he’s an assistant professor at Harvard Medical School in Boston..
He is most at home in the emergency room at Massachusetts General Hospital, where he works as an emergency medical specialist. For him, the ER is the first line of defense for meeting the community’s health needs. Growing up in Neptune, the ER “was where poor folks got their care,” he says. His mom worked two jobs and when she got off work at 8 p.m. there was no pediatrician open. “When I was sick as a kid we always went to the emergency room,” he says.
While at Harvard, he also pursued a degree from the Kennedy School of Government, because of the huge role he feels that politics play in our health care system and especially in bringing care to impoverished communities. And since then he’s taken numerous steps to bridge the gap.
Addiction, for example, became an important issue for Martin, ever since a patient he encountered in his first week as an internist. She was a mom of two who had recently gotten surgery because she broke her ankle falling down the stairs at her child’s daycare, he says. Prescribed oxycodone, she feared she was becoming addicted and needed help. But at the time, there was nothing the ER could do.
“I remember that look in her eyes when we had to turn her away,” he says.
Martin has worked to change protocol at his hospital and others throughout the nation so they can be better set up to treat opioid addiction. He’s the founder of GetWaivered, an organization that trains doctors throughout the country to use evidence-based medicine to manage opioid addiction. In the U.S. doctors need what’s called a DEA X waiver to be able to prescribe buprenorphine to opioid-addicted patients. That means that currently only about 1% of all emergency room doctors nationwide have the waiver and without it, it’s impossible to help patients when they need it the most.
Shuhan He, MD, an internist with Martin at Massachusetts General Hospital who also works on the GetWaivered program, says Martin has a particular trait that helps him be successful.
“He’s a doer and when he sees a problem, he’s gonna try and fix it.”
A version of this article first appeared on Medscape.com.
It’s not often that a high school brawl with gang members sets you down a path to becoming a Harvard-trained doctor. But that’s exactly how Alister Martin’s life unfolded.
In retrospect, he should have seen the whole thing coming. That night at the party, his best friend was attacked by a gang member from a nearby high school. Martin was not in a gang but he jumped into the fray to defend his friend.
“I wanted to save the day, but that’s not what happened,” he says. “There were just too many of them.”
When his mother rushed to the hospital, he was so bruised and bloody that she couldn’t recognize him at first. Ever since he was a baby, she had done her best to shield him from the neighborhood where gang violence was a regular disruption. But it hadn’t worked.
“My high school had a zero-tolerance policy for gang violence,” Martin says, “so even though I wasn’t in a gang, I was kicked out.”
Now expelled from high school, his mother wanted him out of town, fearing gang retaliation, or that Martin might seek vengeance on the boy who had brutally beaten him. So, the biology teacher and single mom who worked numerous jobs to keep them afloat, came up with a plan to get him far away from any temptations.
Martin had loved tennis since middle school, when his 8th-grade math teacher, Billie Weise, also a tennis pro, got him a job as a court sweeper at an upscale tennis club nearby. He knew nothing then about tennis but would come to fall in love with the sport. To get her son out of town, Martin’s mother took out loans for $30,000 and sent him to a Florida tennis training camp.
After 6 months of training, Martin, who earned a GED degree while attending the camp, was offered a scholarship to play tennis at Rutgers University in New Brunswick, N.J. The transition to college was tough, however. He was nervous and felt out of place. “I could have died that first day. It became so obvious how poorly my high school education had prepared me for this.”
But the unease he felt was also motivating in a way. Worried about failure, “he locked himself in a room with another student and they studied day and night,” recalls Kamal Khan, director of the office for diversity and academic success at Rutgers. “I’ve never seen anything like it.”
And Martin displayed other attributes that would draw others to him – and later prove important in his career as a doctor. His ability to display empathy and interact with students and teachers separated him from his peers, Mr. Khan says. “There’re a lot of really smart students out there,” he says, “but not many who understand people like Martin.”
After graduating, he decided to pursue his dream of becoming a doctor. He’d wanted to be a doctor since he was 10 years old after his mom was diagnosed with metastatic breast cancer. He remembers overhearing a conversation she was having with a family friend about where he would go if she died.
“That’s when I knew it was serious,” he says.
Doctors saved her life, and it’s something he’ll never forget. But it wasn’t until his time at Rutgers that he finally had the confidence to think he could succeed in medical school.
Martin went on to attend Harvard Medical School and Harvard Kennedy School of Government as well as serving as chief resident at Brigham and Women’s Hospital. He was also a fellow at the White House in the Office of the Vice President and today, he’s an assistant professor at Harvard Medical School in Boston..
He is most at home in the emergency room at Massachusetts General Hospital, where he works as an emergency medical specialist. For him, the ER is the first line of defense for meeting the community’s health needs. Growing up in Neptune, the ER “was where poor folks got their care,” he says. His mom worked two jobs and when she got off work at 8 p.m. there was no pediatrician open. “When I was sick as a kid we always went to the emergency room,” he says.
While at Harvard, he also pursued a degree from the Kennedy School of Government, because of the huge role he feels that politics play in our health care system and especially in bringing care to impoverished communities. And since then he’s taken numerous steps to bridge the gap.
Addiction, for example, became an important issue for Martin, ever since a patient he encountered in his first week as an internist. She was a mom of two who had recently gotten surgery because she broke her ankle falling down the stairs at her child’s daycare, he says. Prescribed oxycodone, she feared she was becoming addicted and needed help. But at the time, there was nothing the ER could do.
“I remember that look in her eyes when we had to turn her away,” he says.
Martin has worked to change protocol at his hospital and others throughout the nation so they can be better set up to treat opioid addiction. He’s the founder of GetWaivered, an organization that trains doctors throughout the country to use evidence-based medicine to manage opioid addiction. In the U.S. doctors need what’s called a DEA X waiver to be able to prescribe buprenorphine to opioid-addicted patients. That means that currently only about 1% of all emergency room doctors nationwide have the waiver and without it, it’s impossible to help patients when they need it the most.
Shuhan He, MD, an internist with Martin at Massachusetts General Hospital who also works on the GetWaivered program, says Martin has a particular trait that helps him be successful.
“He’s a doer and when he sees a problem, he’s gonna try and fix it.”
A version of this article first appeared on Medscape.com.