User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
AI at the office: Are clinicians prepared?
AURORA, COLO. – Artificial Intelligence has arrived at medical offices, whether or not clinicians feel ready for it.
AI might result in more accurate, efficient, and cost-effective care. But it’s possible it could cause harm. That’s according to Benjamin Collins, MD, at Vanderbilt University Medical Center, Nashville, Tenn., who spoke on the subject at the annual meeting of the Society of General Internal Medicine.
Understanding the nuances of AI is even more important because of the quick development of the algorithms.
“When I submitted this workshop, there was no ChatGPT,” said Dr. Collins, referring to Chat Generative Pre-trained Transformer, a recently released natural language processing model. “A lot has already changed.”
Biased data
Biased data are perhaps the biggest pitfall of AI algorithms, Dr. Collins said. If garbage data go in, garbage predictions come out.
If the dataset that trains the algorithm underrepresents a particular gender or ethnic group, for example, the algorithm may not respond accurately to prompts. When an AI tool compounds existing inequalities related to socioeconomic status, ethnicity, or sexual orientation, the algorithm is biased, according to Harvard researchers.
“People often assume that artificial intelligence is free of bias due to the use of scientific processes and its development,” he said. “But whatever flaws exist in data collection and old data can lead to poor representation or underrepresentation in the data used to train the AI tool.”
Racial minorities are underrepresented in studies; therefore, data input into an AI tool might skew results for these patients.
The Framingham Heart Study, for example, which began in 1948, examined heart disease in mainly White participants. The findings from the study resulted in the creation of a sex-specific algorithm that was used to estimate the 10-year cardiovascular risk of a patient. While the cardiovascular risk score was accurate for White persons, it was less accurate for Black patients.
A study published in Science in 2019 revealed bias in an algorithm that used health care costs as a proxy for health needs. Because less money was spent on Black patients who had the same level of need as their White counterparts, the output inaccurately showed that Black patients were healthier and thus did not require extra care.
Developers can also be a source of bias, inasmuch as AI often reflects preexisting human biases, Dr. Collins said.
“Algorithmic bias presents a clear risk of harm that clinicians must play against the benefits of using AI,” Dr. Collins said. “That risk of harm is often disproportionately distributed to marginalized populations.”
As clinicians use AI algorithms to diagnose and detect disease, predict outcomes, and guide treatment, trouble comes when those algorithms perform well for some patients and poorly for others. This gap can exacerbate existing disparities in health care outcomes.
Dr. Collins advised clinicians to push to find out what data were used to train AI algorithms to determine how bias could have influenced the model and whether the developers risk-adjusted for bias. If the training data are not available, clinicians should ask their employers and AI developers to know more about the system.
Clinicians may face the so-called black box phenomenon, which occurs when developers cannot or will not explain what data went into an AI model, Dr. Collins said.
According to Stanford (Calif.) University, AI must be trained on large datasets of images that have been annotated by human experts. Those datasets can cost millions of dollars to create, meaning corporations often fund them and do not always share the data publicly.
Some groups, such as Stanford’s Center for Artificial Intelligence in Medicine and Imaging, are working to acquire annotated datasets so researchers who train AI models can know where the data came from.
Paul Haidet, MD, MPH, an internist at Penn State College of Medicine, Hershey, sees the technology as a tool that requires careful handling.
“It takes a while to learn how to use a stethoscope, and AI is like that,” Dr. Haidet said. “The thing about AI, though, is that it can be just dropped into a system and no one knows how it works.”
Dr. Haidet said he likes knowing how the sausage is made, something AI developers are often reticent to make known.
“If you’re just putting blind faith in a tool, that’s scary,” Dr. Haidet said.
Transparency and ‘explainability’
The ability to explain what goes into tools is essential to maintaining trust in the health care system, Dr. Collins said.
“Part of knowing how much trust to place in the system is the transparency of those systems and the ability to audit how well the algorithm is performing,” Dr. Collins said. “The system should also regularly report to users the level of certainty with which it is providing an output rather than providing a simple binary output.”
Dr. Collins recommends that providers develop an understanding of the limits of AI regulations as well, which might including learning how the system was approved and how it is monitored.
“The FDA has oversight over some applications of AI and health care for software as a medical device, but there’s currently no dedicated process to evaluate the systems for the presence of bias,” Dr. Collins said. “The gaps in regulation leave the door open for the use of AI in clinical care that contain significant biases.”
Dr. Haidet likened AI tools to the Global Positioning System: A good GPS system will let users see alternate routes, opt out of toll roads or highways, and will highlight why routes have changed. But users need to understand how to read the map so they can tell when something seems amiss.
Dr. Collins and Dr. Haidet report no relevant financial relationships
A version of this article first appeared on Medscape.com.
AURORA, COLO. – Artificial Intelligence has arrived at medical offices, whether or not clinicians feel ready for it.
AI might result in more accurate, efficient, and cost-effective care. But it’s possible it could cause harm. That’s according to Benjamin Collins, MD, at Vanderbilt University Medical Center, Nashville, Tenn., who spoke on the subject at the annual meeting of the Society of General Internal Medicine.
Understanding the nuances of AI is even more important because of the quick development of the algorithms.
“When I submitted this workshop, there was no ChatGPT,” said Dr. Collins, referring to Chat Generative Pre-trained Transformer, a recently released natural language processing model. “A lot has already changed.”
Biased data
Biased data are perhaps the biggest pitfall of AI algorithms, Dr. Collins said. If garbage data go in, garbage predictions come out.
If the dataset that trains the algorithm underrepresents a particular gender or ethnic group, for example, the algorithm may not respond accurately to prompts. When an AI tool compounds existing inequalities related to socioeconomic status, ethnicity, or sexual orientation, the algorithm is biased, according to Harvard researchers.
“People often assume that artificial intelligence is free of bias due to the use of scientific processes and its development,” he said. “But whatever flaws exist in data collection and old data can lead to poor representation or underrepresentation in the data used to train the AI tool.”
Racial minorities are underrepresented in studies; therefore, data input into an AI tool might skew results for these patients.
The Framingham Heart Study, for example, which began in 1948, examined heart disease in mainly White participants. The findings from the study resulted in the creation of a sex-specific algorithm that was used to estimate the 10-year cardiovascular risk of a patient. While the cardiovascular risk score was accurate for White persons, it was less accurate for Black patients.
A study published in Science in 2019 revealed bias in an algorithm that used health care costs as a proxy for health needs. Because less money was spent on Black patients who had the same level of need as their White counterparts, the output inaccurately showed that Black patients were healthier and thus did not require extra care.
Developers can also be a source of bias, inasmuch as AI often reflects preexisting human biases, Dr. Collins said.
“Algorithmic bias presents a clear risk of harm that clinicians must play against the benefits of using AI,” Dr. Collins said. “That risk of harm is often disproportionately distributed to marginalized populations.”
As clinicians use AI algorithms to diagnose and detect disease, predict outcomes, and guide treatment, trouble comes when those algorithms perform well for some patients and poorly for others. This gap can exacerbate existing disparities in health care outcomes.
Dr. Collins advised clinicians to push to find out what data were used to train AI algorithms to determine how bias could have influenced the model and whether the developers risk-adjusted for bias. If the training data are not available, clinicians should ask their employers and AI developers to know more about the system.
Clinicians may face the so-called black box phenomenon, which occurs when developers cannot or will not explain what data went into an AI model, Dr. Collins said.
According to Stanford (Calif.) University, AI must be trained on large datasets of images that have been annotated by human experts. Those datasets can cost millions of dollars to create, meaning corporations often fund them and do not always share the data publicly.
Some groups, such as Stanford’s Center for Artificial Intelligence in Medicine and Imaging, are working to acquire annotated datasets so researchers who train AI models can know where the data came from.
Paul Haidet, MD, MPH, an internist at Penn State College of Medicine, Hershey, sees the technology as a tool that requires careful handling.
“It takes a while to learn how to use a stethoscope, and AI is like that,” Dr. Haidet said. “The thing about AI, though, is that it can be just dropped into a system and no one knows how it works.”
Dr. Haidet said he likes knowing how the sausage is made, something AI developers are often reticent to make known.
“If you’re just putting blind faith in a tool, that’s scary,” Dr. Haidet said.
Transparency and ‘explainability’
The ability to explain what goes into tools is essential to maintaining trust in the health care system, Dr. Collins said.
“Part of knowing how much trust to place in the system is the transparency of those systems and the ability to audit how well the algorithm is performing,” Dr. Collins said. “The system should also regularly report to users the level of certainty with which it is providing an output rather than providing a simple binary output.”
Dr. Collins recommends that providers develop an understanding of the limits of AI regulations as well, which might including learning how the system was approved and how it is monitored.
“The FDA has oversight over some applications of AI and health care for software as a medical device, but there’s currently no dedicated process to evaluate the systems for the presence of bias,” Dr. Collins said. “The gaps in regulation leave the door open for the use of AI in clinical care that contain significant biases.”
Dr. Haidet likened AI tools to the Global Positioning System: A good GPS system will let users see alternate routes, opt out of toll roads or highways, and will highlight why routes have changed. But users need to understand how to read the map so they can tell when something seems amiss.
Dr. Collins and Dr. Haidet report no relevant financial relationships
A version of this article first appeared on Medscape.com.
AURORA, COLO. – Artificial Intelligence has arrived at medical offices, whether or not clinicians feel ready for it.
AI might result in more accurate, efficient, and cost-effective care. But it’s possible it could cause harm. That’s according to Benjamin Collins, MD, at Vanderbilt University Medical Center, Nashville, Tenn., who spoke on the subject at the annual meeting of the Society of General Internal Medicine.
Understanding the nuances of AI is even more important because of the quick development of the algorithms.
“When I submitted this workshop, there was no ChatGPT,” said Dr. Collins, referring to Chat Generative Pre-trained Transformer, a recently released natural language processing model. “A lot has already changed.”
Biased data
Biased data are perhaps the biggest pitfall of AI algorithms, Dr. Collins said. If garbage data go in, garbage predictions come out.
If the dataset that trains the algorithm underrepresents a particular gender or ethnic group, for example, the algorithm may not respond accurately to prompts. When an AI tool compounds existing inequalities related to socioeconomic status, ethnicity, or sexual orientation, the algorithm is biased, according to Harvard researchers.
“People often assume that artificial intelligence is free of bias due to the use of scientific processes and its development,” he said. “But whatever flaws exist in data collection and old data can lead to poor representation or underrepresentation in the data used to train the AI tool.”
Racial minorities are underrepresented in studies; therefore, data input into an AI tool might skew results for these patients.
The Framingham Heart Study, for example, which began in 1948, examined heart disease in mainly White participants. The findings from the study resulted in the creation of a sex-specific algorithm that was used to estimate the 10-year cardiovascular risk of a patient. While the cardiovascular risk score was accurate for White persons, it was less accurate for Black patients.
A study published in Science in 2019 revealed bias in an algorithm that used health care costs as a proxy for health needs. Because less money was spent on Black patients who had the same level of need as their White counterparts, the output inaccurately showed that Black patients were healthier and thus did not require extra care.
Developers can also be a source of bias, inasmuch as AI often reflects preexisting human biases, Dr. Collins said.
“Algorithmic bias presents a clear risk of harm that clinicians must play against the benefits of using AI,” Dr. Collins said. “That risk of harm is often disproportionately distributed to marginalized populations.”
As clinicians use AI algorithms to diagnose and detect disease, predict outcomes, and guide treatment, trouble comes when those algorithms perform well for some patients and poorly for others. This gap can exacerbate existing disparities in health care outcomes.
Dr. Collins advised clinicians to push to find out what data were used to train AI algorithms to determine how bias could have influenced the model and whether the developers risk-adjusted for bias. If the training data are not available, clinicians should ask their employers and AI developers to know more about the system.
Clinicians may face the so-called black box phenomenon, which occurs when developers cannot or will not explain what data went into an AI model, Dr. Collins said.
According to Stanford (Calif.) University, AI must be trained on large datasets of images that have been annotated by human experts. Those datasets can cost millions of dollars to create, meaning corporations often fund them and do not always share the data publicly.
Some groups, such as Stanford’s Center for Artificial Intelligence in Medicine and Imaging, are working to acquire annotated datasets so researchers who train AI models can know where the data came from.
Paul Haidet, MD, MPH, an internist at Penn State College of Medicine, Hershey, sees the technology as a tool that requires careful handling.
“It takes a while to learn how to use a stethoscope, and AI is like that,” Dr. Haidet said. “The thing about AI, though, is that it can be just dropped into a system and no one knows how it works.”
Dr. Haidet said he likes knowing how the sausage is made, something AI developers are often reticent to make known.
“If you’re just putting blind faith in a tool, that’s scary,” Dr. Haidet said.
Transparency and ‘explainability’
The ability to explain what goes into tools is essential to maintaining trust in the health care system, Dr. Collins said.
“Part of knowing how much trust to place in the system is the transparency of those systems and the ability to audit how well the algorithm is performing,” Dr. Collins said. “The system should also regularly report to users the level of certainty with which it is providing an output rather than providing a simple binary output.”
Dr. Collins recommends that providers develop an understanding of the limits of AI regulations as well, which might including learning how the system was approved and how it is monitored.
“The FDA has oversight over some applications of AI and health care for software as a medical device, but there’s currently no dedicated process to evaluate the systems for the presence of bias,” Dr. Collins said. “The gaps in regulation leave the door open for the use of AI in clinical care that contain significant biases.”
Dr. Haidet likened AI tools to the Global Positioning System: A good GPS system will let users see alternate routes, opt out of toll roads or highways, and will highlight why routes have changed. But users need to understand how to read the map so they can tell when something seems amiss.
Dr. Collins and Dr. Haidet report no relevant financial relationships
A version of this article first appeared on Medscape.com.
AT SGIM 2023
Pop this question to improve medication adherence
AURORA, COLO. – How often do you talk with patients about how to lower their out-of-pocket costs for medical care?
For most clinicians, the answer is: not often enough. But having those conversations can improve medication adherence and strengthen the patient-clinician relationship, according to panelists at the annual meeting of the Society of General Internal Medicine.
The inverse association between out-of-pocket expenditures and fidelity to prescriptions is clear. A 2020 study by the IQVIA Institute for Human Data Science, for example, found that rates of prescription abandonment are less than 5% when a given medication carries no out-of-pocket cost for patients. That figure rises to 45% when the cost is more than $125, and to 60% when it exceeds $500. One in five Americans said cost prevented them from adhering to medication regimens, according to a new study in JAMA Network Open.
The researchers surveyed more than 2,000 men and women, 40.4% of whom were aged 75 or older. They found that nearly 90% of respondents said they would not be uncomfortable being asked about drug costs before a visit with a physician. A similar share (89.5%) said they would welcome the use by their physician of a real-time tool to determine the cost of their medication.
But the survey results contained a note of warning for clinicians: A significant number of respondents said they would be “extremely” upset if the cost of their medication exceeded the estimate from the pricing tool. And many also said they would be “moderately” or “extremely” angry if their physician used a pricing tool but failed to share the results with them.
“Real-time benefit tools may support medication cost conversations and cost-conscious prescribing, and patients are enthusiastic about their use,” the authors write. “However, if disclosed prices are inaccurate, there is potential for harm through loss of confidence in the physician and nonadherence to prescribed medications.”
While having conversations about cost can be difficult for both clinicians and patients, studies have shown that patients who discuss cost concerns with their doctors feel as if they have stronger relationships as a result.
Clinicians often avoid conversations about out-of-pocket expenses because they don’t know specific price information, they lack solutions to address cost, or they are uncomfortable bringing up the issue.
One member of the audience at the SGIM meeting recalled a patient who worked in a warehouse for a large company. The man, who had type 2 diabetes, had medical insurance, but even with insurance, insulin was going to cost him $150 per month. He struggled to afford the necessary treatment.
“He looked at me and said, ‘What do they want me to do? Do they want me to actually not be able to work for them and not manage my diabetes?’ ”
The clinician said he offered empathy in the moment but felt he could do little else.
Panelists acknowledged that clinicians are crunched on time when seeing patients, but being willing to initiate conversations about cost with patients and to offer resources can help patients get necessary treatment.
Start the conversation
Panel member Caroline Sloan, MD, an assistant professor of medicine at Duke University, Durham, N.C., said making patients aware that you know cost can make a big difference.
The American College of Physicians advises clinicians to ask patients whether they are worried about the cost of care and to not assume which patients may have concerns.
The conversation could be started like this: “I’d like to discuss any concerns you might have about the cost of your health care.”
Normalize the concern by making it more general, and reassure your patient that your goal is to get them the best care. Say something like, “I’ve heard from many patients the cost of medications or tests is becoming hard to manage.”
Once a patient’s concerns are clear, you can direct them to resources for assistance in reducing their costs, Dr. Sloan said, such as ClearHealthCosts, FAIR Health, Healthcare Bluebook, New Choice Health, GoodRx, PharmacyChecker, HealthWell Foundation, Patient Advocate Foundation, Good Days, Good Health Will, Mercy Medical Angels, and the American Association of Family Physicians Neighborhood Navigator.
Dr. Sloan said she knows clinicians don’t have time to understand every insurance plan and other issues related to cost. “But at least know to ask about costs,” she said. “Practice, practice, practice. It feels awkward at first, but it gets easier every time.”
A version of this article first appeared on Medscape.com.
AURORA, COLO. – How often do you talk with patients about how to lower their out-of-pocket costs for medical care?
For most clinicians, the answer is: not often enough. But having those conversations can improve medication adherence and strengthen the patient-clinician relationship, according to panelists at the annual meeting of the Society of General Internal Medicine.
The inverse association between out-of-pocket expenditures and fidelity to prescriptions is clear. A 2020 study by the IQVIA Institute for Human Data Science, for example, found that rates of prescription abandonment are less than 5% when a given medication carries no out-of-pocket cost for patients. That figure rises to 45% when the cost is more than $125, and to 60% when it exceeds $500. One in five Americans said cost prevented them from adhering to medication regimens, according to a new study in JAMA Network Open.
The researchers surveyed more than 2,000 men and women, 40.4% of whom were aged 75 or older. They found that nearly 90% of respondents said they would not be uncomfortable being asked about drug costs before a visit with a physician. A similar share (89.5%) said they would welcome the use by their physician of a real-time tool to determine the cost of their medication.
But the survey results contained a note of warning for clinicians: A significant number of respondents said they would be “extremely” upset if the cost of their medication exceeded the estimate from the pricing tool. And many also said they would be “moderately” or “extremely” angry if their physician used a pricing tool but failed to share the results with them.
“Real-time benefit tools may support medication cost conversations and cost-conscious prescribing, and patients are enthusiastic about their use,” the authors write. “However, if disclosed prices are inaccurate, there is potential for harm through loss of confidence in the physician and nonadherence to prescribed medications.”
While having conversations about cost can be difficult for both clinicians and patients, studies have shown that patients who discuss cost concerns with their doctors feel as if they have stronger relationships as a result.
Clinicians often avoid conversations about out-of-pocket expenses because they don’t know specific price information, they lack solutions to address cost, or they are uncomfortable bringing up the issue.
One member of the audience at the SGIM meeting recalled a patient who worked in a warehouse for a large company. The man, who had type 2 diabetes, had medical insurance, but even with insurance, insulin was going to cost him $150 per month. He struggled to afford the necessary treatment.
“He looked at me and said, ‘What do they want me to do? Do they want me to actually not be able to work for them and not manage my diabetes?’ ”
The clinician said he offered empathy in the moment but felt he could do little else.
Panelists acknowledged that clinicians are crunched on time when seeing patients, but being willing to initiate conversations about cost with patients and to offer resources can help patients get necessary treatment.
Start the conversation
Panel member Caroline Sloan, MD, an assistant professor of medicine at Duke University, Durham, N.C., said making patients aware that you know cost can make a big difference.
The American College of Physicians advises clinicians to ask patients whether they are worried about the cost of care and to not assume which patients may have concerns.
The conversation could be started like this: “I’d like to discuss any concerns you might have about the cost of your health care.”
Normalize the concern by making it more general, and reassure your patient that your goal is to get them the best care. Say something like, “I’ve heard from many patients the cost of medications or tests is becoming hard to manage.”
Once a patient’s concerns are clear, you can direct them to resources for assistance in reducing their costs, Dr. Sloan said, such as ClearHealthCosts, FAIR Health, Healthcare Bluebook, New Choice Health, GoodRx, PharmacyChecker, HealthWell Foundation, Patient Advocate Foundation, Good Days, Good Health Will, Mercy Medical Angels, and the American Association of Family Physicians Neighborhood Navigator.
Dr. Sloan said she knows clinicians don’t have time to understand every insurance plan and other issues related to cost. “But at least know to ask about costs,” she said. “Practice, practice, practice. It feels awkward at first, but it gets easier every time.”
A version of this article first appeared on Medscape.com.
AURORA, COLO. – How often do you talk with patients about how to lower their out-of-pocket costs for medical care?
For most clinicians, the answer is: not often enough. But having those conversations can improve medication adherence and strengthen the patient-clinician relationship, according to panelists at the annual meeting of the Society of General Internal Medicine.
The inverse association between out-of-pocket expenditures and fidelity to prescriptions is clear. A 2020 study by the IQVIA Institute for Human Data Science, for example, found that rates of prescription abandonment are less than 5% when a given medication carries no out-of-pocket cost for patients. That figure rises to 45% when the cost is more than $125, and to 60% when it exceeds $500. One in five Americans said cost prevented them from adhering to medication regimens, according to a new study in JAMA Network Open.
The researchers surveyed more than 2,000 men and women, 40.4% of whom were aged 75 or older. They found that nearly 90% of respondents said they would not be uncomfortable being asked about drug costs before a visit with a physician. A similar share (89.5%) said they would welcome the use by their physician of a real-time tool to determine the cost of their medication.
But the survey results contained a note of warning for clinicians: A significant number of respondents said they would be “extremely” upset if the cost of their medication exceeded the estimate from the pricing tool. And many also said they would be “moderately” or “extremely” angry if their physician used a pricing tool but failed to share the results with them.
“Real-time benefit tools may support medication cost conversations and cost-conscious prescribing, and patients are enthusiastic about their use,” the authors write. “However, if disclosed prices are inaccurate, there is potential for harm through loss of confidence in the physician and nonadherence to prescribed medications.”
While having conversations about cost can be difficult for both clinicians and patients, studies have shown that patients who discuss cost concerns with their doctors feel as if they have stronger relationships as a result.
Clinicians often avoid conversations about out-of-pocket expenses because they don’t know specific price information, they lack solutions to address cost, or they are uncomfortable bringing up the issue.
One member of the audience at the SGIM meeting recalled a patient who worked in a warehouse for a large company. The man, who had type 2 diabetes, had medical insurance, but even with insurance, insulin was going to cost him $150 per month. He struggled to afford the necessary treatment.
“He looked at me and said, ‘What do they want me to do? Do they want me to actually not be able to work for them and not manage my diabetes?’ ”
The clinician said he offered empathy in the moment but felt he could do little else.
Panelists acknowledged that clinicians are crunched on time when seeing patients, but being willing to initiate conversations about cost with patients and to offer resources can help patients get necessary treatment.
Start the conversation
Panel member Caroline Sloan, MD, an assistant professor of medicine at Duke University, Durham, N.C., said making patients aware that you know cost can make a big difference.
The American College of Physicians advises clinicians to ask patients whether they are worried about the cost of care and to not assume which patients may have concerns.
The conversation could be started like this: “I’d like to discuss any concerns you might have about the cost of your health care.”
Normalize the concern by making it more general, and reassure your patient that your goal is to get them the best care. Say something like, “I’ve heard from many patients the cost of medications or tests is becoming hard to manage.”
Once a patient’s concerns are clear, you can direct them to resources for assistance in reducing their costs, Dr. Sloan said, such as ClearHealthCosts, FAIR Health, Healthcare Bluebook, New Choice Health, GoodRx, PharmacyChecker, HealthWell Foundation, Patient Advocate Foundation, Good Days, Good Health Will, Mercy Medical Angels, and the American Association of Family Physicians Neighborhood Navigator.
Dr. Sloan said she knows clinicians don’t have time to understand every insurance plan and other issues related to cost. “But at least know to ask about costs,” she said. “Practice, practice, practice. It feels awkward at first, but it gets easier every time.”
A version of this article first appeared on Medscape.com.
AT SGIM 2023
No expiration date for sex
For health professionals, the thought that our parents and grandparents don’t have sex – or didn’t – might be comforting.
The reality is that, for a significant proportion of our older patients, sex has no use-by date. Humans are sexual beings throughout their lives, yet the culture has concealed that fact.
According to Rome, the purpose of sex is to make children. According to Hollywood, sex is only for the young, the healthy, and the beautiful. For the medical profession, sex consists mainly of risks or dysfunctions.
The results of these biases? Sexuality and intimacy are essential elements for quality of life, with clear physical, emotional, and relational benefits.
Let’s look at the data when researchers dared to ask seniors about their sexuality.
We start with the 2015 U.K. national research on sexuality. The study found a link between age and a decline in various aspects of sexual activity – but not a zeroing-out. For example, among men aged 70-79, 59% reported having had sex in the past year, with 19% having intercourse at least twice a month and 18% masturbating at least that often. Above age 80, those numbers dropped to 39%, 6%, and 5%, respectively. The reason behind the declines? A combination of taboo, fear of disease, use of medications or other interventions that disrupt sexual function or cause disfigurement, and a little bit of age itself.
What about women? Among women ages 70-79, 39% said they’d had sex in the past year, with 6% having intercourse at least twice per month and 5% masturbating two times or more monthly. Above age 80, those numbers were 10%, 4.5%, and 1%, respectively. Driving the falloff in women were the same factors as for men, plus the sad reality that many heterosexual women become widowed because their older male partners die earlier.
The male-female difference also reflects lower levels of testosterone in women. And, because women say they value intimacy more than performance, we have two explanations for their lower frequency of masturbation. After all, a lot of intimacy occurs without either intercourse or masturbation.
Surprising and relevant is the amount of distress – or rather, their relative lack thereof – older patients report because of sexual problems. At age 18-44, 11% of U.S. women indicated sexual distress; at age 45-64, the figure was 15%; and at age 65 and up, 9%.
For clinicians, those figures should prompt us to look more closely at alternative forms of sexual expression – those not involving intercourse or masturbation – in the aged, a field physicians typically do not consider.
Although dyspareunia or erectile problems affect many in long-standing relationships, neither is a reason to abstain from sexual pleasure. Indeed, in many couples, oral sex will replace vaginal intercourse, and if urinary, fecal, or flatal incontinence intrude, couples often waive oral sex in favor of more cuddling, kissing, digital stimulation, and other forms of sexual pleasure.
What about the expiry date for sex?
Fascinating research from Nils Beckman, PhD, and colleagues found that the sex drive persists even as people (and men in particular) reach their 100th year. Dr. Beckman’s group interviewed 269 Swedish seniors, all without dementia, at age 97. Sexual desire was affirmed by 27% of men and 5% of women in the survey. Among the men, 32% said they still had sexual thoughts, compared with 18% of women. Meanwhile, 26% of the men and 15% of the women said they missed sexual activity.
What should clinicians do with this information? First, we could start talking about sex with our older patients. According to the 97-year-old Swedes, most want us to! More than 8 in 10 of both women and men in the survey expressed positive views about questions on sexuality. And please don’t be scared to address the subject in the single senior. They, too, can have a sexual or relationship issue and are happy when we raise the subject. They’re not scared to talk about masturbation, either.
When caring for those with chronic diseases, cancer, in the course of physical rehabilitation, and even in the last phase of life, the clinical experience indicates that our patients are happy when we address sexuality and intimacy. Doing so can open the door to the admission of a problem and a corresponding solution, a lubricant or a PDE5 inhibitor.
But sometimes the solution is the conversation itself: Roughly 25% of patients are sufficiently helped simply by talking about sex. Addressing the importance of sexual pleasure is nearly always valuable.
Here are a few ice-breakers I find helpful:
- Did taking this medication change aspects of sexuality? If so, does that bother you?
- Knowing that continuing intimacy is healthy, do you mind if I address that subject?
- We know that aspects of sexuality and intimacy are healthy. Without a partner, some people become sexually isolated. Would you like to talk about that?’
If addressing sexuality has benefits, what about sex itself?
We are gradually learning more about the many short-, intermediate-, and long-term health benefits of solo and joint sexual activity. Short-term benefits include muscle relaxation, pain relief (even, perhaps ironically, for headaches), and better sleep – all pretty valuable for older adults. Examples of intermediate-term benefits include stress relief and less depression. Research from the United States has found that hugging can reduce the concentrations of proinflammatory cytokines, and kissing positively influences cholesterol levels.
Finally, while the long-term benefits of sex might be less relevant for seniors, they do exist.
Among them are delayed onset of dementia and a substantial reduction in cardiovascular and cerebrovascular problems in men. More sex has been linked to longevity, with men benefiting a bit more than women from going through the entire process, including an orgasm, whereas women appear to gain from having a “satisfying” sex life, which does not always require an orgasm.
Let us not forget that these benefits apply to both patients and clinicians alike. Addressing intimacy and sexuality can ease eventual sexual concerns and potentially create a stronger clinician-patient relationship.
Dr. Gianotten, MD is emeritus senior lecturer in medical sexology, Erasmus University Medical Centre, Rotterdam, the Netherlands. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
For health professionals, the thought that our parents and grandparents don’t have sex – or didn’t – might be comforting.
The reality is that, for a significant proportion of our older patients, sex has no use-by date. Humans are sexual beings throughout their lives, yet the culture has concealed that fact.
According to Rome, the purpose of sex is to make children. According to Hollywood, sex is only for the young, the healthy, and the beautiful. For the medical profession, sex consists mainly of risks or dysfunctions.
The results of these biases? Sexuality and intimacy are essential elements for quality of life, with clear physical, emotional, and relational benefits.
Let’s look at the data when researchers dared to ask seniors about their sexuality.
We start with the 2015 U.K. national research on sexuality. The study found a link between age and a decline in various aspects of sexual activity – but not a zeroing-out. For example, among men aged 70-79, 59% reported having had sex in the past year, with 19% having intercourse at least twice a month and 18% masturbating at least that often. Above age 80, those numbers dropped to 39%, 6%, and 5%, respectively. The reason behind the declines? A combination of taboo, fear of disease, use of medications or other interventions that disrupt sexual function or cause disfigurement, and a little bit of age itself.
What about women? Among women ages 70-79, 39% said they’d had sex in the past year, with 6% having intercourse at least twice per month and 5% masturbating two times or more monthly. Above age 80, those numbers were 10%, 4.5%, and 1%, respectively. Driving the falloff in women were the same factors as for men, plus the sad reality that many heterosexual women become widowed because their older male partners die earlier.
The male-female difference also reflects lower levels of testosterone in women. And, because women say they value intimacy more than performance, we have two explanations for their lower frequency of masturbation. After all, a lot of intimacy occurs without either intercourse or masturbation.
Surprising and relevant is the amount of distress – or rather, their relative lack thereof – older patients report because of sexual problems. At age 18-44, 11% of U.S. women indicated sexual distress; at age 45-64, the figure was 15%; and at age 65 and up, 9%.
For clinicians, those figures should prompt us to look more closely at alternative forms of sexual expression – those not involving intercourse or masturbation – in the aged, a field physicians typically do not consider.
Although dyspareunia or erectile problems affect many in long-standing relationships, neither is a reason to abstain from sexual pleasure. Indeed, in many couples, oral sex will replace vaginal intercourse, and if urinary, fecal, or flatal incontinence intrude, couples often waive oral sex in favor of more cuddling, kissing, digital stimulation, and other forms of sexual pleasure.
What about the expiry date for sex?
Fascinating research from Nils Beckman, PhD, and colleagues found that the sex drive persists even as people (and men in particular) reach their 100th year. Dr. Beckman’s group interviewed 269 Swedish seniors, all without dementia, at age 97. Sexual desire was affirmed by 27% of men and 5% of women in the survey. Among the men, 32% said they still had sexual thoughts, compared with 18% of women. Meanwhile, 26% of the men and 15% of the women said they missed sexual activity.
What should clinicians do with this information? First, we could start talking about sex with our older patients. According to the 97-year-old Swedes, most want us to! More than 8 in 10 of both women and men in the survey expressed positive views about questions on sexuality. And please don’t be scared to address the subject in the single senior. They, too, can have a sexual or relationship issue and are happy when we raise the subject. They’re not scared to talk about masturbation, either.
When caring for those with chronic diseases, cancer, in the course of physical rehabilitation, and even in the last phase of life, the clinical experience indicates that our patients are happy when we address sexuality and intimacy. Doing so can open the door to the admission of a problem and a corresponding solution, a lubricant or a PDE5 inhibitor.
But sometimes the solution is the conversation itself: Roughly 25% of patients are sufficiently helped simply by talking about sex. Addressing the importance of sexual pleasure is nearly always valuable.
Here are a few ice-breakers I find helpful:
- Did taking this medication change aspects of sexuality? If so, does that bother you?
- Knowing that continuing intimacy is healthy, do you mind if I address that subject?
- We know that aspects of sexuality and intimacy are healthy. Without a partner, some people become sexually isolated. Would you like to talk about that?’
If addressing sexuality has benefits, what about sex itself?
We are gradually learning more about the many short-, intermediate-, and long-term health benefits of solo and joint sexual activity. Short-term benefits include muscle relaxation, pain relief (even, perhaps ironically, for headaches), and better sleep – all pretty valuable for older adults. Examples of intermediate-term benefits include stress relief and less depression. Research from the United States has found that hugging can reduce the concentrations of proinflammatory cytokines, and kissing positively influences cholesterol levels.
Finally, while the long-term benefits of sex might be less relevant for seniors, they do exist.
Among them are delayed onset of dementia and a substantial reduction in cardiovascular and cerebrovascular problems in men. More sex has been linked to longevity, with men benefiting a bit more than women from going through the entire process, including an orgasm, whereas women appear to gain from having a “satisfying” sex life, which does not always require an orgasm.
Let us not forget that these benefits apply to both patients and clinicians alike. Addressing intimacy and sexuality can ease eventual sexual concerns and potentially create a stronger clinician-patient relationship.
Dr. Gianotten, MD is emeritus senior lecturer in medical sexology, Erasmus University Medical Centre, Rotterdam, the Netherlands. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
For health professionals, the thought that our parents and grandparents don’t have sex – or didn’t – might be comforting.
The reality is that, for a significant proportion of our older patients, sex has no use-by date. Humans are sexual beings throughout their lives, yet the culture has concealed that fact.
According to Rome, the purpose of sex is to make children. According to Hollywood, sex is only for the young, the healthy, and the beautiful. For the medical profession, sex consists mainly of risks or dysfunctions.
The results of these biases? Sexuality and intimacy are essential elements for quality of life, with clear physical, emotional, and relational benefits.
Let’s look at the data when researchers dared to ask seniors about their sexuality.
We start with the 2015 U.K. national research on sexuality. The study found a link between age and a decline in various aspects of sexual activity – but not a zeroing-out. For example, among men aged 70-79, 59% reported having had sex in the past year, with 19% having intercourse at least twice a month and 18% masturbating at least that often. Above age 80, those numbers dropped to 39%, 6%, and 5%, respectively. The reason behind the declines? A combination of taboo, fear of disease, use of medications or other interventions that disrupt sexual function or cause disfigurement, and a little bit of age itself.
What about women? Among women ages 70-79, 39% said they’d had sex in the past year, with 6% having intercourse at least twice per month and 5% masturbating two times or more monthly. Above age 80, those numbers were 10%, 4.5%, and 1%, respectively. Driving the falloff in women were the same factors as for men, plus the sad reality that many heterosexual women become widowed because their older male partners die earlier.
The male-female difference also reflects lower levels of testosterone in women. And, because women say they value intimacy more than performance, we have two explanations for their lower frequency of masturbation. After all, a lot of intimacy occurs without either intercourse or masturbation.
Surprising and relevant is the amount of distress – or rather, their relative lack thereof – older patients report because of sexual problems. At age 18-44, 11% of U.S. women indicated sexual distress; at age 45-64, the figure was 15%; and at age 65 and up, 9%.
For clinicians, those figures should prompt us to look more closely at alternative forms of sexual expression – those not involving intercourse or masturbation – in the aged, a field physicians typically do not consider.
Although dyspareunia or erectile problems affect many in long-standing relationships, neither is a reason to abstain from sexual pleasure. Indeed, in many couples, oral sex will replace vaginal intercourse, and if urinary, fecal, or flatal incontinence intrude, couples often waive oral sex in favor of more cuddling, kissing, digital stimulation, and other forms of sexual pleasure.
What about the expiry date for sex?
Fascinating research from Nils Beckman, PhD, and colleagues found that the sex drive persists even as people (and men in particular) reach their 100th year. Dr. Beckman’s group interviewed 269 Swedish seniors, all without dementia, at age 97. Sexual desire was affirmed by 27% of men and 5% of women in the survey. Among the men, 32% said they still had sexual thoughts, compared with 18% of women. Meanwhile, 26% of the men and 15% of the women said they missed sexual activity.
What should clinicians do with this information? First, we could start talking about sex with our older patients. According to the 97-year-old Swedes, most want us to! More than 8 in 10 of both women and men in the survey expressed positive views about questions on sexuality. And please don’t be scared to address the subject in the single senior. They, too, can have a sexual or relationship issue and are happy when we raise the subject. They’re not scared to talk about masturbation, either.
When caring for those with chronic diseases, cancer, in the course of physical rehabilitation, and even in the last phase of life, the clinical experience indicates that our patients are happy when we address sexuality and intimacy. Doing so can open the door to the admission of a problem and a corresponding solution, a lubricant or a PDE5 inhibitor.
But sometimes the solution is the conversation itself: Roughly 25% of patients are sufficiently helped simply by talking about sex. Addressing the importance of sexual pleasure is nearly always valuable.
Here are a few ice-breakers I find helpful:
- Did taking this medication change aspects of sexuality? If so, does that bother you?
- Knowing that continuing intimacy is healthy, do you mind if I address that subject?
- We know that aspects of sexuality and intimacy are healthy. Without a partner, some people become sexually isolated. Would you like to talk about that?’
If addressing sexuality has benefits, what about sex itself?
We are gradually learning more about the many short-, intermediate-, and long-term health benefits of solo and joint sexual activity. Short-term benefits include muscle relaxation, pain relief (even, perhaps ironically, for headaches), and better sleep – all pretty valuable for older adults. Examples of intermediate-term benefits include stress relief and less depression. Research from the United States has found that hugging can reduce the concentrations of proinflammatory cytokines, and kissing positively influences cholesterol levels.
Finally, while the long-term benefits of sex might be less relevant for seniors, they do exist.
Among them are delayed onset of dementia and a substantial reduction in cardiovascular and cerebrovascular problems in men. More sex has been linked to longevity, with men benefiting a bit more than women from going through the entire process, including an orgasm, whereas women appear to gain from having a “satisfying” sex life, which does not always require an orgasm.
Let us not forget that these benefits apply to both patients and clinicians alike. Addressing intimacy and sexuality can ease eventual sexual concerns and potentially create a stronger clinician-patient relationship.
Dr. Gianotten, MD is emeritus senior lecturer in medical sexology, Erasmus University Medical Centre, Rotterdam, the Netherlands. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Breast cancer survivors need a comprehensive care plan, says doctor
said Patricia A. Ganz, MD, during a presentation at the European Society for Medical Oncology Breast Cancer annual congress.
Several studies suggest that many breast cancer patients are not well prepared to move forward after a breast cancer diagnosis and subsequent treatments, continued Dr. Ganz, who works at the UCLA Jonsson Comprehensive Cancer Center, Los Angeles.
Meeting the survivorship needs of breast cancer patients requires addressing both their physical and psychosocial needs, Dr. Ganz said. She explained how to achieve that, but first pointed to research elaborating on what's missing from some breast cancer survivors' care and barriers to these patients having their variety of health-related needs met.
In a 2021 study published in the Journal of Cancer Survivorship, Dr. Ganz and colleagues conducted a survey of approximately 200 medical oncologists in the United States. They determined that less than 50% provide survivorship care plans to patients at the end of treatment or communicate with patients’ other physicians about follow-up care.
In a secondary analysis of data from the same survey published in 2022 in Breast Cancer Research and Treatment, Dr. Ganz and colleagues examined medical oncologists’ perceived barriers to addressing both physical and psychosocial long-term effects in breast cancer survivors. For both, lack of time was the greatest perceived barrier, cited by nearly two-thirds of oncologists. Other barriers to addressing physical effects included lack of evidence-based, effective interventions, lack of clinical algorithms to guide care, and ambiguity regarding professional responsibility at the end of treatment. Other top barriers to addressing psychosocial issues included lack of mental health providers, lack of psychosocial resources, and lack of clinician knowledge and skills.
Data from additional studies suggest that, overall, cancer patients with greater physical burdens, such as more complex and lengthy treatment regimens, also have greater psychosocial needs, Dr. Ganz noted. Plus, approximately 15%-20% of cancer survivors have ongoing anxiety and depressive symptoms.
Shift to primary care
As more breast cancer and other cancer patients survive for longer periods, more care will likely occur in general medical settings, Dr. Ganz said. Issues to be addressed will include the potential increased risk of comorbid conditions for these survivors, and whether survivorship interventions earlier in the disease trajectory will impact survivorship. For cancer patients who achieve remission after treatment, the first 5 years after a diagnosis involves treatment and short-term surveillance for late effects. Beyond 5 years, care for cancer survivors mainly involves primary care and management of any comorbid conditions, as well as surveillance for late effects and recurrences, and awareness of new research.
A patient consultation early in the process after diagnosis is the start of a continuum of care, Dr. Ganz said. A patient consultation should address symptoms related to initial treatments, such as neuropathy, pain, fatigue, and insomnia, as well as the psychological symptoms of anxiety and depression. An early consultation also should evaluate adherence to endocrine therapy and management of symptoms, if needed, with the larger goal of preparing patients for recovery and the transition to survivorship, and what to expect for long-term follow-up.
Delivering the three P’s
The “Three P’s” of survivor care for breast cancer patients are palliation, prevention, and promotion of health, according to Dr. Ganz .
The first “P,” for palliative, is a key part of survivorship care, said Dr. Ganz. Palliative care is defined as care that focuses on reducing symptom severity and improving quality of life. The biological effects of cancer treatment can be associated with physical effects, such as functional limitations and frailty, and behavioral/cognitive effects such as depression, fatigue, and cognitive deficits, she said. To manage these effects and provide palliative care, consultation is needed with specialists in relevant areas including mental health, pain management, physical medicine/rehabilitation, endocrinology, cardiology, and neurology.
The second “P,” which is for prevention in survivorship care, refers to ongoing follow-up screening to identify any potentially serious late-onset complications such as osteoporosis or cardiac disease so they can be addressed, said Dr. Ganz. Other considerations include chemoprevention if available and genetic counseling for patients with hereditary cancers. Prevention also includes counseling patients about lifestyle modifications to help prevent additional cancer.
The goal of the third “P,” which is for health promotion, is to promote risk reduction for the health problems associated with accelerated aging that may arise in cancer survivors, said Dr. Ganz.
Health promotion strategies include maintaining a healthy weight, increasing physical activity, and avoiding harmful exposures, she said. Healthy lifestyle interventions can also reduce the risk of other chronic diseases such as diabetes and heart disease.
To that end, Dr. Ganz outlined several behavioral interventions that may mitigate the effects of cancer treatment on the accelerated aging process, including stress reduction in the form of meditation or yoga, cognitive behavioral therapy, improving sleep, increasing physical activity, reducing obesity, and decreasing tobacco and alcohol use. These interventions may help reduce inflammation and promote tissue repair and healing.
For cancer survivors, the life span may be longer than the health span, and these patients may benefit from an integrated model of care, with systematic screening and consolidated appointments, rather than a fragmented model in which departments and referrals are siloed, which may result in conflicting advice or redundancy, said Dr. Ganz.
Looking ahead, more research is needed to explore models of care delivery, as requirements for survivor care will vary among patients and care settings, Dr. Ganz said.
However, regardless of setting, treatment plans and shared decision-making can help reduce potential long-term or late-emerging effects, she said. Developing a survivorship care plan can help patients learn how to enhance their recovery.
During a question and answer session, Dr. Ganz was asked about whether hormone therapy could be used for patients with hormone negative breast cancer. “I think vaginal estrogen can be used if someone is on tamoxifen,” she said. However, “we need to be cautious” in case there are remaining estrogen positive cells, in order to avoid potential metastases, and use of hormone therapy in breast cancer survivors is an individualized decision based in part on quality of life.
Engaging a patient’s partner early can be helpful
If possible, engage the patient’s partner in survivorship discussions, said Luzia Travado, PhD, head of psycho-oncology at the Champalimaud Foundation, Lisbon, who presented on the topic of sexuality and commented on survivorship during the discussion. For those women with partners, engaging the partner early in treatment often means they are more likely to play a larger role in the post treatment and long term by providing stability and emotional support.
“Make sure partners are engaged and understand that they have a role, and that this role is valued,” she said. Unfortunately, there are a lot of divorced women with breast cancer, as the disease can take a toll on relationships. However, remember “sexuality is not just sex; it is caring, loving, and intimacy.”
“To end on a positive note, it is important to empower patients, and to give them self-management skills so they can make things even better in their survivorship,” said Dr. Ganz. In spite of discussing difficulties and challenges, one of the goals of the session was to offer potential solutions and answers.
Dr. Ganz disclosed serving as editor of the cancer survivorship section on Up-to-Date, and serving as a consultant for Blue Note Therapeutics, GRAIL, InformedDNA, and Roche-Genentech. Dr. Travado had no relevant financial conflicts to disclose.
said Patricia A. Ganz, MD, during a presentation at the European Society for Medical Oncology Breast Cancer annual congress.
Several studies suggest that many breast cancer patients are not well prepared to move forward after a breast cancer diagnosis and subsequent treatments, continued Dr. Ganz, who works at the UCLA Jonsson Comprehensive Cancer Center, Los Angeles.
Meeting the survivorship needs of breast cancer patients requires addressing both their physical and psychosocial needs, Dr. Ganz said. She explained how to achieve that, but first pointed to research elaborating on what's missing from some breast cancer survivors' care and barriers to these patients having their variety of health-related needs met.
In a 2021 study published in the Journal of Cancer Survivorship, Dr. Ganz and colleagues conducted a survey of approximately 200 medical oncologists in the United States. They determined that less than 50% provide survivorship care plans to patients at the end of treatment or communicate with patients’ other physicians about follow-up care.
In a secondary analysis of data from the same survey published in 2022 in Breast Cancer Research and Treatment, Dr. Ganz and colleagues examined medical oncologists’ perceived barriers to addressing both physical and psychosocial long-term effects in breast cancer survivors. For both, lack of time was the greatest perceived barrier, cited by nearly two-thirds of oncologists. Other barriers to addressing physical effects included lack of evidence-based, effective interventions, lack of clinical algorithms to guide care, and ambiguity regarding professional responsibility at the end of treatment. Other top barriers to addressing psychosocial issues included lack of mental health providers, lack of psychosocial resources, and lack of clinician knowledge and skills.
Data from additional studies suggest that, overall, cancer patients with greater physical burdens, such as more complex and lengthy treatment regimens, also have greater psychosocial needs, Dr. Ganz noted. Plus, approximately 15%-20% of cancer survivors have ongoing anxiety and depressive symptoms.
Shift to primary care
As more breast cancer and other cancer patients survive for longer periods, more care will likely occur in general medical settings, Dr. Ganz said. Issues to be addressed will include the potential increased risk of comorbid conditions for these survivors, and whether survivorship interventions earlier in the disease trajectory will impact survivorship. For cancer patients who achieve remission after treatment, the first 5 years after a diagnosis involves treatment and short-term surveillance for late effects. Beyond 5 years, care for cancer survivors mainly involves primary care and management of any comorbid conditions, as well as surveillance for late effects and recurrences, and awareness of new research.
A patient consultation early in the process after diagnosis is the start of a continuum of care, Dr. Ganz said. A patient consultation should address symptoms related to initial treatments, such as neuropathy, pain, fatigue, and insomnia, as well as the psychological symptoms of anxiety and depression. An early consultation also should evaluate adherence to endocrine therapy and management of symptoms, if needed, with the larger goal of preparing patients for recovery and the transition to survivorship, and what to expect for long-term follow-up.
Delivering the three P’s
The “Three P’s” of survivor care for breast cancer patients are palliation, prevention, and promotion of health, according to Dr. Ganz .
The first “P,” for palliative, is a key part of survivorship care, said Dr. Ganz. Palliative care is defined as care that focuses on reducing symptom severity and improving quality of life. The biological effects of cancer treatment can be associated with physical effects, such as functional limitations and frailty, and behavioral/cognitive effects such as depression, fatigue, and cognitive deficits, she said. To manage these effects and provide palliative care, consultation is needed with specialists in relevant areas including mental health, pain management, physical medicine/rehabilitation, endocrinology, cardiology, and neurology.
The second “P,” which is for prevention in survivorship care, refers to ongoing follow-up screening to identify any potentially serious late-onset complications such as osteoporosis or cardiac disease so they can be addressed, said Dr. Ganz. Other considerations include chemoprevention if available and genetic counseling for patients with hereditary cancers. Prevention also includes counseling patients about lifestyle modifications to help prevent additional cancer.
The goal of the third “P,” which is for health promotion, is to promote risk reduction for the health problems associated with accelerated aging that may arise in cancer survivors, said Dr. Ganz.
Health promotion strategies include maintaining a healthy weight, increasing physical activity, and avoiding harmful exposures, she said. Healthy lifestyle interventions can also reduce the risk of other chronic diseases such as diabetes and heart disease.
To that end, Dr. Ganz outlined several behavioral interventions that may mitigate the effects of cancer treatment on the accelerated aging process, including stress reduction in the form of meditation or yoga, cognitive behavioral therapy, improving sleep, increasing physical activity, reducing obesity, and decreasing tobacco and alcohol use. These interventions may help reduce inflammation and promote tissue repair and healing.
For cancer survivors, the life span may be longer than the health span, and these patients may benefit from an integrated model of care, with systematic screening and consolidated appointments, rather than a fragmented model in which departments and referrals are siloed, which may result in conflicting advice or redundancy, said Dr. Ganz.
Looking ahead, more research is needed to explore models of care delivery, as requirements for survivor care will vary among patients and care settings, Dr. Ganz said.
However, regardless of setting, treatment plans and shared decision-making can help reduce potential long-term or late-emerging effects, she said. Developing a survivorship care plan can help patients learn how to enhance their recovery.
During a question and answer session, Dr. Ganz was asked about whether hormone therapy could be used for patients with hormone negative breast cancer. “I think vaginal estrogen can be used if someone is on tamoxifen,” she said. However, “we need to be cautious” in case there are remaining estrogen positive cells, in order to avoid potential metastases, and use of hormone therapy in breast cancer survivors is an individualized decision based in part on quality of life.
Engaging a patient’s partner early can be helpful
If possible, engage the patient’s partner in survivorship discussions, said Luzia Travado, PhD, head of psycho-oncology at the Champalimaud Foundation, Lisbon, who presented on the topic of sexuality and commented on survivorship during the discussion. For those women with partners, engaging the partner early in treatment often means they are more likely to play a larger role in the post treatment and long term by providing stability and emotional support.
“Make sure partners are engaged and understand that they have a role, and that this role is valued,” she said. Unfortunately, there are a lot of divorced women with breast cancer, as the disease can take a toll on relationships. However, remember “sexuality is not just sex; it is caring, loving, and intimacy.”
“To end on a positive note, it is important to empower patients, and to give them self-management skills so they can make things even better in their survivorship,” said Dr. Ganz. In spite of discussing difficulties and challenges, one of the goals of the session was to offer potential solutions and answers.
Dr. Ganz disclosed serving as editor of the cancer survivorship section on Up-to-Date, and serving as a consultant for Blue Note Therapeutics, GRAIL, InformedDNA, and Roche-Genentech. Dr. Travado had no relevant financial conflicts to disclose.
said Patricia A. Ganz, MD, during a presentation at the European Society for Medical Oncology Breast Cancer annual congress.
Several studies suggest that many breast cancer patients are not well prepared to move forward after a breast cancer diagnosis and subsequent treatments, continued Dr. Ganz, who works at the UCLA Jonsson Comprehensive Cancer Center, Los Angeles.
Meeting the survivorship needs of breast cancer patients requires addressing both their physical and psychosocial needs, Dr. Ganz said. She explained how to achieve that, but first pointed to research elaborating on what's missing from some breast cancer survivors' care and barriers to these patients having their variety of health-related needs met.
In a 2021 study published in the Journal of Cancer Survivorship, Dr. Ganz and colleagues conducted a survey of approximately 200 medical oncologists in the United States. They determined that less than 50% provide survivorship care plans to patients at the end of treatment or communicate with patients’ other physicians about follow-up care.
In a secondary analysis of data from the same survey published in 2022 in Breast Cancer Research and Treatment, Dr. Ganz and colleagues examined medical oncologists’ perceived barriers to addressing both physical and psychosocial long-term effects in breast cancer survivors. For both, lack of time was the greatest perceived barrier, cited by nearly two-thirds of oncologists. Other barriers to addressing physical effects included lack of evidence-based, effective interventions, lack of clinical algorithms to guide care, and ambiguity regarding professional responsibility at the end of treatment. Other top barriers to addressing psychosocial issues included lack of mental health providers, lack of psychosocial resources, and lack of clinician knowledge and skills.
Data from additional studies suggest that, overall, cancer patients with greater physical burdens, such as more complex and lengthy treatment regimens, also have greater psychosocial needs, Dr. Ganz noted. Plus, approximately 15%-20% of cancer survivors have ongoing anxiety and depressive symptoms.
Shift to primary care
As more breast cancer and other cancer patients survive for longer periods, more care will likely occur in general medical settings, Dr. Ganz said. Issues to be addressed will include the potential increased risk of comorbid conditions for these survivors, and whether survivorship interventions earlier in the disease trajectory will impact survivorship. For cancer patients who achieve remission after treatment, the first 5 years after a diagnosis involves treatment and short-term surveillance for late effects. Beyond 5 years, care for cancer survivors mainly involves primary care and management of any comorbid conditions, as well as surveillance for late effects and recurrences, and awareness of new research.
A patient consultation early in the process after diagnosis is the start of a continuum of care, Dr. Ganz said. A patient consultation should address symptoms related to initial treatments, such as neuropathy, pain, fatigue, and insomnia, as well as the psychological symptoms of anxiety and depression. An early consultation also should evaluate adherence to endocrine therapy and management of symptoms, if needed, with the larger goal of preparing patients for recovery and the transition to survivorship, and what to expect for long-term follow-up.
Delivering the three P’s
The “Three P’s” of survivor care for breast cancer patients are palliation, prevention, and promotion of health, according to Dr. Ganz .
The first “P,” for palliative, is a key part of survivorship care, said Dr. Ganz. Palliative care is defined as care that focuses on reducing symptom severity and improving quality of life. The biological effects of cancer treatment can be associated with physical effects, such as functional limitations and frailty, and behavioral/cognitive effects such as depression, fatigue, and cognitive deficits, she said. To manage these effects and provide palliative care, consultation is needed with specialists in relevant areas including mental health, pain management, physical medicine/rehabilitation, endocrinology, cardiology, and neurology.
The second “P,” which is for prevention in survivorship care, refers to ongoing follow-up screening to identify any potentially serious late-onset complications such as osteoporosis or cardiac disease so they can be addressed, said Dr. Ganz. Other considerations include chemoprevention if available and genetic counseling for patients with hereditary cancers. Prevention also includes counseling patients about lifestyle modifications to help prevent additional cancer.
The goal of the third “P,” which is for health promotion, is to promote risk reduction for the health problems associated with accelerated aging that may arise in cancer survivors, said Dr. Ganz.
Health promotion strategies include maintaining a healthy weight, increasing physical activity, and avoiding harmful exposures, she said. Healthy lifestyle interventions can also reduce the risk of other chronic diseases such as diabetes and heart disease.
To that end, Dr. Ganz outlined several behavioral interventions that may mitigate the effects of cancer treatment on the accelerated aging process, including stress reduction in the form of meditation or yoga, cognitive behavioral therapy, improving sleep, increasing physical activity, reducing obesity, and decreasing tobacco and alcohol use. These interventions may help reduce inflammation and promote tissue repair and healing.
For cancer survivors, the life span may be longer than the health span, and these patients may benefit from an integrated model of care, with systematic screening and consolidated appointments, rather than a fragmented model in which departments and referrals are siloed, which may result in conflicting advice or redundancy, said Dr. Ganz.
Looking ahead, more research is needed to explore models of care delivery, as requirements for survivor care will vary among patients and care settings, Dr. Ganz said.
However, regardless of setting, treatment plans and shared decision-making can help reduce potential long-term or late-emerging effects, she said. Developing a survivorship care plan can help patients learn how to enhance their recovery.
During a question and answer session, Dr. Ganz was asked about whether hormone therapy could be used for patients with hormone negative breast cancer. “I think vaginal estrogen can be used if someone is on tamoxifen,” she said. However, “we need to be cautious” in case there are remaining estrogen positive cells, in order to avoid potential metastases, and use of hormone therapy in breast cancer survivors is an individualized decision based in part on quality of life.
Engaging a patient’s partner early can be helpful
If possible, engage the patient’s partner in survivorship discussions, said Luzia Travado, PhD, head of psycho-oncology at the Champalimaud Foundation, Lisbon, who presented on the topic of sexuality and commented on survivorship during the discussion. For those women with partners, engaging the partner early in treatment often means they are more likely to play a larger role in the post treatment and long term by providing stability and emotional support.
“Make sure partners are engaged and understand that they have a role, and that this role is valued,” she said. Unfortunately, there are a lot of divorced women with breast cancer, as the disease can take a toll on relationships. However, remember “sexuality is not just sex; it is caring, loving, and intimacy.”
“To end on a positive note, it is important to empower patients, and to give them self-management skills so they can make things even better in their survivorship,” said Dr. Ganz. In spite of discussing difficulties and challenges, one of the goals of the session was to offer potential solutions and answers.
Dr. Ganz disclosed serving as editor of the cancer survivorship section on Up-to-Date, and serving as a consultant for Blue Note Therapeutics, GRAIL, InformedDNA, and Roche-Genentech. Dr. Travado had no relevant financial conflicts to disclose.
FROM ESMO BREAST CANCER 2023
Morning PT
Tuesdays and Fridays are tough. Not so much because of clinic, but rather because of the 32 minutes before clinic that I’m on the Peloton bike. They are the mornings I dedicate to training VO2max.
Training VO2max, or maximal oxygen consumption, is simple. Spin for a leisurely, easy-breathing, 4 minutes, then for 4 minutes push yourself until you see the light of heaven and wish for death to come. Then relax for 4 minutes again. Repeat this cycle four to six times. Done justly, you will dread Tuesdays and Fridays too. The punishing cycle of a 4-minute push, then 4-minute recovery is, however, an excellent way to improve cardiovascular fitness. And no, I’m not training for the Boston Marathon, so why am I working so hard? Because I’m training for marathon clinic days for the next 20 years.
Now more than ever, I feel we have to be physically fit to deal with a physicians’ day’s work. It’s exhausting. The root cause is too much work, yes, but I believe being physically fit could help.
I was talking to an 86-year-old patient about this very topic recently. He was short, with a well-manicured goatee and shiny head. He stuck his arm out to shake my hand. “Glad we’re back to handshakes again, doc.” His grip was that of a 30-year-old. “Buff” you’d likely describe him: He is noticeably muscular, not a skinny old man. He’s an old Navy Master Chief who started a business in wholesale flowers, which distributes all over the United States. And he’s still working full time. Impressed, I asked his secret for such vigor. PT, he replied.
PT, or physical training, is a foundational element of the Navy. Every sailor starts his or her day with morning PT before carrying out their duties. Some 30 years later, this guy is still getting after it. He does push-ups, sit-ups, and pull-ups nearly every morning. Morning PT is what he attributes to his success not only in health, but also business. As he sees it, he has the business savvy and experience of an old guy and the energy and stamina of a college kid. A good combination for a successful life.
I’ve always been pretty fit. Lately, I’ve been trying to take it to the next level, to not just be “physically active,” but rather “high-performance fit.” There are plenty of sources for instruction; how to stay young and healthy isn’t a new idea after all. I mean, Herodotus wrote of finding the Fountain of Youth in the 5th century BCE. A couple thousand years later, it’s still on trend. One of my favorite sages giving health span advice is Peter Attia, MD. I’ve been a fan since I met him at TEDMED in 2013 and I marvel at the astounding body of work he has created since. A Johns Hopkins–trained surgeon, he has spent his career reviewing the scientific literature about longevity and sharing it as actionable content. His book, “Outlive: The Science and Art of Longevity” (New York: Penguin Random House, 2023) is a nice summary of his work. I recommend it.
Right now I’m switching between type 2 muscle fiber work (lots of jumping like my 2-year-old) and cardiovascular training including the aforementioned VO2max work. I cannot say that my patient inbox is any cleaner, or that I’m faster in the office, but I’m not flagging by the end of the day anymore. Master Chief challenged me to match his 10 pull-ups before he returns for his follow up visit. I’ll gladly give up Peloton sprints to work on that.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Tuesdays and Fridays are tough. Not so much because of clinic, but rather because of the 32 minutes before clinic that I’m on the Peloton bike. They are the mornings I dedicate to training VO2max.
Training VO2max, or maximal oxygen consumption, is simple. Spin for a leisurely, easy-breathing, 4 minutes, then for 4 minutes push yourself until you see the light of heaven and wish for death to come. Then relax for 4 minutes again. Repeat this cycle four to six times. Done justly, you will dread Tuesdays and Fridays too. The punishing cycle of a 4-minute push, then 4-minute recovery is, however, an excellent way to improve cardiovascular fitness. And no, I’m not training for the Boston Marathon, so why am I working so hard? Because I’m training for marathon clinic days for the next 20 years.
Now more than ever, I feel we have to be physically fit to deal with a physicians’ day’s work. It’s exhausting. The root cause is too much work, yes, but I believe being physically fit could help.
I was talking to an 86-year-old patient about this very topic recently. He was short, with a well-manicured goatee and shiny head. He stuck his arm out to shake my hand. “Glad we’re back to handshakes again, doc.” His grip was that of a 30-year-old. “Buff” you’d likely describe him: He is noticeably muscular, not a skinny old man. He’s an old Navy Master Chief who started a business in wholesale flowers, which distributes all over the United States. And he’s still working full time. Impressed, I asked his secret for such vigor. PT, he replied.
PT, or physical training, is a foundational element of the Navy. Every sailor starts his or her day with morning PT before carrying out their duties. Some 30 years later, this guy is still getting after it. He does push-ups, sit-ups, and pull-ups nearly every morning. Morning PT is what he attributes to his success not only in health, but also business. As he sees it, he has the business savvy and experience of an old guy and the energy and stamina of a college kid. A good combination for a successful life.
I’ve always been pretty fit. Lately, I’ve been trying to take it to the next level, to not just be “physically active,” but rather “high-performance fit.” There are plenty of sources for instruction; how to stay young and healthy isn’t a new idea after all. I mean, Herodotus wrote of finding the Fountain of Youth in the 5th century BCE. A couple thousand years later, it’s still on trend. One of my favorite sages giving health span advice is Peter Attia, MD. I’ve been a fan since I met him at TEDMED in 2013 and I marvel at the astounding body of work he has created since. A Johns Hopkins–trained surgeon, he has spent his career reviewing the scientific literature about longevity and sharing it as actionable content. His book, “Outlive: The Science and Art of Longevity” (New York: Penguin Random House, 2023) is a nice summary of his work. I recommend it.
Right now I’m switching between type 2 muscle fiber work (lots of jumping like my 2-year-old) and cardiovascular training including the aforementioned VO2max work. I cannot say that my patient inbox is any cleaner, or that I’m faster in the office, but I’m not flagging by the end of the day anymore. Master Chief challenged me to match his 10 pull-ups before he returns for his follow up visit. I’ll gladly give up Peloton sprints to work on that.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Tuesdays and Fridays are tough. Not so much because of clinic, but rather because of the 32 minutes before clinic that I’m on the Peloton bike. They are the mornings I dedicate to training VO2max.
Training VO2max, or maximal oxygen consumption, is simple. Spin for a leisurely, easy-breathing, 4 minutes, then for 4 minutes push yourself until you see the light of heaven and wish for death to come. Then relax for 4 minutes again. Repeat this cycle four to six times. Done justly, you will dread Tuesdays and Fridays too. The punishing cycle of a 4-minute push, then 4-minute recovery is, however, an excellent way to improve cardiovascular fitness. And no, I’m not training for the Boston Marathon, so why am I working so hard? Because I’m training for marathon clinic days for the next 20 years.
Now more than ever, I feel we have to be physically fit to deal with a physicians’ day’s work. It’s exhausting. The root cause is too much work, yes, but I believe being physically fit could help.
I was talking to an 86-year-old patient about this very topic recently. He was short, with a well-manicured goatee and shiny head. He stuck his arm out to shake my hand. “Glad we’re back to handshakes again, doc.” His grip was that of a 30-year-old. “Buff” you’d likely describe him: He is noticeably muscular, not a skinny old man. He’s an old Navy Master Chief who started a business in wholesale flowers, which distributes all over the United States. And he’s still working full time. Impressed, I asked his secret for such vigor. PT, he replied.
PT, or physical training, is a foundational element of the Navy. Every sailor starts his or her day with morning PT before carrying out their duties. Some 30 years later, this guy is still getting after it. He does push-ups, sit-ups, and pull-ups nearly every morning. Morning PT is what he attributes to his success not only in health, but also business. As he sees it, he has the business savvy and experience of an old guy and the energy and stamina of a college kid. A good combination for a successful life.
I’ve always been pretty fit. Lately, I’ve been trying to take it to the next level, to not just be “physically active,” but rather “high-performance fit.” There are plenty of sources for instruction; how to stay young and healthy isn’t a new idea after all. I mean, Herodotus wrote of finding the Fountain of Youth in the 5th century BCE. A couple thousand years later, it’s still on trend. One of my favorite sages giving health span advice is Peter Attia, MD. I’ve been a fan since I met him at TEDMED in 2013 and I marvel at the astounding body of work he has created since. A Johns Hopkins–trained surgeon, he has spent his career reviewing the scientific literature about longevity and sharing it as actionable content. His book, “Outlive: The Science and Art of Longevity” (New York: Penguin Random House, 2023) is a nice summary of his work. I recommend it.
Right now I’m switching between type 2 muscle fiber work (lots of jumping like my 2-year-old) and cardiovascular training including the aforementioned VO2max work. I cannot say that my patient inbox is any cleaner, or that I’m faster in the office, but I’m not flagging by the end of the day anymore. Master Chief challenged me to match his 10 pull-ups before he returns for his follow up visit. I’ll gladly give up Peloton sprints to work on that.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Review supports continued mask-wearing in health care visits
A new study urges people to continue wearing protective masks in medical settings, even though the U.S. public health emergency declaration around COVID-19 has expired.
Masks continue to lower the risk of catching the virus during medical visits, according to the study, published in Annals of Internal Medicine. And there was not much difference between wearing surgical masks and N95 respirators in health care settings.
The researchers reviewed 3 randomized trials and 21 observational studies to compare the effectiveness of those and cloth masks in reducing COVID-19 transmission.
Tara N. Palmore, MD, of George Washington University, Washington, and David K. Henderson, MD, of the National Institutes of Health, Bethesda, Md., wrote in an opinion article accompanying the study.
“In our enthusiasm to return to the appearance and feeling of normalcy, and as institutions decide which mitigation strategies to discontinue, we strongly advocate not discarding this important lesson learned for the sake of our patients’ safety,” Dr. Palmore and Dr. Henderson wrote.
Surgical masks limit the spread of aerosols and droplets from people who have the flu, coronaviruses or other respiratory viruses, CNN reported. And while masks are not 100% effective, they substantially lower the amount of virus put into the air via coughing and talking.
The study said one reason people should wear masks to medical settings is because “health care personnel are notorious for coming to work while ill.” Transmission from patient to staff and staff to patient is still possible, but rare, when both are masked.
The review authors reported no conflicts of interest. Dr. Palmore has received grants from the NIH, Rigel, Gilead, and AbbVie, and Dr. Henderson is a past president of the Society for Healthcare Epidemiology of America.
A version of this article first appeared on WebMD.com.
A new study urges people to continue wearing protective masks in medical settings, even though the U.S. public health emergency declaration around COVID-19 has expired.
Masks continue to lower the risk of catching the virus during medical visits, according to the study, published in Annals of Internal Medicine. And there was not much difference between wearing surgical masks and N95 respirators in health care settings.
The researchers reviewed 3 randomized trials and 21 observational studies to compare the effectiveness of those and cloth masks in reducing COVID-19 transmission.
Tara N. Palmore, MD, of George Washington University, Washington, and David K. Henderson, MD, of the National Institutes of Health, Bethesda, Md., wrote in an opinion article accompanying the study.
“In our enthusiasm to return to the appearance and feeling of normalcy, and as institutions decide which mitigation strategies to discontinue, we strongly advocate not discarding this important lesson learned for the sake of our patients’ safety,” Dr. Palmore and Dr. Henderson wrote.
Surgical masks limit the spread of aerosols and droplets from people who have the flu, coronaviruses or other respiratory viruses, CNN reported. And while masks are not 100% effective, they substantially lower the amount of virus put into the air via coughing and talking.
The study said one reason people should wear masks to medical settings is because “health care personnel are notorious for coming to work while ill.” Transmission from patient to staff and staff to patient is still possible, but rare, when both are masked.
The review authors reported no conflicts of interest. Dr. Palmore has received grants from the NIH, Rigel, Gilead, and AbbVie, and Dr. Henderson is a past president of the Society for Healthcare Epidemiology of America.
A version of this article first appeared on WebMD.com.
A new study urges people to continue wearing protective masks in medical settings, even though the U.S. public health emergency declaration around COVID-19 has expired.
Masks continue to lower the risk of catching the virus during medical visits, according to the study, published in Annals of Internal Medicine. And there was not much difference between wearing surgical masks and N95 respirators in health care settings.
The researchers reviewed 3 randomized trials and 21 observational studies to compare the effectiveness of those and cloth masks in reducing COVID-19 transmission.
Tara N. Palmore, MD, of George Washington University, Washington, and David K. Henderson, MD, of the National Institutes of Health, Bethesda, Md., wrote in an opinion article accompanying the study.
“In our enthusiasm to return to the appearance and feeling of normalcy, and as institutions decide which mitigation strategies to discontinue, we strongly advocate not discarding this important lesson learned for the sake of our patients’ safety,” Dr. Palmore and Dr. Henderson wrote.
Surgical masks limit the spread of aerosols and droplets from people who have the flu, coronaviruses or other respiratory viruses, CNN reported. And while masks are not 100% effective, they substantially lower the amount of virus put into the air via coughing and talking.
The study said one reason people should wear masks to medical settings is because “health care personnel are notorious for coming to work while ill.” Transmission from patient to staff and staff to patient is still possible, but rare, when both are masked.
The review authors reported no conflicts of interest. Dr. Palmore has received grants from the NIH, Rigel, Gilead, and AbbVie, and Dr. Henderson is a past president of the Society for Healthcare Epidemiology of America.
A version of this article first appeared on WebMD.com.
FROM ANNALS OF INTERNAL MEDICINE
U.S. adults report depression at record rates: Survey
In a survey, 29% of adults said they had been diagnosed with depression during their lifetime, and 18% said they currently have depression or are being treated for it. Those rates are up from the baseline 2015 rates of 20% of people ever having depression and 11% of people with a current diagnosis.
Depression had been steadily rising before the pandemic, and the Gallup analysts wrote that “social isolation, loneliness, fear of infection, psychological exhaustion (particularly among frontline responders such as health care workers), elevated substance abuse, and disruptions in mental health services have all likely played a role” in the increase.
“The fact that Americans are more depressed and struggling after this time of incredible stress and isolation is perhaps not surprising,” American Psychiatric Association president Rebecca Brendel, MD, told CNN. “There are lingering effects on our health, especially our mental health, from the past 3 years that disrupted everything we knew.”
The new estimates are based on online survey responses collected in February from 5,167 adults in the United States who answered the questions:
- Has a doctor or nurse ever told you that you have depression?
- Do you currently have or are you currently being treated for depression?
Depression, which is also called major depressive disorder, is a treatable illness that negatively affects how someone feels, thinks, and acts. The symptoms can be both emotional (such as sadness or loss of interest in activities) and physical (such as fatigue or slowed movements or speech).
The latest study found that depression rates increased the most among women, young adults, Black people, and Hispanic people. For the first time, more Black and Hispanic people than White people reported ever being diagnosed with depression. The lifetime depression rate among Black people was 34%, compared with 31% for Hispanic people and 29% for White people.
The rate of lifetime depression among women jumped 10 percentage points in the past 5 years, to 37%, in February, the survey results showed. About 1 in 4 women said they currently had depression or were being treated for it, up 6 percentage points compared with 5 years ago.
When responses were analyzed by age, those 18-44 years old were the most likely to report ever being diagnosed with depression or currently having the illness. About one-third of younger adults have ever been diagnosed, and more than 1 in 5 said they currently have depression.
Dr. Brendel said awareness and reduced stigma could be adding to the rising rates of depression.
“We’re making it easier to talk about mental health and looking at it as part of our overall wellness, just like physical health,” she said. “People are aware of depression, and people are seeking help for it.”
If you or someone you know needs help, dial 988 for support from the national Suicide & Crisis Lifeline. It’s free, confidential, and available 24 hours a day, 7 days a week. You can also visit 988lifeline.org and choose the chat feature.
A version of this article first appeared on Medscape.com.
In a survey, 29% of adults said they had been diagnosed with depression during their lifetime, and 18% said they currently have depression or are being treated for it. Those rates are up from the baseline 2015 rates of 20% of people ever having depression and 11% of people with a current diagnosis.
Depression had been steadily rising before the pandemic, and the Gallup analysts wrote that “social isolation, loneliness, fear of infection, psychological exhaustion (particularly among frontline responders such as health care workers), elevated substance abuse, and disruptions in mental health services have all likely played a role” in the increase.
“The fact that Americans are more depressed and struggling after this time of incredible stress and isolation is perhaps not surprising,” American Psychiatric Association president Rebecca Brendel, MD, told CNN. “There are lingering effects on our health, especially our mental health, from the past 3 years that disrupted everything we knew.”
The new estimates are based on online survey responses collected in February from 5,167 adults in the United States who answered the questions:
- Has a doctor or nurse ever told you that you have depression?
- Do you currently have or are you currently being treated for depression?
Depression, which is also called major depressive disorder, is a treatable illness that negatively affects how someone feels, thinks, and acts. The symptoms can be both emotional (such as sadness or loss of interest in activities) and physical (such as fatigue or slowed movements or speech).
The latest study found that depression rates increased the most among women, young adults, Black people, and Hispanic people. For the first time, more Black and Hispanic people than White people reported ever being diagnosed with depression. The lifetime depression rate among Black people was 34%, compared with 31% for Hispanic people and 29% for White people.
The rate of lifetime depression among women jumped 10 percentage points in the past 5 years, to 37%, in February, the survey results showed. About 1 in 4 women said they currently had depression or were being treated for it, up 6 percentage points compared with 5 years ago.
When responses were analyzed by age, those 18-44 years old were the most likely to report ever being diagnosed with depression or currently having the illness. About one-third of younger adults have ever been diagnosed, and more than 1 in 5 said they currently have depression.
Dr. Brendel said awareness and reduced stigma could be adding to the rising rates of depression.
“We’re making it easier to talk about mental health and looking at it as part of our overall wellness, just like physical health,” she said. “People are aware of depression, and people are seeking help for it.”
If you or someone you know needs help, dial 988 for support from the national Suicide & Crisis Lifeline. It’s free, confidential, and available 24 hours a day, 7 days a week. You can also visit 988lifeline.org and choose the chat feature.
A version of this article first appeared on Medscape.com.
In a survey, 29% of adults said they had been diagnosed with depression during their lifetime, and 18% said they currently have depression or are being treated for it. Those rates are up from the baseline 2015 rates of 20% of people ever having depression and 11% of people with a current diagnosis.
Depression had been steadily rising before the pandemic, and the Gallup analysts wrote that “social isolation, loneliness, fear of infection, psychological exhaustion (particularly among frontline responders such as health care workers), elevated substance abuse, and disruptions in mental health services have all likely played a role” in the increase.
“The fact that Americans are more depressed and struggling after this time of incredible stress and isolation is perhaps not surprising,” American Psychiatric Association president Rebecca Brendel, MD, told CNN. “There are lingering effects on our health, especially our mental health, from the past 3 years that disrupted everything we knew.”
The new estimates are based on online survey responses collected in February from 5,167 adults in the United States who answered the questions:
- Has a doctor or nurse ever told you that you have depression?
- Do you currently have or are you currently being treated for depression?
Depression, which is also called major depressive disorder, is a treatable illness that negatively affects how someone feels, thinks, and acts. The symptoms can be both emotional (such as sadness or loss of interest in activities) and physical (such as fatigue or slowed movements or speech).
The latest study found that depression rates increased the most among women, young adults, Black people, and Hispanic people. For the first time, more Black and Hispanic people than White people reported ever being diagnosed with depression. The lifetime depression rate among Black people was 34%, compared with 31% for Hispanic people and 29% for White people.
The rate of lifetime depression among women jumped 10 percentage points in the past 5 years, to 37%, in February, the survey results showed. About 1 in 4 women said they currently had depression or were being treated for it, up 6 percentage points compared with 5 years ago.
When responses were analyzed by age, those 18-44 years old were the most likely to report ever being diagnosed with depression or currently having the illness. About one-third of younger adults have ever been diagnosed, and more than 1 in 5 said they currently have depression.
Dr. Brendel said awareness and reduced stigma could be adding to the rising rates of depression.
“We’re making it easier to talk about mental health and looking at it as part of our overall wellness, just like physical health,” she said. “People are aware of depression, and people are seeking help for it.”
If you or someone you know needs help, dial 988 for support from the national Suicide & Crisis Lifeline. It’s free, confidential, and available 24 hours a day, 7 days a week. You can also visit 988lifeline.org and choose the chat feature.
A version of this article first appeared on Medscape.com.
The antimicrobial peptide that even Pharma can love
Fastest peptide north, south, east, aaaaand west of the Pecos
Bacterial infections are supposed to be simple. You get infected, you get an antibiotic to treat it. Easy. Some bacteria, though, don’t play by the rules. Those antibiotics may kill 99.9% of germs, but what about the 0.1% that gets left behind? With their fallen comrades out of the way, the accidentally drug resistant species are free to inherit the Earth.
Antibiotic resistance is thus a major concern for the medical community. Naturally, anything that prevents doctors from successfully curing sick people is a priority. Unless you’re a major pharmaceutical company that has been loath to develop new drugs that can beat antibiotic-resistant bacteria. Blah blah, time and money, blah blah, long time between development and market application, blah blah, no profit. We all know the story with pharmaceutical companies.
Research from other sources has continued, however, and Brazilian scientists recently published research involving a peptide known as plantaricin 149. This peptide, derived from the bacterium Lactobacillus plantarum, has been known for nearly 30 years to have antibacterial properties. Pln149 in its natural state, though, is not particularly efficient at bacteria-killing. Fortunately, we have science and technology on our side.
The researchers synthesized 20 analogs of Pln149, of which Pln149-PEP20 had the best results. The elegantly named compound is less than half the size of the original peptide, less toxic, and far better at killing any and all drug-resistant bacteria the researchers threw at it. How much better? Pln149-PEP20 started killing bacteria less than an hour after being introduced in lab trials.
The research is just in its early days – just because something is less toxic doesn’t necessarily mean you want to go and help yourself to it – but we can only hope that those lovely pharmaceutical companies deign to look down upon us and actually develop a drug utilizing Pln149-PEP20 to, you know, actually help sick people, instead of trying to build monopolies or avoiding paying billions in taxes. Yeah, we couldn’t keep a straight face through that last sentence either.
Speed healing: The wavy wound gets the swirl
Did you know that wavy wounds heal faster than straight wounds? Well, we didn’t, but apparently quite a few people did, because somebody has been trying to figure out why wavy wounds heal faster than straight ones. Do the surgeons know about this? How about you dermatologists? Wavy over straight? We’re the media. We’re supposed to report this kind of stuff. Maybe hit us with a tweet next time you do something important, or push a TikTok our way, okay?
You could be more like the investigators at Nanyang Technological University in Singapore, who figured out the why and then released a statement about it.
They created synthetic wounds – some straight, some wavy – in micropatterned hydrogel substrates that mimicked human skin. Then they used an advanced optical technique known as particle image velocimetry to measure fluid flow and learn how cells moved to close the wound gaps.
The wavy wounds “induced more complex collective cell movements, such as a swirly, vortex-like motion,” according to the written statement from NTU Singapore. In the straight wounds, cell movements paralleled the wound front, “moving in straight lines like a marching band,” they pointed out, unlike some researchers who never call us unless they need money.
Complex epithelial cell movements are better, it turns out. Over an observation period of 64 hours the NTU team found that the healing efficiency of wavy gaps – measured by the area covered by the cells over time – is nearly five times faster than straight gaps.
The complex motion “enabled cells to quickly connect with similar cells on the opposite site of the wound edge, forming a bridge and closing the wavy wound gaps faster than straight gaps,” explained lead author Xu Hongmei, a doctoral student at NTU’s School of Mechanical and Aerospace Engineering, who seems to have time to toss out a tumblr or two to keep the press informed.
As for the rest of you, would it kill you to pick up a phone once in a while? Maybe let a journalist know that you’re still alive? We have feelings too, you know, and we worry.
A little Jekyll, a little Hyde, and a little shop of horrors
More “Little Shop of Horrors” references are coming, so be prepared.
We begin with Triphyophyllum peltatum. This woody vine is of great interest to medical and pharmaceutical researchers because its constituents have shown promise against pancreatic cancer and leukemia cells, among others, along with the pathogens that cause malaria and other diseases. There is another side, however. T. peltatum also has a tendency to turn into a realistic Audrey II when deprived.
No, of course they’re not craving human flesh, but it does become … carnivorous in its appetite.
T. peltatum, native to the West African tropics and not found in a New York florist shop, has the unique ability to change its diet and development based on the environmental circumstances. For some unknown reason, the leaves would develop adhesive traps in the form of sticky drops that capture insect prey. The plant is notoriously hard to grow, however, so no one could study the transformation under lab conditions. Until now.
A group of German scientists “exposed the plant to different stress factors, including deficiencies of various nutrients, and studied how it responded to each,” said Dr. Traud Winkelmann of Leibniz University Hannover. “Only in one case were we able to observe the formation of traps: in the case of a lack of phosphorus.”
Well, there you have it: phosphorus. We need it for healthy bones and teeth, which this plant doesn’t have to worry about, unlike its Tony Award–nominated counterpart. The investigators hope that their findings could lead to “future molecular analyses that will help understand the origins of carnivory,” but we’re guessing that a certain singing alien species will be left out of that research.
Fastest peptide north, south, east, aaaaand west of the Pecos
Bacterial infections are supposed to be simple. You get infected, you get an antibiotic to treat it. Easy. Some bacteria, though, don’t play by the rules. Those antibiotics may kill 99.9% of germs, but what about the 0.1% that gets left behind? With their fallen comrades out of the way, the accidentally drug resistant species are free to inherit the Earth.
Antibiotic resistance is thus a major concern for the medical community. Naturally, anything that prevents doctors from successfully curing sick people is a priority. Unless you’re a major pharmaceutical company that has been loath to develop new drugs that can beat antibiotic-resistant bacteria. Blah blah, time and money, blah blah, long time between development and market application, blah blah, no profit. We all know the story with pharmaceutical companies.
Research from other sources has continued, however, and Brazilian scientists recently published research involving a peptide known as plantaricin 149. This peptide, derived from the bacterium Lactobacillus plantarum, has been known for nearly 30 years to have antibacterial properties. Pln149 in its natural state, though, is not particularly efficient at bacteria-killing. Fortunately, we have science and technology on our side.
The researchers synthesized 20 analogs of Pln149, of which Pln149-PEP20 had the best results. The elegantly named compound is less than half the size of the original peptide, less toxic, and far better at killing any and all drug-resistant bacteria the researchers threw at it. How much better? Pln149-PEP20 started killing bacteria less than an hour after being introduced in lab trials.
The research is just in its early days – just because something is less toxic doesn’t necessarily mean you want to go and help yourself to it – but we can only hope that those lovely pharmaceutical companies deign to look down upon us and actually develop a drug utilizing Pln149-PEP20 to, you know, actually help sick people, instead of trying to build monopolies or avoiding paying billions in taxes. Yeah, we couldn’t keep a straight face through that last sentence either.
Speed healing: The wavy wound gets the swirl
Did you know that wavy wounds heal faster than straight wounds? Well, we didn’t, but apparently quite a few people did, because somebody has been trying to figure out why wavy wounds heal faster than straight ones. Do the surgeons know about this? How about you dermatologists? Wavy over straight? We’re the media. We’re supposed to report this kind of stuff. Maybe hit us with a tweet next time you do something important, or push a TikTok our way, okay?
You could be more like the investigators at Nanyang Technological University in Singapore, who figured out the why and then released a statement about it.
They created synthetic wounds – some straight, some wavy – in micropatterned hydrogel substrates that mimicked human skin. Then they used an advanced optical technique known as particle image velocimetry to measure fluid flow and learn how cells moved to close the wound gaps.
The wavy wounds “induced more complex collective cell movements, such as a swirly, vortex-like motion,” according to the written statement from NTU Singapore. In the straight wounds, cell movements paralleled the wound front, “moving in straight lines like a marching band,” they pointed out, unlike some researchers who never call us unless they need money.
Complex epithelial cell movements are better, it turns out. Over an observation period of 64 hours the NTU team found that the healing efficiency of wavy gaps – measured by the area covered by the cells over time – is nearly five times faster than straight gaps.
The complex motion “enabled cells to quickly connect with similar cells on the opposite site of the wound edge, forming a bridge and closing the wavy wound gaps faster than straight gaps,” explained lead author Xu Hongmei, a doctoral student at NTU’s School of Mechanical and Aerospace Engineering, who seems to have time to toss out a tumblr or two to keep the press informed.
As for the rest of you, would it kill you to pick up a phone once in a while? Maybe let a journalist know that you’re still alive? We have feelings too, you know, and we worry.
A little Jekyll, a little Hyde, and a little shop of horrors
More “Little Shop of Horrors” references are coming, so be prepared.
We begin with Triphyophyllum peltatum. This woody vine is of great interest to medical and pharmaceutical researchers because its constituents have shown promise against pancreatic cancer and leukemia cells, among others, along with the pathogens that cause malaria and other diseases. There is another side, however. T. peltatum also has a tendency to turn into a realistic Audrey II when deprived.
No, of course they’re not craving human flesh, but it does become … carnivorous in its appetite.
T. peltatum, native to the West African tropics and not found in a New York florist shop, has the unique ability to change its diet and development based on the environmental circumstances. For some unknown reason, the leaves would develop adhesive traps in the form of sticky drops that capture insect prey. The plant is notoriously hard to grow, however, so no one could study the transformation under lab conditions. Until now.
A group of German scientists “exposed the plant to different stress factors, including deficiencies of various nutrients, and studied how it responded to each,” said Dr. Traud Winkelmann of Leibniz University Hannover. “Only in one case were we able to observe the formation of traps: in the case of a lack of phosphorus.”
Well, there you have it: phosphorus. We need it for healthy bones and teeth, which this plant doesn’t have to worry about, unlike its Tony Award–nominated counterpart. The investigators hope that their findings could lead to “future molecular analyses that will help understand the origins of carnivory,” but we’re guessing that a certain singing alien species will be left out of that research.
Fastest peptide north, south, east, aaaaand west of the Pecos
Bacterial infections are supposed to be simple. You get infected, you get an antibiotic to treat it. Easy. Some bacteria, though, don’t play by the rules. Those antibiotics may kill 99.9% of germs, but what about the 0.1% that gets left behind? With their fallen comrades out of the way, the accidentally drug resistant species are free to inherit the Earth.
Antibiotic resistance is thus a major concern for the medical community. Naturally, anything that prevents doctors from successfully curing sick people is a priority. Unless you’re a major pharmaceutical company that has been loath to develop new drugs that can beat antibiotic-resistant bacteria. Blah blah, time and money, blah blah, long time between development and market application, blah blah, no profit. We all know the story with pharmaceutical companies.
Research from other sources has continued, however, and Brazilian scientists recently published research involving a peptide known as plantaricin 149. This peptide, derived from the bacterium Lactobacillus plantarum, has been known for nearly 30 years to have antibacterial properties. Pln149 in its natural state, though, is not particularly efficient at bacteria-killing. Fortunately, we have science and technology on our side.
The researchers synthesized 20 analogs of Pln149, of which Pln149-PEP20 had the best results. The elegantly named compound is less than half the size of the original peptide, less toxic, and far better at killing any and all drug-resistant bacteria the researchers threw at it. How much better? Pln149-PEP20 started killing bacteria less than an hour after being introduced in lab trials.
The research is just in its early days – just because something is less toxic doesn’t necessarily mean you want to go and help yourself to it – but we can only hope that those lovely pharmaceutical companies deign to look down upon us and actually develop a drug utilizing Pln149-PEP20 to, you know, actually help sick people, instead of trying to build monopolies or avoiding paying billions in taxes. Yeah, we couldn’t keep a straight face through that last sentence either.
Speed healing: The wavy wound gets the swirl
Did you know that wavy wounds heal faster than straight wounds? Well, we didn’t, but apparently quite a few people did, because somebody has been trying to figure out why wavy wounds heal faster than straight ones. Do the surgeons know about this? How about you dermatologists? Wavy over straight? We’re the media. We’re supposed to report this kind of stuff. Maybe hit us with a tweet next time you do something important, or push a TikTok our way, okay?
You could be more like the investigators at Nanyang Technological University in Singapore, who figured out the why and then released a statement about it.
They created synthetic wounds – some straight, some wavy – in micropatterned hydrogel substrates that mimicked human skin. Then they used an advanced optical technique known as particle image velocimetry to measure fluid flow and learn how cells moved to close the wound gaps.
The wavy wounds “induced more complex collective cell movements, such as a swirly, vortex-like motion,” according to the written statement from NTU Singapore. In the straight wounds, cell movements paralleled the wound front, “moving in straight lines like a marching band,” they pointed out, unlike some researchers who never call us unless they need money.
Complex epithelial cell movements are better, it turns out. Over an observation period of 64 hours the NTU team found that the healing efficiency of wavy gaps – measured by the area covered by the cells over time – is nearly five times faster than straight gaps.
The complex motion “enabled cells to quickly connect with similar cells on the opposite site of the wound edge, forming a bridge and closing the wavy wound gaps faster than straight gaps,” explained lead author Xu Hongmei, a doctoral student at NTU’s School of Mechanical and Aerospace Engineering, who seems to have time to toss out a tumblr or two to keep the press informed.
As for the rest of you, would it kill you to pick up a phone once in a while? Maybe let a journalist know that you’re still alive? We have feelings too, you know, and we worry.
A little Jekyll, a little Hyde, and a little shop of horrors
More “Little Shop of Horrors” references are coming, so be prepared.
We begin with Triphyophyllum peltatum. This woody vine is of great interest to medical and pharmaceutical researchers because its constituents have shown promise against pancreatic cancer and leukemia cells, among others, along with the pathogens that cause malaria and other diseases. There is another side, however. T. peltatum also has a tendency to turn into a realistic Audrey II when deprived.
No, of course they’re not craving human flesh, but it does become … carnivorous in its appetite.
T. peltatum, native to the West African tropics and not found in a New York florist shop, has the unique ability to change its diet and development based on the environmental circumstances. For some unknown reason, the leaves would develop adhesive traps in the form of sticky drops that capture insect prey. The plant is notoriously hard to grow, however, so no one could study the transformation under lab conditions. Until now.
A group of German scientists “exposed the plant to different stress factors, including deficiencies of various nutrients, and studied how it responded to each,” said Dr. Traud Winkelmann of Leibniz University Hannover. “Only in one case were we able to observe the formation of traps: in the case of a lack of phosphorus.”
Well, there you have it: phosphorus. We need it for healthy bones and teeth, which this plant doesn’t have to worry about, unlike its Tony Award–nominated counterpart. The investigators hope that their findings could lead to “future molecular analyses that will help understand the origins of carnivory,” but we’re guessing that a certain singing alien species will be left out of that research.
Mailed HPV test kits boost cervical cancer screening
The self-sampling kits, which detect human papillomavirus (HPV), are available only for use in clinical trials, but the researchers hope that eventually these kits will be approved for use by the general public.
The researchers, from the University of North Carolina, explored use of these kits in the My Body, My Test-3 study, which was published online in The Lancet Public Health.
In a commentary published with the study, Runzhi Wang, MD, and Jennell Coleman, MD, MPH, both of Johns Hopkins University, Baltimore, said it “provides the required evidence that ... self-collected samples can be an effective strategy for hard-to-reach populations.”
The study involved 665 women (aged 25-64) in North Carolina who were either uninsured or enrolled in Medicaid or Medicare. The patients had low-income backgrounds and lived in urban areas. More than half self-reported as Black or Hispanic (55%), uninsured (78%) or unemployed (57%). None had a Pap smear in at least 4 years or a high-risk HPV test in the last 6 years.
Two-thirds of the women were mailed an HPV self-collection kit and received assistance with scheduling an in-person screening appointment. The kit included a Viba-Brush device, which is inserted into the vagina like a tampon to collect the sample.
The other third of women, the control group, only received scheduling assistance.
The team found that mailing the self-collection tests along with helping women book in-clinic appointments improved screening rates twofold, compared with just assisting patients to schedule an appointment.
Screening success among those who received the at-home collection kit was 72%, compared with 37% in the control group.
Of those who received the kits, 78% returned them. This is “impressive,” said Dr. Wang and Dr. Coleman, as previous studies have reported return rates of only 8%-20%.
About 23% of eligible women are overdue for cervical cancer screening by at least a year, according to the National Cancer Institute. Jennifer Smith, PhD, MPH, professor of epidemiology at the University of North Carolina at Chapel Hill and an author of the study, believes every woman deserves equal access to cervical screening.
“I think we really need to make efforts to increase cervical cancer screening among women who are overdue for screening by a year or more from the recommended guidelines,” Dr. Smith said. “We’ve proven along with the wide evidence both in the U.S. and globally that self-collection intervention works well and can motivate screening uptake by breaking down barriers for populations that have less access to care.”
“We’re hoping this research in combination with all of the extensive evidence on the positive performance of HPV self-collection will provide additional information to be considered by the FDA for approval of the kits for primary screening,” Dr. Smith said.
“Government approval of at-home HPV tests would have a huge impact,” said coauthor Noel Brewer, PhD, also of UNC Chapel Hill. “We could better reach those in rural areas where cervical cancer screening is hard to come by.”
Dr. Smith has received research grants, supply donations, and consultancies for Hologic and BD Diagnostics. Dr. Brewer, Dr. Wang, and Dr. Coleman reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
The self-sampling kits, which detect human papillomavirus (HPV), are available only for use in clinical trials, but the researchers hope that eventually these kits will be approved for use by the general public.
The researchers, from the University of North Carolina, explored use of these kits in the My Body, My Test-3 study, which was published online in The Lancet Public Health.
In a commentary published with the study, Runzhi Wang, MD, and Jennell Coleman, MD, MPH, both of Johns Hopkins University, Baltimore, said it “provides the required evidence that ... self-collected samples can be an effective strategy for hard-to-reach populations.”
The study involved 665 women (aged 25-64) in North Carolina who were either uninsured or enrolled in Medicaid or Medicare. The patients had low-income backgrounds and lived in urban areas. More than half self-reported as Black or Hispanic (55%), uninsured (78%) or unemployed (57%). None had a Pap smear in at least 4 years or a high-risk HPV test in the last 6 years.
Two-thirds of the women were mailed an HPV self-collection kit and received assistance with scheduling an in-person screening appointment. The kit included a Viba-Brush device, which is inserted into the vagina like a tampon to collect the sample.
The other third of women, the control group, only received scheduling assistance.
The team found that mailing the self-collection tests along with helping women book in-clinic appointments improved screening rates twofold, compared with just assisting patients to schedule an appointment.
Screening success among those who received the at-home collection kit was 72%, compared with 37% in the control group.
Of those who received the kits, 78% returned them. This is “impressive,” said Dr. Wang and Dr. Coleman, as previous studies have reported return rates of only 8%-20%.
About 23% of eligible women are overdue for cervical cancer screening by at least a year, according to the National Cancer Institute. Jennifer Smith, PhD, MPH, professor of epidemiology at the University of North Carolina at Chapel Hill and an author of the study, believes every woman deserves equal access to cervical screening.
“I think we really need to make efforts to increase cervical cancer screening among women who are overdue for screening by a year or more from the recommended guidelines,” Dr. Smith said. “We’ve proven along with the wide evidence both in the U.S. and globally that self-collection intervention works well and can motivate screening uptake by breaking down barriers for populations that have less access to care.”
“We’re hoping this research in combination with all of the extensive evidence on the positive performance of HPV self-collection will provide additional information to be considered by the FDA for approval of the kits for primary screening,” Dr. Smith said.
“Government approval of at-home HPV tests would have a huge impact,” said coauthor Noel Brewer, PhD, also of UNC Chapel Hill. “We could better reach those in rural areas where cervical cancer screening is hard to come by.”
Dr. Smith has received research grants, supply donations, and consultancies for Hologic and BD Diagnostics. Dr. Brewer, Dr. Wang, and Dr. Coleman reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
The self-sampling kits, which detect human papillomavirus (HPV), are available only for use in clinical trials, but the researchers hope that eventually these kits will be approved for use by the general public.
The researchers, from the University of North Carolina, explored use of these kits in the My Body, My Test-3 study, which was published online in The Lancet Public Health.
In a commentary published with the study, Runzhi Wang, MD, and Jennell Coleman, MD, MPH, both of Johns Hopkins University, Baltimore, said it “provides the required evidence that ... self-collected samples can be an effective strategy for hard-to-reach populations.”
The study involved 665 women (aged 25-64) in North Carolina who were either uninsured or enrolled in Medicaid or Medicare. The patients had low-income backgrounds and lived in urban areas. More than half self-reported as Black or Hispanic (55%), uninsured (78%) or unemployed (57%). None had a Pap smear in at least 4 years or a high-risk HPV test in the last 6 years.
Two-thirds of the women were mailed an HPV self-collection kit and received assistance with scheduling an in-person screening appointment. The kit included a Viba-Brush device, which is inserted into the vagina like a tampon to collect the sample.
The other third of women, the control group, only received scheduling assistance.
The team found that mailing the self-collection tests along with helping women book in-clinic appointments improved screening rates twofold, compared with just assisting patients to schedule an appointment.
Screening success among those who received the at-home collection kit was 72%, compared with 37% in the control group.
Of those who received the kits, 78% returned them. This is “impressive,” said Dr. Wang and Dr. Coleman, as previous studies have reported return rates of only 8%-20%.
About 23% of eligible women are overdue for cervical cancer screening by at least a year, according to the National Cancer Institute. Jennifer Smith, PhD, MPH, professor of epidemiology at the University of North Carolina at Chapel Hill and an author of the study, believes every woman deserves equal access to cervical screening.
“I think we really need to make efforts to increase cervical cancer screening among women who are overdue for screening by a year or more from the recommended guidelines,” Dr. Smith said. “We’ve proven along with the wide evidence both in the U.S. and globally that self-collection intervention works well and can motivate screening uptake by breaking down barriers for populations that have less access to care.”
“We’re hoping this research in combination with all of the extensive evidence on the positive performance of HPV self-collection will provide additional information to be considered by the FDA for approval of the kits for primary screening,” Dr. Smith said.
“Government approval of at-home HPV tests would have a huge impact,” said coauthor Noel Brewer, PhD, also of UNC Chapel Hill. “We could better reach those in rural areas where cervical cancer screening is hard to come by.”
Dr. Smith has received research grants, supply donations, and consultancies for Hologic and BD Diagnostics. Dr. Brewer, Dr. Wang, and Dr. Coleman reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
FROM THE LANCET PUBLIC HEALTH
Would you prescribe antenatal steroids to a pregnant patient at high risk for delivering at 22 weeks’ gestation?

For many decades, the limit of newborn viability was at approximately 24 weeks’ gestation. Recent advances in pregnancy and neonatal care suggest that the new limit of viability is 22 (22 weeks and 0 days to 22 weeks and 6 days) or 23 (23 weeks and 0 days to 23 weeks and 6 days) weeks of gestation. In addition, data from observational cohort studies indicate that for infants born at 22 and 23 weeks’ gestation, survival is dependent on a course of antenatal steroids administered prior to birth plus intensive respiratory and cardiovascular support at delivery and in the neonatal intensive care unit (NICU).
Antenatal steroids: Critical for survival at 22 and 23 weeks of gestation
Most studies of birth outcomes at 22 and 23 weeks’ gestation rely on observational cohorts where unmeasured differences among the maternal-fetal dyads that received or did not receive a specific treatment confounds the interpretation of the data. However, data from multiple large observational cohorts suggest that between 22 and 24 weeks of gestation, completion of a course of antenatal steroids will optimize infant outcomes. Particularly noteworthy was the observation that the incremental survival benefit of antenatal steroids was greatest at 22 and 23 weeks’ gestation (TABLE 1).1 Similar results have been reported by Rossi and colleagues (TABLE 2).2
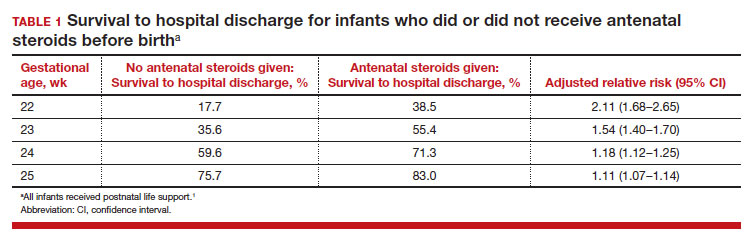
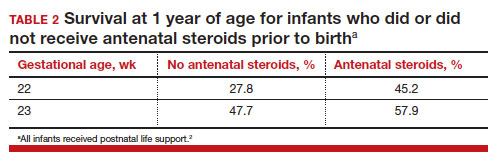
The importance of a completed course of antenatal steroids before birth was confirmed in another cohort study of 431 infants born in 2016 to 2019 at 22 weeks and 0 days’ to 23 weeks and 6 days’ gestation.3 Survival to discharge occurred in 53.9% of infants who received a full course of antenatal steroids before birth and 35.5% among those who did not receive antenatal steroids..3 Survival to discharge without major neonatal morbidities was 26.9% in those who received a full course of antenatal steroids and 10% among those who did not. In this cohort, major neonatal morbidities included severe intracranial hemorrhage, cystic periventricular leukomalacia, severe bronchopulmonary dysplasia, surgical necrotizing enterocolitis, or severe retinopathy of prematurity requiring treatment.
The American College of Obstetricians and Gynecologists (ACOG) recommends against antenatal steroids prior to 22 weeks and 0 days gestation.4 However, some neonatologists might recommend that antenatal steroids be given starting at 21 weeks and 5 days of gestation if birth is anticipated in the 22nd week of gestation and the patient prefers aggressive treatment of the newborn.
Active respiratory and cardiovascular support improves newborn outcomes
To maximize survival, infants born at 22 and 23 weeks’ gestation always require intensive active treatment at birth and in the following days in the NICU. Active treatment may include respiratory support, surfactant treatment, pressors, closure of a patent ductus arteriosus, transfusion of red blood cells, and parenteral nutrition. In one observational cohort study, active treatment at birth was not routinely provided at 22 and 23 weeks’ gestation but was routinely provided at later gestational ages (TABLE 3A).5 Not surprisingly, active treatment, especially at early gestational ages, is associated with improved survival to discharge. For example, at 22 weeks’ gestation, survival to discharge in infants who received or did not receive intensive active treatment was 28% and 0%, respectively.5 However, specific clinical characteristics of the pregnant patient and newborn may have influenced which infants were actively treated, confounding interpretation of the observation. In this cohort of extremely premature newborns, survival to hospital discharge increased substantially between 22 weeks and 26 weeks of gestational age (TABLE 3B).5
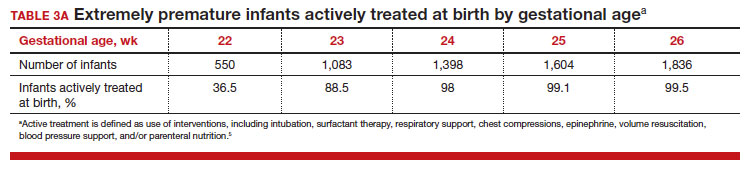
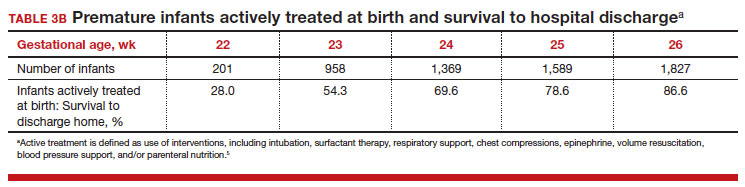
Many of the surviving infants needed chronic support treatment. Among surviving infants born at 22 weeks and 26 weeks, chronic support treatments were being used by 22.6% and 10.6% of infants, respectively, 2 years after birth.5 For surviving infants born at 22 weeks, the specific chronic support treatments included gastrostomy or feeding tube (19.4%), oxygen (9.7%), pulse oximeter (9.7%), and/or tracheostomy (3.2%). For surviving infants born at 26 weeks’ gestation, the specific chronic support treatments included gastrotomy or feeding tube (8.5%), pulse oximeter (4.4%), oxygen (3.2%), tracheostomy (2.3%), an apnea monitor (1.5%), and/or ventilator or continuous positive airway pressure (1.1%).5
Continue to: Evolving improvement in infant outcomes...
Evolving improvement in infant outcomes
In 1963, Jacqueline Bouvier Kennedy went into preterm labor at 34 weeks of gestation and delivered her son Patrick at a community facility. Due to severe respiratory distress syndrome, Patrick was transferred to the Boston Children’s Hospital, and he died shortly thereafter.6 Sixty years later, due to advances in obstetric and neonatal care, death from respiratory distress syndrome at 34 weeks of gestation is uncommon in the United States.
Infant outcomes following birth at 22 and 23 weeks’ gestation continue to improve. An observational cohort study from Sweden reported that at 22 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 10% and 30%, respectively.7 Similarly, at 23 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 52% and 61%, respectively.7 However, most of the surviving infants in this cohort had one or more major neonatal morbidities, including intraventricular hemorrhage grade 3 or 4; periventricular leukomalacia; necrotizing enterocolitis; retinopathy of prematurity grade 3, 4, or 5; or severe bronchopulmonary dysplasia.7
In a cohort of infants born in Japan at 22 to 24 weeks of gestation, there was a notable decrease in major neurodisability at 3 years of age for births occurring in 2 epochs, 2003 to 2007 and 2008 to 2012.8 When comparing outcomes in 2003 to 2007 versus 2008 to 2012, the change in rate of various major complications included the following: cerebral palsy (15.9% vs 9.5%), visual impairment (13.6% vs 4.4%), blindness (4.8% vs 1.3%), and hearing impairment (2.6% vs 1.0%). In contrast, the rate of cognitive impairment, defined as less than 70% of standard test performance for chronological age, was similar in the 2 time periods (36.5% and 37.9%, respectively).8 Based on data reported between 2000 and 2020, a systematic review and meta-analysis by Backes and colleagues concluded that there has been substantial improvement in the survival of infants born at 22 weeks of gestation.9
The small baby unit
A feature of modern medicine is the relentless evolution of new clinical subspecialties and sub-subspecialties. NICUs evolved from newborn nurseries to serve the needs of the most severely ill newborns, with care provided by a cadre of highly trained subspecialized neonatologists and neonatal nurses. A new era is dawning, with some NICUs developing a sub-subspecialized small baby unit to care for infants born between 22 and 26 weeks of gestation. These units often are staffed by clinicians with a specific interest in optimizing the care of extremely preterm infants, providing continuity of care over a long hospitalization.10 The benefits of a small baby unit may include:
- relentless standardization and adherence to the best intensive care practices
- daily use of checklists
- strict adherence to central line care
- timely extubation and transition to continuous positive airway pressure
- adherence to breastfeeding guidelines
- limiting the number of clinicians responsible for the patient
- promotion of kangaroo care
- avoidance of noxious stimuli.10,11
Continue to: Ethical and clinical issues...
Ethical and clinical issues
Providing clinical care to infants born at the edge of viability is challenging and raises many ethical and clinical concerns.12,13 For an infant born at the edge of viability, clinicians and parents do not want to initiate a care process that improves survival but results in an extremely poor quality of life. At the same time, clinicians and parents do not want to withhold care that could help an extremely premature newborn survive and thrive. Consequently, the counseling process is complex and requires coordination between the obstetrical and neonatology disciplines, involving physicians and nurses from both. A primary consideration in deciding to institute active treatment at birth is the preference of the pregnant patient and the patient’s trusted family members. A thorough discussion of these issues is beyond the scope of this editorial. ACOG provides detailed advice about the approach to counseling patients who face the possibility of a periviable birth.14
To help standardize the counseling process, institutions may find it helpful to recommend that clinicians consistently use a calculator to provide newborn outcome data to patients. The National Institute of Child Health and Human Development’s Extremely Preterm Birth Outcomes calculator uses the following inputs:
- gestational age
- estimated birth weight
- sex
- singleton/multiple gestation
- antenatal steroid treatment.
It also provides the following outputs as percentages:
- survival with active treatment at birth
- survival without active treatment at birth
- profound neurodevelopmental impairment
- moderate to severe neurodevelopmental impairment
- blindness
- deafness
- moderate to severe cerebral palsy
- cognitive developmental delay.15
A full assessment of all known clinical factors should influence the interpretation of the output from the clinical calculator. An alternativeis to use data from the Vermont Oxford Network. NICUs with sufficient clinical volume may prefer to use their own outcome data in the counseling process.
Institutions and clinical teams may improve the consistency of the counseling process by identifying criteria for 3 main treatment options:
- clinical situations where active treatment at birth is not generally offered (eg, <22 weeks’ gestation)
- clinical situations where active treatment at birth is almost always routinely provided (eg, >25 weeks’ gestation)
- clinical situations where patient preferences are especially important in guiding the use of active treatment.
Most institutions do not routinely offer active treatment of the newborn at a gestational age of less than 22 weeks and 0 days. Instead, comfort care often is provided for these newborns. Most institutions routinely provide active treatment at birth beginning at 24 or 25 weeks’ gestation unless unique risk factors or comorbidities warrant not providing active treatment (TABLE 3A). Some professional societies recommend setting a threshold for recommending active treatment at birth. For example, the British Association of Perinatal Medicine recommends that if there is 50% or higher probability of survival without severe disability, active treatment at birth should be considered because it is in the best interest of the newborn.16 In the hours and days following birth, the clinical course of the newborn greatly influences the treatment plan and care goals. After the initial resuscitation, if the clinical condition of an extremely preterm infant worsens and the prognosis is grim, a pivot to palliative care may be considered.
Final thoughts
Periviability is the earliest stage of fetal development where there is a reasonable chance, but not a high likelihood, of survival outside the womb. For decades, the threshold for periviability was approximately 24 weeks of gestation. With current obstetrical and neonatal practice, the new threshold for periviability is 22 to 23 weeks of gestation, but death prior to hospital discharge occurs in approximately half of these newborns. For the survivors, lifelong neurodevelopmental complications and pulmonary disease are common. Obstetricians play a key role in counseling patients who are at risk of giving birth before 24 weeks of gestation. Given the challenges faced by an infant born at 22 and 23 weeks’ gestation, pregnant patients and trusted family members should approach the decision to actively resuscitate the newborn with caution. However, if the clinical team, patient, and trusted family members agree to pursue active treatment, completion of a course of antenatal steroids and appropriate respiratory and cardiovascular support at birth are key to improving long-term outcomes. ●
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks gestation. JAMA Network Open. 2018;E183235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks [published online November 28, 2021]. Am J Perinatol. doi:10.1055/s-004-1740062
- Chawla S, Wyckoff MH, Rysavy MA, et al. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Network Open. 2022;5:E2233331.
- Use of antenatal corticosteroids at 22 weeks of gestation. ACOG website. Published September 2021. Accessed April 10, 2023. https://www.acog .org/clinical/clinical-guidance/practice -advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation
- Bell EF, Hintz SR, Hansen NI, et al. Mortality, in-hospital morbidity, care practices and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 2022;327:248-263.
- The tragic death of Patrick, JFK and Jackie’s newborn son, in 1963. Irish Central website. Published November 6, 2022. Accessed April 10, 2023. https://www.irishcentral.com/roots/history /tragic-death-patrick-kennedy-jfk-jackie
- Norman M, Hallberg B, Abrahamsson T, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004-2007 and 2014-2016. JAMA. 2019;32:1188-1199.
- Kono Y, Yonemoto N, Nakanishi H, et al. Changes in survival and neurodevelopmental outcomes of infants born at <25 weeks gestation: a retrospective observational study in tertiary centres in Japan. BMJ Paediatrics Open. 2018;2:E000211.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Morris M, Cleary JP, Soliman A. Small baby unit improves quality and outcomes in extremely low birth weight infants. Pediatrics. 2015;136:E1007-E1015.
- Fathi O, Nelin LD, Shephard EG, et al. Development of a small baby unit to improve outcomes for the extremely premature infant. J Perinatology. 2002;42:157-164.
- Lantos JD. Ethical issues in treatment of babies born at 22 weeks of gestation. Arch Dis Child. 2021;106:1155-1157.
- Shinwell ES. Ethics of birth at the limit of viability: the risky business of prediction. Neonatology. 2015;107:317-320.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No 6. periviable birth. Obstet Gynecol. 2017;E187-E199.
- Extremely preterm birth outcomes tool. NICHD website. Updated March 2, 2020. Accessed April 10, 2023. https://www.nichd.nih.gov/research /supported/EPBO/use#
- Mactier H, Bates SE, Johnston T, et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch Dis Child Fetal Neonatal Ed. 2020;105:F232-F239.

For many decades, the limit of newborn viability was at approximately 24 weeks’ gestation. Recent advances in pregnancy and neonatal care suggest that the new limit of viability is 22 (22 weeks and 0 days to 22 weeks and 6 days) or 23 (23 weeks and 0 days to 23 weeks and 6 days) weeks of gestation. In addition, data from observational cohort studies indicate that for infants born at 22 and 23 weeks’ gestation, survival is dependent on a course of antenatal steroids administered prior to birth plus intensive respiratory and cardiovascular support at delivery and in the neonatal intensive care unit (NICU).
Antenatal steroids: Critical for survival at 22 and 23 weeks of gestation
Most studies of birth outcomes at 22 and 23 weeks’ gestation rely on observational cohorts where unmeasured differences among the maternal-fetal dyads that received or did not receive a specific treatment confounds the interpretation of the data. However, data from multiple large observational cohorts suggest that between 22 and 24 weeks of gestation, completion of a course of antenatal steroids will optimize infant outcomes. Particularly noteworthy was the observation that the incremental survival benefit of antenatal steroids was greatest at 22 and 23 weeks’ gestation (TABLE 1).1 Similar results have been reported by Rossi and colleagues (TABLE 2).2
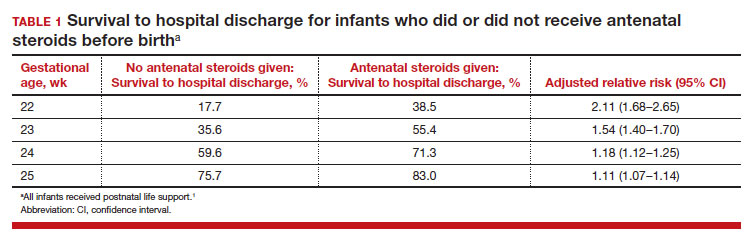
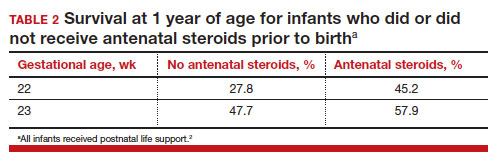
The importance of a completed course of antenatal steroids before birth was confirmed in another cohort study of 431 infants born in 2016 to 2019 at 22 weeks and 0 days’ to 23 weeks and 6 days’ gestation.3 Survival to discharge occurred in 53.9% of infants who received a full course of antenatal steroids before birth and 35.5% among those who did not receive antenatal steroids..3 Survival to discharge without major neonatal morbidities was 26.9% in those who received a full course of antenatal steroids and 10% among those who did not. In this cohort, major neonatal morbidities included severe intracranial hemorrhage, cystic periventricular leukomalacia, severe bronchopulmonary dysplasia, surgical necrotizing enterocolitis, or severe retinopathy of prematurity requiring treatment.
The American College of Obstetricians and Gynecologists (ACOG) recommends against antenatal steroids prior to 22 weeks and 0 days gestation.4 However, some neonatologists might recommend that antenatal steroids be given starting at 21 weeks and 5 days of gestation if birth is anticipated in the 22nd week of gestation and the patient prefers aggressive treatment of the newborn.
Active respiratory and cardiovascular support improves newborn outcomes
To maximize survival, infants born at 22 and 23 weeks’ gestation always require intensive active treatment at birth and in the following days in the NICU. Active treatment may include respiratory support, surfactant treatment, pressors, closure of a patent ductus arteriosus, transfusion of red blood cells, and parenteral nutrition. In one observational cohort study, active treatment at birth was not routinely provided at 22 and 23 weeks’ gestation but was routinely provided at later gestational ages (TABLE 3A).5 Not surprisingly, active treatment, especially at early gestational ages, is associated with improved survival to discharge. For example, at 22 weeks’ gestation, survival to discharge in infants who received or did not receive intensive active treatment was 28% and 0%, respectively.5 However, specific clinical characteristics of the pregnant patient and newborn may have influenced which infants were actively treated, confounding interpretation of the observation. In this cohort of extremely premature newborns, survival to hospital discharge increased substantially between 22 weeks and 26 weeks of gestational age (TABLE 3B).5
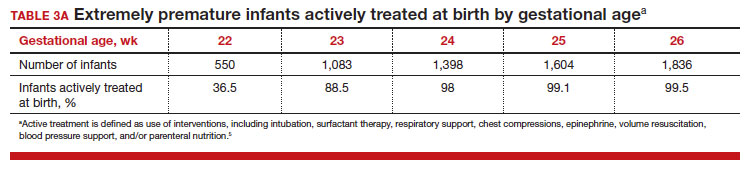
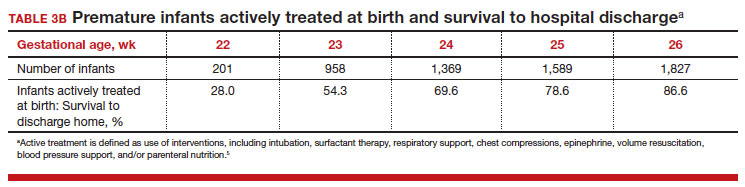
Many of the surviving infants needed chronic support treatment. Among surviving infants born at 22 weeks and 26 weeks, chronic support treatments were being used by 22.6% and 10.6% of infants, respectively, 2 years after birth.5 For surviving infants born at 22 weeks, the specific chronic support treatments included gastrostomy or feeding tube (19.4%), oxygen (9.7%), pulse oximeter (9.7%), and/or tracheostomy (3.2%). For surviving infants born at 26 weeks’ gestation, the specific chronic support treatments included gastrotomy or feeding tube (8.5%), pulse oximeter (4.4%), oxygen (3.2%), tracheostomy (2.3%), an apnea monitor (1.5%), and/or ventilator or continuous positive airway pressure (1.1%).5
Continue to: Evolving improvement in infant outcomes...
Evolving improvement in infant outcomes
In 1963, Jacqueline Bouvier Kennedy went into preterm labor at 34 weeks of gestation and delivered her son Patrick at a community facility. Due to severe respiratory distress syndrome, Patrick was transferred to the Boston Children’s Hospital, and he died shortly thereafter.6 Sixty years later, due to advances in obstetric and neonatal care, death from respiratory distress syndrome at 34 weeks of gestation is uncommon in the United States.
Infant outcomes following birth at 22 and 23 weeks’ gestation continue to improve. An observational cohort study from Sweden reported that at 22 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 10% and 30%, respectively.7 Similarly, at 23 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 52% and 61%, respectively.7 However, most of the surviving infants in this cohort had one or more major neonatal morbidities, including intraventricular hemorrhage grade 3 or 4; periventricular leukomalacia; necrotizing enterocolitis; retinopathy of prematurity grade 3, 4, or 5; or severe bronchopulmonary dysplasia.7
In a cohort of infants born in Japan at 22 to 24 weeks of gestation, there was a notable decrease in major neurodisability at 3 years of age for births occurring in 2 epochs, 2003 to 2007 and 2008 to 2012.8 When comparing outcomes in 2003 to 2007 versus 2008 to 2012, the change in rate of various major complications included the following: cerebral palsy (15.9% vs 9.5%), visual impairment (13.6% vs 4.4%), blindness (4.8% vs 1.3%), and hearing impairment (2.6% vs 1.0%). In contrast, the rate of cognitive impairment, defined as less than 70% of standard test performance for chronological age, was similar in the 2 time periods (36.5% and 37.9%, respectively).8 Based on data reported between 2000 and 2020, a systematic review and meta-analysis by Backes and colleagues concluded that there has been substantial improvement in the survival of infants born at 22 weeks of gestation.9
The small baby unit
A feature of modern medicine is the relentless evolution of new clinical subspecialties and sub-subspecialties. NICUs evolved from newborn nurseries to serve the needs of the most severely ill newborns, with care provided by a cadre of highly trained subspecialized neonatologists and neonatal nurses. A new era is dawning, with some NICUs developing a sub-subspecialized small baby unit to care for infants born between 22 and 26 weeks of gestation. These units often are staffed by clinicians with a specific interest in optimizing the care of extremely preterm infants, providing continuity of care over a long hospitalization.10 The benefits of a small baby unit may include:
- relentless standardization and adherence to the best intensive care practices
- daily use of checklists
- strict adherence to central line care
- timely extubation and transition to continuous positive airway pressure
- adherence to breastfeeding guidelines
- limiting the number of clinicians responsible for the patient
- promotion of kangaroo care
- avoidance of noxious stimuli.10,11
Continue to: Ethical and clinical issues...
Ethical and clinical issues
Providing clinical care to infants born at the edge of viability is challenging and raises many ethical and clinical concerns.12,13 For an infant born at the edge of viability, clinicians and parents do not want to initiate a care process that improves survival but results in an extremely poor quality of life. At the same time, clinicians and parents do not want to withhold care that could help an extremely premature newborn survive and thrive. Consequently, the counseling process is complex and requires coordination between the obstetrical and neonatology disciplines, involving physicians and nurses from both. A primary consideration in deciding to institute active treatment at birth is the preference of the pregnant patient and the patient’s trusted family members. A thorough discussion of these issues is beyond the scope of this editorial. ACOG provides detailed advice about the approach to counseling patients who face the possibility of a periviable birth.14
To help standardize the counseling process, institutions may find it helpful to recommend that clinicians consistently use a calculator to provide newborn outcome data to patients. The National Institute of Child Health and Human Development’s Extremely Preterm Birth Outcomes calculator uses the following inputs:
- gestational age
- estimated birth weight
- sex
- singleton/multiple gestation
- antenatal steroid treatment.
It also provides the following outputs as percentages:
- survival with active treatment at birth
- survival without active treatment at birth
- profound neurodevelopmental impairment
- moderate to severe neurodevelopmental impairment
- blindness
- deafness
- moderate to severe cerebral palsy
- cognitive developmental delay.15
A full assessment of all known clinical factors should influence the interpretation of the output from the clinical calculator. An alternativeis to use data from the Vermont Oxford Network. NICUs with sufficient clinical volume may prefer to use their own outcome data in the counseling process.
Institutions and clinical teams may improve the consistency of the counseling process by identifying criteria for 3 main treatment options:
- clinical situations where active treatment at birth is not generally offered (eg, <22 weeks’ gestation)
- clinical situations where active treatment at birth is almost always routinely provided (eg, >25 weeks’ gestation)
- clinical situations where patient preferences are especially important in guiding the use of active treatment.
Most institutions do not routinely offer active treatment of the newborn at a gestational age of less than 22 weeks and 0 days. Instead, comfort care often is provided for these newborns. Most institutions routinely provide active treatment at birth beginning at 24 or 25 weeks’ gestation unless unique risk factors or comorbidities warrant not providing active treatment (TABLE 3A). Some professional societies recommend setting a threshold for recommending active treatment at birth. For example, the British Association of Perinatal Medicine recommends that if there is 50% or higher probability of survival without severe disability, active treatment at birth should be considered because it is in the best interest of the newborn.16 In the hours and days following birth, the clinical course of the newborn greatly influences the treatment plan and care goals. After the initial resuscitation, if the clinical condition of an extremely preterm infant worsens and the prognosis is grim, a pivot to palliative care may be considered.
Final thoughts
Periviability is the earliest stage of fetal development where there is a reasonable chance, but not a high likelihood, of survival outside the womb. For decades, the threshold for periviability was approximately 24 weeks of gestation. With current obstetrical and neonatal practice, the new threshold for periviability is 22 to 23 weeks of gestation, but death prior to hospital discharge occurs in approximately half of these newborns. For the survivors, lifelong neurodevelopmental complications and pulmonary disease are common. Obstetricians play a key role in counseling patients who are at risk of giving birth before 24 weeks of gestation. Given the challenges faced by an infant born at 22 and 23 weeks’ gestation, pregnant patients and trusted family members should approach the decision to actively resuscitate the newborn with caution. However, if the clinical team, patient, and trusted family members agree to pursue active treatment, completion of a course of antenatal steroids and appropriate respiratory and cardiovascular support at birth are key to improving long-term outcomes. ●

For many decades, the limit of newborn viability was at approximately 24 weeks’ gestation. Recent advances in pregnancy and neonatal care suggest that the new limit of viability is 22 (22 weeks and 0 days to 22 weeks and 6 days) or 23 (23 weeks and 0 days to 23 weeks and 6 days) weeks of gestation. In addition, data from observational cohort studies indicate that for infants born at 22 and 23 weeks’ gestation, survival is dependent on a course of antenatal steroids administered prior to birth plus intensive respiratory and cardiovascular support at delivery and in the neonatal intensive care unit (NICU).
Antenatal steroids: Critical for survival at 22 and 23 weeks of gestation
Most studies of birth outcomes at 22 and 23 weeks’ gestation rely on observational cohorts where unmeasured differences among the maternal-fetal dyads that received or did not receive a specific treatment confounds the interpretation of the data. However, data from multiple large observational cohorts suggest that between 22 and 24 weeks of gestation, completion of a course of antenatal steroids will optimize infant outcomes. Particularly noteworthy was the observation that the incremental survival benefit of antenatal steroids was greatest at 22 and 23 weeks’ gestation (TABLE 1).1 Similar results have been reported by Rossi and colleagues (TABLE 2).2
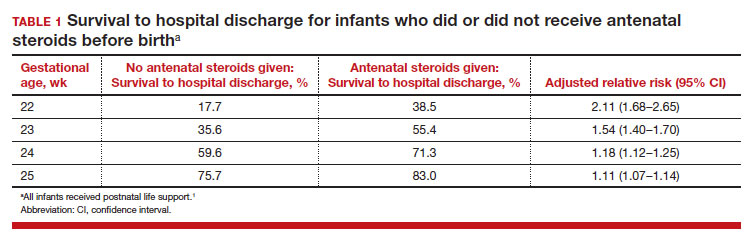
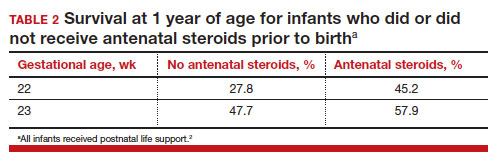
The importance of a completed course of antenatal steroids before birth was confirmed in another cohort study of 431 infants born in 2016 to 2019 at 22 weeks and 0 days’ to 23 weeks and 6 days’ gestation.3 Survival to discharge occurred in 53.9% of infants who received a full course of antenatal steroids before birth and 35.5% among those who did not receive antenatal steroids..3 Survival to discharge without major neonatal morbidities was 26.9% in those who received a full course of antenatal steroids and 10% among those who did not. In this cohort, major neonatal morbidities included severe intracranial hemorrhage, cystic periventricular leukomalacia, severe bronchopulmonary dysplasia, surgical necrotizing enterocolitis, or severe retinopathy of prematurity requiring treatment.
The American College of Obstetricians and Gynecologists (ACOG) recommends against antenatal steroids prior to 22 weeks and 0 days gestation.4 However, some neonatologists might recommend that antenatal steroids be given starting at 21 weeks and 5 days of gestation if birth is anticipated in the 22nd week of gestation and the patient prefers aggressive treatment of the newborn.
Active respiratory and cardiovascular support improves newborn outcomes
To maximize survival, infants born at 22 and 23 weeks’ gestation always require intensive active treatment at birth and in the following days in the NICU. Active treatment may include respiratory support, surfactant treatment, pressors, closure of a patent ductus arteriosus, transfusion of red blood cells, and parenteral nutrition. In one observational cohort study, active treatment at birth was not routinely provided at 22 and 23 weeks’ gestation but was routinely provided at later gestational ages (TABLE 3A).5 Not surprisingly, active treatment, especially at early gestational ages, is associated with improved survival to discharge. For example, at 22 weeks’ gestation, survival to discharge in infants who received or did not receive intensive active treatment was 28% and 0%, respectively.5 However, specific clinical characteristics of the pregnant patient and newborn may have influenced which infants were actively treated, confounding interpretation of the observation. In this cohort of extremely premature newborns, survival to hospital discharge increased substantially between 22 weeks and 26 weeks of gestational age (TABLE 3B).5
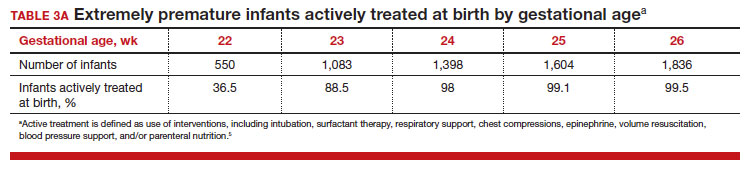
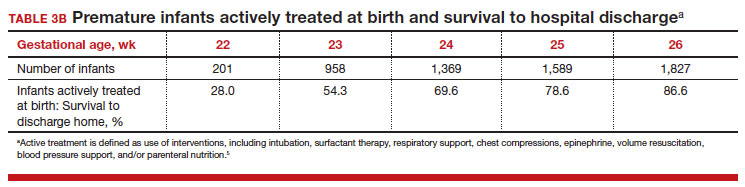
Many of the surviving infants needed chronic support treatment. Among surviving infants born at 22 weeks and 26 weeks, chronic support treatments were being used by 22.6% and 10.6% of infants, respectively, 2 years after birth.5 For surviving infants born at 22 weeks, the specific chronic support treatments included gastrostomy or feeding tube (19.4%), oxygen (9.7%), pulse oximeter (9.7%), and/or tracheostomy (3.2%). For surviving infants born at 26 weeks’ gestation, the specific chronic support treatments included gastrotomy or feeding tube (8.5%), pulse oximeter (4.4%), oxygen (3.2%), tracheostomy (2.3%), an apnea monitor (1.5%), and/or ventilator or continuous positive airway pressure (1.1%).5
Continue to: Evolving improvement in infant outcomes...
Evolving improvement in infant outcomes
In 1963, Jacqueline Bouvier Kennedy went into preterm labor at 34 weeks of gestation and delivered her son Patrick at a community facility. Due to severe respiratory distress syndrome, Patrick was transferred to the Boston Children’s Hospital, and he died shortly thereafter.6 Sixty years later, due to advances in obstetric and neonatal care, death from respiratory distress syndrome at 34 weeks of gestation is uncommon in the United States.
Infant outcomes following birth at 22 and 23 weeks’ gestation continue to improve. An observational cohort study from Sweden reported that at 22 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 10% and 30%, respectively.7 Similarly, at 23 weeks’ gestation, the percentage of live-born infants who survived to 1-year post birth in 2004 to 2007 and 2014 to 2016 was 52% and 61%, respectively.7 However, most of the surviving infants in this cohort had one or more major neonatal morbidities, including intraventricular hemorrhage grade 3 or 4; periventricular leukomalacia; necrotizing enterocolitis; retinopathy of prematurity grade 3, 4, or 5; or severe bronchopulmonary dysplasia.7
In a cohort of infants born in Japan at 22 to 24 weeks of gestation, there was a notable decrease in major neurodisability at 3 years of age for births occurring in 2 epochs, 2003 to 2007 and 2008 to 2012.8 When comparing outcomes in 2003 to 2007 versus 2008 to 2012, the change in rate of various major complications included the following: cerebral palsy (15.9% vs 9.5%), visual impairment (13.6% vs 4.4%), blindness (4.8% vs 1.3%), and hearing impairment (2.6% vs 1.0%). In contrast, the rate of cognitive impairment, defined as less than 70% of standard test performance for chronological age, was similar in the 2 time periods (36.5% and 37.9%, respectively).8 Based on data reported between 2000 and 2020, a systematic review and meta-analysis by Backes and colleagues concluded that there has been substantial improvement in the survival of infants born at 22 weeks of gestation.9
The small baby unit
A feature of modern medicine is the relentless evolution of new clinical subspecialties and sub-subspecialties. NICUs evolved from newborn nurseries to serve the needs of the most severely ill newborns, with care provided by a cadre of highly trained subspecialized neonatologists and neonatal nurses. A new era is dawning, with some NICUs developing a sub-subspecialized small baby unit to care for infants born between 22 and 26 weeks of gestation. These units often are staffed by clinicians with a specific interest in optimizing the care of extremely preterm infants, providing continuity of care over a long hospitalization.10 The benefits of a small baby unit may include:
- relentless standardization and adherence to the best intensive care practices
- daily use of checklists
- strict adherence to central line care
- timely extubation and transition to continuous positive airway pressure
- adherence to breastfeeding guidelines
- limiting the number of clinicians responsible for the patient
- promotion of kangaroo care
- avoidance of noxious stimuli.10,11
Continue to: Ethical and clinical issues...
Ethical and clinical issues
Providing clinical care to infants born at the edge of viability is challenging and raises many ethical and clinical concerns.12,13 For an infant born at the edge of viability, clinicians and parents do not want to initiate a care process that improves survival but results in an extremely poor quality of life. At the same time, clinicians and parents do not want to withhold care that could help an extremely premature newborn survive and thrive. Consequently, the counseling process is complex and requires coordination between the obstetrical and neonatology disciplines, involving physicians and nurses from both. A primary consideration in deciding to institute active treatment at birth is the preference of the pregnant patient and the patient’s trusted family members. A thorough discussion of these issues is beyond the scope of this editorial. ACOG provides detailed advice about the approach to counseling patients who face the possibility of a periviable birth.14
To help standardize the counseling process, institutions may find it helpful to recommend that clinicians consistently use a calculator to provide newborn outcome data to patients. The National Institute of Child Health and Human Development’s Extremely Preterm Birth Outcomes calculator uses the following inputs:
- gestational age
- estimated birth weight
- sex
- singleton/multiple gestation
- antenatal steroid treatment.
It also provides the following outputs as percentages:
- survival with active treatment at birth
- survival without active treatment at birth
- profound neurodevelopmental impairment
- moderate to severe neurodevelopmental impairment
- blindness
- deafness
- moderate to severe cerebral palsy
- cognitive developmental delay.15
A full assessment of all known clinical factors should influence the interpretation of the output from the clinical calculator. An alternativeis to use data from the Vermont Oxford Network. NICUs with sufficient clinical volume may prefer to use their own outcome data in the counseling process.
Institutions and clinical teams may improve the consistency of the counseling process by identifying criteria for 3 main treatment options:
- clinical situations where active treatment at birth is not generally offered (eg, <22 weeks’ gestation)
- clinical situations where active treatment at birth is almost always routinely provided (eg, >25 weeks’ gestation)
- clinical situations where patient preferences are especially important in guiding the use of active treatment.
Most institutions do not routinely offer active treatment of the newborn at a gestational age of less than 22 weeks and 0 days. Instead, comfort care often is provided for these newborns. Most institutions routinely provide active treatment at birth beginning at 24 or 25 weeks’ gestation unless unique risk factors or comorbidities warrant not providing active treatment (TABLE 3A). Some professional societies recommend setting a threshold for recommending active treatment at birth. For example, the British Association of Perinatal Medicine recommends that if there is 50% or higher probability of survival without severe disability, active treatment at birth should be considered because it is in the best interest of the newborn.16 In the hours and days following birth, the clinical course of the newborn greatly influences the treatment plan and care goals. After the initial resuscitation, if the clinical condition of an extremely preterm infant worsens and the prognosis is grim, a pivot to palliative care may be considered.
Final thoughts
Periviability is the earliest stage of fetal development where there is a reasonable chance, but not a high likelihood, of survival outside the womb. For decades, the threshold for periviability was approximately 24 weeks of gestation. With current obstetrical and neonatal practice, the new threshold for periviability is 22 to 23 weeks of gestation, but death prior to hospital discharge occurs in approximately half of these newborns. For the survivors, lifelong neurodevelopmental complications and pulmonary disease are common. Obstetricians play a key role in counseling patients who are at risk of giving birth before 24 weeks of gestation. Given the challenges faced by an infant born at 22 and 23 weeks’ gestation, pregnant patients and trusted family members should approach the decision to actively resuscitate the newborn with caution. However, if the clinical team, patient, and trusted family members agree to pursue active treatment, completion of a course of antenatal steroids and appropriate respiratory and cardiovascular support at birth are key to improving long-term outcomes. ●
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks gestation. JAMA Network Open. 2018;E183235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks [published online November 28, 2021]. Am J Perinatol. doi:10.1055/s-004-1740062
- Chawla S, Wyckoff MH, Rysavy MA, et al. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Network Open. 2022;5:E2233331.
- Use of antenatal corticosteroids at 22 weeks of gestation. ACOG website. Published September 2021. Accessed April 10, 2023. https://www.acog .org/clinical/clinical-guidance/practice -advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation
- Bell EF, Hintz SR, Hansen NI, et al. Mortality, in-hospital morbidity, care practices and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 2022;327:248-263.
- The tragic death of Patrick, JFK and Jackie’s newborn son, in 1963. Irish Central website. Published November 6, 2022. Accessed April 10, 2023. https://www.irishcentral.com/roots/history /tragic-death-patrick-kennedy-jfk-jackie
- Norman M, Hallberg B, Abrahamsson T, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004-2007 and 2014-2016. JAMA. 2019;32:1188-1199.
- Kono Y, Yonemoto N, Nakanishi H, et al. Changes in survival and neurodevelopmental outcomes of infants born at <25 weeks gestation: a retrospective observational study in tertiary centres in Japan. BMJ Paediatrics Open. 2018;2:E000211.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Morris M, Cleary JP, Soliman A. Small baby unit improves quality and outcomes in extremely low birth weight infants. Pediatrics. 2015;136:E1007-E1015.
- Fathi O, Nelin LD, Shephard EG, et al. Development of a small baby unit to improve outcomes for the extremely premature infant. J Perinatology. 2002;42:157-164.
- Lantos JD. Ethical issues in treatment of babies born at 22 weeks of gestation. Arch Dis Child. 2021;106:1155-1157.
- Shinwell ES. Ethics of birth at the limit of viability: the risky business of prediction. Neonatology. 2015;107:317-320.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No 6. periviable birth. Obstet Gynecol. 2017;E187-E199.
- Extremely preterm birth outcomes tool. NICHD website. Updated March 2, 2020. Accessed April 10, 2023. https://www.nichd.nih.gov/research /supported/EPBO/use#
- Mactier H, Bates SE, Johnston T, et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch Dis Child Fetal Neonatal Ed. 2020;105:F232-F239.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks gestation. JAMA Network Open. 2018;E183235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks [published online November 28, 2021]. Am J Perinatol. doi:10.1055/s-004-1740062
- Chawla S, Wyckoff MH, Rysavy MA, et al. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Network Open. 2022;5:E2233331.
- Use of antenatal corticosteroids at 22 weeks of gestation. ACOG website. Published September 2021. Accessed April 10, 2023. https://www.acog .org/clinical/clinical-guidance/practice -advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation
- Bell EF, Hintz SR, Hansen NI, et al. Mortality, in-hospital morbidity, care practices and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 2022;327:248-263.
- The tragic death of Patrick, JFK and Jackie’s newborn son, in 1963. Irish Central website. Published November 6, 2022. Accessed April 10, 2023. https://www.irishcentral.com/roots/history /tragic-death-patrick-kennedy-jfk-jackie
- Norman M, Hallberg B, Abrahamsson T, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004-2007 and 2014-2016. JAMA. 2019;32:1188-1199.
- Kono Y, Yonemoto N, Nakanishi H, et al. Changes in survival and neurodevelopmental outcomes of infants born at <25 weeks gestation: a retrospective observational study in tertiary centres in Japan. BMJ Paediatrics Open. 2018;2:E000211.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Morris M, Cleary JP, Soliman A. Small baby unit improves quality and outcomes in extremely low birth weight infants. Pediatrics. 2015;136:E1007-E1015.
- Fathi O, Nelin LD, Shephard EG, et al. Development of a small baby unit to improve outcomes for the extremely premature infant. J Perinatology. 2002;42:157-164.
- Lantos JD. Ethical issues in treatment of babies born at 22 weeks of gestation. Arch Dis Child. 2021;106:1155-1157.
- Shinwell ES. Ethics of birth at the limit of viability: the risky business of prediction. Neonatology. 2015;107:317-320.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No 6. periviable birth. Obstet Gynecol. 2017;E187-E199.
- Extremely preterm birth outcomes tool. NICHD website. Updated March 2, 2020. Accessed April 10, 2023. https://www.nichd.nih.gov/research /supported/EPBO/use#
- Mactier H, Bates SE, Johnston T, et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch Dis Child Fetal Neonatal Ed. 2020;105:F232-F239.