User login
Other Pediatric Literature of Interest
1. Esper F, Shapiro ED, Weibel C, et al. Association between a novel human coronavirus and Kawasaki disease. J Infect Dis. 2005;191:499-502.
Kawasaki disease, a systemic vasculitis of childhood, is the most common cause of childhood acquired heart disease in developed countries and frequently a diagnosis made in the inpatient setting. Although the etiology of Kawasaki disease is not known, there is evidence to suggest the disease may be triggered by an infectious agent. This evidence includes wavelike spread in countries, seasonal epidemics, and the rarity of Kawasaki disease in adults and infants less than 3 months old. Even more compelling is the recent identification by Rowley et al. Of an antigen of unknown origin in respiratory epithelial cells and macrophages from children with Kawasaki disease (1).
Despite suggestion that retroviruses, Epstein–Barr virus, parvovirus B19, or chlamydia may be important in the pathogenesis of Kawasaki disease, no infectious etiology has been proven. In this brief report, Esper et al. document the interesting finding of a novel human coronavirus, “New Haven coronavirus” (HCoVNH), in the respiratory secretions of a 6-month old infant diagnosed with Kawasaki disease. Subsequently, the authors performed a retrospective, case-controlled study of 11 Kawasaki disease patients less than 5 years of age from whom respiratory secretions were archived but had tested negative for respiratory syncytial virus, influenza viruses A and B, parainfluenza viruses 1–3, and adenovirus by direct fluorescent antibody assay. These patients were matched with 2 control subjects. Eight (72.7%) of 11 case subjects and 1 (4.5%) of the 22 control subjects tested positive for HCoVNH by reverse transcriptase polymerase chain reaction (p=.0015). Further studies are needed to determine the precise role this, or other infectious pathogens, may have in the pathogenesis of the disease.
Reference
- Rowley AH, Baker SC, Shulman ST, et al. Detection of antigen in bronchial epithelium and macrophages in acute Kawasaki disease by use of synthetic antibody. J Infect Dis. 2004;190:856-65.
2. Eyaid WM, AlNouri DM, Rashed MS, et al. An inborn error of metabolism presenting as hypoxicischemic insult. Pediatr Neurol. 2005;32:134-6.
Inborn error of metabolism is frequently on the “bottom” of many differential diagnoses lists for common pediatric presenting complaints. Relative infrequency coupled with the occasional difficulty of making an accurate diagnosis presents unique challenges. Nonetheless, the importance of making this diagnosis is essential, given the frequent opportunity for pharmacologic and/ or dietary intervention to be therapeutic.
These authors present an interesting case of siblings presenting with seizures and central nervous system imaging consistent with hypoxicischemic insult who were subsequently diagnosed with isolated sulfite oxidase deficiency.
1. Esper F, Shapiro ED, Weibel C, et al. Association between a novel human coronavirus and Kawasaki disease. J Infect Dis. 2005;191:499-502.
Kawasaki disease, a systemic vasculitis of childhood, is the most common cause of childhood acquired heart disease in developed countries and frequently a diagnosis made in the inpatient setting. Although the etiology of Kawasaki disease is not known, there is evidence to suggest the disease may be triggered by an infectious agent. This evidence includes wavelike spread in countries, seasonal epidemics, and the rarity of Kawasaki disease in adults and infants less than 3 months old. Even more compelling is the recent identification by Rowley et al. Of an antigen of unknown origin in respiratory epithelial cells and macrophages from children with Kawasaki disease (1).
Despite suggestion that retroviruses, Epstein–Barr virus, parvovirus B19, or chlamydia may be important in the pathogenesis of Kawasaki disease, no infectious etiology has been proven. In this brief report, Esper et al. document the interesting finding of a novel human coronavirus, “New Haven coronavirus” (HCoVNH), in the respiratory secretions of a 6-month old infant diagnosed with Kawasaki disease. Subsequently, the authors performed a retrospective, case-controlled study of 11 Kawasaki disease patients less than 5 years of age from whom respiratory secretions were archived but had tested negative for respiratory syncytial virus, influenza viruses A and B, parainfluenza viruses 1–3, and adenovirus by direct fluorescent antibody assay. These patients were matched with 2 control subjects. Eight (72.7%) of 11 case subjects and 1 (4.5%) of the 22 control subjects tested positive for HCoVNH by reverse transcriptase polymerase chain reaction (p=.0015). Further studies are needed to determine the precise role this, or other infectious pathogens, may have in the pathogenesis of the disease.
Reference
- Rowley AH, Baker SC, Shulman ST, et al. Detection of antigen in bronchial epithelium and macrophages in acute Kawasaki disease by use of synthetic antibody. J Infect Dis. 2004;190:856-65.
2. Eyaid WM, AlNouri DM, Rashed MS, et al. An inborn error of metabolism presenting as hypoxicischemic insult. Pediatr Neurol. 2005;32:134-6.
Inborn error of metabolism is frequently on the “bottom” of many differential diagnoses lists for common pediatric presenting complaints. Relative infrequency coupled with the occasional difficulty of making an accurate diagnosis presents unique challenges. Nonetheless, the importance of making this diagnosis is essential, given the frequent opportunity for pharmacologic and/ or dietary intervention to be therapeutic.
These authors present an interesting case of siblings presenting with seizures and central nervous system imaging consistent with hypoxicischemic insult who were subsequently diagnosed with isolated sulfite oxidase deficiency.
1. Esper F, Shapiro ED, Weibel C, et al. Association between a novel human coronavirus and Kawasaki disease. J Infect Dis. 2005;191:499-502.
Kawasaki disease, a systemic vasculitis of childhood, is the most common cause of childhood acquired heart disease in developed countries and frequently a diagnosis made in the inpatient setting. Although the etiology of Kawasaki disease is not known, there is evidence to suggest the disease may be triggered by an infectious agent. This evidence includes wavelike spread in countries, seasonal epidemics, and the rarity of Kawasaki disease in adults and infants less than 3 months old. Even more compelling is the recent identification by Rowley et al. Of an antigen of unknown origin in respiratory epithelial cells and macrophages from children with Kawasaki disease (1).
Despite suggestion that retroviruses, Epstein–Barr virus, parvovirus B19, or chlamydia may be important in the pathogenesis of Kawasaki disease, no infectious etiology has been proven. In this brief report, Esper et al. document the interesting finding of a novel human coronavirus, “New Haven coronavirus” (HCoVNH), in the respiratory secretions of a 6-month old infant diagnosed with Kawasaki disease. Subsequently, the authors performed a retrospective, case-controlled study of 11 Kawasaki disease patients less than 5 years of age from whom respiratory secretions were archived but had tested negative for respiratory syncytial virus, influenza viruses A and B, parainfluenza viruses 1–3, and adenovirus by direct fluorescent antibody assay. These patients were matched with 2 control subjects. Eight (72.7%) of 11 case subjects and 1 (4.5%) of the 22 control subjects tested positive for HCoVNH by reverse transcriptase polymerase chain reaction (p=.0015). Further studies are needed to determine the precise role this, or other infectious pathogens, may have in the pathogenesis of the disease.
Reference
- Rowley AH, Baker SC, Shulman ST, et al. Detection of antigen in bronchial epithelium and macrophages in acute Kawasaki disease by use of synthetic antibody. J Infect Dis. 2004;190:856-65.
2. Eyaid WM, AlNouri DM, Rashed MS, et al. An inborn error of metabolism presenting as hypoxicischemic insult. Pediatr Neurol. 2005;32:134-6.
Inborn error of metabolism is frequently on the “bottom” of many differential diagnoses lists for common pediatric presenting complaints. Relative infrequency coupled with the occasional difficulty of making an accurate diagnosis presents unique challenges. Nonetheless, the importance of making this diagnosis is essential, given the frequent opportunity for pharmacologic and/ or dietary intervention to be therapeutic.
These authors present an interesting case of siblings presenting with seizures and central nervous system imaging consistent with hypoxicischemic insult who were subsequently diagnosed with isolated sulfite oxidase deficiency.
Pediatric in the Literature
Calicitonin Precusors and IL-8 as a Screen Panel for Bacterial Sepsis
Stryjewski GR, Nylen ES, Bell MJ, et al. Interleukin-6, interleukin-8, and a rapid and sensitive assay for calcitonin precursors for the determination of bacterial sepsis in febrile neutropenic children. Pediatr Crit Care Med. 2005;6:129-35.
Identification of sensitive and specific markers for serious bacterial infection (SBI) in children has commanded significant attention in recent literature. These researchers present a prospective cohort study of 56 children aged 5 months to 17 years (median 6.7 years) with fever (axillary temperature ≥37.5°C or oral temperature ≥38°C) and neutropenia (absolute neutrophil count ≤500/mm3) admitted to Children’s National Medical Center during a 15-month period. Researchers hypothesized that a highly sensitive assay for calcitonin precursors (CTpr) would detect levels of CTpr early in the course of illness, and that these levels in conjunction with measured levels of the cytokines interleukin (IL)-6 and IL-8 would provide a sensitive and specific set of markers for diagnosing bacterial sepsis in the study population. Markers were measured at admission, at 24 hours and at 48 hours. CTpr at 24 hours (adjusted odds ratio [95% confidence interval], 1.8 [1.2–2.8], p=.001) and IL8 (at 48 hours 1.08 [1.2–2.8], p=.02) were found to have association with bacterial sepsis. The authors conclude that based on the data generated, using cutoff values of 500 pg/mL for CTpr at 24 hours and 20 pg/mL for IL-8 at 48 hours would provide a sensitivity of 94% and specificity of 90%. Reliable biochemical markers that are highly associated with SBI and/or sepsis will likely improve the care of pediatric patients by guiding more specific therapy and potentially limiting exposure to unnecessary antibiotic . The results of this study cannot be generalized to all pediatric patients with fever and risk for SBI, due to the unique attributes of the study population. However, the study does provide information for future research into the development of markers and/or scoring systems to aid in the early diagnosis of SBI/sepsis in the general pediatric population.
Which Tests are Helpful and Cost-Effective in the Evaluation of Pediatric Syncope?
Steinberg LA, Knilans TK. Syncope in children: diagnostic tests have a high cost and low yield. J Pediatr. 2005;146:355-8.
Evaluation of syncope in children is not uncommon. This evaluation can often include multiple expensive tests, and evidence defining the most efficacious and cost-effective course of evaluation is lacking. Researchers from the Children’s Heart Center at St. Vincent Hospital in Indianapolis and the Division of Cardiology at Children’s Hospital Medical Center in Cincinnati present a retrospective review of 169 patients aged 4.5 to 18.7 years (mean, 13.1 ± 3.6) presenting to a tertiary care center for evaluation of transient loss of consciousness associated with loss of postural tone to describe the cost and utility of testing used to make a diagnosis. Costs were based on hospital costs for 1999 and did not include professional fees, the cost of clinic evaluations, or hospital admissions. There are significant limitations in the study design, and these are adequately discussed by the authors. A diagnosis was established in 128 patients (76%), and neurocardiogenic syncope was the most common diagnosis occurring in 116 patients (68%). Other diagnoses included seizure disorder (3 patients), pseudoseizure (2), anxiety disorder (2), psychogenic syncope (2) and 1 patient each with breathholding spells, long QT syndrome, and exertonal ventricular tachycardia. Tilt-testing had the highest diagnostic yield, although the researchers aptly point out that in the literature the specificity of tilt-testing ranges from 48 to 100% and that this test is rarely required to diagnose neurocardiogenic syncope, the most frequent diagnosis in this review. Loop memory cardiac monitoring had the lowest cost per diagnostic result. Electrocardiography had the lowest diagnostic yield and highest cost per test. Echocardiogram, chest radiograph, cardiac catheterization, electrophysiology studies, and evaluation of serum and body fluids were not diagnostic in this series. This respective review highlights the need for a consistent, evidence-based approach to this common presenting problem while emphasizing the importance of judicious testing guided by a thorough history and physical exam.
An Increase in Severe Community Acquired MRSA Infections in Texas
Gonzales BE, Martinez-Aguilar G, Hulten KG, et al. Severe staphylococcal sepsis in adolescents in the era of community-acquired methicillin-resistant Staphylococcus aureus. Pediatrics. 2005;115:642-8.
Gonzales et al. describe data prospectively gathered since August 1, 2001, showing an increase in the number of severely ill patients with community acquired (CA) Staphylococcus aureus infections. Fourteen patients with a mean age of 12.9 years (range: 10–15 years) were admitted to the PICU with sepsis. Twelve patients had CA methicillin-resistant S. aureus (CAMRSA). Thirteen patients (93%) had bone and joint infections. Thirteen patients had pulmonary involvement. Acute prerenal failure and peripheral vascular thrombosis were present in 50% and 29% of patients, respectively. Thirteen patients were bacteremic. All CAMRSA isolates were resistant to erythromycin, without inducible resistance to clindamycin. The review is interesting in light of the other literature reviewed by the authors suggesting a trend toward more severe infections caused by CAMRSA.
TheoPhylline vs. Terubutaline in Critically III Asthmatics
Wheeler DS, Jacobs BR, Kenreigh CA, et al. Theophylline versus terbutaline in treating critically ill children with status asthmaticus: A prospective, randomized, controlled trial. Pediatr Crit Care Med. 2005;6:142-7.
Status asthmaticus is a common diagnosis on the pediatric inpatient unit and in the pediatric intensive care unit (PICU). Inhaled beta-2 agonists, systemic corticosteroids, and supplemental oxygen are accepted as the standard of care for children with status asthmaticus who require admission. For critically ill children who are poorly responsive to the aforementioned triad of therapy, both theophylline and terbutaline are considered possible adjunctive therapies. Wheeler et al. suggest that the many studies failing to demonstrate added benefit of theophylline in non–critically ill patients has decreased the use of theophylline in the critical care setting, but point out that recent studies involving critically ill populations with status asthmaticus treated with theophylline have suggested benefit with comparison to placebo. Therefore, these researchers present a randomized, prospective, controlled, double-blind trial comparing the efficacy of theophylline alone, terbutaline alone, and theophylline and terbutaline together in critically ill pediatric patients receiving continuous nebulized albuterol and intravenous steroids. Forty patients with impending respiratory failure between the ages of 3 and 15 years were randomized to 1 of 3 groups: theophylline plus placebo (group 1), terbutaline plus placebo (group 2), or theophylline and terbutaline together (group 3). Thirty-six patients completed the study; 3 patients from group 1 were withdrawn due to parental request secondary to agitation (2 patients) and being inadvertently placed on a terbutaline infusion (1 patient). One patient from group 3 was withdrawn by the treating physician due to lack of improvement. All study participants, with the exception of the study pharmacist, were blinded to group assignment. Adjunctive therapies, including magnesium, ipatropium bromide and ketamine, were utilized at the discretion of the treating physician and were not controlled for. The primary outcome variable was change in a clinical scoring tool. Secondary outcomes variables included time to a specific clinical score, length of stay in the PICU, progression to mechanical ventilation, and incidence of adverse events. In addition, a cost analysis was performed isolating the 3 groups based on fiscal year 2003 cost estimates for theophylline and terbutaline. Results demonstrated no difference in the primary or secondary clinical outcome measures, with the exception of a higher incidence of nausea in group 3. The hospital costs were significantly lower in group 1 compared with groups 2 and 3 ($280 vs. $3,908 vs. $4,045, respectively, p<.0001). Significant limitations to the study include the lack of control of adjunctive therapies, a small sample size that confounds the ability to conclude no clinical difference between groups, and a baseline Pediatric Risk of Mortality (PRISM) Score in group 3 compared with groups 1 and 2. Despite these limitations the researchers suggest that the addition of intravenous theophylline to continuous nebulized albuterol and corticosteroids in the management of critically ill children with status asthmaticus is as safe and effective as adding intravenous terbutaline while being more cost-effective. Subsequent larger, well-controlled studies are required to support this conclusion.
Can Computerized Physician Ordering Create Errors?
Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293:1197-203.
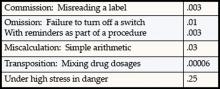
Adverse drug events are a frequent etiology of inpatient morbidity and prescribing errors are the most frequent source. Computerized physician order entry (CPOE) is touted as a potential remedy for some types of adverse drug events. Few studies have investigated the potential for novel medication errors generated by a change to CPOE from conventional ordering. Koppel et al. present a quantitative and qualitative study of medication errors caused or exacerbated by a CPOE system. Interviews, surveys, and focus groups were the primary means of data collection. Housestaff who typically enter more than 9 orders per month were the primary study population, but data collection also included pharmacists, nursing staff , information technology managers, and attending physicians. The study was conducted in a tertiary-care teaching hospital between 2002 and 2004 utilizing a CPOE system in place since 1997. The CPOE system utilized is described as “monochromatic” and having “pre-Windows interfaces.” While not integrated with all hospital functions, the system was integrated with pharmacy and nursing medication lists. Researchers grouped errors into two broad categories: (1) information errors (fragmentation and systems integration failure) and (2) human-machine interface flaws (machine rules that do not correspond to work organization or usual behaviors). In total, 22 types of errors were recorded.
An example of an “information error” is assumed and incorrect dose information based on viewing doses intended only to describe pharmacy stocking practice―i.e. assuming that because the pharmacy stocks a 10mg dose of a medication, 10mg is an appropriate “minimally effective” dose. A “human-machine interface error” example is selecting an incorrect patient for ordering due to properties of the CPOE screen, such as the patient name not appearing on all screens. There are several important limitations to this study, but perhaps most important is the inability to generalize this data to other settings with potentially different physician users and software. Also important is a lack of description regarding physician user training and/or correlation of errors with amount of training or frequency of use, considering that the study population was defined as housestaff who may only use the system for 9 orders each . Despite these limitations, the study represents a requisite component to the growing trend toward the complete electronic record―namely, the use of objective investigations to study the safety and effectiveness of CPOE and the electronic record to promote the most optimal implementation and evolution of this new clinical tool.
Single-Dose Azithromycin for Acute Otitis Media
Arguedas A, Emparanza P, Schwartz RH, et al. A randomized, multicenter, double blind, double dummy trial of single dose azithromycin versus high dose amoxicillin for treatment of uncomplicated acute otitis media. Pediatr Infect Dis J. 2005;24: 153-61.
Acute otitis media is a common comorbid condition in pediatric inpatients. Patients at risk of having AOM with drug-resistant Streptococcus pneumoniae can be treated with high-dose amoxicillin as a first-line therapy according to recent American Academy of Pediatrics (AAP) recommendations. Despite this recommendation, there is evidence of reduced in vitro activity of amoxicillin against β-lactamase-producing Haemophilus influenzae and Moraxella catarrhalis, as well as a lack of data from controlled and blinded studies demonstrating efficacy, adverse events and compliance for high-dose regimens. Azithromycin has in vitro activity against the 4 pathogens of clinical significance in AOM, and studies have shown that a single-dose regimen of azithromycin by the oral route is pharmacokinetically feasible, safe, and comparable in success rate to 3- and 5-day azithromycin regimens. With these considerations in mind, Arguedas et al. designed this study to compare single-dose (30 mg/kg) azithromycin with high-dose (90 mg/kg/day) amoxicillin in uncomplicated AOM.
In this double-blind, double-dummy, multinational, clinical trial, children between the ages of 6 and 30 months with uncomplicated AOM were randomized to treatment with single-dose azithromycin or high-dose amoxicillin (90 mg/kg/day, in 2 div doses) for 10 days. The primary outcome measure was clinical efficacy assessed at the end of treatment on the basis of a modified intent-to-treat (MITT) population. Secondary outcomes were analyses of safety and compliance. Three hundred thirteen patients were enrolled, of whom 83% were <2 years old, with 158 patients randomized to receive azithromycin and 154 to receive amoxicillin. Tympanocentesis was performed at baseline, and clinical responses were assessed at days 12–14 (end of therapy) and 25–28 (end of study). A middle-ear pathogen was detected in 212 patients (68%). H. Influenzae was the most common pathogen isolated (96 cases), followed by S. pneumoniae (92), M. catarrhalis (23), and S. pyogenes (23). At the end of therapy, clinical success rates for azithromycin and amoxicillin were comparable for all patients (84% and 84%, respectively) and for children <2 years of age (82% and 82%, respectively). At the end of the study, clinical efficacies among all microbiologic modified intent-to-treat evaluable subjects were comparable for patients treated with azithro(80%) and patients treated with amoxicillin (83%). The rates of adverse events for azithromycin and amoxicillin were 20% and 29%, respectively (p=.064). Diarrhea was more common in the amoxicillin group (17.5%) as compared to the azithromycin group (8.2%) (p=.017). Compliance, defined as completion of >80% of the study medications, was higher in the azithromycin group (100%) then in the amoxicillin group (90%) (p=.001). For practitioners ordering medications, compliance and efficacy are uppermost considerations. Single-dose azithromycin ensured 100% compliance, decreased adverse reactions, and equal efficacy, compared to high-dose amoxicillin in this well designed, randomized, controlled trial. (Jadad Score = 4/5) all patients (84% and 84%, respectively) and for children <2 years of age (82% and 82%, respectively). At the end of the study, clinical efficacies among all microbiologic modified intent-to-treat evaluable subjects were comparable for patients treated with azithromycin (80%) and patients treated with amoxicillin (83%). The rates of adverse events for azithromycin and amoxicillin were 20% and 29%, respectively
(p=.064). Diarrhea was more common in the amoxicillin group (17.5%) as compared to the azithromycin group (8.2%) (p=.017). Compliance, defined as completion of >80% of the study medications, was higher in the azithromycin group (100%) then in the amoxicillin group (90%) (p=.001). For practitioners ordering medications, compliance and efficacy are uppermost considerations. Single-dose azithromycin ensured 100% compliance, decreased adverse reactions, and equal efficacy, compared to high-dose amoxicillin in this well-designed, randomized, controlled trial. (Jadad Score = 4/5)
Calicitonin Precusors and IL-8 as a Screen Panel for Bacterial Sepsis
Stryjewski GR, Nylen ES, Bell MJ, et al. Interleukin-6, interleukin-8, and a rapid and sensitive assay for calcitonin precursors for the determination of bacterial sepsis in febrile neutropenic children. Pediatr Crit Care Med. 2005;6:129-35.
Identification of sensitive and specific markers for serious bacterial infection (SBI) in children has commanded significant attention in recent literature. These researchers present a prospective cohort study of 56 children aged 5 months to 17 years (median 6.7 years) with fever (axillary temperature ≥37.5°C or oral temperature ≥38°C) and neutropenia (absolute neutrophil count ≤500/mm3) admitted to Children’s National Medical Center during a 15-month period. Researchers hypothesized that a highly sensitive assay for calcitonin precursors (CTpr) would detect levels of CTpr early in the course of illness, and that these levels in conjunction with measured levels of the cytokines interleukin (IL)-6 and IL-8 would provide a sensitive and specific set of markers for diagnosing bacterial sepsis in the study population. Markers were measured at admission, at 24 hours and at 48 hours. CTpr at 24 hours (adjusted odds ratio [95% confidence interval], 1.8 [1.2–2.8], p=.001) and IL8 (at 48 hours 1.08 [1.2–2.8], p=.02) were found to have association with bacterial sepsis. The authors conclude that based on the data generated, using cutoff values of 500 pg/mL for CTpr at 24 hours and 20 pg/mL for IL-8 at 48 hours would provide a sensitivity of 94% and specificity of 90%. Reliable biochemical markers that are highly associated with SBI and/or sepsis will likely improve the care of pediatric patients by guiding more specific therapy and potentially limiting exposure to unnecessary antibiotic . The results of this study cannot be generalized to all pediatric patients with fever and risk for SBI, due to the unique attributes of the study population. However, the study does provide information for future research into the development of markers and/or scoring systems to aid in the early diagnosis of SBI/sepsis in the general pediatric population.
Which Tests are Helpful and Cost-Effective in the Evaluation of Pediatric Syncope?
Steinberg LA, Knilans TK. Syncope in children: diagnostic tests have a high cost and low yield. J Pediatr. 2005;146:355-8.
Evaluation of syncope in children is not uncommon. This evaluation can often include multiple expensive tests, and evidence defining the most efficacious and cost-effective course of evaluation is lacking. Researchers from the Children’s Heart Center at St. Vincent Hospital in Indianapolis and the Division of Cardiology at Children’s Hospital Medical Center in Cincinnati present a retrospective review of 169 patients aged 4.5 to 18.7 years (mean, 13.1 ± 3.6) presenting to a tertiary care center for evaluation of transient loss of consciousness associated with loss of postural tone to describe the cost and utility of testing used to make a diagnosis. Costs were based on hospital costs for 1999 and did not include professional fees, the cost of clinic evaluations, or hospital admissions. There are significant limitations in the study design, and these are adequately discussed by the authors. A diagnosis was established in 128 patients (76%), and neurocardiogenic syncope was the most common diagnosis occurring in 116 patients (68%). Other diagnoses included seizure disorder (3 patients), pseudoseizure (2), anxiety disorder (2), psychogenic syncope (2) and 1 patient each with breathholding spells, long QT syndrome, and exertonal ventricular tachycardia. Tilt-testing had the highest diagnostic yield, although the researchers aptly point out that in the literature the specificity of tilt-testing ranges from 48 to 100% and that this test is rarely required to diagnose neurocardiogenic syncope, the most frequent diagnosis in this review. Loop memory cardiac monitoring had the lowest cost per diagnostic result. Electrocardiography had the lowest diagnostic yield and highest cost per test. Echocardiogram, chest radiograph, cardiac catheterization, electrophysiology studies, and evaluation of serum and body fluids were not diagnostic in this series. This respective review highlights the need for a consistent, evidence-based approach to this common presenting problem while emphasizing the importance of judicious testing guided by a thorough history and physical exam.
An Increase in Severe Community Acquired MRSA Infections in Texas
Gonzales BE, Martinez-Aguilar G, Hulten KG, et al. Severe staphylococcal sepsis in adolescents in the era of community-acquired methicillin-resistant Staphylococcus aureus. Pediatrics. 2005;115:642-8.
Gonzales et al. describe data prospectively gathered since August 1, 2001, showing an increase in the number of severely ill patients with community acquired (CA) Staphylococcus aureus infections. Fourteen patients with a mean age of 12.9 years (range: 10–15 years) were admitted to the PICU with sepsis. Twelve patients had CA methicillin-resistant S. aureus (CAMRSA). Thirteen patients (93%) had bone and joint infections. Thirteen patients had pulmonary involvement. Acute prerenal failure and peripheral vascular thrombosis were present in 50% and 29% of patients, respectively. Thirteen patients were bacteremic. All CAMRSA isolates were resistant to erythromycin, without inducible resistance to clindamycin. The review is interesting in light of the other literature reviewed by the authors suggesting a trend toward more severe infections caused by CAMRSA.
TheoPhylline vs. Terubutaline in Critically III Asthmatics
Wheeler DS, Jacobs BR, Kenreigh CA, et al. Theophylline versus terbutaline in treating critically ill children with status asthmaticus: A prospective, randomized, controlled trial. Pediatr Crit Care Med. 2005;6:142-7.
Status asthmaticus is a common diagnosis on the pediatric inpatient unit and in the pediatric intensive care unit (PICU). Inhaled beta-2 agonists, systemic corticosteroids, and supplemental oxygen are accepted as the standard of care for children with status asthmaticus who require admission. For critically ill children who are poorly responsive to the aforementioned triad of therapy, both theophylline and terbutaline are considered possible adjunctive therapies. Wheeler et al. suggest that the many studies failing to demonstrate added benefit of theophylline in non–critically ill patients has decreased the use of theophylline in the critical care setting, but point out that recent studies involving critically ill populations with status asthmaticus treated with theophylline have suggested benefit with comparison to placebo. Therefore, these researchers present a randomized, prospective, controlled, double-blind trial comparing the efficacy of theophylline alone, terbutaline alone, and theophylline and terbutaline together in critically ill pediatric patients receiving continuous nebulized albuterol and intravenous steroids. Forty patients with impending respiratory failure between the ages of 3 and 15 years were randomized to 1 of 3 groups: theophylline plus placebo (group 1), terbutaline plus placebo (group 2), or theophylline and terbutaline together (group 3). Thirty-six patients completed the study; 3 patients from group 1 were withdrawn due to parental request secondary to agitation (2 patients) and being inadvertently placed on a terbutaline infusion (1 patient). One patient from group 3 was withdrawn by the treating physician due to lack of improvement. All study participants, with the exception of the study pharmacist, were blinded to group assignment. Adjunctive therapies, including magnesium, ipatropium bromide and ketamine, were utilized at the discretion of the treating physician and were not controlled for. The primary outcome variable was change in a clinical scoring tool. Secondary outcomes variables included time to a specific clinical score, length of stay in the PICU, progression to mechanical ventilation, and incidence of adverse events. In addition, a cost analysis was performed isolating the 3 groups based on fiscal year 2003 cost estimates for theophylline and terbutaline. Results demonstrated no difference in the primary or secondary clinical outcome measures, with the exception of a higher incidence of nausea in group 3. The hospital costs were significantly lower in group 1 compared with groups 2 and 3 ($280 vs. $3,908 vs. $4,045, respectively, p<.0001). Significant limitations to the study include the lack of control of adjunctive therapies, a small sample size that confounds the ability to conclude no clinical difference between groups, and a baseline Pediatric Risk of Mortality (PRISM) Score in group 3 compared with groups 1 and 2. Despite these limitations the researchers suggest that the addition of intravenous theophylline to continuous nebulized albuterol and corticosteroids in the management of critically ill children with status asthmaticus is as safe and effective as adding intravenous terbutaline while being more cost-effective. Subsequent larger, well-controlled studies are required to support this conclusion.
Can Computerized Physician Ordering Create Errors?
Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293:1197-203.
Adverse drug events are a frequent etiology of inpatient morbidity and prescribing errors are the most frequent source. Computerized physician order entry (CPOE) is touted as a potential remedy for some types of adverse drug events. Few studies have investigated the potential for novel medication errors generated by a change to CPOE from conventional ordering. Koppel et al. present a quantitative and qualitative study of medication errors caused or exacerbated by a CPOE system. Interviews, surveys, and focus groups were the primary means of data collection. Housestaff who typically enter more than 9 orders per month were the primary study population, but data collection also included pharmacists, nursing staff , information technology managers, and attending physicians. The study was conducted in a tertiary-care teaching hospital between 2002 and 2004 utilizing a CPOE system in place since 1997. The CPOE system utilized is described as “monochromatic” and having “pre-Windows interfaces.” While not integrated with all hospital functions, the system was integrated with pharmacy and nursing medication lists. Researchers grouped errors into two broad categories: (1) information errors (fragmentation and systems integration failure) and (2) human-machine interface flaws (machine rules that do not correspond to work organization or usual behaviors). In total, 22 types of errors were recorded.
An example of an “information error” is assumed and incorrect dose information based on viewing doses intended only to describe pharmacy stocking practice―i.e. assuming that because the pharmacy stocks a 10mg dose of a medication, 10mg is an appropriate “minimally effective” dose. A “human-machine interface error” example is selecting an incorrect patient for ordering due to properties of the CPOE screen, such as the patient name not appearing on all screens. There are several important limitations to this study, but perhaps most important is the inability to generalize this data to other settings with potentially different physician users and software. Also important is a lack of description regarding physician user training and/or correlation of errors with amount of training or frequency of use, considering that the study population was defined as housestaff who may only use the system for 9 orders each . Despite these limitations, the study represents a requisite component to the growing trend toward the complete electronic record―namely, the use of objective investigations to study the safety and effectiveness of CPOE and the electronic record to promote the most optimal implementation and evolution of this new clinical tool.
Single-Dose Azithromycin for Acute Otitis Media
Arguedas A, Emparanza P, Schwartz RH, et al. A randomized, multicenter, double blind, double dummy trial of single dose azithromycin versus high dose amoxicillin for treatment of uncomplicated acute otitis media. Pediatr Infect Dis J. 2005;24: 153-61.
Acute otitis media is a common comorbid condition in pediatric inpatients. Patients at risk of having AOM with drug-resistant Streptococcus pneumoniae can be treated with high-dose amoxicillin as a first-line therapy according to recent American Academy of Pediatrics (AAP) recommendations. Despite this recommendation, there is evidence of reduced in vitro activity of amoxicillin against β-lactamase-producing Haemophilus influenzae and Moraxella catarrhalis, as well as a lack of data from controlled and blinded studies demonstrating efficacy, adverse events and compliance for high-dose regimens. Azithromycin has in vitro activity against the 4 pathogens of clinical significance in AOM, and studies have shown that a single-dose regimen of azithromycin by the oral route is pharmacokinetically feasible, safe, and comparable in success rate to 3- and 5-day azithromycin regimens. With these considerations in mind, Arguedas et al. designed this study to compare single-dose (30 mg/kg) azithromycin with high-dose (90 mg/kg/day) amoxicillin in uncomplicated AOM.
In this double-blind, double-dummy, multinational, clinical trial, children between the ages of 6 and 30 months with uncomplicated AOM were randomized to treatment with single-dose azithromycin or high-dose amoxicillin (90 mg/kg/day, in 2 div doses) for 10 days. The primary outcome measure was clinical efficacy assessed at the end of treatment on the basis of a modified intent-to-treat (MITT) population. Secondary outcomes were analyses of safety and compliance. Three hundred thirteen patients were enrolled, of whom 83% were <2 years old, with 158 patients randomized to receive azithromycin and 154 to receive amoxicillin. Tympanocentesis was performed at baseline, and clinical responses were assessed at days 12–14 (end of therapy) and 25–28 (end of study). A middle-ear pathogen was detected in 212 patients (68%). H. Influenzae was the most common pathogen isolated (96 cases), followed by S. pneumoniae (92), M. catarrhalis (23), and S. pyogenes (23). At the end of therapy, clinical success rates for azithromycin and amoxicillin were comparable for all patients (84% and 84%, respectively) and for children <2 years of age (82% and 82%, respectively). At the end of the study, clinical efficacies among all microbiologic modified intent-to-treat evaluable subjects were comparable for patients treated with azithro(80%) and patients treated with amoxicillin (83%). The rates of adverse events for azithromycin and amoxicillin were 20% and 29%, respectively (p=.064). Diarrhea was more common in the amoxicillin group (17.5%) as compared to the azithromycin group (8.2%) (p=.017). Compliance, defined as completion of >80% of the study medications, was higher in the azithromycin group (100%) then in the amoxicillin group (90%) (p=.001). For practitioners ordering medications, compliance and efficacy are uppermost considerations. Single-dose azithromycin ensured 100% compliance, decreased adverse reactions, and equal efficacy, compared to high-dose amoxicillin in this well designed, randomized, controlled trial. (Jadad Score = 4/5) all patients (84% and 84%, respectively) and for children <2 years of age (82% and 82%, respectively). At the end of the study, clinical efficacies among all microbiologic modified intent-to-treat evaluable subjects were comparable for patients treated with azithromycin (80%) and patients treated with amoxicillin (83%). The rates of adverse events for azithromycin and amoxicillin were 20% and 29%, respectively
(p=.064). Diarrhea was more common in the amoxicillin group (17.5%) as compared to the azithromycin group (8.2%) (p=.017). Compliance, defined as completion of >80% of the study medications, was higher in the azithromycin group (100%) then in the amoxicillin group (90%) (p=.001). For practitioners ordering medications, compliance and efficacy are uppermost considerations. Single-dose azithromycin ensured 100% compliance, decreased adverse reactions, and equal efficacy, compared to high-dose amoxicillin in this well-designed, randomized, controlled trial. (Jadad Score = 4/5)
Calicitonin Precusors and IL-8 as a Screen Panel for Bacterial Sepsis
Stryjewski GR, Nylen ES, Bell MJ, et al. Interleukin-6, interleukin-8, and a rapid and sensitive assay for calcitonin precursors for the determination of bacterial sepsis in febrile neutropenic children. Pediatr Crit Care Med. 2005;6:129-35.
Identification of sensitive and specific markers for serious bacterial infection (SBI) in children has commanded significant attention in recent literature. These researchers present a prospective cohort study of 56 children aged 5 months to 17 years (median 6.7 years) with fever (axillary temperature ≥37.5°C or oral temperature ≥38°C) and neutropenia (absolute neutrophil count ≤500/mm3) admitted to Children’s National Medical Center during a 15-month period. Researchers hypothesized that a highly sensitive assay for calcitonin precursors (CTpr) would detect levels of CTpr early in the course of illness, and that these levels in conjunction with measured levels of the cytokines interleukin (IL)-6 and IL-8 would provide a sensitive and specific set of markers for diagnosing bacterial sepsis in the study population. Markers were measured at admission, at 24 hours and at 48 hours. CTpr at 24 hours (adjusted odds ratio [95% confidence interval], 1.8 [1.2–2.8], p=.001) and IL8 (at 48 hours 1.08 [1.2–2.8], p=.02) were found to have association with bacterial sepsis. The authors conclude that based on the data generated, using cutoff values of 500 pg/mL for CTpr at 24 hours and 20 pg/mL for IL-8 at 48 hours would provide a sensitivity of 94% and specificity of 90%. Reliable biochemical markers that are highly associated with SBI and/or sepsis will likely improve the care of pediatric patients by guiding more specific therapy and potentially limiting exposure to unnecessary antibiotic . The results of this study cannot be generalized to all pediatric patients with fever and risk for SBI, due to the unique attributes of the study population. However, the study does provide information for future research into the development of markers and/or scoring systems to aid in the early diagnosis of SBI/sepsis in the general pediatric population.
Which Tests are Helpful and Cost-Effective in the Evaluation of Pediatric Syncope?
Steinberg LA, Knilans TK. Syncope in children: diagnostic tests have a high cost and low yield. J Pediatr. 2005;146:355-8.
Evaluation of syncope in children is not uncommon. This evaluation can often include multiple expensive tests, and evidence defining the most efficacious and cost-effective course of evaluation is lacking. Researchers from the Children’s Heart Center at St. Vincent Hospital in Indianapolis and the Division of Cardiology at Children’s Hospital Medical Center in Cincinnati present a retrospective review of 169 patients aged 4.5 to 18.7 years (mean, 13.1 ± 3.6) presenting to a tertiary care center for evaluation of transient loss of consciousness associated with loss of postural tone to describe the cost and utility of testing used to make a diagnosis. Costs were based on hospital costs for 1999 and did not include professional fees, the cost of clinic evaluations, or hospital admissions. There are significant limitations in the study design, and these are adequately discussed by the authors. A diagnosis was established in 128 patients (76%), and neurocardiogenic syncope was the most common diagnosis occurring in 116 patients (68%). Other diagnoses included seizure disorder (3 patients), pseudoseizure (2), anxiety disorder (2), psychogenic syncope (2) and 1 patient each with breathholding spells, long QT syndrome, and exertonal ventricular tachycardia. Tilt-testing had the highest diagnostic yield, although the researchers aptly point out that in the literature the specificity of tilt-testing ranges from 48 to 100% and that this test is rarely required to diagnose neurocardiogenic syncope, the most frequent diagnosis in this review. Loop memory cardiac monitoring had the lowest cost per diagnostic result. Electrocardiography had the lowest diagnostic yield and highest cost per test. Echocardiogram, chest radiograph, cardiac catheterization, electrophysiology studies, and evaluation of serum and body fluids were not diagnostic in this series. This respective review highlights the need for a consistent, evidence-based approach to this common presenting problem while emphasizing the importance of judicious testing guided by a thorough history and physical exam.
An Increase in Severe Community Acquired MRSA Infections in Texas
Gonzales BE, Martinez-Aguilar G, Hulten KG, et al. Severe staphylococcal sepsis in adolescents in the era of community-acquired methicillin-resistant Staphylococcus aureus. Pediatrics. 2005;115:642-8.
Gonzales et al. describe data prospectively gathered since August 1, 2001, showing an increase in the number of severely ill patients with community acquired (CA) Staphylococcus aureus infections. Fourteen patients with a mean age of 12.9 years (range: 10–15 years) were admitted to the PICU with sepsis. Twelve patients had CA methicillin-resistant S. aureus (CAMRSA). Thirteen patients (93%) had bone and joint infections. Thirteen patients had pulmonary involvement. Acute prerenal failure and peripheral vascular thrombosis were present in 50% and 29% of patients, respectively. Thirteen patients were bacteremic. All CAMRSA isolates were resistant to erythromycin, without inducible resistance to clindamycin. The review is interesting in light of the other literature reviewed by the authors suggesting a trend toward more severe infections caused by CAMRSA.
TheoPhylline vs. Terubutaline in Critically III Asthmatics
Wheeler DS, Jacobs BR, Kenreigh CA, et al. Theophylline versus terbutaline in treating critically ill children with status asthmaticus: A prospective, randomized, controlled trial. Pediatr Crit Care Med. 2005;6:142-7.
Status asthmaticus is a common diagnosis on the pediatric inpatient unit and in the pediatric intensive care unit (PICU). Inhaled beta-2 agonists, systemic corticosteroids, and supplemental oxygen are accepted as the standard of care for children with status asthmaticus who require admission. For critically ill children who are poorly responsive to the aforementioned triad of therapy, both theophylline and terbutaline are considered possible adjunctive therapies. Wheeler et al. suggest that the many studies failing to demonstrate added benefit of theophylline in non–critically ill patients has decreased the use of theophylline in the critical care setting, but point out that recent studies involving critically ill populations with status asthmaticus treated with theophylline have suggested benefit with comparison to placebo. Therefore, these researchers present a randomized, prospective, controlled, double-blind trial comparing the efficacy of theophylline alone, terbutaline alone, and theophylline and terbutaline together in critically ill pediatric patients receiving continuous nebulized albuterol and intravenous steroids. Forty patients with impending respiratory failure between the ages of 3 and 15 years were randomized to 1 of 3 groups: theophylline plus placebo (group 1), terbutaline plus placebo (group 2), or theophylline and terbutaline together (group 3). Thirty-six patients completed the study; 3 patients from group 1 were withdrawn due to parental request secondary to agitation (2 patients) and being inadvertently placed on a terbutaline infusion (1 patient). One patient from group 3 was withdrawn by the treating physician due to lack of improvement. All study participants, with the exception of the study pharmacist, were blinded to group assignment. Adjunctive therapies, including magnesium, ipatropium bromide and ketamine, were utilized at the discretion of the treating physician and were not controlled for. The primary outcome variable was change in a clinical scoring tool. Secondary outcomes variables included time to a specific clinical score, length of stay in the PICU, progression to mechanical ventilation, and incidence of adverse events. In addition, a cost analysis was performed isolating the 3 groups based on fiscal year 2003 cost estimates for theophylline and terbutaline. Results demonstrated no difference in the primary or secondary clinical outcome measures, with the exception of a higher incidence of nausea in group 3. The hospital costs were significantly lower in group 1 compared with groups 2 and 3 ($280 vs. $3,908 vs. $4,045, respectively, p<.0001). Significant limitations to the study include the lack of control of adjunctive therapies, a small sample size that confounds the ability to conclude no clinical difference between groups, and a baseline Pediatric Risk of Mortality (PRISM) Score in group 3 compared with groups 1 and 2. Despite these limitations the researchers suggest that the addition of intravenous theophylline to continuous nebulized albuterol and corticosteroids in the management of critically ill children with status asthmaticus is as safe and effective as adding intravenous terbutaline while being more cost-effective. Subsequent larger, well-controlled studies are required to support this conclusion.
Can Computerized Physician Ordering Create Errors?
Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293:1197-203.
Adverse drug events are a frequent etiology of inpatient morbidity and prescribing errors are the most frequent source. Computerized physician order entry (CPOE) is touted as a potential remedy for some types of adverse drug events. Few studies have investigated the potential for novel medication errors generated by a change to CPOE from conventional ordering. Koppel et al. present a quantitative and qualitative study of medication errors caused or exacerbated by a CPOE system. Interviews, surveys, and focus groups were the primary means of data collection. Housestaff who typically enter more than 9 orders per month were the primary study population, but data collection also included pharmacists, nursing staff , information technology managers, and attending physicians. The study was conducted in a tertiary-care teaching hospital between 2002 and 2004 utilizing a CPOE system in place since 1997. The CPOE system utilized is described as “monochromatic” and having “pre-Windows interfaces.” While not integrated with all hospital functions, the system was integrated with pharmacy and nursing medication lists. Researchers grouped errors into two broad categories: (1) information errors (fragmentation and systems integration failure) and (2) human-machine interface flaws (machine rules that do not correspond to work organization or usual behaviors). In total, 22 types of errors were recorded.
An example of an “information error” is assumed and incorrect dose information based on viewing doses intended only to describe pharmacy stocking practice―i.e. assuming that because the pharmacy stocks a 10mg dose of a medication, 10mg is an appropriate “minimally effective” dose. A “human-machine interface error” example is selecting an incorrect patient for ordering due to properties of the CPOE screen, such as the patient name not appearing on all screens. There are several important limitations to this study, but perhaps most important is the inability to generalize this data to other settings with potentially different physician users and software. Also important is a lack of description regarding physician user training and/or correlation of errors with amount of training or frequency of use, considering that the study population was defined as housestaff who may only use the system for 9 orders each . Despite these limitations, the study represents a requisite component to the growing trend toward the complete electronic record―namely, the use of objective investigations to study the safety and effectiveness of CPOE and the electronic record to promote the most optimal implementation and evolution of this new clinical tool.
Single-Dose Azithromycin for Acute Otitis Media
Arguedas A, Emparanza P, Schwartz RH, et al. A randomized, multicenter, double blind, double dummy trial of single dose azithromycin versus high dose amoxicillin for treatment of uncomplicated acute otitis media. Pediatr Infect Dis J. 2005;24: 153-61.
Acute otitis media is a common comorbid condition in pediatric inpatients. Patients at risk of having AOM with drug-resistant Streptococcus pneumoniae can be treated with high-dose amoxicillin as a first-line therapy according to recent American Academy of Pediatrics (AAP) recommendations. Despite this recommendation, there is evidence of reduced in vitro activity of amoxicillin against β-lactamase-producing Haemophilus influenzae and Moraxella catarrhalis, as well as a lack of data from controlled and blinded studies demonstrating efficacy, adverse events and compliance for high-dose regimens. Azithromycin has in vitro activity against the 4 pathogens of clinical significance in AOM, and studies have shown that a single-dose regimen of azithromycin by the oral route is pharmacokinetically feasible, safe, and comparable in success rate to 3- and 5-day azithromycin regimens. With these considerations in mind, Arguedas et al. designed this study to compare single-dose (30 mg/kg) azithromycin with high-dose (90 mg/kg/day) amoxicillin in uncomplicated AOM.
In this double-blind, double-dummy, multinational, clinical trial, children between the ages of 6 and 30 months with uncomplicated AOM were randomized to treatment with single-dose azithromycin or high-dose amoxicillin (90 mg/kg/day, in 2 div doses) for 10 days. The primary outcome measure was clinical efficacy assessed at the end of treatment on the basis of a modified intent-to-treat (MITT) population. Secondary outcomes were analyses of safety and compliance. Three hundred thirteen patients were enrolled, of whom 83% were <2 years old, with 158 patients randomized to receive azithromycin and 154 to receive amoxicillin. Tympanocentesis was performed at baseline, and clinical responses were assessed at days 12–14 (end of therapy) and 25–28 (end of study). A middle-ear pathogen was detected in 212 patients (68%). H. Influenzae was the most common pathogen isolated (96 cases), followed by S. pneumoniae (92), M. catarrhalis (23), and S. pyogenes (23). At the end of therapy, clinical success rates for azithromycin and amoxicillin were comparable for all patients (84% and 84%, respectively) and for children <2 years of age (82% and 82%, respectively). At the end of the study, clinical efficacies among all microbiologic modified intent-to-treat evaluable subjects were comparable for patients treated with azithro(80%) and patients treated with amoxicillin (83%). The rates of adverse events for azithromycin and amoxicillin were 20% and 29%, respectively (p=.064). Diarrhea was more common in the amoxicillin group (17.5%) as compared to the azithromycin group (8.2%) (p=.017). Compliance, defined as completion of >80% of the study medications, was higher in the azithromycin group (100%) then in the amoxicillin group (90%) (p=.001). For practitioners ordering medications, compliance and efficacy are uppermost considerations. Single-dose azithromycin ensured 100% compliance, decreased adverse reactions, and equal efficacy, compared to high-dose amoxicillin in this well designed, randomized, controlled trial. (Jadad Score = 4/5) all patients (84% and 84%, respectively) and for children <2 years of age (82% and 82%, respectively). At the end of the study, clinical efficacies among all microbiologic modified intent-to-treat evaluable subjects were comparable for patients treated with azithromycin (80%) and patients treated with amoxicillin (83%). The rates of adverse events for azithromycin and amoxicillin were 20% and 29%, respectively
(p=.064). Diarrhea was more common in the amoxicillin group (17.5%) as compared to the azithromycin group (8.2%) (p=.017). Compliance, defined as completion of >80% of the study medications, was higher in the azithromycin group (100%) then in the amoxicillin group (90%) (p=.001). For practitioners ordering medications, compliance and efficacy are uppermost considerations. Single-dose azithromycin ensured 100% compliance, decreased adverse reactions, and equal efficacy, compared to high-dose amoxicillin in this well-designed, randomized, controlled trial. (Jadad Score = 4/5)
In the Literature
Coronary-Artery Revascularization Before Elective Major Vascular Sugery
McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2861-3.
Cardiac risk stratification and treatment prior to non-cardiac surgery is a frequent reason for medical consultation, and yet the optimal approach to managing these patients remains controversial. National guidelines, based on expert opinion and inferred from published data, suggest that preoperative cardiac revascularization be reserved for patients with unstable coronary syndromes or for whom coronary artery bypass grad ing has been shown to improve mortality. Despite these recommendations, there remains considerable variability in clinical practice, which is compounded by a paucity of prospective randomized trials to validate one approach over another.
In this multicenter randomized controlled trial, McFalls et al. studied whether coronary artery revascularization prior to elective vascular surgery would reduce mortality among a cohort of patients with angiographically documented stable coronary artery disease. The investigators evaluated 5859 patients from 18 centers scheduled for abdominal aortic aneurysm or lower extremity vascular surgery. Patients felt to be at high risk for perioperative cardiac complications based on cardiology consultation, established clinical criteria, or the presence of ischemia on stress imaging studies were referred for coronary angiography. Of this cohort, 4669 (80%) were excluded due to subsequent determination of insufficient cardiac risk (28%), urgent need for vascular surgery (18%), severe comorbid illness (13%), patient preference (11%), or prior revascularization without new ischemia (11%). Of the 1190 patients who underwent angiography, 680 were excluded due to protocol criteria including: the absence of obstructive coronary artery disease (54%), coronary disease not amenable to revascularization (32%), led main artery stenosis ≥ 50% (8%), led ventricular ejection fraction <20% (2%), or severe aortic stenosis (AVA<1.0 cm2) (1%).
Of the 510 patients who remained, 252 were randomized to proceed with vascular surgery with optimal medical management, of which 9 crossed over due to the need for urgent cardiac revascularization. Two hundred fifty-eight patients were randomized to elective preoperative revascularization; 99 underwent CABG, 141 underwent PCI, and 18 were excluded due to need for urgent vascular surgery, patient preference, or in one case, stroke. Both groups were similar with respect to baseline clinical variables, including the incidence of previous myocardial infarction, congestive heart failure, diabetes mellitus, led ventricular ejection fraction, and 3vessel coronary artery disease. They were also similar in the use of perioperative betablockers (~ 85%), statins, and aspirin.
At 2.7 years after randomization, mortality was 22% in the revascularization group and 22% in the medical management group, the relative risk was 0.98 (95% CI 0.7-1.37; p=.92), which was not statistically significant. The median time from randomization to vascular surgery was 54 days in the revascularization group and 18 days in the medical management group not undergoing revascularization (p<.001). Although not designed to address short-term outcomes, there were no differences in the rates of early postoperative myocardial infarction, death, or hospital length of stay. It is also worth noting that 316 of the 510 patients who were ultimately randomized had undergone nuclear imaging studies, of which 226 (72%) had moderate to large reversible perfusion defects detected. These outcome data suggest that the presence of reversible perfusions defects is not in itself a reason for preoperative revascularization.
This well-designed study demonstrates that in the absence of unstable coronary syndromes, led main disease, severe aortic stenosis, or severely depressed led ventricular ejection fraction, there is no morbidity or mortality benefit to revascularization among patients with stable coronary artery disease prior to vascular surgery. Because vascular surgery is the highest risk category among non-cardiac procedures, it may be reasonable to extend these findings to lower risk surgeries as well, and in this sense this study is particularly relevant to consultative practice. While this study provides clear evidence on how to manage this cohort of patients, it remains unclear what the optimal strategy is to identify and manage those patients who were excluded from the trial. (DF)
Amiodarone or a Implantable Cardioverter-Defibrilator for Congestive Heart Failure
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005 20;352:225-37.
Ventricular arrhythmias are the leading cause of sudden cardiac death in patients with systolic heart failure. Treatment with antiarrhythmic drug therapy has failed to improve survival in these patients, due to their proarrhythmic effects. Unlike other antiarrhythmics, amiodarone is a drug with low proarrhythmic effects. Some studies have suggested that amiodarone may be beneficial in patients with systolic heart failure. Conversely, several primary and secondary prevention trials have demonstrated that placement of an implantable cardioverter-defibrillator (ICD) confers a survival benefit in patients with ischemic cardiomyopathy. However, the role of ICDs in nonischemic heart failure remained unproven.
Bardy and colleagues developed the Sudden Cardiac Death in Heart Failure Trial (SCDHeFT) to evaluate the hypothesis that treatment with amiodarone or a shock-only, single-lead ICD would decrease death from any cause in a population of patients with mild to moderate heart failure. They randomly assigned 2521 patients with New York Heart Association (NYHA) class II or II heart failure (and a led ventricular ejection fraction (LVEF) of 35% or less to conventional medical therapy plus placebo, conventional therapy plus treatment with amiodarone or conventional therapy plus a conservatively programmed, shock-only, single-lead ICD.
Fifty-two percent of patients had ischemic heart failure and 48% had nonischemic heart failure. Placebo and amiodarone were given in double-blind fashion. The primary endpoint was death from any cause with a median followup of 45.5 months. The results were as follows:
Placebo Group - 244 deaths (29% Death Rate)
Amiodarone Group - 240 deaths (28% Death Rate)
ICD Group - 182 deaths (22% Death Rate)
Patients treated with amiodarone had a similar risk of death as those who received placebo (hazard ratio, 1.06; 97.5% CI: 0.86–1.30; p=0.53). Patients implanted with an ICD had a 23% decreased risk of death when compared with those who received placebo (0.77; 97.5% CI: 0.62–0.96; p=.007). This resulted in an absolute risk reduction of 7.2% at 5 years. The authors concluded that in patients with NYHA class II or III heart failure and a LVEF of 35% or less, implantation of a single-lead, shock-only ICD reduced overall mortality by 23%, while treatment with amiodarone had no effect on survival. The benefit of ICD placement reached or approached significance in both the ischemic (hazard ratio .79, CI: 0.60–1.04, p= .05) and nonischemic (hazard ratio 0.73, CI: 0.50–1.07, p= 0.06) subgroups.
It is important to note that an additional subgroup analysis showed that ICD therapy had a significant survival benefit only in NYHA class II patients but not in NYHA class III patients. Amiodarone therapy had no benefit in class II patients and actually decreased survival in class III patients compared to those receiving placebo. In light of results from previous trials that demonstrated a greater survival benefit from ICD placement with worsening ejection fraction in patients with ischemic heart failure, the authors were unable to explain whether the differences in subclasses were biologically plausible.
This study is important for several reasons. First, it suggested that patients with systolic heart failure due to either ischemic or non ischemic causes would benefit from placement of an ICD. Second, these results support the conclusions of previous trials that demonstrate a survival advantage of ICD placement in patients with ischemic heart failure. Finally, this study also demonstrates that amiodarone therapy offers no survival benefit in this population of patients. (JL)
Clopidogrel versus Aspirin and Esomeprazole to Prevent Recurrent Ulcer Bleeding
Chan F, Ching J, Hung L, et al. Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding. N Engl J Med. 2005;352:238-44.
The optimal choice of antiplatelet therapy for patients with coronary heart disease who have had a recent upper gastrointestinal hemorrhage has not been well studied. Clopidogrel has been shown to cause fewer episodes of gastrointestinal hemorrhage than aspirin, but it is unknown whether clopidogrel monotherapy is in fact superior to aspirin plus a protonpump inhibitor. In this prospective, randomized, doubleblind trial, Chan and colleagues hypothesize that clopidogrel monotherapy would “not be inferior” to aspirin plus esomeprazole in a population of patients who had recovered from aspirin-induced hemorrhagic ulcers.
The study population was drawn from patients taking aspirin who were evaluated for an upper gastrointestinal bleed and had ulcer disease documented on endoscopy. Patients with documented Helicobacter pylori infection were treated with a 1-week course of a standard triple-drug regimen. All subjects, regardless of H. pylori status, were treated with an 8-week course of proton-pump inhibitors (PPI). Inclusion criteria included endoscopic confirmation of ulcer healing and successful eradication of H. pylori, if it was present. The location of the ulcers was not specified in the study.
Exclusion criteria included use of nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2 inhibitors, anticoagulant drugs, corticosteroids, or other anti-platelet agents; history of gastric surgery; presence of erosive esophagitis; gastric outlet obstruction; cancer; need for dialysis; or terminal illness.
Subjects who met the inclusion criteria were randomized to receive either 75 mg of clopidogrel and placebo or 80 mg of aspirin daily plus 20 mg of esomeprazole twice a day for a 12 months. Patients returned for evaluation every 3 months during the 1-year study period. The primary endpoint was recurrence of ulcer bleeding, which was predefined as clinical or laboratory evidence of gastrointestinal hemorrhage with a documented recurrence of ulcers on endoscopy. Lower gastrointestinal bleeding was a secondary endpoint.
Of 492 consecutive patients who were evaluated, 320 met inclusion criteria and were evenly divided into the clopidogrel plus placebo or the aspirin plus esomeprazole arms. Only 3 patients were lost to followup. During the study period, 34 cases of suspected gastrointestinal hemorrhage (defined as hematemesis, melena, or 2 g/dL decrease of hemoglobin) were identified. During endoscopy,14 cases were confirmed to be due to recurrent ulcer bleeding. Of these, 13 ulcers were in the clopidogrel arm (6 gastric ulcers, 5 duodenal, and 2 both) and 1 ulcer (duodenal) in the aspirin plus esomeprazole arm, a statistically significant difference (p=.001).
Fourteen patients were determined to have a lower gastrointestinal hemorrhage. Interestingly, these cases were evenly divided between the clopidogrel group (7 cases) and the aspirin plus esomeprazole (7 cases). This finding suggests the effect of esomeprazole in this study may be specific in preventing recurrent upper gastrointestinal ulcer formation and hemorrhage. The 2 groups had equivalent rates of recurrent ischemic events.
This study addresses an important clinical question, frequently encountered by hospitalists. The recommendation that clopidogrel be used instead of aspirin in patients who require antiplatelet therapy but have a history of upper gastrointestinal hemorrhage is based on studies using high-dose (325 mg) aspirin and excluded patients on acid-suppressing therapy. However, this study failed to prove noninferiority of clopidogrel to aspirin and esomeprazole for this indication. Although this study was not designed to show superiority of aspirin and esomeprazole over clopidogrel, these results indicate that this may be the case, and such a study would be timely. (CG)
Coronary-Artery Revascularization Before Elective Major Vascular Sugery
McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2861-3.
Cardiac risk stratification and treatment prior to non-cardiac surgery is a frequent reason for medical consultation, and yet the optimal approach to managing these patients remains controversial. National guidelines, based on expert opinion and inferred from published data, suggest that preoperative cardiac revascularization be reserved for patients with unstable coronary syndromes or for whom coronary artery bypass grad ing has been shown to improve mortality. Despite these recommendations, there remains considerable variability in clinical practice, which is compounded by a paucity of prospective randomized trials to validate one approach over another.
In this multicenter randomized controlled trial, McFalls et al. studied whether coronary artery revascularization prior to elective vascular surgery would reduce mortality among a cohort of patients with angiographically documented stable coronary artery disease. The investigators evaluated 5859 patients from 18 centers scheduled for abdominal aortic aneurysm or lower extremity vascular surgery. Patients felt to be at high risk for perioperative cardiac complications based on cardiology consultation, established clinical criteria, or the presence of ischemia on stress imaging studies were referred for coronary angiography. Of this cohort, 4669 (80%) were excluded due to subsequent determination of insufficient cardiac risk (28%), urgent need for vascular surgery (18%), severe comorbid illness (13%), patient preference (11%), or prior revascularization without new ischemia (11%). Of the 1190 patients who underwent angiography, 680 were excluded due to protocol criteria including: the absence of obstructive coronary artery disease (54%), coronary disease not amenable to revascularization (32%), led main artery stenosis ≥ 50% (8%), led ventricular ejection fraction <20% (2%), or severe aortic stenosis (AVA<1.0 cm2) (1%).
Of the 510 patients who remained, 252 were randomized to proceed with vascular surgery with optimal medical management, of which 9 crossed over due to the need for urgent cardiac revascularization. Two hundred fifty-eight patients were randomized to elective preoperative revascularization; 99 underwent CABG, 141 underwent PCI, and 18 were excluded due to need for urgent vascular surgery, patient preference, or in one case, stroke. Both groups were similar with respect to baseline clinical variables, including the incidence of previous myocardial infarction, congestive heart failure, diabetes mellitus, led ventricular ejection fraction, and 3vessel coronary artery disease. They were also similar in the use of perioperative betablockers (~ 85%), statins, and aspirin.
At 2.7 years after randomization, mortality was 22% in the revascularization group and 22% in the medical management group, the relative risk was 0.98 (95% CI 0.7-1.37; p=.92), which was not statistically significant. The median time from randomization to vascular surgery was 54 days in the revascularization group and 18 days in the medical management group not undergoing revascularization (p<.001). Although not designed to address short-term outcomes, there were no differences in the rates of early postoperative myocardial infarction, death, or hospital length of stay. It is also worth noting that 316 of the 510 patients who were ultimately randomized had undergone nuclear imaging studies, of which 226 (72%) had moderate to large reversible perfusion defects detected. These outcome data suggest that the presence of reversible perfusions defects is not in itself a reason for preoperative revascularization.
This well-designed study demonstrates that in the absence of unstable coronary syndromes, led main disease, severe aortic stenosis, or severely depressed led ventricular ejection fraction, there is no morbidity or mortality benefit to revascularization among patients with stable coronary artery disease prior to vascular surgery. Because vascular surgery is the highest risk category among non-cardiac procedures, it may be reasonable to extend these findings to lower risk surgeries as well, and in this sense this study is particularly relevant to consultative practice. While this study provides clear evidence on how to manage this cohort of patients, it remains unclear what the optimal strategy is to identify and manage those patients who were excluded from the trial. (DF)
Amiodarone or a Implantable Cardioverter-Defibrilator for Congestive Heart Failure
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005 20;352:225-37.
Ventricular arrhythmias are the leading cause of sudden cardiac death in patients with systolic heart failure. Treatment with antiarrhythmic drug therapy has failed to improve survival in these patients, due to their proarrhythmic effects. Unlike other antiarrhythmics, amiodarone is a drug with low proarrhythmic effects. Some studies have suggested that amiodarone may be beneficial in patients with systolic heart failure. Conversely, several primary and secondary prevention trials have demonstrated that placement of an implantable cardioverter-defibrillator (ICD) confers a survival benefit in patients with ischemic cardiomyopathy. However, the role of ICDs in nonischemic heart failure remained unproven.
Bardy and colleagues developed the Sudden Cardiac Death in Heart Failure Trial (SCDHeFT) to evaluate the hypothesis that treatment with amiodarone or a shock-only, single-lead ICD would decrease death from any cause in a population of patients with mild to moderate heart failure. They randomly assigned 2521 patients with New York Heart Association (NYHA) class II or II heart failure (and a led ventricular ejection fraction (LVEF) of 35% or less to conventional medical therapy plus placebo, conventional therapy plus treatment with amiodarone or conventional therapy plus a conservatively programmed, shock-only, single-lead ICD.
Fifty-two percent of patients had ischemic heart failure and 48% had nonischemic heart failure. Placebo and amiodarone were given in double-blind fashion. The primary endpoint was death from any cause with a median followup of 45.5 months. The results were as follows:
Placebo Group - 244 deaths (29% Death Rate)
Amiodarone Group - 240 deaths (28% Death Rate)
ICD Group - 182 deaths (22% Death Rate)
Patients treated with amiodarone had a similar risk of death as those who received placebo (hazard ratio, 1.06; 97.5% CI: 0.86–1.30; p=0.53). Patients implanted with an ICD had a 23% decreased risk of death when compared with those who received placebo (0.77; 97.5% CI: 0.62–0.96; p=.007). This resulted in an absolute risk reduction of 7.2% at 5 years. The authors concluded that in patients with NYHA class II or III heart failure and a LVEF of 35% or less, implantation of a single-lead, shock-only ICD reduced overall mortality by 23%, while treatment with amiodarone had no effect on survival. The benefit of ICD placement reached or approached significance in both the ischemic (hazard ratio .79, CI: 0.60–1.04, p= .05) and nonischemic (hazard ratio 0.73, CI: 0.50–1.07, p= 0.06) subgroups.
It is important to note that an additional subgroup analysis showed that ICD therapy had a significant survival benefit only in NYHA class II patients but not in NYHA class III patients. Amiodarone therapy had no benefit in class II patients and actually decreased survival in class III patients compared to those receiving placebo. In light of results from previous trials that demonstrated a greater survival benefit from ICD placement with worsening ejection fraction in patients with ischemic heart failure, the authors were unable to explain whether the differences in subclasses were biologically plausible.
This study is important for several reasons. First, it suggested that patients with systolic heart failure due to either ischemic or non ischemic causes would benefit from placement of an ICD. Second, these results support the conclusions of previous trials that demonstrate a survival advantage of ICD placement in patients with ischemic heart failure. Finally, this study also demonstrates that amiodarone therapy offers no survival benefit in this population of patients. (JL)
Clopidogrel versus Aspirin and Esomeprazole to Prevent Recurrent Ulcer Bleeding
Chan F, Ching J, Hung L, et al. Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding. N Engl J Med. 2005;352:238-44.
The optimal choice of antiplatelet therapy for patients with coronary heart disease who have had a recent upper gastrointestinal hemorrhage has not been well studied. Clopidogrel has been shown to cause fewer episodes of gastrointestinal hemorrhage than aspirin, but it is unknown whether clopidogrel monotherapy is in fact superior to aspirin plus a protonpump inhibitor. In this prospective, randomized, doubleblind trial, Chan and colleagues hypothesize that clopidogrel monotherapy would “not be inferior” to aspirin plus esomeprazole in a population of patients who had recovered from aspirin-induced hemorrhagic ulcers.
The study population was drawn from patients taking aspirin who were evaluated for an upper gastrointestinal bleed and had ulcer disease documented on endoscopy. Patients with documented Helicobacter pylori infection were treated with a 1-week course of a standard triple-drug regimen. All subjects, regardless of H. pylori status, were treated with an 8-week course of proton-pump inhibitors (PPI). Inclusion criteria included endoscopic confirmation of ulcer healing and successful eradication of H. pylori, if it was present. The location of the ulcers was not specified in the study.
Exclusion criteria included use of nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2 inhibitors, anticoagulant drugs, corticosteroids, or other anti-platelet agents; history of gastric surgery; presence of erosive esophagitis; gastric outlet obstruction; cancer; need for dialysis; or terminal illness.
Subjects who met the inclusion criteria were randomized to receive either 75 mg of clopidogrel and placebo or 80 mg of aspirin daily plus 20 mg of esomeprazole twice a day for a 12 months. Patients returned for evaluation every 3 months during the 1-year study period. The primary endpoint was recurrence of ulcer bleeding, which was predefined as clinical or laboratory evidence of gastrointestinal hemorrhage with a documented recurrence of ulcers on endoscopy. Lower gastrointestinal bleeding was a secondary endpoint.
Of 492 consecutive patients who were evaluated, 320 met inclusion criteria and were evenly divided into the clopidogrel plus placebo or the aspirin plus esomeprazole arms. Only 3 patients were lost to followup. During the study period, 34 cases of suspected gastrointestinal hemorrhage (defined as hematemesis, melena, or 2 g/dL decrease of hemoglobin) were identified. During endoscopy,14 cases were confirmed to be due to recurrent ulcer bleeding. Of these, 13 ulcers were in the clopidogrel arm (6 gastric ulcers, 5 duodenal, and 2 both) and 1 ulcer (duodenal) in the aspirin plus esomeprazole arm, a statistically significant difference (p=.001).
Fourteen patients were determined to have a lower gastrointestinal hemorrhage. Interestingly, these cases were evenly divided between the clopidogrel group (7 cases) and the aspirin plus esomeprazole (7 cases). This finding suggests the effect of esomeprazole in this study may be specific in preventing recurrent upper gastrointestinal ulcer formation and hemorrhage. The 2 groups had equivalent rates of recurrent ischemic events.
This study addresses an important clinical question, frequently encountered by hospitalists. The recommendation that clopidogrel be used instead of aspirin in patients who require antiplatelet therapy but have a history of upper gastrointestinal hemorrhage is based on studies using high-dose (325 mg) aspirin and excluded patients on acid-suppressing therapy. However, this study failed to prove noninferiority of clopidogrel to aspirin and esomeprazole for this indication. Although this study was not designed to show superiority of aspirin and esomeprazole over clopidogrel, these results indicate that this may be the case, and such a study would be timely. (CG)
Coronary-Artery Revascularization Before Elective Major Vascular Sugery
McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2861-3.
Cardiac risk stratification and treatment prior to non-cardiac surgery is a frequent reason for medical consultation, and yet the optimal approach to managing these patients remains controversial. National guidelines, based on expert opinion and inferred from published data, suggest that preoperative cardiac revascularization be reserved for patients with unstable coronary syndromes or for whom coronary artery bypass grad ing has been shown to improve mortality. Despite these recommendations, there remains considerable variability in clinical practice, which is compounded by a paucity of prospective randomized trials to validate one approach over another.
In this multicenter randomized controlled trial, McFalls et al. studied whether coronary artery revascularization prior to elective vascular surgery would reduce mortality among a cohort of patients with angiographically documented stable coronary artery disease. The investigators evaluated 5859 patients from 18 centers scheduled for abdominal aortic aneurysm or lower extremity vascular surgery. Patients felt to be at high risk for perioperative cardiac complications based on cardiology consultation, established clinical criteria, or the presence of ischemia on stress imaging studies were referred for coronary angiography. Of this cohort, 4669 (80%) were excluded due to subsequent determination of insufficient cardiac risk (28%), urgent need for vascular surgery (18%), severe comorbid illness (13%), patient preference (11%), or prior revascularization without new ischemia (11%). Of the 1190 patients who underwent angiography, 680 were excluded due to protocol criteria including: the absence of obstructive coronary artery disease (54%), coronary disease not amenable to revascularization (32%), led main artery stenosis ≥ 50% (8%), led ventricular ejection fraction <20% (2%), or severe aortic stenosis (AVA<1.0 cm2) (1%).
Of the 510 patients who remained, 252 were randomized to proceed with vascular surgery with optimal medical management, of which 9 crossed over due to the need for urgent cardiac revascularization. Two hundred fifty-eight patients were randomized to elective preoperative revascularization; 99 underwent CABG, 141 underwent PCI, and 18 were excluded due to need for urgent vascular surgery, patient preference, or in one case, stroke. Both groups were similar with respect to baseline clinical variables, including the incidence of previous myocardial infarction, congestive heart failure, diabetes mellitus, led ventricular ejection fraction, and 3vessel coronary artery disease. They were also similar in the use of perioperative betablockers (~ 85%), statins, and aspirin.
At 2.7 years after randomization, mortality was 22% in the revascularization group and 22% in the medical management group, the relative risk was 0.98 (95% CI 0.7-1.37; p=.92), which was not statistically significant. The median time from randomization to vascular surgery was 54 days in the revascularization group and 18 days in the medical management group not undergoing revascularization (p<.001). Although not designed to address short-term outcomes, there were no differences in the rates of early postoperative myocardial infarction, death, or hospital length of stay. It is also worth noting that 316 of the 510 patients who were ultimately randomized had undergone nuclear imaging studies, of which 226 (72%) had moderate to large reversible perfusion defects detected. These outcome data suggest that the presence of reversible perfusions defects is not in itself a reason for preoperative revascularization.
This well-designed study demonstrates that in the absence of unstable coronary syndromes, led main disease, severe aortic stenosis, or severely depressed led ventricular ejection fraction, there is no morbidity or mortality benefit to revascularization among patients with stable coronary artery disease prior to vascular surgery. Because vascular surgery is the highest risk category among non-cardiac procedures, it may be reasonable to extend these findings to lower risk surgeries as well, and in this sense this study is particularly relevant to consultative practice. While this study provides clear evidence on how to manage this cohort of patients, it remains unclear what the optimal strategy is to identify and manage those patients who were excluded from the trial. (DF)
Amiodarone or a Implantable Cardioverter-Defibrilator for Congestive Heart Failure
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005 20;352:225-37.
Ventricular arrhythmias are the leading cause of sudden cardiac death in patients with systolic heart failure. Treatment with antiarrhythmic drug therapy has failed to improve survival in these patients, due to their proarrhythmic effects. Unlike other antiarrhythmics, amiodarone is a drug with low proarrhythmic effects. Some studies have suggested that amiodarone may be beneficial in patients with systolic heart failure. Conversely, several primary and secondary prevention trials have demonstrated that placement of an implantable cardioverter-defibrillator (ICD) confers a survival benefit in patients with ischemic cardiomyopathy. However, the role of ICDs in nonischemic heart failure remained unproven.
Bardy and colleagues developed the Sudden Cardiac Death in Heart Failure Trial (SCDHeFT) to evaluate the hypothesis that treatment with amiodarone or a shock-only, single-lead ICD would decrease death from any cause in a population of patients with mild to moderate heart failure. They randomly assigned 2521 patients with New York Heart Association (NYHA) class II or II heart failure (and a led ventricular ejection fraction (LVEF) of 35% or less to conventional medical therapy plus placebo, conventional therapy plus treatment with amiodarone or conventional therapy plus a conservatively programmed, shock-only, single-lead ICD.
Fifty-two percent of patients had ischemic heart failure and 48% had nonischemic heart failure. Placebo and amiodarone were given in double-blind fashion. The primary endpoint was death from any cause with a median followup of 45.5 months. The results were as follows:
Placebo Group - 244 deaths (29% Death Rate)
Amiodarone Group - 240 deaths (28% Death Rate)
ICD Group - 182 deaths (22% Death Rate)
Patients treated with amiodarone had a similar risk of death as those who received placebo (hazard ratio, 1.06; 97.5% CI: 0.86–1.30; p=0.53). Patients implanted with an ICD had a 23% decreased risk of death when compared with those who received placebo (0.77; 97.5% CI: 0.62–0.96; p=.007). This resulted in an absolute risk reduction of 7.2% at 5 years. The authors concluded that in patients with NYHA class II or III heart failure and a LVEF of 35% or less, implantation of a single-lead, shock-only ICD reduced overall mortality by 23%, while treatment with amiodarone had no effect on survival. The benefit of ICD placement reached or approached significance in both the ischemic (hazard ratio .79, CI: 0.60–1.04, p= .05) and nonischemic (hazard ratio 0.73, CI: 0.50–1.07, p= 0.06) subgroups.
It is important to note that an additional subgroup analysis showed that ICD therapy had a significant survival benefit only in NYHA class II patients but not in NYHA class III patients. Amiodarone therapy had no benefit in class II patients and actually decreased survival in class III patients compared to those receiving placebo. In light of results from previous trials that demonstrated a greater survival benefit from ICD placement with worsening ejection fraction in patients with ischemic heart failure, the authors were unable to explain whether the differences in subclasses were biologically plausible.
This study is important for several reasons. First, it suggested that patients with systolic heart failure due to either ischemic or non ischemic causes would benefit from placement of an ICD. Second, these results support the conclusions of previous trials that demonstrate a survival advantage of ICD placement in patients with ischemic heart failure. Finally, this study also demonstrates that amiodarone therapy offers no survival benefit in this population of patients. (JL)
Clopidogrel versus Aspirin and Esomeprazole to Prevent Recurrent Ulcer Bleeding
Chan F, Ching J, Hung L, et al. Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding. N Engl J Med. 2005;352:238-44.
The optimal choice of antiplatelet therapy for patients with coronary heart disease who have had a recent upper gastrointestinal hemorrhage has not been well studied. Clopidogrel has been shown to cause fewer episodes of gastrointestinal hemorrhage than aspirin, but it is unknown whether clopidogrel monotherapy is in fact superior to aspirin plus a protonpump inhibitor. In this prospective, randomized, doubleblind trial, Chan and colleagues hypothesize that clopidogrel monotherapy would “not be inferior” to aspirin plus esomeprazole in a population of patients who had recovered from aspirin-induced hemorrhagic ulcers.
The study population was drawn from patients taking aspirin who were evaluated for an upper gastrointestinal bleed and had ulcer disease documented on endoscopy. Patients with documented Helicobacter pylori infection were treated with a 1-week course of a standard triple-drug regimen. All subjects, regardless of H. pylori status, were treated with an 8-week course of proton-pump inhibitors (PPI). Inclusion criteria included endoscopic confirmation of ulcer healing and successful eradication of H. pylori, if it was present. The location of the ulcers was not specified in the study.
Exclusion criteria included use of nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2 inhibitors, anticoagulant drugs, corticosteroids, or other anti-platelet agents; history of gastric surgery; presence of erosive esophagitis; gastric outlet obstruction; cancer; need for dialysis; or terminal illness.
Subjects who met the inclusion criteria were randomized to receive either 75 mg of clopidogrel and placebo or 80 mg of aspirin daily plus 20 mg of esomeprazole twice a day for a 12 months. Patients returned for evaluation every 3 months during the 1-year study period. The primary endpoint was recurrence of ulcer bleeding, which was predefined as clinical or laboratory evidence of gastrointestinal hemorrhage with a documented recurrence of ulcers on endoscopy. Lower gastrointestinal bleeding was a secondary endpoint.
Of 492 consecutive patients who were evaluated, 320 met inclusion criteria and were evenly divided into the clopidogrel plus placebo or the aspirin plus esomeprazole arms. Only 3 patients were lost to followup. During the study period, 34 cases of suspected gastrointestinal hemorrhage (defined as hematemesis, melena, or 2 g/dL decrease of hemoglobin) were identified. During endoscopy,14 cases were confirmed to be due to recurrent ulcer bleeding. Of these, 13 ulcers were in the clopidogrel arm (6 gastric ulcers, 5 duodenal, and 2 both) and 1 ulcer (duodenal) in the aspirin plus esomeprazole arm, a statistically significant difference (p=.001).
Fourteen patients were determined to have a lower gastrointestinal hemorrhage. Interestingly, these cases were evenly divided between the clopidogrel group (7 cases) and the aspirin plus esomeprazole (7 cases). This finding suggests the effect of esomeprazole in this study may be specific in preventing recurrent upper gastrointestinal ulcer formation and hemorrhage. The 2 groups had equivalent rates of recurrent ischemic events.
This study addresses an important clinical question, frequently encountered by hospitalists. The recommendation that clopidogrel be used instead of aspirin in patients who require antiplatelet therapy but have a history of upper gastrointestinal hemorrhage is based on studies using high-dose (325 mg) aspirin and excluded patients on acid-suppressing therapy. However, this study failed to prove noninferiority of clopidogrel to aspirin and esomeprazole for this indication. Although this study was not designed to show superiority of aspirin and esomeprazole over clopidogrel, these results indicate that this may be the case, and such a study would be timely. (CG)
Practice Profile
Contact
Mark Kulaga, MD
Associate Program Director
Internal Medicine Residency
Norwalk Hospital
Norwalk, CT 06856
Physician Staff
Pamela Charney, MD
Joseph Cleary, MD
Mark Kulaga, MD
Eric Mazur, MD
Stephen O’Mahony, MD
Jason Orlinick, MD, PhD
Andrea Peterson, MD
Other Staff
Michael Marotta, PA
Start Up
July 1999
Hospital Setting
Norwalk Hospital, Norwalk, CT
Academic Community Hospital with 250 beds
Affiliated with Yale University
Patient Population
Our patient population is wonderfully diverse, both economically and socially. Located in the heart of affluent Fairfield County, Norwalk is nevertheless a true small city and home to vibrant communities of African Americans, Latinos, and multiple other immigrant groups. The Hospitalist Clinician-Educator program was originally created to provide inpatient care for indigent patients (who predominantly attend the Norwalk Community Health Center) and for those patients without a local primary care physician. In recent years, as more community internists have chosen to use the hospital medicine service, our payer mix has substantially changed to include many more patients with private insurance and/or Medicare.
Employer
All physicians are general internists employed by the Norwalk Hospital.
Organization/Management
Dr. Eric Mazur, Chairman of the Department of Internal Medicine, is the program founder and administrative leader. He serves as the primary liaison between the hospitalists and the Chief Executive and Operating Officers of the hospital.
Total Number of Patients Served Each Year
On average, each hospitalist admits 350 patients per year. When this threshold is exceeded, a new hospitalist has been added to the group. In the first few years of service, our hospitalists covered 20-25% of the total number of medical admissions to the Norwalk Hospital. As use of the service by local internists has increased, this percentage has grown to 40–45%. It is projected that the Norwalk Hospital hospital medicine service will admit over 2200 patients this year.
Compensation/Schedules
All hospitalists receive a fixed annual salary. The hospital subsidizes 50% of each Hospitalist Clinician Educator position and bills the faculty practice income for the remaining 50%. Faculty practice income is generated through direct patient billing facilitated by a billing agency not affiliated with the hospital. The hospital also provides an annual stipend to the faculty practice for the indigent care supplied by the hospital medicine group. Our compensation model does not utilize an incentive bonus system, although yearly bonuses derived from surplus faculty practice revenue are provided at the discretion of the Chairman.
All hospitalists admit and co-manage patients with resident teams who provide 24/7 in-house coverage. Each hospitalist typically works Monday through Friday from approximately 7–8 a.m. until 5:30–6:30 p.m. depending on patient census. Hospitalists, along with other members of the full time faculty, provide nighttime backup coverage from home for the residents. Weekend coverage responsibilities are also shared with other members of the teaching faculty. Weekend moonlighters, all of whom are board-certified or board-eligible internists from nearby communities, assist full-time faculty members with coverage on Saturdays and Sundays.
Communication Strategies/Role in Education
All of our hospitalists are highly rated by medical residents for their effectiveness as teachers and supervisors. For many, they also serve as important mentors and role models. In addition to traditional educational roles on the inpatient service, our hospitalists have developed several innovative teaching conferences, which include: teaching skills workshops; weekly medical informatics sessions; a monthly medical quiz game incorporating content from core educational conferences; a multidisciplinary Morbidity and Mortality Conference in which residents from the internal medicine and radiology departments are key participants; and a series of conferences in which end-of-life issues and physician professional development are explored in great depth.
Our hospitalists have also established a formal medical consultation service with a specially designed curriculum for the residents. We have also developed a hospital medicine elective where medical residents experience what being a hospitalist is “really like.” This elective has also been used to remediate struggling residents. Our hospitalists also have prominent administrative hospital roles; one is the Director of Graduate Medical Education, and 2 others serve as Associate Program Directors for the Internal Medicine residency. In addition, they have presented their academic work at regional and national meetings of the American College of Physicians and the Society of General Internal Medicine.
Challenges Now and in the Future
Our biggest challenge can be summed up with one word: growth. Up to this point in time, a major strength of our program is that it has been able to grow incrementally and deliberately. We have never “rushed” the hiring of new hospitalists and thus have been able to recruit physicians with similar academic backgrounds and career goals. This has resulted in a cohesive group of hospitalists who support each other in every way and work extremely well together.
A major concern in hospitalist medicine is the concept of “hospitalist burnout.” We have successfully addressed this issue by limiting the number of hospitalist admissions and weekends on call, actively participating in medical education with resident physicians, and serving in important administrative roles within the hospital. As we expand to meet the growing demand for our inpatient care services by primary care physicians, we are finding it more difficult to strike a balance between our service duties and academic interests. We are working closely with our department chairman, who is a true advocate of “hospitalist career building,” to find creative ways to achieve this goal. We believe that it is the balance between service and education that has allowed us to attain a hospitalist retention rate of 100% since the inception of the group.
Goals of Hospital Medicine Group
In addition to providing outstanding patient care and resident teaching, the goals of our group are commensurate with many of the current trends affecting the field of medicine and include:
- Quality. As quality moves to the forefront of medicine, we believe that hospitalists are the logical champions and effectors of inpatient quality care. Our hospitalists have been involved in a number of quality improvement projects, such as the establishment of multidisciplinary patient rounds, which serve to advance care and achieve high levels of core measure compliance; stroke center development; and the design of inpatient diabetes management protocols. Our hospitalists have also been heavily involved in the implementation of computerized physician order entry at the Norwalk Hospital and have written numerous order sets for specific diagnoses. We expect these projects to result in demonstrably improved quality beyond the improvements in length-of-stay and core-measures adherence already achieved. We believe that our involvement in quality, both now and in the future, adds value to our role as hospitalists from the point of view of hospital administrators. It also provides us with enhanced job satisfaction and multiple opportunities for career development.
- Patient safety. This is another “hot topic” in the field of medicine where we feel that hospitalists can and should have a substantial impact. As mentioned before, our hospitalists have played prominent roles in the successful implementation of computerized physician order entry, a process that has been shown to result in major improvements in patient safety. Our hospitalists also serve on the patient safety committee and are an important link between residents and ancillary staff when housestaff raise safety concerns. In the future, our hospitalists hope to have an even greater role in such important safety areas as infection control, management of delirium in the elderly, venous thromboembolism prophylaxis in the medical inpatient, and the prevention of patient falls.
- Research. Clinically and educationally oriented research is encouraged among all full-time hospitalist faculty. We recently published data on the financial and educational benefits of our hospitalist model in the April 2004 issue of the Journal of General Internal Medicine, but we feel that more needs to be done. In particular, we plan to better quantify how hospitalists achieve the reported cost-saving benefits. We also plan to further assess the roles of hospitalists in the education of medical residents in the community setting, a topic that is vastly underrepresented in the medical literature. Hospitalist faculty will also participate in a formal evaluation of the Multidisciplinary Rounds Process and will mentor residents in their personal research projects.
Contact
Mark Kulaga, MD
Associate Program Director
Internal Medicine Residency
Norwalk Hospital
Norwalk, CT 06856
Physician Staff
Pamela Charney, MD
Joseph Cleary, MD
Mark Kulaga, MD
Eric Mazur, MD
Stephen O’Mahony, MD
Jason Orlinick, MD, PhD
Andrea Peterson, MD
Other Staff
Michael Marotta, PA
Start Up
July 1999
Hospital Setting
Norwalk Hospital, Norwalk, CT
Academic Community Hospital with 250 beds
Affiliated with Yale University
Patient Population
Our patient population is wonderfully diverse, both economically and socially. Located in the heart of affluent Fairfield County, Norwalk is nevertheless a true small city and home to vibrant communities of African Americans, Latinos, and multiple other immigrant groups. The Hospitalist Clinician-Educator program was originally created to provide inpatient care for indigent patients (who predominantly attend the Norwalk Community Health Center) and for those patients without a local primary care physician. In recent years, as more community internists have chosen to use the hospital medicine service, our payer mix has substantially changed to include many more patients with private insurance and/or Medicare.
Employer
All physicians are general internists employed by the Norwalk Hospital.
Organization/Management
Dr. Eric Mazur, Chairman of the Department of Internal Medicine, is the program founder and administrative leader. He serves as the primary liaison between the hospitalists and the Chief Executive and Operating Officers of the hospital.
Total Number of Patients Served Each Year
On average, each hospitalist admits 350 patients per year. When this threshold is exceeded, a new hospitalist has been added to the group. In the first few years of service, our hospitalists covered 20-25% of the total number of medical admissions to the Norwalk Hospital. As use of the service by local internists has increased, this percentage has grown to 40–45%. It is projected that the Norwalk Hospital hospital medicine service will admit over 2200 patients this year.
Compensation/Schedules
All hospitalists receive a fixed annual salary. The hospital subsidizes 50% of each Hospitalist Clinician Educator position and bills the faculty practice income for the remaining 50%. Faculty practice income is generated through direct patient billing facilitated by a billing agency not affiliated with the hospital. The hospital also provides an annual stipend to the faculty practice for the indigent care supplied by the hospital medicine group. Our compensation model does not utilize an incentive bonus system, although yearly bonuses derived from surplus faculty practice revenue are provided at the discretion of the Chairman.
All hospitalists admit and co-manage patients with resident teams who provide 24/7 in-house coverage. Each hospitalist typically works Monday through Friday from approximately 7–8 a.m. until 5:30–6:30 p.m. depending on patient census. Hospitalists, along with other members of the full time faculty, provide nighttime backup coverage from home for the residents. Weekend coverage responsibilities are also shared with other members of the teaching faculty. Weekend moonlighters, all of whom are board-certified or board-eligible internists from nearby communities, assist full-time faculty members with coverage on Saturdays and Sundays.
Communication Strategies/Role in Education
All of our hospitalists are highly rated by medical residents for their effectiveness as teachers and supervisors. For many, they also serve as important mentors and role models. In addition to traditional educational roles on the inpatient service, our hospitalists have developed several innovative teaching conferences, which include: teaching skills workshops; weekly medical informatics sessions; a monthly medical quiz game incorporating content from core educational conferences; a multidisciplinary Morbidity and Mortality Conference in which residents from the internal medicine and radiology departments are key participants; and a series of conferences in which end-of-life issues and physician professional development are explored in great depth.
Our hospitalists have also established a formal medical consultation service with a specially designed curriculum for the residents. We have also developed a hospital medicine elective where medical residents experience what being a hospitalist is “really like.” This elective has also been used to remediate struggling residents. Our hospitalists also have prominent administrative hospital roles; one is the Director of Graduate Medical Education, and 2 others serve as Associate Program Directors for the Internal Medicine residency. In addition, they have presented their academic work at regional and national meetings of the American College of Physicians and the Society of General Internal Medicine.
Challenges Now and in the Future
Our biggest challenge can be summed up with one word: growth. Up to this point in time, a major strength of our program is that it has been able to grow incrementally and deliberately. We have never “rushed” the hiring of new hospitalists and thus have been able to recruit physicians with similar academic backgrounds and career goals. This has resulted in a cohesive group of hospitalists who support each other in every way and work extremely well together.
A major concern in hospitalist medicine is the concept of “hospitalist burnout.” We have successfully addressed this issue by limiting the number of hospitalist admissions and weekends on call, actively participating in medical education with resident physicians, and serving in important administrative roles within the hospital. As we expand to meet the growing demand for our inpatient care services by primary care physicians, we are finding it more difficult to strike a balance between our service duties and academic interests. We are working closely with our department chairman, who is a true advocate of “hospitalist career building,” to find creative ways to achieve this goal. We believe that it is the balance between service and education that has allowed us to attain a hospitalist retention rate of 100% since the inception of the group.
Goals of Hospital Medicine Group
In addition to providing outstanding patient care and resident teaching, the goals of our group are commensurate with many of the current trends affecting the field of medicine and include:
- Quality. As quality moves to the forefront of medicine, we believe that hospitalists are the logical champions and effectors of inpatient quality care. Our hospitalists have been involved in a number of quality improvement projects, such as the establishment of multidisciplinary patient rounds, which serve to advance care and achieve high levels of core measure compliance; stroke center development; and the design of inpatient diabetes management protocols. Our hospitalists have also been heavily involved in the implementation of computerized physician order entry at the Norwalk Hospital and have written numerous order sets for specific diagnoses. We expect these projects to result in demonstrably improved quality beyond the improvements in length-of-stay and core-measures adherence already achieved. We believe that our involvement in quality, both now and in the future, adds value to our role as hospitalists from the point of view of hospital administrators. It also provides us with enhanced job satisfaction and multiple opportunities for career development.
- Patient safety. This is another “hot topic” in the field of medicine where we feel that hospitalists can and should have a substantial impact. As mentioned before, our hospitalists have played prominent roles in the successful implementation of computerized physician order entry, a process that has been shown to result in major improvements in patient safety. Our hospitalists also serve on the patient safety committee and are an important link between residents and ancillary staff when housestaff raise safety concerns. In the future, our hospitalists hope to have an even greater role in such important safety areas as infection control, management of delirium in the elderly, venous thromboembolism prophylaxis in the medical inpatient, and the prevention of patient falls.
- Research. Clinically and educationally oriented research is encouraged among all full-time hospitalist faculty. We recently published data on the financial and educational benefits of our hospitalist model in the April 2004 issue of the Journal of General Internal Medicine, but we feel that more needs to be done. In particular, we plan to better quantify how hospitalists achieve the reported cost-saving benefits. We also plan to further assess the roles of hospitalists in the education of medical residents in the community setting, a topic that is vastly underrepresented in the medical literature. Hospitalist faculty will also participate in a formal evaluation of the Multidisciplinary Rounds Process and will mentor residents in their personal research projects.
Contact
Mark Kulaga, MD
Associate Program Director
Internal Medicine Residency
Norwalk Hospital
Norwalk, CT 06856
Physician Staff
Pamela Charney, MD
Joseph Cleary, MD
Mark Kulaga, MD
Eric Mazur, MD
Stephen O’Mahony, MD
Jason Orlinick, MD, PhD
Andrea Peterson, MD
Other Staff
Michael Marotta, PA
Start Up
July 1999
Hospital Setting
Norwalk Hospital, Norwalk, CT
Academic Community Hospital with 250 beds
Affiliated with Yale University
Patient Population
Our patient population is wonderfully diverse, both economically and socially. Located in the heart of affluent Fairfield County, Norwalk is nevertheless a true small city and home to vibrant communities of African Americans, Latinos, and multiple other immigrant groups. The Hospitalist Clinician-Educator program was originally created to provide inpatient care for indigent patients (who predominantly attend the Norwalk Community Health Center) and for those patients without a local primary care physician. In recent years, as more community internists have chosen to use the hospital medicine service, our payer mix has substantially changed to include many more patients with private insurance and/or Medicare.
Employer
All physicians are general internists employed by the Norwalk Hospital.
Organization/Management
Dr. Eric Mazur, Chairman of the Department of Internal Medicine, is the program founder and administrative leader. He serves as the primary liaison between the hospitalists and the Chief Executive and Operating Officers of the hospital.
Total Number of Patients Served Each Year
On average, each hospitalist admits 350 patients per year. When this threshold is exceeded, a new hospitalist has been added to the group. In the first few years of service, our hospitalists covered 20-25% of the total number of medical admissions to the Norwalk Hospital. As use of the service by local internists has increased, this percentage has grown to 40–45%. It is projected that the Norwalk Hospital hospital medicine service will admit over 2200 patients this year.
Compensation/Schedules
All hospitalists receive a fixed annual salary. The hospital subsidizes 50% of each Hospitalist Clinician Educator position and bills the faculty practice income for the remaining 50%. Faculty practice income is generated through direct patient billing facilitated by a billing agency not affiliated with the hospital. The hospital also provides an annual stipend to the faculty practice for the indigent care supplied by the hospital medicine group. Our compensation model does not utilize an incentive bonus system, although yearly bonuses derived from surplus faculty practice revenue are provided at the discretion of the Chairman.
All hospitalists admit and co-manage patients with resident teams who provide 24/7 in-house coverage. Each hospitalist typically works Monday through Friday from approximately 7–8 a.m. until 5:30–6:30 p.m. depending on patient census. Hospitalists, along with other members of the full time faculty, provide nighttime backup coverage from home for the residents. Weekend coverage responsibilities are also shared with other members of the teaching faculty. Weekend moonlighters, all of whom are board-certified or board-eligible internists from nearby communities, assist full-time faculty members with coverage on Saturdays and Sundays.
Communication Strategies/Role in Education
All of our hospitalists are highly rated by medical residents for their effectiveness as teachers and supervisors. For many, they also serve as important mentors and role models. In addition to traditional educational roles on the inpatient service, our hospitalists have developed several innovative teaching conferences, which include: teaching skills workshops; weekly medical informatics sessions; a monthly medical quiz game incorporating content from core educational conferences; a multidisciplinary Morbidity and Mortality Conference in which residents from the internal medicine and radiology departments are key participants; and a series of conferences in which end-of-life issues and physician professional development are explored in great depth.
Our hospitalists have also established a formal medical consultation service with a specially designed curriculum for the residents. We have also developed a hospital medicine elective where medical residents experience what being a hospitalist is “really like.” This elective has also been used to remediate struggling residents. Our hospitalists also have prominent administrative hospital roles; one is the Director of Graduate Medical Education, and 2 others serve as Associate Program Directors for the Internal Medicine residency. In addition, they have presented their academic work at regional and national meetings of the American College of Physicians and the Society of General Internal Medicine.
Challenges Now and in the Future
Our biggest challenge can be summed up with one word: growth. Up to this point in time, a major strength of our program is that it has been able to grow incrementally and deliberately. We have never “rushed” the hiring of new hospitalists and thus have been able to recruit physicians with similar academic backgrounds and career goals. This has resulted in a cohesive group of hospitalists who support each other in every way and work extremely well together.
A major concern in hospitalist medicine is the concept of “hospitalist burnout.” We have successfully addressed this issue by limiting the number of hospitalist admissions and weekends on call, actively participating in medical education with resident physicians, and serving in important administrative roles within the hospital. As we expand to meet the growing demand for our inpatient care services by primary care physicians, we are finding it more difficult to strike a balance between our service duties and academic interests. We are working closely with our department chairman, who is a true advocate of “hospitalist career building,” to find creative ways to achieve this goal. We believe that it is the balance between service and education that has allowed us to attain a hospitalist retention rate of 100% since the inception of the group.
Goals of Hospital Medicine Group
In addition to providing outstanding patient care and resident teaching, the goals of our group are commensurate with many of the current trends affecting the field of medicine and include:
- Quality. As quality moves to the forefront of medicine, we believe that hospitalists are the logical champions and effectors of inpatient quality care. Our hospitalists have been involved in a number of quality improvement projects, such as the establishment of multidisciplinary patient rounds, which serve to advance care and achieve high levels of core measure compliance; stroke center development; and the design of inpatient diabetes management protocols. Our hospitalists have also been heavily involved in the implementation of computerized physician order entry at the Norwalk Hospital and have written numerous order sets for specific diagnoses. We expect these projects to result in demonstrably improved quality beyond the improvements in length-of-stay and core-measures adherence already achieved. We believe that our involvement in quality, both now and in the future, adds value to our role as hospitalists from the point of view of hospital administrators. It also provides us with enhanced job satisfaction and multiple opportunities for career development.
- Patient safety. This is another “hot topic” in the field of medicine where we feel that hospitalists can and should have a substantial impact. As mentioned before, our hospitalists have played prominent roles in the successful implementation of computerized physician order entry, a process that has been shown to result in major improvements in patient safety. Our hospitalists also serve on the patient safety committee and are an important link between residents and ancillary staff when housestaff raise safety concerns. In the future, our hospitalists hope to have an even greater role in such important safety areas as infection control, management of delirium in the elderly, venous thromboembolism prophylaxis in the medical inpatient, and the prevention of patient falls.
- Research. Clinically and educationally oriented research is encouraged among all full-time hospitalist faculty. We recently published data on the financial and educational benefits of our hospitalist model in the April 2004 issue of the Journal of General Internal Medicine, but we feel that more needs to be done. In particular, we plan to better quantify how hospitalists achieve the reported cost-saving benefits. We also plan to further assess the roles of hospitalists in the education of medical residents in the community setting, a topic that is vastly underrepresented in the medical literature. Hospitalist faculty will also participate in a formal evaluation of the Multidisciplinary Rounds Process and will mentor residents in their personal research projects.
Life as a Nocturnist
Jackson Memorial Hospital is an accredited, nonprofit, tertiary care hospital and the major teaching facility for the University of Miami School of Medicine. Jackson Memorial Hospital is one of the busiest centers in the country, with approximately 1500 licensed beds, 225,000 emergency and urgent care visits, and nearly 60,000 admissions to the hospital each year. Furthermore, JMH is the only full-service provider for the uninsured and medically indigent in Miami-Dade County, Florida.
Jackson Memorial Hospital has a broad range of tertiary services and clinical programs designed to serve the entire community. Its medical staff is recognized nationally for the quality of its patient care, teaching, and research. The hospital has over 11,000 full-time employees, approximately 1000 house staff, and nearly 700 clinical attending physicians from the University of Miami School of Medicine alone.
Our medicine department is composed of the following inpatient services: eight general medical teaching teams, three HIV/AIDS teams, one cardiology team, an acute care for the elderly (ACE) unit, one oncology team, and a hospitalist run (non-teaching) service.
Over the last several years a combination of the pressures from outside regulatory agencies and an increasing number of patient admissions brought the admitting process to a breaking point. Teaching services were being held to the admission cap guidelines by the Residency Review Committee (RRC). Furthermore, the Accreditation Council for Graduate Medical Education (ACGME) began to enforce strict work-hour rules for all training programs. With these restrictions a fixed number of admissions were admitted to a fixed number of services within a shorter period of the day. In fact, many patients were being held in the emergency department (ED) for as long as 15 hours before an internal medicine service saw the patient or wrote admission orders. We had concerns about safety and the provision of high quality of care for these patients. One of the concerns was that ED physicians were caring for patients who were essentially inpatients while continuing to treat new ED cases.
In an attempt to provide excellent care to our patients, we developed the Emergency Medical Hospitalist Service (EMHS), a nocturnist service. The goals of this service are to: (1) provide attendinglevel care to patients requiring admission, (2) allow the hospital to operate within the admission cap guideline set forth by the RRC, (3) function during the time in which the ACGME work hour limits were affecting the hospital, and (4) operate in a manner that would be at least cost neutral for the institution. We hired two internists (myself and Dr. Roshan K. Rao) to admit patients overnight and begin their inpatient work-up. During this shift, we admit and initiate the inpatient care of all medical admissions for the inpatient services, including the housestaff covered teams. During a typical 12-hour shift, we will admit an average of 10–12 new patients from the ED. In addition to this, there is one resident on each night (termed “night relief”), who provides cross-coverage of existing medical inpatients. We also work in close concert with the newly developed “Patient Placement Coordinator,” who facilitates prompt bed assignments and movement of these patients to in-house beds.
Currently there are two of us, so we make our own schedule depending on each others’ needs. We currently work one week on/one week off, from 8 p.m. To 8 a.m. Towards the end of the shift, we sign out the newly admitted patients to the appropriate services. Typically, the resident will come into the ED and take their sign-out from one of us. The geriatrics fellows and non-teaching hospitalists usually take sign-out over the phone. The entire sign-out process occurs anytime from 6:00 a.m. to 8:00 a.m. We also reserve this part of the shift to follow up laboratory studies and other diagnostic procedures. Occasionally, we are able to discharge some patients by the end of the shift as well.
On occasion, we will call in the other nocturnist to help out when admissions are too numerous for one physician to handle. This typically occurs towards the end of the work week. We usually require “double coverage” approximately 6–8 nights per month.
Since we instituted the nocturnist program 2 years ago, we have seen great improvements in ED throughput, inpatient bed utilization, patient satisfaction, average length of stay (both in the ED and inpatient), and quality of care. As soon as the emergency physician makes their decision to admit the patient, one of us is already interviewing, examining, and writing admission orders on the patient. This speeds up the process of the patient’s evaluation and allows the patient to be immediately transferred to a quiet room. Furthermore, this allows us to develop a rapport with the patient in the middle of the night, instead of feeling rushed in the morning to round on as many as 20 new patients. This also ensures a good night’s rest for the patient and improves the bed utilization. Moving patients to the floor in a timely fashion also allows for the ED to treat more patients.
Having a nocturnist in the hospital throughout the night allows for a more precise and accurate physical exam, formulation of an impression, and execution of a treatment plan. Physicians who are on-call at home often do not get the complete or correct story from the ED, which can lead to incomplete admission orders and delayed treatment plans. This can lead to unnecessary increases in length of stay. For example, I often admit “chest pain” patients, who by morning have already “ruled out” for an acute coronary event, had a stress test, and are ready for discharge before the “daytime” physician has seen the patient. Another example is diabetic ketoacidosis. I am able to be very aggressive with the treatment plan throughout the night, again decreasing length of stay and hospital costs.
Nocturnism is not only advantageous to the hospital and patients, but also to the nocturnist himself/herself. Dedicated nocturnists have less fatigue and stress. I work only nights, so I do not become excessively tired. My sleep schedule is completely reversed from the norm. This also has many advantages to my personal life. One of these is that I never miss a package delivered to my home!
Indeed, developing this program was a challenge. Initially we sold the idea through a combination of patient safety and revenue. The hospital cannot bill for holding patients in the ED. If we admit patients and move them to an inpatient bed, the hospital can generate this otherwise lost revenue. As with any new idea, we did meet resistance and opposition along the way. However, we were able to overcome these obstacles and build upon them. Once the administration saw the improvements and our productivity, they were immensely pleased. In fact, the administration is already looking at expanding our staffing and our services. Our billing and collections have shown we pay for our cost and generate additional funds for the hospital, despite a poor payer mix. I am excited to see what the future holds for nocturnists, not only in our institution, but across the country. Groups that employ nocturnists probably wonder how they ever survived without them in the past.
Dr. Sabharwal can be contacted at [email protected].
Jackson Memorial Hospital is an accredited, nonprofit, tertiary care hospital and the major teaching facility for the University of Miami School of Medicine. Jackson Memorial Hospital is one of the busiest centers in the country, with approximately 1500 licensed beds, 225,000 emergency and urgent care visits, and nearly 60,000 admissions to the hospital each year. Furthermore, JMH is the only full-service provider for the uninsured and medically indigent in Miami-Dade County, Florida.
Jackson Memorial Hospital has a broad range of tertiary services and clinical programs designed to serve the entire community. Its medical staff is recognized nationally for the quality of its patient care, teaching, and research. The hospital has over 11,000 full-time employees, approximately 1000 house staff, and nearly 700 clinical attending physicians from the University of Miami School of Medicine alone.
Our medicine department is composed of the following inpatient services: eight general medical teaching teams, three HIV/AIDS teams, one cardiology team, an acute care for the elderly (ACE) unit, one oncology team, and a hospitalist run (non-teaching) service.
Over the last several years a combination of the pressures from outside regulatory agencies and an increasing number of patient admissions brought the admitting process to a breaking point. Teaching services were being held to the admission cap guidelines by the Residency Review Committee (RRC). Furthermore, the Accreditation Council for Graduate Medical Education (ACGME) began to enforce strict work-hour rules for all training programs. With these restrictions a fixed number of admissions were admitted to a fixed number of services within a shorter period of the day. In fact, many patients were being held in the emergency department (ED) for as long as 15 hours before an internal medicine service saw the patient or wrote admission orders. We had concerns about safety and the provision of high quality of care for these patients. One of the concerns was that ED physicians were caring for patients who were essentially inpatients while continuing to treat new ED cases.
In an attempt to provide excellent care to our patients, we developed the Emergency Medical Hospitalist Service (EMHS), a nocturnist service. The goals of this service are to: (1) provide attendinglevel care to patients requiring admission, (2) allow the hospital to operate within the admission cap guideline set forth by the RRC, (3) function during the time in which the ACGME work hour limits were affecting the hospital, and (4) operate in a manner that would be at least cost neutral for the institution. We hired two internists (myself and Dr. Roshan K. Rao) to admit patients overnight and begin their inpatient work-up. During this shift, we admit and initiate the inpatient care of all medical admissions for the inpatient services, including the housestaff covered teams. During a typical 12-hour shift, we will admit an average of 10–12 new patients from the ED. In addition to this, there is one resident on each night (termed “night relief”), who provides cross-coverage of existing medical inpatients. We also work in close concert with the newly developed “Patient Placement Coordinator,” who facilitates prompt bed assignments and movement of these patients to in-house beds.
Currently there are two of us, so we make our own schedule depending on each others’ needs. We currently work one week on/one week off, from 8 p.m. To 8 a.m. Towards the end of the shift, we sign out the newly admitted patients to the appropriate services. Typically, the resident will come into the ED and take their sign-out from one of us. The geriatrics fellows and non-teaching hospitalists usually take sign-out over the phone. The entire sign-out process occurs anytime from 6:00 a.m. to 8:00 a.m. We also reserve this part of the shift to follow up laboratory studies and other diagnostic procedures. Occasionally, we are able to discharge some patients by the end of the shift as well.
On occasion, we will call in the other nocturnist to help out when admissions are too numerous for one physician to handle. This typically occurs towards the end of the work week. We usually require “double coverage” approximately 6–8 nights per month.
Since we instituted the nocturnist program 2 years ago, we have seen great improvements in ED throughput, inpatient bed utilization, patient satisfaction, average length of stay (both in the ED and inpatient), and quality of care. As soon as the emergency physician makes their decision to admit the patient, one of us is already interviewing, examining, and writing admission orders on the patient. This speeds up the process of the patient’s evaluation and allows the patient to be immediately transferred to a quiet room. Furthermore, this allows us to develop a rapport with the patient in the middle of the night, instead of feeling rushed in the morning to round on as many as 20 new patients. This also ensures a good night’s rest for the patient and improves the bed utilization. Moving patients to the floor in a timely fashion also allows for the ED to treat more patients.
Having a nocturnist in the hospital throughout the night allows for a more precise and accurate physical exam, formulation of an impression, and execution of a treatment plan. Physicians who are on-call at home often do not get the complete or correct story from the ED, which can lead to incomplete admission orders and delayed treatment plans. This can lead to unnecessary increases in length of stay. For example, I often admit “chest pain” patients, who by morning have already “ruled out” for an acute coronary event, had a stress test, and are ready for discharge before the “daytime” physician has seen the patient. Another example is diabetic ketoacidosis. I am able to be very aggressive with the treatment plan throughout the night, again decreasing length of stay and hospital costs.
Nocturnism is not only advantageous to the hospital and patients, but also to the nocturnist himself/herself. Dedicated nocturnists have less fatigue and stress. I work only nights, so I do not become excessively tired. My sleep schedule is completely reversed from the norm. This also has many advantages to my personal life. One of these is that I never miss a package delivered to my home!
Indeed, developing this program was a challenge. Initially we sold the idea through a combination of patient safety and revenue. The hospital cannot bill for holding patients in the ED. If we admit patients and move them to an inpatient bed, the hospital can generate this otherwise lost revenue. As with any new idea, we did meet resistance and opposition along the way. However, we were able to overcome these obstacles and build upon them. Once the administration saw the improvements and our productivity, they were immensely pleased. In fact, the administration is already looking at expanding our staffing and our services. Our billing and collections have shown we pay for our cost and generate additional funds for the hospital, despite a poor payer mix. I am excited to see what the future holds for nocturnists, not only in our institution, but across the country. Groups that employ nocturnists probably wonder how they ever survived without them in the past.
Dr. Sabharwal can be contacted at [email protected].
Jackson Memorial Hospital is an accredited, nonprofit, tertiary care hospital and the major teaching facility for the University of Miami School of Medicine. Jackson Memorial Hospital is one of the busiest centers in the country, with approximately 1500 licensed beds, 225,000 emergency and urgent care visits, and nearly 60,000 admissions to the hospital each year. Furthermore, JMH is the only full-service provider for the uninsured and medically indigent in Miami-Dade County, Florida.
Jackson Memorial Hospital has a broad range of tertiary services and clinical programs designed to serve the entire community. Its medical staff is recognized nationally for the quality of its patient care, teaching, and research. The hospital has over 11,000 full-time employees, approximately 1000 house staff, and nearly 700 clinical attending physicians from the University of Miami School of Medicine alone.
Our medicine department is composed of the following inpatient services: eight general medical teaching teams, three HIV/AIDS teams, one cardiology team, an acute care for the elderly (ACE) unit, one oncology team, and a hospitalist run (non-teaching) service.
Over the last several years a combination of the pressures from outside regulatory agencies and an increasing number of patient admissions brought the admitting process to a breaking point. Teaching services were being held to the admission cap guidelines by the Residency Review Committee (RRC). Furthermore, the Accreditation Council for Graduate Medical Education (ACGME) began to enforce strict work-hour rules for all training programs. With these restrictions a fixed number of admissions were admitted to a fixed number of services within a shorter period of the day. In fact, many patients were being held in the emergency department (ED) for as long as 15 hours before an internal medicine service saw the patient or wrote admission orders. We had concerns about safety and the provision of high quality of care for these patients. One of the concerns was that ED physicians were caring for patients who were essentially inpatients while continuing to treat new ED cases.
In an attempt to provide excellent care to our patients, we developed the Emergency Medical Hospitalist Service (EMHS), a nocturnist service. The goals of this service are to: (1) provide attendinglevel care to patients requiring admission, (2) allow the hospital to operate within the admission cap guideline set forth by the RRC, (3) function during the time in which the ACGME work hour limits were affecting the hospital, and (4) operate in a manner that would be at least cost neutral for the institution. We hired two internists (myself and Dr. Roshan K. Rao) to admit patients overnight and begin their inpatient work-up. During this shift, we admit and initiate the inpatient care of all medical admissions for the inpatient services, including the housestaff covered teams. During a typical 12-hour shift, we will admit an average of 10–12 new patients from the ED. In addition to this, there is one resident on each night (termed “night relief”), who provides cross-coverage of existing medical inpatients. We also work in close concert with the newly developed “Patient Placement Coordinator,” who facilitates prompt bed assignments and movement of these patients to in-house beds.
Currently there are two of us, so we make our own schedule depending on each others’ needs. We currently work one week on/one week off, from 8 p.m. To 8 a.m. Towards the end of the shift, we sign out the newly admitted patients to the appropriate services. Typically, the resident will come into the ED and take their sign-out from one of us. The geriatrics fellows and non-teaching hospitalists usually take sign-out over the phone. The entire sign-out process occurs anytime from 6:00 a.m. to 8:00 a.m. We also reserve this part of the shift to follow up laboratory studies and other diagnostic procedures. Occasionally, we are able to discharge some patients by the end of the shift as well.
On occasion, we will call in the other nocturnist to help out when admissions are too numerous for one physician to handle. This typically occurs towards the end of the work week. We usually require “double coverage” approximately 6–8 nights per month.
Since we instituted the nocturnist program 2 years ago, we have seen great improvements in ED throughput, inpatient bed utilization, patient satisfaction, average length of stay (both in the ED and inpatient), and quality of care. As soon as the emergency physician makes their decision to admit the patient, one of us is already interviewing, examining, and writing admission orders on the patient. This speeds up the process of the patient’s evaluation and allows the patient to be immediately transferred to a quiet room. Furthermore, this allows us to develop a rapport with the patient in the middle of the night, instead of feeling rushed in the morning to round on as many as 20 new patients. This also ensures a good night’s rest for the patient and improves the bed utilization. Moving patients to the floor in a timely fashion also allows for the ED to treat more patients.
Having a nocturnist in the hospital throughout the night allows for a more precise and accurate physical exam, formulation of an impression, and execution of a treatment plan. Physicians who are on-call at home often do not get the complete or correct story from the ED, which can lead to incomplete admission orders and delayed treatment plans. This can lead to unnecessary increases in length of stay. For example, I often admit “chest pain” patients, who by morning have already “ruled out” for an acute coronary event, had a stress test, and are ready for discharge before the “daytime” physician has seen the patient. Another example is diabetic ketoacidosis. I am able to be very aggressive with the treatment plan throughout the night, again decreasing length of stay and hospital costs.
Nocturnism is not only advantageous to the hospital and patients, but also to the nocturnist himself/herself. Dedicated nocturnists have less fatigue and stress. I work only nights, so I do not become excessively tired. My sleep schedule is completely reversed from the norm. This also has many advantages to my personal life. One of these is that I never miss a package delivered to my home!
Indeed, developing this program was a challenge. Initially we sold the idea through a combination of patient safety and revenue. The hospital cannot bill for holding patients in the ED. If we admit patients and move them to an inpatient bed, the hospital can generate this otherwise lost revenue. As with any new idea, we did meet resistance and opposition along the way. However, we were able to overcome these obstacles and build upon them. Once the administration saw the improvements and our productivity, they were immensely pleased. In fact, the administration is already looking at expanding our staffing and our services. Our billing and collections have shown we pay for our cost and generate additional funds for the hospital, despite a poor payer mix. I am excited to see what the future holds for nocturnists, not only in our institution, but across the country. Groups that employ nocturnists probably wonder how they ever survived without them in the past.
Dr. Sabharwal can be contacted at [email protected].
Medical Student Teaching on a “Non-Teaching” Service
At many academic institutions, hospitalists are increasingly acting as the teaching attendings on inpatient general medicine rotations. There have been multiple studies demonstrating perceived benefits of hospitalist faculty on housestaff education in academic and community hospitals (1-6). Measured benefits have included improved trainee satisfaction with the educational experience, improved teaching, and higher quality of attending rounds (3,4). There is growing evidence that hospitalist physicians attending on medicine wards provide educational advantages for medical students as well (5-7).
The majority of published studies thus far have focused on trainee education on a traditional medicine ward rotation, with a team including housestaff and medical students. A few medical centers have developed a resident or medical student rotation on a primary hospitalist service (8). With recent restrictions on resident work hours, many more academic programs are developing a “non-covered” hospitalist service similar to the community model (9). While the outcomes of many such programs are not yet entirely clear, this type of service may provide opportunities for an alternative learning experience for medical students. The author is not aware of any published accounts of the medical student experience on such rotations.
Barnes-Jewish Hospital is an urban, 904-bed academic center. The hospitalist program at our institution was initiated as a community model in 2000, with a private service managing patients independent of the internal medicine teaching service. Since then, members of the group have become integrally involved in multiple other teaching roles throughout the institution. The private inpatient service has remained a portion of the practice. During this time period, fourth-year medical students have had the opportunity to participate in a 4-week clinical elective on our primary hospitalist service as a substitute for, or in addition to, the traditional internal medicine sub-internship.
This rotation differs from the traditional medicine rotation in that students have the opportunity to be exposed to more patients, as multiple patients are admitted each day, rather than on a rotating call schedule. Students work directly with hospitalists on the service without the involvement of housestaff. They are not assigned to a specific attending, and therefore work with several attendings over the course of the rotation. A single student rotates on any given 4-week block. There are no other support staff involved in patient care, such as physician assistants or nurse practitioners. Over the last 4 years, over 30 students have participated in this rotation.
In 4 years, students have enrolled in approximately 75% of the elective block rotations available. Overall, written feedback has been obtained from 21 students. Students have been asked to rate the quality of teaching, meaningful participation in patient care, and overall satisfaction with the rotation, as well as to provide additional comments on their experience. Ratings were on a five-point scale, ranging from poor to excellent. Review of student evaluations of this rotation over the past 4 years reveals a majority rating of excellent or very good in all three categories (17/21).
In the students’ narrative comments, several themes were predominant. Positive feedback included the opportunity for one-on-one interactions with several attendings. Students valued the exposure to multiple role models with unique patient care styles. In addition, many students appreciated the opportunity to see a larger number of patients, given the multiple daily admissions. Students see an average of 16 new admissions during the rotation compared to an average of 10 patients on the traditional sub-internship over the course of 4 weeks.
Students also commented on the diversity of patients seen. Given the high patient census on the service (an average of 30 each day), we are able to be selective and choose learning cases with interesting and varied diagnoses. Several students appreciated the opportunity to perform more procedures, which may be preferentially performed by the housestaff on a traditional medicine rotation.
Many students noted an increased level of independence experienced on this rotation compared with traditional teaching rotations. In other studies, concerns have been voiced regarding resident lack of autonomy while working with a hospitalist attending, who tends to have a more visible presence on the inpatient medicine floors (1,4). These concerns have not been validated by resident or medical student feedback of actual experiences (1,4). At the training level of a third- or fourth-year medical student, not having a resident intermediary may lead to more perceived autonomy, adding to the overall learning experience.
The main reservation expressed by students pertained to the challenge of scheduling dedicated teaching time while attending physicians are busy with patient care. Serving as the primary inpatient caregiver for patients can often lead to an unpredictable daily schedule. This year our hospital has instituted a designated floor for patients on the< hospitalist service. This has allowed centralization of most patient care, providing more time for teaching and more visibility of attending physicians to medical students on the rotation. Another solution may involve the increased use of non-physician practitioners, as are being incorporated into many hospital medicine practices. This could allow the physicians to focus on teaching and on patients with more complex medical issues.
From the physician perspective, having medical students rotate on the service is consistent with our mission as clinician educators. Hospitalists choose a position at an academic institution in part because teaching is a priority. For community hospitalists, working with medical students may offer an option to incorporate teaching into clinical patient care. For academic hospitalists facing more “nonteaching” duties, a similar rotation may allow physicians to incorporate an additional teaching role into such duties. Based on the limited experience at this institution, a hospitalist rotation appears to offer a distinct and positive learning experience for medical students compared with a traditional medicine rotation. More extensive experience in the future may support this as a viable option at more centers. Further study will be necessary to identify an optimal curriculum for such a rotation and to evaluate the impact on students’ career choices and perceptions of the field of internal medicine.
Dr. Quartarolo can be contacted at [email protected].
References
- Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560-5.
- Kulaga ME, Charney P, O’Mahony SP. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Hauer KE, Wachter RM, McCulloch CE, Woo GA, Auerbach AD. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004;164:1866-71.
- Chung P, Morrison J, Jin L, Levinson W. Humphrey H. Meltzer D. Resident satisfaction on an academic hospitalist service: Time to teach. Am J Med. 2002;112: 597-601.
- Kripalani S, Pope AC, Rask K. Hospitalists as teachers. J Gen Intern Med. 2004;19:8-15.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations. Acad Med. 2004;79:78-82.
- Hauer KE and Wachter RM. Implications of the hospitalist model for medical students’ education. Acad Med. 2001;76:324-330.
- Amin AN. A successful hospitalist rotation for senior medicine residents. Med Educ. 2003;37:1042.
- Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19:392-3.
At many academic institutions, hospitalists are increasingly acting as the teaching attendings on inpatient general medicine rotations. There have been multiple studies demonstrating perceived benefits of hospitalist faculty on housestaff education in academic and community hospitals (1-6). Measured benefits have included improved trainee satisfaction with the educational experience, improved teaching, and higher quality of attending rounds (3,4). There is growing evidence that hospitalist physicians attending on medicine wards provide educational advantages for medical students as well (5-7).
The majority of published studies thus far have focused on trainee education on a traditional medicine ward rotation, with a team including housestaff and medical students. A few medical centers have developed a resident or medical student rotation on a primary hospitalist service (8). With recent restrictions on resident work hours, many more academic programs are developing a “non-covered” hospitalist service similar to the community model (9). While the outcomes of many such programs are not yet entirely clear, this type of service may provide opportunities for an alternative learning experience for medical students. The author is not aware of any published accounts of the medical student experience on such rotations.
Barnes-Jewish Hospital is an urban, 904-bed academic center. The hospitalist program at our institution was initiated as a community model in 2000, with a private service managing patients independent of the internal medicine teaching service. Since then, members of the group have become integrally involved in multiple other teaching roles throughout the institution. The private inpatient service has remained a portion of the practice. During this time period, fourth-year medical students have had the opportunity to participate in a 4-week clinical elective on our primary hospitalist service as a substitute for, or in addition to, the traditional internal medicine sub-internship.
This rotation differs from the traditional medicine rotation in that students have the opportunity to be exposed to more patients, as multiple patients are admitted each day, rather than on a rotating call schedule. Students work directly with hospitalists on the service without the involvement of housestaff. They are not assigned to a specific attending, and therefore work with several attendings over the course of the rotation. A single student rotates on any given 4-week block. There are no other support staff involved in patient care, such as physician assistants or nurse practitioners. Over the last 4 years, over 30 students have participated in this rotation.
In 4 years, students have enrolled in approximately 75% of the elective block rotations available. Overall, written feedback has been obtained from 21 students. Students have been asked to rate the quality of teaching, meaningful participation in patient care, and overall satisfaction with the rotation, as well as to provide additional comments on their experience. Ratings were on a five-point scale, ranging from poor to excellent. Review of student evaluations of this rotation over the past 4 years reveals a majority rating of excellent or very good in all three categories (17/21).
In the students’ narrative comments, several themes were predominant. Positive feedback included the opportunity for one-on-one interactions with several attendings. Students valued the exposure to multiple role models with unique patient care styles. In addition, many students appreciated the opportunity to see a larger number of patients, given the multiple daily admissions. Students see an average of 16 new admissions during the rotation compared to an average of 10 patients on the traditional sub-internship over the course of 4 weeks.
Students also commented on the diversity of patients seen. Given the high patient census on the service (an average of 30 each day), we are able to be selective and choose learning cases with interesting and varied diagnoses. Several students appreciated the opportunity to perform more procedures, which may be preferentially performed by the housestaff on a traditional medicine rotation.
Many students noted an increased level of independence experienced on this rotation compared with traditional teaching rotations. In other studies, concerns have been voiced regarding resident lack of autonomy while working with a hospitalist attending, who tends to have a more visible presence on the inpatient medicine floors (1,4). These concerns have not been validated by resident or medical student feedback of actual experiences (1,4). At the training level of a third- or fourth-year medical student, not having a resident intermediary may lead to more perceived autonomy, adding to the overall learning experience.
The main reservation expressed by students pertained to the challenge of scheduling dedicated teaching time while attending physicians are busy with patient care. Serving as the primary inpatient caregiver for patients can often lead to an unpredictable daily schedule. This year our hospital has instituted a designated floor for patients on the< hospitalist service. This has allowed centralization of most patient care, providing more time for teaching and more visibility of attending physicians to medical students on the rotation. Another solution may involve the increased use of non-physician practitioners, as are being incorporated into many hospital medicine practices. This could allow the physicians to focus on teaching and on patients with more complex medical issues.
From the physician perspective, having medical students rotate on the service is consistent with our mission as clinician educators. Hospitalists choose a position at an academic institution in part because teaching is a priority. For community hospitalists, working with medical students may offer an option to incorporate teaching into clinical patient care. For academic hospitalists facing more “nonteaching” duties, a similar rotation may allow physicians to incorporate an additional teaching role into such duties. Based on the limited experience at this institution, a hospitalist rotation appears to offer a distinct and positive learning experience for medical students compared with a traditional medicine rotation. More extensive experience in the future may support this as a viable option at more centers. Further study will be necessary to identify an optimal curriculum for such a rotation and to evaluate the impact on students’ career choices and perceptions of the field of internal medicine.
Dr. Quartarolo can be contacted at [email protected].
References
- Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560-5.
- Kulaga ME, Charney P, O’Mahony SP. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Hauer KE, Wachter RM, McCulloch CE, Woo GA, Auerbach AD. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004;164:1866-71.
- Chung P, Morrison J, Jin L, Levinson W. Humphrey H. Meltzer D. Resident satisfaction on an academic hospitalist service: Time to teach. Am J Med. 2002;112: 597-601.
- Kripalani S, Pope AC, Rask K. Hospitalists as teachers. J Gen Intern Med. 2004;19:8-15.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations. Acad Med. 2004;79:78-82.
- Hauer KE and Wachter RM. Implications of the hospitalist model for medical students’ education. Acad Med. 2001;76:324-330.
- Amin AN. A successful hospitalist rotation for senior medicine residents. Med Educ. 2003;37:1042.
- Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19:392-3.
At many academic institutions, hospitalists are increasingly acting as the teaching attendings on inpatient general medicine rotations. There have been multiple studies demonstrating perceived benefits of hospitalist faculty on housestaff education in academic and community hospitals (1-6). Measured benefits have included improved trainee satisfaction with the educational experience, improved teaching, and higher quality of attending rounds (3,4). There is growing evidence that hospitalist physicians attending on medicine wards provide educational advantages for medical students as well (5-7).
The majority of published studies thus far have focused on trainee education on a traditional medicine ward rotation, with a team including housestaff and medical students. A few medical centers have developed a resident or medical student rotation on a primary hospitalist service (8). With recent restrictions on resident work hours, many more academic programs are developing a “non-covered” hospitalist service similar to the community model (9). While the outcomes of many such programs are not yet entirely clear, this type of service may provide opportunities for an alternative learning experience for medical students. The author is not aware of any published accounts of the medical student experience on such rotations.
Barnes-Jewish Hospital is an urban, 904-bed academic center. The hospitalist program at our institution was initiated as a community model in 2000, with a private service managing patients independent of the internal medicine teaching service. Since then, members of the group have become integrally involved in multiple other teaching roles throughout the institution. The private inpatient service has remained a portion of the practice. During this time period, fourth-year medical students have had the opportunity to participate in a 4-week clinical elective on our primary hospitalist service as a substitute for, or in addition to, the traditional internal medicine sub-internship.
This rotation differs from the traditional medicine rotation in that students have the opportunity to be exposed to more patients, as multiple patients are admitted each day, rather than on a rotating call schedule. Students work directly with hospitalists on the service without the involvement of housestaff. They are not assigned to a specific attending, and therefore work with several attendings over the course of the rotation. A single student rotates on any given 4-week block. There are no other support staff involved in patient care, such as physician assistants or nurse practitioners. Over the last 4 years, over 30 students have participated in this rotation.
In 4 years, students have enrolled in approximately 75% of the elective block rotations available. Overall, written feedback has been obtained from 21 students. Students have been asked to rate the quality of teaching, meaningful participation in patient care, and overall satisfaction with the rotation, as well as to provide additional comments on their experience. Ratings were on a five-point scale, ranging from poor to excellent. Review of student evaluations of this rotation over the past 4 years reveals a majority rating of excellent or very good in all three categories (17/21).
In the students’ narrative comments, several themes were predominant. Positive feedback included the opportunity for one-on-one interactions with several attendings. Students valued the exposure to multiple role models with unique patient care styles. In addition, many students appreciated the opportunity to see a larger number of patients, given the multiple daily admissions. Students see an average of 16 new admissions during the rotation compared to an average of 10 patients on the traditional sub-internship over the course of 4 weeks.
Students also commented on the diversity of patients seen. Given the high patient census on the service (an average of 30 each day), we are able to be selective and choose learning cases with interesting and varied diagnoses. Several students appreciated the opportunity to perform more procedures, which may be preferentially performed by the housestaff on a traditional medicine rotation.
Many students noted an increased level of independence experienced on this rotation compared with traditional teaching rotations. In other studies, concerns have been voiced regarding resident lack of autonomy while working with a hospitalist attending, who tends to have a more visible presence on the inpatient medicine floors (1,4). These concerns have not been validated by resident or medical student feedback of actual experiences (1,4). At the training level of a third- or fourth-year medical student, not having a resident intermediary may lead to more perceived autonomy, adding to the overall learning experience.
The main reservation expressed by students pertained to the challenge of scheduling dedicated teaching time while attending physicians are busy with patient care. Serving as the primary inpatient caregiver for patients can often lead to an unpredictable daily schedule. This year our hospital has instituted a designated floor for patients on the< hospitalist service. This has allowed centralization of most patient care, providing more time for teaching and more visibility of attending physicians to medical students on the rotation. Another solution may involve the increased use of non-physician practitioners, as are being incorporated into many hospital medicine practices. This could allow the physicians to focus on teaching and on patients with more complex medical issues.
From the physician perspective, having medical students rotate on the service is consistent with our mission as clinician educators. Hospitalists choose a position at an academic institution in part because teaching is a priority. For community hospitalists, working with medical students may offer an option to incorporate teaching into clinical patient care. For academic hospitalists facing more “nonteaching” duties, a similar rotation may allow physicians to incorporate an additional teaching role into such duties. Based on the limited experience at this institution, a hospitalist rotation appears to offer a distinct and positive learning experience for medical students compared with a traditional medicine rotation. More extensive experience in the future may support this as a viable option at more centers. Further study will be necessary to identify an optimal curriculum for such a rotation and to evaluate the impact on students’ career choices and perceptions of the field of internal medicine.
Dr. Quartarolo can be contacted at [email protected].
References
- Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560-5.
- Kulaga ME, Charney P, O’Mahony SP. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Hauer KE, Wachter RM, McCulloch CE, Woo GA, Auerbach AD. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004;164:1866-71.
- Chung P, Morrison J, Jin L, Levinson W. Humphrey H. Meltzer D. Resident satisfaction on an academic hospitalist service: Time to teach. Am J Med. 2002;112: 597-601.
- Kripalani S, Pope AC, Rask K. Hospitalists as teachers. J Gen Intern Med. 2004;19:8-15.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations. Acad Med. 2004;79:78-82.
- Hauer KE and Wachter RM. Implications of the hospitalist model for medical students’ education. Acad Med. 2001;76:324-330.
- Amin AN. A successful hospitalist rotation for senior medicine residents. Med Educ. 2003;37:1042.
- Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19:392-3.
SHM’s Scott Flanders, MD and Sanjay Saint, MD, MPH
SHM’s scott Flanders, MD, of the University of Michigan Health System, and Sanjay Saint, MD, MPH, a hospitalist at the Ann Arbor VA Medical Center and University of Michigan Health System, are spearheading the nation’s first multi-hospital patient safety project to protect hospital patients from errors and oversights. The project, called Hospitalists as Emerging Leaders in Patient Safety, or HELPS, will coordinate the efforts of nine southeast Michigan health systems, allowing hospitalists from around the region to share tips, tools and techniques. It also will help doctors put proven safety ideas into motion at their hospitals and measure how well this pooled effort can prevent such problems as medication errors, hospital-acquired infections and dangerous falls.
The patient safety project was launched in April via an $117,000 grant to the University of Michigan Health System from the Blue Cross Blue Shield of Michigan Foundation. This is the latest of several recent patient safety-related grants awarded to the University of Michigan by the Blue Cross Blue Shield of Michigan Foundation.
“Although patient safety relies on every member of the hospital staff to take appropriate actions and to speak up when something goes wrong, the buck stops with the physician who leads the inpatient team – and increasingly that physician is a hospitalist,” said Dr. Flanders, chief of the hospitalist service at UMHS, associate professor of medicine and member of the SHM board of directors. “Health systems are hiring hospitalists to maximize inpatient care efficiency, coordination and patient satisfaction, while lowering the costs of care,” added Dr. Flanders. “An integral part of these goals should be to improve patient safety by reducing medical errors.”
Dr. Saint, an associate professor who heads the Patient Safety Enhancement Program at the Ann Arbor VA Medical Center and UMHS, credits much of the impetus for HELPS to the Agency for Healthcare Research and Quality and the VA’s Health Services Research and Development Program, both of which have supported previous patient safety work that forms much of the basis of this new project. Dr. Saint and hospitalists at the University of Michigan have already shown that they can reduce urinary tract and bloodstream infections among hospitalized patients by using reminders and automatic orders to prompt doctors, and by standardizing the use of new site disinfectants and novel antibacterial catheters. This effort alone is saving UMHS hospital patients considerable pain and risk, while lowering UMHS costs, despite the fact that the new technology costs more initially. Drs. Flanders and Saint will attempt to repeat this success in hospitals across the southeast region in nine different areas of medicine, including:
- Techniques for performing quality-improvement research, so that doctors can accurately assess the effects of their efforts;
- Preventing device-related infections;
- Eliminating medication errors and creating a culture of safety;
- Improving the use of preventive medications for surgical patients;
- Closing gaps in care between different services in the hospital and gaps that exist as patients are discharged from the hospital;
- Improving intensive-care practices, including pneumonia prevention;
- End-of-life care, including pain and advance directives;
- Safety for older patients, including prevention of falls and delirium; and
- Learning lessons from patient safety efforts.
The nine participating Michigan health systems include:
- University of Michigan Health System
- VA Ann Arbor Healthcare System
- St. Joseph Mercy Healthcare System
- Oakwood Healthcare System
- Beaumont Hospital
- Detroit Medical Center
- Henry Ford Health System
- Chelsea Community Hospital and
- Michigan Hospitalists, who practice throughout the St. John Health System.
In all, the hospitalists in the new consortium care for about 80,000 patients each year.
“Linking these key hospitals, where hospitalists care for so many patients, will make a huge difference in patient safety in southeast Michigan,” said Dr. Saint. “We’ll all now have the advantage of cross-sharing patient safety tactics that work, instead of allowing that knowledge to stay within one hospital or health system. We will also focus on which implementation strategies are likely to work and which ones should be abandoned.”
In addition to its cross-sharing of patient safety information, UMHS will also provide expertise in patient-safety research and statistical analysis that will boost the project’s impact. The hospitalist team hopes to publish its data about safety-enhancing practices that show the most promise―and about how to persuade and remind doctors to use safety-enhancing practices. The team has already begun publishing work related to HELPS. The manuscript describing this unique consortium was recently accepted in the Journal of Patient Safety.
The UMHS hospitalist practice currently cares for nearly half of the adult patients admitted to the internal medicine services of University Hospital. UMHS has also added a team of pediatric hospitalists. In addition to the patient safety project, UMHS hospitalists are pioneering co-management of surgical patients with orthopaedic surgeons.
Drs. Flanders and Saint also anticipate that their nine-hospital consortium will eventually develop into a multicenter collaborative in which clinical studies―both experimental and observational―will be conducted. They expect that hospitalists, working closely with specialist colleagues, will be actively engaged in creating the new knowledge that is increasingly required to care for hospitalized patients. Importantly, this knowledge will come not just from patients admitted to tertiary-care academic medical centers, but also community hospitals, the venue in which the majority of hospitalized patients receive care. Similar to the success of cardiologists and oncologists in establishing regional, national, and international networks of clinical investigators, Drs. Flanders and Saint would be thrilled if HELPS is viewed in a decade as birthing a hospitalist network of clinical research excellence. Given the high level of support that has been provided by the UMHS and the enthusiastic response HELPS has received from each of the participating sites, Saint feels they are well on their way.
Flanders says that more and more, hospitalists will become the linchpins to patient safety improvement. “It would be extremely difficult to coordinate the efforts of the thousands of independent, community-based doctors who spend part of their time caring for inpatients,” he said. “By spearheading this effort through hospitalists, we can change the system from the inside out, and help spread patient safety best practices to other physician specialists, primary care doctors, nurses and every member of the patient care team.”
SHM’s scott Flanders, MD, of the University of Michigan Health System, and Sanjay Saint, MD, MPH, a hospitalist at the Ann Arbor VA Medical Center and University of Michigan Health System, are spearheading the nation’s first multi-hospital patient safety project to protect hospital patients from errors and oversights. The project, called Hospitalists as Emerging Leaders in Patient Safety, or HELPS, will coordinate the efforts of nine southeast Michigan health systems, allowing hospitalists from around the region to share tips, tools and techniques. It also will help doctors put proven safety ideas into motion at their hospitals and measure how well this pooled effort can prevent such problems as medication errors, hospital-acquired infections and dangerous falls.
The patient safety project was launched in April via an $117,000 grant to the University of Michigan Health System from the Blue Cross Blue Shield of Michigan Foundation. This is the latest of several recent patient safety-related grants awarded to the University of Michigan by the Blue Cross Blue Shield of Michigan Foundation.
“Although patient safety relies on every member of the hospital staff to take appropriate actions and to speak up when something goes wrong, the buck stops with the physician who leads the inpatient team – and increasingly that physician is a hospitalist,” said Dr. Flanders, chief of the hospitalist service at UMHS, associate professor of medicine and member of the SHM board of directors. “Health systems are hiring hospitalists to maximize inpatient care efficiency, coordination and patient satisfaction, while lowering the costs of care,” added Dr. Flanders. “An integral part of these goals should be to improve patient safety by reducing medical errors.”
Dr. Saint, an associate professor who heads the Patient Safety Enhancement Program at the Ann Arbor VA Medical Center and UMHS, credits much of the impetus for HELPS to the Agency for Healthcare Research and Quality and the VA’s Health Services Research and Development Program, both of which have supported previous patient safety work that forms much of the basis of this new project. Dr. Saint and hospitalists at the University of Michigan have already shown that they can reduce urinary tract and bloodstream infections among hospitalized patients by using reminders and automatic orders to prompt doctors, and by standardizing the use of new site disinfectants and novel antibacterial catheters. This effort alone is saving UMHS hospital patients considerable pain and risk, while lowering UMHS costs, despite the fact that the new technology costs more initially. Drs. Flanders and Saint will attempt to repeat this success in hospitals across the southeast region in nine different areas of medicine, including:
- Techniques for performing quality-improvement research, so that doctors can accurately assess the effects of their efforts;
- Preventing device-related infections;
- Eliminating medication errors and creating a culture of safety;
- Improving the use of preventive medications for surgical patients;
- Closing gaps in care between different services in the hospital and gaps that exist as patients are discharged from the hospital;
- Improving intensive-care practices, including pneumonia prevention;
- End-of-life care, including pain and advance directives;
- Safety for older patients, including prevention of falls and delirium; and
- Learning lessons from patient safety efforts.
The nine participating Michigan health systems include:
- University of Michigan Health System
- VA Ann Arbor Healthcare System
- St. Joseph Mercy Healthcare System
- Oakwood Healthcare System
- Beaumont Hospital
- Detroit Medical Center
- Henry Ford Health System
- Chelsea Community Hospital and
- Michigan Hospitalists, who practice throughout the St. John Health System.
In all, the hospitalists in the new consortium care for about 80,000 patients each year.
“Linking these key hospitals, where hospitalists care for so many patients, will make a huge difference in patient safety in southeast Michigan,” said Dr. Saint. “We’ll all now have the advantage of cross-sharing patient safety tactics that work, instead of allowing that knowledge to stay within one hospital or health system. We will also focus on which implementation strategies are likely to work and which ones should be abandoned.”
In addition to its cross-sharing of patient safety information, UMHS will also provide expertise in patient-safety research and statistical analysis that will boost the project’s impact. The hospitalist team hopes to publish its data about safety-enhancing practices that show the most promise―and about how to persuade and remind doctors to use safety-enhancing practices. The team has already begun publishing work related to HELPS. The manuscript describing this unique consortium was recently accepted in the Journal of Patient Safety.
The UMHS hospitalist practice currently cares for nearly half of the adult patients admitted to the internal medicine services of University Hospital. UMHS has also added a team of pediatric hospitalists. In addition to the patient safety project, UMHS hospitalists are pioneering co-management of surgical patients with orthopaedic surgeons.
Drs. Flanders and Saint also anticipate that their nine-hospital consortium will eventually develop into a multicenter collaborative in which clinical studies―both experimental and observational―will be conducted. They expect that hospitalists, working closely with specialist colleagues, will be actively engaged in creating the new knowledge that is increasingly required to care for hospitalized patients. Importantly, this knowledge will come not just from patients admitted to tertiary-care academic medical centers, but also community hospitals, the venue in which the majority of hospitalized patients receive care. Similar to the success of cardiologists and oncologists in establishing regional, national, and international networks of clinical investigators, Drs. Flanders and Saint would be thrilled if HELPS is viewed in a decade as birthing a hospitalist network of clinical research excellence. Given the high level of support that has been provided by the UMHS and the enthusiastic response HELPS has received from each of the participating sites, Saint feels they are well on their way.
Flanders says that more and more, hospitalists will become the linchpins to patient safety improvement. “It would be extremely difficult to coordinate the efforts of the thousands of independent, community-based doctors who spend part of their time caring for inpatients,” he said. “By spearheading this effort through hospitalists, we can change the system from the inside out, and help spread patient safety best practices to other physician specialists, primary care doctors, nurses and every member of the patient care team.”
SHM’s scott Flanders, MD, of the University of Michigan Health System, and Sanjay Saint, MD, MPH, a hospitalist at the Ann Arbor VA Medical Center and University of Michigan Health System, are spearheading the nation’s first multi-hospital patient safety project to protect hospital patients from errors and oversights. The project, called Hospitalists as Emerging Leaders in Patient Safety, or HELPS, will coordinate the efforts of nine southeast Michigan health systems, allowing hospitalists from around the region to share tips, tools and techniques. It also will help doctors put proven safety ideas into motion at their hospitals and measure how well this pooled effort can prevent such problems as medication errors, hospital-acquired infections and dangerous falls.
The patient safety project was launched in April via an $117,000 grant to the University of Michigan Health System from the Blue Cross Blue Shield of Michigan Foundation. This is the latest of several recent patient safety-related grants awarded to the University of Michigan by the Blue Cross Blue Shield of Michigan Foundation.
“Although patient safety relies on every member of the hospital staff to take appropriate actions and to speak up when something goes wrong, the buck stops with the physician who leads the inpatient team – and increasingly that physician is a hospitalist,” said Dr. Flanders, chief of the hospitalist service at UMHS, associate professor of medicine and member of the SHM board of directors. “Health systems are hiring hospitalists to maximize inpatient care efficiency, coordination and patient satisfaction, while lowering the costs of care,” added Dr. Flanders. “An integral part of these goals should be to improve patient safety by reducing medical errors.”
Dr. Saint, an associate professor who heads the Patient Safety Enhancement Program at the Ann Arbor VA Medical Center and UMHS, credits much of the impetus for HELPS to the Agency for Healthcare Research and Quality and the VA’s Health Services Research and Development Program, both of which have supported previous patient safety work that forms much of the basis of this new project. Dr. Saint and hospitalists at the University of Michigan have already shown that they can reduce urinary tract and bloodstream infections among hospitalized patients by using reminders and automatic orders to prompt doctors, and by standardizing the use of new site disinfectants and novel antibacterial catheters. This effort alone is saving UMHS hospital patients considerable pain and risk, while lowering UMHS costs, despite the fact that the new technology costs more initially. Drs. Flanders and Saint will attempt to repeat this success in hospitals across the southeast region in nine different areas of medicine, including:
- Techniques for performing quality-improvement research, so that doctors can accurately assess the effects of their efforts;
- Preventing device-related infections;
- Eliminating medication errors and creating a culture of safety;
- Improving the use of preventive medications for surgical patients;
- Closing gaps in care between different services in the hospital and gaps that exist as patients are discharged from the hospital;
- Improving intensive-care practices, including pneumonia prevention;
- End-of-life care, including pain and advance directives;
- Safety for older patients, including prevention of falls and delirium; and
- Learning lessons from patient safety efforts.
The nine participating Michigan health systems include:
- University of Michigan Health System
- VA Ann Arbor Healthcare System
- St. Joseph Mercy Healthcare System
- Oakwood Healthcare System
- Beaumont Hospital
- Detroit Medical Center
- Henry Ford Health System
- Chelsea Community Hospital and
- Michigan Hospitalists, who practice throughout the St. John Health System.
In all, the hospitalists in the new consortium care for about 80,000 patients each year.
“Linking these key hospitals, where hospitalists care for so many patients, will make a huge difference in patient safety in southeast Michigan,” said Dr. Saint. “We’ll all now have the advantage of cross-sharing patient safety tactics that work, instead of allowing that knowledge to stay within one hospital or health system. We will also focus on which implementation strategies are likely to work and which ones should be abandoned.”
In addition to its cross-sharing of patient safety information, UMHS will also provide expertise in patient-safety research and statistical analysis that will boost the project’s impact. The hospitalist team hopes to publish its data about safety-enhancing practices that show the most promise―and about how to persuade and remind doctors to use safety-enhancing practices. The team has already begun publishing work related to HELPS. The manuscript describing this unique consortium was recently accepted in the Journal of Patient Safety.
The UMHS hospitalist practice currently cares for nearly half of the adult patients admitted to the internal medicine services of University Hospital. UMHS has also added a team of pediatric hospitalists. In addition to the patient safety project, UMHS hospitalists are pioneering co-management of surgical patients with orthopaedic surgeons.
Drs. Flanders and Saint also anticipate that their nine-hospital consortium will eventually develop into a multicenter collaborative in which clinical studies―both experimental and observational―will be conducted. They expect that hospitalists, working closely with specialist colleagues, will be actively engaged in creating the new knowledge that is increasingly required to care for hospitalized patients. Importantly, this knowledge will come not just from patients admitted to tertiary-care academic medical centers, but also community hospitals, the venue in which the majority of hospitalized patients receive care. Similar to the success of cardiologists and oncologists in establishing regional, national, and international networks of clinical investigators, Drs. Flanders and Saint would be thrilled if HELPS is viewed in a decade as birthing a hospitalist network of clinical research excellence. Given the high level of support that has been provided by the UMHS and the enthusiastic response HELPS has received from each of the participating sites, Saint feels they are well on their way.
Flanders says that more and more, hospitalists will become the linchpins to patient safety improvement. “It would be extremely difficult to coordinate the efforts of the thousands of independent, community-based doctors who spend part of their time caring for inpatients,” he said. “By spearheading this effort through hospitalists, we can change the system from the inside out, and help spread patient safety best practices to other physician specialists, primary care doctors, nurses and every member of the patient care team.”
Seven Effective Strategies of Highly Successful Resuscitations (or A New Look at an Ancient Practice)
Despite more intensive guidelines and advances in resuscitation research, the survival rate for victims of cardiopulmonary arrest remains virtually unchanged from forty years ago when modern cardiopulmonary resuscitation (CPR) was first described (1). Perhaps in part because the guidelines for ACLS set forth by the American Heart Association (AHA) and the International Liaison Committee on Resuscitation (ILCOR) have become so complex―and continue to increase in breadth and scope into topics well beyond cardiopulmonary arrest with each revision―the critical aspects of resuscitation have become diluted by unnecessarily difficult algorithms. Critical skill sets―such as proper performance of CPR and rapid defibrillation―have become dwarfed by less critical aspects of acute resuscitation. Remarkably common errors usurp the dual fundamental goals of ACLS: neurological preservation and prevention of early death. This review will address the historical context of resuscitation and then will focus on seven of the most essential, evidence-based strategies for improving outcomes in ACLS.
History of Resuscitation
The modern resuscitation era began in 1960 when Kouwenhoven, Jude, and Knickerbocker published a pair of landmark papers on the use of closed chest compressions (CCC) as a means to resuscitate patients in cardiopulmonary arrest (2,3). Interestingly, the culmination of their three and a half decades of work was initially motivated and sponsored by an electric company seeking to reduce the death rate of its linemen from ventricular fibrillation. While innovative, their technique built on millennia of creative, and sometimes bizarre ancient practices geared at reversing death. Given the lack of in-depth knowledge of anatomy and physiology combined with a rich overlap between shamanism and medicine, it is perhaps stunning to realize that the oldest recorded reasonably physiologic approach to resuscitation stems from over 3500 years ago. Egyptian hieroglyphs show the story of the healing goddess, Isis, reviving her husband Osiris using mouth-to-mouth ventilation (4). Still other Egyptian texts advocated hanging drowned victims upside down, compressing and releasing the thorax with the goal to ventilate and revive the patient (5). Hebrew midwives were documented as having performed mouth-to-mouth on deceased newborns as early as 1300 BCE (6). And even the Bible tells of the prophet Elishah’s successful resuscitation of a deceased child through artificial respiration:
...And he went up, and lay upon the child, and put his mouth upon his mouth, and his eyes upon his eyes, and his hands upon his hands; and he stretched himself upon the child; and the flesh of the child waxed warm (7).
One of the forefathers of modern medicine, the Greek physician Galen, was the first doctor to use an artificial ventilation strategy in 177, filling dead animals’ lungs with air from a bellows (8).
In 1628, physician William Harvey, the first to accurately describe circulation, used his newfound knowledge to successfully stop ventricular fibrillation in a pigeon using open heart massage (9 ). John Hunter created a bellows that could deliver positive and negative pressure ventilation, which he used to resuscitate dogs in 1755 (10). The Dutch Humane Society immediately tapped Hunter’s knowledge to help reduce the death rate of drowning victims (11). The resultant 1767 publication was the first ever to advocate the use of “artificial respiration”:
…the operator closed the patient’s nostrils, applied his mouth to the patient’s mouth, inflated the lungs and expanded the chest and belly, and produced expiration by compressing the abdomen with his free hand (12).
Despite giving ventilation equal measure with another popular technique at the time called fumigation―the use of tobacco smoke to fill the colon of drowned victims via a rectal tube―scientists rapidly began to use true physiologic practices to advance resuscitation.
Within eight years, Priestly would discover the element oxygen and Squires of London would record the first-ever use of electricity in resuscitation:
…he tried the effects of electricity. Twenty minutes elapsed before he could apply the shock [to the 3 year old child who had fallen out of a 1st story window], which he gave to various parts of the body in vain; but upon transmitting a few shocks through the thorax, he perceived a small pulsation; in a few minutes the child began to breathe….her health was restored (4).
Resuscitation became a legitimate science during the 19th century with literature replete of experimental successes in laboratory animal resuscitations. Techniques included using closed and open heart massage, manual ventilation using specialized medical bellows, and then finally, in 1899, documented cessation of ventricular fibrillation by electricity. Jean Louis Prevost and Frederic Batelli reported that they had defibrillated a dog successfully with the use of two electrodes―one on the head and one in the rectum―with high voltage AC current (13).
As the 20th century dawned, George Washington Crile―the cofounder of the Cleveland Clinic and considered by many as the most innovative researcher in the field of resuscitation―described successful closed chest cardiac massage in man and the first use of saline and epinephrine infusion in cardiac arrest in 1903. after the Russians Gurvich and Yuniev had demonstrated the superiority of DC current to AC current in defibrillation in 1939, Beck (1947) and Zoll (1956) published their successes in humans of open and closed chest defibrillation respectively.13 Even though the advent of the modern defibrillator loomed imminently, the practicality of widespread dissemination of the cumbersome equipment needed to provide these shocks was not yet manifest. Thus, Kouwenhoven and colleagues created a technique of closed chest cardiac massage that could keep patients alive long enough to receive definitive treatment, and modern CPR was born (14).
Epidemiology of Cardiopulmonary Arrest
In the United States an estimated 375,000 to 750,000 hospitalized patients suffer a cardiopulmonary arrest (CA) requiring advanced cardiac life support (ACLS) annually (15). The incidence of CA is estimated to be as high as 1–2% of all patients admitted to academic hospitals with a prevalence of 58 to 71 people per 100,000 nationally (16,17). The demographics of over 14,000 patients resuscitated for a CA are summarized in Table 1; patient comorbidities are listed in Figure 1.18 The typical CA patient is a white male in his seventh decade of life with a history of cardiac, pulmonary, or renal disease suffering from a pre-arrest arrhythmia or respiratory problem. Over 86% of patients are either on continuous cardiac monitoring (telemetry) or have a witnessed CA.
When primary respiratory arrests are excluded (such as from opiate overdose or post-anesthesia), only approximately 1 in 7 patients will survive an in-hospital resuscitation to discharge (1,19). Survivors’ initial rhythms are typically either pulseless ventricular tachycardia (VT) (35%) or ventricular fibrillation (VF) (34%), but fully 20% of survivors have initial “rhythms” of asystole or pulseless electrical activity (PEA)―which comprise virtually two–thirds of all arrests―suggesting a meager benefit to resuscitation of this subgroup of patients. Almost one third of survivors who lived independently pre-arrest are unable to be discharged home and between 14-23% of survivors―whose pre-arrest neurological function was normal―develop moderate to severe cognitive deficits after resuscitation (18,20). Fewer than 2% of survivors suffer coma or a persistent vegetative state. Neither gender nor advanced age appears to be a negative predictor of survival (1,21).
Time is Life Lost
The goals of resuscitation are two-fold: preservation of neurological function and prevention of early death. Expedient resuscitation maximizes the likelihood of positive outcomes, but too often, precious time is life lost spent performing unnecessary diagnostic maneuvers or unimportant interventions that have little impact on prognosis. The overarching target in in-hospital adult resuscitation is minimizing the time it takes for patients to receive defibrillation. All other activities are only a mean to this end. The remainder of this review will focus on seven highly effective strategies for successful resuscitations.
Primary Survey
Guidelines continue to stress the importance of airway, breathing, and circulation as the basic tenets of initial response to a CA. While this approach has merit in out-of-hospital arrests, it is an anathema in hospitalized patients. Valuable time is often lost trying to ascertain the presence or absence of respirations or pulse. Earle et al. designed a very creative way to gauge the operating characteristics of the carotid pulse check. Providers were asked to assess randomized patients who were to undergo open-heart surgery; some of the patients were already on cardiopulmonary bypass (“true negatives” with no spontaneous pulse) and the remainder were not (“true positives” with a pulse). With a median time of over 30 seconds, care providers could only accurately determine pulselessness 65% of the time (90% sensitivity and 55% specificity).22 Given that this study occurred in a very controlled environment without the drama of a real CA, it is likely that these data would even be worse in the chaos of resuscitation.
First Effective Stratagem: If an unresponsive adult inpatient clinically appears to be suffering a cardiopulmonary arrest, treatment (activation of a “code team” and application of CPR) should be initiated immediately without performing a pulse check.
CPR Physiology and Impact
CPR is a critical bridge to defibrillation but is not an end unto itself. The physiology that occurs during CPR is remarkably complex, and our current understanding is incomplete. Kouwenhoven posited that chest compressions result in a functional equivalent to open cardiac massage (2). In this “cardiac pump model,” the physiology is similar to a surgeon’s hands squeezing the non-beating heart: artificial systole from the down stroke of a compression compresses the heart against the spinal column forcing blood from the ventricles and forcing closure of the mitral and tricuspid valves. During artificial diastole, reversing pressure gradients result in closure of the aortic and pulmonic valves resulting in bi-ventricular filling of blood and perfusion of the coronary arteries.
An alternative model, the “thoracic pump model,” looks at the entire thoracic cavity as a pump with functional “valves” at the thoracic inlet preventing back-flow from the intrathoracic veins into the extrathoracic veins (23). The intrathoracic pressure rapidly increases during artificial systole leading to antegrade flow of blood from vessels under relatively higher pressure (the aorta and the pulmonary vasculature) to blood vessels under relatively lower pressure (the carotid arteries). The elevated intrathoracic pressure collapses the comparably weak vena cava, and, combined with tricuspid valve closure, prevents simultaneous retrograde venous flow. With three of the cardiac valves open during artificial systole, the heart is relegated to the role of a passive conduit for blood rather than providing any meaningful pumping action. During artificial diastole, intrathoracic pressure drops to near zero resulting in transient back flow of blood from the carotid arteries toward the heart. This induces aortic valve closure and generates only meager coronary artery perfusion.
Subsequent work by Paradis et al. shows that, in essence, both “pump” models have equal validity, and one or the other physiology dominates in any given patient (24). Regardless of which type of physiology occurs during resuscitation, neither provides physiologically sufficient circulation to maintain organ viability for long. When performed ideally, chest compressions during actual resuscitations in humans yield systolic blood pressures of only 60–80mmHg; and blood flow of less than one third the normal cardiac output, less than 10–15% of normal cerebral blood flow, and less than 1–5% of normal coronary artery blood flow (25).
Such subphysiologic circulation leaves little latitude for improper technique. Yet, care providers rarely perform chest compressions properly, erring towards too shallow a compression depth 62.6% of the time and too slow a compression rate 71.9% of the time on actual resuscitations―errors that increase in frequency the longer it has been since the caregiver was trained (26,27). Observational data on the quality of CPR suggest that these are not just esoteric technical deviations, but that compared with those in whom CPR is correctly performed, 14-day survival was almost 75% lower in those on whom CPR was incorrectly performed (16% vs. 4%)(28).
Furthermore, routine interruptions in chest compressions― such as for positive pressure ventilations in non-intubated patients―likely further hinder survival rather than contribute meaningfully to outcome. For example, medical students performing traditional CPR took an average of 14 seconds to administer two mouth-to-mouth ventilations after each group of 15 compressions. This effectively reduced the number of compressions to a mere 43 per minute, or less than half the guideline-mandated 100 per minute, thus theoretically reducing circulation to the heart and brain by a similar percentage (29). Yu et al demonstrated that swine receiving more than 80 compressions per minute during CPR had a 100% survival at 24 hours compared with a dismal 10% survival in animals that had less than 80 compressions per minute (30). Kern et al found statistically significantly higher coronary artery perfusion pressures and markedly higher neurological normal 24 hour survival in swine receiving continuous chest compressions compared with controls receiving traditional CPR (31).
Increasingly data such as these do raise the question of what―if any―benefit rescue breathing has in adult resuscitation. Human data show that a strategy of continuous chest compressions―without rescue breathing―is equally efficacious to traditional CPR in terms of outcome (32). Two physiologic theories prevail: 1) the mechanics of chest wall compression may be sufficient to provide a limited minute ventilation independent of supplemental ventilation (author’s speculation); and 2) the improved oxygenation that occurs in those receiving artificial ventilation is offset by the deleterious impact on hemodynamics that occur when chest compressions are interrupted for ventilation (34).
Second Effective Stratagem: Until an adult inpatient can be defibrillated, the focus of resuscitation should be on proper continuous chest compression depth and rate, not on ventilation.
Ventilations are Harmful
Cardiopulmonary collapse has immediate consequences on cellular physiology. Both due to a lack of expiration of carbon dioxide and the development of lactatemia due to the shift to anaerobic metabolism, blood pH drops precipitously. As the pH shifts out of the physiologic range, drugs begin to perform in unexpected ways or fail altogether; ion trapping occurs; and many electrolytes begin to shift in or out of cells affecting their serum concentration. Diminished or absent cardiac output accelerates these derangements in a relentless positive feedback loop. Logic, therefore, dictates that anything that can improve oxygenation and ventilation would be helpful at slowing or reversing this pathophysiology. Surprisingly, however, clinicians’ lack of knowledge of both equipment and technique often promotes, rather than mitigates, the physiologic derangements.
The bag-valve-mask (BVM) is one of the least understood resuscitation devices. For example, clinicians occasionally place a BVM over spontaneously breathing patients who are exceptionally ill with the goal of augmenting patients’ meager ventilations. However, the BVM is constructed only for positive pressure ventilation and thus, unless the clinician squeezes the bag in perfect coordination with the patient’s ventilatory effort, the BVM will paradoxically smother the patient.
The bag portion of the BVM is designed for a one-handed squeeze to deliver a tidal volume that is roughly 750cc; this volume is in keeping with guideline recommendations of positive pressure ventilation volumes of roughly 10cc/kg/ventilation (29). Yet, clinicians commonly use two hands to compress the BVM maximally during resuscitation (theoretically delivering upwards of double the recommended volume).
In addition to excessive volume, clinicians also deliver ventilations too rapidly. Abella et al. showed that during human resuscitations, ventilation rate exceeded the recommended goal of 20 ventilations/minute 60.9% of the time (27). Theoretically, high minute ventilations lead to an increased incidence of gastric insufflation, regurgitation, and post-resuscitation aspiration.
Though no studies have ever been performed to understand why clinicians hyperventilate patients during resuscitation, it is interesting to speculate that clinicians are not only trying to raise blood oxygen levels rapidly, but also to reverse the profound metabolic and respiratory acidosis that occur during CA. While seemingly mechanistically sound, the logic that supraphysiologic minute ventilations will profoundly change blood pH without other physiologic costs is specious at best. Aufderheide et al. Demonstrated that hyperventilation during resuscitation in swine resulted in increased intrathoracic pressures, markedly reduced coronary artery perfusion pressures, and resultant proportional reductions in survival rates as hyperventilation increased (35). Clinically these findings are known as auto-PEEP, a known complication of artificial ventilation that results in systemic arterial hypotension. Thus the paradox: aggressive attempts to overcorrect systemic acidoses via higher minute ventilations leads to worsening systemic blood pressures and thus worsening lactic acidosis. I believe that iatrogenic hypotension is one of the most common problems to complicate an otherwise successful resuscitation and that more research is urgently needed on this issue.
Third Effective Stratagem: Bag-valve-mask ventilations should be performed with precision; when used, the bag should be compressed with only one hand and delivered no faster than one breath every 3–5 seconds.
Fourth Effective Stratagem: In cases of pulseless electrical activity (PEA) or post-resuscitation hypotension, auto-PEEP should be considered foremost as a proximal cause.
Fifth Effective Stratagem: Ventilations in resuscitation should be viewed primarily as a means to oxygenate the patient rather than as a means to compensate from a systemic acidemia.
Shocking Revelations
Even though patients in ventricular fibrillation (VF) and pulseless ventricular tachycardia (PVT) together only comprise about one–third of all inpatient cardiac arrests, they account for almost 70% of survivors of CA. Survival in these arrhythmias is predicated solely on rapid defibrillation: the simultaneous depolarization of a critical mass of myocytes by an electrical current with resultant resumption of normal cardiac conduction (36). Perhaps the best attestation to the importance of rapid defibrillation actually comes from the survival of patients with cardiac arrest at casinos: security cameras provided exact documentation of time of collapse and defibrillation. Survival to hospital discharge was cut in half when the time-from-collapse-to-defibrillation was greater than 3 minutes (74% vs. 49%)(37).
Sixth Effective Stratagem: Since patients in VF/PVT are the most likely to survive CA―and that rate is directly related to immediacy of defibrillation―all patients should be presumptively treated as if they are in VF/PVT and should be defibrillated within 3 minutes of collapse unless there are data to support another arrhythmia or cause of collapse.
Much of the electrical current delivered during a defibrillation attempt is either dissipated as heat or is conducted around the thorax without penetrating the myocardium; Lerman and Deale have shown that the amount of current reaching the heart may be as little as 4% during a defibrillation attempt (38). From Ohm’s Law, the current that reaches the heart is directly proportional to the voltage across the chest and inversely related to the resistance of the supervening tissues. Interestingly, increasing the voltage of a shock only increases the amount of heat produced without a commensurate increase in current delivered. Therefore, techniques that reduce thoracic resistance yield the highest current delivery: the use of manual defibrillator paddles (as opposed to self adhesive defibrillation pads), the amount of pressure applied to the paddles (>25 pounds), the correct placement (underneath, rather than on top of breast tissue), the use of a conduction material (gel or pads), and the rapid delivery of a stacked shock (resistance transiently decreases after a counter-shock) all improve current delivery and thus may improve defibrillation outcome (36).
Physician leadership during resuscitations is critical for maximizing likelihood of patient survival. Perhaps due to physicians’ lack of familiarity with defibrillators, the mechanics of defibrillation are often deferred unnecessarily to nursing staff. Unfortunately, this may have profoundly negative effects on the resuscitation. Since many hospitals reduce educational expenses by foregoing training nurses in ACLS unless they work in intensive care units, nurses on a code may have even less comfort in using defibrillators than physicians. One study showed nearly a 72.5% decrease in patient survival when the nurse who arrived first at the resuscitation was untrained in ACLS (37.5% vs. 10.3%); a difference that probably is related to delayed defibrillation though the study could not establish direct causality (39).
A separate study showed that 85% of patients on cardiac monitored wards were defibrillated in the target time of 3 minutes from collapse, while only 28% of patients on unmonitored wards were defibrillated within the target time; this led to an adjusted odds ratio for survival-to-discharge in patients on monitored versus non-monitored wards of 1.45 (95% CI, 0.95–2.20)(40). While at first these data seem to indicate faster responses on monitored wards, these data were specific to time-from-collapse-to-defibrillation and therefore should be location-independent once the need for resuscitation was identified. Instead, I interpret these data as showing the lower comfort nurses on non-monitored wards have with rapid defibrillation. Rather than serving as an indictment against nurses, these data in aggregate underscore the vital role physician responders have to ensure rapid defibrillation of patients in cardiac arrest.
Seventh Effective Stratagem: Physicians should aggressively pursue defibrillation as early as possible during resuscitation especially on non-monitored wards where nurses are less likely to be ACLS trained and less likely to be familiar with defibrillator operation.
Conclusions
Resuscitation, the act of bringing back life from imminent death, is one of the most sensationalized practices in medicine and dates almost to the beginning of recorded history. In the past two decades, increasingly evidence-based guidelines have tried to provide a guide to help practitioners treat patients effectively in the minutes after cardiopulmonary collapse. Unfortunately, with each new iteration of the guidelines, it has become increasingly difficult to determine which strategies offer the highest yield or the most import. As ILCOR meets in 2005 to revise the guidelines once again, hopefully the most important strategies will be given their proper highlight, providing clinicians with increased comfort and confidence with cardiopulmonary resuscitation.
Bibliography
- Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following inhospital adult cardiopulmonary resuscitation. CMAJ. 2002;167:343-8.
- Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed chest cardiac massage. JAMA. 1960;173:1064-7.
- Jude JR, Kouwenhoven WB, Knickerbocker GG. Cardiac arrest; report of application of external cardiac massage on 118 patients. JAMA. 1961;178:1063-71.
- Varon J, Sternback GL. Cardiopulmonary resuscitation: lessons from the past. J Emerg Med. 1991;9:5037.
- Liss HP. A history of resuscitation. Ann Emerg Med.1986;15: 65-72.
- Thangam S, Weil MH, Rackow EC. Cardiopulmonary resuscitation: a historical review. Acute Care. 1986;12:63-94.
- Kings II, 4:34-35 (KJV).
- Baker AB. Artificial respiration: the history of an idea. Med Hist. 1971;15:336-46.
- Stephenson HE. Cardiac Arrest and Resuscitation. St Louis: CV Mosby; 1969.
- Lee RV. Cardiopulmonary resuscitation in the eighteenth century: a historical perspective on present practice. J Hist Med. 1972;27:418-33.
- Varon J, Marik PE, Fromm RE. Cardiopulmonary resuscitation: a review for clinicians. Resuscitation. 1998;36: 133-45.
- Keith A. Three Hunterian lectures on the various mechanisms underlying the various methods of artificial respiration. Lancet. 1909;1:895-9.
- DeBard ML. The history of cardiopulmonary resuscitation. Ann Emerg Med. 1980;9:273-5.
- Acosta P, Varion J, Sternbach GL, BaskeQ P. Resuscitation great. Kouwenhoven, Jude and Knickerbocker: the introduction of defibrillation and external chest compressions into modern resuscitation. Resuscitation. 2005;64:139-43.
- US Congress, Office of Technology Assessment. Life-sustaining technologies and the elderly. Washington, DC: US Government Printing Office, 1987; 11, Publication OTA-BA-306.
- DeBard ML. Cardiopulmonary resuscitation: analysis of six years’ experience and review of the literature. Ann Emerg Med. 1981;10:408-11.
- Cassel CK, et al. Cardiopulmonary resuscitation in the elderly. Office of Technology Assessment, U.S. Congress, Washington, DC, November, 1985.
- Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58297-308.
- Valentin A, Karnik R, Donath P, Winkler WB, Slany J. Outcome of cardiopulmonary resuscitation in hospitalized patients. Resuscitation. 1995;30:217-21.
- Robinson GR, Hess D. Postdischarge survival and functional status following in-hospital cardiopulmonary resuscitation. Chest. 1994;105:991-6.
- Murphy DI, Murray AM, Robinson BE. Outcomes of cardiopulmonary resuscitation in the elderly. Ann Int Med. 1989;111:199-205.
- Eberle B, Dick WF, Schneider T, Wisser G, Doetsch S, Tzanova I. Checking the carotid pulse check: diagnostic accuracy of first responders in patients with and without a pulse. Resuscitation. 1996;33:107-16.
- Rudikoff MT, Maughan WL, Effron M, Freund P, Weisfeldt ML. Mechanisms of blood flow during cardiopulmonary resuscitation. Circulation. 1980;61:345-52.
- Paradis NA, Martin GB, Goetting MG, et al. Simultaneous aortic, jugular bulb, and right atrial pressures during cardiopulmonary resuscitation in humans: insight into mechanisms. Circulation. 1989;80:361-8.
- Sanders AB, Ogle M, Ewy GA. Coronary perfusion pressure during cardiopulmonary resuscitation. Am J Emerg Med. 1985;3:11-4.
- Heidenreich JW, Higdon TA, Kern KB, et al. Single-rescuer cardiopulmonary resuscitation: “two quick breaths”―an oxymoron. Resuscitation. 2004;62:283-89.
- Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305-10.
- Van Hoeyweghen RJ, Bossaert LL, Mullie A, et al. (Belgian Cerebral Resuscitation Study Group.) Quality and efficiency of bystander CPR. Resuscitation. 1993;26:47-52.
- American Heart Association in collaboration with the International Liaison Committee on Resuscitation (ILCOR). International Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care―a consensus on science. Resuscitation. 2000.46:1-448.
- Yu T, Weil MH, Tang W, et al. Adverse outcomes of interrupted precordial compression during automated defibrillation. Circulation. 2002;106:368-72.
- Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation. 2002;105:645-649.
- Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with to-mouth ventilation. N Engl J Med. ;342: 154-653.
- Berg RA, Sanders AB, Kern KB, et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation. 2001;104:2465-70.
- Aufderheide TP, Sigurdsson G, Pirallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960-5.
- Dalzell GWN. Determinants of successful defibrillation. Heart. ;80:405-7.
- Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW,Hardman RG. Outcomes of rapid defibrillation by security ad er cardiac arrest in casinos. N Engl J Med. ;343:120-69.
- Lerman BB, Deale C. Relation between transcardiac and thransthoracic current during defibrillation in humans. Circ Res. 1990;67:1420-6.
- Dane FC, RussellLindgren KS, Parish DC, Durham MD, Brown TD. Inhospital resuscitation: association between ACLS training and survival to discharge. Resuscitation. 2000;47:83-7.
- Herlitz J, Bang A, Aune S, Ekstrom L, Lundstrom G, Holmberg S. Characteristics and outcome among patients suffering inhospital cardiac arrest in monitored and nonmonitored areas. Resuscitation. ;48:125-35.
Despite more intensive guidelines and advances in resuscitation research, the survival rate for victims of cardiopulmonary arrest remains virtually unchanged from forty years ago when modern cardiopulmonary resuscitation (CPR) was first described (1). Perhaps in part because the guidelines for ACLS set forth by the American Heart Association (AHA) and the International Liaison Committee on Resuscitation (ILCOR) have become so complex―and continue to increase in breadth and scope into topics well beyond cardiopulmonary arrest with each revision―the critical aspects of resuscitation have become diluted by unnecessarily difficult algorithms. Critical skill sets―such as proper performance of CPR and rapid defibrillation―have become dwarfed by less critical aspects of acute resuscitation. Remarkably common errors usurp the dual fundamental goals of ACLS: neurological preservation and prevention of early death. This review will address the historical context of resuscitation and then will focus on seven of the most essential, evidence-based strategies for improving outcomes in ACLS.
History of Resuscitation
The modern resuscitation era began in 1960 when Kouwenhoven, Jude, and Knickerbocker published a pair of landmark papers on the use of closed chest compressions (CCC) as a means to resuscitate patients in cardiopulmonary arrest (2,3). Interestingly, the culmination of their three and a half decades of work was initially motivated and sponsored by an electric company seeking to reduce the death rate of its linemen from ventricular fibrillation. While innovative, their technique built on millennia of creative, and sometimes bizarre ancient practices geared at reversing death. Given the lack of in-depth knowledge of anatomy and physiology combined with a rich overlap between shamanism and medicine, it is perhaps stunning to realize that the oldest recorded reasonably physiologic approach to resuscitation stems from over 3500 years ago. Egyptian hieroglyphs show the story of the healing goddess, Isis, reviving her husband Osiris using mouth-to-mouth ventilation (4). Still other Egyptian texts advocated hanging drowned victims upside down, compressing and releasing the thorax with the goal to ventilate and revive the patient (5). Hebrew midwives were documented as having performed mouth-to-mouth on deceased newborns as early as 1300 BCE (6). And even the Bible tells of the prophet Elishah’s successful resuscitation of a deceased child through artificial respiration:
...And he went up, and lay upon the child, and put his mouth upon his mouth, and his eyes upon his eyes, and his hands upon his hands; and he stretched himself upon the child; and the flesh of the child waxed warm (7).
One of the forefathers of modern medicine, the Greek physician Galen, was the first doctor to use an artificial ventilation strategy in 177, filling dead animals’ lungs with air from a bellows (8).
In 1628, physician William Harvey, the first to accurately describe circulation, used his newfound knowledge to successfully stop ventricular fibrillation in a pigeon using open heart massage (9 ). John Hunter created a bellows that could deliver positive and negative pressure ventilation, which he used to resuscitate dogs in 1755 (10). The Dutch Humane Society immediately tapped Hunter’s knowledge to help reduce the death rate of drowning victims (11). The resultant 1767 publication was the first ever to advocate the use of “artificial respiration”:
…the operator closed the patient’s nostrils, applied his mouth to the patient’s mouth, inflated the lungs and expanded the chest and belly, and produced expiration by compressing the abdomen with his free hand (12).
Despite giving ventilation equal measure with another popular technique at the time called fumigation―the use of tobacco smoke to fill the colon of drowned victims via a rectal tube―scientists rapidly began to use true physiologic practices to advance resuscitation.
Within eight years, Priestly would discover the element oxygen and Squires of London would record the first-ever use of electricity in resuscitation:
…he tried the effects of electricity. Twenty minutes elapsed before he could apply the shock [to the 3 year old child who had fallen out of a 1st story window], which he gave to various parts of the body in vain; but upon transmitting a few shocks through the thorax, he perceived a small pulsation; in a few minutes the child began to breathe….her health was restored (4).
Resuscitation became a legitimate science during the 19th century with literature replete of experimental successes in laboratory animal resuscitations. Techniques included using closed and open heart massage, manual ventilation using specialized medical bellows, and then finally, in 1899, documented cessation of ventricular fibrillation by electricity. Jean Louis Prevost and Frederic Batelli reported that they had defibrillated a dog successfully with the use of two electrodes―one on the head and one in the rectum―with high voltage AC current (13).
As the 20th century dawned, George Washington Crile―the cofounder of the Cleveland Clinic and considered by many as the most innovative researcher in the field of resuscitation―described successful closed chest cardiac massage in man and the first use of saline and epinephrine infusion in cardiac arrest in 1903. after the Russians Gurvich and Yuniev had demonstrated the superiority of DC current to AC current in defibrillation in 1939, Beck (1947) and Zoll (1956) published their successes in humans of open and closed chest defibrillation respectively.13 Even though the advent of the modern defibrillator loomed imminently, the practicality of widespread dissemination of the cumbersome equipment needed to provide these shocks was not yet manifest. Thus, Kouwenhoven and colleagues created a technique of closed chest cardiac massage that could keep patients alive long enough to receive definitive treatment, and modern CPR was born (14).
Epidemiology of Cardiopulmonary Arrest
In the United States an estimated 375,000 to 750,000 hospitalized patients suffer a cardiopulmonary arrest (CA) requiring advanced cardiac life support (ACLS) annually (15). The incidence of CA is estimated to be as high as 1–2% of all patients admitted to academic hospitals with a prevalence of 58 to 71 people per 100,000 nationally (16,17). The demographics of over 14,000 patients resuscitated for a CA are summarized in Table 1; patient comorbidities are listed in Figure 1.18 The typical CA patient is a white male in his seventh decade of life with a history of cardiac, pulmonary, or renal disease suffering from a pre-arrest arrhythmia or respiratory problem. Over 86% of patients are either on continuous cardiac monitoring (telemetry) or have a witnessed CA.
When primary respiratory arrests are excluded (such as from opiate overdose or post-anesthesia), only approximately 1 in 7 patients will survive an in-hospital resuscitation to discharge (1,19). Survivors’ initial rhythms are typically either pulseless ventricular tachycardia (VT) (35%) or ventricular fibrillation (VF) (34%), but fully 20% of survivors have initial “rhythms” of asystole or pulseless electrical activity (PEA)―which comprise virtually two–thirds of all arrests―suggesting a meager benefit to resuscitation of this subgroup of patients. Almost one third of survivors who lived independently pre-arrest are unable to be discharged home and between 14-23% of survivors―whose pre-arrest neurological function was normal―develop moderate to severe cognitive deficits after resuscitation (18,20). Fewer than 2% of survivors suffer coma or a persistent vegetative state. Neither gender nor advanced age appears to be a negative predictor of survival (1,21).
Time is Life Lost
The goals of resuscitation are two-fold: preservation of neurological function and prevention of early death. Expedient resuscitation maximizes the likelihood of positive outcomes, but too often, precious time is life lost spent performing unnecessary diagnostic maneuvers or unimportant interventions that have little impact on prognosis. The overarching target in in-hospital adult resuscitation is minimizing the time it takes for patients to receive defibrillation. All other activities are only a mean to this end. The remainder of this review will focus on seven highly effective strategies for successful resuscitations.
Primary Survey
Guidelines continue to stress the importance of airway, breathing, and circulation as the basic tenets of initial response to a CA. While this approach has merit in out-of-hospital arrests, it is an anathema in hospitalized patients. Valuable time is often lost trying to ascertain the presence or absence of respirations or pulse. Earle et al. designed a very creative way to gauge the operating characteristics of the carotid pulse check. Providers were asked to assess randomized patients who were to undergo open-heart surgery; some of the patients were already on cardiopulmonary bypass (“true negatives” with no spontaneous pulse) and the remainder were not (“true positives” with a pulse). With a median time of over 30 seconds, care providers could only accurately determine pulselessness 65% of the time (90% sensitivity and 55% specificity).22 Given that this study occurred in a very controlled environment without the drama of a real CA, it is likely that these data would even be worse in the chaos of resuscitation.
First Effective Stratagem: If an unresponsive adult inpatient clinically appears to be suffering a cardiopulmonary arrest, treatment (activation of a “code team” and application of CPR) should be initiated immediately without performing a pulse check.
CPR Physiology and Impact
CPR is a critical bridge to defibrillation but is not an end unto itself. The physiology that occurs during CPR is remarkably complex, and our current understanding is incomplete. Kouwenhoven posited that chest compressions result in a functional equivalent to open cardiac massage (2). In this “cardiac pump model,” the physiology is similar to a surgeon’s hands squeezing the non-beating heart: artificial systole from the down stroke of a compression compresses the heart against the spinal column forcing blood from the ventricles and forcing closure of the mitral and tricuspid valves. During artificial diastole, reversing pressure gradients result in closure of the aortic and pulmonic valves resulting in bi-ventricular filling of blood and perfusion of the coronary arteries.
An alternative model, the “thoracic pump model,” looks at the entire thoracic cavity as a pump with functional “valves” at the thoracic inlet preventing back-flow from the intrathoracic veins into the extrathoracic veins (23). The intrathoracic pressure rapidly increases during artificial systole leading to antegrade flow of blood from vessels under relatively higher pressure (the aorta and the pulmonary vasculature) to blood vessels under relatively lower pressure (the carotid arteries). The elevated intrathoracic pressure collapses the comparably weak vena cava, and, combined with tricuspid valve closure, prevents simultaneous retrograde venous flow. With three of the cardiac valves open during artificial systole, the heart is relegated to the role of a passive conduit for blood rather than providing any meaningful pumping action. During artificial diastole, intrathoracic pressure drops to near zero resulting in transient back flow of blood from the carotid arteries toward the heart. This induces aortic valve closure and generates only meager coronary artery perfusion.
Subsequent work by Paradis et al. shows that, in essence, both “pump” models have equal validity, and one or the other physiology dominates in any given patient (24). Regardless of which type of physiology occurs during resuscitation, neither provides physiologically sufficient circulation to maintain organ viability for long. When performed ideally, chest compressions during actual resuscitations in humans yield systolic blood pressures of only 60–80mmHg; and blood flow of less than one third the normal cardiac output, less than 10–15% of normal cerebral blood flow, and less than 1–5% of normal coronary artery blood flow (25).
Such subphysiologic circulation leaves little latitude for improper technique. Yet, care providers rarely perform chest compressions properly, erring towards too shallow a compression depth 62.6% of the time and too slow a compression rate 71.9% of the time on actual resuscitations―errors that increase in frequency the longer it has been since the caregiver was trained (26,27). Observational data on the quality of CPR suggest that these are not just esoteric technical deviations, but that compared with those in whom CPR is correctly performed, 14-day survival was almost 75% lower in those on whom CPR was incorrectly performed (16% vs. 4%)(28).
Furthermore, routine interruptions in chest compressions― such as for positive pressure ventilations in non-intubated patients―likely further hinder survival rather than contribute meaningfully to outcome. For example, medical students performing traditional CPR took an average of 14 seconds to administer two mouth-to-mouth ventilations after each group of 15 compressions. This effectively reduced the number of compressions to a mere 43 per minute, or less than half the guideline-mandated 100 per minute, thus theoretically reducing circulation to the heart and brain by a similar percentage (29). Yu et al demonstrated that swine receiving more than 80 compressions per minute during CPR had a 100% survival at 24 hours compared with a dismal 10% survival in animals that had less than 80 compressions per minute (30). Kern et al found statistically significantly higher coronary artery perfusion pressures and markedly higher neurological normal 24 hour survival in swine receiving continuous chest compressions compared with controls receiving traditional CPR (31).
Increasingly data such as these do raise the question of what―if any―benefit rescue breathing has in adult resuscitation. Human data show that a strategy of continuous chest compressions―without rescue breathing―is equally efficacious to traditional CPR in terms of outcome (32). Two physiologic theories prevail: 1) the mechanics of chest wall compression may be sufficient to provide a limited minute ventilation independent of supplemental ventilation (author’s speculation); and 2) the improved oxygenation that occurs in those receiving artificial ventilation is offset by the deleterious impact on hemodynamics that occur when chest compressions are interrupted for ventilation (34).
Second Effective Stratagem: Until an adult inpatient can be defibrillated, the focus of resuscitation should be on proper continuous chest compression depth and rate, not on ventilation.
Ventilations are Harmful
Cardiopulmonary collapse has immediate consequences on cellular physiology. Both due to a lack of expiration of carbon dioxide and the development of lactatemia due to the shift to anaerobic metabolism, blood pH drops precipitously. As the pH shifts out of the physiologic range, drugs begin to perform in unexpected ways or fail altogether; ion trapping occurs; and many electrolytes begin to shift in or out of cells affecting their serum concentration. Diminished or absent cardiac output accelerates these derangements in a relentless positive feedback loop. Logic, therefore, dictates that anything that can improve oxygenation and ventilation would be helpful at slowing or reversing this pathophysiology. Surprisingly, however, clinicians’ lack of knowledge of both equipment and technique often promotes, rather than mitigates, the physiologic derangements.
The bag-valve-mask (BVM) is one of the least understood resuscitation devices. For example, clinicians occasionally place a BVM over spontaneously breathing patients who are exceptionally ill with the goal of augmenting patients’ meager ventilations. However, the BVM is constructed only for positive pressure ventilation and thus, unless the clinician squeezes the bag in perfect coordination with the patient’s ventilatory effort, the BVM will paradoxically smother the patient.
The bag portion of the BVM is designed for a one-handed squeeze to deliver a tidal volume that is roughly 750cc; this volume is in keeping with guideline recommendations of positive pressure ventilation volumes of roughly 10cc/kg/ventilation (29). Yet, clinicians commonly use two hands to compress the BVM maximally during resuscitation (theoretically delivering upwards of double the recommended volume).
In addition to excessive volume, clinicians also deliver ventilations too rapidly. Abella et al. showed that during human resuscitations, ventilation rate exceeded the recommended goal of 20 ventilations/minute 60.9% of the time (27). Theoretically, high minute ventilations lead to an increased incidence of gastric insufflation, regurgitation, and post-resuscitation aspiration.
Though no studies have ever been performed to understand why clinicians hyperventilate patients during resuscitation, it is interesting to speculate that clinicians are not only trying to raise blood oxygen levels rapidly, but also to reverse the profound metabolic and respiratory acidosis that occur during CA. While seemingly mechanistically sound, the logic that supraphysiologic minute ventilations will profoundly change blood pH without other physiologic costs is specious at best. Aufderheide et al. Demonstrated that hyperventilation during resuscitation in swine resulted in increased intrathoracic pressures, markedly reduced coronary artery perfusion pressures, and resultant proportional reductions in survival rates as hyperventilation increased (35). Clinically these findings are known as auto-PEEP, a known complication of artificial ventilation that results in systemic arterial hypotension. Thus the paradox: aggressive attempts to overcorrect systemic acidoses via higher minute ventilations leads to worsening systemic blood pressures and thus worsening lactic acidosis. I believe that iatrogenic hypotension is one of the most common problems to complicate an otherwise successful resuscitation and that more research is urgently needed on this issue.
Third Effective Stratagem: Bag-valve-mask ventilations should be performed with precision; when used, the bag should be compressed with only one hand and delivered no faster than one breath every 3–5 seconds.
Fourth Effective Stratagem: In cases of pulseless electrical activity (PEA) or post-resuscitation hypotension, auto-PEEP should be considered foremost as a proximal cause.
Fifth Effective Stratagem: Ventilations in resuscitation should be viewed primarily as a means to oxygenate the patient rather than as a means to compensate from a systemic acidemia.
Shocking Revelations
Even though patients in ventricular fibrillation (VF) and pulseless ventricular tachycardia (PVT) together only comprise about one–third of all inpatient cardiac arrests, they account for almost 70% of survivors of CA. Survival in these arrhythmias is predicated solely on rapid defibrillation: the simultaneous depolarization of a critical mass of myocytes by an electrical current with resultant resumption of normal cardiac conduction (36). Perhaps the best attestation to the importance of rapid defibrillation actually comes from the survival of patients with cardiac arrest at casinos: security cameras provided exact documentation of time of collapse and defibrillation. Survival to hospital discharge was cut in half when the time-from-collapse-to-defibrillation was greater than 3 minutes (74% vs. 49%)(37).
Sixth Effective Stratagem: Since patients in VF/PVT are the most likely to survive CA―and that rate is directly related to immediacy of defibrillation―all patients should be presumptively treated as if they are in VF/PVT and should be defibrillated within 3 minutes of collapse unless there are data to support another arrhythmia or cause of collapse.
Much of the electrical current delivered during a defibrillation attempt is either dissipated as heat or is conducted around the thorax without penetrating the myocardium; Lerman and Deale have shown that the amount of current reaching the heart may be as little as 4% during a defibrillation attempt (38). From Ohm’s Law, the current that reaches the heart is directly proportional to the voltage across the chest and inversely related to the resistance of the supervening tissues. Interestingly, increasing the voltage of a shock only increases the amount of heat produced without a commensurate increase in current delivered. Therefore, techniques that reduce thoracic resistance yield the highest current delivery: the use of manual defibrillator paddles (as opposed to self adhesive defibrillation pads), the amount of pressure applied to the paddles (>25 pounds), the correct placement (underneath, rather than on top of breast tissue), the use of a conduction material (gel or pads), and the rapid delivery of a stacked shock (resistance transiently decreases after a counter-shock) all improve current delivery and thus may improve defibrillation outcome (36).
Physician leadership during resuscitations is critical for maximizing likelihood of patient survival. Perhaps due to physicians’ lack of familiarity with defibrillators, the mechanics of defibrillation are often deferred unnecessarily to nursing staff. Unfortunately, this may have profoundly negative effects on the resuscitation. Since many hospitals reduce educational expenses by foregoing training nurses in ACLS unless they work in intensive care units, nurses on a code may have even less comfort in using defibrillators than physicians. One study showed nearly a 72.5% decrease in patient survival when the nurse who arrived first at the resuscitation was untrained in ACLS (37.5% vs. 10.3%); a difference that probably is related to delayed defibrillation though the study could not establish direct causality (39).
A separate study showed that 85% of patients on cardiac monitored wards were defibrillated in the target time of 3 minutes from collapse, while only 28% of patients on unmonitored wards were defibrillated within the target time; this led to an adjusted odds ratio for survival-to-discharge in patients on monitored versus non-monitored wards of 1.45 (95% CI, 0.95–2.20)(40). While at first these data seem to indicate faster responses on monitored wards, these data were specific to time-from-collapse-to-defibrillation and therefore should be location-independent once the need for resuscitation was identified. Instead, I interpret these data as showing the lower comfort nurses on non-monitored wards have with rapid defibrillation. Rather than serving as an indictment against nurses, these data in aggregate underscore the vital role physician responders have to ensure rapid defibrillation of patients in cardiac arrest.
Seventh Effective Stratagem: Physicians should aggressively pursue defibrillation as early as possible during resuscitation especially on non-monitored wards where nurses are less likely to be ACLS trained and less likely to be familiar with defibrillator operation.
Conclusions
Resuscitation, the act of bringing back life from imminent death, is one of the most sensationalized practices in medicine and dates almost to the beginning of recorded history. In the past two decades, increasingly evidence-based guidelines have tried to provide a guide to help practitioners treat patients effectively in the minutes after cardiopulmonary collapse. Unfortunately, with each new iteration of the guidelines, it has become increasingly difficult to determine which strategies offer the highest yield or the most import. As ILCOR meets in 2005 to revise the guidelines once again, hopefully the most important strategies will be given their proper highlight, providing clinicians with increased comfort and confidence with cardiopulmonary resuscitation.
Bibliography
- Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following inhospital adult cardiopulmonary resuscitation. CMAJ. 2002;167:343-8.
- Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed chest cardiac massage. JAMA. 1960;173:1064-7.
- Jude JR, Kouwenhoven WB, Knickerbocker GG. Cardiac arrest; report of application of external cardiac massage on 118 patients. JAMA. 1961;178:1063-71.
- Varon J, Sternback GL. Cardiopulmonary resuscitation: lessons from the past. J Emerg Med. 1991;9:5037.
- Liss HP. A history of resuscitation. Ann Emerg Med.1986;15: 65-72.
- Thangam S, Weil MH, Rackow EC. Cardiopulmonary resuscitation: a historical review. Acute Care. 1986;12:63-94.
- Kings II, 4:34-35 (KJV).
- Baker AB. Artificial respiration: the history of an idea. Med Hist. 1971;15:336-46.
- Stephenson HE. Cardiac Arrest and Resuscitation. St Louis: CV Mosby; 1969.
- Lee RV. Cardiopulmonary resuscitation in the eighteenth century: a historical perspective on present practice. J Hist Med. 1972;27:418-33.
- Varon J, Marik PE, Fromm RE. Cardiopulmonary resuscitation: a review for clinicians. Resuscitation. 1998;36: 133-45.
- Keith A. Three Hunterian lectures on the various mechanisms underlying the various methods of artificial respiration. Lancet. 1909;1:895-9.
- DeBard ML. The history of cardiopulmonary resuscitation. Ann Emerg Med. 1980;9:273-5.
- Acosta P, Varion J, Sternbach GL, BaskeQ P. Resuscitation great. Kouwenhoven, Jude and Knickerbocker: the introduction of defibrillation and external chest compressions into modern resuscitation. Resuscitation. 2005;64:139-43.
- US Congress, Office of Technology Assessment. Life-sustaining technologies and the elderly. Washington, DC: US Government Printing Office, 1987; 11, Publication OTA-BA-306.
- DeBard ML. Cardiopulmonary resuscitation: analysis of six years’ experience and review of the literature. Ann Emerg Med. 1981;10:408-11.
- Cassel CK, et al. Cardiopulmonary resuscitation in the elderly. Office of Technology Assessment, U.S. Congress, Washington, DC, November, 1985.
- Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58297-308.
- Valentin A, Karnik R, Donath P, Winkler WB, Slany J. Outcome of cardiopulmonary resuscitation in hospitalized patients. Resuscitation. 1995;30:217-21.
- Robinson GR, Hess D. Postdischarge survival and functional status following in-hospital cardiopulmonary resuscitation. Chest. 1994;105:991-6.
- Murphy DI, Murray AM, Robinson BE. Outcomes of cardiopulmonary resuscitation in the elderly. Ann Int Med. 1989;111:199-205.
- Eberle B, Dick WF, Schneider T, Wisser G, Doetsch S, Tzanova I. Checking the carotid pulse check: diagnostic accuracy of first responders in patients with and without a pulse. Resuscitation. 1996;33:107-16.
- Rudikoff MT, Maughan WL, Effron M, Freund P, Weisfeldt ML. Mechanisms of blood flow during cardiopulmonary resuscitation. Circulation. 1980;61:345-52.
- Paradis NA, Martin GB, Goetting MG, et al. Simultaneous aortic, jugular bulb, and right atrial pressures during cardiopulmonary resuscitation in humans: insight into mechanisms. Circulation. 1989;80:361-8.
- Sanders AB, Ogle M, Ewy GA. Coronary perfusion pressure during cardiopulmonary resuscitation. Am J Emerg Med. 1985;3:11-4.
- Heidenreich JW, Higdon TA, Kern KB, et al. Single-rescuer cardiopulmonary resuscitation: “two quick breaths”―an oxymoron. Resuscitation. 2004;62:283-89.
- Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305-10.
- Van Hoeyweghen RJ, Bossaert LL, Mullie A, et al. (Belgian Cerebral Resuscitation Study Group.) Quality and efficiency of bystander CPR. Resuscitation. 1993;26:47-52.
- American Heart Association in collaboration with the International Liaison Committee on Resuscitation (ILCOR). International Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care―a consensus on science. Resuscitation. 2000.46:1-448.
- Yu T, Weil MH, Tang W, et al. Adverse outcomes of interrupted precordial compression during automated defibrillation. Circulation. 2002;106:368-72.
- Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation. 2002;105:645-649.
- Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with to-mouth ventilation. N Engl J Med. ;342: 154-653.
- Berg RA, Sanders AB, Kern KB, et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation. 2001;104:2465-70.
- Aufderheide TP, Sigurdsson G, Pirallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960-5.
- Dalzell GWN. Determinants of successful defibrillation. Heart. ;80:405-7.
- Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW,Hardman RG. Outcomes of rapid defibrillation by security ad er cardiac arrest in casinos. N Engl J Med. ;343:120-69.
- Lerman BB, Deale C. Relation between transcardiac and thransthoracic current during defibrillation in humans. Circ Res. 1990;67:1420-6.
- Dane FC, RussellLindgren KS, Parish DC, Durham MD, Brown TD. Inhospital resuscitation: association between ACLS training and survival to discharge. Resuscitation. 2000;47:83-7.
- Herlitz J, Bang A, Aune S, Ekstrom L, Lundstrom G, Holmberg S. Characteristics and outcome among patients suffering inhospital cardiac arrest in monitored and nonmonitored areas. Resuscitation. ;48:125-35.
Despite more intensive guidelines and advances in resuscitation research, the survival rate for victims of cardiopulmonary arrest remains virtually unchanged from forty years ago when modern cardiopulmonary resuscitation (CPR) was first described (1). Perhaps in part because the guidelines for ACLS set forth by the American Heart Association (AHA) and the International Liaison Committee on Resuscitation (ILCOR) have become so complex―and continue to increase in breadth and scope into topics well beyond cardiopulmonary arrest with each revision―the critical aspects of resuscitation have become diluted by unnecessarily difficult algorithms. Critical skill sets―such as proper performance of CPR and rapid defibrillation―have become dwarfed by less critical aspects of acute resuscitation. Remarkably common errors usurp the dual fundamental goals of ACLS: neurological preservation and prevention of early death. This review will address the historical context of resuscitation and then will focus on seven of the most essential, evidence-based strategies for improving outcomes in ACLS.
History of Resuscitation
The modern resuscitation era began in 1960 when Kouwenhoven, Jude, and Knickerbocker published a pair of landmark papers on the use of closed chest compressions (CCC) as a means to resuscitate patients in cardiopulmonary arrest (2,3). Interestingly, the culmination of their three and a half decades of work was initially motivated and sponsored by an electric company seeking to reduce the death rate of its linemen from ventricular fibrillation. While innovative, their technique built on millennia of creative, and sometimes bizarre ancient practices geared at reversing death. Given the lack of in-depth knowledge of anatomy and physiology combined with a rich overlap between shamanism and medicine, it is perhaps stunning to realize that the oldest recorded reasonably physiologic approach to resuscitation stems from over 3500 years ago. Egyptian hieroglyphs show the story of the healing goddess, Isis, reviving her husband Osiris using mouth-to-mouth ventilation (4). Still other Egyptian texts advocated hanging drowned victims upside down, compressing and releasing the thorax with the goal to ventilate and revive the patient (5). Hebrew midwives were documented as having performed mouth-to-mouth on deceased newborns as early as 1300 BCE (6). And even the Bible tells of the prophet Elishah’s successful resuscitation of a deceased child through artificial respiration:
...And he went up, and lay upon the child, and put his mouth upon his mouth, and his eyes upon his eyes, and his hands upon his hands; and he stretched himself upon the child; and the flesh of the child waxed warm (7).
One of the forefathers of modern medicine, the Greek physician Galen, was the first doctor to use an artificial ventilation strategy in 177, filling dead animals’ lungs with air from a bellows (8).
In 1628, physician William Harvey, the first to accurately describe circulation, used his newfound knowledge to successfully stop ventricular fibrillation in a pigeon using open heart massage (9 ). John Hunter created a bellows that could deliver positive and negative pressure ventilation, which he used to resuscitate dogs in 1755 (10). The Dutch Humane Society immediately tapped Hunter’s knowledge to help reduce the death rate of drowning victims (11). The resultant 1767 publication was the first ever to advocate the use of “artificial respiration”:
…the operator closed the patient’s nostrils, applied his mouth to the patient’s mouth, inflated the lungs and expanded the chest and belly, and produced expiration by compressing the abdomen with his free hand (12).
Despite giving ventilation equal measure with another popular technique at the time called fumigation―the use of tobacco smoke to fill the colon of drowned victims via a rectal tube―scientists rapidly began to use true physiologic practices to advance resuscitation.
Within eight years, Priestly would discover the element oxygen and Squires of London would record the first-ever use of electricity in resuscitation:
…he tried the effects of electricity. Twenty minutes elapsed before he could apply the shock [to the 3 year old child who had fallen out of a 1st story window], which he gave to various parts of the body in vain; but upon transmitting a few shocks through the thorax, he perceived a small pulsation; in a few minutes the child began to breathe….her health was restored (4).
Resuscitation became a legitimate science during the 19th century with literature replete of experimental successes in laboratory animal resuscitations. Techniques included using closed and open heart massage, manual ventilation using specialized medical bellows, and then finally, in 1899, documented cessation of ventricular fibrillation by electricity. Jean Louis Prevost and Frederic Batelli reported that they had defibrillated a dog successfully with the use of two electrodes―one on the head and one in the rectum―with high voltage AC current (13).
As the 20th century dawned, George Washington Crile―the cofounder of the Cleveland Clinic and considered by many as the most innovative researcher in the field of resuscitation―described successful closed chest cardiac massage in man and the first use of saline and epinephrine infusion in cardiac arrest in 1903. after the Russians Gurvich and Yuniev had demonstrated the superiority of DC current to AC current in defibrillation in 1939, Beck (1947) and Zoll (1956) published their successes in humans of open and closed chest defibrillation respectively.13 Even though the advent of the modern defibrillator loomed imminently, the practicality of widespread dissemination of the cumbersome equipment needed to provide these shocks was not yet manifest. Thus, Kouwenhoven and colleagues created a technique of closed chest cardiac massage that could keep patients alive long enough to receive definitive treatment, and modern CPR was born (14).
Epidemiology of Cardiopulmonary Arrest
In the United States an estimated 375,000 to 750,000 hospitalized patients suffer a cardiopulmonary arrest (CA) requiring advanced cardiac life support (ACLS) annually (15). The incidence of CA is estimated to be as high as 1–2% of all patients admitted to academic hospitals with a prevalence of 58 to 71 people per 100,000 nationally (16,17). The demographics of over 14,000 patients resuscitated for a CA are summarized in Table 1; patient comorbidities are listed in Figure 1.18 The typical CA patient is a white male in his seventh decade of life with a history of cardiac, pulmonary, or renal disease suffering from a pre-arrest arrhythmia or respiratory problem. Over 86% of patients are either on continuous cardiac monitoring (telemetry) or have a witnessed CA.
When primary respiratory arrests are excluded (such as from opiate overdose or post-anesthesia), only approximately 1 in 7 patients will survive an in-hospital resuscitation to discharge (1,19). Survivors’ initial rhythms are typically either pulseless ventricular tachycardia (VT) (35%) or ventricular fibrillation (VF) (34%), but fully 20% of survivors have initial “rhythms” of asystole or pulseless electrical activity (PEA)―which comprise virtually two–thirds of all arrests―suggesting a meager benefit to resuscitation of this subgroup of patients. Almost one third of survivors who lived independently pre-arrest are unable to be discharged home and between 14-23% of survivors―whose pre-arrest neurological function was normal―develop moderate to severe cognitive deficits after resuscitation (18,20). Fewer than 2% of survivors suffer coma or a persistent vegetative state. Neither gender nor advanced age appears to be a negative predictor of survival (1,21).
Time is Life Lost
The goals of resuscitation are two-fold: preservation of neurological function and prevention of early death. Expedient resuscitation maximizes the likelihood of positive outcomes, but too often, precious time is life lost spent performing unnecessary diagnostic maneuvers or unimportant interventions that have little impact on prognosis. The overarching target in in-hospital adult resuscitation is minimizing the time it takes for patients to receive defibrillation. All other activities are only a mean to this end. The remainder of this review will focus on seven highly effective strategies for successful resuscitations.
Primary Survey
Guidelines continue to stress the importance of airway, breathing, and circulation as the basic tenets of initial response to a CA. While this approach has merit in out-of-hospital arrests, it is an anathema in hospitalized patients. Valuable time is often lost trying to ascertain the presence or absence of respirations or pulse. Earle et al. designed a very creative way to gauge the operating characteristics of the carotid pulse check. Providers were asked to assess randomized patients who were to undergo open-heart surgery; some of the patients were already on cardiopulmonary bypass (“true negatives” with no spontaneous pulse) and the remainder were not (“true positives” with a pulse). With a median time of over 30 seconds, care providers could only accurately determine pulselessness 65% of the time (90% sensitivity and 55% specificity).22 Given that this study occurred in a very controlled environment without the drama of a real CA, it is likely that these data would even be worse in the chaos of resuscitation.
First Effective Stratagem: If an unresponsive adult inpatient clinically appears to be suffering a cardiopulmonary arrest, treatment (activation of a “code team” and application of CPR) should be initiated immediately without performing a pulse check.
CPR Physiology and Impact
CPR is a critical bridge to defibrillation but is not an end unto itself. The physiology that occurs during CPR is remarkably complex, and our current understanding is incomplete. Kouwenhoven posited that chest compressions result in a functional equivalent to open cardiac massage (2). In this “cardiac pump model,” the physiology is similar to a surgeon’s hands squeezing the non-beating heart: artificial systole from the down stroke of a compression compresses the heart against the spinal column forcing blood from the ventricles and forcing closure of the mitral and tricuspid valves. During artificial diastole, reversing pressure gradients result in closure of the aortic and pulmonic valves resulting in bi-ventricular filling of blood and perfusion of the coronary arteries.
An alternative model, the “thoracic pump model,” looks at the entire thoracic cavity as a pump with functional “valves” at the thoracic inlet preventing back-flow from the intrathoracic veins into the extrathoracic veins (23). The intrathoracic pressure rapidly increases during artificial systole leading to antegrade flow of blood from vessels under relatively higher pressure (the aorta and the pulmonary vasculature) to blood vessels under relatively lower pressure (the carotid arteries). The elevated intrathoracic pressure collapses the comparably weak vena cava, and, combined with tricuspid valve closure, prevents simultaneous retrograde venous flow. With three of the cardiac valves open during artificial systole, the heart is relegated to the role of a passive conduit for blood rather than providing any meaningful pumping action. During artificial diastole, intrathoracic pressure drops to near zero resulting in transient back flow of blood from the carotid arteries toward the heart. This induces aortic valve closure and generates only meager coronary artery perfusion.
Subsequent work by Paradis et al. shows that, in essence, both “pump” models have equal validity, and one or the other physiology dominates in any given patient (24). Regardless of which type of physiology occurs during resuscitation, neither provides physiologically sufficient circulation to maintain organ viability for long. When performed ideally, chest compressions during actual resuscitations in humans yield systolic blood pressures of only 60–80mmHg; and blood flow of less than one third the normal cardiac output, less than 10–15% of normal cerebral blood flow, and less than 1–5% of normal coronary artery blood flow (25).
Such subphysiologic circulation leaves little latitude for improper technique. Yet, care providers rarely perform chest compressions properly, erring towards too shallow a compression depth 62.6% of the time and too slow a compression rate 71.9% of the time on actual resuscitations―errors that increase in frequency the longer it has been since the caregiver was trained (26,27). Observational data on the quality of CPR suggest that these are not just esoteric technical deviations, but that compared with those in whom CPR is correctly performed, 14-day survival was almost 75% lower in those on whom CPR was incorrectly performed (16% vs. 4%)(28).
Furthermore, routine interruptions in chest compressions― such as for positive pressure ventilations in non-intubated patients―likely further hinder survival rather than contribute meaningfully to outcome. For example, medical students performing traditional CPR took an average of 14 seconds to administer two mouth-to-mouth ventilations after each group of 15 compressions. This effectively reduced the number of compressions to a mere 43 per minute, or less than half the guideline-mandated 100 per minute, thus theoretically reducing circulation to the heart and brain by a similar percentage (29). Yu et al demonstrated that swine receiving more than 80 compressions per minute during CPR had a 100% survival at 24 hours compared with a dismal 10% survival in animals that had less than 80 compressions per minute (30). Kern et al found statistically significantly higher coronary artery perfusion pressures and markedly higher neurological normal 24 hour survival in swine receiving continuous chest compressions compared with controls receiving traditional CPR (31).
Increasingly data such as these do raise the question of what―if any―benefit rescue breathing has in adult resuscitation. Human data show that a strategy of continuous chest compressions―without rescue breathing―is equally efficacious to traditional CPR in terms of outcome (32). Two physiologic theories prevail: 1) the mechanics of chest wall compression may be sufficient to provide a limited minute ventilation independent of supplemental ventilation (author’s speculation); and 2) the improved oxygenation that occurs in those receiving artificial ventilation is offset by the deleterious impact on hemodynamics that occur when chest compressions are interrupted for ventilation (34).
Second Effective Stratagem: Until an adult inpatient can be defibrillated, the focus of resuscitation should be on proper continuous chest compression depth and rate, not on ventilation.
Ventilations are Harmful
Cardiopulmonary collapse has immediate consequences on cellular physiology. Both due to a lack of expiration of carbon dioxide and the development of lactatemia due to the shift to anaerobic metabolism, blood pH drops precipitously. As the pH shifts out of the physiologic range, drugs begin to perform in unexpected ways or fail altogether; ion trapping occurs; and many electrolytes begin to shift in or out of cells affecting their serum concentration. Diminished or absent cardiac output accelerates these derangements in a relentless positive feedback loop. Logic, therefore, dictates that anything that can improve oxygenation and ventilation would be helpful at slowing or reversing this pathophysiology. Surprisingly, however, clinicians’ lack of knowledge of both equipment and technique often promotes, rather than mitigates, the physiologic derangements.
The bag-valve-mask (BVM) is one of the least understood resuscitation devices. For example, clinicians occasionally place a BVM over spontaneously breathing patients who are exceptionally ill with the goal of augmenting patients’ meager ventilations. However, the BVM is constructed only for positive pressure ventilation and thus, unless the clinician squeezes the bag in perfect coordination with the patient’s ventilatory effort, the BVM will paradoxically smother the patient.
The bag portion of the BVM is designed for a one-handed squeeze to deliver a tidal volume that is roughly 750cc; this volume is in keeping with guideline recommendations of positive pressure ventilation volumes of roughly 10cc/kg/ventilation (29). Yet, clinicians commonly use two hands to compress the BVM maximally during resuscitation (theoretically delivering upwards of double the recommended volume).
In addition to excessive volume, clinicians also deliver ventilations too rapidly. Abella et al. showed that during human resuscitations, ventilation rate exceeded the recommended goal of 20 ventilations/minute 60.9% of the time (27). Theoretically, high minute ventilations lead to an increased incidence of gastric insufflation, regurgitation, and post-resuscitation aspiration.
Though no studies have ever been performed to understand why clinicians hyperventilate patients during resuscitation, it is interesting to speculate that clinicians are not only trying to raise blood oxygen levels rapidly, but also to reverse the profound metabolic and respiratory acidosis that occur during CA. While seemingly mechanistically sound, the logic that supraphysiologic minute ventilations will profoundly change blood pH without other physiologic costs is specious at best. Aufderheide et al. Demonstrated that hyperventilation during resuscitation in swine resulted in increased intrathoracic pressures, markedly reduced coronary artery perfusion pressures, and resultant proportional reductions in survival rates as hyperventilation increased (35). Clinically these findings are known as auto-PEEP, a known complication of artificial ventilation that results in systemic arterial hypotension. Thus the paradox: aggressive attempts to overcorrect systemic acidoses via higher minute ventilations leads to worsening systemic blood pressures and thus worsening lactic acidosis. I believe that iatrogenic hypotension is one of the most common problems to complicate an otherwise successful resuscitation and that more research is urgently needed on this issue.
Third Effective Stratagem: Bag-valve-mask ventilations should be performed with precision; when used, the bag should be compressed with only one hand and delivered no faster than one breath every 3–5 seconds.
Fourth Effective Stratagem: In cases of pulseless electrical activity (PEA) or post-resuscitation hypotension, auto-PEEP should be considered foremost as a proximal cause.
Fifth Effective Stratagem: Ventilations in resuscitation should be viewed primarily as a means to oxygenate the patient rather than as a means to compensate from a systemic acidemia.
Shocking Revelations
Even though patients in ventricular fibrillation (VF) and pulseless ventricular tachycardia (PVT) together only comprise about one–third of all inpatient cardiac arrests, they account for almost 70% of survivors of CA. Survival in these arrhythmias is predicated solely on rapid defibrillation: the simultaneous depolarization of a critical mass of myocytes by an electrical current with resultant resumption of normal cardiac conduction (36). Perhaps the best attestation to the importance of rapid defibrillation actually comes from the survival of patients with cardiac arrest at casinos: security cameras provided exact documentation of time of collapse and defibrillation. Survival to hospital discharge was cut in half when the time-from-collapse-to-defibrillation was greater than 3 minutes (74% vs. 49%)(37).
Sixth Effective Stratagem: Since patients in VF/PVT are the most likely to survive CA―and that rate is directly related to immediacy of defibrillation―all patients should be presumptively treated as if they are in VF/PVT and should be defibrillated within 3 minutes of collapse unless there are data to support another arrhythmia or cause of collapse.
Much of the electrical current delivered during a defibrillation attempt is either dissipated as heat or is conducted around the thorax without penetrating the myocardium; Lerman and Deale have shown that the amount of current reaching the heart may be as little as 4% during a defibrillation attempt (38). From Ohm’s Law, the current that reaches the heart is directly proportional to the voltage across the chest and inversely related to the resistance of the supervening tissues. Interestingly, increasing the voltage of a shock only increases the amount of heat produced without a commensurate increase in current delivered. Therefore, techniques that reduce thoracic resistance yield the highest current delivery: the use of manual defibrillator paddles (as opposed to self adhesive defibrillation pads), the amount of pressure applied to the paddles (>25 pounds), the correct placement (underneath, rather than on top of breast tissue), the use of a conduction material (gel or pads), and the rapid delivery of a stacked shock (resistance transiently decreases after a counter-shock) all improve current delivery and thus may improve defibrillation outcome (36).
Physician leadership during resuscitations is critical for maximizing likelihood of patient survival. Perhaps due to physicians’ lack of familiarity with defibrillators, the mechanics of defibrillation are often deferred unnecessarily to nursing staff. Unfortunately, this may have profoundly negative effects on the resuscitation. Since many hospitals reduce educational expenses by foregoing training nurses in ACLS unless they work in intensive care units, nurses on a code may have even less comfort in using defibrillators than physicians. One study showed nearly a 72.5% decrease in patient survival when the nurse who arrived first at the resuscitation was untrained in ACLS (37.5% vs. 10.3%); a difference that probably is related to delayed defibrillation though the study could not establish direct causality (39).
A separate study showed that 85% of patients on cardiac monitored wards were defibrillated in the target time of 3 minutes from collapse, while only 28% of patients on unmonitored wards were defibrillated within the target time; this led to an adjusted odds ratio for survival-to-discharge in patients on monitored versus non-monitored wards of 1.45 (95% CI, 0.95–2.20)(40). While at first these data seem to indicate faster responses on monitored wards, these data were specific to time-from-collapse-to-defibrillation and therefore should be location-independent once the need for resuscitation was identified. Instead, I interpret these data as showing the lower comfort nurses on non-monitored wards have with rapid defibrillation. Rather than serving as an indictment against nurses, these data in aggregate underscore the vital role physician responders have to ensure rapid defibrillation of patients in cardiac arrest.
Seventh Effective Stratagem: Physicians should aggressively pursue defibrillation as early as possible during resuscitation especially on non-monitored wards where nurses are less likely to be ACLS trained and less likely to be familiar with defibrillator operation.
Conclusions
Resuscitation, the act of bringing back life from imminent death, is one of the most sensationalized practices in medicine and dates almost to the beginning of recorded history. In the past two decades, increasingly evidence-based guidelines have tried to provide a guide to help practitioners treat patients effectively in the minutes after cardiopulmonary collapse. Unfortunately, with each new iteration of the guidelines, it has become increasingly difficult to determine which strategies offer the highest yield or the most import. As ILCOR meets in 2005 to revise the guidelines once again, hopefully the most important strategies will be given their proper highlight, providing clinicians with increased comfort and confidence with cardiopulmonary resuscitation.
Bibliography
- Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following inhospital adult cardiopulmonary resuscitation. CMAJ. 2002;167:343-8.
- Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed chest cardiac massage. JAMA. 1960;173:1064-7.
- Jude JR, Kouwenhoven WB, Knickerbocker GG. Cardiac arrest; report of application of external cardiac massage on 118 patients. JAMA. 1961;178:1063-71.
- Varon J, Sternback GL. Cardiopulmonary resuscitation: lessons from the past. J Emerg Med. 1991;9:5037.
- Liss HP. A history of resuscitation. Ann Emerg Med.1986;15: 65-72.
- Thangam S, Weil MH, Rackow EC. Cardiopulmonary resuscitation: a historical review. Acute Care. 1986;12:63-94.
- Kings II, 4:34-35 (KJV).
- Baker AB. Artificial respiration: the history of an idea. Med Hist. 1971;15:336-46.
- Stephenson HE. Cardiac Arrest and Resuscitation. St Louis: CV Mosby; 1969.
- Lee RV. Cardiopulmonary resuscitation in the eighteenth century: a historical perspective on present practice. J Hist Med. 1972;27:418-33.
- Varon J, Marik PE, Fromm RE. Cardiopulmonary resuscitation: a review for clinicians. Resuscitation. 1998;36: 133-45.
- Keith A. Three Hunterian lectures on the various mechanisms underlying the various methods of artificial respiration. Lancet. 1909;1:895-9.
- DeBard ML. The history of cardiopulmonary resuscitation. Ann Emerg Med. 1980;9:273-5.
- Acosta P, Varion J, Sternbach GL, BaskeQ P. Resuscitation great. Kouwenhoven, Jude and Knickerbocker: the introduction of defibrillation and external chest compressions into modern resuscitation. Resuscitation. 2005;64:139-43.
- US Congress, Office of Technology Assessment. Life-sustaining technologies and the elderly. Washington, DC: US Government Printing Office, 1987; 11, Publication OTA-BA-306.
- DeBard ML. Cardiopulmonary resuscitation: analysis of six years’ experience and review of the literature. Ann Emerg Med. 1981;10:408-11.
- Cassel CK, et al. Cardiopulmonary resuscitation in the elderly. Office of Technology Assessment, U.S. Congress, Washington, DC, November, 1985.
- Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58297-308.
- Valentin A, Karnik R, Donath P, Winkler WB, Slany J. Outcome of cardiopulmonary resuscitation in hospitalized patients. Resuscitation. 1995;30:217-21.
- Robinson GR, Hess D. Postdischarge survival and functional status following in-hospital cardiopulmonary resuscitation. Chest. 1994;105:991-6.
- Murphy DI, Murray AM, Robinson BE. Outcomes of cardiopulmonary resuscitation in the elderly. Ann Int Med. 1989;111:199-205.
- Eberle B, Dick WF, Schneider T, Wisser G, Doetsch S, Tzanova I. Checking the carotid pulse check: diagnostic accuracy of first responders in patients with and without a pulse. Resuscitation. 1996;33:107-16.
- Rudikoff MT, Maughan WL, Effron M, Freund P, Weisfeldt ML. Mechanisms of blood flow during cardiopulmonary resuscitation. Circulation. 1980;61:345-52.
- Paradis NA, Martin GB, Goetting MG, et al. Simultaneous aortic, jugular bulb, and right atrial pressures during cardiopulmonary resuscitation in humans: insight into mechanisms. Circulation. 1989;80:361-8.
- Sanders AB, Ogle M, Ewy GA. Coronary perfusion pressure during cardiopulmonary resuscitation. Am J Emerg Med. 1985;3:11-4.
- Heidenreich JW, Higdon TA, Kern KB, et al. Single-rescuer cardiopulmonary resuscitation: “two quick breaths”―an oxymoron. Resuscitation. 2004;62:283-89.
- Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305-10.
- Van Hoeyweghen RJ, Bossaert LL, Mullie A, et al. (Belgian Cerebral Resuscitation Study Group.) Quality and efficiency of bystander CPR. Resuscitation. 1993;26:47-52.
- American Heart Association in collaboration with the International Liaison Committee on Resuscitation (ILCOR). International Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care―a consensus on science. Resuscitation. 2000.46:1-448.
- Yu T, Weil MH, Tang W, et al. Adverse outcomes of interrupted precordial compression during automated defibrillation. Circulation. 2002;106:368-72.
- Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation. 2002;105:645-649.
- Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with to-mouth ventilation. N Engl J Med. ;342: 154-653.
- Berg RA, Sanders AB, Kern KB, et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation. 2001;104:2465-70.
- Aufderheide TP, Sigurdsson G, Pirallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960-5.
- Dalzell GWN. Determinants of successful defibrillation. Heart. ;80:405-7.
- Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW,Hardman RG. Outcomes of rapid defibrillation by security ad er cardiac arrest in casinos. N Engl J Med. ;343:120-69.
- Lerman BB, Deale C. Relation between transcardiac and thransthoracic current during defibrillation in humans. Circ Res. 1990;67:1420-6.
- Dane FC, RussellLindgren KS, Parish DC, Durham MD, Brown TD. Inhospital resuscitation: association between ACLS training and survival to discharge. Resuscitation. 2000;47:83-7.
- Herlitz J, Bang A, Aune S, Ekstrom L, Lundstrom G, Holmberg S. Characteristics and outcome among patients suffering inhospital cardiac arrest in monitored and nonmonitored areas. Resuscitation. ;48:125-35.
Advancing Toward the Ideal Hospital Discharge for the Elderly Patient
The interval between hospital discharge and the continuity provider’s first post-hospital patient visit is being increasingly recognized as a hazardous hiatus (1). The patient is vulnerable to a variety of factors that may result in morbidity or hospital readmission, including the recurrence of symptoms that prompted the initial hospitalization, adverse drug events from new medications, new drug-drug interactions, or issues of care coordination, such as followup visits and tests. Inadequate social support can further exacerbate the medical complexity of care transition from the inpatient to the outpatient setting.
Many post-discharge adverse events are preventable or “ameliorable” by careful discharge planning and timely followup (1). However, existing guidelines and standards regarding the discharge process have been disease specific and have not focused on populations, such as the elderly, that may be at especially high risk regardless of their specific medical issues. For example, CMS currently requires that all patients have an assessment of cognition, mobility, and family support before final discharge plans are set. Experienced hospitalists know that these basic elements are only the beginning of a more complex and robust algorithm of discharge planning; including trimming and reconciling medications; planning followup tests; engineering followup appointments; and activating any required community resources, durable medical good needs, or home health care. In fact, many SHM members have already begun to implement local strategies to ease the care transition at the time of discharge.
The SHM Hospital Quality & Patient Safety (HQPS) Committee believes that hospitalists will play an important role in shaping the ideal discharge process. With support from the Hartford foundation, HQPS has formulated a strategy to develop “discharge best practices,” integrating evidence-based care with the experience and expert opinion of hospitalist leaders. To our knowledge, no national society or professional organization has undertaken such an activity to improve the quality of care at discharge and after hospitalization.
The process began with a literature review in 2004 that showed no commonly accepted compendium or consolidated list of activities that could form the basis for the ideal discharge. Drawing upon SHM member experience and the literature, HQPS committee members formulated a list of potential best practices, which are presented in Table 1. Although many discharge activities are required and many are done automatically (such as writing a discharge order or prescriptions) the committee chose to focus on important but discretionary activities that may be overlooked by a busy physician. To complement this checklist of activities, the committee is developing a discharge framework with the input of experts in the area of care transitions.
The committee held a consensus-building workshop at the SHM annual meeting entitled “Developing the Ideal Discharge Process.” This session provided a forum to discuss the checklist of best practices and discharge framework with attendees, receive their feedback, and identify hospitalists interested in validating and refining the materials over time. The committee will continue revising the materials in 2005, with the goal of developing a usable and valuable consensus statement addressing the steps involved in the ideal hospital discharge.
References
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161-7.
- Guidelines for appropriate use of “Do-Not-Resuscitate” orders. Council on Ethical and Judicial Affairs. American Medical Association. JAMA. 1991;265:1868-71.
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “getup and go” test. Arch Phys Med Rehabil. 1986;67:387-9.
- Manning DM, Keller AS, Frank DL. Independent Mobility Validation Exam (IMOVE): A tool for periodic reassessment of fallrisk and discharge planning. Abstract and poster presentation at SHM (formerly NAIP) 5th Annual Meeting in Philadelphia, PA, on April 9, 2002.
- van Walraven C, Mamdani M, Fang J, Austin PC. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med. 2004;19:624-31.
- van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during the post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17:186-92.
- Whitford K, Huddleston JM. Specific appointments after pneumonia hospitalization reduce readmissions. Abstract and Poster presentation at SHM (formerly NAIP) 5th Annual Meeting in Philadelphia, PA, on April 9, 2002.
- JCAHO Manual: Information Management (IM) 6.10 and Patient Care (PC) 15.30.
- Lewis T. Using the NO TEARS tool for medication review. BMJ. 2004;329:434.
- Whittington J, Cohen H. OSF healthcare’s journey in patient safety. Qual Manag Health Care. 2004;13:53-9.
- Kucukarslan SN, Peters M, Mlynarek M, Nafziger D. Pharmacists on rounding teams reduce preventable adverse events in hospital general medicine units. Arch Intern Med. 2003;163:2014-18.
- Dudas V, Bookwalter T, Kerr K, Pantilat SZ. The impact of followup telephone calls to patients after hospitalization. Am J Med. 2001;111(9B):26S-30S.
- Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
- Manning DM. Toward safer warfarin therapy: does precise daily dosing improve international normalized ratio control? Mayo Clin Proc. 2002;77:873-5.
Resources (including Medline Search: “patient discharge” and/ or “quality indicators” and “quality of care”):
- Bull MJ, Hansen HE, Gross CR. Predictors of elder and family caregiver satisfaction with discharge planning. J Cardiovasc Nurs. 2000;14:76-87.
- Charles C, Gauld M, Chambers L, O’Brien B, Haynes RB, Labelle R. How was your hospital stay? Patients’ report about their care in Canadian hospitals. CMAJ. 1994; 150:1813-22.
- Cleary PD. A hospitalization from hell: a patient’s perspective on quality. Ann Intern Med. 2003:138:33-9.
- Demlo LK, Campbell PM. Improving hospital discharge data: lessons from the National Hospital Discharge Survey. Med Care. 1981 Oct;19(10):1030-40.
- Felden JM, scott S, Horne JG. An investigation of patient satisfaction following discharge after total hip replacement surgery. Orthop Nurs. 2003;22:429-36.
- Frain JP, Frain AE, Carr PH. Experience of medical senior house officers in preparing discharge summaries. BMJ. 1996;312:350.
- Gombeski WR, Miller PJ, Hahn JH, et al. Patient callback program. J Health Care Mark 1993;13:60-5.
- Hickey ML, Kleefield SF, Pearson SD, et al. Payer-hospital collaboration to improve patient satisfaction with hospital discharge. Jt Comm J Qual Improv. 1996;22:336-44.
- Kroenke K, Stump T, Clark DO, Callahan CM, McDonald CJ. Symptoms in hospitalized patients: outcome and satisfaction with care. Am J Med 1999;107: 425-31.
- Macaulay EM, Cooper GC, Engeset J, Naylor AR. Prospective audit of discharge summary errors. Br J Surg. 1996;83:788-90.
- Moher D, Weinberg A, Hanlon R, Runnalls K. Effects of a medical team coordinator on length of hospital stay. CMAJ. 1992;146:511-5.
- Minnick A, Young WB. Comparison between reports of care obtained by post-discharge telephone interview and pre-discharge personal interview. Outcomes Manag Nurs Pract 1999;3:32-7.
- Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home followup of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613-20.
- Parkes J, Shepperd S. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004. Review.
- Reiley P, Pike A, Phipps M, et al. Learning from patients: a discharge planning improvement project. Jt Comm J Qual Improv. 1996;22:31122.
- van Walraven C, Weinberg AL. Quality assessment of a discharge summary system. CMAJ. 1995;152:1437-42.
- van Walraven C, Rokosh E. What is necessary for high-quality discharge summaries? Am J Med Qual. 1999;14: 160-9.
- Zwicker D, Picariello G. Discharge planning for the older adult. In: Mezey M, Fulmer T, Abraaham I, Zwicker D, eds. Geriatric Nursing Protocols for Best Practice. 2nd ed. New York: Springer Publishing 2003;292-316.
The interval between hospital discharge and the continuity provider’s first post-hospital patient visit is being increasingly recognized as a hazardous hiatus (1). The patient is vulnerable to a variety of factors that may result in morbidity or hospital readmission, including the recurrence of symptoms that prompted the initial hospitalization, adverse drug events from new medications, new drug-drug interactions, or issues of care coordination, such as followup visits and tests. Inadequate social support can further exacerbate the medical complexity of care transition from the inpatient to the outpatient setting.
Many post-discharge adverse events are preventable or “ameliorable” by careful discharge planning and timely followup (1). However, existing guidelines and standards regarding the discharge process have been disease specific and have not focused on populations, such as the elderly, that may be at especially high risk regardless of their specific medical issues. For example, CMS currently requires that all patients have an assessment of cognition, mobility, and family support before final discharge plans are set. Experienced hospitalists know that these basic elements are only the beginning of a more complex and robust algorithm of discharge planning; including trimming and reconciling medications; planning followup tests; engineering followup appointments; and activating any required community resources, durable medical good needs, or home health care. In fact, many SHM members have already begun to implement local strategies to ease the care transition at the time of discharge.
The SHM Hospital Quality & Patient Safety (HQPS) Committee believes that hospitalists will play an important role in shaping the ideal discharge process. With support from the Hartford foundation, HQPS has formulated a strategy to develop “discharge best practices,” integrating evidence-based care with the experience and expert opinion of hospitalist leaders. To our knowledge, no national society or professional organization has undertaken such an activity to improve the quality of care at discharge and after hospitalization.
The process began with a literature review in 2004 that showed no commonly accepted compendium or consolidated list of activities that could form the basis for the ideal discharge. Drawing upon SHM member experience and the literature, HQPS committee members formulated a list of potential best practices, which are presented in Table 1. Although many discharge activities are required and many are done automatically (such as writing a discharge order or prescriptions) the committee chose to focus on important but discretionary activities that may be overlooked by a busy physician. To complement this checklist of activities, the committee is developing a discharge framework with the input of experts in the area of care transitions.
The committee held a consensus-building workshop at the SHM annual meeting entitled “Developing the Ideal Discharge Process.” This session provided a forum to discuss the checklist of best practices and discharge framework with attendees, receive their feedback, and identify hospitalists interested in validating and refining the materials over time. The committee will continue revising the materials in 2005, with the goal of developing a usable and valuable consensus statement addressing the steps involved in the ideal hospital discharge.
References
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161-7.
- Guidelines for appropriate use of “Do-Not-Resuscitate” orders. Council on Ethical and Judicial Affairs. American Medical Association. JAMA. 1991;265:1868-71.
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “getup and go” test. Arch Phys Med Rehabil. 1986;67:387-9.
- Manning DM, Keller AS, Frank DL. Independent Mobility Validation Exam (IMOVE): A tool for periodic reassessment of fallrisk and discharge planning. Abstract and poster presentation at SHM (formerly NAIP) 5th Annual Meeting in Philadelphia, PA, on April 9, 2002.
- van Walraven C, Mamdani M, Fang J, Austin PC. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med. 2004;19:624-31.
- van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during the post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17:186-92.
- Whitford K, Huddleston JM. Specific appointments after pneumonia hospitalization reduce readmissions. Abstract and Poster presentation at SHM (formerly NAIP) 5th Annual Meeting in Philadelphia, PA, on April 9, 2002.
- JCAHO Manual: Information Management (IM) 6.10 and Patient Care (PC) 15.30.
- Lewis T. Using the NO TEARS tool for medication review. BMJ. 2004;329:434.
- Whittington J, Cohen H. OSF healthcare’s journey in patient safety. Qual Manag Health Care. 2004;13:53-9.
- Kucukarslan SN, Peters M, Mlynarek M, Nafziger D. Pharmacists on rounding teams reduce preventable adverse events in hospital general medicine units. Arch Intern Med. 2003;163:2014-18.
- Dudas V, Bookwalter T, Kerr K, Pantilat SZ. The impact of followup telephone calls to patients after hospitalization. Am J Med. 2001;111(9B):26S-30S.
- Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
- Manning DM. Toward safer warfarin therapy: does precise daily dosing improve international normalized ratio control? Mayo Clin Proc. 2002;77:873-5.
Resources (including Medline Search: “patient discharge” and/ or “quality indicators” and “quality of care”):
- Bull MJ, Hansen HE, Gross CR. Predictors of elder and family caregiver satisfaction with discharge planning. J Cardiovasc Nurs. 2000;14:76-87.
- Charles C, Gauld M, Chambers L, O’Brien B, Haynes RB, Labelle R. How was your hospital stay? Patients’ report about their care in Canadian hospitals. CMAJ. 1994; 150:1813-22.
- Cleary PD. A hospitalization from hell: a patient’s perspective on quality. Ann Intern Med. 2003:138:33-9.
- Demlo LK, Campbell PM. Improving hospital discharge data: lessons from the National Hospital Discharge Survey. Med Care. 1981 Oct;19(10):1030-40.
- Felden JM, scott S, Horne JG. An investigation of patient satisfaction following discharge after total hip replacement surgery. Orthop Nurs. 2003;22:429-36.
- Frain JP, Frain AE, Carr PH. Experience of medical senior house officers in preparing discharge summaries. BMJ. 1996;312:350.
- Gombeski WR, Miller PJ, Hahn JH, et al. Patient callback program. J Health Care Mark 1993;13:60-5.
- Hickey ML, Kleefield SF, Pearson SD, et al. Payer-hospital collaboration to improve patient satisfaction with hospital discharge. Jt Comm J Qual Improv. 1996;22:336-44.
- Kroenke K, Stump T, Clark DO, Callahan CM, McDonald CJ. Symptoms in hospitalized patients: outcome and satisfaction with care. Am J Med 1999;107: 425-31.
- Macaulay EM, Cooper GC, Engeset J, Naylor AR. Prospective audit of discharge summary errors. Br J Surg. 1996;83:788-90.
- Moher D, Weinberg A, Hanlon R, Runnalls K. Effects of a medical team coordinator on length of hospital stay. CMAJ. 1992;146:511-5.
- Minnick A, Young WB. Comparison between reports of care obtained by post-discharge telephone interview and pre-discharge personal interview. Outcomes Manag Nurs Pract 1999;3:32-7.
- Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home followup of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613-20.
- Parkes J, Shepperd S. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004. Review.
- Reiley P, Pike A, Phipps M, et al. Learning from patients: a discharge planning improvement project. Jt Comm J Qual Improv. 1996;22:31122.
- van Walraven C, Weinberg AL. Quality assessment of a discharge summary system. CMAJ. 1995;152:1437-42.
- van Walraven C, Rokosh E. What is necessary for high-quality discharge summaries? Am J Med Qual. 1999;14: 160-9.
- Zwicker D, Picariello G. Discharge planning for the older adult. In: Mezey M, Fulmer T, Abraaham I, Zwicker D, eds. Geriatric Nursing Protocols for Best Practice. 2nd ed. New York: Springer Publishing 2003;292-316.
The interval between hospital discharge and the continuity provider’s first post-hospital patient visit is being increasingly recognized as a hazardous hiatus (1). The patient is vulnerable to a variety of factors that may result in morbidity or hospital readmission, including the recurrence of symptoms that prompted the initial hospitalization, adverse drug events from new medications, new drug-drug interactions, or issues of care coordination, such as followup visits and tests. Inadequate social support can further exacerbate the medical complexity of care transition from the inpatient to the outpatient setting.
Many post-discharge adverse events are preventable or “ameliorable” by careful discharge planning and timely followup (1). However, existing guidelines and standards regarding the discharge process have been disease specific and have not focused on populations, such as the elderly, that may be at especially high risk regardless of their specific medical issues. For example, CMS currently requires that all patients have an assessment of cognition, mobility, and family support before final discharge plans are set. Experienced hospitalists know that these basic elements are only the beginning of a more complex and robust algorithm of discharge planning; including trimming and reconciling medications; planning followup tests; engineering followup appointments; and activating any required community resources, durable medical good needs, or home health care. In fact, many SHM members have already begun to implement local strategies to ease the care transition at the time of discharge.
The SHM Hospital Quality & Patient Safety (HQPS) Committee believes that hospitalists will play an important role in shaping the ideal discharge process. With support from the Hartford foundation, HQPS has formulated a strategy to develop “discharge best practices,” integrating evidence-based care with the experience and expert opinion of hospitalist leaders. To our knowledge, no national society or professional organization has undertaken such an activity to improve the quality of care at discharge and after hospitalization.
The process began with a literature review in 2004 that showed no commonly accepted compendium or consolidated list of activities that could form the basis for the ideal discharge. Drawing upon SHM member experience and the literature, HQPS committee members formulated a list of potential best practices, which are presented in Table 1. Although many discharge activities are required and many are done automatically (such as writing a discharge order or prescriptions) the committee chose to focus on important but discretionary activities that may be overlooked by a busy physician. To complement this checklist of activities, the committee is developing a discharge framework with the input of experts in the area of care transitions.
The committee held a consensus-building workshop at the SHM annual meeting entitled “Developing the Ideal Discharge Process.” This session provided a forum to discuss the checklist of best practices and discharge framework with attendees, receive their feedback, and identify hospitalists interested in validating and refining the materials over time. The committee will continue revising the materials in 2005, with the goal of developing a usable and valuable consensus statement addressing the steps involved in the ideal hospital discharge.
References
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161-7.
- Guidelines for appropriate use of “Do-Not-Resuscitate” orders. Council on Ethical and Judicial Affairs. American Medical Association. JAMA. 1991;265:1868-71.
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “getup and go” test. Arch Phys Med Rehabil. 1986;67:387-9.
- Manning DM, Keller AS, Frank DL. Independent Mobility Validation Exam (IMOVE): A tool for periodic reassessment of fallrisk and discharge planning. Abstract and poster presentation at SHM (formerly NAIP) 5th Annual Meeting in Philadelphia, PA, on April 9, 2002.
- van Walraven C, Mamdani M, Fang J, Austin PC. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med. 2004;19:624-31.
- van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during the post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17:186-92.
- Whitford K, Huddleston JM. Specific appointments after pneumonia hospitalization reduce readmissions. Abstract and Poster presentation at SHM (formerly NAIP) 5th Annual Meeting in Philadelphia, PA, on April 9, 2002.
- JCAHO Manual: Information Management (IM) 6.10 and Patient Care (PC) 15.30.
- Lewis T. Using the NO TEARS tool for medication review. BMJ. 2004;329:434.
- Whittington J, Cohen H. OSF healthcare’s journey in patient safety. Qual Manag Health Care. 2004;13:53-9.
- Kucukarslan SN, Peters M, Mlynarek M, Nafziger D. Pharmacists on rounding teams reduce preventable adverse events in hospital general medicine units. Arch Intern Med. 2003;163:2014-18.
- Dudas V, Bookwalter T, Kerr K, Pantilat SZ. The impact of followup telephone calls to patients after hospitalization. Am J Med. 2001;111(9B):26S-30S.
- Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
- Manning DM. Toward safer warfarin therapy: does precise daily dosing improve international normalized ratio control? Mayo Clin Proc. 2002;77:873-5.
Resources (including Medline Search: “patient discharge” and/ or “quality indicators” and “quality of care”):
- Bull MJ, Hansen HE, Gross CR. Predictors of elder and family caregiver satisfaction with discharge planning. J Cardiovasc Nurs. 2000;14:76-87.
- Charles C, Gauld M, Chambers L, O’Brien B, Haynes RB, Labelle R. How was your hospital stay? Patients’ report about their care in Canadian hospitals. CMAJ. 1994; 150:1813-22.
- Cleary PD. A hospitalization from hell: a patient’s perspective on quality. Ann Intern Med. 2003:138:33-9.
- Demlo LK, Campbell PM. Improving hospital discharge data: lessons from the National Hospital Discharge Survey. Med Care. 1981 Oct;19(10):1030-40.
- Felden JM, scott S, Horne JG. An investigation of patient satisfaction following discharge after total hip replacement surgery. Orthop Nurs. 2003;22:429-36.
- Frain JP, Frain AE, Carr PH. Experience of medical senior house officers in preparing discharge summaries. BMJ. 1996;312:350.
- Gombeski WR, Miller PJ, Hahn JH, et al. Patient callback program. J Health Care Mark 1993;13:60-5.
- Hickey ML, Kleefield SF, Pearson SD, et al. Payer-hospital collaboration to improve patient satisfaction with hospital discharge. Jt Comm J Qual Improv. 1996;22:336-44.
- Kroenke K, Stump T, Clark DO, Callahan CM, McDonald CJ. Symptoms in hospitalized patients: outcome and satisfaction with care. Am J Med 1999;107: 425-31.
- Macaulay EM, Cooper GC, Engeset J, Naylor AR. Prospective audit of discharge summary errors. Br J Surg. 1996;83:788-90.
- Moher D, Weinberg A, Hanlon R, Runnalls K. Effects of a medical team coordinator on length of hospital stay. CMAJ. 1992;146:511-5.
- Minnick A, Young WB. Comparison between reports of care obtained by post-discharge telephone interview and pre-discharge personal interview. Outcomes Manag Nurs Pract 1999;3:32-7.
- Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home followup of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613-20.
- Parkes J, Shepperd S. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004. Review.
- Reiley P, Pike A, Phipps M, et al. Learning from patients: a discharge planning improvement project. Jt Comm J Qual Improv. 1996;22:31122.
- van Walraven C, Weinberg AL. Quality assessment of a discharge summary system. CMAJ. 1995;152:1437-42.
- van Walraven C, Rokosh E. What is necessary for high-quality discharge summaries? Am J Med Qual. 1999;14: 160-9.
- Zwicker D, Picariello G. Discharge planning for the older adult. In: Mezey M, Fulmer T, Abraaham I, Zwicker D, eds. Geriatric Nursing Protocols for Best Practice. 2nd ed. New York: Springer Publishing 2003;292-316.
Quality Tools: Root Cause Analysis (RCA) and Failure Modes and Effects Analysis (FMEA)
When we speak of “quality” in health care, we generally think of mortality outcomes or regulatory requirements that are mandated by the JCAHO (Joint Commission for Accreditation of Healthcare Organizations). But how do these relate to and impact our everyday lives as hospitalists? At the 8th Annual Meeting of SHM we presented a workshop on RCA and FMEA, taking a practical approach to illustrate how these two JCAHO required methodologies can improve patient care as well as improve the work environment for hospitalists by addressing the systemic issues that can compromise care.
The workshop starts by stepping into the life of a hospitalist and something we all fear: “Something bad happens. Then what?” Depending on the severity of the event, the options include peer review, notifying the Department Chief, calling the Risk Manager, calling your lawyer, or doing nothing. You’ve probably had many experiences when “something wasn’t quite right,” but often there is no obvious bad outcome or obvious solution, so we shrug our shoulders and say, “Oh well, we got lucky this time; no harm, no foul.” The problem is, there are recurring patterns to these types of events, and the same issues may affect the next patient, who may not be so lucky.
Defining “Something Bad”
These types of cases, which have outcomes ranging from no effect on the patient to death, may be approached several different ways. The terms “near miss” or “close call” refer to an incident where a mistake was made but caught in time, so no harm was done to the patient. An example of this is when a physician makes a mistake on a medication order, but it is caught and corrected by a pharmacist or nurse.
When adverse outcomes do occur, think about and define etiologies so that you identify and address underlying causes. Is the outcome an expected or unexpected complication of therapy? Was there an error involved? In asking these questions, remember that you can have harm without error and error without harm. Error is defined as “failure of a planned action to be completed as intended or use of a wrong plan to achieve an aim; the accumulation of errors results in accidents” (Kohn, et al). This definition points out that usually a chain of events rather than a single individual or event results in a bad outcome. The purpose of defining etiologies is not to assign blame but to identify underlying issues and surrounding circumstances that may have contributed to the adverse outcome.
Significant adverse events are called “sentinel events” and defined as an “unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes loss of limb or function” (JCAHO 1998).
How We Approach Error
Unfortunately, as humans we are fallible and make errors quite reliably. Table 1 demonstrates types of errors and expected rates of errors. For example, we make errors of omission 0.01% of the time, but the good news is that with reminders or ticklers, we can reduce this rate to 0.003%. Unfortunately, when humans are under high stress in danger, research from the military indicates error rates of 25% (Salvendy 1997). In a complex ICU setting, researchers have documented an average of 178 activities per patient per day with an error rate of 0.95%. Despite an error rate of less than 1%, the yield of errors during the 4-month period of observation was still over 1000 errors, 29% of which were considered to have severe or potentially severe consequences (Donchin, et al).
The reality is that we err. Having the unrealistic expectations developed in medical training of being perfect in all our actions perpetuates the blame cycle when the inevitable mistake occurs, and it prevents us from implementing solutions that prevent errors from ever occurring or catching them before they cause harm.
RCA and FMEA Help Us Create Solutions That Make a Difference
Briefly, Root Cause Analysis (RCA) is a retrospective investigation that is required by JCAHO after a sentinel event: “Root cause analysis is a process for identifying the basic or causal factor(s) that underlies variation in performance, including the occurrence or possible occurrence of a sentinel event. A root cause is that most fundamental reason a problem―a situation where performance does not meet expectations―has occurred” (JCAHO 1998). An RCA looks back in time at an event and asks the question “What
happened?” The utility of this methodology lies in the fact that it not only asks what happened but also asks “Why did this happen” rather than focus on “Who is to blame?” Some hospitals use this methodology for cases that are not sentinel events, because the knowledge gained from these investigations often uncovers system issues previously not known and that negatively impact many departments, not just the departments involved in a particular case.
Failure Modes and Effects Analysis (FMEA) is a prospective investigation aimed at identifying vulnerabilities and preventing failures in the future. It looks forward and asks what could go wrong? Performance of an FMEA is also required yearly by JCAHO and focuses on improving risky processes such as blood transfusions, chemotherapy, and other high risk medications.
Approaching a clinical case clearly demonstrates the differences between RCA and FMEA. Imagine a 72-year-old patient admitted to your hospital with findings of an acute abdomen requiring surgery. The patient is a smoker, with Type 2 diabetes and an admission blood sugar of 465, but no evidence of DKA. She normally takes an oral hypoglycemic to control her diabetes and an ACE inhibitor for high blood pressure but no other medications. She is taken to the OR emergently, where surgery seems to go well, and post-operatively is admitted to the ICU. Subsequently, her blood glucose ranges from 260 to 370 and is “controlled” with sliding scale insulin. Unfortunately, within 18 hours of surgery she suffers an MI and develops a postoperative wound infection 4 days after surgery. She eventually dies from sepsis.
An RCA of this case might reveal causal factors such as lack of use of a beta-blocker preoperatively and lack of use of IV insulin to lower her blood sugars to the 80–110 range. While possibly identifying the root cause of this adverse outcome, an RCA is limited by its hindsight bias and the labor-intensive nature of the investigation that may or may not have broad application, since it is an in-depth study of one case. However, RCA’s do have the salutary effects of building teamwork, identifying needed changes, and if carried out impartially without assigning blame can facilitate a culture of patient safety.
FMEA takes a different approach and proactively aims to prevent failure. It is a systematic method of identifying and preventing product and process failures before they occur. It does not require a specific case or adverse event. Rather, a high-risk process is chosen for study, and an interdisciplinary team asks the question “What can go wrong with this process and how can we prevent failures?” Considering the above case, imagine that before it ever occurred you as the hospitalist concerned with patient safety decided to conduct an FMEA on controlling blood sugar in the ICU or administering beta-blockers perioperatively to patients who are appropriate candidates.
For example, using FMEA methodology to study the process of intensive insulin therapy to achieve tight control of glucose in the ICU would identify potential barriers and failures preventing successful implementation. A significant risk encountered in achieving tight glucose control in the range of 80–110 includes hypoglycemia. Common pitfalls of insulin administration include administration and calculation errors that can result in 10-fold differences in doses of insulin. Other details of administration, such as type of IV tubing used and how the IV tubing is primed, can greatly affect the amount of insulin delivered to the patient and thus the glucose levels. If an inadequate amount of solution is flushed through to prime the tubing, the patient may receive saline rather than insulin for a few hours, resulting in higher-than-expected glucose levels and titration of insulin to higher doses. The result would then be an unexpectedly low glucose several hours later. Once failure modes such as these are identified, a fail-safe system can be designed so that failures are less likely to occur.
The advantages of FMEA include its focus on system design rather than on a single incident such as in RCA. By focusing on systems and processes, the learning and changes implemented are likely to impact a larger number of patients.
Summary and Discussion
To summarize, RCA is retrospective and dissects a case, while FMEA is prospective and dissects a process. It is important to remember that given the right set of circumstances, any physician can make a mistake. It makes sense to apply methodologies that probe into surrounding circumstances and contributing factors so that knowledge gained can be used to prevent the same mistakes from happening to different individuals and have broader impact on healthcare systems.
Resources
- www.patientsafety.gov: VA National Center for Patient Safety. Excellent website with very helpful, practical tools.
- www.ihi.org: Institute for Healthcare Improvement website. Has a nice FMEA toolkit.
- www.jcaho.com: The Joint Commission for Accreditation of Healthcare Organizations website. Has information on sentinel events and use of RCA.
Bibliography
- Kohn LT, Corrigan JM, Eds. To Err is Human. Building a Safer Helath System. Washington, DC: National Academy Press; 1999.
- Joint Commission on Accreditation of Healthcare Organizations. Sentinel events: evaluating cause and planning improvement. 1998. Library of congress catalog number 97-80531.
- Salvendy G, ed. Handbook of Human Factors and Ergonomics. New York: John Wiley & Sons;1997:163
- Donchin Y, Gopher D, Olin M, et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23:294-300.
- McNutt R, Abrams R, Hasler S, et al. Determining medical error: three case reports. Eff Clin Pract. 2002;5:23-8.
- Senders JW. FMEA and RCA: the mantras of modern risk management. Qual Saf Health Care. 2004;13:249-50.
- Spath PL. Investigating Sentinel Events: How to Find and Resolve Root Causes. Forest Grove, OR: Brown Spath and Associates; 1997.
- Wald H, Shojania KG. Root cause analysis. In: Shojania KG, McDonald KM, Wachter RM, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment No. 43, AHRQ Publication No. 01-E058; July 2001. Available at http://www.ahrq.gov.
- Woodhouse S, Burney B, Coste K. To err is human: improving patient safety through failure mode and effect analysis. Clin leadersh Manag Rev. 2004;18:32-6.
When we speak of “quality” in health care, we generally think of mortality outcomes or regulatory requirements that are mandated by the JCAHO (Joint Commission for Accreditation of Healthcare Organizations). But how do these relate to and impact our everyday lives as hospitalists? At the 8th Annual Meeting of SHM we presented a workshop on RCA and FMEA, taking a practical approach to illustrate how these two JCAHO required methodologies can improve patient care as well as improve the work environment for hospitalists by addressing the systemic issues that can compromise care.
The workshop starts by stepping into the life of a hospitalist and something we all fear: “Something bad happens. Then what?” Depending on the severity of the event, the options include peer review, notifying the Department Chief, calling the Risk Manager, calling your lawyer, or doing nothing. You’ve probably had many experiences when “something wasn’t quite right,” but often there is no obvious bad outcome or obvious solution, so we shrug our shoulders and say, “Oh well, we got lucky this time; no harm, no foul.” The problem is, there are recurring patterns to these types of events, and the same issues may affect the next patient, who may not be so lucky.
Defining “Something Bad”
These types of cases, which have outcomes ranging from no effect on the patient to death, may be approached several different ways. The terms “near miss” or “close call” refer to an incident where a mistake was made but caught in time, so no harm was done to the patient. An example of this is when a physician makes a mistake on a medication order, but it is caught and corrected by a pharmacist or nurse.
When adverse outcomes do occur, think about and define etiologies so that you identify and address underlying causes. Is the outcome an expected or unexpected complication of therapy? Was there an error involved? In asking these questions, remember that you can have harm without error and error without harm. Error is defined as “failure of a planned action to be completed as intended or use of a wrong plan to achieve an aim; the accumulation of errors results in accidents” (Kohn, et al). This definition points out that usually a chain of events rather than a single individual or event results in a bad outcome. The purpose of defining etiologies is not to assign blame but to identify underlying issues and surrounding circumstances that may have contributed to the adverse outcome.
Significant adverse events are called “sentinel events” and defined as an “unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes loss of limb or function” (JCAHO 1998).
How We Approach Error
Unfortunately, as humans we are fallible and make errors quite reliably. Table 1 demonstrates types of errors and expected rates of errors. For example, we make errors of omission 0.01% of the time, but the good news is that with reminders or ticklers, we can reduce this rate to 0.003%. Unfortunately, when humans are under high stress in danger, research from the military indicates error rates of 25% (Salvendy 1997). In a complex ICU setting, researchers have documented an average of 178 activities per patient per day with an error rate of 0.95%. Despite an error rate of less than 1%, the yield of errors during the 4-month period of observation was still over 1000 errors, 29% of which were considered to have severe or potentially severe consequences (Donchin, et al).
The reality is that we err. Having the unrealistic expectations developed in medical training of being perfect in all our actions perpetuates the blame cycle when the inevitable mistake occurs, and it prevents us from implementing solutions that prevent errors from ever occurring or catching them before they cause harm.
RCA and FMEA Help Us Create Solutions That Make a Difference
Briefly, Root Cause Analysis (RCA) is a retrospective investigation that is required by JCAHO after a sentinel event: “Root cause analysis is a process for identifying the basic or causal factor(s) that underlies variation in performance, including the occurrence or possible occurrence of a sentinel event. A root cause is that most fundamental reason a problem―a situation where performance does not meet expectations―has occurred” (JCAHO 1998). An RCA looks back in time at an event and asks the question “What
happened?” The utility of this methodology lies in the fact that it not only asks what happened but also asks “Why did this happen” rather than focus on “Who is to blame?” Some hospitals use this methodology for cases that are not sentinel events, because the knowledge gained from these investigations often uncovers system issues previously not known and that negatively impact many departments, not just the departments involved in a particular case.
Failure Modes and Effects Analysis (FMEA) is a prospective investigation aimed at identifying vulnerabilities and preventing failures in the future. It looks forward and asks what could go wrong? Performance of an FMEA is also required yearly by JCAHO and focuses on improving risky processes such as blood transfusions, chemotherapy, and other high risk medications.
Approaching a clinical case clearly demonstrates the differences between RCA and FMEA. Imagine a 72-year-old patient admitted to your hospital with findings of an acute abdomen requiring surgery. The patient is a smoker, with Type 2 diabetes and an admission blood sugar of 465, but no evidence of DKA. She normally takes an oral hypoglycemic to control her diabetes and an ACE inhibitor for high blood pressure but no other medications. She is taken to the OR emergently, where surgery seems to go well, and post-operatively is admitted to the ICU. Subsequently, her blood glucose ranges from 260 to 370 and is “controlled” with sliding scale insulin. Unfortunately, within 18 hours of surgery she suffers an MI and develops a postoperative wound infection 4 days after surgery. She eventually dies from sepsis.
An RCA of this case might reveal causal factors such as lack of use of a beta-blocker preoperatively and lack of use of IV insulin to lower her blood sugars to the 80–110 range. While possibly identifying the root cause of this adverse outcome, an RCA is limited by its hindsight bias and the labor-intensive nature of the investigation that may or may not have broad application, since it is an in-depth study of one case. However, RCA’s do have the salutary effects of building teamwork, identifying needed changes, and if carried out impartially without assigning blame can facilitate a culture of patient safety.
FMEA takes a different approach and proactively aims to prevent failure. It is a systematic method of identifying and preventing product and process failures before they occur. It does not require a specific case or adverse event. Rather, a high-risk process is chosen for study, and an interdisciplinary team asks the question “What can go wrong with this process and how can we prevent failures?” Considering the above case, imagine that before it ever occurred you as the hospitalist concerned with patient safety decided to conduct an FMEA on controlling blood sugar in the ICU or administering beta-blockers perioperatively to patients who are appropriate candidates.
For example, using FMEA methodology to study the process of intensive insulin therapy to achieve tight control of glucose in the ICU would identify potential barriers and failures preventing successful implementation. A significant risk encountered in achieving tight glucose control in the range of 80–110 includes hypoglycemia. Common pitfalls of insulin administration include administration and calculation errors that can result in 10-fold differences in doses of insulin. Other details of administration, such as type of IV tubing used and how the IV tubing is primed, can greatly affect the amount of insulin delivered to the patient and thus the glucose levels. If an inadequate amount of solution is flushed through to prime the tubing, the patient may receive saline rather than insulin for a few hours, resulting in higher-than-expected glucose levels and titration of insulin to higher doses. The result would then be an unexpectedly low glucose several hours later. Once failure modes such as these are identified, a fail-safe system can be designed so that failures are less likely to occur.
The advantages of FMEA include its focus on system design rather than on a single incident such as in RCA. By focusing on systems and processes, the learning and changes implemented are likely to impact a larger number of patients.
Summary and Discussion
To summarize, RCA is retrospective and dissects a case, while FMEA is prospective and dissects a process. It is important to remember that given the right set of circumstances, any physician can make a mistake. It makes sense to apply methodologies that probe into surrounding circumstances and contributing factors so that knowledge gained can be used to prevent the same mistakes from happening to different individuals and have broader impact on healthcare systems.
Resources
- www.patientsafety.gov: VA National Center for Patient Safety. Excellent website with very helpful, practical tools.
- www.ihi.org: Institute for Healthcare Improvement website. Has a nice FMEA toolkit.
- www.jcaho.com: The Joint Commission for Accreditation of Healthcare Organizations website. Has information on sentinel events and use of RCA.
Bibliography
- Kohn LT, Corrigan JM, Eds. To Err is Human. Building a Safer Helath System. Washington, DC: National Academy Press; 1999.
- Joint Commission on Accreditation of Healthcare Organizations. Sentinel events: evaluating cause and planning improvement. 1998. Library of congress catalog number 97-80531.
- Salvendy G, ed. Handbook of Human Factors and Ergonomics. New York: John Wiley & Sons;1997:163
- Donchin Y, Gopher D, Olin M, et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23:294-300.
- McNutt R, Abrams R, Hasler S, et al. Determining medical error: three case reports. Eff Clin Pract. 2002;5:23-8.
- Senders JW. FMEA and RCA: the mantras of modern risk management. Qual Saf Health Care. 2004;13:249-50.
- Spath PL. Investigating Sentinel Events: How to Find and Resolve Root Causes. Forest Grove, OR: Brown Spath and Associates; 1997.
- Wald H, Shojania KG. Root cause analysis. In: Shojania KG, McDonald KM, Wachter RM, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment No. 43, AHRQ Publication No. 01-E058; July 2001. Available at http://www.ahrq.gov.
- Woodhouse S, Burney B, Coste K. To err is human: improving patient safety through failure mode and effect analysis. Clin leadersh Manag Rev. 2004;18:32-6.
When we speak of “quality” in health care, we generally think of mortality outcomes or regulatory requirements that are mandated by the JCAHO (Joint Commission for Accreditation of Healthcare Organizations). But how do these relate to and impact our everyday lives as hospitalists? At the 8th Annual Meeting of SHM we presented a workshop on RCA and FMEA, taking a practical approach to illustrate how these two JCAHO required methodologies can improve patient care as well as improve the work environment for hospitalists by addressing the systemic issues that can compromise care.
The workshop starts by stepping into the life of a hospitalist and something we all fear: “Something bad happens. Then what?” Depending on the severity of the event, the options include peer review, notifying the Department Chief, calling the Risk Manager, calling your lawyer, or doing nothing. You’ve probably had many experiences when “something wasn’t quite right,” but often there is no obvious bad outcome or obvious solution, so we shrug our shoulders and say, “Oh well, we got lucky this time; no harm, no foul.” The problem is, there are recurring patterns to these types of events, and the same issues may affect the next patient, who may not be so lucky.
Defining “Something Bad”
These types of cases, which have outcomes ranging from no effect on the patient to death, may be approached several different ways. The terms “near miss” or “close call” refer to an incident where a mistake was made but caught in time, so no harm was done to the patient. An example of this is when a physician makes a mistake on a medication order, but it is caught and corrected by a pharmacist or nurse.
When adverse outcomes do occur, think about and define etiologies so that you identify and address underlying causes. Is the outcome an expected or unexpected complication of therapy? Was there an error involved? In asking these questions, remember that you can have harm without error and error without harm. Error is defined as “failure of a planned action to be completed as intended or use of a wrong plan to achieve an aim; the accumulation of errors results in accidents” (Kohn, et al). This definition points out that usually a chain of events rather than a single individual or event results in a bad outcome. The purpose of defining etiologies is not to assign blame but to identify underlying issues and surrounding circumstances that may have contributed to the adverse outcome.
Significant adverse events are called “sentinel events” and defined as an “unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes loss of limb or function” (JCAHO 1998).
How We Approach Error
Unfortunately, as humans we are fallible and make errors quite reliably. Table 1 demonstrates types of errors and expected rates of errors. For example, we make errors of omission 0.01% of the time, but the good news is that with reminders or ticklers, we can reduce this rate to 0.003%. Unfortunately, when humans are under high stress in danger, research from the military indicates error rates of 25% (Salvendy 1997). In a complex ICU setting, researchers have documented an average of 178 activities per patient per day with an error rate of 0.95%. Despite an error rate of less than 1%, the yield of errors during the 4-month period of observation was still over 1000 errors, 29% of which were considered to have severe or potentially severe consequences (Donchin, et al).
The reality is that we err. Having the unrealistic expectations developed in medical training of being perfect in all our actions perpetuates the blame cycle when the inevitable mistake occurs, and it prevents us from implementing solutions that prevent errors from ever occurring or catching them before they cause harm.
RCA and FMEA Help Us Create Solutions That Make a Difference
Briefly, Root Cause Analysis (RCA) is a retrospective investigation that is required by JCAHO after a sentinel event: “Root cause analysis is a process for identifying the basic or causal factor(s) that underlies variation in performance, including the occurrence or possible occurrence of a sentinel event. A root cause is that most fundamental reason a problem―a situation where performance does not meet expectations―has occurred” (JCAHO 1998). An RCA looks back in time at an event and asks the question “What
happened?” The utility of this methodology lies in the fact that it not only asks what happened but also asks “Why did this happen” rather than focus on “Who is to blame?” Some hospitals use this methodology for cases that are not sentinel events, because the knowledge gained from these investigations often uncovers system issues previously not known and that negatively impact many departments, not just the departments involved in a particular case.
Failure Modes and Effects Analysis (FMEA) is a prospective investigation aimed at identifying vulnerabilities and preventing failures in the future. It looks forward and asks what could go wrong? Performance of an FMEA is also required yearly by JCAHO and focuses on improving risky processes such as blood transfusions, chemotherapy, and other high risk medications.
Approaching a clinical case clearly demonstrates the differences between RCA and FMEA. Imagine a 72-year-old patient admitted to your hospital with findings of an acute abdomen requiring surgery. The patient is a smoker, with Type 2 diabetes and an admission blood sugar of 465, but no evidence of DKA. She normally takes an oral hypoglycemic to control her diabetes and an ACE inhibitor for high blood pressure but no other medications. She is taken to the OR emergently, where surgery seems to go well, and post-operatively is admitted to the ICU. Subsequently, her blood glucose ranges from 260 to 370 and is “controlled” with sliding scale insulin. Unfortunately, within 18 hours of surgery she suffers an MI and develops a postoperative wound infection 4 days after surgery. She eventually dies from sepsis.
An RCA of this case might reveal causal factors such as lack of use of a beta-blocker preoperatively and lack of use of IV insulin to lower her blood sugars to the 80–110 range. While possibly identifying the root cause of this adverse outcome, an RCA is limited by its hindsight bias and the labor-intensive nature of the investigation that may or may not have broad application, since it is an in-depth study of one case. However, RCA’s do have the salutary effects of building teamwork, identifying needed changes, and if carried out impartially without assigning blame can facilitate a culture of patient safety.
FMEA takes a different approach and proactively aims to prevent failure. It is a systematic method of identifying and preventing product and process failures before they occur. It does not require a specific case or adverse event. Rather, a high-risk process is chosen for study, and an interdisciplinary team asks the question “What can go wrong with this process and how can we prevent failures?” Considering the above case, imagine that before it ever occurred you as the hospitalist concerned with patient safety decided to conduct an FMEA on controlling blood sugar in the ICU or administering beta-blockers perioperatively to patients who are appropriate candidates.
For example, using FMEA methodology to study the process of intensive insulin therapy to achieve tight control of glucose in the ICU would identify potential barriers and failures preventing successful implementation. A significant risk encountered in achieving tight glucose control in the range of 80–110 includes hypoglycemia. Common pitfalls of insulin administration include administration and calculation errors that can result in 10-fold differences in doses of insulin. Other details of administration, such as type of IV tubing used and how the IV tubing is primed, can greatly affect the amount of insulin delivered to the patient and thus the glucose levels. If an inadequate amount of solution is flushed through to prime the tubing, the patient may receive saline rather than insulin for a few hours, resulting in higher-than-expected glucose levels and titration of insulin to higher doses. The result would then be an unexpectedly low glucose several hours later. Once failure modes such as these are identified, a fail-safe system can be designed so that failures are less likely to occur.
The advantages of FMEA include its focus on system design rather than on a single incident such as in RCA. By focusing on systems and processes, the learning and changes implemented are likely to impact a larger number of patients.
Summary and Discussion
To summarize, RCA is retrospective and dissects a case, while FMEA is prospective and dissects a process. It is important to remember that given the right set of circumstances, any physician can make a mistake. It makes sense to apply methodologies that probe into surrounding circumstances and contributing factors so that knowledge gained can be used to prevent the same mistakes from happening to different individuals and have broader impact on healthcare systems.
Resources
- www.patientsafety.gov: VA National Center for Patient Safety. Excellent website with very helpful, practical tools.
- www.ihi.org: Institute for Healthcare Improvement website. Has a nice FMEA toolkit.
- www.jcaho.com: The Joint Commission for Accreditation of Healthcare Organizations website. Has information on sentinel events and use of RCA.
Bibliography
- Kohn LT, Corrigan JM, Eds. To Err is Human. Building a Safer Helath System. Washington, DC: National Academy Press; 1999.
- Joint Commission on Accreditation of Healthcare Organizations. Sentinel events: evaluating cause and planning improvement. 1998. Library of congress catalog number 97-80531.
- Salvendy G, ed. Handbook of Human Factors and Ergonomics. New York: John Wiley & Sons;1997:163
- Donchin Y, Gopher D, Olin M, et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23:294-300.
- McNutt R, Abrams R, Hasler S, et al. Determining medical error: three case reports. Eff Clin Pract. 2002;5:23-8.
- Senders JW. FMEA and RCA: the mantras of modern risk management. Qual Saf Health Care. 2004;13:249-50.
- Spath PL. Investigating Sentinel Events: How to Find and Resolve Root Causes. Forest Grove, OR: Brown Spath and Associates; 1997.
- Wald H, Shojania KG. Root cause analysis. In: Shojania KG, McDonald KM, Wachter RM, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment No. 43, AHRQ Publication No. 01-E058; July 2001. Available at http://www.ahrq.gov.
- Woodhouse S, Burney B, Coste K. To err is human: improving patient safety through failure mode and effect analysis. Clin leadersh Manag Rev. 2004;18:32-6.