User login
Electronic nose may sniff out early lung cancer in COPD
, based on data from a prospective study of approximately 800 individuals.
Lung cancer remains a major cause of death in patients with chronic obstructive pulmonary disease (COPD), but many cases may go undetected in the early stage because of lack of screening and lack of validated predictive biomarkers, wrote Rianne de Vries, PhD, of the University of Amsterdam, and colleagues.
Accurate, noninvasive tests to screen patients with COPD for lung cancer are needed, and molecular profiling of exhaled breath using electronic nose (eNose) technology has shown potential as a method of early detection by identifying patterns of exhaled volatile organic compounds (VOCs), they said.
In a study published in the journal Chest, the researchers reviewed data from 682 adults with COPD and 211 with lung cancer who were enrolled in BreathCloud, a multicenter, observational study of healthy controls and individuals with suspected or confirmed diagnosis of asthma, COPD, or lung cancer.
Patients’ breath profiles were collected at study enrollment, between May 2017 and November 2018, using a metal oxide semiconductor eNose (SpiroNose).
Data from the eNose included the highest sensor peak normalized to the most stable sensor and the ratio between sensor peak and breath hold point. These variables were combined into four principal components (PCs) that captured 78.4% of variance in the dataset, and training and validation sets were constructed for all subjects. The researchers calculated a receiver operating characteristic (ROC) curve, including the area under the curve (AUC).
All patients were treated with standard clinical care and were monitored for development of clinically diagnosed lung cancer for 2 years, confirmed via CT imaging. The mean age of the patients was 64 years, and demographics at baseline were similar for patients with and without lung cancer.
After exclusion of 116 patients with both COPD and lung cancer, the analysis showed an accuracy of 90% and a ROC-AUC of 0.95.
Within 2 years of study enrollment, 37 patients with COPD (5.4%) developed lung cancer. In training sets and validation sets, the principal components one, two, and three were significantly different in patients with COPD who developed lung cancer and those who did not, (P = .002, P < .001, P < .001, respectively). The ROC-AUCs of the testing and validation sets were 0.89 and 0.86, respectively.
“Interestingly, the VOC pattern associated with early development of lung cancer in COPD did not match to the pattern related to lung cancer stages, as the former was mainly captured by PC2 and the latter by PC3,” the researchers wrote in their discussion. “This suggests that early identification of upcoming clinically manifest lung cancer in patients with COPD by eNose is not driven by VOCs that are predominantly associated with a particular stage of the disease,” they said.
The findings were limited by several factors including the lack of CT scanning at baseline because of the real-world design, so the presence of any baseline tumors was unknown, although none of the COPD patients showed symptoms indicative of lung cancer at baseline, the researchers noted.
However, the results suggest that eNose technology can identify lung cancer-specific VOC patterns early in cancer development in COPD patients, which provides a possible opportunity for early intervention, they concluded.
The study received no outside funding. De Vries disclosed personal fees and a substantial interest in the start-up company Breathomix.
A version of this article first appeared on Medscape.com.
, based on data from a prospective study of approximately 800 individuals.
Lung cancer remains a major cause of death in patients with chronic obstructive pulmonary disease (COPD), but many cases may go undetected in the early stage because of lack of screening and lack of validated predictive biomarkers, wrote Rianne de Vries, PhD, of the University of Amsterdam, and colleagues.
Accurate, noninvasive tests to screen patients with COPD for lung cancer are needed, and molecular profiling of exhaled breath using electronic nose (eNose) technology has shown potential as a method of early detection by identifying patterns of exhaled volatile organic compounds (VOCs), they said.
In a study published in the journal Chest, the researchers reviewed data from 682 adults with COPD and 211 with lung cancer who were enrolled in BreathCloud, a multicenter, observational study of healthy controls and individuals with suspected or confirmed diagnosis of asthma, COPD, or lung cancer.
Patients’ breath profiles were collected at study enrollment, between May 2017 and November 2018, using a metal oxide semiconductor eNose (SpiroNose).
Data from the eNose included the highest sensor peak normalized to the most stable sensor and the ratio between sensor peak and breath hold point. These variables were combined into four principal components (PCs) that captured 78.4% of variance in the dataset, and training and validation sets were constructed for all subjects. The researchers calculated a receiver operating characteristic (ROC) curve, including the area under the curve (AUC).
All patients were treated with standard clinical care and were monitored for development of clinically diagnosed lung cancer for 2 years, confirmed via CT imaging. The mean age of the patients was 64 years, and demographics at baseline were similar for patients with and without lung cancer.
After exclusion of 116 patients with both COPD and lung cancer, the analysis showed an accuracy of 90% and a ROC-AUC of 0.95.
Within 2 years of study enrollment, 37 patients with COPD (5.4%) developed lung cancer. In training sets and validation sets, the principal components one, two, and three were significantly different in patients with COPD who developed lung cancer and those who did not, (P = .002, P < .001, P < .001, respectively). The ROC-AUCs of the testing and validation sets were 0.89 and 0.86, respectively.
“Interestingly, the VOC pattern associated with early development of lung cancer in COPD did not match to the pattern related to lung cancer stages, as the former was mainly captured by PC2 and the latter by PC3,” the researchers wrote in their discussion. “This suggests that early identification of upcoming clinically manifest lung cancer in patients with COPD by eNose is not driven by VOCs that are predominantly associated with a particular stage of the disease,” they said.
The findings were limited by several factors including the lack of CT scanning at baseline because of the real-world design, so the presence of any baseline tumors was unknown, although none of the COPD patients showed symptoms indicative of lung cancer at baseline, the researchers noted.
However, the results suggest that eNose technology can identify lung cancer-specific VOC patterns early in cancer development in COPD patients, which provides a possible opportunity for early intervention, they concluded.
The study received no outside funding. De Vries disclosed personal fees and a substantial interest in the start-up company Breathomix.
A version of this article first appeared on Medscape.com.
, based on data from a prospective study of approximately 800 individuals.
Lung cancer remains a major cause of death in patients with chronic obstructive pulmonary disease (COPD), but many cases may go undetected in the early stage because of lack of screening and lack of validated predictive biomarkers, wrote Rianne de Vries, PhD, of the University of Amsterdam, and colleagues.
Accurate, noninvasive tests to screen patients with COPD for lung cancer are needed, and molecular profiling of exhaled breath using electronic nose (eNose) technology has shown potential as a method of early detection by identifying patterns of exhaled volatile organic compounds (VOCs), they said.
In a study published in the journal Chest, the researchers reviewed data from 682 adults with COPD and 211 with lung cancer who were enrolled in BreathCloud, a multicenter, observational study of healthy controls and individuals with suspected or confirmed diagnosis of asthma, COPD, or lung cancer.
Patients’ breath profiles were collected at study enrollment, between May 2017 and November 2018, using a metal oxide semiconductor eNose (SpiroNose).
Data from the eNose included the highest sensor peak normalized to the most stable sensor and the ratio between sensor peak and breath hold point. These variables were combined into four principal components (PCs) that captured 78.4% of variance in the dataset, and training and validation sets were constructed for all subjects. The researchers calculated a receiver operating characteristic (ROC) curve, including the area under the curve (AUC).
All patients were treated with standard clinical care and were monitored for development of clinically diagnosed lung cancer for 2 years, confirmed via CT imaging. The mean age of the patients was 64 years, and demographics at baseline were similar for patients with and without lung cancer.
After exclusion of 116 patients with both COPD and lung cancer, the analysis showed an accuracy of 90% and a ROC-AUC of 0.95.
Within 2 years of study enrollment, 37 patients with COPD (5.4%) developed lung cancer. In training sets and validation sets, the principal components one, two, and three were significantly different in patients with COPD who developed lung cancer and those who did not, (P = .002, P < .001, P < .001, respectively). The ROC-AUCs of the testing and validation sets were 0.89 and 0.86, respectively.
“Interestingly, the VOC pattern associated with early development of lung cancer in COPD did not match to the pattern related to lung cancer stages, as the former was mainly captured by PC2 and the latter by PC3,” the researchers wrote in their discussion. “This suggests that early identification of upcoming clinically manifest lung cancer in patients with COPD by eNose is not driven by VOCs that are predominantly associated with a particular stage of the disease,” they said.
The findings were limited by several factors including the lack of CT scanning at baseline because of the real-world design, so the presence of any baseline tumors was unknown, although none of the COPD patients showed symptoms indicative of lung cancer at baseline, the researchers noted.
However, the results suggest that eNose technology can identify lung cancer-specific VOC patterns early in cancer development in COPD patients, which provides a possible opportunity for early intervention, they concluded.
The study received no outside funding. De Vries disclosed personal fees and a substantial interest in the start-up company Breathomix.
A version of this article first appeared on Medscape.com.
FROM CHEST
Abrocitinib improves outcomes in severe or difficult-to-treat atopic dermatitis
Key clinical point: Abrocitinib led to greater and rapid improvements in itch and skin clearance compared with placebo in patients with severe or difficult-to-treat atopic dermatitis (AD).
Major finding: At week 16, a significantly higher proportion of patients achieved an Investigator’s Global Assessment score of 0 or 1, Eczema Area and Severity Index-75 and -90 responses, and a ≥4-point improvement in Peak Pruritus Numerical Rating Scale score with abrocitinib 200-mg vs placebo across all subgroups (all nominal P < .05).
Study details: This post hoc analysis of the JADE COMPARE trial (n = 837) included a subset of patients with severe or difficult-to-treat AD who were randomly assigned to receive oral abrocitinib (200 or 100 mg), subcutaneous dupilumab (300 mg), or placebo with medicated topical therapy for 16 weeks.
Disclosures: This study was funded by Pfizer Inc. Some authors declared receiving grants or personal fees or serving as consultants, speakers, board members, or investigators for various organizations, including Pfizer. Five authors declared being employees of or shareholders in Pfizer.
Source: Simpson EL et al. Efficacy and safety of abrocitinib in patients with severe and/or difficult‑to‑treat atopic dermatitis: A post hoc analysis of the randomized phase 3 JADE COMPARE trial. Am J Clin Dermatol. 2023 (May 22). doi: 10.1007/s40257-023-00785-5
Key clinical point: Abrocitinib led to greater and rapid improvements in itch and skin clearance compared with placebo in patients with severe or difficult-to-treat atopic dermatitis (AD).
Major finding: At week 16, a significantly higher proportion of patients achieved an Investigator’s Global Assessment score of 0 or 1, Eczema Area and Severity Index-75 and -90 responses, and a ≥4-point improvement in Peak Pruritus Numerical Rating Scale score with abrocitinib 200-mg vs placebo across all subgroups (all nominal P < .05).
Study details: This post hoc analysis of the JADE COMPARE trial (n = 837) included a subset of patients with severe or difficult-to-treat AD who were randomly assigned to receive oral abrocitinib (200 or 100 mg), subcutaneous dupilumab (300 mg), or placebo with medicated topical therapy for 16 weeks.
Disclosures: This study was funded by Pfizer Inc. Some authors declared receiving grants or personal fees or serving as consultants, speakers, board members, or investigators for various organizations, including Pfizer. Five authors declared being employees of or shareholders in Pfizer.
Source: Simpson EL et al. Efficacy and safety of abrocitinib in patients with severe and/or difficult‑to‑treat atopic dermatitis: A post hoc analysis of the randomized phase 3 JADE COMPARE trial. Am J Clin Dermatol. 2023 (May 22). doi: 10.1007/s40257-023-00785-5
Key clinical point: Abrocitinib led to greater and rapid improvements in itch and skin clearance compared with placebo in patients with severe or difficult-to-treat atopic dermatitis (AD).
Major finding: At week 16, a significantly higher proportion of patients achieved an Investigator’s Global Assessment score of 0 or 1, Eczema Area and Severity Index-75 and -90 responses, and a ≥4-point improvement in Peak Pruritus Numerical Rating Scale score with abrocitinib 200-mg vs placebo across all subgroups (all nominal P < .05).
Study details: This post hoc analysis of the JADE COMPARE trial (n = 837) included a subset of patients with severe or difficult-to-treat AD who were randomly assigned to receive oral abrocitinib (200 or 100 mg), subcutaneous dupilumab (300 mg), or placebo with medicated topical therapy for 16 weeks.
Disclosures: This study was funded by Pfizer Inc. Some authors declared receiving grants or personal fees or serving as consultants, speakers, board members, or investigators for various organizations, including Pfizer. Five authors declared being employees of or shareholders in Pfizer.
Source: Simpson EL et al. Efficacy and safety of abrocitinib in patients with severe and/or difficult‑to‑treat atopic dermatitis: A post hoc analysis of the randomized phase 3 JADE COMPARE trial. Am J Clin Dermatol. 2023 (May 22). doi: 10.1007/s40257-023-00785-5
Successful dupilumab dose tapering in controlled atopic dermatitis
Key clinical point: Dupilumab dose was successfully tapered while maintaining controlled disease in the majority of patients with atopic dermatitis (AD) using a patient-centered dosing regimen in a large daily practice cohort study.
Major finding: Dose reduction was successful in 83.3% of patients who prolonged dupilumab interval while maintaining controlled disease, with most patients receiving dupilumab every 3 or 4 weeks. Although a significant small increase was observed in the highest mean Eczema Area and Severity Index and Numeric Rating Scale-Pruritis scores (both P < .001), the scores remained low.
Study details: Findings are from a prospective, multicenter study including 595 adult patients with controlled AD treated with dupilumab for ≥1 yearfrom the BioDay registry, of which 401 patients prolonged the dupilumab interval.
Disclosures: The BioDay registry was sponsored by Sanofi, AbbVie, and others. Some authors declared serving as investigators, speakers, advisors, or consultants for various sources, including the BioDay registry sponsors.
Source: Spekhorst LS, Boesjes CM, et al. Successful tapering of dupilumab in atopic dermatitis patients with low disease activity: A large pragmatic daily practice study from the BioDay registry. Br J Dermatol. 2023 (May 13). doi: 10.1093/bjd/ljad159
Key clinical point: Dupilumab dose was successfully tapered while maintaining controlled disease in the majority of patients with atopic dermatitis (AD) using a patient-centered dosing regimen in a large daily practice cohort study.
Major finding: Dose reduction was successful in 83.3% of patients who prolonged dupilumab interval while maintaining controlled disease, with most patients receiving dupilumab every 3 or 4 weeks. Although a significant small increase was observed in the highest mean Eczema Area and Severity Index and Numeric Rating Scale-Pruritis scores (both P < .001), the scores remained low.
Study details: Findings are from a prospective, multicenter study including 595 adult patients with controlled AD treated with dupilumab for ≥1 yearfrom the BioDay registry, of which 401 patients prolonged the dupilumab interval.
Disclosures: The BioDay registry was sponsored by Sanofi, AbbVie, and others. Some authors declared serving as investigators, speakers, advisors, or consultants for various sources, including the BioDay registry sponsors.
Source: Spekhorst LS, Boesjes CM, et al. Successful tapering of dupilumab in atopic dermatitis patients with low disease activity: A large pragmatic daily practice study from the BioDay registry. Br J Dermatol. 2023 (May 13). doi: 10.1093/bjd/ljad159
Key clinical point: Dupilumab dose was successfully tapered while maintaining controlled disease in the majority of patients with atopic dermatitis (AD) using a patient-centered dosing regimen in a large daily practice cohort study.
Major finding: Dose reduction was successful in 83.3% of patients who prolonged dupilumab interval while maintaining controlled disease, with most patients receiving dupilumab every 3 or 4 weeks. Although a significant small increase was observed in the highest mean Eczema Area and Severity Index and Numeric Rating Scale-Pruritis scores (both P < .001), the scores remained low.
Study details: Findings are from a prospective, multicenter study including 595 adult patients with controlled AD treated with dupilumab for ≥1 yearfrom the BioDay registry, of which 401 patients prolonged the dupilumab interval.
Disclosures: The BioDay registry was sponsored by Sanofi, AbbVie, and others. Some authors declared serving as investigators, speakers, advisors, or consultants for various sources, including the BioDay registry sponsors.
Source: Spekhorst LS, Boesjes CM, et al. Successful tapering of dupilumab in atopic dermatitis patients with low disease activity: A large pragmatic daily practice study from the BioDay registry. Br J Dermatol. 2023 (May 13). doi: 10.1093/bjd/ljad159
Switching to upadacitinib from dupilumab improves atopic dermatitis
Key clinical point: In patients with moderate-to-severe atopic dermatitis (AD), continuous upadacitinib treatment was safe and provided sustained responses through 40 weeks and switch to upadacitinib treatment improved outcomes irrespective of prior dupilumab response.
Major finding: At open-label extension week 16 vs Heads Up week 24, the mean Eczema Area and Severity Index scores were similar with continuous upadacitinib treatment (2.7 vs 2.6) and improved with a switch to upadacitinib from dupilumab (1.09 vs 3.29). Most patients without minimal threshold or adequate response with dupilumab achieved it with upadacitinib. No new safety signals were reported.
Study details: This 16-week interim analysis of a 52-week open-label extension study of the Heads Up trial included adults with moderate-to-severe AD who were assigned to continue receiving upadacitinib (n = 239) or switch to upadacitinib after 24 weeks of dupilumab (n = 245).
Disclosures: This study was supported by AbbVie Inc. Some authors reported ties with various organizations, including AbbVie. Eight authors declared being employees of or holding stock or stock options in AbbVie.
Source: Blauvelt A et al. Efficacy and safety of switching from dupilumab to upadacitinib versus continuous upadacitinib in moderate-to-severe atopic dermatitis: Results from an open-label extension of the phase 3, randomized, controlled trial (Heads Up). J Am Acad Dermatol. 2023 (May 22). doi: 10.1016/j.jaad.2023.05.033
Key clinical point: In patients with moderate-to-severe atopic dermatitis (AD), continuous upadacitinib treatment was safe and provided sustained responses through 40 weeks and switch to upadacitinib treatment improved outcomes irrespective of prior dupilumab response.
Major finding: At open-label extension week 16 vs Heads Up week 24, the mean Eczema Area and Severity Index scores were similar with continuous upadacitinib treatment (2.7 vs 2.6) and improved with a switch to upadacitinib from dupilumab (1.09 vs 3.29). Most patients without minimal threshold or adequate response with dupilumab achieved it with upadacitinib. No new safety signals were reported.
Study details: This 16-week interim analysis of a 52-week open-label extension study of the Heads Up trial included adults with moderate-to-severe AD who were assigned to continue receiving upadacitinib (n = 239) or switch to upadacitinib after 24 weeks of dupilumab (n = 245).
Disclosures: This study was supported by AbbVie Inc. Some authors reported ties with various organizations, including AbbVie. Eight authors declared being employees of or holding stock or stock options in AbbVie.
Source: Blauvelt A et al. Efficacy and safety of switching from dupilumab to upadacitinib versus continuous upadacitinib in moderate-to-severe atopic dermatitis: Results from an open-label extension of the phase 3, randomized, controlled trial (Heads Up). J Am Acad Dermatol. 2023 (May 22). doi: 10.1016/j.jaad.2023.05.033
Key clinical point: In patients with moderate-to-severe atopic dermatitis (AD), continuous upadacitinib treatment was safe and provided sustained responses through 40 weeks and switch to upadacitinib treatment improved outcomes irrespective of prior dupilumab response.
Major finding: At open-label extension week 16 vs Heads Up week 24, the mean Eczema Area and Severity Index scores were similar with continuous upadacitinib treatment (2.7 vs 2.6) and improved with a switch to upadacitinib from dupilumab (1.09 vs 3.29). Most patients without minimal threshold or adequate response with dupilumab achieved it with upadacitinib. No new safety signals were reported.
Study details: This 16-week interim analysis of a 52-week open-label extension study of the Heads Up trial included adults with moderate-to-severe AD who were assigned to continue receiving upadacitinib (n = 239) or switch to upadacitinib after 24 weeks of dupilumab (n = 245).
Disclosures: This study was supported by AbbVie Inc. Some authors reported ties with various organizations, including AbbVie. Eight authors declared being employees of or holding stock or stock options in AbbVie.
Source: Blauvelt A et al. Efficacy and safety of switching from dupilumab to upadacitinib versus continuous upadacitinib in moderate-to-severe atopic dermatitis: Results from an open-label extension of the phase 3, randomized, controlled trial (Heads Up). J Am Acad Dermatol. 2023 (May 22). doi: 10.1016/j.jaad.2023.05.033
Crisaborole once daily an effective long-term maintenance therapy for atopic dermatitis
Key clinical point: Maintenance therapy with once-daily crisaborole is safe and effective in adult and pediatric patients with mild-to-moderate atopic dermatitis (AD) who have previously responded to twice-daily crisaborole treatment.
Major finding: The crisaborole vs vehicle group had a significantly longer median flare-free maintenance time (111 vs 30 days; P = .0034), higher mean number of flare-free days (234.0 vs 199.4 days; P = .0346), and lower mean number of flares (0.95 vs 1.36; P = .0042). No new safety signals were reported.
Study details: This phase 3 study (CrisADe CONTROL) included 270 patients age ≥3 months with mild-to-moderate AD who received twice-daily crisaborole for a maximum of 8 weeks; the responders were randomly assigned to receive once-daily crisaborole 2% ointment (n = 135) or vehicle (n = 135) for 52 weeks.
Disclosures: This study was funded by Pfizer Inc. Some authors declared serving as investigators, speakers, or consultants for or receiving research grants from various sources, including Pfizer. Six authors declared being employees of and shareholders in Pfizer.
Source: Eichenfield LF et al. Once‑daily crisaborole ointment, 2%, as a long‑term maintenance treatment in patients aged ≥ 3 months with mild‑to‑moderate atopic dermatitis: A 52-week clinical study. Am J Clin Dermatol. 2023 (May 15). doi: 10.1007/s40257-023-00780-w
Key clinical point: Maintenance therapy with once-daily crisaborole is safe and effective in adult and pediatric patients with mild-to-moderate atopic dermatitis (AD) who have previously responded to twice-daily crisaborole treatment.
Major finding: The crisaborole vs vehicle group had a significantly longer median flare-free maintenance time (111 vs 30 days; P = .0034), higher mean number of flare-free days (234.0 vs 199.4 days; P = .0346), and lower mean number of flares (0.95 vs 1.36; P = .0042). No new safety signals were reported.
Study details: This phase 3 study (CrisADe CONTROL) included 270 patients age ≥3 months with mild-to-moderate AD who received twice-daily crisaborole for a maximum of 8 weeks; the responders were randomly assigned to receive once-daily crisaborole 2% ointment (n = 135) or vehicle (n = 135) for 52 weeks.
Disclosures: This study was funded by Pfizer Inc. Some authors declared serving as investigators, speakers, or consultants for or receiving research grants from various sources, including Pfizer. Six authors declared being employees of and shareholders in Pfizer.
Source: Eichenfield LF et al. Once‑daily crisaborole ointment, 2%, as a long‑term maintenance treatment in patients aged ≥ 3 months with mild‑to‑moderate atopic dermatitis: A 52-week clinical study. Am J Clin Dermatol. 2023 (May 15). doi: 10.1007/s40257-023-00780-w
Key clinical point: Maintenance therapy with once-daily crisaborole is safe and effective in adult and pediatric patients with mild-to-moderate atopic dermatitis (AD) who have previously responded to twice-daily crisaborole treatment.
Major finding: The crisaborole vs vehicle group had a significantly longer median flare-free maintenance time (111 vs 30 days; P = .0034), higher mean number of flare-free days (234.0 vs 199.4 days; P = .0346), and lower mean number of flares (0.95 vs 1.36; P = .0042). No new safety signals were reported.
Study details: This phase 3 study (CrisADe CONTROL) included 270 patients age ≥3 months with mild-to-moderate AD who received twice-daily crisaborole for a maximum of 8 weeks; the responders were randomly assigned to receive once-daily crisaborole 2% ointment (n = 135) or vehicle (n = 135) for 52 weeks.
Disclosures: This study was funded by Pfizer Inc. Some authors declared serving as investigators, speakers, or consultants for or receiving research grants from various sources, including Pfizer. Six authors declared being employees of and shareholders in Pfizer.
Source: Eichenfield LF et al. Once‑daily crisaborole ointment, 2%, as a long‑term maintenance treatment in patients aged ≥ 3 months with mild‑to‑moderate atopic dermatitis: A 52-week clinical study. Am J Clin Dermatol. 2023 (May 15). doi: 10.1007/s40257-023-00780-w
Atopic dermatitis positively linked with the risk for incident venous thromboembolism
Key clinical point: Adults with atopic dermatitis (AD) have a 1.28-fold increased risk for incident venous thromboembolism (VTE) compared with those without AD.
Major finding: Patients with AD vs control individuals without AD had an increased risk for incident VTE (hazard ratio [HR] 1.28; 95% CI 1.17-1.40), with the risk being elevated for both deep vein thrombosis (HR 1.26; 95% CI 1.14-1.40) and pulmonary embolism (HR 1.30; 95% CI 1.08-1.57).
Study details: The data come from a retrospective cohort study that included 142,429 patients age ≥ 20 years with AD and 142,429 matched control individuals without AD.
Disclosures: This study was funded by Hualien Tzu Chi Hospital, Taiwan. The authors declared no conflicts of interest.
Source: Chen TL et al. Risk of venous thromboembolism among adults with atopic dermatitis. JAMA Dermatol. 2023 (May 31). doi: 10.1001/jamadermatol.2023.1300.
Key clinical point: Adults with atopic dermatitis (AD) have a 1.28-fold increased risk for incident venous thromboembolism (VTE) compared with those without AD.
Major finding: Patients with AD vs control individuals without AD had an increased risk for incident VTE (hazard ratio [HR] 1.28; 95% CI 1.17-1.40), with the risk being elevated for both deep vein thrombosis (HR 1.26; 95% CI 1.14-1.40) and pulmonary embolism (HR 1.30; 95% CI 1.08-1.57).
Study details: The data come from a retrospective cohort study that included 142,429 patients age ≥ 20 years with AD and 142,429 matched control individuals without AD.
Disclosures: This study was funded by Hualien Tzu Chi Hospital, Taiwan. The authors declared no conflicts of interest.
Source: Chen TL et al. Risk of venous thromboembolism among adults with atopic dermatitis. JAMA Dermatol. 2023 (May 31). doi: 10.1001/jamadermatol.2023.1300.
Key clinical point: Adults with atopic dermatitis (AD) have a 1.28-fold increased risk for incident venous thromboembolism (VTE) compared with those without AD.
Major finding: Patients with AD vs control individuals without AD had an increased risk for incident VTE (hazard ratio [HR] 1.28; 95% CI 1.17-1.40), with the risk being elevated for both deep vein thrombosis (HR 1.26; 95% CI 1.14-1.40) and pulmonary embolism (HR 1.30; 95% CI 1.08-1.57).
Study details: The data come from a retrospective cohort study that included 142,429 patients age ≥ 20 years with AD and 142,429 matched control individuals without AD.
Disclosures: This study was funded by Hualien Tzu Chi Hospital, Taiwan. The authors declared no conflicts of interest.
Source: Chen TL et al. Risk of venous thromboembolism among adults with atopic dermatitis. JAMA Dermatol. 2023 (May 31). doi: 10.1001/jamadermatol.2023.1300.
A live topical biotherapeutic spray improves pruritus in atopic dermatitis
Key clinical point: A topical biotherapeutic spray containing live ammonia-oxidizing bacteria (B244) was safe and meaningfully improved pruritus at both high and low dose levels in patients with mild-to-moderate atopic dermatitis (AD) and moderate-to-severe pruritus.
Major finding: At week 4, treatment with low dose (optical density [OD] at 600 nm 5.0) and high dose (OD at 600 nm 20.0) spray vs vehicle showed a significant treatment effect (P = .015 and P = .014, respectively), with a 34% mean reduction in Worst Itch Numeric Rating Scale scores from baseline in both treatment groups. No serious adverse events were reported.
Study details: This multicenter phase 2b randomized controlled trial included 547 adult patients with mild-to-moderate AD and moderate-to-severe pruritus who were randomly assigned to receive low dose B244, high dose B244, or vehicle for 4 weeks.
Disclosures: This study was funded by AOBiome Therapeutics. Some authors reported ties with various organizations, including AOBiome. Six authors declared being current or former employees of or holding stock or stock options in AOBiome.
Source: Silverberg JI et al. Efficacy and safety of topically applied therapeutic ammonia oxidising bacteria in adults with mild-to-moderate atopic dermatitis and moderate-to-severe pruritus: A randomised, double-blind, placebo-controlled, dose-ranging, phase 2b trial. EClinicalMedicine. 2023 (May 16). doi:10.1016/j.eclinm.2023.102002
Key clinical point: A topical biotherapeutic spray containing live ammonia-oxidizing bacteria (B244) was safe and meaningfully improved pruritus at both high and low dose levels in patients with mild-to-moderate atopic dermatitis (AD) and moderate-to-severe pruritus.
Major finding: At week 4, treatment with low dose (optical density [OD] at 600 nm 5.0) and high dose (OD at 600 nm 20.0) spray vs vehicle showed a significant treatment effect (P = .015 and P = .014, respectively), with a 34% mean reduction in Worst Itch Numeric Rating Scale scores from baseline in both treatment groups. No serious adverse events were reported.
Study details: This multicenter phase 2b randomized controlled trial included 547 adult patients with mild-to-moderate AD and moderate-to-severe pruritus who were randomly assigned to receive low dose B244, high dose B244, or vehicle for 4 weeks.
Disclosures: This study was funded by AOBiome Therapeutics. Some authors reported ties with various organizations, including AOBiome. Six authors declared being current or former employees of or holding stock or stock options in AOBiome.
Source: Silverberg JI et al. Efficacy and safety of topically applied therapeutic ammonia oxidising bacteria in adults with mild-to-moderate atopic dermatitis and moderate-to-severe pruritus: A randomised, double-blind, placebo-controlled, dose-ranging, phase 2b trial. EClinicalMedicine. 2023 (May 16). doi:10.1016/j.eclinm.2023.102002
Key clinical point: A topical biotherapeutic spray containing live ammonia-oxidizing bacteria (B244) was safe and meaningfully improved pruritus at both high and low dose levels in patients with mild-to-moderate atopic dermatitis (AD) and moderate-to-severe pruritus.
Major finding: At week 4, treatment with low dose (optical density [OD] at 600 nm 5.0) and high dose (OD at 600 nm 20.0) spray vs vehicle showed a significant treatment effect (P = .015 and P = .014, respectively), with a 34% mean reduction in Worst Itch Numeric Rating Scale scores from baseline in both treatment groups. No serious adverse events were reported.
Study details: This multicenter phase 2b randomized controlled trial included 547 adult patients with mild-to-moderate AD and moderate-to-severe pruritus who were randomly assigned to receive low dose B244, high dose B244, or vehicle for 4 weeks.
Disclosures: This study was funded by AOBiome Therapeutics. Some authors reported ties with various organizations, including AOBiome. Six authors declared being current or former employees of or holding stock or stock options in AOBiome.
Source: Silverberg JI et al. Efficacy and safety of topically applied therapeutic ammonia oxidising bacteria in adults with mild-to-moderate atopic dermatitis and moderate-to-severe pruritus: A randomised, double-blind, placebo-controlled, dose-ranging, phase 2b trial. EClinicalMedicine. 2023 (May 16). doi:10.1016/j.eclinm.2023.102002
Cancer drug shortages spur worry, rationing, and tough choices
CHICAGO – Oncologist Denise Yardley, MD, isn’t used to expressing uncertainty when she tells patients about what’s in store for them in terms of drug treatment. But things are dramatically different now amid a severe national shortage of carboplatin and cisplatin, two common and crucial cancer drugs.
“There’s a regimen I’m thinking about,” Dr. Yardley told a new patient recently, “but we’ll have to wait until you finish your staging evaluation to see whether I can deliver this. Another regimen that’s a little more toxic is my second choice.” And, she added, the alternative chemotherapy treatment – anthracycline instead of carboplatin – requires a longer treatment period.
This ambiguity is hardly ideal, said Dr. Yardley, of Tennessee Oncology and Sarah Cannon Research Institute in Nashville. “It’s another factor in being overwhelmed in a first-time visit and wanting to know the details about what your treatment is going to look like. You’re not walking out knowing exactly what you’re going to take or the exact timing so you can start mapping out your calendar and work schedule.”
This kind of scenario is becoming all too familiar this spring, according to oncologists who gathered at the annual meeting of the American Society of Clinical Oncology (ASCO). In interviews, these physicians said the limited supply of multiple cancer drugs – including the chemotherapies carboplatin and cisplatin – is having an unprecedented negative effect since their use is so widespread in cancer care.
“Every patient could get impacted. That’s why we need to address this sooner rather than later,” said oncologist Aditya Baria, MBBS, MPH, director of the Breast Cancer Research Program at Massachusetts General Hospital, Boston.
Shortages of cancer drugs are not unusual. Three-quarters of oncology pharmacists at 68 organizations surveyed from 2019 to 2020 said shortages prompted treatment delays, reduced doses, or alternative regimens. But the current shortages are having a much wider impact.
The National Comprehensive Cancer Network recently reported that 93% of 27 member institutions surveyed in late May are short on carboplatin, and 70% have reported a shortage of cisplatin. Plus, 20% of 19 centers said they weren’t able to continue carboplatin regimens for all patients.
The drugs are mainstays of multiple types of treatment for a long list of cancer types including lung, breast, gynecologic, and many others.
Several scenarios are possible when the drugs are in short supply, said Dr. Yardley, who noted that the shortage is more severe than any she’s seen in her medical career of more than 3 decades. Patients may need to be switched to regimens with more side effects, even when they’re in the middle of a treatment, she said. Or patients might have to go longer between treatments.
In some cases, Dr. Yardley said, the shortage is forcing patients to go without an important component of a larger combination therapy regimen. “The Keynote 522 neoadjuvant regimen for triple-negative breast cancer has carboplatin given with Taxol [paclitaxel] and Keytruda [pembrolizumab]. We are just deleting the carboplatin.”
She added that carboplatin is part of the following so-called TCHP regimen for HER2+ early-stage breast cancer: Taxotere (docetaxel), carboplatin, Herceptin (trastuzumab), and Perjeta (pertuzumab).
“You can delete [carboplatin] or consider substituting cyclophosphamide for carboplatin,” she said. But she cautioned the Keynote 522 and TCHP regimens haven’t been tested without carboplatin in curative-intent trials.
At Duke University in Durham, N.C., doses of carboplatin for many patients are being lowered by a third to the level that’s commonly used for older and frail patients, said oncologist Arif Kamal, MD, MBA, MHS, who works at the academic center and is the chief patient officer at the American Cancer Society.
“We don’t know if [the lower doses will negatively affect cancer patients’ outcomes]. What’s amazing is how many patients [are understanding about having to take smaller amounts of the chemotherapy],” he said.
Medical organizations are offering guidance. The Society of Gynecologic Oncology, for example, in late April recommended that oncologists increase intervals between chemotherapy treatments when appropriate, round down vial sizes to ensure “efficient use,” and eliminate or minimize use of cisplatin and carboplatin in certain platinum-resistant cancers.
In early June, ASCO published guidance regarding alternatives to cisplatin, carboplatin, and 5-fluorouracil, which is also in short supply, in gastrointestinal cancer. As the guidance notes, some alternatives are more untested or more toxic than ideal treatments.
In addition, ASCO has a webpage devoted to news and resources about shortages of cancer drugs. It offers drug availability updates, general guidance, and breast cancer guidance. ASCO also offers ethical guidance about handling drug shortages.
Patients in clinical trials and those who hope to join them are especially vulnerable to the drug shortage, oncologists interviewed for this story said. Cisplatin and carboplatin are the backbones of many clinical trials, Dr. Yardley said. “When you can’t supply a drug in one of the [trial] arms, that puts the whole trial on pause.”
Even clinics that have managed to find adequate supplies of the drugs are planning for when they run out.
“Our institution and other institutions are trying to come up with a rationing protocol, deciding which patients are going to get access, and which ones have reasonable alternatives,” radiation oncologist Corey Speers MD, PhD, of University Hospitals Seidman Cancer Center and Case Western Reserve University, Cleveland, said in an interview. “In some settings, there really isn’t an effective alternative. Or the alternatives are tens of thousands of dollars more expensive.”
Oncologists also noted that cisplatin and carboplatin aren’t the only cancer drugs in short supply.
“Methotrexate is critically low, and 5FU [fluorouracil] is critically low,” Dr. Yardley said, referring to drugs that each treat several types of cancer. According to the May NCNN survey, 67% of respondents reported low supplies of methotrexate, and 26% said they were low on 5FU.
“Viscous lidocaine is a component of many supportive care mouth rinses for the stomatitis caused by our drugs but is not available at all,” Dr. Yardley said.
She added that there are also low supplies of fludarabine, which is used to treat chronic lymphocytic lymphom; clofarabine, which is used to treat acute lymphoblastic leukemia; and rasburicase, which is used to treat high levels of uric acid in patients on chemotherapy.
Dr. Speers said his institution is facing a shortage of capecitabine, which is used to treat several types of cancer.
“Numerous trials have demonstrated the improved, safety, efficacy, and convenience of oral capecitabine. With the shortage we’re having to use infusional 5FU, which not only is less convenient but also ends up being more costly and requires infusion room space or continuous infusion pumps. This impacts our ability to treat cancer patients,” he said. “Our capacity is becoming more limited to accommodate these added patients, and we have to use infusional formulations of a drug that previously was readily available via an oral formulation. Patients and caregivers now have to come to the cancer center for appointments and infusions that previously weren’t needed as they could take an oral pill.”
Dr. Speers added that his institution is rationing methotrexate. “We are now prioritizing patients being treated with curative intent and adjusting protocols to use the lowest allowable doses to conserve supply,” he said.
The roots of the platinum chemotherapy drug shortage link back to the India-based Intas Pharmaceuticals company, a major manufacturer of cisplatin and carboplatin. According to Kellyann Zuzulo, spokeperson for Accord Healthcare, an Instas U.S. subsidiary, a facility inspection in December 2022 prompted a decision to temporarily stop making the drugs. The inspection identified multiple problems.
“Intas and Accord are working with the FDA on a plan to return to manufacturing,” Ms. Zuzulo said in an interview. “This will allow for continued production of products that will be prioritized based on medical necessity. A date has not yet been confirmed in which the facility will return to manufacturing for cisplatin, carboplatin or any other products.”
Ms. Zuzulo said the company is not a health care provider and cannot offer advice to patients about alternatives.
Other companies that make cisplatin and carboplatin have also reported shortages. In interviews, representatives for Fresenius Kabi and Pfizer said the companies have limited supplies because of increased demand – not because of manufacturing problems.
On June 12, the American Society of Health-System Pharmacists (ASHP) reported that carboplatin remains in short supply, with all five companies that sell the drug listed as having limited or back-ordered supplies. Cisplatin is also in short supply, the organization reported in a June 9 update, although some is available.
In a June 12 update on methotrexate, ASHP said manufacturing delays at Accord have caused a shortage, and other companies are running low due to increased demand.
As for the future, Congress and the Biden administration, according to a report by Bloomberg, are trying to figure out what to do regarding shortages of cheap generic drugs such as cisplatin and carboplatin. The FDA is exploring a partnership with a Chinese drugmaker to make cisplatin, NBC News reported.
However, fixes will be challenging, according to former FDA commissioner and Pfizer board member, Scott Gottlieb, MD.
“This generic business, particularly for these complex drugs, these complex formulations, is not a healthy business right now. Yet it’s a vital business from a public standpoint,” he told CBS News.
In an interview, Dr. Kamal said that there is even talk about boosting the prices of cheap generic drugs “to ensure that there’s enough incentive for multiple manufacturers to be involved.”
Dr. Kamal said he is crossing his fingers that cutting chemotherapy doses at his clinic doesn’t result in worse outcomes for his patients.
“Right now, I think dropping someone by 25% or 30% is okay. And for some patients, particularly in a curative setting, we try to keep them at as much as 100% as possible. But there’s just a lot of unknowns,” he said.
CHICAGO – Oncologist Denise Yardley, MD, isn’t used to expressing uncertainty when she tells patients about what’s in store for them in terms of drug treatment. But things are dramatically different now amid a severe national shortage of carboplatin and cisplatin, two common and crucial cancer drugs.
“There’s a regimen I’m thinking about,” Dr. Yardley told a new patient recently, “but we’ll have to wait until you finish your staging evaluation to see whether I can deliver this. Another regimen that’s a little more toxic is my second choice.” And, she added, the alternative chemotherapy treatment – anthracycline instead of carboplatin – requires a longer treatment period.
This ambiguity is hardly ideal, said Dr. Yardley, of Tennessee Oncology and Sarah Cannon Research Institute in Nashville. “It’s another factor in being overwhelmed in a first-time visit and wanting to know the details about what your treatment is going to look like. You’re not walking out knowing exactly what you’re going to take or the exact timing so you can start mapping out your calendar and work schedule.”
This kind of scenario is becoming all too familiar this spring, according to oncologists who gathered at the annual meeting of the American Society of Clinical Oncology (ASCO). In interviews, these physicians said the limited supply of multiple cancer drugs – including the chemotherapies carboplatin and cisplatin – is having an unprecedented negative effect since their use is so widespread in cancer care.
“Every patient could get impacted. That’s why we need to address this sooner rather than later,” said oncologist Aditya Baria, MBBS, MPH, director of the Breast Cancer Research Program at Massachusetts General Hospital, Boston.
Shortages of cancer drugs are not unusual. Three-quarters of oncology pharmacists at 68 organizations surveyed from 2019 to 2020 said shortages prompted treatment delays, reduced doses, or alternative regimens. But the current shortages are having a much wider impact.
The National Comprehensive Cancer Network recently reported that 93% of 27 member institutions surveyed in late May are short on carboplatin, and 70% have reported a shortage of cisplatin. Plus, 20% of 19 centers said they weren’t able to continue carboplatin regimens for all patients.
The drugs are mainstays of multiple types of treatment for a long list of cancer types including lung, breast, gynecologic, and many others.
Several scenarios are possible when the drugs are in short supply, said Dr. Yardley, who noted that the shortage is more severe than any she’s seen in her medical career of more than 3 decades. Patients may need to be switched to regimens with more side effects, even when they’re in the middle of a treatment, she said. Or patients might have to go longer between treatments.
In some cases, Dr. Yardley said, the shortage is forcing patients to go without an important component of a larger combination therapy regimen. “The Keynote 522 neoadjuvant regimen for triple-negative breast cancer has carboplatin given with Taxol [paclitaxel] and Keytruda [pembrolizumab]. We are just deleting the carboplatin.”
She added that carboplatin is part of the following so-called TCHP regimen for HER2+ early-stage breast cancer: Taxotere (docetaxel), carboplatin, Herceptin (trastuzumab), and Perjeta (pertuzumab).
“You can delete [carboplatin] or consider substituting cyclophosphamide for carboplatin,” she said. But she cautioned the Keynote 522 and TCHP regimens haven’t been tested without carboplatin in curative-intent trials.
At Duke University in Durham, N.C., doses of carboplatin for many patients are being lowered by a third to the level that’s commonly used for older and frail patients, said oncologist Arif Kamal, MD, MBA, MHS, who works at the academic center and is the chief patient officer at the American Cancer Society.
“We don’t know if [the lower doses will negatively affect cancer patients’ outcomes]. What’s amazing is how many patients [are understanding about having to take smaller amounts of the chemotherapy],” he said.
Medical organizations are offering guidance. The Society of Gynecologic Oncology, for example, in late April recommended that oncologists increase intervals between chemotherapy treatments when appropriate, round down vial sizes to ensure “efficient use,” and eliminate or minimize use of cisplatin and carboplatin in certain platinum-resistant cancers.
In early June, ASCO published guidance regarding alternatives to cisplatin, carboplatin, and 5-fluorouracil, which is also in short supply, in gastrointestinal cancer. As the guidance notes, some alternatives are more untested or more toxic than ideal treatments.
In addition, ASCO has a webpage devoted to news and resources about shortages of cancer drugs. It offers drug availability updates, general guidance, and breast cancer guidance. ASCO also offers ethical guidance about handling drug shortages.
Patients in clinical trials and those who hope to join them are especially vulnerable to the drug shortage, oncologists interviewed for this story said. Cisplatin and carboplatin are the backbones of many clinical trials, Dr. Yardley said. “When you can’t supply a drug in one of the [trial] arms, that puts the whole trial on pause.”
Even clinics that have managed to find adequate supplies of the drugs are planning for when they run out.
“Our institution and other institutions are trying to come up with a rationing protocol, deciding which patients are going to get access, and which ones have reasonable alternatives,” radiation oncologist Corey Speers MD, PhD, of University Hospitals Seidman Cancer Center and Case Western Reserve University, Cleveland, said in an interview. “In some settings, there really isn’t an effective alternative. Or the alternatives are tens of thousands of dollars more expensive.”
Oncologists also noted that cisplatin and carboplatin aren’t the only cancer drugs in short supply.
“Methotrexate is critically low, and 5FU [fluorouracil] is critically low,” Dr. Yardley said, referring to drugs that each treat several types of cancer. According to the May NCNN survey, 67% of respondents reported low supplies of methotrexate, and 26% said they were low on 5FU.
“Viscous lidocaine is a component of many supportive care mouth rinses for the stomatitis caused by our drugs but is not available at all,” Dr. Yardley said.
She added that there are also low supplies of fludarabine, which is used to treat chronic lymphocytic lymphom; clofarabine, which is used to treat acute lymphoblastic leukemia; and rasburicase, which is used to treat high levels of uric acid in patients on chemotherapy.
Dr. Speers said his institution is facing a shortage of capecitabine, which is used to treat several types of cancer.
“Numerous trials have demonstrated the improved, safety, efficacy, and convenience of oral capecitabine. With the shortage we’re having to use infusional 5FU, which not only is less convenient but also ends up being more costly and requires infusion room space or continuous infusion pumps. This impacts our ability to treat cancer patients,” he said. “Our capacity is becoming more limited to accommodate these added patients, and we have to use infusional formulations of a drug that previously was readily available via an oral formulation. Patients and caregivers now have to come to the cancer center for appointments and infusions that previously weren’t needed as they could take an oral pill.”
Dr. Speers added that his institution is rationing methotrexate. “We are now prioritizing patients being treated with curative intent and adjusting protocols to use the lowest allowable doses to conserve supply,” he said.
The roots of the platinum chemotherapy drug shortage link back to the India-based Intas Pharmaceuticals company, a major manufacturer of cisplatin and carboplatin. According to Kellyann Zuzulo, spokeperson for Accord Healthcare, an Instas U.S. subsidiary, a facility inspection in December 2022 prompted a decision to temporarily stop making the drugs. The inspection identified multiple problems.
“Intas and Accord are working with the FDA on a plan to return to manufacturing,” Ms. Zuzulo said in an interview. “This will allow for continued production of products that will be prioritized based on medical necessity. A date has not yet been confirmed in which the facility will return to manufacturing for cisplatin, carboplatin or any other products.”
Ms. Zuzulo said the company is not a health care provider and cannot offer advice to patients about alternatives.
Other companies that make cisplatin and carboplatin have also reported shortages. In interviews, representatives for Fresenius Kabi and Pfizer said the companies have limited supplies because of increased demand – not because of manufacturing problems.
On June 12, the American Society of Health-System Pharmacists (ASHP) reported that carboplatin remains in short supply, with all five companies that sell the drug listed as having limited or back-ordered supplies. Cisplatin is also in short supply, the organization reported in a June 9 update, although some is available.
In a June 12 update on methotrexate, ASHP said manufacturing delays at Accord have caused a shortage, and other companies are running low due to increased demand.
As for the future, Congress and the Biden administration, according to a report by Bloomberg, are trying to figure out what to do regarding shortages of cheap generic drugs such as cisplatin and carboplatin. The FDA is exploring a partnership with a Chinese drugmaker to make cisplatin, NBC News reported.
However, fixes will be challenging, according to former FDA commissioner and Pfizer board member, Scott Gottlieb, MD.
“This generic business, particularly for these complex drugs, these complex formulations, is not a healthy business right now. Yet it’s a vital business from a public standpoint,” he told CBS News.
In an interview, Dr. Kamal said that there is even talk about boosting the prices of cheap generic drugs “to ensure that there’s enough incentive for multiple manufacturers to be involved.”
Dr. Kamal said he is crossing his fingers that cutting chemotherapy doses at his clinic doesn’t result in worse outcomes for his patients.
“Right now, I think dropping someone by 25% or 30% is okay. And for some patients, particularly in a curative setting, we try to keep them at as much as 100% as possible. But there’s just a lot of unknowns,” he said.
CHICAGO – Oncologist Denise Yardley, MD, isn’t used to expressing uncertainty when she tells patients about what’s in store for them in terms of drug treatment. But things are dramatically different now amid a severe national shortage of carboplatin and cisplatin, two common and crucial cancer drugs.
“There’s a regimen I’m thinking about,” Dr. Yardley told a new patient recently, “but we’ll have to wait until you finish your staging evaluation to see whether I can deliver this. Another regimen that’s a little more toxic is my second choice.” And, she added, the alternative chemotherapy treatment – anthracycline instead of carboplatin – requires a longer treatment period.
This ambiguity is hardly ideal, said Dr. Yardley, of Tennessee Oncology and Sarah Cannon Research Institute in Nashville. “It’s another factor in being overwhelmed in a first-time visit and wanting to know the details about what your treatment is going to look like. You’re not walking out knowing exactly what you’re going to take or the exact timing so you can start mapping out your calendar and work schedule.”
This kind of scenario is becoming all too familiar this spring, according to oncologists who gathered at the annual meeting of the American Society of Clinical Oncology (ASCO). In interviews, these physicians said the limited supply of multiple cancer drugs – including the chemotherapies carboplatin and cisplatin – is having an unprecedented negative effect since their use is so widespread in cancer care.
“Every patient could get impacted. That’s why we need to address this sooner rather than later,” said oncologist Aditya Baria, MBBS, MPH, director of the Breast Cancer Research Program at Massachusetts General Hospital, Boston.
Shortages of cancer drugs are not unusual. Three-quarters of oncology pharmacists at 68 organizations surveyed from 2019 to 2020 said shortages prompted treatment delays, reduced doses, or alternative regimens. But the current shortages are having a much wider impact.
The National Comprehensive Cancer Network recently reported that 93% of 27 member institutions surveyed in late May are short on carboplatin, and 70% have reported a shortage of cisplatin. Plus, 20% of 19 centers said they weren’t able to continue carboplatin regimens for all patients.
The drugs are mainstays of multiple types of treatment for a long list of cancer types including lung, breast, gynecologic, and many others.
Several scenarios are possible when the drugs are in short supply, said Dr. Yardley, who noted that the shortage is more severe than any she’s seen in her medical career of more than 3 decades. Patients may need to be switched to regimens with more side effects, even when they’re in the middle of a treatment, she said. Or patients might have to go longer between treatments.
In some cases, Dr. Yardley said, the shortage is forcing patients to go without an important component of a larger combination therapy regimen. “The Keynote 522 neoadjuvant regimen for triple-negative breast cancer has carboplatin given with Taxol [paclitaxel] and Keytruda [pembrolizumab]. We are just deleting the carboplatin.”
She added that carboplatin is part of the following so-called TCHP regimen for HER2+ early-stage breast cancer: Taxotere (docetaxel), carboplatin, Herceptin (trastuzumab), and Perjeta (pertuzumab).
“You can delete [carboplatin] or consider substituting cyclophosphamide for carboplatin,” she said. But she cautioned the Keynote 522 and TCHP regimens haven’t been tested without carboplatin in curative-intent trials.
At Duke University in Durham, N.C., doses of carboplatin for many patients are being lowered by a third to the level that’s commonly used for older and frail patients, said oncologist Arif Kamal, MD, MBA, MHS, who works at the academic center and is the chief patient officer at the American Cancer Society.
“We don’t know if [the lower doses will negatively affect cancer patients’ outcomes]. What’s amazing is how many patients [are understanding about having to take smaller amounts of the chemotherapy],” he said.
Medical organizations are offering guidance. The Society of Gynecologic Oncology, for example, in late April recommended that oncologists increase intervals between chemotherapy treatments when appropriate, round down vial sizes to ensure “efficient use,” and eliminate or minimize use of cisplatin and carboplatin in certain platinum-resistant cancers.
In early June, ASCO published guidance regarding alternatives to cisplatin, carboplatin, and 5-fluorouracil, which is also in short supply, in gastrointestinal cancer. As the guidance notes, some alternatives are more untested or more toxic than ideal treatments.
In addition, ASCO has a webpage devoted to news and resources about shortages of cancer drugs. It offers drug availability updates, general guidance, and breast cancer guidance. ASCO also offers ethical guidance about handling drug shortages.
Patients in clinical trials and those who hope to join them are especially vulnerable to the drug shortage, oncologists interviewed for this story said. Cisplatin and carboplatin are the backbones of many clinical trials, Dr. Yardley said. “When you can’t supply a drug in one of the [trial] arms, that puts the whole trial on pause.”
Even clinics that have managed to find adequate supplies of the drugs are planning for when they run out.
“Our institution and other institutions are trying to come up with a rationing protocol, deciding which patients are going to get access, and which ones have reasonable alternatives,” radiation oncologist Corey Speers MD, PhD, of University Hospitals Seidman Cancer Center and Case Western Reserve University, Cleveland, said in an interview. “In some settings, there really isn’t an effective alternative. Or the alternatives are tens of thousands of dollars more expensive.”
Oncologists also noted that cisplatin and carboplatin aren’t the only cancer drugs in short supply.
“Methotrexate is critically low, and 5FU [fluorouracil] is critically low,” Dr. Yardley said, referring to drugs that each treat several types of cancer. According to the May NCNN survey, 67% of respondents reported low supplies of methotrexate, and 26% said they were low on 5FU.
“Viscous lidocaine is a component of many supportive care mouth rinses for the stomatitis caused by our drugs but is not available at all,” Dr. Yardley said.
She added that there are also low supplies of fludarabine, which is used to treat chronic lymphocytic lymphom; clofarabine, which is used to treat acute lymphoblastic leukemia; and rasburicase, which is used to treat high levels of uric acid in patients on chemotherapy.
Dr. Speers said his institution is facing a shortage of capecitabine, which is used to treat several types of cancer.
“Numerous trials have demonstrated the improved, safety, efficacy, and convenience of oral capecitabine. With the shortage we’re having to use infusional 5FU, which not only is less convenient but also ends up being more costly and requires infusion room space or continuous infusion pumps. This impacts our ability to treat cancer patients,” he said. “Our capacity is becoming more limited to accommodate these added patients, and we have to use infusional formulations of a drug that previously was readily available via an oral formulation. Patients and caregivers now have to come to the cancer center for appointments and infusions that previously weren’t needed as they could take an oral pill.”
Dr. Speers added that his institution is rationing methotrexate. “We are now prioritizing patients being treated with curative intent and adjusting protocols to use the lowest allowable doses to conserve supply,” he said.
The roots of the platinum chemotherapy drug shortage link back to the India-based Intas Pharmaceuticals company, a major manufacturer of cisplatin and carboplatin. According to Kellyann Zuzulo, spokeperson for Accord Healthcare, an Instas U.S. subsidiary, a facility inspection in December 2022 prompted a decision to temporarily stop making the drugs. The inspection identified multiple problems.
“Intas and Accord are working with the FDA on a plan to return to manufacturing,” Ms. Zuzulo said in an interview. “This will allow for continued production of products that will be prioritized based on medical necessity. A date has not yet been confirmed in which the facility will return to manufacturing for cisplatin, carboplatin or any other products.”
Ms. Zuzulo said the company is not a health care provider and cannot offer advice to patients about alternatives.
Other companies that make cisplatin and carboplatin have also reported shortages. In interviews, representatives for Fresenius Kabi and Pfizer said the companies have limited supplies because of increased demand – not because of manufacturing problems.
On June 12, the American Society of Health-System Pharmacists (ASHP) reported that carboplatin remains in short supply, with all five companies that sell the drug listed as having limited or back-ordered supplies. Cisplatin is also in short supply, the organization reported in a June 9 update, although some is available.
In a June 12 update on methotrexate, ASHP said manufacturing delays at Accord have caused a shortage, and other companies are running low due to increased demand.
As for the future, Congress and the Biden administration, according to a report by Bloomberg, are trying to figure out what to do regarding shortages of cheap generic drugs such as cisplatin and carboplatin. The FDA is exploring a partnership with a Chinese drugmaker to make cisplatin, NBC News reported.
However, fixes will be challenging, according to former FDA commissioner and Pfizer board member, Scott Gottlieb, MD.
“This generic business, particularly for these complex drugs, these complex formulations, is not a healthy business right now. Yet it’s a vital business from a public standpoint,” he told CBS News.
In an interview, Dr. Kamal said that there is even talk about boosting the prices of cheap generic drugs “to ensure that there’s enough incentive for multiple manufacturers to be involved.”
Dr. Kamal said he is crossing his fingers that cutting chemotherapy doses at his clinic doesn’t result in worse outcomes for his patients.
“Right now, I think dropping someone by 25% or 30% is okay. And for some patients, particularly in a curative setting, we try to keep them at as much as 100% as possible. But there’s just a lot of unknowns,” he said.
AT ASCO 2023
Annual physical exam
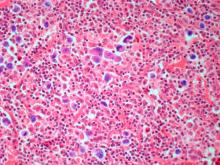
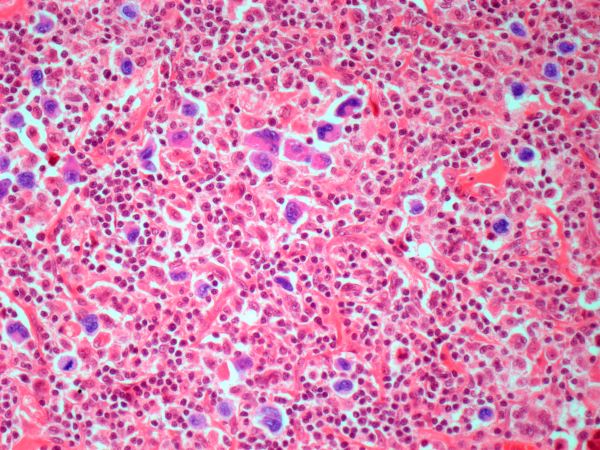
The history and findings in this case are suggestive of leukemic non-nodal mantle cell lymphoma (MCL).
MCL is a rare mature B-cell neoplasm characterized by t(11;14) (q13;q32) and cyclin D1 overexpression in more than 95% of cases. It accounts for approximately 5%-7% of all lymphomas, with an annual incidence of one case per 200,000 people. In North America and Europe, the incidence of MCL is like that of noncutaneous peripheral T-cell lymphomas. MCL occurs more frequently in men than in women (3:1), and the median age at diagnosis ranges from ages 60-70 years.
In recent years, MCL has been categorized into two major subgroups that have distinct clinical presentation and molecular features: nodal MCL and leukemic non-nodal MCL. Nodal MCL is a common variant with an aggressive disease course. Unmutated IGHV gene rearrangement, SOX11 overexpression, a higher degree of genomic instability (eg, ATM, CDKN2A, chromatin modifier mutations), and other oncogenic mutations and epigenetic modifications are seen in patients with this variant.
Leukemic non-nodal MCL is seen in 10%-20% of patients with MCL. Patients frequently present with lymphocytosis and splenomegaly. In most cases, it is associated with an indolent disease course and superior outcome. This subtype is largely IGHV mutated and mostly SOX11-negative, with positive expression of CD200, peripheral blood, bone marrow, and splenic involvement, low tumor burden, and a low Ki-67 index.
Recognition of the leukemic non-nodal MCL immunophenotype enables it to be differentiated from other CD5-positive B-cell cancers, particularly classical MCL and chronic lymphocytic leukemia (CLL). The overexpression of cyclin D1, the presence of the t(11;14) translocation, and the absence of chromosomal markers typically present in CLL differentiate leukemic non-nodal MCL from CLL. Moreover, CLL has high expression of CD23 and is negative for SOX11 and CD200.
Pathologic features of MCL include small- to medium-size lymphocytes with scant cytoplasm, clumped chromatin, inconspicuous nucleoli, and prominent nuclear clefts. Observed growth patterns include diffuse, nodular (more vague and less discrete than that found in follicular lymphomas), mantle-zone lymphoma with expansion of mantle zones, and in situ mantle-cell neoplasia [typical cells with the characteristic t(11;14) translocation, scattered in the mantle zone of otherwise normal-appearing lymph nodes]. Cytologic subtypes include classic MCL, the blastoid subtype (large cells, dispersed chromatin, and a high mitotic rate), and the pleomorphic subtype (cells of variable sizes, although many are large, with pale cytoplasm, oval irregular nuclei, and prominent nucleoli).
MCL is a challenging disease to treat. Despite treatment advances, it is largely incurable, with a median overall survival of 1.8-9.4 years, depending on whether it is aggressive or indolent MCL. The aggressiveness of the disease, the patient's performance status, age, and mantle cell international prognostic index score should all be considered when selecting treatment because there is no standard curative treatment.
According to the 2023 guidelines from the National Comprehensive Cancer Network (NCCN), for patients with indolent disease (eg, IGHV mutated and mostly SOX11-negative with leukemic and non-nodal presentation), observation is reasonable when patients are asymptomatic and have no indications for treatment. For patients with symptomatic disease or other indications for treatment, induction therapy with aggressive regimens is recommended when patients do not have a TP53 mutation. The optimum approach for patients with TP53 mutation is not yet known; induction therapy followed by high-dose therapy with autologous stem cell transplant or less aggressive regimens could be an option for these patients.
Treatment options for relapsed/refractory MCL include radiotherapy; traditional chemotherapy regimens, with or without rituximab; and newer targeted therapies. These include Bruton tyrosine kinase inhibitors (ibrutinib, zanubrutinib, acalabrutinib, pirtobrutinib), lenalidomide, bortezomib, the mammalian target of rapamycin inhibitors temsirolimus and everolimus, the phosphatidylinositol 3–kinase inhibitors idelalisib and umbralisib, and the B-cell lymphoma 2 inhibitor venetoclax. These agents are frequently administered in combination with rituximab or another anti-CD20 antibody.
For comprehensive guidance on the treatment of MCL, consult the complete NCCN guidelines.
Timothy J. Voorhees, MD, MSCR, Assistant Professor of Internal Medicine - Clinical, Division of Hematology, The Ohio State University James Comprehensive Cancer Center, Columbus, OH.
Timothy J. Voorhees, MD, MSCR, has disclosed the following relevant financial relationships:
Received research grant from: AstraZeneca; Morphosys; Incyte; Recordati.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The history and findings in this case are suggestive of leukemic non-nodal mantle cell lymphoma (MCL).
MCL is a rare mature B-cell neoplasm characterized by t(11;14) (q13;q32) and cyclin D1 overexpression in more than 95% of cases. It accounts for approximately 5%-7% of all lymphomas, with an annual incidence of one case per 200,000 people. In North America and Europe, the incidence of MCL is like that of noncutaneous peripheral T-cell lymphomas. MCL occurs more frequently in men than in women (3:1), and the median age at diagnosis ranges from ages 60-70 years.
In recent years, MCL has been categorized into two major subgroups that have distinct clinical presentation and molecular features: nodal MCL and leukemic non-nodal MCL. Nodal MCL is a common variant with an aggressive disease course. Unmutated IGHV gene rearrangement, SOX11 overexpression, a higher degree of genomic instability (eg, ATM, CDKN2A, chromatin modifier mutations), and other oncogenic mutations and epigenetic modifications are seen in patients with this variant.
Leukemic non-nodal MCL is seen in 10%-20% of patients with MCL. Patients frequently present with lymphocytosis and splenomegaly. In most cases, it is associated with an indolent disease course and superior outcome. This subtype is largely IGHV mutated and mostly SOX11-negative, with positive expression of CD200, peripheral blood, bone marrow, and splenic involvement, low tumor burden, and a low Ki-67 index.
Recognition of the leukemic non-nodal MCL immunophenotype enables it to be differentiated from other CD5-positive B-cell cancers, particularly classical MCL and chronic lymphocytic leukemia (CLL). The overexpression of cyclin D1, the presence of the t(11;14) translocation, and the absence of chromosomal markers typically present in CLL differentiate leukemic non-nodal MCL from CLL. Moreover, CLL has high expression of CD23 and is negative for SOX11 and CD200.
Pathologic features of MCL include small- to medium-size lymphocytes with scant cytoplasm, clumped chromatin, inconspicuous nucleoli, and prominent nuclear clefts. Observed growth patterns include diffuse, nodular (more vague and less discrete than that found in follicular lymphomas), mantle-zone lymphoma with expansion of mantle zones, and in situ mantle-cell neoplasia [typical cells with the characteristic t(11;14) translocation, scattered in the mantle zone of otherwise normal-appearing lymph nodes]. Cytologic subtypes include classic MCL, the blastoid subtype (large cells, dispersed chromatin, and a high mitotic rate), and the pleomorphic subtype (cells of variable sizes, although many are large, with pale cytoplasm, oval irregular nuclei, and prominent nucleoli).
MCL is a challenging disease to treat. Despite treatment advances, it is largely incurable, with a median overall survival of 1.8-9.4 years, depending on whether it is aggressive or indolent MCL. The aggressiveness of the disease, the patient's performance status, age, and mantle cell international prognostic index score should all be considered when selecting treatment because there is no standard curative treatment.
According to the 2023 guidelines from the National Comprehensive Cancer Network (NCCN), for patients with indolent disease (eg, IGHV mutated and mostly SOX11-negative with leukemic and non-nodal presentation), observation is reasonable when patients are asymptomatic and have no indications for treatment. For patients with symptomatic disease or other indications for treatment, induction therapy with aggressive regimens is recommended when patients do not have a TP53 mutation. The optimum approach for patients with TP53 mutation is not yet known; induction therapy followed by high-dose therapy with autologous stem cell transplant or less aggressive regimens could be an option for these patients.
Treatment options for relapsed/refractory MCL include radiotherapy; traditional chemotherapy regimens, with or without rituximab; and newer targeted therapies. These include Bruton tyrosine kinase inhibitors (ibrutinib, zanubrutinib, acalabrutinib, pirtobrutinib), lenalidomide, bortezomib, the mammalian target of rapamycin inhibitors temsirolimus and everolimus, the phosphatidylinositol 3–kinase inhibitors idelalisib and umbralisib, and the B-cell lymphoma 2 inhibitor venetoclax. These agents are frequently administered in combination with rituximab or another anti-CD20 antibody.
For comprehensive guidance on the treatment of MCL, consult the complete NCCN guidelines.
Timothy J. Voorhees, MD, MSCR, Assistant Professor of Internal Medicine - Clinical, Division of Hematology, The Ohio State University James Comprehensive Cancer Center, Columbus, OH.
Timothy J. Voorhees, MD, MSCR, has disclosed the following relevant financial relationships:
Received research grant from: AstraZeneca; Morphosys; Incyte; Recordati.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The history and findings in this case are suggestive of leukemic non-nodal mantle cell lymphoma (MCL).
MCL is a rare mature B-cell neoplasm characterized by t(11;14) (q13;q32) and cyclin D1 overexpression in more than 95% of cases. It accounts for approximately 5%-7% of all lymphomas, with an annual incidence of one case per 200,000 people. In North America and Europe, the incidence of MCL is like that of noncutaneous peripheral T-cell lymphomas. MCL occurs more frequently in men than in women (3:1), and the median age at diagnosis ranges from ages 60-70 years.
In recent years, MCL has been categorized into two major subgroups that have distinct clinical presentation and molecular features: nodal MCL and leukemic non-nodal MCL. Nodal MCL is a common variant with an aggressive disease course. Unmutated IGHV gene rearrangement, SOX11 overexpression, a higher degree of genomic instability (eg, ATM, CDKN2A, chromatin modifier mutations), and other oncogenic mutations and epigenetic modifications are seen in patients with this variant.
Leukemic non-nodal MCL is seen in 10%-20% of patients with MCL. Patients frequently present with lymphocytosis and splenomegaly. In most cases, it is associated with an indolent disease course and superior outcome. This subtype is largely IGHV mutated and mostly SOX11-negative, with positive expression of CD200, peripheral blood, bone marrow, and splenic involvement, low tumor burden, and a low Ki-67 index.
Recognition of the leukemic non-nodal MCL immunophenotype enables it to be differentiated from other CD5-positive B-cell cancers, particularly classical MCL and chronic lymphocytic leukemia (CLL). The overexpression of cyclin D1, the presence of the t(11;14) translocation, and the absence of chromosomal markers typically present in CLL differentiate leukemic non-nodal MCL from CLL. Moreover, CLL has high expression of CD23 and is negative for SOX11 and CD200.
Pathologic features of MCL include small- to medium-size lymphocytes with scant cytoplasm, clumped chromatin, inconspicuous nucleoli, and prominent nuclear clefts. Observed growth patterns include diffuse, nodular (more vague and less discrete than that found in follicular lymphomas), mantle-zone lymphoma with expansion of mantle zones, and in situ mantle-cell neoplasia [typical cells with the characteristic t(11;14) translocation, scattered in the mantle zone of otherwise normal-appearing lymph nodes]. Cytologic subtypes include classic MCL, the blastoid subtype (large cells, dispersed chromatin, and a high mitotic rate), and the pleomorphic subtype (cells of variable sizes, although many are large, with pale cytoplasm, oval irregular nuclei, and prominent nucleoli).
MCL is a challenging disease to treat. Despite treatment advances, it is largely incurable, with a median overall survival of 1.8-9.4 years, depending on whether it is aggressive or indolent MCL. The aggressiveness of the disease, the patient's performance status, age, and mantle cell international prognostic index score should all be considered when selecting treatment because there is no standard curative treatment.
According to the 2023 guidelines from the National Comprehensive Cancer Network (NCCN), for patients with indolent disease (eg, IGHV mutated and mostly SOX11-negative with leukemic and non-nodal presentation), observation is reasonable when patients are asymptomatic and have no indications for treatment. For patients with symptomatic disease or other indications for treatment, induction therapy with aggressive regimens is recommended when patients do not have a TP53 mutation. The optimum approach for patients with TP53 mutation is not yet known; induction therapy followed by high-dose therapy with autologous stem cell transplant or less aggressive regimens could be an option for these patients.
Treatment options for relapsed/refractory MCL include radiotherapy; traditional chemotherapy regimens, with or without rituximab; and newer targeted therapies. These include Bruton tyrosine kinase inhibitors (ibrutinib, zanubrutinib, acalabrutinib, pirtobrutinib), lenalidomide, bortezomib, the mammalian target of rapamycin inhibitors temsirolimus and everolimus, the phosphatidylinositol 3–kinase inhibitors idelalisib and umbralisib, and the B-cell lymphoma 2 inhibitor venetoclax. These agents are frequently administered in combination with rituximab or another anti-CD20 antibody.
For comprehensive guidance on the treatment of MCL, consult the complete NCCN guidelines.
Timothy J. Voorhees, MD, MSCR, Assistant Professor of Internal Medicine - Clinical, Division of Hematology, The Ohio State University James Comprehensive Cancer Center, Columbus, OH.
Timothy J. Voorhees, MD, MSCR, has disclosed the following relevant financial relationships:
Received research grant from: AstraZeneca; Morphosys; Incyte; Recordati.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 67-year-old White man presents for his annual physical examination. The patient is a physical therapist and reports regular exercise and adherence to a healthy diet. His previous medical history is unremarkable. There is a family history of non-Hodgkin lymphoma (paternal uncle). The patient has no complaints or concerns about his health.
Physical examination reveals non-tender abdominal distention and splenomegaly. Pertinent laboratory findings include hemoglobin = 10/g/dL; red blood cell = 3.28 M/mcL; mean corpuscular volume = 54.2 fL, hematocrit = 34%; and absolute lymphocyte count = 4820/µL.
Flow cytometry showed high positivity for CD5, no expression of SOX11, low expression of CD23 and CD200, and overexpression of cyclin D1. A bone marrow biopsy is performed and show an abnormal B-lymphoid infiltrate. Fluorescence in situ hybridization analysis revealed t(11;14)(q13;q32) and mutated IGHV. A blood smear showed abnormal mononuclear cells and atypical lymphocytes.
Upadacitinib shows promise in treatment-resistant UC and Crohn’s
according to results from a real-world study at a Chicago treatment center.
The results suggest that upadacitinib may be an appropriate salvage treatment for patients who have failed other advanced therapies, including tofacitinib.
For their research, published in Clinical Gastroenterology and Hepatology, Scott Friedberg, MD, and colleagues at the University of Chicago’s Inflammatory Bowel Disease Center, looked at results from 44 patients diagnosed with ulcerative colitis and 40 with Crohn’s disease, all with active luminal or perianal disease. All patients in the study had previous exposure to tumor necrosis factor inhibitors, and nearly 90% had exposure to two or more advanced therapies, including tofacitinib (n = 17), before being switched to upadacitinib.
Upadacitinib (Rinvoq, AbbVie) is the second small-molecule Janus kinase (JAK) inhibitor approved for ulcerative colitis by the Food and Drug Administration in March 2022 after tofacitinib (Xeljanz, Pfizer) in 2018. Upadacitinib received an additional indication in May 2023 as a treatment for Crohn’s disease. It selectively inhibits JAK1, while tofacitinib inhibits JAK1 and JAK3.
Among the ulcerative colitis patients in Dr. Friedberg and colleagues’ study (mean age, 39 years; 48% female), 85% had a clinical response and 82% achieved clinical remission by week 8. Of nine patients previously treated with tofacitinib, seven (78%) achieved remission at 8 weeks.
Some 76% of the Crohn’s disease patients in the study (mean age, 37 years; 53% female) saw clinical response by 8 weeks, and 71% achieved remission by that time. More than 60% of all participants who had increased fecal calprotectin and C-reactive protein levels at baseline saw normalization of these biomarkers by week 8.
Some patients saw an especially fast response, with 36% of the ulcerative colitis patients and 56% of the Crohn’s patients experiencing clinical remission by week 2.
Acne was the most common reported adverse event, occurring in 23% of patients. Only one serious adverse event, an anemia requiring hospitalization, occurred during the study.
No wash-out period occurred before starting patients on upadacitinib. There were no adverse events seen associated with this strategy, Dr. Friedberg and colleagues noted, a finding with important implications for real-world practice.
“When patients with active IBD are sick, starting a new therapy as soon as it is available is not only reasonable, it is required,” the investigators wrote. Additionally, the findings support the use of upadacitinib in ulcerative colitis patients with previous exposure to tofacitinib, as “selectivity of JAK targets may have different effectiveness profiles.”
Upadacitinib’s rapid onset “has multiple advantages,” the investigators wrote, “not only by being an option for severely active disease but also by allowing for a rapid taper or complete avoidance of corticosteroids.”
The authors noted their study’s small sample size as a key limitation. Several of Dr. Friedberg’s coauthors disclosed financial relationships with drug manufacturers, including AbbVie.
Understanding the efficacy, onset of action and safety of newly approved inflammatory bowel disease (IBD) therapies is difficult in the absence of real-world data as clinical trial populations are much more restrictive and typically do not reflect the patient populations seen in most IBD clinics. This single-center study by Friedberg and colleagues reports on their experience with upadacitinib use in patients with ulcerative colitis (UC) and Crohn’s disease (CD). One key finding of this study is the rapid onset of action with high rates of clinical response and remission within 2 weeks of initiation (60% and 36%) for UC and (50% and 56%) for CD. Further, these high rates of clinical response and remission were noted despite exposure to multiple prior therapies (including prior tofacitinib use), which has been a limitation with other IBD therapies.
With the concerns for safety of tofacitinib use, another Janus kinase inhibitor, raised by the ORAL surveillance study, many patients and practitioners are concerned about the safety of upadacitinib use. This study highlighted the low rate of adverse events including no incidences of herpes zoster infection, venous thromboembolism or major adverse cardiovascular events. Acne was noted to be the most common adverse event, occurring in 22% of the study population.
Further research is needed to assess the long term clinical and endoscopic response rates as well as long-term safety assessments, however these results will facilitate conversations with patients who could potentially benefit from treatment with this new therapy.
Jill K. J. Gaidos, MD, FACG, AGAF, is associate professor of medicine, vice chief of clinical research, section of digestive diseases, Yale University, and director of clinical research, Yale Inflammatory Bowel Disease Program, New Haven, Conn.
Understanding the efficacy, onset of action and safety of newly approved inflammatory bowel disease (IBD) therapies is difficult in the absence of real-world data as clinical trial populations are much more restrictive and typically do not reflect the patient populations seen in most IBD clinics. This single-center study by Friedberg and colleagues reports on their experience with upadacitinib use in patients with ulcerative colitis (UC) and Crohn’s disease (CD). One key finding of this study is the rapid onset of action with high rates of clinical response and remission within 2 weeks of initiation (60% and 36%) for UC and (50% and 56%) for CD. Further, these high rates of clinical response and remission were noted despite exposure to multiple prior therapies (including prior tofacitinib use), which has been a limitation with other IBD therapies.
With the concerns for safety of tofacitinib use, another Janus kinase inhibitor, raised by the ORAL surveillance study, many patients and practitioners are concerned about the safety of upadacitinib use. This study highlighted the low rate of adverse events including no incidences of herpes zoster infection, venous thromboembolism or major adverse cardiovascular events. Acne was noted to be the most common adverse event, occurring in 22% of the study population.
Further research is needed to assess the long term clinical and endoscopic response rates as well as long-term safety assessments, however these results will facilitate conversations with patients who could potentially benefit from treatment with this new therapy.
Jill K. J. Gaidos, MD, FACG, AGAF, is associate professor of medicine, vice chief of clinical research, section of digestive diseases, Yale University, and director of clinical research, Yale Inflammatory Bowel Disease Program, New Haven, Conn.
Understanding the efficacy, onset of action and safety of newly approved inflammatory bowel disease (IBD) therapies is difficult in the absence of real-world data as clinical trial populations are much more restrictive and typically do not reflect the patient populations seen in most IBD clinics. This single-center study by Friedberg and colleagues reports on their experience with upadacitinib use in patients with ulcerative colitis (UC) and Crohn’s disease (CD). One key finding of this study is the rapid onset of action with high rates of clinical response and remission within 2 weeks of initiation (60% and 36%) for UC and (50% and 56%) for CD. Further, these high rates of clinical response and remission were noted despite exposure to multiple prior therapies (including prior tofacitinib use), which has been a limitation with other IBD therapies.
With the concerns for safety of tofacitinib use, another Janus kinase inhibitor, raised by the ORAL surveillance study, many patients and practitioners are concerned about the safety of upadacitinib use. This study highlighted the low rate of adverse events including no incidences of herpes zoster infection, venous thromboembolism or major adverse cardiovascular events. Acne was noted to be the most common adverse event, occurring in 22% of the study population.
Further research is needed to assess the long term clinical and endoscopic response rates as well as long-term safety assessments, however these results will facilitate conversations with patients who could potentially benefit from treatment with this new therapy.
Jill K. J. Gaidos, MD, FACG, AGAF, is associate professor of medicine, vice chief of clinical research, section of digestive diseases, Yale University, and director of clinical research, Yale Inflammatory Bowel Disease Program, New Haven, Conn.
according to results from a real-world study at a Chicago treatment center.
The results suggest that upadacitinib may be an appropriate salvage treatment for patients who have failed other advanced therapies, including tofacitinib.
For their research, published in Clinical Gastroenterology and Hepatology, Scott Friedberg, MD, and colleagues at the University of Chicago’s Inflammatory Bowel Disease Center, looked at results from 44 patients diagnosed with ulcerative colitis and 40 with Crohn’s disease, all with active luminal or perianal disease. All patients in the study had previous exposure to tumor necrosis factor inhibitors, and nearly 90% had exposure to two or more advanced therapies, including tofacitinib (n = 17), before being switched to upadacitinib.
Upadacitinib (Rinvoq, AbbVie) is the second small-molecule Janus kinase (JAK) inhibitor approved for ulcerative colitis by the Food and Drug Administration in March 2022 after tofacitinib (Xeljanz, Pfizer) in 2018. Upadacitinib received an additional indication in May 2023 as a treatment for Crohn’s disease. It selectively inhibits JAK1, while tofacitinib inhibits JAK1 and JAK3.
Among the ulcerative colitis patients in Dr. Friedberg and colleagues’ study (mean age, 39 years; 48% female), 85% had a clinical response and 82% achieved clinical remission by week 8. Of nine patients previously treated with tofacitinib, seven (78%) achieved remission at 8 weeks.
Some 76% of the Crohn’s disease patients in the study (mean age, 37 years; 53% female) saw clinical response by 8 weeks, and 71% achieved remission by that time. More than 60% of all participants who had increased fecal calprotectin and C-reactive protein levels at baseline saw normalization of these biomarkers by week 8.
Some patients saw an especially fast response, with 36% of the ulcerative colitis patients and 56% of the Crohn’s patients experiencing clinical remission by week 2.
Acne was the most common reported adverse event, occurring in 23% of patients. Only one serious adverse event, an anemia requiring hospitalization, occurred during the study.
No wash-out period occurred before starting patients on upadacitinib. There were no adverse events seen associated with this strategy, Dr. Friedberg and colleagues noted, a finding with important implications for real-world practice.
“When patients with active IBD are sick, starting a new therapy as soon as it is available is not only reasonable, it is required,” the investigators wrote. Additionally, the findings support the use of upadacitinib in ulcerative colitis patients with previous exposure to tofacitinib, as “selectivity of JAK targets may have different effectiveness profiles.”
Upadacitinib’s rapid onset “has multiple advantages,” the investigators wrote, “not only by being an option for severely active disease but also by allowing for a rapid taper or complete avoidance of corticosteroids.”
The authors noted their study’s small sample size as a key limitation. Several of Dr. Friedberg’s coauthors disclosed financial relationships with drug manufacturers, including AbbVie.
according to results from a real-world study at a Chicago treatment center.
The results suggest that upadacitinib may be an appropriate salvage treatment for patients who have failed other advanced therapies, including tofacitinib.
For their research, published in Clinical Gastroenterology and Hepatology, Scott Friedberg, MD, and colleagues at the University of Chicago’s Inflammatory Bowel Disease Center, looked at results from 44 patients diagnosed with ulcerative colitis and 40 with Crohn’s disease, all with active luminal or perianal disease. All patients in the study had previous exposure to tumor necrosis factor inhibitors, and nearly 90% had exposure to two or more advanced therapies, including tofacitinib (n = 17), before being switched to upadacitinib.
Upadacitinib (Rinvoq, AbbVie) is the second small-molecule Janus kinase (JAK) inhibitor approved for ulcerative colitis by the Food and Drug Administration in March 2022 after tofacitinib (Xeljanz, Pfizer) in 2018. Upadacitinib received an additional indication in May 2023 as a treatment for Crohn’s disease. It selectively inhibits JAK1, while tofacitinib inhibits JAK1 and JAK3.
Among the ulcerative colitis patients in Dr. Friedberg and colleagues’ study (mean age, 39 years; 48% female), 85% had a clinical response and 82% achieved clinical remission by week 8. Of nine patients previously treated with tofacitinib, seven (78%) achieved remission at 8 weeks.
Some 76% of the Crohn’s disease patients in the study (mean age, 37 years; 53% female) saw clinical response by 8 weeks, and 71% achieved remission by that time. More than 60% of all participants who had increased fecal calprotectin and C-reactive protein levels at baseline saw normalization of these biomarkers by week 8.
Some patients saw an especially fast response, with 36% of the ulcerative colitis patients and 56% of the Crohn’s patients experiencing clinical remission by week 2.
Acne was the most common reported adverse event, occurring in 23% of patients. Only one serious adverse event, an anemia requiring hospitalization, occurred during the study.
No wash-out period occurred before starting patients on upadacitinib. There were no adverse events seen associated with this strategy, Dr. Friedberg and colleagues noted, a finding with important implications for real-world practice.
“When patients with active IBD are sick, starting a new therapy as soon as it is available is not only reasonable, it is required,” the investigators wrote. Additionally, the findings support the use of upadacitinib in ulcerative colitis patients with previous exposure to tofacitinib, as “selectivity of JAK targets may have different effectiveness profiles.”
Upadacitinib’s rapid onset “has multiple advantages,” the investigators wrote, “not only by being an option for severely active disease but also by allowing for a rapid taper or complete avoidance of corticosteroids.”
The authors noted their study’s small sample size as a key limitation. Several of Dr. Friedberg’s coauthors disclosed financial relationships with drug manufacturers, including AbbVie.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY