User login
A 47-year-old man with chest and neck pain
A 47-year-old man presented with acute shortness of breath and chest and neck pain, which began after he heard popping sounds while boarding a bus. The pain was right-sided, sharp, worse with deep breathing, and associated with a sensation of fullness over the right chest.
His medical conditions included controlled hypertension, gastroesophageal reflux disease, and chronic obstructive pulmonary disease (COPD). The COPD was managed with an albuterol inhaler only. He had a 50-pack-year history of smoking, and he drank alcohol occasionally.
On arrival, he was in mild respiratory distress, but his vital signs were stable. We could hear wheezing on both sides of his chest and feel subcutaneous crepitation on both sides of his chest and neck, the latter more on the right side. The rest of the examination was unremarkable.
Results of a complete blood cell count and metabolic panel were within normal limits. Because of the above findings, nasopharyngeal radiogragraphy was ordered (Figures 1 and 2).
Q: What is the most likely cause of this presentation?
- Esophageal rupture
- Gas gangrene
- Asthma exacerbation
- Ruptured emphysematous bullae
A: This patient had a history of COPD, which put him at risk of developing bullous emphysematous bullae that can rupture and cause subcutaneous emphysema. His nasopharyngeal radiograph (Figure1) showed bilateral extensive subcutaneous emphysema. His lateral nasopharyngeal radiograph (Figure 2) showed air-tracking within the mediastinum and into the retropharyngeal space (arrow). Computed tomography (Figure 3) showed extensive subcutaneous emphysema in the right lateral chest wall (arrow) and large bullae in the right upper lobe (arrow heads). As for the other possibilities:
Esophageal ruptures and tears are iatrogenic in most cases and usually occur after endoscopic procedures, but they can also occur in patients with intractable vomiting. Computed tomography often shows esophageal thickening, periesophageal fluid, mediastinal widening, and extraluminal air. However, in most cases, it is seen as pneumomediastinum and subcutaneous emphysema.1
Gas gangrene is a life-threatening soft-tissue and muscle infection caused by Clostridium perfringens in most cases.2 The pain is out of proportion to the findings on physical examination. Patients usually have toxic signs and symptoms such as fever and hypotension. Our patient was hemodynamically stable, with no changes in skin color.
Severe exacerbations of asthma can lead to alveolar rupture, pneumothorax, and subcutaneous emphysema, although this is a rare complication. Air can dissect along the bronchovascular sheaths into the neck and cause subcutaneous emphysema, or into the pleural space and cause pneumothorax. Our patient had no history of asthma and plainly had emphysematous bullae.3
SUBCUTANEOUS EMPHYSEMA
Subcutaneous emphysema is a collection of air within subcutaneous tissues. It usually presents as bloating of the skin around the neck and the chest wall. It is often seen in patients with pneumothorax.
The most common cause of subcutaneous emphysema is traumatic injury to the chest wall, such as from a motor vehicle accident or a stab wound,4 but it can also occur spontaneously in patients who have severe emphysema with large bullae. As the emphysema progresses, the bullae can easily rupture, and this can lead to pneumothorax, which can lead to subcutaneous emphysema. Primary spontaneous pneumothorax and subcutaneous emphysema can occur in people who have unrecognized lung disease and genetic disorders such as Marfan syndrome and Ehler-Danlos syndrome.5 Other causes include iatrogenic injury, Pneumocystis jirovecii pneumonia (common in patients with human immunodeficiency virus infection), and cystic fibrosis. Pneumothorax occurs in about 30% of cases of P jirovecii pneumonia,6 and in about 6% of patients with cystic fibrosis.7 Bronchocutaneous fistula is an extremely rare complication of lung cancer and can cause subcutaneous emphysema.8 Tuberculosis is another possible cause.9
Subcutaneous emphysema mainly presents with chest or neck pain and wheezing. In severe cases, air can track to the face, causing facial swelling and difficulty breathing due to compression of the larynx. Also, it can track down to the thighs, causing leg pain and swelling.10
On examination, subcutaneous emphysema can be detected by palpating the chest wall, which causes the air bubble to move and produce crackling sounds. Most cases of subcutaneous emphysema are diagnosed clinically. Chest radiography and computed tomography help identify the source of air leak. Ultrasonography is usually used in cases of blunt trauma to the chest as part of the Focal Assessment With Sonography for Trauma protocol.11
Subcutaneous emphysema can resolve spontaneously, requiring only pain management and supplemental oxygen.12 In severe cases, air collection can lead to what is called “massive subcutaneous emphysema,” which requires surgical drainage.
Our patient had large emphysematous bullae in the apical region of the right lung that ruptured and led to subcutaneous emphysema. After placement of a chest tube, he underwent right-sided thoracotomy with bullectomy. His postoperative course was uneventful, and he was discharged a few days later. Three weeks later, repeated chest radiography showed resolution of his subcutaneous emphysema (Figure 4).
- White CS, Templeton PA, Attar S. Esophageal perforation: CT findings. AJR Am J Roentgenol 1993; 160:767–770.
- Aggelidakis J, Lasithiotakis K, Topalidou A, Koutroumpas J, Kouvidis G, Katonis P. Limb salvage after gas gangrene: a case report and review of the literature. World J Emerg Surg 2011; 6:28.
- Romero KJ, Trujillo MH. Spontaneous pneumomediastinum and subcutaneous emphysema in asthma exacerbation: the Macklin effect. Heart Lung 2010; 39:444–447.
- Peart O. Subcutaneous emphysema. Radiol Technol 2006; 77:296.
- Chiu HT, Garcia CK. Familial spontaneous pneumothorax. Curr Opin Pulm Med 2006; 12:268–272.
- Sepkowitz KA, Telzak EE, Gold JW, et al. Pneumothorax in AIDS. Ann Intern Med 1991; 114:455–459.
- Flume PA, Strange C, Ye X, Ebeling M, Hulsey T, Clark LL. Pneumothorax in cystic fibrosis. Chest 2005; 128:720–728.
- Yalçinkaya S, Vural AH, Göncü MT, Özyazicioglu AF. Cavitary lung cancer presenting as subcutaneous emphysema on the contralateral side. Interact Cardiovasc Thorac Surg 2012; 14:338–339.
- Shamaei M, Tabarsi P, Pojhan S, et al. Tuberculosis-associated secondary pneumothorax: a retrospective study of 53 patients. Respir Care 2011; 56:298–302.
- Sherif HM, Ott DA. The use of subcutaneous drains to manage subcutaneous emphysema. Tex Heart Inst J 1999; 26:129–131.
- Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med 2010; 17:11–17.
- Mattox KL, Allen MK. Systematic approach to pneumothorax, haemothorax, pneumomediastinum and subcutaneous emphysema. Injury 1986; 17:309–312.
A 47-year-old man presented with acute shortness of breath and chest and neck pain, which began after he heard popping sounds while boarding a bus. The pain was right-sided, sharp, worse with deep breathing, and associated with a sensation of fullness over the right chest.
His medical conditions included controlled hypertension, gastroesophageal reflux disease, and chronic obstructive pulmonary disease (COPD). The COPD was managed with an albuterol inhaler only. He had a 50-pack-year history of smoking, and he drank alcohol occasionally.
On arrival, he was in mild respiratory distress, but his vital signs were stable. We could hear wheezing on both sides of his chest and feel subcutaneous crepitation on both sides of his chest and neck, the latter more on the right side. The rest of the examination was unremarkable.
Results of a complete blood cell count and metabolic panel were within normal limits. Because of the above findings, nasopharyngeal radiogragraphy was ordered (Figures 1 and 2).
Q: What is the most likely cause of this presentation?
- Esophageal rupture
- Gas gangrene
- Asthma exacerbation
- Ruptured emphysematous bullae
A: This patient had a history of COPD, which put him at risk of developing bullous emphysematous bullae that can rupture and cause subcutaneous emphysema. His nasopharyngeal radiograph (Figure1) showed bilateral extensive subcutaneous emphysema. His lateral nasopharyngeal radiograph (Figure 2) showed air-tracking within the mediastinum and into the retropharyngeal space (arrow). Computed tomography (Figure 3) showed extensive subcutaneous emphysema in the right lateral chest wall (arrow) and large bullae in the right upper lobe (arrow heads). As for the other possibilities:
Esophageal ruptures and tears are iatrogenic in most cases and usually occur after endoscopic procedures, but they can also occur in patients with intractable vomiting. Computed tomography often shows esophageal thickening, periesophageal fluid, mediastinal widening, and extraluminal air. However, in most cases, it is seen as pneumomediastinum and subcutaneous emphysema.1
Gas gangrene is a life-threatening soft-tissue and muscle infection caused by Clostridium perfringens in most cases.2 The pain is out of proportion to the findings on physical examination. Patients usually have toxic signs and symptoms such as fever and hypotension. Our patient was hemodynamically stable, with no changes in skin color.
Severe exacerbations of asthma can lead to alveolar rupture, pneumothorax, and subcutaneous emphysema, although this is a rare complication. Air can dissect along the bronchovascular sheaths into the neck and cause subcutaneous emphysema, or into the pleural space and cause pneumothorax. Our patient had no history of asthma and plainly had emphysematous bullae.3
SUBCUTANEOUS EMPHYSEMA
Subcutaneous emphysema is a collection of air within subcutaneous tissues. It usually presents as bloating of the skin around the neck and the chest wall. It is often seen in patients with pneumothorax.
The most common cause of subcutaneous emphysema is traumatic injury to the chest wall, such as from a motor vehicle accident or a stab wound,4 but it can also occur spontaneously in patients who have severe emphysema with large bullae. As the emphysema progresses, the bullae can easily rupture, and this can lead to pneumothorax, which can lead to subcutaneous emphysema. Primary spontaneous pneumothorax and subcutaneous emphysema can occur in people who have unrecognized lung disease and genetic disorders such as Marfan syndrome and Ehler-Danlos syndrome.5 Other causes include iatrogenic injury, Pneumocystis jirovecii pneumonia (common in patients with human immunodeficiency virus infection), and cystic fibrosis. Pneumothorax occurs in about 30% of cases of P jirovecii pneumonia,6 and in about 6% of patients with cystic fibrosis.7 Bronchocutaneous fistula is an extremely rare complication of lung cancer and can cause subcutaneous emphysema.8 Tuberculosis is another possible cause.9
Subcutaneous emphysema mainly presents with chest or neck pain and wheezing. In severe cases, air can track to the face, causing facial swelling and difficulty breathing due to compression of the larynx. Also, it can track down to the thighs, causing leg pain and swelling.10
On examination, subcutaneous emphysema can be detected by palpating the chest wall, which causes the air bubble to move and produce crackling sounds. Most cases of subcutaneous emphysema are diagnosed clinically. Chest radiography and computed tomography help identify the source of air leak. Ultrasonography is usually used in cases of blunt trauma to the chest as part of the Focal Assessment With Sonography for Trauma protocol.11
Subcutaneous emphysema can resolve spontaneously, requiring only pain management and supplemental oxygen.12 In severe cases, air collection can lead to what is called “massive subcutaneous emphysema,” which requires surgical drainage.
Our patient had large emphysematous bullae in the apical region of the right lung that ruptured and led to subcutaneous emphysema. After placement of a chest tube, he underwent right-sided thoracotomy with bullectomy. His postoperative course was uneventful, and he was discharged a few days later. Three weeks later, repeated chest radiography showed resolution of his subcutaneous emphysema (Figure 4).
A 47-year-old man presented with acute shortness of breath and chest and neck pain, which began after he heard popping sounds while boarding a bus. The pain was right-sided, sharp, worse with deep breathing, and associated with a sensation of fullness over the right chest.
His medical conditions included controlled hypertension, gastroesophageal reflux disease, and chronic obstructive pulmonary disease (COPD). The COPD was managed with an albuterol inhaler only. He had a 50-pack-year history of smoking, and he drank alcohol occasionally.
On arrival, he was in mild respiratory distress, but his vital signs were stable. We could hear wheezing on both sides of his chest and feel subcutaneous crepitation on both sides of his chest and neck, the latter more on the right side. The rest of the examination was unremarkable.
Results of a complete blood cell count and metabolic panel were within normal limits. Because of the above findings, nasopharyngeal radiogragraphy was ordered (Figures 1 and 2).
Q: What is the most likely cause of this presentation?
- Esophageal rupture
- Gas gangrene
- Asthma exacerbation
- Ruptured emphysematous bullae
A: This patient had a history of COPD, which put him at risk of developing bullous emphysematous bullae that can rupture and cause subcutaneous emphysema. His nasopharyngeal radiograph (Figure1) showed bilateral extensive subcutaneous emphysema. His lateral nasopharyngeal radiograph (Figure 2) showed air-tracking within the mediastinum and into the retropharyngeal space (arrow). Computed tomography (Figure 3) showed extensive subcutaneous emphysema in the right lateral chest wall (arrow) and large bullae in the right upper lobe (arrow heads). As for the other possibilities:
Esophageal ruptures and tears are iatrogenic in most cases and usually occur after endoscopic procedures, but they can also occur in patients with intractable vomiting. Computed tomography often shows esophageal thickening, periesophageal fluid, mediastinal widening, and extraluminal air. However, in most cases, it is seen as pneumomediastinum and subcutaneous emphysema.1
Gas gangrene is a life-threatening soft-tissue and muscle infection caused by Clostridium perfringens in most cases.2 The pain is out of proportion to the findings on physical examination. Patients usually have toxic signs and symptoms such as fever and hypotension. Our patient was hemodynamically stable, with no changes in skin color.
Severe exacerbations of asthma can lead to alveolar rupture, pneumothorax, and subcutaneous emphysema, although this is a rare complication. Air can dissect along the bronchovascular sheaths into the neck and cause subcutaneous emphysema, or into the pleural space and cause pneumothorax. Our patient had no history of asthma and plainly had emphysematous bullae.3
SUBCUTANEOUS EMPHYSEMA
Subcutaneous emphysema is a collection of air within subcutaneous tissues. It usually presents as bloating of the skin around the neck and the chest wall. It is often seen in patients with pneumothorax.
The most common cause of subcutaneous emphysema is traumatic injury to the chest wall, such as from a motor vehicle accident or a stab wound,4 but it can also occur spontaneously in patients who have severe emphysema with large bullae. As the emphysema progresses, the bullae can easily rupture, and this can lead to pneumothorax, which can lead to subcutaneous emphysema. Primary spontaneous pneumothorax and subcutaneous emphysema can occur in people who have unrecognized lung disease and genetic disorders such as Marfan syndrome and Ehler-Danlos syndrome.5 Other causes include iatrogenic injury, Pneumocystis jirovecii pneumonia (common in patients with human immunodeficiency virus infection), and cystic fibrosis. Pneumothorax occurs in about 30% of cases of P jirovecii pneumonia,6 and in about 6% of patients with cystic fibrosis.7 Bronchocutaneous fistula is an extremely rare complication of lung cancer and can cause subcutaneous emphysema.8 Tuberculosis is another possible cause.9
Subcutaneous emphysema mainly presents with chest or neck pain and wheezing. In severe cases, air can track to the face, causing facial swelling and difficulty breathing due to compression of the larynx. Also, it can track down to the thighs, causing leg pain and swelling.10
On examination, subcutaneous emphysema can be detected by palpating the chest wall, which causes the air bubble to move and produce crackling sounds. Most cases of subcutaneous emphysema are diagnosed clinically. Chest radiography and computed tomography help identify the source of air leak. Ultrasonography is usually used in cases of blunt trauma to the chest as part of the Focal Assessment With Sonography for Trauma protocol.11
Subcutaneous emphysema can resolve spontaneously, requiring only pain management and supplemental oxygen.12 In severe cases, air collection can lead to what is called “massive subcutaneous emphysema,” which requires surgical drainage.
Our patient had large emphysematous bullae in the apical region of the right lung that ruptured and led to subcutaneous emphysema. After placement of a chest tube, he underwent right-sided thoracotomy with bullectomy. His postoperative course was uneventful, and he was discharged a few days later. Three weeks later, repeated chest radiography showed resolution of his subcutaneous emphysema (Figure 4).
- White CS, Templeton PA, Attar S. Esophageal perforation: CT findings. AJR Am J Roentgenol 1993; 160:767–770.
- Aggelidakis J, Lasithiotakis K, Topalidou A, Koutroumpas J, Kouvidis G, Katonis P. Limb salvage after gas gangrene: a case report and review of the literature. World J Emerg Surg 2011; 6:28.
- Romero KJ, Trujillo MH. Spontaneous pneumomediastinum and subcutaneous emphysema in asthma exacerbation: the Macklin effect. Heart Lung 2010; 39:444–447.
- Peart O. Subcutaneous emphysema. Radiol Technol 2006; 77:296.
- Chiu HT, Garcia CK. Familial spontaneous pneumothorax. Curr Opin Pulm Med 2006; 12:268–272.
- Sepkowitz KA, Telzak EE, Gold JW, et al. Pneumothorax in AIDS. Ann Intern Med 1991; 114:455–459.
- Flume PA, Strange C, Ye X, Ebeling M, Hulsey T, Clark LL. Pneumothorax in cystic fibrosis. Chest 2005; 128:720–728.
- Yalçinkaya S, Vural AH, Göncü MT, Özyazicioglu AF. Cavitary lung cancer presenting as subcutaneous emphysema on the contralateral side. Interact Cardiovasc Thorac Surg 2012; 14:338–339.
- Shamaei M, Tabarsi P, Pojhan S, et al. Tuberculosis-associated secondary pneumothorax: a retrospective study of 53 patients. Respir Care 2011; 56:298–302.
- Sherif HM, Ott DA. The use of subcutaneous drains to manage subcutaneous emphysema. Tex Heart Inst J 1999; 26:129–131.
- Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med 2010; 17:11–17.
- Mattox KL, Allen MK. Systematic approach to pneumothorax, haemothorax, pneumomediastinum and subcutaneous emphysema. Injury 1986; 17:309–312.
- White CS, Templeton PA, Attar S. Esophageal perforation: CT findings. AJR Am J Roentgenol 1993; 160:767–770.
- Aggelidakis J, Lasithiotakis K, Topalidou A, Koutroumpas J, Kouvidis G, Katonis P. Limb salvage after gas gangrene: a case report and review of the literature. World J Emerg Surg 2011; 6:28.
- Romero KJ, Trujillo MH. Spontaneous pneumomediastinum and subcutaneous emphysema in asthma exacerbation: the Macklin effect. Heart Lung 2010; 39:444–447.
- Peart O. Subcutaneous emphysema. Radiol Technol 2006; 77:296.
- Chiu HT, Garcia CK. Familial spontaneous pneumothorax. Curr Opin Pulm Med 2006; 12:268–272.
- Sepkowitz KA, Telzak EE, Gold JW, et al. Pneumothorax in AIDS. Ann Intern Med 1991; 114:455–459.
- Flume PA, Strange C, Ye X, Ebeling M, Hulsey T, Clark LL. Pneumothorax in cystic fibrosis. Chest 2005; 128:720–728.
- Yalçinkaya S, Vural AH, Göncü MT, Özyazicioglu AF. Cavitary lung cancer presenting as subcutaneous emphysema on the contralateral side. Interact Cardiovasc Thorac Surg 2012; 14:338–339.
- Shamaei M, Tabarsi P, Pojhan S, et al. Tuberculosis-associated secondary pneumothorax: a retrospective study of 53 patients. Respir Care 2011; 56:298–302.
- Sherif HM, Ott DA. The use of subcutaneous drains to manage subcutaneous emphysema. Tex Heart Inst J 1999; 26:129–131.
- Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med 2010; 17:11–17.
- Mattox KL, Allen MK. Systematic approach to pneumothorax, haemothorax, pneumomediastinum and subcutaneous emphysema. Injury 1986; 17:309–312.
A guideline is like a prescription
Before we write a prescription, we review the patient’s diagnosis, the known evidence, and our own experience. Then we discuss the risks and benefits with the patient. If he or she chooses to fill the prescription, we are responsible for the outcome. But patients may choose to not take the medication, feeling that the accumulated evidence does not apply to them or not fully understanding the balance of potential benefit and harm.
When a group of expert physicians writes practice guidelines, they review the literature and their own experience and then summarize key practices that they believe should be followed or avoided. These guidelines are offered to practicing physicians to accept or reject. Unlike the physician writing an individual prescription, the authors of the guidelines are not held directly responsible for the outcome in a specific patient.
Guidelines seem to be accepted on an academic level, not as a prescriptive approach to care but as a way of evaluating the relevant evidence and its practical application. But many practicing clinicians fear that guidelines are leading to the algorithmic practice of medicine and to reimbursement according to adherence to the guidelines, regardless of patient outcomes.
In this issue, Roland Moskowitz, an expert in osteoarthritis, comments on the 2012 American College of Rheumatology “recommendations” for the treatment of this disease.1 He notes that these recommendations are not a cookbook, points out areas in which his own practices differ from them, and emphasizes the need to individualize our recommendations. For instance, he notes that some of his patients have relief of pain after hyaluronan injections into their osteoarthritic knees, even though the guidelines do not recommend this therapy1 and structured reviews suggest it has little benefit (in groups of patients) beyond that of placebo injections. This apparent paradox suggests that this therapy is not appropriate for everyone, but also that it should not be removed from our toolkit. Certainly, the patient’s response to an injection (outcome) should be evaluated before repeating this therapy.
We should not worship the idol of guidelines alone, but neither should we ignore them and make decisions only on the basis of anecdote and experience. When making individual treatment decisions, we must assess external validity before applying pooled trial data. And administrators need to understand that clinicians may choose to not follow practice guidelines in individual patients for very valid reasons.
Most studies of the impact of guidelines have focused on how well physicians comply with them, not on patient outcomes. Compliance—of patients with physicians’ advice and of physicians with guidelines—is a complicated process. Compliance should not be considered a cookbook expectation—for patients or for doctors.
- Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of non-pharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012; 64:465–474.
Before we write a prescription, we review the patient’s diagnosis, the known evidence, and our own experience. Then we discuss the risks and benefits with the patient. If he or she chooses to fill the prescription, we are responsible for the outcome. But patients may choose to not take the medication, feeling that the accumulated evidence does not apply to them or not fully understanding the balance of potential benefit and harm.
When a group of expert physicians writes practice guidelines, they review the literature and their own experience and then summarize key practices that they believe should be followed or avoided. These guidelines are offered to practicing physicians to accept or reject. Unlike the physician writing an individual prescription, the authors of the guidelines are not held directly responsible for the outcome in a specific patient.
Guidelines seem to be accepted on an academic level, not as a prescriptive approach to care but as a way of evaluating the relevant evidence and its practical application. But many practicing clinicians fear that guidelines are leading to the algorithmic practice of medicine and to reimbursement according to adherence to the guidelines, regardless of patient outcomes.
In this issue, Roland Moskowitz, an expert in osteoarthritis, comments on the 2012 American College of Rheumatology “recommendations” for the treatment of this disease.1 He notes that these recommendations are not a cookbook, points out areas in which his own practices differ from them, and emphasizes the need to individualize our recommendations. For instance, he notes that some of his patients have relief of pain after hyaluronan injections into their osteoarthritic knees, even though the guidelines do not recommend this therapy1 and structured reviews suggest it has little benefit (in groups of patients) beyond that of placebo injections. This apparent paradox suggests that this therapy is not appropriate for everyone, but also that it should not be removed from our toolkit. Certainly, the patient’s response to an injection (outcome) should be evaluated before repeating this therapy.
We should not worship the idol of guidelines alone, but neither should we ignore them and make decisions only on the basis of anecdote and experience. When making individual treatment decisions, we must assess external validity before applying pooled trial data. And administrators need to understand that clinicians may choose to not follow practice guidelines in individual patients for very valid reasons.
Most studies of the impact of guidelines have focused on how well physicians comply with them, not on patient outcomes. Compliance—of patients with physicians’ advice and of physicians with guidelines—is a complicated process. Compliance should not be considered a cookbook expectation—for patients or for doctors.
Before we write a prescription, we review the patient’s diagnosis, the known evidence, and our own experience. Then we discuss the risks and benefits with the patient. If he or she chooses to fill the prescription, we are responsible for the outcome. But patients may choose to not take the medication, feeling that the accumulated evidence does not apply to them or not fully understanding the balance of potential benefit and harm.
When a group of expert physicians writes practice guidelines, they review the literature and their own experience and then summarize key practices that they believe should be followed or avoided. These guidelines are offered to practicing physicians to accept or reject. Unlike the physician writing an individual prescription, the authors of the guidelines are not held directly responsible for the outcome in a specific patient.
Guidelines seem to be accepted on an academic level, not as a prescriptive approach to care but as a way of evaluating the relevant evidence and its practical application. But many practicing clinicians fear that guidelines are leading to the algorithmic practice of medicine and to reimbursement according to adherence to the guidelines, regardless of patient outcomes.
In this issue, Roland Moskowitz, an expert in osteoarthritis, comments on the 2012 American College of Rheumatology “recommendations” for the treatment of this disease.1 He notes that these recommendations are not a cookbook, points out areas in which his own practices differ from them, and emphasizes the need to individualize our recommendations. For instance, he notes that some of his patients have relief of pain after hyaluronan injections into their osteoarthritic knees, even though the guidelines do not recommend this therapy1 and structured reviews suggest it has little benefit (in groups of patients) beyond that of placebo injections. This apparent paradox suggests that this therapy is not appropriate for everyone, but also that it should not be removed from our toolkit. Certainly, the patient’s response to an injection (outcome) should be evaluated before repeating this therapy.
We should not worship the idol of guidelines alone, but neither should we ignore them and make decisions only on the basis of anecdote and experience. When making individual treatment decisions, we must assess external validity before applying pooled trial data. And administrators need to understand that clinicians may choose to not follow practice guidelines in individual patients for very valid reasons.
Most studies of the impact of guidelines have focused on how well physicians comply with them, not on patient outcomes. Compliance—of patients with physicians’ advice and of physicians with guidelines—is a complicated process. Compliance should not be considered a cookbook expectation—for patients or for doctors.
- Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of non-pharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012; 64:465–474.
- Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of non-pharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012; 64:465–474.
The 2012 ACR guidelines for osteoarthritis: Not a cookbook
“When I see a patient with arthritis coming in the front door, I leave by the back door.”
—Sir William Ostler
Fortunately for today’s physicians treating patients with osteoarthritis, we need not be as pessimistic as Osler was more than a century ago when he uttered his now-famous words. Still, there is no magic bullet for the contemporary clinician treating an elderly patient with osteoarthritis. Instead, there are many imperfect bullets, and choosing between them is always a balancing act between benefit and risk from various agents: nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics such as acetaminophen and tramadol, opioids, and supplements such as glucosamine and chondroitin sulfate.
So there was great interest when, in 2012,1 the American College of Rheumatology (ACR) updated its previous guidelines (from 2000) on drug and nondrug therapies for osteoarthritis of the hip and the knee2 and added new recommendations on osteoarthritis of the hand.
Revising the guidelines was appropriate, since new therapies have become available. But, as the guideline authors state, with osteoarthritis, as with other diseases, guidelines cannot be a “cookbook.”
The treatment approach differs depending on the patient’s clinical presentation and on the preferences of the patient and the physician. Often, more than one approach is possible, and more than one approach may be appropriate in a given patient at a given time. The guideline authors also point out that some physicians may disagree with some of the recommendations.
I wish to review here several of the key recommendations. But I also provide some of my personal perspective and experience after 4 decades of treating patients with osteoarthritis.
HOW THE GUIDELINES WERE MADE
The new ACR guidelines were developed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, a formal process to develop recommendations that are as evidence-based as possible.3
The authors are outstanding experts in the field of osteoarthritis from throughout the United States and Canada. Further, the recommendations were voted on by a “technical expert panel” representing the fields of rheumatology, orthopedics, physical medicine, and rehabilitation, from both academic medicine and private practice. This representation provides a balance of input from the types of clinicians frequently involved in managing osteoarthritis.
The initial literature searches for drug therapies were conducted during late 2008, and those for nonpharmacologic treatments were conducted during the second and third quarters of 2009. The goal of the literature searches was to identify the most current systematic reviews and meta-analyses that would provide reliable estimates of benefits of intervention for the prespecified clinically relevant outcomes of pain and function, as well as data on safety.
Recommendations: For or against, strong or weak—and the informed patient’s perspective
Therapies received the following possible recommendations:
- Strong recommendation to use
- Weak (or conditional) recommendation to use
- No recommendation
- Weak (or conditional) recommendation not to use
- Strong recommendation not to use.
A strong recommendation required high-quality evidence and evidence of a large difference between desirable and undesirable effects of the treatment. A conditional recommendation was based on the absence of high-quality evidence, evidence of only a small difference between desirable and undesirable effects of the treatment, or both.
One interesting feature of these recommendations is that they took into account how informed patients might themselves evaluate the data with their medical condition.
For instance, if a therapy received a strong favorable recommendation, we can assume that most informed patients would choose to receive it, and we can shape our interaction with the patient accordingly. A conditional recommendation means that most informed patients would choose the treatment—but many would not, and physicians should keep the patient’s values and preferences in mind.
I admit I had a problem with the meaning of the word “conditional” in the context of these guidelines. When evaluating a treatment, the term “weak” is readily understood and clearer. By using the word “weak,” one is making a positive statement in support of use but letting you know that the data and recommendation are weak. The word “conditional” is less readily defined and does not necessarily imply support for use.
Recommendations were drafted after discussion of the evidence at each meeting of the technical expert panel. Consensus was defined as 75% or more of the members of the panel voting to either strongly or conditionally recommend using a therapy, to either strongly or conditionally recommend not using it, or to choose not to make a recommendation on its use.
OSTEOARTHRITIS OF THE HAND: NO STRONG RECOMMENDATIONS
The technical expert panel gave no strong recommendations for any nondrug or drug treatment for osteoarthritis of the hand.
Conditional recommendations for nondrug treatments
The panel conditionally recommended the following:
- All patients with osteoarthritis of the hand should be evaluated either by their primary physician or by an occupational or physical therapist, particularly with respect to ability to perform activities of daily living.
- Assistive devices such as jar openers, key turners, and pull tabs for zippers should be recommended, as needed.
- Patients should be instructed in joint protection and in the use of thermal treatments (eg, heating pads, ultrasound devices, hot packs, and ice packs).
Comments. Appliances are often beneficial in patients who have involvement of the first carpometacarpal (trapeziometacarpal) joint. Although over-the-counter thumb splints are an option, referral to an occupational therapist for splint prescription is advantageous to achieve a comfortable fit and, importantly, for instructions to the patient on how to avoid joint trauma.
It would be unrealistic to expect primary care physicians and internists to have the expertise to make detailed recommendations about orthopedic appliances. Accordingly, referral to an occupational therapist or an orthopedist is advisable for these situations. It is important, however, that the physician be aware of what treatments are available and most effective, and of the indications for referral.
As for heat treatment, elastic stretch gloves may relieve symptoms through their warming and massaging effects.4
Some drugs for hand osteoarthritis got conditional recommendations in favor
The expert panel gave conditional recommendations in favor of:
- Topical capsaicin
- Topical NSAIDs
- Oral NSAIDs (including both nonselective and selective agents)
- Tramadol (Ultram)
- Topical rather than oral NSAIDs for patients age 75 and older.
Other drug treatments got conditional recommendations against their use
The expert panel gave conditional recommendations against using:
- Intra-articular injections, and in particular, corticosteroid injections in the trapeziometacarpal (first carpometacarpal) joint
- Opioid analgesics
- Oral methotrexate or sulfasalazine in patients with erosive inflammatory interphalangeal osteoarthritis.
No recommendation for or against
- Hydroxychloroquine.
Comments—Intra-articular injections, opioids, and oral NSAIDs
I differ with these recommendations on several points.
Although the guidelines committee conditionally recommended against using intra-articular therapies for hand osteoarthritis, I find that intra-articular corticosteroid injections are often effective, particularly in patients who have inflammatory forms of the disease, ie, “erosive inflammatory osteoarthritis.” Most nonspecialist physicians probably have limited experience in giving injections into small joints, and referral to a rheumatologist or orthopedist would be appropriate.
I disagree as well with the conditional recommendation that intra-articular corticosteroid injections not be used for involvement of the trapeziometacarpal (first carpometacarpal) joint. I find that many patients with osteoarthritis of this joint experience improvement with intra-articular corticosteroid injections.
I agree that there are limited data on the use of intra-articular hyaluronan injections in this situation and do not routinely use them in this joint.
Opioid analgesics also received a conditional recommendation against their use. The same caveats apply here as for these drugs elsewhere.5 If used, opioids should be used at the lowest dose possible and for as short a time as possible. If the physician is uncomfortable prescribing opioids for patients with osteoarthritis, referral to a pain specialist is recommended.
I disagree to some extent with the conditional recommendation that people age 75 and older should use topical rather than oral NSAIDs. I understand the recommendation, given that older people have a higher frequency of gastrointestinal, renal, and cardiac disease and are best served by avoiding NSAIDs. However, we all see patients over age 75 who are physiologically younger than their numerical age. Accordingly, I feel that the judgment of the physician plays a role in whether NSAIDs are reasonable for some older patients.
The committee recommended not using oral methotrexate or sulfasalazine in patients with erosive inflammatory interphalangeal osteoarthritis. I have used oral hydroxychloroquine off-label in such patients and find that they respond in a very rewarding fashion.
Given that this is an off-label use of hydroxychloroquine, the drug should be used only with appropriate consideration and after discussion with the patient about toxicity, especially about the risk of ocular manifestations.
OSTEOARTHRITIS OF THE KNEE
Some nondrug therapies got strong recommendations
The expert panel strongly recommended:
- Exercise (aerobic, resistance, land-based, and aquatic)
- Weight loss (for patients who are overweight).
Other nondrug therapies got conditional recommendations
The panel conditionally recommended:
- Self-management programs
- Manual therapy in combination with supervised exercise
- Psychosocial interventions
- Medially directed patellar taping
- Medially wedged insoles (if the patient has lateral compartment osteoarthritis)
- Laterally wedged subtalar strapped insoles (if the patient has medial compartment osteoarthritis)
- Heat therapy
- Walking aids, as needed
- Tai chi
- Chinese acupuncture
- Transcutaneous electrical nerve stimulation.
Comments. The ACR panel appropriately noted that Chinese acupuncture or transcutaneous electrical stimulation should be recommended only if the patient has chronic moderate to severe pain and is a candidate for total knee arthroplasty but is unwilling to undergo the procedure or has comorbid medical conditions that rule out surgery.
Nondrug therapies for knee osteoarthritis that got no recommendation for or against
- Balance exercise
- Laterally wedged insoles
- Manual therapy alone
- Knee braces
- Laterally directed patellar taping.
Comments. It was somewhat surprising that there were no recommendations about laterally wedged insoles or knee braces. Laterally wedged insoles have been recommended for patients who have medial compartment knee osteoarthritis6; being thinner at the instep and thicker at the outer edge of the foot, they reduce load on the medial aspect of the knee. One has to be cautious in using knee wedging in patients who have concomitant ankle or hip angle deformities, lest these joints be compromised.
Some of these treatments would be out of the realm of the nonspecialist physician.
Conditional recommendations for initial drug therapy for knee osteoarthritis
The panel conditionally recommended that patients who have osteoarthritis of the knee use one of the following:
- Acetaminophen (contained in Tylenol and a host of other products)
- Oral NSAIDs
- Topical NSAIDs (with a strong recommendation for topical NSAIDs rather than oral NSAIDs in patients age 75 and older)
- Tramadol
- Intra-articular corticosteroid injections.
Comments. In the past, it was recommended that acetaminophen in full doses of up to 4,000 mg per day be considered.7 Current dogma, however, is that doses of acetaminophen should not exceed 3,000 mg per day to avoid damaging the liver. This concern led the US Food and Drug Administration (FDA) in 2011 to advise that the maximum daily dose be limited.8 The ACR panel recommended that patients be counseled to avoid all other products that contain acetaminophen, which is especially cogent, given the presence of this agent in many over-the-counter medications.9
The panel conditionally recommended that people age 75 and older use topical rather than oral NSAIDs. As mentioned earlier, a specific age limit does not take into account that many people age 75 and older may actually be physiologically younger than some in their 50s or 60s. Accordingly, it is recommended that the physician use judgment in this regard so that NSAIDs will not be denied to patients for whom they might be of significant value.
Strong recommendation for gastric protection in patients at risk on NSAIDs
If a patient with knee osteoarthritis has a history of a symptomatic or complicated upper gastrointestinal ulcer but has not had an upper gastrointestinal bleed in the past year and the physician chooses to prescribe an oral NSAID, the expert panel strongly recommended using either a cyclooxygenase (COX)-2-selective inhibitor or a nonselective NSAID in combination with a proton pump inhibitor.
Comment. The suggestion that patients who have had a complicated upper gastrointestinal ulcer in the past year could be considered for treatment with a COX-2-selective inhibitor or nonselective NSAID in combination with a proton pump inhibitor seemed a bit aggressive. My own inclination would be to avoid both nonselective and selective inhibitors in this situation. Alternative agents such as acetaminophen in full doses, tramadol, intra-articular hyaluronan injections, and intra-articular corticosteroid injections seem preferable with respect to safety in such patients.
The suggestion that a proton pump inhibitor be used whenever an NSAID is given for chronic management of knee or hip osteoarthritis is reasonable.10,11 Although some studies have suggested that chronic use of proton pump inhibitors may predispose to osteopenia or osteoporosis, others have not, and gastric protection should be considered in patients at gastrointestinal risk.
Strong recommendation against ibuprofen in patients taking aspirin
The ACR panel strongly recommended that ibuprofen (Advil) not be prescribed to patients with knee osteoarthritis who are using aspirin in low doses for cardioprotection, and strongly recommended using another nonselective NSAID plus a proton pump inhibitor instead. The panel also strongly recommended against using a COX-2-selective inhibitor in this situation.12,13
Comment. The rationale for these recommendations is that ibuprofen may render aspirin ineffective as a cardioprotective agent. Ibuprofen interferes with the aspirin-binding site on platelets, so that the protective effect of aspirin is lost.14,15 Celecoxib (Celebrex)16 and diclofenac (Voltaren) have binding sites different from that of aspirin, although the ACR recommends against using COX-2-selective inhibitors such as celecoxib in the situation and gives no recommendation about other NSAIDs.
No recommendations for or against
The panel issued no recommendations for or against the following treatments for patients with knee osteoarthritis:
- Intra-articular hyaluronan injections
- Duloxetine (Cymbalta)
- Opioid analgesics.
Comments on knee injections
Intra-articular injections of corticosteroids or hyaluronan are commonly used for knee osteoarthritis. As noted, corticosteroid injections received a conditional recommendation, while hyaluronan injections received no recommendation for or against.
How often to inject corticosteroids? In general, too-frequent injection of corticosteroids is to be avoided, in view of the risk of promoting joint breakdown. There is no “magic” number of injections that is safe, although more than 4 per year in the same joint should generally be avoided. In some situations, however, repeat injections may be reasonable if alternative therapies are associated with higher risk.
Raynauld et al,17 in a randomized, double-blind, placebo-controlled trial, demonstrated that intra-articular corticosteroid injections at 3-month intervals for 2 years were not deleterious to knees.
My philosophy is generally not to inject on a regular basis, but to be selective and be guided by the patient’s clinical condition and response to prior injections.
Are hyaluronan injections effective? Although experts differ in their enthusiasm for intra-articular hyaluronan injections in the knee, I have found that many patients benefit from this treatment. Multiple studies have found it efficacious and safe overall.18–21 However, some systematic reviews have called its efficacy into question.7
Although differences in efficacy have been noted, this therapy was approved as being useful in patients with knee osteoarthritis in the Osteoarthritis Research Society International (OARSI) recommendations.7 The effect sizes were smaller in later assessments.22
Hyaluronan injections do not pose the risk of joint breakdown that corticosteroid injections do, but their clinical efficacy is not as dramatic. Adverse reactions to most intraarticular hyaluronans are limited, with slight increases in pain and stiffness after injection. Significant inflammatory reactions characterized as “postinjection flares” are more commonly seen with high-molecular-weight crosslinked preparations. These reactions can be severe and can mimic joint infection clinically. Joint aspiration with synovial fluid analysis and culture may be necessary to exclude infection. Response to aspiration and nonsteroidal inflammatory agents or intra-articular corticosteroids is usually excellent.
Ultrasonographic guidance. As with intraarticular injections in other areas, ultrasonographic guidance is becoming more common, as it allows for more accurate drug administration.
Pes anserine bursitis must be ruled out as a cause of the patient’s knee symptoms—misdiagnosis is not uncommon. The bursa is located on the medial aspect of the tibia, and inflammation of the bursa is a common cause of pain in this area. Local steroid injection is extremely effective in symptomatic therapy. Physical therapy and NSAIDs may be adequate to treat milder cases.
Conditional recommendation against glucosamine, chondroitin, capsaicin
The ACR panel conditionally recommended that patients with knee osteoarthritis not use:
- Chondroitin sulfate
- Glucosamine
- Topical capsaicin.
Comment. Evidence is mixed about the efficacy of glucosamine and chondroitin sulfate, which are so-called nutraceuticals. Some studies found them useful23–25 but some did not,26 and a meta-analysis concluded that they do not help.27 The OARSI guidelines published in 2008 stated that these agents may relieve symptoms of osteoarthritis of the knee.7 The OARSI update published in 2010 found that glucosamine was effective, but less so than in previous studies.22 If glucosamine is effective, some studies suggest that glucosamine sulfate is more effective than glucosamine hydrochloride.22
The same OARSI review revealed that chondroitin sulfate relieved pain but with heterogeneous, dissimilar effect sizes. Of interest was the finding that the 5-year incidence of total knee replacement was lower in patients treated with glucosamine sulfate 1,500 mg/day than with placebo. Also, the rate of decline of joint space narrowing was reported to be reduced in chondroitin sulfate-treated patients.22
In practice, a conditional recommendation against a treatment means that most informed patients would not want the treatment, but some would. Accordingly, if patients still want to take chondroitin or glucosamine after being informed of the limited evidence of benefit, I feel a trial of their use is reasonable.
OSTEOARTHRITIS OF THE HIP
Indications for therapy of osteoarthritis of the hip are similar to those for osteoarthritis of the knee.
As in the knee, nonpharmacologic therapies are important. Loss of weight for overweight patients is extremely important; supervised exercise is especially valuable. Use of canes or crutches as needed is conditionally recommended.
Pharmacologic management is similar to that of osteoarthritis of the knee, with particular use of acetaminophen, NSAIDs, tramadol, and intra-articular corticosteroid injections.
Comment. Intra-articular injection of corticosteroids into the hip would be out of the realm of most nonspecialist practices. Although some rheumatologists are expert in such injections, this treatment is generally best left to an orthopedist or invasive radiologist. The use of ultrasonographic guidance is becoming more frequent, with many rheumatologists having developed expertise in this approach to the knee and the hip. Since most studies were in patients with osteoarthritis of the knee, fewer data are available as to the efficacy of these agents in patients with hip osteoarthritis.
Fewer data are available also with respect to the benefit of chondroitin sulfate and glucosamine in patients with osteoarthritis of the hip. Total joint replacement is extremely effective if conservative therapy does not help.
FIRST, DO NO HARM
Guidelines from the ACR,1,2 the European League Against Rheumatism (EULAR),28,29 the American Academy of Orthopedic Surgeons (AAOS),30 and the OARSI7,22 all differ somewhat, owing to the different evidence available at the time each guideline was developed and to different geographic and cultural backgrounds.
The compositions of these various panels also differ sufficiently to affect their overall recommendations. For example, the EULAR panel consisted of only rheumatologists and an orthopedic surgeon; for the hand osteoarthritis recommendations they added a physiatrist and two allied health professionals.28,29 The OARSI panel included two primary care physicians in addition to rheumatologists and an orthopedic surgeon.7 The ACR was the only professional society to include primary care physicians, physiatrists, and geriatricians along with rheumatologists, an orthopedic surgeon, and physical and occupational therapists.
Although it is to be expected that there will not be universal agreement on all points of management of osteoarthritis by diverse groups, it is essential that input from all these experts representing various subspecialties be recognized. Therapeutic approaches will vary depending on patient characteristics and the experience of the treating physician. As long as therapy is based on reasonable supportive data, beneficial effects can be anticipated. Therapies that received conditional recommendations are not to be discounted if a reasonable percent of patients respond in positive fashion. Obviously, strong recommendations are more likely to be universally accepted since the likelihood that they will be beneficial is stronger.
In any approach to therapy, the caveat primum non nocere—first, do no harm—must always be kept in mind.
- Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of non-pharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012; 64:465–474.
- American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum 2000; 43:1905–1915.
- Atkins D, Best D, Briss PA, et al; GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004; 328:1490.
- Askari A, Moskowitz RW, Ryan C. Stretch gloves. A study of objective and subjective effectiveness in arthritis of the hands. Arthritis Rheum 1974; 17:263–265.
- Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009; 10:113–130.
- Fang MA, Taylor CE, Nouvong A, Masih S, Kao KC, Perell KL. Effects of footwear on medial compartment knee osteoarthritis. J Rehabil Res Dev 2006; 43:427–434.
- Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008; 16:137–162.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: Prescription Acetaminophen Products to be Limited to 325 mg Per Dosage Unit; Boxed Warning Will Highlight Potential for Severe Liver Failure. January 13, 2011. http://www.fda.gov/Drugs/DrugSafety/ucm239821.htm. Accessed November 28, 2012.
- Schilling A, Corey R, Leonard M, Eghtesad B. Acetaminophen: old drug, new warnings. Cleve Clin J Med 2010; 77:19–27.
- Bolten WW. Rational use of nonsteroidal anti-inflammatory drugs and proton pump inhibitors in combination for rheumatic diseases. Orthopedic Research and Reviews 2010; 2:75–84.
- Graham DY, Agrawal NM, Campbell DR, et al; NSAID-Associated Gastric Ulcer Prevention Study Group. Ulcer prevention in long-term users of nonsteroidal anti-inflammatory drugs: results of a double-blind, randomized, multicenter, active- and placebo-controlled study of misoprostol vs lansoprazole. Arch Intern Med 2002; 162:169–175.
- American College of Rheumatology Ad Hoc Group on Use of Selective and Nonselective Nonsteroidal Antiinflammatory Drugs. Recommendations for use of selective and nonselective nonsteroidal antiinflammatory drugs: an American College of Rheumatology white paper. Arthritis Rheum 2008; 59:1058–1073.
- Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA; American Heart Association. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation 2007; 115:1634–1642.
- Ellison J, Dager W. Recent FDA warning of the concomitant use of aspirin and ibuprofen and the effects on platelet aggregation. Prev Cardiol 2007; 10:61–63.
- Schuijt MP, Huntjens-Fleuren HW, de Metz M, Vollaard EJ. The interaction of ibuprofen and diclofenac with aspirin in healthy volunteers. Br J Pharmacol 2009; 157:931–934.
- Wilner KD, Rushing M, Walden C, et al. Celecoxib does not affect the antiplatelet activity of aspirin in healthy volunteers. J Clin Pharmacol 2002; 42:1027–1030.
- Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum 2003; 48:370–377.
- Berenbaum F, Grifka J, Cazzaniga S, et al. A randomised, double-blind, controlled trial comparing two intra-articular hyaluronic acid preparations differing by their molecular weight in symptomatic knee osteoarthritis. Ann Rheum Dis 2012; 71:1454–1460.
- Colen S, van den Bekerom MP, Mulier M, Haverkamp D. Hyaluronic acid in the treatment of knee osteoarthritis: a systematic review and meta-analysis with emphasis on the efficacy of different products. BioDrugs 2012; 26:257–268.
- Wang CT, Lin J, Chang CJ, Lin YT, Hou SM. Therapeutic effects of hyaluronic acid on osteoarthritis of the knee. A meta-analysis of randomized controlled trials. J Bone Joint Surg Am 2004; 86-A:538–545.
- Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S. Visco-supplementation for osteoarthritis of the knee: a systematic review and meta-analysis. Ann Intern Med 2012; 157:180–191.
- Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage 2010; 18:476–499.
- Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treat-ment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage 2007; 15:981–1000.
- Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev 2005; 2:CD002946.
- Vlad SC, LaValley MP, McAlindon TE, Felson DT. Glucosamine for pain in osteoarthritis: why do trial results differ? Arthritis Rheum 2007; 56:2267–2277.
- Clegg DO, Reda DJ, Harris CL, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med 2006; 354:795–808.
- Wandel S, Jüni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ 2010; 341:c4675.
- Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2003;62:1145–55. Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2005; 64:669–681.
- Zhang W, Doherty M, Leeb BF, et al. EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 2007; 66:377–388.
- American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee (non-arthroplasty). Rosemont, IL: American Academy of Orthopaedic Surgeons; 2008.
“When I see a patient with arthritis coming in the front door, I leave by the back door.”
—Sir William Ostler
Fortunately for today’s physicians treating patients with osteoarthritis, we need not be as pessimistic as Osler was more than a century ago when he uttered his now-famous words. Still, there is no magic bullet for the contemporary clinician treating an elderly patient with osteoarthritis. Instead, there are many imperfect bullets, and choosing between them is always a balancing act between benefit and risk from various agents: nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics such as acetaminophen and tramadol, opioids, and supplements such as glucosamine and chondroitin sulfate.
So there was great interest when, in 2012,1 the American College of Rheumatology (ACR) updated its previous guidelines (from 2000) on drug and nondrug therapies for osteoarthritis of the hip and the knee2 and added new recommendations on osteoarthritis of the hand.
Revising the guidelines was appropriate, since new therapies have become available. But, as the guideline authors state, with osteoarthritis, as with other diseases, guidelines cannot be a “cookbook.”
The treatment approach differs depending on the patient’s clinical presentation and on the preferences of the patient and the physician. Often, more than one approach is possible, and more than one approach may be appropriate in a given patient at a given time. The guideline authors also point out that some physicians may disagree with some of the recommendations.
I wish to review here several of the key recommendations. But I also provide some of my personal perspective and experience after 4 decades of treating patients with osteoarthritis.
HOW THE GUIDELINES WERE MADE
The new ACR guidelines were developed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, a formal process to develop recommendations that are as evidence-based as possible.3
The authors are outstanding experts in the field of osteoarthritis from throughout the United States and Canada. Further, the recommendations were voted on by a “technical expert panel” representing the fields of rheumatology, orthopedics, physical medicine, and rehabilitation, from both academic medicine and private practice. This representation provides a balance of input from the types of clinicians frequently involved in managing osteoarthritis.
The initial literature searches for drug therapies were conducted during late 2008, and those for nonpharmacologic treatments were conducted during the second and third quarters of 2009. The goal of the literature searches was to identify the most current systematic reviews and meta-analyses that would provide reliable estimates of benefits of intervention for the prespecified clinically relevant outcomes of pain and function, as well as data on safety.
Recommendations: For or against, strong or weak—and the informed patient’s perspective
Therapies received the following possible recommendations:
- Strong recommendation to use
- Weak (or conditional) recommendation to use
- No recommendation
- Weak (or conditional) recommendation not to use
- Strong recommendation not to use.
A strong recommendation required high-quality evidence and evidence of a large difference between desirable and undesirable effects of the treatment. A conditional recommendation was based on the absence of high-quality evidence, evidence of only a small difference between desirable and undesirable effects of the treatment, or both.
One interesting feature of these recommendations is that they took into account how informed patients might themselves evaluate the data with their medical condition.
For instance, if a therapy received a strong favorable recommendation, we can assume that most informed patients would choose to receive it, and we can shape our interaction with the patient accordingly. A conditional recommendation means that most informed patients would choose the treatment—but many would not, and physicians should keep the patient’s values and preferences in mind.
I admit I had a problem with the meaning of the word “conditional” in the context of these guidelines. When evaluating a treatment, the term “weak” is readily understood and clearer. By using the word “weak,” one is making a positive statement in support of use but letting you know that the data and recommendation are weak. The word “conditional” is less readily defined and does not necessarily imply support for use.
Recommendations were drafted after discussion of the evidence at each meeting of the technical expert panel. Consensus was defined as 75% or more of the members of the panel voting to either strongly or conditionally recommend using a therapy, to either strongly or conditionally recommend not using it, or to choose not to make a recommendation on its use.
OSTEOARTHRITIS OF THE HAND: NO STRONG RECOMMENDATIONS
The technical expert panel gave no strong recommendations for any nondrug or drug treatment for osteoarthritis of the hand.
Conditional recommendations for nondrug treatments
The panel conditionally recommended the following:
- All patients with osteoarthritis of the hand should be evaluated either by their primary physician or by an occupational or physical therapist, particularly with respect to ability to perform activities of daily living.
- Assistive devices such as jar openers, key turners, and pull tabs for zippers should be recommended, as needed.
- Patients should be instructed in joint protection and in the use of thermal treatments (eg, heating pads, ultrasound devices, hot packs, and ice packs).
Comments. Appliances are often beneficial in patients who have involvement of the first carpometacarpal (trapeziometacarpal) joint. Although over-the-counter thumb splints are an option, referral to an occupational therapist for splint prescription is advantageous to achieve a comfortable fit and, importantly, for instructions to the patient on how to avoid joint trauma.
It would be unrealistic to expect primary care physicians and internists to have the expertise to make detailed recommendations about orthopedic appliances. Accordingly, referral to an occupational therapist or an orthopedist is advisable for these situations. It is important, however, that the physician be aware of what treatments are available and most effective, and of the indications for referral.
As for heat treatment, elastic stretch gloves may relieve symptoms through their warming and massaging effects.4
Some drugs for hand osteoarthritis got conditional recommendations in favor
The expert panel gave conditional recommendations in favor of:
- Topical capsaicin
- Topical NSAIDs
- Oral NSAIDs (including both nonselective and selective agents)
- Tramadol (Ultram)
- Topical rather than oral NSAIDs for patients age 75 and older.
Other drug treatments got conditional recommendations against their use
The expert panel gave conditional recommendations against using:
- Intra-articular injections, and in particular, corticosteroid injections in the trapeziometacarpal (first carpometacarpal) joint
- Opioid analgesics
- Oral methotrexate or sulfasalazine in patients with erosive inflammatory interphalangeal osteoarthritis.
No recommendation for or against
- Hydroxychloroquine.
Comments—Intra-articular injections, opioids, and oral NSAIDs
I differ with these recommendations on several points.
Although the guidelines committee conditionally recommended against using intra-articular therapies for hand osteoarthritis, I find that intra-articular corticosteroid injections are often effective, particularly in patients who have inflammatory forms of the disease, ie, “erosive inflammatory osteoarthritis.” Most nonspecialist physicians probably have limited experience in giving injections into small joints, and referral to a rheumatologist or orthopedist would be appropriate.
I disagree as well with the conditional recommendation that intra-articular corticosteroid injections not be used for involvement of the trapeziometacarpal (first carpometacarpal) joint. I find that many patients with osteoarthritis of this joint experience improvement with intra-articular corticosteroid injections.
I agree that there are limited data on the use of intra-articular hyaluronan injections in this situation and do not routinely use them in this joint.
Opioid analgesics also received a conditional recommendation against their use. The same caveats apply here as for these drugs elsewhere.5 If used, opioids should be used at the lowest dose possible and for as short a time as possible. If the physician is uncomfortable prescribing opioids for patients with osteoarthritis, referral to a pain specialist is recommended.
I disagree to some extent with the conditional recommendation that people age 75 and older should use topical rather than oral NSAIDs. I understand the recommendation, given that older people have a higher frequency of gastrointestinal, renal, and cardiac disease and are best served by avoiding NSAIDs. However, we all see patients over age 75 who are physiologically younger than their numerical age. Accordingly, I feel that the judgment of the physician plays a role in whether NSAIDs are reasonable for some older patients.
The committee recommended not using oral methotrexate or sulfasalazine in patients with erosive inflammatory interphalangeal osteoarthritis. I have used oral hydroxychloroquine off-label in such patients and find that they respond in a very rewarding fashion.
Given that this is an off-label use of hydroxychloroquine, the drug should be used only with appropriate consideration and after discussion with the patient about toxicity, especially about the risk of ocular manifestations.
OSTEOARTHRITIS OF THE KNEE
Some nondrug therapies got strong recommendations
The expert panel strongly recommended:
- Exercise (aerobic, resistance, land-based, and aquatic)
- Weight loss (for patients who are overweight).
Other nondrug therapies got conditional recommendations
The panel conditionally recommended:
- Self-management programs
- Manual therapy in combination with supervised exercise
- Psychosocial interventions
- Medially directed patellar taping
- Medially wedged insoles (if the patient has lateral compartment osteoarthritis)
- Laterally wedged subtalar strapped insoles (if the patient has medial compartment osteoarthritis)
- Heat therapy
- Walking aids, as needed
- Tai chi
- Chinese acupuncture
- Transcutaneous electrical nerve stimulation.
Comments. The ACR panel appropriately noted that Chinese acupuncture or transcutaneous electrical stimulation should be recommended only if the patient has chronic moderate to severe pain and is a candidate for total knee arthroplasty but is unwilling to undergo the procedure or has comorbid medical conditions that rule out surgery.
Nondrug therapies for knee osteoarthritis that got no recommendation for or against
- Balance exercise
- Laterally wedged insoles
- Manual therapy alone
- Knee braces
- Laterally directed patellar taping.
Comments. It was somewhat surprising that there were no recommendations about laterally wedged insoles or knee braces. Laterally wedged insoles have been recommended for patients who have medial compartment knee osteoarthritis6; being thinner at the instep and thicker at the outer edge of the foot, they reduce load on the medial aspect of the knee. One has to be cautious in using knee wedging in patients who have concomitant ankle or hip angle deformities, lest these joints be compromised.
Some of these treatments would be out of the realm of the nonspecialist physician.
Conditional recommendations for initial drug therapy for knee osteoarthritis
The panel conditionally recommended that patients who have osteoarthritis of the knee use one of the following:
- Acetaminophen (contained in Tylenol and a host of other products)
- Oral NSAIDs
- Topical NSAIDs (with a strong recommendation for topical NSAIDs rather than oral NSAIDs in patients age 75 and older)
- Tramadol
- Intra-articular corticosteroid injections.
Comments. In the past, it was recommended that acetaminophen in full doses of up to 4,000 mg per day be considered.7 Current dogma, however, is that doses of acetaminophen should not exceed 3,000 mg per day to avoid damaging the liver. This concern led the US Food and Drug Administration (FDA) in 2011 to advise that the maximum daily dose be limited.8 The ACR panel recommended that patients be counseled to avoid all other products that contain acetaminophen, which is especially cogent, given the presence of this agent in many over-the-counter medications.9
The panel conditionally recommended that people age 75 and older use topical rather than oral NSAIDs. As mentioned earlier, a specific age limit does not take into account that many people age 75 and older may actually be physiologically younger than some in their 50s or 60s. Accordingly, it is recommended that the physician use judgment in this regard so that NSAIDs will not be denied to patients for whom they might be of significant value.
Strong recommendation for gastric protection in patients at risk on NSAIDs
If a patient with knee osteoarthritis has a history of a symptomatic or complicated upper gastrointestinal ulcer but has not had an upper gastrointestinal bleed in the past year and the physician chooses to prescribe an oral NSAID, the expert panel strongly recommended using either a cyclooxygenase (COX)-2-selective inhibitor or a nonselective NSAID in combination with a proton pump inhibitor.
Comment. The suggestion that patients who have had a complicated upper gastrointestinal ulcer in the past year could be considered for treatment with a COX-2-selective inhibitor or nonselective NSAID in combination with a proton pump inhibitor seemed a bit aggressive. My own inclination would be to avoid both nonselective and selective inhibitors in this situation. Alternative agents such as acetaminophen in full doses, tramadol, intra-articular hyaluronan injections, and intra-articular corticosteroid injections seem preferable with respect to safety in such patients.
The suggestion that a proton pump inhibitor be used whenever an NSAID is given for chronic management of knee or hip osteoarthritis is reasonable.10,11 Although some studies have suggested that chronic use of proton pump inhibitors may predispose to osteopenia or osteoporosis, others have not, and gastric protection should be considered in patients at gastrointestinal risk.
Strong recommendation against ibuprofen in patients taking aspirin
The ACR panel strongly recommended that ibuprofen (Advil) not be prescribed to patients with knee osteoarthritis who are using aspirin in low doses for cardioprotection, and strongly recommended using another nonselective NSAID plus a proton pump inhibitor instead. The panel also strongly recommended against using a COX-2-selective inhibitor in this situation.12,13
Comment. The rationale for these recommendations is that ibuprofen may render aspirin ineffective as a cardioprotective agent. Ibuprofen interferes with the aspirin-binding site on platelets, so that the protective effect of aspirin is lost.14,15 Celecoxib (Celebrex)16 and diclofenac (Voltaren) have binding sites different from that of aspirin, although the ACR recommends against using COX-2-selective inhibitors such as celecoxib in the situation and gives no recommendation about other NSAIDs.
No recommendations for or against
The panel issued no recommendations for or against the following treatments for patients with knee osteoarthritis:
- Intra-articular hyaluronan injections
- Duloxetine (Cymbalta)
- Opioid analgesics.
Comments on knee injections
Intra-articular injections of corticosteroids or hyaluronan are commonly used for knee osteoarthritis. As noted, corticosteroid injections received a conditional recommendation, while hyaluronan injections received no recommendation for or against.
How often to inject corticosteroids? In general, too-frequent injection of corticosteroids is to be avoided, in view of the risk of promoting joint breakdown. There is no “magic” number of injections that is safe, although more than 4 per year in the same joint should generally be avoided. In some situations, however, repeat injections may be reasonable if alternative therapies are associated with higher risk.
Raynauld et al,17 in a randomized, double-blind, placebo-controlled trial, demonstrated that intra-articular corticosteroid injections at 3-month intervals for 2 years were not deleterious to knees.
My philosophy is generally not to inject on a regular basis, but to be selective and be guided by the patient’s clinical condition and response to prior injections.
Are hyaluronan injections effective? Although experts differ in their enthusiasm for intra-articular hyaluronan injections in the knee, I have found that many patients benefit from this treatment. Multiple studies have found it efficacious and safe overall.18–21 However, some systematic reviews have called its efficacy into question.7
Although differences in efficacy have been noted, this therapy was approved as being useful in patients with knee osteoarthritis in the Osteoarthritis Research Society International (OARSI) recommendations.7 The effect sizes were smaller in later assessments.22
Hyaluronan injections do not pose the risk of joint breakdown that corticosteroid injections do, but their clinical efficacy is not as dramatic. Adverse reactions to most intraarticular hyaluronans are limited, with slight increases in pain and stiffness after injection. Significant inflammatory reactions characterized as “postinjection flares” are more commonly seen with high-molecular-weight crosslinked preparations. These reactions can be severe and can mimic joint infection clinically. Joint aspiration with synovial fluid analysis and culture may be necessary to exclude infection. Response to aspiration and nonsteroidal inflammatory agents or intra-articular corticosteroids is usually excellent.
Ultrasonographic guidance. As with intraarticular injections in other areas, ultrasonographic guidance is becoming more common, as it allows for more accurate drug administration.
Pes anserine bursitis must be ruled out as a cause of the patient’s knee symptoms—misdiagnosis is not uncommon. The bursa is located on the medial aspect of the tibia, and inflammation of the bursa is a common cause of pain in this area. Local steroid injection is extremely effective in symptomatic therapy. Physical therapy and NSAIDs may be adequate to treat milder cases.
Conditional recommendation against glucosamine, chondroitin, capsaicin
The ACR panel conditionally recommended that patients with knee osteoarthritis not use:
- Chondroitin sulfate
- Glucosamine
- Topical capsaicin.
Comment. Evidence is mixed about the efficacy of glucosamine and chondroitin sulfate, which are so-called nutraceuticals. Some studies found them useful23–25 but some did not,26 and a meta-analysis concluded that they do not help.27 The OARSI guidelines published in 2008 stated that these agents may relieve symptoms of osteoarthritis of the knee.7 The OARSI update published in 2010 found that glucosamine was effective, but less so than in previous studies.22 If glucosamine is effective, some studies suggest that glucosamine sulfate is more effective than glucosamine hydrochloride.22
The same OARSI review revealed that chondroitin sulfate relieved pain but with heterogeneous, dissimilar effect sizes. Of interest was the finding that the 5-year incidence of total knee replacement was lower in patients treated with glucosamine sulfate 1,500 mg/day than with placebo. Also, the rate of decline of joint space narrowing was reported to be reduced in chondroitin sulfate-treated patients.22
In practice, a conditional recommendation against a treatment means that most informed patients would not want the treatment, but some would. Accordingly, if patients still want to take chondroitin or glucosamine after being informed of the limited evidence of benefit, I feel a trial of their use is reasonable.
OSTEOARTHRITIS OF THE HIP
Indications for therapy of osteoarthritis of the hip are similar to those for osteoarthritis of the knee.
As in the knee, nonpharmacologic therapies are important. Loss of weight for overweight patients is extremely important; supervised exercise is especially valuable. Use of canes or crutches as needed is conditionally recommended.
Pharmacologic management is similar to that of osteoarthritis of the knee, with particular use of acetaminophen, NSAIDs, tramadol, and intra-articular corticosteroid injections.
Comment. Intra-articular injection of corticosteroids into the hip would be out of the realm of most nonspecialist practices. Although some rheumatologists are expert in such injections, this treatment is generally best left to an orthopedist or invasive radiologist. The use of ultrasonographic guidance is becoming more frequent, with many rheumatologists having developed expertise in this approach to the knee and the hip. Since most studies were in patients with osteoarthritis of the knee, fewer data are available as to the efficacy of these agents in patients with hip osteoarthritis.
Fewer data are available also with respect to the benefit of chondroitin sulfate and glucosamine in patients with osteoarthritis of the hip. Total joint replacement is extremely effective if conservative therapy does not help.
FIRST, DO NO HARM
Guidelines from the ACR,1,2 the European League Against Rheumatism (EULAR),28,29 the American Academy of Orthopedic Surgeons (AAOS),30 and the OARSI7,22 all differ somewhat, owing to the different evidence available at the time each guideline was developed and to different geographic and cultural backgrounds.
The compositions of these various panels also differ sufficiently to affect their overall recommendations. For example, the EULAR panel consisted of only rheumatologists and an orthopedic surgeon; for the hand osteoarthritis recommendations they added a physiatrist and two allied health professionals.28,29 The OARSI panel included two primary care physicians in addition to rheumatologists and an orthopedic surgeon.7 The ACR was the only professional society to include primary care physicians, physiatrists, and geriatricians along with rheumatologists, an orthopedic surgeon, and physical and occupational therapists.
Although it is to be expected that there will not be universal agreement on all points of management of osteoarthritis by diverse groups, it is essential that input from all these experts representing various subspecialties be recognized. Therapeutic approaches will vary depending on patient characteristics and the experience of the treating physician. As long as therapy is based on reasonable supportive data, beneficial effects can be anticipated. Therapies that received conditional recommendations are not to be discounted if a reasonable percent of patients respond in positive fashion. Obviously, strong recommendations are more likely to be universally accepted since the likelihood that they will be beneficial is stronger.
In any approach to therapy, the caveat primum non nocere—first, do no harm—must always be kept in mind.
“When I see a patient with arthritis coming in the front door, I leave by the back door.”
—Sir William Ostler
Fortunately for today’s physicians treating patients with osteoarthritis, we need not be as pessimistic as Osler was more than a century ago when he uttered his now-famous words. Still, there is no magic bullet for the contemporary clinician treating an elderly patient with osteoarthritis. Instead, there are many imperfect bullets, and choosing between them is always a balancing act between benefit and risk from various agents: nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics such as acetaminophen and tramadol, opioids, and supplements such as glucosamine and chondroitin sulfate.
So there was great interest when, in 2012,1 the American College of Rheumatology (ACR) updated its previous guidelines (from 2000) on drug and nondrug therapies for osteoarthritis of the hip and the knee2 and added new recommendations on osteoarthritis of the hand.
Revising the guidelines was appropriate, since new therapies have become available. But, as the guideline authors state, with osteoarthritis, as with other diseases, guidelines cannot be a “cookbook.”
The treatment approach differs depending on the patient’s clinical presentation and on the preferences of the patient and the physician. Often, more than one approach is possible, and more than one approach may be appropriate in a given patient at a given time. The guideline authors also point out that some physicians may disagree with some of the recommendations.
I wish to review here several of the key recommendations. But I also provide some of my personal perspective and experience after 4 decades of treating patients with osteoarthritis.
HOW THE GUIDELINES WERE MADE
The new ACR guidelines were developed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, a formal process to develop recommendations that are as evidence-based as possible.3
The authors are outstanding experts in the field of osteoarthritis from throughout the United States and Canada. Further, the recommendations were voted on by a “technical expert panel” representing the fields of rheumatology, orthopedics, physical medicine, and rehabilitation, from both academic medicine and private practice. This representation provides a balance of input from the types of clinicians frequently involved in managing osteoarthritis.
The initial literature searches for drug therapies were conducted during late 2008, and those for nonpharmacologic treatments were conducted during the second and third quarters of 2009. The goal of the literature searches was to identify the most current systematic reviews and meta-analyses that would provide reliable estimates of benefits of intervention for the prespecified clinically relevant outcomes of pain and function, as well as data on safety.
Recommendations: For or against, strong or weak—and the informed patient’s perspective
Therapies received the following possible recommendations:
- Strong recommendation to use
- Weak (or conditional) recommendation to use
- No recommendation
- Weak (or conditional) recommendation not to use
- Strong recommendation not to use.
A strong recommendation required high-quality evidence and evidence of a large difference between desirable and undesirable effects of the treatment. A conditional recommendation was based on the absence of high-quality evidence, evidence of only a small difference between desirable and undesirable effects of the treatment, or both.
One interesting feature of these recommendations is that they took into account how informed patients might themselves evaluate the data with their medical condition.
For instance, if a therapy received a strong favorable recommendation, we can assume that most informed patients would choose to receive it, and we can shape our interaction with the patient accordingly. A conditional recommendation means that most informed patients would choose the treatment—but many would not, and physicians should keep the patient’s values and preferences in mind.
I admit I had a problem with the meaning of the word “conditional” in the context of these guidelines. When evaluating a treatment, the term “weak” is readily understood and clearer. By using the word “weak,” one is making a positive statement in support of use but letting you know that the data and recommendation are weak. The word “conditional” is less readily defined and does not necessarily imply support for use.
Recommendations were drafted after discussion of the evidence at each meeting of the technical expert panel. Consensus was defined as 75% or more of the members of the panel voting to either strongly or conditionally recommend using a therapy, to either strongly or conditionally recommend not using it, or to choose not to make a recommendation on its use.
OSTEOARTHRITIS OF THE HAND: NO STRONG RECOMMENDATIONS
The technical expert panel gave no strong recommendations for any nondrug or drug treatment for osteoarthritis of the hand.
Conditional recommendations for nondrug treatments
The panel conditionally recommended the following:
- All patients with osteoarthritis of the hand should be evaluated either by their primary physician or by an occupational or physical therapist, particularly with respect to ability to perform activities of daily living.
- Assistive devices such as jar openers, key turners, and pull tabs for zippers should be recommended, as needed.
- Patients should be instructed in joint protection and in the use of thermal treatments (eg, heating pads, ultrasound devices, hot packs, and ice packs).
Comments. Appliances are often beneficial in patients who have involvement of the first carpometacarpal (trapeziometacarpal) joint. Although over-the-counter thumb splints are an option, referral to an occupational therapist for splint prescription is advantageous to achieve a comfortable fit and, importantly, for instructions to the patient on how to avoid joint trauma.
It would be unrealistic to expect primary care physicians and internists to have the expertise to make detailed recommendations about orthopedic appliances. Accordingly, referral to an occupational therapist or an orthopedist is advisable for these situations. It is important, however, that the physician be aware of what treatments are available and most effective, and of the indications for referral.
As for heat treatment, elastic stretch gloves may relieve symptoms through their warming and massaging effects.4
Some drugs for hand osteoarthritis got conditional recommendations in favor
The expert panel gave conditional recommendations in favor of:
- Topical capsaicin
- Topical NSAIDs
- Oral NSAIDs (including both nonselective and selective agents)
- Tramadol (Ultram)
- Topical rather than oral NSAIDs for patients age 75 and older.
Other drug treatments got conditional recommendations against their use
The expert panel gave conditional recommendations against using:
- Intra-articular injections, and in particular, corticosteroid injections in the trapeziometacarpal (first carpometacarpal) joint
- Opioid analgesics
- Oral methotrexate or sulfasalazine in patients with erosive inflammatory interphalangeal osteoarthritis.
No recommendation for or against
- Hydroxychloroquine.
Comments—Intra-articular injections, opioids, and oral NSAIDs
I differ with these recommendations on several points.
Although the guidelines committee conditionally recommended against using intra-articular therapies for hand osteoarthritis, I find that intra-articular corticosteroid injections are often effective, particularly in patients who have inflammatory forms of the disease, ie, “erosive inflammatory osteoarthritis.” Most nonspecialist physicians probably have limited experience in giving injections into small joints, and referral to a rheumatologist or orthopedist would be appropriate.
I disagree as well with the conditional recommendation that intra-articular corticosteroid injections not be used for involvement of the trapeziometacarpal (first carpometacarpal) joint. I find that many patients with osteoarthritis of this joint experience improvement with intra-articular corticosteroid injections.
I agree that there are limited data on the use of intra-articular hyaluronan injections in this situation and do not routinely use them in this joint.
Opioid analgesics also received a conditional recommendation against their use. The same caveats apply here as for these drugs elsewhere.5 If used, opioids should be used at the lowest dose possible and for as short a time as possible. If the physician is uncomfortable prescribing opioids for patients with osteoarthritis, referral to a pain specialist is recommended.
I disagree to some extent with the conditional recommendation that people age 75 and older should use topical rather than oral NSAIDs. I understand the recommendation, given that older people have a higher frequency of gastrointestinal, renal, and cardiac disease and are best served by avoiding NSAIDs. However, we all see patients over age 75 who are physiologically younger than their numerical age. Accordingly, I feel that the judgment of the physician plays a role in whether NSAIDs are reasonable for some older patients.
The committee recommended not using oral methotrexate or sulfasalazine in patients with erosive inflammatory interphalangeal osteoarthritis. I have used oral hydroxychloroquine off-label in such patients and find that they respond in a very rewarding fashion.
Given that this is an off-label use of hydroxychloroquine, the drug should be used only with appropriate consideration and after discussion with the patient about toxicity, especially about the risk of ocular manifestations.
OSTEOARTHRITIS OF THE KNEE
Some nondrug therapies got strong recommendations
The expert panel strongly recommended:
- Exercise (aerobic, resistance, land-based, and aquatic)
- Weight loss (for patients who are overweight).
Other nondrug therapies got conditional recommendations
The panel conditionally recommended:
- Self-management programs
- Manual therapy in combination with supervised exercise
- Psychosocial interventions
- Medially directed patellar taping
- Medially wedged insoles (if the patient has lateral compartment osteoarthritis)
- Laterally wedged subtalar strapped insoles (if the patient has medial compartment osteoarthritis)
- Heat therapy
- Walking aids, as needed
- Tai chi
- Chinese acupuncture
- Transcutaneous electrical nerve stimulation.
Comments. The ACR panel appropriately noted that Chinese acupuncture or transcutaneous electrical stimulation should be recommended only if the patient has chronic moderate to severe pain and is a candidate for total knee arthroplasty but is unwilling to undergo the procedure or has comorbid medical conditions that rule out surgery.
Nondrug therapies for knee osteoarthritis that got no recommendation for or against
- Balance exercise
- Laterally wedged insoles
- Manual therapy alone
- Knee braces
- Laterally directed patellar taping.
Comments. It was somewhat surprising that there were no recommendations about laterally wedged insoles or knee braces. Laterally wedged insoles have been recommended for patients who have medial compartment knee osteoarthritis6; being thinner at the instep and thicker at the outer edge of the foot, they reduce load on the medial aspect of the knee. One has to be cautious in using knee wedging in patients who have concomitant ankle or hip angle deformities, lest these joints be compromised.
Some of these treatments would be out of the realm of the nonspecialist physician.
Conditional recommendations for initial drug therapy for knee osteoarthritis
The panel conditionally recommended that patients who have osteoarthritis of the knee use one of the following:
- Acetaminophen (contained in Tylenol and a host of other products)
- Oral NSAIDs
- Topical NSAIDs (with a strong recommendation for topical NSAIDs rather than oral NSAIDs in patients age 75 and older)
- Tramadol
- Intra-articular corticosteroid injections.
Comments. In the past, it was recommended that acetaminophen in full doses of up to 4,000 mg per day be considered.7 Current dogma, however, is that doses of acetaminophen should not exceed 3,000 mg per day to avoid damaging the liver. This concern led the US Food and Drug Administration (FDA) in 2011 to advise that the maximum daily dose be limited.8 The ACR panel recommended that patients be counseled to avoid all other products that contain acetaminophen, which is especially cogent, given the presence of this agent in many over-the-counter medications.9
The panel conditionally recommended that people age 75 and older use topical rather than oral NSAIDs. As mentioned earlier, a specific age limit does not take into account that many people age 75 and older may actually be physiologically younger than some in their 50s or 60s. Accordingly, it is recommended that the physician use judgment in this regard so that NSAIDs will not be denied to patients for whom they might be of significant value.
Strong recommendation for gastric protection in patients at risk on NSAIDs
If a patient with knee osteoarthritis has a history of a symptomatic or complicated upper gastrointestinal ulcer but has not had an upper gastrointestinal bleed in the past year and the physician chooses to prescribe an oral NSAID, the expert panel strongly recommended using either a cyclooxygenase (COX)-2-selective inhibitor or a nonselective NSAID in combination with a proton pump inhibitor.
Comment. The suggestion that patients who have had a complicated upper gastrointestinal ulcer in the past year could be considered for treatment with a COX-2-selective inhibitor or nonselective NSAID in combination with a proton pump inhibitor seemed a bit aggressive. My own inclination would be to avoid both nonselective and selective inhibitors in this situation. Alternative agents such as acetaminophen in full doses, tramadol, intra-articular hyaluronan injections, and intra-articular corticosteroid injections seem preferable with respect to safety in such patients.
The suggestion that a proton pump inhibitor be used whenever an NSAID is given for chronic management of knee or hip osteoarthritis is reasonable.10,11 Although some studies have suggested that chronic use of proton pump inhibitors may predispose to osteopenia or osteoporosis, others have not, and gastric protection should be considered in patients at gastrointestinal risk.
Strong recommendation against ibuprofen in patients taking aspirin
The ACR panel strongly recommended that ibuprofen (Advil) not be prescribed to patients with knee osteoarthritis who are using aspirin in low doses for cardioprotection, and strongly recommended using another nonselective NSAID plus a proton pump inhibitor instead. The panel also strongly recommended against using a COX-2-selective inhibitor in this situation.12,13
Comment. The rationale for these recommendations is that ibuprofen may render aspirin ineffective as a cardioprotective agent. Ibuprofen interferes with the aspirin-binding site on platelets, so that the protective effect of aspirin is lost.14,15 Celecoxib (Celebrex)16 and diclofenac (Voltaren) have binding sites different from that of aspirin, although the ACR recommends against using COX-2-selective inhibitors such as celecoxib in the situation and gives no recommendation about other NSAIDs.
No recommendations for or against
The panel issued no recommendations for or against the following treatments for patients with knee osteoarthritis:
- Intra-articular hyaluronan injections
- Duloxetine (Cymbalta)
- Opioid analgesics.
Comments on knee injections
Intra-articular injections of corticosteroids or hyaluronan are commonly used for knee osteoarthritis. As noted, corticosteroid injections received a conditional recommendation, while hyaluronan injections received no recommendation for or against.
How often to inject corticosteroids? In general, too-frequent injection of corticosteroids is to be avoided, in view of the risk of promoting joint breakdown. There is no “magic” number of injections that is safe, although more than 4 per year in the same joint should generally be avoided. In some situations, however, repeat injections may be reasonable if alternative therapies are associated with higher risk.
Raynauld et al,17 in a randomized, double-blind, placebo-controlled trial, demonstrated that intra-articular corticosteroid injections at 3-month intervals for 2 years were not deleterious to knees.
My philosophy is generally not to inject on a regular basis, but to be selective and be guided by the patient’s clinical condition and response to prior injections.
Are hyaluronan injections effective? Although experts differ in their enthusiasm for intra-articular hyaluronan injections in the knee, I have found that many patients benefit from this treatment. Multiple studies have found it efficacious and safe overall.18–21 However, some systematic reviews have called its efficacy into question.7
Although differences in efficacy have been noted, this therapy was approved as being useful in patients with knee osteoarthritis in the Osteoarthritis Research Society International (OARSI) recommendations.7 The effect sizes were smaller in later assessments.22
Hyaluronan injections do not pose the risk of joint breakdown that corticosteroid injections do, but their clinical efficacy is not as dramatic. Adverse reactions to most intraarticular hyaluronans are limited, with slight increases in pain and stiffness after injection. Significant inflammatory reactions characterized as “postinjection flares” are more commonly seen with high-molecular-weight crosslinked preparations. These reactions can be severe and can mimic joint infection clinically. Joint aspiration with synovial fluid analysis and culture may be necessary to exclude infection. Response to aspiration and nonsteroidal inflammatory agents or intra-articular corticosteroids is usually excellent.
Ultrasonographic guidance. As with intraarticular injections in other areas, ultrasonographic guidance is becoming more common, as it allows for more accurate drug administration.
Pes anserine bursitis must be ruled out as a cause of the patient’s knee symptoms—misdiagnosis is not uncommon. The bursa is located on the medial aspect of the tibia, and inflammation of the bursa is a common cause of pain in this area. Local steroid injection is extremely effective in symptomatic therapy. Physical therapy and NSAIDs may be adequate to treat milder cases.
Conditional recommendation against glucosamine, chondroitin, capsaicin
The ACR panel conditionally recommended that patients with knee osteoarthritis not use:
- Chondroitin sulfate
- Glucosamine
- Topical capsaicin.
Comment. Evidence is mixed about the efficacy of glucosamine and chondroitin sulfate, which are so-called nutraceuticals. Some studies found them useful23–25 but some did not,26 and a meta-analysis concluded that they do not help.27 The OARSI guidelines published in 2008 stated that these agents may relieve symptoms of osteoarthritis of the knee.7 The OARSI update published in 2010 found that glucosamine was effective, but less so than in previous studies.22 If glucosamine is effective, some studies suggest that glucosamine sulfate is more effective than glucosamine hydrochloride.22
The same OARSI review revealed that chondroitin sulfate relieved pain but with heterogeneous, dissimilar effect sizes. Of interest was the finding that the 5-year incidence of total knee replacement was lower in patients treated with glucosamine sulfate 1,500 mg/day than with placebo. Also, the rate of decline of joint space narrowing was reported to be reduced in chondroitin sulfate-treated patients.22
In practice, a conditional recommendation against a treatment means that most informed patients would not want the treatment, but some would. Accordingly, if patients still want to take chondroitin or glucosamine after being informed of the limited evidence of benefit, I feel a trial of their use is reasonable.
OSTEOARTHRITIS OF THE HIP
Indications for therapy of osteoarthritis of the hip are similar to those for osteoarthritis of the knee.
As in the knee, nonpharmacologic therapies are important. Loss of weight for overweight patients is extremely important; supervised exercise is especially valuable. Use of canes or crutches as needed is conditionally recommended.
Pharmacologic management is similar to that of osteoarthritis of the knee, with particular use of acetaminophen, NSAIDs, tramadol, and intra-articular corticosteroid injections.
Comment. Intra-articular injection of corticosteroids into the hip would be out of the realm of most nonspecialist practices. Although some rheumatologists are expert in such injections, this treatment is generally best left to an orthopedist or invasive radiologist. The use of ultrasonographic guidance is becoming more frequent, with many rheumatologists having developed expertise in this approach to the knee and the hip. Since most studies were in patients with osteoarthritis of the knee, fewer data are available as to the efficacy of these agents in patients with hip osteoarthritis.
Fewer data are available also with respect to the benefit of chondroitin sulfate and glucosamine in patients with osteoarthritis of the hip. Total joint replacement is extremely effective if conservative therapy does not help.
FIRST, DO NO HARM
Guidelines from the ACR,1,2 the European League Against Rheumatism (EULAR),28,29 the American Academy of Orthopedic Surgeons (AAOS),30 and the OARSI7,22 all differ somewhat, owing to the different evidence available at the time each guideline was developed and to different geographic and cultural backgrounds.
The compositions of these various panels also differ sufficiently to affect their overall recommendations. For example, the EULAR panel consisted of only rheumatologists and an orthopedic surgeon; for the hand osteoarthritis recommendations they added a physiatrist and two allied health professionals.28,29 The OARSI panel included two primary care physicians in addition to rheumatologists and an orthopedic surgeon.7 The ACR was the only professional society to include primary care physicians, physiatrists, and geriatricians along with rheumatologists, an orthopedic surgeon, and physical and occupational therapists.
Although it is to be expected that there will not be universal agreement on all points of management of osteoarthritis by diverse groups, it is essential that input from all these experts representing various subspecialties be recognized. Therapeutic approaches will vary depending on patient characteristics and the experience of the treating physician. As long as therapy is based on reasonable supportive data, beneficial effects can be anticipated. Therapies that received conditional recommendations are not to be discounted if a reasonable percent of patients respond in positive fashion. Obviously, strong recommendations are more likely to be universally accepted since the likelihood that they will be beneficial is stronger.
In any approach to therapy, the caveat primum non nocere—first, do no harm—must always be kept in mind.
- Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of non-pharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012; 64:465–474.
- American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum 2000; 43:1905–1915.
- Atkins D, Best D, Briss PA, et al; GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004; 328:1490.
- Askari A, Moskowitz RW, Ryan C. Stretch gloves. A study of objective and subjective effectiveness in arthritis of the hands. Arthritis Rheum 1974; 17:263–265.
- Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009; 10:113–130.
- Fang MA, Taylor CE, Nouvong A, Masih S, Kao KC, Perell KL. Effects of footwear on medial compartment knee osteoarthritis. J Rehabil Res Dev 2006; 43:427–434.
- Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008; 16:137–162.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: Prescription Acetaminophen Products to be Limited to 325 mg Per Dosage Unit; Boxed Warning Will Highlight Potential for Severe Liver Failure. January 13, 2011. http://www.fda.gov/Drugs/DrugSafety/ucm239821.htm. Accessed November 28, 2012.
- Schilling A, Corey R, Leonard M, Eghtesad B. Acetaminophen: old drug, new warnings. Cleve Clin J Med 2010; 77:19–27.
- Bolten WW. Rational use of nonsteroidal anti-inflammatory drugs and proton pump inhibitors in combination for rheumatic diseases. Orthopedic Research and Reviews 2010; 2:75–84.
- Graham DY, Agrawal NM, Campbell DR, et al; NSAID-Associated Gastric Ulcer Prevention Study Group. Ulcer prevention in long-term users of nonsteroidal anti-inflammatory drugs: results of a double-blind, randomized, multicenter, active- and placebo-controlled study of misoprostol vs lansoprazole. Arch Intern Med 2002; 162:169–175.
- American College of Rheumatology Ad Hoc Group on Use of Selective and Nonselective Nonsteroidal Antiinflammatory Drugs. Recommendations for use of selective and nonselective nonsteroidal antiinflammatory drugs: an American College of Rheumatology white paper. Arthritis Rheum 2008; 59:1058–1073.
- Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA; American Heart Association. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation 2007; 115:1634–1642.
- Ellison J, Dager W. Recent FDA warning of the concomitant use of aspirin and ibuprofen and the effects on platelet aggregation. Prev Cardiol 2007; 10:61–63.
- Schuijt MP, Huntjens-Fleuren HW, de Metz M, Vollaard EJ. The interaction of ibuprofen and diclofenac with aspirin in healthy volunteers. Br J Pharmacol 2009; 157:931–934.
- Wilner KD, Rushing M, Walden C, et al. Celecoxib does not affect the antiplatelet activity of aspirin in healthy volunteers. J Clin Pharmacol 2002; 42:1027–1030.
- Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum 2003; 48:370–377.
- Berenbaum F, Grifka J, Cazzaniga S, et al. A randomised, double-blind, controlled trial comparing two intra-articular hyaluronic acid preparations differing by their molecular weight in symptomatic knee osteoarthritis. Ann Rheum Dis 2012; 71:1454–1460.
- Colen S, van den Bekerom MP, Mulier M, Haverkamp D. Hyaluronic acid in the treatment of knee osteoarthritis: a systematic review and meta-analysis with emphasis on the efficacy of different products. BioDrugs 2012; 26:257–268.
- Wang CT, Lin J, Chang CJ, Lin YT, Hou SM. Therapeutic effects of hyaluronic acid on osteoarthritis of the knee. A meta-analysis of randomized controlled trials. J Bone Joint Surg Am 2004; 86-A:538–545.
- Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S. Visco-supplementation for osteoarthritis of the knee: a systematic review and meta-analysis. Ann Intern Med 2012; 157:180–191.
- Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage 2010; 18:476–499.
- Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treat-ment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage 2007; 15:981–1000.
- Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev 2005; 2:CD002946.
- Vlad SC, LaValley MP, McAlindon TE, Felson DT. Glucosamine for pain in osteoarthritis: why do trial results differ? Arthritis Rheum 2007; 56:2267–2277.
- Clegg DO, Reda DJ, Harris CL, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med 2006; 354:795–808.
- Wandel S, Jüni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ 2010; 341:c4675.
- Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2003;62:1145–55. Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2005; 64:669–681.
- Zhang W, Doherty M, Leeb BF, et al. EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 2007; 66:377–388.
- American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee (non-arthroplasty). Rosemont, IL: American Academy of Orthopaedic Surgeons; 2008.
- Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of non-pharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012; 64:465–474.
- American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum 2000; 43:1905–1915.
- Atkins D, Best D, Briss PA, et al; GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004; 328:1490.
- Askari A, Moskowitz RW, Ryan C. Stretch gloves. A study of objective and subjective effectiveness in arthritis of the hands. Arthritis Rheum 1974; 17:263–265.
- Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009; 10:113–130.
- Fang MA, Taylor CE, Nouvong A, Masih S, Kao KC, Perell KL. Effects of footwear on medial compartment knee osteoarthritis. J Rehabil Res Dev 2006; 43:427–434.
- Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008; 16:137–162.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: Prescription Acetaminophen Products to be Limited to 325 mg Per Dosage Unit; Boxed Warning Will Highlight Potential for Severe Liver Failure. January 13, 2011. http://www.fda.gov/Drugs/DrugSafety/ucm239821.htm. Accessed November 28, 2012.
- Schilling A, Corey R, Leonard M, Eghtesad B. Acetaminophen: old drug, new warnings. Cleve Clin J Med 2010; 77:19–27.
- Bolten WW. Rational use of nonsteroidal anti-inflammatory drugs and proton pump inhibitors in combination for rheumatic diseases. Orthopedic Research and Reviews 2010; 2:75–84.
- Graham DY, Agrawal NM, Campbell DR, et al; NSAID-Associated Gastric Ulcer Prevention Study Group. Ulcer prevention in long-term users of nonsteroidal anti-inflammatory drugs: results of a double-blind, randomized, multicenter, active- and placebo-controlled study of misoprostol vs lansoprazole. Arch Intern Med 2002; 162:169–175.
- American College of Rheumatology Ad Hoc Group on Use of Selective and Nonselective Nonsteroidal Antiinflammatory Drugs. Recommendations for use of selective and nonselective nonsteroidal antiinflammatory drugs: an American College of Rheumatology white paper. Arthritis Rheum 2008; 59:1058–1073.
- Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA; American Heart Association. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation 2007; 115:1634–1642.
- Ellison J, Dager W. Recent FDA warning of the concomitant use of aspirin and ibuprofen and the effects on platelet aggregation. Prev Cardiol 2007; 10:61–63.
- Schuijt MP, Huntjens-Fleuren HW, de Metz M, Vollaard EJ. The interaction of ibuprofen and diclofenac with aspirin in healthy volunteers. Br J Pharmacol 2009; 157:931–934.
- Wilner KD, Rushing M, Walden C, et al. Celecoxib does not affect the antiplatelet activity of aspirin in healthy volunteers. J Clin Pharmacol 2002; 42:1027–1030.
- Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum 2003; 48:370–377.
- Berenbaum F, Grifka J, Cazzaniga S, et al. A randomised, double-blind, controlled trial comparing two intra-articular hyaluronic acid preparations differing by their molecular weight in symptomatic knee osteoarthritis. Ann Rheum Dis 2012; 71:1454–1460.
- Colen S, van den Bekerom MP, Mulier M, Haverkamp D. Hyaluronic acid in the treatment of knee osteoarthritis: a systematic review and meta-analysis with emphasis on the efficacy of different products. BioDrugs 2012; 26:257–268.
- Wang CT, Lin J, Chang CJ, Lin YT, Hou SM. Therapeutic effects of hyaluronic acid on osteoarthritis of the knee. A meta-analysis of randomized controlled trials. J Bone Joint Surg Am 2004; 86-A:538–545.
- Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S. Visco-supplementation for osteoarthritis of the knee: a systematic review and meta-analysis. Ann Intern Med 2012; 157:180–191.
- Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage 2010; 18:476–499.
- Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treat-ment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage 2007; 15:981–1000.
- Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev 2005; 2:CD002946.
- Vlad SC, LaValley MP, McAlindon TE, Felson DT. Glucosamine for pain in osteoarthritis: why do trial results differ? Arthritis Rheum 2007; 56:2267–2277.
- Clegg DO, Reda DJ, Harris CL, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med 2006; 354:795–808.
- Wandel S, Jüni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ 2010; 341:c4675.
- Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2003;62:1145–55. Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2005; 64:669–681.
- Zhang W, Doherty M, Leeb BF, et al. EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 2007; 66:377–388.
- American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee (non-arthroplasty). Rosemont, IL: American Academy of Orthopaedic Surgeons; 2008.
Correction: Androgen deficiency in older men
In an article in the November 2012 issue (McGill JJ, Shoskes DA, Sabanegh ES Jr. Androgen deficiency in older men: Indications, advantages, and pitfalls of testosterone replacement therapy. Cleve Clin J Med 2012; 79:797–806), the final sentence of the abstract was omitted. The missing sentence should read as follows: “This article reviews androgen decline in men, focusing on those over age 40, and covers symptoms, indications, contraindications, diagnosis, treatments, and the risks and benefits of treatment.” The online version of the article has been corrected.
In an article in the November 2012 issue (McGill JJ, Shoskes DA, Sabanegh ES Jr. Androgen deficiency in older men: Indications, advantages, and pitfalls of testosterone replacement therapy. Cleve Clin J Med 2012; 79:797–806), the final sentence of the abstract was omitted. The missing sentence should read as follows: “This article reviews androgen decline in men, focusing on those over age 40, and covers symptoms, indications, contraindications, diagnosis, treatments, and the risks and benefits of treatment.” The online version of the article has been corrected.
In an article in the November 2012 issue (McGill JJ, Shoskes DA, Sabanegh ES Jr. Androgen deficiency in older men: Indications, advantages, and pitfalls of testosterone replacement therapy. Cleve Clin J Med 2012; 79:797–806), the final sentence of the abstract was omitted. The missing sentence should read as follows: “This article reviews androgen decline in men, focusing on those over age 40, and covers symptoms, indications, contraindications, diagnosis, treatments, and the risks and benefits of treatment.” The online version of the article has been corrected.
Tackling a Delicate Subject With Heart Failure Patients
New and Noteworthy Information—January
Patients with multiple sclerosis (MS) disease activity have a higher rate of thinning of the ganglion cell/inner plexiform (GCIP) layer of the eye, researchers reported in the January 1 Neurology. Annual rates of GCIP thinning may be highest among patients with new gadolinium-enhancing lesions, new T2 lesions, and disease duration of less than five years. The investigators performed spectral-domain optical coherence tomography scans every six months on 164 patients with MS and 59 healthy controls. The mean follow-up time was 21.1 months. Annual GCIP thinning occurred 42% faster in patients with relapses, 54% faster in patients with new gadolinium-enhanced lesions, and 36% faster in patients with new T2 lesions.
Vaccination with a monovalent AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine does not appear to be associated with an increased risk of epileptic seizures, according to research published in the December 28, 2012, BMJ. Researchers studied 373,398 people with and without epilepsy who had received the vaccine. The primary end point was admission to a hospital or outpatient hospital care with epileptic seizures. The investigators found no increased risk of seizures in patients with epilepsy and a nonsignificantly decreased risk of seizures in persons without epilepsy during the initial seven-day risk period. During the subsequent 23-day risk period, people without epilepsy had a nonsignificantly increased risk of seizures, but patients with epilepsy had no increase in risk of seizures.
Variations in some genes associated with risk for psychiatric disorders may be observed as differences in brain structure in neonates, according to a study published in the January 2 online Cerebral Cortex. Investigators performed automated region-of-interest volumetry and tensor-based morphometry on 272 newborns who had had high-resolution MRI scans. The group found that estrogen receptor alpha (rs9340799) predicted intracranial volume. Polymorphisms in estrogen receptor alpha (rs9340799), as well as in disrupted-in-schizophrenia 1 (DISC1, rs821616), catechol-O-methyltransferase (COMT), neuregulin 1, apolipoprotein E, and brain-derived neurotrophic factor, were significantly associated with local variation in gray matter volume. “The results highlight the importance of prenatal brain development in mediating psychiatric risk,” noted the authors.
Four months after mild traumatic brain injury (TBI), white matter abnormalities may persist in children, even if cognitive symptoms have resolved, according to research published in the December 12, 2012, Journal of Neuroscience. The magnitude and duration of these abnormalities also appear to be greater in children with mild TBI than in adults with mild TBI. Researchers performed fractional anisotropy, axial diffusivity, and radial diffusivity on 15 children with semiacute mild TBI and 15 matched controls. Post-TBI cognitive dysfunction was observed in the domains of attention and processing speed. Increased anisotropy identified patients with pediatric mild TBI with 90% accuracy but was not associated with neuropsychologic deficits. Anisotropic diffusion may provide an objective biomarker of pediatric mild TBI.
The FDA has approved Eliquis (apixaban) for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. In a phase III clinical trial, Eliquis, an oral anticoagulant, reduced the risk of stroke or systemic embolism by 21%, compared with warfarin. The drug primarily reduced the risk of hemorrhagic stroke and ischemic stroke that converted to hemorrhagic stroke, and it also decreased the risks of major bleeding and all-cause mortality, compared with warfarin. Eliquis inhibits Factor Xa, a blood-clotting protein, thus decreasing thrombin generation and blood clots. The recommended dose is 5 mg twice daily. For patients age 80 or older and those who weigh 60 kg or less, the recommended dose is 2.5 mg twice daily. Eliquis is manufactured by Bristol-Myers Squibb (New York City) and comarketed with Pfizer (New York City).
Intermittent fasting, together with a ketogenic diet, may reduce seizures in children with epilepsy to a greater extent than the ketogenic diet alone, investigators reported in the November 30, 2012, online Epilepsy Research. The researchers placed six children with an incomplete response to a ketogenic diet on an intermittent fasting regimen. The children, ages 2 to 7, fasted on alternate days. Four children had transient improvement in seizure control, but they also had hunger-related adverse reactions. Three patients adhered to the combined intermittent fasting and ketogenic diet regimen for two months. The ketogenic diet and intermittent fasting may not share the same anticonvulsant mechanisms, noted the authors.
The available evidence does not support the use of cannabis extract to treat multiple sclerosis (MS), according to a review published in the December 2012 Drug and Therapeutics Bulletin. Researchers concluded that the trial data for nabiximols, a mouth spray for patients with MS containing dronabinol and cannabidiol, were limited. In the trials, which were the basis for the drug’s approval, symptoms decreased in a slightly higher number of patients taking nabiximols, compared with patients taking placebo. The drug was used for relatively short periods (ie, six weeks to four months) in many of these studies, however, and no study compared nabiximols with another active ingredient. One properly designed trial with a sufficient number of patients showed no difference in symptom relief between participants who took nabiximols and those who did not.
Baseline depression was associated with mild cognitive impairment (MCI) and dementia in individuals 65 or older, researchers reported in the December 31, 2012, Archives of Neurology. Depression may coincide with cognitive impairment, but may not precede it, the study authors noted. The investigators studied 2,160 community-dwelling Medicare recipients in New York City. The team defined depression as a score of 4 or more on the Center for Epidemiological Studies Depression scale. MCI, dementia, and progression from MCI to dementia were the study’s main outcome measures. Baseline depression was associated with an increased risk of incident dementia, but not with incident MCI. Participants with MCI and comorbid depression at baseline had a higher risk of progression to dementia, but not Alzheimer’s disease.
Consumption of fructose resulted in a smaller increase in systemic glucose, insulin, and glucagon-like polypeptide 1 levels than consumption of glucose, according to research published in the January 2 JAMA. Glucose ingestion was associated with a significantly greater reduction in hypothalamic cerebral blood flow than fructose ingestion. Researchers performed MRIs of 20 healthy adults at baseline and after ingestion of a glucose or fructose drink. The blinded study had a random-order crossover design. Compared with baseline, glucose ingestion increased functional connectivity between the hypothalamus and the thalamus and striatum. Fructose increased connectivity between the hypothalamus and thalamus, but not the striatum. Fructose reduced regional cerebral blood flow in the thalamus, hippocampus, posterior cingulate cortex, fusiform, and visual cortex.
Research published in the January 7 online Epilepsia provides evidence for a shared genetic susceptibility to epilespsy and migraine with aura. Compared with migraine without aura, the prevalence of migraine with aura was significantly increased among patients with epilepsy who have two or more first-degree relatives with epilepsy. Investigators studied the prevalence of a history of migraine in 730 participants in the Epilepsy Phenome/Genome Project. Eligible participants were 12 or older, had nonacquired focal epilepsy or generalized epilepsy, and had one or more relative epilepsy of unknown cause. The researchers collected information on migraine with and without aura using an instrument validated for individuals 12 and older. The team also interviewed participants about the history of seizure disorders in nonenrolled family members.
Higher exposure to benomyl is associated with an increased risk for Parkinson’s disease, according to an epidemiologic study published in the December 24, 2012, online Proceedings of the National Academy of Sciences. In primary mesencephalic neurons, benomyl exposure inhibits aldehyde dehydrogenase (ALDH) and alters dopamine homeostasis. Investigators tested the effects of benomyl in cell cultures and confirmed that the chemical damaged or destroyed dopaminergic neurons. The researchers also found that benomyl caused the loss of dopaminergic neurons in zebrafish. The ALDH model for Parkinson’s disease etiology may help explain the selective vulnerability of dopaminergic neurons and describe the mechanism through which environmental toxicants contribute to Parkinson’s disease pathogenesis, the authors theorized.
Patients with a history of traumatic brain injury (TBI) and loss of consciousness may have an increased risk for future TBI and loss of consciousness, according to a study published in the November 21, 2012, online Journal of Neurology, Neurosurgery, and Psychiatry. Researchers are conducting an ongoing study of 4,225 nondemented adults age 65 and older. Participants are seen every two years, and 14% have reported a lifetime history of TBI and loss of consciousness. Individuals reporting a first injury before age 25 had an adjusted hazard ratio of 2.54 for TBI and loss of consciousness, compared with a hazard ratio of 3.79 for adults with first injury after age 55.
—Erik Greb
Patients with multiple sclerosis (MS) disease activity have a higher rate of thinning of the ganglion cell/inner plexiform (GCIP) layer of the eye, researchers reported in the January 1 Neurology. Annual rates of GCIP thinning may be highest among patients with new gadolinium-enhancing lesions, new T2 lesions, and disease duration of less than five years. The investigators performed spectral-domain optical coherence tomography scans every six months on 164 patients with MS and 59 healthy controls. The mean follow-up time was 21.1 months. Annual GCIP thinning occurred 42% faster in patients with relapses, 54% faster in patients with new gadolinium-enhanced lesions, and 36% faster in patients with new T2 lesions.
Vaccination with a monovalent AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine does not appear to be associated with an increased risk of epileptic seizures, according to research published in the December 28, 2012, BMJ. Researchers studied 373,398 people with and without epilepsy who had received the vaccine. The primary end point was admission to a hospital or outpatient hospital care with epileptic seizures. The investigators found no increased risk of seizures in patients with epilepsy and a nonsignificantly decreased risk of seizures in persons without epilepsy during the initial seven-day risk period. During the subsequent 23-day risk period, people without epilepsy had a nonsignificantly increased risk of seizures, but patients with epilepsy had no increase in risk of seizures.
Variations in some genes associated with risk for psychiatric disorders may be observed as differences in brain structure in neonates, according to a study published in the January 2 online Cerebral Cortex. Investigators performed automated region-of-interest volumetry and tensor-based morphometry on 272 newborns who had had high-resolution MRI scans. The group found that estrogen receptor alpha (rs9340799) predicted intracranial volume. Polymorphisms in estrogen receptor alpha (rs9340799), as well as in disrupted-in-schizophrenia 1 (DISC1, rs821616), catechol-O-methyltransferase (COMT), neuregulin 1, apolipoprotein E, and brain-derived neurotrophic factor, were significantly associated with local variation in gray matter volume. “The results highlight the importance of prenatal brain development in mediating psychiatric risk,” noted the authors.
Four months after mild traumatic brain injury (TBI), white matter abnormalities may persist in children, even if cognitive symptoms have resolved, according to research published in the December 12, 2012, Journal of Neuroscience. The magnitude and duration of these abnormalities also appear to be greater in children with mild TBI than in adults with mild TBI. Researchers performed fractional anisotropy, axial diffusivity, and radial diffusivity on 15 children with semiacute mild TBI and 15 matched controls. Post-TBI cognitive dysfunction was observed in the domains of attention and processing speed. Increased anisotropy identified patients with pediatric mild TBI with 90% accuracy but was not associated with neuropsychologic deficits. Anisotropic diffusion may provide an objective biomarker of pediatric mild TBI.
The FDA has approved Eliquis (apixaban) for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. In a phase III clinical trial, Eliquis, an oral anticoagulant, reduced the risk of stroke or systemic embolism by 21%, compared with warfarin. The drug primarily reduced the risk of hemorrhagic stroke and ischemic stroke that converted to hemorrhagic stroke, and it also decreased the risks of major bleeding and all-cause mortality, compared with warfarin. Eliquis inhibits Factor Xa, a blood-clotting protein, thus decreasing thrombin generation and blood clots. The recommended dose is 5 mg twice daily. For patients age 80 or older and those who weigh 60 kg or less, the recommended dose is 2.5 mg twice daily. Eliquis is manufactured by Bristol-Myers Squibb (New York City) and comarketed with Pfizer (New York City).
Intermittent fasting, together with a ketogenic diet, may reduce seizures in children with epilepsy to a greater extent than the ketogenic diet alone, investigators reported in the November 30, 2012, online Epilepsy Research. The researchers placed six children with an incomplete response to a ketogenic diet on an intermittent fasting regimen. The children, ages 2 to 7, fasted on alternate days. Four children had transient improvement in seizure control, but they also had hunger-related adverse reactions. Three patients adhered to the combined intermittent fasting and ketogenic diet regimen for two months. The ketogenic diet and intermittent fasting may not share the same anticonvulsant mechanisms, noted the authors.
The available evidence does not support the use of cannabis extract to treat multiple sclerosis (MS), according to a review published in the December 2012 Drug and Therapeutics Bulletin. Researchers concluded that the trial data for nabiximols, a mouth spray for patients with MS containing dronabinol and cannabidiol, were limited. In the trials, which were the basis for the drug’s approval, symptoms decreased in a slightly higher number of patients taking nabiximols, compared with patients taking placebo. The drug was used for relatively short periods (ie, six weeks to four months) in many of these studies, however, and no study compared nabiximols with another active ingredient. One properly designed trial with a sufficient number of patients showed no difference in symptom relief between participants who took nabiximols and those who did not.
Baseline depression was associated with mild cognitive impairment (MCI) and dementia in individuals 65 or older, researchers reported in the December 31, 2012, Archives of Neurology. Depression may coincide with cognitive impairment, but may not precede it, the study authors noted. The investigators studied 2,160 community-dwelling Medicare recipients in New York City. The team defined depression as a score of 4 or more on the Center for Epidemiological Studies Depression scale. MCI, dementia, and progression from MCI to dementia were the study’s main outcome measures. Baseline depression was associated with an increased risk of incident dementia, but not with incident MCI. Participants with MCI and comorbid depression at baseline had a higher risk of progression to dementia, but not Alzheimer’s disease.
Consumption of fructose resulted in a smaller increase in systemic glucose, insulin, and glucagon-like polypeptide 1 levels than consumption of glucose, according to research published in the January 2 JAMA. Glucose ingestion was associated with a significantly greater reduction in hypothalamic cerebral blood flow than fructose ingestion. Researchers performed MRIs of 20 healthy adults at baseline and after ingestion of a glucose or fructose drink. The blinded study had a random-order crossover design. Compared with baseline, glucose ingestion increased functional connectivity between the hypothalamus and the thalamus and striatum. Fructose increased connectivity between the hypothalamus and thalamus, but not the striatum. Fructose reduced regional cerebral blood flow in the thalamus, hippocampus, posterior cingulate cortex, fusiform, and visual cortex.
Research published in the January 7 online Epilepsia provides evidence for a shared genetic susceptibility to epilespsy and migraine with aura. Compared with migraine without aura, the prevalence of migraine with aura was significantly increased among patients with epilepsy who have two or more first-degree relatives with epilepsy. Investigators studied the prevalence of a history of migraine in 730 participants in the Epilepsy Phenome/Genome Project. Eligible participants were 12 or older, had nonacquired focal epilepsy or generalized epilepsy, and had one or more relative epilepsy of unknown cause. The researchers collected information on migraine with and without aura using an instrument validated for individuals 12 and older. The team also interviewed participants about the history of seizure disorders in nonenrolled family members.
Higher exposure to benomyl is associated with an increased risk for Parkinson’s disease, according to an epidemiologic study published in the December 24, 2012, online Proceedings of the National Academy of Sciences. In primary mesencephalic neurons, benomyl exposure inhibits aldehyde dehydrogenase (ALDH) and alters dopamine homeostasis. Investigators tested the effects of benomyl in cell cultures and confirmed that the chemical damaged or destroyed dopaminergic neurons. The researchers also found that benomyl caused the loss of dopaminergic neurons in zebrafish. The ALDH model for Parkinson’s disease etiology may help explain the selective vulnerability of dopaminergic neurons and describe the mechanism through which environmental toxicants contribute to Parkinson’s disease pathogenesis, the authors theorized.
Patients with a history of traumatic brain injury (TBI) and loss of consciousness may have an increased risk for future TBI and loss of consciousness, according to a study published in the November 21, 2012, online Journal of Neurology, Neurosurgery, and Psychiatry. Researchers are conducting an ongoing study of 4,225 nondemented adults age 65 and older. Participants are seen every two years, and 14% have reported a lifetime history of TBI and loss of consciousness. Individuals reporting a first injury before age 25 had an adjusted hazard ratio of 2.54 for TBI and loss of consciousness, compared with a hazard ratio of 3.79 for adults with first injury after age 55.
—Erik Greb
Patients with multiple sclerosis (MS) disease activity have a higher rate of thinning of the ganglion cell/inner plexiform (GCIP) layer of the eye, researchers reported in the January 1 Neurology. Annual rates of GCIP thinning may be highest among patients with new gadolinium-enhancing lesions, new T2 lesions, and disease duration of less than five years. The investigators performed spectral-domain optical coherence tomography scans every six months on 164 patients with MS and 59 healthy controls. The mean follow-up time was 21.1 months. Annual GCIP thinning occurred 42% faster in patients with relapses, 54% faster in patients with new gadolinium-enhanced lesions, and 36% faster in patients with new T2 lesions.
Vaccination with a monovalent AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine does not appear to be associated with an increased risk of epileptic seizures, according to research published in the December 28, 2012, BMJ. Researchers studied 373,398 people with and without epilepsy who had received the vaccine. The primary end point was admission to a hospital or outpatient hospital care with epileptic seizures. The investigators found no increased risk of seizures in patients with epilepsy and a nonsignificantly decreased risk of seizures in persons without epilepsy during the initial seven-day risk period. During the subsequent 23-day risk period, people without epilepsy had a nonsignificantly increased risk of seizures, but patients with epilepsy had no increase in risk of seizures.
Variations in some genes associated with risk for psychiatric disorders may be observed as differences in brain structure in neonates, according to a study published in the January 2 online Cerebral Cortex. Investigators performed automated region-of-interest volumetry and tensor-based morphometry on 272 newborns who had had high-resolution MRI scans. The group found that estrogen receptor alpha (rs9340799) predicted intracranial volume. Polymorphisms in estrogen receptor alpha (rs9340799), as well as in disrupted-in-schizophrenia 1 (DISC1, rs821616), catechol-O-methyltransferase (COMT), neuregulin 1, apolipoprotein E, and brain-derived neurotrophic factor, were significantly associated with local variation in gray matter volume. “The results highlight the importance of prenatal brain development in mediating psychiatric risk,” noted the authors.
Four months after mild traumatic brain injury (TBI), white matter abnormalities may persist in children, even if cognitive symptoms have resolved, according to research published in the December 12, 2012, Journal of Neuroscience. The magnitude and duration of these abnormalities also appear to be greater in children with mild TBI than in adults with mild TBI. Researchers performed fractional anisotropy, axial diffusivity, and radial diffusivity on 15 children with semiacute mild TBI and 15 matched controls. Post-TBI cognitive dysfunction was observed in the domains of attention and processing speed. Increased anisotropy identified patients with pediatric mild TBI with 90% accuracy but was not associated with neuropsychologic deficits. Anisotropic diffusion may provide an objective biomarker of pediatric mild TBI.
The FDA has approved Eliquis (apixaban) for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. In a phase III clinical trial, Eliquis, an oral anticoagulant, reduced the risk of stroke or systemic embolism by 21%, compared with warfarin. The drug primarily reduced the risk of hemorrhagic stroke and ischemic stroke that converted to hemorrhagic stroke, and it also decreased the risks of major bleeding and all-cause mortality, compared with warfarin. Eliquis inhibits Factor Xa, a blood-clotting protein, thus decreasing thrombin generation and blood clots. The recommended dose is 5 mg twice daily. For patients age 80 or older and those who weigh 60 kg or less, the recommended dose is 2.5 mg twice daily. Eliquis is manufactured by Bristol-Myers Squibb (New York City) and comarketed with Pfizer (New York City).
Intermittent fasting, together with a ketogenic diet, may reduce seizures in children with epilepsy to a greater extent than the ketogenic diet alone, investigators reported in the November 30, 2012, online Epilepsy Research. The researchers placed six children with an incomplete response to a ketogenic diet on an intermittent fasting regimen. The children, ages 2 to 7, fasted on alternate days. Four children had transient improvement in seizure control, but they also had hunger-related adverse reactions. Three patients adhered to the combined intermittent fasting and ketogenic diet regimen for two months. The ketogenic diet and intermittent fasting may not share the same anticonvulsant mechanisms, noted the authors.
The available evidence does not support the use of cannabis extract to treat multiple sclerosis (MS), according to a review published in the December 2012 Drug and Therapeutics Bulletin. Researchers concluded that the trial data for nabiximols, a mouth spray for patients with MS containing dronabinol and cannabidiol, were limited. In the trials, which were the basis for the drug’s approval, symptoms decreased in a slightly higher number of patients taking nabiximols, compared with patients taking placebo. The drug was used for relatively short periods (ie, six weeks to four months) in many of these studies, however, and no study compared nabiximols with another active ingredient. One properly designed trial with a sufficient number of patients showed no difference in symptom relief between participants who took nabiximols and those who did not.
Baseline depression was associated with mild cognitive impairment (MCI) and dementia in individuals 65 or older, researchers reported in the December 31, 2012, Archives of Neurology. Depression may coincide with cognitive impairment, but may not precede it, the study authors noted. The investigators studied 2,160 community-dwelling Medicare recipients in New York City. The team defined depression as a score of 4 or more on the Center for Epidemiological Studies Depression scale. MCI, dementia, and progression from MCI to dementia were the study’s main outcome measures. Baseline depression was associated with an increased risk of incident dementia, but not with incident MCI. Participants with MCI and comorbid depression at baseline had a higher risk of progression to dementia, but not Alzheimer’s disease.
Consumption of fructose resulted in a smaller increase in systemic glucose, insulin, and glucagon-like polypeptide 1 levels than consumption of glucose, according to research published in the January 2 JAMA. Glucose ingestion was associated with a significantly greater reduction in hypothalamic cerebral blood flow than fructose ingestion. Researchers performed MRIs of 20 healthy adults at baseline and after ingestion of a glucose or fructose drink. The blinded study had a random-order crossover design. Compared with baseline, glucose ingestion increased functional connectivity between the hypothalamus and the thalamus and striatum. Fructose increased connectivity between the hypothalamus and thalamus, but not the striatum. Fructose reduced regional cerebral blood flow in the thalamus, hippocampus, posterior cingulate cortex, fusiform, and visual cortex.
Research published in the January 7 online Epilepsia provides evidence for a shared genetic susceptibility to epilespsy and migraine with aura. Compared with migraine without aura, the prevalence of migraine with aura was significantly increased among patients with epilepsy who have two or more first-degree relatives with epilepsy. Investigators studied the prevalence of a history of migraine in 730 participants in the Epilepsy Phenome/Genome Project. Eligible participants were 12 or older, had nonacquired focal epilepsy or generalized epilepsy, and had one or more relative epilepsy of unknown cause. The researchers collected information on migraine with and without aura using an instrument validated for individuals 12 and older. The team also interviewed participants about the history of seizure disorders in nonenrolled family members.
Higher exposure to benomyl is associated with an increased risk for Parkinson’s disease, according to an epidemiologic study published in the December 24, 2012, online Proceedings of the National Academy of Sciences. In primary mesencephalic neurons, benomyl exposure inhibits aldehyde dehydrogenase (ALDH) and alters dopamine homeostasis. Investigators tested the effects of benomyl in cell cultures and confirmed that the chemical damaged or destroyed dopaminergic neurons. The researchers also found that benomyl caused the loss of dopaminergic neurons in zebrafish. The ALDH model for Parkinson’s disease etiology may help explain the selective vulnerability of dopaminergic neurons and describe the mechanism through which environmental toxicants contribute to Parkinson’s disease pathogenesis, the authors theorized.
Patients with a history of traumatic brain injury (TBI) and loss of consciousness may have an increased risk for future TBI and loss of consciousness, according to a study published in the November 21, 2012, online Journal of Neurology, Neurosurgery, and Psychiatry. Researchers are conducting an ongoing study of 4,225 nondemented adults age 65 and older. Participants are seen every two years, and 14% have reported a lifetime history of TBI and loss of consciousness. Individuals reporting a first injury before age 25 had an adjusted hazard ratio of 2.54 for TBI and loss of consciousness, compared with a hazard ratio of 3.79 for adults with first injury after age 55.
—Erik Greb
Man, 56, With Wrist Pain After a Fall
A white man, age 56, presented to his primary care clinician with wrist pain and swelling. Two days earlier, he had fallen from a step stool and landed on his right wrist. He treated the pain by resting, elevating his arm, applying ice, and taking ibuprofen 800 mg tid. He said he had lost strength in his hand and arm and was experiencing numbness and tingling in his right hand and fingers.
The patient’s medical history included hypertension, type 2 diabetes mellitus, morbid obesity, obstructive sleep apnea, asthma, carpel tunnel syndrome, and peripheral neuropathy. His surgical history was significant for duodenal switch gastric bypass surgery, performed eight years earlier, and his weight at the time of presentation was 200 lb; before his gastric bypass, he weighed 385 lb. Since the surgery, his hypertension, diabetes, asthma, and sleep apnea had all resolved. Table 1 shows a list of medications he was taking at the time of presentation.
The patient, a registered nurse, had been married for 30 years and had one child. He had quit smoking 15 years earlier, with a 43–pack-year smoking history. He reported social drinking but denied any recreational drug use. He was unaware of having any allergies to food or medication.
His vital signs on presentation were blood pressure, 110/75 mm Hg; heart rate, 53 beats/min; respiration, 18 breaths/min; O2 saturation, 97% on room air; and temperature, 97.5°F.
Physical exam revealed that the patient’s right wrist was ecchymotic and swollen with +1 pitting edema. The skin was warm and dry to the touch. Decreased range of motion was noted in the right wrist, compared with the left. Pain with point tenderness was noted at the right lateral wrist. Pulses were +3 with capillary refill of less than 3 seconds. The rest of the exam was unremarkable.
The differential diagnosis included fracture secondary to the fall, osteoporosis, osteopenia, osteomalacia, Paget’s disease, tumor, infection, and sprain or strain of the wrist. A wrist x-ray was ordered, as were the following baseline labs: complete blood count with differential (CBC), vitamin B12 and folate levels, blood chemistry, lipid profile, liver profile, total vitamin D, and sensitive thyroid-stimulating hormone. Test results are shown in Table 2.
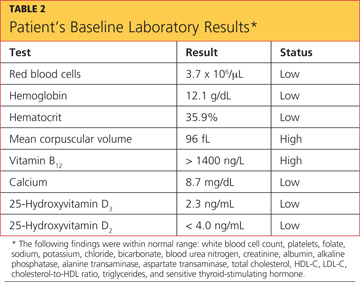
X-ray of the wrist showed fracture only, making it possible to rule out Paget’s disease (ie, no patchy white areas noted in the bone) and tumor (no masses seen) as the immediate cause of fracture. Normal body temperature and normal white blood cell count eliminated the possibility of infection.
Because the patient was only 56 and had a history of bariatric surgery, further testing was pursued to investigate a cause for the weakened bone. Bone mineral density (BMD) testing revealed the following results:
• The lumbar spine in frontal projection measured 0.968 g/cm2 with a T-score of –2.2 and a Z-score of –2.2.
• Total BMD of the left hip was 0.863 g/cm2 with a T-score of –1.7 and a Z-score of –1.4.
• Total BMD of the left femoral neck was 0.863 g/cm2 with a T-score of 1.7 and a Z-score of –1.1.
These findings suggested osteopenia1,2 (not osteoporosis) in all sites, with a 12% decrease of BMD in the spine (suggesting increased risk for spinal fracture) and a 16.3% decrease of BMD in the hip since the patient’s most recent bone scan five years earlier (radiologist’s report). Other abnormal findings were elevated parathyroid hormone (PTH) serum, 95.7 pg/mL (reference range, 10 to 65 pg/mL); low total calcium serum, 8.7 mg/dL (reference range, 8.9 to 10.2 mg/dL), and low 25-hydroxyvitamin D total, 12.3 ng/mL (reference range, 25 to 80 ng/mL).
A 2010 clinical practice guideline from the Endocrine Society3 specifies that after malabsorptive surgery, vitamin D and calcium supplementation should be adjusted by a qualified medical professional, based on serum markers and measures of bone density. An endocrinologist who was consulted at the patient’s initial visit prescribed the following medications: vitamin D2, 50,000 U/wk PO; combined calcium citrate (vitamin D3) 500 IU with calcium 630 mg, 1 tab bid; and calcitriol 0.5 μg bid.
The patient’s final diagnosis was osteomalacia secondary to gastric bypass surgery. (See “Making the Diagnosis of Osteomalacia.”4-6)
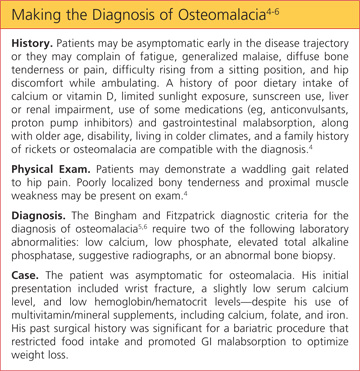
DISCUSSION
According to 2008 data from the World Health Organization (WHO),7 1.4 billion persons older than 20 worldwide were overweight, and 200 million men and 300 million women were considered obese—meaning that one in every 10 adults worldwide is overweight or obese. In 2010, the WHO reports, 40 million children younger than 5 worldwide were considered overweight.7 Health care providers need to be prepared to care for the increasing number of patients who will undergo bariatric surgeries to treat obesity and its related comorbidities.8
Postoperative follow-up for the malabsorption deficiencies related to bariatric procedures should be performed every six months, including obtaining levels of alkaline phosphatase and others previously discussed. In addition, the Endocrine Society guideline3 recommends measuring levels of vitamin B12, albumin, pre-albumin, iron, and ferritin, and obtaining a CBC, a liver profile, glucose reading, creatinine measurement, and a metabolic profile at one month and two months after surgery, then every six months until two years after surgery, then annually if findings are stable.
Furthermore, the Endocrine Society3 recommends obtaining zinc levels every six months for the first year, then annually. An annual vitamin A level is optional.9 Yearly bone density testing is recommended until the patient’s BMD is deemed stable.3
Additionally, Koch and Finelli10 recommend performing the following labs postoperatively: hemoglobin A1C every three months; copper, magnesium, whole blood thiamine, vitamin B12, and a 24-hour urinary calcium every six months for the first three years, then once a year if findings remain stable.
Use of alcohol should be discouraged among patients who have undergone bariatric surgery, as its use alters micronutrient requirements and metabolism. Alcohol consumption may also contribute to dumping syndrome (ie, rapid gastric emptying).11
Any patient with a history of malabsorptive bypass surgery who complains of neurologic, visual, or skin disorders, anemia, or edema may require a further workup to rule out other absorptive deficiencies. These include vitamins A, E, and B12, zinc, folate, thiamine, niacin, selenium, and ferritin.10
Osteomalacia
Metabolic bone diseases can result from genetics, dietary factors, medication use, surgery, or hormonal irregularities. They alter the normal biochemical reactions in bone structure.
The three most common forms of metabolic bone disease are osteoporosis, osteopenia, and osteomalacia. The WHO diagnostic classifications and associated T-scores for bone mineral density1,2 indicate a T-score above –1.0 as normal. A score between –1.0 and –2.5 is indicative of osteopenia, and a score below –2.5 indicates osteoporosis. A T-score below –2.5 in the patient with a history of fragility fracture indicates severe osteoporosis.1,2
In osteomalacia, bone volume remains unchanged, but mineralization of osteoid in the mature compact and spongy bone is either delayed or inadequate. The remolding cycle continues unchanged in the formation of osteoid, but mineral calcification and deposition do not occur.3-5
Osteomalacia is normally considered a rare disorder, but it may become more common as increasing numbers of patients undergo gastric bypass operations.12,13 Primary care practitioners should monitor for this condition in such patients before serious bone loss or other problems develop.9,13,14
Vitamin D deficiency (see “Vitamin D Metabolism,”4,15-19 below), whether or not the result of gastric bypass surgery, is a major risk factor for osteomalacia. Disorders of the small bowel, the hepatobiliary system, and the pancreas are all common causes of vitamin D deficiency. Liver disease interferes with the metabolism of vitamin D. Diseases of the pancreas may cause a deficiency of bile salts, which are vital for the intestinal absorption of vitamin D.17

Restriction and Malabsorption
The case patient had undergone a gastric bypass (duodenal switch), in which a large portion of the stomach is removed and a large part of the small bowel rerouted—with both parts of the procedure causing malabsorption.11 It is in the small bowel that absorption of vitamin D and calcium takes place.
The duodenal switch gastric bypass surgery causes both restriction and malabsorption. Though similar to a biliopancreatic diversion, the duodenal switch preserves the distal stomach and the pylorus20 by way of a sleeve gastrectomy that is performed to reduce the gastric reservoir; the common channel length after revision is 100 cm, not 50 cm (as in conventional biliopancreatic diversion).13 The sleeve gastrectomy involves removal of parietal cells, reducing production of hydrochloric acid (which is necessary to break down food), and hindering the absorption of certain nutrients, including the fat-soluble vitamins, vitamin B12, and iron.12 Patients who take H2-blockers or proton pump inhibitors experience an additional decrease in the production and availability of HCl and may have an increased risk for fracture.14,20,21
In addition to its biliopancreatic diversion component, the duodenal switch diverts a large portion of the small bowel, with food restricted from moving through it. Vitamin D and protein are normally absorbed at the jejunum and ileum, but only when bile salts are present; after a duodenal switch, bile and pancreatic enzymes are not introduced into the small intestines until 75 to 100 cm before they reach the large intestine. Thus, absorption of vitamin D, protein, calcium, and other nutrients is impaired.20,22
Since phosphorus and magnesium are also absorbed at the sites of the duodenum and jejunum, malabsorption of these nutrients may occur in a patient who has undergone a duodenal switch. Although vitamin B12 is absorbed at the site of the distal ileum, it also requires gastric acid to free it from the food. Zinc absorption, which normally occurs at the site of the jejunum, may be impaired after duodenal switch surgery, and calcium supplementation, though essential, may further reduce zinc absorption.9 Iron absorption requires HCl, facilitated by the presence of vitamin C. Use of H2-blockers and proton pump inhibitors may impair iron metabolism, resulting in anemia.20
In a randomized controlled trial, Aasheim et al23 compared the effects of Roux-en-Y gastric bypass with those of duodenal switch gastric bypass on patients’ vitamin metabolism. The researchers concluded that patients who undergo a duodenal switch are at greater risk for vitamin A and D deficiencies in the first year after surgery; and for thiamine deficiency in the months following surgery as a result of malabsorption, compared with patients who undergo Roux-en-Y gastric bypass.20,23
Patient Management
The case patient’s care necessitated consultations with endocrinology, dermatology, and gastroenterology (GI). Table 3 (below) shows the laboratory findings and the medication changes prompted by the patient’s physical exam and lab results. Table 4 lists the findings from other lab studies ordered throughout the patient’s course of treatment.
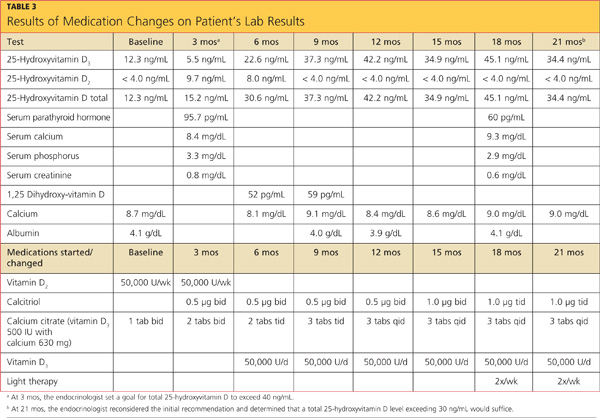
The endocrinologist was consulted at the first sign of osteopenia, and a workup was soon initiated, followed by treatment. GI was consulted six months after the beginning of treatment, when the patient began to complain of reflux while sleeping and frequent diarrhea throughout the day.
Results of esophagogastroduodenoscopy with biopsy ruled out celiac disease and mucosal ulceration, but a small hiatal hernia that was detected (< 3 cm) was determined to be an aggravating factor for the patient’s reflux. The patient was instructed in lifestyle modifications for hiatal hernia, including the need to remain upright one to two hours after eating before going to sleep to prevent aspiration. The patient was instructed to avoid taking iron and calcium within two hours of each other and to limit his alcohol intake. He was also educated in precautions against falls.
Dermatology was consulted nine months into treatment so that light therapy could be initiated, allowing the patient to take advantage of the body’s natural pathway to manufacture vitamin D3.
CONCLUSION
For post–bariatric surgery patients, primary care practitioners are in a position to coordinate care recommendations from multiple specialists, including those in nutrition, to determine the best course of action.
This case illustrates complications of bariatric surgery (malabsorption of key vitamins and minerals, wrist fracture, osteopenia, osteomalacia) that require diagnosis and treatment. The specialists and the primary care practitioner, along with the patient, had to weigh the risks and benefits of continued proton pump inhibitor use, as such medications can increase the risk for fracture. They also addressed the patient’s anemia and remained attentive to his preventive health care needs.
REFERENCES
1. Brusin JH. Update on bone densitometry. Radiol Technol. 2009;81(2):153BD-170BD.
2. Wilson CR. Essentials of bone densitometry for the medical physicist. Presented at: The American Association of Physicists in Medicine 2003 Annual Meeting; July 22-26, 2003; San Diego, CA.
3. Heber D, Greenway FL, Kaplan LM. et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(11):4825-4843.
4. Osteomalacia: step-by-step diagnostic approach (2011). http://bestpractice.bmj.com/best-practice/monograph/517/diagnosis/step-by-step.html. Accessed December 18, 2012.
5. Gifre L, Peris P, Monegal A, et al. Osteomalacia revisited : a report on 28 cases. Clin Rheumatol. 2011;30(5):639-645.
6. Bingham CT, Fitzpatrick LA. Noninvasive testing in the diagnosis of osteomalacia. Am J Med. 1993;95(5):519-523.
7. World Health Organization. Obesity and overweight (May 2012). Fact Sheet No 311. www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 18, 2012.
8. Tanner BD, Allen JW. Complications of bariatric surgery: implications for the covering physician. Am Surg. 2009;75(2):103-112.
9. Soleymani T, Tejavanija S, Morgan S. Obesity, bariatric surgery, and bone. Curr Opin Rheumatol. 2011;23(4):396-405.
10. Koch TR, Finelli FC. Postoperative metabolic and nutritional complications of bariatric surgery. Gastroenterol Clin North Am. 2010;39(1):109-124.
11. Manchester S, Roye GD. Bariatric surgery: an overview for dietetics professionals. Nutr Today. 2011;46(6):264-275.
12. Bal BS, Finelli FC, Shope TR, Koch TR. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544-546.
13. Iannelli A, Schneck AS, Dahman M, et al. Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc. 2009;23(10):2385-2389.
14. Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085.
15. Holrick MF. Vitamin D: important for prevention of osteoporosis, cardiovascular heart disease, type 1 diabetes, autoimmune diseases, and some cancers. South Med J. 2005;98 (10):1024-1027.
16. Kalro BN. Vitamin D and the skeleton. Alt Ther Womens Health. 2009;2(4):25-32.
17. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1568-1617.
18. Huether SE. Structure and function of the renal and urologic systems. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1344-1364.
19. Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am. 2010;39(2):321-331.
20. Decker GA, Swain JM, Crowell MD. Gastrointestinal and nutritional complications after bariatric surgery. Am J Gastroenterol. 2007;102(11):2571-2580.
21. Targownik LE, Lix LM, Metge C, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179(4):319-326.
22. Ybarra J, Sánchez-Hernández J, Pérez A. Hypovitaminosis D and morbid obesity. Nurs Clin North Am. 2007;42(1):19-27.
23. Aasheim ET, Björkman S, Søvik TT, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90(1):15-22.
A white man, age 56, presented to his primary care clinician with wrist pain and swelling. Two days earlier, he had fallen from a step stool and landed on his right wrist. He treated the pain by resting, elevating his arm, applying ice, and taking ibuprofen 800 mg tid. He said he had lost strength in his hand and arm and was experiencing numbness and tingling in his right hand and fingers.
The patient’s medical history included hypertension, type 2 diabetes mellitus, morbid obesity, obstructive sleep apnea, asthma, carpel tunnel syndrome, and peripheral neuropathy. His surgical history was significant for duodenal switch gastric bypass surgery, performed eight years earlier, and his weight at the time of presentation was 200 lb; before his gastric bypass, he weighed 385 lb. Since the surgery, his hypertension, diabetes, asthma, and sleep apnea had all resolved. Table 1 shows a list of medications he was taking at the time of presentation.
The patient, a registered nurse, had been married for 30 years and had one child. He had quit smoking 15 years earlier, with a 43–pack-year smoking history. He reported social drinking but denied any recreational drug use. He was unaware of having any allergies to food or medication.
His vital signs on presentation were blood pressure, 110/75 mm Hg; heart rate, 53 beats/min; respiration, 18 breaths/min; O2 saturation, 97% on room air; and temperature, 97.5°F.
Physical exam revealed that the patient’s right wrist was ecchymotic and swollen with +1 pitting edema. The skin was warm and dry to the touch. Decreased range of motion was noted in the right wrist, compared with the left. Pain with point tenderness was noted at the right lateral wrist. Pulses were +3 with capillary refill of less than 3 seconds. The rest of the exam was unremarkable.
The differential diagnosis included fracture secondary to the fall, osteoporosis, osteopenia, osteomalacia, Paget’s disease, tumor, infection, and sprain or strain of the wrist. A wrist x-ray was ordered, as were the following baseline labs: complete blood count with differential (CBC), vitamin B12 and folate levels, blood chemistry, lipid profile, liver profile, total vitamin D, and sensitive thyroid-stimulating hormone. Test results are shown in Table 2.
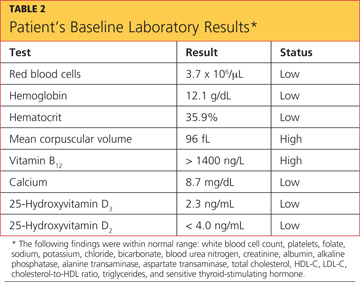
X-ray of the wrist showed fracture only, making it possible to rule out Paget’s disease (ie, no patchy white areas noted in the bone) and tumor (no masses seen) as the immediate cause of fracture. Normal body temperature and normal white blood cell count eliminated the possibility of infection.
Because the patient was only 56 and had a history of bariatric surgery, further testing was pursued to investigate a cause for the weakened bone. Bone mineral density (BMD) testing revealed the following results:
• The lumbar spine in frontal projection measured 0.968 g/cm2 with a T-score of –2.2 and a Z-score of –2.2.
• Total BMD of the left hip was 0.863 g/cm2 with a T-score of –1.7 and a Z-score of –1.4.
• Total BMD of the left femoral neck was 0.863 g/cm2 with a T-score of 1.7 and a Z-score of –1.1.
These findings suggested osteopenia1,2 (not osteoporosis) in all sites, with a 12% decrease of BMD in the spine (suggesting increased risk for spinal fracture) and a 16.3% decrease of BMD in the hip since the patient’s most recent bone scan five years earlier (radiologist’s report). Other abnormal findings were elevated parathyroid hormone (PTH) serum, 95.7 pg/mL (reference range, 10 to 65 pg/mL); low total calcium serum, 8.7 mg/dL (reference range, 8.9 to 10.2 mg/dL), and low 25-hydroxyvitamin D total, 12.3 ng/mL (reference range, 25 to 80 ng/mL).
A 2010 clinical practice guideline from the Endocrine Society3 specifies that after malabsorptive surgery, vitamin D and calcium supplementation should be adjusted by a qualified medical professional, based on serum markers and measures of bone density. An endocrinologist who was consulted at the patient’s initial visit prescribed the following medications: vitamin D2, 50,000 U/wk PO; combined calcium citrate (vitamin D3) 500 IU with calcium 630 mg, 1 tab bid; and calcitriol 0.5 μg bid.
The patient’s final diagnosis was osteomalacia secondary to gastric bypass surgery. (See “Making the Diagnosis of Osteomalacia.”4-6)
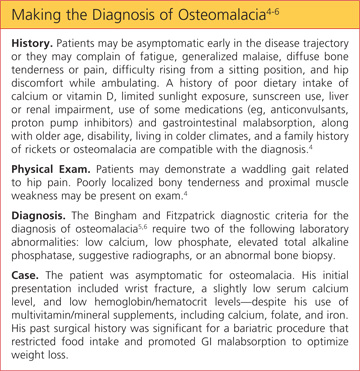
DISCUSSION
According to 2008 data from the World Health Organization (WHO),7 1.4 billion persons older than 20 worldwide were overweight, and 200 million men and 300 million women were considered obese—meaning that one in every 10 adults worldwide is overweight or obese. In 2010, the WHO reports, 40 million children younger than 5 worldwide were considered overweight.7 Health care providers need to be prepared to care for the increasing number of patients who will undergo bariatric surgeries to treat obesity and its related comorbidities.8
Postoperative follow-up for the malabsorption deficiencies related to bariatric procedures should be performed every six months, including obtaining levels of alkaline phosphatase and others previously discussed. In addition, the Endocrine Society guideline3 recommends measuring levels of vitamin B12, albumin, pre-albumin, iron, and ferritin, and obtaining a CBC, a liver profile, glucose reading, creatinine measurement, and a metabolic profile at one month and two months after surgery, then every six months until two years after surgery, then annually if findings are stable.
Furthermore, the Endocrine Society3 recommends obtaining zinc levels every six months for the first year, then annually. An annual vitamin A level is optional.9 Yearly bone density testing is recommended until the patient’s BMD is deemed stable.3
Additionally, Koch and Finelli10 recommend performing the following labs postoperatively: hemoglobin A1C every three months; copper, magnesium, whole blood thiamine, vitamin B12, and a 24-hour urinary calcium every six months for the first three years, then once a year if findings remain stable.
Use of alcohol should be discouraged among patients who have undergone bariatric surgery, as its use alters micronutrient requirements and metabolism. Alcohol consumption may also contribute to dumping syndrome (ie, rapid gastric emptying).11
Any patient with a history of malabsorptive bypass surgery who complains of neurologic, visual, or skin disorders, anemia, or edema may require a further workup to rule out other absorptive deficiencies. These include vitamins A, E, and B12, zinc, folate, thiamine, niacin, selenium, and ferritin.10
Osteomalacia
Metabolic bone diseases can result from genetics, dietary factors, medication use, surgery, or hormonal irregularities. They alter the normal biochemical reactions in bone structure.
The three most common forms of metabolic bone disease are osteoporosis, osteopenia, and osteomalacia. The WHO diagnostic classifications and associated T-scores for bone mineral density1,2 indicate a T-score above –1.0 as normal. A score between –1.0 and –2.5 is indicative of osteopenia, and a score below –2.5 indicates osteoporosis. A T-score below –2.5 in the patient with a history of fragility fracture indicates severe osteoporosis.1,2
In osteomalacia, bone volume remains unchanged, but mineralization of osteoid in the mature compact and spongy bone is either delayed or inadequate. The remolding cycle continues unchanged in the formation of osteoid, but mineral calcification and deposition do not occur.3-5
Osteomalacia is normally considered a rare disorder, but it may become more common as increasing numbers of patients undergo gastric bypass operations.12,13 Primary care practitioners should monitor for this condition in such patients before serious bone loss or other problems develop.9,13,14
Vitamin D deficiency (see “Vitamin D Metabolism,”4,15-19 below), whether or not the result of gastric bypass surgery, is a major risk factor for osteomalacia. Disorders of the small bowel, the hepatobiliary system, and the pancreas are all common causes of vitamin D deficiency. Liver disease interferes with the metabolism of vitamin D. Diseases of the pancreas may cause a deficiency of bile salts, which are vital for the intestinal absorption of vitamin D.17

Restriction and Malabsorption
The case patient had undergone a gastric bypass (duodenal switch), in which a large portion of the stomach is removed and a large part of the small bowel rerouted—with both parts of the procedure causing malabsorption.11 It is in the small bowel that absorption of vitamin D and calcium takes place.
The duodenal switch gastric bypass surgery causes both restriction and malabsorption. Though similar to a biliopancreatic diversion, the duodenal switch preserves the distal stomach and the pylorus20 by way of a sleeve gastrectomy that is performed to reduce the gastric reservoir; the common channel length after revision is 100 cm, not 50 cm (as in conventional biliopancreatic diversion).13 The sleeve gastrectomy involves removal of parietal cells, reducing production of hydrochloric acid (which is necessary to break down food), and hindering the absorption of certain nutrients, including the fat-soluble vitamins, vitamin B12, and iron.12 Patients who take H2-blockers or proton pump inhibitors experience an additional decrease in the production and availability of HCl and may have an increased risk for fracture.14,20,21
In addition to its biliopancreatic diversion component, the duodenal switch diverts a large portion of the small bowel, with food restricted from moving through it. Vitamin D and protein are normally absorbed at the jejunum and ileum, but only when bile salts are present; after a duodenal switch, bile and pancreatic enzymes are not introduced into the small intestines until 75 to 100 cm before they reach the large intestine. Thus, absorption of vitamin D, protein, calcium, and other nutrients is impaired.20,22
Since phosphorus and magnesium are also absorbed at the sites of the duodenum and jejunum, malabsorption of these nutrients may occur in a patient who has undergone a duodenal switch. Although vitamin B12 is absorbed at the site of the distal ileum, it also requires gastric acid to free it from the food. Zinc absorption, which normally occurs at the site of the jejunum, may be impaired after duodenal switch surgery, and calcium supplementation, though essential, may further reduce zinc absorption.9 Iron absorption requires HCl, facilitated by the presence of vitamin C. Use of H2-blockers and proton pump inhibitors may impair iron metabolism, resulting in anemia.20
In a randomized controlled trial, Aasheim et al23 compared the effects of Roux-en-Y gastric bypass with those of duodenal switch gastric bypass on patients’ vitamin metabolism. The researchers concluded that patients who undergo a duodenal switch are at greater risk for vitamin A and D deficiencies in the first year after surgery; and for thiamine deficiency in the months following surgery as a result of malabsorption, compared with patients who undergo Roux-en-Y gastric bypass.20,23
Patient Management
The case patient’s care necessitated consultations with endocrinology, dermatology, and gastroenterology (GI). Table 3 (below) shows the laboratory findings and the medication changes prompted by the patient’s physical exam and lab results. Table 4 lists the findings from other lab studies ordered throughout the patient’s course of treatment.
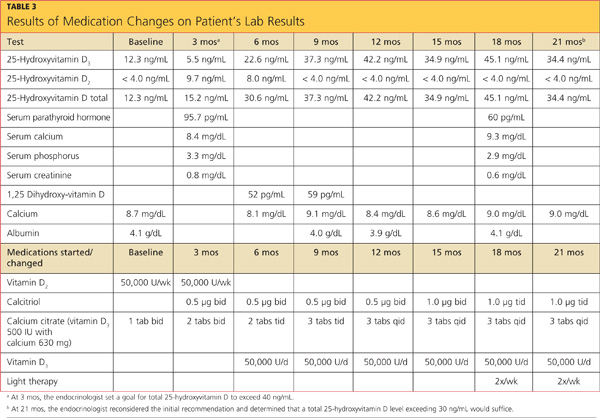
The endocrinologist was consulted at the first sign of osteopenia, and a workup was soon initiated, followed by treatment. GI was consulted six months after the beginning of treatment, when the patient began to complain of reflux while sleeping and frequent diarrhea throughout the day.
Results of esophagogastroduodenoscopy with biopsy ruled out celiac disease and mucosal ulceration, but a small hiatal hernia that was detected (< 3 cm) was determined to be an aggravating factor for the patient’s reflux. The patient was instructed in lifestyle modifications for hiatal hernia, including the need to remain upright one to two hours after eating before going to sleep to prevent aspiration. The patient was instructed to avoid taking iron and calcium within two hours of each other and to limit his alcohol intake. He was also educated in precautions against falls.
Dermatology was consulted nine months into treatment so that light therapy could be initiated, allowing the patient to take advantage of the body’s natural pathway to manufacture vitamin D3.
CONCLUSION
For post–bariatric surgery patients, primary care practitioners are in a position to coordinate care recommendations from multiple specialists, including those in nutrition, to determine the best course of action.
This case illustrates complications of bariatric surgery (malabsorption of key vitamins and minerals, wrist fracture, osteopenia, osteomalacia) that require diagnosis and treatment. The specialists and the primary care practitioner, along with the patient, had to weigh the risks and benefits of continued proton pump inhibitor use, as such medications can increase the risk for fracture. They also addressed the patient’s anemia and remained attentive to his preventive health care needs.
REFERENCES
1. Brusin JH. Update on bone densitometry. Radiol Technol. 2009;81(2):153BD-170BD.
2. Wilson CR. Essentials of bone densitometry for the medical physicist. Presented at: The American Association of Physicists in Medicine 2003 Annual Meeting; July 22-26, 2003; San Diego, CA.
3. Heber D, Greenway FL, Kaplan LM. et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(11):4825-4843.
4. Osteomalacia: step-by-step diagnostic approach (2011). http://bestpractice.bmj.com/best-practice/monograph/517/diagnosis/step-by-step.html. Accessed December 18, 2012.
5. Gifre L, Peris P, Monegal A, et al. Osteomalacia revisited : a report on 28 cases. Clin Rheumatol. 2011;30(5):639-645.
6. Bingham CT, Fitzpatrick LA. Noninvasive testing in the diagnosis of osteomalacia. Am J Med. 1993;95(5):519-523.
7. World Health Organization. Obesity and overweight (May 2012). Fact Sheet No 311. www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 18, 2012.
8. Tanner BD, Allen JW. Complications of bariatric surgery: implications for the covering physician. Am Surg. 2009;75(2):103-112.
9. Soleymani T, Tejavanija S, Morgan S. Obesity, bariatric surgery, and bone. Curr Opin Rheumatol. 2011;23(4):396-405.
10. Koch TR, Finelli FC. Postoperative metabolic and nutritional complications of bariatric surgery. Gastroenterol Clin North Am. 2010;39(1):109-124.
11. Manchester S, Roye GD. Bariatric surgery: an overview for dietetics professionals. Nutr Today. 2011;46(6):264-275.
12. Bal BS, Finelli FC, Shope TR, Koch TR. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544-546.
13. Iannelli A, Schneck AS, Dahman M, et al. Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc. 2009;23(10):2385-2389.
14. Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085.
15. Holrick MF. Vitamin D: important for prevention of osteoporosis, cardiovascular heart disease, type 1 diabetes, autoimmune diseases, and some cancers. South Med J. 2005;98 (10):1024-1027.
16. Kalro BN. Vitamin D and the skeleton. Alt Ther Womens Health. 2009;2(4):25-32.
17. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1568-1617.
18. Huether SE. Structure and function of the renal and urologic systems. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1344-1364.
19. Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am. 2010;39(2):321-331.
20. Decker GA, Swain JM, Crowell MD. Gastrointestinal and nutritional complications after bariatric surgery. Am J Gastroenterol. 2007;102(11):2571-2580.
21. Targownik LE, Lix LM, Metge C, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179(4):319-326.
22. Ybarra J, Sánchez-Hernández J, Pérez A. Hypovitaminosis D and morbid obesity. Nurs Clin North Am. 2007;42(1):19-27.
23. Aasheim ET, Björkman S, Søvik TT, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90(1):15-22.
A white man, age 56, presented to his primary care clinician with wrist pain and swelling. Two days earlier, he had fallen from a step stool and landed on his right wrist. He treated the pain by resting, elevating his arm, applying ice, and taking ibuprofen 800 mg tid. He said he had lost strength in his hand and arm and was experiencing numbness and tingling in his right hand and fingers.
The patient’s medical history included hypertension, type 2 diabetes mellitus, morbid obesity, obstructive sleep apnea, asthma, carpel tunnel syndrome, and peripheral neuropathy. His surgical history was significant for duodenal switch gastric bypass surgery, performed eight years earlier, and his weight at the time of presentation was 200 lb; before his gastric bypass, he weighed 385 lb. Since the surgery, his hypertension, diabetes, asthma, and sleep apnea had all resolved. Table 1 shows a list of medications he was taking at the time of presentation.
The patient, a registered nurse, had been married for 30 years and had one child. He had quit smoking 15 years earlier, with a 43–pack-year smoking history. He reported social drinking but denied any recreational drug use. He was unaware of having any allergies to food or medication.
His vital signs on presentation were blood pressure, 110/75 mm Hg; heart rate, 53 beats/min; respiration, 18 breaths/min; O2 saturation, 97% on room air; and temperature, 97.5°F.
Physical exam revealed that the patient’s right wrist was ecchymotic and swollen with +1 pitting edema. The skin was warm and dry to the touch. Decreased range of motion was noted in the right wrist, compared with the left. Pain with point tenderness was noted at the right lateral wrist. Pulses were +3 with capillary refill of less than 3 seconds. The rest of the exam was unremarkable.
The differential diagnosis included fracture secondary to the fall, osteoporosis, osteopenia, osteomalacia, Paget’s disease, tumor, infection, and sprain or strain of the wrist. A wrist x-ray was ordered, as were the following baseline labs: complete blood count with differential (CBC), vitamin B12 and folate levels, blood chemistry, lipid profile, liver profile, total vitamin D, and sensitive thyroid-stimulating hormone. Test results are shown in Table 2.
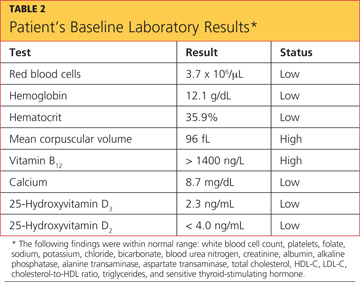
X-ray of the wrist showed fracture only, making it possible to rule out Paget’s disease (ie, no patchy white areas noted in the bone) and tumor (no masses seen) as the immediate cause of fracture. Normal body temperature and normal white blood cell count eliminated the possibility of infection.
Because the patient was only 56 and had a history of bariatric surgery, further testing was pursued to investigate a cause for the weakened bone. Bone mineral density (BMD) testing revealed the following results:
• The lumbar spine in frontal projection measured 0.968 g/cm2 with a T-score of –2.2 and a Z-score of –2.2.
• Total BMD of the left hip was 0.863 g/cm2 with a T-score of –1.7 and a Z-score of –1.4.
• Total BMD of the left femoral neck was 0.863 g/cm2 with a T-score of 1.7 and a Z-score of –1.1.
These findings suggested osteopenia1,2 (not osteoporosis) in all sites, with a 12% decrease of BMD in the spine (suggesting increased risk for spinal fracture) and a 16.3% decrease of BMD in the hip since the patient’s most recent bone scan five years earlier (radiologist’s report). Other abnormal findings were elevated parathyroid hormone (PTH) serum, 95.7 pg/mL (reference range, 10 to 65 pg/mL); low total calcium serum, 8.7 mg/dL (reference range, 8.9 to 10.2 mg/dL), and low 25-hydroxyvitamin D total, 12.3 ng/mL (reference range, 25 to 80 ng/mL).
A 2010 clinical practice guideline from the Endocrine Society3 specifies that after malabsorptive surgery, vitamin D and calcium supplementation should be adjusted by a qualified medical professional, based on serum markers and measures of bone density. An endocrinologist who was consulted at the patient’s initial visit prescribed the following medications: vitamin D2, 50,000 U/wk PO; combined calcium citrate (vitamin D3) 500 IU with calcium 630 mg, 1 tab bid; and calcitriol 0.5 μg bid.
The patient’s final diagnosis was osteomalacia secondary to gastric bypass surgery. (See “Making the Diagnosis of Osteomalacia.”4-6)
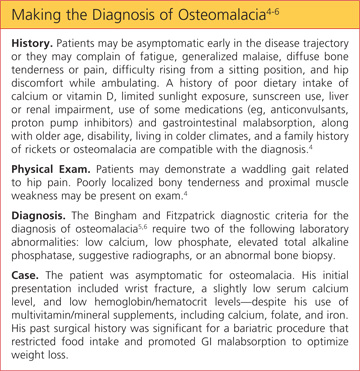
DISCUSSION
According to 2008 data from the World Health Organization (WHO),7 1.4 billion persons older than 20 worldwide were overweight, and 200 million men and 300 million women were considered obese—meaning that one in every 10 adults worldwide is overweight or obese. In 2010, the WHO reports, 40 million children younger than 5 worldwide were considered overweight.7 Health care providers need to be prepared to care for the increasing number of patients who will undergo bariatric surgeries to treat obesity and its related comorbidities.8
Postoperative follow-up for the malabsorption deficiencies related to bariatric procedures should be performed every six months, including obtaining levels of alkaline phosphatase and others previously discussed. In addition, the Endocrine Society guideline3 recommends measuring levels of vitamin B12, albumin, pre-albumin, iron, and ferritin, and obtaining a CBC, a liver profile, glucose reading, creatinine measurement, and a metabolic profile at one month and two months after surgery, then every six months until two years after surgery, then annually if findings are stable.
Furthermore, the Endocrine Society3 recommends obtaining zinc levels every six months for the first year, then annually. An annual vitamin A level is optional.9 Yearly bone density testing is recommended until the patient’s BMD is deemed stable.3
Additionally, Koch and Finelli10 recommend performing the following labs postoperatively: hemoglobin A1C every three months; copper, magnesium, whole blood thiamine, vitamin B12, and a 24-hour urinary calcium every six months for the first three years, then once a year if findings remain stable.
Use of alcohol should be discouraged among patients who have undergone bariatric surgery, as its use alters micronutrient requirements and metabolism. Alcohol consumption may also contribute to dumping syndrome (ie, rapid gastric emptying).11
Any patient with a history of malabsorptive bypass surgery who complains of neurologic, visual, or skin disorders, anemia, or edema may require a further workup to rule out other absorptive deficiencies. These include vitamins A, E, and B12, zinc, folate, thiamine, niacin, selenium, and ferritin.10
Osteomalacia
Metabolic bone diseases can result from genetics, dietary factors, medication use, surgery, or hormonal irregularities. They alter the normal biochemical reactions in bone structure.
The three most common forms of metabolic bone disease are osteoporosis, osteopenia, and osteomalacia. The WHO diagnostic classifications and associated T-scores for bone mineral density1,2 indicate a T-score above –1.0 as normal. A score between –1.0 and –2.5 is indicative of osteopenia, and a score below –2.5 indicates osteoporosis. A T-score below –2.5 in the patient with a history of fragility fracture indicates severe osteoporosis.1,2
In osteomalacia, bone volume remains unchanged, but mineralization of osteoid in the mature compact and spongy bone is either delayed or inadequate. The remolding cycle continues unchanged in the formation of osteoid, but mineral calcification and deposition do not occur.3-5
Osteomalacia is normally considered a rare disorder, but it may become more common as increasing numbers of patients undergo gastric bypass operations.12,13 Primary care practitioners should monitor for this condition in such patients before serious bone loss or other problems develop.9,13,14
Vitamin D deficiency (see “Vitamin D Metabolism,”4,15-19 below), whether or not the result of gastric bypass surgery, is a major risk factor for osteomalacia. Disorders of the small bowel, the hepatobiliary system, and the pancreas are all common causes of vitamin D deficiency. Liver disease interferes with the metabolism of vitamin D. Diseases of the pancreas may cause a deficiency of bile salts, which are vital for the intestinal absorption of vitamin D.17

Restriction and Malabsorption
The case patient had undergone a gastric bypass (duodenal switch), in which a large portion of the stomach is removed and a large part of the small bowel rerouted—with both parts of the procedure causing malabsorption.11 It is in the small bowel that absorption of vitamin D and calcium takes place.
The duodenal switch gastric bypass surgery causes both restriction and malabsorption. Though similar to a biliopancreatic diversion, the duodenal switch preserves the distal stomach and the pylorus20 by way of a sleeve gastrectomy that is performed to reduce the gastric reservoir; the common channel length after revision is 100 cm, not 50 cm (as in conventional biliopancreatic diversion).13 The sleeve gastrectomy involves removal of parietal cells, reducing production of hydrochloric acid (which is necessary to break down food), and hindering the absorption of certain nutrients, including the fat-soluble vitamins, vitamin B12, and iron.12 Patients who take H2-blockers or proton pump inhibitors experience an additional decrease in the production and availability of HCl and may have an increased risk for fracture.14,20,21
In addition to its biliopancreatic diversion component, the duodenal switch diverts a large portion of the small bowel, with food restricted from moving through it. Vitamin D and protein are normally absorbed at the jejunum and ileum, but only when bile salts are present; after a duodenal switch, bile and pancreatic enzymes are not introduced into the small intestines until 75 to 100 cm before they reach the large intestine. Thus, absorption of vitamin D, protein, calcium, and other nutrients is impaired.20,22
Since phosphorus and magnesium are also absorbed at the sites of the duodenum and jejunum, malabsorption of these nutrients may occur in a patient who has undergone a duodenal switch. Although vitamin B12 is absorbed at the site of the distal ileum, it also requires gastric acid to free it from the food. Zinc absorption, which normally occurs at the site of the jejunum, may be impaired after duodenal switch surgery, and calcium supplementation, though essential, may further reduce zinc absorption.9 Iron absorption requires HCl, facilitated by the presence of vitamin C. Use of H2-blockers and proton pump inhibitors may impair iron metabolism, resulting in anemia.20
In a randomized controlled trial, Aasheim et al23 compared the effects of Roux-en-Y gastric bypass with those of duodenal switch gastric bypass on patients’ vitamin metabolism. The researchers concluded that patients who undergo a duodenal switch are at greater risk for vitamin A and D deficiencies in the first year after surgery; and for thiamine deficiency in the months following surgery as a result of malabsorption, compared with patients who undergo Roux-en-Y gastric bypass.20,23
Patient Management
The case patient’s care necessitated consultations with endocrinology, dermatology, and gastroenterology (GI). Table 3 (below) shows the laboratory findings and the medication changes prompted by the patient’s physical exam and lab results. Table 4 lists the findings from other lab studies ordered throughout the patient’s course of treatment.
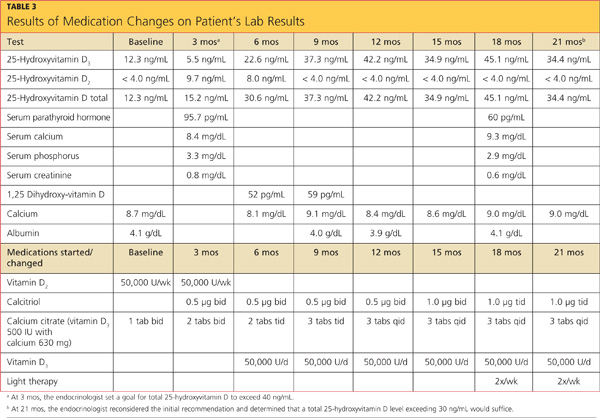
The endocrinologist was consulted at the first sign of osteopenia, and a workup was soon initiated, followed by treatment. GI was consulted six months after the beginning of treatment, when the patient began to complain of reflux while sleeping and frequent diarrhea throughout the day.
Results of esophagogastroduodenoscopy with biopsy ruled out celiac disease and mucosal ulceration, but a small hiatal hernia that was detected (< 3 cm) was determined to be an aggravating factor for the patient’s reflux. The patient was instructed in lifestyle modifications for hiatal hernia, including the need to remain upright one to two hours after eating before going to sleep to prevent aspiration. The patient was instructed to avoid taking iron and calcium within two hours of each other and to limit his alcohol intake. He was also educated in precautions against falls.
Dermatology was consulted nine months into treatment so that light therapy could be initiated, allowing the patient to take advantage of the body’s natural pathway to manufacture vitamin D3.
CONCLUSION
For post–bariatric surgery patients, primary care practitioners are in a position to coordinate care recommendations from multiple specialists, including those in nutrition, to determine the best course of action.
This case illustrates complications of bariatric surgery (malabsorption of key vitamins and minerals, wrist fracture, osteopenia, osteomalacia) that require diagnosis and treatment. The specialists and the primary care practitioner, along with the patient, had to weigh the risks and benefits of continued proton pump inhibitor use, as such medications can increase the risk for fracture. They also addressed the patient’s anemia and remained attentive to his preventive health care needs.
REFERENCES
1. Brusin JH. Update on bone densitometry. Radiol Technol. 2009;81(2):153BD-170BD.
2. Wilson CR. Essentials of bone densitometry for the medical physicist. Presented at: The American Association of Physicists in Medicine 2003 Annual Meeting; July 22-26, 2003; San Diego, CA.
3. Heber D, Greenway FL, Kaplan LM. et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(11):4825-4843.
4. Osteomalacia: step-by-step diagnostic approach (2011). http://bestpractice.bmj.com/best-practice/monograph/517/diagnosis/step-by-step.html. Accessed December 18, 2012.
5. Gifre L, Peris P, Monegal A, et al. Osteomalacia revisited : a report on 28 cases. Clin Rheumatol. 2011;30(5):639-645.
6. Bingham CT, Fitzpatrick LA. Noninvasive testing in the diagnosis of osteomalacia. Am J Med. 1993;95(5):519-523.
7. World Health Organization. Obesity and overweight (May 2012). Fact Sheet No 311. www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 18, 2012.
8. Tanner BD, Allen JW. Complications of bariatric surgery: implications for the covering physician. Am Surg. 2009;75(2):103-112.
9. Soleymani T, Tejavanija S, Morgan S. Obesity, bariatric surgery, and bone. Curr Opin Rheumatol. 2011;23(4):396-405.
10. Koch TR, Finelli FC. Postoperative metabolic and nutritional complications of bariatric surgery. Gastroenterol Clin North Am. 2010;39(1):109-124.
11. Manchester S, Roye GD. Bariatric surgery: an overview for dietetics professionals. Nutr Today. 2011;46(6):264-275.
12. Bal BS, Finelli FC, Shope TR, Koch TR. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544-546.
13. Iannelli A, Schneck AS, Dahman M, et al. Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc. 2009;23(10):2385-2389.
14. Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085.
15. Holrick MF. Vitamin D: important for prevention of osteoporosis, cardiovascular heart disease, type 1 diabetes, autoimmune diseases, and some cancers. South Med J. 2005;98 (10):1024-1027.
16. Kalro BN. Vitamin D and the skeleton. Alt Ther Womens Health. 2009;2(4):25-32.
17. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1568-1617.
18. Huether SE. Structure and function of the renal and urologic systems. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1344-1364.
19. Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am. 2010;39(2):321-331.
20. Decker GA, Swain JM, Crowell MD. Gastrointestinal and nutritional complications after bariatric surgery. Am J Gastroenterol. 2007;102(11):2571-2580.
21. Targownik LE, Lix LM, Metge C, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179(4):319-326.
22. Ybarra J, Sánchez-Hernández J, Pérez A. Hypovitaminosis D and morbid obesity. Nurs Clin North Am. 2007;42(1):19-27.
23. Aasheim ET, Björkman S, Søvik TT, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90(1):15-22.
Underlying Factors Influence Insulin's Effect
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.