User login
Normal enzyme aids mutated FLT3 to fuel AML

Results of preclinical research suggest the wild-type version of SYK pairs with mutated FLT3 to promote progression of acute myelogenous leukemia (AML).
And this molecular partnership promotes AML cells’ resistance to FLT3 inhibitors.
However, adding a SYK inhibitor to the mix can override this resistance. In an animal model of AML, treatment with a combination of FLT3 and SYK inhibitors was significantly more effective than either inhibitor alone.
These findings, published in Cancer Cell, raise hopes that treatment strategies focusing on both enzymes simultaneously could improve outcomes for patients with FLT3-ITD AML.
“Patients whose AML cells express FLT3-ITD are among the highest-risk group of patients with AML,” said study author Kimberly Stegmaier, MD, of the Dana-Farber Cancer Institute in Boston. “Their AML is particularly difficult to treat.”
In 2009, researchers in Dr Stegmaier’s lab discovered that SYK, a kinase that had attracted attention for its role in other malignancies, could be a potential drug target in AML. Unlike other cancer-associated kinases, SYK rarely undergoes mutations or other genomic alterations in cancer cells, remaining in its wild-type form.
With the current study, Dr Stegmaier and her colleagues set out to better understand SYK’s role in AML. The team screened AML cell lines to reveal the full scope of the enzyme’s molecular interactions. And they found evidence of strong interactions between wild-type SYK and mutated FLT3, particularly FLT3-ITD.
“We wanted to understand the cooperative oncologic effects by which SYK contributes to AML,” Dr Stegmaier said. “The concept of a normal enzyme aiding a mutant one has not yet been widely explored, and so we were both surprised and pleased to see FLT3-ITD come up as a high-priority hit in our screens.”
Through experiments in cell lines, primary patient samples, and animal models, the researchers found that SYK and FLT3-ITD’s interactions are a key ingredient in the progression of myeloproliferative neoplasms into AML. AML cells’ continued growth after turning malignant also relied on these interactions.
In addition, the team found that SYK’s hyperactivated form can promote resistance to the FLT3-targeting drug quizartinib. However, a combination of quizartinib and the SYK inhibitor PRT062607 overcame this resistance, significantly increasing survival and reducing signs of disease in a FLT3-ITD AML mouse model.
Highlighting their findings’ clinical relevance, the researchers found strong SYK activity in cells from FLT3-ITD AML patients. The cells were also highly sensitive to SYK inhibition.
“These data affirm that SYK is an important target in AML,” Dr Stegmaier said. “They also suggest that interactions between oncologic kinases and SYK or other wild-type enzymes may contribute to resistance of kinase inhibitors more broadly.”
Dr Stegmaier added that, over the course of this research, the team has developed a suite of tools that could prove useful for future clinical studies of treatments with SYK inhibitors or SYK inhibitors in combination with FLT3 inhibitors.
“We have not only identified SYK as a candidate treatment target in AML, but we have also identified a specific population of patients with AML more likely to respond to SYK inhibitors: patients with FLT3 mutations,” she said.
“Moreover, we have developed tools for identifying patients with high levels of SYK and FLT3 activation and can monitor these 2 targets while patients are receiving treatment. Predictive biomarkers of response are becoming increasingly important in the development of effective clinical trials of targeted therapies.” ![]()

Results of preclinical research suggest the wild-type version of SYK pairs with mutated FLT3 to promote progression of acute myelogenous leukemia (AML).
And this molecular partnership promotes AML cells’ resistance to FLT3 inhibitors.
However, adding a SYK inhibitor to the mix can override this resistance. In an animal model of AML, treatment with a combination of FLT3 and SYK inhibitors was significantly more effective than either inhibitor alone.
These findings, published in Cancer Cell, raise hopes that treatment strategies focusing on both enzymes simultaneously could improve outcomes for patients with FLT3-ITD AML.
“Patients whose AML cells express FLT3-ITD are among the highest-risk group of patients with AML,” said study author Kimberly Stegmaier, MD, of the Dana-Farber Cancer Institute in Boston. “Their AML is particularly difficult to treat.”
In 2009, researchers in Dr Stegmaier’s lab discovered that SYK, a kinase that had attracted attention for its role in other malignancies, could be a potential drug target in AML. Unlike other cancer-associated kinases, SYK rarely undergoes mutations or other genomic alterations in cancer cells, remaining in its wild-type form.
With the current study, Dr Stegmaier and her colleagues set out to better understand SYK’s role in AML. The team screened AML cell lines to reveal the full scope of the enzyme’s molecular interactions. And they found evidence of strong interactions between wild-type SYK and mutated FLT3, particularly FLT3-ITD.
“We wanted to understand the cooperative oncologic effects by which SYK contributes to AML,” Dr Stegmaier said. “The concept of a normal enzyme aiding a mutant one has not yet been widely explored, and so we were both surprised and pleased to see FLT3-ITD come up as a high-priority hit in our screens.”
Through experiments in cell lines, primary patient samples, and animal models, the researchers found that SYK and FLT3-ITD’s interactions are a key ingredient in the progression of myeloproliferative neoplasms into AML. AML cells’ continued growth after turning malignant also relied on these interactions.
In addition, the team found that SYK’s hyperactivated form can promote resistance to the FLT3-targeting drug quizartinib. However, a combination of quizartinib and the SYK inhibitor PRT062607 overcame this resistance, significantly increasing survival and reducing signs of disease in a FLT3-ITD AML mouse model.
Highlighting their findings’ clinical relevance, the researchers found strong SYK activity in cells from FLT3-ITD AML patients. The cells were also highly sensitive to SYK inhibition.
“These data affirm that SYK is an important target in AML,” Dr Stegmaier said. “They also suggest that interactions between oncologic kinases and SYK or other wild-type enzymes may contribute to resistance of kinase inhibitors more broadly.”
Dr Stegmaier added that, over the course of this research, the team has developed a suite of tools that could prove useful for future clinical studies of treatments with SYK inhibitors or SYK inhibitors in combination with FLT3 inhibitors.
“We have not only identified SYK as a candidate treatment target in AML, but we have also identified a specific population of patients with AML more likely to respond to SYK inhibitors: patients with FLT3 mutations,” she said.
“Moreover, we have developed tools for identifying patients with high levels of SYK and FLT3 activation and can monitor these 2 targets while patients are receiving treatment. Predictive biomarkers of response are becoming increasingly important in the development of effective clinical trials of targeted therapies.” ![]()

Results of preclinical research suggest the wild-type version of SYK pairs with mutated FLT3 to promote progression of acute myelogenous leukemia (AML).
And this molecular partnership promotes AML cells’ resistance to FLT3 inhibitors.
However, adding a SYK inhibitor to the mix can override this resistance. In an animal model of AML, treatment with a combination of FLT3 and SYK inhibitors was significantly more effective than either inhibitor alone.
These findings, published in Cancer Cell, raise hopes that treatment strategies focusing on both enzymes simultaneously could improve outcomes for patients with FLT3-ITD AML.
“Patients whose AML cells express FLT3-ITD are among the highest-risk group of patients with AML,” said study author Kimberly Stegmaier, MD, of the Dana-Farber Cancer Institute in Boston. “Their AML is particularly difficult to treat.”
In 2009, researchers in Dr Stegmaier’s lab discovered that SYK, a kinase that had attracted attention for its role in other malignancies, could be a potential drug target in AML. Unlike other cancer-associated kinases, SYK rarely undergoes mutations or other genomic alterations in cancer cells, remaining in its wild-type form.
With the current study, Dr Stegmaier and her colleagues set out to better understand SYK’s role in AML. The team screened AML cell lines to reveal the full scope of the enzyme’s molecular interactions. And they found evidence of strong interactions between wild-type SYK and mutated FLT3, particularly FLT3-ITD.
“We wanted to understand the cooperative oncologic effects by which SYK contributes to AML,” Dr Stegmaier said. “The concept of a normal enzyme aiding a mutant one has not yet been widely explored, and so we were both surprised and pleased to see FLT3-ITD come up as a high-priority hit in our screens.”
Through experiments in cell lines, primary patient samples, and animal models, the researchers found that SYK and FLT3-ITD’s interactions are a key ingredient in the progression of myeloproliferative neoplasms into AML. AML cells’ continued growth after turning malignant also relied on these interactions.
In addition, the team found that SYK’s hyperactivated form can promote resistance to the FLT3-targeting drug quizartinib. However, a combination of quizartinib and the SYK inhibitor PRT062607 overcame this resistance, significantly increasing survival and reducing signs of disease in a FLT3-ITD AML mouse model.
Highlighting their findings’ clinical relevance, the researchers found strong SYK activity in cells from FLT3-ITD AML patients. The cells were also highly sensitive to SYK inhibition.
“These data affirm that SYK is an important target in AML,” Dr Stegmaier said. “They also suggest that interactions between oncologic kinases and SYK or other wild-type enzymes may contribute to resistance of kinase inhibitors more broadly.”
Dr Stegmaier added that, over the course of this research, the team has developed a suite of tools that could prove useful for future clinical studies of treatments with SYK inhibitors or SYK inhibitors in combination with FLT3 inhibitors.
“We have not only identified SYK as a candidate treatment target in AML, but we have also identified a specific population of patients with AML more likely to respond to SYK inhibitors: patients with FLT3 mutations,” she said.
“Moreover, we have developed tools for identifying patients with high levels of SYK and FLT3 activation and can monitor these 2 targets while patients are receiving treatment. Predictive biomarkers of response are becoming increasingly important in the development of effective clinical trials of targeted therapies.” ![]()
Proteins may help explain PEL pathogenesis

Researchers say they’ve identified 20 proteins specific to primary effusion lymphoma (PEL).
The proteins, which were found by growing PEL cells in culture and analyzing the secretome, may explain PEL pathogenesis, its peculiar cell adhesion, and migration patterns.
The investigators also uncovered related oncogenic pathways, which could pave the way for more individualized treatment of PEL.
These findings appear in The American Journal of Pathology.
The researchers analyzed secretomes from 4 established PEL cell lines—CRO-AP2, CRO-AP3, CRO-AP5, and CRO-AP6—as well as from 4 PEL clinical samples and 3 primary solid lymphomas. PEL cells are characterized by Kaposi’s sarcoma-associated herpesvirus (KSHV) infection, and the primary solid lymphomas were KSHV-positive as well.
The investigators measured protein content using 2 complementary mass spectrometry platforms. The experiments allowed cells to grow for 16 to 18 hours and were performed under serum-free conditions to increase the ability to detect secreted proteins.
Of the 266 proteins identified, 139 (52%) were secreted, and 127 were considered to have an intracellular origin or were secreted in an unconventional fashion.
“Most of the proteins we recognized in the secretome of PEL are new with respect to previous studies utilizing conventional proteomic analysis and gene expression profiling,” said study author Annunziata Gloghini, PhD, of Istituto Nazionale dei Tumori in Milan, Italy.
“Importantly, 27 proteins were shared by secretomes from all PEL cell lines.”
The PEL secretomes were enriched with proteins specifically involved in inflammation and the immune response—such as HMGB1, GRAA, and PCBP2—as well as cell growth—such as LEG1, STMN1, and S10A6.
Other proteins are known to play roles in mRNA processing—such as ANM1 and PCBP2—or cell structure, adhesion, migration, and organization—such as EZRI and MOES. Some of the proteins have enzymatic activity—such as CATA and GSTK1.
A comparison of secretomes from PEL with those from other tumor cell lines revealed 20 proteins specific to the PEL cell lines. This suggests secretome profiling provides a source of tumor biomarkers and may ultimately improve patient management, the researchers said.
The group also conducted pathway/network enrichment analyses and found that the pathways most activated in PEL cell lines were involved with the regulation of autophagy through LRRK2-mediated signaling pathways and with apoptosis and survival through granzyme A signaling.
“The extracellular functions of granzyme A might be involved in the particular tropism of PEL and its cell growth,” said study author Italia Bongarzone, PhD, also of the Istituto Nazionale dei Tumori.
“Further studies are needed to confirm and validate the importance of these pathways/processes and their roles in lymphoma tumorigenesis and progression.” ![]()

Researchers say they’ve identified 20 proteins specific to primary effusion lymphoma (PEL).
The proteins, which were found by growing PEL cells in culture and analyzing the secretome, may explain PEL pathogenesis, its peculiar cell adhesion, and migration patterns.
The investigators also uncovered related oncogenic pathways, which could pave the way for more individualized treatment of PEL.
These findings appear in The American Journal of Pathology.
The researchers analyzed secretomes from 4 established PEL cell lines—CRO-AP2, CRO-AP3, CRO-AP5, and CRO-AP6—as well as from 4 PEL clinical samples and 3 primary solid lymphomas. PEL cells are characterized by Kaposi’s sarcoma-associated herpesvirus (KSHV) infection, and the primary solid lymphomas were KSHV-positive as well.
The investigators measured protein content using 2 complementary mass spectrometry platforms. The experiments allowed cells to grow for 16 to 18 hours and were performed under serum-free conditions to increase the ability to detect secreted proteins.
Of the 266 proteins identified, 139 (52%) were secreted, and 127 were considered to have an intracellular origin or were secreted in an unconventional fashion.
“Most of the proteins we recognized in the secretome of PEL are new with respect to previous studies utilizing conventional proteomic analysis and gene expression profiling,” said study author Annunziata Gloghini, PhD, of Istituto Nazionale dei Tumori in Milan, Italy.
“Importantly, 27 proteins were shared by secretomes from all PEL cell lines.”
The PEL secretomes were enriched with proteins specifically involved in inflammation and the immune response—such as HMGB1, GRAA, and PCBP2—as well as cell growth—such as LEG1, STMN1, and S10A6.
Other proteins are known to play roles in mRNA processing—such as ANM1 and PCBP2—or cell structure, adhesion, migration, and organization—such as EZRI and MOES. Some of the proteins have enzymatic activity—such as CATA and GSTK1.
A comparison of secretomes from PEL with those from other tumor cell lines revealed 20 proteins specific to the PEL cell lines. This suggests secretome profiling provides a source of tumor biomarkers and may ultimately improve patient management, the researchers said.
The group also conducted pathway/network enrichment analyses and found that the pathways most activated in PEL cell lines were involved with the regulation of autophagy through LRRK2-mediated signaling pathways and with apoptosis and survival through granzyme A signaling.
“The extracellular functions of granzyme A might be involved in the particular tropism of PEL and its cell growth,” said study author Italia Bongarzone, PhD, also of the Istituto Nazionale dei Tumori.
“Further studies are needed to confirm and validate the importance of these pathways/processes and their roles in lymphoma tumorigenesis and progression.” ![]()

Researchers say they’ve identified 20 proteins specific to primary effusion lymphoma (PEL).
The proteins, which were found by growing PEL cells in culture and analyzing the secretome, may explain PEL pathogenesis, its peculiar cell adhesion, and migration patterns.
The investigators also uncovered related oncogenic pathways, which could pave the way for more individualized treatment of PEL.
These findings appear in The American Journal of Pathology.
The researchers analyzed secretomes from 4 established PEL cell lines—CRO-AP2, CRO-AP3, CRO-AP5, and CRO-AP6—as well as from 4 PEL clinical samples and 3 primary solid lymphomas. PEL cells are characterized by Kaposi’s sarcoma-associated herpesvirus (KSHV) infection, and the primary solid lymphomas were KSHV-positive as well.
The investigators measured protein content using 2 complementary mass spectrometry platforms. The experiments allowed cells to grow for 16 to 18 hours and were performed under serum-free conditions to increase the ability to detect secreted proteins.
Of the 266 proteins identified, 139 (52%) were secreted, and 127 were considered to have an intracellular origin or were secreted in an unconventional fashion.
“Most of the proteins we recognized in the secretome of PEL are new with respect to previous studies utilizing conventional proteomic analysis and gene expression profiling,” said study author Annunziata Gloghini, PhD, of Istituto Nazionale dei Tumori in Milan, Italy.
“Importantly, 27 proteins were shared by secretomes from all PEL cell lines.”
The PEL secretomes were enriched with proteins specifically involved in inflammation and the immune response—such as HMGB1, GRAA, and PCBP2—as well as cell growth—such as LEG1, STMN1, and S10A6.
Other proteins are known to play roles in mRNA processing—such as ANM1 and PCBP2—or cell structure, adhesion, migration, and organization—such as EZRI and MOES. Some of the proteins have enzymatic activity—such as CATA and GSTK1.
A comparison of secretomes from PEL with those from other tumor cell lines revealed 20 proteins specific to the PEL cell lines. This suggests secretome profiling provides a source of tumor biomarkers and may ultimately improve patient management, the researchers said.
The group also conducted pathway/network enrichment analyses and found that the pathways most activated in PEL cell lines were involved with the regulation of autophagy through LRRK2-mediated signaling pathways and with apoptosis and survival through granzyme A signaling.
“The extracellular functions of granzyme A might be involved in the particular tropism of PEL and its cell growth,” said study author Italia Bongarzone, PhD, also of the Istituto Nazionale dei Tumori.
“Further studies are needed to confirm and validate the importance of these pathways/processes and their roles in lymphoma tumorigenesis and progression.” ![]()
Team develops new live-cell printing technology

Credit: Lidong Qin lab
A new technique allows scientists to print living cells onto any surface in virtually any shape, according to a paper published in Proceedings of the National Academy of Sciences.
The approach, called Block-Cell-Printing (BloC-Printing), produces 2-D cell arrays in as little as half an hour, prints the cells as close together as 5 μm, and allows for the use of different cell types.
And unlike similar work using inkjet printing approaches, almost all cells survive BloC-Printing.
“Cell printing is used in so many different ways now—for drug development and in studies of tissue regeneration, cell function, and cell-cell communication,” said study author Lidong Qin, PhD, of Houston Methodist Research Institute in Texas.
“Such things can only be done when cells are alive and active. A survival rate of 50% to 80% is typical as cells exit the inkjet nozzles. By comparison, we are seeing close to 100% of cells in BloC-Printing survive the printing process.”
On the other hand, Dr Qin noted that inkjet printing remains faster than BloC-Printing. And BloC-Printing cannot yet print multi-layer structures as inkjetting can.
BloC-Printing manipulates microfluidic physics to guide living cells into hook-like traps in a silicone mold. Cells flow down a column in the mold, past trapped cells to the next available slot, eventually creating a line of cells (in a grid of such lines).
The position and spacing of the traps and the shape of the channel navigated by the cells is fully configurable during the mold’s creation. When the mold is lifted away, the living cells remain behind, adhering to the growth medium or other substrate in prescribed formation.
Dr Qin’s group tested BloC-Printing for its utility in studying breast cancer cells and primary neurons.
By arranging the cancer cells in a grid and examining their growth in comparison with a non-metastatic control, the researchers found they could easily characterize the metastatic potential of the cancer cells.
“We looked at cancer cells for their protrusion generation capability, which correlates to their malignancy level,” Dr Qin said. “Longer protrusion means more aggressive cancer cells. The measurement may help to diagnose a cancer’s stage.”
The researchers also printed a grid of brain cells and gave the cells time to form synaptic and autaptic junctions.
“The cell junctions we created may be useful for future neuron signal transduction and axon regeneration studies,” Dr Qin said. “Such work could be helpful in understanding Alzheimer’s disease and other neurodegenerative diseases.”
While it is too early to predict the market cost of BloC-Printing, Dr Qin said the materials of a single BloC mold cost about $1. After the mold has been fabricated and delivered, a researcher only needs a syringe, a carefully prepared suspension of living cells, a Petri dish, and a steady hand.
“BloC-Printing can be combined with molecular printing for many types of drug screening, RNA interference, and molecule-cell interaction studies,” Dr Qin said. “We believe the technology has big potential.” ![]()

Credit: Lidong Qin lab
A new technique allows scientists to print living cells onto any surface in virtually any shape, according to a paper published in Proceedings of the National Academy of Sciences.
The approach, called Block-Cell-Printing (BloC-Printing), produces 2-D cell arrays in as little as half an hour, prints the cells as close together as 5 μm, and allows for the use of different cell types.
And unlike similar work using inkjet printing approaches, almost all cells survive BloC-Printing.
“Cell printing is used in so many different ways now—for drug development and in studies of tissue regeneration, cell function, and cell-cell communication,” said study author Lidong Qin, PhD, of Houston Methodist Research Institute in Texas.
“Such things can only be done when cells are alive and active. A survival rate of 50% to 80% is typical as cells exit the inkjet nozzles. By comparison, we are seeing close to 100% of cells in BloC-Printing survive the printing process.”
On the other hand, Dr Qin noted that inkjet printing remains faster than BloC-Printing. And BloC-Printing cannot yet print multi-layer structures as inkjetting can.
BloC-Printing manipulates microfluidic physics to guide living cells into hook-like traps in a silicone mold. Cells flow down a column in the mold, past trapped cells to the next available slot, eventually creating a line of cells (in a grid of such lines).
The position and spacing of the traps and the shape of the channel navigated by the cells is fully configurable during the mold’s creation. When the mold is lifted away, the living cells remain behind, adhering to the growth medium or other substrate in prescribed formation.
Dr Qin’s group tested BloC-Printing for its utility in studying breast cancer cells and primary neurons.
By arranging the cancer cells in a grid and examining their growth in comparison with a non-metastatic control, the researchers found they could easily characterize the metastatic potential of the cancer cells.
“We looked at cancer cells for their protrusion generation capability, which correlates to their malignancy level,” Dr Qin said. “Longer protrusion means more aggressive cancer cells. The measurement may help to diagnose a cancer’s stage.”
The researchers also printed a grid of brain cells and gave the cells time to form synaptic and autaptic junctions.
“The cell junctions we created may be useful for future neuron signal transduction and axon regeneration studies,” Dr Qin said. “Such work could be helpful in understanding Alzheimer’s disease and other neurodegenerative diseases.”
While it is too early to predict the market cost of BloC-Printing, Dr Qin said the materials of a single BloC mold cost about $1. After the mold has been fabricated and delivered, a researcher only needs a syringe, a carefully prepared suspension of living cells, a Petri dish, and a steady hand.
“BloC-Printing can be combined with molecular printing for many types of drug screening, RNA interference, and molecule-cell interaction studies,” Dr Qin said. “We believe the technology has big potential.” ![]()

Credit: Lidong Qin lab
A new technique allows scientists to print living cells onto any surface in virtually any shape, according to a paper published in Proceedings of the National Academy of Sciences.
The approach, called Block-Cell-Printing (BloC-Printing), produces 2-D cell arrays in as little as half an hour, prints the cells as close together as 5 μm, and allows for the use of different cell types.
And unlike similar work using inkjet printing approaches, almost all cells survive BloC-Printing.
“Cell printing is used in so many different ways now—for drug development and in studies of tissue regeneration, cell function, and cell-cell communication,” said study author Lidong Qin, PhD, of Houston Methodist Research Institute in Texas.
“Such things can only be done when cells are alive and active. A survival rate of 50% to 80% is typical as cells exit the inkjet nozzles. By comparison, we are seeing close to 100% of cells in BloC-Printing survive the printing process.”
On the other hand, Dr Qin noted that inkjet printing remains faster than BloC-Printing. And BloC-Printing cannot yet print multi-layer structures as inkjetting can.
BloC-Printing manipulates microfluidic physics to guide living cells into hook-like traps in a silicone mold. Cells flow down a column in the mold, past trapped cells to the next available slot, eventually creating a line of cells (in a grid of such lines).
The position and spacing of the traps and the shape of the channel navigated by the cells is fully configurable during the mold’s creation. When the mold is lifted away, the living cells remain behind, adhering to the growth medium or other substrate in prescribed formation.
Dr Qin’s group tested BloC-Printing for its utility in studying breast cancer cells and primary neurons.
By arranging the cancer cells in a grid and examining their growth in comparison with a non-metastatic control, the researchers found they could easily characterize the metastatic potential of the cancer cells.
“We looked at cancer cells for their protrusion generation capability, which correlates to their malignancy level,” Dr Qin said. “Longer protrusion means more aggressive cancer cells. The measurement may help to diagnose a cancer’s stage.”
The researchers also printed a grid of brain cells and gave the cells time to form synaptic and autaptic junctions.
“The cell junctions we created may be useful for future neuron signal transduction and axon regeneration studies,” Dr Qin said. “Such work could be helpful in understanding Alzheimer’s disease and other neurodegenerative diseases.”
While it is too early to predict the market cost of BloC-Printing, Dr Qin said the materials of a single BloC mold cost about $1. After the mold has been fabricated and delivered, a researcher only needs a syringe, a carefully prepared suspension of living cells, a Petri dish, and a steady hand.
“BloC-Printing can be combined with molecular printing for many types of drug screening, RNA interference, and molecule-cell interaction studies,” Dr Qin said. “We believe the technology has big potential.” ![]()
Actinic keratoses: The cold truth
Actinic keratosis, or solar keratosis, results from the proliferation of atypical epidermal keratinocytes. When we can take the time to do a skin examination, we all see a lot of them especially among our older and middle-aged sun worshippers and sunscreen agnostics. My traditional approach, for better or for worse, has been to acquire the liquid nitrogen bottle on the floor and go to work. But my recent review of guidelines prepared on behalf of the British Association of Dermatologists and published several years ago have prompted me to open my eyes a bit more to other possible approaches.
Reassuringly, the likelihood of progression of an AK to squamous cell carcinoma (SCC) is low. Estimates from a large U.S. cohort revealed a rate of transformation to invasive or in situ SCC of 0.6% after 1 year and 2.6 % after 4 years. But we have to remember that although the progression rate is low, 60% of SCC arise from AKs.
The AK guideline authors synthesized and graded published evidence. Topical therapies receiving an "A grade" (i.e., good evidence) included no therapy or emollients for mild AKs and 5-fluorouracil. Therapies with a "B grade" (i.e., fair evidence) include diclofenac gel and imiquimod.
Other treatments include cryosurgery (A grade) and photodynamic therapy (B grade). We do a lot of cryotherapy in our practice but patients need to be informed of the scarring and possible hyper- or hypopigmentation that can occur with treatment. Photodynamic therapy will, in most cases, be administered by dermatologists.
According to a recent paper in the Drugs and Therapeutic Bulletin, patients should be referred to a dermatologist if there is diagnostic uncertainty, concerns about malignancy, treatment failure or management concerns, or if the patient is at high risk (e.g., organ transplant recipients, multiple large lesions, or previous SCC).
The guideline authors suggest that most patients can be evaluated and treated in the primary care setting. They go on to say that there is inadequate evidence to justify treatment of all AKs in an attempt to prevent malignant transformation. While reassuring, this requires us to consider all possible treatment approaches. One liquid nitrogen bottle does not fit all.
Dr. Ebbert is professor of medicine and general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no conflicts of interest.
Actinic keratosis, or solar keratosis, results from the proliferation of atypical epidermal keratinocytes. When we can take the time to do a skin examination, we all see a lot of them especially among our older and middle-aged sun worshippers and sunscreen agnostics. My traditional approach, for better or for worse, has been to acquire the liquid nitrogen bottle on the floor and go to work. But my recent review of guidelines prepared on behalf of the British Association of Dermatologists and published several years ago have prompted me to open my eyes a bit more to other possible approaches.
Reassuringly, the likelihood of progression of an AK to squamous cell carcinoma (SCC) is low. Estimates from a large U.S. cohort revealed a rate of transformation to invasive or in situ SCC of 0.6% after 1 year and 2.6 % after 4 years. But we have to remember that although the progression rate is low, 60% of SCC arise from AKs.
The AK guideline authors synthesized and graded published evidence. Topical therapies receiving an "A grade" (i.e., good evidence) included no therapy or emollients for mild AKs and 5-fluorouracil. Therapies with a "B grade" (i.e., fair evidence) include diclofenac gel and imiquimod.
Other treatments include cryosurgery (A grade) and photodynamic therapy (B grade). We do a lot of cryotherapy in our practice but patients need to be informed of the scarring and possible hyper- or hypopigmentation that can occur with treatment. Photodynamic therapy will, in most cases, be administered by dermatologists.
According to a recent paper in the Drugs and Therapeutic Bulletin, patients should be referred to a dermatologist if there is diagnostic uncertainty, concerns about malignancy, treatment failure or management concerns, or if the patient is at high risk (e.g., organ transplant recipients, multiple large lesions, or previous SCC).
The guideline authors suggest that most patients can be evaluated and treated in the primary care setting. They go on to say that there is inadequate evidence to justify treatment of all AKs in an attempt to prevent malignant transformation. While reassuring, this requires us to consider all possible treatment approaches. One liquid nitrogen bottle does not fit all.
Dr. Ebbert is professor of medicine and general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no conflicts of interest.
Actinic keratosis, or solar keratosis, results from the proliferation of atypical epidermal keratinocytes. When we can take the time to do a skin examination, we all see a lot of them especially among our older and middle-aged sun worshippers and sunscreen agnostics. My traditional approach, for better or for worse, has been to acquire the liquid nitrogen bottle on the floor and go to work. But my recent review of guidelines prepared on behalf of the British Association of Dermatologists and published several years ago have prompted me to open my eyes a bit more to other possible approaches.
Reassuringly, the likelihood of progression of an AK to squamous cell carcinoma (SCC) is low. Estimates from a large U.S. cohort revealed a rate of transformation to invasive or in situ SCC of 0.6% after 1 year and 2.6 % after 4 years. But we have to remember that although the progression rate is low, 60% of SCC arise from AKs.
The AK guideline authors synthesized and graded published evidence. Topical therapies receiving an "A grade" (i.e., good evidence) included no therapy or emollients for mild AKs and 5-fluorouracil. Therapies with a "B grade" (i.e., fair evidence) include diclofenac gel and imiquimod.
Other treatments include cryosurgery (A grade) and photodynamic therapy (B grade). We do a lot of cryotherapy in our practice but patients need to be informed of the scarring and possible hyper- or hypopigmentation that can occur with treatment. Photodynamic therapy will, in most cases, be administered by dermatologists.
According to a recent paper in the Drugs and Therapeutic Bulletin, patients should be referred to a dermatologist if there is diagnostic uncertainty, concerns about malignancy, treatment failure or management concerns, or if the patient is at high risk (e.g., organ transplant recipients, multiple large lesions, or previous SCC).
The guideline authors suggest that most patients can be evaluated and treated in the primary care setting. They go on to say that there is inadequate evidence to justify treatment of all AKs in an attempt to prevent malignant transformation. While reassuring, this requires us to consider all possible treatment approaches. One liquid nitrogen bottle does not fit all.
Dr. Ebbert is professor of medicine and general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no conflicts of interest.
'I'm going to live forever': the guarantee-time bias
Some study findings are more probably due to a bias in terms of who is included in the studies than to the miraculous effects of occupation, winning awards, or ER status, or whatever is being studied. How should investigators go about avoiding this bias, and more specifically, what should readers look for when they’re reading about some new miracle cure?
Click on the PDF icon above to read the full article.
Some study findings are more probably due to a bias in terms of who is included in the studies than to the miraculous effects of occupation, winning awards, or ER status, or whatever is being studied. How should investigators go about avoiding this bias, and more specifically, what should readers look for when they’re reading about some new miracle cure?
Click on the PDF icon above to read the full article.
Some study findings are more probably due to a bias in terms of who is included in the studies than to the miraculous effects of occupation, winning awards, or ER status, or whatever is being studied. How should investigators go about avoiding this bias, and more specifically, what should readers look for when they’re reading about some new miracle cure?
Click on the PDF icon above to read the full article.
Power lines don’t raise leukemia risk in kids
Living near overhead power lines in early life does not increase a child’s risk of developing leukemia, according to a study published in the British Journal of Cancer.
An earlier study using information on childhood leukemia diagnosed between 1962 and 1995 suggested there was an elevated risk for children born within 600 meters of overhead power lines.
But now, updated data indicate that children born after the 1980s don’t have an increased risk.
According to researchers, this strongly suggests there is no direct biological effect of power lines on leukemia risk.
They believe the previous findings could be explained by changes in the characteristics of people living near power lines. The results might also be a chance finding or have resulted from problems with the study design.
“It’s very encouraging to see that, in recent decades, there has been no increased risk of leukemia among children born near overhead power lines,” said lead study author Kathryn Bunch, of the University of Oxford.
“More research is needed to determine precisely why previous evidence suggested a risk prior to 1980, but parents can be reassured from the findings of this study that overhead power lines don’t increase their child’s risk of leukemia.”
Expanding on previous findings
Several years ago, Dr Bunch’s colleagues at the University of Oxford set out to determine if proximity to high-voltage power lines affected the risk of childhood cancers in England and Wales, using data spanning the period from 1962 to 1995.
The team found evidence to suggest a relationship between childhood leukemia risk and the proximity to power lines of the mother’s residence at the time of the child’s birth. This included all 400 kV and 275 kV power lines and a small fraction of 132 kV lines (Draper et al, BMJ 2005).
Dr Bunch and her colleagues decided to extend this study by including more recent data, as well as cases and control subjects from Scotland. The group evaluated 132 kV, 275 kV, and 400 kV power lines and looked at subjects living greater distances from the power lines than those included in the previous study.
The researchers analyzed 53,515 children enrolled in the National Registry of Childhood Tumours from 1962 to 2008 and a group of matched controls.
The team found that, for the entire study period, there was no evidence of an increased risk of leukemia among subjects living closer to power lines. The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines (for all voltages), was 1.12.
There did appear to be an increased risk of leukemia when the researchers analyzed data according to decade. However, this risk declined over time.
The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines, was 4.50 in the 1960s, 2.46 in the 1970s, 1.54 in the 1980s, 0.99 in the 1990s, and 0.71 in the 2000s.
The elevated risk in the 1980s was not statistically significant, the researchers noted. They also pointed out that, even in the decades when the risk appears to be present, there is no evidence that it extended beyond the 600 m limit of the original analysis.
The fact that the risk declined over time suggests the leukemia is unlikely to have arisen from any physical effect of the power lines, the researchers said. They believe it’s more likely the result of changing population characteristics. ![]()
Living near overhead power lines in early life does not increase a child’s risk of developing leukemia, according to a study published in the British Journal of Cancer.
An earlier study using information on childhood leukemia diagnosed between 1962 and 1995 suggested there was an elevated risk for children born within 600 meters of overhead power lines.
But now, updated data indicate that children born after the 1980s don’t have an increased risk.
According to researchers, this strongly suggests there is no direct biological effect of power lines on leukemia risk.
They believe the previous findings could be explained by changes in the characteristics of people living near power lines. The results might also be a chance finding or have resulted from problems with the study design.
“It’s very encouraging to see that, in recent decades, there has been no increased risk of leukemia among children born near overhead power lines,” said lead study author Kathryn Bunch, of the University of Oxford.
“More research is needed to determine precisely why previous evidence suggested a risk prior to 1980, but parents can be reassured from the findings of this study that overhead power lines don’t increase their child’s risk of leukemia.”
Expanding on previous findings
Several years ago, Dr Bunch’s colleagues at the University of Oxford set out to determine if proximity to high-voltage power lines affected the risk of childhood cancers in England and Wales, using data spanning the period from 1962 to 1995.
The team found evidence to suggest a relationship between childhood leukemia risk and the proximity to power lines of the mother’s residence at the time of the child’s birth. This included all 400 kV and 275 kV power lines and a small fraction of 132 kV lines (Draper et al, BMJ 2005).
Dr Bunch and her colleagues decided to extend this study by including more recent data, as well as cases and control subjects from Scotland. The group evaluated 132 kV, 275 kV, and 400 kV power lines and looked at subjects living greater distances from the power lines than those included in the previous study.
The researchers analyzed 53,515 children enrolled in the National Registry of Childhood Tumours from 1962 to 2008 and a group of matched controls.
The team found that, for the entire study period, there was no evidence of an increased risk of leukemia among subjects living closer to power lines. The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines (for all voltages), was 1.12.
There did appear to be an increased risk of leukemia when the researchers analyzed data according to decade. However, this risk declined over time.
The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines, was 4.50 in the 1960s, 2.46 in the 1970s, 1.54 in the 1980s, 0.99 in the 1990s, and 0.71 in the 2000s.
The elevated risk in the 1980s was not statistically significant, the researchers noted. They also pointed out that, even in the decades when the risk appears to be present, there is no evidence that it extended beyond the 600 m limit of the original analysis.
The fact that the risk declined over time suggests the leukemia is unlikely to have arisen from any physical effect of the power lines, the researchers said. They believe it’s more likely the result of changing population characteristics. ![]()
Living near overhead power lines in early life does not increase a child’s risk of developing leukemia, according to a study published in the British Journal of Cancer.
An earlier study using information on childhood leukemia diagnosed between 1962 and 1995 suggested there was an elevated risk for children born within 600 meters of overhead power lines.
But now, updated data indicate that children born after the 1980s don’t have an increased risk.
According to researchers, this strongly suggests there is no direct biological effect of power lines on leukemia risk.
They believe the previous findings could be explained by changes in the characteristics of people living near power lines. The results might also be a chance finding or have resulted from problems with the study design.
“It’s very encouraging to see that, in recent decades, there has been no increased risk of leukemia among children born near overhead power lines,” said lead study author Kathryn Bunch, of the University of Oxford.
“More research is needed to determine precisely why previous evidence suggested a risk prior to 1980, but parents can be reassured from the findings of this study that overhead power lines don’t increase their child’s risk of leukemia.”
Expanding on previous findings
Several years ago, Dr Bunch’s colleagues at the University of Oxford set out to determine if proximity to high-voltage power lines affected the risk of childhood cancers in England and Wales, using data spanning the period from 1962 to 1995.
The team found evidence to suggest a relationship between childhood leukemia risk and the proximity to power lines of the mother’s residence at the time of the child’s birth. This included all 400 kV and 275 kV power lines and a small fraction of 132 kV lines (Draper et al, BMJ 2005).
Dr Bunch and her colleagues decided to extend this study by including more recent data, as well as cases and control subjects from Scotland. The group evaluated 132 kV, 275 kV, and 400 kV power lines and looked at subjects living greater distances from the power lines than those included in the previous study.
The researchers analyzed 53,515 children enrolled in the National Registry of Childhood Tumours from 1962 to 2008 and a group of matched controls.
The team found that, for the entire study period, there was no evidence of an increased risk of leukemia among subjects living closer to power lines. The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines (for all voltages), was 1.12.
There did appear to be an increased risk of leukemia when the researchers analyzed data according to decade. However, this risk declined over time.
The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines, was 4.50 in the 1960s, 2.46 in the 1970s, 1.54 in the 1980s, 0.99 in the 1990s, and 0.71 in the 2000s.
The elevated risk in the 1980s was not statistically significant, the researchers noted. They also pointed out that, even in the decades when the risk appears to be present, there is no evidence that it extended beyond the 600 m limit of the original analysis.
The fact that the risk declined over time suggests the leukemia is unlikely to have arisen from any physical effect of the power lines, the researchers said. They believe it’s more likely the result of changing population characteristics. ![]()
Improving the efficacy of etoposide

after treatment with etoposide
Credit: CNIO
A compound that interferes with the cell cycle can increase the antineoplastic effects of etoposide, according to research published in Cell Reports.
Etoposide works by inhibiting topoisomerase II (TOP2), a protein needed for DNA repair during cell division.
Researchers discovered a relationship between TOP2 and Cdh1, a protein that (along with Cdc20) controls cell division by activating the anaphase-promoting complex/cyclosome (APC/C).
So the team hypothesized that combining etoposide with a compound that inhibits Cdh1 might improve etoposide’s antineoplastic effects. Experiments in cancer cell lines confirmed this theory.
Marcos Malumbres, PhD, of the Spanish National Cancer Research Centre (CNIO) in Madrid, and his colleagues began this research by investigating Cdh1 in vitro and in mouse models.
The team found that a decrease in Cdh1 activity increases cells’ TOP2 levels. So they decided to combine etoposide with a Cdh1 inhibitor and evaluate the effect on cancer cells, which divide more than normal cells and therefore have a greater dependency on TOP2 to maintain DNA integrity.
The researchers tested proTAME, a small molecule that targets APC/C-Cdh1 and APC/C-Cdc20, in combination with etoposide. And they found the drugs had a synergistic effect against cancer cells.
In experiments with a lung cancer cell line (A549) and 2 breast cancer cell lines (HeLa and MCF7), administering proTAME and etoposide together proved more effective than administering either compound alone.
The researchers believe these findings could apply to other malignancies as well. Etoposide has demonstrated activity against a number of cancers, including leukemias, lymphomas, and multiple myeloma.
The team said their next step is to study the etoposide-proTAME combination in patients and investigate the malignancies in which this therapeutic strategy would be most effective.
The researchers also noted that previous studies have shown Cdh1 is inactive in some patients due to various oncogenic mutations. So stratifying patients according to their tumor’s Cdh1 status could optimize treatment with etoposide. ![]()

after treatment with etoposide
Credit: CNIO
A compound that interferes with the cell cycle can increase the antineoplastic effects of etoposide, according to research published in Cell Reports.
Etoposide works by inhibiting topoisomerase II (TOP2), a protein needed for DNA repair during cell division.
Researchers discovered a relationship between TOP2 and Cdh1, a protein that (along with Cdc20) controls cell division by activating the anaphase-promoting complex/cyclosome (APC/C).
So the team hypothesized that combining etoposide with a compound that inhibits Cdh1 might improve etoposide’s antineoplastic effects. Experiments in cancer cell lines confirmed this theory.
Marcos Malumbres, PhD, of the Spanish National Cancer Research Centre (CNIO) in Madrid, and his colleagues began this research by investigating Cdh1 in vitro and in mouse models.
The team found that a decrease in Cdh1 activity increases cells’ TOP2 levels. So they decided to combine etoposide with a Cdh1 inhibitor and evaluate the effect on cancer cells, which divide more than normal cells and therefore have a greater dependency on TOP2 to maintain DNA integrity.
The researchers tested proTAME, a small molecule that targets APC/C-Cdh1 and APC/C-Cdc20, in combination with etoposide. And they found the drugs had a synergistic effect against cancer cells.
In experiments with a lung cancer cell line (A549) and 2 breast cancer cell lines (HeLa and MCF7), administering proTAME and etoposide together proved more effective than administering either compound alone.
The researchers believe these findings could apply to other malignancies as well. Etoposide has demonstrated activity against a number of cancers, including leukemias, lymphomas, and multiple myeloma.
The team said their next step is to study the etoposide-proTAME combination in patients and investigate the malignancies in which this therapeutic strategy would be most effective.
The researchers also noted that previous studies have shown Cdh1 is inactive in some patients due to various oncogenic mutations. So stratifying patients according to their tumor’s Cdh1 status could optimize treatment with etoposide. ![]()

after treatment with etoposide
Credit: CNIO
A compound that interferes with the cell cycle can increase the antineoplastic effects of etoposide, according to research published in Cell Reports.
Etoposide works by inhibiting topoisomerase II (TOP2), a protein needed for DNA repair during cell division.
Researchers discovered a relationship between TOP2 and Cdh1, a protein that (along with Cdc20) controls cell division by activating the anaphase-promoting complex/cyclosome (APC/C).
So the team hypothesized that combining etoposide with a compound that inhibits Cdh1 might improve etoposide’s antineoplastic effects. Experiments in cancer cell lines confirmed this theory.
Marcos Malumbres, PhD, of the Spanish National Cancer Research Centre (CNIO) in Madrid, and his colleagues began this research by investigating Cdh1 in vitro and in mouse models.
The team found that a decrease in Cdh1 activity increases cells’ TOP2 levels. So they decided to combine etoposide with a Cdh1 inhibitor and evaluate the effect on cancer cells, which divide more than normal cells and therefore have a greater dependency on TOP2 to maintain DNA integrity.
The researchers tested proTAME, a small molecule that targets APC/C-Cdh1 and APC/C-Cdc20, in combination with etoposide. And they found the drugs had a synergistic effect against cancer cells.
In experiments with a lung cancer cell line (A549) and 2 breast cancer cell lines (HeLa and MCF7), administering proTAME and etoposide together proved more effective than administering either compound alone.
The researchers believe these findings could apply to other malignancies as well. Etoposide has demonstrated activity against a number of cancers, including leukemias, lymphomas, and multiple myeloma.
The team said their next step is to study the etoposide-proTAME combination in patients and investigate the malignancies in which this therapeutic strategy would be most effective.
The researchers also noted that previous studies have shown Cdh1 is inactive in some patients due to various oncogenic mutations. So stratifying patients according to their tumor’s Cdh1 status could optimize treatment with etoposide. ![]()
National plan to lower HAIs shows signs of success, investigators find

Credit: CDC
New research suggests a federally sponsored plan to decrease the incidence of healthcare-acquired infections (HAIs) in the US was successful in addressing the challenges of prioritizing and coordinating strategies.
The plan has also been associated with reductions in the rates of HAIs, with progress made toward most targets where data are available.
Descriptions of the plan and its initial results appear in a series of articles published in a supplement to the February issue of Medical Care.
“Much progress has been made in raising awareness of and developing strategies for curbing the life-threatening infections that strike patients too often when they are receiving medical care,” said Katherine Kahn, MD, a leader of the project and professor at the Geffen School of Medicine at the University of California, Los Angeles.
“In order to make even more progress, we need to build our systems of care to be safer within and across hospitals, nursing homes, clinics, and community settings.”
In 2009, the US Department of Health and Humans Services released a national plan aimed at preventing HAIs, called “National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.”
Researchers performed an evaluation of the first few years of the plan, reviewing the structure of the effort, as well as the results thus far.
The plan focuses on evidence-based strategies, such as considering the benefits and risks when deciding about the use and duration of treatments like antibiotics.
Most of the prevention initiatives have focused on hospital settings, but the action plan has focused attention on efforts in other care settings, such as outpatient surgery centers, kidney dialysis centers, and long-term care facilities.
The investigators said these efforts have likely contributed to stakeholders’ reported perceptions of greater momentum in adopting strategies to prevent HAIs.
The national plan has generated clinical, political, and financial support for the complex efforts required to eliminate HAIs across federal, regional, state, and local settings.
Despite an influx of federal funding to support elimination of HAIs, the researchers said ongoing dedicated resources will be required to maintain momentum and sustain efforts made to date.
On the other hand, because future funding for efforts to further reduce HAIs is unclear, the investigators said it may be best to incorporate the efforts into the overall movement to improve patient safety. ![]()

Credit: CDC
New research suggests a federally sponsored plan to decrease the incidence of healthcare-acquired infections (HAIs) in the US was successful in addressing the challenges of prioritizing and coordinating strategies.
The plan has also been associated with reductions in the rates of HAIs, with progress made toward most targets where data are available.
Descriptions of the plan and its initial results appear in a series of articles published in a supplement to the February issue of Medical Care.
“Much progress has been made in raising awareness of and developing strategies for curbing the life-threatening infections that strike patients too often when they are receiving medical care,” said Katherine Kahn, MD, a leader of the project and professor at the Geffen School of Medicine at the University of California, Los Angeles.
“In order to make even more progress, we need to build our systems of care to be safer within and across hospitals, nursing homes, clinics, and community settings.”
In 2009, the US Department of Health and Humans Services released a national plan aimed at preventing HAIs, called “National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.”
Researchers performed an evaluation of the first few years of the plan, reviewing the structure of the effort, as well as the results thus far.
The plan focuses on evidence-based strategies, such as considering the benefits and risks when deciding about the use and duration of treatments like antibiotics.
Most of the prevention initiatives have focused on hospital settings, but the action plan has focused attention on efforts in other care settings, such as outpatient surgery centers, kidney dialysis centers, and long-term care facilities.
The investigators said these efforts have likely contributed to stakeholders’ reported perceptions of greater momentum in adopting strategies to prevent HAIs.
The national plan has generated clinical, political, and financial support for the complex efforts required to eliminate HAIs across federal, regional, state, and local settings.
Despite an influx of federal funding to support elimination of HAIs, the researchers said ongoing dedicated resources will be required to maintain momentum and sustain efforts made to date.
On the other hand, because future funding for efforts to further reduce HAIs is unclear, the investigators said it may be best to incorporate the efforts into the overall movement to improve patient safety. ![]()

Credit: CDC
New research suggests a federally sponsored plan to decrease the incidence of healthcare-acquired infections (HAIs) in the US was successful in addressing the challenges of prioritizing and coordinating strategies.
The plan has also been associated with reductions in the rates of HAIs, with progress made toward most targets where data are available.
Descriptions of the plan and its initial results appear in a series of articles published in a supplement to the February issue of Medical Care.
“Much progress has been made in raising awareness of and developing strategies for curbing the life-threatening infections that strike patients too often when they are receiving medical care,” said Katherine Kahn, MD, a leader of the project and professor at the Geffen School of Medicine at the University of California, Los Angeles.
“In order to make even more progress, we need to build our systems of care to be safer within and across hospitals, nursing homes, clinics, and community settings.”
In 2009, the US Department of Health and Humans Services released a national plan aimed at preventing HAIs, called “National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.”
Researchers performed an evaluation of the first few years of the plan, reviewing the structure of the effort, as well as the results thus far.
The plan focuses on evidence-based strategies, such as considering the benefits and risks when deciding about the use and duration of treatments like antibiotics.
Most of the prevention initiatives have focused on hospital settings, but the action plan has focused attention on efforts in other care settings, such as outpatient surgery centers, kidney dialysis centers, and long-term care facilities.
The investigators said these efforts have likely contributed to stakeholders’ reported perceptions of greater momentum in adopting strategies to prevent HAIs.
The national plan has generated clinical, political, and financial support for the complex efforts required to eliminate HAIs across federal, regional, state, and local settings.
Despite an influx of federal funding to support elimination of HAIs, the researchers said ongoing dedicated resources will be required to maintain momentum and sustain efforts made to date.
On the other hand, because future funding for efforts to further reduce HAIs is unclear, the investigators said it may be best to incorporate the efforts into the overall movement to improve patient safety. ![]()
Unique protein found in MM patients

Credit: Rhoda Baer
Researchers say they have discovered a bacterial protein that attaches to virtually any antibody and prevents it from binding to its target.
It appears that this molecule, called mycoplasma protein (or protein M), helps some bacteria evade the immune response and establish long-term infections.
The researchers discovered protein M in samples from multiple myeloma (MM) patients.
And the team believes the protein could be engineered to target cancerous B cells in patients with MM and other B-cell malignancies.
Protein M might also become a target for new antibacterial drugs, and it could prove useful for preparing highly pure antibodies for research and drug manufacturing.
Richard A. Lerner, MD, of The Scripps Research Institute (TSRI) in La Jolla, California, and his colleagues described their discovery of protein M in Science.
The discovery originated from an effort to understand the origin of MM. Clonal B-cell proliferation, as well as MM and lymphomas, can result from chronic infections by organisms such as Escherichia coli, Helicobacter pylori, and hepatitis C virus.
To better understand this process, Dr Lerner and his colleagues investigated mycoplasma, a parasite that infects people chronically and is largely confined to the cell surface.
In a search for factors associated with long-term mycoplasma infection, the team tested samples of antibodies from MM patients’ blood against a variety of mycoplasma species. One of the proteins recognized by the antibodies was from Mycoplasma genitalium, which causes sexually transmitted infections.
To the researchers’ surprise, every antibody sample tested showed reactivity to this protein. But further tests made it clear that these antibody reactions were not in response to mass infection with M genitalium.
Instead, the M genitalium protein, which the team named protein M, appeared to have evolved simply to bind to any antibody it encounters.
“It binds to every antibody generically—capable of hijacking the entire diversity of antibody repertoire—but, at the same time, it blocks the specific interaction between that antibody and its intended biomolecular target,” said Rajesh Grover, PhD, of TSRI.
To better understand how protein M works, the researchers took a structural biology approach. Using X-ray crystallography and other techniques, the team determined the protein’s 3D atomic structure while it was bound to various human antibodies.
Compared to thousands of known structures in the Protein Data Bank, the worldwide structure database, protein M appeared to be unique. The data also revealed that protein M binds to a small, conserved region at the outer tip of every antibody’s antigen-binding arm.
“It likely extends the other end of itself, like a tail, over the antibody’s main antigen-binding region,” said Xueyong Zhu, PhD, of TSRI.
The team is now studying protein M’s function during M genitalium infections. It seems likely that the protein evolved to help M genitalium cope with the immune response, as it has one of the smallest bacterial genomes in nature.
“It appears to represent an elegant evolutionary solution to the special problem that mycoplasma have in evading the adaptive immune system,” Dr Grover said. “The smallest parasitic [bacterium] on planet Earth seems to have evolved the most sophisticated invading molecular machine.”
If protein M is confirmed as a universal “decoy” for antibodies, it will become a target for new drugs, the researchers said. This could make it easier to treat chronic, sometimes silent, infections by M genitalium and any other microbes that have evolved a similar antibody-thwarting defense.
In principle, protein M also could be engineered to target specific groups of B cells, delivering cytotoxic agents to cancerous B cells in patients with MM and lymphomas.
But the most immediate use of protein M, according to the researchers, is likely to be as a tool for grabbing antibodies in test tubes and cell cultures. This would allow the preparation of highly pure antibodies for research and drug manufacturing. Other generic antibody-binding proteins have been put to use in this way, but, so far, it appears that none does the job quite as well as protein M.
“It may be the most useful antibody purification device ever found,” said Dr Lerner, who is now working to commercialize the protein. ![]()

Credit: Rhoda Baer
Researchers say they have discovered a bacterial protein that attaches to virtually any antibody and prevents it from binding to its target.
It appears that this molecule, called mycoplasma protein (or protein M), helps some bacteria evade the immune response and establish long-term infections.
The researchers discovered protein M in samples from multiple myeloma (MM) patients.
And the team believes the protein could be engineered to target cancerous B cells in patients with MM and other B-cell malignancies.
Protein M might also become a target for new antibacterial drugs, and it could prove useful for preparing highly pure antibodies for research and drug manufacturing.
Richard A. Lerner, MD, of The Scripps Research Institute (TSRI) in La Jolla, California, and his colleagues described their discovery of protein M in Science.
The discovery originated from an effort to understand the origin of MM. Clonal B-cell proliferation, as well as MM and lymphomas, can result from chronic infections by organisms such as Escherichia coli, Helicobacter pylori, and hepatitis C virus.
To better understand this process, Dr Lerner and his colleagues investigated mycoplasma, a parasite that infects people chronically and is largely confined to the cell surface.
In a search for factors associated with long-term mycoplasma infection, the team tested samples of antibodies from MM patients’ blood against a variety of mycoplasma species. One of the proteins recognized by the antibodies was from Mycoplasma genitalium, which causes sexually transmitted infections.
To the researchers’ surprise, every antibody sample tested showed reactivity to this protein. But further tests made it clear that these antibody reactions were not in response to mass infection with M genitalium.
Instead, the M genitalium protein, which the team named protein M, appeared to have evolved simply to bind to any antibody it encounters.
“It binds to every antibody generically—capable of hijacking the entire diversity of antibody repertoire—but, at the same time, it blocks the specific interaction between that antibody and its intended biomolecular target,” said Rajesh Grover, PhD, of TSRI.
To better understand how protein M works, the researchers took a structural biology approach. Using X-ray crystallography and other techniques, the team determined the protein’s 3D atomic structure while it was bound to various human antibodies.
Compared to thousands of known structures in the Protein Data Bank, the worldwide structure database, protein M appeared to be unique. The data also revealed that protein M binds to a small, conserved region at the outer tip of every antibody’s antigen-binding arm.
“It likely extends the other end of itself, like a tail, over the antibody’s main antigen-binding region,” said Xueyong Zhu, PhD, of TSRI.
The team is now studying protein M’s function during M genitalium infections. It seems likely that the protein evolved to help M genitalium cope with the immune response, as it has one of the smallest bacterial genomes in nature.
“It appears to represent an elegant evolutionary solution to the special problem that mycoplasma have in evading the adaptive immune system,” Dr Grover said. “The smallest parasitic [bacterium] on planet Earth seems to have evolved the most sophisticated invading molecular machine.”
If protein M is confirmed as a universal “decoy” for antibodies, it will become a target for new drugs, the researchers said. This could make it easier to treat chronic, sometimes silent, infections by M genitalium and any other microbes that have evolved a similar antibody-thwarting defense.
In principle, protein M also could be engineered to target specific groups of B cells, delivering cytotoxic agents to cancerous B cells in patients with MM and lymphomas.
But the most immediate use of protein M, according to the researchers, is likely to be as a tool for grabbing antibodies in test tubes and cell cultures. This would allow the preparation of highly pure antibodies for research and drug manufacturing. Other generic antibody-binding proteins have been put to use in this way, but, so far, it appears that none does the job quite as well as protein M.
“It may be the most useful antibody purification device ever found,” said Dr Lerner, who is now working to commercialize the protein. ![]()

Credit: Rhoda Baer
Researchers say they have discovered a bacterial protein that attaches to virtually any antibody and prevents it from binding to its target.
It appears that this molecule, called mycoplasma protein (or protein M), helps some bacteria evade the immune response and establish long-term infections.
The researchers discovered protein M in samples from multiple myeloma (MM) patients.
And the team believes the protein could be engineered to target cancerous B cells in patients with MM and other B-cell malignancies.
Protein M might also become a target for new antibacterial drugs, and it could prove useful for preparing highly pure antibodies for research and drug manufacturing.
Richard A. Lerner, MD, of The Scripps Research Institute (TSRI) in La Jolla, California, and his colleagues described their discovery of protein M in Science.
The discovery originated from an effort to understand the origin of MM. Clonal B-cell proliferation, as well as MM and lymphomas, can result from chronic infections by organisms such as Escherichia coli, Helicobacter pylori, and hepatitis C virus.
To better understand this process, Dr Lerner and his colleagues investigated mycoplasma, a parasite that infects people chronically and is largely confined to the cell surface.
In a search for factors associated with long-term mycoplasma infection, the team tested samples of antibodies from MM patients’ blood against a variety of mycoplasma species. One of the proteins recognized by the antibodies was from Mycoplasma genitalium, which causes sexually transmitted infections.
To the researchers’ surprise, every antibody sample tested showed reactivity to this protein. But further tests made it clear that these antibody reactions were not in response to mass infection with M genitalium.
Instead, the M genitalium protein, which the team named protein M, appeared to have evolved simply to bind to any antibody it encounters.
“It binds to every antibody generically—capable of hijacking the entire diversity of antibody repertoire—but, at the same time, it blocks the specific interaction between that antibody and its intended biomolecular target,” said Rajesh Grover, PhD, of TSRI.
To better understand how protein M works, the researchers took a structural biology approach. Using X-ray crystallography and other techniques, the team determined the protein’s 3D atomic structure while it was bound to various human antibodies.
Compared to thousands of known structures in the Protein Data Bank, the worldwide structure database, protein M appeared to be unique. The data also revealed that protein M binds to a small, conserved region at the outer tip of every antibody’s antigen-binding arm.
“It likely extends the other end of itself, like a tail, over the antibody’s main antigen-binding region,” said Xueyong Zhu, PhD, of TSRI.
The team is now studying protein M’s function during M genitalium infections. It seems likely that the protein evolved to help M genitalium cope with the immune response, as it has one of the smallest bacterial genomes in nature.
“It appears to represent an elegant evolutionary solution to the special problem that mycoplasma have in evading the adaptive immune system,” Dr Grover said. “The smallest parasitic [bacterium] on planet Earth seems to have evolved the most sophisticated invading molecular machine.”
If protein M is confirmed as a universal “decoy” for antibodies, it will become a target for new drugs, the researchers said. This could make it easier to treat chronic, sometimes silent, infections by M genitalium and any other microbes that have evolved a similar antibody-thwarting defense.
In principle, protein M also could be engineered to target specific groups of B cells, delivering cytotoxic agents to cancerous B cells in patients with MM and lymphomas.
But the most immediate use of protein M, according to the researchers, is likely to be as a tool for grabbing antibodies in test tubes and cell cultures. This would allow the preparation of highly pure antibodies for research and drug manufacturing. Other generic antibody-binding proteins have been put to use in this way, but, so far, it appears that none does the job quite as well as protein M.
“It may be the most useful antibody purification device ever found,” said Dr Lerner, who is now working to commercialize the protein.
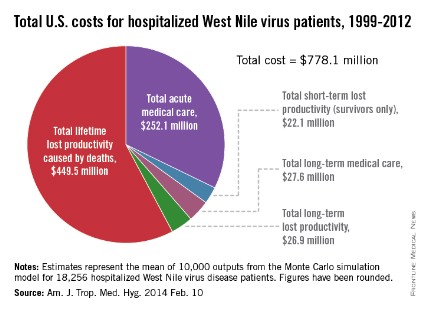
West Nile virus has cost the United States nearly $800 million
Since the West Nile virus was first detected in New York in 1999, hospitalized patients in the United States have cost an estimated $778.1 million in health care expenditures and lost productivity, according to a study published online Feb. 10 in the American Journal of Tropical Medicine and Hygiene.
Of that $778.1 million, the largest share – $449.5 million, or almost 58% – represents mean lifetime lost productivity from deaths caused by infection. Hospitalization for acute illness was estimated at $252.1 million, long-term medical care cost $27.6 million, long-term lost productivity cost $26.9 million, and short-term lost productivity (survivors only) totaled $22.1 million, investigators from the Centers for Disease Control and Prevention reported.
From 1999 through 2012, there were 37,088 cases of West Nile virus disease reported to the CDC’s ArboNET surveillance system, resulting in more than 18,000 hospitalizations and 1,529 deaths, the investigators said (Am. J. Trop. Med. Hyg. 2014 Feb. 10).
They determined the cost of initial hospitalization for 80 patients in a 2003 West Nile virus outbreak in Colorado, then calculated the cost of additional medical care and missed work for 38 patients who had 5 years of follow-up data available after the initial infection. These costs were then extrapolated to the total number of hospitalized cases in the United States since 1999.

Since the West Nile virus was first detected in New York in 1999, hospitalized patients in the United States have cost an estimated $778.1 million in health care expenditures and lost productivity, according to a study published online Feb. 10 in the American Journal of Tropical Medicine and Hygiene.
Of that $778.1 million, the largest share – $449.5 million, or almost 58% – represents mean lifetime lost productivity from deaths caused by infection. Hospitalization for acute illness was estimated at $252.1 million, long-term medical care cost $27.6 million, long-term lost productivity cost $26.9 million, and short-term lost productivity (survivors only) totaled $22.1 million, investigators from the Centers for Disease Control and Prevention reported.
From 1999 through 2012, there were 37,088 cases of West Nile virus disease reported to the CDC’s ArboNET surveillance system, resulting in more than 18,000 hospitalizations and 1,529 deaths, the investigators said (Am. J. Trop. Med. Hyg. 2014 Feb. 10).
They determined the cost of initial hospitalization for 80 patients in a 2003 West Nile virus outbreak in Colorado, then calculated the cost of additional medical care and missed work for 38 patients who had 5 years of follow-up data available after the initial infection. These costs were then extrapolated to the total number of hospitalized cases in the United States since 1999.

Since the West Nile virus was first detected in New York in 1999, hospitalized patients in the United States have cost an estimated $778.1 million in health care expenditures and lost productivity, according to a study published online Feb. 10 in the American Journal of Tropical Medicine and Hygiene.
Of that $778.1 million, the largest share – $449.5 million, or almost 58% – represents mean lifetime lost productivity from deaths caused by infection. Hospitalization for acute illness was estimated at $252.1 million, long-term medical care cost $27.6 million, long-term lost productivity cost $26.9 million, and short-term lost productivity (survivors only) totaled $22.1 million, investigators from the Centers for Disease Control and Prevention reported.
From 1999 through 2012, there were 37,088 cases of West Nile virus disease reported to the CDC’s ArboNET surveillance system, resulting in more than 18,000 hospitalizations and 1,529 deaths, the investigators said (Am. J. Trop. Med. Hyg. 2014 Feb. 10).
They determined the cost of initial hospitalization for 80 patients in a 2003 West Nile virus outbreak in Colorado, then calculated the cost of additional medical care and missed work for 38 patients who had 5 years of follow-up data available after the initial infection. These costs were then extrapolated to the total number of hospitalized cases in the United States since 1999.

FROM AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE