User login
Rural residency offers tool to address ob.gyn. shortages
In 2021, the first obstetrician-gynecologist trained on a separate rural residency track will graduate from the University of Wisconsin.
Program leaders are gambling that the investment in specialized training – including a quarter of the training time spent in smaller, community hospitals – will eventually pay off in terms of more ob.gyns. living and practicing in Wisconsin’s underserved rural settings.
“The key premise that we’re working on and that’s been borne out in the literature on rural training in family medicine is that people who are ultimately going to practice in a rural setting are people who are interested in it, who have a rural background, and people who have experience in a clinical environment in the rural setting,” said Ellen Hartenbach, MD, ob.gyn. residency program director at the University of Wisconsin, Madison.
For now, the program is starting slowly. It matched its first and only rural resident – Laura McDowell of the University of Minnesota – in the 2017 National Resident Match. The new rural-track resident joins the six residents in the school’s main ob.gyn. training program. New residents will be added to the rural track based on the availability of funding. The university relied on a development grant from the state, as well as funding from local community hospitals, to help finance the new position.
Dr. Hartenbach said the selection of the rural-track resident centered around finding someone who had both interest and prior experience in a rural setting, as well as someone who wanted to eventually live in a rural community. The university also had to ensure that applicants weren’t trying to game the system, looking for a way to break into the competitive ob.gyn. residency field, which had a 100% fill rate in 2017. More than 100 medical students applied for the single rural track position.
University of Wisconsin’s program is thought to be the country’s first dedicated, sanctioned rural ob.gyn. residency track. The university has been working for the last 2 years to develop the program and get approval from the Accreditation Council for Graduate Medical Education’s Residency Review Committee.
When the first resident starts on July 1, she will receive 75% of her training in the university hospital in Madison and 25% split among four smaller, community hospitals. The rural resident will receive the same clinical and cognitive skills training as the other residents, with the same number of required procedures. The big difference, Dr. Hartenbach said, comes from the experience gained in working in smaller hospitals.
“There’s a pretty big difference with the ob.gyn. unit in a 50-bed hospital, compared to a 500-bed hospital,” she said. “There’s a difference in terms of the types of patients that come in to smaller medical centers.”
Dr. Hartenbach said she hopes having real-world experience in the rural setting will help to dispel common misperceptions, including that rural physicians are always on call.
The Wisconsin program could be a model for other states by giving residents a chance to understand the dynamics of smaller hospitals, said Thomas Gellhaus, MD, president of the American Congress of Obstetricians and Gynecologists (ACOG). But its success would depend on the presence of community hospitals that have an adequate number of physicians to supervise residents and a case mix that matches up with training requirements. “It can’t just be anywhere,” said Dr. Gellhaus, clinical associate professor at the University of Iowa, Iowa City.
Dr. Hartenbach said the goal behind the new training design is to help bolster the rural OB workforce.
“There’s a lot of rural health disparities in a lot of medical fields, in particular in maternity health services,” she said. “There have been a lot of reports showing that we’re not going to have enough ob.gyns. and a lot of rural hospitals are closing down their maternity services.”
About one out of three Wisconsin counties don’t have an ob.gyn, according to ACOG. In the past, family medicine physicians and nurse midwives have helped to pick up the slack on maternity care in rural settings, but the number of family physicians who offer obstetric services is on the decline. One study showed that the proportion of family physicians providing maternity care dropped from 23% in 2000 to less than 10% in 2010 (J Am Board Fam Med. 2012 May-Jun;25[3]:270-1). That development has contributed to an “acute” crisis in the provision of rural maternity care, Dr. Hartenbach said.
Maldistribution
This trend is national as well. Nearly half of the 3,107 U.S. counties lack ob.gyns. These counties are located in all states but primarily in the Midwest and Mountain West, according to a 2011 workforce report from ACOG.
As of 2010, the national ratio of ob.gyns. per 10,000 women was 2.1, but that ratio decreases from 2.9 in metropolitan counties to 0.7 in rural counties.
William F. Rayburn, MD, distinguished professor and emeritus chair of obstetrics and gynecology at the University of New Mexico, Albuquerque, is working on an update to the workforce report, expected to be released in May 2017 at ACOG’s annual scientific meeting in San Diego.
The maldistribution trend is likely to continue over the next decade for several reasons, said Dr. Rayburn, associate dean for continuing medical education and professional development at the university.
At the top of the list is the stagnant number of residency training slots across the country. While medical schools in the United States and abroad are graduating more students, the number of first-year ob.gyn. residency positions has remained at about 1,200 since 1980. In 2017, there were 1,288 positions offered in the Main Residency Match.
Gender is another factor. Ob.gyn. is now a majority female specialty and by 2025 women will make up about two-thirds of the workforce, Dr. Rayburn said. While women are just as productive as men, they don’t work as many hours and they tend to drop obstetrics from their practices earlier, he added.
In addition, research indicates that women ob.gyns. are more likely to stay in urban areas after training.
“The movement, generally speaking, when people relocate is often to urban areas, from one urban area to another or from a rural area to a more urban area,” Dr. Rayburn said.
There is growing demand for health care from a population of adult women that is increasing at a greater rate than the number of ob.gyn. residents, he said.
The rural residency option being explored in Wisconsin is a great idea, Dr. Rayburn said, provided the trainees receive enough experience in the rural environment to prepare them for the change in practice. “The more you can get people to train in more rural areas, the more likely they are to eventually go there. But that’s far from a guarantee,” he said.
Going forward Dr. Rayburn said he expects to see loan repayment used to draw physicians to underserved areas.
“The problem is that the rural areas tend to have less of a good payer mix,” he said. “In other words, there are more poor people in rural areas. And the health care delivery is more limited in terms of resources, types of surgical equipment, and being able to take care of complicated pregnancies.”
GME funding cap
The Association of American Medical Colleges is focused on easing physician shortages by getting lawmakers to lift the cap on federal funding for graduate medical education (GME) positions that was put in place as part of the Balanced Budget Act of 1997.
“The population is getting larger and aging, which increases the need for more physicians and thus we have to work with Congress to lift the cap,” said Janis Orlowski, MD, Chief Health Care Officer at the Association of American Medical Colleges.
Specifically, the association is calling for funding to train at least 3,000 more physicians each year. In the last Congress, lawmakers introduced bills that would have provided those positions, with one of those bills directing that a portion of those new positions be dedicated to specialties with physician shortages.
Dr. Orlowski said bipartisan support still exists for lifting the cap, though new legislation probably won’t be introduced until after the summer recess when Congress won’t be bogged down with efforts to repeal and replace the Affordable Care Act.
Getting the GME cap lifted is mostly about coming up with the funding, she said. But some lawmakers have expressed concerns about how to ensure that increases go to the specialties with the greatest needs or that physicians trained in these spots will ultimately practice in the areas where care is needed, such as rural America.
“Those are issues that we need to continue to work on and address,” she said.
ACOG supports efforts to lift the GME funding cap and is pushing federal legislation that would establish maternity care health professionals shortage areas, allowing the National Health Service Corps to offer scholarships and loan repayment benefits to providers who work in those areas. Similar programs are already in place for primary care, and dental and mental health. Like the GME funding bill, legislation on this topic was introduced in the last session of Congress but will need to be reintroduced in the current Congress.
“We have to work on the workforce,” Dr. Gellhaus said. “It’s going to be a concern.”
[email protected]
On Twitter @maryellenny
In 2021, the first obstetrician-gynecologist trained on a separate rural residency track will graduate from the University of Wisconsin.
Program leaders are gambling that the investment in specialized training – including a quarter of the training time spent in smaller, community hospitals – will eventually pay off in terms of more ob.gyns. living and practicing in Wisconsin’s underserved rural settings.
“The key premise that we’re working on and that’s been borne out in the literature on rural training in family medicine is that people who are ultimately going to practice in a rural setting are people who are interested in it, who have a rural background, and people who have experience in a clinical environment in the rural setting,” said Ellen Hartenbach, MD, ob.gyn. residency program director at the University of Wisconsin, Madison.
For now, the program is starting slowly. It matched its first and only rural resident – Laura McDowell of the University of Minnesota – in the 2017 National Resident Match. The new rural-track resident joins the six residents in the school’s main ob.gyn. training program. New residents will be added to the rural track based on the availability of funding. The university relied on a development grant from the state, as well as funding from local community hospitals, to help finance the new position.
Dr. Hartenbach said the selection of the rural-track resident centered around finding someone who had both interest and prior experience in a rural setting, as well as someone who wanted to eventually live in a rural community. The university also had to ensure that applicants weren’t trying to game the system, looking for a way to break into the competitive ob.gyn. residency field, which had a 100% fill rate in 2017. More than 100 medical students applied for the single rural track position.
University of Wisconsin’s program is thought to be the country’s first dedicated, sanctioned rural ob.gyn. residency track. The university has been working for the last 2 years to develop the program and get approval from the Accreditation Council for Graduate Medical Education’s Residency Review Committee.
When the first resident starts on July 1, she will receive 75% of her training in the university hospital in Madison and 25% split among four smaller, community hospitals. The rural resident will receive the same clinical and cognitive skills training as the other residents, with the same number of required procedures. The big difference, Dr. Hartenbach said, comes from the experience gained in working in smaller hospitals.
“There’s a pretty big difference with the ob.gyn. unit in a 50-bed hospital, compared to a 500-bed hospital,” she said. “There’s a difference in terms of the types of patients that come in to smaller medical centers.”
Dr. Hartenbach said she hopes having real-world experience in the rural setting will help to dispel common misperceptions, including that rural physicians are always on call.
The Wisconsin program could be a model for other states by giving residents a chance to understand the dynamics of smaller hospitals, said Thomas Gellhaus, MD, president of the American Congress of Obstetricians and Gynecologists (ACOG). But its success would depend on the presence of community hospitals that have an adequate number of physicians to supervise residents and a case mix that matches up with training requirements. “It can’t just be anywhere,” said Dr. Gellhaus, clinical associate professor at the University of Iowa, Iowa City.
Dr. Hartenbach said the goal behind the new training design is to help bolster the rural OB workforce.
“There’s a lot of rural health disparities in a lot of medical fields, in particular in maternity health services,” she said. “There have been a lot of reports showing that we’re not going to have enough ob.gyns. and a lot of rural hospitals are closing down their maternity services.”
About one out of three Wisconsin counties don’t have an ob.gyn, according to ACOG. In the past, family medicine physicians and nurse midwives have helped to pick up the slack on maternity care in rural settings, but the number of family physicians who offer obstetric services is on the decline. One study showed that the proportion of family physicians providing maternity care dropped from 23% in 2000 to less than 10% in 2010 (J Am Board Fam Med. 2012 May-Jun;25[3]:270-1). That development has contributed to an “acute” crisis in the provision of rural maternity care, Dr. Hartenbach said.
Maldistribution
This trend is national as well. Nearly half of the 3,107 U.S. counties lack ob.gyns. These counties are located in all states but primarily in the Midwest and Mountain West, according to a 2011 workforce report from ACOG.
As of 2010, the national ratio of ob.gyns. per 10,000 women was 2.1, but that ratio decreases from 2.9 in metropolitan counties to 0.7 in rural counties.
William F. Rayburn, MD, distinguished professor and emeritus chair of obstetrics and gynecology at the University of New Mexico, Albuquerque, is working on an update to the workforce report, expected to be released in May 2017 at ACOG’s annual scientific meeting in San Diego.
The maldistribution trend is likely to continue over the next decade for several reasons, said Dr. Rayburn, associate dean for continuing medical education and professional development at the university.
At the top of the list is the stagnant number of residency training slots across the country. While medical schools in the United States and abroad are graduating more students, the number of first-year ob.gyn. residency positions has remained at about 1,200 since 1980. In 2017, there were 1,288 positions offered in the Main Residency Match.
Gender is another factor. Ob.gyn. is now a majority female specialty and by 2025 women will make up about two-thirds of the workforce, Dr. Rayburn said. While women are just as productive as men, they don’t work as many hours and they tend to drop obstetrics from their practices earlier, he added.
In addition, research indicates that women ob.gyns. are more likely to stay in urban areas after training.
“The movement, generally speaking, when people relocate is often to urban areas, from one urban area to another or from a rural area to a more urban area,” Dr. Rayburn said.
There is growing demand for health care from a population of adult women that is increasing at a greater rate than the number of ob.gyn. residents, he said.
The rural residency option being explored in Wisconsin is a great idea, Dr. Rayburn said, provided the trainees receive enough experience in the rural environment to prepare them for the change in practice. “The more you can get people to train in more rural areas, the more likely they are to eventually go there. But that’s far from a guarantee,” he said.
Going forward Dr. Rayburn said he expects to see loan repayment used to draw physicians to underserved areas.
“The problem is that the rural areas tend to have less of a good payer mix,” he said. “In other words, there are more poor people in rural areas. And the health care delivery is more limited in terms of resources, types of surgical equipment, and being able to take care of complicated pregnancies.”
GME funding cap
The Association of American Medical Colleges is focused on easing physician shortages by getting lawmakers to lift the cap on federal funding for graduate medical education (GME) positions that was put in place as part of the Balanced Budget Act of 1997.
“The population is getting larger and aging, which increases the need for more physicians and thus we have to work with Congress to lift the cap,” said Janis Orlowski, MD, Chief Health Care Officer at the Association of American Medical Colleges.
Specifically, the association is calling for funding to train at least 3,000 more physicians each year. In the last Congress, lawmakers introduced bills that would have provided those positions, with one of those bills directing that a portion of those new positions be dedicated to specialties with physician shortages.
Dr. Orlowski said bipartisan support still exists for lifting the cap, though new legislation probably won’t be introduced until after the summer recess when Congress won’t be bogged down with efforts to repeal and replace the Affordable Care Act.
Getting the GME cap lifted is mostly about coming up with the funding, she said. But some lawmakers have expressed concerns about how to ensure that increases go to the specialties with the greatest needs or that physicians trained in these spots will ultimately practice in the areas where care is needed, such as rural America.
“Those are issues that we need to continue to work on and address,” she said.
ACOG supports efforts to lift the GME funding cap and is pushing federal legislation that would establish maternity care health professionals shortage areas, allowing the National Health Service Corps to offer scholarships and loan repayment benefits to providers who work in those areas. Similar programs are already in place for primary care, and dental and mental health. Like the GME funding bill, legislation on this topic was introduced in the last session of Congress but will need to be reintroduced in the current Congress.
“We have to work on the workforce,” Dr. Gellhaus said. “It’s going to be a concern.”
[email protected]
On Twitter @maryellenny
In 2021, the first obstetrician-gynecologist trained on a separate rural residency track will graduate from the University of Wisconsin.
Program leaders are gambling that the investment in specialized training – including a quarter of the training time spent in smaller, community hospitals – will eventually pay off in terms of more ob.gyns. living and practicing in Wisconsin’s underserved rural settings.
“The key premise that we’re working on and that’s been borne out in the literature on rural training in family medicine is that people who are ultimately going to practice in a rural setting are people who are interested in it, who have a rural background, and people who have experience in a clinical environment in the rural setting,” said Ellen Hartenbach, MD, ob.gyn. residency program director at the University of Wisconsin, Madison.
For now, the program is starting slowly. It matched its first and only rural resident – Laura McDowell of the University of Minnesota – in the 2017 National Resident Match. The new rural-track resident joins the six residents in the school’s main ob.gyn. training program. New residents will be added to the rural track based on the availability of funding. The university relied on a development grant from the state, as well as funding from local community hospitals, to help finance the new position.
Dr. Hartenbach said the selection of the rural-track resident centered around finding someone who had both interest and prior experience in a rural setting, as well as someone who wanted to eventually live in a rural community. The university also had to ensure that applicants weren’t trying to game the system, looking for a way to break into the competitive ob.gyn. residency field, which had a 100% fill rate in 2017. More than 100 medical students applied for the single rural track position.
University of Wisconsin’s program is thought to be the country’s first dedicated, sanctioned rural ob.gyn. residency track. The university has been working for the last 2 years to develop the program and get approval from the Accreditation Council for Graduate Medical Education’s Residency Review Committee.
When the first resident starts on July 1, she will receive 75% of her training in the university hospital in Madison and 25% split among four smaller, community hospitals. The rural resident will receive the same clinical and cognitive skills training as the other residents, with the same number of required procedures. The big difference, Dr. Hartenbach said, comes from the experience gained in working in smaller hospitals.
“There’s a pretty big difference with the ob.gyn. unit in a 50-bed hospital, compared to a 500-bed hospital,” she said. “There’s a difference in terms of the types of patients that come in to smaller medical centers.”
Dr. Hartenbach said she hopes having real-world experience in the rural setting will help to dispel common misperceptions, including that rural physicians are always on call.
The Wisconsin program could be a model for other states by giving residents a chance to understand the dynamics of smaller hospitals, said Thomas Gellhaus, MD, president of the American Congress of Obstetricians and Gynecologists (ACOG). But its success would depend on the presence of community hospitals that have an adequate number of physicians to supervise residents and a case mix that matches up with training requirements. “It can’t just be anywhere,” said Dr. Gellhaus, clinical associate professor at the University of Iowa, Iowa City.
Dr. Hartenbach said the goal behind the new training design is to help bolster the rural OB workforce.
“There’s a lot of rural health disparities in a lot of medical fields, in particular in maternity health services,” she said. “There have been a lot of reports showing that we’re not going to have enough ob.gyns. and a lot of rural hospitals are closing down their maternity services.”
About one out of three Wisconsin counties don’t have an ob.gyn, according to ACOG. In the past, family medicine physicians and nurse midwives have helped to pick up the slack on maternity care in rural settings, but the number of family physicians who offer obstetric services is on the decline. One study showed that the proportion of family physicians providing maternity care dropped from 23% in 2000 to less than 10% in 2010 (J Am Board Fam Med. 2012 May-Jun;25[3]:270-1). That development has contributed to an “acute” crisis in the provision of rural maternity care, Dr. Hartenbach said.
Maldistribution
This trend is national as well. Nearly half of the 3,107 U.S. counties lack ob.gyns. These counties are located in all states but primarily in the Midwest and Mountain West, according to a 2011 workforce report from ACOG.
As of 2010, the national ratio of ob.gyns. per 10,000 women was 2.1, but that ratio decreases from 2.9 in metropolitan counties to 0.7 in rural counties.
William F. Rayburn, MD, distinguished professor and emeritus chair of obstetrics and gynecology at the University of New Mexico, Albuquerque, is working on an update to the workforce report, expected to be released in May 2017 at ACOG’s annual scientific meeting in San Diego.
The maldistribution trend is likely to continue over the next decade for several reasons, said Dr. Rayburn, associate dean for continuing medical education and professional development at the university.
At the top of the list is the stagnant number of residency training slots across the country. While medical schools in the United States and abroad are graduating more students, the number of first-year ob.gyn. residency positions has remained at about 1,200 since 1980. In 2017, there were 1,288 positions offered in the Main Residency Match.
Gender is another factor. Ob.gyn. is now a majority female specialty and by 2025 women will make up about two-thirds of the workforce, Dr. Rayburn said. While women are just as productive as men, they don’t work as many hours and they tend to drop obstetrics from their practices earlier, he added.
In addition, research indicates that women ob.gyns. are more likely to stay in urban areas after training.
“The movement, generally speaking, when people relocate is often to urban areas, from one urban area to another or from a rural area to a more urban area,” Dr. Rayburn said.
There is growing demand for health care from a population of adult women that is increasing at a greater rate than the number of ob.gyn. residents, he said.
The rural residency option being explored in Wisconsin is a great idea, Dr. Rayburn said, provided the trainees receive enough experience in the rural environment to prepare them for the change in practice. “The more you can get people to train in more rural areas, the more likely they are to eventually go there. But that’s far from a guarantee,” he said.
Going forward Dr. Rayburn said he expects to see loan repayment used to draw physicians to underserved areas.
“The problem is that the rural areas tend to have less of a good payer mix,” he said. “In other words, there are more poor people in rural areas. And the health care delivery is more limited in terms of resources, types of surgical equipment, and being able to take care of complicated pregnancies.”
GME funding cap
The Association of American Medical Colleges is focused on easing physician shortages by getting lawmakers to lift the cap on federal funding for graduate medical education (GME) positions that was put in place as part of the Balanced Budget Act of 1997.
“The population is getting larger and aging, which increases the need for more physicians and thus we have to work with Congress to lift the cap,” said Janis Orlowski, MD, Chief Health Care Officer at the Association of American Medical Colleges.
Specifically, the association is calling for funding to train at least 3,000 more physicians each year. In the last Congress, lawmakers introduced bills that would have provided those positions, with one of those bills directing that a portion of those new positions be dedicated to specialties with physician shortages.
Dr. Orlowski said bipartisan support still exists for lifting the cap, though new legislation probably won’t be introduced until after the summer recess when Congress won’t be bogged down with efforts to repeal and replace the Affordable Care Act.
Getting the GME cap lifted is mostly about coming up with the funding, she said. But some lawmakers have expressed concerns about how to ensure that increases go to the specialties with the greatest needs or that physicians trained in these spots will ultimately practice in the areas where care is needed, such as rural America.
“Those are issues that we need to continue to work on and address,” she said.
ACOG supports efforts to lift the GME funding cap and is pushing federal legislation that would establish maternity care health professionals shortage areas, allowing the National Health Service Corps to offer scholarships and loan repayment benefits to providers who work in those areas. Similar programs are already in place for primary care, and dental and mental health. Like the GME funding bill, legislation on this topic was introduced in the last session of Congress but will need to be reintroduced in the current Congress.
“We have to work on the workforce,” Dr. Gellhaus said. “It’s going to be a concern.”
[email protected]
On Twitter @maryellenny
Intensive ventilation precedes lesser pulmonary complications
Addition of 10 cm H2O to positive end-expiratory volume (PEEP) during mechanical ventilation was followed by significantly lessened pulmonary complications in hospitalized patients who developed hypoxemia after cardiac surgery, participating in a single-center, randomized trial.
This “intensive” alveolar recruitment strategy yielded a median pulmonary complications score of 1.7 (interquartile range, 1.0-2.0), compared with 2.0 (IQR, 1.5-3.0) among patients who underwent ventilation with a PEEP of 20 cm H2O, Alcino Costa Leme, RRT, PhD, said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously online March 21 in JAMA.
Intensive alveolar recruitment nearly doubled the odds of a lower pulmonary complications score (common odds ratio, 1.9; 95% confidence interval, 1.2-2.8; P = .003), Dr. Leme and his associates reported.
The study comprised 320 adults who developed hypoxemia immediately after undergoing elective cardiac surgery at the Heart Institute (Incor) of the University of São Paulo. The median age of the patients was 62 years, and none had a history of lung disease. Pulmonary complications were scored between 0 (no signs or symptoms) and 5 (death), the investigators noted (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2297).
The intensive alveolar recruitment strategy consisted of three 60-second cycles of lung inflation with a positive end-expiratory pressure (PEEP) of 30 cm H2O, pressure-controlled ventilation, driving pressure of 15 cm H2O, respiratory rate of 15/min, inspiratory time of 1.5 seconds, and FIO2 of 0.40. Between and after inflations, patients received assist-controlled or pressure-controlled ventilation, with driving pressures set to achieve a tidal volume of 6 mL/kg of predicted body weight, an inspiratory time of 1 second, PEEP of 13 cm H2O, and minimum respiratory rate to maintain PaCO2 between 35 and 45 mm Hg.
The “moderate strategy” consisted of three 30-second inflations under continuous positive airway pressure mode at 20 cm H2O and FIO2 of 0.60. Between and after inflations, patients received assist or control volume-controlled ventilation (decelerating-flow waveform), tidal volume of 6 mL/kg of predicted body weight, inspiratory time of 1 second, PEEP of 8 cm H2O, and FIO2 of 0.60, at a minimum respiratory rate that maintained PaCO2 at 35-45 mm Hg.
“[The] use of an intensive alveolar recruitment strategy compared with a moderate recruitment strategy resulted in less severe pulmonary complications during the hospital stay,” the investigators wrote. On average, intensively managed patients had shorter stays in the hospital (10.9 vs. 12.4 days; P = .04) and in the intensive care unit (3.8 vs. 4.8 days; P = .01) than did moderately managed patients. Intensive management also was associated with lower rates of hospital mortality and barotrauma, but the differences in these less common outcomes did not reach statistical significance.
“To our knowledge, this is the first study to show a significant effect of lung recruitment maneuvers on clinical outcomes, which objectively resulted in modest reductions in ICU and hospital length of stay,” the researchers wrote. “This is especially noteworthy considering that the control group was also receiving protective lung ventilation with low [tidal volume] and moderate PEEP levels. Thus, the major difference between treatment groups was the intensity of lung recruitment.”
FAPESP (Fundação de Amparo e Pesquisa do Estado de São Paulo) and FINEP (Financiadora de Estudos e Projetos) provided partial funding. Dr. Leme had no disclosures. Senior author Marcelo Britto Passos Amato, MD, PhD, disclosed research funding from Covidien/Medtronics, Dixtal Biomedica Ltd, and Timpel SA.
High PEEP “not only recruits collapsed lung tissue, but can also lead to lung overdistension. If lung collapse is extensive, as in patients with ARDS [acute respiratory distress syndrome], and maybe also in patients with postoperative ARDS, the balance between benefit (i.e., recruitment of lung tissue), and harm (i.e., lung overdistension), tips toward benefit. If there is very little lung collapse, as in critically ill patients without ARDS or patients during surgery, this balance could go in the other direction.”
The clinical trial by Leme and his colleagues “provides another brick in the evidence wall of lung protection. However, it remains unclear which patients benefit most from ventilation with a high [positive end-expiratory pressure] level.”
Ary Serpa Neto, MD, MSc, PhD, and Marcus J. Schultz, MD, PhD, are at the Academic Medical Center, Amsterdam. They reported having no conflicts of interest. These comments are from their editorial (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2570).
High PEEP “not only recruits collapsed lung tissue, but can also lead to lung overdistension. If lung collapse is extensive, as in patients with ARDS [acute respiratory distress syndrome], and maybe also in patients with postoperative ARDS, the balance between benefit (i.e., recruitment of lung tissue), and harm (i.e., lung overdistension), tips toward benefit. If there is very little lung collapse, as in critically ill patients without ARDS or patients during surgery, this balance could go in the other direction.”
The clinical trial by Leme and his colleagues “provides another brick in the evidence wall of lung protection. However, it remains unclear which patients benefit most from ventilation with a high [positive end-expiratory pressure] level.”
Ary Serpa Neto, MD, MSc, PhD, and Marcus J. Schultz, MD, PhD, are at the Academic Medical Center, Amsterdam. They reported having no conflicts of interest. These comments are from their editorial (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2570).
High PEEP “not only recruits collapsed lung tissue, but can also lead to lung overdistension. If lung collapse is extensive, as in patients with ARDS [acute respiratory distress syndrome], and maybe also in patients with postoperative ARDS, the balance between benefit (i.e., recruitment of lung tissue), and harm (i.e., lung overdistension), tips toward benefit. If there is very little lung collapse, as in critically ill patients without ARDS or patients during surgery, this balance could go in the other direction.”
The clinical trial by Leme and his colleagues “provides another brick in the evidence wall of lung protection. However, it remains unclear which patients benefit most from ventilation with a high [positive end-expiratory pressure] level.”
Ary Serpa Neto, MD, MSc, PhD, and Marcus J. Schultz, MD, PhD, are at the Academic Medical Center, Amsterdam. They reported having no conflicts of interest. These comments are from their editorial (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2570).
Addition of 10 cm H2O to positive end-expiratory volume (PEEP) during mechanical ventilation was followed by significantly lessened pulmonary complications in hospitalized patients who developed hypoxemia after cardiac surgery, participating in a single-center, randomized trial.
This “intensive” alveolar recruitment strategy yielded a median pulmonary complications score of 1.7 (interquartile range, 1.0-2.0), compared with 2.0 (IQR, 1.5-3.0) among patients who underwent ventilation with a PEEP of 20 cm H2O, Alcino Costa Leme, RRT, PhD, said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously online March 21 in JAMA.
Intensive alveolar recruitment nearly doubled the odds of a lower pulmonary complications score (common odds ratio, 1.9; 95% confidence interval, 1.2-2.8; P = .003), Dr. Leme and his associates reported.
The study comprised 320 adults who developed hypoxemia immediately after undergoing elective cardiac surgery at the Heart Institute (Incor) of the University of São Paulo. The median age of the patients was 62 years, and none had a history of lung disease. Pulmonary complications were scored between 0 (no signs or symptoms) and 5 (death), the investigators noted (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2297).
The intensive alveolar recruitment strategy consisted of three 60-second cycles of lung inflation with a positive end-expiratory pressure (PEEP) of 30 cm H2O, pressure-controlled ventilation, driving pressure of 15 cm H2O, respiratory rate of 15/min, inspiratory time of 1.5 seconds, and FIO2 of 0.40. Between and after inflations, patients received assist-controlled or pressure-controlled ventilation, with driving pressures set to achieve a tidal volume of 6 mL/kg of predicted body weight, an inspiratory time of 1 second, PEEP of 13 cm H2O, and minimum respiratory rate to maintain PaCO2 between 35 and 45 mm Hg.
The “moderate strategy” consisted of three 30-second inflations under continuous positive airway pressure mode at 20 cm H2O and FIO2 of 0.60. Between and after inflations, patients received assist or control volume-controlled ventilation (decelerating-flow waveform), tidal volume of 6 mL/kg of predicted body weight, inspiratory time of 1 second, PEEP of 8 cm H2O, and FIO2 of 0.60, at a minimum respiratory rate that maintained PaCO2 at 35-45 mm Hg.
“[The] use of an intensive alveolar recruitment strategy compared with a moderate recruitment strategy resulted in less severe pulmonary complications during the hospital stay,” the investigators wrote. On average, intensively managed patients had shorter stays in the hospital (10.9 vs. 12.4 days; P = .04) and in the intensive care unit (3.8 vs. 4.8 days; P = .01) than did moderately managed patients. Intensive management also was associated with lower rates of hospital mortality and barotrauma, but the differences in these less common outcomes did not reach statistical significance.
“To our knowledge, this is the first study to show a significant effect of lung recruitment maneuvers on clinical outcomes, which objectively resulted in modest reductions in ICU and hospital length of stay,” the researchers wrote. “This is especially noteworthy considering that the control group was also receiving protective lung ventilation with low [tidal volume] and moderate PEEP levels. Thus, the major difference between treatment groups was the intensity of lung recruitment.”
FAPESP (Fundação de Amparo e Pesquisa do Estado de São Paulo) and FINEP (Financiadora de Estudos e Projetos) provided partial funding. Dr. Leme had no disclosures. Senior author Marcelo Britto Passos Amato, MD, PhD, disclosed research funding from Covidien/Medtronics, Dixtal Biomedica Ltd, and Timpel SA.
Addition of 10 cm H2O to positive end-expiratory volume (PEEP) during mechanical ventilation was followed by significantly lessened pulmonary complications in hospitalized patients who developed hypoxemia after cardiac surgery, participating in a single-center, randomized trial.
This “intensive” alveolar recruitment strategy yielded a median pulmonary complications score of 1.7 (interquartile range, 1.0-2.0), compared with 2.0 (IQR, 1.5-3.0) among patients who underwent ventilation with a PEEP of 20 cm H2O, Alcino Costa Leme, RRT, PhD, said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously online March 21 in JAMA.
Intensive alveolar recruitment nearly doubled the odds of a lower pulmonary complications score (common odds ratio, 1.9; 95% confidence interval, 1.2-2.8; P = .003), Dr. Leme and his associates reported.
The study comprised 320 adults who developed hypoxemia immediately after undergoing elective cardiac surgery at the Heart Institute (Incor) of the University of São Paulo. The median age of the patients was 62 years, and none had a history of lung disease. Pulmonary complications were scored between 0 (no signs or symptoms) and 5 (death), the investigators noted (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2297).
The intensive alveolar recruitment strategy consisted of three 60-second cycles of lung inflation with a positive end-expiratory pressure (PEEP) of 30 cm H2O, pressure-controlled ventilation, driving pressure of 15 cm H2O, respiratory rate of 15/min, inspiratory time of 1.5 seconds, and FIO2 of 0.40. Between and after inflations, patients received assist-controlled or pressure-controlled ventilation, with driving pressures set to achieve a tidal volume of 6 mL/kg of predicted body weight, an inspiratory time of 1 second, PEEP of 13 cm H2O, and minimum respiratory rate to maintain PaCO2 between 35 and 45 mm Hg.
The “moderate strategy” consisted of three 30-second inflations under continuous positive airway pressure mode at 20 cm H2O and FIO2 of 0.60. Between and after inflations, patients received assist or control volume-controlled ventilation (decelerating-flow waveform), tidal volume of 6 mL/kg of predicted body weight, inspiratory time of 1 second, PEEP of 8 cm H2O, and FIO2 of 0.60, at a minimum respiratory rate that maintained PaCO2 at 35-45 mm Hg.
“[The] use of an intensive alveolar recruitment strategy compared with a moderate recruitment strategy resulted in less severe pulmonary complications during the hospital stay,” the investigators wrote. On average, intensively managed patients had shorter stays in the hospital (10.9 vs. 12.4 days; P = .04) and in the intensive care unit (3.8 vs. 4.8 days; P = .01) than did moderately managed patients. Intensive management also was associated with lower rates of hospital mortality and barotrauma, but the differences in these less common outcomes did not reach statistical significance.
“To our knowledge, this is the first study to show a significant effect of lung recruitment maneuvers on clinical outcomes, which objectively resulted in modest reductions in ICU and hospital length of stay,” the researchers wrote. “This is especially noteworthy considering that the control group was also receiving protective lung ventilation with low [tidal volume] and moderate PEEP levels. Thus, the major difference between treatment groups was the intensity of lung recruitment.”
FAPESP (Fundação de Amparo e Pesquisa do Estado de São Paulo) and FINEP (Financiadora de Estudos e Projetos) provided partial funding. Dr. Leme had no disclosures. Senior author Marcelo Britto Passos Amato, MD, PhD, disclosed research funding from Covidien/Medtronics, Dixtal Biomedica Ltd, and Timpel SA.
FROM ISICEM
Key clinical point: Intensive lung recruitment during mechanical ventilation of hypoxemic cardiac surgery patients was followed by less severe pulmonary complications, compared with moderate lung recruitment.
Major finding: Compared with moderate alveolar recruitment, intensive recruitment nearly doubled the odds that patients had a lower pulmonary complications score (odds ratio, 1.9; 95% confidence interval, 1.2 to 2.8; P = .003).
Data source: A single-center randomized trial of 320 adults with no history of pulmonary disease who developed hypoxemia after undergoing elective cardiac surgery.
Disclosures: FAPESP (Fundação de Amparo e Pesquisa do Estado de São Paulo) and FINEP (Financiadora de Estudos e Projetos) provided partial funding. Dr. Leme had no disclosures. Senior author Marcelo Britto Passos Amato, MD, PhD, disclosed research funding from Covidien/Medtronics, Dixtal Biomedica Ltd, and Timpel SA.
Levosimendan does not improve 30-day mortality following cardiac surgery
Adding a low dose of levosimendan to the standard care for patients on perioperative hemodynamic support does not improve outcomes to any significant extent, according to the findings of a new study presented at the annual congress of the European Society of Intensive Care Medicine and published simultaneously online in the New England Journal of Medicine.
“Levosimendan (Simdax, Orion) is an inotropic agent that has been shown to be associated with a higher rate of survival than other inotropic agents in meta-analyses, especially those involving patients undergoing cardiac surgery,” wrote the authors of the study, led by Giovanni Landoni, MD, of Vita-Salute San Raffaele University in Milan, adding, “Considering the pharmacologic properties of levosimendan and the results of previous studies, we hypothesized that the administration of levosimendan, in addition to standard treatment, might result in lower mortality in this context.”
Dr. Landoni and his colleagues conducted the Levosimendan to Reduce Mortality in High Risk Cardiac Surgery Patients: A Multicenter Randomized Controlled Trial, known more commonly as CHEETAH. Written consent was given by 4,725 patients from 14 centers located in Italy, Russia, and Brazil between November 2009 and April 2016. The investigators recruited a total of 506 patients. All subjects included in the study underwent cardiac surgery and experienced a perioperative cardiovascular dysfunction (N Engl J Med. 2017 Mar 21. doi: 10.1056/NEJMoa1616325).
Subjects were then randomized into a cohort receiving either a placebo or a low dose of levosimendan, which varied between 0.025 to 0.2 mcg/kg of body weight per minute continuously for up to 48 hours. A total of 248 subjects received levosimendan and 258 received placebo. All patients were administered the treatment while in the ICU; patients were taken off their regimen prior to 48 hours if they were discharged from the ICU. Anyone screened for inclusion who already had experienced a negative reaction to levosimendan was excluded from the study.
“We collected preoperative data on baseline characteristics and coexisting conditions, intraoperative and postoperative treatment data, postoperative laboratory values, duration of mechanical ventilation, durations of ICU and hospital stays, and major outcomes,” the authors explained, adding that “telephone follow-up was performed at 30 days and 180 days after randomization by an investigator who was unaware of the trial group assignments.”
The primary outcome of the study was 30-day mortality. The levosimendan cohort experienced 32 deaths (12.9%), while the placebo cohort saw 33 (12.8%), a nonsignificant difference (P = .97) between the two groups. Similarly, the median time spent on mechanical ventilation was 19 hours for those on levosimendan, versus 21 hours for those on placebo (P = .48), and median length of hospital stay was 14 days in both groups (P = .39).
“Previous meta-analyses of randomized, controlled trials showed a higher rate of survival with levosimendan than with other treatment regimens among patients undergoing cardiac surgery,” Dr. Landoni and his coauthors noted. Previous studies also had a number of key differences, such as the number of subjects who underwent coronary artery bypass grafting, the dosing of levosimendan, and inclusion of patients who had reduced preoperative ejection fraction instead of ones with myocardial dysfunction who needed inotropic support, which the current study used.
The study was funded by the Italian Ministry of Health. Dr. Landoni reported receiving nonfinancial support from the Orion Corporation while the study was ongoing; several other coauthors reported similar disclosures.
Adding a low dose of levosimendan to the standard care for patients on perioperative hemodynamic support does not improve outcomes to any significant extent, according to the findings of a new study presented at the annual congress of the European Society of Intensive Care Medicine and published simultaneously online in the New England Journal of Medicine.
“Levosimendan (Simdax, Orion) is an inotropic agent that has been shown to be associated with a higher rate of survival than other inotropic agents in meta-analyses, especially those involving patients undergoing cardiac surgery,” wrote the authors of the study, led by Giovanni Landoni, MD, of Vita-Salute San Raffaele University in Milan, adding, “Considering the pharmacologic properties of levosimendan and the results of previous studies, we hypothesized that the administration of levosimendan, in addition to standard treatment, might result in lower mortality in this context.”
Dr. Landoni and his colleagues conducted the Levosimendan to Reduce Mortality in High Risk Cardiac Surgery Patients: A Multicenter Randomized Controlled Trial, known more commonly as CHEETAH. Written consent was given by 4,725 patients from 14 centers located in Italy, Russia, and Brazil between November 2009 and April 2016. The investigators recruited a total of 506 patients. All subjects included in the study underwent cardiac surgery and experienced a perioperative cardiovascular dysfunction (N Engl J Med. 2017 Mar 21. doi: 10.1056/NEJMoa1616325).
Subjects were then randomized into a cohort receiving either a placebo or a low dose of levosimendan, which varied between 0.025 to 0.2 mcg/kg of body weight per minute continuously for up to 48 hours. A total of 248 subjects received levosimendan and 258 received placebo. All patients were administered the treatment while in the ICU; patients were taken off their regimen prior to 48 hours if they were discharged from the ICU. Anyone screened for inclusion who already had experienced a negative reaction to levosimendan was excluded from the study.
“We collected preoperative data on baseline characteristics and coexisting conditions, intraoperative and postoperative treatment data, postoperative laboratory values, duration of mechanical ventilation, durations of ICU and hospital stays, and major outcomes,” the authors explained, adding that “telephone follow-up was performed at 30 days and 180 days after randomization by an investigator who was unaware of the trial group assignments.”
The primary outcome of the study was 30-day mortality. The levosimendan cohort experienced 32 deaths (12.9%), while the placebo cohort saw 33 (12.8%), a nonsignificant difference (P = .97) between the two groups. Similarly, the median time spent on mechanical ventilation was 19 hours for those on levosimendan, versus 21 hours for those on placebo (P = .48), and median length of hospital stay was 14 days in both groups (P = .39).
“Previous meta-analyses of randomized, controlled trials showed a higher rate of survival with levosimendan than with other treatment regimens among patients undergoing cardiac surgery,” Dr. Landoni and his coauthors noted. Previous studies also had a number of key differences, such as the number of subjects who underwent coronary artery bypass grafting, the dosing of levosimendan, and inclusion of patients who had reduced preoperative ejection fraction instead of ones with myocardial dysfunction who needed inotropic support, which the current study used.
The study was funded by the Italian Ministry of Health. Dr. Landoni reported receiving nonfinancial support from the Orion Corporation while the study was ongoing; several other coauthors reported similar disclosures.
Adding a low dose of levosimendan to the standard care for patients on perioperative hemodynamic support does not improve outcomes to any significant extent, according to the findings of a new study presented at the annual congress of the European Society of Intensive Care Medicine and published simultaneously online in the New England Journal of Medicine.
“Levosimendan (Simdax, Orion) is an inotropic agent that has been shown to be associated with a higher rate of survival than other inotropic agents in meta-analyses, especially those involving patients undergoing cardiac surgery,” wrote the authors of the study, led by Giovanni Landoni, MD, of Vita-Salute San Raffaele University in Milan, adding, “Considering the pharmacologic properties of levosimendan and the results of previous studies, we hypothesized that the administration of levosimendan, in addition to standard treatment, might result in lower mortality in this context.”
Dr. Landoni and his colleagues conducted the Levosimendan to Reduce Mortality in High Risk Cardiac Surgery Patients: A Multicenter Randomized Controlled Trial, known more commonly as CHEETAH. Written consent was given by 4,725 patients from 14 centers located in Italy, Russia, and Brazil between November 2009 and April 2016. The investigators recruited a total of 506 patients. All subjects included in the study underwent cardiac surgery and experienced a perioperative cardiovascular dysfunction (N Engl J Med. 2017 Mar 21. doi: 10.1056/NEJMoa1616325).
Subjects were then randomized into a cohort receiving either a placebo or a low dose of levosimendan, which varied between 0.025 to 0.2 mcg/kg of body weight per minute continuously for up to 48 hours. A total of 248 subjects received levosimendan and 258 received placebo. All patients were administered the treatment while in the ICU; patients were taken off their regimen prior to 48 hours if they were discharged from the ICU. Anyone screened for inclusion who already had experienced a negative reaction to levosimendan was excluded from the study.
“We collected preoperative data on baseline characteristics and coexisting conditions, intraoperative and postoperative treatment data, postoperative laboratory values, duration of mechanical ventilation, durations of ICU and hospital stays, and major outcomes,” the authors explained, adding that “telephone follow-up was performed at 30 days and 180 days after randomization by an investigator who was unaware of the trial group assignments.”
The primary outcome of the study was 30-day mortality. The levosimendan cohort experienced 32 deaths (12.9%), while the placebo cohort saw 33 (12.8%), a nonsignificant difference (P = .97) between the two groups. Similarly, the median time spent on mechanical ventilation was 19 hours for those on levosimendan, versus 21 hours for those on placebo (P = .48), and median length of hospital stay was 14 days in both groups (P = .39).
“Previous meta-analyses of randomized, controlled trials showed a higher rate of survival with levosimendan than with other treatment regimens among patients undergoing cardiac surgery,” Dr. Landoni and his coauthors noted. Previous studies also had a number of key differences, such as the number of subjects who underwent coronary artery bypass grafting, the dosing of levosimendan, and inclusion of patients who had reduced preoperative ejection fraction instead of ones with myocardial dysfunction who needed inotropic support, which the current study used.
The study was funded by the Italian Ministry of Health. Dr. Landoni reported receiving nonfinancial support from the Orion Corporation while the study was ongoing; several other coauthors reported similar disclosures.
Key clinical point:
Major finding: Among other things, 30-day mortality rates between levosimendan (12.9%) and placebo (12.8%) cohorts were not significantly different (P = .97).
Data source: The CHEETAH study is a multicenter, randomized, double-blind, placebo-controlled trial of 506 cardiac surgery patients recommended for perioperative hemodynamic support.
Disclosures: Funded by the Italian Ministry of Health. Several coauthors reported potentially relevant conflicts of interest.
Dexmedetomidine improves sedation in sepsis
Use of dexmedetomidine improved sedation among ventilated patients with sepsis, but did not significantly cut mortality rates or increase ventilator-free days in a multicenter, open-label randomized controlled trial.
Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2), Yu Kawazoe, MD, PhD, and his associates reported at the International Symposium on Intensive Care and Emergency Medicine. The report was simultaneously published in JAMA.
“The study may have identified a clinically important benefit of dexmedetomidine – an 8% reduction in 28-day mortality – that did not demonstrate statistical significance ... ” wrote Dr. Kawazoe of Tohoku University Graduate School of Medicine, Sendai, Japan. “Physicians may consider an 8% difference in 28-day mortality to be clinically significant, but this study was underpowered to detect this difference.”
Dexmedetomidine often is used for sedation during ventilation, but its effects on mortality and ventilator weaning are poorly understood, the researchers noted. However, this highly selective alpha2-adrenergic agonist has been found to suppress inflammation and to protect organs, and “can improve patients’ ability to communicate pain compared with midazolam and propofol,” the researchers wrote. Therefore, they randomly assigned 201 patients with sepsis at eight intensive care units in Japan to receive sedation with or without dexmedetomidine. Both arms received fentanyl, propofol, and midazolam, dosed to achieve Richmond Agitation-Sedation Scale (RASS) scores of 0 (calm) during the day and –2 (lightly sedated) at night (JAMA. 2017 March 21. doi: 10.1001/jama.2017.2088).
The dexmedetomidine group spent a median of 20 days off the ventilator, compared with 18 days for controls (P = .20), the investigators reported. However, dexmedetomidine led to significantly higher rates of well-controlled sedation. The highest rate of well-controlled sedation (defined as having a RASS scores between –3 and 1 throughout 1 day in the ICU) in treated patients was 58%, while the highest rate of well-controlled sedation in the control group was 39% (P = .01).
Rates of adverse events did not significantly differ between groups. Bradycardia was most common, affecting 7% of the intervention group and 2% of controls (P = .1) the researchers said.
Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved in the research project. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Use of dexmedetomidine improved sedation among ventilated patients with sepsis, but did not significantly cut mortality rates or increase ventilator-free days in a multicenter, open-label randomized controlled trial.
Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2), Yu Kawazoe, MD, PhD, and his associates reported at the International Symposium on Intensive Care and Emergency Medicine. The report was simultaneously published in JAMA.
“The study may have identified a clinically important benefit of dexmedetomidine – an 8% reduction in 28-day mortality – that did not demonstrate statistical significance ... ” wrote Dr. Kawazoe of Tohoku University Graduate School of Medicine, Sendai, Japan. “Physicians may consider an 8% difference in 28-day mortality to be clinically significant, but this study was underpowered to detect this difference.”
Dexmedetomidine often is used for sedation during ventilation, but its effects on mortality and ventilator weaning are poorly understood, the researchers noted. However, this highly selective alpha2-adrenergic agonist has been found to suppress inflammation and to protect organs, and “can improve patients’ ability to communicate pain compared with midazolam and propofol,” the researchers wrote. Therefore, they randomly assigned 201 patients with sepsis at eight intensive care units in Japan to receive sedation with or without dexmedetomidine. Both arms received fentanyl, propofol, and midazolam, dosed to achieve Richmond Agitation-Sedation Scale (RASS) scores of 0 (calm) during the day and –2 (lightly sedated) at night (JAMA. 2017 March 21. doi: 10.1001/jama.2017.2088).
The dexmedetomidine group spent a median of 20 days off the ventilator, compared with 18 days for controls (P = .20), the investigators reported. However, dexmedetomidine led to significantly higher rates of well-controlled sedation. The highest rate of well-controlled sedation (defined as having a RASS scores between –3 and 1 throughout 1 day in the ICU) in treated patients was 58%, while the highest rate of well-controlled sedation in the control group was 39% (P = .01).
Rates of adverse events did not significantly differ between groups. Bradycardia was most common, affecting 7% of the intervention group and 2% of controls (P = .1) the researchers said.
Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved in the research project. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Use of dexmedetomidine improved sedation among ventilated patients with sepsis, but did not significantly cut mortality rates or increase ventilator-free days in a multicenter, open-label randomized controlled trial.
Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2), Yu Kawazoe, MD, PhD, and his associates reported at the International Symposium on Intensive Care and Emergency Medicine. The report was simultaneously published in JAMA.
“The study may have identified a clinically important benefit of dexmedetomidine – an 8% reduction in 28-day mortality – that did not demonstrate statistical significance ... ” wrote Dr. Kawazoe of Tohoku University Graduate School of Medicine, Sendai, Japan. “Physicians may consider an 8% difference in 28-day mortality to be clinically significant, but this study was underpowered to detect this difference.”
Dexmedetomidine often is used for sedation during ventilation, but its effects on mortality and ventilator weaning are poorly understood, the researchers noted. However, this highly selective alpha2-adrenergic agonist has been found to suppress inflammation and to protect organs, and “can improve patients’ ability to communicate pain compared with midazolam and propofol,” the researchers wrote. Therefore, they randomly assigned 201 patients with sepsis at eight intensive care units in Japan to receive sedation with or without dexmedetomidine. Both arms received fentanyl, propofol, and midazolam, dosed to achieve Richmond Agitation-Sedation Scale (RASS) scores of 0 (calm) during the day and –2 (lightly sedated) at night (JAMA. 2017 March 21. doi: 10.1001/jama.2017.2088).
The dexmedetomidine group spent a median of 20 days off the ventilator, compared with 18 days for controls (P = .20), the investigators reported. However, dexmedetomidine led to significantly higher rates of well-controlled sedation. The highest rate of well-controlled sedation (defined as having a RASS scores between –3 and 1 throughout 1 day in the ICU) in treated patients was 58%, while the highest rate of well-controlled sedation in the control group was 39% (P = .01).
Rates of adverse events did not significantly differ between groups. Bradycardia was most common, affecting 7% of the intervention group and 2% of controls (P = .1) the researchers said.
Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved in the research project. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Key clinical point. Use of dexmedetomidine improved sedation but did not significantly cut mortality rates or increase ventilator-free days among hospitalized patients with sepsis.
Major finding: Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2).
Data source: A multicenter, open-label randomized controlled trial of 201 ventilated patients with sepsis.
Disclosures: Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Osteoarthritis’ link to metabolic syndrome tied to body weight, BMI
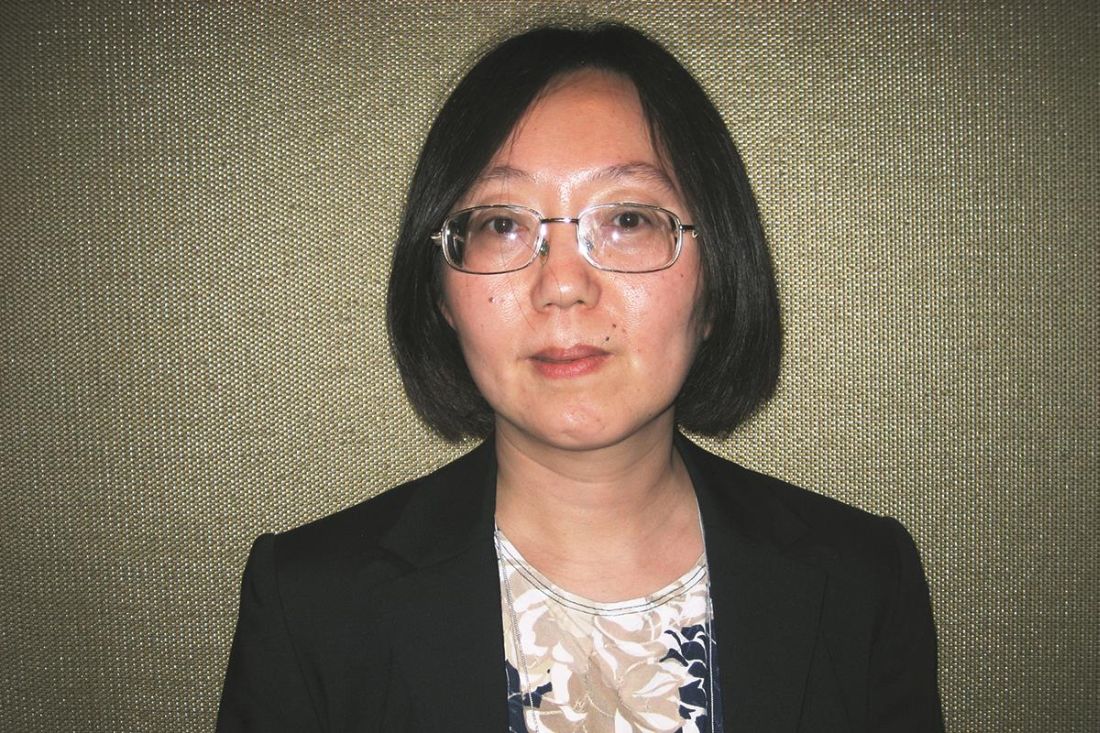
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: There is no strong association between the metabolic syndrome (MetS) and OA after adjustment for BMI or body weight.
Major finding: Components of MetS were initially associated with incident radiographic and symptomatic OA, but after adjustment for BMI or body weight, most of the associations were weak and insignificant. However, an association between the MetS and high blood pressure persisted in both sexes.
Data source: An analysis of 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline and were followed for 10 years.
Disclosures: The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The power of words in aesthetic procedures and healing patients
The words we choose to use prior to procedures can positively or negatively impact a patient’s experience during a procedure and their decision to have the procedure performed. A practical example would include using the word discomfort instead of pain to describe pain that may be associated with a procedure. The root word of discomfort is comfort, which the mind focuses on and creates less of an anxious state than pain.
Obviously, the need to provide proper and realistic expectations, as well as risks and benefits, is of utmost importance when obtaining informed consent. The words used can put a patient’s mind at ease or cause further anxiety about ideas of needles, scalpels, pain, risk of infection, and bleeding that are part of our everyday procedures.
Judith Thomas, DDS, a dentist in Virginia who is trained in clinical hypnosis, once described the power of the word but. People will often put more emphasis in their minds on what is said after the word but than on what is said before. For example, in a romantic relationship context, saying “I love you, but you drive me crazy” has a different impact than “You drive me crazy, but I love you.” The focus tends to stay on the “I love you” portion more when it is said last, after the “but.”
The same phenomenon can happen when we discuss procedures with our patients. When a medical assistant performs phlebotomy or when we as doctors are about to perform an injection, instead of saying this is going to hurt, another way to phrase it would be “In a moment you may feel something, but it doesn’t have to bother you” or “You may experience some discomfort, but it will resolve quickly.” Something I’ve said for years to patients before surgery is “You may feel a little stinging as the anesthetic goes in, after that you may feel me touching you, but nothing uncomfortable.” I guess I had been intuitively using this technique for years, without knowing the impact of the word “but.” Perhaps now that I am more mindful of it, I will be even more mindful of how I phrase these terms. We, in addition to our nurses and medical assistants, can use these techniques to enhance patient comfort and the patient’s experience.
According to the American Society of Clinical Hypnosis, physicians and dentists used the power of words through hypnosis as anesthesia before the first chemical general anesthetic agent, ether, was used for surgery in the 1840s, followed by chloroform. Prior to this time, British and Scottish physicians John Elliotson, James Esdaile, and James Braid performed over 3,000 procedures and surgeries with clinical hypnosis alone. Some may argue that the ancient Egyptians also used hypnosis for their well-described surgeries, as no other anesthetic has been documented. Moreover, there is evidence of “sleep temples” that the ancient Egyptians used for healing.1
This article is not to suggest that our words should replace anesthesia. Many advances in anesthesia and pain control have been made since the time of chloroform. However, being mindful of our words can aid and assist in our surgical and aesthetic procedures where less anesthesia is used: Patients feel more comfortable, they heal faster, and overall, they have a more positive outcome and pleasant physician-patient experience.2
For patients, the skill of the doctor and the outcome of the procedure are of the utmost importance, but, especially in aesthetic dermatology, where some of our procedures are repeated or performed periodically, the positive impact of the entire experience will entrust them with your care long term.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References
1. Mutter, C.B. (1998). History of Hypnosis. (pp. 10-12) “Hypnotic Induction and Suggestion.” Chicago: American Society of Clinical Hypnosis.
2. Burns. 2010 Aug;36(5):639-46.
The words we choose to use prior to procedures can positively or negatively impact a patient’s experience during a procedure and their decision to have the procedure performed. A practical example would include using the word discomfort instead of pain to describe pain that may be associated with a procedure. The root word of discomfort is comfort, which the mind focuses on and creates less of an anxious state than pain.
Obviously, the need to provide proper and realistic expectations, as well as risks and benefits, is of utmost importance when obtaining informed consent. The words used can put a patient’s mind at ease or cause further anxiety about ideas of needles, scalpels, pain, risk of infection, and bleeding that are part of our everyday procedures.
Judith Thomas, DDS, a dentist in Virginia who is trained in clinical hypnosis, once described the power of the word but. People will often put more emphasis in their minds on what is said after the word but than on what is said before. For example, in a romantic relationship context, saying “I love you, but you drive me crazy” has a different impact than “You drive me crazy, but I love you.” The focus tends to stay on the “I love you” portion more when it is said last, after the “but.”
The same phenomenon can happen when we discuss procedures with our patients. When a medical assistant performs phlebotomy or when we as doctors are about to perform an injection, instead of saying this is going to hurt, another way to phrase it would be “In a moment you may feel something, but it doesn’t have to bother you” or “You may experience some discomfort, but it will resolve quickly.” Something I’ve said for years to patients before surgery is “You may feel a little stinging as the anesthetic goes in, after that you may feel me touching you, but nothing uncomfortable.” I guess I had been intuitively using this technique for years, without knowing the impact of the word “but.” Perhaps now that I am more mindful of it, I will be even more mindful of how I phrase these terms. We, in addition to our nurses and medical assistants, can use these techniques to enhance patient comfort and the patient’s experience.
According to the American Society of Clinical Hypnosis, physicians and dentists used the power of words through hypnosis as anesthesia before the first chemical general anesthetic agent, ether, was used for surgery in the 1840s, followed by chloroform. Prior to this time, British and Scottish physicians John Elliotson, James Esdaile, and James Braid performed over 3,000 procedures and surgeries with clinical hypnosis alone. Some may argue that the ancient Egyptians also used hypnosis for their well-described surgeries, as no other anesthetic has been documented. Moreover, there is evidence of “sleep temples” that the ancient Egyptians used for healing.1
This article is not to suggest that our words should replace anesthesia. Many advances in anesthesia and pain control have been made since the time of chloroform. However, being mindful of our words can aid and assist in our surgical and aesthetic procedures where less anesthesia is used: Patients feel more comfortable, they heal faster, and overall, they have a more positive outcome and pleasant physician-patient experience.2
For patients, the skill of the doctor and the outcome of the procedure are of the utmost importance, but, especially in aesthetic dermatology, where some of our procedures are repeated or performed periodically, the positive impact of the entire experience will entrust them with your care long term.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References
1. Mutter, C.B. (1998). History of Hypnosis. (pp. 10-12) “Hypnotic Induction and Suggestion.” Chicago: American Society of Clinical Hypnosis.
2. Burns. 2010 Aug;36(5):639-46.
The words we choose to use prior to procedures can positively or negatively impact a patient’s experience during a procedure and their decision to have the procedure performed. A practical example would include using the word discomfort instead of pain to describe pain that may be associated with a procedure. The root word of discomfort is comfort, which the mind focuses on and creates less of an anxious state than pain.
Obviously, the need to provide proper and realistic expectations, as well as risks and benefits, is of utmost importance when obtaining informed consent. The words used can put a patient’s mind at ease or cause further anxiety about ideas of needles, scalpels, pain, risk of infection, and bleeding that are part of our everyday procedures.
Judith Thomas, DDS, a dentist in Virginia who is trained in clinical hypnosis, once described the power of the word but. People will often put more emphasis in their minds on what is said after the word but than on what is said before. For example, in a romantic relationship context, saying “I love you, but you drive me crazy” has a different impact than “You drive me crazy, but I love you.” The focus tends to stay on the “I love you” portion more when it is said last, after the “but.”
The same phenomenon can happen when we discuss procedures with our patients. When a medical assistant performs phlebotomy or when we as doctors are about to perform an injection, instead of saying this is going to hurt, another way to phrase it would be “In a moment you may feel something, but it doesn’t have to bother you” or “You may experience some discomfort, but it will resolve quickly.” Something I’ve said for years to patients before surgery is “You may feel a little stinging as the anesthetic goes in, after that you may feel me touching you, but nothing uncomfortable.” I guess I had been intuitively using this technique for years, without knowing the impact of the word “but.” Perhaps now that I am more mindful of it, I will be even more mindful of how I phrase these terms. We, in addition to our nurses and medical assistants, can use these techniques to enhance patient comfort and the patient’s experience.
According to the American Society of Clinical Hypnosis, physicians and dentists used the power of words through hypnosis as anesthesia before the first chemical general anesthetic agent, ether, was used for surgery in the 1840s, followed by chloroform. Prior to this time, British and Scottish physicians John Elliotson, James Esdaile, and James Braid performed over 3,000 procedures and surgeries with clinical hypnosis alone. Some may argue that the ancient Egyptians also used hypnosis for their well-described surgeries, as no other anesthetic has been documented. Moreover, there is evidence of “sleep temples” that the ancient Egyptians used for healing.1
This article is not to suggest that our words should replace anesthesia. Many advances in anesthesia and pain control have been made since the time of chloroform. However, being mindful of our words can aid and assist in our surgical and aesthetic procedures where less anesthesia is used: Patients feel more comfortable, they heal faster, and overall, they have a more positive outcome and pleasant physician-patient experience.2
For patients, the skill of the doctor and the outcome of the procedure are of the utmost importance, but, especially in aesthetic dermatology, where some of our procedures are repeated or performed periodically, the positive impact of the entire experience will entrust them with your care long term.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References
1. Mutter, C.B. (1998). History of Hypnosis. (pp. 10-12) “Hypnotic Induction and Suggestion.” Chicago: American Society of Clinical Hypnosis.
2. Burns. 2010 Aug;36(5):639-46.
Norepinephrine shortage linked to mortality in patients with septic shock
A national shortage of norepinephrine in the United States was associated with higher rates of mortality among patients hospitalized with septic shock, investigators reported.
Rates of in-hospital mortality in 2011 were 40% during quarters when hospitals were facing shortages and 36% when they were not, Emily Vail, MD, and her associates said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously in JAMA.
The link between norepinephrine shortage and death from septic shock persisted even after the researchers accounted for numerous clinical and demographic factors (adjusted odds ratio, 1.2; 95% confidence interval, 1.01 to 1.30; P = .03), wrote Dr. Vail of Columbia University, New York (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2841).
Drug shortages are common in the United States, but few studies have explored their effects on patient outcomes. Investigators compared mortality rates among affected patients during 3-month intervals when hospitals were and were not using at least 20% less norepinephrine than baseline. The researchers used Premier Healthcare Database, which includes both standard claims and detailed, dated logs of all services billed to patients or insurance, with minimal missing data.
A total of 77% patients admitted with septic shock received norepinephrine before the shortage. During the lowest point of the shortage, 56% of patients received it, the researchers reported. Clinicians most often used phenylephrine instead, prescribing it to up to 54% of patients during the worst time of the shortage. The absolute increase in mortality during the quarters of shortage was 3.7% (95% CI, 1.5%-6.0%).
Several factors might explain the link between norepinephrine shortage and mortality, said the investigators. The vasopressors chosen to replace norepinephrine might result directly in worse outcomes, but a decrease in norepinephrine use also might be a proxy for relevant variables such as delayed use of vasopressors, lack of knowledge of how to optimally dose vasopressors besides norepinephrine, or the absence of a pharmacist dedicated to helping optimize the use of limited supplies.
The study did not uncover a dose-response association between greater decreases in norepinephrine use and increased mortality, the researchers noted. “This may be due to a threshold effect of vasopressor shortage on mortality, or lack of power due to relatively few hospital quarters at the extreme levels of vasopressor shortage,” they wrote.
Because the deaths captured included only those that occurred in-hospital, “the results may have underestimated mortality, particularly for hospitals that tend transfer patients early to other skilled care facilities,” the researchers noted.
The cohort of patients was limited to those who received vasopressors for 2 or more days and excluded patients who died on the first day of vasopressor treatment, the researchers said.
The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
A national shortage of norepinephrine in the United States was associated with higher rates of mortality among patients hospitalized with septic shock, investigators reported.
Rates of in-hospital mortality in 2011 were 40% during quarters when hospitals were facing shortages and 36% when they were not, Emily Vail, MD, and her associates said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously in JAMA.
The link between norepinephrine shortage and death from septic shock persisted even after the researchers accounted for numerous clinical and demographic factors (adjusted odds ratio, 1.2; 95% confidence interval, 1.01 to 1.30; P = .03), wrote Dr. Vail of Columbia University, New York (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2841).
Drug shortages are common in the United States, but few studies have explored their effects on patient outcomes. Investigators compared mortality rates among affected patients during 3-month intervals when hospitals were and were not using at least 20% less norepinephrine than baseline. The researchers used Premier Healthcare Database, which includes both standard claims and detailed, dated logs of all services billed to patients or insurance, with minimal missing data.
A total of 77% patients admitted with septic shock received norepinephrine before the shortage. During the lowest point of the shortage, 56% of patients received it, the researchers reported. Clinicians most often used phenylephrine instead, prescribing it to up to 54% of patients during the worst time of the shortage. The absolute increase in mortality during the quarters of shortage was 3.7% (95% CI, 1.5%-6.0%).
Several factors might explain the link between norepinephrine shortage and mortality, said the investigators. The vasopressors chosen to replace norepinephrine might result directly in worse outcomes, but a decrease in norepinephrine use also might be a proxy for relevant variables such as delayed use of vasopressors, lack of knowledge of how to optimally dose vasopressors besides norepinephrine, or the absence of a pharmacist dedicated to helping optimize the use of limited supplies.
The study did not uncover a dose-response association between greater decreases in norepinephrine use and increased mortality, the researchers noted. “This may be due to a threshold effect of vasopressor shortage on mortality, or lack of power due to relatively few hospital quarters at the extreme levels of vasopressor shortage,” they wrote.
Because the deaths captured included only those that occurred in-hospital, “the results may have underestimated mortality, particularly for hospitals that tend transfer patients early to other skilled care facilities,” the researchers noted.
The cohort of patients was limited to those who received vasopressors for 2 or more days and excluded patients who died on the first day of vasopressor treatment, the researchers said.
The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
A national shortage of norepinephrine in the United States was associated with higher rates of mortality among patients hospitalized with septic shock, investigators reported.
Rates of in-hospital mortality in 2011 were 40% during quarters when hospitals were facing shortages and 36% when they were not, Emily Vail, MD, and her associates said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously in JAMA.
The link between norepinephrine shortage and death from septic shock persisted even after the researchers accounted for numerous clinical and demographic factors (adjusted odds ratio, 1.2; 95% confidence interval, 1.01 to 1.30; P = .03), wrote Dr. Vail of Columbia University, New York (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2841).
Drug shortages are common in the United States, but few studies have explored their effects on patient outcomes. Investigators compared mortality rates among affected patients during 3-month intervals when hospitals were and were not using at least 20% less norepinephrine than baseline. The researchers used Premier Healthcare Database, which includes both standard claims and detailed, dated logs of all services billed to patients or insurance, with minimal missing data.
A total of 77% patients admitted with septic shock received norepinephrine before the shortage. During the lowest point of the shortage, 56% of patients received it, the researchers reported. Clinicians most often used phenylephrine instead, prescribing it to up to 54% of patients during the worst time of the shortage. The absolute increase in mortality during the quarters of shortage was 3.7% (95% CI, 1.5%-6.0%).
Several factors might explain the link between norepinephrine shortage and mortality, said the investigators. The vasopressors chosen to replace norepinephrine might result directly in worse outcomes, but a decrease in norepinephrine use also might be a proxy for relevant variables such as delayed use of vasopressors, lack of knowledge of how to optimally dose vasopressors besides norepinephrine, or the absence of a pharmacist dedicated to helping optimize the use of limited supplies.
The study did not uncover a dose-response association between greater decreases in norepinephrine use and increased mortality, the researchers noted. “This may be due to a threshold effect of vasopressor shortage on mortality, or lack of power due to relatively few hospital quarters at the extreme levels of vasopressor shortage,” they wrote.
Because the deaths captured included only those that occurred in-hospital, “the results may have underestimated mortality, particularly for hospitals that tend transfer patients early to other skilled care facilities,” the researchers noted.
The cohort of patients was limited to those who received vasopressors for 2 or more days and excluded patients who died on the first day of vasopressor treatment, the researchers said.
The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
FROM ISICEM
Key clinical point. The 2011 norepinephrine shortage was associated with mortality among patients hospitalized with septic shock.
Major finding: Rates of in-hospital mortality were 36% during quarters of normal norepinephrine use and 40% during quarters of decreased use (adjusted odds ratio, 1.2; P = .03).
Data source: A retrospective cohort study of 27,835 patients at 26 hospitals in the United States that were affected by the shortage.
Disclosures: The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
Pretreatment Imaging May Help Prevent Hodgkin Lymphoma Recurrence
Advances in radiation treatment have led to better targeting, minimizing the dose to healthy tissue. For patients with Hodgkin lymphoma (HL), pretreatment scanning with positron emission tomography and computed tomography (PET/CT) has become the gold standard, say researchers from University of Florida, in determining the extent of HL. Because HL may recur at the site of the original cancer, the scans are important to accurately capture the scope of the disease. Moreover, the researchers say pretreatment PET/CT may reduce disease progression.
Related: Study Points to Risk Factors for Lymphoma
In their study of 37 patients with stage I or II HL, 31 had PET/CT before chemotherapy. Two of the remaining 6 had PET/CT done within 5 days after chemotherapy was started. Median follow-up was 46 months.
The 4-year rate of relapse-free survival was 92%. Patients who did not receive pretreatment PET/CT were more likely to have a relapse (67%). Of 4 recurrences, 3 were within 12 months of follow-up; 1 developed 5 years after treatment.
Among the 6 patients who did not have a baseline PET/CT scan, all 3 recurrences were in lymph node regions outside of, but adjacent to, the radiation field. None of the 6 experienced an in-field treatment failure.
Related: Development and Implementation of a Veterans’ Cancer Survivorship Program
Long-term survivors of HL are vulnerable to late adverse effects, the researchers note, and that fact is “the impetus behind efforts to reduce radiation exposure to organs at risk.” They cite studies that have found that PET/CT scans, compared with using only pretreatment contrast-enhanced CT scans, can alter the staging in 10% to 30% of patients with HL. Their study, the researchers add, helps support the National Comprehensive Cancer Network guidelines that advise prechemotherapy PET/CT imaging in staging all HL patients. Not doing complete staging, the researchers say, puts patients at “unnecessary, and in some instances preventable, risk for recurrence.”
Source:
Figura N, Flampouri S, Mendenhall NP, et al. Adv Radiat Oncol. 2017;1-16.
Advances in radiation treatment have led to better targeting, minimizing the dose to healthy tissue. For patients with Hodgkin lymphoma (HL), pretreatment scanning with positron emission tomography and computed tomography (PET/CT) has become the gold standard, say researchers from University of Florida, in determining the extent of HL. Because HL may recur at the site of the original cancer, the scans are important to accurately capture the scope of the disease. Moreover, the researchers say pretreatment PET/CT may reduce disease progression.
Related: Study Points to Risk Factors for Lymphoma
In their study of 37 patients with stage I or II HL, 31 had PET/CT before chemotherapy. Two of the remaining 6 had PET/CT done within 5 days after chemotherapy was started. Median follow-up was 46 months.
The 4-year rate of relapse-free survival was 92%. Patients who did not receive pretreatment PET/CT were more likely to have a relapse (67%). Of 4 recurrences, 3 were within 12 months of follow-up; 1 developed 5 years after treatment.
Among the 6 patients who did not have a baseline PET/CT scan, all 3 recurrences were in lymph node regions outside of, but adjacent to, the radiation field. None of the 6 experienced an in-field treatment failure.
Related: Development and Implementation of a Veterans’ Cancer Survivorship Program
Long-term survivors of HL are vulnerable to late adverse effects, the researchers note, and that fact is “the impetus behind efforts to reduce radiation exposure to organs at risk.” They cite studies that have found that PET/CT scans, compared with using only pretreatment contrast-enhanced CT scans, can alter the staging in 10% to 30% of patients with HL. Their study, the researchers add, helps support the National Comprehensive Cancer Network guidelines that advise prechemotherapy PET/CT imaging in staging all HL patients. Not doing complete staging, the researchers say, puts patients at “unnecessary, and in some instances preventable, risk for recurrence.”
Source:
Figura N, Flampouri S, Mendenhall NP, et al. Adv Radiat Oncol. 2017;1-16.
Advances in radiation treatment have led to better targeting, minimizing the dose to healthy tissue. For patients with Hodgkin lymphoma (HL), pretreatment scanning with positron emission tomography and computed tomography (PET/CT) has become the gold standard, say researchers from University of Florida, in determining the extent of HL. Because HL may recur at the site of the original cancer, the scans are important to accurately capture the scope of the disease. Moreover, the researchers say pretreatment PET/CT may reduce disease progression.
Related: Study Points to Risk Factors for Lymphoma
In their study of 37 patients with stage I or II HL, 31 had PET/CT before chemotherapy. Two of the remaining 6 had PET/CT done within 5 days after chemotherapy was started. Median follow-up was 46 months.
The 4-year rate of relapse-free survival was 92%. Patients who did not receive pretreatment PET/CT were more likely to have a relapse (67%). Of 4 recurrences, 3 were within 12 months of follow-up; 1 developed 5 years after treatment.
Among the 6 patients who did not have a baseline PET/CT scan, all 3 recurrences were in lymph node regions outside of, but adjacent to, the radiation field. None of the 6 experienced an in-field treatment failure.
Related: Development and Implementation of a Veterans’ Cancer Survivorship Program
Long-term survivors of HL are vulnerable to late adverse effects, the researchers note, and that fact is “the impetus behind efforts to reduce radiation exposure to organs at risk.” They cite studies that have found that PET/CT scans, compared with using only pretreatment contrast-enhanced CT scans, can alter the staging in 10% to 30% of patients with HL. Their study, the researchers add, helps support the National Comprehensive Cancer Network guidelines that advise prechemotherapy PET/CT imaging in staging all HL patients. Not doing complete staging, the researchers say, puts patients at “unnecessary, and in some instances preventable, risk for recurrence.”
Source:
Figura N, Flampouri S, Mendenhall NP, et al. Adv Radiat Oncol. 2017;1-16.
Study supports use of rivaroxaban to prevent VTE recurrence
WASHINGTON, DC—Results of the EINSTEIN CHOICE study suggest rivaroxaban is more effective than, and just as safe as, aspirin for long-term anticoagulation in patients with venous thromboembolism (VTE).
In this phase 3 study, patients who had completed 6 to 12 months of anticoagulant therapy were randomized to receive rivaroxaban or aspirin.
Those who received rivaroxaban had a significantly lower risk of recurrent VTE, and the rates of major bleeding were similar between the treatment arms.
“How best to extend anticoagulant use beyond the initial treatment window has been a constant source of debate, with physicians carefully balancing patients’ risk of another VTE with the risk of anticoagulant-related bleeding,” said study investigator Philip S. Wells, MD, of The Ottawa Hospital in Ontario, Canada.
“With EINSTEIN CHOICE, for the first time, we have clinical evidence confirming rivaroxaban is superior to aspirin in reducing recurrent VTE, with no significant impact on safety. These important results have the potential to trigger a paradigm shift in how physicians manage their patients and protect them from VTE recurrence over the long term.”
These results were presented at the American College of Cardiology’s 66th Annual Scientific Session and published in NEJM. The research was funded by Bayer Pharmaceuticals.
The study enrolled 3365 patients with confirmed deep vein thrombosis or pulmonary embolism who were initially treated with anticoagulant therapy for 6 to 12 months.
Patients who required extended anticoagulation at therapeutic doses were not included in this trial, as the objective was to investigate those patients for whom the treating physician was uncertain about the need for continuing anticoagulant therapy.
Patients were randomized in a 1:1:1 ratio to receive a prophylactic dose of rivaroxaban (10 mg once daily), a treatment dose of rivaroxaban (20 mg once daily), or aspirin (100 mg once daily) for up to 12 months. Sixty percent of patients completed the full 12 months of treatment.
Efficacy
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2%, respectively.
For the primary endpoint, the HR for the comparison between the 20 mg and 10 mg rivaroxaban arms was 1.34 (95% CI, 0.65 to 2.75, P=0.42). However, the researchers noted that the comparison of these 2 arms was not powered for significance.
The researchers also found that rivaroxaban reduced patients’ risk of experiencing one of the following events: recurrent VTE, heart attack, ischemic stroke, systemic embolism, or venous thrombosis in another location.
This endpoint occurred in 1.9% of patients in the 10 mg rivaroxaban group (HR=0.33; 95% CI, 0.20 to 0.54; P<0.001), 2.0% of patients in the 20 mg rivaroxaban group (HR=0.35; 95% CI, 0.22 to 0.57; P<0.001), and 5.6% of patients in the aspirin group.
Recurrent VTE or all-cause mortality occurred in 1.3% of patients in the 10 mg rivaroxaban group (HR=0.27; 95% CI, 0.15 to 0.47; P<0.001), 2.1% of patients in the 20 mg rivaroxaban group (HR=0.42; 95% CI, 0.26 to 0.68; P<0.001), and 4.9% of patients in the aspirin group.
Safety
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group.
Rates of clinically relevant non-major bleeding were 2.0%, 2.7%, and 1.8%, respectively (no significant difference).
“We know from previous studies that only about 40% of venous thromboembolism patients are actually on long-term blood thinners,” Dr Wells said.
“We hope that this study, which shows the blood thinner rivaroxaban is as safe as aspirin but much more effective at preventing future clots, will convince patients and their physicians to continue life-long medication that can prevent potentially dangerous blood clots.” ![]()
WASHINGTON, DC—Results of the EINSTEIN CHOICE study suggest rivaroxaban is more effective than, and just as safe as, aspirin for long-term anticoagulation in patients with venous thromboembolism (VTE).
In this phase 3 study, patients who had completed 6 to 12 months of anticoagulant therapy were randomized to receive rivaroxaban or aspirin.
Those who received rivaroxaban had a significantly lower risk of recurrent VTE, and the rates of major bleeding were similar between the treatment arms.
“How best to extend anticoagulant use beyond the initial treatment window has been a constant source of debate, with physicians carefully balancing patients’ risk of another VTE with the risk of anticoagulant-related bleeding,” said study investigator Philip S. Wells, MD, of The Ottawa Hospital in Ontario, Canada.
“With EINSTEIN CHOICE, for the first time, we have clinical evidence confirming rivaroxaban is superior to aspirin in reducing recurrent VTE, with no significant impact on safety. These important results have the potential to trigger a paradigm shift in how physicians manage their patients and protect them from VTE recurrence over the long term.”
These results were presented at the American College of Cardiology’s 66th Annual Scientific Session and published in NEJM. The research was funded by Bayer Pharmaceuticals.
The study enrolled 3365 patients with confirmed deep vein thrombosis or pulmonary embolism who were initially treated with anticoagulant therapy for 6 to 12 months.
Patients who required extended anticoagulation at therapeutic doses were not included in this trial, as the objective was to investigate those patients for whom the treating physician was uncertain about the need for continuing anticoagulant therapy.
Patients were randomized in a 1:1:1 ratio to receive a prophylactic dose of rivaroxaban (10 mg once daily), a treatment dose of rivaroxaban (20 mg once daily), or aspirin (100 mg once daily) for up to 12 months. Sixty percent of patients completed the full 12 months of treatment.
Efficacy
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2%, respectively.
For the primary endpoint, the HR for the comparison between the 20 mg and 10 mg rivaroxaban arms was 1.34 (95% CI, 0.65 to 2.75, P=0.42). However, the researchers noted that the comparison of these 2 arms was not powered for significance.
The researchers also found that rivaroxaban reduced patients’ risk of experiencing one of the following events: recurrent VTE, heart attack, ischemic stroke, systemic embolism, or venous thrombosis in another location.
This endpoint occurred in 1.9% of patients in the 10 mg rivaroxaban group (HR=0.33; 95% CI, 0.20 to 0.54; P<0.001), 2.0% of patients in the 20 mg rivaroxaban group (HR=0.35; 95% CI, 0.22 to 0.57; P<0.001), and 5.6% of patients in the aspirin group.
Recurrent VTE or all-cause mortality occurred in 1.3% of patients in the 10 mg rivaroxaban group (HR=0.27; 95% CI, 0.15 to 0.47; P<0.001), 2.1% of patients in the 20 mg rivaroxaban group (HR=0.42; 95% CI, 0.26 to 0.68; P<0.001), and 4.9% of patients in the aspirin group.
Safety
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group.
Rates of clinically relevant non-major bleeding were 2.0%, 2.7%, and 1.8%, respectively (no significant difference).
“We know from previous studies that only about 40% of venous thromboembolism patients are actually on long-term blood thinners,” Dr Wells said.
“We hope that this study, which shows the blood thinner rivaroxaban is as safe as aspirin but much more effective at preventing future clots, will convince patients and their physicians to continue life-long medication that can prevent potentially dangerous blood clots.” ![]()
WASHINGTON, DC—Results of the EINSTEIN CHOICE study suggest rivaroxaban is more effective than, and just as safe as, aspirin for long-term anticoagulation in patients with venous thromboembolism (VTE).
In this phase 3 study, patients who had completed 6 to 12 months of anticoagulant therapy were randomized to receive rivaroxaban or aspirin.
Those who received rivaroxaban had a significantly lower risk of recurrent VTE, and the rates of major bleeding were similar between the treatment arms.
“How best to extend anticoagulant use beyond the initial treatment window has been a constant source of debate, with physicians carefully balancing patients’ risk of another VTE with the risk of anticoagulant-related bleeding,” said study investigator Philip S. Wells, MD, of The Ottawa Hospital in Ontario, Canada.
“With EINSTEIN CHOICE, for the first time, we have clinical evidence confirming rivaroxaban is superior to aspirin in reducing recurrent VTE, with no significant impact on safety. These important results have the potential to trigger a paradigm shift in how physicians manage their patients and protect them from VTE recurrence over the long term.”
These results were presented at the American College of Cardiology’s 66th Annual Scientific Session and published in NEJM. The research was funded by Bayer Pharmaceuticals.
The study enrolled 3365 patients with confirmed deep vein thrombosis or pulmonary embolism who were initially treated with anticoagulant therapy for 6 to 12 months.
Patients who required extended anticoagulation at therapeutic doses were not included in this trial, as the objective was to investigate those patients for whom the treating physician was uncertain about the need for continuing anticoagulant therapy.
Patients were randomized in a 1:1:1 ratio to receive a prophylactic dose of rivaroxaban (10 mg once daily), a treatment dose of rivaroxaban (20 mg once daily), or aspirin (100 mg once daily) for up to 12 months. Sixty percent of patients completed the full 12 months of treatment.
Efficacy
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2%, respectively.
For the primary endpoint, the HR for the comparison between the 20 mg and 10 mg rivaroxaban arms was 1.34 (95% CI, 0.65 to 2.75, P=0.42). However, the researchers noted that the comparison of these 2 arms was not powered for significance.
The researchers also found that rivaroxaban reduced patients’ risk of experiencing one of the following events: recurrent VTE, heart attack, ischemic stroke, systemic embolism, or venous thrombosis in another location.
This endpoint occurred in 1.9% of patients in the 10 mg rivaroxaban group (HR=0.33; 95% CI, 0.20 to 0.54; P<0.001), 2.0% of patients in the 20 mg rivaroxaban group (HR=0.35; 95% CI, 0.22 to 0.57; P<0.001), and 5.6% of patients in the aspirin group.
Recurrent VTE or all-cause mortality occurred in 1.3% of patients in the 10 mg rivaroxaban group (HR=0.27; 95% CI, 0.15 to 0.47; P<0.001), 2.1% of patients in the 20 mg rivaroxaban group (HR=0.42; 95% CI, 0.26 to 0.68; P<0.001), and 4.9% of patients in the aspirin group.
Safety
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group.
Rates of clinically relevant non-major bleeding were 2.0%, 2.7%, and 1.8%, respectively (no significant difference).
“We know from previous studies that only about 40% of venous thromboembolism patients are actually on long-term blood thinners,” Dr Wells said.
“We hope that this study, which shows the blood thinner rivaroxaban is as safe as aspirin but much more effective at preventing future clots, will convince patients and their physicians to continue life-long medication that can prevent potentially dangerous blood clots.” ![]()
Proteins may be therapeutic targets for TKI-resistant CML, ALL
Researchers say they have identified 2 signaling proteins that enable resistance to tyrosine kinase inhibitors (TKIs) and could be therapeutic targets for acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML).
The team found that by deleting these proteins—c-Fos and Dusp1—they could eradicate BCR-ABL-induced B-cell ALL in mice.
And treatment combining c-Fos and Dusp1 inhibitors with the TKI imatinib was able to cure mice with BCR-ABL-driven CML.
The researchers reported these findings in Nature Medicine.
“We think that, within the next 5 years, our data will change the way people think about cancer development and targeted therapy,” said study author Mohammad Azam, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This study identifies a potential Achilles’ heel of kinase-driven cancers, and what we propose is intended to be curative, not just treatment.”
The potential Achilles’ heel is a common point of passage in cells—a signaling node—that appears to be required to generate cancer cells. The node is formed by the signaling proteins c-Fos and Dusp1, according to the researchers.
The team identified c-Fos and Dusp1 by conducting global gene-expression analysis of mouse leukemia cells and human CML cells. Analysis of the human cells revealed extremely high levels of c-FOS and DUSP1 in BCR-ABL-positive, TKI-resistant cells.
Dr Azam and his colleagues found that signaling from tyrosine kinase and growth factor proteins that support cell expansion (such as IL-3 and IL-6) converge to elevate c-Fos and Dusp1 levels in leukemia cells.
Working together, these molecules maintain the survival of leukemia stem cells (LSCs), which translates to minimal residual disease (MRD) after treatment.
Dr Azam said Dusp1 and c-Fos support the survival of LSCs by increasing the toxic threshold needed to kill them. This means imatinib and other TKIs cannot eliminate the residual LSCs.
After describing the roles of c-Fos and Dusp1, Dr Azam and his colleagues put their ideas to the test in mouse models of CML.
The team tested several treatments in these mice, including:
- monotherapy with imatinib
- inhibitors of c-Fos and Dusp1
- treatment with imatinib and inhibitors of c-Fos and Dusp1.
As suspected, treatment with imatinib alone initially stopped CML progression, but mice ultimately relapsed.
Treatment with c-Fos and Dusp1 inhibitors significantly slowed CML progression and prolonged survival in a majority of mice, but this treatment wasn’t curative.
However, a month of treatment with c-Fos and Dusp1 inhibitors as well as imatinib cured about 90% of mice with CML, and there were no signs of MRD.
The researchers also found that simply deleting c-Fos and Dusp1 was sufficient to block the development of B-cell ALL in mice.
The team said they are following up this study by testing c-Fos and Dusp1 as treatment targets for different kinase-fueled cancers. ![]()
Researchers say they have identified 2 signaling proteins that enable resistance to tyrosine kinase inhibitors (TKIs) and could be therapeutic targets for acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML).
The team found that by deleting these proteins—c-Fos and Dusp1—they could eradicate BCR-ABL-induced B-cell ALL in mice.
And treatment combining c-Fos and Dusp1 inhibitors with the TKI imatinib was able to cure mice with BCR-ABL-driven CML.
The researchers reported these findings in Nature Medicine.
“We think that, within the next 5 years, our data will change the way people think about cancer development and targeted therapy,” said study author Mohammad Azam, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This study identifies a potential Achilles’ heel of kinase-driven cancers, and what we propose is intended to be curative, not just treatment.”
The potential Achilles’ heel is a common point of passage in cells—a signaling node—that appears to be required to generate cancer cells. The node is formed by the signaling proteins c-Fos and Dusp1, according to the researchers.
The team identified c-Fos and Dusp1 by conducting global gene-expression analysis of mouse leukemia cells and human CML cells. Analysis of the human cells revealed extremely high levels of c-FOS and DUSP1 in BCR-ABL-positive, TKI-resistant cells.
Dr Azam and his colleagues found that signaling from tyrosine kinase and growth factor proteins that support cell expansion (such as IL-3 and IL-6) converge to elevate c-Fos and Dusp1 levels in leukemia cells.
Working together, these molecules maintain the survival of leukemia stem cells (LSCs), which translates to minimal residual disease (MRD) after treatment.
Dr Azam said Dusp1 and c-Fos support the survival of LSCs by increasing the toxic threshold needed to kill them. This means imatinib and other TKIs cannot eliminate the residual LSCs.
After describing the roles of c-Fos and Dusp1, Dr Azam and his colleagues put their ideas to the test in mouse models of CML.
The team tested several treatments in these mice, including:
- monotherapy with imatinib
- inhibitors of c-Fos and Dusp1
- treatment with imatinib and inhibitors of c-Fos and Dusp1.
As suspected, treatment with imatinib alone initially stopped CML progression, but mice ultimately relapsed.
Treatment with c-Fos and Dusp1 inhibitors significantly slowed CML progression and prolonged survival in a majority of mice, but this treatment wasn’t curative.
However, a month of treatment with c-Fos and Dusp1 inhibitors as well as imatinib cured about 90% of mice with CML, and there were no signs of MRD.
The researchers also found that simply deleting c-Fos and Dusp1 was sufficient to block the development of B-cell ALL in mice.
The team said they are following up this study by testing c-Fos and Dusp1 as treatment targets for different kinase-fueled cancers. ![]()
Researchers say they have identified 2 signaling proteins that enable resistance to tyrosine kinase inhibitors (TKIs) and could be therapeutic targets for acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML).
The team found that by deleting these proteins—c-Fos and Dusp1—they could eradicate BCR-ABL-induced B-cell ALL in mice.
And treatment combining c-Fos and Dusp1 inhibitors with the TKI imatinib was able to cure mice with BCR-ABL-driven CML.
The researchers reported these findings in Nature Medicine.
“We think that, within the next 5 years, our data will change the way people think about cancer development and targeted therapy,” said study author Mohammad Azam, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This study identifies a potential Achilles’ heel of kinase-driven cancers, and what we propose is intended to be curative, not just treatment.”
The potential Achilles’ heel is a common point of passage in cells—a signaling node—that appears to be required to generate cancer cells. The node is formed by the signaling proteins c-Fos and Dusp1, according to the researchers.
The team identified c-Fos and Dusp1 by conducting global gene-expression analysis of mouse leukemia cells and human CML cells. Analysis of the human cells revealed extremely high levels of c-FOS and DUSP1 in BCR-ABL-positive, TKI-resistant cells.
Dr Azam and his colleagues found that signaling from tyrosine kinase and growth factor proteins that support cell expansion (such as IL-3 and IL-6) converge to elevate c-Fos and Dusp1 levels in leukemia cells.
Working together, these molecules maintain the survival of leukemia stem cells (LSCs), which translates to minimal residual disease (MRD) after treatment.
Dr Azam said Dusp1 and c-Fos support the survival of LSCs by increasing the toxic threshold needed to kill them. This means imatinib and other TKIs cannot eliminate the residual LSCs.
After describing the roles of c-Fos and Dusp1, Dr Azam and his colleagues put their ideas to the test in mouse models of CML.
The team tested several treatments in these mice, including:
- monotherapy with imatinib
- inhibitors of c-Fos and Dusp1
- treatment with imatinib and inhibitors of c-Fos and Dusp1.
As suspected, treatment with imatinib alone initially stopped CML progression, but mice ultimately relapsed.
Treatment with c-Fos and Dusp1 inhibitors significantly slowed CML progression and prolonged survival in a majority of mice, but this treatment wasn’t curative.
However, a month of treatment with c-Fos and Dusp1 inhibitors as well as imatinib cured about 90% of mice with CML, and there were no signs of MRD.
The researchers also found that simply deleting c-Fos and Dusp1 was sufficient to block the development of B-cell ALL in mice.
The team said they are following up this study by testing c-Fos and Dusp1 as treatment targets for different kinase-fueled cancers. ![]()