User login
Patient and physician outreach boost CRC screening rates
Can outreach improve the globally low rates of adherence to colorectal cancer screening? Yes, according to two recent studies in JAMA; the studies found that both patient-focused and physician-focused outreach approaches can result in significantly better patient participation in colorectal cancer (CRC) screening.
The first study (JAMA. 2017;318[9]:806-15) compared a colonoscopy outreach program and a fecal immunochemical test (FIT) outreach program both with each other and with usual care. The results of the pragmatic, single-site, randomized, clinical trial showed that completed screenings were higher for both outreach groups, compared with the usual care group.
The primary outcome measure of the study was completion of the screening process, wrote Amit Singal, MD, and his coauthors. This was defined as any adherence to colonoscopy completion, the completion of annual testing for patients who had a normal FIT test, or treatment evaluation if CRC was detected during the screening process. Screenings were considered complete even if, for example, a patient in the colonoscopy arm eventually went on to have three consecutive annual FIT tests rather than a colonoscopy.
A total of 5,999 patients eligible for screening were initially randomized to one of the three study arms. Across all study arms, approximately half were lost to follow-up. These patients were excluded from the primary analysis but were included in an additional intention-to-screen analysis. A total of 2,400 patients received a colonoscopy outreach mailing; 2,400 received FIT outreach, including a letter, the home FIT testing kit and instructions; 1,199 received usual care. Patients in both intervention arms also received up to two phone calls if they didn’t respond to the initial mailing within 2 weeks. Mailings and phone calls were conducted in English or Spanish, according to the patients’ stated language preferences (those whose spoke neither language were excluded from the study).
Of the patients in the colonoscopy outreach group, 922 (38.4%) completed the screening process, compared with 671 (28.0%) in the FIT outreach group and 128 (10.7%) in the usual care group.
Compared with the group receiving usual care, completion of the screening process was 27.7% higher in the colonoscopy outreach group and 17.3% higher in the FIT outreach group. Screening process completion was 10.4% higher for the colonoscopy outreach group, compared with the FIT outreach group (P less than .001 for all).
Dr. Singal, who is with the department of internal medicine at UT Southwestern Medical Center, Dallas, and his colleagues also performed several post-hoc secondary analyses. In one, they used a less-stringent definition of screening process completion in which biennial FIT testing was considered satisfactory. When this definition was applied, the colonoscopy outreach group had 0.5% lower screening process completion than the FIT outreach group. The chances of a patient receiving any screening during the study period was highest in the FIT group (65%), with 51.7% of those in the colonoscopy outreach group and 39% of those in the usual care group receiving any screening.
“FIT has lower barriers to one-time participation but requires annual screening and diagnostic evaluation of abnormal results,” wrote Dr. Singal and his colleagues.
Strengths of the study, said Dr. Singal and his colleagues, included the fact that the study took place at a “safety net” institution with a racially and socioeconomically diverse population. Also, the study design avoided volunteer bias, and offered a pragmatic head-to-head comparison of colonoscopy and FIT.
The second study took place in western France, and targeted outreach to physicians rather than patients (JAMA. 2017;318[9];816-84). When physicians were given a list of their own patients who were not up to date on CRC screening, investigators saw a small, but significant, uptick in patient participation in FIT screening.
One year after the reminders went out, FIT screening had been initiated in 24.8% of patients whose physicians had received the list, compared with 21.7% of patients of physicians who had received a more generic notice and 20.6% of patients whose physicians received no notification, according to first author Cedric Rat, MD, and his colleagues.
The study examined which notification approach was most effective in increasing FIT screening among the physicians’ patient panels: sending general practitioners (GPs) letters that included a list of their own patients who had not undergone CRC screening, or sending them generic letters describing CRC screening adherence rates specific to their region. A usual care group of practices received no notifications in this 3-group randomized cluster design.
Patients in the patient-specific reminders group had an odds ratio of 1.27 for participation in FIT screening (P less than .001) compared to the usual care group. The odds ratio for the generic reminders group was 1.09, a nonsignificant difference.
Between-group comparison showed statistical significance for both the 3.1% difference between the patient-specific and generic reminders groups, and for the 4.2% difference between the patient-specific and usual care groups (P less than .001 for both). There was no significant difference between the generic reminders group and the usual care group.
Dr. Rat, professor of medicine at the Faculty of Medicine, Nantes, France, and his colleagues enrolled GPs in a total of 801 practices that included patients aged 50participating GPs caring for 33,044 patients who met study criteria.
Physician characteristics that were associated with higher FIT participation included younger age and an initially smaller number of unscreened patients. Patients with low socioeconomic status and those with a higher chronic disease burden were less likely to participate in FIT screening.
Also, Dr. Rat and his colleagues noted that the busiest practices actually had higher CRC screening rates. The investigators hypothesized that a recent physician pay-for-performance grant for CRC completion might be more appealing for some busy physicians.
This was the largest study of CRC screening participation to date, according to Dr. Rat and his coauthors, and showed the small but detectable efficacy of an inexpensive intervention that, given complete patient records, is relatively easy to effect. Though the effect size was smaller than the 12% difference the investigators had anticipated seeing for the patient-specific reminders group, the study still showed that targeting physicians can be an effective public health intervention to increase CRC screening rates, said Dr. Rat and his colleagues.
None of the investigators in either study reported conflicts of interest.
Both studies, though they used different outreach interventions, highlight the same problem: the need to identify and execute effective colorectal cancer (CRC) screening programs. Effective screening has great lifesaving potential; if screening rates were elevated to greater than 80% in the United States, an estimated 200,000 deaths would be prevented within the next 2 decades.
The nature of CRC screening options means that a home fecal sample collection is inexpensive, and will result in an initial higher screening rate; however, complete screening via fecal occult blood testing requires annual repeats of negative tests, and patients with positive fecal occult blood tests still need colonoscopy.
Colonoscopy, although it’s burdensome for patients and perhaps cost prohibitive for those without health insurance, offers a one-time test that, if negative, provides patients with a 10-year window of screening coverage.
Any effective programs to increase CRC screening rates will need to use a systems change approach, with creative interventions that take patient education, and even delivery of preventive health services, out of the context of the already too-full office visit.
Staff supports, such as the follow-up telephone calls used in the patient-targeted intervention, are key to effective interventions, especially for vulnerable populations. Additionally, institutions must ensure that they have adequate physical and staff resources to support the increased screening they are seeking to achieve.
Dr. Michael Pignone is a professor of medicine at the University of Texas at Austin. Dr. David Miller is a professor of internal medicine, Wake Forest University, Winston-Salem, N.C. Dr. Pignone is a medical director for Healthwise; Dr. Miller reported no relevant conflicts of interest These remarks were drawn from an editorial accompanying the two clinical trials.
Both studies, though they used different outreach interventions, highlight the same problem: the need to identify and execute effective colorectal cancer (CRC) screening programs. Effective screening has great lifesaving potential; if screening rates were elevated to greater than 80% in the United States, an estimated 200,000 deaths would be prevented within the next 2 decades.
The nature of CRC screening options means that a home fecal sample collection is inexpensive, and will result in an initial higher screening rate; however, complete screening via fecal occult blood testing requires annual repeats of negative tests, and patients with positive fecal occult blood tests still need colonoscopy.
Colonoscopy, although it’s burdensome for patients and perhaps cost prohibitive for those without health insurance, offers a one-time test that, if negative, provides patients with a 10-year window of screening coverage.
Any effective programs to increase CRC screening rates will need to use a systems change approach, with creative interventions that take patient education, and even delivery of preventive health services, out of the context of the already too-full office visit.
Staff supports, such as the follow-up telephone calls used in the patient-targeted intervention, are key to effective interventions, especially for vulnerable populations. Additionally, institutions must ensure that they have adequate physical and staff resources to support the increased screening they are seeking to achieve.
Dr. Michael Pignone is a professor of medicine at the University of Texas at Austin. Dr. David Miller is a professor of internal medicine, Wake Forest University, Winston-Salem, N.C. Dr. Pignone is a medical director for Healthwise; Dr. Miller reported no relevant conflicts of interest These remarks were drawn from an editorial accompanying the two clinical trials.
Both studies, though they used different outreach interventions, highlight the same problem: the need to identify and execute effective colorectal cancer (CRC) screening programs. Effective screening has great lifesaving potential; if screening rates were elevated to greater than 80% in the United States, an estimated 200,000 deaths would be prevented within the next 2 decades.
The nature of CRC screening options means that a home fecal sample collection is inexpensive, and will result in an initial higher screening rate; however, complete screening via fecal occult blood testing requires annual repeats of negative tests, and patients with positive fecal occult blood tests still need colonoscopy.
Colonoscopy, although it’s burdensome for patients and perhaps cost prohibitive for those without health insurance, offers a one-time test that, if negative, provides patients with a 10-year window of screening coverage.
Any effective programs to increase CRC screening rates will need to use a systems change approach, with creative interventions that take patient education, and even delivery of preventive health services, out of the context of the already too-full office visit.
Staff supports, such as the follow-up telephone calls used in the patient-targeted intervention, are key to effective interventions, especially for vulnerable populations. Additionally, institutions must ensure that they have adequate physical and staff resources to support the increased screening they are seeking to achieve.
Dr. Michael Pignone is a professor of medicine at the University of Texas at Austin. Dr. David Miller is a professor of internal medicine, Wake Forest University, Winston-Salem, N.C. Dr. Pignone is a medical director for Healthwise; Dr. Miller reported no relevant conflicts of interest These remarks were drawn from an editorial accompanying the two clinical trials.
Can outreach improve the globally low rates of adherence to colorectal cancer screening? Yes, according to two recent studies in JAMA; the studies found that both patient-focused and physician-focused outreach approaches can result in significantly better patient participation in colorectal cancer (CRC) screening.
The first study (JAMA. 2017;318[9]:806-15) compared a colonoscopy outreach program and a fecal immunochemical test (FIT) outreach program both with each other and with usual care. The results of the pragmatic, single-site, randomized, clinical trial showed that completed screenings were higher for both outreach groups, compared with the usual care group.
The primary outcome measure of the study was completion of the screening process, wrote Amit Singal, MD, and his coauthors. This was defined as any adherence to colonoscopy completion, the completion of annual testing for patients who had a normal FIT test, or treatment evaluation if CRC was detected during the screening process. Screenings were considered complete even if, for example, a patient in the colonoscopy arm eventually went on to have three consecutive annual FIT tests rather than a colonoscopy.
A total of 5,999 patients eligible for screening were initially randomized to one of the three study arms. Across all study arms, approximately half were lost to follow-up. These patients were excluded from the primary analysis but were included in an additional intention-to-screen analysis. A total of 2,400 patients received a colonoscopy outreach mailing; 2,400 received FIT outreach, including a letter, the home FIT testing kit and instructions; 1,199 received usual care. Patients in both intervention arms also received up to two phone calls if they didn’t respond to the initial mailing within 2 weeks. Mailings and phone calls were conducted in English or Spanish, according to the patients’ stated language preferences (those whose spoke neither language were excluded from the study).
Of the patients in the colonoscopy outreach group, 922 (38.4%) completed the screening process, compared with 671 (28.0%) in the FIT outreach group and 128 (10.7%) in the usual care group.
Compared with the group receiving usual care, completion of the screening process was 27.7% higher in the colonoscopy outreach group and 17.3% higher in the FIT outreach group. Screening process completion was 10.4% higher for the colonoscopy outreach group, compared with the FIT outreach group (P less than .001 for all).
Dr. Singal, who is with the department of internal medicine at UT Southwestern Medical Center, Dallas, and his colleagues also performed several post-hoc secondary analyses. In one, they used a less-stringent definition of screening process completion in which biennial FIT testing was considered satisfactory. When this definition was applied, the colonoscopy outreach group had 0.5% lower screening process completion than the FIT outreach group. The chances of a patient receiving any screening during the study period was highest in the FIT group (65%), with 51.7% of those in the colonoscopy outreach group and 39% of those in the usual care group receiving any screening.
“FIT has lower barriers to one-time participation but requires annual screening and diagnostic evaluation of abnormal results,” wrote Dr. Singal and his colleagues.
Strengths of the study, said Dr. Singal and his colleagues, included the fact that the study took place at a “safety net” institution with a racially and socioeconomically diverse population. Also, the study design avoided volunteer bias, and offered a pragmatic head-to-head comparison of colonoscopy and FIT.
The second study took place in western France, and targeted outreach to physicians rather than patients (JAMA. 2017;318[9];816-84). When physicians were given a list of their own patients who were not up to date on CRC screening, investigators saw a small, but significant, uptick in patient participation in FIT screening.
One year after the reminders went out, FIT screening had been initiated in 24.8% of patients whose physicians had received the list, compared with 21.7% of patients of physicians who had received a more generic notice and 20.6% of patients whose physicians received no notification, according to first author Cedric Rat, MD, and his colleagues.
The study examined which notification approach was most effective in increasing FIT screening among the physicians’ patient panels: sending general practitioners (GPs) letters that included a list of their own patients who had not undergone CRC screening, or sending them generic letters describing CRC screening adherence rates specific to their region. A usual care group of practices received no notifications in this 3-group randomized cluster design.
Patients in the patient-specific reminders group had an odds ratio of 1.27 for participation in FIT screening (P less than .001) compared to the usual care group. The odds ratio for the generic reminders group was 1.09, a nonsignificant difference.
Between-group comparison showed statistical significance for both the 3.1% difference between the patient-specific and generic reminders groups, and for the 4.2% difference between the patient-specific and usual care groups (P less than .001 for both). There was no significant difference between the generic reminders group and the usual care group.
Dr. Rat, professor of medicine at the Faculty of Medicine, Nantes, France, and his colleagues enrolled GPs in a total of 801 practices that included patients aged 50participating GPs caring for 33,044 patients who met study criteria.
Physician characteristics that were associated with higher FIT participation included younger age and an initially smaller number of unscreened patients. Patients with low socioeconomic status and those with a higher chronic disease burden were less likely to participate in FIT screening.
Also, Dr. Rat and his colleagues noted that the busiest practices actually had higher CRC screening rates. The investigators hypothesized that a recent physician pay-for-performance grant for CRC completion might be more appealing for some busy physicians.
This was the largest study of CRC screening participation to date, according to Dr. Rat and his coauthors, and showed the small but detectable efficacy of an inexpensive intervention that, given complete patient records, is relatively easy to effect. Though the effect size was smaller than the 12% difference the investigators had anticipated seeing for the patient-specific reminders group, the study still showed that targeting physicians can be an effective public health intervention to increase CRC screening rates, said Dr. Rat and his colleagues.
None of the investigators in either study reported conflicts of interest.
Can outreach improve the globally low rates of adherence to colorectal cancer screening? Yes, according to two recent studies in JAMA; the studies found that both patient-focused and physician-focused outreach approaches can result in significantly better patient participation in colorectal cancer (CRC) screening.
The first study (JAMA. 2017;318[9]:806-15) compared a colonoscopy outreach program and a fecal immunochemical test (FIT) outreach program both with each other and with usual care. The results of the pragmatic, single-site, randomized, clinical trial showed that completed screenings were higher for both outreach groups, compared with the usual care group.
The primary outcome measure of the study was completion of the screening process, wrote Amit Singal, MD, and his coauthors. This was defined as any adherence to colonoscopy completion, the completion of annual testing for patients who had a normal FIT test, or treatment evaluation if CRC was detected during the screening process. Screenings were considered complete even if, for example, a patient in the colonoscopy arm eventually went on to have three consecutive annual FIT tests rather than a colonoscopy.
A total of 5,999 patients eligible for screening were initially randomized to one of the three study arms. Across all study arms, approximately half were lost to follow-up. These patients were excluded from the primary analysis but were included in an additional intention-to-screen analysis. A total of 2,400 patients received a colonoscopy outreach mailing; 2,400 received FIT outreach, including a letter, the home FIT testing kit and instructions; 1,199 received usual care. Patients in both intervention arms also received up to two phone calls if they didn’t respond to the initial mailing within 2 weeks. Mailings and phone calls were conducted in English or Spanish, according to the patients’ stated language preferences (those whose spoke neither language were excluded from the study).
Of the patients in the colonoscopy outreach group, 922 (38.4%) completed the screening process, compared with 671 (28.0%) in the FIT outreach group and 128 (10.7%) in the usual care group.
Compared with the group receiving usual care, completion of the screening process was 27.7% higher in the colonoscopy outreach group and 17.3% higher in the FIT outreach group. Screening process completion was 10.4% higher for the colonoscopy outreach group, compared with the FIT outreach group (P less than .001 for all).
Dr. Singal, who is with the department of internal medicine at UT Southwestern Medical Center, Dallas, and his colleagues also performed several post-hoc secondary analyses. In one, they used a less-stringent definition of screening process completion in which biennial FIT testing was considered satisfactory. When this definition was applied, the colonoscopy outreach group had 0.5% lower screening process completion than the FIT outreach group. The chances of a patient receiving any screening during the study period was highest in the FIT group (65%), with 51.7% of those in the colonoscopy outreach group and 39% of those in the usual care group receiving any screening.
“FIT has lower barriers to one-time participation but requires annual screening and diagnostic evaluation of abnormal results,” wrote Dr. Singal and his colleagues.
Strengths of the study, said Dr. Singal and his colleagues, included the fact that the study took place at a “safety net” institution with a racially and socioeconomically diverse population. Also, the study design avoided volunteer bias, and offered a pragmatic head-to-head comparison of colonoscopy and FIT.
The second study took place in western France, and targeted outreach to physicians rather than patients (JAMA. 2017;318[9];816-84). When physicians were given a list of their own patients who were not up to date on CRC screening, investigators saw a small, but significant, uptick in patient participation in FIT screening.
One year after the reminders went out, FIT screening had been initiated in 24.8% of patients whose physicians had received the list, compared with 21.7% of patients of physicians who had received a more generic notice and 20.6% of patients whose physicians received no notification, according to first author Cedric Rat, MD, and his colleagues.
The study examined which notification approach was most effective in increasing FIT screening among the physicians’ patient panels: sending general practitioners (GPs) letters that included a list of their own patients who had not undergone CRC screening, or sending them generic letters describing CRC screening adherence rates specific to their region. A usual care group of practices received no notifications in this 3-group randomized cluster design.
Patients in the patient-specific reminders group had an odds ratio of 1.27 for participation in FIT screening (P less than .001) compared to the usual care group. The odds ratio for the generic reminders group was 1.09, a nonsignificant difference.
Between-group comparison showed statistical significance for both the 3.1% difference between the patient-specific and generic reminders groups, and for the 4.2% difference between the patient-specific and usual care groups (P less than .001 for both). There was no significant difference between the generic reminders group and the usual care group.
Dr. Rat, professor of medicine at the Faculty of Medicine, Nantes, France, and his colleagues enrolled GPs in a total of 801 practices that included patients aged 50participating GPs caring for 33,044 patients who met study criteria.
Physician characteristics that were associated with higher FIT participation included younger age and an initially smaller number of unscreened patients. Patients with low socioeconomic status and those with a higher chronic disease burden were less likely to participate in FIT screening.
Also, Dr. Rat and his colleagues noted that the busiest practices actually had higher CRC screening rates. The investigators hypothesized that a recent physician pay-for-performance grant for CRC completion might be more appealing for some busy physicians.
This was the largest study of CRC screening participation to date, according to Dr. Rat and his coauthors, and showed the small but detectable efficacy of an inexpensive intervention that, given complete patient records, is relatively easy to effect. Though the effect size was smaller than the 12% difference the investigators had anticipated seeing for the patient-specific reminders group, the study still showed that targeting physicians can be an effective public health intervention to increase CRC screening rates, said Dr. Rat and his colleagues.
None of the investigators in either study reported conflicts of interest.
FROM JAMA
Key clinical point: Both a physician-directed outreach effort and one that targeted patients increased CRC screening rates.
Major finding: The patient-directed effort increased CRC screening completion by 17%-28%, compared with usual care; a single physician-directed outreach intervention increased screening by 4.2% compared to usual care.
Study details: A single-center pragmatic study of 5,999 patients eligible for CRC screening, and a three-group randomized cluster study of 1,446 general practitioners caring for 33,044 patients eligible for CRC screening.
Disclosures: No study authors reported conflicts of interest.
Keeping Up-to-Date on Health Disparity Data
The DATA2020 HealthyPeople.gov data search function just got more user friendly. The Office of Disease Prevention and Health Promotion, National Center for Health Statistics, and Office of Minority Health, partners in DATA2020, have released a shareable widget that gives users easy access to regularly updated information.
The health disparities tool at DATA2020 lets users sort and view health disparities by demographic groups, including race/ethnicity, age, disability status, and geographic location. Users also can easily navigate and visualize data and changes in disparities over time; compare data points for each population group; and see all rates, rate ratios, confidence intervals and other technical details about data collection.
The new widget is an easy way (by simply copying the provided code) to share health disparities information on individual websites. Users can browse by disparity type or by Leading Health Indicator. The widget needs no maintenance; content updates automatically.
The DATA2020 HealthyPeople.gov data search function just got more user friendly. The Office of Disease Prevention and Health Promotion, National Center for Health Statistics, and Office of Minority Health, partners in DATA2020, have released a shareable widget that gives users easy access to regularly updated information.
The health disparities tool at DATA2020 lets users sort and view health disparities by demographic groups, including race/ethnicity, age, disability status, and geographic location. Users also can easily navigate and visualize data and changes in disparities over time; compare data points for each population group; and see all rates, rate ratios, confidence intervals and other technical details about data collection.
The new widget is an easy way (by simply copying the provided code) to share health disparities information on individual websites. Users can browse by disparity type or by Leading Health Indicator. The widget needs no maintenance; content updates automatically.
The DATA2020 HealthyPeople.gov data search function just got more user friendly. The Office of Disease Prevention and Health Promotion, National Center for Health Statistics, and Office of Minority Health, partners in DATA2020, have released a shareable widget that gives users easy access to regularly updated information.
The health disparities tool at DATA2020 lets users sort and view health disparities by demographic groups, including race/ethnicity, age, disability status, and geographic location. Users also can easily navigate and visualize data and changes in disparities over time; compare data points for each population group; and see all rates, rate ratios, confidence intervals and other technical details about data collection.
The new widget is an easy way (by simply copying the provided code) to share health disparities information on individual websites. Users can browse by disparity type or by Leading Health Indicator. The widget needs no maintenance; content updates automatically.
R&D costs for cancer drugs may be lower than previously thought
New research has provided an updated estimate of the spending needed to bring a cancer drug to the US market.
In analyzing data from 10 companies bringing a cancer drug to market, researchers found that sales revenue from these drugs was roughly 7 times higher than the research and development (R&D) costs.
The total sales revenue for the drugs—during a median follow-up of 4 years—was $67.0 billion, and the total R&D spending was $9.1 billion (including 7% opportunity costs).
Researchers reported these figures in JAMA Internal Medicine.
“[T]he price of cancer drugs is currently rising higher and higher each year,” said study author Vinay Prasad, MD, of Oregon Health and Science University in Portland.
“The cost of 1 drug for 1 year of treatment is now routinely in excess of $100,000 . . . . One of the often-cited reasons why cancer drugs cost so much—one of the justifications for the high price—is that the outlay by the biopharmaceutical industry to bring these drugs to market is sizable, and there have been a wide range of estimates for what that R&D outlay is.”
“The most-cited estimate is one that comes out of the Tufts Medical Group1 that puts the cost to bring a cancer drug to market, when adjusted for 2017 dollars, at $2.7 billion. Another estimate is from the group Public Citizen.2 And that is a much lower estimate, finding the cost to bring a drug to market of $320 million.”
“Both of these estimates have limitations in the methods for how they estimated the cost to bring a drug to market. Notably, the Tufts group is rather non-transparent. Because of confidentiality agreements, we don’t know what drugs and what companies they’re looking at, and we can’t independently verify their analysis.”
“The Public Citizen group, in contrast, is comparing expenditures over a period of time against the number of drugs in a different period of time to make an estimate of the cost to bring a drug to market, but this isn’t exactly the cost of bringing those particular drugs to market.”
These issues prompted Dr Prasad and Sham Mailankody, MBBS, of the Memorial Sloan Kettering Cancer Center in New York, to conduct the current study.
Analysis
The researchers analyzed US Securities and Exchange Commission filings for 10 drug companies that received approval from the US Food and Drug Administration for a cancer drug from 2006 through 2015.
Prior to this, none of the companies had any drugs approved for use in the US. However, the companies had a median of 3.5 (range, 2-11) drugs in development during the study period.
The researchers said the fact that these companies had no prior drug approvals eliminated biases that may be present when analyzing larger drug companies, such as redundancies in R&D development and tax incentives for listing different endeavors as R&D spending.
In addition, the fact that the 10 companies were developing other drugs during the study period means this study takes into account the cost of failure in bringing a drug to market.
Results
For the 10 companies and drugs analyzed, the median duration of drug development was 7.3 years (range, 5.8 to 15.2 years).
The median cost of drug development (in 2017 US dollars) was $648.0 million (range, $157.3 to $1950.8 million). For a 7% per annum cost of capital (or opportunity costs), the median cost was $757.4 million (range, $203.6 to $2601.7 million).
The median time from approval to analysis in December 2016 (or until the company sold or licensed the compound to another company) was 4.0 years (range, 0.8 years to 8.8 years).
The total revenue from sales of the 10 drugs during this time was $67.0 billion.
The total R&D spending was $7.2 billion, or $9.1 billion when including 7% opportunity costs.
The following table includes data broken down by drug.
| Drug and company | Approval date | Indication | Total R&D costs | Revenue since approval |
|---|---|---|---|---|
| Eculizumab (Soliris)
Alexion Pharmaceuticals |
2007 | Paroxysmal nocturnal hemoglobinuria | $817.6 million | $12,987.8 million |
| Pralatrexate (Folotyn)*
Allos Therapeutics |
2009 | Relapsed/refractory peripheral T-cell lymphoma | $178.2 million | $304.8 million |
| Brentuximab vedotin (Adcetris)*
Seattle Genetics |
2011 | Certain patients with Hodgkin lymphoma and systemic anaplastic large cell lymphoma | $899.2 million | $1034.3 million |
| Ruxolitinib (Jakafi)
Incyte Corporation |
2011 | Intermediate- and high-risk myelofibrosis | $1097.8 million | $2251.5 million |
| Enzalutamide (Xtandi)**
Medivation |
2012 | Metastatic castration-resistant prostate cancer | $473.3 million | $21,068.3 million |
| Vincristine liposome (Marqibo)*
Talon Therapeutics |
2012 | Ph- acute lymphoblastic leukemia | $157.3 million | $204.1 million |
| Cabozantinib (Cometriq)
Exelixis |
2012 | Metastatic medullary thyroid cancer | $1950.8 million | $341.9 million |
| Ponatinib (Iclusig)*
Ariad Pharmaceuticals |
2012 | Chronic myeloid leukemia and Ph+ acute lymphoblastic leukemia
|
$480.1 million | $5457.98 million |
| Ibrutinib (Imbruvica)*
Pharmacyclics |
2013 | Previously treated mantle cell lymphoma | $328.1 million | $22,275.0 million |
| Irinotecan liposome (Onivyde)
Merrimack Pharmaceuticals |
2015 | Advanced pancreatic cancer previously treated with gemcitabine-based chemotherapy | $815.8 million | $1065.2 million |
*Received accelerated approval. (The other 5 drugs received regular approval.)
**Did not receive orphan designation. (Nine of the 10 drugs received orphan designation.)
“So I think what we’re showing is . . . a transparent analysis of cancer drugs and companies, looking at the cost to bring a drug to market,” Dr Mailankody said. “And our estimate of $648 million is substantially lower than the often-cited number of $2.7 billion.”
“We’re also showing that, for these 10 drugs, revenue since approval is quite a bit higher than the R&D spending, almost 7-fold higher, and some of these companies have already had revenue of 10-fold or higher, compared to the R&D expenses.”
The researchers acknowledged that this study is limited by a small data set and the fact that the findings cannot be extrapolated to other types of drugs. ![]()
1. DiMasi JA et al. Innovation in the pharmaceutical industry: new estimates of R&D costs. J Health Econ. 2016;47:20-33.
2. Young B et al. Rx R&D Myths: The Case Against the Drug Industry’s R&D “Scare Card.” Washington, DC: Public Citizen’s Congress Watch; 2001. https://www.citizen.org/sites/default/files/rdmyths.pdf.
New research has provided an updated estimate of the spending needed to bring a cancer drug to the US market.
In analyzing data from 10 companies bringing a cancer drug to market, researchers found that sales revenue from these drugs was roughly 7 times higher than the research and development (R&D) costs.
The total sales revenue for the drugs—during a median follow-up of 4 years—was $67.0 billion, and the total R&D spending was $9.1 billion (including 7% opportunity costs).
Researchers reported these figures in JAMA Internal Medicine.
“[T]he price of cancer drugs is currently rising higher and higher each year,” said study author Vinay Prasad, MD, of Oregon Health and Science University in Portland.
“The cost of 1 drug for 1 year of treatment is now routinely in excess of $100,000 . . . . One of the often-cited reasons why cancer drugs cost so much—one of the justifications for the high price—is that the outlay by the biopharmaceutical industry to bring these drugs to market is sizable, and there have been a wide range of estimates for what that R&D outlay is.”
“The most-cited estimate is one that comes out of the Tufts Medical Group1 that puts the cost to bring a cancer drug to market, when adjusted for 2017 dollars, at $2.7 billion. Another estimate is from the group Public Citizen.2 And that is a much lower estimate, finding the cost to bring a drug to market of $320 million.”
“Both of these estimates have limitations in the methods for how they estimated the cost to bring a drug to market. Notably, the Tufts group is rather non-transparent. Because of confidentiality agreements, we don’t know what drugs and what companies they’re looking at, and we can’t independently verify their analysis.”
“The Public Citizen group, in contrast, is comparing expenditures over a period of time against the number of drugs in a different period of time to make an estimate of the cost to bring a drug to market, but this isn’t exactly the cost of bringing those particular drugs to market.”
These issues prompted Dr Prasad and Sham Mailankody, MBBS, of the Memorial Sloan Kettering Cancer Center in New York, to conduct the current study.
Analysis
The researchers analyzed US Securities and Exchange Commission filings for 10 drug companies that received approval from the US Food and Drug Administration for a cancer drug from 2006 through 2015.
Prior to this, none of the companies had any drugs approved for use in the US. However, the companies had a median of 3.5 (range, 2-11) drugs in development during the study period.
The researchers said the fact that these companies had no prior drug approvals eliminated biases that may be present when analyzing larger drug companies, such as redundancies in R&D development and tax incentives for listing different endeavors as R&D spending.
In addition, the fact that the 10 companies were developing other drugs during the study period means this study takes into account the cost of failure in bringing a drug to market.
Results
For the 10 companies and drugs analyzed, the median duration of drug development was 7.3 years (range, 5.8 to 15.2 years).
The median cost of drug development (in 2017 US dollars) was $648.0 million (range, $157.3 to $1950.8 million). For a 7% per annum cost of capital (or opportunity costs), the median cost was $757.4 million (range, $203.6 to $2601.7 million).
The median time from approval to analysis in December 2016 (or until the company sold or licensed the compound to another company) was 4.0 years (range, 0.8 years to 8.8 years).
The total revenue from sales of the 10 drugs during this time was $67.0 billion.
The total R&D spending was $7.2 billion, or $9.1 billion when including 7% opportunity costs.
The following table includes data broken down by drug.
| Drug and company | Approval date | Indication | Total R&D costs | Revenue since approval |
|---|---|---|---|---|
| Eculizumab (Soliris)
Alexion Pharmaceuticals |
2007 | Paroxysmal nocturnal hemoglobinuria | $817.6 million | $12,987.8 million |
| Pralatrexate (Folotyn)*
Allos Therapeutics |
2009 | Relapsed/refractory peripheral T-cell lymphoma | $178.2 million | $304.8 million |
| Brentuximab vedotin (Adcetris)*
Seattle Genetics |
2011 | Certain patients with Hodgkin lymphoma and systemic anaplastic large cell lymphoma | $899.2 million | $1034.3 million |
| Ruxolitinib (Jakafi)
Incyte Corporation |
2011 | Intermediate- and high-risk myelofibrosis | $1097.8 million | $2251.5 million |
| Enzalutamide (Xtandi)**
Medivation |
2012 | Metastatic castration-resistant prostate cancer | $473.3 million | $21,068.3 million |
| Vincristine liposome (Marqibo)*
Talon Therapeutics |
2012 | Ph- acute lymphoblastic leukemia | $157.3 million | $204.1 million |
| Cabozantinib (Cometriq)
Exelixis |
2012 | Metastatic medullary thyroid cancer | $1950.8 million | $341.9 million |
| Ponatinib (Iclusig)*
Ariad Pharmaceuticals |
2012 | Chronic myeloid leukemia and Ph+ acute lymphoblastic leukemia
|
$480.1 million | $5457.98 million |
| Ibrutinib (Imbruvica)*
Pharmacyclics |
2013 | Previously treated mantle cell lymphoma | $328.1 million | $22,275.0 million |
| Irinotecan liposome (Onivyde)
Merrimack Pharmaceuticals |
2015 | Advanced pancreatic cancer previously treated with gemcitabine-based chemotherapy | $815.8 million | $1065.2 million |
*Received accelerated approval. (The other 5 drugs received regular approval.)
**Did not receive orphan designation. (Nine of the 10 drugs received orphan designation.)
“So I think what we’re showing is . . . a transparent analysis of cancer drugs and companies, looking at the cost to bring a drug to market,” Dr Mailankody said. “And our estimate of $648 million is substantially lower than the often-cited number of $2.7 billion.”
“We’re also showing that, for these 10 drugs, revenue since approval is quite a bit higher than the R&D spending, almost 7-fold higher, and some of these companies have already had revenue of 10-fold or higher, compared to the R&D expenses.”
The researchers acknowledged that this study is limited by a small data set and the fact that the findings cannot be extrapolated to other types of drugs. ![]()
1. DiMasi JA et al. Innovation in the pharmaceutical industry: new estimates of R&D costs. J Health Econ. 2016;47:20-33.
2. Young B et al. Rx R&D Myths: The Case Against the Drug Industry’s R&D “Scare Card.” Washington, DC: Public Citizen’s Congress Watch; 2001. https://www.citizen.org/sites/default/files/rdmyths.pdf.
New research has provided an updated estimate of the spending needed to bring a cancer drug to the US market.
In analyzing data from 10 companies bringing a cancer drug to market, researchers found that sales revenue from these drugs was roughly 7 times higher than the research and development (R&D) costs.
The total sales revenue for the drugs—during a median follow-up of 4 years—was $67.0 billion, and the total R&D spending was $9.1 billion (including 7% opportunity costs).
Researchers reported these figures in JAMA Internal Medicine.
“[T]he price of cancer drugs is currently rising higher and higher each year,” said study author Vinay Prasad, MD, of Oregon Health and Science University in Portland.
“The cost of 1 drug for 1 year of treatment is now routinely in excess of $100,000 . . . . One of the often-cited reasons why cancer drugs cost so much—one of the justifications for the high price—is that the outlay by the biopharmaceutical industry to bring these drugs to market is sizable, and there have been a wide range of estimates for what that R&D outlay is.”
“The most-cited estimate is one that comes out of the Tufts Medical Group1 that puts the cost to bring a cancer drug to market, when adjusted for 2017 dollars, at $2.7 billion. Another estimate is from the group Public Citizen.2 And that is a much lower estimate, finding the cost to bring a drug to market of $320 million.”
“Both of these estimates have limitations in the methods for how they estimated the cost to bring a drug to market. Notably, the Tufts group is rather non-transparent. Because of confidentiality agreements, we don’t know what drugs and what companies they’re looking at, and we can’t independently verify their analysis.”
“The Public Citizen group, in contrast, is comparing expenditures over a period of time against the number of drugs in a different period of time to make an estimate of the cost to bring a drug to market, but this isn’t exactly the cost of bringing those particular drugs to market.”
These issues prompted Dr Prasad and Sham Mailankody, MBBS, of the Memorial Sloan Kettering Cancer Center in New York, to conduct the current study.
Analysis
The researchers analyzed US Securities and Exchange Commission filings for 10 drug companies that received approval from the US Food and Drug Administration for a cancer drug from 2006 through 2015.
Prior to this, none of the companies had any drugs approved for use in the US. However, the companies had a median of 3.5 (range, 2-11) drugs in development during the study period.
The researchers said the fact that these companies had no prior drug approvals eliminated biases that may be present when analyzing larger drug companies, such as redundancies in R&D development and tax incentives for listing different endeavors as R&D spending.
In addition, the fact that the 10 companies were developing other drugs during the study period means this study takes into account the cost of failure in bringing a drug to market.
Results
For the 10 companies and drugs analyzed, the median duration of drug development was 7.3 years (range, 5.8 to 15.2 years).
The median cost of drug development (in 2017 US dollars) was $648.0 million (range, $157.3 to $1950.8 million). For a 7% per annum cost of capital (or opportunity costs), the median cost was $757.4 million (range, $203.6 to $2601.7 million).
The median time from approval to analysis in December 2016 (or until the company sold or licensed the compound to another company) was 4.0 years (range, 0.8 years to 8.8 years).
The total revenue from sales of the 10 drugs during this time was $67.0 billion.
The total R&D spending was $7.2 billion, or $9.1 billion when including 7% opportunity costs.
The following table includes data broken down by drug.
| Drug and company | Approval date | Indication | Total R&D costs | Revenue since approval |
|---|---|---|---|---|
| Eculizumab (Soliris)
Alexion Pharmaceuticals |
2007 | Paroxysmal nocturnal hemoglobinuria | $817.6 million | $12,987.8 million |
| Pralatrexate (Folotyn)*
Allos Therapeutics |
2009 | Relapsed/refractory peripheral T-cell lymphoma | $178.2 million | $304.8 million |
| Brentuximab vedotin (Adcetris)*
Seattle Genetics |
2011 | Certain patients with Hodgkin lymphoma and systemic anaplastic large cell lymphoma | $899.2 million | $1034.3 million |
| Ruxolitinib (Jakafi)
Incyte Corporation |
2011 | Intermediate- and high-risk myelofibrosis | $1097.8 million | $2251.5 million |
| Enzalutamide (Xtandi)**
Medivation |
2012 | Metastatic castration-resistant prostate cancer | $473.3 million | $21,068.3 million |
| Vincristine liposome (Marqibo)*
Talon Therapeutics |
2012 | Ph- acute lymphoblastic leukemia | $157.3 million | $204.1 million |
| Cabozantinib (Cometriq)
Exelixis |
2012 | Metastatic medullary thyroid cancer | $1950.8 million | $341.9 million |
| Ponatinib (Iclusig)*
Ariad Pharmaceuticals |
2012 | Chronic myeloid leukemia and Ph+ acute lymphoblastic leukemia
|
$480.1 million | $5457.98 million |
| Ibrutinib (Imbruvica)*
Pharmacyclics |
2013 | Previously treated mantle cell lymphoma | $328.1 million | $22,275.0 million |
| Irinotecan liposome (Onivyde)
Merrimack Pharmaceuticals |
2015 | Advanced pancreatic cancer previously treated with gemcitabine-based chemotherapy | $815.8 million | $1065.2 million |
*Received accelerated approval. (The other 5 drugs received regular approval.)
**Did not receive orphan designation. (Nine of the 10 drugs received orphan designation.)
“So I think what we’re showing is . . . a transparent analysis of cancer drugs and companies, looking at the cost to bring a drug to market,” Dr Mailankody said. “And our estimate of $648 million is substantially lower than the often-cited number of $2.7 billion.”
“We’re also showing that, for these 10 drugs, revenue since approval is quite a bit higher than the R&D spending, almost 7-fold higher, and some of these companies have already had revenue of 10-fold or higher, compared to the R&D expenses.”
The researchers acknowledged that this study is limited by a small data set and the fact that the findings cannot be extrapolated to other types of drugs. ![]()
1. DiMasi JA et al. Innovation in the pharmaceutical industry: new estimates of R&D costs. J Health Econ. 2016;47:20-33.
2. Young B et al. Rx R&D Myths: The Case Against the Drug Industry’s R&D “Scare Card.” Washington, DC: Public Citizen’s Congress Watch; 2001. https://www.citizen.org/sites/default/files/rdmyths.pdf.
New drug proves effective against malaria
A new drug is effective against non-severe cases of malaria, according to results from a phase 2 trial published in The Lancet Infectious Diseases.
The drug, AQ-13, was able to clear patients of the malaria parasite Plasmodium falciparum within a week, matching the effectiveness of combination treatment with artemether and lumefantrine.
“The clinical trial results are extraordinarily encouraging,” said study author Donald Krogstad, MD, of Tulane University in New Orleans, Louisiana.
“Compared to the current first-line recommendation for treatment of malaria, the new drug comes out very well.”
For this study, Dr Krogstad and his colleagues recruited 66 adult men in Mali with uncomplicated malaria. Half of the subjects were randomized to receive AQ-13, and the other half received combination treatment with artemether and lumefantrine.
The researchers found that asexual parasites were cleared by day 7 in both treatment groups.
In a per-protocol analysis, the cure rate was 100% (28/28) in the AQ-13 group and 93.9% (28/31) in the combination group (P=0.50, difference −6.1%, 95% CI −14.7 to 2.4).
In the intention-to-treat analysis, the cure rate was 84.8% (28/33) in the AQ-13 group and 93.9% in the combination group (P=0.43, difference 9.1%, 95% CI −5.6 to 23.8).
Grade 1 or lower adverse events (AEs) occurred in 239 patients in the AQ-13 group and 214 in the combination group. There were no grade 2-4 AEs.
The most common AEs (in the AQ-13 and combination groups, respectively) were fever (97% and 88%), weakness (82% and 85%), myalgias and arthralgias (82% and 76%), headache (97% and 94%), and anorexia (73% and 61%).
Two subjects in AQ-13 group left the study, and 3 were lost to follow-up. Two subjects in the combination group had late treatment failures with recurrence of their original infections.
The researchers hope to expand testing of AQ-13 to more participants, including women and children.
Dr Krogstad said the same biotechnology that helped the researchers develop AQ-13 has also revealed similar drugs that hold promise against drug-resistant parasites.
“The potential long-term implications are bigger than one drug,” Dr Krogstad said. “The conceptual step here is that if you understand the resistance well enough, you may actually be able to develop others as well. We synthesized over 200 analogues and, of those, 66 worked against the resistant parasites.” ![]()
A new drug is effective against non-severe cases of malaria, according to results from a phase 2 trial published in The Lancet Infectious Diseases.
The drug, AQ-13, was able to clear patients of the malaria parasite Plasmodium falciparum within a week, matching the effectiveness of combination treatment with artemether and lumefantrine.
“The clinical trial results are extraordinarily encouraging,” said study author Donald Krogstad, MD, of Tulane University in New Orleans, Louisiana.
“Compared to the current first-line recommendation for treatment of malaria, the new drug comes out very well.”
For this study, Dr Krogstad and his colleagues recruited 66 adult men in Mali with uncomplicated malaria. Half of the subjects were randomized to receive AQ-13, and the other half received combination treatment with artemether and lumefantrine.
The researchers found that asexual parasites were cleared by day 7 in both treatment groups.
In a per-protocol analysis, the cure rate was 100% (28/28) in the AQ-13 group and 93.9% (28/31) in the combination group (P=0.50, difference −6.1%, 95% CI −14.7 to 2.4).
In the intention-to-treat analysis, the cure rate was 84.8% (28/33) in the AQ-13 group and 93.9% in the combination group (P=0.43, difference 9.1%, 95% CI −5.6 to 23.8).
Grade 1 or lower adverse events (AEs) occurred in 239 patients in the AQ-13 group and 214 in the combination group. There were no grade 2-4 AEs.
The most common AEs (in the AQ-13 and combination groups, respectively) were fever (97% and 88%), weakness (82% and 85%), myalgias and arthralgias (82% and 76%), headache (97% and 94%), and anorexia (73% and 61%).
Two subjects in AQ-13 group left the study, and 3 were lost to follow-up. Two subjects in the combination group had late treatment failures with recurrence of their original infections.
The researchers hope to expand testing of AQ-13 to more participants, including women and children.
Dr Krogstad said the same biotechnology that helped the researchers develop AQ-13 has also revealed similar drugs that hold promise against drug-resistant parasites.
“The potential long-term implications are bigger than one drug,” Dr Krogstad said. “The conceptual step here is that if you understand the resistance well enough, you may actually be able to develop others as well. We synthesized over 200 analogues and, of those, 66 worked against the resistant parasites.” ![]()
A new drug is effective against non-severe cases of malaria, according to results from a phase 2 trial published in The Lancet Infectious Diseases.
The drug, AQ-13, was able to clear patients of the malaria parasite Plasmodium falciparum within a week, matching the effectiveness of combination treatment with artemether and lumefantrine.
“The clinical trial results are extraordinarily encouraging,” said study author Donald Krogstad, MD, of Tulane University in New Orleans, Louisiana.
“Compared to the current first-line recommendation for treatment of malaria, the new drug comes out very well.”
For this study, Dr Krogstad and his colleagues recruited 66 adult men in Mali with uncomplicated malaria. Half of the subjects were randomized to receive AQ-13, and the other half received combination treatment with artemether and lumefantrine.
The researchers found that asexual parasites were cleared by day 7 in both treatment groups.
In a per-protocol analysis, the cure rate was 100% (28/28) in the AQ-13 group and 93.9% (28/31) in the combination group (P=0.50, difference −6.1%, 95% CI −14.7 to 2.4).
In the intention-to-treat analysis, the cure rate was 84.8% (28/33) in the AQ-13 group and 93.9% in the combination group (P=0.43, difference 9.1%, 95% CI −5.6 to 23.8).
Grade 1 or lower adverse events (AEs) occurred in 239 patients in the AQ-13 group and 214 in the combination group. There were no grade 2-4 AEs.
The most common AEs (in the AQ-13 and combination groups, respectively) were fever (97% and 88%), weakness (82% and 85%), myalgias and arthralgias (82% and 76%), headache (97% and 94%), and anorexia (73% and 61%).
Two subjects in AQ-13 group left the study, and 3 were lost to follow-up. Two subjects in the combination group had late treatment failures with recurrence of their original infections.
The researchers hope to expand testing of AQ-13 to more participants, including women and children.
Dr Krogstad said the same biotechnology that helped the researchers develop AQ-13 has also revealed similar drugs that hold promise against drug-resistant parasites.
“The potential long-term implications are bigger than one drug,” Dr Krogstad said. “The conceptual step here is that if you understand the resistance well enough, you may actually be able to develop others as well. We synthesized over 200 analogues and, of those, 66 worked against the resistant parasites.” ![]()
Clinical trials may go unregistered, unpublished
A new study has revealed a lack of registration and publication of clinical trials, as well as discrepancies in the reporting of primary outcomes.
However, this study is limited in that it only included 113 clinical trials approved in Finland.
An-Wen Chan, MD, DPhil, of the University of Toronto in Ontario, Canada, and his colleagues reported findings from the study in JAMA.
The results were also presented at the Eighth International Congress on Peer Review and Scientific Publication.
The researchers examined adherence to trial registration and its association with subsequent publication and reporting of primary outcomes.
The team looked at 113 clinical trial protocols approved in 2007 by the research ethics committee for the region of Helsinki and Uusimaa, Finland.
Sixty-one percent of the trials were prospectively registered, which was defined as registration within 1 month of the trial start date to allow for incomplete start dates and processing delays in the registry.
Fifty-seven percent of the trials were published, and 80% had a defined primary outcome.
Prospective registration was significantly associated with subsequent publication, with 68% of registered trials and 39% of unregistered trials getting published (adjusted odds ratio=4.53 [95% CI, 1.12-18.34]).
In addition, registered trials were significantly more likely than unregistered trials to be published with the same primary outcomes as defined in the protocol—64% and 25%, respectively (adjusted odds ratio=5.79 [95% CI, 1.42-23.65]).
The researchers assessed discrepancies in primary outcomes between the protocol and the registry/publication. These were defined as:
- A new primary outcome being reported that was not specified as primary in the protocol
- A protocol-defined primary outcome being omitted or downgraded (reported as secondary or unspecified) in the registry or publication.
The researchers found discrepancies between the registry and the protocol in 23% of the prospectively registered trials. There were discrepancies between the publication and the protocol for 16% of published trials.
Discrepancies between the protocol and publication were more common in unregistered trials than registered trials—55% and 6%, respectively (P<0.001).
Based on these results, the researchers concluded that prospective registration should be mandatory for all clinical trials. ![]()
A new study has revealed a lack of registration and publication of clinical trials, as well as discrepancies in the reporting of primary outcomes.
However, this study is limited in that it only included 113 clinical trials approved in Finland.
An-Wen Chan, MD, DPhil, of the University of Toronto in Ontario, Canada, and his colleagues reported findings from the study in JAMA.
The results were also presented at the Eighth International Congress on Peer Review and Scientific Publication.
The researchers examined adherence to trial registration and its association with subsequent publication and reporting of primary outcomes.
The team looked at 113 clinical trial protocols approved in 2007 by the research ethics committee for the region of Helsinki and Uusimaa, Finland.
Sixty-one percent of the trials were prospectively registered, which was defined as registration within 1 month of the trial start date to allow for incomplete start dates and processing delays in the registry.
Fifty-seven percent of the trials were published, and 80% had a defined primary outcome.
Prospective registration was significantly associated with subsequent publication, with 68% of registered trials and 39% of unregistered trials getting published (adjusted odds ratio=4.53 [95% CI, 1.12-18.34]).
In addition, registered trials were significantly more likely than unregistered trials to be published with the same primary outcomes as defined in the protocol—64% and 25%, respectively (adjusted odds ratio=5.79 [95% CI, 1.42-23.65]).
The researchers assessed discrepancies in primary outcomes between the protocol and the registry/publication. These were defined as:
- A new primary outcome being reported that was not specified as primary in the protocol
- A protocol-defined primary outcome being omitted or downgraded (reported as secondary or unspecified) in the registry or publication.
The researchers found discrepancies between the registry and the protocol in 23% of the prospectively registered trials. There were discrepancies between the publication and the protocol for 16% of published trials.
Discrepancies between the protocol and publication were more common in unregistered trials than registered trials—55% and 6%, respectively (P<0.001).
Based on these results, the researchers concluded that prospective registration should be mandatory for all clinical trials. ![]()
A new study has revealed a lack of registration and publication of clinical trials, as well as discrepancies in the reporting of primary outcomes.
However, this study is limited in that it only included 113 clinical trials approved in Finland.
An-Wen Chan, MD, DPhil, of the University of Toronto in Ontario, Canada, and his colleagues reported findings from the study in JAMA.
The results were also presented at the Eighth International Congress on Peer Review and Scientific Publication.
The researchers examined adherence to trial registration and its association with subsequent publication and reporting of primary outcomes.
The team looked at 113 clinical trial protocols approved in 2007 by the research ethics committee for the region of Helsinki and Uusimaa, Finland.
Sixty-one percent of the trials were prospectively registered, which was defined as registration within 1 month of the trial start date to allow for incomplete start dates and processing delays in the registry.
Fifty-seven percent of the trials were published, and 80% had a defined primary outcome.
Prospective registration was significantly associated with subsequent publication, with 68% of registered trials and 39% of unregistered trials getting published (adjusted odds ratio=4.53 [95% CI, 1.12-18.34]).
In addition, registered trials were significantly more likely than unregistered trials to be published with the same primary outcomes as defined in the protocol—64% and 25%, respectively (adjusted odds ratio=5.79 [95% CI, 1.42-23.65]).
The researchers assessed discrepancies in primary outcomes between the protocol and the registry/publication. These were defined as:
- A new primary outcome being reported that was not specified as primary in the protocol
- A protocol-defined primary outcome being omitted or downgraded (reported as secondary or unspecified) in the registry or publication.
The researchers found discrepancies between the registry and the protocol in 23% of the prospectively registered trials. There were discrepancies between the publication and the protocol for 16% of published trials.
Discrepancies between the protocol and publication were more common in unregistered trials than registered trials—55% and 6%, respectively (P<0.001).
Based on these results, the researchers concluded that prospective registration should be mandatory for all clinical trials. ![]()
New assay helps differentiate between viral and bacterial infections in children
An assay testing the presence of three blood-borne host-proteins shows promise in accurately identifying viral and bacterial infections in febrile children, a validation study found.
The three proteins that the ImmunoXpert assay uses to differentiate between viral and bacterial infections are: viral-induced tumor necrosis factor-related apoptosis–inducing ligand (TRAIL), interferon gamma-induced protein-10 (IP-10), and bacterial-induced C-reactive protein (CRP). TRAIL and IP-10 are novel identifiers, while CRP has been used in traditional bacterial detecting assays, Isaac Srugo, MD, and his colleagues reported.
Of the 361 patients whose samples were selected for testing, the assay identified 209 patients (58%) with a viral infection, 99 patients (27%) with a bacterial infection, and the remaining 53 patients (15%) with an equivocal outcome, according to Dr. Srugo of the Ruth and Bruce Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel, and his colleagues. The 307 patients with a bacterial or viral diagnosis had sensitivity of 93.8% (95% confidence interval, 87.8%-99.8%) and specificity of 89.8% (CI, 85.6%-94.0%). There were 4 false-negative and 21 false-positive findings.
The levels of TRAIL and IP-10 were present in higher levels in children with viral infections than children with bacterial infections. The opposite was true of CRP results, with levels being drastically lower in children with viral infections than in children with bacterial infections.
“Notably, among the indeterminate diagnosis patients without a reference standard, the assay gave a bacterial or viral outcome for 69% of the cases (the rest were equivocal), with half of these yielding a score associated with a particularly high degree of assay diagnostic confidence,” investigators said. “This finding suggests that the assay may be applicable to ‘harder to diagnose’ cases in real-life clinical settings.”
Also, the assay “exhibits consistent performance across a wide range of ages [3 months to 18 years], time from symptom onset, and clinical syndromes,” Dr. Srugo and his associates said.
Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
Being able to accurately determine if a child is suffering from a serious bacterial infection that requires hospitalization or a viral infection that can be treated at home is a difficult decision. Physicians are wary of prescribing antibiotics due to overuse, resulting in poor outcomes for patients, society, and the health care system, but have not had the diagnostic tests to accurately determine infection types in pediatric patients.
The work of Srugo et al. and the development of the ImmunoXpert assay have added another diagnostic tool to help physicians more effectively treat infections in children. When determining the effectiveness of a diagnostic test, the sensitivity and specificity of the test must be scrutinized. Compared with traditional laboratory tests, the ImmunoXpert assay displayed higher specificity and sensitivity and a superior positive likelihood ratio. With a positive likelihood near 10 and a negative likelihood ratio of 0.07, the “test results may be able to be used meaningfully in the management of patients to a degree that currently does not exist.”
Although the ImmunoXpert assay shows promise as a diagnostic tool, confirmatory investigations must be done to determine if the assay will work in a more real world manner, using refrigerated instead of frozen specimens, and testing the assay in children under 3 months of age.
David Kimberlin, MD, is a professor of pediatrics, vice chair for clinical and translational research, as well as the codirector of the division of pediatric infections diseases at the University of Alabama, Birmingham. Claudette L. Poole, MD, is a Dixon Fellow of Infections Diseases at the university. These comments were published in a commentary accompanying the Srugo et al. article in Pediatrics (2017;140[4]:e20171210).
Being able to accurately determine if a child is suffering from a serious bacterial infection that requires hospitalization or a viral infection that can be treated at home is a difficult decision. Physicians are wary of prescribing antibiotics due to overuse, resulting in poor outcomes for patients, society, and the health care system, but have not had the diagnostic tests to accurately determine infection types in pediatric patients.
The work of Srugo et al. and the development of the ImmunoXpert assay have added another diagnostic tool to help physicians more effectively treat infections in children. When determining the effectiveness of a diagnostic test, the sensitivity and specificity of the test must be scrutinized. Compared with traditional laboratory tests, the ImmunoXpert assay displayed higher specificity and sensitivity and a superior positive likelihood ratio. With a positive likelihood near 10 and a negative likelihood ratio of 0.07, the “test results may be able to be used meaningfully in the management of patients to a degree that currently does not exist.”
Although the ImmunoXpert assay shows promise as a diagnostic tool, confirmatory investigations must be done to determine if the assay will work in a more real world manner, using refrigerated instead of frozen specimens, and testing the assay in children under 3 months of age.
David Kimberlin, MD, is a professor of pediatrics, vice chair for clinical and translational research, as well as the codirector of the division of pediatric infections diseases at the University of Alabama, Birmingham. Claudette L. Poole, MD, is a Dixon Fellow of Infections Diseases at the university. These comments were published in a commentary accompanying the Srugo et al. article in Pediatrics (2017;140[4]:e20171210).
Being able to accurately determine if a child is suffering from a serious bacterial infection that requires hospitalization or a viral infection that can be treated at home is a difficult decision. Physicians are wary of prescribing antibiotics due to overuse, resulting in poor outcomes for patients, society, and the health care system, but have not had the diagnostic tests to accurately determine infection types in pediatric patients.
The work of Srugo et al. and the development of the ImmunoXpert assay have added another diagnostic tool to help physicians more effectively treat infections in children. When determining the effectiveness of a diagnostic test, the sensitivity and specificity of the test must be scrutinized. Compared with traditional laboratory tests, the ImmunoXpert assay displayed higher specificity and sensitivity and a superior positive likelihood ratio. With a positive likelihood near 10 and a negative likelihood ratio of 0.07, the “test results may be able to be used meaningfully in the management of patients to a degree that currently does not exist.”
Although the ImmunoXpert assay shows promise as a diagnostic tool, confirmatory investigations must be done to determine if the assay will work in a more real world manner, using refrigerated instead of frozen specimens, and testing the assay in children under 3 months of age.
David Kimberlin, MD, is a professor of pediatrics, vice chair for clinical and translational research, as well as the codirector of the division of pediatric infections diseases at the University of Alabama, Birmingham. Claudette L. Poole, MD, is a Dixon Fellow of Infections Diseases at the university. These comments were published in a commentary accompanying the Srugo et al. article in Pediatrics (2017;140[4]:e20171210).
An assay testing the presence of three blood-borne host-proteins shows promise in accurately identifying viral and bacterial infections in febrile children, a validation study found.
The three proteins that the ImmunoXpert assay uses to differentiate between viral and bacterial infections are: viral-induced tumor necrosis factor-related apoptosis–inducing ligand (TRAIL), interferon gamma-induced protein-10 (IP-10), and bacterial-induced C-reactive protein (CRP). TRAIL and IP-10 are novel identifiers, while CRP has been used in traditional bacterial detecting assays, Isaac Srugo, MD, and his colleagues reported.
Of the 361 patients whose samples were selected for testing, the assay identified 209 patients (58%) with a viral infection, 99 patients (27%) with a bacterial infection, and the remaining 53 patients (15%) with an equivocal outcome, according to Dr. Srugo of the Ruth and Bruce Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel, and his colleagues. The 307 patients with a bacterial or viral diagnosis had sensitivity of 93.8% (95% confidence interval, 87.8%-99.8%) and specificity of 89.8% (CI, 85.6%-94.0%). There were 4 false-negative and 21 false-positive findings.
The levels of TRAIL and IP-10 were present in higher levels in children with viral infections than children with bacterial infections. The opposite was true of CRP results, with levels being drastically lower in children with viral infections than in children with bacterial infections.
“Notably, among the indeterminate diagnosis patients without a reference standard, the assay gave a bacterial or viral outcome for 69% of the cases (the rest were equivocal), with half of these yielding a score associated with a particularly high degree of assay diagnostic confidence,” investigators said. “This finding suggests that the assay may be applicable to ‘harder to diagnose’ cases in real-life clinical settings.”
Also, the assay “exhibits consistent performance across a wide range of ages [3 months to 18 years], time from symptom onset, and clinical syndromes,” Dr. Srugo and his associates said.
Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
An assay testing the presence of three blood-borne host-proteins shows promise in accurately identifying viral and bacterial infections in febrile children, a validation study found.
The three proteins that the ImmunoXpert assay uses to differentiate between viral and bacterial infections are: viral-induced tumor necrosis factor-related apoptosis–inducing ligand (TRAIL), interferon gamma-induced protein-10 (IP-10), and bacterial-induced C-reactive protein (CRP). TRAIL and IP-10 are novel identifiers, while CRP has been used in traditional bacterial detecting assays, Isaac Srugo, MD, and his colleagues reported.
Of the 361 patients whose samples were selected for testing, the assay identified 209 patients (58%) with a viral infection, 99 patients (27%) with a bacterial infection, and the remaining 53 patients (15%) with an equivocal outcome, according to Dr. Srugo of the Ruth and Bruce Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel, and his colleagues. The 307 patients with a bacterial or viral diagnosis had sensitivity of 93.8% (95% confidence interval, 87.8%-99.8%) and specificity of 89.8% (CI, 85.6%-94.0%). There were 4 false-negative and 21 false-positive findings.
The levels of TRAIL and IP-10 were present in higher levels in children with viral infections than children with bacterial infections. The opposite was true of CRP results, with levels being drastically lower in children with viral infections than in children with bacterial infections.
“Notably, among the indeterminate diagnosis patients without a reference standard, the assay gave a bacterial or viral outcome for 69% of the cases (the rest were equivocal), with half of these yielding a score associated with a particularly high degree of assay diagnostic confidence,” investigators said. “This finding suggests that the assay may be applicable to ‘harder to diagnose’ cases in real-life clinical settings.”
Also, the assay “exhibits consistent performance across a wide range of ages [3 months to 18 years], time from symptom onset, and clinical syndromes,” Dr. Srugo and his associates said.
Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: In 361 patients, the assay identified infections as 209 (58%) viral, 99 (27%) bacterial, and 53 (15%) equivocal with high sensitivity and specificity.
Data source: Double-blind study with multiple evaluation sites using frozen serum sample from five pediatric emergency departments and two wards. Of 529 potential candidates, only 361 met selection criteria.
Disclosures: Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
Advance Care Planning: Making It Easier for Patients (and You)
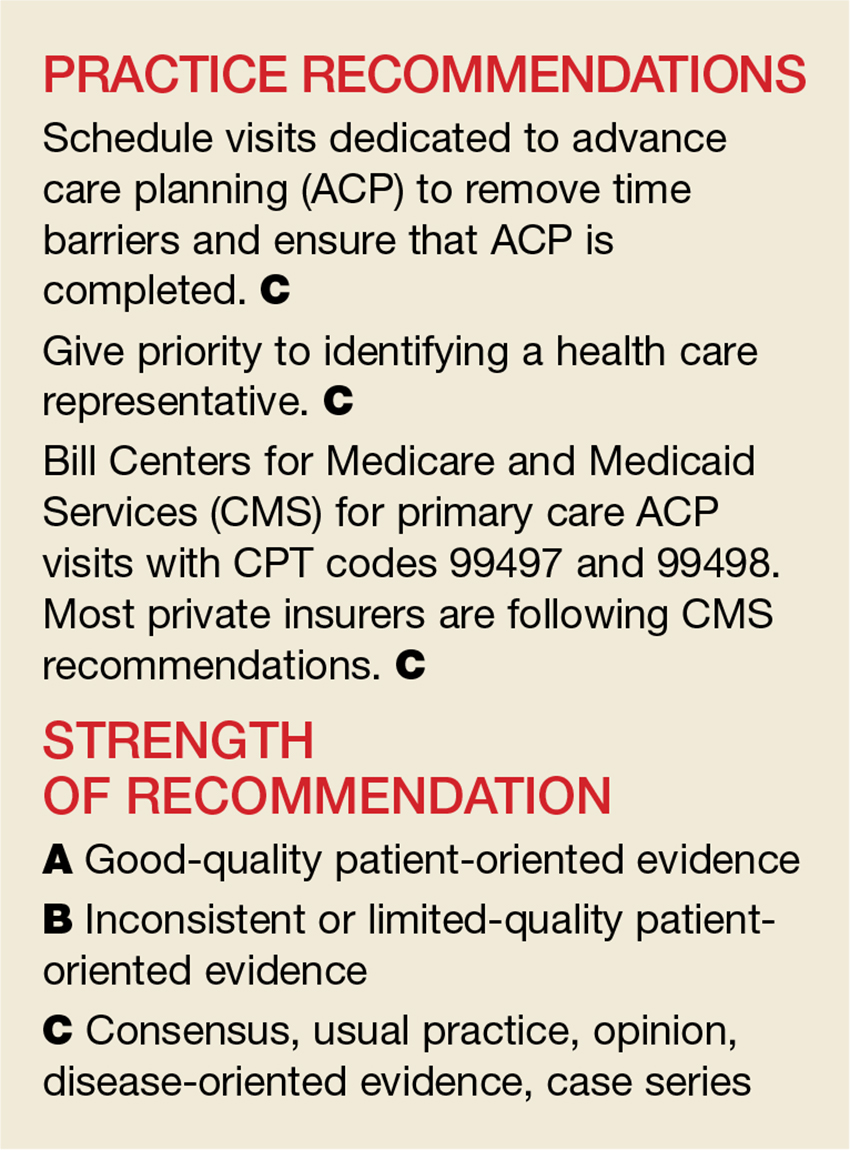
With the number of aging Americans projected to grow dramatically in the next several years, the need for primary palliative care and advance care planning (ACP) is more important than ever. Patients and their families want and expect palliative care when needed, but initial conversations about ACP can be difficult for them. Appropriate timing in raising this subject and clear communication can give patients the opportunity, while they are still independent, to set their goals for medical care.
For the past several decades, political decisions and judicial cases have shaped palliative care as we know it today. And its shape is still evolving. In support of ACP, advocacy groups at a national level are developing models that practitioners can use to engage patients in setting goals. And Medicare is now reimbursing primary care providers for this work that they have been doing for years (although many still may not be billing for the service).
Finally, the busy primary care office may have its own set of challenges in addressing ACP. Our aim in this review is to identify the barriers we face and the solutions we can implement to make a difference in our patients’ end-of-life care planning.
LANDMARK EVENTS HAVE DEFINED ACP TODAY
In 1969, Luis Kutner, an Illinois attorney, proposed the idea of a “living will,” envisioned as a document specifying the types of treatment a person would be willing to receive were he or she unable at a later time to participate in making a decision.1 In 1976, California became the first state to give living wills the power of the law through the Natural Death Act.2
Throughout the 1970s and ‘80s, several high-profile court cases brought this idea into the national spotlight. In 1975, the New Jersey Supreme Court granted the parents of 21-year-old Karen Ann Quinlan the right to discontinue the treatment sustaining her in a persistent vegetative state. Ms. Quinlan was removed from the ventilator and lived nine more months before dying in a nursing home.
In 1983, age 25, Nancy Cruzan was involved in a motor vehicle accident that left her in a persistent vegetative state. She remained so until 1988, when her parents asked that her feeding tube be removed. The hospital refused, indicating that it would lead to her death. The family sued, and the case eventually went to the US Supreme Court in 1989.
In a 5-to-4 decision, the Supreme Court ruled that a state was legally able to require “clear and convincing evidence” of a patient’s wish for removal of life-sustaining therapies. Cruzan’s family was able to provide such evidence, and her artificial nutrition was withheld. She died 12 days later.
The Cruzan case was instrumental in furthering ACP, leading to the passage of the Patient Self Determination Act by Congress in 1990. All federally funded health care facilities were now required to educate patients of their rights in determining their medical care and to ask about advance directives.3 The ACP movement gained additional momentum from the landmark SUPPORT study that documented shortcomings in communication between physicians and patients/families about treatment preferences and end-of-life care in US hospitals.4
In the Terri Schiavo case, the patient’s husband disagreed with the life-sustaining decisions of his wife’s parents, given her persistent vegetative state and the fact that she had no chance of meaningful recovery. After a prolonged national debate, it was ultimately decided that the husband could elect to withhold artificial nutrition. (She died in 2005.) The Schiavo case, as well as the Institute of Medicine’s report on Dying in America, influenced Congress in 2016 to pass legislation funding ACP conversations.5
THE DEMONSTRATED BENEFITS OF ACP
When done comprehensively, ACP yields many benefits for patients and families and for the health care system. A systematic review demonstrated that, despite the few studies examining the economic cost of ACP, the process may lead to decreased health care costs in certain populations (nursing home residents, community-dwelling adults with dementia, and those living in high health care–spending regions) and at the very least does not increase health care costs.6 ACP has increased the number of do-not-resuscitate orders and has decreased hospitalizations, admissions to intensive care units, and rates of cardiopulmonary resuscitation, mechanical ventilation, and use of tube feeding.6-8
More noteworthy than the decrease in resource utilization and potential cost savings is the impact that ACP can have on a patient’s quality of life. Patients who receive aggressive care at the end of life tend to experience decreased quality of life compared with those receiving hospice care.7 Quality-of-life scores for patients in hospice improved with the length of enrollment in that care.7 When ACP discussions have taken place, the care patients receive at the end of life tends to conform more closely to their wishes and to increase family satisfaction.9-11
One reason that practitioners often give for not completing ACP is the fear of increasing patient or family anxiety or post-traumatic stress disorder (PTSD). However, studies have shown this concern to be unfounded.7,12 While ACP studies have not shown a decrease in rates of anxiety or PTSD, no study has shown an increase in these psychologic morbidities.8
Caveats to keep in mind. Not all studies have shown unambiguous benefits related to ACP. Among the systematic reviews previously noted, there was significant variability in quality of data. Additionally, some experts argue that the traditional view of ACP (ie, completion of a single advance directive/living will) is outdated and should be replaced with a method that prepares patients and families to anticipate “in-the-moment decision making.”13 While we still believe that completion of an advance directive is useful, the experts’ point is well taken, especially since many patients change their preferences over time (and typically toward more aggressive care).14,15 While the advance directive serves a role, it is more important to help patients recognize their goals and preferences and to facilitate ongoing discussions between the patient and his or her family/surrogate decision-maker and providers.
A SNAPSHOT OF PARTICIPATION IN ACP
Despite the ACP movement and the likely benefits associated with it, most individuals have not participated. Rates of completion do seem to be rising, but there is still room for improvement. Among all individuals older than 18, only 26.3% have an advance directive.16 In a cohort of older patients seen in an emergency department, only 40% had a living will, while nearly 54% had a designated health care power of attorney.17 Perhaps more alarming is the lack of ACP for those patients almost all providers would agree need it: the long-term care population. The National Center for Health Statistics has reported that only 28% of home health care patients, 65% of nursing home residents, and 88% of hospice patients have an advance directive on file.18
PROVIDER AND PATIENT BARRIERS TO ACP
If ACP can decrease resource utilization and improve caregiver compliance with a patient’s wishes for end of life, the obvious question is: Why isn’t it done more often? A longstanding barrier for providers has been that these types of discussions are time intensive and have not been billable. However, since January 1, 2016, we are now able to bill for these discussions. (More on this in a bit.) Providers do cite other barriers, though.
A recent systematic review showed that ACP is hindered by time constraints imposed by other clinical and administrative tasks that are heavily monitored.19 Barriers to engaging in ACP reported by patients include a reluctance to think about dying, a belief that family or providers will know what to do, difficulty understanding ACP forms, and the absence of a person who can serve as a surrogate decision-maker.20,21
NATIONAL MODELS TO HELP WITH IMPLEMENTATION
The percentage of individuals with an advance directive in the US has not increased significantly over the past decade.22 The lack of traction in completion and use of advance directives has led several authors to question the utility of this older model of ACP.22 Several experts in the field believe that more robust, ongoing goals-of-care conversations between patients, families, and providers are equally, or even more, important than the completion of actual advance directive documents.23,24
National models such as the POLST (Physician Orders for Life-Sustaining Treatment) paradigm have become popular in several states (www.polst.org). Intended for those with estimated life expectancy of less than one year, POLST is not an advance directive but a physician order for these seriously ill patients. Emergency medical service workers are legally able to follow a POLST document but not a living will or advance directive—a significant reason for those with end-stage illness to consider completing a POLST document with their health care provider. Programs such as “Respecting Choices” have incorporated POLST documentation as part of ongoing goals-of-care conversations between patients and health care providers (www.gundersenhealth.org/respecting-choices).
Many groups have developed products to encourage patients and their families to initiate conversations at home. An example is the Conversation Project, a free online resource available in multiple languages that can help break the ice for patients and get them talking about their wishes for end-of-life care (www.theconversationproject.org). It poses simple stimulating questions such as “What kind of role do you want to have in the decision-making process?” and “What are your concerns about treatment?”
HOW-TO TIPS FOR ACP IN OUTPATIENT SETTINGS
When approaching the topic of ACP with patients, it’s important to do so over time, starting as soon as possible with older patients and those with chronic illness that confers a high risk for significant morbidity or mortality. Assess each patient’s understanding of ACP and readiness to discuss the topic. Many patients think of ACP in the context of a document (eg, living will), so asking about the existence of a living will may help to start the conversation. Alternatively, consider inquiring about whether the patient has had experience with family or friends at the end of life or during a difficult medical situation, and whether the patient has thought about making personal plans for such a situation.25
When a patient is ready to have this conversation, your goal should be three-fold:26
- Help the patient articulate personal values, goals, and preferences.
- Ask the patient to formally assign health care power of attorney (POA) to a trusted individual or to name a surrogate decision-maker. Document this decision in the medical record.
- Help the patient translate expressed values into specific medical care plans, if applicable.
Because ACP conversations are often time consuming, it’s a good idea to schedule separate appointments to focus on this alone. If, however, a patient is unable to return for a dedicated ACP visit, a first step that can be completed in a reasonably short period would be choosing a surrogate decision-maker.
Helping a patient articulate personal values may be eased by asking such questions as, “Have you ever thought about what kind of care you would want if the time came when you could not make your own decisions?” or “What worries you the most about possibly not being able to make your own decisions?”27 If the patient is able to identify a surrogate decision-maker before the ACP appointment, ask that this person attend. A family member or close friend may remember instances in which the patient expressed health care preferences, and their presence can help to minimize gaps in communication.
Once the patient’s preferences are clear, document them in the medical record. Some preferences may be suitable for translation into POLST orders or an advance directive, but this is less important than the overall discussion. ACP should be an ongoing conversation, since a patient’s goals may change over time. And encourage the patient to share any desired change in plans with their surrogate decision-maker or update the POA document.
BE SURE TO BILL FOR ACP SERVICES
To encourage office-based providers to conduct ACP, the Centers for Medicare and Medicaid Services (CMS) implemented payment for CPT codes 99497 and 99498.
CPT code 99497 covers the first 30 minutes of face-to-face time with patients or their family members or medical decision-makers. This time can be used to discuss living wills or advance directives.
CPT code 99498 can be applied to each additional 30 minutes of ACP services. Typically, this billing code would be used as an add-on for a particular diagnosis, such as heart failure, chronic obstructive pulmonary disease, or pancreatic cancer.
CPT Code 99497 equates to 2.40 relative-value units (RVU) with an estimated payment of $85.99, while CPT code 99498 equates to 2.09 RVU with an estimated payment of $74.88.28
According to CMS, there is no annual limit to the number of times the ACP codes can be billed for a particular patient. And there are no restrictions regarding location of service, meaning a provider could perform this in an outpatient setting, an inpatient setting, or a long-term care facility. All health care providers are allowed to bill with this code. Also worth noting: You don’t need to complete any particular documentation for a visit to be billed as an ACP service. CMS provides a helpful Q & A at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/FAQ-Advance-Care-Planning.pdf.
1. Kutner L. Due process of euthanasia: the living will, a proposal. Indiana Law J. 1969;44:539-554.
2. California Law Revision Commission. 2000 Health Care Decisions Law and Revised Power of Attorney Law. www.clrc.ca.gov/pub/Printed-Reports/Pub208.pdf. Accessed August 14, 2017.
3. H.R. 5067 - 101st Congress. Patient Self Determination Act of 1990. www.govtrack.us/congress/bills/101/hr5067. Accessed August 14, 2017.
4. The SUPPORT Principle Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT). JAMA. 1995;274:1591-1598.
5. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: National Academies Press; 2015.
6. Dixon J, Matosevic T, Knapp M. The economic evidence for advance care planning: systematic review of evidence. Palliat Med. 2015;29:869-884.
7. Wright AA, Ray A, Mack JW, et al. Associations between end-of-life discussions, patient mental-health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665-1673.
8. Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28:1000-1025.
9. Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345.
10. Morrison RS, Chichin E, Carter J, et al. The effect of a social work intervention to enhance advance care planning documentation in the nursing home. J Am Geriatr Soc. 2005;53:290-294.
11. Schamp R, Tenkku L. Managed death in a PACE: pathways in present and advance directives. J Am Med Dir Assoc. 2006;7:339-344.
12. Walczak A, Butow PN, Bu S, et al. A systematic review of evidence for end-of-life communication interventions: who do they target, how are they structured and do they work? Patient Educ Couns. 2016;99:3-16.
13. Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153:256-261.
14. Straton JB, Wang NY, Meoni LA, et al. Physical functioning, depression, and preferences for treatment at the end of life: the Johns Hopkins Precursors study. J Am Geriatr Soc. 2004;52:577-582.
15. Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med. 2006;166:890-895.
16. Rao JK, Anderson LA, Lin F, et al. Completion of advance directives among U.S. consumers. Am J Prev Med. 2014;46:65-70.
17. Grudzen CR, Buonocore P, Steinberg J, et al; AAHPM Research Committee Writing Group. Concordance of advance care plans with inpatient directives in the electronic medical record for older patients admitted from the emergency department. J Pain Symptom Manage. 2016;51:647-651.
18. Jones AL, Moss AJ, Harris-Kojetin LD. Use of advance directives in long-term care populations. NCHS Data Brief. 2011;(54):1-8.
19. Lund S, Richardson A, May C. Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLoS One. 2015;10:e0116629.
20. Fried TR, Bullock K, Iannone L, et al. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc. 2009;57:1547-1555.
21. Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. 2009;57:31-39.
22. Winter L, Parks SM, Diamond JJ. Ask a different question, get a different answer: why living wills are poor guides to care preferences at the end of life. J Palliat Med. 2010;13:567-572.
23. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. www.nap.edu/read/18748/chapter/1. Accessed August 14, 2017.
24. Sudore RL, Schickedanz AD, Landefeld CS, et al. Engagement in multiple steps of the advance care planning process: a descriptive study of diverse older adults. J Am Geriatr Soc. 2008;56:1006-1013.
25. McMahan RD, Knight SJ, Fried TR, et al. Advance care planning beyond advance directives: perspectives from patients and surrogates. J Pain Symptom Manage. 2013;46:355-365.
26. Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin North Am. 2015;99:391-403.
27. Lum HD, Sudore RL. Advance care planning and goals of care communication in older adults with cardiovascular disease and multi-morbidity. Clin Geriatr Med. 2016;32:247-260.
28. American College of Physicians. Advanced Care Planning: Implementation for practices. www.acponline.org/system/files/documents/practice-resources/business-resources/payment/advance_care_planning_toolkit.pdf. Accessed August 14, 2017.
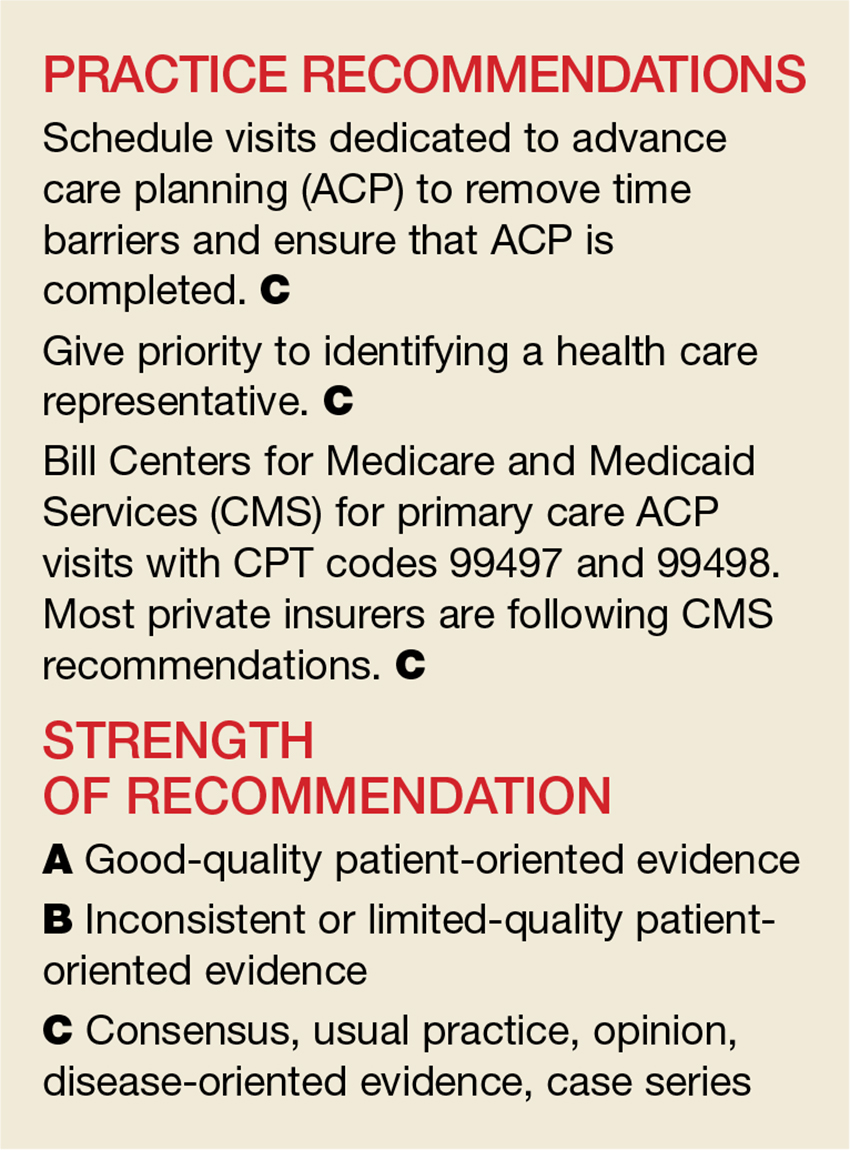
With the number of aging Americans projected to grow dramatically in the next several years, the need for primary palliative care and advance care planning (ACP) is more important than ever. Patients and their families want and expect palliative care when needed, but initial conversations about ACP can be difficult for them. Appropriate timing in raising this subject and clear communication can give patients the opportunity, while they are still independent, to set their goals for medical care.
For the past several decades, political decisions and judicial cases have shaped palliative care as we know it today. And its shape is still evolving. In support of ACP, advocacy groups at a national level are developing models that practitioners can use to engage patients in setting goals. And Medicare is now reimbursing primary care providers for this work that they have been doing for years (although many still may not be billing for the service).
Finally, the busy primary care office may have its own set of challenges in addressing ACP. Our aim in this review is to identify the barriers we face and the solutions we can implement to make a difference in our patients’ end-of-life care planning.
LANDMARK EVENTS HAVE DEFINED ACP TODAY
In 1969, Luis Kutner, an Illinois attorney, proposed the idea of a “living will,” envisioned as a document specifying the types of treatment a person would be willing to receive were he or she unable at a later time to participate in making a decision.1 In 1976, California became the first state to give living wills the power of the law through the Natural Death Act.2
Throughout the 1970s and ‘80s, several high-profile court cases brought this idea into the national spotlight. In 1975, the New Jersey Supreme Court granted the parents of 21-year-old Karen Ann Quinlan the right to discontinue the treatment sustaining her in a persistent vegetative state. Ms. Quinlan was removed from the ventilator and lived nine more months before dying in a nursing home.
In 1983, age 25, Nancy Cruzan was involved in a motor vehicle accident that left her in a persistent vegetative state. She remained so until 1988, when her parents asked that her feeding tube be removed. The hospital refused, indicating that it would lead to her death. The family sued, and the case eventually went to the US Supreme Court in 1989.
In a 5-to-4 decision, the Supreme Court ruled that a state was legally able to require “clear and convincing evidence” of a patient’s wish for removal of life-sustaining therapies. Cruzan’s family was able to provide such evidence, and her artificial nutrition was withheld. She died 12 days later.
The Cruzan case was instrumental in furthering ACP, leading to the passage of the Patient Self Determination Act by Congress in 1990. All federally funded health care facilities were now required to educate patients of their rights in determining their medical care and to ask about advance directives.3 The ACP movement gained additional momentum from the landmark SUPPORT study that documented shortcomings in communication between physicians and patients/families about treatment preferences and end-of-life care in US hospitals.4
In the Terri Schiavo case, the patient’s husband disagreed with the life-sustaining decisions of his wife’s parents, given her persistent vegetative state and the fact that she had no chance of meaningful recovery. After a prolonged national debate, it was ultimately decided that the husband could elect to withhold artificial nutrition. (She died in 2005.) The Schiavo case, as well as the Institute of Medicine’s report on Dying in America, influenced Congress in 2016 to pass legislation funding ACP conversations.5
THE DEMONSTRATED BENEFITS OF ACP
When done comprehensively, ACP yields many benefits for patients and families and for the health care system. A systematic review demonstrated that, despite the few studies examining the economic cost of ACP, the process may lead to decreased health care costs in certain populations (nursing home residents, community-dwelling adults with dementia, and those living in high health care–spending regions) and at the very least does not increase health care costs.6 ACP has increased the number of do-not-resuscitate orders and has decreased hospitalizations, admissions to intensive care units, and rates of cardiopulmonary resuscitation, mechanical ventilation, and use of tube feeding.6-8
More noteworthy than the decrease in resource utilization and potential cost savings is the impact that ACP can have on a patient’s quality of life. Patients who receive aggressive care at the end of life tend to experience decreased quality of life compared with those receiving hospice care.7 Quality-of-life scores for patients in hospice improved with the length of enrollment in that care.7 When ACP discussions have taken place, the care patients receive at the end of life tends to conform more closely to their wishes and to increase family satisfaction.9-11
One reason that practitioners often give for not completing ACP is the fear of increasing patient or family anxiety or post-traumatic stress disorder (PTSD). However, studies have shown this concern to be unfounded.7,12 While ACP studies have not shown a decrease in rates of anxiety or PTSD, no study has shown an increase in these psychologic morbidities.8
Caveats to keep in mind. Not all studies have shown unambiguous benefits related to ACP. Among the systematic reviews previously noted, there was significant variability in quality of data. Additionally, some experts argue that the traditional view of ACP (ie, completion of a single advance directive/living will) is outdated and should be replaced with a method that prepares patients and families to anticipate “in-the-moment decision making.”13 While we still believe that completion of an advance directive is useful, the experts’ point is well taken, especially since many patients change their preferences over time (and typically toward more aggressive care).14,15 While the advance directive serves a role, it is more important to help patients recognize their goals and preferences and to facilitate ongoing discussions between the patient and his or her family/surrogate decision-maker and providers.
A SNAPSHOT OF PARTICIPATION IN ACP
Despite the ACP movement and the likely benefits associated with it, most individuals have not participated. Rates of completion do seem to be rising, but there is still room for improvement. Among all individuals older than 18, only 26.3% have an advance directive.16 In a cohort of older patients seen in an emergency department, only 40% had a living will, while nearly 54% had a designated health care power of attorney.17 Perhaps more alarming is the lack of ACP for those patients almost all providers would agree need it: the long-term care population. The National Center for Health Statistics has reported that only 28% of home health care patients, 65% of nursing home residents, and 88% of hospice patients have an advance directive on file.18
PROVIDER AND PATIENT BARRIERS TO ACP
If ACP can decrease resource utilization and improve caregiver compliance with a patient’s wishes for end of life, the obvious question is: Why isn’t it done more often? A longstanding barrier for providers has been that these types of discussions are time intensive and have not been billable. However, since January 1, 2016, we are now able to bill for these discussions. (More on this in a bit.) Providers do cite other barriers, though.
A recent systematic review showed that ACP is hindered by time constraints imposed by other clinical and administrative tasks that are heavily monitored.19 Barriers to engaging in ACP reported by patients include a reluctance to think about dying, a belief that family or providers will know what to do, difficulty understanding ACP forms, and the absence of a person who can serve as a surrogate decision-maker.20,21
NATIONAL MODELS TO HELP WITH IMPLEMENTATION
The percentage of individuals with an advance directive in the US has not increased significantly over the past decade.22 The lack of traction in completion and use of advance directives has led several authors to question the utility of this older model of ACP.22 Several experts in the field believe that more robust, ongoing goals-of-care conversations between patients, families, and providers are equally, or even more, important than the completion of actual advance directive documents.23,24
National models such as the POLST (Physician Orders for Life-Sustaining Treatment) paradigm have become popular in several states (www.polst.org). Intended for those with estimated life expectancy of less than one year, POLST is not an advance directive but a physician order for these seriously ill patients. Emergency medical service workers are legally able to follow a POLST document but not a living will or advance directive—a significant reason for those with end-stage illness to consider completing a POLST document with their health care provider. Programs such as “Respecting Choices” have incorporated POLST documentation as part of ongoing goals-of-care conversations between patients and health care providers (www.gundersenhealth.org/respecting-choices).
Many groups have developed products to encourage patients and their families to initiate conversations at home. An example is the Conversation Project, a free online resource available in multiple languages that can help break the ice for patients and get them talking about their wishes for end-of-life care (www.theconversationproject.org). It poses simple stimulating questions such as “What kind of role do you want to have in the decision-making process?” and “What are your concerns about treatment?”
HOW-TO TIPS FOR ACP IN OUTPATIENT SETTINGS
When approaching the topic of ACP with patients, it’s important to do so over time, starting as soon as possible with older patients and those with chronic illness that confers a high risk for significant morbidity or mortality. Assess each patient’s understanding of ACP and readiness to discuss the topic. Many patients think of ACP in the context of a document (eg, living will), so asking about the existence of a living will may help to start the conversation. Alternatively, consider inquiring about whether the patient has had experience with family or friends at the end of life or during a difficult medical situation, and whether the patient has thought about making personal plans for such a situation.25
When a patient is ready to have this conversation, your goal should be three-fold:26
- Help the patient articulate personal values, goals, and preferences.
- Ask the patient to formally assign health care power of attorney (POA) to a trusted individual or to name a surrogate decision-maker. Document this decision in the medical record.
- Help the patient translate expressed values into specific medical care plans, if applicable.
Because ACP conversations are often time consuming, it’s a good idea to schedule separate appointments to focus on this alone. If, however, a patient is unable to return for a dedicated ACP visit, a first step that can be completed in a reasonably short period would be choosing a surrogate decision-maker.
Helping a patient articulate personal values may be eased by asking such questions as, “Have you ever thought about what kind of care you would want if the time came when you could not make your own decisions?” or “What worries you the most about possibly not being able to make your own decisions?”27 If the patient is able to identify a surrogate decision-maker before the ACP appointment, ask that this person attend. A family member or close friend may remember instances in which the patient expressed health care preferences, and their presence can help to minimize gaps in communication.
Once the patient’s preferences are clear, document them in the medical record. Some preferences may be suitable for translation into POLST orders or an advance directive, but this is less important than the overall discussion. ACP should be an ongoing conversation, since a patient’s goals may change over time. And encourage the patient to share any desired change in plans with their surrogate decision-maker or update the POA document.
BE SURE TO BILL FOR ACP SERVICES
To encourage office-based providers to conduct ACP, the Centers for Medicare and Medicaid Services (CMS) implemented payment for CPT codes 99497 and 99498.
CPT code 99497 covers the first 30 minutes of face-to-face time with patients or their family members or medical decision-makers. This time can be used to discuss living wills or advance directives.
CPT code 99498 can be applied to each additional 30 minutes of ACP services. Typically, this billing code would be used as an add-on for a particular diagnosis, such as heart failure, chronic obstructive pulmonary disease, or pancreatic cancer.
CPT Code 99497 equates to 2.40 relative-value units (RVU) with an estimated payment of $85.99, while CPT code 99498 equates to 2.09 RVU with an estimated payment of $74.88.28
According to CMS, there is no annual limit to the number of times the ACP codes can be billed for a particular patient. And there are no restrictions regarding location of service, meaning a provider could perform this in an outpatient setting, an inpatient setting, or a long-term care facility. All health care providers are allowed to bill with this code. Also worth noting: You don’t need to complete any particular documentation for a visit to be billed as an ACP service. CMS provides a helpful Q & A at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/FAQ-Advance-Care-Planning.pdf.
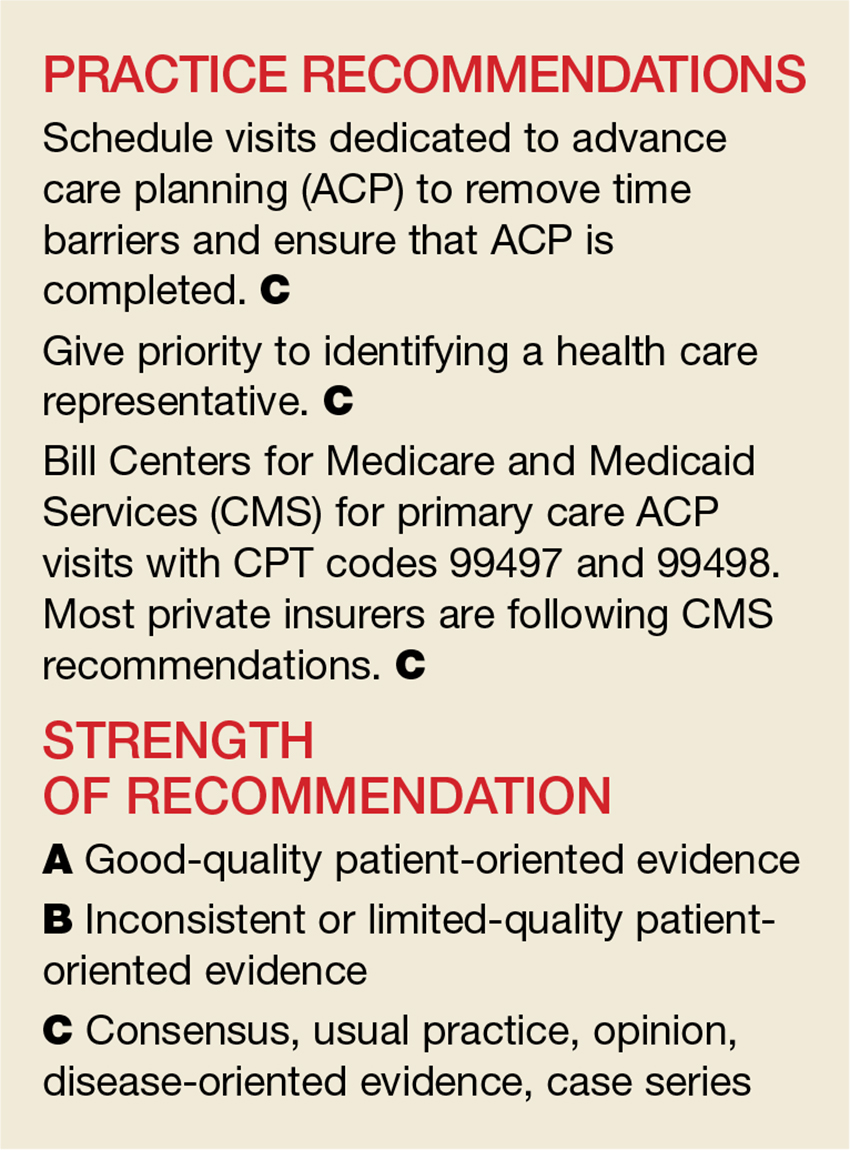
With the number of aging Americans projected to grow dramatically in the next several years, the need for primary palliative care and advance care planning (ACP) is more important than ever. Patients and their families want and expect palliative care when needed, but initial conversations about ACP can be difficult for them. Appropriate timing in raising this subject and clear communication can give patients the opportunity, while they are still independent, to set their goals for medical care.
For the past several decades, political decisions and judicial cases have shaped palliative care as we know it today. And its shape is still evolving. In support of ACP, advocacy groups at a national level are developing models that practitioners can use to engage patients in setting goals. And Medicare is now reimbursing primary care providers for this work that they have been doing for years (although many still may not be billing for the service).
Finally, the busy primary care office may have its own set of challenges in addressing ACP. Our aim in this review is to identify the barriers we face and the solutions we can implement to make a difference in our patients’ end-of-life care planning.
LANDMARK EVENTS HAVE DEFINED ACP TODAY
In 1969, Luis Kutner, an Illinois attorney, proposed the idea of a “living will,” envisioned as a document specifying the types of treatment a person would be willing to receive were he or she unable at a later time to participate in making a decision.1 In 1976, California became the first state to give living wills the power of the law through the Natural Death Act.2
Throughout the 1970s and ‘80s, several high-profile court cases brought this idea into the national spotlight. In 1975, the New Jersey Supreme Court granted the parents of 21-year-old Karen Ann Quinlan the right to discontinue the treatment sustaining her in a persistent vegetative state. Ms. Quinlan was removed from the ventilator and lived nine more months before dying in a nursing home.
In 1983, age 25, Nancy Cruzan was involved in a motor vehicle accident that left her in a persistent vegetative state. She remained so until 1988, when her parents asked that her feeding tube be removed. The hospital refused, indicating that it would lead to her death. The family sued, and the case eventually went to the US Supreme Court in 1989.
In a 5-to-4 decision, the Supreme Court ruled that a state was legally able to require “clear and convincing evidence” of a patient’s wish for removal of life-sustaining therapies. Cruzan’s family was able to provide such evidence, and her artificial nutrition was withheld. She died 12 days later.
The Cruzan case was instrumental in furthering ACP, leading to the passage of the Patient Self Determination Act by Congress in 1990. All federally funded health care facilities were now required to educate patients of their rights in determining their medical care and to ask about advance directives.3 The ACP movement gained additional momentum from the landmark SUPPORT study that documented shortcomings in communication between physicians and patients/families about treatment preferences and end-of-life care in US hospitals.4
In the Terri Schiavo case, the patient’s husband disagreed with the life-sustaining decisions of his wife’s parents, given her persistent vegetative state and the fact that she had no chance of meaningful recovery. After a prolonged national debate, it was ultimately decided that the husband could elect to withhold artificial nutrition. (She died in 2005.) The Schiavo case, as well as the Institute of Medicine’s report on Dying in America, influenced Congress in 2016 to pass legislation funding ACP conversations.5
THE DEMONSTRATED BENEFITS OF ACP
When done comprehensively, ACP yields many benefits for patients and families and for the health care system. A systematic review demonstrated that, despite the few studies examining the economic cost of ACP, the process may lead to decreased health care costs in certain populations (nursing home residents, community-dwelling adults with dementia, and those living in high health care–spending regions) and at the very least does not increase health care costs.6 ACP has increased the number of do-not-resuscitate orders and has decreased hospitalizations, admissions to intensive care units, and rates of cardiopulmonary resuscitation, mechanical ventilation, and use of tube feeding.6-8
More noteworthy than the decrease in resource utilization and potential cost savings is the impact that ACP can have on a patient’s quality of life. Patients who receive aggressive care at the end of life tend to experience decreased quality of life compared with those receiving hospice care.7 Quality-of-life scores for patients in hospice improved with the length of enrollment in that care.7 When ACP discussions have taken place, the care patients receive at the end of life tends to conform more closely to their wishes and to increase family satisfaction.9-11
One reason that practitioners often give for not completing ACP is the fear of increasing patient or family anxiety or post-traumatic stress disorder (PTSD). However, studies have shown this concern to be unfounded.7,12 While ACP studies have not shown a decrease in rates of anxiety or PTSD, no study has shown an increase in these psychologic morbidities.8
Caveats to keep in mind. Not all studies have shown unambiguous benefits related to ACP. Among the systematic reviews previously noted, there was significant variability in quality of data. Additionally, some experts argue that the traditional view of ACP (ie, completion of a single advance directive/living will) is outdated and should be replaced with a method that prepares patients and families to anticipate “in-the-moment decision making.”13 While we still believe that completion of an advance directive is useful, the experts’ point is well taken, especially since many patients change their preferences over time (and typically toward more aggressive care).14,15 While the advance directive serves a role, it is more important to help patients recognize their goals and preferences and to facilitate ongoing discussions between the patient and his or her family/surrogate decision-maker and providers.
A SNAPSHOT OF PARTICIPATION IN ACP
Despite the ACP movement and the likely benefits associated with it, most individuals have not participated. Rates of completion do seem to be rising, but there is still room for improvement. Among all individuals older than 18, only 26.3% have an advance directive.16 In a cohort of older patients seen in an emergency department, only 40% had a living will, while nearly 54% had a designated health care power of attorney.17 Perhaps more alarming is the lack of ACP for those patients almost all providers would agree need it: the long-term care population. The National Center for Health Statistics has reported that only 28% of home health care patients, 65% of nursing home residents, and 88% of hospice patients have an advance directive on file.18
PROVIDER AND PATIENT BARRIERS TO ACP
If ACP can decrease resource utilization and improve caregiver compliance with a patient’s wishes for end of life, the obvious question is: Why isn’t it done more often? A longstanding barrier for providers has been that these types of discussions are time intensive and have not been billable. However, since January 1, 2016, we are now able to bill for these discussions. (More on this in a bit.) Providers do cite other barriers, though.
A recent systematic review showed that ACP is hindered by time constraints imposed by other clinical and administrative tasks that are heavily monitored.19 Barriers to engaging in ACP reported by patients include a reluctance to think about dying, a belief that family or providers will know what to do, difficulty understanding ACP forms, and the absence of a person who can serve as a surrogate decision-maker.20,21
NATIONAL MODELS TO HELP WITH IMPLEMENTATION
The percentage of individuals with an advance directive in the US has not increased significantly over the past decade.22 The lack of traction in completion and use of advance directives has led several authors to question the utility of this older model of ACP.22 Several experts in the field believe that more robust, ongoing goals-of-care conversations between patients, families, and providers are equally, or even more, important than the completion of actual advance directive documents.23,24
National models such as the POLST (Physician Orders for Life-Sustaining Treatment) paradigm have become popular in several states (www.polst.org). Intended for those with estimated life expectancy of less than one year, POLST is not an advance directive but a physician order for these seriously ill patients. Emergency medical service workers are legally able to follow a POLST document but not a living will or advance directive—a significant reason for those with end-stage illness to consider completing a POLST document with their health care provider. Programs such as “Respecting Choices” have incorporated POLST documentation as part of ongoing goals-of-care conversations between patients and health care providers (www.gundersenhealth.org/respecting-choices).
Many groups have developed products to encourage patients and their families to initiate conversations at home. An example is the Conversation Project, a free online resource available in multiple languages that can help break the ice for patients and get them talking about their wishes for end-of-life care (www.theconversationproject.org). It poses simple stimulating questions such as “What kind of role do you want to have in the decision-making process?” and “What are your concerns about treatment?”
HOW-TO TIPS FOR ACP IN OUTPATIENT SETTINGS
When approaching the topic of ACP with patients, it’s important to do so over time, starting as soon as possible with older patients and those with chronic illness that confers a high risk for significant morbidity or mortality. Assess each patient’s understanding of ACP and readiness to discuss the topic. Many patients think of ACP in the context of a document (eg, living will), so asking about the existence of a living will may help to start the conversation. Alternatively, consider inquiring about whether the patient has had experience with family or friends at the end of life or during a difficult medical situation, and whether the patient has thought about making personal plans for such a situation.25
When a patient is ready to have this conversation, your goal should be three-fold:26
- Help the patient articulate personal values, goals, and preferences.
- Ask the patient to formally assign health care power of attorney (POA) to a trusted individual or to name a surrogate decision-maker. Document this decision in the medical record.
- Help the patient translate expressed values into specific medical care plans, if applicable.
Because ACP conversations are often time consuming, it’s a good idea to schedule separate appointments to focus on this alone. If, however, a patient is unable to return for a dedicated ACP visit, a first step that can be completed in a reasonably short period would be choosing a surrogate decision-maker.
Helping a patient articulate personal values may be eased by asking such questions as, “Have you ever thought about what kind of care you would want if the time came when you could not make your own decisions?” or “What worries you the most about possibly not being able to make your own decisions?”27 If the patient is able to identify a surrogate decision-maker before the ACP appointment, ask that this person attend. A family member or close friend may remember instances in which the patient expressed health care preferences, and their presence can help to minimize gaps in communication.
Once the patient’s preferences are clear, document them in the medical record. Some preferences may be suitable for translation into POLST orders or an advance directive, but this is less important than the overall discussion. ACP should be an ongoing conversation, since a patient’s goals may change over time. And encourage the patient to share any desired change in plans with their surrogate decision-maker or update the POA document.
BE SURE TO BILL FOR ACP SERVICES
To encourage office-based providers to conduct ACP, the Centers for Medicare and Medicaid Services (CMS) implemented payment for CPT codes 99497 and 99498.
CPT code 99497 covers the first 30 minutes of face-to-face time with patients or their family members or medical decision-makers. This time can be used to discuss living wills or advance directives.
CPT code 99498 can be applied to each additional 30 minutes of ACP services. Typically, this billing code would be used as an add-on for a particular diagnosis, such as heart failure, chronic obstructive pulmonary disease, or pancreatic cancer.
CPT Code 99497 equates to 2.40 relative-value units (RVU) with an estimated payment of $85.99, while CPT code 99498 equates to 2.09 RVU with an estimated payment of $74.88.28
According to CMS, there is no annual limit to the number of times the ACP codes can be billed for a particular patient. And there are no restrictions regarding location of service, meaning a provider could perform this in an outpatient setting, an inpatient setting, or a long-term care facility. All health care providers are allowed to bill with this code. Also worth noting: You don’t need to complete any particular documentation for a visit to be billed as an ACP service. CMS provides a helpful Q & A at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/FAQ-Advance-Care-Planning.pdf.
1. Kutner L. Due process of euthanasia: the living will, a proposal. Indiana Law J. 1969;44:539-554.
2. California Law Revision Commission. 2000 Health Care Decisions Law and Revised Power of Attorney Law. www.clrc.ca.gov/pub/Printed-Reports/Pub208.pdf. Accessed August 14, 2017.
3. H.R. 5067 - 101st Congress. Patient Self Determination Act of 1990. www.govtrack.us/congress/bills/101/hr5067. Accessed August 14, 2017.
4. The SUPPORT Principle Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT). JAMA. 1995;274:1591-1598.
5. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: National Academies Press; 2015.
6. Dixon J, Matosevic T, Knapp M. The economic evidence for advance care planning: systematic review of evidence. Palliat Med. 2015;29:869-884.
7. Wright AA, Ray A, Mack JW, et al. Associations between end-of-life discussions, patient mental-health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665-1673.
8. Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28:1000-1025.
9. Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345.
10. Morrison RS, Chichin E, Carter J, et al. The effect of a social work intervention to enhance advance care planning documentation in the nursing home. J Am Geriatr Soc. 2005;53:290-294.
11. Schamp R, Tenkku L. Managed death in a PACE: pathways in present and advance directives. J Am Med Dir Assoc. 2006;7:339-344.
12. Walczak A, Butow PN, Bu S, et al. A systematic review of evidence for end-of-life communication interventions: who do they target, how are they structured and do they work? Patient Educ Couns. 2016;99:3-16.
13. Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153:256-261.
14. Straton JB, Wang NY, Meoni LA, et al. Physical functioning, depression, and preferences for treatment at the end of life: the Johns Hopkins Precursors study. J Am Geriatr Soc. 2004;52:577-582.
15. Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med. 2006;166:890-895.
16. Rao JK, Anderson LA, Lin F, et al. Completion of advance directives among U.S. consumers. Am J Prev Med. 2014;46:65-70.
17. Grudzen CR, Buonocore P, Steinberg J, et al; AAHPM Research Committee Writing Group. Concordance of advance care plans with inpatient directives in the electronic medical record for older patients admitted from the emergency department. J Pain Symptom Manage. 2016;51:647-651.
18. Jones AL, Moss AJ, Harris-Kojetin LD. Use of advance directives in long-term care populations. NCHS Data Brief. 2011;(54):1-8.
19. Lund S, Richardson A, May C. Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLoS One. 2015;10:e0116629.
20. Fried TR, Bullock K, Iannone L, et al. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc. 2009;57:1547-1555.
21. Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. 2009;57:31-39.
22. Winter L, Parks SM, Diamond JJ. Ask a different question, get a different answer: why living wills are poor guides to care preferences at the end of life. J Palliat Med. 2010;13:567-572.
23. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. www.nap.edu/read/18748/chapter/1. Accessed August 14, 2017.
24. Sudore RL, Schickedanz AD, Landefeld CS, et al. Engagement in multiple steps of the advance care planning process: a descriptive study of diverse older adults. J Am Geriatr Soc. 2008;56:1006-1013.
25. McMahan RD, Knight SJ, Fried TR, et al. Advance care planning beyond advance directives: perspectives from patients and surrogates. J Pain Symptom Manage. 2013;46:355-365.
26. Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin North Am. 2015;99:391-403.
27. Lum HD, Sudore RL. Advance care planning and goals of care communication in older adults with cardiovascular disease and multi-morbidity. Clin Geriatr Med. 2016;32:247-260.
28. American College of Physicians. Advanced Care Planning: Implementation for practices. www.acponline.org/system/files/documents/practice-resources/business-resources/payment/advance_care_planning_toolkit.pdf. Accessed August 14, 2017.
1. Kutner L. Due process of euthanasia: the living will, a proposal. Indiana Law J. 1969;44:539-554.
2. California Law Revision Commission. 2000 Health Care Decisions Law and Revised Power of Attorney Law. www.clrc.ca.gov/pub/Printed-Reports/Pub208.pdf. Accessed August 14, 2017.
3. H.R. 5067 - 101st Congress. Patient Self Determination Act of 1990. www.govtrack.us/congress/bills/101/hr5067. Accessed August 14, 2017.
4. The SUPPORT Principle Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT). JAMA. 1995;274:1591-1598.
5. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: National Academies Press; 2015.
6. Dixon J, Matosevic T, Knapp M. The economic evidence for advance care planning: systematic review of evidence. Palliat Med. 2015;29:869-884.
7. Wright AA, Ray A, Mack JW, et al. Associations between end-of-life discussions, patient mental-health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665-1673.
8. Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28:1000-1025.
9. Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345.
10. Morrison RS, Chichin E, Carter J, et al. The effect of a social work intervention to enhance advance care planning documentation in the nursing home. J Am Geriatr Soc. 2005;53:290-294.
11. Schamp R, Tenkku L. Managed death in a PACE: pathways in present and advance directives. J Am Med Dir Assoc. 2006;7:339-344.
12. Walczak A, Butow PN, Bu S, et al. A systematic review of evidence for end-of-life communication interventions: who do they target, how are they structured and do they work? Patient Educ Couns. 2016;99:3-16.
13. Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153:256-261.
14. Straton JB, Wang NY, Meoni LA, et al. Physical functioning, depression, and preferences for treatment at the end of life: the Johns Hopkins Precursors study. J Am Geriatr Soc. 2004;52:577-582.
15. Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med. 2006;166:890-895.
16. Rao JK, Anderson LA, Lin F, et al. Completion of advance directives among U.S. consumers. Am J Prev Med. 2014;46:65-70.
17. Grudzen CR, Buonocore P, Steinberg J, et al; AAHPM Research Committee Writing Group. Concordance of advance care plans with inpatient directives in the electronic medical record for older patients admitted from the emergency department. J Pain Symptom Manage. 2016;51:647-651.
18. Jones AL, Moss AJ, Harris-Kojetin LD. Use of advance directives in long-term care populations. NCHS Data Brief. 2011;(54):1-8.
19. Lund S, Richardson A, May C. Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLoS One. 2015;10:e0116629.
20. Fried TR, Bullock K, Iannone L, et al. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc. 2009;57:1547-1555.
21. Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. 2009;57:31-39.
22. Winter L, Parks SM, Diamond JJ. Ask a different question, get a different answer: why living wills are poor guides to care preferences at the end of life. J Palliat Med. 2010;13:567-572.
23. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. www.nap.edu/read/18748/chapter/1. Accessed August 14, 2017.
24. Sudore RL, Schickedanz AD, Landefeld CS, et al. Engagement in multiple steps of the advance care planning process: a descriptive study of diverse older adults. J Am Geriatr Soc. 2008;56:1006-1013.
25. McMahan RD, Knight SJ, Fried TR, et al. Advance care planning beyond advance directives: perspectives from patients and surrogates. J Pain Symptom Manage. 2013;46:355-365.
26. Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin North Am. 2015;99:391-403.
27. Lum HD, Sudore RL. Advance care planning and goals of care communication in older adults with cardiovascular disease and multi-morbidity. Clin Geriatr Med. 2016;32:247-260.
28. American College of Physicians. Advanced Care Planning: Implementation for practices. www.acponline.org/system/files/documents/practice-resources/business-resources/payment/advance_care_planning_toolkit.pdf. Accessed August 14, 2017.
Review of plant phenolics, Part 2: flavonoid compounds
This column picks up with a recent literature review suggesting potential benefits of topically applied or orally administered flavonoid polyphenolic substances. The discussion is based on at least one sample compound from each flavonoid category.
Flavonols: quercetin
Known to exert substantial antioxidant and anti-inflammatory activities, quercetin has been shown in various cellular and animal-based models to deliver photoprotection from UV and contribute to wound healing.1 In a single center, single-blind trial with 30 healthy volunteers, a 1% topical quercetin cream was found to be effective in reducing erythema, itching, and wheal diameter in experimentally-induced skin stress.2 Quercetin also has been reported to have the capacity to inhibit melanin production.3
Flavones: apigenin
Flavanones: naringenin
The citrus flavanone naringenin shows promise as a preventive agent against cutaneous aging as well as carcinogenesis. In a 2008 study, naringenin exerted an anti-apoptotic effect in UVB-damaged cells, significantly extending long-term cellular survival, and facilitating the removal of cyclobutane pyrimidine dimers from the genome.7 More recently, topical naringenin has been shown in mice to mitigate the cutaneous inflammation and oxidative stress caused by UVB irradiation,8 and, present in Lippia graveolens, to protect against chronic UVB-induced damage including phototumorigenesis.9
Isoflavones: red clover, genistein, and daidzein
Red clover, the isoflavones of which have been demonstrated – in high dietary concentrations – to contribute to low incidence of osteoporosis and menopausal symptoms, was shown in a 2006 study to exert anti-aging effects in mice, indicating potential for alleviating the cutaneous aging brought on by declines in estrogen.10 In 2011, Lipovac et al. showed that oral supplementation with red clover extract improved scalp hair and skin status as well as libido, mood, sleep, and fatigue in a study with 109 postmenopausal women.11
The topical application of the soy isoflavones genistein, daidzein, and glycitein has shown promise as a treatment for photoaging and photodamage.12 Genistein has been noted for its antioxidant and antibrowning activity, and has exhibited anti-aging properties in mouse studies and photoprotective activity in humans.13 A 2015 study by Zhao et al. in cultured skin fibroblasts and nude mouse skin indicated that daidzein treatment appears to increase skin collagen production and suppress collagen degradation.14
Flavan-3-ols (catechins): epigallocatechin 3-gallate
Already considered a potent antioxidant, epigallocatechin 3-gallate (EGCG) continues to receive attention for conferring an expanding range of health benefits. This catechin, which is the most abundant and potent of such compounds in green tea, has exhibited the capacity to hinder UVB-induced collagen-degrading matrix metalloproteinases (MMPs).15 EGCG also has been proposed as a preventive and therapeutic agent for keloids, given findings indicating that it hampered the proliferation and migration of keloid fibroblasts in vitro, as well as in vivo by interrupting the signal transducer and activator of transcription 3 (STAT3) signaling pathway.16 Further, EGCG has been suggested as a potential therapeutic approach to atopic dermatitis (AD) given success against AD-like skin lesions in a murine model.17 An investigation of the anti-aging cutaneous effects of EGCG on d-galactose-induced aging in mice revealed that subcutaneously injected EGCG yielded overall improvement in the structure and function of the skin.18 EGCG also is known to yield improvements in skin condition by providing DNA protection, reactivating damaged cells, and increasing cellular energy production.3
Perhaps most importantly, formulations containing green tea extracts have been shown in a small study of 20 volunteers to exert protection against photoaging and photoimmunosuppression, with the extract hindering the expression of MMP-9 and MMP-2.19 Wrinkle reduction also was observed in another clinical study involving topical green tea.20 The tea plant Camellia sinensis is one of the best sources of antioxidant catechins, particularly green tea (unfermented), but also white (unfermented), black (fermented), and oolong (semifermented) tea.21
Anthocyanins: cyanidin
A 2017 in vivo study in mice found that cyanidin hindered the binding of the cytokine interleukin-17A to the IL-17RA subunit to reduce inflammation.22 In a 2007 study, methanol extracts of black raspberries, strawberries, and blueberries were tested for the capacity to inhibit UV-induced activation of nuclear factor–kappa B (NF-kappaB) and activator protein–1 (AP-1) in mouse epidermal cells. The methanol fractions of black raspberries, which contain the anthocyanin cyanidin-3-rutinoside, were found to time- and dose-dependently inhibit the UV effects on NF-kappaB and AP-1, unlike the other berries, which do not contain cyanidin-3-rutinoside.23 The pretreatment of human keratinocytes with the anthocyanin cyanidin-3-O-glucoside also has been demonstrated to protect against a wide array of UVB-induced damage,24 and acai fruit–derived cyanidin and malvidin have been shown recently to thwart UVA-induced stress in immortalized fibroblasts.25 Further, cyanidin derived from elderberries has exhibited antiproliferative and apoptotic potential on melanoma cells in a 2017 mouse model, indicating a potential role in skin cancer treatment.26
Conclusion
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Eur J Pharm Biopharm. 2016 Nov;108:41-53.
2. Clin Cosmet Investig Dermatol. 2016 Feb 26;9:55-62.
3. Int J Mol Sci. 2016 Feb 18;17(2):160-201.
4. Cancer Res. 2008 Apr 15:68(8):3057-65.
5. J Acupunct Meridian Stud. 2013 Oct;6(5):252-62.
6. Evid Based Complement Alternat Med. 2012;2012:912028.
7. Photochem Photobiol. 2008 Mar-Apr;84(2):307-16.
8. PLoS One. 2016 Jan 7;11(1):e0146296.
9. J Photochem Photobiol B. 2017 Feb;167:72-81.
10. Phytother Res. 2006 Dec;20(12):1096-9.
11. Obstet Gynecol Int. 2011;2011:949302.
12. Int J Pharm. 2008 Nov 19;364(1):36-44.
13. Biomed Pharmacother. 2016 Aug;82:379-92.
14. Australas J Dermatol. 2015 Feb;56(1):e7-14.
15. Food Chem Toxicol. 2008 Apr;46(4):1298-307.
16. J Invest Dermatol. 2008 Oct;128(10):2429-41.
17. Int Immunopharmacol. 2008 Sep;8(9):1172-82.
18. Mech Ageing Dev. 2017 Mar 24;164:1-7.
19. Skin Res Technol. 2009 Aug;15(3):338-45.
20. Int J Cosmet Sci. 2010 Apr;32(2):99-106.
21. Int J Cosmet Sci. 2015 Oct;37(5):455-64.
22. Sci Signal. 2017 Feb 21;10(467). eaaf8823.
23. Nutr Cancer. 2007;58(2):205-12.
24. J Agric Food Chem. 2006 May 31;54(11):4041-7.
25. J Photochem Photobiol B. 2017 Jul;172:42-51.
26. Int J Mol Sci. 2017 Apr 30;18(5):949.
This column picks up with a recent literature review suggesting potential benefits of topically applied or orally administered flavonoid polyphenolic substances. The discussion is based on at least one sample compound from each flavonoid category.
Flavonols: quercetin
Known to exert substantial antioxidant and anti-inflammatory activities, quercetin has been shown in various cellular and animal-based models to deliver photoprotection from UV and contribute to wound healing.1 In a single center, single-blind trial with 30 healthy volunteers, a 1% topical quercetin cream was found to be effective in reducing erythema, itching, and wheal diameter in experimentally-induced skin stress.2 Quercetin also has been reported to have the capacity to inhibit melanin production.3
Flavones: apigenin
Flavanones: naringenin
The citrus flavanone naringenin shows promise as a preventive agent against cutaneous aging as well as carcinogenesis. In a 2008 study, naringenin exerted an anti-apoptotic effect in UVB-damaged cells, significantly extending long-term cellular survival, and facilitating the removal of cyclobutane pyrimidine dimers from the genome.7 More recently, topical naringenin has been shown in mice to mitigate the cutaneous inflammation and oxidative stress caused by UVB irradiation,8 and, present in Lippia graveolens, to protect against chronic UVB-induced damage including phototumorigenesis.9
Isoflavones: red clover, genistein, and daidzein
Red clover, the isoflavones of which have been demonstrated – in high dietary concentrations – to contribute to low incidence of osteoporosis and menopausal symptoms, was shown in a 2006 study to exert anti-aging effects in mice, indicating potential for alleviating the cutaneous aging brought on by declines in estrogen.10 In 2011, Lipovac et al. showed that oral supplementation with red clover extract improved scalp hair and skin status as well as libido, mood, sleep, and fatigue in a study with 109 postmenopausal women.11
The topical application of the soy isoflavones genistein, daidzein, and glycitein has shown promise as a treatment for photoaging and photodamage.12 Genistein has been noted for its antioxidant and antibrowning activity, and has exhibited anti-aging properties in mouse studies and photoprotective activity in humans.13 A 2015 study by Zhao et al. in cultured skin fibroblasts and nude mouse skin indicated that daidzein treatment appears to increase skin collagen production and suppress collagen degradation.14
Flavan-3-ols (catechins): epigallocatechin 3-gallate
Already considered a potent antioxidant, epigallocatechin 3-gallate (EGCG) continues to receive attention for conferring an expanding range of health benefits. This catechin, which is the most abundant and potent of such compounds in green tea, has exhibited the capacity to hinder UVB-induced collagen-degrading matrix metalloproteinases (MMPs).15 EGCG also has been proposed as a preventive and therapeutic agent for keloids, given findings indicating that it hampered the proliferation and migration of keloid fibroblasts in vitro, as well as in vivo by interrupting the signal transducer and activator of transcription 3 (STAT3) signaling pathway.16 Further, EGCG has been suggested as a potential therapeutic approach to atopic dermatitis (AD) given success against AD-like skin lesions in a murine model.17 An investigation of the anti-aging cutaneous effects of EGCG on d-galactose-induced aging in mice revealed that subcutaneously injected EGCG yielded overall improvement in the structure and function of the skin.18 EGCG also is known to yield improvements in skin condition by providing DNA protection, reactivating damaged cells, and increasing cellular energy production.3
Perhaps most importantly, formulations containing green tea extracts have been shown in a small study of 20 volunteers to exert protection against photoaging and photoimmunosuppression, with the extract hindering the expression of MMP-9 and MMP-2.19 Wrinkle reduction also was observed in another clinical study involving topical green tea.20 The tea plant Camellia sinensis is one of the best sources of antioxidant catechins, particularly green tea (unfermented), but also white (unfermented), black (fermented), and oolong (semifermented) tea.21
Anthocyanins: cyanidin
A 2017 in vivo study in mice found that cyanidin hindered the binding of the cytokine interleukin-17A to the IL-17RA subunit to reduce inflammation.22 In a 2007 study, methanol extracts of black raspberries, strawberries, and blueberries were tested for the capacity to inhibit UV-induced activation of nuclear factor–kappa B (NF-kappaB) and activator protein–1 (AP-1) in mouse epidermal cells. The methanol fractions of black raspberries, which contain the anthocyanin cyanidin-3-rutinoside, were found to time- and dose-dependently inhibit the UV effects on NF-kappaB and AP-1, unlike the other berries, which do not contain cyanidin-3-rutinoside.23 The pretreatment of human keratinocytes with the anthocyanin cyanidin-3-O-glucoside also has been demonstrated to protect against a wide array of UVB-induced damage,24 and acai fruit–derived cyanidin and malvidin have been shown recently to thwart UVA-induced stress in immortalized fibroblasts.25 Further, cyanidin derived from elderberries has exhibited antiproliferative and apoptotic potential on melanoma cells in a 2017 mouse model, indicating a potential role in skin cancer treatment.26
Conclusion
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Eur J Pharm Biopharm. 2016 Nov;108:41-53.
2. Clin Cosmet Investig Dermatol. 2016 Feb 26;9:55-62.
3. Int J Mol Sci. 2016 Feb 18;17(2):160-201.
4. Cancer Res. 2008 Apr 15:68(8):3057-65.
5. J Acupunct Meridian Stud. 2013 Oct;6(5):252-62.
6. Evid Based Complement Alternat Med. 2012;2012:912028.
7. Photochem Photobiol. 2008 Mar-Apr;84(2):307-16.
8. PLoS One. 2016 Jan 7;11(1):e0146296.
9. J Photochem Photobiol B. 2017 Feb;167:72-81.
10. Phytother Res. 2006 Dec;20(12):1096-9.
11. Obstet Gynecol Int. 2011;2011:949302.
12. Int J Pharm. 2008 Nov 19;364(1):36-44.
13. Biomed Pharmacother. 2016 Aug;82:379-92.
14. Australas J Dermatol. 2015 Feb;56(1):e7-14.
15. Food Chem Toxicol. 2008 Apr;46(4):1298-307.
16. J Invest Dermatol. 2008 Oct;128(10):2429-41.
17. Int Immunopharmacol. 2008 Sep;8(9):1172-82.
18. Mech Ageing Dev. 2017 Mar 24;164:1-7.
19. Skin Res Technol. 2009 Aug;15(3):338-45.
20. Int J Cosmet Sci. 2010 Apr;32(2):99-106.
21. Int J Cosmet Sci. 2015 Oct;37(5):455-64.
22. Sci Signal. 2017 Feb 21;10(467). eaaf8823.
23. Nutr Cancer. 2007;58(2):205-12.
24. J Agric Food Chem. 2006 May 31;54(11):4041-7.
25. J Photochem Photobiol B. 2017 Jul;172:42-51.
26. Int J Mol Sci. 2017 Apr 30;18(5):949.
This column picks up with a recent literature review suggesting potential benefits of topically applied or orally administered flavonoid polyphenolic substances. The discussion is based on at least one sample compound from each flavonoid category.
Flavonols: quercetin
Known to exert substantial antioxidant and anti-inflammatory activities, quercetin has been shown in various cellular and animal-based models to deliver photoprotection from UV and contribute to wound healing.1 In a single center, single-blind trial with 30 healthy volunteers, a 1% topical quercetin cream was found to be effective in reducing erythema, itching, and wheal diameter in experimentally-induced skin stress.2 Quercetin also has been reported to have the capacity to inhibit melanin production.3
Flavones: apigenin
Flavanones: naringenin
The citrus flavanone naringenin shows promise as a preventive agent against cutaneous aging as well as carcinogenesis. In a 2008 study, naringenin exerted an anti-apoptotic effect in UVB-damaged cells, significantly extending long-term cellular survival, and facilitating the removal of cyclobutane pyrimidine dimers from the genome.7 More recently, topical naringenin has been shown in mice to mitigate the cutaneous inflammation and oxidative stress caused by UVB irradiation,8 and, present in Lippia graveolens, to protect against chronic UVB-induced damage including phototumorigenesis.9
Isoflavones: red clover, genistein, and daidzein
Red clover, the isoflavones of which have been demonstrated – in high dietary concentrations – to contribute to low incidence of osteoporosis and menopausal symptoms, was shown in a 2006 study to exert anti-aging effects in mice, indicating potential for alleviating the cutaneous aging brought on by declines in estrogen.10 In 2011, Lipovac et al. showed that oral supplementation with red clover extract improved scalp hair and skin status as well as libido, mood, sleep, and fatigue in a study with 109 postmenopausal women.11
The topical application of the soy isoflavones genistein, daidzein, and glycitein has shown promise as a treatment for photoaging and photodamage.12 Genistein has been noted for its antioxidant and antibrowning activity, and has exhibited anti-aging properties in mouse studies and photoprotective activity in humans.13 A 2015 study by Zhao et al. in cultured skin fibroblasts and nude mouse skin indicated that daidzein treatment appears to increase skin collagen production and suppress collagen degradation.14
Flavan-3-ols (catechins): epigallocatechin 3-gallate
Already considered a potent antioxidant, epigallocatechin 3-gallate (EGCG) continues to receive attention for conferring an expanding range of health benefits. This catechin, which is the most abundant and potent of such compounds in green tea, has exhibited the capacity to hinder UVB-induced collagen-degrading matrix metalloproteinases (MMPs).15 EGCG also has been proposed as a preventive and therapeutic agent for keloids, given findings indicating that it hampered the proliferation and migration of keloid fibroblasts in vitro, as well as in vivo by interrupting the signal transducer and activator of transcription 3 (STAT3) signaling pathway.16 Further, EGCG has been suggested as a potential therapeutic approach to atopic dermatitis (AD) given success against AD-like skin lesions in a murine model.17 An investigation of the anti-aging cutaneous effects of EGCG on d-galactose-induced aging in mice revealed that subcutaneously injected EGCG yielded overall improvement in the structure and function of the skin.18 EGCG also is known to yield improvements in skin condition by providing DNA protection, reactivating damaged cells, and increasing cellular energy production.3
Perhaps most importantly, formulations containing green tea extracts have been shown in a small study of 20 volunteers to exert protection against photoaging and photoimmunosuppression, with the extract hindering the expression of MMP-9 and MMP-2.19 Wrinkle reduction also was observed in another clinical study involving topical green tea.20 The tea plant Camellia sinensis is one of the best sources of antioxidant catechins, particularly green tea (unfermented), but also white (unfermented), black (fermented), and oolong (semifermented) tea.21
Anthocyanins: cyanidin
A 2017 in vivo study in mice found that cyanidin hindered the binding of the cytokine interleukin-17A to the IL-17RA subunit to reduce inflammation.22 In a 2007 study, methanol extracts of black raspberries, strawberries, and blueberries were tested for the capacity to inhibit UV-induced activation of nuclear factor–kappa B (NF-kappaB) and activator protein–1 (AP-1) in mouse epidermal cells. The methanol fractions of black raspberries, which contain the anthocyanin cyanidin-3-rutinoside, were found to time- and dose-dependently inhibit the UV effects on NF-kappaB and AP-1, unlike the other berries, which do not contain cyanidin-3-rutinoside.23 The pretreatment of human keratinocytes with the anthocyanin cyanidin-3-O-glucoside also has been demonstrated to protect against a wide array of UVB-induced damage,24 and acai fruit–derived cyanidin and malvidin have been shown recently to thwart UVA-induced stress in immortalized fibroblasts.25 Further, cyanidin derived from elderberries has exhibited antiproliferative and apoptotic potential on melanoma cells in a 2017 mouse model, indicating a potential role in skin cancer treatment.26
Conclusion
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Eur J Pharm Biopharm. 2016 Nov;108:41-53.
2. Clin Cosmet Investig Dermatol. 2016 Feb 26;9:55-62.
3. Int J Mol Sci. 2016 Feb 18;17(2):160-201.
4. Cancer Res. 2008 Apr 15:68(8):3057-65.
5. J Acupunct Meridian Stud. 2013 Oct;6(5):252-62.
6. Evid Based Complement Alternat Med. 2012;2012:912028.
7. Photochem Photobiol. 2008 Mar-Apr;84(2):307-16.
8. PLoS One. 2016 Jan 7;11(1):e0146296.
9. J Photochem Photobiol B. 2017 Feb;167:72-81.
10. Phytother Res. 2006 Dec;20(12):1096-9.
11. Obstet Gynecol Int. 2011;2011:949302.
12. Int J Pharm. 2008 Nov 19;364(1):36-44.
13. Biomed Pharmacother. 2016 Aug;82:379-92.
14. Australas J Dermatol. 2015 Feb;56(1):e7-14.
15. Food Chem Toxicol. 2008 Apr;46(4):1298-307.
16. J Invest Dermatol. 2008 Oct;128(10):2429-41.
17. Int Immunopharmacol. 2008 Sep;8(9):1172-82.
18. Mech Ageing Dev. 2017 Mar 24;164:1-7.
19. Skin Res Technol. 2009 Aug;15(3):338-45.
20. Int J Cosmet Sci. 2010 Apr;32(2):99-106.
21. Int J Cosmet Sci. 2015 Oct;37(5):455-64.
22. Sci Signal. 2017 Feb 21;10(467). eaaf8823.
23. Nutr Cancer. 2007;58(2):205-12.
24. J Agric Food Chem. 2006 May 31;54(11):4041-7.
25. J Photochem Photobiol B. 2017 Jul;172:42-51.
26. Int J Mol Sci. 2017 Apr 30;18(5):949.
Regional differences in surgical outcomes could unfairly skew bundled payments
Risk-adjusted adverse outcomes for elective colorectal surgery vary significantly across regions in the United States, and, therefore, regionally based Medicare payments could disadvantage some hospitals.
The findings, presented at the annual Central Surgical Association meeting, suggest that alternative payment models (APMs) should consider regional benchmarks as a variable when evaluating quality and pricing of episodes of care to level the playing field among hospitals, the study authors said.
All hospitals with a minimum of 20 evaluable colorectal resection cases from the master data set regardless of coding quality were identified for comparative outcomes. For hospital analysis, the total number of patients with one or more adverse outcomes (AOs) was tabulated. The total predicted AOs were then set equal to the number of observed events for each hospital by multiplication of the hospital-specific predicted value by the ratio of observed-to-predicted events for the entire final hospital population of patients.
Hospitals were then sorted by the nine Census Bureau regions: region 1 (New England), region 2 (Middle Atlantic), region 3 (South Atlantic), region 4 (East South Central), region 5 (West South Central), region 6 (East North Central), region 7 (West North Central), region 8 (Mountain), and region 9 (Pacific).
Within each region, total patients, total observed AOs, and total predicted AOs were derived from the prediction models. Region-specific standard deviations (SDs) were computed and overall region z scores and risk-adjusted AO rates were calculated for comparison.
A total of 1,497 hospitals had 86,624 patients for the comparative analysis of hospitals with 20 or more qualifying cases. Hospitals averaged 57.9 cases with a median of 43 for the study period. Among the AOs, there were 947 IpD (1.1%), 7,268 prLOS (8.4%), 762 PD90 (0.9%), and 14,552 RA90 (16.8%) patients. An additional 1,130 patients died during or following readmission within the 90-day postdischarge period for total postoperative deaths including inpatient and 90 days following discharge of 2,839 (3.3%). Total patients with one or more AOs were 21,064 (24.3%).
Among the hospitals, 49 (3.3%) had z scores of –2.0 or less. These best-performing hospitals had a median z score of –2.24 and a median risk-adjusted AO rate of 10.8%. A total of 159 hospitals (10.6%) had z scores that were greater than –2.0 but less than or equal to –1.0. These hospitals had a median risk-adjusted AO rate of 15.1%. There were 66 hospitals (4.4%) with z scores greater than +2.0. These suboptimal-performing hospitals had a z score of +2.39 and a median risk-adjusted AO rate of 38.8%. A total of 209 hospitals (14.0%) had z scores greater than or equal to +1.0 but less than +2.0. They had a median risk-adjusted AO rate of 32.5%.
Findings showed a nearly 5-SD difference between the Pacific region and the New England region. In addition, the results showed a 2.5% absolute risk–adjusted adverse outcome rate difference between the top- and the lowest-performing regions.
What findings could mean for bundled payments
The findings raise concerns about a lopsided playing field for hospitals when it comes to bundled payments, according to the study authors.
“What that means is if you have more readmissions and more complications and your historical profile is being used to pay for care going forward, regions of the country with poorer outcomes would get higher prices than those areas with better outcomes,” Dr. Fry, executive vice president, clinical outcomes management, MPA Healthcare Solutions, Chicago, said in an interview.
The Centers for Medicare & Medicaid Services has used performance of the Census Bureau region as a major factor in defining target price at the beginning of the Comprehensive Care for Joint Replacement bundled payment program. Regional performance will become the exclusive basis for the target price as the program matures into successive years, the study authors noted. A colorectal surgery bundle has not yet been proposed by Medicare, but because it’s a common operation with relatively high adverse outcomes rates, it is expected to be included in a future bundled payment strategy, according to the investigators.
Dr. Fry and his coauthors concluded that hospitals and surgeons may find meeting the target price of a bundled payment to improve margins or avoid losses more difficult for any inpatient operation if they are in a best-performing region.
A 2.5% adverse outcome rate difference between regions may not seem like much, but the variance could mean a wide disparity in payments, Dr. Fry said.
“We have done previous research with colon operations and identified that a readmission after an elective colon operation costs about an additional $30,000,” he said. “If cases being done in poorer-performing areas of the country have two or three more readmissions per 100 patients, then it means those areas are going to be paid on average $1,000 more per case than would be the circumstance for those areas where outcomes are better.”
By these parameters, the CMS would basically be rewarding care that is suboptimal in the regions with high adverse outcome rates, he said.
“APMs are going to evolve in health care,” Dr. Fry said. “I feel that regional and local outcomes, as illustrated in this article, are different, and that a national standard for expected outcomes needs to be the benchmark. The national benchmark becomes a method to stimulate hospitals and surgeons to know what the results of their care really are and how they compare nationally.”
Perspectives on the study
However, it remains unclear whether adjustment for quality measures should be based on regions, and, if so, how those regions should be broken down, said Dr. Whitcomb, who is cofounder and past president of the Society of Hospital Medicine. Another question is whether adjustments should take into consideration the characteristics of hospitals, he said, for example, the general demographics of patients who visit academic medical centers, compared with the demographics of community hospitals. Dr. Whitcomb also noted that programs such as the Hospital Readmissions Reduction Program has faced criticism for not factoring in the disproportionately high share of low socioeconomic status patients at some hospitals.
“The paper raises the important issue of comparing apples to apples when quality measures are used to determine payment under alternative payment models,” Dr. Whitcomb said in an interview. “But a number of questions remain about how risk should be adjusted and how benchmarking should occur between hospitals.”
“The overall average adverse outcome in the study was 24.3%, but 16.8% of that 24% is due to readmissions,” he said in an interview. “Length of stay and readmissions are correlated – people who tend to have long lengths of stay tend to be readmitted. If you add those two rates together in the study, almost all of the outcome rate is the length of stay and readmissions. You could argue [that] mortality [should] be more heavily weighted than length of stay and readmissions.”
In regard to adjusting risk by region, there is good research that utilization of procedures varies dramatically by region and that some of this variation may have more to do with overutilization of procedures, Dr. Pitt added.
“I would think that risk adjusting for type of operation, diagnosis, and socioeconomic status –across the country – would be more appropriate than risk adjusting by region where there may be major differences in patient selection and indication for operation,” he said.
For example, there is currently an international debate about the management of diverticulitis, including whether and when to operate as well as what procedure(s) to perform.
“It may be in one region, there’s a very low threshold to operate, whereas in another region, there’s a high threshold to operate,” he said. “And the operations that are done may be very different in one region than another.”
Dr. Fry and his colleagues are planning future research in this area, and he said he hopes their studies will impact how the CMS rolls out its bundled payment programs in the future.
“What we’re trying to stimulate is for payment models to be nationally indexed and not regionally indexed,” he said. “CMS is doing that now with [Medicare Severity–Diagnosis Related Groups]. They are paying a price for a total joint replacement, a price for a colon resection, a price for a heart operation – and they do make adjustments based on the local wage and price index, but the core payment is linked to a national payment model, and that’s what we would like to see happen with the bundled payment initiative.”
[email protected]
On Twitter @legal_med
Risk-adjusted adverse outcomes for elective colorectal surgery vary significantly across regions in the United States, and, therefore, regionally based Medicare payments could disadvantage some hospitals.
The findings, presented at the annual Central Surgical Association meeting, suggest that alternative payment models (APMs) should consider regional benchmarks as a variable when evaluating quality and pricing of episodes of care to level the playing field among hospitals, the study authors said.
All hospitals with a minimum of 20 evaluable colorectal resection cases from the master data set regardless of coding quality were identified for comparative outcomes. For hospital analysis, the total number of patients with one or more adverse outcomes (AOs) was tabulated. The total predicted AOs were then set equal to the number of observed events for each hospital by multiplication of the hospital-specific predicted value by the ratio of observed-to-predicted events for the entire final hospital population of patients.
Hospitals were then sorted by the nine Census Bureau regions: region 1 (New England), region 2 (Middle Atlantic), region 3 (South Atlantic), region 4 (East South Central), region 5 (West South Central), region 6 (East North Central), region 7 (West North Central), region 8 (Mountain), and region 9 (Pacific).
Within each region, total patients, total observed AOs, and total predicted AOs were derived from the prediction models. Region-specific standard deviations (SDs) were computed and overall region z scores and risk-adjusted AO rates were calculated for comparison.
A total of 1,497 hospitals had 86,624 patients for the comparative analysis of hospitals with 20 or more qualifying cases. Hospitals averaged 57.9 cases with a median of 43 for the study period. Among the AOs, there were 947 IpD (1.1%), 7,268 prLOS (8.4%), 762 PD90 (0.9%), and 14,552 RA90 (16.8%) patients. An additional 1,130 patients died during or following readmission within the 90-day postdischarge period for total postoperative deaths including inpatient and 90 days following discharge of 2,839 (3.3%). Total patients with one or more AOs were 21,064 (24.3%).
Among the hospitals, 49 (3.3%) had z scores of –2.0 or less. These best-performing hospitals had a median z score of –2.24 and a median risk-adjusted AO rate of 10.8%. A total of 159 hospitals (10.6%) had z scores that were greater than –2.0 but less than or equal to –1.0. These hospitals had a median risk-adjusted AO rate of 15.1%. There were 66 hospitals (4.4%) with z scores greater than +2.0. These suboptimal-performing hospitals had a z score of +2.39 and a median risk-adjusted AO rate of 38.8%. A total of 209 hospitals (14.0%) had z scores greater than or equal to +1.0 but less than +2.0. They had a median risk-adjusted AO rate of 32.5%.
Findings showed a nearly 5-SD difference between the Pacific region and the New England region. In addition, the results showed a 2.5% absolute risk–adjusted adverse outcome rate difference between the top- and the lowest-performing regions.
What findings could mean for bundled payments
The findings raise concerns about a lopsided playing field for hospitals when it comes to bundled payments, according to the study authors.
“What that means is if you have more readmissions and more complications and your historical profile is being used to pay for care going forward, regions of the country with poorer outcomes would get higher prices than those areas with better outcomes,” Dr. Fry, executive vice president, clinical outcomes management, MPA Healthcare Solutions, Chicago, said in an interview.
The Centers for Medicare & Medicaid Services has used performance of the Census Bureau region as a major factor in defining target price at the beginning of the Comprehensive Care for Joint Replacement bundled payment program. Regional performance will become the exclusive basis for the target price as the program matures into successive years, the study authors noted. A colorectal surgery bundle has not yet been proposed by Medicare, but because it’s a common operation with relatively high adverse outcomes rates, it is expected to be included in a future bundled payment strategy, according to the investigators.
Dr. Fry and his coauthors concluded that hospitals and surgeons may find meeting the target price of a bundled payment to improve margins or avoid losses more difficult for any inpatient operation if they are in a best-performing region.
A 2.5% adverse outcome rate difference between regions may not seem like much, but the variance could mean a wide disparity in payments, Dr. Fry said.
“We have done previous research with colon operations and identified that a readmission after an elective colon operation costs about an additional $30,000,” he said. “If cases being done in poorer-performing areas of the country have two or three more readmissions per 100 patients, then it means those areas are going to be paid on average $1,000 more per case than would be the circumstance for those areas where outcomes are better.”
By these parameters, the CMS would basically be rewarding care that is suboptimal in the regions with high adverse outcome rates, he said.
“APMs are going to evolve in health care,” Dr. Fry said. “I feel that regional and local outcomes, as illustrated in this article, are different, and that a national standard for expected outcomes needs to be the benchmark. The national benchmark becomes a method to stimulate hospitals and surgeons to know what the results of their care really are and how they compare nationally.”
Perspectives on the study
However, it remains unclear whether adjustment for quality measures should be based on regions, and, if so, how those regions should be broken down, said Dr. Whitcomb, who is cofounder and past president of the Society of Hospital Medicine. Another question is whether adjustments should take into consideration the characteristics of hospitals, he said, for example, the general demographics of patients who visit academic medical centers, compared with the demographics of community hospitals. Dr. Whitcomb also noted that programs such as the Hospital Readmissions Reduction Program has faced criticism for not factoring in the disproportionately high share of low socioeconomic status patients at some hospitals.
“The paper raises the important issue of comparing apples to apples when quality measures are used to determine payment under alternative payment models,” Dr. Whitcomb said in an interview. “But a number of questions remain about how risk should be adjusted and how benchmarking should occur between hospitals.”
“The overall average adverse outcome in the study was 24.3%, but 16.8% of that 24% is due to readmissions,” he said in an interview. “Length of stay and readmissions are correlated – people who tend to have long lengths of stay tend to be readmitted. If you add those two rates together in the study, almost all of the outcome rate is the length of stay and readmissions. You could argue [that] mortality [should] be more heavily weighted than length of stay and readmissions.”
In regard to adjusting risk by region, there is good research that utilization of procedures varies dramatically by region and that some of this variation may have more to do with overutilization of procedures, Dr. Pitt added.
“I would think that risk adjusting for type of operation, diagnosis, and socioeconomic status –across the country – would be more appropriate than risk adjusting by region where there may be major differences in patient selection and indication for operation,” he said.
For example, there is currently an international debate about the management of diverticulitis, including whether and when to operate as well as what procedure(s) to perform.
“It may be in one region, there’s a very low threshold to operate, whereas in another region, there’s a high threshold to operate,” he said. “And the operations that are done may be very different in one region than another.”
Dr. Fry and his colleagues are planning future research in this area, and he said he hopes their studies will impact how the CMS rolls out its bundled payment programs in the future.
“What we’re trying to stimulate is for payment models to be nationally indexed and not regionally indexed,” he said. “CMS is doing that now with [Medicare Severity–Diagnosis Related Groups]. They are paying a price for a total joint replacement, a price for a colon resection, a price for a heart operation – and they do make adjustments based on the local wage and price index, but the core payment is linked to a national payment model, and that’s what we would like to see happen with the bundled payment initiative.”
[email protected]
On Twitter @legal_med
Risk-adjusted adverse outcomes for elective colorectal surgery vary significantly across regions in the United States, and, therefore, regionally based Medicare payments could disadvantage some hospitals.
The findings, presented at the annual Central Surgical Association meeting, suggest that alternative payment models (APMs) should consider regional benchmarks as a variable when evaluating quality and pricing of episodes of care to level the playing field among hospitals, the study authors said.
All hospitals with a minimum of 20 evaluable colorectal resection cases from the master data set regardless of coding quality were identified for comparative outcomes. For hospital analysis, the total number of patients with one or more adverse outcomes (AOs) was tabulated. The total predicted AOs were then set equal to the number of observed events for each hospital by multiplication of the hospital-specific predicted value by the ratio of observed-to-predicted events for the entire final hospital population of patients.
Hospitals were then sorted by the nine Census Bureau regions: region 1 (New England), region 2 (Middle Atlantic), region 3 (South Atlantic), region 4 (East South Central), region 5 (West South Central), region 6 (East North Central), region 7 (West North Central), region 8 (Mountain), and region 9 (Pacific).
Within each region, total patients, total observed AOs, and total predicted AOs were derived from the prediction models. Region-specific standard deviations (SDs) were computed and overall region z scores and risk-adjusted AO rates were calculated for comparison.
A total of 1,497 hospitals had 86,624 patients for the comparative analysis of hospitals with 20 or more qualifying cases. Hospitals averaged 57.9 cases with a median of 43 for the study period. Among the AOs, there were 947 IpD (1.1%), 7,268 prLOS (8.4%), 762 PD90 (0.9%), and 14,552 RA90 (16.8%) patients. An additional 1,130 patients died during or following readmission within the 90-day postdischarge period for total postoperative deaths including inpatient and 90 days following discharge of 2,839 (3.3%). Total patients with one or more AOs were 21,064 (24.3%).
Among the hospitals, 49 (3.3%) had z scores of –2.0 or less. These best-performing hospitals had a median z score of –2.24 and a median risk-adjusted AO rate of 10.8%. A total of 159 hospitals (10.6%) had z scores that were greater than –2.0 but less than or equal to –1.0. These hospitals had a median risk-adjusted AO rate of 15.1%. There were 66 hospitals (4.4%) with z scores greater than +2.0. These suboptimal-performing hospitals had a z score of +2.39 and a median risk-adjusted AO rate of 38.8%. A total of 209 hospitals (14.0%) had z scores greater than or equal to +1.0 but less than +2.0. They had a median risk-adjusted AO rate of 32.5%.
Findings showed a nearly 5-SD difference between the Pacific region and the New England region. In addition, the results showed a 2.5% absolute risk–adjusted adverse outcome rate difference between the top- and the lowest-performing regions.
What findings could mean for bundled payments
The findings raise concerns about a lopsided playing field for hospitals when it comes to bundled payments, according to the study authors.
“What that means is if you have more readmissions and more complications and your historical profile is being used to pay for care going forward, regions of the country with poorer outcomes would get higher prices than those areas with better outcomes,” Dr. Fry, executive vice president, clinical outcomes management, MPA Healthcare Solutions, Chicago, said in an interview.
The Centers for Medicare & Medicaid Services has used performance of the Census Bureau region as a major factor in defining target price at the beginning of the Comprehensive Care for Joint Replacement bundled payment program. Regional performance will become the exclusive basis for the target price as the program matures into successive years, the study authors noted. A colorectal surgery bundle has not yet been proposed by Medicare, but because it’s a common operation with relatively high adverse outcomes rates, it is expected to be included in a future bundled payment strategy, according to the investigators.
Dr. Fry and his coauthors concluded that hospitals and surgeons may find meeting the target price of a bundled payment to improve margins or avoid losses more difficult for any inpatient operation if they are in a best-performing region.
A 2.5% adverse outcome rate difference between regions may not seem like much, but the variance could mean a wide disparity in payments, Dr. Fry said.
“We have done previous research with colon operations and identified that a readmission after an elective colon operation costs about an additional $30,000,” he said. “If cases being done in poorer-performing areas of the country have two or three more readmissions per 100 patients, then it means those areas are going to be paid on average $1,000 more per case than would be the circumstance for those areas where outcomes are better.”
By these parameters, the CMS would basically be rewarding care that is suboptimal in the regions with high adverse outcome rates, he said.
“APMs are going to evolve in health care,” Dr. Fry said. “I feel that regional and local outcomes, as illustrated in this article, are different, and that a national standard for expected outcomes needs to be the benchmark. The national benchmark becomes a method to stimulate hospitals and surgeons to know what the results of their care really are and how they compare nationally.”
Perspectives on the study
However, it remains unclear whether adjustment for quality measures should be based on regions, and, if so, how those regions should be broken down, said Dr. Whitcomb, who is cofounder and past president of the Society of Hospital Medicine. Another question is whether adjustments should take into consideration the characteristics of hospitals, he said, for example, the general demographics of patients who visit academic medical centers, compared with the demographics of community hospitals. Dr. Whitcomb also noted that programs such as the Hospital Readmissions Reduction Program has faced criticism for not factoring in the disproportionately high share of low socioeconomic status patients at some hospitals.
“The paper raises the important issue of comparing apples to apples when quality measures are used to determine payment under alternative payment models,” Dr. Whitcomb said in an interview. “But a number of questions remain about how risk should be adjusted and how benchmarking should occur between hospitals.”
“The overall average adverse outcome in the study was 24.3%, but 16.8% of that 24% is due to readmissions,” he said in an interview. “Length of stay and readmissions are correlated – people who tend to have long lengths of stay tend to be readmitted. If you add those two rates together in the study, almost all of the outcome rate is the length of stay and readmissions. You could argue [that] mortality [should] be more heavily weighted than length of stay and readmissions.”
In regard to adjusting risk by region, there is good research that utilization of procedures varies dramatically by region and that some of this variation may have more to do with overutilization of procedures, Dr. Pitt added.
“I would think that risk adjusting for type of operation, diagnosis, and socioeconomic status –across the country – would be more appropriate than risk adjusting by region where there may be major differences in patient selection and indication for operation,” he said.
For example, there is currently an international debate about the management of diverticulitis, including whether and when to operate as well as what procedure(s) to perform.
“It may be in one region, there’s a very low threshold to operate, whereas in another region, there’s a high threshold to operate,” he said. “And the operations that are done may be very different in one region than another.”
Dr. Fry and his colleagues are planning future research in this area, and he said he hopes their studies will impact how the CMS rolls out its bundled payment programs in the future.
“What we’re trying to stimulate is for payment models to be nationally indexed and not regionally indexed,” he said. “CMS is doing that now with [Medicare Severity–Diagnosis Related Groups]. They are paying a price for a total joint replacement, a price for a colon resection, a price for a heart operation – and they do make adjustments based on the local wage and price index, but the core payment is linked to a national payment model, and that’s what we would like to see happen with the bundled payment initiative.”
[email protected]
On Twitter @legal_med
Pembrolizumab and Nivolumab May Cause Neurologic Events
Approximately 3% of patients developed adverse neurologic events within 12 months of receiving nivolumab or pembrolizumab, according to the results of a single-center retrospective study published online ahead of print September 5 in JAMA Neurology.
These syndromes included myopathy, axonal thoracolumbar polyradiculopathy, severe demyelinating length-dependent peripheral neuropathy with axonal loss, asymmetric vasculitic neuropathy, cerebellar ataxia, autoimmune retinopathy, bilateral internuclear ophthalmoplegia, and headache, said Justin C. Kao, MBChB, a neurologist at Mayo Clinic in Rochester, Minnesota, and his coinvestigators.
Nivolumab and pembrolizumab are anti-programmed death–1 (PD-1) antibodies. In response to an increase in reports of neurologic events associated with anti–PD-1 therapy, the investigators searched the Mayo Cancer Pharmacy Database and identified 347 patients treated with pembrolizumab or nivolumab between 2014 and 2016. Ten patients (2.9%, two women) developed neurologic complications within 12 months of anti–PD-1 exposure. The median age was 71. None of their neurologic symptoms could be attributed directly to other treatments or to metastatic disease. Median modified Rankin Scale (mRS) score was 2.5. Symptom severity peaked at between one day and more than three months after starting anti–PD-1 treatment.
Stopping anti–PD-1 treatment and starting high-dose corticosteroids led to neurologic improvements (median mRS score, 2). A patient with necrotizing myopathy who had been receiving pembrolizumab for stage 4 melanoma developed extraocular, bulbar, and respiratory muscle weakness. These symptoms worsened over three weeks and did not respond to prednisone (80 mg/day) or to three sessions of plasmapheresis. The patient subsequently died.
If a patient on anti–PD-1 therapy develops neurologic symptoms, clinicians should promptly stop treatment and pursue a full workup, including electrodiagnostic studies and consideration of muscle or nerve biopsy to clarify the underlying pathophysiologic mechanisms, the researchers said. “If the clinical examination demonstrates severe clinical deficits at onset or worsens despite medication discontinuation, additional immune suppressant treatment should be considered,” they said.
—Amy Karon
Suggested Reading
Kao JC, Liao B, Markovic SN, et al. Neurological complications associated with anti-programmed death 1 (PD-1) antibodies. JAMA Neurol. 2017 Sep 5 [Epub ahead of print].
Approximately 3% of patients developed adverse neurologic events within 12 months of receiving nivolumab or pembrolizumab, according to the results of a single-center retrospective study published online ahead of print September 5 in JAMA Neurology.
These syndromes included myopathy, axonal thoracolumbar polyradiculopathy, severe demyelinating length-dependent peripheral neuropathy with axonal loss, asymmetric vasculitic neuropathy, cerebellar ataxia, autoimmune retinopathy, bilateral internuclear ophthalmoplegia, and headache, said Justin C. Kao, MBChB, a neurologist at Mayo Clinic in Rochester, Minnesota, and his coinvestigators.
Nivolumab and pembrolizumab are anti-programmed death–1 (PD-1) antibodies. In response to an increase in reports of neurologic events associated with anti–PD-1 therapy, the investigators searched the Mayo Cancer Pharmacy Database and identified 347 patients treated with pembrolizumab or nivolumab between 2014 and 2016. Ten patients (2.9%, two women) developed neurologic complications within 12 months of anti–PD-1 exposure. The median age was 71. None of their neurologic symptoms could be attributed directly to other treatments or to metastatic disease. Median modified Rankin Scale (mRS) score was 2.5. Symptom severity peaked at between one day and more than three months after starting anti–PD-1 treatment.
Stopping anti–PD-1 treatment and starting high-dose corticosteroids led to neurologic improvements (median mRS score, 2). A patient with necrotizing myopathy who had been receiving pembrolizumab for stage 4 melanoma developed extraocular, bulbar, and respiratory muscle weakness. These symptoms worsened over three weeks and did not respond to prednisone (80 mg/day) or to three sessions of plasmapheresis. The patient subsequently died.
If a patient on anti–PD-1 therapy develops neurologic symptoms, clinicians should promptly stop treatment and pursue a full workup, including electrodiagnostic studies and consideration of muscle or nerve biopsy to clarify the underlying pathophysiologic mechanisms, the researchers said. “If the clinical examination demonstrates severe clinical deficits at onset or worsens despite medication discontinuation, additional immune suppressant treatment should be considered,” they said.
—Amy Karon
Suggested Reading
Kao JC, Liao B, Markovic SN, et al. Neurological complications associated with anti-programmed death 1 (PD-1) antibodies. JAMA Neurol. 2017 Sep 5 [Epub ahead of print].
Approximately 3% of patients developed adverse neurologic events within 12 months of receiving nivolumab or pembrolizumab, according to the results of a single-center retrospective study published online ahead of print September 5 in JAMA Neurology.
These syndromes included myopathy, axonal thoracolumbar polyradiculopathy, severe demyelinating length-dependent peripheral neuropathy with axonal loss, asymmetric vasculitic neuropathy, cerebellar ataxia, autoimmune retinopathy, bilateral internuclear ophthalmoplegia, and headache, said Justin C. Kao, MBChB, a neurologist at Mayo Clinic in Rochester, Minnesota, and his coinvestigators.
Nivolumab and pembrolizumab are anti-programmed death–1 (PD-1) antibodies. In response to an increase in reports of neurologic events associated with anti–PD-1 therapy, the investigators searched the Mayo Cancer Pharmacy Database and identified 347 patients treated with pembrolizumab or nivolumab between 2014 and 2016. Ten patients (2.9%, two women) developed neurologic complications within 12 months of anti–PD-1 exposure. The median age was 71. None of their neurologic symptoms could be attributed directly to other treatments or to metastatic disease. Median modified Rankin Scale (mRS) score was 2.5. Symptom severity peaked at between one day and more than three months after starting anti–PD-1 treatment.
Stopping anti–PD-1 treatment and starting high-dose corticosteroids led to neurologic improvements (median mRS score, 2). A patient with necrotizing myopathy who had been receiving pembrolizumab for stage 4 melanoma developed extraocular, bulbar, and respiratory muscle weakness. These symptoms worsened over three weeks and did not respond to prednisone (80 mg/day) or to three sessions of plasmapheresis. The patient subsequently died.
If a patient on anti–PD-1 therapy develops neurologic symptoms, clinicians should promptly stop treatment and pursue a full workup, including electrodiagnostic studies and consideration of muscle or nerve biopsy to clarify the underlying pathophysiologic mechanisms, the researchers said. “If the clinical examination demonstrates severe clinical deficits at onset or worsens despite medication discontinuation, additional immune suppressant treatment should be considered,” they said.
—Amy Karon
Suggested Reading
Kao JC, Liao B, Markovic SN, et al. Neurological complications associated with anti-programmed death 1 (PD-1) antibodies. JAMA Neurol. 2017 Sep 5 [Epub ahead of print].