User login
Agent exhibits activity in leukemias, MDS
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
EC expands indication for denosumab to MM
The European Commission (EC) has approved an expanded indication for denosumab (Xgeva).
The drug is now approved for the prevention of skeletal-related events (SREs) in adults with advanced malignancies involving bone, which includes patients with multiple myeloma (MM).
Approval from the EC provides a centralized marketing authorization with unified labeling in all member countries of the European Union.
Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
Denosumab was previously approved by the EC to prevent SREs—defined as radiation to bone, pathologic fracture, surgery to bone, and spinal cord compression—in adults with bone metastases from solid tumors.
Denosumab also received EC approval for the treatment of adults and skeletally mature adolescents with giant cell tumor of bone that is unresectable or where surgical resection is likely to result in severe morbidity.
The EC’s approval for denosumab in MM patients is based on data from the ’482 study, which were recently published in The Lancet Oncology.
In this phase 3 trial, denosumab proved non-inferior to zoledronic acid for delaying SREs in patients with newly diagnosed MM and bone disease.
Researchers randomized 1718 patients to receive subcutaneous denosumab at 120 mg and intravenous placebo every 4 weeks (n=859) or intravenous zoledronic acid at 4 mg (adjusted for renal function at baseline) and subcutaneous placebo every 4 weeks (n=859).
All patients also received investigators’ choice of first-line MM therapy.
The median time to first on-study SRE was 22.8 months for patients in the denosumab arm and 24 months for those in the zoledronic acid arm (hazard ratio=0.98; 95% confidence interval: 0.85-1.14; P for non-inferiority=0.010).
There were fewer renal treatment-emergent adverse events in the denosumab arm than the zoledronic acid arm—10% and 17%, respectively.
But there were more hypocalcemia adverse events in the denosumab arm than the zoledronic acid arm—17% and 12%, respectively.
The European Commission (EC) has approved an expanded indication for denosumab (Xgeva).
The drug is now approved for the prevention of skeletal-related events (SREs) in adults with advanced malignancies involving bone, which includes patients with multiple myeloma (MM).
Approval from the EC provides a centralized marketing authorization with unified labeling in all member countries of the European Union.
Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
Denosumab was previously approved by the EC to prevent SREs—defined as radiation to bone, pathologic fracture, surgery to bone, and spinal cord compression—in adults with bone metastases from solid tumors.
Denosumab also received EC approval for the treatment of adults and skeletally mature adolescents with giant cell tumor of bone that is unresectable or where surgical resection is likely to result in severe morbidity.
The EC’s approval for denosumab in MM patients is based on data from the ’482 study, which were recently published in The Lancet Oncology.
In this phase 3 trial, denosumab proved non-inferior to zoledronic acid for delaying SREs in patients with newly diagnosed MM and bone disease.
Researchers randomized 1718 patients to receive subcutaneous denosumab at 120 mg and intravenous placebo every 4 weeks (n=859) or intravenous zoledronic acid at 4 mg (adjusted for renal function at baseline) and subcutaneous placebo every 4 weeks (n=859).
All patients also received investigators’ choice of first-line MM therapy.
The median time to first on-study SRE was 22.8 months for patients in the denosumab arm and 24 months for those in the zoledronic acid arm (hazard ratio=0.98; 95% confidence interval: 0.85-1.14; P for non-inferiority=0.010).
There were fewer renal treatment-emergent adverse events in the denosumab arm than the zoledronic acid arm—10% and 17%, respectively.
But there were more hypocalcemia adverse events in the denosumab arm than the zoledronic acid arm—17% and 12%, respectively.
The European Commission (EC) has approved an expanded indication for denosumab (Xgeva).
The drug is now approved for the prevention of skeletal-related events (SREs) in adults with advanced malignancies involving bone, which includes patients with multiple myeloma (MM).
Approval from the EC provides a centralized marketing authorization with unified labeling in all member countries of the European Union.
Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
Denosumab was previously approved by the EC to prevent SREs—defined as radiation to bone, pathologic fracture, surgery to bone, and spinal cord compression—in adults with bone metastases from solid tumors.
Denosumab also received EC approval for the treatment of adults and skeletally mature adolescents with giant cell tumor of bone that is unresectable or where surgical resection is likely to result in severe morbidity.
The EC’s approval for denosumab in MM patients is based on data from the ’482 study, which were recently published in The Lancet Oncology.
In this phase 3 trial, denosumab proved non-inferior to zoledronic acid for delaying SREs in patients with newly diagnosed MM and bone disease.
Researchers randomized 1718 patients to receive subcutaneous denosumab at 120 mg and intravenous placebo every 4 weeks (n=859) or intravenous zoledronic acid at 4 mg (adjusted for renal function at baseline) and subcutaneous placebo every 4 weeks (n=859).
All patients also received investigators’ choice of first-line MM therapy.
The median time to first on-study SRE was 22.8 months for patients in the denosumab arm and 24 months for those in the zoledronic acid arm (hazard ratio=0.98; 95% confidence interval: 0.85-1.14; P for non-inferiority=0.010).
There were fewer renal treatment-emergent adverse events in the denosumab arm than the zoledronic acid arm—10% and 17%, respectively.
But there were more hypocalcemia adverse events in the denosumab arm than the zoledronic acid arm—17% and 12%, respectively.
Drug nets orphan designation for SCD
The European Commission (EC) has granted orphan designation to Altemia (formerly SC411) for the treatment of pediatric patients with sickle cell disease (SCD).
Altemia gelatin capsules are designed to replenish the lipids destroyed by sickle hemoglobin.
Altemia is intended to be taken once daily to reduce vaso-occlusive crises, anemia, organ damage, and other complications of SCD.
Altemia consists of a mixture of fatty acids, primarily in the form of Ethyl Cervonate (a proprietary blend of docosahexaenoic acid and other omega-3 fatty acids), and surface active agents formulated using Advanced Lipid Technologies.
Advanced Lipid Technologies are proprietary formulation and manufacturing techniques used by Sancilio Pharmaceuticals Company, Inc. (SPCI) to create lipophilic drug products.
Last November, SPCI reported topline data from its phase 2 study of Altemia, the SCOT trial (NCT02973360). The trial included pediatric patients, ages 5 to 17, with SCD.
The study’s primary endpoint was the change from baseline in blood cell membranes’ fatty acids concentration. SPCI said Altemia showed a significant improvement in this endpoint, compared to placebo, within 4 weeks of treatment initiation.
Patients who received Altemia also had significant improvements in markers of coagulation (D-dimer), inflammation (C-reactive protein), and adhesion (E-selectin) after 8 weeks of treatment.
And patients treated with Altemia had a “clinically meaningful” reduction in vaso-occlusive events, according to SPCI.
There were no treatment-related serious adverse events reported.
Ninety-four percent of patients completed the study, and most have chosen to participate in the open-label extension phase, in which researchers will continue monitoring the safety and effectiveness of Altemia.
SPCI said additional analyses of SCOT data are ongoing, and the company plans to present detailed data from the study in journals and at upcoming scientific conferences.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Commission (EC) has granted orphan designation to Altemia (formerly SC411) for the treatment of pediatric patients with sickle cell disease (SCD).
Altemia gelatin capsules are designed to replenish the lipids destroyed by sickle hemoglobin.
Altemia is intended to be taken once daily to reduce vaso-occlusive crises, anemia, organ damage, and other complications of SCD.
Altemia consists of a mixture of fatty acids, primarily in the form of Ethyl Cervonate (a proprietary blend of docosahexaenoic acid and other omega-3 fatty acids), and surface active agents formulated using Advanced Lipid Technologies.
Advanced Lipid Technologies are proprietary formulation and manufacturing techniques used by Sancilio Pharmaceuticals Company, Inc. (SPCI) to create lipophilic drug products.
Last November, SPCI reported topline data from its phase 2 study of Altemia, the SCOT trial (NCT02973360). The trial included pediatric patients, ages 5 to 17, with SCD.
The study’s primary endpoint was the change from baseline in blood cell membranes’ fatty acids concentration. SPCI said Altemia showed a significant improvement in this endpoint, compared to placebo, within 4 weeks of treatment initiation.
Patients who received Altemia also had significant improvements in markers of coagulation (D-dimer), inflammation (C-reactive protein), and adhesion (E-selectin) after 8 weeks of treatment.
And patients treated with Altemia had a “clinically meaningful” reduction in vaso-occlusive events, according to SPCI.
There were no treatment-related serious adverse events reported.
Ninety-four percent of patients completed the study, and most have chosen to participate in the open-label extension phase, in which researchers will continue monitoring the safety and effectiveness of Altemia.
SPCI said additional analyses of SCOT data are ongoing, and the company plans to present detailed data from the study in journals and at upcoming scientific conferences.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Commission (EC) has granted orphan designation to Altemia (formerly SC411) for the treatment of pediatric patients with sickle cell disease (SCD).
Altemia gelatin capsules are designed to replenish the lipids destroyed by sickle hemoglobin.
Altemia is intended to be taken once daily to reduce vaso-occlusive crises, anemia, organ damage, and other complications of SCD.
Altemia consists of a mixture of fatty acids, primarily in the form of Ethyl Cervonate (a proprietary blend of docosahexaenoic acid and other omega-3 fatty acids), and surface active agents formulated using Advanced Lipid Technologies.
Advanced Lipid Technologies are proprietary formulation and manufacturing techniques used by Sancilio Pharmaceuticals Company, Inc. (SPCI) to create lipophilic drug products.
Last November, SPCI reported topline data from its phase 2 study of Altemia, the SCOT trial (NCT02973360). The trial included pediatric patients, ages 5 to 17, with SCD.
The study’s primary endpoint was the change from baseline in blood cell membranes’ fatty acids concentration. SPCI said Altemia showed a significant improvement in this endpoint, compared to placebo, within 4 weeks of treatment initiation.
Patients who received Altemia also had significant improvements in markers of coagulation (D-dimer), inflammation (C-reactive protein), and adhesion (E-selectin) after 8 weeks of treatment.
And patients treated with Altemia had a “clinically meaningful” reduction in vaso-occlusive events, according to SPCI.
There were no treatment-related serious adverse events reported.
Ninety-four percent of patients completed the study, and most have chosen to participate in the open-label extension phase, in which researchers will continue monitoring the safety and effectiveness of Altemia.
SPCI said additional analyses of SCOT data are ongoing, and the company plans to present detailed data from the study in journals and at upcoming scientific conferences.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
Test for HIT receives CE mark
HIT Confirm, a test used to diagnose heparin-induced thrombocytopenia (HIT), has received the CE mark.
This means the test meets regulatory requirements and health, safety, and environmental protection standards for products sold within the European Economic Area.
HIT Confirm is a flow cytometry-based test developed by Emosis. The test can be performed on any flow cytometer and provides results within 30 minutes.
HIT Confirm requires a low-volume sample (microliters) of platelet-rich plasma to confirm the presence of HIT antibodies that lead to the formation of a heparin-antibody-PF4 complex that will bind to platelets and activate them.
HIT Confirm requires a single incubation with 2 fluorophores against a marker of platelets (CD41) and a marker of activated platelets (CD62).
After 30 minutes of incubation with 2 dose levels of heparin (0.3 U/mL and 100 U/mL), the proportion of activated platelets is obtained via flow cytometry.
Results are interpreted using a platelet activation index called HEPLA, which was developed by Emosis.
Research presented at the 2017 ISTH Congress (abstract OC 34.3*) indicated that HIT Confirm produces results comparable to those provided by the serotonin release assay (SRA).
Researchers tested the sensitivity and specificity of SRA and HIT Confirm when analyzing plasma from 290 patients—131 of whom were deemed HIT-positive by experts.
When compared to expert opinion, HIT Confirm provided 90% sensitivity and 94% specificity. SRA provided 80% sensitivity and 94% specificity compared to expert opinion.
For more information on HIT Confirm, visit the Emosis website.
*Data in the abstract differ from data provided by Emosis. The data used here were provided by Emosis.
HIT Confirm, a test used to diagnose heparin-induced thrombocytopenia (HIT), has received the CE mark.
This means the test meets regulatory requirements and health, safety, and environmental protection standards for products sold within the European Economic Area.
HIT Confirm is a flow cytometry-based test developed by Emosis. The test can be performed on any flow cytometer and provides results within 30 minutes.
HIT Confirm requires a low-volume sample (microliters) of platelet-rich plasma to confirm the presence of HIT antibodies that lead to the formation of a heparin-antibody-PF4 complex that will bind to platelets and activate them.
HIT Confirm requires a single incubation with 2 fluorophores against a marker of platelets (CD41) and a marker of activated platelets (CD62).
After 30 minutes of incubation with 2 dose levels of heparin (0.3 U/mL and 100 U/mL), the proportion of activated platelets is obtained via flow cytometry.
Results are interpreted using a platelet activation index called HEPLA, which was developed by Emosis.
Research presented at the 2017 ISTH Congress (abstract OC 34.3*) indicated that HIT Confirm produces results comparable to those provided by the serotonin release assay (SRA).
Researchers tested the sensitivity and specificity of SRA and HIT Confirm when analyzing plasma from 290 patients—131 of whom were deemed HIT-positive by experts.
When compared to expert opinion, HIT Confirm provided 90% sensitivity and 94% specificity. SRA provided 80% sensitivity and 94% specificity compared to expert opinion.
For more information on HIT Confirm, visit the Emosis website.
*Data in the abstract differ from data provided by Emosis. The data used here were provided by Emosis.
HIT Confirm, a test used to diagnose heparin-induced thrombocytopenia (HIT), has received the CE mark.
This means the test meets regulatory requirements and health, safety, and environmental protection standards for products sold within the European Economic Area.
HIT Confirm is a flow cytometry-based test developed by Emosis. The test can be performed on any flow cytometer and provides results within 30 minutes.
HIT Confirm requires a low-volume sample (microliters) of platelet-rich plasma to confirm the presence of HIT antibodies that lead to the formation of a heparin-antibody-PF4 complex that will bind to platelets and activate them.
HIT Confirm requires a single incubation with 2 fluorophores against a marker of platelets (CD41) and a marker of activated platelets (CD62).
After 30 minutes of incubation with 2 dose levels of heparin (0.3 U/mL and 100 U/mL), the proportion of activated platelets is obtained via flow cytometry.
Results are interpreted using a platelet activation index called HEPLA, which was developed by Emosis.
Research presented at the 2017 ISTH Congress (abstract OC 34.3*) indicated that HIT Confirm produces results comparable to those provided by the serotonin release assay (SRA).
Researchers tested the sensitivity and specificity of SRA and HIT Confirm when analyzing plasma from 290 patients—131 of whom were deemed HIT-positive by experts.
When compared to expert opinion, HIT Confirm provided 90% sensitivity and 94% specificity. SRA provided 80% sensitivity and 94% specificity compared to expert opinion.
For more information on HIT Confirm, visit the Emosis website.
*Data in the abstract differ from data provided by Emosis. The data used here were provided by Emosis.
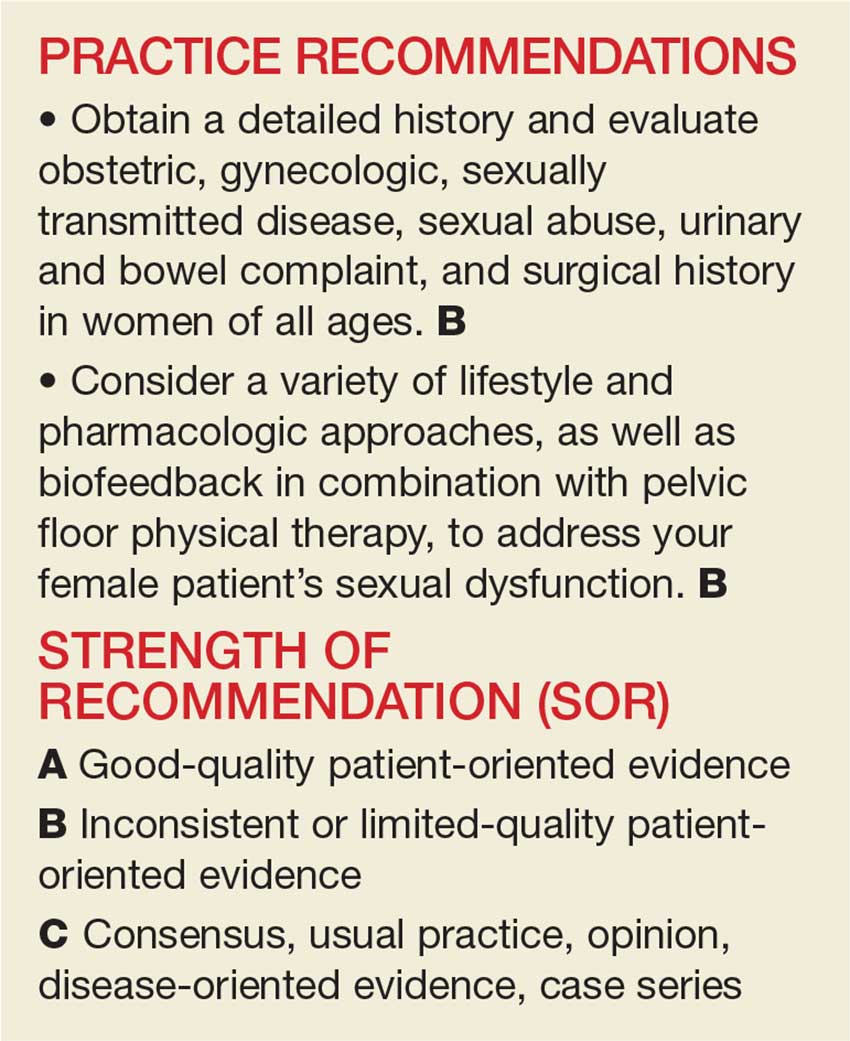
Evaluation and Management of Female Sexual Dysfunction
IN THIS ARTICLE
- Causes of pain
- Screening
- Multimodal treatment
Care of women with sexual disorders has made great strides since Masters and Johnson began their study in 1957. In 2000, the Sexual Function Health Council of the American Foundation for Urologic Disease devised the classification system for female sexual dysfunction, which was officially defined in the Diagnostic and Statistical Manual of Mental Disorders-IV-TR.1 There are now definitions for sexual desire disorders, sexual arousal disorders, orgasmic disorder, and sexual pain disorders.
Female sexual dysfunction (FSD) has complex physiologic and psychologic components that require a detailed screening, history, and physical examination. Our goal in this review is to provide primary care providers with insights and practical advice to help screen, diagnose, and treat FSD, which can have a profound impact on patients’ most intimate relationships.
UNDERSTANDING THE TYPES OF FSD
Most women consider sexual health an important part of their overall health.2 Factors that can disrupt normal sexual function include aging, socioeconomics, and other medical comorbidities. FSD is common in women throughout their lives and refers to various sexual dysfunctions including diminished arousal, problems achieving orgasm, dyspareunia, and low desire. Its prevalence is reported to be as high as 20% to 43%.3,4
The World Health Organization and the US Surgeon General have released statements encouraging health care providers to address sexual health during a patient’s annual visits.5 Unfortunately, despite this call to action, many patients and providers are initially hesitant to discuss these problems.6
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the definition and diagnostic guidelines for the different components of FSD. Its classification of sexual disorders was simplified and published in May 2013.7 There are now only three female dysfunctions (as opposed to five in DSM-IV):
- Female hypoactive desire dysfunction and female arousal dysfunction were merged into a single syndrome labeled female sexual interest/arousal disorder.
- The formerly separate dyspareunia (painful intercourse) and vaginismus are now called genitopelvic pain/penetration disorder.
- Female orgasmic disorder remains as a category and is unchanged.
To qualify as a dysfunction, the problem must be present more than 75% of the time, for more than six months, causing significant distress, and must not be explained by a nonsexual mental disorder, relationship distress, substance abuse, or a medical condition.
Substance- or medication-induced sexual dysfunction falls under “Other Dysfunctions” and is defined as a clinically significant disturbance in sexual function that is predominant in the clinical picture. The criteria for substance- and medication-induced sexual dysfunction are unchanged and include neither the 75% nor the six-month requirement. The diagnosis of sexual dysfunction due to a general medical condition and sexual aversion disorder are absent from the DSM-5.7
Continue to: A common symptom
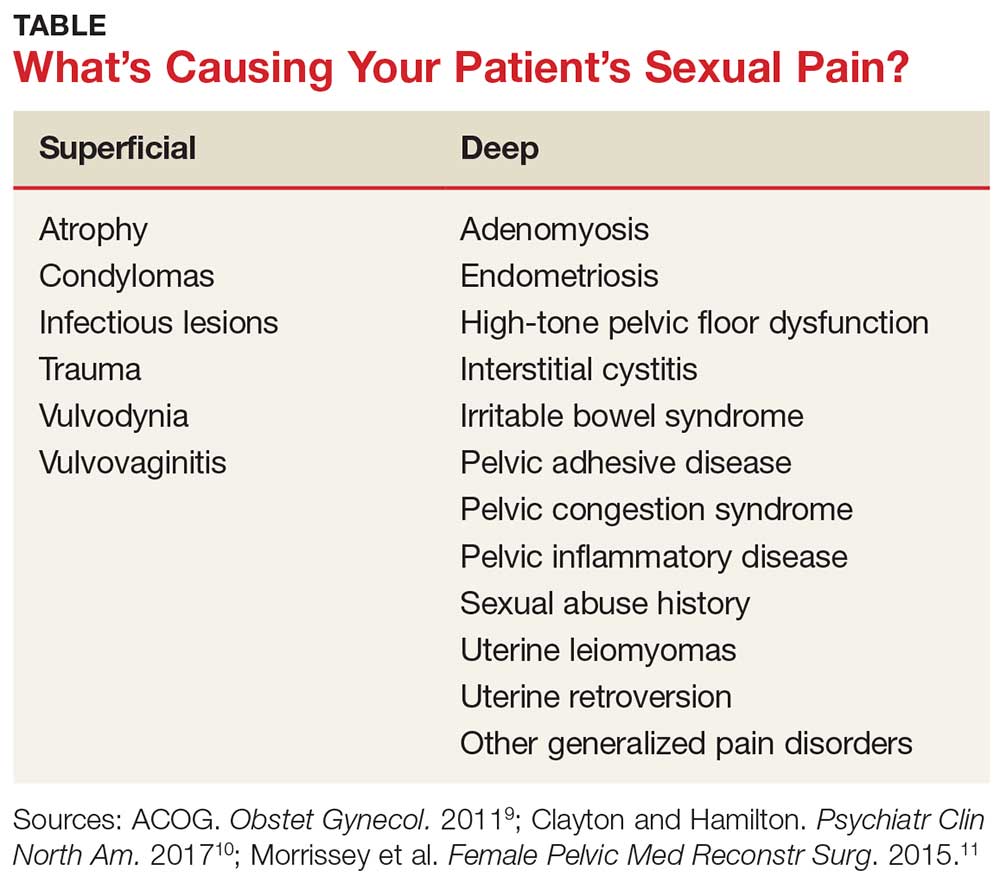
A common symptom. Female sexual disorders can be caused by several complex physiologic and psychologic factors. A common symptom among many women is dyspareunia. It is seen more often in postmenopausal women, and its prevalence ranges from 8% to 22%.8 Pain on vaginal entry usually indicates vaginal atrophy, vaginal dermatitis, or provoked vestibulodynia. Pain on deep penetration could be caused by endometriosis, interstitial cystitis, or uterine leiomyomas.9
The physical examination will reproduce the pain when the vulva or vagina is touched with a cotton swab or when you insert a finger into the vagina. The differential diagnosis is listed in the Table.9-11
EVALUATING THE PATIENT
Initially, many patients and providers may hesitate to discuss sexual dysfunction, but the annual exam is a good opportunity to broach the topic of sexual health.
Screening and history
Clinicians can screen all patients, regardless of age, with the help of a validated sex questionnaire or during a routine review of systems. There are many validated screening tools available. A simple, integrated screening tool to use is the Brief Sexual Symptom Checklist for Women (BSSC-W), created by the International Consultation on Sexual Medicine.12 Although recommended by the American Congress of Obstetricians and Gynecologists, the BSSC-W is not validated.9 The four items in the questionnaire ascertain personal information regarding an individual’s overall sexual function satisfaction, the problem causing dysfunction, how bothersome the symptoms are, and whether the patient is interested in discussing it with her provider.12
It’s important to obtain a detailed obstetric and gynecologic history that includes any sexually transmitted diseases, sexual abuse, urinary and bowel complaints, or surgeries. In addition, you’ll want to differentiate between various types of dysfunctions. A thorough physical examination, including an external and internal pelvic exam, can help to rule out other causes of sexual dysfunction.
Continue to: General exam: What to look for
General exam: What to look for
The external pelvic examination begins with visual inspection of the vulva, labia majora, and labia minora. Often, this is best accomplished gently with a gloved hand and a cotton swab. This inspection may reveal changes in pubic hair distribution, vulvar skin disorders, lesions, masses, cracks, or fissures. Inspection may also reveal redness and pain typical of vestibulitis, a flattening and pallor of the labia that suggests estrogen deficiency, or pelvic organ prolapse.
The internal pelvic examination begins with a manual evaluation of the muscles of the pelvic floor, uterus, bladder, urethra, anus, and adnexa. Make careful note of any unusual tenderness or pelvic masses. Pelvic floor muscles (PFMs) should voluntarily contract and relax and are not normally tender to palpation. Pelvic organ prolapse and/or hypermobility of the bladder may indicate a weakening of the endopelvic fascia and may cause sexual pain. The size and flexion of the uterus, tenderness in the vaginal fornix possibly indicating endometriosis, and adnexal fullness and/or masses should be identified and evaluated.
Neurologic exam of the pelvis will involve evaluation of sensory and motor function of both lower extremities and include a screening lumbosacral neurologic examination. Lumbosacral examination includes assessment of PFM strength, anal sphincter resting tone, voluntary anal contraction, and perineal sensation. If abnormalities are noted in the screening assessment, a complete comprehensive neurologic examination should be performed.
It’s important to assess pelvic floor muscle strength
Sexual function is associated with normal PFM function.13,14 The PFMs, particularly the pubococcygeus and iliococcygeus, are responsible for involuntary contractions during orgasm.13 Orgasm has been considered a reflex, which is preceded by increased blood flow to the genital organs, tumescence of the vulva and vagina, increased secretions during sexual arousal, and increased tension and contractions of the PFMs.15
Lowenstein et al found that women with strong or moderate PFM contractions scored significantly higher on both orgasm and arousal domains of the Female Sexual Function Index (FSFI), compared with women with weak PFM contractions.16 Orgasm and arousal functions may be associated with PFM strength, with a positive association between pelvic floor strength and sexual activity and function.17,18
The function and dysfunction of the PFMs have been characterized as normal, overactive (high tone), underactive (low tone), and nonfunctioning.
Continue to: Normal PFMs
Normal PFMs are those that can voluntarily and involuntarily contract and relax.19,20
Overactive (high-tone) muscles are those that do not relax and possibly contract during times of relaxation for micturition or defecation. This type of dysfunction can lead to voiding dysfunction, defecatory dysfunction, and dyspareunia.19
Underactive, or low-tone, PFMs cannot contract voluntarily. This can be associated with urinary and anal incontinence and pelvic organ prolapse.
Nonfunctioning muscles are completely inactive.19
How to assess. There are several ways to assess PFM tone and strength.20 The first is intravaginal or intrarectal digital palpation, which can be performed when the patient is in a supine or standing position. This examination evaluates PFM tone, squeeze pressure during contraction, symmetry, and relaxation. However, there is no validated scale to quantify PFM strength. Contractions can be further divided into voluntary and involuntary.19
During the exam, ask the patient to contract as much as she can to evaluate the maximum strength and sustained contraction for endurance. This measurement can be done with digital palpation or with pressure manometry or dynamometry.
Examination can be focused on the levator ani, piriformis, and internal obturator muscles bilaterally and rated by the patient’s reactions. Pelvic muscle tenderness, which can be highly prevalent in women with chronic pelvic pain, is associated with higher degrees of dyspareunia.21 Digital evaluation of the pelvic floor musculature varies in scale, number of fingers used, and parameters evaluated.
Lukban et al have described a 0 to 4 numbered scale that evaluates tenderness in the pelvic floor.22 The scale denotes “1” as comfortable pressure associated with the exam, “2” as uncomfortable pressure associated with the exam, “3” as moderate pain associated with the exam that intensifies with contraction, and “4” indicating severe pain with the exam and inability to perform the contraction maneuver due to pain.
Continue to: EFFECTIVE TREATMENT INCLUDES MULTIPLE OPTIONS
EFFECTIVE TREATMENT INCLUDES MULTIPLE OPTIONS
Lifestyle modifications can help
Lifestyle changes may help improve sexual function. These modifications include physical activity, healthy diet, nutrition counseling, and adequate sleep.23,24
Identifying medical conditions such as depression and anxiety will help delineate differential diagnoses of sexual dysfunction. Cardiovascular diseases may contribute to arousal disorder as a result of atherosclerosis of the vessels supplying the vagina and clitoris. Neurologic diseases such as multiple sclerosis and diabetes can affect sexual dysfunction by impairing arousal and orgasm.
Identification of concurrent comorbidities and implementation of lifestyle changes will help improve overall health and may improve sexual function.25
In addition, Herati et al found food sensitivities to grapefruit juice, spicy foods, alcohol, and caffeine were more prevalent in patients with interstitial cystitis and chronic pelvic pain.26 Avoiding irritants such as soap and other detergents in the perineal region may help decrease dysfunction.27 Finally, foods high in oxalate and other acidic items may cause bladder pain and worsening symptoms of vulvodynia.28
Topical therapies worth considering
Lubricants and moisturizers may help women with dyspareunia or symptoms of vaginal atrophy. For instance
Zestra, which contains a patented blend of botanical oils and extracts and is applied to the vulva prior to sexual activity, has been proven more effective than placebo for improving desire and arousal.29
Neogyn, a nonhormonal cream containing cutaneous lysate, has been shown to improve vulvar pain in women with vulvodynia. A double-blind placebo-controlled randomized crossover trial followed 30 patients for three months and found a significant reduction in pain during sexual activity and a significant reduction in erythema.30
Alprostadil, a prostaglandin E1 analogue that increases genital vasodilation when applied topically, is currently undergoing investigational trials.31,32
Patients can also choose from many OTC lubricants that contain water-based, oil-based, or silicone-based ingredients.
Continue to: Don't overlook physical therapy
Don’t overlook physical therapy
Manual therapies, including the transvaginal technique, are used for FSD that results from a variety of causes, including high-tone pelvic floor dysfunction. The transvaginal technique can identify myofascial pain; treatment involves internal release of the PFMs and external trigger-point identification and alleviation.
One pilot study examined use of transvaginal Thiele massage twice a week for five weeks in 21 symptomatic women with interstitial cystitis and high-tone pelvic floor dysfunction. The researchers found it decreased hypertonicity of the pelvic floor and generated statistically significant improvement in the Symptom and Problem Indexes of the O’Leary-Sant Questionnaire, Likert Visual Analogue Scales for urgency and pain, and the Physical and Mental Component Summary from the SF-12 Quality-of-Life Scale.33 Transvaginal physical therapy is also an effective treatment for myofascial pelvic pain.34
Biofeedback, which can be used in combination with pelvic floor physical therapy, teaches the patient to control the PFMs by visualizing the activity to achieve conscious control over contraction of the pelvic floor and ceasing the cycle of spasm.35 Ger et al investigated patients with levator spasm and found biofeedback decreased pain; relief was rated as good or excellent at 15-month follow-up in six of 14 patients (43%).36
Home devices such as Eros Therapy, an FDA-approved, nonpharmacologic battery-operated device, provide vacuum suction to the clitoris with vibratory sensation. Eros Therapy has been shown to increase blood flow to the clitoris, vagina, and pelvic floor and increase sensation, orgasm, lubrication, and satisfaction.37
Vaginal dilators allow increasing lengths and girths designed to treat vaginal and pelvic floor pain.38 In our practice, we encourage pelvic muscle strengthening tools in the form of Kegel trainers and other insertion devices that may improve PFM coordination and strength.
Continue to: Pharmacotherapy has its place
Pharmacotherapy has its place
The treatment of FSD may require a multimodal systematic approach targeting genitopelvic pain. But before the best options can be found, it is important to first establish the cause of the pain. Several drug formulations have been effectively used, including hormonal and nonhormonal options.
Conjugated estrogens are FDA approved for the treatment of dyspareunia, which can contribute to decreased desire. Systemic estrogen in oral form, transdermal preparations, and topical formulations may increase sexual desire and arousal and decrease dyspareunia.39 Even synthetic steroid compounds such as tibolone may improve sexual function, although it is not FDA approved for that purpose.40
Ospemifene is a selective estrogen receptor modulator that acts as an estrogen agonist in select tissues, including vaginal epithelium. It is FDA approved for dyspareunia in postmenopausal women.41,42 A daily dose of 60 mg is effective and safe, with minimal adverse effects.42 Studies suggest that testosterone, although not FDA approved in the United States for this purpose, improves sexual desire, pleasure, orgasm, and arousal satisfaction.39 The hormone has not gained FDA approval because of concerns about long-term safety and efficacy.42
Nonhormonal drugs including flibanserin, a well-tolerated serotonin receptor 1A agonist, 2A antagonist shown to improve sexual desire, increase the number of satisfying sexual events and reduce distress associated with low sexual desire when compared with placebo.43 The FDA has approved flibanserin as the first treatment targeted for women with hypoactive sexual desire disorder (HSDD). It can, however, cause severe hypotension and syncope, is not well tolerated with alcohol, and is contraindicated in patients who take strong CYP3A4 inhibitors, such as fluconazole, verapamil, and erythromycin, or who have liver impairment.
Bupropion, a mild dopamine and norepinephrine reuptake inhibitor and acetylcholine receptor antagonist, has been shown to improve desire in women with and without depression. Although it is FDA approved for major depressive disorder, it is not approved for female sexual dysfunction and is still under investigation.
Tricyclic antidepressants, such as nortriptyline and amitriptyline, may be effective in treating neuropathic pain. Starting doses of both amitriptyline and nortriptyline are 10 mg/d and can be increased to a maximum of 100 mg/d.44 Tricyclic antidepressants are still under investigation for the treatment of FSD.
Muscle relaxants in oral and topical compounded form are used to treat increased pelvic floor tension and spasticity. Cyclobenzaprine and tizanidine are FDA-approved muscle relaxants indicated for muscle spasticity.
Cyclobenzaprine, at a starting dose of 10 mg, can be taken up to three times a day for pelvic floor tension. Tizanidine is a centrally active alpha 2 agonist that’s superior to placebo in treating high-tone pelvic floor dysfunction.44
Other medications include benzodiazepines, such as oral clonazepam and intravaginal diazepam, although they are not FDA approved for high-tone pelvic floor dysfunction. Rogalski et al evaluated data for 26 patients who received vaginal diazepam for bladder pain, sexual pain, and levator hypertonus.45 They found subjective and sexual pain improvement assessed on FSFI and the visual analog pain scale. PFM tone significantly improved during resting, squeezing, and relaxation phases. Multimodal therapy can be used for muscle spasticity and high-tone pelvic floor dysfunction.
Continue to: Trigger point and Botox injections
Trigger point and Botox injections
Although drug therapy has its place in the management of sexual dysfunction, other modalities that involve trigger-point injections or botulinum toxin injections to the PFMs may prove helpful for patients with high-tone pelvic floor dysfunction.
A prospective study investigated the role of trigger-point injections in 18 women with levator ani muscle spasm using a mixture of 0.25% bupivacaine in 10 mL, 2% lidocaine in 10 mL, and 40 mg of triamcinolone in 1 mL combined and used for injection of 5 mL per trigger point.46 Three months after injections, 13 of the 18 women showed improvement, resulting in a success rate of 72%. Trigger point injections can be applied externally or transvaginally.
OnabotulinumtoxinA (Botox) has also been tested for relief of levator ani muscle spasm. Botox is FDA approved for upper and lower limb spasticity but is not approved for pelvic floor spasticity or tension. It may reduce pressure in the PFMs and may be useful in women with high-tone pelvic floor dysfunction.47
In a prospective six-month pilot study, 28 patients with pelvic pain for whom conservative treatment did not work received up to 300 U Botox into the pelvic floor.11 The study, which used needle electromyography guidance and a transperineal approach, found that the dyspareunia visual analog scale improved significantly at weeks 12 and 24. Keep in mind, however, that onabotulinumtoxinA should be reserved for patients for whom conventional treatments fail.47,48
Addressing psychologic issues
Sex therapy is a traditional approach that aims to improve individual or couples’ sexual experiences and help reduce anxiety related to sex.42 Cognitive behavioral sex therapy includes traditional sex therapy components but puts greater emphasis on modifying thought patterns that interfere with intimacy and sex.42
Mindfulness-based cognitive behavioral treatments have shown promise for sexual desire problems. It is an ancient eastern practice with Buddhist roots. This therapy is a nonjudgmental, present-moment awareness comprised of self-regulation of attention and accepting orientation to the present.49 Although there is little evidence from prospective studies, it may benefit women with sexual dysfunction after intervention with sex therapy and cognitive behavioral therapy.
CONCLUSION
Female sexual dysfunction is common and affects women of all ages. It can negatively impact a woman’s quality of life and overall well-being. The etiology of FSD is complex, and treatments are based on the causes of the dysfunction. Difficult cases warrant referral to a specialist in sexual health and female pelvic medicine. Future prospective trials, randomized controlled trials, the use of validated questionnaires, and meta-analyses will continue to move us forward as we find better ways to understand, identify, and treat female sexual dysfunction.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed, text revision). Washington, DC; 1994.
2. Shifren JL, Monz BU, Russo PA, et al. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112:970-978.
3. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1:35-39.
4. Laumann E, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537-544.
5. Office of the Surgeon General. The Surgeon General’s Call to Action to Promote Sexual Health and Responsible Sexual Behavior. Rockville, MD; 2001.
6. Pauls RN, Kleeman SD, Segal JL, et al. Practice patterns of physician members of the American Urogynecologic Society regarding female sexual dysfunction: results of a national survey. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:460-467.
7. American Psychiatric Association. Sexual dysfunction. In: Diagnostic and Statistical Manual of Mental Disorders (5th ed). Washington, DC; 2013.
8. Steege JF, Zolnoun DA. Evaluation and treatment of dyspareunia. Obstet Gynecol. 2009;113:1124-1136.
9. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 119: Female sexual dysfunction. Obstet Gynecol. 2011;117:996-1007.
10. Clayton AH, Hamilton DV. Female sexual dysfunction. Psychiatr Clin North Am. 2017;40:267-284.
11. Morrissey D, El-Khawand D, Ginzburg N, et al. Botulinum Toxin A injections into pelvic floor muscles under electromyographic guidance for women with refractory high-tone pelvic floor dysfunction: a 6-month prospective pilot study. Female Pelvic Med Reconstr Surg. 2015;21:277-282.
12. Hatzichristou D, Rosen RC, Derogatis LR, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7(1 pt 2):337-348.
13. Kegel A. Sexual functions of the pubococcygeus muscle. West J Surg Obstet Gynecol. 1952;60:521-524.
14. Shafik A. The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J. 2000;11:361-376.
15. Kinsey A, Pomeroy WB, Martin CE, et al. Sexual Behavior in the Human Female. Philadelphia, PA: WB Saunders; 1998.
16. Lowenstein L, Gruenwald I, Gartman I, et al. Can stronger pelvic muscle floor improve sexual function? Int Urogynecol J. 2010;21:553-556.
17. Kanter G, Rogers RG, Pauls RN, et al. A strong pelvic floor is associated with higher rates of sexual activity in women with pelvic floor disorders. Int Urogynecol J. 2015;26:991-996.
18. Wehbe SA, Kellogg-Spadt S, Whitmore K. Urogenital complaints and female sexual dysfunction. Part 2. J Sex Med. 2010;7:2304-2317.
19. Messelink B, Benson T, Berghmans B, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the Pelvic Floor Clinical Assessment Group of the International Continence Society. Neurourol Urodyn. 2005;24:374-380.
20. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4-20.
21. Montenegro ML, Mateus-Vasconcelos EC, Rosa e Silva JC, et al. Importance of pelvic muscle tenderness evaluation in women with chronic pelvic pain. Pain Med. 2010;11:224-228.
22. Lukban JC, Whitmore KE. Pelvic floor muscle re-education treatment of the overactive bladder and painful bladder syndrome. Clin Obstet Gynecol. 2002;45:273-285.
23. Kalmbach DA, Arnedt JT, Pillai V, et al. The impact of sleep on female sexual response and behavior: a pilot study. J Sex Med. 2015;12:1221-1232.
24. Aversa A, Bruzziches R, Francomano D, et al. Weight loss by multidisciplinary intervention improves endothelial and sexual function in obese fertile women. J Sex Med. 2013;10:1024-1033.
25. Pauls RN, Kleeman SD, Karram MM. Female sexual dysfunction: principles of diagnosis and therapy. Obstet Gynecol Surv. 2005;60:196-205.
26. Herati AS, Shorter B, Tai J, et al. Differences in food sensitivities between female interstitial cystitis/painful bladder syndrome (IC/PBS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) patients. J Urol. 2009;181(4)(suppl):22.
27. Farrell J, Cacchioni T. The medicalization of women’s sexual pain. J Sex Res. 2012;49:328-336.
28. De Andres J, Sanchis-Lopez NM, Asensio-Samper JM, et al. Vulvodynia—an evidence-based literature review and proposed treatment algorithm. Pain Pract. 2016;16:204-236.
29. Herbenick D, Reece M, Schick V, et al. Women’s use and perceptions of commercial lubricants: prevalence and characteristics in a nationally representative sample of American adults. J Sex Med. 2014;11:642-652.
30. Donders GG, Bellen G. Cream with cutaneous fibroblast lysate for the treatment of provoked vestibulodynia: a double-blind randomized placebo-controlled crossover study. J Low Genit Tract Dis. 2012;16:427-436.
31. Belkin ZR, Krapf JM, Goldstein AT. Drugs in early clinical development for the treatment of female sexual dysfunction. Expert Opin Investig Drugs. 2015;24:159-167.
32. Islam A, Mitchel J, Rosen R, et al. Topical alprostadil in the treatment of female sexual arousal disorder: a pilot study. J Sex Marital Ther. 2001;27:531-540.
33. Oyama IA, Rejba A, Lukban JC, et al. Modified Thiele massage as therapeutic intervention for female patients with interstitial cystitis and high-tone pelvic floor dysfunction. Urology. 2004;64:862-865.
34. Bedaiwy MA, Patterson B, Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med. 2013;58:504-510.
35. Wehbe SA, Fariello JY, Whitmore K. Minimally invasive therapies for chronic pelvic pain syndrome. Curr Urol Rep. 2010;11:276-285.
36. Ger GC, Wexner SD, Jorge JM, et al. Evaluation and treatment of chronic intractable rectal pain—a frustrating endeavor. Dis Colon Rectum. 1993;36:139-145.
37. Billups KL, Berman L, Berman J, et al. A new non-pharmacological vacuum therapy for female sexual dysfunction. J Sex Marital Ther. 2001;27:435-441.
38. Miles T, Johnson N. Vaginal dilator therapy for women receiving pelvic radiotherapy. Cochrane Database Syst Rev. 2014;9:CD007291.
39. Goldstein I. Current management strategies of the postmenopausal patient with sexual health problems. J Sex Med. 2007;4(suppl 3):235-253.
40. Modelska K, Cummings S. Female sexual dysfunction in postmenopausal women: systematic review of placebo-controlled trials. Am J Obstet Gynecol. 2003;188:286-293.
41. Constantine G, Graham S, Portman DJ, et al. Female sexual function improved with ospemifene in postmenopausal women with vulvar and vaginal atrophy: results of a randomized, placebo-controlled trial. Climacteric. 2015;18:226-232.
42. Kingsberg SA, Woodard T. Female sexual dysfunction: focus on low desire. Obstet Gynecol. 2015;125:477-486.
43. Simon JA, Kingsberg SA, Shumel B, et al. Efficacy and safety of flibanserin in postmenopausal women with hypoactive sexual desire disorder: results of the SNOWDROP trial. Menopause. 2014;21:633-640.
44. Curtis Nickel J, Baranowski AP, Pontari M, et al. Management of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome who have failed traditional management. Rev Urol. 2007;9:63-72.
45. Rogalski MJ, Kellogg-Spadt S, Hoffmann AR, et al. Retrospective chart review of vaginal diazepam suppository use in high-tone pelvic floor dysfunction. Int Urogynecol J. 2010;21:895-899.
46. Langford CF, Udvari Nagy S, Ghoniem GM. Levator ani trigger point injections: an underutilized treatment for chronic pelvic pain. Neurourol Urodyn. 2007;26:59-62.
47. Abbott JA, Jarvis SK, Lyons SD, et al. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol. 2006;108:915-923.
48. Kamanli A, Kaya A, Ardicoglu O, et al. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int. 2005;25:604-611.
49. Brotto LA, Erskine Y, Carey M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012;125:320-325.
IN THIS ARTICLE
- Causes of pain
- Screening
- Multimodal treatment
Care of women with sexual disorders has made great strides since Masters and Johnson began their study in 1957. In 2000, the Sexual Function Health Council of the American Foundation for Urologic Disease devised the classification system for female sexual dysfunction, which was officially defined in the Diagnostic and Statistical Manual of Mental Disorders-IV-TR.1 There are now definitions for sexual desire disorders, sexual arousal disorders, orgasmic disorder, and sexual pain disorders.
Female sexual dysfunction (FSD) has complex physiologic and psychologic components that require a detailed screening, history, and physical examination. Our goal in this review is to provide primary care providers with insights and practical advice to help screen, diagnose, and treat FSD, which can have a profound impact on patients’ most intimate relationships.
UNDERSTANDING THE TYPES OF FSD
Most women consider sexual health an important part of their overall health.2 Factors that can disrupt normal sexual function include aging, socioeconomics, and other medical comorbidities. FSD is common in women throughout their lives and refers to various sexual dysfunctions including diminished arousal, problems achieving orgasm, dyspareunia, and low desire. Its prevalence is reported to be as high as 20% to 43%.3,4
The World Health Organization and the US Surgeon General have released statements encouraging health care providers to address sexual health during a patient’s annual visits.5 Unfortunately, despite this call to action, many patients and providers are initially hesitant to discuss these problems.6
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the definition and diagnostic guidelines for the different components of FSD. Its classification of sexual disorders was simplified and published in May 2013.7 There are now only three female dysfunctions (as opposed to five in DSM-IV):
- Female hypoactive desire dysfunction and female arousal dysfunction were merged into a single syndrome labeled female sexual interest/arousal disorder.
- The formerly separate dyspareunia (painful intercourse) and vaginismus are now called genitopelvic pain/penetration disorder.
- Female orgasmic disorder remains as a category and is unchanged.
To qualify as a dysfunction, the problem must be present more than 75% of the time, for more than six months, causing significant distress, and must not be explained by a nonsexual mental disorder, relationship distress, substance abuse, or a medical condition.
Substance- or medication-induced sexual dysfunction falls under “Other Dysfunctions” and is defined as a clinically significant disturbance in sexual function that is predominant in the clinical picture. The criteria for substance- and medication-induced sexual dysfunction are unchanged and include neither the 75% nor the six-month requirement. The diagnosis of sexual dysfunction due to a general medical condition and sexual aversion disorder are absent from the DSM-5.7
Continue to: A common symptom
A common symptom. Female sexual disorders can be caused by several complex physiologic and psychologic factors. A common symptom among many women is dyspareunia. It is seen more often in postmenopausal women, and its prevalence ranges from 8% to 22%.8 Pain on vaginal entry usually indicates vaginal atrophy, vaginal dermatitis, or provoked vestibulodynia. Pain on deep penetration could be caused by endometriosis, interstitial cystitis, or uterine leiomyomas.9
The physical examination will reproduce the pain when the vulva or vagina is touched with a cotton swab or when you insert a finger into the vagina. The differential diagnosis is listed in the Table.9-11
EVALUATING THE PATIENT
Initially, many patients and providers may hesitate to discuss sexual dysfunction, but the annual exam is a good opportunity to broach the topic of sexual health.
Screening and history
Clinicians can screen all patients, regardless of age, with the help of a validated sex questionnaire or during a routine review of systems. There are many validated screening tools available. A simple, integrated screening tool to use is the Brief Sexual Symptom Checklist for Women (BSSC-W), created by the International Consultation on Sexual Medicine.12 Although recommended by the American Congress of Obstetricians and Gynecologists, the BSSC-W is not validated.9 The four items in the questionnaire ascertain personal information regarding an individual’s overall sexual function satisfaction, the problem causing dysfunction, how bothersome the symptoms are, and whether the patient is interested in discussing it with her provider.12
It’s important to obtain a detailed obstetric and gynecologic history that includes any sexually transmitted diseases, sexual abuse, urinary and bowel complaints, or surgeries. In addition, you’ll want to differentiate between various types of dysfunctions. A thorough physical examination, including an external and internal pelvic exam, can help to rule out other causes of sexual dysfunction.
Continue to: General exam: What to look for
General exam: What to look for
The external pelvic examination begins with visual inspection of the vulva, labia majora, and labia minora. Often, this is best accomplished gently with a gloved hand and a cotton swab. This inspection may reveal changes in pubic hair distribution, vulvar skin disorders, lesions, masses, cracks, or fissures. Inspection may also reveal redness and pain typical of vestibulitis, a flattening and pallor of the labia that suggests estrogen deficiency, or pelvic organ prolapse.
The internal pelvic examination begins with a manual evaluation of the muscles of the pelvic floor, uterus, bladder, urethra, anus, and adnexa. Make careful note of any unusual tenderness or pelvic masses. Pelvic floor muscles (PFMs) should voluntarily contract and relax and are not normally tender to palpation. Pelvic organ prolapse and/or hypermobility of the bladder may indicate a weakening of the endopelvic fascia and may cause sexual pain. The size and flexion of the uterus, tenderness in the vaginal fornix possibly indicating endometriosis, and adnexal fullness and/or masses should be identified and evaluated.
Neurologic exam of the pelvis will involve evaluation of sensory and motor function of both lower extremities and include a screening lumbosacral neurologic examination. Lumbosacral examination includes assessment of PFM strength, anal sphincter resting tone, voluntary anal contraction, and perineal sensation. If abnormalities are noted in the screening assessment, a complete comprehensive neurologic examination should be performed.
It’s important to assess pelvic floor muscle strength
Sexual function is associated with normal PFM function.13,14 The PFMs, particularly the pubococcygeus and iliococcygeus, are responsible for involuntary contractions during orgasm.13 Orgasm has been considered a reflex, which is preceded by increased blood flow to the genital organs, tumescence of the vulva and vagina, increased secretions during sexual arousal, and increased tension and contractions of the PFMs.15
Lowenstein et al found that women with strong or moderate PFM contractions scored significantly higher on both orgasm and arousal domains of the Female Sexual Function Index (FSFI), compared with women with weak PFM contractions.16 Orgasm and arousal functions may be associated with PFM strength, with a positive association between pelvic floor strength and sexual activity and function.17,18
The function and dysfunction of the PFMs have been characterized as normal, overactive (high tone), underactive (low tone), and nonfunctioning.
Continue to: Normal PFMs
Normal PFMs are those that can voluntarily and involuntarily contract and relax.19,20
Overactive (high-tone) muscles are those that do not relax and possibly contract during times of relaxation for micturition or defecation. This type of dysfunction can lead to voiding dysfunction, defecatory dysfunction, and dyspareunia.19
Underactive, or low-tone, PFMs cannot contract voluntarily. This can be associated with urinary and anal incontinence and pelvic organ prolapse.
Nonfunctioning muscles are completely inactive.19
How to assess. There are several ways to assess PFM tone and strength.20 The first is intravaginal or intrarectal digital palpation, which can be performed when the patient is in a supine or standing position. This examination evaluates PFM tone, squeeze pressure during contraction, symmetry, and relaxation. However, there is no validated scale to quantify PFM strength. Contractions can be further divided into voluntary and involuntary.19
During the exam, ask the patient to contract as much as she can to evaluate the maximum strength and sustained contraction for endurance. This measurement can be done with digital palpation or with pressure manometry or dynamometry.
Examination can be focused on the levator ani, piriformis, and internal obturator muscles bilaterally and rated by the patient’s reactions. Pelvic muscle tenderness, which can be highly prevalent in women with chronic pelvic pain, is associated with higher degrees of dyspareunia.21 Digital evaluation of the pelvic floor musculature varies in scale, number of fingers used, and parameters evaluated.
Lukban et al have described a 0 to 4 numbered scale that evaluates tenderness in the pelvic floor.22 The scale denotes “1” as comfortable pressure associated with the exam, “2” as uncomfortable pressure associated with the exam, “3” as moderate pain associated with the exam that intensifies with contraction, and “4” indicating severe pain with the exam and inability to perform the contraction maneuver due to pain.
Continue to: EFFECTIVE TREATMENT INCLUDES MULTIPLE OPTIONS
EFFECTIVE TREATMENT INCLUDES MULTIPLE OPTIONS
Lifestyle modifications can help
Lifestyle changes may help improve sexual function. These modifications include physical activity, healthy diet, nutrition counseling, and adequate sleep.23,24
Identifying medical conditions such as depression and anxiety will help delineate differential diagnoses of sexual dysfunction. Cardiovascular diseases may contribute to arousal disorder as a result of atherosclerosis of the vessels supplying the vagina and clitoris. Neurologic diseases such as multiple sclerosis and diabetes can affect sexual dysfunction by impairing arousal and orgasm.
Identification of concurrent comorbidities and implementation of lifestyle changes will help improve overall health and may improve sexual function.25
In addition, Herati et al found food sensitivities to grapefruit juice, spicy foods, alcohol, and caffeine were more prevalent in patients with interstitial cystitis and chronic pelvic pain.26 Avoiding irritants such as soap and other detergents in the perineal region may help decrease dysfunction.27 Finally, foods high in oxalate and other acidic items may cause bladder pain and worsening symptoms of vulvodynia.28
Topical therapies worth considering
Lubricants and moisturizers may help women with dyspareunia or symptoms of vaginal atrophy. For instance
Zestra, which contains a patented blend of botanical oils and extracts and is applied to the vulva prior to sexual activity, has been proven more effective than placebo for improving desire and arousal.29
Neogyn, a nonhormonal cream containing cutaneous lysate, has been shown to improve vulvar pain in women with vulvodynia. A double-blind placebo-controlled randomized crossover trial followed 30 patients for three months and found a significant reduction in pain during sexual activity and a significant reduction in erythema.30
Alprostadil, a prostaglandin E1 analogue that increases genital vasodilation when applied topically, is currently undergoing investigational trials.31,32
Patients can also choose from many OTC lubricants that contain water-based, oil-based, or silicone-based ingredients.
Continue to: Don't overlook physical therapy
Don’t overlook physical therapy
Manual therapies, including the transvaginal technique, are used for FSD that results from a variety of causes, including high-tone pelvic floor dysfunction. The transvaginal technique can identify myofascial pain; treatment involves internal release of the PFMs and external trigger-point identification and alleviation.
One pilot study examined use of transvaginal Thiele massage twice a week for five weeks in 21 symptomatic women with interstitial cystitis and high-tone pelvic floor dysfunction. The researchers found it decreased hypertonicity of the pelvic floor and generated statistically significant improvement in the Symptom and Problem Indexes of the O’Leary-Sant Questionnaire, Likert Visual Analogue Scales for urgency and pain, and the Physical and Mental Component Summary from the SF-12 Quality-of-Life Scale.33 Transvaginal physical therapy is also an effective treatment for myofascial pelvic pain.34
Biofeedback, which can be used in combination with pelvic floor physical therapy, teaches the patient to control the PFMs by visualizing the activity to achieve conscious control over contraction of the pelvic floor and ceasing the cycle of spasm.35 Ger et al investigated patients with levator spasm and found biofeedback decreased pain; relief was rated as good or excellent at 15-month follow-up in six of 14 patients (43%).36
Home devices such as Eros Therapy, an FDA-approved, nonpharmacologic battery-operated device, provide vacuum suction to the clitoris with vibratory sensation. Eros Therapy has been shown to increase blood flow to the clitoris, vagina, and pelvic floor and increase sensation, orgasm, lubrication, and satisfaction.37
Vaginal dilators allow increasing lengths and girths designed to treat vaginal and pelvic floor pain.38 In our practice, we encourage pelvic muscle strengthening tools in the form of Kegel trainers and other insertion devices that may improve PFM coordination and strength.
Continue to: Pharmacotherapy has its place
Pharmacotherapy has its place
The treatment of FSD may require a multimodal systematic approach targeting genitopelvic pain. But before the best options can be found, it is important to first establish the cause of the pain. Several drug formulations have been effectively used, including hormonal and nonhormonal options.
Conjugated estrogens are FDA approved for the treatment of dyspareunia, which can contribute to decreased desire. Systemic estrogen in oral form, transdermal preparations, and topical formulations may increase sexual desire and arousal and decrease dyspareunia.39 Even synthetic steroid compounds such as tibolone may improve sexual function, although it is not FDA approved for that purpose.40
Ospemifene is a selective estrogen receptor modulator that acts as an estrogen agonist in select tissues, including vaginal epithelium. It is FDA approved for dyspareunia in postmenopausal women.41,42 A daily dose of 60 mg is effective and safe, with minimal adverse effects.42 Studies suggest that testosterone, although not FDA approved in the United States for this purpose, improves sexual desire, pleasure, orgasm, and arousal satisfaction.39 The hormone has not gained FDA approval because of concerns about long-term safety and efficacy.42
Nonhormonal drugs including flibanserin, a well-tolerated serotonin receptor 1A agonist, 2A antagonist shown to improve sexual desire, increase the number of satisfying sexual events and reduce distress associated with low sexual desire when compared with placebo.43 The FDA has approved flibanserin as the first treatment targeted for women with hypoactive sexual desire disorder (HSDD). It can, however, cause severe hypotension and syncope, is not well tolerated with alcohol, and is contraindicated in patients who take strong CYP3A4 inhibitors, such as fluconazole, verapamil, and erythromycin, or who have liver impairment.
Bupropion, a mild dopamine and norepinephrine reuptake inhibitor and acetylcholine receptor antagonist, has been shown to improve desire in women with and without depression. Although it is FDA approved for major depressive disorder, it is not approved for female sexual dysfunction and is still under investigation.
Tricyclic antidepressants, such as nortriptyline and amitriptyline, may be effective in treating neuropathic pain. Starting doses of both amitriptyline and nortriptyline are 10 mg/d and can be increased to a maximum of 100 mg/d.44 Tricyclic antidepressants are still under investigation for the treatment of FSD.
Muscle relaxants in oral and topical compounded form are used to treat increased pelvic floor tension and spasticity. Cyclobenzaprine and tizanidine are FDA-approved muscle relaxants indicated for muscle spasticity.
Cyclobenzaprine, at a starting dose of 10 mg, can be taken up to three times a day for pelvic floor tension. Tizanidine is a centrally active alpha 2 agonist that’s superior to placebo in treating high-tone pelvic floor dysfunction.44
Other medications include benzodiazepines, such as oral clonazepam and intravaginal diazepam, although they are not FDA approved for high-tone pelvic floor dysfunction. Rogalski et al evaluated data for 26 patients who received vaginal diazepam for bladder pain, sexual pain, and levator hypertonus.45 They found subjective and sexual pain improvement assessed on FSFI and the visual analog pain scale. PFM tone significantly improved during resting, squeezing, and relaxation phases. Multimodal therapy can be used for muscle spasticity and high-tone pelvic floor dysfunction.
Continue to: Trigger point and Botox injections
Trigger point and Botox injections
Although drug therapy has its place in the management of sexual dysfunction, other modalities that involve trigger-point injections or botulinum toxin injections to the PFMs may prove helpful for patients with high-tone pelvic floor dysfunction.
A prospective study investigated the role of trigger-point injections in 18 women with levator ani muscle spasm using a mixture of 0.25% bupivacaine in 10 mL, 2% lidocaine in 10 mL, and 40 mg of triamcinolone in 1 mL combined and used for injection of 5 mL per trigger point.46 Three months after injections, 13 of the 18 women showed improvement, resulting in a success rate of 72%. Trigger point injections can be applied externally or transvaginally.
OnabotulinumtoxinA (Botox) has also been tested for relief of levator ani muscle spasm. Botox is FDA approved for upper and lower limb spasticity but is not approved for pelvic floor spasticity or tension. It may reduce pressure in the PFMs and may be useful in women with high-tone pelvic floor dysfunction.47
In a prospective six-month pilot study, 28 patients with pelvic pain for whom conservative treatment did not work received up to 300 U Botox into the pelvic floor.11 The study, which used needle electromyography guidance and a transperineal approach, found that the dyspareunia visual analog scale improved significantly at weeks 12 and 24. Keep in mind, however, that onabotulinumtoxinA should be reserved for patients for whom conventional treatments fail.47,48
Addressing psychologic issues
Sex therapy is a traditional approach that aims to improve individual or couples’ sexual experiences and help reduce anxiety related to sex.42 Cognitive behavioral sex therapy includes traditional sex therapy components but puts greater emphasis on modifying thought patterns that interfere with intimacy and sex.42
Mindfulness-based cognitive behavioral treatments have shown promise for sexual desire problems. It is an ancient eastern practice with Buddhist roots. This therapy is a nonjudgmental, present-moment awareness comprised of self-regulation of attention and accepting orientation to the present.49 Although there is little evidence from prospective studies, it may benefit women with sexual dysfunction after intervention with sex therapy and cognitive behavioral therapy.
CONCLUSION
Female sexual dysfunction is common and affects women of all ages. It can negatively impact a woman’s quality of life and overall well-being. The etiology of FSD is complex, and treatments are based on the causes of the dysfunction. Difficult cases warrant referral to a specialist in sexual health and female pelvic medicine. Future prospective trials, randomized controlled trials, the use of validated questionnaires, and meta-analyses will continue to move us forward as we find better ways to understand, identify, and treat female sexual dysfunction.
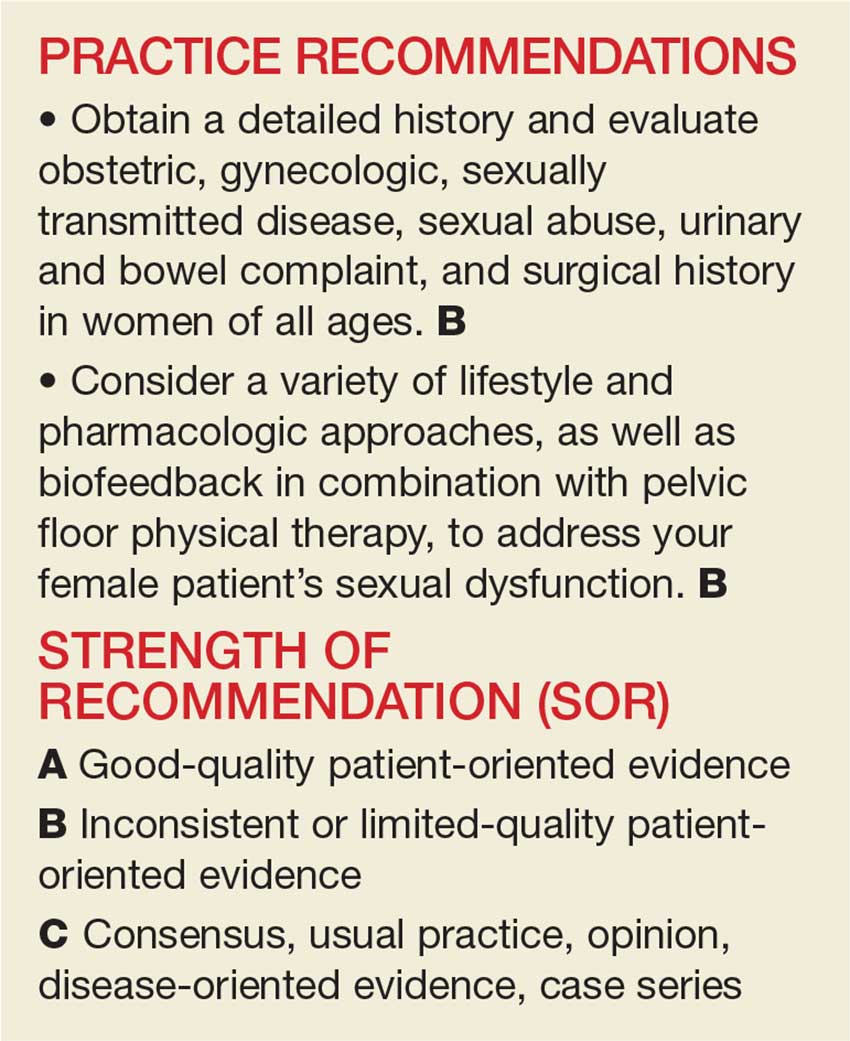
IN THIS ARTICLE
- Causes of pain
- Screening
- Multimodal treatment
Care of women with sexual disorders has made great strides since Masters and Johnson began their study in 1957. In 2000, the Sexual Function Health Council of the American Foundation for Urologic Disease devised the classification system for female sexual dysfunction, which was officially defined in the Diagnostic and Statistical Manual of Mental Disorders-IV-TR.1 There are now definitions for sexual desire disorders, sexual arousal disorders, orgasmic disorder, and sexual pain disorders.
Female sexual dysfunction (FSD) has complex physiologic and psychologic components that require a detailed screening, history, and physical examination. Our goal in this review is to provide primary care providers with insights and practical advice to help screen, diagnose, and treat FSD, which can have a profound impact on patients’ most intimate relationships.
UNDERSTANDING THE TYPES OF FSD
Most women consider sexual health an important part of their overall health.2 Factors that can disrupt normal sexual function include aging, socioeconomics, and other medical comorbidities. FSD is common in women throughout their lives and refers to various sexual dysfunctions including diminished arousal, problems achieving orgasm, dyspareunia, and low desire. Its prevalence is reported to be as high as 20% to 43%.3,4
The World Health Organization and the US Surgeon General have released statements encouraging health care providers to address sexual health during a patient’s annual visits.5 Unfortunately, despite this call to action, many patients and providers are initially hesitant to discuss these problems.6
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the definition and diagnostic guidelines for the different components of FSD. Its classification of sexual disorders was simplified and published in May 2013.7 There are now only three female dysfunctions (as opposed to five in DSM-IV):
- Female hypoactive desire dysfunction and female arousal dysfunction were merged into a single syndrome labeled female sexual interest/arousal disorder.
- The formerly separate dyspareunia (painful intercourse) and vaginismus are now called genitopelvic pain/penetration disorder.
- Female orgasmic disorder remains as a category and is unchanged.
To qualify as a dysfunction, the problem must be present more than 75% of the time, for more than six months, causing significant distress, and must not be explained by a nonsexual mental disorder, relationship distress, substance abuse, or a medical condition.
Substance- or medication-induced sexual dysfunction falls under “Other Dysfunctions” and is defined as a clinically significant disturbance in sexual function that is predominant in the clinical picture. The criteria for substance- and medication-induced sexual dysfunction are unchanged and include neither the 75% nor the six-month requirement. The diagnosis of sexual dysfunction due to a general medical condition and sexual aversion disorder are absent from the DSM-5.7
Continue to: A common symptom
A common symptom. Female sexual disorders can be caused by several complex physiologic and psychologic factors. A common symptom among many women is dyspareunia. It is seen more often in postmenopausal women, and its prevalence ranges from 8% to 22%.8 Pain on vaginal entry usually indicates vaginal atrophy, vaginal dermatitis, or provoked vestibulodynia. Pain on deep penetration could be caused by endometriosis, interstitial cystitis, or uterine leiomyomas.9
The physical examination will reproduce the pain when the vulva or vagina is touched with a cotton swab or when you insert a finger into the vagina. The differential diagnosis is listed in the Table.9-11
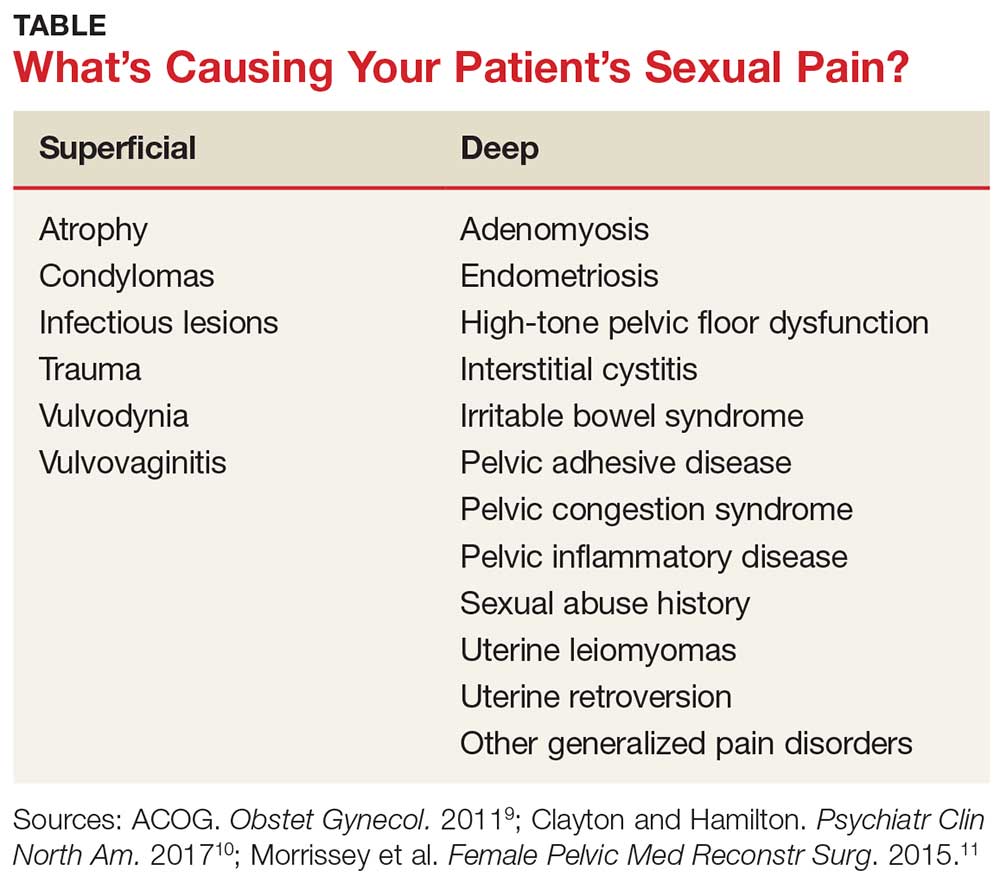
EVALUATING THE PATIENT
Initially, many patients and providers may hesitate to discuss sexual dysfunction, but the annual exam is a good opportunity to broach the topic of sexual health.
Screening and history
Clinicians can screen all patients, regardless of age, with the help of a validated sex questionnaire or during a routine review of systems. There are many validated screening tools available. A simple, integrated screening tool to use is the Brief Sexual Symptom Checklist for Women (BSSC-W), created by the International Consultation on Sexual Medicine.12 Although recommended by the American Congress of Obstetricians and Gynecologists, the BSSC-W is not validated.9 The four items in the questionnaire ascertain personal information regarding an individual’s overall sexual function satisfaction, the problem causing dysfunction, how bothersome the symptoms are, and whether the patient is interested in discussing it with her provider.12
It’s important to obtain a detailed obstetric and gynecologic history that includes any sexually transmitted diseases, sexual abuse, urinary and bowel complaints, or surgeries. In addition, you’ll want to differentiate between various types of dysfunctions. A thorough physical examination, including an external and internal pelvic exam, can help to rule out other causes of sexual dysfunction.
Continue to: General exam: What to look for
General exam: What to look for
The external pelvic examination begins with visual inspection of the vulva, labia majora, and labia minora. Often, this is best accomplished gently with a gloved hand and a cotton swab. This inspection may reveal changes in pubic hair distribution, vulvar skin disorders, lesions, masses, cracks, or fissures. Inspection may also reveal redness and pain typical of vestibulitis, a flattening and pallor of the labia that suggests estrogen deficiency, or pelvic organ prolapse.
The internal pelvic examination begins with a manual evaluation of the muscles of the pelvic floor, uterus, bladder, urethra, anus, and adnexa. Make careful note of any unusual tenderness or pelvic masses. Pelvic floor muscles (PFMs) should voluntarily contract and relax and are not normally tender to palpation. Pelvic organ prolapse and/or hypermobility of the bladder may indicate a weakening of the endopelvic fascia and may cause sexual pain. The size and flexion of the uterus, tenderness in the vaginal fornix possibly indicating endometriosis, and adnexal fullness and/or masses should be identified and evaluated.
Neurologic exam of the pelvis will involve evaluation of sensory and motor function of both lower extremities and include a screening lumbosacral neurologic examination. Lumbosacral examination includes assessment of PFM strength, anal sphincter resting tone, voluntary anal contraction, and perineal sensation. If abnormalities are noted in the screening assessment, a complete comprehensive neurologic examination should be performed.
It’s important to assess pelvic floor muscle strength
Sexual function is associated with normal PFM function.13,14 The PFMs, particularly the pubococcygeus and iliococcygeus, are responsible for involuntary contractions during orgasm.13 Orgasm has been considered a reflex, which is preceded by increased blood flow to the genital organs, tumescence of the vulva and vagina, increased secretions during sexual arousal, and increased tension and contractions of the PFMs.15
Lowenstein et al found that women with strong or moderate PFM contractions scored significantly higher on both orgasm and arousal domains of the Female Sexual Function Index (FSFI), compared with women with weak PFM contractions.16 Orgasm and arousal functions may be associated with PFM strength, with a positive association between pelvic floor strength and sexual activity and function.17,18
The function and dysfunction of the PFMs have been characterized as normal, overactive (high tone), underactive (low tone), and nonfunctioning.
Continue to: Normal PFMs
Normal PFMs are those that can voluntarily and involuntarily contract and relax.19,20
Overactive (high-tone) muscles are those that do not relax and possibly contract during times of relaxation for micturition or defecation. This type of dysfunction can lead to voiding dysfunction, defecatory dysfunction, and dyspareunia.19
Underactive, or low-tone, PFMs cannot contract voluntarily. This can be associated with urinary and anal incontinence and pelvic organ prolapse.
Nonfunctioning muscles are completely inactive.19
How to assess. There are several ways to assess PFM tone and strength.20 The first is intravaginal or intrarectal digital palpation, which can be performed when the patient is in a supine or standing position. This examination evaluates PFM tone, squeeze pressure during contraction, symmetry, and relaxation. However, there is no validated scale to quantify PFM strength. Contractions can be further divided into voluntary and involuntary.19
During the exam, ask the patient to contract as much as she can to evaluate the maximum strength and sustained contraction for endurance. This measurement can be done with digital palpation or with pressure manometry or dynamometry.
Examination can be focused on the levator ani, piriformis, and internal obturator muscles bilaterally and rated by the patient’s reactions. Pelvic muscle tenderness, which can be highly prevalent in women with chronic pelvic pain, is associated with higher degrees of dyspareunia.21 Digital evaluation of the pelvic floor musculature varies in scale, number of fingers used, and parameters evaluated.
Lukban et al have described a 0 to 4 numbered scale that evaluates tenderness in the pelvic floor.22 The scale denotes “1” as comfortable pressure associated with the exam, “2” as uncomfortable pressure associated with the exam, “3” as moderate pain associated with the exam that intensifies with contraction, and “4” indicating severe pain with the exam and inability to perform the contraction maneuver due to pain.
Continue to: EFFECTIVE TREATMENT INCLUDES MULTIPLE OPTIONS
EFFECTIVE TREATMENT INCLUDES MULTIPLE OPTIONS
Lifestyle modifications can help
Lifestyle changes may help improve sexual function. These modifications include physical activity, healthy diet, nutrition counseling, and adequate sleep.23,24
Identifying medical conditions such as depression and anxiety will help delineate differential diagnoses of sexual dysfunction. Cardiovascular diseases may contribute to arousal disorder as a result of atherosclerosis of the vessels supplying the vagina and clitoris. Neurologic diseases such as multiple sclerosis and diabetes can affect sexual dysfunction by impairing arousal and orgasm.
Identification of concurrent comorbidities and implementation of lifestyle changes will help improve overall health and may improve sexual function.25
In addition, Herati et al found food sensitivities to grapefruit juice, spicy foods, alcohol, and caffeine were more prevalent in patients with interstitial cystitis and chronic pelvic pain.26 Avoiding irritants such as soap and other detergents in the perineal region may help decrease dysfunction.27 Finally, foods high in oxalate and other acidic items may cause bladder pain and worsening symptoms of vulvodynia.28
Topical therapies worth considering
Lubricants and moisturizers may help women with dyspareunia or symptoms of vaginal atrophy. For instance
Zestra, which contains a patented blend of botanical oils and extracts and is applied to the vulva prior to sexual activity, has been proven more effective than placebo for improving desire and arousal.29
Neogyn, a nonhormonal cream containing cutaneous lysate, has been shown to improve vulvar pain in women with vulvodynia. A double-blind placebo-controlled randomized crossover trial followed 30 patients for three months and found a significant reduction in pain during sexual activity and a significant reduction in erythema.30
Alprostadil, a prostaglandin E1 analogue that increases genital vasodilation when applied topically, is currently undergoing investigational trials.31,32
Patients can also choose from many OTC lubricants that contain water-based, oil-based, or silicone-based ingredients.
Continue to: Don't overlook physical therapy
Don’t overlook physical therapy
Manual therapies, including the transvaginal technique, are used for FSD that results from a variety of causes, including high-tone pelvic floor dysfunction. The transvaginal technique can identify myofascial pain; treatment involves internal release of the PFMs and external trigger-point identification and alleviation.
One pilot study examined use of transvaginal Thiele massage twice a week for five weeks in 21 symptomatic women with interstitial cystitis and high-tone pelvic floor dysfunction. The researchers found it decreased hypertonicity of the pelvic floor and generated statistically significant improvement in the Symptom and Problem Indexes of the O’Leary-Sant Questionnaire, Likert Visual Analogue Scales for urgency and pain, and the Physical and Mental Component Summary from the SF-12 Quality-of-Life Scale.33 Transvaginal physical therapy is also an effective treatment for myofascial pelvic pain.34
Biofeedback, which can be used in combination with pelvic floor physical therapy, teaches the patient to control the PFMs by visualizing the activity to achieve conscious control over contraction of the pelvic floor and ceasing the cycle of spasm.35 Ger et al investigated patients with levator spasm and found biofeedback decreased pain; relief was rated as good or excellent at 15-month follow-up in six of 14 patients (43%).36
Home devices such as Eros Therapy, an FDA-approved, nonpharmacologic battery-operated device, provide vacuum suction to the clitoris with vibratory sensation. Eros Therapy has been shown to increase blood flow to the clitoris, vagina, and pelvic floor and increase sensation, orgasm, lubrication, and satisfaction.37
Vaginal dilators allow increasing lengths and girths designed to treat vaginal and pelvic floor pain.38 In our practice, we encourage pelvic muscle strengthening tools in the form of Kegel trainers and other insertion devices that may improve PFM coordination and strength.
Continue to: Pharmacotherapy has its place
Pharmacotherapy has its place
The treatment of FSD may require a multimodal systematic approach targeting genitopelvic pain. But before the best options can be found, it is important to first establish the cause of the pain. Several drug formulations have been effectively used, including hormonal and nonhormonal options.
Conjugated estrogens are FDA approved for the treatment of dyspareunia, which can contribute to decreased desire. Systemic estrogen in oral form, transdermal preparations, and topical formulations may increase sexual desire and arousal and decrease dyspareunia.39 Even synthetic steroid compounds such as tibolone may improve sexual function, although it is not FDA approved for that purpose.40
Ospemifene is a selective estrogen receptor modulator that acts as an estrogen agonist in select tissues, including vaginal epithelium. It is FDA approved for dyspareunia in postmenopausal women.41,42 A daily dose of 60 mg is effective and safe, with minimal adverse effects.42 Studies suggest that testosterone, although not FDA approved in the United States for this purpose, improves sexual desire, pleasure, orgasm, and arousal satisfaction.39 The hormone has not gained FDA approval because of concerns about long-term safety and efficacy.42
Nonhormonal drugs including flibanserin, a well-tolerated serotonin receptor 1A agonist, 2A antagonist shown to improve sexual desire, increase the number of satisfying sexual events and reduce distress associated with low sexual desire when compared with placebo.43 The FDA has approved flibanserin as the first treatment targeted for women with hypoactive sexual desire disorder (HSDD). It can, however, cause severe hypotension and syncope, is not well tolerated with alcohol, and is contraindicated in patients who take strong CYP3A4 inhibitors, such as fluconazole, verapamil, and erythromycin, or who have liver impairment.
Bupropion, a mild dopamine and norepinephrine reuptake inhibitor and acetylcholine receptor antagonist, has been shown to improve desire in women with and without depression. Although it is FDA approved for major depressive disorder, it is not approved for female sexual dysfunction and is still under investigation.
Tricyclic antidepressants, such as nortriptyline and amitriptyline, may be effective in treating neuropathic pain. Starting doses of both amitriptyline and nortriptyline are 10 mg/d and can be increased to a maximum of 100 mg/d.44 Tricyclic antidepressants are still under investigation for the treatment of FSD.
Muscle relaxants in oral and topical compounded form are used to treat increased pelvic floor tension and spasticity. Cyclobenzaprine and tizanidine are FDA-approved muscle relaxants indicated for muscle spasticity.
Cyclobenzaprine, at a starting dose of 10 mg, can be taken up to three times a day for pelvic floor tension. Tizanidine is a centrally active alpha 2 agonist that’s superior to placebo in treating high-tone pelvic floor dysfunction.44
Other medications include benzodiazepines, such as oral clonazepam and intravaginal diazepam, although they are not FDA approved for high-tone pelvic floor dysfunction. Rogalski et al evaluated data for 26 patients who received vaginal diazepam for bladder pain, sexual pain, and levator hypertonus.45 They found subjective and sexual pain improvement assessed on FSFI and the visual analog pain scale. PFM tone significantly improved during resting, squeezing, and relaxation phases. Multimodal therapy can be used for muscle spasticity and high-tone pelvic floor dysfunction.
Continue to: Trigger point and Botox injections
Trigger point and Botox injections
Although drug therapy has its place in the management of sexual dysfunction, other modalities that involve trigger-point injections or botulinum toxin injections to the PFMs may prove helpful for patients with high-tone pelvic floor dysfunction.
A prospective study investigated the role of trigger-point injections in 18 women with levator ani muscle spasm using a mixture of 0.25% bupivacaine in 10 mL, 2% lidocaine in 10 mL, and 40 mg of triamcinolone in 1 mL combined and used for injection of 5 mL per trigger point.46 Three months after injections, 13 of the 18 women showed improvement, resulting in a success rate of 72%. Trigger point injections can be applied externally or transvaginally.
OnabotulinumtoxinA (Botox) has also been tested for relief of levator ani muscle spasm. Botox is FDA approved for upper and lower limb spasticity but is not approved for pelvic floor spasticity or tension. It may reduce pressure in the PFMs and may be useful in women with high-tone pelvic floor dysfunction.47
In a prospective six-month pilot study, 28 patients with pelvic pain for whom conservative treatment did not work received up to 300 U Botox into the pelvic floor.11 The study, which used needle electromyography guidance and a transperineal approach, found that the dyspareunia visual analog scale improved significantly at weeks 12 and 24. Keep in mind, however, that onabotulinumtoxinA should be reserved for patients for whom conventional treatments fail.47,48
Addressing psychologic issues
Sex therapy is a traditional approach that aims to improve individual or couples’ sexual experiences and help reduce anxiety related to sex.42 Cognitive behavioral sex therapy includes traditional sex therapy components but puts greater emphasis on modifying thought patterns that interfere with intimacy and sex.42
Mindfulness-based cognitive behavioral treatments have shown promise for sexual desire problems. It is an ancient eastern practice with Buddhist roots. This therapy is a nonjudgmental, present-moment awareness comprised of self-regulation of attention and accepting orientation to the present.49 Although there is little evidence from prospective studies, it may benefit women with sexual dysfunction after intervention with sex therapy and cognitive behavioral therapy.
CONCLUSION
Female sexual dysfunction is common and affects women of all ages. It can negatively impact a woman’s quality of life and overall well-being. The etiology of FSD is complex, and treatments are based on the causes of the dysfunction. Difficult cases warrant referral to a specialist in sexual health and female pelvic medicine. Future prospective trials, randomized controlled trials, the use of validated questionnaires, and meta-analyses will continue to move us forward as we find better ways to understand, identify, and treat female sexual dysfunction.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed, text revision). Washington, DC; 1994.
2. Shifren JL, Monz BU, Russo PA, et al. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112:970-978.
3. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1:35-39.
4. Laumann E, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537-544.
5. Office of the Surgeon General. The Surgeon General’s Call to Action to Promote Sexual Health and Responsible Sexual Behavior. Rockville, MD; 2001.
6. Pauls RN, Kleeman SD, Segal JL, et al. Practice patterns of physician members of the American Urogynecologic Society regarding female sexual dysfunction: results of a national survey. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:460-467.
7. American Psychiatric Association. Sexual dysfunction. In: Diagnostic and Statistical Manual of Mental Disorders (5th ed). Washington, DC; 2013.
8. Steege JF, Zolnoun DA. Evaluation and treatment of dyspareunia. Obstet Gynecol. 2009;113:1124-1136.
9. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 119: Female sexual dysfunction. Obstet Gynecol. 2011;117:996-1007.
10. Clayton AH, Hamilton DV. Female sexual dysfunction. Psychiatr Clin North Am. 2017;40:267-284.
11. Morrissey D, El-Khawand D, Ginzburg N, et al. Botulinum Toxin A injections into pelvic floor muscles under electromyographic guidance for women with refractory high-tone pelvic floor dysfunction: a 6-month prospective pilot study. Female Pelvic Med Reconstr Surg. 2015;21:277-282.
12. Hatzichristou D, Rosen RC, Derogatis LR, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7(1 pt 2):337-348.
13. Kegel A. Sexual functions of the pubococcygeus muscle. West J Surg Obstet Gynecol. 1952;60:521-524.
14. Shafik A. The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J. 2000;11:361-376.
15. Kinsey A, Pomeroy WB, Martin CE, et al. Sexual Behavior in the Human Female. Philadelphia, PA: WB Saunders; 1998.
16. Lowenstein L, Gruenwald I, Gartman I, et al. Can stronger pelvic muscle floor improve sexual function? Int Urogynecol J. 2010;21:553-556.
17. Kanter G, Rogers RG, Pauls RN, et al. A strong pelvic floor is associated with higher rates of sexual activity in women with pelvic floor disorders. Int Urogynecol J. 2015;26:991-996.
18. Wehbe SA, Kellogg-Spadt S, Whitmore K. Urogenital complaints and female sexual dysfunction. Part 2. J Sex Med. 2010;7:2304-2317.
19. Messelink B, Benson T, Berghmans B, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the Pelvic Floor Clinical Assessment Group of the International Continence Society. Neurourol Urodyn. 2005;24:374-380.
20. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4-20.
21. Montenegro ML, Mateus-Vasconcelos EC, Rosa e Silva JC, et al. Importance of pelvic muscle tenderness evaluation in women with chronic pelvic pain. Pain Med. 2010;11:224-228.
22. Lukban JC, Whitmore KE. Pelvic floor muscle re-education treatment of the overactive bladder and painful bladder syndrome. Clin Obstet Gynecol. 2002;45:273-285.
23. Kalmbach DA, Arnedt JT, Pillai V, et al. The impact of sleep on female sexual response and behavior: a pilot study. J Sex Med. 2015;12:1221-1232.
24. Aversa A, Bruzziches R, Francomano D, et al. Weight loss by multidisciplinary intervention improves endothelial and sexual function in obese fertile women. J Sex Med. 2013;10:1024-1033.
25. Pauls RN, Kleeman SD, Karram MM. Female sexual dysfunction: principles of diagnosis and therapy. Obstet Gynecol Surv. 2005;60:196-205.
26. Herati AS, Shorter B, Tai J, et al. Differences in food sensitivities between female interstitial cystitis/painful bladder syndrome (IC/PBS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) patients. J Urol. 2009;181(4)(suppl):22.
27. Farrell J, Cacchioni T. The medicalization of women’s sexual pain. J Sex Res. 2012;49:328-336.
28. De Andres J, Sanchis-Lopez NM, Asensio-Samper JM, et al. Vulvodynia—an evidence-based literature review and proposed treatment algorithm. Pain Pract. 2016;16:204-236.
29. Herbenick D, Reece M, Schick V, et al. Women’s use and perceptions of commercial lubricants: prevalence and characteristics in a nationally representative sample of American adults. J Sex Med. 2014;11:642-652.
30. Donders GG, Bellen G. Cream with cutaneous fibroblast lysate for the treatment of provoked vestibulodynia: a double-blind randomized placebo-controlled crossover study. J Low Genit Tract Dis. 2012;16:427-436.
31. Belkin ZR, Krapf JM, Goldstein AT. Drugs in early clinical development for the treatment of female sexual dysfunction. Expert Opin Investig Drugs. 2015;24:159-167.
32. Islam A, Mitchel J, Rosen R, et al. Topical alprostadil in the treatment of female sexual arousal disorder: a pilot study. J Sex Marital Ther. 2001;27:531-540.
33. Oyama IA, Rejba A, Lukban JC, et al. Modified Thiele massage as therapeutic intervention for female patients with interstitial cystitis and high-tone pelvic floor dysfunction. Urology. 2004;64:862-865.
34. Bedaiwy MA, Patterson B, Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med. 2013;58:504-510.
35. Wehbe SA, Fariello JY, Whitmore K. Minimally invasive therapies for chronic pelvic pain syndrome. Curr Urol Rep. 2010;11:276-285.
36. Ger GC, Wexner SD, Jorge JM, et al. Evaluation and treatment of chronic intractable rectal pain—a frustrating endeavor. Dis Colon Rectum. 1993;36:139-145.
37. Billups KL, Berman L, Berman J, et al. A new non-pharmacological vacuum therapy for female sexual dysfunction. J Sex Marital Ther. 2001;27:435-441.
38. Miles T, Johnson N. Vaginal dilator therapy for women receiving pelvic radiotherapy. Cochrane Database Syst Rev. 2014;9:CD007291.
39. Goldstein I. Current management strategies of the postmenopausal patient with sexual health problems. J Sex Med. 2007;4(suppl 3):235-253.
40. Modelska K, Cummings S. Female sexual dysfunction in postmenopausal women: systematic review of placebo-controlled trials. Am J Obstet Gynecol. 2003;188:286-293.
41. Constantine G, Graham S, Portman DJ, et al. Female sexual function improved with ospemifene in postmenopausal women with vulvar and vaginal atrophy: results of a randomized, placebo-controlled trial. Climacteric. 2015;18:226-232.
42. Kingsberg SA, Woodard T. Female sexual dysfunction: focus on low desire. Obstet Gynecol. 2015;125:477-486.
43. Simon JA, Kingsberg SA, Shumel B, et al. Efficacy and safety of flibanserin in postmenopausal women with hypoactive sexual desire disorder: results of the SNOWDROP trial. Menopause. 2014;21:633-640.
44. Curtis Nickel J, Baranowski AP, Pontari M, et al. Management of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome who have failed traditional management. Rev Urol. 2007;9:63-72.
45. Rogalski MJ, Kellogg-Spadt S, Hoffmann AR, et al. Retrospective chart review of vaginal diazepam suppository use in high-tone pelvic floor dysfunction. Int Urogynecol J. 2010;21:895-899.
46. Langford CF, Udvari Nagy S, Ghoniem GM. Levator ani trigger point injections: an underutilized treatment for chronic pelvic pain. Neurourol Urodyn. 2007;26:59-62.
47. Abbott JA, Jarvis SK, Lyons SD, et al. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol. 2006;108:915-923.
48. Kamanli A, Kaya A, Ardicoglu O, et al. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int. 2005;25:604-611.
49. Brotto LA, Erskine Y, Carey M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012;125:320-325.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed, text revision). Washington, DC; 1994.
2. Shifren JL, Monz BU, Russo PA, et al. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112:970-978.
3. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1:35-39.
4. Laumann E, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537-544.
5. Office of the Surgeon General. The Surgeon General’s Call to Action to Promote Sexual Health and Responsible Sexual Behavior. Rockville, MD; 2001.
6. Pauls RN, Kleeman SD, Segal JL, et al. Practice patterns of physician members of the American Urogynecologic Society regarding female sexual dysfunction: results of a national survey. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:460-467.
7. American Psychiatric Association. Sexual dysfunction. In: Diagnostic and Statistical Manual of Mental Disorders (5th ed). Washington, DC; 2013.
8. Steege JF, Zolnoun DA. Evaluation and treatment of dyspareunia. Obstet Gynecol. 2009;113:1124-1136.
9. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 119: Female sexual dysfunction. Obstet Gynecol. 2011;117:996-1007.
10. Clayton AH, Hamilton DV. Female sexual dysfunction. Psychiatr Clin North Am. 2017;40:267-284.
11. Morrissey D, El-Khawand D, Ginzburg N, et al. Botulinum Toxin A injections into pelvic floor muscles under electromyographic guidance for women with refractory high-tone pelvic floor dysfunction: a 6-month prospective pilot study. Female Pelvic Med Reconstr Surg. 2015;21:277-282.
12. Hatzichristou D, Rosen RC, Derogatis LR, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7(1 pt 2):337-348.
13. Kegel A. Sexual functions of the pubococcygeus muscle. West J Surg Obstet Gynecol. 1952;60:521-524.
14. Shafik A. The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J. 2000;11:361-376.
15. Kinsey A, Pomeroy WB, Martin CE, et al. Sexual Behavior in the Human Female. Philadelphia, PA: WB Saunders; 1998.
16. Lowenstein L, Gruenwald I, Gartman I, et al. Can stronger pelvic muscle floor improve sexual function? Int Urogynecol J. 2010;21:553-556.
17. Kanter G, Rogers RG, Pauls RN, et al. A strong pelvic floor is associated with higher rates of sexual activity in women with pelvic floor disorders. Int Urogynecol J. 2015;26:991-996.
18. Wehbe SA, Kellogg-Spadt S, Whitmore K. Urogenital complaints and female sexual dysfunction. Part 2. J Sex Med. 2010;7:2304-2317.
19. Messelink B, Benson T, Berghmans B, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the Pelvic Floor Clinical Assessment Group of the International Continence Society. Neurourol Urodyn. 2005;24:374-380.
20. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4-20.
21. Montenegro ML, Mateus-Vasconcelos EC, Rosa e Silva JC, et al. Importance of pelvic muscle tenderness evaluation in women with chronic pelvic pain. Pain Med. 2010;11:224-228.
22. Lukban JC, Whitmore KE. Pelvic floor muscle re-education treatment of the overactive bladder and painful bladder syndrome. Clin Obstet Gynecol. 2002;45:273-285.
23. Kalmbach DA, Arnedt JT, Pillai V, et al. The impact of sleep on female sexual response and behavior: a pilot study. J Sex Med. 2015;12:1221-1232.
24. Aversa A, Bruzziches R, Francomano D, et al. Weight loss by multidisciplinary intervention improves endothelial and sexual function in obese fertile women. J Sex Med. 2013;10:1024-1033.
25. Pauls RN, Kleeman SD, Karram MM. Female sexual dysfunction: principles of diagnosis and therapy. Obstet Gynecol Surv. 2005;60:196-205.
26. Herati AS, Shorter B, Tai J, et al. Differences in food sensitivities between female interstitial cystitis/painful bladder syndrome (IC/PBS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) patients. J Urol. 2009;181(4)(suppl):22.
27. Farrell J, Cacchioni T. The medicalization of women’s sexual pain. J Sex Res. 2012;49:328-336.
28. De Andres J, Sanchis-Lopez NM, Asensio-Samper JM, et al. Vulvodynia—an evidence-based literature review and proposed treatment algorithm. Pain Pract. 2016;16:204-236.
29. Herbenick D, Reece M, Schick V, et al. Women’s use and perceptions of commercial lubricants: prevalence and characteristics in a nationally representative sample of American adults. J Sex Med. 2014;11:642-652.
30. Donders GG, Bellen G. Cream with cutaneous fibroblast lysate for the treatment of provoked vestibulodynia: a double-blind randomized placebo-controlled crossover study. J Low Genit Tract Dis. 2012;16:427-436.
31. Belkin ZR, Krapf JM, Goldstein AT. Drugs in early clinical development for the treatment of female sexual dysfunction. Expert Opin Investig Drugs. 2015;24:159-167.
32. Islam A, Mitchel J, Rosen R, et al. Topical alprostadil in the treatment of female sexual arousal disorder: a pilot study. J Sex Marital Ther. 2001;27:531-540.
33. Oyama IA, Rejba A, Lukban JC, et al. Modified Thiele massage as therapeutic intervention for female patients with interstitial cystitis and high-tone pelvic floor dysfunction. Urology. 2004;64:862-865.
34. Bedaiwy MA, Patterson B, Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med. 2013;58:504-510.
35. Wehbe SA, Fariello JY, Whitmore K. Minimally invasive therapies for chronic pelvic pain syndrome. Curr Urol Rep. 2010;11:276-285.
36. Ger GC, Wexner SD, Jorge JM, et al. Evaluation and treatment of chronic intractable rectal pain—a frustrating endeavor. Dis Colon Rectum. 1993;36:139-145.
37. Billups KL, Berman L, Berman J, et al. A new non-pharmacological vacuum therapy for female sexual dysfunction. J Sex Marital Ther. 2001;27:435-441.
38. Miles T, Johnson N. Vaginal dilator therapy for women receiving pelvic radiotherapy. Cochrane Database Syst Rev. 2014;9:CD007291.
39. Goldstein I. Current management strategies of the postmenopausal patient with sexual health problems. J Sex Med. 2007;4(suppl 3):235-253.
40. Modelska K, Cummings S. Female sexual dysfunction in postmenopausal women: systematic review of placebo-controlled trials. Am J Obstet Gynecol. 2003;188:286-293.
41. Constantine G, Graham S, Portman DJ, et al. Female sexual function improved with ospemifene in postmenopausal women with vulvar and vaginal atrophy: results of a randomized, placebo-controlled trial. Climacteric. 2015;18:226-232.
42. Kingsberg SA, Woodard T. Female sexual dysfunction: focus on low desire. Obstet Gynecol. 2015;125:477-486.
43. Simon JA, Kingsberg SA, Shumel B, et al. Efficacy and safety of flibanserin in postmenopausal women with hypoactive sexual desire disorder: results of the SNOWDROP trial. Menopause. 2014;21:633-640.
44. Curtis Nickel J, Baranowski AP, Pontari M, et al. Management of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome who have failed traditional management. Rev Urol. 2007;9:63-72.
45. Rogalski MJ, Kellogg-Spadt S, Hoffmann AR, et al. Retrospective chart review of vaginal diazepam suppository use in high-tone pelvic floor dysfunction. Int Urogynecol J. 2010;21:895-899.
46. Langford CF, Udvari Nagy S, Ghoniem GM. Levator ani trigger point injections: an underutilized treatment for chronic pelvic pain. Neurourol Urodyn. 2007;26:59-62.
47. Abbott JA, Jarvis SK, Lyons SD, et al. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol. 2006;108:915-923.
48. Kamanli A, Kaya A, Ardicoglu O, et al. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int. 2005;25:604-611.
49. Brotto LA, Erskine Y, Carey M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012;125:320-325.
Always get culture in symptomatic children with neurogenic bladder
In the symptomatic child with neurogenic bladder at risk for urinary tract infection (UTI), urine culture should be performed regardless of the results of urinalysis, recommended Catherine S. Forster, MD, of Cincinnati Children’s Hospital Medical Center, and her associates.
In a general pediatric population, studies have found that certain uropathogens – such as Enterococcus species, Klebsiella species, and Pseudomonas aeruginosa – are less likely to be associated with pyuria than Escherichia coli.
According to the guidelines of the Infectious Disease Society of America guidelines for the diagnosis of catheter-associated UTI, pyuria is not considered diagnostic of UTI in patients who require CIC.
Children with neurogenic bladder requiring CIC often have bacteriuria and often undergo urinalyses to determine if empirical antibiotics are warranted until urine culture results are available. “Although timely initiation of antibiotics can prevent the progression of infection and decrease the risk of renal scars, unnecessary antimicrobial agents contribute to the emergence of bacterial resistance,” Dr. Forster and her associates said.
So the researchers designed a study to find out if the presence of pyuria was associated with particular uropathogens in children with neurogenic bladders.
In an analysis of 2,420 urinalysis and urine culture results from EHRs between Jan.1, 2008, and Dec. 31, 2014, for patients aged 18 years and younger with neurogenic bladders requiring CIC, the most frequently isolated uropathogen was E. coli (37%), followed by Enterococcus species (14%), Klebsiella species (11%), and various other uropathogen species (38%).
In children needing CIC for neurogenic bladder, growth of Enterococcus species on urine culture was linked with lower odds of both microscopic pyuria (0.44) and leukocyte esterase (0.45).
“With these results, we suggest that the current markers of UTI evidenced on urinalysis and urine microscopy are insufficient for predicting bacteriuria in this population,” Dr. Forster and her colleagues said, leading to their recommendation to perform a culture in symptomatic children with neurogenic bladders irrespective of urinalysis results.
Dr. Forster received a research grant from the National Institutes of Health. The investigators said they had no relevant conflicts of interest.
SOURCE: Forster CS et al. Pediatrics. 2018;141(5):e20173006.
In the symptomatic child with neurogenic bladder at risk for urinary tract infection (UTI), urine culture should be performed regardless of the results of urinalysis, recommended Catherine S. Forster, MD, of Cincinnati Children’s Hospital Medical Center, and her associates.
In a general pediatric population, studies have found that certain uropathogens – such as Enterococcus species, Klebsiella species, and Pseudomonas aeruginosa – are less likely to be associated with pyuria than Escherichia coli.
According to the guidelines of the Infectious Disease Society of America guidelines for the diagnosis of catheter-associated UTI, pyuria is not considered diagnostic of UTI in patients who require CIC.
Children with neurogenic bladder requiring CIC often have bacteriuria and often undergo urinalyses to determine if empirical antibiotics are warranted until urine culture results are available. “Although timely initiation of antibiotics can prevent the progression of infection and decrease the risk of renal scars, unnecessary antimicrobial agents contribute to the emergence of bacterial resistance,” Dr. Forster and her associates said.
So the researchers designed a study to find out if the presence of pyuria was associated with particular uropathogens in children with neurogenic bladders.
In an analysis of 2,420 urinalysis and urine culture results from EHRs between Jan.1, 2008, and Dec. 31, 2014, for patients aged 18 years and younger with neurogenic bladders requiring CIC, the most frequently isolated uropathogen was E. coli (37%), followed by Enterococcus species (14%), Klebsiella species (11%), and various other uropathogen species (38%).
In children needing CIC for neurogenic bladder, growth of Enterococcus species on urine culture was linked with lower odds of both microscopic pyuria (0.44) and leukocyte esterase (0.45).
“With these results, we suggest that the current markers of UTI evidenced on urinalysis and urine microscopy are insufficient for predicting bacteriuria in this population,” Dr. Forster and her colleagues said, leading to their recommendation to perform a culture in symptomatic children with neurogenic bladders irrespective of urinalysis results.
Dr. Forster received a research grant from the National Institutes of Health. The investigators said they had no relevant conflicts of interest.
SOURCE: Forster CS et al. Pediatrics. 2018;141(5):e20173006.
In the symptomatic child with neurogenic bladder at risk for urinary tract infection (UTI), urine culture should be performed regardless of the results of urinalysis, recommended Catherine S. Forster, MD, of Cincinnati Children’s Hospital Medical Center, and her associates.
In a general pediatric population, studies have found that certain uropathogens – such as Enterococcus species, Klebsiella species, and Pseudomonas aeruginosa – are less likely to be associated with pyuria than Escherichia coli.
According to the guidelines of the Infectious Disease Society of America guidelines for the diagnosis of catheter-associated UTI, pyuria is not considered diagnostic of UTI in patients who require CIC.
Children with neurogenic bladder requiring CIC often have bacteriuria and often undergo urinalyses to determine if empirical antibiotics are warranted until urine culture results are available. “Although timely initiation of antibiotics can prevent the progression of infection and decrease the risk of renal scars, unnecessary antimicrobial agents contribute to the emergence of bacterial resistance,” Dr. Forster and her associates said.
So the researchers designed a study to find out if the presence of pyuria was associated with particular uropathogens in children with neurogenic bladders.
In an analysis of 2,420 urinalysis and urine culture results from EHRs between Jan.1, 2008, and Dec. 31, 2014, for patients aged 18 years and younger with neurogenic bladders requiring CIC, the most frequently isolated uropathogen was E. coli (37%), followed by Enterococcus species (14%), Klebsiella species (11%), and various other uropathogen species (38%).
In children needing CIC for neurogenic bladder, growth of Enterococcus species on urine culture was linked with lower odds of both microscopic pyuria (0.44) and leukocyte esterase (0.45).
“With these results, we suggest that the current markers of UTI evidenced on urinalysis and urine microscopy are insufficient for predicting bacteriuria in this population,” Dr. Forster and her colleagues said, leading to their recommendation to perform a culture in symptomatic children with neurogenic bladders irrespective of urinalysis results.
Dr. Forster received a research grant from the National Institutes of Health. The investigators said they had no relevant conflicts of interest.
SOURCE: Forster CS et al. Pediatrics. 2018;141(5):e20173006.
FROM PEDIATRICS
Key clinical point:
Major finding: In children needing CIC for neurogenic bladder, growth of Enterococcus species on urine culture was linked with lower odds of both microscopic pyuria (0.44) and leukocyte esterase (0.45).
Study details: Assessment of 2,420 urinalyses and urine cultures in children with neurogenic bladders.
Disclosures: Dr. Forster received a research grant from the National Institutes of Health. The investigators said they had no relevant conflicts of interest.
Source: Forster CS et al. Pediatrics. 2018;141(5):e20173006.
Which Headache Features May Help Identify Subarachnoid Hemorrhage?
Headaches that reach peak intensity in less than one second of onset are significantly more common in patients with subarachnoid hemorrhage (SAH) than in patients who present to a hospital with headaches caused by other conditions, according to a prospective, observational study published in the March issue of Headache. Other headache characteristics, including occipital location and a stabbing
“Our study suggests a number of features of the clinical history that may aid in identifying those patients presenting with headache at high likelihood of having an SAH,” said Brian Mac Grory, MB, BCh, BAO, Assistant Professor of Neurology at Warren Alpert Medical School of Brown University in Providence, Rhode Island, and colleagues. “This points to the possibility that we may be able to more accurately triage patients in the acute setting based on readily obtainable clinical metrics, which has the potential to reduce the number of expensive and invasive diagnostic tests performed, as well as the number of missed diagnoses.”
SAH is a life-threatening emergency. Patients most commonly present with a severe headache, but the presentation of SAH varies and is often subtle, the researchers said.
To characterize the headache associated with SAH, Dr. Mac Grory and colleagues performed a prospective, observational study examining the clinical features of the presenting headache in people with and without SAH in the emergency department and in the neurosciences intensive care unit of a tertiary referral center. They sought to assess whether any easily obtainable features of the clinical history might allow clinicians to predict whether a person has an SAH in the acute setting. The investigators documented clinical features of the headache, including the time to peak intensity, location, associated symptoms, and activities that caused worsening.
The researchers enrolled 158 subjects, of whom 20 had SAH. Distinguishing features included occipital location (55% in the SAH group vs 22% in the non-SAH group), stabbing quality (35% in the SAH group vs 5% in the non-SAH group), presence of prior headache (50% in the SAH group vs 83% in the non-SAH group), associated meningismus (80% in the SAH group vs 42% in the non-SAH group), and headache that reached peak intensity within 1 second (65% in the SAH group vs 10% in the non-SAH group).
—Jake Remaly
Suggested Reading
Mac Grory B, Vu L, Cutting S, et al. Distinguishing characteristics of headache in nontraumatic subarachnoid hemorrhage. Headache. 2018;58(3):364-370.
Headaches that reach peak intensity in less than one second of onset are significantly more common in patients with subarachnoid hemorrhage (SAH) than in patients who present to a hospital with headaches caused by other conditions, according to a prospective, observational study published in the March issue of Headache. Other headache characteristics, including occipital location and a stabbing
“Our study suggests a number of features of the clinical history that may aid in identifying those patients presenting with headache at high likelihood of having an SAH,” said Brian Mac Grory, MB, BCh, BAO, Assistant Professor of Neurology at Warren Alpert Medical School of Brown University in Providence, Rhode Island, and colleagues. “This points to the possibility that we may be able to more accurately triage patients in the acute setting based on readily obtainable clinical metrics, which has the potential to reduce the number of expensive and invasive diagnostic tests performed, as well as the number of missed diagnoses.”
SAH is a life-threatening emergency. Patients most commonly present with a severe headache, but the presentation of SAH varies and is often subtle, the researchers said.
To characterize the headache associated with SAH, Dr. Mac Grory and colleagues performed a prospective, observational study examining the clinical features of the presenting headache in people with and without SAH in the emergency department and in the neurosciences intensive care unit of a tertiary referral center. They sought to assess whether any easily obtainable features of the clinical history might allow clinicians to predict whether a person has an SAH in the acute setting. The investigators documented clinical features of the headache, including the time to peak intensity, location, associated symptoms, and activities that caused worsening.
The researchers enrolled 158 subjects, of whom 20 had SAH. Distinguishing features included occipital location (55% in the SAH group vs 22% in the non-SAH group), stabbing quality (35% in the SAH group vs 5% in the non-SAH group), presence of prior headache (50% in the SAH group vs 83% in the non-SAH group), associated meningismus (80% in the SAH group vs 42% in the non-SAH group), and headache that reached peak intensity within 1 second (65% in the SAH group vs 10% in the non-SAH group).
—Jake Remaly
Suggested Reading
Mac Grory B, Vu L, Cutting S, et al. Distinguishing characteristics of headache in nontraumatic subarachnoid hemorrhage. Headache. 2018;58(3):364-370.
Headaches that reach peak intensity in less than one second of onset are significantly more common in patients with subarachnoid hemorrhage (SAH) than in patients who present to a hospital with headaches caused by other conditions, according to a prospective, observational study published in the March issue of Headache. Other headache characteristics, including occipital location and a stabbing
“Our study suggests a number of features of the clinical history that may aid in identifying those patients presenting with headache at high likelihood of having an SAH,” said Brian Mac Grory, MB, BCh, BAO, Assistant Professor of Neurology at Warren Alpert Medical School of Brown University in Providence, Rhode Island, and colleagues. “This points to the possibility that we may be able to more accurately triage patients in the acute setting based on readily obtainable clinical metrics, which has the potential to reduce the number of expensive and invasive diagnostic tests performed, as well as the number of missed diagnoses.”
SAH is a life-threatening emergency. Patients most commonly present with a severe headache, but the presentation of SAH varies and is often subtle, the researchers said.
To characterize the headache associated with SAH, Dr. Mac Grory and colleagues performed a prospective, observational study examining the clinical features of the presenting headache in people with and without SAH in the emergency department and in the neurosciences intensive care unit of a tertiary referral center. They sought to assess whether any easily obtainable features of the clinical history might allow clinicians to predict whether a person has an SAH in the acute setting. The investigators documented clinical features of the headache, including the time to peak intensity, location, associated symptoms, and activities that caused worsening.
The researchers enrolled 158 subjects, of whom 20 had SAH. Distinguishing features included occipital location (55% in the SAH group vs 22% in the non-SAH group), stabbing quality (35% in the SAH group vs 5% in the non-SAH group), presence of prior headache (50% in the SAH group vs 83% in the non-SAH group), associated meningismus (80% in the SAH group vs 42% in the non-SAH group), and headache that reached peak intensity within 1 second (65% in the SAH group vs 10% in the non-SAH group).
—Jake Remaly
Suggested Reading
Mac Grory B, Vu L, Cutting S, et al. Distinguishing characteristics of headache in nontraumatic subarachnoid hemorrhage. Headache. 2018;58(3):364-370.
Conference News Roundup—American College of Cardiology
Drug Stops Dangerous Bleeding in Patients Taking Factor Xa Inhibitors
The experimental drug andexanet is associated with control of serious bleeding in patients taking a common class of anticoagulants known as Factor Xa inhibitors, according to interim clinical trial results. Factor Xa inhibitors elevate the risk of serious bleeding. If approved by the FDA, andexanet would be the first agent available to directly reverse the effects of Factor Xa inhibition if bleeding occurs.
Factor Xa inhibitors, which inhibit a protein involved in the formation of blood clots, are commonly prescribed for patients who are at high risk for stroke and venous thrombosis. Because Factor Xa inhibitors and other anticoagulants reduce the body’s ability to form a blood clot, these drugs can also increase the risk of uncontrolled bleeding. When this happens, it can be challenging for doctors to stop the bleeding. About 25% of patients who experience bleeding in the brain while taking a Factor Xa inhibitor die.
“Unlike for some other anticoagulants, there is currently no approved reversal agent for Factor Xa inhibitors,” said Stuart Connolly, MD, Professor of Medicine at McMaster University in Hamilton, Ontario. “Factor Xa inhibitors are already widely used because of their excellent efficacy and safety profile. However, some physicians and patients may choose to use other anticoagulant drugs because they have a reversal agent, rather than using one of the Factor Xa inhibitors. Having a safe and effective reversal agent available will benefit patients with acute bleeding.”
About 2.9 million people in the United States currently take Factor Xa inhibitors. Of these people, most are older and have illnesses, such as heart failure, that put them at high risk for cardiovascular problems. Approximately 84,000 patients taking Factor Xa inhibitors are hospitalized for major bleeding each year, according to a recent analysis of the MarketScan Commercial and Medicare databases. The most common types of major bleeds include bleeding in the brain, sometimes resulting from a fall, and gastrointestinal bleeding.
Andexanet is a recombinant modified Factor Xa molecule designed to bind to and disable Factor Xa inhibitors, thereby allowing Factor Xa produced by the body to play its normal role in the formation of blood clots. In earlier trials performed in healthy volunteers, andexanet rapidly reversed the anticoagulant effect of Factor Xa inhibitors without causing any significant safety problems.
ANNEXA-4 is an ongoing clinical trial that uses andexanet to help treat patients experiencing major bleeding while taking Factor Xa inhibitors. The interim analysis includes data on safety outcomes for 227 patients and adjudicated efficacy outcomes for 132 patients enrolled at centers in the US, Canada, and Europe. All trial participants presented with acute major bleeding within 18 hours of taking one of four Factor Xa inhibitors (ie, apixaban, rivaroxaban, edoxaban, or enoxaparin). Patients received an injection of andexanet followed by a two-hour infusion of the drug, with the dosage determined based on the specific Factor Xa inhibitor the patient was taking and how long it had been since the last dose.
The trial assesses the drug’s efficacy in terms of the following two coprimary endpoints: reduction in anti-Factor Xa inhibitor activity and achievement of clinical hemostasis by 12 hours after administration. The interim results show that median anti-Factor Xa inhibitor activity was reduced by 88% for patients taking rivaroxaban, 91% for patients taking apixaban, and 75% for patients taking enoxaparin. Few patients in the study had received edoxaban. Excellent or good clinical hemostasis was achieved in 83% of patients overall.
Safety of andexanet was assessed in all 227 patients. At 30 days, 12% of patients had died, and 11% had a thrombotic event (ie, stroke, heart attack, or blood clot in the legs). These rates of adverse events are in line with what would be expected, given the underlying medical condition of the patients in the trial and the fact that many had not resumed anticoagulant treatment during the 30 days after receiving andexanet, Dr. Connolly said. The trial was funded by Portola Pharmaceuticals, maker of andexanet.
Low-Dose Triple Pill Lowers Blood Pressure More Than Usual Care
A pill combining low doses of three blood pressure–lowering medications significantly increased the number of patients reaching blood pressure targets, compared with usual care, said researchers. The combination therapy was not associated with a significant increase in adverse effects.
“Most people—70%—reached blood pressure targets with the triple pill. The benefits were seen straight away and maintained until six months, whereas with usual care, control rates were 55% at six months and even lower earlier in the trial,” said Ruth Webster, MBBS, Head of Research Programs at the George Institute for Global Health at the University of New South Wales in Sydney. “Based on our findings, we conclude that this new method of using blood pressure–lowering drugs was more effective and just as safe as current approaches.”
Despite the availability of effective blood pressure–lowering drugs, high blood pressure remains a major problem around the world, said Dr. Webster. Effectively treating high blood pressure can help to prevent strokes, heart attacks, and kidney problems. Globally, however, many people with high blood pressure receive no treatment, and only about a third of those who are treated achieve recommended reductions in blood pressure. Achieving desired reductions in blood pressure often requires treatment with more than one medication, which increases the complexity of treatment. Patients often have difficulty adhering to regimens that involve taking multiple pills every day.
This study was the first large trial designed to test the theory that starting treatment with low doses of three drugs could achieve better blood pressure control, compared with usual care, and that combining these drugs in a single pill would make it easier for doctors to prescribe treatment and for patients to adhere to it, said Dr. Webster.
The TRIUMPH trial, which was conducted in Sri Lanka, enrolled 700 patients (58% women) whose average age was 56. Trial participants had an average blood pressure of 154/90 mm Hg. Approximately 59% were receiving no treatment for high blood pressure before they enrolled in the trial. In addition to high blood pressure, 32% of participants had diabetes or chronic kidney disease.
Patients were randomly assigned to receive either the combination pill or usual care. The combination pill, or triple pill, consisted of the blood pressure medications telmisartan (20 mg), amlodipine (2.5 mg), and chlorthalidone (12.5 mg). These medications use different mechanisms to reduce blood pressure by relaxing the blood vessels. Usual care meant that patients received their doctors’ choice of blood pressure–lowering medication.
The trial’s primary end point was the proportion of patients who achieved a blood pressure target of 140/90 mm Hg or less (130/80 mm Hg or less in those with diabetes or chronic kidney disease) at six months.
Compared with patients receiving usual care, a significantly higher proportion of patients receiving the triple pill achieved their target blood pressure at six months. The average reduction in blood pressure was 8.7 mm Hg for participants receiving the triple pill and 4.5 mm Hg for those receiving usual care. At six months, 83% of participants in the triple pill group were still receiving the combination pill, and one-third of those in the usual-care group was receiving at least two blood pressure–lowering drugs.
The maximum difference between the two groups of patients was observed at six weeks after starting treatment, when 68% of those receiving the triple pill had achieved a blood pressure within their target range, compared with 44% of those receiving usual care. This result represented a 53% reduction in the risk for high blood pressure for patients receiving the triple pill, said Dr. Webster.
Rates of participants having to change treatment due to side effects were not significantly different between the two groups (6.6% for the triple pill and 6.8% for usual care). This finding should allay concerns that use of the three-drug combination pill could lead to an unacceptable increase in adverse medication side effects, said Dr. Webster.
Each of the drugs in the triple pill is highly effective in reducing blood pressure and preventing deaths and illness due to heart disease and strokes, she added. Each drug represents a different class of blood pressure medication, and previous studies have shown that combining such drugs results in synergistic effects.
“The most urgent need for innovative strategies to control blood pressure is in low- and middle-income countries,” said Dr. Webster.
The study’s findings are also important for high-income countries, she said. “A control rate of 70% would be a considerable improvement even in high-income settings. Most hypertension guidelines in these countries do not recommend combination blood pressure–lowering therapy for initial treatment in all people,” she said. “Our findings should prompt reconsideration of recommendations around the use of combination therapy.”
An inevitable consequence of a necessarily unblinded study is that doctors might manage patients differently, depending on the assigned treatment. It is important to note, however, that this trial was designed to evaluate a new strategy of care in a real-world setting, said Dr. Webster. To minimize the risk of bias in measuring the main outcomes, the number of patient visits was identical in both groups, and all outcomes were standardized and objectively documented, she said.
Metoprolol May Increase Postsurgical Risk of Stroke or Death
During the 12 months after undergoing noncardiac surgery, patients with heart disease or at risk for heart disease who are treated with the beta blocker metoprolol for 30 days are less likely than patients who receive a placebo to have a heart attack, but more likely to die or have a stroke, said researchers.
These follow-up findings confirm that an increased risk for death or stroke persists at one year post surgery in patients treated with metoprolol, said P. J. Devereaux, MD, PhD, Director of Cardiology at McMaster University in Hamilton, Ontario. Previously reported results from the same study at 30 days post surgery showed a similar pattern, with a reduction in heart attacks, but increases in deaths and strokes.
“Our results suggest at one year, for every 1,000 patients having noncardiac surgery, treatment with metoprolol would prevent heart attacks in 12 patients, but would result in an excess of 13 deaths and six strokes,” said Dr. Devereaux.
“While there is little doubt that some patients benefit from receiving beta blockers during the period immediately before and after noncardiac surgery, these data show that at least as many patients are seriously harmed,” he said. “These data tell us that we need to exercise caution when using beta blockers in this setting until we figure out how to mitigate the substantial risks and enable all patients to obtain the potential benefits of this intervention.”
Beta blockers work by slowing the heart rate and relaxing the blood vessels, which, in turn, reduces blood pressure. The problem is that during the period immediately after major noncardiac surgery (such as a hip or knee replacement, bowel resection, or abdominal aortic aneurysm repair), patients are usually treated with opioid medications to relieve pain, said Dr. Devereaux. The effects of those medications may mask drops in blood pressure or heart rate to dangerously low levels. “Hypotension is common in this setting and is a main contributor to the adverse effects resulting from perioperative beta blockers,” he said.
Patients who become hypotensive for whatever reason after surgery (eg, sepsis, bleeding, or heart failure) find their problem exacerbated when they are receiving a beta blocker, which further lowers blood pressure and makes treating hypotension more challenging.
The PeriOperative Ischemic Evaluation (POISE) trial enrolled 8,351 patients in 23 countries. Eligible patients were age 45 or older and had a history of heart disease, blood-vessel disease, stroke, congestive heart failure, or other health problems such as diabetes or impaired kidney function. Patients’ median age was 69, and 63% were men.
Patients were randomly assigned to receive metoprolol or a placebo, beginning a few hours before surgery and for 30 days afterward. Patients, health care providers, and research staff, except those analyzing data, were blinded to which group received metoprolol and which received a placebo. The study’s primary end point was a composite of the combined rate of death from heart disease, nonfatal heart attack, and nonfatal cardiac arrest after 30 days.
At one-year follow-up, fewer patients in the metoprolol group than in the placebo group had heart attacks (5% vs 6.2%), but more patients in the metoprolol group had died (9.8% vs 8.5%) or had a stroke (2% vs 1.4%).
These results followed the same pattern that had previously been seen at the 30-day follow-up: statistically fewer heart attacks in the metoprolol group (4.2% vs 5.7% in the placebo group), but statistically more deaths (3.1% vs 2.3% in the placebo group) and strokes (1% vs 0.5% in the placebo group).
Observers have suggested that the metoprolol dose in the POISE trial (200 mg/day) was too high and that a lower dose would have produced fewer adverse effects. But a lower dose might also have decreased the drug’s effectiveness in reducing heart attacks, said Dr. Devereaux, noting that the metoprolol dose in POISE only resulted in a 7-bpm lower heart rate, compared with placebo. More continuous monitoring “I believe the answer is more continuous patient monitoring during the immediate postsurgical period so that dangerous drops in heart rate or blood pressure are promptly identified and treated.”
Managing Blood Pressure in Barbershops Yields Improvements
African American men who received medical intervention aimed at controlling their high blood pressure while at the barber saw a marked drop in blood pressure in six months, according to researchers. Specifically, men who received frequent monitoring and medication management from a specially trained pharmacist who met them monthly in their barbershop lowered their systolic blood pressure by 21 mm Hg more, on average, compared with men who were encouraged by their barber to follow up with a doctor and to make healthy lifestyle choices.
While high blood pressure is a common problem among many American adults, African American men are more likely than other groups to have high blood pressure that is not adequately controlled and tend to have less contact with the health care system.
“By bringing state-of-the-art medicine directly to the people who need it on their home turf, in this case, in a barbershop, and making it both convenient and rigorous, blood pressure can be controlled just as well in African American men as in other groups,” said Ronald G. Victor, MD, Associate Director of the Smidt Heart Institute at Cedars-Sinai in Los Angeles. “If this model were scaled up and sustained, millions of lives could be saved, and many heart attacks and strokes could be prevented.”
Previous studies have shown that equipping barbers—who remain trusted, consistent, and convenient figures for many African American men—with health information can positively affect health. The new study is unique because it combined barbershop-based health outreach with the delivery of care by medical professionals at the barbershop and evaluated subsequent efficacy with a randomized trial.
The study recruited 319 men at 52 Los Angeles County barbershops. All the men had systolic blood pressure over 140 mm Hg, based on multiple measurements taken on two different days. The men ranged in age from 35 to 71 and, on average, had patronized their barbershop for more than a decade and had their hair cut twice a month.
In total, 303 men completed the study—representing a 95% cohort retention—and all received an intervention designed to help them lower their blood pressure.
A little over half of the men (171) were randomly assigned to receive health education from their barbers, who were trained to use a National Heart, Lung, and Blood Institute–developed script to encourage the men to visit their doctors and get their blood pressure under control.
The remaining men (132) were randomly assigned to receive regular monitoring (at least once per month) and active medication management by a pharmacist who met them at the barbershop. During each pharmacist visit, the men in this group received a blood pressure evaluation and a finger-stick blood test, which the pharmacist used to evaluate each man’s response to blood pressure medications and adjust prescriptions as needed. The pharmacists worked directly with the men under a collaborative care agreement with their primary care doctors.
On average, men who interacted only with their barber and were referred to their own doctor saw their systolic blood pressure decrease from 155 mm Hg at the start of the study to 145 mm Hg after six months. Diastolic blood pressured decreased by 4 mm Hg in this group. By contrast, men who interacted with their barber and a pharmacist saw their systolic blood pressure decrease from 153 mm Hg at the start of the study to 126 mm Hg after six months, along with a decrease in diastolic blood pressure of 18 mm Hg.
Under current American College of Cardiology–American Heart Association guidelines, blood pressure below 130/80 mm Hg is considered normal. At the end of six months, 64% of participants who saw a pharmacist had blood pressure in the normal range, compared with 12% of participants who were referred to their own doctor. “This is a large effect for a hypertension trial of any kind,” said Dr. Victor. “We are excited about the results.” Researchers are studying whether the effects can be sustained for an additional six months.
Drug Stops Dangerous Bleeding in Patients Taking Factor Xa Inhibitors
The experimental drug andexanet is associated with control of serious bleeding in patients taking a common class of anticoagulants known as Factor Xa inhibitors, according to interim clinical trial results. Factor Xa inhibitors elevate the risk of serious bleeding. If approved by the FDA, andexanet would be the first agent available to directly reverse the effects of Factor Xa inhibition if bleeding occurs.
Factor Xa inhibitors, which inhibit a protein involved in the formation of blood clots, are commonly prescribed for patients who are at high risk for stroke and venous thrombosis. Because Factor Xa inhibitors and other anticoagulants reduce the body’s ability to form a blood clot, these drugs can also increase the risk of uncontrolled bleeding. When this happens, it can be challenging for doctors to stop the bleeding. About 25% of patients who experience bleeding in the brain while taking a Factor Xa inhibitor die.
“Unlike for some other anticoagulants, there is currently no approved reversal agent for Factor Xa inhibitors,” said Stuart Connolly, MD, Professor of Medicine at McMaster University in Hamilton, Ontario. “Factor Xa inhibitors are already widely used because of their excellent efficacy and safety profile. However, some physicians and patients may choose to use other anticoagulant drugs because they have a reversal agent, rather than using one of the Factor Xa inhibitors. Having a safe and effective reversal agent available will benefit patients with acute bleeding.”
About 2.9 million people in the United States currently take Factor Xa inhibitors. Of these people, most are older and have illnesses, such as heart failure, that put them at high risk for cardiovascular problems. Approximately 84,000 patients taking Factor Xa inhibitors are hospitalized for major bleeding each year, according to a recent analysis of the MarketScan Commercial and Medicare databases. The most common types of major bleeds include bleeding in the brain, sometimes resulting from a fall, and gastrointestinal bleeding.
Andexanet is a recombinant modified Factor Xa molecule designed to bind to and disable Factor Xa inhibitors, thereby allowing Factor Xa produced by the body to play its normal role in the formation of blood clots. In earlier trials performed in healthy volunteers, andexanet rapidly reversed the anticoagulant effect of Factor Xa inhibitors without causing any significant safety problems.
ANNEXA-4 is an ongoing clinical trial that uses andexanet to help treat patients experiencing major bleeding while taking Factor Xa inhibitors. The interim analysis includes data on safety outcomes for 227 patients and adjudicated efficacy outcomes for 132 patients enrolled at centers in the US, Canada, and Europe. All trial participants presented with acute major bleeding within 18 hours of taking one of four Factor Xa inhibitors (ie, apixaban, rivaroxaban, edoxaban, or enoxaparin). Patients received an injection of andexanet followed by a two-hour infusion of the drug, with the dosage determined based on the specific Factor Xa inhibitor the patient was taking and how long it had been since the last dose.
The trial assesses the drug’s efficacy in terms of the following two coprimary endpoints: reduction in anti-Factor Xa inhibitor activity and achievement of clinical hemostasis by 12 hours after administration. The interim results show that median anti-Factor Xa inhibitor activity was reduced by 88% for patients taking rivaroxaban, 91% for patients taking apixaban, and 75% for patients taking enoxaparin. Few patients in the study had received edoxaban. Excellent or good clinical hemostasis was achieved in 83% of patients overall.
Safety of andexanet was assessed in all 227 patients. At 30 days, 12% of patients had died, and 11% had a thrombotic event (ie, stroke, heart attack, or blood clot in the legs). These rates of adverse events are in line with what would be expected, given the underlying medical condition of the patients in the trial and the fact that many had not resumed anticoagulant treatment during the 30 days after receiving andexanet, Dr. Connolly said. The trial was funded by Portola Pharmaceuticals, maker of andexanet.
Low-Dose Triple Pill Lowers Blood Pressure More Than Usual Care
A pill combining low doses of three blood pressure–lowering medications significantly increased the number of patients reaching blood pressure targets, compared with usual care, said researchers. The combination therapy was not associated with a significant increase in adverse effects.
“Most people—70%—reached blood pressure targets with the triple pill. The benefits were seen straight away and maintained until six months, whereas with usual care, control rates were 55% at six months and even lower earlier in the trial,” said Ruth Webster, MBBS, Head of Research Programs at the George Institute for Global Health at the University of New South Wales in Sydney. “Based on our findings, we conclude that this new method of using blood pressure–lowering drugs was more effective and just as safe as current approaches.”
Despite the availability of effective blood pressure–lowering drugs, high blood pressure remains a major problem around the world, said Dr. Webster. Effectively treating high blood pressure can help to prevent strokes, heart attacks, and kidney problems. Globally, however, many people with high blood pressure receive no treatment, and only about a third of those who are treated achieve recommended reductions in blood pressure. Achieving desired reductions in blood pressure often requires treatment with more than one medication, which increases the complexity of treatment. Patients often have difficulty adhering to regimens that involve taking multiple pills every day.
This study was the first large trial designed to test the theory that starting treatment with low doses of three drugs could achieve better blood pressure control, compared with usual care, and that combining these drugs in a single pill would make it easier for doctors to prescribe treatment and for patients to adhere to it, said Dr. Webster.
The TRIUMPH trial, which was conducted in Sri Lanka, enrolled 700 patients (58% women) whose average age was 56. Trial participants had an average blood pressure of 154/90 mm Hg. Approximately 59% were receiving no treatment for high blood pressure before they enrolled in the trial. In addition to high blood pressure, 32% of participants had diabetes or chronic kidney disease.
Patients were randomly assigned to receive either the combination pill or usual care. The combination pill, or triple pill, consisted of the blood pressure medications telmisartan (20 mg), amlodipine (2.5 mg), and chlorthalidone (12.5 mg). These medications use different mechanisms to reduce blood pressure by relaxing the blood vessels. Usual care meant that patients received their doctors’ choice of blood pressure–lowering medication.
The trial’s primary end point was the proportion of patients who achieved a blood pressure target of 140/90 mm Hg or less (130/80 mm Hg or less in those with diabetes or chronic kidney disease) at six months.
Compared with patients receiving usual care, a significantly higher proportion of patients receiving the triple pill achieved their target blood pressure at six months. The average reduction in blood pressure was 8.7 mm Hg for participants receiving the triple pill and 4.5 mm Hg for those receiving usual care. At six months, 83% of participants in the triple pill group were still receiving the combination pill, and one-third of those in the usual-care group was receiving at least two blood pressure–lowering drugs.
The maximum difference between the two groups of patients was observed at six weeks after starting treatment, when 68% of those receiving the triple pill had achieved a blood pressure within their target range, compared with 44% of those receiving usual care. This result represented a 53% reduction in the risk for high blood pressure for patients receiving the triple pill, said Dr. Webster.
Rates of participants having to change treatment due to side effects were not significantly different between the two groups (6.6% for the triple pill and 6.8% for usual care). This finding should allay concerns that use of the three-drug combination pill could lead to an unacceptable increase in adverse medication side effects, said Dr. Webster.
Each of the drugs in the triple pill is highly effective in reducing blood pressure and preventing deaths and illness due to heart disease and strokes, she added. Each drug represents a different class of blood pressure medication, and previous studies have shown that combining such drugs results in synergistic effects.
“The most urgent need for innovative strategies to control blood pressure is in low- and middle-income countries,” said Dr. Webster.
The study’s findings are also important for high-income countries, she said. “A control rate of 70% would be a considerable improvement even in high-income settings. Most hypertension guidelines in these countries do not recommend combination blood pressure–lowering therapy for initial treatment in all people,” she said. “Our findings should prompt reconsideration of recommendations around the use of combination therapy.”
An inevitable consequence of a necessarily unblinded study is that doctors might manage patients differently, depending on the assigned treatment. It is important to note, however, that this trial was designed to evaluate a new strategy of care in a real-world setting, said Dr. Webster. To minimize the risk of bias in measuring the main outcomes, the number of patient visits was identical in both groups, and all outcomes were standardized and objectively documented, she said.
Metoprolol May Increase Postsurgical Risk of Stroke or Death
During the 12 months after undergoing noncardiac surgery, patients with heart disease or at risk for heart disease who are treated with the beta blocker metoprolol for 30 days are less likely than patients who receive a placebo to have a heart attack, but more likely to die or have a stroke, said researchers.
These follow-up findings confirm that an increased risk for death or stroke persists at one year post surgery in patients treated with metoprolol, said P. J. Devereaux, MD, PhD, Director of Cardiology at McMaster University in Hamilton, Ontario. Previously reported results from the same study at 30 days post surgery showed a similar pattern, with a reduction in heart attacks, but increases in deaths and strokes.
“Our results suggest at one year, for every 1,000 patients having noncardiac surgery, treatment with metoprolol would prevent heart attacks in 12 patients, but would result in an excess of 13 deaths and six strokes,” said Dr. Devereaux.
“While there is little doubt that some patients benefit from receiving beta blockers during the period immediately before and after noncardiac surgery, these data show that at least as many patients are seriously harmed,” he said. “These data tell us that we need to exercise caution when using beta blockers in this setting until we figure out how to mitigate the substantial risks and enable all patients to obtain the potential benefits of this intervention.”
Beta blockers work by slowing the heart rate and relaxing the blood vessels, which, in turn, reduces blood pressure. The problem is that during the period immediately after major noncardiac surgery (such as a hip or knee replacement, bowel resection, or abdominal aortic aneurysm repair), patients are usually treated with opioid medications to relieve pain, said Dr. Devereaux. The effects of those medications may mask drops in blood pressure or heart rate to dangerously low levels. “Hypotension is common in this setting and is a main contributor to the adverse effects resulting from perioperative beta blockers,” he said.
Patients who become hypotensive for whatever reason after surgery (eg, sepsis, bleeding, or heart failure) find their problem exacerbated when they are receiving a beta blocker, which further lowers blood pressure and makes treating hypotension more challenging.
The PeriOperative Ischemic Evaluation (POISE) trial enrolled 8,351 patients in 23 countries. Eligible patients were age 45 or older and had a history of heart disease, blood-vessel disease, stroke, congestive heart failure, or other health problems such as diabetes or impaired kidney function. Patients’ median age was 69, and 63% were men.
Patients were randomly assigned to receive metoprolol or a placebo, beginning a few hours before surgery and for 30 days afterward. Patients, health care providers, and research staff, except those analyzing data, were blinded to which group received metoprolol and which received a placebo. The study’s primary end point was a composite of the combined rate of death from heart disease, nonfatal heart attack, and nonfatal cardiac arrest after 30 days.
At one-year follow-up, fewer patients in the metoprolol group than in the placebo group had heart attacks (5% vs 6.2%), but more patients in the metoprolol group had died (9.8% vs 8.5%) or had a stroke (2% vs 1.4%).
These results followed the same pattern that had previously been seen at the 30-day follow-up: statistically fewer heart attacks in the metoprolol group (4.2% vs 5.7% in the placebo group), but statistically more deaths (3.1% vs 2.3% in the placebo group) and strokes (1% vs 0.5% in the placebo group).
Observers have suggested that the metoprolol dose in the POISE trial (200 mg/day) was too high and that a lower dose would have produced fewer adverse effects. But a lower dose might also have decreased the drug’s effectiveness in reducing heart attacks, said Dr. Devereaux, noting that the metoprolol dose in POISE only resulted in a 7-bpm lower heart rate, compared with placebo. More continuous monitoring “I believe the answer is more continuous patient monitoring during the immediate postsurgical period so that dangerous drops in heart rate or blood pressure are promptly identified and treated.”
Managing Blood Pressure in Barbershops Yields Improvements
African American men who received medical intervention aimed at controlling their high blood pressure while at the barber saw a marked drop in blood pressure in six months, according to researchers. Specifically, men who received frequent monitoring and medication management from a specially trained pharmacist who met them monthly in their barbershop lowered their systolic blood pressure by 21 mm Hg more, on average, compared with men who were encouraged by their barber to follow up with a doctor and to make healthy lifestyle choices.
While high blood pressure is a common problem among many American adults, African American men are more likely than other groups to have high blood pressure that is not adequately controlled and tend to have less contact with the health care system.
“By bringing state-of-the-art medicine directly to the people who need it on their home turf, in this case, in a barbershop, and making it both convenient and rigorous, blood pressure can be controlled just as well in African American men as in other groups,” said Ronald G. Victor, MD, Associate Director of the Smidt Heart Institute at Cedars-Sinai in Los Angeles. “If this model were scaled up and sustained, millions of lives could be saved, and many heart attacks and strokes could be prevented.”
Previous studies have shown that equipping barbers—who remain trusted, consistent, and convenient figures for many African American men—with health information can positively affect health. The new study is unique because it combined barbershop-based health outreach with the delivery of care by medical professionals at the barbershop and evaluated subsequent efficacy with a randomized trial.
The study recruited 319 men at 52 Los Angeles County barbershops. All the men had systolic blood pressure over 140 mm Hg, based on multiple measurements taken on two different days. The men ranged in age from 35 to 71 and, on average, had patronized their barbershop for more than a decade and had their hair cut twice a month.
In total, 303 men completed the study—representing a 95% cohort retention—and all received an intervention designed to help them lower their blood pressure.
A little over half of the men (171) were randomly assigned to receive health education from their barbers, who were trained to use a National Heart, Lung, and Blood Institute–developed script to encourage the men to visit their doctors and get their blood pressure under control.
The remaining men (132) were randomly assigned to receive regular monitoring (at least once per month) and active medication management by a pharmacist who met them at the barbershop. During each pharmacist visit, the men in this group received a blood pressure evaluation and a finger-stick blood test, which the pharmacist used to evaluate each man’s response to blood pressure medications and adjust prescriptions as needed. The pharmacists worked directly with the men under a collaborative care agreement with their primary care doctors.
On average, men who interacted only with their barber and were referred to their own doctor saw their systolic blood pressure decrease from 155 mm Hg at the start of the study to 145 mm Hg after six months. Diastolic blood pressured decreased by 4 mm Hg in this group. By contrast, men who interacted with their barber and a pharmacist saw their systolic blood pressure decrease from 153 mm Hg at the start of the study to 126 mm Hg after six months, along with a decrease in diastolic blood pressure of 18 mm Hg.
Under current American College of Cardiology–American Heart Association guidelines, blood pressure below 130/80 mm Hg is considered normal. At the end of six months, 64% of participants who saw a pharmacist had blood pressure in the normal range, compared with 12% of participants who were referred to their own doctor. “This is a large effect for a hypertension trial of any kind,” said Dr. Victor. “We are excited about the results.” Researchers are studying whether the effects can be sustained for an additional six months.
Drug Stops Dangerous Bleeding in Patients Taking Factor Xa Inhibitors
The experimental drug andexanet is associated with control of serious bleeding in patients taking a common class of anticoagulants known as Factor Xa inhibitors, according to interim clinical trial results. Factor Xa inhibitors elevate the risk of serious bleeding. If approved by the FDA, andexanet would be the first agent available to directly reverse the effects of Factor Xa inhibition if bleeding occurs.
Factor Xa inhibitors, which inhibit a protein involved in the formation of blood clots, are commonly prescribed for patients who are at high risk for stroke and venous thrombosis. Because Factor Xa inhibitors and other anticoagulants reduce the body’s ability to form a blood clot, these drugs can also increase the risk of uncontrolled bleeding. When this happens, it can be challenging for doctors to stop the bleeding. About 25% of patients who experience bleeding in the brain while taking a Factor Xa inhibitor die.
“Unlike for some other anticoagulants, there is currently no approved reversal agent for Factor Xa inhibitors,” said Stuart Connolly, MD, Professor of Medicine at McMaster University in Hamilton, Ontario. “Factor Xa inhibitors are already widely used because of their excellent efficacy and safety profile. However, some physicians and patients may choose to use other anticoagulant drugs because they have a reversal agent, rather than using one of the Factor Xa inhibitors. Having a safe and effective reversal agent available will benefit patients with acute bleeding.”
About 2.9 million people in the United States currently take Factor Xa inhibitors. Of these people, most are older and have illnesses, such as heart failure, that put them at high risk for cardiovascular problems. Approximately 84,000 patients taking Factor Xa inhibitors are hospitalized for major bleeding each year, according to a recent analysis of the MarketScan Commercial and Medicare databases. The most common types of major bleeds include bleeding in the brain, sometimes resulting from a fall, and gastrointestinal bleeding.
Andexanet is a recombinant modified Factor Xa molecule designed to bind to and disable Factor Xa inhibitors, thereby allowing Factor Xa produced by the body to play its normal role in the formation of blood clots. In earlier trials performed in healthy volunteers, andexanet rapidly reversed the anticoagulant effect of Factor Xa inhibitors without causing any significant safety problems.
ANNEXA-4 is an ongoing clinical trial that uses andexanet to help treat patients experiencing major bleeding while taking Factor Xa inhibitors. The interim analysis includes data on safety outcomes for 227 patients and adjudicated efficacy outcomes for 132 patients enrolled at centers in the US, Canada, and Europe. All trial participants presented with acute major bleeding within 18 hours of taking one of four Factor Xa inhibitors (ie, apixaban, rivaroxaban, edoxaban, or enoxaparin). Patients received an injection of andexanet followed by a two-hour infusion of the drug, with the dosage determined based on the specific Factor Xa inhibitor the patient was taking and how long it had been since the last dose.
The trial assesses the drug’s efficacy in terms of the following two coprimary endpoints: reduction in anti-Factor Xa inhibitor activity and achievement of clinical hemostasis by 12 hours after administration. The interim results show that median anti-Factor Xa inhibitor activity was reduced by 88% for patients taking rivaroxaban, 91% for patients taking apixaban, and 75% for patients taking enoxaparin. Few patients in the study had received edoxaban. Excellent or good clinical hemostasis was achieved in 83% of patients overall.
Safety of andexanet was assessed in all 227 patients. At 30 days, 12% of patients had died, and 11% had a thrombotic event (ie, stroke, heart attack, or blood clot in the legs). These rates of adverse events are in line with what would be expected, given the underlying medical condition of the patients in the trial and the fact that many had not resumed anticoagulant treatment during the 30 days after receiving andexanet, Dr. Connolly said. The trial was funded by Portola Pharmaceuticals, maker of andexanet.
Low-Dose Triple Pill Lowers Blood Pressure More Than Usual Care
A pill combining low doses of three blood pressure–lowering medications significantly increased the number of patients reaching blood pressure targets, compared with usual care, said researchers. The combination therapy was not associated with a significant increase in adverse effects.
“Most people—70%—reached blood pressure targets with the triple pill. The benefits were seen straight away and maintained until six months, whereas with usual care, control rates were 55% at six months and even lower earlier in the trial,” said Ruth Webster, MBBS, Head of Research Programs at the George Institute for Global Health at the University of New South Wales in Sydney. “Based on our findings, we conclude that this new method of using blood pressure–lowering drugs was more effective and just as safe as current approaches.”
Despite the availability of effective blood pressure–lowering drugs, high blood pressure remains a major problem around the world, said Dr. Webster. Effectively treating high blood pressure can help to prevent strokes, heart attacks, and kidney problems. Globally, however, many people with high blood pressure receive no treatment, and only about a third of those who are treated achieve recommended reductions in blood pressure. Achieving desired reductions in blood pressure often requires treatment with more than one medication, which increases the complexity of treatment. Patients often have difficulty adhering to regimens that involve taking multiple pills every day.
This study was the first large trial designed to test the theory that starting treatment with low doses of three drugs could achieve better blood pressure control, compared with usual care, and that combining these drugs in a single pill would make it easier for doctors to prescribe treatment and for patients to adhere to it, said Dr. Webster.
The TRIUMPH trial, which was conducted in Sri Lanka, enrolled 700 patients (58% women) whose average age was 56. Trial participants had an average blood pressure of 154/90 mm Hg. Approximately 59% were receiving no treatment for high blood pressure before they enrolled in the trial. In addition to high blood pressure, 32% of participants had diabetes or chronic kidney disease.
Patients were randomly assigned to receive either the combination pill or usual care. The combination pill, or triple pill, consisted of the blood pressure medications telmisartan (20 mg), amlodipine (2.5 mg), and chlorthalidone (12.5 mg). These medications use different mechanisms to reduce blood pressure by relaxing the blood vessels. Usual care meant that patients received their doctors’ choice of blood pressure–lowering medication.
The trial’s primary end point was the proportion of patients who achieved a blood pressure target of 140/90 mm Hg or less (130/80 mm Hg or less in those with diabetes or chronic kidney disease) at six months.
Compared with patients receiving usual care, a significantly higher proportion of patients receiving the triple pill achieved their target blood pressure at six months. The average reduction in blood pressure was 8.7 mm Hg for participants receiving the triple pill and 4.5 mm Hg for those receiving usual care. At six months, 83% of participants in the triple pill group were still receiving the combination pill, and one-third of those in the usual-care group was receiving at least two blood pressure–lowering drugs.
The maximum difference between the two groups of patients was observed at six weeks after starting treatment, when 68% of those receiving the triple pill had achieved a blood pressure within their target range, compared with 44% of those receiving usual care. This result represented a 53% reduction in the risk for high blood pressure for patients receiving the triple pill, said Dr. Webster.
Rates of participants having to change treatment due to side effects were not significantly different between the two groups (6.6% for the triple pill and 6.8% for usual care). This finding should allay concerns that use of the three-drug combination pill could lead to an unacceptable increase in adverse medication side effects, said Dr. Webster.
Each of the drugs in the triple pill is highly effective in reducing blood pressure and preventing deaths and illness due to heart disease and strokes, she added. Each drug represents a different class of blood pressure medication, and previous studies have shown that combining such drugs results in synergistic effects.
“The most urgent need for innovative strategies to control blood pressure is in low- and middle-income countries,” said Dr. Webster.
The study’s findings are also important for high-income countries, she said. “A control rate of 70% would be a considerable improvement even in high-income settings. Most hypertension guidelines in these countries do not recommend combination blood pressure–lowering therapy for initial treatment in all people,” she said. “Our findings should prompt reconsideration of recommendations around the use of combination therapy.”
An inevitable consequence of a necessarily unblinded study is that doctors might manage patients differently, depending on the assigned treatment. It is important to note, however, that this trial was designed to evaluate a new strategy of care in a real-world setting, said Dr. Webster. To minimize the risk of bias in measuring the main outcomes, the number of patient visits was identical in both groups, and all outcomes were standardized and objectively documented, she said.
Metoprolol May Increase Postsurgical Risk of Stroke or Death
During the 12 months after undergoing noncardiac surgery, patients with heart disease or at risk for heart disease who are treated with the beta blocker metoprolol for 30 days are less likely than patients who receive a placebo to have a heart attack, but more likely to die or have a stroke, said researchers.
These follow-up findings confirm that an increased risk for death or stroke persists at one year post surgery in patients treated with metoprolol, said P. J. Devereaux, MD, PhD, Director of Cardiology at McMaster University in Hamilton, Ontario. Previously reported results from the same study at 30 days post surgery showed a similar pattern, with a reduction in heart attacks, but increases in deaths and strokes.
“Our results suggest at one year, for every 1,000 patients having noncardiac surgery, treatment with metoprolol would prevent heart attacks in 12 patients, but would result in an excess of 13 deaths and six strokes,” said Dr. Devereaux.
“While there is little doubt that some patients benefit from receiving beta blockers during the period immediately before and after noncardiac surgery, these data show that at least as many patients are seriously harmed,” he said. “These data tell us that we need to exercise caution when using beta blockers in this setting until we figure out how to mitigate the substantial risks and enable all patients to obtain the potential benefits of this intervention.”
Beta blockers work by slowing the heart rate and relaxing the blood vessels, which, in turn, reduces blood pressure. The problem is that during the period immediately after major noncardiac surgery (such as a hip or knee replacement, bowel resection, or abdominal aortic aneurysm repair), patients are usually treated with opioid medications to relieve pain, said Dr. Devereaux. The effects of those medications may mask drops in blood pressure or heart rate to dangerously low levels. “Hypotension is common in this setting and is a main contributor to the adverse effects resulting from perioperative beta blockers,” he said.
Patients who become hypotensive for whatever reason after surgery (eg, sepsis, bleeding, or heart failure) find their problem exacerbated when they are receiving a beta blocker, which further lowers blood pressure and makes treating hypotension more challenging.
The PeriOperative Ischemic Evaluation (POISE) trial enrolled 8,351 patients in 23 countries. Eligible patients were age 45 or older and had a history of heart disease, blood-vessel disease, stroke, congestive heart failure, or other health problems such as diabetes or impaired kidney function. Patients’ median age was 69, and 63% were men.
Patients were randomly assigned to receive metoprolol or a placebo, beginning a few hours before surgery and for 30 days afterward. Patients, health care providers, and research staff, except those analyzing data, were blinded to which group received metoprolol and which received a placebo. The study’s primary end point was a composite of the combined rate of death from heart disease, nonfatal heart attack, and nonfatal cardiac arrest after 30 days.
At one-year follow-up, fewer patients in the metoprolol group than in the placebo group had heart attacks (5% vs 6.2%), but more patients in the metoprolol group had died (9.8% vs 8.5%) or had a stroke (2% vs 1.4%).
These results followed the same pattern that had previously been seen at the 30-day follow-up: statistically fewer heart attacks in the metoprolol group (4.2% vs 5.7% in the placebo group), but statistically more deaths (3.1% vs 2.3% in the placebo group) and strokes (1% vs 0.5% in the placebo group).
Observers have suggested that the metoprolol dose in the POISE trial (200 mg/day) was too high and that a lower dose would have produced fewer adverse effects. But a lower dose might also have decreased the drug’s effectiveness in reducing heart attacks, said Dr. Devereaux, noting that the metoprolol dose in POISE only resulted in a 7-bpm lower heart rate, compared with placebo. More continuous monitoring “I believe the answer is more continuous patient monitoring during the immediate postsurgical period so that dangerous drops in heart rate or blood pressure are promptly identified and treated.”
Managing Blood Pressure in Barbershops Yields Improvements
African American men who received medical intervention aimed at controlling their high blood pressure while at the barber saw a marked drop in blood pressure in six months, according to researchers. Specifically, men who received frequent monitoring and medication management from a specially trained pharmacist who met them monthly in their barbershop lowered their systolic blood pressure by 21 mm Hg more, on average, compared with men who were encouraged by their barber to follow up with a doctor and to make healthy lifestyle choices.
While high blood pressure is a common problem among many American adults, African American men are more likely than other groups to have high blood pressure that is not adequately controlled and tend to have less contact with the health care system.
“By bringing state-of-the-art medicine directly to the people who need it on their home turf, in this case, in a barbershop, and making it both convenient and rigorous, blood pressure can be controlled just as well in African American men as in other groups,” said Ronald G. Victor, MD, Associate Director of the Smidt Heart Institute at Cedars-Sinai in Los Angeles. “If this model were scaled up and sustained, millions of lives could be saved, and many heart attacks and strokes could be prevented.”
Previous studies have shown that equipping barbers—who remain trusted, consistent, and convenient figures for many African American men—with health information can positively affect health. The new study is unique because it combined barbershop-based health outreach with the delivery of care by medical professionals at the barbershop and evaluated subsequent efficacy with a randomized trial.
The study recruited 319 men at 52 Los Angeles County barbershops. All the men had systolic blood pressure over 140 mm Hg, based on multiple measurements taken on two different days. The men ranged in age from 35 to 71 and, on average, had patronized their barbershop for more than a decade and had their hair cut twice a month.
In total, 303 men completed the study—representing a 95% cohort retention—and all received an intervention designed to help them lower their blood pressure.
A little over half of the men (171) were randomly assigned to receive health education from their barbers, who were trained to use a National Heart, Lung, and Blood Institute–developed script to encourage the men to visit their doctors and get their blood pressure under control.
The remaining men (132) were randomly assigned to receive regular monitoring (at least once per month) and active medication management by a pharmacist who met them at the barbershop. During each pharmacist visit, the men in this group received a blood pressure evaluation and a finger-stick blood test, which the pharmacist used to evaluate each man’s response to blood pressure medications and adjust prescriptions as needed. The pharmacists worked directly with the men under a collaborative care agreement with their primary care doctors.
On average, men who interacted only with their barber and were referred to their own doctor saw their systolic blood pressure decrease from 155 mm Hg at the start of the study to 145 mm Hg after six months. Diastolic blood pressured decreased by 4 mm Hg in this group. By contrast, men who interacted with their barber and a pharmacist saw their systolic blood pressure decrease from 153 mm Hg at the start of the study to 126 mm Hg after six months, along with a decrease in diastolic blood pressure of 18 mm Hg.
Under current American College of Cardiology–American Heart Association guidelines, blood pressure below 130/80 mm Hg is considered normal. At the end of six months, 64% of participants who saw a pharmacist had blood pressure in the normal range, compared with 12% of participants who were referred to their own doctor. “This is a large effect for a hypertension trial of any kind,” said Dr. Victor. “We are excited about the results.” Researchers are studying whether the effects can be sustained for an additional six months.
Neuro-Ophthalmology: No Longer Diagnose and Adios
Deborah I. Friedman, MD, MPH
Dr. Friedman is a Professor in the Departments of Neurology and Ophthalmology at the University of Texas Southwestern Medical Center in Dallas.
Neuro-ophthalmology is a small subspecialty that had its origins in ophthalmology but has always included neurologists. National neuro-ophthalmology meetings in North America began with the Rocky Mountain Neuro-Ophthalmology Course in 1975, which led to the formation of the Rocky Mountain Neuro-Ophthalmology Society in 1980. By 1986, it had 240 members and changed its name to the North American Neuro-Ophthalmology Society (NANOS). Already existing was the 1.5-day annual Frank Walsh Society meeting with its clinical-pathological correlation format, which originated at Johns Hopkins Medical School. The two societies merged in 1992. Currently, NANOS has grown to more than 650 members and is the premier organization for neuro-ophthalmology worldwide. The society’s journal, the Journal of Neuro-Ophthalmology, commenced publication in 1994, one year after the inaugural issue of Neurology Reviews.
Overcoming an early reputation for “admiring” disease, neuro-ophthalmology has evolved considerably over the past 25 years, with advances in neuroimaging, genomics, proteomics, office-based technologies, and immunology. The first multicenter, randomized trial in neuro-ophthalmology—the Optic Neuritis Treatment Trial (ONTT),1 published 25 years ago—showed that intravenous methylprednisolone 250 mg QID for three days followed by an 11-day prednisone taper was superior to either oral prednisone (1 mg/kg for 14 days) or oral placebo (14 days), speeding the recovery of vision with slightly better vision at six months. There was a higher rate of relapse in the group assigned to receive oral prednisone. The ONTT was a pivotal event for neuro-ophthalmology, heralding a paradigm shift from observational reporting to randomized clinical trials.
Three years later, the Ischemic Optic Neuropathy Decompression Trial (IONDT)2 showed that optic nerve sheath fenestration surgery, performed within 14 days of symptom onset for acute non-arteritic ischemic optic neuropathy or within 30 days in participants with a progressive course, did not improve visual acuity or visual field compared to careful follow-up and medical management at six months. Enrollees randomized to undergo surgery had a lower rate of improvement and were more likely to lose three or more lines of vision than the control group.
With this momentum, the Neuro-Ophthalmology Research Disease Investigators Consortium was formed to create infrastructure for future clinical trials of neuro-ophthalmic disorders. The Idiopathic Intracranial Hypertension Treatment Trial (IIHTT)3 studied patients with idiopathic intracranial hypertension and mild visual field loss. IIHTT confirmed that acetazolamide (500 mg BID, increasing to a maximum dose of 4 grams daily) was superior to placebo treatment when combined with a supervised weight loss program, resulting in improved visual field loss, papilledema grade, weight reduction, lumbar puncture opening pressure, and quality of life. Ongoing research efforts are investigating treatments for Leber hereditary optic neuropathy, non-arteritic ischemic optic neuropathy, thyroid eye disease, rehabilitation for poststroke homonymous hemianopia and giant cell arteritis in adults, and idiopathic intracranial hypertension and optic nerve gliomas in children.
Attendance at the NANOS annual meeting continues to grow, emphasizing scientific as well as clinical neuro-ophthalmic topics. Vibrant and active neuro-ophthalmology societies in other parts of the world (eg, Europe, Japan, Australia, British Isles) contribute to the camaraderie, collegiality, collaboration, and discovery that advance our field.
Happy 25th anniversary to Neurology Reviews! The next 25 years will likely transform the field of neuro-ophthalmology as we better understand the molecular and genetic basis of neuro-ophthalmic disorders. No longer “diagnose and adios,” we anticipate significant therapeutic advancements—and perhaps cures—for individuals with severe, sight-impairing, neuro-ophthalmic conditions.
References
2. The Ischemic Optic Neuropathy Decompression Trial Research Group. Optic nerve decompression surgery for nonarteritic anterior ischemic optic neuropathy (NAION) is not effective and may be harmful. JAMA. 1995;273(8):625-632.
3. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss. JAMA. 2014;311(16):1641-1651.
Deborah I. Friedman, MD, MPH
Dr. Friedman is a Professor in the Departments of Neurology and Ophthalmology at the University of Texas Southwestern Medical Center in Dallas.
Neuro-ophthalmology is a small subspecialty that had its origins in ophthalmology but has always included neurologists. National neuro-ophthalmology meetings in North America began with the Rocky Mountain Neuro-Ophthalmology Course in 1975, which led to the formation of the Rocky Mountain Neuro-Ophthalmology Society in 1980. By 1986, it had 240 members and changed its name to the North American Neuro-Ophthalmology Society (NANOS). Already existing was the 1.5-day annual Frank Walsh Society meeting with its clinical-pathological correlation format, which originated at Johns Hopkins Medical School. The two societies merged in 1992. Currently, NANOS has grown to more than 650 members and is the premier organization for neuro-ophthalmology worldwide. The society’s journal, the Journal of Neuro-Ophthalmology, commenced publication in 1994, one year after the inaugural issue of Neurology Reviews.
Overcoming an early reputation for “admiring” disease, neuro-ophthalmology has evolved considerably over the past 25 years, with advances in neuroimaging, genomics, proteomics, office-based technologies, and immunology. The first multicenter, randomized trial in neuro-ophthalmology—the Optic Neuritis Treatment Trial (ONTT),1 published 25 years ago—showed that intravenous methylprednisolone 250 mg QID for three days followed by an 11-day prednisone taper was superior to either oral prednisone (1 mg/kg for 14 days) or oral placebo (14 days), speeding the recovery of vision with slightly better vision at six months. There was a higher rate of relapse in the group assigned to receive oral prednisone. The ONTT was a pivotal event for neuro-ophthalmology, heralding a paradigm shift from observational reporting to randomized clinical trials.
Three years later, the Ischemic Optic Neuropathy Decompression Trial (IONDT)2 showed that optic nerve sheath fenestration surgery, performed within 14 days of symptom onset for acute non-arteritic ischemic optic neuropathy or within 30 days in participants with a progressive course, did not improve visual acuity or visual field compared to careful follow-up and medical management at six months. Enrollees randomized to undergo surgery had a lower rate of improvement and were more likely to lose three or more lines of vision than the control group.
With this momentum, the Neuro-Ophthalmology Research Disease Investigators Consortium was formed to create infrastructure for future clinical trials of neuro-ophthalmic disorders. The Idiopathic Intracranial Hypertension Treatment Trial (IIHTT)3 studied patients with idiopathic intracranial hypertension and mild visual field loss. IIHTT confirmed that acetazolamide (500 mg BID, increasing to a maximum dose of 4 grams daily) was superior to placebo treatment when combined with a supervised weight loss program, resulting in improved visual field loss, papilledema grade, weight reduction, lumbar puncture opening pressure, and quality of life. Ongoing research efforts are investigating treatments for Leber hereditary optic neuropathy, non-arteritic ischemic optic neuropathy, thyroid eye disease, rehabilitation for poststroke homonymous hemianopia and giant cell arteritis in adults, and idiopathic intracranial hypertension and optic nerve gliomas in children.
Attendance at the NANOS annual meeting continues to grow, emphasizing scientific as well as clinical neuro-ophthalmic topics. Vibrant and active neuro-ophthalmology societies in other parts of the world (eg, Europe, Japan, Australia, British Isles) contribute to the camaraderie, collegiality, collaboration, and discovery that advance our field.
Happy 25th anniversary to Neurology Reviews! The next 25 years will likely transform the field of neuro-ophthalmology as we better understand the molecular and genetic basis of neuro-ophthalmic disorders. No longer “diagnose and adios,” we anticipate significant therapeutic advancements—and perhaps cures—for individuals with severe, sight-impairing, neuro-ophthalmic conditions.
References
2. The Ischemic Optic Neuropathy Decompression Trial Research Group. Optic nerve decompression surgery for nonarteritic anterior ischemic optic neuropathy (NAION) is not effective and may be harmful. JAMA. 1995;273(8):625-632.
3. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss. JAMA. 2014;311(16):1641-1651.
Deborah I. Friedman, MD, MPH
Dr. Friedman is a Professor in the Departments of Neurology and Ophthalmology at the University of Texas Southwestern Medical Center in Dallas.
Neuro-ophthalmology is a small subspecialty that had its origins in ophthalmology but has always included neurologists. National neuro-ophthalmology meetings in North America began with the Rocky Mountain Neuro-Ophthalmology Course in 1975, which led to the formation of the Rocky Mountain Neuro-Ophthalmology Society in 1980. By 1986, it had 240 members and changed its name to the North American Neuro-Ophthalmology Society (NANOS). Already existing was the 1.5-day annual Frank Walsh Society meeting with its clinical-pathological correlation format, which originated at Johns Hopkins Medical School. The two societies merged in 1992. Currently, NANOS has grown to more than 650 members and is the premier organization for neuro-ophthalmology worldwide. The society’s journal, the Journal of Neuro-Ophthalmology, commenced publication in 1994, one year after the inaugural issue of Neurology Reviews.
Overcoming an early reputation for “admiring” disease, neuro-ophthalmology has evolved considerably over the past 25 years, with advances in neuroimaging, genomics, proteomics, office-based technologies, and immunology. The first multicenter, randomized trial in neuro-ophthalmology—the Optic Neuritis Treatment Trial (ONTT),1 published 25 years ago—showed that intravenous methylprednisolone 250 mg QID for three days followed by an 11-day prednisone taper was superior to either oral prednisone (1 mg/kg for 14 days) or oral placebo (14 days), speeding the recovery of vision with slightly better vision at six months. There was a higher rate of relapse in the group assigned to receive oral prednisone. The ONTT was a pivotal event for neuro-ophthalmology, heralding a paradigm shift from observational reporting to randomized clinical trials.
Three years later, the Ischemic Optic Neuropathy Decompression Trial (IONDT)2 showed that optic nerve sheath fenestration surgery, performed within 14 days of symptom onset for acute non-arteritic ischemic optic neuropathy or within 30 days in participants with a progressive course, did not improve visual acuity or visual field compared to careful follow-up and medical management at six months. Enrollees randomized to undergo surgery had a lower rate of improvement and were more likely to lose three or more lines of vision than the control group.
With this momentum, the Neuro-Ophthalmology Research Disease Investigators Consortium was formed to create infrastructure for future clinical trials of neuro-ophthalmic disorders. The Idiopathic Intracranial Hypertension Treatment Trial (IIHTT)3 studied patients with idiopathic intracranial hypertension and mild visual field loss. IIHTT confirmed that acetazolamide (500 mg BID, increasing to a maximum dose of 4 grams daily) was superior to placebo treatment when combined with a supervised weight loss program, resulting in improved visual field loss, papilledema grade, weight reduction, lumbar puncture opening pressure, and quality of life. Ongoing research efforts are investigating treatments for Leber hereditary optic neuropathy, non-arteritic ischemic optic neuropathy, thyroid eye disease, rehabilitation for poststroke homonymous hemianopia and giant cell arteritis in adults, and idiopathic intracranial hypertension and optic nerve gliomas in children.
Attendance at the NANOS annual meeting continues to grow, emphasizing scientific as well as clinical neuro-ophthalmic topics. Vibrant and active neuro-ophthalmology societies in other parts of the world (eg, Europe, Japan, Australia, British Isles) contribute to the camaraderie, collegiality, collaboration, and discovery that advance our field.
Happy 25th anniversary to Neurology Reviews! The next 25 years will likely transform the field of neuro-ophthalmology as we better understand the molecular and genetic basis of neuro-ophthalmic disorders. No longer “diagnose and adios,” we anticipate significant therapeutic advancements—and perhaps cures—for individuals with severe, sight-impairing, neuro-ophthalmic conditions.
References
2. The Ischemic Optic Neuropathy Decompression Trial Research Group. Optic nerve decompression surgery for nonarteritic anterior ischemic optic neuropathy (NAION) is not effective and may be harmful. JAMA. 1995;273(8):625-632.
3. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss. JAMA. 2014;311(16):1641-1651.
Admitting medicine patients to off-service, nonmedicine units linked with increased in-hospital mortality
Background: Increased saturation of hospital capacity compromises patient outcomes. This creates additional challenges for the provision of appropriate specialized care. In some hospitals, patients are “bed-spaced,” or admitted to non–internal medicine service locations, such as a surgical ward, in order to free up space in the emergency department. Whether bed-spacing reduces quality of care or patient outcomes has not been previously studied.
Study design: Retrospective cohort study.
Setting: Large tertiary care academic hospital in Canada, during Jan. 1, 2015-Jan. 1, 2016.
Synopsis: There were 3,243 patients included in the analysis, of which 1,125 (35%) were bed-spaced to the off-service wards. The remaining 2,118 patients (65%) were admitted to the assigned internal medicine units. In the first week of hospitalization, in-hospital mortality among bed-spaced patients was approximately three times that of patients admitted to the assigned internal medicine wards. Upon admission, in-hospital mortality for the bed-spaced patients had a hazard ratio of 3.42 (95% confidence interval, 2.23-5.26; P less than .0001) with subsequent decrease by 0.97 (95% CI, 0.94-0.99; P = .0133) per day in the hospital. By the third week of hospitalization, the mortality risks had equalized. Sensitivity analyses revealed similar results.
Bottom line: This retrospective study is based on a single center; however, the observed increased mortality among the bed-spaced patients merits further investigation. Assessment of study generalizability and formulation of strategies for improving patient safety are needed.
Citation: Bai AD et al. Mortality of hospitalised internal medicine patients bed-spaced to non–internal medicine inpatient units: Retrospective cohort study. BMJ Qual Saf. 2018 Jan;27(1):11-20. doi: 10.1136/bmjqs-2017-006925.
Dr. Burklin is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Background: Increased saturation of hospital capacity compromises patient outcomes. This creates additional challenges for the provision of appropriate specialized care. In some hospitals, patients are “bed-spaced,” or admitted to non–internal medicine service locations, such as a surgical ward, in order to free up space in the emergency department. Whether bed-spacing reduces quality of care or patient outcomes has not been previously studied.
Study design: Retrospective cohort study.
Setting: Large tertiary care academic hospital in Canada, during Jan. 1, 2015-Jan. 1, 2016.
Synopsis: There were 3,243 patients included in the analysis, of which 1,125 (35%) were bed-spaced to the off-service wards. The remaining 2,118 patients (65%) were admitted to the assigned internal medicine units. In the first week of hospitalization, in-hospital mortality among bed-spaced patients was approximately three times that of patients admitted to the assigned internal medicine wards. Upon admission, in-hospital mortality for the bed-spaced patients had a hazard ratio of 3.42 (95% confidence interval, 2.23-5.26; P less than .0001) with subsequent decrease by 0.97 (95% CI, 0.94-0.99; P = .0133) per day in the hospital. By the third week of hospitalization, the mortality risks had equalized. Sensitivity analyses revealed similar results.
Bottom line: This retrospective study is based on a single center; however, the observed increased mortality among the bed-spaced patients merits further investigation. Assessment of study generalizability and formulation of strategies for improving patient safety are needed.
Citation: Bai AD et al. Mortality of hospitalised internal medicine patients bed-spaced to non–internal medicine inpatient units: Retrospective cohort study. BMJ Qual Saf. 2018 Jan;27(1):11-20. doi: 10.1136/bmjqs-2017-006925.
Dr. Burklin is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Background: Increased saturation of hospital capacity compromises patient outcomes. This creates additional challenges for the provision of appropriate specialized care. In some hospitals, patients are “bed-spaced,” or admitted to non–internal medicine service locations, such as a surgical ward, in order to free up space in the emergency department. Whether bed-spacing reduces quality of care or patient outcomes has not been previously studied.
Study design: Retrospective cohort study.
Setting: Large tertiary care academic hospital in Canada, during Jan. 1, 2015-Jan. 1, 2016.
Synopsis: There were 3,243 patients included in the analysis, of which 1,125 (35%) were bed-spaced to the off-service wards. The remaining 2,118 patients (65%) were admitted to the assigned internal medicine units. In the first week of hospitalization, in-hospital mortality among bed-spaced patients was approximately three times that of patients admitted to the assigned internal medicine wards. Upon admission, in-hospital mortality for the bed-spaced patients had a hazard ratio of 3.42 (95% confidence interval, 2.23-5.26; P less than .0001) with subsequent decrease by 0.97 (95% CI, 0.94-0.99; P = .0133) per day in the hospital. By the third week of hospitalization, the mortality risks had equalized. Sensitivity analyses revealed similar results.
Bottom line: This retrospective study is based on a single center; however, the observed increased mortality among the bed-spaced patients merits further investigation. Assessment of study generalizability and formulation of strategies for improving patient safety are needed.
Citation: Bai AD et al. Mortality of hospitalised internal medicine patients bed-spaced to non–internal medicine inpatient units: Retrospective cohort study. BMJ Qual Saf. 2018 Jan;27(1):11-20. doi: 10.1136/bmjqs-2017-006925.
Dr. Burklin is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.