User login
Baricitinib found effective for moderate to severe AD out to 52 weeks
“With long-term therapy, the baricitinib 2 mg response remains stable or slightly improved, compared with week 16 for skin inflammation, itch, sleep, and quality of life,” presenting study author Eric L. Simpson, MD, said during the Revolutionizing Atopic Dermatitis symposium.
Baricitinib is an oral selective Janus kinase 1/JAK2 inhibitor being developed for the treatment of moderate to severe AD in adults who are candidates for systemic therapy. The drug is already approved for AD in Europe at the 2-mg and 4-mg doses. A 16-week placebo-controlled study conducted in North America known as BREEZE-AD5 found that 2 mg of baricitinib improved disease in adults with moderate to severe AD.
For the current analysis, Dr. Simpson, professor of dermatology at Oregon Health and Science University, Portland, and colleagues integrated data from BREEZE-AD5 and BREEZE-AD6, an ongoing, open-label study of BREEZE-AD5, to evaluate the long-term efficacy and safety of baricitinib 2 mg in patients with moderate to severe AD.
At week 16, patients from BREEZE-AD5 who were on baricitinib 2 mg could either continue the trial out to week 52, or they could transition to BREEZE-AD6 if they were nonresponders. The use of low-potency corticosteroids was permitted after week 16 in BREEZE-AD5 and throughout BREEZE-AD6. Endpoints of interest at week 52 in both trials were the proportions of patients with 75% or greater improvement from baseline in the Eczema and Severity Index (EASI75), a Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) score of 0 or 1, a Dermatology Life Quality Index (DLQI) score of 5 or less, as well as mean SCORing AD (SCORAD) visual analog scales of itch and sleeplessness scores, and the mean percent change from baseline in EASI score.
Dr. Simpson presented data on 146 patients from both trials who were randomized to baricitinib 2 mg. Their mean age was 40 years, 53% were female, 58% were White, 21% were Black, 15% were Asian, and the remainder were from other backgrounds. Their mean duration of AD was 16 years and their average EASI score was 26.6. At weeks 16, 32, and 52, the proportion of patients who achieved an EASI75 response was 40%, 51%, and 49%, respectively, while the mean percent change from baseline in EASI score was –50%, –59%, and –57%.
At weeks 16, 32, and 52, the vIGA-AD responses of 0 or 1 were observed in 27%, 38%, and 31% of patients. The mean SCORAD pruritus score improved from 7.7 at baseline to 4.8 at week 16 and was maintained at weeks 32 (3.8) and 52 (4.3). The mean SCORAD sleeplessness score also improved from 6.5 at baseline to 3.9 at week 16 and remained stable through weeks 32 (3.4) and 52 (3.7).
Finally, among 129 patients who had a baseline DLQI of greater than 5, 39% had DLQI scores of 5 or lower at week 16, compared with 49% at week 32 and 45% at week 52, indicating a small or no effect of AD on quality of life.
The study was sponsored by Eli Lilly, which is developing baricitinib. Dr. Simpson disclosed that he is a consultant to and/or an investigator for several pharmaceutical companies, including Eli Lilly.
“With long-term therapy, the baricitinib 2 mg response remains stable or slightly improved, compared with week 16 for skin inflammation, itch, sleep, and quality of life,” presenting study author Eric L. Simpson, MD, said during the Revolutionizing Atopic Dermatitis symposium.
Baricitinib is an oral selective Janus kinase 1/JAK2 inhibitor being developed for the treatment of moderate to severe AD in adults who are candidates for systemic therapy. The drug is already approved for AD in Europe at the 2-mg and 4-mg doses. A 16-week placebo-controlled study conducted in North America known as BREEZE-AD5 found that 2 mg of baricitinib improved disease in adults with moderate to severe AD.
For the current analysis, Dr. Simpson, professor of dermatology at Oregon Health and Science University, Portland, and colleagues integrated data from BREEZE-AD5 and BREEZE-AD6, an ongoing, open-label study of BREEZE-AD5, to evaluate the long-term efficacy and safety of baricitinib 2 mg in patients with moderate to severe AD.
At week 16, patients from BREEZE-AD5 who were on baricitinib 2 mg could either continue the trial out to week 52, or they could transition to BREEZE-AD6 if they were nonresponders. The use of low-potency corticosteroids was permitted after week 16 in BREEZE-AD5 and throughout BREEZE-AD6. Endpoints of interest at week 52 in both trials were the proportions of patients with 75% or greater improvement from baseline in the Eczema and Severity Index (EASI75), a Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) score of 0 or 1, a Dermatology Life Quality Index (DLQI) score of 5 or less, as well as mean SCORing AD (SCORAD) visual analog scales of itch and sleeplessness scores, and the mean percent change from baseline in EASI score.
Dr. Simpson presented data on 146 patients from both trials who were randomized to baricitinib 2 mg. Their mean age was 40 years, 53% were female, 58% were White, 21% were Black, 15% were Asian, and the remainder were from other backgrounds. Their mean duration of AD was 16 years and their average EASI score was 26.6. At weeks 16, 32, and 52, the proportion of patients who achieved an EASI75 response was 40%, 51%, and 49%, respectively, while the mean percent change from baseline in EASI score was –50%, –59%, and –57%.
At weeks 16, 32, and 52, the vIGA-AD responses of 0 or 1 were observed in 27%, 38%, and 31% of patients. The mean SCORAD pruritus score improved from 7.7 at baseline to 4.8 at week 16 and was maintained at weeks 32 (3.8) and 52 (4.3). The mean SCORAD sleeplessness score also improved from 6.5 at baseline to 3.9 at week 16 and remained stable through weeks 32 (3.4) and 52 (3.7).
Finally, among 129 patients who had a baseline DLQI of greater than 5, 39% had DLQI scores of 5 or lower at week 16, compared with 49% at week 32 and 45% at week 52, indicating a small or no effect of AD on quality of life.
The study was sponsored by Eli Lilly, which is developing baricitinib. Dr. Simpson disclosed that he is a consultant to and/or an investigator for several pharmaceutical companies, including Eli Lilly.
“With long-term therapy, the baricitinib 2 mg response remains stable or slightly improved, compared with week 16 for skin inflammation, itch, sleep, and quality of life,” presenting study author Eric L. Simpson, MD, said during the Revolutionizing Atopic Dermatitis symposium.
Baricitinib is an oral selective Janus kinase 1/JAK2 inhibitor being developed for the treatment of moderate to severe AD in adults who are candidates for systemic therapy. The drug is already approved for AD in Europe at the 2-mg and 4-mg doses. A 16-week placebo-controlled study conducted in North America known as BREEZE-AD5 found that 2 mg of baricitinib improved disease in adults with moderate to severe AD.
For the current analysis, Dr. Simpson, professor of dermatology at Oregon Health and Science University, Portland, and colleagues integrated data from BREEZE-AD5 and BREEZE-AD6, an ongoing, open-label study of BREEZE-AD5, to evaluate the long-term efficacy and safety of baricitinib 2 mg in patients with moderate to severe AD.
At week 16, patients from BREEZE-AD5 who were on baricitinib 2 mg could either continue the trial out to week 52, or they could transition to BREEZE-AD6 if they were nonresponders. The use of low-potency corticosteroids was permitted after week 16 in BREEZE-AD5 and throughout BREEZE-AD6. Endpoints of interest at week 52 in both trials were the proportions of patients with 75% or greater improvement from baseline in the Eczema and Severity Index (EASI75), a Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) score of 0 or 1, a Dermatology Life Quality Index (DLQI) score of 5 or less, as well as mean SCORing AD (SCORAD) visual analog scales of itch and sleeplessness scores, and the mean percent change from baseline in EASI score.
Dr. Simpson presented data on 146 patients from both trials who were randomized to baricitinib 2 mg. Their mean age was 40 years, 53% were female, 58% were White, 21% were Black, 15% were Asian, and the remainder were from other backgrounds. Their mean duration of AD was 16 years and their average EASI score was 26.6. At weeks 16, 32, and 52, the proportion of patients who achieved an EASI75 response was 40%, 51%, and 49%, respectively, while the mean percent change from baseline in EASI score was –50%, –59%, and –57%.
At weeks 16, 32, and 52, the vIGA-AD responses of 0 or 1 were observed in 27%, 38%, and 31% of patients. The mean SCORAD pruritus score improved from 7.7 at baseline to 4.8 at week 16 and was maintained at weeks 32 (3.8) and 52 (4.3). The mean SCORAD sleeplessness score also improved from 6.5 at baseline to 3.9 at week 16 and remained stable through weeks 32 (3.4) and 52 (3.7).
Finally, among 129 patients who had a baseline DLQI of greater than 5, 39% had DLQI scores of 5 or lower at week 16, compared with 49% at week 32 and 45% at week 52, indicating a small or no effect of AD on quality of life.
The study was sponsored by Eli Lilly, which is developing baricitinib. Dr. Simpson disclosed that he is a consultant to and/or an investigator for several pharmaceutical companies, including Eli Lilly.
FROM REVOLUTIONIZING AD 2021
Maintain OMT for 5 years after revascularization, boost survival at 10 years: SYNTAXES
When it comes to medical therapy after a coronary revascularization procedure, more is better. Patients started and then maintained indefinitely on more rather than fewer of the drugs identified as optimal medical therapy (OMT) achieve a major survival benefit 10 years later, according to long-term follow-up from an extended analysis of the SYNTAX trial.
For the survival benefit at 10 years, “the present study suggests that at least three types of optimal medical therapy should be maintained for at least 5 years after revascularization,” reported a multinational team of cardiovascular specialists led by Hideyuki Kawashima, MD and Patrick Serruys, MD, who both have affiliations with the department of cardiology of the National University of Ireland, Galway.
The SYNTAX trial was conducted to compare percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) for patients with previously untreated three-vessel and/or left main disease (N Engl J Med 2009;360:961-72). The conclusion from that study, published in 2009 and subsequently reinforced by a 5-year follow-up, was that CABG should remain the standard of care for complex lesions.
Optimal medical therapy defined
In the course of SYNTAX, the impact of OMT on outcome was also evaluated in a subanalysis. At 5 years, there was a mortality advantage for those receiving an antiplatelet drug, a statin, a renin-angiotensin system inhibitor (ACE inhibitor or angiotensin receptor blocker), and a beta-blocker when compared with fewer of these agents.
When an investigator-initiated extension of SYNTAX, called SYNTAXES, was conducted to compare the outcomes of PCI and CABG at 10 years, it also permitted an extended analysis of OMT. Although the primary comparison of SYNTAXES, reported 2 years ago, did not show a significant difference between PCI and CABG for mortality at 10 years, there was a difference for OMT.
When investigators compared treatment with three or more OMT agents with that with two or fewer OMT drugs at 5 years, the result for all-cause death at 10 years translated into a more than 50% relative reduction (hazard ratio, 0.47; P = .002). The absolute difference in mortality was a more than 6% reduction (13.1% vs. 19.9%).
OMT data offer major message
The current study is considered to have a major message for patients as well as physicians.
“OMT even outweighs the survival benefit from revascularization alone, so our patients should convince themselves of the value of rigorous adherence and compliance,” Dr. Serruys said in an interview. According to him, these are compelling data for telling patients that OMT “is the best insurance for extended survival.” We now know from these data “the longer, the better.”
The same message from these data extends to physicians.
“I wish I could understand the apparent blind spot physicians have with respect to prescribing OMT despite the overwhelming benefit from multiple clinical trials,” said William E. Boden, MD, professor of medicine, Boston University.
Dr. Boden was a coauthor of an editorial accompanying the newly published SYNTAXES subanalysis. In the editorial, he noted that OMT following revascularization and in other high-risk patients “has been unacceptably low,” but he was asked to expand on the lessons from the newly released SYNTAXES subanalysis in an interview.
“There has often been a belief that revascularization negates the need for OMT and that’s why the SYNTAXES trial 10-year mortality reduction – which builds upon an earlier 5-year mortality reduction analysis – is so important,” he said.
Patients should take OMT long term
These data “should be both a motivator for physicians to prescribe OMT and for patients to remain adherent to OMT,” he said. “It is the best warranty to blunt the progression of atherosclerosis and to reduce subsequent cardiac events.”
For the 10-year subanalysis of OMT in SYNTAXES, the patients were stratified by the number of OMTs they were taking at 5 years after revascularization and then evaluated for survival at 10 years. Of the 1,472 patients available for analysis at 5 years, only 678 (46%) were on OMT. The other 794 patients were not.
Graphically, the Kaplan-Meier survival curve for those on three types of OMT was consistently beneath that of those on four OMTs, but the gap narrowed over time. At the end of 10 years, the advantage of the four-drug OMT was not statistically significant relative to three or fewer (13.1% vs. 12.7%).
Statins and antiplatelets show largest effect
When analyzed individually and in different combinations, the agents with OMT did not appear to be equal. For example, the biggest survival gap at 10 years was for those who were on an antiplatelet therapy and a statin at 5 years relative to those who were not on either (13.2% vs. 22.6%; P = .006). Even after adjustment, there was nearly 45% survival benefit for these two agents (HR, 0.556; P = .02).
Conversely, the 10-year survival advantage for being on a renin-angiotensin system inhibitor at 5 years versus not being exposed to this therapy was small and nonsignificant (14.7% vs. 13.7%; P = .651).
The precise proportion of patients who were prescribed and adhered to OMT between 5 years and 10 years is unknown, acknowledged the authors, so conclusions are limited about the added benefit of 10- versus 5-year OMT, although the authors presume that a substantial proportion of those adherent for 5 years would likely continue on these therapies.
It can be said with confidence that those adherent for at least 5 years are more likely to be alive at 10 years than those who are not, according to Dr. Boden. He considers these data a call for physicians and all high-risk patients, not just those who have undergone revascularization, to take these standard therapies.
There are plenty of data to “show how poorly we treat patients with OMT,” said Dr. Boden, citing several studies. In one, which looked at OMT in a nationally representative sample in the United States, only a third of patients with angina were taking an antiplatelet, a statin, and a beta-blocker, all of which are indicated.
“Hospitalization for revascularization provides an opportune time to capture the attention of patients and their physicians,” he wrote in his editorial. He called OMT “an imperative to optimize clinical outcomes.”
Many of the investigators involved in the SYNTAXES subanalysis, including Dr. Serruys, have financial relationships with multiple pharmaceutical companies, including Boston Scientific, which provided the initial funding for the SYNTAX trial. Dr. Boden reports no potential conflicts of interest.
When it comes to medical therapy after a coronary revascularization procedure, more is better. Patients started and then maintained indefinitely on more rather than fewer of the drugs identified as optimal medical therapy (OMT) achieve a major survival benefit 10 years later, according to long-term follow-up from an extended analysis of the SYNTAX trial.
For the survival benefit at 10 years, “the present study suggests that at least three types of optimal medical therapy should be maintained for at least 5 years after revascularization,” reported a multinational team of cardiovascular specialists led by Hideyuki Kawashima, MD and Patrick Serruys, MD, who both have affiliations with the department of cardiology of the National University of Ireland, Galway.
The SYNTAX trial was conducted to compare percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) for patients with previously untreated three-vessel and/or left main disease (N Engl J Med 2009;360:961-72). The conclusion from that study, published in 2009 and subsequently reinforced by a 5-year follow-up, was that CABG should remain the standard of care for complex lesions.
Optimal medical therapy defined
In the course of SYNTAX, the impact of OMT on outcome was also evaluated in a subanalysis. At 5 years, there was a mortality advantage for those receiving an antiplatelet drug, a statin, a renin-angiotensin system inhibitor (ACE inhibitor or angiotensin receptor blocker), and a beta-blocker when compared with fewer of these agents.
When an investigator-initiated extension of SYNTAX, called SYNTAXES, was conducted to compare the outcomes of PCI and CABG at 10 years, it also permitted an extended analysis of OMT. Although the primary comparison of SYNTAXES, reported 2 years ago, did not show a significant difference between PCI and CABG for mortality at 10 years, there was a difference for OMT.
When investigators compared treatment with three or more OMT agents with that with two or fewer OMT drugs at 5 years, the result for all-cause death at 10 years translated into a more than 50% relative reduction (hazard ratio, 0.47; P = .002). The absolute difference in mortality was a more than 6% reduction (13.1% vs. 19.9%).
OMT data offer major message
The current study is considered to have a major message for patients as well as physicians.
“OMT even outweighs the survival benefit from revascularization alone, so our patients should convince themselves of the value of rigorous adherence and compliance,” Dr. Serruys said in an interview. According to him, these are compelling data for telling patients that OMT “is the best insurance for extended survival.” We now know from these data “the longer, the better.”
The same message from these data extends to physicians.
“I wish I could understand the apparent blind spot physicians have with respect to prescribing OMT despite the overwhelming benefit from multiple clinical trials,” said William E. Boden, MD, professor of medicine, Boston University.
Dr. Boden was a coauthor of an editorial accompanying the newly published SYNTAXES subanalysis. In the editorial, he noted that OMT following revascularization and in other high-risk patients “has been unacceptably low,” but he was asked to expand on the lessons from the newly released SYNTAXES subanalysis in an interview.
“There has often been a belief that revascularization negates the need for OMT and that’s why the SYNTAXES trial 10-year mortality reduction – which builds upon an earlier 5-year mortality reduction analysis – is so important,” he said.
Patients should take OMT long term
These data “should be both a motivator for physicians to prescribe OMT and for patients to remain adherent to OMT,” he said. “It is the best warranty to blunt the progression of atherosclerosis and to reduce subsequent cardiac events.”
For the 10-year subanalysis of OMT in SYNTAXES, the patients were stratified by the number of OMTs they were taking at 5 years after revascularization and then evaluated for survival at 10 years. Of the 1,472 patients available for analysis at 5 years, only 678 (46%) were on OMT. The other 794 patients were not.
Graphically, the Kaplan-Meier survival curve for those on three types of OMT was consistently beneath that of those on four OMTs, but the gap narrowed over time. At the end of 10 years, the advantage of the four-drug OMT was not statistically significant relative to three or fewer (13.1% vs. 12.7%).
Statins and antiplatelets show largest effect
When analyzed individually and in different combinations, the agents with OMT did not appear to be equal. For example, the biggest survival gap at 10 years was for those who were on an antiplatelet therapy and a statin at 5 years relative to those who were not on either (13.2% vs. 22.6%; P = .006). Even after adjustment, there was nearly 45% survival benefit for these two agents (HR, 0.556; P = .02).
Conversely, the 10-year survival advantage for being on a renin-angiotensin system inhibitor at 5 years versus not being exposed to this therapy was small and nonsignificant (14.7% vs. 13.7%; P = .651).
The precise proportion of patients who were prescribed and adhered to OMT between 5 years and 10 years is unknown, acknowledged the authors, so conclusions are limited about the added benefit of 10- versus 5-year OMT, although the authors presume that a substantial proportion of those adherent for 5 years would likely continue on these therapies.
It can be said with confidence that those adherent for at least 5 years are more likely to be alive at 10 years than those who are not, according to Dr. Boden. He considers these data a call for physicians and all high-risk patients, not just those who have undergone revascularization, to take these standard therapies.
There are plenty of data to “show how poorly we treat patients with OMT,” said Dr. Boden, citing several studies. In one, which looked at OMT in a nationally representative sample in the United States, only a third of patients with angina were taking an antiplatelet, a statin, and a beta-blocker, all of which are indicated.
“Hospitalization for revascularization provides an opportune time to capture the attention of patients and their physicians,” he wrote in his editorial. He called OMT “an imperative to optimize clinical outcomes.”
Many of the investigators involved in the SYNTAXES subanalysis, including Dr. Serruys, have financial relationships with multiple pharmaceutical companies, including Boston Scientific, which provided the initial funding for the SYNTAX trial. Dr. Boden reports no potential conflicts of interest.
When it comes to medical therapy after a coronary revascularization procedure, more is better. Patients started and then maintained indefinitely on more rather than fewer of the drugs identified as optimal medical therapy (OMT) achieve a major survival benefit 10 years later, according to long-term follow-up from an extended analysis of the SYNTAX trial.
For the survival benefit at 10 years, “the present study suggests that at least three types of optimal medical therapy should be maintained for at least 5 years after revascularization,” reported a multinational team of cardiovascular specialists led by Hideyuki Kawashima, MD and Patrick Serruys, MD, who both have affiliations with the department of cardiology of the National University of Ireland, Galway.
The SYNTAX trial was conducted to compare percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) for patients with previously untreated three-vessel and/or left main disease (N Engl J Med 2009;360:961-72). The conclusion from that study, published in 2009 and subsequently reinforced by a 5-year follow-up, was that CABG should remain the standard of care for complex lesions.
Optimal medical therapy defined
In the course of SYNTAX, the impact of OMT on outcome was also evaluated in a subanalysis. At 5 years, there was a mortality advantage for those receiving an antiplatelet drug, a statin, a renin-angiotensin system inhibitor (ACE inhibitor or angiotensin receptor blocker), and a beta-blocker when compared with fewer of these agents.
When an investigator-initiated extension of SYNTAX, called SYNTAXES, was conducted to compare the outcomes of PCI and CABG at 10 years, it also permitted an extended analysis of OMT. Although the primary comparison of SYNTAXES, reported 2 years ago, did not show a significant difference between PCI and CABG for mortality at 10 years, there was a difference for OMT.
When investigators compared treatment with three or more OMT agents with that with two or fewer OMT drugs at 5 years, the result for all-cause death at 10 years translated into a more than 50% relative reduction (hazard ratio, 0.47; P = .002). The absolute difference in mortality was a more than 6% reduction (13.1% vs. 19.9%).
OMT data offer major message
The current study is considered to have a major message for patients as well as physicians.
“OMT even outweighs the survival benefit from revascularization alone, so our patients should convince themselves of the value of rigorous adherence and compliance,” Dr. Serruys said in an interview. According to him, these are compelling data for telling patients that OMT “is the best insurance for extended survival.” We now know from these data “the longer, the better.”
The same message from these data extends to physicians.
“I wish I could understand the apparent blind spot physicians have with respect to prescribing OMT despite the overwhelming benefit from multiple clinical trials,” said William E. Boden, MD, professor of medicine, Boston University.
Dr. Boden was a coauthor of an editorial accompanying the newly published SYNTAXES subanalysis. In the editorial, he noted that OMT following revascularization and in other high-risk patients “has been unacceptably low,” but he was asked to expand on the lessons from the newly released SYNTAXES subanalysis in an interview.
“There has often been a belief that revascularization negates the need for OMT and that’s why the SYNTAXES trial 10-year mortality reduction – which builds upon an earlier 5-year mortality reduction analysis – is so important,” he said.
Patients should take OMT long term
These data “should be both a motivator for physicians to prescribe OMT and for patients to remain adherent to OMT,” he said. “It is the best warranty to blunt the progression of atherosclerosis and to reduce subsequent cardiac events.”
For the 10-year subanalysis of OMT in SYNTAXES, the patients were stratified by the number of OMTs they were taking at 5 years after revascularization and then evaluated for survival at 10 years. Of the 1,472 patients available for analysis at 5 years, only 678 (46%) were on OMT. The other 794 patients were not.
Graphically, the Kaplan-Meier survival curve for those on three types of OMT was consistently beneath that of those on four OMTs, but the gap narrowed over time. At the end of 10 years, the advantage of the four-drug OMT was not statistically significant relative to three or fewer (13.1% vs. 12.7%).
Statins and antiplatelets show largest effect
When analyzed individually and in different combinations, the agents with OMT did not appear to be equal. For example, the biggest survival gap at 10 years was for those who were on an antiplatelet therapy and a statin at 5 years relative to those who were not on either (13.2% vs. 22.6%; P = .006). Even after adjustment, there was nearly 45% survival benefit for these two agents (HR, 0.556; P = .02).
Conversely, the 10-year survival advantage for being on a renin-angiotensin system inhibitor at 5 years versus not being exposed to this therapy was small and nonsignificant (14.7% vs. 13.7%; P = .651).
The precise proportion of patients who were prescribed and adhered to OMT between 5 years and 10 years is unknown, acknowledged the authors, so conclusions are limited about the added benefit of 10- versus 5-year OMT, although the authors presume that a substantial proportion of those adherent for 5 years would likely continue on these therapies.
It can be said with confidence that those adherent for at least 5 years are more likely to be alive at 10 years than those who are not, according to Dr. Boden. He considers these data a call for physicians and all high-risk patients, not just those who have undergone revascularization, to take these standard therapies.
There are plenty of data to “show how poorly we treat patients with OMT,” said Dr. Boden, citing several studies. In one, which looked at OMT in a nationally representative sample in the United States, only a third of patients with angina were taking an antiplatelet, a statin, and a beta-blocker, all of which are indicated.
“Hospitalization for revascularization provides an opportune time to capture the attention of patients and their physicians,” he wrote in his editorial. He called OMT “an imperative to optimize clinical outcomes.”
Many of the investigators involved in the SYNTAXES subanalysis, including Dr. Serruys, have financial relationships with multiple pharmaceutical companies, including Boston Scientific, which provided the initial funding for the SYNTAX trial. Dr. Boden reports no potential conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
'Full throttle': 'Diabetes Garage' workshops boost Mexican American men's self-management
Automotive-themed workshops that refer to doctor visits as “tune-ups” and nutritious food as “high-performance fuel” are showing promise as a strategy to better explain diabetes self-management to Mexican American men, an investigator has reported.
The workshops, which started out in person and transitioned online because of the COVID-19 pandemic, have improved self-care behaviors among Mexican American men with diabetes, said Jeannie Belinda Concha, PhD, MPH, of the University of Texas, El Paso.
After participating in the workshops, known as The Diabetes Garage, men more often measured food portions and counted carbohydrates, and had improved confidence in their ability to self-manage their diabetes, Dr. Concha said in a virtual presentation on the study.
Although those improvements in self-care behaviors didn’t translate into significant improvements in blood pressure or hemoglobin A1c, she said, they could be predecessors to improved physical health outcomes with longer follow-up.
”We know it takes some time to move those numbers, but they are going in the right direction,” Dr. Concha said in her presentation, which took place during the annual scientific sessions of the American Diabetes Association.
Meeting Mexican American men where they’re at
Robert Gabbay, MD, PhD, chief scientific and medical officer of the ADA, said The Diabetes Garage is an “innovative” approach to tailoring diabetes self-care message for a specific of individuals.
“It’s such a wonderful example of something that we believe so strongly, which is that you’ve got to meet people where they’re at,” Dr. Gabbay said in an interview.
“We know that people learn in different ways, and people and with different backgrounds have different things that resonate with them,” he continued. “For better or worse, one size doesn’t fit all, and that in a sense is one of the challenges around diabetes, because we’re really trying to help everybody.”
Unmet needs for diabetes education
The prevalence of diabetes in the United States is high among Hispanics, higher among Mexican Americans, and even higher still among Mexican-American men, according to Dr. Concha.
The age-adjusted prevalence of diabetes is 16.2% among Mexican-American men, as compared with 12.8% for Mexican American women, and 8.6% for White non-Hispanic men, according to 2018 data from the Centers for Disease Control and Prevention that Dr. Concha highlighted in her presentation.
Moreover, only 25% of participants in diabetes education are men, highlighting another disparity that needs to be addressed, she said.
Infusing diabetes self-management with car culture
The Diabetes Garage leverages a positive “car culture” that is prevalent in Mexican American communities in general, and cities like El Paso in particular, Dr. Concha said.
This culture brings Mexican American people together at numerous car shows, and is viewed as a form of family identification for enthusiasts, who will illustrate their own pride by customizing their cars with cultural symbols, according to Dr. Concha.
The diabetes education intervention consists of four workshops delivered as 2-hour weekly sessions that include a diabetes educator and an automotive instructor:
In the first session, men learn about “starting and operating” their body with diabetes, and checking their “gauges” when it comes to blood pressure, cholesterol, and other measures, according to Dr. Concha.
The second session stresses the importance of physical activity (“using all your gears”) and of managing stress (“full throttle”).
The third session highlights medication as a tool (“to keep your battery charged”) and the importance of diabetes complications (“catastrophic failure”) as well as visiting the doctor (“tune ups and inspections”).
Finally, men learn about nutrition (high-performance fuel) in a workshop on eating well with diabetes. “We ask them to invite their family and friends, and they do,” said Dr. Concha.
Rubber hits the road
Since 2018, 16 workshops have been completed in El Paso, San Antonio, and Harlingen, Tex., of which 9 were in English, 5 were in Spanish, and 2 were bilingual. Due to the COVID-19 pandemic, 10 of the workshops were completed online, Dr. Concha said.
In total, 97 men engaged in the workshops, of whom 91% were Hispanic/Latino; 71% were employed, 71% were married, and 84% had health insurance. Eighty-six percent completed all four workshops, while 89% completed at least three workshops.
The number of days men measured food portions increased significantly from pre- to postworkshop assessment, from a mean of 2.1 days to 2.74 days, Dr. Concha reported. Similarly, the mean number of days counting carbohydrate portions increased significantly, from 1.92 to 2.64 days.
The proportion of men agreeing or strongly agreeing they were confident they could manage diabetes increased from 74% before the intervention to 93% afterward, according to Dr. Concha’s presentation.
By contrast, there were no statistically significant increases in physical outcomes including physical activity, weight, waist circumference, A1c, or blood pressure from before the workshop to after, though outcomes trended in an improved direction, according to Dr. Concha.
Postactivity satisfaction survey results showed that 86%of men said the automotive analogies in the program helped them understand the importance of diabetes management. “I am looking forward to better managing my human-mobile for a long, long time with a good quality of life,” one of the men wrote in survey feedback.
Dr. Concha and coauthors reported no conflicts of interest related to the study.
Automotive-themed workshops that refer to doctor visits as “tune-ups” and nutritious food as “high-performance fuel” are showing promise as a strategy to better explain diabetes self-management to Mexican American men, an investigator has reported.
The workshops, which started out in person and transitioned online because of the COVID-19 pandemic, have improved self-care behaviors among Mexican American men with diabetes, said Jeannie Belinda Concha, PhD, MPH, of the University of Texas, El Paso.
After participating in the workshops, known as The Diabetes Garage, men more often measured food portions and counted carbohydrates, and had improved confidence in their ability to self-manage their diabetes, Dr. Concha said in a virtual presentation on the study.
Although those improvements in self-care behaviors didn’t translate into significant improvements in blood pressure or hemoglobin A1c, she said, they could be predecessors to improved physical health outcomes with longer follow-up.
”We know it takes some time to move those numbers, but they are going in the right direction,” Dr. Concha said in her presentation, which took place during the annual scientific sessions of the American Diabetes Association.
Meeting Mexican American men where they’re at
Robert Gabbay, MD, PhD, chief scientific and medical officer of the ADA, said The Diabetes Garage is an “innovative” approach to tailoring diabetes self-care message for a specific of individuals.
“It’s such a wonderful example of something that we believe so strongly, which is that you’ve got to meet people where they’re at,” Dr. Gabbay said in an interview.
“We know that people learn in different ways, and people and with different backgrounds have different things that resonate with them,” he continued. “For better or worse, one size doesn’t fit all, and that in a sense is one of the challenges around diabetes, because we’re really trying to help everybody.”
Unmet needs for diabetes education
The prevalence of diabetes in the United States is high among Hispanics, higher among Mexican Americans, and even higher still among Mexican-American men, according to Dr. Concha.
The age-adjusted prevalence of diabetes is 16.2% among Mexican-American men, as compared with 12.8% for Mexican American women, and 8.6% for White non-Hispanic men, according to 2018 data from the Centers for Disease Control and Prevention that Dr. Concha highlighted in her presentation.
Moreover, only 25% of participants in diabetes education are men, highlighting another disparity that needs to be addressed, she said.
Infusing diabetes self-management with car culture
The Diabetes Garage leverages a positive “car culture” that is prevalent in Mexican American communities in general, and cities like El Paso in particular, Dr. Concha said.
This culture brings Mexican American people together at numerous car shows, and is viewed as a form of family identification for enthusiasts, who will illustrate their own pride by customizing their cars with cultural symbols, according to Dr. Concha.
The diabetes education intervention consists of four workshops delivered as 2-hour weekly sessions that include a diabetes educator and an automotive instructor:
In the first session, men learn about “starting and operating” their body with diabetes, and checking their “gauges” when it comes to blood pressure, cholesterol, and other measures, according to Dr. Concha.
The second session stresses the importance of physical activity (“using all your gears”) and of managing stress (“full throttle”).
The third session highlights medication as a tool (“to keep your battery charged”) and the importance of diabetes complications (“catastrophic failure”) as well as visiting the doctor (“tune ups and inspections”).
Finally, men learn about nutrition (high-performance fuel) in a workshop on eating well with diabetes. “We ask them to invite their family and friends, and they do,” said Dr. Concha.
Rubber hits the road
Since 2018, 16 workshops have been completed in El Paso, San Antonio, and Harlingen, Tex., of which 9 were in English, 5 were in Spanish, and 2 were bilingual. Due to the COVID-19 pandemic, 10 of the workshops were completed online, Dr. Concha said.
In total, 97 men engaged in the workshops, of whom 91% were Hispanic/Latino; 71% were employed, 71% were married, and 84% had health insurance. Eighty-six percent completed all four workshops, while 89% completed at least three workshops.
The number of days men measured food portions increased significantly from pre- to postworkshop assessment, from a mean of 2.1 days to 2.74 days, Dr. Concha reported. Similarly, the mean number of days counting carbohydrate portions increased significantly, from 1.92 to 2.64 days.
The proportion of men agreeing or strongly agreeing they were confident they could manage diabetes increased from 74% before the intervention to 93% afterward, according to Dr. Concha’s presentation.
By contrast, there were no statistically significant increases in physical outcomes including physical activity, weight, waist circumference, A1c, or blood pressure from before the workshop to after, though outcomes trended in an improved direction, according to Dr. Concha.
Postactivity satisfaction survey results showed that 86%of men said the automotive analogies in the program helped them understand the importance of diabetes management. “I am looking forward to better managing my human-mobile for a long, long time with a good quality of life,” one of the men wrote in survey feedback.
Dr. Concha and coauthors reported no conflicts of interest related to the study.
Automotive-themed workshops that refer to doctor visits as “tune-ups” and nutritious food as “high-performance fuel” are showing promise as a strategy to better explain diabetes self-management to Mexican American men, an investigator has reported.
The workshops, which started out in person and transitioned online because of the COVID-19 pandemic, have improved self-care behaviors among Mexican American men with diabetes, said Jeannie Belinda Concha, PhD, MPH, of the University of Texas, El Paso.
After participating in the workshops, known as The Diabetes Garage, men more often measured food portions and counted carbohydrates, and had improved confidence in their ability to self-manage their diabetes, Dr. Concha said in a virtual presentation on the study.
Although those improvements in self-care behaviors didn’t translate into significant improvements in blood pressure or hemoglobin A1c, she said, they could be predecessors to improved physical health outcomes with longer follow-up.
”We know it takes some time to move those numbers, but they are going in the right direction,” Dr. Concha said in her presentation, which took place during the annual scientific sessions of the American Diabetes Association.
Meeting Mexican American men where they’re at
Robert Gabbay, MD, PhD, chief scientific and medical officer of the ADA, said The Diabetes Garage is an “innovative” approach to tailoring diabetes self-care message for a specific of individuals.
“It’s such a wonderful example of something that we believe so strongly, which is that you’ve got to meet people where they’re at,” Dr. Gabbay said in an interview.
“We know that people learn in different ways, and people and with different backgrounds have different things that resonate with them,” he continued. “For better or worse, one size doesn’t fit all, and that in a sense is one of the challenges around diabetes, because we’re really trying to help everybody.”
Unmet needs for diabetes education
The prevalence of diabetes in the United States is high among Hispanics, higher among Mexican Americans, and even higher still among Mexican-American men, according to Dr. Concha.
The age-adjusted prevalence of diabetes is 16.2% among Mexican-American men, as compared with 12.8% for Mexican American women, and 8.6% for White non-Hispanic men, according to 2018 data from the Centers for Disease Control and Prevention that Dr. Concha highlighted in her presentation.
Moreover, only 25% of participants in diabetes education are men, highlighting another disparity that needs to be addressed, she said.
Infusing diabetes self-management with car culture
The Diabetes Garage leverages a positive “car culture” that is prevalent in Mexican American communities in general, and cities like El Paso in particular, Dr. Concha said.
This culture brings Mexican American people together at numerous car shows, and is viewed as a form of family identification for enthusiasts, who will illustrate their own pride by customizing their cars with cultural symbols, according to Dr. Concha.
The diabetes education intervention consists of four workshops delivered as 2-hour weekly sessions that include a diabetes educator and an automotive instructor:
In the first session, men learn about “starting and operating” their body with diabetes, and checking their “gauges” when it comes to blood pressure, cholesterol, and other measures, according to Dr. Concha.
The second session stresses the importance of physical activity (“using all your gears”) and of managing stress (“full throttle”).
The third session highlights medication as a tool (“to keep your battery charged”) and the importance of diabetes complications (“catastrophic failure”) as well as visiting the doctor (“tune ups and inspections”).
Finally, men learn about nutrition (high-performance fuel) in a workshop on eating well with diabetes. “We ask them to invite their family and friends, and they do,” said Dr. Concha.
Rubber hits the road
Since 2018, 16 workshops have been completed in El Paso, San Antonio, and Harlingen, Tex., of which 9 were in English, 5 were in Spanish, and 2 were bilingual. Due to the COVID-19 pandemic, 10 of the workshops were completed online, Dr. Concha said.
In total, 97 men engaged in the workshops, of whom 91% were Hispanic/Latino; 71% were employed, 71% were married, and 84% had health insurance. Eighty-six percent completed all four workshops, while 89% completed at least three workshops.
The number of days men measured food portions increased significantly from pre- to postworkshop assessment, from a mean of 2.1 days to 2.74 days, Dr. Concha reported. Similarly, the mean number of days counting carbohydrate portions increased significantly, from 1.92 to 2.64 days.
The proportion of men agreeing or strongly agreeing they were confident they could manage diabetes increased from 74% before the intervention to 93% afterward, according to Dr. Concha’s presentation.
By contrast, there were no statistically significant increases in physical outcomes including physical activity, weight, waist circumference, A1c, or blood pressure from before the workshop to after, though outcomes trended in an improved direction, according to Dr. Concha.
Postactivity satisfaction survey results showed that 86%of men said the automotive analogies in the program helped them understand the importance of diabetes management. “I am looking forward to better managing my human-mobile for a long, long time with a good quality of life,” one of the men wrote in survey feedback.
Dr. Concha and coauthors reported no conflicts of interest related to the study.
FROM ADA 2021
Advances in hepatocellular carcinoma at ASCO 2021
Dr. Laura Goff presents treatment updates in hepatocellular carcinoma (HCC) that were presented at the ASCO 2021 Annual Meeting.
Updated data from the phase 3 KEYNOTE-240 study demonstrated that overall survival, progression-free survival, and objective response rate were maintained over 3 years with pembrolizumab compared to placebo in patients with advanced HCC previously treated with sorafenib.
An exploratory analysis of IMBRAVE150 examined the association between best overall response and overall survival, as well as independent predictors of survival in patients with unresectable HCC treated with atezolizumab plus bevacizumab versus sorafenib. In the study treatment population, confirmed response by RECIST 1.1 and by HCC mRECIST were associated with improved overall survival. Data suggested that both confirmed response and stable disease are associated with improved clinical outcomes in patients treated with this regimen.
Lastly, a retrospective cohort study comparing sorafenib, and nivolumab as first-line systemic therapies for patients with advanced HCC and Child-Pugh class B cirrhosis found that nivolumab was associated with better overall survival as a first-line treatment.
--
Laura W. Goff, MD is an Associate Professor at Vanderbilt University Medical Center in Nashville, Tennessee.
Dr. Goff discloses previous work with: Agios, ArQule; ASLAN Pharmaceuticals; Astellas Pharma; Basilea Pharmaceutica; BeiGene; Bristol Myers Squibb; Eli Lilly and Company; H3 Biomedicine; Incyte; Leap Therapeutics; Merck; Onyx Pharmaceuticals; Pfizer; SunPharma.
Dr. Laura Goff presents treatment updates in hepatocellular carcinoma (HCC) that were presented at the ASCO 2021 Annual Meeting.
Updated data from the phase 3 KEYNOTE-240 study demonstrated that overall survival, progression-free survival, and objective response rate were maintained over 3 years with pembrolizumab compared to placebo in patients with advanced HCC previously treated with sorafenib.
An exploratory analysis of IMBRAVE150 examined the association between best overall response and overall survival, as well as independent predictors of survival in patients with unresectable HCC treated with atezolizumab plus bevacizumab versus sorafenib. In the study treatment population, confirmed response by RECIST 1.1 and by HCC mRECIST were associated with improved overall survival. Data suggested that both confirmed response and stable disease are associated with improved clinical outcomes in patients treated with this regimen.
Lastly, a retrospective cohort study comparing sorafenib, and nivolumab as first-line systemic therapies for patients with advanced HCC and Child-Pugh class B cirrhosis found that nivolumab was associated with better overall survival as a first-line treatment.
--
Laura W. Goff, MD is an Associate Professor at Vanderbilt University Medical Center in Nashville, Tennessee.
Dr. Goff discloses previous work with: Agios, ArQule; ASLAN Pharmaceuticals; Astellas Pharma; Basilea Pharmaceutica; BeiGene; Bristol Myers Squibb; Eli Lilly and Company; H3 Biomedicine; Incyte; Leap Therapeutics; Merck; Onyx Pharmaceuticals; Pfizer; SunPharma.
Dr. Laura Goff presents treatment updates in hepatocellular carcinoma (HCC) that were presented at the ASCO 2021 Annual Meeting.
Updated data from the phase 3 KEYNOTE-240 study demonstrated that overall survival, progression-free survival, and objective response rate were maintained over 3 years with pembrolizumab compared to placebo in patients with advanced HCC previously treated with sorafenib.
An exploratory analysis of IMBRAVE150 examined the association between best overall response and overall survival, as well as independent predictors of survival in patients with unresectable HCC treated with atezolizumab plus bevacizumab versus sorafenib. In the study treatment population, confirmed response by RECIST 1.1 and by HCC mRECIST were associated with improved overall survival. Data suggested that both confirmed response and stable disease are associated with improved clinical outcomes in patients treated with this regimen.
Lastly, a retrospective cohort study comparing sorafenib, and nivolumab as first-line systemic therapies for patients with advanced HCC and Child-Pugh class B cirrhosis found that nivolumab was associated with better overall survival as a first-line treatment.
--
Laura W. Goff, MD is an Associate Professor at Vanderbilt University Medical Center in Nashville, Tennessee.
Dr. Goff discloses previous work with: Agios, ArQule; ASLAN Pharmaceuticals; Astellas Pharma; Basilea Pharmaceutica; BeiGene; Bristol Myers Squibb; Eli Lilly and Company; H3 Biomedicine; Incyte; Leap Therapeutics; Merck; Onyx Pharmaceuticals; Pfizer; SunPharma.

Top Abstracts in Locally Advanced NSCLC From ASCO 2021
Dr Thomas Stinchcombe, from Duke Cancer Center in Durham, North Carolina, highlights key abstracts in locally advanced non–small cell lung cancer (NSCLC) presented at the 2021 annual meeting of the American Society of Clinical Oncology.
First, he reviews the IMpower010 trial, which compares atezolizumab vs best supportive care in patients with surgically resected NSCLC who had received adjuvant chemotherapy.
He then discusses surgical outcomes from the CheckMate 816 trial in patients with resectable NSCLC who had been treated with nivolumab plus platinum-doublet chemotherapy vs chemotherapy alone.
Finally, Dr Stinchcombe discusses the IMPACT trial, which looked at adjuvant gefitinib vs cisplatin/vinorelbine in completely resected NSCLC patients with EGFR mutations.
--
Thomas E. Stinchcombe, MD, Medical Oncology, Duke Cancer Center, Durham, North Carolina.
Thomas E. Stinchcombe, MD, has disclosed the following relevant financial relationships:
Received research funding from: Genentech/Roche; Blueprint Medicines; AstraZeneca
Received income in an amount equal to or greater than $250 from: Takeda; AstraZeneca; Genentech/Roche; Foundation Medicine; Pfizer; EMD Serono; Novartis; Daiichi Sankyo; Eli Lilly and Company; Medtronic.
Dr Thomas Stinchcombe, from Duke Cancer Center in Durham, North Carolina, highlights key abstracts in locally advanced non–small cell lung cancer (NSCLC) presented at the 2021 annual meeting of the American Society of Clinical Oncology.
First, he reviews the IMpower010 trial, which compares atezolizumab vs best supportive care in patients with surgically resected NSCLC who had received adjuvant chemotherapy.
He then discusses surgical outcomes from the CheckMate 816 trial in patients with resectable NSCLC who had been treated with nivolumab plus platinum-doublet chemotherapy vs chemotherapy alone.
Finally, Dr Stinchcombe discusses the IMPACT trial, which looked at adjuvant gefitinib vs cisplatin/vinorelbine in completely resected NSCLC patients with EGFR mutations.
--
Thomas E. Stinchcombe, MD, Medical Oncology, Duke Cancer Center, Durham, North Carolina.
Thomas E. Stinchcombe, MD, has disclosed the following relevant financial relationships:
Received research funding from: Genentech/Roche; Blueprint Medicines; AstraZeneca
Received income in an amount equal to or greater than $250 from: Takeda; AstraZeneca; Genentech/Roche; Foundation Medicine; Pfizer; EMD Serono; Novartis; Daiichi Sankyo; Eli Lilly and Company; Medtronic.
Dr Thomas Stinchcombe, from Duke Cancer Center in Durham, North Carolina, highlights key abstracts in locally advanced non–small cell lung cancer (NSCLC) presented at the 2021 annual meeting of the American Society of Clinical Oncology.
First, he reviews the IMpower010 trial, which compares atezolizumab vs best supportive care in patients with surgically resected NSCLC who had received adjuvant chemotherapy.
He then discusses surgical outcomes from the CheckMate 816 trial in patients with resectable NSCLC who had been treated with nivolumab plus platinum-doublet chemotherapy vs chemotherapy alone.
Finally, Dr Stinchcombe discusses the IMPACT trial, which looked at adjuvant gefitinib vs cisplatin/vinorelbine in completely resected NSCLC patients with EGFR mutations.
--
Thomas E. Stinchcombe, MD, Medical Oncology, Duke Cancer Center, Durham, North Carolina.
Thomas E. Stinchcombe, MD, has disclosed the following relevant financial relationships:
Received research funding from: Genentech/Roche; Blueprint Medicines; AstraZeneca
Received income in an amount equal to or greater than $250 from: Takeda; AstraZeneca; Genentech/Roche; Foundation Medicine; Pfizer; EMD Serono; Novartis; Daiichi Sankyo; Eli Lilly and Company; Medtronic.

Real-world CAR T outcomes for DLBCL mimic clinical trials
Data from a large French registry on a multicenter experience with chimeric antigen receptor T-cell (CAR T) therapy for aggressive lymphoma suggests that the favorable outcomes seen in clinical trials can be replicated in the real world.
Among 481 patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) treated with either of two commercially available CAR T products – tisagenlecleucel (Kymriah) or axicabtagene ciloleucel (Yescarta) – the duration of responses, progression-free survival (PFS), and overall survival (OS) rates at 6 months mirror those seen in clinical trials, reported Steven LeGouill, MD, PhD, from the University of Nantes (France), on behalf of colleagues in the DESCAR-T (Dispositive d’Evaluation et de Suivi des CAR-T) registry.
“CAR T has now become a standard of care in a lot of French centers, with more than 640 patients treated with CAR T in less than 2 years. The DESCAR-T real-life experience mimics the experience that had been previously by other real-life registries but also in clinical trials. We didn’t see new emerging toxicity signals in real life,” he said in an oral abstract session during the European Hematology Association annual congress (Abstract S216).
“I am convinced that a population registry about CAR T–treated patients is needed,” commented Pieter Sonneveld, MD, from Erasmus Medical Center in Rotterdam, the Netherlands, who was not involved in the study.
“Selection criteria for CAR T trials have been incredibly restrictive, and academic trials have not gained ground yet. It is important to collect and analyze more data, include non-trial patients and analyze long-term follow-up in order to determine the real effects of this innovative treatment in lymphoma and other diseases,” he said.
Dr. Sonneveld, EHA past president, was the moderator a briefing where Dr. LeGouill presented the DESCAR-T study findings.
Natalie Sophia Grover, MD, a leukemia and lymphoma specialist at the University of North Carolina at Chapel Hill, noted in an interview that “there have been several publications recently that have shown that these promising outcomes for these really refractory, high-risk patients with diffuse large B-cell lymphoma seem to be similar with what we’ve seen in trials, which is definitely exciting.”
She noted that the median time from CAR T order to treatment in the study, 50 days, was longer than in her experience.
“Generally, from collection to treatment is less than a month. Looking at that, I would have expected more patients not to make it CAR T, but nearly 90% of patients who had collections got treatment, which is pretty good. Those patients that didn’t make it to treatment had really poor outcomes,” she said.
Dr. Grover was not involved in the study.
More data, s’il vous plait
The DESCAR-T registry was created in response to a request from French health authorities for data beyond that provided in the EBMT patient registry. The health authorities asked for characterization of the CAR T–eligible population in an intention to treat, 15-year follow-up of both CAR T recipients and candidates who were not treated for whatever reasons, and a full accounting of previous lines of therapy.
Dr. LeGouill presented the first analysis of data from the registry involving 19 enrolling site and 647 patients with DLBCL for whom CAR T cells were ordered from January 2018 to March 2021.
Of the 647 candidates, 10 did not have CAR T ordered for reasons that included patient deaths or disease progression, infection, and patient refusal. An additional 30 patients either had leukapheresis performed or pending, and 607 had CAR T ordered.
Of the 607 patients, 53 did not receive CAR T infusions because of disease progression, death before product administration, manufacturing or leukapheresis failures, uncontrolled infections, patient choice, or progression of other malignancies.
That left 550 patients (85%) who received a CAR T product, either tisagenlecleucel (200 patients) or axicabtagene ciloleucel (350 patients).
Among all patients, the median age at CAR T order was 63 for patients who received tisagenlecleucel, and 65 for patients receiving axicabtagene ciloleucel. Patients 65 and older comprised 44% and 51% of the population, respectively.
Patients treated with each CAR T product had a median of three prior lines of therapy.
Manageable toxicities
Toxicities within 10 days of CAR T infusion included 418 cases among 515 patients (81.2%) of cytokine release syndrome, with most being grade 1 or 2 in severity; 44 patients had grade 3 or 4 CRS.
Any-grade neurotoxicity was seen in 184 patients (35.7%), primarily grade 1 or 2 in severity; 50 patients had grade 3 or greater neurotoxicity.
Of 427 patients with at least one CAR T–specific toxicity within 10 days, 139 (32.8%) required ICU admission, 325 (76,1%) were treated for CAR T–specific toxicities, 278 (65.1%) received tocilizumab, 13 (3%) received siltuximab, and 176 (41.2%) received corticosteroids.
Favorable outcomes
Overall response rates, at 1, 3, and 6 months post infusions were 70.6%, 56.3%, and 60%, respectively, with the majority of response at each time point being complete responses (CR).
The 6-month overall survival (OS) rate among all patients who were treated was 83.7%, compared with 5.5% for patients who did not receive CAR T infusions.
Progression-free survival (PFS) at 6 months was 44.5%, and 57.7% of patients had an ongoing response at the same time point.
Among patients who received bridging therapy between leukapheresis and CAR T infusion, the 6-month PFS was 58.4% for patients with either a CR, partial response, or stable disease, compared with 63.3% for patients who did not receive bridging therapy, and 29.8% for those with disease progression.
The respective 6 months OS rates were 87.4%, 82.3%, and 65.5%.
The results showed that patients who do not have at least stable disease at the time of CAR T infusion are at risk for early relapse, but approximately 30% of these patients still had long-term disease control, Dr. LeGouill said.
He acknowledged that longer follow-up will be need to see whether the plateaus in the PFS and OS curves the investigators observed can be maintained over time. Questions that still need to be answered include the impact of bridging therapy or disease status at the start of treatment on outcomes, and how to improve CAR T efficacy based on individual patient characteristics.
The registry will be extended to include data on patients treated with CAR T for mantle cell lymphoma and multiple myeloma, investigators announced.
The study is supported by participating centers and Gilead/Kite and Novartis. Dr. LeGouill disclosed advisory board activity and honoraria from the companies and others. Dr. Grover disclosed advisory board participating for Kite and others. Dr. Sonneveld has disclosed research grants and honoraria from several companies, not including Kite or Novartis.
Data from a large French registry on a multicenter experience with chimeric antigen receptor T-cell (CAR T) therapy for aggressive lymphoma suggests that the favorable outcomes seen in clinical trials can be replicated in the real world.
Among 481 patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) treated with either of two commercially available CAR T products – tisagenlecleucel (Kymriah) or axicabtagene ciloleucel (Yescarta) – the duration of responses, progression-free survival (PFS), and overall survival (OS) rates at 6 months mirror those seen in clinical trials, reported Steven LeGouill, MD, PhD, from the University of Nantes (France), on behalf of colleagues in the DESCAR-T (Dispositive d’Evaluation et de Suivi des CAR-T) registry.
“CAR T has now become a standard of care in a lot of French centers, with more than 640 patients treated with CAR T in less than 2 years. The DESCAR-T real-life experience mimics the experience that had been previously by other real-life registries but also in clinical trials. We didn’t see new emerging toxicity signals in real life,” he said in an oral abstract session during the European Hematology Association annual congress (Abstract S216).
“I am convinced that a population registry about CAR T–treated patients is needed,” commented Pieter Sonneveld, MD, from Erasmus Medical Center in Rotterdam, the Netherlands, who was not involved in the study.
“Selection criteria for CAR T trials have been incredibly restrictive, and academic trials have not gained ground yet. It is important to collect and analyze more data, include non-trial patients and analyze long-term follow-up in order to determine the real effects of this innovative treatment in lymphoma and other diseases,” he said.
Dr. Sonneveld, EHA past president, was the moderator a briefing where Dr. LeGouill presented the DESCAR-T study findings.
Natalie Sophia Grover, MD, a leukemia and lymphoma specialist at the University of North Carolina at Chapel Hill, noted in an interview that “there have been several publications recently that have shown that these promising outcomes for these really refractory, high-risk patients with diffuse large B-cell lymphoma seem to be similar with what we’ve seen in trials, which is definitely exciting.”
She noted that the median time from CAR T order to treatment in the study, 50 days, was longer than in her experience.
“Generally, from collection to treatment is less than a month. Looking at that, I would have expected more patients not to make it CAR T, but nearly 90% of patients who had collections got treatment, which is pretty good. Those patients that didn’t make it to treatment had really poor outcomes,” she said.
Dr. Grover was not involved in the study.
More data, s’il vous plait
The DESCAR-T registry was created in response to a request from French health authorities for data beyond that provided in the EBMT patient registry. The health authorities asked for characterization of the CAR T–eligible population in an intention to treat, 15-year follow-up of both CAR T recipients and candidates who were not treated for whatever reasons, and a full accounting of previous lines of therapy.
Dr. LeGouill presented the first analysis of data from the registry involving 19 enrolling site and 647 patients with DLBCL for whom CAR T cells were ordered from January 2018 to March 2021.
Of the 647 candidates, 10 did not have CAR T ordered for reasons that included patient deaths or disease progression, infection, and patient refusal. An additional 30 patients either had leukapheresis performed or pending, and 607 had CAR T ordered.
Of the 607 patients, 53 did not receive CAR T infusions because of disease progression, death before product administration, manufacturing or leukapheresis failures, uncontrolled infections, patient choice, or progression of other malignancies.
That left 550 patients (85%) who received a CAR T product, either tisagenlecleucel (200 patients) or axicabtagene ciloleucel (350 patients).
Among all patients, the median age at CAR T order was 63 for patients who received tisagenlecleucel, and 65 for patients receiving axicabtagene ciloleucel. Patients 65 and older comprised 44% and 51% of the population, respectively.
Patients treated with each CAR T product had a median of three prior lines of therapy.
Manageable toxicities
Toxicities within 10 days of CAR T infusion included 418 cases among 515 patients (81.2%) of cytokine release syndrome, with most being grade 1 or 2 in severity; 44 patients had grade 3 or 4 CRS.
Any-grade neurotoxicity was seen in 184 patients (35.7%), primarily grade 1 or 2 in severity; 50 patients had grade 3 or greater neurotoxicity.
Of 427 patients with at least one CAR T–specific toxicity within 10 days, 139 (32.8%) required ICU admission, 325 (76,1%) were treated for CAR T–specific toxicities, 278 (65.1%) received tocilizumab, 13 (3%) received siltuximab, and 176 (41.2%) received corticosteroids.
Favorable outcomes
Overall response rates, at 1, 3, and 6 months post infusions were 70.6%, 56.3%, and 60%, respectively, with the majority of response at each time point being complete responses (CR).
The 6-month overall survival (OS) rate among all patients who were treated was 83.7%, compared with 5.5% for patients who did not receive CAR T infusions.
Progression-free survival (PFS) at 6 months was 44.5%, and 57.7% of patients had an ongoing response at the same time point.
Among patients who received bridging therapy between leukapheresis and CAR T infusion, the 6-month PFS was 58.4% for patients with either a CR, partial response, or stable disease, compared with 63.3% for patients who did not receive bridging therapy, and 29.8% for those with disease progression.
The respective 6 months OS rates were 87.4%, 82.3%, and 65.5%.
The results showed that patients who do not have at least stable disease at the time of CAR T infusion are at risk for early relapse, but approximately 30% of these patients still had long-term disease control, Dr. LeGouill said.
He acknowledged that longer follow-up will be need to see whether the plateaus in the PFS and OS curves the investigators observed can be maintained over time. Questions that still need to be answered include the impact of bridging therapy or disease status at the start of treatment on outcomes, and how to improve CAR T efficacy based on individual patient characteristics.
The registry will be extended to include data on patients treated with CAR T for mantle cell lymphoma and multiple myeloma, investigators announced.
The study is supported by participating centers and Gilead/Kite and Novartis. Dr. LeGouill disclosed advisory board activity and honoraria from the companies and others. Dr. Grover disclosed advisory board participating for Kite and others. Dr. Sonneveld has disclosed research grants and honoraria from several companies, not including Kite or Novartis.
Data from a large French registry on a multicenter experience with chimeric antigen receptor T-cell (CAR T) therapy for aggressive lymphoma suggests that the favorable outcomes seen in clinical trials can be replicated in the real world.
Among 481 patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) treated with either of two commercially available CAR T products – tisagenlecleucel (Kymriah) or axicabtagene ciloleucel (Yescarta) – the duration of responses, progression-free survival (PFS), and overall survival (OS) rates at 6 months mirror those seen in clinical trials, reported Steven LeGouill, MD, PhD, from the University of Nantes (France), on behalf of colleagues in the DESCAR-T (Dispositive d’Evaluation et de Suivi des CAR-T) registry.
“CAR T has now become a standard of care in a lot of French centers, with more than 640 patients treated with CAR T in less than 2 years. The DESCAR-T real-life experience mimics the experience that had been previously by other real-life registries but also in clinical trials. We didn’t see new emerging toxicity signals in real life,” he said in an oral abstract session during the European Hematology Association annual congress (Abstract S216).
“I am convinced that a population registry about CAR T–treated patients is needed,” commented Pieter Sonneveld, MD, from Erasmus Medical Center in Rotterdam, the Netherlands, who was not involved in the study.
“Selection criteria for CAR T trials have been incredibly restrictive, and academic trials have not gained ground yet. It is important to collect and analyze more data, include non-trial patients and analyze long-term follow-up in order to determine the real effects of this innovative treatment in lymphoma and other diseases,” he said.
Dr. Sonneveld, EHA past president, was the moderator a briefing where Dr. LeGouill presented the DESCAR-T study findings.
Natalie Sophia Grover, MD, a leukemia and lymphoma specialist at the University of North Carolina at Chapel Hill, noted in an interview that “there have been several publications recently that have shown that these promising outcomes for these really refractory, high-risk patients with diffuse large B-cell lymphoma seem to be similar with what we’ve seen in trials, which is definitely exciting.”
She noted that the median time from CAR T order to treatment in the study, 50 days, was longer than in her experience.
“Generally, from collection to treatment is less than a month. Looking at that, I would have expected more patients not to make it CAR T, but nearly 90% of patients who had collections got treatment, which is pretty good. Those patients that didn’t make it to treatment had really poor outcomes,” she said.
Dr. Grover was not involved in the study.
More data, s’il vous plait
The DESCAR-T registry was created in response to a request from French health authorities for data beyond that provided in the EBMT patient registry. The health authorities asked for characterization of the CAR T–eligible population in an intention to treat, 15-year follow-up of both CAR T recipients and candidates who were not treated for whatever reasons, and a full accounting of previous lines of therapy.
Dr. LeGouill presented the first analysis of data from the registry involving 19 enrolling site and 647 patients with DLBCL for whom CAR T cells were ordered from January 2018 to March 2021.
Of the 647 candidates, 10 did not have CAR T ordered for reasons that included patient deaths or disease progression, infection, and patient refusal. An additional 30 patients either had leukapheresis performed or pending, and 607 had CAR T ordered.
Of the 607 patients, 53 did not receive CAR T infusions because of disease progression, death before product administration, manufacturing or leukapheresis failures, uncontrolled infections, patient choice, or progression of other malignancies.
That left 550 patients (85%) who received a CAR T product, either tisagenlecleucel (200 patients) or axicabtagene ciloleucel (350 patients).
Among all patients, the median age at CAR T order was 63 for patients who received tisagenlecleucel, and 65 for patients receiving axicabtagene ciloleucel. Patients 65 and older comprised 44% and 51% of the population, respectively.
Patients treated with each CAR T product had a median of three prior lines of therapy.
Manageable toxicities
Toxicities within 10 days of CAR T infusion included 418 cases among 515 patients (81.2%) of cytokine release syndrome, with most being grade 1 or 2 in severity; 44 patients had grade 3 or 4 CRS.
Any-grade neurotoxicity was seen in 184 patients (35.7%), primarily grade 1 or 2 in severity; 50 patients had grade 3 or greater neurotoxicity.
Of 427 patients with at least one CAR T–specific toxicity within 10 days, 139 (32.8%) required ICU admission, 325 (76,1%) were treated for CAR T–specific toxicities, 278 (65.1%) received tocilizumab, 13 (3%) received siltuximab, and 176 (41.2%) received corticosteroids.
Favorable outcomes
Overall response rates, at 1, 3, and 6 months post infusions were 70.6%, 56.3%, and 60%, respectively, with the majority of response at each time point being complete responses (CR).
The 6-month overall survival (OS) rate among all patients who were treated was 83.7%, compared with 5.5% for patients who did not receive CAR T infusions.
Progression-free survival (PFS) at 6 months was 44.5%, and 57.7% of patients had an ongoing response at the same time point.
Among patients who received bridging therapy between leukapheresis and CAR T infusion, the 6-month PFS was 58.4% for patients with either a CR, partial response, or stable disease, compared with 63.3% for patients who did not receive bridging therapy, and 29.8% for those with disease progression.
The respective 6 months OS rates were 87.4%, 82.3%, and 65.5%.
The results showed that patients who do not have at least stable disease at the time of CAR T infusion are at risk for early relapse, but approximately 30% of these patients still had long-term disease control, Dr. LeGouill said.
He acknowledged that longer follow-up will be need to see whether the plateaus in the PFS and OS curves the investigators observed can be maintained over time. Questions that still need to be answered include the impact of bridging therapy or disease status at the start of treatment on outcomes, and how to improve CAR T efficacy based on individual patient characteristics.
The registry will be extended to include data on patients treated with CAR T for mantle cell lymphoma and multiple myeloma, investigators announced.
The study is supported by participating centers and Gilead/Kite and Novartis. Dr. LeGouill disclosed advisory board activity and honoraria from the companies and others. Dr. Grover disclosed advisory board participating for Kite and others. Dr. Sonneveld has disclosed research grants and honoraria from several companies, not including Kite or Novartis.
FROM EHA 2021
New! Spotlight on medical power couples: Their extraordinary lives
When people started dying from lethal anthrax spores sent through the mail in 2001, infectious disease expert Jeannette Guarner, MD, was called to Florida and Connecticut to analyze the bodies. She and her pathology team investigated how the bacteria had entered the victims and examined tissue samples from across the country to discern the scale of the attacks.

After conducting autopsies and identifying that inhalation anthrax had caused the deaths, Dr. Guarner rushed home to Atlanta just in time for Thanksgiving. Exhausted, the beloved family chef still managed to cook the big turkey that holiday, but she enlisted help with dessert.
“She returned home on Thanksgiving at like three in the morning,” recalls Carlos del Rio, MD. “She said to me, ‘In order for us to have Thanksgiving, you have to be in charge of the pies.’ When I told my daughter, she said, ‘This is going to be a disaster! If mom’s not cooking, this is not going to be good.’”
“It didn’t turn out that bad,” Dr. Guarner laughs. “There was dessert.”
As two of the top infectious disease experts in the country, Dr. Guarner and Dr. del Rio are no strangers to juggling their personal lives around disease outbreaks, last-minute travel, and pressing research.
Former director of the clinical laboratory at Mexico’s National Cancer Institute, Dr. Guarner worked for the Centers for Disease Control and Prevention for 10 years, where she played an integral part in the discovery of SARS. She and her team identified that a coronavirus was in cultures taken from a health care worker who died after working in Asia and determined through molecular testing that the virus was different from any other coronaviruses at the time.
Dr. Guarner went on to search for the novel virus in tissue samples and determine that it was SARS that had caused the damage. She is now a professor in the department of pathology and laboratory medicine at Emory University, Atlanta, medical director of the clinical laboratory at Emory University Hospital Midtown, and vice chair for faculty affairs.
Dr. Del Rio, who served as director of the National AIDS Council of Mexico, is a distinguished professor of medicine in Emory University’s division of infectious diseases and a professor of global health and epidemiology in the Rollins School of Public Health at Emory University. He is also co-director of the Emory Center for AIDS Research and co-principal investigator of the Emory-CDC HIV Clinical Trials Unit and the Emory Vaccine and Treatment Evaluation Unit.
Dr. Del Rio’s work in HIV prevention and care has made great strides, including developing the concept for the HIV Care Continuum, a public health model that outlines the stages that HIV patients go through, from diagnosis to achieving viral suppression. Dr. Del Rio, who is foreign secretary of the National Academy of Medicine, has also worked on emerging infections such as pandemic influenza and was a member of the WHO Influenza A (H1N1) Clinical Advisory Group and of the CDC Influenza A Task Force during the 2009 pandemic.
Dr. Del Rio and Dr. Guarner met during medical school in Mexico City. At first, the two carpooled to classes, but when Dr. Guarner fell ill with hepatitis A, Dr. del Rio brought Dr. Guarner the class notes so she wouldn’t fall behind. The study buddies later became a couple and married just before coming to the United States for residency.
With their expertise in infectious disease, Dr. del Rio and Dr. Guarner have worked collaboratively in the past, but the couple says they’ve always maintained separate professional identities.
“We try to create our own spaces,” Dr. del Rio said. “You try to keep your personal and professional identity independent as much as possible. You don’t want people to say, ‘Oh, you got this or you’re doing this because you are married to this other person.’ You want, to a certain degree, intellectual independence.”
This has been easier in some ways because Dr. del Rio and Dr. Guarner have different last names. Over the years they have frequently encountered people who had no idea that they are married.
“One time, we were both down in the lab and Jeanette was discussing a case, and she started teasing me or poking me, making fun,” recalls Dr. del Rio. “Some of the ID fellows were like, ‘Oh my God, who the hell is this woman?’ They didn’t realize she was my wife.”
Since the COVID-19 outbreak, both Dr. Guarner and Dr. del Rio have been involved in different ways with the pandemic. Dr. Del Rio has seen patients, conducted clinical trials, and given hundreds of local and national interviews about the virus. As a laboratory director, Dr. Guarner has validated tests for the diagnosis of COVID-19 and counseled staff on exposure concerns.
“An important aspect has also been to make sure that our laboratory technologists understand the disease and the need for the different protection elements we have had to use in the hospital,” she said. “In many ways I have had to scale down fears the techs have had when handling specimens from these patients.”
In their own words
What was one of your most surprising discoveries?
Jeannette: During the anthrax attacks, we received lots of tissues on live patients, particularly skin biopsies from different parts of the country where pathologists had concerns that there was anthrax. From New York, we received more than 50 skin biopsies and discovered that the necrotic lesions suspected of anthrax had Rickettsia in them. In other words, we discovered that rickettsialpox – a mite-borne infectious disease – was circulating in the city, which was unknown at the time.
Describe a challenge that you overcame:
Carlos: When I was appointed as director of the National AIDS Council of Mexico (CONASIDA), I was quite young, only 32 years old. I had to learn to listen to others who had expertise and institutional memory, to respect their opinions, and at the same time to push for change. A huge challenge was the role of the Catholic Church and conservative groups that were adamantly against condom promotion. Thus, I learned how to advance policies based in science without being confrontational.
Have you ever been famous for anything other than your work?
Jeannette: In 2017, a tree fell on our house during Hurricane Irma. It fell right on my husband’s office a few minutes after he left the room. Fortunately, I have always been small and flexible, and I crawled through the rubble to save our valuables before they were ruined by the rain. Later, a local Atlanta TV news crew was in the neighborhood reporting on the damage, and I told them to come to our house if they wanted to see real damage. That night, we were on the local news.
Power couple Paul and Mary Klotman
When Mary Klotman, MD, was offered an opportunity with the National Institutes of Health in 1991, Paul Klotman, MD, didn’t hesitate to resign his post at Duke University, Durham, N.C., and join his wife in Washington. Paul says he wanted to support Mary’s aspirations, even though it meant an uncertain track for his own career.

Fortunately for the Klotmans, the move proved instrumental for both of their careers and spurred one of their proudest scientific breakthroughs.
At NIH, Mary was a member of the Public Health Service and worked in the laboratory of tumor cell biology, and Paul became chief of the institute’s molecular medicine section in the laboratory of developmental biology. Together, their work led to the first animal model of HIV-associated nephropathy using transgenic techniques. The Klotmans and their team demonstrated that HIV resides in and evolves separately in kidney cells, a critical step in HIV-associated kidney disease.
“That’s where our longstanding collaboration around HIV-associated nephropathy started,” Mary says. “Paul and I have a passion for research, and we’ve had the same grant together for 25 years.”
After their successful stint at NIH, the Klotmans next climbed the ranks at the Icahn School of Medicine at Mount Sinai, where Paul started as chief of the nephrology division and became chair of medicine, and Mary became chief of infectious diseases and co-director of Mount Sinai’s Global Health and Emerging Pathogens Institute.
Today, Mary and Paul are the first – and only – married couple in the United States to lead separate medical schools. Mary is dean and vice chancellor for health affairs at Duke, and Paul is president and executive dean of Baylor College of Medicine, Houston.
Despite their 1,100-mile separation, the Klotmans manage their relationship in an unconventional way that some might balk at: Every Friday, one spouse hops on a plane and travels to the other for a date night and weekend.
“When we started this crazy lifestyle, we committed to being together every weekend,” says Mary. “And in 10 years – before COVID – we missed only one weekend together.”
The Klotmans say the scheduled time together places a hard end to each work week and enables them to truly enjoy their quality time.
“Friday at noon, I’m on the plane going to Durham, and I know that in 2 hours I’m going to have a date with my wife,” Paul said. “There are institutions that we’ve run into that think you have to be 7 days a week on site. But Duke and Baylor have been very supportive [of our situation].”
No doubt, the arrangement means a lot of time in the air for the couple. Paul says he travels about 150,000 miles every year by plane.
Having dual leadership positions in academic medicine has kept the Klotmans tightly connected, and the couple says their strong partnership has contributed to their success.
“It’s really been helpful having a deep understanding of our career paths, because we’ve been able to understand when one of us needed to be really focused on work and the other one would step back a bit with the kids and vice versa,” Mary said.
“There’s no question that we wouldn’t be in the positions we are in now if it weren’t for the fact that we’ve had each other,” Paul said.
In their own words
What is a little-known title that you have?
Paul: Purse-carrier for my wife. When she is honored at a national meeting or event, she often stands up and hands me her purse. I now make sure I have on an appropriate outfit that matches the purse.
Tell us about your children.
Mary: We had a very traumatic first pregnancy that we lost. Six years later, we adopted our first child, which was an amazing blessing. Our second son was Duke’s first successful frozen embryo transfer.
Describe a memorable moment in your relationship.
Paul: As we were leaving for our honeymoon, Mary’s dad handed me this booklet. It was the receipts for Mary’s medical school loans for the next 10 years. He said, “Congratulations, she’s all yours!”
A version of this article first appeared on Medscape.com.
When people started dying from lethal anthrax spores sent through the mail in 2001, infectious disease expert Jeannette Guarner, MD, was called to Florida and Connecticut to analyze the bodies. She and her pathology team investigated how the bacteria had entered the victims and examined tissue samples from across the country to discern the scale of the attacks.

After conducting autopsies and identifying that inhalation anthrax had caused the deaths, Dr. Guarner rushed home to Atlanta just in time for Thanksgiving. Exhausted, the beloved family chef still managed to cook the big turkey that holiday, but she enlisted help with dessert.
“She returned home on Thanksgiving at like three in the morning,” recalls Carlos del Rio, MD. “She said to me, ‘In order for us to have Thanksgiving, you have to be in charge of the pies.’ When I told my daughter, she said, ‘This is going to be a disaster! If mom’s not cooking, this is not going to be good.’”
“It didn’t turn out that bad,” Dr. Guarner laughs. “There was dessert.”
As two of the top infectious disease experts in the country, Dr. Guarner and Dr. del Rio are no strangers to juggling their personal lives around disease outbreaks, last-minute travel, and pressing research.
Former director of the clinical laboratory at Mexico’s National Cancer Institute, Dr. Guarner worked for the Centers for Disease Control and Prevention for 10 years, where she played an integral part in the discovery of SARS. She and her team identified that a coronavirus was in cultures taken from a health care worker who died after working in Asia and determined through molecular testing that the virus was different from any other coronaviruses at the time.
Dr. Guarner went on to search for the novel virus in tissue samples and determine that it was SARS that had caused the damage. She is now a professor in the department of pathology and laboratory medicine at Emory University, Atlanta, medical director of the clinical laboratory at Emory University Hospital Midtown, and vice chair for faculty affairs.
Dr. Del Rio, who served as director of the National AIDS Council of Mexico, is a distinguished professor of medicine in Emory University’s division of infectious diseases and a professor of global health and epidemiology in the Rollins School of Public Health at Emory University. He is also co-director of the Emory Center for AIDS Research and co-principal investigator of the Emory-CDC HIV Clinical Trials Unit and the Emory Vaccine and Treatment Evaluation Unit.
Dr. Del Rio’s work in HIV prevention and care has made great strides, including developing the concept for the HIV Care Continuum, a public health model that outlines the stages that HIV patients go through, from diagnosis to achieving viral suppression. Dr. Del Rio, who is foreign secretary of the National Academy of Medicine, has also worked on emerging infections such as pandemic influenza and was a member of the WHO Influenza A (H1N1) Clinical Advisory Group and of the CDC Influenza A Task Force during the 2009 pandemic.
Dr. Del Rio and Dr. Guarner met during medical school in Mexico City. At first, the two carpooled to classes, but when Dr. Guarner fell ill with hepatitis A, Dr. del Rio brought Dr. Guarner the class notes so she wouldn’t fall behind. The study buddies later became a couple and married just before coming to the United States for residency.
With their expertise in infectious disease, Dr. del Rio and Dr. Guarner have worked collaboratively in the past, but the couple says they’ve always maintained separate professional identities.
“We try to create our own spaces,” Dr. del Rio said. “You try to keep your personal and professional identity independent as much as possible. You don’t want people to say, ‘Oh, you got this or you’re doing this because you are married to this other person.’ You want, to a certain degree, intellectual independence.”
This has been easier in some ways because Dr. del Rio and Dr. Guarner have different last names. Over the years they have frequently encountered people who had no idea that they are married.
“One time, we were both down in the lab and Jeanette was discussing a case, and she started teasing me or poking me, making fun,” recalls Dr. del Rio. “Some of the ID fellows were like, ‘Oh my God, who the hell is this woman?’ They didn’t realize she was my wife.”
Since the COVID-19 outbreak, both Dr. Guarner and Dr. del Rio have been involved in different ways with the pandemic. Dr. Del Rio has seen patients, conducted clinical trials, and given hundreds of local and national interviews about the virus. As a laboratory director, Dr. Guarner has validated tests for the diagnosis of COVID-19 and counseled staff on exposure concerns.
“An important aspect has also been to make sure that our laboratory technologists understand the disease and the need for the different protection elements we have had to use in the hospital,” she said. “In many ways I have had to scale down fears the techs have had when handling specimens from these patients.”
In their own words
What was one of your most surprising discoveries?
Jeannette: During the anthrax attacks, we received lots of tissues on live patients, particularly skin biopsies from different parts of the country where pathologists had concerns that there was anthrax. From New York, we received more than 50 skin biopsies and discovered that the necrotic lesions suspected of anthrax had Rickettsia in them. In other words, we discovered that rickettsialpox – a mite-borne infectious disease – was circulating in the city, which was unknown at the time.
Describe a challenge that you overcame:
Carlos: When I was appointed as director of the National AIDS Council of Mexico (CONASIDA), I was quite young, only 32 years old. I had to learn to listen to others who had expertise and institutional memory, to respect their opinions, and at the same time to push for change. A huge challenge was the role of the Catholic Church and conservative groups that were adamantly against condom promotion. Thus, I learned how to advance policies based in science without being confrontational.
Have you ever been famous for anything other than your work?
Jeannette: In 2017, a tree fell on our house during Hurricane Irma. It fell right on my husband’s office a few minutes after he left the room. Fortunately, I have always been small and flexible, and I crawled through the rubble to save our valuables before they were ruined by the rain. Later, a local Atlanta TV news crew was in the neighborhood reporting on the damage, and I told them to come to our house if they wanted to see real damage. That night, we were on the local news.
Power couple Paul and Mary Klotman
When Mary Klotman, MD, was offered an opportunity with the National Institutes of Health in 1991, Paul Klotman, MD, didn’t hesitate to resign his post at Duke University, Durham, N.C., and join his wife in Washington. Paul says he wanted to support Mary’s aspirations, even though it meant an uncertain track for his own career.

Fortunately for the Klotmans, the move proved instrumental for both of their careers and spurred one of their proudest scientific breakthroughs.
At NIH, Mary was a member of the Public Health Service and worked in the laboratory of tumor cell biology, and Paul became chief of the institute’s molecular medicine section in the laboratory of developmental biology. Together, their work led to the first animal model of HIV-associated nephropathy using transgenic techniques. The Klotmans and their team demonstrated that HIV resides in and evolves separately in kidney cells, a critical step in HIV-associated kidney disease.
“That’s where our longstanding collaboration around HIV-associated nephropathy started,” Mary says. “Paul and I have a passion for research, and we’ve had the same grant together for 25 years.”
After their successful stint at NIH, the Klotmans next climbed the ranks at the Icahn School of Medicine at Mount Sinai, where Paul started as chief of the nephrology division and became chair of medicine, and Mary became chief of infectious diseases and co-director of Mount Sinai’s Global Health and Emerging Pathogens Institute.
Today, Mary and Paul are the first – and only – married couple in the United States to lead separate medical schools. Mary is dean and vice chancellor for health affairs at Duke, and Paul is president and executive dean of Baylor College of Medicine, Houston.
Despite their 1,100-mile separation, the Klotmans manage their relationship in an unconventional way that some might balk at: Every Friday, one spouse hops on a plane and travels to the other for a date night and weekend.
“When we started this crazy lifestyle, we committed to being together every weekend,” says Mary. “And in 10 years – before COVID – we missed only one weekend together.”
The Klotmans say the scheduled time together places a hard end to each work week and enables them to truly enjoy their quality time.
“Friday at noon, I’m on the plane going to Durham, and I know that in 2 hours I’m going to have a date with my wife,” Paul said. “There are institutions that we’ve run into that think you have to be 7 days a week on site. But Duke and Baylor have been very supportive [of our situation].”
No doubt, the arrangement means a lot of time in the air for the couple. Paul says he travels about 150,000 miles every year by plane.
Having dual leadership positions in academic medicine has kept the Klotmans tightly connected, and the couple says their strong partnership has contributed to their success.
“It’s really been helpful having a deep understanding of our career paths, because we’ve been able to understand when one of us needed to be really focused on work and the other one would step back a bit with the kids and vice versa,” Mary said.
“There’s no question that we wouldn’t be in the positions we are in now if it weren’t for the fact that we’ve had each other,” Paul said.
In their own words
What is a little-known title that you have?
Paul: Purse-carrier for my wife. When she is honored at a national meeting or event, she often stands up and hands me her purse. I now make sure I have on an appropriate outfit that matches the purse.
Tell us about your children.
Mary: We had a very traumatic first pregnancy that we lost. Six years later, we adopted our first child, which was an amazing blessing. Our second son was Duke’s first successful frozen embryo transfer.
Describe a memorable moment in your relationship.
Paul: As we were leaving for our honeymoon, Mary’s dad handed me this booklet. It was the receipts for Mary’s medical school loans for the next 10 years. He said, “Congratulations, she’s all yours!”
A version of this article first appeared on Medscape.com.
When people started dying from lethal anthrax spores sent through the mail in 2001, infectious disease expert Jeannette Guarner, MD, was called to Florida and Connecticut to analyze the bodies. She and her pathology team investigated how the bacteria had entered the victims and examined tissue samples from across the country to discern the scale of the attacks.

After conducting autopsies and identifying that inhalation anthrax had caused the deaths, Dr. Guarner rushed home to Atlanta just in time for Thanksgiving. Exhausted, the beloved family chef still managed to cook the big turkey that holiday, but she enlisted help with dessert.
“She returned home on Thanksgiving at like three in the morning,” recalls Carlos del Rio, MD. “She said to me, ‘In order for us to have Thanksgiving, you have to be in charge of the pies.’ When I told my daughter, she said, ‘This is going to be a disaster! If mom’s not cooking, this is not going to be good.’”
“It didn’t turn out that bad,” Dr. Guarner laughs. “There was dessert.”
As two of the top infectious disease experts in the country, Dr. Guarner and Dr. del Rio are no strangers to juggling their personal lives around disease outbreaks, last-minute travel, and pressing research.
Former director of the clinical laboratory at Mexico’s National Cancer Institute, Dr. Guarner worked for the Centers for Disease Control and Prevention for 10 years, where she played an integral part in the discovery of SARS. She and her team identified that a coronavirus was in cultures taken from a health care worker who died after working in Asia and determined through molecular testing that the virus was different from any other coronaviruses at the time.
Dr. Guarner went on to search for the novel virus in tissue samples and determine that it was SARS that had caused the damage. She is now a professor in the department of pathology and laboratory medicine at Emory University, Atlanta, medical director of the clinical laboratory at Emory University Hospital Midtown, and vice chair for faculty affairs.
Dr. Del Rio, who served as director of the National AIDS Council of Mexico, is a distinguished professor of medicine in Emory University’s division of infectious diseases and a professor of global health and epidemiology in the Rollins School of Public Health at Emory University. He is also co-director of the Emory Center for AIDS Research and co-principal investigator of the Emory-CDC HIV Clinical Trials Unit and the Emory Vaccine and Treatment Evaluation Unit.
Dr. Del Rio’s work in HIV prevention and care has made great strides, including developing the concept for the HIV Care Continuum, a public health model that outlines the stages that HIV patients go through, from diagnosis to achieving viral suppression. Dr. Del Rio, who is foreign secretary of the National Academy of Medicine, has also worked on emerging infections such as pandemic influenza and was a member of the WHO Influenza A (H1N1) Clinical Advisory Group and of the CDC Influenza A Task Force during the 2009 pandemic.
Dr. Del Rio and Dr. Guarner met during medical school in Mexico City. At first, the two carpooled to classes, but when Dr. Guarner fell ill with hepatitis A, Dr. del Rio brought Dr. Guarner the class notes so she wouldn’t fall behind. The study buddies later became a couple and married just before coming to the United States for residency.
With their expertise in infectious disease, Dr. del Rio and Dr. Guarner have worked collaboratively in the past, but the couple says they’ve always maintained separate professional identities.
“We try to create our own spaces,” Dr. del Rio said. “You try to keep your personal and professional identity independent as much as possible. You don’t want people to say, ‘Oh, you got this or you’re doing this because you are married to this other person.’ You want, to a certain degree, intellectual independence.”
This has been easier in some ways because Dr. del Rio and Dr. Guarner have different last names. Over the years they have frequently encountered people who had no idea that they are married.
“One time, we were both down in the lab and Jeanette was discussing a case, and she started teasing me or poking me, making fun,” recalls Dr. del Rio. “Some of the ID fellows were like, ‘Oh my God, who the hell is this woman?’ They didn’t realize she was my wife.”
Since the COVID-19 outbreak, both Dr. Guarner and Dr. del Rio have been involved in different ways with the pandemic. Dr. Del Rio has seen patients, conducted clinical trials, and given hundreds of local and national interviews about the virus. As a laboratory director, Dr. Guarner has validated tests for the diagnosis of COVID-19 and counseled staff on exposure concerns.
“An important aspect has also been to make sure that our laboratory technologists understand the disease and the need for the different protection elements we have had to use in the hospital,” she said. “In many ways I have had to scale down fears the techs have had when handling specimens from these patients.”
In their own words
What was one of your most surprising discoveries?
Jeannette: During the anthrax attacks, we received lots of tissues on live patients, particularly skin biopsies from different parts of the country where pathologists had concerns that there was anthrax. From New York, we received more than 50 skin biopsies and discovered that the necrotic lesions suspected of anthrax had Rickettsia in them. In other words, we discovered that rickettsialpox – a mite-borne infectious disease – was circulating in the city, which was unknown at the time.
Describe a challenge that you overcame:
Carlos: When I was appointed as director of the National AIDS Council of Mexico (CONASIDA), I was quite young, only 32 years old. I had to learn to listen to others who had expertise and institutional memory, to respect their opinions, and at the same time to push for change. A huge challenge was the role of the Catholic Church and conservative groups that were adamantly against condom promotion. Thus, I learned how to advance policies based in science without being confrontational.
Have you ever been famous for anything other than your work?
Jeannette: In 2017, a tree fell on our house during Hurricane Irma. It fell right on my husband’s office a few minutes after he left the room. Fortunately, I have always been small and flexible, and I crawled through the rubble to save our valuables before they were ruined by the rain. Later, a local Atlanta TV news crew was in the neighborhood reporting on the damage, and I told them to come to our house if they wanted to see real damage. That night, we were on the local news.
Power couple Paul and Mary Klotman
When Mary Klotman, MD, was offered an opportunity with the National Institutes of Health in 1991, Paul Klotman, MD, didn’t hesitate to resign his post at Duke University, Durham, N.C., and join his wife in Washington. Paul says he wanted to support Mary’s aspirations, even though it meant an uncertain track for his own career.

Fortunately for the Klotmans, the move proved instrumental for both of their careers and spurred one of their proudest scientific breakthroughs.
At NIH, Mary was a member of the Public Health Service and worked in the laboratory of tumor cell biology, and Paul became chief of the institute’s molecular medicine section in the laboratory of developmental biology. Together, their work led to the first animal model of HIV-associated nephropathy using transgenic techniques. The Klotmans and their team demonstrated that HIV resides in and evolves separately in kidney cells, a critical step in HIV-associated kidney disease.
“That’s where our longstanding collaboration around HIV-associated nephropathy started,” Mary says. “Paul and I have a passion for research, and we’ve had the same grant together for 25 years.”
After their successful stint at NIH, the Klotmans next climbed the ranks at the Icahn School of Medicine at Mount Sinai, where Paul started as chief of the nephrology division and became chair of medicine, and Mary became chief of infectious diseases and co-director of Mount Sinai’s Global Health and Emerging Pathogens Institute.
Today, Mary and Paul are the first – and only – married couple in the United States to lead separate medical schools. Mary is dean and vice chancellor for health affairs at Duke, and Paul is president and executive dean of Baylor College of Medicine, Houston.
Despite their 1,100-mile separation, the Klotmans manage their relationship in an unconventional way that some might balk at: Every Friday, one spouse hops on a plane and travels to the other for a date night and weekend.
“When we started this crazy lifestyle, we committed to being together every weekend,” says Mary. “And in 10 years – before COVID – we missed only one weekend together.”
The Klotmans say the scheduled time together places a hard end to each work week and enables them to truly enjoy their quality time.
“Friday at noon, I’m on the plane going to Durham, and I know that in 2 hours I’m going to have a date with my wife,” Paul said. “There are institutions that we’ve run into that think you have to be 7 days a week on site. But Duke and Baylor have been very supportive [of our situation].”
No doubt, the arrangement means a lot of time in the air for the couple. Paul says he travels about 150,000 miles every year by plane.
Having dual leadership positions in academic medicine has kept the Klotmans tightly connected, and the couple says their strong partnership has contributed to their success.
“It’s really been helpful having a deep understanding of our career paths, because we’ve been able to understand when one of us needed to be really focused on work and the other one would step back a bit with the kids and vice versa,” Mary said.
“There’s no question that we wouldn’t be in the positions we are in now if it weren’t for the fact that we’ve had each other,” Paul said.
In their own words
What is a little-known title that you have?
Paul: Purse-carrier for my wife. When she is honored at a national meeting or event, she often stands up and hands me her purse. I now make sure I have on an appropriate outfit that matches the purse.
Tell us about your children.
Mary: We had a very traumatic first pregnancy that we lost. Six years later, we adopted our first child, which was an amazing blessing. Our second son was Duke’s first successful frozen embryo transfer.
Describe a memorable moment in your relationship.
Paul: As we were leaving for our honeymoon, Mary’s dad handed me this booklet. It was the receipts for Mary’s medical school loans for the next 10 years. He said, “Congratulations, she’s all yours!”
A version of this article first appeared on Medscape.com.
Even a pandemic can’t stop teens’ alcohol and marijuana use
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
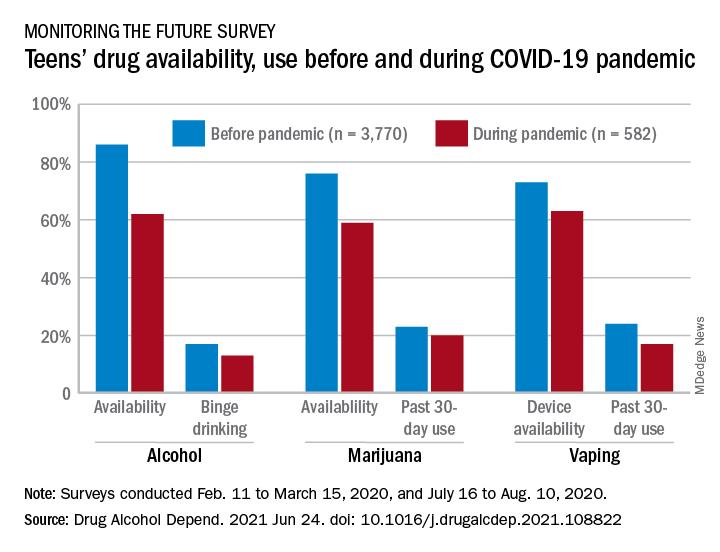
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
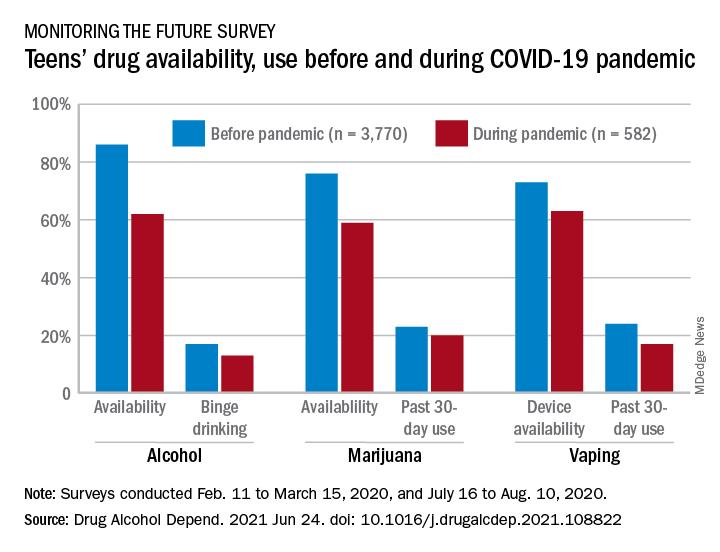
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
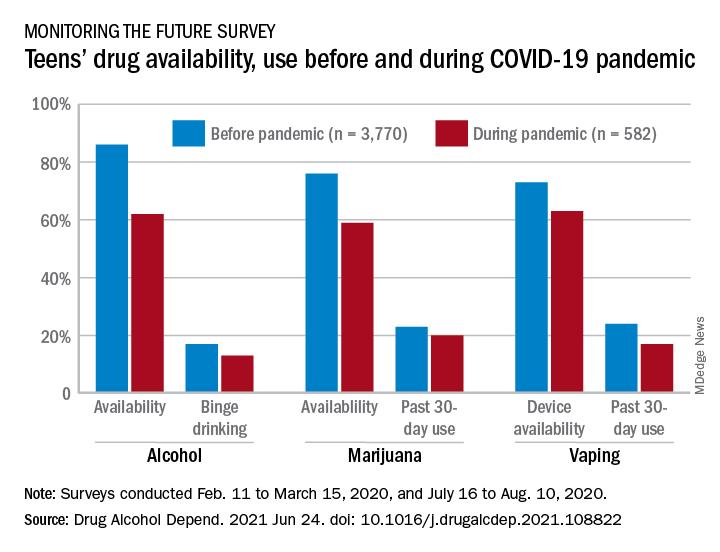
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
FROM DRUG AND ALCOHOL DEPENDENCE
Nocturnal hypoglycemia halved with insulin degludec vs. glargine
Patients with type 1 diabetes who used insulin degludec as their basal insulin had fewer than half the number of nocturnal hypoglycemia events, compared with patients who used insulin glargine U100, in a head-to-head crossover study with 51 patients who had a history of nighttime hypoglycemia episodes.
Patients with type 1 diabetes who are “struggling with nocturnal hypoglycemia would benefit from insulin degludec treatment,” said Julie M. Brøsen, MD, at the annual scientific sessions of the American Diabetes Association.
Accumulating evidence for less hypoglycemia with insulin degludec
Results from several studies comparing insulin degludec (Tresiba), a second-generation, longer-acting insulin with more stable steady-state performance, with the first-generation basal insulin analogue glargine (Lantus), have built the case that degludec produces fewer hypoglycemia events.
The landmark SWITCH 1 crossover study published in 2017 showed in about 500 patients with type 1 diabetes and a risk factor for hypoglycemia that treatment with insulin degludec led to significantly few total hypoglycemia episodes and significantly fewer nocturnal episodes, compared with insulin glargine.
Next came similar findings from ReFLeCT, a multicenter observational study that followed 556 unselected patients with type 1 diabetes in routine practice settings who switched to insulin degludec following treatment with a different basal insulin. The results again showed a significant drop-off in total, nonsevere, severe, and nocturnal hypoglycemia events.
Homing in on higher-risk patients
The current study, HypoDeg (Insulin Degludec and Symptomatic Nocturnal Hypoglycaemia), ran at 10 Danish centers and enrolled 149 adults with type 1 diabetes who had at least one episode of severe nocturnal hypoglycemia within the prior 2 years, focusing on patients most at risk for future nocturnal hypoglycemia events. In an unusual study design, researchers identified nocturnal hypoglycemic episodes with hourly venous blood samples drawn from a subcutaneous line.
They randomized the patients to basal insulin treatment with either insulin degludec or to insulin glargine U100, allowed their treatment to stabilize for 3 months, and then tallied nocturnal hypoglycemia events for 9 months. They then crossed patients to the alternative basal insulin and repeated the process.
Results from the full study have not yet appeared in published form but were in a pair of reports at the 2020 scientific sessions of the ADA.
One report included findings based on 136 episodes of severe hypoglycemia identified clinically and showed these events occurred 35% less often during treatment with insulin degludec, a significant difference. The overall finding was primarily driven by 48% fewer episodes of severe nocturnal hypoglycemia, but this difference was not significant.
The second report identified hypoglycemia events with continuous glucose monitoring in 74 of the study participants, which identified 193 episodes of nonsevere nocturnal hypoglycemia and found that treatment with insulin degludec cut the rate by 47%, primarily by reducing asymptomatic episodes.
Hourly blood draws track overnight hypoglycemia
The current study included 51 of the 149 HypoDeg patients who agreed to undergo overnight blood sampling and had this done at least once while treated with each of the two study insulins. (The study design called for two blood sampling nights for each willing patient during each of the two treatment periods.) The 51 patients had type 1 diabetes for an average of 28 years and an average age of 58 years. Two-thirds were men, their baseline A1c was 7.8%, and on average had 2.6 episodes of severe nocturnal hypoglycemia during the prior 2 years.
The researchers drew hourly blood specimens on a total of 196 nights from the 51 participating patients and identified 57 nights when blood glucose levels reached hypoglycemia thresholds in 33 patients. One-third of the events occurred when patients were on insulin degludec treatment, and two-thirds when they were on insulin glargine, reported Dr. Brøsen.
She presented three separate analyses of the data. One analysis focused on level 1 hypoglycemia events, when blood glucose dips to 70 mg/dL or less, which occurred 54% less often when patients were on insulin degludec. A second analysis looked at level 2 events, when blood glucose falls below 54 mg/dL, and treatment with insulin degludec cut this by 64% compared with insulin glargine. The third analysis focused on symptomatic events when blood glucose was 70 mg/dL or less, and treatment with insulin degludec linked with a 62% cut in this metric. All three between-group differences were significant.
Evidence supports already-changed practice
This new evidence “supports recommending” insulin degludec over insulin glargine, commented Bastiaan E. de Galan, MD, PhD, an endocrinologist and professor at Maastrict (the Netherlands) University Medical Center. The new results “extend those from previous trials in populations with type 1 diabetes that were unselected for the risk of hypoglycemia. In clinical practice, insulin degludec is already considered for patients who reported nocturnal hypoglycemia while on insulin glargine U100, but it’s great this study provides the scientific evidence,” said Dr. de Galan in an interview.
“The lower rate of nocturnal hypoglycemia with degludec, compared with glargine U100 is well established. Inpatient assessment of hypoglycemia with measurement of hourly plasma glucose allowed HypoDeg to provide stronger evidence than prior studies. The benefit of delgudec versus glargine U100 was significant and clinically meaningful, in hypo-prone patients who would benefit the most” by using insulin degludec, commented Gian Paolo Fadini, MD, an endocrinologist at the University of Padova (Italy), and a lead investigator on the ReFLeCT study.
But insulin degludec is not a completely silver bullet. Its prolonged duration of action and stability that may in part explain why it limits hypoglycemia events can also be a drawback: “It probably offers fewer options for flexibility. Any change in dose takes at least a day or 2 to settle, which may be unfavorable in certain circumstances,” noted Dr. de Galan.
“I wouldn’t recommend insulin degludec for all patients with type 1 diabetes. It’s an individual evaluation in each patient,” said Dr. Brøsen. “We will be looking into whether some patients are better off on insulin glargine.”
Cost makes a difference
Another, potentially more consequential flaw is insulin degludec’s relative expense.
“To date, use of degludec in routine practice has been limited by its cost, compared with older basal insulins,” observed Dr. Fadini in an interview. “In several countries, including the United States, degludec is substantially more expensive than glargine.”
The ADA’s Standards of Medical Care in Diabetes–2021 includes table 9.3 that lists the costs of various insulins and shows the median average wholesale price of insulin glargine U100 follow-on products as $190/vial, compared with a $407 price for a similar vial of insulin degludec.
Insulin degludec “is clearly superior from a hypoglycemia standpoint. Patients with type 1 diabetes like the reduction because hypoglycemia is scary, and dangerous. The main issue is cost, and the extent to which it may be covered by insurance,” commented Lisa Chow, MD, an endocrinologist at the University of Minnesota, Minneapolis. “We generally won’t prescribe degludec unless it is at a price affordable to the patient. We try to use patient assistance programs sponsored by the company [that markets insulin degludec: Novo Nordisk] to try to make it more affordable.”
Dr. Chow also highlighted that a new wrinkle has been introduction of a more concentrated formulation of insulin glargine, U300, which appears to cause less hypoglycemia than insulin glargine U100. Recent study results indicated that no significant difference exists in the incidence of hypoglycemia among patients treated with insulin glargine U300 and those treated with insulin degludec, such as findings from the BRIGHT trial, which included just over 900 patients, and in the CONCLUDE trial, which randomized more than 1,600 patients.
The HypoDeg study was sponsored by Novo Nordisk, the company that markets insulin degludec. Dr. Brøsen had no personal disclosures, but several of her coauthors were either Novo Nordisk employees or had financial relationships with the company. Dr. de Galan has received research funding from Novo Nordisk. Dr. Fadini has received lecture fees and research funding from Novo Nordisk, from Sanofi, the company that markets insulin glargine, and from several other companies. Dr. Chow has received research funding from Dexcom.
Patients with type 1 diabetes who used insulin degludec as their basal insulin had fewer than half the number of nocturnal hypoglycemia events, compared with patients who used insulin glargine U100, in a head-to-head crossover study with 51 patients who had a history of nighttime hypoglycemia episodes.
Patients with type 1 diabetes who are “struggling with nocturnal hypoglycemia would benefit from insulin degludec treatment,” said Julie M. Brøsen, MD, at the annual scientific sessions of the American Diabetes Association.
Accumulating evidence for less hypoglycemia with insulin degludec
Results from several studies comparing insulin degludec (Tresiba), a second-generation, longer-acting insulin with more stable steady-state performance, with the first-generation basal insulin analogue glargine (Lantus), have built the case that degludec produces fewer hypoglycemia events.
The landmark SWITCH 1 crossover study published in 2017 showed in about 500 patients with type 1 diabetes and a risk factor for hypoglycemia that treatment with insulin degludec led to significantly few total hypoglycemia episodes and significantly fewer nocturnal episodes, compared with insulin glargine.
Next came similar findings from ReFLeCT, a multicenter observational study that followed 556 unselected patients with type 1 diabetes in routine practice settings who switched to insulin degludec following treatment with a different basal insulin. The results again showed a significant drop-off in total, nonsevere, severe, and nocturnal hypoglycemia events.
Homing in on higher-risk patients
The current study, HypoDeg (Insulin Degludec and Symptomatic Nocturnal Hypoglycaemia), ran at 10 Danish centers and enrolled 149 adults with type 1 diabetes who had at least one episode of severe nocturnal hypoglycemia within the prior 2 years, focusing on patients most at risk for future nocturnal hypoglycemia events. In an unusual study design, researchers identified nocturnal hypoglycemic episodes with hourly venous blood samples drawn from a subcutaneous line.
They randomized the patients to basal insulin treatment with either insulin degludec or to insulin glargine U100, allowed their treatment to stabilize for 3 months, and then tallied nocturnal hypoglycemia events for 9 months. They then crossed patients to the alternative basal insulin and repeated the process.
Results from the full study have not yet appeared in published form but were in a pair of reports at the 2020 scientific sessions of the ADA.
One report included findings based on 136 episodes of severe hypoglycemia identified clinically and showed these events occurred 35% less often during treatment with insulin degludec, a significant difference. The overall finding was primarily driven by 48% fewer episodes of severe nocturnal hypoglycemia, but this difference was not significant.
The second report identified hypoglycemia events with continuous glucose monitoring in 74 of the study participants, which identified 193 episodes of nonsevere nocturnal hypoglycemia and found that treatment with insulin degludec cut the rate by 47%, primarily by reducing asymptomatic episodes.
Hourly blood draws track overnight hypoglycemia
The current study included 51 of the 149 HypoDeg patients who agreed to undergo overnight blood sampling and had this done at least once while treated with each of the two study insulins. (The study design called for two blood sampling nights for each willing patient during each of the two treatment periods.) The 51 patients had type 1 diabetes for an average of 28 years and an average age of 58 years. Two-thirds were men, their baseline A1c was 7.8%, and on average had 2.6 episodes of severe nocturnal hypoglycemia during the prior 2 years.
The researchers drew hourly blood specimens on a total of 196 nights from the 51 participating patients and identified 57 nights when blood glucose levels reached hypoglycemia thresholds in 33 patients. One-third of the events occurred when patients were on insulin degludec treatment, and two-thirds when they were on insulin glargine, reported Dr. Brøsen.
She presented three separate analyses of the data. One analysis focused on level 1 hypoglycemia events, when blood glucose dips to 70 mg/dL or less, which occurred 54% less often when patients were on insulin degludec. A second analysis looked at level 2 events, when blood glucose falls below 54 mg/dL, and treatment with insulin degludec cut this by 64% compared with insulin glargine. The third analysis focused on symptomatic events when blood glucose was 70 mg/dL or less, and treatment with insulin degludec linked with a 62% cut in this metric. All three between-group differences were significant.
Evidence supports already-changed practice
This new evidence “supports recommending” insulin degludec over insulin glargine, commented Bastiaan E. de Galan, MD, PhD, an endocrinologist and professor at Maastrict (the Netherlands) University Medical Center. The new results “extend those from previous trials in populations with type 1 diabetes that were unselected for the risk of hypoglycemia. In clinical practice, insulin degludec is already considered for patients who reported nocturnal hypoglycemia while on insulin glargine U100, but it’s great this study provides the scientific evidence,” said Dr. de Galan in an interview.
“The lower rate of nocturnal hypoglycemia with degludec, compared with glargine U100 is well established. Inpatient assessment of hypoglycemia with measurement of hourly plasma glucose allowed HypoDeg to provide stronger evidence than prior studies. The benefit of delgudec versus glargine U100 was significant and clinically meaningful, in hypo-prone patients who would benefit the most” by using insulin degludec, commented Gian Paolo Fadini, MD, an endocrinologist at the University of Padova (Italy), and a lead investigator on the ReFLeCT study.
But insulin degludec is not a completely silver bullet. Its prolonged duration of action and stability that may in part explain why it limits hypoglycemia events can also be a drawback: “It probably offers fewer options for flexibility. Any change in dose takes at least a day or 2 to settle, which may be unfavorable in certain circumstances,” noted Dr. de Galan.
“I wouldn’t recommend insulin degludec for all patients with type 1 diabetes. It’s an individual evaluation in each patient,” said Dr. Brøsen. “We will be looking into whether some patients are better off on insulin glargine.”
Cost makes a difference
Another, potentially more consequential flaw is insulin degludec’s relative expense.
“To date, use of degludec in routine practice has been limited by its cost, compared with older basal insulins,” observed Dr. Fadini in an interview. “In several countries, including the United States, degludec is substantially more expensive than glargine.”
The ADA’s Standards of Medical Care in Diabetes–2021 includes table 9.3 that lists the costs of various insulins and shows the median average wholesale price of insulin glargine U100 follow-on products as $190/vial, compared with a $407 price for a similar vial of insulin degludec.
Insulin degludec “is clearly superior from a hypoglycemia standpoint. Patients with type 1 diabetes like the reduction because hypoglycemia is scary, and dangerous. The main issue is cost, and the extent to which it may be covered by insurance,” commented Lisa Chow, MD, an endocrinologist at the University of Minnesota, Minneapolis. “We generally won’t prescribe degludec unless it is at a price affordable to the patient. We try to use patient assistance programs sponsored by the company [that markets insulin degludec: Novo Nordisk] to try to make it more affordable.”
Dr. Chow also highlighted that a new wrinkle has been introduction of a more concentrated formulation of insulin glargine, U300, which appears to cause less hypoglycemia than insulin glargine U100. Recent study results indicated that no significant difference exists in the incidence of hypoglycemia among patients treated with insulin glargine U300 and those treated with insulin degludec, such as findings from the BRIGHT trial, which included just over 900 patients, and in the CONCLUDE trial, which randomized more than 1,600 patients.
The HypoDeg study was sponsored by Novo Nordisk, the company that markets insulin degludec. Dr. Brøsen had no personal disclosures, but several of her coauthors were either Novo Nordisk employees or had financial relationships with the company. Dr. de Galan has received research funding from Novo Nordisk. Dr. Fadini has received lecture fees and research funding from Novo Nordisk, from Sanofi, the company that markets insulin glargine, and from several other companies. Dr. Chow has received research funding from Dexcom.
Patients with type 1 diabetes who used insulin degludec as their basal insulin had fewer than half the number of nocturnal hypoglycemia events, compared with patients who used insulin glargine U100, in a head-to-head crossover study with 51 patients who had a history of nighttime hypoglycemia episodes.
Patients with type 1 diabetes who are “struggling with nocturnal hypoglycemia would benefit from insulin degludec treatment,” said Julie M. Brøsen, MD, at the annual scientific sessions of the American Diabetes Association.
Accumulating evidence for less hypoglycemia with insulin degludec
Results from several studies comparing insulin degludec (Tresiba), a second-generation, longer-acting insulin with more stable steady-state performance, with the first-generation basal insulin analogue glargine (Lantus), have built the case that degludec produces fewer hypoglycemia events.
The landmark SWITCH 1 crossover study published in 2017 showed in about 500 patients with type 1 diabetes and a risk factor for hypoglycemia that treatment with insulin degludec led to significantly few total hypoglycemia episodes and significantly fewer nocturnal episodes, compared with insulin glargine.
Next came similar findings from ReFLeCT, a multicenter observational study that followed 556 unselected patients with type 1 diabetes in routine practice settings who switched to insulin degludec following treatment with a different basal insulin. The results again showed a significant drop-off in total, nonsevere, severe, and nocturnal hypoglycemia events.
Homing in on higher-risk patients
The current study, HypoDeg (Insulin Degludec and Symptomatic Nocturnal Hypoglycaemia), ran at 10 Danish centers and enrolled 149 adults with type 1 diabetes who had at least one episode of severe nocturnal hypoglycemia within the prior 2 years, focusing on patients most at risk for future nocturnal hypoglycemia events. In an unusual study design, researchers identified nocturnal hypoglycemic episodes with hourly venous blood samples drawn from a subcutaneous line.
They randomized the patients to basal insulin treatment with either insulin degludec or to insulin glargine U100, allowed their treatment to stabilize for 3 months, and then tallied nocturnal hypoglycemia events for 9 months. They then crossed patients to the alternative basal insulin and repeated the process.
Results from the full study have not yet appeared in published form but were in a pair of reports at the 2020 scientific sessions of the ADA.
One report included findings based on 136 episodes of severe hypoglycemia identified clinically and showed these events occurred 35% less often during treatment with insulin degludec, a significant difference. The overall finding was primarily driven by 48% fewer episodes of severe nocturnal hypoglycemia, but this difference was not significant.
The second report identified hypoglycemia events with continuous glucose monitoring in 74 of the study participants, which identified 193 episodes of nonsevere nocturnal hypoglycemia and found that treatment with insulin degludec cut the rate by 47%, primarily by reducing asymptomatic episodes.
Hourly blood draws track overnight hypoglycemia
The current study included 51 of the 149 HypoDeg patients who agreed to undergo overnight blood sampling and had this done at least once while treated with each of the two study insulins. (The study design called for two blood sampling nights for each willing patient during each of the two treatment periods.) The 51 patients had type 1 diabetes for an average of 28 years and an average age of 58 years. Two-thirds were men, their baseline A1c was 7.8%, and on average had 2.6 episodes of severe nocturnal hypoglycemia during the prior 2 years.
The researchers drew hourly blood specimens on a total of 196 nights from the 51 participating patients and identified 57 nights when blood glucose levels reached hypoglycemia thresholds in 33 patients. One-third of the events occurred when patients were on insulin degludec treatment, and two-thirds when they were on insulin glargine, reported Dr. Brøsen.
She presented three separate analyses of the data. One analysis focused on level 1 hypoglycemia events, when blood glucose dips to 70 mg/dL or less, which occurred 54% less often when patients were on insulin degludec. A second analysis looked at level 2 events, when blood glucose falls below 54 mg/dL, and treatment with insulin degludec cut this by 64% compared with insulin glargine. The third analysis focused on symptomatic events when blood glucose was 70 mg/dL or less, and treatment with insulin degludec linked with a 62% cut in this metric. All three between-group differences were significant.
Evidence supports already-changed practice
This new evidence “supports recommending” insulin degludec over insulin glargine, commented Bastiaan E. de Galan, MD, PhD, an endocrinologist and professor at Maastrict (the Netherlands) University Medical Center. The new results “extend those from previous trials in populations with type 1 diabetes that were unselected for the risk of hypoglycemia. In clinical practice, insulin degludec is already considered for patients who reported nocturnal hypoglycemia while on insulin glargine U100, but it’s great this study provides the scientific evidence,” said Dr. de Galan in an interview.
“The lower rate of nocturnal hypoglycemia with degludec, compared with glargine U100 is well established. Inpatient assessment of hypoglycemia with measurement of hourly plasma glucose allowed HypoDeg to provide stronger evidence than prior studies. The benefit of delgudec versus glargine U100 was significant and clinically meaningful, in hypo-prone patients who would benefit the most” by using insulin degludec, commented Gian Paolo Fadini, MD, an endocrinologist at the University of Padova (Italy), and a lead investigator on the ReFLeCT study.
But insulin degludec is not a completely silver bullet. Its prolonged duration of action and stability that may in part explain why it limits hypoglycemia events can also be a drawback: “It probably offers fewer options for flexibility. Any change in dose takes at least a day or 2 to settle, which may be unfavorable in certain circumstances,” noted Dr. de Galan.
“I wouldn’t recommend insulin degludec for all patients with type 1 diabetes. It’s an individual evaluation in each patient,” said Dr. Brøsen. “We will be looking into whether some patients are better off on insulin glargine.”
Cost makes a difference
Another, potentially more consequential flaw is insulin degludec’s relative expense.
“To date, use of degludec in routine practice has been limited by its cost, compared with older basal insulins,” observed Dr. Fadini in an interview. “In several countries, including the United States, degludec is substantially more expensive than glargine.”
The ADA’s Standards of Medical Care in Diabetes–2021 includes table 9.3 that lists the costs of various insulins and shows the median average wholesale price of insulin glargine U100 follow-on products as $190/vial, compared with a $407 price for a similar vial of insulin degludec.
Insulin degludec “is clearly superior from a hypoglycemia standpoint. Patients with type 1 diabetes like the reduction because hypoglycemia is scary, and dangerous. The main issue is cost, and the extent to which it may be covered by insurance,” commented Lisa Chow, MD, an endocrinologist at the University of Minnesota, Minneapolis. “We generally won’t prescribe degludec unless it is at a price affordable to the patient. We try to use patient assistance programs sponsored by the company [that markets insulin degludec: Novo Nordisk] to try to make it more affordable.”
Dr. Chow also highlighted that a new wrinkle has been introduction of a more concentrated formulation of insulin glargine, U300, which appears to cause less hypoglycemia than insulin glargine U100. Recent study results indicated that no significant difference exists in the incidence of hypoglycemia among patients treated with insulin glargine U300 and those treated with insulin degludec, such as findings from the BRIGHT trial, which included just over 900 patients, and in the CONCLUDE trial, which randomized more than 1,600 patients.
The HypoDeg study was sponsored by Novo Nordisk, the company that markets insulin degludec. Dr. Brøsen had no personal disclosures, but several of her coauthors were either Novo Nordisk employees or had financial relationships with the company. Dr. de Galan has received research funding from Novo Nordisk. Dr. Fadini has received lecture fees and research funding from Novo Nordisk, from Sanofi, the company that markets insulin glargine, and from several other companies. Dr. Chow has received research funding from Dexcom.
FROM ADA 2021
Calories may outweigh nutrients in diets for fatty liver
Intermittent calorie restriction offers only modest advantages over a low-carbohydrate, high-fat (LCHF) diet for treating nonalcoholic fatty liver disease (NAFLD), researchers say.
The intermittent diet offers more benefit for liver stiffness and LDL cholesterol, and might be easier to maintain, said Magnus Holmer, MD, head of the hepatology unit at the Karolinska Institute in Stockholm.
But the intermittent diet also has drawbacks and the differences between the two were slight, he said in an interview.
“They were more or less identically effective in reducing liver steatosis in NAFLD and also reducing body weight,” he said. “And from this, we can say that the composition of macronutrients such as fat or sugar seems to be less important than how many calories you eat.”
Dr. Holmer and colleagues presented their findings at the meeting sponsored by the European Association for the Study of the Liver and published them in JHEP Reports
While previous studies have shown that dieting can effectively treat NAFLD, researchers have debated whether popular LCHF diets might cause more harm than good.
At the same time, intermittent-calorie restriction diets have also been gaining in popularity, particularly the 5:2 diet in which participants eat normally for 5 days a week and restrict their calories the other 2 days.
How do the two diets compare?
To see if one was more effective than the other, the researchers recruited 74 people with NAFLD. They diagnosed the patients either by radiologic assessment or a combination of controlled attenuation parameter (CAP) greater than 280 dB/m and obesity, or a CAP greater than 280 dB/m, elevated ALT, and overweight. Sixteen of the patients were being treated with statins.
The researchers randomly assigned 25 people to an LCHF diet, 25 to a 5:2 diet, and 24 to standard care. The groups were similar in diet, age, body mass index, liver stiffness, and most other criteria at baseline, although there were more women in the standard-care group.
At the start of the study, the participants in the standard-care group consulted with a hepatologist who advised them to avoid sweets and saturated fats, eat three meals a day, and avoid large portions.
The researchers asked women in the 5:2 diet to eat up to 500 kcal/day each of 2 days per week and up to 2,000 kcal/day each of the other 5 days. They asked men in the group to eat up to 600 kcal/day each of 2 days per week and up to 2,400 kcal/day the other 5 days.
They provided all the 5:2 participants with recipes that followed the Nordic Nutrition Recommendations, an adaptation of the Mediterranean diet that emphasizes foods traditional in Nordic countries, particularly grains such as whole-grain rye, oats, and barley; fruits such as apples, pears, berries, and plums; root vegetables, cabbages, onions, peas, beans, fish, boiled potatoes, and dairy products; and the use of rapeseed (canola) oil. The calories provided in the recipes were composed of 45%-60% carbohydrates, 25% fat, and 10%-20% protein.
The researchers asked women in the LCHF diet to eat an average of 1,600 kcal/day and men to eat an average of 1,900 kcal/day. All the participants used recipes based on meat, fish, eggs, low-carbohydrate vegetables, and dairy fat. Participants avoided sugar, bread, pasta, rice, pies, potatoes, and fruit. The calories in the recipes were composed of 5%-10% carbohydrates, 50%-80% fat, and 15%-40% protein.
All the participants reported what they ate over the previous 3 days, both at the start of the study and after 12 weeks. Participants in the 5:2 and LCHF groups also received follow-up calls to report their past 24 hours of eating at 2, 4, 8, and 12 weeks, and also at week 6, when they visited a dietitian.
In addition, the researchers measured the participants’ linoleic acid and alpha-linolenic acid intake to verify that the participants’ diets were different among the groups.
After 12 weeks, all three groups lost a significant amount of liver fat, but the LCHF and 5:2 groups lost more than the standard care group. Liver stiffness decreased significantly in the 5:2 and standard care groups, but not in the LCHF group.
The differences in steatosis change between the standard care and LCHF groups was statistically significant (P = .001), as it was between the standard care and 5:2 groups (P = .029). The differences between the LCHF and 5:2 groups were not statistically significant for weight or steatosis, but they were statistically significant for liver stiffness.
In addition, the 5:2 group significantly reduced total and LDL cholesterol, while the standard care group did not. In the LCHF group, levels of LDL cholesterol, HDL cholesterol, and total cholesterol all increased.
The long-term implications of the cholesterol findings are unclear, Dr. Holmer said. He hopes to follow up on these patients after 18-24 months. But the initial cholesterol findings are perhaps enough to constitute a red flag for anyone with a history of cardiovascular disease.
Diet adherence
Only one person dropped out of the 5:2 group, compared with five in the LCHF group and four in the standard-care group. More people in the LCHF group reported adverse events, such as gastrointestinal upset.
“With LCHF, it’s a drastic change for most people,” Dr. Holmer said. “Many patients are a bit shocked when they realize how much fat they are supposed to eat for breakfast, for lunch, and for dinner. They might eat bacon and eggs for breakfast every day.” The diet could be challenging for people who want to reduce their consumption of meat for environmental reasons.
The 5:2 group offers the advantage that people can choose what they want to eat as long as they adhere to the calorie restrictions, he pointed out. Still, he cautioned that the diet would not work well for people with insulin-dependent diabetes because of the difficulty of adjusting insulin levels on fasting days. He also recommended against this diet for people with cirrhosis because they need to eat frequent meals.
LCHF and 5:2 diets can work
But for most people the good news is that a variety of diets will work to treat NAFLD, Dr. Holmer said.
“I begin with saying to my patients that this can be completely cured, as long as you’re able to lose weight,” he said. “Then the next question is, how are they going to go ahead with that task? And if they’re already interested in some sort of specific diet, then I can, based on these findings, encourage that.”
Stephen Harrison, MD, a visiting professor of hepatology at Radcliffe Department of Medicine, University of Oxford, England, said that longer-term results will be important. For example, it will be interesting to see if the diets had effects on ballooning or inflammation.
Another limitation of the study is that it is relatively small in size, he said. He pointed out that people with NAFLD should increase their physical activity as well as eating less.
Still, Dr. Harrison greeted the findings enthusiastically, saying: “This is an important study.”
It’s useful to compare two popular diets head to head, and it’s also encouraging to get confirmation that either one can work, he added.
The study was supported by grants from the Stockholm County Council, the Dietary Science Foundation (Kostfonden), the Skandia Research Foundation, and the Åke Wiberg Foundation. Dr. Holmer has disclosed no relevant financial relationships. Harrison is a consultant to Madrigal Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Intermittent calorie restriction offers only modest advantages over a low-carbohydrate, high-fat (LCHF) diet for treating nonalcoholic fatty liver disease (NAFLD), researchers say.
The intermittent diet offers more benefit for liver stiffness and LDL cholesterol, and might be easier to maintain, said Magnus Holmer, MD, head of the hepatology unit at the Karolinska Institute in Stockholm.
But the intermittent diet also has drawbacks and the differences between the two were slight, he said in an interview.
“They were more or less identically effective in reducing liver steatosis in NAFLD and also reducing body weight,” he said. “And from this, we can say that the composition of macronutrients such as fat or sugar seems to be less important than how many calories you eat.”
Dr. Holmer and colleagues presented their findings at the meeting sponsored by the European Association for the Study of the Liver and published them in JHEP Reports
While previous studies have shown that dieting can effectively treat NAFLD, researchers have debated whether popular LCHF diets might cause more harm than good.
At the same time, intermittent-calorie restriction diets have also been gaining in popularity, particularly the 5:2 diet in which participants eat normally for 5 days a week and restrict their calories the other 2 days.
How do the two diets compare?
To see if one was more effective than the other, the researchers recruited 74 people with NAFLD. They diagnosed the patients either by radiologic assessment or a combination of controlled attenuation parameter (CAP) greater than 280 dB/m and obesity, or a CAP greater than 280 dB/m, elevated ALT, and overweight. Sixteen of the patients were being treated with statins.
The researchers randomly assigned 25 people to an LCHF diet, 25 to a 5:2 diet, and 24 to standard care. The groups were similar in diet, age, body mass index, liver stiffness, and most other criteria at baseline, although there were more women in the standard-care group.
At the start of the study, the participants in the standard-care group consulted with a hepatologist who advised them to avoid sweets and saturated fats, eat three meals a day, and avoid large portions.
The researchers asked women in the 5:2 diet to eat up to 500 kcal/day each of 2 days per week and up to 2,000 kcal/day each of the other 5 days. They asked men in the group to eat up to 600 kcal/day each of 2 days per week and up to 2,400 kcal/day the other 5 days.
They provided all the 5:2 participants with recipes that followed the Nordic Nutrition Recommendations, an adaptation of the Mediterranean diet that emphasizes foods traditional in Nordic countries, particularly grains such as whole-grain rye, oats, and barley; fruits such as apples, pears, berries, and plums; root vegetables, cabbages, onions, peas, beans, fish, boiled potatoes, and dairy products; and the use of rapeseed (canola) oil. The calories provided in the recipes were composed of 45%-60% carbohydrates, 25% fat, and 10%-20% protein.
The researchers asked women in the LCHF diet to eat an average of 1,600 kcal/day and men to eat an average of 1,900 kcal/day. All the participants used recipes based on meat, fish, eggs, low-carbohydrate vegetables, and dairy fat. Participants avoided sugar, bread, pasta, rice, pies, potatoes, and fruit. The calories in the recipes were composed of 5%-10% carbohydrates, 50%-80% fat, and 15%-40% protein.
All the participants reported what they ate over the previous 3 days, both at the start of the study and after 12 weeks. Participants in the 5:2 and LCHF groups also received follow-up calls to report their past 24 hours of eating at 2, 4, 8, and 12 weeks, and also at week 6, when they visited a dietitian.
In addition, the researchers measured the participants’ linoleic acid and alpha-linolenic acid intake to verify that the participants’ diets were different among the groups.
After 12 weeks, all three groups lost a significant amount of liver fat, but the LCHF and 5:2 groups lost more than the standard care group. Liver stiffness decreased significantly in the 5:2 and standard care groups, but not in the LCHF group.
The differences in steatosis change between the standard care and LCHF groups was statistically significant (P = .001), as it was between the standard care and 5:2 groups (P = .029). The differences between the LCHF and 5:2 groups were not statistically significant for weight or steatosis, but they were statistically significant for liver stiffness.
In addition, the 5:2 group significantly reduced total and LDL cholesterol, while the standard care group did not. In the LCHF group, levels of LDL cholesterol, HDL cholesterol, and total cholesterol all increased.
The long-term implications of the cholesterol findings are unclear, Dr. Holmer said. He hopes to follow up on these patients after 18-24 months. But the initial cholesterol findings are perhaps enough to constitute a red flag for anyone with a history of cardiovascular disease.
Diet adherence
Only one person dropped out of the 5:2 group, compared with five in the LCHF group and four in the standard-care group. More people in the LCHF group reported adverse events, such as gastrointestinal upset.
“With LCHF, it’s a drastic change for most people,” Dr. Holmer said. “Many patients are a bit shocked when they realize how much fat they are supposed to eat for breakfast, for lunch, and for dinner. They might eat bacon and eggs for breakfast every day.” The diet could be challenging for people who want to reduce their consumption of meat for environmental reasons.
The 5:2 group offers the advantage that people can choose what they want to eat as long as they adhere to the calorie restrictions, he pointed out. Still, he cautioned that the diet would not work well for people with insulin-dependent diabetes because of the difficulty of adjusting insulin levels on fasting days. He also recommended against this diet for people with cirrhosis because they need to eat frequent meals.
LCHF and 5:2 diets can work
But for most people the good news is that a variety of diets will work to treat NAFLD, Dr. Holmer said.
“I begin with saying to my patients that this can be completely cured, as long as you’re able to lose weight,” he said. “Then the next question is, how are they going to go ahead with that task? And if they’re already interested in some sort of specific diet, then I can, based on these findings, encourage that.”
Stephen Harrison, MD, a visiting professor of hepatology at Radcliffe Department of Medicine, University of Oxford, England, said that longer-term results will be important. For example, it will be interesting to see if the diets had effects on ballooning or inflammation.
Another limitation of the study is that it is relatively small in size, he said. He pointed out that people with NAFLD should increase their physical activity as well as eating less.
Still, Dr. Harrison greeted the findings enthusiastically, saying: “This is an important study.”
It’s useful to compare two popular diets head to head, and it’s also encouraging to get confirmation that either one can work, he added.
The study was supported by grants from the Stockholm County Council, the Dietary Science Foundation (Kostfonden), the Skandia Research Foundation, and the Åke Wiberg Foundation. Dr. Holmer has disclosed no relevant financial relationships. Harrison is a consultant to Madrigal Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Intermittent calorie restriction offers only modest advantages over a low-carbohydrate, high-fat (LCHF) diet for treating nonalcoholic fatty liver disease (NAFLD), researchers say.
The intermittent diet offers more benefit for liver stiffness and LDL cholesterol, and might be easier to maintain, said Magnus Holmer, MD, head of the hepatology unit at the Karolinska Institute in Stockholm.
But the intermittent diet also has drawbacks and the differences between the two were slight, he said in an interview.
“They were more or less identically effective in reducing liver steatosis in NAFLD and also reducing body weight,” he said. “And from this, we can say that the composition of macronutrients such as fat or sugar seems to be less important than how many calories you eat.”
Dr. Holmer and colleagues presented their findings at the meeting sponsored by the European Association for the Study of the Liver and published them in JHEP Reports
While previous studies have shown that dieting can effectively treat NAFLD, researchers have debated whether popular LCHF diets might cause more harm than good.
At the same time, intermittent-calorie restriction diets have also been gaining in popularity, particularly the 5:2 diet in which participants eat normally for 5 days a week and restrict their calories the other 2 days.
How do the two diets compare?
To see if one was more effective than the other, the researchers recruited 74 people with NAFLD. They diagnosed the patients either by radiologic assessment or a combination of controlled attenuation parameter (CAP) greater than 280 dB/m and obesity, or a CAP greater than 280 dB/m, elevated ALT, and overweight. Sixteen of the patients were being treated with statins.
The researchers randomly assigned 25 people to an LCHF diet, 25 to a 5:2 diet, and 24 to standard care. The groups were similar in diet, age, body mass index, liver stiffness, and most other criteria at baseline, although there were more women in the standard-care group.
At the start of the study, the participants in the standard-care group consulted with a hepatologist who advised them to avoid sweets and saturated fats, eat three meals a day, and avoid large portions.
The researchers asked women in the 5:2 diet to eat up to 500 kcal/day each of 2 days per week and up to 2,000 kcal/day each of the other 5 days. They asked men in the group to eat up to 600 kcal/day each of 2 days per week and up to 2,400 kcal/day the other 5 days.
They provided all the 5:2 participants with recipes that followed the Nordic Nutrition Recommendations, an adaptation of the Mediterranean diet that emphasizes foods traditional in Nordic countries, particularly grains such as whole-grain rye, oats, and barley; fruits such as apples, pears, berries, and plums; root vegetables, cabbages, onions, peas, beans, fish, boiled potatoes, and dairy products; and the use of rapeseed (canola) oil. The calories provided in the recipes were composed of 45%-60% carbohydrates, 25% fat, and 10%-20% protein.
The researchers asked women in the LCHF diet to eat an average of 1,600 kcal/day and men to eat an average of 1,900 kcal/day. All the participants used recipes based on meat, fish, eggs, low-carbohydrate vegetables, and dairy fat. Participants avoided sugar, bread, pasta, rice, pies, potatoes, and fruit. The calories in the recipes were composed of 5%-10% carbohydrates, 50%-80% fat, and 15%-40% protein.
All the participants reported what they ate over the previous 3 days, both at the start of the study and after 12 weeks. Participants in the 5:2 and LCHF groups also received follow-up calls to report their past 24 hours of eating at 2, 4, 8, and 12 weeks, and also at week 6, when they visited a dietitian.
In addition, the researchers measured the participants’ linoleic acid and alpha-linolenic acid intake to verify that the participants’ diets were different among the groups.
After 12 weeks, all three groups lost a significant amount of liver fat, but the LCHF and 5:2 groups lost more than the standard care group. Liver stiffness decreased significantly in the 5:2 and standard care groups, but not in the LCHF group.
The differences in steatosis change between the standard care and LCHF groups was statistically significant (P = .001), as it was between the standard care and 5:2 groups (P = .029). The differences between the LCHF and 5:2 groups were not statistically significant for weight or steatosis, but they were statistically significant for liver stiffness.
In addition, the 5:2 group significantly reduced total and LDL cholesterol, while the standard care group did not. In the LCHF group, levels of LDL cholesterol, HDL cholesterol, and total cholesterol all increased.
The long-term implications of the cholesterol findings are unclear, Dr. Holmer said. He hopes to follow up on these patients after 18-24 months. But the initial cholesterol findings are perhaps enough to constitute a red flag for anyone with a history of cardiovascular disease.
Diet adherence
Only one person dropped out of the 5:2 group, compared with five in the LCHF group and four in the standard-care group. More people in the LCHF group reported adverse events, such as gastrointestinal upset.
“With LCHF, it’s a drastic change for most people,” Dr. Holmer said. “Many patients are a bit shocked when they realize how much fat they are supposed to eat for breakfast, for lunch, and for dinner. They might eat bacon and eggs for breakfast every day.” The diet could be challenging for people who want to reduce their consumption of meat for environmental reasons.
The 5:2 group offers the advantage that people can choose what they want to eat as long as they adhere to the calorie restrictions, he pointed out. Still, he cautioned that the diet would not work well for people with insulin-dependent diabetes because of the difficulty of adjusting insulin levels on fasting days. He also recommended against this diet for people with cirrhosis because they need to eat frequent meals.
LCHF and 5:2 diets can work
But for most people the good news is that a variety of diets will work to treat NAFLD, Dr. Holmer said.
“I begin with saying to my patients that this can be completely cured, as long as you’re able to lose weight,” he said. “Then the next question is, how are they going to go ahead with that task? And if they’re already interested in some sort of specific diet, then I can, based on these findings, encourage that.”
Stephen Harrison, MD, a visiting professor of hepatology at Radcliffe Department of Medicine, University of Oxford, England, said that longer-term results will be important. For example, it will be interesting to see if the diets had effects on ballooning or inflammation.
Another limitation of the study is that it is relatively small in size, he said. He pointed out that people with NAFLD should increase their physical activity as well as eating less.
Still, Dr. Harrison greeted the findings enthusiastically, saying: “This is an important study.”
It’s useful to compare two popular diets head to head, and it’s also encouraging to get confirmation that either one can work, he added.
The study was supported by grants from the Stockholm County Council, the Dietary Science Foundation (Kostfonden), the Skandia Research Foundation, and the Åke Wiberg Foundation. Dr. Holmer has disclosed no relevant financial relationships. Harrison is a consultant to Madrigal Pharmaceuticals.
A version of this article first appeared on Medscape.com.








