User login
AAP approves CDC’s child/adolescent vax schedule for 2022
In a policy statement published online Feb. 17 in Pediatrics, the AAP said the updated recommendations differ little from those released last year by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
“The only significant change this year was to add the dengue vaccine to the schedule,” Sean T. O’Leary, MD, MPH, vice chair of the AAP’s 2021-2022 Committee on Infectious Diseases and a coauthor of the statement, told this news organization. “But that is really only relevant for children living in endemic areas, primarily Puerto Rico but some other smaller U.S .territories as well.”
Dengue fever also is endemic in American Samoa and the U.S. Virgin Islands.
Notably, a new section has been added on routine recommendations for use of the Dengvaxia vaccine.
The 2022 policy statement addresses regular immunization of children from birth to 18 years and catch-up vaccination for those aged 4 months to 18 years. In addition to the AAP, multiple complementary physician and nurse organizations have approved the updates. The ACIP schedule is revised annually to reflect current recommendations on vaccines licensed by the U.S. Food and Drug Administration.
Most of the other changes this year involve minor updates to clarify language or improve usability. “CDC and AAP are always working to make the schedule as user-friendly as possible, with improvements made every year,” Dr. O’Leary, professor of pediatric infectious diseases at the University of Colorado at Denver, Aurora, said.
In terms of physician acceptance, he added, “I don’t think any of the changes would be considered controversial.”
Among other updates and clarifications:
- For Haemophilus influenzae type b (Hib) vaccination, the text now includes recommendations for the hexavalent Vaxelis vaccine (diphtheria, tetanus, pertussis, polio, Hib, and hepatitis B) for both routine and catch-up vaccination.
- For hepatitis A, the relevant note has been updated to clarify the age for routine vaccination.
- For human papillomavirus (HPV), the note now clarifies when an HPV series is complete with no additional dose recommended.
- The special situations section has been amended to specify which persons with immunocompromising conditions such as HIV should receive three doses of HPV vaccine regardless of age at initial vaccination.
- For measles, mumps, and rubella, routine vaccination now includes recommendations on the combination measles, mumps, rubella, and varicella vaccine.
- For meningococcal serogroup A, C, W, and Y vaccines, the augmented text explains when these can be simultaneously administered with serogroup B meningococcal vaccines, preferably at different anatomic sites. The language for the dosing schedule for Menveo vaccination in infants also has been clarified.
- In the catch-up immunization schedule for late-starting children aged 4 months to 18 years, the text on Hib has been changed so that the minimum interval between dose two and dose three now refers to Vaxelis, while reference to the discontinued Comvax (Hib-Hep B) vaccine has been removed.
As in other years, graphic changes have been made to table coloration and layout to improve accessibility. And as before, the 2022 childhood and adolescent immunization schedule has been updated to ensure consistency between its format and that of the 2022 adult immunization schedules.
The AAP committee stressed that clinically significant adverse events after immunization should be reported to the Vaccine Adverse Event Reporting System.
The full 2022 schedule can be found on the CDC’s website.
A version of this article first appeared on Medscape.com.
In a policy statement published online Feb. 17 in Pediatrics, the AAP said the updated recommendations differ little from those released last year by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
“The only significant change this year was to add the dengue vaccine to the schedule,” Sean T. O’Leary, MD, MPH, vice chair of the AAP’s 2021-2022 Committee on Infectious Diseases and a coauthor of the statement, told this news organization. “But that is really only relevant for children living in endemic areas, primarily Puerto Rico but some other smaller U.S .territories as well.”
Dengue fever also is endemic in American Samoa and the U.S. Virgin Islands.
Notably, a new section has been added on routine recommendations for use of the Dengvaxia vaccine.
The 2022 policy statement addresses regular immunization of children from birth to 18 years and catch-up vaccination for those aged 4 months to 18 years. In addition to the AAP, multiple complementary physician and nurse organizations have approved the updates. The ACIP schedule is revised annually to reflect current recommendations on vaccines licensed by the U.S. Food and Drug Administration.
Most of the other changes this year involve minor updates to clarify language or improve usability. “CDC and AAP are always working to make the schedule as user-friendly as possible, with improvements made every year,” Dr. O’Leary, professor of pediatric infectious diseases at the University of Colorado at Denver, Aurora, said.
In terms of physician acceptance, he added, “I don’t think any of the changes would be considered controversial.”
Among other updates and clarifications:
- For Haemophilus influenzae type b (Hib) vaccination, the text now includes recommendations for the hexavalent Vaxelis vaccine (diphtheria, tetanus, pertussis, polio, Hib, and hepatitis B) for both routine and catch-up vaccination.
- For hepatitis A, the relevant note has been updated to clarify the age for routine vaccination.
- For human papillomavirus (HPV), the note now clarifies when an HPV series is complete with no additional dose recommended.
- The special situations section has been amended to specify which persons with immunocompromising conditions such as HIV should receive three doses of HPV vaccine regardless of age at initial vaccination.
- For measles, mumps, and rubella, routine vaccination now includes recommendations on the combination measles, mumps, rubella, and varicella vaccine.
- For meningococcal serogroup A, C, W, and Y vaccines, the augmented text explains when these can be simultaneously administered with serogroup B meningococcal vaccines, preferably at different anatomic sites. The language for the dosing schedule for Menveo vaccination in infants also has been clarified.
- In the catch-up immunization schedule for late-starting children aged 4 months to 18 years, the text on Hib has been changed so that the minimum interval between dose two and dose three now refers to Vaxelis, while reference to the discontinued Comvax (Hib-Hep B) vaccine has been removed.
As in other years, graphic changes have been made to table coloration and layout to improve accessibility. And as before, the 2022 childhood and adolescent immunization schedule has been updated to ensure consistency between its format and that of the 2022 adult immunization schedules.
The AAP committee stressed that clinically significant adverse events after immunization should be reported to the Vaccine Adverse Event Reporting System.
The full 2022 schedule can be found on the CDC’s website.
A version of this article first appeared on Medscape.com.
In a policy statement published online Feb. 17 in Pediatrics, the AAP said the updated recommendations differ little from those released last year by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
“The only significant change this year was to add the dengue vaccine to the schedule,” Sean T. O’Leary, MD, MPH, vice chair of the AAP’s 2021-2022 Committee on Infectious Diseases and a coauthor of the statement, told this news organization. “But that is really only relevant for children living in endemic areas, primarily Puerto Rico but some other smaller U.S .territories as well.”
Dengue fever also is endemic in American Samoa and the U.S. Virgin Islands.
Notably, a new section has been added on routine recommendations for use of the Dengvaxia vaccine.
The 2022 policy statement addresses regular immunization of children from birth to 18 years and catch-up vaccination for those aged 4 months to 18 years. In addition to the AAP, multiple complementary physician and nurse organizations have approved the updates. The ACIP schedule is revised annually to reflect current recommendations on vaccines licensed by the U.S. Food and Drug Administration.
Most of the other changes this year involve minor updates to clarify language or improve usability. “CDC and AAP are always working to make the schedule as user-friendly as possible, with improvements made every year,” Dr. O’Leary, professor of pediatric infectious diseases at the University of Colorado at Denver, Aurora, said.
In terms of physician acceptance, he added, “I don’t think any of the changes would be considered controversial.”
Among other updates and clarifications:
- For Haemophilus influenzae type b (Hib) vaccination, the text now includes recommendations for the hexavalent Vaxelis vaccine (diphtheria, tetanus, pertussis, polio, Hib, and hepatitis B) for both routine and catch-up vaccination.
- For hepatitis A, the relevant note has been updated to clarify the age for routine vaccination.
- For human papillomavirus (HPV), the note now clarifies when an HPV series is complete with no additional dose recommended.
- The special situations section has been amended to specify which persons with immunocompromising conditions such as HIV should receive three doses of HPV vaccine regardless of age at initial vaccination.
- For measles, mumps, and rubella, routine vaccination now includes recommendations on the combination measles, mumps, rubella, and varicella vaccine.
- For meningococcal serogroup A, C, W, and Y vaccines, the augmented text explains when these can be simultaneously administered with serogroup B meningococcal vaccines, preferably at different anatomic sites. The language for the dosing schedule for Menveo vaccination in infants also has been clarified.
- In the catch-up immunization schedule for late-starting children aged 4 months to 18 years, the text on Hib has been changed so that the minimum interval between dose two and dose three now refers to Vaxelis, while reference to the discontinued Comvax (Hib-Hep B) vaccine has been removed.
As in other years, graphic changes have been made to table coloration and layout to improve accessibility. And as before, the 2022 childhood and adolescent immunization schedule has been updated to ensure consistency between its format and that of the 2022 adult immunization schedules.
The AAP committee stressed that clinically significant adverse events after immunization should be reported to the Vaccine Adverse Event Reporting System.
The full 2022 schedule can be found on the CDC’s website.
A version of this article first appeared on Medscape.com.
Slow-Growing Pink Nodule in an Active-Duty Service Member
The Diagnosis: Leishmaniasis
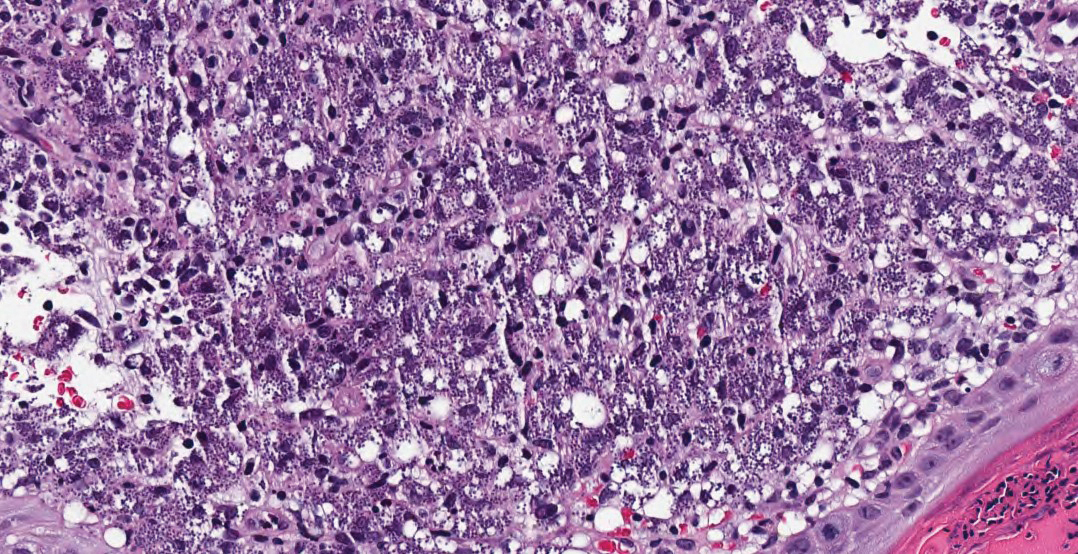
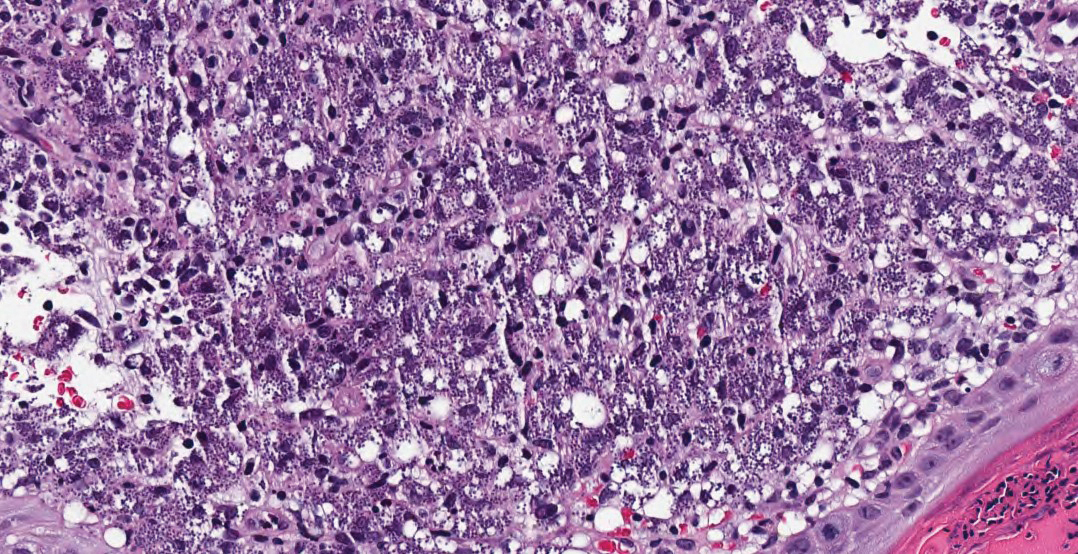
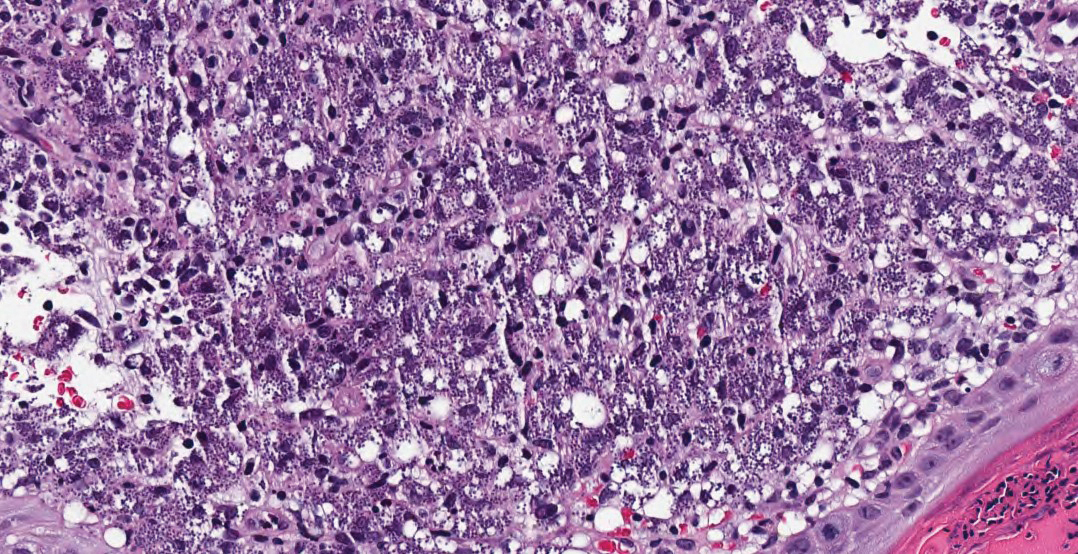
Hematoxylin and eosin staining of the tissue specimen revealed a dense histiocytic infiltrate with scattered lymphocytes and neutrophils. There were round to oval basophilic structures within the macrophages consistent with amastigotes. Giemsa staining was not necessary to visualize the organisms. The infiltrate abutted the overlying epidermis, which was acanthotic with pseudoepitheliomatous hyperplasia. There were collections of neutrophils, parakeratosis, and a serum crust overlying the epidermis (Figure). Clinical and histologic findings, as well as travel history, led to a diagnosis of cutaneous leishmaniasis (CL).
Leishmaniases is a group of diseases caused by a parasitic infection with flagellated protozoa of the genus Leishmania. There are more than 20 different Leishmania species that are pathogenic to humans, all presenting with cutaneous findings. The presentation depends on the inoculating species and the host cellular immune response and includes cutaneous, mucosal, and visceral involvement. The disease is transmitted via the bite of an infected bloodsucking female sand fly.1 There are approximately 30 different species of sand flies that are proven to be vectors of the disease, with up to 40 more suspected of involvement in transmission, predominantly from the genera Phlebotomus (Old World) and Lutzomyia (New World).1,2 There are an estimated 1 to 2 million new cases of cutaneous leishmaniasis diagnosed annually in 70 endemic countries of the tropics, subtropics, and southern Europe.1,3,4
The differential diagnosis included cutaneous tuberculosis, which can have a similar progression and clinical appearance. Cutaneous tuberculosis starts as firm, reddish-brown, painless papules that slowly enlarge and ulcerate.5 It may be further differentiated on histopathology by the presence of tuberculoid granulomas, caseating necrosis, and acid-fast bacilli, which are easily detected in early lesions but are less prevalent after the granuloma develops.6 Sporotrichosis presents as a nodule, which may or may not ulcerate, on the extremities. However, the classic morphology is a sporotrichoid pattern, which describes the initial lesion plus subcutaneous nodular spread along the lymphatics.7 On histology, sporotrichosis has a characteristic “sporotrichoid asteroid” comprised of the yeast form surrounded by eosinophilic hyaline material in raylike processes that are found in the center of suppurative granulomas or foci.8
Atypical mycobacteria, principally Mycobacterium marinum (swimming pool granuloma) and Mycobacterium ulcerans (Buruli ulcer), are capable of causing cutaneous infections. They may be differentiated histologically by a neutrophilic infiltrate of poorly formed granulomas without caseation and extensive coagulative necrosis with little cellular infiltrate, respectively.6 Histoplasma capsulatum also infects histiocytes and may appear similar in size and shape; however, histoplasmosis is surrounded by a pseudocapsule and evenly spaced.8
Conversely, the histology of leishmaniasis lacks a pseudocapsule. The amastigotes may form the classic marquee sign by lining the periphery of the macrophage or they can be randomly spaced. Classically, the epidermis shows hyperkeratosis and acanthosis. Sometimes atrophy, ulceration, or intraepidermal abscesses also can be observed. Pseudoepitheliomatous hyperplasia can be seen in some long-standing lesions.1,4 Many of these findings were observed on hematoxylin and eosin staining from a punch biopsy obtained from the center of the lesion in our patient. For further delineation, a speciation kit was obtained from Walter Reed National Military Medical Center (Bethesda, Maryland). A second punch biopsy was obtained from the lesion edge, sectioned into 4 individual pieces, and placed in Schneider tissue culture medium. It was sent for tissue culture, polymerase chain reaction, and histology. Polymerase chain reaction analysis was positive for Leishmania, which was further identified as Leishmania tropica by tissue culture.
Leishmania tropica (Old World CL) commonly causes CL and is endemic to Central Asia, the Middle East, parts of North Africa, and Southeast Asia. Old and New World CL start as a small erythematous papule after a bite from an infected female sand fly. The papule develops into a nodule over weeks to months. The lesion may ulcerate and typically heals leaving an atrophic scar in months to years.1 Speciation of CL is important to guide therapy.
Leishmania mexicana, a New World species that commonly causes CL, classically is found in Central and South America, but there also have been documented cases in Texas. A 2008 case series identified 9 cases in northern Texas in residents without a travel history to endemic locations.9 Similarly, a cross-sectional study identified 41 locally endemic cases of CL over a 10-year period (2007-2017) in Texas; 22 of these cases had speciation by polymerase chain reaction, and all cases were attributed to L mexicana.10
In the United States, CL classically has been associated with travelers and military personnel returning from the Middle East; however, a growing body of literature suggests that it may be endemic to Texas, where it is now a reportable disease. Physicians should have an increased awareness of this entity and a high index of suspicion when treating patients with nonhealing cutaneous lesions.
- Bravo F. Protozoa and worms. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1470-1502.
- Killick-Kendrick R. The biology and control of phlebotomine sandflies. Clin Dermatol. 1999;17:279-289.
- Reithinger R, Dujardin JC, Louzir H, et al. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-596.
- Patterson J. Protozoal infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:787-795.
- Ramos-e-Silva M, Ribeiro de Castro MC. Mycobacterial infections. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1296-1318.
- Patterson J. Bacterial and rickettsial infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:673-709.
- Elewski B, Hughey L, Hunt K, et al. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1329-1363.
- Patterson J. Mycoses and algal infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:721-755.
- Wright NA, Davis LE, Aftergut KS, et al. Cutaneous leishmaniasis in Texas: a northern spread of endemic areas [published online February 4, 2008]. J Am Acad Dermatol. 2008;58:650-652. doi:10.1016/j .jaad.2007.11.008.
- McIlwee BE, Weis SE, Hosler GA. Incidence of endemic human cutaneous leishmaniasis in the United States. JAMA Dermatol. 2018;154:1032-1039. doi:10.1001/jamadermatol.2018.2133
The Diagnosis: Leishmaniasis
Hematoxylin and eosin staining of the tissue specimen revealed a dense histiocytic infiltrate with scattered lymphocytes and neutrophils. There were round to oval basophilic structures within the macrophages consistent with amastigotes. Giemsa staining was not necessary to visualize the organisms. The infiltrate abutted the overlying epidermis, which was acanthotic with pseudoepitheliomatous hyperplasia. There were collections of neutrophils, parakeratosis, and a serum crust overlying the epidermis (Figure). Clinical and histologic findings, as well as travel history, led to a diagnosis of cutaneous leishmaniasis (CL).
Leishmaniases is a group of diseases caused by a parasitic infection with flagellated protozoa of the genus Leishmania. There are more than 20 different Leishmania species that are pathogenic to humans, all presenting with cutaneous findings. The presentation depends on the inoculating species and the host cellular immune response and includes cutaneous, mucosal, and visceral involvement. The disease is transmitted via the bite of an infected bloodsucking female sand fly.1 There are approximately 30 different species of sand flies that are proven to be vectors of the disease, with up to 40 more suspected of involvement in transmission, predominantly from the genera Phlebotomus (Old World) and Lutzomyia (New World).1,2 There are an estimated 1 to 2 million new cases of cutaneous leishmaniasis diagnosed annually in 70 endemic countries of the tropics, subtropics, and southern Europe.1,3,4
The differential diagnosis included cutaneous tuberculosis, which can have a similar progression and clinical appearance. Cutaneous tuberculosis starts as firm, reddish-brown, painless papules that slowly enlarge and ulcerate.5 It may be further differentiated on histopathology by the presence of tuberculoid granulomas, caseating necrosis, and acid-fast bacilli, which are easily detected in early lesions but are less prevalent after the granuloma develops.6 Sporotrichosis presents as a nodule, which may or may not ulcerate, on the extremities. However, the classic morphology is a sporotrichoid pattern, which describes the initial lesion plus subcutaneous nodular spread along the lymphatics.7 On histology, sporotrichosis has a characteristic “sporotrichoid asteroid” comprised of the yeast form surrounded by eosinophilic hyaline material in raylike processes that are found in the center of suppurative granulomas or foci.8
Atypical mycobacteria, principally Mycobacterium marinum (swimming pool granuloma) and Mycobacterium ulcerans (Buruli ulcer), are capable of causing cutaneous infections. They may be differentiated histologically by a neutrophilic infiltrate of poorly formed granulomas without caseation and extensive coagulative necrosis with little cellular infiltrate, respectively.6 Histoplasma capsulatum also infects histiocytes and may appear similar in size and shape; however, histoplasmosis is surrounded by a pseudocapsule and evenly spaced.8
Conversely, the histology of leishmaniasis lacks a pseudocapsule. The amastigotes may form the classic marquee sign by lining the periphery of the macrophage or they can be randomly spaced. Classically, the epidermis shows hyperkeratosis and acanthosis. Sometimes atrophy, ulceration, or intraepidermal abscesses also can be observed. Pseudoepitheliomatous hyperplasia can be seen in some long-standing lesions.1,4 Many of these findings were observed on hematoxylin and eosin staining from a punch biopsy obtained from the center of the lesion in our patient. For further delineation, a speciation kit was obtained from Walter Reed National Military Medical Center (Bethesda, Maryland). A second punch biopsy was obtained from the lesion edge, sectioned into 4 individual pieces, and placed in Schneider tissue culture medium. It was sent for tissue culture, polymerase chain reaction, and histology. Polymerase chain reaction analysis was positive for Leishmania, which was further identified as Leishmania tropica by tissue culture.
Leishmania tropica (Old World CL) commonly causes CL and is endemic to Central Asia, the Middle East, parts of North Africa, and Southeast Asia. Old and New World CL start as a small erythematous papule after a bite from an infected female sand fly. The papule develops into a nodule over weeks to months. The lesion may ulcerate and typically heals leaving an atrophic scar in months to years.1 Speciation of CL is important to guide therapy.
Leishmania mexicana, a New World species that commonly causes CL, classically is found in Central and South America, but there also have been documented cases in Texas. A 2008 case series identified 9 cases in northern Texas in residents without a travel history to endemic locations.9 Similarly, a cross-sectional study identified 41 locally endemic cases of CL over a 10-year period (2007-2017) in Texas; 22 of these cases had speciation by polymerase chain reaction, and all cases were attributed to L mexicana.10
In the United States, CL classically has been associated with travelers and military personnel returning from the Middle East; however, a growing body of literature suggests that it may be endemic to Texas, where it is now a reportable disease. Physicians should have an increased awareness of this entity and a high index of suspicion when treating patients with nonhealing cutaneous lesions.
The Diagnosis: Leishmaniasis
Hematoxylin and eosin staining of the tissue specimen revealed a dense histiocytic infiltrate with scattered lymphocytes and neutrophils. There were round to oval basophilic structures within the macrophages consistent with amastigotes. Giemsa staining was not necessary to visualize the organisms. The infiltrate abutted the overlying epidermis, which was acanthotic with pseudoepitheliomatous hyperplasia. There were collections of neutrophils, parakeratosis, and a serum crust overlying the epidermis (Figure). Clinical and histologic findings, as well as travel history, led to a diagnosis of cutaneous leishmaniasis (CL).
Leishmaniases is a group of diseases caused by a parasitic infection with flagellated protozoa of the genus Leishmania. There are more than 20 different Leishmania species that are pathogenic to humans, all presenting with cutaneous findings. The presentation depends on the inoculating species and the host cellular immune response and includes cutaneous, mucosal, and visceral involvement. The disease is transmitted via the bite of an infected bloodsucking female sand fly.1 There are approximately 30 different species of sand flies that are proven to be vectors of the disease, with up to 40 more suspected of involvement in transmission, predominantly from the genera Phlebotomus (Old World) and Lutzomyia (New World).1,2 There are an estimated 1 to 2 million new cases of cutaneous leishmaniasis diagnosed annually in 70 endemic countries of the tropics, subtropics, and southern Europe.1,3,4
The differential diagnosis included cutaneous tuberculosis, which can have a similar progression and clinical appearance. Cutaneous tuberculosis starts as firm, reddish-brown, painless papules that slowly enlarge and ulcerate.5 It may be further differentiated on histopathology by the presence of tuberculoid granulomas, caseating necrosis, and acid-fast bacilli, which are easily detected in early lesions but are less prevalent after the granuloma develops.6 Sporotrichosis presents as a nodule, which may or may not ulcerate, on the extremities. However, the classic morphology is a sporotrichoid pattern, which describes the initial lesion plus subcutaneous nodular spread along the lymphatics.7 On histology, sporotrichosis has a characteristic “sporotrichoid asteroid” comprised of the yeast form surrounded by eosinophilic hyaline material in raylike processes that are found in the center of suppurative granulomas or foci.8
Atypical mycobacteria, principally Mycobacterium marinum (swimming pool granuloma) and Mycobacterium ulcerans (Buruli ulcer), are capable of causing cutaneous infections. They may be differentiated histologically by a neutrophilic infiltrate of poorly formed granulomas without caseation and extensive coagulative necrosis with little cellular infiltrate, respectively.6 Histoplasma capsulatum also infects histiocytes and may appear similar in size and shape; however, histoplasmosis is surrounded by a pseudocapsule and evenly spaced.8
Conversely, the histology of leishmaniasis lacks a pseudocapsule. The amastigotes may form the classic marquee sign by lining the periphery of the macrophage or they can be randomly spaced. Classically, the epidermis shows hyperkeratosis and acanthosis. Sometimes atrophy, ulceration, or intraepidermal abscesses also can be observed. Pseudoepitheliomatous hyperplasia can be seen in some long-standing lesions.1,4 Many of these findings were observed on hematoxylin and eosin staining from a punch biopsy obtained from the center of the lesion in our patient. For further delineation, a speciation kit was obtained from Walter Reed National Military Medical Center (Bethesda, Maryland). A second punch biopsy was obtained from the lesion edge, sectioned into 4 individual pieces, and placed in Schneider tissue culture medium. It was sent for tissue culture, polymerase chain reaction, and histology. Polymerase chain reaction analysis was positive for Leishmania, which was further identified as Leishmania tropica by tissue culture.
Leishmania tropica (Old World CL) commonly causes CL and is endemic to Central Asia, the Middle East, parts of North Africa, and Southeast Asia. Old and New World CL start as a small erythematous papule after a bite from an infected female sand fly. The papule develops into a nodule over weeks to months. The lesion may ulcerate and typically heals leaving an atrophic scar in months to years.1 Speciation of CL is important to guide therapy.
Leishmania mexicana, a New World species that commonly causes CL, classically is found in Central and South America, but there also have been documented cases in Texas. A 2008 case series identified 9 cases in northern Texas in residents without a travel history to endemic locations.9 Similarly, a cross-sectional study identified 41 locally endemic cases of CL over a 10-year period (2007-2017) in Texas; 22 of these cases had speciation by polymerase chain reaction, and all cases were attributed to L mexicana.10
In the United States, CL classically has been associated with travelers and military personnel returning from the Middle East; however, a growing body of literature suggests that it may be endemic to Texas, where it is now a reportable disease. Physicians should have an increased awareness of this entity and a high index of suspicion when treating patients with nonhealing cutaneous lesions.
- Bravo F. Protozoa and worms. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1470-1502.
- Killick-Kendrick R. The biology and control of phlebotomine sandflies. Clin Dermatol. 1999;17:279-289.
- Reithinger R, Dujardin JC, Louzir H, et al. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-596.
- Patterson J. Protozoal infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:787-795.
- Ramos-e-Silva M, Ribeiro de Castro MC. Mycobacterial infections. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1296-1318.
- Patterson J. Bacterial and rickettsial infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:673-709.
- Elewski B, Hughey L, Hunt K, et al. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1329-1363.
- Patterson J. Mycoses and algal infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:721-755.
- Wright NA, Davis LE, Aftergut KS, et al. Cutaneous leishmaniasis in Texas: a northern spread of endemic areas [published online February 4, 2008]. J Am Acad Dermatol. 2008;58:650-652. doi:10.1016/j .jaad.2007.11.008.
- McIlwee BE, Weis SE, Hosler GA. Incidence of endemic human cutaneous leishmaniasis in the United States. JAMA Dermatol. 2018;154:1032-1039. doi:10.1001/jamadermatol.2018.2133
- Bravo F. Protozoa and worms. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1470-1502.
- Killick-Kendrick R. The biology and control of phlebotomine sandflies. Clin Dermatol. 1999;17:279-289.
- Reithinger R, Dujardin JC, Louzir H, et al. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-596.
- Patterson J. Protozoal infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:787-795.
- Ramos-e-Silva M, Ribeiro de Castro MC. Mycobacterial infections. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1296-1318.
- Patterson J. Bacterial and rickettsial infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:673-709.
- Elewski B, Hughey L, Hunt K, et al. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. WB Saunders Co; 2018:1329-1363.
- Patterson J. Mycoses and algal infections. Weedon’s Skin Pathology. 5th ed. Elsevier; 2021:721-755.
- Wright NA, Davis LE, Aftergut KS, et al. Cutaneous leishmaniasis in Texas: a northern spread of endemic areas [published online February 4, 2008]. J Am Acad Dermatol. 2008;58:650-652. doi:10.1016/j .jaad.2007.11.008.
- McIlwee BE, Weis SE, Hosler GA. Incidence of endemic human cutaneous leishmaniasis in the United States. JAMA Dermatol. 2018;154:1032-1039. doi:10.1001/jamadermatol.2018.2133
A 36-year-old active-duty male service member with no notable medical history presented to the dermatology clinic with an asymptomatic nodule on the right forearm that he initially noticed approximately 1 year prior while deployed in Syria and thought that it was a mosquito bite; it continued to enlarge slowly since that time. He attempted self-extraction but was only able to express a small amount of clear fluid. No other therapies had been used. He denied any other symptoms on a review of systems and was not taking any medications. Physical examination revealed a 1.5-cm, erythematous, nonulcerated, pink nodule on the right distal volar forearm without other cutaneous findings. A 4-mm punch biopsy was performed.

Gene therapy: A ‘one and done’ hemophilia B treatment?
The report on the gene therapy treatment, known as etranacogene dezaparvovec (EtranaDez), was released at the Feb. 2-4, 2022, annual meeting of the European Association of Hemophilia and Allied Disorders.
In an interview, study lead author Wolfgang Miesbach, MD, PhD, of University Hospital Frankfurt in Germany, touted the decline in ABR. “This statistically significant reduction not only met the primary endpoint for non-inferiority but also demonstrates clear superiority of etranacogene dezaparvovec to prophylaxis in the lead-in period,” he said. “In addition to that, the quality of life improved significantly, [and] there was an overall favorable safety profile.”
Hemophilia B is much rarer than hemophilia A. In a 2020 report, the CDC estimated that type A accounted for less than a quarter of the 29,761-32,985 cases of U.S. males who had hemophilia from 2012-2018. The rest had type B. Most of the males with hemophilia were white (81.2%) and fairly young (just 20.6% were older than 39).
High adherence and high prices
Factor IX (FIX) replacement therapy aims to boost levels of the blood-clotting protein in patients with severe hepatitis B. However, the intravenous prophylactic treatment requires a “high level of adherence” due to the need for self-administration several times a week, Dr. Miesbach said, adding that the treatment does not reliably prevent bleeding and joint destruction.
Also, the price of FIX replacement therapy in the United States is exorbitant, costing an average of $397,491 a year for the conventional treatment and an average of $788,861 a year for an extended half-life treatment, according to a 2019 report.
The gene therapy treatment, formerly known as AMT-061, “consists of a functional FIX gene with higher activity than the wild-type FIX (Padua variant), together with an AAV (AAV5),” Dr. Miesbach said. “AAV 5 is a vector with high liver tropism to transduce the liver cells and lead to the production of the functional FIX gene there.”
For the new open-label, single-dose, single-arm HOPE-B study, researchers treated 54 adult men with severe or moderately severe HB (FIX ≤2%), 31 with and 23 without preexisting AAV5 neutralizing antibodies. The average age was 41.5, 81.5% had severe cases (FIX<1%), and 25.9% had no bleeds at lead-in.
The participants began 12 months of treatment with gene therapy following a 6-month lead-in period of FIX prophylaxis. All but one completed follow-up.
“Mean FIX activity was 39.0 IU/dL (±18.7; 8.2, 97.1) (standard deviation; min, max) at month 6 and 36.9 IU/dL (±21.4; 4.5, 122.9) at month 18,” the researchers reported. ABR dropped by 64% from the lead-in period to the 12-month treatment period (4.19 vs. 1.51, P = .0002), and FIX-treated bleeds fell by 77% (ABR=3.65 vs. 0.83, P < .0001).
Fifty-two of 54 patients stopped full-dose prophylaxis and didn’t return to it. Mean unadjusted annualized FIX use dropped by 97% overall from the lead-in period to months 13-18 (257,338.8 vs. 8,486.6 IU/year/participant).
Thirty-seven participants experienced 92 treatment-related adverse events such as abnormal alanine aminotransferase (16.7%), headache (14.8%), influenza-like illness (13.0%), infusion-related infection (13.0%), and abnormal aspartate aminotransferase (9.3). Researchers determined 74 (80.4%) of the adverse effects were mild.
“Transaminase increases were reported, and corticosteroids were required in nine participants, but the mean duration of corticosteroids, including taper, was only 79 days,” Dr. Miesbach said.
“There was no prophylactic use of steroids in this study. FIX expression was maintained. One death was found to be unrelated to study treatment. One case of hepatocellular carcinoma, which has been reported in detail previously, was reported. But after detailed molecular analysis, this was found to be unrelated to study treatment,” he noted.
Quality of life scores improved by 21.5%-28.78%. The P values, ranging from < .0001 to .0036, were considered to be “nominally significant” due to analysis limitations.
A ‘one and done’ treatment
While the trial is expected to continue until 2025, no further treatment with etranacogene dezaparvovec was given. “Gene therapy is a ‘one and done’ treatment,” Dr. Miesbach said. “According to our current knowledge, it cannot be repeated.”
No information about the expected cost of the treatment is available. CSL Behring, which licensed global rights for the gene therapy from developer uniQure, is expected to seek Food and Drug Administration approval this year.
The trial was funded by CSL Behring. Dr. Miesbach and other study authors report various disclosures including support from CSL Behring and uniQure. Some authors are employees of CSL Behring and uniQure.
The report on the gene therapy treatment, known as etranacogene dezaparvovec (EtranaDez), was released at the Feb. 2-4, 2022, annual meeting of the European Association of Hemophilia and Allied Disorders.
In an interview, study lead author Wolfgang Miesbach, MD, PhD, of University Hospital Frankfurt in Germany, touted the decline in ABR. “This statistically significant reduction not only met the primary endpoint for non-inferiority but also demonstrates clear superiority of etranacogene dezaparvovec to prophylaxis in the lead-in period,” he said. “In addition to that, the quality of life improved significantly, [and] there was an overall favorable safety profile.”
Hemophilia B is much rarer than hemophilia A. In a 2020 report, the CDC estimated that type A accounted for less than a quarter of the 29,761-32,985 cases of U.S. males who had hemophilia from 2012-2018. The rest had type B. Most of the males with hemophilia were white (81.2%) and fairly young (just 20.6% were older than 39).
High adherence and high prices
Factor IX (FIX) replacement therapy aims to boost levels of the blood-clotting protein in patients with severe hepatitis B. However, the intravenous prophylactic treatment requires a “high level of adherence” due to the need for self-administration several times a week, Dr. Miesbach said, adding that the treatment does not reliably prevent bleeding and joint destruction.
Also, the price of FIX replacement therapy in the United States is exorbitant, costing an average of $397,491 a year for the conventional treatment and an average of $788,861 a year for an extended half-life treatment, according to a 2019 report.
The gene therapy treatment, formerly known as AMT-061, “consists of a functional FIX gene with higher activity than the wild-type FIX (Padua variant), together with an AAV (AAV5),” Dr. Miesbach said. “AAV 5 is a vector with high liver tropism to transduce the liver cells and lead to the production of the functional FIX gene there.”
For the new open-label, single-dose, single-arm HOPE-B study, researchers treated 54 adult men with severe or moderately severe HB (FIX ≤2%), 31 with and 23 without preexisting AAV5 neutralizing antibodies. The average age was 41.5, 81.5% had severe cases (FIX<1%), and 25.9% had no bleeds at lead-in.
The participants began 12 months of treatment with gene therapy following a 6-month lead-in period of FIX prophylaxis. All but one completed follow-up.
“Mean FIX activity was 39.0 IU/dL (±18.7; 8.2, 97.1) (standard deviation; min, max) at month 6 and 36.9 IU/dL (±21.4; 4.5, 122.9) at month 18,” the researchers reported. ABR dropped by 64% from the lead-in period to the 12-month treatment period (4.19 vs. 1.51, P = .0002), and FIX-treated bleeds fell by 77% (ABR=3.65 vs. 0.83, P < .0001).
Fifty-two of 54 patients stopped full-dose prophylaxis and didn’t return to it. Mean unadjusted annualized FIX use dropped by 97% overall from the lead-in period to months 13-18 (257,338.8 vs. 8,486.6 IU/year/participant).
Thirty-seven participants experienced 92 treatment-related adverse events such as abnormal alanine aminotransferase (16.7%), headache (14.8%), influenza-like illness (13.0%), infusion-related infection (13.0%), and abnormal aspartate aminotransferase (9.3). Researchers determined 74 (80.4%) of the adverse effects were mild.
“Transaminase increases were reported, and corticosteroids were required in nine participants, but the mean duration of corticosteroids, including taper, was only 79 days,” Dr. Miesbach said.
“There was no prophylactic use of steroids in this study. FIX expression was maintained. One death was found to be unrelated to study treatment. One case of hepatocellular carcinoma, which has been reported in detail previously, was reported. But after detailed molecular analysis, this was found to be unrelated to study treatment,” he noted.
Quality of life scores improved by 21.5%-28.78%. The P values, ranging from < .0001 to .0036, were considered to be “nominally significant” due to analysis limitations.
A ‘one and done’ treatment
While the trial is expected to continue until 2025, no further treatment with etranacogene dezaparvovec was given. “Gene therapy is a ‘one and done’ treatment,” Dr. Miesbach said. “According to our current knowledge, it cannot be repeated.”
No information about the expected cost of the treatment is available. CSL Behring, which licensed global rights for the gene therapy from developer uniQure, is expected to seek Food and Drug Administration approval this year.
The trial was funded by CSL Behring. Dr. Miesbach and other study authors report various disclosures including support from CSL Behring and uniQure. Some authors are employees of CSL Behring and uniQure.
The report on the gene therapy treatment, known as etranacogene dezaparvovec (EtranaDez), was released at the Feb. 2-4, 2022, annual meeting of the European Association of Hemophilia and Allied Disorders.
In an interview, study lead author Wolfgang Miesbach, MD, PhD, of University Hospital Frankfurt in Germany, touted the decline in ABR. “This statistically significant reduction not only met the primary endpoint for non-inferiority but also demonstrates clear superiority of etranacogene dezaparvovec to prophylaxis in the lead-in period,” he said. “In addition to that, the quality of life improved significantly, [and] there was an overall favorable safety profile.”
Hemophilia B is much rarer than hemophilia A. In a 2020 report, the CDC estimated that type A accounted for less than a quarter of the 29,761-32,985 cases of U.S. males who had hemophilia from 2012-2018. The rest had type B. Most of the males with hemophilia were white (81.2%) and fairly young (just 20.6% were older than 39).
High adherence and high prices
Factor IX (FIX) replacement therapy aims to boost levels of the blood-clotting protein in patients with severe hepatitis B. However, the intravenous prophylactic treatment requires a “high level of adherence” due to the need for self-administration several times a week, Dr. Miesbach said, adding that the treatment does not reliably prevent bleeding and joint destruction.
Also, the price of FIX replacement therapy in the United States is exorbitant, costing an average of $397,491 a year for the conventional treatment and an average of $788,861 a year for an extended half-life treatment, according to a 2019 report.
The gene therapy treatment, formerly known as AMT-061, “consists of a functional FIX gene with higher activity than the wild-type FIX (Padua variant), together with an AAV (AAV5),” Dr. Miesbach said. “AAV 5 is a vector with high liver tropism to transduce the liver cells and lead to the production of the functional FIX gene there.”
For the new open-label, single-dose, single-arm HOPE-B study, researchers treated 54 adult men with severe or moderately severe HB (FIX ≤2%), 31 with and 23 without preexisting AAV5 neutralizing antibodies. The average age was 41.5, 81.5% had severe cases (FIX<1%), and 25.9% had no bleeds at lead-in.
The participants began 12 months of treatment with gene therapy following a 6-month lead-in period of FIX prophylaxis. All but one completed follow-up.
“Mean FIX activity was 39.0 IU/dL (±18.7; 8.2, 97.1) (standard deviation; min, max) at month 6 and 36.9 IU/dL (±21.4; 4.5, 122.9) at month 18,” the researchers reported. ABR dropped by 64% from the lead-in period to the 12-month treatment period (4.19 vs. 1.51, P = .0002), and FIX-treated bleeds fell by 77% (ABR=3.65 vs. 0.83, P < .0001).
Fifty-two of 54 patients stopped full-dose prophylaxis and didn’t return to it. Mean unadjusted annualized FIX use dropped by 97% overall from the lead-in period to months 13-18 (257,338.8 vs. 8,486.6 IU/year/participant).
Thirty-seven participants experienced 92 treatment-related adverse events such as abnormal alanine aminotransferase (16.7%), headache (14.8%), influenza-like illness (13.0%), infusion-related infection (13.0%), and abnormal aspartate aminotransferase (9.3). Researchers determined 74 (80.4%) of the adverse effects were mild.
“Transaminase increases were reported, and corticosteroids were required in nine participants, but the mean duration of corticosteroids, including taper, was only 79 days,” Dr. Miesbach said.
“There was no prophylactic use of steroids in this study. FIX expression was maintained. One death was found to be unrelated to study treatment. One case of hepatocellular carcinoma, which has been reported in detail previously, was reported. But after detailed molecular analysis, this was found to be unrelated to study treatment,” he noted.
Quality of life scores improved by 21.5%-28.78%. The P values, ranging from < .0001 to .0036, were considered to be “nominally significant” due to analysis limitations.
A ‘one and done’ treatment
While the trial is expected to continue until 2025, no further treatment with etranacogene dezaparvovec was given. “Gene therapy is a ‘one and done’ treatment,” Dr. Miesbach said. “According to our current knowledge, it cannot be repeated.”
No information about the expected cost of the treatment is available. CSL Behring, which licensed global rights for the gene therapy from developer uniQure, is expected to seek Food and Drug Administration approval this year.
The trial was funded by CSL Behring. Dr. Miesbach and other study authors report various disclosures including support from CSL Behring and uniQure. Some authors are employees of CSL Behring and uniQure.
REPORTING FROM EAHAD
ACIP issues adult vaccination schedule 2022
by the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC).
The Clinical Guideline on the “Recommended Adult Immunization Schedule, United States, 2022” appears online Feb. 17 in Annals of Internal Medicine and in the CDC’s Morbidity and Mortality Weekly Report.
The document features changes to the zoster, pneumococcal, and hepatitis B vaccines. COVID-19 vaccinations are now included in the notes section of the schedule and can be co-administered with other vaccines, according to ACIP.
The 2022 schedule is particularly important because the pandemic has caused many adults to fall behind in routine vaccinations, according to lead author Neil Murthy, MD, MPH, MSJ, of the CDC’s immunization services division, National Center for Immunization and Respiratory Diseases, and colleagues.
“Providers should administer all due and overdue vaccines according to the routine immunization schedule during the same visit,” the group wrote. “In addition, providers should implement strategies to catch up all patients on any overdue vaccines.”
Among other changes appearing in the 2022 recommendations:
- A new step 4 in the form of an appendix lists all the contraindications and precautions for each vaccine.
- The zoster vaccine now is recommended for use in everyone aged 19 years and older who are or will be immunodeficient or immunosuppressed through disease or therapy. The new purple color bar reflects ACIP’s new two-dose series regimen for immunocompromised adults aged 19 to 49.
- The simplified pneumococcal recommendation includes guidance on using the new PCV15 and PCV20 vaccines.
- The hepatitis B recommendation has been made more inclusive, with vaccination recommended for all adults aged 19 to 59. The Special Situations section in the Notes outlines the risk-based recommendations for the hepatitis B vaccine in adults aged 60 and older. The schedule has been harmonized with the 2022 Child and Adolescent Immunization Schedule.
A welcome change
Sandra A. Fryhofer, MD, a member of the ACIP Combined Immunization Work Group, said the new pneumococcal recommendation is a particularly welcome change.
“The old recommendation was complicated and confusing. The new one is much more straightforward,” Dr. Fryhofer, an internist in Atlanta, said in an interview. Now there are only two options: a two-vaccine series of PCV15 (Vaxneuvance), in combination with the already familiar PPSV23 polysaccharide vaccine (Pneumovax 23), and a single dose of the new PCV20, Prevnar 20.
“Some work group members favored a universal age-based recommendation starting at 50 instead of 65,” Fryhofer said. “This would provide more opportunities to vaccinate adults but could lead to waning immunity later in life when risk of disease is higher.”
Although none of the updates is likely to stir controversy, discussion among ACIP members was particularly lively around hepatitis B vaccination, Dr. Fryhofer said. This vaccine has historically been recommended based on risk and has had poor uptake, while age-based vaccine recommendations generally have greater uptake.
“ACIP approved hepatitis B vaccine universally for those up to age 60, but for those 60 and older, the recommendation remains risk-based with a loophole: Anyone 60 and older who wants it can get it,” she told this news organization. “Some of the risk indications for hepatitis B vaccination may be uncomfortable or embarrassing to disclose, especially for older patients. The loophole takes care of that, but patients may have to ask for the vaccine.”
As usual, the graphics have been fine-tuned for greater accuracy and readability. “You can print a color copy to have in the exam room or at your workspace or give it a bookmark and check it online,” Dr. Fryhofer said. “It’s a great resource to have at your fingertips.”
Dr. Fryhofer has made a series of videos explaining ACIP’s approval process, the use of the schedule, and changes to vaccines including influenza. These can be accessed on the American College of Physicians website.
The authors of the recommendations stress that physicians should pay careful attention to the notes section for each vaccine, as these details clarify who needs what vaccine, when, and at what dose.
Co-author Henry Bernstein, DO, reported that he is the editor of Current Opinion in Pediatrics Office Pediatrics Series and received a presentation honorarium from the Florida chapter of the American Academy of Pediatrics. Co-author Kevin Ault, MD, reported having received a grant from the National Cancer Institute, consulting fees from PathoVax, and payments supporting attending meetings and/or travel from the American College of Obstetricians and Gynecologists.
A version of this article first appeared on Medscape.com.
by the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC).
The Clinical Guideline on the “Recommended Adult Immunization Schedule, United States, 2022” appears online Feb. 17 in Annals of Internal Medicine and in the CDC’s Morbidity and Mortality Weekly Report.
The document features changes to the zoster, pneumococcal, and hepatitis B vaccines. COVID-19 vaccinations are now included in the notes section of the schedule and can be co-administered with other vaccines, according to ACIP.
The 2022 schedule is particularly important because the pandemic has caused many adults to fall behind in routine vaccinations, according to lead author Neil Murthy, MD, MPH, MSJ, of the CDC’s immunization services division, National Center for Immunization and Respiratory Diseases, and colleagues.
“Providers should administer all due and overdue vaccines according to the routine immunization schedule during the same visit,” the group wrote. “In addition, providers should implement strategies to catch up all patients on any overdue vaccines.”
Among other changes appearing in the 2022 recommendations:
- A new step 4 in the form of an appendix lists all the contraindications and precautions for each vaccine.
- The zoster vaccine now is recommended for use in everyone aged 19 years and older who are or will be immunodeficient or immunosuppressed through disease or therapy. The new purple color bar reflects ACIP’s new two-dose series regimen for immunocompromised adults aged 19 to 49.
- The simplified pneumococcal recommendation includes guidance on using the new PCV15 and PCV20 vaccines.
- The hepatitis B recommendation has been made more inclusive, with vaccination recommended for all adults aged 19 to 59. The Special Situations section in the Notes outlines the risk-based recommendations for the hepatitis B vaccine in adults aged 60 and older. The schedule has been harmonized with the 2022 Child and Adolescent Immunization Schedule.
A welcome change
Sandra A. Fryhofer, MD, a member of the ACIP Combined Immunization Work Group, said the new pneumococcal recommendation is a particularly welcome change.
“The old recommendation was complicated and confusing. The new one is much more straightforward,” Dr. Fryhofer, an internist in Atlanta, said in an interview. Now there are only two options: a two-vaccine series of PCV15 (Vaxneuvance), in combination with the already familiar PPSV23 polysaccharide vaccine (Pneumovax 23), and a single dose of the new PCV20, Prevnar 20.
“Some work group members favored a universal age-based recommendation starting at 50 instead of 65,” Fryhofer said. “This would provide more opportunities to vaccinate adults but could lead to waning immunity later in life when risk of disease is higher.”
Although none of the updates is likely to stir controversy, discussion among ACIP members was particularly lively around hepatitis B vaccination, Dr. Fryhofer said. This vaccine has historically been recommended based on risk and has had poor uptake, while age-based vaccine recommendations generally have greater uptake.
“ACIP approved hepatitis B vaccine universally for those up to age 60, but for those 60 and older, the recommendation remains risk-based with a loophole: Anyone 60 and older who wants it can get it,” she told this news organization. “Some of the risk indications for hepatitis B vaccination may be uncomfortable or embarrassing to disclose, especially for older patients. The loophole takes care of that, but patients may have to ask for the vaccine.”
As usual, the graphics have been fine-tuned for greater accuracy and readability. “You can print a color copy to have in the exam room or at your workspace or give it a bookmark and check it online,” Dr. Fryhofer said. “It’s a great resource to have at your fingertips.”
Dr. Fryhofer has made a series of videos explaining ACIP’s approval process, the use of the schedule, and changes to vaccines including influenza. These can be accessed on the American College of Physicians website.
The authors of the recommendations stress that physicians should pay careful attention to the notes section for each vaccine, as these details clarify who needs what vaccine, when, and at what dose.
Co-author Henry Bernstein, DO, reported that he is the editor of Current Opinion in Pediatrics Office Pediatrics Series and received a presentation honorarium from the Florida chapter of the American Academy of Pediatrics. Co-author Kevin Ault, MD, reported having received a grant from the National Cancer Institute, consulting fees from PathoVax, and payments supporting attending meetings and/or travel from the American College of Obstetricians and Gynecologists.
A version of this article first appeared on Medscape.com.
by the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC).
The Clinical Guideline on the “Recommended Adult Immunization Schedule, United States, 2022” appears online Feb. 17 in Annals of Internal Medicine and in the CDC’s Morbidity and Mortality Weekly Report.
The document features changes to the zoster, pneumococcal, and hepatitis B vaccines. COVID-19 vaccinations are now included in the notes section of the schedule and can be co-administered with other vaccines, according to ACIP.
The 2022 schedule is particularly important because the pandemic has caused many adults to fall behind in routine vaccinations, according to lead author Neil Murthy, MD, MPH, MSJ, of the CDC’s immunization services division, National Center for Immunization and Respiratory Diseases, and colleagues.
“Providers should administer all due and overdue vaccines according to the routine immunization schedule during the same visit,” the group wrote. “In addition, providers should implement strategies to catch up all patients on any overdue vaccines.”
Among other changes appearing in the 2022 recommendations:
- A new step 4 in the form of an appendix lists all the contraindications and precautions for each vaccine.
- The zoster vaccine now is recommended for use in everyone aged 19 years and older who are or will be immunodeficient or immunosuppressed through disease or therapy. The new purple color bar reflects ACIP’s new two-dose series regimen for immunocompromised adults aged 19 to 49.
- The simplified pneumococcal recommendation includes guidance on using the new PCV15 and PCV20 vaccines.
- The hepatitis B recommendation has been made more inclusive, with vaccination recommended for all adults aged 19 to 59. The Special Situations section in the Notes outlines the risk-based recommendations for the hepatitis B vaccine in adults aged 60 and older. The schedule has been harmonized with the 2022 Child and Adolescent Immunization Schedule.
A welcome change
Sandra A. Fryhofer, MD, a member of the ACIP Combined Immunization Work Group, said the new pneumococcal recommendation is a particularly welcome change.
“The old recommendation was complicated and confusing. The new one is much more straightforward,” Dr. Fryhofer, an internist in Atlanta, said in an interview. Now there are only two options: a two-vaccine series of PCV15 (Vaxneuvance), in combination with the already familiar PPSV23 polysaccharide vaccine (Pneumovax 23), and a single dose of the new PCV20, Prevnar 20.
“Some work group members favored a universal age-based recommendation starting at 50 instead of 65,” Fryhofer said. “This would provide more opportunities to vaccinate adults but could lead to waning immunity later in life when risk of disease is higher.”
Although none of the updates is likely to stir controversy, discussion among ACIP members was particularly lively around hepatitis B vaccination, Dr. Fryhofer said. This vaccine has historically been recommended based on risk and has had poor uptake, while age-based vaccine recommendations generally have greater uptake.
“ACIP approved hepatitis B vaccine universally for those up to age 60, but for those 60 and older, the recommendation remains risk-based with a loophole: Anyone 60 and older who wants it can get it,” she told this news organization. “Some of the risk indications for hepatitis B vaccination may be uncomfortable or embarrassing to disclose, especially for older patients. The loophole takes care of that, but patients may have to ask for the vaccine.”
As usual, the graphics have been fine-tuned for greater accuracy and readability. “You can print a color copy to have in the exam room or at your workspace or give it a bookmark and check it online,” Dr. Fryhofer said. “It’s a great resource to have at your fingertips.”
Dr. Fryhofer has made a series of videos explaining ACIP’s approval process, the use of the schedule, and changes to vaccines including influenza. These can be accessed on the American College of Physicians website.
The authors of the recommendations stress that physicians should pay careful attention to the notes section for each vaccine, as these details clarify who needs what vaccine, when, and at what dose.
Co-author Henry Bernstein, DO, reported that he is the editor of Current Opinion in Pediatrics Office Pediatrics Series and received a presentation honorarium from the Florida chapter of the American Academy of Pediatrics. Co-author Kevin Ault, MD, reported having received a grant from the National Cancer Institute, consulting fees from PathoVax, and payments supporting attending meetings and/or travel from the American College of Obstetricians and Gynecologists.
A version of this article first appeared on Medscape.com.
High praise, condemnation for CMS Aduhelm coverage plan
Medicare has received a key endorsement of its plan to restrict payment for the controversial Alzheimer’s disease (AD) drug aducanumab (Aduhelm) – but also drew pleas from other groups for more generous reimbursement of the drug, as well as expected similar medications currently in development.
The Centers for Medicare & Medicaid Services received more than 9,900 comments on its plan, according to the current tally posted on its website. However, it is unclear when the final count will be available.
CMS intends to limit federal payment for monoclonal antibodies that target amyloid to clinical trials. Among supporters of this approach is the influential Medicare Payment Advisory Commission, an expert panel that helps Congress and CMS manage the federal health program.
Opponents of the CMS plan include several pharmaceutical companies. Patient and consumer groups, individuals, and lawmakers had mixed views.
CMS officials will weigh the feedback provided in the comments when setting a final coverage policy for aducanumab. It is expected the agency’s final decision will be announced on April 11.
Ongoing debate
The Food and Drug Administration’s unusual approach to clearing the drug for U.S. sales triggered a review of its management of the accelerated approval process by the Office of Inspector General for the Department of Health & Human Services.
The FDA granted an accelerated approval for aducanumab in June based on evidence that the drug clears amyloid in the brain. However, it is unclear whether clearing the protein from the brain results in clinical benefit.
Usually, accelerated approvals precede the completion of phase 3 drug trials, with the FDA allowing early access to a medicine while awaiting confirmatory trials.
In the case of aducanumab, results of the phase 3 confirmatory trials ENGAGE and EMERGE were available at the time of FDA approval. However, interpretation of the findings is controversial.
Biogen contends that the amyloid-clearing effect of the higher dose of aducanumab shown in EMERGE indicates the drug has clinical potential. However, others argue that amyloid clearance does not indicate clinical benefit.
Limiting Medicare coverage of aducanumab for treatment of AD means “the progression of disease, for nearly all beneficiaries, would continue unabated,” Biogen wrote in its comment to CMS.
Conflicting data
Supporters of the CMS plan have a different view of the trial data. They note the failure of aducanumab in the companion ENGAGE trial, while also questioning the magnitude of benefit suggested by even the most positive data cited for the drug in the EMERGE trial.
Both studies used the Clinical Dementia Rating-Sum of Boxes (CDR-SB) score, an 18-point scale measuring cognition and function.
In his comment to CMS, MedPAC chairman Michael E. Chernew, PhD, noted the change in CDR-SB score of 0.39 in EMERGE’s high-dose aducanumab group. CMS has described this as being “less than the 1-2 point change that has been suggested as a minimal clinically important difference,” Dr. Chernew wrote.
MedPAC does not normally comment on Medicare coverage decisions, but did so in this case because of its significance and because of the potential fiscal implications, he noted.
“Though there is only limited, conflicting data on Aduhelm’s clinical effectiveness, Medicare would pay a high price for the product,” Dr. Chernew wrote, pointing out the $28,200 annual U.S. price of the drug.
MedPAC thus endorsed the coverage-with-evidence-development (CED) pathway. Under this approach, Medicare would pay for these drugs when used in clinical trials that meet certain criteria.
Legal challenge?
In its comment to CMS, Biogen questioned the agency’s legal grounds for limiting coverage of aducanumab. A mandate on clinical trials as part of the CED proposal “runs afoul of the Administrative Procedure Act’s prohibition against arbitrary and capricious agency action,” Biogen said.
The drug company argued that its own planned follow-on studies would provide the kind of data Medicare officials want to see. It also argued for greater use of observational data, including real-world evidence, and of information from Medicare claims.
Roche’s Genentech, which is also developing antiamyloid drugs for AD, echoed some of Biogen’s concerns about the aducanumab plan.
CMS’ CED plan would be “unnecessarily restrictive and discouraging for patients living with this destructive disease,” David Burt, executive director for federal government affairs at Genentech, wrote in a comment to CMS.
CMS should clarify that the CED requirement would not apply to cases of FDA-approved antiamyloid therapies that have demonstrated “clinically meaningful improvement,” Mr. Burt added. He noted there are phase 3 trials of drugs in this class that could soon produce data.
CMS should “fully consider the broad ramifications and significant unintended consequences of prematurely placing unduly severe restrictions on the entire class of antiamyloid monoclonal antibodies,” Mr. Burt wrote.
Health care inequity
In its comment to CMS, Biogen also noted the Medicare proposal would “compound the already pervasive inequities in access to treatment and will ultimately prove highly detrimental to health equity.”
There are already concerns about the access of Black and Latinx patients to clinical trials. The planned CED approach would tightly restrict access to aducanumab, as well as expected follow-ons in the amyloid-directed monoclonal antibody (mAb) drug class, the company said.
“Many of the trial sites for Aduhelm, as well as for other amyloid-directed [monoclonal antibodies] are not hospital-based outpatient settings, but include infusion centers, private practices, and medical research centers,” Biogen wrote.
Patient groups such as UsAgainstAlzheimer’s told CMS the CED approach would worsen disparities, despite the aim of Medicare officials to increase participation of Black and Latinx patients in future testing.
“CMS will be hard-pressed to achieve diversity if such hospitals are the only locations where Medicare beneficiaries are able to access mAbs,” USAgainstAlzheimer’s wrote in a Feb. 10 comment.
In contrast, the nonprofit National Center for Health Research praised CMS for what it described as an effort to address a lack of representation of Black and Latinx patients in earlier aducanumab research.
However, the NCHR also suggested CMS revise its plan to mandate that clinical trials include patients who are representative of the national population diagnosed with AD.
“Rather than being concerned about the percentage of patients in specific racial and ethnic groups, we propose that CMS include sufficient numbers of patients in different racial, ethnic, and age groups to ensure that there is enough statistical power for subgroup analyses to determine safety and efficacy for each of the major demographic groups,” the NCHR wrote.
Patient health, Medicare at risk
On Feb. 8, a group of House Republican lawmakers asked CMS to reverse its stance. In a publicly released letter, Rep. Cathy McMorris Rodgers of Washington state, the ranking Republican on the House Energy and Commerce Committee, and colleagues urged broader coverage of aducanumab.
In the letter, the group emphasized the idea of aducanumab as a potential treatment for patients with Down syndrome who are at risk for AD.
“The link between Down Syndrome and AD is still being researched by scientists,” Rep. Rodgers and colleagues wrote.
“However, there appears to be a correlation between the additional 21st chromosome present in people with Down Syndrome and the chromosome’s gene that makes amyloid precursor proteins and can cause a build-up of the beta-amyloid plaques common amongst those with AD,” they add.
On the other hand, CMS garnered earlier support from influential Democrats. On Jan. 13, House Energy and Commerce Chairman Frank Pallone Jr (D-N.J.) and House Oversight and Reform Chairwoman Carolyn B. Maloney (D-N.Y.) released a letter praising CMS for its plan for covering aducanumab.
In addition to the HHS-OIG review of the FDA’s approval of the drug, the two House committees are in the midst of their own investigation of the agency’s decision to clear the drug.
“Any broader coverage determination before there is clarity on Aduhelm’s approval process and findings from the myriad ongoing investigations may put the health of millions of Alzheimer’s patients on the line and the financial stability of the nation’s health insurance program for American seniors at risk,” Rep. Pallone and Rep. Maloney wrote.
A version of this article first appeared on Medscape.com.
Medicare has received a key endorsement of its plan to restrict payment for the controversial Alzheimer’s disease (AD) drug aducanumab (Aduhelm) – but also drew pleas from other groups for more generous reimbursement of the drug, as well as expected similar medications currently in development.
The Centers for Medicare & Medicaid Services received more than 9,900 comments on its plan, according to the current tally posted on its website. However, it is unclear when the final count will be available.
CMS intends to limit federal payment for monoclonal antibodies that target amyloid to clinical trials. Among supporters of this approach is the influential Medicare Payment Advisory Commission, an expert panel that helps Congress and CMS manage the federal health program.
Opponents of the CMS plan include several pharmaceutical companies. Patient and consumer groups, individuals, and lawmakers had mixed views.
CMS officials will weigh the feedback provided in the comments when setting a final coverage policy for aducanumab. It is expected the agency’s final decision will be announced on April 11.
Ongoing debate
The Food and Drug Administration’s unusual approach to clearing the drug for U.S. sales triggered a review of its management of the accelerated approval process by the Office of Inspector General for the Department of Health & Human Services.
The FDA granted an accelerated approval for aducanumab in June based on evidence that the drug clears amyloid in the brain. However, it is unclear whether clearing the protein from the brain results in clinical benefit.
Usually, accelerated approvals precede the completion of phase 3 drug trials, with the FDA allowing early access to a medicine while awaiting confirmatory trials.
In the case of aducanumab, results of the phase 3 confirmatory trials ENGAGE and EMERGE were available at the time of FDA approval. However, interpretation of the findings is controversial.
Biogen contends that the amyloid-clearing effect of the higher dose of aducanumab shown in EMERGE indicates the drug has clinical potential. However, others argue that amyloid clearance does not indicate clinical benefit.
Limiting Medicare coverage of aducanumab for treatment of AD means “the progression of disease, for nearly all beneficiaries, would continue unabated,” Biogen wrote in its comment to CMS.
Conflicting data
Supporters of the CMS plan have a different view of the trial data. They note the failure of aducanumab in the companion ENGAGE trial, while also questioning the magnitude of benefit suggested by even the most positive data cited for the drug in the EMERGE trial.
Both studies used the Clinical Dementia Rating-Sum of Boxes (CDR-SB) score, an 18-point scale measuring cognition and function.
In his comment to CMS, MedPAC chairman Michael E. Chernew, PhD, noted the change in CDR-SB score of 0.39 in EMERGE’s high-dose aducanumab group. CMS has described this as being “less than the 1-2 point change that has been suggested as a minimal clinically important difference,” Dr. Chernew wrote.
MedPAC does not normally comment on Medicare coverage decisions, but did so in this case because of its significance and because of the potential fiscal implications, he noted.
“Though there is only limited, conflicting data on Aduhelm’s clinical effectiveness, Medicare would pay a high price for the product,” Dr. Chernew wrote, pointing out the $28,200 annual U.S. price of the drug.
MedPAC thus endorsed the coverage-with-evidence-development (CED) pathway. Under this approach, Medicare would pay for these drugs when used in clinical trials that meet certain criteria.
Legal challenge?
In its comment to CMS, Biogen questioned the agency’s legal grounds for limiting coverage of aducanumab. A mandate on clinical trials as part of the CED proposal “runs afoul of the Administrative Procedure Act’s prohibition against arbitrary and capricious agency action,” Biogen said.
The drug company argued that its own planned follow-on studies would provide the kind of data Medicare officials want to see. It also argued for greater use of observational data, including real-world evidence, and of information from Medicare claims.
Roche’s Genentech, which is also developing antiamyloid drugs for AD, echoed some of Biogen’s concerns about the aducanumab plan.
CMS’ CED plan would be “unnecessarily restrictive and discouraging for patients living with this destructive disease,” David Burt, executive director for federal government affairs at Genentech, wrote in a comment to CMS.
CMS should clarify that the CED requirement would not apply to cases of FDA-approved antiamyloid therapies that have demonstrated “clinically meaningful improvement,” Mr. Burt added. He noted there are phase 3 trials of drugs in this class that could soon produce data.
CMS should “fully consider the broad ramifications and significant unintended consequences of prematurely placing unduly severe restrictions on the entire class of antiamyloid monoclonal antibodies,” Mr. Burt wrote.
Health care inequity
In its comment to CMS, Biogen also noted the Medicare proposal would “compound the already pervasive inequities in access to treatment and will ultimately prove highly detrimental to health equity.”
There are already concerns about the access of Black and Latinx patients to clinical trials. The planned CED approach would tightly restrict access to aducanumab, as well as expected follow-ons in the amyloid-directed monoclonal antibody (mAb) drug class, the company said.
“Many of the trial sites for Aduhelm, as well as for other amyloid-directed [monoclonal antibodies] are not hospital-based outpatient settings, but include infusion centers, private practices, and medical research centers,” Biogen wrote.
Patient groups such as UsAgainstAlzheimer’s told CMS the CED approach would worsen disparities, despite the aim of Medicare officials to increase participation of Black and Latinx patients in future testing.
“CMS will be hard-pressed to achieve diversity if such hospitals are the only locations where Medicare beneficiaries are able to access mAbs,” USAgainstAlzheimer’s wrote in a Feb. 10 comment.
In contrast, the nonprofit National Center for Health Research praised CMS for what it described as an effort to address a lack of representation of Black and Latinx patients in earlier aducanumab research.
However, the NCHR also suggested CMS revise its plan to mandate that clinical trials include patients who are representative of the national population diagnosed with AD.
“Rather than being concerned about the percentage of patients in specific racial and ethnic groups, we propose that CMS include sufficient numbers of patients in different racial, ethnic, and age groups to ensure that there is enough statistical power for subgroup analyses to determine safety and efficacy for each of the major demographic groups,” the NCHR wrote.
Patient health, Medicare at risk
On Feb. 8, a group of House Republican lawmakers asked CMS to reverse its stance. In a publicly released letter, Rep. Cathy McMorris Rodgers of Washington state, the ranking Republican on the House Energy and Commerce Committee, and colleagues urged broader coverage of aducanumab.
In the letter, the group emphasized the idea of aducanumab as a potential treatment for patients with Down syndrome who are at risk for AD.
“The link between Down Syndrome and AD is still being researched by scientists,” Rep. Rodgers and colleagues wrote.
“However, there appears to be a correlation between the additional 21st chromosome present in people with Down Syndrome and the chromosome’s gene that makes amyloid precursor proteins and can cause a build-up of the beta-amyloid plaques common amongst those with AD,” they add.
On the other hand, CMS garnered earlier support from influential Democrats. On Jan. 13, House Energy and Commerce Chairman Frank Pallone Jr (D-N.J.) and House Oversight and Reform Chairwoman Carolyn B. Maloney (D-N.Y.) released a letter praising CMS for its plan for covering aducanumab.
In addition to the HHS-OIG review of the FDA’s approval of the drug, the two House committees are in the midst of their own investigation of the agency’s decision to clear the drug.
“Any broader coverage determination before there is clarity on Aduhelm’s approval process and findings from the myriad ongoing investigations may put the health of millions of Alzheimer’s patients on the line and the financial stability of the nation’s health insurance program for American seniors at risk,” Rep. Pallone and Rep. Maloney wrote.
A version of this article first appeared on Medscape.com.
Medicare has received a key endorsement of its plan to restrict payment for the controversial Alzheimer’s disease (AD) drug aducanumab (Aduhelm) – but also drew pleas from other groups for more generous reimbursement of the drug, as well as expected similar medications currently in development.
The Centers for Medicare & Medicaid Services received more than 9,900 comments on its plan, according to the current tally posted on its website. However, it is unclear when the final count will be available.
CMS intends to limit federal payment for monoclonal antibodies that target amyloid to clinical trials. Among supporters of this approach is the influential Medicare Payment Advisory Commission, an expert panel that helps Congress and CMS manage the federal health program.
Opponents of the CMS plan include several pharmaceutical companies. Patient and consumer groups, individuals, and lawmakers had mixed views.
CMS officials will weigh the feedback provided in the comments when setting a final coverage policy for aducanumab. It is expected the agency’s final decision will be announced on April 11.
Ongoing debate
The Food and Drug Administration’s unusual approach to clearing the drug for U.S. sales triggered a review of its management of the accelerated approval process by the Office of Inspector General for the Department of Health & Human Services.
The FDA granted an accelerated approval for aducanumab in June based on evidence that the drug clears amyloid in the brain. However, it is unclear whether clearing the protein from the brain results in clinical benefit.
Usually, accelerated approvals precede the completion of phase 3 drug trials, with the FDA allowing early access to a medicine while awaiting confirmatory trials.
In the case of aducanumab, results of the phase 3 confirmatory trials ENGAGE and EMERGE were available at the time of FDA approval. However, interpretation of the findings is controversial.
Biogen contends that the amyloid-clearing effect of the higher dose of aducanumab shown in EMERGE indicates the drug has clinical potential. However, others argue that amyloid clearance does not indicate clinical benefit.
Limiting Medicare coverage of aducanumab for treatment of AD means “the progression of disease, for nearly all beneficiaries, would continue unabated,” Biogen wrote in its comment to CMS.
Conflicting data
Supporters of the CMS plan have a different view of the trial data. They note the failure of aducanumab in the companion ENGAGE trial, while also questioning the magnitude of benefit suggested by even the most positive data cited for the drug in the EMERGE trial.
Both studies used the Clinical Dementia Rating-Sum of Boxes (CDR-SB) score, an 18-point scale measuring cognition and function.
In his comment to CMS, MedPAC chairman Michael E. Chernew, PhD, noted the change in CDR-SB score of 0.39 in EMERGE’s high-dose aducanumab group. CMS has described this as being “less than the 1-2 point change that has been suggested as a minimal clinically important difference,” Dr. Chernew wrote.
MedPAC does not normally comment on Medicare coverage decisions, but did so in this case because of its significance and because of the potential fiscal implications, he noted.
“Though there is only limited, conflicting data on Aduhelm’s clinical effectiveness, Medicare would pay a high price for the product,” Dr. Chernew wrote, pointing out the $28,200 annual U.S. price of the drug.
MedPAC thus endorsed the coverage-with-evidence-development (CED) pathway. Under this approach, Medicare would pay for these drugs when used in clinical trials that meet certain criteria.
Legal challenge?
In its comment to CMS, Biogen questioned the agency’s legal grounds for limiting coverage of aducanumab. A mandate on clinical trials as part of the CED proposal “runs afoul of the Administrative Procedure Act’s prohibition against arbitrary and capricious agency action,” Biogen said.
The drug company argued that its own planned follow-on studies would provide the kind of data Medicare officials want to see. It also argued for greater use of observational data, including real-world evidence, and of information from Medicare claims.
Roche’s Genentech, which is also developing antiamyloid drugs for AD, echoed some of Biogen’s concerns about the aducanumab plan.
CMS’ CED plan would be “unnecessarily restrictive and discouraging for patients living with this destructive disease,” David Burt, executive director for federal government affairs at Genentech, wrote in a comment to CMS.
CMS should clarify that the CED requirement would not apply to cases of FDA-approved antiamyloid therapies that have demonstrated “clinically meaningful improvement,” Mr. Burt added. He noted there are phase 3 trials of drugs in this class that could soon produce data.
CMS should “fully consider the broad ramifications and significant unintended consequences of prematurely placing unduly severe restrictions on the entire class of antiamyloid monoclonal antibodies,” Mr. Burt wrote.
Health care inequity
In its comment to CMS, Biogen also noted the Medicare proposal would “compound the already pervasive inequities in access to treatment and will ultimately prove highly detrimental to health equity.”
There are already concerns about the access of Black and Latinx patients to clinical trials. The planned CED approach would tightly restrict access to aducanumab, as well as expected follow-ons in the amyloid-directed monoclonal antibody (mAb) drug class, the company said.
“Many of the trial sites for Aduhelm, as well as for other amyloid-directed [monoclonal antibodies] are not hospital-based outpatient settings, but include infusion centers, private practices, and medical research centers,” Biogen wrote.
Patient groups such as UsAgainstAlzheimer’s told CMS the CED approach would worsen disparities, despite the aim of Medicare officials to increase participation of Black and Latinx patients in future testing.
“CMS will be hard-pressed to achieve diversity if such hospitals are the only locations where Medicare beneficiaries are able to access mAbs,” USAgainstAlzheimer’s wrote in a Feb. 10 comment.
In contrast, the nonprofit National Center for Health Research praised CMS for what it described as an effort to address a lack of representation of Black and Latinx patients in earlier aducanumab research.
However, the NCHR also suggested CMS revise its plan to mandate that clinical trials include patients who are representative of the national population diagnosed with AD.
“Rather than being concerned about the percentage of patients in specific racial and ethnic groups, we propose that CMS include sufficient numbers of patients in different racial, ethnic, and age groups to ensure that there is enough statistical power for subgroup analyses to determine safety and efficacy for each of the major demographic groups,” the NCHR wrote.
Patient health, Medicare at risk
On Feb. 8, a group of House Republican lawmakers asked CMS to reverse its stance. In a publicly released letter, Rep. Cathy McMorris Rodgers of Washington state, the ranking Republican on the House Energy and Commerce Committee, and colleagues urged broader coverage of aducanumab.
In the letter, the group emphasized the idea of aducanumab as a potential treatment for patients with Down syndrome who are at risk for AD.
“The link between Down Syndrome and AD is still being researched by scientists,” Rep. Rodgers and colleagues wrote.
“However, there appears to be a correlation between the additional 21st chromosome present in people with Down Syndrome and the chromosome’s gene that makes amyloid precursor proteins and can cause a build-up of the beta-amyloid plaques common amongst those with AD,” they add.
On the other hand, CMS garnered earlier support from influential Democrats. On Jan. 13, House Energy and Commerce Chairman Frank Pallone Jr (D-N.J.) and House Oversight and Reform Chairwoman Carolyn B. Maloney (D-N.Y.) released a letter praising CMS for its plan for covering aducanumab.
In addition to the HHS-OIG review of the FDA’s approval of the drug, the two House committees are in the midst of their own investigation of the agency’s decision to clear the drug.
“Any broader coverage determination before there is clarity on Aduhelm’s approval process and findings from the myriad ongoing investigations may put the health of millions of Alzheimer’s patients on the line and the financial stability of the nation’s health insurance program for American seniors at risk,” Rep. Pallone and Rep. Maloney wrote.
A version of this article first appeared on Medscape.com.
Radioactive iodine therapy linked to later malignancy
, including breast cancer, according to a new analysis of the United States SEER cancer registries.
The study included data from 36,311 patients between 1975 and 2017. Among 5-year differentiated thyroid cancer survivors, over a median follow-up of 15.6 years, radioactive iodine treatment was linked to a 23% increased risk of solid tumors. Among 20-year survivors, there was a 47% increased risk in solid tumors and a 46% increased risk of breast cancer. Two-year survivors had a 51% increased risk of hematologic malignancies, including a 92% increased risk of leukemia. The researchers estimate that 6% of all solid tumors, 5% of breast tumors, and 14% of hematologic malignancies among differentiated thyroid cancer patients who have survived at least 1 year are attributable to radioactive iodine (RAI).
“Our study is not the first to show an increased risk of leukemia or solid cancer after RAI therapy, although some may be surprised about the increased risk of breast cancer, which was not observed in some earlier studies on this topic. The large size of our study, our focus on younger patients (who are more susceptible to the late effects of radiation therapy than older patients), and more than 40 years of follow-up, enabled us to provide more precise estimates of these risks. Our findings were not surprising given current understanding of the long-term, carcinogenic effects of radiation exposure,” said lead author Cari Kitahara, PhD, senior investigator in the division of cancer epidemiology and genetics at National Cancer Institute. The risk estimates also are similar to previous studies of exposure to medial and nonmedical radiation sources, she added.
Although radioactive iodine has seen an increase in use for treatment of differentiated thyroid cancer, there is little evidence that it improves outcomes in localized differentiated thyroid cancer, and the American Thyroid Association guidelines recommend against radioactive iodine therapy for low-risk differentiated thyroid cancers smaller than 1 cm, and lower radiation levels for larger tumors. The pediatric guideline suggests a similar approach, except that it doesn’t discourage use of RAI in low-risk differentiated thyroid cancers.
“Physicians should discuss the overall balance of risks and benefits of RAI therapy with their patients. Although RAI has been used in the management of thyroid cancer for many decades, clinical practice guidelines have changed over time and now encourage avoidance of unnecessary or excessive use of RAI therapy for low-risk tumors. Our results suggest that even greater caution and more consideration of the late effects of RAI therapy are needed for younger patients, who are more vulnerable to the carcinogenic effects of radiation exposure and are more likely to experience these long-term effects than older adults,” Dr. Kitahara said.
The study was funded by the National Cancer Institute. Dr. Kitahara has no relevant financial disclosures.
, including breast cancer, according to a new analysis of the United States SEER cancer registries.
The study included data from 36,311 patients between 1975 and 2017. Among 5-year differentiated thyroid cancer survivors, over a median follow-up of 15.6 years, radioactive iodine treatment was linked to a 23% increased risk of solid tumors. Among 20-year survivors, there was a 47% increased risk in solid tumors and a 46% increased risk of breast cancer. Two-year survivors had a 51% increased risk of hematologic malignancies, including a 92% increased risk of leukemia. The researchers estimate that 6% of all solid tumors, 5% of breast tumors, and 14% of hematologic malignancies among differentiated thyroid cancer patients who have survived at least 1 year are attributable to radioactive iodine (RAI).
“Our study is not the first to show an increased risk of leukemia or solid cancer after RAI therapy, although some may be surprised about the increased risk of breast cancer, which was not observed in some earlier studies on this topic. The large size of our study, our focus on younger patients (who are more susceptible to the late effects of radiation therapy than older patients), and more than 40 years of follow-up, enabled us to provide more precise estimates of these risks. Our findings were not surprising given current understanding of the long-term, carcinogenic effects of radiation exposure,” said lead author Cari Kitahara, PhD, senior investigator in the division of cancer epidemiology and genetics at National Cancer Institute. The risk estimates also are similar to previous studies of exposure to medial and nonmedical radiation sources, she added.
Although radioactive iodine has seen an increase in use for treatment of differentiated thyroid cancer, there is little evidence that it improves outcomes in localized differentiated thyroid cancer, and the American Thyroid Association guidelines recommend against radioactive iodine therapy for low-risk differentiated thyroid cancers smaller than 1 cm, and lower radiation levels for larger tumors. The pediatric guideline suggests a similar approach, except that it doesn’t discourage use of RAI in low-risk differentiated thyroid cancers.
“Physicians should discuss the overall balance of risks and benefits of RAI therapy with their patients. Although RAI has been used in the management of thyroid cancer for many decades, clinical practice guidelines have changed over time and now encourage avoidance of unnecessary or excessive use of RAI therapy for low-risk tumors. Our results suggest that even greater caution and more consideration of the late effects of RAI therapy are needed for younger patients, who are more vulnerable to the carcinogenic effects of radiation exposure and are more likely to experience these long-term effects than older adults,” Dr. Kitahara said.
The study was funded by the National Cancer Institute. Dr. Kitahara has no relevant financial disclosures.
, including breast cancer, according to a new analysis of the United States SEER cancer registries.
The study included data from 36,311 patients between 1975 and 2017. Among 5-year differentiated thyroid cancer survivors, over a median follow-up of 15.6 years, radioactive iodine treatment was linked to a 23% increased risk of solid tumors. Among 20-year survivors, there was a 47% increased risk in solid tumors and a 46% increased risk of breast cancer. Two-year survivors had a 51% increased risk of hematologic malignancies, including a 92% increased risk of leukemia. The researchers estimate that 6% of all solid tumors, 5% of breast tumors, and 14% of hematologic malignancies among differentiated thyroid cancer patients who have survived at least 1 year are attributable to radioactive iodine (RAI).
“Our study is not the first to show an increased risk of leukemia or solid cancer after RAI therapy, although some may be surprised about the increased risk of breast cancer, which was not observed in some earlier studies on this topic. The large size of our study, our focus on younger patients (who are more susceptible to the late effects of radiation therapy than older patients), and more than 40 years of follow-up, enabled us to provide more precise estimates of these risks. Our findings were not surprising given current understanding of the long-term, carcinogenic effects of radiation exposure,” said lead author Cari Kitahara, PhD, senior investigator in the division of cancer epidemiology and genetics at National Cancer Institute. The risk estimates also are similar to previous studies of exposure to medial and nonmedical radiation sources, she added.
Although radioactive iodine has seen an increase in use for treatment of differentiated thyroid cancer, there is little evidence that it improves outcomes in localized differentiated thyroid cancer, and the American Thyroid Association guidelines recommend against radioactive iodine therapy for low-risk differentiated thyroid cancers smaller than 1 cm, and lower radiation levels for larger tumors. The pediatric guideline suggests a similar approach, except that it doesn’t discourage use of RAI in low-risk differentiated thyroid cancers.
“Physicians should discuss the overall balance of risks and benefits of RAI therapy with their patients. Although RAI has been used in the management of thyroid cancer for many decades, clinical practice guidelines have changed over time and now encourage avoidance of unnecessary or excessive use of RAI therapy for low-risk tumors. Our results suggest that even greater caution and more consideration of the late effects of RAI therapy are needed for younger patients, who are more vulnerable to the carcinogenic effects of radiation exposure and are more likely to experience these long-term effects than older adults,” Dr. Kitahara said.
The study was funded by the National Cancer Institute. Dr. Kitahara has no relevant financial disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Nedaplatin chemo proves to be a less toxic option for nasopharyngeal carcinoma
Patients with stage II to IVB nasopharyngeal carcinoma who were treated with nedaplatin-based concurrent chemoradiotherapy, achieved 5-year survival rates comparable to those of patients treated with cisplatin chemoradiotherapy, but with fewer toxic effects, shows a study in JAMA Network Open.
The findings confirm that , wrote authors who were led by Lin-Quan Tang, MD, PhD, Sun Yat-sen University Cancer Center, Guangzhou, China.
While the National Comprehensive Cancer Network recommends radiotherapy administered concurrently with 100 mg/m2 of cisplatin every 3 weeks for patients with stage II to IVB nasopharyngeal carcinoma, the addition of cisplatin-based chemotherapy to radiotherapy increases the frequency of treatment-related toxic effects. They include severe gastrointestinal responses, hearing deficits, renal toxic effects, and neurotoxic effects, decreasing treatment adherence and patient quality of life. An antitumor drug with similar therapeutic efficacy to cisplatin but with reduced adverse effects is needed urgently, authors wrote.
The cisplatin analogue nedaplatin, designed to decrease the nephrotoxic and gastrointestinal toxic effects seen with cisplatin, has antitumor mechanisms and efficacy similar to cisplatin. It has demonstrated effectiveness and tolerability in various malignant tumors, and has, in vitro, shown potential as a radiosensitizing agent with nasopharyngeal carcinoma and cervical squamous cell carcinoma cells.
In the initial 2-year results of the phase 3 randomized trial in this population of patients with stage II to IVB nasopharyngeal carcinoma, nedaplatin-based concurrent chemoradiotherapy was noninferior to cisplatin-based concurrent chemoradiotherapy with differences of 1.9% and 1.0% (P = .005 and P = .002), in the intention-to-treat and per-protocol analyses of progression-free survival, respectively. Patients (n = 402) were randomly assigned (1:1) to receive nedaplatin (100 mg/m2)– or cisplatin (100 mg/m2)–based chemotherapy every 3 weeks for three cycles concurrently with intensity-modulated radiotherapy. Information on long-term follow-up and late toxic effects was limited.
In the current analysis of 402 patients (about 25% female, median age 44.5 years), the intention-to-treat 5-year progression-free survival rate was 81.4% (95% CI, 75.9%-86.9%) for the cisplatin group and 79.8% (95% CI, 74.1%-85.5%) for the nedaplatin group, with a difference of 1.6% (95% CI, −6.3% to 9.5%; P = .002 for noninferiority). No significant survival differences were observed between the cisplatin and nedaplatin groups for 5-year overall survival (89.4% vs. 88.8%; P = .63), distant metastasis–free survival (85.9% vs. 90.4%, P = .17), and locoregional relapse–free survival (92.6% vs. 89.6%; P = .17) rates.
The incidence of grade 3 and 4 auditory toxic effects was higher in the cisplatin group than in the nedaplatin group (35 [17.7%] vs. 21 [10.5%], P = .04). Also, the cumulative incidence of grade 3-4 auditory toxic effects was higher in the cisplatin group versus patients in the nedaplatin group (19.9% vs. 12.0%; P = .42). The odds ratio, in a post hoc regression analysis, for auditory toxic effects was 0.51 (0.51; 95% CI, 0.28-0.93; P = .03) for patients in the nedaplatin group.
The findings, the authors concluded, confirm that nedaplatin-based concurrent chemoradiotherapy could be an alternative to cisplatin-based concurrent chemoradiotherapy as doublet therapy for II to IVB nasopharyngeal carcinoma. The potential of nedaplatin in combination drug chemotherapy for nasopharyngeal carcinoma in the induction or adjuvant phase needs to be explored in further investigations, the authors added.
The study was funded by multiple grants; the study investigator reported no conflicts of interest.
Patients with stage II to IVB nasopharyngeal carcinoma who were treated with nedaplatin-based concurrent chemoradiotherapy, achieved 5-year survival rates comparable to those of patients treated with cisplatin chemoradiotherapy, but with fewer toxic effects, shows a study in JAMA Network Open.
The findings confirm that , wrote authors who were led by Lin-Quan Tang, MD, PhD, Sun Yat-sen University Cancer Center, Guangzhou, China.
While the National Comprehensive Cancer Network recommends radiotherapy administered concurrently with 100 mg/m2 of cisplatin every 3 weeks for patients with stage II to IVB nasopharyngeal carcinoma, the addition of cisplatin-based chemotherapy to radiotherapy increases the frequency of treatment-related toxic effects. They include severe gastrointestinal responses, hearing deficits, renal toxic effects, and neurotoxic effects, decreasing treatment adherence and patient quality of life. An antitumor drug with similar therapeutic efficacy to cisplatin but with reduced adverse effects is needed urgently, authors wrote.
The cisplatin analogue nedaplatin, designed to decrease the nephrotoxic and gastrointestinal toxic effects seen with cisplatin, has antitumor mechanisms and efficacy similar to cisplatin. It has demonstrated effectiveness and tolerability in various malignant tumors, and has, in vitro, shown potential as a radiosensitizing agent with nasopharyngeal carcinoma and cervical squamous cell carcinoma cells.
In the initial 2-year results of the phase 3 randomized trial in this population of patients with stage II to IVB nasopharyngeal carcinoma, nedaplatin-based concurrent chemoradiotherapy was noninferior to cisplatin-based concurrent chemoradiotherapy with differences of 1.9% and 1.0% (P = .005 and P = .002), in the intention-to-treat and per-protocol analyses of progression-free survival, respectively. Patients (n = 402) were randomly assigned (1:1) to receive nedaplatin (100 mg/m2)– or cisplatin (100 mg/m2)–based chemotherapy every 3 weeks for three cycles concurrently with intensity-modulated radiotherapy. Information on long-term follow-up and late toxic effects was limited.
In the current analysis of 402 patients (about 25% female, median age 44.5 years), the intention-to-treat 5-year progression-free survival rate was 81.4% (95% CI, 75.9%-86.9%) for the cisplatin group and 79.8% (95% CI, 74.1%-85.5%) for the nedaplatin group, with a difference of 1.6% (95% CI, −6.3% to 9.5%; P = .002 for noninferiority). No significant survival differences were observed between the cisplatin and nedaplatin groups for 5-year overall survival (89.4% vs. 88.8%; P = .63), distant metastasis–free survival (85.9% vs. 90.4%, P = .17), and locoregional relapse–free survival (92.6% vs. 89.6%; P = .17) rates.
The incidence of grade 3 and 4 auditory toxic effects was higher in the cisplatin group than in the nedaplatin group (35 [17.7%] vs. 21 [10.5%], P = .04). Also, the cumulative incidence of grade 3-4 auditory toxic effects was higher in the cisplatin group versus patients in the nedaplatin group (19.9% vs. 12.0%; P = .42). The odds ratio, in a post hoc regression analysis, for auditory toxic effects was 0.51 (0.51; 95% CI, 0.28-0.93; P = .03) for patients in the nedaplatin group.
The findings, the authors concluded, confirm that nedaplatin-based concurrent chemoradiotherapy could be an alternative to cisplatin-based concurrent chemoradiotherapy as doublet therapy for II to IVB nasopharyngeal carcinoma. The potential of nedaplatin in combination drug chemotherapy for nasopharyngeal carcinoma in the induction or adjuvant phase needs to be explored in further investigations, the authors added.
The study was funded by multiple grants; the study investigator reported no conflicts of interest.
Patients with stage II to IVB nasopharyngeal carcinoma who were treated with nedaplatin-based concurrent chemoradiotherapy, achieved 5-year survival rates comparable to those of patients treated with cisplatin chemoradiotherapy, but with fewer toxic effects, shows a study in JAMA Network Open.
The findings confirm that , wrote authors who were led by Lin-Quan Tang, MD, PhD, Sun Yat-sen University Cancer Center, Guangzhou, China.
While the National Comprehensive Cancer Network recommends radiotherapy administered concurrently with 100 mg/m2 of cisplatin every 3 weeks for patients with stage II to IVB nasopharyngeal carcinoma, the addition of cisplatin-based chemotherapy to radiotherapy increases the frequency of treatment-related toxic effects. They include severe gastrointestinal responses, hearing deficits, renal toxic effects, and neurotoxic effects, decreasing treatment adherence and patient quality of life. An antitumor drug with similar therapeutic efficacy to cisplatin but with reduced adverse effects is needed urgently, authors wrote.
The cisplatin analogue nedaplatin, designed to decrease the nephrotoxic and gastrointestinal toxic effects seen with cisplatin, has antitumor mechanisms and efficacy similar to cisplatin. It has demonstrated effectiveness and tolerability in various malignant tumors, and has, in vitro, shown potential as a radiosensitizing agent with nasopharyngeal carcinoma and cervical squamous cell carcinoma cells.
In the initial 2-year results of the phase 3 randomized trial in this population of patients with stage II to IVB nasopharyngeal carcinoma, nedaplatin-based concurrent chemoradiotherapy was noninferior to cisplatin-based concurrent chemoradiotherapy with differences of 1.9% and 1.0% (P = .005 and P = .002), in the intention-to-treat and per-protocol analyses of progression-free survival, respectively. Patients (n = 402) were randomly assigned (1:1) to receive nedaplatin (100 mg/m2)– or cisplatin (100 mg/m2)–based chemotherapy every 3 weeks for three cycles concurrently with intensity-modulated radiotherapy. Information on long-term follow-up and late toxic effects was limited.
In the current analysis of 402 patients (about 25% female, median age 44.5 years), the intention-to-treat 5-year progression-free survival rate was 81.4% (95% CI, 75.9%-86.9%) for the cisplatin group and 79.8% (95% CI, 74.1%-85.5%) for the nedaplatin group, with a difference of 1.6% (95% CI, −6.3% to 9.5%; P = .002 for noninferiority). No significant survival differences were observed between the cisplatin and nedaplatin groups for 5-year overall survival (89.4% vs. 88.8%; P = .63), distant metastasis–free survival (85.9% vs. 90.4%, P = .17), and locoregional relapse–free survival (92.6% vs. 89.6%; P = .17) rates.
The incidence of grade 3 and 4 auditory toxic effects was higher in the cisplatin group than in the nedaplatin group (35 [17.7%] vs. 21 [10.5%], P = .04). Also, the cumulative incidence of grade 3-4 auditory toxic effects was higher in the cisplatin group versus patients in the nedaplatin group (19.9% vs. 12.0%; P = .42). The odds ratio, in a post hoc regression analysis, for auditory toxic effects was 0.51 (0.51; 95% CI, 0.28-0.93; P = .03) for patients in the nedaplatin group.
The findings, the authors concluded, confirm that nedaplatin-based concurrent chemoradiotherapy could be an alternative to cisplatin-based concurrent chemoradiotherapy as doublet therapy for II to IVB nasopharyngeal carcinoma. The potential of nedaplatin in combination drug chemotherapy for nasopharyngeal carcinoma in the induction or adjuvant phase needs to be explored in further investigations, the authors added.
The study was funded by multiple grants; the study investigator reported no conflicts of interest.
FROM JAMA NETWORK OPEN
Patients are interrupting DMARD use well into the COVID-19 pandemic
The COVID-19 pandemic led to a decrease in the proportion of patients with rheumatic diseases who stopped taking their disease-modifying antirheumatic drugs (DMARDs), but the percentage who interrupted DMARD treatment increased later in the pandemic, according to speakers at the 2022 Rheumatology Winter Clinical Symposium.
“People seem to be less anxious, but they’re interrupting their DMARD therapy more, more recently than in the pits of COVID, if you will,” said Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, and director of RWCS.
Dr. Kavanaugh and his copresenter Jack Cush, MD, were discussing the results of a recent study published in Arthritis Care & Research that evaluated 2,424 patients with rheumatic diseases who completed a baseline and at least one follow-up survey issued by patient organizations between March 2020 and May 2021, with a median of five follow-up surveys completed. The patients included in the study were aged a mean of 57 years, 86.6% were women, 90.5% were White, 41.8% had rheumatoid arthritis (RA), 14.8% had antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, and 12.4% had psoriatic arthritis. Overall, 52.6% were on biologics or a Janus kinase (JAK) inhibitor, 30.0% were receiving methotrexate, 21.4% were taking hydroxychloroquine, and 28.6% were receiving low-dose (24.0%) or high-dose (4.6%) glucocorticoids.
Patients’ T-scores on the anxiety short form Patient-Reported Outcomes Measurement Information System (PROMIS) survey significantly decreased from a score of 58.7 in April 2020 to a score of 53.7 in May 2021 (P < .001), but there was a significant decrease in the interruption of DMARD treatment between April and December 2020 (11.2% vs. 7.5%; P < .001). This percentage rose significantly to 14.0% by May 2021 (P < .001). Patients who stopped using DMARDs were significantly associated with predicted incidence of severe flare in the next survey in adjusted models (12.9% vs. 8.0%; odds ratio, 1.71; 95% confidence interval, 1.23-2.36).
The results tell us “that we as a discipline are not doing a good job educating our patients,” said Dr. Cush, a rheumatologist based in Dallas, Tex., and executive editor of RheumNow.com.
“I wish we – and I’m really talking about myself – but myself and my practice were more proactive when COVID happened [in] sending out regular bulletins: ‘Don’t stop your therapy; these are the things you get; get the test that you need to get done,’ ” he said. “We let a lot of things go on autopilot with the patient driving throughout COVID. Even now, it’s happening. And this is a problem, and there are going to be consequences to this.”
Dr. Kavanaugh agreed with Dr. Cush’s assessment, suggesting that the pandemic came up quickly enough that it was difficult to be proactive with the situation.
Patients on JAK inhibitors as new COVID-19 risk group?
Another standout study on COVID-19 from 2021 was an analysis of the COVID-19 Global Rheumatology Alliance physician registry that examined risk of COVID-19 severity for patients with RA taking biologic or targeted synthetic DMARDs (tsDMARDs), which was presented at the 2021 EULAR congress and later published in Annals of the Rheumatic Diseases.
The researchers evaluated 2,869 patients March 2020 and April 2021 who were receiving abatacept (237 patients), rituximab (364 patients), interleukin (IL)-6 inhibitors (317 patients), JAK inhibitors (563 patients), or tumor necrosis factor (TNF) inhibitors such as infliximab, etanercept, adalimumab, certolizumab pegol, and golimumab (1,388 patients) before developing COVID-19. Data about biologics or tsDMARDs were collected as a drug class. Patients in the study were mostly White (69.0%) women (80.8%) with a mean age of 56.7 years who lived in Europe (51.8%) or North America (35.0%). The researchers examined the severity of COVID-19 among all patients studied and calculated odds ratios based on drug class, with the TNF inhibitor group serving as a reference.
“[I]n this case, they said that the baseline use of rituximab was associated with more severity, and you see the severity being hospitalization and ICU and deaths. They found a signal for the JAK inhibitors that is not found in the other studies,” Dr. Kavanaugh said.
Overall, they found 21% of patients in the registry were hospitalized and 5.5% died, with rituximab (OR, 4.15; 95% CI, 3.16-5.44) and JAK inhibitors (OR, 2.06; 95% CI, 1.60-2.65) associated with more severe COVID-19 outcomes. Specifically, rituximab was associated with greater likelihood of hospitalization (OR, 4.53; 95% CI, 3.32-6.18), hospitalization with oxygen/ventilation (OR, 2.87; 95% CI, 2.03-4.06), need for mechanical ventilation (OR, 4.05; 95% CI, 3.08-5.33), and mortality (OR, 4.57; 95% CI, 3.32-9.01), compared with TNF inhibitors. For JAK inhibitors, there was also a greater likelihood of hospitalization (OR, 2.40; 95% CI, 1.78-3.24), hospitalization with oxygen/ventilation (OR, 1.55; 95% CI, 1.04-2.18), need for mechanical ventilation (OR, 2.03; 95% CI, 1.56-2.62), and mortality (OR, 2.04; 95% CI, 1.58-2.65), compared with the TNF inhibitors group. Associations between COVID-19 severity and abatacept or IL-6 inhibitors were not identified.
Commenting on the study in a question-and-answer session, Roy Fleischmann, MD, said the part of the study that identified a signal for JAK inhibitors was “very interesting.” He called attention to a rapid response comment to the study, which questioned if it was the drug class itself that caused the risk for severe disease. “This is very important, because actually, the patients who stop the JAK [inhibitor], that’s what drove the illness. The patients [who] continued the JAK [inhibitor], very few of them had illness,” said Dr. Fleischmann, clinical professor of medicine at the University of Texas Southwestern Medical School and codirector of the Metroplex Clinical Research Center, both in Dallas, Tex.
Confusion among patients during COVID-19
Alvin Wells, MD, PhD, asked the copresenters during the Q&A session whether they had any clinical pearls for the audience on how they manage treatment of patients with rheumatic disease with potential COVID-19 risk. “I think the confusion with our patients and COVID is what the ACR has put out with their guidelines,” said Dr. Wells, director of the department of rheumatology at Advocate Aurora Health in Franklin, Wisc.
Dr. Cush said he has three rules he follows: lower and discontinue steroids, avoid rituximab as a starting treatment and negotiate if patients are already taking it, and don’t stop any therapy.
“I want disease control. I think being under control is what keeps you away from risk of COVID and hospitalization,” Dr. Cush said. “I think being uncontrolled and inflamed, whether it’s our [patients with] inflammatory arthritis or lupus or, worse, vasculitis [or] myositis, those are the ones at high risk of progression from being just infected to being sick and in the hospital.”
Eric Ruderman, MD, professor of rheumatology at Northwestern University, Chicago, posed the question of getting somewhat back to normal during COVID-19 with regard to recently infected patients presenting at infusion centers, whether patients are more likely to continue testing positive, and when patients are cleared to come back. Dr. Ruderman said his center has a 20-day rule for returning after having COVID-19, while Dr. Cush said his center allows patients to come in if they test negative after 7-10 days.
“One of the things we’re struggling with is our infusion center, and one of the questions that keeps coming up is when can people come back after a COVID infection?” he said. “If you’re on a drug at home, that’s up to you and the patient. But in the infusion [center], then you have other people sitting around there.”
Dr. Kavanaugh said there is no current data for how long patients with rheumatic disease shed virus, or how long a positive test can be measured. “You definitely will continue to shed, and you’ll be detectable for a while,” he said.
Dr. Cush and Dr. Kavanaugh reported having financial relationships with numerous pharmaceutical companies.
The COVID-19 pandemic led to a decrease in the proportion of patients with rheumatic diseases who stopped taking their disease-modifying antirheumatic drugs (DMARDs), but the percentage who interrupted DMARD treatment increased later in the pandemic, according to speakers at the 2022 Rheumatology Winter Clinical Symposium.
“People seem to be less anxious, but they’re interrupting their DMARD therapy more, more recently than in the pits of COVID, if you will,” said Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, and director of RWCS.
Dr. Kavanaugh and his copresenter Jack Cush, MD, were discussing the results of a recent study published in Arthritis Care & Research that evaluated 2,424 patients with rheumatic diseases who completed a baseline and at least one follow-up survey issued by patient organizations between March 2020 and May 2021, with a median of five follow-up surveys completed. The patients included in the study were aged a mean of 57 years, 86.6% were women, 90.5% were White, 41.8% had rheumatoid arthritis (RA), 14.8% had antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, and 12.4% had psoriatic arthritis. Overall, 52.6% were on biologics or a Janus kinase (JAK) inhibitor, 30.0% were receiving methotrexate, 21.4% were taking hydroxychloroquine, and 28.6% were receiving low-dose (24.0%) or high-dose (4.6%) glucocorticoids.
Patients’ T-scores on the anxiety short form Patient-Reported Outcomes Measurement Information System (PROMIS) survey significantly decreased from a score of 58.7 in April 2020 to a score of 53.7 in May 2021 (P < .001), but there was a significant decrease in the interruption of DMARD treatment between April and December 2020 (11.2% vs. 7.5%; P < .001). This percentage rose significantly to 14.0% by May 2021 (P < .001). Patients who stopped using DMARDs were significantly associated with predicted incidence of severe flare in the next survey in adjusted models (12.9% vs. 8.0%; odds ratio, 1.71; 95% confidence interval, 1.23-2.36).
The results tell us “that we as a discipline are not doing a good job educating our patients,” said Dr. Cush, a rheumatologist based in Dallas, Tex., and executive editor of RheumNow.com.
“I wish we – and I’m really talking about myself – but myself and my practice were more proactive when COVID happened [in] sending out regular bulletins: ‘Don’t stop your therapy; these are the things you get; get the test that you need to get done,’ ” he said. “We let a lot of things go on autopilot with the patient driving throughout COVID. Even now, it’s happening. And this is a problem, and there are going to be consequences to this.”
Dr. Kavanaugh agreed with Dr. Cush’s assessment, suggesting that the pandemic came up quickly enough that it was difficult to be proactive with the situation.
Patients on JAK inhibitors as new COVID-19 risk group?
Another standout study on COVID-19 from 2021 was an analysis of the COVID-19 Global Rheumatology Alliance physician registry that examined risk of COVID-19 severity for patients with RA taking biologic or targeted synthetic DMARDs (tsDMARDs), which was presented at the 2021 EULAR congress and later published in Annals of the Rheumatic Diseases.
The researchers evaluated 2,869 patients March 2020 and April 2021 who were receiving abatacept (237 patients), rituximab (364 patients), interleukin (IL)-6 inhibitors (317 patients), JAK inhibitors (563 patients), or tumor necrosis factor (TNF) inhibitors such as infliximab, etanercept, adalimumab, certolizumab pegol, and golimumab (1,388 patients) before developing COVID-19. Data about biologics or tsDMARDs were collected as a drug class. Patients in the study were mostly White (69.0%) women (80.8%) with a mean age of 56.7 years who lived in Europe (51.8%) or North America (35.0%). The researchers examined the severity of COVID-19 among all patients studied and calculated odds ratios based on drug class, with the TNF inhibitor group serving as a reference.
“[I]n this case, they said that the baseline use of rituximab was associated with more severity, and you see the severity being hospitalization and ICU and deaths. They found a signal for the JAK inhibitors that is not found in the other studies,” Dr. Kavanaugh said.
Overall, they found 21% of patients in the registry were hospitalized and 5.5% died, with rituximab (OR, 4.15; 95% CI, 3.16-5.44) and JAK inhibitors (OR, 2.06; 95% CI, 1.60-2.65) associated with more severe COVID-19 outcomes. Specifically, rituximab was associated with greater likelihood of hospitalization (OR, 4.53; 95% CI, 3.32-6.18), hospitalization with oxygen/ventilation (OR, 2.87; 95% CI, 2.03-4.06), need for mechanical ventilation (OR, 4.05; 95% CI, 3.08-5.33), and mortality (OR, 4.57; 95% CI, 3.32-9.01), compared with TNF inhibitors. For JAK inhibitors, there was also a greater likelihood of hospitalization (OR, 2.40; 95% CI, 1.78-3.24), hospitalization with oxygen/ventilation (OR, 1.55; 95% CI, 1.04-2.18), need for mechanical ventilation (OR, 2.03; 95% CI, 1.56-2.62), and mortality (OR, 2.04; 95% CI, 1.58-2.65), compared with the TNF inhibitors group. Associations between COVID-19 severity and abatacept or IL-6 inhibitors were not identified.
Commenting on the study in a question-and-answer session, Roy Fleischmann, MD, said the part of the study that identified a signal for JAK inhibitors was “very interesting.” He called attention to a rapid response comment to the study, which questioned if it was the drug class itself that caused the risk for severe disease. “This is very important, because actually, the patients who stop the JAK [inhibitor], that’s what drove the illness. The patients [who] continued the JAK [inhibitor], very few of them had illness,” said Dr. Fleischmann, clinical professor of medicine at the University of Texas Southwestern Medical School and codirector of the Metroplex Clinical Research Center, both in Dallas, Tex.
Confusion among patients during COVID-19
Alvin Wells, MD, PhD, asked the copresenters during the Q&A session whether they had any clinical pearls for the audience on how they manage treatment of patients with rheumatic disease with potential COVID-19 risk. “I think the confusion with our patients and COVID is what the ACR has put out with their guidelines,” said Dr. Wells, director of the department of rheumatology at Advocate Aurora Health in Franklin, Wisc.
Dr. Cush said he has three rules he follows: lower and discontinue steroids, avoid rituximab as a starting treatment and negotiate if patients are already taking it, and don’t stop any therapy.
“I want disease control. I think being under control is what keeps you away from risk of COVID and hospitalization,” Dr. Cush said. “I think being uncontrolled and inflamed, whether it’s our [patients with] inflammatory arthritis or lupus or, worse, vasculitis [or] myositis, those are the ones at high risk of progression from being just infected to being sick and in the hospital.”
Eric Ruderman, MD, professor of rheumatology at Northwestern University, Chicago, posed the question of getting somewhat back to normal during COVID-19 with regard to recently infected patients presenting at infusion centers, whether patients are more likely to continue testing positive, and when patients are cleared to come back. Dr. Ruderman said his center has a 20-day rule for returning after having COVID-19, while Dr. Cush said his center allows patients to come in if they test negative after 7-10 days.
“One of the things we’re struggling with is our infusion center, and one of the questions that keeps coming up is when can people come back after a COVID infection?” he said. “If you’re on a drug at home, that’s up to you and the patient. But in the infusion [center], then you have other people sitting around there.”
Dr. Kavanaugh said there is no current data for how long patients with rheumatic disease shed virus, or how long a positive test can be measured. “You definitely will continue to shed, and you’ll be detectable for a while,” he said.
Dr. Cush and Dr. Kavanaugh reported having financial relationships with numerous pharmaceutical companies.
The COVID-19 pandemic led to a decrease in the proportion of patients with rheumatic diseases who stopped taking their disease-modifying antirheumatic drugs (DMARDs), but the percentage who interrupted DMARD treatment increased later in the pandemic, according to speakers at the 2022 Rheumatology Winter Clinical Symposium.
“People seem to be less anxious, but they’re interrupting their DMARD therapy more, more recently than in the pits of COVID, if you will,” said Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, and director of RWCS.
Dr. Kavanaugh and his copresenter Jack Cush, MD, were discussing the results of a recent study published in Arthritis Care & Research that evaluated 2,424 patients with rheumatic diseases who completed a baseline and at least one follow-up survey issued by patient organizations between March 2020 and May 2021, with a median of five follow-up surveys completed. The patients included in the study were aged a mean of 57 years, 86.6% were women, 90.5% were White, 41.8% had rheumatoid arthritis (RA), 14.8% had antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, and 12.4% had psoriatic arthritis. Overall, 52.6% were on biologics or a Janus kinase (JAK) inhibitor, 30.0% were receiving methotrexate, 21.4% were taking hydroxychloroquine, and 28.6% were receiving low-dose (24.0%) or high-dose (4.6%) glucocorticoids.
Patients’ T-scores on the anxiety short form Patient-Reported Outcomes Measurement Information System (PROMIS) survey significantly decreased from a score of 58.7 in April 2020 to a score of 53.7 in May 2021 (P < .001), but there was a significant decrease in the interruption of DMARD treatment between April and December 2020 (11.2% vs. 7.5%; P < .001). This percentage rose significantly to 14.0% by May 2021 (P < .001). Patients who stopped using DMARDs were significantly associated with predicted incidence of severe flare in the next survey in adjusted models (12.9% vs. 8.0%; odds ratio, 1.71; 95% confidence interval, 1.23-2.36).
The results tell us “that we as a discipline are not doing a good job educating our patients,” said Dr. Cush, a rheumatologist based in Dallas, Tex., and executive editor of RheumNow.com.
“I wish we – and I’m really talking about myself – but myself and my practice were more proactive when COVID happened [in] sending out regular bulletins: ‘Don’t stop your therapy; these are the things you get; get the test that you need to get done,’ ” he said. “We let a lot of things go on autopilot with the patient driving throughout COVID. Even now, it’s happening. And this is a problem, and there are going to be consequences to this.”
Dr. Kavanaugh agreed with Dr. Cush’s assessment, suggesting that the pandemic came up quickly enough that it was difficult to be proactive with the situation.
Patients on JAK inhibitors as new COVID-19 risk group?
Another standout study on COVID-19 from 2021 was an analysis of the COVID-19 Global Rheumatology Alliance physician registry that examined risk of COVID-19 severity for patients with RA taking biologic or targeted synthetic DMARDs (tsDMARDs), which was presented at the 2021 EULAR congress and later published in Annals of the Rheumatic Diseases.
The researchers evaluated 2,869 patients March 2020 and April 2021 who were receiving abatacept (237 patients), rituximab (364 patients), interleukin (IL)-6 inhibitors (317 patients), JAK inhibitors (563 patients), or tumor necrosis factor (TNF) inhibitors such as infliximab, etanercept, adalimumab, certolizumab pegol, and golimumab (1,388 patients) before developing COVID-19. Data about biologics or tsDMARDs were collected as a drug class. Patients in the study were mostly White (69.0%) women (80.8%) with a mean age of 56.7 years who lived in Europe (51.8%) or North America (35.0%). The researchers examined the severity of COVID-19 among all patients studied and calculated odds ratios based on drug class, with the TNF inhibitor group serving as a reference.
“[I]n this case, they said that the baseline use of rituximab was associated with more severity, and you see the severity being hospitalization and ICU and deaths. They found a signal for the JAK inhibitors that is not found in the other studies,” Dr. Kavanaugh said.
Overall, they found 21% of patients in the registry were hospitalized and 5.5% died, with rituximab (OR, 4.15; 95% CI, 3.16-5.44) and JAK inhibitors (OR, 2.06; 95% CI, 1.60-2.65) associated with more severe COVID-19 outcomes. Specifically, rituximab was associated with greater likelihood of hospitalization (OR, 4.53; 95% CI, 3.32-6.18), hospitalization with oxygen/ventilation (OR, 2.87; 95% CI, 2.03-4.06), need for mechanical ventilation (OR, 4.05; 95% CI, 3.08-5.33), and mortality (OR, 4.57; 95% CI, 3.32-9.01), compared with TNF inhibitors. For JAK inhibitors, there was also a greater likelihood of hospitalization (OR, 2.40; 95% CI, 1.78-3.24), hospitalization with oxygen/ventilation (OR, 1.55; 95% CI, 1.04-2.18), need for mechanical ventilation (OR, 2.03; 95% CI, 1.56-2.62), and mortality (OR, 2.04; 95% CI, 1.58-2.65), compared with the TNF inhibitors group. Associations between COVID-19 severity and abatacept or IL-6 inhibitors were not identified.
Commenting on the study in a question-and-answer session, Roy Fleischmann, MD, said the part of the study that identified a signal for JAK inhibitors was “very interesting.” He called attention to a rapid response comment to the study, which questioned if it was the drug class itself that caused the risk for severe disease. “This is very important, because actually, the patients who stop the JAK [inhibitor], that’s what drove the illness. The patients [who] continued the JAK [inhibitor], very few of them had illness,” said Dr. Fleischmann, clinical professor of medicine at the University of Texas Southwestern Medical School and codirector of the Metroplex Clinical Research Center, both in Dallas, Tex.
Confusion among patients during COVID-19
Alvin Wells, MD, PhD, asked the copresenters during the Q&A session whether they had any clinical pearls for the audience on how they manage treatment of patients with rheumatic disease with potential COVID-19 risk. “I think the confusion with our patients and COVID is what the ACR has put out with their guidelines,” said Dr. Wells, director of the department of rheumatology at Advocate Aurora Health in Franklin, Wisc.
Dr. Cush said he has three rules he follows: lower and discontinue steroids, avoid rituximab as a starting treatment and negotiate if patients are already taking it, and don’t stop any therapy.
“I want disease control. I think being under control is what keeps you away from risk of COVID and hospitalization,” Dr. Cush said. “I think being uncontrolled and inflamed, whether it’s our [patients with] inflammatory arthritis or lupus or, worse, vasculitis [or] myositis, those are the ones at high risk of progression from being just infected to being sick and in the hospital.”
Eric Ruderman, MD, professor of rheumatology at Northwestern University, Chicago, posed the question of getting somewhat back to normal during COVID-19 with regard to recently infected patients presenting at infusion centers, whether patients are more likely to continue testing positive, and when patients are cleared to come back. Dr. Ruderman said his center has a 20-day rule for returning after having COVID-19, while Dr. Cush said his center allows patients to come in if they test negative after 7-10 days.
“One of the things we’re struggling with is our infusion center, and one of the questions that keeps coming up is when can people come back after a COVID infection?” he said. “If you’re on a drug at home, that’s up to you and the patient. But in the infusion [center], then you have other people sitting around there.”
Dr. Kavanaugh said there is no current data for how long patients with rheumatic disease shed virus, or how long a positive test can be measured. “You definitely will continue to shed, and you’ll be detectable for a while,” he said.
Dr. Cush and Dr. Kavanaugh reported having financial relationships with numerous pharmaceutical companies.
FROM RWCS 2022
Diversity among oncologists has not kept pace with the U.S. population
in these fields, according to a cross-sectional study of data from the Association of American Medical Colleges.
“Creating and maintaining a diverse health care workforce is a priority to help combat societal inequities and health disparities, particularly in light of the evolving demographic characteristics of the general U.S. population,” wrote authors who were led by Sophia C. Kamran, MD, a radiation oncologist with Massachusetts General Hospital, Boston.
The study, which was published Dec. 9 in JAMA Oncology, surveyed full-time U.S.-based faculty in radiation and medical oncology departments from 1970 through 2019.
Improved patient satisfaction, compliance, and outcomes have been documented when a health care workforce better reflects the demographic traits of those whom it serves, Dr. Kamran and associates wrote.
They point to recent increases in the number and urgency of calls for improved diversity in the health care workforce, citing also higher incidence and mortality of new cancer cases among Black, indigenous, and Hispanic populations, compared with their non-Hispanic White counterparts. Prior calls for health care work force diversity have led to some creation of opportunities and pathways for increased representation of women and racial and ethnic minority groups in medicine, and the overall diversity of medical school faculty has been increasing by race and ethnicity and sex.
The change, however, is of lesser magnitude than what has been seen among medical school applicants, students, and graduates, and the gains in medical school faculty diversity have not kept pace with increasing diversity of the U.S. population. It has remained unclear whether corresponding progress has occurred in the composition of radiation oncology and medical oncology departments during the last 5 decades.
Despite lack of diversity, total faculty numbers have increased
Dr. Kamran and associates’ analysis revealed that total faculty numbers increased over time in both radiation oncology and medical oncology, with faculty representation of underrepresented-in-medicine (URM) women proportionally increased by 0.1% per decade in both radiation oncology (95% confidence interval, 0.005%-0.110%; P < . 001 for trend) and medical oncology (95% CI, −0.03% to 0.16%; P = .06 for trend), compared with non–URM women faculty, which increased by 0.4% (95% CI, 0.25%-0.80%) per decade in radiation oncology and 0.7% (95% CI, 0.47%-0.87%) per decade in medical oncology (P < .001 for trend for both). Faculty representation of URM men did not significantly change for radiation oncology (0.03% per decade [95% CI, −0.008% to 0.065%]; P = .09 for trend) or for medical oncology (0.003% per decade [95% CI, −0.13% to 0.14%]; P = .94 for trend).
In both 2009 and 2019, representation of both women and URM individuals for both specialties was less than their representation in the U.S. population. Radiation oncology faculty had the lowest URM representation in 2019 at 5.1%. The number of total URM faculty represented among both medical oncology and radiation oncology remained low for every rank in 2019 (Medical oncology: instructor, 2 of 44 [5%]; assistant professor, 18 of 274 [7%]; associate professor, 13 of 177 [7%]; full professor, 13 of 276 [5%]. Radiation oncology: instructor, 9 of 147 [6%]; assistant professor, 57 of 927 [6%]; associate professor, 20 of 510 [4%]; full professor, 18 of 452 [4%]).
“Our results highlight significant diversity differences along the career ladder in both specialties, with women having lower academic rank than men throughout the study period, and underrepresented [racial and ethnic groups] at every rank,” the authors wrote.
And, although Black, Hispanic, and indigenous people make up about 31% of the U.S. population, their inclusion in the health care workforce trails at all stages in the pipeline, the investigators found.
Diversity among radiation and medical oncologists lags behind that of medical school diversity in general, which has grown through efforts by the Association of American Medical Colleges.
Despite some improvements, the authors suggest the need for more initiatives to retain racial and ethnic minorities in an effort to reflect the diversity of the U.S. cancer population.
“This is a multifactorial issue, with focus not only on increasing diversity of the upstream pipeline but maintaining diversity throughout the entire pipeline, requiring difficult but necessary conversations about racial and ethnic systemic bias, lack of exposure and opportunities, and financial toxicities and pressures, to name a few. Until these factors are further delineated and better addressed, focused and targeted mentorship is key,” the authors wrote.
Small steps can have a collective impact
In a commentary published with the study, Frederick Lansigan, MD, and Charles R. Thomas Jr, MD, both of the Norris Cotton Cancer Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., called for a systemic change in hiring practices.
“Any small steps of change that contribute to supporting the issues highlighted by the Kamran et al. study can have a collective positive impact. A holistic evaluation of [underrepresented] applicants at all stages of education and training is paramount, and joining selection committees is necessary to ensure fair processes. Mentoring programs, leadership courses, and addressing microaggressions and mistreatment may improve retention of [underrepresented] medical school matriculants and trainees in oncology. Cancer centers can build and lead visible and tangible diversity, equity, inclusion, justice, and belonging efforts as we are doing at our institution,” the physicians wrote.
But above all, Dr. Lansigan and Dr. Thomas said that the oncology community needs to agree that intentionally increasing the number of underrepresented physicians in the U.S. workforce is necessary to better address health care inequities.
“We need all hands on deck to reduce structural barriers in early education. We need STEM programs that start in elementary school and offer support through college. Oncologists can mentor these early learners to highlight the positive aspects of a career in oncology, the importance of [underrepresented] physicians in oncology, and the resilience required in caring for those with serious illness, many of whom will come from underserved populations. “Physicians and public health experts themselves who are interested in tackling the discrepancy between [underrepresented] and [non-underrepresented] medical school [students] and oncology trainees need to seek and be elected into positions that can start to balance this equation. If more are willing to acknowledge the structural inequities that exist in the oncology workforce pipeline, we can start to solve the complex equation of structural inequities.”
Dr Lansigan reported being the Interim Associate Dean of Diversity, Equity, and Inclusion at the Geisel School of Medicine and the Principal of Diversity, Equity, and Inclusion for the department of medicine at Dartmouth-Hitchcock Medical Center. No other disclosures were reported.
in these fields, according to a cross-sectional study of data from the Association of American Medical Colleges.
“Creating and maintaining a diverse health care workforce is a priority to help combat societal inequities and health disparities, particularly in light of the evolving demographic characteristics of the general U.S. population,” wrote authors who were led by Sophia C. Kamran, MD, a radiation oncologist with Massachusetts General Hospital, Boston.
The study, which was published Dec. 9 in JAMA Oncology, surveyed full-time U.S.-based faculty in radiation and medical oncology departments from 1970 through 2019.
Improved patient satisfaction, compliance, and outcomes have been documented when a health care workforce better reflects the demographic traits of those whom it serves, Dr. Kamran and associates wrote.
They point to recent increases in the number and urgency of calls for improved diversity in the health care workforce, citing also higher incidence and mortality of new cancer cases among Black, indigenous, and Hispanic populations, compared with their non-Hispanic White counterparts. Prior calls for health care work force diversity have led to some creation of opportunities and pathways for increased representation of women and racial and ethnic minority groups in medicine, and the overall diversity of medical school faculty has been increasing by race and ethnicity and sex.
The change, however, is of lesser magnitude than what has been seen among medical school applicants, students, and graduates, and the gains in medical school faculty diversity have not kept pace with increasing diversity of the U.S. population. It has remained unclear whether corresponding progress has occurred in the composition of radiation oncology and medical oncology departments during the last 5 decades.
Despite lack of diversity, total faculty numbers have increased
Dr. Kamran and associates’ analysis revealed that total faculty numbers increased over time in both radiation oncology and medical oncology, with faculty representation of underrepresented-in-medicine (URM) women proportionally increased by 0.1% per decade in both radiation oncology (95% confidence interval, 0.005%-0.110%; P < . 001 for trend) and medical oncology (95% CI, −0.03% to 0.16%; P = .06 for trend), compared with non–URM women faculty, which increased by 0.4% (95% CI, 0.25%-0.80%) per decade in radiation oncology and 0.7% (95% CI, 0.47%-0.87%) per decade in medical oncology (P < .001 for trend for both). Faculty representation of URM men did not significantly change for radiation oncology (0.03% per decade [95% CI, −0.008% to 0.065%]; P = .09 for trend) or for medical oncology (0.003% per decade [95% CI, −0.13% to 0.14%]; P = .94 for trend).
In both 2009 and 2019, representation of both women and URM individuals for both specialties was less than their representation in the U.S. population. Radiation oncology faculty had the lowest URM representation in 2019 at 5.1%. The number of total URM faculty represented among both medical oncology and radiation oncology remained low for every rank in 2019 (Medical oncology: instructor, 2 of 44 [5%]; assistant professor, 18 of 274 [7%]; associate professor, 13 of 177 [7%]; full professor, 13 of 276 [5%]. Radiation oncology: instructor, 9 of 147 [6%]; assistant professor, 57 of 927 [6%]; associate professor, 20 of 510 [4%]; full professor, 18 of 452 [4%]).
“Our results highlight significant diversity differences along the career ladder in both specialties, with women having lower academic rank than men throughout the study period, and underrepresented [racial and ethnic groups] at every rank,” the authors wrote.
And, although Black, Hispanic, and indigenous people make up about 31% of the U.S. population, their inclusion in the health care workforce trails at all stages in the pipeline, the investigators found.
Diversity among radiation and medical oncologists lags behind that of medical school diversity in general, which has grown through efforts by the Association of American Medical Colleges.
Despite some improvements, the authors suggest the need for more initiatives to retain racial and ethnic minorities in an effort to reflect the diversity of the U.S. cancer population.
“This is a multifactorial issue, with focus not only on increasing diversity of the upstream pipeline but maintaining diversity throughout the entire pipeline, requiring difficult but necessary conversations about racial and ethnic systemic bias, lack of exposure and opportunities, and financial toxicities and pressures, to name a few. Until these factors are further delineated and better addressed, focused and targeted mentorship is key,” the authors wrote.
Small steps can have a collective impact
In a commentary published with the study, Frederick Lansigan, MD, and Charles R. Thomas Jr, MD, both of the Norris Cotton Cancer Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., called for a systemic change in hiring practices.
“Any small steps of change that contribute to supporting the issues highlighted by the Kamran et al. study can have a collective positive impact. A holistic evaluation of [underrepresented] applicants at all stages of education and training is paramount, and joining selection committees is necessary to ensure fair processes. Mentoring programs, leadership courses, and addressing microaggressions and mistreatment may improve retention of [underrepresented] medical school matriculants and trainees in oncology. Cancer centers can build and lead visible and tangible diversity, equity, inclusion, justice, and belonging efforts as we are doing at our institution,” the physicians wrote.
But above all, Dr. Lansigan and Dr. Thomas said that the oncology community needs to agree that intentionally increasing the number of underrepresented physicians in the U.S. workforce is necessary to better address health care inequities.
“We need all hands on deck to reduce structural barriers in early education. We need STEM programs that start in elementary school and offer support through college. Oncologists can mentor these early learners to highlight the positive aspects of a career in oncology, the importance of [underrepresented] physicians in oncology, and the resilience required in caring for those with serious illness, many of whom will come from underserved populations. “Physicians and public health experts themselves who are interested in tackling the discrepancy between [underrepresented] and [non-underrepresented] medical school [students] and oncology trainees need to seek and be elected into positions that can start to balance this equation. If more are willing to acknowledge the structural inequities that exist in the oncology workforce pipeline, we can start to solve the complex equation of structural inequities.”
Dr Lansigan reported being the Interim Associate Dean of Diversity, Equity, and Inclusion at the Geisel School of Medicine and the Principal of Diversity, Equity, and Inclusion for the department of medicine at Dartmouth-Hitchcock Medical Center. No other disclosures were reported.
in these fields, according to a cross-sectional study of data from the Association of American Medical Colleges.
“Creating and maintaining a diverse health care workforce is a priority to help combat societal inequities and health disparities, particularly in light of the evolving demographic characteristics of the general U.S. population,” wrote authors who were led by Sophia C. Kamran, MD, a radiation oncologist with Massachusetts General Hospital, Boston.
The study, which was published Dec. 9 in JAMA Oncology, surveyed full-time U.S.-based faculty in radiation and medical oncology departments from 1970 through 2019.
Improved patient satisfaction, compliance, and outcomes have been documented when a health care workforce better reflects the demographic traits of those whom it serves, Dr. Kamran and associates wrote.
They point to recent increases in the number and urgency of calls for improved diversity in the health care workforce, citing also higher incidence and mortality of new cancer cases among Black, indigenous, and Hispanic populations, compared with their non-Hispanic White counterparts. Prior calls for health care work force diversity have led to some creation of opportunities and pathways for increased representation of women and racial and ethnic minority groups in medicine, and the overall diversity of medical school faculty has been increasing by race and ethnicity and sex.
The change, however, is of lesser magnitude than what has been seen among medical school applicants, students, and graduates, and the gains in medical school faculty diversity have not kept pace with increasing diversity of the U.S. population. It has remained unclear whether corresponding progress has occurred in the composition of radiation oncology and medical oncology departments during the last 5 decades.
Despite lack of diversity, total faculty numbers have increased
Dr. Kamran and associates’ analysis revealed that total faculty numbers increased over time in both radiation oncology and medical oncology, with faculty representation of underrepresented-in-medicine (URM) women proportionally increased by 0.1% per decade in both radiation oncology (95% confidence interval, 0.005%-0.110%; P < . 001 for trend) and medical oncology (95% CI, −0.03% to 0.16%; P = .06 for trend), compared with non–URM women faculty, which increased by 0.4% (95% CI, 0.25%-0.80%) per decade in radiation oncology and 0.7% (95% CI, 0.47%-0.87%) per decade in medical oncology (P < .001 for trend for both). Faculty representation of URM men did not significantly change for radiation oncology (0.03% per decade [95% CI, −0.008% to 0.065%]; P = .09 for trend) or for medical oncology (0.003% per decade [95% CI, −0.13% to 0.14%]; P = .94 for trend).
In both 2009 and 2019, representation of both women and URM individuals for both specialties was less than their representation in the U.S. population. Radiation oncology faculty had the lowest URM representation in 2019 at 5.1%. The number of total URM faculty represented among both medical oncology and radiation oncology remained low for every rank in 2019 (Medical oncology: instructor, 2 of 44 [5%]; assistant professor, 18 of 274 [7%]; associate professor, 13 of 177 [7%]; full professor, 13 of 276 [5%]. Radiation oncology: instructor, 9 of 147 [6%]; assistant professor, 57 of 927 [6%]; associate professor, 20 of 510 [4%]; full professor, 18 of 452 [4%]).
“Our results highlight significant diversity differences along the career ladder in both specialties, with women having lower academic rank than men throughout the study period, and underrepresented [racial and ethnic groups] at every rank,” the authors wrote.
And, although Black, Hispanic, and indigenous people make up about 31% of the U.S. population, their inclusion in the health care workforce trails at all stages in the pipeline, the investigators found.
Diversity among radiation and medical oncologists lags behind that of medical school diversity in general, which has grown through efforts by the Association of American Medical Colleges.
Despite some improvements, the authors suggest the need for more initiatives to retain racial and ethnic minorities in an effort to reflect the diversity of the U.S. cancer population.
“This is a multifactorial issue, with focus not only on increasing diversity of the upstream pipeline but maintaining diversity throughout the entire pipeline, requiring difficult but necessary conversations about racial and ethnic systemic bias, lack of exposure and opportunities, and financial toxicities and pressures, to name a few. Until these factors are further delineated and better addressed, focused and targeted mentorship is key,” the authors wrote.
Small steps can have a collective impact
In a commentary published with the study, Frederick Lansigan, MD, and Charles R. Thomas Jr, MD, both of the Norris Cotton Cancer Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., called for a systemic change in hiring practices.
“Any small steps of change that contribute to supporting the issues highlighted by the Kamran et al. study can have a collective positive impact. A holistic evaluation of [underrepresented] applicants at all stages of education and training is paramount, and joining selection committees is necessary to ensure fair processes. Mentoring programs, leadership courses, and addressing microaggressions and mistreatment may improve retention of [underrepresented] medical school matriculants and trainees in oncology. Cancer centers can build and lead visible and tangible diversity, equity, inclusion, justice, and belonging efforts as we are doing at our institution,” the physicians wrote.
But above all, Dr. Lansigan and Dr. Thomas said that the oncology community needs to agree that intentionally increasing the number of underrepresented physicians in the U.S. workforce is necessary to better address health care inequities.
“We need all hands on deck to reduce structural barriers in early education. We need STEM programs that start in elementary school and offer support through college. Oncologists can mentor these early learners to highlight the positive aspects of a career in oncology, the importance of [underrepresented] physicians in oncology, and the resilience required in caring for those with serious illness, many of whom will come from underserved populations. “Physicians and public health experts themselves who are interested in tackling the discrepancy between [underrepresented] and [non-underrepresented] medical school [students] and oncology trainees need to seek and be elected into positions that can start to balance this equation. If more are willing to acknowledge the structural inequities that exist in the oncology workforce pipeline, we can start to solve the complex equation of structural inequities.”
Dr Lansigan reported being the Interim Associate Dean of Diversity, Equity, and Inclusion at the Geisel School of Medicine and the Principal of Diversity, Equity, and Inclusion for the department of medicine at Dartmouth-Hitchcock Medical Center. No other disclosures were reported.
FROM JAMA ONCOLOGY
Biden’s FDA chief nominee narrowly wins Senate confirmation
On Feb. 15, Robert Califf, MD, narrowly won Senate confirmation to once again serve as the commissioner of the Food and Drug Administration, overcoming protest votes from lawmakers about abortion and opioid issues.
The Senate voted 50-46 in favor of Dr. Califf’s nomination. A cardiologist long affiliated with Duke University and a noted expert on clinical trials, Dr. Califf also led the FDA from February 2016 through January 2017.
In 2016, the Senate confirmed him as FDA chief in an 89-4 vote. At that time, Sen. Joe Manchin, D-WV, and a few other senators said they were concerned that Dr. Califf’s links to the drug industry would hamper his ability to regulate drugmakers, particularly in terms of rules on prescription painkillers.
Sen. Manchin also objected to Dr. Califf’s second nomination as FDA commissioner, as did several fellow Democrats, including Sen. Edward Markey of Massachusetts. In a statement issued after the Feb. 15 vote, Sen. Markey said he has “consistently raised concerns about the FDA’s egregious mishandling of opioid approvals and its role in enabling the current opioid epidemic.”
“To date, the FDA still has not implemented many of the reforms necessary to ensure that it is fulfilling its role as our nation’s top pharmaceutical cop on the beat,” Sen. Markey said. “I have not received any real commitment from Dr. Califf to truly reform the FDA or to learn from the failures that fueled this public health crisis.”
This time, Dr. Califf lost support among Republican senators due to objections raised by groups seeking to end women’s access to abortion. Susan B. Anthony List and National Right to Life asked senators in a January letter to oppose Dr. Califf’s nomination, citing their objections to how the FDA handled reporting of adverse events from abortions by medication during Dr. Califf’s Tenure.
But some Republicans supported Califf in the Tuesday vote. Sens. Roy Blunt of Missouri, Richard Burr of North Carolina, Susan Collins of Maine, Lisa Murkowski of Alaska, Mitt Romney of Utah, and Pat Toomey of Pennsylvania all voted in his favor.
On Feb. 14, Sen. Patty Murray, D-WA, chairwoman of the Senate Health, Education, Labor, and Pensions Committee, urged her colleagues to vote for Dr. Califf to give the FDA strong leadership to tackle urgent health needs such as the opioid crisis, youth tobacco use, antimicrobial resistance, and inequities in health care.
“At this critical moment, we need a trusted hand to lead the FDA,” she said in a floor speech. Dr. Califf’s previous service at the FDA and his years spent as a research scientist “give him the experience to take on this challenge.”
Separately, three former FDA commissioners on Feb. 15 published an opinion article that appeared in The Hill. Republican presidents nominated two of these former FDA chiefs: Scott Gottlieb, MD, and Mark McClellan, MD. The third, Margaret Hamburg, MD, was nominated by President Barack Obama, as was Dr. Califf for his first time as FDA chief.
There’s an urgent need for a confirmed leader at the FDA as the United States seeks to move beyond the pandemic, the former FDA chiefs wrote. The work ahead includes continued efforts with vaccines as well as efforts to bolster medical supply chains, they said.
Dr. Califf “knows how to advance the safe development and use of medical products and to bring a sound, science-based foundation to the FDA’s regulatory actions. Because of this, he has earned the confidence of FDA’s professional career staff, as well as a broad base of patient groups, academic experts, medical professionals, and public health organizations,” Dr. Gottlieb, Dr. Hamburg, and Dr. McClellan wrote.
The article also was signed by former Centers for Medicare and Medicaid Services Administrator Andy Slavitt, who served in the Obama administration.
Support of medical community
The American Heart Association issued a statement on Feb.15, congratulating Dr. Califf on his second confirmation after the Senate vote.
“With a distinguished career in public service and a long-time volunteer leader at the American Heart Association, Dr. Califf has honed his ability to communicate and build trust with diverse constituencies,” CEO Nancy Brown said in the statement. “He will use his experience as a cardiologist to safeguard the health and well-being of people throughout the country, and his background in research to prioritize science and evidence-based policymaking.”
Dr. Califf was also backed by the Association of American Medical Colleges, the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians when he was nominated for the role last year by President Joe Biden.
A version of this article first appeared on Medscape.com.
On Feb. 15, Robert Califf, MD, narrowly won Senate confirmation to once again serve as the commissioner of the Food and Drug Administration, overcoming protest votes from lawmakers about abortion and opioid issues.
The Senate voted 50-46 in favor of Dr. Califf’s nomination. A cardiologist long affiliated with Duke University and a noted expert on clinical trials, Dr. Califf also led the FDA from February 2016 through January 2017.
In 2016, the Senate confirmed him as FDA chief in an 89-4 vote. At that time, Sen. Joe Manchin, D-WV, and a few other senators said they were concerned that Dr. Califf’s links to the drug industry would hamper his ability to regulate drugmakers, particularly in terms of rules on prescription painkillers.
Sen. Manchin also objected to Dr. Califf’s second nomination as FDA commissioner, as did several fellow Democrats, including Sen. Edward Markey of Massachusetts. In a statement issued after the Feb. 15 vote, Sen. Markey said he has “consistently raised concerns about the FDA’s egregious mishandling of opioid approvals and its role in enabling the current opioid epidemic.”
“To date, the FDA still has not implemented many of the reforms necessary to ensure that it is fulfilling its role as our nation’s top pharmaceutical cop on the beat,” Sen. Markey said. “I have not received any real commitment from Dr. Califf to truly reform the FDA or to learn from the failures that fueled this public health crisis.”
This time, Dr. Califf lost support among Republican senators due to objections raised by groups seeking to end women’s access to abortion. Susan B. Anthony List and National Right to Life asked senators in a January letter to oppose Dr. Califf’s nomination, citing their objections to how the FDA handled reporting of adverse events from abortions by medication during Dr. Califf’s Tenure.
But some Republicans supported Califf in the Tuesday vote. Sens. Roy Blunt of Missouri, Richard Burr of North Carolina, Susan Collins of Maine, Lisa Murkowski of Alaska, Mitt Romney of Utah, and Pat Toomey of Pennsylvania all voted in his favor.
On Feb. 14, Sen. Patty Murray, D-WA, chairwoman of the Senate Health, Education, Labor, and Pensions Committee, urged her colleagues to vote for Dr. Califf to give the FDA strong leadership to tackle urgent health needs such as the opioid crisis, youth tobacco use, antimicrobial resistance, and inequities in health care.
“At this critical moment, we need a trusted hand to lead the FDA,” she said in a floor speech. Dr. Califf’s previous service at the FDA and his years spent as a research scientist “give him the experience to take on this challenge.”
Separately, three former FDA commissioners on Feb. 15 published an opinion article that appeared in The Hill. Republican presidents nominated two of these former FDA chiefs: Scott Gottlieb, MD, and Mark McClellan, MD. The third, Margaret Hamburg, MD, was nominated by President Barack Obama, as was Dr. Califf for his first time as FDA chief.
There’s an urgent need for a confirmed leader at the FDA as the United States seeks to move beyond the pandemic, the former FDA chiefs wrote. The work ahead includes continued efforts with vaccines as well as efforts to bolster medical supply chains, they said.
Dr. Califf “knows how to advance the safe development and use of medical products and to bring a sound, science-based foundation to the FDA’s regulatory actions. Because of this, he has earned the confidence of FDA’s professional career staff, as well as a broad base of patient groups, academic experts, medical professionals, and public health organizations,” Dr. Gottlieb, Dr. Hamburg, and Dr. McClellan wrote.
The article also was signed by former Centers for Medicare and Medicaid Services Administrator Andy Slavitt, who served in the Obama administration.
Support of medical community
The American Heart Association issued a statement on Feb.15, congratulating Dr. Califf on his second confirmation after the Senate vote.
“With a distinguished career in public service and a long-time volunteer leader at the American Heart Association, Dr. Califf has honed his ability to communicate and build trust with diverse constituencies,” CEO Nancy Brown said in the statement. “He will use his experience as a cardiologist to safeguard the health and well-being of people throughout the country, and his background in research to prioritize science and evidence-based policymaking.”
Dr. Califf was also backed by the Association of American Medical Colleges, the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians when he was nominated for the role last year by President Joe Biden.
A version of this article first appeared on Medscape.com.
On Feb. 15, Robert Califf, MD, narrowly won Senate confirmation to once again serve as the commissioner of the Food and Drug Administration, overcoming protest votes from lawmakers about abortion and opioid issues.
The Senate voted 50-46 in favor of Dr. Califf’s nomination. A cardiologist long affiliated with Duke University and a noted expert on clinical trials, Dr. Califf also led the FDA from February 2016 through January 2017.
In 2016, the Senate confirmed him as FDA chief in an 89-4 vote. At that time, Sen. Joe Manchin, D-WV, and a few other senators said they were concerned that Dr. Califf’s links to the drug industry would hamper his ability to regulate drugmakers, particularly in terms of rules on prescription painkillers.
Sen. Manchin also objected to Dr. Califf’s second nomination as FDA commissioner, as did several fellow Democrats, including Sen. Edward Markey of Massachusetts. In a statement issued after the Feb. 15 vote, Sen. Markey said he has “consistently raised concerns about the FDA’s egregious mishandling of opioid approvals and its role in enabling the current opioid epidemic.”
“To date, the FDA still has not implemented many of the reforms necessary to ensure that it is fulfilling its role as our nation’s top pharmaceutical cop on the beat,” Sen. Markey said. “I have not received any real commitment from Dr. Califf to truly reform the FDA or to learn from the failures that fueled this public health crisis.”
This time, Dr. Califf lost support among Republican senators due to objections raised by groups seeking to end women’s access to abortion. Susan B. Anthony List and National Right to Life asked senators in a January letter to oppose Dr. Califf’s nomination, citing their objections to how the FDA handled reporting of adverse events from abortions by medication during Dr. Califf’s Tenure.
But some Republicans supported Califf in the Tuesday vote. Sens. Roy Blunt of Missouri, Richard Burr of North Carolina, Susan Collins of Maine, Lisa Murkowski of Alaska, Mitt Romney of Utah, and Pat Toomey of Pennsylvania all voted in his favor.
On Feb. 14, Sen. Patty Murray, D-WA, chairwoman of the Senate Health, Education, Labor, and Pensions Committee, urged her colleagues to vote for Dr. Califf to give the FDA strong leadership to tackle urgent health needs such as the opioid crisis, youth tobacco use, antimicrobial resistance, and inequities in health care.
“At this critical moment, we need a trusted hand to lead the FDA,” she said in a floor speech. Dr. Califf’s previous service at the FDA and his years spent as a research scientist “give him the experience to take on this challenge.”
Separately, three former FDA commissioners on Feb. 15 published an opinion article that appeared in The Hill. Republican presidents nominated two of these former FDA chiefs: Scott Gottlieb, MD, and Mark McClellan, MD. The third, Margaret Hamburg, MD, was nominated by President Barack Obama, as was Dr. Califf for his first time as FDA chief.
There’s an urgent need for a confirmed leader at the FDA as the United States seeks to move beyond the pandemic, the former FDA chiefs wrote. The work ahead includes continued efforts with vaccines as well as efforts to bolster medical supply chains, they said.
Dr. Califf “knows how to advance the safe development and use of medical products and to bring a sound, science-based foundation to the FDA’s regulatory actions. Because of this, he has earned the confidence of FDA’s professional career staff, as well as a broad base of patient groups, academic experts, medical professionals, and public health organizations,” Dr. Gottlieb, Dr. Hamburg, and Dr. McClellan wrote.
The article also was signed by former Centers for Medicare and Medicaid Services Administrator Andy Slavitt, who served in the Obama administration.
Support of medical community
The American Heart Association issued a statement on Feb.15, congratulating Dr. Califf on his second confirmation after the Senate vote.
“With a distinguished career in public service and a long-time volunteer leader at the American Heart Association, Dr. Califf has honed his ability to communicate and build trust with diverse constituencies,” CEO Nancy Brown said in the statement. “He will use his experience as a cardiologist to safeguard the health and well-being of people throughout the country, and his background in research to prioritize science and evidence-based policymaking.”
Dr. Califf was also backed by the Association of American Medical Colleges, the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians when he was nominated for the role last year by President Joe Biden.
A version of this article first appeared on Medscape.com.




