User login
For cancer prevention, not all plant-based diets are equal
researchers have found.
The study of more than 65,000 people showed that plant-based diets that were high in whole grains, fruits, and vegetables appear to be more protective against breast cancer than diets rich in processed plant-based products, such as juice and chips.
“Results suggest that the best plant-based diet for breast cancer prevention could be a healthy plant-based diet comprising fruit, vegetables, whole grains, nuts, and legumes,” said Sanam Shah, MBBS, FCPS, MPH, a doctoral candidate in epidemiology at Paris-Saclay University, who is the lead author of the new study. “In contrast, an unhealthy plant-based diet comprising higher intakes of primarily processed products of plant origin, such as refined grains, fruit juices, sweets, desserts, and potatoes, would be worse for breast cancer prevention.”
Dr. Shah’s group is presenting their research online at the annual meeting of the American Society for Nutrition.
Although the role of plant-based diets in cancer prevention has received extensive attention, Dr. Shah said few studies have assessed the influence of the quality of those diets on the risk of breast cancer.
Dr. Shah and colleagues conducted a prospective cohort study to investigate the link between healthy and unhealthy plant-based diets and breast cancer risk. Unlike other studies, the researchers also evaluated the effect of a gradual decrease in animal products in diets on health.
Dr. Shah’s group followed 65,574 postmenopausal women in France (mean age, 52.8 years) from 1993 to 2014. The researchers used self-reported food questionnaires to classify women into groups on the basis of adherence to a mostly plant or animal diet. Plant-based diets did not exclude meat but had more plant than animal products, Dr. Shah said. The researchers also grouped women on the basis of how healthy the plant-based diets were.
Over the 21-year study period, 3,968 women were diagnosed with breast cancer. Those who adhered to a more healthful plant-based diet had a 14% lower risk than average of developing breast cancer, while those who adhered to a less healthful plant-based diet had a 20% greater risk of developing the disease.
Nutritional quality varies greatly across plant-based foods. Quality plant-based diets should focus on variety to avoid nutritional deficiencies in iron, zinc, calcium, and vitamin B12, Dr. Shah said.
“The study by Shah and coworkers underscores the importance of considering more global aspects of the diet rather than single components when examining relationships between diet and health,” said Megan McCrory, PhD, research associate professor of nutrition at Boston University. “As the study illustrates, plant-based diets as a whole are not always healthy and may also contain less desirable nutrients and foods.”
Abstracts in the conference have been selected by a board of experts for presentation but have not yet been peer reviewed. All findings are to be regarded as preliminary until they are published in peer-reviewed articles. Dr. Shah and Dr. McCrory disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
The study of more than 65,000 people showed that plant-based diets that were high in whole grains, fruits, and vegetables appear to be more protective against breast cancer than diets rich in processed plant-based products, such as juice and chips.
“Results suggest that the best plant-based diet for breast cancer prevention could be a healthy plant-based diet comprising fruit, vegetables, whole grains, nuts, and legumes,” said Sanam Shah, MBBS, FCPS, MPH, a doctoral candidate in epidemiology at Paris-Saclay University, who is the lead author of the new study. “In contrast, an unhealthy plant-based diet comprising higher intakes of primarily processed products of plant origin, such as refined grains, fruit juices, sweets, desserts, and potatoes, would be worse for breast cancer prevention.”
Dr. Shah’s group is presenting their research online at the annual meeting of the American Society for Nutrition.
Although the role of plant-based diets in cancer prevention has received extensive attention, Dr. Shah said few studies have assessed the influence of the quality of those diets on the risk of breast cancer.
Dr. Shah and colleagues conducted a prospective cohort study to investigate the link between healthy and unhealthy plant-based diets and breast cancer risk. Unlike other studies, the researchers also evaluated the effect of a gradual decrease in animal products in diets on health.
Dr. Shah’s group followed 65,574 postmenopausal women in France (mean age, 52.8 years) from 1993 to 2014. The researchers used self-reported food questionnaires to classify women into groups on the basis of adherence to a mostly plant or animal diet. Plant-based diets did not exclude meat but had more plant than animal products, Dr. Shah said. The researchers also grouped women on the basis of how healthy the plant-based diets were.
Over the 21-year study period, 3,968 women were diagnosed with breast cancer. Those who adhered to a more healthful plant-based diet had a 14% lower risk than average of developing breast cancer, while those who adhered to a less healthful plant-based diet had a 20% greater risk of developing the disease.
Nutritional quality varies greatly across plant-based foods. Quality plant-based diets should focus on variety to avoid nutritional deficiencies in iron, zinc, calcium, and vitamin B12, Dr. Shah said.
“The study by Shah and coworkers underscores the importance of considering more global aspects of the diet rather than single components when examining relationships between diet and health,” said Megan McCrory, PhD, research associate professor of nutrition at Boston University. “As the study illustrates, plant-based diets as a whole are not always healthy and may also contain less desirable nutrients and foods.”
Abstracts in the conference have been selected by a board of experts for presentation but have not yet been peer reviewed. All findings are to be regarded as preliminary until they are published in peer-reviewed articles. Dr. Shah and Dr. McCrory disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
The study of more than 65,000 people showed that plant-based diets that were high in whole grains, fruits, and vegetables appear to be more protective against breast cancer than diets rich in processed plant-based products, such as juice and chips.
“Results suggest that the best plant-based diet for breast cancer prevention could be a healthy plant-based diet comprising fruit, vegetables, whole grains, nuts, and legumes,” said Sanam Shah, MBBS, FCPS, MPH, a doctoral candidate in epidemiology at Paris-Saclay University, who is the lead author of the new study. “In contrast, an unhealthy plant-based diet comprising higher intakes of primarily processed products of plant origin, such as refined grains, fruit juices, sweets, desserts, and potatoes, would be worse for breast cancer prevention.”
Dr. Shah’s group is presenting their research online at the annual meeting of the American Society for Nutrition.
Although the role of plant-based diets in cancer prevention has received extensive attention, Dr. Shah said few studies have assessed the influence of the quality of those diets on the risk of breast cancer.
Dr. Shah and colleagues conducted a prospective cohort study to investigate the link between healthy and unhealthy plant-based diets and breast cancer risk. Unlike other studies, the researchers also evaluated the effect of a gradual decrease in animal products in diets on health.
Dr. Shah’s group followed 65,574 postmenopausal women in France (mean age, 52.8 years) from 1993 to 2014. The researchers used self-reported food questionnaires to classify women into groups on the basis of adherence to a mostly plant or animal diet. Plant-based diets did not exclude meat but had more plant than animal products, Dr. Shah said. The researchers also grouped women on the basis of how healthy the plant-based diets were.
Over the 21-year study period, 3,968 women were diagnosed with breast cancer. Those who adhered to a more healthful plant-based diet had a 14% lower risk than average of developing breast cancer, while those who adhered to a less healthful plant-based diet had a 20% greater risk of developing the disease.
Nutritional quality varies greatly across plant-based foods. Quality plant-based diets should focus on variety to avoid nutritional deficiencies in iron, zinc, calcium, and vitamin B12, Dr. Shah said.
“The study by Shah and coworkers underscores the importance of considering more global aspects of the diet rather than single components when examining relationships between diet and health,” said Megan McCrory, PhD, research associate professor of nutrition at Boston University. “As the study illustrates, plant-based diets as a whole are not always healthy and may also contain less desirable nutrients and foods.”
Abstracts in the conference have been selected by a board of experts for presentation but have not yet been peer reviewed. All findings are to be regarded as preliminary until they are published in peer-reviewed articles. Dr. Shah and Dr. McCrory disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NUTRITION 2022
Sleep, not smoke, the key to COPD exacerbations?
, according to a study reported online in the journal Sleep.
Researchers followed 1,647 patients with confirmed COPD who were enrolled in the Subpopulations and Intermediate Outcome Measures in COPD Study (SPIROMICS). SPIROMICS is a multicenter study funded by the National Heart, Lung, and Blood Institute and the COPD Foundation and is designed to evaluate COPD subpopulations, outcomes, and biomarkers. All participants in the study were current or former smokers with confirmed COPD.
COPD exacerbations over a 3-year follow-up period were compared against reported sleep quality. The researchers used the Pittsburgh Sleep Quality Index (PSQI), a combination of seven sleep measures, including sleep duration, timing of sleep, and frequency of disturbances. The higher the score, the worse the quality of sleep.
Individuals who self-reported having poor-quality sleep had a 25%-95% higher risk of COPD exacerbations, compared with those who reported good-quality sleep, according to the results.
There was a significant association between PSQI score and total and mean exacerbations in the unadjusted analysis (incidence rate ratios, 1.09; 95% confidence interval, 1.05-1.13) and the analysis adjusted for demographics, medical comorbidities, disease severity, medication usage, and socioeconomic environmental exposure (IRR, 1.08; 95% CI, 1.03-1.13).
In addition, the PSQI score was independently associated with an increased risk of hospitalization, with a 7% increase in risk of hospitalization with each 1-point increase in PSQI, according to the researchers.
Surprising findings
These findings suggest that sleep quality may be a better predictor of flare-ups than the patient’s history of smoking, according to the researchers.
“Among those who already have COPD, knowing how they sleep at night will tell me much more about their risk of a flare-up than knowing whether they smoked for 40 versus 60 years. … That is very surprising and is not necessarily what I expected going into this study. Smoking is such a central process to COPD that I would have predicted it would be the more important predictor in the case of exacerbations,” said lead study author Aaron Baugh, MD, a practicing pulmonologist, and a clinical fellow at the University of California, San Francisco, in a National Institutes of Health press release on the study.
The study findings were applicable to all races and ethnicities studied, however the results may be particularly relevant to Black Americans, Dr. Baugh indicated, because past studies have shown that Black Americans tend to have poorer sleep quality than other races and ethnicities. With poorer sleep linked to worse COPD outcomes, the current study may help explain why Black Americans as a group tend to do worse when they have COPD, compared with other racial and ethnic groups, the researchers suggested.
The study was supported by the National Institutes of Health and the COPD Foundation. SPIROMICS was supported by NIH and the COPD Foundation as well as numerous pharmaceutical and biotechnology companies. The authors reported no other financial disclosures.
, according to a study reported online in the journal Sleep.
Researchers followed 1,647 patients with confirmed COPD who were enrolled in the Subpopulations and Intermediate Outcome Measures in COPD Study (SPIROMICS). SPIROMICS is a multicenter study funded by the National Heart, Lung, and Blood Institute and the COPD Foundation and is designed to evaluate COPD subpopulations, outcomes, and biomarkers. All participants in the study were current or former smokers with confirmed COPD.
COPD exacerbations over a 3-year follow-up period were compared against reported sleep quality. The researchers used the Pittsburgh Sleep Quality Index (PSQI), a combination of seven sleep measures, including sleep duration, timing of sleep, and frequency of disturbances. The higher the score, the worse the quality of sleep.
Individuals who self-reported having poor-quality sleep had a 25%-95% higher risk of COPD exacerbations, compared with those who reported good-quality sleep, according to the results.
There was a significant association between PSQI score and total and mean exacerbations in the unadjusted analysis (incidence rate ratios, 1.09; 95% confidence interval, 1.05-1.13) and the analysis adjusted for demographics, medical comorbidities, disease severity, medication usage, and socioeconomic environmental exposure (IRR, 1.08; 95% CI, 1.03-1.13).
In addition, the PSQI score was independently associated with an increased risk of hospitalization, with a 7% increase in risk of hospitalization with each 1-point increase in PSQI, according to the researchers.
Surprising findings
These findings suggest that sleep quality may be a better predictor of flare-ups than the patient’s history of smoking, according to the researchers.
“Among those who already have COPD, knowing how they sleep at night will tell me much more about their risk of a flare-up than knowing whether they smoked for 40 versus 60 years. … That is very surprising and is not necessarily what I expected going into this study. Smoking is such a central process to COPD that I would have predicted it would be the more important predictor in the case of exacerbations,” said lead study author Aaron Baugh, MD, a practicing pulmonologist, and a clinical fellow at the University of California, San Francisco, in a National Institutes of Health press release on the study.
The study findings were applicable to all races and ethnicities studied, however the results may be particularly relevant to Black Americans, Dr. Baugh indicated, because past studies have shown that Black Americans tend to have poorer sleep quality than other races and ethnicities. With poorer sleep linked to worse COPD outcomes, the current study may help explain why Black Americans as a group tend to do worse when they have COPD, compared with other racial and ethnic groups, the researchers suggested.
The study was supported by the National Institutes of Health and the COPD Foundation. SPIROMICS was supported by NIH and the COPD Foundation as well as numerous pharmaceutical and biotechnology companies. The authors reported no other financial disclosures.
, according to a study reported online in the journal Sleep.
Researchers followed 1,647 patients with confirmed COPD who were enrolled in the Subpopulations and Intermediate Outcome Measures in COPD Study (SPIROMICS). SPIROMICS is a multicenter study funded by the National Heart, Lung, and Blood Institute and the COPD Foundation and is designed to evaluate COPD subpopulations, outcomes, and biomarkers. All participants in the study were current or former smokers with confirmed COPD.
COPD exacerbations over a 3-year follow-up period were compared against reported sleep quality. The researchers used the Pittsburgh Sleep Quality Index (PSQI), a combination of seven sleep measures, including sleep duration, timing of sleep, and frequency of disturbances. The higher the score, the worse the quality of sleep.
Individuals who self-reported having poor-quality sleep had a 25%-95% higher risk of COPD exacerbations, compared with those who reported good-quality sleep, according to the results.
There was a significant association between PSQI score and total and mean exacerbations in the unadjusted analysis (incidence rate ratios, 1.09; 95% confidence interval, 1.05-1.13) and the analysis adjusted for demographics, medical comorbidities, disease severity, medication usage, and socioeconomic environmental exposure (IRR, 1.08; 95% CI, 1.03-1.13).
In addition, the PSQI score was independently associated with an increased risk of hospitalization, with a 7% increase in risk of hospitalization with each 1-point increase in PSQI, according to the researchers.
Surprising findings
These findings suggest that sleep quality may be a better predictor of flare-ups than the patient’s history of smoking, according to the researchers.
“Among those who already have COPD, knowing how they sleep at night will tell me much more about their risk of a flare-up than knowing whether they smoked for 40 versus 60 years. … That is very surprising and is not necessarily what I expected going into this study. Smoking is such a central process to COPD that I would have predicted it would be the more important predictor in the case of exacerbations,” said lead study author Aaron Baugh, MD, a practicing pulmonologist, and a clinical fellow at the University of California, San Francisco, in a National Institutes of Health press release on the study.
The study findings were applicable to all races and ethnicities studied, however the results may be particularly relevant to Black Americans, Dr. Baugh indicated, because past studies have shown that Black Americans tend to have poorer sleep quality than other races and ethnicities. With poorer sleep linked to worse COPD outcomes, the current study may help explain why Black Americans as a group tend to do worse when they have COPD, compared with other racial and ethnic groups, the researchers suggested.
The study was supported by the National Institutes of Health and the COPD Foundation. SPIROMICS was supported by NIH and the COPD Foundation as well as numerous pharmaceutical and biotechnology companies. The authors reported no other financial disclosures.
FROM SLEEP
Can too much sleep raise the risk of cancer?
The findings reveal that sleeping 10-plus hours may increase a woman’s risk of getting cancer and both men and women’s risk of dying from cancer.
The researchers say their findings may help refine sleep recommendations in Japan, which currently advise working, middle-aged adults to sleep “as long as they can.”
Based on the new findings, a sleep duration of 6-8 hours for men and 6-9 hours for women “may be the safest” regarding cancer incidence and mortality risk among Japanese adults, the authors conclude.
The findings were published online in the International Journal of Cancer.
The literature on sleep time and cancer risk is mixed. A trio of meta-analyses conducted between 2016 and 2019 found that long sleep duration, but not short, was associated with a slightly elevated risk of all cancer mortality in Asians.
A separate meta-analysis conducted in 2018 found that both short and long sleep durations were not related to cancer incidence. But in the stratified analysis, shorter sleep time was associated with 36% increased cancer risk among Asians.
To investigate further, the researchers pooled data from six population-based cohorts that included 271,694 adults – 126,930 men and 144,764 women – with 40,751 total incident cancer cases and 18,323 total cancer deaths during a follow-up lasting about 5.9 million person-years.
In the multivariable analysis, longer sleep duration was not associated with total cancer incidence in men. In women, however, sleeping 10 or more hours vs. 7 was associated with a 19% increased risk of cancer.
In addition, sleeping 10 or more hours was associated with an increased risk of dying from cancer in women (hazard ratio, 1.44) and men (HR, 1.18).
Sleeping for 5 hours or fewer, compared with 7, was not associated with cancer incidence and mortality. However, among postmenopausal women, shorter sleep durations did increase the risk of dying from cancer (HR, 1.15).
The authors highlight several strengths of the analysis, including a large sample size as well as stratification of the results by body mass index and menopause status, which has rarely been done in previous studies.
Limitations include self-reported sleep durations and lack of data on sleep quality. The researchers note that the mechanism by which sleep time may influence cancer incidence and mortality is unclear but likely to be complex and cancer site specific.
It’s also possible that reverse causation could explain associations between sleep duration and cancer occurrence and mortality – with pain from cancer, for instance, impairing sleep duration and quality. However, the sensitivity analysis found no evidence of reverse causality or other confounding factors.
Based on these findings, the researchers say sleep duration “may be an important variable to include in cancer incidence and mortality risk prediction models.”
The study had no specific funding. The authors declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The findings reveal that sleeping 10-plus hours may increase a woman’s risk of getting cancer and both men and women’s risk of dying from cancer.
The researchers say their findings may help refine sleep recommendations in Japan, which currently advise working, middle-aged adults to sleep “as long as they can.”
Based on the new findings, a sleep duration of 6-8 hours for men and 6-9 hours for women “may be the safest” regarding cancer incidence and mortality risk among Japanese adults, the authors conclude.
The findings were published online in the International Journal of Cancer.
The literature on sleep time and cancer risk is mixed. A trio of meta-analyses conducted between 2016 and 2019 found that long sleep duration, but not short, was associated with a slightly elevated risk of all cancer mortality in Asians.
A separate meta-analysis conducted in 2018 found that both short and long sleep durations were not related to cancer incidence. But in the stratified analysis, shorter sleep time was associated with 36% increased cancer risk among Asians.
To investigate further, the researchers pooled data from six population-based cohorts that included 271,694 adults – 126,930 men and 144,764 women – with 40,751 total incident cancer cases and 18,323 total cancer deaths during a follow-up lasting about 5.9 million person-years.
In the multivariable analysis, longer sleep duration was not associated with total cancer incidence in men. In women, however, sleeping 10 or more hours vs. 7 was associated with a 19% increased risk of cancer.
In addition, sleeping 10 or more hours was associated with an increased risk of dying from cancer in women (hazard ratio, 1.44) and men (HR, 1.18).
Sleeping for 5 hours or fewer, compared with 7, was not associated with cancer incidence and mortality. However, among postmenopausal women, shorter sleep durations did increase the risk of dying from cancer (HR, 1.15).
The authors highlight several strengths of the analysis, including a large sample size as well as stratification of the results by body mass index and menopause status, which has rarely been done in previous studies.
Limitations include self-reported sleep durations and lack of data on sleep quality. The researchers note that the mechanism by which sleep time may influence cancer incidence and mortality is unclear but likely to be complex and cancer site specific.
It’s also possible that reverse causation could explain associations between sleep duration and cancer occurrence and mortality – with pain from cancer, for instance, impairing sleep duration and quality. However, the sensitivity analysis found no evidence of reverse causality or other confounding factors.
Based on these findings, the researchers say sleep duration “may be an important variable to include in cancer incidence and mortality risk prediction models.”
The study had no specific funding. The authors declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The findings reveal that sleeping 10-plus hours may increase a woman’s risk of getting cancer and both men and women’s risk of dying from cancer.
The researchers say their findings may help refine sleep recommendations in Japan, which currently advise working, middle-aged adults to sleep “as long as they can.”
Based on the new findings, a sleep duration of 6-8 hours for men and 6-9 hours for women “may be the safest” regarding cancer incidence and mortality risk among Japanese adults, the authors conclude.
The findings were published online in the International Journal of Cancer.
The literature on sleep time and cancer risk is mixed. A trio of meta-analyses conducted between 2016 and 2019 found that long sleep duration, but not short, was associated with a slightly elevated risk of all cancer mortality in Asians.
A separate meta-analysis conducted in 2018 found that both short and long sleep durations were not related to cancer incidence. But in the stratified analysis, shorter sleep time was associated with 36% increased cancer risk among Asians.
To investigate further, the researchers pooled data from six population-based cohorts that included 271,694 adults – 126,930 men and 144,764 women – with 40,751 total incident cancer cases and 18,323 total cancer deaths during a follow-up lasting about 5.9 million person-years.
In the multivariable analysis, longer sleep duration was not associated with total cancer incidence in men. In women, however, sleeping 10 or more hours vs. 7 was associated with a 19% increased risk of cancer.
In addition, sleeping 10 or more hours was associated with an increased risk of dying from cancer in women (hazard ratio, 1.44) and men (HR, 1.18).
Sleeping for 5 hours or fewer, compared with 7, was not associated with cancer incidence and mortality. However, among postmenopausal women, shorter sleep durations did increase the risk of dying from cancer (HR, 1.15).
The authors highlight several strengths of the analysis, including a large sample size as well as stratification of the results by body mass index and menopause status, which has rarely been done in previous studies.
Limitations include self-reported sleep durations and lack of data on sleep quality. The researchers note that the mechanism by which sleep time may influence cancer incidence and mortality is unclear but likely to be complex and cancer site specific.
It’s also possible that reverse causation could explain associations between sleep duration and cancer occurrence and mortality – with pain from cancer, for instance, impairing sleep duration and quality. However, the sensitivity analysis found no evidence of reverse causality or other confounding factors.
Based on these findings, the researchers say sleep duration “may be an important variable to include in cancer incidence and mortality risk prediction models.”
The study had no specific funding. The authors declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE INTERNATIONAL JOURNAL OF CANCER
‘Forever chemicals’ linked to hypertension in middle-aged women
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
Registered Dietitian Nutritionists’ Role in Hospital in Home
Hospital in Home (HIH) is the delivery of acute care services in a patient’s home as an alternative to hospitalization.1 Compared with traditional inpatient care, HIH programs have been associated with reduced costs, as well as patient and caregiver satisfaction, diseasespecific outcomes, and mortality rates that were similar or improved compared with inpatient admissions.1-4
The US Department of Veterans Affairs (VA) Veterans Health Administration (VHA) and other hospital systems are increasingly adopting HIH models.2-4 At the time of this writing, there were 12 HIH programs in VHA (personal communication, D. Cooper, 2/28/2022). In addition to physicians and nurses, the interdisciplinary HIH team may include a pharmacist, social worker, and registered dietitian nutritionist (RDN).2,5 HIH programs have been shown to improve nutritional status as measured by the Mini Nutritional Assessment Score, but overall, there is a paucity of published information regarding the provision of nutrition care in HIH.6 The role of the RDN has varied within VHA. Some sites, such as the Sacramento VA Medical Center in California, include a distinct RDN position on the HIH team, whereas others, such as the Spark M. Matsunaga VA Medical Center in Honolulu, Hawaii, and the James A. Haley Veterans’ Hospital in Tampa, Florida, consult clinic RDNs.
Since HIH programs typically treat conditions for which diet is an inherent part of the treatment (eg, congestive heart failure [CHF]), there is a need to precisely define the role of the RDN within the HIH model.2,3,7 Drawing from my experience as an HIH RDN, I will describe how the inclusion of an RDN position within the HIH team is optimal for health care delivery and how HIH practitioners can best utilize RDN services.
RDN Role in HIH Team
Delegating nutrition services to an RDN enhances patient care by empowering HIH team members to function at the highest level of their scope of practice. RDNs have been recognized by physicians as the most qualified health care professionals to help patients with diet-related conditions, such as obesity, and physicians also have reported a desire for additional training in nutrition.8 Although home-health nurses have frequently performed nutrition assessments and interventions, survey results have indicated that many nurses do not feel confident in teaching complex nutritional information.9 In my experience, many HIH patients are nutritionally complex, with more than one condition requiring nutrition intervention. For example, patients may be admitted to HIH for management of CHF, but they may also have diabetes mellitus (DM), obesity, and low socioeconomic status. The HIH RDN can address the nutrition aspects of these conditions, freeing time for physicians and nurses to focus on their respective areas of expertise.9,10 Moreover, the RDN can also provide dietary education to the HIH team to increase their knowledge of nutritional topics and promote consistent messaging to patients.
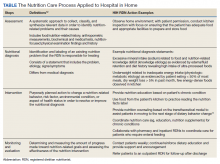
Including an RDN on the HIH team enables patients to have comprehensive, personalized nutrition care. Rather than merely offering generalized nutrition education, RDNs are trained to provide medical nutrition therapy (MNT), which has been shown to improve health outcomes and be cost-effective for conditions such as type 2 DM, chronic kidney disease, hypertension, and obesity.10,11 In MNT, RDNs use the standardized 4-stepnutrition care process (NCP).12 The Table shows examples of how the NCP can be applied in HIH settings. Furthermore, in my experience, MNT from an RDN also contributes to patient satisfaction. Subjective observations from my team have indicated that patients often express more confidence in managing their diets by the time of HIH discharge.
RDNs can guide physicians and pharmacists in ordering oral nutrition supplements (ONS). Within the VHA, a “food first” approach is preferred to increase caloric intake, and patients must meet specific criteria for prescription of an ONS.13 Furthermore, ONS designed for specific medical conditions (eg, chronic kidney disease) are considered nonformulary and require an RDN evaluation.13 Including an RDN on the HIH team allows this evaluation process to begin early in the patient’s admission to the program and ensures that provision of ONS is clinically appropriate and cost-effective.
Care Coordination
HIH is highly interdisciplinary. Team members perform their respective roles and communicate with the team throughout the day. RDNs can help monitor patients and alert physicians for changes in blood glucose, gastrointestinal concerns, and weight. This is especially helpful for patients who do not have a planned nursing visit on the day of an RDN evaluation. The HIH RDN can also collaborate with other team members to address patient needs. For example, for patients with limited financial resources, the HIH RDN can provide nutrition education regarding cooking on a budget, and the HIH social worker can arrange free or low-cost meal services.
Tips
When hiring an HIH RDN, seek candidates with experience in inpatient, outpatient, and home care settings. As a hybrid of these 3 areas, the HIH RDN position requires a unique combination of acute care skills and health coaching. Additionally, in my experience, the HIH RDN interacts more frequently with the HIH team than other RDN colleagues, so it is important that candidates can work independently and take initiative. This type of position would not be suitable for entry-level RDNs.
Stagger HIH team visits to prevent overwhelming the patient and caregivers. Early in our program, my team quickly learned that patients and caregivers can feel overwhelmed with too many home visits upon admission to HIH. After seeing multiple HIH team members the same day, they were often too tired to focus well on diet education during my visit. Staggering visits (eg, completing the initial nutrition assessment 1 day to 1 week after the initial medical and pharmacy visits) has been an effective strategy to address this problem. Furthermore, some patients prefer that the initial RDN appointment is conducted by telephone, with an inperson reassessment the following week. In my experience, HIH workflow is dynamic by nature, so it is crucial to remain flexible and accommodate individual patient needs as much as possible.
Dietary behavior change is a long-term process, and restrictive hospital diets can be challenging to replicate at home. In a hospital setting, clinicians can order a specialized diet (eg, low sodium with fluid restriction for CHF patients), whereas efforts to implement these restrictions in the home setting can be cumbersome and negatively impact quality of life.7,14 Nevertheless, the effectiveness of medical treatment is compromised when patients do not adhere to dietary recommendations. Meal delivery services that offer specialized diets can be a useful resource for patients and caregivers who are unable to cook, and the HIH RDN can assist patients in ordering these services.
HIH patients may vary in terms of readiness to make dietary changes, and in addition to nutrition education, nutrition counseling is usually needed to effect behavior change. My team has found that consideration of the transtheoretical/ stages of change model can be a helpful approach. 15 The HIH RDN can tailor nutrition interventions to the patient’s stage of change. For example, for patients in the precontemplation stage, the HIH RDN would focus on providing information and addressing emotional aspects of dietary change. In contrast, for patients in the action stage of change, the HIH RDN might emphasize behavioral skill training and social support.15 Particularly for patients in the early stages of change, it may be unrealistic to expect full adoption of the recommended diet within the 30 days of the HIH program. However, by acknowledging the reality of the patient’s stage of change, the HIH RDN and team can then collaborate to support the patient in moving toward the next stage. Patients who are not ready for dietary behavior change during the 30 days of HIH may benefit from longer-term support, and the HIH RDN can arrange followup care with an outpatient RDN.
Conclusions
As the HIH model continues to be adopted across the VHA and other health care systems, it is crucial to consider the value and expertise of an RDN for guiding nutrition care in the HIH setting. The HIH RDN contributes to optimal health care delivery by leading nutritional aspects of patient care, offering personalized MNT, and coordinating and collaborating with team members to meet individual patient needs. An RDN can serve as a valuable resource for nutrition information and enhance the team’s overall services, with the potential to impact clinical outcomes and patient satisfaction.
1. Levine DM, Ouchi K, Blanchfield B, et al. Hospitallevel care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77-85. doi:10.7326/M19-0600
2. Cai S, Grubbs A, Makineni R, Kinosian B, Phibbs CS, Intrator O. Evaluation of the Cincinnati Veterans Affairs medical center hospital-in-home program. J Am Geriatr Soc. 2018;66(7):1392-1398. doi:10.1111/jgs.15382
3. Cai S, Laurel PA, Makineni R, Marks ML. Evaluation of a hospital-in-home program implemented among veterans. Am J Manag Care. 2017;23(8):482-487.
4. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. doi:10.1001/jamainternmed.2016.5974
5. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1144: Hospital in Home program, Appendix A, Hospital in Home program standards. January 19, 2021. Accessed May 5, 2022. https://www .va.gov/VHApublications/ViewPublication.asp?pub _ID=9157
6. Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569-1575. doi:10.1001/archinternmed.2009.267
7. Abshire M, Xu J, Baptiste D, et al. Nutritional interventions in heart failure: a systematic review of the literature. J Card Fail. 2015;21(12):989-999. doi:10.1016/j.cardfail.2015.10.004
8. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871. Published 2012 Dec 20. doi:10.1136/bmjopen-2012-001871
9. Sousa AM. Benefits of dietitian home visits. J Am Diet Assoc. 1994;94(10):1149-1151. doi:10.1016/0002-8223(94)91136-3
10. Casas-Agustench P, Megías-Rangil I, Babio N. Economic benefit of dietetic-nutritional treatment in the multidisciplinary primary care team. Beneficio económico del tratamiento dietético-nutricional en el equipo multidisciplinario de atención primaria. Nutr Hosp. 2020;37(4):863-874. doi:10.20960/nh.03025
11. Lee J, Briggs Early K, Kovesdy CP, Lancaster K, Brown N, Steiber AL. The impact of RDNs on non-communicable diseases: proceedings from The State of Food and Nutrition Series Forum. J Acad Nutr Diet. 2022;122(1):166-174. doi:10.1016/j.jand.2021.02.021
12. Academy of Nutrition and Dietetics. Evidence analysis library, nutrition care process. Accessed May 5, 2022. https://www.andeal.org/ncp
13. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1438, clinical nutrition management and therapy. Appendix A, nutrition support therapy. September 19, 2019. Accessed January 20, 2022. https://www.va.gov/VHAPUBLICATIONS/ViewPublication .asp?pub_ID=8512
14. Vogelzang JL. Fifteen ways to enhance client outcomes by using your registered dietitian. Home Healthc Nurse. 2002;20(4):227-229. doi:10.1097/00004045-200204000-00005
15. Kristal AR, Glanz K, Curry SJ, Patterson RE. How can stages of change be best used in dietary interventions?. J Am Diet Assoc. 1999;99(6):679-684. doi:10.1016/S0002-8223(99)00165-0
Hospital in Home (HIH) is the delivery of acute care services in a patient’s home as an alternative to hospitalization.1 Compared with traditional inpatient care, HIH programs have been associated with reduced costs, as well as patient and caregiver satisfaction, diseasespecific outcomes, and mortality rates that were similar or improved compared with inpatient admissions.1-4
The US Department of Veterans Affairs (VA) Veterans Health Administration (VHA) and other hospital systems are increasingly adopting HIH models.2-4 At the time of this writing, there were 12 HIH programs in VHA (personal communication, D. Cooper, 2/28/2022). In addition to physicians and nurses, the interdisciplinary HIH team may include a pharmacist, social worker, and registered dietitian nutritionist (RDN).2,5 HIH programs have been shown to improve nutritional status as measured by the Mini Nutritional Assessment Score, but overall, there is a paucity of published information regarding the provision of nutrition care in HIH.6 The role of the RDN has varied within VHA. Some sites, such as the Sacramento VA Medical Center in California, include a distinct RDN position on the HIH team, whereas others, such as the Spark M. Matsunaga VA Medical Center in Honolulu, Hawaii, and the James A. Haley Veterans’ Hospital in Tampa, Florida, consult clinic RDNs.
Since HIH programs typically treat conditions for which diet is an inherent part of the treatment (eg, congestive heart failure [CHF]), there is a need to precisely define the role of the RDN within the HIH model.2,3,7 Drawing from my experience as an HIH RDN, I will describe how the inclusion of an RDN position within the HIH team is optimal for health care delivery and how HIH practitioners can best utilize RDN services.
RDN Role in HIH Team
Delegating nutrition services to an RDN enhances patient care by empowering HIH team members to function at the highest level of their scope of practice. RDNs have been recognized by physicians as the most qualified health care professionals to help patients with diet-related conditions, such as obesity, and physicians also have reported a desire for additional training in nutrition.8 Although home-health nurses have frequently performed nutrition assessments and interventions, survey results have indicated that many nurses do not feel confident in teaching complex nutritional information.9 In my experience, many HIH patients are nutritionally complex, with more than one condition requiring nutrition intervention. For example, patients may be admitted to HIH for management of CHF, but they may also have diabetes mellitus (DM), obesity, and low socioeconomic status. The HIH RDN can address the nutrition aspects of these conditions, freeing time for physicians and nurses to focus on their respective areas of expertise.9,10 Moreover, the RDN can also provide dietary education to the HIH team to increase their knowledge of nutritional topics and promote consistent messaging to patients.
Including an RDN on the HIH team enables patients to have comprehensive, personalized nutrition care. Rather than merely offering generalized nutrition education, RDNs are trained to provide medical nutrition therapy (MNT), which has been shown to improve health outcomes and be cost-effective for conditions such as type 2 DM, chronic kidney disease, hypertension, and obesity.10,11 In MNT, RDNs use the standardized 4-stepnutrition care process (NCP).12 The Table shows examples of how the NCP can be applied in HIH settings. Furthermore, in my experience, MNT from an RDN also contributes to patient satisfaction. Subjective observations from my team have indicated that patients often express more confidence in managing their diets by the time of HIH discharge.
RDNs can guide physicians and pharmacists in ordering oral nutrition supplements (ONS). Within the VHA, a “food first” approach is preferred to increase caloric intake, and patients must meet specific criteria for prescription of an ONS.13 Furthermore, ONS designed for specific medical conditions (eg, chronic kidney disease) are considered nonformulary and require an RDN evaluation.13 Including an RDN on the HIH team allows this evaluation process to begin early in the patient’s admission to the program and ensures that provision of ONS is clinically appropriate and cost-effective.
Care Coordination
HIH is highly interdisciplinary. Team members perform their respective roles and communicate with the team throughout the day. RDNs can help monitor patients and alert physicians for changes in blood glucose, gastrointestinal concerns, and weight. This is especially helpful for patients who do not have a planned nursing visit on the day of an RDN evaluation. The HIH RDN can also collaborate with other team members to address patient needs. For example, for patients with limited financial resources, the HIH RDN can provide nutrition education regarding cooking on a budget, and the HIH social worker can arrange free or low-cost meal services.
Tips
When hiring an HIH RDN, seek candidates with experience in inpatient, outpatient, and home care settings. As a hybrid of these 3 areas, the HIH RDN position requires a unique combination of acute care skills and health coaching. Additionally, in my experience, the HIH RDN interacts more frequently with the HIH team than other RDN colleagues, so it is important that candidates can work independently and take initiative. This type of position would not be suitable for entry-level RDNs.
Stagger HIH team visits to prevent overwhelming the patient and caregivers. Early in our program, my team quickly learned that patients and caregivers can feel overwhelmed with too many home visits upon admission to HIH. After seeing multiple HIH team members the same day, they were often too tired to focus well on diet education during my visit. Staggering visits (eg, completing the initial nutrition assessment 1 day to 1 week after the initial medical and pharmacy visits) has been an effective strategy to address this problem. Furthermore, some patients prefer that the initial RDN appointment is conducted by telephone, with an inperson reassessment the following week. In my experience, HIH workflow is dynamic by nature, so it is crucial to remain flexible and accommodate individual patient needs as much as possible.
Dietary behavior change is a long-term process, and restrictive hospital diets can be challenging to replicate at home. In a hospital setting, clinicians can order a specialized diet (eg, low sodium with fluid restriction for CHF patients), whereas efforts to implement these restrictions in the home setting can be cumbersome and negatively impact quality of life.7,14 Nevertheless, the effectiveness of medical treatment is compromised when patients do not adhere to dietary recommendations. Meal delivery services that offer specialized diets can be a useful resource for patients and caregivers who are unable to cook, and the HIH RDN can assist patients in ordering these services.
HIH patients may vary in terms of readiness to make dietary changes, and in addition to nutrition education, nutrition counseling is usually needed to effect behavior change. My team has found that consideration of the transtheoretical/ stages of change model can be a helpful approach. 15 The HIH RDN can tailor nutrition interventions to the patient’s stage of change. For example, for patients in the precontemplation stage, the HIH RDN would focus on providing information and addressing emotional aspects of dietary change. In contrast, for patients in the action stage of change, the HIH RDN might emphasize behavioral skill training and social support.15 Particularly for patients in the early stages of change, it may be unrealistic to expect full adoption of the recommended diet within the 30 days of the HIH program. However, by acknowledging the reality of the patient’s stage of change, the HIH RDN and team can then collaborate to support the patient in moving toward the next stage. Patients who are not ready for dietary behavior change during the 30 days of HIH may benefit from longer-term support, and the HIH RDN can arrange followup care with an outpatient RDN.
Conclusions
As the HIH model continues to be adopted across the VHA and other health care systems, it is crucial to consider the value and expertise of an RDN for guiding nutrition care in the HIH setting. The HIH RDN contributes to optimal health care delivery by leading nutritional aspects of patient care, offering personalized MNT, and coordinating and collaborating with team members to meet individual patient needs. An RDN can serve as a valuable resource for nutrition information and enhance the team’s overall services, with the potential to impact clinical outcomes and patient satisfaction.
Hospital in Home (HIH) is the delivery of acute care services in a patient’s home as an alternative to hospitalization.1 Compared with traditional inpatient care, HIH programs have been associated with reduced costs, as well as patient and caregiver satisfaction, diseasespecific outcomes, and mortality rates that were similar or improved compared with inpatient admissions.1-4
The US Department of Veterans Affairs (VA) Veterans Health Administration (VHA) and other hospital systems are increasingly adopting HIH models.2-4 At the time of this writing, there were 12 HIH programs in VHA (personal communication, D. Cooper, 2/28/2022). In addition to physicians and nurses, the interdisciplinary HIH team may include a pharmacist, social worker, and registered dietitian nutritionist (RDN).2,5 HIH programs have been shown to improve nutritional status as measured by the Mini Nutritional Assessment Score, but overall, there is a paucity of published information regarding the provision of nutrition care in HIH.6 The role of the RDN has varied within VHA. Some sites, such as the Sacramento VA Medical Center in California, include a distinct RDN position on the HIH team, whereas others, such as the Spark M. Matsunaga VA Medical Center in Honolulu, Hawaii, and the James A. Haley Veterans’ Hospital in Tampa, Florida, consult clinic RDNs.
Since HIH programs typically treat conditions for which diet is an inherent part of the treatment (eg, congestive heart failure [CHF]), there is a need to precisely define the role of the RDN within the HIH model.2,3,7 Drawing from my experience as an HIH RDN, I will describe how the inclusion of an RDN position within the HIH team is optimal for health care delivery and how HIH practitioners can best utilize RDN services.
RDN Role in HIH Team
Delegating nutrition services to an RDN enhances patient care by empowering HIH team members to function at the highest level of their scope of practice. RDNs have been recognized by physicians as the most qualified health care professionals to help patients with diet-related conditions, such as obesity, and physicians also have reported a desire for additional training in nutrition.8 Although home-health nurses have frequently performed nutrition assessments and interventions, survey results have indicated that many nurses do not feel confident in teaching complex nutritional information.9 In my experience, many HIH patients are nutritionally complex, with more than one condition requiring nutrition intervention. For example, patients may be admitted to HIH for management of CHF, but they may also have diabetes mellitus (DM), obesity, and low socioeconomic status. The HIH RDN can address the nutrition aspects of these conditions, freeing time for physicians and nurses to focus on their respective areas of expertise.9,10 Moreover, the RDN can also provide dietary education to the HIH team to increase their knowledge of nutritional topics and promote consistent messaging to patients.
Including an RDN on the HIH team enables patients to have comprehensive, personalized nutrition care. Rather than merely offering generalized nutrition education, RDNs are trained to provide medical nutrition therapy (MNT), which has been shown to improve health outcomes and be cost-effective for conditions such as type 2 DM, chronic kidney disease, hypertension, and obesity.10,11 In MNT, RDNs use the standardized 4-stepnutrition care process (NCP).12 The Table shows examples of how the NCP can be applied in HIH settings. Furthermore, in my experience, MNT from an RDN also contributes to patient satisfaction. Subjective observations from my team have indicated that patients often express more confidence in managing their diets by the time of HIH discharge.
RDNs can guide physicians and pharmacists in ordering oral nutrition supplements (ONS). Within the VHA, a “food first” approach is preferred to increase caloric intake, and patients must meet specific criteria for prescription of an ONS.13 Furthermore, ONS designed for specific medical conditions (eg, chronic kidney disease) are considered nonformulary and require an RDN evaluation.13 Including an RDN on the HIH team allows this evaluation process to begin early in the patient’s admission to the program and ensures that provision of ONS is clinically appropriate and cost-effective.
Care Coordination
HIH is highly interdisciplinary. Team members perform their respective roles and communicate with the team throughout the day. RDNs can help monitor patients and alert physicians for changes in blood glucose, gastrointestinal concerns, and weight. This is especially helpful for patients who do not have a planned nursing visit on the day of an RDN evaluation. The HIH RDN can also collaborate with other team members to address patient needs. For example, for patients with limited financial resources, the HIH RDN can provide nutrition education regarding cooking on a budget, and the HIH social worker can arrange free or low-cost meal services.
Tips
When hiring an HIH RDN, seek candidates with experience in inpatient, outpatient, and home care settings. As a hybrid of these 3 areas, the HIH RDN position requires a unique combination of acute care skills and health coaching. Additionally, in my experience, the HIH RDN interacts more frequently with the HIH team than other RDN colleagues, so it is important that candidates can work independently and take initiative. This type of position would not be suitable for entry-level RDNs.
Stagger HIH team visits to prevent overwhelming the patient and caregivers. Early in our program, my team quickly learned that patients and caregivers can feel overwhelmed with too many home visits upon admission to HIH. After seeing multiple HIH team members the same day, they were often too tired to focus well on diet education during my visit. Staggering visits (eg, completing the initial nutrition assessment 1 day to 1 week after the initial medical and pharmacy visits) has been an effective strategy to address this problem. Furthermore, some patients prefer that the initial RDN appointment is conducted by telephone, with an inperson reassessment the following week. In my experience, HIH workflow is dynamic by nature, so it is crucial to remain flexible and accommodate individual patient needs as much as possible.
Dietary behavior change is a long-term process, and restrictive hospital diets can be challenging to replicate at home. In a hospital setting, clinicians can order a specialized diet (eg, low sodium with fluid restriction for CHF patients), whereas efforts to implement these restrictions in the home setting can be cumbersome and negatively impact quality of life.7,14 Nevertheless, the effectiveness of medical treatment is compromised when patients do not adhere to dietary recommendations. Meal delivery services that offer specialized diets can be a useful resource for patients and caregivers who are unable to cook, and the HIH RDN can assist patients in ordering these services.
HIH patients may vary in terms of readiness to make dietary changes, and in addition to nutrition education, nutrition counseling is usually needed to effect behavior change. My team has found that consideration of the transtheoretical/ stages of change model can be a helpful approach. 15 The HIH RDN can tailor nutrition interventions to the patient’s stage of change. For example, for patients in the precontemplation stage, the HIH RDN would focus on providing information and addressing emotional aspects of dietary change. In contrast, for patients in the action stage of change, the HIH RDN might emphasize behavioral skill training and social support.15 Particularly for patients in the early stages of change, it may be unrealistic to expect full adoption of the recommended diet within the 30 days of the HIH program. However, by acknowledging the reality of the patient’s stage of change, the HIH RDN and team can then collaborate to support the patient in moving toward the next stage. Patients who are not ready for dietary behavior change during the 30 days of HIH may benefit from longer-term support, and the HIH RDN can arrange followup care with an outpatient RDN.
Conclusions
As the HIH model continues to be adopted across the VHA and other health care systems, it is crucial to consider the value and expertise of an RDN for guiding nutrition care in the HIH setting. The HIH RDN contributes to optimal health care delivery by leading nutritional aspects of patient care, offering personalized MNT, and coordinating and collaborating with team members to meet individual patient needs. An RDN can serve as a valuable resource for nutrition information and enhance the team’s overall services, with the potential to impact clinical outcomes and patient satisfaction.
1. Levine DM, Ouchi K, Blanchfield B, et al. Hospitallevel care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77-85. doi:10.7326/M19-0600
2. Cai S, Grubbs A, Makineni R, Kinosian B, Phibbs CS, Intrator O. Evaluation of the Cincinnati Veterans Affairs medical center hospital-in-home program. J Am Geriatr Soc. 2018;66(7):1392-1398. doi:10.1111/jgs.15382
3. Cai S, Laurel PA, Makineni R, Marks ML. Evaluation of a hospital-in-home program implemented among veterans. Am J Manag Care. 2017;23(8):482-487.
4. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. doi:10.1001/jamainternmed.2016.5974
5. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1144: Hospital in Home program, Appendix A, Hospital in Home program standards. January 19, 2021. Accessed May 5, 2022. https://www .va.gov/VHApublications/ViewPublication.asp?pub _ID=9157
6. Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569-1575. doi:10.1001/archinternmed.2009.267
7. Abshire M, Xu J, Baptiste D, et al. Nutritional interventions in heart failure: a systematic review of the literature. J Card Fail. 2015;21(12):989-999. doi:10.1016/j.cardfail.2015.10.004
8. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871. Published 2012 Dec 20. doi:10.1136/bmjopen-2012-001871
9. Sousa AM. Benefits of dietitian home visits. J Am Diet Assoc. 1994;94(10):1149-1151. doi:10.1016/0002-8223(94)91136-3
10. Casas-Agustench P, Megías-Rangil I, Babio N. Economic benefit of dietetic-nutritional treatment in the multidisciplinary primary care team. Beneficio económico del tratamiento dietético-nutricional en el equipo multidisciplinario de atención primaria. Nutr Hosp. 2020;37(4):863-874. doi:10.20960/nh.03025
11. Lee J, Briggs Early K, Kovesdy CP, Lancaster K, Brown N, Steiber AL. The impact of RDNs on non-communicable diseases: proceedings from The State of Food and Nutrition Series Forum. J Acad Nutr Diet. 2022;122(1):166-174. doi:10.1016/j.jand.2021.02.021
12. Academy of Nutrition and Dietetics. Evidence analysis library, nutrition care process. Accessed May 5, 2022. https://www.andeal.org/ncp
13. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1438, clinical nutrition management and therapy. Appendix A, nutrition support therapy. September 19, 2019. Accessed January 20, 2022. https://www.va.gov/VHAPUBLICATIONS/ViewPublication .asp?pub_ID=8512
14. Vogelzang JL. Fifteen ways to enhance client outcomes by using your registered dietitian. Home Healthc Nurse. 2002;20(4):227-229. doi:10.1097/00004045-200204000-00005
15. Kristal AR, Glanz K, Curry SJ, Patterson RE. How can stages of change be best used in dietary interventions?. J Am Diet Assoc. 1999;99(6):679-684. doi:10.1016/S0002-8223(99)00165-0
1. Levine DM, Ouchi K, Blanchfield B, et al. Hospitallevel care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77-85. doi:10.7326/M19-0600
2. Cai S, Grubbs A, Makineni R, Kinosian B, Phibbs CS, Intrator O. Evaluation of the Cincinnati Veterans Affairs medical center hospital-in-home program. J Am Geriatr Soc. 2018;66(7):1392-1398. doi:10.1111/jgs.15382
3. Cai S, Laurel PA, Makineni R, Marks ML. Evaluation of a hospital-in-home program implemented among veterans. Am J Manag Care. 2017;23(8):482-487.
4. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. doi:10.1001/jamainternmed.2016.5974
5. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1144: Hospital in Home program, Appendix A, Hospital in Home program standards. January 19, 2021. Accessed May 5, 2022. https://www .va.gov/VHApublications/ViewPublication.asp?pub _ID=9157
6. Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569-1575. doi:10.1001/archinternmed.2009.267
7. Abshire M, Xu J, Baptiste D, et al. Nutritional interventions in heart failure: a systematic review of the literature. J Card Fail. 2015;21(12):989-999. doi:10.1016/j.cardfail.2015.10.004
8. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871. Published 2012 Dec 20. doi:10.1136/bmjopen-2012-001871
9. Sousa AM. Benefits of dietitian home visits. J Am Diet Assoc. 1994;94(10):1149-1151. doi:10.1016/0002-8223(94)91136-3
10. Casas-Agustench P, Megías-Rangil I, Babio N. Economic benefit of dietetic-nutritional treatment in the multidisciplinary primary care team. Beneficio económico del tratamiento dietético-nutricional en el equipo multidisciplinario de atención primaria. Nutr Hosp. 2020;37(4):863-874. doi:10.20960/nh.03025
11. Lee J, Briggs Early K, Kovesdy CP, Lancaster K, Brown N, Steiber AL. The impact of RDNs on non-communicable diseases: proceedings from The State of Food and Nutrition Series Forum. J Acad Nutr Diet. 2022;122(1):166-174. doi:10.1016/j.jand.2021.02.021
12. Academy of Nutrition and Dietetics. Evidence analysis library, nutrition care process. Accessed May 5, 2022. https://www.andeal.org/ncp
13. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1438, clinical nutrition management and therapy. Appendix A, nutrition support therapy. September 19, 2019. Accessed January 20, 2022. https://www.va.gov/VHAPUBLICATIONS/ViewPublication .asp?pub_ID=8512
14. Vogelzang JL. Fifteen ways to enhance client outcomes by using your registered dietitian. Home Healthc Nurse. 2002;20(4):227-229. doi:10.1097/00004045-200204000-00005
15. Kristal AR, Glanz K, Curry SJ, Patterson RE. How can stages of change be best used in dietary interventions?. J Am Diet Assoc. 1999;99(6):679-684. doi:10.1016/S0002-8223(99)00165-0
Don’t overlook this cause of falls
I enjoyed reading “How to identify balance disorders and reduce fall risk” (J Fam Pract. 2022;71:20-30) from the January/February issue. I was, however, disappointed to see that normal pressure hydrocephalus (NPH) was not discussed in the article or tables.
Recently, I took care of a 72-year-old patient who presented after multiple falls. In conjunction with Neurology, the presumptive diagnosis of Parkinson disease was made. However, the patient continued to experience a health decline that included cognitive changes, nocturia, and the classic “magnetic gait” of NPH (mnemonic for diagnosing this triad of symptoms: weird, wet, wobbly). The presumptive diagnosis was then changed when the results of a fluorodopa F18 positron emission tomography scan (also known as a DaT scan) returned as normal, essentially excluding the diagnosis of Parkinson disease.
The patient has since seen a dramatic improvement in gait and cognitive and urinary symptoms following a high-volume lumbar puncture and placement of a ventriculoperitoneal shunt.
This case demonstrates the importance of considering NPH in the differential diagnosis for patients with balance disorders. Prompt diagnosis and management can result in a variable, but at times dramatic, reversal of symptoms.
Ernestine Lee, MD, MPH
Austin, TX
I enjoyed reading “How to identify balance disorders and reduce fall risk” (J Fam Pract. 2022;71:20-30) from the January/February issue. I was, however, disappointed to see that normal pressure hydrocephalus (NPH) was not discussed in the article or tables.
Recently, I took care of a 72-year-old patient who presented after multiple falls. In conjunction with Neurology, the presumptive diagnosis of Parkinson disease was made. However, the patient continued to experience a health decline that included cognitive changes, nocturia, and the classic “magnetic gait” of NPH (mnemonic for diagnosing this triad of symptoms: weird, wet, wobbly). The presumptive diagnosis was then changed when the results of a fluorodopa F18 positron emission tomography scan (also known as a DaT scan) returned as normal, essentially excluding the diagnosis of Parkinson disease.
The patient has since seen a dramatic improvement in gait and cognitive and urinary symptoms following a high-volume lumbar puncture and placement of a ventriculoperitoneal shunt.
This case demonstrates the importance of considering NPH in the differential diagnosis for patients with balance disorders. Prompt diagnosis and management can result in a variable, but at times dramatic, reversal of symptoms.
Ernestine Lee, MD, MPH
Austin, TX
I enjoyed reading “How to identify balance disorders and reduce fall risk” (J Fam Pract. 2022;71:20-30) from the January/February issue. I was, however, disappointed to see that normal pressure hydrocephalus (NPH) was not discussed in the article or tables.
Recently, I took care of a 72-year-old patient who presented after multiple falls. In conjunction with Neurology, the presumptive diagnosis of Parkinson disease was made. However, the patient continued to experience a health decline that included cognitive changes, nocturia, and the classic “magnetic gait” of NPH (mnemonic for diagnosing this triad of symptoms: weird, wet, wobbly). The presumptive diagnosis was then changed when the results of a fluorodopa F18 positron emission tomography scan (also known as a DaT scan) returned as normal, essentially excluding the diagnosis of Parkinson disease.
The patient has since seen a dramatic improvement in gait and cognitive and urinary symptoms following a high-volume lumbar puncture and placement of a ventriculoperitoneal shunt.
This case demonstrates the importance of considering NPH in the differential diagnosis for patients with balance disorders. Prompt diagnosis and management can result in a variable, but at times dramatic, reversal of symptoms.
Ernestine Lee, MD, MPH
Austin, TX
Findings raise questions about migraine and sleep
CHARLOTTE, N.C. – What may be the largest case-based study of patients with migraine and sleep-disordered breathing to date has found that, counter to prevailing thought, they may not be at higher risk of having obstructive sleep apnea (OSA) than nonmigraine patients, although further prospective studies are needed to validate that finding.
“This in no way for me changes the fact that, for patients that complain of headaches, sleep apnea remains to be something that should be considered as possible cause of their headaches,” neurologist and Cleveland Clinic postdoctoral fellow Eric Gruenthal, MD, said in an interview after he presented his results at the annual meeting of the Associated Professional Sleep Societies.
The study suggested that patients with migraine may have an OSA risk that “may be a little lower” than their nonmigraine counterparts, Dr. Gruenthal said. “But we have really yet to determine whether that’s true or not.”
Large case-based study
The retrospective case study included 4,783 migraine cases from the Cleveland Clinic electronic health record database who were case matched on a 1:3 basis with 14,287 controls. Patients with migraine had an average age of 47.5 years (±13.3) and body mass index of 33.7 kg/m2 (±8.6), and 76.4% were White. All patients had polysomnography (PSG) at a Cleveland Clinic facility from 1998 to 2021.
The analysis evaluated the collected data in two domains: sleep architecture, consisting of arousal index (AI), total sleep time (TST) and percentage of sleep stage time; and sleep-disordered breathing, including apnea hypopnea index (AHI) and mean oxygen saturation. The key findings of the migraine patients versus controls include:
- Lower AI, 19.6 (95% confidence interval, 12.8-30.9) versus 22.6 (95% CI, 14.7-34.9; P < .001).
- Shorter TST, 359 (95% CI, 307-421) versus 363 (95% CI, 306-432.5) minutes (P = .01).
- With regard to sleep stage, the percentage of N2 sleep was higher, 67.8% (95% CI, 59.6%-75.6%) versus 67% (95% CI, 58.4%-74.8%; P < .001); but the percentage of REM was lower at 16.7% (95% CI, 10%-22%) versus 17% (95% CI, 11.1%-22.2%; P = .012).
- Lower AHI, 7.4 (95% CI, 2.6-17) versus 9.5 (95% CI, 3.7-22.1, P < .001).
- Higher mean oxygen saturation, 93.7 (±2.4) versus 93.3% (±2.6; P < .001).
“Also,” Dr. Gruenthal added, “we found that the percentage of sleep time with oxygen saturation below 90% was lower among patients with migraine, at 1.3% versus 2.4%” (P < .001).
A unique profile?
The goal of the study was to determine whether migraine patients would have a unique PSG profile, Dr. Gruenthal said. “We were trying to overcome some of the limitations of previous studies, most notably those that use small sample sizes, and in some cases a lack of controls.”
The findings that migraine patients would have higher AI and elevated AHI ran counter to the study’s hypotheses, but fell in line with the expectation that they would have reduced TST, Dr. Gruenthal said.
Patients with migraine “may, in fact, exhibit a lower burden of sleep-disordered breathing, and that’s based on our findings such as the lower AHI and decreased burden of hypoxemia,” he said. “We theorized that this may be related to patients with migraine having a unique CGRP [calcitonin gene-related peptide] and serotonin physiology.” He noted that previously published research has shown that sleep CGRP and serotonin have a central role in causing arousal in response to rising CO2 levels during sleep, which can occur during apneas and hypopneas.
Dr. Gruenthal noted that the researchers are still analyzing the findings. “We theorized that possible indication bias may be present in our study,” he said. “It may be the case that patients with migraine are more likely to get their PSG done because of their headache and not for things like snoring and witnessed apneas, which may be more predictive of significant sleep apnea.” They’re also evaluating the “question of medicine confounding.”
Dr. Gruenthal added that “the big unanswered question out there is, if you have a patient with migraine who also has sleep apnea, by treating the sleep apnea will that improve their migraine?”
More questions than answers
Commenting on the study, Donald Bliwise, PhD, professor of neurology at Emory Sleep Center, Atlanta, said the study findings shouldn’t change how clinicians approach migraine in relation to sleep.
“It’s a case series, it’s retrospective,” said Dr. Bliwise, who was not involved in the study. “It’s the largest study that I know of that has ever looked at the diagnosis of migraine in relation to polysomnographic measures of sleep, but it’s imprecise to the extent that migraine is a clinical diagnosis, so not everyone that carries the diagnosis of migraine has the diagnosis made by a neurologist.”
The study raises more questions than it answers, he said, “but that’s not necessarily a bad thing. I think we need more prospective studies.” Those studies should be more granular in how they analyze sleep in migraine patients “Since migraine is an intermittent event, and sleep quality and length, and percentage of REM sleep and even sleep apnea can vary from night to night, it would be fascinating to look at headaches over a month in relation to sleep over a month.”
Dr. Gruenthal and Dr. Bliwise have no disclosures. The Association of Migraine Disorders provided funding for the study.
CHARLOTTE, N.C. – What may be the largest case-based study of patients with migraine and sleep-disordered breathing to date has found that, counter to prevailing thought, they may not be at higher risk of having obstructive sleep apnea (OSA) than nonmigraine patients, although further prospective studies are needed to validate that finding.
“This in no way for me changes the fact that, for patients that complain of headaches, sleep apnea remains to be something that should be considered as possible cause of their headaches,” neurologist and Cleveland Clinic postdoctoral fellow Eric Gruenthal, MD, said in an interview after he presented his results at the annual meeting of the Associated Professional Sleep Societies.
The study suggested that patients with migraine may have an OSA risk that “may be a little lower” than their nonmigraine counterparts, Dr. Gruenthal said. “But we have really yet to determine whether that’s true or not.”
Large case-based study
The retrospective case study included 4,783 migraine cases from the Cleveland Clinic electronic health record database who were case matched on a 1:3 basis with 14,287 controls. Patients with migraine had an average age of 47.5 years (±13.3) and body mass index of 33.7 kg/m2 (±8.6), and 76.4% were White. All patients had polysomnography (PSG) at a Cleveland Clinic facility from 1998 to 2021.
The analysis evaluated the collected data in two domains: sleep architecture, consisting of arousal index (AI), total sleep time (TST) and percentage of sleep stage time; and sleep-disordered breathing, including apnea hypopnea index (AHI) and mean oxygen saturation. The key findings of the migraine patients versus controls include:
- Lower AI, 19.6 (95% confidence interval, 12.8-30.9) versus 22.6 (95% CI, 14.7-34.9; P < .001).
- Shorter TST, 359 (95% CI, 307-421) versus 363 (95% CI, 306-432.5) minutes (P = .01).
- With regard to sleep stage, the percentage of N2 sleep was higher, 67.8% (95% CI, 59.6%-75.6%) versus 67% (95% CI, 58.4%-74.8%; P < .001); but the percentage of REM was lower at 16.7% (95% CI, 10%-22%) versus 17% (95% CI, 11.1%-22.2%; P = .012).
- Lower AHI, 7.4 (95% CI, 2.6-17) versus 9.5 (95% CI, 3.7-22.1, P < .001).
- Higher mean oxygen saturation, 93.7 (±2.4) versus 93.3% (±2.6; P < .001).
“Also,” Dr. Gruenthal added, “we found that the percentage of sleep time with oxygen saturation below 90% was lower among patients with migraine, at 1.3% versus 2.4%” (P < .001).
A unique profile?
The goal of the study was to determine whether migraine patients would have a unique PSG profile, Dr. Gruenthal said. “We were trying to overcome some of the limitations of previous studies, most notably those that use small sample sizes, and in some cases a lack of controls.”
The findings that migraine patients would have higher AI and elevated AHI ran counter to the study’s hypotheses, but fell in line with the expectation that they would have reduced TST, Dr. Gruenthal said.
Patients with migraine “may, in fact, exhibit a lower burden of sleep-disordered breathing, and that’s based on our findings such as the lower AHI and decreased burden of hypoxemia,” he said. “We theorized that this may be related to patients with migraine having a unique CGRP [calcitonin gene-related peptide] and serotonin physiology.” He noted that previously published research has shown that sleep CGRP and serotonin have a central role in causing arousal in response to rising CO2 levels during sleep, which can occur during apneas and hypopneas.
Dr. Gruenthal noted that the researchers are still analyzing the findings. “We theorized that possible indication bias may be present in our study,” he said. “It may be the case that patients with migraine are more likely to get their PSG done because of their headache and not for things like snoring and witnessed apneas, which may be more predictive of significant sleep apnea.” They’re also evaluating the “question of medicine confounding.”
Dr. Gruenthal added that “the big unanswered question out there is, if you have a patient with migraine who also has sleep apnea, by treating the sleep apnea will that improve their migraine?”
More questions than answers
Commenting on the study, Donald Bliwise, PhD, professor of neurology at Emory Sleep Center, Atlanta, said the study findings shouldn’t change how clinicians approach migraine in relation to sleep.
“It’s a case series, it’s retrospective,” said Dr. Bliwise, who was not involved in the study. “It’s the largest study that I know of that has ever looked at the diagnosis of migraine in relation to polysomnographic measures of sleep, but it’s imprecise to the extent that migraine is a clinical diagnosis, so not everyone that carries the diagnosis of migraine has the diagnosis made by a neurologist.”
The study raises more questions than it answers, he said, “but that’s not necessarily a bad thing. I think we need more prospective studies.” Those studies should be more granular in how they analyze sleep in migraine patients “Since migraine is an intermittent event, and sleep quality and length, and percentage of REM sleep and even sleep apnea can vary from night to night, it would be fascinating to look at headaches over a month in relation to sleep over a month.”
Dr. Gruenthal and Dr. Bliwise have no disclosures. The Association of Migraine Disorders provided funding for the study.
CHARLOTTE, N.C. – What may be the largest case-based study of patients with migraine and sleep-disordered breathing to date has found that, counter to prevailing thought, they may not be at higher risk of having obstructive sleep apnea (OSA) than nonmigraine patients, although further prospective studies are needed to validate that finding.
“This in no way for me changes the fact that, for patients that complain of headaches, sleep apnea remains to be something that should be considered as possible cause of their headaches,” neurologist and Cleveland Clinic postdoctoral fellow Eric Gruenthal, MD, said in an interview after he presented his results at the annual meeting of the Associated Professional Sleep Societies.
The study suggested that patients with migraine may have an OSA risk that “may be a little lower” than their nonmigraine counterparts, Dr. Gruenthal said. “But we have really yet to determine whether that’s true or not.”
Large case-based study
The retrospective case study included 4,783 migraine cases from the Cleveland Clinic electronic health record database who were case matched on a 1:3 basis with 14,287 controls. Patients with migraine had an average age of 47.5 years (±13.3) and body mass index of 33.7 kg/m2 (±8.6), and 76.4% were White. All patients had polysomnography (PSG) at a Cleveland Clinic facility from 1998 to 2021.
The analysis evaluated the collected data in two domains: sleep architecture, consisting of arousal index (AI), total sleep time (TST) and percentage of sleep stage time; and sleep-disordered breathing, including apnea hypopnea index (AHI) and mean oxygen saturation. The key findings of the migraine patients versus controls include:
- Lower AI, 19.6 (95% confidence interval, 12.8-30.9) versus 22.6 (95% CI, 14.7-34.9; P < .001).
- Shorter TST, 359 (95% CI, 307-421) versus 363 (95% CI, 306-432.5) minutes (P = .01).
- With regard to sleep stage, the percentage of N2 sleep was higher, 67.8% (95% CI, 59.6%-75.6%) versus 67% (95% CI, 58.4%-74.8%; P < .001); but the percentage of REM was lower at 16.7% (95% CI, 10%-22%) versus 17% (95% CI, 11.1%-22.2%; P = .012).
- Lower AHI, 7.4 (95% CI, 2.6-17) versus 9.5 (95% CI, 3.7-22.1, P < .001).
- Higher mean oxygen saturation, 93.7 (±2.4) versus 93.3% (±2.6; P < .001).
“Also,” Dr. Gruenthal added, “we found that the percentage of sleep time with oxygen saturation below 90% was lower among patients with migraine, at 1.3% versus 2.4%” (P < .001).
A unique profile?
The goal of the study was to determine whether migraine patients would have a unique PSG profile, Dr. Gruenthal said. “We were trying to overcome some of the limitations of previous studies, most notably those that use small sample sizes, and in some cases a lack of controls.”
The findings that migraine patients would have higher AI and elevated AHI ran counter to the study’s hypotheses, but fell in line with the expectation that they would have reduced TST, Dr. Gruenthal said.
Patients with migraine “may, in fact, exhibit a lower burden of sleep-disordered breathing, and that’s based on our findings such as the lower AHI and decreased burden of hypoxemia,” he said. “We theorized that this may be related to patients with migraine having a unique CGRP [calcitonin gene-related peptide] and serotonin physiology.” He noted that previously published research has shown that sleep CGRP and serotonin have a central role in causing arousal in response to rising CO2 levels during sleep, which can occur during apneas and hypopneas.
Dr. Gruenthal noted that the researchers are still analyzing the findings. “We theorized that possible indication bias may be present in our study,” he said. “It may be the case that patients with migraine are more likely to get their PSG done because of their headache and not for things like snoring and witnessed apneas, which may be more predictive of significant sleep apnea.” They’re also evaluating the “question of medicine confounding.”
Dr. Gruenthal added that “the big unanswered question out there is, if you have a patient with migraine who also has sleep apnea, by treating the sleep apnea will that improve their migraine?”
More questions than answers
Commenting on the study, Donald Bliwise, PhD, professor of neurology at Emory Sleep Center, Atlanta, said the study findings shouldn’t change how clinicians approach migraine in relation to sleep.
“It’s a case series, it’s retrospective,” said Dr. Bliwise, who was not involved in the study. “It’s the largest study that I know of that has ever looked at the diagnosis of migraine in relation to polysomnographic measures of sleep, but it’s imprecise to the extent that migraine is a clinical diagnosis, so not everyone that carries the diagnosis of migraine has the diagnosis made by a neurologist.”
The study raises more questions than it answers, he said, “but that’s not necessarily a bad thing. I think we need more prospective studies.” Those studies should be more granular in how they analyze sleep in migraine patients “Since migraine is an intermittent event, and sleep quality and length, and percentage of REM sleep and even sleep apnea can vary from night to night, it would be fascinating to look at headaches over a month in relation to sleep over a month.”
Dr. Gruenthal and Dr. Bliwise have no disclosures. The Association of Migraine Disorders provided funding for the study.
AT SLEEP 2022
Taking the time to get it right
I cannot agree more with Dr. Hickner’s editorial, “The power of the pause to prevent diagnostic error” (J Fam Pract. 2022;71:102). In 1974, when I started at the Medical College of Virginia, I thought I was going to be a medical researcher. By mid-1978, I had completely changed my focus to family medicine. Fortunately, my drive for detail and accuracy remained, albeit at odds with a whirlwind residency and solo practice. I drove my staff (and wife) crazy because I frequently spent more than the “allotted” time with a patient. The time was not wasted; it was most important for me to gain the trust of the patient and then to get it right—or find a path to the answer.
Jeff Ginther, MD
Bristol, VA
I cannot agree more with Dr. Hickner’s editorial, “The power of the pause to prevent diagnostic error” (J Fam Pract. 2022;71:102). In 1974, when I started at the Medical College of Virginia, I thought I was going to be a medical researcher. By mid-1978, I had completely changed my focus to family medicine. Fortunately, my drive for detail and accuracy remained, albeit at odds with a whirlwind residency and solo practice. I drove my staff (and wife) crazy because I frequently spent more than the “allotted” time with a patient. The time was not wasted; it was most important for me to gain the trust of the patient and then to get it right—or find a path to the answer.
Jeff Ginther, MD
Bristol, VA
I cannot agree more with Dr. Hickner’s editorial, “The power of the pause to prevent diagnostic error” (J Fam Pract. 2022;71:102). In 1974, when I started at the Medical College of Virginia, I thought I was going to be a medical researcher. By mid-1978, I had completely changed my focus to family medicine. Fortunately, my drive for detail and accuracy remained, albeit at odds with a whirlwind residency and solo practice. I drove my staff (and wife) crazy because I frequently spent more than the “allotted” time with a patient. The time was not wasted; it was most important for me to gain the trust of the patient and then to get it right—or find a path to the answer.
Jeff Ginther, MD
Bristol, VA
Center-based childcare associated with healthier body weight
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
FROM NUTRITION 2022
FTC decision to investigate pharmacy benefit managers applauded by rheumatologists
The Federal Trade Commission’s announcement June 7 of a plan to investigate the business practices of pharmacy benefit managers (PBMs) was welcome news to rheumatologists. Widespread concern about the cost of prescription drugs and an additional 24,000 comments from the public prompted the agency’s decision to examine PBMs, which act as intermediaries between insurers, manufacturers, and pharmacies.
PBMs negotiate drug prices and rebates with manufacturers, reimburse pharmacies for drug costs, and create insurers’ drug formularies. But it’s widely held that instead of managing and leveling costs, PBMs have ratcheted up prices at multiple junctures to gain more profit.
The FTC’s investigation will focus on the six largest PBMs: CVS Caremark, Express Scripts, OptumRx, Humana, Prime Therapeutics, and MedImpact Healthcare Systems. CVS Caremark is owned by CVS, Express Scripts is owned by Cigna, and OptumRx is owned by UnitedHealth. The companies will have 90 days to respond to the commission’s official request for information.
Some of the information the FTC plans to ask about includes how the companies may be pushing patients toward using PBM-owned pharmacies and how rebates affect insurers’ formularies and the cost of drugs for patients.
The purchase or establishment of PBMs by the largest insurance companies – known as vertical integration – makes it nearly impossible for outsiders to determine what’s really causing price increases for prescription drugs. “The black box of secretive contracts and monies changing hands between manufacturers and PBMs has grown quite large since the Department of Justice and the FTC allowed the big three PBMs to be part of the three largest health insurance companies,” Madelaine A. Feldman, MD, a rheumatologist at the Rheumatology Group, New Orleans, and president of the Coalition of State Rheumatology Organizations, told this news organization.
Dr. Feldman and fellow rheumatologists at the American College of Rheumatology are happy that the FTC has decided to pursue this investigation. They note that rheumatologists have been calling for action for years and are eager to see change.
This probe aims to determine not only how the PBM industry affects pharmacists but also how their practices create ripple effects across the prescription drug industry, said Dr. Feldman. “I was very happy to see that they will be investigating how rebates and other manufacturer price concessions affect formulary construction and utilization management tools, ultimately increasing drug prices and patient cost share.”
A version of this article first appeared on Medscape.com.
The Federal Trade Commission’s announcement June 7 of a plan to investigate the business practices of pharmacy benefit managers (PBMs) was welcome news to rheumatologists. Widespread concern about the cost of prescription drugs and an additional 24,000 comments from the public prompted the agency’s decision to examine PBMs, which act as intermediaries between insurers, manufacturers, and pharmacies.
PBMs negotiate drug prices and rebates with manufacturers, reimburse pharmacies for drug costs, and create insurers’ drug formularies. But it’s widely held that instead of managing and leveling costs, PBMs have ratcheted up prices at multiple junctures to gain more profit.
The FTC’s investigation will focus on the six largest PBMs: CVS Caremark, Express Scripts, OptumRx, Humana, Prime Therapeutics, and MedImpact Healthcare Systems. CVS Caremark is owned by CVS, Express Scripts is owned by Cigna, and OptumRx is owned by UnitedHealth. The companies will have 90 days to respond to the commission’s official request for information.
Some of the information the FTC plans to ask about includes how the companies may be pushing patients toward using PBM-owned pharmacies and how rebates affect insurers’ formularies and the cost of drugs for patients.
The purchase or establishment of PBMs by the largest insurance companies – known as vertical integration – makes it nearly impossible for outsiders to determine what’s really causing price increases for prescription drugs. “The black box of secretive contracts and monies changing hands between manufacturers and PBMs has grown quite large since the Department of Justice and the FTC allowed the big three PBMs to be part of the three largest health insurance companies,” Madelaine A. Feldman, MD, a rheumatologist at the Rheumatology Group, New Orleans, and president of the Coalition of State Rheumatology Organizations, told this news organization.
Dr. Feldman and fellow rheumatologists at the American College of Rheumatology are happy that the FTC has decided to pursue this investigation. They note that rheumatologists have been calling for action for years and are eager to see change.
This probe aims to determine not only how the PBM industry affects pharmacists but also how their practices create ripple effects across the prescription drug industry, said Dr. Feldman. “I was very happy to see that they will be investigating how rebates and other manufacturer price concessions affect formulary construction and utilization management tools, ultimately increasing drug prices and patient cost share.”
A version of this article first appeared on Medscape.com.
The Federal Trade Commission’s announcement June 7 of a plan to investigate the business practices of pharmacy benefit managers (PBMs) was welcome news to rheumatologists. Widespread concern about the cost of prescription drugs and an additional 24,000 comments from the public prompted the agency’s decision to examine PBMs, which act as intermediaries between insurers, manufacturers, and pharmacies.
PBMs negotiate drug prices and rebates with manufacturers, reimburse pharmacies for drug costs, and create insurers’ drug formularies. But it’s widely held that instead of managing and leveling costs, PBMs have ratcheted up prices at multiple junctures to gain more profit.
The FTC’s investigation will focus on the six largest PBMs: CVS Caremark, Express Scripts, OptumRx, Humana, Prime Therapeutics, and MedImpact Healthcare Systems. CVS Caremark is owned by CVS, Express Scripts is owned by Cigna, and OptumRx is owned by UnitedHealth. The companies will have 90 days to respond to the commission’s official request for information.
Some of the information the FTC plans to ask about includes how the companies may be pushing patients toward using PBM-owned pharmacies and how rebates affect insurers’ formularies and the cost of drugs for patients.
The purchase or establishment of PBMs by the largest insurance companies – known as vertical integration – makes it nearly impossible for outsiders to determine what’s really causing price increases for prescription drugs. “The black box of secretive contracts and monies changing hands between manufacturers and PBMs has grown quite large since the Department of Justice and the FTC allowed the big three PBMs to be part of the three largest health insurance companies,” Madelaine A. Feldman, MD, a rheumatologist at the Rheumatology Group, New Orleans, and president of the Coalition of State Rheumatology Organizations, told this news organization.
Dr. Feldman and fellow rheumatologists at the American College of Rheumatology are happy that the FTC has decided to pursue this investigation. They note that rheumatologists have been calling for action for years and are eager to see change.
This probe aims to determine not only how the PBM industry affects pharmacists but also how their practices create ripple effects across the prescription drug industry, said Dr. Feldman. “I was very happy to see that they will be investigating how rebates and other manufacturer price concessions affect formulary construction and utilization management tools, ultimately increasing drug prices and patient cost share.”
A version of this article first appeared on Medscape.com.