User login
Neurology Reviews covers innovative and emerging news in neurology and neuroscience every month, with a focus on practical approaches to treating Parkinson's disease, epilepsy, headache, stroke, multiple sclerosis, Alzheimer's disease, and other neurologic disorders.
PML
Progressive multifocal leukoencephalopathy
Rituxan
The leading independent newspaper covering neurology news and commentary.
Quiet quitting: Are physicians dying inside bit by bit? Or setting healthy boundaries?
In the past few months, “quiet quitting” has garnered increasing traction across social media platforms. My morning review of social media revealed thousands of posts ranging from “Why doing less at work could be good for you – and your employer” to “After ‘quiet quitting’ here comes ‘quiet firing.’ ”
But quiet quitting is neither quiet nor quitting.
Quiet quitting is a misnomer. In addition, quiet quitters are firmer with their boundaries, do not take on work above and beyond clearly stated expectations, do not respond after hours, and do not feel like they are “not doing their job” when they are not immediately available.
Individuals who “quiet quit” continue to meet the demands of their job but reject the hustle-culture mentality that you must always be available for more work and, most importantly, that your value as person and self-worth are defined and determined by your work. Quiet quitters believe that it is possible to have good boundaries and yet remain productive, engaged, and active within the workplace.
Earlier this month, NPR’s posted tutorial on how to set better boundaries at work garnered 491,000 views, reflecting employees’ difficulties in communicating their needs, thoughts, and availability to their employers. Quiet quitting refers to not only rejecting the idea of going above and beyond in the workplace but also feeling confident that there will not be negative ramifications for not consistently working beyond the expected requirements.
A focus on balance, life, loves, and family is rarely addressed or emphasized by traditional employers; employees have little skill in addressing boundaries and clarifying their value and availability. For decades, “needing” flexibility of any kind or valuing activities as much as your job were viewed as negative attributes, making those individuals less-desired employees.
Data support the quiet quitting trend. Gallup data reveal that employee engagement has fallen for 2 consecutive years in the U.S. workforce. Across the first quarter of 2022, Generation Z and younger Millennials report the lowest engagement across populations at 31%. More than half of this cohort, 54%, classified as “not engaged” in their workplace.
Why is quiet quitting gaining prominence now? COVID may play a role.
Many suggest that self-evaluation and establishing firmer boundaries is a logical response to emotional sequelae caused by COVID. Quiet quitting appears to have been fueled by the pandemic. Employees were forced into crisis mode by COVID; the lines between work, life, and home evaporated, allowing or forcing workers to evaluate their efficacy and satisfaction. With the structural impact of COVID reducing and a return to more standard work practices, it is expected that the job “rules” once held as truths come under evaluation and scrutiny.
Perhaps COVID has forced, and provided, another opportunity for us to closely examine our routines and habits and take stock of what really matters. Generations expectedly differ in their values and definitions of success. COVID has set prior established rules on fire, by forcing patterns and expectations that were neither expected nor wanted, within the context of a global health crisis. Within this backdrop, should we really believe our worth is determined by our job?
The truth is, we are still grieving what we lost during COVID and we have expectedly not assimilated to “the new normal.” Psychology has long recognized that losing structures and supports, routines and habits, causes symptoms of significant discomfort.
The idea that we would return to prior workplace expectations is naive. The idea we would “return to life as it was” is naive. It seems expected, then, that both employers and employees should evaluate their goals and communicate more openly about how each can be met.
It is incumbent upon the employers to set up clear guidelines regarding expectations, including rewards for performance and expectations for time, both within and outside of the work schedule. Employers must recognize symptoms of detachment in their employees and engage in the process of continuing clarifying roles and expectations while providing necessities for employees to succeed at their highest level. Employees, in turn, must self-examine their goals, communicate their needs, meet their responsibilities fully, and take on the challenge of determining their own definition of balance.
Maybe instead of quiet quitting, we should call it this new movement “self-awareness, growth, and evolution.” Hmmm, there’s an intriguing thought.
Dr. Calvery is professor of pediatrics at the University of Louisville (Ky.) She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
In the past few months, “quiet quitting” has garnered increasing traction across social media platforms. My morning review of social media revealed thousands of posts ranging from “Why doing less at work could be good for you – and your employer” to “After ‘quiet quitting’ here comes ‘quiet firing.’ ”
But quiet quitting is neither quiet nor quitting.
Quiet quitting is a misnomer. In addition, quiet quitters are firmer with their boundaries, do not take on work above and beyond clearly stated expectations, do not respond after hours, and do not feel like they are “not doing their job” when they are not immediately available.
Individuals who “quiet quit” continue to meet the demands of their job but reject the hustle-culture mentality that you must always be available for more work and, most importantly, that your value as person and self-worth are defined and determined by your work. Quiet quitters believe that it is possible to have good boundaries and yet remain productive, engaged, and active within the workplace.
Earlier this month, NPR’s posted tutorial on how to set better boundaries at work garnered 491,000 views, reflecting employees’ difficulties in communicating their needs, thoughts, and availability to their employers. Quiet quitting refers to not only rejecting the idea of going above and beyond in the workplace but also feeling confident that there will not be negative ramifications for not consistently working beyond the expected requirements.
A focus on balance, life, loves, and family is rarely addressed or emphasized by traditional employers; employees have little skill in addressing boundaries and clarifying their value and availability. For decades, “needing” flexibility of any kind or valuing activities as much as your job were viewed as negative attributes, making those individuals less-desired employees.
Data support the quiet quitting trend. Gallup data reveal that employee engagement has fallen for 2 consecutive years in the U.S. workforce. Across the first quarter of 2022, Generation Z and younger Millennials report the lowest engagement across populations at 31%. More than half of this cohort, 54%, classified as “not engaged” in their workplace.
Why is quiet quitting gaining prominence now? COVID may play a role.
Many suggest that self-evaluation and establishing firmer boundaries is a logical response to emotional sequelae caused by COVID. Quiet quitting appears to have been fueled by the pandemic. Employees were forced into crisis mode by COVID; the lines between work, life, and home evaporated, allowing or forcing workers to evaluate their efficacy and satisfaction. With the structural impact of COVID reducing and a return to more standard work practices, it is expected that the job “rules” once held as truths come under evaluation and scrutiny.
Perhaps COVID has forced, and provided, another opportunity for us to closely examine our routines and habits and take stock of what really matters. Generations expectedly differ in their values and definitions of success. COVID has set prior established rules on fire, by forcing patterns and expectations that were neither expected nor wanted, within the context of a global health crisis. Within this backdrop, should we really believe our worth is determined by our job?
The truth is, we are still grieving what we lost during COVID and we have expectedly not assimilated to “the new normal.” Psychology has long recognized that losing structures and supports, routines and habits, causes symptoms of significant discomfort.
The idea that we would return to prior workplace expectations is naive. The idea we would “return to life as it was” is naive. It seems expected, then, that both employers and employees should evaluate their goals and communicate more openly about how each can be met.
It is incumbent upon the employers to set up clear guidelines regarding expectations, including rewards for performance and expectations for time, both within and outside of the work schedule. Employers must recognize symptoms of detachment in their employees and engage in the process of continuing clarifying roles and expectations while providing necessities for employees to succeed at their highest level. Employees, in turn, must self-examine their goals, communicate their needs, meet their responsibilities fully, and take on the challenge of determining their own definition of balance.
Maybe instead of quiet quitting, we should call it this new movement “self-awareness, growth, and evolution.” Hmmm, there’s an intriguing thought.
Dr. Calvery is professor of pediatrics at the University of Louisville (Ky.) She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
In the past few months, “quiet quitting” has garnered increasing traction across social media platforms. My morning review of social media revealed thousands of posts ranging from “Why doing less at work could be good for you – and your employer” to “After ‘quiet quitting’ here comes ‘quiet firing.’ ”
But quiet quitting is neither quiet nor quitting.
Quiet quitting is a misnomer. In addition, quiet quitters are firmer with their boundaries, do not take on work above and beyond clearly stated expectations, do not respond after hours, and do not feel like they are “not doing their job” when they are not immediately available.
Individuals who “quiet quit” continue to meet the demands of their job but reject the hustle-culture mentality that you must always be available for more work and, most importantly, that your value as person and self-worth are defined and determined by your work. Quiet quitters believe that it is possible to have good boundaries and yet remain productive, engaged, and active within the workplace.
Earlier this month, NPR’s posted tutorial on how to set better boundaries at work garnered 491,000 views, reflecting employees’ difficulties in communicating their needs, thoughts, and availability to their employers. Quiet quitting refers to not only rejecting the idea of going above and beyond in the workplace but also feeling confident that there will not be negative ramifications for not consistently working beyond the expected requirements.
A focus on balance, life, loves, and family is rarely addressed or emphasized by traditional employers; employees have little skill in addressing boundaries and clarifying their value and availability. For decades, “needing” flexibility of any kind or valuing activities as much as your job were viewed as negative attributes, making those individuals less-desired employees.
Data support the quiet quitting trend. Gallup data reveal that employee engagement has fallen for 2 consecutive years in the U.S. workforce. Across the first quarter of 2022, Generation Z and younger Millennials report the lowest engagement across populations at 31%. More than half of this cohort, 54%, classified as “not engaged” in their workplace.
Why is quiet quitting gaining prominence now? COVID may play a role.
Many suggest that self-evaluation and establishing firmer boundaries is a logical response to emotional sequelae caused by COVID. Quiet quitting appears to have been fueled by the pandemic. Employees were forced into crisis mode by COVID; the lines between work, life, and home evaporated, allowing or forcing workers to evaluate their efficacy and satisfaction. With the structural impact of COVID reducing and a return to more standard work practices, it is expected that the job “rules” once held as truths come under evaluation and scrutiny.
Perhaps COVID has forced, and provided, another opportunity for us to closely examine our routines and habits and take stock of what really matters. Generations expectedly differ in their values and definitions of success. COVID has set prior established rules on fire, by forcing patterns and expectations that were neither expected nor wanted, within the context of a global health crisis. Within this backdrop, should we really believe our worth is determined by our job?
The truth is, we are still grieving what we lost during COVID and we have expectedly not assimilated to “the new normal.” Psychology has long recognized that losing structures and supports, routines and habits, causes symptoms of significant discomfort.
The idea that we would return to prior workplace expectations is naive. The idea we would “return to life as it was” is naive. It seems expected, then, that both employers and employees should evaluate their goals and communicate more openly about how each can be met.
It is incumbent upon the employers to set up clear guidelines regarding expectations, including rewards for performance and expectations for time, both within and outside of the work schedule. Employers must recognize symptoms of detachment in their employees and engage in the process of continuing clarifying roles and expectations while providing necessities for employees to succeed at their highest level. Employees, in turn, must self-examine their goals, communicate their needs, meet their responsibilities fully, and take on the challenge of determining their own definition of balance.
Maybe instead of quiet quitting, we should call it this new movement “self-awareness, growth, and evolution.” Hmmm, there’s an intriguing thought.
Dr. Calvery is professor of pediatrics at the University of Louisville (Ky.) She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Novel combination treatment improves function in early Parkinson’s disease
Results from a phase 3 trial found that P2B001 was superior to its components in improving motor symptoms and daily function and was comparable with marketed doses of pramipexole.
P2B001 also produced less daytime sleepiness and fewer dopaminergic effects, said the investigators, who presented findings at the International Congress of Parkinson’s Disease and Movement Disorders.
The treatment studied, P2B001, is a proprietary, fixed-dose combination of extended-release (ER) formulations of pramipexole and rasagiline. Neither dose is currently available on the market.
Investigators wanted to test the hypothesis that two anti-Parkinsonian drugs that act through different mechanisms could work synergistically, providing benefits comparable with pramipexole but with fewer side effects, said lead study author Warren Olanow, MD, professor emeritus in the neurology and neuroscience departments at the Icahn School of Medicine at Mount Sinai, New York.
Pramipexole is problematic in that it causes dopaminergic and sleep-related side effects.
Laboratory studies have shown that low doses of pramipexole and rasagiline act synergistically, said Dr. Olanow. “A previous double-blind controlled study demonstrated that P2B001 was significantly superior to placebo with respect to efficacy (P < .001) and had a good safety and tolerability profile.”
P2B001 outperforms other formulations
The multicenter phase 3 study (NCT03329508) enrolled 544 patients aged 35-80 with early Parkinson’s disease to assess efficacy and safety of a daily dose of P2B001, compared with its components. Patients were randomized 2:2:2:1 to 12 weeks of treatment with P2B001; pramipexole ER 0.6 mg; rasagiline ER 0.75 mg, or to a calibration arm of marketed pramipexole-ER titrated to optimal dose (mean dose, 3.2 mg).
The primary endpoint compared baseline with week 12 changes in Unified Parkinson’s Disease Rating Scale total scores for P2B001 versus its individual components. The secondary endpoint compared baseline changes in Epworth Sleepiness Scale (ESS) for P2B001 versus pramipexole-ER.
P2B001 showed superior efficacy to each of its individual components and comparable efficacy with marketed doses of pramipexole-ER. It also yielded fewer adverse events related to dopaminergic side effects and less daytime sleepiness as measured by ESS. “Further, the drug is administered once a day and does not require titration,” said Dr. Olanow.
Levodopa-related benefits
Another advantage of starting early-stage patients on P2B001 is that it would give patients more time to be on an effective therapy with fewer side effects before going on levodopa, the current gold standard for Parkinson’s disease treatment.
Although the American Academy of Neurology recommends levodopa as initial therapy for Parkinson’s disease, the drug has been associated with a risk of developing motor complications.
“This opinion, however, was formulated prior to the availability of the results of the P2B001 study and should be reassessed in the light of the present study,” said Dr. Olanow. Longer-term studies should assess when and if patients will require levodopa therapy, as well as the long-term effects of P2B001 on the development of motor complications in patients with early Parkinson’s disease patients.
Investigators are preparing a regulatory market approval filing for P2B001 with the Food and Drug Administration.
Dr. Olanow is CEO of Clintrex Research Corporation, which has provided services to Pharma2B, sponsor of the phase 3 study. Pharma Two B is a private, late clinical-stage pharmaceutical company in Rehovot, Israel, that owns worldwide granted patents for P2B001 pharmaceutical composition and method of treatment.
Results from a phase 3 trial found that P2B001 was superior to its components in improving motor symptoms and daily function and was comparable with marketed doses of pramipexole.
P2B001 also produced less daytime sleepiness and fewer dopaminergic effects, said the investigators, who presented findings at the International Congress of Parkinson’s Disease and Movement Disorders.
The treatment studied, P2B001, is a proprietary, fixed-dose combination of extended-release (ER) formulations of pramipexole and rasagiline. Neither dose is currently available on the market.
Investigators wanted to test the hypothesis that two anti-Parkinsonian drugs that act through different mechanisms could work synergistically, providing benefits comparable with pramipexole but with fewer side effects, said lead study author Warren Olanow, MD, professor emeritus in the neurology and neuroscience departments at the Icahn School of Medicine at Mount Sinai, New York.
Pramipexole is problematic in that it causes dopaminergic and sleep-related side effects.
Laboratory studies have shown that low doses of pramipexole and rasagiline act synergistically, said Dr. Olanow. “A previous double-blind controlled study demonstrated that P2B001 was significantly superior to placebo with respect to efficacy (P < .001) and had a good safety and tolerability profile.”
P2B001 outperforms other formulations
The multicenter phase 3 study (NCT03329508) enrolled 544 patients aged 35-80 with early Parkinson’s disease to assess efficacy and safety of a daily dose of P2B001, compared with its components. Patients were randomized 2:2:2:1 to 12 weeks of treatment with P2B001; pramipexole ER 0.6 mg; rasagiline ER 0.75 mg, or to a calibration arm of marketed pramipexole-ER titrated to optimal dose (mean dose, 3.2 mg).
The primary endpoint compared baseline with week 12 changes in Unified Parkinson’s Disease Rating Scale total scores for P2B001 versus its individual components. The secondary endpoint compared baseline changes in Epworth Sleepiness Scale (ESS) for P2B001 versus pramipexole-ER.
P2B001 showed superior efficacy to each of its individual components and comparable efficacy with marketed doses of pramipexole-ER. It also yielded fewer adverse events related to dopaminergic side effects and less daytime sleepiness as measured by ESS. “Further, the drug is administered once a day and does not require titration,” said Dr. Olanow.
Levodopa-related benefits
Another advantage of starting early-stage patients on P2B001 is that it would give patients more time to be on an effective therapy with fewer side effects before going on levodopa, the current gold standard for Parkinson’s disease treatment.
Although the American Academy of Neurology recommends levodopa as initial therapy for Parkinson’s disease, the drug has been associated with a risk of developing motor complications.
“This opinion, however, was formulated prior to the availability of the results of the P2B001 study and should be reassessed in the light of the present study,” said Dr. Olanow. Longer-term studies should assess when and if patients will require levodopa therapy, as well as the long-term effects of P2B001 on the development of motor complications in patients with early Parkinson’s disease patients.
Investigators are preparing a regulatory market approval filing for P2B001 with the Food and Drug Administration.
Dr. Olanow is CEO of Clintrex Research Corporation, which has provided services to Pharma2B, sponsor of the phase 3 study. Pharma Two B is a private, late clinical-stage pharmaceutical company in Rehovot, Israel, that owns worldwide granted patents for P2B001 pharmaceutical composition and method of treatment.
Results from a phase 3 trial found that P2B001 was superior to its components in improving motor symptoms and daily function and was comparable with marketed doses of pramipexole.
P2B001 also produced less daytime sleepiness and fewer dopaminergic effects, said the investigators, who presented findings at the International Congress of Parkinson’s Disease and Movement Disorders.
The treatment studied, P2B001, is a proprietary, fixed-dose combination of extended-release (ER) formulations of pramipexole and rasagiline. Neither dose is currently available on the market.
Investigators wanted to test the hypothesis that two anti-Parkinsonian drugs that act through different mechanisms could work synergistically, providing benefits comparable with pramipexole but with fewer side effects, said lead study author Warren Olanow, MD, professor emeritus in the neurology and neuroscience departments at the Icahn School of Medicine at Mount Sinai, New York.
Pramipexole is problematic in that it causes dopaminergic and sleep-related side effects.
Laboratory studies have shown that low doses of pramipexole and rasagiline act synergistically, said Dr. Olanow. “A previous double-blind controlled study demonstrated that P2B001 was significantly superior to placebo with respect to efficacy (P < .001) and had a good safety and tolerability profile.”
P2B001 outperforms other formulations
The multicenter phase 3 study (NCT03329508) enrolled 544 patients aged 35-80 with early Parkinson’s disease to assess efficacy and safety of a daily dose of P2B001, compared with its components. Patients were randomized 2:2:2:1 to 12 weeks of treatment with P2B001; pramipexole ER 0.6 mg; rasagiline ER 0.75 mg, or to a calibration arm of marketed pramipexole-ER titrated to optimal dose (mean dose, 3.2 mg).
The primary endpoint compared baseline with week 12 changes in Unified Parkinson’s Disease Rating Scale total scores for P2B001 versus its individual components. The secondary endpoint compared baseline changes in Epworth Sleepiness Scale (ESS) for P2B001 versus pramipexole-ER.
P2B001 showed superior efficacy to each of its individual components and comparable efficacy with marketed doses of pramipexole-ER. It also yielded fewer adverse events related to dopaminergic side effects and less daytime sleepiness as measured by ESS. “Further, the drug is administered once a day and does not require titration,” said Dr. Olanow.
Levodopa-related benefits
Another advantage of starting early-stage patients on P2B001 is that it would give patients more time to be on an effective therapy with fewer side effects before going on levodopa, the current gold standard for Parkinson’s disease treatment.
Although the American Academy of Neurology recommends levodopa as initial therapy for Parkinson’s disease, the drug has been associated with a risk of developing motor complications.
“This opinion, however, was formulated prior to the availability of the results of the P2B001 study and should be reassessed in the light of the present study,” said Dr. Olanow. Longer-term studies should assess when and if patients will require levodopa therapy, as well as the long-term effects of P2B001 on the development of motor complications in patients with early Parkinson’s disease patients.
Investigators are preparing a regulatory market approval filing for P2B001 with the Food and Drug Administration.
Dr. Olanow is CEO of Clintrex Research Corporation, which has provided services to Pharma2B, sponsor of the phase 3 study. Pharma Two B is a private, late clinical-stage pharmaceutical company in Rehovot, Israel, that owns worldwide granted patents for P2B001 pharmaceutical composition and method of treatment.
From MDS 2022
Vitamins or cocoa: Which preserves cognition?
Unexpected results from a phase 3 trial exploring the effect of multivitamins and cognition have now been published.
Originally presented last November at the 14th Clinical Trials on Alzheimer’s Disease (CTAD) conference, this is the first large-scale, long-term randomized controlled trial to examine the effects of cocoa extract and multivitamins on global cognition. The trial’s primary focus was on cocoa extract, which earlier studies suggest may preserve cognitive function. Analyzing the effect of multivitamins was a secondary outcome.
Showing vitamins, but not cocoa, were beneficial is the exact opposite of what researchers expected. Still, the results offer an interesting new direction for future study, lead investigator Laura D. Baker, PhD, professor of gerontology and geriatric medicine at Wake Forest University, Winston-Salem, N.C., said in an interview.
“This study made us take notice of a pathway for possible cognitive protection,” Dr. Baker said. “Without this study, we would never have looked down that road.”
The full results were published online in Alzheimer’s and Dementia.
Unexpected effect
The COSMOS-Mind study is a substudy to a larger parent trial called COSMOS. It investigated the effects of cocoa extract and a standard multivitamin-mineral on cardiovascular and cancer outcomes in more than 21,000 older participants.
In COSMOS-Mind, researchers tested whether daily intake of cocoa extract vs. placebo and a multivitamin-mineral vs. placebo improved cognition in older adults.
More than 2,200 participants aged 65 and older were enrolled and followed for 3 years. They completed tests over the telephone at baseline and annually to evaluate memory and other cognitive abilities.
Results showed cocoa extract had no effect on global cognition compared with placebo (mean z-score, 0.03; P = .28). Daily multivitamin use, however, did show significant benefits on global cognition vs. placebo (mean z, 0.07, P = .007).
The beneficial effect was most pronounced in participants with a history of cardiovascular disease (no history 0.06 vs. history 0.14; P = .01).
Researchers found similar protective effects for memory and executive function.
Dr. Baker suggested one possible explanation for the positive effects of multivitamins may be the boost in micronutrients and essential minerals they provided.
“With nutrient-deficient diets plus a high prevalence of cardiovascular disease, diabetes, and other medical comorbidities that we know impact the bioavailability of these nutrients, we are possibly dealing with older adults who are at below optimum in terms of their essential micronutrients and minerals,” she said.
“Even suboptimum levels of micronutrients and essential minerals can have significant consequences for brain health,” she added.
More research needed
Intriguing as the results may be, more work is needed before the findings could affect nutritional guidance, according to Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association.
“While the Alzheimer’s Association is encouraged by these results, we are not ready to recommend widespread use of a multivitamin supplement to reduce risk of cognitive decline in older adults,” Dr. Carrillo said in a statement.
“For now, and until there is more data, people should talk with their health care providers about the benefits and risks of all dietary supplements, including multivitamins,” she added.
Dr. Baker agreed, noting that the study was not designed to measure multivitamin use as a primary outcome. In addition, nearly 90% of the participants were non-Hispanic White, which is not representative of the overall population demographics.
The investigators are now designing another, larger trial that would include a more diverse participant pool. It will be aimed specifically at learning more about how and why multivitamins seem to offer a protective effect on cognition, Dr. Baker noted.
The study was funded by the National Institute on Aging of the National Institutes of Health. Dr. Baker and Dr. Carrillo report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unexpected results from a phase 3 trial exploring the effect of multivitamins and cognition have now been published.
Originally presented last November at the 14th Clinical Trials on Alzheimer’s Disease (CTAD) conference, this is the first large-scale, long-term randomized controlled trial to examine the effects of cocoa extract and multivitamins on global cognition. The trial’s primary focus was on cocoa extract, which earlier studies suggest may preserve cognitive function. Analyzing the effect of multivitamins was a secondary outcome.
Showing vitamins, but not cocoa, were beneficial is the exact opposite of what researchers expected. Still, the results offer an interesting new direction for future study, lead investigator Laura D. Baker, PhD, professor of gerontology and geriatric medicine at Wake Forest University, Winston-Salem, N.C., said in an interview.
“This study made us take notice of a pathway for possible cognitive protection,” Dr. Baker said. “Without this study, we would never have looked down that road.”
The full results were published online in Alzheimer’s and Dementia.
Unexpected effect
The COSMOS-Mind study is a substudy to a larger parent trial called COSMOS. It investigated the effects of cocoa extract and a standard multivitamin-mineral on cardiovascular and cancer outcomes in more than 21,000 older participants.
In COSMOS-Mind, researchers tested whether daily intake of cocoa extract vs. placebo and a multivitamin-mineral vs. placebo improved cognition in older adults.
More than 2,200 participants aged 65 and older were enrolled and followed for 3 years. They completed tests over the telephone at baseline and annually to evaluate memory and other cognitive abilities.
Results showed cocoa extract had no effect on global cognition compared with placebo (mean z-score, 0.03; P = .28). Daily multivitamin use, however, did show significant benefits on global cognition vs. placebo (mean z, 0.07, P = .007).
The beneficial effect was most pronounced in participants with a history of cardiovascular disease (no history 0.06 vs. history 0.14; P = .01).
Researchers found similar protective effects for memory and executive function.
Dr. Baker suggested one possible explanation for the positive effects of multivitamins may be the boost in micronutrients and essential minerals they provided.
“With nutrient-deficient diets plus a high prevalence of cardiovascular disease, diabetes, and other medical comorbidities that we know impact the bioavailability of these nutrients, we are possibly dealing with older adults who are at below optimum in terms of their essential micronutrients and minerals,” she said.
“Even suboptimum levels of micronutrients and essential minerals can have significant consequences for brain health,” she added.
More research needed
Intriguing as the results may be, more work is needed before the findings could affect nutritional guidance, according to Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association.
“While the Alzheimer’s Association is encouraged by these results, we are not ready to recommend widespread use of a multivitamin supplement to reduce risk of cognitive decline in older adults,” Dr. Carrillo said in a statement.
“For now, and until there is more data, people should talk with their health care providers about the benefits and risks of all dietary supplements, including multivitamins,” she added.
Dr. Baker agreed, noting that the study was not designed to measure multivitamin use as a primary outcome. In addition, nearly 90% of the participants were non-Hispanic White, which is not representative of the overall population demographics.
The investigators are now designing another, larger trial that would include a more diverse participant pool. It will be aimed specifically at learning more about how and why multivitamins seem to offer a protective effect on cognition, Dr. Baker noted.
The study was funded by the National Institute on Aging of the National Institutes of Health. Dr. Baker and Dr. Carrillo report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unexpected results from a phase 3 trial exploring the effect of multivitamins and cognition have now been published.
Originally presented last November at the 14th Clinical Trials on Alzheimer’s Disease (CTAD) conference, this is the first large-scale, long-term randomized controlled trial to examine the effects of cocoa extract and multivitamins on global cognition. The trial’s primary focus was on cocoa extract, which earlier studies suggest may preserve cognitive function. Analyzing the effect of multivitamins was a secondary outcome.
Showing vitamins, but not cocoa, were beneficial is the exact opposite of what researchers expected. Still, the results offer an interesting new direction for future study, lead investigator Laura D. Baker, PhD, professor of gerontology and geriatric medicine at Wake Forest University, Winston-Salem, N.C., said in an interview.
“This study made us take notice of a pathway for possible cognitive protection,” Dr. Baker said. “Without this study, we would never have looked down that road.”
The full results were published online in Alzheimer’s and Dementia.
Unexpected effect
The COSMOS-Mind study is a substudy to a larger parent trial called COSMOS. It investigated the effects of cocoa extract and a standard multivitamin-mineral on cardiovascular and cancer outcomes in more than 21,000 older participants.
In COSMOS-Mind, researchers tested whether daily intake of cocoa extract vs. placebo and a multivitamin-mineral vs. placebo improved cognition in older adults.
More than 2,200 participants aged 65 and older were enrolled and followed for 3 years. They completed tests over the telephone at baseline and annually to evaluate memory and other cognitive abilities.
Results showed cocoa extract had no effect on global cognition compared with placebo (mean z-score, 0.03; P = .28). Daily multivitamin use, however, did show significant benefits on global cognition vs. placebo (mean z, 0.07, P = .007).
The beneficial effect was most pronounced in participants with a history of cardiovascular disease (no history 0.06 vs. history 0.14; P = .01).
Researchers found similar protective effects for memory and executive function.
Dr. Baker suggested one possible explanation for the positive effects of multivitamins may be the boost in micronutrients and essential minerals they provided.
“With nutrient-deficient diets plus a high prevalence of cardiovascular disease, diabetes, and other medical comorbidities that we know impact the bioavailability of these nutrients, we are possibly dealing with older adults who are at below optimum in terms of their essential micronutrients and minerals,” she said.
“Even suboptimum levels of micronutrients and essential minerals can have significant consequences for brain health,” she added.
More research needed
Intriguing as the results may be, more work is needed before the findings could affect nutritional guidance, according to Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association.
“While the Alzheimer’s Association is encouraged by these results, we are not ready to recommend widespread use of a multivitamin supplement to reduce risk of cognitive decline in older adults,” Dr. Carrillo said in a statement.
“For now, and until there is more data, people should talk with their health care providers about the benefits and risks of all dietary supplements, including multivitamins,” she added.
Dr. Baker agreed, noting that the study was not designed to measure multivitamin use as a primary outcome. In addition, nearly 90% of the participants were non-Hispanic White, which is not representative of the overall population demographics.
The investigators are now designing another, larger trial that would include a more diverse participant pool. It will be aimed specifically at learning more about how and why multivitamins seem to offer a protective effect on cognition, Dr. Baker noted.
The study was funded by the National Institute on Aging of the National Institutes of Health. Dr. Baker and Dr. Carrillo report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ALZHEIMER’S AND DEMENTIA
‘Dr. Caveman’ had a leg up on amputation
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
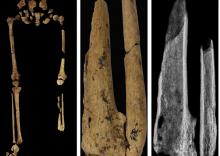
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
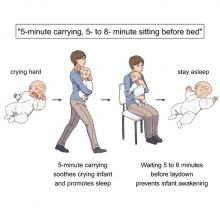
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
One in three MS patients reports chronic itch
, according to investigators.
Itch is historically underrecognized as a symptom of MS, but physicians should know that it is common and may negatively impact quality of life, reported lead author Giuseppe Ingrasci, MD, a dermatology research fellow at the University of Miami, Miller School of Medicine, and colleagues.
While previous publications suggest that pruritus occurs in just 2%-6% of patients with MS, principal author Gil Yosipovitch, MD, professor, Stiefel Chair of Medical Dermatology, and director of the Miami Itch Center in the Dr. Phillip Frost department of dermatology and cutaneous surgery at the University of Miami Miller School of Medicine, encountered itch in enough patients with MS that he presented his observations to a group of neurologists.
Most of them dismissed him, he recalled in an interview: “The neurologists said, ‘Very interesting, but we don’t really see it.’ ”
One of those neurologists, however, decided to take a closer look.
Andrew Brown, MD, assistant professor of clinical neurology and chief of the general neurology division at the University of Miami, Miller School of Medicine, began asking his patients with MS if they were experiencing itch and soon found that it was “a very common problem,” according to Dr. Yosipovitch.
Dr. Yosipovitch, who was the first to report pruritus in patients with psoriasis, launched the present investigation with Dr. Brown to determine if itch is also a blind spot in the world of MS. Their results, and their uphill battle to publication, suggest that it very well could be.
After being rejected from six neurology journals, with one editor suggesting that itch is “not relevant at all to neurology,” their findings were published in the Journal of the European Academy of Dermatology & Venereology.
A common problem that may indicate more severe disease
At the Multiple Sclerosis Center of Excellence in Miami, 27 out of 79 outpatients with MS (35%) reported pruritus, with an average severity of 5.42 out of 10. Among those with itch, the extremities were affected in about half of the patients, while the face, scalp, and trunk were affected in about one-third of the patients. Many described paroxysmal itch that was aggravated by heat, and about half experienced itch on a weekly basis.
Further investigation showed that itch was associated with more severe MS. Compared with patients not experiencing itch, those with itch were significantly more likely to report fatigue (77% vs. 44%), anxiety or depression (48% vs. 16%), and cognitive impairment (62% vs. 26%).
MRI findings backed up these clinical results. Compared with patients not experiencing itch, patients with itch had significantly more T2 hyperintensities in the posterior cervical cord (74.1% vs. 46.0%) and anterior pons/ventromedial medulla (62% vs. 26%). These hyperintensities in the medulla were also associated with an 11-fold increased rate of itch on the face or scalp (odds ratio, 11.3; 95% confidence interval, 1.6-78.6, P = 0.025).
“Health care providers should be aware of episodes of localized, neuropathic itch in MS patients, as they appear to be more prevalent than previously thought and may impair these patients’ quality of life,” the investigators concluded.
Challenges with symptom characterization, management
“This is an important study for both patients and clinicians,” said Justin Abbatemarco, MD, of Cleveland Clinic’s Mellen Center for Multiple Sclerosis, in a written comment. “As the authors mention, many of our patients experience transient symptoms, including many different types of sensory disturbance (that is, pins & needles, burning, electrical shocks, and itching). These symptoms can be really distressing for patients and their caregivers.”
While Dr. Abbatemarco has encountered severe itching in “several patients” with MS, he maintained that it is “relatively uncommon” and noted that MS symptomatology is an inherently cloudy subject.
“I think it is difficult to be definite in any opinion on this topic,” Dr. Abbatemarco said. “How patients experience these symptoms is very subjective and can be difficult to describe/characterize.”
Dr. Abbatemarco emphasized that transient symptoms “do not usually represent MS relapse/flare or new inflammatory disease activity. Instead, we believe these symptoms are related to old areas of injury or demyelination.”
Symptom management can be challenging, he added. He recommended setting realistic expectations, and in the case of pruritus, asking dermatologists to rule out other causes of itch, and to offer “unique treatment approaches.”
Cool the itch?
Noting how heat appears to aggravate itch in patients with MS, Dr. Yosipovitch suggested that one of those unique – and simple – treatment approaches may be cooling itchy areas. Alternatively, clinicians may consider oral agents, like gabapentin to dampen neural transmission, or compounded formulations applied to the skin to reduce neural sensitivity, such as topical ketamine. Finally, Dr. Yosipovitch speculated that newer antibody agents for MS could potentially reduce itch.
All these treatment suggestions are purely hypothetical, he said, and require further investigation before they can be recommended with confidence.
The investigators disclosed relationships with Galderma, Pfizer, Novartis, and others. Dr. Abbatemarco disclosed no conflicts of interest.
Correction, 9/19/22: An earlier version of this article misidentified the photo of Dr. Justin Abbatemarco.
, according to investigators.
Itch is historically underrecognized as a symptom of MS, but physicians should know that it is common and may negatively impact quality of life, reported lead author Giuseppe Ingrasci, MD, a dermatology research fellow at the University of Miami, Miller School of Medicine, and colleagues.
While previous publications suggest that pruritus occurs in just 2%-6% of patients with MS, principal author Gil Yosipovitch, MD, professor, Stiefel Chair of Medical Dermatology, and director of the Miami Itch Center in the Dr. Phillip Frost department of dermatology and cutaneous surgery at the University of Miami Miller School of Medicine, encountered itch in enough patients with MS that he presented his observations to a group of neurologists.
Most of them dismissed him, he recalled in an interview: “The neurologists said, ‘Very interesting, but we don’t really see it.’ ”
One of those neurologists, however, decided to take a closer look.
Andrew Brown, MD, assistant professor of clinical neurology and chief of the general neurology division at the University of Miami, Miller School of Medicine, began asking his patients with MS if they were experiencing itch and soon found that it was “a very common problem,” according to Dr. Yosipovitch.
Dr. Yosipovitch, who was the first to report pruritus in patients with psoriasis, launched the present investigation with Dr. Brown to determine if itch is also a blind spot in the world of MS. Their results, and their uphill battle to publication, suggest that it very well could be.
After being rejected from six neurology journals, with one editor suggesting that itch is “not relevant at all to neurology,” their findings were published in the Journal of the European Academy of Dermatology & Venereology.
A common problem that may indicate more severe disease
At the Multiple Sclerosis Center of Excellence in Miami, 27 out of 79 outpatients with MS (35%) reported pruritus, with an average severity of 5.42 out of 10. Among those with itch, the extremities were affected in about half of the patients, while the face, scalp, and trunk were affected in about one-third of the patients. Many described paroxysmal itch that was aggravated by heat, and about half experienced itch on a weekly basis.
Further investigation showed that itch was associated with more severe MS. Compared with patients not experiencing itch, those with itch were significantly more likely to report fatigue (77% vs. 44%), anxiety or depression (48% vs. 16%), and cognitive impairment (62% vs. 26%).
MRI findings backed up these clinical results. Compared with patients not experiencing itch, patients with itch had significantly more T2 hyperintensities in the posterior cervical cord (74.1% vs. 46.0%) and anterior pons/ventromedial medulla (62% vs. 26%). These hyperintensities in the medulla were also associated with an 11-fold increased rate of itch on the face or scalp (odds ratio, 11.3; 95% confidence interval, 1.6-78.6, P = 0.025).
“Health care providers should be aware of episodes of localized, neuropathic itch in MS patients, as they appear to be more prevalent than previously thought and may impair these patients’ quality of life,” the investigators concluded.
Challenges with symptom characterization, management
“This is an important study for both patients and clinicians,” said Justin Abbatemarco, MD, of Cleveland Clinic’s Mellen Center for Multiple Sclerosis, in a written comment. “As the authors mention, many of our patients experience transient symptoms, including many different types of sensory disturbance (that is, pins & needles, burning, electrical shocks, and itching). These symptoms can be really distressing for patients and their caregivers.”
While Dr. Abbatemarco has encountered severe itching in “several patients” with MS, he maintained that it is “relatively uncommon” and noted that MS symptomatology is an inherently cloudy subject.
“I think it is difficult to be definite in any opinion on this topic,” Dr. Abbatemarco said. “How patients experience these symptoms is very subjective and can be difficult to describe/characterize.”
Dr. Abbatemarco emphasized that transient symptoms “do not usually represent MS relapse/flare or new inflammatory disease activity. Instead, we believe these symptoms are related to old areas of injury or demyelination.”
Symptom management can be challenging, he added. He recommended setting realistic expectations, and in the case of pruritus, asking dermatologists to rule out other causes of itch, and to offer “unique treatment approaches.”
Cool the itch?
Noting how heat appears to aggravate itch in patients with MS, Dr. Yosipovitch suggested that one of those unique – and simple – treatment approaches may be cooling itchy areas. Alternatively, clinicians may consider oral agents, like gabapentin to dampen neural transmission, or compounded formulations applied to the skin to reduce neural sensitivity, such as topical ketamine. Finally, Dr. Yosipovitch speculated that newer antibody agents for MS could potentially reduce itch.
All these treatment suggestions are purely hypothetical, he said, and require further investigation before they can be recommended with confidence.
The investigators disclosed relationships with Galderma, Pfizer, Novartis, and others. Dr. Abbatemarco disclosed no conflicts of interest.
Correction, 9/19/22: An earlier version of this article misidentified the photo of Dr. Justin Abbatemarco.
, according to investigators.
Itch is historically underrecognized as a symptom of MS, but physicians should know that it is common and may negatively impact quality of life, reported lead author Giuseppe Ingrasci, MD, a dermatology research fellow at the University of Miami, Miller School of Medicine, and colleagues.
While previous publications suggest that pruritus occurs in just 2%-6% of patients with MS, principal author Gil Yosipovitch, MD, professor, Stiefel Chair of Medical Dermatology, and director of the Miami Itch Center in the Dr. Phillip Frost department of dermatology and cutaneous surgery at the University of Miami Miller School of Medicine, encountered itch in enough patients with MS that he presented his observations to a group of neurologists.
Most of them dismissed him, he recalled in an interview: “The neurologists said, ‘Very interesting, but we don’t really see it.’ ”
One of those neurologists, however, decided to take a closer look.
Andrew Brown, MD, assistant professor of clinical neurology and chief of the general neurology division at the University of Miami, Miller School of Medicine, began asking his patients with MS if they were experiencing itch and soon found that it was “a very common problem,” according to Dr. Yosipovitch.
Dr. Yosipovitch, who was the first to report pruritus in patients with psoriasis, launched the present investigation with Dr. Brown to determine if itch is also a blind spot in the world of MS. Their results, and their uphill battle to publication, suggest that it very well could be.
After being rejected from six neurology journals, with one editor suggesting that itch is “not relevant at all to neurology,” their findings were published in the Journal of the European Academy of Dermatology & Venereology.
A common problem that may indicate more severe disease
At the Multiple Sclerosis Center of Excellence in Miami, 27 out of 79 outpatients with MS (35%) reported pruritus, with an average severity of 5.42 out of 10. Among those with itch, the extremities were affected in about half of the patients, while the face, scalp, and trunk were affected in about one-third of the patients. Many described paroxysmal itch that was aggravated by heat, and about half experienced itch on a weekly basis.
Further investigation showed that itch was associated with more severe MS. Compared with patients not experiencing itch, those with itch were significantly more likely to report fatigue (77% vs. 44%), anxiety or depression (48% vs. 16%), and cognitive impairment (62% vs. 26%).
MRI findings backed up these clinical results. Compared with patients not experiencing itch, patients with itch had significantly more T2 hyperintensities in the posterior cervical cord (74.1% vs. 46.0%) and anterior pons/ventromedial medulla (62% vs. 26%). These hyperintensities in the medulla were also associated with an 11-fold increased rate of itch on the face or scalp (odds ratio, 11.3; 95% confidence interval, 1.6-78.6, P = 0.025).
“Health care providers should be aware of episodes of localized, neuropathic itch in MS patients, as they appear to be more prevalent than previously thought and may impair these patients’ quality of life,” the investigators concluded.
Challenges with symptom characterization, management
“This is an important study for both patients and clinicians,” said Justin Abbatemarco, MD, of Cleveland Clinic’s Mellen Center for Multiple Sclerosis, in a written comment. “As the authors mention, many of our patients experience transient symptoms, including many different types of sensory disturbance (that is, pins & needles, burning, electrical shocks, and itching). These symptoms can be really distressing for patients and their caregivers.”
While Dr. Abbatemarco has encountered severe itching in “several patients” with MS, he maintained that it is “relatively uncommon” and noted that MS symptomatology is an inherently cloudy subject.
“I think it is difficult to be definite in any opinion on this topic,” Dr. Abbatemarco said. “How patients experience these symptoms is very subjective and can be difficult to describe/characterize.”
Dr. Abbatemarco emphasized that transient symptoms “do not usually represent MS relapse/flare or new inflammatory disease activity. Instead, we believe these symptoms are related to old areas of injury or demyelination.”
Symptom management can be challenging, he added. He recommended setting realistic expectations, and in the case of pruritus, asking dermatologists to rule out other causes of itch, and to offer “unique treatment approaches.”
Cool the itch?
Noting how heat appears to aggravate itch in patients with MS, Dr. Yosipovitch suggested that one of those unique – and simple – treatment approaches may be cooling itchy areas. Alternatively, clinicians may consider oral agents, like gabapentin to dampen neural transmission, or compounded formulations applied to the skin to reduce neural sensitivity, such as topical ketamine. Finally, Dr. Yosipovitch speculated that newer antibody agents for MS could potentially reduce itch.
All these treatment suggestions are purely hypothetical, he said, and require further investigation before they can be recommended with confidence.
The investigators disclosed relationships with Galderma, Pfizer, Novartis, and others. Dr. Abbatemarco disclosed no conflicts of interest.
Correction, 9/19/22: An earlier version of this article misidentified the photo of Dr. Justin Abbatemarco.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY & VENEREOLOGY
TBI is an unrecognized risk factor for cardiovascular disease
(CVD). More severe TBI is associated with higher risk of CVD, new research shows.
Given the relatively young age of post-9/11–era veterans with TBI, there may be an increased burden of heart disease in the future as these veterans age and develop traditional risk factors for CVD, the investigators, led by Ian J. Stewart, MD, with Uniformed Services University, Bethesda, Md., wrote.
The study was published online in JAMA Neurology.
Novel data
Since Sept. 11, 2001, 4.5 million people have served in the U.S. military, with their time in service defined by the long-running wars in Iraq and Afghanistan. Estimates suggest that up to 20% of post-9/11 veterans sustained a TBI.
While some evidence suggests that TBI increases the risk of CVD, prior reports have focused mainly on cerebrovascular outcomes. Until now, the potential association of TBI with CVD has not been comprehensively examined in post-9/11–era veterans.
The retrospective cohort study included 1,559,928 predominantly male post-9/11 veterans, including 301,169 (19.3%) with a history of TBI and 1,258,759 (81%) with no TBI history.
In fully adjusted models, compared with veterans with no TBI history, a history of mild, moderate/severe, or penetrating TBI was associated with increased risk of developing the composite CVD endpoint (coronary artery disease, stroke, peripheral artery disease, and CVD death).

TBIs of all severities were associated with the individual components of the composite outcome, except penetrating TBI and CVD death.
“The association of TBI with subsequent CVD was not attenuated in multivariable models, suggesting that TBI may be accounting for risk that is independent from the other variables,” Dr. Stewart and colleagues wrote.
They noted that the risk was highest shortly after injury, but TBI remained significantly associated with CVD for years after the initial insult.
Why TBI may raise the risk of subsequent CVD remains unclear.
It’s possible that patients with TBI develop more traditional risk factors for CVD through time than do patients without TBI. A study in mice found that TBI led to increased rates of atherosclerosis, the researchers said.
An additional mechanism may be disruption of autonomic regulation, which has been known to occur after TBI.
Another potential pathway is through mental health diagnoses, such as posttraumatic stress disorder; a large body of work has identified associations between PTSD and CVD, including among post-9/11 veterans.
Further work is needed to determine how this risk can be modified to improve outcomes for post-9/11–era veterans, the researchers write.
Unrecognized CVD risk factor?
Reached for comment, Shaheen E. Lakhan, MD, PhD, a neurologist and researcher from Boston who wasn’t involved in the study, said the effects of TBI on heart health are “very underreported, and most clinicians would not make the link.”
“When the brain suffers a traumatic injury, it activates a cascade of neuro-inflammation that goes haywire in an attempt to protect further brain damage. Oftentimes, these inflammatory by-products leak into the body, especially in trauma, when the barriers are broken between brain and body, and can cause systemic body inflammation, which is well associated with heart disease,” Dr. Lakhan said.
In addition, Dr. Lakhan said, “TBI itself localized to just the brain can negatively affect good health habits, leading to worsening heart health, too.”
“Research like this brings light where not much exists and underscores the importance of protecting our brains from physical trauma,” he said.
The study was supported by the assistant secretary of defense for health affairs, endorsed by the Department of Defense through the Psychological Health/Traumatic Brain Injury Research Program Long-Term Impact of Military-Relevant Brain Injury Consortium, and by the U.S. Department of Veterans Affairs. Dr. Stewart and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(CVD). More severe TBI is associated with higher risk of CVD, new research shows.
Given the relatively young age of post-9/11–era veterans with TBI, there may be an increased burden of heart disease in the future as these veterans age and develop traditional risk factors for CVD, the investigators, led by Ian J. Stewart, MD, with Uniformed Services University, Bethesda, Md., wrote.
The study was published online in JAMA Neurology.
Novel data
Since Sept. 11, 2001, 4.5 million people have served in the U.S. military, with their time in service defined by the long-running wars in Iraq and Afghanistan. Estimates suggest that up to 20% of post-9/11 veterans sustained a TBI.
While some evidence suggests that TBI increases the risk of CVD, prior reports have focused mainly on cerebrovascular outcomes. Until now, the potential association of TBI with CVD has not been comprehensively examined in post-9/11–era veterans.
The retrospective cohort study included 1,559,928 predominantly male post-9/11 veterans, including 301,169 (19.3%) with a history of TBI and 1,258,759 (81%) with no TBI history.
In fully adjusted models, compared with veterans with no TBI history, a history of mild, moderate/severe, or penetrating TBI was associated with increased risk of developing the composite CVD endpoint (coronary artery disease, stroke, peripheral artery disease, and CVD death).

TBIs of all severities were associated with the individual components of the composite outcome, except penetrating TBI and CVD death.
“The association of TBI with subsequent CVD was not attenuated in multivariable models, suggesting that TBI may be accounting for risk that is independent from the other variables,” Dr. Stewart and colleagues wrote.
They noted that the risk was highest shortly after injury, but TBI remained significantly associated with CVD for years after the initial insult.
Why TBI may raise the risk of subsequent CVD remains unclear.
It’s possible that patients with TBI develop more traditional risk factors for CVD through time than do patients without TBI. A study in mice found that TBI led to increased rates of atherosclerosis, the researchers said.
An additional mechanism may be disruption of autonomic regulation, which has been known to occur after TBI.
Another potential pathway is through mental health diagnoses, such as posttraumatic stress disorder; a large body of work has identified associations between PTSD and CVD, including among post-9/11 veterans.
Further work is needed to determine how this risk can be modified to improve outcomes for post-9/11–era veterans, the researchers write.
Unrecognized CVD risk factor?
Reached for comment, Shaheen E. Lakhan, MD, PhD, a neurologist and researcher from Boston who wasn’t involved in the study, said the effects of TBI on heart health are “very underreported, and most clinicians would not make the link.”
“When the brain suffers a traumatic injury, it activates a cascade of neuro-inflammation that goes haywire in an attempt to protect further brain damage. Oftentimes, these inflammatory by-products leak into the body, especially in trauma, when the barriers are broken between brain and body, and can cause systemic body inflammation, which is well associated with heart disease,” Dr. Lakhan said.
In addition, Dr. Lakhan said, “TBI itself localized to just the brain can negatively affect good health habits, leading to worsening heart health, too.”
“Research like this brings light where not much exists and underscores the importance of protecting our brains from physical trauma,” he said.
The study was supported by the assistant secretary of defense for health affairs, endorsed by the Department of Defense through the Psychological Health/Traumatic Brain Injury Research Program Long-Term Impact of Military-Relevant Brain Injury Consortium, and by the U.S. Department of Veterans Affairs. Dr. Stewart and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(CVD). More severe TBI is associated with higher risk of CVD, new research shows.
Given the relatively young age of post-9/11–era veterans with TBI, there may be an increased burden of heart disease in the future as these veterans age and develop traditional risk factors for CVD, the investigators, led by Ian J. Stewart, MD, with Uniformed Services University, Bethesda, Md., wrote.
The study was published online in JAMA Neurology.
Novel data
Since Sept. 11, 2001, 4.5 million people have served in the U.S. military, with their time in service defined by the long-running wars in Iraq and Afghanistan. Estimates suggest that up to 20% of post-9/11 veterans sustained a TBI.
While some evidence suggests that TBI increases the risk of CVD, prior reports have focused mainly on cerebrovascular outcomes. Until now, the potential association of TBI with CVD has not been comprehensively examined in post-9/11–era veterans.
The retrospective cohort study included 1,559,928 predominantly male post-9/11 veterans, including 301,169 (19.3%) with a history of TBI and 1,258,759 (81%) with no TBI history.
In fully adjusted models, compared with veterans with no TBI history, a history of mild, moderate/severe, or penetrating TBI was associated with increased risk of developing the composite CVD endpoint (coronary artery disease, stroke, peripheral artery disease, and CVD death).

TBIs of all severities were associated with the individual components of the composite outcome, except penetrating TBI and CVD death.
“The association of TBI with subsequent CVD was not attenuated in multivariable models, suggesting that TBI may be accounting for risk that is independent from the other variables,” Dr. Stewart and colleagues wrote.
They noted that the risk was highest shortly after injury, but TBI remained significantly associated with CVD for years after the initial insult.
Why TBI may raise the risk of subsequent CVD remains unclear.
It’s possible that patients with TBI develop more traditional risk factors for CVD through time than do patients without TBI. A study in mice found that TBI led to increased rates of atherosclerosis, the researchers said.
An additional mechanism may be disruption of autonomic regulation, which has been known to occur after TBI.
Another potential pathway is through mental health diagnoses, such as posttraumatic stress disorder; a large body of work has identified associations between PTSD and CVD, including among post-9/11 veterans.
Further work is needed to determine how this risk can be modified to improve outcomes for post-9/11–era veterans, the researchers write.
Unrecognized CVD risk factor?
Reached for comment, Shaheen E. Lakhan, MD, PhD, a neurologist and researcher from Boston who wasn’t involved in the study, said the effects of TBI on heart health are “very underreported, and most clinicians would not make the link.”
“When the brain suffers a traumatic injury, it activates a cascade of neuro-inflammation that goes haywire in an attempt to protect further brain damage. Oftentimes, these inflammatory by-products leak into the body, especially in trauma, when the barriers are broken between brain and body, and can cause systemic body inflammation, which is well associated with heart disease,” Dr. Lakhan said.
In addition, Dr. Lakhan said, “TBI itself localized to just the brain can negatively affect good health habits, leading to worsening heart health, too.”
“Research like this brings light where not much exists and underscores the importance of protecting our brains from physical trauma,” he said.
The study was supported by the assistant secretary of defense for health affairs, endorsed by the Department of Defense through the Psychological Health/Traumatic Brain Injury Research Program Long-Term Impact of Military-Relevant Brain Injury Consortium, and by the U.S. Department of Veterans Affairs. Dr. Stewart and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ketamine promising for rare condition linked to autism
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
From Human Genetics and Genomic Advances
The doctor circuit
A long time ago, as a fourth-year medical student, I did a neurology rotation at a large academic center.
One of the attendings was talking to me about reading, and how, once learned, it became innate: a function that, like breathing, couldn’t be turned off.
He was right, as is obvious to anyone. Driving down the road, walking past a newsstand, even opening a fridge covered with magnets from various other medical businesses ... it’s impossible NOT to process the letters into words and words into meanings, even if just for a second. Advertisers and headline-writers figured this out long ago. The key is to make those few words something that grabs our attention and interest, so we’ll either want to read more or retain it.
So too is being a doctor. Once that switch is on, you can’t flip it off.
Recently Queen Elizabeth II died. In reading the news stories, without intending to, I found my mind trying to pick out details about her medical condition, formulate a differential ... after all these years of being in medicine it’s second nature to do that.
Of course, it’s none of my business, and I greatly respect personal privacy. But the point is there. At some point, like reading, we can’t turn off the doctor circuit (for lack of a better term). We do it all the time, analyzing gait patterns and arm swings as people go by. Noticing facial asymmetries, tremors, speech patterns. It may be turned down a few notches from when we’re in the office or hospital, but it’s still there.
It becomes second nature, a part of who we are.
It’s not just doctors. Architects casually notice building details that no one else would. Software engineers off-handedly see program features (good and bad) that the rest of us wouldn’t. Teachers and editors pick up on grammatical errors even when they’re not trying to.
None of these (aside from basic observation) are things that brains originally started out to do. But through training and experience we’ve adapted them to do this. We never stop observing, collecting data, and processing it, in ways peculiar to our backgrounds.
Which, if you think about it, is pretty remarkable.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A long time ago, as a fourth-year medical student, I did a neurology rotation at a large academic center.
One of the attendings was talking to me about reading, and how, once learned, it became innate: a function that, like breathing, couldn’t be turned off.
He was right, as is obvious to anyone. Driving down the road, walking past a newsstand, even opening a fridge covered with magnets from various other medical businesses ... it’s impossible NOT to process the letters into words and words into meanings, even if just for a second. Advertisers and headline-writers figured this out long ago. The key is to make those few words something that grabs our attention and interest, so we’ll either want to read more or retain it.
So too is being a doctor. Once that switch is on, you can’t flip it off.
Recently Queen Elizabeth II died. In reading the news stories, without intending to, I found my mind trying to pick out details about her medical condition, formulate a differential ... after all these years of being in medicine it’s second nature to do that.
Of course, it’s none of my business, and I greatly respect personal privacy. But the point is there. At some point, like reading, we can’t turn off the doctor circuit (for lack of a better term). We do it all the time, analyzing gait patterns and arm swings as people go by. Noticing facial asymmetries, tremors, speech patterns. It may be turned down a few notches from when we’re in the office or hospital, but it’s still there.
It becomes second nature, a part of who we are.
It’s not just doctors. Architects casually notice building details that no one else would. Software engineers off-handedly see program features (good and bad) that the rest of us wouldn’t. Teachers and editors pick up on grammatical errors even when they’re not trying to.
None of these (aside from basic observation) are things that brains originally started out to do. But through training and experience we’ve adapted them to do this. We never stop observing, collecting data, and processing it, in ways peculiar to our backgrounds.
Which, if you think about it, is pretty remarkable.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A long time ago, as a fourth-year medical student, I did a neurology rotation at a large academic center.
One of the attendings was talking to me about reading, and how, once learned, it became innate: a function that, like breathing, couldn’t be turned off.
He was right, as is obvious to anyone. Driving down the road, walking past a newsstand, even opening a fridge covered with magnets from various other medical businesses ... it’s impossible NOT to process the letters into words and words into meanings, even if just for a second. Advertisers and headline-writers figured this out long ago. The key is to make those few words something that grabs our attention and interest, so we’ll either want to read more or retain it.
So too is being a doctor. Once that switch is on, you can’t flip it off.
Recently Queen Elizabeth II died. In reading the news stories, without intending to, I found my mind trying to pick out details about her medical condition, formulate a differential ... after all these years of being in medicine it’s second nature to do that.
Of course, it’s none of my business, and I greatly respect personal privacy. But the point is there. At some point, like reading, we can’t turn off the doctor circuit (for lack of a better term). We do it all the time, analyzing gait patterns and arm swings as people go by. Noticing facial asymmetries, tremors, speech patterns. It may be turned down a few notches from when we’re in the office or hospital, but it’s still there.
It becomes second nature, a part of who we are.
It’s not just doctors. Architects casually notice building details that no one else would. Software engineers off-handedly see program features (good and bad) that the rest of us wouldn’t. Teachers and editors pick up on grammatical errors even when they’re not trying to.
None of these (aside from basic observation) are things that brains originally started out to do. But through training and experience we’ve adapted them to do this. We never stop observing, collecting data, and processing it, in ways peculiar to our backgrounds.
Which, if you think about it, is pretty remarkable.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Post-COVID fatigue, exercise intolerance signal ME/CFS
A new study provides yet more evidence that a significant subset of people who experience persistent fatigue and exercise intolerance following COVID-19 will meet diagnostic criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Data from the prospective observational study of 42 patients with “post-COVID-19 syndrome (PCS),” including persistent fatigue and exercise intolerance, suggest that a large proportion will meet strict diagnostic criteria for ME/CFS, including the hallmark postexertional malaise (PEM). Still others may experience similar disability but lack duration and/or severity requirements for the diagnosis.
Moreover, disease severity and symptom burden were found similar in those with ME/CFS following COVID-19 and in a group of 19 age- and sex-matched individuals with ME/CFS that wasn’t associated with COVID-19.
“The major finding is that ME/CFS is indeed part of the spectrum of the post-COVID syndrome and very similar to the ME/CFS we know after other infectious triggers,” senior author Carmen Scheibenbogen, MD, acting director of the Institute for Medical Immunology at the Charité University Medicine Campus Virchow-Klinikum, Berlin, told this news organization.
Importantly, from a clinical standpoint, both diminished hand-grip strength (HGS) and orthostatic intolerance were common across all patient groups, as were several laboratory values, Claudia Kedor, MD, and colleagues at Charité report in the paper, published online in Nature Communications.
Of the 42 with PCS, including persistent fatigue and exercise intolerance lasting at least 6 months, 19 met the rigorous Canadian Consensus Criteria (CCC) for ME/CFS, established in 2003, which require PEM, along with sleep dysfunction, significant persistent fatigue, pain, and several other symptoms from neurological/cognitive, autonomic, neuroendocrine, and immune categories that persist for at least 6 months.
Of the 23 who did not meet the CCC criteria, 18 still experienced PEM but for less than the required 14 hours set by the authors based on recent data. The original CCC had suggested 24 hours as the PEM duration. Eight subjects met all the Canadian criteria except for the neurological/cognitive symptoms. None of the 42 had evidence of severe depression.
The previously widely used 1994 “Fukuda” criteria for ME/CFS are no longer recommended because they don’t require PEM, which is now considered a key symptom. The more recent 2015 Institute (now Academy) of Medicine criteria don’t define the length of PEM, the authors note in the paper.
Dr. Scheibenbogen said, “Post-COVID has a spectrum of syndromes and conditions. We see that a subset of patients have similar symptoms of ME/CFS but don’t fulfill the CCC, although they may meet less stringent criteria. We think this is of relevance for both diagnostic markers and development of therapy, because there may be different pathomechanisms between the subsets of post-COVID patients.”
She pointed to other studies from her group suggesting that inflammation is present early in post-COVID (not yet published), while in the subset that goes on to ME/CFS, autoantibodies or endothelial dysfunction play a more important role. «At the moment, it’s quite complex, and I don’t think in the end we will have just one pathomechanism. So I think we’ll need to develop various treatment strategies.”
Asked to comment on the new data, Anthony L. Komaroff, MD, professor of medicine at Harvard Medical School, senior physician at Brigham and Women’s Hospital, both in Boston, and editor in chief of the Harvard Health Letter, told this news organization, “This paper adds to the evidence that an illness with symptoms that meet criteria for ME/CFS can follow COVID-19 in nearly half of those patients who have lingering symptoms. This can occur even in people who initially have only mild symptoms from COVID-19, although it is more likely to happen in the people who are sickest when they first get COVID-19. And those who meet criteria for ME/CFS were seriously impaired in their ability to function, [both] at work and at home.”
But, Dr. Komaroff also cautioned, “the study does not help in determining what fraction of all people who are infected with SARS-CoV-2 go on to develop a condition like ME/CFS, nor how long that condition will last. It is crucial that we get answers to these questions, as the impact on the economy, the health care system, and the disability system could be substantial.”
He pointed to a recent report from the Brookings Institution (2022 Aug 24. “New data shows long Covid is keeping as many as 4 million people out of work” Katie Bach) “finding that “long COVID may be a major contributor to the shortage of job applicants plaguing many businesses.”
Biomarkers include hand-grip strength, orthostatic intolerance, lab measures
Hand-grip strength, as assessed by 10 repeat grips at maximum force and repeated after 60 minutes, were lower for all those meeting ME/CFS criteria, compared with the healthy controls. Hand-grip strength parameters were also positively correlated with laboratory hemoglobin measures in both PCS groups who did and didn’t meet the Canadian ME/CFS criteria.
A total of three patients with PCS who didn’t meet ME/CFS criteria and seven with PCS who met ME/CFS criteria had sitting blood pressures of greater than 140 mm Hg systolic and/or greater than 90 mm Hg diastolic. Five patients with PCS – four who met ME/CFS criteria and one who didn’t – fulfilled criteria for postural orthostatic tachycardia syndrome. Orthostatic hypotension was diagnosed in a total of seven with PCS, including one who did not meet ME/CFS criteria and the rest who did.
Among significant laboratory findings, mannose-binding lectin deficiency, which is associated with increased infection susceptibility and found in only about 6% of historical controls, was found more frequently in both of the PCS cohorts (17% of those with ME/CFS and 23% of those without) than it has been in the past among those with ME/CFS, compared with historical controls (15%).
There was only slight elevation in C-reactive protein, the most commonly measured marker of inflammation. However, another marker indicating inflammation within the last 3-4 months, interleukin 8 assessed in erythrocytes, was above normal in 37% with PCS and ME/CFS and in 48% with PCS who did not meet the ME/CFS criteria.
Elevated antinuclear antibodies, anti–thyroid peroxidase antibodies, vitamin D deficiencies, and folic acid deficiencies were all seen in small numbers of the PCS patients. Angiotensin-converting enzyme 1 levels were below the normal range in 31% of all patients.
“We must anticipate that this pandemic has the potential to dramatically increase the number of ME/CFS patients,” Dr. Kedor and colleagues write. “At the same time, it offers the unique chance to identify ME/CFS patients in a very early stage of disease and apply interventions such as pacing and coping early with a better therapeutic prognosis. Further, it is an unprecedented opportunity to understand the underlying pathomechanism and characterize targets for specific treatment approaches.”
Dr. Scheibenbogen and Dr. Komaroff reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study provides yet more evidence that a significant subset of people who experience persistent fatigue and exercise intolerance following COVID-19 will meet diagnostic criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Data from the prospective observational study of 42 patients with “post-COVID-19 syndrome (PCS),” including persistent fatigue and exercise intolerance, suggest that a large proportion will meet strict diagnostic criteria for ME/CFS, including the hallmark postexertional malaise (PEM). Still others may experience similar disability but lack duration and/or severity requirements for the diagnosis.
Moreover, disease severity and symptom burden were found similar in those with ME/CFS following COVID-19 and in a group of 19 age- and sex-matched individuals with ME/CFS that wasn’t associated with COVID-19.
“The major finding is that ME/CFS is indeed part of the spectrum of the post-COVID syndrome and very similar to the ME/CFS we know after other infectious triggers,” senior author Carmen Scheibenbogen, MD, acting director of the Institute for Medical Immunology at the Charité University Medicine Campus Virchow-Klinikum, Berlin, told this news organization.
Importantly, from a clinical standpoint, both diminished hand-grip strength (HGS) and orthostatic intolerance were common across all patient groups, as were several laboratory values, Claudia Kedor, MD, and colleagues at Charité report in the paper, published online in Nature Communications.
Of the 42 with PCS, including persistent fatigue and exercise intolerance lasting at least 6 months, 19 met the rigorous Canadian Consensus Criteria (CCC) for ME/CFS, established in 2003, which require PEM, along with sleep dysfunction, significant persistent fatigue, pain, and several other symptoms from neurological/cognitive, autonomic, neuroendocrine, and immune categories that persist for at least 6 months.
Of the 23 who did not meet the CCC criteria, 18 still experienced PEM but for less than the required 14 hours set by the authors based on recent data. The original CCC had suggested 24 hours as the PEM duration. Eight subjects met all the Canadian criteria except for the neurological/cognitive symptoms. None of the 42 had evidence of severe depression.
The previously widely used 1994 “Fukuda” criteria for ME/CFS are no longer recommended because they don’t require PEM, which is now considered a key symptom. The more recent 2015 Institute (now Academy) of Medicine criteria don’t define the length of PEM, the authors note in the paper.
Dr. Scheibenbogen said, “Post-COVID has a spectrum of syndromes and conditions. We see that a subset of patients have similar symptoms of ME/CFS but don’t fulfill the CCC, although they may meet less stringent criteria. We think this is of relevance for both diagnostic markers and development of therapy, because there may be different pathomechanisms between the subsets of post-COVID patients.”
She pointed to other studies from her group suggesting that inflammation is present early in post-COVID (not yet published), while in the subset that goes on to ME/CFS, autoantibodies or endothelial dysfunction play a more important role. «At the moment, it’s quite complex, and I don’t think in the end we will have just one pathomechanism. So I think we’ll need to develop various treatment strategies.”
Asked to comment on the new data, Anthony L. Komaroff, MD, professor of medicine at Harvard Medical School, senior physician at Brigham and Women’s Hospital, both in Boston, and editor in chief of the Harvard Health Letter, told this news organization, “This paper adds to the evidence that an illness with symptoms that meet criteria for ME/CFS can follow COVID-19 in nearly half of those patients who have lingering symptoms. This can occur even in people who initially have only mild symptoms from COVID-19, although it is more likely to happen in the people who are sickest when they first get COVID-19. And those who meet criteria for ME/CFS were seriously impaired in their ability to function, [both] at work and at home.”
But, Dr. Komaroff also cautioned, “the study does not help in determining what fraction of all people who are infected with SARS-CoV-2 go on to develop a condition like ME/CFS, nor how long that condition will last. It is crucial that we get answers to these questions, as the impact on the economy, the health care system, and the disability system could be substantial.”
He pointed to a recent report from the Brookings Institution (2022 Aug 24. “New data shows long Covid is keeping as many as 4 million people out of work” Katie Bach) “finding that “long COVID may be a major contributor to the shortage of job applicants plaguing many businesses.”
Biomarkers include hand-grip strength, orthostatic intolerance, lab measures
Hand-grip strength, as assessed by 10 repeat grips at maximum force and repeated after 60 minutes, were lower for all those meeting ME/CFS criteria, compared with the healthy controls. Hand-grip strength parameters were also positively correlated with laboratory hemoglobin measures in both PCS groups who did and didn’t meet the Canadian ME/CFS criteria.
A total of three patients with PCS who didn’t meet ME/CFS criteria and seven with PCS who met ME/CFS criteria had sitting blood pressures of greater than 140 mm Hg systolic and/or greater than 90 mm Hg diastolic. Five patients with PCS – four who met ME/CFS criteria and one who didn’t – fulfilled criteria for postural orthostatic tachycardia syndrome. Orthostatic hypotension was diagnosed in a total of seven with PCS, including one who did not meet ME/CFS criteria and the rest who did.
Among significant laboratory findings, mannose-binding lectin deficiency, which is associated with increased infection susceptibility and found in only about 6% of historical controls, was found more frequently in both of the PCS cohorts (17% of those with ME/CFS and 23% of those without) than it has been in the past among those with ME/CFS, compared with historical controls (15%).
There was only slight elevation in C-reactive protein, the most commonly measured marker of inflammation. However, another marker indicating inflammation within the last 3-4 months, interleukin 8 assessed in erythrocytes, was above normal in 37% with PCS and ME/CFS and in 48% with PCS who did not meet the ME/CFS criteria.
Elevated antinuclear antibodies, anti–thyroid peroxidase antibodies, vitamin D deficiencies, and folic acid deficiencies were all seen in small numbers of the PCS patients. Angiotensin-converting enzyme 1 levels were below the normal range in 31% of all patients.
“We must anticipate that this pandemic has the potential to dramatically increase the number of ME/CFS patients,” Dr. Kedor and colleagues write. “At the same time, it offers the unique chance to identify ME/CFS patients in a very early stage of disease and apply interventions such as pacing and coping early with a better therapeutic prognosis. Further, it is an unprecedented opportunity to understand the underlying pathomechanism and characterize targets for specific treatment approaches.”
Dr. Scheibenbogen and Dr. Komaroff reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study provides yet more evidence that a significant subset of people who experience persistent fatigue and exercise intolerance following COVID-19 will meet diagnostic criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Data from the prospective observational study of 42 patients with “post-COVID-19 syndrome (PCS),” including persistent fatigue and exercise intolerance, suggest that a large proportion will meet strict diagnostic criteria for ME/CFS, including the hallmark postexertional malaise (PEM). Still others may experience similar disability but lack duration and/or severity requirements for the diagnosis.
Moreover, disease severity and symptom burden were found similar in those with ME/CFS following COVID-19 and in a group of 19 age- and sex-matched individuals with ME/CFS that wasn’t associated with COVID-19.
“The major finding is that ME/CFS is indeed part of the spectrum of the post-COVID syndrome and very similar to the ME/CFS we know after other infectious triggers,” senior author Carmen Scheibenbogen, MD, acting director of the Institute for Medical Immunology at the Charité University Medicine Campus Virchow-Klinikum, Berlin, told this news organization.
Importantly, from a clinical standpoint, both diminished hand-grip strength (HGS) and orthostatic intolerance were common across all patient groups, as were several laboratory values, Claudia Kedor, MD, and colleagues at Charité report in the paper, published online in Nature Communications.
Of the 42 with PCS, including persistent fatigue and exercise intolerance lasting at least 6 months, 19 met the rigorous Canadian Consensus Criteria (CCC) for ME/CFS, established in 2003, which require PEM, along with sleep dysfunction, significant persistent fatigue, pain, and several other symptoms from neurological/cognitive, autonomic, neuroendocrine, and immune categories that persist for at least 6 months.
Of the 23 who did not meet the CCC criteria, 18 still experienced PEM but for less than the required 14 hours set by the authors based on recent data. The original CCC had suggested 24 hours as the PEM duration. Eight subjects met all the Canadian criteria except for the neurological/cognitive symptoms. None of the 42 had evidence of severe depression.
The previously widely used 1994 “Fukuda” criteria for ME/CFS are no longer recommended because they don’t require PEM, which is now considered a key symptom. The more recent 2015 Institute (now Academy) of Medicine criteria don’t define the length of PEM, the authors note in the paper.
Dr. Scheibenbogen said, “Post-COVID has a spectrum of syndromes and conditions. We see that a subset of patients have similar symptoms of ME/CFS but don’t fulfill the CCC, although they may meet less stringent criteria. We think this is of relevance for both diagnostic markers and development of therapy, because there may be different pathomechanisms between the subsets of post-COVID patients.”
She pointed to other studies from her group suggesting that inflammation is present early in post-COVID (not yet published), while in the subset that goes on to ME/CFS, autoantibodies or endothelial dysfunction play a more important role. «At the moment, it’s quite complex, and I don’t think in the end we will have just one pathomechanism. So I think we’ll need to develop various treatment strategies.”
Asked to comment on the new data, Anthony L. Komaroff, MD, professor of medicine at Harvard Medical School, senior physician at Brigham and Women’s Hospital, both in Boston, and editor in chief of the Harvard Health Letter, told this news organization, “This paper adds to the evidence that an illness with symptoms that meet criteria for ME/CFS can follow COVID-19 in nearly half of those patients who have lingering symptoms. This can occur even in people who initially have only mild symptoms from COVID-19, although it is more likely to happen in the people who are sickest when they first get COVID-19. And those who meet criteria for ME/CFS were seriously impaired in their ability to function, [both] at work and at home.”
But, Dr. Komaroff also cautioned, “the study does not help in determining what fraction of all people who are infected with SARS-CoV-2 go on to develop a condition like ME/CFS, nor how long that condition will last. It is crucial that we get answers to these questions, as the impact on the economy, the health care system, and the disability system could be substantial.”
He pointed to a recent report from the Brookings Institution (2022 Aug 24. “New data shows long Covid is keeping as many as 4 million people out of work” Katie Bach) “finding that “long COVID may be a major contributor to the shortage of job applicants plaguing many businesses.”
Biomarkers include hand-grip strength, orthostatic intolerance, lab measures
Hand-grip strength, as assessed by 10 repeat grips at maximum force and repeated after 60 minutes, were lower for all those meeting ME/CFS criteria, compared with the healthy controls. Hand-grip strength parameters were also positively correlated with laboratory hemoglobin measures in both PCS groups who did and didn’t meet the Canadian ME/CFS criteria.
A total of three patients with PCS who didn’t meet ME/CFS criteria and seven with PCS who met ME/CFS criteria had sitting blood pressures of greater than 140 mm Hg systolic and/or greater than 90 mm Hg diastolic. Five patients with PCS – four who met ME/CFS criteria and one who didn’t – fulfilled criteria for postural orthostatic tachycardia syndrome. Orthostatic hypotension was diagnosed in a total of seven with PCS, including one who did not meet ME/CFS criteria and the rest who did.
Among significant laboratory findings, mannose-binding lectin deficiency, which is associated with increased infection susceptibility and found in only about 6% of historical controls, was found more frequently in both of the PCS cohorts (17% of those with ME/CFS and 23% of those without) than it has been in the past among those with ME/CFS, compared with historical controls (15%).
There was only slight elevation in C-reactive protein, the most commonly measured marker of inflammation. However, another marker indicating inflammation within the last 3-4 months, interleukin 8 assessed in erythrocytes, was above normal in 37% with PCS and ME/CFS and in 48% with PCS who did not meet the ME/CFS criteria.
Elevated antinuclear antibodies, anti–thyroid peroxidase antibodies, vitamin D deficiencies, and folic acid deficiencies were all seen in small numbers of the PCS patients. Angiotensin-converting enzyme 1 levels were below the normal range in 31% of all patients.
“We must anticipate that this pandemic has the potential to dramatically increase the number of ME/CFS patients,” Dr. Kedor and colleagues write. “At the same time, it offers the unique chance to identify ME/CFS patients in a very early stage of disease and apply interventions such as pacing and coping early with a better therapeutic prognosis. Further, it is an unprecedented opportunity to understand the underlying pathomechanism and characterize targets for specific treatment approaches.”
Dr. Scheibenbogen and Dr. Komaroff reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NATURE COMMUNICATIONS
Flashy, blingy doc sabotages his own malpractice trial in rural farm town
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.