User login
Faster multiplex PCR improved management of pediatric acute respiratory illness
SAN DIEGO – Switching to a faster, more comprehensive multiplex PCR viral respiratory assay enabled a hospital to discharge young children with acute respiratory illnesses sooner, prescribe oseltamivir more often, and curtail the use of antibiotics and thoracic radiography, Rangaraj Selvarangan, PhD, reported at an annual meeting on infectious disease.
The study shows how rapid multiplex PCR testing can facilitate antimicrobial stewardship, said Dr. Selvarangan, who is a professor at the University of Missouri Kansas City School of Medicine and director of the microbiology laboratory at Children’s Mercy Kansas City. “Our antimicrobial stewardship programs monitors these test results daily, add notes, and make recommendations on antibiotic choices,” he said.
For the study, the researchers compared hospital records from December 2008 through May 2012, when Children’s Mercy hospital used the Luminex xTAG Respiratory Viral Panel, with records from August 2012 through June 2015, after the hospital had switched over to the Biofire FilmArray Respiratory Panel. FilmArray targets the same 17 viral pathogens as the Luminex panel, but also targets Bordetella pertussis, Chlamydia pneumoniae, and Mycoplasma pneumoniae, seasonal influenza A, parainfluenza type 4, and four coronaviruses.
The study included children aged up to 2 years who were not on immunosuppressive medications, in the NICU, or hospitalized for more than 7 days. For this population, the two panels yielded similar rates of positivity overall (about 60%) and for individual viruses, Dr. Selvarangan said. A total of 810 patients tested positive for at least one virus on the Luminex panel, and 2,096 patients tested positive on FilmArray. Results for FilmArray were available within a median of 4 hours, versus 29 hours for Luminex (P less than .001). The prevalence of empiric antibiotic therapy was 44% during the Luminex era and 28% after the hospital switched to FilmArray (P less than .001). Rates of antibiotic discontinuation rose from 16% with Luminex to 23% with FilmArray (P less than .01). Strikingly, oseltamivir prescriptions rose five-fold (from 17% to 85%; P less than .001) after the hospital began using FilmArray, which covers seasonal influenza. Finally, use of chest radiography fell significantly in both infants and older children after the hospital began using FilmArray instead of Luminex.
Clinicians might have become more comfortable interpreting molecular test results over time, which could have altered their clinical decision-making and thereby biased the study results, Dr. Selvarangan noted. Although at least four other single-center retrospective studies have linked multiplex PCR assays to better antibiotic stewardship, this study is one of the first to directly compare clinical outcomes between two assays, he added. More studies are needed to help guide choice of multiplex assays, whose cost remains a major barrier to widespread use, he concluded.
Dr. Selvarangan disclosed grant support from both Biofire Diagnostics and Luminex corporation, and an advisory relationship with BioFire.
SAN DIEGO – Switching to a faster, more comprehensive multiplex PCR viral respiratory assay enabled a hospital to discharge young children with acute respiratory illnesses sooner, prescribe oseltamivir more often, and curtail the use of antibiotics and thoracic radiography, Rangaraj Selvarangan, PhD, reported at an annual meeting on infectious disease.
The study shows how rapid multiplex PCR testing can facilitate antimicrobial stewardship, said Dr. Selvarangan, who is a professor at the University of Missouri Kansas City School of Medicine and director of the microbiology laboratory at Children’s Mercy Kansas City. “Our antimicrobial stewardship programs monitors these test results daily, add notes, and make recommendations on antibiotic choices,” he said.
For the study, the researchers compared hospital records from December 2008 through May 2012, when Children’s Mercy hospital used the Luminex xTAG Respiratory Viral Panel, with records from August 2012 through June 2015, after the hospital had switched over to the Biofire FilmArray Respiratory Panel. FilmArray targets the same 17 viral pathogens as the Luminex panel, but also targets Bordetella pertussis, Chlamydia pneumoniae, and Mycoplasma pneumoniae, seasonal influenza A, parainfluenza type 4, and four coronaviruses.
The study included children aged up to 2 years who were not on immunosuppressive medications, in the NICU, or hospitalized for more than 7 days. For this population, the two panels yielded similar rates of positivity overall (about 60%) and for individual viruses, Dr. Selvarangan said. A total of 810 patients tested positive for at least one virus on the Luminex panel, and 2,096 patients tested positive on FilmArray. Results for FilmArray were available within a median of 4 hours, versus 29 hours for Luminex (P less than .001). The prevalence of empiric antibiotic therapy was 44% during the Luminex era and 28% after the hospital switched to FilmArray (P less than .001). Rates of antibiotic discontinuation rose from 16% with Luminex to 23% with FilmArray (P less than .01). Strikingly, oseltamivir prescriptions rose five-fold (from 17% to 85%; P less than .001) after the hospital began using FilmArray, which covers seasonal influenza. Finally, use of chest radiography fell significantly in both infants and older children after the hospital began using FilmArray instead of Luminex.
Clinicians might have become more comfortable interpreting molecular test results over time, which could have altered their clinical decision-making and thereby biased the study results, Dr. Selvarangan noted. Although at least four other single-center retrospective studies have linked multiplex PCR assays to better antibiotic stewardship, this study is one of the first to directly compare clinical outcomes between two assays, he added. More studies are needed to help guide choice of multiplex assays, whose cost remains a major barrier to widespread use, he concluded.
Dr. Selvarangan disclosed grant support from both Biofire Diagnostics and Luminex corporation, and an advisory relationship with BioFire.
SAN DIEGO – Switching to a faster, more comprehensive multiplex PCR viral respiratory assay enabled a hospital to discharge young children with acute respiratory illnesses sooner, prescribe oseltamivir more often, and curtail the use of antibiotics and thoracic radiography, Rangaraj Selvarangan, PhD, reported at an annual meeting on infectious disease.
The study shows how rapid multiplex PCR testing can facilitate antimicrobial stewardship, said Dr. Selvarangan, who is a professor at the University of Missouri Kansas City School of Medicine and director of the microbiology laboratory at Children’s Mercy Kansas City. “Our antimicrobial stewardship programs monitors these test results daily, add notes, and make recommendations on antibiotic choices,” he said.
For the study, the researchers compared hospital records from December 2008 through May 2012, when Children’s Mercy hospital used the Luminex xTAG Respiratory Viral Panel, with records from August 2012 through June 2015, after the hospital had switched over to the Biofire FilmArray Respiratory Panel. FilmArray targets the same 17 viral pathogens as the Luminex panel, but also targets Bordetella pertussis, Chlamydia pneumoniae, and Mycoplasma pneumoniae, seasonal influenza A, parainfluenza type 4, and four coronaviruses.
The study included children aged up to 2 years who were not on immunosuppressive medications, in the NICU, or hospitalized for more than 7 days. For this population, the two panels yielded similar rates of positivity overall (about 60%) and for individual viruses, Dr. Selvarangan said. A total of 810 patients tested positive for at least one virus on the Luminex panel, and 2,096 patients tested positive on FilmArray. Results for FilmArray were available within a median of 4 hours, versus 29 hours for Luminex (P less than .001). The prevalence of empiric antibiotic therapy was 44% during the Luminex era and 28% after the hospital switched to FilmArray (P less than .001). Rates of antibiotic discontinuation rose from 16% with Luminex to 23% with FilmArray (P less than .01). Strikingly, oseltamivir prescriptions rose five-fold (from 17% to 85%; P less than .001) after the hospital began using FilmArray, which covers seasonal influenza. Finally, use of chest radiography fell significantly in both infants and older children after the hospital began using FilmArray instead of Luminex.
Clinicians might have become more comfortable interpreting molecular test results over time, which could have altered their clinical decision-making and thereby biased the study results, Dr. Selvarangan noted. Although at least four other single-center retrospective studies have linked multiplex PCR assays to better antibiotic stewardship, this study is one of the first to directly compare clinical outcomes between two assays, he added. More studies are needed to help guide choice of multiplex assays, whose cost remains a major barrier to widespread use, he concluded.
Dr. Selvarangan disclosed grant support from both Biofire Diagnostics and Luminex corporation, and an advisory relationship with BioFire.
AT IDWEEK 2017
Key clinical point: Faster multiplex PCR respiratory panel results helped guide management of young children hospitalized with acute respiratory illness.
Major finding: Empiric antibiotic therapy, thoracic radiography, and median length of stay all decreased.
Data source: A descriptive single-center retrospective study of 2,905 children up to 24 months old who were hospitalized with acute respiratory illness and tested positive for at least one virus on a multiplex PCR.
Disclosures: Dr. Selvarangan disclosed grant support from both Biofire Diagnostics and Luminex corporation, and an advisory relationship with BioFire.
Study eyes factors that may trigger breakthrough bacteremia
SAN DIEGO – , according to a detailed study of six isolates.
“Both patient and microbe factors can contribute to treatment failure, even involving pan-susceptible isolates,” Andrew Berti, PharmD, PhD, said in an interview prior to an annual scientific meeting on infectious diseases.

The researchers presented the case of a patient who experienced multiple episodes of breakthrough Staphylococcus aureus bacteremia over a period of 5 years in the setting of appropriately dosed antimicrobial suppressive therapy. They recovered six clinical bloodstream isolates from the patient during distinct episodes of methicillin-susceptible S. aureus (MSSA) bacteremia, and it was determined that a central line infection was the source for each episode. Isolates recovered were susceptible to the individual therapies received, which included oxacillin, daptomycin, and dalbavancin. The researchers used Illumina technology to collect bacterial whole genome sequence data. “Relatively little is known about bacterial evolution during human infection as these tend to be acute, rapidly resolved events,” Dr. Berti said. “This case was unique in that we could observe changes to a pathogen over a more than 6 years period as it adapted to survive host defenses and multiple antibiotic interventions.”
The researchers discovered that the first two isolates (ST256) and the last four isolates (ST5) “represent distinct populations and suggest that a distinct MSSA strain displaced the previous population between bacteremia episodes 2 and 3,” they wrote in their abstract. “Of note, all of these strains were able to survive and establish breakthrough bacteremias despite favorable susceptibility profiles to the agents used as suppressive therapy. Although the MICs remain low and in the susceptible range to oxacillin, daptomycin, and dalbavancin, these isolates progressively developed significant antimicrobial tolerance phenotypes, which coincided with mutations in walK (yycG), htrA2, ftsW, ebh, and ileS that may be advantageous to survival under antibiotic pressure.”
Dr. Berti acknowledged certain limitations of the analysis, including the inability to test for heteroresistance to some antibiotics, which may also contribute to treatment failure. “Specific therapeutic interventions that coincide with bacterial population changes are not necessarily causative of those changes,” he said. One of the study authors, Warren Rose, PharmD, disclosed having received research grants, speaker honoraria, and/or consulting fees from Theravance, Merck, The Medicines Company and Visante, Inc. All other authors reported having no financial disclosures.
SAN DIEGO – , according to a detailed study of six isolates.
“Both patient and microbe factors can contribute to treatment failure, even involving pan-susceptible isolates,” Andrew Berti, PharmD, PhD, said in an interview prior to an annual scientific meeting on infectious diseases.

The researchers presented the case of a patient who experienced multiple episodes of breakthrough Staphylococcus aureus bacteremia over a period of 5 years in the setting of appropriately dosed antimicrobial suppressive therapy. They recovered six clinical bloodstream isolates from the patient during distinct episodes of methicillin-susceptible S. aureus (MSSA) bacteremia, and it was determined that a central line infection was the source for each episode. Isolates recovered were susceptible to the individual therapies received, which included oxacillin, daptomycin, and dalbavancin. The researchers used Illumina technology to collect bacterial whole genome sequence data. “Relatively little is known about bacterial evolution during human infection as these tend to be acute, rapidly resolved events,” Dr. Berti said. “This case was unique in that we could observe changes to a pathogen over a more than 6 years period as it adapted to survive host defenses and multiple antibiotic interventions.”
The researchers discovered that the first two isolates (ST256) and the last four isolates (ST5) “represent distinct populations and suggest that a distinct MSSA strain displaced the previous population between bacteremia episodes 2 and 3,” they wrote in their abstract. “Of note, all of these strains were able to survive and establish breakthrough bacteremias despite favorable susceptibility profiles to the agents used as suppressive therapy. Although the MICs remain low and in the susceptible range to oxacillin, daptomycin, and dalbavancin, these isolates progressively developed significant antimicrobial tolerance phenotypes, which coincided with mutations in walK (yycG), htrA2, ftsW, ebh, and ileS that may be advantageous to survival under antibiotic pressure.”
Dr. Berti acknowledged certain limitations of the analysis, including the inability to test for heteroresistance to some antibiotics, which may also contribute to treatment failure. “Specific therapeutic interventions that coincide with bacterial population changes are not necessarily causative of those changes,” he said. One of the study authors, Warren Rose, PharmD, disclosed having received research grants, speaker honoraria, and/or consulting fees from Theravance, Merck, The Medicines Company and Visante, Inc. All other authors reported having no financial disclosures.
SAN DIEGO – , according to a detailed study of six isolates.
“Both patient and microbe factors can contribute to treatment failure, even involving pan-susceptible isolates,” Andrew Berti, PharmD, PhD, said in an interview prior to an annual scientific meeting on infectious diseases.

The researchers presented the case of a patient who experienced multiple episodes of breakthrough Staphylococcus aureus bacteremia over a period of 5 years in the setting of appropriately dosed antimicrobial suppressive therapy. They recovered six clinical bloodstream isolates from the patient during distinct episodes of methicillin-susceptible S. aureus (MSSA) bacteremia, and it was determined that a central line infection was the source for each episode. Isolates recovered were susceptible to the individual therapies received, which included oxacillin, daptomycin, and dalbavancin. The researchers used Illumina technology to collect bacterial whole genome sequence data. “Relatively little is known about bacterial evolution during human infection as these tend to be acute, rapidly resolved events,” Dr. Berti said. “This case was unique in that we could observe changes to a pathogen over a more than 6 years period as it adapted to survive host defenses and multiple antibiotic interventions.”
The researchers discovered that the first two isolates (ST256) and the last four isolates (ST5) “represent distinct populations and suggest that a distinct MSSA strain displaced the previous population between bacteremia episodes 2 and 3,” they wrote in their abstract. “Of note, all of these strains were able to survive and establish breakthrough bacteremias despite favorable susceptibility profiles to the agents used as suppressive therapy. Although the MICs remain low and in the susceptible range to oxacillin, daptomycin, and dalbavancin, these isolates progressively developed significant antimicrobial tolerance phenotypes, which coincided with mutations in walK (yycG), htrA2, ftsW, ebh, and ileS that may be advantageous to survival under antibiotic pressure.”
Dr. Berti acknowledged certain limitations of the analysis, including the inability to test for heteroresistance to some antibiotics, which may also contribute to treatment failure. “Specific therapeutic interventions that coincide with bacterial population changes are not necessarily causative of those changes,” he said. One of the study authors, Warren Rose, PharmD, disclosed having received research grants, speaker honoraria, and/or consulting fees from Theravance, Merck, The Medicines Company and Visante, Inc. All other authors reported having no financial disclosures.
REPORTING FROM ID WEEK 2017
Key clinical point: Both patient and microbe factors can contribute to antibitoic treatment failure.
Major finding: Two distinct Staphylococcus aureus lineages were islolated over a period of 5 years, and each was able to persist despite appropriate antibitoic interventions.
Study details: Clinical analysis of six bloodstream isolates from a singles patient over a 5-year period.
Disclosures: One of the study authors, Warren Rose, PharmD, disclosed having received research grants, speaker honoraria and/or consulting fees from Theravance, Merck, The Medicines Company and Visante. All other authors reported having no financial disclosures.
Dentist-prescribed antibiotics implicated in community-acquired C. diff
SAN DIEGO – Antibiotic prescriptions written by dentists make a substantial but largely unrecognized contribution to the risk of community-acquired Clostridium difficile (CA-CDI) infections, according to results of a public health initiative that was presented at an annual scientific meeting on infectious diseases.
When nearly 1,000 cases of CA-CDI suspected of being the result of antibiotic exposure were evaluated, it was found that 15% of the prescriptions were written by dentists, often for indications that are counter to current guidelines, reported Maria Bye, MPH, an officer in the Infectious Disease Epidemiology, Prevention, and Control Division of the Minnesota Department of Health, St. Paul.
In another finding from this study relevant to infection control, a substantial proportion of dentist-prescribed antibiotics associated with CA-CDI were not in the medical record. Rather, they were discovered in interviews conducted to isolate risk factors. “This is concerning since clinicians unaware of these exposures will not think about CA-CDI or other complications of antibiotic use, possibly delaying therapy,” Ms. Bye said.
The importance of dental antibiotic prescriptions in CA-CDI was identified in an ongoing infectious disease program managed by the Minnesota Department of Health in collaboration with the Centers for Disease Control and Prevention. In the years 2009-2015, medical records and interviews were conducted to identify risk factors in 1,626 confirmed cases of CA-CDI in five Minnesota counties. All cases were among patients without an overnight stay in a health care facility in the previous 12 weeks, which was an exclusion criterion.
After the review of medical records and patient interviews, 926 (57%) of the CA-CDI cases were deemed likely to be related to antibiotic exposure. Of these antibiotic exposures, 136 (15%) were from prescriptions written by dentists, a figure reached only when patients were interviewed. According to Ms. Bye, 34% of the antibiotics prescribed by dentists were not in the medical record.
There were also notable differences in antibiotic exposures stemming from dentist prescriptions relative to prescriptions from other sources. Perhaps most significantly, dental-related antibiotic prescriptions were far more likely to be for clindamycin (50% vs. 10%; P less than .001), which is commonly associated with increased risk of C. difficile, according to Ms. Bye. Fluoroquinolones (6% vs. 19%; P less than .001) and cephalosporins (7% vs. 30%; P less than .001) were significantly less likely to be prescribed by dentists. Patients who developed CA-CDI associated with antibiotics prescribed by dentists were also significantly older than were those receiving antibiotics from another source (mean age 57 years vs. 45 years; P less than .001).
For the first years of this analysis, information on the indication for dentist-prescribed antibiotics was not collected, but these data were collected beginning in 2015. In the data collected so far, a substantial proportion of prescriptions were written for prophylaxis against systemic infections, including prevention of endocarditis or infection of prosthetic joints. However, few of these prescriptions were indicated.
“The American Dental Association stated that antibiotic prophylaxis is not generally recommended in patients with prosthetic joints,” said Ms. Bye, noting that this is consistent with similar statements issued by the American Academy of Orthopedic Surgery. In 2007, the American Heart Association narrowed its recommendations for prophylactic antibiotics to patients at the highest risk of adverse consequences from endocarditis.
Of the four patients who received prophylactic antibiotics from their dentists for a cardiovascular or orthopedic indication, only one met current criteria, Ms. Bye reported.
The contribution of antibiotic exposures from dentist prescriptions to CA-CDI should not be surprising, according to Ms. Bye. In the United States, dentists prescribe 10% of all outpatient antibiotics. Although there are many valid indications for these prescriptions, Ms. Bye cited a survey that found that the proportion of dentists familiar with current guidelines and the risks of adverse events produced by antibiotics, including CA-CDI, is less than 50%.
“Dentists need to be included in antibiotic stewardship programs,” she advised. This will include educating dentists about the indications for antibiotic prophylaxis for medical conditions. She also suggested that clinicians should routinely ask patients about whether they have received antibiotics from a dentist so that this information gets into the medical record.
The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Antibiotic prescriptions written by dentists make a substantial but largely unrecognized contribution to the risk of community-acquired Clostridium difficile (CA-CDI) infections, according to results of a public health initiative that was presented at an annual scientific meeting on infectious diseases.
When nearly 1,000 cases of CA-CDI suspected of being the result of antibiotic exposure were evaluated, it was found that 15% of the prescriptions were written by dentists, often for indications that are counter to current guidelines, reported Maria Bye, MPH, an officer in the Infectious Disease Epidemiology, Prevention, and Control Division of the Minnesota Department of Health, St. Paul.
In another finding from this study relevant to infection control, a substantial proportion of dentist-prescribed antibiotics associated with CA-CDI were not in the medical record. Rather, they were discovered in interviews conducted to isolate risk factors. “This is concerning since clinicians unaware of these exposures will not think about CA-CDI or other complications of antibiotic use, possibly delaying therapy,” Ms. Bye said.
The importance of dental antibiotic prescriptions in CA-CDI was identified in an ongoing infectious disease program managed by the Minnesota Department of Health in collaboration with the Centers for Disease Control and Prevention. In the years 2009-2015, medical records and interviews were conducted to identify risk factors in 1,626 confirmed cases of CA-CDI in five Minnesota counties. All cases were among patients without an overnight stay in a health care facility in the previous 12 weeks, which was an exclusion criterion.
After the review of medical records and patient interviews, 926 (57%) of the CA-CDI cases were deemed likely to be related to antibiotic exposure. Of these antibiotic exposures, 136 (15%) were from prescriptions written by dentists, a figure reached only when patients were interviewed. According to Ms. Bye, 34% of the antibiotics prescribed by dentists were not in the medical record.
There were also notable differences in antibiotic exposures stemming from dentist prescriptions relative to prescriptions from other sources. Perhaps most significantly, dental-related antibiotic prescriptions were far more likely to be for clindamycin (50% vs. 10%; P less than .001), which is commonly associated with increased risk of C. difficile, according to Ms. Bye. Fluoroquinolones (6% vs. 19%; P less than .001) and cephalosporins (7% vs. 30%; P less than .001) were significantly less likely to be prescribed by dentists. Patients who developed CA-CDI associated with antibiotics prescribed by dentists were also significantly older than were those receiving antibiotics from another source (mean age 57 years vs. 45 years; P less than .001).
For the first years of this analysis, information on the indication for dentist-prescribed antibiotics was not collected, but these data were collected beginning in 2015. In the data collected so far, a substantial proportion of prescriptions were written for prophylaxis against systemic infections, including prevention of endocarditis or infection of prosthetic joints. However, few of these prescriptions were indicated.
“The American Dental Association stated that antibiotic prophylaxis is not generally recommended in patients with prosthetic joints,” said Ms. Bye, noting that this is consistent with similar statements issued by the American Academy of Orthopedic Surgery. In 2007, the American Heart Association narrowed its recommendations for prophylactic antibiotics to patients at the highest risk of adverse consequences from endocarditis.
Of the four patients who received prophylactic antibiotics from their dentists for a cardiovascular or orthopedic indication, only one met current criteria, Ms. Bye reported.
The contribution of antibiotic exposures from dentist prescriptions to CA-CDI should not be surprising, according to Ms. Bye. In the United States, dentists prescribe 10% of all outpatient antibiotics. Although there are many valid indications for these prescriptions, Ms. Bye cited a survey that found that the proportion of dentists familiar with current guidelines and the risks of adverse events produced by antibiotics, including CA-CDI, is less than 50%.
“Dentists need to be included in antibiotic stewardship programs,” she advised. This will include educating dentists about the indications for antibiotic prophylaxis for medical conditions. She also suggested that clinicians should routinely ask patients about whether they have received antibiotics from a dentist so that this information gets into the medical record.
The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Antibiotic prescriptions written by dentists make a substantial but largely unrecognized contribution to the risk of community-acquired Clostridium difficile (CA-CDI) infections, according to results of a public health initiative that was presented at an annual scientific meeting on infectious diseases.
When nearly 1,000 cases of CA-CDI suspected of being the result of antibiotic exposure were evaluated, it was found that 15% of the prescriptions were written by dentists, often for indications that are counter to current guidelines, reported Maria Bye, MPH, an officer in the Infectious Disease Epidemiology, Prevention, and Control Division of the Minnesota Department of Health, St. Paul.
In another finding from this study relevant to infection control, a substantial proportion of dentist-prescribed antibiotics associated with CA-CDI were not in the medical record. Rather, they were discovered in interviews conducted to isolate risk factors. “This is concerning since clinicians unaware of these exposures will not think about CA-CDI or other complications of antibiotic use, possibly delaying therapy,” Ms. Bye said.
The importance of dental antibiotic prescriptions in CA-CDI was identified in an ongoing infectious disease program managed by the Minnesota Department of Health in collaboration with the Centers for Disease Control and Prevention. In the years 2009-2015, medical records and interviews were conducted to identify risk factors in 1,626 confirmed cases of CA-CDI in five Minnesota counties. All cases were among patients without an overnight stay in a health care facility in the previous 12 weeks, which was an exclusion criterion.
After the review of medical records and patient interviews, 926 (57%) of the CA-CDI cases were deemed likely to be related to antibiotic exposure. Of these antibiotic exposures, 136 (15%) were from prescriptions written by dentists, a figure reached only when patients were interviewed. According to Ms. Bye, 34% of the antibiotics prescribed by dentists were not in the medical record.
There were also notable differences in antibiotic exposures stemming from dentist prescriptions relative to prescriptions from other sources. Perhaps most significantly, dental-related antibiotic prescriptions were far more likely to be for clindamycin (50% vs. 10%; P less than .001), which is commonly associated with increased risk of C. difficile, according to Ms. Bye. Fluoroquinolones (6% vs. 19%; P less than .001) and cephalosporins (7% vs. 30%; P less than .001) were significantly less likely to be prescribed by dentists. Patients who developed CA-CDI associated with antibiotics prescribed by dentists were also significantly older than were those receiving antibiotics from another source (mean age 57 years vs. 45 years; P less than .001).
For the first years of this analysis, information on the indication for dentist-prescribed antibiotics was not collected, but these data were collected beginning in 2015. In the data collected so far, a substantial proportion of prescriptions were written for prophylaxis against systemic infections, including prevention of endocarditis or infection of prosthetic joints. However, few of these prescriptions were indicated.
“The American Dental Association stated that antibiotic prophylaxis is not generally recommended in patients with prosthetic joints,” said Ms. Bye, noting that this is consistent with similar statements issued by the American Academy of Orthopedic Surgery. In 2007, the American Heart Association narrowed its recommendations for prophylactic antibiotics to patients at the highest risk of adverse consequences from endocarditis.
Of the four patients who received prophylactic antibiotics from their dentists for a cardiovascular or orthopedic indication, only one met current criteria, Ms. Bye reported.
The contribution of antibiotic exposures from dentist prescriptions to CA-CDI should not be surprising, according to Ms. Bye. In the United States, dentists prescribe 10% of all outpatient antibiotics. Although there are many valid indications for these prescriptions, Ms. Bye cited a survey that found that the proportion of dentists familiar with current guidelines and the risks of adverse events produced by antibiotics, including CA-CDI, is less than 50%.
“Dentists need to be included in antibiotic stewardship programs,” she advised. This will include educating dentists about the indications for antibiotic prophylaxis for medical conditions. She also suggested that clinicians should routinely ask patients about whether they have received antibiotics from a dentist so that this information gets into the medical record.
The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
AT ID WEEK 2017
Key clinical point: A public health initiative tracking community-acquired Clostridium difficile infections suggests dental antibiotic prescribing is a significant source.
Major finding: When traced, 15% of the antibiotics related to community-acquired C. difficile infections were from a dentist prescription.
Data source: Population-based surveillance study.
Disclosures: Ms. Bye reported that she has no financial relationships relevant to this topic.
PrEP is not main driver in STI epidemic, says expert
SAN DIEGO – Increased use of pre-exposure prophylaxis (PrEP) to prevent HIV transmission has accelerated but is not the main reason for surging rates of sexually transmitted infections in the United States, Kenneth Mayer, MD, said during an oral presentation at an annual scientific meeting on infectious diseases.
Public health officials are seeing unprecedented rises in STIs such as syphilis and gonorrhea in both HIV-negative and HIV-positive individuals, and these trends predate the advent of PrEP, said Dr. Mayer of the Fenway Institute and Harvard University in Boston, Mass. “An overall level of behavioral disinhibition is fueling this epidemic and is not necessarily associated with PrEP,” he said.
Several studies suggest that being on PrEP does not increase the likelihood of acquiring or transmitting an STI, Dr. Mayer emphasized. In the open-label PROUD trial of PrEP in men who have sex with men (MSM), “rates of STI were extremely high and remained so, but did not go up after PrEP was initiated,” he noted. Importantly, the incidence of HIV infection was only 1.6 per 100 person-years when MSM received PrEP immediately but was 9.4 cases per 100 person-years when MSM were randomly assigned to a 1-year wait list (rate ratio, 6.0). In the randomized ANRS IPERGAY trial, 70% of high-risk MSM prescribed PrEP reported engaging in condomless anal intercourse during their most recent sexual encounter, but that proportion remained stable over 24 subsequent months of follow-up.
Providers also should understand that oral PrEP is just as effective at preventing HIV transmission when patients have STIs, Dr. Mayer said. In five recent studies, PrEP was equally efficacious among MSM regardless of whether they had syphilis or other STIs, and bacterial vaginosis in women also did not decrease the efficacy of oral PrEP. “There is no evidence to indicate that the efficacy of PrEP is lower among persons with STIs,” Dr. Mayer said.
Finally, providers should consider screening high-risk individuals for STIs more frequently than every 6 months as recommended by the Centers for Disease Control and Prevention, said Dr. Mayer. “For men who have sex with men, who are sexually active, and are on PrEP, quarterly screening makes exceedingly good sense from a cost-effectiveness standpoint,” he said.
“Screening less frequently than quarterly means that these individuals are having STIs for a longer period of time. When they are sexually active, we have a better chance of interrupting the transmission chain if we detect closer to the time of infection.”
Dr. Mayer disclosed support from the National Institutes of Health and Gilead Sciences, which makes some of the medications used in PrEP regimens.
SAN DIEGO – Increased use of pre-exposure prophylaxis (PrEP) to prevent HIV transmission has accelerated but is not the main reason for surging rates of sexually transmitted infections in the United States, Kenneth Mayer, MD, said during an oral presentation at an annual scientific meeting on infectious diseases.
Public health officials are seeing unprecedented rises in STIs such as syphilis and gonorrhea in both HIV-negative and HIV-positive individuals, and these trends predate the advent of PrEP, said Dr. Mayer of the Fenway Institute and Harvard University in Boston, Mass. “An overall level of behavioral disinhibition is fueling this epidemic and is not necessarily associated with PrEP,” he said.
Several studies suggest that being on PrEP does not increase the likelihood of acquiring or transmitting an STI, Dr. Mayer emphasized. In the open-label PROUD trial of PrEP in men who have sex with men (MSM), “rates of STI were extremely high and remained so, but did not go up after PrEP was initiated,” he noted. Importantly, the incidence of HIV infection was only 1.6 per 100 person-years when MSM received PrEP immediately but was 9.4 cases per 100 person-years when MSM were randomly assigned to a 1-year wait list (rate ratio, 6.0). In the randomized ANRS IPERGAY trial, 70% of high-risk MSM prescribed PrEP reported engaging in condomless anal intercourse during their most recent sexual encounter, but that proportion remained stable over 24 subsequent months of follow-up.
Providers also should understand that oral PrEP is just as effective at preventing HIV transmission when patients have STIs, Dr. Mayer said. In five recent studies, PrEP was equally efficacious among MSM regardless of whether they had syphilis or other STIs, and bacterial vaginosis in women also did not decrease the efficacy of oral PrEP. “There is no evidence to indicate that the efficacy of PrEP is lower among persons with STIs,” Dr. Mayer said.
Finally, providers should consider screening high-risk individuals for STIs more frequently than every 6 months as recommended by the Centers for Disease Control and Prevention, said Dr. Mayer. “For men who have sex with men, who are sexually active, and are on PrEP, quarterly screening makes exceedingly good sense from a cost-effectiveness standpoint,” he said.
“Screening less frequently than quarterly means that these individuals are having STIs for a longer period of time. When they are sexually active, we have a better chance of interrupting the transmission chain if we detect closer to the time of infection.”
Dr. Mayer disclosed support from the National Institutes of Health and Gilead Sciences, which makes some of the medications used in PrEP regimens.
SAN DIEGO – Increased use of pre-exposure prophylaxis (PrEP) to prevent HIV transmission has accelerated but is not the main reason for surging rates of sexually transmitted infections in the United States, Kenneth Mayer, MD, said during an oral presentation at an annual scientific meeting on infectious diseases.
Public health officials are seeing unprecedented rises in STIs such as syphilis and gonorrhea in both HIV-negative and HIV-positive individuals, and these trends predate the advent of PrEP, said Dr. Mayer of the Fenway Institute and Harvard University in Boston, Mass. “An overall level of behavioral disinhibition is fueling this epidemic and is not necessarily associated with PrEP,” he said.
Several studies suggest that being on PrEP does not increase the likelihood of acquiring or transmitting an STI, Dr. Mayer emphasized. In the open-label PROUD trial of PrEP in men who have sex with men (MSM), “rates of STI were extremely high and remained so, but did not go up after PrEP was initiated,” he noted. Importantly, the incidence of HIV infection was only 1.6 per 100 person-years when MSM received PrEP immediately but was 9.4 cases per 100 person-years when MSM were randomly assigned to a 1-year wait list (rate ratio, 6.0). In the randomized ANRS IPERGAY trial, 70% of high-risk MSM prescribed PrEP reported engaging in condomless anal intercourse during their most recent sexual encounter, but that proportion remained stable over 24 subsequent months of follow-up.
Providers also should understand that oral PrEP is just as effective at preventing HIV transmission when patients have STIs, Dr. Mayer said. In five recent studies, PrEP was equally efficacious among MSM regardless of whether they had syphilis or other STIs, and bacterial vaginosis in women also did not decrease the efficacy of oral PrEP. “There is no evidence to indicate that the efficacy of PrEP is lower among persons with STIs,” Dr. Mayer said.
Finally, providers should consider screening high-risk individuals for STIs more frequently than every 6 months as recommended by the Centers for Disease Control and Prevention, said Dr. Mayer. “For men who have sex with men, who are sexually active, and are on PrEP, quarterly screening makes exceedingly good sense from a cost-effectiveness standpoint,” he said.
“Screening less frequently than quarterly means that these individuals are having STIs for a longer period of time. When they are sexually active, we have a better chance of interrupting the transmission chain if we detect closer to the time of infection.”
Dr. Mayer disclosed support from the National Institutes of Health and Gilead Sciences, which makes some of the medications used in PrEP regimens.
AT IDWEEK 2017
HIV antiretroviral resistance can affect more than 10% of pregnant women
SAN DIEGO – HIV antiretroviral resistance can affect more than 10% of pregnant women, even if they are previously treatment naive, results of a case-control study demonstrated.
“Furthermore, if there is an HIV-infected infant who received HIV prophylaxis with zidovudine and nevirapine, the infant may have developed resistance to the nonnucleoside reverse transcriptase inhibitors [NNRTIs] class of medications, and timely antiretroviral-resistant testing is an important step prior to choosing an appropriate regimen,” Nava Yeganeh, MD, said in an interview prior to an annual scientific meeting on infectious diseases.
In all, 140 infants were HIV infected, and 13 had drug-resistant mutations. Of the 606 women who had sufficient nucleic acid amplification for resistance testing, 63 (10.4%) had drug-resistant mutations against one or more classes of antiretrovirals. “These mothers may have been infected with a drug-resistant strain of HIV, which they then may have passed on to their infants,” Dr. Yeganeh said. “We also found that 3 of the 13 HIV-infected infants with drug-resistant mutations against NNRTIs were born to mothers who did not have a resistant strain of HIV. These three infants likely developed resistance because of the infant prophylaxis they received with nevirapine.”
Univariate and multivariate analyses revealed that drug-resistant mutation in mothers was not associated with increased risk of HIV mother-to-child transmission (adjusted odds ratio, 0.79). The only predictors of mother-to-child transmission were log HIV viral load (OR, 1.4) and infant prophylaxis arm with a two-drug regimen (OR, 1.6). In addition, the presence of drug-resistant mutations in mothers who transmitted was strongly associated with presence of drug-resistant mutations in infants (P less than .001).
A key limitation of the trial, Dr. Yeganeh said, was that it was completed in 2011. “Antiretroviral-resistant HIV may be even more common now that antiretrovirals are more available,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. She reported having no financial disclosures.
SAN DIEGO – HIV antiretroviral resistance can affect more than 10% of pregnant women, even if they are previously treatment naive, results of a case-control study demonstrated.
“Furthermore, if there is an HIV-infected infant who received HIV prophylaxis with zidovudine and nevirapine, the infant may have developed resistance to the nonnucleoside reverse transcriptase inhibitors [NNRTIs] class of medications, and timely antiretroviral-resistant testing is an important step prior to choosing an appropriate regimen,” Nava Yeganeh, MD, said in an interview prior to an annual scientific meeting on infectious diseases.
In all, 140 infants were HIV infected, and 13 had drug-resistant mutations. Of the 606 women who had sufficient nucleic acid amplification for resistance testing, 63 (10.4%) had drug-resistant mutations against one or more classes of antiretrovirals. “These mothers may have been infected with a drug-resistant strain of HIV, which they then may have passed on to their infants,” Dr. Yeganeh said. “We also found that 3 of the 13 HIV-infected infants with drug-resistant mutations against NNRTIs were born to mothers who did not have a resistant strain of HIV. These three infants likely developed resistance because of the infant prophylaxis they received with nevirapine.”
Univariate and multivariate analyses revealed that drug-resistant mutation in mothers was not associated with increased risk of HIV mother-to-child transmission (adjusted odds ratio, 0.79). The only predictors of mother-to-child transmission were log HIV viral load (OR, 1.4) and infant prophylaxis arm with a two-drug regimen (OR, 1.6). In addition, the presence of drug-resistant mutations in mothers who transmitted was strongly associated with presence of drug-resistant mutations in infants (P less than .001).
A key limitation of the trial, Dr. Yeganeh said, was that it was completed in 2011. “Antiretroviral-resistant HIV may be even more common now that antiretrovirals are more available,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. She reported having no financial disclosures.
SAN DIEGO – HIV antiretroviral resistance can affect more than 10% of pregnant women, even if they are previously treatment naive, results of a case-control study demonstrated.
“Furthermore, if there is an HIV-infected infant who received HIV prophylaxis with zidovudine and nevirapine, the infant may have developed resistance to the nonnucleoside reverse transcriptase inhibitors [NNRTIs] class of medications, and timely antiretroviral-resistant testing is an important step prior to choosing an appropriate regimen,” Nava Yeganeh, MD, said in an interview prior to an annual scientific meeting on infectious diseases.
In all, 140 infants were HIV infected, and 13 had drug-resistant mutations. Of the 606 women who had sufficient nucleic acid amplification for resistance testing, 63 (10.4%) had drug-resistant mutations against one or more classes of antiretrovirals. “These mothers may have been infected with a drug-resistant strain of HIV, which they then may have passed on to their infants,” Dr. Yeganeh said. “We also found that 3 of the 13 HIV-infected infants with drug-resistant mutations against NNRTIs were born to mothers who did not have a resistant strain of HIV. These three infants likely developed resistance because of the infant prophylaxis they received with nevirapine.”
Univariate and multivariate analyses revealed that drug-resistant mutation in mothers was not associated with increased risk of HIV mother-to-child transmission (adjusted odds ratio, 0.79). The only predictors of mother-to-child transmission were log HIV viral load (OR, 1.4) and infant prophylaxis arm with a two-drug regimen (OR, 1.6). In addition, the presence of drug-resistant mutations in mothers who transmitted was strongly associated with presence of drug-resistant mutations in infants (P less than .001).
A key limitation of the trial, Dr. Yeganeh said, was that it was completed in 2011. “Antiretroviral-resistant HIV may be even more common now that antiretrovirals are more available,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. She reported having no financial disclosures.
AT IDWEEK 2017
Key clinical point:
Major finding: Of 606 women who had sufficient nucleic acid amplification for resistance testing, 63 (10.4%) had drug-resistant mutations against one or more classes of antiretrovirals.
Study details: A case-control study of blood samples from 606 HIV-infected pregnant women and their infants.
Disclosures: Dr. Yeganeh reported having no financial disclosures.
In the reemergence of typhus, the challenge is early diagnosis
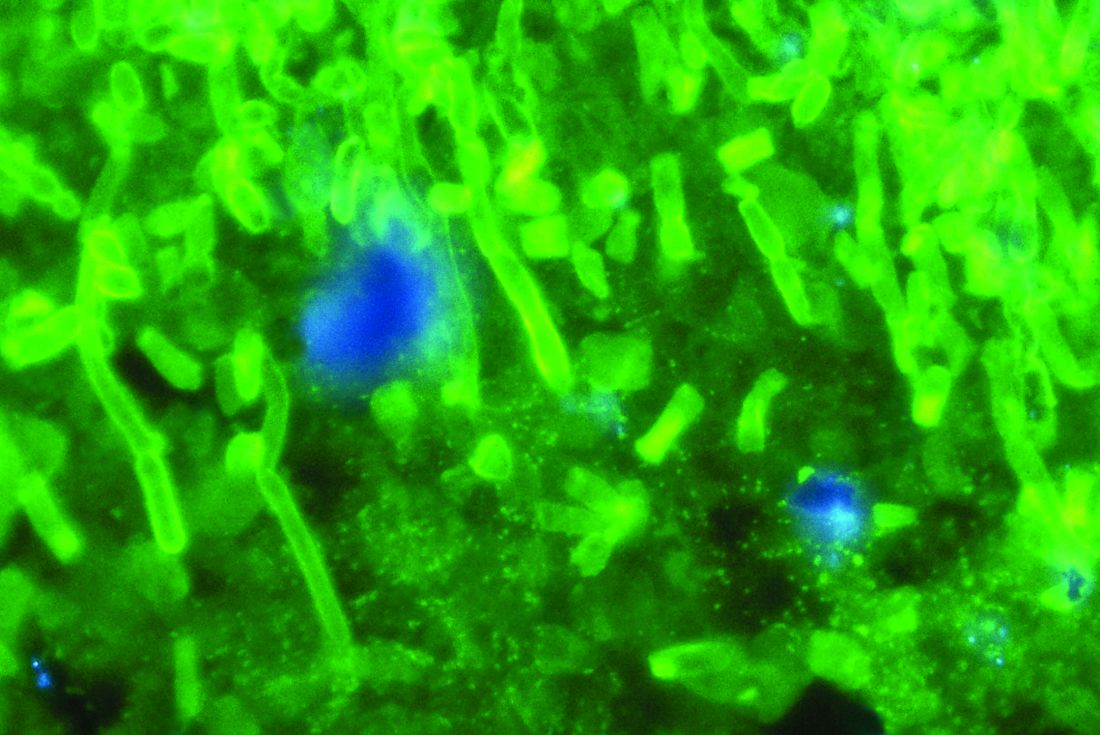
SAN DIEGO – Typhus in many forms, particularly scrub typhus, has reemerged worldwide, but none of these rickettsial infections poses a significant public health threat if promptly diagnosed, according to an update presented at an annual scientific meeting on infectious diseases.
Scrub typhus, which is spread by several species of trombiculid mites or chiggers, poses a large threat in regard to typhus epidemics, particularly in Asia, but sporadic cases of different types of typhus are being seen everywhere, including in the United States, according to George M. Varghese, MD, department of infectious diseases, Christian Medical College, Vellore, India.
“The typhus diseases are clinically similar but epidemiologically and etiologically distinct,” reported Dr. Varghese, “but doxycycline is the drug of choice for almost all of the rickettsial infections.”

The bacteria responsible for scrub typhus is Orientia tsutsugamushi, which is no longer included in the genus Rickettsia, but Dr. Varghese, who has published frequently on the epidemiology of scrub typhus, said that it is still appropriately grouped among rickettsial infections. It shares many features with the other rickettsioses, which were considered to be fading but are now resurging after the large epidemics that occurred prior to the introduction of antibiotics.
In the World Wars, Rickettsia prowazekii – which is carried and spread by body lice – was the most well known typhus threat. According to Dr. Varghese, this bacterium may have killed more soldiers in these conflicts than did firearms. Although R. prowazekii has not disappeared as a source of typhus outbreaks, particularly in South America and Africa, there are current epidemics produced from rickettsial infections carried by fleas, such as R. typhi, or ticks, like R. rickettsii, or mice, like R. felis.
For clinical detection of these forms of typhus, there are differences. Although all are associated with a rapid onset of fever, headache, and myalgia, subtle signs can be helpful in making a diagnosis while waiting for laboratory confirmation. For example, scrub typhus, unlike Rocky Mountain Fever, which is caused by tick bites, does not generally include a rash. Rather, eschars, which are small patches of necrotic skin, are far more characteristic.
“Serological tests are the most common diagnostic tool for typhus, but serology may not allow early diagnosis. You can obtain a false positive in the early stages of disease,” Dr. Varghese warned. To speed the diagnosis, he said that looking for the clinical clues characteristic of the suspected form of typhus, such as the scrub typhus-associated eschar, “is valuable.” However, he also emphasized that even with positive serology results, “good epidemiology and history is helpful for laboratory interpretation.”
A variety of serological tests can identify typhus pathogens, but ELISA is now the most widely used, according to Dr. Varghese, noting that this test offers a sensitivity of 93% and a specificity of 91%. Both are higher than those provided by alternatives. As a result of improved sensitivity of diagnostic tests, prevalence rates of some forms of typhus have proved to be unexpectedly high. For example, in a study undertaken in his region of India, the seroprevalence of scrub typhus was 31.8% (Trop Med Int Health. 2017;22:576-82. doi: 10.1111/tmi.12853).
Of unmet needs in the clinical management of typhus, Dr. Varghese listed better strategies for point-of-care diagnosis and treatment and better data on how to manage patients who are severely ill. Advanced disease, which is common to rural areas with limited access to health care, is the source of almost all typhus mortality, according to Dr. Varghese. He described a trial now being initiated in severe disease that will compare intravenous doxycycline to IV azithromycin and to a combination of both IV doxycycline and azithromycin.
Although Dr. Varghese cautioned that reports of resistant typhus infections, particularly in Thailand, might prove to be the next big clinical challenge in typhus, he said that progress is being made toward reducing the burden of this disease in his area of the world. In a disease associated with a mortality of 50% if left untreated, he attributes gains to earlier diagnosis and prompt treatment.
At his medical center, “we have been working with this disease for a decade and a half,” he said, referring to scrub typhus. “When we started off, the mortality was around 15% after diagnosis. Today, the mortality is about 5%-7%.”
Dr. Varghese reported that he has no financial relationships relevant to this topic. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Typhus in many forms, particularly scrub typhus, has reemerged worldwide, but none of these rickettsial infections poses a significant public health threat if promptly diagnosed, according to an update presented at an annual scientific meeting on infectious diseases.
Scrub typhus, which is spread by several species of trombiculid mites or chiggers, poses a large threat in regard to typhus epidemics, particularly in Asia, but sporadic cases of different types of typhus are being seen everywhere, including in the United States, according to George M. Varghese, MD, department of infectious diseases, Christian Medical College, Vellore, India.
“The typhus diseases are clinically similar but epidemiologically and etiologically distinct,” reported Dr. Varghese, “but doxycycline is the drug of choice for almost all of the rickettsial infections.”

The bacteria responsible for scrub typhus is Orientia tsutsugamushi, which is no longer included in the genus Rickettsia, but Dr. Varghese, who has published frequently on the epidemiology of scrub typhus, said that it is still appropriately grouped among rickettsial infections. It shares many features with the other rickettsioses, which were considered to be fading but are now resurging after the large epidemics that occurred prior to the introduction of antibiotics.
In the World Wars, Rickettsia prowazekii – which is carried and spread by body lice – was the most well known typhus threat. According to Dr. Varghese, this bacterium may have killed more soldiers in these conflicts than did firearms. Although R. prowazekii has not disappeared as a source of typhus outbreaks, particularly in South America and Africa, there are current epidemics produced from rickettsial infections carried by fleas, such as R. typhi, or ticks, like R. rickettsii, or mice, like R. felis.
For clinical detection of these forms of typhus, there are differences. Although all are associated with a rapid onset of fever, headache, and myalgia, subtle signs can be helpful in making a diagnosis while waiting for laboratory confirmation. For example, scrub typhus, unlike Rocky Mountain Fever, which is caused by tick bites, does not generally include a rash. Rather, eschars, which are small patches of necrotic skin, are far more characteristic.
“Serological tests are the most common diagnostic tool for typhus, but serology may not allow early diagnosis. You can obtain a false positive in the early stages of disease,” Dr. Varghese warned. To speed the diagnosis, he said that looking for the clinical clues characteristic of the suspected form of typhus, such as the scrub typhus-associated eschar, “is valuable.” However, he also emphasized that even with positive serology results, “good epidemiology and history is helpful for laboratory interpretation.”
A variety of serological tests can identify typhus pathogens, but ELISA is now the most widely used, according to Dr. Varghese, noting that this test offers a sensitivity of 93% and a specificity of 91%. Both are higher than those provided by alternatives. As a result of improved sensitivity of diagnostic tests, prevalence rates of some forms of typhus have proved to be unexpectedly high. For example, in a study undertaken in his region of India, the seroprevalence of scrub typhus was 31.8% (Trop Med Int Health. 2017;22:576-82. doi: 10.1111/tmi.12853).
Of unmet needs in the clinical management of typhus, Dr. Varghese listed better strategies for point-of-care diagnosis and treatment and better data on how to manage patients who are severely ill. Advanced disease, which is common to rural areas with limited access to health care, is the source of almost all typhus mortality, according to Dr. Varghese. He described a trial now being initiated in severe disease that will compare intravenous doxycycline to IV azithromycin and to a combination of both IV doxycycline and azithromycin.
Although Dr. Varghese cautioned that reports of resistant typhus infections, particularly in Thailand, might prove to be the next big clinical challenge in typhus, he said that progress is being made toward reducing the burden of this disease in his area of the world. In a disease associated with a mortality of 50% if left untreated, he attributes gains to earlier diagnosis and prompt treatment.
At his medical center, “we have been working with this disease for a decade and a half,” he said, referring to scrub typhus. “When we started off, the mortality was around 15% after diagnosis. Today, the mortality is about 5%-7%.”
Dr. Varghese reported that he has no financial relationships relevant to this topic. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Typhus in many forms, particularly scrub typhus, has reemerged worldwide, but none of these rickettsial infections poses a significant public health threat if promptly diagnosed, according to an update presented at an annual scientific meeting on infectious diseases.
Scrub typhus, which is spread by several species of trombiculid mites or chiggers, poses a large threat in regard to typhus epidemics, particularly in Asia, but sporadic cases of different types of typhus are being seen everywhere, including in the United States, according to George M. Varghese, MD, department of infectious diseases, Christian Medical College, Vellore, India.
“The typhus diseases are clinically similar but epidemiologically and etiologically distinct,” reported Dr. Varghese, “but doxycycline is the drug of choice for almost all of the rickettsial infections.”

The bacteria responsible for scrub typhus is Orientia tsutsugamushi, which is no longer included in the genus Rickettsia, but Dr. Varghese, who has published frequently on the epidemiology of scrub typhus, said that it is still appropriately grouped among rickettsial infections. It shares many features with the other rickettsioses, which were considered to be fading but are now resurging after the large epidemics that occurred prior to the introduction of antibiotics.
In the World Wars, Rickettsia prowazekii – which is carried and spread by body lice – was the most well known typhus threat. According to Dr. Varghese, this bacterium may have killed more soldiers in these conflicts than did firearms. Although R. prowazekii has not disappeared as a source of typhus outbreaks, particularly in South America and Africa, there are current epidemics produced from rickettsial infections carried by fleas, such as R. typhi, or ticks, like R. rickettsii, or mice, like R. felis.
For clinical detection of these forms of typhus, there are differences. Although all are associated with a rapid onset of fever, headache, and myalgia, subtle signs can be helpful in making a diagnosis while waiting for laboratory confirmation. For example, scrub typhus, unlike Rocky Mountain Fever, which is caused by tick bites, does not generally include a rash. Rather, eschars, which are small patches of necrotic skin, are far more characteristic.
“Serological tests are the most common diagnostic tool for typhus, but serology may not allow early diagnosis. You can obtain a false positive in the early stages of disease,” Dr. Varghese warned. To speed the diagnosis, he said that looking for the clinical clues characteristic of the suspected form of typhus, such as the scrub typhus-associated eschar, “is valuable.” However, he also emphasized that even with positive serology results, “good epidemiology and history is helpful for laboratory interpretation.”
A variety of serological tests can identify typhus pathogens, but ELISA is now the most widely used, according to Dr. Varghese, noting that this test offers a sensitivity of 93% and a specificity of 91%. Both are higher than those provided by alternatives. As a result of improved sensitivity of diagnostic tests, prevalence rates of some forms of typhus have proved to be unexpectedly high. For example, in a study undertaken in his region of India, the seroprevalence of scrub typhus was 31.8% (Trop Med Int Health. 2017;22:576-82. doi: 10.1111/tmi.12853).
Of unmet needs in the clinical management of typhus, Dr. Varghese listed better strategies for point-of-care diagnosis and treatment and better data on how to manage patients who are severely ill. Advanced disease, which is common to rural areas with limited access to health care, is the source of almost all typhus mortality, according to Dr. Varghese. He described a trial now being initiated in severe disease that will compare intravenous doxycycline to IV azithromycin and to a combination of both IV doxycycline and azithromycin.
Although Dr. Varghese cautioned that reports of resistant typhus infections, particularly in Thailand, might prove to be the next big clinical challenge in typhus, he said that progress is being made toward reducing the burden of this disease in his area of the world. In a disease associated with a mortality of 50% if left untreated, he attributes gains to earlier diagnosis and prompt treatment.
At his medical center, “we have been working with this disease for a decade and a half,” he said, referring to scrub typhus. “When we started off, the mortality was around 15% after diagnosis. Today, the mortality is about 5%-7%.”
Dr. Varghese reported that he has no financial relationships relevant to this topic. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
AT IDWEEK 2017
Key clinical point:
Major finding: Almost all of the estimated 15,000 annual global deaths attributed to rickettsial infections could be eliminated with prompt doxycycline therapy.
Data source: Topic review.
Disclosures: Dr. Varghese reported that he has no relevant conflicts to disclose.
Study: Macrolide treatment lowers risk of failure in pediatric CAP patients
SAN DIEGO – Macrolide use showed lower treatment failure rates than did amoxicillin or beta-lactam treatment for pediatric community acquired pneumonia (CAP) patients, according to a study presented at an annual scientific meeting on infectious diseases.
While guidelines recommend amoxicillin as the first-line therapy against CAP, investigators have noticed an increase in macrolide prescriptions to pediatric outpatients, despite reported shortcomings in its use against atypical pneumonia.
“Macrolides are probably prescribed out of proportion to the presence of atypical pneumonia in that practice setting,” said Lori Handy, MD, of Children’s Hospital of Philadelphia. This could be an issue, according to Dr. Handy: “We also know that depending on the study, up to 40% of Streptococcus pneumoniae is resistant to macrolides, meaning there are children out there who may have S. pneumoniae who are receiving therapy not targeted at their disease pathogen.”
To examine the possible impact of an increase in macrolide prescriptions, the investigators conducted a retrospective cohort study of 10,470 CAP pediatric patients across 31 primary care practices in the Children’s Hospital of Philadelphia network who were diagnosed between January 2009 and December 2013.
The studied cohort was split into three groups based on treatment options: amoxicillin monotherapy (4,252, 40.6%), macrolide monotherapy (4,459, 42.6%), and broad-spectrum beta-lactams (1,759, 16.8%).
Patient age ranged from 3 months to 18 years, the majority were white, with a roughly equal number of each sex. Of the children studied, 634 (6.1%) experienced treatment failure, defined as a change in antibiotics, an emergency department visit for related symptoms, or hospitalization for pneumonia, all of which had to occur more than 24 hours after a pediatric visit, according to Dr. Handy.
Of the children who failed treatment, 341 (54%) were in the amoxicillin group, 145 (23%) were in the macrolide group, and 147 (23%) were in the broad-spectrum group.
Patients younger than 5 years old who received macrolide therapy were half as likely to experience treatment failure compared with those given amoxicillin (odds ratio [OR] .52 [95% confidence interval (CI), 0.34-0.78]).
“What this translates to in practice is that about 32 children would need to treated with macrolides to prevent one failure in the amoxicillin group,” said Dr. Handy.
Patients 5 years and older showed even lower odds of treatment failure, at approximately one-third the rate of amoxicillin treated patients (OR .31 [95% CI, 0.23-0.92]).
Dr. Handy stated that the retrospective nature of the study and the possibility of changes in the epidemiology of CAP occurring since 2013 should be considered when evaluating the findings.
In addition, she pointed out, CAP is a clinical diagnosis, and there is generally no microbiological data associated with it in order to determine the etiology of the infection.
Overall, in healthy children with CAP, it would be better to use macrolide antibiotics compared with amoxicillin, Dr. Handy concluded. However, without the microbiological data, a more randomized, controlled trial would be needed to determine how to best treat these patients, she added.
During discussion, members of the audience asked about the appropriateness of measuring a change in antibiotics as an endpoint, especially in children with viral pneumonia, who may have had parents request stronger medication when their children did not improve quickly enough.
The 47 patients who were hospitalized would not have provided enough control to properly test the results, Dr. Handy replied, although she did acknowledge the potential issue of viral infections.
She stated the need for further study to assess its possible impact, saying she didn’t know whether viral infections may have skewed their results. “Either they’ve done nothing because they’re equally distributed among the groups or they’ve pushed them one way or the other way,” she said.
Dr. Handy and her colleagues reported having no relevant financial disclosures. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
[email protected]
On Twitter @eaztweets
SAN DIEGO – Macrolide use showed lower treatment failure rates than did amoxicillin or beta-lactam treatment for pediatric community acquired pneumonia (CAP) patients, according to a study presented at an annual scientific meeting on infectious diseases.
While guidelines recommend amoxicillin as the first-line therapy against CAP, investigators have noticed an increase in macrolide prescriptions to pediatric outpatients, despite reported shortcomings in its use against atypical pneumonia.
“Macrolides are probably prescribed out of proportion to the presence of atypical pneumonia in that practice setting,” said Lori Handy, MD, of Children’s Hospital of Philadelphia. This could be an issue, according to Dr. Handy: “We also know that depending on the study, up to 40% of Streptococcus pneumoniae is resistant to macrolides, meaning there are children out there who may have S. pneumoniae who are receiving therapy not targeted at their disease pathogen.”
To examine the possible impact of an increase in macrolide prescriptions, the investigators conducted a retrospective cohort study of 10,470 CAP pediatric patients across 31 primary care practices in the Children’s Hospital of Philadelphia network who were diagnosed between January 2009 and December 2013.
The studied cohort was split into three groups based on treatment options: amoxicillin monotherapy (4,252, 40.6%), macrolide monotherapy (4,459, 42.6%), and broad-spectrum beta-lactams (1,759, 16.8%).
Patient age ranged from 3 months to 18 years, the majority were white, with a roughly equal number of each sex. Of the children studied, 634 (6.1%) experienced treatment failure, defined as a change in antibiotics, an emergency department visit for related symptoms, or hospitalization for pneumonia, all of which had to occur more than 24 hours after a pediatric visit, according to Dr. Handy.
Of the children who failed treatment, 341 (54%) were in the amoxicillin group, 145 (23%) were in the macrolide group, and 147 (23%) were in the broad-spectrum group.
Patients younger than 5 years old who received macrolide therapy were half as likely to experience treatment failure compared with those given amoxicillin (odds ratio [OR] .52 [95% confidence interval (CI), 0.34-0.78]).
“What this translates to in practice is that about 32 children would need to treated with macrolides to prevent one failure in the amoxicillin group,” said Dr. Handy.
Patients 5 years and older showed even lower odds of treatment failure, at approximately one-third the rate of amoxicillin treated patients (OR .31 [95% CI, 0.23-0.92]).
Dr. Handy stated that the retrospective nature of the study and the possibility of changes in the epidemiology of CAP occurring since 2013 should be considered when evaluating the findings.
In addition, she pointed out, CAP is a clinical diagnosis, and there is generally no microbiological data associated with it in order to determine the etiology of the infection.
Overall, in healthy children with CAP, it would be better to use macrolide antibiotics compared with amoxicillin, Dr. Handy concluded. However, without the microbiological data, a more randomized, controlled trial would be needed to determine how to best treat these patients, she added.
During discussion, members of the audience asked about the appropriateness of measuring a change in antibiotics as an endpoint, especially in children with viral pneumonia, who may have had parents request stronger medication when their children did not improve quickly enough.
The 47 patients who were hospitalized would not have provided enough control to properly test the results, Dr. Handy replied, although she did acknowledge the potential issue of viral infections.
She stated the need for further study to assess its possible impact, saying she didn’t know whether viral infections may have skewed their results. “Either they’ve done nothing because they’re equally distributed among the groups or they’ve pushed them one way or the other way,” she said.
Dr. Handy and her colleagues reported having no relevant financial disclosures. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
[email protected]
On Twitter @eaztweets
SAN DIEGO – Macrolide use showed lower treatment failure rates than did amoxicillin or beta-lactam treatment for pediatric community acquired pneumonia (CAP) patients, according to a study presented at an annual scientific meeting on infectious diseases.
While guidelines recommend amoxicillin as the first-line therapy against CAP, investigators have noticed an increase in macrolide prescriptions to pediatric outpatients, despite reported shortcomings in its use against atypical pneumonia.
“Macrolides are probably prescribed out of proportion to the presence of atypical pneumonia in that practice setting,” said Lori Handy, MD, of Children’s Hospital of Philadelphia. This could be an issue, according to Dr. Handy: “We also know that depending on the study, up to 40% of Streptococcus pneumoniae is resistant to macrolides, meaning there are children out there who may have S. pneumoniae who are receiving therapy not targeted at their disease pathogen.”
To examine the possible impact of an increase in macrolide prescriptions, the investigators conducted a retrospective cohort study of 10,470 CAP pediatric patients across 31 primary care practices in the Children’s Hospital of Philadelphia network who were diagnosed between January 2009 and December 2013.
The studied cohort was split into three groups based on treatment options: amoxicillin monotherapy (4,252, 40.6%), macrolide monotherapy (4,459, 42.6%), and broad-spectrum beta-lactams (1,759, 16.8%).
Patient age ranged from 3 months to 18 years, the majority were white, with a roughly equal number of each sex. Of the children studied, 634 (6.1%) experienced treatment failure, defined as a change in antibiotics, an emergency department visit for related symptoms, or hospitalization for pneumonia, all of which had to occur more than 24 hours after a pediatric visit, according to Dr. Handy.
Of the children who failed treatment, 341 (54%) were in the amoxicillin group, 145 (23%) were in the macrolide group, and 147 (23%) were in the broad-spectrum group.
Patients younger than 5 years old who received macrolide therapy were half as likely to experience treatment failure compared with those given amoxicillin (odds ratio [OR] .52 [95% confidence interval (CI), 0.34-0.78]).
“What this translates to in practice is that about 32 children would need to treated with macrolides to prevent one failure in the amoxicillin group,” said Dr. Handy.
Patients 5 years and older showed even lower odds of treatment failure, at approximately one-third the rate of amoxicillin treated patients (OR .31 [95% CI, 0.23-0.92]).
Dr. Handy stated that the retrospective nature of the study and the possibility of changes in the epidemiology of CAP occurring since 2013 should be considered when evaluating the findings.
In addition, she pointed out, CAP is a clinical diagnosis, and there is generally no microbiological data associated with it in order to determine the etiology of the infection.
Overall, in healthy children with CAP, it would be better to use macrolide antibiotics compared with amoxicillin, Dr. Handy concluded. However, without the microbiological data, a more randomized, controlled trial would be needed to determine how to best treat these patients, she added.
During discussion, members of the audience asked about the appropriateness of measuring a change in antibiotics as an endpoint, especially in children with viral pneumonia, who may have had parents request stronger medication when their children did not improve quickly enough.
The 47 patients who were hospitalized would not have provided enough control to properly test the results, Dr. Handy replied, although she did acknowledge the potential issue of viral infections.
She stated the need for further study to assess its possible impact, saying she didn’t know whether viral infections may have skewed their results. “Either they’ve done nothing because they’re equally distributed among the groups or they’ve pushed them one way or the other way,” she said.
Dr. Handy and her colleagues reported having no relevant financial disclosures. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
[email protected]
On Twitter @eaztweets
AT ID WEEK 2017
Key clinical point:
Major finding: Macrolide treatment was associated with treatment failure OR of .52 in patients younger than 5 years and .31 among patients older than 5 years.
Data source: Retrospective study of 10,460 pediatric patients receiving antibiotics for community acquired pneumonia during 2009-2013.
Disclosures: Dr. Handy and her colleagues reported having no relevant financial disclosures.
Expanding treatment options to deal with antibiotic resistance
SAN DIEGO – In an era of rising antibiotic resistance, new potential treatment options and policy changes took the stage at the start of an annual scientific meeting on infectious diseases.
Presenters covered emerging topics addressing infectious diseases, with a strong focus on HIV. A common emphasis, among all presentations, was the pressing need to update availability of newer and more effective drugs.
“There’s always something hot in ID, and often it’s transient. But what isn’t transient is the overwhelming problem of antibiotic resistance,” said Stan Deresinski, MD, infectious disease specialist from Stanford (Calif.) University. He added that: “A fear come true is the merger of antibiotic resistance and increased virulence.”
While long-term solutions are needed, a short-term answer is the increase in the kinds of antibiotics available, Dr. Deresinski said.
“As we look at this sort of event, we begin to look at ourselves in the near future as plague doctors,” warned Dr. Deresinski. “We need to deal with this, and the thing that can be done in the short term is the development of new antibiotics.”
The Food and Drug Administration has several avenues that could be used to provide for expedited antibiotics approval, such as fast tracking and priority approval of drugs. An additional program called Generating Antibiotic Incentives Now (GAIN) that allows the FDA to designate an antibiotic as an anti-infectious disease product, making it eligible for fast tracking and priority approval, as well as the addition of 5 years of market exclusivity, may be used to incentivize the development of newer drugs.
In addition, Combating Antibiotic Resistant Bacteria Biopharmaceutical Accelerator (CARB-X) and the Antibacterial Resistance Leadership Group (ARLG) are two groups that will be essential for accelerating antibiotic development, Dr. Deresinski said.
CARB-X, which is a public-private partnership created by a White House executive order in 2014, focuses on preclinical discovery and development, and ARLG works under the mission statement, “prioritize, design, and execute clinical research that will reduce public health threat of antibacterial resistance.”
Among the hot topics in HIV, presenters described a series of studies conducted throughout the year assessing prexposure prophylaxis (PrEP), and how interventions, such as the use of the drug tenofovir, can increase efficacy of oral prophylaxis in preventing HIV-1 transmission.
In a test of antiretroviral therapy, the use of long-acting intramuscular injectable therapy every 4 and 8 weeks had huge improvement in patient approval, 88% and 89% respectively, compared with the 43% approval rate that oral HIV-1 medications received, said Wendy Armstrong, MD, of Emory University, Atlanta.
“[This] therapy is really getting to the point that we dreamed of 25 years ago, when our goals were finding an effective agent: to have simple agents, less frequent dosing schemes, limited adverse effects, and limited drug-to-drug interaction,” said Dr. Armstrong.
Among other topics to be addressed at the conference, Dr. Deresinski noted that the recent drop in Zika infections, as well as an uptick seen in hepatitis A outbreaks among the homeless and drug-user populations, would be discussed later in the week.
[email protected]
On Twitter @eaztweets
SAN DIEGO – In an era of rising antibiotic resistance, new potential treatment options and policy changes took the stage at the start of an annual scientific meeting on infectious diseases.
Presenters covered emerging topics addressing infectious diseases, with a strong focus on HIV. A common emphasis, among all presentations, was the pressing need to update availability of newer and more effective drugs.
“There’s always something hot in ID, and often it’s transient. But what isn’t transient is the overwhelming problem of antibiotic resistance,” said Stan Deresinski, MD, infectious disease specialist from Stanford (Calif.) University. He added that: “A fear come true is the merger of antibiotic resistance and increased virulence.”
While long-term solutions are needed, a short-term answer is the increase in the kinds of antibiotics available, Dr. Deresinski said.
“As we look at this sort of event, we begin to look at ourselves in the near future as plague doctors,” warned Dr. Deresinski. “We need to deal with this, and the thing that can be done in the short term is the development of new antibiotics.”
The Food and Drug Administration has several avenues that could be used to provide for expedited antibiotics approval, such as fast tracking and priority approval of drugs. An additional program called Generating Antibiotic Incentives Now (GAIN) that allows the FDA to designate an antibiotic as an anti-infectious disease product, making it eligible for fast tracking and priority approval, as well as the addition of 5 years of market exclusivity, may be used to incentivize the development of newer drugs.
In addition, Combating Antibiotic Resistant Bacteria Biopharmaceutical Accelerator (CARB-X) and the Antibacterial Resistance Leadership Group (ARLG) are two groups that will be essential for accelerating antibiotic development, Dr. Deresinski said.
CARB-X, which is a public-private partnership created by a White House executive order in 2014, focuses on preclinical discovery and development, and ARLG works under the mission statement, “prioritize, design, and execute clinical research that will reduce public health threat of antibacterial resistance.”
Among the hot topics in HIV, presenters described a series of studies conducted throughout the year assessing prexposure prophylaxis (PrEP), and how interventions, such as the use of the drug tenofovir, can increase efficacy of oral prophylaxis in preventing HIV-1 transmission.
In a test of antiretroviral therapy, the use of long-acting intramuscular injectable therapy every 4 and 8 weeks had huge improvement in patient approval, 88% and 89% respectively, compared with the 43% approval rate that oral HIV-1 medications received, said Wendy Armstrong, MD, of Emory University, Atlanta.
“[This] therapy is really getting to the point that we dreamed of 25 years ago, when our goals were finding an effective agent: to have simple agents, less frequent dosing schemes, limited adverse effects, and limited drug-to-drug interaction,” said Dr. Armstrong.
Among other topics to be addressed at the conference, Dr. Deresinski noted that the recent drop in Zika infections, as well as an uptick seen in hepatitis A outbreaks among the homeless and drug-user populations, would be discussed later in the week.
[email protected]
On Twitter @eaztweets
SAN DIEGO – In an era of rising antibiotic resistance, new potential treatment options and policy changes took the stage at the start of an annual scientific meeting on infectious diseases.
Presenters covered emerging topics addressing infectious diseases, with a strong focus on HIV. A common emphasis, among all presentations, was the pressing need to update availability of newer and more effective drugs.
“There’s always something hot in ID, and often it’s transient. But what isn’t transient is the overwhelming problem of antibiotic resistance,” said Stan Deresinski, MD, infectious disease specialist from Stanford (Calif.) University. He added that: “A fear come true is the merger of antibiotic resistance and increased virulence.”
While long-term solutions are needed, a short-term answer is the increase in the kinds of antibiotics available, Dr. Deresinski said.
“As we look at this sort of event, we begin to look at ourselves in the near future as plague doctors,” warned Dr. Deresinski. “We need to deal with this, and the thing that can be done in the short term is the development of new antibiotics.”
The Food and Drug Administration has several avenues that could be used to provide for expedited antibiotics approval, such as fast tracking and priority approval of drugs. An additional program called Generating Antibiotic Incentives Now (GAIN) that allows the FDA to designate an antibiotic as an anti-infectious disease product, making it eligible for fast tracking and priority approval, as well as the addition of 5 years of market exclusivity, may be used to incentivize the development of newer drugs.
In addition, Combating Antibiotic Resistant Bacteria Biopharmaceutical Accelerator (CARB-X) and the Antibacterial Resistance Leadership Group (ARLG) are two groups that will be essential for accelerating antibiotic development, Dr. Deresinski said.
CARB-X, which is a public-private partnership created by a White House executive order in 2014, focuses on preclinical discovery and development, and ARLG works under the mission statement, “prioritize, design, and execute clinical research that will reduce public health threat of antibacterial resistance.”
Among the hot topics in HIV, presenters described a series of studies conducted throughout the year assessing prexposure prophylaxis (PrEP), and how interventions, such as the use of the drug tenofovir, can increase efficacy of oral prophylaxis in preventing HIV-1 transmission.
In a test of antiretroviral therapy, the use of long-acting intramuscular injectable therapy every 4 and 8 weeks had huge improvement in patient approval, 88% and 89% respectively, compared with the 43% approval rate that oral HIV-1 medications received, said Wendy Armstrong, MD, of Emory University, Atlanta.
“[This] therapy is really getting to the point that we dreamed of 25 years ago, when our goals were finding an effective agent: to have simple agents, less frequent dosing schemes, limited adverse effects, and limited drug-to-drug interaction,” said Dr. Armstrong.
Among other topics to be addressed at the conference, Dr. Deresinski noted that the recent drop in Zika infections, as well as an uptick seen in hepatitis A outbreaks among the homeless and drug-user populations, would be discussed later in the week.
[email protected]
On Twitter @eaztweets
AT IDWEEK 2017
Anidulafungin effectively treated invasive pediatric candidiasis in open-label trial
SAN DIEGO – The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in a single-arm, multicenter, open-label trial of 47 children aged 2-17 years.
The overall global response rate of 72% resembled that from the prior adult registry study (76%), Emmanuel Roilides, MD, PhD, and his associates reported in a poster presented at an annual scientific meeting on infectious diseases.
At 6-week follow-up, two patients (4%) had relapsed, both with Candida parapsilosis, which was more resistant to treatment with anidulafungin (Eraxis) than other Candida species, the researchers reported. Treating the children with 3.0 mg/kg anidulafungin on day 1, followed by 1.5 mg/kg every 24 hours, yielded similar pharmacokinetics as the 200/100 mg regimen used in adults. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%), which also reflected findings in adults, the investigators said. Five patients (10%) developed at least one severe treatment-emergent adverse event, including neutropenia, gastrointestinal hemorrhage, increased hepatic transaminases, hyponatremia, and myalgia. The study (NCT00761267) is ongoing and continues to recruit patients in 11 states in the United States and nine other countries, with final top-line results expected in 2019.
Although rates of invasive candidiasis appear to be decreasing in children overall, the population at risk is expanding, experts have noted. Relevant guidelines from the Infectious Disease Society of America and the European Society of Clinical Microbiology and Infectious Diseases list amphotericin B, echinocandins, and azoles as treatment options, but these recommendations are extrapolated mainly from adult studies, noted Dr. Roilides, who is a pediatric infectious disease specialist at Aristotle University School of Health Sciences and Hippokration General Hospital in Thessaloniki, Greece.
To better characterize the safety and efficacy of anidulafungin in children, the researchers enrolled patients up to 17 years of age who had signs and symptoms of invasive candidiasis and Candida cultured from a normally sterile site. Patients received intravenous anidulafungin (3 mg/kg on day 1, followed by 1.5 mg/kg every 24 hours) for at least 10 days, after which they could switch to oral fluconazole. Treatment continued for at least 14 days after blood cultures were negative and signs and symptoms resolved.
At interim data cutoff in October 2016, patients were exposed to anidulafungin for a median of 11.5 days (range, 1-28 days). Among 47 patients who received at least one dose of anidulafungin, about two-thirds were male, about 70% were white, and the average age was 8 years (standard deviation, 4.7 years). Rates of global success – a combination of clinical and microbiological response – were 82% in patients up to 5 years old and 67% in older children. Children whose baseline neutrophil count was at least 500 per mm3 had a 78% global response rate versus 50% among those with more severe neutropenia. C. parapsilosis had higher minimum inhibitory concentrations than other Candida species, and in vitro susceptibility rates of 85% for C. parapsilosis versus 100% for other species.
All patients experienced at least one treatment-emergent adverse effect. In addition to diarrhea, vomiting, and pyrexia, adverse events affecting more than 10% of patients included epistaxis (17%), headache (15%), and abdominal pain (13%). Half of patients switched to oral fluconazole. Four patients stopped treatment because of vomiting, generalized pruritus, or increased transaminases. A total of 15% of patients died, although no deaths were considered treatment related. The patient who stopped treatment because of pruritus later died of septic shock secondary to invasive candidiasis, despite having started treatment with fluconazole and micafungin, the investigators reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Nearly all patients had bloodstream infections, and catheters also cultured positive in more than two-thirds of cases, the researchers said. Many patients had multiple risk factors for infection such as central venous catheters, broad-spectrum antibiotic therapy, total parenteral nutrition, and chemotherapy. Cultures were most often positive for Candida albicans (38%), followed by C. parapsilosis (26%) and C. tropicalis (13%).
Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
SAN DIEGO – The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in a single-arm, multicenter, open-label trial of 47 children aged 2-17 years.
The overall global response rate of 72% resembled that from the prior adult registry study (76%), Emmanuel Roilides, MD, PhD, and his associates reported in a poster presented at an annual scientific meeting on infectious diseases.
At 6-week follow-up, two patients (4%) had relapsed, both with Candida parapsilosis, which was more resistant to treatment with anidulafungin (Eraxis) than other Candida species, the researchers reported. Treating the children with 3.0 mg/kg anidulafungin on day 1, followed by 1.5 mg/kg every 24 hours, yielded similar pharmacokinetics as the 200/100 mg regimen used in adults. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%), which also reflected findings in adults, the investigators said. Five patients (10%) developed at least one severe treatment-emergent adverse event, including neutropenia, gastrointestinal hemorrhage, increased hepatic transaminases, hyponatremia, and myalgia. The study (NCT00761267) is ongoing and continues to recruit patients in 11 states in the United States and nine other countries, with final top-line results expected in 2019.
Although rates of invasive candidiasis appear to be decreasing in children overall, the population at risk is expanding, experts have noted. Relevant guidelines from the Infectious Disease Society of America and the European Society of Clinical Microbiology and Infectious Diseases list amphotericin B, echinocandins, and azoles as treatment options, but these recommendations are extrapolated mainly from adult studies, noted Dr. Roilides, who is a pediatric infectious disease specialist at Aristotle University School of Health Sciences and Hippokration General Hospital in Thessaloniki, Greece.
To better characterize the safety and efficacy of anidulafungin in children, the researchers enrolled patients up to 17 years of age who had signs and symptoms of invasive candidiasis and Candida cultured from a normally sterile site. Patients received intravenous anidulafungin (3 mg/kg on day 1, followed by 1.5 mg/kg every 24 hours) for at least 10 days, after which they could switch to oral fluconazole. Treatment continued for at least 14 days after blood cultures were negative and signs and symptoms resolved.
At interim data cutoff in October 2016, patients were exposed to anidulafungin for a median of 11.5 days (range, 1-28 days). Among 47 patients who received at least one dose of anidulafungin, about two-thirds were male, about 70% were white, and the average age was 8 years (standard deviation, 4.7 years). Rates of global success – a combination of clinical and microbiological response – were 82% in patients up to 5 years old and 67% in older children. Children whose baseline neutrophil count was at least 500 per mm3 had a 78% global response rate versus 50% among those with more severe neutropenia. C. parapsilosis had higher minimum inhibitory concentrations than other Candida species, and in vitro susceptibility rates of 85% for C. parapsilosis versus 100% for other species.
All patients experienced at least one treatment-emergent adverse effect. In addition to diarrhea, vomiting, and pyrexia, adverse events affecting more than 10% of patients included epistaxis (17%), headache (15%), and abdominal pain (13%). Half of patients switched to oral fluconazole. Four patients stopped treatment because of vomiting, generalized pruritus, or increased transaminases. A total of 15% of patients died, although no deaths were considered treatment related. The patient who stopped treatment because of pruritus later died of septic shock secondary to invasive candidiasis, despite having started treatment with fluconazole and micafungin, the investigators reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Nearly all patients had bloodstream infections, and catheters also cultured positive in more than two-thirds of cases, the researchers said. Many patients had multiple risk factors for infection such as central venous catheters, broad-spectrum antibiotic therapy, total parenteral nutrition, and chemotherapy. Cultures were most often positive for Candida albicans (38%), followed by C. parapsilosis (26%) and C. tropicalis (13%).
Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
SAN DIEGO – The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in a single-arm, multicenter, open-label trial of 47 children aged 2-17 years.
The overall global response rate of 72% resembled that from the prior adult registry study (76%), Emmanuel Roilides, MD, PhD, and his associates reported in a poster presented at an annual scientific meeting on infectious diseases.
At 6-week follow-up, two patients (4%) had relapsed, both with Candida parapsilosis, which was more resistant to treatment with anidulafungin (Eraxis) than other Candida species, the researchers reported. Treating the children with 3.0 mg/kg anidulafungin on day 1, followed by 1.5 mg/kg every 24 hours, yielded similar pharmacokinetics as the 200/100 mg regimen used in adults. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%), which also reflected findings in adults, the investigators said. Five patients (10%) developed at least one severe treatment-emergent adverse event, including neutropenia, gastrointestinal hemorrhage, increased hepatic transaminases, hyponatremia, and myalgia. The study (NCT00761267) is ongoing and continues to recruit patients in 11 states in the United States and nine other countries, with final top-line results expected in 2019.
Although rates of invasive candidiasis appear to be decreasing in children overall, the population at risk is expanding, experts have noted. Relevant guidelines from the Infectious Disease Society of America and the European Society of Clinical Microbiology and Infectious Diseases list amphotericin B, echinocandins, and azoles as treatment options, but these recommendations are extrapolated mainly from adult studies, noted Dr. Roilides, who is a pediatric infectious disease specialist at Aristotle University School of Health Sciences and Hippokration General Hospital in Thessaloniki, Greece.
To better characterize the safety and efficacy of anidulafungin in children, the researchers enrolled patients up to 17 years of age who had signs and symptoms of invasive candidiasis and Candida cultured from a normally sterile site. Patients received intravenous anidulafungin (3 mg/kg on day 1, followed by 1.5 mg/kg every 24 hours) for at least 10 days, after which they could switch to oral fluconazole. Treatment continued for at least 14 days after blood cultures were negative and signs and symptoms resolved.
At interim data cutoff in October 2016, patients were exposed to anidulafungin for a median of 11.5 days (range, 1-28 days). Among 47 patients who received at least one dose of anidulafungin, about two-thirds were male, about 70% were white, and the average age was 8 years (standard deviation, 4.7 years). Rates of global success – a combination of clinical and microbiological response – were 82% in patients up to 5 years old and 67% in older children. Children whose baseline neutrophil count was at least 500 per mm3 had a 78% global response rate versus 50% among those with more severe neutropenia. C. parapsilosis had higher minimum inhibitory concentrations than other Candida species, and in vitro susceptibility rates of 85% for C. parapsilosis versus 100% for other species.
All patients experienced at least one treatment-emergent adverse effect. In addition to diarrhea, vomiting, and pyrexia, adverse events affecting more than 10% of patients included epistaxis (17%), headache (15%), and abdominal pain (13%). Half of patients switched to oral fluconazole. Four patients stopped treatment because of vomiting, generalized pruritus, or increased transaminases. A total of 15% of patients died, although no deaths were considered treatment related. The patient who stopped treatment because of pruritus later died of septic shock secondary to invasive candidiasis, despite having started treatment with fluconazole and micafungin, the investigators reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Nearly all patients had bloodstream infections, and catheters also cultured positive in more than two-thirds of cases, the researchers said. Many patients had multiple risk factors for infection such as central venous catheters, broad-spectrum antibiotic therapy, total parenteral nutrition, and chemotherapy. Cultures were most often positive for Candida albicans (38%), followed by C. parapsilosis (26%) and C. tropicalis (13%).
Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
AT IDWEEK 2017
Key clinical point: The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in children, with a safety profile resembling what has been previously reported for adults.
Major finding: The overall global response rate was 72%. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%). Five patients (10%) developed at least one severe treatment-emergent adverse event.
Data source: A multicenter, single-arm, open-label study of 47 patients aged 2-17 years.
Disclosures: Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
High percentage of nursing home residents found to harbor MDROs
SAN DIEGO – Nearly half of nursing home residents harbored multi-drug resistant organisms on their skin, results from a large multi-center surveillance study showed.
“Residents in skilled nursing homes are the most vulnerable patients in the health care system,” lead study author James A. McKinnell, MD, said in an interview in advance of an annual scientific meeting on infectious diseases. “Many residents depend on help from health care workers for routine needs like eating or bathing. Skilled nursing facilities have an obligation to optimize the personal hygiene and environmental cleanliness in skilled nursing facilities.”

The researchers obtained 2,797 body swabs from 1,400 residents in all. Swabs were processed for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus spp. (VRE), extended spectrum beta-lactamase producers (ESBLs), and carbapenem-resistant Enterobacteriaceae (CRE). “MRSA is a relatively well known bacteria, but CRE is the new pathogen that the CDC has defined as an urgent public health threat,” Dr. McKinnell said.
The researchers also conducted environmental surveillance of commonly touched items in skilled nursing facilities. The five surfaces tested in resident rooms were the bedside table, TV remote, door knobs, light switch, and bathrooms. The five surfaces tested in common areas were the nursing station counter, tables, chairs, hallway hand rails, and drinking fountains.
Overall, 49% of residents harbored MDROs. MRSA was found in 37% of residents, followed by ESBL in 16%, VRE in 7%, and CRE in 1%. Resident MDRO status was known for 11% of MRSA carriers, compared with 18% of ESBL, 4% of VRE, and none of the CRE carriers. Rates of colonization did not differ whether residents had long stays at the facility or postacute stays (49% vs. 48%, respectively), but bed-bound residents were more likely to be MDRO colonized, compared with ambulatory residents (59% vs. 46%; P less than .001). In the analysis of environmental swabs, 93% of common areas and 74% of resident rooms had an MDRO-positive object, with an average of 2.5 and 1.9 objects, respectively, found to be contaminated.
“The fact that about half of patients were carrying a bacteria that could cause infection on their skin was very high,” said Dr. McKinnell, who is a member of the Infectious Disease Clinical Outcome Research Unit at the Los Angeles Biomedical Research Institute at Harbor-UCLA. “Studies conducted in other care settings, we would typically see less than a quarter of patients carry these types of bacteria. I was also surprised to see that 1% of patients were carrying the CRE bacteria on their skin.”
He acknowledged certain limitations of the study, including the fact that the data were taken from a select group of nursing homes that are participating in an interventional study to improve personal hygiene for skilled nursing facility residents. “They may not be representative of all skilled nursing facilities,” he said.
The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Nearly half of nursing home residents harbored multi-drug resistant organisms on their skin, results from a large multi-center surveillance study showed.
“Residents in skilled nursing homes are the most vulnerable patients in the health care system,” lead study author James A. McKinnell, MD, said in an interview in advance of an annual scientific meeting on infectious diseases. “Many residents depend on help from health care workers for routine needs like eating or bathing. Skilled nursing facilities have an obligation to optimize the personal hygiene and environmental cleanliness in skilled nursing facilities.”

The researchers obtained 2,797 body swabs from 1,400 residents in all. Swabs were processed for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus spp. (VRE), extended spectrum beta-lactamase producers (ESBLs), and carbapenem-resistant Enterobacteriaceae (CRE). “MRSA is a relatively well known bacteria, but CRE is the new pathogen that the CDC has defined as an urgent public health threat,” Dr. McKinnell said.
The researchers also conducted environmental surveillance of commonly touched items in skilled nursing facilities. The five surfaces tested in resident rooms were the bedside table, TV remote, door knobs, light switch, and bathrooms. The five surfaces tested in common areas were the nursing station counter, tables, chairs, hallway hand rails, and drinking fountains.
Overall, 49% of residents harbored MDROs. MRSA was found in 37% of residents, followed by ESBL in 16%, VRE in 7%, and CRE in 1%. Resident MDRO status was known for 11% of MRSA carriers, compared with 18% of ESBL, 4% of VRE, and none of the CRE carriers. Rates of colonization did not differ whether residents had long stays at the facility or postacute stays (49% vs. 48%, respectively), but bed-bound residents were more likely to be MDRO colonized, compared with ambulatory residents (59% vs. 46%; P less than .001). In the analysis of environmental swabs, 93% of common areas and 74% of resident rooms had an MDRO-positive object, with an average of 2.5 and 1.9 objects, respectively, found to be contaminated.
“The fact that about half of patients were carrying a bacteria that could cause infection on their skin was very high,” said Dr. McKinnell, who is a member of the Infectious Disease Clinical Outcome Research Unit at the Los Angeles Biomedical Research Institute at Harbor-UCLA. “Studies conducted in other care settings, we would typically see less than a quarter of patients carry these types of bacteria. I was also surprised to see that 1% of patients were carrying the CRE bacteria on their skin.”
He acknowledged certain limitations of the study, including the fact that the data were taken from a select group of nursing homes that are participating in an interventional study to improve personal hygiene for skilled nursing facility residents. “They may not be representative of all skilled nursing facilities,” he said.
The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Nearly half of nursing home residents harbored multi-drug resistant organisms on their skin, results from a large multi-center surveillance study showed.
“Residents in skilled nursing homes are the most vulnerable patients in the health care system,” lead study author James A. McKinnell, MD, said in an interview in advance of an annual scientific meeting on infectious diseases. “Many residents depend on help from health care workers for routine needs like eating or bathing. Skilled nursing facilities have an obligation to optimize the personal hygiene and environmental cleanliness in skilled nursing facilities.”

The researchers obtained 2,797 body swabs from 1,400 residents in all. Swabs were processed for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus spp. (VRE), extended spectrum beta-lactamase producers (ESBLs), and carbapenem-resistant Enterobacteriaceae (CRE). “MRSA is a relatively well known bacteria, but CRE is the new pathogen that the CDC has defined as an urgent public health threat,” Dr. McKinnell said.
The researchers also conducted environmental surveillance of commonly touched items in skilled nursing facilities. The five surfaces tested in resident rooms were the bedside table, TV remote, door knobs, light switch, and bathrooms. The five surfaces tested in common areas were the nursing station counter, tables, chairs, hallway hand rails, and drinking fountains.
Overall, 49% of residents harbored MDROs. MRSA was found in 37% of residents, followed by ESBL in 16%, VRE in 7%, and CRE in 1%. Resident MDRO status was known for 11% of MRSA carriers, compared with 18% of ESBL, 4% of VRE, and none of the CRE carriers. Rates of colonization did not differ whether residents had long stays at the facility or postacute stays (49% vs. 48%, respectively), but bed-bound residents were more likely to be MDRO colonized, compared with ambulatory residents (59% vs. 46%; P less than .001). In the analysis of environmental swabs, 93% of common areas and 74% of resident rooms had an MDRO-positive object, with an average of 2.5 and 1.9 objects, respectively, found to be contaminated.
“The fact that about half of patients were carrying a bacteria that could cause infection on their skin was very high,” said Dr. McKinnell, who is a member of the Infectious Disease Clinical Outcome Research Unit at the Los Angeles Biomedical Research Institute at Harbor-UCLA. “Studies conducted in other care settings, we would typically see less than a quarter of patients carry these types of bacteria. I was also surprised to see that 1% of patients were carrying the CRE bacteria on their skin.”
He acknowledged certain limitations of the study, including the fact that the data were taken from a select group of nursing homes that are participating in an interventional study to improve personal hygiene for skilled nursing facility residents. “They may not be representative of all skilled nursing facilities,” he said.
The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
AT ID WEEK 2017
Key clinical point: About one of every two nursing home residents is colonized with multidrug resistant organisms.
Major finding:
Study details: A surveillance study of 1,400 residents at 28 skilled nursing facilities in Southern California.
Disclosures: The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry.