User login
British Society for Rheumatology (BSR): Annual Conference (Rheumatology 2015)
Rate ratio of comorbidity high in SLE patients under 40
MANCHESTER, U.K. – When systemic lupus erythematosus (SLE) occurs before age 40, patients run a high relative risk of end-stage renal disease, data from a retrospective U.K.-based cohort study have shown.
While the risk for cardiovascular disease and stroke has been reported previously, particularly in younger SLE patients, the risks for comorbidities such as end-stage renal failure (ESRF), osteoporosis, and infection were not as clear. “We know that comorbidities are increased in patients with lupus, but we didn’t know by how much,” Dr. Frances Rees of Nottingham University Hospitals NHS Trust, Nottingham, England, explained at the British Society for Rheumatology annual conference.The adjusted incidence rate ratio (IRR) for ESRF was greater than 60 for lupus patients under age 40 and about 10 for those aged 40-69 years.“Although the absolute risk increased with age, the relative risk difference between cases and controls was highest in those at younger ages, so don’t forget primary prevention and screening in younger patients,” Dr. Rees said.
The risk was based on data obtained from the Clinical Practice Research Datalink, an anonymized database of primary care records for approximately 12 million people, on all prevalent cases of SLE occurring between 1999 and 2012 in the United Kingdom. Each of the 7,732 cases was matched to up to four patients who did not have lupus and were seen at the same practice. The control population exceeded 28,000 individuals.
Around 55% of lupus patients had a Charlson Comorbidity Index (CCI) of zero while around 75% of patients without lupus had no comorbidities. About 33% of lupus patients had a CCI of 1-2 as did about 20% of controls; less than 10% of patients had a CCI of 3-5 or more than 5.
“The highest difference between the two groups was for end-stage renal failure even after adjusting for confounders,” she added. IRRs for the other comorbidities were around or just under 2.“When we compared men and women, men had higher risks of cardiovascular disease, stroke, and cancer, but women had higher rates of infection and osteoporosis, which would fit with the underlying population,” Dr. Rees observed.
“What was interesting, however, was the difference in the incidence rates for osteoporosis between cases and controls in men, which was of a bigger relative risk than it was in women,” Dr. Rees noted. “So don’t forget to consider osteoporosis in men,” she advised. For cardiovascular disease, the IRR was much higher in patients under age 40 years than for the older patients (IRR <5).In an interview, Dr. Rees explained that while these data partly confirm what was already known, the research is the first to look at comorbidity in SLE from a community perspective. “Also, some of the previous studies done in hospitals have only really shown that the risk of cardiovascular disease and stroke was in younger people, but we have found that the risk was increased across all age groups.”
The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
MANCHESTER, U.K. – When systemic lupus erythematosus (SLE) occurs before age 40, patients run a high relative risk of end-stage renal disease, data from a retrospective U.K.-based cohort study have shown.
While the risk for cardiovascular disease and stroke has been reported previously, particularly in younger SLE patients, the risks for comorbidities such as end-stage renal failure (ESRF), osteoporosis, and infection were not as clear. “We know that comorbidities are increased in patients with lupus, but we didn’t know by how much,” Dr. Frances Rees of Nottingham University Hospitals NHS Trust, Nottingham, England, explained at the British Society for Rheumatology annual conference.The adjusted incidence rate ratio (IRR) for ESRF was greater than 60 for lupus patients under age 40 and about 10 for those aged 40-69 years.“Although the absolute risk increased with age, the relative risk difference between cases and controls was highest in those at younger ages, so don’t forget primary prevention and screening in younger patients,” Dr. Rees said.
The risk was based on data obtained from the Clinical Practice Research Datalink, an anonymized database of primary care records for approximately 12 million people, on all prevalent cases of SLE occurring between 1999 and 2012 in the United Kingdom. Each of the 7,732 cases was matched to up to four patients who did not have lupus and were seen at the same practice. The control population exceeded 28,000 individuals.
Around 55% of lupus patients had a Charlson Comorbidity Index (CCI) of zero while around 75% of patients without lupus had no comorbidities. About 33% of lupus patients had a CCI of 1-2 as did about 20% of controls; less than 10% of patients had a CCI of 3-5 or more than 5.
“The highest difference between the two groups was for end-stage renal failure even after adjusting for confounders,” she added. IRRs for the other comorbidities were around or just under 2.“When we compared men and women, men had higher risks of cardiovascular disease, stroke, and cancer, but women had higher rates of infection and osteoporosis, which would fit with the underlying population,” Dr. Rees observed.
“What was interesting, however, was the difference in the incidence rates for osteoporosis between cases and controls in men, which was of a bigger relative risk than it was in women,” Dr. Rees noted. “So don’t forget to consider osteoporosis in men,” she advised. For cardiovascular disease, the IRR was much higher in patients under age 40 years than for the older patients (IRR <5).In an interview, Dr. Rees explained that while these data partly confirm what was already known, the research is the first to look at comorbidity in SLE from a community perspective. “Also, some of the previous studies done in hospitals have only really shown that the risk of cardiovascular disease and stroke was in younger people, but we have found that the risk was increased across all age groups.”
The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
MANCHESTER, U.K. – When systemic lupus erythematosus (SLE) occurs before age 40, patients run a high relative risk of end-stage renal disease, data from a retrospective U.K.-based cohort study have shown.
While the risk for cardiovascular disease and stroke has been reported previously, particularly in younger SLE patients, the risks for comorbidities such as end-stage renal failure (ESRF), osteoporosis, and infection were not as clear. “We know that comorbidities are increased in patients with lupus, but we didn’t know by how much,” Dr. Frances Rees of Nottingham University Hospitals NHS Trust, Nottingham, England, explained at the British Society for Rheumatology annual conference.The adjusted incidence rate ratio (IRR) for ESRF was greater than 60 for lupus patients under age 40 and about 10 for those aged 40-69 years.“Although the absolute risk increased with age, the relative risk difference between cases and controls was highest in those at younger ages, so don’t forget primary prevention and screening in younger patients,” Dr. Rees said.
The risk was based on data obtained from the Clinical Practice Research Datalink, an anonymized database of primary care records for approximately 12 million people, on all prevalent cases of SLE occurring between 1999 and 2012 in the United Kingdom. Each of the 7,732 cases was matched to up to four patients who did not have lupus and were seen at the same practice. The control population exceeded 28,000 individuals.
Around 55% of lupus patients had a Charlson Comorbidity Index (CCI) of zero while around 75% of patients without lupus had no comorbidities. About 33% of lupus patients had a CCI of 1-2 as did about 20% of controls; less than 10% of patients had a CCI of 3-5 or more than 5.
“The highest difference between the two groups was for end-stage renal failure even after adjusting for confounders,” she added. IRRs for the other comorbidities were around or just under 2.“When we compared men and women, men had higher risks of cardiovascular disease, stroke, and cancer, but women had higher rates of infection and osteoporosis, which would fit with the underlying population,” Dr. Rees observed.
“What was interesting, however, was the difference in the incidence rates for osteoporosis between cases and controls in men, which was of a bigger relative risk than it was in women,” Dr. Rees noted. “So don’t forget to consider osteoporosis in men,” she advised. For cardiovascular disease, the IRR was much higher in patients under age 40 years than for the older patients (IRR <5).In an interview, Dr. Rees explained that while these data partly confirm what was already known, the research is the first to look at comorbidity in SLE from a community perspective. “Also, some of the previous studies done in hospitals have only really shown that the risk of cardiovascular disease and stroke was in younger people, but we have found that the risk was increased across all age groups.”
The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
Key clinical point: The relative comorbidity burden is highest in SLE patients under age 40.
Major finding: The adjusted incidence rate ratio (IRR) for end-stage renal failure was 60-fold higher in patients under age 40 years and 10-fold higher in patients aged 40-69 years, compared to controls.
Data source: Retrospective cohort study of 7,732 patients with systemic lupus erythematosus and 29,079 lupus-free individuals.
Disclosures: The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
BSR: Flagging early symptoms could diagnose lupus sooner
MANCHESTER, U.K. – In a general practice setting, people who developed systemic lupus erythematosus were more than twice as likely to consult a primary care physician in the 5-year run-up to their diagnosis, according to the results of a case-control study.
The median annual consultation rates were 9.2 times for systemic lupus erythematosus (SLE) patients versus 3.8 times for controls (P < .001).
Lupus patients also started to exhibit telltale symptoms during this time, providing an opportunity for making a diagnosis sooner through better recognition of these early symptoms.
The aim of the study was “to find out whether people with lupus came to see their GP [general practitioner] more frequently and what they were going to see their GP for,” Dr. Frances Rees of Nottingham (England) University Hospitals NHS Trust explained in a poster session on connective tissue disease at the British Society for Rheumatology annual conference.
“After that, we developed a risk-prediction model which was a multivariate analysis taking some of the variables that we decided in advance would be most significant,” she added. These variables included age, gender, arthritis or arthralgia, rash, fatigue, alopecia, serositis, sicca, Raynaud’s phenomenon, and the consultation rate.
“We found that the model performed well in both the model development data set and in the model validation data set,” Dr. Rees said.
The rationale for the study was that SLE can be difficult to diagnose early, and that delays of more than 7 years have been found between symptom onset and diagnosis. Perhaps, if SLE is diagnosed earlier, outcomes could be improved, Dr. Rees and her coauthors reasoned.
Using the UK Clinical Practice Research Datalink, an anonymized database of general practice records for approximately 12 million people, all incident cases of SLE occurring between 1999 and 2012 were identified and matched to four individuals without lupus who were seen at the same primary care practices.
A total of 1,739 patients with lupus and 6,952 controls were identified and separated into two cohorts: approximately two-thirds formed the development cohort and the remainder a validation cohort.
Individual odds ratios (OR) were calculated for age, gender, consultation rates, 27 clinical features, and five previous diagnoses of rheumatic disease in the 5 years preceding SLE diagnosis. Some of the clinical features considered were arthritis or arthralgia, rash, fatigue, alopecia, serositis, and sicca; the associated diseases were another connective tissue disease, rheumatoid arthritis (RA), fibromyalgia, chronic fatigue syndrome (CFS), and Epstein-Barr virus (EBV) infection.
Results showed that cases were more than five times more likely than controls to be female (84% vs. 51%; OR, 5.23; P < .001).
Early symptoms suggestive of SLE occurred more often in cases than in controls, with arthritis or arthralgia in 36% vs. 10% (OR, 4.77; P < .001), rash in 43% vs. 10% (OR, 6.84; P < .001), fatigue in 17% vs. 7% (OR, 2.76; P < .001), alopecia in 4% vs. 1% (OR, 4.77; P < .001), serositis in 4% vs. 1% (OR, 5.05; P < .001), and sicca in 6% vs 1% (OR, 4.97; P < .001). Raynaud’s phenomenon was seen in 4% vs. 0%, with an OR of 15.29, which was significant (P < .001), but the confidence interval (CI) was wide (CI, 9.41-24.85).
Patients with SLE also were more than 20 times more likely to have a prior diagnosis of another connective tissue disease (OR, 21.68; P < .001) and 10 times more likely to have been diagnosed with RA (OR, 10.77; P < .001). Fibromyalgia (OR, 7.89; P < .001) and CFS (OR, 6.39; P < .001) also were more frequent among those who developed lupus than in those who did not.
“This suggests that, although there probably is a delay in diagnosis, patients are getting other diagnoses first,” Dr. Rees noted. “So, we would propose that, in the future, our risk-prediction model may be able to reduce that delay in conjunction with educational programs to say if you have a combination of these symptoms think about testing for [antinuclear antibodies] and/or referring to rheumatology.”
The team’s risk-prediction model now needs further external and economic validation, but the hope is that perhaps it could be incorporated into electronic systems used in primary care to flag potential lupus cases.
“The clinical message is to keep SLE in mind if someone is presenting multiple times with these kind of symptoms,” Dr. Rees said in an interview.
“Lupus is very rare,” she acknowledged, nothing that some primary care physicians may only see one or two cases of lupus in their career. So the risk-prediction model would aim to be an aid to help them consider SLE as a possibility in patients with several symptoms that, on their own, might not be suggestive of lupus.
The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
MANCHESTER, U.K. – In a general practice setting, people who developed systemic lupus erythematosus were more than twice as likely to consult a primary care physician in the 5-year run-up to their diagnosis, according to the results of a case-control study.
The median annual consultation rates were 9.2 times for systemic lupus erythematosus (SLE) patients versus 3.8 times for controls (P < .001).
Lupus patients also started to exhibit telltale symptoms during this time, providing an opportunity for making a diagnosis sooner through better recognition of these early symptoms.
The aim of the study was “to find out whether people with lupus came to see their GP [general practitioner] more frequently and what they were going to see their GP for,” Dr. Frances Rees of Nottingham (England) University Hospitals NHS Trust explained in a poster session on connective tissue disease at the British Society for Rheumatology annual conference.
“After that, we developed a risk-prediction model which was a multivariate analysis taking some of the variables that we decided in advance would be most significant,” she added. These variables included age, gender, arthritis or arthralgia, rash, fatigue, alopecia, serositis, sicca, Raynaud’s phenomenon, and the consultation rate.
“We found that the model performed well in both the model development data set and in the model validation data set,” Dr. Rees said.
The rationale for the study was that SLE can be difficult to diagnose early, and that delays of more than 7 years have been found between symptom onset and diagnosis. Perhaps, if SLE is diagnosed earlier, outcomes could be improved, Dr. Rees and her coauthors reasoned.
Using the UK Clinical Practice Research Datalink, an anonymized database of general practice records for approximately 12 million people, all incident cases of SLE occurring between 1999 and 2012 were identified and matched to four individuals without lupus who were seen at the same primary care practices.
A total of 1,739 patients with lupus and 6,952 controls were identified and separated into two cohorts: approximately two-thirds formed the development cohort and the remainder a validation cohort.
Individual odds ratios (OR) were calculated for age, gender, consultation rates, 27 clinical features, and five previous diagnoses of rheumatic disease in the 5 years preceding SLE diagnosis. Some of the clinical features considered were arthritis or arthralgia, rash, fatigue, alopecia, serositis, and sicca; the associated diseases were another connective tissue disease, rheumatoid arthritis (RA), fibromyalgia, chronic fatigue syndrome (CFS), and Epstein-Barr virus (EBV) infection.
Results showed that cases were more than five times more likely than controls to be female (84% vs. 51%; OR, 5.23; P < .001).
Early symptoms suggestive of SLE occurred more often in cases than in controls, with arthritis or arthralgia in 36% vs. 10% (OR, 4.77; P < .001), rash in 43% vs. 10% (OR, 6.84; P < .001), fatigue in 17% vs. 7% (OR, 2.76; P < .001), alopecia in 4% vs. 1% (OR, 4.77; P < .001), serositis in 4% vs. 1% (OR, 5.05; P < .001), and sicca in 6% vs 1% (OR, 4.97; P < .001). Raynaud’s phenomenon was seen in 4% vs. 0%, with an OR of 15.29, which was significant (P < .001), but the confidence interval (CI) was wide (CI, 9.41-24.85).
Patients with SLE also were more than 20 times more likely to have a prior diagnosis of another connective tissue disease (OR, 21.68; P < .001) and 10 times more likely to have been diagnosed with RA (OR, 10.77; P < .001). Fibromyalgia (OR, 7.89; P < .001) and CFS (OR, 6.39; P < .001) also were more frequent among those who developed lupus than in those who did not.
“This suggests that, although there probably is a delay in diagnosis, patients are getting other diagnoses first,” Dr. Rees noted. “So, we would propose that, in the future, our risk-prediction model may be able to reduce that delay in conjunction with educational programs to say if you have a combination of these symptoms think about testing for [antinuclear antibodies] and/or referring to rheumatology.”
The team’s risk-prediction model now needs further external and economic validation, but the hope is that perhaps it could be incorporated into electronic systems used in primary care to flag potential lupus cases.
“The clinical message is to keep SLE in mind if someone is presenting multiple times with these kind of symptoms,” Dr. Rees said in an interview.
“Lupus is very rare,” she acknowledged, nothing that some primary care physicians may only see one or two cases of lupus in their career. So the risk-prediction model would aim to be an aid to help them consider SLE as a possibility in patients with several symptoms that, on their own, might not be suggestive of lupus.
The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
MANCHESTER, U.K. – In a general practice setting, people who developed systemic lupus erythematosus were more than twice as likely to consult a primary care physician in the 5-year run-up to their diagnosis, according to the results of a case-control study.
The median annual consultation rates were 9.2 times for systemic lupus erythematosus (SLE) patients versus 3.8 times for controls (P < .001).
Lupus patients also started to exhibit telltale symptoms during this time, providing an opportunity for making a diagnosis sooner through better recognition of these early symptoms.
The aim of the study was “to find out whether people with lupus came to see their GP [general practitioner] more frequently and what they were going to see their GP for,” Dr. Frances Rees of Nottingham (England) University Hospitals NHS Trust explained in a poster session on connective tissue disease at the British Society for Rheumatology annual conference.
“After that, we developed a risk-prediction model which was a multivariate analysis taking some of the variables that we decided in advance would be most significant,” she added. These variables included age, gender, arthritis or arthralgia, rash, fatigue, alopecia, serositis, sicca, Raynaud’s phenomenon, and the consultation rate.
“We found that the model performed well in both the model development data set and in the model validation data set,” Dr. Rees said.
The rationale for the study was that SLE can be difficult to diagnose early, and that delays of more than 7 years have been found between symptom onset and diagnosis. Perhaps, if SLE is diagnosed earlier, outcomes could be improved, Dr. Rees and her coauthors reasoned.
Using the UK Clinical Practice Research Datalink, an anonymized database of general practice records for approximately 12 million people, all incident cases of SLE occurring between 1999 and 2012 were identified and matched to four individuals without lupus who were seen at the same primary care practices.
A total of 1,739 patients with lupus and 6,952 controls were identified and separated into two cohorts: approximately two-thirds formed the development cohort and the remainder a validation cohort.
Individual odds ratios (OR) were calculated for age, gender, consultation rates, 27 clinical features, and five previous diagnoses of rheumatic disease in the 5 years preceding SLE diagnosis. Some of the clinical features considered were arthritis or arthralgia, rash, fatigue, alopecia, serositis, and sicca; the associated diseases were another connective tissue disease, rheumatoid arthritis (RA), fibromyalgia, chronic fatigue syndrome (CFS), and Epstein-Barr virus (EBV) infection.
Results showed that cases were more than five times more likely than controls to be female (84% vs. 51%; OR, 5.23; P < .001).
Early symptoms suggestive of SLE occurred more often in cases than in controls, with arthritis or arthralgia in 36% vs. 10% (OR, 4.77; P < .001), rash in 43% vs. 10% (OR, 6.84; P < .001), fatigue in 17% vs. 7% (OR, 2.76; P < .001), alopecia in 4% vs. 1% (OR, 4.77; P < .001), serositis in 4% vs. 1% (OR, 5.05; P < .001), and sicca in 6% vs 1% (OR, 4.97; P < .001). Raynaud’s phenomenon was seen in 4% vs. 0%, with an OR of 15.29, which was significant (P < .001), but the confidence interval (CI) was wide (CI, 9.41-24.85).
Patients with SLE also were more than 20 times more likely to have a prior diagnosis of another connective tissue disease (OR, 21.68; P < .001) and 10 times more likely to have been diagnosed with RA (OR, 10.77; P < .001). Fibromyalgia (OR, 7.89; P < .001) and CFS (OR, 6.39; P < .001) also were more frequent among those who developed lupus than in those who did not.
“This suggests that, although there probably is a delay in diagnosis, patients are getting other diagnoses first,” Dr. Rees noted. “So, we would propose that, in the future, our risk-prediction model may be able to reduce that delay in conjunction with educational programs to say if you have a combination of these symptoms think about testing for [antinuclear antibodies] and/or referring to rheumatology.”
The team’s risk-prediction model now needs further external and economic validation, but the hope is that perhaps it could be incorporated into electronic systems used in primary care to flag potential lupus cases.
“The clinical message is to keep SLE in mind if someone is presenting multiple times with these kind of symptoms,” Dr. Rees said in an interview.
“Lupus is very rare,” she acknowledged, nothing that some primary care physicians may only see one or two cases of lupus in their career. So the risk-prediction model would aim to be an aid to help them consider SLE as a possibility in patients with several symptoms that, on their own, might not be suggestive of lupus.
The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
AT RHEUMATOLOGY 2015
Key clinical point: A risk-prediction model may help primary care physicians diagnose lupus earlier.
Major finding: Lupus patients consulted more frequently than controls (median of 9.2 vs.<b/>3.8 times a year, P < .001).
Data source: 1,739 patients with newly diagnosed systemic lupus erythematosus and 6,952 practice-matched controls.
Disclosures: The work was supported by a research grant from Lupus UK. Dr. Rees had no conflicts of interest.
Anti-CarP antibodies linked to worse outcome in early arthritis
MANCHESTER, ENGLAND – Anti–carbamylated protein antibodies were associated with both increased disability and greater disease progression over time in patients with early inflammatory arthritis, data from a 20-year retrospective, observational analysis showed.
According to the research, presented at the British Society for Rheumatology annual conference, patients who were also positive for anti–citrullinated protein antibodies (ACPAs) fared worse long term than those who were ACPA negative.
The results showed that anti–carbamylated protein (anti-CarP) antibodies may provide additional prognostic information to current antibody tests in inflammatory arthritis (IA), but their measurement is not yet ready for general use, said Dr. Jennifer Humphreys of the Arthritis Research UK Centre for Epidemiology at the University of Manchester.
“We know that inflammatory arthritis patients who are rheumatoid factor [RF] or ACPA positive have an increased risk of persistent disease and a poor prognosis,” she said.
“In particular, ACPA[s] are associated with severe radiological progression [and] increased disability and mortality. However, not all patients who lack these antibodies do well,” Dr. Humphreys said.
Research at the University of Leiden (the Netherlands) has found that ACPA-negative patients have anti-CarP antibodies in their sera and that these autoantibodies precede the onset of symptoms and predict the development of rheumatoid arthritis (RA) in patients with arthralgia. These antibodies have also been associated with radiological damage, she said.
Because there were few data on the relationship to disease activity and long-term outcomes in the presence of these antibodies, Dr. Humphreys and her associates decided to look at this using data from the Norfolk Arthritis Register (NOAR), she said. The U.K. team worked in collaboration with the Dutch researchers who performed the anti-CarP tests on serum samples taken from 1,995 patients with early IA enrolled in NOAR from 1990 onward.
At baseline, 1,222 patients met American College of Rheumatology/European League Against Rheumatism 2010 criteria for RA. The mean age of onset was 55 years for both the total population with IA and for those with RA. About two-thirds of the participants were women, and their median symptom duration at enrollment was 33 weeks.
Long-term disability was assessed using the health assessment questionnaire (HAQ), and disease activity was evaluated using the disease activity in 28 joints (DAS28) score. The median baseline DAS28 score was 3.81 for the total cohort and 4.45 for patients with RA, and the median baseline HAQ scores were a respective 0.875 and 1.125.
When the team looked at patient baseline characteristics according to baseline anti-CarP status, they found that the 460 (23%) patients who were positive for these autoantibodies were more likely to have higher baseline DAS28 scores (4.23 vs. 3.73), HAQ scores (1.125 vs. 0.875), and C-reactive protein levels (14 mg/L vs. 7 mg/L) than the 1,543 patients who tested anti-CarP negative. Patients positive for anti-Carp antibodies were also less likely to be female (58% vs 68%) and were slightly older at onset (55 vs. 53 years).
Dr. Humphreys noted that there was a lot of overlap among the presence of anti-CarP, ACPA, and RF. Of the 460 who were anti-CarP positive, 124 were positive only for anti-CarP, 148 were also RF positive, 30 were also ACPA positive, and 158 had all three antibodies.
“Patients who were anti-CarP antibody positive had higher HAQ scores at baseline, and this higher level of disability persisted throughout follow-up, and that association remained significant in the multivariate model,” Dr. Humphreys said.
“When we stratified by ACPA status, there was a statistically significant association in the ACPA-negative subgroup but not in the ACPA-positive subgroup,” she added. However, she noted that the beta coefficients for the association between anti-CarP antibodies and HAQ scores over time were similar (0.12 for the total cohort, 0.14 for the ACPA-negative patients, and 0.09 for the ACPA-positive patients) and that confidence intervals were wide.
Similar findings were seen for the association between anti-CarP antibodies and the DAS28 over time, with respective beta coefficients of 0.23, 01.18, and 0.25 for the total cohort, the ACPA-negative subgroup, and the ACPA-positive subgroup. Again, confidence intervals were wide.
The researchers looked at the additive effect of having anti-CarP and ACPA, and found that while there is no association between RF positivity and long-term disability, there were independent associations with both ACPA positivity and anti-CarP antibody positivity, with respective beta coefficients of –0.05, 0.12, and 0.14.
“And we see the exact same pattern with disease activity over time,” Dr. Humphreys reported.
Thus, measuring anti-CarP antibodies “may be a useful test to do in addition to both RF and ACPA,” she suggested, adding that measuring these antibodies “may be particularly valuable in patients who lack other antibodies.”
NOAR is funded by Arthritis Research UK. Dr. Humphreys had no relevant financial disclosures.
MANCHESTER, ENGLAND – Anti–carbamylated protein antibodies were associated with both increased disability and greater disease progression over time in patients with early inflammatory arthritis, data from a 20-year retrospective, observational analysis showed.
According to the research, presented at the British Society for Rheumatology annual conference, patients who were also positive for anti–citrullinated protein antibodies (ACPAs) fared worse long term than those who were ACPA negative.
The results showed that anti–carbamylated protein (anti-CarP) antibodies may provide additional prognostic information to current antibody tests in inflammatory arthritis (IA), but their measurement is not yet ready for general use, said Dr. Jennifer Humphreys of the Arthritis Research UK Centre for Epidemiology at the University of Manchester.
“We know that inflammatory arthritis patients who are rheumatoid factor [RF] or ACPA positive have an increased risk of persistent disease and a poor prognosis,” she said.
“In particular, ACPA[s] are associated with severe radiological progression [and] increased disability and mortality. However, not all patients who lack these antibodies do well,” Dr. Humphreys said.
Research at the University of Leiden (the Netherlands) has found that ACPA-negative patients have anti-CarP antibodies in their sera and that these autoantibodies precede the onset of symptoms and predict the development of rheumatoid arthritis (RA) in patients with arthralgia. These antibodies have also been associated with radiological damage, she said.
Because there were few data on the relationship to disease activity and long-term outcomes in the presence of these antibodies, Dr. Humphreys and her associates decided to look at this using data from the Norfolk Arthritis Register (NOAR), she said. The U.K. team worked in collaboration with the Dutch researchers who performed the anti-CarP tests on serum samples taken from 1,995 patients with early IA enrolled in NOAR from 1990 onward.
At baseline, 1,222 patients met American College of Rheumatology/European League Against Rheumatism 2010 criteria for RA. The mean age of onset was 55 years for both the total population with IA and for those with RA. About two-thirds of the participants were women, and their median symptom duration at enrollment was 33 weeks.
Long-term disability was assessed using the health assessment questionnaire (HAQ), and disease activity was evaluated using the disease activity in 28 joints (DAS28) score. The median baseline DAS28 score was 3.81 for the total cohort and 4.45 for patients with RA, and the median baseline HAQ scores were a respective 0.875 and 1.125.
When the team looked at patient baseline characteristics according to baseline anti-CarP status, they found that the 460 (23%) patients who were positive for these autoantibodies were more likely to have higher baseline DAS28 scores (4.23 vs. 3.73), HAQ scores (1.125 vs. 0.875), and C-reactive protein levels (14 mg/L vs. 7 mg/L) than the 1,543 patients who tested anti-CarP negative. Patients positive for anti-Carp antibodies were also less likely to be female (58% vs 68%) and were slightly older at onset (55 vs. 53 years).
Dr. Humphreys noted that there was a lot of overlap among the presence of anti-CarP, ACPA, and RF. Of the 460 who were anti-CarP positive, 124 were positive only for anti-CarP, 148 were also RF positive, 30 were also ACPA positive, and 158 had all three antibodies.
“Patients who were anti-CarP antibody positive had higher HAQ scores at baseline, and this higher level of disability persisted throughout follow-up, and that association remained significant in the multivariate model,” Dr. Humphreys said.
“When we stratified by ACPA status, there was a statistically significant association in the ACPA-negative subgroup but not in the ACPA-positive subgroup,” she added. However, she noted that the beta coefficients for the association between anti-CarP antibodies and HAQ scores over time were similar (0.12 for the total cohort, 0.14 for the ACPA-negative patients, and 0.09 for the ACPA-positive patients) and that confidence intervals were wide.
Similar findings were seen for the association between anti-CarP antibodies and the DAS28 over time, with respective beta coefficients of 0.23, 01.18, and 0.25 for the total cohort, the ACPA-negative subgroup, and the ACPA-positive subgroup. Again, confidence intervals were wide.
The researchers looked at the additive effect of having anti-CarP and ACPA, and found that while there is no association between RF positivity and long-term disability, there were independent associations with both ACPA positivity and anti-CarP antibody positivity, with respective beta coefficients of –0.05, 0.12, and 0.14.
“And we see the exact same pattern with disease activity over time,” Dr. Humphreys reported.
Thus, measuring anti-CarP antibodies “may be a useful test to do in addition to both RF and ACPA,” she suggested, adding that measuring these antibodies “may be particularly valuable in patients who lack other antibodies.”
NOAR is funded by Arthritis Research UK. Dr. Humphreys had no relevant financial disclosures.
MANCHESTER, ENGLAND – Anti–carbamylated protein antibodies were associated with both increased disability and greater disease progression over time in patients with early inflammatory arthritis, data from a 20-year retrospective, observational analysis showed.
According to the research, presented at the British Society for Rheumatology annual conference, patients who were also positive for anti–citrullinated protein antibodies (ACPAs) fared worse long term than those who were ACPA negative.
The results showed that anti–carbamylated protein (anti-CarP) antibodies may provide additional prognostic information to current antibody tests in inflammatory arthritis (IA), but their measurement is not yet ready for general use, said Dr. Jennifer Humphreys of the Arthritis Research UK Centre for Epidemiology at the University of Manchester.
“We know that inflammatory arthritis patients who are rheumatoid factor [RF] or ACPA positive have an increased risk of persistent disease and a poor prognosis,” she said.
“In particular, ACPA[s] are associated with severe radiological progression [and] increased disability and mortality. However, not all patients who lack these antibodies do well,” Dr. Humphreys said.
Research at the University of Leiden (the Netherlands) has found that ACPA-negative patients have anti-CarP antibodies in their sera and that these autoantibodies precede the onset of symptoms and predict the development of rheumatoid arthritis (RA) in patients with arthralgia. These antibodies have also been associated with radiological damage, she said.
Because there were few data on the relationship to disease activity and long-term outcomes in the presence of these antibodies, Dr. Humphreys and her associates decided to look at this using data from the Norfolk Arthritis Register (NOAR), she said. The U.K. team worked in collaboration with the Dutch researchers who performed the anti-CarP tests on serum samples taken from 1,995 patients with early IA enrolled in NOAR from 1990 onward.
At baseline, 1,222 patients met American College of Rheumatology/European League Against Rheumatism 2010 criteria for RA. The mean age of onset was 55 years for both the total population with IA and for those with RA. About two-thirds of the participants were women, and their median symptom duration at enrollment was 33 weeks.
Long-term disability was assessed using the health assessment questionnaire (HAQ), and disease activity was evaluated using the disease activity in 28 joints (DAS28) score. The median baseline DAS28 score was 3.81 for the total cohort and 4.45 for patients with RA, and the median baseline HAQ scores were a respective 0.875 and 1.125.
When the team looked at patient baseline characteristics according to baseline anti-CarP status, they found that the 460 (23%) patients who were positive for these autoantibodies were more likely to have higher baseline DAS28 scores (4.23 vs. 3.73), HAQ scores (1.125 vs. 0.875), and C-reactive protein levels (14 mg/L vs. 7 mg/L) than the 1,543 patients who tested anti-CarP negative. Patients positive for anti-Carp antibodies were also less likely to be female (58% vs 68%) and were slightly older at onset (55 vs. 53 years).
Dr. Humphreys noted that there was a lot of overlap among the presence of anti-CarP, ACPA, and RF. Of the 460 who were anti-CarP positive, 124 were positive only for anti-CarP, 148 were also RF positive, 30 were also ACPA positive, and 158 had all three antibodies.
“Patients who were anti-CarP antibody positive had higher HAQ scores at baseline, and this higher level of disability persisted throughout follow-up, and that association remained significant in the multivariate model,” Dr. Humphreys said.
“When we stratified by ACPA status, there was a statistically significant association in the ACPA-negative subgroup but not in the ACPA-positive subgroup,” she added. However, she noted that the beta coefficients for the association between anti-CarP antibodies and HAQ scores over time were similar (0.12 for the total cohort, 0.14 for the ACPA-negative patients, and 0.09 for the ACPA-positive patients) and that confidence intervals were wide.
Similar findings were seen for the association between anti-CarP antibodies and the DAS28 over time, with respective beta coefficients of 0.23, 01.18, and 0.25 for the total cohort, the ACPA-negative subgroup, and the ACPA-positive subgroup. Again, confidence intervals were wide.
The researchers looked at the additive effect of having anti-CarP and ACPA, and found that while there is no association between RF positivity and long-term disability, there were independent associations with both ACPA positivity and anti-CarP antibody positivity, with respective beta coefficients of –0.05, 0.12, and 0.14.
“And we see the exact same pattern with disease activity over time,” Dr. Humphreys reported.
Thus, measuring anti-CarP antibodies “may be a useful test to do in addition to both RF and ACPA,” she suggested, adding that measuring these antibodies “may be particularly valuable in patients who lack other antibodies.”
NOAR is funded by Arthritis Research UK. Dr. Humphreys had no relevant financial disclosures.
AT RHEUMATOLOGY 2015
Key clinical point: Anti-CarP antibodies may provide additional prognostic information to current antibody tests in early inflammatory arthritis.
Major finding: Anti-CarP antibodies were associated with both increased disability and higher disease progression over time.
Data source: A 20-year retrospective, observational study of 1,995 patients who were a median of 55 years old at diagnosis of early IA and who were enrolled in the Norfolk Arthritis Register.
Disclosures: NOAR is funded by Arthritis Research UK. Dr. Humphreys had no relevant financial disclosures.
BSR: Subclinical synovitis common in RA remission
MANCHESTER, U.K. – Subclinical synovitis on ultrasound was apparent in almost half of patients with early rheumatoid arthritis deemed to be in clinical remission and in two-thirds of those with low-disease activity in an observational study.
Power Doppler ultrasound changes were seen in 43% of patients in remission and in 65% of those with LDA. Grey-scale ultrasound changes also were found in 78% of the cohort studied, suggesting synovial hypertrophy. The changes correlated with disease activity. Alterations in synovial T-cell populations also were observed.
Attaining and maintaining clinical remission is a long-established primary treatment goal in rheumatoid arthritis (RA), but current criteria used to determine if this is being achieved are largely subjective, noted Dr. Hanna Gul, who presented the research at the for Rheumatology annual conference.
“Over the years there have been many attempts to define clinical remission criteria using disease activity indices,” said Dr. Gul, a clinical research fellow and specialist registrar at the Leeds Institute of Rheumatic and Musculoskeletal Medicine at the University of Leeds (England).
However, current criteria used in clinical practice and in clinical trials – most commonly the DAS28 – tend to be based on composite scores of disease, can vary in their interpretation, and do not include objective imaging or immunological assessments, she said.
While patients do seem to be increasingly achieving remission, this is not always associated with good outcomes as structural and functional progression still occurs, Dr. Gul said.
“This raises the question regarding the validity of clinical criteria,” she suggested. “Subsequently, the concept of ‘true remission’ has arisen, which is described as the absence of intra- and extra-articular inflammation, immunologic activity, and structural and functional progression.”
To look at the true remission state in more depth using disease activity criteria, imaging, and immunologic markers, Dr. Gul and her colleagues conducted a retrospective, cross-sectional study of 632 patients with early inflammatory arthritis who were considered to be in clinical remission.
Clinical remission was defined as a DAS28-CRP of less than 3.2. A total of 512 patients had a score of less than 2.6, considered as being in ‘strict’ remission, and the remaining 120 had a score of 2.6 to 3.2, having low disease activity (LDA).
The mean age of patients in the strict remission group was 58 years, and in the LDA group it was 57 years. Most of study subjects were female (70% vs. 67%), had anti-citrullinated antibodies (70% and 68%), and were rheumatoid factor positive (59% and 67%).
The median duration of disease was 6.7 months longer in the patients achieving clinical remission, at 12.9 months versus 6.2 months in the LDA group, and patients in the strict remission group had been in remission for an average of 7.6 months (in the LDA group no patient was in strict remission by definition).
The majority (75% in both groups) had been or was being treated with conventional disease-modifying drugs (csDMARDs) either alone (40%-45%) or in combination (30%-34%). About 12.5% of patients in the remission group, and 7.5% of those in the LDA group were being treated with biologics, mostly in combination with a csDMARD.
“In terms of clinical characteristics, the levels of CRP and swollen and tender joints were generally low,” Dr. Gul reported. “There was also overlap between remission and low disease activity states.”
Various patient-reported outcomes were assessed and showed that the levels of disability and functional impairment were generally low, but that there were differences between the remission and LDA states, with the best outcomes reported in patients with a CRP, tender and swollen joint count of zero.
Flow cytometry was used to analyze T-cell populations in 51 patients compared to 120 healthy controls. Results showed that there was a 9% decrease from the normal range in the percentage of naive CD4+ T-cells, a 26% increase in inflammation-related cells, and a 50% decrease in regulatory T-cells.
“This is the most extensive examination of T-cell abnormalities in RA and confirms T-regulatory abnormalities in patients with clinical remission,” Dr. Gul observed.
“Further research is required for understanding the implications, specifically with regard to T-cell abnormalities as predictors of flare,” she said.
The research was supported by the U.K. National Institute for Health Research. Dr. Gul had no disclosures.
MANCHESTER, U.K. – Subclinical synovitis on ultrasound was apparent in almost half of patients with early rheumatoid arthritis deemed to be in clinical remission and in two-thirds of those with low-disease activity in an observational study.
Power Doppler ultrasound changes were seen in 43% of patients in remission and in 65% of those with LDA. Grey-scale ultrasound changes also were found in 78% of the cohort studied, suggesting synovial hypertrophy. The changes correlated with disease activity. Alterations in synovial T-cell populations also were observed.
Attaining and maintaining clinical remission is a long-established primary treatment goal in rheumatoid arthritis (RA), but current criteria used to determine if this is being achieved are largely subjective, noted Dr. Hanna Gul, who presented the research at the for Rheumatology annual conference.
“Over the years there have been many attempts to define clinical remission criteria using disease activity indices,” said Dr. Gul, a clinical research fellow and specialist registrar at the Leeds Institute of Rheumatic and Musculoskeletal Medicine at the University of Leeds (England).
However, current criteria used in clinical practice and in clinical trials – most commonly the DAS28 – tend to be based on composite scores of disease, can vary in their interpretation, and do not include objective imaging or immunological assessments, she said.
While patients do seem to be increasingly achieving remission, this is not always associated with good outcomes as structural and functional progression still occurs, Dr. Gul said.
“This raises the question regarding the validity of clinical criteria,” she suggested. “Subsequently, the concept of ‘true remission’ has arisen, which is described as the absence of intra- and extra-articular inflammation, immunologic activity, and structural and functional progression.”
To look at the true remission state in more depth using disease activity criteria, imaging, and immunologic markers, Dr. Gul and her colleagues conducted a retrospective, cross-sectional study of 632 patients with early inflammatory arthritis who were considered to be in clinical remission.
Clinical remission was defined as a DAS28-CRP of less than 3.2. A total of 512 patients had a score of less than 2.6, considered as being in ‘strict’ remission, and the remaining 120 had a score of 2.6 to 3.2, having low disease activity (LDA).
The mean age of patients in the strict remission group was 58 years, and in the LDA group it was 57 years. Most of study subjects were female (70% vs. 67%), had anti-citrullinated antibodies (70% and 68%), and were rheumatoid factor positive (59% and 67%).
The median duration of disease was 6.7 months longer in the patients achieving clinical remission, at 12.9 months versus 6.2 months in the LDA group, and patients in the strict remission group had been in remission for an average of 7.6 months (in the LDA group no patient was in strict remission by definition).
The majority (75% in both groups) had been or was being treated with conventional disease-modifying drugs (csDMARDs) either alone (40%-45%) or in combination (30%-34%). About 12.5% of patients in the remission group, and 7.5% of those in the LDA group were being treated with biologics, mostly in combination with a csDMARD.
“In terms of clinical characteristics, the levels of CRP and swollen and tender joints were generally low,” Dr. Gul reported. “There was also overlap between remission and low disease activity states.”
Various patient-reported outcomes were assessed and showed that the levels of disability and functional impairment were generally low, but that there were differences between the remission and LDA states, with the best outcomes reported in patients with a CRP, tender and swollen joint count of zero.
Flow cytometry was used to analyze T-cell populations in 51 patients compared to 120 healthy controls. Results showed that there was a 9% decrease from the normal range in the percentage of naive CD4+ T-cells, a 26% increase in inflammation-related cells, and a 50% decrease in regulatory T-cells.
“This is the most extensive examination of T-cell abnormalities in RA and confirms T-regulatory abnormalities in patients with clinical remission,” Dr. Gul observed.
“Further research is required for understanding the implications, specifically with regard to T-cell abnormalities as predictors of flare,” she said.
The research was supported by the U.K. National Institute for Health Research. Dr. Gul had no disclosures.
MANCHESTER, U.K. – Subclinical synovitis on ultrasound was apparent in almost half of patients with early rheumatoid arthritis deemed to be in clinical remission and in two-thirds of those with low-disease activity in an observational study.
Power Doppler ultrasound changes were seen in 43% of patients in remission and in 65% of those with LDA. Grey-scale ultrasound changes also were found in 78% of the cohort studied, suggesting synovial hypertrophy. The changes correlated with disease activity. Alterations in synovial T-cell populations also were observed.
Attaining and maintaining clinical remission is a long-established primary treatment goal in rheumatoid arthritis (RA), but current criteria used to determine if this is being achieved are largely subjective, noted Dr. Hanna Gul, who presented the research at the for Rheumatology annual conference.
“Over the years there have been many attempts to define clinical remission criteria using disease activity indices,” said Dr. Gul, a clinical research fellow and specialist registrar at the Leeds Institute of Rheumatic and Musculoskeletal Medicine at the University of Leeds (England).
However, current criteria used in clinical practice and in clinical trials – most commonly the DAS28 – tend to be based on composite scores of disease, can vary in their interpretation, and do not include objective imaging or immunological assessments, she said.
While patients do seem to be increasingly achieving remission, this is not always associated with good outcomes as structural and functional progression still occurs, Dr. Gul said.
“This raises the question regarding the validity of clinical criteria,” she suggested. “Subsequently, the concept of ‘true remission’ has arisen, which is described as the absence of intra- and extra-articular inflammation, immunologic activity, and structural and functional progression.”
To look at the true remission state in more depth using disease activity criteria, imaging, and immunologic markers, Dr. Gul and her colleagues conducted a retrospective, cross-sectional study of 632 patients with early inflammatory arthritis who were considered to be in clinical remission.
Clinical remission was defined as a DAS28-CRP of less than 3.2. A total of 512 patients had a score of less than 2.6, considered as being in ‘strict’ remission, and the remaining 120 had a score of 2.6 to 3.2, having low disease activity (LDA).
The mean age of patients in the strict remission group was 58 years, and in the LDA group it was 57 years. Most of study subjects were female (70% vs. 67%), had anti-citrullinated antibodies (70% and 68%), and were rheumatoid factor positive (59% and 67%).
The median duration of disease was 6.7 months longer in the patients achieving clinical remission, at 12.9 months versus 6.2 months in the LDA group, and patients in the strict remission group had been in remission for an average of 7.6 months (in the LDA group no patient was in strict remission by definition).
The majority (75% in both groups) had been or was being treated with conventional disease-modifying drugs (csDMARDs) either alone (40%-45%) or in combination (30%-34%). About 12.5% of patients in the remission group, and 7.5% of those in the LDA group were being treated with biologics, mostly in combination with a csDMARD.
“In terms of clinical characteristics, the levels of CRP and swollen and tender joints were generally low,” Dr. Gul reported. “There was also overlap between remission and low disease activity states.”
Various patient-reported outcomes were assessed and showed that the levels of disability and functional impairment were generally low, but that there were differences between the remission and LDA states, with the best outcomes reported in patients with a CRP, tender and swollen joint count of zero.
Flow cytometry was used to analyze T-cell populations in 51 patients compared to 120 healthy controls. Results showed that there was a 9% decrease from the normal range in the percentage of naive CD4+ T-cells, a 26% increase in inflammation-related cells, and a 50% decrease in regulatory T-cells.
“This is the most extensive examination of T-cell abnormalities in RA and confirms T-regulatory abnormalities in patients with clinical remission,” Dr. Gul observed.
“Further research is required for understanding the implications, specifically with regard to T-cell abnormalities as predictors of flare,” she said.
The research was supported by the U.K. National Institute for Health Research. Dr. Gul had no disclosures.
AT RHEUMATOLOGY 2015
Key clinical point: Patients with RA in clinical remission defined via clinical criteria alone may still have subclinical inflammation.
Major finding: Power Doppler ultrasound changes were seen in 43% of patients in remission and in 65% of those with LDA.
Data source: Retrospective, cross-sectional, observational study of 632 patients with early inflammatory arthritis in clinical remission (DAS28-CRP < 3.2).
Disclosures: The research was supported by the U.K. National Institute for Health Research. Dr. Gul had no disclosures.
Ultrasound sign could help diagnose giant cell arteritis
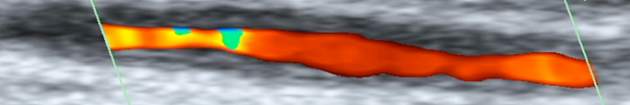
MANCHESTER, U.K. – An early halo sign on ultrasound is both diagnostic and prognostic according to the findings of a substudy of the ongoing TABUL trial.
In newly diagnosed giant cell arteritis (GCA), halo on ultrasound was seen in 46% of cases, and its presence correlated significantly with both ischemic symptoms and abnormal physical examination of the temporal arteries.
The finding “supports the early use of the halo as a diagnostic and potentially prognostic marker,” Dr. Raashid Luqmani, professor of rheumatology at the University of Oxford, England, said at the British Society for Rheumatology annual conference.
The halo sign is an abnormal shadow seen around the temporal arteries on ultrasound, Dr. Luqmani explained.
“The value of halo size change over time in individual patients is being investigated as a marker of response to treatment,” he added, noting that the size of the halo decreased rapidly with longer duration of early, high-dose steroid treatment.
The main TABUL (Temporal Artery Biopsy Versus Ultrasound for the Diagnosis of Giant Cell Arteritis) trial is looking at the overall diagnostic performance, accuracy, and cost-effectiveness of ultrasound versus biopsy in patients with newly suspected GCA. A total of 430 patients have been recruited and have undergone a single ultrasound scan of the temporal and axillary arteries followed by temporal artery biopsy within 7 days of commencing steroids.
Clinicians are blinded to the results of the ultrasound scan until 2 weeks after a treatment decision has been made and they intend to start rapid steroid withdrawal. Following this, patients are seen at a 6-month follow-up visit.
The aim of the substudy reported by Dr. Luqmani was to describe the features of the early halo sign in response to steroid therapy and whether it correlated to ischemic symptoms.
A cross-sectional analysis was performed on data from 312 patients to look at the extent of arterial involvement, the maximum thickness of the halo, the duration of steroid treatment when the ultrasound was performed, and what ischemic symptoms were present.
The mean age of the 220 women studied was 72.5 years, and that of the 92 men was 71.2 years.
Most patients had one (30.6%), two (22.2%), or three (13.9%) temporal arterial segments involved, with the remaining third having four or more. Bilateral halos were seen in 30% of patients, temporal or axillary artery halos in 13.5%, and isolated axillary halos in 2.6%.
The fact that 13.5% had both temporal and axillary artery involvement and 2.6% had only isolated axillary halos suggests a role for scanning both the axillary and temporal arteries, Dr. Luqmani suggested.
The likelihood of finding a halo diminished with the duration of steroid therapy, he reported. “Patients who received no steroid therapy had a much bigger halo and it got progressively smaller and significantly less by day 4,” he observed.
“Although there are still some patients who still have a halo at days 5 and 6 of steroid treatment, the likelihood of finding that halo is much, much less,” he added.
Looking at the presence of halo in relation to ischemic symptoms, there did appear to be an association but it was only significant (P < .004) for jaw claudication.
“If you have a patient with newly suspected GCA, you are likely to see a significant halo, but you need to be quick, you need to be seeing that halo within 4 days of starting steroids or evaluating patients who have not had any steroid treatment,” Dr. Luqmani said.
The TABUL study is funded by the U.K. Health Technology Assessment, a program of the National Institute for Health Research,and sponsored by the University of Oxford. Dr. Luqmani had received consulting fees from GlaxoSmithKline, Novartis, Roche, and Pfizer.
MANCHESTER, U.K. – An early halo sign on ultrasound is both diagnostic and prognostic according to the findings of a substudy of the ongoing TABUL trial.
In newly diagnosed giant cell arteritis (GCA), halo on ultrasound was seen in 46% of cases, and its presence correlated significantly with both ischemic symptoms and abnormal physical examination of the temporal arteries.
The finding “supports the early use of the halo as a diagnostic and potentially prognostic marker,” Dr. Raashid Luqmani, professor of rheumatology at the University of Oxford, England, said at the British Society for Rheumatology annual conference.
The halo sign is an abnormal shadow seen around the temporal arteries on ultrasound, Dr. Luqmani explained.
“The value of halo size change over time in individual patients is being investigated as a marker of response to treatment,” he added, noting that the size of the halo decreased rapidly with longer duration of early, high-dose steroid treatment.
The main TABUL (Temporal Artery Biopsy Versus Ultrasound for the Diagnosis of Giant Cell Arteritis) trial is looking at the overall diagnostic performance, accuracy, and cost-effectiveness of ultrasound versus biopsy in patients with newly suspected GCA. A total of 430 patients have been recruited and have undergone a single ultrasound scan of the temporal and axillary arteries followed by temporal artery biopsy within 7 days of commencing steroids.
Clinicians are blinded to the results of the ultrasound scan until 2 weeks after a treatment decision has been made and they intend to start rapid steroid withdrawal. Following this, patients are seen at a 6-month follow-up visit.
The aim of the substudy reported by Dr. Luqmani was to describe the features of the early halo sign in response to steroid therapy and whether it correlated to ischemic symptoms.
A cross-sectional analysis was performed on data from 312 patients to look at the extent of arterial involvement, the maximum thickness of the halo, the duration of steroid treatment when the ultrasound was performed, and what ischemic symptoms were present.
The mean age of the 220 women studied was 72.5 years, and that of the 92 men was 71.2 years.
Most patients had one (30.6%), two (22.2%), or three (13.9%) temporal arterial segments involved, with the remaining third having four or more. Bilateral halos were seen in 30% of patients, temporal or axillary artery halos in 13.5%, and isolated axillary halos in 2.6%.
The fact that 13.5% had both temporal and axillary artery involvement and 2.6% had only isolated axillary halos suggests a role for scanning both the axillary and temporal arteries, Dr. Luqmani suggested.
The likelihood of finding a halo diminished with the duration of steroid therapy, he reported. “Patients who received no steroid therapy had a much bigger halo and it got progressively smaller and significantly less by day 4,” he observed.
“Although there are still some patients who still have a halo at days 5 and 6 of steroid treatment, the likelihood of finding that halo is much, much less,” he added.
Looking at the presence of halo in relation to ischemic symptoms, there did appear to be an association but it was only significant (P < .004) for jaw claudication.
“If you have a patient with newly suspected GCA, you are likely to see a significant halo, but you need to be quick, you need to be seeing that halo within 4 days of starting steroids or evaluating patients who have not had any steroid treatment,” Dr. Luqmani said.
The TABUL study is funded by the U.K. Health Technology Assessment, a program of the National Institute for Health Research,and sponsored by the University of Oxford. Dr. Luqmani had received consulting fees from GlaxoSmithKline, Novartis, Roche, and Pfizer.
MANCHESTER, U.K. – An early halo sign on ultrasound is both diagnostic and prognostic according to the findings of a substudy of the ongoing TABUL trial.
In newly diagnosed giant cell arteritis (GCA), halo on ultrasound was seen in 46% of cases, and its presence correlated significantly with both ischemic symptoms and abnormal physical examination of the temporal arteries.
The finding “supports the early use of the halo as a diagnostic and potentially prognostic marker,” Dr. Raashid Luqmani, professor of rheumatology at the University of Oxford, England, said at the British Society for Rheumatology annual conference.
The halo sign is an abnormal shadow seen around the temporal arteries on ultrasound, Dr. Luqmani explained.
“The value of halo size change over time in individual patients is being investigated as a marker of response to treatment,” he added, noting that the size of the halo decreased rapidly with longer duration of early, high-dose steroid treatment.
The main TABUL (Temporal Artery Biopsy Versus Ultrasound for the Diagnosis of Giant Cell Arteritis) trial is looking at the overall diagnostic performance, accuracy, and cost-effectiveness of ultrasound versus biopsy in patients with newly suspected GCA. A total of 430 patients have been recruited and have undergone a single ultrasound scan of the temporal and axillary arteries followed by temporal artery biopsy within 7 days of commencing steroids.
Clinicians are blinded to the results of the ultrasound scan until 2 weeks after a treatment decision has been made and they intend to start rapid steroid withdrawal. Following this, patients are seen at a 6-month follow-up visit.
The aim of the substudy reported by Dr. Luqmani was to describe the features of the early halo sign in response to steroid therapy and whether it correlated to ischemic symptoms.
A cross-sectional analysis was performed on data from 312 patients to look at the extent of arterial involvement, the maximum thickness of the halo, the duration of steroid treatment when the ultrasound was performed, and what ischemic symptoms were present.
The mean age of the 220 women studied was 72.5 years, and that of the 92 men was 71.2 years.
Most patients had one (30.6%), two (22.2%), or three (13.9%) temporal arterial segments involved, with the remaining third having four or more. Bilateral halos were seen in 30% of patients, temporal or axillary artery halos in 13.5%, and isolated axillary halos in 2.6%.
The fact that 13.5% had both temporal and axillary artery involvement and 2.6% had only isolated axillary halos suggests a role for scanning both the axillary and temporal arteries, Dr. Luqmani suggested.
The likelihood of finding a halo diminished with the duration of steroid therapy, he reported. “Patients who received no steroid therapy had a much bigger halo and it got progressively smaller and significantly less by day 4,” he observed.
“Although there are still some patients who still have a halo at days 5 and 6 of steroid treatment, the likelihood of finding that halo is much, much less,” he added.
Looking at the presence of halo in relation to ischemic symptoms, there did appear to be an association but it was only significant (P < .004) for jaw claudication.
“If you have a patient with newly suspected GCA, you are likely to see a significant halo, but you need to be quick, you need to be seeing that halo within 4 days of starting steroids or evaluating patients who have not had any steroid treatment,” Dr. Luqmani said.
The TABUL study is funded by the U.K. Health Technology Assessment, a program of the National Institute for Health Research,and sponsored by the University of Oxford. Dr. Luqmani had received consulting fees from GlaxoSmithKline, Novartis, Roche, and Pfizer.
AT RHEUMATOLOGY 2015
Key clinical point: The halo sign on ultrasound is a diagnostic and potentially prognostic marker, but its use is limited by the effect of early high-dose steroids from about day 4 onward.
Major finding: Halo on ultrasound was seen in 46% of cases; its presence correlated with both ischemic symptoms and abnormal physical examination of the temporal arteries.
Data source: The TABUL trial, involving 312 patients suspected of giant cell arteritis.
Disclosures: TABUL is funded by the U.K. Health Technology Assessment, a program of the National Institute for Health Research, and sponsored by the University of Oxford. Dr. Luqmani had received consulting fees from GlaxoSmithKline, Novartis, Roche, and Pfizer.
Synovial pathotype could help guide anti-TNF therapy
MANCHESTER, U.K. – Analysis of synovial tissue taken by ultrasound-guided biopsy could help stratify patients with rheumatoid arthritis and decide if treatment with a tumor necrosis factor inhibitor is appropriate, according to research presented at the British Society for Rheumatology annual conference.
In a small yet intriguing study, Dr. Maria Di Cicco of Queen Mary University of London and her colleagues found that patients who had a lymphoid synovial pathotype were more likely to respond to treatment with the anti-TNF inhibitor certolizumab pegol than if they had other synovial pathotypes.
“Rheumatoid arthritis is a clinically heterogeneous disease to the extent that we should think of it as a syndrome rather than a disease,” Dr. Di Cicco said. “This heterogeneity is expressed as a variable outcome and response to treatment,” she added.
Although biologic drugs have dramatically changed how patients are treated, 30%-40% of patients do not respond to treatment and the way biologic treatment is selected for RA is more down to trial and error than personalized medicine, Dr. Di Cicco observed. This is concerning, as the number of biologic medicines available is exponentially increasing and ways of matching the right drug to the right patient need to be found.
The aim of the current study was to see if different synovial subtypes could influence patients’ first response to treatment with anti-TNF therapy. Recent research looking at synovial tissue suggests that there are three clear synovial subtypes: myeloid, Pauci-immune, and lymphoid.
The myeloid and Pauci-immune pathotypes are characterized by diffuse cellular infiltration distributed evenly through the synovium. The lymphoid synovial pathotype, on the other hand, is characterized by the presence of large lymphocytic aggregates that are known as ectopic lymphoid structures (ELS). Dr. Di Cicco noted that ELS had been linked to B-cell proliferation within the synovium and to promoting in situ autoantibody production and class switching.
For the study, 28 patients with RA on stable doses of methotrexate who qualified for anti-TNF treatment according to U.K. National Institute for Health and Care Excellence guidance were recruited at a single center. All patients underwent ultrasound-guided biopsy of an active joint, which tended to be a small joint such as the wrist or metacarpophalangeal, before they were treated with certolizumab pegol. Twenty patients had a repeat synovial biopsy when the clinical efficacy of treatment was assessed at 12 weeks.
A minimum of six samples were taken from each biopsied joint, and this material underwent immunohistochemical analysis for the presence of T cells expressing CD3, B cells expressing CD20, macrophages expressing CD68, and plasma cells expressing CD138.
Samples were then classified as being the lymphoid pathotype if they contained mainly B and T cells and formed large lymphocytic aggregates or ELS. Myeloid subtype was defined as the presence of sublining macrophages and Pauci-immune if none of these features was present.
Thirteen (46.4%) patients were found to the have the Pauci-immune pathotype, with the lymphoid pathotype being the next most common (39.3% of patients), and four (14.3%) had the myeloid pathotype.
Apart from no prior oral steroid use in patients with the lymphoid pathotype versus 75% of patients with the myeloid pathotype and 38.5% of patients with the Pauci-immune pathotype, there were no significant differences among the groups in terms of demographics, clinical features, inflammatory markers, antibody or erosive status, or other treatments.
“After 12 weeks of therapy, the myeloid and the lymphoid groups showed a significantly higher fall in [Disease Activity Score] 28 compared to the Pauci-immune group,” Dr. Di Cicco reported.
“We also assessed achievement of EULAR response, and 71% of patients did respond. Half of them were good responders and half of them were moderate responders,” she added.
EULAR response by synovial pathotype was 100% for patients with the lymphoid pathotype, 75% for those with the myeloid pathotype, and 46% for those with the Pauci-immune pathotype.
Greater decreases in synovial thickening and power Doppler ultrasound also were seen in the myeloid and lymphoid pathotypes, compared with the Pauci-immune pathotype, which appeared more resistant to change in response to the anti-TNF therapy.
In the 20 patients who had a repeat biopsy, 9 had ELS at baseline. After treatment, three patients were ELS negative, four remained ELS positive, and two were ungraded.
“Our work shows that the presence of synovial ectopic lymphoid structures defining a lymphoid pathotype is a predictor of clinical response to anti-TNF-alpha,” Dr. Di Cicco said. Although further research and confirmation is needed, “we think that synovial tissue analysis could be considered as a promising tool to stratify RA patients and guide therapeutic decision,” she said.
Dr. Di Cicco had no disclosures.
MANCHESTER, U.K. – Analysis of synovial tissue taken by ultrasound-guided biopsy could help stratify patients with rheumatoid arthritis and decide if treatment with a tumor necrosis factor inhibitor is appropriate, according to research presented at the British Society for Rheumatology annual conference.
In a small yet intriguing study, Dr. Maria Di Cicco of Queen Mary University of London and her colleagues found that patients who had a lymphoid synovial pathotype were more likely to respond to treatment with the anti-TNF inhibitor certolizumab pegol than if they had other synovial pathotypes.
“Rheumatoid arthritis is a clinically heterogeneous disease to the extent that we should think of it as a syndrome rather than a disease,” Dr. Di Cicco said. “This heterogeneity is expressed as a variable outcome and response to treatment,” she added.
Although biologic drugs have dramatically changed how patients are treated, 30%-40% of patients do not respond to treatment and the way biologic treatment is selected for RA is more down to trial and error than personalized medicine, Dr. Di Cicco observed. This is concerning, as the number of biologic medicines available is exponentially increasing and ways of matching the right drug to the right patient need to be found.
The aim of the current study was to see if different synovial subtypes could influence patients’ first response to treatment with anti-TNF therapy. Recent research looking at synovial tissue suggests that there are three clear synovial subtypes: myeloid, Pauci-immune, and lymphoid.
The myeloid and Pauci-immune pathotypes are characterized by diffuse cellular infiltration distributed evenly through the synovium. The lymphoid synovial pathotype, on the other hand, is characterized by the presence of large lymphocytic aggregates that are known as ectopic lymphoid structures (ELS). Dr. Di Cicco noted that ELS had been linked to B-cell proliferation within the synovium and to promoting in situ autoantibody production and class switching.
For the study, 28 patients with RA on stable doses of methotrexate who qualified for anti-TNF treatment according to U.K. National Institute for Health and Care Excellence guidance were recruited at a single center. All patients underwent ultrasound-guided biopsy of an active joint, which tended to be a small joint such as the wrist or metacarpophalangeal, before they were treated with certolizumab pegol. Twenty patients had a repeat synovial biopsy when the clinical efficacy of treatment was assessed at 12 weeks.
A minimum of six samples were taken from each biopsied joint, and this material underwent immunohistochemical analysis for the presence of T cells expressing CD3, B cells expressing CD20, macrophages expressing CD68, and plasma cells expressing CD138.
Samples were then classified as being the lymphoid pathotype if they contained mainly B and T cells and formed large lymphocytic aggregates or ELS. Myeloid subtype was defined as the presence of sublining macrophages and Pauci-immune if none of these features was present.
Thirteen (46.4%) patients were found to the have the Pauci-immune pathotype, with the lymphoid pathotype being the next most common (39.3% of patients), and four (14.3%) had the myeloid pathotype.
Apart from no prior oral steroid use in patients with the lymphoid pathotype versus 75% of patients with the myeloid pathotype and 38.5% of patients with the Pauci-immune pathotype, there were no significant differences among the groups in terms of demographics, clinical features, inflammatory markers, antibody or erosive status, or other treatments.
“After 12 weeks of therapy, the myeloid and the lymphoid groups showed a significantly higher fall in [Disease Activity Score] 28 compared to the Pauci-immune group,” Dr. Di Cicco reported.
“We also assessed achievement of EULAR response, and 71% of patients did respond. Half of them were good responders and half of them were moderate responders,” she added.
EULAR response by synovial pathotype was 100% for patients with the lymphoid pathotype, 75% for those with the myeloid pathotype, and 46% for those with the Pauci-immune pathotype.
Greater decreases in synovial thickening and power Doppler ultrasound also were seen in the myeloid and lymphoid pathotypes, compared with the Pauci-immune pathotype, which appeared more resistant to change in response to the anti-TNF therapy.
In the 20 patients who had a repeat biopsy, 9 had ELS at baseline. After treatment, three patients were ELS negative, four remained ELS positive, and two were ungraded.
“Our work shows that the presence of synovial ectopic lymphoid structures defining a lymphoid pathotype is a predictor of clinical response to anti-TNF-alpha,” Dr. Di Cicco said. Although further research and confirmation is needed, “we think that synovial tissue analysis could be considered as a promising tool to stratify RA patients and guide therapeutic decision,” she said.
Dr. Di Cicco had no disclosures.
MANCHESTER, U.K. – Analysis of synovial tissue taken by ultrasound-guided biopsy could help stratify patients with rheumatoid arthritis and decide if treatment with a tumor necrosis factor inhibitor is appropriate, according to research presented at the British Society for Rheumatology annual conference.
In a small yet intriguing study, Dr. Maria Di Cicco of Queen Mary University of London and her colleagues found that patients who had a lymphoid synovial pathotype were more likely to respond to treatment with the anti-TNF inhibitor certolizumab pegol than if they had other synovial pathotypes.
“Rheumatoid arthritis is a clinically heterogeneous disease to the extent that we should think of it as a syndrome rather than a disease,” Dr. Di Cicco said. “This heterogeneity is expressed as a variable outcome and response to treatment,” she added.
Although biologic drugs have dramatically changed how patients are treated, 30%-40% of patients do not respond to treatment and the way biologic treatment is selected for RA is more down to trial and error than personalized medicine, Dr. Di Cicco observed. This is concerning, as the number of biologic medicines available is exponentially increasing and ways of matching the right drug to the right patient need to be found.
The aim of the current study was to see if different synovial subtypes could influence patients’ first response to treatment with anti-TNF therapy. Recent research looking at synovial tissue suggests that there are three clear synovial subtypes: myeloid, Pauci-immune, and lymphoid.
The myeloid and Pauci-immune pathotypes are characterized by diffuse cellular infiltration distributed evenly through the synovium. The lymphoid synovial pathotype, on the other hand, is characterized by the presence of large lymphocytic aggregates that are known as ectopic lymphoid structures (ELS). Dr. Di Cicco noted that ELS had been linked to B-cell proliferation within the synovium and to promoting in situ autoantibody production and class switching.
For the study, 28 patients with RA on stable doses of methotrexate who qualified for anti-TNF treatment according to U.K. National Institute for Health and Care Excellence guidance were recruited at a single center. All patients underwent ultrasound-guided biopsy of an active joint, which tended to be a small joint such as the wrist or metacarpophalangeal, before they were treated with certolizumab pegol. Twenty patients had a repeat synovial biopsy when the clinical efficacy of treatment was assessed at 12 weeks.
A minimum of six samples were taken from each biopsied joint, and this material underwent immunohistochemical analysis for the presence of T cells expressing CD3, B cells expressing CD20, macrophages expressing CD68, and plasma cells expressing CD138.
Samples were then classified as being the lymphoid pathotype if they contained mainly B and T cells and formed large lymphocytic aggregates or ELS. Myeloid subtype was defined as the presence of sublining macrophages and Pauci-immune if none of these features was present.
Thirteen (46.4%) patients were found to the have the Pauci-immune pathotype, with the lymphoid pathotype being the next most common (39.3% of patients), and four (14.3%) had the myeloid pathotype.
Apart from no prior oral steroid use in patients with the lymphoid pathotype versus 75% of patients with the myeloid pathotype and 38.5% of patients with the Pauci-immune pathotype, there were no significant differences among the groups in terms of demographics, clinical features, inflammatory markers, antibody or erosive status, or other treatments.
“After 12 weeks of therapy, the myeloid and the lymphoid groups showed a significantly higher fall in [Disease Activity Score] 28 compared to the Pauci-immune group,” Dr. Di Cicco reported.
“We also assessed achievement of EULAR response, and 71% of patients did respond. Half of them were good responders and half of them were moderate responders,” she added.
EULAR response by synovial pathotype was 100% for patients with the lymphoid pathotype, 75% for those with the myeloid pathotype, and 46% for those with the Pauci-immune pathotype.
Greater decreases in synovial thickening and power Doppler ultrasound also were seen in the myeloid and lymphoid pathotypes, compared with the Pauci-immune pathotype, which appeared more resistant to change in response to the anti-TNF therapy.
In the 20 patients who had a repeat biopsy, 9 had ELS at baseline. After treatment, three patients were ELS negative, four remained ELS positive, and two were ungraded.
“Our work shows that the presence of synovial ectopic lymphoid structures defining a lymphoid pathotype is a predictor of clinical response to anti-TNF-alpha,” Dr. Di Cicco said. Although further research and confirmation is needed, “we think that synovial tissue analysis could be considered as a promising tool to stratify RA patients and guide therapeutic decision,” she said.
Dr. Di Cicco had no disclosures.
AT RHEUMATOLOGY 2015
Key clinical point: Early data suggest that synovial tissue analysis may be a potential tool to guide anti-TNF therapy, although more data are needed.
Major finding: EULAR response by synovial pathotype was 100% for patients with the lymphoid pathotype, 75% for those with the myeloid pathotype, and 46% for those with the Pauci-immune pathotype.
Data source: 28 patients with rheumatoid arthritis needing first anti-TNF treatment.
Disclosures: Dr. Di Cicco had no disclosures.
BSR: Patient selection key to using rituximab in lupus
MANCHESTER, U.K. – Although around half of patients with refractory systemic lupus erythematous (SLE) benefit from rituximab treatment at 6 months, there is a subgroup of patients that appears to do worse, according to research presented at the British Society for Rheumatology annual conference.
Data from the British Isles Lupus Assessment Group Biologic Registry (BILAG BR) showed that 58.75% of patients showed an improvement in disease activity measured using the BILAG 2004 Index System at 3 months and 48.75% showed improvement at 6 months.
Persistent disease, however, remained in 20% of patients at 3 and 6 months, and deteriorating disease occurred in 15% at 3 months and 22.5% at 6 months.
“A similar pattern was seen with the SLEDAI-2K response, although a higher percentage of patients seemed to improve with this measure,” said BILAG BR study coordinator Emily Sutton of the Centre for Musculoskeletal Research at the University of Manchester, England, where the registry is based.
Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) responses at 3 and 6 months showed around 70% of patients had improved at both time points, 16%-18% had persistent disease, and 11%-13% had worsening disease.
BILAG BR is a UK-based, multicenter, prospective, observational study of patients with SLE who are refractory to standard immunosuppressive therapy and are starting treatment with a biologic drug or a conventional, nonbiologic therapy.
The registry was set up in 2010 with the aim of recruiting 220 patients into the biologic cohort and 220 patients into the conventional, nonbiologic therapy cohort to enable monitoring of the real-world safety and effectiveness of biologics, compared with standard immunosuppressive therapies in the treatment of SLE.
Prior data on rituximab therapy in SLE were inconclusive, Dr. Sutton noted, with two clinical trials – EXPLORER (Arthritis Rheum. 2010;62:222-33) and LUNAR (Arthritis Rheum. 2012;64:1215-26) failing to hit their primary endpoints and show a clear benefit for rituximab.
Nevertheless, data from an open-label, single-center study of 50 patients treated with rituximab show that around 42% of patients achieved remission at 6 months (Arthritis Rheum. 2009;61:482-7).
The current analysis of BILAG BR data looked at the response to rituximab at 3 and 6 months in a total of 80 patients. Most (92.5%) of the study subjects were female, with a median age at diagnosis of 29.4 years and a median age at enrollment into the registry of 39.5 years. Approximately 60% were white, 13.7% were of South Asian descent, 13.7% of African ancestry, and the remainder was of mixed ethnicity.
The BILAG 2004 Index System scores disease activity across nine organ systems, and Dr. Sutton noted that all organ systems were involved at baseline, but the most common systems involved were the mucocutaneous (41% of patients), renal (35%), and musculoskeletal (31%) systems.
“When we looked at the disease activity at 6 months by BILAG organ system, there were a number of new flares in systems not previously involved,” Dr. Sutton reported.
“SLE patients demonstrated a variable response to rituximab, not just in the organ system involved, but also in the magnitude of response and the duration of remission,” she said.
“It is, therefore, essential that we work towards a position where we are able to select those patients who are most likely to respond well to treatment,” Dr. Sutton observed.
Patients continue to be enrolled into the registry, and future work will look at whether there are any factors predictive of a response to rituximab and try to stratify patients for B-cell depletion therapy, she added.
BILAG BR is supported by unconditional educational grants from Roche and GlaxoSmithKline. Dr. Sutton has received research funding from Roche and GlaxoSmithKline.
MANCHESTER, U.K. – Although around half of patients with refractory systemic lupus erythematous (SLE) benefit from rituximab treatment at 6 months, there is a subgroup of patients that appears to do worse, according to research presented at the British Society for Rheumatology annual conference.
Data from the British Isles Lupus Assessment Group Biologic Registry (BILAG BR) showed that 58.75% of patients showed an improvement in disease activity measured using the BILAG 2004 Index System at 3 months and 48.75% showed improvement at 6 months.
Persistent disease, however, remained in 20% of patients at 3 and 6 months, and deteriorating disease occurred in 15% at 3 months and 22.5% at 6 months.
“A similar pattern was seen with the SLEDAI-2K response, although a higher percentage of patients seemed to improve with this measure,” said BILAG BR study coordinator Emily Sutton of the Centre for Musculoskeletal Research at the University of Manchester, England, where the registry is based.
Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) responses at 3 and 6 months showed around 70% of patients had improved at both time points, 16%-18% had persistent disease, and 11%-13% had worsening disease.
BILAG BR is a UK-based, multicenter, prospective, observational study of patients with SLE who are refractory to standard immunosuppressive therapy and are starting treatment with a biologic drug or a conventional, nonbiologic therapy.
The registry was set up in 2010 with the aim of recruiting 220 patients into the biologic cohort and 220 patients into the conventional, nonbiologic therapy cohort to enable monitoring of the real-world safety and effectiveness of biologics, compared with standard immunosuppressive therapies in the treatment of SLE.
Prior data on rituximab therapy in SLE were inconclusive, Dr. Sutton noted, with two clinical trials – EXPLORER (Arthritis Rheum. 2010;62:222-33) and LUNAR (Arthritis Rheum. 2012;64:1215-26) failing to hit their primary endpoints and show a clear benefit for rituximab.
Nevertheless, data from an open-label, single-center study of 50 patients treated with rituximab show that around 42% of patients achieved remission at 6 months (Arthritis Rheum. 2009;61:482-7).
The current analysis of BILAG BR data looked at the response to rituximab at 3 and 6 months in a total of 80 patients. Most (92.5%) of the study subjects were female, with a median age at diagnosis of 29.4 years and a median age at enrollment into the registry of 39.5 years. Approximately 60% were white, 13.7% were of South Asian descent, 13.7% of African ancestry, and the remainder was of mixed ethnicity.
The BILAG 2004 Index System scores disease activity across nine organ systems, and Dr. Sutton noted that all organ systems were involved at baseline, but the most common systems involved were the mucocutaneous (41% of patients), renal (35%), and musculoskeletal (31%) systems.
“When we looked at the disease activity at 6 months by BILAG organ system, there were a number of new flares in systems not previously involved,” Dr. Sutton reported.
“SLE patients demonstrated a variable response to rituximab, not just in the organ system involved, but also in the magnitude of response and the duration of remission,” she said.
“It is, therefore, essential that we work towards a position where we are able to select those patients who are most likely to respond well to treatment,” Dr. Sutton observed.
Patients continue to be enrolled into the registry, and future work will look at whether there are any factors predictive of a response to rituximab and try to stratify patients for B-cell depletion therapy, she added.
BILAG BR is supported by unconditional educational grants from Roche and GlaxoSmithKline. Dr. Sutton has received research funding from Roche and GlaxoSmithKline.
MANCHESTER, U.K. – Although around half of patients with refractory systemic lupus erythematous (SLE) benefit from rituximab treatment at 6 months, there is a subgroup of patients that appears to do worse, according to research presented at the British Society for Rheumatology annual conference.
Data from the British Isles Lupus Assessment Group Biologic Registry (BILAG BR) showed that 58.75% of patients showed an improvement in disease activity measured using the BILAG 2004 Index System at 3 months and 48.75% showed improvement at 6 months.
Persistent disease, however, remained in 20% of patients at 3 and 6 months, and deteriorating disease occurred in 15% at 3 months and 22.5% at 6 months.
“A similar pattern was seen with the SLEDAI-2K response, although a higher percentage of patients seemed to improve with this measure,” said BILAG BR study coordinator Emily Sutton of the Centre for Musculoskeletal Research at the University of Manchester, England, where the registry is based.
Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) responses at 3 and 6 months showed around 70% of patients had improved at both time points, 16%-18% had persistent disease, and 11%-13% had worsening disease.
BILAG BR is a UK-based, multicenter, prospective, observational study of patients with SLE who are refractory to standard immunosuppressive therapy and are starting treatment with a biologic drug or a conventional, nonbiologic therapy.
The registry was set up in 2010 with the aim of recruiting 220 patients into the biologic cohort and 220 patients into the conventional, nonbiologic therapy cohort to enable monitoring of the real-world safety and effectiveness of biologics, compared with standard immunosuppressive therapies in the treatment of SLE.
Prior data on rituximab therapy in SLE were inconclusive, Dr. Sutton noted, with two clinical trials – EXPLORER (Arthritis Rheum. 2010;62:222-33) and LUNAR (Arthritis Rheum. 2012;64:1215-26) failing to hit their primary endpoints and show a clear benefit for rituximab.
Nevertheless, data from an open-label, single-center study of 50 patients treated with rituximab show that around 42% of patients achieved remission at 6 months (Arthritis Rheum. 2009;61:482-7).
The current analysis of BILAG BR data looked at the response to rituximab at 3 and 6 months in a total of 80 patients. Most (92.5%) of the study subjects were female, with a median age at diagnosis of 29.4 years and a median age at enrollment into the registry of 39.5 years. Approximately 60% were white, 13.7% were of South Asian descent, 13.7% of African ancestry, and the remainder was of mixed ethnicity.
The BILAG 2004 Index System scores disease activity across nine organ systems, and Dr. Sutton noted that all organ systems were involved at baseline, but the most common systems involved were the mucocutaneous (41% of patients), renal (35%), and musculoskeletal (31%) systems.
“When we looked at the disease activity at 6 months by BILAG organ system, there were a number of new flares in systems not previously involved,” Dr. Sutton reported.
“SLE patients demonstrated a variable response to rituximab, not just in the organ system involved, but also in the magnitude of response and the duration of remission,” she said.
“It is, therefore, essential that we work towards a position where we are able to select those patients who are most likely to respond well to treatment,” Dr. Sutton observed.
Patients continue to be enrolled into the registry, and future work will look at whether there are any factors predictive of a response to rituximab and try to stratify patients for B-cell depletion therapy, she added.
BILAG BR is supported by unconditional educational grants from Roche and GlaxoSmithKline. Dr. Sutton has received research funding from Roche and GlaxoSmithKline.
AT RHEUMATOLOGY 2015
Key clinical point: Although the majority of patients benefited from rituximab, a significant proportion did not, highlighting the need to identify predictive factors to help stratify patients suitable for this therapy.
Major finding: At 6 months, around 50% of patients had improved, 20% had persistent disease, and 22.5% had deteriorating disease using the BILAG 2004 System Index.
Data source: The BILAG BR is a prospective, observational cohort study of patients with systemic lupus erythematosus who are starting treatment with a biologic drug or a conventional, nonbiologic therapy.
Disclosures: The BILAG BR is supported by unconditional educational grants from Roche and GlaxoSmithKline. Dr. Sutton has received research funding from Roche and GlaxoSmithKline.
BSR: Lengthy SLE remission is possible, late relapses occur
MANCHESTER – Complete remissions of at least 3 years were achieved by nearly 15% of patients with systemic lupus erythematous, based on a retrospective analysis of an observational, single-center cohort of 624 patients treated over a 32-year span.
Nearly 5% of the patients achieved complete remissions of at least 10 years.
“Systemic lupus erythematosus is an unpredictable disease with many periods of exacerbations and remissions, but patients can achieve complete remission,” said Dr. Carmen Medina-Quiñones, of Ramón y Cajal Hospital in Madrid, at the British Society for Rheumatology annual conference.
Nevertheless, a patient with SLE can relapse after many years of remission, she noted during a poster tour.
Indeed, SLE flared in 22% of patients who had achieved complete remission, and 3 of these 15 patients relapsed more than a decade later. One patient relapsed after 12 years, another after 16 years, and the remaining patient after 18 years.
The findings indicate that all SLE patients need to be monitored and that long-term strategies are needed to control lupus activity, Dr. Medina-Quiñones said.
The analysis consisted of patients enrolled for a minimum period of 3 years in the SLE cohort at University College Hospital, London, from January 1978 to December 2010. The main aim was to determine how many patients in the cohort were able to achieve a complete remission over the follow-up period of 32 years.
Complete remission was defined as achieving BILAG (British Isles Lupus Assessment Group) scores of C, D, or E signifying the absence of clinical features and having normal laboratory findings, including normal complement levels. The definition also required that patients were off treatment for at least 3 years, meaning no corticosteroid or immunosuppressive therapies, although antimalarial and nonsteroidal anti-inflammatory drugs were allowed.
It was found that 45 (8.5%) achieved clinical but not serologic remission, and 66 (12.4%) patients achieved only serologic remission. “Interestingly, 29 patients achieved complete remission even without any antimalarial or nonsteroidal treatment,” Dr. Medina-Quiñones said.
The researchers also found that remissions were less likely in patients who had renal (P < .001), neurologic (P = .002), or cardiopulmonary involvement (P < .001).
Dr. Anisur Rahman of University College London who moderated the poster tour commented: “Many patients ask, ‘Will I ever be free of this disease?’ and ‘Will I ever not have to take any medication?’ The message here seems to be that it is quite unlikely for people with lupus.”
Dr. Medina-Quiñones commented: “Nowadays, we have a lot of new technologies and we have had a lot of success with different kinds of treatment, so it is likely that patients’ quality of life will improve and that they will have more chances to achieve remission.”
Dr. Medina-Quiñones has no relevant financial disclosures.
MANCHESTER – Complete remissions of at least 3 years were achieved by nearly 15% of patients with systemic lupus erythematous, based on a retrospective analysis of an observational, single-center cohort of 624 patients treated over a 32-year span.
Nearly 5% of the patients achieved complete remissions of at least 10 years.
“Systemic lupus erythematosus is an unpredictable disease with many periods of exacerbations and remissions, but patients can achieve complete remission,” said Dr. Carmen Medina-Quiñones, of Ramón y Cajal Hospital in Madrid, at the British Society for Rheumatology annual conference.
Nevertheless, a patient with SLE can relapse after many years of remission, she noted during a poster tour.
Indeed, SLE flared in 22% of patients who had achieved complete remission, and 3 of these 15 patients relapsed more than a decade later. One patient relapsed after 12 years, another after 16 years, and the remaining patient after 18 years.
The findings indicate that all SLE patients need to be monitored and that long-term strategies are needed to control lupus activity, Dr. Medina-Quiñones said.
The analysis consisted of patients enrolled for a minimum period of 3 years in the SLE cohort at University College Hospital, London, from January 1978 to December 2010. The main aim was to determine how many patients in the cohort were able to achieve a complete remission over the follow-up period of 32 years.
Complete remission was defined as achieving BILAG (British Isles Lupus Assessment Group) scores of C, D, or E signifying the absence of clinical features and having normal laboratory findings, including normal complement levels. The definition also required that patients were off treatment for at least 3 years, meaning no corticosteroid or immunosuppressive therapies, although antimalarial and nonsteroidal anti-inflammatory drugs were allowed.
It was found that 45 (8.5%) achieved clinical but not serologic remission, and 66 (12.4%) patients achieved only serologic remission. “Interestingly, 29 patients achieved complete remission even without any antimalarial or nonsteroidal treatment,” Dr. Medina-Quiñones said.
The researchers also found that remissions were less likely in patients who had renal (P < .001), neurologic (P = .002), or cardiopulmonary involvement (P < .001).
Dr. Anisur Rahman of University College London who moderated the poster tour commented: “Many patients ask, ‘Will I ever be free of this disease?’ and ‘Will I ever not have to take any medication?’ The message here seems to be that it is quite unlikely for people with lupus.”
Dr. Medina-Quiñones commented: “Nowadays, we have a lot of new technologies and we have had a lot of success with different kinds of treatment, so it is likely that patients’ quality of life will improve and that they will have more chances to achieve remission.”
Dr. Medina-Quiñones has no relevant financial disclosures.
MANCHESTER – Complete remissions of at least 3 years were achieved by nearly 15% of patients with systemic lupus erythematous, based on a retrospective analysis of an observational, single-center cohort of 624 patients treated over a 32-year span.
Nearly 5% of the patients achieved complete remissions of at least 10 years.
“Systemic lupus erythematosus is an unpredictable disease with many periods of exacerbations and remissions, but patients can achieve complete remission,” said Dr. Carmen Medina-Quiñones, of Ramón y Cajal Hospital in Madrid, at the British Society for Rheumatology annual conference.
Nevertheless, a patient with SLE can relapse after many years of remission, she noted during a poster tour.
Indeed, SLE flared in 22% of patients who had achieved complete remission, and 3 of these 15 patients relapsed more than a decade later. One patient relapsed after 12 years, another after 16 years, and the remaining patient after 18 years.
The findings indicate that all SLE patients need to be monitored and that long-term strategies are needed to control lupus activity, Dr. Medina-Quiñones said.
The analysis consisted of patients enrolled for a minimum period of 3 years in the SLE cohort at University College Hospital, London, from January 1978 to December 2010. The main aim was to determine how many patients in the cohort were able to achieve a complete remission over the follow-up period of 32 years.
Complete remission was defined as achieving BILAG (British Isles Lupus Assessment Group) scores of C, D, or E signifying the absence of clinical features and having normal laboratory findings, including normal complement levels. The definition also required that patients were off treatment for at least 3 years, meaning no corticosteroid or immunosuppressive therapies, although antimalarial and nonsteroidal anti-inflammatory drugs were allowed.
It was found that 45 (8.5%) achieved clinical but not serologic remission, and 66 (12.4%) patients achieved only serologic remission. “Interestingly, 29 patients achieved complete remission even without any antimalarial or nonsteroidal treatment,” Dr. Medina-Quiñones said.
The researchers also found that remissions were less likely in patients who had renal (P < .001), neurologic (P = .002), or cardiopulmonary involvement (P < .001).
Dr. Anisur Rahman of University College London who moderated the poster tour commented: “Many patients ask, ‘Will I ever be free of this disease?’ and ‘Will I ever not have to take any medication?’ The message here seems to be that it is quite unlikely for people with lupus.”
Dr. Medina-Quiñones commented: “Nowadays, we have a lot of new technologies and we have had a lot of success with different kinds of treatment, so it is likely that patients’ quality of life will improve and that they will have more chances to achieve remission.”
Dr. Medina-Quiñones has no relevant financial disclosures.
AT RHEUMATOLOGY 2015
Key clinical point: Patients with systemic lupus erythematosus can achieve complete remission for many years, but relapse can occur decades later, so long-term follow-up and monitoring are required.
Major finding: Complete remission was achieved by 15% of patients for at least 3 years and by 5% of patients for at least 10 years.
Data source: A 32-year retrospective analysis of an observational, single-center cohort of 624 patients with SLE treated for a minimum period of 3 years.
Disclosures: Dr. Medina-Quiñones has no relevant financial disclosures.
Tocilizumab shows promise as systemic sclerosis treatment
MANCHESTER, U.K. – Tocilizumab showed signs of improving skin and other symptoms in patients with systemic sclerosis (SSc) in an ongoing proof-of-concept study.
Although the primary endpoint of a significant change in the modified Rodan skin score (mRSS) at 24 weeks was not met, there was a numerically greater decrease in mRSS among patients who took tocilizumab versus those who took placebo. The mean change in mRSS was –3.92 units vs. –1.22 units, respectively, giving a difference of –2.70 units (P = .09).
“We were more encouraged by the 48-week data because we saw a much clearer fall in the mRSS,” said Dr. Christopher P. Denton, who presented these early findings from the phase II/III faSScinate trial at the British Society for Rheumatology annual conference.
At 48 weeks, there was a decrease of 6.33 units in the tocilizumab-treated patients vs. a decrease of 2.77 units in the placebo arm (mean change of –3.55 units; P = .06). A drop of 4 units in the mRSS is deemed to be a minimally clinically important difference.
“There is a reasonable rationale for looking at the IL [interleukin]-6 axis in systemic sclerosis as a target for therapy,” explained Dr. Denton, who is a consultant rheumatologist and professor of experimental rheumatology at University College London.
Indeed, preclinical data have indicated that IL-6 expression is elevated in SSc skin and that an antibody targeting IL-6 inhibited collagen synthesis in cultured fibroblasts and IL-6 receptor antibody reduced skin fibrosis in an animal model.
There also were early clinical data in SSc patients from Dr. Denton’s group that supported conducting a phase II study with tocilizumab (Ann. Rheum. Dis. 2012;71:1235-42).
The faSScinate trial started in 2012 and included 87 patients with active diffuse SSc of 5 years’ or less duration. For inclusion, patients had to have an mRSS of between 15 and 40 units at baseline and elevated acute phase reactants. Patients were randomized to treatment with tocilizumab, which was given at a dose of 162 mg by subcutaneous injection every week, or matching placebo. Treatment was blinded for 48 weeks, followed by an open-label period for a further 48 weeks, during which all patients received tocilizumab.
Dr. Denton said that there were clear and consistent trends towards continuous improvement in skin scores from baseline out to week 48 in the tocilizumab arm. There also were “encouraging trends” favoring tocilizumab in improvement in a number of secondary endpoints, including the Health Assessment Questionnaire-Disability Index (HAQ-DI), Patient and Clinician Global Assessment, FACIT-Fatigue score, and pruritus measured using the 5-D Itch Scale.
More patients treated with placebo than with tocilizumab experienced a worsening in lung function during the trial. This was an exploratory endpoint with an “intriguing” result, Dr. Denton said. A clinically meaningful drop of 10% or more in forced vital capacity was seen in just 3.3% of tocilizumab-treated patients, compared with 19.4% of placebo-treated patients (P = .009).
“Treatment was not entirely benign,” he acknowledged, adding that “noninfective adverse events were more common in the placebo-treatment arm and infective adverse events were more common in the tocilizumab-treated arm.” The increase in infective side effects was not surprising and generally treatable, he said, and serious adverse events were potentially due to complications of SSc rather than treatment.
“This was a small study, but relatively large for a proof-of-concept trial in systemic sclerosis,” Dr. Denton observed.
“We do feel the benefit-to-safety ratio does favor further investigation and that tocilizumab is likely to benefit a subset of patients with SSc who would otherwise have a particularly poor outcome.”
A phase III study is now being planned, with recruitment likely to start later this year.
Tocilizumab is currently indicated for use in the United States as Actemra and in Europe as RoActemra in combination with methotrexate for the treatment of severe, active, and progressive rheumatoid arthritis and for active juvenile idiopathic systemic or polyarthritis.
The faSScinate study was funded by F. Hoffman La Roche. Dr. Denton has acted as a consultant for Actelion Pharmaceuticals US, Biogen-Idec, CSL Behring, Genentech/Roche, GlaxoSmithKline, and Sanofi-Aventis. His coinvestigators also reported financial relationships with other pharmaceutical companies, including Roche.
MANCHESTER, U.K. – Tocilizumab showed signs of improving skin and other symptoms in patients with systemic sclerosis (SSc) in an ongoing proof-of-concept study.
Although the primary endpoint of a significant change in the modified Rodan skin score (mRSS) at 24 weeks was not met, there was a numerically greater decrease in mRSS among patients who took tocilizumab versus those who took placebo. The mean change in mRSS was –3.92 units vs. –1.22 units, respectively, giving a difference of –2.70 units (P = .09).
“We were more encouraged by the 48-week data because we saw a much clearer fall in the mRSS,” said Dr. Christopher P. Denton, who presented these early findings from the phase II/III faSScinate trial at the British Society for Rheumatology annual conference.
At 48 weeks, there was a decrease of 6.33 units in the tocilizumab-treated patients vs. a decrease of 2.77 units in the placebo arm (mean change of –3.55 units; P = .06). A drop of 4 units in the mRSS is deemed to be a minimally clinically important difference.
“There is a reasonable rationale for looking at the IL [interleukin]-6 axis in systemic sclerosis as a target for therapy,” explained Dr. Denton, who is a consultant rheumatologist and professor of experimental rheumatology at University College London.
Indeed, preclinical data have indicated that IL-6 expression is elevated in SSc skin and that an antibody targeting IL-6 inhibited collagen synthesis in cultured fibroblasts and IL-6 receptor antibody reduced skin fibrosis in an animal model.
There also were early clinical data in SSc patients from Dr. Denton’s group that supported conducting a phase II study with tocilizumab (Ann. Rheum. Dis. 2012;71:1235-42).
The faSScinate trial started in 2012 and included 87 patients with active diffuse SSc of 5 years’ or less duration. For inclusion, patients had to have an mRSS of between 15 and 40 units at baseline and elevated acute phase reactants. Patients were randomized to treatment with tocilizumab, which was given at a dose of 162 mg by subcutaneous injection every week, or matching placebo. Treatment was blinded for 48 weeks, followed by an open-label period for a further 48 weeks, during which all patients received tocilizumab.
Dr. Denton said that there were clear and consistent trends towards continuous improvement in skin scores from baseline out to week 48 in the tocilizumab arm. There also were “encouraging trends” favoring tocilizumab in improvement in a number of secondary endpoints, including the Health Assessment Questionnaire-Disability Index (HAQ-DI), Patient and Clinician Global Assessment, FACIT-Fatigue score, and pruritus measured using the 5-D Itch Scale.
More patients treated with placebo than with tocilizumab experienced a worsening in lung function during the trial. This was an exploratory endpoint with an “intriguing” result, Dr. Denton said. A clinically meaningful drop of 10% or more in forced vital capacity was seen in just 3.3% of tocilizumab-treated patients, compared with 19.4% of placebo-treated patients (P = .009).
“Treatment was not entirely benign,” he acknowledged, adding that “noninfective adverse events were more common in the placebo-treatment arm and infective adverse events were more common in the tocilizumab-treated arm.” The increase in infective side effects was not surprising and generally treatable, he said, and serious adverse events were potentially due to complications of SSc rather than treatment.
“This was a small study, but relatively large for a proof-of-concept trial in systemic sclerosis,” Dr. Denton observed.
“We do feel the benefit-to-safety ratio does favor further investigation and that tocilizumab is likely to benefit a subset of patients with SSc who would otherwise have a particularly poor outcome.”
A phase III study is now being planned, with recruitment likely to start later this year.
Tocilizumab is currently indicated for use in the United States as Actemra and in Europe as RoActemra in combination with methotrexate for the treatment of severe, active, and progressive rheumatoid arthritis and for active juvenile idiopathic systemic or polyarthritis.
The faSScinate study was funded by F. Hoffman La Roche. Dr. Denton has acted as a consultant for Actelion Pharmaceuticals US, Biogen-Idec, CSL Behring, Genentech/Roche, GlaxoSmithKline, and Sanofi-Aventis. His coinvestigators also reported financial relationships with other pharmaceutical companies, including Roche.
MANCHESTER, U.K. – Tocilizumab showed signs of improving skin and other symptoms in patients with systemic sclerosis (SSc) in an ongoing proof-of-concept study.
Although the primary endpoint of a significant change in the modified Rodan skin score (mRSS) at 24 weeks was not met, there was a numerically greater decrease in mRSS among patients who took tocilizumab versus those who took placebo. The mean change in mRSS was –3.92 units vs. –1.22 units, respectively, giving a difference of –2.70 units (P = .09).
“We were more encouraged by the 48-week data because we saw a much clearer fall in the mRSS,” said Dr. Christopher P. Denton, who presented these early findings from the phase II/III faSScinate trial at the British Society for Rheumatology annual conference.
At 48 weeks, there was a decrease of 6.33 units in the tocilizumab-treated patients vs. a decrease of 2.77 units in the placebo arm (mean change of –3.55 units; P = .06). A drop of 4 units in the mRSS is deemed to be a minimally clinically important difference.
“There is a reasonable rationale for looking at the IL [interleukin]-6 axis in systemic sclerosis as a target for therapy,” explained Dr. Denton, who is a consultant rheumatologist and professor of experimental rheumatology at University College London.
Indeed, preclinical data have indicated that IL-6 expression is elevated in SSc skin and that an antibody targeting IL-6 inhibited collagen synthesis in cultured fibroblasts and IL-6 receptor antibody reduced skin fibrosis in an animal model.
There also were early clinical data in SSc patients from Dr. Denton’s group that supported conducting a phase II study with tocilizumab (Ann. Rheum. Dis. 2012;71:1235-42).
The faSScinate trial started in 2012 and included 87 patients with active diffuse SSc of 5 years’ or less duration. For inclusion, patients had to have an mRSS of between 15 and 40 units at baseline and elevated acute phase reactants. Patients were randomized to treatment with tocilizumab, which was given at a dose of 162 mg by subcutaneous injection every week, or matching placebo. Treatment was blinded for 48 weeks, followed by an open-label period for a further 48 weeks, during which all patients received tocilizumab.
Dr. Denton said that there were clear and consistent trends towards continuous improvement in skin scores from baseline out to week 48 in the tocilizumab arm. There also were “encouraging trends” favoring tocilizumab in improvement in a number of secondary endpoints, including the Health Assessment Questionnaire-Disability Index (HAQ-DI), Patient and Clinician Global Assessment, FACIT-Fatigue score, and pruritus measured using the 5-D Itch Scale.
More patients treated with placebo than with tocilizumab experienced a worsening in lung function during the trial. This was an exploratory endpoint with an “intriguing” result, Dr. Denton said. A clinically meaningful drop of 10% or more in forced vital capacity was seen in just 3.3% of tocilizumab-treated patients, compared with 19.4% of placebo-treated patients (P = .009).
“Treatment was not entirely benign,” he acknowledged, adding that “noninfective adverse events were more common in the placebo-treatment arm and infective adverse events were more common in the tocilizumab-treated arm.” The increase in infective side effects was not surprising and generally treatable, he said, and serious adverse events were potentially due to complications of SSc rather than treatment.
“This was a small study, but relatively large for a proof-of-concept trial in systemic sclerosis,” Dr. Denton observed.
“We do feel the benefit-to-safety ratio does favor further investigation and that tocilizumab is likely to benefit a subset of patients with SSc who would otherwise have a particularly poor outcome.”
A phase III study is now being planned, with recruitment likely to start later this year.
Tocilizumab is currently indicated for use in the United States as Actemra and in Europe as RoActemra in combination with methotrexate for the treatment of severe, active, and progressive rheumatoid arthritis and for active juvenile idiopathic systemic or polyarthritis.
The faSScinate study was funded by F. Hoffman La Roche. Dr. Denton has acted as a consultant for Actelion Pharmaceuticals US, Biogen-Idec, CSL Behring, Genentech/Roche, GlaxoSmithKline, and Sanofi-Aventis. His coinvestigators also reported financial relationships with other pharmaceutical companies, including Roche.
AT RHEUMATOLOGY 2015
Key clinical point: Targeting interleukin-6 with tocilizumab has shown some early clinical promise in treating patients with systemic scleroderma.
Major finding: The mean change in mRSS at 24 weeks was –3.92 for tocilizumab and –1.22 for placebo, giving a numerically favorable difference of –2.70 (P = .09).
Data source: Phase II/III, randomized, double blind, placebo-controlled multicenter study assessing the safety and efficacy of 24 weeks’ tocilizumab treatment in 87 patients with systemic scleroderma.
Disclosures: The faSScinate study was funded by F. Hoffman La Roche. Dr. Denton has acted as a paid consultant for Actelion Pharmaceuticals, Biogen-Idec, CSL Behring, Genentech/Roche, GlaxoSmithKline, and Sanofi-Aventis. His coinvestigators also reported financial relationships with other pharmaceutical companies, including Roche.
TRACE-RA: Statin therapy may prevent CVD in RA
MANCHESTER, ENGLAND – Results of the Trial of Atorvastatin for the Primary Prevention of Cardiovascular Events in Patients with Rheumatoid Arthritis (TRACE-RA) suggest that daily treatment with atorvastatin may have a primary protective effect on the development of cardiovascular disease in patients with rheumatoid arthritis.
There was a 34% reduction in the primary composite cardiovascular endpoint, which, although not significant, showed a trend for benefit that was similar to that seen with other statin studies in the general population, according to Dr. George Kitas, a consultant rheumatologist and director of research and development at the Dudley (England) Group NHS Foundation Trust.
“The event rate we observed was actually lower than we had calculated on,” Dr. Kitas said in an interview at the British Society for Rheumatology annual conference. The anticipated event rate was 1.8%, but the observed event rate was 0.76%, he explained. As a result, the trial was terminated early as there would not be sufficient events over the planned time course of the trial.
“However, if you correct for a couple of baseline differences, particularly smoking and ethnicity, and also for compliance, the effect on the CVD event rate is actually statistically significant,” Dr. Kitas observed.
He noted that low-density lipoprotein cholesterol (LDL-C) was lowered by a significant 1.07 mmol/L (19.26 mg/dL) in the 1,492 patients randomized to atorvastatin versus a 0.14 mmol/L (2.52 mg/dL) decrease in the 1,492 patients randomized to placebo (P < .001).
Statins are established as a means of both primary and secondary prevention of CVD in the general population, but few patients with RA were included in the seminal statin trials. The aim of TRACE-RA was therefore to look at statins as a possible means for primary prevention in patients with high-grade inflammation such as RA.
TRACE-RA was a prospective, double-blind trial of 2,986 patients with RA aged 50 years or older or who had a disease duration of more than 10 years and who had been recruited at 102 participating centers between 2007 and 2012.
Patients had been randomized to treatment with atorvastatin 40 mg/day or placebo for the primary prevention of cardiovascular events and the median follow-up was 2.53 years, with an overall 7,908 years of patient follow-up. All patients were given lifestyle advice on how to reduce their cardiovascular risk.
The primary endpoint was a composite of CVD death, nonfatal myocardial infarction, cerebrovascular accident (excluding hemorrhagic stroke), transient ischemic attack, hospitalized angina, and coronary and noncoronary revascularization. A total of 33 of these CVD events occurred in 24 atorvastatin-treated patients and 52 events occurred in 36 patients on placebo. Of these, the majority were coronary events.
Adverse event rates in the atorvastatin and placebo arms were a respective 19.7% and 19.5%. “The side effects that were observed in the statin arm were virtually identical to the side effects that were observed in the placebo arm,” Dr. Kitas noted.
“So, what we think we can say from TRACE-RA is firstly that statins are ‘safe’ in people with rheumatoid arthritis. Secondly, that they have virtually identical effects, both in terms of LDL-C reduction and in terms of hard cardiovascular events, as what one would expect with equivalent doses of statins in the general population,” Dr. Kitas said.
“In practical terms, I would suggest that we all assess our patients regularly for their cardiovascular risk and make sure that we do not hesitate to start a statin in those who fulfill criteria according to the relevant national guidelines.”
Commenting on the study, Dr. Ernest Choy of Cardiff University, Wales, said that this is the largest randomized, controlled trial to look at preventing cardiovascular mortality in patients with RA.
“The message is that cardiovascular risk can potentially be reduced by a statin, especially in high-risk patients,” Dr. Choy said, noting that it also “highlights the importance of monitoring for cardiovascular disease.”
TRACE-RA was funded by Arthritis Research UK and the British Heart Foundation. Pfizer UK provided the study medication and an unrestricted grant for the TRACE-RA biobank. Dr. Kitas had no financial conflicts of interest to disclose.
MANCHESTER, ENGLAND – Results of the Trial of Atorvastatin for the Primary Prevention of Cardiovascular Events in Patients with Rheumatoid Arthritis (TRACE-RA) suggest that daily treatment with atorvastatin may have a primary protective effect on the development of cardiovascular disease in patients with rheumatoid arthritis.
There was a 34% reduction in the primary composite cardiovascular endpoint, which, although not significant, showed a trend for benefit that was similar to that seen with other statin studies in the general population, according to Dr. George Kitas, a consultant rheumatologist and director of research and development at the Dudley (England) Group NHS Foundation Trust.
“The event rate we observed was actually lower than we had calculated on,” Dr. Kitas said in an interview at the British Society for Rheumatology annual conference. The anticipated event rate was 1.8%, but the observed event rate was 0.76%, he explained. As a result, the trial was terminated early as there would not be sufficient events over the planned time course of the trial.
“However, if you correct for a couple of baseline differences, particularly smoking and ethnicity, and also for compliance, the effect on the CVD event rate is actually statistically significant,” Dr. Kitas observed.
He noted that low-density lipoprotein cholesterol (LDL-C) was lowered by a significant 1.07 mmol/L (19.26 mg/dL) in the 1,492 patients randomized to atorvastatin versus a 0.14 mmol/L (2.52 mg/dL) decrease in the 1,492 patients randomized to placebo (P < .001).
Statins are established as a means of both primary and secondary prevention of CVD in the general population, but few patients with RA were included in the seminal statin trials. The aim of TRACE-RA was therefore to look at statins as a possible means for primary prevention in patients with high-grade inflammation such as RA.
TRACE-RA was a prospective, double-blind trial of 2,986 patients with RA aged 50 years or older or who had a disease duration of more than 10 years and who had been recruited at 102 participating centers between 2007 and 2012.
Patients had been randomized to treatment with atorvastatin 40 mg/day or placebo for the primary prevention of cardiovascular events and the median follow-up was 2.53 years, with an overall 7,908 years of patient follow-up. All patients were given lifestyle advice on how to reduce their cardiovascular risk.
The primary endpoint was a composite of CVD death, nonfatal myocardial infarction, cerebrovascular accident (excluding hemorrhagic stroke), transient ischemic attack, hospitalized angina, and coronary and noncoronary revascularization. A total of 33 of these CVD events occurred in 24 atorvastatin-treated patients and 52 events occurred in 36 patients on placebo. Of these, the majority were coronary events.
Adverse event rates in the atorvastatin and placebo arms were a respective 19.7% and 19.5%. “The side effects that were observed in the statin arm were virtually identical to the side effects that were observed in the placebo arm,” Dr. Kitas noted.
“So, what we think we can say from TRACE-RA is firstly that statins are ‘safe’ in people with rheumatoid arthritis. Secondly, that they have virtually identical effects, both in terms of LDL-C reduction and in terms of hard cardiovascular events, as what one would expect with equivalent doses of statins in the general population,” Dr. Kitas said.
“In practical terms, I would suggest that we all assess our patients regularly for their cardiovascular risk and make sure that we do not hesitate to start a statin in those who fulfill criteria according to the relevant national guidelines.”
Commenting on the study, Dr. Ernest Choy of Cardiff University, Wales, said that this is the largest randomized, controlled trial to look at preventing cardiovascular mortality in patients with RA.
“The message is that cardiovascular risk can potentially be reduced by a statin, especially in high-risk patients,” Dr. Choy said, noting that it also “highlights the importance of monitoring for cardiovascular disease.”
TRACE-RA was funded by Arthritis Research UK and the British Heart Foundation. Pfizer UK provided the study medication and an unrestricted grant for the TRACE-RA biobank. Dr. Kitas had no financial conflicts of interest to disclose.
MANCHESTER, ENGLAND – Results of the Trial of Atorvastatin for the Primary Prevention of Cardiovascular Events in Patients with Rheumatoid Arthritis (TRACE-RA) suggest that daily treatment with atorvastatin may have a primary protective effect on the development of cardiovascular disease in patients with rheumatoid arthritis.
There was a 34% reduction in the primary composite cardiovascular endpoint, which, although not significant, showed a trend for benefit that was similar to that seen with other statin studies in the general population, according to Dr. George Kitas, a consultant rheumatologist and director of research and development at the Dudley (England) Group NHS Foundation Trust.
“The event rate we observed was actually lower than we had calculated on,” Dr. Kitas said in an interview at the British Society for Rheumatology annual conference. The anticipated event rate was 1.8%, but the observed event rate was 0.76%, he explained. As a result, the trial was terminated early as there would not be sufficient events over the planned time course of the trial.
“However, if you correct for a couple of baseline differences, particularly smoking and ethnicity, and also for compliance, the effect on the CVD event rate is actually statistically significant,” Dr. Kitas observed.
He noted that low-density lipoprotein cholesterol (LDL-C) was lowered by a significant 1.07 mmol/L (19.26 mg/dL) in the 1,492 patients randomized to atorvastatin versus a 0.14 mmol/L (2.52 mg/dL) decrease in the 1,492 patients randomized to placebo (P < .001).
Statins are established as a means of both primary and secondary prevention of CVD in the general population, but few patients with RA were included in the seminal statin trials. The aim of TRACE-RA was therefore to look at statins as a possible means for primary prevention in patients with high-grade inflammation such as RA.
TRACE-RA was a prospective, double-blind trial of 2,986 patients with RA aged 50 years or older or who had a disease duration of more than 10 years and who had been recruited at 102 participating centers between 2007 and 2012.
Patients had been randomized to treatment with atorvastatin 40 mg/day or placebo for the primary prevention of cardiovascular events and the median follow-up was 2.53 years, with an overall 7,908 years of patient follow-up. All patients were given lifestyle advice on how to reduce their cardiovascular risk.
The primary endpoint was a composite of CVD death, nonfatal myocardial infarction, cerebrovascular accident (excluding hemorrhagic stroke), transient ischemic attack, hospitalized angina, and coronary and noncoronary revascularization. A total of 33 of these CVD events occurred in 24 atorvastatin-treated patients and 52 events occurred in 36 patients on placebo. Of these, the majority were coronary events.
Adverse event rates in the atorvastatin and placebo arms were a respective 19.7% and 19.5%. “The side effects that were observed in the statin arm were virtually identical to the side effects that were observed in the placebo arm,” Dr. Kitas noted.
“So, what we think we can say from TRACE-RA is firstly that statins are ‘safe’ in people with rheumatoid arthritis. Secondly, that they have virtually identical effects, both in terms of LDL-C reduction and in terms of hard cardiovascular events, as what one would expect with equivalent doses of statins in the general population,” Dr. Kitas said.
“In practical terms, I would suggest that we all assess our patients regularly for their cardiovascular risk and make sure that we do not hesitate to start a statin in those who fulfill criteria according to the relevant national guidelines.”
Commenting on the study, Dr. Ernest Choy of Cardiff University, Wales, said that this is the largest randomized, controlled trial to look at preventing cardiovascular mortality in patients with RA.
“The message is that cardiovascular risk can potentially be reduced by a statin, especially in high-risk patients,” Dr. Choy said, noting that it also “highlights the importance of monitoring for cardiovascular disease.”
TRACE-RA was funded by Arthritis Research UK and the British Heart Foundation. Pfizer UK provided the study medication and an unrestricted grant for the TRACE-RA biobank. Dr. Kitas had no financial conflicts of interest to disclose.
AT RHEUMATOLOGY 2015
Key clinical point: Statin therapy may be as beneficial in patients with RA as it is in the general population for the primary prevention of cardiovascular events.
Major finding: The hazard ratio for the reduction in the primary composite cardiovascular endpoint was 0.66 (P = .0119).
Data source: Multicenter, double-blind trial of 2,986 patients with RA aged older than 50 years or with more than 10 years’ disease duration randomized to treatment with atorvastatin 40 mg/day or placebo for the primary prevention of cardiovascular events.
Disclosures: TRACE-RA was funded by Arthritis Research UK and the British Heart Foundation. Pfizer UK provided the study medication and an unrestricted grant for the TRACE-RA biobank. Dr. Kitas had no financial conflicts of interest to disclose.