User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Trastuzumab deruxtecan proves active in HER2-mutated NSCLC
, an investigator reported.
The overall response rate (ORR) exceeded 60% among these heavily pretreated patients, with an estimated median progression-free survival (PFS) of 14 months, according to Egbert F. Smit, MD, PhD, of the Netherlands Cancer Institute.
Interstitial lung disease is an identified risk associated with T-DXd treatment, though the events in the DESTINY-Lung01 trial have been low-grade and have not resulted in any deaths, Dr. Smit said when presenting results from the trial as part of the American Society of Clinical Oncology virtual scientific program.
“These data demonstrate the potential of T-DXd as a new treatment option for patients with HER2-mutated non–small-cell lung cancer,” Dr. Smit said.
‘A good targeted therapy’
The findings are a “nice early confirmation” of the initial results seen with T-DXd in an earlier, smaller, phase 1 population, said invited discussant Grace K. Dy, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
“Trastuzumab-DXd showed clinical outcomes that meet the standards of what we expect a good targeted therapy should have in terms of overall response rate and progression free survival,” Dr. Dy said.
She noted that the ORR in DESTINY-Lung01 exceeds a 23% ORR seen among NSCLC patients treated with dual HER2-targeted therapy – trastuzumab plus pertuzumab – in a basket trial (J Clin Oncol. 2018 Feb 20;36[6]:536-42). Moreover, the response and PFS data “far surpass” results seen to date with oral tyrosine kinase inhibitors, including pyrotinib, poziotinib, neratinib, and afatinib.
The T-DXd results also look favorable in comparison to another antibody-drug conjugate, ado trastuzumab emtansine, Dr. Dy added, referencing another basket trial in which investigators reported an ORR of 44% and a median PFS of 5 months among 18 patients with advanced HER2-mutant lung adenocarcinomas (J Clin Oncol. 2018 Aug 20;36[24]:2532-7).
“Although T-DM1 [ado trastuzumab emtansine] demonstrated some degree of activity, its lower dosing, which was limited by the payload, lower drug-antibody ratio, and shorter half-life likely explain why results were better with T-DXd,” Dr. Dy said.
T-DXd was, in fact, designed to deliver an optimal antitumor effect, according to Dr. Smit.
The treatment incorporates a humanized anti-HER2 IgG1 monoclonal antibody that has the same amino acid sequence as trastuzumab. The antibody is attached via a cleavable, tumor-selective linker to a payload of deruxtecan, a topoisomerase I inhibitor.
The resulting antibody-drug conjugate has a high drug-to-antibody ratio, with 8 DXd molecules per monoclonal antibody, according to Dr. Smit.
Study details
The DESTINY-Lung01 trial included 42 patients with HER2-mutated NSCLC who received T-DXd at a dose of 6.4 mg/kg every 3 weeks. The patients’ median age was 63 years, and about 64% were female. Eastern Cooperative Oncology Group performance status was 0 in about one-quarter of the patients, and 1 in the remainder.
Patients had received up to six prior lines of treatment, including platinum-based chemotherapy in about 91%, a PD-1 or PD-L1 inhibitor in 55%, and docetaxel in 19%.
The confirmed ORR by independent central review was 61.9% (26/42). That included a single complete response (2.4%) and 25 partial responses (59.5%).
The duration of response was not reached (95% CI, 5.3 months to not estimable), and the median PFS was 14.0 months (95% CI, 6.4-14.0 months).
All patients experienced a treatment-related adverse event. Treatment-related events of grade 3 or greater were seen in 22 patients (52%). These mainly included decreased neutrophil count, anemia, nausea, vomiting, and fatigue.
There were five cases of interstitial lung disease, all of which were grade 2. In four cases, T-DXd was withdrawn. In one case, the drug was interrupted. All patients were treated with steroids.
“Two [patients] recovered, one recovered with sequelae, one was recovering, and one had not recovered by data cutoff,” Dr. Smit said.
DESTINY-Lung01 also includes a cohort of patients with HER2-expressing NSCLC not reported at the meeting. Enrollment in the HER2-mutated cohort that was reported has been expanded with another 50 patients to “better characterize the risk-benefit ratio,” Dr. Smit said.
The DESTINY-Lung01 study is sponsored by Daiichi Sankyo Inc. Dr. Smit reported relationships with Daiichi Sankyo and many other companies. Dr. Dy reported disclosures related to Amgen, AstraZeneca/Medimmune, GlaxoSmithKline, Takeda, and Tesaro.
SOURCE: Smit EF et al. ASCO 2020, Abstract 9504.
, an investigator reported.
The overall response rate (ORR) exceeded 60% among these heavily pretreated patients, with an estimated median progression-free survival (PFS) of 14 months, according to Egbert F. Smit, MD, PhD, of the Netherlands Cancer Institute.
Interstitial lung disease is an identified risk associated with T-DXd treatment, though the events in the DESTINY-Lung01 trial have been low-grade and have not resulted in any deaths, Dr. Smit said when presenting results from the trial as part of the American Society of Clinical Oncology virtual scientific program.
“These data demonstrate the potential of T-DXd as a new treatment option for patients with HER2-mutated non–small-cell lung cancer,” Dr. Smit said.
‘A good targeted therapy’
The findings are a “nice early confirmation” of the initial results seen with T-DXd in an earlier, smaller, phase 1 population, said invited discussant Grace K. Dy, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
“Trastuzumab-DXd showed clinical outcomes that meet the standards of what we expect a good targeted therapy should have in terms of overall response rate and progression free survival,” Dr. Dy said.
She noted that the ORR in DESTINY-Lung01 exceeds a 23% ORR seen among NSCLC patients treated with dual HER2-targeted therapy – trastuzumab plus pertuzumab – in a basket trial (J Clin Oncol. 2018 Feb 20;36[6]:536-42). Moreover, the response and PFS data “far surpass” results seen to date with oral tyrosine kinase inhibitors, including pyrotinib, poziotinib, neratinib, and afatinib.
The T-DXd results also look favorable in comparison to another antibody-drug conjugate, ado trastuzumab emtansine, Dr. Dy added, referencing another basket trial in which investigators reported an ORR of 44% and a median PFS of 5 months among 18 patients with advanced HER2-mutant lung adenocarcinomas (J Clin Oncol. 2018 Aug 20;36[24]:2532-7).
“Although T-DM1 [ado trastuzumab emtansine] demonstrated some degree of activity, its lower dosing, which was limited by the payload, lower drug-antibody ratio, and shorter half-life likely explain why results were better with T-DXd,” Dr. Dy said.
T-DXd was, in fact, designed to deliver an optimal antitumor effect, according to Dr. Smit.
The treatment incorporates a humanized anti-HER2 IgG1 monoclonal antibody that has the same amino acid sequence as trastuzumab. The antibody is attached via a cleavable, tumor-selective linker to a payload of deruxtecan, a topoisomerase I inhibitor.
The resulting antibody-drug conjugate has a high drug-to-antibody ratio, with 8 DXd molecules per monoclonal antibody, according to Dr. Smit.
Study details
The DESTINY-Lung01 trial included 42 patients with HER2-mutated NSCLC who received T-DXd at a dose of 6.4 mg/kg every 3 weeks. The patients’ median age was 63 years, and about 64% were female. Eastern Cooperative Oncology Group performance status was 0 in about one-quarter of the patients, and 1 in the remainder.
Patients had received up to six prior lines of treatment, including platinum-based chemotherapy in about 91%, a PD-1 or PD-L1 inhibitor in 55%, and docetaxel in 19%.
The confirmed ORR by independent central review was 61.9% (26/42). That included a single complete response (2.4%) and 25 partial responses (59.5%).
The duration of response was not reached (95% CI, 5.3 months to not estimable), and the median PFS was 14.0 months (95% CI, 6.4-14.0 months).
All patients experienced a treatment-related adverse event. Treatment-related events of grade 3 or greater were seen in 22 patients (52%). These mainly included decreased neutrophil count, anemia, nausea, vomiting, and fatigue.
There were five cases of interstitial lung disease, all of which were grade 2. In four cases, T-DXd was withdrawn. In one case, the drug was interrupted. All patients were treated with steroids.
“Two [patients] recovered, one recovered with sequelae, one was recovering, and one had not recovered by data cutoff,” Dr. Smit said.
DESTINY-Lung01 also includes a cohort of patients with HER2-expressing NSCLC not reported at the meeting. Enrollment in the HER2-mutated cohort that was reported has been expanded with another 50 patients to “better characterize the risk-benefit ratio,” Dr. Smit said.
The DESTINY-Lung01 study is sponsored by Daiichi Sankyo Inc. Dr. Smit reported relationships with Daiichi Sankyo and many other companies. Dr. Dy reported disclosures related to Amgen, AstraZeneca/Medimmune, GlaxoSmithKline, Takeda, and Tesaro.
SOURCE: Smit EF et al. ASCO 2020, Abstract 9504.
, an investigator reported.
The overall response rate (ORR) exceeded 60% among these heavily pretreated patients, with an estimated median progression-free survival (PFS) of 14 months, according to Egbert F. Smit, MD, PhD, of the Netherlands Cancer Institute.
Interstitial lung disease is an identified risk associated with T-DXd treatment, though the events in the DESTINY-Lung01 trial have been low-grade and have not resulted in any deaths, Dr. Smit said when presenting results from the trial as part of the American Society of Clinical Oncology virtual scientific program.
“These data demonstrate the potential of T-DXd as a new treatment option for patients with HER2-mutated non–small-cell lung cancer,” Dr. Smit said.
‘A good targeted therapy’
The findings are a “nice early confirmation” of the initial results seen with T-DXd in an earlier, smaller, phase 1 population, said invited discussant Grace K. Dy, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
“Trastuzumab-DXd showed clinical outcomes that meet the standards of what we expect a good targeted therapy should have in terms of overall response rate and progression free survival,” Dr. Dy said.
She noted that the ORR in DESTINY-Lung01 exceeds a 23% ORR seen among NSCLC patients treated with dual HER2-targeted therapy – trastuzumab plus pertuzumab – in a basket trial (J Clin Oncol. 2018 Feb 20;36[6]:536-42). Moreover, the response and PFS data “far surpass” results seen to date with oral tyrosine kinase inhibitors, including pyrotinib, poziotinib, neratinib, and afatinib.
The T-DXd results also look favorable in comparison to another antibody-drug conjugate, ado trastuzumab emtansine, Dr. Dy added, referencing another basket trial in which investigators reported an ORR of 44% and a median PFS of 5 months among 18 patients with advanced HER2-mutant lung adenocarcinomas (J Clin Oncol. 2018 Aug 20;36[24]:2532-7).
“Although T-DM1 [ado trastuzumab emtansine] demonstrated some degree of activity, its lower dosing, which was limited by the payload, lower drug-antibody ratio, and shorter half-life likely explain why results were better with T-DXd,” Dr. Dy said.
T-DXd was, in fact, designed to deliver an optimal antitumor effect, according to Dr. Smit.
The treatment incorporates a humanized anti-HER2 IgG1 monoclonal antibody that has the same amino acid sequence as trastuzumab. The antibody is attached via a cleavable, tumor-selective linker to a payload of deruxtecan, a topoisomerase I inhibitor.
The resulting antibody-drug conjugate has a high drug-to-antibody ratio, with 8 DXd molecules per monoclonal antibody, according to Dr. Smit.
Study details
The DESTINY-Lung01 trial included 42 patients with HER2-mutated NSCLC who received T-DXd at a dose of 6.4 mg/kg every 3 weeks. The patients’ median age was 63 years, and about 64% were female. Eastern Cooperative Oncology Group performance status was 0 in about one-quarter of the patients, and 1 in the remainder.
Patients had received up to six prior lines of treatment, including platinum-based chemotherapy in about 91%, a PD-1 or PD-L1 inhibitor in 55%, and docetaxel in 19%.
The confirmed ORR by independent central review was 61.9% (26/42). That included a single complete response (2.4%) and 25 partial responses (59.5%).
The duration of response was not reached (95% CI, 5.3 months to not estimable), and the median PFS was 14.0 months (95% CI, 6.4-14.0 months).
All patients experienced a treatment-related adverse event. Treatment-related events of grade 3 or greater were seen in 22 patients (52%). These mainly included decreased neutrophil count, anemia, nausea, vomiting, and fatigue.
There were five cases of interstitial lung disease, all of which were grade 2. In four cases, T-DXd was withdrawn. In one case, the drug was interrupted. All patients were treated with steroids.
“Two [patients] recovered, one recovered with sequelae, one was recovering, and one had not recovered by data cutoff,” Dr. Smit said.
DESTINY-Lung01 also includes a cohort of patients with HER2-expressing NSCLC not reported at the meeting. Enrollment in the HER2-mutated cohort that was reported has been expanded with another 50 patients to “better characterize the risk-benefit ratio,” Dr. Smit said.
The DESTINY-Lung01 study is sponsored by Daiichi Sankyo Inc. Dr. Smit reported relationships with Daiichi Sankyo and many other companies. Dr. Dy reported disclosures related to Amgen, AstraZeneca/Medimmune, GlaxoSmithKline, Takeda, and Tesaro.
SOURCE: Smit EF et al. ASCO 2020, Abstract 9504.
FROM ASCO 2020
Oral relugolix works to a T against advanced prostate cancer
according to investigators from the phase 3 HERO trial.
Relugolix was also associated with a significantly lower incidence of major adverse cardiovascular events (MACE), reported Neal D. Shore, MD, of the Carolina Urologic Research Center in Myrtle Beach, S.C., in a presentation made as a part of the American Society of Clinical Oncology virtual scientific program. The study was published simultaneously in The New England Journal of Medicine.
“Relugolix is a novel oral GnRH antagonist that has the potential to become a new standard for ADT [androgen-deprivation therapy] in advanced prostate cancer,” Dr. Shore said. He added that a potential advantage of relugolix compared with the leutenizing hormone-releasing hormone (LHRH) agonist leuprolide is the oral agent’s adverse event profile.
“Of note, and importantly, cardiovascular mortality is the leading cause of death for patients with prostate cancer. The percentage of patients with prostate cancer dying of cardiovascular disease has surpassed the percentage of patients dying from prostate cancer itself since the early 1990s. Approximately 30% of men with prostate cancer have known cardiovascular disease, and many more of these patients have comorbid risk factors, including obesity, diabetes, hypertension, and hyperlipidemia,” Dr. Shore said.
LHRH agonists also cause an initial testosterone surge that may cause an early but transient symptom flare. In contrast, relugolix has a direct inhibitory effect on pituitary GnRH receptors, leading to suppression of both leutenizing hormone and follicle-stimulating hormone, with no testosterone flare.
Study details
In the HERO trial, men with advanced prostate cancer were randomized in a 2:1 ratio to receive either relugolix at a 360-mg loading dose on day 1 followed by a 120-mg oral dose once daily (n = 622) or leuprolide delivered via depot injection every 3 months (n = 308) for a total of 48 weeks.
About half of all patients in each arm had biochemical (prostate-specific antigen, or “PSA”) relapse, 23% had newly diagnosed androgen-sensitive metastatic disease, and the remaining men (26%-28%) had advanced localized disease.
Patients with a history of a MACE event – a composite of nonfatal myocardial infarction, nonfatal stroke, and death from any cause – within 6 months were excluded.
The median PSA level at baseline was 11.7 mg/mL in the relugolix arm and 9.4 ng/mL in the leuprolide arm. Respective median testosterone levels were 415.8 ng/dL and 395.9 ng/dL.
“Of note, more than 90% of men enrolled in this study had at least one cardiovascular risk factor,” Dr. Shore said. “Tobacco use and obesity were common, as were diabetes and hypertension. Fourteen percent of men reported a prior history of major adverse cardiovascular event, such as a heart attack or stroke; this is lower than the 30% expected in a typical population of men with advanced prostate cancer given the study’s cardiovascular exclusion criteria.”
Efficacy
Sustained testosterone suppression to castration levels (less than 50 ng/dL) was achieved through 48 weeks in 96.7% of patients on relugolix, compared with 88.8% of men on leuprolide.
The absolute difference of 7.9% reached the statistical definitions for both noninferiority and superiority of relugolix over leuprolide (P for superiority < .001).
Mean testosterone levels on day 4 had decreased to below 50 ng/dL for relugolix and were maintained at castration levels until the end of treatment. In the leuprolide group, the mean testosterone level on day 4 was 625 ng/dL, which declined to castration levels by day 29 and remained below 50 ng/dL after the end of treatment at week 53. In contrast, testosterone levels in the relugolix arm began to recover immediately after the cessation of therapy.
Results with relugolix were significantly better than with leuprolide for the following endpoints (P < .0001 for all comparisons):
- Proportion of patients with PSA response at day 15 and confirmed at day 29 (79.4% vs. 19.8%)
- Cumulative probability of testosterone suppression to less than 50 ng/dL on day 15 (98.7% vs. 12.05%)
- Cumulative probability of profound testosterone suppression to less than 20 ng/dL on day 15 (78.38% vs. 0.98%)
- Mean follicle-stimulating hormone level at the end of week 24 (1.72 vs. 5.95 IU/L).
Safety
Treatment-related adverse events occurred in 73.6% of patients treated with relugolix and 68.8% of those who received leuprolide. Grade 3 or greater adverse events occurred in 3.4% and 2.6%, respectively. The respective incidences of fatal adverse events were 1.1% and 2.9%.
At 48 weeks, MACE had occurred in 2.9% of patients on relugolix and 6.2% on leuprolide. Among men with a history of a MACE event more than 6 months before study entry, leuprolide was associated with a nearly sixfold increased risk for a new MACE.
The investigators also found that compliance with the assigned medication was greater than 99% in each study arm, allaying concerns that men assigned to the oral therapy might be less likely to faithfully take their medicine.
Antagonists vs. agonists
Agents such as relugolix, which are, in effect, LHRH antagonists, have several advantages over LHRH agonists, according to invited discussant Elahe Mostaghel, MD, PhD, of the VA Puget Sound Health Care System and Fred Hutchinson Cancer Research Center, both in Seattle.
“Cost and access aside, antagonists have potential benefits over agonists, each of which may be more or less important, depending on context,” she said.
Antagonists have a more rapid onset of castration, lack the flare response seen with agonists such as leuprolide, and are associated with a significant decrease in risk for MACE.
“Differences in depth and consistency of androgen suppression may also be important. LHRH antagonists may be superior to LHRH agonists in this regard, although this remains to be fully proven, while rapid testosterone recovery and oral administration may also have benefits in particular contexts,” Dr. Mostaghel said.
“It is likely that the anticancer effects of a GnRH antagonist will not be inferior to those of a GnRH agonist and may be beneficial in terms of cardiovascular events that may be life-limiting,” Celestia S. Higano, MD, of the University of Washington in Seattle wrote in an editorial accompanying the HERO study in The New England Journal of Medicine.
“Close monitoring will be required because exposure to oral relugolix for longer than 48 weeks has not been studied and many oral agents are associated with adherence problems, especially if they cause adverse effects,” Dr. Higano added.
The HERO study was supported by Myovant. Dr. Shore disclosed relationships with Myovant and other companies. Dr. Mostaghel disclosed affiliations with Context Therapeutics. Dr. Hinago disclosed grants and fees from various companies, not including Myovant.
SOURCES: Shore ND et al. ASCO 2020, Abstract 5602; N Engl J Med. 2020 May 29. doi: 10.1056/NEJMoa2004325.
according to investigators from the phase 3 HERO trial.
Relugolix was also associated with a significantly lower incidence of major adverse cardiovascular events (MACE), reported Neal D. Shore, MD, of the Carolina Urologic Research Center in Myrtle Beach, S.C., in a presentation made as a part of the American Society of Clinical Oncology virtual scientific program. The study was published simultaneously in The New England Journal of Medicine.
“Relugolix is a novel oral GnRH antagonist that has the potential to become a new standard for ADT [androgen-deprivation therapy] in advanced prostate cancer,” Dr. Shore said. He added that a potential advantage of relugolix compared with the leutenizing hormone-releasing hormone (LHRH) agonist leuprolide is the oral agent’s adverse event profile.
“Of note, and importantly, cardiovascular mortality is the leading cause of death for patients with prostate cancer. The percentage of patients with prostate cancer dying of cardiovascular disease has surpassed the percentage of patients dying from prostate cancer itself since the early 1990s. Approximately 30% of men with prostate cancer have known cardiovascular disease, and many more of these patients have comorbid risk factors, including obesity, diabetes, hypertension, and hyperlipidemia,” Dr. Shore said.
LHRH agonists also cause an initial testosterone surge that may cause an early but transient symptom flare. In contrast, relugolix has a direct inhibitory effect on pituitary GnRH receptors, leading to suppression of both leutenizing hormone and follicle-stimulating hormone, with no testosterone flare.
Study details
In the HERO trial, men with advanced prostate cancer were randomized in a 2:1 ratio to receive either relugolix at a 360-mg loading dose on day 1 followed by a 120-mg oral dose once daily (n = 622) or leuprolide delivered via depot injection every 3 months (n = 308) for a total of 48 weeks.
About half of all patients in each arm had biochemical (prostate-specific antigen, or “PSA”) relapse, 23% had newly diagnosed androgen-sensitive metastatic disease, and the remaining men (26%-28%) had advanced localized disease.
Patients with a history of a MACE event – a composite of nonfatal myocardial infarction, nonfatal stroke, and death from any cause – within 6 months were excluded.
The median PSA level at baseline was 11.7 mg/mL in the relugolix arm and 9.4 ng/mL in the leuprolide arm. Respective median testosterone levels were 415.8 ng/dL and 395.9 ng/dL.
“Of note, more than 90% of men enrolled in this study had at least one cardiovascular risk factor,” Dr. Shore said. “Tobacco use and obesity were common, as were diabetes and hypertension. Fourteen percent of men reported a prior history of major adverse cardiovascular event, such as a heart attack or stroke; this is lower than the 30% expected in a typical population of men with advanced prostate cancer given the study’s cardiovascular exclusion criteria.”
Efficacy
Sustained testosterone suppression to castration levels (less than 50 ng/dL) was achieved through 48 weeks in 96.7% of patients on relugolix, compared with 88.8% of men on leuprolide.
The absolute difference of 7.9% reached the statistical definitions for both noninferiority and superiority of relugolix over leuprolide (P for superiority < .001).
Mean testosterone levels on day 4 had decreased to below 50 ng/dL for relugolix and were maintained at castration levels until the end of treatment. In the leuprolide group, the mean testosterone level on day 4 was 625 ng/dL, which declined to castration levels by day 29 and remained below 50 ng/dL after the end of treatment at week 53. In contrast, testosterone levels in the relugolix arm began to recover immediately after the cessation of therapy.
Results with relugolix were significantly better than with leuprolide for the following endpoints (P < .0001 for all comparisons):
- Proportion of patients with PSA response at day 15 and confirmed at day 29 (79.4% vs. 19.8%)
- Cumulative probability of testosterone suppression to less than 50 ng/dL on day 15 (98.7% vs. 12.05%)
- Cumulative probability of profound testosterone suppression to less than 20 ng/dL on day 15 (78.38% vs. 0.98%)
- Mean follicle-stimulating hormone level at the end of week 24 (1.72 vs. 5.95 IU/L).
Safety
Treatment-related adverse events occurred in 73.6% of patients treated with relugolix and 68.8% of those who received leuprolide. Grade 3 or greater adverse events occurred in 3.4% and 2.6%, respectively. The respective incidences of fatal adverse events were 1.1% and 2.9%.
At 48 weeks, MACE had occurred in 2.9% of patients on relugolix and 6.2% on leuprolide. Among men with a history of a MACE event more than 6 months before study entry, leuprolide was associated with a nearly sixfold increased risk for a new MACE.
The investigators also found that compliance with the assigned medication was greater than 99% in each study arm, allaying concerns that men assigned to the oral therapy might be less likely to faithfully take their medicine.
Antagonists vs. agonists
Agents such as relugolix, which are, in effect, LHRH antagonists, have several advantages over LHRH agonists, according to invited discussant Elahe Mostaghel, MD, PhD, of the VA Puget Sound Health Care System and Fred Hutchinson Cancer Research Center, both in Seattle.
“Cost and access aside, antagonists have potential benefits over agonists, each of which may be more or less important, depending on context,” she said.
Antagonists have a more rapid onset of castration, lack the flare response seen with agonists such as leuprolide, and are associated with a significant decrease in risk for MACE.
“Differences in depth and consistency of androgen suppression may also be important. LHRH antagonists may be superior to LHRH agonists in this regard, although this remains to be fully proven, while rapid testosterone recovery and oral administration may also have benefits in particular contexts,” Dr. Mostaghel said.
“It is likely that the anticancer effects of a GnRH antagonist will not be inferior to those of a GnRH agonist and may be beneficial in terms of cardiovascular events that may be life-limiting,” Celestia S. Higano, MD, of the University of Washington in Seattle wrote in an editorial accompanying the HERO study in The New England Journal of Medicine.
“Close monitoring will be required because exposure to oral relugolix for longer than 48 weeks has not been studied and many oral agents are associated with adherence problems, especially if they cause adverse effects,” Dr. Higano added.
The HERO study was supported by Myovant. Dr. Shore disclosed relationships with Myovant and other companies. Dr. Mostaghel disclosed affiliations with Context Therapeutics. Dr. Hinago disclosed grants and fees from various companies, not including Myovant.
SOURCES: Shore ND et al. ASCO 2020, Abstract 5602; N Engl J Med. 2020 May 29. doi: 10.1056/NEJMoa2004325.
according to investigators from the phase 3 HERO trial.
Relugolix was also associated with a significantly lower incidence of major adverse cardiovascular events (MACE), reported Neal D. Shore, MD, of the Carolina Urologic Research Center in Myrtle Beach, S.C., in a presentation made as a part of the American Society of Clinical Oncology virtual scientific program. The study was published simultaneously in The New England Journal of Medicine.
“Relugolix is a novel oral GnRH antagonist that has the potential to become a new standard for ADT [androgen-deprivation therapy] in advanced prostate cancer,” Dr. Shore said. He added that a potential advantage of relugolix compared with the leutenizing hormone-releasing hormone (LHRH) agonist leuprolide is the oral agent’s adverse event profile.
“Of note, and importantly, cardiovascular mortality is the leading cause of death for patients with prostate cancer. The percentage of patients with prostate cancer dying of cardiovascular disease has surpassed the percentage of patients dying from prostate cancer itself since the early 1990s. Approximately 30% of men with prostate cancer have known cardiovascular disease, and many more of these patients have comorbid risk factors, including obesity, diabetes, hypertension, and hyperlipidemia,” Dr. Shore said.
LHRH agonists also cause an initial testosterone surge that may cause an early but transient symptom flare. In contrast, relugolix has a direct inhibitory effect on pituitary GnRH receptors, leading to suppression of both leutenizing hormone and follicle-stimulating hormone, with no testosterone flare.
Study details
In the HERO trial, men with advanced prostate cancer were randomized in a 2:1 ratio to receive either relugolix at a 360-mg loading dose on day 1 followed by a 120-mg oral dose once daily (n = 622) or leuprolide delivered via depot injection every 3 months (n = 308) for a total of 48 weeks.
About half of all patients in each arm had biochemical (prostate-specific antigen, or “PSA”) relapse, 23% had newly diagnosed androgen-sensitive metastatic disease, and the remaining men (26%-28%) had advanced localized disease.
Patients with a history of a MACE event – a composite of nonfatal myocardial infarction, nonfatal stroke, and death from any cause – within 6 months were excluded.
The median PSA level at baseline was 11.7 mg/mL in the relugolix arm and 9.4 ng/mL in the leuprolide arm. Respective median testosterone levels were 415.8 ng/dL and 395.9 ng/dL.
“Of note, more than 90% of men enrolled in this study had at least one cardiovascular risk factor,” Dr. Shore said. “Tobacco use and obesity were common, as were diabetes and hypertension. Fourteen percent of men reported a prior history of major adverse cardiovascular event, such as a heart attack or stroke; this is lower than the 30% expected in a typical population of men with advanced prostate cancer given the study’s cardiovascular exclusion criteria.”
Efficacy
Sustained testosterone suppression to castration levels (less than 50 ng/dL) was achieved through 48 weeks in 96.7% of patients on relugolix, compared with 88.8% of men on leuprolide.
The absolute difference of 7.9% reached the statistical definitions for both noninferiority and superiority of relugolix over leuprolide (P for superiority < .001).
Mean testosterone levels on day 4 had decreased to below 50 ng/dL for relugolix and were maintained at castration levels until the end of treatment. In the leuprolide group, the mean testosterone level on day 4 was 625 ng/dL, which declined to castration levels by day 29 and remained below 50 ng/dL after the end of treatment at week 53. In contrast, testosterone levels in the relugolix arm began to recover immediately after the cessation of therapy.
Results with relugolix were significantly better than with leuprolide for the following endpoints (P < .0001 for all comparisons):
- Proportion of patients with PSA response at day 15 and confirmed at day 29 (79.4% vs. 19.8%)
- Cumulative probability of testosterone suppression to less than 50 ng/dL on day 15 (98.7% vs. 12.05%)
- Cumulative probability of profound testosterone suppression to less than 20 ng/dL on day 15 (78.38% vs. 0.98%)
- Mean follicle-stimulating hormone level at the end of week 24 (1.72 vs. 5.95 IU/L).
Safety
Treatment-related adverse events occurred in 73.6% of patients treated with relugolix and 68.8% of those who received leuprolide. Grade 3 or greater adverse events occurred in 3.4% and 2.6%, respectively. The respective incidences of fatal adverse events were 1.1% and 2.9%.
At 48 weeks, MACE had occurred in 2.9% of patients on relugolix and 6.2% on leuprolide. Among men with a history of a MACE event more than 6 months before study entry, leuprolide was associated with a nearly sixfold increased risk for a new MACE.
The investigators also found that compliance with the assigned medication was greater than 99% in each study arm, allaying concerns that men assigned to the oral therapy might be less likely to faithfully take their medicine.
Antagonists vs. agonists
Agents such as relugolix, which are, in effect, LHRH antagonists, have several advantages over LHRH agonists, according to invited discussant Elahe Mostaghel, MD, PhD, of the VA Puget Sound Health Care System and Fred Hutchinson Cancer Research Center, both in Seattle.
“Cost and access aside, antagonists have potential benefits over agonists, each of which may be more or less important, depending on context,” she said.
Antagonists have a more rapid onset of castration, lack the flare response seen with agonists such as leuprolide, and are associated with a significant decrease in risk for MACE.
“Differences in depth and consistency of androgen suppression may also be important. LHRH antagonists may be superior to LHRH agonists in this regard, although this remains to be fully proven, while rapid testosterone recovery and oral administration may also have benefits in particular contexts,” Dr. Mostaghel said.
“It is likely that the anticancer effects of a GnRH antagonist will not be inferior to those of a GnRH agonist and may be beneficial in terms of cardiovascular events that may be life-limiting,” Celestia S. Higano, MD, of the University of Washington in Seattle wrote in an editorial accompanying the HERO study in The New England Journal of Medicine.
“Close monitoring will be required because exposure to oral relugolix for longer than 48 weeks has not been studied and many oral agents are associated with adherence problems, especially if they cause adverse effects,” Dr. Higano added.
The HERO study was supported by Myovant. Dr. Shore disclosed relationships with Myovant and other companies. Dr. Mostaghel disclosed affiliations with Context Therapeutics. Dr. Hinago disclosed grants and fees from various companies, not including Myovant.
SOURCES: Shore ND et al. ASCO 2020, Abstract 5602; N Engl J Med. 2020 May 29. doi: 10.1056/NEJMoa2004325.
FROM ASCO 2020
Capecitabine maintenance improved DFS, not OS, in TNBC patients
according to results of a phase 3 trial.
Patients who received metronomic capecitabine maintenance had significantly higher rates of 5-year DFS and distant DFS, but not OS, when compared with patients who did not receive capecitabine, reported Xi Wang, PhD, of Sun Yat-sen University Cancer Center in Guangzhou, China, who presented the findings as part of the American Society of Clinical Oncology virtual scientific program.
“TNBC has the worst outcomes among all subtypes of breast cancer,” Dr. Wang said. “Effective strategies to reduce risk of relapse are a critical clinical need.”
He went on to describe capecitabine as a “potential ideal drug for metronomic administration,” particularly among patients with high risk of distant metastasis.
With that in mind, Dr. Wang and colleagues tested metronomic capecitabine maintenance in the phase 3 SYSUCC-001 trial. The trial included 434 patients with invasive ductal carcinoma. They had undergone standard therapy, which included surgery, neoadjuvant/adjuvant chemotherapy, and radiation therapy.
Patients were randomized to receive capecitabine at 650 mg/m2 twice daily for 1 year (n = 221) or undergo observation (n = 213). The primary endpoint was DFS, while secondary endpoints included safety, distant DFS, and OS.
According to Dr. Wang, the two patient groups were “well balanced,” with similar baseline characteristics. Most patients underwent adjuvant chemotherapy (93%), had histological grade 3 tumors (71%-74%), had a Ki-67 index of at least 30% (73%-80%), had negative lymph node status (61%-62%), had a tumor size of 2.1-5 cm (55%-58%), and/or pathologic stage II disease (54%-55%).
Survival and safety
At a median follow-up of 56.5 months, the median 5-year DFS rate was 83% in the capecitabine group, compared with 73% in the observation group (P = .027). Similarly, capecitabine use correlated with a significantly better rate of distant DFS (85% vs. 76%; P = .016).
Although the capecitabine group demonstrated a slight trend toward improved OS at 5 years, this finding was not statistically significant (86% vs. 81%; P = .203).
Capecitabine was generally well tolerated, with 91% of patients completing 1 year of therapy, and 75% completing therapy at the full dose.
Almost half of patients in the capecitabine group experienced hand-foot syndrome (45%), and one in four developed leukopenia (24%). Less common adverse events included hyperbilirubinemia (13%), gastrointestinal pain (7%), and elevated serum transaminases (5%). No unexpected serious adverse events occurred.
Effects on practice
Amy Tiersten, MD, of the Icahn School of Medicine at Mount Sinai in New York, suggested these findings may lead to broader use of capecitabine among patients with TNBC.
“[This is a] very exciting study showing an impressive disease-free survival benefit in the adjuvant setting for capecitabine in patients with early stage TNBC,” Dr. Tiersten said. “Presently, we only have positive data for capecitabine in patients with residual disease after neoadjuvant therapy, but this current study now suggests that this benefit could extend to all comers.”
Dr. Tiersten advised that the medical community stay tuned, since longer-term data may provide a clearer picture of survival benefit.
“It will be interesting to see if there is an impact on overall survival with further follow-up,” she said.
According to invited discussant Naamit Kurshan Gerber, MD, of New York University, the results support previous findings from the CREATE-X trial, along with meta-analyses that have shown a “preferential benefit” of capecitabine when used to treat TNBC, compared with estrogen receptor–positive disease.
Still, Dr. Gerber noted that, for most patients, the findings from the SYSUCC-001 trial are unlikely to influence clinical decision-making since most patients with TNBC receive neoadjuvant chemotherapy followed by treatment based on pathologic response. However, she also suggested that, after peer review, the findings could influence treatment for a select few.
“For the small population of patients who receive adjuvant chemotherapy for higher-stage TNBC and who would have met eligibility criteria, this approach may be considered,” Dr. Gerber said.
The study was funded by the Sun Yat-sen University Clinical Research 5010 Program. The investigators disclosed no conflicts of interest. Dr. Gerber reported a relationship with OncLive. Dr. Tiersten reported no relevant disclosures.
SOURCE: Wang X et al. ASCO 2020, Abstract 507.
according to results of a phase 3 trial.
Patients who received metronomic capecitabine maintenance had significantly higher rates of 5-year DFS and distant DFS, but not OS, when compared with patients who did not receive capecitabine, reported Xi Wang, PhD, of Sun Yat-sen University Cancer Center in Guangzhou, China, who presented the findings as part of the American Society of Clinical Oncology virtual scientific program.
“TNBC has the worst outcomes among all subtypes of breast cancer,” Dr. Wang said. “Effective strategies to reduce risk of relapse are a critical clinical need.”
He went on to describe capecitabine as a “potential ideal drug for metronomic administration,” particularly among patients with high risk of distant metastasis.
With that in mind, Dr. Wang and colleagues tested metronomic capecitabine maintenance in the phase 3 SYSUCC-001 trial. The trial included 434 patients with invasive ductal carcinoma. They had undergone standard therapy, which included surgery, neoadjuvant/adjuvant chemotherapy, and radiation therapy.
Patients were randomized to receive capecitabine at 650 mg/m2 twice daily for 1 year (n = 221) or undergo observation (n = 213). The primary endpoint was DFS, while secondary endpoints included safety, distant DFS, and OS.
According to Dr. Wang, the two patient groups were “well balanced,” with similar baseline characteristics. Most patients underwent adjuvant chemotherapy (93%), had histological grade 3 tumors (71%-74%), had a Ki-67 index of at least 30% (73%-80%), had negative lymph node status (61%-62%), had a tumor size of 2.1-5 cm (55%-58%), and/or pathologic stage II disease (54%-55%).
Survival and safety
At a median follow-up of 56.5 months, the median 5-year DFS rate was 83% in the capecitabine group, compared with 73% in the observation group (P = .027). Similarly, capecitabine use correlated with a significantly better rate of distant DFS (85% vs. 76%; P = .016).
Although the capecitabine group demonstrated a slight trend toward improved OS at 5 years, this finding was not statistically significant (86% vs. 81%; P = .203).
Capecitabine was generally well tolerated, with 91% of patients completing 1 year of therapy, and 75% completing therapy at the full dose.
Almost half of patients in the capecitabine group experienced hand-foot syndrome (45%), and one in four developed leukopenia (24%). Less common adverse events included hyperbilirubinemia (13%), gastrointestinal pain (7%), and elevated serum transaminases (5%). No unexpected serious adverse events occurred.
Effects on practice
Amy Tiersten, MD, of the Icahn School of Medicine at Mount Sinai in New York, suggested these findings may lead to broader use of capecitabine among patients with TNBC.
“[This is a] very exciting study showing an impressive disease-free survival benefit in the adjuvant setting for capecitabine in patients with early stage TNBC,” Dr. Tiersten said. “Presently, we only have positive data for capecitabine in patients with residual disease after neoadjuvant therapy, but this current study now suggests that this benefit could extend to all comers.”
Dr. Tiersten advised that the medical community stay tuned, since longer-term data may provide a clearer picture of survival benefit.
“It will be interesting to see if there is an impact on overall survival with further follow-up,” she said.
According to invited discussant Naamit Kurshan Gerber, MD, of New York University, the results support previous findings from the CREATE-X trial, along with meta-analyses that have shown a “preferential benefit” of capecitabine when used to treat TNBC, compared with estrogen receptor–positive disease.
Still, Dr. Gerber noted that, for most patients, the findings from the SYSUCC-001 trial are unlikely to influence clinical decision-making since most patients with TNBC receive neoadjuvant chemotherapy followed by treatment based on pathologic response. However, she also suggested that, after peer review, the findings could influence treatment for a select few.
“For the small population of patients who receive adjuvant chemotherapy for higher-stage TNBC and who would have met eligibility criteria, this approach may be considered,” Dr. Gerber said.
The study was funded by the Sun Yat-sen University Clinical Research 5010 Program. The investigators disclosed no conflicts of interest. Dr. Gerber reported a relationship with OncLive. Dr. Tiersten reported no relevant disclosures.
SOURCE: Wang X et al. ASCO 2020, Abstract 507.
according to results of a phase 3 trial.
Patients who received metronomic capecitabine maintenance had significantly higher rates of 5-year DFS and distant DFS, but not OS, when compared with patients who did not receive capecitabine, reported Xi Wang, PhD, of Sun Yat-sen University Cancer Center in Guangzhou, China, who presented the findings as part of the American Society of Clinical Oncology virtual scientific program.
“TNBC has the worst outcomes among all subtypes of breast cancer,” Dr. Wang said. “Effective strategies to reduce risk of relapse are a critical clinical need.”
He went on to describe capecitabine as a “potential ideal drug for metronomic administration,” particularly among patients with high risk of distant metastasis.
With that in mind, Dr. Wang and colleagues tested metronomic capecitabine maintenance in the phase 3 SYSUCC-001 trial. The trial included 434 patients with invasive ductal carcinoma. They had undergone standard therapy, which included surgery, neoadjuvant/adjuvant chemotherapy, and radiation therapy.
Patients were randomized to receive capecitabine at 650 mg/m2 twice daily for 1 year (n = 221) or undergo observation (n = 213). The primary endpoint was DFS, while secondary endpoints included safety, distant DFS, and OS.
According to Dr. Wang, the two patient groups were “well balanced,” with similar baseline characteristics. Most patients underwent adjuvant chemotherapy (93%), had histological grade 3 tumors (71%-74%), had a Ki-67 index of at least 30% (73%-80%), had negative lymph node status (61%-62%), had a tumor size of 2.1-5 cm (55%-58%), and/or pathologic stage II disease (54%-55%).
Survival and safety
At a median follow-up of 56.5 months, the median 5-year DFS rate was 83% in the capecitabine group, compared with 73% in the observation group (P = .027). Similarly, capecitabine use correlated with a significantly better rate of distant DFS (85% vs. 76%; P = .016).
Although the capecitabine group demonstrated a slight trend toward improved OS at 5 years, this finding was not statistically significant (86% vs. 81%; P = .203).
Capecitabine was generally well tolerated, with 91% of patients completing 1 year of therapy, and 75% completing therapy at the full dose.
Almost half of patients in the capecitabine group experienced hand-foot syndrome (45%), and one in four developed leukopenia (24%). Less common adverse events included hyperbilirubinemia (13%), gastrointestinal pain (7%), and elevated serum transaminases (5%). No unexpected serious adverse events occurred.
Effects on practice
Amy Tiersten, MD, of the Icahn School of Medicine at Mount Sinai in New York, suggested these findings may lead to broader use of capecitabine among patients with TNBC.
“[This is a] very exciting study showing an impressive disease-free survival benefit in the adjuvant setting for capecitabine in patients with early stage TNBC,” Dr. Tiersten said. “Presently, we only have positive data for capecitabine in patients with residual disease after neoadjuvant therapy, but this current study now suggests that this benefit could extend to all comers.”
Dr. Tiersten advised that the medical community stay tuned, since longer-term data may provide a clearer picture of survival benefit.
“It will be interesting to see if there is an impact on overall survival with further follow-up,” she said.
According to invited discussant Naamit Kurshan Gerber, MD, of New York University, the results support previous findings from the CREATE-X trial, along with meta-analyses that have shown a “preferential benefit” of capecitabine when used to treat TNBC, compared with estrogen receptor–positive disease.
Still, Dr. Gerber noted that, for most patients, the findings from the SYSUCC-001 trial are unlikely to influence clinical decision-making since most patients with TNBC receive neoadjuvant chemotherapy followed by treatment based on pathologic response. However, she also suggested that, after peer review, the findings could influence treatment for a select few.
“For the small population of patients who receive adjuvant chemotherapy for higher-stage TNBC and who would have met eligibility criteria, this approach may be considered,” Dr. Gerber said.
The study was funded by the Sun Yat-sen University Clinical Research 5010 Program. The investigators disclosed no conflicts of interest. Dr. Gerber reported a relationship with OncLive. Dr. Tiersten reported no relevant disclosures.
SOURCE: Wang X et al. ASCO 2020, Abstract 507.
FROM ASCO 2020
PPI added to chemo improves breast tumor response rate
The proton pump inhibitor (PPI) omeprazole may be a useful addition to treatment for triple-negative breast cancer, as it boosted the expected rate of tumor disappearance among women with early-stage disease, according to the results of a phase 2 trial.
The trial results are presented online at the 2020 virtual annual meeting of the American Society of Clinical Oncology.
The rationale behind the approach includes the fact that PPIs inhibit fatty acid synthase (FASN), an enzyme overexpressed in 70% of newly diagnosed triple-negative breast cancers (TNBC) and associated with poor prognosis.
In the study, omeprazole, a generic drug for gastroesophageal reflux, was added to standard chemotherapy. Both were given to 42 women as neoadjuvant treatment in the weeks before breast surgery at five US centers in the single-arm study.
The pathologic complete response (pCR) rate was 71% in the study population, which is higher than the typical 40% seen in patients treated with standard AC-T (adriamycin and cyclophosphamide plus a taxane), said lead author Sagar D. Sardesai, MBBS, a medical oncologist at Ohio State Comprehensive Cancer Center in Columbus.
“It’s exciting,” said Dr. Sardesai in an interview. “Overall, triple-negative patients who achieve a pCR have a very good outcome.”
That complete disappearance of the tumor is a surrogate for overall survival in TNBC, and patients who achieve it have a greatly reduced risk of recurrence or death, he explained.
Natalie Berger, MD, medical oncologist, Icahn School of Medicine at Mount Sinai, New York City, said the study’s pCR rates were “much higher” than expected and “intriguing and hypothesis generating.”
But Dr. Berger, who was not involved in the study, wanted to see more data.
“Having a non-chemotherapeutic agent to offer our patients with TNBC that improves pCR rates without added toxicity would be an exciting finding, but we need a larger randomized study,” she said in an email.
The researchers, who include high-profile breast cancer specialist Kathy Miller, MD, of Indiana University, are seeking a National Cancer Institute or Department of Defense grant to mount a 100-plus patient randomized trial.
Potential Drug Target for Some Years
Dr. Sardesai explained that FASN, which is an enzyme, helps generate fatty acids that are a key to cancer cell survival. FASN is primarily found in hormone-dominated tissue such as those of the endometrium, prostate, and breast.
PPIs “selectively inhibit FASN activity and induce apoptosis in breast cancer cell lines with minimal effect on non-malignant cells,” wrote the study authors in their meeting abstract.
The only other known agent known to inhibit FASN is the weight loss drug orlistat, which is poorly absorbed by the body and unlikely to impact cancer cells, Dr. Sardesai said.
FASN has been a potential drug target in TNBC for 10 to 15 years, but the first clinical evidence of efficacy in solid tumors was only seen in the last 5 years, he commented.
In 2015, Chinese investigators reported that the PPI esomeprazole in combination with chemotherapy produced a 5-month improvement in progression-free survival (vs. chemo alone) among a subset of 15 TNBC patients in a randomized trial of 94 patients with a variety of breast cancer types.
No Added Toxicity, But Some Unexpected Findings
The study was conducted in patients with early-stage, operable TNBC (with and without baseline FASN expression) and no prior PPI use within 12 months.
All patients started daily high-dose omeprazole 4 to 7 days prior to start of AC-T neoadjuvant chemotherapy (the addition of carboplatin was allowed per physician discretion) and continued until surgery.
The primary endpoint was pCR, defined as no residual invasive disease in breast or axilla, in patients with baseline FASN expression (FASN+). The pCR rate was 71.4% in the 28 FASN+ patients and 71.8% in all 42 enrolled patients. The researchers had targeted a pCR rate of 60% in the FASN+ patients. Also, among the subset of 15 patients who received carboplatin with AC-T, the pCR was 73%.
These two findings both have limitations, commented Dr. Berger. She pointed out that it is “unexplained” as to why the pCR rates were similar among the FASN+ patients and the total population (including 14 FASN– patients); the pCR rate would be expected to be lower in the total population, she suggested.
Further, it was also unexplained as to why there were similar pCR rates with or without carboplatin; other research has demonstrated improved pCR rates in patients receiving additional carboplatin (compared to AC-T alone) but at the cost of increased toxicity, she said.
Dr. Sardesai said that omeprazole was well tolerated with no known grade 3 or 4 toxicities and that the chemotherapy toxicity was similar to prior studies of AC-T. PPIs have side effects if taken for longer than a year, including a higher risk of infections, osteoporosis, and low magnesium, he also commented.
“Omeprazole can be safely administered in doses that inhibit FASN. The addition of high-dose omeprazole to neoadjuvant AC-T yields a promising pCR rate without adding toxicity,” the authors concluded in their abstract.
Dr. Sardesai also highlighted the fact that using a PPI for breast cancer is an example of drug repurposing. The approach offers a way of rapid drug development because PPIs have complete safety and pharmacokinetics data available, he said. “If we can prove the efficacy, the treatment can move forward quickly and be available in clinical practice much sooner than with traditional drug development.”
The study was funded by the Breast Cancer Research Foundation. Dr. Sardesai disclosed financial ties to Novartis and Immunomedics. Other study authors have ties to industry. Dr. Berger disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The proton pump inhibitor (PPI) omeprazole may be a useful addition to treatment for triple-negative breast cancer, as it boosted the expected rate of tumor disappearance among women with early-stage disease, according to the results of a phase 2 trial.
The trial results are presented online at the 2020 virtual annual meeting of the American Society of Clinical Oncology.
The rationale behind the approach includes the fact that PPIs inhibit fatty acid synthase (FASN), an enzyme overexpressed in 70% of newly diagnosed triple-negative breast cancers (TNBC) and associated with poor prognosis.
In the study, omeprazole, a generic drug for gastroesophageal reflux, was added to standard chemotherapy. Both were given to 42 women as neoadjuvant treatment in the weeks before breast surgery at five US centers in the single-arm study.
The pathologic complete response (pCR) rate was 71% in the study population, which is higher than the typical 40% seen in patients treated with standard AC-T (adriamycin and cyclophosphamide plus a taxane), said lead author Sagar D. Sardesai, MBBS, a medical oncologist at Ohio State Comprehensive Cancer Center in Columbus.
“It’s exciting,” said Dr. Sardesai in an interview. “Overall, triple-negative patients who achieve a pCR have a very good outcome.”
That complete disappearance of the tumor is a surrogate for overall survival in TNBC, and patients who achieve it have a greatly reduced risk of recurrence or death, he explained.
Natalie Berger, MD, medical oncologist, Icahn School of Medicine at Mount Sinai, New York City, said the study’s pCR rates were “much higher” than expected and “intriguing and hypothesis generating.”
But Dr. Berger, who was not involved in the study, wanted to see more data.
“Having a non-chemotherapeutic agent to offer our patients with TNBC that improves pCR rates without added toxicity would be an exciting finding, but we need a larger randomized study,” she said in an email.
The researchers, who include high-profile breast cancer specialist Kathy Miller, MD, of Indiana University, are seeking a National Cancer Institute or Department of Defense grant to mount a 100-plus patient randomized trial.
Potential Drug Target for Some Years
Dr. Sardesai explained that FASN, which is an enzyme, helps generate fatty acids that are a key to cancer cell survival. FASN is primarily found in hormone-dominated tissue such as those of the endometrium, prostate, and breast.
PPIs “selectively inhibit FASN activity and induce apoptosis in breast cancer cell lines with minimal effect on non-malignant cells,” wrote the study authors in their meeting abstract.
The only other known agent known to inhibit FASN is the weight loss drug orlistat, which is poorly absorbed by the body and unlikely to impact cancer cells, Dr. Sardesai said.
FASN has been a potential drug target in TNBC for 10 to 15 years, but the first clinical evidence of efficacy in solid tumors was only seen in the last 5 years, he commented.
In 2015, Chinese investigators reported that the PPI esomeprazole in combination with chemotherapy produced a 5-month improvement in progression-free survival (vs. chemo alone) among a subset of 15 TNBC patients in a randomized trial of 94 patients with a variety of breast cancer types.
No Added Toxicity, But Some Unexpected Findings
The study was conducted in patients with early-stage, operable TNBC (with and without baseline FASN expression) and no prior PPI use within 12 months.
All patients started daily high-dose omeprazole 4 to 7 days prior to start of AC-T neoadjuvant chemotherapy (the addition of carboplatin was allowed per physician discretion) and continued until surgery.
The primary endpoint was pCR, defined as no residual invasive disease in breast or axilla, in patients with baseline FASN expression (FASN+). The pCR rate was 71.4% in the 28 FASN+ patients and 71.8% in all 42 enrolled patients. The researchers had targeted a pCR rate of 60% in the FASN+ patients. Also, among the subset of 15 patients who received carboplatin with AC-T, the pCR was 73%.
These two findings both have limitations, commented Dr. Berger. She pointed out that it is “unexplained” as to why the pCR rates were similar among the FASN+ patients and the total population (including 14 FASN– patients); the pCR rate would be expected to be lower in the total population, she suggested.
Further, it was also unexplained as to why there were similar pCR rates with or without carboplatin; other research has demonstrated improved pCR rates in patients receiving additional carboplatin (compared to AC-T alone) but at the cost of increased toxicity, she said.
Dr. Sardesai said that omeprazole was well tolerated with no known grade 3 or 4 toxicities and that the chemotherapy toxicity was similar to prior studies of AC-T. PPIs have side effects if taken for longer than a year, including a higher risk of infections, osteoporosis, and low magnesium, he also commented.
“Omeprazole can be safely administered in doses that inhibit FASN. The addition of high-dose omeprazole to neoadjuvant AC-T yields a promising pCR rate without adding toxicity,” the authors concluded in their abstract.
Dr. Sardesai also highlighted the fact that using a PPI for breast cancer is an example of drug repurposing. The approach offers a way of rapid drug development because PPIs have complete safety and pharmacokinetics data available, he said. “If we can prove the efficacy, the treatment can move forward quickly and be available in clinical practice much sooner than with traditional drug development.”
The study was funded by the Breast Cancer Research Foundation. Dr. Sardesai disclosed financial ties to Novartis and Immunomedics. Other study authors have ties to industry. Dr. Berger disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The proton pump inhibitor (PPI) omeprazole may be a useful addition to treatment for triple-negative breast cancer, as it boosted the expected rate of tumor disappearance among women with early-stage disease, according to the results of a phase 2 trial.
The trial results are presented online at the 2020 virtual annual meeting of the American Society of Clinical Oncology.
The rationale behind the approach includes the fact that PPIs inhibit fatty acid synthase (FASN), an enzyme overexpressed in 70% of newly diagnosed triple-negative breast cancers (TNBC) and associated with poor prognosis.
In the study, omeprazole, a generic drug for gastroesophageal reflux, was added to standard chemotherapy. Both were given to 42 women as neoadjuvant treatment in the weeks before breast surgery at five US centers in the single-arm study.
The pathologic complete response (pCR) rate was 71% in the study population, which is higher than the typical 40% seen in patients treated with standard AC-T (adriamycin and cyclophosphamide plus a taxane), said lead author Sagar D. Sardesai, MBBS, a medical oncologist at Ohio State Comprehensive Cancer Center in Columbus.
“It’s exciting,” said Dr. Sardesai in an interview. “Overall, triple-negative patients who achieve a pCR have a very good outcome.”
That complete disappearance of the tumor is a surrogate for overall survival in TNBC, and patients who achieve it have a greatly reduced risk of recurrence or death, he explained.
Natalie Berger, MD, medical oncologist, Icahn School of Medicine at Mount Sinai, New York City, said the study’s pCR rates were “much higher” than expected and “intriguing and hypothesis generating.”
But Dr. Berger, who was not involved in the study, wanted to see more data.
“Having a non-chemotherapeutic agent to offer our patients with TNBC that improves pCR rates without added toxicity would be an exciting finding, but we need a larger randomized study,” she said in an email.
The researchers, who include high-profile breast cancer specialist Kathy Miller, MD, of Indiana University, are seeking a National Cancer Institute or Department of Defense grant to mount a 100-plus patient randomized trial.
Potential Drug Target for Some Years
Dr. Sardesai explained that FASN, which is an enzyme, helps generate fatty acids that are a key to cancer cell survival. FASN is primarily found in hormone-dominated tissue such as those of the endometrium, prostate, and breast.
PPIs “selectively inhibit FASN activity and induce apoptosis in breast cancer cell lines with minimal effect on non-malignant cells,” wrote the study authors in their meeting abstract.
The only other known agent known to inhibit FASN is the weight loss drug orlistat, which is poorly absorbed by the body and unlikely to impact cancer cells, Dr. Sardesai said.
FASN has been a potential drug target in TNBC for 10 to 15 years, but the first clinical evidence of efficacy in solid tumors was only seen in the last 5 years, he commented.
In 2015, Chinese investigators reported that the PPI esomeprazole in combination with chemotherapy produced a 5-month improvement in progression-free survival (vs. chemo alone) among a subset of 15 TNBC patients in a randomized trial of 94 patients with a variety of breast cancer types.
No Added Toxicity, But Some Unexpected Findings
The study was conducted in patients with early-stage, operable TNBC (with and without baseline FASN expression) and no prior PPI use within 12 months.
All patients started daily high-dose omeprazole 4 to 7 days prior to start of AC-T neoadjuvant chemotherapy (the addition of carboplatin was allowed per physician discretion) and continued until surgery.
The primary endpoint was pCR, defined as no residual invasive disease in breast or axilla, in patients with baseline FASN expression (FASN+). The pCR rate was 71.4% in the 28 FASN+ patients and 71.8% in all 42 enrolled patients. The researchers had targeted a pCR rate of 60% in the FASN+ patients. Also, among the subset of 15 patients who received carboplatin with AC-T, the pCR was 73%.
These two findings both have limitations, commented Dr. Berger. She pointed out that it is “unexplained” as to why the pCR rates were similar among the FASN+ patients and the total population (including 14 FASN– patients); the pCR rate would be expected to be lower in the total population, she suggested.
Further, it was also unexplained as to why there were similar pCR rates with or without carboplatin; other research has demonstrated improved pCR rates in patients receiving additional carboplatin (compared to AC-T alone) but at the cost of increased toxicity, she said.
Dr. Sardesai said that omeprazole was well tolerated with no known grade 3 or 4 toxicities and that the chemotherapy toxicity was similar to prior studies of AC-T. PPIs have side effects if taken for longer than a year, including a higher risk of infections, osteoporosis, and low magnesium, he also commented.
“Omeprazole can be safely administered in doses that inhibit FASN. The addition of high-dose omeprazole to neoadjuvant AC-T yields a promising pCR rate without adding toxicity,” the authors concluded in their abstract.
Dr. Sardesai also highlighted the fact that using a PPI for breast cancer is an example of drug repurposing. The approach offers a way of rapid drug development because PPIs have complete safety and pharmacokinetics data available, he said. “If we can prove the efficacy, the treatment can move forward quickly and be available in clinical practice much sooner than with traditional drug development.”
The study was funded by the Breast Cancer Research Foundation. Dr. Sardesai disclosed financial ties to Novartis and Immunomedics. Other study authors have ties to industry. Dr. Berger disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
FROM ASCO 2020
First-line nivolumab plus platinum/etoposide effective in extensive-stage SCLC
While nivolumab plus doublet chemotherapy was effective in extensive-stage small-cell lung cancer (ES-SCLC) in a recent randomized trial, the results might not be sufficient to change current clinical practice, in which two first-line chemo-immunotherapies are already approved and recommended, sources said.
Nivolumab added to platinum/etoposide doublet chemotherapy was well tolerated and significantly improved progression-free survival (PFS) and overall survival (OS) compared to chemotherapy alone, according to results of ECOG-ACRIN EA5161, a randomized, phase 2 trial including 160 patients with ES-SCLC.
Risks of progression and death were reduced by 32% and 27%, respectively, when the immune checkpoint inhibitor was given along with chemotherapy, according to data presented by investigator Ticiana A. Leal, MD, of the University of Wisconsin Carbone Cancer Center in Madison.
“Our study, EA5161, confirms the efficacy of nivolumab in extensive-stage small cell lung cancer,” Dr. Leal said in a presentation she gave as part of the American Society of Clinical Oncology virtual scientific program.
Nivolumab did demonstrate a clear PFS advantage in EA5161, but “more surprisingly for a small trial” it also showed a clear OS advantage, said Taofeek K. Owonikoko, MD, PhD, in a commentary on the study.
“While the study as currently reported is insufficient to change practice, it does however provide very strong data to make the combination of nivolumab and platinum doublet acceptable as a platform for future clinical trials,” he said in the commentary, which was also included in the virtual ASCO proceedings.
Going forward, it would be difficult to justify another nondefinitive randomized phase 2 chemo-immunotherapy trial, especially if there are no “immediate plans” for a confirmatory phase 3 trial, added Dr. Owonikoko, who is director of thoracic oncology at Winship Cancer Institute of Emory University in Atlanta.
Nivolumab wasn’t the only immune checkpoint with new first-line data in ES-SCLC at ASCO. In the randomized, double-blind, phase 3 KEYNOTE-604 trial, pembrolizumab added to etoposide and platinum significantly prolonged PFS and showed a trend toward improved OS. However, the significance threshold for OS was missed, according to the report.
While these pembrolizumab data are also insufficient to change today’s practice standards, results for both the pembrolizumab- and nivolumab-containing regimens are nevertheless compelling to support their use as a platform for new treatment strategies, according to Dr. Owonikoko.
With these new ASCO data, there are now randomized data confirming a benefit of immune checkpoint inhibitor–based regimens in ES-SCLC, according to Lauren A. Byers, MD, from the department of thoracic/head and neck medical oncology at The University of Texas MD Anderson Cancer Center in Houston.
Immune checkpoint inhibitors that are approved by the Food and Drug Administration for first-line treatment of ES-SCLC include atezolizumab (in combination with carboplatin and etoposide) and durvalumab (in combination with either carboplatin or cisplatin plus etoposide). In current National Comprehensive Cancer Network (NCCN) guidelines, both are described as “preferred” regimens for primary or adjuvant therapy.
“A lot of times in oncology we have trials with similar drugs, and you get somewhat different answers in terms of the outcome of the trials, so we’re kind of trying to tease them apart,” Dr. Byers said in an interview.
“I think in this situation, we’ve got four studies, and they essentially are extremely similar in terms of the result, which just gives us even more confidence that there is benefit, at least for a subset of patients.”
The EA5161 study was developed to evaluate the role of nivolumab in ES-SCLC, Dr. Leal said in her virtual ASCO presentation.
Of the 160 patients enrolled and randomized, 145 were eligible and treated, including 75 in the nivolumab plus chemotherapy arm and 70 in the chemotherapy arm. Participants were evenly split between performance status 0 and 1, and little more than half of patients were women, and a median of five treatment cycles were delivered in each arm.
Median PFS, the primary end point of the trial, was 5.5 months for nivolumab plus chemotherapy versus 4.7 months for chemotherapy alone for all eligible and treated patients (hazard ratio, 0.68; 95% confidence interval, 0.48-1.00; P = .047). In the intent-to-treat population, median PFS was 5.5 and 4.6 months in the respective arms (HR, 0.65; 95% CI, 0.46-0.91; P = .012).
Median overall survival was 11.3 months and 9.3 months for the nivolumab plus chemotherapy and chemotherapy-only arms, respectively, for all eligible and treated patients (HR, 0.73; 95% CI, 0.49-1.1), and in the intent-to-treat population, median OS was 11.3 and 8.5 months for the respective arms (HR, 0.67; 95% CI, 0.46-0.98; P = .038).
The overall response rate was 52% for nivolumab plus chemotherapy and 47% for chemotherapy alone, with a median duration of response of 5.6 and 3.3 months, respectively, Dr. Leal reported.
Treatment was generally well tolerated in both arms, according to the investigator, with no safety signals observed. Toxicities resulting in death occurred in nine patients in the nivolumab plus chemotherapy arm and seven in the chemotherapy-only arm. “Most of the events were related to progression of disease,” Dr. Leal said.
While nivolumab and pembrolizumab’s use in the first-line setting may be uncertain, it is currently approved for metastatic SCLC that has progressed following platinum-based chemotherapy and at least one more line of therapy, according to the drug’s package insert.
The EA5161 study was sponsored by the National Cancer Institute. Dr. Leal provided disclosures related to AbbVie, AstraZeneca, Bayer, BeyondSpring, Bristol-Myers Squibb, Genentech, InvisionFirst Lung, Merck, Mirati, Novocure, and Takeda.
Dr. Owonikoko provided disclosures related to Bristol-Myers Squibb, Novartis, Celgene, Lilly, Sandoz, AbbVie, Eisai, and Takeda, among others. Dr. Byers reported disclosures related to Bristol-Myers Squibb, AstraZeneca, AbbVie, GenMab, PharmaMar, and Sierra Oncology, Tolero, Alethia, Merck, Jazz Pharmaceuticals, and Pfizer.
SOURCE: Leal TA et al. ASCO 2020, Abstract 9000.
While nivolumab plus doublet chemotherapy was effective in extensive-stage small-cell lung cancer (ES-SCLC) in a recent randomized trial, the results might not be sufficient to change current clinical practice, in which two first-line chemo-immunotherapies are already approved and recommended, sources said.
Nivolumab added to platinum/etoposide doublet chemotherapy was well tolerated and significantly improved progression-free survival (PFS) and overall survival (OS) compared to chemotherapy alone, according to results of ECOG-ACRIN EA5161, a randomized, phase 2 trial including 160 patients with ES-SCLC.
Risks of progression and death were reduced by 32% and 27%, respectively, when the immune checkpoint inhibitor was given along with chemotherapy, according to data presented by investigator Ticiana A. Leal, MD, of the University of Wisconsin Carbone Cancer Center in Madison.
“Our study, EA5161, confirms the efficacy of nivolumab in extensive-stage small cell lung cancer,” Dr. Leal said in a presentation she gave as part of the American Society of Clinical Oncology virtual scientific program.
Nivolumab did demonstrate a clear PFS advantage in EA5161, but “more surprisingly for a small trial” it also showed a clear OS advantage, said Taofeek K. Owonikoko, MD, PhD, in a commentary on the study.
“While the study as currently reported is insufficient to change practice, it does however provide very strong data to make the combination of nivolumab and platinum doublet acceptable as a platform for future clinical trials,” he said in the commentary, which was also included in the virtual ASCO proceedings.
Going forward, it would be difficult to justify another nondefinitive randomized phase 2 chemo-immunotherapy trial, especially if there are no “immediate plans” for a confirmatory phase 3 trial, added Dr. Owonikoko, who is director of thoracic oncology at Winship Cancer Institute of Emory University in Atlanta.
Nivolumab wasn’t the only immune checkpoint with new first-line data in ES-SCLC at ASCO. In the randomized, double-blind, phase 3 KEYNOTE-604 trial, pembrolizumab added to etoposide and platinum significantly prolonged PFS and showed a trend toward improved OS. However, the significance threshold for OS was missed, according to the report.
While these pembrolizumab data are also insufficient to change today’s practice standards, results for both the pembrolizumab- and nivolumab-containing regimens are nevertheless compelling to support their use as a platform for new treatment strategies, according to Dr. Owonikoko.
With these new ASCO data, there are now randomized data confirming a benefit of immune checkpoint inhibitor–based regimens in ES-SCLC, according to Lauren A. Byers, MD, from the department of thoracic/head and neck medical oncology at The University of Texas MD Anderson Cancer Center in Houston.
Immune checkpoint inhibitors that are approved by the Food and Drug Administration for first-line treatment of ES-SCLC include atezolizumab (in combination with carboplatin and etoposide) and durvalumab (in combination with either carboplatin or cisplatin plus etoposide). In current National Comprehensive Cancer Network (NCCN) guidelines, both are described as “preferred” regimens for primary or adjuvant therapy.
“A lot of times in oncology we have trials with similar drugs, and you get somewhat different answers in terms of the outcome of the trials, so we’re kind of trying to tease them apart,” Dr. Byers said in an interview.
“I think in this situation, we’ve got four studies, and they essentially are extremely similar in terms of the result, which just gives us even more confidence that there is benefit, at least for a subset of patients.”
The EA5161 study was developed to evaluate the role of nivolumab in ES-SCLC, Dr. Leal said in her virtual ASCO presentation.
Of the 160 patients enrolled and randomized, 145 were eligible and treated, including 75 in the nivolumab plus chemotherapy arm and 70 in the chemotherapy arm. Participants were evenly split between performance status 0 and 1, and little more than half of patients were women, and a median of five treatment cycles were delivered in each arm.
Median PFS, the primary end point of the trial, was 5.5 months for nivolumab plus chemotherapy versus 4.7 months for chemotherapy alone for all eligible and treated patients (hazard ratio, 0.68; 95% confidence interval, 0.48-1.00; P = .047). In the intent-to-treat population, median PFS was 5.5 and 4.6 months in the respective arms (HR, 0.65; 95% CI, 0.46-0.91; P = .012).
Median overall survival was 11.3 months and 9.3 months for the nivolumab plus chemotherapy and chemotherapy-only arms, respectively, for all eligible and treated patients (HR, 0.73; 95% CI, 0.49-1.1), and in the intent-to-treat population, median OS was 11.3 and 8.5 months for the respective arms (HR, 0.67; 95% CI, 0.46-0.98; P = .038).
The overall response rate was 52% for nivolumab plus chemotherapy and 47% for chemotherapy alone, with a median duration of response of 5.6 and 3.3 months, respectively, Dr. Leal reported.
Treatment was generally well tolerated in both arms, according to the investigator, with no safety signals observed. Toxicities resulting in death occurred in nine patients in the nivolumab plus chemotherapy arm and seven in the chemotherapy-only arm. “Most of the events were related to progression of disease,” Dr. Leal said.
While nivolumab and pembrolizumab’s use in the first-line setting may be uncertain, it is currently approved for metastatic SCLC that has progressed following platinum-based chemotherapy and at least one more line of therapy, according to the drug’s package insert.
The EA5161 study was sponsored by the National Cancer Institute. Dr. Leal provided disclosures related to AbbVie, AstraZeneca, Bayer, BeyondSpring, Bristol-Myers Squibb, Genentech, InvisionFirst Lung, Merck, Mirati, Novocure, and Takeda.
Dr. Owonikoko provided disclosures related to Bristol-Myers Squibb, Novartis, Celgene, Lilly, Sandoz, AbbVie, Eisai, and Takeda, among others. Dr. Byers reported disclosures related to Bristol-Myers Squibb, AstraZeneca, AbbVie, GenMab, PharmaMar, and Sierra Oncology, Tolero, Alethia, Merck, Jazz Pharmaceuticals, and Pfizer.
SOURCE: Leal TA et al. ASCO 2020, Abstract 9000.
While nivolumab plus doublet chemotherapy was effective in extensive-stage small-cell lung cancer (ES-SCLC) in a recent randomized trial, the results might not be sufficient to change current clinical practice, in which two first-line chemo-immunotherapies are already approved and recommended, sources said.
Nivolumab added to platinum/etoposide doublet chemotherapy was well tolerated and significantly improved progression-free survival (PFS) and overall survival (OS) compared to chemotherapy alone, according to results of ECOG-ACRIN EA5161, a randomized, phase 2 trial including 160 patients with ES-SCLC.
Risks of progression and death were reduced by 32% and 27%, respectively, when the immune checkpoint inhibitor was given along with chemotherapy, according to data presented by investigator Ticiana A. Leal, MD, of the University of Wisconsin Carbone Cancer Center in Madison.
“Our study, EA5161, confirms the efficacy of nivolumab in extensive-stage small cell lung cancer,” Dr. Leal said in a presentation she gave as part of the American Society of Clinical Oncology virtual scientific program.
Nivolumab did demonstrate a clear PFS advantage in EA5161, but “more surprisingly for a small trial” it also showed a clear OS advantage, said Taofeek K. Owonikoko, MD, PhD, in a commentary on the study.
“While the study as currently reported is insufficient to change practice, it does however provide very strong data to make the combination of nivolumab and platinum doublet acceptable as a platform for future clinical trials,” he said in the commentary, which was also included in the virtual ASCO proceedings.
Going forward, it would be difficult to justify another nondefinitive randomized phase 2 chemo-immunotherapy trial, especially if there are no “immediate plans” for a confirmatory phase 3 trial, added Dr. Owonikoko, who is director of thoracic oncology at Winship Cancer Institute of Emory University in Atlanta.
Nivolumab wasn’t the only immune checkpoint with new first-line data in ES-SCLC at ASCO. In the randomized, double-blind, phase 3 KEYNOTE-604 trial, pembrolizumab added to etoposide and platinum significantly prolonged PFS and showed a trend toward improved OS. However, the significance threshold for OS was missed, according to the report.
While these pembrolizumab data are also insufficient to change today’s practice standards, results for both the pembrolizumab- and nivolumab-containing regimens are nevertheless compelling to support their use as a platform for new treatment strategies, according to Dr. Owonikoko.
With these new ASCO data, there are now randomized data confirming a benefit of immune checkpoint inhibitor–based regimens in ES-SCLC, according to Lauren A. Byers, MD, from the department of thoracic/head and neck medical oncology at The University of Texas MD Anderson Cancer Center in Houston.
Immune checkpoint inhibitors that are approved by the Food and Drug Administration for first-line treatment of ES-SCLC include atezolizumab (in combination with carboplatin and etoposide) and durvalumab (in combination with either carboplatin or cisplatin plus etoposide). In current National Comprehensive Cancer Network (NCCN) guidelines, both are described as “preferred” regimens for primary or adjuvant therapy.
“A lot of times in oncology we have trials with similar drugs, and you get somewhat different answers in terms of the outcome of the trials, so we’re kind of trying to tease them apart,” Dr. Byers said in an interview.
“I think in this situation, we’ve got four studies, and they essentially are extremely similar in terms of the result, which just gives us even more confidence that there is benefit, at least for a subset of patients.”
The EA5161 study was developed to evaluate the role of nivolumab in ES-SCLC, Dr. Leal said in her virtual ASCO presentation.
Of the 160 patients enrolled and randomized, 145 were eligible and treated, including 75 in the nivolumab plus chemotherapy arm and 70 in the chemotherapy arm. Participants were evenly split between performance status 0 and 1, and little more than half of patients were women, and a median of five treatment cycles were delivered in each arm.
Median PFS, the primary end point of the trial, was 5.5 months for nivolumab plus chemotherapy versus 4.7 months for chemotherapy alone for all eligible and treated patients (hazard ratio, 0.68; 95% confidence interval, 0.48-1.00; P = .047). In the intent-to-treat population, median PFS was 5.5 and 4.6 months in the respective arms (HR, 0.65; 95% CI, 0.46-0.91; P = .012).
Median overall survival was 11.3 months and 9.3 months for the nivolumab plus chemotherapy and chemotherapy-only arms, respectively, for all eligible and treated patients (HR, 0.73; 95% CI, 0.49-1.1), and in the intent-to-treat population, median OS was 11.3 and 8.5 months for the respective arms (HR, 0.67; 95% CI, 0.46-0.98; P = .038).
The overall response rate was 52% for nivolumab plus chemotherapy and 47% for chemotherapy alone, with a median duration of response of 5.6 and 3.3 months, respectively, Dr. Leal reported.
Treatment was generally well tolerated in both arms, according to the investigator, with no safety signals observed. Toxicities resulting in death occurred in nine patients in the nivolumab plus chemotherapy arm and seven in the chemotherapy-only arm. “Most of the events were related to progression of disease,” Dr. Leal said.
While nivolumab and pembrolizumab’s use in the first-line setting may be uncertain, it is currently approved for metastatic SCLC that has progressed following platinum-based chemotherapy and at least one more line of therapy, according to the drug’s package insert.
The EA5161 study was sponsored by the National Cancer Institute. Dr. Leal provided disclosures related to AbbVie, AstraZeneca, Bayer, BeyondSpring, Bristol-Myers Squibb, Genentech, InvisionFirst Lung, Merck, Mirati, Novocure, and Takeda.
Dr. Owonikoko provided disclosures related to Bristol-Myers Squibb, Novartis, Celgene, Lilly, Sandoz, AbbVie, Eisai, and Takeda, among others. Dr. Byers reported disclosures related to Bristol-Myers Squibb, AstraZeneca, AbbVie, GenMab, PharmaMar, and Sierra Oncology, Tolero, Alethia, Merck, Jazz Pharmaceuticals, and Pfizer.
SOURCE: Leal TA et al. ASCO 2020, Abstract 9000.
FROM ASCO 2020
Despite guidelines, controversy remains over corticosteroids in COVID-19
Three main reasons have been put forth for using corticosteroids in critically ill patients with COVID-19, but only one – the hope of preventing lung fibrosis in patients with unresolved acute respiratory distress syndrome – is reasonable to employ now outside of formal randomized trials, Peter Pickkers, MD, PhD, asserted at a webinar on COVID-19 sponsored by the European Society of Intensive Care Medicine.
The most commonly invoked rationale for giving steroids in patients with severe COVID-19 is to modulate the destructive inflammatory immune response that occurs with advancing disease. Another justification cited for giving steroids is to treat suspected adrenal insufficiency in those with refractory shock. Of note, both practices are endorsed in the recent Surviving Sepsis Campaign guidelines on management of critically ill patients with COVID-19 (Intensive Care Med. 2020 May;46[5]:854-87).
But those recommendations – numbers 22 and 42 out of a total of 50 recommendations included in the guidelines – should never have been made, according to Dr. Pickkers, professor of experimental intensive care medicine at Radboud University Medical Center in Nijmegen, the Netherlands.
Dueling guidelines
The Surviving Sepsis Campaign guidelines, which were developed by a panel comprising 36 experts in 12 countries, are quite frank in conceding that the guidance in favor of corticosteroids are weak recommendations based on low-quality evidence.
The guidelines recommend against using corticosteroids to try to modulate the immune system in mechanically ventilated COVID-19 patients without acute respiratory distress syndrome (ARDS), but do recommend steroids in those with COVID-19 and ARDS. However, the guidelines also note that, because of the very low quality of the evidence, some experts on the panel preferred not to issue a pro-steroids recommendation at all until higher-quality evidence becomes available. Dr. Pickkers said he believes that the minority view should have prevailed. Moreover, current COVID-19 guidance from the World Health Organization is at odds with the Surviving Sepsis Campaign recommendations; the WHO advises against corticosteroids unless the treatment is indicated for a reason other than immunomodulation, he noted.
The evidence in favor of steroids in an effort to blunt the immune response in COVID patients with ARDS is based largely upon a single small, retrospective, non–peer-reviewed report that 5-7 days of treatment with 1-2 mg/kg per day of methylprednisolone was associated with shortened fever duration and need for supplemental oxygen.
The evidence against steroids for immunomodulation comes mainly from earlier studies of the SARS and MERS novel coronaviruses. For example, in a multicenter study of 309 patients with the MERS (Middle East respiratory syndrome) virus, those who received corticosteroids received no benefit and experienced delayed viral clearance (Am J Respir Crit Care Med. 2018 Mar 15;197[6]:757-67).
“The thing is, virtually all COVID-19 patients in the ICU fulfill the criteria for ARDS, so following the Surviving Sepsis Campaign guidelines would have far-reaching consequences,” Dr. Pickkers said.
Those consequences include a theoretic potential for serious harm arising from dampening the immune response at a point in the course of COVID-19 when the virus is still present, which could result in slowed viral clearance and prolonged viral shedding. Moreover so far no one has been able to identify a sweet spot in the disease course where the viral load has waned and the immune response is sufficiently early that intervention with corticosteroids might have an optimal benefit/risk ratio, he continued.
“My opinion is that at this moment there is no benefit at all for corticosteroids for immunomodulation in patients with COVID-19,” Dr. Pickkers said. “My personal recommendation, in contrast to the Surviving Sepsis Campaign recommendation, is not to use this therapy outside of a study.”
He added that randomized, controlled trials of corticosteroid therapy in critically ill patients with COVID-19 are ongoing in Europe and the United States, including the large RECOVERY study of dexamethasone in the United Kingdom.
As for the Surviving Sepsis Campaign recommendation to use corticosteroids to treat refractory shock in COVID-19, Dr. Pickkers dismissed this guidance as largely irrelevant. That’s because few patients with COVID-19 who need mechanical ventilation have refractory shock as evidenced by the need for a high infusion rate of norepinephrine. Anyway, he noted, that Surviving Sepsis recommendation is based upon extrapolation from evidence of benefit in bacterial septic shock patients, which he deemed to be of questionable relevance to the COVID-19 pandemic.
Attacking the fibroproliferative phase of ARDS
First off, Dr. Pickkers conceded, there is no evidence that treatment with corticosteroids to prevent lung fibrosis in COVID-19 patients with nonresolving ARDS is an effective strategy; the pandemic is simply too new at this point for the appropriate studies to have been done. But this much is known: Postmortem pathologic studies show fibroplastic proliferation is present in the lungs of COVID-19 patients, as in those who die of ARDS of other causes. Also, COVID-19 patients typically aren’t admitted to the ICU until day 11 or 12 after developing their first symptoms, so by the time they display indications that their ARDS is not resolving, the virus has typically left the scene; thus, there is little risk at that point that corticosteroids will promote viral proliferation. Additionally, studies in critically ill patients with nonresolving ARDS of other causes show clinically meaningful benefits for corticosteroid therapy.
Dr. Pickkers cited as “must reading” an analysis of five randomized trials of corticosteroid therapy in a total of 518 patients with acute lung injury ARDS of non–COVID-19 origin. The analysis by investigators at the University of Tennessee, Memphis, concluded that treatment resulted in clinically meaningful reductions in duration of mechanical ventilation and ICU length of stay. Moreover, in the 400 patients whose steroid therapy commenced before day 14 of ARDS, there was a statistically significant 22% reduction in risk of death, compared with patients in whom corticosteroids were started later (Intensive Care Med. 2008 Jan;34[1]:61-9).
Session cochair Jan De Waele, MD, PhD, struck a cautious note, remarking, “It’s my perception that we’re using the evidence that we’ve gathered in other conditions and are now trying to apply it in COVID-19. But quality data on patients with COVID-19 itself is pretty scare, and it’s really hard to say whether this disease behaves similarly to bacterial septic shock or to other viral infections.”
“We need more information about the use of corticosteroids in COVID-19, although I think a lot of people are using it at this moment,” added Dr. De Waele, a surgical intensivist at Ghent (Belgium) University.
That being said, he asked Dr. Pickkers when he considers using corticosteroids to prevent pulmonary fibrosis.
Dr. Pickkers said that when he notices that a COVID-19 patient’s lung compliance is worsening, that stiff lung is a clue that fibrosis is occurring and is having clinical consequences. “We also measure blood procollagen, a not very sensitive but moderately specific marker of fibroproliferation. If we see an increase in this biomarker and the lung mechanics are changing, then we do treat these patients with corticosteroids,” Dr. Pickkers replied.
He and his colleagues try to start steroids before day 14 of ARDS, and they continue treatment for longer than 7 days in order to prevent a rebound inflammatory response upon treatment discontinuation. They also avoid using neuromuscular agents and engage in meticulous infection surveillance in order to minimize potential complications of corticosteroid therapy in the ICU.
Dr. Pickkers reported having no financial conflicts regarding his presentation.
Three main reasons have been put forth for using corticosteroids in critically ill patients with COVID-19, but only one – the hope of preventing lung fibrosis in patients with unresolved acute respiratory distress syndrome – is reasonable to employ now outside of formal randomized trials, Peter Pickkers, MD, PhD, asserted at a webinar on COVID-19 sponsored by the European Society of Intensive Care Medicine.
The most commonly invoked rationale for giving steroids in patients with severe COVID-19 is to modulate the destructive inflammatory immune response that occurs with advancing disease. Another justification cited for giving steroids is to treat suspected adrenal insufficiency in those with refractory shock. Of note, both practices are endorsed in the recent Surviving Sepsis Campaign guidelines on management of critically ill patients with COVID-19 (Intensive Care Med. 2020 May;46[5]:854-87).
But those recommendations – numbers 22 and 42 out of a total of 50 recommendations included in the guidelines – should never have been made, according to Dr. Pickkers, professor of experimental intensive care medicine at Radboud University Medical Center in Nijmegen, the Netherlands.
Dueling guidelines
The Surviving Sepsis Campaign guidelines, which were developed by a panel comprising 36 experts in 12 countries, are quite frank in conceding that the guidance in favor of corticosteroids are weak recommendations based on low-quality evidence.
The guidelines recommend against using corticosteroids to try to modulate the immune system in mechanically ventilated COVID-19 patients without acute respiratory distress syndrome (ARDS), but do recommend steroids in those with COVID-19 and ARDS. However, the guidelines also note that, because of the very low quality of the evidence, some experts on the panel preferred not to issue a pro-steroids recommendation at all until higher-quality evidence becomes available. Dr. Pickkers said he believes that the minority view should have prevailed. Moreover, current COVID-19 guidance from the World Health Organization is at odds with the Surviving Sepsis Campaign recommendations; the WHO advises against corticosteroids unless the treatment is indicated for a reason other than immunomodulation, he noted.
The evidence in favor of steroids in an effort to blunt the immune response in COVID patients with ARDS is based largely upon a single small, retrospective, non–peer-reviewed report that 5-7 days of treatment with 1-2 mg/kg per day of methylprednisolone was associated with shortened fever duration and need for supplemental oxygen.
The evidence against steroids for immunomodulation comes mainly from earlier studies of the SARS and MERS novel coronaviruses. For example, in a multicenter study of 309 patients with the MERS (Middle East respiratory syndrome) virus, those who received corticosteroids received no benefit and experienced delayed viral clearance (Am J Respir Crit Care Med. 2018 Mar 15;197[6]:757-67).
“The thing is, virtually all COVID-19 patients in the ICU fulfill the criteria for ARDS, so following the Surviving Sepsis Campaign guidelines would have far-reaching consequences,” Dr. Pickkers said.
Those consequences include a theoretic potential for serious harm arising from dampening the immune response at a point in the course of COVID-19 when the virus is still present, which could result in slowed viral clearance and prolonged viral shedding. Moreover so far no one has been able to identify a sweet spot in the disease course where the viral load has waned and the immune response is sufficiently early that intervention with corticosteroids might have an optimal benefit/risk ratio, he continued.
“My opinion is that at this moment there is no benefit at all for corticosteroids for immunomodulation in patients with COVID-19,” Dr. Pickkers said. “My personal recommendation, in contrast to the Surviving Sepsis Campaign recommendation, is not to use this therapy outside of a study.”
He added that randomized, controlled trials of corticosteroid therapy in critically ill patients with COVID-19 are ongoing in Europe and the United States, including the large RECOVERY study of dexamethasone in the United Kingdom.
As for the Surviving Sepsis Campaign recommendation to use corticosteroids to treat refractory shock in COVID-19, Dr. Pickkers dismissed this guidance as largely irrelevant. That’s because few patients with COVID-19 who need mechanical ventilation have refractory shock as evidenced by the need for a high infusion rate of norepinephrine. Anyway, he noted, that Surviving Sepsis recommendation is based upon extrapolation from evidence of benefit in bacterial septic shock patients, which he deemed to be of questionable relevance to the COVID-19 pandemic.
Attacking the fibroproliferative phase of ARDS
First off, Dr. Pickkers conceded, there is no evidence that treatment with corticosteroids to prevent lung fibrosis in COVID-19 patients with nonresolving ARDS is an effective strategy; the pandemic is simply too new at this point for the appropriate studies to have been done. But this much is known: Postmortem pathologic studies show fibroplastic proliferation is present in the lungs of COVID-19 patients, as in those who die of ARDS of other causes. Also, COVID-19 patients typically aren’t admitted to the ICU until day 11 or 12 after developing their first symptoms, so by the time they display indications that their ARDS is not resolving, the virus has typically left the scene; thus, there is little risk at that point that corticosteroids will promote viral proliferation. Additionally, studies in critically ill patients with nonresolving ARDS of other causes show clinically meaningful benefits for corticosteroid therapy.
Dr. Pickkers cited as “must reading” an analysis of five randomized trials of corticosteroid therapy in a total of 518 patients with acute lung injury ARDS of non–COVID-19 origin. The analysis by investigators at the University of Tennessee, Memphis, concluded that treatment resulted in clinically meaningful reductions in duration of mechanical ventilation and ICU length of stay. Moreover, in the 400 patients whose steroid therapy commenced before day 14 of ARDS, there was a statistically significant 22% reduction in risk of death, compared with patients in whom corticosteroids were started later (Intensive Care Med. 2008 Jan;34[1]:61-9).
Session cochair Jan De Waele, MD, PhD, struck a cautious note, remarking, “It’s my perception that we’re using the evidence that we’ve gathered in other conditions and are now trying to apply it in COVID-19. But quality data on patients with COVID-19 itself is pretty scare, and it’s really hard to say whether this disease behaves similarly to bacterial septic shock or to other viral infections.”
“We need more information about the use of corticosteroids in COVID-19, although I think a lot of people are using it at this moment,” added Dr. De Waele, a surgical intensivist at Ghent (Belgium) University.
That being said, he asked Dr. Pickkers when he considers using corticosteroids to prevent pulmonary fibrosis.
Dr. Pickkers said that when he notices that a COVID-19 patient’s lung compliance is worsening, that stiff lung is a clue that fibrosis is occurring and is having clinical consequences. “We also measure blood procollagen, a not very sensitive but moderately specific marker of fibroproliferation. If we see an increase in this biomarker and the lung mechanics are changing, then we do treat these patients with corticosteroids,” Dr. Pickkers replied.
He and his colleagues try to start steroids before day 14 of ARDS, and they continue treatment for longer than 7 days in order to prevent a rebound inflammatory response upon treatment discontinuation. They also avoid using neuromuscular agents and engage in meticulous infection surveillance in order to minimize potential complications of corticosteroid therapy in the ICU.
Dr. Pickkers reported having no financial conflicts regarding his presentation.
Three main reasons have been put forth for using corticosteroids in critically ill patients with COVID-19, but only one – the hope of preventing lung fibrosis in patients with unresolved acute respiratory distress syndrome – is reasonable to employ now outside of formal randomized trials, Peter Pickkers, MD, PhD, asserted at a webinar on COVID-19 sponsored by the European Society of Intensive Care Medicine.
The most commonly invoked rationale for giving steroids in patients with severe COVID-19 is to modulate the destructive inflammatory immune response that occurs with advancing disease. Another justification cited for giving steroids is to treat suspected adrenal insufficiency in those with refractory shock. Of note, both practices are endorsed in the recent Surviving Sepsis Campaign guidelines on management of critically ill patients with COVID-19 (Intensive Care Med. 2020 May;46[5]:854-87).
But those recommendations – numbers 22 and 42 out of a total of 50 recommendations included in the guidelines – should never have been made, according to Dr. Pickkers, professor of experimental intensive care medicine at Radboud University Medical Center in Nijmegen, the Netherlands.
Dueling guidelines
The Surviving Sepsis Campaign guidelines, which were developed by a panel comprising 36 experts in 12 countries, are quite frank in conceding that the guidance in favor of corticosteroids are weak recommendations based on low-quality evidence.
The guidelines recommend against using corticosteroids to try to modulate the immune system in mechanically ventilated COVID-19 patients without acute respiratory distress syndrome (ARDS), but do recommend steroids in those with COVID-19 and ARDS. However, the guidelines also note that, because of the very low quality of the evidence, some experts on the panel preferred not to issue a pro-steroids recommendation at all until higher-quality evidence becomes available. Dr. Pickkers said he believes that the minority view should have prevailed. Moreover, current COVID-19 guidance from the World Health Organization is at odds with the Surviving Sepsis Campaign recommendations; the WHO advises against corticosteroids unless the treatment is indicated for a reason other than immunomodulation, he noted.
The evidence in favor of steroids in an effort to blunt the immune response in COVID patients with ARDS is based largely upon a single small, retrospective, non–peer-reviewed report that 5-7 days of treatment with 1-2 mg/kg per day of methylprednisolone was associated with shortened fever duration and need for supplemental oxygen.
The evidence against steroids for immunomodulation comes mainly from earlier studies of the SARS and MERS novel coronaviruses. For example, in a multicenter study of 309 patients with the MERS (Middle East respiratory syndrome) virus, those who received corticosteroids received no benefit and experienced delayed viral clearance (Am J Respir Crit Care Med. 2018 Mar 15;197[6]:757-67).
“The thing is, virtually all COVID-19 patients in the ICU fulfill the criteria for ARDS, so following the Surviving Sepsis Campaign guidelines would have far-reaching consequences,” Dr. Pickkers said.
Those consequences include a theoretic potential for serious harm arising from dampening the immune response at a point in the course of COVID-19 when the virus is still present, which could result in slowed viral clearance and prolonged viral shedding. Moreover so far no one has been able to identify a sweet spot in the disease course where the viral load has waned and the immune response is sufficiently early that intervention with corticosteroids might have an optimal benefit/risk ratio, he continued.
“My opinion is that at this moment there is no benefit at all for corticosteroids for immunomodulation in patients with COVID-19,” Dr. Pickkers said. “My personal recommendation, in contrast to the Surviving Sepsis Campaign recommendation, is not to use this therapy outside of a study.”
He added that randomized, controlled trials of corticosteroid therapy in critically ill patients with COVID-19 are ongoing in Europe and the United States, including the large RECOVERY study of dexamethasone in the United Kingdom.
As for the Surviving Sepsis Campaign recommendation to use corticosteroids to treat refractory shock in COVID-19, Dr. Pickkers dismissed this guidance as largely irrelevant. That’s because few patients with COVID-19 who need mechanical ventilation have refractory shock as evidenced by the need for a high infusion rate of norepinephrine. Anyway, he noted, that Surviving Sepsis recommendation is based upon extrapolation from evidence of benefit in bacterial septic shock patients, which he deemed to be of questionable relevance to the COVID-19 pandemic.
Attacking the fibroproliferative phase of ARDS
First off, Dr. Pickkers conceded, there is no evidence that treatment with corticosteroids to prevent lung fibrosis in COVID-19 patients with nonresolving ARDS is an effective strategy; the pandemic is simply too new at this point for the appropriate studies to have been done. But this much is known: Postmortem pathologic studies show fibroplastic proliferation is present in the lungs of COVID-19 patients, as in those who die of ARDS of other causes. Also, COVID-19 patients typically aren’t admitted to the ICU until day 11 or 12 after developing their first symptoms, so by the time they display indications that their ARDS is not resolving, the virus has typically left the scene; thus, there is little risk at that point that corticosteroids will promote viral proliferation. Additionally, studies in critically ill patients with nonresolving ARDS of other causes show clinically meaningful benefits for corticosteroid therapy.
Dr. Pickkers cited as “must reading” an analysis of five randomized trials of corticosteroid therapy in a total of 518 patients with acute lung injury ARDS of non–COVID-19 origin. The analysis by investigators at the University of Tennessee, Memphis, concluded that treatment resulted in clinically meaningful reductions in duration of mechanical ventilation and ICU length of stay. Moreover, in the 400 patients whose steroid therapy commenced before day 14 of ARDS, there was a statistically significant 22% reduction in risk of death, compared with patients in whom corticosteroids were started later (Intensive Care Med. 2008 Jan;34[1]:61-9).
Session cochair Jan De Waele, MD, PhD, struck a cautious note, remarking, “It’s my perception that we’re using the evidence that we’ve gathered in other conditions and are now trying to apply it in COVID-19. But quality data on patients with COVID-19 itself is pretty scare, and it’s really hard to say whether this disease behaves similarly to bacterial septic shock or to other viral infections.”
“We need more information about the use of corticosteroids in COVID-19, although I think a lot of people are using it at this moment,” added Dr. De Waele, a surgical intensivist at Ghent (Belgium) University.
That being said, he asked Dr. Pickkers when he considers using corticosteroids to prevent pulmonary fibrosis.
Dr. Pickkers said that when he notices that a COVID-19 patient’s lung compliance is worsening, that stiff lung is a clue that fibrosis is occurring and is having clinical consequences. “We also measure blood procollagen, a not very sensitive but moderately specific marker of fibroproliferation. If we see an increase in this biomarker and the lung mechanics are changing, then we do treat these patients with corticosteroids,” Dr. Pickkers replied.
He and his colleagues try to start steroids before day 14 of ARDS, and they continue treatment for longer than 7 days in order to prevent a rebound inflammatory response upon treatment discontinuation. They also avoid using neuromuscular agents and engage in meticulous infection surveillance in order to minimize potential complications of corticosteroid therapy in the ICU.
Dr. Pickkers reported having no financial conflicts regarding his presentation.
Today’s top news highlights: Cancer makes COVID-19 more dangerous, treatment for heavy menstrual bleeding, and more
Here are the stories our MDedge editors across specialties think you need to know about today:
Active cancer ups death risk for patients with COVID-19
New data show that patients with COVID-19 and progressing cancer had a significantly higher risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer. Interestingly, one of the independent risk factor for death in patients with COVID-19 and cancer was treatment with hydroxychloroquine plus azithromycin. This finding, however, was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville. Read more.
Two new studies indicate that social distancing successfully flattened the curve on COVID-19 hospitalizations. One study, published in JAMA, showed significantly lower numbers of observed cases versus worst-case projections in four states: Colorado, Minnesota, Ohio, and Virginia. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In a separate study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention. Read more.
FDA approves treatment for heavy menstrual bleeding
The Food and Drug Administration has approved a medication for the management of heavy menstrual bleeding associated with uterine fibroids in premenopausal women. The medication, marketed as Oriahnn, is an estrogen and progestin combination product that consists of elagolix, estradiol, and norethindrone acetate capsules packaged together for oral use. The most common side effects of the drug included hot flushes, headache, fatigue, and irregular vaginal bleeding. The drug’s label includes a boxed warning about a risk of strokes and blood clots, especially in women at increased risk for these events. Read more.
Lessons from a drive-through COVID testing center
Chris Notte, MD, and Neil Skolnik, MD, were part of a team of clinicians charged with launching a drive-through COVID-19 testing center. Their task was to get the operation up and running in 2 days. It took them 3 days. While the launch was a success, the experience taught them some lessons about the limits of medical technology and the importance of personal protective equipment. “Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site,” they wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Active cancer ups death risk for patients with COVID-19
New data show that patients with COVID-19 and progressing cancer had a significantly higher risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer. Interestingly, one of the independent risk factor for death in patients with COVID-19 and cancer was treatment with hydroxychloroquine plus azithromycin. This finding, however, was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville. Read more.
Two new studies indicate that social distancing successfully flattened the curve on COVID-19 hospitalizations. One study, published in JAMA, showed significantly lower numbers of observed cases versus worst-case projections in four states: Colorado, Minnesota, Ohio, and Virginia. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In a separate study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention. Read more.
FDA approves treatment for heavy menstrual bleeding
The Food and Drug Administration has approved a medication for the management of heavy menstrual bleeding associated with uterine fibroids in premenopausal women. The medication, marketed as Oriahnn, is an estrogen and progestin combination product that consists of elagolix, estradiol, and norethindrone acetate capsules packaged together for oral use. The most common side effects of the drug included hot flushes, headache, fatigue, and irregular vaginal bleeding. The drug’s label includes a boxed warning about a risk of strokes and blood clots, especially in women at increased risk for these events. Read more.
Lessons from a drive-through COVID testing center
Chris Notte, MD, and Neil Skolnik, MD, were part of a team of clinicians charged with launching a drive-through COVID-19 testing center. Their task was to get the operation up and running in 2 days. It took them 3 days. While the launch was a success, the experience taught them some lessons about the limits of medical technology and the importance of personal protective equipment. “Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site,” they wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Active cancer ups death risk for patients with COVID-19
New data show that patients with COVID-19 and progressing cancer had a significantly higher risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer. Interestingly, one of the independent risk factor for death in patients with COVID-19 and cancer was treatment with hydroxychloroquine plus azithromycin. This finding, however, was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville. Read more.
Two new studies indicate that social distancing successfully flattened the curve on COVID-19 hospitalizations. One study, published in JAMA, showed significantly lower numbers of observed cases versus worst-case projections in four states: Colorado, Minnesota, Ohio, and Virginia. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In a separate study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention. Read more.
FDA approves treatment for heavy menstrual bleeding
The Food and Drug Administration has approved a medication for the management of heavy menstrual bleeding associated with uterine fibroids in premenopausal women. The medication, marketed as Oriahnn, is an estrogen and progestin combination product that consists of elagolix, estradiol, and norethindrone acetate capsules packaged together for oral use. The most common side effects of the drug included hot flushes, headache, fatigue, and irregular vaginal bleeding. The drug’s label includes a boxed warning about a risk of strokes and blood clots, especially in women at increased risk for these events. Read more.
Lessons from a drive-through COVID testing center
Chris Notte, MD, and Neil Skolnik, MD, were part of a team of clinicians charged with launching a drive-through COVID-19 testing center. Their task was to get the operation up and running in 2 days. It took them 3 days. While the launch was a success, the experience taught them some lessons about the limits of medical technology and the importance of personal protective equipment. “Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site,” they wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Upfront pembrolizumab doubles PFS in MSI-H/dMMR metastatic colorectal cancer
The median PFS was 16.5 months for patients who received pembrolizumab and 8.2 months for those who received investigators’ choice of chemotherapy (one of six regimens).
“In the past, no medical treatment has shown such difference in terms of improvement of PFS in metastatic colorectal cancer,” said study investigator Thierry André, MD, of Hôpital Saint Antoine in Paris.
“Today, this study demonstrates that the majority of the 5% of patients with metastatic colorectal cancer selected by MSI-high status benefited greatly from anti–PD-1 [programmed death-1] pembrolizumab, compared with standard of care,” he added.
Dr. André discussed the study in a press briefing prior to his presentation of the data as part of the American Society of Clinical Oncology virtual scientific program.
“I think this is setting a new standard of care,” said Michael J. Overman, MD, of the University of Texas MD Anderson Cancer Center in Houston. Dr. Overman, the invited discussant, commented on the KEYNOTE-177 study in an interview prior to the presentation.
Dr. Overman noted that, although the overall response rate was higher with pembrolizumab, the rate of progressive disease was higher in the pembrolizumab arm than in the chemotherapy arm. Progressive disease was the best response in 29.4% of patients on pembrolizumab and 12.3% of patients on chemotherapy.
“The only area where I think the question on pembrolizumab is still open would be in the group of patients where we’re saying ‘I care about the near future – this patient has so many symptoms and so much disease burden that I care what happens in the short term,’” Dr. Overman said. He added that, for this subgroup of patients, chemotherapy or pembrolizumab in combination with another immunotherapy, such as ipilimumab, might be more appropriate.
KEYNOTE-177 details
Investigators enrolled 307 patients with confirmed, untreated MSI-H/dMMR metastatic colorectal cancer and good performance status (Eastern Cooperative Oncology Group performance status 0 or 1).
Patients were randomized to pembrolizumab at 200 mg every 3 weeks for up to 35 cycles (n = 153) or to the investigators’ choice of chemotherapy (n = 154). Chemotherapy regimens were modified FOLFOX (5-fluorouracil, leucovorin, oxaliplatin) alone or in combination with either bevacizumab or cetuximab, or FOLFIRI (leucovorin, fluorouracil, irinotecan) alone or in combination with either bevacizumab or cetuximab.
Patients assigned to the chemotherapy arm were allowed to cross over to pembrolizumab for up to 35 cycles if they had disease progression confirmed by central review.
PFS is a coprimary endpoint with overall survival. The trial was deemed to be successful if either of the coprimary endpoints was met. Overall survival results are not yet available.
The median PFS was 16.5 months with pembrolizumab and 8.2 months with chemotherapy (hazard ratio, 0.60; P = .0002). The 12-month PFS rates were 55% and 37%, respectively. The 24-month PFS rates were 48% and 19%, respectively.
Overall response rates were 43.8% with pembrolizumab, consisting of 11.1% complete responses and 32.7% partial responses. The overall response rate with chemotherapy was 33.1%, consisting of 3.9% complete responses and 29.2% partial responses.
In all, 20.9% of patients on pembrolizumab and 42.2% of those on chemotherapy had stable disease. Rates of progressive disease were 29.4% and 12.3%, respectively.
The median duration of response was not reached in the pembrolizumab arm and was 10.6 months in the chemotherapy arm. At 2 years, 83% of patients treated with pembrolizumab and 35% treated with chemotherapy had ongoing responses.
Grade 3 or greater treatment-related adverse events occurred in 22% of patients on pembrolizumab and 66% on chemotherapy.
Immune-mediated adverse events and infusion reactions were more common with pembrolizumab than with chemotherapy (31% and 13%, respectively). Adverse events that were common with chemotherapy included gastrointestinal events, fatigue, neutropenia, and peripheral sensory neuropathy.
The study was funded by Merck. Dr. André disclosed relationships with multiple companies, including MSD Oncology. Dr. Overman disclosed consulting activities with various companies, not including Merck.
SOURCE: André T et al. ASCO 2020, Abstract LBA4.
The median PFS was 16.5 months for patients who received pembrolizumab and 8.2 months for those who received investigators’ choice of chemotherapy (one of six regimens).
“In the past, no medical treatment has shown such difference in terms of improvement of PFS in metastatic colorectal cancer,” said study investigator Thierry André, MD, of Hôpital Saint Antoine in Paris.
“Today, this study demonstrates that the majority of the 5% of patients with metastatic colorectal cancer selected by MSI-high status benefited greatly from anti–PD-1 [programmed death-1] pembrolizumab, compared with standard of care,” he added.
Dr. André discussed the study in a press briefing prior to his presentation of the data as part of the American Society of Clinical Oncology virtual scientific program.
“I think this is setting a new standard of care,” said Michael J. Overman, MD, of the University of Texas MD Anderson Cancer Center in Houston. Dr. Overman, the invited discussant, commented on the KEYNOTE-177 study in an interview prior to the presentation.
Dr. Overman noted that, although the overall response rate was higher with pembrolizumab, the rate of progressive disease was higher in the pembrolizumab arm than in the chemotherapy arm. Progressive disease was the best response in 29.4% of patients on pembrolizumab and 12.3% of patients on chemotherapy.
“The only area where I think the question on pembrolizumab is still open would be in the group of patients where we’re saying ‘I care about the near future – this patient has so many symptoms and so much disease burden that I care what happens in the short term,’” Dr. Overman said. He added that, for this subgroup of patients, chemotherapy or pembrolizumab in combination with another immunotherapy, such as ipilimumab, might be more appropriate.
KEYNOTE-177 details
Investigators enrolled 307 patients with confirmed, untreated MSI-H/dMMR metastatic colorectal cancer and good performance status (Eastern Cooperative Oncology Group performance status 0 or 1).
Patients were randomized to pembrolizumab at 200 mg every 3 weeks for up to 35 cycles (n = 153) or to the investigators’ choice of chemotherapy (n = 154). Chemotherapy regimens were modified FOLFOX (5-fluorouracil, leucovorin, oxaliplatin) alone or in combination with either bevacizumab or cetuximab, or FOLFIRI (leucovorin, fluorouracil, irinotecan) alone or in combination with either bevacizumab or cetuximab.
Patients assigned to the chemotherapy arm were allowed to cross over to pembrolizumab for up to 35 cycles if they had disease progression confirmed by central review.
PFS is a coprimary endpoint with overall survival. The trial was deemed to be successful if either of the coprimary endpoints was met. Overall survival results are not yet available.
The median PFS was 16.5 months with pembrolizumab and 8.2 months with chemotherapy (hazard ratio, 0.60; P = .0002). The 12-month PFS rates were 55% and 37%, respectively. The 24-month PFS rates were 48% and 19%, respectively.
Overall response rates were 43.8% with pembrolizumab, consisting of 11.1% complete responses and 32.7% partial responses. The overall response rate with chemotherapy was 33.1%, consisting of 3.9% complete responses and 29.2% partial responses.
In all, 20.9% of patients on pembrolizumab and 42.2% of those on chemotherapy had stable disease. Rates of progressive disease were 29.4% and 12.3%, respectively.
The median duration of response was not reached in the pembrolizumab arm and was 10.6 months in the chemotherapy arm. At 2 years, 83% of patients treated with pembrolizumab and 35% treated with chemotherapy had ongoing responses.
Grade 3 or greater treatment-related adverse events occurred in 22% of patients on pembrolizumab and 66% on chemotherapy.
Immune-mediated adverse events and infusion reactions were more common with pembrolizumab than with chemotherapy (31% and 13%, respectively). Adverse events that were common with chemotherapy included gastrointestinal events, fatigue, neutropenia, and peripheral sensory neuropathy.
The study was funded by Merck. Dr. André disclosed relationships with multiple companies, including MSD Oncology. Dr. Overman disclosed consulting activities with various companies, not including Merck.
SOURCE: André T et al. ASCO 2020, Abstract LBA4.
The median PFS was 16.5 months for patients who received pembrolizumab and 8.2 months for those who received investigators’ choice of chemotherapy (one of six regimens).
“In the past, no medical treatment has shown such difference in terms of improvement of PFS in metastatic colorectal cancer,” said study investigator Thierry André, MD, of Hôpital Saint Antoine in Paris.
“Today, this study demonstrates that the majority of the 5% of patients with metastatic colorectal cancer selected by MSI-high status benefited greatly from anti–PD-1 [programmed death-1] pembrolizumab, compared with standard of care,” he added.
Dr. André discussed the study in a press briefing prior to his presentation of the data as part of the American Society of Clinical Oncology virtual scientific program.
“I think this is setting a new standard of care,” said Michael J. Overman, MD, of the University of Texas MD Anderson Cancer Center in Houston. Dr. Overman, the invited discussant, commented on the KEYNOTE-177 study in an interview prior to the presentation.
Dr. Overman noted that, although the overall response rate was higher with pembrolizumab, the rate of progressive disease was higher in the pembrolizumab arm than in the chemotherapy arm. Progressive disease was the best response in 29.4% of patients on pembrolizumab and 12.3% of patients on chemotherapy.
“The only area where I think the question on pembrolizumab is still open would be in the group of patients where we’re saying ‘I care about the near future – this patient has so many symptoms and so much disease burden that I care what happens in the short term,’” Dr. Overman said. He added that, for this subgroup of patients, chemotherapy or pembrolizumab in combination with another immunotherapy, such as ipilimumab, might be more appropriate.
KEYNOTE-177 details
Investigators enrolled 307 patients with confirmed, untreated MSI-H/dMMR metastatic colorectal cancer and good performance status (Eastern Cooperative Oncology Group performance status 0 or 1).
Patients were randomized to pembrolizumab at 200 mg every 3 weeks for up to 35 cycles (n = 153) or to the investigators’ choice of chemotherapy (n = 154). Chemotherapy regimens were modified FOLFOX (5-fluorouracil, leucovorin, oxaliplatin) alone or in combination with either bevacizumab or cetuximab, or FOLFIRI (leucovorin, fluorouracil, irinotecan) alone or in combination with either bevacizumab or cetuximab.
Patients assigned to the chemotherapy arm were allowed to cross over to pembrolizumab for up to 35 cycles if they had disease progression confirmed by central review.
PFS is a coprimary endpoint with overall survival. The trial was deemed to be successful if either of the coprimary endpoints was met. Overall survival results are not yet available.
The median PFS was 16.5 months with pembrolizumab and 8.2 months with chemotherapy (hazard ratio, 0.60; P = .0002). The 12-month PFS rates were 55% and 37%, respectively. The 24-month PFS rates were 48% and 19%, respectively.
Overall response rates were 43.8% with pembrolizumab, consisting of 11.1% complete responses and 32.7% partial responses. The overall response rate with chemotherapy was 33.1%, consisting of 3.9% complete responses and 29.2% partial responses.
In all, 20.9% of patients on pembrolizumab and 42.2% of those on chemotherapy had stable disease. Rates of progressive disease were 29.4% and 12.3%, respectively.
The median duration of response was not reached in the pembrolizumab arm and was 10.6 months in the chemotherapy arm. At 2 years, 83% of patients treated with pembrolizumab and 35% treated with chemotherapy had ongoing responses.
Grade 3 or greater treatment-related adverse events occurred in 22% of patients on pembrolizumab and 66% on chemotherapy.
Immune-mediated adverse events and infusion reactions were more common with pembrolizumab than with chemotherapy (31% and 13%, respectively). Adverse events that were common with chemotherapy included gastrointestinal events, fatigue, neutropenia, and peripheral sensory neuropathy.
The study was funded by Merck. Dr. André disclosed relationships with multiple companies, including MSD Oncology. Dr. Overman disclosed consulting activities with various companies, not including Merck.
SOURCE: André T et al. ASCO 2020, Abstract LBA4.
FROM ASCO 2020
COVID-19 effect: Prescription fills mostly down for leading drugs
Prescription fills for hydroxychloroquine/chloroquine spiked right after COVID-19 was declared a national emergency in March, but use of the drugs still remains well above 2019 levels, based on data from more than 58,000 U.S. pharmacies.
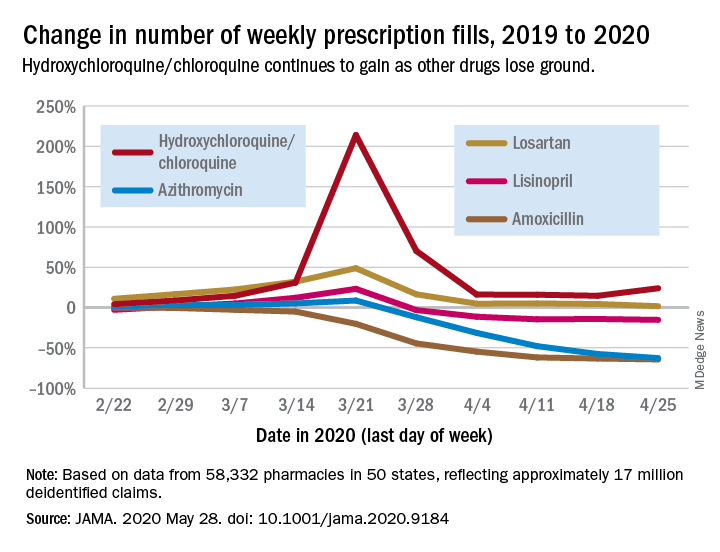
Hydroxychloroquine/chloroquine are also doing better than any of the prescription drugs in the top 10 based on total claims in 2019, Muthiah Vaduganathan, MD, MPH, of Brigham and Women’s Hospital, Boston, and associates reported May 28 in a research letter in JAMA.
Prescription fills for hydroxychloroquine/chloroquine have been above 2019 levels every week since the national emergency was declared on March 13, with the high occurring during the week of March 15-21, when fills were 214% higher than the corresponding week in 2019. The lowest level in that time came during the week of April 12-18, with growth of 14.6% over 2019, the investigators said.
The drugs occupying the top 10 – amlodipine, amoxicillin, atorvastatin, gabapentin, hydrocodone-acetaminophen, levothyroxine, lisinopril, losartan, omeprazole, and sertraline – have not done as well. Losartan, the only one that hasn’t lost ground in any week since March 13, rose by almost 49% during March 15-21, but was down to a 1.7% rise by the end of the study period, they reported.
Meanwhile, the other drug touted as a treatment for COVID-19, azithromycin, has fallen farther than most of the top 10. By April 19-25, the last week of the study period, fills for the antibiotic were down 62.7%, compared with last year, the analysis showed. Only amoxicillin had dropped more (64.4%).
“The modest decline for most common long-term therapies after peak could represent reduced contact with prescribing clinicians, restricted access to pharmacies, pharmacist rationing, loss of insurance from unemployment, or replete supplies from early stockpiling,” Dr. Vaduganathan and associates wrote.
The investigators “used all-payer U.S. pharmacy data from 58,332 chain, independent, and mail-order pharmacies across 14,421 zip codes in 50 states, reflecting approximately 17 million deidentified claims,” to estimate national prescription fills, they explained.
SOURCE: Vaduganathan M et al. JAMA 2020 May 28. doi: 10.1001/jama.2020.9184.
Prescription fills for hydroxychloroquine/chloroquine spiked right after COVID-19 was declared a national emergency in March, but use of the drugs still remains well above 2019 levels, based on data from more than 58,000 U.S. pharmacies.
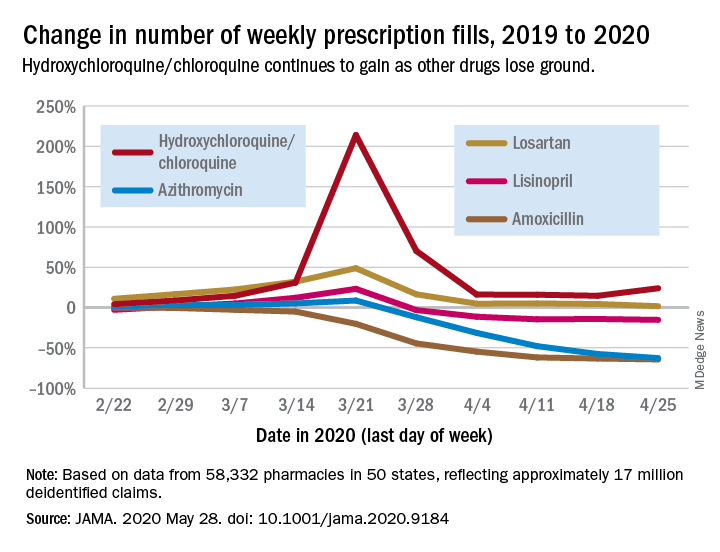
Hydroxychloroquine/chloroquine are also doing better than any of the prescription drugs in the top 10 based on total claims in 2019, Muthiah Vaduganathan, MD, MPH, of Brigham and Women’s Hospital, Boston, and associates reported May 28 in a research letter in JAMA.
Prescription fills for hydroxychloroquine/chloroquine have been above 2019 levels every week since the national emergency was declared on March 13, with the high occurring during the week of March 15-21, when fills were 214% higher than the corresponding week in 2019. The lowest level in that time came during the week of April 12-18, with growth of 14.6% over 2019, the investigators said.
The drugs occupying the top 10 – amlodipine, amoxicillin, atorvastatin, gabapentin, hydrocodone-acetaminophen, levothyroxine, lisinopril, losartan, omeprazole, and sertraline – have not done as well. Losartan, the only one that hasn’t lost ground in any week since March 13, rose by almost 49% during March 15-21, but was down to a 1.7% rise by the end of the study period, they reported.
Meanwhile, the other drug touted as a treatment for COVID-19, azithromycin, has fallen farther than most of the top 10. By April 19-25, the last week of the study period, fills for the antibiotic were down 62.7%, compared with last year, the analysis showed. Only amoxicillin had dropped more (64.4%).
“The modest decline for most common long-term therapies after peak could represent reduced contact with prescribing clinicians, restricted access to pharmacies, pharmacist rationing, loss of insurance from unemployment, or replete supplies from early stockpiling,” Dr. Vaduganathan and associates wrote.
The investigators “used all-payer U.S. pharmacy data from 58,332 chain, independent, and mail-order pharmacies across 14,421 zip codes in 50 states, reflecting approximately 17 million deidentified claims,” to estimate national prescription fills, they explained.
SOURCE: Vaduganathan M et al. JAMA 2020 May 28. doi: 10.1001/jama.2020.9184.
Prescription fills for hydroxychloroquine/chloroquine spiked right after COVID-19 was declared a national emergency in March, but use of the drugs still remains well above 2019 levels, based on data from more than 58,000 U.S. pharmacies.
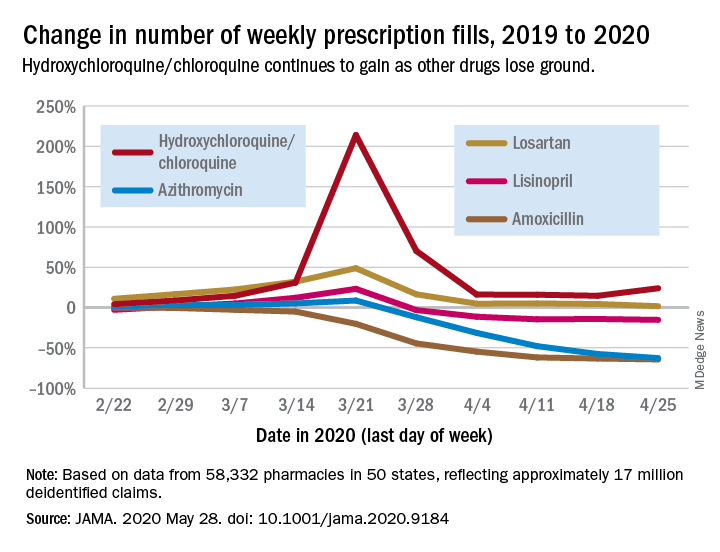
Hydroxychloroquine/chloroquine are also doing better than any of the prescription drugs in the top 10 based on total claims in 2019, Muthiah Vaduganathan, MD, MPH, of Brigham and Women’s Hospital, Boston, and associates reported May 28 in a research letter in JAMA.
Prescription fills for hydroxychloroquine/chloroquine have been above 2019 levels every week since the national emergency was declared on March 13, with the high occurring during the week of March 15-21, when fills were 214% higher than the corresponding week in 2019. The lowest level in that time came during the week of April 12-18, with growth of 14.6% over 2019, the investigators said.
The drugs occupying the top 10 – amlodipine, amoxicillin, atorvastatin, gabapentin, hydrocodone-acetaminophen, levothyroxine, lisinopril, losartan, omeprazole, and sertraline – have not done as well. Losartan, the only one that hasn’t lost ground in any week since March 13, rose by almost 49% during March 15-21, but was down to a 1.7% rise by the end of the study period, they reported.
Meanwhile, the other drug touted as a treatment for COVID-19, azithromycin, has fallen farther than most of the top 10. By April 19-25, the last week of the study period, fills for the antibiotic were down 62.7%, compared with last year, the analysis showed. Only amoxicillin had dropped more (64.4%).
“The modest decline for most common long-term therapies after peak could represent reduced contact with prescribing clinicians, restricted access to pharmacies, pharmacist rationing, loss of insurance from unemployment, or replete supplies from early stockpiling,” Dr. Vaduganathan and associates wrote.
The investigators “used all-payer U.S. pharmacy data from 58,332 chain, independent, and mail-order pharmacies across 14,421 zip codes in 50 states, reflecting approximately 17 million deidentified claims,” to estimate national prescription fills, they explained.
SOURCE: Vaduganathan M et al. JAMA 2020 May 28. doi: 10.1001/jama.2020.9184.
FROM JAMA
APA, others lobby to make COVID-19 telehealth waivers permanent
The American Psychiatric Association (APA) is calling on Congress to permanently lift restrictions that have allowed unfettered delivery of telehealth services during the COVID-19 pandemic, which experts say has been a boon to patients and physicians alike.
“We ask Congress to extend the telehealth waiver authority under COVID-19 beyond the emergency and to study its impact while doing so,” said APA President Jeffrey Geller, MD, in a May 27 video briefing with congressional staff and reporters.
The APA is also seeking to make permanent certain waivers granted by the Centers for Medicare & Medicaid Services on April 30, including elimination of geographic restrictions on behavioral health and allowing patients be seen at home, said Dr. Geller.
The APA also is asking for the elimination of the rule that requires clinicians to have an initial face-to-face meeting with patients before they can prescribe controlled substances, Dr. Geller said. The Drug Enforcement Administration waived that requirement, known as the Ryan Haight Act, on March 17 for the duration of the national emergency.
Telemedicine has supporters on both sides of the aisle in Congress, including Rep. Paul Tonko (D-N.Y.) who said at the APA briefing he would fight to make the waivers permanent.
“The expanded use of telehealth has enormous potential during normal times as well, especially in behavioral health,” said Mr. Tonko. “I am pushing fiercely for these current flexibilities to be extended for a reasonable time after the public health emergency so that we can have time to evaluate which should be made permanent,” he said.
Dr. Geller, other clinicians, and advocates in the briefing praised CMS for facilitating telepsychiatry for Medicare. That follows in the footsteps of most private insurers, who have also relaxed requirements into the summer, according to the Medical Group Management Association.
Game changer
The Medicare waivers “have dramatically changed the entire scene for someone like myself as a clinician to allow me to see my patients in a much easier way,” said Peter Yellowlees, MBBS, MD, chief wellness officer, University of California Davis Health. Within 2 weeks in March, the health system converted almost all of its regular outpatient visits to telemedicine, he said.
Dr. Yellowlees added government still needs to address, what he called, outdated HIPAA regulations that ban certain technologies.
“It makes no sense that I can talk to someone on an iPhone, but the moment I talk to them on FaceTime, it’s illegal,” said Dr. Yellowlees, a former president of the American Telemedicine Association.
Dr. Geller said that “psychiatric care provided by telehealth is as effective as in-person psychiatric services,” adding that “some patients prefer telepsychiatry because of its convenience and as a means of reducing stigma associated with seeking help for mental health.”
Shabana Khan, MD, a child psychiatrist and director of telepsychiatry at New York University Langone Health, said audio and video conferencing are helping address a shortage and maldistribution of child and adolescent psychiatrists.
Americans’ mental health is suffering during the pandemic. The U.S. Census Bureau recently released data showing that half of those surveyed reported depressed mood and that one-third are reporting anxiety, depression, or both, as reported by the Washington Post.
“At this very time that anxiety, depression, substance use, and other mental health problems are rising, our nation’s already strained mental health system is really being pushed to the brink,” said Jodi Kwarciany, manager for mental health policy for the National Alliance on Mental Illness, during the briefing.
Telemedicine can help “by connecting people to providers at the time and the place and using the technology that works best for them,” she said, adding that NAMI would press policymakers to address barriers to access.
The clinicians on the briefing said they’ve observed that some patients are more comfortable with video or audio interactions than with in-person visits.
Increased access to care
Telepsychiatry seems to be convincing some to reconsider therapy, since they can do it at home, said Dr. Yellowlees. he said.
For instance, he said, he has been able to consult by phone and video with several patients who receive care through the Indian Health Service who had not be able to get into the physical clinic.
Dr. Yellowlees said video sessions also may encourage patients to be more, not less, talkative. “Video is actually counterintuitively a very intimate experience,” he said, in part because of the perceived distance and people’s tendency to be less inhibited on technology platforms.“It’s less embarrassing,” he said. “If you’ve got really dramatic, difficult, traumatic things to talk about, it’s slightly easier to talk to someone who’s slightly further apart from you on video,” said Dr. Yellowlees.
“Individuals who have a significant amount of anxiety may actually feel more comfortable with the distance that this technology affords,” agreed Dr. Khan. She said telemedicine had made sessions more comfortable for some of her patients with autism spectrum disorder.
Dr. Geller said audio and video have been important to his practice during the pandemic. One of his patients never leaves the house and does not use computers. “He spends his time sequestered at home listening to records on his record player,” said Dr. Geller. But he’s been amenable to phone sessions. “What I’ve found with him, and I’ve found with several other patients, is that they actually talk more easily when they’re not face to face,” he said.
Far fewer no-shows
Another plus for his New England–based practice during the last few months: patients have not been anxious about missing sessions because of the weather. The clinicians all noted that telepsychiatry seemed to reduce missed visits.
Dr. Yellowlees said that no-show rates had decreased by half at UC Davis. “That means no significant loss of income,” during the pandemic, he said.
“The no-show rate is incredibly low, particularly because when you call the patients and they don’t remember they had an appointment, you have the appointment anyway, most of the time,” said Dr. Geller.
For Dr. Khan, being able to conduct audio and video sessions during the pandemic has meant keeping up continuity of care.
As a result of the pandemic, many college students in New York City had to go home – often to another state. The waivers granted by New York’s Medicaid program and other insurers have allowed Dr. Khan to continue care for these patients.
The NYU clinic also operates day programs in rural areas 5 hours from the city. Dr. Khan recently evaluated a 12-year-old girl with significant anxiety and low mood, both of which had worsened.
“She would not have been able to access care otherwise,” said Dr. Khan. And for rural patients who do not have access to broadband or smartphones, audio visits “have been immensely helpful,” she said.
Dr. Khan, Dr. Geller, and Dr. Yellowlees have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The American Psychiatric Association (APA) is calling on Congress to permanently lift restrictions that have allowed unfettered delivery of telehealth services during the COVID-19 pandemic, which experts say has been a boon to patients and physicians alike.
“We ask Congress to extend the telehealth waiver authority under COVID-19 beyond the emergency and to study its impact while doing so,” said APA President Jeffrey Geller, MD, in a May 27 video briefing with congressional staff and reporters.
The APA is also seeking to make permanent certain waivers granted by the Centers for Medicare & Medicaid Services on April 30, including elimination of geographic restrictions on behavioral health and allowing patients be seen at home, said Dr. Geller.
The APA also is asking for the elimination of the rule that requires clinicians to have an initial face-to-face meeting with patients before they can prescribe controlled substances, Dr. Geller said. The Drug Enforcement Administration waived that requirement, known as the Ryan Haight Act, on March 17 for the duration of the national emergency.
Telemedicine has supporters on both sides of the aisle in Congress, including Rep. Paul Tonko (D-N.Y.) who said at the APA briefing he would fight to make the waivers permanent.
“The expanded use of telehealth has enormous potential during normal times as well, especially in behavioral health,” said Mr. Tonko. “I am pushing fiercely for these current flexibilities to be extended for a reasonable time after the public health emergency so that we can have time to evaluate which should be made permanent,” he said.
Dr. Geller, other clinicians, and advocates in the briefing praised CMS for facilitating telepsychiatry for Medicare. That follows in the footsteps of most private insurers, who have also relaxed requirements into the summer, according to the Medical Group Management Association.
Game changer
The Medicare waivers “have dramatically changed the entire scene for someone like myself as a clinician to allow me to see my patients in a much easier way,” said Peter Yellowlees, MBBS, MD, chief wellness officer, University of California Davis Health. Within 2 weeks in March, the health system converted almost all of its regular outpatient visits to telemedicine, he said.
Dr. Yellowlees added government still needs to address, what he called, outdated HIPAA regulations that ban certain technologies.
“It makes no sense that I can talk to someone on an iPhone, but the moment I talk to them on FaceTime, it’s illegal,” said Dr. Yellowlees, a former president of the American Telemedicine Association.
Dr. Geller said that “psychiatric care provided by telehealth is as effective as in-person psychiatric services,” adding that “some patients prefer telepsychiatry because of its convenience and as a means of reducing stigma associated with seeking help for mental health.”
Shabana Khan, MD, a child psychiatrist and director of telepsychiatry at New York University Langone Health, said audio and video conferencing are helping address a shortage and maldistribution of child and adolescent psychiatrists.
Americans’ mental health is suffering during the pandemic. The U.S. Census Bureau recently released data showing that half of those surveyed reported depressed mood and that one-third are reporting anxiety, depression, or both, as reported by the Washington Post.
“At this very time that anxiety, depression, substance use, and other mental health problems are rising, our nation’s already strained mental health system is really being pushed to the brink,” said Jodi Kwarciany, manager for mental health policy for the National Alliance on Mental Illness, during the briefing.
Telemedicine can help “by connecting people to providers at the time and the place and using the technology that works best for them,” she said, adding that NAMI would press policymakers to address barriers to access.
The clinicians on the briefing said they’ve observed that some patients are more comfortable with video or audio interactions than with in-person visits.
Increased access to care
Telepsychiatry seems to be convincing some to reconsider therapy, since they can do it at home, said Dr. Yellowlees. he said.
For instance, he said, he has been able to consult by phone and video with several patients who receive care through the Indian Health Service who had not be able to get into the physical clinic.
Dr. Yellowlees said video sessions also may encourage patients to be more, not less, talkative. “Video is actually counterintuitively a very intimate experience,” he said, in part because of the perceived distance and people’s tendency to be less inhibited on technology platforms.“It’s less embarrassing,” he said. “If you’ve got really dramatic, difficult, traumatic things to talk about, it’s slightly easier to talk to someone who’s slightly further apart from you on video,” said Dr. Yellowlees.
“Individuals who have a significant amount of anxiety may actually feel more comfortable with the distance that this technology affords,” agreed Dr. Khan. She said telemedicine had made sessions more comfortable for some of her patients with autism spectrum disorder.
Dr. Geller said audio and video have been important to his practice during the pandemic. One of his patients never leaves the house and does not use computers. “He spends his time sequestered at home listening to records on his record player,” said Dr. Geller. But he’s been amenable to phone sessions. “What I’ve found with him, and I’ve found with several other patients, is that they actually talk more easily when they’re not face to face,” he said.
Far fewer no-shows
Another plus for his New England–based practice during the last few months: patients have not been anxious about missing sessions because of the weather. The clinicians all noted that telepsychiatry seemed to reduce missed visits.
Dr. Yellowlees said that no-show rates had decreased by half at UC Davis. “That means no significant loss of income,” during the pandemic, he said.
“The no-show rate is incredibly low, particularly because when you call the patients and they don’t remember they had an appointment, you have the appointment anyway, most of the time,” said Dr. Geller.
For Dr. Khan, being able to conduct audio and video sessions during the pandemic has meant keeping up continuity of care.
As a result of the pandemic, many college students in New York City had to go home – often to another state. The waivers granted by New York’s Medicaid program and other insurers have allowed Dr. Khan to continue care for these patients.
The NYU clinic also operates day programs in rural areas 5 hours from the city. Dr. Khan recently evaluated a 12-year-old girl with significant anxiety and low mood, both of which had worsened.
“She would not have been able to access care otherwise,” said Dr. Khan. And for rural patients who do not have access to broadband or smartphones, audio visits “have been immensely helpful,” she said.
Dr. Khan, Dr. Geller, and Dr. Yellowlees have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The American Psychiatric Association (APA) is calling on Congress to permanently lift restrictions that have allowed unfettered delivery of telehealth services during the COVID-19 pandemic, which experts say has been a boon to patients and physicians alike.
“We ask Congress to extend the telehealth waiver authority under COVID-19 beyond the emergency and to study its impact while doing so,” said APA President Jeffrey Geller, MD, in a May 27 video briefing with congressional staff and reporters.
The APA is also seeking to make permanent certain waivers granted by the Centers for Medicare & Medicaid Services on April 30, including elimination of geographic restrictions on behavioral health and allowing patients be seen at home, said Dr. Geller.
The APA also is asking for the elimination of the rule that requires clinicians to have an initial face-to-face meeting with patients before they can prescribe controlled substances, Dr. Geller said. The Drug Enforcement Administration waived that requirement, known as the Ryan Haight Act, on March 17 for the duration of the national emergency.
Telemedicine has supporters on both sides of the aisle in Congress, including Rep. Paul Tonko (D-N.Y.) who said at the APA briefing he would fight to make the waivers permanent.
“The expanded use of telehealth has enormous potential during normal times as well, especially in behavioral health,” said Mr. Tonko. “I am pushing fiercely for these current flexibilities to be extended for a reasonable time after the public health emergency so that we can have time to evaluate which should be made permanent,” he said.
Dr. Geller, other clinicians, and advocates in the briefing praised CMS for facilitating telepsychiatry for Medicare. That follows in the footsteps of most private insurers, who have also relaxed requirements into the summer, according to the Medical Group Management Association.
Game changer
The Medicare waivers “have dramatically changed the entire scene for someone like myself as a clinician to allow me to see my patients in a much easier way,” said Peter Yellowlees, MBBS, MD, chief wellness officer, University of California Davis Health. Within 2 weeks in March, the health system converted almost all of its regular outpatient visits to telemedicine, he said.
Dr. Yellowlees added government still needs to address, what he called, outdated HIPAA regulations that ban certain technologies.
“It makes no sense that I can talk to someone on an iPhone, but the moment I talk to them on FaceTime, it’s illegal,” said Dr. Yellowlees, a former president of the American Telemedicine Association.
Dr. Geller said that “psychiatric care provided by telehealth is as effective as in-person psychiatric services,” adding that “some patients prefer telepsychiatry because of its convenience and as a means of reducing stigma associated with seeking help for mental health.”
Shabana Khan, MD, a child psychiatrist and director of telepsychiatry at New York University Langone Health, said audio and video conferencing are helping address a shortage and maldistribution of child and adolescent psychiatrists.
Americans’ mental health is suffering during the pandemic. The U.S. Census Bureau recently released data showing that half of those surveyed reported depressed mood and that one-third are reporting anxiety, depression, or both, as reported by the Washington Post.
“At this very time that anxiety, depression, substance use, and other mental health problems are rising, our nation’s already strained mental health system is really being pushed to the brink,” said Jodi Kwarciany, manager for mental health policy for the National Alliance on Mental Illness, during the briefing.
Telemedicine can help “by connecting people to providers at the time and the place and using the technology that works best for them,” she said, adding that NAMI would press policymakers to address barriers to access.
The clinicians on the briefing said they’ve observed that some patients are more comfortable with video or audio interactions than with in-person visits.
Increased access to care
Telepsychiatry seems to be convincing some to reconsider therapy, since they can do it at home, said Dr. Yellowlees. he said.
For instance, he said, he has been able to consult by phone and video with several patients who receive care through the Indian Health Service who had not be able to get into the physical clinic.
Dr. Yellowlees said video sessions also may encourage patients to be more, not less, talkative. “Video is actually counterintuitively a very intimate experience,” he said, in part because of the perceived distance and people’s tendency to be less inhibited on technology platforms.“It’s less embarrassing,” he said. “If you’ve got really dramatic, difficult, traumatic things to talk about, it’s slightly easier to talk to someone who’s slightly further apart from you on video,” said Dr. Yellowlees.
“Individuals who have a significant amount of anxiety may actually feel more comfortable with the distance that this technology affords,” agreed Dr. Khan. She said telemedicine had made sessions more comfortable for some of her patients with autism spectrum disorder.
Dr. Geller said audio and video have been important to his practice during the pandemic. One of his patients never leaves the house and does not use computers. “He spends his time sequestered at home listening to records on his record player,” said Dr. Geller. But he’s been amenable to phone sessions. “What I’ve found with him, and I’ve found with several other patients, is that they actually talk more easily when they’re not face to face,” he said.
Far fewer no-shows
Another plus for his New England–based practice during the last few months: patients have not been anxious about missing sessions because of the weather. The clinicians all noted that telepsychiatry seemed to reduce missed visits.
Dr. Yellowlees said that no-show rates had decreased by half at UC Davis. “That means no significant loss of income,” during the pandemic, he said.
“The no-show rate is incredibly low, particularly because when you call the patients and they don’t remember they had an appointment, you have the appointment anyway, most of the time,” said Dr. Geller.
For Dr. Khan, being able to conduct audio and video sessions during the pandemic has meant keeping up continuity of care.
As a result of the pandemic, many college students in New York City had to go home – often to another state. The waivers granted by New York’s Medicaid program and other insurers have allowed Dr. Khan to continue care for these patients.
The NYU clinic also operates day programs in rural areas 5 hours from the city. Dr. Khan recently evaluated a 12-year-old girl with significant anxiety and low mood, both of which had worsened.
“She would not have been able to access care otherwise,” said Dr. Khan. And for rural patients who do not have access to broadband or smartphones, audio visits “have been immensely helpful,” she said.
Dr. Khan, Dr. Geller, and Dr. Yellowlees have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.

