User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Lancet, NEJM retract studies on hydroxychloroquine for COVID-19
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
Should healthcare workers wear masks at home?
Wearing a mask at home, even when everyone is feeling fine, might reduce the risk of frontline healthcare workers transmitting SARS-CoV-2 infection to their families, a recent study from China suggests. But the benefits might not outweigh the costs, according to several physicians interviewed.
“My gut reaction is that home mask use for healthcare workers would place an inordinately high burden on those healthcare workers and their families,” said Jeanne Noble, MD, an emergency care physician at the University of California, San Francisco. “Wearing a mask for a 10-hour shift already represents significant physical discomfort, causing sores across the nose and behind the ears. The emotional toll of the physical distance that comes with mask use, with limited facial expression, is also quite real.”
The suggested benefit of home mask use comes from research published online May 28 in BMJ Global Health. To assess predictors of household transmission of SARS-CoV-2 infection, Yu Wang, MD, of the Beijing Center for Disease Prevention and Control and colleagues conducted a retrospective study of 124 families in Beijing in which there was a confirmed case of COVID-19 as of February 21. The researchers surveyed family members by telephone about household hygiene and behaviors during the pandemic to examine risk factors for transmission.
During the 2 weeks following onset of the primary case, secondary transmission occurred in 41 families. Overall, 77 of 335 family members developed COVID-19.
A multivariable logistic regression analysis found that in households in which family members wore masks at home before the first person became ill, there was less likelihood of transmission of disease to a family member, compared with families in which no one wore a mask prior to illness onset.
“Facemasks were 79% effective and disinfection was 77% effective in preventing transmission,” the researchers report, “whilst close frequent contact in the household increased the risk of transmission 18 times, and diarrhea in the index patient increased the risk by four times.
However, wearing masks after symptom onset was not protective, according to the analysis. The findings support “universal face mask use, and also provides guidance on risk reduction for families living with someone in quarantine or isolation, and families of health workers, who may face ongoing risk,” the authors write.
Still, other precautions may be more important, experts say.
“I think by far the best way for healthcare professionals to protect their families is to carefully employ appropriate infection prevention measures at work,” said Mark E. Rupp, MD, chief of the Division of Infectious Diseases at Nebraska Medical Center in Omaha. “The combination of administrative interventions, engineering improvements, and personal protective equipment is very effective in preventing SARS-CoV-2 acquisition in the workplace.”
Many physicians already wear masks at home, and this study “only reemphasized the importance of doing so,” said Raghavendra Tirupathi, MD, medical director of Keystone Infectious Diseases in Chambersburg, Pennsylvania, who recently reviewed studies about masks and COVID-19.
Home mask use provides “one more layer of protection that might help mitigate the risk of transmission to family members,” Tirupathi said. But it does not obviate the need to follow other preventive measures, such as social distancing and proper hygiene.
But Rupp, whose advice on how healthcare workers can protect their families was recently highlighted by the American Medical Association, isn’t convinced. He said he won’t be adding home mask use to his list of recommendations. “It would be intrusive, cumbersome, and impractical to wear a mask in the home setting,” Rupp said in an interview.
However, when out in the community, all family members must protect one another by practicing social distancing, wearing masks, and practicing proper hand hygiene. “I also think that it is a good idea to have some masks on hand in case anyone does develop symptoms in the household and to wear them if a family member falls ill ― at least until testing can confirm COVID-19,” Rupp said. “If a family member does fall ill, masks for the ill person as well as the well persons would be indicated along with other home quarantine measures.”
For her part, Noble, who has provided guidance about proper mask use, said that targeted use of masks at home, such as around older visiting relatives or other more vulnerable family members, may be more realistic than continuous in-home use.
When a household member becomes ill, recommendations for preventing disease spread include having a sick family member sleep in a separate bedroom, using a separate bathroom, and wearing a mask when within 6 feet of other household members. They also should avoid sharing meals. “For a household member who is a medical provider, to follow these self-isolation precautions while at home for months on end would have a significant emotional toll,” Noble said in an email. “With no end in sight for the pandemic, perpetual mask use in both the private and public sphere strikes me as overwhelming ― I write this near the end of my 10-hour shift wearing both an N95 and surgical mask and counting the minutes before I can take them off!”
A limitation of the study was its reliance on telephone interviews, which are subject to recall bias, the authors note.
The study was funded by the Beijing Science and Technology Planning Project. The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Wearing a mask at home, even when everyone is feeling fine, might reduce the risk of frontline healthcare workers transmitting SARS-CoV-2 infection to their families, a recent study from China suggests. But the benefits might not outweigh the costs, according to several physicians interviewed.
“My gut reaction is that home mask use for healthcare workers would place an inordinately high burden on those healthcare workers and their families,” said Jeanne Noble, MD, an emergency care physician at the University of California, San Francisco. “Wearing a mask for a 10-hour shift already represents significant physical discomfort, causing sores across the nose and behind the ears. The emotional toll of the physical distance that comes with mask use, with limited facial expression, is also quite real.”
The suggested benefit of home mask use comes from research published online May 28 in BMJ Global Health. To assess predictors of household transmission of SARS-CoV-2 infection, Yu Wang, MD, of the Beijing Center for Disease Prevention and Control and colleagues conducted a retrospective study of 124 families in Beijing in which there was a confirmed case of COVID-19 as of February 21. The researchers surveyed family members by telephone about household hygiene and behaviors during the pandemic to examine risk factors for transmission.
During the 2 weeks following onset of the primary case, secondary transmission occurred in 41 families. Overall, 77 of 335 family members developed COVID-19.
A multivariable logistic regression analysis found that in households in which family members wore masks at home before the first person became ill, there was less likelihood of transmission of disease to a family member, compared with families in which no one wore a mask prior to illness onset.
“Facemasks were 79% effective and disinfection was 77% effective in preventing transmission,” the researchers report, “whilst close frequent contact in the household increased the risk of transmission 18 times, and diarrhea in the index patient increased the risk by four times.
However, wearing masks after symptom onset was not protective, according to the analysis. The findings support “universal face mask use, and also provides guidance on risk reduction for families living with someone in quarantine or isolation, and families of health workers, who may face ongoing risk,” the authors write.
Still, other precautions may be more important, experts say.
“I think by far the best way for healthcare professionals to protect their families is to carefully employ appropriate infection prevention measures at work,” said Mark E. Rupp, MD, chief of the Division of Infectious Diseases at Nebraska Medical Center in Omaha. “The combination of administrative interventions, engineering improvements, and personal protective equipment is very effective in preventing SARS-CoV-2 acquisition in the workplace.”
Many physicians already wear masks at home, and this study “only reemphasized the importance of doing so,” said Raghavendra Tirupathi, MD, medical director of Keystone Infectious Diseases in Chambersburg, Pennsylvania, who recently reviewed studies about masks and COVID-19.
Home mask use provides “one more layer of protection that might help mitigate the risk of transmission to family members,” Tirupathi said. But it does not obviate the need to follow other preventive measures, such as social distancing and proper hygiene.
But Rupp, whose advice on how healthcare workers can protect their families was recently highlighted by the American Medical Association, isn’t convinced. He said he won’t be adding home mask use to his list of recommendations. “It would be intrusive, cumbersome, and impractical to wear a mask in the home setting,” Rupp said in an interview.
However, when out in the community, all family members must protect one another by practicing social distancing, wearing masks, and practicing proper hand hygiene. “I also think that it is a good idea to have some masks on hand in case anyone does develop symptoms in the household and to wear them if a family member falls ill ― at least until testing can confirm COVID-19,” Rupp said. “If a family member does fall ill, masks for the ill person as well as the well persons would be indicated along with other home quarantine measures.”
For her part, Noble, who has provided guidance about proper mask use, said that targeted use of masks at home, such as around older visiting relatives or other more vulnerable family members, may be more realistic than continuous in-home use.
When a household member becomes ill, recommendations for preventing disease spread include having a sick family member sleep in a separate bedroom, using a separate bathroom, and wearing a mask when within 6 feet of other household members. They also should avoid sharing meals. “For a household member who is a medical provider, to follow these self-isolation precautions while at home for months on end would have a significant emotional toll,” Noble said in an email. “With no end in sight for the pandemic, perpetual mask use in both the private and public sphere strikes me as overwhelming ― I write this near the end of my 10-hour shift wearing both an N95 and surgical mask and counting the minutes before I can take them off!”
A limitation of the study was its reliance on telephone interviews, which are subject to recall bias, the authors note.
The study was funded by the Beijing Science and Technology Planning Project. The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Wearing a mask at home, even when everyone is feeling fine, might reduce the risk of frontline healthcare workers transmitting SARS-CoV-2 infection to their families, a recent study from China suggests. But the benefits might not outweigh the costs, according to several physicians interviewed.
“My gut reaction is that home mask use for healthcare workers would place an inordinately high burden on those healthcare workers and their families,” said Jeanne Noble, MD, an emergency care physician at the University of California, San Francisco. “Wearing a mask for a 10-hour shift already represents significant physical discomfort, causing sores across the nose and behind the ears. The emotional toll of the physical distance that comes with mask use, with limited facial expression, is also quite real.”
The suggested benefit of home mask use comes from research published online May 28 in BMJ Global Health. To assess predictors of household transmission of SARS-CoV-2 infection, Yu Wang, MD, of the Beijing Center for Disease Prevention and Control and colleagues conducted a retrospective study of 124 families in Beijing in which there was a confirmed case of COVID-19 as of February 21. The researchers surveyed family members by telephone about household hygiene and behaviors during the pandemic to examine risk factors for transmission.
During the 2 weeks following onset of the primary case, secondary transmission occurred in 41 families. Overall, 77 of 335 family members developed COVID-19.
A multivariable logistic regression analysis found that in households in which family members wore masks at home before the first person became ill, there was less likelihood of transmission of disease to a family member, compared with families in which no one wore a mask prior to illness onset.
“Facemasks were 79% effective and disinfection was 77% effective in preventing transmission,” the researchers report, “whilst close frequent contact in the household increased the risk of transmission 18 times, and diarrhea in the index patient increased the risk by four times.
However, wearing masks after symptom onset was not protective, according to the analysis. The findings support “universal face mask use, and also provides guidance on risk reduction for families living with someone in quarantine or isolation, and families of health workers, who may face ongoing risk,” the authors write.
Still, other precautions may be more important, experts say.
“I think by far the best way for healthcare professionals to protect their families is to carefully employ appropriate infection prevention measures at work,” said Mark E. Rupp, MD, chief of the Division of Infectious Diseases at Nebraska Medical Center in Omaha. “The combination of administrative interventions, engineering improvements, and personal protective equipment is very effective in preventing SARS-CoV-2 acquisition in the workplace.”
Many physicians already wear masks at home, and this study “only reemphasized the importance of doing so,” said Raghavendra Tirupathi, MD, medical director of Keystone Infectious Diseases in Chambersburg, Pennsylvania, who recently reviewed studies about masks and COVID-19.
Home mask use provides “one more layer of protection that might help mitigate the risk of transmission to family members,” Tirupathi said. But it does not obviate the need to follow other preventive measures, such as social distancing and proper hygiene.
But Rupp, whose advice on how healthcare workers can protect their families was recently highlighted by the American Medical Association, isn’t convinced. He said he won’t be adding home mask use to his list of recommendations. “It would be intrusive, cumbersome, and impractical to wear a mask in the home setting,” Rupp said in an interview.
However, when out in the community, all family members must protect one another by practicing social distancing, wearing masks, and practicing proper hand hygiene. “I also think that it is a good idea to have some masks on hand in case anyone does develop symptoms in the household and to wear them if a family member falls ill ― at least until testing can confirm COVID-19,” Rupp said. “If a family member does fall ill, masks for the ill person as well as the well persons would be indicated along with other home quarantine measures.”
For her part, Noble, who has provided guidance about proper mask use, said that targeted use of masks at home, such as around older visiting relatives or other more vulnerable family members, may be more realistic than continuous in-home use.
When a household member becomes ill, recommendations for preventing disease spread include having a sick family member sleep in a separate bedroom, using a separate bathroom, and wearing a mask when within 6 feet of other household members. They also should avoid sharing meals. “For a household member who is a medical provider, to follow these self-isolation precautions while at home for months on end would have a significant emotional toll,” Noble said in an email. “With no end in sight for the pandemic, perpetual mask use in both the private and public sphere strikes me as overwhelming ― I write this near the end of my 10-hour shift wearing both an N95 and surgical mask and counting the minutes before I can take them off!”
A limitation of the study was its reliance on telephone interviews, which are subject to recall bias, the authors note.
The study was funded by the Beijing Science and Technology Planning Project. The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Most rheumatology drugs don’t increase COVID-19 hospitalization risk
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
Parenting special needs children: An unlikely model
COVID-19 can give physicians a window into lives of families
The last few months have tested the stamina of most families. Many people are struggling to keep some semblance of normalcy amid a radical transformation of everyday life. It seems as if everything changed overnight.
In a similar way, when a child with many needs is born into a family, adjustments also have to take place to receive the new baby. Families are, in most cases, not prepared for what is to come. Their expectations usually are not in sync with how their lives end up. They are crunched for time. They need to adjust, and at the same time, they mourn the loss of their previous less demanding lifestyle. More importantly, these parents learn that this might be an adjustment that they might need to make for a long time – in some instances, for a lifetime.
Stress load over time can correlate with a sense of burnout, and mental health professionals need to be prepared to address these issues in our patients.
Here is a list of some chronic struggles with which many special needs parents must contend. These strongly resemble the challenges parents in the general population have been facing with their families during this pandemic:
- Bypassing breaks to unwind and having to be always “on” while at home: These parents take care of children who need to be chronically tube fed, can’t sleep well at night because they are often sick, have recurrent seizures or maladaptive behaviors that affect the caretakers and the rest of the family. For parents of children who are on the autism spectrum, these challenges can be a constant struggle. Almost 60% of children with autism spectrum disorder (ASD) experience bodily difficulties, such as trouble breathing. However, nearly 100% of children with ASD experienced difficulties with their abilities and activities, such as self-care tasks like eating and dressing, and emotional or behavioral health, according to a 2016 report on child and adolescent health by the Johns Hopkins Bloomberg School of Public Health.
- Taking on roles for which they are not trained: Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time. There are about 1.17 million children in the United States living with ASD and more than 12% of children with ASD have severe cases, the Hopkins report said. Parents frequently are forced to take on the role of “therapist” to meet the needs of their child.
- Staying home often: Some parents are unable to have a “regular sitter” to provide respite, because the needs of the child require a higher level of care, training, and consideration. Caring for a special child means parents often don’t have the option of leaving their older child alone. As a result, they may end up spending more time at home than their counterpart parents with children who are the same age.
- Struggling to meet everyone’s demands for attention while at home: The child might require full-time attention or prolonged hospitalizations, and the needs of other siblings are sometimes put on hold until time or energy are available for all.
- Not traveling unless absolutely necessary: Families have a hard time leaving home for vacations or for other reasons. They may have to travel with medical supplies and equipment. They need to make sure that their destination is ready to welcome their child with all needs taken into consideration (special diets, activities, and facilities). Will the vacation set them back because it might take more effort to go than to stay home?
- Avoiding unnecessary exposures: Trying to avoid infections (even the ones that may be innocuous to others) if their child is immunocompromised. These children may readily decompensate and end up hospitalized with a more serious medical complication.
- Being very aware of remaining physically distant from others: Parents must go to great lengths not to impinge on other people’s space if the child is being loud or moving in a disruptive way, or if other people negatively affect how the child responds. Some families are apprehensive because they have felt judged by others when they are in the community, restaurants, or other places of gathering.
- Feeling concerned about having the right food, medicines, and supplements in the house: Parents are constantly trying to fulfill special dietary requirements and have the reserve to make sure that all meals and treatments are accounted for in the near future. They might need oxygen or specialized formulas that are hard to find in local stores. Some treatments, when withdrawn or unavailable, can prove life threatening.
- Restricting social circles: Some families with children with severe autism may self-isolate when they feel it is hard to be around them and be friends with them, since they can’t readily participate in “usual family activities,” and the regular norms of socialization can’t apply to their family’s set of behaviors. Their child might seem to be disruptive, or loud, nonverbal, mute, or unable to easily relate to others.
- Experiencing a pervasive sense of uncertainty about the future: A child might continue to miss milestones, or might have a rare condition that hasn’t been diagnosed. When thinking of the future, parents can’t predict what level of care they need to plan and budget for.
- Being concerned about dying early and not being able to provide for their child: Parents worry about who would take care of their child for life. Who would take care of their aging adult “child” after parents are gone? They might have concerns about having a will in place early on.
- Facing financial stress secondary to losing a job or the cost of treatments: Absenteeism might be the end result of having to care for their child’s ongoing needs, appointments, and medical emergencies. Sometimes, they might depend on a caretaker who might be very difficult to replace. It might take extensive training once a candidate is found. Direct costs include medical care, hospitalizations, special education, special therapies (occupational, speech, and physical therapy), and paid caregivers. Indirect costs include lost productivity for family caregivers because of the inability to maintain employment while caring for affected individuals, as well as lost wages and benefits, the Hopkins report said.
- Struggling to coordinate daily schedules: Parents face this challenge not only with young children but with those who are chronically ill and might need ongoing 24/7 care. The schedule might include educational and therapeutic (physical, occupational, speech, language therapy, recreational) interventions regularly or daily. This schedule is to be superimposed on all the other necessary responsibilities parents already have to contend with. Forty-eight percent of school-aged children with ASD use three or more services. In addition, children with moderate or severe cases of ASD used three or more services at almost twice the rate of children with mild cases of ASD (60% vs. 35%).
- Longing for a cure or a medicine that will improve the outcome: Often, parents search for treatments so that their child could live a more comfortable or healthier life. For children who have a rare condition, there may not be sufficient research dedicated to their cause or diagnostic pursuits. Currently, it is estimated that 1 in 10 Americans has a rare disease – about 80% of which are genetically based. Of the nearly 7,000 rare diseases known to exist, less than 500 – roughly 5% – have a known treatment approved by the U.S. Food and Drug Administration, reports the National Center for Advancing Translational Diseases and the Genetic and Rare Diseases Information Center.
- Hoping for better times to come: It is difficult at times to appreciate the present when it happens to be so chronically challenging and exhausting for everyone.
Parents of children with significant special needs experience many hurdles that they learn to endure, overcome, and master. This pandemic can provide physicians with a window into the lives of these families.
Dr. Sotir is a psychiatrist in private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. In Part 2, she will explore how psychiatrists as a specialty can support these families. She has no disclosures.
COVID-19 can give physicians a window into lives of families
COVID-19 can give physicians a window into lives of families
The last few months have tested the stamina of most families. Many people are struggling to keep some semblance of normalcy amid a radical transformation of everyday life. It seems as if everything changed overnight.
In a similar way, when a child with many needs is born into a family, adjustments also have to take place to receive the new baby. Families are, in most cases, not prepared for what is to come. Their expectations usually are not in sync with how their lives end up. They are crunched for time. They need to adjust, and at the same time, they mourn the loss of their previous less demanding lifestyle. More importantly, these parents learn that this might be an adjustment that they might need to make for a long time – in some instances, for a lifetime.
Stress load over time can correlate with a sense of burnout, and mental health professionals need to be prepared to address these issues in our patients.
Here is a list of some chronic struggles with which many special needs parents must contend. These strongly resemble the challenges parents in the general population have been facing with their families during this pandemic:
- Bypassing breaks to unwind and having to be always “on” while at home: These parents take care of children who need to be chronically tube fed, can’t sleep well at night because they are often sick, have recurrent seizures or maladaptive behaviors that affect the caretakers and the rest of the family. For parents of children who are on the autism spectrum, these challenges can be a constant struggle. Almost 60% of children with autism spectrum disorder (ASD) experience bodily difficulties, such as trouble breathing. However, nearly 100% of children with ASD experienced difficulties with their abilities and activities, such as self-care tasks like eating and dressing, and emotional or behavioral health, according to a 2016 report on child and adolescent health by the Johns Hopkins Bloomberg School of Public Health.
- Taking on roles for which they are not trained: Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time. There are about 1.17 million children in the United States living with ASD and more than 12% of children with ASD have severe cases, the Hopkins report said. Parents frequently are forced to take on the role of “therapist” to meet the needs of their child.
- Staying home often: Some parents are unable to have a “regular sitter” to provide respite, because the needs of the child require a higher level of care, training, and consideration. Caring for a special child means parents often don’t have the option of leaving their older child alone. As a result, they may end up spending more time at home than their counterpart parents with children who are the same age.
- Struggling to meet everyone’s demands for attention while at home: The child might require full-time attention or prolonged hospitalizations, and the needs of other siblings are sometimes put on hold until time or energy are available for all.
- Not traveling unless absolutely necessary: Families have a hard time leaving home for vacations or for other reasons. They may have to travel with medical supplies and equipment. They need to make sure that their destination is ready to welcome their child with all needs taken into consideration (special diets, activities, and facilities). Will the vacation set them back because it might take more effort to go than to stay home?
- Avoiding unnecessary exposures: Trying to avoid infections (even the ones that may be innocuous to others) if their child is immunocompromised. These children may readily decompensate and end up hospitalized with a more serious medical complication.
- Being very aware of remaining physically distant from others: Parents must go to great lengths not to impinge on other people’s space if the child is being loud or moving in a disruptive way, or if other people negatively affect how the child responds. Some families are apprehensive because they have felt judged by others when they are in the community, restaurants, or other places of gathering.
- Feeling concerned about having the right food, medicines, and supplements in the house: Parents are constantly trying to fulfill special dietary requirements and have the reserve to make sure that all meals and treatments are accounted for in the near future. They might need oxygen or specialized formulas that are hard to find in local stores. Some treatments, when withdrawn or unavailable, can prove life threatening.
- Restricting social circles: Some families with children with severe autism may self-isolate when they feel it is hard to be around them and be friends with them, since they can’t readily participate in “usual family activities,” and the regular norms of socialization can’t apply to their family’s set of behaviors. Their child might seem to be disruptive, or loud, nonverbal, mute, or unable to easily relate to others.
- Experiencing a pervasive sense of uncertainty about the future: A child might continue to miss milestones, or might have a rare condition that hasn’t been diagnosed. When thinking of the future, parents can’t predict what level of care they need to plan and budget for.
- Being concerned about dying early and not being able to provide for their child: Parents worry about who would take care of their child for life. Who would take care of their aging adult “child” after parents are gone? They might have concerns about having a will in place early on.
- Facing financial stress secondary to losing a job or the cost of treatments: Absenteeism might be the end result of having to care for their child’s ongoing needs, appointments, and medical emergencies. Sometimes, they might depend on a caretaker who might be very difficult to replace. It might take extensive training once a candidate is found. Direct costs include medical care, hospitalizations, special education, special therapies (occupational, speech, and physical therapy), and paid caregivers. Indirect costs include lost productivity for family caregivers because of the inability to maintain employment while caring for affected individuals, as well as lost wages and benefits, the Hopkins report said.
- Struggling to coordinate daily schedules: Parents face this challenge not only with young children but with those who are chronically ill and might need ongoing 24/7 care. The schedule might include educational and therapeutic (physical, occupational, speech, language therapy, recreational) interventions regularly or daily. This schedule is to be superimposed on all the other necessary responsibilities parents already have to contend with. Forty-eight percent of school-aged children with ASD use three or more services. In addition, children with moderate or severe cases of ASD used three or more services at almost twice the rate of children with mild cases of ASD (60% vs. 35%).
- Longing for a cure or a medicine that will improve the outcome: Often, parents search for treatments so that their child could live a more comfortable or healthier life. For children who have a rare condition, there may not be sufficient research dedicated to their cause or diagnostic pursuits. Currently, it is estimated that 1 in 10 Americans has a rare disease – about 80% of which are genetically based. Of the nearly 7,000 rare diseases known to exist, less than 500 – roughly 5% – have a known treatment approved by the U.S. Food and Drug Administration, reports the National Center for Advancing Translational Diseases and the Genetic and Rare Diseases Information Center.
- Hoping for better times to come: It is difficult at times to appreciate the present when it happens to be so chronically challenging and exhausting for everyone.
Parents of children with significant special needs experience many hurdles that they learn to endure, overcome, and master. This pandemic can provide physicians with a window into the lives of these families.
Dr. Sotir is a psychiatrist in private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. In Part 2, she will explore how psychiatrists as a specialty can support these families. She has no disclosures.
The last few months have tested the stamina of most families. Many people are struggling to keep some semblance of normalcy amid a radical transformation of everyday life. It seems as if everything changed overnight.
In a similar way, when a child with many needs is born into a family, adjustments also have to take place to receive the new baby. Families are, in most cases, not prepared for what is to come. Their expectations usually are not in sync with how their lives end up. They are crunched for time. They need to adjust, and at the same time, they mourn the loss of their previous less demanding lifestyle. More importantly, these parents learn that this might be an adjustment that they might need to make for a long time – in some instances, for a lifetime.
Stress load over time can correlate with a sense of burnout, and mental health professionals need to be prepared to address these issues in our patients.
Here is a list of some chronic struggles with which many special needs parents must contend. These strongly resemble the challenges parents in the general population have been facing with their families during this pandemic:
- Bypassing breaks to unwind and having to be always “on” while at home: These parents take care of children who need to be chronically tube fed, can’t sleep well at night because they are often sick, have recurrent seizures or maladaptive behaviors that affect the caretakers and the rest of the family. For parents of children who are on the autism spectrum, these challenges can be a constant struggle. Almost 60% of children with autism spectrum disorder (ASD) experience bodily difficulties, such as trouble breathing. However, nearly 100% of children with ASD experienced difficulties with their abilities and activities, such as self-care tasks like eating and dressing, and emotional or behavioral health, according to a 2016 report on child and adolescent health by the Johns Hopkins Bloomberg School of Public Health.
- Taking on roles for which they are not trained: Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time. There are about 1.17 million children in the United States living with ASD and more than 12% of children with ASD have severe cases, the Hopkins report said. Parents frequently are forced to take on the role of “therapist” to meet the needs of their child.
- Staying home often: Some parents are unable to have a “regular sitter” to provide respite, because the needs of the child require a higher level of care, training, and consideration. Caring for a special child means parents often don’t have the option of leaving their older child alone. As a result, they may end up spending more time at home than their counterpart parents with children who are the same age.
- Struggling to meet everyone’s demands for attention while at home: The child might require full-time attention or prolonged hospitalizations, and the needs of other siblings are sometimes put on hold until time or energy are available for all.
- Not traveling unless absolutely necessary: Families have a hard time leaving home for vacations or for other reasons. They may have to travel with medical supplies and equipment. They need to make sure that their destination is ready to welcome their child with all needs taken into consideration (special diets, activities, and facilities). Will the vacation set them back because it might take more effort to go than to stay home?
- Avoiding unnecessary exposures: Trying to avoid infections (even the ones that may be innocuous to others) if their child is immunocompromised. These children may readily decompensate and end up hospitalized with a more serious medical complication.
- Being very aware of remaining physically distant from others: Parents must go to great lengths not to impinge on other people’s space if the child is being loud or moving in a disruptive way, or if other people negatively affect how the child responds. Some families are apprehensive because they have felt judged by others when they are in the community, restaurants, or other places of gathering.
- Feeling concerned about having the right food, medicines, and supplements in the house: Parents are constantly trying to fulfill special dietary requirements and have the reserve to make sure that all meals and treatments are accounted for in the near future. They might need oxygen or specialized formulas that are hard to find in local stores. Some treatments, when withdrawn or unavailable, can prove life threatening.
- Restricting social circles: Some families with children with severe autism may self-isolate when they feel it is hard to be around them and be friends with them, since they can’t readily participate in “usual family activities,” and the regular norms of socialization can’t apply to their family’s set of behaviors. Their child might seem to be disruptive, or loud, nonverbal, mute, or unable to easily relate to others.
- Experiencing a pervasive sense of uncertainty about the future: A child might continue to miss milestones, or might have a rare condition that hasn’t been diagnosed. When thinking of the future, parents can’t predict what level of care they need to plan and budget for.
- Being concerned about dying early and not being able to provide for their child: Parents worry about who would take care of their child for life. Who would take care of their aging adult “child” after parents are gone? They might have concerns about having a will in place early on.
- Facing financial stress secondary to losing a job or the cost of treatments: Absenteeism might be the end result of having to care for their child’s ongoing needs, appointments, and medical emergencies. Sometimes, they might depend on a caretaker who might be very difficult to replace. It might take extensive training once a candidate is found. Direct costs include medical care, hospitalizations, special education, special therapies (occupational, speech, and physical therapy), and paid caregivers. Indirect costs include lost productivity for family caregivers because of the inability to maintain employment while caring for affected individuals, as well as lost wages and benefits, the Hopkins report said.
- Struggling to coordinate daily schedules: Parents face this challenge not only with young children but with those who are chronically ill and might need ongoing 24/7 care. The schedule might include educational and therapeutic (physical, occupational, speech, language therapy, recreational) interventions regularly or daily. This schedule is to be superimposed on all the other necessary responsibilities parents already have to contend with. Forty-eight percent of school-aged children with ASD use three or more services. In addition, children with moderate or severe cases of ASD used three or more services at almost twice the rate of children with mild cases of ASD (60% vs. 35%).
- Longing for a cure or a medicine that will improve the outcome: Often, parents search for treatments so that their child could live a more comfortable or healthier life. For children who have a rare condition, there may not be sufficient research dedicated to their cause or diagnostic pursuits. Currently, it is estimated that 1 in 10 Americans has a rare disease – about 80% of which are genetically based. Of the nearly 7,000 rare diseases known to exist, less than 500 – roughly 5% – have a known treatment approved by the U.S. Food and Drug Administration, reports the National Center for Advancing Translational Diseases and the Genetic and Rare Diseases Information Center.
- Hoping for better times to come: It is difficult at times to appreciate the present when it happens to be so chronically challenging and exhausting for everyone.
Parents of children with significant special needs experience many hurdles that they learn to endure, overcome, and master. This pandemic can provide physicians with a window into the lives of these families.
Dr. Sotir is a psychiatrist in private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. In Part 2, she will explore how psychiatrists as a specialty can support these families. She has no disclosures.
More fatalities in heart transplant patients with COVID-19
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
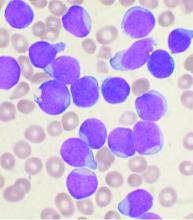
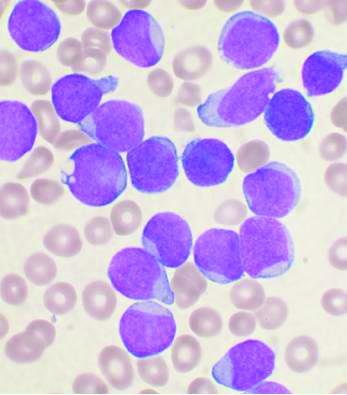
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.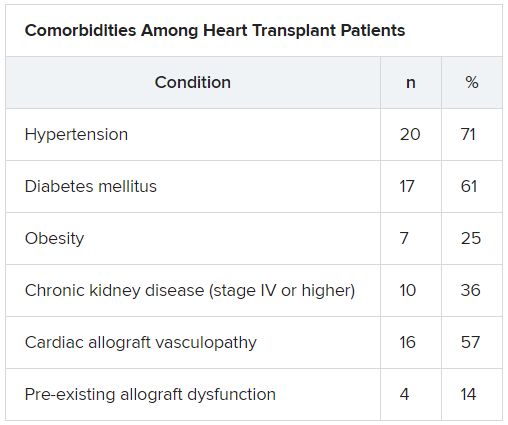
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.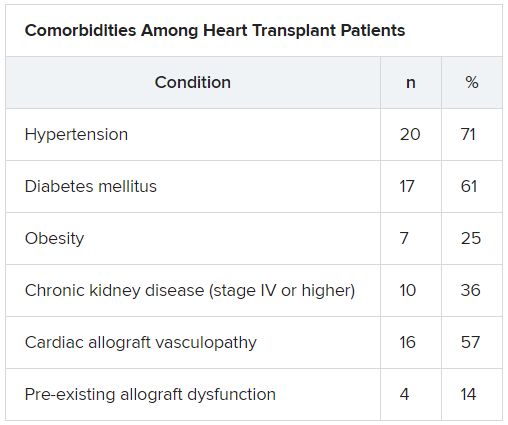
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.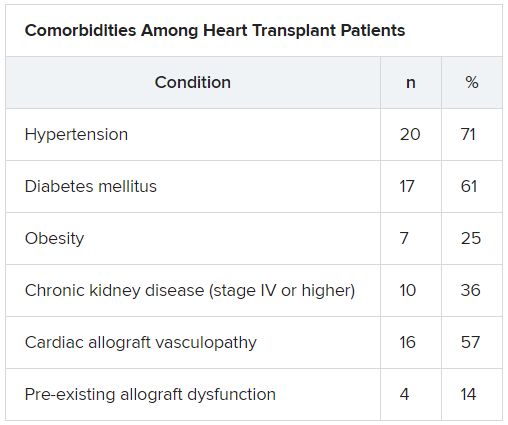
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Americans avoided emergency departments early in the pandemic
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
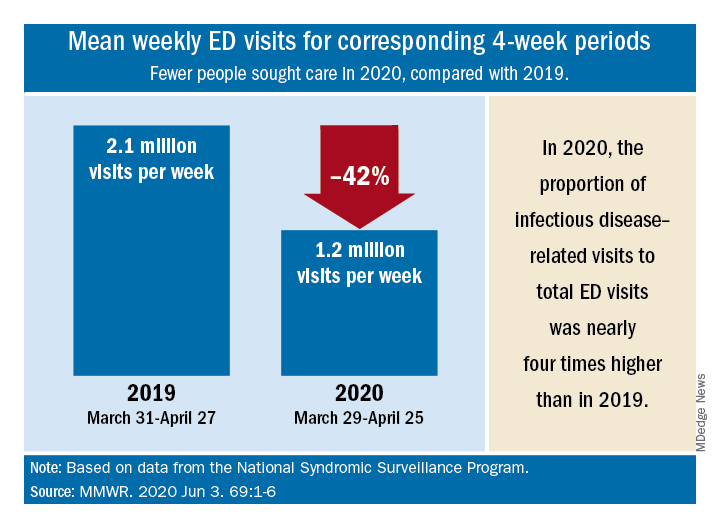
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
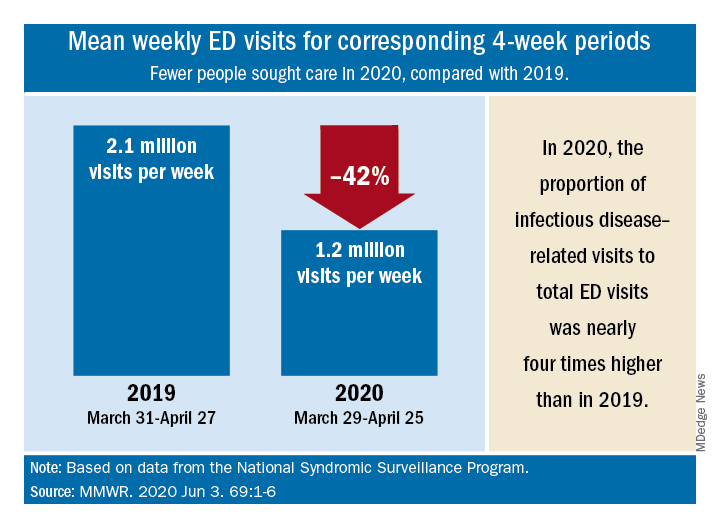
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
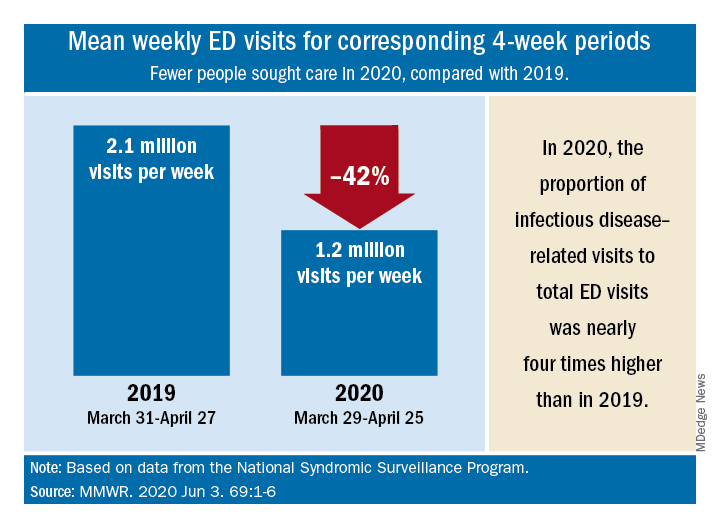
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
FROM MMWR
The grocery store hug
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Acute lymphoblastic leukemia can be successfully treated in the frail elderly
A treatment schedule of very attenuated chemotherapy using standard drugs is feasible and effective in frail and elderly patients with acute lymphoblastic leukemia (ALL), according to a prospective study published in Clinical Lymphoma, Myeloma & Leukemia.
The study comprised 67 previously untreated patients with B- or T-lineage Philadelphia chromosome–negative ALL from 30 Spanish hospitals who were enrolled in the prospective, multicenter ALL-07FRAIL trial (NCT01358201) from the Spanish PETHEMA (Programa Español de Tratamientos en Hematologia) group from January 2008 to October 2019.
The median patient age in this analysis was 67 years and 51 patients (76%) were older than 70 years. The median Charlson Comorbidity Index was 5, with the main comorbidities being cardiovascular (47 patients), other neoplasia (24), diabetes (17), and very advanced age (>80 years; 12).
The attenuated treatment regimen consisted of a prephase with dexamethasone and intrathecal therapy with methotrexate was given for a maximum of 1 week. Then weekly induction therapy consisted of weekly vincristine (capped at 1 mg/week) and daily dexamethasone with a progressively decreasing dose along 4 weeks, as well as two additional doses of intrathecal methotrexate.
Those patients who achieved complete remission received maintenance therapy with mercaptopurine and methotrexate to complete 2 years of treatment. In addition, reinduction pulses with vincristine and dexamethasone were given every 3 months during the first year, according to Josep-Maria Ribera, MD, of the Universitat Autònoma de Barcelona, Badalona, Spain and colleagues on behalf of the PETHEMA group of the Spanish Society of Hematology.
The complete remission rate was 54% (36/67 patients). The median disease-free survival and overall survival were 6.9 months and 7.6 months, respectively.
Of the 32 patients who initiated maintenance therapy, 5 patients died of infection (2), hemorrhage (2), and acute cognitive impairment (1), and 23 relapsed, with a cumulative incidence of relapse of 74% and a median time to relapse of 12.3 months.
The most frequent toxic events reported were hematologic (neutropenia 77% and thrombocytopenia 54%, of grade III-IV in all cases) followed by infections, metabolic (mainly hyperglycemia), and neurologic, according to the researchers.
“The lack of similar trials specifically directed to this frail population is one of the major strengths of this study, and we consider that this minimal chemotherapy approach could be used as a backbone for addition of immuno/targeted therapy in this subset of infirm patients,” the researchers concluded.
The study was supported by the CERCA Program/Generalitat de Catalunya and the Josep Carreras Leukemia Research Institute. The authors reported having no disclosures.
SOURCE: Ribera J-M et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 5. doi: 10.1016/j.clml.2020.03.011.
A treatment schedule of very attenuated chemotherapy using standard drugs is feasible and effective in frail and elderly patients with acute lymphoblastic leukemia (ALL), according to a prospective study published in Clinical Lymphoma, Myeloma & Leukemia.
The study comprised 67 previously untreated patients with B- or T-lineage Philadelphia chromosome–negative ALL from 30 Spanish hospitals who were enrolled in the prospective, multicenter ALL-07FRAIL trial (NCT01358201) from the Spanish PETHEMA (Programa Español de Tratamientos en Hematologia) group from January 2008 to October 2019.
The median patient age in this analysis was 67 years and 51 patients (76%) were older than 70 years. The median Charlson Comorbidity Index was 5, with the main comorbidities being cardiovascular (47 patients), other neoplasia (24), diabetes (17), and very advanced age (>80 years; 12).
The attenuated treatment regimen consisted of a prephase with dexamethasone and intrathecal therapy with methotrexate was given for a maximum of 1 week. Then weekly induction therapy consisted of weekly vincristine (capped at 1 mg/week) and daily dexamethasone with a progressively decreasing dose along 4 weeks, as well as two additional doses of intrathecal methotrexate.
Those patients who achieved complete remission received maintenance therapy with mercaptopurine and methotrexate to complete 2 years of treatment. In addition, reinduction pulses with vincristine and dexamethasone were given every 3 months during the first year, according to Josep-Maria Ribera, MD, of the Universitat Autònoma de Barcelona, Badalona, Spain and colleagues on behalf of the PETHEMA group of the Spanish Society of Hematology.
The complete remission rate was 54% (36/67 patients). The median disease-free survival and overall survival were 6.9 months and 7.6 months, respectively.
Of the 32 patients who initiated maintenance therapy, 5 patients died of infection (2), hemorrhage (2), and acute cognitive impairment (1), and 23 relapsed, with a cumulative incidence of relapse of 74% and a median time to relapse of 12.3 months.
The most frequent toxic events reported were hematologic (neutropenia 77% and thrombocytopenia 54%, of grade III-IV in all cases) followed by infections, metabolic (mainly hyperglycemia), and neurologic, according to the researchers.
“The lack of similar trials specifically directed to this frail population is one of the major strengths of this study, and we consider that this minimal chemotherapy approach could be used as a backbone for addition of immuno/targeted therapy in this subset of infirm patients,” the researchers concluded.
The study was supported by the CERCA Program/Generalitat de Catalunya and the Josep Carreras Leukemia Research Institute. The authors reported having no disclosures.
SOURCE: Ribera J-M et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 5. doi: 10.1016/j.clml.2020.03.011.
A treatment schedule of very attenuated chemotherapy using standard drugs is feasible and effective in frail and elderly patients with acute lymphoblastic leukemia (ALL), according to a prospective study published in Clinical Lymphoma, Myeloma & Leukemia.
The study comprised 67 previously untreated patients with B- or T-lineage Philadelphia chromosome–negative ALL from 30 Spanish hospitals who were enrolled in the prospective, multicenter ALL-07FRAIL trial (NCT01358201) from the Spanish PETHEMA (Programa Español de Tratamientos en Hematologia) group from January 2008 to October 2019.
The median patient age in this analysis was 67 years and 51 patients (76%) were older than 70 years. The median Charlson Comorbidity Index was 5, with the main comorbidities being cardiovascular (47 patients), other neoplasia (24), diabetes (17), and very advanced age (>80 years; 12).
The attenuated treatment regimen consisted of a prephase with dexamethasone and intrathecal therapy with methotrexate was given for a maximum of 1 week. Then weekly induction therapy consisted of weekly vincristine (capped at 1 mg/week) and daily dexamethasone with a progressively decreasing dose along 4 weeks, as well as two additional doses of intrathecal methotrexate.
Those patients who achieved complete remission received maintenance therapy with mercaptopurine and methotrexate to complete 2 years of treatment. In addition, reinduction pulses with vincristine and dexamethasone were given every 3 months during the first year, according to Josep-Maria Ribera, MD, of the Universitat Autònoma de Barcelona, Badalona, Spain and colleagues on behalf of the PETHEMA group of the Spanish Society of Hematology.
The complete remission rate was 54% (36/67 patients). The median disease-free survival and overall survival were 6.9 months and 7.6 months, respectively.
Of the 32 patients who initiated maintenance therapy, 5 patients died of infection (2), hemorrhage (2), and acute cognitive impairment (1), and 23 relapsed, with a cumulative incidence of relapse of 74% and a median time to relapse of 12.3 months.
The most frequent toxic events reported were hematologic (neutropenia 77% and thrombocytopenia 54%, of grade III-IV in all cases) followed by infections, metabolic (mainly hyperglycemia), and neurologic, according to the researchers.
“The lack of similar trials specifically directed to this frail population is one of the major strengths of this study, and we consider that this minimal chemotherapy approach could be used as a backbone for addition of immuno/targeted therapy in this subset of infirm patients,” the researchers concluded.
The study was supported by the CERCA Program/Generalitat de Catalunya and the Josep Carreras Leukemia Research Institute. The authors reported having no disclosures.
SOURCE: Ribera J-M et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 5. doi: 10.1016/j.clml.2020.03.011.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
COVID-19: New group stands up for health professionals facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
FDA okays emergency use for Impella RP in COVID-19 right heart failure
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.