User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Children’s share of COVID-19 burden has never been higher
For the first time since the pandemic began, children’s share of weekly COVID-19 cases topped 20% in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
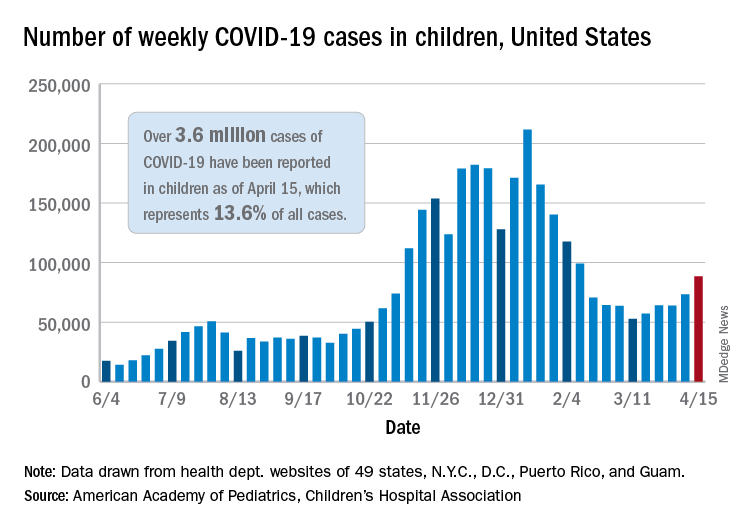
That represented 20.6% of all new cases for the week, eclipsing the previous high of 19.1% recorded just 3 weeks ago, based on data collected by the AAP and CHA from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Cumulative cases of COVID-19 in children exceed 3.6 million in those jurisdictions, which is 13.6% of the total reported among all ages, and the overall rate of coronavirus infection is 4,824 cases per 100,000 children in the population, the AAP and CHA said in their weekly COVID-19 report.
Among the 53 reporting jurisdictions, North Dakota has the highest cumulative rate, 9,167 per 100,000 children, followed by Tennessee (8,580), South Carolina (7,948), South Dakota (7,938), and Connecticut (7,707). Children’s share of cumulative cases is highest in Vermont, at 21.9%, with Alaska next at 20.0% and Wyoming at 19.2%, the AAP and CHA said.
Since the beginning of April, the largest local increases in cases reported came in Michigan (21.6%), Vermont (15.9%), and Maine (15.6%). Nationally, the increase over those same 2 weeks is just under 5%, the two organizations noted.
There were 5 deaths among children during the week of April 9-15, bringing the total to 297, but the recent increases in cases have not affected the long-term trends for serious illness. The death rate for children with COVID-19 has been 0.01% since early November – 43 states, New York City, Puerto Rico, and Guam are reporting such data – and the hospitalization rate has been 0.8% since mid-January in 24 states and New York City, the AAP/CHA data show.
For the first time since the pandemic began, children’s share of weekly COVID-19 cases topped 20% in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
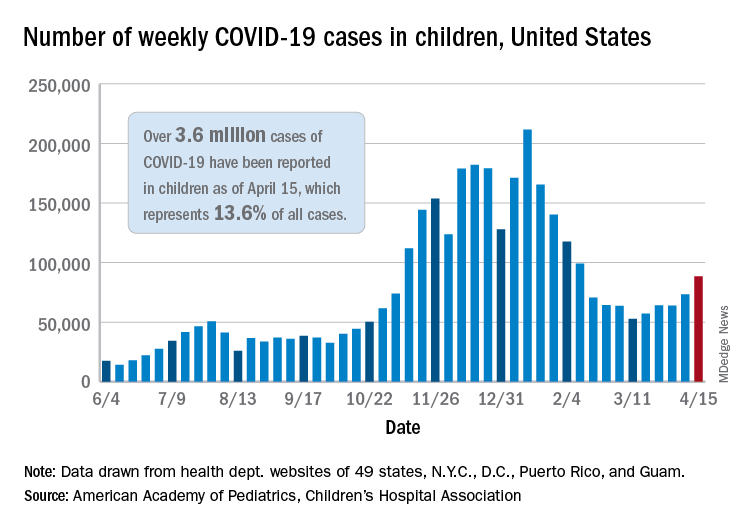
That represented 20.6% of all new cases for the week, eclipsing the previous high of 19.1% recorded just 3 weeks ago, based on data collected by the AAP and CHA from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Cumulative cases of COVID-19 in children exceed 3.6 million in those jurisdictions, which is 13.6% of the total reported among all ages, and the overall rate of coronavirus infection is 4,824 cases per 100,000 children in the population, the AAP and CHA said in their weekly COVID-19 report.
Among the 53 reporting jurisdictions, North Dakota has the highest cumulative rate, 9,167 per 100,000 children, followed by Tennessee (8,580), South Carolina (7,948), South Dakota (7,938), and Connecticut (7,707). Children’s share of cumulative cases is highest in Vermont, at 21.9%, with Alaska next at 20.0% and Wyoming at 19.2%, the AAP and CHA said.
Since the beginning of April, the largest local increases in cases reported came in Michigan (21.6%), Vermont (15.9%), and Maine (15.6%). Nationally, the increase over those same 2 weeks is just under 5%, the two organizations noted.
There were 5 deaths among children during the week of April 9-15, bringing the total to 297, but the recent increases in cases have not affected the long-term trends for serious illness. The death rate for children with COVID-19 has been 0.01% since early November – 43 states, New York City, Puerto Rico, and Guam are reporting such data – and the hospitalization rate has been 0.8% since mid-January in 24 states and New York City, the AAP/CHA data show.
For the first time since the pandemic began, children’s share of weekly COVID-19 cases topped 20% in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
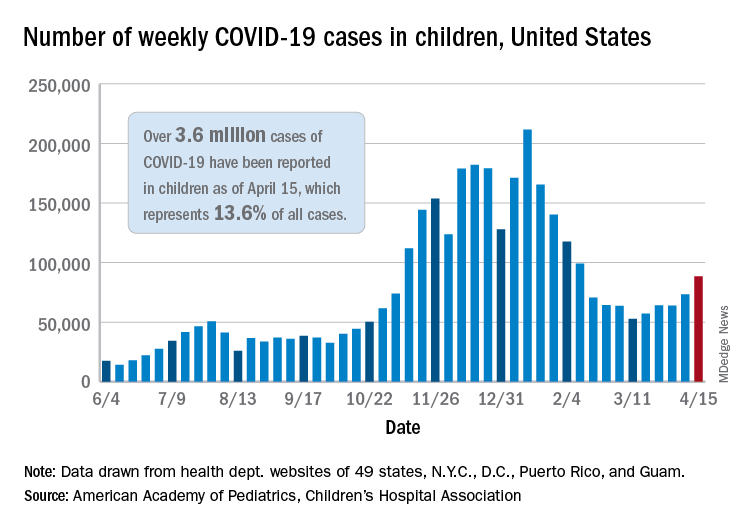
That represented 20.6% of all new cases for the week, eclipsing the previous high of 19.1% recorded just 3 weeks ago, based on data collected by the AAP and CHA from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Cumulative cases of COVID-19 in children exceed 3.6 million in those jurisdictions, which is 13.6% of the total reported among all ages, and the overall rate of coronavirus infection is 4,824 cases per 100,000 children in the population, the AAP and CHA said in their weekly COVID-19 report.
Among the 53 reporting jurisdictions, North Dakota has the highest cumulative rate, 9,167 per 100,000 children, followed by Tennessee (8,580), South Carolina (7,948), South Dakota (7,938), and Connecticut (7,707). Children’s share of cumulative cases is highest in Vermont, at 21.9%, with Alaska next at 20.0% and Wyoming at 19.2%, the AAP and CHA said.
Since the beginning of April, the largest local increases in cases reported came in Michigan (21.6%), Vermont (15.9%), and Maine (15.6%). Nationally, the increase over those same 2 weeks is just under 5%, the two organizations noted.
There were 5 deaths among children during the week of April 9-15, bringing the total to 297, but the recent increases in cases have not affected the long-term trends for serious illness. The death rate for children with COVID-19 has been 0.01% since early November – 43 states, New York City, Puerto Rico, and Guam are reporting such data – and the hospitalization rate has been 0.8% since mid-January in 24 states and New York City, the AAP/CHA data show.
Common MS treatment wears off more quickly in Black patients
new research suggests. In a study of almost 200 patients, Black participants with MS or NMOSD showed significantly more rapid B-cell repopulation 6-12 months after receiving anti-CD20 infusion therapy with rituximab or ocrelizumab (Rituxan, Ocrevus, Genentech) than did White participants.
“The results showed that this B-cell targeted therapy wore off more quickly in African Americans,” said study coinvestigator Gregg J. Silverman, MD, a professor at New York University.
He said that, although the study was more observational in design, “over time when people come back to the clinic, it gives you an idea of whether the agent is still working in their bodies.”
Overall, “our findings raise the question of whether the same therapy dose may be equally effective for all people,” coinvestigator Ilya Kister, MD, also from NYU, added in a press release.
Dr. Kister noted that this could have implications for the way Black patients with autoimmune diseases are treated in the future.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More severe disease in Black patients
Anti-CD20 infusion therapy, or B-cell depletion therapy, is commonly used to treat autoimmune diseases, including MS and NMOSD. “While previous research has shown that this type of infusion therapy is effective for people with these diseases, we also know that Black people tend to have more severe courses of MS,” Dr. Kister said.
“We wanted to compare how quickly the B cells came back in Black people and White people after treatment,” he added.
Dr. Silverman noted that he has been “studying this agent in autoimmune disease for many years. And from all the different studies, I don’t think we had the right population to ask this question. Demographics were just reviewed as they were.”
The current study included 168 participants (mean age, 44 years; 71% women) who had a diagnosis of MS (n = 134) or NMOSD (n = 32) or who were considered to have MS or NMOSD (n = 2). In addition, 36% of the participants self-identified as Black or African American, 36% self-identified as White, and 28% self-identified as another race.
Flow cytometry results were available for all patients after undergoing anti-CD20 infusions at the NYU MS Care Center. Cluster analyses were conducted on the following B-cell subsets: CD19, CD20, IgD, and CD27. “B-cell repopulation was defined as any detectable number of CD19+ cells on flow cytometry,” the investigators reported.
Clinical implications?
Results showed that 29.8% of the full study group showed B-cell repopulation a mean of 6.8 months after infusion. In those with B-cell repopulation, 80.3% had IgD+/CD27– subsets, 11.6% had IgD–/CD27+, 6.2% had IgD–/CD27–, and 1.8% had IgD+/CD27+. These B-cell subset ratios did not differ significantly between the Black and White participants.
Interestingly, no patients showed B-cell repopulation before 4 months after infusion. From 4 to 6 months after infusion, there were no significant differences between the Black and White participants in terms of frequency of B-cell repopulation (20.8% vs. 17.9%, respectively; P = .79).
However, repopulation was significantly more frequent in the Black patients 6-12 months after infusion (76.2% vs. 33.3%; P = .02).
Overall, the findings “may have implications for clinical management of MS/NMOSD” in Black individuals, the investigators wrote.
“I was impressed by the differences we saw in responses of patients that were self-declaring as African Americans versus those who were Whites,” Dr. Silverman said. However, “as we say in science: it gives us an answer but it raises even more questions, which may well be important for helping us understand how the agent works and how the disease affects different people.”
Still, Dr. Silverman noted that the findings give clinicians using the agent “a signal that they should be very vigilant. It was an observation at one center, but we’re asking our colleagues [at other clinics] to think about being more careful as they review data with their patients.”
He added that future multicenter studies will allow these issues to be assessed more comprehensively. “This was a discovery study; it now needs validation; and maybe the next step would be looking into the mechanism.”
Dr. Silverman pointed out that the Food and Drug Administration–approved label for this type of therapy “allows for somewhat more frequent dosing. So that might be indicated if it’s found that it’s wearing off in an individual. Perhaps they should be treated more frequently?”
“At a minimum, this has raised our vigilance – and we’re interested to see what the feedback will be at the [AAN] meeting,” he added.
Real-world data
Commenting on the findings, Eric Klawiter, MD, associate professor of neurology at Harvard Medical School and director of the Multiple Sclerosis and NMO unit at Massachusetts General Hospital, both in Boston, noted that an important study factor was the focus on repopulation to identify specific groups “who may be early repopulators” as it relates to disease activity and disability progression in MS.
“I thought this was a nicely designed study that made good use of real-world data in MS and NMOSD,” added Dr. Klawiter, who was not involved with the research. He pointed out that timing was another interesting aspect of the study. “As we typically use these cell-depleting agents on an ‘every-6-month’ basis, the most pertinent time frame surrounds those that repopulate prior to 6 months.”
If the current study would have shown differences between the Black and White participants at that time point, “I think that would have been most pertinent from a clinical standpoint and a greater opportunity for intervention,” Dr. Klawiter said. “But we saw that, before 4 and 6 months, [the difference] wasn’t significant.”
Still, “after 6 months, the study demonstrates that Black people with MS and NMOSD may repopulate faster,” he added.
“The only real change a clinician could make would be to modify the frequency of the dosing. So if we can identify certain characteristics that would lead you to want to evaluate for the need of redosing sooner, I think that would be useful,” he said.
Specific characteristics identified in previous research include body mass index. “If there are also ethnicity factors, that would be an additional demographic factor that a clinician should pay close attention to,” said Dr. Klawiter.
He noted that his current practice is to check flow cytometry and B-cell counts at the time of a patient’s next infusion. “And if I’m seeing that B-cell levels are repleting at that time point, I am already then making adjustments with their next infusion as to the dosing frequency,” he added.
“This [study] may elucidate some of the potential reasons why we see some people replete their B cells faster than others, but I think additional studies are necessary to make that determination,” Dr. Klawiter concluded.
Genentech provided funding for the study. Dr. Silverman reported no relevant financial relationships. Dr. Klawiter reported having received research funds and consulting fees from Genentech.
A version of this article first appeared on Medscape.com.
new research suggests. In a study of almost 200 patients, Black participants with MS or NMOSD showed significantly more rapid B-cell repopulation 6-12 months after receiving anti-CD20 infusion therapy with rituximab or ocrelizumab (Rituxan, Ocrevus, Genentech) than did White participants.
“The results showed that this B-cell targeted therapy wore off more quickly in African Americans,” said study coinvestigator Gregg J. Silverman, MD, a professor at New York University.
He said that, although the study was more observational in design, “over time when people come back to the clinic, it gives you an idea of whether the agent is still working in their bodies.”
Overall, “our findings raise the question of whether the same therapy dose may be equally effective for all people,” coinvestigator Ilya Kister, MD, also from NYU, added in a press release.
Dr. Kister noted that this could have implications for the way Black patients with autoimmune diseases are treated in the future.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More severe disease in Black patients
Anti-CD20 infusion therapy, or B-cell depletion therapy, is commonly used to treat autoimmune diseases, including MS and NMOSD. “While previous research has shown that this type of infusion therapy is effective for people with these diseases, we also know that Black people tend to have more severe courses of MS,” Dr. Kister said.
“We wanted to compare how quickly the B cells came back in Black people and White people after treatment,” he added.
Dr. Silverman noted that he has been “studying this agent in autoimmune disease for many years. And from all the different studies, I don’t think we had the right population to ask this question. Demographics were just reviewed as they were.”
The current study included 168 participants (mean age, 44 years; 71% women) who had a diagnosis of MS (n = 134) or NMOSD (n = 32) or who were considered to have MS or NMOSD (n = 2). In addition, 36% of the participants self-identified as Black or African American, 36% self-identified as White, and 28% self-identified as another race.
Flow cytometry results were available for all patients after undergoing anti-CD20 infusions at the NYU MS Care Center. Cluster analyses were conducted on the following B-cell subsets: CD19, CD20, IgD, and CD27. “B-cell repopulation was defined as any detectable number of CD19+ cells on flow cytometry,” the investigators reported.
Clinical implications?
Results showed that 29.8% of the full study group showed B-cell repopulation a mean of 6.8 months after infusion. In those with B-cell repopulation, 80.3% had IgD+/CD27– subsets, 11.6% had IgD–/CD27+, 6.2% had IgD–/CD27–, and 1.8% had IgD+/CD27+. These B-cell subset ratios did not differ significantly between the Black and White participants.
Interestingly, no patients showed B-cell repopulation before 4 months after infusion. From 4 to 6 months after infusion, there were no significant differences between the Black and White participants in terms of frequency of B-cell repopulation (20.8% vs. 17.9%, respectively; P = .79).
However, repopulation was significantly more frequent in the Black patients 6-12 months after infusion (76.2% vs. 33.3%; P = .02).
Overall, the findings “may have implications for clinical management of MS/NMOSD” in Black individuals, the investigators wrote.
“I was impressed by the differences we saw in responses of patients that were self-declaring as African Americans versus those who were Whites,” Dr. Silverman said. However, “as we say in science: it gives us an answer but it raises even more questions, which may well be important for helping us understand how the agent works and how the disease affects different people.”
Still, Dr. Silverman noted that the findings give clinicians using the agent “a signal that they should be very vigilant. It was an observation at one center, but we’re asking our colleagues [at other clinics] to think about being more careful as they review data with their patients.”
He added that future multicenter studies will allow these issues to be assessed more comprehensively. “This was a discovery study; it now needs validation; and maybe the next step would be looking into the mechanism.”
Dr. Silverman pointed out that the Food and Drug Administration–approved label for this type of therapy “allows for somewhat more frequent dosing. So that might be indicated if it’s found that it’s wearing off in an individual. Perhaps they should be treated more frequently?”
“At a minimum, this has raised our vigilance – and we’re interested to see what the feedback will be at the [AAN] meeting,” he added.
Real-world data
Commenting on the findings, Eric Klawiter, MD, associate professor of neurology at Harvard Medical School and director of the Multiple Sclerosis and NMO unit at Massachusetts General Hospital, both in Boston, noted that an important study factor was the focus on repopulation to identify specific groups “who may be early repopulators” as it relates to disease activity and disability progression in MS.
“I thought this was a nicely designed study that made good use of real-world data in MS and NMOSD,” added Dr. Klawiter, who was not involved with the research. He pointed out that timing was another interesting aspect of the study. “As we typically use these cell-depleting agents on an ‘every-6-month’ basis, the most pertinent time frame surrounds those that repopulate prior to 6 months.”
If the current study would have shown differences between the Black and White participants at that time point, “I think that would have been most pertinent from a clinical standpoint and a greater opportunity for intervention,” Dr. Klawiter said. “But we saw that, before 4 and 6 months, [the difference] wasn’t significant.”
Still, “after 6 months, the study demonstrates that Black people with MS and NMOSD may repopulate faster,” he added.
“The only real change a clinician could make would be to modify the frequency of the dosing. So if we can identify certain characteristics that would lead you to want to evaluate for the need of redosing sooner, I think that would be useful,” he said.
Specific characteristics identified in previous research include body mass index. “If there are also ethnicity factors, that would be an additional demographic factor that a clinician should pay close attention to,” said Dr. Klawiter.
He noted that his current practice is to check flow cytometry and B-cell counts at the time of a patient’s next infusion. “And if I’m seeing that B-cell levels are repleting at that time point, I am already then making adjustments with their next infusion as to the dosing frequency,” he added.
“This [study] may elucidate some of the potential reasons why we see some people replete their B cells faster than others, but I think additional studies are necessary to make that determination,” Dr. Klawiter concluded.
Genentech provided funding for the study. Dr. Silverman reported no relevant financial relationships. Dr. Klawiter reported having received research funds and consulting fees from Genentech.
A version of this article first appeared on Medscape.com.
new research suggests. In a study of almost 200 patients, Black participants with MS or NMOSD showed significantly more rapid B-cell repopulation 6-12 months after receiving anti-CD20 infusion therapy with rituximab or ocrelizumab (Rituxan, Ocrevus, Genentech) than did White participants.
“The results showed that this B-cell targeted therapy wore off more quickly in African Americans,” said study coinvestigator Gregg J. Silverman, MD, a professor at New York University.
He said that, although the study was more observational in design, “over time when people come back to the clinic, it gives you an idea of whether the agent is still working in their bodies.”
Overall, “our findings raise the question of whether the same therapy dose may be equally effective for all people,” coinvestigator Ilya Kister, MD, also from NYU, added in a press release.
Dr. Kister noted that this could have implications for the way Black patients with autoimmune diseases are treated in the future.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More severe disease in Black patients
Anti-CD20 infusion therapy, or B-cell depletion therapy, is commonly used to treat autoimmune diseases, including MS and NMOSD. “While previous research has shown that this type of infusion therapy is effective for people with these diseases, we also know that Black people tend to have more severe courses of MS,” Dr. Kister said.
“We wanted to compare how quickly the B cells came back in Black people and White people after treatment,” he added.
Dr. Silverman noted that he has been “studying this agent in autoimmune disease for many years. And from all the different studies, I don’t think we had the right population to ask this question. Demographics were just reviewed as they were.”
The current study included 168 participants (mean age, 44 years; 71% women) who had a diagnosis of MS (n = 134) or NMOSD (n = 32) or who were considered to have MS or NMOSD (n = 2). In addition, 36% of the participants self-identified as Black or African American, 36% self-identified as White, and 28% self-identified as another race.
Flow cytometry results were available for all patients after undergoing anti-CD20 infusions at the NYU MS Care Center. Cluster analyses were conducted on the following B-cell subsets: CD19, CD20, IgD, and CD27. “B-cell repopulation was defined as any detectable number of CD19+ cells on flow cytometry,” the investigators reported.
Clinical implications?
Results showed that 29.8% of the full study group showed B-cell repopulation a mean of 6.8 months after infusion. In those with B-cell repopulation, 80.3% had IgD+/CD27– subsets, 11.6% had IgD–/CD27+, 6.2% had IgD–/CD27–, and 1.8% had IgD+/CD27+. These B-cell subset ratios did not differ significantly between the Black and White participants.
Interestingly, no patients showed B-cell repopulation before 4 months after infusion. From 4 to 6 months after infusion, there were no significant differences between the Black and White participants in terms of frequency of B-cell repopulation (20.8% vs. 17.9%, respectively; P = .79).
However, repopulation was significantly more frequent in the Black patients 6-12 months after infusion (76.2% vs. 33.3%; P = .02).
Overall, the findings “may have implications for clinical management of MS/NMOSD” in Black individuals, the investigators wrote.
“I was impressed by the differences we saw in responses of patients that were self-declaring as African Americans versus those who were Whites,” Dr. Silverman said. However, “as we say in science: it gives us an answer but it raises even more questions, which may well be important for helping us understand how the agent works and how the disease affects different people.”
Still, Dr. Silverman noted that the findings give clinicians using the agent “a signal that they should be very vigilant. It was an observation at one center, but we’re asking our colleagues [at other clinics] to think about being more careful as they review data with their patients.”
He added that future multicenter studies will allow these issues to be assessed more comprehensively. “This was a discovery study; it now needs validation; and maybe the next step would be looking into the mechanism.”
Dr. Silverman pointed out that the Food and Drug Administration–approved label for this type of therapy “allows for somewhat more frequent dosing. So that might be indicated if it’s found that it’s wearing off in an individual. Perhaps they should be treated more frequently?”
“At a minimum, this has raised our vigilance – and we’re interested to see what the feedback will be at the [AAN] meeting,” he added.
Real-world data
Commenting on the findings, Eric Klawiter, MD, associate professor of neurology at Harvard Medical School and director of the Multiple Sclerosis and NMO unit at Massachusetts General Hospital, both in Boston, noted that an important study factor was the focus on repopulation to identify specific groups “who may be early repopulators” as it relates to disease activity and disability progression in MS.
“I thought this was a nicely designed study that made good use of real-world data in MS and NMOSD,” added Dr. Klawiter, who was not involved with the research. He pointed out that timing was another interesting aspect of the study. “As we typically use these cell-depleting agents on an ‘every-6-month’ basis, the most pertinent time frame surrounds those that repopulate prior to 6 months.”
If the current study would have shown differences between the Black and White participants at that time point, “I think that would have been most pertinent from a clinical standpoint and a greater opportunity for intervention,” Dr. Klawiter said. “But we saw that, before 4 and 6 months, [the difference] wasn’t significant.”
Still, “after 6 months, the study demonstrates that Black people with MS and NMOSD may repopulate faster,” he added.
“The only real change a clinician could make would be to modify the frequency of the dosing. So if we can identify certain characteristics that would lead you to want to evaluate for the need of redosing sooner, I think that would be useful,” he said.
Specific characteristics identified in previous research include body mass index. “If there are also ethnicity factors, that would be an additional demographic factor that a clinician should pay close attention to,” said Dr. Klawiter.
He noted that his current practice is to check flow cytometry and B-cell counts at the time of a patient’s next infusion. “And if I’m seeing that B-cell levels are repleting at that time point, I am already then making adjustments with their next infusion as to the dosing frequency,” he added.
“This [study] may elucidate some of the potential reasons why we see some people replete their B cells faster than others, but I think additional studies are necessary to make that determination,” Dr. Klawiter concluded.
Genentech provided funding for the study. Dr. Silverman reported no relevant financial relationships. Dr. Klawiter reported having received research funds and consulting fees from Genentech.
A version of this article first appeared on Medscape.com.
FROM AAN 2021
What COVID did to MD income in 2020
, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Almost 18,000 physicians in more than 29 specialties told Medscape about their income, hours worked, greatest challenges, and the unexpected impact of COVID-19 on their compensation.
How many physicians avoided massive losses
When the pandemic started around March 2020, “a great many physicians saw reductions in volume at first,” says Robert Pearl, MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University.
Medscape’s survey report shows that a staggering 44% saw a 1%-25% reduction in patient volume, and 9% saw a 26%-50% decline. “That is indeed breathtaking,” Dr. Pearl says.
Several key factors saved many practices from hemorrhaging money, says Michael Belkin, JD, divisional vice president at Merritt Hawkins and Associates in Dallas. “Many physicians used the federal Paycheck Protection Program [PPP] to help keep themselves afloat,” he says. “A large percentage reduced their staff, which reduced their expenses, and many got some of their volume back by transitioning to telemedicine.”
In a 2020 survey for the Physicians Foundation, conducted by Merritt Hawkins, 48% of physicians said their practice had received PPP support, and most of those said the support was enough to allow them to stay open without reducing staff. Only 6% of practices that received PPP support did not stay open.
Telemedicine helped many practices
Early in the pandemic, Medicare reimbursements for telemedicine were equal with those for face-to-face visits. “Since telemedicine takes a third less time than an inpatient visit, doctors could see more patients,” Dr. Pearl says.
The switch was almost instantaneous in some practices. Within 3 days, a 200-provider multispecialty practice in Wilmington, N.C., went from not using telehealth to its being used by all physicians, the Medical Group Management Association reported. By late April, the practice was already back up to about 70% of normal overall production.
However, telemedicine could not help every specialty equally. “Generally, allergists can’t do their allergy testing virtually, and patients with mild problems probably put off visits,” Dr. Pearl says. Allergists experienced a large percentage decline in compensation, according to Medscape’s survey. For some, income fell from $301,000 the prior year to $274,000 this year.
Primary care struggled
Primary care physicians posted lower compensation than they did the prior year, but most rebounded to some degree. A study released in June 2020 projected that, even with telemedicine, primary care physicians would lose an average of $67,774 for the year.
However, Medscape’s survey found that internists’ average compensation declined from $251,000 in the prior year to $248,000, and average family physicians’ compensation actually rose from $234,000.
Pediatricians had a harder slog. Their average compensation sank from $232,000 to $221,000, according to the report. Even with telemedicine, parents of young children were not contacting the doctor. In May 2020, visits by children aged 3-5 years were down by 56%.
Many proceduralists recovered
Procedure-oriented specialties were particularly hard-hit at first, because many hospitals and some states banned all elective surgeries at the beginning of the pandemic.
“In March and April, ophthalmology practices were virtually at a standstill,” says John B. Pinto, an ophthalmology practice management consultant in San Diego. “But by the fourth quarter, operations were back to normal. Practices were fully open, and patients were coming back in.”
Medscape’s survey shows that, by year’s end, compensation was about the same as the year before for orthopedic surgeons ($511,000 in both the 2020 and 2021 reports); cardiologists actually did better ($438,000 in our 2020 report and $459,000 in 2021); and ophthalmologists’ compensation was about the same ($378,000 in our prior report and $379,000 in 2021).
Some other proceduralists, however, did not do as well. Otolaryngologists’ compensation fell to $417,000, the second-biggest percentage drop. “This may be because otolaryngologists’ chief procedures are tonsillectomies, sinus surgery, and nasal surgery, which can be put off,” Dr. Pearl says.
Anesthesiologists, who depend on surgical volume, also did not earn as much in 2020. Their compensation declined from $398,000 in our 2020 report to $378,000 in Medscape’s 2021 report.
“Not only has 70% of our revenue disappeared, but our physicians are still working every day,” an independent anesthesiology practice in Alabama told the MGMA early in the pandemic.
Plastic surgeons now the top earners
The biggest increase in compensation by far was made by plastic surgeons, whose income rose 9.8% over the year before, to $526,000. This put them at the top of the list
Dr. Pearl adds that plastic surgeons can perform their procedures in their offices, rather than in a hospital, where elective surgeries were often canceled.
Mr. Belkin says specialties other than plastic surgery had been offering more boutique cosmetic care even before the pandemic. In 2020, nonsurgical cosmetic procedures such as neurotoxin therapy, dermal filler procedures, chemical peels, and hair removal earned $3.1 billion in revenue, according to a survey by the Aesthetic Society.
Other specialties that earned more even during COVID
In Medscape’s survey, several specialties actually earned more during the pandemic than in 2019. Some specialties, such as critical care and public health, were integral in managing COVID patients and the pandemic.
However, some specialties involved in COVID care did not see an increase. Compensation for infectious disease specialists (at $245,000) and emergency medicine specialists (at $354,000) remained basically unchanged from the prior year, and for pulmonologists, it was slightly down.
Emergency departments reported decreases in volume of 40% or more early in the pandemic, according to the American College of Emergency Physicians. It was reported that patients were avoiding EDs for fear of contracting COVID, and car accidents were down because people ventured out less.
In this year’s report, psychiatrists saw a modest rise in compensation, to $275,000. “There has been an increase in mental health visits in the pandemic,” Dr. Pearl says. In 2020, about 4 in 10 adults in the United States reported symptoms of anxiety or depressive disorder, up from 1 in 10 adults the prior year. In addition, psychiatrists were third on the list of Merritt Hawkins’ most requested recruiting engagements.
Oncologists saw a rise in compensation, from $377,000 to $403,000. “Volume likely did not fall because cancer patients would go through with their chemotherapy in spite of the pandemic,” Dr. Pearl says. “The increase in income might have to do with the usual inflation in the cost of chemotherapy drugs.” Dr. Pinto saw the same trend for retinal surgeons, whose care also cannot be delayed.
Medscape’s survey also reports increases in compensation for rheumatologists, endocrinologists, and neurologists, but it reports small declines among dermatologists, radiologists, and gastroenterologists.
Gender-based pay gap remains in place
The gender-based pay gap in this year’s report is similar to that seen in Medscape’s report for the prior year. Men earned 27% more than women in 2021, compared with 25% more the year before. Some physicians commented that more women physicians maintained flexible or shorter work schedules to help with children who could not go into school.
“Having to be a full-time physician, full-time mom, and full-time teacher during our surge was unbelievable,” a primary care pediatrician in group practice and mother of two reported in November. “I felt pulled in all directions and didn’t do anything well.”
In addition, “men dominate some specialties that seem to have seen a smaller drop in volume in the pandemic, such as emergency medicine, infectious disease, pulmonology, and oncology,” says Halee Fischer-Wright, MD, CEO of MGMA.
Employed physicians shared their employers’ pain
Employed physicians, who typically work at hospitals, shared the financial pains of their institutions, particularly in the early stages of the pandemic. In April, hospital admissions were 34.1% below prepandemic levels, according to a study published in Health Affairs. That figure had risen by June, but it was still 8.3% below prepandemic volume.
By the end of the year, many hospitals and hospital systems were in the black, thanks in large part to generous federal subsidies, but actual operations still lost money for the year. Altogether, 42% of them posted an operational loss in 2020, up from the 23% in 2019, according to a survey by Moody’s Investors Service.
Medscape’s report shows that many employed physicians lost pay in 2020, and for many, pay had not returned to pre-COVID levels. Only 28% of primary care physicians and 32% of specialists who lost pay have seen it restored, according to the report. In addition, 15% of surveyed physicians did not receive an annual raise.
Many employed doctors are paid on the basis of relative value units (RVUs), which is a measure of the value of their work. In many cases, there was not enough work to reach RVU thresholds. Would hospitals and other employers lower RVU targets to meet the problem? “I haven’t seen our clients make concessions to providers along those lines,” Mr. Belkin says.
Physicians had to work longer hours
The Medscape report also found that in 2020, physicians saw fewer patients because each visit took longer.
“With the threat of COVID, in-person visits take more time than before,” Mr. Belkin says. “Physicians and staff have to prepare the exam room after each visit, and doctors must spend more time answering patients’ questions about COVID.”
“The new protocols to keep everyone safe add time between patients, and physicians have to answer patients’ questions about the pandemic and vaccines,” Dr. Fischer-Wright says. “You might see a 20% increase in time spent just on these non–revenue-generating COVID activities.”
Physicians still like their specialty
Although 2020 was a challenging year for physicians, the percentage of those who were satisfied with their specialty choice generally did not slip from the year before. It actually rose for several specialties – most notably, rheumatology, pulmonology, physical medicine and rehabilitation, and nephrology.
One specialty saw a decline in satisfaction with their specialty choice, and that was public health and preventive medicine, which plummeted 16 percentage points to 67% – putting it at the bottom of the list.
Even before the pandemic, many public health departments were chronically underfunded. This problem was possibly exacerbated by the pressures to keep up with COVID reporting and testing responsibilities.
Conclusion
Although 2020 was a wild ride for many physicians, many came out of it with only minor reductions in overall compensation, and some saw increases. Still, some specialties and many individuals experienced terrible financial stress and had to make changes in their lives and their spending in order to stay afloat.
“The biggest inhibitor to getting back to normal had to do with doctors who did not want to return because they did not want to risk getting COVID,” Dr. Pinto reports. But he notes that by February 2021 most doctors were completely vaccinated and could feel safe again.
A version of this article first appeared on Medscape.com.
, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Almost 18,000 physicians in more than 29 specialties told Medscape about their income, hours worked, greatest challenges, and the unexpected impact of COVID-19 on their compensation.
How many physicians avoided massive losses
When the pandemic started around March 2020, “a great many physicians saw reductions in volume at first,” says Robert Pearl, MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University.
Medscape’s survey report shows that a staggering 44% saw a 1%-25% reduction in patient volume, and 9% saw a 26%-50% decline. “That is indeed breathtaking,” Dr. Pearl says.
Several key factors saved many practices from hemorrhaging money, says Michael Belkin, JD, divisional vice president at Merritt Hawkins and Associates in Dallas. “Many physicians used the federal Paycheck Protection Program [PPP] to help keep themselves afloat,” he says. “A large percentage reduced their staff, which reduced their expenses, and many got some of their volume back by transitioning to telemedicine.”
In a 2020 survey for the Physicians Foundation, conducted by Merritt Hawkins, 48% of physicians said their practice had received PPP support, and most of those said the support was enough to allow them to stay open without reducing staff. Only 6% of practices that received PPP support did not stay open.
Telemedicine helped many practices
Early in the pandemic, Medicare reimbursements for telemedicine were equal with those for face-to-face visits. “Since telemedicine takes a third less time than an inpatient visit, doctors could see more patients,” Dr. Pearl says.
The switch was almost instantaneous in some practices. Within 3 days, a 200-provider multispecialty practice in Wilmington, N.C., went from not using telehealth to its being used by all physicians, the Medical Group Management Association reported. By late April, the practice was already back up to about 70% of normal overall production.
However, telemedicine could not help every specialty equally. “Generally, allergists can’t do their allergy testing virtually, and patients with mild problems probably put off visits,” Dr. Pearl says. Allergists experienced a large percentage decline in compensation, according to Medscape’s survey. For some, income fell from $301,000 the prior year to $274,000 this year.
Primary care struggled
Primary care physicians posted lower compensation than they did the prior year, but most rebounded to some degree. A study released in June 2020 projected that, even with telemedicine, primary care physicians would lose an average of $67,774 for the year.
However, Medscape’s survey found that internists’ average compensation declined from $251,000 in the prior year to $248,000, and average family physicians’ compensation actually rose from $234,000.
Pediatricians had a harder slog. Their average compensation sank from $232,000 to $221,000, according to the report. Even with telemedicine, parents of young children were not contacting the doctor. In May 2020, visits by children aged 3-5 years were down by 56%.
Many proceduralists recovered
Procedure-oriented specialties were particularly hard-hit at first, because many hospitals and some states banned all elective surgeries at the beginning of the pandemic.
“In March and April, ophthalmology practices were virtually at a standstill,” says John B. Pinto, an ophthalmology practice management consultant in San Diego. “But by the fourth quarter, operations were back to normal. Practices were fully open, and patients were coming back in.”
Medscape’s survey shows that, by year’s end, compensation was about the same as the year before for orthopedic surgeons ($511,000 in both the 2020 and 2021 reports); cardiologists actually did better ($438,000 in our 2020 report and $459,000 in 2021); and ophthalmologists’ compensation was about the same ($378,000 in our prior report and $379,000 in 2021).
Some other proceduralists, however, did not do as well. Otolaryngologists’ compensation fell to $417,000, the second-biggest percentage drop. “This may be because otolaryngologists’ chief procedures are tonsillectomies, sinus surgery, and nasal surgery, which can be put off,” Dr. Pearl says.
Anesthesiologists, who depend on surgical volume, also did not earn as much in 2020. Their compensation declined from $398,000 in our 2020 report to $378,000 in Medscape’s 2021 report.
“Not only has 70% of our revenue disappeared, but our physicians are still working every day,” an independent anesthesiology practice in Alabama told the MGMA early in the pandemic.
Plastic surgeons now the top earners
The biggest increase in compensation by far was made by plastic surgeons, whose income rose 9.8% over the year before, to $526,000. This put them at the top of the list
Dr. Pearl adds that plastic surgeons can perform their procedures in their offices, rather than in a hospital, where elective surgeries were often canceled.
Mr. Belkin says specialties other than plastic surgery had been offering more boutique cosmetic care even before the pandemic. In 2020, nonsurgical cosmetic procedures such as neurotoxin therapy, dermal filler procedures, chemical peels, and hair removal earned $3.1 billion in revenue, according to a survey by the Aesthetic Society.
Other specialties that earned more even during COVID
In Medscape’s survey, several specialties actually earned more during the pandemic than in 2019. Some specialties, such as critical care and public health, were integral in managing COVID patients and the pandemic.
However, some specialties involved in COVID care did not see an increase. Compensation for infectious disease specialists (at $245,000) and emergency medicine specialists (at $354,000) remained basically unchanged from the prior year, and for pulmonologists, it was slightly down.
Emergency departments reported decreases in volume of 40% or more early in the pandemic, according to the American College of Emergency Physicians. It was reported that patients were avoiding EDs for fear of contracting COVID, and car accidents were down because people ventured out less.
In this year’s report, psychiatrists saw a modest rise in compensation, to $275,000. “There has been an increase in mental health visits in the pandemic,” Dr. Pearl says. In 2020, about 4 in 10 adults in the United States reported symptoms of anxiety or depressive disorder, up from 1 in 10 adults the prior year. In addition, psychiatrists were third on the list of Merritt Hawkins’ most requested recruiting engagements.
Oncologists saw a rise in compensation, from $377,000 to $403,000. “Volume likely did not fall because cancer patients would go through with their chemotherapy in spite of the pandemic,” Dr. Pearl says. “The increase in income might have to do with the usual inflation in the cost of chemotherapy drugs.” Dr. Pinto saw the same trend for retinal surgeons, whose care also cannot be delayed.
Medscape’s survey also reports increases in compensation for rheumatologists, endocrinologists, and neurologists, but it reports small declines among dermatologists, radiologists, and gastroenterologists.
Gender-based pay gap remains in place
The gender-based pay gap in this year’s report is similar to that seen in Medscape’s report for the prior year. Men earned 27% more than women in 2021, compared with 25% more the year before. Some physicians commented that more women physicians maintained flexible or shorter work schedules to help with children who could not go into school.
“Having to be a full-time physician, full-time mom, and full-time teacher during our surge was unbelievable,” a primary care pediatrician in group practice and mother of two reported in November. “I felt pulled in all directions and didn’t do anything well.”
In addition, “men dominate some specialties that seem to have seen a smaller drop in volume in the pandemic, such as emergency medicine, infectious disease, pulmonology, and oncology,” says Halee Fischer-Wright, MD, CEO of MGMA.
Employed physicians shared their employers’ pain
Employed physicians, who typically work at hospitals, shared the financial pains of their institutions, particularly in the early stages of the pandemic. In April, hospital admissions were 34.1% below prepandemic levels, according to a study published in Health Affairs. That figure had risen by June, but it was still 8.3% below prepandemic volume.
By the end of the year, many hospitals and hospital systems were in the black, thanks in large part to generous federal subsidies, but actual operations still lost money for the year. Altogether, 42% of them posted an operational loss in 2020, up from the 23% in 2019, according to a survey by Moody’s Investors Service.
Medscape’s report shows that many employed physicians lost pay in 2020, and for many, pay had not returned to pre-COVID levels. Only 28% of primary care physicians and 32% of specialists who lost pay have seen it restored, according to the report. In addition, 15% of surveyed physicians did not receive an annual raise.
Many employed doctors are paid on the basis of relative value units (RVUs), which is a measure of the value of their work. In many cases, there was not enough work to reach RVU thresholds. Would hospitals and other employers lower RVU targets to meet the problem? “I haven’t seen our clients make concessions to providers along those lines,” Mr. Belkin says.
Physicians had to work longer hours
The Medscape report also found that in 2020, physicians saw fewer patients because each visit took longer.
“With the threat of COVID, in-person visits take more time than before,” Mr. Belkin says. “Physicians and staff have to prepare the exam room after each visit, and doctors must spend more time answering patients’ questions about COVID.”
“The new protocols to keep everyone safe add time between patients, and physicians have to answer patients’ questions about the pandemic and vaccines,” Dr. Fischer-Wright says. “You might see a 20% increase in time spent just on these non–revenue-generating COVID activities.”
Physicians still like their specialty
Although 2020 was a challenging year for physicians, the percentage of those who were satisfied with their specialty choice generally did not slip from the year before. It actually rose for several specialties – most notably, rheumatology, pulmonology, physical medicine and rehabilitation, and nephrology.
One specialty saw a decline in satisfaction with their specialty choice, and that was public health and preventive medicine, which plummeted 16 percentage points to 67% – putting it at the bottom of the list.
Even before the pandemic, many public health departments were chronically underfunded. This problem was possibly exacerbated by the pressures to keep up with COVID reporting and testing responsibilities.
Conclusion
Although 2020 was a wild ride for many physicians, many came out of it with only minor reductions in overall compensation, and some saw increases. Still, some specialties and many individuals experienced terrible financial stress and had to make changes in their lives and their spending in order to stay afloat.
“The biggest inhibitor to getting back to normal had to do with doctors who did not want to return because they did not want to risk getting COVID,” Dr. Pinto reports. But he notes that by February 2021 most doctors were completely vaccinated and could feel safe again.
A version of this article first appeared on Medscape.com.
, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Almost 18,000 physicians in more than 29 specialties told Medscape about their income, hours worked, greatest challenges, and the unexpected impact of COVID-19 on their compensation.
How many physicians avoided massive losses
When the pandemic started around March 2020, “a great many physicians saw reductions in volume at first,” says Robert Pearl, MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University.
Medscape’s survey report shows that a staggering 44% saw a 1%-25% reduction in patient volume, and 9% saw a 26%-50% decline. “That is indeed breathtaking,” Dr. Pearl says.
Several key factors saved many practices from hemorrhaging money, says Michael Belkin, JD, divisional vice president at Merritt Hawkins and Associates in Dallas. “Many physicians used the federal Paycheck Protection Program [PPP] to help keep themselves afloat,” he says. “A large percentage reduced their staff, which reduced their expenses, and many got some of their volume back by transitioning to telemedicine.”
In a 2020 survey for the Physicians Foundation, conducted by Merritt Hawkins, 48% of physicians said their practice had received PPP support, and most of those said the support was enough to allow them to stay open without reducing staff. Only 6% of practices that received PPP support did not stay open.
Telemedicine helped many practices
Early in the pandemic, Medicare reimbursements for telemedicine were equal with those for face-to-face visits. “Since telemedicine takes a third less time than an inpatient visit, doctors could see more patients,” Dr. Pearl says.
The switch was almost instantaneous in some practices. Within 3 days, a 200-provider multispecialty practice in Wilmington, N.C., went from not using telehealth to its being used by all physicians, the Medical Group Management Association reported. By late April, the practice was already back up to about 70% of normal overall production.
However, telemedicine could not help every specialty equally. “Generally, allergists can’t do their allergy testing virtually, and patients with mild problems probably put off visits,” Dr. Pearl says. Allergists experienced a large percentage decline in compensation, according to Medscape’s survey. For some, income fell from $301,000 the prior year to $274,000 this year.
Primary care struggled
Primary care physicians posted lower compensation than they did the prior year, but most rebounded to some degree. A study released in June 2020 projected that, even with telemedicine, primary care physicians would lose an average of $67,774 for the year.
However, Medscape’s survey found that internists’ average compensation declined from $251,000 in the prior year to $248,000, and average family physicians’ compensation actually rose from $234,000.
Pediatricians had a harder slog. Their average compensation sank from $232,000 to $221,000, according to the report. Even with telemedicine, parents of young children were not contacting the doctor. In May 2020, visits by children aged 3-5 years were down by 56%.
Many proceduralists recovered
Procedure-oriented specialties were particularly hard-hit at first, because many hospitals and some states banned all elective surgeries at the beginning of the pandemic.
“In March and April, ophthalmology practices were virtually at a standstill,” says John B. Pinto, an ophthalmology practice management consultant in San Diego. “But by the fourth quarter, operations were back to normal. Practices were fully open, and patients were coming back in.”
Medscape’s survey shows that, by year’s end, compensation was about the same as the year before for orthopedic surgeons ($511,000 in both the 2020 and 2021 reports); cardiologists actually did better ($438,000 in our 2020 report and $459,000 in 2021); and ophthalmologists’ compensation was about the same ($378,000 in our prior report and $379,000 in 2021).
Some other proceduralists, however, did not do as well. Otolaryngologists’ compensation fell to $417,000, the second-biggest percentage drop. “This may be because otolaryngologists’ chief procedures are tonsillectomies, sinus surgery, and nasal surgery, which can be put off,” Dr. Pearl says.
Anesthesiologists, who depend on surgical volume, also did not earn as much in 2020. Their compensation declined from $398,000 in our 2020 report to $378,000 in Medscape’s 2021 report.
“Not only has 70% of our revenue disappeared, but our physicians are still working every day,” an independent anesthesiology practice in Alabama told the MGMA early in the pandemic.
Plastic surgeons now the top earners
The biggest increase in compensation by far was made by plastic surgeons, whose income rose 9.8% over the year before, to $526,000. This put them at the top of the list
Dr. Pearl adds that plastic surgeons can perform their procedures in their offices, rather than in a hospital, where elective surgeries were often canceled.
Mr. Belkin says specialties other than plastic surgery had been offering more boutique cosmetic care even before the pandemic. In 2020, nonsurgical cosmetic procedures such as neurotoxin therapy, dermal filler procedures, chemical peels, and hair removal earned $3.1 billion in revenue, according to a survey by the Aesthetic Society.
Other specialties that earned more even during COVID
In Medscape’s survey, several specialties actually earned more during the pandemic than in 2019. Some specialties, such as critical care and public health, were integral in managing COVID patients and the pandemic.
However, some specialties involved in COVID care did not see an increase. Compensation for infectious disease specialists (at $245,000) and emergency medicine specialists (at $354,000) remained basically unchanged from the prior year, and for pulmonologists, it was slightly down.
Emergency departments reported decreases in volume of 40% or more early in the pandemic, according to the American College of Emergency Physicians. It was reported that patients were avoiding EDs for fear of contracting COVID, and car accidents were down because people ventured out less.
In this year’s report, psychiatrists saw a modest rise in compensation, to $275,000. “There has been an increase in mental health visits in the pandemic,” Dr. Pearl says. In 2020, about 4 in 10 adults in the United States reported symptoms of anxiety or depressive disorder, up from 1 in 10 adults the prior year. In addition, psychiatrists were third on the list of Merritt Hawkins’ most requested recruiting engagements.
Oncologists saw a rise in compensation, from $377,000 to $403,000. “Volume likely did not fall because cancer patients would go through with their chemotherapy in spite of the pandemic,” Dr. Pearl says. “The increase in income might have to do with the usual inflation in the cost of chemotherapy drugs.” Dr. Pinto saw the same trend for retinal surgeons, whose care also cannot be delayed.
Medscape’s survey also reports increases in compensation for rheumatologists, endocrinologists, and neurologists, but it reports small declines among dermatologists, radiologists, and gastroenterologists.
Gender-based pay gap remains in place
The gender-based pay gap in this year’s report is similar to that seen in Medscape’s report for the prior year. Men earned 27% more than women in 2021, compared with 25% more the year before. Some physicians commented that more women physicians maintained flexible or shorter work schedules to help with children who could not go into school.
“Having to be a full-time physician, full-time mom, and full-time teacher during our surge was unbelievable,” a primary care pediatrician in group practice and mother of two reported in November. “I felt pulled in all directions and didn’t do anything well.”
In addition, “men dominate some specialties that seem to have seen a smaller drop in volume in the pandemic, such as emergency medicine, infectious disease, pulmonology, and oncology,” says Halee Fischer-Wright, MD, CEO of MGMA.
Employed physicians shared their employers’ pain
Employed physicians, who typically work at hospitals, shared the financial pains of their institutions, particularly in the early stages of the pandemic. In April, hospital admissions were 34.1% below prepandemic levels, according to a study published in Health Affairs. That figure had risen by June, but it was still 8.3% below prepandemic volume.
By the end of the year, many hospitals and hospital systems were in the black, thanks in large part to generous federal subsidies, but actual operations still lost money for the year. Altogether, 42% of them posted an operational loss in 2020, up from the 23% in 2019, according to a survey by Moody’s Investors Service.
Medscape’s report shows that many employed physicians lost pay in 2020, and for many, pay had not returned to pre-COVID levels. Only 28% of primary care physicians and 32% of specialists who lost pay have seen it restored, according to the report. In addition, 15% of surveyed physicians did not receive an annual raise.
Many employed doctors are paid on the basis of relative value units (RVUs), which is a measure of the value of their work. In many cases, there was not enough work to reach RVU thresholds. Would hospitals and other employers lower RVU targets to meet the problem? “I haven’t seen our clients make concessions to providers along those lines,” Mr. Belkin says.
Physicians had to work longer hours
The Medscape report also found that in 2020, physicians saw fewer patients because each visit took longer.
“With the threat of COVID, in-person visits take more time than before,” Mr. Belkin says. “Physicians and staff have to prepare the exam room after each visit, and doctors must spend more time answering patients’ questions about COVID.”
“The new protocols to keep everyone safe add time between patients, and physicians have to answer patients’ questions about the pandemic and vaccines,” Dr. Fischer-Wright says. “You might see a 20% increase in time spent just on these non–revenue-generating COVID activities.”
Physicians still like their specialty
Although 2020 was a challenging year for physicians, the percentage of those who were satisfied with their specialty choice generally did not slip from the year before. It actually rose for several specialties – most notably, rheumatology, pulmonology, physical medicine and rehabilitation, and nephrology.
One specialty saw a decline in satisfaction with their specialty choice, and that was public health and preventive medicine, which plummeted 16 percentage points to 67% – putting it at the bottom of the list.
Even before the pandemic, many public health departments were chronically underfunded. This problem was possibly exacerbated by the pressures to keep up with COVID reporting and testing responsibilities.
Conclusion
Although 2020 was a wild ride for many physicians, many came out of it with only minor reductions in overall compensation, and some saw increases. Still, some specialties and many individuals experienced terrible financial stress and had to make changes in their lives and their spending in order to stay afloat.
“The biggest inhibitor to getting back to normal had to do with doctors who did not want to return because they did not want to risk getting COVID,” Dr. Pinto reports. But he notes that by February 2021 most doctors were completely vaccinated and could feel safe again.
A version of this article first appeared on Medscape.com.
Watch for abnormal movements in hospitalized COVID-19 patients
Myoclonus was diagnosed in about half of hospitalized COVID-19 patients who were evaluated for movement disorders, data from 50 cases show.
Abnormal movements often occur as complications from critical illness, and neurologic consultation can determine whether patients have experienced a seizure or stroke. However, restriction of bedside assessment in the wake of the COVID-19 pandemic increases the risk that abnormal movements will be missed, Jeffrey R. Clark and Eric M. Liotta, MD, of Northwestern University, Chicago, and colleagues wrote.
“Given the limited reports of abnormal movements in hospitalized COVID-19 patients and increased recognition of neurologic manifestations of COVID-19, we sought to examine the frequency and etiology of this finding as an indication of neurologic consultation,” they said.
In a study published in the Journal of the Neurological Sciences, the researchers reviewed data from the first 50 consecutive patients with COVID-19 symptoms who were hospitalized at a single center and underwent neurologic consultation between March 17, 2020, and May 18, 2020.
Overall, 11 patients (22.0%) of patients experienced abnormal movement, and all were admitted to the ICU within 7 days of meeting criteria for severe COVID-19. These patients included nine men and two women with an age range of 36-78 years. The most common comorbidities were obesity, hypertension, diabetes, chronic kidney disease, and coronary artery disease.
Myoclonus (generalized and focal) was the most common abnormal movement, and present in 6 of the 11 patients. Three cases were attributed to high-intensity sedation, and three to toxic-metabolic disturbances. In two patients, abnormal movements were attributed to focal seizures in the setting of encephalopathy, with focal facial twitching. An additional two patients experienced tremors; one showed an acute subdural hemorrhage on CT imaging. The second patient showed no sign of stroke or other abnormality on MRI and the tremor improved during the hospital stay. One patient who experienced abnormal high-amplitude nonrhythmic movements of the lower extremities was diagnosed with serotonin syndrome that resolved after discontinuing high-dose fentanyl.
The study findings were limited by several factors, including the small study population and limited availability of MRI, the researchers noted. Assessing severe COVID-19 cases in the ICU setting presents a challenge because of limited patient participation and the potentially confounding effects of sedation and mechanical ventilation.
However, the researchers said.
“A heightened awareness of abnormal eye movements, or subtle facial tremoring, may be the first steps in recognizing potentially dangerous neurologic manifestations,” and clinicians caring for patients with severe COVID-19 should be able to recognize abnormal movements and seek neurologic consultation when indicated, they emphasized.
The study was supported in part by grants to coauthors Nicholas J. Reish, MD, and Dr. Liotta from the National Institutes of Health. The researchers had no financial conflicts to disclose.
Myoclonus was diagnosed in about half of hospitalized COVID-19 patients who were evaluated for movement disorders, data from 50 cases show.
Abnormal movements often occur as complications from critical illness, and neurologic consultation can determine whether patients have experienced a seizure or stroke. However, restriction of bedside assessment in the wake of the COVID-19 pandemic increases the risk that abnormal movements will be missed, Jeffrey R. Clark and Eric M. Liotta, MD, of Northwestern University, Chicago, and colleagues wrote.
“Given the limited reports of abnormal movements in hospitalized COVID-19 patients and increased recognition of neurologic manifestations of COVID-19, we sought to examine the frequency and etiology of this finding as an indication of neurologic consultation,” they said.
In a study published in the Journal of the Neurological Sciences, the researchers reviewed data from the first 50 consecutive patients with COVID-19 symptoms who were hospitalized at a single center and underwent neurologic consultation between March 17, 2020, and May 18, 2020.
Overall, 11 patients (22.0%) of patients experienced abnormal movement, and all were admitted to the ICU within 7 days of meeting criteria for severe COVID-19. These patients included nine men and two women with an age range of 36-78 years. The most common comorbidities were obesity, hypertension, diabetes, chronic kidney disease, and coronary artery disease.
Myoclonus (generalized and focal) was the most common abnormal movement, and present in 6 of the 11 patients. Three cases were attributed to high-intensity sedation, and three to toxic-metabolic disturbances. In two patients, abnormal movements were attributed to focal seizures in the setting of encephalopathy, with focal facial twitching. An additional two patients experienced tremors; one showed an acute subdural hemorrhage on CT imaging. The second patient showed no sign of stroke or other abnormality on MRI and the tremor improved during the hospital stay. One patient who experienced abnormal high-amplitude nonrhythmic movements of the lower extremities was diagnosed with serotonin syndrome that resolved after discontinuing high-dose fentanyl.
The study findings were limited by several factors, including the small study population and limited availability of MRI, the researchers noted. Assessing severe COVID-19 cases in the ICU setting presents a challenge because of limited patient participation and the potentially confounding effects of sedation and mechanical ventilation.
However, the researchers said.
“A heightened awareness of abnormal eye movements, or subtle facial tremoring, may be the first steps in recognizing potentially dangerous neurologic manifestations,” and clinicians caring for patients with severe COVID-19 should be able to recognize abnormal movements and seek neurologic consultation when indicated, they emphasized.
The study was supported in part by grants to coauthors Nicholas J. Reish, MD, and Dr. Liotta from the National Institutes of Health. The researchers had no financial conflicts to disclose.
Myoclonus was diagnosed in about half of hospitalized COVID-19 patients who were evaluated for movement disorders, data from 50 cases show.
Abnormal movements often occur as complications from critical illness, and neurologic consultation can determine whether patients have experienced a seizure or stroke. However, restriction of bedside assessment in the wake of the COVID-19 pandemic increases the risk that abnormal movements will be missed, Jeffrey R. Clark and Eric M. Liotta, MD, of Northwestern University, Chicago, and colleagues wrote.
“Given the limited reports of abnormal movements in hospitalized COVID-19 patients and increased recognition of neurologic manifestations of COVID-19, we sought to examine the frequency and etiology of this finding as an indication of neurologic consultation,” they said.
In a study published in the Journal of the Neurological Sciences, the researchers reviewed data from the first 50 consecutive patients with COVID-19 symptoms who were hospitalized at a single center and underwent neurologic consultation between March 17, 2020, and May 18, 2020.
Overall, 11 patients (22.0%) of patients experienced abnormal movement, and all were admitted to the ICU within 7 days of meeting criteria for severe COVID-19. These patients included nine men and two women with an age range of 36-78 years. The most common comorbidities were obesity, hypertension, diabetes, chronic kidney disease, and coronary artery disease.
Myoclonus (generalized and focal) was the most common abnormal movement, and present in 6 of the 11 patients. Three cases were attributed to high-intensity sedation, and three to toxic-metabolic disturbances. In two patients, abnormal movements were attributed to focal seizures in the setting of encephalopathy, with focal facial twitching. An additional two patients experienced tremors; one showed an acute subdural hemorrhage on CT imaging. The second patient showed no sign of stroke or other abnormality on MRI and the tremor improved during the hospital stay. One patient who experienced abnormal high-amplitude nonrhythmic movements of the lower extremities was diagnosed with serotonin syndrome that resolved after discontinuing high-dose fentanyl.
The study findings were limited by several factors, including the small study population and limited availability of MRI, the researchers noted. Assessing severe COVID-19 cases in the ICU setting presents a challenge because of limited patient participation and the potentially confounding effects of sedation and mechanical ventilation.
However, the researchers said.
“A heightened awareness of abnormal eye movements, or subtle facial tremoring, may be the first steps in recognizing potentially dangerous neurologic manifestations,” and clinicians caring for patients with severe COVID-19 should be able to recognize abnormal movements and seek neurologic consultation when indicated, they emphasized.
The study was supported in part by grants to coauthors Nicholas J. Reish, MD, and Dr. Liotta from the National Institutes of Health. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF THE NEUROLOGICAL SCIENCES
Cardiologists can perform stroke thrombectomy to fill ‘unmet need’
Cardiologists experienced in cardiac interventions can competently perform stroke thrombectomy after a short period of training, with outcomes comparable to those achieved by neuroradiology centers, a new study suggests.
“Using interventional cardiologists in this way will help address the huge unmet need for stroke thrombectomy that currently exists,” senior author Petr Widimsky, MD, said in an interview.
Although this may be a feasible way forward in Europe, there is strong opposition to such a proposal from U.S. neurointerventionalists.
The study, published in the April 12 issue of JACC: Cardiovascular Interventions, describes the establishment of a stroke thrombectomy program in University Hospital Kralovske Vinohrady, a large tertiary hospital in Prague, Czech Republic.
The hospital did not have a neurointerventional program until 2012 when a joint program was started involving an experienced team of cardiologists, angiologists, and one interventional radiologist who trained the cardiologists on the thrombectomy procedure.
The current paper reports on the outcomes of the 333 patients with large vessel occlusion stroke treated under this program between October 2012 and December 2019.
The decision to perform catheter-based thrombectomy was made by a neurologist and was based on acute stroke clinical symptoms and CT angiographic findings.
Results show that functional clinical outcomes, assessed via the Modified Rankin Scale (mRS) score at 3 months, did not vary significantly across years 2012 to 2019, with a favorable outcome (mRS 0 to 2) achieved in 47.9% of patients.
Symptomatic intracerebral hemorrhage occurred in 19 patients (5.7%) and embolization in a new vascular territory occurred in 6 patients (1.8%), outcomes similar to those of neuroradiology centers.
The desired clinical results were achieved from the onset of the program, without any signs of a learning curve effect, they reported.
“These findings support the potential role of interventional cardiac cath labs in the treatment of acute stroke in regions where this therapy is not readily available due to the lack of neurointerventionalists,” the authors concluded.
“Our main message is that our results were excellent from the beginning,” Dr. Widimsky said. “When centers prepare properly, they can achieve excellent results from the beginning with cardiologists who are experienced in interventional procedures and who have spent sufficient time learning about the brain.”
The authors noted that despite thrombectomy being an extremely beneficial treatment for severe stroke, many eligible patients remain untreated, largely because of a lack of neurointerventionalists in many regions worldwide. They estimate that about 15% of all stroke patients are eligible for thrombectomy but only around 2% of stroke patients in Europe actually receive such treatment.
Dr. Widimsky, an interventional cardiologist, first thought of the idea of using cardiologists to perform stroke thrombectomies after a good friend and colleague suffered a severe stroke in 2010.
“This made us realize that our hospital needed to be more active in the stroke field,” he said. “We decided that we needed to start doing stroke interventions.”
But the major problem was the lack of neurointerventionalists.
“There are not enough neurointerventionalists in Europe. Interventional cardiologists can perform thousands of procedures every year whereas a neurointerventionalist will at best perform hundreds a year. It is quicker and simpler to train the cardiologist to do it,” Dr. Widimsky said.
They hired one neurointerventionalist to lead the program. “He was our tutor, he taught us his skills,” Dr. Widimsky said. “The cath lab is open 24/7, but if we only have one neurointerventionalist we cannot offer a 24/7 service for stroke thrombectomy. But if we merge with cardiology then we can,” he added.
Their hospital is a very busy center for myocardial infarction, percutaneous coronary intervention, and carotid stenting, he noted. “It is not difficult to make the step from that to stroke thrombectomy. Interventional cardiologists are used to performing carotid and coronary artery stenting. Stroke thrombectomy is a similar technique. The thrombectomy procedure is different from coronary angioplasty but it is not more difficult. Actually, I think coronary angioplasty can be more difficult.”
Dr. Widimsky explained that cardiologists need to learn about the brain anatomy and physiology and learn the stroke imaging techniques. “I spent 1 month in the U.S. learning stroke interventions working with simulators,” he said. “I think interventional cardiologists can learn what they need to know in about 6 months. I would recommend they should watch about 50 procedures and perform at least 25 under supervision.”
He said this model is the way forward and hopes it will become routine. Thrombectomy is “tremendously effective” in improving outcomes in severe strokes, with a number needed to treat (NNT) of just 2.6 to prevent long-term disability in one patient, he said, while other procedures can have NNTs of 50 or more.
“But millions of patients with acute severe stroke are not getting this life-changing treatment,” he added. “We must do everything we can to make this service available to as many patients as possible.”
Dr. Widimsky acknowledges that there has been opposition to this idea from the neurointerventionalist professional bodies but this has lessened recently, at least in Europe. And a program that allows interventionalists with experience in extracranial carotid and vertebral endovascular procedures to “fast-track” technical training has now been proposed.
“There is an enormous unmet need for stroke thrombectomy in Europe, with some countries needing to increase the number of procedures done by 10 or 20 times. These include the U.K., Sweden, Italy, Spain, and Portugal. This cannot be done without cardiology,” Dr. Widimsky said.
Editorial strongly supportive
An accompanying editorial strongly endorses the idea of using interdisciplinary teams to deliver high standard stroke care.
Marius Hornung, MD, and Horst Sievert, MD, from CardioVascular Center Frankfurt (Germany), point out that many experienced cardiologists are trained in performing carotid artery interventions and are therefore experienced in accessing the supra-aortic arteries.
“To be able to guarantee optimized stroke therapy as soon as possible, disputes over competence among the individual medical societies involved must be ended,” they wrote.
They advocate for the creation of interdisciplinary teams, with diagnostics, patient selection, and follow-up care remaining the core competencies and tasks of neurology; in addition, they call for appropriately trained and experienced physicians – regardless of their specialties – performing acute stroke interventions and endovascular thrombectomy.
“Such a network must be installed as soon as possible to fulfill the mantra ‘time is brain’ ... and not losing unnecessary time to patient transfer, or continuing to offer only the second-best therapy,” they concluded.
Opposition in the United States
Dr. Widimsky explained that this proposal may not be so applicable to the United States, where the need for more clinicians capable of performing stroke thrombectomies does not appear to be as critical, possibly because vascular neurosurgeons as well as neuroradiologists are qualified to undertake these procedures.
In an interview, J. Mocco, MD, director of the cerebrovascular center, department of neurological surgery, at Mount Sinai Health System, New York, confirmed that this was the case.
“There is no legitimate data to support the claim that there is a lack of an adequate workforce to provide stroke thrombectomy, at least in the U.S.,” he said, adding that, rather, the primary limitation to patient access is a lack of adequate systems of care. “We should learn from the trauma model, which is strongly evidence based, and provide emergency stroke care in a similarly regionalized manner.”
Dr. Mocco, vice president of the Society of NeuroInterventional Surgery, was not impressed with the current study.
“This paper is a retrospective, single-center, unadjudicated, nonindependent assessor case series and therefore, as the authors acknowledge in the limitations section of their paper, it is invalid to compare these data to the results from high-quality, prospective, core-lab, and independent assessor adjudicated randomized trials,” he said. “The supposition that this trial provides evidence that the reported model should be widely considered lacks scientific rigor.”
Furthermore, “the interventional cardiology literature is replete with data regarding the importance of technical expertise and content knowledge,” he added. “Why would that community now propose that such expertise and knowledge is not necessary for the brain?”
Dr. Mocco argues that the concept that interventional cardiologists should be fast-tracked to perform stroke interventions because they use similar tools, navigate blood vessels, and are comfortable working in critical situations, does not hold up.
“Liver surgeons and brain surgeons are both familiar with tissue manipulation, are used to operating in critical situations, and use cautery, scissors, and scalpels; but no one would argue that a brain surgeon should be fast-tracked to perform liver surgery, or vice versa.”
He added: “Stroke patients do not have the luxury of choosing the physician who provides their thrombectomy. We should do everything reasonable to ensure that our systems of care are organized so that these vulnerable patients are treated by physicians who have appropriate knowledge and expertise.”
This study was supported by the Charles University Research program. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiologists experienced in cardiac interventions can competently perform stroke thrombectomy after a short period of training, with outcomes comparable to those achieved by neuroradiology centers, a new study suggests.
“Using interventional cardiologists in this way will help address the huge unmet need for stroke thrombectomy that currently exists,” senior author Petr Widimsky, MD, said in an interview.
Although this may be a feasible way forward in Europe, there is strong opposition to such a proposal from U.S. neurointerventionalists.
The study, published in the April 12 issue of JACC: Cardiovascular Interventions, describes the establishment of a stroke thrombectomy program in University Hospital Kralovske Vinohrady, a large tertiary hospital in Prague, Czech Republic.
The hospital did not have a neurointerventional program until 2012 when a joint program was started involving an experienced team of cardiologists, angiologists, and one interventional radiologist who trained the cardiologists on the thrombectomy procedure.
The current paper reports on the outcomes of the 333 patients with large vessel occlusion stroke treated under this program between October 2012 and December 2019.
The decision to perform catheter-based thrombectomy was made by a neurologist and was based on acute stroke clinical symptoms and CT angiographic findings.
Results show that functional clinical outcomes, assessed via the Modified Rankin Scale (mRS) score at 3 months, did not vary significantly across years 2012 to 2019, with a favorable outcome (mRS 0 to 2) achieved in 47.9% of patients.
Symptomatic intracerebral hemorrhage occurred in 19 patients (5.7%) and embolization in a new vascular territory occurred in 6 patients (1.8%), outcomes similar to those of neuroradiology centers.
The desired clinical results were achieved from the onset of the program, without any signs of a learning curve effect, they reported.
“These findings support the potential role of interventional cardiac cath labs in the treatment of acute stroke in regions where this therapy is not readily available due to the lack of neurointerventionalists,” the authors concluded.
“Our main message is that our results were excellent from the beginning,” Dr. Widimsky said. “When centers prepare properly, they can achieve excellent results from the beginning with cardiologists who are experienced in interventional procedures and who have spent sufficient time learning about the brain.”
The authors noted that despite thrombectomy being an extremely beneficial treatment for severe stroke, many eligible patients remain untreated, largely because of a lack of neurointerventionalists in many regions worldwide. They estimate that about 15% of all stroke patients are eligible for thrombectomy but only around 2% of stroke patients in Europe actually receive such treatment.
Dr. Widimsky, an interventional cardiologist, first thought of the idea of using cardiologists to perform stroke thrombectomies after a good friend and colleague suffered a severe stroke in 2010.
“This made us realize that our hospital needed to be more active in the stroke field,” he said. “We decided that we needed to start doing stroke interventions.”
But the major problem was the lack of neurointerventionalists.
“There are not enough neurointerventionalists in Europe. Interventional cardiologists can perform thousands of procedures every year whereas a neurointerventionalist will at best perform hundreds a year. It is quicker and simpler to train the cardiologist to do it,” Dr. Widimsky said.
They hired one neurointerventionalist to lead the program. “He was our tutor, he taught us his skills,” Dr. Widimsky said. “The cath lab is open 24/7, but if we only have one neurointerventionalist we cannot offer a 24/7 service for stroke thrombectomy. But if we merge with cardiology then we can,” he added.
Their hospital is a very busy center for myocardial infarction, percutaneous coronary intervention, and carotid stenting, he noted. “It is not difficult to make the step from that to stroke thrombectomy. Interventional cardiologists are used to performing carotid and coronary artery stenting. Stroke thrombectomy is a similar technique. The thrombectomy procedure is different from coronary angioplasty but it is not more difficult. Actually, I think coronary angioplasty can be more difficult.”
Dr. Widimsky explained that cardiologists need to learn about the brain anatomy and physiology and learn the stroke imaging techniques. “I spent 1 month in the U.S. learning stroke interventions working with simulators,” he said. “I think interventional cardiologists can learn what they need to know in about 6 months. I would recommend they should watch about 50 procedures and perform at least 25 under supervision.”
He said this model is the way forward and hopes it will become routine. Thrombectomy is “tremendously effective” in improving outcomes in severe strokes, with a number needed to treat (NNT) of just 2.6 to prevent long-term disability in one patient, he said, while other procedures can have NNTs of 50 or more.
“But millions of patients with acute severe stroke are not getting this life-changing treatment,” he added. “We must do everything we can to make this service available to as many patients as possible.”
Dr. Widimsky acknowledges that there has been opposition to this idea from the neurointerventionalist professional bodies but this has lessened recently, at least in Europe. And a program that allows interventionalists with experience in extracranial carotid and vertebral endovascular procedures to “fast-track” technical training has now been proposed.
“There is an enormous unmet need for stroke thrombectomy in Europe, with some countries needing to increase the number of procedures done by 10 or 20 times. These include the U.K., Sweden, Italy, Spain, and Portugal. This cannot be done without cardiology,” Dr. Widimsky said.
Editorial strongly supportive
An accompanying editorial strongly endorses the idea of using interdisciplinary teams to deliver high standard stroke care.
Marius Hornung, MD, and Horst Sievert, MD, from CardioVascular Center Frankfurt (Germany), point out that many experienced cardiologists are trained in performing carotid artery interventions and are therefore experienced in accessing the supra-aortic arteries.
“To be able to guarantee optimized stroke therapy as soon as possible, disputes over competence among the individual medical societies involved must be ended,” they wrote.
They advocate for the creation of interdisciplinary teams, with diagnostics, patient selection, and follow-up care remaining the core competencies and tasks of neurology; in addition, they call for appropriately trained and experienced physicians – regardless of their specialties – performing acute stroke interventions and endovascular thrombectomy.
“Such a network must be installed as soon as possible to fulfill the mantra ‘time is brain’ ... and not losing unnecessary time to patient transfer, or continuing to offer only the second-best therapy,” they concluded.
Opposition in the United States
Dr. Widimsky explained that this proposal may not be so applicable to the United States, where the need for more clinicians capable of performing stroke thrombectomies does not appear to be as critical, possibly because vascular neurosurgeons as well as neuroradiologists are qualified to undertake these procedures.
In an interview, J. Mocco, MD, director of the cerebrovascular center, department of neurological surgery, at Mount Sinai Health System, New York, confirmed that this was the case.
“There is no legitimate data to support the claim that there is a lack of an adequate workforce to provide stroke thrombectomy, at least in the U.S.,” he said, adding that, rather, the primary limitation to patient access is a lack of adequate systems of care. “We should learn from the trauma model, which is strongly evidence based, and provide emergency stroke care in a similarly regionalized manner.”
Dr. Mocco, vice president of the Society of NeuroInterventional Surgery, was not impressed with the current study.
“This paper is a retrospective, single-center, unadjudicated, nonindependent assessor case series and therefore, as the authors acknowledge in the limitations section of their paper, it is invalid to compare these data to the results from high-quality, prospective, core-lab, and independent assessor adjudicated randomized trials,” he said. “The supposition that this trial provides evidence that the reported model should be widely considered lacks scientific rigor.”
Furthermore, “the interventional cardiology literature is replete with data regarding the importance of technical expertise and content knowledge,” he added. “Why would that community now propose that such expertise and knowledge is not necessary for the brain?”
Dr. Mocco argues that the concept that interventional cardiologists should be fast-tracked to perform stroke interventions because they use similar tools, navigate blood vessels, and are comfortable working in critical situations, does not hold up.
“Liver surgeons and brain surgeons are both familiar with tissue manipulation, are used to operating in critical situations, and use cautery, scissors, and scalpels; but no one would argue that a brain surgeon should be fast-tracked to perform liver surgery, or vice versa.”
He added: “Stroke patients do not have the luxury of choosing the physician who provides their thrombectomy. We should do everything reasonable to ensure that our systems of care are organized so that these vulnerable patients are treated by physicians who have appropriate knowledge and expertise.”
This study was supported by the Charles University Research program. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiologists experienced in cardiac interventions can competently perform stroke thrombectomy after a short period of training, with outcomes comparable to those achieved by neuroradiology centers, a new study suggests.
“Using interventional cardiologists in this way will help address the huge unmet need for stroke thrombectomy that currently exists,” senior author Petr Widimsky, MD, said in an interview.
Although this may be a feasible way forward in Europe, there is strong opposition to such a proposal from U.S. neurointerventionalists.
The study, published in the April 12 issue of JACC: Cardiovascular Interventions, describes the establishment of a stroke thrombectomy program in University Hospital Kralovske Vinohrady, a large tertiary hospital in Prague, Czech Republic.
The hospital did not have a neurointerventional program until 2012 when a joint program was started involving an experienced team of cardiologists, angiologists, and one interventional radiologist who trained the cardiologists on the thrombectomy procedure.
The current paper reports on the outcomes of the 333 patients with large vessel occlusion stroke treated under this program between October 2012 and December 2019.
The decision to perform catheter-based thrombectomy was made by a neurologist and was based on acute stroke clinical symptoms and CT angiographic findings.
Results show that functional clinical outcomes, assessed via the Modified Rankin Scale (mRS) score at 3 months, did not vary significantly across years 2012 to 2019, with a favorable outcome (mRS 0 to 2) achieved in 47.9% of patients.
Symptomatic intracerebral hemorrhage occurred in 19 patients (5.7%) and embolization in a new vascular territory occurred in 6 patients (1.8%), outcomes similar to those of neuroradiology centers.
The desired clinical results were achieved from the onset of the program, without any signs of a learning curve effect, they reported.
“These findings support the potential role of interventional cardiac cath labs in the treatment of acute stroke in regions where this therapy is not readily available due to the lack of neurointerventionalists,” the authors concluded.
“Our main message is that our results were excellent from the beginning,” Dr. Widimsky said. “When centers prepare properly, they can achieve excellent results from the beginning with cardiologists who are experienced in interventional procedures and who have spent sufficient time learning about the brain.”
The authors noted that despite thrombectomy being an extremely beneficial treatment for severe stroke, many eligible patients remain untreated, largely because of a lack of neurointerventionalists in many regions worldwide. They estimate that about 15% of all stroke patients are eligible for thrombectomy but only around 2% of stroke patients in Europe actually receive such treatment.
Dr. Widimsky, an interventional cardiologist, first thought of the idea of using cardiologists to perform stroke thrombectomies after a good friend and colleague suffered a severe stroke in 2010.
“This made us realize that our hospital needed to be more active in the stroke field,” he said. “We decided that we needed to start doing stroke interventions.”
But the major problem was the lack of neurointerventionalists.
“There are not enough neurointerventionalists in Europe. Interventional cardiologists can perform thousands of procedures every year whereas a neurointerventionalist will at best perform hundreds a year. It is quicker and simpler to train the cardiologist to do it,” Dr. Widimsky said.
They hired one neurointerventionalist to lead the program. “He was our tutor, he taught us his skills,” Dr. Widimsky said. “The cath lab is open 24/7, but if we only have one neurointerventionalist we cannot offer a 24/7 service for stroke thrombectomy. But if we merge with cardiology then we can,” he added.
Their hospital is a very busy center for myocardial infarction, percutaneous coronary intervention, and carotid stenting, he noted. “It is not difficult to make the step from that to stroke thrombectomy. Interventional cardiologists are used to performing carotid and coronary artery stenting. Stroke thrombectomy is a similar technique. The thrombectomy procedure is different from coronary angioplasty but it is not more difficult. Actually, I think coronary angioplasty can be more difficult.”
Dr. Widimsky explained that cardiologists need to learn about the brain anatomy and physiology and learn the stroke imaging techniques. “I spent 1 month in the U.S. learning stroke interventions working with simulators,” he said. “I think interventional cardiologists can learn what they need to know in about 6 months. I would recommend they should watch about 50 procedures and perform at least 25 under supervision.”
He said this model is the way forward and hopes it will become routine. Thrombectomy is “tremendously effective” in improving outcomes in severe strokes, with a number needed to treat (NNT) of just 2.6 to prevent long-term disability in one patient, he said, while other procedures can have NNTs of 50 or more.
“But millions of patients with acute severe stroke are not getting this life-changing treatment,” he added. “We must do everything we can to make this service available to as many patients as possible.”
Dr. Widimsky acknowledges that there has been opposition to this idea from the neurointerventionalist professional bodies but this has lessened recently, at least in Europe. And a program that allows interventionalists with experience in extracranial carotid and vertebral endovascular procedures to “fast-track” technical training has now been proposed.
“There is an enormous unmet need for stroke thrombectomy in Europe, with some countries needing to increase the number of procedures done by 10 or 20 times. These include the U.K., Sweden, Italy, Spain, and Portugal. This cannot be done without cardiology,” Dr. Widimsky said.
Editorial strongly supportive
An accompanying editorial strongly endorses the idea of using interdisciplinary teams to deliver high standard stroke care.
Marius Hornung, MD, and Horst Sievert, MD, from CardioVascular Center Frankfurt (Germany), point out that many experienced cardiologists are trained in performing carotid artery interventions and are therefore experienced in accessing the supra-aortic arteries.
“To be able to guarantee optimized stroke therapy as soon as possible, disputes over competence among the individual medical societies involved must be ended,” they wrote.
They advocate for the creation of interdisciplinary teams, with diagnostics, patient selection, and follow-up care remaining the core competencies and tasks of neurology; in addition, they call for appropriately trained and experienced physicians – regardless of their specialties – performing acute stroke interventions and endovascular thrombectomy.
“Such a network must be installed as soon as possible to fulfill the mantra ‘time is brain’ ... and not losing unnecessary time to patient transfer, or continuing to offer only the second-best therapy,” they concluded.
Opposition in the United States
Dr. Widimsky explained that this proposal may not be so applicable to the United States, where the need for more clinicians capable of performing stroke thrombectomies does not appear to be as critical, possibly because vascular neurosurgeons as well as neuroradiologists are qualified to undertake these procedures.
In an interview, J. Mocco, MD, director of the cerebrovascular center, department of neurological surgery, at Mount Sinai Health System, New York, confirmed that this was the case.
“There is no legitimate data to support the claim that there is a lack of an adequate workforce to provide stroke thrombectomy, at least in the U.S.,” he said, adding that, rather, the primary limitation to patient access is a lack of adequate systems of care. “We should learn from the trauma model, which is strongly evidence based, and provide emergency stroke care in a similarly regionalized manner.”
Dr. Mocco, vice president of the Society of NeuroInterventional Surgery, was not impressed with the current study.
“This paper is a retrospective, single-center, unadjudicated, nonindependent assessor case series and therefore, as the authors acknowledge in the limitations section of their paper, it is invalid to compare these data to the results from high-quality, prospective, core-lab, and independent assessor adjudicated randomized trials,” he said. “The supposition that this trial provides evidence that the reported model should be widely considered lacks scientific rigor.”
Furthermore, “the interventional cardiology literature is replete with data regarding the importance of technical expertise and content knowledge,” he added. “Why would that community now propose that such expertise and knowledge is not necessary for the brain?”
Dr. Mocco argues that the concept that interventional cardiologists should be fast-tracked to perform stroke interventions because they use similar tools, navigate blood vessels, and are comfortable working in critical situations, does not hold up.
“Liver surgeons and brain surgeons are both familiar with tissue manipulation, are used to operating in critical situations, and use cautery, scissors, and scalpels; but no one would argue that a brain surgeon should be fast-tracked to perform liver surgery, or vice versa.”
He added: “Stroke patients do not have the luxury of choosing the physician who provides their thrombectomy. We should do everything reasonable to ensure that our systems of care are organized so that these vulnerable patients are treated by physicians who have appropriate knowledge and expertise.”
This study was supported by the Charles University Research program. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pneumonia risk soars in heart failure patients, especially HFpEF
Patients with heart failure get pneumonia at a rate almost three times greater than expected and, once they do get pneumonia, have about a fourfold greater risk of death, investigators for a retrospective analysis of 13,000 patients from two landmark randomized HF trials have found.
The investigators also found that HF patients with preserved ejection fraction (HFpEF) are at the highest risk of developing pneumonia. The findings underscore the importance of patients with HF getting a pneumonia vaccination, they found.
The analysis showed that 6.3% of patients in the PARADIGM-HF trial and 10.6% of those in the PARAGON-HF trial developed pneumonia, reported the study authors, led by John J.V. McMurray, MD, of the British Heart Foundation Cardiovascular Research Center at the University of Glasgow in Scotland (J Am Coll Cardiol. 2021;77:1961-73).
“The main reason for doing this study was the fact that many heart failure patients are not vaccinated, as they should be, against pneumonia – both pneumococcus and influenza vaccination,” Dr. McMurray said in an interview. “We wanted to document the frequency and consequences of pneumonia in patients with heart failure to help highlight this deficiency in care.”
Dr. McMurray said he believes this is the first study to document the incidence of pneumonia and pneumonia-related outcomes according to the two major ejection fraction phenotypes.
PARADIGM-HF and PARAGON-HF
The post hoc analysis consisted of 8,399 patients with HF with reduced ejection fraction (HFrEF) in PARADIGM-HF (Eur J Heart Fail. 2013 Sep;15[9]:1062-73) and 4,796 patients with HFpEF in PARAGON-HF (N Engl J Med. 2014 Sep 11;371[11]:993-1004). The analysis focused on the 528 and 510 patients in each study, respectively, who developed pneumonia. Those rates translated to an incidence rate of 29 per 1,000 patient-years (95% confidence interval, 27-31) in PARADIGM-HF and 39 per 1,000 patient-years (95% CI, 36-42) in PARAGON-HF.
After pneumonia, the risk of death in patients increased substantially. In PARADIGM-HF, the adjusted hazard ratio for the risk of death from any cause after pneumonia was 4.34 (95% CI, 3.73-5.05). In PARAGON-HF, it was 3.76 (95% CI, 3.09-4.58). HF patients who contracted pneumonia also tended to have HF longer than their counterparts who didn’t develop pneumonia, but the frequency of previous hospitalization for HF didn’t vary between the pneumonia and no-pneumonia groups.
Patients who developed pneumonia tended to be older (average age of 66.9 years vs. 64.6 years, P < .001) and male (83.9% vs. 77.8%, P < .001). The mean age of patients in PARADIGM-HF was almost a decade younger than those in PARAGON-HF, 64 vs. 73 years.
Pneumonia patients also had worse Kansas City Cardiomyopathy Questionnaire scores (76 vs. 80 on average), but no difference in New York Heart Association functional class. “In general, patients who developed pneumonia had more symptoms and signs and HF than those who did not develop pneumonia,” Dr. McMurray and colleagues wrote.
Pneumonia patients also had higher rates of chronic obstructive pulmonary disease (26% vs. 12%), diabetes (43% vs. 34%), and atrial fibrillation (46% vs. 36%).
Another reason for conducting the study, Dr. McMurray said, “was the prior findings in patients with coronary disease and acute myocardial infarction that the risk associated with an episode of pneumonia [e.g., in subsequent vascular events and deaths] persisted long after the acute event. We wanted to see if this was also the case for heart failure, and indeed it was.”
For example, the adjusted HR for cardiovascular death or hospitalization in the first month following an episode of pneumonia was 9.48 (range of 6.85-13.12, P < .001), leveling off to 1.59 after 3 months or more.
Vaccination crucial in HF patients
Dr. McMurray noted that this study emphasizes the importance of pneumonia vaccination for patients with HF. “Given that we have so few treatments to offer patients with HFpEF, this makes the potential value of vaccination in these patients all the greater,” he said.
The COVID-19 pandemic, Dr. McMurray said, is a “good reminder of the dangers of a respiratory infection and the importance of vaccination in these patients. COVID-19 has interesting parallels in being a systemic disease and one with postacute, persisting effects.”
The persistent risk for adverse cardiovascular events 3 months and later after pneumonia is a novel finding of the study, wrote Donna Mancini, MD, and Gregory Gibson, MD, in an invited commentary (J Am Coll Cardiol. 2021;77:1974-6). Both are with the Icahn School of Medicine at Mt. Sinai in New York. The post hoc study also “serves as an important reminder” of pneumonia risk in patients with HF, especially during the pandemic, they wrote.
“Although vaccination alone appears unlikely to be a panacea, it is a readily accessible tool for mitigating disease severity and improving outcomes,” Dr. Mancini and Dr. Gibson wrote. “After all, an ounce of prevention is worth a pound of cure.”
Novartis provided funding for the PARADIGM-HF and PARAGON-HF trials, and Dr. McMurray and coauthors disclosed financial relationships with Novartis. Dr. Mancini and Dr. Gibson have no relevant financial relationships to disclose.
Patients with heart failure get pneumonia at a rate almost three times greater than expected and, once they do get pneumonia, have about a fourfold greater risk of death, investigators for a retrospective analysis of 13,000 patients from two landmark randomized HF trials have found.
The investigators also found that HF patients with preserved ejection fraction (HFpEF) are at the highest risk of developing pneumonia. The findings underscore the importance of patients with HF getting a pneumonia vaccination, they found.
The analysis showed that 6.3% of patients in the PARADIGM-HF trial and 10.6% of those in the PARAGON-HF trial developed pneumonia, reported the study authors, led by John J.V. McMurray, MD, of the British Heart Foundation Cardiovascular Research Center at the University of Glasgow in Scotland (J Am Coll Cardiol. 2021;77:1961-73).
“The main reason for doing this study was the fact that many heart failure patients are not vaccinated, as they should be, against pneumonia – both pneumococcus and influenza vaccination,” Dr. McMurray said in an interview. “We wanted to document the frequency and consequences of pneumonia in patients with heart failure to help highlight this deficiency in care.”
Dr. McMurray said he believes this is the first study to document the incidence of pneumonia and pneumonia-related outcomes according to the two major ejection fraction phenotypes.
PARADIGM-HF and PARAGON-HF
The post hoc analysis consisted of 8,399 patients with HF with reduced ejection fraction (HFrEF) in PARADIGM-HF (Eur J Heart Fail. 2013 Sep;15[9]:1062-73) and 4,796 patients with HFpEF in PARAGON-HF (N Engl J Med. 2014 Sep 11;371[11]:993-1004). The analysis focused on the 528 and 510 patients in each study, respectively, who developed pneumonia. Those rates translated to an incidence rate of 29 per 1,000 patient-years (95% confidence interval, 27-31) in PARADIGM-HF and 39 per 1,000 patient-years (95% CI, 36-42) in PARAGON-HF.
After pneumonia, the risk of death in patients increased substantially. In PARADIGM-HF, the adjusted hazard ratio for the risk of death from any cause after pneumonia was 4.34 (95% CI, 3.73-5.05). In PARAGON-HF, it was 3.76 (95% CI, 3.09-4.58). HF patients who contracted pneumonia also tended to have HF longer than their counterparts who didn’t develop pneumonia, but the frequency of previous hospitalization for HF didn’t vary between the pneumonia and no-pneumonia groups.
Patients who developed pneumonia tended to be older (average age of 66.9 years vs. 64.6 years, P < .001) and male (83.9% vs. 77.8%, P < .001). The mean age of patients in PARADIGM-HF was almost a decade younger than those in PARAGON-HF, 64 vs. 73 years.
Pneumonia patients also had worse Kansas City Cardiomyopathy Questionnaire scores (76 vs. 80 on average), but no difference in New York Heart Association functional class. “In general, patients who developed pneumonia had more symptoms and signs and HF than those who did not develop pneumonia,” Dr. McMurray and colleagues wrote.
Pneumonia patients also had higher rates of chronic obstructive pulmonary disease (26% vs. 12%), diabetes (43% vs. 34%), and atrial fibrillation (46% vs. 36%).
Another reason for conducting the study, Dr. McMurray said, “was the prior findings in patients with coronary disease and acute myocardial infarction that the risk associated with an episode of pneumonia [e.g., in subsequent vascular events and deaths] persisted long after the acute event. We wanted to see if this was also the case for heart failure, and indeed it was.”
For example, the adjusted HR for cardiovascular death or hospitalization in the first month following an episode of pneumonia was 9.48 (range of 6.85-13.12, P < .001), leveling off to 1.59 after 3 months or more.
Vaccination crucial in HF patients
Dr. McMurray noted that this study emphasizes the importance of pneumonia vaccination for patients with HF. “Given that we have so few treatments to offer patients with HFpEF, this makes the potential value of vaccination in these patients all the greater,” he said.
The COVID-19 pandemic, Dr. McMurray said, is a “good reminder of the dangers of a respiratory infection and the importance of vaccination in these patients. COVID-19 has interesting parallels in being a systemic disease and one with postacute, persisting effects.”
The persistent risk for adverse cardiovascular events 3 months and later after pneumonia is a novel finding of the study, wrote Donna Mancini, MD, and Gregory Gibson, MD, in an invited commentary (J Am Coll Cardiol. 2021;77:1974-6). Both are with the Icahn School of Medicine at Mt. Sinai in New York. The post hoc study also “serves as an important reminder” of pneumonia risk in patients with HF, especially during the pandemic, they wrote.
“Although vaccination alone appears unlikely to be a panacea, it is a readily accessible tool for mitigating disease severity and improving outcomes,” Dr. Mancini and Dr. Gibson wrote. “After all, an ounce of prevention is worth a pound of cure.”
Novartis provided funding for the PARADIGM-HF and PARAGON-HF trials, and Dr. McMurray and coauthors disclosed financial relationships with Novartis. Dr. Mancini and Dr. Gibson have no relevant financial relationships to disclose.
Patients with heart failure get pneumonia at a rate almost three times greater than expected and, once they do get pneumonia, have about a fourfold greater risk of death, investigators for a retrospective analysis of 13,000 patients from two landmark randomized HF trials have found.
The investigators also found that HF patients with preserved ejection fraction (HFpEF) are at the highest risk of developing pneumonia. The findings underscore the importance of patients with HF getting a pneumonia vaccination, they found.
The analysis showed that 6.3% of patients in the PARADIGM-HF trial and 10.6% of those in the PARAGON-HF trial developed pneumonia, reported the study authors, led by John J.V. McMurray, MD, of the British Heart Foundation Cardiovascular Research Center at the University of Glasgow in Scotland (J Am Coll Cardiol. 2021;77:1961-73).
“The main reason for doing this study was the fact that many heart failure patients are not vaccinated, as they should be, against pneumonia – both pneumococcus and influenza vaccination,” Dr. McMurray said in an interview. “We wanted to document the frequency and consequences of pneumonia in patients with heart failure to help highlight this deficiency in care.”
Dr. McMurray said he believes this is the first study to document the incidence of pneumonia and pneumonia-related outcomes according to the two major ejection fraction phenotypes.
PARADIGM-HF and PARAGON-HF
The post hoc analysis consisted of 8,399 patients with HF with reduced ejection fraction (HFrEF) in PARADIGM-HF (Eur J Heart Fail. 2013 Sep;15[9]:1062-73) and 4,796 patients with HFpEF in PARAGON-HF (N Engl J Med. 2014 Sep 11;371[11]:993-1004). The analysis focused on the 528 and 510 patients in each study, respectively, who developed pneumonia. Those rates translated to an incidence rate of 29 per 1,000 patient-years (95% confidence interval, 27-31) in PARADIGM-HF and 39 per 1,000 patient-years (95% CI, 36-42) in PARAGON-HF.
After pneumonia, the risk of death in patients increased substantially. In PARADIGM-HF, the adjusted hazard ratio for the risk of death from any cause after pneumonia was 4.34 (95% CI, 3.73-5.05). In PARAGON-HF, it was 3.76 (95% CI, 3.09-4.58). HF patients who contracted pneumonia also tended to have HF longer than their counterparts who didn’t develop pneumonia, but the frequency of previous hospitalization for HF didn’t vary between the pneumonia and no-pneumonia groups.
Patients who developed pneumonia tended to be older (average age of 66.9 years vs. 64.6 years, P < .001) and male (83.9% vs. 77.8%, P < .001). The mean age of patients in PARADIGM-HF was almost a decade younger than those in PARAGON-HF, 64 vs. 73 years.
Pneumonia patients also had worse Kansas City Cardiomyopathy Questionnaire scores (76 vs. 80 on average), but no difference in New York Heart Association functional class. “In general, patients who developed pneumonia had more symptoms and signs and HF than those who did not develop pneumonia,” Dr. McMurray and colleagues wrote.
Pneumonia patients also had higher rates of chronic obstructive pulmonary disease (26% vs. 12%), diabetes (43% vs. 34%), and atrial fibrillation (46% vs. 36%).
Another reason for conducting the study, Dr. McMurray said, “was the prior findings in patients with coronary disease and acute myocardial infarction that the risk associated with an episode of pneumonia [e.g., in subsequent vascular events and deaths] persisted long after the acute event. We wanted to see if this was also the case for heart failure, and indeed it was.”
For example, the adjusted HR for cardiovascular death or hospitalization in the first month following an episode of pneumonia was 9.48 (range of 6.85-13.12, P < .001), leveling off to 1.59 after 3 months or more.
Vaccination crucial in HF patients
Dr. McMurray noted that this study emphasizes the importance of pneumonia vaccination for patients with HF. “Given that we have so few treatments to offer patients with HFpEF, this makes the potential value of vaccination in these patients all the greater,” he said.
The COVID-19 pandemic, Dr. McMurray said, is a “good reminder of the dangers of a respiratory infection and the importance of vaccination in these patients. COVID-19 has interesting parallels in being a systemic disease and one with postacute, persisting effects.”
The persistent risk for adverse cardiovascular events 3 months and later after pneumonia is a novel finding of the study, wrote Donna Mancini, MD, and Gregory Gibson, MD, in an invited commentary (J Am Coll Cardiol. 2021;77:1974-6). Both are with the Icahn School of Medicine at Mt. Sinai in New York. The post hoc study also “serves as an important reminder” of pneumonia risk in patients with HF, especially during the pandemic, they wrote.
“Although vaccination alone appears unlikely to be a panacea, it is a readily accessible tool for mitigating disease severity and improving outcomes,” Dr. Mancini and Dr. Gibson wrote. “After all, an ounce of prevention is worth a pound of cure.”
Novartis provided funding for the PARADIGM-HF and PARAGON-HF trials, and Dr. McMurray and coauthors disclosed financial relationships with Novartis. Dr. Mancini and Dr. Gibson have no relevant financial relationships to disclose.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Eating more fat may boost borderline low testosterone
Low-fat diets appear to decrease testosterone levels in men, but further randomized, controlled trials are needed to confirm this effect, the authors of a meta-analysis of six small intervention studies concluded.
A total of 206 healthy men with normal testosterone received a high-fat diet followed by a low-fat diet (or vice versa), and their mean total testosterone levels were 10%-15% lower (but still in the normal range) during the low-fat diet.
The study by registered nutritionist Joseph Whittaker, MSc, University of Worcester (England), and statistician Kexin Wu, MSc, University of Warwick, Coventry, England, was published online in the Journal of Steroid Biochemistry and Molecular Biology.
“I think our results are consistent and fairly strong, but they are not strong enough to give blanket recommendations,” Mr. Whittaker said in an interview.
However, “if somebody has low testosterone, particularly borderline, they could try increasing their fat intake, maybe on a Mediterranean diet,” he said, and see if that works to increase their testosterone by 60 ng/dL, the weighted mean difference in total testosterone levels between the low-fat versus high-fat diet interventions in this meta-analysis.
“A Mediterranean diet is a good way to increase ‘healthy fats,’ mono- and polyunsaturated fatty acids, which will likely decrease cardiovascular disease risk, and boost testosterone at the same time,” Mr. Whittaker noted.
Olive oil has been shown to boost testosterone more than butter, and it also reduces CVD, he continued. Nuts are high in “healthy fats” and consistently decrease CVD and mortality and may boost testosterone. Other sources of “good fat” in a healthy diet include avocado, and red meat and poultry in moderation.
“It is controversial, but our results also indicate that foods with saturated fatty acids may boost testosterone,” he added, noting however that such foods are also associated with an increase in cholesterol.
Is waning testosterone explained by leaner diet?
Men need healthy testosterone levels for good physical performance, mental health, and sexual health, and low levels are associated with a higher risk of heart disease, diabetes, and Alzheimer’s disease, according to a statement about this research issued by the University of Worcester.
Although testosterone levels do decline with advancing age, there has also been an additional age-independent and persistent decline in testosterone levels that began roughly after nutrition guidelines began recommending a lower-fat diet in 1965.
Fat consumption dropped from 45% of the diet in 1965 to 35% of the diet in 1991, and stayed around that lower level through to 2011.
However, it is not clear if this decrease in dietary fat intake might explain part of the concurrent decline in men’s testosterone levels.
Mr. Whittaker and Mr. Wu conducted a systematic literature review and identified six crossover intervention studies that compared testosterone levels during low-fat versus high-fat diets – Dorgan 1996, Wang 2005, Hamalainen 1984, Hill 1980, Reed 1987, and Hill 1979 – and then they combined these studies in a meta-analysis.
Five studies each enrolled 6-43 healthy men from North America, the United Kingdom, and Scandinavia, and the sixth study (Hill 1980) enrolled 34 healthy men from North America and 39 farm laborers from South Africa.
Overall, on average, the men were aged 34-54 years and slightly overweight (a mean body mass index of roughly 27 kg/m2) with normal testosterone (i.e., >300 ng/dL, based on the 2018 American Urological Association guidelines criteria).
Most men received a high-fat diet (40% of calories from fat) first, followed by a low-fat diet (on average 20% of calories from fat; range, 7%-25%), but the subgroup of men from South Africa received the low-fat diet first.
To put this into context, U.K. guidelines recommend a fat intake of less than 35% of daily calories, and U.S. guidelines recommend a fat intake of 20%-35% of daily calories.
The low-and high-fat interventions ranged from 2 to 10 weeks.
Lowest testosterone levels with low-fat vegetarian diets
Overall, on average, the men’s total testosterone was 475 mg/dL when they were consuming a low-fat diet and 532 mg/dL when they were consuming a high-fat diet.
However, the South African men had higher testosterone levels when they consumed a low-fat diet. This suggests that “men with European ancestry may experience a greater decrease in testosterone in response to a low-fat diet,” the researchers wrote.
The decrease in total testosterone in the low-fat versus high-fat diet was largest (26%) in the two studies of men who consumed a vegetarian diet (Hill 1979 and Hill 1980). These diets may have been low in zinc, since a marginal zinc deficiency has been shown to decrease total testosterone, Mr. Whittaker and Mr. Wu speculated.
The meta-analysis also showed that levels of free testosterone, urinary testosterone, and dihydrotestosterone declined during the low-fat diet, whereas levels of luteinizing hormone or sex hormone binding globulin were similar with both diets.
Men with low testosterone and overweight, obesity
What nutritional advice should practitioners give to men who have low testosterone and overweight/obesity?
“If you are very overweight, losing weight is going to dramatically improve your testosterone,” Mr. Whittaker said.
However, proponents of various diets are often in stark disagreement about the merits of a low-fat versus low-carbohydrate diet to lose weight.
“In general,” he continued, “the literature shows low-carb (high-fat) diets are better for weight loss [although many will disagree with that statement].”
Although nutrition guidelines have stressed the importance of limiting fat intake, fat in the diet is also associated with lower triglyceride levels and blood pressure and higher HDL cholesterol levels, and now in this study, higher testosterone levels.
More research needed
The researchers acknowledge study limitations: The meta-analysis included just a few small studies with heterogeneous designs and findings, and there was possible bias from confounding variables.
“Ideally, we would like to see a few more studies to confirm our results,” Mr. Whittaker said in the statement. “However, these studies may never come; normally researchers want to find new results, not replicate old ones. In the meantime, men with low testosterone would be wise to avoid low-fat diets.”
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Low-fat diets appear to decrease testosterone levels in men, but further randomized, controlled trials are needed to confirm this effect, the authors of a meta-analysis of six small intervention studies concluded.
A total of 206 healthy men with normal testosterone received a high-fat diet followed by a low-fat diet (or vice versa), and their mean total testosterone levels were 10%-15% lower (but still in the normal range) during the low-fat diet.
The study by registered nutritionist Joseph Whittaker, MSc, University of Worcester (England), and statistician Kexin Wu, MSc, University of Warwick, Coventry, England, was published online in the Journal of Steroid Biochemistry and Molecular Biology.
“I think our results are consistent and fairly strong, but they are not strong enough to give blanket recommendations,” Mr. Whittaker said in an interview.
However, “if somebody has low testosterone, particularly borderline, they could try increasing their fat intake, maybe on a Mediterranean diet,” he said, and see if that works to increase their testosterone by 60 ng/dL, the weighted mean difference in total testosterone levels between the low-fat versus high-fat diet interventions in this meta-analysis.
“A Mediterranean diet is a good way to increase ‘healthy fats,’ mono- and polyunsaturated fatty acids, which will likely decrease cardiovascular disease risk, and boost testosterone at the same time,” Mr. Whittaker noted.
Olive oil has been shown to boost testosterone more than butter, and it also reduces CVD, he continued. Nuts are high in “healthy fats” and consistently decrease CVD and mortality and may boost testosterone. Other sources of “good fat” in a healthy diet include avocado, and red meat and poultry in moderation.
“It is controversial, but our results also indicate that foods with saturated fatty acids may boost testosterone,” he added, noting however that such foods are also associated with an increase in cholesterol.
Is waning testosterone explained by leaner diet?
Men need healthy testosterone levels for good physical performance, mental health, and sexual health, and low levels are associated with a higher risk of heart disease, diabetes, and Alzheimer’s disease, according to a statement about this research issued by the University of Worcester.
Although testosterone levels do decline with advancing age, there has also been an additional age-independent and persistent decline in testosterone levels that began roughly after nutrition guidelines began recommending a lower-fat diet in 1965.
Fat consumption dropped from 45% of the diet in 1965 to 35% of the diet in 1991, and stayed around that lower level through to 2011.
However, it is not clear if this decrease in dietary fat intake might explain part of the concurrent decline in men’s testosterone levels.
Mr. Whittaker and Mr. Wu conducted a systematic literature review and identified six crossover intervention studies that compared testosterone levels during low-fat versus high-fat diets – Dorgan 1996, Wang 2005, Hamalainen 1984, Hill 1980, Reed 1987, and Hill 1979 – and then they combined these studies in a meta-analysis.
Five studies each enrolled 6-43 healthy men from North America, the United Kingdom, and Scandinavia, and the sixth study (Hill 1980) enrolled 34 healthy men from North America and 39 farm laborers from South Africa.
Overall, on average, the men were aged 34-54 years and slightly overweight (a mean body mass index of roughly 27 kg/m2) with normal testosterone (i.e., >300 ng/dL, based on the 2018 American Urological Association guidelines criteria).
Most men received a high-fat diet (40% of calories from fat) first, followed by a low-fat diet (on average 20% of calories from fat; range, 7%-25%), but the subgroup of men from South Africa received the low-fat diet first.
To put this into context, U.K. guidelines recommend a fat intake of less than 35% of daily calories, and U.S. guidelines recommend a fat intake of 20%-35% of daily calories.
The low-and high-fat interventions ranged from 2 to 10 weeks.
Lowest testosterone levels with low-fat vegetarian diets
Overall, on average, the men’s total testosterone was 475 mg/dL when they were consuming a low-fat diet and 532 mg/dL when they were consuming a high-fat diet.
However, the South African men had higher testosterone levels when they consumed a low-fat diet. This suggests that “men with European ancestry may experience a greater decrease in testosterone in response to a low-fat diet,” the researchers wrote.
The decrease in total testosterone in the low-fat versus high-fat diet was largest (26%) in the two studies of men who consumed a vegetarian diet (Hill 1979 and Hill 1980). These diets may have been low in zinc, since a marginal zinc deficiency has been shown to decrease total testosterone, Mr. Whittaker and Mr. Wu speculated.
The meta-analysis also showed that levels of free testosterone, urinary testosterone, and dihydrotestosterone declined during the low-fat diet, whereas levels of luteinizing hormone or sex hormone binding globulin were similar with both diets.
Men with low testosterone and overweight, obesity
What nutritional advice should practitioners give to men who have low testosterone and overweight/obesity?
“If you are very overweight, losing weight is going to dramatically improve your testosterone,” Mr. Whittaker said.
However, proponents of various diets are often in stark disagreement about the merits of a low-fat versus low-carbohydrate diet to lose weight.
“In general,” he continued, “the literature shows low-carb (high-fat) diets are better for weight loss [although many will disagree with that statement].”
Although nutrition guidelines have stressed the importance of limiting fat intake, fat in the diet is also associated with lower triglyceride levels and blood pressure and higher HDL cholesterol levels, and now in this study, higher testosterone levels.
More research needed
The researchers acknowledge study limitations: The meta-analysis included just a few small studies with heterogeneous designs and findings, and there was possible bias from confounding variables.
“Ideally, we would like to see a few more studies to confirm our results,” Mr. Whittaker said in the statement. “However, these studies may never come; normally researchers want to find new results, not replicate old ones. In the meantime, men with low testosterone would be wise to avoid low-fat diets.”
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Low-fat diets appear to decrease testosterone levels in men, but further randomized, controlled trials are needed to confirm this effect, the authors of a meta-analysis of six small intervention studies concluded.
A total of 206 healthy men with normal testosterone received a high-fat diet followed by a low-fat diet (or vice versa), and their mean total testosterone levels were 10%-15% lower (but still in the normal range) during the low-fat diet.
The study by registered nutritionist Joseph Whittaker, MSc, University of Worcester (England), and statistician Kexin Wu, MSc, University of Warwick, Coventry, England, was published online in the Journal of Steroid Biochemistry and Molecular Biology.
“I think our results are consistent and fairly strong, but they are not strong enough to give blanket recommendations,” Mr. Whittaker said in an interview.
However, “if somebody has low testosterone, particularly borderline, they could try increasing their fat intake, maybe on a Mediterranean diet,” he said, and see if that works to increase their testosterone by 60 ng/dL, the weighted mean difference in total testosterone levels between the low-fat versus high-fat diet interventions in this meta-analysis.
“A Mediterranean diet is a good way to increase ‘healthy fats,’ mono- and polyunsaturated fatty acids, which will likely decrease cardiovascular disease risk, and boost testosterone at the same time,” Mr. Whittaker noted.
Olive oil has been shown to boost testosterone more than butter, and it also reduces CVD, he continued. Nuts are high in “healthy fats” and consistently decrease CVD and mortality and may boost testosterone. Other sources of “good fat” in a healthy diet include avocado, and red meat and poultry in moderation.
“It is controversial, but our results also indicate that foods with saturated fatty acids may boost testosterone,” he added, noting however that such foods are also associated with an increase in cholesterol.
Is waning testosterone explained by leaner diet?
Men need healthy testosterone levels for good physical performance, mental health, and sexual health, and low levels are associated with a higher risk of heart disease, diabetes, and Alzheimer’s disease, according to a statement about this research issued by the University of Worcester.
Although testosterone levels do decline with advancing age, there has also been an additional age-independent and persistent decline in testosterone levels that began roughly after nutrition guidelines began recommending a lower-fat diet in 1965.
Fat consumption dropped from 45% of the diet in 1965 to 35% of the diet in 1991, and stayed around that lower level through to 2011.
However, it is not clear if this decrease in dietary fat intake might explain part of the concurrent decline in men’s testosterone levels.
Mr. Whittaker and Mr. Wu conducted a systematic literature review and identified six crossover intervention studies that compared testosterone levels during low-fat versus high-fat diets – Dorgan 1996, Wang 2005, Hamalainen 1984, Hill 1980, Reed 1987, and Hill 1979 – and then they combined these studies in a meta-analysis.
Five studies each enrolled 6-43 healthy men from North America, the United Kingdom, and Scandinavia, and the sixth study (Hill 1980) enrolled 34 healthy men from North America and 39 farm laborers from South Africa.
Overall, on average, the men were aged 34-54 years and slightly overweight (a mean body mass index of roughly 27 kg/m2) with normal testosterone (i.e., >300 ng/dL, based on the 2018 American Urological Association guidelines criteria).
Most men received a high-fat diet (40% of calories from fat) first, followed by a low-fat diet (on average 20% of calories from fat; range, 7%-25%), but the subgroup of men from South Africa received the low-fat diet first.
To put this into context, U.K. guidelines recommend a fat intake of less than 35% of daily calories, and U.S. guidelines recommend a fat intake of 20%-35% of daily calories.
The low-and high-fat interventions ranged from 2 to 10 weeks.
Lowest testosterone levels with low-fat vegetarian diets
Overall, on average, the men’s total testosterone was 475 mg/dL when they were consuming a low-fat diet and 532 mg/dL when they were consuming a high-fat diet.
However, the South African men had higher testosterone levels when they consumed a low-fat diet. This suggests that “men with European ancestry may experience a greater decrease in testosterone in response to a low-fat diet,” the researchers wrote.
The decrease in total testosterone in the low-fat versus high-fat diet was largest (26%) in the two studies of men who consumed a vegetarian diet (Hill 1979 and Hill 1980). These diets may have been low in zinc, since a marginal zinc deficiency has been shown to decrease total testosterone, Mr. Whittaker and Mr. Wu speculated.
The meta-analysis also showed that levels of free testosterone, urinary testosterone, and dihydrotestosterone declined during the low-fat diet, whereas levels of luteinizing hormone or sex hormone binding globulin were similar with both diets.
Men with low testosterone and overweight, obesity
What nutritional advice should practitioners give to men who have low testosterone and overweight/obesity?
“If you are very overweight, losing weight is going to dramatically improve your testosterone,” Mr. Whittaker said.
However, proponents of various diets are often in stark disagreement about the merits of a low-fat versus low-carbohydrate diet to lose weight.
“In general,” he continued, “the literature shows low-carb (high-fat) diets are better for weight loss [although many will disagree with that statement].”
Although nutrition guidelines have stressed the importance of limiting fat intake, fat in the diet is also associated with lower triglyceride levels and blood pressure and higher HDL cholesterol levels, and now in this study, higher testosterone levels.
More research needed
The researchers acknowledge study limitations: The meta-analysis included just a few small studies with heterogeneous designs and findings, and there was possible bias from confounding variables.
“Ideally, we would like to see a few more studies to confirm our results,” Mr. Whittaker said in the statement. “However, these studies may never come; normally researchers want to find new results, not replicate old ones. In the meantime, men with low testosterone would be wise to avoid low-fat diets.”
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Study aims to enhance understanding of ‘tremendously understudied’ prurigo nodularis
compared with age-matched controls, as well those with atopic dermatitis and psoriasis.
Those are key findings from a retrospective analysis of claims data that was published online April 3, 2021, in the Journal of Investigative Dermatology.
“Prurigo nodularis is a tremendously understudied inflammatory skin disease,” one of the study’s cosenior authors, Shawn G. Kwatra, MD, of the department of dermatology, Johns Hopkins University, Baltimore, said in an interview. “Prurigo nodularis patients have uncontrolled itch, which leads to reduced quality of life, and the association with many disease comorbidities. We focused on better understanding in this work the unique comorbidities of prurigo nodularis, compared to other inflammatory skin diseases.”
For the study, Dr. Kwatra, cosenior author Yevgeniy R. Semenov, MD, of the department of dermatology, Massachusetts General Hospital, Boston, and colleagues evaluated nationally representative, private insurance claims data from October 2015 to December 2019 to identify prurigo nodularis (PN) patients, who were defined as individuals with two or more medical claims for PN using ICD-10-CM codes. For comparison with patients with inflammatory skin diseases, they used the same claims data to identify patients with atopic dermatitis (AD) and psoriasis as well as to select controls who were age and gender matched to PN patients. Next, they quantified the overall comorbidity burden with the Charlson Comorbidity Index (CCI).
In 2016, the claims database included 2,658 patients with PN, 21,482 patients with AD, 21,073 patients with psoriasis, and 13,290 controls. The number of patients in each category rose each subsequent year, so that by the end of 2019 there were 9,426 patients with PN, 70,298 patients with AD, 59,509 patients with psoriasis, and 47,130 controls. Between 2016 and 2019 the mean age of PN patients increased from 57.5 to 59.8 years and the percent of male patients rose from 44.5% to 46.5%.
Between 2016 and 2019, the overall PN prevalence rates rose from 18 per 100,000 to 58 per 100,000, while the PN prevalence rates among adults increased from 22 per 100,000 to 70 per 100,000, and the rates among children rose grew from 2 per 100,000 to 7 per 100,000. “Our report shows an estimated disease prevalence of around 335,000 cases of PN in the United States,” said Dr. Kwatra, who was among a group of researchers to recently report on systemic Th22-polarized inflammation in PN patients.
The researchers also found that patients with PN had the highest mean CCI in both 2016 and 2019. In 2016, their mean CCI was 1.53, compared with 0.98 among controls, 0.53 among those with AD, and 1.16 among those with psoriasis. In 2019, the mean CCI had increased in all groups of patients, to 2.32 among those with PN, 1.57 among controls, 0.75 among those with AD patients, and 1.71 among those with psoriasis.
The top five medical specialties who cared for PN patients, defined as the estimated number of visits per year per patient, were internal medicine (2.01 visits), dermatology (1.87 visits), family practice (1.60 visits), cardiology or cardiovascular disease (0.85 visits), and orthopedics or orthopedic surgery (0.49 visits).
“If you encounter a patient with prurigo nodularis, it’s important to perform a screening for chronic kidney disease, diabetes, and liver disease,” Dr. Kwatra said. “These comorbidities along with emerging studies on circulating blood biomarkers suggest prurigo nodularis is a systemic inflammatory disorder; thus systemic agents are needed for most patients as part of multimodal therapy in prurigo nodularis.”
The researchers acknowledged certain limitations of the study, including its retrospective design and the identification of patients with PN with the ICD-10-CM code, which require further validation. “Furthermore, the increase in annual prevalence estimates for PN, AD, and psoriasis observed in the study could also be a result of increasing coding of these diagnoses in the claims data along with rising awareness by the medical profession,” they wrote.
Dr. Kwatra disclosed that he is an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron, and Kiniksa Pharmaceuticals, and has received grant funding from Galderma, Pfizer, and Kiniksa. He has also received a Dermatology Foundation Medical Dermatology Career Development Award, a research grant from the Skin of Color Society, and is supported by the National Institutes of Health. One coauthor has been funded by NIH grants.
compared with age-matched controls, as well those with atopic dermatitis and psoriasis.
Those are key findings from a retrospective analysis of claims data that was published online April 3, 2021, in the Journal of Investigative Dermatology.
“Prurigo nodularis is a tremendously understudied inflammatory skin disease,” one of the study’s cosenior authors, Shawn G. Kwatra, MD, of the department of dermatology, Johns Hopkins University, Baltimore, said in an interview. “Prurigo nodularis patients have uncontrolled itch, which leads to reduced quality of life, and the association with many disease comorbidities. We focused on better understanding in this work the unique comorbidities of prurigo nodularis, compared to other inflammatory skin diseases.”
For the study, Dr. Kwatra, cosenior author Yevgeniy R. Semenov, MD, of the department of dermatology, Massachusetts General Hospital, Boston, and colleagues evaluated nationally representative, private insurance claims data from October 2015 to December 2019 to identify prurigo nodularis (PN) patients, who were defined as individuals with two or more medical claims for PN using ICD-10-CM codes. For comparison with patients with inflammatory skin diseases, they used the same claims data to identify patients with atopic dermatitis (AD) and psoriasis as well as to select controls who were age and gender matched to PN patients. Next, they quantified the overall comorbidity burden with the Charlson Comorbidity Index (CCI).
In 2016, the claims database included 2,658 patients with PN, 21,482 patients with AD, 21,073 patients with psoriasis, and 13,290 controls. The number of patients in each category rose each subsequent year, so that by the end of 2019 there were 9,426 patients with PN, 70,298 patients with AD, 59,509 patients with psoriasis, and 47,130 controls. Between 2016 and 2019 the mean age of PN patients increased from 57.5 to 59.8 years and the percent of male patients rose from 44.5% to 46.5%.
Between 2016 and 2019, the overall PN prevalence rates rose from 18 per 100,000 to 58 per 100,000, while the PN prevalence rates among adults increased from 22 per 100,000 to 70 per 100,000, and the rates among children rose grew from 2 per 100,000 to 7 per 100,000. “Our report shows an estimated disease prevalence of around 335,000 cases of PN in the United States,” said Dr. Kwatra, who was among a group of researchers to recently report on systemic Th22-polarized inflammation in PN patients.
The researchers also found that patients with PN had the highest mean CCI in both 2016 and 2019. In 2016, their mean CCI was 1.53, compared with 0.98 among controls, 0.53 among those with AD, and 1.16 among those with psoriasis. In 2019, the mean CCI had increased in all groups of patients, to 2.32 among those with PN, 1.57 among controls, 0.75 among those with AD patients, and 1.71 among those with psoriasis.
The top five medical specialties who cared for PN patients, defined as the estimated number of visits per year per patient, were internal medicine (2.01 visits), dermatology (1.87 visits), family practice (1.60 visits), cardiology or cardiovascular disease (0.85 visits), and orthopedics or orthopedic surgery (0.49 visits).
“If you encounter a patient with prurigo nodularis, it’s important to perform a screening for chronic kidney disease, diabetes, and liver disease,” Dr. Kwatra said. “These comorbidities along with emerging studies on circulating blood biomarkers suggest prurigo nodularis is a systemic inflammatory disorder; thus systemic agents are needed for most patients as part of multimodal therapy in prurigo nodularis.”
The researchers acknowledged certain limitations of the study, including its retrospective design and the identification of patients with PN with the ICD-10-CM code, which require further validation. “Furthermore, the increase in annual prevalence estimates for PN, AD, and psoriasis observed in the study could also be a result of increasing coding of these diagnoses in the claims data along with rising awareness by the medical profession,” they wrote.
Dr. Kwatra disclosed that he is an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron, and Kiniksa Pharmaceuticals, and has received grant funding from Galderma, Pfizer, and Kiniksa. He has also received a Dermatology Foundation Medical Dermatology Career Development Award, a research grant from the Skin of Color Society, and is supported by the National Institutes of Health. One coauthor has been funded by NIH grants.
compared with age-matched controls, as well those with atopic dermatitis and psoriasis.
Those are key findings from a retrospective analysis of claims data that was published online April 3, 2021, in the Journal of Investigative Dermatology.
“Prurigo nodularis is a tremendously understudied inflammatory skin disease,” one of the study’s cosenior authors, Shawn G. Kwatra, MD, of the department of dermatology, Johns Hopkins University, Baltimore, said in an interview. “Prurigo nodularis patients have uncontrolled itch, which leads to reduced quality of life, and the association with many disease comorbidities. We focused on better understanding in this work the unique comorbidities of prurigo nodularis, compared to other inflammatory skin diseases.”
For the study, Dr. Kwatra, cosenior author Yevgeniy R. Semenov, MD, of the department of dermatology, Massachusetts General Hospital, Boston, and colleagues evaluated nationally representative, private insurance claims data from October 2015 to December 2019 to identify prurigo nodularis (PN) patients, who were defined as individuals with two or more medical claims for PN using ICD-10-CM codes. For comparison with patients with inflammatory skin diseases, they used the same claims data to identify patients with atopic dermatitis (AD) and psoriasis as well as to select controls who were age and gender matched to PN patients. Next, they quantified the overall comorbidity burden with the Charlson Comorbidity Index (CCI).
In 2016, the claims database included 2,658 patients with PN, 21,482 patients with AD, 21,073 patients with psoriasis, and 13,290 controls. The number of patients in each category rose each subsequent year, so that by the end of 2019 there were 9,426 patients with PN, 70,298 patients with AD, 59,509 patients with psoriasis, and 47,130 controls. Between 2016 and 2019 the mean age of PN patients increased from 57.5 to 59.8 years and the percent of male patients rose from 44.5% to 46.5%.
Between 2016 and 2019, the overall PN prevalence rates rose from 18 per 100,000 to 58 per 100,000, while the PN prevalence rates among adults increased from 22 per 100,000 to 70 per 100,000, and the rates among children rose grew from 2 per 100,000 to 7 per 100,000. “Our report shows an estimated disease prevalence of around 335,000 cases of PN in the United States,” said Dr. Kwatra, who was among a group of researchers to recently report on systemic Th22-polarized inflammation in PN patients.
The researchers also found that patients with PN had the highest mean CCI in both 2016 and 2019. In 2016, their mean CCI was 1.53, compared with 0.98 among controls, 0.53 among those with AD, and 1.16 among those with psoriasis. In 2019, the mean CCI had increased in all groups of patients, to 2.32 among those with PN, 1.57 among controls, 0.75 among those with AD patients, and 1.71 among those with psoriasis.
The top five medical specialties who cared for PN patients, defined as the estimated number of visits per year per patient, were internal medicine (2.01 visits), dermatology (1.87 visits), family practice (1.60 visits), cardiology or cardiovascular disease (0.85 visits), and orthopedics or orthopedic surgery (0.49 visits).
“If you encounter a patient with prurigo nodularis, it’s important to perform a screening for chronic kidney disease, diabetes, and liver disease,” Dr. Kwatra said. “These comorbidities along with emerging studies on circulating blood biomarkers suggest prurigo nodularis is a systemic inflammatory disorder; thus systemic agents are needed for most patients as part of multimodal therapy in prurigo nodularis.”
The researchers acknowledged certain limitations of the study, including its retrospective design and the identification of patients with PN with the ICD-10-CM code, which require further validation. “Furthermore, the increase in annual prevalence estimates for PN, AD, and psoriasis observed in the study could also be a result of increasing coding of these diagnoses in the claims data along with rising awareness by the medical profession,” they wrote.
Dr. Kwatra disclosed that he is an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron, and Kiniksa Pharmaceuticals, and has received grant funding from Galderma, Pfizer, and Kiniksa. He has also received a Dermatology Foundation Medical Dermatology Career Development Award, a research grant from the Skin of Color Society, and is supported by the National Institutes of Health. One coauthor has been funded by NIH grants.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
CDC: STI rates rise for sixth year in a row
Annual cases of sexually transmitted infections in the United States jumped for the sixth year in a row in 2019, according to a new Centers for Disease Control and Prevention report that highlights an increase in congenital syphilis and rising rates of syphilis, chlamydia, and gonorrhea in men, especially men who have sex with men (MSM).
The report says nothing about STI rates during the COVID-19 pandemic, when both casual sex and disease screening and surveillance declined significantly, at least in the early months. But epidemiologist Patricia Kissinger, PhD, MPH, from Tulane University School, New Orleans, said in an interview that the findings reflect how “a confluence of factors” drove up rates before the age of COVID. Those factors include online dating, the opioid epidemic, the decline in condom use in the MSM community as HIV became more preventable, and indifference among policy makers and the community at large.
The CDC report, based on data from local health departments, says there were 129,813 cases of syphilis in 2019, up 74% since 2015. Almost 2,000 cases of congenital syphilis were reported, up 279% since 2015, and 128 infants died.
“There’s no reason for us to have congenital syphilis,” said Dr. Kissinger, who noted that the disease can cause birth defects and meningitis in addition to death. “Women should be screened, and it’s relatively easy to treat via penicillin injections.”
Indeed, medical guidelines suggest that pregnant women be routinely tested for syphilis. But that doesn’t always happen because “it falls through the cracks,” Dr. Kissinger said. Or, she added, women might not be tested enough times during their pregnancies: “You have to screen women in the third trimester. You can’t just do it in the first trimester because people do have sex when they’re pregnant.”
Rising congenital syphilis numbers have convinced at least one health system to take action. As of June 1, the University of California, San Diego, will routinely test pregnant women in the emergency department for syphilis in addition to HIV and hepatitis C, Martin Hoenigl, MD, a UCSF infectious disease specialist, said in an interview.
The CDC report also notes 1.8 million cases of chlamydia in 2019, a jump of 19% in 4 years, and a 56% increase in gonorrhea in that time period, to a total of 616,392 cases.
The report says increasing gonorrhea and chlamydia cases in men, especially MSM, could be caused by increased testing/screening, increased transmission, or both. Although women are generally diagnosed with chlamydia more often than men, the report says, numbers among men grew by 32% from 2015 to 2019. And since 2013, rates of gonorrhea among men have risen at a much faster clip than among women.
MSM accounted for most male cases of primary and secondary syphilis in 2019, although the report said the apparent long-term rise in these cases might be slowing.
Many MSM no longer use condoms because they’re using pre-exposure prophylaxis (PrEP) or have undetectable levels of HIV because of treatment, said Jeffrey Klausner, MD, MPH, an STI specialist at the University of Southern California in Los Angeles, said in an interview.
Many MSM might be getting screened much more often for STIs than in the past because frequent screening is required for those on PrEP. However, Dr. Kissinger said some clinics weren’t able to test at times during the pandemic because of a swab shortage. In addition, patients of all types avoided routine medical care during the pandemic, and some medical professionals in the infectious disease field were redirected to COVID care.
Clinical trials have been investigating a possible preventive STI strategy in MSM who don’t wear condoms – prophylaxis, either before or after exposure, with the antibiotic doxycycline. “That’s a very good solution,” Dr. Klausner said, but he believes bigger challenges remain. According to him, the existence of the report itself – which offers statistics from 2 years ago instead of more relevant recent numbers – is evidence of how the federal government isn’t doing enough to fight STIs. “If we’re taking the STD epidemic seriously, there should be timely and regular reporting.” Dr. Klausner said he likes the idea of monthly reports, as well as more funding for prevention.
Instead, he noted, the federal government cut STI prevention funding by 40% in inflation-adjusted dollars from 2002-2003 to 2018-2019, according to the National Coalition of STD Directors. “Burying your head in the sand and hoping the problem goes away is not an effective strategy,” he said.
It’s not clear whether STI rates are on the decline because of pandemic restrictions and stay-at-home orders. Surveys suggest that a dip in casual sex early in pandemic – when much of society shut down – was only temporary, Dr. Klausner said.
Dr. Kissinger disclosed no relevant financial relationships. Dr. Hoenigl reported receiving research funding via his university from Gilead. Dr. Klausner has recently provided consulting services to Danaher, Cepheid, Roche, GlaxoSmithKline, Talis Bio, SpeeDx, and Visby Medical, all manufacturers of diagnostic assays for STIs.
A version of this article first appeared on Medscape.com.
Annual cases of sexually transmitted infections in the United States jumped for the sixth year in a row in 2019, according to a new Centers for Disease Control and Prevention report that highlights an increase in congenital syphilis and rising rates of syphilis, chlamydia, and gonorrhea in men, especially men who have sex with men (MSM).
The report says nothing about STI rates during the COVID-19 pandemic, when both casual sex and disease screening and surveillance declined significantly, at least in the early months. But epidemiologist Patricia Kissinger, PhD, MPH, from Tulane University School, New Orleans, said in an interview that the findings reflect how “a confluence of factors” drove up rates before the age of COVID. Those factors include online dating, the opioid epidemic, the decline in condom use in the MSM community as HIV became more preventable, and indifference among policy makers and the community at large.
The CDC report, based on data from local health departments, says there were 129,813 cases of syphilis in 2019, up 74% since 2015. Almost 2,000 cases of congenital syphilis were reported, up 279% since 2015, and 128 infants died.
“There’s no reason for us to have congenital syphilis,” said Dr. Kissinger, who noted that the disease can cause birth defects and meningitis in addition to death. “Women should be screened, and it’s relatively easy to treat via penicillin injections.”
Indeed, medical guidelines suggest that pregnant women be routinely tested for syphilis. But that doesn’t always happen because “it falls through the cracks,” Dr. Kissinger said. Or, she added, women might not be tested enough times during their pregnancies: “You have to screen women in the third trimester. You can’t just do it in the first trimester because people do have sex when they’re pregnant.”
Rising congenital syphilis numbers have convinced at least one health system to take action. As of June 1, the University of California, San Diego, will routinely test pregnant women in the emergency department for syphilis in addition to HIV and hepatitis C, Martin Hoenigl, MD, a UCSF infectious disease specialist, said in an interview.
The CDC report also notes 1.8 million cases of chlamydia in 2019, a jump of 19% in 4 years, and a 56% increase in gonorrhea in that time period, to a total of 616,392 cases.
The report says increasing gonorrhea and chlamydia cases in men, especially MSM, could be caused by increased testing/screening, increased transmission, or both. Although women are generally diagnosed with chlamydia more often than men, the report says, numbers among men grew by 32% from 2015 to 2019. And since 2013, rates of gonorrhea among men have risen at a much faster clip than among women.
MSM accounted for most male cases of primary and secondary syphilis in 2019, although the report said the apparent long-term rise in these cases might be slowing.
Many MSM no longer use condoms because they’re using pre-exposure prophylaxis (PrEP) or have undetectable levels of HIV because of treatment, said Jeffrey Klausner, MD, MPH, an STI specialist at the University of Southern California in Los Angeles, said in an interview.
Many MSM might be getting screened much more often for STIs than in the past because frequent screening is required for those on PrEP. However, Dr. Kissinger said some clinics weren’t able to test at times during the pandemic because of a swab shortage. In addition, patients of all types avoided routine medical care during the pandemic, and some medical professionals in the infectious disease field were redirected to COVID care.
Clinical trials have been investigating a possible preventive STI strategy in MSM who don’t wear condoms – prophylaxis, either before or after exposure, with the antibiotic doxycycline. “That’s a very good solution,” Dr. Klausner said, but he believes bigger challenges remain. According to him, the existence of the report itself – which offers statistics from 2 years ago instead of more relevant recent numbers – is evidence of how the federal government isn’t doing enough to fight STIs. “If we’re taking the STD epidemic seriously, there should be timely and regular reporting.” Dr. Klausner said he likes the idea of monthly reports, as well as more funding for prevention.
Instead, he noted, the federal government cut STI prevention funding by 40% in inflation-adjusted dollars from 2002-2003 to 2018-2019, according to the National Coalition of STD Directors. “Burying your head in the sand and hoping the problem goes away is not an effective strategy,” he said.
It’s not clear whether STI rates are on the decline because of pandemic restrictions and stay-at-home orders. Surveys suggest that a dip in casual sex early in pandemic – when much of society shut down – was only temporary, Dr. Klausner said.
Dr. Kissinger disclosed no relevant financial relationships. Dr. Hoenigl reported receiving research funding via his university from Gilead. Dr. Klausner has recently provided consulting services to Danaher, Cepheid, Roche, GlaxoSmithKline, Talis Bio, SpeeDx, and Visby Medical, all manufacturers of diagnostic assays for STIs.
A version of this article first appeared on Medscape.com.
Annual cases of sexually transmitted infections in the United States jumped for the sixth year in a row in 2019, according to a new Centers for Disease Control and Prevention report that highlights an increase in congenital syphilis and rising rates of syphilis, chlamydia, and gonorrhea in men, especially men who have sex with men (MSM).
The report says nothing about STI rates during the COVID-19 pandemic, when both casual sex and disease screening and surveillance declined significantly, at least in the early months. But epidemiologist Patricia Kissinger, PhD, MPH, from Tulane University School, New Orleans, said in an interview that the findings reflect how “a confluence of factors” drove up rates before the age of COVID. Those factors include online dating, the opioid epidemic, the decline in condom use in the MSM community as HIV became more preventable, and indifference among policy makers and the community at large.
The CDC report, based on data from local health departments, says there were 129,813 cases of syphilis in 2019, up 74% since 2015. Almost 2,000 cases of congenital syphilis were reported, up 279% since 2015, and 128 infants died.
“There’s no reason for us to have congenital syphilis,” said Dr. Kissinger, who noted that the disease can cause birth defects and meningitis in addition to death. “Women should be screened, and it’s relatively easy to treat via penicillin injections.”
Indeed, medical guidelines suggest that pregnant women be routinely tested for syphilis. But that doesn’t always happen because “it falls through the cracks,” Dr. Kissinger said. Or, she added, women might not be tested enough times during their pregnancies: “You have to screen women in the third trimester. You can’t just do it in the first trimester because people do have sex when they’re pregnant.”
Rising congenital syphilis numbers have convinced at least one health system to take action. As of June 1, the University of California, San Diego, will routinely test pregnant women in the emergency department for syphilis in addition to HIV and hepatitis C, Martin Hoenigl, MD, a UCSF infectious disease specialist, said in an interview.
The CDC report also notes 1.8 million cases of chlamydia in 2019, a jump of 19% in 4 years, and a 56% increase in gonorrhea in that time period, to a total of 616,392 cases.
The report says increasing gonorrhea and chlamydia cases in men, especially MSM, could be caused by increased testing/screening, increased transmission, or both. Although women are generally diagnosed with chlamydia more often than men, the report says, numbers among men grew by 32% from 2015 to 2019. And since 2013, rates of gonorrhea among men have risen at a much faster clip than among women.
MSM accounted for most male cases of primary and secondary syphilis in 2019, although the report said the apparent long-term rise in these cases might be slowing.
Many MSM no longer use condoms because they’re using pre-exposure prophylaxis (PrEP) or have undetectable levels of HIV because of treatment, said Jeffrey Klausner, MD, MPH, an STI specialist at the University of Southern California in Los Angeles, said in an interview.
Many MSM might be getting screened much more often for STIs than in the past because frequent screening is required for those on PrEP. However, Dr. Kissinger said some clinics weren’t able to test at times during the pandemic because of a swab shortage. In addition, patients of all types avoided routine medical care during the pandemic, and some medical professionals in the infectious disease field were redirected to COVID care.
Clinical trials have been investigating a possible preventive STI strategy in MSM who don’t wear condoms – prophylaxis, either before or after exposure, with the antibiotic doxycycline. “That’s a very good solution,” Dr. Klausner said, but he believes bigger challenges remain. According to him, the existence of the report itself – which offers statistics from 2 years ago instead of more relevant recent numbers – is evidence of how the federal government isn’t doing enough to fight STIs. “If we’re taking the STD epidemic seriously, there should be timely and regular reporting.” Dr. Klausner said he likes the idea of monthly reports, as well as more funding for prevention.
Instead, he noted, the federal government cut STI prevention funding by 40% in inflation-adjusted dollars from 2002-2003 to 2018-2019, according to the National Coalition of STD Directors. “Burying your head in the sand and hoping the problem goes away is not an effective strategy,” he said.
It’s not clear whether STI rates are on the decline because of pandemic restrictions and stay-at-home orders. Surveys suggest that a dip in casual sex early in pandemic – when much of society shut down – was only temporary, Dr. Klausner said.
Dr. Kissinger disclosed no relevant financial relationships. Dr. Hoenigl reported receiving research funding via his university from Gilead. Dr. Klausner has recently provided consulting services to Danaher, Cepheid, Roche, GlaxoSmithKline, Talis Bio, SpeeDx, and Visby Medical, all manufacturers of diagnostic assays for STIs.
A version of this article first appeared on Medscape.com.
COVID-19–related inflammatory syndrome tied to neurologic symptoms in children
About half of children with pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) have new-onset neurologic symptoms, research shows.
These symptoms involve the central and peripheral nervous systems but do not always affect the respiratory system. In addition, neurologic symptoms appear to be more common in severe presentations of this syndrome.
“These new data consolidate the initial findings in our JAMA Neurology publication on the neurological problems that children with PIMS-TS can present with, even in the absence of respiratory systems,” study investigator Omar Abdel-Mannan, MD, clinical research fellow at University College London Institute of Neurology and senior resident at Great Ormond Street Hospital for children in London, said in an interview.
He added that the findings are in keeping with other recent research studies on PIMS-TS, which is known more commonly in the United States as multisystem inflammatory syndrome in children (MIS-C).
The findings will be presented April 18 at the American Academy of Neurology (AAN) 2021 Annual Meeting.
Neurologic manifestations common
Many children and adults with COVID-19 have developed neurologic manifestations. PIMS-TS is a severe, postinfectious, immune-mediated disorder characterized by persistent fever and extreme inflammation.
Patients may have acute diarrhea or vomiting, rash or bilateral conjunctivitis, and low blood pressure. They should be examined by a pediatric specialist, and most children with this disorder need intensive care.
To report the neurologic manifestations in children with PIMS-TS, the researchers retrospectively examined data for children and adolescents younger than 18 years who had the disorder and presented to a single center between April 4, 2020, and Sept. 1, 2020.
Forty-six patients (median age, 10.2 years) were included in the analysis. Thirty (65.2%) were male, and 37 (80.4%) were of non-White ethnicities.
Twenty-four (52.2%) patients had new-onset neurologic symptoms, which included headache (n = 24), encephalopathy (n = 14 patients), dysarthria/dysphonia (n = 6), hallucinations (n = 6), ataxia (n = 4), peripheral nerve involvement (n = 3), and seizures (n=1).
Laboratory and imaging results provided further information. One patient had 118 leukocytes in cerebrospinal fluid. Children with neurologic involvement had higher levels of peak inflammatory markers and were more likely to be ventilated and require inotropic support in the PICU (P < .05).
Four of 16 patients who underwent brain MRI had splenium signal changes. Of 15 patients who underwent electroencephalogram (EEG), 14 had an excess of slow activity. Four of 7 patients who underwent nerve conduction studies and electromyography (EMG) had myopathic and neuropathic changes.
Response to SARS-CoV-2
Central neurologic problems of the brain and peripheral nerve involvement rarely occur at the same time in children.
“This makes it highly possible that the syndrome is secondary to cytokine release in response to the SARS-CoV-2 virus, as there is significant clinical overlap with both genetic and acquired forms of another immune-mediated condition known as hemophagocytic lymphohistiocytosis,” said Dr. Abdel-Mannan.
The researchers found no demographic differences between children with neurologic involvement at presentation and those without.
“However, the numbers are small given the rarity of this condition, which makes it difficult to extrapolate associations and differences between the two groups, and will require future collaborative larger scale studies to look at what potentially makes some children more susceptible to neurologic involvement than others,” said Dr. Abdel-Mannan.
Excluding potential causes of the symptoms other than COVID-19 also is important, he added.
The preponderance of ethnic minorities in the current study population mirrors that in other PIMS-TS cohorts in other countries, said Dr. Abdel-Mannan. It reflects the higher incidence of COVID-19 in ethnic minority groups. However, presentation, investigations, and management did not differ between White and non-White children in the current study.
“Although PIMS-TS patients with neurologic involvement are initially sicker, our center’s preliminary follow-up data up to 6 months post discharge from hospital demonstrates that most of these children make an almost complete functional recovery, which is reassuring,” said Dr. Abdel-Mannan.
The data underscore how important it is that clinicians be aware that children with PIMS-TS can present with neurologic symptoms, even in the absence of respiratory involvement, he added.
The researchers will soon begin a multicenter research study that will involve longitudinal clinical and cognitive assessments and advanced neuroimaging. The objective will be to determine whether all children with PIMS-TS, or only those with neurologic symptoms, are at risk of chronic longer-term neurocognitive and psychiatric outcomes.
Unanswered questions
John B. Bodensteiner, MD, professor of neurology and pediatrics at Mayo Clinic, Rochester, Minn., said in an interview that the findings help flesh out the range of neurologic involvement that PIMS-TS entails.
“It’s not a surprise to us as neurologists, but it’s not been emphasized in the general literature and in the public health sector,” he said.
The study’s most important implication is that neurologic conditions are not uncommon among children with PIMS-TS, Dr. Bodensteiner added.
“We have no idea how long or what the long-term effects of that are,” he said. Not enough time has elapsed to enable a clear understanding of the syndrome’s lasting effects on cognition, he said, “but I think this certainly raises a flag that this is a real entity. This is nothing to sniff at.”
He noted that the study has the limitations of any retrospective case series. The researchers did not perform prospective and systematic evaluations of children with the syndrome
The findings also raise unanswered questions.
“They had 14 kids with encephalopathy, but not all of them got the same evaluation,” said Dr. Bodensteiner. Although the researchers mention peripheral nerve involvement in three children, they do not describe it. “They said that the EMG showed myopathic and neuropathic changes, but peripheral nerve involvement wouldn’t give you myopathic changes, so maybe there’s some direct involvement of the muscle in this inflammatory process.”
The study also focused on a select group of patients, said Dr. Bodensteiner. “These are all patients admitted to Great Ormond Street Hospital, and we don’t know what percentage of kids who get COVID are hospitalized, which is an important issue.”
It is necessary to know what proportion of children with COVID-19 develop encephalopathy and MRI changes, he added. The findings do confirm that this coronavirus-related inflammatory condition is real and may have long-term sequelae. “We should be careful about kids getting this disease,” said Dr. Bodensteiner
The study had no funding. Dr. Abdel-Mannan and Dr. Bodensteiner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
About half of children with pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) have new-onset neurologic symptoms, research shows.
These symptoms involve the central and peripheral nervous systems but do not always affect the respiratory system. In addition, neurologic symptoms appear to be more common in severe presentations of this syndrome.
“These new data consolidate the initial findings in our JAMA Neurology publication on the neurological problems that children with PIMS-TS can present with, even in the absence of respiratory systems,” study investigator Omar Abdel-Mannan, MD, clinical research fellow at University College London Institute of Neurology and senior resident at Great Ormond Street Hospital for children in London, said in an interview.
He added that the findings are in keeping with other recent research studies on PIMS-TS, which is known more commonly in the United States as multisystem inflammatory syndrome in children (MIS-C).
The findings will be presented April 18 at the American Academy of Neurology (AAN) 2021 Annual Meeting.
Neurologic manifestations common
Many children and adults with COVID-19 have developed neurologic manifestations. PIMS-TS is a severe, postinfectious, immune-mediated disorder characterized by persistent fever and extreme inflammation.
Patients may have acute diarrhea or vomiting, rash or bilateral conjunctivitis, and low blood pressure. They should be examined by a pediatric specialist, and most children with this disorder need intensive care.
To report the neurologic manifestations in children with PIMS-TS, the researchers retrospectively examined data for children and adolescents younger than 18 years who had the disorder and presented to a single center between April 4, 2020, and Sept. 1, 2020.
Forty-six patients (median age, 10.2 years) were included in the analysis. Thirty (65.2%) were male, and 37 (80.4%) were of non-White ethnicities.
Twenty-four (52.2%) patients had new-onset neurologic symptoms, which included headache (n = 24), encephalopathy (n = 14 patients), dysarthria/dysphonia (n = 6), hallucinations (n = 6), ataxia (n = 4), peripheral nerve involvement (n = 3), and seizures (n=1).
Laboratory and imaging results provided further information. One patient had 118 leukocytes in cerebrospinal fluid. Children with neurologic involvement had higher levels of peak inflammatory markers and were more likely to be ventilated and require inotropic support in the PICU (P < .05).
Four of 16 patients who underwent brain MRI had splenium signal changes. Of 15 patients who underwent electroencephalogram (EEG), 14 had an excess of slow activity. Four of 7 patients who underwent nerve conduction studies and electromyography (EMG) had myopathic and neuropathic changes.
Response to SARS-CoV-2
Central neurologic problems of the brain and peripheral nerve involvement rarely occur at the same time in children.
“This makes it highly possible that the syndrome is secondary to cytokine release in response to the SARS-CoV-2 virus, as there is significant clinical overlap with both genetic and acquired forms of another immune-mediated condition known as hemophagocytic lymphohistiocytosis,” said Dr. Abdel-Mannan.
The researchers found no demographic differences between children with neurologic involvement at presentation and those without.
“However, the numbers are small given the rarity of this condition, which makes it difficult to extrapolate associations and differences between the two groups, and will require future collaborative larger scale studies to look at what potentially makes some children more susceptible to neurologic involvement than others,” said Dr. Abdel-Mannan.
Excluding potential causes of the symptoms other than COVID-19 also is important, he added.
The preponderance of ethnic minorities in the current study population mirrors that in other PIMS-TS cohorts in other countries, said Dr. Abdel-Mannan. It reflects the higher incidence of COVID-19 in ethnic minority groups. However, presentation, investigations, and management did not differ between White and non-White children in the current study.
“Although PIMS-TS patients with neurologic involvement are initially sicker, our center’s preliminary follow-up data up to 6 months post discharge from hospital demonstrates that most of these children make an almost complete functional recovery, which is reassuring,” said Dr. Abdel-Mannan.
The data underscore how important it is that clinicians be aware that children with PIMS-TS can present with neurologic symptoms, even in the absence of respiratory involvement, he added.
The researchers will soon begin a multicenter research study that will involve longitudinal clinical and cognitive assessments and advanced neuroimaging. The objective will be to determine whether all children with PIMS-TS, or only those with neurologic symptoms, are at risk of chronic longer-term neurocognitive and psychiatric outcomes.
Unanswered questions
John B. Bodensteiner, MD, professor of neurology and pediatrics at Mayo Clinic, Rochester, Minn., said in an interview that the findings help flesh out the range of neurologic involvement that PIMS-TS entails.
“It’s not a surprise to us as neurologists, but it’s not been emphasized in the general literature and in the public health sector,” he said.
The study’s most important implication is that neurologic conditions are not uncommon among children with PIMS-TS, Dr. Bodensteiner added.
“We have no idea how long or what the long-term effects of that are,” he said. Not enough time has elapsed to enable a clear understanding of the syndrome’s lasting effects on cognition, he said, “but I think this certainly raises a flag that this is a real entity. This is nothing to sniff at.”
He noted that the study has the limitations of any retrospective case series. The researchers did not perform prospective and systematic evaluations of children with the syndrome
The findings also raise unanswered questions.
“They had 14 kids with encephalopathy, but not all of them got the same evaluation,” said Dr. Bodensteiner. Although the researchers mention peripheral nerve involvement in three children, they do not describe it. “They said that the EMG showed myopathic and neuropathic changes, but peripheral nerve involvement wouldn’t give you myopathic changes, so maybe there’s some direct involvement of the muscle in this inflammatory process.”
The study also focused on a select group of patients, said Dr. Bodensteiner. “These are all patients admitted to Great Ormond Street Hospital, and we don’t know what percentage of kids who get COVID are hospitalized, which is an important issue.”
It is necessary to know what proportion of children with COVID-19 develop encephalopathy and MRI changes, he added. The findings do confirm that this coronavirus-related inflammatory condition is real and may have long-term sequelae. “We should be careful about kids getting this disease,” said Dr. Bodensteiner
The study had no funding. Dr. Abdel-Mannan and Dr. Bodensteiner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
About half of children with pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) have new-onset neurologic symptoms, research shows.
These symptoms involve the central and peripheral nervous systems but do not always affect the respiratory system. In addition, neurologic symptoms appear to be more common in severe presentations of this syndrome.
“These new data consolidate the initial findings in our JAMA Neurology publication on the neurological problems that children with PIMS-TS can present with, even in the absence of respiratory systems,” study investigator Omar Abdel-Mannan, MD, clinical research fellow at University College London Institute of Neurology and senior resident at Great Ormond Street Hospital for children in London, said in an interview.
He added that the findings are in keeping with other recent research studies on PIMS-TS, which is known more commonly in the United States as multisystem inflammatory syndrome in children (MIS-C).
The findings will be presented April 18 at the American Academy of Neurology (AAN) 2021 Annual Meeting.
Neurologic manifestations common
Many children and adults with COVID-19 have developed neurologic manifestations. PIMS-TS is a severe, postinfectious, immune-mediated disorder characterized by persistent fever and extreme inflammation.
Patients may have acute diarrhea or vomiting, rash or bilateral conjunctivitis, and low blood pressure. They should be examined by a pediatric specialist, and most children with this disorder need intensive care.
To report the neurologic manifestations in children with PIMS-TS, the researchers retrospectively examined data for children and adolescents younger than 18 years who had the disorder and presented to a single center between April 4, 2020, and Sept. 1, 2020.
Forty-six patients (median age, 10.2 years) were included in the analysis. Thirty (65.2%) were male, and 37 (80.4%) were of non-White ethnicities.
Twenty-four (52.2%) patients had new-onset neurologic symptoms, which included headache (n = 24), encephalopathy (n = 14 patients), dysarthria/dysphonia (n = 6), hallucinations (n = 6), ataxia (n = 4), peripheral nerve involvement (n = 3), and seizures (n=1).
Laboratory and imaging results provided further information. One patient had 118 leukocytes in cerebrospinal fluid. Children with neurologic involvement had higher levels of peak inflammatory markers and were more likely to be ventilated and require inotropic support in the PICU (P < .05).
Four of 16 patients who underwent brain MRI had splenium signal changes. Of 15 patients who underwent electroencephalogram (EEG), 14 had an excess of slow activity. Four of 7 patients who underwent nerve conduction studies and electromyography (EMG) had myopathic and neuropathic changes.
Response to SARS-CoV-2
Central neurologic problems of the brain and peripheral nerve involvement rarely occur at the same time in children.
“This makes it highly possible that the syndrome is secondary to cytokine release in response to the SARS-CoV-2 virus, as there is significant clinical overlap with both genetic and acquired forms of another immune-mediated condition known as hemophagocytic lymphohistiocytosis,” said Dr. Abdel-Mannan.
The researchers found no demographic differences between children with neurologic involvement at presentation and those without.
“However, the numbers are small given the rarity of this condition, which makes it difficult to extrapolate associations and differences between the two groups, and will require future collaborative larger scale studies to look at what potentially makes some children more susceptible to neurologic involvement than others,” said Dr. Abdel-Mannan.
Excluding potential causes of the symptoms other than COVID-19 also is important, he added.
The preponderance of ethnic minorities in the current study population mirrors that in other PIMS-TS cohorts in other countries, said Dr. Abdel-Mannan. It reflects the higher incidence of COVID-19 in ethnic minority groups. However, presentation, investigations, and management did not differ between White and non-White children in the current study.
“Although PIMS-TS patients with neurologic involvement are initially sicker, our center’s preliminary follow-up data up to 6 months post discharge from hospital demonstrates that most of these children make an almost complete functional recovery, which is reassuring,” said Dr. Abdel-Mannan.
The data underscore how important it is that clinicians be aware that children with PIMS-TS can present with neurologic symptoms, even in the absence of respiratory involvement, he added.
The researchers will soon begin a multicenter research study that will involve longitudinal clinical and cognitive assessments and advanced neuroimaging. The objective will be to determine whether all children with PIMS-TS, or only those with neurologic symptoms, are at risk of chronic longer-term neurocognitive and psychiatric outcomes.
Unanswered questions
John B. Bodensteiner, MD, professor of neurology and pediatrics at Mayo Clinic, Rochester, Minn., said in an interview that the findings help flesh out the range of neurologic involvement that PIMS-TS entails.
“It’s not a surprise to us as neurologists, but it’s not been emphasized in the general literature and in the public health sector,” he said.
The study’s most important implication is that neurologic conditions are not uncommon among children with PIMS-TS, Dr. Bodensteiner added.
“We have no idea how long or what the long-term effects of that are,” he said. Not enough time has elapsed to enable a clear understanding of the syndrome’s lasting effects on cognition, he said, “but I think this certainly raises a flag that this is a real entity. This is nothing to sniff at.”
He noted that the study has the limitations of any retrospective case series. The researchers did not perform prospective and systematic evaluations of children with the syndrome
The findings also raise unanswered questions.
“They had 14 kids with encephalopathy, but not all of them got the same evaluation,” said Dr. Bodensteiner. Although the researchers mention peripheral nerve involvement in three children, they do not describe it. “They said that the EMG showed myopathic and neuropathic changes, but peripheral nerve involvement wouldn’t give you myopathic changes, so maybe there’s some direct involvement of the muscle in this inflammatory process.”
The study also focused on a select group of patients, said Dr. Bodensteiner. “These are all patients admitted to Great Ormond Street Hospital, and we don’t know what percentage of kids who get COVID are hospitalized, which is an important issue.”
It is necessary to know what proportion of children with COVID-19 develop encephalopathy and MRI changes, he added. The findings do confirm that this coronavirus-related inflammatory condition is real and may have long-term sequelae. “We should be careful about kids getting this disease,” said Dr. Bodensteiner
The study had no funding. Dr. Abdel-Mannan and Dr. Bodensteiner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.









