User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
FDA OKs first fecal transplant therapy for recurrent C. difficile
Rebyota (fecal microbiota, live-jslm), from Ferring Pharmaceuticals, is intended for use after an individual has completed antibiotic treatment for recurrent CDI. It is not indicated for the first occurrence of CDI.
“Recurrent CDI impacts an individual’s quality of life and can also potentially be life-threatening,” Peter Marks, MD, PhD, director, FDA Center for Biologics Evaluation and Research, said in a statement announcing approval.
As the first FDA-approved fecal microbiota product, this approval “represents an important milestone, as it provides an additional approved option to prevent recurrent CDI,” Dr. Marks added.
A panel of FDA advisors recommended approval of Rebyota in September.
The application for Rebyota received priority review and had orphan drug and breakthrough therapy designation.
A vicious cycle
Treatment options for recurrent CDI are limited. It’s been estimated that up to one-third of CDI cases recur, and people who suffer a recurrent bout of CDI are at a significantly higher risk for further infections.
Following the first recurrence, up to two-thirds of patients may experience a subsequent recurrence. Antibiotics used to treat CDI may contribute to a cycle of recurrence by altering the gut flora. The administration of fecal microbiota helps restore the gut flora to prevent further episodes of CDI.
Rebyota is a microbiota-based live biotherapeutic prepared from human stool collected from prescreened, qualified donors. It comes prepackaged in a single dose that is administered rectally.
The safety and efficacy of Rebyota were assessed in five clinical trials with more than 1,000 participants, the company notes in a press release.
In one trial, following a standard course of antibiotics, a one-time treatment with Rebyota was successful for three-quarters of participants at 8 weeks.
The treatment also prevented additional bouts; 84% of these initial responders remaining free of CDI at 6 months.
Two-thirds of participants reported treatment-emergent adverse events. Most events were mild to moderate in severity. Diarrhea and abdominal pain were the most common.
The data, from the ongoing PUNCH CD3-OLS study, were presented in October at the annual meeting of the American College of Gastroenterology and were published simultaneously in the journal Drugs.
“This is a positive adjunct to our current therapies for C. difficile in terms of trying to knock it out once a standard course of antibiotics has been administered,” Lisa Malter, MD, a gastroenterologist and professor of medicine at New York University Langone Health, said in an interview.
Dr. Malter acknowledged that because it’s delivered rectally, there could be “some hesitation” on the patient’s part to undergo the therapy.
However, C. difficile can be “excruciating” for patients, and they “may be more than willing to take [this agent] because it gets them feeling better,” Dr. Malter said.
Full prescribing information for Rebyota is available online.
Dr. Malter reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rebyota (fecal microbiota, live-jslm), from Ferring Pharmaceuticals, is intended for use after an individual has completed antibiotic treatment for recurrent CDI. It is not indicated for the first occurrence of CDI.
“Recurrent CDI impacts an individual’s quality of life and can also potentially be life-threatening,” Peter Marks, MD, PhD, director, FDA Center for Biologics Evaluation and Research, said in a statement announcing approval.
As the first FDA-approved fecal microbiota product, this approval “represents an important milestone, as it provides an additional approved option to prevent recurrent CDI,” Dr. Marks added.
A panel of FDA advisors recommended approval of Rebyota in September.
The application for Rebyota received priority review and had orphan drug and breakthrough therapy designation.
A vicious cycle
Treatment options for recurrent CDI are limited. It’s been estimated that up to one-third of CDI cases recur, and people who suffer a recurrent bout of CDI are at a significantly higher risk for further infections.
Following the first recurrence, up to two-thirds of patients may experience a subsequent recurrence. Antibiotics used to treat CDI may contribute to a cycle of recurrence by altering the gut flora. The administration of fecal microbiota helps restore the gut flora to prevent further episodes of CDI.
Rebyota is a microbiota-based live biotherapeutic prepared from human stool collected from prescreened, qualified donors. It comes prepackaged in a single dose that is administered rectally.
The safety and efficacy of Rebyota were assessed in five clinical trials with more than 1,000 participants, the company notes in a press release.
In one trial, following a standard course of antibiotics, a one-time treatment with Rebyota was successful for three-quarters of participants at 8 weeks.
The treatment also prevented additional bouts; 84% of these initial responders remaining free of CDI at 6 months.
Two-thirds of participants reported treatment-emergent adverse events. Most events were mild to moderate in severity. Diarrhea and abdominal pain were the most common.
The data, from the ongoing PUNCH CD3-OLS study, were presented in October at the annual meeting of the American College of Gastroenterology and were published simultaneously in the journal Drugs.
“This is a positive adjunct to our current therapies for C. difficile in terms of trying to knock it out once a standard course of antibiotics has been administered,” Lisa Malter, MD, a gastroenterologist and professor of medicine at New York University Langone Health, said in an interview.
Dr. Malter acknowledged that because it’s delivered rectally, there could be “some hesitation” on the patient’s part to undergo the therapy.
However, C. difficile can be “excruciating” for patients, and they “may be more than willing to take [this agent] because it gets them feeling better,” Dr. Malter said.
Full prescribing information for Rebyota is available online.
Dr. Malter reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rebyota (fecal microbiota, live-jslm), from Ferring Pharmaceuticals, is intended for use after an individual has completed antibiotic treatment for recurrent CDI. It is not indicated for the first occurrence of CDI.
“Recurrent CDI impacts an individual’s quality of life and can also potentially be life-threatening,” Peter Marks, MD, PhD, director, FDA Center for Biologics Evaluation and Research, said in a statement announcing approval.
As the first FDA-approved fecal microbiota product, this approval “represents an important milestone, as it provides an additional approved option to prevent recurrent CDI,” Dr. Marks added.
A panel of FDA advisors recommended approval of Rebyota in September.
The application for Rebyota received priority review and had orphan drug and breakthrough therapy designation.
A vicious cycle
Treatment options for recurrent CDI are limited. It’s been estimated that up to one-third of CDI cases recur, and people who suffer a recurrent bout of CDI are at a significantly higher risk for further infections.
Following the first recurrence, up to two-thirds of patients may experience a subsequent recurrence. Antibiotics used to treat CDI may contribute to a cycle of recurrence by altering the gut flora. The administration of fecal microbiota helps restore the gut flora to prevent further episodes of CDI.
Rebyota is a microbiota-based live biotherapeutic prepared from human stool collected from prescreened, qualified donors. It comes prepackaged in a single dose that is administered rectally.
The safety and efficacy of Rebyota were assessed in five clinical trials with more than 1,000 participants, the company notes in a press release.
In one trial, following a standard course of antibiotics, a one-time treatment with Rebyota was successful for three-quarters of participants at 8 weeks.
The treatment also prevented additional bouts; 84% of these initial responders remaining free of CDI at 6 months.
Two-thirds of participants reported treatment-emergent adverse events. Most events were mild to moderate in severity. Diarrhea and abdominal pain were the most common.
The data, from the ongoing PUNCH CD3-OLS study, were presented in October at the annual meeting of the American College of Gastroenterology and were published simultaneously in the journal Drugs.
“This is a positive adjunct to our current therapies for C. difficile in terms of trying to knock it out once a standard course of antibiotics has been administered,” Lisa Malter, MD, a gastroenterologist and professor of medicine at New York University Langone Health, said in an interview.
Dr. Malter acknowledged that because it’s delivered rectally, there could be “some hesitation” on the patient’s part to undergo the therapy.
However, C. difficile can be “excruciating” for patients, and they “may be more than willing to take [this agent] because it gets them feeling better,” Dr. Malter said.
Full prescribing information for Rebyota is available online.
Dr. Malter reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Looking for a healthy meat substitute? Consider the potato
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Newer agents for nosocomial pneumonia: The right drug for the right bug
“The right drug at the right time with the right dose for the right bug for the right duration.” That, said professor Kristina Crothers, MD, is the general guidance for optimizing antibiotic use (while awaiting an infectious disease consult). In her oral presentation at the annual meeting of the American College of Chest Physicians, “Choosing newer antibiotics for nosocomial pneumonia,” Dr. Crothers asked the question: “Beyond the guidelines: When should novel antimicrobials be used?”
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) are the most common nosocomial infections at 22%, and are the leading cause of death attributable to hospital-acquired infections. They increase mortality by 20%-50%, with an economic burden of about $40,000 per patient. The incidence of multidrug-resistant (MDR) organism infections varies widely by locality, but several factors increase the likelihood: prior broad-spectrum antibiotic exposure within the past 90 days; longer hospitalization; indwelling vascular devices; tracheostomy; and ventilator dependence. The Centers for Disease Control and Prevention lists as “Serious Threat” the HAP/VAP MDR organisms methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa (PSA) with difficult-to-treat-resistance, and beta-lactamase producing Enterobacterales (ESBL). In the category of “Urgent Threat” the CDC lists: carbapenamase-resistant Enterobacterales (CRE) (carbapenamase producing or non–carbapenemase producing), and carbapenem-resistant Acinetobacter (CRAB), according to Dr. Crothers who is at the University of Washington Veterans Affairs Puget Sound Health Care System, Seattle.
Newer antibiotics for HAP/VAP that are still beyond the guidelines include telavancin and tedizolid as gram-positive agents, and as gram-negative ones: ceftazidime-avibactam, ceftolozane-tazobactam, cefiderocol, imipenem-cilastatin-relebactam and meropenem-vaborbactam, she added.
Tedizolid, Dr. Crothers stated, is a novel oxazolidinone, and is an alternative to vancomycin and linezolid for gram-positive HAP/VAP. In the VITAL noninferiority study versus linezolid with 726 patients, it was noninferior to linezolid for 28-day all-cause mortality (28% vs. 26%), but did not achieve noninferiority for investigator-assessed clinical cure (56% vs. 64%).
Televancin, a semisynthetic derivative of vancomycin, in the ATTAIN studies vs. vancomycin had overall similar cure rates. It is FDA-approved for S. aureus HAP/VAP but not other bacterial causes. It should be reserved for those who cannot receive vancomycin or linezolid, with normal renal function, according to Dr. Crothers. Excluded from first-line treatment of gram-positive HAP/VAP are daptomycin, ceftaroline, ceftobiprole, and tigecycline.
Ceftazidime-avibactam, a third-generation cephalosporin-plus novel beta-lactamase inhibitor has wide activity (Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, PSA and Haemophilus influenzae. It is also active against some extended-spectrum beta-lactamases (ESBLs), ampC beta-lactamases (AmpCs), and K. pneumoniae carbapenemase (KPC)–producing Enterobacterales, but not with metallo-beta-lactamases). Ceftazidime-avibactam is also indicated for HAP/VAP, and has a toxicity profile including nausea, vomiting, and diarrhea.
In the REPROVE trial of ceftazidime-avibactam vs. meropenem for 7-14 days with 527 clinically evaluable patients (37% K. pneumoniae, 30% P. aeruginosa, and 33%-35% VAP), the clinical cure at 21-25 days post randomization was 69% vs. 73%, respectively, with similar adverse events.
Ceftolozane-tazobactam, a novel fifth-generation cephalosporin plus a beta-lactamase inhibitor has activity against PSA including extensively drug-resistant PSA, AmpC, and ESBL-E, but it has limited activity against Acinetobacter and Stenotrophomonas. It is indicated for HAP/VAP, has reduced efficacy with creatine clearance of 50 mL/min or less, increases transaminases and renal impairment, and causes diarrhea. In ASPECT-NP (n = 726) ceftolozane-tazobactam versus meropenem for 8-14 days (HAP/VAP), showed a 28 day-mortality of 24% vs. 25%, respectively, with test of cure at 54% vs. 53% at 7-14 days post therapy. Adverse events were similar between groups.
Imipenem-cilastatin-relebactam, a novel beta-lactamase inhibitor plus carbapenem, is indicated for HAP/VAP and has activity against ESBL, CRE: KPC-producing Enterobacterales, PSA including AmpC. It can cause seizures (requires caution with central nervous system disorders and renal impairment). It increases transaminases, anemia, diarrhea, and reduces potassium and sodium. In RESTORE-IMI 2 (n = 537 with HAP/VAP) it was noninferior for 28-day all-cause mortality vs. piperacillin and tazobactam (16% vs. 21%), with similar adverse events.
Cefiderocol, a siderophore cephalosporin, is indicated for HAP/VAP. It has a wide spectrum of activity: ESBL, CRE, CR PSA, Stenotrophomonas maltophilia, Acinetobacter baumanii, Streptococcus.) It increases transaminases, diarrhea, and atrial fibrillation, and it reduces potassium and magnesium. In APEKS-NP versus linezolid plus cefiderocol or extended meropenem infusion (HAP/VAP n = 292; gram-negative pneumonia = 251; 60% invasive mechanical ventilation) it was noninferior for 14-day all-cause mortality (12.4% vs. 11.6%) with similar adverse events. In CREDIBLE-CR vs. best available therapy for carbapenem-resistant gram-negative infections, clinical cure rates were similar (50% vs. 53% in 59 HAP/VAP patients at 7 days), but with more deaths in the cefiderocol arm. Adverse events were > 90% in both groups and 34% vs. 19% died, mostly with Acinetobacter.
Meropenem-vaborbactam, a novel beta-lactamase inhibitor plus carbapenem, is approved and indicated for HAP/VAP in Europe. It has activity against MDR, Enterobacterales including CRE. Its toxicities include headache, phlebitis/infusion-site reactions and diarrhea. In TANGO-2 versus best available treatment for carbapenem-resistant Enterobacteriaceae (CRE) (n = 77, 47 with confirmed CRE), clinical cure was increased and mortality decreased compared with best available therapy. Treatment- and renal-related adverse events were lower for meropenem-vaborbactam.
In closing, Dr. Crothers cited advice from the paper by Tamma et al. (“Rethinking how Antibiotics are Prescribed” JAMA. 2018) about the need to review findings after therapy has been initiated to confirm the pneumonia diagnosis: Novel agents should be kept in reserve in the absence of MDR risk factors for MRSA and gram-negative bacilli; therapy should be deescalated after 48-72 hours if MDR organisms are not detected; and therapy should be directed to the specific organism detected. Most HAP and VAP in adults can be treated for 7 days, she added.
“Know indications for new therapeutic agents approved for nosocomial pneumonia,” she concluded.
Dr. Crothers reported having no disclosures.
“The right drug at the right time with the right dose for the right bug for the right duration.” That, said professor Kristina Crothers, MD, is the general guidance for optimizing antibiotic use (while awaiting an infectious disease consult). In her oral presentation at the annual meeting of the American College of Chest Physicians, “Choosing newer antibiotics for nosocomial pneumonia,” Dr. Crothers asked the question: “Beyond the guidelines: When should novel antimicrobials be used?”
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) are the most common nosocomial infections at 22%, and are the leading cause of death attributable to hospital-acquired infections. They increase mortality by 20%-50%, with an economic burden of about $40,000 per patient. The incidence of multidrug-resistant (MDR) organism infections varies widely by locality, but several factors increase the likelihood: prior broad-spectrum antibiotic exposure within the past 90 days; longer hospitalization; indwelling vascular devices; tracheostomy; and ventilator dependence. The Centers for Disease Control and Prevention lists as “Serious Threat” the HAP/VAP MDR organisms methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa (PSA) with difficult-to-treat-resistance, and beta-lactamase producing Enterobacterales (ESBL). In the category of “Urgent Threat” the CDC lists: carbapenamase-resistant Enterobacterales (CRE) (carbapenamase producing or non–carbapenemase producing), and carbapenem-resistant Acinetobacter (CRAB), according to Dr. Crothers who is at the University of Washington Veterans Affairs Puget Sound Health Care System, Seattle.
Newer antibiotics for HAP/VAP that are still beyond the guidelines include telavancin and tedizolid as gram-positive agents, and as gram-negative ones: ceftazidime-avibactam, ceftolozane-tazobactam, cefiderocol, imipenem-cilastatin-relebactam and meropenem-vaborbactam, she added.
Tedizolid, Dr. Crothers stated, is a novel oxazolidinone, and is an alternative to vancomycin and linezolid for gram-positive HAP/VAP. In the VITAL noninferiority study versus linezolid with 726 patients, it was noninferior to linezolid for 28-day all-cause mortality (28% vs. 26%), but did not achieve noninferiority for investigator-assessed clinical cure (56% vs. 64%).
Televancin, a semisynthetic derivative of vancomycin, in the ATTAIN studies vs. vancomycin had overall similar cure rates. It is FDA-approved for S. aureus HAP/VAP but not other bacterial causes. It should be reserved for those who cannot receive vancomycin or linezolid, with normal renal function, according to Dr. Crothers. Excluded from first-line treatment of gram-positive HAP/VAP are daptomycin, ceftaroline, ceftobiprole, and tigecycline.
Ceftazidime-avibactam, a third-generation cephalosporin-plus novel beta-lactamase inhibitor has wide activity (Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, PSA and Haemophilus influenzae. It is also active against some extended-spectrum beta-lactamases (ESBLs), ampC beta-lactamases (AmpCs), and K. pneumoniae carbapenemase (KPC)–producing Enterobacterales, but not with metallo-beta-lactamases). Ceftazidime-avibactam is also indicated for HAP/VAP, and has a toxicity profile including nausea, vomiting, and diarrhea.
In the REPROVE trial of ceftazidime-avibactam vs. meropenem for 7-14 days with 527 clinically evaluable patients (37% K. pneumoniae, 30% P. aeruginosa, and 33%-35% VAP), the clinical cure at 21-25 days post randomization was 69% vs. 73%, respectively, with similar adverse events.
Ceftolozane-tazobactam, a novel fifth-generation cephalosporin plus a beta-lactamase inhibitor has activity against PSA including extensively drug-resistant PSA, AmpC, and ESBL-E, but it has limited activity against Acinetobacter and Stenotrophomonas. It is indicated for HAP/VAP, has reduced efficacy with creatine clearance of 50 mL/min or less, increases transaminases and renal impairment, and causes diarrhea. In ASPECT-NP (n = 726) ceftolozane-tazobactam versus meropenem for 8-14 days (HAP/VAP), showed a 28 day-mortality of 24% vs. 25%, respectively, with test of cure at 54% vs. 53% at 7-14 days post therapy. Adverse events were similar between groups.
Imipenem-cilastatin-relebactam, a novel beta-lactamase inhibitor plus carbapenem, is indicated for HAP/VAP and has activity against ESBL, CRE: KPC-producing Enterobacterales, PSA including AmpC. It can cause seizures (requires caution with central nervous system disorders and renal impairment). It increases transaminases, anemia, diarrhea, and reduces potassium and sodium. In RESTORE-IMI 2 (n = 537 with HAP/VAP) it was noninferior for 28-day all-cause mortality vs. piperacillin and tazobactam (16% vs. 21%), with similar adverse events.
Cefiderocol, a siderophore cephalosporin, is indicated for HAP/VAP. It has a wide spectrum of activity: ESBL, CRE, CR PSA, Stenotrophomonas maltophilia, Acinetobacter baumanii, Streptococcus.) It increases transaminases, diarrhea, and atrial fibrillation, and it reduces potassium and magnesium. In APEKS-NP versus linezolid plus cefiderocol or extended meropenem infusion (HAP/VAP n = 292; gram-negative pneumonia = 251; 60% invasive mechanical ventilation) it was noninferior for 14-day all-cause mortality (12.4% vs. 11.6%) with similar adverse events. In CREDIBLE-CR vs. best available therapy for carbapenem-resistant gram-negative infections, clinical cure rates were similar (50% vs. 53% in 59 HAP/VAP patients at 7 days), but with more deaths in the cefiderocol arm. Adverse events were > 90% in both groups and 34% vs. 19% died, mostly with Acinetobacter.
Meropenem-vaborbactam, a novel beta-lactamase inhibitor plus carbapenem, is approved and indicated for HAP/VAP in Europe. It has activity against MDR, Enterobacterales including CRE. Its toxicities include headache, phlebitis/infusion-site reactions and diarrhea. In TANGO-2 versus best available treatment for carbapenem-resistant Enterobacteriaceae (CRE) (n = 77, 47 with confirmed CRE), clinical cure was increased and mortality decreased compared with best available therapy. Treatment- and renal-related adverse events were lower for meropenem-vaborbactam.
In closing, Dr. Crothers cited advice from the paper by Tamma et al. (“Rethinking how Antibiotics are Prescribed” JAMA. 2018) about the need to review findings after therapy has been initiated to confirm the pneumonia diagnosis: Novel agents should be kept in reserve in the absence of MDR risk factors for MRSA and gram-negative bacilli; therapy should be deescalated after 48-72 hours if MDR organisms are not detected; and therapy should be directed to the specific organism detected. Most HAP and VAP in adults can be treated for 7 days, she added.
“Know indications for new therapeutic agents approved for nosocomial pneumonia,” she concluded.
Dr. Crothers reported having no disclosures.
“The right drug at the right time with the right dose for the right bug for the right duration.” That, said professor Kristina Crothers, MD, is the general guidance for optimizing antibiotic use (while awaiting an infectious disease consult). In her oral presentation at the annual meeting of the American College of Chest Physicians, “Choosing newer antibiotics for nosocomial pneumonia,” Dr. Crothers asked the question: “Beyond the guidelines: When should novel antimicrobials be used?”
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) are the most common nosocomial infections at 22%, and are the leading cause of death attributable to hospital-acquired infections. They increase mortality by 20%-50%, with an economic burden of about $40,000 per patient. The incidence of multidrug-resistant (MDR) organism infections varies widely by locality, but several factors increase the likelihood: prior broad-spectrum antibiotic exposure within the past 90 days; longer hospitalization; indwelling vascular devices; tracheostomy; and ventilator dependence. The Centers for Disease Control and Prevention lists as “Serious Threat” the HAP/VAP MDR organisms methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa (PSA) with difficult-to-treat-resistance, and beta-lactamase producing Enterobacterales (ESBL). In the category of “Urgent Threat” the CDC lists: carbapenamase-resistant Enterobacterales (CRE) (carbapenamase producing or non–carbapenemase producing), and carbapenem-resistant Acinetobacter (CRAB), according to Dr. Crothers who is at the University of Washington Veterans Affairs Puget Sound Health Care System, Seattle.
Newer antibiotics for HAP/VAP that are still beyond the guidelines include telavancin and tedizolid as gram-positive agents, and as gram-negative ones: ceftazidime-avibactam, ceftolozane-tazobactam, cefiderocol, imipenem-cilastatin-relebactam and meropenem-vaborbactam, she added.
Tedizolid, Dr. Crothers stated, is a novel oxazolidinone, and is an alternative to vancomycin and linezolid for gram-positive HAP/VAP. In the VITAL noninferiority study versus linezolid with 726 patients, it was noninferior to linezolid for 28-day all-cause mortality (28% vs. 26%), but did not achieve noninferiority for investigator-assessed clinical cure (56% vs. 64%).
Televancin, a semisynthetic derivative of vancomycin, in the ATTAIN studies vs. vancomycin had overall similar cure rates. It is FDA-approved for S. aureus HAP/VAP but not other bacterial causes. It should be reserved for those who cannot receive vancomycin or linezolid, with normal renal function, according to Dr. Crothers. Excluded from first-line treatment of gram-positive HAP/VAP are daptomycin, ceftaroline, ceftobiprole, and tigecycline.
Ceftazidime-avibactam, a third-generation cephalosporin-plus novel beta-lactamase inhibitor has wide activity (Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, PSA and Haemophilus influenzae. It is also active against some extended-spectrum beta-lactamases (ESBLs), ampC beta-lactamases (AmpCs), and K. pneumoniae carbapenemase (KPC)–producing Enterobacterales, but not with metallo-beta-lactamases). Ceftazidime-avibactam is also indicated for HAP/VAP, and has a toxicity profile including nausea, vomiting, and diarrhea.
In the REPROVE trial of ceftazidime-avibactam vs. meropenem for 7-14 days with 527 clinically evaluable patients (37% K. pneumoniae, 30% P. aeruginosa, and 33%-35% VAP), the clinical cure at 21-25 days post randomization was 69% vs. 73%, respectively, with similar adverse events.
Ceftolozane-tazobactam, a novel fifth-generation cephalosporin plus a beta-lactamase inhibitor has activity against PSA including extensively drug-resistant PSA, AmpC, and ESBL-E, but it has limited activity against Acinetobacter and Stenotrophomonas. It is indicated for HAP/VAP, has reduced efficacy with creatine clearance of 50 mL/min or less, increases transaminases and renal impairment, and causes diarrhea. In ASPECT-NP (n = 726) ceftolozane-tazobactam versus meropenem for 8-14 days (HAP/VAP), showed a 28 day-mortality of 24% vs. 25%, respectively, with test of cure at 54% vs. 53% at 7-14 days post therapy. Adverse events were similar between groups.
Imipenem-cilastatin-relebactam, a novel beta-lactamase inhibitor plus carbapenem, is indicated for HAP/VAP and has activity against ESBL, CRE: KPC-producing Enterobacterales, PSA including AmpC. It can cause seizures (requires caution with central nervous system disorders and renal impairment). It increases transaminases, anemia, diarrhea, and reduces potassium and sodium. In RESTORE-IMI 2 (n = 537 with HAP/VAP) it was noninferior for 28-day all-cause mortality vs. piperacillin and tazobactam (16% vs. 21%), with similar adverse events.
Cefiderocol, a siderophore cephalosporin, is indicated for HAP/VAP. It has a wide spectrum of activity: ESBL, CRE, CR PSA, Stenotrophomonas maltophilia, Acinetobacter baumanii, Streptococcus.) It increases transaminases, diarrhea, and atrial fibrillation, and it reduces potassium and magnesium. In APEKS-NP versus linezolid plus cefiderocol or extended meropenem infusion (HAP/VAP n = 292; gram-negative pneumonia = 251; 60% invasive mechanical ventilation) it was noninferior for 14-day all-cause mortality (12.4% vs. 11.6%) with similar adverse events. In CREDIBLE-CR vs. best available therapy for carbapenem-resistant gram-negative infections, clinical cure rates were similar (50% vs. 53% in 59 HAP/VAP patients at 7 days), but with more deaths in the cefiderocol arm. Adverse events were > 90% in both groups and 34% vs. 19% died, mostly with Acinetobacter.
Meropenem-vaborbactam, a novel beta-lactamase inhibitor plus carbapenem, is approved and indicated for HAP/VAP in Europe. It has activity against MDR, Enterobacterales including CRE. Its toxicities include headache, phlebitis/infusion-site reactions and diarrhea. In TANGO-2 versus best available treatment for carbapenem-resistant Enterobacteriaceae (CRE) (n = 77, 47 with confirmed CRE), clinical cure was increased and mortality decreased compared with best available therapy. Treatment- and renal-related adverse events were lower for meropenem-vaborbactam.
In closing, Dr. Crothers cited advice from the paper by Tamma et al. (“Rethinking how Antibiotics are Prescribed” JAMA. 2018) about the need to review findings after therapy has been initiated to confirm the pneumonia diagnosis: Novel agents should be kept in reserve in the absence of MDR risk factors for MRSA and gram-negative bacilli; therapy should be deescalated after 48-72 hours if MDR organisms are not detected; and therapy should be directed to the specific organism detected. Most HAP and VAP in adults can be treated for 7 days, she added.
“Know indications for new therapeutic agents approved for nosocomial pneumonia,” she concluded.
Dr. Crothers reported having no disclosures.
FROM CHEST 2022
Will a one-dose drug mean the end of sleeping sickness?
A single dose of oral acoziborole resulted in a greater than 95% cure or probable cure rate for human African trypanosomiasis (HAT), also known as sleeping sickness, according to results from a clinical trial testing a one-dose experimental drug.
The drug has “the potential to revolutionize treatment” for the disease, which remains endemic in sub-Saharan Africa, said Antoine Tarral, MD, head of the human African trypanosomiasis clinical program at the Drugs for Neglected Diseases initiative, based in Geneva, and senior author of the study, in a press release.
he told this news organization. “It’s the first drug we can use without hospitalization. ... All the previous medications needed hospitalization, and therefore we could not treat the population early before they started expressing symptoms.”
The World Health Organization “has been working for decades for such a possibility to implement a new strategy for this disease,” Dr. Tarral said.
Current (2019) WHO guidelines recommend oral fexinidazole as first-line treatment for any stage of the disease. The 10-day course often requires hospitalization and skilled staff. Previous recommendations required disease-staging with cerebrospinal fluid (CSF) sampling and 7 days of intramuscular pentamidine for early-stage disease or nifurtimox-eflornithine combination therapy (NECT) with hospitalization for late-stage disease.
By contrast, acoziborole, which was codeveloped by the DND initiative and Sanofi, “is administered in a single dose and is effective across every stage of the disease, thereby eliminating the many barriers currently in place for people most vulnerable to the diseases, such as invasive treatments and long travel distances to a hospital or clinic, and opening the door to screen-and-treat approaches at the village level,” Dr. Tarral said in the statement.
“Today, and in the future, we will have less and less support to do this long and costly diagnostic process and treatment in the hospital,” he said in an interview. “This development means we can go for a simple test and a simple treatment, which means we can meet the WHO 2030 goal for ending transmission of this disease.”
Results from the multicenter, prospective, open-label, single-arm, noncomparative, phase 2/3 study were published in The Lancet.
Pragmatic study design
Sleeping sickness is caused by Trypanosoma brucei gambiense (gambiense HAT). It is transmitted by the tsetse fly and mostly fatal when left untreated.
The study enrolled 208 adults and adolescents (167 with late-stage, and 41 with early-stage or intermediate-stage disease) from 10 hospitals in the Democratic Republic of the Congo and Guinea. All patients were treated with acoziborole 960 mg – an unusual study design.
“Due to the substantial decline in incidence, enrolling patients with gambiense HAT into clinical trials is challenging,” the authors wrote. “Following advice from the European Medicines Agency, this study was designed as an open-label, single-arm trial with no comparator or control group.”
After 18 months of follow-up, treatment success, defined as absence of trypanosomes and less than 20 white blood cells per mcL of CSF, occurred in 159 (95.2%) of the late-stage patients, and 100% of the early- and intermediate-stage patients, “which was similar to the estimated historical results for NECT,” the authors noted.
Serious treatment-emergent adverse events were reported in 21 (10%) of patients, “but none of these events were considered drug-related,” they added.
The DND initiative and the WHO are currently nearing completion of a much larger, double-blind, placebo-controlled trial of acoziborole to “increase the safety database,” Dr. Tarral explained.
“Purists will say that acoziborole has not been evaluated according to current standards, because the study was not a randomized trial, there was no control group, and the number of participants was small,” said Jacques Pépin, MD, from the University of Sherbrooke (Que.), in a linked commentary.
“But these were difficult challenges to overcome, considering the drastic reduction in the number of patients with HAT and dispersion over a vast territory, particularly in the Democratic Republic of the Congo. For these reasons, the authors took a pragmatic approach instead,” he wrote.
A potential new tool for eradication of sleeping sickness
“This is really an exciting development, which will be useful in the drive for eradication/interruption of transmission of this disease,” Dr. Pépin told this news organization.
Dr. Pépin treated around 1,000 trypanosomiasis patients during an outbreak in Zaire in the early 1980s. Because the asymptomatic incubation period for the disease can be several months or even years, “the core strategy for controlling the disease is active screening,” he said in an interview.
“You try to convince the whole population of endemic villages to show up on a given day, and then you have a mobile team of nurses who examine everybody, trying to find those with early trypanosomiasis. This includes physical examination for lymph nodes in the neck, but also a blood test whose results are available within minutes,” he said.
“Until now, these persons with a positive serology would undergo additional and labor-intensive examinations of blood to try to find trypanosomes and prove that they have the disease. So far those with a positive serology and negative parasitological assays (‘serological suspects’) were left untreated, because the treatments were toxic and cumbersome, and because a substantial but unknown proportion of these ‘suspects’ just have a false positive of their serological test, without having the disease,” Dr. Pépin said.
“Now with acoziborole, which seems to have little serious toxicity ... and can be given as a single-dose oral med, it might be reasonable to treat the ‘serological suspects,’ ” he said.
“Take it one step further, it might be possible to do the serological test only and treat all individuals with a positive serology without bothering to do parasitological assays. This is what they call ‘test-and-treat’ strategy. It would make sense, provided that we are sure that the drug is very well tolerated.”
Dr. Pépin added that he is “just slightly worried” about three patients described in the paper who had psychiatric adverse events 3 months after treatment. “If that happens to patients who indeed have trypanosomiasis, that’s a reasonable price to pay considering the toxicity of other drugs,” he said. “If that happens to serological suspects, many of whom don’t have any disease, this becomes a preoccupation.”
But Dr. Tarral said, “We have no indication that the drug can provoke psychiatric symptoms. In fact, the psychiatric symptoms did not emerge – they re-emerged after 3 months due to some patients’ refusal to be followed up.”
“We included patients in very advanced stages of the disease, and these symptoms are considered disease sequelae,” Dr. Tarral said. “The majority of patients who have such psychiatric symptoms need follow-up after treatment. If not, they can relapse very early. There were a lot of patients who had such symptoms and the investigators proposed they should be followed by a psychiatrist and some of them refused. And due to that only three of our patients had this relapse, and they were cured after psychiatric support.”
The study was funded through the DND initiative and was supported by grants from the Bill & Melinda Gates Foundation; UK Aid; the Federal Ministry of Education and Research through Kreditanstalt für Wiederaufbau, Germany; the Swiss Agency for Development and Cooperation; Médecins Sans Frontières; the Dutch Ministry of Foreign Affairs; the Norwegian Agency for Development Cooperation; the Stavros Niarchos Foundation; the Spanish Agency for International Development Cooperation; and the Banco Bilbao Vizcaya Argentaria Foundation.
A number of study investigators, including Dr. Tarral, report employment at the DND initiative. Other investigators report fees from the DND initiative for the statistical report, consulting fees from CEMAG, D&A Pharma, Inventiva, and OT4B Pharma. The Swiss Tropical and Public Health Institute acted as a service provider for the DND initiative by monitoring the study sites. Dr. Pépin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A single dose of oral acoziborole resulted in a greater than 95% cure or probable cure rate for human African trypanosomiasis (HAT), also known as sleeping sickness, according to results from a clinical trial testing a one-dose experimental drug.
The drug has “the potential to revolutionize treatment” for the disease, which remains endemic in sub-Saharan Africa, said Antoine Tarral, MD, head of the human African trypanosomiasis clinical program at the Drugs for Neglected Diseases initiative, based in Geneva, and senior author of the study, in a press release.
he told this news organization. “It’s the first drug we can use without hospitalization. ... All the previous medications needed hospitalization, and therefore we could not treat the population early before they started expressing symptoms.”
The World Health Organization “has been working for decades for such a possibility to implement a new strategy for this disease,” Dr. Tarral said.
Current (2019) WHO guidelines recommend oral fexinidazole as first-line treatment for any stage of the disease. The 10-day course often requires hospitalization and skilled staff. Previous recommendations required disease-staging with cerebrospinal fluid (CSF) sampling and 7 days of intramuscular pentamidine for early-stage disease or nifurtimox-eflornithine combination therapy (NECT) with hospitalization for late-stage disease.
By contrast, acoziborole, which was codeveloped by the DND initiative and Sanofi, “is administered in a single dose and is effective across every stage of the disease, thereby eliminating the many barriers currently in place for people most vulnerable to the diseases, such as invasive treatments and long travel distances to a hospital or clinic, and opening the door to screen-and-treat approaches at the village level,” Dr. Tarral said in the statement.
“Today, and in the future, we will have less and less support to do this long and costly diagnostic process and treatment in the hospital,” he said in an interview. “This development means we can go for a simple test and a simple treatment, which means we can meet the WHO 2030 goal for ending transmission of this disease.”
Results from the multicenter, prospective, open-label, single-arm, noncomparative, phase 2/3 study were published in The Lancet.
Pragmatic study design
Sleeping sickness is caused by Trypanosoma brucei gambiense (gambiense HAT). It is transmitted by the tsetse fly and mostly fatal when left untreated.
The study enrolled 208 adults and adolescents (167 with late-stage, and 41 with early-stage or intermediate-stage disease) from 10 hospitals in the Democratic Republic of the Congo and Guinea. All patients were treated with acoziborole 960 mg – an unusual study design.
“Due to the substantial decline in incidence, enrolling patients with gambiense HAT into clinical trials is challenging,” the authors wrote. “Following advice from the European Medicines Agency, this study was designed as an open-label, single-arm trial with no comparator or control group.”
After 18 months of follow-up, treatment success, defined as absence of trypanosomes and less than 20 white blood cells per mcL of CSF, occurred in 159 (95.2%) of the late-stage patients, and 100% of the early- and intermediate-stage patients, “which was similar to the estimated historical results for NECT,” the authors noted.
Serious treatment-emergent adverse events were reported in 21 (10%) of patients, “but none of these events were considered drug-related,” they added.
The DND initiative and the WHO are currently nearing completion of a much larger, double-blind, placebo-controlled trial of acoziborole to “increase the safety database,” Dr. Tarral explained.
“Purists will say that acoziborole has not been evaluated according to current standards, because the study was not a randomized trial, there was no control group, and the number of participants was small,” said Jacques Pépin, MD, from the University of Sherbrooke (Que.), in a linked commentary.
“But these were difficult challenges to overcome, considering the drastic reduction in the number of patients with HAT and dispersion over a vast territory, particularly in the Democratic Republic of the Congo. For these reasons, the authors took a pragmatic approach instead,” he wrote.
A potential new tool for eradication of sleeping sickness
“This is really an exciting development, which will be useful in the drive for eradication/interruption of transmission of this disease,” Dr. Pépin told this news organization.
Dr. Pépin treated around 1,000 trypanosomiasis patients during an outbreak in Zaire in the early 1980s. Because the asymptomatic incubation period for the disease can be several months or even years, “the core strategy for controlling the disease is active screening,” he said in an interview.
“You try to convince the whole population of endemic villages to show up on a given day, and then you have a mobile team of nurses who examine everybody, trying to find those with early trypanosomiasis. This includes physical examination for lymph nodes in the neck, but also a blood test whose results are available within minutes,” he said.
“Until now, these persons with a positive serology would undergo additional and labor-intensive examinations of blood to try to find trypanosomes and prove that they have the disease. So far those with a positive serology and negative parasitological assays (‘serological suspects’) were left untreated, because the treatments were toxic and cumbersome, and because a substantial but unknown proportion of these ‘suspects’ just have a false positive of their serological test, without having the disease,” Dr. Pépin said.
“Now with acoziborole, which seems to have little serious toxicity ... and can be given as a single-dose oral med, it might be reasonable to treat the ‘serological suspects,’ ” he said.
“Take it one step further, it might be possible to do the serological test only and treat all individuals with a positive serology without bothering to do parasitological assays. This is what they call ‘test-and-treat’ strategy. It would make sense, provided that we are sure that the drug is very well tolerated.”
Dr. Pépin added that he is “just slightly worried” about three patients described in the paper who had psychiatric adverse events 3 months after treatment. “If that happens to patients who indeed have trypanosomiasis, that’s a reasonable price to pay considering the toxicity of other drugs,” he said. “If that happens to serological suspects, many of whom don’t have any disease, this becomes a preoccupation.”
But Dr. Tarral said, “We have no indication that the drug can provoke psychiatric symptoms. In fact, the psychiatric symptoms did not emerge – they re-emerged after 3 months due to some patients’ refusal to be followed up.”
“We included patients in very advanced stages of the disease, and these symptoms are considered disease sequelae,” Dr. Tarral said. “The majority of patients who have such psychiatric symptoms need follow-up after treatment. If not, they can relapse very early. There were a lot of patients who had such symptoms and the investigators proposed they should be followed by a psychiatrist and some of them refused. And due to that only three of our patients had this relapse, and they were cured after psychiatric support.”
The study was funded through the DND initiative and was supported by grants from the Bill & Melinda Gates Foundation; UK Aid; the Federal Ministry of Education and Research through Kreditanstalt für Wiederaufbau, Germany; the Swiss Agency for Development and Cooperation; Médecins Sans Frontières; the Dutch Ministry of Foreign Affairs; the Norwegian Agency for Development Cooperation; the Stavros Niarchos Foundation; the Spanish Agency for International Development Cooperation; and the Banco Bilbao Vizcaya Argentaria Foundation.
A number of study investigators, including Dr. Tarral, report employment at the DND initiative. Other investigators report fees from the DND initiative for the statistical report, consulting fees from CEMAG, D&A Pharma, Inventiva, and OT4B Pharma. The Swiss Tropical and Public Health Institute acted as a service provider for the DND initiative by monitoring the study sites. Dr. Pépin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A single dose of oral acoziborole resulted in a greater than 95% cure or probable cure rate for human African trypanosomiasis (HAT), also known as sleeping sickness, according to results from a clinical trial testing a one-dose experimental drug.
The drug has “the potential to revolutionize treatment” for the disease, which remains endemic in sub-Saharan Africa, said Antoine Tarral, MD, head of the human African trypanosomiasis clinical program at the Drugs for Neglected Diseases initiative, based in Geneva, and senior author of the study, in a press release.
he told this news organization. “It’s the first drug we can use without hospitalization. ... All the previous medications needed hospitalization, and therefore we could not treat the population early before they started expressing symptoms.”
The World Health Organization “has been working for decades for such a possibility to implement a new strategy for this disease,” Dr. Tarral said.
Current (2019) WHO guidelines recommend oral fexinidazole as first-line treatment for any stage of the disease. The 10-day course often requires hospitalization and skilled staff. Previous recommendations required disease-staging with cerebrospinal fluid (CSF) sampling and 7 days of intramuscular pentamidine for early-stage disease or nifurtimox-eflornithine combination therapy (NECT) with hospitalization for late-stage disease.
By contrast, acoziborole, which was codeveloped by the DND initiative and Sanofi, “is administered in a single dose and is effective across every stage of the disease, thereby eliminating the many barriers currently in place for people most vulnerable to the diseases, such as invasive treatments and long travel distances to a hospital or clinic, and opening the door to screen-and-treat approaches at the village level,” Dr. Tarral said in the statement.
“Today, and in the future, we will have less and less support to do this long and costly diagnostic process and treatment in the hospital,” he said in an interview. “This development means we can go for a simple test and a simple treatment, which means we can meet the WHO 2030 goal for ending transmission of this disease.”
Results from the multicenter, prospective, open-label, single-arm, noncomparative, phase 2/3 study were published in The Lancet.
Pragmatic study design
Sleeping sickness is caused by Trypanosoma brucei gambiense (gambiense HAT). It is transmitted by the tsetse fly and mostly fatal when left untreated.
The study enrolled 208 adults and adolescents (167 with late-stage, and 41 with early-stage or intermediate-stage disease) from 10 hospitals in the Democratic Republic of the Congo and Guinea. All patients were treated with acoziborole 960 mg – an unusual study design.
“Due to the substantial decline in incidence, enrolling patients with gambiense HAT into clinical trials is challenging,” the authors wrote. “Following advice from the European Medicines Agency, this study was designed as an open-label, single-arm trial with no comparator or control group.”
After 18 months of follow-up, treatment success, defined as absence of trypanosomes and less than 20 white blood cells per mcL of CSF, occurred in 159 (95.2%) of the late-stage patients, and 100% of the early- and intermediate-stage patients, “which was similar to the estimated historical results for NECT,” the authors noted.
Serious treatment-emergent adverse events were reported in 21 (10%) of patients, “but none of these events were considered drug-related,” they added.
The DND initiative and the WHO are currently nearing completion of a much larger, double-blind, placebo-controlled trial of acoziborole to “increase the safety database,” Dr. Tarral explained.
“Purists will say that acoziborole has not been evaluated according to current standards, because the study was not a randomized trial, there was no control group, and the number of participants was small,” said Jacques Pépin, MD, from the University of Sherbrooke (Que.), in a linked commentary.
“But these were difficult challenges to overcome, considering the drastic reduction in the number of patients with HAT and dispersion over a vast territory, particularly in the Democratic Republic of the Congo. For these reasons, the authors took a pragmatic approach instead,” he wrote.
A potential new tool for eradication of sleeping sickness
“This is really an exciting development, which will be useful in the drive for eradication/interruption of transmission of this disease,” Dr. Pépin told this news organization.
Dr. Pépin treated around 1,000 trypanosomiasis patients during an outbreak in Zaire in the early 1980s. Because the asymptomatic incubation period for the disease can be several months or even years, “the core strategy for controlling the disease is active screening,” he said in an interview.
“You try to convince the whole population of endemic villages to show up on a given day, and then you have a mobile team of nurses who examine everybody, trying to find those with early trypanosomiasis. This includes physical examination for lymph nodes in the neck, but also a blood test whose results are available within minutes,” he said.
“Until now, these persons with a positive serology would undergo additional and labor-intensive examinations of blood to try to find trypanosomes and prove that they have the disease. So far those with a positive serology and negative parasitological assays (‘serological suspects’) were left untreated, because the treatments were toxic and cumbersome, and because a substantial but unknown proportion of these ‘suspects’ just have a false positive of their serological test, without having the disease,” Dr. Pépin said.
“Now with acoziborole, which seems to have little serious toxicity ... and can be given as a single-dose oral med, it might be reasonable to treat the ‘serological suspects,’ ” he said.
“Take it one step further, it might be possible to do the serological test only and treat all individuals with a positive serology without bothering to do parasitological assays. This is what they call ‘test-and-treat’ strategy. It would make sense, provided that we are sure that the drug is very well tolerated.”
Dr. Pépin added that he is “just slightly worried” about three patients described in the paper who had psychiatric adverse events 3 months after treatment. “If that happens to patients who indeed have trypanosomiasis, that’s a reasonable price to pay considering the toxicity of other drugs,” he said. “If that happens to serological suspects, many of whom don’t have any disease, this becomes a preoccupation.”
But Dr. Tarral said, “We have no indication that the drug can provoke psychiatric symptoms. In fact, the psychiatric symptoms did not emerge – they re-emerged after 3 months due to some patients’ refusal to be followed up.”
“We included patients in very advanced stages of the disease, and these symptoms are considered disease sequelae,” Dr. Tarral said. “The majority of patients who have such psychiatric symptoms need follow-up after treatment. If not, they can relapse very early. There were a lot of patients who had such symptoms and the investigators proposed they should be followed by a psychiatrist and some of them refused. And due to that only three of our patients had this relapse, and they were cured after psychiatric support.”
The study was funded through the DND initiative and was supported by grants from the Bill & Melinda Gates Foundation; UK Aid; the Federal Ministry of Education and Research through Kreditanstalt für Wiederaufbau, Germany; the Swiss Agency for Development and Cooperation; Médecins Sans Frontières; the Dutch Ministry of Foreign Affairs; the Norwegian Agency for Development Cooperation; the Stavros Niarchos Foundation; the Spanish Agency for International Development Cooperation; and the Banco Bilbao Vizcaya Argentaria Foundation.
A number of study investigators, including Dr. Tarral, report employment at the DND initiative. Other investigators report fees from the DND initiative for the statistical report, consulting fees from CEMAG, D&A Pharma, Inventiva, and OT4B Pharma. The Swiss Tropical and Public Health Institute acted as a service provider for the DND initiative by monitoring the study sites. Dr. Pépin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
What is the genetic influence on the severity of COVID-19?
A striking characteristic of COVID-19 is that the severity of clinical outcomes is remarkably variable. Establishing a prognosis for individuals infected with COVID-19 remains a challenge.
Since the start of the COVID-19 pandemic, the heterogeneity of individuals who progress toward severe disease or death, along with the fact that individuals directly exposed to the virus do not necessarily become sick, supports the hypothesis that genetic risk or protective factors are at play.
In an interview with this news organization, Mayana Zatz, PhD, head professor of genetics and coordinator of the Human Genome and Stem Cell Study Center at the University of São Paulo, explained: “The first case that caught my eye was the case of my neighbors, a couple. He presented COVID-19 symptoms, but his wife, who took care of him, had absolutely no symptoms. I thought that it was strange, but we received 3,000 emails from people saying, ‘This happened to me, too.’”
Reports in the media about seven pairs of monozygotic (MZ) twins who died from COVID-19 within days of one another in Brazil also stood out, said the researcher.
, as well as their pathology. Dr. Zatz’s team analyzed the case of a 31-year-old Brazilian MZ twin brother pair who presented simultaneously with severe COVID-19 and the need for oxygen support, despite their age and good health conditions. Curiously, they were admitted and intubated on the same day, but neither of the twins knew about the other’s situation; they found out only when they were extubated.
The study was carried out at the USP with the collaboration of the State University of São Paulo. The authors mapped the genetic profile (by sequencing the genome responsible for coding proteins, or whole-exome sequencing) and the immune cell profile to evaluate innate and adaptive immunity.
The MZ twin brothers shared the same two rare genetic mutations, which may be associated with their increased risk of developing severe COVID-19. However, since these variants were not studied at the protein or functional level, their pathogenicity has yet to be determined. The twins also had [human leukocyte antigen (HLA)] alleles associated with severe COVID-19, which are important candidates for the mechanisms of innate and adaptive immunity and susceptibility to COVID-19 infection and manifestation.
But one particular oddity stood out to the researchers: One of the brothers required longer hospitalization, and only he reported symptoms of long COVID.
In the authors’ eyes, even though the patients shared genetic mutations potentially associated with the risk of developing severe COVID-19, the differences in clinical progression emphasize that, beyond genetic risk factors, continuous exposure to pathogens over a lifetime and other environmental factors mean that each individual’s immune response is unique, even in twins.
“There is no doubt that genetics contribute to the severity of COVID-19, and environmental factors sometimes give us the opportunity to study the disease, too. Such [is the case with] MZ twins who have genetic similarities, even with changes that take place over a lifetime,” José Eduardo Krieger, MD, PhD, professor of molecular medicine at the University of São Paulo Medical School (FMUSP), told this news organization. “Examining MZ twins is a strategy that may help, but, with n = 2, luck really needs to be on your side to get straight to the problem. You need to combine [these findings] with other studies to solve this conundrum,” said Dr. Krieger, who did not take part in the research.
Large cohorts
Genomic and computer resources allow for the study of large sets of data from thousands of individuals. In each of those sets of data, the signal offered by thousands of markers distributed throughout the genome can be studied. This is the possibility offered by various genomic studies of large cohorts of patients with different clinical manifestations.
“Researchers examine thousands of genetic variants throughout the genome from a large sample of individuals and have the chance, for example, to identify genetic variants that are more prevalent in patients who have presented with severe disease than in those who presented with milder disease,” said Dr. Krieger. “These associations highlight a chromosome region in which one or more genes explain, at least in part, the differences observed.”
Genomewide association studies have identified some genetic variants that indicate severity of COVID-19, with potential impact on the virus entering the cell, the immune response, or the development of cytokine storms.
One of these studies, COVID-19 Host Genetics Initiative (COVID-19 HGI), is an international, open-science collaboration for sharing scientific methods and resources with research groups across the world, with the goal of robustly mapping the host genetic determinants of SARS-CoV-2 infection and the severity of the resulting COVID-19 disease. At the start of 2021, the COVID-19 HGI combined genetic data from 49,562 cases and 2 million controls from 46 studies in 19 countries. A total of 853 samples from the BRACOVID study were included in the meta-analysis. The endeavor enabled the identification of 13 genomewide significant loci that are associated with SARS-CoV-2 infection or severe manifestations of COVID-19.
The BRACOVID study, in which Dr. Krieger participates, aims to identify host genetic factors that determine the severity of COVID-19. It is currently the largest project of its kind in Latin America. An article provides the analysis of the first 5,233 participants in the BRACOVID study, who were recruited in São Paulo. Of these participants, 3,533 had been infected with COVID-19 and hospitalized at either the Heart Institute or the Central Institute of the FMUSP General Hospital. The remaining 1,700 made up the control group, which included health care professionals and members of the general population. The controls were recruited through serology assays or PCR tests for SARS-CoV-2.
The researchers discovered a region of chromosome 1 that could play a role in modulating immune response and that could lead to an increase in the likelihood of hospitalization across a wide range of COVID-19 risk factors. This region of chromosome 1 was observed only in Brazilians with a strong European ancestry; however, this finding had not been mentioned in previous studies, suggesting that it could harbor a risk allele specific to the Brazilian population.
The study also confirmed most, but not all, of the regions recorded in the literature, which may be significant in identifying factors determining severity that are specific to a given population.
Including information from the BRACOVID study, other studies have enhanced the knowledge on affected organs. Combined data from 14,000 patients from nine countries evaluated a region of a single chromosome and found that carriers of a certain allele had a higher probability of experiencing various COVID-19 complications, such as severe respiratory failure, venous thromboembolism, and liver damage. The risk was even higher for individuals aged 60 years and over.
Discordant couples
Smaller sample sizes of underrepresented populations also provide relevant data for genomic studies. Dr. Zatz’s team carried out genomic studies on smaller groups, comparing serodiscordant couples (where one was infected and symptomatic while the partner remained asymptomatic and seronegative despite sharing the same bedroom during the infection). Their research found genetic variants related to immune response that were associated with susceptibility to infection and progression to severe COVID-19.
The team also went on to study a group of patients older than 90 years who recovered from COVID-19 with mild symptoms or who remained asymptomatic following a positive test for SARS-CoV-2. They compared these patients with a sample of elderly patients from the same city (São Paulo), sampled before the current pandemic. The researchers identified a genetic variant related to mucin production. “In individuals with mild COVID-19, the degradation of these mucins would be more efficient,” said Dr. Zatz. It is possible for this variant to interfere not only with the production of mucus, but also in its composition, as there is an exchange of amino acids in the protein.
“We continued the study by comparing the extremes, i.e., those in their 90s with mild COVID-19 and younger patients with severe COVID-19, including several who died,” said Dr. Zatz.
More personalized medicine
The specialists agreed that a genetic test to predict COVID-19 severity is still a long way away. The genetic component is too little understood to enable the evaluation of individual risk. It has been possible to identify several important areas but, as Dr. Krieger pointed out, a variant identified in a certain chromosome interval may not be just one gene. There may be various candidate genes, or there may be a regulatory sequence for a distant gene. Furthermore, there are regions with genes that make sense as moderators of COVID-19 severity, because they regulate an inflammatory or immunologic reaction, but evidence is still lacking.
Reaching the molecular mechanism would, in future, allow a medicine to be chosen for a given patient, as already happens with other diseases. It also could enable the discovery of new medicines following as-yet-unexplored lines of research. Dr. Zatz also considers the possibility of genetic therapy.
Even with the knowledge of human genetics, one part of the equation is missing: viral genetics. “Many of the individuals who were resistant to the Delta variant were later affected by Omicron,” she pointed out.
Significance of Brazil
“We have an infinite amount of genomic data worldwide, but the vast majority originates from White Americans of European origin,” said Dr. Krieger. Moreover, genomic associations of COVID-19 severity discovered in the Chinese population were not significant in the European population. Besides underscoring the importance of collaborating with international studies, this situation supports scientists’ interest in carrying out genetic studies within Brazil, he added.
“In the genomic study of the Brazilian population, we found 2 million variants that were not present in the European populations,” said Dr. Zatz.
Dr. Krieger mentioned a technical advantage that Brazil has. “Having been colonized by different ethnic groups and mixed many generations ago, Brazil has a population with a unique genetic structure; the recombinations are different. When preparing the samples, the regions break differently.” This factor could help to separate, in a candidate region, the gene that is significant from those that might not be.
In general, severe COVID-19 would be a complex phenomenon involving several genes and interactions with environmental factors. The Brazilian studies tried to find a factor that was unique to Brazil, but the significance of the differences remained unclear. “We found some signs that were specific to our population,” concluded Dr. Krieger. “But the reason that more people in Brazil died as a result of COVID-19 was not genetic,” he added.
Dr. Zatz and Dr. Krieger reported no conflicts of interest. This article was translated from the Medscape Portuguese edition.
A version of this article first appeared on Medscape.com.
A striking characteristic of COVID-19 is that the severity of clinical outcomes is remarkably variable. Establishing a prognosis for individuals infected with COVID-19 remains a challenge.
Since the start of the COVID-19 pandemic, the heterogeneity of individuals who progress toward severe disease or death, along with the fact that individuals directly exposed to the virus do not necessarily become sick, supports the hypothesis that genetic risk or protective factors are at play.
In an interview with this news organization, Mayana Zatz, PhD, head professor of genetics and coordinator of the Human Genome and Stem Cell Study Center at the University of São Paulo, explained: “The first case that caught my eye was the case of my neighbors, a couple. He presented COVID-19 symptoms, but his wife, who took care of him, had absolutely no symptoms. I thought that it was strange, but we received 3,000 emails from people saying, ‘This happened to me, too.’”
Reports in the media about seven pairs of monozygotic (MZ) twins who died from COVID-19 within days of one another in Brazil also stood out, said the researcher.
, as well as their pathology. Dr. Zatz’s team analyzed the case of a 31-year-old Brazilian MZ twin brother pair who presented simultaneously with severe COVID-19 and the need for oxygen support, despite their age and good health conditions. Curiously, they were admitted and intubated on the same day, but neither of the twins knew about the other’s situation; they found out only when they were extubated.
The study was carried out at the USP with the collaboration of the State University of São Paulo. The authors mapped the genetic profile (by sequencing the genome responsible for coding proteins, or whole-exome sequencing) and the immune cell profile to evaluate innate and adaptive immunity.
The MZ twin brothers shared the same two rare genetic mutations, which may be associated with their increased risk of developing severe COVID-19. However, since these variants were not studied at the protein or functional level, their pathogenicity has yet to be determined. The twins also had [human leukocyte antigen (HLA)] alleles associated with severe COVID-19, which are important candidates for the mechanisms of innate and adaptive immunity and susceptibility to COVID-19 infection and manifestation.
But one particular oddity stood out to the researchers: One of the brothers required longer hospitalization, and only he reported symptoms of long COVID.
In the authors’ eyes, even though the patients shared genetic mutations potentially associated with the risk of developing severe COVID-19, the differences in clinical progression emphasize that, beyond genetic risk factors, continuous exposure to pathogens over a lifetime and other environmental factors mean that each individual’s immune response is unique, even in twins.
“There is no doubt that genetics contribute to the severity of COVID-19, and environmental factors sometimes give us the opportunity to study the disease, too. Such [is the case with] MZ twins who have genetic similarities, even with changes that take place over a lifetime,” José Eduardo Krieger, MD, PhD, professor of molecular medicine at the University of São Paulo Medical School (FMUSP), told this news organization. “Examining MZ twins is a strategy that may help, but, with n = 2, luck really needs to be on your side to get straight to the problem. You need to combine [these findings] with other studies to solve this conundrum,” said Dr. Krieger, who did not take part in the research.
Large cohorts
Genomic and computer resources allow for the study of large sets of data from thousands of individuals. In each of those sets of data, the signal offered by thousands of markers distributed throughout the genome can be studied. This is the possibility offered by various genomic studies of large cohorts of patients with different clinical manifestations.
“Researchers examine thousands of genetic variants throughout the genome from a large sample of individuals and have the chance, for example, to identify genetic variants that are more prevalent in patients who have presented with severe disease than in those who presented with milder disease,” said Dr. Krieger. “These associations highlight a chromosome region in which one or more genes explain, at least in part, the differences observed.”
Genomewide association studies have identified some genetic variants that indicate severity of COVID-19, with potential impact on the virus entering the cell, the immune response, or the development of cytokine storms.
One of these studies, COVID-19 Host Genetics Initiative (COVID-19 HGI), is an international, open-science collaboration for sharing scientific methods and resources with research groups across the world, with the goal of robustly mapping the host genetic determinants of SARS-CoV-2 infection and the severity of the resulting COVID-19 disease. At the start of 2021, the COVID-19 HGI combined genetic data from 49,562 cases and 2 million controls from 46 studies in 19 countries. A total of 853 samples from the BRACOVID study were included in the meta-analysis. The endeavor enabled the identification of 13 genomewide significant loci that are associated with SARS-CoV-2 infection or severe manifestations of COVID-19.
The BRACOVID study, in which Dr. Krieger participates, aims to identify host genetic factors that determine the severity of COVID-19. It is currently the largest project of its kind in Latin America. An article provides the analysis of the first 5,233 participants in the BRACOVID study, who were recruited in São Paulo. Of these participants, 3,533 had been infected with COVID-19 and hospitalized at either the Heart Institute or the Central Institute of the FMUSP General Hospital. The remaining 1,700 made up the control group, which included health care professionals and members of the general population. The controls were recruited through serology assays or PCR tests for SARS-CoV-2.
The researchers discovered a region of chromosome 1 that could play a role in modulating immune response and that could lead to an increase in the likelihood of hospitalization across a wide range of COVID-19 risk factors. This region of chromosome 1 was observed only in Brazilians with a strong European ancestry; however, this finding had not been mentioned in previous studies, suggesting that it could harbor a risk allele specific to the Brazilian population.
The study also confirmed most, but not all, of the regions recorded in the literature, which may be significant in identifying factors determining severity that are specific to a given population.
Including information from the BRACOVID study, other studies have enhanced the knowledge on affected organs. Combined data from 14,000 patients from nine countries evaluated a region of a single chromosome and found that carriers of a certain allele had a higher probability of experiencing various COVID-19 complications, such as severe respiratory failure, venous thromboembolism, and liver damage. The risk was even higher for individuals aged 60 years and over.
Discordant couples
Smaller sample sizes of underrepresented populations also provide relevant data for genomic studies. Dr. Zatz’s team carried out genomic studies on smaller groups, comparing serodiscordant couples (where one was infected and symptomatic while the partner remained asymptomatic and seronegative despite sharing the same bedroom during the infection). Their research found genetic variants related to immune response that were associated with susceptibility to infection and progression to severe COVID-19.
The team also went on to study a group of patients older than 90 years who recovered from COVID-19 with mild symptoms or who remained asymptomatic following a positive test for SARS-CoV-2. They compared these patients with a sample of elderly patients from the same city (São Paulo), sampled before the current pandemic. The researchers identified a genetic variant related to mucin production. “In individuals with mild COVID-19, the degradation of these mucins would be more efficient,” said Dr. Zatz. It is possible for this variant to interfere not only with the production of mucus, but also in its composition, as there is an exchange of amino acids in the protein.
“We continued the study by comparing the extremes, i.e., those in their 90s with mild COVID-19 and younger patients with severe COVID-19, including several who died,” said Dr. Zatz.
More personalized medicine
The specialists agreed that a genetic test to predict COVID-19 severity is still a long way away. The genetic component is too little understood to enable the evaluation of individual risk. It has been possible to identify several important areas but, as Dr. Krieger pointed out, a variant identified in a certain chromosome interval may not be just one gene. There may be various candidate genes, or there may be a regulatory sequence for a distant gene. Furthermore, there are regions with genes that make sense as moderators of COVID-19 severity, because they regulate an inflammatory or immunologic reaction, but evidence is still lacking.
Reaching the molecular mechanism would, in future, allow a medicine to be chosen for a given patient, as already happens with other diseases. It also could enable the discovery of new medicines following as-yet-unexplored lines of research. Dr. Zatz also considers the possibility of genetic therapy.
Even with the knowledge of human genetics, one part of the equation is missing: viral genetics. “Many of the individuals who were resistant to the Delta variant were later affected by Omicron,” she pointed out.
Significance of Brazil
“We have an infinite amount of genomic data worldwide, but the vast majority originates from White Americans of European origin,” said Dr. Krieger. Moreover, genomic associations of COVID-19 severity discovered in the Chinese population were not significant in the European population. Besides underscoring the importance of collaborating with international studies, this situation supports scientists’ interest in carrying out genetic studies within Brazil, he added.
“In the genomic study of the Brazilian population, we found 2 million variants that were not present in the European populations,” said Dr. Zatz.
Dr. Krieger mentioned a technical advantage that Brazil has. “Having been colonized by different ethnic groups and mixed many generations ago, Brazil has a population with a unique genetic structure; the recombinations are different. When preparing the samples, the regions break differently.” This factor could help to separate, in a candidate region, the gene that is significant from those that might not be.
In general, severe COVID-19 would be a complex phenomenon involving several genes and interactions with environmental factors. The Brazilian studies tried to find a factor that was unique to Brazil, but the significance of the differences remained unclear. “We found some signs that were specific to our population,” concluded Dr. Krieger. “But the reason that more people in Brazil died as a result of COVID-19 was not genetic,” he added.
Dr. Zatz and Dr. Krieger reported no conflicts of interest. This article was translated from the Medscape Portuguese edition.
A version of this article first appeared on Medscape.com.
A striking characteristic of COVID-19 is that the severity of clinical outcomes is remarkably variable. Establishing a prognosis for individuals infected with COVID-19 remains a challenge.
Since the start of the COVID-19 pandemic, the heterogeneity of individuals who progress toward severe disease or death, along with the fact that individuals directly exposed to the virus do not necessarily become sick, supports the hypothesis that genetic risk or protective factors are at play.
In an interview with this news organization, Mayana Zatz, PhD, head professor of genetics and coordinator of the Human Genome and Stem Cell Study Center at the University of São Paulo, explained: “The first case that caught my eye was the case of my neighbors, a couple. He presented COVID-19 symptoms, but his wife, who took care of him, had absolutely no symptoms. I thought that it was strange, but we received 3,000 emails from people saying, ‘This happened to me, too.’”
Reports in the media about seven pairs of monozygotic (MZ) twins who died from COVID-19 within days of one another in Brazil also stood out, said the researcher.
, as well as their pathology. Dr. Zatz’s team analyzed the case of a 31-year-old Brazilian MZ twin brother pair who presented simultaneously with severe COVID-19 and the need for oxygen support, despite their age and good health conditions. Curiously, they were admitted and intubated on the same day, but neither of the twins knew about the other’s situation; they found out only when they were extubated.
The study was carried out at the USP with the collaboration of the State University of São Paulo. The authors mapped the genetic profile (by sequencing the genome responsible for coding proteins, or whole-exome sequencing) and the immune cell profile to evaluate innate and adaptive immunity.
The MZ twin brothers shared the same two rare genetic mutations, which may be associated with their increased risk of developing severe COVID-19. However, since these variants were not studied at the protein or functional level, their pathogenicity has yet to be determined. The twins also had [human leukocyte antigen (HLA)] alleles associated with severe COVID-19, which are important candidates for the mechanisms of innate and adaptive immunity and susceptibility to COVID-19 infection and manifestation.
But one particular oddity stood out to the researchers: One of the brothers required longer hospitalization, and only he reported symptoms of long COVID.
In the authors’ eyes, even though the patients shared genetic mutations potentially associated with the risk of developing severe COVID-19, the differences in clinical progression emphasize that, beyond genetic risk factors, continuous exposure to pathogens over a lifetime and other environmental factors mean that each individual’s immune response is unique, even in twins.
“There is no doubt that genetics contribute to the severity of COVID-19, and environmental factors sometimes give us the opportunity to study the disease, too. Such [is the case with] MZ twins who have genetic similarities, even with changes that take place over a lifetime,” José Eduardo Krieger, MD, PhD, professor of molecular medicine at the University of São Paulo Medical School (FMUSP), told this news organization. “Examining MZ twins is a strategy that may help, but, with n = 2, luck really needs to be on your side to get straight to the problem. You need to combine [these findings] with other studies to solve this conundrum,” said Dr. Krieger, who did not take part in the research.
Large cohorts
Genomic and computer resources allow for the study of large sets of data from thousands of individuals. In each of those sets of data, the signal offered by thousands of markers distributed throughout the genome can be studied. This is the possibility offered by various genomic studies of large cohorts of patients with different clinical manifestations.
“Researchers examine thousands of genetic variants throughout the genome from a large sample of individuals and have the chance, for example, to identify genetic variants that are more prevalent in patients who have presented with severe disease than in those who presented with milder disease,” said Dr. Krieger. “These associations highlight a chromosome region in which one or more genes explain, at least in part, the differences observed.”
Genomewide association studies have identified some genetic variants that indicate severity of COVID-19, with potential impact on the virus entering the cell, the immune response, or the development of cytokine storms.
One of these studies, COVID-19 Host Genetics Initiative (COVID-19 HGI), is an international, open-science collaboration for sharing scientific methods and resources with research groups across the world, with the goal of robustly mapping the host genetic determinants of SARS-CoV-2 infection and the severity of the resulting COVID-19 disease. At the start of 2021, the COVID-19 HGI combined genetic data from 49,562 cases and 2 million controls from 46 studies in 19 countries. A total of 853 samples from the BRACOVID study were included in the meta-analysis. The endeavor enabled the identification of 13 genomewide significant loci that are associated with SARS-CoV-2 infection or severe manifestations of COVID-19.
The BRACOVID study, in which Dr. Krieger participates, aims to identify host genetic factors that determine the severity of COVID-19. It is currently the largest project of its kind in Latin America. An article provides the analysis of the first 5,233 participants in the BRACOVID study, who were recruited in São Paulo. Of these participants, 3,533 had been infected with COVID-19 and hospitalized at either the Heart Institute or the Central Institute of the FMUSP General Hospital. The remaining 1,700 made up the control group, which included health care professionals and members of the general population. The controls were recruited through serology assays or PCR tests for SARS-CoV-2.
The researchers discovered a region of chromosome 1 that could play a role in modulating immune response and that could lead to an increase in the likelihood of hospitalization across a wide range of COVID-19 risk factors. This region of chromosome 1 was observed only in Brazilians with a strong European ancestry; however, this finding had not been mentioned in previous studies, suggesting that it could harbor a risk allele specific to the Brazilian population.
The study also confirmed most, but not all, of the regions recorded in the literature, which may be significant in identifying factors determining severity that are specific to a given population.
Including information from the BRACOVID study, other studies have enhanced the knowledge on affected organs. Combined data from 14,000 patients from nine countries evaluated a region of a single chromosome and found that carriers of a certain allele had a higher probability of experiencing various COVID-19 complications, such as severe respiratory failure, venous thromboembolism, and liver damage. The risk was even higher for individuals aged 60 years and over.
Discordant couples
Smaller sample sizes of underrepresented populations also provide relevant data for genomic studies. Dr. Zatz’s team carried out genomic studies on smaller groups, comparing serodiscordant couples (where one was infected and symptomatic while the partner remained asymptomatic and seronegative despite sharing the same bedroom during the infection). Their research found genetic variants related to immune response that were associated with susceptibility to infection and progression to severe COVID-19.
The team also went on to study a group of patients older than 90 years who recovered from COVID-19 with mild symptoms or who remained asymptomatic following a positive test for SARS-CoV-2. They compared these patients with a sample of elderly patients from the same city (São Paulo), sampled before the current pandemic. The researchers identified a genetic variant related to mucin production. “In individuals with mild COVID-19, the degradation of these mucins would be more efficient,” said Dr. Zatz. It is possible for this variant to interfere not only with the production of mucus, but also in its composition, as there is an exchange of amino acids in the protein.
“We continued the study by comparing the extremes, i.e., those in their 90s with mild COVID-19 and younger patients with severe COVID-19, including several who died,” said Dr. Zatz.
More personalized medicine
The specialists agreed that a genetic test to predict COVID-19 severity is still a long way away. The genetic component is too little understood to enable the evaluation of individual risk. It has been possible to identify several important areas but, as Dr. Krieger pointed out, a variant identified in a certain chromosome interval may not be just one gene. There may be various candidate genes, or there may be a regulatory sequence for a distant gene. Furthermore, there are regions with genes that make sense as moderators of COVID-19 severity, because they regulate an inflammatory or immunologic reaction, but evidence is still lacking.
Reaching the molecular mechanism would, in future, allow a medicine to be chosen for a given patient, as already happens with other diseases. It also could enable the discovery of new medicines following as-yet-unexplored lines of research. Dr. Zatz also considers the possibility of genetic therapy.
Even with the knowledge of human genetics, one part of the equation is missing: viral genetics. “Many of the individuals who were resistant to the Delta variant were later affected by Omicron,” she pointed out.
Significance of Brazil
“We have an infinite amount of genomic data worldwide, but the vast majority originates from White Americans of European origin,” said Dr. Krieger. Moreover, genomic associations of COVID-19 severity discovered in the Chinese population were not significant in the European population. Besides underscoring the importance of collaborating with international studies, this situation supports scientists’ interest in carrying out genetic studies within Brazil, he added.
“In the genomic study of the Brazilian population, we found 2 million variants that were not present in the European populations,” said Dr. Zatz.
Dr. Krieger mentioned a technical advantage that Brazil has. “Having been colonized by different ethnic groups and mixed many generations ago, Brazil has a population with a unique genetic structure; the recombinations are different. When preparing the samples, the regions break differently.” This factor could help to separate, in a candidate region, the gene that is significant from those that might not be.
In general, severe COVID-19 would be a complex phenomenon involving several genes and interactions with environmental factors. The Brazilian studies tried to find a factor that was unique to Brazil, but the significance of the differences remained unclear. “We found some signs that were specific to our population,” concluded Dr. Krieger. “But the reason that more people in Brazil died as a result of COVID-19 was not genetic,” he added.
Dr. Zatz and Dr. Krieger reported no conflicts of interest. This article was translated from the Medscape Portuguese edition.
A version of this article first appeared on Medscape.com.
The surprising failure of vitamin D in deficient kids
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
U.S. flu activity already at mid-season levels
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.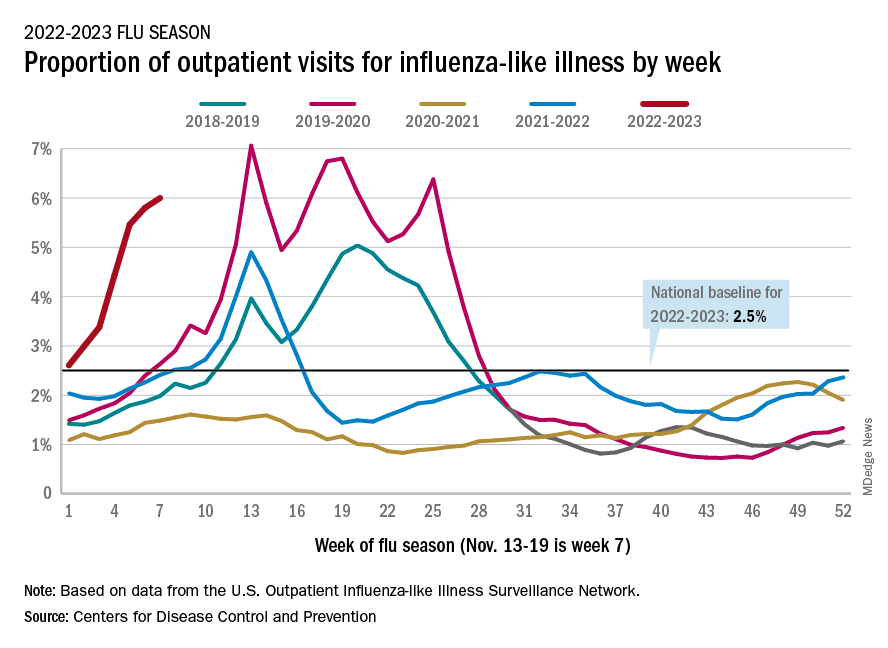
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.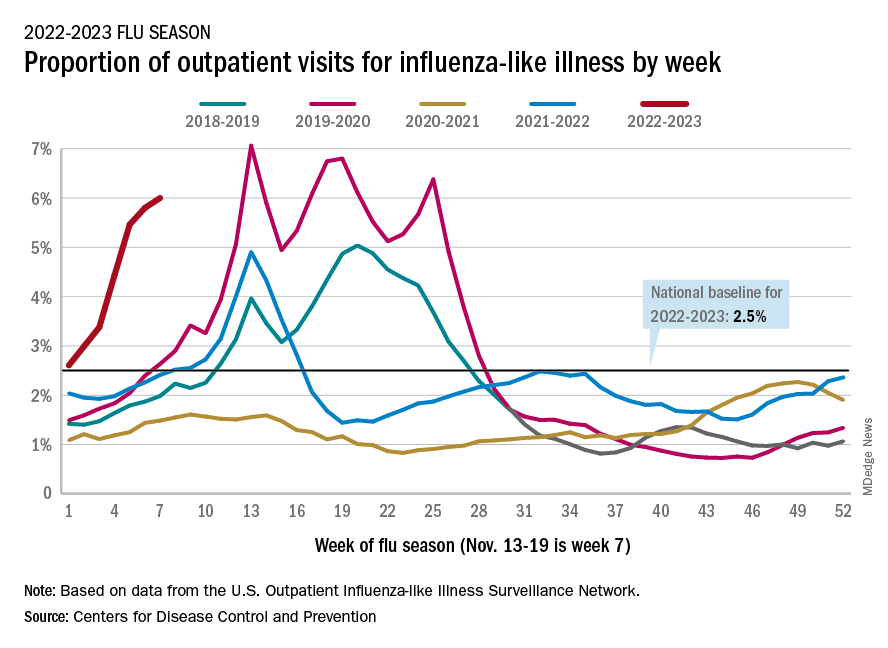
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.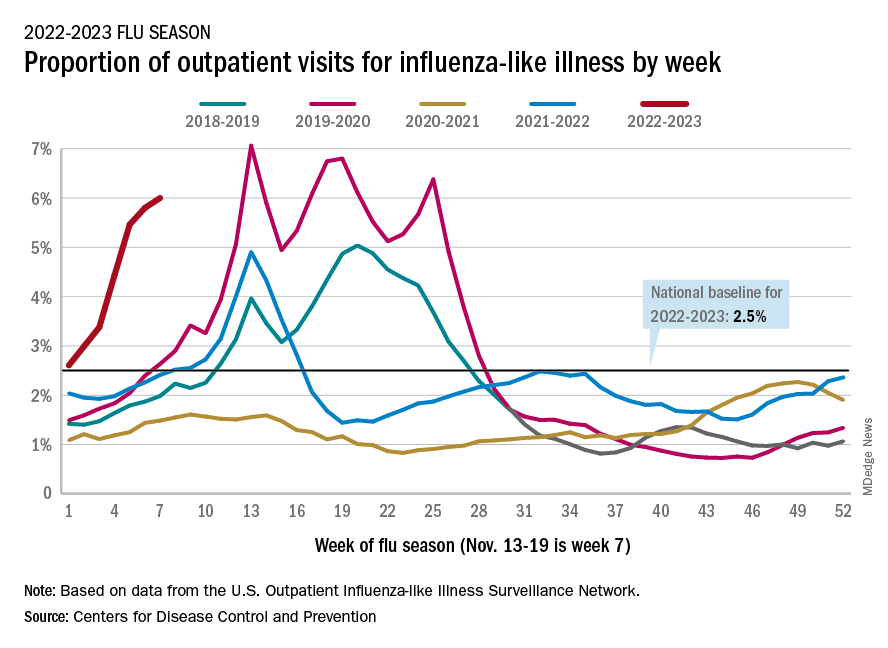
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
Is it long COVID, or dementia, or both?
In early September, about a week after recovering from COVID-19, Barri Sanders went to the bank to pay a bill. But by mistake, she transferred a large amount of money from the wrong account.
“I’m talking about $20,000,” she said. “I had to go back [later] and fix it.”
Ms. Sanders, 83, had not had confusion like that before. Suddenly, the Albuquerque, N.M., resident found herself looking up from a book and not remembering what she had just read. She would stand up from her chair and forget what she meant to do.
“I kind of thought it was just the aging process,” she said. Combined with sudden balance issues, insomnia, and a nagging postnasal drip, the overall effect was “subtle, but scary,” she said.
After 5 days of this, she went to bed and slept the whole night through. She woke up in the morning to find her balanced restored, her sinuses clear, and the mental fog gone. What she’d had, she realized, wasn’t a rapid start of dementia, but rather a mercifully short form of long COVID.
Somewhere between 22% and 32% of people who recover from COVID-19 get “brain fog,” a nonscientific term used to describe slow or sluggish thinking. While this is disturbing at any age, And some scientists are starting to confirm what doctors, patients, and their families can already see: Older patients who have had COVID-19 have a higher risk of getting dementia or, if they already have mental confusion, the illness may worsen their condition.
British scientists who studied medical records from around the world reported in the journal The Lancet Psychiatry that people who recovered from COVID-19 had a higher risk of problems with their thinking and dementia even after 2 years had passed.
Another 2022 study, published in JAMA Neurology, looked at older COVID-19 patients for a year after they were discharged from hospitals in Wuhan, China. Compared with uninfected people, those who survived a severe case of COVID-19 were at higher risk for early onset, late-onset, and progressive decline in their thinking skills. Those who survived a mild infection were at a higher risk for early onset decline, the study found.
Eran Metzger, MD, assistant professor of psychiatry at Beth Israel Deaconess Medical Center in Boston, said he’s noticed that COVID-19 makes some older patients confused, and their brains don’t regain their former clarity.
“We see a stepwise decline in their cognition during the COVID episode, and then they never get back up to their baseline,” said Dr. Metzger, medical director at Hebrew SeniorLife.
New research is beginning to back up such findings.
People who got COVID-19 were twice as likely to receive a diagnosis of Alzheimer’s disease in the 12 months after infection, compared to those who didn’t get COVID, according to a study published in the journal Nature Medicine , which analyzed the health care databases of the U.S. Department of Veterans Affairs.
Joshua Cahan, MD, a cognitive neurologist at Northwestern University, Chicago, advises caution about applying such a specific label simply from a patient’s medical chart. After all, he noted, few patients get tested to confirm that they have the proteins linked to Alzheimer’s.
“Probably the most appropriate conclusion from that is that there’s an increased risk of dementia after a COVID infection,” he said, “but we don’t know whether it’s truly Alzheimer’s disease or not.”
There could be a number of reasons why COVID-19 triggers a decline in thinking skills, says Michelle Monje, MD, a neuroscientist and neuro-oncologist at Stanford (Calif.) University.
In a paper published in the journal Neuron, Dr. Monje and her coauthor, Akiko Iwasaki, PhD, professor of immunobiology at Yale University, New Haven, Conn., propose possible triggers for brain fog caused by COVID: inflammation in the lungs and respiratory passages that leads to inflammation and dysregulation of the central nervous system; autoimmune reactions that damage the central nervous system; brain infection directly caused by the coronavirus (though, they note, this appears rare); a reactivation of an Epstein-Barr virus, which can lead to neuroinflammation; triggered by the coronavirus; and/or complications from severe cases of COVID-19, possibly involving periods of low blood oxygen and multi-organ failure.
Scientific understanding of brain fog is “part of an emerging picture that inflammation elsewhere in the body can be transmitted to become inflammation in the brain,” Dr. Monje said. “And once there’s inflammation in the brain … that can dysregulate other cell types that normally support healthy cognitive function.”
One issue with the concept of brain fog is that, like the term itself, the condition can be tough to define for doctors and patients alike and difficult, if not impossible, to capture on common cognition tests.
These days, patients often arrive at the Center of Excellence for Alzheimer’s Disease, in Syracuse, N.Y., complaining that they “don’t feel the same” as they did before contracting COVID-19, said Sharon Brangman, MD, the center’s director and the chair of the geriatrics department at Upstate Medical University.
But the evidence of diminished cognition just isn’t there.
“There’s nothing that we can find, objectively, that’s wrong with them,” she said. “They’re not severe enough to score low on mental status testing.”
But specialized, directed testing can find some probable signs, said Dr. Cahan, who evaluates patient cognition in a long COVID clinic at Northwestern University.
He often finds that his long COVID patients score in the low normal range on cognitive testing.
“Patients do have a complaint that something’s changed, and we don’t have prior testing,” he said. “So it’s possible that they were maybe in the high normal range or the superior range, but you just don’t know.”
He said he has seen very high-performing people, such as lawyers, executives, PhDs, and other professionals, who have tests that might be interpreted as normal, but given their level of achievement, “you would expect [higher scores].”
Like Ms. Sanders, many of those who do have muddled thinking after a COVID infection return to their former mental status. A study published in the journal Brain Communications found that people who had recovered from COVID-19, even if they had a mild illness, were significantly more likely to have memory and other cognition issues in the months after infection. But after 9 months, the former COVID patients had returned to their normal level of cognition, the team at Britain’s University of Oxford reported.
Notably, though, the average age of the people in the study was 28.6.
At the Northwestern clinic, Dr. Cahan treats patients who have struggled with COVID-induced cognition issues for months or even years. A rehabilitation program involves working with patients to come up with ways to compensate for cognitive deficits – such as making lists – as well as brain exercises, Dr. Cahan said. Over time, patients may achieve a 75% to 85% improvement, he said.
Dr. Monje hopes that one day, science will come up with ways to fully reverse the decline.
“I think what is likely the most common contributor to brain fog is this neuroinflammation, causing dysfunction of other cell types,” she said. “And, at least in the laboratory, we can rescue that in mouse models of chemotherapy brain fog, which gives me hope that we can rescue that for people.”
A version of this article first appeared on WebMD.com.
In early September, about a week after recovering from COVID-19, Barri Sanders went to the bank to pay a bill. But by mistake, she transferred a large amount of money from the wrong account.
“I’m talking about $20,000,” she said. “I had to go back [later] and fix it.”
Ms. Sanders, 83, had not had confusion like that before. Suddenly, the Albuquerque, N.M., resident found herself looking up from a book and not remembering what she had just read. She would stand up from her chair and forget what she meant to do.
“I kind of thought it was just the aging process,” she said. Combined with sudden balance issues, insomnia, and a nagging postnasal drip, the overall effect was “subtle, but scary,” she said.
After 5 days of this, she went to bed and slept the whole night through. She woke up in the morning to find her balanced restored, her sinuses clear, and the mental fog gone. What she’d had, she realized, wasn’t a rapid start of dementia, but rather a mercifully short form of long COVID.
Somewhere between 22% and 32% of people who recover from COVID-19 get “brain fog,” a nonscientific term used to describe slow or sluggish thinking. While this is disturbing at any age, And some scientists are starting to confirm what doctors, patients, and their families can already see: Older patients who have had COVID-19 have a higher risk of getting dementia or, if they already have mental confusion, the illness may worsen their condition.
British scientists who studied medical records from around the world reported in the journal The Lancet Psychiatry that people who recovered from COVID-19 had a higher risk of problems with their thinking and dementia even after 2 years had passed.
Another 2022 study, published in JAMA Neurology, looked at older COVID-19 patients for a year after they were discharged from hospitals in Wuhan, China. Compared with uninfected people, those who survived a severe case of COVID-19 were at higher risk for early onset, late-onset, and progressive decline in their thinking skills. Those who survived a mild infection were at a higher risk for early onset decline, the study found.
Eran Metzger, MD, assistant professor of psychiatry at Beth Israel Deaconess Medical Center in Boston, said he’s noticed that COVID-19 makes some older patients confused, and their brains don’t regain their former clarity.
“We see a stepwise decline in their cognition during the COVID episode, and then they never get back up to their baseline,” said Dr. Metzger, medical director at Hebrew SeniorLife.
New research is beginning to back up such findings.
People who got COVID-19 were twice as likely to receive a diagnosis of Alzheimer’s disease in the 12 months after infection, compared to those who didn’t get COVID, according to a study published in the journal Nature Medicine , which analyzed the health care databases of the U.S. Department of Veterans Affairs.
Joshua Cahan, MD, a cognitive neurologist at Northwestern University, Chicago, advises caution about applying such a specific label simply from a patient’s medical chart. After all, he noted, few patients get tested to confirm that they have the proteins linked to Alzheimer’s.
“Probably the most appropriate conclusion from that is that there’s an increased risk of dementia after a COVID infection,” he said, “but we don’t know whether it’s truly Alzheimer’s disease or not.”
There could be a number of reasons why COVID-19 triggers a decline in thinking skills, says Michelle Monje, MD, a neuroscientist and neuro-oncologist at Stanford (Calif.) University.
In a paper published in the journal Neuron, Dr. Monje and her coauthor, Akiko Iwasaki, PhD, professor of immunobiology at Yale University, New Haven, Conn., propose possible triggers for brain fog caused by COVID: inflammation in the lungs and respiratory passages that leads to inflammation and dysregulation of the central nervous system; autoimmune reactions that damage the central nervous system; brain infection directly caused by the coronavirus (though, they note, this appears rare); a reactivation of an Epstein-Barr virus, which can lead to neuroinflammation; triggered by the coronavirus; and/or complications from severe cases of COVID-19, possibly involving periods of low blood oxygen and multi-organ failure.
Scientific understanding of brain fog is “part of an emerging picture that inflammation elsewhere in the body can be transmitted to become inflammation in the brain,” Dr. Monje said. “And once there’s inflammation in the brain … that can dysregulate other cell types that normally support healthy cognitive function.”
One issue with the concept of brain fog is that, like the term itself, the condition can be tough to define for doctors and patients alike and difficult, if not impossible, to capture on common cognition tests.
These days, patients often arrive at the Center of Excellence for Alzheimer’s Disease, in Syracuse, N.Y., complaining that they “don’t feel the same” as they did before contracting COVID-19, said Sharon Brangman, MD, the center’s director and the chair of the geriatrics department at Upstate Medical University.
But the evidence of diminished cognition just isn’t there.
“There’s nothing that we can find, objectively, that’s wrong with them,” she said. “They’re not severe enough to score low on mental status testing.”
But specialized, directed testing can find some probable signs, said Dr. Cahan, who evaluates patient cognition in a long COVID clinic at Northwestern University.
He often finds that his long COVID patients score in the low normal range on cognitive testing.
“Patients do have a complaint that something’s changed, and we don’t have prior testing,” he said. “So it’s possible that they were maybe in the high normal range or the superior range, but you just don’t know.”
He said he has seen very high-performing people, such as lawyers, executives, PhDs, and other professionals, who have tests that might be interpreted as normal, but given their level of achievement, “you would expect [higher scores].”
Like Ms. Sanders, many of those who do have muddled thinking after a COVID infection return to their former mental status. A study published in the journal Brain Communications found that people who had recovered from COVID-19, even if they had a mild illness, were significantly more likely to have memory and other cognition issues in the months after infection. But after 9 months, the former COVID patients had returned to their normal level of cognition, the team at Britain’s University of Oxford reported.
Notably, though, the average age of the people in the study was 28.6.
At the Northwestern clinic, Dr. Cahan treats patients who have struggled with COVID-induced cognition issues for months or even years. A rehabilitation program involves working with patients to come up with ways to compensate for cognitive deficits – such as making lists – as well as brain exercises, Dr. Cahan said. Over time, patients may achieve a 75% to 85% improvement, he said.
Dr. Monje hopes that one day, science will come up with ways to fully reverse the decline.
“I think what is likely the most common contributor to brain fog is this neuroinflammation, causing dysfunction of other cell types,” she said. “And, at least in the laboratory, we can rescue that in mouse models of chemotherapy brain fog, which gives me hope that we can rescue that for people.”
A version of this article first appeared on WebMD.com.
In early September, about a week after recovering from COVID-19, Barri Sanders went to the bank to pay a bill. But by mistake, she transferred a large amount of money from the wrong account.
“I’m talking about $20,000,” she said. “I had to go back [later] and fix it.”
Ms. Sanders, 83, had not had confusion like that before. Suddenly, the Albuquerque, N.M., resident found herself looking up from a book and not remembering what she had just read. She would stand up from her chair and forget what she meant to do.
“I kind of thought it was just the aging process,” she said. Combined with sudden balance issues, insomnia, and a nagging postnasal drip, the overall effect was “subtle, but scary,” she said.
After 5 days of this, she went to bed and slept the whole night through. She woke up in the morning to find her balanced restored, her sinuses clear, and the mental fog gone. What she’d had, she realized, wasn’t a rapid start of dementia, but rather a mercifully short form of long COVID.
Somewhere between 22% and 32% of people who recover from COVID-19 get “brain fog,” a nonscientific term used to describe slow or sluggish thinking. While this is disturbing at any age, And some scientists are starting to confirm what doctors, patients, and their families can already see: Older patients who have had COVID-19 have a higher risk of getting dementia or, if they already have mental confusion, the illness may worsen their condition.
British scientists who studied medical records from around the world reported in the journal The Lancet Psychiatry that people who recovered from COVID-19 had a higher risk of problems with their thinking and dementia even after 2 years had passed.
Another 2022 study, published in JAMA Neurology, looked at older COVID-19 patients for a year after they were discharged from hospitals in Wuhan, China. Compared with uninfected people, those who survived a severe case of COVID-19 were at higher risk for early onset, late-onset, and progressive decline in their thinking skills. Those who survived a mild infection were at a higher risk for early onset decline, the study found.
Eran Metzger, MD, assistant professor of psychiatry at Beth Israel Deaconess Medical Center in Boston, said he’s noticed that COVID-19 makes some older patients confused, and their brains don’t regain their former clarity.
“We see a stepwise decline in their cognition during the COVID episode, and then they never get back up to their baseline,” said Dr. Metzger, medical director at Hebrew SeniorLife.
New research is beginning to back up such findings.
People who got COVID-19 were twice as likely to receive a diagnosis of Alzheimer’s disease in the 12 months after infection, compared to those who didn’t get COVID, according to a study published in the journal Nature Medicine , which analyzed the health care databases of the U.S. Department of Veterans Affairs.
Joshua Cahan, MD, a cognitive neurologist at Northwestern University, Chicago, advises caution about applying such a specific label simply from a patient’s medical chart. After all, he noted, few patients get tested to confirm that they have the proteins linked to Alzheimer’s.
“Probably the most appropriate conclusion from that is that there’s an increased risk of dementia after a COVID infection,” he said, “but we don’t know whether it’s truly Alzheimer’s disease or not.”
There could be a number of reasons why COVID-19 triggers a decline in thinking skills, says Michelle Monje, MD, a neuroscientist and neuro-oncologist at Stanford (Calif.) University.
In a paper published in the journal Neuron, Dr. Monje and her coauthor, Akiko Iwasaki, PhD, professor of immunobiology at Yale University, New Haven, Conn., propose possible triggers for brain fog caused by COVID: inflammation in the lungs and respiratory passages that leads to inflammation and dysregulation of the central nervous system; autoimmune reactions that damage the central nervous system; brain infection directly caused by the coronavirus (though, they note, this appears rare); a reactivation of an Epstein-Barr virus, which can lead to neuroinflammation; triggered by the coronavirus; and/or complications from severe cases of COVID-19, possibly involving periods of low blood oxygen and multi-organ failure.
Scientific understanding of brain fog is “part of an emerging picture that inflammation elsewhere in the body can be transmitted to become inflammation in the brain,” Dr. Monje said. “And once there’s inflammation in the brain … that can dysregulate other cell types that normally support healthy cognitive function.”
One issue with the concept of brain fog is that, like the term itself, the condition can be tough to define for doctors and patients alike and difficult, if not impossible, to capture on common cognition tests.
These days, patients often arrive at the Center of Excellence for Alzheimer’s Disease, in Syracuse, N.Y., complaining that they “don’t feel the same” as they did before contracting COVID-19, said Sharon Brangman, MD, the center’s director and the chair of the geriatrics department at Upstate Medical University.
But the evidence of diminished cognition just isn’t there.
“There’s nothing that we can find, objectively, that’s wrong with them,” she said. “They’re not severe enough to score low on mental status testing.”
But specialized, directed testing can find some probable signs, said Dr. Cahan, who evaluates patient cognition in a long COVID clinic at Northwestern University.
He often finds that his long COVID patients score in the low normal range on cognitive testing.
“Patients do have a complaint that something’s changed, and we don’t have prior testing,” he said. “So it’s possible that they were maybe in the high normal range or the superior range, but you just don’t know.”
He said he has seen very high-performing people, such as lawyers, executives, PhDs, and other professionals, who have tests that might be interpreted as normal, but given their level of achievement, “you would expect [higher scores].”
Like Ms. Sanders, many of those who do have muddled thinking after a COVID infection return to their former mental status. A study published in the journal Brain Communications found that people who had recovered from COVID-19, even if they had a mild illness, were significantly more likely to have memory and other cognition issues in the months after infection. But after 9 months, the former COVID patients had returned to their normal level of cognition, the team at Britain’s University of Oxford reported.
Notably, though, the average age of the people in the study was 28.6.
At the Northwestern clinic, Dr. Cahan treats patients who have struggled with COVID-induced cognition issues for months or even years. A rehabilitation program involves working with patients to come up with ways to compensate for cognitive deficits – such as making lists – as well as brain exercises, Dr. Cahan said. Over time, patients may achieve a 75% to 85% improvement, he said.
Dr. Monje hopes that one day, science will come up with ways to fully reverse the decline.
“I think what is likely the most common contributor to brain fog is this neuroinflammation, causing dysfunction of other cell types,” she said. “And, at least in the laboratory, we can rescue that in mouse models of chemotherapy brain fog, which gives me hope that we can rescue that for people.”
A version of this article first appeared on WebMD.com.
More work needed to optimize STI screening in primary care settings
TAMPA – Boosting screening for sexually transmitted infections in primary care settings could help alleviate some of the barriers to optimal testing and treatment, a new quality improvement initiative suggests.
Many primary care doctors are challenged for time and send people to other health care settings, such as a local health department or a clinic that specializes in STI diagnosis and treatment, said Wendy Kays, DNP, APRN, AGNP-BC, AAHIVS, a nurse practitioner and researcher at Care Resource, Miami.
However, for multiple reasons, many patients do not follow up and are not screened or treated, Dr. Kays said at the Association of Nurses in AIDS Care annual meeting. Some people can afford the copay to see a primary care provider, for example, but do not have the resources to pay for a second clinical visit or laboratory testing.
In other instances, transportation can be a problem. “People, especially in the neighborhood where we are located, depend a lot on buses to go to their primary care,” Dr. Kays told this news organization. But “follow-up is very important. It can promote early treatment and prevent the spread of disease.”
Primary care is critical as a gateway into health care that could help address low rates of STI screening, she said. There is also evidence that STIs are on the rise because of the COVID-19 pandemic.
If more primary care doctors tested and treated STIs using standardized Centers for Disease Control and Prevention guidelines, patients would not have to make a trip to another location, Dr. Kays said.
“The primary health setting … is actually the perfect place to get your screening,” said Jimmie Leckliter, MSN-Ed, RN, PHN, in an interview. He was not affiliated with the presentation. “I’m a former ER nurse, and a lot of people are using the ER as primary care, and it’s not really set up to do that screening.”
Mr. Leckliter suggested that primary care doctors incorporate some questions about sexual health during a regular head-to-toe checkup and ask questions in a very clinical, nonjudgmental way.
He also acknowledged that for some physicians it can be uncomfortable to raise the issues. “Unfortunately, I think in our society, talking to people about sex is taboo, and people become uncomfortable. We need to be able to learn to put our biases aside and treat our patients. That’s what our job is, added Mr. Leckliter, an adjunct faculty member at the College of the Desert’s School of Nursing and Allied Health Programs, Palm Springs, Calif.
Clinicians should be aware of the stigma associated with sending a person to an STD clinic for further workup, Mr. Leckliter advised. “You have to look at the stigma in the community in which you’re located. It makes a big difference,” he said. “Is it mainly a Latino or African American community?”
Compliance was a challenge
Dr. Kays and colleague performed a quality improvement project focused on implementing the CDC’s STI treatment guidelines at Care Resource. One goal was to educate a multidisciplinary team on the importance of screening in the primary care setting. The clientele at Care Resource consists primarily of underprivileged minorities, including the Latino, Black, gay, and transgender communities.
Six health care providers participated – two medical doctors and four advanced-practice providers. They evaluated patient charts from the electronic health record system 4 weeks before the intervention and 4 weeks after.
The education had a positive impact, the researchers reported, even though three providers were compliant with the CDC-recommended screening protocol and three others were not.
The quality improvement initiative had some limitations, Dr. Kays noted. “The hope is that the [quality improvement] process will continue moving forward, and early diagnosis and treatment of STIs will be standardized in this primary care practice.”
An evidence-based tool to screen for STIs in primary care is “crucial,” she added. Using a standardized, evidence-based protocol in primary care “can create positive change in patients’ outcomes.”
The study was independently supported. Dr. Kays and Mr. Leckliter report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TAMPA – Boosting screening for sexually transmitted infections in primary care settings could help alleviate some of the barriers to optimal testing and treatment, a new quality improvement initiative suggests.
Many primary care doctors are challenged for time and send people to other health care settings, such as a local health department or a clinic that specializes in STI diagnosis and treatment, said Wendy Kays, DNP, APRN, AGNP-BC, AAHIVS, a nurse practitioner and researcher at Care Resource, Miami.
However, for multiple reasons, many patients do not follow up and are not screened or treated, Dr. Kays said at the Association of Nurses in AIDS Care annual meeting. Some people can afford the copay to see a primary care provider, for example, but do not have the resources to pay for a second clinical visit or laboratory testing.
In other instances, transportation can be a problem. “People, especially in the neighborhood where we are located, depend a lot on buses to go to their primary care,” Dr. Kays told this news organization. But “follow-up is very important. It can promote early treatment and prevent the spread of disease.”
Primary care is critical as a gateway into health care that could help address low rates of STI screening, she said. There is also evidence that STIs are on the rise because of the COVID-19 pandemic.
If more primary care doctors tested and treated STIs using standardized Centers for Disease Control and Prevention guidelines, patients would not have to make a trip to another location, Dr. Kays said.
“The primary health setting … is actually the perfect place to get your screening,” said Jimmie Leckliter, MSN-Ed, RN, PHN, in an interview. He was not affiliated with the presentation. “I’m a former ER nurse, and a lot of people are using the ER as primary care, and it’s not really set up to do that screening.”
Mr. Leckliter suggested that primary care doctors incorporate some questions about sexual health during a regular head-to-toe checkup and ask questions in a very clinical, nonjudgmental way.
He also acknowledged that for some physicians it can be uncomfortable to raise the issues. “Unfortunately, I think in our society, talking to people about sex is taboo, and people become uncomfortable. We need to be able to learn to put our biases aside and treat our patients. That’s what our job is, added Mr. Leckliter, an adjunct faculty member at the College of the Desert’s School of Nursing and Allied Health Programs, Palm Springs, Calif.
Clinicians should be aware of the stigma associated with sending a person to an STD clinic for further workup, Mr. Leckliter advised. “You have to look at the stigma in the community in which you’re located. It makes a big difference,” he said. “Is it mainly a Latino or African American community?”
Compliance was a challenge
Dr. Kays and colleague performed a quality improvement project focused on implementing the CDC’s STI treatment guidelines at Care Resource. One goal was to educate a multidisciplinary team on the importance of screening in the primary care setting. The clientele at Care Resource consists primarily of underprivileged minorities, including the Latino, Black, gay, and transgender communities.
Six health care providers participated – two medical doctors and four advanced-practice providers. They evaluated patient charts from the electronic health record system 4 weeks before the intervention and 4 weeks after.
The education had a positive impact, the researchers reported, even though three providers were compliant with the CDC-recommended screening protocol and three others were not.
The quality improvement initiative had some limitations, Dr. Kays noted. “The hope is that the [quality improvement] process will continue moving forward, and early diagnosis and treatment of STIs will be standardized in this primary care practice.”
An evidence-based tool to screen for STIs in primary care is “crucial,” she added. Using a standardized, evidence-based protocol in primary care “can create positive change in patients’ outcomes.”
The study was independently supported. Dr. Kays and Mr. Leckliter report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TAMPA – Boosting screening for sexually transmitted infections in primary care settings could help alleviate some of the barriers to optimal testing and treatment, a new quality improvement initiative suggests.
Many primary care doctors are challenged for time and send people to other health care settings, such as a local health department or a clinic that specializes in STI diagnosis and treatment, said Wendy Kays, DNP, APRN, AGNP-BC, AAHIVS, a nurse practitioner and researcher at Care Resource, Miami.
However, for multiple reasons, many patients do not follow up and are not screened or treated, Dr. Kays said at the Association of Nurses in AIDS Care annual meeting. Some people can afford the copay to see a primary care provider, for example, but do not have the resources to pay for a second clinical visit or laboratory testing.
In other instances, transportation can be a problem. “People, especially in the neighborhood where we are located, depend a lot on buses to go to their primary care,” Dr. Kays told this news organization. But “follow-up is very important. It can promote early treatment and prevent the spread of disease.”
Primary care is critical as a gateway into health care that could help address low rates of STI screening, she said. There is also evidence that STIs are on the rise because of the COVID-19 pandemic.
If more primary care doctors tested and treated STIs using standardized Centers for Disease Control and Prevention guidelines, patients would not have to make a trip to another location, Dr. Kays said.
“The primary health setting … is actually the perfect place to get your screening,” said Jimmie Leckliter, MSN-Ed, RN, PHN, in an interview. He was not affiliated with the presentation. “I’m a former ER nurse, and a lot of people are using the ER as primary care, and it’s not really set up to do that screening.”
Mr. Leckliter suggested that primary care doctors incorporate some questions about sexual health during a regular head-to-toe checkup and ask questions in a very clinical, nonjudgmental way.
He also acknowledged that for some physicians it can be uncomfortable to raise the issues. “Unfortunately, I think in our society, talking to people about sex is taboo, and people become uncomfortable. We need to be able to learn to put our biases aside and treat our patients. That’s what our job is, added Mr. Leckliter, an adjunct faculty member at the College of the Desert’s School of Nursing and Allied Health Programs, Palm Springs, Calif.
Clinicians should be aware of the stigma associated with sending a person to an STD clinic for further workup, Mr. Leckliter advised. “You have to look at the stigma in the community in which you’re located. It makes a big difference,” he said. “Is it mainly a Latino or African American community?”
Compliance was a challenge
Dr. Kays and colleague performed a quality improvement project focused on implementing the CDC’s STI treatment guidelines at Care Resource. One goal was to educate a multidisciplinary team on the importance of screening in the primary care setting. The clientele at Care Resource consists primarily of underprivileged minorities, including the Latino, Black, gay, and transgender communities.
Six health care providers participated – two medical doctors and four advanced-practice providers. They evaluated patient charts from the electronic health record system 4 weeks before the intervention and 4 weeks after.
The education had a positive impact, the researchers reported, even though three providers were compliant with the CDC-recommended screening protocol and three others were not.
The quality improvement initiative had some limitations, Dr. Kays noted. “The hope is that the [quality improvement] process will continue moving forward, and early diagnosis and treatment of STIs will be standardized in this primary care practice.”
An evidence-based tool to screen for STIs in primary care is “crucial,” she added. Using a standardized, evidence-based protocol in primary care “can create positive change in patients’ outcomes.”
The study was independently supported. Dr. Kays and Mr. Leckliter report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Study affirms shorter regimens for drug-resistant tuberculosis
Two short-course bedaquiline-containing treatment regimens for rifampicin-resistant tuberculosis showed “robust evidence” for superior efficacy and less ototoxicity compared to a 9-month injectable control regimen, researchers report.
The findings validate the World Health Organization’s current recommendation of a 9-month, bedaquiline-based oral regimen, “which was based only on observational data,” noted lead author Ruth Goodall, PhD, from the Medical Research Council Clinical Trials Unit at University College London, and colleagues.
The study was published in The Lancet.
The Standard Treatment Regimen of Anti-tuberculosis Drugs for Patients With MDR-TB (STREAM) stage 2 study was a randomized, phase 3, noninferiority trial conducted at 13 hospital clinics in seven countries that had prespecified tests for superiority if noninferiority was shown. The study enrolled individuals aged 15 years or older who had rifampicin-resistant TB without fluoroquinolone or aminoglycoside resistance.
The study’s first stage, STREAM stage 1, showed that The 9-month regimen was recommended by the WHO in 2016. That recommendation was superceded in 2020 when concerns of hearing loss associated with aminoglycosides prompted the WHO to endorse a 9-month bedaquiline-containing, injectable-free alternative, the authors write.
Seeking shorter treatment for better outcomes
STREAM stage 2 used a 9-month injectable regimen as its control. The investigators measured it against a fully oral 9-month bedaquiline-based treatment (primary comparison), as well as a 6-month oral bedaquiline regimen that included 8 weeks of a second-line injectable (secondary comparison).
The 9-month fully oral treatment included levofloxacin, clofazimine, ethambutol, and pyrazinamide for 40 weeks; bedaquiline, high-dose isoniazid, and prothionamide were given for the 16-week intensive phase.
The 6-month regimen included bedaquiline, clofazimine, pyrazinamide, and levofloxacin for 28 weeks, supplemented by high-dose isoniazid with kanamycin for an 8-week intensive phase.
For both comparisons, the primary outcome was favorable status at 76 weeks, defined as cultures that were negative for Mycobacterium tuberculosis without a preceding unfavorable outcome (defined as any death, bacteriologic failure or recurrence, or major treatment change).
Among 517 participants in the modified intention-to-treat population across the study groups, 62% were men, and 38% were women (median age, 32.5 years).
For the primary comparison, 71% of the control group and 83% of the oral regimen group had a favorable outcome.
In the secondary comparison, 69% had a favorable outcome in the control group, compared with 91% of those receiving the 6-month regimen.
Although the rate of grade 3 or 4 adverse events was similar in all three groups, there was significantly less ototoxicity among patients who received the oral regimen, compared with control patients (2% vs. 9%); 4% of those taking the 6-month regimen had hearing loss, compared with 8% of control patients.
Exploratory analyses comparing both bedaquiline-containing regimens revealed a significantly higher proportion of favorable outcomes among participants receiving the 6-month regimen (91%), compared with patients taking the fully oral 9-month regimen (79%). There were no significant differences in the rate of grade 3 or 4 adverse events.
The trial’s main limitation was its open-label design, which might have influenced decisions about treatment change, note the investigators.
“STREAM stage 2 has shown that two short-course, bedaquiline-containing regimens are not only non-inferior but superior to a 9-month injectable-containing regimen,” they conclude.
“The STREAM stage 2 fully oral regimen avoided the toxicity of aminoglycosides, and the 6-month regimen was highly effective, with reduced levels of ototoxicity. These two regimens offer promising treatment options for patients with MDR or rifampicin-resistant tuberculosis,” the authors write.
Dr. Goodall added, “Although both STREAM regimens were very effective, participants experienced relatively high levels of adverse events during the trial (though many of these were likely due to the close laboratory monitoring of the trial).
“While hearing loss was reduced on the 6-month regimen, it was not entirely eliminated,” she said. “Other new regimens in the field containing the medicine linezolid report side effects such as anemia and peripheral neuropathy. So more work needs to be done to ensure the treatment regimens are as safe and tolerable for patients as possible. In addition, even 6 months’ treatment is long for patients to tolerate, and further regimen shortening would be a welcome development for patients and health systems.”
‘A revolution in MDR tuberculosis’
“The authors must be commended on completing this challenging high-quality, phase 3, non-inferiority, randomized controlled trial involving 13 health care facilities across Ethiopia, Georgia, India, Moldova, Mongolia, South Africa, and Uganda ... despite the COVID-19 pandemic,” noted Keertan Dheda, MD, PhD, and Christoph Lange, MD, PhD, in an accompanying comment titled, “A Revolution in the Management of Multidrug-Resistant Tuberculosis”.
Although the WHO recently approved an all-oral 6-month bedaquiline, pretomanid, and linezolid plus moxifloxacin (BPaLM) regimen, results from the alternate 6-month regimen examined in STREAM stage 2 “do provide confidence in using 2 months of an injectable as part of a salvage regimen in patients for whom MDR tuberculosis treatment is not successful” or in those with extensively drug-resistant (XDR) or pre-XDR TB, “for whom therapeutic options are few,” noted Dr. Dheda, from the University of Cape Town (South Africa) and the London School of Hygiene and Tropical Medicine, and Dr. Lange, from the University of Lübeck (Germany), Baylor College of Medicine, and Texas Children’s Hospital, both in Houston.
The study authors and the commentators stress that safer and simpler treatments are still needed for MDR TB. “The search is now on for regimens that could further reduce duration, toxicity, and pill burden,” note Dr. Dheda and Dr. Lange.
However, they also note that “substantial resistance” to bedaquiline is already emerging. “Therefore, if we are to protect key drugs from becoming functionally redundant, drug-susceptibility testing capacity will need to be rapidly improved to minimize resistance amplification and onward disease transmission.”
The study was funded by USAID and Janssen Research and Development. Dr. Goodall has disclosed no relevant financial relationships. Dr. Dheda has received funding from the EU and the South African Medical Research Council for studies related to the diagnosis or management of drug-resistant tuberculosis. Dr. Lange is supported by the German Center for Infection Research and has received funding from the European Commission for studies on the development of novel antituberculosis medicines and for studies related to novel diagnostics of tuberculosis; consulting fees from INSMED; speaker’s fees from INSMED, GILEAD, and Janssen; and is a member of the data safety board of trials from Medicines sans Frontiers, all of which are unrelated to the current study.
A version of this article first appeared on Medscape.com.
Two short-course bedaquiline-containing treatment regimens for rifampicin-resistant tuberculosis showed “robust evidence” for superior efficacy and less ototoxicity compared to a 9-month injectable control regimen, researchers report.
The findings validate the World Health Organization’s current recommendation of a 9-month, bedaquiline-based oral regimen, “which was based only on observational data,” noted lead author Ruth Goodall, PhD, from the Medical Research Council Clinical Trials Unit at University College London, and colleagues.
The study was published in The Lancet.
The Standard Treatment Regimen of Anti-tuberculosis Drugs for Patients With MDR-TB (STREAM) stage 2 study was a randomized, phase 3, noninferiority trial conducted at 13 hospital clinics in seven countries that had prespecified tests for superiority if noninferiority was shown. The study enrolled individuals aged 15 years or older who had rifampicin-resistant TB without fluoroquinolone or aminoglycoside resistance.
The study’s first stage, STREAM stage 1, showed that The 9-month regimen was recommended by the WHO in 2016. That recommendation was superceded in 2020 when concerns of hearing loss associated with aminoglycosides prompted the WHO to endorse a 9-month bedaquiline-containing, injectable-free alternative, the authors write.
Seeking shorter treatment for better outcomes
STREAM stage 2 used a 9-month injectable regimen as its control. The investigators measured it against a fully oral 9-month bedaquiline-based treatment (primary comparison), as well as a 6-month oral bedaquiline regimen that included 8 weeks of a second-line injectable (secondary comparison).
The 9-month fully oral treatment included levofloxacin, clofazimine, ethambutol, and pyrazinamide for 40 weeks; bedaquiline, high-dose isoniazid, and prothionamide were given for the 16-week intensive phase.
The 6-month regimen included bedaquiline, clofazimine, pyrazinamide, and levofloxacin for 28 weeks, supplemented by high-dose isoniazid with kanamycin for an 8-week intensive phase.
For both comparisons, the primary outcome was favorable status at 76 weeks, defined as cultures that were negative for Mycobacterium tuberculosis without a preceding unfavorable outcome (defined as any death, bacteriologic failure or recurrence, or major treatment change).
Among 517 participants in the modified intention-to-treat population across the study groups, 62% were men, and 38% were women (median age, 32.5 years).
For the primary comparison, 71% of the control group and 83% of the oral regimen group had a favorable outcome.
In the secondary comparison, 69% had a favorable outcome in the control group, compared with 91% of those receiving the 6-month regimen.
Although the rate of grade 3 or 4 adverse events was similar in all three groups, there was significantly less ototoxicity among patients who received the oral regimen, compared with control patients (2% vs. 9%); 4% of those taking the 6-month regimen had hearing loss, compared with 8% of control patients.
Exploratory analyses comparing both bedaquiline-containing regimens revealed a significantly higher proportion of favorable outcomes among participants receiving the 6-month regimen (91%), compared with patients taking the fully oral 9-month regimen (79%). There were no significant differences in the rate of grade 3 or 4 adverse events.
The trial’s main limitation was its open-label design, which might have influenced decisions about treatment change, note the investigators.
“STREAM stage 2 has shown that two short-course, bedaquiline-containing regimens are not only non-inferior but superior to a 9-month injectable-containing regimen,” they conclude.
“The STREAM stage 2 fully oral regimen avoided the toxicity of aminoglycosides, and the 6-month regimen was highly effective, with reduced levels of ototoxicity. These two regimens offer promising treatment options for patients with MDR or rifampicin-resistant tuberculosis,” the authors write.
Dr. Goodall added, “Although both STREAM regimens were very effective, participants experienced relatively high levels of adverse events during the trial (though many of these were likely due to the close laboratory monitoring of the trial).
“While hearing loss was reduced on the 6-month regimen, it was not entirely eliminated,” she said. “Other new regimens in the field containing the medicine linezolid report side effects such as anemia and peripheral neuropathy. So more work needs to be done to ensure the treatment regimens are as safe and tolerable for patients as possible. In addition, even 6 months’ treatment is long for patients to tolerate, and further regimen shortening would be a welcome development for patients and health systems.”
‘A revolution in MDR tuberculosis’
“The authors must be commended on completing this challenging high-quality, phase 3, non-inferiority, randomized controlled trial involving 13 health care facilities across Ethiopia, Georgia, India, Moldova, Mongolia, South Africa, and Uganda ... despite the COVID-19 pandemic,” noted Keertan Dheda, MD, PhD, and Christoph Lange, MD, PhD, in an accompanying comment titled, “A Revolution in the Management of Multidrug-Resistant Tuberculosis”.
Although the WHO recently approved an all-oral 6-month bedaquiline, pretomanid, and linezolid plus moxifloxacin (BPaLM) regimen, results from the alternate 6-month regimen examined in STREAM stage 2 “do provide confidence in using 2 months of an injectable as part of a salvage regimen in patients for whom MDR tuberculosis treatment is not successful” or in those with extensively drug-resistant (XDR) or pre-XDR TB, “for whom therapeutic options are few,” noted Dr. Dheda, from the University of Cape Town (South Africa) and the London School of Hygiene and Tropical Medicine, and Dr. Lange, from the University of Lübeck (Germany), Baylor College of Medicine, and Texas Children’s Hospital, both in Houston.
The study authors and the commentators stress that safer and simpler treatments are still needed for MDR TB. “The search is now on for regimens that could further reduce duration, toxicity, and pill burden,” note Dr. Dheda and Dr. Lange.
However, they also note that “substantial resistance” to bedaquiline is already emerging. “Therefore, if we are to protect key drugs from becoming functionally redundant, drug-susceptibility testing capacity will need to be rapidly improved to minimize resistance amplification and onward disease transmission.”
The study was funded by USAID and Janssen Research and Development. Dr. Goodall has disclosed no relevant financial relationships. Dr. Dheda has received funding from the EU and the South African Medical Research Council for studies related to the diagnosis or management of drug-resistant tuberculosis. Dr. Lange is supported by the German Center for Infection Research and has received funding from the European Commission for studies on the development of novel antituberculosis medicines and for studies related to novel diagnostics of tuberculosis; consulting fees from INSMED; speaker’s fees from INSMED, GILEAD, and Janssen; and is a member of the data safety board of trials from Medicines sans Frontiers, all of which are unrelated to the current study.
A version of this article first appeared on Medscape.com.
Two short-course bedaquiline-containing treatment regimens for rifampicin-resistant tuberculosis showed “robust evidence” for superior efficacy and less ototoxicity compared to a 9-month injectable control regimen, researchers report.
The findings validate the World Health Organization’s current recommendation of a 9-month, bedaquiline-based oral regimen, “which was based only on observational data,” noted lead author Ruth Goodall, PhD, from the Medical Research Council Clinical Trials Unit at University College London, and colleagues.
The study was published in The Lancet.
The Standard Treatment Regimen of Anti-tuberculosis Drugs for Patients With MDR-TB (STREAM) stage 2 study was a randomized, phase 3, noninferiority trial conducted at 13 hospital clinics in seven countries that had prespecified tests for superiority if noninferiority was shown. The study enrolled individuals aged 15 years or older who had rifampicin-resistant TB without fluoroquinolone or aminoglycoside resistance.
The study’s first stage, STREAM stage 1, showed that The 9-month regimen was recommended by the WHO in 2016. That recommendation was superceded in 2020 when concerns of hearing loss associated with aminoglycosides prompted the WHO to endorse a 9-month bedaquiline-containing, injectable-free alternative, the authors write.
Seeking shorter treatment for better outcomes
STREAM stage 2 used a 9-month injectable regimen as its control. The investigators measured it against a fully oral 9-month bedaquiline-based treatment (primary comparison), as well as a 6-month oral bedaquiline regimen that included 8 weeks of a second-line injectable (secondary comparison).
The 9-month fully oral treatment included levofloxacin, clofazimine, ethambutol, and pyrazinamide for 40 weeks; bedaquiline, high-dose isoniazid, and prothionamide were given for the 16-week intensive phase.
The 6-month regimen included bedaquiline, clofazimine, pyrazinamide, and levofloxacin for 28 weeks, supplemented by high-dose isoniazid with kanamycin for an 8-week intensive phase.
For both comparisons, the primary outcome was favorable status at 76 weeks, defined as cultures that were negative for Mycobacterium tuberculosis without a preceding unfavorable outcome (defined as any death, bacteriologic failure or recurrence, or major treatment change).
Among 517 participants in the modified intention-to-treat population across the study groups, 62% were men, and 38% were women (median age, 32.5 years).
For the primary comparison, 71% of the control group and 83% of the oral regimen group had a favorable outcome.
In the secondary comparison, 69% had a favorable outcome in the control group, compared with 91% of those receiving the 6-month regimen.
Although the rate of grade 3 or 4 adverse events was similar in all three groups, there was significantly less ototoxicity among patients who received the oral regimen, compared with control patients (2% vs. 9%); 4% of those taking the 6-month regimen had hearing loss, compared with 8% of control patients.
Exploratory analyses comparing both bedaquiline-containing regimens revealed a significantly higher proportion of favorable outcomes among participants receiving the 6-month regimen (91%), compared with patients taking the fully oral 9-month regimen (79%). There were no significant differences in the rate of grade 3 or 4 adverse events.
The trial’s main limitation was its open-label design, which might have influenced decisions about treatment change, note the investigators.
“STREAM stage 2 has shown that two short-course, bedaquiline-containing regimens are not only non-inferior but superior to a 9-month injectable-containing regimen,” they conclude.
“The STREAM stage 2 fully oral regimen avoided the toxicity of aminoglycosides, and the 6-month regimen was highly effective, with reduced levels of ototoxicity. These two regimens offer promising treatment options for patients with MDR or rifampicin-resistant tuberculosis,” the authors write.
Dr. Goodall added, “Although both STREAM regimens were very effective, participants experienced relatively high levels of adverse events during the trial (though many of these were likely due to the close laboratory monitoring of the trial).
“While hearing loss was reduced on the 6-month regimen, it was not entirely eliminated,” she said. “Other new regimens in the field containing the medicine linezolid report side effects such as anemia and peripheral neuropathy. So more work needs to be done to ensure the treatment regimens are as safe and tolerable for patients as possible. In addition, even 6 months’ treatment is long for patients to tolerate, and further regimen shortening would be a welcome development for patients and health systems.”
‘A revolution in MDR tuberculosis’
“The authors must be commended on completing this challenging high-quality, phase 3, non-inferiority, randomized controlled trial involving 13 health care facilities across Ethiopia, Georgia, India, Moldova, Mongolia, South Africa, and Uganda ... despite the COVID-19 pandemic,” noted Keertan Dheda, MD, PhD, and Christoph Lange, MD, PhD, in an accompanying comment titled, “A Revolution in the Management of Multidrug-Resistant Tuberculosis”.
Although the WHO recently approved an all-oral 6-month bedaquiline, pretomanid, and linezolid plus moxifloxacin (BPaLM) regimen, results from the alternate 6-month regimen examined in STREAM stage 2 “do provide confidence in using 2 months of an injectable as part of a salvage regimen in patients for whom MDR tuberculosis treatment is not successful” or in those with extensively drug-resistant (XDR) or pre-XDR TB, “for whom therapeutic options are few,” noted Dr. Dheda, from the University of Cape Town (South Africa) and the London School of Hygiene and Tropical Medicine, and Dr. Lange, from the University of Lübeck (Germany), Baylor College of Medicine, and Texas Children’s Hospital, both in Houston.
The study authors and the commentators stress that safer and simpler treatments are still needed for MDR TB. “The search is now on for regimens that could further reduce duration, toxicity, and pill burden,” note Dr. Dheda and Dr. Lange.
However, they also note that “substantial resistance” to bedaquiline is already emerging. “Therefore, if we are to protect key drugs from becoming functionally redundant, drug-susceptibility testing capacity will need to be rapidly improved to minimize resistance amplification and onward disease transmission.”
The study was funded by USAID and Janssen Research and Development. Dr. Goodall has disclosed no relevant financial relationships. Dr. Dheda has received funding from the EU and the South African Medical Research Council for studies related to the diagnosis or management of drug-resistant tuberculosis. Dr. Lange is supported by the German Center for Infection Research and has received funding from the European Commission for studies on the development of novel antituberculosis medicines and for studies related to novel diagnostics of tuberculosis; consulting fees from INSMED; speaker’s fees from INSMED, GILEAD, and Janssen; and is a member of the data safety board of trials from Medicines sans Frontiers, all of which are unrelated to the current study.
A version of this article first appeared on Medscape.com.




