User login
-
Blood group O linked to decreased risk of SARS-CoV-2 infection
Blood group O was associated with a decreased risk for contracting SARS-CoV-2 infection, according to the results of large retrospective analysis of the Danish population.
Researchers Mike Bogetofte Barnkob, MD, of the Department of Clinical Immunology, Odense (Denmark) University Hospital, and colleagues performed a retrospective cohort analysis of all Danish individuals with a known ABO blood group who were tested for SARS-CoV-2 between Feb. 27, 2020, and July 30, 2020.
Of the 841,327 people tested, ABO and RhD blood groups could be identified for 473,654 individuals. ABO and RhD data from 2,204,742 (38% of the entire Danish population) were used as a reference, according to the online report in Blood Advances.
The primary outcome was status of ABO and RhD blood groups and test results for SARS-CoV-2. The secondary outcomes followed were hospitalization and death from COVID-19.
Reduced prevalence
The study found that ABO blood groups varied significantly between patients and the reference group, with only 38.41% (95% confidence interval, 37.30%-39.50%) of the patients belonging to blood group O, compared with 41.70% (95% CI, 41.60%-41.80%) in the controls, corresponding to a relative risk of 0.87 (95% CI, 0.83-0.91) for acquiring COVID-19.
There was a slight, but statistically significant, difference in blood group distribution between the SARS-CoV-22 individuals and the reference population (P < .001), according to the authors.
Among the SARS-CoV-2 individuals, fewer group O individuals were found (P < .001); while more A, B, and AB individuals were seen (P < .001, P = .011, and P = .091, respectively). There was no significant difference seen among A, B, and AB blood groups (P = .30). The RR for contracting SARS-CoV-2 were 1.09 (95% CI, 1.04-1.14) for A group individuals; 1.06 (95% CI, 0.99-1.14) for B group; and 1.15 (95% CI, 1.03-1.27) for AB group, respectively.
There was no difference found in the RhD group between positive test cases and the reference population (P = .15). In addition, there was no statistical difference (all P > .40) between ABO blood groups and clinical severity of COVID-19 for nonhospitalized patients versus hospitalized patients or for deceased patients versus living patients, the researchers added.
Possible causes
The authors speculated on two possible causes of the lower prevalence of SARS-CoV-2 infection in the blood group O population. The first is that anti-A and anti-B antibodies may have an effect on neutralizing SARS-CoV viruses and that anti-A and anti-B are present on mucosal surfaces in some individuals lacking the corresponding ABO blood group. The second is that the association between ABO blood groups and levels of von Willebrand factor, which is higher in non-O individuals and is tied to an increased likelihood of arterial and venous thrombosis, could have an indirect or unknown impact on susceptibility to infection, according to the authors.
“Given the known increased risk of thrombosis in non-O individuals and the evolving central role for thrombosis in the pathogenesis of COVID-19, it is important to explore this aspect more closely in larger patient cohorts (e.g., by examining ABO blood type and viral load, the severity of symptoms, and the long-term effects following COVID-19),” the researchers concluded.
One author reported receiving fees from Bristol Myers Squibb, Novartis, and Roche. The remaining authors reported they had no competing financial interests.
SOURCE: Barnkob MB et al. Blood Adv. 2020 Oct 14. doi: 10.1182/bloodadvances.2020002657.
Blood group O was associated with a decreased risk for contracting SARS-CoV-2 infection, according to the results of large retrospective analysis of the Danish population.
Researchers Mike Bogetofte Barnkob, MD, of the Department of Clinical Immunology, Odense (Denmark) University Hospital, and colleagues performed a retrospective cohort analysis of all Danish individuals with a known ABO blood group who were tested for SARS-CoV-2 between Feb. 27, 2020, and July 30, 2020.
Of the 841,327 people tested, ABO and RhD blood groups could be identified for 473,654 individuals. ABO and RhD data from 2,204,742 (38% of the entire Danish population) were used as a reference, according to the online report in Blood Advances.
The primary outcome was status of ABO and RhD blood groups and test results for SARS-CoV-2. The secondary outcomes followed were hospitalization and death from COVID-19.
Reduced prevalence
The study found that ABO blood groups varied significantly between patients and the reference group, with only 38.41% (95% confidence interval, 37.30%-39.50%) of the patients belonging to blood group O, compared with 41.70% (95% CI, 41.60%-41.80%) in the controls, corresponding to a relative risk of 0.87 (95% CI, 0.83-0.91) for acquiring COVID-19.
There was a slight, but statistically significant, difference in blood group distribution between the SARS-CoV-22 individuals and the reference population (P < .001), according to the authors.
Among the SARS-CoV-2 individuals, fewer group O individuals were found (P < .001); while more A, B, and AB individuals were seen (P < .001, P = .011, and P = .091, respectively). There was no significant difference seen among A, B, and AB blood groups (P = .30). The RR for contracting SARS-CoV-2 were 1.09 (95% CI, 1.04-1.14) for A group individuals; 1.06 (95% CI, 0.99-1.14) for B group; and 1.15 (95% CI, 1.03-1.27) for AB group, respectively.
There was no difference found in the RhD group between positive test cases and the reference population (P = .15). In addition, there was no statistical difference (all P > .40) between ABO blood groups and clinical severity of COVID-19 for nonhospitalized patients versus hospitalized patients or for deceased patients versus living patients, the researchers added.
Possible causes
The authors speculated on two possible causes of the lower prevalence of SARS-CoV-2 infection in the blood group O population. The first is that anti-A and anti-B antibodies may have an effect on neutralizing SARS-CoV viruses and that anti-A and anti-B are present on mucosal surfaces in some individuals lacking the corresponding ABO blood group. The second is that the association between ABO blood groups and levels of von Willebrand factor, which is higher in non-O individuals and is tied to an increased likelihood of arterial and venous thrombosis, could have an indirect or unknown impact on susceptibility to infection, according to the authors.
“Given the known increased risk of thrombosis in non-O individuals and the evolving central role for thrombosis in the pathogenesis of COVID-19, it is important to explore this aspect more closely in larger patient cohorts (e.g., by examining ABO blood type and viral load, the severity of symptoms, and the long-term effects following COVID-19),” the researchers concluded.
One author reported receiving fees from Bristol Myers Squibb, Novartis, and Roche. The remaining authors reported they had no competing financial interests.
SOURCE: Barnkob MB et al. Blood Adv. 2020 Oct 14. doi: 10.1182/bloodadvances.2020002657.
Blood group O was associated with a decreased risk for contracting SARS-CoV-2 infection, according to the results of large retrospective analysis of the Danish population.
Researchers Mike Bogetofte Barnkob, MD, of the Department of Clinical Immunology, Odense (Denmark) University Hospital, and colleagues performed a retrospective cohort analysis of all Danish individuals with a known ABO blood group who were tested for SARS-CoV-2 between Feb. 27, 2020, and July 30, 2020.
Of the 841,327 people tested, ABO and RhD blood groups could be identified for 473,654 individuals. ABO and RhD data from 2,204,742 (38% of the entire Danish population) were used as a reference, according to the online report in Blood Advances.
The primary outcome was status of ABO and RhD blood groups and test results for SARS-CoV-2. The secondary outcomes followed were hospitalization and death from COVID-19.
Reduced prevalence
The study found that ABO blood groups varied significantly between patients and the reference group, with only 38.41% (95% confidence interval, 37.30%-39.50%) of the patients belonging to blood group O, compared with 41.70% (95% CI, 41.60%-41.80%) in the controls, corresponding to a relative risk of 0.87 (95% CI, 0.83-0.91) for acquiring COVID-19.
There was a slight, but statistically significant, difference in blood group distribution between the SARS-CoV-22 individuals and the reference population (P < .001), according to the authors.
Among the SARS-CoV-2 individuals, fewer group O individuals were found (P < .001); while more A, B, and AB individuals were seen (P < .001, P = .011, and P = .091, respectively). There was no significant difference seen among A, B, and AB blood groups (P = .30). The RR for contracting SARS-CoV-2 were 1.09 (95% CI, 1.04-1.14) for A group individuals; 1.06 (95% CI, 0.99-1.14) for B group; and 1.15 (95% CI, 1.03-1.27) for AB group, respectively.
There was no difference found in the RhD group between positive test cases and the reference population (P = .15). In addition, there was no statistical difference (all P > .40) between ABO blood groups and clinical severity of COVID-19 for nonhospitalized patients versus hospitalized patients or for deceased patients versus living patients, the researchers added.
Possible causes
The authors speculated on two possible causes of the lower prevalence of SARS-CoV-2 infection in the blood group O population. The first is that anti-A and anti-B antibodies may have an effect on neutralizing SARS-CoV viruses and that anti-A and anti-B are present on mucosal surfaces in some individuals lacking the corresponding ABO blood group. The second is that the association between ABO blood groups and levels of von Willebrand factor, which is higher in non-O individuals and is tied to an increased likelihood of arterial and venous thrombosis, could have an indirect or unknown impact on susceptibility to infection, according to the authors.
“Given the known increased risk of thrombosis in non-O individuals and the evolving central role for thrombosis in the pathogenesis of COVID-19, it is important to explore this aspect more closely in larger patient cohorts (e.g., by examining ABO blood type and viral load, the severity of symptoms, and the long-term effects following COVID-19),” the researchers concluded.
One author reported receiving fees from Bristol Myers Squibb, Novartis, and Roche. The remaining authors reported they had no competing financial interests.
SOURCE: Barnkob MB et al. Blood Adv. 2020 Oct 14. doi: 10.1182/bloodadvances.2020002657.
FROM BLOOD ADVANCES
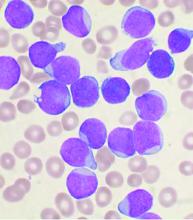
Study: Complications from childhood ALL and its treatment are common, but can be managed
Despite survival after treatment of acute lymphoblastic leukemia (ALL), a high percentage of children suffered acute complications, even without relapse, according to a report published online in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study of 110 children with acute lymphoblastic leukemia (ALL), Ayse Pınar Öztürk, MD, and colleagues at Istanbul University, Cerrahpasa Faculty of Medicine, evaluated the acute complications that occurred during the treatment of childhood ALL and documented their survival rates. The 110 patients, comprising 65 boys and 45 girls, were all treated with the Children’s Oncology Group protocol from 1999 to 2014.
The mean age at admission was 8.3 years and 97 patients (88.2%) were diagnosed with pre–B-cell ALL, 11 (10%) with T-cell ALL, 1 (0.9%) with mixed phenotype acute leukemia, and 1 (0.9%) with mature B-cell acute leukemia. A total of 36.3% were evaluated to be in the standard-risk group and the rest were in the high-risk group. Regular follow-up and evaluation for acute complications was available for 105 of the patients.
Survival and complications
Of the 110 patients, 98 were assessed in the survival analyses. The 5- and 10-year overall survival rates were both 85.9%, while the relapse-free survival rates at 1, 3, and 5 years were 97.9%, 91.3%, and 86.3%, respectively. These results are favorable and in line with good results reported in the literature, according to the researchers.
In terms of acute complications, infection was the most common (88.5%), followed by gastrointestinal (27.6%), neurologic (26.6%), metabolic/endocrine (15.2%), drug-related hypersensitivity (15.2%), avascular necrosis (12.3%), thrombotic (10.4%), severe psychiatric (1.9%), and various other complications (11.4%).
In the present study, 13 of the 98 patients (13.3%) died. All 13 patients had been in the high-risk group and 9 had had relapsed ALL. Of the 13 deaths, 8 (8.2%) had resulted from treatment resistance and toxicity and 5 (5.1%) from severe infection (sepsis).
During ALL treatment, various complications can occur related to the disease itself or the treatment, according to the authors. However, they added that in regularly and closely monitored patients, complications can be effectively prevented, treated, and eliminated by aggressive observation and prompt intervention.
“In our study, the short hospitalization period, prompt implementation of protocol updates, rapid analysis of laboratory tests, continuous supportive care, efficient education given to the parents of children, and consistently undertaking patient care and treatment management by the same expert team increased the success of the therapy and ensured low complication rates,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Öztürk AP et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 17. doi: 10.1016/j.clml.2020.08.025.
Despite survival after treatment of acute lymphoblastic leukemia (ALL), a high percentage of children suffered acute complications, even without relapse, according to a report published online in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study of 110 children with acute lymphoblastic leukemia (ALL), Ayse Pınar Öztürk, MD, and colleagues at Istanbul University, Cerrahpasa Faculty of Medicine, evaluated the acute complications that occurred during the treatment of childhood ALL and documented their survival rates. The 110 patients, comprising 65 boys and 45 girls, were all treated with the Children’s Oncology Group protocol from 1999 to 2014.
The mean age at admission was 8.3 years and 97 patients (88.2%) were diagnosed with pre–B-cell ALL, 11 (10%) with T-cell ALL, 1 (0.9%) with mixed phenotype acute leukemia, and 1 (0.9%) with mature B-cell acute leukemia. A total of 36.3% were evaluated to be in the standard-risk group and the rest were in the high-risk group. Regular follow-up and evaluation for acute complications was available for 105 of the patients.
Survival and complications
Of the 110 patients, 98 were assessed in the survival analyses. The 5- and 10-year overall survival rates were both 85.9%, while the relapse-free survival rates at 1, 3, and 5 years were 97.9%, 91.3%, and 86.3%, respectively. These results are favorable and in line with good results reported in the literature, according to the researchers.
In terms of acute complications, infection was the most common (88.5%), followed by gastrointestinal (27.6%), neurologic (26.6%), metabolic/endocrine (15.2%), drug-related hypersensitivity (15.2%), avascular necrosis (12.3%), thrombotic (10.4%), severe psychiatric (1.9%), and various other complications (11.4%).
In the present study, 13 of the 98 patients (13.3%) died. All 13 patients had been in the high-risk group and 9 had had relapsed ALL. Of the 13 deaths, 8 (8.2%) had resulted from treatment resistance and toxicity and 5 (5.1%) from severe infection (sepsis).
During ALL treatment, various complications can occur related to the disease itself or the treatment, according to the authors. However, they added that in regularly and closely monitored patients, complications can be effectively prevented, treated, and eliminated by aggressive observation and prompt intervention.
“In our study, the short hospitalization period, prompt implementation of protocol updates, rapid analysis of laboratory tests, continuous supportive care, efficient education given to the parents of children, and consistently undertaking patient care and treatment management by the same expert team increased the success of the therapy and ensured low complication rates,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Öztürk AP et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 17. doi: 10.1016/j.clml.2020.08.025.
Despite survival after treatment of acute lymphoblastic leukemia (ALL), a high percentage of children suffered acute complications, even without relapse, according to a report published online in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study of 110 children with acute lymphoblastic leukemia (ALL), Ayse Pınar Öztürk, MD, and colleagues at Istanbul University, Cerrahpasa Faculty of Medicine, evaluated the acute complications that occurred during the treatment of childhood ALL and documented their survival rates. The 110 patients, comprising 65 boys and 45 girls, were all treated with the Children’s Oncology Group protocol from 1999 to 2014.
The mean age at admission was 8.3 years and 97 patients (88.2%) were diagnosed with pre–B-cell ALL, 11 (10%) with T-cell ALL, 1 (0.9%) with mixed phenotype acute leukemia, and 1 (0.9%) with mature B-cell acute leukemia. A total of 36.3% were evaluated to be in the standard-risk group and the rest were in the high-risk group. Regular follow-up and evaluation for acute complications was available for 105 of the patients.
Survival and complications
Of the 110 patients, 98 were assessed in the survival analyses. The 5- and 10-year overall survival rates were both 85.9%, while the relapse-free survival rates at 1, 3, and 5 years were 97.9%, 91.3%, and 86.3%, respectively. These results are favorable and in line with good results reported in the literature, according to the researchers.
In terms of acute complications, infection was the most common (88.5%), followed by gastrointestinal (27.6%), neurologic (26.6%), metabolic/endocrine (15.2%), drug-related hypersensitivity (15.2%), avascular necrosis (12.3%), thrombotic (10.4%), severe psychiatric (1.9%), and various other complications (11.4%).
In the present study, 13 of the 98 patients (13.3%) died. All 13 patients had been in the high-risk group and 9 had had relapsed ALL. Of the 13 deaths, 8 (8.2%) had resulted from treatment resistance and toxicity and 5 (5.1%) from severe infection (sepsis).
During ALL treatment, various complications can occur related to the disease itself or the treatment, according to the authors. However, they added that in regularly and closely monitored patients, complications can be effectively prevented, treated, and eliminated by aggressive observation and prompt intervention.
“In our study, the short hospitalization period, prompt implementation of protocol updates, rapid analysis of laboratory tests, continuous supportive care, efficient education given to the parents of children, and consistently undertaking patient care and treatment management by the same expert team increased the success of the therapy and ensured low complication rates,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Öztürk AP et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 17. doi: 10.1016/j.clml.2020.08.025.
FROM Clinical Lymphoma, Myeloma & Leukemia
A uniquely patient-focused take on treating AML in older adults
A diagnosis of acute myeloid leukemia (AML) is particularly challenging in older adults, whose age makes them highly susceptible to the disease and treatment-related toxicity. To help patients and practitioners navigate the clinical decision-making process, the American Society of Hematology convened a panel of experts who conducted a thorough review of the literature. The result of their work can be found in a new set of guidelines for the treatment of newly diagnosed AML in older adults.
In an interview, Mikkael Sekeres, MD, chair of the ASH AML guideline panel and director of the Leukemia Program at Cleveland Clinic Taussig Cancer Institute in Cleveland, Ohio, shared the rationale behind the panel’s key recommendations and the importance of keeping the patient’s goals in mind.
Question: What is the average life expectancy of a 75-year-old developing AML compared with someone of the same age without AML?
Dr. Sekeres: A 75-year-old developing AML has an average life expectancy measured in fewer than 6 months. Somebody who is 75 without leukemia in the United States has a life expectancy that can be measured in a decade or more. AML is a really serious diagnosis when someone is older and significantly truncates expected survival.
Q: What is the median age at AML diagnosis in the United States?
Dr. Sekeres: About 67 years.
Q: What are the biological underpinnings for poor outcomes in older AML patients?
Dr. Sekeres: There are a few of them. Older adults with AML tend to have a leukemia that has evolved from a known or unknown previous bone marrow condition such as myelodysplastic syndrome. Older adults also have worse genetics driving their leukemia, which makes the leukemia cells more resistant to chemotherapy. And the leukemia cells may even have drug efflux pumps that extrude chemotherapy that tries to enter the cell. Finally, older adults are more likely to have comorbidities that make their ability to tolerate chemotherapy much lower than for younger adults.
Q: In someone who is newly diagnosed with AML, what initial options are they routinely given?
Dr. Sekeres: For someone who is older, we divide those options into three main categories.
The first is to take intensive chemotherapy, which requires a 4-6 week hospitalization and has a chance of getting somebody who is older into a remission of approximately 50%-60%. But this also carries with it significant treatment-related mortality that may be as high as 10%-20%. So I have to look my older patients in the eyes when I talk about intensive chemotherapy and say, “There is a 1 in 10 or 1 in 5 chance that you might not make it out of the hospital alive.”
The second prong is lower-dose therapy. While the more-intensive therapy requiring hospitalization does have a low, but real, chance of curing that person, less-intensive therapy is not curative. Our best hope with less-intensive therapy is that our patients enter a remission and live longer. With less-intensive therapy, the chance that someone will go into remission is probably around 20%, but again it is not curative. The flip side to that is that it improves a person’s immediate quality of life because they’re not in the hospital for 4-6 weeks.
The final prong is to discuss palliative care or hospice upfront. We designed these guidelines to be focused on a patient’s goals of therapy and to constantly revisit those goals to make sure that the treatment options we are offering are aligning with them.
Q: The panel’s first recommendation is to offer antileukemic therapy over best supportive care in patients who are appropriate candidates. Can you provide some context for this recommendation?
Dr. Sekeres: Doesn’t that strike you as funny that we even have to make a recommendation about getting chemotherapy? Some database studies conducted over the past 2 decades show that, as recently as 15 years ago, only one-third of patients who were over the age of 65 years received any type of chemotherapy for AML. More recently, as we have had a few more drugs available that allow us to use lower-dose approaches, that number has crept up to probably about 50%. We still have half the patients offered no therapy at all. So we felt that we had to deliberately make a recommendation saying that, if it aligns with the patients’ goals, they should be offered chemotherapy.
Q: The second recommendation is that patients considered candidates for intensive antileukemic therapy should receive it over less-intensive antileukemic therapy. How did you get to that recommendation?
Dr. Sekeres: There is a debate in our field about whether older adults should be offered intensive inpatient chemotherapy at all or whether we should be treating all of them with less-intensive therapy. There is not a huge amount of high-quality studies out there to answer some of these questions, in particular whether intensive chemotherapy should be recommended over less-intensive therapy. But with the available evidence, what we believe is that patients live longer if they are offered intensive antileukemic chemotherapy. So again, if it aligns with a patient’s goals, we support that patient receiving more-intensive therapy in the hospital.
Q: What does the panel recommend for patients who achieve remission after at least a single cycle of intensive antileukemic therapy and who are not candidates for allogeneic hematopoietic stem cell transplantation?
Dr. Sekeres: Once again, this may seem at first blush to be an obvious recommendation. The standard treatment of someone who is younger with AML is to offer intensive inpatient chemotherapy to induce remission. This is followed by a few cycles of chemotherapy, mostly in an outpatient setting, to consolidate that remission.
Q: What is the underlying philosophy for this approach?
Dr. Sekeres: Every time we give chemotherapy, we probably get about a 3-4 log kill of leukemia cells. Imagine when patients first present with AML, they may have 10 billion leukemia cells in their body. We are reducing that 3-4 log with the first course of chemotherapy.
When we then look at a bone marrow biopsy, it may appear to be normal. When leukemia is at a lower level in the body, we simply can’t see it using standard techniques. But that doesn’t mean the leukemia is gone. For younger patients, we give another cycle of chemotherapy, then another, then another, and then even another to reduce the number of leukemia cells left over in the body until that person has a durable remission and hopefully cure.
For someone who is older, the data are less clear. While some studies have shown that, if you give too much chemotherapy after the initial course, it doesn’t help that much, there is a paucity of studies that show that any chemotherapy at all after the first induction course is helpful. Consequently, we have to use indirect data. Older people who are long-term survivors from their acute leukemia always seem to have gotten more than one course of chemotherapy. In other words, the initial course of chemotherapy that a patient receives in the hospital isn’t enough. They should receive more than that.
Q: What about older adults with AML considered appropriate for antileukemic therapy but not for intensive antileukemic therapy?
Dr. Sekeres: This again gets to the question of what are a patient’s goals. It takes a very involved conversation with patients at the time of their AML diagnosis to determine whether they would want to pursue an aggressive approach or a less-aggressive approach. If a patients want a less-aggressive approach, and want nothing to do with a hospital stay, then they are also prioritizing initial quality of life. In this recommendation, based on existing studies, we didn’t have a preference for which of the available less-aggressive chemotherapies a person selects.
There’s also debate about what to do in those considered appropriate for antileukemic therapy, such as hypomethylating agents (azacitidine and decitabine) or low-dose cytarabine, but not for intensive antileukemic therapy. What did the available evidence seem to indicate about this issue?
There has been a lot of studies trying to add two drugs together to see if those do better than one drug alone in patients who are older and who choose less-intensive therapy. The majority of those studies have shown no advantage to getting two drugs over one drug.
Our recommendation is that in these situations a patient gets one drug, not two, but there are a couple of caveats. One caveat is that there has been a small study showing the effectiveness of one of those low-dose chemotherapies combined with the drug glasdegib. The second caveat is that there have been results presented combining one of these low-dose chemotherapies with the drug venetoclax. One of those was a negative study, and another was a positive study showing a survival advantage to the combination vs. the low-dose therapy alone. We had to couch our recommendation a little bit because we knew this other study had been presented at a conference, but it hadn’t come out in final form yet. It did recently, however, and we will now revisit this recommendation.
The other complicated aspect to this is that we weren’t 100% convinced that the combination of venetoclax with one of these lower-dose therapies is truly less-intensive therapy. We think it is starting to creep up toward more-intensive chemotherapy, even though it is commonly given to patients in the outpatient setting. It gets into the very complicated area of what are we defining as more-intensive therapy and less-intensive therapy.
Q: Is there a recommended strategy for older adults with AML who achieve a response after receiving less-intensive therapy?
Dr. Sekeres: This is also challenging because there are no randomized studies in which patients received less-intensive therapy for a finite period of time vs. receiving those therapies ad infinitum. Given the lack of data and also given a lot of anecdotal data out there about patients who stopped a certain therapy and relapsed thereafter, we recommended that patients continue the less-intensive therapy ad infinitum. So as long as they are receiving a response to that therapy, they continue on the drug.
Q: Of course, there are also unique considerations faced by older patients who are no longer receiving antileukemic therapy and have moved on to receiving end-of-life care or hospice care. What advice do the guidelines offer in this situation?
Dr. Sekeres: There are a lot of aspects of these recommendations that I think are special. The first is the focus on patient goals of care at every point in these guidelines. The second is that the guidelines follow the real disease course and a real conversation that doctors and patients have at every step of the way to help guide the decisions that have to be made in real time.
A problem we have in the United States is that once patients enter a hospice, most will not allow blood transfusions. One reason is that some say it is antithetical to their philosophy and consider it aggressive care. The second reason is that, to be completely blunt, economically it doesn’t make sense for hospices to allow blood transfusions. The amount that they are reimbursed by Medicare is much lower than the cost of receiving blood in an infusion center.
We wanted to make a clear recommendation that we consider transfusions in a patient who is in a palliative care or hospice mode to be supportive and necessary, and that these should be provided to patients even if they are in hospice and, as always, if consistent with a patient’s goals of care.
Q: How does a patient’s age inform the discussion surrounding what intensity treatment to offer?
Dr. Sekeres: With younger adults, this is not as complicated a conversation. A younger person has a better chance of being cured with intensive chemotherapy and is much more likely to tolerate that intensive chemotherapy. For someone who is younger, we offer intensive chemotherapy and the chance of going into remission is higher, at 70%-80%. The chance of dying is lower, usually less than 5%. It is an easy decision to make.
For an older adult, the risk-benefit ratio shifts and it becomes a more complicated option. Less-intensive therapy or best supportive care or hospice become viable.
Q: Are there other factors confounding the treatment decision-making process in older adults with AML that practitioners should consider?
Dr. Sekeres: Someone who is older is making a different decision than I would. I have school-aged children and believe that my job as a parent is to successfully get them to adulthood, so I would take any treatment under the sun to make sure that happens. People who have lived a longer life than I have may have children and even grandchildren who are adults, and they might have different goals of care. My goals are not going to be the same as my patient’s goals.
It is also harder because patients who are older may feel that they have lived a good life and don’t need to go through heroic measures to try to be around as long as possible, and those goals may not align with the goals of that person’s children who want their parent to be around as long as possible. One of the confounding factors in this is navigating the different goals of the different family members.
Dr. Sekeres has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A diagnosis of acute myeloid leukemia (AML) is particularly challenging in older adults, whose age makes them highly susceptible to the disease and treatment-related toxicity. To help patients and practitioners navigate the clinical decision-making process, the American Society of Hematology convened a panel of experts who conducted a thorough review of the literature. The result of their work can be found in a new set of guidelines for the treatment of newly diagnosed AML in older adults.
In an interview, Mikkael Sekeres, MD, chair of the ASH AML guideline panel and director of the Leukemia Program at Cleveland Clinic Taussig Cancer Institute in Cleveland, Ohio, shared the rationale behind the panel’s key recommendations and the importance of keeping the patient’s goals in mind.
Question: What is the average life expectancy of a 75-year-old developing AML compared with someone of the same age without AML?
Dr. Sekeres: A 75-year-old developing AML has an average life expectancy measured in fewer than 6 months. Somebody who is 75 without leukemia in the United States has a life expectancy that can be measured in a decade or more. AML is a really serious diagnosis when someone is older and significantly truncates expected survival.
Q: What is the median age at AML diagnosis in the United States?
Dr. Sekeres: About 67 years.
Q: What are the biological underpinnings for poor outcomes in older AML patients?
Dr. Sekeres: There are a few of them. Older adults with AML tend to have a leukemia that has evolved from a known or unknown previous bone marrow condition such as myelodysplastic syndrome. Older adults also have worse genetics driving their leukemia, which makes the leukemia cells more resistant to chemotherapy. And the leukemia cells may even have drug efflux pumps that extrude chemotherapy that tries to enter the cell. Finally, older adults are more likely to have comorbidities that make their ability to tolerate chemotherapy much lower than for younger adults.
Q: In someone who is newly diagnosed with AML, what initial options are they routinely given?
Dr. Sekeres: For someone who is older, we divide those options into three main categories.
The first is to take intensive chemotherapy, which requires a 4-6 week hospitalization and has a chance of getting somebody who is older into a remission of approximately 50%-60%. But this also carries with it significant treatment-related mortality that may be as high as 10%-20%. So I have to look my older patients in the eyes when I talk about intensive chemotherapy and say, “There is a 1 in 10 or 1 in 5 chance that you might not make it out of the hospital alive.”
The second prong is lower-dose therapy. While the more-intensive therapy requiring hospitalization does have a low, but real, chance of curing that person, less-intensive therapy is not curative. Our best hope with less-intensive therapy is that our patients enter a remission and live longer. With less-intensive therapy, the chance that someone will go into remission is probably around 20%, but again it is not curative. The flip side to that is that it improves a person’s immediate quality of life because they’re not in the hospital for 4-6 weeks.
The final prong is to discuss palliative care or hospice upfront. We designed these guidelines to be focused on a patient’s goals of therapy and to constantly revisit those goals to make sure that the treatment options we are offering are aligning with them.
Q: The panel’s first recommendation is to offer antileukemic therapy over best supportive care in patients who are appropriate candidates. Can you provide some context for this recommendation?
Dr. Sekeres: Doesn’t that strike you as funny that we even have to make a recommendation about getting chemotherapy? Some database studies conducted over the past 2 decades show that, as recently as 15 years ago, only one-third of patients who were over the age of 65 years received any type of chemotherapy for AML. More recently, as we have had a few more drugs available that allow us to use lower-dose approaches, that number has crept up to probably about 50%. We still have half the patients offered no therapy at all. So we felt that we had to deliberately make a recommendation saying that, if it aligns with the patients’ goals, they should be offered chemotherapy.
Q: The second recommendation is that patients considered candidates for intensive antileukemic therapy should receive it over less-intensive antileukemic therapy. How did you get to that recommendation?
Dr. Sekeres: There is a debate in our field about whether older adults should be offered intensive inpatient chemotherapy at all or whether we should be treating all of them with less-intensive therapy. There is not a huge amount of high-quality studies out there to answer some of these questions, in particular whether intensive chemotherapy should be recommended over less-intensive therapy. But with the available evidence, what we believe is that patients live longer if they are offered intensive antileukemic chemotherapy. So again, if it aligns with a patient’s goals, we support that patient receiving more-intensive therapy in the hospital.
Q: What does the panel recommend for patients who achieve remission after at least a single cycle of intensive antileukemic therapy and who are not candidates for allogeneic hematopoietic stem cell transplantation?
Dr. Sekeres: Once again, this may seem at first blush to be an obvious recommendation. The standard treatment of someone who is younger with AML is to offer intensive inpatient chemotherapy to induce remission. This is followed by a few cycles of chemotherapy, mostly in an outpatient setting, to consolidate that remission.
Q: What is the underlying philosophy for this approach?
Dr. Sekeres: Every time we give chemotherapy, we probably get about a 3-4 log kill of leukemia cells. Imagine when patients first present with AML, they may have 10 billion leukemia cells in their body. We are reducing that 3-4 log with the first course of chemotherapy.
When we then look at a bone marrow biopsy, it may appear to be normal. When leukemia is at a lower level in the body, we simply can’t see it using standard techniques. But that doesn’t mean the leukemia is gone. For younger patients, we give another cycle of chemotherapy, then another, then another, and then even another to reduce the number of leukemia cells left over in the body until that person has a durable remission and hopefully cure.
For someone who is older, the data are less clear. While some studies have shown that, if you give too much chemotherapy after the initial course, it doesn’t help that much, there is a paucity of studies that show that any chemotherapy at all after the first induction course is helpful. Consequently, we have to use indirect data. Older people who are long-term survivors from their acute leukemia always seem to have gotten more than one course of chemotherapy. In other words, the initial course of chemotherapy that a patient receives in the hospital isn’t enough. They should receive more than that.
Q: What about older adults with AML considered appropriate for antileukemic therapy but not for intensive antileukemic therapy?
Dr. Sekeres: This again gets to the question of what are a patient’s goals. It takes a very involved conversation with patients at the time of their AML diagnosis to determine whether they would want to pursue an aggressive approach or a less-aggressive approach. If a patients want a less-aggressive approach, and want nothing to do with a hospital stay, then they are also prioritizing initial quality of life. In this recommendation, based on existing studies, we didn’t have a preference for which of the available less-aggressive chemotherapies a person selects.
There’s also debate about what to do in those considered appropriate for antileukemic therapy, such as hypomethylating agents (azacitidine and decitabine) or low-dose cytarabine, but not for intensive antileukemic therapy. What did the available evidence seem to indicate about this issue?
There has been a lot of studies trying to add two drugs together to see if those do better than one drug alone in patients who are older and who choose less-intensive therapy. The majority of those studies have shown no advantage to getting two drugs over one drug.
Our recommendation is that in these situations a patient gets one drug, not two, but there are a couple of caveats. One caveat is that there has been a small study showing the effectiveness of one of those low-dose chemotherapies combined with the drug glasdegib. The second caveat is that there have been results presented combining one of these low-dose chemotherapies with the drug venetoclax. One of those was a negative study, and another was a positive study showing a survival advantage to the combination vs. the low-dose therapy alone. We had to couch our recommendation a little bit because we knew this other study had been presented at a conference, but it hadn’t come out in final form yet. It did recently, however, and we will now revisit this recommendation.
The other complicated aspect to this is that we weren’t 100% convinced that the combination of venetoclax with one of these lower-dose therapies is truly less-intensive therapy. We think it is starting to creep up toward more-intensive chemotherapy, even though it is commonly given to patients in the outpatient setting. It gets into the very complicated area of what are we defining as more-intensive therapy and less-intensive therapy.
Q: Is there a recommended strategy for older adults with AML who achieve a response after receiving less-intensive therapy?
Dr. Sekeres: This is also challenging because there are no randomized studies in which patients received less-intensive therapy for a finite period of time vs. receiving those therapies ad infinitum. Given the lack of data and also given a lot of anecdotal data out there about patients who stopped a certain therapy and relapsed thereafter, we recommended that patients continue the less-intensive therapy ad infinitum. So as long as they are receiving a response to that therapy, they continue on the drug.
Q: Of course, there are also unique considerations faced by older patients who are no longer receiving antileukemic therapy and have moved on to receiving end-of-life care or hospice care. What advice do the guidelines offer in this situation?
Dr. Sekeres: There are a lot of aspects of these recommendations that I think are special. The first is the focus on patient goals of care at every point in these guidelines. The second is that the guidelines follow the real disease course and a real conversation that doctors and patients have at every step of the way to help guide the decisions that have to be made in real time.
A problem we have in the United States is that once patients enter a hospice, most will not allow blood transfusions. One reason is that some say it is antithetical to their philosophy and consider it aggressive care. The second reason is that, to be completely blunt, economically it doesn’t make sense for hospices to allow blood transfusions. The amount that they are reimbursed by Medicare is much lower than the cost of receiving blood in an infusion center.
We wanted to make a clear recommendation that we consider transfusions in a patient who is in a palliative care or hospice mode to be supportive and necessary, and that these should be provided to patients even if they are in hospice and, as always, if consistent with a patient’s goals of care.
Q: How does a patient’s age inform the discussion surrounding what intensity treatment to offer?
Dr. Sekeres: With younger adults, this is not as complicated a conversation. A younger person has a better chance of being cured with intensive chemotherapy and is much more likely to tolerate that intensive chemotherapy. For someone who is younger, we offer intensive chemotherapy and the chance of going into remission is higher, at 70%-80%. The chance of dying is lower, usually less than 5%. It is an easy decision to make.
For an older adult, the risk-benefit ratio shifts and it becomes a more complicated option. Less-intensive therapy or best supportive care or hospice become viable.
Q: Are there other factors confounding the treatment decision-making process in older adults with AML that practitioners should consider?
Dr. Sekeres: Someone who is older is making a different decision than I would. I have school-aged children and believe that my job as a parent is to successfully get them to adulthood, so I would take any treatment under the sun to make sure that happens. People who have lived a longer life than I have may have children and even grandchildren who are adults, and they might have different goals of care. My goals are not going to be the same as my patient’s goals.
It is also harder because patients who are older may feel that they have lived a good life and don’t need to go through heroic measures to try to be around as long as possible, and those goals may not align with the goals of that person’s children who want their parent to be around as long as possible. One of the confounding factors in this is navigating the different goals of the different family members.
Dr. Sekeres has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A diagnosis of acute myeloid leukemia (AML) is particularly challenging in older adults, whose age makes them highly susceptible to the disease and treatment-related toxicity. To help patients and practitioners navigate the clinical decision-making process, the American Society of Hematology convened a panel of experts who conducted a thorough review of the literature. The result of their work can be found in a new set of guidelines for the treatment of newly diagnosed AML in older adults.
In an interview, Mikkael Sekeres, MD, chair of the ASH AML guideline panel and director of the Leukemia Program at Cleveland Clinic Taussig Cancer Institute in Cleveland, Ohio, shared the rationale behind the panel’s key recommendations and the importance of keeping the patient’s goals in mind.
Question: What is the average life expectancy of a 75-year-old developing AML compared with someone of the same age without AML?
Dr. Sekeres: A 75-year-old developing AML has an average life expectancy measured in fewer than 6 months. Somebody who is 75 without leukemia in the United States has a life expectancy that can be measured in a decade or more. AML is a really serious diagnosis when someone is older and significantly truncates expected survival.
Q: What is the median age at AML diagnosis in the United States?
Dr. Sekeres: About 67 years.
Q: What are the biological underpinnings for poor outcomes in older AML patients?
Dr. Sekeres: There are a few of them. Older adults with AML tend to have a leukemia that has evolved from a known or unknown previous bone marrow condition such as myelodysplastic syndrome. Older adults also have worse genetics driving their leukemia, which makes the leukemia cells more resistant to chemotherapy. And the leukemia cells may even have drug efflux pumps that extrude chemotherapy that tries to enter the cell. Finally, older adults are more likely to have comorbidities that make their ability to tolerate chemotherapy much lower than for younger adults.
Q: In someone who is newly diagnosed with AML, what initial options are they routinely given?
Dr. Sekeres: For someone who is older, we divide those options into three main categories.
The first is to take intensive chemotherapy, which requires a 4-6 week hospitalization and has a chance of getting somebody who is older into a remission of approximately 50%-60%. But this also carries with it significant treatment-related mortality that may be as high as 10%-20%. So I have to look my older patients in the eyes when I talk about intensive chemotherapy and say, “There is a 1 in 10 or 1 in 5 chance that you might not make it out of the hospital alive.”
The second prong is lower-dose therapy. While the more-intensive therapy requiring hospitalization does have a low, but real, chance of curing that person, less-intensive therapy is not curative. Our best hope with less-intensive therapy is that our patients enter a remission and live longer. With less-intensive therapy, the chance that someone will go into remission is probably around 20%, but again it is not curative. The flip side to that is that it improves a person’s immediate quality of life because they’re not in the hospital for 4-6 weeks.
The final prong is to discuss palliative care or hospice upfront. We designed these guidelines to be focused on a patient’s goals of therapy and to constantly revisit those goals to make sure that the treatment options we are offering are aligning with them.
Q: The panel’s first recommendation is to offer antileukemic therapy over best supportive care in patients who are appropriate candidates. Can you provide some context for this recommendation?
Dr. Sekeres: Doesn’t that strike you as funny that we even have to make a recommendation about getting chemotherapy? Some database studies conducted over the past 2 decades show that, as recently as 15 years ago, only one-third of patients who were over the age of 65 years received any type of chemotherapy for AML. More recently, as we have had a few more drugs available that allow us to use lower-dose approaches, that number has crept up to probably about 50%. We still have half the patients offered no therapy at all. So we felt that we had to deliberately make a recommendation saying that, if it aligns with the patients’ goals, they should be offered chemotherapy.
Q: The second recommendation is that patients considered candidates for intensive antileukemic therapy should receive it over less-intensive antileukemic therapy. How did you get to that recommendation?
Dr. Sekeres: There is a debate in our field about whether older adults should be offered intensive inpatient chemotherapy at all or whether we should be treating all of them with less-intensive therapy. There is not a huge amount of high-quality studies out there to answer some of these questions, in particular whether intensive chemotherapy should be recommended over less-intensive therapy. But with the available evidence, what we believe is that patients live longer if they are offered intensive antileukemic chemotherapy. So again, if it aligns with a patient’s goals, we support that patient receiving more-intensive therapy in the hospital.
Q: What does the panel recommend for patients who achieve remission after at least a single cycle of intensive antileukemic therapy and who are not candidates for allogeneic hematopoietic stem cell transplantation?
Dr. Sekeres: Once again, this may seem at first blush to be an obvious recommendation. The standard treatment of someone who is younger with AML is to offer intensive inpatient chemotherapy to induce remission. This is followed by a few cycles of chemotherapy, mostly in an outpatient setting, to consolidate that remission.
Q: What is the underlying philosophy for this approach?
Dr. Sekeres: Every time we give chemotherapy, we probably get about a 3-4 log kill of leukemia cells. Imagine when patients first present with AML, they may have 10 billion leukemia cells in their body. We are reducing that 3-4 log with the first course of chemotherapy.
When we then look at a bone marrow biopsy, it may appear to be normal. When leukemia is at a lower level in the body, we simply can’t see it using standard techniques. But that doesn’t mean the leukemia is gone. For younger patients, we give another cycle of chemotherapy, then another, then another, and then even another to reduce the number of leukemia cells left over in the body until that person has a durable remission and hopefully cure.
For someone who is older, the data are less clear. While some studies have shown that, if you give too much chemotherapy after the initial course, it doesn’t help that much, there is a paucity of studies that show that any chemotherapy at all after the first induction course is helpful. Consequently, we have to use indirect data. Older people who are long-term survivors from their acute leukemia always seem to have gotten more than one course of chemotherapy. In other words, the initial course of chemotherapy that a patient receives in the hospital isn’t enough. They should receive more than that.
Q: What about older adults with AML considered appropriate for antileukemic therapy but not for intensive antileukemic therapy?
Dr. Sekeres: This again gets to the question of what are a patient’s goals. It takes a very involved conversation with patients at the time of their AML diagnosis to determine whether they would want to pursue an aggressive approach or a less-aggressive approach. If a patients want a less-aggressive approach, and want nothing to do with a hospital stay, then they are also prioritizing initial quality of life. In this recommendation, based on existing studies, we didn’t have a preference for which of the available less-aggressive chemotherapies a person selects.
There’s also debate about what to do in those considered appropriate for antileukemic therapy, such as hypomethylating agents (azacitidine and decitabine) or low-dose cytarabine, but not for intensive antileukemic therapy. What did the available evidence seem to indicate about this issue?
There has been a lot of studies trying to add two drugs together to see if those do better than one drug alone in patients who are older and who choose less-intensive therapy. The majority of those studies have shown no advantage to getting two drugs over one drug.
Our recommendation is that in these situations a patient gets one drug, not two, but there are a couple of caveats. One caveat is that there has been a small study showing the effectiveness of one of those low-dose chemotherapies combined with the drug glasdegib. The second caveat is that there have been results presented combining one of these low-dose chemotherapies with the drug venetoclax. One of those was a negative study, and another was a positive study showing a survival advantage to the combination vs. the low-dose therapy alone. We had to couch our recommendation a little bit because we knew this other study had been presented at a conference, but it hadn’t come out in final form yet. It did recently, however, and we will now revisit this recommendation.
The other complicated aspect to this is that we weren’t 100% convinced that the combination of venetoclax with one of these lower-dose therapies is truly less-intensive therapy. We think it is starting to creep up toward more-intensive chemotherapy, even though it is commonly given to patients in the outpatient setting. It gets into the very complicated area of what are we defining as more-intensive therapy and less-intensive therapy.
Q: Is there a recommended strategy for older adults with AML who achieve a response after receiving less-intensive therapy?
Dr. Sekeres: This is also challenging because there are no randomized studies in which patients received less-intensive therapy for a finite period of time vs. receiving those therapies ad infinitum. Given the lack of data and also given a lot of anecdotal data out there about patients who stopped a certain therapy and relapsed thereafter, we recommended that patients continue the less-intensive therapy ad infinitum. So as long as they are receiving a response to that therapy, they continue on the drug.
Q: Of course, there are also unique considerations faced by older patients who are no longer receiving antileukemic therapy and have moved on to receiving end-of-life care or hospice care. What advice do the guidelines offer in this situation?
Dr. Sekeres: There are a lot of aspects of these recommendations that I think are special. The first is the focus on patient goals of care at every point in these guidelines. The second is that the guidelines follow the real disease course and a real conversation that doctors and patients have at every step of the way to help guide the decisions that have to be made in real time.
A problem we have in the United States is that once patients enter a hospice, most will not allow blood transfusions. One reason is that some say it is antithetical to their philosophy and consider it aggressive care. The second reason is that, to be completely blunt, economically it doesn’t make sense for hospices to allow blood transfusions. The amount that they are reimbursed by Medicare is much lower than the cost of receiving blood in an infusion center.
We wanted to make a clear recommendation that we consider transfusions in a patient who is in a palliative care or hospice mode to be supportive and necessary, and that these should be provided to patients even if they are in hospice and, as always, if consistent with a patient’s goals of care.
Q: How does a patient’s age inform the discussion surrounding what intensity treatment to offer?
Dr. Sekeres: With younger adults, this is not as complicated a conversation. A younger person has a better chance of being cured with intensive chemotherapy and is much more likely to tolerate that intensive chemotherapy. For someone who is younger, we offer intensive chemotherapy and the chance of going into remission is higher, at 70%-80%. The chance of dying is lower, usually less than 5%. It is an easy decision to make.
For an older adult, the risk-benefit ratio shifts and it becomes a more complicated option. Less-intensive therapy or best supportive care or hospice become viable.
Q: Are there other factors confounding the treatment decision-making process in older adults with AML that practitioners should consider?
Dr. Sekeres: Someone who is older is making a different decision than I would. I have school-aged children and believe that my job as a parent is to successfully get them to adulthood, so I would take any treatment under the sun to make sure that happens. People who have lived a longer life than I have may have children and even grandchildren who are adults, and they might have different goals of care. My goals are not going to be the same as my patient’s goals.
It is also harder because patients who are older may feel that they have lived a good life and don’t need to go through heroic measures to try to be around as long as possible, and those goals may not align with the goals of that person’s children who want their parent to be around as long as possible. One of the confounding factors in this is navigating the different goals of the different family members.
Dr. Sekeres has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
‘Profound human toll’ in excess deaths from COVID-19 calculated in two studies
However, additional deaths could be indirectly related because people avoided emergency care during the pandemic, new research shows.
Deaths linked to COVID-19 varied by state and phase of the pandemic, as reported in a study from researchers at Virginia Commonwealth University and Yale University that was published online October 12 in JAMA.
Another study published online simultaneously in JAMA took more of an international perspective. Investigators from the University of Pennsylvania and Harvard University found that in America there were more excess deaths and there was higher all-cause mortality during the pandemic than in 18 other countries.
Although the ongoing number of deaths attributable to COVID-19 continues to garner attention, there can be a lag of weeks or months in how long it takes some public health agencies to update their figures.
“For the public at large, the take-home message is twofold: that the number of deaths caused by the pandemic exceeds publicly reported COVID-19 death counts by 20% and that states that reopened or lifted restrictions early suffered a protracted surge in excess deaths that extended into the summer,” lead author of the US-focused study, Steven H. Woolf, MD, MPH, told Medscape Medical News.
The take-away for physicians is in the bigger picture – it is likely that the COVID-19 pandemic is responsible for deaths from other conditions as well. “Surges in COVID-19 were accompanied by an increase in deaths attributed to other causes, such as heart disease and Alzheimer’s disease and dementia,” said Woolf, director emeritus and senior adviser at the Center on Society and Health and professor in the Department of Family Medicine and Population Health at the Virginia Commonwealth University School of Medicine in Richmond, Virginia.
The investigators identified 225,530 excess US deaths in the 5 months from March to July. They report that 67% were directly attributable to COVID-19.
Deaths linked to COVID-19 included those in which the disease was listed as an underlying or contributing cause. US total death rates are “remarkably consistent” year after year, and the investigators calculated a 20% overall jump in mortality.
The study included data from the National Center for Health Statistics and the US Census Bureau for 48 states and the District of Columbia. Connecticut and North Carolina were excluded because of missing data.
Woolf and colleagues also found statistically higher rates of deaths from two other causes, heart disease and Alzheimer’s disease/dementia.
Altered states
New York, New Jersey, Massachusetts, Louisiana, Arizona, Mississippi, Maryland, Delaware, Rhode Island, and Michigan had the highest per capita excess death rates. Three states experienced the shortest epidemics during the study period: New York, New Jersey, and Massachusetts.
Some lessons could be learned by looking at how individual states managed large numbers of people with COVID-19. “Although we suspected that states that reopened early might have put themselves at risk of a pandemic surge, the consistency with which that occurred and the devastating numbers of deaths they suffered was a surprise,” Woolf said.
“The goal of our study is not to look in the rearview mirror and lament what happened months ago but to learn the lesson going forward: Our country will be unable to take control of this pandemic without more robust efforts to control community spread,” Woolf said. “Our study found that states that did this well, such as New York and New Jersey, experienced large surges but bent the curve and were back to baseline in less than 10 weeks.
“If we could do this as a country, countless lives could be saved.”
A global perspective
The United States experienced high mortality linked to COVID-19, as well as high all-cause mortality, compared with 18 other countries, as reported in the study by University of Pennsylvania and Harvard University researchers.
The United States ranked third, with 72 deaths per 100,000 people, among countries with moderate or high mortality. Although perhaps not surprising given the state of SARS-CoV-2 infection across the United States, a question remains as to what extent the relatively high mortality rate is linked to early outbreaks vs “poor long-term response,” the researchers note.
Alyssa Bilinski, MSc, and lead author Ezekiel J. Emanuel, MD, PhD, chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania Perelman School of Medicine in Philadelphia, calculated the difference in COVID-19 deaths among countries through Sept. 19, 2020. On this date, the United States reported a total 198,589 COVID-19 deaths.
They calculated that, if the US death rates were similar to those in Australia, the United States would have experienced 187,661 fewer COVID-19 deaths. If similar to those of Canada, there would have been 117,622 fewer deaths in the United States.
The US death rate was lower than six other countries with high COVID-19 mortality in the early spring, including Belgium, Spain, and the United Kingdom. However, after May 10, the per capita mortality rate in the United States exceeded the others.
Between May 10 and Sept. 19, the death rate in Italy was 9.1 per 100,000, vs 36.9 per 100,000.
“After the first peak in early spring, US death rates from COVID-19 and from all causes remained higher than even countries with high COVID-19 mortality,” the researchers note. “This may have been a result of several factors, including weak public health infrastructure and a decentralized, inconsistent US response to the pandemic.”
“Mortifying and motivating”
Woolf and colleagues estimate that more than 225,000 excess deaths occurred in recent months; this represents a 20% increase over expected deaths, note Harvey V. Fineberg, MD, PhD, of the Gordon and Betty Moore Foundation, in an accompanying editorial in JAMA.
“Importantly, a condition such as COVID-19 can contribute both directly and indirectly to excess mortality,” he writes.
Although the direct contribution to the mortality rates by those infected is straightforward, “the indirect contribution may relate to circumstances or choices due to the COVID-19 pandemic: for example, a patient who develops symptoms of a stroke is too concerned about COVID-19 to go to the emergency department, and a potentially reversible condition becomes fatal.”
Fineberg notes that “a general indication of the death toll from COVID-19 and the excess deaths related to the pandemic, as presented by Woolf et al, are sufficiently mortifying and motivating.”
“Profound human toll”
“The importance of the estimate by Woolf et al – which suggests that for the entirety of 2020, more than 400,000 excess deaths will occur – cannot be overstated, because it accounts for what could be declines in some causes of death, like motor vehicle crashes, but increases in others, like myocardial infarction,” write Howard Bauchner, MD, editor in chief of JAMA, and Phil B. Fontanarosa, MD, MBA, executive editor of JAMA, in another accompanying editorial.
“These deaths reflect a true measure of the human cost of the Great Pandemic of 2020,” they add.
The study from Emanuel and Bilinski was notable for calculating the excess COVID-19 and all-cause mortality to Sept. 2020, they note. “After the initial peak in early spring, US death rates from COVID-19 and from all causes remained higher than rates in countries with high COVID-19 mortality.”
“Few people will forget the Great Pandemic of 2020, where and how they lived, how it substantially changed their lives, and for many, the profound human toll it has taken,” Bauchner and Fontanarosa write.
The study by Woolf and colleagues was supported by National Center for Advancing Translational Sciences, the National Institute on Aging, and the National Institute of Allergy and Infectious Diseases. The study by Bilinski and Emanuel was partially funded by the Colton Foundation. Woolf, Emanuel, Fineberg, Bauchner, and Fontanarosa have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
However, additional deaths could be indirectly related because people avoided emergency care during the pandemic, new research shows.
Deaths linked to COVID-19 varied by state and phase of the pandemic, as reported in a study from researchers at Virginia Commonwealth University and Yale University that was published online October 12 in JAMA.
Another study published online simultaneously in JAMA took more of an international perspective. Investigators from the University of Pennsylvania and Harvard University found that in America there were more excess deaths and there was higher all-cause mortality during the pandemic than in 18 other countries.
Although the ongoing number of deaths attributable to COVID-19 continues to garner attention, there can be a lag of weeks or months in how long it takes some public health agencies to update their figures.
“For the public at large, the take-home message is twofold: that the number of deaths caused by the pandemic exceeds publicly reported COVID-19 death counts by 20% and that states that reopened or lifted restrictions early suffered a protracted surge in excess deaths that extended into the summer,” lead author of the US-focused study, Steven H. Woolf, MD, MPH, told Medscape Medical News.
The take-away for physicians is in the bigger picture – it is likely that the COVID-19 pandemic is responsible for deaths from other conditions as well. “Surges in COVID-19 were accompanied by an increase in deaths attributed to other causes, such as heart disease and Alzheimer’s disease and dementia,” said Woolf, director emeritus and senior adviser at the Center on Society and Health and professor in the Department of Family Medicine and Population Health at the Virginia Commonwealth University School of Medicine in Richmond, Virginia.
The investigators identified 225,530 excess US deaths in the 5 months from March to July. They report that 67% were directly attributable to COVID-19.
Deaths linked to COVID-19 included those in which the disease was listed as an underlying or contributing cause. US total death rates are “remarkably consistent” year after year, and the investigators calculated a 20% overall jump in mortality.
The study included data from the National Center for Health Statistics and the US Census Bureau for 48 states and the District of Columbia. Connecticut and North Carolina were excluded because of missing data.
Woolf and colleagues also found statistically higher rates of deaths from two other causes, heart disease and Alzheimer’s disease/dementia.
Altered states
New York, New Jersey, Massachusetts, Louisiana, Arizona, Mississippi, Maryland, Delaware, Rhode Island, and Michigan had the highest per capita excess death rates. Three states experienced the shortest epidemics during the study period: New York, New Jersey, and Massachusetts.
Some lessons could be learned by looking at how individual states managed large numbers of people with COVID-19. “Although we suspected that states that reopened early might have put themselves at risk of a pandemic surge, the consistency with which that occurred and the devastating numbers of deaths they suffered was a surprise,” Woolf said.
“The goal of our study is not to look in the rearview mirror and lament what happened months ago but to learn the lesson going forward: Our country will be unable to take control of this pandemic without more robust efforts to control community spread,” Woolf said. “Our study found that states that did this well, such as New York and New Jersey, experienced large surges but bent the curve and were back to baseline in less than 10 weeks.
“If we could do this as a country, countless lives could be saved.”
A global perspective
The United States experienced high mortality linked to COVID-19, as well as high all-cause mortality, compared with 18 other countries, as reported in the study by University of Pennsylvania and Harvard University researchers.
The United States ranked third, with 72 deaths per 100,000 people, among countries with moderate or high mortality. Although perhaps not surprising given the state of SARS-CoV-2 infection across the United States, a question remains as to what extent the relatively high mortality rate is linked to early outbreaks vs “poor long-term response,” the researchers note.
Alyssa Bilinski, MSc, and lead author Ezekiel J. Emanuel, MD, PhD, chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania Perelman School of Medicine in Philadelphia, calculated the difference in COVID-19 deaths among countries through Sept. 19, 2020. On this date, the United States reported a total 198,589 COVID-19 deaths.
They calculated that, if the US death rates were similar to those in Australia, the United States would have experienced 187,661 fewer COVID-19 deaths. If similar to those of Canada, there would have been 117,622 fewer deaths in the United States.
The US death rate was lower than six other countries with high COVID-19 mortality in the early spring, including Belgium, Spain, and the United Kingdom. However, after May 10, the per capita mortality rate in the United States exceeded the others.
Between May 10 and Sept. 19, the death rate in Italy was 9.1 per 100,000, vs 36.9 per 100,000.
“After the first peak in early spring, US death rates from COVID-19 and from all causes remained higher than even countries with high COVID-19 mortality,” the researchers note. “This may have been a result of several factors, including weak public health infrastructure and a decentralized, inconsistent US response to the pandemic.”
“Mortifying and motivating”
Woolf and colleagues estimate that more than 225,000 excess deaths occurred in recent months; this represents a 20% increase over expected deaths, note Harvey V. Fineberg, MD, PhD, of the Gordon and Betty Moore Foundation, in an accompanying editorial in JAMA.
“Importantly, a condition such as COVID-19 can contribute both directly and indirectly to excess mortality,” he writes.
Although the direct contribution to the mortality rates by those infected is straightforward, “the indirect contribution may relate to circumstances or choices due to the COVID-19 pandemic: for example, a patient who develops symptoms of a stroke is too concerned about COVID-19 to go to the emergency department, and a potentially reversible condition becomes fatal.”
Fineberg notes that “a general indication of the death toll from COVID-19 and the excess deaths related to the pandemic, as presented by Woolf et al, are sufficiently mortifying and motivating.”
“Profound human toll”
“The importance of the estimate by Woolf et al – which suggests that for the entirety of 2020, more than 400,000 excess deaths will occur – cannot be overstated, because it accounts for what could be declines in some causes of death, like motor vehicle crashes, but increases in others, like myocardial infarction,” write Howard Bauchner, MD, editor in chief of JAMA, and Phil B. Fontanarosa, MD, MBA, executive editor of JAMA, in another accompanying editorial.
“These deaths reflect a true measure of the human cost of the Great Pandemic of 2020,” they add.
The study from Emanuel and Bilinski was notable for calculating the excess COVID-19 and all-cause mortality to Sept. 2020, they note. “After the initial peak in early spring, US death rates from COVID-19 and from all causes remained higher than rates in countries with high COVID-19 mortality.”
“Few people will forget the Great Pandemic of 2020, where and how they lived, how it substantially changed their lives, and for many, the profound human toll it has taken,” Bauchner and Fontanarosa write.
The study by Woolf and colleagues was supported by National Center for Advancing Translational Sciences, the National Institute on Aging, and the National Institute of Allergy and Infectious Diseases. The study by Bilinski and Emanuel was partially funded by the Colton Foundation. Woolf, Emanuel, Fineberg, Bauchner, and Fontanarosa have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
However, additional deaths could be indirectly related because people avoided emergency care during the pandemic, new research shows.
Deaths linked to COVID-19 varied by state and phase of the pandemic, as reported in a study from researchers at Virginia Commonwealth University and Yale University that was published online October 12 in JAMA.
Another study published online simultaneously in JAMA took more of an international perspective. Investigators from the University of Pennsylvania and Harvard University found that in America there were more excess deaths and there was higher all-cause mortality during the pandemic than in 18 other countries.
Although the ongoing number of deaths attributable to COVID-19 continues to garner attention, there can be a lag of weeks or months in how long it takes some public health agencies to update their figures.
“For the public at large, the take-home message is twofold: that the number of deaths caused by the pandemic exceeds publicly reported COVID-19 death counts by 20% and that states that reopened or lifted restrictions early suffered a protracted surge in excess deaths that extended into the summer,” lead author of the US-focused study, Steven H. Woolf, MD, MPH, told Medscape Medical News.
The take-away for physicians is in the bigger picture – it is likely that the COVID-19 pandemic is responsible for deaths from other conditions as well. “Surges in COVID-19 were accompanied by an increase in deaths attributed to other causes, such as heart disease and Alzheimer’s disease and dementia,” said Woolf, director emeritus and senior adviser at the Center on Society and Health and professor in the Department of Family Medicine and Population Health at the Virginia Commonwealth University School of Medicine in Richmond, Virginia.
The investigators identified 225,530 excess US deaths in the 5 months from March to July. They report that 67% were directly attributable to COVID-19.
Deaths linked to COVID-19 included those in which the disease was listed as an underlying or contributing cause. US total death rates are “remarkably consistent” year after year, and the investigators calculated a 20% overall jump in mortality.
The study included data from the National Center for Health Statistics and the US Census Bureau for 48 states and the District of Columbia. Connecticut and North Carolina were excluded because of missing data.
Woolf and colleagues also found statistically higher rates of deaths from two other causes, heart disease and Alzheimer’s disease/dementia.
Altered states
New York, New Jersey, Massachusetts, Louisiana, Arizona, Mississippi, Maryland, Delaware, Rhode Island, and Michigan had the highest per capita excess death rates. Three states experienced the shortest epidemics during the study period: New York, New Jersey, and Massachusetts.
Some lessons could be learned by looking at how individual states managed large numbers of people with COVID-19. “Although we suspected that states that reopened early might have put themselves at risk of a pandemic surge, the consistency with which that occurred and the devastating numbers of deaths they suffered was a surprise,” Woolf said.
“The goal of our study is not to look in the rearview mirror and lament what happened months ago but to learn the lesson going forward: Our country will be unable to take control of this pandemic without more robust efforts to control community spread,” Woolf said. “Our study found that states that did this well, such as New York and New Jersey, experienced large surges but bent the curve and were back to baseline in less than 10 weeks.
“If we could do this as a country, countless lives could be saved.”
A global perspective
The United States experienced high mortality linked to COVID-19, as well as high all-cause mortality, compared with 18 other countries, as reported in the study by University of Pennsylvania and Harvard University researchers.
The United States ranked third, with 72 deaths per 100,000 people, among countries with moderate or high mortality. Although perhaps not surprising given the state of SARS-CoV-2 infection across the United States, a question remains as to what extent the relatively high mortality rate is linked to early outbreaks vs “poor long-term response,” the researchers note.
Alyssa Bilinski, MSc, and lead author Ezekiel J. Emanuel, MD, PhD, chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania Perelman School of Medicine in Philadelphia, calculated the difference in COVID-19 deaths among countries through Sept. 19, 2020. On this date, the United States reported a total 198,589 COVID-19 deaths.
They calculated that, if the US death rates were similar to those in Australia, the United States would have experienced 187,661 fewer COVID-19 deaths. If similar to those of Canada, there would have been 117,622 fewer deaths in the United States.
The US death rate was lower than six other countries with high COVID-19 mortality in the early spring, including Belgium, Spain, and the United Kingdom. However, after May 10, the per capita mortality rate in the United States exceeded the others.
Between May 10 and Sept. 19, the death rate in Italy was 9.1 per 100,000, vs 36.9 per 100,000.
“After the first peak in early spring, US death rates from COVID-19 and from all causes remained higher than even countries with high COVID-19 mortality,” the researchers note. “This may have been a result of several factors, including weak public health infrastructure and a decentralized, inconsistent US response to the pandemic.”
“Mortifying and motivating”
Woolf and colleagues estimate that more than 225,000 excess deaths occurred in recent months; this represents a 20% increase over expected deaths, note Harvey V. Fineberg, MD, PhD, of the Gordon and Betty Moore Foundation, in an accompanying editorial in JAMA.
“Importantly, a condition such as COVID-19 can contribute both directly and indirectly to excess mortality,” he writes.
Although the direct contribution to the mortality rates by those infected is straightforward, “the indirect contribution may relate to circumstances or choices due to the COVID-19 pandemic: for example, a patient who develops symptoms of a stroke is too concerned about COVID-19 to go to the emergency department, and a potentially reversible condition becomes fatal.”
Fineberg notes that “a general indication of the death toll from COVID-19 and the excess deaths related to the pandemic, as presented by Woolf et al, are sufficiently mortifying and motivating.”
“Profound human toll”
“The importance of the estimate by Woolf et al – which suggests that for the entirety of 2020, more than 400,000 excess deaths will occur – cannot be overstated, because it accounts for what could be declines in some causes of death, like motor vehicle crashes, but increases in others, like myocardial infarction,” write Howard Bauchner, MD, editor in chief of JAMA, and Phil B. Fontanarosa, MD, MBA, executive editor of JAMA, in another accompanying editorial.
“These deaths reflect a true measure of the human cost of the Great Pandemic of 2020,” they add.
The study from Emanuel and Bilinski was notable for calculating the excess COVID-19 and all-cause mortality to Sept. 2020, they note. “After the initial peak in early spring, US death rates from COVID-19 and from all causes remained higher than rates in countries with high COVID-19 mortality.”
“Few people will forget the Great Pandemic of 2020, where and how they lived, how it substantially changed their lives, and for many, the profound human toll it has taken,” Bauchner and Fontanarosa write.
The study by Woolf and colleagues was supported by National Center for Advancing Translational Sciences, the National Institute on Aging, and the National Institute of Allergy and Infectious Diseases. The study by Bilinski and Emanuel was partially funded by the Colton Foundation. Woolf, Emanuel, Fineberg, Bauchner, and Fontanarosa have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Fourteen-day sports hiatus recommended for children after COVID-19
Children should not return to sports for 14 days after exposure to COVID-19, and those with moderate symptoms should undergo an electrocardiogram before returning, according to the American Academy of Pediatrics.
said Susannah Briskin, MD, a pediatric sports medicine specialist at Rainbow Babies and Children’s Hospital in Cleveland.
“There has been emerging evidence about cases of myocarditis occurring in athletes, including athletes who are asymptomatic with COVID-19,” she said in an interview.
The update aligns the AAP recommendations with those from the American College of Cardiologists, she added.
Recent imaging studies have turned up signs of myocarditis in athletes recovering from mild or asymptomatic cases of COVID-19 and have prompted calls for clearer guidelines about imaging studies and return to play.
Viral myocarditis poses a risk to athletes because it can lead to potentially fatal arrhythmias, Dr. Briskin said.
Although children benefit from participating in sports, these activities also put them at risk of contracting COVID-19 and spreading it to others, the guidance noted.
To balance the risks and benefits, the academy proposed guidelines that vary depending on the severity of the presentation.
In the first category are patients with a severe presentation (hypotension, arrhythmias, need for intubation or extracorporeal membrane oxygenation support, kidney or cardiac failure) or with multisystem inflammatory syndrome. Clinicians should treat these patients as though they have myocarditis. Patients should be restricted from engaging in sports and other exercise for 3-6 months, the guidance stated.
The primary care physician and “appropriate pediatric medical subspecialist, preferably in consultation with a pediatric cardiologist,” should clear them before they return to activities. In examining patients for return to play, clinicians should focus on cardiac symptoms, including chest pain, shortness of breath, fatigue, palpitations, or syncope, the guidance said.
In another category are patients with cardiac symptoms, those with concerning findings on examination, and those with moderate symptoms of COVID-19, including prolonged fever. These patients should undergo an ECG and possibly be referred to a pediatric cardiologist, the guidelines said. These symptoms must be absent for at least 14 days before these patients can return to sports, and the athletes should obtain clearance from their primary care physicians before they resume.
In a third category are patients who have been infected with SARS-CoV-2 or who have had close contact with someone who was infected but who have not themselves experienced symptoms. These athletes should refrain from sports for at least 14 days, the guidelines said.
Children who don’t fall into any of these categories should not be tested for the virus or antibodies to it before participation in sports, the academy said.
The guidelines don’t vary depending on the sport. But the academy has issued separate guidance for parents and guardians to help them evaluate the risk for COVID-19 transmission by sport.
Athletes participating in “sports that have greater amount of contact time or proximity to people would be at higher risk for contracting COVID-19,” Dr. Briskin said. “But I think that’s all fairly common sense, given the recommendations for non–sport-related activity just in terms of social distancing and masking.”
The new guidance called on sports organizers to minimize contact by, for example, modifying drills and conditioning. It recommended that athletes wear masks except during vigorous exercise or when participating in water sports, as well as in other circumstances in which the mask could become a safety hazard.
They also recommended using handwashing stations or hand sanitizer, avoiding contact with shared surfaces, and avoiding small rooms and areas with poor ventilation.
Dr. Briskin disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Children should not return to sports for 14 days after exposure to COVID-19, and those with moderate symptoms should undergo an electrocardiogram before returning, according to the American Academy of Pediatrics.
said Susannah Briskin, MD, a pediatric sports medicine specialist at Rainbow Babies and Children’s Hospital in Cleveland.
“There has been emerging evidence about cases of myocarditis occurring in athletes, including athletes who are asymptomatic with COVID-19,” she said in an interview.
The update aligns the AAP recommendations with those from the American College of Cardiologists, she added.
Recent imaging studies have turned up signs of myocarditis in athletes recovering from mild or asymptomatic cases of COVID-19 and have prompted calls for clearer guidelines about imaging studies and return to play.
Viral myocarditis poses a risk to athletes because it can lead to potentially fatal arrhythmias, Dr. Briskin said.
Although children benefit from participating in sports, these activities also put them at risk of contracting COVID-19 and spreading it to others, the guidance noted.
To balance the risks and benefits, the academy proposed guidelines that vary depending on the severity of the presentation.
In the first category are patients with a severe presentation (hypotension, arrhythmias, need for intubation or extracorporeal membrane oxygenation support, kidney or cardiac failure) or with multisystem inflammatory syndrome. Clinicians should treat these patients as though they have myocarditis. Patients should be restricted from engaging in sports and other exercise for 3-6 months, the guidance stated.
The primary care physician and “appropriate pediatric medical subspecialist, preferably in consultation with a pediatric cardiologist,” should clear them before they return to activities. In examining patients for return to play, clinicians should focus on cardiac symptoms, including chest pain, shortness of breath, fatigue, palpitations, or syncope, the guidance said.
In another category are patients with cardiac symptoms, those with concerning findings on examination, and those with moderate symptoms of COVID-19, including prolonged fever. These patients should undergo an ECG and possibly be referred to a pediatric cardiologist, the guidelines said. These symptoms must be absent for at least 14 days before these patients can return to sports, and the athletes should obtain clearance from their primary care physicians before they resume.
In a third category are patients who have been infected with SARS-CoV-2 or who have had close contact with someone who was infected but who have not themselves experienced symptoms. These athletes should refrain from sports for at least 14 days, the guidelines said.
Children who don’t fall into any of these categories should not be tested for the virus or antibodies to it before participation in sports, the academy said.
The guidelines don’t vary depending on the sport. But the academy has issued separate guidance for parents and guardians to help them evaluate the risk for COVID-19 transmission by sport.
Athletes participating in “sports that have greater amount of contact time or proximity to people would be at higher risk for contracting COVID-19,” Dr. Briskin said. “But I think that’s all fairly common sense, given the recommendations for non–sport-related activity just in terms of social distancing and masking.”
The new guidance called on sports organizers to minimize contact by, for example, modifying drills and conditioning. It recommended that athletes wear masks except during vigorous exercise or when participating in water sports, as well as in other circumstances in which the mask could become a safety hazard.
They also recommended using handwashing stations or hand sanitizer, avoiding contact with shared surfaces, and avoiding small rooms and areas with poor ventilation.
Dr. Briskin disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Children should not return to sports for 14 days after exposure to COVID-19, and those with moderate symptoms should undergo an electrocardiogram before returning, according to the American Academy of Pediatrics.
said Susannah Briskin, MD, a pediatric sports medicine specialist at Rainbow Babies and Children’s Hospital in Cleveland.
“There has been emerging evidence about cases of myocarditis occurring in athletes, including athletes who are asymptomatic with COVID-19,” she said in an interview.
The update aligns the AAP recommendations with those from the American College of Cardiologists, she added.
Recent imaging studies have turned up signs of myocarditis in athletes recovering from mild or asymptomatic cases of COVID-19 and have prompted calls for clearer guidelines about imaging studies and return to play.
Viral myocarditis poses a risk to athletes because it can lead to potentially fatal arrhythmias, Dr. Briskin said.
Although children benefit from participating in sports, these activities also put them at risk of contracting COVID-19 and spreading it to others, the guidance noted.
To balance the risks and benefits, the academy proposed guidelines that vary depending on the severity of the presentation.
In the first category are patients with a severe presentation (hypotension, arrhythmias, need for intubation or extracorporeal membrane oxygenation support, kidney or cardiac failure) or with multisystem inflammatory syndrome. Clinicians should treat these patients as though they have myocarditis. Patients should be restricted from engaging in sports and other exercise for 3-6 months, the guidance stated.
The primary care physician and “appropriate pediatric medical subspecialist, preferably in consultation with a pediatric cardiologist,” should clear them before they return to activities. In examining patients for return to play, clinicians should focus on cardiac symptoms, including chest pain, shortness of breath, fatigue, palpitations, or syncope, the guidance said.
In another category are patients with cardiac symptoms, those with concerning findings on examination, and those with moderate symptoms of COVID-19, including prolonged fever. These patients should undergo an ECG and possibly be referred to a pediatric cardiologist, the guidelines said. These symptoms must be absent for at least 14 days before these patients can return to sports, and the athletes should obtain clearance from their primary care physicians before they resume.
In a third category are patients who have been infected with SARS-CoV-2 or who have had close contact with someone who was infected but who have not themselves experienced symptoms. These athletes should refrain from sports for at least 14 days, the guidelines said.
Children who don’t fall into any of these categories should not be tested for the virus or antibodies to it before participation in sports, the academy said.
The guidelines don’t vary depending on the sport. But the academy has issued separate guidance for parents and guardians to help them evaluate the risk for COVID-19 transmission by sport.
Athletes participating in “sports that have greater amount of contact time or proximity to people would be at higher risk for contracting COVID-19,” Dr. Briskin said. “But I think that’s all fairly common sense, given the recommendations for non–sport-related activity just in terms of social distancing and masking.”
The new guidance called on sports organizers to minimize contact by, for example, modifying drills and conditioning. It recommended that athletes wear masks except during vigorous exercise or when participating in water sports, as well as in other circumstances in which the mask could become a safety hazard.
They also recommended using handwashing stations or hand sanitizer, avoiding contact with shared surfaces, and avoiding small rooms and areas with poor ventilation.
Dr. Briskin disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Access to care: A nurse practitioner’s plea
Having been a reader of Pediatric News for years, I want to bring to light access-to-care issues involving COVID-19 medical facility restrictions for pediatric patients and their parents.
On March 27, 2020, I received a phone call from the Department of Human Services pleading with me to take a medically fragile child who was entering the foster care system that day. He had very specific needs, and they had no one available who could medically meet those needs. The week prior was my kids’ scheduled spring break; the week I got the call was the week that I was voluntarily furloughed from my job as a pediatric nurse practitioner so that I could stay home with my kids as their school would not be reopening for the year, and someone had to be with them. I was already home with my 3-year-old and 6-year-old, so why not add another?
Leo (name changed for privacy) came to me with a multitude of diagnoses, to say the least. Not only did he require physical, speech, and occupational therapy twice weekly, but he often had appointments with 10 different specialists at the local children’s hospital. The first few weeks he was in my care, we had almost daily visits to either therapists or specialists. Keeping up with these types of appointments in a normal world is difficult ... I was getting the crash course on how to navigate all of it in the COVID-19 world.
So now, I am the primary caregiver during the day for my two children and our medically fragile foster child who has multiple medical appointments a week. Our local children’s hospital allowed only the caregiver to accompany him to his visits. In theory this sounds great, right? Fewer people in a facility equals less exposure, less risk, and fewer COVID-19 infections.
But what about the negative consequences of these hospital policies? I have two other children I was caring for. I couldn’t take them to their grandparents’ house because people over age 65 years are at risk of having COVID-19 complications. I had been furloughed, so our income was half what it typically was. Regardless,
Now imagine if I were a single mom who had three kids and a lesser paying job. Schools are closed and she’s forced to work from home and homeschool her children. Or worse, she’s been laid off and living on unemployment. Do you think she is going to have the time or finances available to hire a babysitter so that she can take her medically fragile child in for his cardiology follow-up? Because not only does she have to pay the copays and whatever insurance doesn’t cover, but now she has to fork over $50 for child care. If you don’t know the answer already, it’s no, she does not have the time or the finances. So her child misses a cardiology appointment, which means that his meds weren’t increased according to his growth, which means his pulmonary hypertension is not controlled, which worsens his heart failure ... you get my drift.
Fast forward to Sept. 22, 2020. I had a cardiology appointment at our local heart hospital for myself. It’s 2020, people, I’ve been having some palpitations that I needed checked out and was going in to have a heart monitor patch placed. I had my 4-year-old son with me because he is on a hybrid schedule where we homeschool 2 days a week. We entered the building wearing masks, and I was immediately stopped by security and informed that, according to the COVID-19 policy for their hospital, children under 16 are not allowed to enter the building. After some discussion, I was ultimately refused care because my son was with me that day. Refused care because I had a masked 4-year-old with a normal temperature at my side.
These policies are not working. We are in health care. It should not matter what pandemic is on the table, we should not be refusing patients access to care based on who is by their side that day. We knew the risks when we entered our profession, and we know the proper measures to protect ourselves. Our patients also know the risks and can protect themselves accordingly.
So this is my plea to all medical facilities out there: Stop. Stop telling people their loved ones can’t accompany them to appointments. Stop telling caregivers to wait in their cars while their elderly, demented mothers have their annual physicals. Stop telling moms they need to leave their other children at home. This is now a huge access-to-care issue nationwide and it needs to stop. Excess deaths in our nation are soaring, and it’s not just because people don’t want to seek medical attention; it’s because medical facilities are making it almost impossible to seek help for many. People are dying, and it’s not only from COVID-19. This is on us as health care providers, and we need to step up to the plate and do what is right.
Ms. Baxendale is a nurse practitioner in Mustang, Okla. Email her at [email protected].
Having been a reader of Pediatric News for years, I want to bring to light access-to-care issues involving COVID-19 medical facility restrictions for pediatric patients and their parents.
On March 27, 2020, I received a phone call from the Department of Human Services pleading with me to take a medically fragile child who was entering the foster care system that day. He had very specific needs, and they had no one available who could medically meet those needs. The week prior was my kids’ scheduled spring break; the week I got the call was the week that I was voluntarily furloughed from my job as a pediatric nurse practitioner so that I could stay home with my kids as their school would not be reopening for the year, and someone had to be with them. I was already home with my 3-year-old and 6-year-old, so why not add another?
Leo (name changed for privacy) came to me with a multitude of diagnoses, to say the least. Not only did he require physical, speech, and occupational therapy twice weekly, but he often had appointments with 10 different specialists at the local children’s hospital. The first few weeks he was in my care, we had almost daily visits to either therapists or specialists. Keeping up with these types of appointments in a normal world is difficult ... I was getting the crash course on how to navigate all of it in the COVID-19 world.
So now, I am the primary caregiver during the day for my two children and our medically fragile foster child who has multiple medical appointments a week. Our local children’s hospital allowed only the caregiver to accompany him to his visits. In theory this sounds great, right? Fewer people in a facility equals less exposure, less risk, and fewer COVID-19 infections.
But what about the negative consequences of these hospital policies? I have two other children I was caring for. I couldn’t take them to their grandparents’ house because people over age 65 years are at risk of having COVID-19 complications. I had been furloughed, so our income was half what it typically was. Regardless,
Now imagine if I were a single mom who had three kids and a lesser paying job. Schools are closed and she’s forced to work from home and homeschool her children. Or worse, she’s been laid off and living on unemployment. Do you think she is going to have the time or finances available to hire a babysitter so that she can take her medically fragile child in for his cardiology follow-up? Because not only does she have to pay the copays and whatever insurance doesn’t cover, but now she has to fork over $50 for child care. If you don’t know the answer already, it’s no, she does not have the time or the finances. So her child misses a cardiology appointment, which means that his meds weren’t increased according to his growth, which means his pulmonary hypertension is not controlled, which worsens his heart failure ... you get my drift.
Fast forward to Sept. 22, 2020. I had a cardiology appointment at our local heart hospital for myself. It’s 2020, people, I’ve been having some palpitations that I needed checked out and was going in to have a heart monitor patch placed. I had my 4-year-old son with me because he is on a hybrid schedule where we homeschool 2 days a week. We entered the building wearing masks, and I was immediately stopped by security and informed that, according to the COVID-19 policy for their hospital, children under 16 are not allowed to enter the building. After some discussion, I was ultimately refused care because my son was with me that day. Refused care because I had a masked 4-year-old with a normal temperature at my side.
These policies are not working. We are in health care. It should not matter what pandemic is on the table, we should not be refusing patients access to care based on who is by their side that day. We knew the risks when we entered our profession, and we know the proper measures to protect ourselves. Our patients also know the risks and can protect themselves accordingly.
So this is my plea to all medical facilities out there: Stop. Stop telling people their loved ones can’t accompany them to appointments. Stop telling caregivers to wait in their cars while their elderly, demented mothers have their annual physicals. Stop telling moms they need to leave their other children at home. This is now a huge access-to-care issue nationwide and it needs to stop. Excess deaths in our nation are soaring, and it’s not just because people don’t want to seek medical attention; it’s because medical facilities are making it almost impossible to seek help for many. People are dying, and it’s not only from COVID-19. This is on us as health care providers, and we need to step up to the plate and do what is right.
Ms. Baxendale is a nurse practitioner in Mustang, Okla. Email her at [email protected].
Having been a reader of Pediatric News for years, I want to bring to light access-to-care issues involving COVID-19 medical facility restrictions for pediatric patients and their parents.
On March 27, 2020, I received a phone call from the Department of Human Services pleading with me to take a medically fragile child who was entering the foster care system that day. He had very specific needs, and they had no one available who could medically meet those needs. The week prior was my kids’ scheduled spring break; the week I got the call was the week that I was voluntarily furloughed from my job as a pediatric nurse practitioner so that I could stay home with my kids as their school would not be reopening for the year, and someone had to be with them. I was already home with my 3-year-old and 6-year-old, so why not add another?
Leo (name changed for privacy) came to me with a multitude of diagnoses, to say the least. Not only did he require physical, speech, and occupational therapy twice weekly, but he often had appointments with 10 different specialists at the local children’s hospital. The first few weeks he was in my care, we had almost daily visits to either therapists or specialists. Keeping up with these types of appointments in a normal world is difficult ... I was getting the crash course on how to navigate all of it in the COVID-19 world.
So now, I am the primary caregiver during the day for my two children and our medically fragile foster child who has multiple medical appointments a week. Our local children’s hospital allowed only the caregiver to accompany him to his visits. In theory this sounds great, right? Fewer people in a facility equals less exposure, less risk, and fewer COVID-19 infections.
But what about the negative consequences of these hospital policies? I have two other children I was caring for. I couldn’t take them to their grandparents’ house because people over age 65 years are at risk of having COVID-19 complications. I had been furloughed, so our income was half what it typically was. Regardless,
Now imagine if I were a single mom who had three kids and a lesser paying job. Schools are closed and she’s forced to work from home and homeschool her children. Or worse, she’s been laid off and living on unemployment. Do you think she is going to have the time or finances available to hire a babysitter so that she can take her medically fragile child in for his cardiology follow-up? Because not only does she have to pay the copays and whatever insurance doesn’t cover, but now she has to fork over $50 for child care. If you don’t know the answer already, it’s no, she does not have the time or the finances. So her child misses a cardiology appointment, which means that his meds weren’t increased according to his growth, which means his pulmonary hypertension is not controlled, which worsens his heart failure ... you get my drift.
Fast forward to Sept. 22, 2020. I had a cardiology appointment at our local heart hospital for myself. It’s 2020, people, I’ve been having some palpitations that I needed checked out and was going in to have a heart monitor patch placed. I had my 4-year-old son with me because he is on a hybrid schedule where we homeschool 2 days a week. We entered the building wearing masks, and I was immediately stopped by security and informed that, according to the COVID-19 policy for their hospital, children under 16 are not allowed to enter the building. After some discussion, I was ultimately refused care because my son was with me that day. Refused care because I had a masked 4-year-old with a normal temperature at my side.
These policies are not working. We are in health care. It should not matter what pandemic is on the table, we should not be refusing patients access to care based on who is by their side that day. We knew the risks when we entered our profession, and we know the proper measures to protect ourselves. Our patients also know the risks and can protect themselves accordingly.
So this is my plea to all medical facilities out there: Stop. Stop telling people their loved ones can’t accompany them to appointments. Stop telling caregivers to wait in their cars while their elderly, demented mothers have their annual physicals. Stop telling moms they need to leave their other children at home. This is now a huge access-to-care issue nationwide and it needs to stop. Excess deaths in our nation are soaring, and it’s not just because people don’t want to seek medical attention; it’s because medical facilities are making it almost impossible to seek help for many. People are dying, and it’s not only from COVID-19. This is on us as health care providers, and we need to step up to the plate and do what is right.
Ms. Baxendale is a nurse practitioner in Mustang, Okla. Email her at [email protected].
Learning about “No”
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Prescribe Halloween safety by region, current conditions
Halloween is fast approaching and retail stores are fully stocked with costumes and candy. Physician dialog is beginning to shift from school access toward how to counsel patients and families on COVID-19 safety around Halloween. advised pediatrician Shelly Vaziri Flais, MD.

Halloween “is going to look very different this year, especially in urban and rural settings, according to Dr. Flais, who is a spokesperson for the American Academy of Pediatrics and assistant professor of clinical pediatrics at Northwestern University, Chicago. The notion that trick-or-treating automatically involves physically distancing is a misconception. Urban celebrations frequently see many people gathering on the streets, and that will be even more likely in a pandemic year when people have been separated for long periods of time.
For pediatricians advising families on COVID-19 safety measures to follow while celebrating Halloween, it’s not going to be a one-size-fits-all approach, said Dr. Flais, who practices pediatrics at Pediatric Health Associates in Naperville, Ill.
The goal for physicians across the board should be “to ensure that we aren’t so cautious that we drive folks to do things that are higher risk,” she said in an interview. “We are now 6-7 months into the pandemic and the public is growing weary of laying low, so it is important for physicians to not recommend safety measures that are too restrictive.”
The balance pediatricians will need to strike in advising their patients is tricky at best. So in dispensing advice, it is important to make sure that it has a benefit to the overall population, cautioned Dr. Flais. Activities such as hosting independently organized, heavily packed indoor gatherings where people are eating, drinking, and not wearing masks is not going to be beneficial for the masses.
“We’re all lucky that we have technology. We’ve gotten used to doing virtual hugs and activities on Zoom,” she said, adding that she has already seen some really creative ideas on social media for enjoying a COVID-conscious Halloween, including a festive candy chute created by an Ohio family that is perfect for distributing candy while minimizing physical contact.
In an AAP press release, Dr. Flais noted that “this is a good time to teach children the importance of protecting not just ourselves but each other.” How we choose to manage our safety and the safety of our children “can have a ripple effect on our family members.” It is possible to make safe, responsible choices when celebrating and still create magical memories for our children.
Francis E. Rushton Jr., MD, of the University of South Carolina, Columbia, said in an interview, “ I certainly support the AAP recommendations. Because of the way COVID-19 virus is spread, I would emphasize with my patients that the No. 1 thing to do is to enforce facial mask wearing while out trick-or-treating.
“I would also err on the side of safety if my child was showing any signs of illness and find an alternative method of celebrating Halloween that would not involve close contact with other individuals,” said Dr. Rushton, who is a member of the Pediatric News editorial advisory board.
AAP-recommended Do’s and Don’ts for celebrating Halloween
DO:
- Avoid large gatherings.
- Maintain 6 feet distance.
- Wear cloth masks and wash hands often.
- Use hand sanitizer before and after visiting pumpkin patches and apple orchards.
DON’T:
- Wear painted cloth masks since paints can contain toxins that should not be breathed.
- Use a costume mask unless it has layers of breathable fabric snugly covering mouth and nose.
- Wear cloth mask under costume mask.
- Attend indoor parties or haunted houses.
CDC safety considerations (supplemental to state and local safety laws)
- Assess current cases and overall spread in your community before making any plans.
- Choose outdoor venues or indoor facilities that are well ventilated.
- Consider the length of the event, how many are attending, where they are coming from, and how they behave before and during the event.
- If you are awaiting test results, have COVID-19 symptoms, or have been exposed to COVID-19, stay home.
- If you are at higher risk, avoid large gatherings and limit exposure to anyone you do not live with.
- Make available to others masks, 60% or greater alcohol-based hand sanitizer, and tissues.
- Avoid touching your nose, eyes, and mouth.
- For a complete set of Centers for Disease Control and Prevention COVID safety recommendations go here.
Suggested safe, fun activities
- Use Zoom and other chat programs to share costumes, play games, and watch festive movies.
- Participate in socially distanced outdoor community events at local parks, zoos, etc.
- Attend haunted forests and corn mazes. Maintain more than 6 feet of distance around screaming patrons.
- Decorate pumpkins.
- Cook a Halloween-themed meal.
- If trick-or-treating has been canceled, try a scavenger hunt in the house or yard.
- When handing out treats, wear gloves and mask. Consider prepackaging treat bags. Line up visitors 6 feet apart and discourage gatherings around entranceways.
- Wipe down all goodies received and consider quarantining them for a few days.
- Always wash hands before and after trick-or-treating and when handling treats.
Halloween is fast approaching and retail stores are fully stocked with costumes and candy. Physician dialog is beginning to shift from school access toward how to counsel patients and families on COVID-19 safety around Halloween. advised pediatrician Shelly Vaziri Flais, MD.

Halloween “is going to look very different this year, especially in urban and rural settings, according to Dr. Flais, who is a spokesperson for the American Academy of Pediatrics and assistant professor of clinical pediatrics at Northwestern University, Chicago. The notion that trick-or-treating automatically involves physically distancing is a misconception. Urban celebrations frequently see many people gathering on the streets, and that will be even more likely in a pandemic year when people have been separated for long periods of time.
For pediatricians advising families on COVID-19 safety measures to follow while celebrating Halloween, it’s not going to be a one-size-fits-all approach, said Dr. Flais, who practices pediatrics at Pediatric Health Associates in Naperville, Ill.
The goal for physicians across the board should be “to ensure that we aren’t so cautious that we drive folks to do things that are higher risk,” she said in an interview. “We are now 6-7 months into the pandemic and the public is growing weary of laying low, so it is important for physicians to not recommend safety measures that are too restrictive.”
The balance pediatricians will need to strike in advising their patients is tricky at best. So in dispensing advice, it is important to make sure that it has a benefit to the overall population, cautioned Dr. Flais. Activities such as hosting independently organized, heavily packed indoor gatherings where people are eating, drinking, and not wearing masks is not going to be beneficial for the masses.
“We’re all lucky that we have technology. We’ve gotten used to doing virtual hugs and activities on Zoom,” she said, adding that she has already seen some really creative ideas on social media for enjoying a COVID-conscious Halloween, including a festive candy chute created by an Ohio family that is perfect for distributing candy while minimizing physical contact.
In an AAP press release, Dr. Flais noted that “this is a good time to teach children the importance of protecting not just ourselves but each other.” How we choose to manage our safety and the safety of our children “can have a ripple effect on our family members.” It is possible to make safe, responsible choices when celebrating and still create magical memories for our children.
Francis E. Rushton Jr., MD, of the University of South Carolina, Columbia, said in an interview, “ I certainly support the AAP recommendations. Because of the way COVID-19 virus is spread, I would emphasize with my patients that the No. 1 thing to do is to enforce facial mask wearing while out trick-or-treating.
“I would also err on the side of safety if my child was showing any signs of illness and find an alternative method of celebrating Halloween that would not involve close contact with other individuals,” said Dr. Rushton, who is a member of the Pediatric News editorial advisory board.
AAP-recommended Do’s and Don’ts for celebrating Halloween
DO:
- Avoid large gatherings.
- Maintain 6 feet distance.
- Wear cloth masks and wash hands often.
- Use hand sanitizer before and after visiting pumpkin patches and apple orchards.
DON’T:
- Wear painted cloth masks since paints can contain toxins that should not be breathed.
- Use a costume mask unless it has layers of breathable fabric snugly covering mouth and nose.
- Wear cloth mask under costume mask.
- Attend indoor parties or haunted houses.
CDC safety considerations (supplemental to state and local safety laws)
- Assess current cases and overall spread in your community before making any plans.
- Choose outdoor venues or indoor facilities that are well ventilated.
- Consider the length of the event, how many are attending, where they are coming from, and how they behave before and during the event.
- If you are awaiting test results, have COVID-19 symptoms, or have been exposed to COVID-19, stay home.
- If you are at higher risk, avoid large gatherings and limit exposure to anyone you do not live with.
- Make available to others masks, 60% or greater alcohol-based hand sanitizer, and tissues.
- Avoid touching your nose, eyes, and mouth.
- For a complete set of Centers for Disease Control and Prevention COVID safety recommendations go here.
Suggested safe, fun activities
- Use Zoom and other chat programs to share costumes, play games, and watch festive movies.
- Participate in socially distanced outdoor community events at local parks, zoos, etc.
- Attend haunted forests and corn mazes. Maintain more than 6 feet of distance around screaming patrons.
- Decorate pumpkins.
- Cook a Halloween-themed meal.
- If trick-or-treating has been canceled, try a scavenger hunt in the house or yard.
- When handing out treats, wear gloves and mask. Consider prepackaging treat bags. Line up visitors 6 feet apart and discourage gatherings around entranceways.
- Wipe down all goodies received and consider quarantining them for a few days.
- Always wash hands before and after trick-or-treating and when handling treats.
Halloween is fast approaching and retail stores are fully stocked with costumes and candy. Physician dialog is beginning to shift from school access toward how to counsel patients and families on COVID-19 safety around Halloween. advised pediatrician Shelly Vaziri Flais, MD.

Halloween “is going to look very different this year, especially in urban and rural settings, according to Dr. Flais, who is a spokesperson for the American Academy of Pediatrics and assistant professor of clinical pediatrics at Northwestern University, Chicago. The notion that trick-or-treating automatically involves physically distancing is a misconception. Urban celebrations frequently see many people gathering on the streets, and that will be even more likely in a pandemic year when people have been separated for long periods of time.
For pediatricians advising families on COVID-19 safety measures to follow while celebrating Halloween, it’s not going to be a one-size-fits-all approach, said Dr. Flais, who practices pediatrics at Pediatric Health Associates in Naperville, Ill.
The goal for physicians across the board should be “to ensure that we aren’t so cautious that we drive folks to do things that are higher risk,” she said in an interview. “We are now 6-7 months into the pandemic and the public is growing weary of laying low, so it is important for physicians to not recommend safety measures that are too restrictive.”
The balance pediatricians will need to strike in advising their patients is tricky at best. So in dispensing advice, it is important to make sure that it has a benefit to the overall population, cautioned Dr. Flais. Activities such as hosting independently organized, heavily packed indoor gatherings where people are eating, drinking, and not wearing masks is not going to be beneficial for the masses.
“We’re all lucky that we have technology. We’ve gotten used to doing virtual hugs and activities on Zoom,” she said, adding that she has already seen some really creative ideas on social media for enjoying a COVID-conscious Halloween, including a festive candy chute created by an Ohio family that is perfect for distributing candy while minimizing physical contact.
In an AAP press release, Dr. Flais noted that “this is a good time to teach children the importance of protecting not just ourselves but each other.” How we choose to manage our safety and the safety of our children “can have a ripple effect on our family members.” It is possible to make safe, responsible choices when celebrating and still create magical memories for our children.
Francis E. Rushton Jr., MD, of the University of South Carolina, Columbia, said in an interview, “ I certainly support the AAP recommendations. Because of the way COVID-19 virus is spread, I would emphasize with my patients that the No. 1 thing to do is to enforce facial mask wearing while out trick-or-treating.
“I would also err on the side of safety if my child was showing any signs of illness and find an alternative method of celebrating Halloween that would not involve close contact with other individuals,” said Dr. Rushton, who is a member of the Pediatric News editorial advisory board.
AAP-recommended Do’s and Don’ts for celebrating Halloween
DO:
- Avoid large gatherings.
- Maintain 6 feet distance.
- Wear cloth masks and wash hands often.
- Use hand sanitizer before and after visiting pumpkin patches and apple orchards.
DON’T:
- Wear painted cloth masks since paints can contain toxins that should not be breathed.
- Use a costume mask unless it has layers of breathable fabric snugly covering mouth and nose.
- Wear cloth mask under costume mask.
- Attend indoor parties or haunted houses.
CDC safety considerations (supplemental to state and local safety laws)
- Assess current cases and overall spread in your community before making any plans.
- Choose outdoor venues or indoor facilities that are well ventilated.
- Consider the length of the event, how many are attending, where they are coming from, and how they behave before and during the event.
- If you are awaiting test results, have COVID-19 symptoms, or have been exposed to COVID-19, stay home.
- If you are at higher risk, avoid large gatherings and limit exposure to anyone you do not live with.
- Make available to others masks, 60% or greater alcohol-based hand sanitizer, and tissues.
- Avoid touching your nose, eyes, and mouth.
- For a complete set of Centers for Disease Control and Prevention COVID safety recommendations go here.
Suggested safe, fun activities
- Use Zoom and other chat programs to share costumes, play games, and watch festive movies.
- Participate in socially distanced outdoor community events at local parks, zoos, etc.
- Attend haunted forests and corn mazes. Maintain more than 6 feet of distance around screaming patrons.
- Decorate pumpkins.
- Cook a Halloween-themed meal.
- If trick-or-treating has been canceled, try a scavenger hunt in the house or yard.
- When handing out treats, wear gloves and mask. Consider prepackaging treat bags. Line up visitors 6 feet apart and discourage gatherings around entranceways.
- Wipe down all goodies received and consider quarantining them for a few days.
- Always wash hands before and after trick-or-treating and when handling treats.
Returning to competition
As we continue to stumble around trying to find our way out of the COVID-19 pandemic, it has become clear that the journey has been a never-ending continuum of exercises in risk/benefit assessment. The population always has sorted itself into a bell-shaped curve from those who are risk averse to those who revel in risk taking. And, of course, with a paucity of facts on which we can base our assessment of risk, the discussion often shifts to our gut feelings about the benefits.
When faced with the question of when it is time for children to return to in-person schooling, there seems to be reasonably good agreement about the benefits of face-to-face learning. The level of risk is still to be determined.
When it comes to the issue of when to return to competitive school sports, the risks are equally indeterminate but there is less agreement on the benefits. This lack of uniformity reflects a long-standing dichotomy between those parents and students with a passion for competitive sports and those who see them as nonessential. This existential tug-of-war has gone on in almost every school system I am aware of when the school budget comes up for a vote.
The debate about a return to competitive sports on a collegiate and professional level unfortunately is colored by enormous revenues from media contracts, which means that high school and middle schools can’t look to what are essentially businesses for guidance. The delay created confusion, fluctuating angst and disappointment, but the end product made some sense. Volleyball (indoor) and football were indefinitely delayed. Heavy breathing between competitors separated by a couple of feet and protected only by a flimsy net or helmet cage seems like a risk not worth taking – at least until we have more information.
Other sports were allowed to start with restrictions based on existing social distancing mandates which include no locker rooms and no fans. Some rules such as no throw-ins for soccer didn’t make sense given what we are learning about the virus. But, for the most part, the compromises should result in a chance to reap the benefits of competition for the students whose families are willing to expose them to the yet to be fully determined risks.
There has been some grumbling from parents who see the no-fans mandate as a step too far. Until we know more about the risk of group gatherings outdoors, having no fans, including parents and grandparents, makes sense. In fact, to me it is a step long overdue and a rare sliver of silver lining to the pandemic. Competitive youth sports are for the kids. They are not meant to be entertainment events. Too often children are exposed to parental pressure (voiced and unvoiced) about their “performance” on the field. Neither my younger sister nor I can remember our parents going to any of my away football games in high school or any of my lacrosse games in college. I never felt the loss.
Will I miss watching my grandchildren compete? Of course I will miss it badly. However, giving kids some space to learn and enjoy the competition for itself in an atmosphere free of parental over-involvement will be a breath of fresh air. Something we need badly during this pandemic.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
As we continue to stumble around trying to find our way out of the COVID-19 pandemic, it has become clear that the journey has been a never-ending continuum of exercises in risk/benefit assessment. The population always has sorted itself into a bell-shaped curve from those who are risk averse to those who revel in risk taking. And, of course, with a paucity of facts on which we can base our assessment of risk, the discussion often shifts to our gut feelings about the benefits.
When faced with the question of when it is time for children to return to in-person schooling, there seems to be reasonably good agreement about the benefits of face-to-face learning. The level of risk is still to be determined.
When it comes to the issue of when to return to competitive school sports, the risks are equally indeterminate but there is less agreement on the benefits. This lack of uniformity reflects a long-standing dichotomy between those parents and students with a passion for competitive sports and those who see them as nonessential. This existential tug-of-war has gone on in almost every school system I am aware of when the school budget comes up for a vote.
The debate about a return to competitive sports on a collegiate and professional level unfortunately is colored by enormous revenues from media contracts, which means that high school and middle schools can’t look to what are essentially businesses for guidance. The delay created confusion, fluctuating angst and disappointment, but the end product made some sense. Volleyball (indoor) and football were indefinitely delayed. Heavy breathing between competitors separated by a couple of feet and protected only by a flimsy net or helmet cage seems like a risk not worth taking – at least until we have more information.
Other sports were allowed to start with restrictions based on existing social distancing mandates which include no locker rooms and no fans. Some rules such as no throw-ins for soccer didn’t make sense given what we are learning about the virus. But, for the most part, the compromises should result in a chance to reap the benefits of competition for the students whose families are willing to expose them to the yet to be fully determined risks.
There has been some grumbling from parents who see the no-fans mandate as a step too far. Until we know more about the risk of group gatherings outdoors, having no fans, including parents and grandparents, makes sense. In fact, to me it is a step long overdue and a rare sliver of silver lining to the pandemic. Competitive youth sports are for the kids. They are not meant to be entertainment events. Too often children are exposed to parental pressure (voiced and unvoiced) about their “performance” on the field. Neither my younger sister nor I can remember our parents going to any of my away football games in high school or any of my lacrosse games in college. I never felt the loss.
Will I miss watching my grandchildren compete? Of course I will miss it badly. However, giving kids some space to learn and enjoy the competition for itself in an atmosphere free of parental over-involvement will be a breath of fresh air. Something we need badly during this pandemic.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
As we continue to stumble around trying to find our way out of the COVID-19 pandemic, it has become clear that the journey has been a never-ending continuum of exercises in risk/benefit assessment. The population always has sorted itself into a bell-shaped curve from those who are risk averse to those who revel in risk taking. And, of course, with a paucity of facts on which we can base our assessment of risk, the discussion often shifts to our gut feelings about the benefits.
When faced with the question of when it is time for children to return to in-person schooling, there seems to be reasonably good agreement about the benefits of face-to-face learning. The level of risk is still to be determined.
When it comes to the issue of when to return to competitive school sports, the risks are equally indeterminate but there is less agreement on the benefits. This lack of uniformity reflects a long-standing dichotomy between those parents and students with a passion for competitive sports and those who see them as nonessential. This existential tug-of-war has gone on in almost every school system I am aware of when the school budget comes up for a vote.
The debate about a return to competitive sports on a collegiate and professional level unfortunately is colored by enormous revenues from media contracts, which means that high school and middle schools can’t look to what are essentially businesses for guidance. The delay created confusion, fluctuating angst and disappointment, but the end product made some sense. Volleyball (indoor) and football were indefinitely delayed. Heavy breathing between competitors separated by a couple of feet and protected only by a flimsy net or helmet cage seems like a risk not worth taking – at least until we have more information.
Other sports were allowed to start with restrictions based on existing social distancing mandates which include no locker rooms and no fans. Some rules such as no throw-ins for soccer didn’t make sense given what we are learning about the virus. But, for the most part, the compromises should result in a chance to reap the benefits of competition for the students whose families are willing to expose them to the yet to be fully determined risks.
There has been some grumbling from parents who see the no-fans mandate as a step too far. Until we know more about the risk of group gatherings outdoors, having no fans, including parents and grandparents, makes sense. In fact, to me it is a step long overdue and a rare sliver of silver lining to the pandemic. Competitive youth sports are for the kids. They are not meant to be entertainment events. Too often children are exposed to parental pressure (voiced and unvoiced) about their “performance” on the field. Neither my younger sister nor I can remember our parents going to any of my away football games in high school or any of my lacrosse games in college. I never felt the loss.
Will I miss watching my grandchildren compete? Of course I will miss it badly. However, giving kids some space to learn and enjoy the competition for itself in an atmosphere free of parental over-involvement will be a breath of fresh air. Something we need badly during this pandemic.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Seven things to know about new lymphoma drug tafasitamab
The Food and Drug Administration recently approved tafasitamab-cxix (Monjuvi) in combination with lenalidomide for the treatment of adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified, including DLBCL arising from low-grade lymphoma, who are not eligible for autologous stem cell transplant (ASCT).
In an interview, Ann S. LaCasce, MD, a lymphoma specialist, associate professor of medicine at Harvard Medical School, and director of the Dana-Farber/Massachusetts General Brigham fellowship in hematology/oncology, discussed the drug and its approval:
Question: How common is relapsed or refractory DLBCL? Have there been any changes in the rates of this disease in recent years?
Dr. LaCasce: Approximately 40% of patients with DLBCL will have relapsed or refractory disease. The rates of lymphoma have been rising over the past several decades for unclear reasons. As this is a disease predominantly of older adults, increasing life expectancy likely plays a role. Environmental factors may also be contributing.
Q: How long do patients with relapsed or refractory DLBCL who are not eligible for stem cell transplant usually survive?
Dr. LaCasce: This is highly variable, though it’s estimated to be approximately 1 year. Some patients will be cured with autologous transplantation or CAR-T cells. The pace of the disease can be highly variable, with some patients responding to multiple lines of therapy whereas others may have rapidly progressive refractory disease.
Q: What makes patients with relapsed or refractory DLBCL ineligible for ASCT?
Dr. LaCasce: To be eligible, patients need to be younger than 70-75 years or so without significant comorbidities and must have chemotherapy-responsive disease. More than half of patients will not fit these criteria.
Q: Can you briefly describe the L-MIND study that led to the approval of tafasitamab-cxix?
Dr. LaCasce: This was a single-arm, phase 2 study of tafasitamab plus lenalidomide in patients with relapsed/refractory DLBCL status after one to three prior regimens who were not candidates for ASCT. Patients received tafasitamab until progression and up to 1 year of lenalidomide. The median age was 72 years, and 50% of patients had received only one prior line of therapy.
The overall and complete response rates in 80 patients treated were 60% and 43%, respectively. The median progression-free survival was approximately 1 year. Nearly half of patients required dose reduction of lenalidomide, and about a quarter discontinued the drug. Twenty-five percent of patients discontinued therapy for adverse events.
Q: What’s the toxicity profile of tafasitamab-cxix?
Dr. LaCasce: The most common adverse events were infusion reactions and myelosuppression, which are managed with standard approaches to incident rate ratios with steroids, antihistamines, etc. Myelosuppression can occur, but in this combination is mostly driven by lenalidomide, which is dose reduced or discontinued.
Q: Where does tafasitamab-cxix fit in the treatment paradigm for relapsed or refractory DLBCL? How does it compare with other available options?
Dr. LaCasce: This is an option for patients who are not candidates for potentially curative approaches, including ASCT and CAR T-cell therapy. There are patients not eligible for ASCT who may be appropriate for CAR-T.
Tafasitamab plus lenalidomide requires frequent visits, particularly during the first 3 months, and then every other week until progression. The dose of lenalidomide will not be tolerable for many of these patients.
Other options in this population include polatuzumab plus bendamustine/rituximab or possibly selinexor. The former has similar activity and is time limited, though many patients will not tolerate the full dose of bendamustine. In the study leading to approval, selinexor had a much lower response rate of approximately 30%, and the patient population was much more favorable, given that eligibility required 60-98 days after last therapy before enrolling.
The only approval specific for nontransplant patients is tafasitamab/lenalidomide.
Q: From a cost standpoint, how does tafasitamab compare with other options in this patient population?
Dr. LaCasce: I don’t have exact figures, but all options are very expensive. CAR-T is the most expensive. Given the ongoing therapy of tafasitamab until progression, the cumulative cost could be very high. Polatuzumab plus bendamustine/rituximab and selinexor are also very costly.
Q: What other drugs are in development for relapsed or refractory DLBCL?
Dr. LaCasce: Novel CAR T-cell therapies, including lisocabtagene maraleucel that is at the FDA, are in development. Bispecific antibodies (REGN1979 and mosunetuzumab), combinations with CD47 antibodies, and loncastuximab tesirine are all in phase 2 trials.
Dr. LaCasce has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration recently approved tafasitamab-cxix (Monjuvi) in combination with lenalidomide for the treatment of adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified, including DLBCL arising from low-grade lymphoma, who are not eligible for autologous stem cell transplant (ASCT).
In an interview, Ann S. LaCasce, MD, a lymphoma specialist, associate professor of medicine at Harvard Medical School, and director of the Dana-Farber/Massachusetts General Brigham fellowship in hematology/oncology, discussed the drug and its approval:
Question: How common is relapsed or refractory DLBCL? Have there been any changes in the rates of this disease in recent years?
Dr. LaCasce: Approximately 40% of patients with DLBCL will have relapsed or refractory disease. The rates of lymphoma have been rising over the past several decades for unclear reasons. As this is a disease predominantly of older adults, increasing life expectancy likely plays a role. Environmental factors may also be contributing.
Q: How long do patients with relapsed or refractory DLBCL who are not eligible for stem cell transplant usually survive?
Dr. LaCasce: This is highly variable, though it’s estimated to be approximately 1 year. Some patients will be cured with autologous transplantation or CAR-T cells. The pace of the disease can be highly variable, with some patients responding to multiple lines of therapy whereas others may have rapidly progressive refractory disease.
Q: What makes patients with relapsed or refractory DLBCL ineligible for ASCT?
Dr. LaCasce: To be eligible, patients need to be younger than 70-75 years or so without significant comorbidities and must have chemotherapy-responsive disease. More than half of patients will not fit these criteria.
Q: Can you briefly describe the L-MIND study that led to the approval of tafasitamab-cxix?
Dr. LaCasce: This was a single-arm, phase 2 study of tafasitamab plus lenalidomide in patients with relapsed/refractory DLBCL status after one to three prior regimens who were not candidates for ASCT. Patients received tafasitamab until progression and up to 1 year of lenalidomide. The median age was 72 years, and 50% of patients had received only one prior line of therapy.
The overall and complete response rates in 80 patients treated were 60% and 43%, respectively. The median progression-free survival was approximately 1 year. Nearly half of patients required dose reduction of lenalidomide, and about a quarter discontinued the drug. Twenty-five percent of patients discontinued therapy for adverse events.
Q: What’s the toxicity profile of tafasitamab-cxix?
Dr. LaCasce: The most common adverse events were infusion reactions and myelosuppression, which are managed with standard approaches to incident rate ratios with steroids, antihistamines, etc. Myelosuppression can occur, but in this combination is mostly driven by lenalidomide, which is dose reduced or discontinued.
Q: Where does tafasitamab-cxix fit in the treatment paradigm for relapsed or refractory DLBCL? How does it compare with other available options?
Dr. LaCasce: This is an option for patients who are not candidates for potentially curative approaches, including ASCT and CAR T-cell therapy. There are patients not eligible for ASCT who may be appropriate for CAR-T.
Tafasitamab plus lenalidomide requires frequent visits, particularly during the first 3 months, and then every other week until progression. The dose of lenalidomide will not be tolerable for many of these patients.
Other options in this population include polatuzumab plus bendamustine/rituximab or possibly selinexor. The former has similar activity and is time limited, though many patients will not tolerate the full dose of bendamustine. In the study leading to approval, selinexor had a much lower response rate of approximately 30%, and the patient population was much more favorable, given that eligibility required 60-98 days after last therapy before enrolling.
The only approval specific for nontransplant patients is tafasitamab/lenalidomide.
Q: From a cost standpoint, how does tafasitamab compare with other options in this patient population?
Dr. LaCasce: I don’t have exact figures, but all options are very expensive. CAR-T is the most expensive. Given the ongoing therapy of tafasitamab until progression, the cumulative cost could be very high. Polatuzumab plus bendamustine/rituximab and selinexor are also very costly.
Q: What other drugs are in development for relapsed or refractory DLBCL?
Dr. LaCasce: Novel CAR T-cell therapies, including lisocabtagene maraleucel that is at the FDA, are in development. Bispecific antibodies (REGN1979 and mosunetuzumab), combinations with CD47 antibodies, and loncastuximab tesirine are all in phase 2 trials.
Dr. LaCasce has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration recently approved tafasitamab-cxix (Monjuvi) in combination with lenalidomide for the treatment of adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified, including DLBCL arising from low-grade lymphoma, who are not eligible for autologous stem cell transplant (ASCT).
In an interview, Ann S. LaCasce, MD, a lymphoma specialist, associate professor of medicine at Harvard Medical School, and director of the Dana-Farber/Massachusetts General Brigham fellowship in hematology/oncology, discussed the drug and its approval:
Question: How common is relapsed or refractory DLBCL? Have there been any changes in the rates of this disease in recent years?
Dr. LaCasce: Approximately 40% of patients with DLBCL will have relapsed or refractory disease. The rates of lymphoma have been rising over the past several decades for unclear reasons. As this is a disease predominantly of older adults, increasing life expectancy likely plays a role. Environmental factors may also be contributing.
Q: How long do patients with relapsed or refractory DLBCL who are not eligible for stem cell transplant usually survive?
Dr. LaCasce: This is highly variable, though it’s estimated to be approximately 1 year. Some patients will be cured with autologous transplantation or CAR-T cells. The pace of the disease can be highly variable, with some patients responding to multiple lines of therapy whereas others may have rapidly progressive refractory disease.
Q: What makes patients with relapsed or refractory DLBCL ineligible for ASCT?
Dr. LaCasce: To be eligible, patients need to be younger than 70-75 years or so without significant comorbidities and must have chemotherapy-responsive disease. More than half of patients will not fit these criteria.
Q: Can you briefly describe the L-MIND study that led to the approval of tafasitamab-cxix?
Dr. LaCasce: This was a single-arm, phase 2 study of tafasitamab plus lenalidomide in patients with relapsed/refractory DLBCL status after one to three prior regimens who were not candidates for ASCT. Patients received tafasitamab until progression and up to 1 year of lenalidomide. The median age was 72 years, and 50% of patients had received only one prior line of therapy.
The overall and complete response rates in 80 patients treated were 60% and 43%, respectively. The median progression-free survival was approximately 1 year. Nearly half of patients required dose reduction of lenalidomide, and about a quarter discontinued the drug. Twenty-five percent of patients discontinued therapy for adverse events.
Q: What’s the toxicity profile of tafasitamab-cxix?
Dr. LaCasce: The most common adverse events were infusion reactions and myelosuppression, which are managed with standard approaches to incident rate ratios with steroids, antihistamines, etc. Myelosuppression can occur, but in this combination is mostly driven by lenalidomide, which is dose reduced or discontinued.
Q: Where does tafasitamab-cxix fit in the treatment paradigm for relapsed or refractory DLBCL? How does it compare with other available options?
Dr. LaCasce: This is an option for patients who are not candidates for potentially curative approaches, including ASCT and CAR T-cell therapy. There are patients not eligible for ASCT who may be appropriate for CAR-T.
Tafasitamab plus lenalidomide requires frequent visits, particularly during the first 3 months, and then every other week until progression. The dose of lenalidomide will not be tolerable for many of these patients.
Other options in this population include polatuzumab plus bendamustine/rituximab or possibly selinexor. The former has similar activity and is time limited, though many patients will not tolerate the full dose of bendamustine. In the study leading to approval, selinexor had a much lower response rate of approximately 30%, and the patient population was much more favorable, given that eligibility required 60-98 days after last therapy before enrolling.
The only approval specific for nontransplant patients is tafasitamab/lenalidomide.
Q: From a cost standpoint, how does tafasitamab compare with other options in this patient population?
Dr. LaCasce: I don’t have exact figures, but all options are very expensive. CAR-T is the most expensive. Given the ongoing therapy of tafasitamab until progression, the cumulative cost could be very high. Polatuzumab plus bendamustine/rituximab and selinexor are also very costly.
Q: What other drugs are in development for relapsed or refractory DLBCL?
Dr. LaCasce: Novel CAR T-cell therapies, including lisocabtagene maraleucel that is at the FDA, are in development. Bispecific antibodies (REGN1979 and mosunetuzumab), combinations with CD47 antibodies, and loncastuximab tesirine are all in phase 2 trials.
Dr. LaCasce has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.