User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Why is vitamin D hype so impervious to evidence?
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
CDC preparing to update mask guidance
, CDC Director Rochelle P. Walensky, MD, said on Feb. 16.
“As we consider future metrics, which will be updated soon, we recognize the importance of not just cases … but critically, medically severe disease that leads to hospitalizations,” Dr. Walensky said at a White House news briefing. “We must consider hospital capacity as an additional important barometer.”
She later added, “We are looking at an overview of much of our guidance, and masking in all settings will be a part of that.”
Coronavirus cases continue to drop nationwide. This week’s 7-day daily average of cases is 147,000, a decrease of 40%. Hospitalizations have dropped 28% to 9,500, and daily deaths are 2,200, a decrease of 9%.
“Omicron cases are declining, and we are all cautiously optimistic about the trajectory we’re on,” Dr. Walensky said. “Things are moving in the right direction, but we want to remain vigilant to do all we can so this trajectory continues.”
Dr. Walensky said public masking remains especially important if someone is symptomatic or not feeling well, or if there has been a COVID-19 exposure. Those who are within 10 days of being diagnosed with the virus should also remain masked in public.
“We all share the same goal: to get to a point where COVID-19 is no longer disrupting our daily lives. A time when it won’t be a constant crisis,” Dr. Walensky said. “Moving from this pandemic will be a process led by science and epidemiological trends, and one that relies on the powerful tools we already have.”
A version of this article first appeared on WebMD.com.
, CDC Director Rochelle P. Walensky, MD, said on Feb. 16.
“As we consider future metrics, which will be updated soon, we recognize the importance of not just cases … but critically, medically severe disease that leads to hospitalizations,” Dr. Walensky said at a White House news briefing. “We must consider hospital capacity as an additional important barometer.”
She later added, “We are looking at an overview of much of our guidance, and masking in all settings will be a part of that.”
Coronavirus cases continue to drop nationwide. This week’s 7-day daily average of cases is 147,000, a decrease of 40%. Hospitalizations have dropped 28% to 9,500, and daily deaths are 2,200, a decrease of 9%.
“Omicron cases are declining, and we are all cautiously optimistic about the trajectory we’re on,” Dr. Walensky said. “Things are moving in the right direction, but we want to remain vigilant to do all we can so this trajectory continues.”
Dr. Walensky said public masking remains especially important if someone is symptomatic or not feeling well, or if there has been a COVID-19 exposure. Those who are within 10 days of being diagnosed with the virus should also remain masked in public.
“We all share the same goal: to get to a point where COVID-19 is no longer disrupting our daily lives. A time when it won’t be a constant crisis,” Dr. Walensky said. “Moving from this pandemic will be a process led by science and epidemiological trends, and one that relies on the powerful tools we already have.”
A version of this article first appeared on WebMD.com.
, CDC Director Rochelle P. Walensky, MD, said on Feb. 16.
“As we consider future metrics, which will be updated soon, we recognize the importance of not just cases … but critically, medically severe disease that leads to hospitalizations,” Dr. Walensky said at a White House news briefing. “We must consider hospital capacity as an additional important barometer.”
She later added, “We are looking at an overview of much of our guidance, and masking in all settings will be a part of that.”
Coronavirus cases continue to drop nationwide. This week’s 7-day daily average of cases is 147,000, a decrease of 40%. Hospitalizations have dropped 28% to 9,500, and daily deaths are 2,200, a decrease of 9%.
“Omicron cases are declining, and we are all cautiously optimistic about the trajectory we’re on,” Dr. Walensky said. “Things are moving in the right direction, but we want to remain vigilant to do all we can so this trajectory continues.”
Dr. Walensky said public masking remains especially important if someone is symptomatic or not feeling well, or if there has been a COVID-19 exposure. Those who are within 10 days of being diagnosed with the virus should also remain masked in public.
“We all share the same goal: to get to a point where COVID-19 is no longer disrupting our daily lives. A time when it won’t be a constant crisis,” Dr. Walensky said. “Moving from this pandemic will be a process led by science and epidemiological trends, and one that relies on the powerful tools we already have.”
A version of this article first appeared on WebMD.com.
Tiny hitchhikers like to ride in the trunk
Junk (germs) in the trunk
It’s been a long drive, and you’ve got a long way to go. You pull into a rest stop to use the bathroom and get some food. Quick, which order do you do those things in?
If you’re not a crazy person, you’d use the bathroom and then get your food. Who would bring food into a dirty bathroom? That’s kind of gross. Most people would take care of business, grab food, then get back in the car, eating along the way. Unfortunately, if you’re searching for a sanitary eating environment, your car may not actually be much better than that bathroom, according to new research from Aston University in Birmingham, England.
Let’s start off with the good news. The steering wheels of the five used cars that were swabbed for bacteria were pretty clean. Definitely cleaner than either of the toilet seats analyzed, likely thanks to increased usage of sanitizer, courtesy of the current pandemic. It’s easy to wipe down the steering wheel. Things break down, though, once we look elsewhere. The interiors of the five cars all contained just as much, if not more, bacteria than the toilet seats, with fecal matter commonly appearing on the driver’s seat.
The car interiors were less than sanitary, but they paled in comparison with the real winner here: the trunk. In each of the five cars, bacteria levels there far exceeded those in the toilets, and included everyone’s favorites – Escherichia coli and Staphylococcus aureus.
So, snacking on a bag of chips as you drive along is probably okay, but the food that popped out of its bag and spent the last 5 minutes rolling around the back? Perhaps less okay. You may want to wash it. Or burn it. Or torch the entire car for good measure like we’re about to do. Next time we’ll buy a car without poop in it.
Shut the lid when you flush
Maybe you’ve never thought about this, but it’s actually extremely important to shut the toilet lid when you flush. Just think of all those germs flying around from the force of the flush. Is your toothbrush anywhere near the toilet? Ew. Those pesky little bacteria and viruses are everywhere, and we know we can’t really escape them, but we should really do our best once we’re made aware of where to find them.
It seems like a no-brainer these days since we’ve all been really focused on cleanliness during the pandemic, but according to a poll in the United Kingdom, 55% of the 2,000 participants said they don’t put the lid down while flushing.
The OnePoll survey commissioned by Harpic, a company that makes toilet-cleaning products, also advised that toilet water isn’t even completely clean after flushed several times and can still be contaminated with many germs. Company researchers took specialized pictures of flushing toilets and they looked like tiny little Fourth of July fireworks shows, minus the sparklers. The pictures proved that droplets can go all over the place, including on bathroom users.
“There has never been a more important time to take extra care around our homes, although the risks associated with germ spread in unhygienic bathrooms are high, the solution to keeping them clean is simple,” a Harpic researcher said. Since other studies have shown that coronavirus can be found in feces, it’s become increasingly important to keep ourselves and others safe. Fireworks are pretty, but not when they come out of your toilet.
The latest in MRI fashion
Do you see that photo just below? Looks like something you could buy at the Lego store, right? Well, it’s not. Nor is it the proverbial thinking cap come to life.
(Did someone just say “come to life”? That reminds us of our favorite scene from Frosty the Snowman.)
Anywaaay, about the photo. That funny-looking chapeau is what we in the science business call a metamaterial.
Nope, metamaterials have nothing to do with Facebook parent company Meta. We checked. According to a statement from Boston University, they are engineered structures “created from small unit cells that might be unspectacular alone, but when grouped together in a precise way, get new superpowers not found in nature.”
Superpowers, eh? Who doesn’t want superpowers? Even if they come with a funny hat.
The unit cells, known as resonators, are just plastic tubes wrapped in copper wiring, but when they are grouped in an array and precisely arranged into a helmet, they can channel the magnetic field of the MRI machine during a scan. In theory, that would create “crisper images that can be captured at twice the normal speed,” Xin Zhang, PhD, and her team at BU’s Photonics Center explained in the university statement.
In the future, the metamaterial device could “be used in conjunction with cheaper low-field MRI machines to make the technology more widely available, particularly in the developing world,” they suggested. Or, like so many other superpowers, it could fall into the wrong hands. Like those of Lex Luthor. Or Mark Zuckerberg. Or Frosty the Snowman.
The highway of the mind
How fast can you think on your feet? Well, according to a recently published study, it could be a legitimate measure of intelligence. Here’s the science.
Researchers from the University of Würzburg in Germany and Indiana University have suggested that a person’s intelligence score measures the ability, based on certain neuronal networks and their communication structures, to switch between resting state and different task states.
The investigators set up a study to observe almost 800 people while they completed seven tasks. By monitoring brain activity with functional magnetic resonance imaging, the teams found that subjects who had higher intelligence scores required “less adjustment when switching between different cognitive states,” they said in a separate statement.
It comes down to the network architecture of their brains.
Kirsten Hilger, PhD, head of the German group, described it in terms of highways. The resting state of the brain is normal traffic. It’s always moving. Holiday traffic is the task. The ability to handle the increased flow of commuters is a function of the highway infrastructure. The better the infrastructure, the higher the intelligence.
So the next time you’re stuck in traffic, think how efficient your brain would be with such a task. The quicker, the better.
Junk (germs) in the trunk
It’s been a long drive, and you’ve got a long way to go. You pull into a rest stop to use the bathroom and get some food. Quick, which order do you do those things in?
If you’re not a crazy person, you’d use the bathroom and then get your food. Who would bring food into a dirty bathroom? That’s kind of gross. Most people would take care of business, grab food, then get back in the car, eating along the way. Unfortunately, if you’re searching for a sanitary eating environment, your car may not actually be much better than that bathroom, according to new research from Aston University in Birmingham, England.
Let’s start off with the good news. The steering wheels of the five used cars that were swabbed for bacteria were pretty clean. Definitely cleaner than either of the toilet seats analyzed, likely thanks to increased usage of sanitizer, courtesy of the current pandemic. It’s easy to wipe down the steering wheel. Things break down, though, once we look elsewhere. The interiors of the five cars all contained just as much, if not more, bacteria than the toilet seats, with fecal matter commonly appearing on the driver’s seat.
The car interiors were less than sanitary, but they paled in comparison with the real winner here: the trunk. In each of the five cars, bacteria levels there far exceeded those in the toilets, and included everyone’s favorites – Escherichia coli and Staphylococcus aureus.
So, snacking on a bag of chips as you drive along is probably okay, but the food that popped out of its bag and spent the last 5 minutes rolling around the back? Perhaps less okay. You may want to wash it. Or burn it. Or torch the entire car for good measure like we’re about to do. Next time we’ll buy a car without poop in it.
Shut the lid when you flush
Maybe you’ve never thought about this, but it’s actually extremely important to shut the toilet lid when you flush. Just think of all those germs flying around from the force of the flush. Is your toothbrush anywhere near the toilet? Ew. Those pesky little bacteria and viruses are everywhere, and we know we can’t really escape them, but we should really do our best once we’re made aware of where to find them.
It seems like a no-brainer these days since we’ve all been really focused on cleanliness during the pandemic, but according to a poll in the United Kingdom, 55% of the 2,000 participants said they don’t put the lid down while flushing.
The OnePoll survey commissioned by Harpic, a company that makes toilet-cleaning products, also advised that toilet water isn’t even completely clean after flushed several times and can still be contaminated with many germs. Company researchers took specialized pictures of flushing toilets and they looked like tiny little Fourth of July fireworks shows, minus the sparklers. The pictures proved that droplets can go all over the place, including on bathroom users.
“There has never been a more important time to take extra care around our homes, although the risks associated with germ spread in unhygienic bathrooms are high, the solution to keeping them clean is simple,” a Harpic researcher said. Since other studies have shown that coronavirus can be found in feces, it’s become increasingly important to keep ourselves and others safe. Fireworks are pretty, but not when they come out of your toilet.
The latest in MRI fashion
Do you see that photo just below? Looks like something you could buy at the Lego store, right? Well, it’s not. Nor is it the proverbial thinking cap come to life.
(Did someone just say “come to life”? That reminds us of our favorite scene from Frosty the Snowman.)
Anywaaay, about the photo. That funny-looking chapeau is what we in the science business call a metamaterial.
Nope, metamaterials have nothing to do with Facebook parent company Meta. We checked. According to a statement from Boston University, they are engineered structures “created from small unit cells that might be unspectacular alone, but when grouped together in a precise way, get new superpowers not found in nature.”
Superpowers, eh? Who doesn’t want superpowers? Even if they come with a funny hat.
The unit cells, known as resonators, are just plastic tubes wrapped in copper wiring, but when they are grouped in an array and precisely arranged into a helmet, they can channel the magnetic field of the MRI machine during a scan. In theory, that would create “crisper images that can be captured at twice the normal speed,” Xin Zhang, PhD, and her team at BU’s Photonics Center explained in the university statement.
In the future, the metamaterial device could “be used in conjunction with cheaper low-field MRI machines to make the technology more widely available, particularly in the developing world,” they suggested. Or, like so many other superpowers, it could fall into the wrong hands. Like those of Lex Luthor. Or Mark Zuckerberg. Or Frosty the Snowman.
The highway of the mind
How fast can you think on your feet? Well, according to a recently published study, it could be a legitimate measure of intelligence. Here’s the science.
Researchers from the University of Würzburg in Germany and Indiana University have suggested that a person’s intelligence score measures the ability, based on certain neuronal networks and their communication structures, to switch between resting state and different task states.
The investigators set up a study to observe almost 800 people while they completed seven tasks. By monitoring brain activity with functional magnetic resonance imaging, the teams found that subjects who had higher intelligence scores required “less adjustment when switching between different cognitive states,” they said in a separate statement.
It comes down to the network architecture of their brains.
Kirsten Hilger, PhD, head of the German group, described it in terms of highways. The resting state of the brain is normal traffic. It’s always moving. Holiday traffic is the task. The ability to handle the increased flow of commuters is a function of the highway infrastructure. The better the infrastructure, the higher the intelligence.
So the next time you’re stuck in traffic, think how efficient your brain would be with such a task. The quicker, the better.
Junk (germs) in the trunk
It’s been a long drive, and you’ve got a long way to go. You pull into a rest stop to use the bathroom and get some food. Quick, which order do you do those things in?
If you’re not a crazy person, you’d use the bathroom and then get your food. Who would bring food into a dirty bathroom? That’s kind of gross. Most people would take care of business, grab food, then get back in the car, eating along the way. Unfortunately, if you’re searching for a sanitary eating environment, your car may not actually be much better than that bathroom, according to new research from Aston University in Birmingham, England.
Let’s start off with the good news. The steering wheels of the five used cars that were swabbed for bacteria were pretty clean. Definitely cleaner than either of the toilet seats analyzed, likely thanks to increased usage of sanitizer, courtesy of the current pandemic. It’s easy to wipe down the steering wheel. Things break down, though, once we look elsewhere. The interiors of the five cars all contained just as much, if not more, bacteria than the toilet seats, with fecal matter commonly appearing on the driver’s seat.
The car interiors were less than sanitary, but they paled in comparison with the real winner here: the trunk. In each of the five cars, bacteria levels there far exceeded those in the toilets, and included everyone’s favorites – Escherichia coli and Staphylococcus aureus.
So, snacking on a bag of chips as you drive along is probably okay, but the food that popped out of its bag and spent the last 5 minutes rolling around the back? Perhaps less okay. You may want to wash it. Or burn it. Or torch the entire car for good measure like we’re about to do. Next time we’ll buy a car without poop in it.
Shut the lid when you flush
Maybe you’ve never thought about this, but it’s actually extremely important to shut the toilet lid when you flush. Just think of all those germs flying around from the force of the flush. Is your toothbrush anywhere near the toilet? Ew. Those pesky little bacteria and viruses are everywhere, and we know we can’t really escape them, but we should really do our best once we’re made aware of where to find them.
It seems like a no-brainer these days since we’ve all been really focused on cleanliness during the pandemic, but according to a poll in the United Kingdom, 55% of the 2,000 participants said they don’t put the lid down while flushing.
The OnePoll survey commissioned by Harpic, a company that makes toilet-cleaning products, also advised that toilet water isn’t even completely clean after flushed several times and can still be contaminated with many germs. Company researchers took specialized pictures of flushing toilets and they looked like tiny little Fourth of July fireworks shows, minus the sparklers. The pictures proved that droplets can go all over the place, including on bathroom users.
“There has never been a more important time to take extra care around our homes, although the risks associated with germ spread in unhygienic bathrooms are high, the solution to keeping them clean is simple,” a Harpic researcher said. Since other studies have shown that coronavirus can be found in feces, it’s become increasingly important to keep ourselves and others safe. Fireworks are pretty, but not when they come out of your toilet.
The latest in MRI fashion
Do you see that photo just below? Looks like something you could buy at the Lego store, right? Well, it’s not. Nor is it the proverbial thinking cap come to life.
(Did someone just say “come to life”? That reminds us of our favorite scene from Frosty the Snowman.)
Anywaaay, about the photo. That funny-looking chapeau is what we in the science business call a metamaterial.
Nope, metamaterials have nothing to do with Facebook parent company Meta. We checked. According to a statement from Boston University, they are engineered structures “created from small unit cells that might be unspectacular alone, but when grouped together in a precise way, get new superpowers not found in nature.”
Superpowers, eh? Who doesn’t want superpowers? Even if they come with a funny hat.
The unit cells, known as resonators, are just plastic tubes wrapped in copper wiring, but when they are grouped in an array and precisely arranged into a helmet, they can channel the magnetic field of the MRI machine during a scan. In theory, that would create “crisper images that can be captured at twice the normal speed,” Xin Zhang, PhD, and her team at BU’s Photonics Center explained in the university statement.
In the future, the metamaterial device could “be used in conjunction with cheaper low-field MRI machines to make the technology more widely available, particularly in the developing world,” they suggested. Or, like so many other superpowers, it could fall into the wrong hands. Like those of Lex Luthor. Or Mark Zuckerberg. Or Frosty the Snowman.
The highway of the mind
How fast can you think on your feet? Well, according to a recently published study, it could be a legitimate measure of intelligence. Here’s the science.
Researchers from the University of Würzburg in Germany and Indiana University have suggested that a person’s intelligence score measures the ability, based on certain neuronal networks and their communication structures, to switch between resting state and different task states.
The investigators set up a study to observe almost 800 people while they completed seven tasks. By monitoring brain activity with functional magnetic resonance imaging, the teams found that subjects who had higher intelligence scores required “less adjustment when switching between different cognitive states,” they said in a separate statement.
It comes down to the network architecture of their brains.
Kirsten Hilger, PhD, head of the German group, described it in terms of highways. The resting state of the brain is normal traffic. It’s always moving. Holiday traffic is the task. The ability to handle the increased flow of commuters is a function of the highway infrastructure. The better the infrastructure, the higher the intelligence.
So the next time you’re stuck in traffic, think how efficient your brain would be with such a task. The quicker, the better.
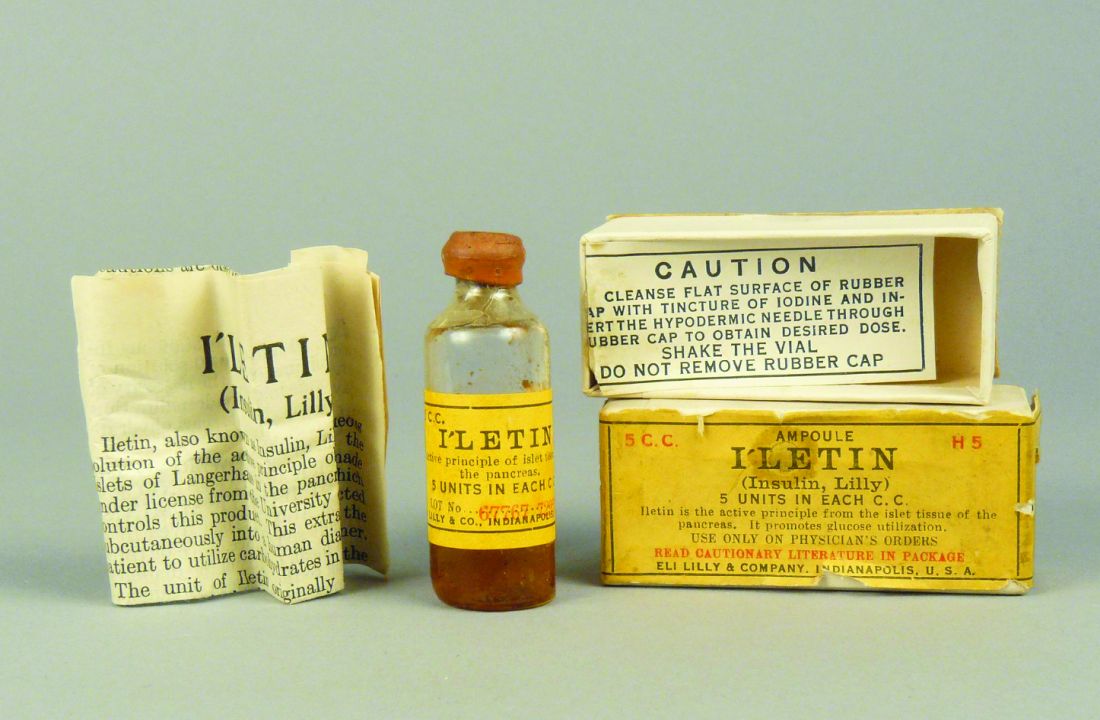
The battle of egos behind the life-saving discovery of insulin
Leonard Thompson’s father was so desperate to save his 14-year-old child from certain death due to diabetes that, on Jan. 11, 1922, he took him to Toronto General Hospital to receive what is arguably the first dose of insulin given to a human. From an anticipated life expectancy of weeks – months at best – Thompson lived for an astonishing further 13 years, eventually dying from pneumonia unrelated to diabetes.
By all accounts, the story is a centenary celebration of a remarkable discovery. Insulin has changed what was once a death sentence to a near-normal life expectancy for the millions of people with type 1 diabetes over the past 100 years.
But behind the life-changing success of the discovery – and the Nobel Prize that went with it – lies a tale blighted by disputed claims, twisted truths, and likely injustices between the scientists involved, as they each vied for an honored place in medical history.
Kersten Hall, PhD, honorary fellow, religion and history of science, at the University of Leeds, England, has scoured archives and personal records held at the University of Toronto to uncover the personal stories behind insulin’s discovery.
Despite the wranglings, Dr. Hall asserts: “There’s a distinction between the science and the scientists. Scientists are wonderfully flawed and complex human beings with all their glorious virtues and vices, as we all are. It’s no surprise that they get greedy, jealous, and insecure.”
At death’s door: Diabetes before the 1920s
Prior to insulin’s discovery in 1921, a diagnosis of type 1 diabetes placed someone at death’s door, with nothing but starvation – albeit a slightly slower death – to mitigate a fast-approaching departure from this world. At that time, most diabetes cases would have been type 1 diabetes because, with less obesogenic diets and shorter lifespans, people were much less likely to develop type 2 diabetes.
Nowadays, it is widely recognized that the prevalence of type 2 diabetes is on a steep upward curve, but so too is type 1 diabetes. In the United States alone, there are 1.5 million people diagnosed with type 1 diabetes, a number expected to rise to around 5 million by 2050, according to JDRF, the type 1 diabetes advocacy organization.
Interestingly, 100 years since the first treated patient, life-long insulin remains the only real effective therapy for patients with type 1 diabetes. Once pancreatic beta cells have ceased to function and insulin production has stopped, insulin replacement is the only way to keep blood glucose levels within the recommended range (A1c ≤ 48 mmol/mol [6.5%]), according to the UK National Institute for Health and Care Excellence (NICE), as well as numerous diabetes organizations, including the American Diabetes Association (ADA).
Preliminary clinical trials have looked at stem cell transplantation, prematurely dubbed as a “cure” for type 1 diabetes, as an alternative to insulin therapy. The procedure involves transplanting stem cell–derived cells, which become functional beta cells when infused into humans, but requires immunosuppression, as reported by this news organization.
Today, the life expectancy of people with type 1 diabetes treated with insulin is close to those without the disease, although this is dependent on how tightly blood glucose is controlled. Some studies show life expectancy of those with type 1 diabetes is around 8-12 years lower than the general population but varies depending on where a person lives.
In some lower-income countries, many with type 1 diabetes still die prematurely either because they are undiagnosed or cannot access insulin. The high cost of insulin in the United States is well publicized, as featured in numerous articles by this news organization, and numerous patients in the United States have died because they cannot afford insulin.
Without insulin, young Leonard Thompson would have been lucky to have reached his 15th birthday.
“Such patients were cachectic and thin and would have weighed around 40-50 pounds (18-23 kg), which is very low for an older child. Survival was short and lasted weeks or months usually,” said Elizabeth Stephens, MD, an endocrinologist in Portland, Ore.
“The discovery of insulin was really a miracle because without it diabetes patients were facing certain death. Even nowadays, if people don’t get their insulin because they can’t afford it or for whatever reason, they can still die,” Dr. Stephens stressed.
Antidiabetic effects of pancreatic extract limited
Back in 1869, Paul Langerhans, MD, discovered pancreatic islet cells, or islets of Langerhans, as a medical student. Researchers tried to produce extracts that lowered blood glucose but they were too toxic for patient use.
In 1908, as detailed in his recent book, Insulin – the Crooked Timber, Dr. Hall also refers to the fact that a German researcher, Georg Zuelzer, MD, demonstrated in six patients that pancreatic extracts could reduce urinary levels of glucose and ketones, and that in one case, the treatment woke the patient from a coma. Dr. Zuelzer had purified the extract with alcohol but patients still experienced convulsions and coma; in fact, they were experiencing hypoglycemic shock, but Dr. Zuelzer had not identified it as such.
“He thought his preparation was full of impurities – and that’s the irony. He had in his hands an insulin prep that was so clean and so potent that it sent the test animals into hypoglycemic shock,” Dr. Hall pointed out.
By 1921, two young researchers, Frederick G. Banting, MD, a practicing medical doctor in Toronto, together with a final year physiology student at the University of Toronto, Charles H. Best, MD, DSc, collaborated on the instruction of Dr. Best’s superior, John James Rickard Macleod, MBChB, professor of physiology at the University of Toronto, to make pancreatic extracts, first from dogs and then from cattle.
Over the months prior to treating Thompson, working together in the laboratory, Dr. Banting and Dr. Best prepared the pancreatic extract from cattle and tested it on dogs with diabetes.
Then, in what amounted to a phase 1 trial of its day, with an “n of one,” a frail and close-to-death Thompson was given 15 cc of pancreatic extract at Toronto General Hospital in January 1922. His blood glucose level dropped by 25%, but unfortunately, his body still produced ketones, indicating the antidiabetic effect was limited. He also experienced an adverse reaction at the injection site with an accumulation of abscesses.
So despite success with isolating the extract and administering it to Thompson, the product remained tainted with impurities.
At this point, colleague James Collip, MD, PhD, came to the rescue. He used his skills as a biochemist to purify the pancreatic extract enough to eliminate impurities.
When Thompson was treated 2 weeks later with the purified extract, he experienced a more positive outcome. Gone was the injection site reaction, gone were the high blood glucose levels, and Thompson “became brighter, more active, looked better, and said he felt stronger,” according to a publication describing the treatment.
Dr. Collip also determined that by over-purifying the product, the animals he experimented on could overreact and experience convulsions, coma, and death due to hypoglycemia from too much insulin.
Fighting talk
Recalling an excerpt from Dr. Banting’s diary, Dr. Hall said that Dr. Banting had a mercurial temper and testified to his loss of patience with Dr. Collip when the chemist refused to share his formula of purification. His diary reads: “I grabbed him in one hand by the overcoat ... and almost lifting him I sat him down hard on the chair ... I remember telling him that it was a good job he was so much smaller – otherwise I would ‘knock hell out of him.’ ”
According to Dr. Hall, in 1923, when Dr. Banting and Dr. Macleod were jointly awarded the Nobel Prize for Medicine, Dr. Best resented being excluded, and despite Dr. Banting’s sharing half his prize money with Dr. Best, animosity prevailed.
At one point, before leaving on a plane for a wartime mission to the United Kingdom, Dr. Banting noted that if he didn’t make it back alive, “and they give my [professorial] chair to that son-of-a-bitch Best, I’ll never rest in my grave.” In a cruel twist of fate, Dr. Banting’s plane crashed and all aboard died.
The Nobel Prize had also been a source of rivalry between Dr. Banting and his boss, Dr. Macleod. In late 1921, while presenting the findings from animal models at the American Physiological Society conference, Dr. Banting’s nerves got the better of him and Dr. Macleod took over at the podium to finish the talk. Dr. Banting perceived this as his boss stealing the limelight.
Only a few months later, at the Association of American Physicians annual conference, Dr. Macleod played to an audience for a second time by making the first formal announcement of the discovery to the scientific community. Notably, Dr. Banting was absent.
The Nobel Prize or a poisoned chalice?
Awarded annually for physics, chemistry, medicine/physiology, literature, peace, and economics, Nobel Prizes are usually considered the holy grail of achievement. In 1895, funds for the prizes were bequeathed by Alfred Nobel in his last will and testament, with each prize worth around $40,000 at the time (approximately $1,000,000 in today’s value).
Writing in 2001 in the journal Diabetes Voice, Professor Sir George Alberti, DPhil, BM BCh, former president of the UK Royal College of Physicians, summarized the burden that accompanies the Nobel Prize: “I personally believe that such prizes and awards do more harm than good and should be abolished. Many a scientist has gone to their grave feeling deeply aggrieved because they were not awarded a Nobel Prize.”
Such high stakes surround the prize that, in the case of insulin, the course of its discovery meant courtesies and truth were swept aside in hot pursuit of fame. After Dr. Macleod died in 1935 and Dr. Banting died in 1941, Dr. Best took the opportunity to try to revise history. There was the small obstacle of Dr. Collip, but Dr. Best managed to play down Dr. Collip’s contribution by focusing on the eureka moment as being the first insulin dose administered, despite the fact that a more complete recovery without side effects was later achieved only with Dr. Collip’s help.
Despite exclusion from the Nobel Prize, Dr. Best nevertheless became recognized as the “go-to-guy” for the discovery of insulin, said Dr. Hall. When Dr. Best spoke about the discovery of insulin at the New York Diabetes Association meeting in 1946, he was introduced as a speaker whose reputation was already so great that he did “not require much of an introduction.”
“And when a new research institute was opened in Toronto in 1953, it was named in his honor. The opening address, by Sir Henry Dale of the UK Medical Research Council, sang Best’s praises to the rafters, much to the disgruntlement of Best’s former colleague, James Collip, who was sitting in the audience,” Dr. Hall pointed out.
Both Dr. Hall and Dr. Stephens live with type 1 diabetes and have benefited from the efforts of Dr. Banting, Dr. Best, Dr. Collip, Dr. Zuelzer, and Dr. Macleod.
“The discovery of insulin was a miracle, it has allowed people to survive,” said Dr. Stephens. “Few medicines can reverse a death sentence like insulin can. It’s easy to forget how it was when insulin wasn’t there – and it wasn’t that long ago.”
Dr. Hall reflects that scientific progress and discovery are often portrayed as being the result of towering geniuses standing on each other’s shoulders.
“But I think that when German philosopher Immanuel Kant remarked that ‘Out of the crooked timber of humanity, no straight thing can ever be made,’ he offered us a much more accurate picture of how science works. And I think that there’s perhaps no more powerful example of this than the story of insulin,” he said.
A version of this article first appeared on Medscape.com.
Leonard Thompson’s father was so desperate to save his 14-year-old child from certain death due to diabetes that, on Jan. 11, 1922, he took him to Toronto General Hospital to receive what is arguably the first dose of insulin given to a human. From an anticipated life expectancy of weeks – months at best – Thompson lived for an astonishing further 13 years, eventually dying from pneumonia unrelated to diabetes.
By all accounts, the story is a centenary celebration of a remarkable discovery. Insulin has changed what was once a death sentence to a near-normal life expectancy for the millions of people with type 1 diabetes over the past 100 years.
But behind the life-changing success of the discovery – and the Nobel Prize that went with it – lies a tale blighted by disputed claims, twisted truths, and likely injustices between the scientists involved, as they each vied for an honored place in medical history.
Kersten Hall, PhD, honorary fellow, religion and history of science, at the University of Leeds, England, has scoured archives and personal records held at the University of Toronto to uncover the personal stories behind insulin’s discovery.
Despite the wranglings, Dr. Hall asserts: “There’s a distinction between the science and the scientists. Scientists are wonderfully flawed and complex human beings with all their glorious virtues and vices, as we all are. It’s no surprise that they get greedy, jealous, and insecure.”
At death’s door: Diabetes before the 1920s
Prior to insulin’s discovery in 1921, a diagnosis of type 1 diabetes placed someone at death’s door, with nothing but starvation – albeit a slightly slower death – to mitigate a fast-approaching departure from this world. At that time, most diabetes cases would have been type 1 diabetes because, with less obesogenic diets and shorter lifespans, people were much less likely to develop type 2 diabetes.
Nowadays, it is widely recognized that the prevalence of type 2 diabetes is on a steep upward curve, but so too is type 1 diabetes. In the United States alone, there are 1.5 million people diagnosed with type 1 diabetes, a number expected to rise to around 5 million by 2050, according to JDRF, the type 1 diabetes advocacy organization.
Interestingly, 100 years since the first treated patient, life-long insulin remains the only real effective therapy for patients with type 1 diabetes. Once pancreatic beta cells have ceased to function and insulin production has stopped, insulin replacement is the only way to keep blood glucose levels within the recommended range (A1c ≤ 48 mmol/mol [6.5%]), according to the UK National Institute for Health and Care Excellence (NICE), as well as numerous diabetes organizations, including the American Diabetes Association (ADA).
Preliminary clinical trials have looked at stem cell transplantation, prematurely dubbed as a “cure” for type 1 diabetes, as an alternative to insulin therapy. The procedure involves transplanting stem cell–derived cells, which become functional beta cells when infused into humans, but requires immunosuppression, as reported by this news organization.
Today, the life expectancy of people with type 1 diabetes treated with insulin is close to those without the disease, although this is dependent on how tightly blood glucose is controlled. Some studies show life expectancy of those with type 1 diabetes is around 8-12 years lower than the general population but varies depending on where a person lives.
In some lower-income countries, many with type 1 diabetes still die prematurely either because they are undiagnosed or cannot access insulin. The high cost of insulin in the United States is well publicized, as featured in numerous articles by this news organization, and numerous patients in the United States have died because they cannot afford insulin.
Without insulin, young Leonard Thompson would have been lucky to have reached his 15th birthday.
“Such patients were cachectic and thin and would have weighed around 40-50 pounds (18-23 kg), which is very low for an older child. Survival was short and lasted weeks or months usually,” said Elizabeth Stephens, MD, an endocrinologist in Portland, Ore.
“The discovery of insulin was really a miracle because without it diabetes patients were facing certain death. Even nowadays, if people don’t get their insulin because they can’t afford it or for whatever reason, they can still die,” Dr. Stephens stressed.
Antidiabetic effects of pancreatic extract limited
Back in 1869, Paul Langerhans, MD, discovered pancreatic islet cells, or islets of Langerhans, as a medical student. Researchers tried to produce extracts that lowered blood glucose but they were too toxic for patient use.
In 1908, as detailed in his recent book, Insulin – the Crooked Timber, Dr. Hall also refers to the fact that a German researcher, Georg Zuelzer, MD, demonstrated in six patients that pancreatic extracts could reduce urinary levels of glucose and ketones, and that in one case, the treatment woke the patient from a coma. Dr. Zuelzer had purified the extract with alcohol but patients still experienced convulsions and coma; in fact, they were experiencing hypoglycemic shock, but Dr. Zuelzer had not identified it as such.
“He thought his preparation was full of impurities – and that’s the irony. He had in his hands an insulin prep that was so clean and so potent that it sent the test animals into hypoglycemic shock,” Dr. Hall pointed out.
By 1921, two young researchers, Frederick G. Banting, MD, a practicing medical doctor in Toronto, together with a final year physiology student at the University of Toronto, Charles H. Best, MD, DSc, collaborated on the instruction of Dr. Best’s superior, John James Rickard Macleod, MBChB, professor of physiology at the University of Toronto, to make pancreatic extracts, first from dogs and then from cattle.
Over the months prior to treating Thompson, working together in the laboratory, Dr. Banting and Dr. Best prepared the pancreatic extract from cattle and tested it on dogs with diabetes.
Then, in what amounted to a phase 1 trial of its day, with an “n of one,” a frail and close-to-death Thompson was given 15 cc of pancreatic extract at Toronto General Hospital in January 1922. His blood glucose level dropped by 25%, but unfortunately, his body still produced ketones, indicating the antidiabetic effect was limited. He also experienced an adverse reaction at the injection site with an accumulation of abscesses.
So despite success with isolating the extract and administering it to Thompson, the product remained tainted with impurities.
At this point, colleague James Collip, MD, PhD, came to the rescue. He used his skills as a biochemist to purify the pancreatic extract enough to eliminate impurities.
When Thompson was treated 2 weeks later with the purified extract, he experienced a more positive outcome. Gone was the injection site reaction, gone were the high blood glucose levels, and Thompson “became brighter, more active, looked better, and said he felt stronger,” according to a publication describing the treatment.
Dr. Collip also determined that by over-purifying the product, the animals he experimented on could overreact and experience convulsions, coma, and death due to hypoglycemia from too much insulin.
Fighting talk
Recalling an excerpt from Dr. Banting’s diary, Dr. Hall said that Dr. Banting had a mercurial temper and testified to his loss of patience with Dr. Collip when the chemist refused to share his formula of purification. His diary reads: “I grabbed him in one hand by the overcoat ... and almost lifting him I sat him down hard on the chair ... I remember telling him that it was a good job he was so much smaller – otherwise I would ‘knock hell out of him.’ ”
According to Dr. Hall, in 1923, when Dr. Banting and Dr. Macleod were jointly awarded the Nobel Prize for Medicine, Dr. Best resented being excluded, and despite Dr. Banting’s sharing half his prize money with Dr. Best, animosity prevailed.
At one point, before leaving on a plane for a wartime mission to the United Kingdom, Dr. Banting noted that if he didn’t make it back alive, “and they give my [professorial] chair to that son-of-a-bitch Best, I’ll never rest in my grave.” In a cruel twist of fate, Dr. Banting’s plane crashed and all aboard died.
The Nobel Prize had also been a source of rivalry between Dr. Banting and his boss, Dr. Macleod. In late 1921, while presenting the findings from animal models at the American Physiological Society conference, Dr. Banting’s nerves got the better of him and Dr. Macleod took over at the podium to finish the talk. Dr. Banting perceived this as his boss stealing the limelight.
Only a few months later, at the Association of American Physicians annual conference, Dr. Macleod played to an audience for a second time by making the first formal announcement of the discovery to the scientific community. Notably, Dr. Banting was absent.
The Nobel Prize or a poisoned chalice?
Awarded annually for physics, chemistry, medicine/physiology, literature, peace, and economics, Nobel Prizes are usually considered the holy grail of achievement. In 1895, funds for the prizes were bequeathed by Alfred Nobel in his last will and testament, with each prize worth around $40,000 at the time (approximately $1,000,000 in today’s value).
Writing in 2001 in the journal Diabetes Voice, Professor Sir George Alberti, DPhil, BM BCh, former president of the UK Royal College of Physicians, summarized the burden that accompanies the Nobel Prize: “I personally believe that such prizes and awards do more harm than good and should be abolished. Many a scientist has gone to their grave feeling deeply aggrieved because they were not awarded a Nobel Prize.”
Such high stakes surround the prize that, in the case of insulin, the course of its discovery meant courtesies and truth were swept aside in hot pursuit of fame. After Dr. Macleod died in 1935 and Dr. Banting died in 1941, Dr. Best took the opportunity to try to revise history. There was the small obstacle of Dr. Collip, but Dr. Best managed to play down Dr. Collip’s contribution by focusing on the eureka moment as being the first insulin dose administered, despite the fact that a more complete recovery without side effects was later achieved only with Dr. Collip’s help.
Despite exclusion from the Nobel Prize, Dr. Best nevertheless became recognized as the “go-to-guy” for the discovery of insulin, said Dr. Hall. When Dr. Best spoke about the discovery of insulin at the New York Diabetes Association meeting in 1946, he was introduced as a speaker whose reputation was already so great that he did “not require much of an introduction.”
“And when a new research institute was opened in Toronto in 1953, it was named in his honor. The opening address, by Sir Henry Dale of the UK Medical Research Council, sang Best’s praises to the rafters, much to the disgruntlement of Best’s former colleague, James Collip, who was sitting in the audience,” Dr. Hall pointed out.
Both Dr. Hall and Dr. Stephens live with type 1 diabetes and have benefited from the efforts of Dr. Banting, Dr. Best, Dr. Collip, Dr. Zuelzer, and Dr. Macleod.
“The discovery of insulin was a miracle, it has allowed people to survive,” said Dr. Stephens. “Few medicines can reverse a death sentence like insulin can. It’s easy to forget how it was when insulin wasn’t there – and it wasn’t that long ago.”
Dr. Hall reflects that scientific progress and discovery are often portrayed as being the result of towering geniuses standing on each other’s shoulders.
“But I think that when German philosopher Immanuel Kant remarked that ‘Out of the crooked timber of humanity, no straight thing can ever be made,’ he offered us a much more accurate picture of how science works. And I think that there’s perhaps no more powerful example of this than the story of insulin,” he said.
A version of this article first appeared on Medscape.com.
Leonard Thompson’s father was so desperate to save his 14-year-old child from certain death due to diabetes that, on Jan. 11, 1922, he took him to Toronto General Hospital to receive what is arguably the first dose of insulin given to a human. From an anticipated life expectancy of weeks – months at best – Thompson lived for an astonishing further 13 years, eventually dying from pneumonia unrelated to diabetes.
By all accounts, the story is a centenary celebration of a remarkable discovery. Insulin has changed what was once a death sentence to a near-normal life expectancy for the millions of people with type 1 diabetes over the past 100 years.
But behind the life-changing success of the discovery – and the Nobel Prize that went with it – lies a tale blighted by disputed claims, twisted truths, and likely injustices between the scientists involved, as they each vied for an honored place in medical history.
Kersten Hall, PhD, honorary fellow, religion and history of science, at the University of Leeds, England, has scoured archives and personal records held at the University of Toronto to uncover the personal stories behind insulin’s discovery.
Despite the wranglings, Dr. Hall asserts: “There’s a distinction between the science and the scientists. Scientists are wonderfully flawed and complex human beings with all their glorious virtues and vices, as we all are. It’s no surprise that they get greedy, jealous, and insecure.”
At death’s door: Diabetes before the 1920s
Prior to insulin’s discovery in 1921, a diagnosis of type 1 diabetes placed someone at death’s door, with nothing but starvation – albeit a slightly slower death – to mitigate a fast-approaching departure from this world. At that time, most diabetes cases would have been type 1 diabetes because, with less obesogenic diets and shorter lifespans, people were much less likely to develop type 2 diabetes.
Nowadays, it is widely recognized that the prevalence of type 2 diabetes is on a steep upward curve, but so too is type 1 diabetes. In the United States alone, there are 1.5 million people diagnosed with type 1 diabetes, a number expected to rise to around 5 million by 2050, according to JDRF, the type 1 diabetes advocacy organization.
Interestingly, 100 years since the first treated patient, life-long insulin remains the only real effective therapy for patients with type 1 diabetes. Once pancreatic beta cells have ceased to function and insulin production has stopped, insulin replacement is the only way to keep blood glucose levels within the recommended range (A1c ≤ 48 mmol/mol [6.5%]), according to the UK National Institute for Health and Care Excellence (NICE), as well as numerous diabetes organizations, including the American Diabetes Association (ADA).
Preliminary clinical trials have looked at stem cell transplantation, prematurely dubbed as a “cure” for type 1 diabetes, as an alternative to insulin therapy. The procedure involves transplanting stem cell–derived cells, which become functional beta cells when infused into humans, but requires immunosuppression, as reported by this news organization.
Today, the life expectancy of people with type 1 diabetes treated with insulin is close to those without the disease, although this is dependent on how tightly blood glucose is controlled. Some studies show life expectancy of those with type 1 diabetes is around 8-12 years lower than the general population but varies depending on where a person lives.
In some lower-income countries, many with type 1 diabetes still die prematurely either because they are undiagnosed or cannot access insulin. The high cost of insulin in the United States is well publicized, as featured in numerous articles by this news organization, and numerous patients in the United States have died because they cannot afford insulin.
Without insulin, young Leonard Thompson would have been lucky to have reached his 15th birthday.
“Such patients were cachectic and thin and would have weighed around 40-50 pounds (18-23 kg), which is very low for an older child. Survival was short and lasted weeks or months usually,” said Elizabeth Stephens, MD, an endocrinologist in Portland, Ore.
“The discovery of insulin was really a miracle because without it diabetes patients were facing certain death. Even nowadays, if people don’t get their insulin because they can’t afford it or for whatever reason, they can still die,” Dr. Stephens stressed.
Antidiabetic effects of pancreatic extract limited
Back in 1869, Paul Langerhans, MD, discovered pancreatic islet cells, or islets of Langerhans, as a medical student. Researchers tried to produce extracts that lowered blood glucose but they were too toxic for patient use.
In 1908, as detailed in his recent book, Insulin – the Crooked Timber, Dr. Hall also refers to the fact that a German researcher, Georg Zuelzer, MD, demonstrated in six patients that pancreatic extracts could reduce urinary levels of glucose and ketones, and that in one case, the treatment woke the patient from a coma. Dr. Zuelzer had purified the extract with alcohol but patients still experienced convulsions and coma; in fact, they were experiencing hypoglycemic shock, but Dr. Zuelzer had not identified it as such.
“He thought his preparation was full of impurities – and that’s the irony. He had in his hands an insulin prep that was so clean and so potent that it sent the test animals into hypoglycemic shock,” Dr. Hall pointed out.
By 1921, two young researchers, Frederick G. Banting, MD, a practicing medical doctor in Toronto, together with a final year physiology student at the University of Toronto, Charles H. Best, MD, DSc, collaborated on the instruction of Dr. Best’s superior, John James Rickard Macleod, MBChB, professor of physiology at the University of Toronto, to make pancreatic extracts, first from dogs and then from cattle.
Over the months prior to treating Thompson, working together in the laboratory, Dr. Banting and Dr. Best prepared the pancreatic extract from cattle and tested it on dogs with diabetes.
Then, in what amounted to a phase 1 trial of its day, with an “n of one,” a frail and close-to-death Thompson was given 15 cc of pancreatic extract at Toronto General Hospital in January 1922. His blood glucose level dropped by 25%, but unfortunately, his body still produced ketones, indicating the antidiabetic effect was limited. He also experienced an adverse reaction at the injection site with an accumulation of abscesses.
So despite success with isolating the extract and administering it to Thompson, the product remained tainted with impurities.
At this point, colleague James Collip, MD, PhD, came to the rescue. He used his skills as a biochemist to purify the pancreatic extract enough to eliminate impurities.
When Thompson was treated 2 weeks later with the purified extract, he experienced a more positive outcome. Gone was the injection site reaction, gone were the high blood glucose levels, and Thompson “became brighter, more active, looked better, and said he felt stronger,” according to a publication describing the treatment.
Dr. Collip also determined that by over-purifying the product, the animals he experimented on could overreact and experience convulsions, coma, and death due to hypoglycemia from too much insulin.
Fighting talk
Recalling an excerpt from Dr. Banting’s diary, Dr. Hall said that Dr. Banting had a mercurial temper and testified to his loss of patience with Dr. Collip when the chemist refused to share his formula of purification. His diary reads: “I grabbed him in one hand by the overcoat ... and almost lifting him I sat him down hard on the chair ... I remember telling him that it was a good job he was so much smaller – otherwise I would ‘knock hell out of him.’ ”
According to Dr. Hall, in 1923, when Dr. Banting and Dr. Macleod were jointly awarded the Nobel Prize for Medicine, Dr. Best resented being excluded, and despite Dr. Banting’s sharing half his prize money with Dr. Best, animosity prevailed.
At one point, before leaving on a plane for a wartime mission to the United Kingdom, Dr. Banting noted that if he didn’t make it back alive, “and they give my [professorial] chair to that son-of-a-bitch Best, I’ll never rest in my grave.” In a cruel twist of fate, Dr. Banting’s plane crashed and all aboard died.
The Nobel Prize had also been a source of rivalry between Dr. Banting and his boss, Dr. Macleod. In late 1921, while presenting the findings from animal models at the American Physiological Society conference, Dr. Banting’s nerves got the better of him and Dr. Macleod took over at the podium to finish the talk. Dr. Banting perceived this as his boss stealing the limelight.
Only a few months later, at the Association of American Physicians annual conference, Dr. Macleod played to an audience for a second time by making the first formal announcement of the discovery to the scientific community. Notably, Dr. Banting was absent.
The Nobel Prize or a poisoned chalice?
Awarded annually for physics, chemistry, medicine/physiology, literature, peace, and economics, Nobel Prizes are usually considered the holy grail of achievement. In 1895, funds for the prizes were bequeathed by Alfred Nobel in his last will and testament, with each prize worth around $40,000 at the time (approximately $1,000,000 in today’s value).
Writing in 2001 in the journal Diabetes Voice, Professor Sir George Alberti, DPhil, BM BCh, former president of the UK Royal College of Physicians, summarized the burden that accompanies the Nobel Prize: “I personally believe that such prizes and awards do more harm than good and should be abolished. Many a scientist has gone to their grave feeling deeply aggrieved because they were not awarded a Nobel Prize.”
Such high stakes surround the prize that, in the case of insulin, the course of its discovery meant courtesies and truth were swept aside in hot pursuit of fame. After Dr. Macleod died in 1935 and Dr. Banting died in 1941, Dr. Best took the opportunity to try to revise history. There was the small obstacle of Dr. Collip, but Dr. Best managed to play down Dr. Collip’s contribution by focusing on the eureka moment as being the first insulin dose administered, despite the fact that a more complete recovery without side effects was later achieved only with Dr. Collip’s help.
Despite exclusion from the Nobel Prize, Dr. Best nevertheless became recognized as the “go-to-guy” for the discovery of insulin, said Dr. Hall. When Dr. Best spoke about the discovery of insulin at the New York Diabetes Association meeting in 1946, he was introduced as a speaker whose reputation was already so great that he did “not require much of an introduction.”
“And when a new research institute was opened in Toronto in 1953, it was named in his honor. The opening address, by Sir Henry Dale of the UK Medical Research Council, sang Best’s praises to the rafters, much to the disgruntlement of Best’s former colleague, James Collip, who was sitting in the audience,” Dr. Hall pointed out.
Both Dr. Hall and Dr. Stephens live with type 1 diabetes and have benefited from the efforts of Dr. Banting, Dr. Best, Dr. Collip, Dr. Zuelzer, and Dr. Macleod.
“The discovery of insulin was a miracle, it has allowed people to survive,” said Dr. Stephens. “Few medicines can reverse a death sentence like insulin can. It’s easy to forget how it was when insulin wasn’t there – and it wasn’t that long ago.”
Dr. Hall reflects that scientific progress and discovery are often portrayed as being the result of towering geniuses standing on each other’s shoulders.
“But I think that when German philosopher Immanuel Kant remarked that ‘Out of the crooked timber of humanity, no straight thing can ever be made,’ he offered us a much more accurate picture of how science works. And I think that there’s perhaps no more powerful example of this than the story of insulin,” he said.
A version of this article first appeared on Medscape.com.
Medical boards pressured to let it slide when doctors spread COVID misinformation
Tennessee’s Board of Medical Examiners unanimously adopted in September 2021 a statement that said doctors spreading COVID misinformation – such as suggesting that vaccines contain microchips – could jeopardize their license to practice.
“I’m very glad that we’re taking this step,” Dr. Stephen Loyd, MD, the panel’s vice president, said at the time. “If you’re spreading this willful misinformation, for me it’s going to be really hard to do anything other than put you on probation or take your license for a year. There has to be a message sent for this. It’s not okay.”
The board’s statement was posted on a government website.
The growing tension in Tennessee between conservative lawmakers and the state’s medical board may be the most prominent example in the country. But the Federation of State Medical Boards, which created the language adopted by at least 15 state boards, is tracking legislation introduced by Republicans in at least 14 states that would restrict a medical board’s authority to discipline doctors for their advice on COVID.
Humayun Chaudhry, DO, the federation’s CEO, called it “an unwelcome trend.” The nonprofit association, based in Euless, Tex., said the statement is merely a COVID-specific restatement of an existing rule: that doctors who engage in behavior that puts patients at risk could face disciplinary action.
Although doctors have leeway to decide which treatments to provide, the medical boards that oversee them have broad authority over licensing. Often, doctors are investigated for violating guidelines on prescribing high-powered drugs. But physicians are sometimes punished for other “unprofessional conduct.” In 2013, Tennessee’s board fined U.S. Rep. Scott DesJarlais for separately having sexual relations with two female patients more than a decade earlier.
Still, stopping doctors from sharing unsound medical advice has proved challenging. Even defining misinformation has been difficult. And during the pandemic, resistance from some state legislatures is complicating the effort.
A relatively small group of physicians peddle COVID misinformation, but many of them associate with America’s Frontline Doctors. Its founder, Simone Gold, MD, has claimed patients are dying from COVID treatments, not the virus itself. Sherri Tenpenny, DO, said in a legislative hearing in Ohio that the COVID vaccine could magnetize patients. Stella Immanuel, MD, has pushed hydroxychloroquine as a COVID cure in Texas, although clinical trials showed that it had no benefit. None of them agreed to requests for comment.
The Texas Medical Board fined Dr. Immanuel $500 for not informing a patient of the risks associated with using hydroxychloroquine as an off-label COVID treatment.
In Tennessee, state lawmakers called a special legislative session in October to address COVID restrictions, and Republican Gov. Bill Lee signed a sweeping package of bills that push back against pandemic rules. One included language directed at the medical board’s recent COVID policy statement, making it more difficult for the panel to investigate complaints about physicians’ advice on COVID vaccines or treatments.
In November, Republican state Rep. John Ragan sent the medical board a letter demanding that the statement be deleted from the state’s website. Rep. Ragan leads a legislative panel that had raised the prospect of defunding the state’s health department over its promotion of COVID vaccines to teens.
Among his demands, Rep. Ragan listed 20 questions he wanted the medical board to answer in writing, including why the misinformation “policy” was proposed nearly two years into the pandemic, which scholars would determine what constitutes misinformation, and how was the “policy” not an infringement on the doctor-patient relationship.
“If you fail to act promptly, your organization will be required to appear before the Joint Government Operations Committee to explain your inaction,” Rep. Ragan wrote in the letter, obtained by Kaiser Health News and Nashville Public Radio.
In response to a request for comment, Rep. Ragan said that “any executive agency, including Board of Medical Examiners, that refuses to follow the law is subject to dissolution.”
He set a deadline of Dec. 7.
In Florida, a Republican-sponsored bill making its way through the state legislature proposes to ban medical boards from revoking or threatening to revoke doctors’ licenses for what they say unless “direct physical harm” of a patient occurred. If the publicized complaint can’t be proved, the board could owe a doctor up to $1.5 million in damages.
Although Florida’s medical board has not adopted the Federation of State Medical Boards’ COVID misinformation statement, the panel has considered misinformation complaints against physicians, including the state’s surgeon general, Joseph Ladapo, MD, PhD.
Dr. Chaudhry said he’s surprised just how many COVID-related complaints are being filed across the country. Often, boards do not publicize investigations before a violation of ethics or standards is confirmed. But in response to a survey by the federation in late 2021, two-thirds of state boards reported an increase in misinformation complaints. And the federation said 12 boards had taken action against a licensed physician.
“At the end of the day, if a physician who is licensed engages in activity that causes harm, the state medical boards are the ones that historically have been set up to look into the situation and make a judgment about what happened or didn’t happen,” Dr. Chaudhry said. “And if you start to chip away at that, it becomes a slippery slope.”
The Georgia Composite Medical Board adopted a version of the federation’s misinformation guidance in early November and has been receiving 10-20 complaints each month, said Debi Dalton, MD, the chairperson. Two months in, no one had been sanctioned.
Dr. Dalton said that even putting out a misinformation policy leaves some “gray” area. Generally, physicians are expected to follow the “consensus,” rather than “the newest information that pops up on social media,” she said.
“We expect physicians to think ethically, professionally, and with the safety of patients in mind,” Dr. Dalton said.
A few physician groups are resisting attempts to root out misinformation, including the Association of American Physicians and Surgeons, known for its stands against government regulation.
Some medical boards have opted against taking a public stand against misinformation.
The Alabama Board of Medical Examiners discussed signing on to the federation’s statement, according to the minutes from an October meeting. But after debating the potential legal ramifications in a private executive session, the board opted not to act.
In Tennessee, the Board of Medical Examiners met on the day Rep. Ragan had set as the deadline and voted to remove the misinformation statement from its website to avoid being called into a legislative hearing. But then, in late January, the board decided to stick with the policy – although it did not republish the statement online immediately – and more specifically defined misinformation, calling it “content that is false, inaccurate or misleading, even if spread unintentionally.”
Board members acknowledged they would likely get more pushback from lawmakers but said they wanted to protect their profession from interference.
“Doctors who are putting forth good evidence-based medicine deserve the protection of this board so they can actually say: ‘Hey, I’m in line with this guideline, and this is a source of truth,’” said Melanie Blake, MD, the board’s president. “We should be a source of truth.”
The medical board was looking into nearly 30 open complaints related to COVID when its misinformation statement came down from its website. As of early February, no Tennessee physician had faced disciplinary action.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. This story is part of a partnership that includes Nashville Public Radio, NPR, and KHN.
Tennessee’s Board of Medical Examiners unanimously adopted in September 2021 a statement that said doctors spreading COVID misinformation – such as suggesting that vaccines contain microchips – could jeopardize their license to practice.
“I’m very glad that we’re taking this step,” Dr. Stephen Loyd, MD, the panel’s vice president, said at the time. “If you’re spreading this willful misinformation, for me it’s going to be really hard to do anything other than put you on probation or take your license for a year. There has to be a message sent for this. It’s not okay.”
The board’s statement was posted on a government website.
The growing tension in Tennessee between conservative lawmakers and the state’s medical board may be the most prominent example in the country. But the Federation of State Medical Boards, which created the language adopted by at least 15 state boards, is tracking legislation introduced by Republicans in at least 14 states that would restrict a medical board’s authority to discipline doctors for their advice on COVID.
Humayun Chaudhry, DO, the federation’s CEO, called it “an unwelcome trend.” The nonprofit association, based in Euless, Tex., said the statement is merely a COVID-specific restatement of an existing rule: that doctors who engage in behavior that puts patients at risk could face disciplinary action.
Although doctors have leeway to decide which treatments to provide, the medical boards that oversee them have broad authority over licensing. Often, doctors are investigated for violating guidelines on prescribing high-powered drugs. But physicians are sometimes punished for other “unprofessional conduct.” In 2013, Tennessee’s board fined U.S. Rep. Scott DesJarlais for separately having sexual relations with two female patients more than a decade earlier.
Still, stopping doctors from sharing unsound medical advice has proved challenging. Even defining misinformation has been difficult. And during the pandemic, resistance from some state legislatures is complicating the effort.
A relatively small group of physicians peddle COVID misinformation, but many of them associate with America’s Frontline Doctors. Its founder, Simone Gold, MD, has claimed patients are dying from COVID treatments, not the virus itself. Sherri Tenpenny, DO, said in a legislative hearing in Ohio that the COVID vaccine could magnetize patients. Stella Immanuel, MD, has pushed hydroxychloroquine as a COVID cure in Texas, although clinical trials showed that it had no benefit. None of them agreed to requests for comment.
The Texas Medical Board fined Dr. Immanuel $500 for not informing a patient of the risks associated with using hydroxychloroquine as an off-label COVID treatment.
In Tennessee, state lawmakers called a special legislative session in October to address COVID restrictions, and Republican Gov. Bill Lee signed a sweeping package of bills that push back against pandemic rules. One included language directed at the medical board’s recent COVID policy statement, making it more difficult for the panel to investigate complaints about physicians’ advice on COVID vaccines or treatments.
In November, Republican state Rep. John Ragan sent the medical board a letter demanding that the statement be deleted from the state’s website. Rep. Ragan leads a legislative panel that had raised the prospect of defunding the state’s health department over its promotion of COVID vaccines to teens.
Among his demands, Rep. Ragan listed 20 questions he wanted the medical board to answer in writing, including why the misinformation “policy” was proposed nearly two years into the pandemic, which scholars would determine what constitutes misinformation, and how was the “policy” not an infringement on the doctor-patient relationship.
“If you fail to act promptly, your organization will be required to appear before the Joint Government Operations Committee to explain your inaction,” Rep. Ragan wrote in the letter, obtained by Kaiser Health News and Nashville Public Radio.
In response to a request for comment, Rep. Ragan said that “any executive agency, including Board of Medical Examiners, that refuses to follow the law is subject to dissolution.”
He set a deadline of Dec. 7.
In Florida, a Republican-sponsored bill making its way through the state legislature proposes to ban medical boards from revoking or threatening to revoke doctors’ licenses for what they say unless “direct physical harm” of a patient occurred. If the publicized complaint can’t be proved, the board could owe a doctor up to $1.5 million in damages.
Although Florida’s medical board has not adopted the Federation of State Medical Boards’ COVID misinformation statement, the panel has considered misinformation complaints against physicians, including the state’s surgeon general, Joseph Ladapo, MD, PhD.
Dr. Chaudhry said he’s surprised just how many COVID-related complaints are being filed across the country. Often, boards do not publicize investigations before a violation of ethics or standards is confirmed. But in response to a survey by the federation in late 2021, two-thirds of state boards reported an increase in misinformation complaints. And the federation said 12 boards had taken action against a licensed physician.
“At the end of the day, if a physician who is licensed engages in activity that causes harm, the state medical boards are the ones that historically have been set up to look into the situation and make a judgment about what happened or didn’t happen,” Dr. Chaudhry said. “And if you start to chip away at that, it becomes a slippery slope.”
The Georgia Composite Medical Board adopted a version of the federation’s misinformation guidance in early November and has been receiving 10-20 complaints each month, said Debi Dalton, MD, the chairperson. Two months in, no one had been sanctioned.
Dr. Dalton said that even putting out a misinformation policy leaves some “gray” area. Generally, physicians are expected to follow the “consensus,” rather than “the newest information that pops up on social media,” she said.
“We expect physicians to think ethically, professionally, and with the safety of patients in mind,” Dr. Dalton said.
A few physician groups are resisting attempts to root out misinformation, including the Association of American Physicians and Surgeons, known for its stands against government regulation.
Some medical boards have opted against taking a public stand against misinformation.
The Alabama Board of Medical Examiners discussed signing on to the federation’s statement, according to the minutes from an October meeting. But after debating the potential legal ramifications in a private executive session, the board opted not to act.
In Tennessee, the Board of Medical Examiners met on the day Rep. Ragan had set as the deadline and voted to remove the misinformation statement from its website to avoid being called into a legislative hearing. But then, in late January, the board decided to stick with the policy – although it did not republish the statement online immediately – and more specifically defined misinformation, calling it “content that is false, inaccurate or misleading, even if spread unintentionally.”
Board members acknowledged they would likely get more pushback from lawmakers but said they wanted to protect their profession from interference.
“Doctors who are putting forth good evidence-based medicine deserve the protection of this board so they can actually say: ‘Hey, I’m in line with this guideline, and this is a source of truth,’” said Melanie Blake, MD, the board’s president. “We should be a source of truth.”
The medical board was looking into nearly 30 open complaints related to COVID when its misinformation statement came down from its website. As of early February, no Tennessee physician had faced disciplinary action.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. This story is part of a partnership that includes Nashville Public Radio, NPR, and KHN.
Tennessee’s Board of Medical Examiners unanimously adopted in September 2021 a statement that said doctors spreading COVID misinformation – such as suggesting that vaccines contain microchips – could jeopardize their license to practice.
“I’m very glad that we’re taking this step,” Dr. Stephen Loyd, MD, the panel’s vice president, said at the time. “If you’re spreading this willful misinformation, for me it’s going to be really hard to do anything other than put you on probation or take your license for a year. There has to be a message sent for this. It’s not okay.”
The board’s statement was posted on a government website.
The growing tension in Tennessee between conservative lawmakers and the state’s medical board may be the most prominent example in the country. But the Federation of State Medical Boards, which created the language adopted by at least 15 state boards, is tracking legislation introduced by Republicans in at least 14 states that would restrict a medical board’s authority to discipline doctors for their advice on COVID.
Humayun Chaudhry, DO, the federation’s CEO, called it “an unwelcome trend.” The nonprofit association, based in Euless, Tex., said the statement is merely a COVID-specific restatement of an existing rule: that doctors who engage in behavior that puts patients at risk could face disciplinary action.
Although doctors have leeway to decide which treatments to provide, the medical boards that oversee them have broad authority over licensing. Often, doctors are investigated for violating guidelines on prescribing high-powered drugs. But physicians are sometimes punished for other “unprofessional conduct.” In 2013, Tennessee’s board fined U.S. Rep. Scott DesJarlais for separately having sexual relations with two female patients more than a decade earlier.
Still, stopping doctors from sharing unsound medical advice has proved challenging. Even defining misinformation has been difficult. And during the pandemic, resistance from some state legislatures is complicating the effort.
A relatively small group of physicians peddle COVID misinformation, but many of them associate with America’s Frontline Doctors. Its founder, Simone Gold, MD, has claimed patients are dying from COVID treatments, not the virus itself. Sherri Tenpenny, DO, said in a legislative hearing in Ohio that the COVID vaccine could magnetize patients. Stella Immanuel, MD, has pushed hydroxychloroquine as a COVID cure in Texas, although clinical trials showed that it had no benefit. None of them agreed to requests for comment.
The Texas Medical Board fined Dr. Immanuel $500 for not informing a patient of the risks associated with using hydroxychloroquine as an off-label COVID treatment.
In Tennessee, state lawmakers called a special legislative session in October to address COVID restrictions, and Republican Gov. Bill Lee signed a sweeping package of bills that push back against pandemic rules. One included language directed at the medical board’s recent COVID policy statement, making it more difficult for the panel to investigate complaints about physicians’ advice on COVID vaccines or treatments.
In November, Republican state Rep. John Ragan sent the medical board a letter demanding that the statement be deleted from the state’s website. Rep. Ragan leads a legislative panel that had raised the prospect of defunding the state’s health department over its promotion of COVID vaccines to teens.
Among his demands, Rep. Ragan listed 20 questions he wanted the medical board to answer in writing, including why the misinformation “policy” was proposed nearly two years into the pandemic, which scholars would determine what constitutes misinformation, and how was the “policy” not an infringement on the doctor-patient relationship.
“If you fail to act promptly, your organization will be required to appear before the Joint Government Operations Committee to explain your inaction,” Rep. Ragan wrote in the letter, obtained by Kaiser Health News and Nashville Public Radio.
In response to a request for comment, Rep. Ragan said that “any executive agency, including Board of Medical Examiners, that refuses to follow the law is subject to dissolution.”
He set a deadline of Dec. 7.
In Florida, a Republican-sponsored bill making its way through the state legislature proposes to ban medical boards from revoking or threatening to revoke doctors’ licenses for what they say unless “direct physical harm” of a patient occurred. If the publicized complaint can’t be proved, the board could owe a doctor up to $1.5 million in damages.
Although Florida’s medical board has not adopted the Federation of State Medical Boards’ COVID misinformation statement, the panel has considered misinformation complaints against physicians, including the state’s surgeon general, Joseph Ladapo, MD, PhD.
Dr. Chaudhry said he’s surprised just how many COVID-related complaints are being filed across the country. Often, boards do not publicize investigations before a violation of ethics or standards is confirmed. But in response to a survey by the federation in late 2021, two-thirds of state boards reported an increase in misinformation complaints. And the federation said 12 boards had taken action against a licensed physician.
“At the end of the day, if a physician who is licensed engages in activity that causes harm, the state medical boards are the ones that historically have been set up to look into the situation and make a judgment about what happened or didn’t happen,” Dr. Chaudhry said. “And if you start to chip away at that, it becomes a slippery slope.”
The Georgia Composite Medical Board adopted a version of the federation’s misinformation guidance in early November and has been receiving 10-20 complaints each month, said Debi Dalton, MD, the chairperson. Two months in, no one had been sanctioned.
Dr. Dalton said that even putting out a misinformation policy leaves some “gray” area. Generally, physicians are expected to follow the “consensus,” rather than “the newest information that pops up on social media,” she said.
“We expect physicians to think ethically, professionally, and with the safety of patients in mind,” Dr. Dalton said.
A few physician groups are resisting attempts to root out misinformation, including the Association of American Physicians and Surgeons, known for its stands against government regulation.
Some medical boards have opted against taking a public stand against misinformation.
The Alabama Board of Medical Examiners discussed signing on to the federation’s statement, according to the minutes from an October meeting. But after debating the potential legal ramifications in a private executive session, the board opted not to act.
In Tennessee, the Board of Medical Examiners met on the day Rep. Ragan had set as the deadline and voted to remove the misinformation statement from its website to avoid being called into a legislative hearing. But then, in late January, the board decided to stick with the policy – although it did not republish the statement online immediately – and more specifically defined misinformation, calling it “content that is false, inaccurate or misleading, even if spread unintentionally.”
Board members acknowledged they would likely get more pushback from lawmakers but said they wanted to protect their profession from interference.
“Doctors who are putting forth good evidence-based medicine deserve the protection of this board so they can actually say: ‘Hey, I’m in line with this guideline, and this is a source of truth,’” said Melanie Blake, MD, the board’s president. “We should be a source of truth.”
The medical board was looking into nearly 30 open complaints related to COVID when its misinformation statement came down from its website. As of early February, no Tennessee physician had faced disciplinary action.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. This story is part of a partnership that includes Nashville Public Radio, NPR, and KHN.
Practice valuation
.
Too often, physicians are not receiving a fair return on the equity they have worked so hard to build over several decades, either because they have waited too long and must accept what is offered, or because they simply take the buyer’s word for their practice’s value. Don’t put yourself in either of those positions, and don’t entertain any offers until you obtain an objective appraisal from a neutral party.
Of course, a medical practice is trickier to value than an ordinary business, and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in 750 words; but three basic yardsticks are essential for determining the equity, or book value, of a practice:
- Tangible assets. Equipment, cash, accounts receivable, and other property owned by the practice.
- Liabilities. Accounts payable, outstanding loans, and anything else owed to others.
- Intangible assets. Sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons why patients come back (if in fact they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place and how well they pay, etcetera), the extent and strength of the referral base, and the presence of supplemental income streams, such as clinical research.
It is also important to determine to what extent intangible assets are transferable. For example, unique skills with a laser, neurotoxins, or filler substances, or extraordinary personal charisma, may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again there are many ways to estimate intangible asset value, and once again you should ask which were used. Cash flow analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques that some consider a better estimate of intangible assets are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings (and thus its overall value) are.
Asset-based valuation is the most popular, but by no means the only method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not its income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced and independent financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
.
Too often, physicians are not receiving a fair return on the equity they have worked so hard to build over several decades, either because they have waited too long and must accept what is offered, or because they simply take the buyer’s word for their practice’s value. Don’t put yourself in either of those positions, and don’t entertain any offers until you obtain an objective appraisal from a neutral party.
Of course, a medical practice is trickier to value than an ordinary business, and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in 750 words; but three basic yardsticks are essential for determining the equity, or book value, of a practice:
- Tangible assets. Equipment, cash, accounts receivable, and other property owned by the practice.
- Liabilities. Accounts payable, outstanding loans, and anything else owed to others.
- Intangible assets. Sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons why patients come back (if in fact they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place and how well they pay, etcetera), the extent and strength of the referral base, and the presence of supplemental income streams, such as clinical research.
It is also important to determine to what extent intangible assets are transferable. For example, unique skills with a laser, neurotoxins, or filler substances, or extraordinary personal charisma, may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again there are many ways to estimate intangible asset value, and once again you should ask which were used. Cash flow analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques that some consider a better estimate of intangible assets are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings (and thus its overall value) are.
Asset-based valuation is the most popular, but by no means the only method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not its income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced and independent financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
.
Too often, physicians are not receiving a fair return on the equity they have worked so hard to build over several decades, either because they have waited too long and must accept what is offered, or because they simply take the buyer’s word for their practice’s value. Don’t put yourself in either of those positions, and don’t entertain any offers until you obtain an objective appraisal from a neutral party.
Of course, a medical practice is trickier to value than an ordinary business, and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in 750 words; but three basic yardsticks are essential for determining the equity, or book value, of a practice:
- Tangible assets. Equipment, cash, accounts receivable, and other property owned by the practice.
- Liabilities. Accounts payable, outstanding loans, and anything else owed to others.
- Intangible assets. Sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons why patients come back (if in fact they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place and how well they pay, etcetera), the extent and strength of the referral base, and the presence of supplemental income streams, such as clinical research.
It is also important to determine to what extent intangible assets are transferable. For example, unique skills with a laser, neurotoxins, or filler substances, or extraordinary personal charisma, may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again there are many ways to estimate intangible asset value, and once again you should ask which were used. Cash flow analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques that some consider a better estimate of intangible assets are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings (and thus its overall value) are.
Asset-based valuation is the most popular, but by no means the only method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not its income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced and independent financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
New study shows natural immunity to COVID has enduring strength
It’s a matter of quality, not quantity. That’s the gist of a new Israeli study that shows that unvaccinated people with a prior SARS-CoV-2 infection create antibodies that are more effective in the long run compared with others who were vaccinated but never infected.
“While the quantity of antibodies decreases with time in both COVID-19 recovered patients and vaccinated individuals, ” lead author Carmit Cohen, PhD, said in an interview.
This difference could explain why previously infected patients appear to be better protected against a new infection than those who have only been vaccinated, according to a news release attached to the research.
One key caveat: This research does not include people from the later part of the pandemic.
This means there is a catch in terms of timing, William Schaffner, MD, Vanderbilt University School of Medicine, Nashville, Tenn., said when asked to comment on the study: “The study involved only the early COVID strains – it has no information on either the Delta or Omicron variants. Thus, the results primarily are of scientific or historical interest but are not immediately relevant to the current situation.”
The findings come from an early release of a study to be presented at the European Congress of Clinical Microbiology & Infectious Diseases in April.
An unexpected finding of the study showed that obese people had better protection – a higher and more sustained immune response – compared with overweight and normal-weight individuals.
“The results in the obese group were indeed unexpected and need further research to confirm or dispute,” Dr. Schaffner said. “Obesity does predispose to more severe disease.”
A focus on earlier strains
Dr. Cohen – a senior research assistant in infectious disease prevention at the Sheba Medical Center in Ramat Gan, Israel – and her colleagues recruited participants between March 25, 2020 and Nov. 25, 2020 and completed analysis in April 2021. This means they assessed people with a history of infection from the original, the Alpha, and some Beta strains of SARS-CoV-2.
Dr. Cohen indicated that the next phase of their research will examine innate and acquired immune responses to the more recent Delta and Omicron variants.
The investigators analyzed the antibody-induced immune response up to 1 year in 130 COVID-19 recovered but unvaccinated individuals versus up to 8 months among 402 others matched by age and body mass index (BMI) and without previous infection who received two doses of the Pfizer vaccine.
The numbers of antibodies a month after vaccination were higher than those in the COVID-19 recovered patients. However, these numbers also declined more steeply in the vaccinated group, they note.
To assess the antibody performance, the investigators used the avidity index. This assay measures antibody function based on the strength of the interactions between the antibody and the viral antigen.
They found that the avidity index was higher in vaccinated individuals than in recovered patients initially but changes over time. At up to 6 months, the index did not significantly change in vaccinated individuals, whereas it gradually increased in recovered patients. This increase would potentially protect them from reinfection, the authors note.
These findings stand in stark contrast to an Oct. 29, 2021, Centers for Disease Control and Prevention study that found that COVID-19 vaccines provided five times the protection of natural immunity.
Those results, published in the organization’s Morbidity and Mortality Weekly Report, suggest that vaccination helps people mount a higher, stronger, and more consistent level of immunity against COVID-19 hospitalization than infection alone for at least 6 months.
Protection linked to obesity
Another finding that ran against the scientific grain was the data about obesity.
There was a higher and more persistent antibody performance among people with a BMI of 30 kg/m2.
This could relate to greater disease severity and/or a more pronounced initial response to infection among the obese group.
“Our hypothesis is that patients with obesity begin with a more pronounced response – reflected also by the disease manifestation – and the trend of decline is similar, therefore the kinetics of immune response remain higher throughout the study,” Dr. Cohen said.
“The results in the obese group were indeed unexpected and need further research to confirm or dispute,” said Dr. Schaffner, who is also the current medical director of the National Foundation for Infectious Diseases. “Obesity does predispose to more severe disease.”
Before the boosters
Along with using participants from only the earlier part of the pandemic, another limitation of the study was that the vaccinated group had only two doses of vaccine; boosters were not given during the time of the study, Dr. Schaffner said.
“Again, not the current situation.”
“That said, the strength and duration of natural immunity provided by the early variants was solid for up to a year, confirming previous reports,” he said.
A version of this article first appeared on Medscape.com.
It’s a matter of quality, not quantity. That’s the gist of a new Israeli study that shows that unvaccinated people with a prior SARS-CoV-2 infection create antibodies that are more effective in the long run compared with others who were vaccinated but never infected.
“While the quantity of antibodies decreases with time in both COVID-19 recovered patients and vaccinated individuals, ” lead author Carmit Cohen, PhD, said in an interview.
This difference could explain why previously infected patients appear to be better protected against a new infection than those who have only been vaccinated, according to a news release attached to the research.
One key caveat: This research does not include people from the later part of the pandemic.
This means there is a catch in terms of timing, William Schaffner, MD, Vanderbilt University School of Medicine, Nashville, Tenn., said when asked to comment on the study: “The study involved only the early COVID strains – it has no information on either the Delta or Omicron variants. Thus, the results primarily are of scientific or historical interest but are not immediately relevant to the current situation.”
The findings come from an early release of a study to be presented at the European Congress of Clinical Microbiology & Infectious Diseases in April.
An unexpected finding of the study showed that obese people had better protection – a higher and more sustained immune response – compared with overweight and normal-weight individuals.
“The results in the obese group were indeed unexpected and need further research to confirm or dispute,” Dr. Schaffner said. “Obesity does predispose to more severe disease.”
A focus on earlier strains
Dr. Cohen – a senior research assistant in infectious disease prevention at the Sheba Medical Center in Ramat Gan, Israel – and her colleagues recruited participants between March 25, 2020 and Nov. 25, 2020 and completed analysis in April 2021. This means they assessed people with a history of infection from the original, the Alpha, and some Beta strains of SARS-CoV-2.
Dr. Cohen indicated that the next phase of their research will examine innate and acquired immune responses to the more recent Delta and Omicron variants.
The investigators analyzed the antibody-induced immune response up to 1 year in 130 COVID-19 recovered but unvaccinated individuals versus up to 8 months among 402 others matched by age and body mass index (BMI) and without previous infection who received two doses of the Pfizer vaccine.
The numbers of antibodies a month after vaccination were higher than those in the COVID-19 recovered patients. However, these numbers also declined more steeply in the vaccinated group, they note.
To assess the antibody performance, the investigators used the avidity index. This assay measures antibody function based on the strength of the interactions between the antibody and the viral antigen.
They found that the avidity index was higher in vaccinated individuals than in recovered patients initially but changes over time. At up to 6 months, the index did not significantly change in vaccinated individuals, whereas it gradually increased in recovered patients. This increase would potentially protect them from reinfection, the authors note.
These findings stand in stark contrast to an Oct. 29, 2021, Centers for Disease Control and Prevention study that found that COVID-19 vaccines provided five times the protection of natural immunity.
Those results, published in the organization’s Morbidity and Mortality Weekly Report, suggest that vaccination helps people mount a higher, stronger, and more consistent level of immunity against COVID-19 hospitalization than infection alone for at least 6 months.
Protection linked to obesity
Another finding that ran against the scientific grain was the data about obesity.
There was a higher and more persistent antibody performance among people with a BMI of 30 kg/m2.
This could relate to greater disease severity and/or a more pronounced initial response to infection among the obese group.
“Our hypothesis is that patients with obesity begin with a more pronounced response – reflected also by the disease manifestation – and the trend of decline is similar, therefore the kinetics of immune response remain higher throughout the study,” Dr. Cohen said.
“The results in the obese group were indeed unexpected and need further research to confirm or dispute,” said Dr. Schaffner, who is also the current medical director of the National Foundation for Infectious Diseases. “Obesity does predispose to more severe disease.”
Before the boosters
Along with using participants from only the earlier part of the pandemic, another limitation of the study was that the vaccinated group had only two doses of vaccine; boosters were not given during the time of the study, Dr. Schaffner said.
“Again, not the current situation.”
“That said, the strength and duration of natural immunity provided by the early variants was solid for up to a year, confirming previous reports,” he said.
A version of this article first appeared on Medscape.com.
It’s a matter of quality, not quantity. That’s the gist of a new Israeli study that shows that unvaccinated people with a prior SARS-CoV-2 infection create antibodies that are more effective in the long run compared with others who were vaccinated but never infected.
“While the quantity of antibodies decreases with time in both COVID-19 recovered patients and vaccinated individuals, ” lead author Carmit Cohen, PhD, said in an interview.
This difference could explain why previously infected patients appear to be better protected against a new infection than those who have only been vaccinated, according to a news release attached to the research.
One key caveat: This research does not include people from the later part of the pandemic.
This means there is a catch in terms of timing, William Schaffner, MD, Vanderbilt University School of Medicine, Nashville, Tenn., said when asked to comment on the study: “The study involved only the early COVID strains – it has no information on either the Delta or Omicron variants. Thus, the results primarily are of scientific or historical interest but are not immediately relevant to the current situation.”
The findings come from an early release of a study to be presented at the European Congress of Clinical Microbiology & Infectious Diseases in April.
An unexpected finding of the study showed that obese people had better protection – a higher and more sustained immune response – compared with overweight and normal-weight individuals.
“The results in the obese group were indeed unexpected and need further research to confirm or dispute,” Dr. Schaffner said. “Obesity does predispose to more severe disease.”
A focus on earlier strains
Dr. Cohen – a senior research assistant in infectious disease prevention at the Sheba Medical Center in Ramat Gan, Israel – and her colleagues recruited participants between March 25, 2020 and Nov. 25, 2020 and completed analysis in April 2021. This means they assessed people with a history of infection from the original, the Alpha, and some Beta strains of SARS-CoV-2.
Dr. Cohen indicated that the next phase of their research will examine innate and acquired immune responses to the more recent Delta and Omicron variants.
The investigators analyzed the antibody-induced immune response up to 1 year in 130 COVID-19 recovered but unvaccinated individuals versus up to 8 months among 402 others matched by age and body mass index (BMI) and without previous infection who received two doses of the Pfizer vaccine.
The numbers of antibodies a month after vaccination were higher than those in the COVID-19 recovered patients. However, these numbers also declined more steeply in the vaccinated group, they note.
To assess the antibody performance, the investigators used the avidity index. This assay measures antibody function based on the strength of the interactions between the antibody and the viral antigen.
They found that the avidity index was higher in vaccinated individuals than in recovered patients initially but changes over time. At up to 6 months, the index did not significantly change in vaccinated individuals, whereas it gradually increased in recovered patients. This increase would potentially protect them from reinfection, the authors note.
These findings stand in stark contrast to an Oct. 29, 2021, Centers for Disease Control and Prevention study that found that COVID-19 vaccines provided five times the protection of natural immunity.
Those results, published in the organization’s Morbidity and Mortality Weekly Report, suggest that vaccination helps people mount a higher, stronger, and more consistent level of immunity against COVID-19 hospitalization than infection alone for at least 6 months.
Protection linked to obesity
Another finding that ran against the scientific grain was the data about obesity.
There was a higher and more persistent antibody performance among people with a BMI of 30 kg/m2.
This could relate to greater disease severity and/or a more pronounced initial response to infection among the obese group.
“Our hypothesis is that patients with obesity begin with a more pronounced response – reflected also by the disease manifestation – and the trend of decline is similar, therefore the kinetics of immune response remain higher throughout the study,” Dr. Cohen said.
“The results in the obese group were indeed unexpected and need further research to confirm or dispute,” said Dr. Schaffner, who is also the current medical director of the National Foundation for Infectious Diseases. “Obesity does predispose to more severe disease.”
Before the boosters
Along with using participants from only the earlier part of the pandemic, another limitation of the study was that the vaccinated group had only two doses of vaccine; boosters were not given during the time of the study, Dr. Schaffner said.
“Again, not the current situation.”
“That said, the strength and duration of natural immunity provided by the early variants was solid for up to a year, confirming previous reports,” he said.
A version of this article first appeared on Medscape.com.
To a perfect day
Motionless, every Olympic skater starts off perfectly. Once the music starts, it’s up to them whether they will continue on perfectly or not. In this way, you’re just like an Olympic skater. Each day, a skating program. The music starts the moment your foot touches the floor in the morning. It’s up to you if the rest of the day will continue on flawlessly or not. To this point, I’ve yet to have a perfect day.
If I’m honest, my “perfect day” streak typically ends once I’ve made coffee. By then, I’ll have spilled a few grains of grounds or clinked mugs together when taking one from the cupboard. (D’oh!) Hardly ever can I make it to backing out of the driveway, let alone through a patient encounter. I’ve had a few procedures that when complete I’ve thought, “well, that looks great.” I can remember encounters that went brilliantly despite a high technical difficulty. I’ve also tagged a 7-iron shot 160 downwind yards to within inches of the cup. But I’ve hardly ever done anything in my life perfectly.
What does it mean to be perfect? Well, there have been 23 perfect baseball games. In 1972, the Miami Dolphins had the only perfect NFL season, 14-0 (although my 2007 Patriots went 18-0 before losing to the – ugh – Giants). Every year, several hundred students score a perfect 1600 on the SAT. In an underground vault somewhere in France is a perfect sphere, a perfectly spherical 1-kg mass of pure silicon. There are at least 51 perfect numbers. And model Bella Hadid’s exactly 1.62-ratioed face is said to be perfectly beautiful. But yet, U.S. skater Nathan Chen’s seemingly flawless 113.97-point short program in Beijing, still imperfect.
Attempting a perfect day or perfect surgery or a perfect pour over coffee is a fun game, but perfectionism has an insidious side. Some of us feel this way every day: We must do it exactly right, every time. Even an insignificant imperfection or error feels like failure. A 3.90 GPA is a fail. 515 on the MCAT, not nearly good enough. For them, the burden of perfection is crushing. It is hard for some to recognize that even if your performance could not be improved, the outcome can still be flawed. A chip in the ice, a patient showing up late, an interviewer with an agenda, a missed referee call can all flub up an otherwise flawless day. It isn’t necessary to abandon hope, all ye who live in the real world. Although achieving perfection is usually impossible, reward comes from the pursuit of perfection, not from holding it. It is called perfectionistic striving and in contrast to perfectionistic concerns, it is associated with resilience and positive mood. To do so you must combine giving your all with acceptance of whatever the outcome.
Keith Jarrett is one of the greatest jazz pianists of all time. He is a true perfectionist, precise in his standards and exacting in expectations. In 1975 in Cologne, Germany, he agreed to play at the behest of a teenage girl who arranged to have him perform at the opera house. Except, there was a miscommunication and only a small, broken rehearsal piano was available. As the story goes, she approached him as he waited to be taken back to his hotel, the concert was canceled and she somehow convinced him to play on the nearly unplayable instrument. The result is the Köln Concert, one of the greatest jazz performances in history. It was perfectly imperfect.
Yes, even the 1-kg sphere has femtogram quantities of other elements mixed in – the universal standard for perfect is itself, imperfect. It doesn’t matter. It’s the pursuit of such that makes life worthwhile. There’s always tomorrow. Have your coffee grinders ready.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Motionless, every Olympic skater starts off perfectly. Once the music starts, it’s up to them whether they will continue on perfectly or not. In this way, you’re just like an Olympic skater. Each day, a skating program. The music starts the moment your foot touches the floor in the morning. It’s up to you if the rest of the day will continue on flawlessly or not. To this point, I’ve yet to have a perfect day.
If I’m honest, my “perfect day” streak typically ends once I’ve made coffee. By then, I’ll have spilled a few grains of grounds or clinked mugs together when taking one from the cupboard. (D’oh!) Hardly ever can I make it to backing out of the driveway, let alone through a patient encounter. I’ve had a few procedures that when complete I’ve thought, “well, that looks great.” I can remember encounters that went brilliantly despite a high technical difficulty. I’ve also tagged a 7-iron shot 160 downwind yards to within inches of the cup. But I’ve hardly ever done anything in my life perfectly.
What does it mean to be perfect? Well, there have been 23 perfect baseball games. In 1972, the Miami Dolphins had the only perfect NFL season, 14-0 (although my 2007 Patriots went 18-0 before losing to the – ugh – Giants). Every year, several hundred students score a perfect 1600 on the SAT. In an underground vault somewhere in France is a perfect sphere, a perfectly spherical 1-kg mass of pure silicon. There are at least 51 perfect numbers. And model Bella Hadid’s exactly 1.62-ratioed face is said to be perfectly beautiful. But yet, U.S. skater Nathan Chen’s seemingly flawless 113.97-point short program in Beijing, still imperfect.
Attempting a perfect day or perfect surgery or a perfect pour over coffee is a fun game, but perfectionism has an insidious side. Some of us feel this way every day: We must do it exactly right, every time. Even an insignificant imperfection or error feels like failure. A 3.90 GPA is a fail. 515 on the MCAT, not nearly good enough. For them, the burden of perfection is crushing. It is hard for some to recognize that even if your performance could not be improved, the outcome can still be flawed. A chip in the ice, a patient showing up late, an interviewer with an agenda, a missed referee call can all flub up an otherwise flawless day. It isn’t necessary to abandon hope, all ye who live in the real world. Although achieving perfection is usually impossible, reward comes from the pursuit of perfection, not from holding it. It is called perfectionistic striving and in contrast to perfectionistic concerns, it is associated with resilience and positive mood. To do so you must combine giving your all with acceptance of whatever the outcome.
Keith Jarrett is one of the greatest jazz pianists of all time. He is a true perfectionist, precise in his standards and exacting in expectations. In 1975 in Cologne, Germany, he agreed to play at the behest of a teenage girl who arranged to have him perform at the opera house. Except, there was a miscommunication and only a small, broken rehearsal piano was available. As the story goes, she approached him as he waited to be taken back to his hotel, the concert was canceled and she somehow convinced him to play on the nearly unplayable instrument. The result is the Köln Concert, one of the greatest jazz performances in history. It was perfectly imperfect.
Yes, even the 1-kg sphere has femtogram quantities of other elements mixed in – the universal standard for perfect is itself, imperfect. It doesn’t matter. It’s the pursuit of such that makes life worthwhile. There’s always tomorrow. Have your coffee grinders ready.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Motionless, every Olympic skater starts off perfectly. Once the music starts, it’s up to them whether they will continue on perfectly or not. In this way, you’re just like an Olympic skater. Each day, a skating program. The music starts the moment your foot touches the floor in the morning. It’s up to you if the rest of the day will continue on flawlessly or not. To this point, I’ve yet to have a perfect day.
If I’m honest, my “perfect day” streak typically ends once I’ve made coffee. By then, I’ll have spilled a few grains of grounds or clinked mugs together when taking one from the cupboard. (D’oh!) Hardly ever can I make it to backing out of the driveway, let alone through a patient encounter. I’ve had a few procedures that when complete I’ve thought, “well, that looks great.” I can remember encounters that went brilliantly despite a high technical difficulty. I’ve also tagged a 7-iron shot 160 downwind yards to within inches of the cup. But I’ve hardly ever done anything in my life perfectly.
What does it mean to be perfect? Well, there have been 23 perfect baseball games. In 1972, the Miami Dolphins had the only perfect NFL season, 14-0 (although my 2007 Patriots went 18-0 before losing to the – ugh – Giants). Every year, several hundred students score a perfect 1600 on the SAT. In an underground vault somewhere in France is a perfect sphere, a perfectly spherical 1-kg mass of pure silicon. There are at least 51 perfect numbers. And model Bella Hadid’s exactly 1.62-ratioed face is said to be perfectly beautiful. But yet, U.S. skater Nathan Chen’s seemingly flawless 113.97-point short program in Beijing, still imperfect.
Attempting a perfect day or perfect surgery or a perfect pour over coffee is a fun game, but perfectionism has an insidious side. Some of us feel this way every day: We must do it exactly right, every time. Even an insignificant imperfection or error feels like failure. A 3.90 GPA is a fail. 515 on the MCAT, not nearly good enough. For them, the burden of perfection is crushing. It is hard for some to recognize that even if your performance could not be improved, the outcome can still be flawed. A chip in the ice, a patient showing up late, an interviewer with an agenda, a missed referee call can all flub up an otherwise flawless day. It isn’t necessary to abandon hope, all ye who live in the real world. Although achieving perfection is usually impossible, reward comes from the pursuit of perfection, not from holding it. It is called perfectionistic striving and in contrast to perfectionistic concerns, it is associated with resilience and positive mood. To do so you must combine giving your all with acceptance of whatever the outcome.
Keith Jarrett is one of the greatest jazz pianists of all time. He is a true perfectionist, precise in his standards and exacting in expectations. In 1975 in Cologne, Germany, he agreed to play at the behest of a teenage girl who arranged to have him perform at the opera house. Except, there was a miscommunication and only a small, broken rehearsal piano was available. As the story goes, she approached him as he waited to be taken back to his hotel, the concert was canceled and she somehow convinced him to play on the nearly unplayable instrument. The result is the Köln Concert, one of the greatest jazz performances in history. It was perfectly imperfect.
Yes, even the 1-kg sphere has femtogram quantities of other elements mixed in – the universal standard for perfect is itself, imperfect. It doesn’t matter. It’s the pursuit of such that makes life worthwhile. There’s always tomorrow. Have your coffee grinders ready.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Tips for connecting with your patients
It is a tough time to be a doctor. With the stresses of the pandemic, the continued unfettered rise of insurance company BS, and so many medical groups being bought up that we often don’t even know who makes the decisions, the patient can sometimes be hidden in the equation.
Be curious
When physicians are curious about why patients have symptoms, how those symptoms will affect their lives, and how worried the patient is about them, patients feel cared about.
Ascertaining how concerned patients are about their symptoms will help you make decisions on whether symptoms you are not concerned about actually need to be treated.
Limit use of EHRs when possible
Use of the electronic health record during visits is essential, but focusing on it too much can put a barrier between the physician and the patient.
Marmor and colleagues found there is an inverse relationship between time spent on the EHR by a patient’s physician and the patient’s satisfaction.1
Eye contact with the patient is important, especially when patients are sharing concerns they are scared about and upsetting experiences. There can be awkward pauses when looking things up on the EHR. Fill those pauses by explaining to the patient what you are doing, or chatting with the patient.
Consider teaching medical students
When a medical student works with you, it doubles the time the patient gets with a concerned listener. Students also can do a great job with timely follow-up and checking in with worried patients.
By having the student present in the clinic room, with the patient present, the patient can really feel heard. The student shares all the details the patient shared, and now their physician is hearing an organized, thoughtful report of the patients concerns.
In fact, I was involved in a study that showed that patients preferred in room presentations, and that they were more satisfied when students presented in the room.2
Use healing words
Some words carry loaded emotions. The word chronic, for example, has negative connotations, whereas the term persisting does not.
I will often ask patients how long they have been suffering from a symptom to imply my concern for what they are going through. The term “chief complaint” is outdated, and upsets patients when they see it in their medical record.
As a patient of mine once said to me: “I never complained about that problem, I just brought it to your attention.” No one wants to be seen as a complainer. Substituting the word concern for complaint works well.
Explain as you examine
People love to hear the term normal. When you are examining a patient, let them know when findings are normal.
I also find it helpful to explain to patients why I am doing certain physical exam maneuvers. This helps them assess how thorough we are in our thought process.
When patients feel their physicians are thorough, they have more confidence in them.
In summary
- Be curious.
- Do not overly focus on the EHR.
- Consider teaching a medical student.
- Be careful of word choice.
- “Overexplain” the physical exam.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Marmor RA et al. Appl Clin Inform. 2018 Jan;9(1):11-4.
2. Rogers HD et al. Acad Med. 2003 Sep;78(9):945-9.
It is a tough time to be a doctor. With the stresses of the pandemic, the continued unfettered rise of insurance company BS, and so many medical groups being bought up that we often don’t even know who makes the decisions, the patient can sometimes be hidden in the equation.
Be curious
When physicians are curious about why patients have symptoms, how those symptoms will affect their lives, and how worried the patient is about them, patients feel cared about.
Ascertaining how concerned patients are about their symptoms will help you make decisions on whether symptoms you are not concerned about actually need to be treated.
Limit use of EHRs when possible
Use of the electronic health record during visits is essential, but focusing on it too much can put a barrier between the physician and the patient.
Marmor and colleagues found there is an inverse relationship between time spent on the EHR by a patient’s physician and the patient’s satisfaction.1
Eye contact with the patient is important, especially when patients are sharing concerns they are scared about and upsetting experiences. There can be awkward pauses when looking things up on the EHR. Fill those pauses by explaining to the patient what you are doing, or chatting with the patient.
Consider teaching medical students
When a medical student works with you, it doubles the time the patient gets with a concerned listener. Students also can do a great job with timely follow-up and checking in with worried patients.
By having the student present in the clinic room, with the patient present, the patient can really feel heard. The student shares all the details the patient shared, and now their physician is hearing an organized, thoughtful report of the patients concerns.
In fact, I was involved in a study that showed that patients preferred in room presentations, and that they were more satisfied when students presented in the room.2
Use healing words
Some words carry loaded emotions. The word chronic, for example, has negative connotations, whereas the term persisting does not.
I will often ask patients how long they have been suffering from a symptom to imply my concern for what they are going through. The term “chief complaint” is outdated, and upsets patients when they see it in their medical record.
As a patient of mine once said to me: “I never complained about that problem, I just brought it to your attention.” No one wants to be seen as a complainer. Substituting the word concern for complaint works well.
Explain as you examine
People love to hear the term normal. When you are examining a patient, let them know when findings are normal.
I also find it helpful to explain to patients why I am doing certain physical exam maneuvers. This helps them assess how thorough we are in our thought process.
When patients feel their physicians are thorough, they have more confidence in them.
In summary
- Be curious.
- Do not overly focus on the EHR.
- Consider teaching a medical student.
- Be careful of word choice.
- “Overexplain” the physical exam.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Marmor RA et al. Appl Clin Inform. 2018 Jan;9(1):11-4.
2. Rogers HD et al. Acad Med. 2003 Sep;78(9):945-9.
It is a tough time to be a doctor. With the stresses of the pandemic, the continued unfettered rise of insurance company BS, and so many medical groups being bought up that we often don’t even know who makes the decisions, the patient can sometimes be hidden in the equation.
Be curious
When physicians are curious about why patients have symptoms, how those symptoms will affect their lives, and how worried the patient is about them, patients feel cared about.
Ascertaining how concerned patients are about their symptoms will help you make decisions on whether symptoms you are not concerned about actually need to be treated.
Limit use of EHRs when possible
Use of the electronic health record during visits is essential, but focusing on it too much can put a barrier between the physician and the patient.
Marmor and colleagues found there is an inverse relationship between time spent on the EHR by a patient’s physician and the patient’s satisfaction.1
Eye contact with the patient is important, especially when patients are sharing concerns they are scared about and upsetting experiences. There can be awkward pauses when looking things up on the EHR. Fill those pauses by explaining to the patient what you are doing, or chatting with the patient.
Consider teaching medical students
When a medical student works with you, it doubles the time the patient gets with a concerned listener. Students also can do a great job with timely follow-up and checking in with worried patients.
By having the student present in the clinic room, with the patient present, the patient can really feel heard. The student shares all the details the patient shared, and now their physician is hearing an organized, thoughtful report of the patients concerns.
In fact, I was involved in a study that showed that patients preferred in room presentations, and that they were more satisfied when students presented in the room.2
Use healing words
Some words carry loaded emotions. The word chronic, for example, has negative connotations, whereas the term persisting does not.
I will often ask patients how long they have been suffering from a symptom to imply my concern for what they are going through. The term “chief complaint” is outdated, and upsets patients when they see it in their medical record.
As a patient of mine once said to me: “I never complained about that problem, I just brought it to your attention.” No one wants to be seen as a complainer. Substituting the word concern for complaint works well.
Explain as you examine
People love to hear the term normal. When you are examining a patient, let them know when findings are normal.
I also find it helpful to explain to patients why I am doing certain physical exam maneuvers. This helps them assess how thorough we are in our thought process.
When patients feel their physicians are thorough, they have more confidence in them.
In summary
- Be curious.
- Do not overly focus on the EHR.
- Consider teaching a medical student.
- Be careful of word choice.
- “Overexplain” the physical exam.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Marmor RA et al. Appl Clin Inform. 2018 Jan;9(1):11-4.
2. Rogers HD et al. Acad Med. 2003 Sep;78(9):945-9.
Growth hormone therapy for certain children may help them reach their potential
“Dr. Lilley, you’ll always be my favorite doctor; you helped me grow.”
These were the parting words from the last patient that I treated during my endocrinology fellowship. I had watched this young man grow from a prepubertal 17-year-old to a young man who had reached his predicted family height as I treated his delayed puberty caused by Kallmann syndrome, a problem that had been missed for years. It was the appropriate bookend for my chosen specialty.
Watching children grow and develop into who they were meant to be is one of my favorite things about endocrinology, as well as forming meaningful relationships with families. Treating detectable deficiencies in logical and measurable ways is also extremely satisfying.
Too little testosterone? That’s a problem I can solve. Too much thyroid hormone? There’s a blocker for that! Endocrinology can be a straightforward field, and when all goes well, everyone leaves happy.
Except when they don’t.
Gatekeepers for treatment for children’s growth
“Nice to meet you. We’re here to get growth hormone.”
“We’re here because his pediatrician made us come. We’ve already decided we’re not going to put hormones into his body.”
These are common statements I hear when I first meet new patients whose parents are concerned about their children’s growth. Pediatric endocrinologists, after all, are the usual gatekeepers for this treatment.
Growth hormone (GH) often makes the news for controversial reasons – most commonly for its abuse by elite athletes hoping to exploit its anabolic effects – causing parents to have varied opinions about its possible use in their children.
Some refuse endocrinology referrals at all owing to concerns that we will push daily injections on their children. Others demand referrals for their children of average height, hoping for every perceived advantage.
GH deficiency (GHD) – a condition where the pituitary gland fails to produce enough GH – can occur because of congenital pituitary malformations; anatomic, surgical, or traumatic interruptions to the gland; or enzyme deficiencies leading to faulty production.
GHD is just one reason for poor growth, however.
Growth is one of the most important indicators of health in children. A waning growth rate may be an early symptom of serious problems. In my clinic, I’ve diagnosed severe hypothyroidism in a marathon runner, a brain tumor, celiac disease in a teenager with no gastrointestinal complaints, autoimmune hepatitis, and several other diseases needing treatment in children who show no symptoms other than poor growth.
Barriers to normal growth
Sometimes, the die is cast for children to have barriers to normal growth. Several genetic conditions can lead to poor GH production or response, and GH treatment is often necessary to approximate normal height.
These may include:
- Turner syndrome (in females who are missing an X chromosome in whole or part) should be considered in every girl with abnormally short stature; mosaic forms of the condition may be subtle and lack classic features.
- Noonan syndrome is important to detect owing to the possibility of cardiac or renal malformations that may also occur in this condition, caused by a mutation in one of the genes in the RAS-MAPK pathway.
- Russell-Silver syndrome can cause intrauterine GH restriction and has been traced to uniparental disomy of chromosome 7 or duplications, mutations, or methylation defects in chromosome 11.
- Individuals with Prader-Willi syndrome, which is characterized by low muscle tone, hyperphagia, and hypogonadism, have demonstrated dramatic benefits from GH therapy, primarily in maintaining a normal body mass index.
Children who are small for their gestational age may be GH resistant, and those who do not catch up to their growth curve by the age of 2 years may require GH treatment to reach their height potential.
GH therapy isn’t entirely benign. Rare adverse effects of overtreatment can include slipped capital femoral epiphysis (a fracture to the growth plate) and pseudotumor cerebri (idiopathic intracranial hypertension).
Overtreatment can cause acromegaly, which results in coarsened features and large hands and feet.
When is GH therapy warranted?
“Growth hormone therapy has been denied by her insurer. They want you to fill out an appeal.”
Insurance approval in the United States can be a herculean effort because GH is expensive: Out-of-pocket costs are prohibitive for most people without insurance assistance, ranging from $7,000 to $30,000 annually.
Pediatric endocrinologists aren’t in the business of cosmetic endocrinology. Treatment of idiopathic short stature has been controversial since this became an indication for GH treatment.
GH isn’t always necessary. Diagnosing the underlying cause for poor growth is the most important step.
Often, we find constitutional delay of growth and puberty, or “late bloomers.” This condition is characterized by a delayed bone age (growth plates more open than expected for age) and delayed pubertal onset. These children will often reach a normal height despite starting as some of the smallest of their peers.
However, GH plays other roles in the body than simply propelling height. Children with congenital GHD will require GH treatment to prevent hypoglycemia, especially in infancy.
GH is needed even in adults with fused growth plates for normal lipid metabolism, bone accrual, and maintaining normal muscle mass.
I have noticed marked improvements in muscle tone in many children with developmental delays who are treated with GH, and research supports cognitive benefits for certain populations.
The most common regimens for GH focus on treatment via subcutaneous injection nightly, when GH is naturally produced; sometimes, injections are given six nights out of seven to provide a break or for splitting time between households.
Newer once-weekly formulations have recently received approval, as reported by this news organization, and are coming into use.
Pediatric endocrinologists measure height and follow growth factors closely with visits every 3-6 months. GH levels are not useful outside of provocative diagnostic (stimulation) testing.
Insulinlike growth factor 1 or insulinlike growth factor binding protein levels are analyzed per Tanner stage of puberty to assess appropriate response and to make dose adjustments.
Annual standardized films of the left hand help predict progress and anticipated adult height. Treatment usually persists through puberty until growth plates are closed; if true GHD is noticed, much smaller doses are continued through adulthood.
Regardless, conversations about GH happen with your friendly local pediatric endocrinologist.
We are thrilled to help shepherd patients through their growing age to meet their potential. For more information about GH treatment for children, the MAGIC Foundation is the perfect place to start.
Dr. Lilley is director of the pediatric diabetes and lipid program, Mississippi Center for Advanced Medicine, Madison. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
“Dr. Lilley, you’ll always be my favorite doctor; you helped me grow.”
These were the parting words from the last patient that I treated during my endocrinology fellowship. I had watched this young man grow from a prepubertal 17-year-old to a young man who had reached his predicted family height as I treated his delayed puberty caused by Kallmann syndrome, a problem that had been missed for years. It was the appropriate bookend for my chosen specialty.
Watching children grow and develop into who they were meant to be is one of my favorite things about endocrinology, as well as forming meaningful relationships with families. Treating detectable deficiencies in logical and measurable ways is also extremely satisfying.
Too little testosterone? That’s a problem I can solve. Too much thyroid hormone? There’s a blocker for that! Endocrinology can be a straightforward field, and when all goes well, everyone leaves happy.
Except when they don’t.
Gatekeepers for treatment for children’s growth
“Nice to meet you. We’re here to get growth hormone.”
“We’re here because his pediatrician made us come. We’ve already decided we’re not going to put hormones into his body.”
These are common statements I hear when I first meet new patients whose parents are concerned about their children’s growth. Pediatric endocrinologists, after all, are the usual gatekeepers for this treatment.
Growth hormone (GH) often makes the news for controversial reasons – most commonly for its abuse by elite athletes hoping to exploit its anabolic effects – causing parents to have varied opinions about its possible use in their children.
Some refuse endocrinology referrals at all owing to concerns that we will push daily injections on their children. Others demand referrals for their children of average height, hoping for every perceived advantage.
GH deficiency (GHD) – a condition where the pituitary gland fails to produce enough GH – can occur because of congenital pituitary malformations; anatomic, surgical, or traumatic interruptions to the gland; or enzyme deficiencies leading to faulty production.
GHD is just one reason for poor growth, however.
Growth is one of the most important indicators of health in children. A waning growth rate may be an early symptom of serious problems. In my clinic, I’ve diagnosed severe hypothyroidism in a marathon runner, a brain tumor, celiac disease in a teenager with no gastrointestinal complaints, autoimmune hepatitis, and several other diseases needing treatment in children who show no symptoms other than poor growth.
Barriers to normal growth
Sometimes, the die is cast for children to have barriers to normal growth. Several genetic conditions can lead to poor GH production or response, and GH treatment is often necessary to approximate normal height.
These may include:
- Turner syndrome (in females who are missing an X chromosome in whole or part) should be considered in every girl with abnormally short stature; mosaic forms of the condition may be subtle and lack classic features.
- Noonan syndrome is important to detect owing to the possibility of cardiac or renal malformations that may also occur in this condition, caused by a mutation in one of the genes in the RAS-MAPK pathway.
- Russell-Silver syndrome can cause intrauterine GH restriction and has been traced to uniparental disomy of chromosome 7 or duplications, mutations, or methylation defects in chromosome 11.
- Individuals with Prader-Willi syndrome, which is characterized by low muscle tone, hyperphagia, and hypogonadism, have demonstrated dramatic benefits from GH therapy, primarily in maintaining a normal body mass index.
Children who are small for their gestational age may be GH resistant, and those who do not catch up to their growth curve by the age of 2 years may require GH treatment to reach their height potential.
GH therapy isn’t entirely benign. Rare adverse effects of overtreatment can include slipped capital femoral epiphysis (a fracture to the growth plate) and pseudotumor cerebri (idiopathic intracranial hypertension).
Overtreatment can cause acromegaly, which results in coarsened features and large hands and feet.
When is GH therapy warranted?
“Growth hormone therapy has been denied by her insurer. They want you to fill out an appeal.”
Insurance approval in the United States can be a herculean effort because GH is expensive: Out-of-pocket costs are prohibitive for most people without insurance assistance, ranging from $7,000 to $30,000 annually.
Pediatric endocrinologists aren’t in the business of cosmetic endocrinology. Treatment of idiopathic short stature has been controversial since this became an indication for GH treatment.
GH isn’t always necessary. Diagnosing the underlying cause for poor growth is the most important step.
Often, we find constitutional delay of growth and puberty, or “late bloomers.” This condition is characterized by a delayed bone age (growth plates more open than expected for age) and delayed pubertal onset. These children will often reach a normal height despite starting as some of the smallest of their peers.
However, GH plays other roles in the body than simply propelling height. Children with congenital GHD will require GH treatment to prevent hypoglycemia, especially in infancy.
GH is needed even in adults with fused growth plates for normal lipid metabolism, bone accrual, and maintaining normal muscle mass.
I have noticed marked improvements in muscle tone in many children with developmental delays who are treated with GH, and research supports cognitive benefits for certain populations.
The most common regimens for GH focus on treatment via subcutaneous injection nightly, when GH is naturally produced; sometimes, injections are given six nights out of seven to provide a break or for splitting time between households.
Newer once-weekly formulations have recently received approval, as reported by this news organization, and are coming into use.
Pediatric endocrinologists measure height and follow growth factors closely with visits every 3-6 months. GH levels are not useful outside of provocative diagnostic (stimulation) testing.
Insulinlike growth factor 1 or insulinlike growth factor binding protein levels are analyzed per Tanner stage of puberty to assess appropriate response and to make dose adjustments.
Annual standardized films of the left hand help predict progress and anticipated adult height. Treatment usually persists through puberty until growth plates are closed; if true GHD is noticed, much smaller doses are continued through adulthood.
Regardless, conversations about GH happen with your friendly local pediatric endocrinologist.
We are thrilled to help shepherd patients through their growing age to meet their potential. For more information about GH treatment for children, the MAGIC Foundation is the perfect place to start.
Dr. Lilley is director of the pediatric diabetes and lipid program, Mississippi Center for Advanced Medicine, Madison. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
“Dr. Lilley, you’ll always be my favorite doctor; you helped me grow.”
These were the parting words from the last patient that I treated during my endocrinology fellowship. I had watched this young man grow from a prepubertal 17-year-old to a young man who had reached his predicted family height as I treated his delayed puberty caused by Kallmann syndrome, a problem that had been missed for years. It was the appropriate bookend for my chosen specialty.
Watching children grow and develop into who they were meant to be is one of my favorite things about endocrinology, as well as forming meaningful relationships with families. Treating detectable deficiencies in logical and measurable ways is also extremely satisfying.
Too little testosterone? That’s a problem I can solve. Too much thyroid hormone? There’s a blocker for that! Endocrinology can be a straightforward field, and when all goes well, everyone leaves happy.
Except when they don’t.
Gatekeepers for treatment for children’s growth
“Nice to meet you. We’re here to get growth hormone.”
“We’re here because his pediatrician made us come. We’ve already decided we’re not going to put hormones into his body.”
These are common statements I hear when I first meet new patients whose parents are concerned about their children’s growth. Pediatric endocrinologists, after all, are the usual gatekeepers for this treatment.
Growth hormone (GH) often makes the news for controversial reasons – most commonly for its abuse by elite athletes hoping to exploit its anabolic effects – causing parents to have varied opinions about its possible use in their children.
Some refuse endocrinology referrals at all owing to concerns that we will push daily injections on their children. Others demand referrals for their children of average height, hoping for every perceived advantage.
GH deficiency (GHD) – a condition where the pituitary gland fails to produce enough GH – can occur because of congenital pituitary malformations; anatomic, surgical, or traumatic interruptions to the gland; or enzyme deficiencies leading to faulty production.
GHD is just one reason for poor growth, however.
Growth is one of the most important indicators of health in children. A waning growth rate may be an early symptom of serious problems. In my clinic, I’ve diagnosed severe hypothyroidism in a marathon runner, a brain tumor, celiac disease in a teenager with no gastrointestinal complaints, autoimmune hepatitis, and several other diseases needing treatment in children who show no symptoms other than poor growth.
Barriers to normal growth
Sometimes, the die is cast for children to have barriers to normal growth. Several genetic conditions can lead to poor GH production or response, and GH treatment is often necessary to approximate normal height.
These may include:
- Turner syndrome (in females who are missing an X chromosome in whole or part) should be considered in every girl with abnormally short stature; mosaic forms of the condition may be subtle and lack classic features.
- Noonan syndrome is important to detect owing to the possibility of cardiac or renal malformations that may also occur in this condition, caused by a mutation in one of the genes in the RAS-MAPK pathway.
- Russell-Silver syndrome can cause intrauterine GH restriction and has been traced to uniparental disomy of chromosome 7 or duplications, mutations, or methylation defects in chromosome 11.
- Individuals with Prader-Willi syndrome, which is characterized by low muscle tone, hyperphagia, and hypogonadism, have demonstrated dramatic benefits from GH therapy, primarily in maintaining a normal body mass index.
Children who are small for their gestational age may be GH resistant, and those who do not catch up to their growth curve by the age of 2 years may require GH treatment to reach their height potential.
GH therapy isn’t entirely benign. Rare adverse effects of overtreatment can include slipped capital femoral epiphysis (a fracture to the growth plate) and pseudotumor cerebri (idiopathic intracranial hypertension).
Overtreatment can cause acromegaly, which results in coarsened features and large hands and feet.
When is GH therapy warranted?
“Growth hormone therapy has been denied by her insurer. They want you to fill out an appeal.”
Insurance approval in the United States can be a herculean effort because GH is expensive: Out-of-pocket costs are prohibitive for most people without insurance assistance, ranging from $7,000 to $30,000 annually.
Pediatric endocrinologists aren’t in the business of cosmetic endocrinology. Treatment of idiopathic short stature has been controversial since this became an indication for GH treatment.
GH isn’t always necessary. Diagnosing the underlying cause for poor growth is the most important step.
Often, we find constitutional delay of growth and puberty, or “late bloomers.” This condition is characterized by a delayed bone age (growth plates more open than expected for age) and delayed pubertal onset. These children will often reach a normal height despite starting as some of the smallest of their peers.
However, GH plays other roles in the body than simply propelling height. Children with congenital GHD will require GH treatment to prevent hypoglycemia, especially in infancy.
GH is needed even in adults with fused growth plates for normal lipid metabolism, bone accrual, and maintaining normal muscle mass.
I have noticed marked improvements in muscle tone in many children with developmental delays who are treated with GH, and research supports cognitive benefits for certain populations.
The most common regimens for GH focus on treatment via subcutaneous injection nightly, when GH is naturally produced; sometimes, injections are given six nights out of seven to provide a break or for splitting time between households.
Newer once-weekly formulations have recently received approval, as reported by this news organization, and are coming into use.
Pediatric endocrinologists measure height and follow growth factors closely with visits every 3-6 months. GH levels are not useful outside of provocative diagnostic (stimulation) testing.
Insulinlike growth factor 1 or insulinlike growth factor binding protein levels are analyzed per Tanner stage of puberty to assess appropriate response and to make dose adjustments.
Annual standardized films of the left hand help predict progress and anticipated adult height. Treatment usually persists through puberty until growth plates are closed; if true GHD is noticed, much smaller doses are continued through adulthood.
Regardless, conversations about GH happen with your friendly local pediatric endocrinologist.
We are thrilled to help shepherd patients through their growing age to meet their potential. For more information about GH treatment for children, the MAGIC Foundation is the perfect place to start.
Dr. Lilley is director of the pediatric diabetes and lipid program, Mississippi Center for Advanced Medicine, Madison. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.