User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Medical coding creates barriers to care for transgender patients
In 2021, Tim Chevalier received the first of many coverage denials from his insurance company for the hair-removal procedure he needed as part of a phalloplasty, the creation of a penis.
Electrolysis is a common procedure among transgender people like Mr. Chevalier, a software developer in Oakland, Calif.. In some cases, it’s used to remove unwanted hair from the face or body. But it’s also required for a phalloplasty or a vaginoplasty, the creation of a vagina, because all hair must be removed from the tissue that will be relocated during surgery.
Mr. Chevalier’s insurer, Anthem Blue Cross, told him he needed what’s known as a prior authorization for the procedure. Even after Mr. Chevalier received the authorization, he said, his reimbursement claims kept getting denied. According to Mr. Chevalier, Anthem said the procedure was considered cosmetic.
Many trans patients have trouble getting their insurers to cover gender-affirming care. One reason is transphobia within the U.S. health care system, but another involves how medical diagnoses and procedures are coded for insurance companies. Nationwide, health care providers use a list of diagnostic codes provided by the ICD-10. And many of those, advocates for transgender people say, haven’t caught up to the needs of patients. Such diagnostic codes provide the basis for determining which procedures, such as electrolysis or surgery, insurance will cover.
“It’s widely regarded that the codes are very limited in ICD-10,” said Johanna Olson-Kennedy, MD, medical director of the Center for Transyouth Health and Development at Children’s Hospital Los Angeles.
She advocates for a move to the 11th edition of the coding system, which was endorsed by the World Health Organization in 2019 and began to be adopted around the globe in February. Today, more than 34 countries use ICD-11.
The new edition has replaced outdated terms like “transsexualism” and “gender identity disorder” with “gender incongruence,” which is no longer classified as a mental health condition, but as a sexual health one. This is crucial in reducing the stigmatization of trans people in health care, said Dr. Olson-Kennedy.
A move away from the mental health classification may also mean more coverage of gender-affirming care by insurance companies, which sometimes question mental health claims more rigorously than those for physical illnesses. WHO officials have said they hope that adding gender incongruence to a sexual health chapter will “help increase access to care for health interventions” and “destigmatize the condition,” according to the WHO website.
However, history suggests that ICD-11 likely won’t be implemented in the United States for years. The WHO first endorsed ICD-10 in 1990, but the United States didn’t implement it for 25 years.
Meanwhile, patients who identify as transgender and their doctors are spending hours trying to get coverage – or using crowdfunding to cover big out-of-pocket bills. Mr. Chevalier estimated he has received 78 hours of electrolysis at $140 per hour, costing $10,920.
Anthem spokesperson Michael Bowman wrote in an email that “there has been no medical denials or denial of coverage” because Anthem “preapproved coverage for these services.”
However, even after the preapproval was given, Anthem responded to Mr. Chevalier’s claims by stating the electrolysis would not be reimbursed because the procedure is considered cosmetic, rather than medically necessary. This is regardless of Mr. Chevalier’s diagnosis of gender dysphoria – the psychological distress felt when someone’s biological sex and gender identity don’t match – which many doctors consider a medically legitimate reason for hair removal.
Bowman wrote that “once this issue was identified, Anthem implemented an internal process which included a manual override in the billing system.”
Still, Mr. Chevalier filed a complaint with the California Department of Managed Health Care, and the state declared Anthem Blue Cross out of compliance. Additionally, after KHN started asking Anthem questions about Chevalier’s bills, two claims that had not been addressed since April were resolved in July. So far, Anthem has reimbursed Chevalier around $8,000.
Some procedures that trans patients receive can also be excluded from coverage because insurance companies consider them “sex specific.” For example, a transgender man’s gynecological visit may not be covered because his insurance plan covers those visits only for people enrolled as women.
“There is always this question of: What gender should you tell the insurance company?” said Nick Gorton, MD, an emergency medicine physician in Davis, Calif. Dr. Gorton, who is trans, recommends his patients with insurance plans that exclude trans care calculate the out-of-pocket costs that would be required for certain procedures based on whether the patient lists themselves as male or female on their insurance paperwork. For example, Dr. Gorton said, the question for a trans man becomes “what’s more expensive – paying for testosterone or paying for a Pap smear?” – since insurance likely won’t cover both.
For years, some physicians helped trans patients get coverage by finding other medical reasons for their trans-related care. Dr. Gorton said that if, for instance, a transgender man wanted a hysterectomy but his insurance didn’t cover gender-affirming care, Dr. Gorton would enter the ICD-10 code for pelvic pain, as opposed to gender dysphoria, into the patient’s billing record. Pelvic pain is a legitimate reason for the surgery and is commonly accepted by insurance providers, Dr. Gorton said. But some insurance companies pushed back, and he had to find other ways to help his patients.
In 2005, California passed a first-of-its-kind law that prohibits discrimination by health insurance on the basis of gender or gender identity. Now, 24 states and Washington, D.C., forbid private insurance from excluding transgender-related health care benefits.
Consequently, Dr. Gorton no longer needs to use different codes for patients seeking gender-affirming care at his practice in California. But physicians in other states are still struggling.
When Eric Meininger, MD, MPH, an internist and pediatrician at Indiana University Health’s gender health program in Indianapolis, treats a trans kid seeking hormone therapy, he commonly uses the ICD-10 code for “medication management” as the primary reason for the patient’s visit. That’s because Indiana has no law providing insurance protections for LGBTQ+ people, and when gender dysphoria is listed as the primary reason, insurance companies have denied coverage.
“It’s frustrating,” Dr. Meininger said. In a patient’s billing record, he sometimes provides multiple diagnoses, including gender dysphoria, to increase the likelihood that a procedure will be covered. “It’s not hard usually to come up with five or seven or eight diagnoses for someone because there’s lots of vague ones out there.”
Implementing ICD-11 won’t fix all the coding problems, as insurance companies may still refuse to cover procedures related to gender incongruence even though it is listed as a sexual health condition. It also won’t change the fact that many states still allow insurance to exclude gender-affirming care. But in terms of reducing stigma, it’s a step forward, Dr. Olson-Kennedy said.
One reason the United States took so long to switch to ICD-10 is that the American Medical Association strongly opposed the move. It argued the new system would put an incredible burden on doctors. Physicians would have to “contend with 68,000 diagnosis codes – a fivefold increase from the approximately 13,000 diagnosis codes in use today,” the AMA wrote in a 2014 letter. Implementing software to update providers’ coding systems would also be costly, dealing a financial blow to small medical practices, the association argued.
Unlike past coding systems, ICD-11 is fully electronic, with no physical manual of codes, and can be incorporated into a medical facility’s current coding system without requiring a new rollout, said Christian Lindmeier, a WHO spokesperson.
Whether these changes will make the adoption of the new edition easier in the United States is yet to be seen. For now, many trans patients in need of gender-affirming care must pay their bills out of pocket, fight their insurance company for coverage, or rely on the generosity of others.
“Even though I did get reimbursed eventually, the reimbursements were delayed, and it burned up a lot of my time,” Mr. Chevalier said. “Most people would have just given up.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
In 2021, Tim Chevalier received the first of many coverage denials from his insurance company for the hair-removal procedure he needed as part of a phalloplasty, the creation of a penis.
Electrolysis is a common procedure among transgender people like Mr. Chevalier, a software developer in Oakland, Calif.. In some cases, it’s used to remove unwanted hair from the face or body. But it’s also required for a phalloplasty or a vaginoplasty, the creation of a vagina, because all hair must be removed from the tissue that will be relocated during surgery.
Mr. Chevalier’s insurer, Anthem Blue Cross, told him he needed what’s known as a prior authorization for the procedure. Even after Mr. Chevalier received the authorization, he said, his reimbursement claims kept getting denied. According to Mr. Chevalier, Anthem said the procedure was considered cosmetic.
Many trans patients have trouble getting their insurers to cover gender-affirming care. One reason is transphobia within the U.S. health care system, but another involves how medical diagnoses and procedures are coded for insurance companies. Nationwide, health care providers use a list of diagnostic codes provided by the ICD-10. And many of those, advocates for transgender people say, haven’t caught up to the needs of patients. Such diagnostic codes provide the basis for determining which procedures, such as electrolysis or surgery, insurance will cover.
“It’s widely regarded that the codes are very limited in ICD-10,” said Johanna Olson-Kennedy, MD, medical director of the Center for Transyouth Health and Development at Children’s Hospital Los Angeles.
She advocates for a move to the 11th edition of the coding system, which was endorsed by the World Health Organization in 2019 and began to be adopted around the globe in February. Today, more than 34 countries use ICD-11.
The new edition has replaced outdated terms like “transsexualism” and “gender identity disorder” with “gender incongruence,” which is no longer classified as a mental health condition, but as a sexual health one. This is crucial in reducing the stigmatization of trans people in health care, said Dr. Olson-Kennedy.
A move away from the mental health classification may also mean more coverage of gender-affirming care by insurance companies, which sometimes question mental health claims more rigorously than those for physical illnesses. WHO officials have said they hope that adding gender incongruence to a sexual health chapter will “help increase access to care for health interventions” and “destigmatize the condition,” according to the WHO website.
However, history suggests that ICD-11 likely won’t be implemented in the United States for years. The WHO first endorsed ICD-10 in 1990, but the United States didn’t implement it for 25 years.
Meanwhile, patients who identify as transgender and their doctors are spending hours trying to get coverage – or using crowdfunding to cover big out-of-pocket bills. Mr. Chevalier estimated he has received 78 hours of electrolysis at $140 per hour, costing $10,920.
Anthem spokesperson Michael Bowman wrote in an email that “there has been no medical denials or denial of coverage” because Anthem “preapproved coverage for these services.”
However, even after the preapproval was given, Anthem responded to Mr. Chevalier’s claims by stating the electrolysis would not be reimbursed because the procedure is considered cosmetic, rather than medically necessary. This is regardless of Mr. Chevalier’s diagnosis of gender dysphoria – the psychological distress felt when someone’s biological sex and gender identity don’t match – which many doctors consider a medically legitimate reason for hair removal.
Bowman wrote that “once this issue was identified, Anthem implemented an internal process which included a manual override in the billing system.”
Still, Mr. Chevalier filed a complaint with the California Department of Managed Health Care, and the state declared Anthem Blue Cross out of compliance. Additionally, after KHN started asking Anthem questions about Chevalier’s bills, two claims that had not been addressed since April were resolved in July. So far, Anthem has reimbursed Chevalier around $8,000.
Some procedures that trans patients receive can also be excluded from coverage because insurance companies consider them “sex specific.” For example, a transgender man’s gynecological visit may not be covered because his insurance plan covers those visits only for people enrolled as women.
“There is always this question of: What gender should you tell the insurance company?” said Nick Gorton, MD, an emergency medicine physician in Davis, Calif. Dr. Gorton, who is trans, recommends his patients with insurance plans that exclude trans care calculate the out-of-pocket costs that would be required for certain procedures based on whether the patient lists themselves as male or female on their insurance paperwork. For example, Dr. Gorton said, the question for a trans man becomes “what’s more expensive – paying for testosterone or paying for a Pap smear?” – since insurance likely won’t cover both.
For years, some physicians helped trans patients get coverage by finding other medical reasons for their trans-related care. Dr. Gorton said that if, for instance, a transgender man wanted a hysterectomy but his insurance didn’t cover gender-affirming care, Dr. Gorton would enter the ICD-10 code for pelvic pain, as opposed to gender dysphoria, into the patient’s billing record. Pelvic pain is a legitimate reason for the surgery and is commonly accepted by insurance providers, Dr. Gorton said. But some insurance companies pushed back, and he had to find other ways to help his patients.
In 2005, California passed a first-of-its-kind law that prohibits discrimination by health insurance on the basis of gender or gender identity. Now, 24 states and Washington, D.C., forbid private insurance from excluding transgender-related health care benefits.
Consequently, Dr. Gorton no longer needs to use different codes for patients seeking gender-affirming care at his practice in California. But physicians in other states are still struggling.
When Eric Meininger, MD, MPH, an internist and pediatrician at Indiana University Health’s gender health program in Indianapolis, treats a trans kid seeking hormone therapy, he commonly uses the ICD-10 code for “medication management” as the primary reason for the patient’s visit. That’s because Indiana has no law providing insurance protections for LGBTQ+ people, and when gender dysphoria is listed as the primary reason, insurance companies have denied coverage.
“It’s frustrating,” Dr. Meininger said. In a patient’s billing record, he sometimes provides multiple diagnoses, including gender dysphoria, to increase the likelihood that a procedure will be covered. “It’s not hard usually to come up with five or seven or eight diagnoses for someone because there’s lots of vague ones out there.”
Implementing ICD-11 won’t fix all the coding problems, as insurance companies may still refuse to cover procedures related to gender incongruence even though it is listed as a sexual health condition. It also won’t change the fact that many states still allow insurance to exclude gender-affirming care. But in terms of reducing stigma, it’s a step forward, Dr. Olson-Kennedy said.
One reason the United States took so long to switch to ICD-10 is that the American Medical Association strongly opposed the move. It argued the new system would put an incredible burden on doctors. Physicians would have to “contend with 68,000 diagnosis codes – a fivefold increase from the approximately 13,000 diagnosis codes in use today,” the AMA wrote in a 2014 letter. Implementing software to update providers’ coding systems would also be costly, dealing a financial blow to small medical practices, the association argued.
Unlike past coding systems, ICD-11 is fully electronic, with no physical manual of codes, and can be incorporated into a medical facility’s current coding system without requiring a new rollout, said Christian Lindmeier, a WHO spokesperson.
Whether these changes will make the adoption of the new edition easier in the United States is yet to be seen. For now, many trans patients in need of gender-affirming care must pay their bills out of pocket, fight their insurance company for coverage, or rely on the generosity of others.
“Even though I did get reimbursed eventually, the reimbursements were delayed, and it burned up a lot of my time,” Mr. Chevalier said. “Most people would have just given up.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
In 2021, Tim Chevalier received the first of many coverage denials from his insurance company for the hair-removal procedure he needed as part of a phalloplasty, the creation of a penis.
Electrolysis is a common procedure among transgender people like Mr. Chevalier, a software developer in Oakland, Calif.. In some cases, it’s used to remove unwanted hair from the face or body. But it’s also required for a phalloplasty or a vaginoplasty, the creation of a vagina, because all hair must be removed from the tissue that will be relocated during surgery.
Mr. Chevalier’s insurer, Anthem Blue Cross, told him he needed what’s known as a prior authorization for the procedure. Even after Mr. Chevalier received the authorization, he said, his reimbursement claims kept getting denied. According to Mr. Chevalier, Anthem said the procedure was considered cosmetic.
Many trans patients have trouble getting their insurers to cover gender-affirming care. One reason is transphobia within the U.S. health care system, but another involves how medical diagnoses and procedures are coded for insurance companies. Nationwide, health care providers use a list of diagnostic codes provided by the ICD-10. And many of those, advocates for transgender people say, haven’t caught up to the needs of patients. Such diagnostic codes provide the basis for determining which procedures, such as electrolysis or surgery, insurance will cover.
“It’s widely regarded that the codes are very limited in ICD-10,” said Johanna Olson-Kennedy, MD, medical director of the Center for Transyouth Health and Development at Children’s Hospital Los Angeles.
She advocates for a move to the 11th edition of the coding system, which was endorsed by the World Health Organization in 2019 and began to be adopted around the globe in February. Today, more than 34 countries use ICD-11.
The new edition has replaced outdated terms like “transsexualism” and “gender identity disorder” with “gender incongruence,” which is no longer classified as a mental health condition, but as a sexual health one. This is crucial in reducing the stigmatization of trans people in health care, said Dr. Olson-Kennedy.
A move away from the mental health classification may also mean more coverage of gender-affirming care by insurance companies, which sometimes question mental health claims more rigorously than those for physical illnesses. WHO officials have said they hope that adding gender incongruence to a sexual health chapter will “help increase access to care for health interventions” and “destigmatize the condition,” according to the WHO website.
However, history suggests that ICD-11 likely won’t be implemented in the United States for years. The WHO first endorsed ICD-10 in 1990, but the United States didn’t implement it for 25 years.
Meanwhile, patients who identify as transgender and their doctors are spending hours trying to get coverage – or using crowdfunding to cover big out-of-pocket bills. Mr. Chevalier estimated he has received 78 hours of electrolysis at $140 per hour, costing $10,920.
Anthem spokesperson Michael Bowman wrote in an email that “there has been no medical denials or denial of coverage” because Anthem “preapproved coverage for these services.”
However, even after the preapproval was given, Anthem responded to Mr. Chevalier’s claims by stating the electrolysis would not be reimbursed because the procedure is considered cosmetic, rather than medically necessary. This is regardless of Mr. Chevalier’s diagnosis of gender dysphoria – the psychological distress felt when someone’s biological sex and gender identity don’t match – which many doctors consider a medically legitimate reason for hair removal.
Bowman wrote that “once this issue was identified, Anthem implemented an internal process which included a manual override in the billing system.”
Still, Mr. Chevalier filed a complaint with the California Department of Managed Health Care, and the state declared Anthem Blue Cross out of compliance. Additionally, after KHN started asking Anthem questions about Chevalier’s bills, two claims that had not been addressed since April were resolved in July. So far, Anthem has reimbursed Chevalier around $8,000.
Some procedures that trans patients receive can also be excluded from coverage because insurance companies consider them “sex specific.” For example, a transgender man’s gynecological visit may not be covered because his insurance plan covers those visits only for people enrolled as women.
“There is always this question of: What gender should you tell the insurance company?” said Nick Gorton, MD, an emergency medicine physician in Davis, Calif. Dr. Gorton, who is trans, recommends his patients with insurance plans that exclude trans care calculate the out-of-pocket costs that would be required for certain procedures based on whether the patient lists themselves as male or female on their insurance paperwork. For example, Dr. Gorton said, the question for a trans man becomes “what’s more expensive – paying for testosterone or paying for a Pap smear?” – since insurance likely won’t cover both.
For years, some physicians helped trans patients get coverage by finding other medical reasons for their trans-related care. Dr. Gorton said that if, for instance, a transgender man wanted a hysterectomy but his insurance didn’t cover gender-affirming care, Dr. Gorton would enter the ICD-10 code for pelvic pain, as opposed to gender dysphoria, into the patient’s billing record. Pelvic pain is a legitimate reason for the surgery and is commonly accepted by insurance providers, Dr. Gorton said. But some insurance companies pushed back, and he had to find other ways to help his patients.
In 2005, California passed a first-of-its-kind law that prohibits discrimination by health insurance on the basis of gender or gender identity. Now, 24 states and Washington, D.C., forbid private insurance from excluding transgender-related health care benefits.
Consequently, Dr. Gorton no longer needs to use different codes for patients seeking gender-affirming care at his practice in California. But physicians in other states are still struggling.
When Eric Meininger, MD, MPH, an internist and pediatrician at Indiana University Health’s gender health program in Indianapolis, treats a trans kid seeking hormone therapy, he commonly uses the ICD-10 code for “medication management” as the primary reason for the patient’s visit. That’s because Indiana has no law providing insurance protections for LGBTQ+ people, and when gender dysphoria is listed as the primary reason, insurance companies have denied coverage.
“It’s frustrating,” Dr. Meininger said. In a patient’s billing record, he sometimes provides multiple diagnoses, including gender dysphoria, to increase the likelihood that a procedure will be covered. “It’s not hard usually to come up with five or seven or eight diagnoses for someone because there’s lots of vague ones out there.”
Implementing ICD-11 won’t fix all the coding problems, as insurance companies may still refuse to cover procedures related to gender incongruence even though it is listed as a sexual health condition. It also won’t change the fact that many states still allow insurance to exclude gender-affirming care. But in terms of reducing stigma, it’s a step forward, Dr. Olson-Kennedy said.
One reason the United States took so long to switch to ICD-10 is that the American Medical Association strongly opposed the move. It argued the new system would put an incredible burden on doctors. Physicians would have to “contend with 68,000 diagnosis codes – a fivefold increase from the approximately 13,000 diagnosis codes in use today,” the AMA wrote in a 2014 letter. Implementing software to update providers’ coding systems would also be costly, dealing a financial blow to small medical practices, the association argued.
Unlike past coding systems, ICD-11 is fully electronic, with no physical manual of codes, and can be incorporated into a medical facility’s current coding system without requiring a new rollout, said Christian Lindmeier, a WHO spokesperson.
Whether these changes will make the adoption of the new edition easier in the United States is yet to be seen. For now, many trans patients in need of gender-affirming care must pay their bills out of pocket, fight their insurance company for coverage, or rely on the generosity of others.
“Even though I did get reimbursed eventually, the reimbursements were delayed, and it burned up a lot of my time,” Mr. Chevalier said. “Most people would have just given up.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Pandemic has helped clinicians to gain better insight on pernio, expert says
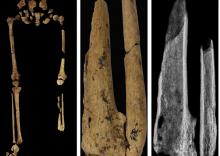
PORTLAND, ORE. – while others are not, according to Lindy P. Fox, MD, professor of dermatology and director of the hospital consultation service at the University of California, San Francisco.
“We’re learning a lot about pernio because of COVID,” Dr. Fox, a member of the American Academy of Dermatology’s Ad Hoc Task Force on COVID-19, said at the annual meeting of the Pacific Dermatologic Association. “Patients with pernio tend to either have bright red or purple individual lesions or an erythromelalgia-like presentation, often waking up in the middle of the night saying ‘my feet hurt. I can’t put sheets over my feet.’ In my experience, the patients with an erythromelalgia-like presentation tend to be a lot harder to treat.”
Establishing terminology to describe pernio-like lesions was a challenge in the early stages of the COVID-19 pandemic, Dr. Fox added, with clinicians using terms like erythema multiforme-like, coxsackie-like, or even necrotic to describe the lesions. “I don’t think pernio is truly necrotic; I think it’s really inflammatory and purpuric,” she said.
Early in the pandemic, studies suggesting a link with these cases and COVID-19 infection include a case series of 318 patients with pernio-like skin lesions who had confirmed or suspected COVID-19. Most of these patients were generally young and healthy and most had relatively mild COVID-19; 7% were laboratory-confirmed COVID-19 positive, and 6% were close contacts of patients with confirmed COVID-19. Pernio-like lesions were the only symptoms in 55% of the patients.
In another study, researchers in France evaluated the clinical, laboratory, and pathologic characteristics of 40 patients who developed chilblain-like lesions (mostly involving the toes) during the COVID-19 pandemic and were seen as outpatients in April 2020 . All were polymerase chain reaction (PCR) negative, 30% were SARS-CoV-2 serology positive, and 60% had elevated D-dimers. Histology obtained from 19 of the patients revealed lymphocytic inflammation and vascular damage, and 8 had IgA positivity.
In a retrospective analysis of seven pediatric chilblains cases during the pandemic, researchers examined the skin biopsies to evaluate histopathological features and explored the presence of SARS-CoV-2 in the tissue. All patients were PCR negative. The authors observed cytoplasmic granular positivity for SARS-CoV-2 spike protein in endothelial cells, a feature that they said showed coronavirus-like particles, consistent with SARS-CoV-2.
Not all studies in the medical literature have demonstrated an association between pernio-like/chilblains-like lesions and COVID-19, though. An analysis of 23 patients, with skin eruptions considered associated with SARS-CoV-2 infections (including 21 cases of chilblains) during the first wave of the pandemic found that the antibody and T-cell response in patients with pandemic chilblains was the same as in negative controls.
“What’s remarkably interesting about this study is that they did autopsies of samples from patients who had died prepandemic, so there was no such thing as COVID-19,” said Dr. Fox, who was not involved with the study. “They stained for viral particles in those patients, and they were positive in a subset of patients. This makes me wonder about what the significance of that staining positivity is.”
Yet another group of investigators looked at what was happening with pernio during the waves of COVID in a study of chilblains cases in children in Spain, and found a stronger association between lockdown and cold temperature, which argues against a direct association between pernio and COVID infection.
In Dr. Fox’s experience, COVID toes can recur, especially upon exposure to cold. “What taught me this in real life is a patient who I saw remotely by video,” she recalled. “It was early on in the pandemic. I could not prove he had COVID no matter how hard I tried, but I do think he had COVID toes at that time.” When he later was confirmed to have COVID, “he got pernio in the same exact location as his original suspected COVID toes.”
According to an analysis of long COVID in the skin, based on cases reported to the American Academy of Dermatology–International League of Dermatological Societies registry from April 8 to Oct. 8, 2020, pernio-like lesions lasted a median of 12 days in patients with lab-confirmed COVID-19 and a median of 15 days in those with suspected COVID-19. But almost 7% of the 103 pernio cases were long-haulers, defined as those with dermatologic signs of COVID that lasted beyond 60 days.
“There are some patients who are resistant to treatment,” Dr. Fox said. “In addition, recurrent lesions make me think that maybe all pernio is triggered by some viral cause. This causes an immunologic phenomenon that’s responding to a viral trigger you’re trying to deal with. That may be the better way to think about COVID toes.”
Different variants of COVID also appear to be changing the characteristics of dermatologic manifestations associated with infection. Results from a large retrospective analysis of nearly 350,000 users of a COVID study App in the United Kingdom found that skin lesions were more predictive of a positive test in the Delta wave, compared with the Omicron wave, while pernio-like lesions were predictive of infection in the Delta wave but not in the Omicron wave.
“And, whether you were vaccinated or unvaccinated really did not influence whether or not you were going to have a skin rash as a presenting sign of COVID, except for the burning rash, which was less in vaccinated patients,” said Dr. Fox, who was not involved with the study.
Dr. Fox reported having no relevant disclosures.
PORTLAND, ORE. – while others are not, according to Lindy P. Fox, MD, professor of dermatology and director of the hospital consultation service at the University of California, San Francisco.
“We’re learning a lot about pernio because of COVID,” Dr. Fox, a member of the American Academy of Dermatology’s Ad Hoc Task Force on COVID-19, said at the annual meeting of the Pacific Dermatologic Association. “Patients with pernio tend to either have bright red or purple individual lesions or an erythromelalgia-like presentation, often waking up in the middle of the night saying ‘my feet hurt. I can’t put sheets over my feet.’ In my experience, the patients with an erythromelalgia-like presentation tend to be a lot harder to treat.”
Establishing terminology to describe pernio-like lesions was a challenge in the early stages of the COVID-19 pandemic, Dr. Fox added, with clinicians using terms like erythema multiforme-like, coxsackie-like, or even necrotic to describe the lesions. “I don’t think pernio is truly necrotic; I think it’s really inflammatory and purpuric,” she said.
Early in the pandemic, studies suggesting a link with these cases and COVID-19 infection include a case series of 318 patients with pernio-like skin lesions who had confirmed or suspected COVID-19. Most of these patients were generally young and healthy and most had relatively mild COVID-19; 7% were laboratory-confirmed COVID-19 positive, and 6% were close contacts of patients with confirmed COVID-19. Pernio-like lesions were the only symptoms in 55% of the patients.
In another study, researchers in France evaluated the clinical, laboratory, and pathologic characteristics of 40 patients who developed chilblain-like lesions (mostly involving the toes) during the COVID-19 pandemic and were seen as outpatients in April 2020 . All were polymerase chain reaction (PCR) negative, 30% were SARS-CoV-2 serology positive, and 60% had elevated D-dimers. Histology obtained from 19 of the patients revealed lymphocytic inflammation and vascular damage, and 8 had IgA positivity.
In a retrospective analysis of seven pediatric chilblains cases during the pandemic, researchers examined the skin biopsies to evaluate histopathological features and explored the presence of SARS-CoV-2 in the tissue. All patients were PCR negative. The authors observed cytoplasmic granular positivity for SARS-CoV-2 spike protein in endothelial cells, a feature that they said showed coronavirus-like particles, consistent with SARS-CoV-2.
Not all studies in the medical literature have demonstrated an association between pernio-like/chilblains-like lesions and COVID-19, though. An analysis of 23 patients, with skin eruptions considered associated with SARS-CoV-2 infections (including 21 cases of chilblains) during the first wave of the pandemic found that the antibody and T-cell response in patients with pandemic chilblains was the same as in negative controls.
“What’s remarkably interesting about this study is that they did autopsies of samples from patients who had died prepandemic, so there was no such thing as COVID-19,” said Dr. Fox, who was not involved with the study. “They stained for viral particles in those patients, and they were positive in a subset of patients. This makes me wonder about what the significance of that staining positivity is.”
Yet another group of investigators looked at what was happening with pernio during the waves of COVID in a study of chilblains cases in children in Spain, and found a stronger association between lockdown and cold temperature, which argues against a direct association between pernio and COVID infection.
In Dr. Fox’s experience, COVID toes can recur, especially upon exposure to cold. “What taught me this in real life is a patient who I saw remotely by video,” she recalled. “It was early on in the pandemic. I could not prove he had COVID no matter how hard I tried, but I do think he had COVID toes at that time.” When he later was confirmed to have COVID, “he got pernio in the same exact location as his original suspected COVID toes.”
According to an analysis of long COVID in the skin, based on cases reported to the American Academy of Dermatology–International League of Dermatological Societies registry from April 8 to Oct. 8, 2020, pernio-like lesions lasted a median of 12 days in patients with lab-confirmed COVID-19 and a median of 15 days in those with suspected COVID-19. But almost 7% of the 103 pernio cases were long-haulers, defined as those with dermatologic signs of COVID that lasted beyond 60 days.
“There are some patients who are resistant to treatment,” Dr. Fox said. “In addition, recurrent lesions make me think that maybe all pernio is triggered by some viral cause. This causes an immunologic phenomenon that’s responding to a viral trigger you’re trying to deal with. That may be the better way to think about COVID toes.”
Different variants of COVID also appear to be changing the characteristics of dermatologic manifestations associated with infection. Results from a large retrospective analysis of nearly 350,000 users of a COVID study App in the United Kingdom found that skin lesions were more predictive of a positive test in the Delta wave, compared with the Omicron wave, while pernio-like lesions were predictive of infection in the Delta wave but not in the Omicron wave.
“And, whether you were vaccinated or unvaccinated really did not influence whether or not you were going to have a skin rash as a presenting sign of COVID, except for the burning rash, which was less in vaccinated patients,” said Dr. Fox, who was not involved with the study.
Dr. Fox reported having no relevant disclosures.
PORTLAND, ORE. – while others are not, according to Lindy P. Fox, MD, professor of dermatology and director of the hospital consultation service at the University of California, San Francisco.
“We’re learning a lot about pernio because of COVID,” Dr. Fox, a member of the American Academy of Dermatology’s Ad Hoc Task Force on COVID-19, said at the annual meeting of the Pacific Dermatologic Association. “Patients with pernio tend to either have bright red or purple individual lesions or an erythromelalgia-like presentation, often waking up in the middle of the night saying ‘my feet hurt. I can’t put sheets over my feet.’ In my experience, the patients with an erythromelalgia-like presentation tend to be a lot harder to treat.”
Establishing terminology to describe pernio-like lesions was a challenge in the early stages of the COVID-19 pandemic, Dr. Fox added, with clinicians using terms like erythema multiforme-like, coxsackie-like, or even necrotic to describe the lesions. “I don’t think pernio is truly necrotic; I think it’s really inflammatory and purpuric,” she said.
Early in the pandemic, studies suggesting a link with these cases and COVID-19 infection include a case series of 318 patients with pernio-like skin lesions who had confirmed or suspected COVID-19. Most of these patients were generally young and healthy and most had relatively mild COVID-19; 7% were laboratory-confirmed COVID-19 positive, and 6% were close contacts of patients with confirmed COVID-19. Pernio-like lesions were the only symptoms in 55% of the patients.
In another study, researchers in France evaluated the clinical, laboratory, and pathologic characteristics of 40 patients who developed chilblain-like lesions (mostly involving the toes) during the COVID-19 pandemic and were seen as outpatients in April 2020 . All were polymerase chain reaction (PCR) negative, 30% were SARS-CoV-2 serology positive, and 60% had elevated D-dimers. Histology obtained from 19 of the patients revealed lymphocytic inflammation and vascular damage, and 8 had IgA positivity.
In a retrospective analysis of seven pediatric chilblains cases during the pandemic, researchers examined the skin biopsies to evaluate histopathological features and explored the presence of SARS-CoV-2 in the tissue. All patients were PCR negative. The authors observed cytoplasmic granular positivity for SARS-CoV-2 spike protein in endothelial cells, a feature that they said showed coronavirus-like particles, consistent with SARS-CoV-2.
Not all studies in the medical literature have demonstrated an association between pernio-like/chilblains-like lesions and COVID-19, though. An analysis of 23 patients, with skin eruptions considered associated with SARS-CoV-2 infections (including 21 cases of chilblains) during the first wave of the pandemic found that the antibody and T-cell response in patients with pandemic chilblains was the same as in negative controls.
“What’s remarkably interesting about this study is that they did autopsies of samples from patients who had died prepandemic, so there was no such thing as COVID-19,” said Dr. Fox, who was not involved with the study. “They stained for viral particles in those patients, and they were positive in a subset of patients. This makes me wonder about what the significance of that staining positivity is.”
Yet another group of investigators looked at what was happening with pernio during the waves of COVID in a study of chilblains cases in children in Spain, and found a stronger association between lockdown and cold temperature, which argues against a direct association between pernio and COVID infection.
In Dr. Fox’s experience, COVID toes can recur, especially upon exposure to cold. “What taught me this in real life is a patient who I saw remotely by video,” she recalled. “It was early on in the pandemic. I could not prove he had COVID no matter how hard I tried, but I do think he had COVID toes at that time.” When he later was confirmed to have COVID, “he got pernio in the same exact location as his original suspected COVID toes.”
According to an analysis of long COVID in the skin, based on cases reported to the American Academy of Dermatology–International League of Dermatological Societies registry from April 8 to Oct. 8, 2020, pernio-like lesions lasted a median of 12 days in patients with lab-confirmed COVID-19 and a median of 15 days in those with suspected COVID-19. But almost 7% of the 103 pernio cases were long-haulers, defined as those with dermatologic signs of COVID that lasted beyond 60 days.
“There are some patients who are resistant to treatment,” Dr. Fox said. “In addition, recurrent lesions make me think that maybe all pernio is triggered by some viral cause. This causes an immunologic phenomenon that’s responding to a viral trigger you’re trying to deal with. That may be the better way to think about COVID toes.”
Different variants of COVID also appear to be changing the characteristics of dermatologic manifestations associated with infection. Results from a large retrospective analysis of nearly 350,000 users of a COVID study App in the United Kingdom found that skin lesions were more predictive of a positive test in the Delta wave, compared with the Omicron wave, while pernio-like lesions were predictive of infection in the Delta wave but not in the Omicron wave.
“And, whether you were vaccinated or unvaccinated really did not influence whether or not you were going to have a skin rash as a presenting sign of COVID, except for the burning rash, which was less in vaccinated patients,” said Dr. Fox, who was not involved with the study.
Dr. Fox reported having no relevant disclosures.
AT PDA 2022
Two states aim to curb diet pill sales to minors
California and New York are on the cusp of going further than the Food and Drug Administration in restricting the sale of nonprescription diet pills to minors as pediatricians and public health advocates try to protect kids from extreme weight-loss gimmicks online.
A bill before Gov. Gavin Newsom would bar anyone under 18 in California from buying over-the-counter weight-loss supplements – whether online or in shops – without a prescription. A similar bill passed by New York lawmakers is on Gov. Kathy Hochul’s desk. Neither Democrat has indicated how he or she will act.
If both bills are signed into law, proponents hope the momentum will build to restrict diet pill sales to children in more states. Massachusetts, New Jersey, and Missouri have introduced similar bills and backers plan to continue their push next year.
Nearly 30 million people in the United States will have an eating disorder in their lifetime; 95% of them are aged between 12 and 25, according to Johns Hopkins All Children’s Hospital. The hospital added that eating disorders pose the highest risk of mortality of any mental health disorder. And it has become easier than ever for minors to get pills that are sold online or on drugstore shelves. All dietary supplements, which include those for weight loss, accounted for nearly 35% of the $63 billion over-the-counter health products industry in 2021, according to Vision Research Reports, a market research firm.
Dietary supplements, which encompass a broad range of vitamins, herbs, and minerals, are classified by the FDA as food and don’t undergo scientific and safety testing as prescription drugs and over-the-counter medicines do.
Public health advocates want to keep weight-loss products – with ads that may promise to “Drop 5 pounds a week!” and pill names like Slim Sense – away from young people, particularly girls, since some research has linked some products to eating disorders. A study in the American Journal of Public Health, which followed more than 10,000 women aged 14-36 over 15 years, found that “those who used diet pills had more than 5 times higher adjusted odds of receiving an eating disorder diagnosis from a health care provider within 1-3 years than those who did not.”
Many pills have been found tainted with banned and dangerous ingredients that may cause cancer, heart attacks, strokes, and other ailments. For example, the FDA advised the public to avoid Slim Sense by Dr. Reade because it contains lorcaserin, which has been found to cause psychiatric disturbances and impairments in attention or memory. The FDA ordered it discontinued and the company couldn’t be reached for comment.
“Unscrupulous manufacturers are willing to take risks with consumers’ health – and they are lacing their products with illegal pharmaceuticals, banned pharmaceuticals, steroids, excessive stimulants, even experimental stimulants,” said S. Bryn Austin, ScD, founding director of the Strategic Training Initiative for the Prevention of Eating Disorders, or STRIPED, which supports the restrictions. “Consumers have no idea that this is what’s in these types of products.”
STRIPED is a public health initiative based at the Harvard School of Public Health, Boston, and Boston Children’s Hospital.
An industry trade group, the Natural Products Association, disputes that diet pills cause eating disorders, citing the lack of consumer complaints to the FDA of adverse events from their members’ products. “According to FDA data, there is no association between the two,” said Kyle Turk, the association’s director of government affairs.
The association contends that its members adhere to safe manufacturing processes, random product testing, and appropriate marketing guidelines. Representatives also worry that if minors can’t buy supplements over the counter, they may buy them from “crooks” on the black market and undermine the integrity of the industry. Under the bills, minors purchasing weight-loss products must show identification along with a prescription.
Not all business groups oppose the ban. The American Herbal Products Association, a trade group representing dietary supplement manufacturers and retailers, dropped its opposition to California’s bill once it was amended to remove ingredient categories that are found in non-diet supplements and vitamins, according to Robert Marriott, director of regulatory affairs.
Children’s advocates have found worrisome trends among young people who envision their ideal body type based on what they see on social media. According to a study commissioned by Fairplay, a nonprofit that seeks to stop harmful marketing practices targeting children, kids as young as 9 were found to be following three or more eating disorder accounts on Instagram, while the median age was 19. The authors called it a “pro–eating disorder bubble.”
Meta, which owns Instagram and Facebook, said the report lacks nuance, such as recognizing the human need to share life’s difficult moments. The company argues that blanket censorship isn’t the answer. “Experts and safety organizations have told us it’s important to strike a balance and allow people to share their personal stories while removing any content that encourages or promotes eating disorders,” Liza Crenshaw, a Meta spokesperson, said in an email.
Jason Nagata, MD, a pediatrician who cares for children and young adults with life-threatening eating disorders, believes that easy access to diet pills contributes to his patients’ conditions at UCSF Benioff Children’s Hospital in San Francisco. That was the case for one of his patients, an emaciated 11-year-old girl.
“She had basically entered a starvation state because she was not getting enough nutrition,” said Dr. Nagata, who provided supporting testimony for the California bill. “She was taking these pills and using other kinds of extreme behaviors to lose weight.”
Dr. Nagata said the number of patients he sees with eating disorders has tripled since the pandemic began. They are desperate to get diet pills, some with modest results. “We’ve had patients who have been so dependent on these products that they will be hospitalized and they’re still ordering these products on Amazon,” he said.
Public health advocates turned to state legislatures in response to the federal government’s limited authority to regulate diet pills. Under a 1994 federal law known as the Dietary Supplement Health and Education Act, the FDA “cannot step in until after there is a clear issue of harm to consumers,” said Dr. Austin.
No match for the supplement industry’s heavy lobbying on Capitol Hill, public health advocates shifted to a state-by-state approach.
There is, however, a push for the FDA to improve oversight of what goes into diet pills. Sen. Dick Durbin (D-Ill.) in April introduced a bill that would require dietary supplement manufacturers to register their products – along with the ingredients – with the regulator.
Proponents say the change is needed because manufacturers have been known to include dangerous ingredients. C. Michael White, PharmD, of the University of Connecticut, Storrs, found 35% of tainted health products came from weight-loss supplements in a review of a health fraud database.
A few ingredients have been banned, including sibutramine, a stimulant. “It was a very commonly used weight-loss supplement that ended up being removed from the U.S. market because of its elevated risk of causing things like heart attacks, strokes, and arrhythmias,” Dr. White said.
Another ingredient was phenolphthalein, which was used in laxatives until it was identified as a suspected carcinogen and banned in 1999. “To think,” he said, “that that product would still be on the U.S. market is just unconscionable.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
California and New York are on the cusp of going further than the Food and Drug Administration in restricting the sale of nonprescription diet pills to minors as pediatricians and public health advocates try to protect kids from extreme weight-loss gimmicks online.
A bill before Gov. Gavin Newsom would bar anyone under 18 in California from buying over-the-counter weight-loss supplements – whether online or in shops – without a prescription. A similar bill passed by New York lawmakers is on Gov. Kathy Hochul’s desk. Neither Democrat has indicated how he or she will act.
If both bills are signed into law, proponents hope the momentum will build to restrict diet pill sales to children in more states. Massachusetts, New Jersey, and Missouri have introduced similar bills and backers plan to continue their push next year.
Nearly 30 million people in the United States will have an eating disorder in their lifetime; 95% of them are aged between 12 and 25, according to Johns Hopkins All Children’s Hospital. The hospital added that eating disorders pose the highest risk of mortality of any mental health disorder. And it has become easier than ever for minors to get pills that are sold online or on drugstore shelves. All dietary supplements, which include those for weight loss, accounted for nearly 35% of the $63 billion over-the-counter health products industry in 2021, according to Vision Research Reports, a market research firm.
Dietary supplements, which encompass a broad range of vitamins, herbs, and minerals, are classified by the FDA as food and don’t undergo scientific and safety testing as prescription drugs and over-the-counter medicines do.
Public health advocates want to keep weight-loss products – with ads that may promise to “Drop 5 pounds a week!” and pill names like Slim Sense – away from young people, particularly girls, since some research has linked some products to eating disorders. A study in the American Journal of Public Health, which followed more than 10,000 women aged 14-36 over 15 years, found that “those who used diet pills had more than 5 times higher adjusted odds of receiving an eating disorder diagnosis from a health care provider within 1-3 years than those who did not.”
Many pills have been found tainted with banned and dangerous ingredients that may cause cancer, heart attacks, strokes, and other ailments. For example, the FDA advised the public to avoid Slim Sense by Dr. Reade because it contains lorcaserin, which has been found to cause psychiatric disturbances and impairments in attention or memory. The FDA ordered it discontinued and the company couldn’t be reached for comment.
“Unscrupulous manufacturers are willing to take risks with consumers’ health – and they are lacing their products with illegal pharmaceuticals, banned pharmaceuticals, steroids, excessive stimulants, even experimental stimulants,” said S. Bryn Austin, ScD, founding director of the Strategic Training Initiative for the Prevention of Eating Disorders, or STRIPED, which supports the restrictions. “Consumers have no idea that this is what’s in these types of products.”
STRIPED is a public health initiative based at the Harvard School of Public Health, Boston, and Boston Children’s Hospital.
An industry trade group, the Natural Products Association, disputes that diet pills cause eating disorders, citing the lack of consumer complaints to the FDA of adverse events from their members’ products. “According to FDA data, there is no association between the two,” said Kyle Turk, the association’s director of government affairs.
The association contends that its members adhere to safe manufacturing processes, random product testing, and appropriate marketing guidelines. Representatives also worry that if minors can’t buy supplements over the counter, they may buy them from “crooks” on the black market and undermine the integrity of the industry. Under the bills, minors purchasing weight-loss products must show identification along with a prescription.
Not all business groups oppose the ban. The American Herbal Products Association, a trade group representing dietary supplement manufacturers and retailers, dropped its opposition to California’s bill once it was amended to remove ingredient categories that are found in non-diet supplements and vitamins, according to Robert Marriott, director of regulatory affairs.
Children’s advocates have found worrisome trends among young people who envision their ideal body type based on what they see on social media. According to a study commissioned by Fairplay, a nonprofit that seeks to stop harmful marketing practices targeting children, kids as young as 9 were found to be following three or more eating disorder accounts on Instagram, while the median age was 19. The authors called it a “pro–eating disorder bubble.”
Meta, which owns Instagram and Facebook, said the report lacks nuance, such as recognizing the human need to share life’s difficult moments. The company argues that blanket censorship isn’t the answer. “Experts and safety organizations have told us it’s important to strike a balance and allow people to share their personal stories while removing any content that encourages or promotes eating disorders,” Liza Crenshaw, a Meta spokesperson, said in an email.
Jason Nagata, MD, a pediatrician who cares for children and young adults with life-threatening eating disorders, believes that easy access to diet pills contributes to his patients’ conditions at UCSF Benioff Children’s Hospital in San Francisco. That was the case for one of his patients, an emaciated 11-year-old girl.
“She had basically entered a starvation state because she was not getting enough nutrition,” said Dr. Nagata, who provided supporting testimony for the California bill. “She was taking these pills and using other kinds of extreme behaviors to lose weight.”
Dr. Nagata said the number of patients he sees with eating disorders has tripled since the pandemic began. They are desperate to get diet pills, some with modest results. “We’ve had patients who have been so dependent on these products that they will be hospitalized and they’re still ordering these products on Amazon,” he said.
Public health advocates turned to state legislatures in response to the federal government’s limited authority to regulate diet pills. Under a 1994 federal law known as the Dietary Supplement Health and Education Act, the FDA “cannot step in until after there is a clear issue of harm to consumers,” said Dr. Austin.
No match for the supplement industry’s heavy lobbying on Capitol Hill, public health advocates shifted to a state-by-state approach.
There is, however, a push for the FDA to improve oversight of what goes into diet pills. Sen. Dick Durbin (D-Ill.) in April introduced a bill that would require dietary supplement manufacturers to register their products – along with the ingredients – with the regulator.
Proponents say the change is needed because manufacturers have been known to include dangerous ingredients. C. Michael White, PharmD, of the University of Connecticut, Storrs, found 35% of tainted health products came from weight-loss supplements in a review of a health fraud database.
A few ingredients have been banned, including sibutramine, a stimulant. “It was a very commonly used weight-loss supplement that ended up being removed from the U.S. market because of its elevated risk of causing things like heart attacks, strokes, and arrhythmias,” Dr. White said.
Another ingredient was phenolphthalein, which was used in laxatives until it was identified as a suspected carcinogen and banned in 1999. “To think,” he said, “that that product would still be on the U.S. market is just unconscionable.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
California and New York are on the cusp of going further than the Food and Drug Administration in restricting the sale of nonprescription diet pills to minors as pediatricians and public health advocates try to protect kids from extreme weight-loss gimmicks online.
A bill before Gov. Gavin Newsom would bar anyone under 18 in California from buying over-the-counter weight-loss supplements – whether online or in shops – without a prescription. A similar bill passed by New York lawmakers is on Gov. Kathy Hochul’s desk. Neither Democrat has indicated how he or she will act.
If both bills are signed into law, proponents hope the momentum will build to restrict diet pill sales to children in more states. Massachusetts, New Jersey, and Missouri have introduced similar bills and backers plan to continue their push next year.
Nearly 30 million people in the United States will have an eating disorder in their lifetime; 95% of them are aged between 12 and 25, according to Johns Hopkins All Children’s Hospital. The hospital added that eating disorders pose the highest risk of mortality of any mental health disorder. And it has become easier than ever for minors to get pills that are sold online or on drugstore shelves. All dietary supplements, which include those for weight loss, accounted for nearly 35% of the $63 billion over-the-counter health products industry in 2021, according to Vision Research Reports, a market research firm.
Dietary supplements, which encompass a broad range of vitamins, herbs, and minerals, are classified by the FDA as food and don’t undergo scientific and safety testing as prescription drugs and over-the-counter medicines do.
Public health advocates want to keep weight-loss products – with ads that may promise to “Drop 5 pounds a week!” and pill names like Slim Sense – away from young people, particularly girls, since some research has linked some products to eating disorders. A study in the American Journal of Public Health, which followed more than 10,000 women aged 14-36 over 15 years, found that “those who used diet pills had more than 5 times higher adjusted odds of receiving an eating disorder diagnosis from a health care provider within 1-3 years than those who did not.”
Many pills have been found tainted with banned and dangerous ingredients that may cause cancer, heart attacks, strokes, and other ailments. For example, the FDA advised the public to avoid Slim Sense by Dr. Reade because it contains lorcaserin, which has been found to cause psychiatric disturbances and impairments in attention or memory. The FDA ordered it discontinued and the company couldn’t be reached for comment.
“Unscrupulous manufacturers are willing to take risks with consumers’ health – and they are lacing their products with illegal pharmaceuticals, banned pharmaceuticals, steroids, excessive stimulants, even experimental stimulants,” said S. Bryn Austin, ScD, founding director of the Strategic Training Initiative for the Prevention of Eating Disorders, or STRIPED, which supports the restrictions. “Consumers have no idea that this is what’s in these types of products.”
STRIPED is a public health initiative based at the Harvard School of Public Health, Boston, and Boston Children’s Hospital.
An industry trade group, the Natural Products Association, disputes that diet pills cause eating disorders, citing the lack of consumer complaints to the FDA of adverse events from their members’ products. “According to FDA data, there is no association between the two,” said Kyle Turk, the association’s director of government affairs.
The association contends that its members adhere to safe manufacturing processes, random product testing, and appropriate marketing guidelines. Representatives also worry that if minors can’t buy supplements over the counter, they may buy them from “crooks” on the black market and undermine the integrity of the industry. Under the bills, minors purchasing weight-loss products must show identification along with a prescription.
Not all business groups oppose the ban. The American Herbal Products Association, a trade group representing dietary supplement manufacturers and retailers, dropped its opposition to California’s bill once it was amended to remove ingredient categories that are found in non-diet supplements and vitamins, according to Robert Marriott, director of regulatory affairs.
Children’s advocates have found worrisome trends among young people who envision their ideal body type based on what they see on social media. According to a study commissioned by Fairplay, a nonprofit that seeks to stop harmful marketing practices targeting children, kids as young as 9 were found to be following three or more eating disorder accounts on Instagram, while the median age was 19. The authors called it a “pro–eating disorder bubble.”
Meta, which owns Instagram and Facebook, said the report lacks nuance, such as recognizing the human need to share life’s difficult moments. The company argues that blanket censorship isn’t the answer. “Experts and safety organizations have told us it’s important to strike a balance and allow people to share their personal stories while removing any content that encourages or promotes eating disorders,” Liza Crenshaw, a Meta spokesperson, said in an email.
Jason Nagata, MD, a pediatrician who cares for children and young adults with life-threatening eating disorders, believes that easy access to diet pills contributes to his patients’ conditions at UCSF Benioff Children’s Hospital in San Francisco. That was the case for one of his patients, an emaciated 11-year-old girl.
“She had basically entered a starvation state because she was not getting enough nutrition,” said Dr. Nagata, who provided supporting testimony for the California bill. “She was taking these pills and using other kinds of extreme behaviors to lose weight.”
Dr. Nagata said the number of patients he sees with eating disorders has tripled since the pandemic began. They are desperate to get diet pills, some with modest results. “We’ve had patients who have been so dependent on these products that they will be hospitalized and they’re still ordering these products on Amazon,” he said.
Public health advocates turned to state legislatures in response to the federal government’s limited authority to regulate diet pills. Under a 1994 federal law known as the Dietary Supplement Health and Education Act, the FDA “cannot step in until after there is a clear issue of harm to consumers,” said Dr. Austin.
No match for the supplement industry’s heavy lobbying on Capitol Hill, public health advocates shifted to a state-by-state approach.
There is, however, a push for the FDA to improve oversight of what goes into diet pills. Sen. Dick Durbin (D-Ill.) in April introduced a bill that would require dietary supplement manufacturers to register their products – along with the ingredients – with the regulator.
Proponents say the change is needed because manufacturers have been known to include dangerous ingredients. C. Michael White, PharmD, of the University of Connecticut, Storrs, found 35% of tainted health products came from weight-loss supplements in a review of a health fraud database.
A few ingredients have been banned, including sibutramine, a stimulant. “It was a very commonly used weight-loss supplement that ended up being removed from the U.S. market because of its elevated risk of causing things like heart attacks, strokes, and arrhythmias,” Dr. White said.
Another ingredient was phenolphthalein, which was used in laxatives until it was identified as a suspected carcinogen and banned in 1999. “To think,” he said, “that that product would still be on the U.S. market is just unconscionable.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Cumulative blood pressure load: A better predictor of CV events?
Cumulative systolic blood pressure load, which can be calculated from serial blood pressure measurements, may provide better prediction of major cardiovascular events, compared with traditional blood pressure measures, a new study suggests.
“Our results suggest that cumulative blood pressure load is an independent predictor of cardiovascular events and should be used in future cardiovascular risk prediction algorithms,” the authors, led by Nelson Wang, MD, George Institute for Global Health, Sydney, conclude.
The study was published online in the Journal of the American College of Cardiology.
The researchers explain that the management of hypertension has traditionally centered around blood pressure measurements taken at a single timepoint, with adequate control defined as those measurements being below a predefined target threshold.
However, this approach fails to recognize blood pressure as a continuous measure that fluctuates over time and does not acknowledge that the most recently recorded measurement may not reflect previous blood pressure control.
More recently, studies have defined the time a patient spends below blood pressure target, or TIme at TaRgEt (TITRE), as a novel marker of cardiovascular risk that is independent of mean blood pressure.
Although TITRE has the added advantage of incorporating duration of control, it is unable to characterize the magnitude of blood pressure elevation, the researchers note.
They point out that an optimal measure as a risk factor for cardiovascular disease would account for both the magnitude and duration of elevated blood pressure.
Such a measure is cumulative blood pressure load, defined as the area under the curve (AUC) expressed in units of mm Hg by time.
The only prior study of this measure was small and retrospective and calculated cumulative blood pressure load from ambulatory blood pressure monitoring estimated over a short (24-hour) period.
Therefore, the aim of the current study was to estimate the association between cumulative systolic blood pressure load over a longer period (24 months) and subsequent major cardiovascular events.
To do this, the researchers conducted a post-hoc analysis of 9,338 patients with type 2 diabetes in the ADVANCE-ON study.
Cumulative systolic blood pressure load was defined as the AUC for systolic blood pressure values above 130 mm Hg divided by the AUC for all measured systolic blood pressure values over a 24-month exposure period.
Over a median 7.6 years of follow-up, 1,469 major cardiovascular events, 1,615 deaths, and 660 cardiovascular deaths occurred.
Results showed that each one standard deviation increase in cumulative systolic blood pressure load was associated with a 14% increase in major cardiovascular events, a 13% increase in all-cause mortality, and a 21% increase in cardiovascular death.
Cumulative systolic blood pressure load outperformed mean systolic blood pressure, time-below-target, and visit-to-visit systolic blood pressure variability for the prediction of cardiovascular events and death and also discriminated risk and reclassified more patients’ risk correctly than the other measures.
“Small improvements in risk prediction can have a major impact when scaled up across large high-risk populations. Furthermore, cumulative systolic pressure load may also prove useful to inform the design of future clinical trials,” the researchers say.
Although the present study only assessed cumulative systolic blood pressure load over 24 months, clinicians should recognize the importance of this measure over a lifetime, they note.
“This approach emphasizes the importance of early blood pressure–lowering interventions to reduce the cumulative systolic blood pressure load that each individual experiences over their lifetime,” they conclude.
The researchers suggest that, based on these results, cumulative systolic blood pressure load and visit-to-visit systolic blood pressure variability “should be used in conjunction in future cardiovascular risk prediction algorithms.”
In an accompanying editorial, Donald Lloyd-Jones, MD, Northwestern Feinberg School of Medicine, Chicago, says that before routinely adopting these new measures, several additional questions need to be addressed.
He notes that many patients in the current study already had cardiovascular disease, and it is not known whether the benefit was consistent among those with and without cardiovascular disease. In addition, longer term data using blood pressure measurements in the real-world clinical setting would be desirable, as well as information on whether these new measures add incremental value to existing risk prediction equations.
“Certainly, the next guidelines should reconsider all types of blood pressure measures, and other potential predictors, to optimize risk estimation and identification of patients with greatest net benefit from risk-reducing therapies,” Dr. Lloyd-Jones comments.
“Ultimately, clinicians should leverage as much information on their patients as possible to understand their blood pressure–related cardiovascular risk, to identify those who may be more likely have occult or emerging subclinical target organ damage, and to identify those who may have particular net benefit from earlier or more intensive treatment,” he concludes.
“These opportunities are more readily available with integration of data that allow for visualization of longer-term blood pressure patterns and incorporation of home monitoring and ambulatory monitoring data to monitor out-of-office blood pressure levels and control.”
A version of this article first appeared on Medscape.com.
Cumulative systolic blood pressure load, which can be calculated from serial blood pressure measurements, may provide better prediction of major cardiovascular events, compared with traditional blood pressure measures, a new study suggests.
“Our results suggest that cumulative blood pressure load is an independent predictor of cardiovascular events and should be used in future cardiovascular risk prediction algorithms,” the authors, led by Nelson Wang, MD, George Institute for Global Health, Sydney, conclude.
The study was published online in the Journal of the American College of Cardiology.
The researchers explain that the management of hypertension has traditionally centered around blood pressure measurements taken at a single timepoint, with adequate control defined as those measurements being below a predefined target threshold.
However, this approach fails to recognize blood pressure as a continuous measure that fluctuates over time and does not acknowledge that the most recently recorded measurement may not reflect previous blood pressure control.
More recently, studies have defined the time a patient spends below blood pressure target, or TIme at TaRgEt (TITRE), as a novel marker of cardiovascular risk that is independent of mean blood pressure.
Although TITRE has the added advantage of incorporating duration of control, it is unable to characterize the magnitude of blood pressure elevation, the researchers note.
They point out that an optimal measure as a risk factor for cardiovascular disease would account for both the magnitude and duration of elevated blood pressure.
Such a measure is cumulative blood pressure load, defined as the area under the curve (AUC) expressed in units of mm Hg by time.
The only prior study of this measure was small and retrospective and calculated cumulative blood pressure load from ambulatory blood pressure monitoring estimated over a short (24-hour) period.
Therefore, the aim of the current study was to estimate the association between cumulative systolic blood pressure load over a longer period (24 months) and subsequent major cardiovascular events.
To do this, the researchers conducted a post-hoc analysis of 9,338 patients with type 2 diabetes in the ADVANCE-ON study.
Cumulative systolic blood pressure load was defined as the AUC for systolic blood pressure values above 130 mm Hg divided by the AUC for all measured systolic blood pressure values over a 24-month exposure period.
Over a median 7.6 years of follow-up, 1,469 major cardiovascular events, 1,615 deaths, and 660 cardiovascular deaths occurred.
Results showed that each one standard deviation increase in cumulative systolic blood pressure load was associated with a 14% increase in major cardiovascular events, a 13% increase in all-cause mortality, and a 21% increase in cardiovascular death.
Cumulative systolic blood pressure load outperformed mean systolic blood pressure, time-below-target, and visit-to-visit systolic blood pressure variability for the prediction of cardiovascular events and death and also discriminated risk and reclassified more patients’ risk correctly than the other measures.
“Small improvements in risk prediction can have a major impact when scaled up across large high-risk populations. Furthermore, cumulative systolic pressure load may also prove useful to inform the design of future clinical trials,” the researchers say.
Although the present study only assessed cumulative systolic blood pressure load over 24 months, clinicians should recognize the importance of this measure over a lifetime, they note.
“This approach emphasizes the importance of early blood pressure–lowering interventions to reduce the cumulative systolic blood pressure load that each individual experiences over their lifetime,” they conclude.
The researchers suggest that, based on these results, cumulative systolic blood pressure load and visit-to-visit systolic blood pressure variability “should be used in conjunction in future cardiovascular risk prediction algorithms.”
In an accompanying editorial, Donald Lloyd-Jones, MD, Northwestern Feinberg School of Medicine, Chicago, says that before routinely adopting these new measures, several additional questions need to be addressed.
He notes that many patients in the current study already had cardiovascular disease, and it is not known whether the benefit was consistent among those with and without cardiovascular disease. In addition, longer term data using blood pressure measurements in the real-world clinical setting would be desirable, as well as information on whether these new measures add incremental value to existing risk prediction equations.
“Certainly, the next guidelines should reconsider all types of blood pressure measures, and other potential predictors, to optimize risk estimation and identification of patients with greatest net benefit from risk-reducing therapies,” Dr. Lloyd-Jones comments.
“Ultimately, clinicians should leverage as much information on their patients as possible to understand their blood pressure–related cardiovascular risk, to identify those who may be more likely have occult or emerging subclinical target organ damage, and to identify those who may have particular net benefit from earlier or more intensive treatment,” he concludes.
“These opportunities are more readily available with integration of data that allow for visualization of longer-term blood pressure patterns and incorporation of home monitoring and ambulatory monitoring data to monitor out-of-office blood pressure levels and control.”
A version of this article first appeared on Medscape.com.
Cumulative systolic blood pressure load, which can be calculated from serial blood pressure measurements, may provide better prediction of major cardiovascular events, compared with traditional blood pressure measures, a new study suggests.
“Our results suggest that cumulative blood pressure load is an independent predictor of cardiovascular events and should be used in future cardiovascular risk prediction algorithms,” the authors, led by Nelson Wang, MD, George Institute for Global Health, Sydney, conclude.
The study was published online in the Journal of the American College of Cardiology.
The researchers explain that the management of hypertension has traditionally centered around blood pressure measurements taken at a single timepoint, with adequate control defined as those measurements being below a predefined target threshold.
However, this approach fails to recognize blood pressure as a continuous measure that fluctuates over time and does not acknowledge that the most recently recorded measurement may not reflect previous blood pressure control.
More recently, studies have defined the time a patient spends below blood pressure target, or TIme at TaRgEt (TITRE), as a novel marker of cardiovascular risk that is independent of mean blood pressure.
Although TITRE has the added advantage of incorporating duration of control, it is unable to characterize the magnitude of blood pressure elevation, the researchers note.
They point out that an optimal measure as a risk factor for cardiovascular disease would account for both the magnitude and duration of elevated blood pressure.
Such a measure is cumulative blood pressure load, defined as the area under the curve (AUC) expressed in units of mm Hg by time.
The only prior study of this measure was small and retrospective and calculated cumulative blood pressure load from ambulatory blood pressure monitoring estimated over a short (24-hour) period.
Therefore, the aim of the current study was to estimate the association between cumulative systolic blood pressure load over a longer period (24 months) and subsequent major cardiovascular events.
To do this, the researchers conducted a post-hoc analysis of 9,338 patients with type 2 diabetes in the ADVANCE-ON study.
Cumulative systolic blood pressure load was defined as the AUC for systolic blood pressure values above 130 mm Hg divided by the AUC for all measured systolic blood pressure values over a 24-month exposure period.
Over a median 7.6 years of follow-up, 1,469 major cardiovascular events, 1,615 deaths, and 660 cardiovascular deaths occurred.
Results showed that each one standard deviation increase in cumulative systolic blood pressure load was associated with a 14% increase in major cardiovascular events, a 13% increase in all-cause mortality, and a 21% increase in cardiovascular death.
Cumulative systolic blood pressure load outperformed mean systolic blood pressure, time-below-target, and visit-to-visit systolic blood pressure variability for the prediction of cardiovascular events and death and also discriminated risk and reclassified more patients’ risk correctly than the other measures.
“Small improvements in risk prediction can have a major impact when scaled up across large high-risk populations. Furthermore, cumulative systolic pressure load may also prove useful to inform the design of future clinical trials,” the researchers say.
Although the present study only assessed cumulative systolic blood pressure load over 24 months, clinicians should recognize the importance of this measure over a lifetime, they note.
“This approach emphasizes the importance of early blood pressure–lowering interventions to reduce the cumulative systolic blood pressure load that each individual experiences over their lifetime,” they conclude.
The researchers suggest that, based on these results, cumulative systolic blood pressure load and visit-to-visit systolic blood pressure variability “should be used in conjunction in future cardiovascular risk prediction algorithms.”
In an accompanying editorial, Donald Lloyd-Jones, MD, Northwestern Feinberg School of Medicine, Chicago, says that before routinely adopting these new measures, several additional questions need to be addressed.
He notes that many patients in the current study already had cardiovascular disease, and it is not known whether the benefit was consistent among those with and without cardiovascular disease. In addition, longer term data using blood pressure measurements in the real-world clinical setting would be desirable, as well as information on whether these new measures add incremental value to existing risk prediction equations.
“Certainly, the next guidelines should reconsider all types of blood pressure measures, and other potential predictors, to optimize risk estimation and identification of patients with greatest net benefit from risk-reducing therapies,” Dr. Lloyd-Jones comments.
“Ultimately, clinicians should leverage as much information on their patients as possible to understand their blood pressure–related cardiovascular risk, to identify those who may be more likely have occult or emerging subclinical target organ damage, and to identify those who may have particular net benefit from earlier or more intensive treatment,” he concludes.
“These opportunities are more readily available with integration of data that allow for visualization of longer-term blood pressure patterns and incorporation of home monitoring and ambulatory monitoring data to monitor out-of-office blood pressure levels and control.”
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Should patients stand for office BP readings?
a new study suggests.
Combining three standing and three seated BP measurements in the same visit may lead to a “quicker diagnosis and save people a trip back to the office,” Wanpen Vongpatanasin, MD, professor of internal medicine and director of the hypertension section, cardiology division, UT Southwestern Medical Center, Dallas, said in an interview.
The study was presented at the Hypertension Scientific Sessions, sponsored by the American Heart Association.
Practice changing?
Clinical guidelines recommend office BP be taken in a seated position for most patients.
However, research has suggested that the sensitivity of seated office BP in diagnosing hypertension is about 50%, with high specificity around 90% during a single visit, Dr. Vongpatanasin explained.
At the follow-up visit, however, the second office BP yielded higher sensitivity to 80% but specificity fell to 55%. Nevertheless, the accuracy of standing BP measurements for diagnosing hypertension has not been investigated.
In a cross-sectional study, Dr. Vongpatanasin and colleagues determined the accuracy of both seated and standing BP for diagnosing hypertension in a single visit in 125 healthy adults who had not had a previous diagnosis of hypertension and were not taking any BP medications. The cohort had a mean age of 49 years, 62% were women, and 24% were Black.
During each office visit, seated BP was measured three times, then standing BP was measured three times using an automated and validated device.
Average seated BP was 123/76 mm Hg and average standing BP was 126/80 mm Hg.
Of the 125 participants, 42 (34%) had hypertension, defined as 24-hour ambulatory systolic/diastolic BP (SBP/DBP) of ≥ 125/75 mm Hg.
The sensitivity and specificity of seated SBP for hypertension was 43% and 92%, respectively.
“Interestingly, with standing SBP, sensitivity was improved to 74% and specificity dropped to 65% – which is okay; you will have to confirm a positive test anyway and when screening for a common disease you’d rather have a high sensitivity rather than low sensitivity to pick it up in this case,” Dr. Vongpatanasin said.
The area under receiver operating characteristic curve (AUROC) of standing SBP was significantly higher than seated SBP (Bayes factor [BF] = 11.8) when hypertension was defined as 24-hour SBP ≥ 125 mm Hg.
Similarly, when hypertension was defined as 24-hour DBP ≥ 75 mm Hg or daytime DBP ≥ 80 mm Hg, the AUROC of standing DBP was higher than seated DBP (all BF > 3).
The addition of standing to seated BP improved detection of hypertension compared with seated BP alone based on 24-hour SBP/DBP ≥ 125/75 mm Hg or daytime SBP/DBP ≥ 130/80 mm Hg (all BF > 3).
“In our hypertension clinic, we always measure both seated and standing BP in all of our patients,” John Giacona, PA-C, a PhD candidate at UT Southwestern Medical Center and coauthor of the study, told this news organization,
Multiple readings most important
Reached for comment, Johanna Contreras, MD, a cardiologist at Mount Sinai Hospital in New York, noted that diagnosing hypertension is “difficult” and she agrees that multiple readings are important.
“I usually take at least two readings in two different visits before I tell the patient they have high blood pressure,” Dr. Contreras said in an interview.
Dr. Contreras said she takes blood pressure both seated and standing.
“I’m not sure standing versus seated makes a big difference. However, when the patient first comes into the office, it is really important to let them rest and calm down before taking the blood pressure,” she said.
The study had no commercial funding. The authors and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new study suggests.
Combining three standing and three seated BP measurements in the same visit may lead to a “quicker diagnosis and save people a trip back to the office,” Wanpen Vongpatanasin, MD, professor of internal medicine and director of the hypertension section, cardiology division, UT Southwestern Medical Center, Dallas, said in an interview.
The study was presented at the Hypertension Scientific Sessions, sponsored by the American Heart Association.
Practice changing?
Clinical guidelines recommend office BP be taken in a seated position for most patients.
However, research has suggested that the sensitivity of seated office BP in diagnosing hypertension is about 50%, with high specificity around 90% during a single visit, Dr. Vongpatanasin explained.
At the follow-up visit, however, the second office BP yielded higher sensitivity to 80% but specificity fell to 55%. Nevertheless, the accuracy of standing BP measurements for diagnosing hypertension has not been investigated.
In a cross-sectional study, Dr. Vongpatanasin and colleagues determined the accuracy of both seated and standing BP for diagnosing hypertension in a single visit in 125 healthy adults who had not had a previous diagnosis of hypertension and were not taking any BP medications. The cohort had a mean age of 49 years, 62% were women, and 24% were Black.
During each office visit, seated BP was measured three times, then standing BP was measured three times using an automated and validated device.
Average seated BP was 123/76 mm Hg and average standing BP was 126/80 mm Hg.
Of the 125 participants, 42 (34%) had hypertension, defined as 24-hour ambulatory systolic/diastolic BP (SBP/DBP) of ≥ 125/75 mm Hg.
The sensitivity and specificity of seated SBP for hypertension was 43% and 92%, respectively.
“Interestingly, with standing SBP, sensitivity was improved to 74% and specificity dropped to 65% – which is okay; you will have to confirm a positive test anyway and when screening for a common disease you’d rather have a high sensitivity rather than low sensitivity to pick it up in this case,” Dr. Vongpatanasin said.
The area under receiver operating characteristic curve (AUROC) of standing SBP was significantly higher than seated SBP (Bayes factor [BF] = 11.8) when hypertension was defined as 24-hour SBP ≥ 125 mm Hg.
Similarly, when hypertension was defined as 24-hour DBP ≥ 75 mm Hg or daytime DBP ≥ 80 mm Hg, the AUROC of standing DBP was higher than seated DBP (all BF > 3).
The addition of standing to seated BP improved detection of hypertension compared with seated BP alone based on 24-hour SBP/DBP ≥ 125/75 mm Hg or daytime SBP/DBP ≥ 130/80 mm Hg (all BF > 3).
“In our hypertension clinic, we always measure both seated and standing BP in all of our patients,” John Giacona, PA-C, a PhD candidate at UT Southwestern Medical Center and coauthor of the study, told this news organization,
Multiple readings most important
Reached for comment, Johanna Contreras, MD, a cardiologist at Mount Sinai Hospital in New York, noted that diagnosing hypertension is “difficult” and she agrees that multiple readings are important.
“I usually take at least two readings in two different visits before I tell the patient they have high blood pressure,” Dr. Contreras said in an interview.
Dr. Contreras said she takes blood pressure both seated and standing.
“I’m not sure standing versus seated makes a big difference. However, when the patient first comes into the office, it is really important to let them rest and calm down before taking the blood pressure,” she said.
The study had no commercial funding. The authors and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new study suggests.
Combining three standing and three seated BP measurements in the same visit may lead to a “quicker diagnosis and save people a trip back to the office,” Wanpen Vongpatanasin, MD, professor of internal medicine and director of the hypertension section, cardiology division, UT Southwestern Medical Center, Dallas, said in an interview.
The study was presented at the Hypertension Scientific Sessions, sponsored by the American Heart Association.
Practice changing?
Clinical guidelines recommend office BP be taken in a seated position for most patients.
However, research has suggested that the sensitivity of seated office BP in diagnosing hypertension is about 50%, with high specificity around 90% during a single visit, Dr. Vongpatanasin explained.
At the follow-up visit, however, the second office BP yielded higher sensitivity to 80% but specificity fell to 55%. Nevertheless, the accuracy of standing BP measurements for diagnosing hypertension has not been investigated.
In a cross-sectional study, Dr. Vongpatanasin and colleagues determined the accuracy of both seated and standing BP for diagnosing hypertension in a single visit in 125 healthy adults who had not had a previous diagnosis of hypertension and were not taking any BP medications. The cohort had a mean age of 49 years, 62% were women, and 24% were Black.
During each office visit, seated BP was measured three times, then standing BP was measured three times using an automated and validated device.
Average seated BP was 123/76 mm Hg and average standing BP was 126/80 mm Hg.
Of the 125 participants, 42 (34%) had hypertension, defined as 24-hour ambulatory systolic/diastolic BP (SBP/DBP) of ≥ 125/75 mm Hg.
The sensitivity and specificity of seated SBP for hypertension was 43% and 92%, respectively.
“Interestingly, with standing SBP, sensitivity was improved to 74% and specificity dropped to 65% – which is okay; you will have to confirm a positive test anyway and when screening for a common disease you’d rather have a high sensitivity rather than low sensitivity to pick it up in this case,” Dr. Vongpatanasin said.
The area under receiver operating characteristic curve (AUROC) of standing SBP was significantly higher than seated SBP (Bayes factor [BF] = 11.8) when hypertension was defined as 24-hour SBP ≥ 125 mm Hg.
Similarly, when hypertension was defined as 24-hour DBP ≥ 75 mm Hg or daytime DBP ≥ 80 mm Hg, the AUROC of standing DBP was higher than seated DBP (all BF > 3).
The addition of standing to seated BP improved detection of hypertension compared with seated BP alone based on 24-hour SBP/DBP ≥ 125/75 mm Hg or daytime SBP/DBP ≥ 130/80 mm Hg (all BF > 3).
“In our hypertension clinic, we always measure both seated and standing BP in all of our patients,” John Giacona, PA-C, a PhD candidate at UT Southwestern Medical Center and coauthor of the study, told this news organization,
Multiple readings most important
Reached for comment, Johanna Contreras, MD, a cardiologist at Mount Sinai Hospital in New York, noted that diagnosing hypertension is “difficult” and she agrees that multiple readings are important.
“I usually take at least two readings in two different visits before I tell the patient they have high blood pressure,” Dr. Contreras said in an interview.
Dr. Contreras said she takes blood pressure both seated and standing.
“I’m not sure standing versus seated makes a big difference. However, when the patient first comes into the office, it is really important to let them rest and calm down before taking the blood pressure,” she said.
The study had no commercial funding. The authors and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION 2022
‘Dr. Caveman’ had a leg up on amputation
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Your poop may hold the secret to long life
Lots of things can disrupt your gut health over the years. A high-sugar diet, stress, antibiotics – all are linked to bad changes in the gut microbiome, the microbes that live in your intestinal tract. And this can raise the risk of diseases.
It could be possible, scientists say, by having people take a sample of their own stool when they are young to be put back into their colons when they are older.
While the science to back this up isn’t quite there yet, some researchers are saying we shouldn’t wait. They are calling on existing stool banks to let people start banking their stool now, so it’s there for them to use if the science becomes available.
But how would that work?
First, you’d go to a stool bank and provide a fresh sample of your poop, which would be screened for diseases, washed, processed, and deposited into a long-term storage facility.
Then, down the road, if you get a condition such as inflammatory bowel disease, heart disease, or type 2 diabetes – or if you have a procedure that wipes out your microbiome, like a course of antibiotics or chemotherapy – doctors could use your preserved stool to “re-colonize” your gut, restoring it to its earlier, healthier state, said Scott Weiss, MD, professor of medicine at Harvard Medical School, Boston, and a coauthor of a recent paper on the topic. They would do that using fecal microbiota transplantation, or FMT.
Timing is everything. You’d want a sample from when you’re healthy – say, between the ages of 18 and 35, or before a chronic condition is likely, said Dr. Weiss. But if you’re still healthy into your late 30s, 40s, or even 50s, providing a sample then could still benefit you later in life.
If we could pull off a banking system like this, it could have the potential to treat autoimmune disease, inflammatory bowel disease, diabetes, obesity, and heart disease – or even reverse the effects of aging. How can we make this happen?
Stool banks of today
While stool banks do exist today, the samples inside are destined not for the original donors but rather for sick patients hoping to treat an illness. Using FMT, doctors transfer the fecal material to the patient’s colon, restoring helpful gut microbiota.
Some research shows FMT may help treat inflammatory bowel diseases, such as Crohn’s or ulcerative colitis. Animal studies suggest it could help treat obesity, lengthen lifespan, and reverse some effects of aging, such as age-related decline in brain function. Other clinical trials are looking into its potential as a cancer treatment, said Dr. Weiss.
But outside the lab, FMT is mainly used for one purpose: to treat Clostridioides difficile infection. It works even better than antibiotics, research shows.
But first you need to find a healthy donor, and that’s harder than you might think.
Finding healthy stool samples
Banking our bodily substances is nothing new. Blood banks, for example, are common throughout the United States, and cord blood banking – preserving blood from a baby’s umbilical cord to aid possible future medical needs of the child – is becoming more popular. Sperm donors are highly sought after, and doctors regularly transplant kidneys and bone marrow to patients in need.
So why are we so particular about poop?
Part of the reason may be because feces (like blood, for that matter) can harbor disease – which is why it’s so important to find healthy stool donors. Problem is, this can be surprisingly hard to do.
To donate fecal matter, people must go through a rigorous screening process, said Majdi Osman, MD, chief medical officer for OpenBiome, a nonprofit microbiome research organization.
Until recently, OpenBiome operated a stool donation program, though it has since shifted its focus to research. Potential donors were screened for diseases and mental health conditions, pathogens, and antibiotic resistance. The pass rate was less than 3%.
“We take a very cautious approach because the association between diseases and the microbiome is still being understood,” Dr. Osman said.
FMT also carries risks – though so far, they seem mild. Side effects include mild diarrhea, nausea, belly pain, and fatigue. (The reason? Even the healthiest donor stool may not mix perfectly with your own.)
That’s where the idea of using your own stool comes in, said Yang-Yu Liu, PhD, a Harvard researcher who studies the microbiome and the lead author of the paper mentioned above. It’s not just more appealing but may also be a better “match” for your body.
Should you bank your stool?
While the researchers say we have reason to be optimistic about the future, it’s important to remember that many challenges remain. FMT is early in development, and there’s a lot about the microbiome we still don’t know.
There’s no guarantee, for example, that restoring a person’s microbiome to its formerly disease-free state will keep diseases at bay forever, said Dr. Weiss. If your genes raise your odds of having Crohn’s, for instance, it’s possible the disease could come back.
We also don’t know how long stool samples can be preserved, said Dr. Liu. Stool banks currently store fecal matter for 1 or 2 years, not decades. To protect the proteins and DNA structures for that long, samples would likely need to be stashed at the liquid nitrogen storage temperature of –196° C. (Currently, samples are stored at about –80° C.) Even then, testing would be needed to confirm if the fragile microorganisms in the stool can survive.
This raises another question: Who’s going to regulate all this?
The FDA regulates the use of FMT as a drug for the treatment of C. diff, but as Dr. Liu pointed out, many gastroenterologists consider the gut microbiota an organ. In that case, human fecal matter could be regulated the same way blood, bone, or even egg cells are.
Cord blood banking may be a helpful model, Dr. Liu said.
“We don’t have to start from scratch.”
Then there’s the question of cost. Cord blood banks could be a point of reference for that too, the researchers say. They charge about $1,500 to $2,820 for the first collection and processing, plus a yearly storage fee of $185 to $370.
Despite the unknowns, one thing is for sure: The interest in fecal banking is real – and growing. At least one microbiome firm, Cordlife Group Limited, based in Singapore, announced that it has started to allow people to bank their stool for future use.
“More people should talk about it and think about it,” said Dr. Liu.
A version of this article first appeared on WebMD.com.
Lots of things can disrupt your gut health over the years. A high-sugar diet, stress, antibiotics – all are linked to bad changes in the gut microbiome, the microbes that live in your intestinal tract. And this can raise the risk of diseases.
It could be possible, scientists say, by having people take a sample of their own stool when they are young to be put back into their colons when they are older.
While the science to back this up isn’t quite there yet, some researchers are saying we shouldn’t wait. They are calling on existing stool banks to let people start banking their stool now, so it’s there for them to use if the science becomes available.
But how would that work?
First, you’d go to a stool bank and provide a fresh sample of your poop, which would be screened for diseases, washed, processed, and deposited into a long-term storage facility.
Then, down the road, if you get a condition such as inflammatory bowel disease, heart disease, or type 2 diabetes – or if you have a procedure that wipes out your microbiome, like a course of antibiotics or chemotherapy – doctors could use your preserved stool to “re-colonize” your gut, restoring it to its earlier, healthier state, said Scott Weiss, MD, professor of medicine at Harvard Medical School, Boston, and a coauthor of a recent paper on the topic. They would do that using fecal microbiota transplantation, or FMT.
Timing is everything. You’d want a sample from when you’re healthy – say, between the ages of 18 and 35, or before a chronic condition is likely, said Dr. Weiss. But if you’re still healthy into your late 30s, 40s, or even 50s, providing a sample then could still benefit you later in life.
If we could pull off a banking system like this, it could have the potential to treat autoimmune disease, inflammatory bowel disease, diabetes, obesity, and heart disease – or even reverse the effects of aging. How can we make this happen?
Stool banks of today
While stool banks do exist today, the samples inside are destined not for the original donors but rather for sick patients hoping to treat an illness. Using FMT, doctors transfer the fecal material to the patient’s colon, restoring helpful gut microbiota.
Some research shows FMT may help treat inflammatory bowel diseases, such as Crohn’s or ulcerative colitis. Animal studies suggest it could help treat obesity, lengthen lifespan, and reverse some effects of aging, such as age-related decline in brain function. Other clinical trials are looking into its potential as a cancer treatment, said Dr. Weiss.
But outside the lab, FMT is mainly used for one purpose: to treat Clostridioides difficile infection. It works even better than antibiotics, research shows.
But first you need to find a healthy donor, and that’s harder than you might think.
Finding healthy stool samples
Banking our bodily substances is nothing new. Blood banks, for example, are common throughout the United States, and cord blood banking – preserving blood from a baby’s umbilical cord to aid possible future medical needs of the child – is becoming more popular. Sperm donors are highly sought after, and doctors regularly transplant kidneys and bone marrow to patients in need.
So why are we so particular about poop?
Part of the reason may be because feces (like blood, for that matter) can harbor disease – which is why it’s so important to find healthy stool donors. Problem is, this can be surprisingly hard to do.
To donate fecal matter, people must go through a rigorous screening process, said Majdi Osman, MD, chief medical officer for OpenBiome, a nonprofit microbiome research organization.
Until recently, OpenBiome operated a stool donation program, though it has since shifted its focus to research. Potential donors were screened for diseases and mental health conditions, pathogens, and antibiotic resistance. The pass rate was less than 3%.
“We take a very cautious approach because the association between diseases and the microbiome is still being understood,” Dr. Osman said.
FMT also carries risks – though so far, they seem mild. Side effects include mild diarrhea, nausea, belly pain, and fatigue. (The reason? Even the healthiest donor stool may not mix perfectly with your own.)
That’s where the idea of using your own stool comes in, said Yang-Yu Liu, PhD, a Harvard researcher who studies the microbiome and the lead author of the paper mentioned above. It’s not just more appealing but may also be a better “match” for your body.
Should you bank your stool?
While the researchers say we have reason to be optimistic about the future, it’s important to remember that many challenges remain. FMT is early in development, and there’s a lot about the microbiome we still don’t know.
There’s no guarantee, for example, that restoring a person’s microbiome to its formerly disease-free state will keep diseases at bay forever, said Dr. Weiss. If your genes raise your odds of having Crohn’s, for instance, it’s possible the disease could come back.
We also don’t know how long stool samples can be preserved, said Dr. Liu. Stool banks currently store fecal matter for 1 or 2 years, not decades. To protect the proteins and DNA structures for that long, samples would likely need to be stashed at the liquid nitrogen storage temperature of –196° C. (Currently, samples are stored at about –80° C.) Even then, testing would be needed to confirm if the fragile microorganisms in the stool can survive.
This raises another question: Who’s going to regulate all this?
The FDA regulates the use of FMT as a drug for the treatment of C. diff, but as Dr. Liu pointed out, many gastroenterologists consider the gut microbiota an organ. In that case, human fecal matter could be regulated the same way blood, bone, or even egg cells are.
Cord blood banking may be a helpful model, Dr. Liu said.
“We don’t have to start from scratch.”
Then there’s the question of cost. Cord blood banks could be a point of reference for that too, the researchers say. They charge about $1,500 to $2,820 for the first collection and processing, plus a yearly storage fee of $185 to $370.
Despite the unknowns, one thing is for sure: The interest in fecal banking is real – and growing. At least one microbiome firm, Cordlife Group Limited, based in Singapore, announced that it has started to allow people to bank their stool for future use.
“More people should talk about it and think about it,” said Dr. Liu.
A version of this article first appeared on WebMD.com.
Lots of things can disrupt your gut health over the years. A high-sugar diet, stress, antibiotics – all are linked to bad changes in the gut microbiome, the microbes that live in your intestinal tract. And this can raise the risk of diseases.
It could be possible, scientists say, by having people take a sample of their own stool when they are young to be put back into their colons when they are older.
While the science to back this up isn’t quite there yet, some researchers are saying we shouldn’t wait. They are calling on existing stool banks to let people start banking their stool now, so it’s there for them to use if the science becomes available.
But how would that work?
First, you’d go to a stool bank and provide a fresh sample of your poop, which would be screened for diseases, washed, processed, and deposited into a long-term storage facility.
Then, down the road, if you get a condition such as inflammatory bowel disease, heart disease, or type 2 diabetes – or if you have a procedure that wipes out your microbiome, like a course of antibiotics or chemotherapy – doctors could use your preserved stool to “re-colonize” your gut, restoring it to its earlier, healthier state, said Scott Weiss, MD, professor of medicine at Harvard Medical School, Boston, and a coauthor of a recent paper on the topic. They would do that using fecal microbiota transplantation, or FMT.
Timing is everything. You’d want a sample from when you’re healthy – say, between the ages of 18 and 35, or before a chronic condition is likely, said Dr. Weiss. But if you’re still healthy into your late 30s, 40s, or even 50s, providing a sample then could still benefit you later in life.
If we could pull off a banking system like this, it could have the potential to treat autoimmune disease, inflammatory bowel disease, diabetes, obesity, and heart disease – or even reverse the effects of aging. How can we make this happen?
Stool banks of today
While stool banks do exist today, the samples inside are destined not for the original donors but rather for sick patients hoping to treat an illness. Using FMT, doctors transfer the fecal material to the patient’s colon, restoring helpful gut microbiota.
Some research shows FMT may help treat inflammatory bowel diseases, such as Crohn’s or ulcerative colitis. Animal studies suggest it could help treat obesity, lengthen lifespan, and reverse some effects of aging, such as age-related decline in brain function. Other clinical trials are looking into its potential as a cancer treatment, said Dr. Weiss.
But outside the lab, FMT is mainly used for one purpose: to treat Clostridioides difficile infection. It works even better than antibiotics, research shows.
But first you need to find a healthy donor, and that’s harder than you might think.
Finding healthy stool samples
Banking our bodily substances is nothing new. Blood banks, for example, are common throughout the United States, and cord blood banking – preserving blood from a baby’s umbilical cord to aid possible future medical needs of the child – is becoming more popular. Sperm donors are highly sought after, and doctors regularly transplant kidneys and bone marrow to patients in need.
So why are we so particular about poop?
Part of the reason may be because feces (like blood, for that matter) can harbor disease – which is why it’s so important to find healthy stool donors. Problem is, this can be surprisingly hard to do.
To donate fecal matter, people must go through a rigorous screening process, said Majdi Osman, MD, chief medical officer for OpenBiome, a nonprofit microbiome research organization.
Until recently, OpenBiome operated a stool donation program, though it has since shifted its focus to research. Potential donors were screened for diseases and mental health conditions, pathogens, and antibiotic resistance. The pass rate was less than 3%.
“We take a very cautious approach because the association between diseases and the microbiome is still being understood,” Dr. Osman said.
FMT also carries risks – though so far, they seem mild. Side effects include mild diarrhea, nausea, belly pain, and fatigue. (The reason? Even the healthiest donor stool may not mix perfectly with your own.)
That’s where the idea of using your own stool comes in, said Yang-Yu Liu, PhD, a Harvard researcher who studies the microbiome and the lead author of the paper mentioned above. It’s not just more appealing but may also be a better “match” for your body.
Should you bank your stool?
While the researchers say we have reason to be optimistic about the future, it’s important to remember that many challenges remain. FMT is early in development, and there’s a lot about the microbiome we still don’t know.
There’s no guarantee, for example, that restoring a person’s microbiome to its formerly disease-free state will keep diseases at bay forever, said Dr. Weiss. If your genes raise your odds of having Crohn’s, for instance, it’s possible the disease could come back.
We also don’t know how long stool samples can be preserved, said Dr. Liu. Stool banks currently store fecal matter for 1 or 2 years, not decades. To protect the proteins and DNA structures for that long, samples would likely need to be stashed at the liquid nitrogen storage temperature of –196° C. (Currently, samples are stored at about –80° C.) Even then, testing would be needed to confirm if the fragile microorganisms in the stool can survive.
This raises another question: Who’s going to regulate all this?
The FDA regulates the use of FMT as a drug for the treatment of C. diff, but as Dr. Liu pointed out, many gastroenterologists consider the gut microbiota an organ. In that case, human fecal matter could be regulated the same way blood, bone, or even egg cells are.
Cord blood banking may be a helpful model, Dr. Liu said.
“We don’t have to start from scratch.”
Then there’s the question of cost. Cord blood banks could be a point of reference for that too, the researchers say. They charge about $1,500 to $2,820 for the first collection and processing, plus a yearly storage fee of $185 to $370.
Despite the unknowns, one thing is for sure: The interest in fecal banking is real – and growing. At least one microbiome firm, Cordlife Group Limited, based in Singapore, announced that it has started to allow people to bank their stool for future use.
“More people should talk about it and think about it,” said Dr. Liu.
A version of this article first appeared on WebMD.com.
Fish oil pills do not reduce fractures in healthy seniors: VITAL
Omega-3 supplements did not reduce fractures during a median 5.3-year follow-up in the more than 25,000 generally healthy men and women (≥ age 50 and ≥ age 55, respectively) in the Vitamin D and Omega-3 Trial (VITAL).
The large randomized controlled trial tested whether omega-3 fatty acid or vitamin D supplements prevented cardiovascular disease or cancer in a representative sample of midlife and older adults from 50 U.S. states – which they did not. In a further analysis of VITAL, vitamin D supplements (cholecalciferol, 2,000 IU/day) did not lower the risk of incident total, nonvertebral, and hip fractures, compared with placebo.
Now this new analysis shows that omega-3 fatty acid supplements (1 g/day of fish oil) did not reduce the risk of such fractures in the VITAL population either. Meryl S. LeBoff, MD, presented the latest findings during an oral session at the annual meeting of the American Society for Bone and Mineral Research.
“In this, the largest randomized controlled trial in the world, we did not find an effect of omega-3 fatty acid supplements on fractures,” Dr. LeBoff, from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, told this news organization.
The current analysis did “unexpectedly” show that among participants who received the omega-3 fatty acid supplements, there was an increase in fractures in men, and fracture risk was higher in people with a normal or low body mass index and lower in people with higher BMI.
However, these subgroup findings need to be interpreted with caution and may be caused by chance, Dr. LeBoff warned. The researchers will be investigating these findings in further analyses.
Should patients take omega-3 supplements or not?
Asked whether, in the meantime, patients should start or keep taking fish oil supplements for possible health benefits, she noted that certain individuals might benefit.
For example, in VITAL, participants who ate less than 1.5 servings of fish per week and received omega-3 fatty acid supplements had a decrease in the combined cardiovascular endpoint, and Black participants who took fish oil supplements had a substantially reduced risk of the outcome, regardless of fish intake.
“I think everybody needs to review [the study findings] with clinicians and make a decision in terms of what would be best for them,” she said.
Session comoderator Bente Langdahl, MD, PhD, commented that “many people take omega-3 because they think it will help” knee, hip, or other joint pain.
Perhaps men are more prone to joint pain because of osteoarthritis and the supplements lessen the pain, so these men became more physically active and more prone to fractures, she speculated.
The current study shows that, “so far, we haven’t been able to demonstrate a reduced rate of fractures with fish oil supplements in clinical randomized trials” conducted in relatively healthy and not the oldest patients, she summarized. “We’re not talking about 80-year-olds.”
In this “well-conducted study, they were not able to see any difference” with omega-3 fatty acid supplements versus placebo, but apparently, there are no harms associated with taking these supplements, she said.
To patients who ask her about such supplements, Dr. Langdahl advised: “Try it out for 3 months. If it really helps you, if it takes away your joint pain or whatever, then that might work for you. But then remember to stop again because it might just be a temporary effect.”
Could fish oil supplements protect against fractures?
An estimated 22% of U.S. adults aged 60 and older take omega-3 fatty acid supplements, Dr. LeBoff noted.
Preclinical studies have shown that omega-3 fatty acids reduce bone resorption and have anti-inflammatory effects, but observational studies have reported conflicting findings.
The researchers conducted this ancillary study of VITAL to fill these knowledge gaps.
VITAL enrolled a national sample of 25,871 U.S. men and women, including 5,106 Black participants, with a mean age of 67 and a mean BMI of 28 kg/m2.
Importantly, participants were not recruited by low bone density, fractures, or vitamin D deficiency. Prior to entry, participants were required to stop taking omega-3 supplements and limit nonstudy vitamin D and calcium supplements.
The omega-3 fatty acid supplements used in the study contained eicosapentaenoic acid and docosahexaenoic acid in a 1.2:1 ratio.
VITAL had a 2x2 factorial design whereby 6,463 participants were randomized to receive the omega-3 fatty acid supplement and 6,474 were randomized to placebo. (Remaining participants were randomized to receive vitamin D or placebo.)
Participants in the omega-3 fatty acid and placebo groups had similar baseline characteristics. For example, about half (50.5%) were women, and on average, they ate 1.1 servings of dark-meat fish (such as salmon) per week.
Participants completed detailed questionnaires at baseline and each year.
Plasma omega-3 levels were measured at baseline and, in 1,583 participants, at 1 year of follow-up. The mean omega-3 index rose 54.7% in the omega-3 fatty acid group and changed less than 2% in the placebo group at 1 year.
Study pill adherence was 87.0% at 2 years and 85.7% at 5 years.
Fractures were self-reported on annual questionnaires and centrally adjudicated in medical record review.
No clinically meaningful effect of omega-3 fatty acids on fractures
During a median 5.3-year follow-up, researchers adjudicated 2,133 total fractures and confirmed 1,991 fractures (93%) in 1551 participants.
Incidences of total, nonvertebral, and hip fractures were similar in both groups.
Compared with placebo, omega-3 fatty acid supplements had no significant effect on risk of total fractures (hazard ratio, 1.02; 95% confidence interval, 0.92-1.13), nonvertebral fractures (HR, 1.01; 95% CI, 0.91-1.12), or hip fractures (HR, 0.89; 95% CI, 0.61-1.30), all adjusted for age, sex, and race.
The “confidence intervals were narrow, likely excluding a clinically meaningful effect,” Dr. LeBoff noted.
Among men, those who received fish oil supplements had a greater risk of fracture than those who received placebo (HR, 1.27; 95% CI, 1.07-1.51), but this result “was not corrected for multiple hypothesis testing,” Dr. LeBoff cautioned.
In the overall population, participants with a BMI less than 25 who received fish oil versus placebo had an increased risk of fracture, and those with a BMI of at least 30 who received fish oil versus placebo had a decreased risk of fracture, but the limits of the confidence intervals crossed 1.00.
After excluding digit, skull, and pathologic fractures, there was no significant reduction in total fractures (HR, 1.02; 95% CI, 0.92-1.14), nonvertebral fractures (HR, 1.02; 95% CI, 0.92-1.14), or hip fractures (HR, 0.90; 95% CI, 0.61-1.33), with omega-3 supplements versus placebo.
Similarly, there was no significant reduction in risk of major osteoporotic fractures (hip, wrist, humerus, and clinical spine fractures) or wrist fractures with omega-3 supplements versus placebo.
VITAL only studied one dose of omega-3 fatty acid supplements, and results may not be generalizable to younger adults, or older adults living in residential communities, Dr. LeBoff noted.
The study was supported by grants from the National Institute of Arthritis Musculoskeletal and Skin Diseases. VITAL was funded by the National Cancer Institute and the National Heart, Lung, and Blood Institute. Dr. LeBoff and Dr. Langdahl have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Omega-3 supplements did not reduce fractures during a median 5.3-year follow-up in the more than 25,000 generally healthy men and women (≥ age 50 and ≥ age 55, respectively) in the Vitamin D and Omega-3 Trial (VITAL).
The large randomized controlled trial tested whether omega-3 fatty acid or vitamin D supplements prevented cardiovascular disease or cancer in a representative sample of midlife and older adults from 50 U.S. states – which they did not. In a further analysis of VITAL, vitamin D supplements (cholecalciferol, 2,000 IU/day) did not lower the risk of incident total, nonvertebral, and hip fractures, compared with placebo.
Now this new analysis shows that omega-3 fatty acid supplements (1 g/day of fish oil) did not reduce the risk of such fractures in the VITAL population either. Meryl S. LeBoff, MD, presented the latest findings during an oral session at the annual meeting of the American Society for Bone and Mineral Research.
“In this, the largest randomized controlled trial in the world, we did not find an effect of omega-3 fatty acid supplements on fractures,” Dr. LeBoff, from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, told this news organization.
The current analysis did “unexpectedly” show that among participants who received the omega-3 fatty acid supplements, there was an increase in fractures in men, and fracture risk was higher in people with a normal or low body mass index and lower in people with higher BMI.
However, these subgroup findings need to be interpreted with caution and may be caused by chance, Dr. LeBoff warned. The researchers will be investigating these findings in further analyses.
Should patients take omega-3 supplements or not?
Asked whether, in the meantime, patients should start or keep taking fish oil supplements for possible health benefits, she noted that certain individuals might benefit.
For example, in VITAL, participants who ate less than 1.5 servings of fish per week and received omega-3 fatty acid supplements had a decrease in the combined cardiovascular endpoint, and Black participants who took fish oil supplements had a substantially reduced risk of the outcome, regardless of fish intake.
“I think everybody needs to review [the study findings] with clinicians and make a decision in terms of what would be best for them,” she said.
Session comoderator Bente Langdahl, MD, PhD, commented that “many people take omega-3 because they think it will help” knee, hip, or other joint pain.
Perhaps men are more prone to joint pain because of osteoarthritis and the supplements lessen the pain, so these men became more physically active and more prone to fractures, she speculated.
The current study shows that, “so far, we haven’t been able to demonstrate a reduced rate of fractures with fish oil supplements in clinical randomized trials” conducted in relatively healthy and not the oldest patients, she summarized. “We’re not talking about 80-year-olds.”
In this “well-conducted study, they were not able to see any difference” with omega-3 fatty acid supplements versus placebo, but apparently, there are no harms associated with taking these supplements, she said.
To patients who ask her about such supplements, Dr. Langdahl advised: “Try it out for 3 months. If it really helps you, if it takes away your joint pain or whatever, then that might work for you. But then remember to stop again because it might just be a temporary effect.”
Could fish oil supplements protect against fractures?
An estimated 22% of U.S. adults aged 60 and older take omega-3 fatty acid supplements, Dr. LeBoff noted.
Preclinical studies have shown that omega-3 fatty acids reduce bone resorption and have anti-inflammatory effects, but observational studies have reported conflicting findings.
The researchers conducted this ancillary study of VITAL to fill these knowledge gaps.
VITAL enrolled a national sample of 25,871 U.S. men and women, including 5,106 Black participants, with a mean age of 67 and a mean BMI of 28 kg/m2.
Importantly, participants were not recruited by low bone density, fractures, or vitamin D deficiency. Prior to entry, participants were required to stop taking omega-3 supplements and limit nonstudy vitamin D and calcium supplements.
The omega-3 fatty acid supplements used in the study contained eicosapentaenoic acid and docosahexaenoic acid in a 1.2:1 ratio.
VITAL had a 2x2 factorial design whereby 6,463 participants were randomized to receive the omega-3 fatty acid supplement and 6,474 were randomized to placebo. (Remaining participants were randomized to receive vitamin D or placebo.)
Participants in the omega-3 fatty acid and placebo groups had similar baseline characteristics. For example, about half (50.5%) were women, and on average, they ate 1.1 servings of dark-meat fish (such as salmon) per week.
Participants completed detailed questionnaires at baseline and each year.
Plasma omega-3 levels were measured at baseline and, in 1,583 participants, at 1 year of follow-up. The mean omega-3 index rose 54.7% in the omega-3 fatty acid group and changed less than 2% in the placebo group at 1 year.
Study pill adherence was 87.0% at 2 years and 85.7% at 5 years.
Fractures were self-reported on annual questionnaires and centrally adjudicated in medical record review.
No clinically meaningful effect of omega-3 fatty acids on fractures
During a median 5.3-year follow-up, researchers adjudicated 2,133 total fractures and confirmed 1,991 fractures (93%) in 1551 participants.
Incidences of total, nonvertebral, and hip fractures were similar in both groups.
Compared with placebo, omega-3 fatty acid supplements had no significant effect on risk of total fractures (hazard ratio, 1.02; 95% confidence interval, 0.92-1.13), nonvertebral fractures (HR, 1.01; 95% CI, 0.91-1.12), or hip fractures (HR, 0.89; 95% CI, 0.61-1.30), all adjusted for age, sex, and race.
The “confidence intervals were narrow, likely excluding a clinically meaningful effect,” Dr. LeBoff noted.
Among men, those who received fish oil supplements had a greater risk of fracture than those who received placebo (HR, 1.27; 95% CI, 1.07-1.51), but this result “was not corrected for multiple hypothesis testing,” Dr. LeBoff cautioned.
In the overall population, participants with a BMI less than 25 who received fish oil versus placebo had an increased risk of fracture, and those with a BMI of at least 30 who received fish oil versus placebo had a decreased risk of fracture, but the limits of the confidence intervals crossed 1.00.
After excluding digit, skull, and pathologic fractures, there was no significant reduction in total fractures (HR, 1.02; 95% CI, 0.92-1.14), nonvertebral fractures (HR, 1.02; 95% CI, 0.92-1.14), or hip fractures (HR, 0.90; 95% CI, 0.61-1.33), with omega-3 supplements versus placebo.
Similarly, there was no significant reduction in risk of major osteoporotic fractures (hip, wrist, humerus, and clinical spine fractures) or wrist fractures with omega-3 supplements versus placebo.
VITAL only studied one dose of omega-3 fatty acid supplements, and results may not be generalizable to younger adults, or older adults living in residential communities, Dr. LeBoff noted.
The study was supported by grants from the National Institute of Arthritis Musculoskeletal and Skin Diseases. VITAL was funded by the National Cancer Institute and the National Heart, Lung, and Blood Institute. Dr. LeBoff and Dr. Langdahl have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Omega-3 supplements did not reduce fractures during a median 5.3-year follow-up in the more than 25,000 generally healthy men and women (≥ age 50 and ≥ age 55, respectively) in the Vitamin D and Omega-3 Trial (VITAL).
The large randomized controlled trial tested whether omega-3 fatty acid or vitamin D supplements prevented cardiovascular disease or cancer in a representative sample of midlife and older adults from 50 U.S. states – which they did not. In a further analysis of VITAL, vitamin D supplements (cholecalciferol, 2,000 IU/day) did not lower the risk of incident total, nonvertebral, and hip fractures, compared with placebo.
Now this new analysis shows that omega-3 fatty acid supplements (1 g/day of fish oil) did not reduce the risk of such fractures in the VITAL population either. Meryl S. LeBoff, MD, presented the latest findings during an oral session at the annual meeting of the American Society for Bone and Mineral Research.
“In this, the largest randomized controlled trial in the world, we did not find an effect of omega-3 fatty acid supplements on fractures,” Dr. LeBoff, from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, told this news organization.
The current analysis did “unexpectedly” show that among participants who received the omega-3 fatty acid supplements, there was an increase in fractures in men, and fracture risk was higher in people with a normal or low body mass index and lower in people with higher BMI.
However, these subgroup findings need to be interpreted with caution and may be caused by chance, Dr. LeBoff warned. The researchers will be investigating these findings in further analyses.
Should patients take omega-3 supplements or not?
Asked whether, in the meantime, patients should start or keep taking fish oil supplements for possible health benefits, she noted that certain individuals might benefit.
For example, in VITAL, participants who ate less than 1.5 servings of fish per week and received omega-3 fatty acid supplements had a decrease in the combined cardiovascular endpoint, and Black participants who took fish oil supplements had a substantially reduced risk of the outcome, regardless of fish intake.
“I think everybody needs to review [the study findings] with clinicians and make a decision in terms of what would be best for them,” she said.
Session comoderator Bente Langdahl, MD, PhD, commented that “many people take omega-3 because they think it will help” knee, hip, or other joint pain.
Perhaps men are more prone to joint pain because of osteoarthritis and the supplements lessen the pain, so these men became more physically active and more prone to fractures, she speculated.
The current study shows that, “so far, we haven’t been able to demonstrate a reduced rate of fractures with fish oil supplements in clinical randomized trials” conducted in relatively healthy and not the oldest patients, she summarized. “We’re not talking about 80-year-olds.”
In this “well-conducted study, they were not able to see any difference” with omega-3 fatty acid supplements versus placebo, but apparently, there are no harms associated with taking these supplements, she said.
To patients who ask her about such supplements, Dr. Langdahl advised: “Try it out for 3 months. If it really helps you, if it takes away your joint pain or whatever, then that might work for you. But then remember to stop again because it might just be a temporary effect.”
Could fish oil supplements protect against fractures?
An estimated 22% of U.S. adults aged 60 and older take omega-3 fatty acid supplements, Dr. LeBoff noted.
Preclinical studies have shown that omega-3 fatty acids reduce bone resorption and have anti-inflammatory effects, but observational studies have reported conflicting findings.
The researchers conducted this ancillary study of VITAL to fill these knowledge gaps.
VITAL enrolled a national sample of 25,871 U.S. men and women, including 5,106 Black participants, with a mean age of 67 and a mean BMI of 28 kg/m2.
Importantly, participants were not recruited by low bone density, fractures, or vitamin D deficiency. Prior to entry, participants were required to stop taking omega-3 supplements and limit nonstudy vitamin D and calcium supplements.
The omega-3 fatty acid supplements used in the study contained eicosapentaenoic acid and docosahexaenoic acid in a 1.2:1 ratio.
VITAL had a 2x2 factorial design whereby 6,463 participants were randomized to receive the omega-3 fatty acid supplement and 6,474 were randomized to placebo. (Remaining participants were randomized to receive vitamin D or placebo.)
Participants in the omega-3 fatty acid and placebo groups had similar baseline characteristics. For example, about half (50.5%) were women, and on average, they ate 1.1 servings of dark-meat fish (such as salmon) per week.
Participants completed detailed questionnaires at baseline and each year.
Plasma omega-3 levels were measured at baseline and, in 1,583 participants, at 1 year of follow-up. The mean omega-3 index rose 54.7% in the omega-3 fatty acid group and changed less than 2% in the placebo group at 1 year.
Study pill adherence was 87.0% at 2 years and 85.7% at 5 years.
Fractures were self-reported on annual questionnaires and centrally adjudicated in medical record review.
No clinically meaningful effect of omega-3 fatty acids on fractures
During a median 5.3-year follow-up, researchers adjudicated 2,133 total fractures and confirmed 1,991 fractures (93%) in 1551 participants.
Incidences of total, nonvertebral, and hip fractures were similar in both groups.
Compared with placebo, omega-3 fatty acid supplements had no significant effect on risk of total fractures (hazard ratio, 1.02; 95% confidence interval, 0.92-1.13), nonvertebral fractures (HR, 1.01; 95% CI, 0.91-1.12), or hip fractures (HR, 0.89; 95% CI, 0.61-1.30), all adjusted for age, sex, and race.
The “confidence intervals were narrow, likely excluding a clinically meaningful effect,” Dr. LeBoff noted.
Among men, those who received fish oil supplements had a greater risk of fracture than those who received placebo (HR, 1.27; 95% CI, 1.07-1.51), but this result “was not corrected for multiple hypothesis testing,” Dr. LeBoff cautioned.
In the overall population, participants with a BMI less than 25 who received fish oil versus placebo had an increased risk of fracture, and those with a BMI of at least 30 who received fish oil versus placebo had a decreased risk of fracture, but the limits of the confidence intervals crossed 1.00.
After excluding digit, skull, and pathologic fractures, there was no significant reduction in total fractures (HR, 1.02; 95% CI, 0.92-1.14), nonvertebral fractures (HR, 1.02; 95% CI, 0.92-1.14), or hip fractures (HR, 0.90; 95% CI, 0.61-1.33), with omega-3 supplements versus placebo.
Similarly, there was no significant reduction in risk of major osteoporotic fractures (hip, wrist, humerus, and clinical spine fractures) or wrist fractures with omega-3 supplements versus placebo.
VITAL only studied one dose of omega-3 fatty acid supplements, and results may not be generalizable to younger adults, or older adults living in residential communities, Dr. LeBoff noted.
The study was supported by grants from the National Institute of Arthritis Musculoskeletal and Skin Diseases. VITAL was funded by the National Cancer Institute and the National Heart, Lung, and Blood Institute. Dr. LeBoff and Dr. Langdahl have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASMBR 2022
Dietary change tops for reducing CVD risk in stage 1 hypertension
Healthy lifestyle changes to reduce systolic blood pressure to below 130 mm Hg may prevent 26,000 heart attacks and strokes and reduce health care costs over the next 10 years, a new simulation study suggests.
Among the various lifestyle changes, adopting the Dietary Approaches to Stop Hypertension diet, known as the DASH diet, may have the greatest impact for young and middle-aged adults with stage 1 hypertension.
“This research reveals that we should look to feasible ways our food system could make healthy eating the default option,” Kendra Sims, PhD, MPH, postdoctoral fellow at University of California, San Francisco, told this news organization.
“Above all, it means collaborating with the patient about nourishing choices that fit best into their culture and lifestyle,” Dr. Sims said.
Be proactive
“What is important is that people not wait until they have hypertension to start thinking about healthful diets,” commented Taylor Wallace, PhD, department of nutrition and food studies, George Mason University, Fairfax, Va., who was not involved in the study.
“It’s all about prevention in my mind. Whether you are hypertensive or are perfectly healthy, the DASH diet or any other dietary pattern that emphasizes consumption of fruits, vegetables, whole grains, lean meats, seafood, nuts/seeds, and low/non-fat dairy and decreased intake of saturated fats, added sugars, and sodium is a good idea,” Dr. Wallace said in an interview.
The study was presented at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Dr. Sims and colleagues used U.S. statistics from multiple sources to simulate CVD events, mortality, and health care costs between 2018 and 2027 in adults aged 35-64 years with untreated stage 1 hypertension, defined as systolic BP of 130 to 139 mm Hg.
The researchers estimate that 8.8 million U.S. adults (5.5 million women) aged 35-64 years have untreated stage 1 hypertension and would be recommended for lifestyle change, such as physical activity, weight loss, moderating alcohol intake, and adoption of the DASH diet.
Controlling blood pressure to less than 130 mm Hg in this population could prevent 26,000 CVD events, avoid 2,900 deaths, and lead to $1.6 billion saved in associated health care costs, the researchers calculate.
The largest benefit would come from adoption of the DASH diet, with an estimated 15,000 CVD events prevented among men and 11,000 among women.
Even small changes can help
“Young and middle-aged adults with stage 1 hypertension aren’t as low risk as you – or even your doctor – might think,” Dr. Sims told this news organization.
“Millions of working-aged people are walking around with elevated blood pressure, which is symptomless but is also a leading preventable cause of disability and death. Most do not follow the recommended DASH diet,” Dr. Sims said.
“Unfortunately, the availability and affordability of healthy food sources does not easily allow people to follow the DASH diet,” Dr. Sims adds in a conference news release.
“Clinicians should consider whether their patients live in food deserts or places with limited walkability. Health counseling should include addressing these specific challenges to blood pressure control,” Dr. Sims says.
Dr. Wallace noted that diet changes don’t have to be drastic.
“Honestly, just increasing fruit and vegetable intake has been shown to displace calories from saturated fats, added sugars, and sodium,” he told this news organization.
“It’s hard for people to stick to ‘diets’ long-term, so shifting toward healthier dietary patterns without having to read a book on the DASH diet or count calories and carbs seems like a more practical solution for the general population, although I have no issues with the DASH diet and think it is a great dietary pattern for heart health,” Dr. Wallace said.
The study had no funding. Dr. Sims reports no relevant financial relationships. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Healthy lifestyle changes to reduce systolic blood pressure to below 130 mm Hg may prevent 26,000 heart attacks and strokes and reduce health care costs over the next 10 years, a new simulation study suggests.
Among the various lifestyle changes, adopting the Dietary Approaches to Stop Hypertension diet, known as the DASH diet, may have the greatest impact for young and middle-aged adults with stage 1 hypertension.
“This research reveals that we should look to feasible ways our food system could make healthy eating the default option,” Kendra Sims, PhD, MPH, postdoctoral fellow at University of California, San Francisco, told this news organization.
“Above all, it means collaborating with the patient about nourishing choices that fit best into their culture and lifestyle,” Dr. Sims said.
Be proactive
“What is important is that people not wait until they have hypertension to start thinking about healthful diets,” commented Taylor Wallace, PhD, department of nutrition and food studies, George Mason University, Fairfax, Va., who was not involved in the study.
“It’s all about prevention in my mind. Whether you are hypertensive or are perfectly healthy, the DASH diet or any other dietary pattern that emphasizes consumption of fruits, vegetables, whole grains, lean meats, seafood, nuts/seeds, and low/non-fat dairy and decreased intake of saturated fats, added sugars, and sodium is a good idea,” Dr. Wallace said in an interview.
The study was presented at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Dr. Sims and colleagues used U.S. statistics from multiple sources to simulate CVD events, mortality, and health care costs between 2018 and 2027 in adults aged 35-64 years with untreated stage 1 hypertension, defined as systolic BP of 130 to 139 mm Hg.
The researchers estimate that 8.8 million U.S. adults (5.5 million women) aged 35-64 years have untreated stage 1 hypertension and would be recommended for lifestyle change, such as physical activity, weight loss, moderating alcohol intake, and adoption of the DASH diet.
Controlling blood pressure to less than 130 mm Hg in this population could prevent 26,000 CVD events, avoid 2,900 deaths, and lead to $1.6 billion saved in associated health care costs, the researchers calculate.
The largest benefit would come from adoption of the DASH diet, with an estimated 15,000 CVD events prevented among men and 11,000 among women.
Even small changes can help
“Young and middle-aged adults with stage 1 hypertension aren’t as low risk as you – or even your doctor – might think,” Dr. Sims told this news organization.
“Millions of working-aged people are walking around with elevated blood pressure, which is symptomless but is also a leading preventable cause of disability and death. Most do not follow the recommended DASH diet,” Dr. Sims said.
“Unfortunately, the availability and affordability of healthy food sources does not easily allow people to follow the DASH diet,” Dr. Sims adds in a conference news release.
“Clinicians should consider whether their patients live in food deserts or places with limited walkability. Health counseling should include addressing these specific challenges to blood pressure control,” Dr. Sims says.
Dr. Wallace noted that diet changes don’t have to be drastic.
“Honestly, just increasing fruit and vegetable intake has been shown to displace calories from saturated fats, added sugars, and sodium,” he told this news organization.
“It’s hard for people to stick to ‘diets’ long-term, so shifting toward healthier dietary patterns without having to read a book on the DASH diet or count calories and carbs seems like a more practical solution for the general population, although I have no issues with the DASH diet and think it is a great dietary pattern for heart health,” Dr. Wallace said.
The study had no funding. Dr. Sims reports no relevant financial relationships. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Healthy lifestyle changes to reduce systolic blood pressure to below 130 mm Hg may prevent 26,000 heart attacks and strokes and reduce health care costs over the next 10 years, a new simulation study suggests.
Among the various lifestyle changes, adopting the Dietary Approaches to Stop Hypertension diet, known as the DASH diet, may have the greatest impact for young and middle-aged adults with stage 1 hypertension.
“This research reveals that we should look to feasible ways our food system could make healthy eating the default option,” Kendra Sims, PhD, MPH, postdoctoral fellow at University of California, San Francisco, told this news organization.
“Above all, it means collaborating with the patient about nourishing choices that fit best into their culture and lifestyle,” Dr. Sims said.
Be proactive
“What is important is that people not wait until they have hypertension to start thinking about healthful diets,” commented Taylor Wallace, PhD, department of nutrition and food studies, George Mason University, Fairfax, Va., who was not involved in the study.
“It’s all about prevention in my mind. Whether you are hypertensive or are perfectly healthy, the DASH diet or any other dietary pattern that emphasizes consumption of fruits, vegetables, whole grains, lean meats, seafood, nuts/seeds, and low/non-fat dairy and decreased intake of saturated fats, added sugars, and sodium is a good idea,” Dr. Wallace said in an interview.
The study was presented at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Dr. Sims and colleagues used U.S. statistics from multiple sources to simulate CVD events, mortality, and health care costs between 2018 and 2027 in adults aged 35-64 years with untreated stage 1 hypertension, defined as systolic BP of 130 to 139 mm Hg.
The researchers estimate that 8.8 million U.S. adults (5.5 million women) aged 35-64 years have untreated stage 1 hypertension and would be recommended for lifestyle change, such as physical activity, weight loss, moderating alcohol intake, and adoption of the DASH diet.
Controlling blood pressure to less than 130 mm Hg in this population could prevent 26,000 CVD events, avoid 2,900 deaths, and lead to $1.6 billion saved in associated health care costs, the researchers calculate.
The largest benefit would come from adoption of the DASH diet, with an estimated 15,000 CVD events prevented among men and 11,000 among women.
Even small changes can help
“Young and middle-aged adults with stage 1 hypertension aren’t as low risk as you – or even your doctor – might think,” Dr. Sims told this news organization.
“Millions of working-aged people are walking around with elevated blood pressure, which is symptomless but is also a leading preventable cause of disability and death. Most do not follow the recommended DASH diet,” Dr. Sims said.
“Unfortunately, the availability and affordability of healthy food sources does not easily allow people to follow the DASH diet,” Dr. Sims adds in a conference news release.
“Clinicians should consider whether their patients live in food deserts or places with limited walkability. Health counseling should include addressing these specific challenges to blood pressure control,” Dr. Sims says.
Dr. Wallace noted that diet changes don’t have to be drastic.
“Honestly, just increasing fruit and vegetable intake has been shown to displace calories from saturated fats, added sugars, and sodium,” he told this news organization.
“It’s hard for people to stick to ‘diets’ long-term, so shifting toward healthier dietary patterns without having to read a book on the DASH diet or count calories and carbs seems like a more practical solution for the general population, although I have no issues with the DASH diet and think it is a great dietary pattern for heart health,” Dr. Wallace said.
The study had no funding. Dr. Sims reports no relevant financial relationships. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Integrase inhibitors and gestational weight gain: Should women worry?
In recent years, increased use of integrase strand transferase inhibitor (INSTI) antiviral treatment (ART) has raised concerns about weight gain and adverse outcomes in patients with HIV. This is especially true regarding possible excessive gestational weight gain, which in women without HIV has been associated with maternal gestational diabetes, hypertensive and liver conditions, as well as related risks for preterm birth, fetal macrosomia, and higher weight after birth.
Unfortunately, few studies in pregnant women with HIV have moved out of the controlled environment into real-world settings, potentially limiting current knowledge about the impact of gestational weight gain – as well as strategies to both prevent it and the associated adverse outcomes.
That is what a team of infectious disease specialists at the Hospital Federal dos Servidores do Estado in Rio de Janeiro recently sought to answer among a cohort of INSTI-experienced and INSTI-naive women with BMIs less than 25 kg/m2 (underweight/normal weight) and higher than 25 kg/m2.
Surprising findings
The investigators determined that rates of excessive weight gain were significantly higher in INSTI-naive women with BMI less than 25 who experienced rates as high as 31.6%, compared with approximately 12% of women who conceived while on INSTIs, regardless of BMI values at baseline (P = .004).
However, rates of unfavorable pregnancy outcomes (for example, small for gestational age, preterm birth, stillbirth, death) appeared to be low overall and similar among all the study groups.
“We had some discussions when we were working on this and thought that the weight gain might have adverse effects,” Trevon Fuller, PhD, lead author and a postdoctoral student at the Hospital Federal dos Servidores do Estado, told this news organization.
“But it looked like the weight gain might actually be good, to the extent that we didn’t see any harm to the mom or the baby of those underweight or normal weight women who were naive to INSTIs,” he explained.
Dr. Fuller and his team enrolled 198 pregnant women living with HIV who sought care at the Hospital Federal dos Servidores do Estado – a national reference center for USAID’s Prevention of Mother to Child Transmission strategic program – between October 2014 and October 2021.
Participants were divided into two primary cohorts: BMI less than 25 at enrollment (n = 74) or BMI of 25 or higher (n = 124), then further divided by timing of INSTI-based combined ART:
- INSTI-naive: women using INSTI-based ART (raltegravir [Isentress] 400 mg twice per day or dolutegravir [Tivicay] 50 mg/day plus 2 non-nucleoside reverse transcriptase inhibitors – lamivudine plus tenofovir disoproxil fumarate or lamivudine plus zidovudine) for 4 weeks between baseline and near delivery.
- INSTI-experienced: women who became pregnant while using INSTIs for at least 6 months before conception.
Among underweight/normal weight participants, 77% (n = 57) were INSTI-naive and 23% (n = 17) INSTI-experienced, and among overweight/obese participants, 81.5% (n = 101) were INSTI-naive, and 18.5% (n = 23) were experienced.
Maternal age, which did not differ significantly by BMI or treatment experience, was a median of 28 years, and most participants were non-White. All participants were virally suppressed near delivery.
Study findings, which were published online in HIV Medicine, highlighted that median weight near delivery in participants who were overweight/obese at baseline was similar regardless of whether they were treatment-experienced (90 kg [198 lb]) or treatment-naive (82.3 kg [181 lb]), P = .026.
However, participants who were underweight/normal weight who were INSTI-naive had significantly higher rates of gestational weight gain (31.5%, 18/57), compared with those of underweight/normal weight who were INSTI-experienced (11.8%, 2/17), P = .004. Notably, this gain was significant in all categories of change (that is, low < 0.18 kg/week, normal 0.18-0.59 kg/week), and high > 0.59 kg/week).
“One of the things that we took away was that this weight gain is primarily happening with women who are starting INSTIs,” said Dr. Fuller.
“The data suggest that [it] might be temporary in the sense that there’s not going to be continuous weight gain but that it will probably approach some type of horizontal asymptote,” he added.
Although obstetric and neonatal outcomes were secondary measures, the investigators did not observe any significantly different outcomes when comparing the groups, and there were no stillbirths, neonatal deaths, or macrosomia.
Preterm delivery rates in underweight/normal weight participants who were INSTI-experienced (11.8%, 2/17) and INSTI-naive (5.3%, 3/57) were similar to overweight/obese participants who were INSTI-experienced (13%, 3/23) and INSTI-naive (6.9%, 7/101).
The same was true for low birthweight.
Still, the study appears to raise more questions than it answers, Sigal Yawetz, MD, an infectious disease specialist at Brigham and Women’s Hospital, Boston, said in an interview – a factor that she said is common also in some of the more recent randomized controlled studies, such as IMPAACT PROMISE.
Dr. Yawetz, who was not involved in the study, also noted, “The groups were small, so comparisons within the groups are difficult, and so many people were excluded that it’s hard to know if there were adverse outcomes related to this ... It’s very confounded.”
The World Health Organization estimates that there are roughly 1.3 million pregnant women with HIV, 81% of whom are on antiretroviral therapy. Although the literature continues to evolve, data suggest that in general, Black women are at greater risk for gestational weight gain.
“We have to remember that women who gain excess weight in pregnancy are still going to be with this weight following pregnancy as well,” Dr. Yawetz said. “So, it might impact their pregnancy but also their health after delivery and for subsequent pregnancies, which we don’t have data for yet.”
Dr. Fuller agrees that more data are needed and mentioned that the team plans to study this further, ideally with larger sample sizes.
Yet, despite the lingering questions, there is a silver lining, one that Dr. Yawetz was emphatic about.
“I really welcome people doing studies on this because we really need the data. By far, integrase inhibitors are the first-line regimen all over the world for pregnant women, and if you look at the gestalt or full picture, this is the best regimen to give pregnant women,” she said.
Dr. Fuller and Dr. Yawetz report no relevant financial relationships. The study was independently supported.
A version of this article first appeared on Medscape.com.
In recent years, increased use of integrase strand transferase inhibitor (INSTI) antiviral treatment (ART) has raised concerns about weight gain and adverse outcomes in patients with HIV. This is especially true regarding possible excessive gestational weight gain, which in women without HIV has been associated with maternal gestational diabetes, hypertensive and liver conditions, as well as related risks for preterm birth, fetal macrosomia, and higher weight after birth.
Unfortunately, few studies in pregnant women with HIV have moved out of the controlled environment into real-world settings, potentially limiting current knowledge about the impact of gestational weight gain – as well as strategies to both prevent it and the associated adverse outcomes.
That is what a team of infectious disease specialists at the Hospital Federal dos Servidores do Estado in Rio de Janeiro recently sought to answer among a cohort of INSTI-experienced and INSTI-naive women with BMIs less than 25 kg/m2 (underweight/normal weight) and higher than 25 kg/m2.
Surprising findings
The investigators determined that rates of excessive weight gain were significantly higher in INSTI-naive women with BMI less than 25 who experienced rates as high as 31.6%, compared with approximately 12% of women who conceived while on INSTIs, regardless of BMI values at baseline (P = .004).
However, rates of unfavorable pregnancy outcomes (for example, small for gestational age, preterm birth, stillbirth, death) appeared to be low overall and similar among all the study groups.
“We had some discussions when we were working on this and thought that the weight gain might have adverse effects,” Trevon Fuller, PhD, lead author and a postdoctoral student at the Hospital Federal dos Servidores do Estado, told this news organization.
“But it looked like the weight gain might actually be good, to the extent that we didn’t see any harm to the mom or the baby of those underweight or normal weight women who were naive to INSTIs,” he explained.
Dr. Fuller and his team enrolled 198 pregnant women living with HIV who sought care at the Hospital Federal dos Servidores do Estado – a national reference center for USAID’s Prevention of Mother to Child Transmission strategic program – between October 2014 and October 2021.
Participants were divided into two primary cohorts: BMI less than 25 at enrollment (n = 74) or BMI of 25 or higher (n = 124), then further divided by timing of INSTI-based combined ART:
- INSTI-naive: women using INSTI-based ART (raltegravir [Isentress] 400 mg twice per day or dolutegravir [Tivicay] 50 mg/day plus 2 non-nucleoside reverse transcriptase inhibitors – lamivudine plus tenofovir disoproxil fumarate or lamivudine plus zidovudine) for 4 weeks between baseline and near delivery.
- INSTI-experienced: women who became pregnant while using INSTIs for at least 6 months before conception.
Among underweight/normal weight participants, 77% (n = 57) were INSTI-naive and 23% (n = 17) INSTI-experienced, and among overweight/obese participants, 81.5% (n = 101) were INSTI-naive, and 18.5% (n = 23) were experienced.
Maternal age, which did not differ significantly by BMI or treatment experience, was a median of 28 years, and most participants were non-White. All participants were virally suppressed near delivery.
Study findings, which were published online in HIV Medicine, highlighted that median weight near delivery in participants who were overweight/obese at baseline was similar regardless of whether they were treatment-experienced (90 kg [198 lb]) or treatment-naive (82.3 kg [181 lb]), P = .026.
However, participants who were underweight/normal weight who were INSTI-naive had significantly higher rates of gestational weight gain (31.5%, 18/57), compared with those of underweight/normal weight who were INSTI-experienced (11.8%, 2/17), P = .004. Notably, this gain was significant in all categories of change (that is, low < 0.18 kg/week, normal 0.18-0.59 kg/week), and high > 0.59 kg/week).
“One of the things that we took away was that this weight gain is primarily happening with women who are starting INSTIs,” said Dr. Fuller.
“The data suggest that [it] might be temporary in the sense that there’s not going to be continuous weight gain but that it will probably approach some type of horizontal asymptote,” he added.
Although obstetric and neonatal outcomes were secondary measures, the investigators did not observe any significantly different outcomes when comparing the groups, and there were no stillbirths, neonatal deaths, or macrosomia.
Preterm delivery rates in underweight/normal weight participants who were INSTI-experienced (11.8%, 2/17) and INSTI-naive (5.3%, 3/57) were similar to overweight/obese participants who were INSTI-experienced (13%, 3/23) and INSTI-naive (6.9%, 7/101).
The same was true for low birthweight.
Still, the study appears to raise more questions than it answers, Sigal Yawetz, MD, an infectious disease specialist at Brigham and Women’s Hospital, Boston, said in an interview – a factor that she said is common also in some of the more recent randomized controlled studies, such as IMPAACT PROMISE.
Dr. Yawetz, who was not involved in the study, also noted, “The groups were small, so comparisons within the groups are difficult, and so many people were excluded that it’s hard to know if there were adverse outcomes related to this ... It’s very confounded.”
The World Health Organization estimates that there are roughly 1.3 million pregnant women with HIV, 81% of whom are on antiretroviral therapy. Although the literature continues to evolve, data suggest that in general, Black women are at greater risk for gestational weight gain.
“We have to remember that women who gain excess weight in pregnancy are still going to be with this weight following pregnancy as well,” Dr. Yawetz said. “So, it might impact their pregnancy but also their health after delivery and for subsequent pregnancies, which we don’t have data for yet.”
Dr. Fuller agrees that more data are needed and mentioned that the team plans to study this further, ideally with larger sample sizes.
Yet, despite the lingering questions, there is a silver lining, one that Dr. Yawetz was emphatic about.
“I really welcome people doing studies on this because we really need the data. By far, integrase inhibitors are the first-line regimen all over the world for pregnant women, and if you look at the gestalt or full picture, this is the best regimen to give pregnant women,” she said.
Dr. Fuller and Dr. Yawetz report no relevant financial relationships. The study was independently supported.
A version of this article first appeared on Medscape.com.
In recent years, increased use of integrase strand transferase inhibitor (INSTI) antiviral treatment (ART) has raised concerns about weight gain and adverse outcomes in patients with HIV. This is especially true regarding possible excessive gestational weight gain, which in women without HIV has been associated with maternal gestational diabetes, hypertensive and liver conditions, as well as related risks for preterm birth, fetal macrosomia, and higher weight after birth.
Unfortunately, few studies in pregnant women with HIV have moved out of the controlled environment into real-world settings, potentially limiting current knowledge about the impact of gestational weight gain – as well as strategies to both prevent it and the associated adverse outcomes.
That is what a team of infectious disease specialists at the Hospital Federal dos Servidores do Estado in Rio de Janeiro recently sought to answer among a cohort of INSTI-experienced and INSTI-naive women with BMIs less than 25 kg/m2 (underweight/normal weight) and higher than 25 kg/m2.
Surprising findings
The investigators determined that rates of excessive weight gain were significantly higher in INSTI-naive women with BMI less than 25 who experienced rates as high as 31.6%, compared with approximately 12% of women who conceived while on INSTIs, regardless of BMI values at baseline (P = .004).
However, rates of unfavorable pregnancy outcomes (for example, small for gestational age, preterm birth, stillbirth, death) appeared to be low overall and similar among all the study groups.
“We had some discussions when we were working on this and thought that the weight gain might have adverse effects,” Trevon Fuller, PhD, lead author and a postdoctoral student at the Hospital Federal dos Servidores do Estado, told this news organization.
“But it looked like the weight gain might actually be good, to the extent that we didn’t see any harm to the mom or the baby of those underweight or normal weight women who were naive to INSTIs,” he explained.
Dr. Fuller and his team enrolled 198 pregnant women living with HIV who sought care at the Hospital Federal dos Servidores do Estado – a national reference center for USAID’s Prevention of Mother to Child Transmission strategic program – between October 2014 and October 2021.
Participants were divided into two primary cohorts: BMI less than 25 at enrollment (n = 74) or BMI of 25 or higher (n = 124), then further divided by timing of INSTI-based combined ART:
- INSTI-naive: women using INSTI-based ART (raltegravir [Isentress] 400 mg twice per day or dolutegravir [Tivicay] 50 mg/day plus 2 non-nucleoside reverse transcriptase inhibitors – lamivudine plus tenofovir disoproxil fumarate or lamivudine plus zidovudine) for 4 weeks between baseline and near delivery.
- INSTI-experienced: women who became pregnant while using INSTIs for at least 6 months before conception.
Among underweight/normal weight participants, 77% (n = 57) were INSTI-naive and 23% (n = 17) INSTI-experienced, and among overweight/obese participants, 81.5% (n = 101) were INSTI-naive, and 18.5% (n = 23) were experienced.
Maternal age, which did not differ significantly by BMI or treatment experience, was a median of 28 years, and most participants were non-White. All participants were virally suppressed near delivery.
Study findings, which were published online in HIV Medicine, highlighted that median weight near delivery in participants who were overweight/obese at baseline was similar regardless of whether they were treatment-experienced (90 kg [198 lb]) or treatment-naive (82.3 kg [181 lb]), P = .026.
However, participants who were underweight/normal weight who were INSTI-naive had significantly higher rates of gestational weight gain (31.5%, 18/57), compared with those of underweight/normal weight who were INSTI-experienced (11.8%, 2/17), P = .004. Notably, this gain was significant in all categories of change (that is, low < 0.18 kg/week, normal 0.18-0.59 kg/week), and high > 0.59 kg/week).
“One of the things that we took away was that this weight gain is primarily happening with women who are starting INSTIs,” said Dr. Fuller.
“The data suggest that [it] might be temporary in the sense that there’s not going to be continuous weight gain but that it will probably approach some type of horizontal asymptote,” he added.
Although obstetric and neonatal outcomes were secondary measures, the investigators did not observe any significantly different outcomes when comparing the groups, and there were no stillbirths, neonatal deaths, or macrosomia.
Preterm delivery rates in underweight/normal weight participants who were INSTI-experienced (11.8%, 2/17) and INSTI-naive (5.3%, 3/57) were similar to overweight/obese participants who were INSTI-experienced (13%, 3/23) and INSTI-naive (6.9%, 7/101).
The same was true for low birthweight.
Still, the study appears to raise more questions than it answers, Sigal Yawetz, MD, an infectious disease specialist at Brigham and Women’s Hospital, Boston, said in an interview – a factor that she said is common also in some of the more recent randomized controlled studies, such as IMPAACT PROMISE.
Dr. Yawetz, who was not involved in the study, also noted, “The groups were small, so comparisons within the groups are difficult, and so many people were excluded that it’s hard to know if there were adverse outcomes related to this ... It’s very confounded.”
The World Health Organization estimates that there are roughly 1.3 million pregnant women with HIV, 81% of whom are on antiretroviral therapy. Although the literature continues to evolve, data suggest that in general, Black women are at greater risk for gestational weight gain.
“We have to remember that women who gain excess weight in pregnancy are still going to be with this weight following pregnancy as well,” Dr. Yawetz said. “So, it might impact their pregnancy but also their health after delivery and for subsequent pregnancies, which we don’t have data for yet.”
Dr. Fuller agrees that more data are needed and mentioned that the team plans to study this further, ideally with larger sample sizes.
Yet, despite the lingering questions, there is a silver lining, one that Dr. Yawetz was emphatic about.
“I really welcome people doing studies on this because we really need the data. By far, integrase inhibitors are the first-line regimen all over the world for pregnant women, and if you look at the gestalt or full picture, this is the best regimen to give pregnant women,” she said.
Dr. Fuller and Dr. Yawetz report no relevant financial relationships. The study was independently supported.
A version of this article first appeared on Medscape.com.