User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Former nurse charged with murder in death of 97-year-old war veteran
A former Kentucky nurse was charged with murder stemming from an incident in which she gave “something special” to a 97-year-old patient who died 5 days later, according to multiple sources, including police and nursing records.
Ms. Hunter allegedly gave lorazepam, typically used for anxiety, to Mr. Morris on April 30. He subsequently developed pneumonia and died on May 5.
Ms. Hunter “intentionally performed actions of medical maltreatment,” according to the Lexington Police Department’s report.
A Baptist Health Lexington spokeswoman told this news organization that the nurse who was charged hasn’t worked at the hospital since the April incident. “We have learned that a former nurse at our hospital has been arrested yesterday on criminal charges,” spokeswoman Ruth Ann Childers stated. “The hospital has fully cooperated with the police investigation. Patient care and safety are always our top priorities. Out of respect for the patient’s family and because this is criminal matter, we are not able to talk about the investigation.”
According to the Kentucky Board of Nursing, which suspended Ms. Hunter’s RN license on a temporary basis on Aug. 22, she allegedly asked the on-duty physician and a nurse practitioner separately for a medication order to calm Mr. Morris, who had become agitated and aggressive. They denied Ms. Hunter’s request, so she withdrew lorazepam intended for another patient and administered it to Mr. Morris, the nursing board suspension order states. “When asked what was administered, she replied ‘something special,’ “ the order states.
Another RN found the patient with labored breathing and “it was determined that respondent had disarmed/lowered the oxygen monitoring system several times as to not set off an alarm at the bedside,” the order continued. “The RN discussed with charge nurse that the patient had been given something intravenously that was causing his decline.”
When the charge nurse entered the room later, she found the patient in “respiratory distress with labored breathing and poor oxygen saturation. ... X-rays would show that the aspiration from the substances ingested by the patient while in his condition caused the patient to develop aspirational pneumonia,” the order continues.
“Despite the rapidly declining condition of the patient, respondent never called for rapid response nor acted with any sense of urgency. Respondent did however edit documentation of administration of Ativan on ‘patient B’ to state ‘not given.’ ”
Mr. Morris’ condition never improved. He was taken to hospice care on May 3 and died 2 days later, the order states.
Ms. Hunter was being held in the Lexington Jail on $100,000 bond, according to jail records.
A version of this article first appeared on Medscape.com.
A former Kentucky nurse was charged with murder stemming from an incident in which she gave “something special” to a 97-year-old patient who died 5 days later, according to multiple sources, including police and nursing records.
Ms. Hunter allegedly gave lorazepam, typically used for anxiety, to Mr. Morris on April 30. He subsequently developed pneumonia and died on May 5.
Ms. Hunter “intentionally performed actions of medical maltreatment,” according to the Lexington Police Department’s report.
A Baptist Health Lexington spokeswoman told this news organization that the nurse who was charged hasn’t worked at the hospital since the April incident. “We have learned that a former nurse at our hospital has been arrested yesterday on criminal charges,” spokeswoman Ruth Ann Childers stated. “The hospital has fully cooperated with the police investigation. Patient care and safety are always our top priorities. Out of respect for the patient’s family and because this is criminal matter, we are not able to talk about the investigation.”
According to the Kentucky Board of Nursing, which suspended Ms. Hunter’s RN license on a temporary basis on Aug. 22, she allegedly asked the on-duty physician and a nurse practitioner separately for a medication order to calm Mr. Morris, who had become agitated and aggressive. They denied Ms. Hunter’s request, so she withdrew lorazepam intended for another patient and administered it to Mr. Morris, the nursing board suspension order states. “When asked what was administered, she replied ‘something special,’ “ the order states.
Another RN found the patient with labored breathing and “it was determined that respondent had disarmed/lowered the oxygen monitoring system several times as to not set off an alarm at the bedside,” the order continued. “The RN discussed with charge nurse that the patient had been given something intravenously that was causing his decline.”
When the charge nurse entered the room later, she found the patient in “respiratory distress with labored breathing and poor oxygen saturation. ... X-rays would show that the aspiration from the substances ingested by the patient while in his condition caused the patient to develop aspirational pneumonia,” the order continues.
“Despite the rapidly declining condition of the patient, respondent never called for rapid response nor acted with any sense of urgency. Respondent did however edit documentation of administration of Ativan on ‘patient B’ to state ‘not given.’ ”
Mr. Morris’ condition never improved. He was taken to hospice care on May 3 and died 2 days later, the order states.
Ms. Hunter was being held in the Lexington Jail on $100,000 bond, according to jail records.
A version of this article first appeared on Medscape.com.
A former Kentucky nurse was charged with murder stemming from an incident in which she gave “something special” to a 97-year-old patient who died 5 days later, according to multiple sources, including police and nursing records.
Ms. Hunter allegedly gave lorazepam, typically used for anxiety, to Mr. Morris on April 30. He subsequently developed pneumonia and died on May 5.
Ms. Hunter “intentionally performed actions of medical maltreatment,” according to the Lexington Police Department’s report.
A Baptist Health Lexington spokeswoman told this news organization that the nurse who was charged hasn’t worked at the hospital since the April incident. “We have learned that a former nurse at our hospital has been arrested yesterday on criminal charges,” spokeswoman Ruth Ann Childers stated. “The hospital has fully cooperated with the police investigation. Patient care and safety are always our top priorities. Out of respect for the patient’s family and because this is criminal matter, we are not able to talk about the investigation.”
According to the Kentucky Board of Nursing, which suspended Ms. Hunter’s RN license on a temporary basis on Aug. 22, she allegedly asked the on-duty physician and a nurse practitioner separately for a medication order to calm Mr. Morris, who had become agitated and aggressive. They denied Ms. Hunter’s request, so she withdrew lorazepam intended for another patient and administered it to Mr. Morris, the nursing board suspension order states. “When asked what was administered, she replied ‘something special,’ “ the order states.
Another RN found the patient with labored breathing and “it was determined that respondent had disarmed/lowered the oxygen monitoring system several times as to not set off an alarm at the bedside,” the order continued. “The RN discussed with charge nurse that the patient had been given something intravenously that was causing his decline.”
When the charge nurse entered the room later, she found the patient in “respiratory distress with labored breathing and poor oxygen saturation. ... X-rays would show that the aspiration from the substances ingested by the patient while in his condition caused the patient to develop aspirational pneumonia,” the order continues.
“Despite the rapidly declining condition of the patient, respondent never called for rapid response nor acted with any sense of urgency. Respondent did however edit documentation of administration of Ativan on ‘patient B’ to state ‘not given.’ ”
Mr. Morris’ condition never improved. He was taken to hospice care on May 3 and died 2 days later, the order states.
Ms. Hunter was being held in the Lexington Jail on $100,000 bond, according to jail records.
A version of this article first appeared on Medscape.com.
COVID to blame as U.S. life expectancy falls
All 50 states and the District of Columbia saw drops in life expectancy, according to the report from the Centers for Disease Control and Prevention’s National Center for Health Statistics.
The declines were mostly because of COVID-19 and “unintentional injuries,” such as drug overdoses.
The overall drop took national life expectancy from 78.8 years in 2019 to 77 years in 2020, the first year of the pandemic, ABC News reported.
States in the West and Northwest generally had higher life expectancy, with states in the South having the lowest.
Hawaii had the highest life expectancy at 80.7 years. It was followed by Washington, Minnesota, California, and Massachusetts. Mississippi had the lowest at 71.9 years, the figures show. The others in the bottom five were West Virginia, Louisiana, Alabama, and Kentucky.
In 2020, COVID-19 was the third-highest cause of death, leading to more than 350,000, the CDC reported earlier this year. At the same time, more people are dying annually from drug overdoses. A record 83,500 fatal overdoses were reported in 2020.
A version of this article first appeared on WebMD.com.
All 50 states and the District of Columbia saw drops in life expectancy, according to the report from the Centers for Disease Control and Prevention’s National Center for Health Statistics.
The declines were mostly because of COVID-19 and “unintentional injuries,” such as drug overdoses.
The overall drop took national life expectancy from 78.8 years in 2019 to 77 years in 2020, the first year of the pandemic, ABC News reported.
States in the West and Northwest generally had higher life expectancy, with states in the South having the lowest.
Hawaii had the highest life expectancy at 80.7 years. It was followed by Washington, Minnesota, California, and Massachusetts. Mississippi had the lowest at 71.9 years, the figures show. The others in the bottom five were West Virginia, Louisiana, Alabama, and Kentucky.
In 2020, COVID-19 was the third-highest cause of death, leading to more than 350,000, the CDC reported earlier this year. At the same time, more people are dying annually from drug overdoses. A record 83,500 fatal overdoses were reported in 2020.
A version of this article first appeared on WebMD.com.
All 50 states and the District of Columbia saw drops in life expectancy, according to the report from the Centers for Disease Control and Prevention’s National Center for Health Statistics.
The declines were mostly because of COVID-19 and “unintentional injuries,” such as drug overdoses.
The overall drop took national life expectancy from 78.8 years in 2019 to 77 years in 2020, the first year of the pandemic, ABC News reported.
States in the West and Northwest generally had higher life expectancy, with states in the South having the lowest.
Hawaii had the highest life expectancy at 80.7 years. It was followed by Washington, Minnesota, California, and Massachusetts. Mississippi had the lowest at 71.9 years, the figures show. The others in the bottom five were West Virginia, Louisiana, Alabama, and Kentucky.
In 2020, COVID-19 was the third-highest cause of death, leading to more than 350,000, the CDC reported earlier this year. At the same time, more people are dying annually from drug overdoses. A record 83,500 fatal overdoses were reported in 2020.
A version of this article first appeared on WebMD.com.
Metformin fails as early COVID-19 treatment but shows potential
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
No fish can escape this net ... of COVID testing
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Are we up the creek without a paddle? What COVID, monkeypox, and nature are trying to tell us
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases fall again, ED rates rebound for some
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.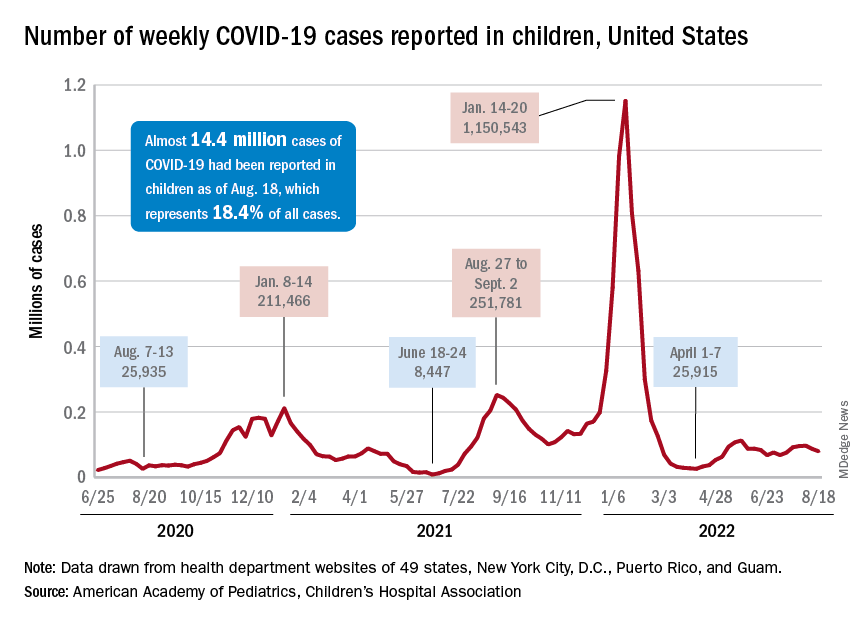
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
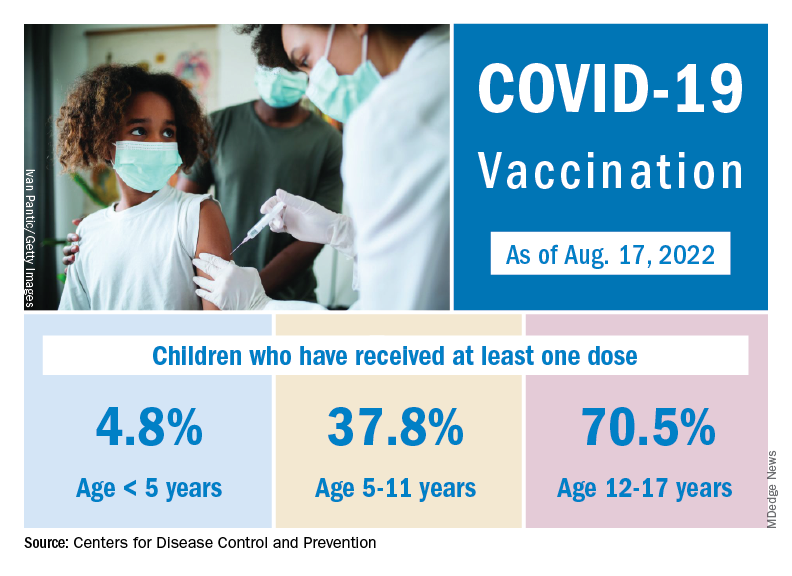
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.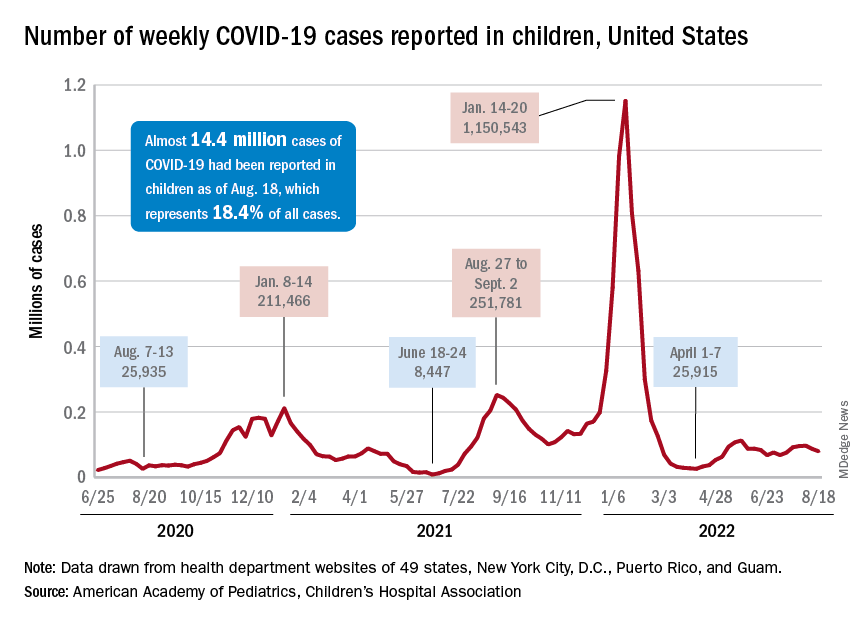
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
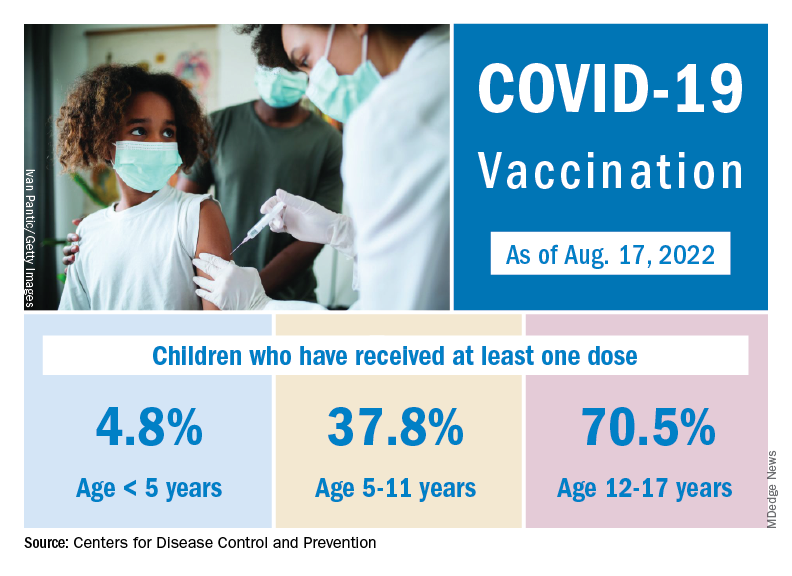
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.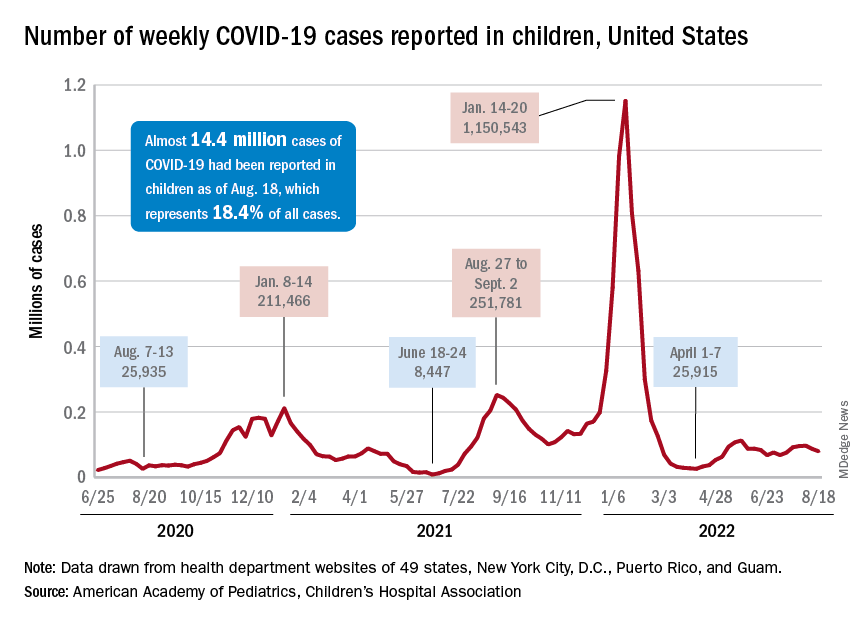
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
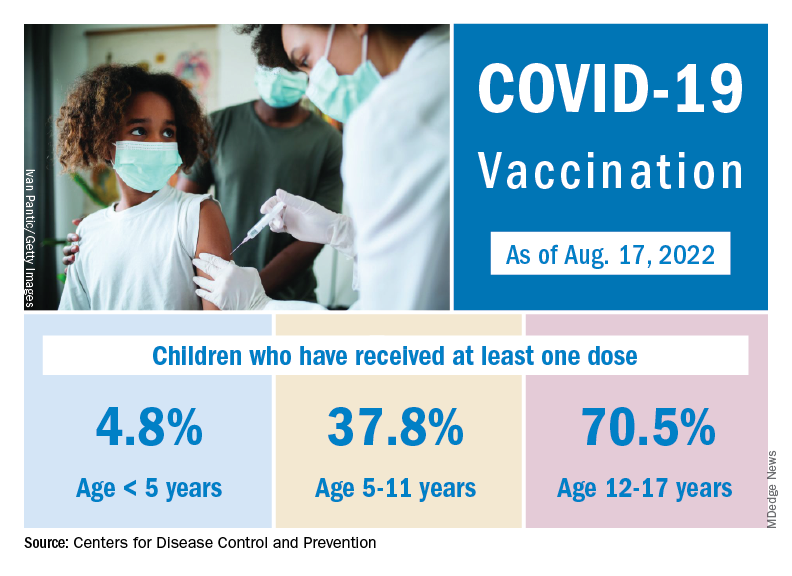
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
Incomplete recovery common 6 months after mild TBI
, new data from the TRACK-TBI study shows.
“Seeing that more than half of the GCS [Glasgow Coma Score] 15, CT-negative TBI cohort in our study were not back to their preinjury baseline at 6 months was surprising and impacts the millions of Americans who suffer from concussions annually,” said lead author Debbie Madhok, MD, with department of emergency medicine, University of California, San Francisco.
“These results highlight the importance of improving care pathways for concussion, particularly from the emergency department,” Dr. Madhok said.
The findings were published online in JAMA Network Open.
The short- and long-term outcomes in the large group of patients who come into the ED with TBI, a GCS of 15, and without acute intracranial traumatic injury (defined as a negative head CT scan) remain poorly understood, the investigators noted. To investigate further, they evaluated outcomes at 2 weeks and 6 months in 991 of these patients (mean age, 38 years; 64% men) from the TRACK-TBI study.
Among the 751 (76%) participants followed up at 2 weeks after the injury, only 204 (27%) had functional recovery – with a Glasgow Outcome Scale-Extended (GOS-E) score of 8. The remaining 547 (73%) had incomplete recovery (GOS-E scores < 8).
Among the 659 patients (66%) followed up at 6 months after the injury, 287 (44%) had functional recovery and 372 (56%) had incomplete recovery.
Most patients who failed to recover completely reported they had not returned to their preinjury life (88%). They described trouble returning to social activities outside the home and disruptions in family relationships and friendships.
The researchers noted that the study population had a high rate of preinjury psychiatric comorbidities, and these patients were more likely to have incomplete recovery than those without psychiatric comorbidities. This aligns with results from previous studies, they added.
The investigators also noted that patients with mild TBI without acute intracranial trauma are typically managed by ED personnel.
“These findings highlight the importance of ED clinicians being aware of the risk of incomplete recovery for patients with a mild TBI (that is, GCS score of 15 and negative head CT scan) and providing accurate education and timely referral information before ED discharge,” they wrote.
The study was funded by grants from the National Foundation of Emergency Medicine, the National Institute of Neurological Disorders and Stroke, and the U.S. Department of Defense Traumatic Brain Injury Endpoints Development Initiative. Dr. Madhok has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new data from the TRACK-TBI study shows.
“Seeing that more than half of the GCS [Glasgow Coma Score] 15, CT-negative TBI cohort in our study were not back to their preinjury baseline at 6 months was surprising and impacts the millions of Americans who suffer from concussions annually,” said lead author Debbie Madhok, MD, with department of emergency medicine, University of California, San Francisco.
“These results highlight the importance of improving care pathways for concussion, particularly from the emergency department,” Dr. Madhok said.
The findings were published online in JAMA Network Open.
The short- and long-term outcomes in the large group of patients who come into the ED with TBI, a GCS of 15, and without acute intracranial traumatic injury (defined as a negative head CT scan) remain poorly understood, the investigators noted. To investigate further, they evaluated outcomes at 2 weeks and 6 months in 991 of these patients (mean age, 38 years; 64% men) from the TRACK-TBI study.
Among the 751 (76%) participants followed up at 2 weeks after the injury, only 204 (27%) had functional recovery – with a Glasgow Outcome Scale-Extended (GOS-E) score of 8. The remaining 547 (73%) had incomplete recovery (GOS-E scores < 8).
Among the 659 patients (66%) followed up at 6 months after the injury, 287 (44%) had functional recovery and 372 (56%) had incomplete recovery.
Most patients who failed to recover completely reported they had not returned to their preinjury life (88%). They described trouble returning to social activities outside the home and disruptions in family relationships and friendships.
The researchers noted that the study population had a high rate of preinjury psychiatric comorbidities, and these patients were more likely to have incomplete recovery than those without psychiatric comorbidities. This aligns with results from previous studies, they added.
The investigators also noted that patients with mild TBI without acute intracranial trauma are typically managed by ED personnel.
“These findings highlight the importance of ED clinicians being aware of the risk of incomplete recovery for patients with a mild TBI (that is, GCS score of 15 and negative head CT scan) and providing accurate education and timely referral information before ED discharge,” they wrote.
The study was funded by grants from the National Foundation of Emergency Medicine, the National Institute of Neurological Disorders and Stroke, and the U.S. Department of Defense Traumatic Brain Injury Endpoints Development Initiative. Dr. Madhok has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new data from the TRACK-TBI study shows.
“Seeing that more than half of the GCS [Glasgow Coma Score] 15, CT-negative TBI cohort in our study were not back to their preinjury baseline at 6 months was surprising and impacts the millions of Americans who suffer from concussions annually,” said lead author Debbie Madhok, MD, with department of emergency medicine, University of California, San Francisco.
“These results highlight the importance of improving care pathways for concussion, particularly from the emergency department,” Dr. Madhok said.
The findings were published online in JAMA Network Open.
The short- and long-term outcomes in the large group of patients who come into the ED with TBI, a GCS of 15, and without acute intracranial traumatic injury (defined as a negative head CT scan) remain poorly understood, the investigators noted. To investigate further, they evaluated outcomes at 2 weeks and 6 months in 991 of these patients (mean age, 38 years; 64% men) from the TRACK-TBI study.
Among the 751 (76%) participants followed up at 2 weeks after the injury, only 204 (27%) had functional recovery – with a Glasgow Outcome Scale-Extended (GOS-E) score of 8. The remaining 547 (73%) had incomplete recovery (GOS-E scores < 8).
Among the 659 patients (66%) followed up at 6 months after the injury, 287 (44%) had functional recovery and 372 (56%) had incomplete recovery.
Most patients who failed to recover completely reported they had not returned to their preinjury life (88%). They described trouble returning to social activities outside the home and disruptions in family relationships and friendships.
The researchers noted that the study population had a high rate of preinjury psychiatric comorbidities, and these patients were more likely to have incomplete recovery than those without psychiatric comorbidities. This aligns with results from previous studies, they added.
The investigators also noted that patients with mild TBI without acute intracranial trauma are typically managed by ED personnel.
“These findings highlight the importance of ED clinicians being aware of the risk of incomplete recovery for patients with a mild TBI (that is, GCS score of 15 and negative head CT scan) and providing accurate education and timely referral information before ED discharge,” they wrote.
The study was funded by grants from the National Foundation of Emergency Medicine, the National Institute of Neurological Disorders and Stroke, and the U.S. Department of Defense Traumatic Brain Injury Endpoints Development Initiative. Dr. Madhok has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Will monkeypox be the ‘syphilis of the 21st century’?
PARIS – France is boosting its vaccination campaign in response to the increase in cases of monkeypox. After a sluggish start, newly appointed French health minister François Braun has announced the release of 42,000 vaccine doses. At the same time, medical students will be able to lend a helping hand at vaccination sites. However, some experts have criticized the measures taken as being too lax to combat what the World Health Organization has designated a global health emergency.
For Benjamin Davido, MD, MSc, PhD, an infectious disease specialist at the Raymond-Poincaré Hospital (Paris Public Hospital Trust, AP-HP, Garches region), the risks of this disease have been minimized and the measures taken are not adequate, despite the ready availability of the tools needed to manage the epidemic. We must remain alert to the risks posed by this monkeypox epidemic, which seems different from the sporadic outbreaks that usually crop up in Central and West Africa, he said. Dr. Davido recently shared his opinions in an interview.
Question: What do you think about the monkeypox vaccination campaign currently underway in France?
Dr. Davido: It doesn’t go far enough, and I am surprised by the lack of a concrete and specific objective. It seems we have to wait until the fire is out of control before we can call the fire department. We should have been more reactive and taken a more drastic approach from the get-go. In France, as in other countries affected by this epidemic, we are still, unfortunately, in a phase of observation, reassuring ourselves that this will surely not become another pandemic, as that would be really bad luck.
Yet we find ourselves in an unprecedented situation: We have known about the disease in question for a long time, the target population has been identified, and we have a vaccine immediately available. So, we have all the tools and knowledge acquired from the COVID-19 pandemic at our disposal, yet we are choosing to wait and see. We have clearly underestimated the risks of failing after a stalled start to the vaccination campaign.
Question: What exactly are the risks, in your opinion? Should we already be worried about how the epidemic is progressing?
Dr. Davido: The situation is definitely worrying. I personally am convinced that this disease will be the syphilis of the 21st century. Although the risk is low, it is not beyond the bounds of possibility that this could be the start of a new pandemic. For the time being, its spread is limited to at-risk populations, mainly men who have sex with other men and who have multiple partners, which accounts for around 300,000 people in France. However, the risk for heterosexuals must not be minimized; we must not forget that this disease can also be transmitted through contact with an infected person and by respiratory droplets from people living in the same household. There have been recent cases of women and children infected with monkeypox. If monkeypox starts to spread in the community, rather than being a sexually transmitted infection, the epidemic could spread to the rest of the population. With the rise in cases, scientists are also concerned about transmission to animals. Monkeypox could become endemic like it is in Africa, where rodents are the main reservoir of the virus.
Question: What do we know about the dynamics of this epidemic? What can be done to effectively improve the situation?
Dr. Davido: Experience gained from African countries affected by monkeypox, as well as from the spate of cases that occurred in the United States in 2003, has shown us that the epidemic can be controlled once the cases have been contained. It is hoped that further waves of the epidemic can be avoided, providing the monkeypox vaccine achieves its objectives.
But we need to give ourselves the means to do so. The expansion of the vaccination program to the most at-risk populations in early July was the right decision. We have seen that ring vaccination targeting close-contact cases does not work with monkeypox. The current problem is that this vaccine is nearly exclusively restricted to hospital settings. We are making the same mistakes as [we did] at the start of the COVID-19 epidemic. We don’t have the right infrastructure in place for this vaccination program. We need to get doctors, paramedics, pharmacists, etc., involved. And cut back on the red tape. After embracing digital procedures during COVID-19, we find ourselves having to complete paper copies of documents for every single person attending a vaccination site. It just doesn’t make sense!
Question: You highlighted the lack of a clear objective with this vaccination campaign. What should we be aiming for?
Dr. Davido: During the COVID-19 vaccination campaign, there was a set number of people to be vaccinated within a given time frame. The approach demanded a fast pace and a desired outcome. Yes, it was an ambitious target from the get-go, but it was one that we stuck to. Currently, no figure, no target, has been set for the monkeypox vaccination program. Ideally, we would have completed the vaccination campaign before the start of the new school year to limit new infections.
As it stands now, only 10% of the target population has received the vaccine. There is talk of the summer period not being favorable. Yet I remember that last year, the COVID-19 vaccination program was strengthened in the middle of August. If the monkeypox vaccination campaign is not given a boost by the end of the summer, we run the risk of encouraging transmission of the virus between close contacts when different groups mix after being on holiday at the start of the new school year. I think that, first and foremost, we must make general practitioners aware of the disease and train them in how to diagnose it so that patients can be isolated and vaccinated as quickly as possible.
Question: There has also been talk of increasing the set 28-day period between the two doses, or even getting rid of it entirely. Would this perhaps lead to better vaccine uptake?
Dr. Davido: The United Kingdom has chosen to give a single dose and recommends a second dose after exposure. I am not sure that this is the best strategy. Although the efficacy data are still limited, the results are not as good after a single dose. According to initial data from the French National Agency for the Safety of Medicines and Health Products (the ANSM), the rate of seroconversion after one dose rises from 10% to 56% on D28 in healthy volunteers, but is between 77% and 89% 2 weeks after the second dose administered on D28.
So, the second dose is needed, especially as immunological memory seems to drop 2 years after the first injection. The U.S. Centers for Disease Control and Prevention proposes leaving 35 days between the two doses. I think this is a reasonable time frame. So, delaying the second dose makes administration of the first dose even easier because the second often fell in the middle of the holiday period and so we also save precious doses. If the time between doses is longer, we risk vaccinated individuals becoming lax and possibly being tempted to skip the “optional” booster or simply forgetting about it.
Question: Are people who have already had the smallpox vaccine better protected against monkeypox?
Dr. Davido: The efficacy of this vaccine against monkeypox is not perfect on a very long-term basis and, to be honest, we don’t really know the level of protection afforded by first-generation vaccines after 20 years. We must not forget that 20% of people infected with monkeypox were vaccinated against smallpox before mandatory vaccination for this disease was abolished [Editor’s note: The requirement of an initial dose of smallpox vaccine was lifted in 1979, once smallpox had been eradicated].
It is hoped that, as a minimum, this vaccine protects against serious illness. Yet in my department, we regularly see severe cases of monkeypox with widespread lesions in the over 45s, who are said to be vaccinated against smallpox.
Question: By comparison, is it likely that a third-generation vaccine would afford better protection against severe illness?
Dr. Davido: We still don’t have enough data or hindsight to assess the real-world impact of third-generation vaccines. This vaccine has a better tolerance profile than its predecessors, but we currently don’t know if it protects against severe forms of monkeypox. We also need to learn more about the disease causing the current epidemic, since it seems different from the sporadic outbreaks that usually crop up in Central and West Africa. The lesions seen are notably milder. The WHO has given this vaccine an efficacy level of 85% against infection by the monkeypox virus, but we must remain cautious: This figure is based on data from Africa. The epidemic in which we find ourselves is not the same. Overall, we must be wary of overly optimistic rhetoric around this new epidemic.
A version of this article appeared on Medscape.com. The article was translated from the Medscape French edition.
PARIS – France is boosting its vaccination campaign in response to the increase in cases of monkeypox. After a sluggish start, newly appointed French health minister François Braun has announced the release of 42,000 vaccine doses. At the same time, medical students will be able to lend a helping hand at vaccination sites. However, some experts have criticized the measures taken as being too lax to combat what the World Health Organization has designated a global health emergency.
For Benjamin Davido, MD, MSc, PhD, an infectious disease specialist at the Raymond-Poincaré Hospital (Paris Public Hospital Trust, AP-HP, Garches region), the risks of this disease have been minimized and the measures taken are not adequate, despite the ready availability of the tools needed to manage the epidemic. We must remain alert to the risks posed by this monkeypox epidemic, which seems different from the sporadic outbreaks that usually crop up in Central and West Africa, he said. Dr. Davido recently shared his opinions in an interview.
Question: What do you think about the monkeypox vaccination campaign currently underway in France?
Dr. Davido: It doesn’t go far enough, and I am surprised by the lack of a concrete and specific objective. It seems we have to wait until the fire is out of control before we can call the fire department. We should have been more reactive and taken a more drastic approach from the get-go. In France, as in other countries affected by this epidemic, we are still, unfortunately, in a phase of observation, reassuring ourselves that this will surely not become another pandemic, as that would be really bad luck.
Yet we find ourselves in an unprecedented situation: We have known about the disease in question for a long time, the target population has been identified, and we have a vaccine immediately available. So, we have all the tools and knowledge acquired from the COVID-19 pandemic at our disposal, yet we are choosing to wait and see. We have clearly underestimated the risks of failing after a stalled start to the vaccination campaign.
Question: What exactly are the risks, in your opinion? Should we already be worried about how the epidemic is progressing?
Dr. Davido: The situation is definitely worrying. I personally am convinced that this disease will be the syphilis of the 21st century. Although the risk is low, it is not beyond the bounds of possibility that this could be the start of a new pandemic. For the time being, its spread is limited to at-risk populations, mainly men who have sex with other men and who have multiple partners, which accounts for around 300,000 people in France. However, the risk for heterosexuals must not be minimized; we must not forget that this disease can also be transmitted through contact with an infected person and by respiratory droplets from people living in the same household. There have been recent cases of women and children infected with monkeypox. If monkeypox starts to spread in the community, rather than being a sexually transmitted infection, the epidemic could spread to the rest of the population. With the rise in cases, scientists are also concerned about transmission to animals. Monkeypox could become endemic like it is in Africa, where rodents are the main reservoir of the virus.
Question: What do we know about the dynamics of this epidemic? What can be done to effectively improve the situation?
Dr. Davido: Experience gained from African countries affected by monkeypox, as well as from the spate of cases that occurred in the United States in 2003, has shown us that the epidemic can be controlled once the cases have been contained. It is hoped that further waves of the epidemic can be avoided, providing the monkeypox vaccine achieves its objectives.
But we need to give ourselves the means to do so. The expansion of the vaccination program to the most at-risk populations in early July was the right decision. We have seen that ring vaccination targeting close-contact cases does not work with monkeypox. The current problem is that this vaccine is nearly exclusively restricted to hospital settings. We are making the same mistakes as [we did] at the start of the COVID-19 epidemic. We don’t have the right infrastructure in place for this vaccination program. We need to get doctors, paramedics, pharmacists, etc., involved. And cut back on the red tape. After embracing digital procedures during COVID-19, we find ourselves having to complete paper copies of documents for every single person attending a vaccination site. It just doesn’t make sense!
Question: You highlighted the lack of a clear objective with this vaccination campaign. What should we be aiming for?
Dr. Davido: During the COVID-19 vaccination campaign, there was a set number of people to be vaccinated within a given time frame. The approach demanded a fast pace and a desired outcome. Yes, it was an ambitious target from the get-go, but it was one that we stuck to. Currently, no figure, no target, has been set for the monkeypox vaccination program. Ideally, we would have completed the vaccination campaign before the start of the new school year to limit new infections.
As it stands now, only 10% of the target population has received the vaccine. There is talk of the summer period not being favorable. Yet I remember that last year, the COVID-19 vaccination program was strengthened in the middle of August. If the monkeypox vaccination campaign is not given a boost by the end of the summer, we run the risk of encouraging transmission of the virus between close contacts when different groups mix after being on holiday at the start of the new school year. I think that, first and foremost, we must make general practitioners aware of the disease and train them in how to diagnose it so that patients can be isolated and vaccinated as quickly as possible.
Question: There has also been talk of increasing the set 28-day period between the two doses, or even getting rid of it entirely. Would this perhaps lead to better vaccine uptake?
Dr. Davido: The United Kingdom has chosen to give a single dose and recommends a second dose after exposure. I am not sure that this is the best strategy. Although the efficacy data are still limited, the results are not as good after a single dose. According to initial data from the French National Agency for the Safety of Medicines and Health Products (the ANSM), the rate of seroconversion after one dose rises from 10% to 56% on D28 in healthy volunteers, but is between 77% and 89% 2 weeks after the second dose administered on D28.
So, the second dose is needed, especially as immunological memory seems to drop 2 years after the first injection. The U.S. Centers for Disease Control and Prevention proposes leaving 35 days between the two doses. I think this is a reasonable time frame. So, delaying the second dose makes administration of the first dose even easier because the second often fell in the middle of the holiday period and so we also save precious doses. If the time between doses is longer, we risk vaccinated individuals becoming lax and possibly being tempted to skip the “optional” booster or simply forgetting about it.
Question: Are people who have already had the smallpox vaccine better protected against monkeypox?
Dr. Davido: The efficacy of this vaccine against monkeypox is not perfect on a very long-term basis and, to be honest, we don’t really know the level of protection afforded by first-generation vaccines after 20 years. We must not forget that 20% of people infected with monkeypox were vaccinated against smallpox before mandatory vaccination for this disease was abolished [Editor’s note: The requirement of an initial dose of smallpox vaccine was lifted in 1979, once smallpox had been eradicated].
It is hoped that, as a minimum, this vaccine protects against serious illness. Yet in my department, we regularly see severe cases of monkeypox with widespread lesions in the over 45s, who are said to be vaccinated against smallpox.
Question: By comparison, is it likely that a third-generation vaccine would afford better protection against severe illness?
Dr. Davido: We still don’t have enough data or hindsight to assess the real-world impact of third-generation vaccines. This vaccine has a better tolerance profile than its predecessors, but we currently don’t know if it protects against severe forms of monkeypox. We also need to learn more about the disease causing the current epidemic, since it seems different from the sporadic outbreaks that usually crop up in Central and West Africa. The lesions seen are notably milder. The WHO has given this vaccine an efficacy level of 85% against infection by the monkeypox virus, but we must remain cautious: This figure is based on data from Africa. The epidemic in which we find ourselves is not the same. Overall, we must be wary of overly optimistic rhetoric around this new epidemic.
A version of this article appeared on Medscape.com. The article was translated from the Medscape French edition.
PARIS – France is boosting its vaccination campaign in response to the increase in cases of monkeypox. After a sluggish start, newly appointed French health minister François Braun has announced the release of 42,000 vaccine doses. At the same time, medical students will be able to lend a helping hand at vaccination sites. However, some experts have criticized the measures taken as being too lax to combat what the World Health Organization has designated a global health emergency.
For Benjamin Davido, MD, MSc, PhD, an infectious disease specialist at the Raymond-Poincaré Hospital (Paris Public Hospital Trust, AP-HP, Garches region), the risks of this disease have been minimized and the measures taken are not adequate, despite the ready availability of the tools needed to manage the epidemic. We must remain alert to the risks posed by this monkeypox epidemic, which seems different from the sporadic outbreaks that usually crop up in Central and West Africa, he said. Dr. Davido recently shared his opinions in an interview.
Question: What do you think about the monkeypox vaccination campaign currently underway in France?
Dr. Davido: It doesn’t go far enough, and I am surprised by the lack of a concrete and specific objective. It seems we have to wait until the fire is out of control before we can call the fire department. We should have been more reactive and taken a more drastic approach from the get-go. In France, as in other countries affected by this epidemic, we are still, unfortunately, in a phase of observation, reassuring ourselves that this will surely not become another pandemic, as that would be really bad luck.
Yet we find ourselves in an unprecedented situation: We have known about the disease in question for a long time, the target population has been identified, and we have a vaccine immediately available. So, we have all the tools and knowledge acquired from the COVID-19 pandemic at our disposal, yet we are choosing to wait and see. We have clearly underestimated the risks of failing after a stalled start to the vaccination campaign.
Question: What exactly are the risks, in your opinion? Should we already be worried about how the epidemic is progressing?
Dr. Davido: The situation is definitely worrying. I personally am convinced that this disease will be the syphilis of the 21st century. Although the risk is low, it is not beyond the bounds of possibility that this could be the start of a new pandemic. For the time being, its spread is limited to at-risk populations, mainly men who have sex with other men and who have multiple partners, which accounts for around 300,000 people in France. However, the risk for heterosexuals must not be minimized; we must not forget that this disease can also be transmitted through contact with an infected person and by respiratory droplets from people living in the same household. There have been recent cases of women and children infected with monkeypox. If monkeypox starts to spread in the community, rather than being a sexually transmitted infection, the epidemic could spread to the rest of the population. With the rise in cases, scientists are also concerned about transmission to animals. Monkeypox could become endemic like it is in Africa, where rodents are the main reservoir of the virus.
Question: What do we know about the dynamics of this epidemic? What can be done to effectively improve the situation?
Dr. Davido: Experience gained from African countries affected by monkeypox, as well as from the spate of cases that occurred in the United States in 2003, has shown us that the epidemic can be controlled once the cases have been contained. It is hoped that further waves of the epidemic can be avoided, providing the monkeypox vaccine achieves its objectives.
But we need to give ourselves the means to do so. The expansion of the vaccination program to the most at-risk populations in early July was the right decision. We have seen that ring vaccination targeting close-contact cases does not work with monkeypox. The current problem is that this vaccine is nearly exclusively restricted to hospital settings. We are making the same mistakes as [we did] at the start of the COVID-19 epidemic. We don’t have the right infrastructure in place for this vaccination program. We need to get doctors, paramedics, pharmacists, etc., involved. And cut back on the red tape. After embracing digital procedures during COVID-19, we find ourselves having to complete paper copies of documents for every single person attending a vaccination site. It just doesn’t make sense!
Question: You highlighted the lack of a clear objective with this vaccination campaign. What should we be aiming for?
Dr. Davido: During the COVID-19 vaccination campaign, there was a set number of people to be vaccinated within a given time frame. The approach demanded a fast pace and a desired outcome. Yes, it was an ambitious target from the get-go, but it was one that we stuck to. Currently, no figure, no target, has been set for the monkeypox vaccination program. Ideally, we would have completed the vaccination campaign before the start of the new school year to limit new infections.
As it stands now, only 10% of the target population has received the vaccine. There is talk of the summer period not being favorable. Yet I remember that last year, the COVID-19 vaccination program was strengthened in the middle of August. If the monkeypox vaccination campaign is not given a boost by the end of the summer, we run the risk of encouraging transmission of the virus between close contacts when different groups mix after being on holiday at the start of the new school year. I think that, first and foremost, we must make general practitioners aware of the disease and train them in how to diagnose it so that patients can be isolated and vaccinated as quickly as possible.
Question: There has also been talk of increasing the set 28-day period between the two doses, or even getting rid of it entirely. Would this perhaps lead to better vaccine uptake?
Dr. Davido: The United Kingdom has chosen to give a single dose and recommends a second dose after exposure. I am not sure that this is the best strategy. Although the efficacy data are still limited, the results are not as good after a single dose. According to initial data from the French National Agency for the Safety of Medicines and Health Products (the ANSM), the rate of seroconversion after one dose rises from 10% to 56% on D28 in healthy volunteers, but is between 77% and 89% 2 weeks after the second dose administered on D28.
So, the second dose is needed, especially as immunological memory seems to drop 2 years after the first injection. The U.S. Centers for Disease Control and Prevention proposes leaving 35 days between the two doses. I think this is a reasonable time frame. So, delaying the second dose makes administration of the first dose even easier because the second often fell in the middle of the holiday period and so we also save precious doses. If the time between doses is longer, we risk vaccinated individuals becoming lax and possibly being tempted to skip the “optional” booster or simply forgetting about it.
Question: Are people who have already had the smallpox vaccine better protected against monkeypox?
Dr. Davido: The efficacy of this vaccine against monkeypox is not perfect on a very long-term basis and, to be honest, we don’t really know the level of protection afforded by first-generation vaccines after 20 years. We must not forget that 20% of people infected with monkeypox were vaccinated against smallpox before mandatory vaccination for this disease was abolished [Editor’s note: The requirement of an initial dose of smallpox vaccine was lifted in 1979, once smallpox had been eradicated].
It is hoped that, as a minimum, this vaccine protects against serious illness. Yet in my department, we regularly see severe cases of monkeypox with widespread lesions in the over 45s, who are said to be vaccinated against smallpox.
Question: By comparison, is it likely that a third-generation vaccine would afford better protection against severe illness?
Dr. Davido: We still don’t have enough data or hindsight to assess the real-world impact of third-generation vaccines. This vaccine has a better tolerance profile than its predecessors, but we currently don’t know if it protects against severe forms of monkeypox. We also need to learn more about the disease causing the current epidemic, since it seems different from the sporadic outbreaks that usually crop up in Central and West Africa. The lesions seen are notably milder. The WHO has given this vaccine an efficacy level of 85% against infection by the monkeypox virus, but we must remain cautious: This figure is based on data from Africa. The epidemic in which we find ourselves is not the same. Overall, we must be wary of overly optimistic rhetoric around this new epidemic.
A version of this article appeared on Medscape.com. The article was translated from the Medscape French edition.
‘I missed it’: Coping with medical error
Thursday night
It was 9 o’clock at night when my phone rang. I didn’t recognize the number but decided to answer it anyway. It was my doctor.
“Chase, I got your labs back and you have a critically low level. I spoke with someone at the hospital, I think I know what is happening, but I need you to go to the pharmacy right now and get a medicine.” She explained further and as I listened electric currents ran through my thighs until I could barely feel my legs.
“I’m so sorry, Chase. I missed it. It was low the last time we did your labs 9 months ago, and I missed it.”
In disbelief, I continued to listen as she instructed me about the next steps I was to take and prepared me for what was to come the next day.
“If you notice any changes overnight, go straight to the ED.”
My chest tingled and I could barely breathe. My mind struggled to comprehend what was happening. I looked at my husband sitting close by on the couch. He looked concerned. I tuned back in and heard her say: “Is your husband there? Can I talk to him?”
“Yes,” is all I could manage, and I handed him the phone. I sat while he listened and asked his questions. My breathing came back under my control, my legs felt wiry, and restlessness set in. “I have to get out of here,” I thought. “I have to go and pick up this medicine.”
Monday afternoon
I am sitting across from a PGY3 resident I have been treating since his intern year, as part of his treatment plan for managing a chronic mental illness that began in medical school. Earlier in the day, I received an urgent message from him requesting an emergency appointment.
Within a few minutes of sitting down, the story from his weekend call shift tumbled out of him. His speech became pressured, and his eyes welled with tears as he recounted in detail the steps he had taken to care for a very sick patient overnight.
“I missed it.” The dam broke and he sat sobbing in front of me, his body trembling.
I sat silently across from him. Willing him to breathe.
In time, his breathing came back under his control, and he slowly regained his composure. He continued: “I got the imaging, and I missed a bleed.”
Failure and shame
I can recall memorable moments from my training when I came to understand that what I initially perceived to be a mistake was instead part of the work. An example from our practice involves a patient whom I was comanaging with her primary care provider (PCP). She was not doing well following a critical work event. When I met with her after the event, she admitted having thoughts of suicide, refused a voluntary inpatient admission, and would not have met criteria for an involuntary admission. My hands were tied.
Together we created a plan to keep her safe, which included paging her PCP after hours if needed. I told her PCP before leaving that night that he might hear from her and that if she reached out, she would require hospitalization.
I arrived at work the following day, and her PCP shared with me that our patient had overdosed on medication, paged him, and was admitted to the unit.
He seemed forlorn.
I was both relieved by the news and confused by his reaction. I had hoped that she would choose a higher level of care than what we could provide her as an outpatient. I said: “This is good. She followed the plan.”
Her overdose was, of course, not part of the plan. She was struggling with several internal conflicts, including having mixed feelings about coming into the hospital; but, when the critical moment happened and she was faced with a decision to call for help or possibly die, she chose to call her PCP and have him paged as we had talked about.
I looked at her PCP. “You helped get her to where she needed to be.”
In the years of working side by side with medically trained colleagues, I have time and again needed to reframe for them that what they perceive to be a “failure” or a “crisis” is often a catalyst for change. The patient I comanaged with the PCP was a highly skilled caregiver and, as such, had been having a hard time asking for help. The hospitalization that her PCP facilitated allowed her to receive the care she needed and created an opportunity for family and friends to show up for her. Their support fed her, and she only made gains from that point on.
My training had taught me that respecting a patient’s autonomy was of the utmost importance. This instills confidence in patients as the authority in their lives. For a clinician to do this, a certain amount of helplessness must be tolerated. As I became better at identifying these moments of helplessness, feelings of failure and shame transformed.
Medical error
Sitting across from the PGY3 resident who I had met with weekly for the past 3 years, I thought about his error.
I thought about my phone call 4 nights earlier. My doctor was called at home by a lab technician, who never met their patients but was simply following protocol and alerted my doctor to the worsening number that she should have been aware of 9 months earlier.
Just like my doctor’s lapse of attention, my patient’s error was not a moment of helplessness to be tolerated. These were mistakes, and there was no way around it.
“People make mistakes.” I said simply.
We sat silently for a time.
I don’t remember who broke the silence. The conversation that followed was centered on our humanity and our capability for both compassion and fallibility. Afterward, I wondered who my doctor confided in and hoped she had a similar conversation.
Dr. Levesque is a clinical psychologist and clinical assistant professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H., where she also serves on the Committee for a Respectful Learning Environment.
A version of this article first appeared on Medscape.com.
Thursday night
It was 9 o’clock at night when my phone rang. I didn’t recognize the number but decided to answer it anyway. It was my doctor.
“Chase, I got your labs back and you have a critically low level. I spoke with someone at the hospital, I think I know what is happening, but I need you to go to the pharmacy right now and get a medicine.” She explained further and as I listened electric currents ran through my thighs until I could barely feel my legs.
“I’m so sorry, Chase. I missed it. It was low the last time we did your labs 9 months ago, and I missed it.”
In disbelief, I continued to listen as she instructed me about the next steps I was to take and prepared me for what was to come the next day.
“If you notice any changes overnight, go straight to the ED.”
My chest tingled and I could barely breathe. My mind struggled to comprehend what was happening. I looked at my husband sitting close by on the couch. He looked concerned. I tuned back in and heard her say: “Is your husband there? Can I talk to him?”
“Yes,” is all I could manage, and I handed him the phone. I sat while he listened and asked his questions. My breathing came back under my control, my legs felt wiry, and restlessness set in. “I have to get out of here,” I thought. “I have to go and pick up this medicine.”
Monday afternoon
I am sitting across from a PGY3 resident I have been treating since his intern year, as part of his treatment plan for managing a chronic mental illness that began in medical school. Earlier in the day, I received an urgent message from him requesting an emergency appointment.
Within a few minutes of sitting down, the story from his weekend call shift tumbled out of him. His speech became pressured, and his eyes welled with tears as he recounted in detail the steps he had taken to care for a very sick patient overnight.
“I missed it.” The dam broke and he sat sobbing in front of me, his body trembling.
I sat silently across from him. Willing him to breathe.
In time, his breathing came back under his control, and he slowly regained his composure. He continued: “I got the imaging, and I missed a bleed.”
Failure and shame
I can recall memorable moments from my training when I came to understand that what I initially perceived to be a mistake was instead part of the work. An example from our practice involves a patient whom I was comanaging with her primary care provider (PCP). She was not doing well following a critical work event. When I met with her after the event, she admitted having thoughts of suicide, refused a voluntary inpatient admission, and would not have met criteria for an involuntary admission. My hands were tied.
Together we created a plan to keep her safe, which included paging her PCP after hours if needed. I told her PCP before leaving that night that he might hear from her and that if she reached out, she would require hospitalization.
I arrived at work the following day, and her PCP shared with me that our patient had overdosed on medication, paged him, and was admitted to the unit.
He seemed forlorn.
I was both relieved by the news and confused by his reaction. I had hoped that she would choose a higher level of care than what we could provide her as an outpatient. I said: “This is good. She followed the plan.”
Her overdose was, of course, not part of the plan. She was struggling with several internal conflicts, including having mixed feelings about coming into the hospital; but, when the critical moment happened and she was faced with a decision to call for help or possibly die, she chose to call her PCP and have him paged as we had talked about.
I looked at her PCP. “You helped get her to where she needed to be.”
In the years of working side by side with medically trained colleagues, I have time and again needed to reframe for them that what they perceive to be a “failure” or a “crisis” is often a catalyst for change. The patient I comanaged with the PCP was a highly skilled caregiver and, as such, had been having a hard time asking for help. The hospitalization that her PCP facilitated allowed her to receive the care she needed and created an opportunity for family and friends to show up for her. Their support fed her, and she only made gains from that point on.
My training had taught me that respecting a patient’s autonomy was of the utmost importance. This instills confidence in patients as the authority in their lives. For a clinician to do this, a certain amount of helplessness must be tolerated. As I became better at identifying these moments of helplessness, feelings of failure and shame transformed.
Medical error
Sitting across from the PGY3 resident who I had met with weekly for the past 3 years, I thought about his error.
I thought about my phone call 4 nights earlier. My doctor was called at home by a lab technician, who never met their patients but was simply following protocol and alerted my doctor to the worsening number that she should have been aware of 9 months earlier.
Just like my doctor’s lapse of attention, my patient’s error was not a moment of helplessness to be tolerated. These were mistakes, and there was no way around it.
“People make mistakes.” I said simply.
We sat silently for a time.
I don’t remember who broke the silence. The conversation that followed was centered on our humanity and our capability for both compassion and fallibility. Afterward, I wondered who my doctor confided in and hoped she had a similar conversation.
Dr. Levesque is a clinical psychologist and clinical assistant professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H., where she also serves on the Committee for a Respectful Learning Environment.
A version of this article first appeared on Medscape.com.
Thursday night
It was 9 o’clock at night when my phone rang. I didn’t recognize the number but decided to answer it anyway. It was my doctor.
“Chase, I got your labs back and you have a critically low level. I spoke with someone at the hospital, I think I know what is happening, but I need you to go to the pharmacy right now and get a medicine.” She explained further and as I listened electric currents ran through my thighs until I could barely feel my legs.
“I’m so sorry, Chase. I missed it. It was low the last time we did your labs 9 months ago, and I missed it.”
In disbelief, I continued to listen as she instructed me about the next steps I was to take and prepared me for what was to come the next day.
“If you notice any changes overnight, go straight to the ED.”
My chest tingled and I could barely breathe. My mind struggled to comprehend what was happening. I looked at my husband sitting close by on the couch. He looked concerned. I tuned back in and heard her say: “Is your husband there? Can I talk to him?”
“Yes,” is all I could manage, and I handed him the phone. I sat while he listened and asked his questions. My breathing came back under my control, my legs felt wiry, and restlessness set in. “I have to get out of here,” I thought. “I have to go and pick up this medicine.”
Monday afternoon
I am sitting across from a PGY3 resident I have been treating since his intern year, as part of his treatment plan for managing a chronic mental illness that began in medical school. Earlier in the day, I received an urgent message from him requesting an emergency appointment.
Within a few minutes of sitting down, the story from his weekend call shift tumbled out of him. His speech became pressured, and his eyes welled with tears as he recounted in detail the steps he had taken to care for a very sick patient overnight.
“I missed it.” The dam broke and he sat sobbing in front of me, his body trembling.
I sat silently across from him. Willing him to breathe.
In time, his breathing came back under his control, and he slowly regained his composure. He continued: “I got the imaging, and I missed a bleed.”
Failure and shame
I can recall memorable moments from my training when I came to understand that what I initially perceived to be a mistake was instead part of the work. An example from our practice involves a patient whom I was comanaging with her primary care provider (PCP). She was not doing well following a critical work event. When I met with her after the event, she admitted having thoughts of suicide, refused a voluntary inpatient admission, and would not have met criteria for an involuntary admission. My hands were tied.
Together we created a plan to keep her safe, which included paging her PCP after hours if needed. I told her PCP before leaving that night that he might hear from her and that if she reached out, she would require hospitalization.
I arrived at work the following day, and her PCP shared with me that our patient had overdosed on medication, paged him, and was admitted to the unit.
He seemed forlorn.
I was both relieved by the news and confused by his reaction. I had hoped that she would choose a higher level of care than what we could provide her as an outpatient. I said: “This is good. She followed the plan.”
Her overdose was, of course, not part of the plan. She was struggling with several internal conflicts, including having mixed feelings about coming into the hospital; but, when the critical moment happened and she was faced with a decision to call for help or possibly die, she chose to call her PCP and have him paged as we had talked about.
I looked at her PCP. “You helped get her to where she needed to be.”
In the years of working side by side with medically trained colleagues, I have time and again needed to reframe for them that what they perceive to be a “failure” or a “crisis” is often a catalyst for change. The patient I comanaged with the PCP was a highly skilled caregiver and, as such, had been having a hard time asking for help. The hospitalization that her PCP facilitated allowed her to receive the care she needed and created an opportunity for family and friends to show up for her. Their support fed her, and she only made gains from that point on.
My training had taught me that respecting a patient’s autonomy was of the utmost importance. This instills confidence in patients as the authority in their lives. For a clinician to do this, a certain amount of helplessness must be tolerated. As I became better at identifying these moments of helplessness, feelings of failure and shame transformed.
Medical error
Sitting across from the PGY3 resident who I had met with weekly for the past 3 years, I thought about his error.
I thought about my phone call 4 nights earlier. My doctor was called at home by a lab technician, who never met their patients but was simply following protocol and alerted my doctor to the worsening number that she should have been aware of 9 months earlier.
Just like my doctor’s lapse of attention, my patient’s error was not a moment of helplessness to be tolerated. These were mistakes, and there was no way around it.
“People make mistakes.” I said simply.
We sat silently for a time.
I don’t remember who broke the silence. The conversation that followed was centered on our humanity and our capability for both compassion and fallibility. Afterward, I wondered who my doctor confided in and hoped she had a similar conversation.
Dr. Levesque is a clinical psychologist and clinical assistant professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H., where she also serves on the Committee for a Respectful Learning Environment.
A version of this article first appeared on Medscape.com.
Regular physical activity may fight infection, illness from COVID: Study
New research suggests that regular physical activity can help lower the risk of COVID-19 infection and its severity, with a weekly tally of 150 minutes of moderate, or 75 minutes of vigorous, physical activity affording the best protection.
“, with potential benefits to reduce the risk of severe COVID-19,” say Antonio García-Hermoso, PhD, Public University of Navarra, Pamplona, Spain, and colleagues.
“Regular physical activity seemed to be related to a lower risk of COVID-19 infection, Dr. García-Hermoso said in an interview. “There is evidence that regular physical activity might contribute to a more effective immune response, providing enhanced protective immunity to infections, which could explain the relationship between exercise consistency with COVID-19 infection.”
Regular exercise may also help to boost the body’s anti-inflammatory responses, as well as cardiorespiratory and muscular fitness, all of which may explain its beneficial effects on COVID-19 severity, the researchers say.
The study was published online in the British Journal of Sports Medicine.
Strong protection from COVID?
A growing body of evidence suggests that increased physical activity may modulate the course of COVID-19 infection and reduce the risk of poor outcomes. The new analysis is the first to systematically evaluate and pool data on the effect of regular physical activity on COVID-19 outcomes.
The findings are based on data from 16 studies with over 1.8 million adults (53% women, mean age 53 years).
Individuals who included regular physical activity in their weekly routine had an 11% lower risk for infection with SARS-CoV-2 (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95), compared with inactive peers.
The physically active adults also had a 36% (HR, 0.64; 95% CI, 0.54-0.76) lower risk of being hospitalized, a 44% (HR, 0.66; 95% CI, 0.58-0.77) lower risk for severe COVID-19 illness, and a 43% (HR, 0.57; 95% CI, 0.46-0.71) lower risk of dying from COVID-19 than their inactive peers.
The greatest protective effect occurs with achieving at least 500 metabolic equivalent of task (MET) minutes per week of physical activity – equivalent to 150 minutes of moderate-intensity or 75 min of vigorous-intensity physical activity per week – with no added benefit beyond this level.
The researchers caution that the analysis included observational studies, differing study designs, subjective assessments of physical activity levels, and concerned only the Beta and Delta variants of SARS-CoV-2, not Omicron.
Despite these limitations, the researchers say their findings “may help guide physicians and health care policymakers in making recommendations and developing guidelines with respect to the degree of physical activity that can help reduce the risk of infectivity, hospitalization, severity, and mortality of COVID-19 at both the individual and the population level, especially in high-risk patients.”
Helpful, but not a panacea
Reached for comment, Sean Heffron, MD, a preventive cardiologist and assistant professor of medicine at NYU Langone Health, New York, said the study “supports the well-established nonlinear association of increasing physical activity with adverse outcomes from a diverse array of diseases, including infectious diseases, such as COVID-19.”
The observation is not particularly surprising, he said.
“It is as I would suspect. They compiled data from a large number of studies published over the past several years that all had consistent findings,” Dr. Heffron said.
“The take-away from a public health standpoint is that being physically active improves health in myriad ways. That being said, it is not a panacea, so additional measures (masking, vaccinations, etc.) are important for everyone,” he said.
Also weighing in, Joseph Herrera, DO, chair of the department of rehabilitation for Mount Sinai Health System, New York, said, “If you are physically fit, your body is more resilient and better prepared to handle the stressors of COVID or any other disease process.”
For now, however, the question of whether physical fitness is actually protective against COVID remains unclear. “I’m just not sure right now,” Dr. Herrera said in an interview.
He said he has treated athletes in professional sports – including the National Football League and Major League Baseball – and some of them have had long COVID and have not returned to play. “These are athletes at the peak of fitness and their career.”
Nonetheless, Dr. Herrera said a good public health message in general is to stay fit or get fit.
“That’s something I preach all the time,” he told this news organization.
Dr. García-Hermoso agreed. “In contrast to the vast majority of drugs, exercise is free of adverse effects. It’s time to consider exercise as medicine. It’s never too late to start being physically active.”
The study had no specific funding. Dr. García-Hermoso, Dr. Heffron, and Dr. Herrera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research suggests that regular physical activity can help lower the risk of COVID-19 infection and its severity, with a weekly tally of 150 minutes of moderate, or 75 minutes of vigorous, physical activity affording the best protection.
“, with potential benefits to reduce the risk of severe COVID-19,” say Antonio García-Hermoso, PhD, Public University of Navarra, Pamplona, Spain, and colleagues.
“Regular physical activity seemed to be related to a lower risk of COVID-19 infection, Dr. García-Hermoso said in an interview. “There is evidence that regular physical activity might contribute to a more effective immune response, providing enhanced protective immunity to infections, which could explain the relationship between exercise consistency with COVID-19 infection.”
Regular exercise may also help to boost the body’s anti-inflammatory responses, as well as cardiorespiratory and muscular fitness, all of which may explain its beneficial effects on COVID-19 severity, the researchers say.
The study was published online in the British Journal of Sports Medicine.
Strong protection from COVID?
A growing body of evidence suggests that increased physical activity may modulate the course of COVID-19 infection and reduce the risk of poor outcomes. The new analysis is the first to systematically evaluate and pool data on the effect of regular physical activity on COVID-19 outcomes.
The findings are based on data from 16 studies with over 1.8 million adults (53% women, mean age 53 years).
Individuals who included regular physical activity in their weekly routine had an 11% lower risk for infection with SARS-CoV-2 (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95), compared with inactive peers.
The physically active adults also had a 36% (HR, 0.64; 95% CI, 0.54-0.76) lower risk of being hospitalized, a 44% (HR, 0.66; 95% CI, 0.58-0.77) lower risk for severe COVID-19 illness, and a 43% (HR, 0.57; 95% CI, 0.46-0.71) lower risk of dying from COVID-19 than their inactive peers.
The greatest protective effect occurs with achieving at least 500 metabolic equivalent of task (MET) minutes per week of physical activity – equivalent to 150 minutes of moderate-intensity or 75 min of vigorous-intensity physical activity per week – with no added benefit beyond this level.
The researchers caution that the analysis included observational studies, differing study designs, subjective assessments of physical activity levels, and concerned only the Beta and Delta variants of SARS-CoV-2, not Omicron.
Despite these limitations, the researchers say their findings “may help guide physicians and health care policymakers in making recommendations and developing guidelines with respect to the degree of physical activity that can help reduce the risk of infectivity, hospitalization, severity, and mortality of COVID-19 at both the individual and the population level, especially in high-risk patients.”
Helpful, but not a panacea
Reached for comment, Sean Heffron, MD, a preventive cardiologist and assistant professor of medicine at NYU Langone Health, New York, said the study “supports the well-established nonlinear association of increasing physical activity with adverse outcomes from a diverse array of diseases, including infectious diseases, such as COVID-19.”
The observation is not particularly surprising, he said.
“It is as I would suspect. They compiled data from a large number of studies published over the past several years that all had consistent findings,” Dr. Heffron said.
“The take-away from a public health standpoint is that being physically active improves health in myriad ways. That being said, it is not a panacea, so additional measures (masking, vaccinations, etc.) are important for everyone,” he said.
Also weighing in, Joseph Herrera, DO, chair of the department of rehabilitation for Mount Sinai Health System, New York, said, “If you are physically fit, your body is more resilient and better prepared to handle the stressors of COVID or any other disease process.”
For now, however, the question of whether physical fitness is actually protective against COVID remains unclear. “I’m just not sure right now,” Dr. Herrera said in an interview.
He said he has treated athletes in professional sports – including the National Football League and Major League Baseball – and some of them have had long COVID and have not returned to play. “These are athletes at the peak of fitness and their career.”
Nonetheless, Dr. Herrera said a good public health message in general is to stay fit or get fit.
“That’s something I preach all the time,” he told this news organization.
Dr. García-Hermoso agreed. “In contrast to the vast majority of drugs, exercise is free of adverse effects. It’s time to consider exercise as medicine. It’s never too late to start being physically active.”
The study had no specific funding. Dr. García-Hermoso, Dr. Heffron, and Dr. Herrera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research suggests that regular physical activity can help lower the risk of COVID-19 infection and its severity, with a weekly tally of 150 minutes of moderate, or 75 minutes of vigorous, physical activity affording the best protection.
“, with potential benefits to reduce the risk of severe COVID-19,” say Antonio García-Hermoso, PhD, Public University of Navarra, Pamplona, Spain, and colleagues.
“Regular physical activity seemed to be related to a lower risk of COVID-19 infection, Dr. García-Hermoso said in an interview. “There is evidence that regular physical activity might contribute to a more effective immune response, providing enhanced protective immunity to infections, which could explain the relationship between exercise consistency with COVID-19 infection.”
Regular exercise may also help to boost the body’s anti-inflammatory responses, as well as cardiorespiratory and muscular fitness, all of which may explain its beneficial effects on COVID-19 severity, the researchers say.
The study was published online in the British Journal of Sports Medicine.
Strong protection from COVID?
A growing body of evidence suggests that increased physical activity may modulate the course of COVID-19 infection and reduce the risk of poor outcomes. The new analysis is the first to systematically evaluate and pool data on the effect of regular physical activity on COVID-19 outcomes.
The findings are based on data from 16 studies with over 1.8 million adults (53% women, mean age 53 years).
Individuals who included regular physical activity in their weekly routine had an 11% lower risk for infection with SARS-CoV-2 (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95), compared with inactive peers.
The physically active adults also had a 36% (HR, 0.64; 95% CI, 0.54-0.76) lower risk of being hospitalized, a 44% (HR, 0.66; 95% CI, 0.58-0.77) lower risk for severe COVID-19 illness, and a 43% (HR, 0.57; 95% CI, 0.46-0.71) lower risk of dying from COVID-19 than their inactive peers.
The greatest protective effect occurs with achieving at least 500 metabolic equivalent of task (MET) minutes per week of physical activity – equivalent to 150 minutes of moderate-intensity or 75 min of vigorous-intensity physical activity per week – with no added benefit beyond this level.
The researchers caution that the analysis included observational studies, differing study designs, subjective assessments of physical activity levels, and concerned only the Beta and Delta variants of SARS-CoV-2, not Omicron.
Despite these limitations, the researchers say their findings “may help guide physicians and health care policymakers in making recommendations and developing guidelines with respect to the degree of physical activity that can help reduce the risk of infectivity, hospitalization, severity, and mortality of COVID-19 at both the individual and the population level, especially in high-risk patients.”
Helpful, but not a panacea
Reached for comment, Sean Heffron, MD, a preventive cardiologist and assistant professor of medicine at NYU Langone Health, New York, said the study “supports the well-established nonlinear association of increasing physical activity with adverse outcomes from a diverse array of diseases, including infectious diseases, such as COVID-19.”
The observation is not particularly surprising, he said.
“It is as I would suspect. They compiled data from a large number of studies published over the past several years that all had consistent findings,” Dr. Heffron said.
“The take-away from a public health standpoint is that being physically active improves health in myriad ways. That being said, it is not a panacea, so additional measures (masking, vaccinations, etc.) are important for everyone,” he said.
Also weighing in, Joseph Herrera, DO, chair of the department of rehabilitation for Mount Sinai Health System, New York, said, “If you are physically fit, your body is more resilient and better prepared to handle the stressors of COVID or any other disease process.”
For now, however, the question of whether physical fitness is actually protective against COVID remains unclear. “I’m just not sure right now,” Dr. Herrera said in an interview.
He said he has treated athletes in professional sports – including the National Football League and Major League Baseball – and some of them have had long COVID and have not returned to play. “These are athletes at the peak of fitness and their career.”
Nonetheless, Dr. Herrera said a good public health message in general is to stay fit or get fit.
“That’s something I preach all the time,” he told this news organization.
Dr. García-Hermoso agreed. “In contrast to the vast majority of drugs, exercise is free of adverse effects. It’s time to consider exercise as medicine. It’s never too late to start being physically active.”
The study had no specific funding. Dr. García-Hermoso, Dr. Heffron, and Dr. Herrera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BRITISH JOURNAL OF SPORTS MEDICINE