User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Study finds genetic factor for COVID smell and taste loss
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
FROM NATURE GENETICS
Fourth vaccine shot less effective against Omicron, Israeli study says
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
Children and COVID: U.S. sees almost 1 million new cases
Another record week for COVID-19 brought almost 1 million new cases to the children of the United States, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
The pre-Omicron high for new cases in a week – 252,000 during the Delta surge of the late summer and early fall – has been surpassed each of the last 3 weeks and now stands at 981,000 (Jan. 7-13), according to the AAP/CHA weekly COVID-19 report. Over the 3-week stretch from Dec. 17 to Jan. 13, weekly cases increased by 394%.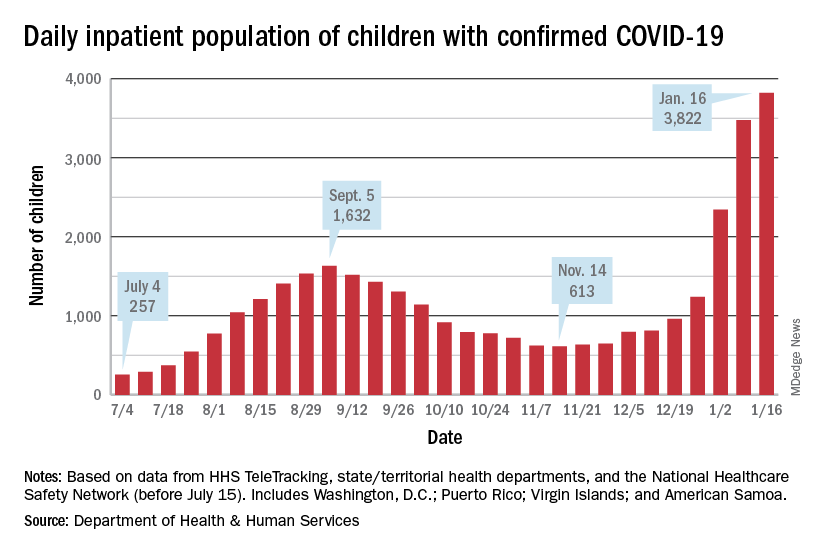
Hospitalizations also climbed to new heights, as daily admissions reached 1.23 per 100,000 children on Jan. 14, an increase of 547% since Nov. 30, when the rate was 0.19 per 100,000. Before Omicron, the highest rate for children was 0.47 per 100,000, based on data from the Centers for Disease Control and Prevention.
The inpatient population count, meanwhile, has followed suit. On Jan. 16, there were 3,822 children hospitalized in pediatric inpatient beds with laboratory-confirmed COVID-19, which is 523% higher than the 613 children who were hospitalized on Nov. 14, according to the Department of Health & Human Services. In the last week, though, the population was up by just 10%.
The one thing that has not surged in the last few weeks is vaccination. Among children aged 5-11 years, the weekly count of those who have received at least one dose dropped by 34% over the last 5 weeks, falling from 527,000 for Dec.11-17 to 347,000 during Jan. 8-14, the CDC said on the COVID Data Tracker, which also noted that just 18.4% of this age group is fully vaccinated.
The situation was reversed in children aged 12-15, who were up by 36% over that same time, but their numbers were much smaller: 78,000 for the week of Dec. 11-17 and 106,000 for Jan. 8-14. Those aged 16-17 were up by just 4% over that 5-week span, the CDC data show.
Over the course of the entire pandemic, almost 9.5 million cases of COVID-19 in children have been reported, and children represent 17.8% of all cases reported in 49 states (excluding New York but including New York City), the District of Columbia, Puerto Rico, and Guam, the AAP and CHA said in their report.
Three states (Alabama, Nebraska, and Texas) stopped public reporting over the summer, but many states count individuals up to age 19 as children, and others (South Carolina, Tennessee, and West Virginia) go up to age 20, the AAP and CHA noted. The CDC, by comparison, puts the number of cases for those aged 0-17 at 8.3 million, but that estimate is based on only 51 million of the nearly 67 million U.S. cases as of Jan. 18.
Another record week for COVID-19 brought almost 1 million new cases to the children of the United States, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
The pre-Omicron high for new cases in a week – 252,000 during the Delta surge of the late summer and early fall – has been surpassed each of the last 3 weeks and now stands at 981,000 (Jan. 7-13), according to the AAP/CHA weekly COVID-19 report. Over the 3-week stretch from Dec. 17 to Jan. 13, weekly cases increased by 394%.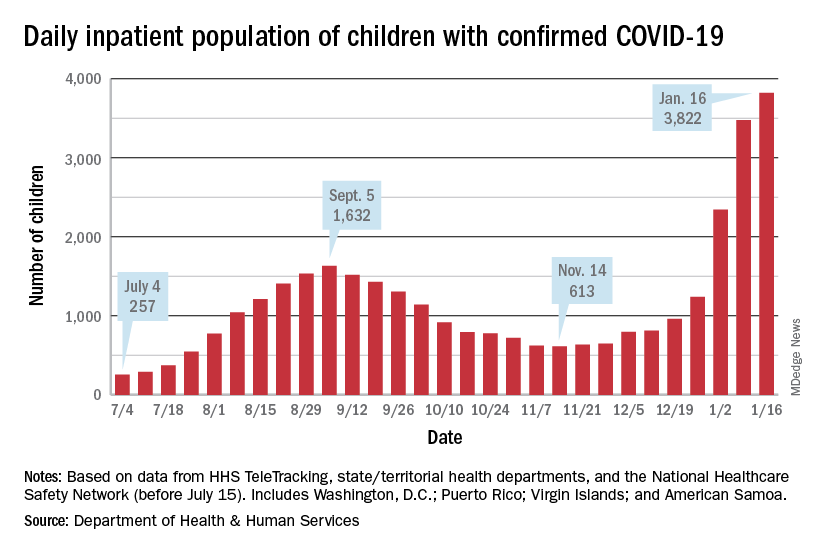
Hospitalizations also climbed to new heights, as daily admissions reached 1.23 per 100,000 children on Jan. 14, an increase of 547% since Nov. 30, when the rate was 0.19 per 100,000. Before Omicron, the highest rate for children was 0.47 per 100,000, based on data from the Centers for Disease Control and Prevention.
The inpatient population count, meanwhile, has followed suit. On Jan. 16, there were 3,822 children hospitalized in pediatric inpatient beds with laboratory-confirmed COVID-19, which is 523% higher than the 613 children who were hospitalized on Nov. 14, according to the Department of Health & Human Services. In the last week, though, the population was up by just 10%.
The one thing that has not surged in the last few weeks is vaccination. Among children aged 5-11 years, the weekly count of those who have received at least one dose dropped by 34% over the last 5 weeks, falling from 527,000 for Dec.11-17 to 347,000 during Jan. 8-14, the CDC said on the COVID Data Tracker, which also noted that just 18.4% of this age group is fully vaccinated.
The situation was reversed in children aged 12-15, who were up by 36% over that same time, but their numbers were much smaller: 78,000 for the week of Dec. 11-17 and 106,000 for Jan. 8-14. Those aged 16-17 were up by just 4% over that 5-week span, the CDC data show.
Over the course of the entire pandemic, almost 9.5 million cases of COVID-19 in children have been reported, and children represent 17.8% of all cases reported in 49 states (excluding New York but including New York City), the District of Columbia, Puerto Rico, and Guam, the AAP and CHA said in their report.
Three states (Alabama, Nebraska, and Texas) stopped public reporting over the summer, but many states count individuals up to age 19 as children, and others (South Carolina, Tennessee, and West Virginia) go up to age 20, the AAP and CHA noted. The CDC, by comparison, puts the number of cases for those aged 0-17 at 8.3 million, but that estimate is based on only 51 million of the nearly 67 million U.S. cases as of Jan. 18.
Another record week for COVID-19 brought almost 1 million new cases to the children of the United States, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
The pre-Omicron high for new cases in a week – 252,000 during the Delta surge of the late summer and early fall – has been surpassed each of the last 3 weeks and now stands at 981,000 (Jan. 7-13), according to the AAP/CHA weekly COVID-19 report. Over the 3-week stretch from Dec. 17 to Jan. 13, weekly cases increased by 394%.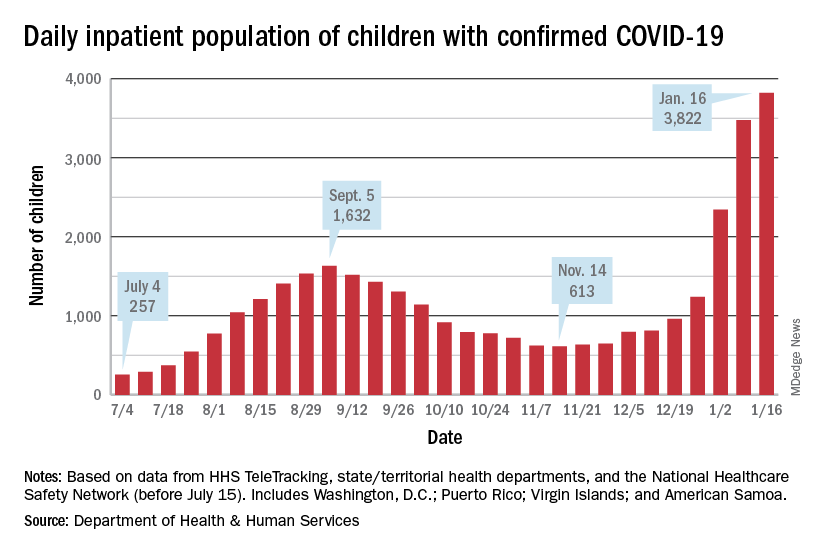
Hospitalizations also climbed to new heights, as daily admissions reached 1.23 per 100,000 children on Jan. 14, an increase of 547% since Nov. 30, when the rate was 0.19 per 100,000. Before Omicron, the highest rate for children was 0.47 per 100,000, based on data from the Centers for Disease Control and Prevention.
The inpatient population count, meanwhile, has followed suit. On Jan. 16, there were 3,822 children hospitalized in pediatric inpatient beds with laboratory-confirmed COVID-19, which is 523% higher than the 613 children who were hospitalized on Nov. 14, according to the Department of Health & Human Services. In the last week, though, the population was up by just 10%.
The one thing that has not surged in the last few weeks is vaccination. Among children aged 5-11 years, the weekly count of those who have received at least one dose dropped by 34% over the last 5 weeks, falling from 527,000 for Dec.11-17 to 347,000 during Jan. 8-14, the CDC said on the COVID Data Tracker, which also noted that just 18.4% of this age group is fully vaccinated.
The situation was reversed in children aged 12-15, who were up by 36% over that same time, but their numbers were much smaller: 78,000 for the week of Dec. 11-17 and 106,000 for Jan. 8-14. Those aged 16-17 were up by just 4% over that 5-week span, the CDC data show.
Over the course of the entire pandemic, almost 9.5 million cases of COVID-19 in children have been reported, and children represent 17.8% of all cases reported in 49 states (excluding New York but including New York City), the District of Columbia, Puerto Rico, and Guam, the AAP and CHA said in their report.
Three states (Alabama, Nebraska, and Texas) stopped public reporting over the summer, but many states count individuals up to age 19 as children, and others (South Carolina, Tennessee, and West Virginia) go up to age 20, the AAP and CHA noted. The CDC, by comparison, puts the number of cases for those aged 0-17 at 8.3 million, but that estimate is based on only 51 million of the nearly 67 million U.S. cases as of Jan. 18.
Feds’ website for free at-home COVID tests launches day early
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
Federal website for free COVID-19 tests opens Jan. 19
The tests will ship within 7 to 12 days after being ordered, senior officials from President Joe Biden’s administration said Jan. 14. The U.S. Postal Service will handle the shipping and delivery through first-class mail.
People will input their name and mailing address on the website and can share an email address to receive updates on the order, according to NPR. People won’t need to pay shipping costs or enter a credit card number to order tests, according to the website’s homepage.
The website will be offered in both English and Spanish. The Biden administration will also set up a phone number so those without internet access can place orders.
Officials didn’t share a specific time that the website will open, according to he New York Times — simply that it will go live sometime on Jan. 19. Each household will be limited to ordering four tests.
Starting Jan. 15, people with private insurance were able to seek reimbursement for tests they purchase on their own. At the same time, some insurers have said it could take weeks to set up a system for smooth reimbursement, the newspaper reported.
Last week’s announcement is the latest step in the president’s pledge to get coronavirus tests to Americans. In December, Biden said his administration would purchase 500 million tests and distribute them to Americans for free. On Jan. 13, he announced that the administration would buy another 500 million tests, bringing the total to 1 billion.
So far, the administration has signed contracts to produce 420 million tests, the newspaper reported. With the website opening this week and the lag in shipping, the tests will likely arrive by the end of January at the earliest, which could be after the peak of the current coronavirus surge in some parts of the country.
At-home tests have been in high demand, with some pharmacies, retailers, and websites reporting no stock in recent weeks. People have lined up at community testing sites for hours to get tested as the national average of daily cases has climbed above 800,000 last week.
Some consumers have also been confused about how or when to use at-home tests. On Jan. 14, Biden administration officials said that people should use rapid tests for three reasons:
- If they begin to experience COVID-19 symptoms;
- When it has been five or more days after being exposed to someone who tests positive;
- If they are gathering indoors with a high-risk person and want to check if they are negative.
A version of this article first appeared on WebMD.com.
The tests will ship within 7 to 12 days after being ordered, senior officials from President Joe Biden’s administration said Jan. 14. The U.S. Postal Service will handle the shipping and delivery through first-class mail.
People will input their name and mailing address on the website and can share an email address to receive updates on the order, according to NPR. People won’t need to pay shipping costs or enter a credit card number to order tests, according to the website’s homepage.
The website will be offered in both English and Spanish. The Biden administration will also set up a phone number so those without internet access can place orders.
Officials didn’t share a specific time that the website will open, according to he New York Times — simply that it will go live sometime on Jan. 19. Each household will be limited to ordering four tests.
Starting Jan. 15, people with private insurance were able to seek reimbursement for tests they purchase on their own. At the same time, some insurers have said it could take weeks to set up a system for smooth reimbursement, the newspaper reported.
Last week’s announcement is the latest step in the president’s pledge to get coronavirus tests to Americans. In December, Biden said his administration would purchase 500 million tests and distribute them to Americans for free. On Jan. 13, he announced that the administration would buy another 500 million tests, bringing the total to 1 billion.
So far, the administration has signed contracts to produce 420 million tests, the newspaper reported. With the website opening this week and the lag in shipping, the tests will likely arrive by the end of January at the earliest, which could be after the peak of the current coronavirus surge in some parts of the country.
At-home tests have been in high demand, with some pharmacies, retailers, and websites reporting no stock in recent weeks. People have lined up at community testing sites for hours to get tested as the national average of daily cases has climbed above 800,000 last week.
Some consumers have also been confused about how or when to use at-home tests. On Jan. 14, Biden administration officials said that people should use rapid tests for three reasons:
- If they begin to experience COVID-19 symptoms;
- When it has been five or more days after being exposed to someone who tests positive;
- If they are gathering indoors with a high-risk person and want to check if they are negative.
A version of this article first appeared on WebMD.com.
The tests will ship within 7 to 12 days after being ordered, senior officials from President Joe Biden’s administration said Jan. 14. The U.S. Postal Service will handle the shipping and delivery through first-class mail.
People will input their name and mailing address on the website and can share an email address to receive updates on the order, according to NPR. People won’t need to pay shipping costs or enter a credit card number to order tests, according to the website’s homepage.
The website will be offered in both English and Spanish. The Biden administration will also set up a phone number so those without internet access can place orders.
Officials didn’t share a specific time that the website will open, according to he New York Times — simply that it will go live sometime on Jan. 19. Each household will be limited to ordering four tests.
Starting Jan. 15, people with private insurance were able to seek reimbursement for tests they purchase on their own. At the same time, some insurers have said it could take weeks to set up a system for smooth reimbursement, the newspaper reported.
Last week’s announcement is the latest step in the president’s pledge to get coronavirus tests to Americans. In December, Biden said his administration would purchase 500 million tests and distribute them to Americans for free. On Jan. 13, he announced that the administration would buy another 500 million tests, bringing the total to 1 billion.
So far, the administration has signed contracts to produce 420 million tests, the newspaper reported. With the website opening this week and the lag in shipping, the tests will likely arrive by the end of January at the earliest, which could be after the peak of the current coronavirus surge in some parts of the country.
At-home tests have been in high demand, with some pharmacies, retailers, and websites reporting no stock in recent weeks. People have lined up at community testing sites for hours to get tested as the national average of daily cases has climbed above 800,000 last week.
Some consumers have also been confused about how or when to use at-home tests. On Jan. 14, Biden administration officials said that people should use rapid tests for three reasons:
- If they begin to experience COVID-19 symptoms;
- When it has been five or more days after being exposed to someone who tests positive;
- If they are gathering indoors with a high-risk person and want to check if they are negative.
A version of this article first appeared on WebMD.com.
ACP advocates outpatient treatment of uncomplicated diverticulitis
The estimated prevalence of acute colonic diverticulitis in the United States appears to be on the rise, wrote Amir Qaseem, MD, and members of the ACP Clinical Guidelines Committee. “Approximately 200,000 hospitalizations for acute left-sided colonic diverticulitis occur in the United States each year, with annual costs of more than $8 billion. Timely and correct diagnosis of acute left-sided colonic diverticulitis is essential for the selection of the most appropriate management options.”
Diverticulitis is becoming increasingly common in patients treated by internal medicine physicians, according to the ACP, and the new clinical guidelines specify a course of treatment focused on outpatient management and minimal medications.
The guidelines, published in Annals of Internal Medicine, were based on a systematic review of evidence from studies published between Jan. 1, 1990, and June 1, 2020. Notably, right-sided diverticulitis was excluded because it is rare in Western countries and involves a different natural history and management options, the authors wrote.
In the guidelines, uncomplicated diverticulitis refers to localized inflammation, and complicated diverticulitis refers to “inflammation associated with an abscess, a phlegmon, a fistula, an obstruction, bleeding, or perforation.”
Guidance on diagnosis and management
In the first guideline, “Diagnosis and Management of Acute Left-Sided Colonic Diverticulitis”, the authors provided three recommendations. First, they recommended that clinicians use abdominal CT imaging in cases of diagnostic uncertainty for patients with suspected acute left-sided colonic diverticulitis. The evidence showed that abdominal CT was associated with appropriate management in patients with suspected acute left-sided colonic diverticulitis, and that misdiagnosis with CT was rare.
Second, the authors of this guidance recommended management of most patients with acute left-sided colonic diverticulitis in an outpatient setting. Evidence showed that the risk for elective surgery and for recurrence were not significantly different based on inpatient or outpatient management.
The third recommendation advised clinicians to manage most patients without antibiotics. This recommendation was based on data showing no significant difference in quality of life at 3, 6, 12, or 24 months; no difference in diverticulitis-related complications; and no difference in the need for surgery in patients treated with antibiotics and those not treated with antibiotics.
All three recommendations are conditional, with low-certainty evidence, according to the authors.
Colonoscopy for diagnostic evaluation and interventions
In the second guideline, “Colonoscopy for Diagnostic Evaluation and Interventions to Prevent Recurrence After Acute Left-Sided Colonic Diverticulitis, the authors advised clinicians to refer patients for a colonoscopy after an initial episode of complicated left-sided colonic diverticulitis if they have not had a recent colonoscopy.
Although acute diverticulitis is usually uncomplicated, approximately 12% of cases are considered complicated, and these patients may have a higher prevalence of colorectal cancer, the authors noted. This recommendation was conditional, with low-certainty evidence. Additional diagnostic colonoscopy is not needed for patients who are up to date on recommended colorectal cancer screening, according to this guideline.
A second recommendation, given as a strong recommendation with high-certainty evidence, advised against using mesalamine to prevent recurrent diverticulitis. Evidence showed that use of mesalamine at doses ranging from 1.2 g/day to 4.8 g/day made no difference in recurrent diverticulitis risk compared with placebo. Mesalamine has no demonstrated clinical benefits, and has been associated with epigastric pain, nausea, diarrhea, dizziness, rash, and renal and hepatic impairment, the authors wrote.
The third recommendation advised the discussion of elective surgery with patients with a history of uncomplicated diverticulitis that persists or recurs frequently. Surgery also may be an option for patients with complicated diverticulitis, according to the guideline. However, “this recommendation does not apply to patients with uncomplicated diverticulitis that is not persistent or frequently recurring,” the authors wrote.
The decision to pursue elective surgery should be informed and personalized according to potential benefits, harms, costs, and patient preferences, they said. This recommendation is conditional, with low-certainty evidence.
This new guideline was designed “to guide care based on the best available evidence and may not apply to all patients or individual clinical situations,” the authors emphasized. “It should not be used as a replacement for a clinician’s judgment.”
Update confirms best practices
“Concerns about inappropriate antimicrobial therapy use and the delay in seeking preventative care such as a colonoscopy have led to poorer outcomes for patients,” ACP president George Abraham, MD, said in an interview. These concerns about a lack of antimicrobial stewardship and of care not being representative of ‘high value care’ “supported the need to reinforce best practices.”
Although most clinicians are aware of the nature of the recommendations in their own clinical practices, “a systematic review helped confirm and codify best practice that everyone can confidently incorporate into their daily decision-making,” Dr. Abraham said.
Compared with previous guidelines, “the single biggest difference is the fact that antimicrobial therapy is not indicated in mild, uncomplicated diverticulitis; we hope this will lead to lesser and more judicious antimicrobial prescribing,” Dr. Abraham emphasized.
Like all guidelines, the current guidelines are meant to be advisory, not mandatory; “they do not replace good clinical judgment and individual patient care decision-making,” Dr. Abraham said. “These guidelines are useful when they are widely read by clinicians, including physicians and advanced practice clinicians, and incorporated into their daily practice.”
Curbing antibiotic use
It is important for clinicians to recognize that uncomplicated diverticulitis in selected patients does not require initial antibiotics, David A. Johnson, MD, chief of gastroenterology at Eastern Virginia School of Medicine, Norfolk, said in an interview. “This paradigm shift began with the AGA guidelines in 2015, and was more recently updated with the 2021 best practice recommendations,” first published in Gastroenterology.
“I was surprised to see this current guideline not mentioning that, if antibiotics are to be used, that amoxicillin-clavulanate alone should be favored over combination of fluoroquinolones and metronidazole,” Dr. Johnson noted. “Furthermore, the U.S. Food and Drug Administration has advised that fluoroquinolones should be reserved for conditions with no alternative treatment options.”
“The initial management approach for the AGA guidelines and best practice are comparable with these most recent ACP recommendations,” said Dr. Johnson. However, “I would suggest that clinicians treating diverticulitis also review the AGA best practice recommendations, which build out important other important points for diverticulitis management including timeframes for colonoscopy, strong effect of genetics, dietary effects, recurrence rates, and the role of surgery.”
As for research gaps, “further data on cost savings would be helpful,” as savings may be likely with significant reduction without antibiotics and imaging in select patients, Dr. Johnson said. “Cost savings and risk reduction of adverse implications of antibiotic and radiation risks should be included in these analyses.”
The guidelines were based on systematic reviews conducted by the Evidence-based Practice Center at Brown University, Providence, R.I., funded by the Agency for Healthcare Research and Quality. The development of the guidelines was supported by the ACP operating budget. The authors, Dr. Abraham, and Dr. Johnson had no financial conflicts to disclose.
The estimated prevalence of acute colonic diverticulitis in the United States appears to be on the rise, wrote Amir Qaseem, MD, and members of the ACP Clinical Guidelines Committee. “Approximately 200,000 hospitalizations for acute left-sided colonic diverticulitis occur in the United States each year, with annual costs of more than $8 billion. Timely and correct diagnosis of acute left-sided colonic diverticulitis is essential for the selection of the most appropriate management options.”
Diverticulitis is becoming increasingly common in patients treated by internal medicine physicians, according to the ACP, and the new clinical guidelines specify a course of treatment focused on outpatient management and minimal medications.
The guidelines, published in Annals of Internal Medicine, were based on a systematic review of evidence from studies published between Jan. 1, 1990, and June 1, 2020. Notably, right-sided diverticulitis was excluded because it is rare in Western countries and involves a different natural history and management options, the authors wrote.
In the guidelines, uncomplicated diverticulitis refers to localized inflammation, and complicated diverticulitis refers to “inflammation associated with an abscess, a phlegmon, a fistula, an obstruction, bleeding, or perforation.”
Guidance on diagnosis and management
In the first guideline, “Diagnosis and Management of Acute Left-Sided Colonic Diverticulitis”, the authors provided three recommendations. First, they recommended that clinicians use abdominal CT imaging in cases of diagnostic uncertainty for patients with suspected acute left-sided colonic diverticulitis. The evidence showed that abdominal CT was associated with appropriate management in patients with suspected acute left-sided colonic diverticulitis, and that misdiagnosis with CT was rare.
Second, the authors of this guidance recommended management of most patients with acute left-sided colonic diverticulitis in an outpatient setting. Evidence showed that the risk for elective surgery and for recurrence were not significantly different based on inpatient or outpatient management.
The third recommendation advised clinicians to manage most patients without antibiotics. This recommendation was based on data showing no significant difference in quality of life at 3, 6, 12, or 24 months; no difference in diverticulitis-related complications; and no difference in the need for surgery in patients treated with antibiotics and those not treated with antibiotics.
All three recommendations are conditional, with low-certainty evidence, according to the authors.
Colonoscopy for diagnostic evaluation and interventions
In the second guideline, “Colonoscopy for Diagnostic Evaluation and Interventions to Prevent Recurrence After Acute Left-Sided Colonic Diverticulitis, the authors advised clinicians to refer patients for a colonoscopy after an initial episode of complicated left-sided colonic diverticulitis if they have not had a recent colonoscopy.
Although acute diverticulitis is usually uncomplicated, approximately 12% of cases are considered complicated, and these patients may have a higher prevalence of colorectal cancer, the authors noted. This recommendation was conditional, with low-certainty evidence. Additional diagnostic colonoscopy is not needed for patients who are up to date on recommended colorectal cancer screening, according to this guideline.
A second recommendation, given as a strong recommendation with high-certainty evidence, advised against using mesalamine to prevent recurrent diverticulitis. Evidence showed that use of mesalamine at doses ranging from 1.2 g/day to 4.8 g/day made no difference in recurrent diverticulitis risk compared with placebo. Mesalamine has no demonstrated clinical benefits, and has been associated with epigastric pain, nausea, diarrhea, dizziness, rash, and renal and hepatic impairment, the authors wrote.
The third recommendation advised the discussion of elective surgery with patients with a history of uncomplicated diverticulitis that persists or recurs frequently. Surgery also may be an option for patients with complicated diverticulitis, according to the guideline. However, “this recommendation does not apply to patients with uncomplicated diverticulitis that is not persistent or frequently recurring,” the authors wrote.
The decision to pursue elective surgery should be informed and personalized according to potential benefits, harms, costs, and patient preferences, they said. This recommendation is conditional, with low-certainty evidence.
This new guideline was designed “to guide care based on the best available evidence and may not apply to all patients or individual clinical situations,” the authors emphasized. “It should not be used as a replacement for a clinician’s judgment.”
Update confirms best practices
“Concerns about inappropriate antimicrobial therapy use and the delay in seeking preventative care such as a colonoscopy have led to poorer outcomes for patients,” ACP president George Abraham, MD, said in an interview. These concerns about a lack of antimicrobial stewardship and of care not being representative of ‘high value care’ “supported the need to reinforce best practices.”
Although most clinicians are aware of the nature of the recommendations in their own clinical practices, “a systematic review helped confirm and codify best practice that everyone can confidently incorporate into their daily decision-making,” Dr. Abraham said.
Compared with previous guidelines, “the single biggest difference is the fact that antimicrobial therapy is not indicated in mild, uncomplicated diverticulitis; we hope this will lead to lesser and more judicious antimicrobial prescribing,” Dr. Abraham emphasized.
Like all guidelines, the current guidelines are meant to be advisory, not mandatory; “they do not replace good clinical judgment and individual patient care decision-making,” Dr. Abraham said. “These guidelines are useful when they are widely read by clinicians, including physicians and advanced practice clinicians, and incorporated into their daily practice.”
Curbing antibiotic use
It is important for clinicians to recognize that uncomplicated diverticulitis in selected patients does not require initial antibiotics, David A. Johnson, MD, chief of gastroenterology at Eastern Virginia School of Medicine, Norfolk, said in an interview. “This paradigm shift began with the AGA guidelines in 2015, and was more recently updated with the 2021 best practice recommendations,” first published in Gastroenterology.
“I was surprised to see this current guideline not mentioning that, if antibiotics are to be used, that amoxicillin-clavulanate alone should be favored over combination of fluoroquinolones and metronidazole,” Dr. Johnson noted. “Furthermore, the U.S. Food and Drug Administration has advised that fluoroquinolones should be reserved for conditions with no alternative treatment options.”
“The initial management approach for the AGA guidelines and best practice are comparable with these most recent ACP recommendations,” said Dr. Johnson. However, “I would suggest that clinicians treating diverticulitis also review the AGA best practice recommendations, which build out important other important points for diverticulitis management including timeframes for colonoscopy, strong effect of genetics, dietary effects, recurrence rates, and the role of surgery.”
As for research gaps, “further data on cost savings would be helpful,” as savings may be likely with significant reduction without antibiotics and imaging in select patients, Dr. Johnson said. “Cost savings and risk reduction of adverse implications of antibiotic and radiation risks should be included in these analyses.”
The guidelines were based on systematic reviews conducted by the Evidence-based Practice Center at Brown University, Providence, R.I., funded by the Agency for Healthcare Research and Quality. The development of the guidelines was supported by the ACP operating budget. The authors, Dr. Abraham, and Dr. Johnson had no financial conflicts to disclose.
The estimated prevalence of acute colonic diverticulitis in the United States appears to be on the rise, wrote Amir Qaseem, MD, and members of the ACP Clinical Guidelines Committee. “Approximately 200,000 hospitalizations for acute left-sided colonic diverticulitis occur in the United States each year, with annual costs of more than $8 billion. Timely and correct diagnosis of acute left-sided colonic diverticulitis is essential for the selection of the most appropriate management options.”
Diverticulitis is becoming increasingly common in patients treated by internal medicine physicians, according to the ACP, and the new clinical guidelines specify a course of treatment focused on outpatient management and minimal medications.
The guidelines, published in Annals of Internal Medicine, were based on a systematic review of evidence from studies published between Jan. 1, 1990, and June 1, 2020. Notably, right-sided diverticulitis was excluded because it is rare in Western countries and involves a different natural history and management options, the authors wrote.
In the guidelines, uncomplicated diverticulitis refers to localized inflammation, and complicated diverticulitis refers to “inflammation associated with an abscess, a phlegmon, a fistula, an obstruction, bleeding, or perforation.”
Guidance on diagnosis and management
In the first guideline, “Diagnosis and Management of Acute Left-Sided Colonic Diverticulitis”, the authors provided three recommendations. First, they recommended that clinicians use abdominal CT imaging in cases of diagnostic uncertainty for patients with suspected acute left-sided colonic diverticulitis. The evidence showed that abdominal CT was associated with appropriate management in patients with suspected acute left-sided colonic diverticulitis, and that misdiagnosis with CT was rare.
Second, the authors of this guidance recommended management of most patients with acute left-sided colonic diverticulitis in an outpatient setting. Evidence showed that the risk for elective surgery and for recurrence were not significantly different based on inpatient or outpatient management.
The third recommendation advised clinicians to manage most patients without antibiotics. This recommendation was based on data showing no significant difference in quality of life at 3, 6, 12, or 24 months; no difference in diverticulitis-related complications; and no difference in the need for surgery in patients treated with antibiotics and those not treated with antibiotics.
All three recommendations are conditional, with low-certainty evidence, according to the authors.
Colonoscopy for diagnostic evaluation and interventions
In the second guideline, “Colonoscopy for Diagnostic Evaluation and Interventions to Prevent Recurrence After Acute Left-Sided Colonic Diverticulitis, the authors advised clinicians to refer patients for a colonoscopy after an initial episode of complicated left-sided colonic diverticulitis if they have not had a recent colonoscopy.
Although acute diverticulitis is usually uncomplicated, approximately 12% of cases are considered complicated, and these patients may have a higher prevalence of colorectal cancer, the authors noted. This recommendation was conditional, with low-certainty evidence. Additional diagnostic colonoscopy is not needed for patients who are up to date on recommended colorectal cancer screening, according to this guideline.
A second recommendation, given as a strong recommendation with high-certainty evidence, advised against using mesalamine to prevent recurrent diverticulitis. Evidence showed that use of mesalamine at doses ranging from 1.2 g/day to 4.8 g/day made no difference in recurrent diverticulitis risk compared with placebo. Mesalamine has no demonstrated clinical benefits, and has been associated with epigastric pain, nausea, diarrhea, dizziness, rash, and renal and hepatic impairment, the authors wrote.
The third recommendation advised the discussion of elective surgery with patients with a history of uncomplicated diverticulitis that persists or recurs frequently. Surgery also may be an option for patients with complicated diverticulitis, according to the guideline. However, “this recommendation does not apply to patients with uncomplicated diverticulitis that is not persistent or frequently recurring,” the authors wrote.
The decision to pursue elective surgery should be informed and personalized according to potential benefits, harms, costs, and patient preferences, they said. This recommendation is conditional, with low-certainty evidence.
This new guideline was designed “to guide care based on the best available evidence and may not apply to all patients or individual clinical situations,” the authors emphasized. “It should not be used as a replacement for a clinician’s judgment.”
Update confirms best practices
“Concerns about inappropriate antimicrobial therapy use and the delay in seeking preventative care such as a colonoscopy have led to poorer outcomes for patients,” ACP president George Abraham, MD, said in an interview. These concerns about a lack of antimicrobial stewardship and of care not being representative of ‘high value care’ “supported the need to reinforce best practices.”
Although most clinicians are aware of the nature of the recommendations in their own clinical practices, “a systematic review helped confirm and codify best practice that everyone can confidently incorporate into their daily decision-making,” Dr. Abraham said.
Compared with previous guidelines, “the single biggest difference is the fact that antimicrobial therapy is not indicated in mild, uncomplicated diverticulitis; we hope this will lead to lesser and more judicious antimicrobial prescribing,” Dr. Abraham emphasized.
Like all guidelines, the current guidelines are meant to be advisory, not mandatory; “they do not replace good clinical judgment and individual patient care decision-making,” Dr. Abraham said. “These guidelines are useful when they are widely read by clinicians, including physicians and advanced practice clinicians, and incorporated into their daily practice.”
Curbing antibiotic use
It is important for clinicians to recognize that uncomplicated diverticulitis in selected patients does not require initial antibiotics, David A. Johnson, MD, chief of gastroenterology at Eastern Virginia School of Medicine, Norfolk, said in an interview. “This paradigm shift began with the AGA guidelines in 2015, and was more recently updated with the 2021 best practice recommendations,” first published in Gastroenterology.
“I was surprised to see this current guideline not mentioning that, if antibiotics are to be used, that amoxicillin-clavulanate alone should be favored over combination of fluoroquinolones and metronidazole,” Dr. Johnson noted. “Furthermore, the U.S. Food and Drug Administration has advised that fluoroquinolones should be reserved for conditions with no alternative treatment options.”
“The initial management approach for the AGA guidelines and best practice are comparable with these most recent ACP recommendations,” said Dr. Johnson. However, “I would suggest that clinicians treating diverticulitis also review the AGA best practice recommendations, which build out important other important points for diverticulitis management including timeframes for colonoscopy, strong effect of genetics, dietary effects, recurrence rates, and the role of surgery.”
As for research gaps, “further data on cost savings would be helpful,” as savings may be likely with significant reduction without antibiotics and imaging in select patients, Dr. Johnson said. “Cost savings and risk reduction of adverse implications of antibiotic and radiation risks should be included in these analyses.”
The guidelines were based on systematic reviews conducted by the Evidence-based Practice Center at Brown University, Providence, R.I., funded by the Agency for Healthcare Research and Quality. The development of the guidelines was supported by the ACP operating budget. The authors, Dr. Abraham, and Dr. Johnson had no financial conflicts to disclose.
FROM ANNALS OF INTERNAL MEDICINE
Docs pen open letter to support Fauci against partisan ‘attacks’
“We deplore the personal attacks on Dr. Fauci. The criticism is inaccurate, unscientific, ill-founded in the facts and, increasingly, motivated by partisan politics,” reads the letter of support, initiated by Ezekiel Emanuel, MD, and signed by almost 300 scientists and public health and medical professionals, including Nobel Laureates, a former Republican senator, and leadership of medical societies and institutions.
Dr. Fauci has led the National Institute for Allergy and Infectious Diseases since 1984 and serves as President Biden’s top medical advisor on the pandemic.
“Dr. Anthony Fauci has served the U.S.A. with wisdom and integrity for nearly 40 years. Through HIV, Ebola, and now COVID, he has unswervingly served the United States guiding the country to very successful outcomes. He has our unreserved respect and trust as a scientist and a national leader,” the letter reads.
Dr. Fauci has repeatedly faced harsh criticism from congressional Republicans, especially Sen. Rand Paul (R-Ky.) and Sen. Roger Marshall (R-Kan.).
At a particularly contentious congressional hearing earlier this week on the federal government’s response to Omicron, Dr. Fauci fought back, telling Sen. Marshall, “You’re so misinformed, it’s extraordinary.”
Dr. Fauci, who has received death threats and harassment of his family, told Sen. Rand that his “completely untrue” statements and rhetoric “kindles the crazies out there.”
‘Sagacious counsel’
The personal attacks on Dr. Fauci are a “distraction from what should be the national focus – working together to finally overcome a pandemic that is killing about 500,000 people a year. We are grateful for Dr. Fauci’s dedication and tireless efforts to help the country through this pandemic and other health crises,” the letter reads.
“Throughout the COVID-19 pandemic, Dr. Fauci has provided the American political leadership and the public with sagacious counsel in these most difficult of times. His advice has been as well informed as data and the rapidly evolving circumstances allowed,” it states.
“Importantly,” Dr. Fauci has given his advice with “humility, being clear about what we know and what is unknown, but requires judgment. He has consistently emphasized the importance of mask-wearing, social distancing, and vaccination. These are standard and necessary public health measures that we all support,” the letter states.
“We are grateful that Dr. Fauci has consistently stated the science in a way that represents the facts as they emerge, without unwarranted speculation.”
“Sadly, in these politically polarized times where misinformation contaminates the United States’ response to the pandemic, routine public health measures have become unnecessarily controversial, undermining the effectiveness of our country’s response,” the letter reads.
A version of this article first appeared on Medscape.com.
“We deplore the personal attacks on Dr. Fauci. The criticism is inaccurate, unscientific, ill-founded in the facts and, increasingly, motivated by partisan politics,” reads the letter of support, initiated by Ezekiel Emanuel, MD, and signed by almost 300 scientists and public health and medical professionals, including Nobel Laureates, a former Republican senator, and leadership of medical societies and institutions.
Dr. Fauci has led the National Institute for Allergy and Infectious Diseases since 1984 and serves as President Biden’s top medical advisor on the pandemic.
“Dr. Anthony Fauci has served the U.S.A. with wisdom and integrity for nearly 40 years. Through HIV, Ebola, and now COVID, he has unswervingly served the United States guiding the country to very successful outcomes. He has our unreserved respect and trust as a scientist and a national leader,” the letter reads.
Dr. Fauci has repeatedly faced harsh criticism from congressional Republicans, especially Sen. Rand Paul (R-Ky.) and Sen. Roger Marshall (R-Kan.).
At a particularly contentious congressional hearing earlier this week on the federal government’s response to Omicron, Dr. Fauci fought back, telling Sen. Marshall, “You’re so misinformed, it’s extraordinary.”
Dr. Fauci, who has received death threats and harassment of his family, told Sen. Rand that his “completely untrue” statements and rhetoric “kindles the crazies out there.”
‘Sagacious counsel’
The personal attacks on Dr. Fauci are a “distraction from what should be the national focus – working together to finally overcome a pandemic that is killing about 500,000 people a year. We are grateful for Dr. Fauci’s dedication and tireless efforts to help the country through this pandemic and other health crises,” the letter reads.
“Throughout the COVID-19 pandemic, Dr. Fauci has provided the American political leadership and the public with sagacious counsel in these most difficult of times. His advice has been as well informed as data and the rapidly evolving circumstances allowed,” it states.
“Importantly,” Dr. Fauci has given his advice with “humility, being clear about what we know and what is unknown, but requires judgment. He has consistently emphasized the importance of mask-wearing, social distancing, and vaccination. These are standard and necessary public health measures that we all support,” the letter states.
“We are grateful that Dr. Fauci has consistently stated the science in a way that represents the facts as they emerge, without unwarranted speculation.”
“Sadly, in these politically polarized times where misinformation contaminates the United States’ response to the pandemic, routine public health measures have become unnecessarily controversial, undermining the effectiveness of our country’s response,” the letter reads.
A version of this article first appeared on Medscape.com.
“We deplore the personal attacks on Dr. Fauci. The criticism is inaccurate, unscientific, ill-founded in the facts and, increasingly, motivated by partisan politics,” reads the letter of support, initiated by Ezekiel Emanuel, MD, and signed by almost 300 scientists and public health and medical professionals, including Nobel Laureates, a former Republican senator, and leadership of medical societies and institutions.
Dr. Fauci has led the National Institute for Allergy and Infectious Diseases since 1984 and serves as President Biden’s top medical advisor on the pandemic.
“Dr. Anthony Fauci has served the U.S.A. with wisdom and integrity for nearly 40 years. Through HIV, Ebola, and now COVID, he has unswervingly served the United States guiding the country to very successful outcomes. He has our unreserved respect and trust as a scientist and a national leader,” the letter reads.
Dr. Fauci has repeatedly faced harsh criticism from congressional Republicans, especially Sen. Rand Paul (R-Ky.) and Sen. Roger Marshall (R-Kan.).
At a particularly contentious congressional hearing earlier this week on the federal government’s response to Omicron, Dr. Fauci fought back, telling Sen. Marshall, “You’re so misinformed, it’s extraordinary.”
Dr. Fauci, who has received death threats and harassment of his family, told Sen. Rand that his “completely untrue” statements and rhetoric “kindles the crazies out there.”
‘Sagacious counsel’
The personal attacks on Dr. Fauci are a “distraction from what should be the national focus – working together to finally overcome a pandemic that is killing about 500,000 people a year. We are grateful for Dr. Fauci’s dedication and tireless efforts to help the country through this pandemic and other health crises,” the letter reads.
“Throughout the COVID-19 pandemic, Dr. Fauci has provided the American political leadership and the public with sagacious counsel in these most difficult of times. His advice has been as well informed as data and the rapidly evolving circumstances allowed,” it states.
“Importantly,” Dr. Fauci has given his advice with “humility, being clear about what we know and what is unknown, but requires judgment. He has consistently emphasized the importance of mask-wearing, social distancing, and vaccination. These are standard and necessary public health measures that we all support,” the letter states.
“We are grateful that Dr. Fauci has consistently stated the science in a way that represents the facts as they emerge, without unwarranted speculation.”
“Sadly, in these politically polarized times where misinformation contaminates the United States’ response to the pandemic, routine public health measures have become unnecessarily controversial, undermining the effectiveness of our country’s response,” the letter reads.
A version of this article first appeared on Medscape.com.
Reducing night-time checks is safe and helps patients sleep
Routine checks of vital signs during the night often prevent hospitalized patients from getting sufficient recuperative sleep. But patients who are judged to be clinically stable by an algorithm that uses real-time data can be safely spared these checks, according to a recent study published in JAMA Internal Medicine.
In their study,
“Sleep is crucial to health,” writes Hyung J. Cho, MD, from the New York University Grossman School of Medicine, in an accompanying editorial. “Ironically, hospitals, where people go to recover from illness, are among the most difficult places to sleep.”
Noise from the surrounding area, night-time examinations, multibed rooms, an unfamiliar environment, early morning blood sample collections, and frequent vital sign checks often prevent patients from sleeping through the night.
The goal of the study was to see if the elimination of one of these disrupting factors – the frequent checks of vital signs – would improve sleep and lead to a reduction in delirium, the primary endpoint.
To do this, the researchers incorporated a predictive algorithm they developed “to identify patients who are at low risk for abnormal night-time vital signs” into the hospitals electronic health records system. Attending physicians received a notification, based on real-time patient data, if it was predicted with a high degree of probability that a patient’s night-time vital signs would be within the normal range. Each physician was free to decide whether they would forgo night-time checks of the vital signs or whether they would turn off the notifications for a specific period.
The randomized clinical trial was conducted at a tertiary care academic teaching hospital from March to November 2019. Half the 1,930 patients were randomized to the algorithm group and half to standard care. None of the patients were receiving intensive care.
Number of night-time checks successfully reduced
The mean number of night-time checks was significantly lower in the algorithm group than in the standard-care group (0.97 vs. 1.41; P < .001).
The reduction in night-time checks had no effect on patient safety. There was no increase in transfers to the intensive care unit in the algorithm or standard-care groups (5% vs 5%; P = .92), and no difference between the number of heart alarms (0.2% vs. 0.9%; P = .07).
However, the reduction also had no effect on the incidence of episodes of delirium in the algorithm or standard-care groups (11% vs. 13%; P = .32).
“The reduction in vital signs checking, although statistically significant, was relatively small,” Dr. Cho explains. But the primary endpoint might have been different had the adherence to intervention been better, he notes.
In fact, the analysis confirmed that changes to routine daily practice in a hospital are not always easy to implement. In 35% of cases, the patients’ vital signs were checked at night, despite the physician’s order to the contrary.
“Busy patient-care assistants and nurses may check vital signs out of habit without noticing that the order has changed for some of the patients,” Dr. Najafi and his coauthors write. Many hospitals are used to thinking that regular measurements of the vital signs are part of good practice.
Include nursing staff
Future projects should use an interdisciplinary approach that includes nursing staff, Dr. Cho recommends. More user-friendly displays and optimized alerts in the electronic patient records could also encourage better implementation of the orders.
Less frequent checks of the vital signs would be welcomed by frontline staff because it would lighten their already heavy workload, he adds.
Although the study didn’t meet its primary endpoint, patients subjected to fewer night-time checks because of the algorithm were able to get a good night’s sleep. Other aspects of hospital care that are based on the patient’s stability, such as cardiac monitoring, could also potentially benefit from this type of intervention, Dr. Najafi and his colleagues suggest.
A version of this article first appeared on Medscape.com.
Routine checks of vital signs during the night often prevent hospitalized patients from getting sufficient recuperative sleep. But patients who are judged to be clinically stable by an algorithm that uses real-time data can be safely spared these checks, according to a recent study published in JAMA Internal Medicine.
In their study,
“Sleep is crucial to health,” writes Hyung J. Cho, MD, from the New York University Grossman School of Medicine, in an accompanying editorial. “Ironically, hospitals, where people go to recover from illness, are among the most difficult places to sleep.”
Noise from the surrounding area, night-time examinations, multibed rooms, an unfamiliar environment, early morning blood sample collections, and frequent vital sign checks often prevent patients from sleeping through the night.
The goal of the study was to see if the elimination of one of these disrupting factors – the frequent checks of vital signs – would improve sleep and lead to a reduction in delirium, the primary endpoint.
To do this, the researchers incorporated a predictive algorithm they developed “to identify patients who are at low risk for abnormal night-time vital signs” into the hospitals electronic health records system. Attending physicians received a notification, based on real-time patient data, if it was predicted with a high degree of probability that a patient’s night-time vital signs would be within the normal range. Each physician was free to decide whether they would forgo night-time checks of the vital signs or whether they would turn off the notifications for a specific period.
The randomized clinical trial was conducted at a tertiary care academic teaching hospital from March to November 2019. Half the 1,930 patients were randomized to the algorithm group and half to standard care. None of the patients were receiving intensive care.
Number of night-time checks successfully reduced
The mean number of night-time checks was significantly lower in the algorithm group than in the standard-care group (0.97 vs. 1.41; P < .001).
The reduction in night-time checks had no effect on patient safety. There was no increase in transfers to the intensive care unit in the algorithm or standard-care groups (5% vs 5%; P = .92), and no difference between the number of heart alarms (0.2% vs. 0.9%; P = .07).
However, the reduction also had no effect on the incidence of episodes of delirium in the algorithm or standard-care groups (11% vs. 13%; P = .32).
“The reduction in vital signs checking, although statistically significant, was relatively small,” Dr. Cho explains. But the primary endpoint might have been different had the adherence to intervention been better, he notes.
In fact, the analysis confirmed that changes to routine daily practice in a hospital are not always easy to implement. In 35% of cases, the patients’ vital signs were checked at night, despite the physician’s order to the contrary.
“Busy patient-care assistants and nurses may check vital signs out of habit without noticing that the order has changed for some of the patients,” Dr. Najafi and his coauthors write. Many hospitals are used to thinking that regular measurements of the vital signs are part of good practice.
Include nursing staff
Future projects should use an interdisciplinary approach that includes nursing staff, Dr. Cho recommends. More user-friendly displays and optimized alerts in the electronic patient records could also encourage better implementation of the orders.
Less frequent checks of the vital signs would be welcomed by frontline staff because it would lighten their already heavy workload, he adds.
Although the study didn’t meet its primary endpoint, patients subjected to fewer night-time checks because of the algorithm were able to get a good night’s sleep. Other aspects of hospital care that are based on the patient’s stability, such as cardiac monitoring, could also potentially benefit from this type of intervention, Dr. Najafi and his colleagues suggest.
A version of this article first appeared on Medscape.com.
Routine checks of vital signs during the night often prevent hospitalized patients from getting sufficient recuperative sleep. But patients who are judged to be clinically stable by an algorithm that uses real-time data can be safely spared these checks, according to a recent study published in JAMA Internal Medicine.
In their study,
“Sleep is crucial to health,” writes Hyung J. Cho, MD, from the New York University Grossman School of Medicine, in an accompanying editorial. “Ironically, hospitals, where people go to recover from illness, are among the most difficult places to sleep.”
Noise from the surrounding area, night-time examinations, multibed rooms, an unfamiliar environment, early morning blood sample collections, and frequent vital sign checks often prevent patients from sleeping through the night.
The goal of the study was to see if the elimination of one of these disrupting factors – the frequent checks of vital signs – would improve sleep and lead to a reduction in delirium, the primary endpoint.
To do this, the researchers incorporated a predictive algorithm they developed “to identify patients who are at low risk for abnormal night-time vital signs” into the hospitals electronic health records system. Attending physicians received a notification, based on real-time patient data, if it was predicted with a high degree of probability that a patient’s night-time vital signs would be within the normal range. Each physician was free to decide whether they would forgo night-time checks of the vital signs or whether they would turn off the notifications for a specific period.
The randomized clinical trial was conducted at a tertiary care academic teaching hospital from March to November 2019. Half the 1,930 patients were randomized to the algorithm group and half to standard care. None of the patients were receiving intensive care.
Number of night-time checks successfully reduced
The mean number of night-time checks was significantly lower in the algorithm group than in the standard-care group (0.97 vs. 1.41; P < .001).
The reduction in night-time checks had no effect on patient safety. There was no increase in transfers to the intensive care unit in the algorithm or standard-care groups (5% vs 5%; P = .92), and no difference between the number of heart alarms (0.2% vs. 0.9%; P = .07).
However, the reduction also had no effect on the incidence of episodes of delirium in the algorithm or standard-care groups (11% vs. 13%; P = .32).
“The reduction in vital signs checking, although statistically significant, was relatively small,” Dr. Cho explains. But the primary endpoint might have been different had the adherence to intervention been better, he notes.
In fact, the analysis confirmed that changes to routine daily practice in a hospital are not always easy to implement. In 35% of cases, the patients’ vital signs were checked at night, despite the physician’s order to the contrary.
“Busy patient-care assistants and nurses may check vital signs out of habit without noticing that the order has changed for some of the patients,” Dr. Najafi and his coauthors write. Many hospitals are used to thinking that regular measurements of the vital signs are part of good practice.
Include nursing staff
Future projects should use an interdisciplinary approach that includes nursing staff, Dr. Cho recommends. More user-friendly displays and optimized alerts in the electronic patient records could also encourage better implementation of the orders.
Less frequent checks of the vital signs would be welcomed by frontline staff because it would lighten their already heavy workload, he adds.
Although the study didn’t meet its primary endpoint, patients subjected to fewer night-time checks because of the algorithm were able to get a good night’s sleep. Other aspects of hospital care that are based on the patient’s stability, such as cardiac monitoring, could also potentially benefit from this type of intervention, Dr. Najafi and his colleagues suggest.
A version of this article first appeared on Medscape.com.
Hand eczema and atopic dermatitis closely linked
An estimated (AD), according to Jacob P. Thyssen, MD, PhD.
“If we look at individuals with AD, the lifetime prevalence of hand eczema reaches 50%, so we see a strong association between hand eczema and AD,” Dr. Thyssen, professor of dermatology at the University of Copenhagen, said at the Revolutionizing Atopic Dermatitis symposium.
Risk factors for hand eczema – defined as eczema on the hand and/or wrists – include AD, which increases the risk by two- to threefold, as well as genetic predisposition beyond AD, exposure to irritants and allergens, female gender, young age, low socioeconomic group, high risk occupations (including construction workers and hairdressers), and tobacco smoking.
“As clinicians, we sometimes need to rule out a few differentials, including psoriasis and T-cell lymphoma. As an example, 10% of T-cell lymphoma patients, a very rare condition, have first onset of the disease on their hands,” Dr. Thyssen said. “Once we see persistent hand eczema, we need to obtain a history of irritant exposure and allergen exposure, both at home and at work, perform a patch test, sometimes a skin prick test, and ask about personal and family history of AD and psoriasis.”
He noted that while formal classification of hand eczema has been a struggle for decades, he favors the “straightforward” clinical approach from the European Environmental and Contact Dermatitis Research Group. Atopic hand eczema, he said, “is very much characterized by dorsal involvement of the hands and fingers and sparse involvement of the palmar aspects of the hands.”
The cheeks and hands are predilection sites for AD in filaggrin mutation carriers (as they are sites of low filaggrin levels), and sometimes harsh environmental exposures, such as cold and dry air. In a study of 3,335 patients in Denmark, Dr. Thyssen and colleagues found that filaggrin mutations and AD were associated with early-onset and persistent hand eczema. In another study of 3,834 adults with AD or psoriasis, he and colleagues found that among those with AD, the wrists, back of the hands, and interdigital areas were often sites of severe eczema, while palmar involvement was more uncommon.
The same findings apply for the feet in filaggrin mutation carriers with AD; the dorsal aspect of the feet was more commonly affected, compared with plantar aspects of the feet.
Medical literature regarding foot eczema is scarce, but a retrospective cohort study from Germany found that foot eczema and hand eczema often co-occur. Among 723 hand eczema patients, 201 (28%) had concomitant foot eczema. The same morphological features were found on the hands and feet in 71% of patients. Foot eczema was significantly associated with male sex, atopic hand eczema, hyperhidrosis, wearing of safety shoes/boots at work, and tobacco smoking.
In addition, a systematic review and meta-analysis of studies of hand eczema and AD found that there was a 4.29-fold increased risk of hand eczema in individuals with AD, and the risk (lifetime prevalence) of occupational hand eczema was increased by more than twofold. “However, this study could not differentiate between irritant contact dermatitis on the hands and atopic dermatitis,” Dr. Thyssen said. “The studies were not accurate enough to allow for any conclusions.”
A multicenter study of adults with hand eczema in Italy found that the proportion of patients with AD was the highest among those with severe and refractory chronic hand eczema. In addition, certain professions, including those of hairdressers, health professionals, and those in trade work, such as plumbing, were more often associated with chronic hand eczema. “This teaches us that we should be very careful about steering these patients from at-risk occupations,” Dr. Thyssen said. “Also, we should remember to treat them aggressively in the beginning to reduce the risk of severe and refractory chronic hand eczema.”
Dr. Thyssen disclosed that he is a speaker, advisory board member, and/or investigator for Asian, Arena, Almirall, AbbVie, Eli Lilly, LEO Pharma, Pfizer, Regeneron, and Sanofi Genzyme.
An estimated (AD), according to Jacob P. Thyssen, MD, PhD.
“If we look at individuals with AD, the lifetime prevalence of hand eczema reaches 50%, so we see a strong association between hand eczema and AD,” Dr. Thyssen, professor of dermatology at the University of Copenhagen, said at the Revolutionizing Atopic Dermatitis symposium.
Risk factors for hand eczema – defined as eczema on the hand and/or wrists – include AD, which increases the risk by two- to threefold, as well as genetic predisposition beyond AD, exposure to irritants and allergens, female gender, young age, low socioeconomic group, high risk occupations (including construction workers and hairdressers), and tobacco smoking.
“As clinicians, we sometimes need to rule out a few differentials, including psoriasis and T-cell lymphoma. As an example, 10% of T-cell lymphoma patients, a very rare condition, have first onset of the disease on their hands,” Dr. Thyssen said. “Once we see persistent hand eczema, we need to obtain a history of irritant exposure and allergen exposure, both at home and at work, perform a patch test, sometimes a skin prick test, and ask about personal and family history of AD and psoriasis.”
He noted that while formal classification of hand eczema has been a struggle for decades, he favors the “straightforward” clinical approach from the European Environmental and Contact Dermatitis Research Group. Atopic hand eczema, he said, “is very much characterized by dorsal involvement of the hands and fingers and sparse involvement of the palmar aspects of the hands.”
The cheeks and hands are predilection sites for AD in filaggrin mutation carriers (as they are sites of low filaggrin levels), and sometimes harsh environmental exposures, such as cold and dry air. In a study of 3,335 patients in Denmark, Dr. Thyssen and colleagues found that filaggrin mutations and AD were associated with early-onset and persistent hand eczema. In another study of 3,834 adults with AD or psoriasis, he and colleagues found that among those with AD, the wrists, back of the hands, and interdigital areas were often sites of severe eczema, while palmar involvement was more uncommon.
The same findings apply for the feet in filaggrin mutation carriers with AD; the dorsal aspect of the feet was more commonly affected, compared with plantar aspects of the feet.
Medical literature regarding foot eczema is scarce, but a retrospective cohort study from Germany found that foot eczema and hand eczema often co-occur. Among 723 hand eczema patients, 201 (28%) had concomitant foot eczema. The same morphological features were found on the hands and feet in 71% of patients. Foot eczema was significantly associated with male sex, atopic hand eczema, hyperhidrosis, wearing of safety shoes/boots at work, and tobacco smoking.
In addition, a systematic review and meta-analysis of studies of hand eczema and AD found that there was a 4.29-fold increased risk of hand eczema in individuals with AD, and the risk (lifetime prevalence) of occupational hand eczema was increased by more than twofold. “However, this study could not differentiate between irritant contact dermatitis on the hands and atopic dermatitis,” Dr. Thyssen said. “The studies were not accurate enough to allow for any conclusions.”
A multicenter study of adults with hand eczema in Italy found that the proportion of patients with AD was the highest among those with severe and refractory chronic hand eczema. In addition, certain professions, including those of hairdressers, health professionals, and those in trade work, such as plumbing, were more often associated with chronic hand eczema. “This teaches us that we should be very careful about steering these patients from at-risk occupations,” Dr. Thyssen said. “Also, we should remember to treat them aggressively in the beginning to reduce the risk of severe and refractory chronic hand eczema.”
Dr. Thyssen disclosed that he is a speaker, advisory board member, and/or investigator for Asian, Arena, Almirall, AbbVie, Eli Lilly, LEO Pharma, Pfizer, Regeneron, and Sanofi Genzyme.
An estimated (AD), according to Jacob P. Thyssen, MD, PhD.
“If we look at individuals with AD, the lifetime prevalence of hand eczema reaches 50%, so we see a strong association between hand eczema and AD,” Dr. Thyssen, professor of dermatology at the University of Copenhagen, said at the Revolutionizing Atopic Dermatitis symposium.
Risk factors for hand eczema – defined as eczema on the hand and/or wrists – include AD, which increases the risk by two- to threefold, as well as genetic predisposition beyond AD, exposure to irritants and allergens, female gender, young age, low socioeconomic group, high risk occupations (including construction workers and hairdressers), and tobacco smoking.
“As clinicians, we sometimes need to rule out a few differentials, including psoriasis and T-cell lymphoma. As an example, 10% of T-cell lymphoma patients, a very rare condition, have first onset of the disease on their hands,” Dr. Thyssen said. “Once we see persistent hand eczema, we need to obtain a history of irritant exposure and allergen exposure, both at home and at work, perform a patch test, sometimes a skin prick test, and ask about personal and family history of AD and psoriasis.”
He noted that while formal classification of hand eczema has been a struggle for decades, he favors the “straightforward” clinical approach from the European Environmental and Contact Dermatitis Research Group. Atopic hand eczema, he said, “is very much characterized by dorsal involvement of the hands and fingers and sparse involvement of the palmar aspects of the hands.”
The cheeks and hands are predilection sites for AD in filaggrin mutation carriers (as they are sites of low filaggrin levels), and sometimes harsh environmental exposures, such as cold and dry air. In a study of 3,335 patients in Denmark, Dr. Thyssen and colleagues found that filaggrin mutations and AD were associated with early-onset and persistent hand eczema. In another study of 3,834 adults with AD or psoriasis, he and colleagues found that among those with AD, the wrists, back of the hands, and interdigital areas were often sites of severe eczema, while palmar involvement was more uncommon.
The same findings apply for the feet in filaggrin mutation carriers with AD; the dorsal aspect of the feet was more commonly affected, compared with plantar aspects of the feet.
Medical literature regarding foot eczema is scarce, but a retrospective cohort study from Germany found that foot eczema and hand eczema often co-occur. Among 723 hand eczema patients, 201 (28%) had concomitant foot eczema. The same morphological features were found on the hands and feet in 71% of patients. Foot eczema was significantly associated with male sex, atopic hand eczema, hyperhidrosis, wearing of safety shoes/boots at work, and tobacco smoking.
In addition, a systematic review and meta-analysis of studies of hand eczema and AD found that there was a 4.29-fold increased risk of hand eczema in individuals with AD, and the risk (lifetime prevalence) of occupational hand eczema was increased by more than twofold. “However, this study could not differentiate between irritant contact dermatitis on the hands and atopic dermatitis,” Dr. Thyssen said. “The studies were not accurate enough to allow for any conclusions.”
A multicenter study of adults with hand eczema in Italy found that the proportion of patients with AD was the highest among those with severe and refractory chronic hand eczema. In addition, certain professions, including those of hairdressers, health professionals, and those in trade work, such as plumbing, were more often associated with chronic hand eczema. “This teaches us that we should be very careful about steering these patients from at-risk occupations,” Dr. Thyssen said. “Also, we should remember to treat them aggressively in the beginning to reduce the risk of severe and refractory chronic hand eczema.”
Dr. Thyssen disclosed that he is a speaker, advisory board member, and/or investigator for Asian, Arena, Almirall, AbbVie, Eli Lilly, LEO Pharma, Pfizer, Regeneron, and Sanofi Genzyme.
FROM REVOLUTIONIZING AD 2021
Cardiac inflammation can be present after mild COVID infection
Myocardial inflammation is present in a small proportion of patients who have recovered from relatively mild cases of COVID-19 infection, a new study shows.
“Our findings suggest that even in patients who have had relatively mild cases of COVID-19, some will have inflammatory changes to the heart, and these changes can be present without any cardiac symptoms,” senior author, Paaladinesh Thavendiranathan, MD, University of Toronto, told this news organization.
“While our data suggest that this inflammation improves over time, and the outcomes seem positive, we don’t know if there will be any long-term consequences,” he added.
Noting that even a short period of inflammation in the heart may be associated with symptoms or arrhythmias in the longer term, Dr. Thavendiranathan said: “I would recommend that it is best to avoid getting the infection if there is any chance of heart inflammation.”
The study was published online in JAMA Cardiology on Jan. 12.
The authors explain that among patients hospitalized with COVID, early studies suggested that approximately one in four experience cardiovascular injury, defined as an elevation in troponin levels, which was associated with a 5- to 10-fold increase in the risk for death. But there is limited information on cardiac injury in patients who do not require hospitalization.
Although a broad range of abnormal myocardial tissue has been reported in several cardiac MRI studies of patients recovered from COVID infection, there is little understanding of persistent changes in myocardial metabolism in recovered patients, which is a potential concern, given that COVID-19 is associated with systemic inflammation during the acute illness, they say.
For the current study, the researchers examined myocardial inflammation measured using two different methods – cardiac MRI and fluorodeoxyglucose–positron emission tomography (FDG-PET) – in individuals who had recovered from COVID-19 infection and looked at how this related to changes in inflammatory blood markers.
Lead author Kate Hanneman, MD, also from the University of Toronto, explained that FDG-PET imaging is more sensitive than MRI in detecting active inflammation. “Inflammatory cells have a higher uptake of glucose, and FDG-PET imaging is used to look for metabolically active inflammatory tissue that takes up glucose. It gives complementary information to MRI. Cardiac MRI shows structural or functional changes, such as scarring or edema, whereas FDG-PET imaging directly measures metabolic activity related to inflammatory cells.”
The study involved 47 individuals, 51% female, with a mean age of 43 years, who had recently recovered from COVID-19 infection. Of these, the majority had had relatively mild COVID disease, with 85% not requiring hospitalization.
Cardiac imaging was performed a mean of 67 days after the diagnosis of COVID-19. At the time of imaging, 19 participants (40%) reported at least one cardiac symptom, including palpitations, chest pain, and shortness of breath.
Results showed that eight patients (17%) had focal FDG uptake on PET consistent with myocardial inflammation. Compared with those without FDG uptake, patients with focal FDG uptake had higher regional T2, T1, and extracellular volume (colocalizing with focal FDG uptake), higher prevalence of late gadolinium enhancement indicating fibrosis, lower left ventricular ejection fraction, worse global longitudinal and circumferential strain, and higher systemic inflammatory blood markers, including interleukin (IL)-6, IL- 8, an high-sensitivity C-reactive protein.
Of the 47 patients in the study, 13 had received at least one dose of a COVID-19 vaccine. There was no significant difference in the proportion of patients who were PET-positive among those who had received a COVID-19 vaccine and those who had not.
There was also no difference in inflammation in patients who had been hospitalized with COVID-19 and those who had managed their infection at home.
Among patients with focal FDG uptake, PET, MRI, and inflammatory blood markers improved at follow-up imaging performed a mean of 52 days after the first imaging. The authors say this suggests that these abnormalities were not related to pre-existing cardiovascular disease.
Of the eight patients with positive FDG-PET results, two did not show any MRI abnormalities. These two patients also had elevated inflammatory biomarkers. “PET is a more sensitive method of measuring cardiac inflammation, and our results show that these changes may not always translate into functional changes seen on MRI,” Dr. Thavendiranathan noted.
The only cardiac risk factor that was more common in participants with FDG uptake was hypertension. Although cardiac symptoms were nearly twice as common in participants with focal FDG uptake, this difference was not statistically significant.
“Given the growing number of survivors with similar symptoms, these interesting findings warrant further investigation,” the authors say.
Noting that FDG uptake correlated with elevations in systemic inflammatory biomarkers, the researchers suggest that “a more intense systemic inflammatory process may be contributing to cardiac inflammation and the consequential alteration to regional and global myocardial function in PET-positive participants.”
On repeat imaging 2 months later, all eight patients who showed FDG uptake showed improvement or resolution of inflammation without any treatment, although two patients still had some signs of inflammation. Blood biomarkers also improved on follow-up.
“This is encouraging information, but we need longer-term data to see if there are any long-term repercussions of this inflammation,” Dr. Hanneman said.
“Overall, the study findings suggest an imaging phenotype that is expected to have good prognosis. However, longer-term follow-up studies are required to understand the need for ongoing cardiac surveillance, relationship to cardiac symptoms, guidance for safe return to exercise and sports participation, and long-term cardiovascular disease risk,” the researchers state.
This study was funded by grants from the Joint Department of Medical Imaging Academic Incentive Fund, Peter Munk Cardiac Center Innovation Committee, and Ted Rogers Center for Heart Research. Dr. Hanneman reports personal fees from Sanofi Genzyme, Amicus, and Medscape outside the submitted work.
A version of this article first appeared on Medscape.com.
Myocardial inflammation is present in a small proportion of patients who have recovered from relatively mild cases of COVID-19 infection, a new study shows.
“Our findings suggest that even in patients who have had relatively mild cases of COVID-19, some will have inflammatory changes to the heart, and these changes can be present without any cardiac symptoms,” senior author, Paaladinesh Thavendiranathan, MD, University of Toronto, told this news organization.
“While our data suggest that this inflammation improves over time, and the outcomes seem positive, we don’t know if there will be any long-term consequences,” he added.
Noting that even a short period of inflammation in the heart may be associated with symptoms or arrhythmias in the longer term, Dr. Thavendiranathan said: “I would recommend that it is best to avoid getting the infection if there is any chance of heart inflammation.”
The study was published online in JAMA Cardiology on Jan. 12.
The authors explain that among patients hospitalized with COVID, early studies suggested that approximately one in four experience cardiovascular injury, defined as an elevation in troponin levels, which was associated with a 5- to 10-fold increase in the risk for death. But there is limited information on cardiac injury in patients who do not require hospitalization.
Although a broad range of abnormal myocardial tissue has been reported in several cardiac MRI studies of patients recovered from COVID infection, there is little understanding of persistent changes in myocardial metabolism in recovered patients, which is a potential concern, given that COVID-19 is associated with systemic inflammation during the acute illness, they say.
For the current study, the researchers examined myocardial inflammation measured using two different methods – cardiac MRI and fluorodeoxyglucose–positron emission tomography (FDG-PET) – in individuals who had recovered from COVID-19 infection and looked at how this related to changes in inflammatory blood markers.
Lead author Kate Hanneman, MD, also from the University of Toronto, explained that FDG-PET imaging is more sensitive than MRI in detecting active inflammation. “Inflammatory cells have a higher uptake of glucose, and FDG-PET imaging is used to look for metabolically active inflammatory tissue that takes up glucose. It gives complementary information to MRI. Cardiac MRI shows structural or functional changes, such as scarring or edema, whereas FDG-PET imaging directly measures metabolic activity related to inflammatory cells.”
The study involved 47 individuals, 51% female, with a mean age of 43 years, who had recently recovered from COVID-19 infection. Of these, the majority had had relatively mild COVID disease, with 85% not requiring hospitalization.
Cardiac imaging was performed a mean of 67 days after the diagnosis of COVID-19. At the time of imaging, 19 participants (40%) reported at least one cardiac symptom, including palpitations, chest pain, and shortness of breath.
Results showed that eight patients (17%) had focal FDG uptake on PET consistent with myocardial inflammation. Compared with those without FDG uptake, patients with focal FDG uptake had higher regional T2, T1, and extracellular volume (colocalizing with focal FDG uptake), higher prevalence of late gadolinium enhancement indicating fibrosis, lower left ventricular ejection fraction, worse global longitudinal and circumferential strain, and higher systemic inflammatory blood markers, including interleukin (IL)-6, IL- 8, an high-sensitivity C-reactive protein.
Of the 47 patients in the study, 13 had received at least one dose of a COVID-19 vaccine. There was no significant difference in the proportion of patients who were PET-positive among those who had received a COVID-19 vaccine and those who had not.
There was also no difference in inflammation in patients who had been hospitalized with COVID-19 and those who had managed their infection at home.
Among patients with focal FDG uptake, PET, MRI, and inflammatory blood markers improved at follow-up imaging performed a mean of 52 days after the first imaging. The authors say this suggests that these abnormalities were not related to pre-existing cardiovascular disease.
Of the eight patients with positive FDG-PET results, two did not show any MRI abnormalities. These two patients also had elevated inflammatory biomarkers. “PET is a more sensitive method of measuring cardiac inflammation, and our results show that these changes may not always translate into functional changes seen on MRI,” Dr. Thavendiranathan noted.
The only cardiac risk factor that was more common in participants with FDG uptake was hypertension. Although cardiac symptoms were nearly twice as common in participants with focal FDG uptake, this difference was not statistically significant.
“Given the growing number of survivors with similar symptoms, these interesting findings warrant further investigation,” the authors say.
Noting that FDG uptake correlated with elevations in systemic inflammatory biomarkers, the researchers suggest that “a more intense systemic inflammatory process may be contributing to cardiac inflammation and the consequential alteration to regional and global myocardial function in PET-positive participants.”
On repeat imaging 2 months later, all eight patients who showed FDG uptake showed improvement or resolution of inflammation without any treatment, although two patients still had some signs of inflammation. Blood biomarkers also improved on follow-up.
“This is encouraging information, but we need longer-term data to see if there are any long-term repercussions of this inflammation,” Dr. Hanneman said.
“Overall, the study findings suggest an imaging phenotype that is expected to have good prognosis. However, longer-term follow-up studies are required to understand the need for ongoing cardiac surveillance, relationship to cardiac symptoms, guidance for safe return to exercise and sports participation, and long-term cardiovascular disease risk,” the researchers state.
This study was funded by grants from the Joint Department of Medical Imaging Academic Incentive Fund, Peter Munk Cardiac Center Innovation Committee, and Ted Rogers Center for Heart Research. Dr. Hanneman reports personal fees from Sanofi Genzyme, Amicus, and Medscape outside the submitted work.
A version of this article first appeared on Medscape.com.
Myocardial inflammation is present in a small proportion of patients who have recovered from relatively mild cases of COVID-19 infection, a new study shows.
“Our findings suggest that even in patients who have had relatively mild cases of COVID-19, some will have inflammatory changes to the heart, and these changes can be present without any cardiac symptoms,” senior author, Paaladinesh Thavendiranathan, MD, University of Toronto, told this news organization.
“While our data suggest that this inflammation improves over time, and the outcomes seem positive, we don’t know if there will be any long-term consequences,” he added.
Noting that even a short period of inflammation in the heart may be associated with symptoms or arrhythmias in the longer term, Dr. Thavendiranathan said: “I would recommend that it is best to avoid getting the infection if there is any chance of heart inflammation.”
The study was published online in JAMA Cardiology on Jan. 12.
The authors explain that among patients hospitalized with COVID, early studies suggested that approximately one in four experience cardiovascular injury, defined as an elevation in troponin levels, which was associated with a 5- to 10-fold increase in the risk for death. But there is limited information on cardiac injury in patients who do not require hospitalization.
Although a broad range of abnormal myocardial tissue has been reported in several cardiac MRI studies of patients recovered from COVID infection, there is little understanding of persistent changes in myocardial metabolism in recovered patients, which is a potential concern, given that COVID-19 is associated with systemic inflammation during the acute illness, they say.
For the current study, the researchers examined myocardial inflammation measured using two different methods – cardiac MRI and fluorodeoxyglucose–positron emission tomography (FDG-PET) – in individuals who had recovered from COVID-19 infection and looked at how this related to changes in inflammatory blood markers.
Lead author Kate Hanneman, MD, also from the University of Toronto, explained that FDG-PET imaging is more sensitive than MRI in detecting active inflammation. “Inflammatory cells have a higher uptake of glucose, and FDG-PET imaging is used to look for metabolically active inflammatory tissue that takes up glucose. It gives complementary information to MRI. Cardiac MRI shows structural or functional changes, such as scarring or edema, whereas FDG-PET imaging directly measures metabolic activity related to inflammatory cells.”
The study involved 47 individuals, 51% female, with a mean age of 43 years, who had recently recovered from COVID-19 infection. Of these, the majority had had relatively mild COVID disease, with 85% not requiring hospitalization.
Cardiac imaging was performed a mean of 67 days after the diagnosis of COVID-19. At the time of imaging, 19 participants (40%) reported at least one cardiac symptom, including palpitations, chest pain, and shortness of breath.
Results showed that eight patients (17%) had focal FDG uptake on PET consistent with myocardial inflammation. Compared with those without FDG uptake, patients with focal FDG uptake had higher regional T2, T1, and extracellular volume (colocalizing with focal FDG uptake), higher prevalence of late gadolinium enhancement indicating fibrosis, lower left ventricular ejection fraction, worse global longitudinal and circumferential strain, and higher systemic inflammatory blood markers, including interleukin (IL)-6, IL- 8, an high-sensitivity C-reactive protein.
Of the 47 patients in the study, 13 had received at least one dose of a COVID-19 vaccine. There was no significant difference in the proportion of patients who were PET-positive among those who had received a COVID-19 vaccine and those who had not.
There was also no difference in inflammation in patients who had been hospitalized with COVID-19 and those who had managed their infection at home.
Among patients with focal FDG uptake, PET, MRI, and inflammatory blood markers improved at follow-up imaging performed a mean of 52 days after the first imaging. The authors say this suggests that these abnormalities were not related to pre-existing cardiovascular disease.
Of the eight patients with positive FDG-PET results, two did not show any MRI abnormalities. These two patients also had elevated inflammatory biomarkers. “PET is a more sensitive method of measuring cardiac inflammation, and our results show that these changes may not always translate into functional changes seen on MRI,” Dr. Thavendiranathan noted.
The only cardiac risk factor that was more common in participants with FDG uptake was hypertension. Although cardiac symptoms were nearly twice as common in participants with focal FDG uptake, this difference was not statistically significant.
“Given the growing number of survivors with similar symptoms, these interesting findings warrant further investigation,” the authors say.
Noting that FDG uptake correlated with elevations in systemic inflammatory biomarkers, the researchers suggest that “a more intense systemic inflammatory process may be contributing to cardiac inflammation and the consequential alteration to regional and global myocardial function in PET-positive participants.”
On repeat imaging 2 months later, all eight patients who showed FDG uptake showed improvement or resolution of inflammation without any treatment, although two patients still had some signs of inflammation. Blood biomarkers also improved on follow-up.
“This is encouraging information, but we need longer-term data to see if there are any long-term repercussions of this inflammation,” Dr. Hanneman said.
“Overall, the study findings suggest an imaging phenotype that is expected to have good prognosis. However, longer-term follow-up studies are required to understand the need for ongoing cardiac surveillance, relationship to cardiac symptoms, guidance for safe return to exercise and sports participation, and long-term cardiovascular disease risk,” the researchers state.
This study was funded by grants from the Joint Department of Medical Imaging Academic Incentive Fund, Peter Munk Cardiac Center Innovation Committee, and Ted Rogers Center for Heart Research. Dr. Hanneman reports personal fees from Sanofi Genzyme, Amicus, and Medscape outside the submitted work.
A version of this article first appeared on Medscape.com.