User login
EMERGENCY MEDICINE is a practical, peer-reviewed monthly publication and Web site that meets the educational needs of emergency clinicians and urgent care clinicians for their practice.
High rates of work-related trauma, PTSD in intern physicians
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”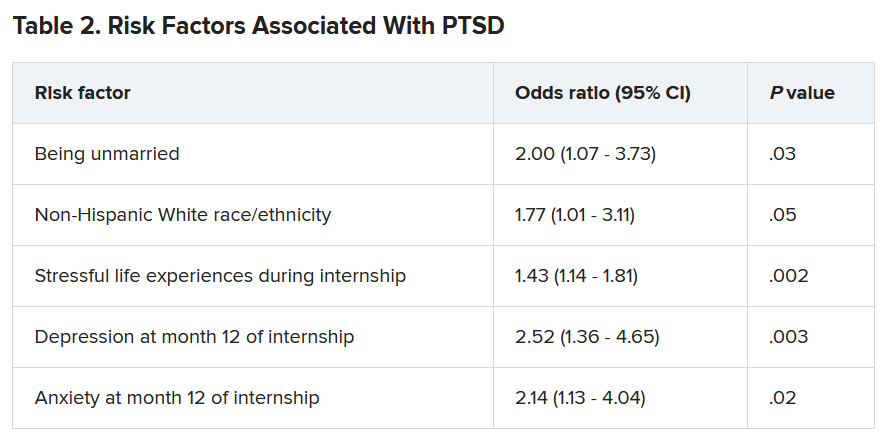
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”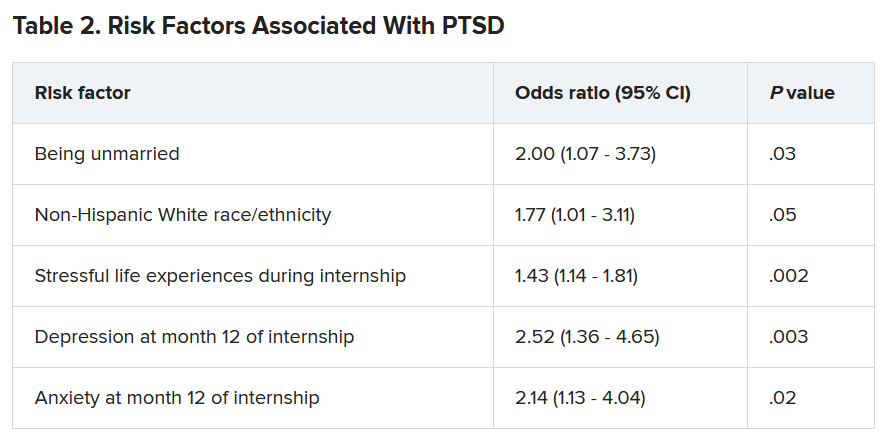
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”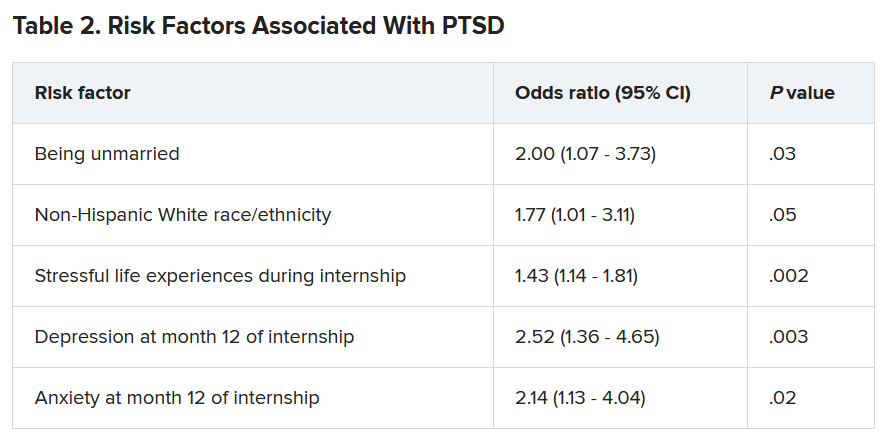
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Incorporating self-care, wellness into routines can prevent doctors’ burnout
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
AMA: ‘Excited delirium’ not a legitimate medical diagnosis
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Inpatient care for HS higher for Black and Hispanic patients
National Inpatient Sample.
The differences occurred despite Black and Hispanic patients being younger at the time of admission than White patients, and may reflect increased disease severity and management challenges in these patients with skin of color, Nishadh Sutaria, BS, a medical student at Tufts University, Boston, said at the annual Skin of Color Society symposium. “They may also reflect social inequities in access to dermatologists, with racial and ethnic minorities using inpatient services in lieu of outpatient care.”
Mr. Sutaria and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified 8,040 HS admissions for White patients, 16,490 Black patients, and 2,405 for Hispanic patients during the 5-year period.
Black and Hispanic patients were significantly younger than White patients, with a mean age of 38.1 years and 35 years, respectively, compared with 42 years for White patients (P < .001 in each case). Compared with White patients, Black patients had more procedures (2.03 vs. 1.84, P = .006), a longer length of stay (5.82 days vs. 4.97 days, P = .001), and higher cost of care ($46,119 vs. $39,862, P = .010). Compared with White patients, Hispanic patients had higher cost of care ($52,334 vs. $39,862, P = .004).
“In these models, Black patients stayed almost a full day longer and accrued a charge of $8,000 more than White patients, and Hispanic patients stayed about a half-day longer and accrued a charge of almost $15,000 more than White patients,” Mr. Sutaria said.
In a multilinear regression analysis adjusting for age, sex, and insurance type, Black race correlated with more procedures, higher length of stay, and higher cost of care, and Hispanic ethnicity with more procedures and higher cost of care.
Prior research has shown that Black patients may be disproportionately affected by HS. A 2017 analysis of electronic health record data for tens of millions of patients nationally, for instance, showed an incidence of HS that was over 2.5 times greater in Blacks than Whites. And a recent analysis of electronic data in Wisconsin for patients with an HS diagnosis and 3 or more encounters for the disease showed that Blacks are more likely to have HS that is Hurley Stage 3, the most severe type.
Increased severity “has not been explicitly shown in Hispanic patients,” Dr. Kwatra said in an interview, “[but] there is a strong relationship between obesity/metabolic syndrome with HS. Because Hispanic patients have higher rates of obesity and metabolic syndrome, it’s [thought] that they may have more severe HS.”
HS patients with skin of color are underrepresented in clinical trials, he said. “Severe HS can be difficult to treat because there are few effective treatments,” he said, noting that adalimumab is the only Food and Drug Administration–approved therapy.
The National Inpatient Sample is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Sutaria is a dermatology research fellow working under the guidance of Dr. Kwatra.
National Inpatient Sample.
The differences occurred despite Black and Hispanic patients being younger at the time of admission than White patients, and may reflect increased disease severity and management challenges in these patients with skin of color, Nishadh Sutaria, BS, a medical student at Tufts University, Boston, said at the annual Skin of Color Society symposium. “They may also reflect social inequities in access to dermatologists, with racial and ethnic minorities using inpatient services in lieu of outpatient care.”
Mr. Sutaria and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified 8,040 HS admissions for White patients, 16,490 Black patients, and 2,405 for Hispanic patients during the 5-year period.
Black and Hispanic patients were significantly younger than White patients, with a mean age of 38.1 years and 35 years, respectively, compared with 42 years for White patients (P < .001 in each case). Compared with White patients, Black patients had more procedures (2.03 vs. 1.84, P = .006), a longer length of stay (5.82 days vs. 4.97 days, P = .001), and higher cost of care ($46,119 vs. $39,862, P = .010). Compared with White patients, Hispanic patients had higher cost of care ($52,334 vs. $39,862, P = .004).
“In these models, Black patients stayed almost a full day longer and accrued a charge of $8,000 more than White patients, and Hispanic patients stayed about a half-day longer and accrued a charge of almost $15,000 more than White patients,” Mr. Sutaria said.
In a multilinear regression analysis adjusting for age, sex, and insurance type, Black race correlated with more procedures, higher length of stay, and higher cost of care, and Hispanic ethnicity with more procedures and higher cost of care.
Prior research has shown that Black patients may be disproportionately affected by HS. A 2017 analysis of electronic health record data for tens of millions of patients nationally, for instance, showed an incidence of HS that was over 2.5 times greater in Blacks than Whites. And a recent analysis of electronic data in Wisconsin for patients with an HS diagnosis and 3 or more encounters for the disease showed that Blacks are more likely to have HS that is Hurley Stage 3, the most severe type.
Increased severity “has not been explicitly shown in Hispanic patients,” Dr. Kwatra said in an interview, “[but] there is a strong relationship between obesity/metabolic syndrome with HS. Because Hispanic patients have higher rates of obesity and metabolic syndrome, it’s [thought] that they may have more severe HS.”
HS patients with skin of color are underrepresented in clinical trials, he said. “Severe HS can be difficult to treat because there are few effective treatments,” he said, noting that adalimumab is the only Food and Drug Administration–approved therapy.
The National Inpatient Sample is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Sutaria is a dermatology research fellow working under the guidance of Dr. Kwatra.
National Inpatient Sample.
The differences occurred despite Black and Hispanic patients being younger at the time of admission than White patients, and may reflect increased disease severity and management challenges in these patients with skin of color, Nishadh Sutaria, BS, a medical student at Tufts University, Boston, said at the annual Skin of Color Society symposium. “They may also reflect social inequities in access to dermatologists, with racial and ethnic minorities using inpatient services in lieu of outpatient care.”
Mr. Sutaria and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified 8,040 HS admissions for White patients, 16,490 Black patients, and 2,405 for Hispanic patients during the 5-year period.
Black and Hispanic patients were significantly younger than White patients, with a mean age of 38.1 years and 35 years, respectively, compared with 42 years for White patients (P < .001 in each case). Compared with White patients, Black patients had more procedures (2.03 vs. 1.84, P = .006), a longer length of stay (5.82 days vs. 4.97 days, P = .001), and higher cost of care ($46,119 vs. $39,862, P = .010). Compared with White patients, Hispanic patients had higher cost of care ($52,334 vs. $39,862, P = .004).
“In these models, Black patients stayed almost a full day longer and accrued a charge of $8,000 more than White patients, and Hispanic patients stayed about a half-day longer and accrued a charge of almost $15,000 more than White patients,” Mr. Sutaria said.
In a multilinear regression analysis adjusting for age, sex, and insurance type, Black race correlated with more procedures, higher length of stay, and higher cost of care, and Hispanic ethnicity with more procedures and higher cost of care.
Prior research has shown that Black patients may be disproportionately affected by HS. A 2017 analysis of electronic health record data for tens of millions of patients nationally, for instance, showed an incidence of HS that was over 2.5 times greater in Blacks than Whites. And a recent analysis of electronic data in Wisconsin for patients with an HS diagnosis and 3 or more encounters for the disease showed that Blacks are more likely to have HS that is Hurley Stage 3, the most severe type.
Increased severity “has not been explicitly shown in Hispanic patients,” Dr. Kwatra said in an interview, “[but] there is a strong relationship between obesity/metabolic syndrome with HS. Because Hispanic patients have higher rates of obesity and metabolic syndrome, it’s [thought] that they may have more severe HS.”
HS patients with skin of color are underrepresented in clinical trials, he said. “Severe HS can be difficult to treat because there are few effective treatments,” he said, noting that adalimumab is the only Food and Drug Administration–approved therapy.
The National Inpatient Sample is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Sutaria is a dermatology research fellow working under the guidance of Dr. Kwatra.
FROM SOC SOCIETY 2021
Minnesota named best place to practice in 2021
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.
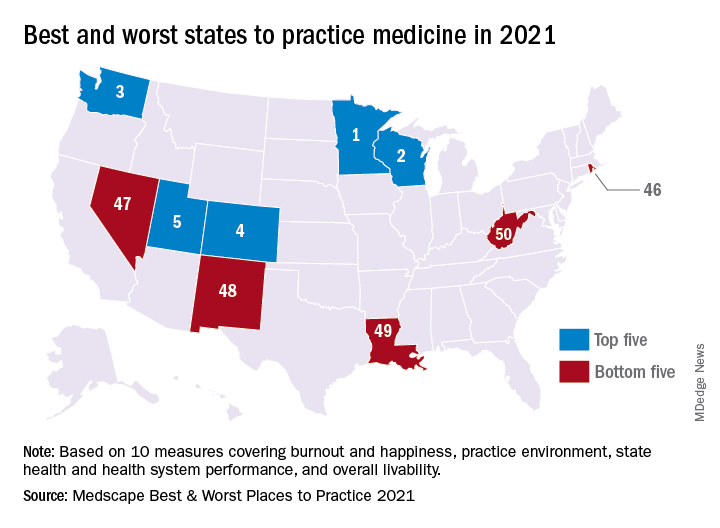
In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.
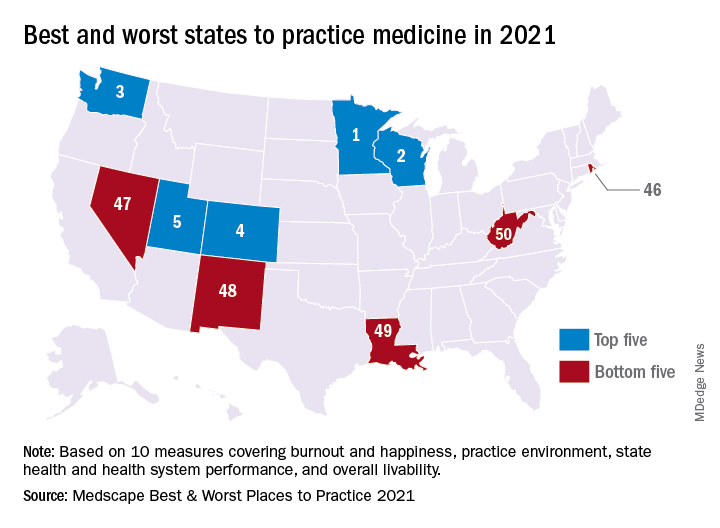
In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.
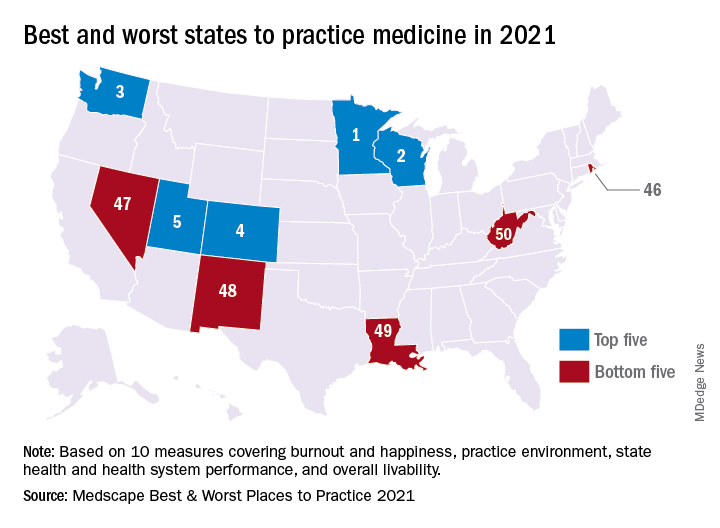
In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
U.S. News releases Best Children’s Hospitals list, with changes
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Bariatric surgery tied to fewer HFpEF hospitalizations
Patients who underwent metabolic and bariatric surgery had fewer than half the number of hospitalizations for both acute and chronic episodes of heart failure with preserved ejection fraction (HFpEF) in a retrospective analysis of more than 2 million Americans collected in a national database.
In a multivariate analysis that adjusted for several variables patients without a history of bariatric surgery had three- to fivefold more hospitalizations for acute events involving HFpEF, and more than double the rate of hospitalizations for chronic HFpEF events, David R. Funes, MD, said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
While this analysis has the limitations of being retrospective, observational, and entirely reliant on procedure codes to define medical histories and outcomes, it had the advantage of using a large database designed to represent the U.S. adult population, said Dr. Funes, a bariatric surgeon at the Cleveland Clinic in Weston, Fla.
HFpEF effects could ‘extend’ surgery’s use
The report “adds an important article to the literature where there is a true void in trying to discern the effect of bariatric surgery on HFpEF,” commented Tammy L. Kindel, MD, PhD, director of the bariatric surgery program at the Medical College of Wisconsin, Milwaukee, and designated discussant for the report. “Minimal studies [up to now] demonstrate that weight loss in any form can modify diastolic dysfunction in patients with HFpEF. Studies that investigate the impact of bariatric surgery on clinical outcomes in patients with HFpEF are probably the most important for extending use of metabolic surgery,” Dr. Kindel said.
She added that “one of the most difficult parts of studying HFpEF” is making a firm diagnosis that often involves excluding other potential causes. She also questioned Dr. Funes about his confidence that his analysis correctly identified patients only with HFpEF. Dr. Funes replied that the diagnostic codes his team used allowed for a clear distinction between patients identified with HFpEF and those with heart failure with reduced ejection fraction, but he also admitted that his study’s complete reliance on these codes introduced a limitation to the analysis.
Including patients with diastolic dysfunction as well as HFpEF
The study used data collected during 2010-2015 by the National Inpatient Sample, run by the U.S. Department of Health & Human Services in a case-control analysis that included 296,041 patients who had undergone some form of bariatric surgery and 2,004,804 people with no history of bariatric surgery selected as controls on the basis of their obesity.
The absolute numbers showed that, during the observation period, the incidence of acute HFpEF hospitalizations was 0.19% among those with prior bariatric surgery and 0.86% among those with no surgery, and the incidence of chronic heart failure hospitalizations was 0.01% among people with prior bariatric surgery and 0.05% among those without prior surgery. Dr. Funes said. He noted that, during the period studied patients, with HFpEF were usually identified as having diastolic heart failure, an older name for the same disease.
In multivariate analyses that adjusted for age, sex, race, hypertension, diabetes, smoking, and coronary artery disease, people without prior bariatric surgery and with hypertension had a 2.8-fold increased rate of acute hospitalizations for HFpEF, while those without hypertension or prior bariatric surgery had a 5.2-fold increased rate. In addition, control patients, regardless of hypertension status, had a 2.9-fold increased rate of hospitalizations for chronic HFpEF events. All these differences were statistically significant.
Dr. Funes also reported results from additional analyses that focused on a roughly 68,000-patient subgroup of those included in the study who had a history of coronary artery disease, including about 62,000 with no prior bariatric surgery and nearly 6,000 people with prior bariatric surgery. In a multivariate analysis of this subgroup, people without prior bariatric surgery had a 2.65-fold increased rate of hospitalization for a HFpEF event (either acute or chronic), compared with those who had undergone bariatric surgery.
Dr. Funes and associates and Dr. Kindel had no relevant disclosures.
Patients who underwent metabolic and bariatric surgery had fewer than half the number of hospitalizations for both acute and chronic episodes of heart failure with preserved ejection fraction (HFpEF) in a retrospective analysis of more than 2 million Americans collected in a national database.
In a multivariate analysis that adjusted for several variables patients without a history of bariatric surgery had three- to fivefold more hospitalizations for acute events involving HFpEF, and more than double the rate of hospitalizations for chronic HFpEF events, David R. Funes, MD, said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
While this analysis has the limitations of being retrospective, observational, and entirely reliant on procedure codes to define medical histories and outcomes, it had the advantage of using a large database designed to represent the U.S. adult population, said Dr. Funes, a bariatric surgeon at the Cleveland Clinic in Weston, Fla.
HFpEF effects could ‘extend’ surgery’s use
The report “adds an important article to the literature where there is a true void in trying to discern the effect of bariatric surgery on HFpEF,” commented Tammy L. Kindel, MD, PhD, director of the bariatric surgery program at the Medical College of Wisconsin, Milwaukee, and designated discussant for the report. “Minimal studies [up to now] demonstrate that weight loss in any form can modify diastolic dysfunction in patients with HFpEF. Studies that investigate the impact of bariatric surgery on clinical outcomes in patients with HFpEF are probably the most important for extending use of metabolic surgery,” Dr. Kindel said.
She added that “one of the most difficult parts of studying HFpEF” is making a firm diagnosis that often involves excluding other potential causes. She also questioned Dr. Funes about his confidence that his analysis correctly identified patients only with HFpEF. Dr. Funes replied that the diagnostic codes his team used allowed for a clear distinction between patients identified with HFpEF and those with heart failure with reduced ejection fraction, but he also admitted that his study’s complete reliance on these codes introduced a limitation to the analysis.
Including patients with diastolic dysfunction as well as HFpEF
The study used data collected during 2010-2015 by the National Inpatient Sample, run by the U.S. Department of Health & Human Services in a case-control analysis that included 296,041 patients who had undergone some form of bariatric surgery and 2,004,804 people with no history of bariatric surgery selected as controls on the basis of their obesity.
The absolute numbers showed that, during the observation period, the incidence of acute HFpEF hospitalizations was 0.19% among those with prior bariatric surgery and 0.86% among those with no surgery, and the incidence of chronic heart failure hospitalizations was 0.01% among people with prior bariatric surgery and 0.05% among those without prior surgery. Dr. Funes said. He noted that, during the period studied patients, with HFpEF were usually identified as having diastolic heart failure, an older name for the same disease.
In multivariate analyses that adjusted for age, sex, race, hypertension, diabetes, smoking, and coronary artery disease, people without prior bariatric surgery and with hypertension had a 2.8-fold increased rate of acute hospitalizations for HFpEF, while those without hypertension or prior bariatric surgery had a 5.2-fold increased rate. In addition, control patients, regardless of hypertension status, had a 2.9-fold increased rate of hospitalizations for chronic HFpEF events. All these differences were statistically significant.
Dr. Funes also reported results from additional analyses that focused on a roughly 68,000-patient subgroup of those included in the study who had a history of coronary artery disease, including about 62,000 with no prior bariatric surgery and nearly 6,000 people with prior bariatric surgery. In a multivariate analysis of this subgroup, people without prior bariatric surgery had a 2.65-fold increased rate of hospitalization for a HFpEF event (either acute or chronic), compared with those who had undergone bariatric surgery.
Dr. Funes and associates and Dr. Kindel had no relevant disclosures.
Patients who underwent metabolic and bariatric surgery had fewer than half the number of hospitalizations for both acute and chronic episodes of heart failure with preserved ejection fraction (HFpEF) in a retrospective analysis of more than 2 million Americans collected in a national database.
In a multivariate analysis that adjusted for several variables patients without a history of bariatric surgery had three- to fivefold more hospitalizations for acute events involving HFpEF, and more than double the rate of hospitalizations for chronic HFpEF events, David R. Funes, MD, said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
While this analysis has the limitations of being retrospective, observational, and entirely reliant on procedure codes to define medical histories and outcomes, it had the advantage of using a large database designed to represent the U.S. adult population, said Dr. Funes, a bariatric surgeon at the Cleveland Clinic in Weston, Fla.
HFpEF effects could ‘extend’ surgery’s use
The report “adds an important article to the literature where there is a true void in trying to discern the effect of bariatric surgery on HFpEF,” commented Tammy L. Kindel, MD, PhD, director of the bariatric surgery program at the Medical College of Wisconsin, Milwaukee, and designated discussant for the report. “Minimal studies [up to now] demonstrate that weight loss in any form can modify diastolic dysfunction in patients with HFpEF. Studies that investigate the impact of bariatric surgery on clinical outcomes in patients with HFpEF are probably the most important for extending use of metabolic surgery,” Dr. Kindel said.
She added that “one of the most difficult parts of studying HFpEF” is making a firm diagnosis that often involves excluding other potential causes. She also questioned Dr. Funes about his confidence that his analysis correctly identified patients only with HFpEF. Dr. Funes replied that the diagnostic codes his team used allowed for a clear distinction between patients identified with HFpEF and those with heart failure with reduced ejection fraction, but he also admitted that his study’s complete reliance on these codes introduced a limitation to the analysis.
Including patients with diastolic dysfunction as well as HFpEF
The study used data collected during 2010-2015 by the National Inpatient Sample, run by the U.S. Department of Health & Human Services in a case-control analysis that included 296,041 patients who had undergone some form of bariatric surgery and 2,004,804 people with no history of bariatric surgery selected as controls on the basis of their obesity.
The absolute numbers showed that, during the observation period, the incidence of acute HFpEF hospitalizations was 0.19% among those with prior bariatric surgery and 0.86% among those with no surgery, and the incidence of chronic heart failure hospitalizations was 0.01% among people with prior bariatric surgery and 0.05% among those without prior surgery. Dr. Funes said. He noted that, during the period studied patients, with HFpEF were usually identified as having diastolic heart failure, an older name for the same disease.
In multivariate analyses that adjusted for age, sex, race, hypertension, diabetes, smoking, and coronary artery disease, people without prior bariatric surgery and with hypertension had a 2.8-fold increased rate of acute hospitalizations for HFpEF, while those without hypertension or prior bariatric surgery had a 5.2-fold increased rate. In addition, control patients, regardless of hypertension status, had a 2.9-fold increased rate of hospitalizations for chronic HFpEF events. All these differences were statistically significant.
Dr. Funes also reported results from additional analyses that focused on a roughly 68,000-patient subgroup of those included in the study who had a history of coronary artery disease, including about 62,000 with no prior bariatric surgery and nearly 6,000 people with prior bariatric surgery. In a multivariate analysis of this subgroup, people without prior bariatric surgery had a 2.65-fold increased rate of hospitalization for a HFpEF event (either acute or chronic), compared with those who had undergone bariatric surgery.
Dr. Funes and associates and Dr. Kindel had no relevant disclosures.
FROM ASMBS 2021
Judge tosses hospital staff suit over vaccine mandate
A federal judge in Texas has dismissed a lawsuit from 117 Houston Methodist Hospital workers who refused to get a COVID-19 vaccine and said it was illegal to require them to do so.
In the ruling issued June 12, U.S. District Judge Lynn Hughes upheld the hospital’s policy and said the vaccination requirement didn’t break any federal laws.
“This is not coercion,” Judge Hughes wrote in the ruling.
“Methodist is trying to do their business of saving lives without giving them the COVID-19 virus,” he wrote. “It is a choice made to keep staff, patients, and their families safer.”
In April, the Houston Methodist Hospital system announced a policy that required employees to be vaccinated by June 7 or request an exemption. After the deadline, 178 of 26,000 employees refused to get inoculated and were placed on suspension without pay. The employees said the vaccine was unsafe and “experimental.” In his ruling, Judge Hughes said their claim was false and irrelevant.
“Texas law only protects employees from being terminated for refusing to commit an act carrying criminal penalties to the worker,” he wrote. “Receiving a COVID-19 vaccination is not an illegal act, and it carries no criminal penalties.”
He denounced the “press-release style of the complaint” and the comparison of the hospital’s vaccine policy to forced experimentation by the Nazis against Jewish people during the Holocaust.
“Equating the injection requirement to medical experimentation in concentration camps is reprehensible,” he wrote. “Nazi doctors conducted medical experiments on victims that caused pain, mutilation, permanent disability, and in many cases, death.”
Judge Hughes also said that employees can “freely choose” to accept or refuse a COVID-19 vaccine. If they refuse, they “simply need to work somewhere else,” he wrote.
“If a worker refuses an assignment, changed office, earlier start time, or other directive, he may be properly fired,” Judge Hughes said. “Every employment includes limits on the worker’s behavior in exchange for his remuneration. This is all part of the bargain.”
The ruling could set a precedent for similar COVID-19 vaccine lawsuits across the country, NPR reported. Houston Methodist was one of the first hospitals to require staff to be vaccinated. After the ruling on June 12, the hospital system wrote in a statement that it was “pleased and reassured” that Judge Hughes dismissed a “frivolous lawsuit.”
The hospital system will begin to terminate the 178 employees who were suspended if they don’t get a vaccine by June 21.
Jennifer Bridges, a nurse who has led the campaign against the vaccine policy, said she and the other plaintiffs will appeal the decision, according to KHOU.
“We’re OK with this decision. We are appealing. This will be taken all the way to the Supreme Court,” she told the news station. “This is far from over. This is literally only the beginning.”
A version of this article first appeared on WebMD.com.
A federal judge in Texas has dismissed a lawsuit from 117 Houston Methodist Hospital workers who refused to get a COVID-19 vaccine and said it was illegal to require them to do so.
In the ruling issued June 12, U.S. District Judge Lynn Hughes upheld the hospital’s policy and said the vaccination requirement didn’t break any federal laws.
“This is not coercion,” Judge Hughes wrote in the ruling.
“Methodist is trying to do their business of saving lives without giving them the COVID-19 virus,” he wrote. “It is a choice made to keep staff, patients, and their families safer.”
In April, the Houston Methodist Hospital system announced a policy that required employees to be vaccinated by June 7 or request an exemption. After the deadline, 178 of 26,000 employees refused to get inoculated and were placed on suspension without pay. The employees said the vaccine was unsafe and “experimental.” In his ruling, Judge Hughes said their claim was false and irrelevant.
“Texas law only protects employees from being terminated for refusing to commit an act carrying criminal penalties to the worker,” he wrote. “Receiving a COVID-19 vaccination is not an illegal act, and it carries no criminal penalties.”
He denounced the “press-release style of the complaint” and the comparison of the hospital’s vaccine policy to forced experimentation by the Nazis against Jewish people during the Holocaust.
“Equating the injection requirement to medical experimentation in concentration camps is reprehensible,” he wrote. “Nazi doctors conducted medical experiments on victims that caused pain, mutilation, permanent disability, and in many cases, death.”
Judge Hughes also said that employees can “freely choose” to accept or refuse a COVID-19 vaccine. If they refuse, they “simply need to work somewhere else,” he wrote.
“If a worker refuses an assignment, changed office, earlier start time, or other directive, he may be properly fired,” Judge Hughes said. “Every employment includes limits on the worker’s behavior in exchange for his remuneration. This is all part of the bargain.”
The ruling could set a precedent for similar COVID-19 vaccine lawsuits across the country, NPR reported. Houston Methodist was one of the first hospitals to require staff to be vaccinated. After the ruling on June 12, the hospital system wrote in a statement that it was “pleased and reassured” that Judge Hughes dismissed a “frivolous lawsuit.”
The hospital system will begin to terminate the 178 employees who were suspended if they don’t get a vaccine by June 21.
Jennifer Bridges, a nurse who has led the campaign against the vaccine policy, said she and the other plaintiffs will appeal the decision, according to KHOU.
“We’re OK with this decision. We are appealing. This will be taken all the way to the Supreme Court,” she told the news station. “This is far from over. This is literally only the beginning.”
A version of this article first appeared on WebMD.com.
A federal judge in Texas has dismissed a lawsuit from 117 Houston Methodist Hospital workers who refused to get a COVID-19 vaccine and said it was illegal to require them to do so.
In the ruling issued June 12, U.S. District Judge Lynn Hughes upheld the hospital’s policy and said the vaccination requirement didn’t break any federal laws.
“This is not coercion,” Judge Hughes wrote in the ruling.
“Methodist is trying to do their business of saving lives without giving them the COVID-19 virus,” he wrote. “It is a choice made to keep staff, patients, and their families safer.”
In April, the Houston Methodist Hospital system announced a policy that required employees to be vaccinated by June 7 or request an exemption. After the deadline, 178 of 26,000 employees refused to get inoculated and were placed on suspension without pay. The employees said the vaccine was unsafe and “experimental.” In his ruling, Judge Hughes said their claim was false and irrelevant.
“Texas law only protects employees from being terminated for refusing to commit an act carrying criminal penalties to the worker,” he wrote. “Receiving a COVID-19 vaccination is not an illegal act, and it carries no criminal penalties.”
He denounced the “press-release style of the complaint” and the comparison of the hospital’s vaccine policy to forced experimentation by the Nazis against Jewish people during the Holocaust.
“Equating the injection requirement to medical experimentation in concentration camps is reprehensible,” he wrote. “Nazi doctors conducted medical experiments on victims that caused pain, mutilation, permanent disability, and in many cases, death.”
Judge Hughes also said that employees can “freely choose” to accept or refuse a COVID-19 vaccine. If they refuse, they “simply need to work somewhere else,” he wrote.
“If a worker refuses an assignment, changed office, earlier start time, or other directive, he may be properly fired,” Judge Hughes said. “Every employment includes limits on the worker’s behavior in exchange for his remuneration. This is all part of the bargain.”
The ruling could set a precedent for similar COVID-19 vaccine lawsuits across the country, NPR reported. Houston Methodist was one of the first hospitals to require staff to be vaccinated. After the ruling on June 12, the hospital system wrote in a statement that it was “pleased and reassured” that Judge Hughes dismissed a “frivolous lawsuit.”
The hospital system will begin to terminate the 178 employees who were suspended if they don’t get a vaccine by June 21.
Jennifer Bridges, a nurse who has led the campaign against the vaccine policy, said she and the other plaintiffs will appeal the decision, according to KHOU.
“We’re OK with this decision. We are appealing. This will be taken all the way to the Supreme Court,” she told the news station. “This is far from over. This is literally only the beginning.”
A version of this article first appeared on WebMD.com.
OSHA issues new rules on COVID-19 safety for health care workers
The U.S. Occupational Safety and Health Administration issued its long-awaited Emergency Temporary Standard (ETS) for COVID-19 June 10, surprising many by including only health care workers in the new emergency workplace safety rules.
“The ETS is an overdue step toward protecting health care workers, especially those working in long-term care facilities and home health care who are at greatly increased risk of infection,” said George Washington University, Washington, professor and former Obama administration Assistant Secretary of Labor David Michaels, PhD, MPH. “OSHA’s failure to issue a COVID-specific standard in other high-risk industries, like meat and poultry processing, corrections, homeless shelters, and retail establishments is disappointing. If exposure is not controlled in these workplaces, they will continue to be important drivers of infections.”
With the new regulations in place, about 10.3 million health care workers at hospitals, nursing homes, and assisted living facilities, as well as emergency responders and home health care workers, should be guaranteed protection standards that replace former guidance.
The new protections include supplying personal protective equipment and ensuring proper usage (for example, mandatory seal checks on respirators); screening everyone who enters the facility for COVID-19; ensuring proper ventilation; and establishing physical distancing requirements (6 feet) for unvaccinated workers. It also requires employers to give workers time off for vaccination. An antiretaliation clause could shield workers who complain about unsafe conditions.
“The science tells us that health care workers, particularly those who come into regular contact with the virus, are most at risk at this point in the pandemic,” Labor Secretary Marty Walsh said on a press call. “So following an extensive review of the science and data, OSHA determined that a health care–specific safety requirement will make the biggest impact.”
But questions remain, said James Brudney, JD, a professor at Fordham Law School in New York and former chief counsel of the U.S. Senate Subcommittee on Labor. The standard doesn’t amplify or address existing rules regarding a right to refuse unsafe work, for example, so employees may still feel they are risking their jobs to complain, despite the antiretaliation clause.
And although vaccinated employees don’t have to adhere to the same distancing and masking standards in many instances, the standard doesn’t spell out how employers should determine their workers’ vaccination status – instead leaving that determination to employers through their own policies and procedures. (California’s state OSHA office rules specify the mechanism for documentation of vaccination.)
The Trump administration did not issue an ETS, saying OSHA’s general duty clause sufficed. President Joe Biden took the opposite approach, calling for an investigation into an ETS on his first day in office. But the process took months longer than promised.
“I know it’s been a long time coming,” Mr. Walsh acknowledged. “Our health care workers from the very beginning have been put at risk.
While health care unions had asked for mandated safety standards sooner, National Nurses United, the country’s largest labor union for registered nurses, still welcomed the rules.
“An ETS is a major step toward requiring accountability for hospitals who consistently put their budget goals and profits over our health and safety,” Zenei Triunfo-Cortez, RN, one of NNU’s three presidents, said in a statement June 9 anticipating the publication of the rules.
The rules do not apply to retail pharmacies, ambulatory care settings that screen nonemployees for COVID-19, or certain other settings in which all employees are vaccinated and people with suspected or confirmed COVID-19 cannot enter.
The agency said it will work with states that have already issued local regulations, including two states that issued temporary standards of their own, Virginia and California.
Employers will have 2 weeks to comply with most of the regulations after they’re published in the Federal Register. The standards will expire in 6 months but could then become permanent, as Virginia’s did in January.
A version of this article first appeared on Medscape.com.
The U.S. Occupational Safety and Health Administration issued its long-awaited Emergency Temporary Standard (ETS) for COVID-19 June 10, surprising many by including only health care workers in the new emergency workplace safety rules.
“The ETS is an overdue step toward protecting health care workers, especially those working in long-term care facilities and home health care who are at greatly increased risk of infection,” said George Washington University, Washington, professor and former Obama administration Assistant Secretary of Labor David Michaels, PhD, MPH. “OSHA’s failure to issue a COVID-specific standard in other high-risk industries, like meat and poultry processing, corrections, homeless shelters, and retail establishments is disappointing. If exposure is not controlled in these workplaces, they will continue to be important drivers of infections.”
With the new regulations in place, about 10.3 million health care workers at hospitals, nursing homes, and assisted living facilities, as well as emergency responders and home health care workers, should be guaranteed protection standards that replace former guidance.
The new protections include supplying personal protective equipment and ensuring proper usage (for example, mandatory seal checks on respirators); screening everyone who enters the facility for COVID-19; ensuring proper ventilation; and establishing physical distancing requirements (6 feet) for unvaccinated workers. It also requires employers to give workers time off for vaccination. An antiretaliation clause could shield workers who complain about unsafe conditions.
“The science tells us that health care workers, particularly those who come into regular contact with the virus, are most at risk at this point in the pandemic,” Labor Secretary Marty Walsh said on a press call. “So following an extensive review of the science and data, OSHA determined that a health care–specific safety requirement will make the biggest impact.”
But questions remain, said James Brudney, JD, a professor at Fordham Law School in New York and former chief counsel of the U.S. Senate Subcommittee on Labor. The standard doesn’t amplify or address existing rules regarding a right to refuse unsafe work, for example, so employees may still feel they are risking their jobs to complain, despite the antiretaliation clause.
And although vaccinated employees don’t have to adhere to the same distancing and masking standards in many instances, the standard doesn’t spell out how employers should determine their workers’ vaccination status – instead leaving that determination to employers through their own policies and procedures. (California’s state OSHA office rules specify the mechanism for documentation of vaccination.)
The Trump administration did not issue an ETS, saying OSHA’s general duty clause sufficed. President Joe Biden took the opposite approach, calling for an investigation into an ETS on his first day in office. But the process took months longer than promised.
“I know it’s been a long time coming,” Mr. Walsh acknowledged. “Our health care workers from the very beginning have been put at risk.
While health care unions had asked for mandated safety standards sooner, National Nurses United, the country’s largest labor union for registered nurses, still welcomed the rules.
“An ETS is a major step toward requiring accountability for hospitals who consistently put their budget goals and profits over our health and safety,” Zenei Triunfo-Cortez, RN, one of NNU’s three presidents, said in a statement June 9 anticipating the publication of the rules.
The rules do not apply to retail pharmacies, ambulatory care settings that screen nonemployees for COVID-19, or certain other settings in which all employees are vaccinated and people with suspected or confirmed COVID-19 cannot enter.
The agency said it will work with states that have already issued local regulations, including two states that issued temporary standards of their own, Virginia and California.
Employers will have 2 weeks to comply with most of the regulations after they’re published in the Federal Register. The standards will expire in 6 months but could then become permanent, as Virginia’s did in January.
A version of this article first appeared on Medscape.com.
The U.S. Occupational Safety and Health Administration issued its long-awaited Emergency Temporary Standard (ETS) for COVID-19 June 10, surprising many by including only health care workers in the new emergency workplace safety rules.
“The ETS is an overdue step toward protecting health care workers, especially those working in long-term care facilities and home health care who are at greatly increased risk of infection,” said George Washington University, Washington, professor and former Obama administration Assistant Secretary of Labor David Michaels, PhD, MPH. “OSHA’s failure to issue a COVID-specific standard in other high-risk industries, like meat and poultry processing, corrections, homeless shelters, and retail establishments is disappointing. If exposure is not controlled in these workplaces, they will continue to be important drivers of infections.”
With the new regulations in place, about 10.3 million health care workers at hospitals, nursing homes, and assisted living facilities, as well as emergency responders and home health care workers, should be guaranteed protection standards that replace former guidance.
The new protections include supplying personal protective equipment and ensuring proper usage (for example, mandatory seal checks on respirators); screening everyone who enters the facility for COVID-19; ensuring proper ventilation; and establishing physical distancing requirements (6 feet) for unvaccinated workers. It also requires employers to give workers time off for vaccination. An antiretaliation clause could shield workers who complain about unsafe conditions.
“The science tells us that health care workers, particularly those who come into regular contact with the virus, are most at risk at this point in the pandemic,” Labor Secretary Marty Walsh said on a press call. “So following an extensive review of the science and data, OSHA determined that a health care–specific safety requirement will make the biggest impact.”
But questions remain, said James Brudney, JD, a professor at Fordham Law School in New York and former chief counsel of the U.S. Senate Subcommittee on Labor. The standard doesn’t amplify or address existing rules regarding a right to refuse unsafe work, for example, so employees may still feel they are risking their jobs to complain, despite the antiretaliation clause.
And although vaccinated employees don’t have to adhere to the same distancing and masking standards in many instances, the standard doesn’t spell out how employers should determine their workers’ vaccination status – instead leaving that determination to employers through their own policies and procedures. (California’s state OSHA office rules specify the mechanism for documentation of vaccination.)
The Trump administration did not issue an ETS, saying OSHA’s general duty clause sufficed. President Joe Biden took the opposite approach, calling for an investigation into an ETS on his first day in office. But the process took months longer than promised.
“I know it’s been a long time coming,” Mr. Walsh acknowledged. “Our health care workers from the very beginning have been put at risk.
While health care unions had asked for mandated safety standards sooner, National Nurses United, the country’s largest labor union for registered nurses, still welcomed the rules.
“An ETS is a major step toward requiring accountability for hospitals who consistently put their budget goals and profits over our health and safety,” Zenei Triunfo-Cortez, RN, one of NNU’s three presidents, said in a statement June 9 anticipating the publication of the rules.
The rules do not apply to retail pharmacies, ambulatory care settings that screen nonemployees for COVID-19, or certain other settings in which all employees are vaccinated and people with suspected or confirmed COVID-19 cannot enter.
The agency said it will work with states that have already issued local regulations, including two states that issued temporary standards of their own, Virginia and California.
Employers will have 2 weeks to comply with most of the regulations after they’re published in the Federal Register. The standards will expire in 6 months but could then become permanent, as Virginia’s did in January.
A version of this article first appeared on Medscape.com.
Improving emergency care for children living outside of urban areas
A new physician workforce study documents that almost all clinically active pediatric emergency physicians in the United States – 99% of them – work in urban areas, and that those who do practice in rural areas are significantly older and closer to retirement age.
The portrait of approximately 2,400 self-identified pediatric emergency medicine (EM) physicians may be unsurprising given the overall propensity of physicians – including board-certified general emergency physicians – to practice in urban areas. Even so, it underscores a decades-long concern that many children do not have access to optimal pediatric emergency care.
And the findings highlight the need, the authors say, to keep pressing to improve emergency care for a population of children with “a mortality rate that is already higher than that of its suburban and urban peers (JAMA Network Open 2021;4[5]:e2110084).”
Emergent care of pediatric patients is well within the scope of practice for physicians with training and board certification in general EM, but children and adolescents have different clinical needs and “there are high-stakes scenarios [in children] that we [as emergency physicians] don’t get exposed to as often because we’re not in a children’s hospital or we just don’t have that additional level of training,” said Christopher L. Bennett, MD, MA, of the department of emergency medicine at Stanford University and lead author of the study.
Researchers have documented that some emergency physicians have some discomfort in caring for very ill pediatric patients, he and his coauthors wrote.
Children account for more than 20% of annual ED visits, and most children who seek emergency care in the United States – upwards of 80% – present to general emergency departments. Yet the vast majority of these EDs care for fewer than 14-15 children a day.
With such low pediatric volume, “there will never be pediatric emergency medicine physicians in the rural hospitals in [our] health care system,” said Kathleen M. Brown, MD, medical director for quality and safety of the Emergency Medicine and Trauma Center at Children’s National Medical Center in Washington.
Redistribution “is not a practical solution, and we’ve known that for a long time,” said Dr. Brown, past chairperson of the American College of Emergency Physicians’ pediatric emergency medicine committee. “That’s why national efforts have focused on better preparing the general emergency department and making sure the hospital workforce is ready to take care of children ... to manage and stabilize [them] and recognize when they need more definitive care.”
Continuing efforts to increase “pediatric readiness” in general EDs is one of the recommendations issued by the American Academy of Pediatrics, ACEP, and Emergency Nurses Association in its most recent joint policy statement on emergency care for children, published in May (Pediatrics 2021;147[5]:e2021050787). A 2018 joint policy statement detailed the resources – medications, equipment, policies, and education – necessary for EDs to provide effective pediatric care (Pediatrics 2018;142[5]:e20182459).
There is some evidence that pediatric readiness has improved and that EDs with higher readiness scores may have better pediatric outcomes and lower mortality, said Dr. Brown, a coauthor of both policy statements. (One study cited in the 2018 policy statement, for example, found that children with extremity immobilization and a pain score of 5 or greater had faster management of their pain and decreased exposure to radiation when they were treated in a better-prepared facility than in a facility with less readiness.)
Yet many hospitals still do not have designated pediatric emergency care coordinators (PECCs) – roles that are widely believed to be central to pediatric readiness. PECCs (physicians and nurses) were recommended in 2006 by the then-Institute of Medicine and have been advocated by the AAP, ACEP, and other organizations.
According to 2013 data from the National Pediatric Readiness Project (NPRP), launched that year by the AAP, ACEP, ENA, and the federal Emergency Medical Services for Children program of the Health Resources and Services Administration, at least 15% of EDs lacked at least 1 piece of recommended equipment, and 81% reported barriers to pediatric emergency care guidelines. The NPRP is currently conducting an updated assessment, Dr. Brown said.
Some experts have proposed a different kind of solution – one in which American Board of Pediatrics–certified pediatric EM physicians would care for selective adult patients with common disease patterns who present to rural EDs, in addition to children. They might provide direct patient care across several hospitals in a region, while also addressing quality improvement and assisting EPs and other providers in the region on pediatric care issues.
The proposal, published in May 2020, comes from the 13-member special subcommittee of the ACEP committee on PEM that was tasked with exploring strategies to improve access to emergency pediatric expertise and disaster preparedness in all settings. The proposal was endorsed by the ACEP board of directors, said Jim Homme, MD, a coauthor of the paper (JACEP Open 2020;1:1520-6.)
“We’re saying, look at the ped-trained pediatric emergency provider more broadly. They can actually successfully care for a broader patient population and make it financially feasible ... [for that physician] to be a part of the system,” said Dr. Homme, program director of the emergency medicine residency at the Mayo Clinic College of Medicine and Science in Rochester, Minn.
“The benefit would be not only having the expertise to see children, but to train up other individuals in the institution, and be advocates for the care of children,” he said.
“We’re not saying we want a pediatrics-trained EM physician in every site so that every child would be seen by one – that’s not the goal,” Dr. Homme said. “The goal is to distribute them more broadly than they currently are, and in doing so, make available the other benefits besides direct patient care.”
Most of the physicians in the United States who identify as pediatric EM physicians have completed either a pediatrics or EM residency, followed by a pediatric EM fellowship. It is much more common to have primary training in pediatrics than in EM, said Dr. Homme and Dr. Bennett. A small number of physicians, like Dr. Homme, are dually trained in pediatrics and EM through the completion of two residencies. Dr. Bennett’s workforce study used the American Medical Association Physician Masterfile database and identified 2,403 clinically active pediatric EPs – 5% of all clinically active emergency physicians. Those practicing in rural areas had a median age of 59, compared with a median age of 46 in urban areas. More than half of the pediatric EPs – 68% – reported having pediatric EM board certification.
Three states – Montana, South Dakota, and Wyoming – had no pediatric EMs at all, Dr. Bennett noted.
Readiness in rural Oregon, New England
Torree McGowan, MD, an emergency physician with the St. Charles Health System in Oregon, works in small critical access hospitals in the rural towns of Madras and Prineville, each several hours by ground to the nearest pediatric hospital. She said she feels well equipped to care for children through her training (a rotation in a pediatric ICU and several months working in pediatric EDs) and through her ongoing work with pediatric patients. Children and adolescents comprise about 20%-30% of her volume.
She sees more pediatric illness – children with respiratory syncytial virus who need respiratory support, for instance, and children with severe asthma or diabetic ketoacidosis – than pediatric trauma. When she faces questions, uncertainties, or wants confirmation of a decision, she consults by phone with pediatric subspecialists.
“I don’t take care of kids on vasopressor drips on a regular basis [for instance],” said Dr. McGowan, who sits on ACEP’s disaster preparedness committee and is an Air Force veteran. “But I know the basics and can phone a colleague to be sure I’m doing it correctly. The ability to outreach is there.”
Telemedicine is valuable, she said, but there may also be value in working alongside a pediatric EM physician. One of her EP colleagues is fellowship-trained in ultrasonography and “leads us in training and quality control,” Dr. McGowan said. “And if she’s on shift with you she’ll teach you all about ultrasound. There’s probably utility in having a pediatric EP who does that as well. But incentivizing that and taking them away from the pediatric hospital is a paradigm shift.”
Either way, she said, “being able to bring that expertise out of urban centers, whether it’s to a hospital group like ours or whether it’s by telemedicine, is really, really helpful.”
Her group does not have official PECCs, but the joint policy statements by AAP/ACEP/ENA on pediatric readiness and the “whole pediatric readiness effort’ have been valuable in “driving conversations” with administrators about needs such as purchasing pediatric-sized video laryngoscope blades and other equipment needed for pediatric emergencies, however infrequently they may occur, Dr. McGowan said.
In New England, researchers leading a grassroots regional intervention to establish a PECC in every ED in the region have reported an increased prevalence of “pediatric champions” from less than 30% 5 years ago to greater than 90% in 2019, investigators have reported (Pediatr Emerg Care. 2021. doi: 10.1097/PEC.0000000000002456).
The initiative involved individual outreach to leaders of each ED – largely through phone and e-mail appeals – and collaboration among the State Emergency Medical Services for Children agencies and ACEP and ENA state chapters. The researchers are currently investigating the direct impact of PECCs on patient outcomes.
More on regionalization of ped-trained EPs
Dr. Bennett sees telemedicine as a primary part of improving pediatric emergency care. “I think that’s where things are going to go in pediatric emergency medicine,” he said, especially in the wake of COVID-19: “I don’t see how it’s not going to become much more common.”
Dr. Homme maintains that a broader integration of ABP-certified pediatric EM physicians into underserved regions would advance ED preparedness in a way that telemedicine, or even the appointment of PECCs, does not, said Dr. Homme.
Institutions would need to acknowledge that many of the current restrictions on pediatric EM physicians’ scope of practice are based on arbitrary age cut-offs, and their leaders would need to expand hospital-defined privileges to better align with training and capabilities, he said. Local credentialing provisions and other policies would also need to be adjusted.
Pediatric EM physicians spend at least 4 months of their graduate EM training in an adult ED, and there is significant overlap in the core competencies and the procedures considered essential for practice between pediatric EM fellowship programs and EM programs, Dr. Homme and his coauthors wrote in their proposal. “The pandemic really reinforced this concept,” Dr. Homme said. “As the number of patients in pediatric EDs plummeted, many of the ped-trained providers had to pivot and help care for adults. ... It worked great.”
The broader integration of pediatrics-trained pediatric EM physicians fits well, he believes, with current workforce dynamics. “There aren’t enough individuals coming out of an EM background and doing that subspecialty training to have any hope that they’d be able to cover these underserved areas,” he said. “And the academic pediatric workforce is getting kind of saturated. So having additional employment opportunities would be great.”
Dr. Homme pursued an EM residency after pediatrics training (rather than a pediatric EM fellowship) because he did not want to be limited geographically and because, while he wanted to focus on children, he also “wanted to be available to a larger population.”
He believes that some pediatrics-trained pediatric EM physicians would choose rural practice options, and hopes that the proposal will gain traction. Some EPs will be opposed, he said, and some pediatrics-trained EPs will not interested, “but if we can find people open to the idea on both sides, I think we can really move the needle in the direction we’re trying to, which is to disseminate an area of expertise into areas that just don’t have it.”
A new physician workforce study documents that almost all clinically active pediatric emergency physicians in the United States – 99% of them – work in urban areas, and that those who do practice in rural areas are significantly older and closer to retirement age.
The portrait of approximately 2,400 self-identified pediatric emergency medicine (EM) physicians may be unsurprising given the overall propensity of physicians – including board-certified general emergency physicians – to practice in urban areas. Even so, it underscores a decades-long concern that many children do not have access to optimal pediatric emergency care.
And the findings highlight the need, the authors say, to keep pressing to improve emergency care for a population of children with “a mortality rate that is already higher than that of its suburban and urban peers (JAMA Network Open 2021;4[5]:e2110084).”
Emergent care of pediatric patients is well within the scope of practice for physicians with training and board certification in general EM, but children and adolescents have different clinical needs and “there are high-stakes scenarios [in children] that we [as emergency physicians] don’t get exposed to as often because we’re not in a children’s hospital or we just don’t have that additional level of training,” said Christopher L. Bennett, MD, MA, of the department of emergency medicine at Stanford University and lead author of the study.
Researchers have documented that some emergency physicians have some discomfort in caring for very ill pediatric patients, he and his coauthors wrote.
Children account for more than 20% of annual ED visits, and most children who seek emergency care in the United States – upwards of 80% – present to general emergency departments. Yet the vast majority of these EDs care for fewer than 14-15 children a day.
With such low pediatric volume, “there will never be pediatric emergency medicine physicians in the rural hospitals in [our] health care system,” said Kathleen M. Brown, MD, medical director for quality and safety of the Emergency Medicine and Trauma Center at Children’s National Medical Center in Washington.
Redistribution “is not a practical solution, and we’ve known that for a long time,” said Dr. Brown, past chairperson of the American College of Emergency Physicians’ pediatric emergency medicine committee. “That’s why national efforts have focused on better preparing the general emergency department and making sure the hospital workforce is ready to take care of children ... to manage and stabilize [them] and recognize when they need more definitive care.”
Continuing efforts to increase “pediatric readiness” in general EDs is one of the recommendations issued by the American Academy of Pediatrics, ACEP, and Emergency Nurses Association in its most recent joint policy statement on emergency care for children, published in May (Pediatrics 2021;147[5]:e2021050787). A 2018 joint policy statement detailed the resources – medications, equipment, policies, and education – necessary for EDs to provide effective pediatric care (Pediatrics 2018;142[5]:e20182459).
There is some evidence that pediatric readiness has improved and that EDs with higher readiness scores may have better pediatric outcomes and lower mortality, said Dr. Brown, a coauthor of both policy statements. (One study cited in the 2018 policy statement, for example, found that children with extremity immobilization and a pain score of 5 or greater had faster management of their pain and decreased exposure to radiation when they were treated in a better-prepared facility than in a facility with less readiness.)
Yet many hospitals still do not have designated pediatric emergency care coordinators (PECCs) – roles that are widely believed to be central to pediatric readiness. PECCs (physicians and nurses) were recommended in 2006 by the then-Institute of Medicine and have been advocated by the AAP, ACEP, and other organizations.
According to 2013 data from the National Pediatric Readiness Project (NPRP), launched that year by the AAP, ACEP, ENA, and the federal Emergency Medical Services for Children program of the Health Resources and Services Administration, at least 15% of EDs lacked at least 1 piece of recommended equipment, and 81% reported barriers to pediatric emergency care guidelines. The NPRP is currently conducting an updated assessment, Dr. Brown said.
Some experts have proposed a different kind of solution – one in which American Board of Pediatrics–certified pediatric EM physicians would care for selective adult patients with common disease patterns who present to rural EDs, in addition to children. They might provide direct patient care across several hospitals in a region, while also addressing quality improvement and assisting EPs and other providers in the region on pediatric care issues.
The proposal, published in May 2020, comes from the 13-member special subcommittee of the ACEP committee on PEM that was tasked with exploring strategies to improve access to emergency pediatric expertise and disaster preparedness in all settings. The proposal was endorsed by the ACEP board of directors, said Jim Homme, MD, a coauthor of the paper (JACEP Open 2020;1:1520-6.)
“We’re saying, look at the ped-trained pediatric emergency provider more broadly. They can actually successfully care for a broader patient population and make it financially feasible ... [for that physician] to be a part of the system,” said Dr. Homme, program director of the emergency medicine residency at the Mayo Clinic College of Medicine and Science in Rochester, Minn.
“The benefit would be not only having the expertise to see children, but to train up other individuals in the institution, and be advocates for the care of children,” he said.
“We’re not saying we want a pediatrics-trained EM physician in every site so that every child would be seen by one – that’s not the goal,” Dr. Homme said. “The goal is to distribute them more broadly than they currently are, and in doing so, make available the other benefits besides direct patient care.”
Most of the physicians in the United States who identify as pediatric EM physicians have completed either a pediatrics or EM residency, followed by a pediatric EM fellowship. It is much more common to have primary training in pediatrics than in EM, said Dr. Homme and Dr. Bennett. A small number of physicians, like Dr. Homme, are dually trained in pediatrics and EM through the completion of two residencies. Dr. Bennett’s workforce study used the American Medical Association Physician Masterfile database and identified 2,403 clinically active pediatric EPs – 5% of all clinically active emergency physicians. Those practicing in rural areas had a median age of 59, compared with a median age of 46 in urban areas. More than half of the pediatric EPs – 68% – reported having pediatric EM board certification.
Three states – Montana, South Dakota, and Wyoming – had no pediatric EMs at all, Dr. Bennett noted.
Readiness in rural Oregon, New England
Torree McGowan, MD, an emergency physician with the St. Charles Health System in Oregon, works in small critical access hospitals in the rural towns of Madras and Prineville, each several hours by ground to the nearest pediatric hospital. She said she feels well equipped to care for children through her training (a rotation in a pediatric ICU and several months working in pediatric EDs) and through her ongoing work with pediatric patients. Children and adolescents comprise about 20%-30% of her volume.
She sees more pediatric illness – children with respiratory syncytial virus who need respiratory support, for instance, and children with severe asthma or diabetic ketoacidosis – than pediatric trauma. When she faces questions, uncertainties, or wants confirmation of a decision, she consults by phone with pediatric subspecialists.
“I don’t take care of kids on vasopressor drips on a regular basis [for instance],” said Dr. McGowan, who sits on ACEP’s disaster preparedness committee and is an Air Force veteran. “But I know the basics and can phone a colleague to be sure I’m doing it correctly. The ability to outreach is there.”
Telemedicine is valuable, she said, but there may also be value in working alongside a pediatric EM physician. One of her EP colleagues is fellowship-trained in ultrasonography and “leads us in training and quality control,” Dr. McGowan said. “And if she’s on shift with you she’ll teach you all about ultrasound. There’s probably utility in having a pediatric EP who does that as well. But incentivizing that and taking them away from the pediatric hospital is a paradigm shift.”
Either way, she said, “being able to bring that expertise out of urban centers, whether it’s to a hospital group like ours or whether it’s by telemedicine, is really, really helpful.”
Her group does not have official PECCs, but the joint policy statements by AAP/ACEP/ENA on pediatric readiness and the “whole pediatric readiness effort’ have been valuable in “driving conversations” with administrators about needs such as purchasing pediatric-sized video laryngoscope blades and other equipment needed for pediatric emergencies, however infrequently they may occur, Dr. McGowan said.
In New England, researchers leading a grassroots regional intervention to establish a PECC in every ED in the region have reported an increased prevalence of “pediatric champions” from less than 30% 5 years ago to greater than 90% in 2019, investigators have reported (Pediatr Emerg Care. 2021. doi: 10.1097/PEC.0000000000002456).
The initiative involved individual outreach to leaders of each ED – largely through phone and e-mail appeals – and collaboration among the State Emergency Medical Services for Children agencies and ACEP and ENA state chapters. The researchers are currently investigating the direct impact of PECCs on patient outcomes.
More on regionalization of ped-trained EPs
Dr. Bennett sees telemedicine as a primary part of improving pediatric emergency care. “I think that’s where things are going to go in pediatric emergency medicine,” he said, especially in the wake of COVID-19: “I don’t see how it’s not going to become much more common.”
Dr. Homme maintains that a broader integration of ABP-certified pediatric EM physicians into underserved regions would advance ED preparedness in a way that telemedicine, or even the appointment of PECCs, does not, said Dr. Homme.
Institutions would need to acknowledge that many of the current restrictions on pediatric EM physicians’ scope of practice are based on arbitrary age cut-offs, and their leaders would need to expand hospital-defined privileges to better align with training and capabilities, he said. Local credentialing provisions and other policies would also need to be adjusted.
Pediatric EM physicians spend at least 4 months of their graduate EM training in an adult ED, and there is significant overlap in the core competencies and the procedures considered essential for practice between pediatric EM fellowship programs and EM programs, Dr. Homme and his coauthors wrote in their proposal. “The pandemic really reinforced this concept,” Dr. Homme said. “As the number of patients in pediatric EDs plummeted, many of the ped-trained providers had to pivot and help care for adults. ... It worked great.”
The broader integration of pediatrics-trained pediatric EM physicians fits well, he believes, with current workforce dynamics. “There aren’t enough individuals coming out of an EM background and doing that subspecialty training to have any hope that they’d be able to cover these underserved areas,” he said. “And the academic pediatric workforce is getting kind of saturated. So having additional employment opportunities would be great.”
Dr. Homme pursued an EM residency after pediatrics training (rather than a pediatric EM fellowship) because he did not want to be limited geographically and because, while he wanted to focus on children, he also “wanted to be available to a larger population.”
He believes that some pediatrics-trained pediatric EM physicians would choose rural practice options, and hopes that the proposal will gain traction. Some EPs will be opposed, he said, and some pediatrics-trained EPs will not interested, “but if we can find people open to the idea on both sides, I think we can really move the needle in the direction we’re trying to, which is to disseminate an area of expertise into areas that just don’t have it.”
A new physician workforce study documents that almost all clinically active pediatric emergency physicians in the United States – 99% of them – work in urban areas, and that those who do practice in rural areas are significantly older and closer to retirement age.
The portrait of approximately 2,400 self-identified pediatric emergency medicine (EM) physicians may be unsurprising given the overall propensity of physicians – including board-certified general emergency physicians – to practice in urban areas. Even so, it underscores a decades-long concern that many children do not have access to optimal pediatric emergency care.
And the findings highlight the need, the authors say, to keep pressing to improve emergency care for a population of children with “a mortality rate that is already higher than that of its suburban and urban peers (JAMA Network Open 2021;4[5]:e2110084).”
Emergent care of pediatric patients is well within the scope of practice for physicians with training and board certification in general EM, but children and adolescents have different clinical needs and “there are high-stakes scenarios [in children] that we [as emergency physicians] don’t get exposed to as often because we’re not in a children’s hospital or we just don’t have that additional level of training,” said Christopher L. Bennett, MD, MA, of the department of emergency medicine at Stanford University and lead author of the study.
Researchers have documented that some emergency physicians have some discomfort in caring for very ill pediatric patients, he and his coauthors wrote.
Children account for more than 20% of annual ED visits, and most children who seek emergency care in the United States – upwards of 80% – present to general emergency departments. Yet the vast majority of these EDs care for fewer than 14-15 children a day.
With such low pediatric volume, “there will never be pediatric emergency medicine physicians in the rural hospitals in [our] health care system,” said Kathleen M. Brown, MD, medical director for quality and safety of the Emergency Medicine and Trauma Center at Children’s National Medical Center in Washington.
Redistribution “is not a practical solution, and we’ve known that for a long time,” said Dr. Brown, past chairperson of the American College of Emergency Physicians’ pediatric emergency medicine committee. “That’s why national efforts have focused on better preparing the general emergency department and making sure the hospital workforce is ready to take care of children ... to manage and stabilize [them] and recognize when they need more definitive care.”
Continuing efforts to increase “pediatric readiness” in general EDs is one of the recommendations issued by the American Academy of Pediatrics, ACEP, and Emergency Nurses Association in its most recent joint policy statement on emergency care for children, published in May (Pediatrics 2021;147[5]:e2021050787). A 2018 joint policy statement detailed the resources – medications, equipment, policies, and education – necessary for EDs to provide effective pediatric care (Pediatrics 2018;142[5]:e20182459).
There is some evidence that pediatric readiness has improved and that EDs with higher readiness scores may have better pediatric outcomes and lower mortality, said Dr. Brown, a coauthor of both policy statements. (One study cited in the 2018 policy statement, for example, found that children with extremity immobilization and a pain score of 5 or greater had faster management of their pain and decreased exposure to radiation when they were treated in a better-prepared facility than in a facility with less readiness.)
Yet many hospitals still do not have designated pediatric emergency care coordinators (PECCs) – roles that are widely believed to be central to pediatric readiness. PECCs (physicians and nurses) were recommended in 2006 by the then-Institute of Medicine and have been advocated by the AAP, ACEP, and other organizations.
According to 2013 data from the National Pediatric Readiness Project (NPRP), launched that year by the AAP, ACEP, ENA, and the federal Emergency Medical Services for Children program of the Health Resources and Services Administration, at least 15% of EDs lacked at least 1 piece of recommended equipment, and 81% reported barriers to pediatric emergency care guidelines. The NPRP is currently conducting an updated assessment, Dr. Brown said.
Some experts have proposed a different kind of solution – one in which American Board of Pediatrics–certified pediatric EM physicians would care for selective adult patients with common disease patterns who present to rural EDs, in addition to children. They might provide direct patient care across several hospitals in a region, while also addressing quality improvement and assisting EPs and other providers in the region on pediatric care issues.
The proposal, published in May 2020, comes from the 13-member special subcommittee of the ACEP committee on PEM that was tasked with exploring strategies to improve access to emergency pediatric expertise and disaster preparedness in all settings. The proposal was endorsed by the ACEP board of directors, said Jim Homme, MD, a coauthor of the paper (JACEP Open 2020;1:1520-6.)
“We’re saying, look at the ped-trained pediatric emergency provider more broadly. They can actually successfully care for a broader patient population and make it financially feasible ... [for that physician] to be a part of the system,” said Dr. Homme, program director of the emergency medicine residency at the Mayo Clinic College of Medicine and Science in Rochester, Minn.
“The benefit would be not only having the expertise to see children, but to train up other individuals in the institution, and be advocates for the care of children,” he said.
“We’re not saying we want a pediatrics-trained EM physician in every site so that every child would be seen by one – that’s not the goal,” Dr. Homme said. “The goal is to distribute them more broadly than they currently are, and in doing so, make available the other benefits besides direct patient care.”
Most of the physicians in the United States who identify as pediatric EM physicians have completed either a pediatrics or EM residency, followed by a pediatric EM fellowship. It is much more common to have primary training in pediatrics than in EM, said Dr. Homme and Dr. Bennett. A small number of physicians, like Dr. Homme, are dually trained in pediatrics and EM through the completion of two residencies. Dr. Bennett’s workforce study used the American Medical Association Physician Masterfile database and identified 2,403 clinically active pediatric EPs – 5% of all clinically active emergency physicians. Those practicing in rural areas had a median age of 59, compared with a median age of 46 in urban areas. More than half of the pediatric EPs – 68% – reported having pediatric EM board certification.
Three states – Montana, South Dakota, and Wyoming – had no pediatric EMs at all, Dr. Bennett noted.
Readiness in rural Oregon, New England
Torree McGowan, MD, an emergency physician with the St. Charles Health System in Oregon, works in small critical access hospitals in the rural towns of Madras and Prineville, each several hours by ground to the nearest pediatric hospital. She said she feels well equipped to care for children through her training (a rotation in a pediatric ICU and several months working in pediatric EDs) and through her ongoing work with pediatric patients. Children and adolescents comprise about 20%-30% of her volume.
She sees more pediatric illness – children with respiratory syncytial virus who need respiratory support, for instance, and children with severe asthma or diabetic ketoacidosis – than pediatric trauma. When she faces questions, uncertainties, or wants confirmation of a decision, she consults by phone with pediatric subspecialists.
“I don’t take care of kids on vasopressor drips on a regular basis [for instance],” said Dr. McGowan, who sits on ACEP’s disaster preparedness committee and is an Air Force veteran. “But I know the basics and can phone a colleague to be sure I’m doing it correctly. The ability to outreach is there.”
Telemedicine is valuable, she said, but there may also be value in working alongside a pediatric EM physician. One of her EP colleagues is fellowship-trained in ultrasonography and “leads us in training and quality control,” Dr. McGowan said. “And if she’s on shift with you she’ll teach you all about ultrasound. There’s probably utility in having a pediatric EP who does that as well. But incentivizing that and taking them away from the pediatric hospital is a paradigm shift.”
Either way, she said, “being able to bring that expertise out of urban centers, whether it’s to a hospital group like ours or whether it’s by telemedicine, is really, really helpful.”
Her group does not have official PECCs, but the joint policy statements by AAP/ACEP/ENA on pediatric readiness and the “whole pediatric readiness effort’ have been valuable in “driving conversations” with administrators about needs such as purchasing pediatric-sized video laryngoscope blades and other equipment needed for pediatric emergencies, however infrequently they may occur, Dr. McGowan said.
In New England, researchers leading a grassroots regional intervention to establish a PECC in every ED in the region have reported an increased prevalence of “pediatric champions” from less than 30% 5 years ago to greater than 90% in 2019, investigators have reported (Pediatr Emerg Care. 2021. doi: 10.1097/PEC.0000000000002456).
The initiative involved individual outreach to leaders of each ED – largely through phone and e-mail appeals – and collaboration among the State Emergency Medical Services for Children agencies and ACEP and ENA state chapters. The researchers are currently investigating the direct impact of PECCs on patient outcomes.
More on regionalization of ped-trained EPs
Dr. Bennett sees telemedicine as a primary part of improving pediatric emergency care. “I think that’s where things are going to go in pediatric emergency medicine,” he said, especially in the wake of COVID-19: “I don’t see how it’s not going to become much more common.”
Dr. Homme maintains that a broader integration of ABP-certified pediatric EM physicians into underserved regions would advance ED preparedness in a way that telemedicine, or even the appointment of PECCs, does not, said Dr. Homme.
Institutions would need to acknowledge that many of the current restrictions on pediatric EM physicians’ scope of practice are based on arbitrary age cut-offs, and their leaders would need to expand hospital-defined privileges to better align with training and capabilities, he said. Local credentialing provisions and other policies would also need to be adjusted.
Pediatric EM physicians spend at least 4 months of their graduate EM training in an adult ED, and there is significant overlap in the core competencies and the procedures considered essential for practice between pediatric EM fellowship programs and EM programs, Dr. Homme and his coauthors wrote in their proposal. “The pandemic really reinforced this concept,” Dr. Homme said. “As the number of patients in pediatric EDs plummeted, many of the ped-trained providers had to pivot and help care for adults. ... It worked great.”
The broader integration of pediatrics-trained pediatric EM physicians fits well, he believes, with current workforce dynamics. “There aren’t enough individuals coming out of an EM background and doing that subspecialty training to have any hope that they’d be able to cover these underserved areas,” he said. “And the academic pediatric workforce is getting kind of saturated. So having additional employment opportunities would be great.”
Dr. Homme pursued an EM residency after pediatrics training (rather than a pediatric EM fellowship) because he did not want to be limited geographically and because, while he wanted to focus on children, he also “wanted to be available to a larger population.”
He believes that some pediatrics-trained pediatric EM physicians would choose rural practice options, and hopes that the proposal will gain traction. Some EPs will be opposed, he said, and some pediatrics-trained EPs will not interested, “but if we can find people open to the idea on both sides, I think we can really move the needle in the direction we’re trying to, which is to disseminate an area of expertise into areas that just don’t have it.”






