User login
EMERGENCY MEDICINE is a practical, peer-reviewed monthly publication and Web site that meets the educational needs of emergency clinicians and urgent care clinicians for their practice.
Troponins touted as ‘ally’ in COVID-19 triage, but message is nuanced
, cardiologists in the United Kingdom advise in a recently published viewpoint.
The tests can be used to “inform the triage of patients to critical care, guide the use of supportive treatments, and facilitate targeted cardiac investigations in those most likely to benefit,” Nicholas Mills, MD, PhD, University of Edinburgh, United Kingdom, told theheart.org | Medscape Cardiology. He is senior author on the viewpoint published online April 6 in the journal Circulation.
Older adults and those with a history of underlying cardiovascular disease appear to be at greatest risk of dying from COVID-19. “From early reports it is clear that elevated cardiac troponin concentrations predict in-hospital mortality,” said Mills.
In a recent report on hospitalized patients with COVID-19 in Wuhan, China, for example, cardiac injury (hs-cTn above the 99th-percentile upper reference limit) was seen in 1 in 5 patients and was an independent predictor of dying in the hospital. Mortality was 10-fold higher in those with cardiac injury on presentation.
Elevated cardiac troponin in the setting of COVID-19, Mills said, “may reflect illness severity with myocardial injury arising due to myocardial oxygen supply–demand imbalance. Or it may be due to direct cardiac involvement through viral myocarditis or stress cardiomyopathy, or where the prothrombotic and proinflammatory state is precipitating acute coronary syndromes.”
In their viewpoint, the authors note that circulating cTn is a marker of myocardial injury, “including but not limited to myocardial infarction or myocarditis, and the clinical relevance of this distinction has never been so clear.”
Therefore, the consequence of not measuring cardiac troponin may be to “ignore the plethora of ischemic and nonischemic causes” of myocardial injury related to COVID-19. “Clinicians who have used troponin measurement as a binary test for myocardial infarction independent of clinical context and those who consider an elevated cardiac troponin concentration to be a mandate for invasive coronary angiography must recalibrate,” they write.
“Rather than encouraging avoidance of troponin testing, we must harness the unheralded engagement from the cardiovascular community due to COVID-19 to better understand the utility of this essential biomarker and to educate clinicians on its interpretation and implications for prognosis and clinical decision making.”
Based on “same logic” as recent ACC guidance
The viewpoint was to some extent a response to a recent informal guidance from the American College of Cardiology (ACC) that advised caution in use of troponin and natriuretic peptide tests in patients with COVID-19.
Even so, that ACC guidance and the new viewpoint in Circulation are based on the “same logic,” James Januzzi Jr, MD, Massachusetts General Hospital, Boston, told theheart.org | Medscape Cardiology. Both documents:
- Point out that troponins are frequently abnormal in patients with severe cases of COVID-19
- Caution that clinicians should not equate an abnormal hs-cTn with acute myocardial infarction
- Note that, in most cases, hs-cTn elevations are a result of noncoronary mechanisms
- Recognize the potential risk to caregivers and the continued unchecked spread of SARS-CoV-2 related to downstream testing that might not be needed
“The Circulation opinion piece states that clinicians often use troponin as a binary test for myocardial infarction and a mandate for downstream testing, suggesting clinicians will need to recalibrate that approach, something I agree with and which is the central message of the ACC position,” Januzzi said.
Probably the biggest difference between the two documents, he said, is in the Circulation authors’ apparent enthusiasm to use hs-cTn as a tool to judge disease severity in patients with COVID-19.
It’s been known for more than a decade that myocardial injury is “an important risk predictor” in critical illness, Januzzi explained. “So the link between cardiac injury and outcomes in critical illness is nothing new. The difference is the fact we are seeing so many patients with COVID-19 all at once, and the authors suggest that using troponin might help in triage decision making.”
“There may be [such] a role here, but the data have not been systematically collected, and whether troponin truly adds something beyond information already available at the bedside — for example, does it add anything not already obvious at the bedside? — has not yet been conclusively proven,” Januzzi cautioned.
“As well, there are no prospective data supporting troponin as a trigger for ICU triage or for deciding on specific treatments.”
Positive cTn status “common” in COVID-19 patients
In his experience, Barry Cohen, MD, Morristown Medical Center, New Jersey, told theheart.org | Medscape Cardiology, that positive cTn status is “common in COVID-19 patients and appears to have prognostic value, not only in type 1 MI due to atherothrombotic disease (related to a proinflammatory and prothrombotic state), but more frequently type 2 MI (supply–demand mismatch), viral myocarditis, coronary microvascular ischemia, stress cardiomyopathy or tachyarrhythmias.”
Moreover, Cohen said, hs-cTn “has identified patients at increased risk for ventilation support (invasive and noninvasive), acute respiratory distress syndrome, acute kidney injury, and mortality.”
Echoing both the ACC document and the Circulation report, Cohen also said hs-cTn measurements “appear to help risk stratify COVID-19 patients, but clearly do not mean that a troponin-positive patient needs to go to the cath lab and be treated as having acute coronary syndrome. Only a minority of these patients require this intervention.”
Mills discloses receiving honoraria from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. Januzzi has previously disclosed receiving personal fees from the American College of Cardiology, Pfizer, Merck, AbbVie, Amgen, Boehringer Ingelheim, and Takeda; grants and personal fees from Novartis, Roche, Abbott, and Janssen; and grants from Singulex and Prevencio. Cohen has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
, cardiologists in the United Kingdom advise in a recently published viewpoint.
The tests can be used to “inform the triage of patients to critical care, guide the use of supportive treatments, and facilitate targeted cardiac investigations in those most likely to benefit,” Nicholas Mills, MD, PhD, University of Edinburgh, United Kingdom, told theheart.org | Medscape Cardiology. He is senior author on the viewpoint published online April 6 in the journal Circulation.
Older adults and those with a history of underlying cardiovascular disease appear to be at greatest risk of dying from COVID-19. “From early reports it is clear that elevated cardiac troponin concentrations predict in-hospital mortality,” said Mills.
In a recent report on hospitalized patients with COVID-19 in Wuhan, China, for example, cardiac injury (hs-cTn above the 99th-percentile upper reference limit) was seen in 1 in 5 patients and was an independent predictor of dying in the hospital. Mortality was 10-fold higher in those with cardiac injury on presentation.
Elevated cardiac troponin in the setting of COVID-19, Mills said, “may reflect illness severity with myocardial injury arising due to myocardial oxygen supply–demand imbalance. Or it may be due to direct cardiac involvement through viral myocarditis or stress cardiomyopathy, or where the prothrombotic and proinflammatory state is precipitating acute coronary syndromes.”
In their viewpoint, the authors note that circulating cTn is a marker of myocardial injury, “including but not limited to myocardial infarction or myocarditis, and the clinical relevance of this distinction has never been so clear.”
Therefore, the consequence of not measuring cardiac troponin may be to “ignore the plethora of ischemic and nonischemic causes” of myocardial injury related to COVID-19. “Clinicians who have used troponin measurement as a binary test for myocardial infarction independent of clinical context and those who consider an elevated cardiac troponin concentration to be a mandate for invasive coronary angiography must recalibrate,” they write.
“Rather than encouraging avoidance of troponin testing, we must harness the unheralded engagement from the cardiovascular community due to COVID-19 to better understand the utility of this essential biomarker and to educate clinicians on its interpretation and implications for prognosis and clinical decision making.”
Based on “same logic” as recent ACC guidance
The viewpoint was to some extent a response to a recent informal guidance from the American College of Cardiology (ACC) that advised caution in use of troponin and natriuretic peptide tests in patients with COVID-19.
Even so, that ACC guidance and the new viewpoint in Circulation are based on the “same logic,” James Januzzi Jr, MD, Massachusetts General Hospital, Boston, told theheart.org | Medscape Cardiology. Both documents:
- Point out that troponins are frequently abnormal in patients with severe cases of COVID-19
- Caution that clinicians should not equate an abnormal hs-cTn with acute myocardial infarction
- Note that, in most cases, hs-cTn elevations are a result of noncoronary mechanisms
- Recognize the potential risk to caregivers and the continued unchecked spread of SARS-CoV-2 related to downstream testing that might not be needed
“The Circulation opinion piece states that clinicians often use troponin as a binary test for myocardial infarction and a mandate for downstream testing, suggesting clinicians will need to recalibrate that approach, something I agree with and which is the central message of the ACC position,” Januzzi said.
Probably the biggest difference between the two documents, he said, is in the Circulation authors’ apparent enthusiasm to use hs-cTn as a tool to judge disease severity in patients with COVID-19.
It’s been known for more than a decade that myocardial injury is “an important risk predictor” in critical illness, Januzzi explained. “So the link between cardiac injury and outcomes in critical illness is nothing new. The difference is the fact we are seeing so many patients with COVID-19 all at once, and the authors suggest that using troponin might help in triage decision making.”
“There may be [such] a role here, but the data have not been systematically collected, and whether troponin truly adds something beyond information already available at the bedside — for example, does it add anything not already obvious at the bedside? — has not yet been conclusively proven,” Januzzi cautioned.
“As well, there are no prospective data supporting troponin as a trigger for ICU triage or for deciding on specific treatments.”
Positive cTn status “common” in COVID-19 patients
In his experience, Barry Cohen, MD, Morristown Medical Center, New Jersey, told theheart.org | Medscape Cardiology, that positive cTn status is “common in COVID-19 patients and appears to have prognostic value, not only in type 1 MI due to atherothrombotic disease (related to a proinflammatory and prothrombotic state), but more frequently type 2 MI (supply–demand mismatch), viral myocarditis, coronary microvascular ischemia, stress cardiomyopathy or tachyarrhythmias.”
Moreover, Cohen said, hs-cTn “has identified patients at increased risk for ventilation support (invasive and noninvasive), acute respiratory distress syndrome, acute kidney injury, and mortality.”
Echoing both the ACC document and the Circulation report, Cohen also said hs-cTn measurements “appear to help risk stratify COVID-19 patients, but clearly do not mean that a troponin-positive patient needs to go to the cath lab and be treated as having acute coronary syndrome. Only a minority of these patients require this intervention.”
Mills discloses receiving honoraria from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. Januzzi has previously disclosed receiving personal fees from the American College of Cardiology, Pfizer, Merck, AbbVie, Amgen, Boehringer Ingelheim, and Takeda; grants and personal fees from Novartis, Roche, Abbott, and Janssen; and grants from Singulex and Prevencio. Cohen has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
, cardiologists in the United Kingdom advise in a recently published viewpoint.
The tests can be used to “inform the triage of patients to critical care, guide the use of supportive treatments, and facilitate targeted cardiac investigations in those most likely to benefit,” Nicholas Mills, MD, PhD, University of Edinburgh, United Kingdom, told theheart.org | Medscape Cardiology. He is senior author on the viewpoint published online April 6 in the journal Circulation.
Older adults and those with a history of underlying cardiovascular disease appear to be at greatest risk of dying from COVID-19. “From early reports it is clear that elevated cardiac troponin concentrations predict in-hospital mortality,” said Mills.
In a recent report on hospitalized patients with COVID-19 in Wuhan, China, for example, cardiac injury (hs-cTn above the 99th-percentile upper reference limit) was seen in 1 in 5 patients and was an independent predictor of dying in the hospital. Mortality was 10-fold higher in those with cardiac injury on presentation.
Elevated cardiac troponin in the setting of COVID-19, Mills said, “may reflect illness severity with myocardial injury arising due to myocardial oxygen supply–demand imbalance. Or it may be due to direct cardiac involvement through viral myocarditis or stress cardiomyopathy, or where the prothrombotic and proinflammatory state is precipitating acute coronary syndromes.”
In their viewpoint, the authors note that circulating cTn is a marker of myocardial injury, “including but not limited to myocardial infarction or myocarditis, and the clinical relevance of this distinction has never been so clear.”
Therefore, the consequence of not measuring cardiac troponin may be to “ignore the plethora of ischemic and nonischemic causes” of myocardial injury related to COVID-19. “Clinicians who have used troponin measurement as a binary test for myocardial infarction independent of clinical context and those who consider an elevated cardiac troponin concentration to be a mandate for invasive coronary angiography must recalibrate,” they write.
“Rather than encouraging avoidance of troponin testing, we must harness the unheralded engagement from the cardiovascular community due to COVID-19 to better understand the utility of this essential biomarker and to educate clinicians on its interpretation and implications for prognosis and clinical decision making.”
Based on “same logic” as recent ACC guidance
The viewpoint was to some extent a response to a recent informal guidance from the American College of Cardiology (ACC) that advised caution in use of troponin and natriuretic peptide tests in patients with COVID-19.
Even so, that ACC guidance and the new viewpoint in Circulation are based on the “same logic,” James Januzzi Jr, MD, Massachusetts General Hospital, Boston, told theheart.org | Medscape Cardiology. Both documents:
- Point out that troponins are frequently abnormal in patients with severe cases of COVID-19
- Caution that clinicians should not equate an abnormal hs-cTn with acute myocardial infarction
- Note that, in most cases, hs-cTn elevations are a result of noncoronary mechanisms
- Recognize the potential risk to caregivers and the continued unchecked spread of SARS-CoV-2 related to downstream testing that might not be needed
“The Circulation opinion piece states that clinicians often use troponin as a binary test for myocardial infarction and a mandate for downstream testing, suggesting clinicians will need to recalibrate that approach, something I agree with and which is the central message of the ACC position,” Januzzi said.
Probably the biggest difference between the two documents, he said, is in the Circulation authors’ apparent enthusiasm to use hs-cTn as a tool to judge disease severity in patients with COVID-19.
It’s been known for more than a decade that myocardial injury is “an important risk predictor” in critical illness, Januzzi explained. “So the link between cardiac injury and outcomes in critical illness is nothing new. The difference is the fact we are seeing so many patients with COVID-19 all at once, and the authors suggest that using troponin might help in triage decision making.”
“There may be [such] a role here, but the data have not been systematically collected, and whether troponin truly adds something beyond information already available at the bedside — for example, does it add anything not already obvious at the bedside? — has not yet been conclusively proven,” Januzzi cautioned.
“As well, there are no prospective data supporting troponin as a trigger for ICU triage or for deciding on specific treatments.”
Positive cTn status “common” in COVID-19 patients
In his experience, Barry Cohen, MD, Morristown Medical Center, New Jersey, told theheart.org | Medscape Cardiology, that positive cTn status is “common in COVID-19 patients and appears to have prognostic value, not only in type 1 MI due to atherothrombotic disease (related to a proinflammatory and prothrombotic state), but more frequently type 2 MI (supply–demand mismatch), viral myocarditis, coronary microvascular ischemia, stress cardiomyopathy or tachyarrhythmias.”
Moreover, Cohen said, hs-cTn “has identified patients at increased risk for ventilation support (invasive and noninvasive), acute respiratory distress syndrome, acute kidney injury, and mortality.”
Echoing both the ACC document and the Circulation report, Cohen also said hs-cTn measurements “appear to help risk stratify COVID-19 patients, but clearly do not mean that a troponin-positive patient needs to go to the cath lab and be treated as having acute coronary syndrome. Only a minority of these patients require this intervention.”
Mills discloses receiving honoraria from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. Januzzi has previously disclosed receiving personal fees from the American College of Cardiology, Pfizer, Merck, AbbVie, Amgen, Boehringer Ingelheim, and Takeda; grants and personal fees from Novartis, Roche, Abbott, and Janssen; and grants from Singulex and Prevencio. Cohen has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
COVID 19: Confessions of an outpatient psychiatrist during the pandemic
It seems that some glitches would be inevitable. With a sudden shift to videoconferencing in private psychiatric practices, there were bound to be issues with both technology and privacy. One friend told me of such a glitch on the very first day she started telemental health: She was meeting with a patient who was sitting at her kitchen table. Unbeknownst to the patient, her husband walked into the kitchen behind her, fully naked, to get something from the refrigerator. “There was a full moon shot!” my friend said, initially quite shocked, and then eventually amused. As we all cope with a national tragedy and the total upheaval to our personal and professional lives, the stories just keep coming.
I left work on Friday, March 13, with plans to return on the following Monday to see patients. I had no idea that, by Sunday evening, I would be persuaded that for the safety of all I would need to shut down my real-life psychiatric practice and switch to a videoconferencing venue. I, along with many psychiatrists in Maryland, made this decision after Amy Huberman, MD, posted the following on the Maryland Psychiatric Society (MPS) listserv on Sunday, March 15:
“I want to make a case for starting video sessions with all your patients NOW. There is increasing evidence that the spread of coronavirus is driven primarily by asymptomatic or mildly ill people infected with the virus. Because of this, it’s not good enough to tell your patients not to come in if they have symptoms, or for you not to come into work if you have no symptoms. Even after I sent out a letter two weeks ago warning people not to come in if they had symptoms or had potentially come in contact with someone with COVID-19, several patients with coughs still came to my office, as well as several people who had just been on trips to New York City.
If we want to help slow the spread of this illness so that our health system has a better chance of being able to offer ventilators to the people who need them, we must limit all contacts as much as possible – even of asymptomatic people, given the emerging data.
I am planning to send out a message to all my patients today that they should do the same. Without the president or the media giving clear advice to people about what to do, it’s our job as physicians to do it.”
By that night, I had set up a home office with a blank wall behind me, windows in front of me, and books propping my computer at a height that would not have my patients looking up my nose. For the first time in over 20 years, I dusted my son’s Little League trophies, moved them and a 40,000 baseball card collection against the wall, carried a desk, chair, rug, houseplant, and a small Buddha into a room in which I would have some privacy, and my telepsychiatry practice found a home.
After some research, I registered for a free site called Doxy.me because it was HIPAA compliant and did not require patients to download an application; anyone with a camera on any Internet-enabled phone, computer, or tablet, could click on a link and enter my virtual waiting room. I soon discovered that images on the Doxy.me site are sometimes grainy and sometimes freeze up; in some sessions, we ended up switching to FaceTime, and as government mandates for HIPAA compliance relaxed, I offered to meet on any site that my patients might be comfortable with: if not Doxy.me (which remains my starting place for most sessions), Facetime, Skype, Zoom, or Whatsapp. I have not offered Bluejeans, Google Hangouts, or WebEx, and no one has requested those applications. I keep the phone next to the computer, and some sessions include a few minutes of tech support as I help patients (or they help me) navigate the various sites. In a few sessions, we could not get the audio to work and we used video on one venue while we talked on the phone. I haven’t figured out if the variations in the quality of the connection has to do with my Comcast connection, the fact that these websites are overloaded with users, or that my household now consists of three people, two large monitors, three laptops, two tablets, three cell phone lines (not to mention one dog and a transplanted cat), all going at the same time. The pets do not require any bandwidth, but all the people are talking to screens throughout the workday.
As my colleagues embarked on the same journey, the listserv questions and comments came quickly. What were the best platforms? Was it a good thing or a bad thing to suddenly be in people’s homes? Some felt the extraneous background to be helpful, others found it distracting and intrusive.
How do these sessions get coded for the purpose of billing? There was a tremendous amount of confusion over that, with the initial verdict being that Medicare wanted the place of service changed to “02” and that private insurers want one of two modifiers, and it was anyone’s guess which company wanted which modifier. Then there was the concern that Medicare was paying 25% less, until the MPS staff clarified that full fees would be paid, but the place of service should be filled in as “11” – not “02” – as with regular office visits, and the modifier “95” should be added on the Health Care Finance Administration claim form. We were left to wait and see what gets reimbursed and for what fees.
Could new patients be seen by videoconferencing? Could patients from other states be seen this way if the psychiatrist was not licensed in the state where the patient was calling from? One psychiatrist reported he had a patient in an adjacent state drive over the border into Maryland, but the patient brought her mother and the evaluation included unwanted input from the mom as the session consisted of the patient and her mother yelling at both each other in the car and at the psychiatrist on the screen!
Psychiatrists on the listserv began to comment that treatment sessions were intense and exhausting. I feel the literal face-to-face contact of another person’s head just inches from my own, with full eye contact, often gets to be a lot. No one asks why I’ve moved a trinket (ah, there are no trinkets) or gazes off around the room. I sometimes sit for long periods of time as I don’t even stand to see the patients to the door. Other patients move about or bounce their devices on their laps, and my stomach starts to feel queasy until I ask to have the device adjusted. In some sessions, I find I’m talking to partial heads, or that computer icons cover the patient’s mouth.
Being in people’s lives via screen has been interesting. Unlike my colleague, I have not had any streaking spouses, but I’ve greeted a few family members – often those serving as technical support – and I’ve toured part of a farm, met dogs, guinea pigs, and even a goat. I’ve made brief daily “visits” to a frightened patient in isolation on a COVID hospital unit and had the joy of celebrating the discharge to home. It’s odd to be in a bedroom with a patient, even virtually, and it is interesting to note where they choose to hold their sessions; I’ve had several patients hold sessions from their cars. Seeing my own image in the corner of the screen is also a bit distracting, and in one session, as I saw my own reaction, my patient said, “I knew you were going to make that face!”
The pandemic has usurped most of the activities of all of our lives, and without social interactions, travel, and work in the usual way, life does not hold its usual richness. In a few cases, I have ended the session after half the time as the patient insisted there was nothing to talk about. Many talk about the medical problems they can’t be seen for, what they are doing to keep safe (or not), how they are washing down their groceries, and who they are meeting with by Zoom. Of those who were terribly anxious before, some feel oddly calmer – the world has ramped up to meet their level of anxiety and they feel vindicated. No one thinks they are odd for worrying about germs on door knobs or elevator buttons. What were once neurotic fears are now our real-life reality. Others have been triggered by a paralyzing fear, often with panic attacks, and these sessions are certainly challenging as I figure out which medications will best help, while responding to requests for reassurance. And there is the troublesome aspect of trying to care for others who are fearful while living with the reality that these fears are not extraneous to our own lives: We, too, are scared for ourselves and our families.
For some people, stay-at-home mandates have been easier than for others. People who are naturally introverted, or those with social anxiety, have told me they find this time at home to be a relief. They no longer feel pressured to go out; there is permission to be alone, to read, or watch Netflix. No one is pressuring them to go to parties or look for a Tinder date. For others, the isolation and loneliness have been devastating, causing a range of emotions from being “stir crazy,” to triggering episodes of major depression and severe anxiety.
Health care workers in therapy talk about their fears of being contaminated with coronavirus, about the exposures they’ve had, their fears of bringing the virus home to family, and about the anger – sometimes rage – that their employers are not doing more to protect them.
Few people these past weeks are looking for insight into their patterns of behavior and emotion. Most of life has come to be about survival and not about personal striving. Students who are driven to excel are disappointed to have their scholastic worlds have switched to pass/fail. And for those struggling with milder forms of depression and anxiety, both the patients and I have all been a bit perplexed by losing the usual measures of what feelings are normal in a tragic world and we no longer use socializing as the hallmark that heralds a return to normalcy after a period of withdrawal.
In some aspects, it is not all been bad. I’ve enjoyed watching my neighbors walk by with their dogs through the window behind my computer screen and I’ve felt part of the daily evolution as the cherry tree outside that same window turns from dead brown wood to vibrant pink blossoms. I like the flexibility of my schedule and the sensation I always carry of being rushed has quelled. I take more walks and spend more time with the family members who are held captive with me. The dog, who no longer is left alone for hours each day, is certainly a winner.
Some of my colleagues tell me they are overwhelmed – patients they have not seen for years have returned, people are asking for more frequent sessions, and they are suddenly trying to work at home while homeschooling children. I have had only a few of those requests for crisis care, while new referrals are much quieter than normal. Some of my patients have even said that they simply aren’t comfortable meeting this way and they will see me at the other end of the pandemic. A few people I would have expected to hear from I have not, and I fear that those who have lost their jobs may avoiding the cost of treatment – this group I will reach out to in the coming weeks. A little extra time, however, has given me the opportunity to join the Johns Hopkins COVID-19 Mental Health team. And my first attempt at teaching a resident seminar by Zoom has gone well.
For some in the medical field, this has been a horrible and traumatic time; they are worked to exhaustion, and surrounded by distress, death, and personal fear with every shift. For others, life has come to a standstill as the elective procedures that fill their days have virtually stopped. For outpatient psychiatry, it’s been a bit of an in-between, we may feel an odd mix of relevant and useless all at the same time, as our services are appreciated by our patients, but as actual soldiers caring for the ill COVID patients, we are leaving that to our colleagues in the EDs, COVID units, and ICUs. As a physician who has not treated a patient in an ICU for decades, I wish I had something more concrete to contribute to the effort, and at the same time, I’m relieved that I don’t.
And what about the patients? How are they doing with remote psychiatry? Some are clearly flustered or frustrated by the technology issues. Other times sessions go smoothly, and the fact that we are talking through screens gets forgotten. Some like the convenience of not having to drive a far distance and no one misses my crowded parking lot.
Kristen, another doctor’s patient in Illinois, commented: “I appreciate the continuity in care, especially if the alternative is delaying appointments. I think that’s most important. The interaction helps manage added anxiety from isolating as well. I don’t think it diminishes the care I receive; it makes me feel that my doctor is still accessible. One other point, since I have had both telemedicine and in-person appointments with my current psychiatrist, is that during in-person meetings, he is usually on his computer and rarely looks at me or makes eye contact. In virtual meetings, I feel he is much more engaged with me.”
In normal times, I spend a good deal of time encouraging patients to work on building their relationships and community – these connections lead people to healthy and fulfilling lives – and now we talk about how to best be socially distant. We see each other as vectors of disease and to greet a friend with a handshake, much less a hug, would be unthinkable. Will our collective psyches ever recover? For those of us who will survive, that remains to be seen. In the meantime, perhaps we are all being forced to be more flexible and innovative.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
It seems that some glitches would be inevitable. With a sudden shift to videoconferencing in private psychiatric practices, there were bound to be issues with both technology and privacy. One friend told me of such a glitch on the very first day she started telemental health: She was meeting with a patient who was sitting at her kitchen table. Unbeknownst to the patient, her husband walked into the kitchen behind her, fully naked, to get something from the refrigerator. “There was a full moon shot!” my friend said, initially quite shocked, and then eventually amused. As we all cope with a national tragedy and the total upheaval to our personal and professional lives, the stories just keep coming.
I left work on Friday, March 13, with plans to return on the following Monday to see patients. I had no idea that, by Sunday evening, I would be persuaded that for the safety of all I would need to shut down my real-life psychiatric practice and switch to a videoconferencing venue. I, along with many psychiatrists in Maryland, made this decision after Amy Huberman, MD, posted the following on the Maryland Psychiatric Society (MPS) listserv on Sunday, March 15:
“I want to make a case for starting video sessions with all your patients NOW. There is increasing evidence that the spread of coronavirus is driven primarily by asymptomatic or mildly ill people infected with the virus. Because of this, it’s not good enough to tell your patients not to come in if they have symptoms, or for you not to come into work if you have no symptoms. Even after I sent out a letter two weeks ago warning people not to come in if they had symptoms or had potentially come in contact with someone with COVID-19, several patients with coughs still came to my office, as well as several people who had just been on trips to New York City.
If we want to help slow the spread of this illness so that our health system has a better chance of being able to offer ventilators to the people who need them, we must limit all contacts as much as possible – even of asymptomatic people, given the emerging data.
I am planning to send out a message to all my patients today that they should do the same. Without the president or the media giving clear advice to people about what to do, it’s our job as physicians to do it.”
By that night, I had set up a home office with a blank wall behind me, windows in front of me, and books propping my computer at a height that would not have my patients looking up my nose. For the first time in over 20 years, I dusted my son’s Little League trophies, moved them and a 40,000 baseball card collection against the wall, carried a desk, chair, rug, houseplant, and a small Buddha into a room in which I would have some privacy, and my telepsychiatry practice found a home.
After some research, I registered for a free site called Doxy.me because it was HIPAA compliant and did not require patients to download an application; anyone with a camera on any Internet-enabled phone, computer, or tablet, could click on a link and enter my virtual waiting room. I soon discovered that images on the Doxy.me site are sometimes grainy and sometimes freeze up; in some sessions, we ended up switching to FaceTime, and as government mandates for HIPAA compliance relaxed, I offered to meet on any site that my patients might be comfortable with: if not Doxy.me (which remains my starting place for most sessions), Facetime, Skype, Zoom, or Whatsapp. I have not offered Bluejeans, Google Hangouts, or WebEx, and no one has requested those applications. I keep the phone next to the computer, and some sessions include a few minutes of tech support as I help patients (or they help me) navigate the various sites. In a few sessions, we could not get the audio to work and we used video on one venue while we talked on the phone. I haven’t figured out if the variations in the quality of the connection has to do with my Comcast connection, the fact that these websites are overloaded with users, or that my household now consists of three people, two large monitors, three laptops, two tablets, three cell phone lines (not to mention one dog and a transplanted cat), all going at the same time. The pets do not require any bandwidth, but all the people are talking to screens throughout the workday.
As my colleagues embarked on the same journey, the listserv questions and comments came quickly. What were the best platforms? Was it a good thing or a bad thing to suddenly be in people’s homes? Some felt the extraneous background to be helpful, others found it distracting and intrusive.
How do these sessions get coded for the purpose of billing? There was a tremendous amount of confusion over that, with the initial verdict being that Medicare wanted the place of service changed to “02” and that private insurers want one of two modifiers, and it was anyone’s guess which company wanted which modifier. Then there was the concern that Medicare was paying 25% less, until the MPS staff clarified that full fees would be paid, but the place of service should be filled in as “11” – not “02” – as with regular office visits, and the modifier “95” should be added on the Health Care Finance Administration claim form. We were left to wait and see what gets reimbursed and for what fees.
Could new patients be seen by videoconferencing? Could patients from other states be seen this way if the psychiatrist was not licensed in the state where the patient was calling from? One psychiatrist reported he had a patient in an adjacent state drive over the border into Maryland, but the patient brought her mother and the evaluation included unwanted input from the mom as the session consisted of the patient and her mother yelling at both each other in the car and at the psychiatrist on the screen!
Psychiatrists on the listserv began to comment that treatment sessions were intense and exhausting. I feel the literal face-to-face contact of another person’s head just inches from my own, with full eye contact, often gets to be a lot. No one asks why I’ve moved a trinket (ah, there are no trinkets) or gazes off around the room. I sometimes sit for long periods of time as I don’t even stand to see the patients to the door. Other patients move about or bounce their devices on their laps, and my stomach starts to feel queasy until I ask to have the device adjusted. In some sessions, I find I’m talking to partial heads, or that computer icons cover the patient’s mouth.
Being in people’s lives via screen has been interesting. Unlike my colleague, I have not had any streaking spouses, but I’ve greeted a few family members – often those serving as technical support – and I’ve toured part of a farm, met dogs, guinea pigs, and even a goat. I’ve made brief daily “visits” to a frightened patient in isolation on a COVID hospital unit and had the joy of celebrating the discharge to home. It’s odd to be in a bedroom with a patient, even virtually, and it is interesting to note where they choose to hold their sessions; I’ve had several patients hold sessions from their cars. Seeing my own image in the corner of the screen is also a bit distracting, and in one session, as I saw my own reaction, my patient said, “I knew you were going to make that face!”
The pandemic has usurped most of the activities of all of our lives, and without social interactions, travel, and work in the usual way, life does not hold its usual richness. In a few cases, I have ended the session after half the time as the patient insisted there was nothing to talk about. Many talk about the medical problems they can’t be seen for, what they are doing to keep safe (or not), how they are washing down their groceries, and who they are meeting with by Zoom. Of those who were terribly anxious before, some feel oddly calmer – the world has ramped up to meet their level of anxiety and they feel vindicated. No one thinks they are odd for worrying about germs on door knobs or elevator buttons. What were once neurotic fears are now our real-life reality. Others have been triggered by a paralyzing fear, often with panic attacks, and these sessions are certainly challenging as I figure out which medications will best help, while responding to requests for reassurance. And there is the troublesome aspect of trying to care for others who are fearful while living with the reality that these fears are not extraneous to our own lives: We, too, are scared for ourselves and our families.
For some people, stay-at-home mandates have been easier than for others. People who are naturally introverted, or those with social anxiety, have told me they find this time at home to be a relief. They no longer feel pressured to go out; there is permission to be alone, to read, or watch Netflix. No one is pressuring them to go to parties or look for a Tinder date. For others, the isolation and loneliness have been devastating, causing a range of emotions from being “stir crazy,” to triggering episodes of major depression and severe anxiety.
Health care workers in therapy talk about their fears of being contaminated with coronavirus, about the exposures they’ve had, their fears of bringing the virus home to family, and about the anger – sometimes rage – that their employers are not doing more to protect them.
Few people these past weeks are looking for insight into their patterns of behavior and emotion. Most of life has come to be about survival and not about personal striving. Students who are driven to excel are disappointed to have their scholastic worlds have switched to pass/fail. And for those struggling with milder forms of depression and anxiety, both the patients and I have all been a bit perplexed by losing the usual measures of what feelings are normal in a tragic world and we no longer use socializing as the hallmark that heralds a return to normalcy after a period of withdrawal.
In some aspects, it is not all been bad. I’ve enjoyed watching my neighbors walk by with their dogs through the window behind my computer screen and I’ve felt part of the daily evolution as the cherry tree outside that same window turns from dead brown wood to vibrant pink blossoms. I like the flexibility of my schedule and the sensation I always carry of being rushed has quelled. I take more walks and spend more time with the family members who are held captive with me. The dog, who no longer is left alone for hours each day, is certainly a winner.
Some of my colleagues tell me they are overwhelmed – patients they have not seen for years have returned, people are asking for more frequent sessions, and they are suddenly trying to work at home while homeschooling children. I have had only a few of those requests for crisis care, while new referrals are much quieter than normal. Some of my patients have even said that they simply aren’t comfortable meeting this way and they will see me at the other end of the pandemic. A few people I would have expected to hear from I have not, and I fear that those who have lost their jobs may avoiding the cost of treatment – this group I will reach out to in the coming weeks. A little extra time, however, has given me the opportunity to join the Johns Hopkins COVID-19 Mental Health team. And my first attempt at teaching a resident seminar by Zoom has gone well.
For some in the medical field, this has been a horrible and traumatic time; they are worked to exhaustion, and surrounded by distress, death, and personal fear with every shift. For others, life has come to a standstill as the elective procedures that fill their days have virtually stopped. For outpatient psychiatry, it’s been a bit of an in-between, we may feel an odd mix of relevant and useless all at the same time, as our services are appreciated by our patients, but as actual soldiers caring for the ill COVID patients, we are leaving that to our colleagues in the EDs, COVID units, and ICUs. As a physician who has not treated a patient in an ICU for decades, I wish I had something more concrete to contribute to the effort, and at the same time, I’m relieved that I don’t.
And what about the patients? How are they doing with remote psychiatry? Some are clearly flustered or frustrated by the technology issues. Other times sessions go smoothly, and the fact that we are talking through screens gets forgotten. Some like the convenience of not having to drive a far distance and no one misses my crowded parking lot.
Kristen, another doctor’s patient in Illinois, commented: “I appreciate the continuity in care, especially if the alternative is delaying appointments. I think that’s most important. The interaction helps manage added anxiety from isolating as well. I don’t think it diminishes the care I receive; it makes me feel that my doctor is still accessible. One other point, since I have had both telemedicine and in-person appointments with my current psychiatrist, is that during in-person meetings, he is usually on his computer and rarely looks at me or makes eye contact. In virtual meetings, I feel he is much more engaged with me.”
In normal times, I spend a good deal of time encouraging patients to work on building their relationships and community – these connections lead people to healthy and fulfilling lives – and now we talk about how to best be socially distant. We see each other as vectors of disease and to greet a friend with a handshake, much less a hug, would be unthinkable. Will our collective psyches ever recover? For those of us who will survive, that remains to be seen. In the meantime, perhaps we are all being forced to be more flexible and innovative.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
It seems that some glitches would be inevitable. With a sudden shift to videoconferencing in private psychiatric practices, there were bound to be issues with both technology and privacy. One friend told me of such a glitch on the very first day she started telemental health: She was meeting with a patient who was sitting at her kitchen table. Unbeknownst to the patient, her husband walked into the kitchen behind her, fully naked, to get something from the refrigerator. “There was a full moon shot!” my friend said, initially quite shocked, and then eventually amused. As we all cope with a national tragedy and the total upheaval to our personal and professional lives, the stories just keep coming.
I left work on Friday, March 13, with plans to return on the following Monday to see patients. I had no idea that, by Sunday evening, I would be persuaded that for the safety of all I would need to shut down my real-life psychiatric practice and switch to a videoconferencing venue. I, along with many psychiatrists in Maryland, made this decision after Amy Huberman, MD, posted the following on the Maryland Psychiatric Society (MPS) listserv on Sunday, March 15:
“I want to make a case for starting video sessions with all your patients NOW. There is increasing evidence that the spread of coronavirus is driven primarily by asymptomatic or mildly ill people infected with the virus. Because of this, it’s not good enough to tell your patients not to come in if they have symptoms, or for you not to come into work if you have no symptoms. Even after I sent out a letter two weeks ago warning people not to come in if they had symptoms or had potentially come in contact with someone with COVID-19, several patients with coughs still came to my office, as well as several people who had just been on trips to New York City.
If we want to help slow the spread of this illness so that our health system has a better chance of being able to offer ventilators to the people who need them, we must limit all contacts as much as possible – even of asymptomatic people, given the emerging data.
I am planning to send out a message to all my patients today that they should do the same. Without the president or the media giving clear advice to people about what to do, it’s our job as physicians to do it.”
By that night, I had set up a home office with a blank wall behind me, windows in front of me, and books propping my computer at a height that would not have my patients looking up my nose. For the first time in over 20 years, I dusted my son’s Little League trophies, moved them and a 40,000 baseball card collection against the wall, carried a desk, chair, rug, houseplant, and a small Buddha into a room in which I would have some privacy, and my telepsychiatry practice found a home.
After some research, I registered for a free site called Doxy.me because it was HIPAA compliant and did not require patients to download an application; anyone with a camera on any Internet-enabled phone, computer, or tablet, could click on a link and enter my virtual waiting room. I soon discovered that images on the Doxy.me site are sometimes grainy and sometimes freeze up; in some sessions, we ended up switching to FaceTime, and as government mandates for HIPAA compliance relaxed, I offered to meet on any site that my patients might be comfortable with: if not Doxy.me (which remains my starting place for most sessions), Facetime, Skype, Zoom, or Whatsapp. I have not offered Bluejeans, Google Hangouts, or WebEx, and no one has requested those applications. I keep the phone next to the computer, and some sessions include a few minutes of tech support as I help patients (or they help me) navigate the various sites. In a few sessions, we could not get the audio to work and we used video on one venue while we talked on the phone. I haven’t figured out if the variations in the quality of the connection has to do with my Comcast connection, the fact that these websites are overloaded with users, or that my household now consists of three people, two large monitors, three laptops, two tablets, three cell phone lines (not to mention one dog and a transplanted cat), all going at the same time. The pets do not require any bandwidth, but all the people are talking to screens throughout the workday.
As my colleagues embarked on the same journey, the listserv questions and comments came quickly. What were the best platforms? Was it a good thing or a bad thing to suddenly be in people’s homes? Some felt the extraneous background to be helpful, others found it distracting and intrusive.
How do these sessions get coded for the purpose of billing? There was a tremendous amount of confusion over that, with the initial verdict being that Medicare wanted the place of service changed to “02” and that private insurers want one of two modifiers, and it was anyone’s guess which company wanted which modifier. Then there was the concern that Medicare was paying 25% less, until the MPS staff clarified that full fees would be paid, but the place of service should be filled in as “11” – not “02” – as with regular office visits, and the modifier “95” should be added on the Health Care Finance Administration claim form. We were left to wait and see what gets reimbursed and for what fees.
Could new patients be seen by videoconferencing? Could patients from other states be seen this way if the psychiatrist was not licensed in the state where the patient was calling from? One psychiatrist reported he had a patient in an adjacent state drive over the border into Maryland, but the patient brought her mother and the evaluation included unwanted input from the mom as the session consisted of the patient and her mother yelling at both each other in the car and at the psychiatrist on the screen!
Psychiatrists on the listserv began to comment that treatment sessions were intense and exhausting. I feel the literal face-to-face contact of another person’s head just inches from my own, with full eye contact, often gets to be a lot. No one asks why I’ve moved a trinket (ah, there are no trinkets) or gazes off around the room. I sometimes sit for long periods of time as I don’t even stand to see the patients to the door. Other patients move about or bounce their devices on their laps, and my stomach starts to feel queasy until I ask to have the device adjusted. In some sessions, I find I’m talking to partial heads, or that computer icons cover the patient’s mouth.
Being in people’s lives via screen has been interesting. Unlike my colleague, I have not had any streaking spouses, but I’ve greeted a few family members – often those serving as technical support – and I’ve toured part of a farm, met dogs, guinea pigs, and even a goat. I’ve made brief daily “visits” to a frightened patient in isolation on a COVID hospital unit and had the joy of celebrating the discharge to home. It’s odd to be in a bedroom with a patient, even virtually, and it is interesting to note where they choose to hold their sessions; I’ve had several patients hold sessions from their cars. Seeing my own image in the corner of the screen is also a bit distracting, and in one session, as I saw my own reaction, my patient said, “I knew you were going to make that face!”
The pandemic has usurped most of the activities of all of our lives, and without social interactions, travel, and work in the usual way, life does not hold its usual richness. In a few cases, I have ended the session after half the time as the patient insisted there was nothing to talk about. Many talk about the medical problems they can’t be seen for, what they are doing to keep safe (or not), how they are washing down their groceries, and who they are meeting with by Zoom. Of those who were terribly anxious before, some feel oddly calmer – the world has ramped up to meet their level of anxiety and they feel vindicated. No one thinks they are odd for worrying about germs on door knobs or elevator buttons. What were once neurotic fears are now our real-life reality. Others have been triggered by a paralyzing fear, often with panic attacks, and these sessions are certainly challenging as I figure out which medications will best help, while responding to requests for reassurance. And there is the troublesome aspect of trying to care for others who are fearful while living with the reality that these fears are not extraneous to our own lives: We, too, are scared for ourselves and our families.
For some people, stay-at-home mandates have been easier than for others. People who are naturally introverted, or those with social anxiety, have told me they find this time at home to be a relief. They no longer feel pressured to go out; there is permission to be alone, to read, or watch Netflix. No one is pressuring them to go to parties or look for a Tinder date. For others, the isolation and loneliness have been devastating, causing a range of emotions from being “stir crazy,” to triggering episodes of major depression and severe anxiety.
Health care workers in therapy talk about their fears of being contaminated with coronavirus, about the exposures they’ve had, their fears of bringing the virus home to family, and about the anger – sometimes rage – that their employers are not doing more to protect them.
Few people these past weeks are looking for insight into their patterns of behavior and emotion. Most of life has come to be about survival and not about personal striving. Students who are driven to excel are disappointed to have their scholastic worlds have switched to pass/fail. And for those struggling with milder forms of depression and anxiety, both the patients and I have all been a bit perplexed by losing the usual measures of what feelings are normal in a tragic world and we no longer use socializing as the hallmark that heralds a return to normalcy after a period of withdrawal.
In some aspects, it is not all been bad. I’ve enjoyed watching my neighbors walk by with their dogs through the window behind my computer screen and I’ve felt part of the daily evolution as the cherry tree outside that same window turns from dead brown wood to vibrant pink blossoms. I like the flexibility of my schedule and the sensation I always carry of being rushed has quelled. I take more walks and spend more time with the family members who are held captive with me. The dog, who no longer is left alone for hours each day, is certainly a winner.
Some of my colleagues tell me they are overwhelmed – patients they have not seen for years have returned, people are asking for more frequent sessions, and they are suddenly trying to work at home while homeschooling children. I have had only a few of those requests for crisis care, while new referrals are much quieter than normal. Some of my patients have even said that they simply aren’t comfortable meeting this way and they will see me at the other end of the pandemic. A few people I would have expected to hear from I have not, and I fear that those who have lost their jobs may avoiding the cost of treatment – this group I will reach out to in the coming weeks. A little extra time, however, has given me the opportunity to join the Johns Hopkins COVID-19 Mental Health team. And my first attempt at teaching a resident seminar by Zoom has gone well.
For some in the medical field, this has been a horrible and traumatic time; they are worked to exhaustion, and surrounded by distress, death, and personal fear with every shift. For others, life has come to a standstill as the elective procedures that fill their days have virtually stopped. For outpatient psychiatry, it’s been a bit of an in-between, we may feel an odd mix of relevant and useless all at the same time, as our services are appreciated by our patients, but as actual soldiers caring for the ill COVID patients, we are leaving that to our colleagues in the EDs, COVID units, and ICUs. As a physician who has not treated a patient in an ICU for decades, I wish I had something more concrete to contribute to the effort, and at the same time, I’m relieved that I don’t.
And what about the patients? How are they doing with remote psychiatry? Some are clearly flustered or frustrated by the technology issues. Other times sessions go smoothly, and the fact that we are talking through screens gets forgotten. Some like the convenience of not having to drive a far distance and no one misses my crowded parking lot.
Kristen, another doctor’s patient in Illinois, commented: “I appreciate the continuity in care, especially if the alternative is delaying appointments. I think that’s most important. The interaction helps manage added anxiety from isolating as well. I don’t think it diminishes the care I receive; it makes me feel that my doctor is still accessible. One other point, since I have had both telemedicine and in-person appointments with my current psychiatrist, is that during in-person meetings, he is usually on his computer and rarely looks at me or makes eye contact. In virtual meetings, I feel he is much more engaged with me.”
In normal times, I spend a good deal of time encouraging patients to work on building their relationships and community – these connections lead people to healthy and fulfilling lives – and now we talk about how to best be socially distant. We see each other as vectors of disease and to greet a friend with a handshake, much less a hug, would be unthinkable. Will our collective psyches ever recover? For those of us who will survive, that remains to be seen. In the meantime, perhaps we are all being forced to be more flexible and innovative.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
TWILIGHT-COMPLEX: Tap ticagrelor monotherapy early after complex PCI
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
FROM ACC 2020
Hypertension goes unmedicated in 40% of adults
Roughly 30% of adults in the United States had hypertension in 2017, and just under 60% of those adults reported using antihypertensive medication, according to the Centers for Disease Control and Prevention.
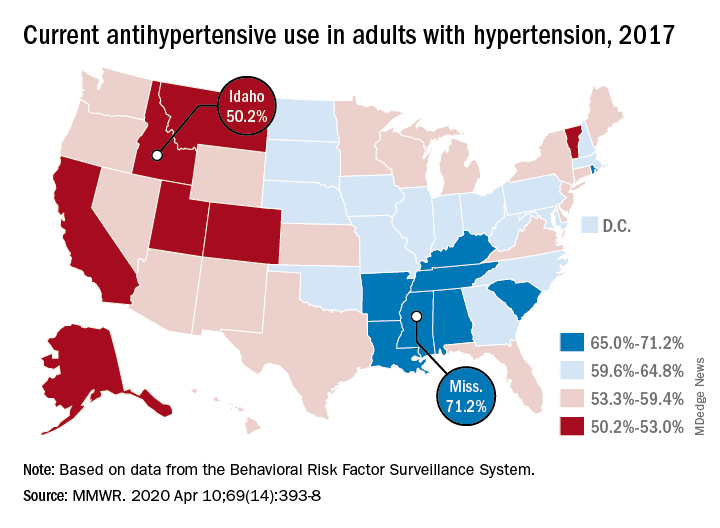
There is, however, quite a bit of variation from those age-standardized national figures when state-level data are considered.
In Alabama and West Virginia, the prevalence of hypertension in 2017 was 38.6%, the highest in the country, with Arkansas (38.5%) and Mississippi (38.2%) not far behind. Meanwhile, Minnesota came in with a lowest-in-the-nation rate of 24.3%, which was nearly matched by Colorado at 24.8%, Claudine M. Samanic, PhD, and associates wrote in the MMWR.
There was also a considerable gap between the states in hypertensive adults’ self-reported use of antihypertensive drugs, which was generally higher in the states with a greater prevalence of disease, they noted.
Adults in Mississippi were the most likely (71.2%) to be taking medication, along with those in Alabama (70.5%) and Arkansas (69.3%). Idaho occupied the other end of the scale with a rate of 50.2%, while Montana and Vermont were slightly better at 51.7%, based on survey data from the Behavioral Risk Factor Surveillance System.
“Prevalence of antihypertensive medication use was higher in older age groups, highest among blacks, and higher among women [64.0%] than men [56.7%]. This overall gender difference has been reported previously, but the reasons are unclear,” wrote Dr. Samanic and associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
The BRFSS data for 2017 are based on based on interviews with 450,016 adults. Respondents were asked, “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” and were considered to have hypertension if they answered yes.
SOURCE: Samanic CM et al. MMWR. 2020 Apr 10;69(14):393-8.
Roughly 30% of adults in the United States had hypertension in 2017, and just under 60% of those adults reported using antihypertensive medication, according to the Centers for Disease Control and Prevention.
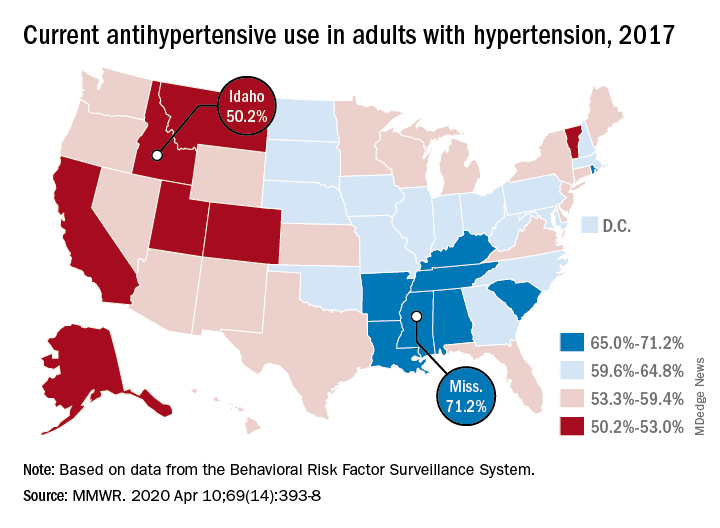
There is, however, quite a bit of variation from those age-standardized national figures when state-level data are considered.
In Alabama and West Virginia, the prevalence of hypertension in 2017 was 38.6%, the highest in the country, with Arkansas (38.5%) and Mississippi (38.2%) not far behind. Meanwhile, Minnesota came in with a lowest-in-the-nation rate of 24.3%, which was nearly matched by Colorado at 24.8%, Claudine M. Samanic, PhD, and associates wrote in the MMWR.
There was also a considerable gap between the states in hypertensive adults’ self-reported use of antihypertensive drugs, which was generally higher in the states with a greater prevalence of disease, they noted.
Adults in Mississippi were the most likely (71.2%) to be taking medication, along with those in Alabama (70.5%) and Arkansas (69.3%). Idaho occupied the other end of the scale with a rate of 50.2%, while Montana and Vermont were slightly better at 51.7%, based on survey data from the Behavioral Risk Factor Surveillance System.
“Prevalence of antihypertensive medication use was higher in older age groups, highest among blacks, and higher among women [64.0%] than men [56.7%]. This overall gender difference has been reported previously, but the reasons are unclear,” wrote Dr. Samanic and associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
The BRFSS data for 2017 are based on based on interviews with 450,016 adults. Respondents were asked, “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” and were considered to have hypertension if they answered yes.
SOURCE: Samanic CM et al. MMWR. 2020 Apr 10;69(14):393-8.
Roughly 30% of adults in the United States had hypertension in 2017, and just under 60% of those adults reported using antihypertensive medication, according to the Centers for Disease Control and Prevention.
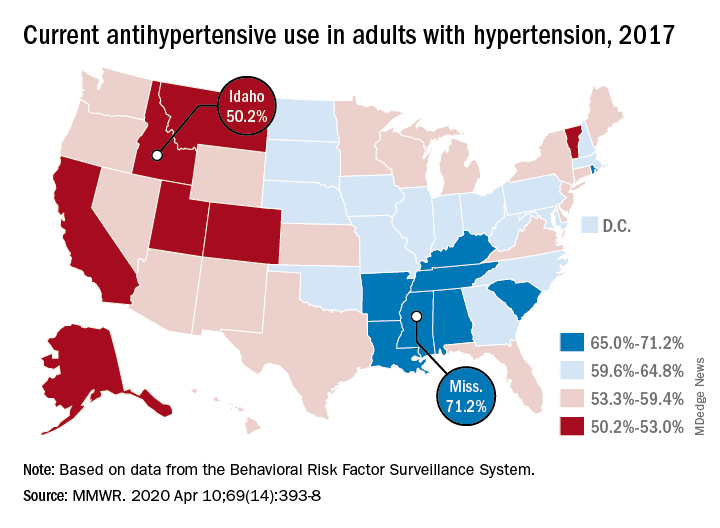
There is, however, quite a bit of variation from those age-standardized national figures when state-level data are considered.
In Alabama and West Virginia, the prevalence of hypertension in 2017 was 38.6%, the highest in the country, with Arkansas (38.5%) and Mississippi (38.2%) not far behind. Meanwhile, Minnesota came in with a lowest-in-the-nation rate of 24.3%, which was nearly matched by Colorado at 24.8%, Claudine M. Samanic, PhD, and associates wrote in the MMWR.
There was also a considerable gap between the states in hypertensive adults’ self-reported use of antihypertensive drugs, which was generally higher in the states with a greater prevalence of disease, they noted.
Adults in Mississippi were the most likely (71.2%) to be taking medication, along with those in Alabama (70.5%) and Arkansas (69.3%). Idaho occupied the other end of the scale with a rate of 50.2%, while Montana and Vermont were slightly better at 51.7%, based on survey data from the Behavioral Risk Factor Surveillance System.
“Prevalence of antihypertensive medication use was higher in older age groups, highest among blacks, and higher among women [64.0%] than men [56.7%]. This overall gender difference has been reported previously, but the reasons are unclear,” wrote Dr. Samanic and associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
The BRFSS data for 2017 are based on based on interviews with 450,016 adults. Respondents were asked, “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” and were considered to have hypertension if they answered yes.
SOURCE: Samanic CM et al. MMWR. 2020 Apr 10;69(14):393-8.
FROM THE MMWR
The 7 strategies of highly effective people facing the COVID-19 pandemic
A few weeks ago, I saw more than 60 responses to a post on Nextdoor.com entitled, “Toilet paper strategies?”
Asking for help is a great coping mechanism when one is struggling to find a strategy, even if it’s for toilet paper. What other kinds of coping strategies can help us through this historic and unprecedented time?
The late Stephen R. Covey, PhD, wrote about the coping strategies of highly effective people in his book, “The 7 Habits of Highly Effective People.”1 For, no matter how smart, perfect, or careful you may be, life will never be trouble free. When trouble comes, it’s important to have coping strategies that help you navigate through choppy waters. Whether you are a practitioner trying to help your patients or someone who wants to maximize their personal resilience during a worldwide pandemic, here are my conceptualizations of the seven top strategies highly effective people use when facing challenges.
Strategy #1: Begin with the end in mind
In 2007, this strategy helped me not only survive but thrive when I battled for my right to practice as a holistic psychiatrist against the Maryland Board of Physicians.2 From the first moment when I read the letter from the board, to the last when I read the administrative law judge’s dismissal, I turned to this strategy to help me cope with unrelenting stress.
I imagined myself remembering being the kind of person I wanted to be, wrote that script for myself, and created those memories for my future self. I wanted to remember myself as being brave, calm, strong, and grounded, so I behaved each day as if I were all of those things.
As Dr. Covey wrote, “ ‘Begin with the end in mind’ is based on the principle that all things are created twice. There’s a mental or first creation, and a physical or second creation to all things.” Imagine who you would like to remember yourself being a year or two down the road. Do you want to remember yourself showing good judgment and being positive and compassionate during this pandemic? Then, follow the script you’ve created in your mind and be that person now, knowing that you are forming memories for your future self. Your future self will look back at who you are right now with appreciation and satisfaction. Of course, this is a habit that you can apply to your entire life.
Strategy #2: Be proactive
Between the event and the outcome is you. You are the interpreter and transformer of the event, with the freedom to apply your will and intention on the event. Whether it is living through a pandemic or dealing with misplaced keys, every day you are revealing your nature through how you deal with life. To be proactive is different from being reactive. Within each of us there is a will, the drive, to rise above our difficult environments.
Dr. Covey wrote, “the ability to subordinate an impulse to a value is the essence of the proactive person.” A woman shared with me that she created an Excel spreadsheet with some of the things she plans to do with her free time while she stays in her NYC apartment. She doesn’t want to slip into a passive state and waste her time. That’s being proactive.
Strategy #3: Set proper priorities
Or, as Dr. Covey would say, “Put first things first.” During a pandemic, when the world seems to be precariously tilting at an angle, it’s easy to cling to outdated standards, expectations, and behavioral patterns. Doing so heightens our sense of regret, fear, and scarcity. Valuing gratitude will empower you to deal with financial loss differently because you can still remain grateful despite uncontrollable losses. We can choose “to have or to be” as psychoanalyst, Erich Fromm, PhD, would say.3 If your happiness is measured by how much money you have, then it would make sense that, when the amount shrinks, so does your happiness. However, if your happiness is a side effect of who you are, you will remain a mountain before the winds and tides of circumstance.
Strategy #4: Create a win/win mentality
This state of mind is built on character. Dr. Covey separates character into three categories: integrity, maturity, and abundance mentality. A lack of character resulted in the hoarding of toilet paper in many communities and the cry for help from Nextdoor.com. I noticed that, in the 60+ responses that included advice about using bidets, old towels, and even leaves, no one offered to share a bag of toilet paper. That’s because people experienced the fear of scarcity, in turn, causing the scarcity they feared.
During a pandemic, a highly effective person or company thinks beyond themselves to create a win/win scenario. At a grocery store in my neighborhood, a man stands at its entrance with a bottle of disinfectant spray in one hand for the shoppers and a sign on the sidewalk with guidelines for purchasing products to avoid hoarding. He tells you where the wipes are for the carts as you enter the store. People line up 6 feet apart, waiting to enter, to limit the number of shoppers inside the store, facilitating proper physical distancing. Instead of maximizing profits at the expense of everyone’s health and safety, the process is a win/win for everyone, from shoppers to employees.
Strategy #5: Develop empathy and understanding
Seeking to first understand and then be understood is one of the most powerful tools of effective people. In my holistic practice, every patient comes in with their own unique needs that evolve and transform over time. I must remain open, or I fail to deliver appropriately.
Learning to listen and then to clearly communicate ideas is essential to effective health care. During this time, it is critical that health care providers and political leaders first listen/understand and then communicate clearly to serve everyone in the best way possible.
In our brains, the frontal lobes (the adult in the room) manages our amygdala (the child in the room) when we get enough sleep, meditate, spend time in nature, exercise, and eat healthy food.4 Stress can interfere with the frontal lobe’s ability to maintain empathy, inhibit unhealthy impulses, and delay gratification. During the pandemic, we can help to shift from the stress response, or “fight-or-flight” response, driven by the sympathetic nervous system to a “rest-and-digest” response driven by the parasympathetic system through coherent breathing, taking slow, deep, relaxed breaths (6 seconds on inhalation and 6 seconds on exhalation). The vagus nerve connected to our diaphragm will help the heart return to a healthy rhythm.5
Strategy #6: Synergize and integrate
All of life is interdependent, each part no more or less important than any other. Is oxygen more important than hydrogen? Is H2O different from the oxygen and hydrogen atoms that make it?
During a pandemic, it’s important for us to appreciate each other’s contributions and work synergistically for the good of the whole. Our survival depends on valuing each other and our planet. This perspective informs the practice of physical distancing and staying home to minimize the spread of the virus and its impact on the health care system, regardless of whether an individual belongs in the high-risk group or not.
Many high-achieving people train in extremely competitive settings in which survival depends on individual performance rather than mutual cooperation. This training process encourages a disregard for others. Good leaders, however, understand that cooperation and mutual respect are essential to personal well-being.
Strategy #7: Practice self-care
There are five aspects of our lives that depend on our self-care: spiritual, mental, emotional, physical, and social. Unfortunately, many kind-hearted people are kinder to others than to themselves. There is really only one person who can truly take care of you properly, and that is yourself. In Seattle, where many suffered early in the pandemic, holistic psychiatrist David Kopacz, MD, is reminding people to nurture themselves in his post, “Nurture Yourself During the Pandemic: Try New Recipes!”6 Indeed, that is what many must do since eating out is not an option now. If you find yourself stuck at home with more time on your hands, take the opportunity to care for yourself. Ask yourself what you really need during this time, and make the effort to provide it to yourself.
After the pandemic is over, will you have grown from the experiences and become a better person from it? Despite our current circumstances, we can continue to grow as individuals and as a community, armed with strategies that can benefit all of us.
References
1. Covey SR. The 7 Habits of Highly Effective People. New York: Simon & Schuster; 1989.
2. Lee AW. Townsend Letter. 2009 Jun;311:22-3.
3. Fromm E. To Have or To Be? New York: Continuum International Publishing; 2005.
4. Rushlau K. Integrative Healthcare Symposium. 2020 Feb 21.
5. Gerbarg PL. Mind Body Practices for Post-Traumatic Stress Disorder. Presentation at Integrative Medicine for Mental Health Conference. 2016 Sep.
6. Kopacz D. Nurture Yourself During the Pandemic: Try New Recipes! Being Fully Human. 2020 Mar 22.
Dr. Lee specializes in integrative and holistic psychiatry and has a private practice in Gaithersburg, Md. She has no disclosures.
A few weeks ago, I saw more than 60 responses to a post on Nextdoor.com entitled, “Toilet paper strategies?”
Asking for help is a great coping mechanism when one is struggling to find a strategy, even if it’s for toilet paper. What other kinds of coping strategies can help us through this historic and unprecedented time?
The late Stephen R. Covey, PhD, wrote about the coping strategies of highly effective people in his book, “The 7 Habits of Highly Effective People.”1 For, no matter how smart, perfect, or careful you may be, life will never be trouble free. When trouble comes, it’s important to have coping strategies that help you navigate through choppy waters. Whether you are a practitioner trying to help your patients or someone who wants to maximize their personal resilience during a worldwide pandemic, here are my conceptualizations of the seven top strategies highly effective people use when facing challenges.
Strategy #1: Begin with the end in mind
In 2007, this strategy helped me not only survive but thrive when I battled for my right to practice as a holistic psychiatrist against the Maryland Board of Physicians.2 From the first moment when I read the letter from the board, to the last when I read the administrative law judge’s dismissal, I turned to this strategy to help me cope with unrelenting stress.
I imagined myself remembering being the kind of person I wanted to be, wrote that script for myself, and created those memories for my future self. I wanted to remember myself as being brave, calm, strong, and grounded, so I behaved each day as if I were all of those things.
As Dr. Covey wrote, “ ‘Begin with the end in mind’ is based on the principle that all things are created twice. There’s a mental or first creation, and a physical or second creation to all things.” Imagine who you would like to remember yourself being a year or two down the road. Do you want to remember yourself showing good judgment and being positive and compassionate during this pandemic? Then, follow the script you’ve created in your mind and be that person now, knowing that you are forming memories for your future self. Your future self will look back at who you are right now with appreciation and satisfaction. Of course, this is a habit that you can apply to your entire life.
Strategy #2: Be proactive
Between the event and the outcome is you. You are the interpreter and transformer of the event, with the freedom to apply your will and intention on the event. Whether it is living through a pandemic or dealing with misplaced keys, every day you are revealing your nature through how you deal with life. To be proactive is different from being reactive. Within each of us there is a will, the drive, to rise above our difficult environments.
Dr. Covey wrote, “the ability to subordinate an impulse to a value is the essence of the proactive person.” A woman shared with me that she created an Excel spreadsheet with some of the things she plans to do with her free time while she stays in her NYC apartment. She doesn’t want to slip into a passive state and waste her time. That’s being proactive.
Strategy #3: Set proper priorities
Or, as Dr. Covey would say, “Put first things first.” During a pandemic, when the world seems to be precariously tilting at an angle, it’s easy to cling to outdated standards, expectations, and behavioral patterns. Doing so heightens our sense of regret, fear, and scarcity. Valuing gratitude will empower you to deal with financial loss differently because you can still remain grateful despite uncontrollable losses. We can choose “to have or to be” as psychoanalyst, Erich Fromm, PhD, would say.3 If your happiness is measured by how much money you have, then it would make sense that, when the amount shrinks, so does your happiness. However, if your happiness is a side effect of who you are, you will remain a mountain before the winds and tides of circumstance.
Strategy #4: Create a win/win mentality
This state of mind is built on character. Dr. Covey separates character into three categories: integrity, maturity, and abundance mentality. A lack of character resulted in the hoarding of toilet paper in many communities and the cry for help from Nextdoor.com. I noticed that, in the 60+ responses that included advice about using bidets, old towels, and even leaves, no one offered to share a bag of toilet paper. That’s because people experienced the fear of scarcity, in turn, causing the scarcity they feared.
During a pandemic, a highly effective person or company thinks beyond themselves to create a win/win scenario. At a grocery store in my neighborhood, a man stands at its entrance with a bottle of disinfectant spray in one hand for the shoppers and a sign on the sidewalk with guidelines for purchasing products to avoid hoarding. He tells you where the wipes are for the carts as you enter the store. People line up 6 feet apart, waiting to enter, to limit the number of shoppers inside the store, facilitating proper physical distancing. Instead of maximizing profits at the expense of everyone’s health and safety, the process is a win/win for everyone, from shoppers to employees.
Strategy #5: Develop empathy and understanding
Seeking to first understand and then be understood is one of the most powerful tools of effective people. In my holistic practice, every patient comes in with their own unique needs that evolve and transform over time. I must remain open, or I fail to deliver appropriately.
Learning to listen and then to clearly communicate ideas is essential to effective health care. During this time, it is critical that health care providers and political leaders first listen/understand and then communicate clearly to serve everyone in the best way possible.
In our brains, the frontal lobes (the adult in the room) manages our amygdala (the child in the room) when we get enough sleep, meditate, spend time in nature, exercise, and eat healthy food.4 Stress can interfere with the frontal lobe’s ability to maintain empathy, inhibit unhealthy impulses, and delay gratification. During the pandemic, we can help to shift from the stress response, or “fight-or-flight” response, driven by the sympathetic nervous system to a “rest-and-digest” response driven by the parasympathetic system through coherent breathing, taking slow, deep, relaxed breaths (6 seconds on inhalation and 6 seconds on exhalation). The vagus nerve connected to our diaphragm will help the heart return to a healthy rhythm.5
Strategy #6: Synergize and integrate
All of life is interdependent, each part no more or less important than any other. Is oxygen more important than hydrogen? Is H2O different from the oxygen and hydrogen atoms that make it?
During a pandemic, it’s important for us to appreciate each other’s contributions and work synergistically for the good of the whole. Our survival depends on valuing each other and our planet. This perspective informs the practice of physical distancing and staying home to minimize the spread of the virus and its impact on the health care system, regardless of whether an individual belongs in the high-risk group or not.
Many high-achieving people train in extremely competitive settings in which survival depends on individual performance rather than mutual cooperation. This training process encourages a disregard for others. Good leaders, however, understand that cooperation and mutual respect are essential to personal well-being.
Strategy #7: Practice self-care
There are five aspects of our lives that depend on our self-care: spiritual, mental, emotional, physical, and social. Unfortunately, many kind-hearted people are kinder to others than to themselves. There is really only one person who can truly take care of you properly, and that is yourself. In Seattle, where many suffered early in the pandemic, holistic psychiatrist David Kopacz, MD, is reminding people to nurture themselves in his post, “Nurture Yourself During the Pandemic: Try New Recipes!”6 Indeed, that is what many must do since eating out is not an option now. If you find yourself stuck at home with more time on your hands, take the opportunity to care for yourself. Ask yourself what you really need during this time, and make the effort to provide it to yourself.
After the pandemic is over, will you have grown from the experiences and become a better person from it? Despite our current circumstances, we can continue to grow as individuals and as a community, armed with strategies that can benefit all of us.
References
1. Covey SR. The 7 Habits of Highly Effective People. New York: Simon & Schuster; 1989.
2. Lee AW. Townsend Letter. 2009 Jun;311:22-3.
3. Fromm E. To Have or To Be? New York: Continuum International Publishing; 2005.
4. Rushlau K. Integrative Healthcare Symposium. 2020 Feb 21.
5. Gerbarg PL. Mind Body Practices for Post-Traumatic Stress Disorder. Presentation at Integrative Medicine for Mental Health Conference. 2016 Sep.
6. Kopacz D. Nurture Yourself During the Pandemic: Try New Recipes! Being Fully Human. 2020 Mar 22.
Dr. Lee specializes in integrative and holistic psychiatry and has a private practice in Gaithersburg, Md. She has no disclosures.
A few weeks ago, I saw more than 60 responses to a post on Nextdoor.com entitled, “Toilet paper strategies?”
Asking for help is a great coping mechanism when one is struggling to find a strategy, even if it’s for toilet paper. What other kinds of coping strategies can help us through this historic and unprecedented time?
The late Stephen R. Covey, PhD, wrote about the coping strategies of highly effective people in his book, “The 7 Habits of Highly Effective People.”1 For, no matter how smart, perfect, or careful you may be, life will never be trouble free. When trouble comes, it’s important to have coping strategies that help you navigate through choppy waters. Whether you are a practitioner trying to help your patients or someone who wants to maximize their personal resilience during a worldwide pandemic, here are my conceptualizations of the seven top strategies highly effective people use when facing challenges.
Strategy #1: Begin with the end in mind
In 2007, this strategy helped me not only survive but thrive when I battled for my right to practice as a holistic psychiatrist against the Maryland Board of Physicians.2 From the first moment when I read the letter from the board, to the last when I read the administrative law judge’s dismissal, I turned to this strategy to help me cope with unrelenting stress.
I imagined myself remembering being the kind of person I wanted to be, wrote that script for myself, and created those memories for my future self. I wanted to remember myself as being brave, calm, strong, and grounded, so I behaved each day as if I were all of those things.
As Dr. Covey wrote, “ ‘Begin with the end in mind’ is based on the principle that all things are created twice. There’s a mental or first creation, and a physical or second creation to all things.” Imagine who you would like to remember yourself being a year or two down the road. Do you want to remember yourself showing good judgment and being positive and compassionate during this pandemic? Then, follow the script you’ve created in your mind and be that person now, knowing that you are forming memories for your future self. Your future self will look back at who you are right now with appreciation and satisfaction. Of course, this is a habit that you can apply to your entire life.
Strategy #2: Be proactive
Between the event and the outcome is you. You are the interpreter and transformer of the event, with the freedom to apply your will and intention on the event. Whether it is living through a pandemic or dealing with misplaced keys, every day you are revealing your nature through how you deal with life. To be proactive is different from being reactive. Within each of us there is a will, the drive, to rise above our difficult environments.
Dr. Covey wrote, “the ability to subordinate an impulse to a value is the essence of the proactive person.” A woman shared with me that she created an Excel spreadsheet with some of the things she plans to do with her free time while she stays in her NYC apartment. She doesn’t want to slip into a passive state and waste her time. That’s being proactive.
Strategy #3: Set proper priorities
Or, as Dr. Covey would say, “Put first things first.” During a pandemic, when the world seems to be precariously tilting at an angle, it’s easy to cling to outdated standards, expectations, and behavioral patterns. Doing so heightens our sense of regret, fear, and scarcity. Valuing gratitude will empower you to deal with financial loss differently because you can still remain grateful despite uncontrollable losses. We can choose “to have or to be” as psychoanalyst, Erich Fromm, PhD, would say.3 If your happiness is measured by how much money you have, then it would make sense that, when the amount shrinks, so does your happiness. However, if your happiness is a side effect of who you are, you will remain a mountain before the winds and tides of circumstance.
Strategy #4: Create a win/win mentality
This state of mind is built on character. Dr. Covey separates character into three categories: integrity, maturity, and abundance mentality. A lack of character resulted in the hoarding of toilet paper in many communities and the cry for help from Nextdoor.com. I noticed that, in the 60+ responses that included advice about using bidets, old towels, and even leaves, no one offered to share a bag of toilet paper. That’s because people experienced the fear of scarcity, in turn, causing the scarcity they feared.
During a pandemic, a highly effective person or company thinks beyond themselves to create a win/win scenario. At a grocery store in my neighborhood, a man stands at its entrance with a bottle of disinfectant spray in one hand for the shoppers and a sign on the sidewalk with guidelines for purchasing products to avoid hoarding. He tells you where the wipes are for the carts as you enter the store. People line up 6 feet apart, waiting to enter, to limit the number of shoppers inside the store, facilitating proper physical distancing. Instead of maximizing profits at the expense of everyone’s health and safety, the process is a win/win for everyone, from shoppers to employees.
Strategy #5: Develop empathy and understanding
Seeking to first understand and then be understood is one of the most powerful tools of effective people. In my holistic practice, every patient comes in with their own unique needs that evolve and transform over time. I must remain open, or I fail to deliver appropriately.
Learning to listen and then to clearly communicate ideas is essential to effective health care. During this time, it is critical that health care providers and political leaders first listen/understand and then communicate clearly to serve everyone in the best way possible.
In our brains, the frontal lobes (the adult in the room) manages our amygdala (the child in the room) when we get enough sleep, meditate, spend time in nature, exercise, and eat healthy food.4 Stress can interfere with the frontal lobe’s ability to maintain empathy, inhibit unhealthy impulses, and delay gratification. During the pandemic, we can help to shift from the stress response, or “fight-or-flight” response, driven by the sympathetic nervous system to a “rest-and-digest” response driven by the parasympathetic system through coherent breathing, taking slow, deep, relaxed breaths (6 seconds on inhalation and 6 seconds on exhalation). The vagus nerve connected to our diaphragm will help the heart return to a healthy rhythm.5
Strategy #6: Synergize and integrate
All of life is interdependent, each part no more or less important than any other. Is oxygen more important than hydrogen? Is H2O different from the oxygen and hydrogen atoms that make it?
During a pandemic, it’s important for us to appreciate each other’s contributions and work synergistically for the good of the whole. Our survival depends on valuing each other and our planet. This perspective informs the practice of physical distancing and staying home to minimize the spread of the virus and its impact on the health care system, regardless of whether an individual belongs in the high-risk group or not.
Many high-achieving people train in extremely competitive settings in which survival depends on individual performance rather than mutual cooperation. This training process encourages a disregard for others. Good leaders, however, understand that cooperation and mutual respect are essential to personal well-being.
Strategy #7: Practice self-care
There are five aspects of our lives that depend on our self-care: spiritual, mental, emotional, physical, and social. Unfortunately, many kind-hearted people are kinder to others than to themselves. There is really only one person who can truly take care of you properly, and that is yourself. In Seattle, where many suffered early in the pandemic, holistic psychiatrist David Kopacz, MD, is reminding people to nurture themselves in his post, “Nurture Yourself During the Pandemic: Try New Recipes!”6 Indeed, that is what many must do since eating out is not an option now. If you find yourself stuck at home with more time on your hands, take the opportunity to care for yourself. Ask yourself what you really need during this time, and make the effort to provide it to yourself.
After the pandemic is over, will you have grown from the experiences and become a better person from it? Despite our current circumstances, we can continue to grow as individuals and as a community, armed with strategies that can benefit all of us.
References
1. Covey SR. The 7 Habits of Highly Effective People. New York: Simon & Schuster; 1989.
2. Lee AW. Townsend Letter. 2009 Jun;311:22-3.
3. Fromm E. To Have or To Be? New York: Continuum International Publishing; 2005.
4. Rushlau K. Integrative Healthcare Symposium. 2020 Feb 21.
5. Gerbarg PL. Mind Body Practices for Post-Traumatic Stress Disorder. Presentation at Integrative Medicine for Mental Health Conference. 2016 Sep.
6. Kopacz D. Nurture Yourself During the Pandemic: Try New Recipes! Being Fully Human. 2020 Mar 22.
Dr. Lee specializes in integrative and holistic psychiatry and has a private practice in Gaithersburg, Md. She has no disclosures.
COVID 19: Psychiatric patients may be among the hardest hit
The COVID-19 pandemic represents a looming crisis for patients with severe mental illness (SMI) and the healthcare systems that serve them, one expert warns.
However, Benjamin Druss, MD, MPH, from Emory University’s Rollins School of Public Health in Atlanta, Georgia, says there are strategies that can help minimize the risk of exposure and transmission of the virus in SMI patients.
In a viewpoint published online April 3 in JAMA Psychiatry, Druss, professor and chair in mental health, notes that “disasters disproportionately affect poor and vulnerable populations, and patients with serious mental illness may be among the hardest hit.”
In an interview with Medscape Medical News, Druss said patients with SMI have “a whole range of vulnerabilities” that put them at higher risk for COVID-19.
These include high rates of smoking, cardiovascular and lung disease, poverty, and homelessness. In fact, estimates show 25% of the US homeless population has a serious mental illness, said Druss.
“You have to keep an eye on these overlapping circles of vulnerable populations: those with disabilities in general and people with serious mental illness in particular; people who are poor; and people who have limited social networks,” he said.
Tailored Communication Vital
It’s important for patients with SMI to have up-to-date, accurate information about mitigating risk and knowing when to seek medical treatment for COVID-19, Druss noted.
Communication materials developed for the general population need to be tailored to address limited health literacy and challenges in implementing physical distancing recommendations, he said.
Patients with SMI also need support in maintaining healthy habits, including diet and physical activity, as well as self-management of chronic mental and physical health conditions, he added.
He noted that even in the face of current constraints on mental health care delivery, ensuring access to services is essential. The increased emphasis on caring for, and keeping in touch with, SMI patients through telepsychiatry is one effective way of addressing this issue, said Druss.
Since mental health clinicians are often the first responders for people with SMI, these professionals need training to recognize the signs and symptoms of COVID-19 and learn basic strategies to mitigate the spread of disease, not only for their patients but also for themselves, he added.
“Any given provider is going to be responsible for many, many patients, so keeping physically and mentally healthy will be vital.”
In order to ease the strain of COVID-19 on community mental health centers and psychiatric hospitals, which are at high risk for outbreaks and have limited capacity to treat medical illness, these institutions need contingency plans to detect and contain outbreaks if they occur.
“Careful planning and execution at multiple levels will be essential for minimizing the adverse outcomes of this pandemic for this vulnerable population,” Druss writes.
Voice of Experience
Commenting on the article for Medscape Medical News, Lloyd I. Sederer, MD, distinguished advisor for the New York State Office of Mental Health and adjunct professor at the Columbia School of Public Health in New York City, commended Druss for highlighting the need for more mental health services during the pandemic.
However, although Druss “has made some very good general statements,” these don’t really apply “in the wake of a real catastrophic event, which is what we’re having here,” Sederer said.
Sederer led Project Liberty, a massive mental health disaster response effort established in the wake of the Sept. 11 attacks in New York. Druss seems to infer that the mental health workforce is capable of expanding, but “what we learned is that the mental health system in this country is vastly undersupplied,” said Sederer.
During a disaster, the system “actually contracts” because clinics close and workforces are reduced. In this environment, some patients with a serious mental illness let their treatment “erode,” Sederer said.
While Druss called for clinics to have protocols for identifying and referring patients at risk for COVID-19, Sederer pointed out that “all the clinics are closed.”
However, he did note that many mental health clinics and hospitals are continuing to reach out to their vulnerable patients during this crisis.
On the 10th anniversary of the 9/11 attacks, Sederer and colleagues published an article in Psychiatric Services that highlighted the “lessons learned” from the Project Liberty experience. One of the biggest lessons was the need for crisis counseling, which is “a recognized, proven intervention,” said Sederer.
Such an initiative involves trained outreach workers, identifying the untreated seriously mentally ill in the community, and “literally shepherding them to services,” he added.
In this current pandemic, it would be up to the federal government to mobilize such a crisis counseling initiative, Sederer explained.
Sederer noted that rapid relief groups like the Federal Emergency Management Agency do not cover mental health services. In order to be effective, disaster-related mental health services need to include funding for treatment, including focused therapies and medication.
Druss and Sederer have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic represents a looming crisis for patients with severe mental illness (SMI) and the healthcare systems that serve them, one expert warns.
However, Benjamin Druss, MD, MPH, from Emory University’s Rollins School of Public Health in Atlanta, Georgia, says there are strategies that can help minimize the risk of exposure and transmission of the virus in SMI patients.
In a viewpoint published online April 3 in JAMA Psychiatry, Druss, professor and chair in mental health, notes that “disasters disproportionately affect poor and vulnerable populations, and patients with serious mental illness may be among the hardest hit.”
In an interview with Medscape Medical News, Druss said patients with SMI have “a whole range of vulnerabilities” that put them at higher risk for COVID-19.
These include high rates of smoking, cardiovascular and lung disease, poverty, and homelessness. In fact, estimates show 25% of the US homeless population has a serious mental illness, said Druss.
“You have to keep an eye on these overlapping circles of vulnerable populations: those with disabilities in general and people with serious mental illness in particular; people who are poor; and people who have limited social networks,” he said.
Tailored Communication Vital
It’s important for patients with SMI to have up-to-date, accurate information about mitigating risk and knowing when to seek medical treatment for COVID-19, Druss noted.
Communication materials developed for the general population need to be tailored to address limited health literacy and challenges in implementing physical distancing recommendations, he said.
Patients with SMI also need support in maintaining healthy habits, including diet and physical activity, as well as self-management of chronic mental and physical health conditions, he added.
He noted that even in the face of current constraints on mental health care delivery, ensuring access to services is essential. The increased emphasis on caring for, and keeping in touch with, SMI patients through telepsychiatry is one effective way of addressing this issue, said Druss.
Since mental health clinicians are often the first responders for people with SMI, these professionals need training to recognize the signs and symptoms of COVID-19 and learn basic strategies to mitigate the spread of disease, not only for their patients but also for themselves, he added.
“Any given provider is going to be responsible for many, many patients, so keeping physically and mentally healthy will be vital.”
In order to ease the strain of COVID-19 on community mental health centers and psychiatric hospitals, which are at high risk for outbreaks and have limited capacity to treat medical illness, these institutions need contingency plans to detect and contain outbreaks if they occur.
“Careful planning and execution at multiple levels will be essential for minimizing the adverse outcomes of this pandemic for this vulnerable population,” Druss writes.
Voice of Experience
Commenting on the article for Medscape Medical News, Lloyd I. Sederer, MD, distinguished advisor for the New York State Office of Mental Health and adjunct professor at the Columbia School of Public Health in New York City, commended Druss for highlighting the need for more mental health services during the pandemic.
However, although Druss “has made some very good general statements,” these don’t really apply “in the wake of a real catastrophic event, which is what we’re having here,” Sederer said.
Sederer led Project Liberty, a massive mental health disaster response effort established in the wake of the Sept. 11 attacks in New York. Druss seems to infer that the mental health workforce is capable of expanding, but “what we learned is that the mental health system in this country is vastly undersupplied,” said Sederer.
During a disaster, the system “actually contracts” because clinics close and workforces are reduced. In this environment, some patients with a serious mental illness let their treatment “erode,” Sederer said.
While Druss called for clinics to have protocols for identifying and referring patients at risk for COVID-19, Sederer pointed out that “all the clinics are closed.”
However, he did note that many mental health clinics and hospitals are continuing to reach out to their vulnerable patients during this crisis.
On the 10th anniversary of the 9/11 attacks, Sederer and colleagues published an article in Psychiatric Services that highlighted the “lessons learned” from the Project Liberty experience. One of the biggest lessons was the need for crisis counseling, which is “a recognized, proven intervention,” said Sederer.
Such an initiative involves trained outreach workers, identifying the untreated seriously mentally ill in the community, and “literally shepherding them to services,” he added.
In this current pandemic, it would be up to the federal government to mobilize such a crisis counseling initiative, Sederer explained.
Sederer noted that rapid relief groups like the Federal Emergency Management Agency do not cover mental health services. In order to be effective, disaster-related mental health services need to include funding for treatment, including focused therapies and medication.
Druss and Sederer have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic represents a looming crisis for patients with severe mental illness (SMI) and the healthcare systems that serve them, one expert warns.
However, Benjamin Druss, MD, MPH, from Emory University’s Rollins School of Public Health in Atlanta, Georgia, says there are strategies that can help minimize the risk of exposure and transmission of the virus in SMI patients.
In a viewpoint published online April 3 in JAMA Psychiatry, Druss, professor and chair in mental health, notes that “disasters disproportionately affect poor and vulnerable populations, and patients with serious mental illness may be among the hardest hit.”
In an interview with Medscape Medical News, Druss said patients with SMI have “a whole range of vulnerabilities” that put them at higher risk for COVID-19.
These include high rates of smoking, cardiovascular and lung disease, poverty, and homelessness. In fact, estimates show 25% of the US homeless population has a serious mental illness, said Druss.
“You have to keep an eye on these overlapping circles of vulnerable populations: those with disabilities in general and people with serious mental illness in particular; people who are poor; and people who have limited social networks,” he said.
Tailored Communication Vital
It’s important for patients with SMI to have up-to-date, accurate information about mitigating risk and knowing when to seek medical treatment for COVID-19, Druss noted.
Communication materials developed for the general population need to be tailored to address limited health literacy and challenges in implementing physical distancing recommendations, he said.
Patients with SMI also need support in maintaining healthy habits, including diet and physical activity, as well as self-management of chronic mental and physical health conditions, he added.
He noted that even in the face of current constraints on mental health care delivery, ensuring access to services is essential. The increased emphasis on caring for, and keeping in touch with, SMI patients through telepsychiatry is one effective way of addressing this issue, said Druss.
Since mental health clinicians are often the first responders for people with SMI, these professionals need training to recognize the signs and symptoms of COVID-19 and learn basic strategies to mitigate the spread of disease, not only for their patients but also for themselves, he added.
“Any given provider is going to be responsible for many, many patients, so keeping physically and mentally healthy will be vital.”
In order to ease the strain of COVID-19 on community mental health centers and psychiatric hospitals, which are at high risk for outbreaks and have limited capacity to treat medical illness, these institutions need contingency plans to detect and contain outbreaks if they occur.
“Careful planning and execution at multiple levels will be essential for minimizing the adverse outcomes of this pandemic for this vulnerable population,” Druss writes.
Voice of Experience
Commenting on the article for Medscape Medical News, Lloyd I. Sederer, MD, distinguished advisor for the New York State Office of Mental Health and adjunct professor at the Columbia School of Public Health in New York City, commended Druss for highlighting the need for more mental health services during the pandemic.
However, although Druss “has made some very good general statements,” these don’t really apply “in the wake of a real catastrophic event, which is what we’re having here,” Sederer said.
Sederer led Project Liberty, a massive mental health disaster response effort established in the wake of the Sept. 11 attacks in New York. Druss seems to infer that the mental health workforce is capable of expanding, but “what we learned is that the mental health system in this country is vastly undersupplied,” said Sederer.
During a disaster, the system “actually contracts” because clinics close and workforces are reduced. In this environment, some patients with a serious mental illness let their treatment “erode,” Sederer said.
While Druss called for clinics to have protocols for identifying and referring patients at risk for COVID-19, Sederer pointed out that “all the clinics are closed.”
However, he did note that many mental health clinics and hospitals are continuing to reach out to their vulnerable patients during this crisis.
On the 10th anniversary of the 9/11 attacks, Sederer and colleagues published an article in Psychiatric Services that highlighted the “lessons learned” from the Project Liberty experience. One of the biggest lessons was the need for crisis counseling, which is “a recognized, proven intervention,” said Sederer.
Such an initiative involves trained outreach workers, identifying the untreated seriously mentally ill in the community, and “literally shepherding them to services,” he added.
In this current pandemic, it would be up to the federal government to mobilize such a crisis counseling initiative, Sederer explained.
Sederer noted that rapid relief groups like the Federal Emergency Management Agency do not cover mental health services. In order to be effective, disaster-related mental health services need to include funding for treatment, including focused therapies and medication.
Druss and Sederer have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Crisis counseling, not therapy, is what’s needed in the wake of COVID-19
In the wake of the attacks on the World Trade Center, the public mental health system in the New York City area mounted the largest mental health disaster response in history. I was New York City’s mental health commissioner at the time. We called the initiative Project Liberty and over 3 years obtained $137 million in funding from the Federal Emergency Management Agency (FEMA) to support it.
Through Project Liberty, New York established the Crisis Counseling Assistance and Training Program (CCP). And it didn’t take us long to realize that what affected people need following a disaster is not necessarily psychotherapy, as might be expected, but in fact crisis counseling, or helping impacted individuals and their families regain control of their anxieties and effectively respond to an immediate disaster. This proved true not only after 9/11 but also after other recent disasters, including hurricanes Katrina and Sandy. The mental health system must now step up again to assuage fears and anxieties—both individual and collective—around the rapidly spreading COVID-19 pandemic.
So, what is crisis counseling?
A person’s usual adaptive, problem-solving capabilities are often compromised after a disaster, but they are there, and if accessed, they can help those afflicted with mental symptoms following a crisis to mentally endure. thereby making it a different approach from traditional psychotherapy.
The five key concepts in crisis counseling are:
- It is strength-based, which means its foundation is rooted in the assumption that resilience and competence are innate human qualities.
- Crisis counseling also employs anonymity. Impacted individuals should not be diagnosed or labeled. As a result, there are no resulting medical records.
- The approach is outreach-oriented, in which counselors provide services out in the community rather than in traditional mental health settings. This occurs primarily in homes, community centers, and settings, as well as in disaster shelters.
- It is culturally attuned, whereby all staff appreciate and respect a community’s cultural beliefs, values, and primary language.
- It is aimed at supporting, not replacing, existing community support systems (eg, a crisis counselor supports but does not organize, deliver, or manage community recovery activities).
Crisis counselors are required to be licensed psychologists or have obtained a bachelor’s degree or higher in psychology, human services, or another health-related field. In other words, crisis counseling draws on a broad, though related, group of individuals. Before deployment into a disaster area, an applicant must complete the FEMA Crisis Counseling Assistance and Training, which is offered in the disaster area by the FEMA-funded CCP.
Crisis counselors provide trustworthy and actionable information about the disaster at hand and where to turn for resources and assistance. They assist with emotional support. And they aim to educate individuals, families, and communities about how to be resilient.
Crisis counseling, however, may not suffice for everyone impacted. We know that a person’s severity of response to a crisis is highly associated with the intensity and duration of exposure to the disaster (especially when it is life-threatening) and/or the degree of a person’s serious loss (of a loved one, home, job, health). We also know that previous trauma (eg, from childhood, domestic violence, or forced immigration) also predicts the gravity of the response to a current crisis. Which is why crisis counselors also are taught to identify those experiencing significant and persistent mental health and addiction problems because they need to be assisted, literally, in obtaining professional treatment.
Only in recent years has trauma been a recognized driver of stress, distress, and mental and addictive disorders. Until relatively recently, skill with, and access to, crisis counseling—and trauma-informed care—was rare among New York’s large and talented mental health professional community. Few had been trained in it in graduate school or practiced it because New York had been spared a disaster on par with 9/11. Following the attacks, Project Liberty’s programs served nearly 1.5 million affected individuals of very diverse ages, races, cultural backgrounds, and socioeconomic status. Their levels of “psychological distress,” the term we used and measured, ranged from low to very high.
The coronavirus pandemic now presents us with a tragically similar, catastrophic moment. The human consequences we face—psychologically, economically, and socially—are just beginning. But this time, the need is not just in New York but throughout our country.
We humans are resilient. We can bend the arc of crisis toward the light, to recovering our existing but overwhelmed capabilities. We can achieve this in a variety of ways. We can practice self-care. This isn’t an act of selfishness but is rather like putting on your own oxygen mask before trying to help your friend or loved one do the same. We can stay connected to the people we care about. We can eat well, get sufficient sleep, take a walk.
Identifying and pursuing practical goals is also important, like obtaining food, housing that is safe and reliable, transportation to where you need to go, and drawing upon financial and other resources that are issued in a disaster area. We can practice positive thinking and recall how we’ve mastered our troubles in the past; we can remind ourselves that “this too will pass.” Crises create an unusually opportune time for change and self-discovery. As Churchill said to the British people in the darkest moments of the start of World War II, “Never give up.”
Worthy of its own itemization are spiritual beliefs, faith—that however we think about a higher power (religious or secular), that power is on our side. Faith can comfort and sustain hope, particularly at a time when doubt about ourselves and humanity is triggered by disaster.
Maya Angelou’s words remind us at this moment of disaster: “...let us try to help before we have to offer therapy. That is to say, let’s see if we can’t prevent being ill by trying to offer a love of prevention before illness.”
Dr. Sederer is the former chief medical officer for the New York State Office of Mental Health and an adjunct professor in the Department of Epidemiology at the Columbia University School of Public Health. His latest book is The Addiction Solution: Treating Our Dependence on Opioids and Other Drugs.
This article first appeared on Medscape.com.
In the wake of the attacks on the World Trade Center, the public mental health system in the New York City area mounted the largest mental health disaster response in history. I was New York City’s mental health commissioner at the time. We called the initiative Project Liberty and over 3 years obtained $137 million in funding from the Federal Emergency Management Agency (FEMA) to support it.
Through Project Liberty, New York established the Crisis Counseling Assistance and Training Program (CCP). And it didn’t take us long to realize that what affected people need following a disaster is not necessarily psychotherapy, as might be expected, but in fact crisis counseling, or helping impacted individuals and their families regain control of their anxieties and effectively respond to an immediate disaster. This proved true not only after 9/11 but also after other recent disasters, including hurricanes Katrina and Sandy. The mental health system must now step up again to assuage fears and anxieties—both individual and collective—around the rapidly spreading COVID-19 pandemic.
So, what is crisis counseling?
A person’s usual adaptive, problem-solving capabilities are often compromised after a disaster, but they are there, and if accessed, they can help those afflicted with mental symptoms following a crisis to mentally endure. thereby making it a different approach from traditional psychotherapy.
The five key concepts in crisis counseling are:
- It is strength-based, which means its foundation is rooted in the assumption that resilience and competence are innate human qualities.
- Crisis counseling also employs anonymity. Impacted individuals should not be diagnosed or labeled. As a result, there are no resulting medical records.
- The approach is outreach-oriented, in which counselors provide services out in the community rather than in traditional mental health settings. This occurs primarily in homes, community centers, and settings, as well as in disaster shelters.
- It is culturally attuned, whereby all staff appreciate and respect a community’s cultural beliefs, values, and primary language.
- It is aimed at supporting, not replacing, existing community support systems (eg, a crisis counselor supports but does not organize, deliver, or manage community recovery activities).
Crisis counselors are required to be licensed psychologists or have obtained a bachelor’s degree or higher in psychology, human services, or another health-related field. In other words, crisis counseling draws on a broad, though related, group of individuals. Before deployment into a disaster area, an applicant must complete the FEMA Crisis Counseling Assistance and Training, which is offered in the disaster area by the FEMA-funded CCP.
Crisis counselors provide trustworthy and actionable information about the disaster at hand and where to turn for resources and assistance. They assist with emotional support. And they aim to educate individuals, families, and communities about how to be resilient.
Crisis counseling, however, may not suffice for everyone impacted. We know that a person’s severity of response to a crisis is highly associated with the intensity and duration of exposure to the disaster (especially when it is life-threatening) and/or the degree of a person’s serious loss (of a loved one, home, job, health). We also know that previous trauma (eg, from childhood, domestic violence, or forced immigration) also predicts the gravity of the response to a current crisis. Which is why crisis counselors also are taught to identify those experiencing significant and persistent mental health and addiction problems because they need to be assisted, literally, in obtaining professional treatment.
Only in recent years has trauma been a recognized driver of stress, distress, and mental and addictive disorders. Until relatively recently, skill with, and access to, crisis counseling—and trauma-informed care—was rare among New York’s large and talented mental health professional community. Few had been trained in it in graduate school or practiced it because New York had been spared a disaster on par with 9/11. Following the attacks, Project Liberty’s programs served nearly 1.5 million affected individuals of very diverse ages, races, cultural backgrounds, and socioeconomic status. Their levels of “psychological distress,” the term we used and measured, ranged from low to very high.
The coronavirus pandemic now presents us with a tragically similar, catastrophic moment. The human consequences we face—psychologically, economically, and socially—are just beginning. But this time, the need is not just in New York but throughout our country.
We humans are resilient. We can bend the arc of crisis toward the light, to recovering our existing but overwhelmed capabilities. We can achieve this in a variety of ways. We can practice self-care. This isn’t an act of selfishness but is rather like putting on your own oxygen mask before trying to help your friend or loved one do the same. We can stay connected to the people we care about. We can eat well, get sufficient sleep, take a walk.
Identifying and pursuing practical goals is also important, like obtaining food, housing that is safe and reliable, transportation to where you need to go, and drawing upon financial and other resources that are issued in a disaster area. We can practice positive thinking and recall how we’ve mastered our troubles in the past; we can remind ourselves that “this too will pass.” Crises create an unusually opportune time for change and self-discovery. As Churchill said to the British people in the darkest moments of the start of World War II, “Never give up.”
Worthy of its own itemization are spiritual beliefs, faith—that however we think about a higher power (religious or secular), that power is on our side. Faith can comfort and sustain hope, particularly at a time when doubt about ourselves and humanity is triggered by disaster.
Maya Angelou’s words remind us at this moment of disaster: “...let us try to help before we have to offer therapy. That is to say, let’s see if we can’t prevent being ill by trying to offer a love of prevention before illness.”
Dr. Sederer is the former chief medical officer for the New York State Office of Mental Health and an adjunct professor in the Department of Epidemiology at the Columbia University School of Public Health. His latest book is The Addiction Solution: Treating Our Dependence on Opioids and Other Drugs.
This article first appeared on Medscape.com.
In the wake of the attacks on the World Trade Center, the public mental health system in the New York City area mounted the largest mental health disaster response in history. I was New York City’s mental health commissioner at the time. We called the initiative Project Liberty and over 3 years obtained $137 million in funding from the Federal Emergency Management Agency (FEMA) to support it.
Through Project Liberty, New York established the Crisis Counseling Assistance and Training Program (CCP). And it didn’t take us long to realize that what affected people need following a disaster is not necessarily psychotherapy, as might be expected, but in fact crisis counseling, or helping impacted individuals and their families regain control of their anxieties and effectively respond to an immediate disaster. This proved true not only after 9/11 but also after other recent disasters, including hurricanes Katrina and Sandy. The mental health system must now step up again to assuage fears and anxieties—both individual and collective—around the rapidly spreading COVID-19 pandemic.
So, what is crisis counseling?
A person’s usual adaptive, problem-solving capabilities are often compromised after a disaster, but they are there, and if accessed, they can help those afflicted with mental symptoms following a crisis to mentally endure. thereby making it a different approach from traditional psychotherapy.
The five key concepts in crisis counseling are:
- It is strength-based, which means its foundation is rooted in the assumption that resilience and competence are innate human qualities.
- Crisis counseling also employs anonymity. Impacted individuals should not be diagnosed or labeled. As a result, there are no resulting medical records.
- The approach is outreach-oriented, in which counselors provide services out in the community rather than in traditional mental health settings. This occurs primarily in homes, community centers, and settings, as well as in disaster shelters.
- It is culturally attuned, whereby all staff appreciate and respect a community’s cultural beliefs, values, and primary language.
- It is aimed at supporting, not replacing, existing community support systems (eg, a crisis counselor supports but does not organize, deliver, or manage community recovery activities).
Crisis counselors are required to be licensed psychologists or have obtained a bachelor’s degree or higher in psychology, human services, or another health-related field. In other words, crisis counseling draws on a broad, though related, group of individuals. Before deployment into a disaster area, an applicant must complete the FEMA Crisis Counseling Assistance and Training, which is offered in the disaster area by the FEMA-funded CCP.
Crisis counselors provide trustworthy and actionable information about the disaster at hand and where to turn for resources and assistance. They assist with emotional support. And they aim to educate individuals, families, and communities about how to be resilient.
Crisis counseling, however, may not suffice for everyone impacted. We know that a person’s severity of response to a crisis is highly associated with the intensity and duration of exposure to the disaster (especially when it is life-threatening) and/or the degree of a person’s serious loss (of a loved one, home, job, health). We also know that previous trauma (eg, from childhood, domestic violence, or forced immigration) also predicts the gravity of the response to a current crisis. Which is why crisis counselors also are taught to identify those experiencing significant and persistent mental health and addiction problems because they need to be assisted, literally, in obtaining professional treatment.
Only in recent years has trauma been a recognized driver of stress, distress, and mental and addictive disorders. Until relatively recently, skill with, and access to, crisis counseling—and trauma-informed care—was rare among New York’s large and talented mental health professional community. Few had been trained in it in graduate school or practiced it because New York had been spared a disaster on par with 9/11. Following the attacks, Project Liberty’s programs served nearly 1.5 million affected individuals of very diverse ages, races, cultural backgrounds, and socioeconomic status. Their levels of “psychological distress,” the term we used and measured, ranged from low to very high.
The coronavirus pandemic now presents us with a tragically similar, catastrophic moment. The human consequences we face—psychologically, economically, and socially—are just beginning. But this time, the need is not just in New York but throughout our country.
We humans are resilient. We can bend the arc of crisis toward the light, to recovering our existing but overwhelmed capabilities. We can achieve this in a variety of ways. We can practice self-care. This isn’t an act of selfishness but is rather like putting on your own oxygen mask before trying to help your friend or loved one do the same. We can stay connected to the people we care about. We can eat well, get sufficient sleep, take a walk.
Identifying and pursuing practical goals is also important, like obtaining food, housing that is safe and reliable, transportation to where you need to go, and drawing upon financial and other resources that are issued in a disaster area. We can practice positive thinking and recall how we’ve mastered our troubles in the past; we can remind ourselves that “this too will pass.” Crises create an unusually opportune time for change and self-discovery. As Churchill said to the British people in the darkest moments of the start of World War II, “Never give up.”
Worthy of its own itemization are spiritual beliefs, faith—that however we think about a higher power (religious or secular), that power is on our side. Faith can comfort and sustain hope, particularly at a time when doubt about ourselves and humanity is triggered by disaster.
Maya Angelou’s words remind us at this moment of disaster: “...let us try to help before we have to offer therapy. That is to say, let’s see if we can’t prevent being ill by trying to offer a love of prevention before illness.”
Dr. Sederer is the former chief medical officer for the New York State Office of Mental Health and an adjunct professor in the Department of Epidemiology at the Columbia University School of Public Health. His latest book is The Addiction Solution: Treating Our Dependence on Opioids and Other Drugs.
This article first appeared on Medscape.com.
COVID-19: A guide to making telepsychiatry work
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
Changes prompted by social distancing could last beyond the pandemic
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
Cardiology groups push back on hydroxychloroquine, azithromycin for COVID-19
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
COVID-19: Dramatic changes to telepsychiatry rules and regs
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.














