User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
How much exercise is needed for maximum heart benefit?
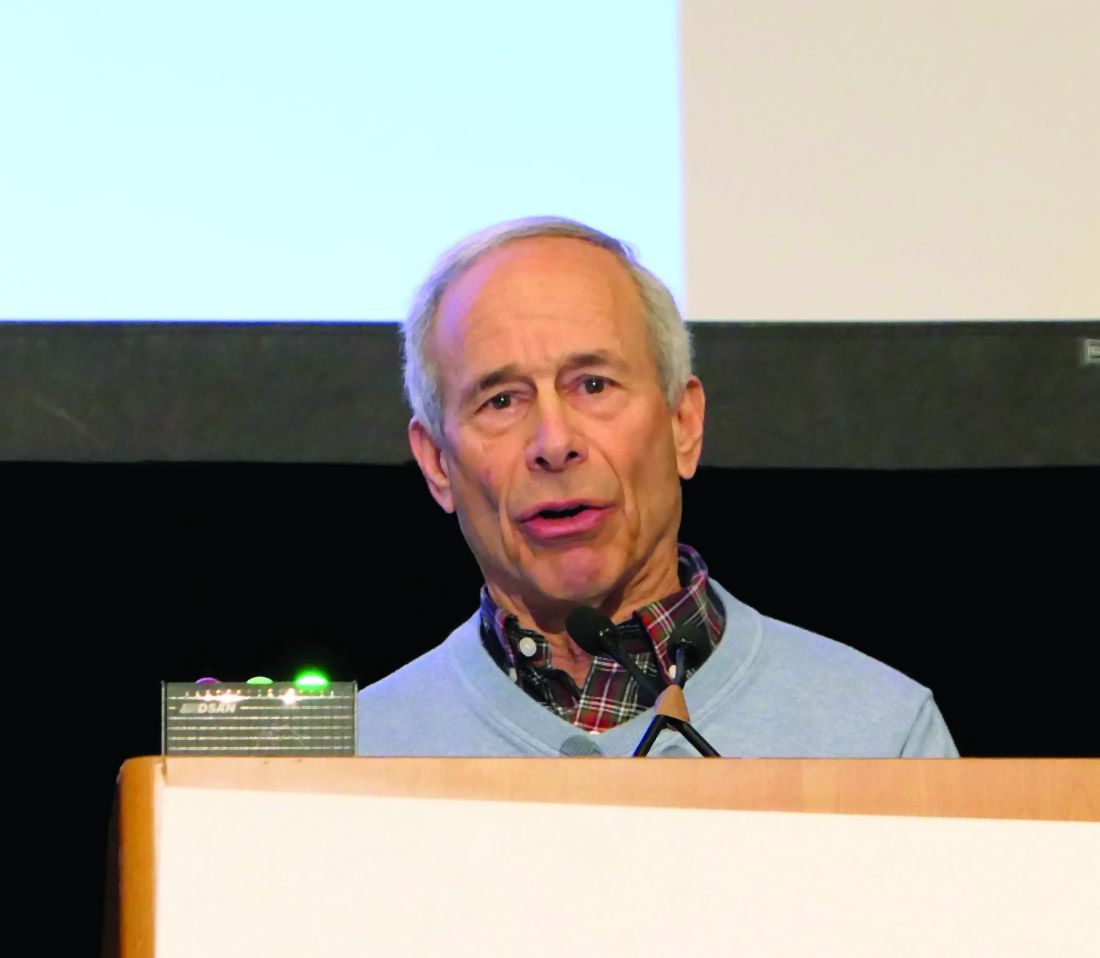
SNOWMASS, COLO. – Physical activity is potent medicine, and it doesn’t take all that much of it to derive the maximum cardiovascular benefit: namely, the equivalent of a brisk hour-long walk 5 days/week or jogging at a 10-minute-per-mile pace for half an hour twice weekly, Robert A. Vogel, MD, asserted at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’m not telling you to run marathons. said Dr. Vogel, a cardiologist at the University of Colorado at Denver, Aurora, with a longstanding interest in preventive cardiology.
He presented selected highlights from the massive evidence base underlying the recommendations put forth in the current comprehensive U.S. Department of Health & Human Services Physical Activity Guidelines for Americans.
One particularly compelling chunk of evidence comes from a Taiwanese government–funded prospective cohort study of more than 416,000 individuals followed for an average of 8 years. A key finding: 15 minutes of moderate-intensity physical activity daily was associated with a 14% reduction in the relative risk of all-cause mortality and a 19% reduction in death caused by cardiovascular disease, compared with that of inactive individuals. Moreover, each additional 15 minutes of daily moderate exercise further reduced mortality by 4%. These benefits extended across the full age spectrum of both sexes and applied to patients with cardiovascular disease (Lancet. 2011 Oct 1;378[9798]:1244-53).
“That’s a very impressive result for modest physical activity,” the cardiologist commented.
Data on more than 50,000 adult participants in the Aerobics Center Longitudinal Study based at the Cooper Clinic in Dallas show that vigorous exercise in the form of running at 6 mph for half an hour twice weekly, or a total of 10 metabolic equivalent of task hours (MET-HR) per week, was associated with a roughly 40% reduction in cardiovascular disease mortality. Importantly, 20, 40, or 50 MET-HR/week of vigorous exercise conferred no further survival benefit (J Am Coll Cardiol. 2014 Aug 5;64[5]:472-81). The same group showed that the sweet spot for moderate physical activity in terms of reduced cardiovascular mortality was brisk walking for an hour daily 5 days/week, for a total of 20 MET-HR, which was also associated with roughly a 40% risk reduction compared to inactivity. At that point the benefit plateaued, with no further mortality reduction noted with additional MET-HR of moderate exercise.
“For more than that, we have no evidence of additional cardiovascular benefit. It’s not going to get you to the Tokyo Olympics, but that’s what we need to be doing,” Dr. Vogel observed.
In another report from the Aerobics Center Longitudinal Study, investigators found that moderate-level cardiorespiratory fitness as defined by METs was associated with a 44% reduction in the risk of sudden cardiac death in men and women after adjustment for potential confounders, while high-level cardiorespiratory fitness was associated with a closely similar 48% reduction in risk. This applied to individuals who were hypertensive, overweight, and/or had poor health status, as well as to others (Mayo Clin Proc. 2016 Jul;91[7]:849-57).
All activity counts
Exercise physiologists speak of NEPA – nonexercise physical activity – such as taking out the garbage. Swedish investigators followed more than 4,200 individuals for an average of 12.5 years and found that high NEPA activity was independently associated with a 30% reduction in all-cause mortality and a 27% lower risk of a first cardiovascular disease event, compared with low NEPA. High NEPA in regular exercisers was associated with a lower rate of metabolic syndrome than in low-NEPA regular exercisers (Br J Sports Med. 2014 Feb;48[3]:233-8).
Don’t just sit there – stand!
The current federal physical activity guidelines place a new emphasis on the detrimental effects of sitting. A report on more than 221,000 participants in the Australian 45 and Up Study, with close to 1 million person-years of follow-up, demonstrated a linear inverse relationship between standing time per day and all-cause mortality. In a multivariate analysis adjusted for potential confounders, individuals who stood for 2-5 hours per day had a 10% lower risk of all-cause mortality than did those who stood for less than 2 hours. Standing for 5-8 hours was associated with a 15% relative risk reduction. And standing for more than 8 hours daily was linked to a 24% reduction in risk (Prev Med. 2014 Dec;69:187-91).
And it’s not just total daily sitting time that’s a risk factor. Prolonged, uninterrupted sedentary time was also associated with a dose-dependent increase in all-cause mortality in a prospective cohort study of nearly 8,000 U.S. adults (Ann Intern Med. 2017 Oct 3;167[7]:465-75).
“If you can’t walk around, talk to your patients standing up. That activity of getting out of your chair is lifesaving,” the cardiologist advised.
Get strong
Muscle-strengthening activity on at least 2 days/week is recommended in the federal guidelines because it’s independently associated with decreased all-cause mortality, even in individuals getting sufficient aerobic exercise, as shown in a large national study with 15-years’ follow-up (Prev Med. 2016 Jun;87:121-127).
“As we get older, we tend to forget about muscle. I work with the National Football League. These folks are pretty strong, but we never see diabetes in these very big players, who are often well over 300 lb. They’ve got a lot of muscle. If you want to prevent diabetes, be strong. It’s a very important factor,” Dr. Vogel said.
For the time constrained
Jogging is more time-efficient than brisk walking as a way to attain the maximum cardiovascular benefit of exercise. And the so-called “Weekend Warrior” study of nearly 64,000 U.K. adults showed that it’s okay to cram the full week’s worth of exercise into one or two sessions and be done with it. Compared with the inactive study participants, the weekend warriors had a 40% reduction in cardiovascular disease mortality, while individuals who split their physical activity up into three or more sessions per week had a nearly identical 41% relative risk reduction (JAMA Intern Med. 2017 Mar 1;177[3]:335-42).
Interval training is a standard way for athletes in training to improve their endurance by alternating short, intense exercise with brief recovery periods. It’s also a time saver: In one classic bicycling study, physically active men were randomized to standardized 2-week programs of sprint interval training or high-volume endurance training on the bike. The training time required to pass a rigorous cycling time trial test was 90% lower in the interval training group (J Physiol. 2006 Sep 15;575(Pt 3):901-11).
The same principle is applicable to the nonathlete interested in physical activity for heart health.
“When I run a couple of miles, I walk for 5 minutes, then maybe run for three-quarters of a mile, then walk again, then run. In interval training you get your heart rate up, and you drop it down. It’s a very good form of exercise. As a vascular biologist I know that if you put endothelial cells in a Petri dish and spin them real fast continuously, you will not get as good an improvement in endothelial function as if you spin the dish, stop it, spin it, stop it,” Dr. Vogel said.
High-volume exercise is safe, even with high coronary calcium
A clinically significant coronary artery calcification score of 100 Agatston units or more is no reason not to exercise. A Cooper Clinic report on nearly 22,000 middle-aged men without baseline cardiovascular disease who were followed for a mean of 10.4 years concluded that those in the highest-volume exercise group, many of whom were marathon runners and engaged in the equivalent of running for at least 5-6 hours/week at a pace of 10 minutes per mile, were 11% more likely to have an elevated baseline coronary artery calcification score than those who exercised less. But these highest-volume exercisers with elevated coronary calcium – their mean level was 807 Agatston units – had risks of all-cause and cardiovascular mortality that weren’t significantly different from those of men with elevated coronary calcium who exercised more moderately (JAMA Cardiol. 2019 Feb 1;4[2]:174-81).
Cardiac rehab
Dr. Vogel had harsh words for his physician colleagues with respect to the widespread underprescribing of cardiac rehabilitation programs.
“You guys are doing a crappy job with exercise in our most vulnerable patients: those who’ve had cardiovascular events,” he charged. “Cardiac rehabilitation is a Class I recommendation in our guidelines. And yet utilization in the United States is just 10%-20%. No other Class I recommendation is in that ballpark.”
A meta-analysis of 34 randomized trials totaling more than 6,000 post-MI patients concluded that those randomized to exercise-based cardiac rehabilitation had a 47% reduction in the risk of reinfarction, 36% lower cardiac mortality, and a 26% reduction in all-cause mortality (Am Heart J. 2011 Oct;162[4]:571-584.e2).
“The data show that cardiac rehabilitation is as effective as anything else we do in cardiovascular medicine. I understand that patients live far away, they don’t like to exercise – I’ve heard every excuse. But I am charging you with the responsibility of meeting a Class I recommendation that gets patients to live longer,” he declared.
Medicare now covers an enhanced, 72-session program called Intensive Cardiac Rehabilitation that teaches comprehensive lifestyle change and provides reasonable reimbursement. “It’s a good thing for our patients,” Dr. Vogel commented.
Yoga
For patients who are reluctant to pound the pavement, yoga may provide an alternative form of physical activity with tangible cardiovascular benefits. Dr. Vogel pointed to the Yoga-CaRe trial presented at the 2018 scientific sessions of the American Heart Association. Yoga-CaRe randomized 3,959 post-MI patients at 29 centers in India to a program of 13 supervised in-hospital yoga classes followed by yoga at home, or to a control group with three educational sessions. The rate of major adverse cardiovascular events over 42 months of follow-up was cut in half, compared with controls, in the 27% of participants who attended at least 10 of the 13 yoga classes. Their quality of life scores were higher, too.
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center. He is on the speaker’s bureau for Sanofi and Regeneron.
SNOWMASS, COLO. – Physical activity is potent medicine, and it doesn’t take all that much of it to derive the maximum cardiovascular benefit: namely, the equivalent of a brisk hour-long walk 5 days/week or jogging at a 10-minute-per-mile pace for half an hour twice weekly, Robert A. Vogel, MD, asserted at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’m not telling you to run marathons. said Dr. Vogel, a cardiologist at the University of Colorado at Denver, Aurora, with a longstanding interest in preventive cardiology.
He presented selected highlights from the massive evidence base underlying the recommendations put forth in the current comprehensive U.S. Department of Health & Human Services Physical Activity Guidelines for Americans.
One particularly compelling chunk of evidence comes from a Taiwanese government–funded prospective cohort study of more than 416,000 individuals followed for an average of 8 years. A key finding: 15 minutes of moderate-intensity physical activity daily was associated with a 14% reduction in the relative risk of all-cause mortality and a 19% reduction in death caused by cardiovascular disease, compared with that of inactive individuals. Moreover, each additional 15 minutes of daily moderate exercise further reduced mortality by 4%. These benefits extended across the full age spectrum of both sexes and applied to patients with cardiovascular disease (Lancet. 2011 Oct 1;378[9798]:1244-53).
“That’s a very impressive result for modest physical activity,” the cardiologist commented.
Data on more than 50,000 adult participants in the Aerobics Center Longitudinal Study based at the Cooper Clinic in Dallas show that vigorous exercise in the form of running at 6 mph for half an hour twice weekly, or a total of 10 metabolic equivalent of task hours (MET-HR) per week, was associated with a roughly 40% reduction in cardiovascular disease mortality. Importantly, 20, 40, or 50 MET-HR/week of vigorous exercise conferred no further survival benefit (J Am Coll Cardiol. 2014 Aug 5;64[5]:472-81). The same group showed that the sweet spot for moderate physical activity in terms of reduced cardiovascular mortality was brisk walking for an hour daily 5 days/week, for a total of 20 MET-HR, which was also associated with roughly a 40% risk reduction compared to inactivity. At that point the benefit plateaued, with no further mortality reduction noted with additional MET-HR of moderate exercise.
“For more than that, we have no evidence of additional cardiovascular benefit. It’s not going to get you to the Tokyo Olympics, but that’s what we need to be doing,” Dr. Vogel observed.
In another report from the Aerobics Center Longitudinal Study, investigators found that moderate-level cardiorespiratory fitness as defined by METs was associated with a 44% reduction in the risk of sudden cardiac death in men and women after adjustment for potential confounders, while high-level cardiorespiratory fitness was associated with a closely similar 48% reduction in risk. This applied to individuals who were hypertensive, overweight, and/or had poor health status, as well as to others (Mayo Clin Proc. 2016 Jul;91[7]:849-57).
All activity counts
Exercise physiologists speak of NEPA – nonexercise physical activity – such as taking out the garbage. Swedish investigators followed more than 4,200 individuals for an average of 12.5 years and found that high NEPA activity was independently associated with a 30% reduction in all-cause mortality and a 27% lower risk of a first cardiovascular disease event, compared with low NEPA. High NEPA in regular exercisers was associated with a lower rate of metabolic syndrome than in low-NEPA regular exercisers (Br J Sports Med. 2014 Feb;48[3]:233-8).
Don’t just sit there – stand!
The current federal physical activity guidelines place a new emphasis on the detrimental effects of sitting. A report on more than 221,000 participants in the Australian 45 and Up Study, with close to 1 million person-years of follow-up, demonstrated a linear inverse relationship between standing time per day and all-cause mortality. In a multivariate analysis adjusted for potential confounders, individuals who stood for 2-5 hours per day had a 10% lower risk of all-cause mortality than did those who stood for less than 2 hours. Standing for 5-8 hours was associated with a 15% relative risk reduction. And standing for more than 8 hours daily was linked to a 24% reduction in risk (Prev Med. 2014 Dec;69:187-91).
And it’s not just total daily sitting time that’s a risk factor. Prolonged, uninterrupted sedentary time was also associated with a dose-dependent increase in all-cause mortality in a prospective cohort study of nearly 8,000 U.S. adults (Ann Intern Med. 2017 Oct 3;167[7]:465-75).
“If you can’t walk around, talk to your patients standing up. That activity of getting out of your chair is lifesaving,” the cardiologist advised.
Get strong
Muscle-strengthening activity on at least 2 days/week is recommended in the federal guidelines because it’s independently associated with decreased all-cause mortality, even in individuals getting sufficient aerobic exercise, as shown in a large national study with 15-years’ follow-up (Prev Med. 2016 Jun;87:121-127).
“As we get older, we tend to forget about muscle. I work with the National Football League. These folks are pretty strong, but we never see diabetes in these very big players, who are often well over 300 lb. They’ve got a lot of muscle. If you want to prevent diabetes, be strong. It’s a very important factor,” Dr. Vogel said.
For the time constrained
Jogging is more time-efficient than brisk walking as a way to attain the maximum cardiovascular benefit of exercise. And the so-called “Weekend Warrior” study of nearly 64,000 U.K. adults showed that it’s okay to cram the full week’s worth of exercise into one or two sessions and be done with it. Compared with the inactive study participants, the weekend warriors had a 40% reduction in cardiovascular disease mortality, while individuals who split their physical activity up into three or more sessions per week had a nearly identical 41% relative risk reduction (JAMA Intern Med. 2017 Mar 1;177[3]:335-42).
Interval training is a standard way for athletes in training to improve their endurance by alternating short, intense exercise with brief recovery periods. It’s also a time saver: In one classic bicycling study, physically active men were randomized to standardized 2-week programs of sprint interval training or high-volume endurance training on the bike. The training time required to pass a rigorous cycling time trial test was 90% lower in the interval training group (J Physiol. 2006 Sep 15;575(Pt 3):901-11).
The same principle is applicable to the nonathlete interested in physical activity for heart health.
“When I run a couple of miles, I walk for 5 minutes, then maybe run for three-quarters of a mile, then walk again, then run. In interval training you get your heart rate up, and you drop it down. It’s a very good form of exercise. As a vascular biologist I know that if you put endothelial cells in a Petri dish and spin them real fast continuously, you will not get as good an improvement in endothelial function as if you spin the dish, stop it, spin it, stop it,” Dr. Vogel said.
High-volume exercise is safe, even with high coronary calcium
A clinically significant coronary artery calcification score of 100 Agatston units or more is no reason not to exercise. A Cooper Clinic report on nearly 22,000 middle-aged men without baseline cardiovascular disease who were followed for a mean of 10.4 years concluded that those in the highest-volume exercise group, many of whom were marathon runners and engaged in the equivalent of running for at least 5-6 hours/week at a pace of 10 minutes per mile, were 11% more likely to have an elevated baseline coronary artery calcification score than those who exercised less. But these highest-volume exercisers with elevated coronary calcium – their mean level was 807 Agatston units – had risks of all-cause and cardiovascular mortality that weren’t significantly different from those of men with elevated coronary calcium who exercised more moderately (JAMA Cardiol. 2019 Feb 1;4[2]:174-81).
Cardiac rehab
Dr. Vogel had harsh words for his physician colleagues with respect to the widespread underprescribing of cardiac rehabilitation programs.
“You guys are doing a crappy job with exercise in our most vulnerable patients: those who’ve had cardiovascular events,” he charged. “Cardiac rehabilitation is a Class I recommendation in our guidelines. And yet utilization in the United States is just 10%-20%. No other Class I recommendation is in that ballpark.”
A meta-analysis of 34 randomized trials totaling more than 6,000 post-MI patients concluded that those randomized to exercise-based cardiac rehabilitation had a 47% reduction in the risk of reinfarction, 36% lower cardiac mortality, and a 26% reduction in all-cause mortality (Am Heart J. 2011 Oct;162[4]:571-584.e2).
“The data show that cardiac rehabilitation is as effective as anything else we do in cardiovascular medicine. I understand that patients live far away, they don’t like to exercise – I’ve heard every excuse. But I am charging you with the responsibility of meeting a Class I recommendation that gets patients to live longer,” he declared.
Medicare now covers an enhanced, 72-session program called Intensive Cardiac Rehabilitation that teaches comprehensive lifestyle change and provides reasonable reimbursement. “It’s a good thing for our patients,” Dr. Vogel commented.
Yoga
For patients who are reluctant to pound the pavement, yoga may provide an alternative form of physical activity with tangible cardiovascular benefits. Dr. Vogel pointed to the Yoga-CaRe trial presented at the 2018 scientific sessions of the American Heart Association. Yoga-CaRe randomized 3,959 post-MI patients at 29 centers in India to a program of 13 supervised in-hospital yoga classes followed by yoga at home, or to a control group with three educational sessions. The rate of major adverse cardiovascular events over 42 months of follow-up was cut in half, compared with controls, in the 27% of participants who attended at least 10 of the 13 yoga classes. Their quality of life scores were higher, too.
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center. He is on the speaker’s bureau for Sanofi and Regeneron.
SNOWMASS, COLO. – Physical activity is potent medicine, and it doesn’t take all that much of it to derive the maximum cardiovascular benefit: namely, the equivalent of a brisk hour-long walk 5 days/week or jogging at a 10-minute-per-mile pace for half an hour twice weekly, Robert A. Vogel, MD, asserted at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’m not telling you to run marathons. said Dr. Vogel, a cardiologist at the University of Colorado at Denver, Aurora, with a longstanding interest in preventive cardiology.
He presented selected highlights from the massive evidence base underlying the recommendations put forth in the current comprehensive U.S. Department of Health & Human Services Physical Activity Guidelines for Americans.
One particularly compelling chunk of evidence comes from a Taiwanese government–funded prospective cohort study of more than 416,000 individuals followed for an average of 8 years. A key finding: 15 minutes of moderate-intensity physical activity daily was associated with a 14% reduction in the relative risk of all-cause mortality and a 19% reduction in death caused by cardiovascular disease, compared with that of inactive individuals. Moreover, each additional 15 minutes of daily moderate exercise further reduced mortality by 4%. These benefits extended across the full age spectrum of both sexes and applied to patients with cardiovascular disease (Lancet. 2011 Oct 1;378[9798]:1244-53).
“That’s a very impressive result for modest physical activity,” the cardiologist commented.
Data on more than 50,000 adult participants in the Aerobics Center Longitudinal Study based at the Cooper Clinic in Dallas show that vigorous exercise in the form of running at 6 mph for half an hour twice weekly, or a total of 10 metabolic equivalent of task hours (MET-HR) per week, was associated with a roughly 40% reduction in cardiovascular disease mortality. Importantly, 20, 40, or 50 MET-HR/week of vigorous exercise conferred no further survival benefit (J Am Coll Cardiol. 2014 Aug 5;64[5]:472-81). The same group showed that the sweet spot for moderate physical activity in terms of reduced cardiovascular mortality was brisk walking for an hour daily 5 days/week, for a total of 20 MET-HR, which was also associated with roughly a 40% risk reduction compared to inactivity. At that point the benefit plateaued, with no further mortality reduction noted with additional MET-HR of moderate exercise.
“For more than that, we have no evidence of additional cardiovascular benefit. It’s not going to get you to the Tokyo Olympics, but that’s what we need to be doing,” Dr. Vogel observed.
In another report from the Aerobics Center Longitudinal Study, investigators found that moderate-level cardiorespiratory fitness as defined by METs was associated with a 44% reduction in the risk of sudden cardiac death in men and women after adjustment for potential confounders, while high-level cardiorespiratory fitness was associated with a closely similar 48% reduction in risk. This applied to individuals who were hypertensive, overweight, and/or had poor health status, as well as to others (Mayo Clin Proc. 2016 Jul;91[7]:849-57).
All activity counts
Exercise physiologists speak of NEPA – nonexercise physical activity – such as taking out the garbage. Swedish investigators followed more than 4,200 individuals for an average of 12.5 years and found that high NEPA activity was independently associated with a 30% reduction in all-cause mortality and a 27% lower risk of a first cardiovascular disease event, compared with low NEPA. High NEPA in regular exercisers was associated with a lower rate of metabolic syndrome than in low-NEPA regular exercisers (Br J Sports Med. 2014 Feb;48[3]:233-8).
Don’t just sit there – stand!
The current federal physical activity guidelines place a new emphasis on the detrimental effects of sitting. A report on more than 221,000 participants in the Australian 45 and Up Study, with close to 1 million person-years of follow-up, demonstrated a linear inverse relationship between standing time per day and all-cause mortality. In a multivariate analysis adjusted for potential confounders, individuals who stood for 2-5 hours per day had a 10% lower risk of all-cause mortality than did those who stood for less than 2 hours. Standing for 5-8 hours was associated with a 15% relative risk reduction. And standing for more than 8 hours daily was linked to a 24% reduction in risk (Prev Med. 2014 Dec;69:187-91).
And it’s not just total daily sitting time that’s a risk factor. Prolonged, uninterrupted sedentary time was also associated with a dose-dependent increase in all-cause mortality in a prospective cohort study of nearly 8,000 U.S. adults (Ann Intern Med. 2017 Oct 3;167[7]:465-75).
“If you can’t walk around, talk to your patients standing up. That activity of getting out of your chair is lifesaving,” the cardiologist advised.
Get strong
Muscle-strengthening activity on at least 2 days/week is recommended in the federal guidelines because it’s independently associated with decreased all-cause mortality, even in individuals getting sufficient aerobic exercise, as shown in a large national study with 15-years’ follow-up (Prev Med. 2016 Jun;87:121-127).
“As we get older, we tend to forget about muscle. I work with the National Football League. These folks are pretty strong, but we never see diabetes in these very big players, who are often well over 300 lb. They’ve got a lot of muscle. If you want to prevent diabetes, be strong. It’s a very important factor,” Dr. Vogel said.
For the time constrained
Jogging is more time-efficient than brisk walking as a way to attain the maximum cardiovascular benefit of exercise. And the so-called “Weekend Warrior” study of nearly 64,000 U.K. adults showed that it’s okay to cram the full week’s worth of exercise into one or two sessions and be done with it. Compared with the inactive study participants, the weekend warriors had a 40% reduction in cardiovascular disease mortality, while individuals who split their physical activity up into three or more sessions per week had a nearly identical 41% relative risk reduction (JAMA Intern Med. 2017 Mar 1;177[3]:335-42).
Interval training is a standard way for athletes in training to improve their endurance by alternating short, intense exercise with brief recovery periods. It’s also a time saver: In one classic bicycling study, physically active men were randomized to standardized 2-week programs of sprint interval training or high-volume endurance training on the bike. The training time required to pass a rigorous cycling time trial test was 90% lower in the interval training group (J Physiol. 2006 Sep 15;575(Pt 3):901-11).
The same principle is applicable to the nonathlete interested in physical activity for heart health.
“When I run a couple of miles, I walk for 5 minutes, then maybe run for three-quarters of a mile, then walk again, then run. In interval training you get your heart rate up, and you drop it down. It’s a very good form of exercise. As a vascular biologist I know that if you put endothelial cells in a Petri dish and spin them real fast continuously, you will not get as good an improvement in endothelial function as if you spin the dish, stop it, spin it, stop it,” Dr. Vogel said.
High-volume exercise is safe, even with high coronary calcium
A clinically significant coronary artery calcification score of 100 Agatston units or more is no reason not to exercise. A Cooper Clinic report on nearly 22,000 middle-aged men without baseline cardiovascular disease who were followed for a mean of 10.4 years concluded that those in the highest-volume exercise group, many of whom were marathon runners and engaged in the equivalent of running for at least 5-6 hours/week at a pace of 10 minutes per mile, were 11% more likely to have an elevated baseline coronary artery calcification score than those who exercised less. But these highest-volume exercisers with elevated coronary calcium – their mean level was 807 Agatston units – had risks of all-cause and cardiovascular mortality that weren’t significantly different from those of men with elevated coronary calcium who exercised more moderately (JAMA Cardiol. 2019 Feb 1;4[2]:174-81).
Cardiac rehab
Dr. Vogel had harsh words for his physician colleagues with respect to the widespread underprescribing of cardiac rehabilitation programs.
“You guys are doing a crappy job with exercise in our most vulnerable patients: those who’ve had cardiovascular events,” he charged. “Cardiac rehabilitation is a Class I recommendation in our guidelines. And yet utilization in the United States is just 10%-20%. No other Class I recommendation is in that ballpark.”
A meta-analysis of 34 randomized trials totaling more than 6,000 post-MI patients concluded that those randomized to exercise-based cardiac rehabilitation had a 47% reduction in the risk of reinfarction, 36% lower cardiac mortality, and a 26% reduction in all-cause mortality (Am Heart J. 2011 Oct;162[4]:571-584.e2).
“The data show that cardiac rehabilitation is as effective as anything else we do in cardiovascular medicine. I understand that patients live far away, they don’t like to exercise – I’ve heard every excuse. But I am charging you with the responsibility of meeting a Class I recommendation that gets patients to live longer,” he declared.
Medicare now covers an enhanced, 72-session program called Intensive Cardiac Rehabilitation that teaches comprehensive lifestyle change and provides reasonable reimbursement. “It’s a good thing for our patients,” Dr. Vogel commented.
Yoga
For patients who are reluctant to pound the pavement, yoga may provide an alternative form of physical activity with tangible cardiovascular benefits. Dr. Vogel pointed to the Yoga-CaRe trial presented at the 2018 scientific sessions of the American Heart Association. Yoga-CaRe randomized 3,959 post-MI patients at 29 centers in India to a program of 13 supervised in-hospital yoga classes followed by yoga at home, or to a control group with three educational sessions. The rate of major adverse cardiovascular events over 42 months of follow-up was cut in half, compared with controls, in the 27% of participants who attended at least 10 of the 13 yoga classes. Their quality of life scores were higher, too.
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center. He is on the speaker’s bureau for Sanofi and Regeneron.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
Trump takes on multiple health topics in State of the Union
President Donald J. Trump took on multiple health care issues in his State of the Union address, imploring Congress to avoid the “socialism” of Medicare-for-all, to pass legislation banning late-term abortions, and to protect insurance coverage for preexisting conditions while joining together to reduce rising drug prices.
Mr. Trump said his administration has already been “taking on the big pharmaceutical companies,” claiming that, in 2019, “for the first time in 51 years, the cost of prescription drugs actually went down.”
That statement was called “misleading” by the New York Times because such efforts have excluded some high-cost drugs, and prices had risen by the end of the year, the publication noted in a fact-check of the president’s speech.
A survey issued in December 2019 found that the United States pays the highest prices in the world for pharmaceuticals, as reported by Medscape Medical News.
But the president did throw down a gauntlet for Congress. “Working together, the Congress can reduce drug prices substantially from current levels,” he said, stating that he had been “speaking to Sen. Chuck Grassley of Iowa and others in the Congress in order to get something on drug pricing done, and done properly.
“Get a bill to my desk, and I will sign it into law without delay,” Mr. Trump said.
A group of House Democrats then stood up in the chamber and loudly chanted, “HR3, HR3,” referring to the Lower Drug Costs Now Act, which the House passed in December 2019.
The bill would give the Department of Health & Human Services the power to negotiate directly with drug companies on up to 250 drugs per year, in particular, the highest-costing and most-utilized drugs.
The Senate has not taken up the legislation, but Sen. Grassley (R) and Sen. Ron Wyden (D-Ore.) introduced a similar bill, the Prescription Drug Pricing Reduction Act. It has been approved by the Senate Finance Committee but has not been moved to the Senate floor.
“I appreciate President Trump recognizing the work we’re doing to lower prescription drug prices,” Sen. Grassley said in a statement after the State of the Union. “Iowans and Americans across the country are demanding reforms that lower sky-high drug costs. A recent poll showed 70% of Americans want Congress to make lowering drug prices its top priority.”
Rep. Greg Walden (R-Ore.), the ranking Republican on the House Energy and Commerce Committee, said he believed Trump was committed to lowering drug costs. “I’ve never seen a president lean in further than President Donald Trump on lowering health care costs,” said Rep. Walden in a statement after the speech.
Trump touted his price transparency rule, which he said would go into effect next January, as a key way to cut health care costs.
Preexisting conditions
The president said that since he’d taken office, insurance had become more affordable and that the quality of health care had improved. He also said that he was making what he called an “iron-clad pledge” to American families.
“We will always protect patients with preexisting conditions – that is a guarantee,” Mr. Trump said.
In a press conference before the speech, Speaker of the House Nancy Pelosi (D-Calif.) took issue with that pledge. “The president swears that he supports protections for people with preexisting conditions, but right now, he is fighting in federal court to eliminate these lifesaving protections and every last protection and benefit of the Affordable Care Act,” she said.
During the speech, Rep. G. K. Butterfield (D-N.C.) tweeted “#FactCheck: Claiming to protect Americans with preexisting conditions, Trump and his administration have repeatedly sought to undermine protections offered by the ACA through executive orders and the courts. He is seeking to strike down the law and its protections entirely.”
Larry Levitt, executive vice president for health policy at the Kaiser Family Foundation, pointed out in a tweet that insurance plans that Trump touted as “affordable alternatives” are in fact missing those protections.
“Ironically, the cheaper health insurance plans that President Trump has expanded are short-term plans that don’t cover preexisting conditions,” Mr. Levitt said.
Socialist takeover
Mr. Trump condemned the Medicare-for-all proposals that have been introduced in Congress and that are being backed in whole or in part by all of the Democratic candidates for president.
“As we work to improve Americans’ health care, there are those who want to take away your health care, take away your doctor, and abolish private insurance entirely,” said Mr. Trump.
He said that 132 members of Congress “have endorsed legislation to impose a socialist takeover of our health care system, wiping out the private health insurance plans of 180 million Americans.”
Added Mr. Trump: “We will never let socialism destroy American health care!”
Medicare-for-all has waxed and waned in popularity among voters, with generally more Democrats than Republicans favoring a single-payer system, with or without a public option.
Preliminary exit polls in Iowa that were conducted during Monday’s caucus found that 57% of Iowa Democratic caucus-goers supported a single-payer plan; 38% opposed such a plan, according to the Washington Post.
Opioids, the coronavirus, and abortion
In some of his final remarks on health care, Mr. Trump cited progress in the opioid crisis, noting that, in 2019, drug overdose deaths declined for the first time in 30 years.
He said that his administration was coordinating with the Chinese government regarding the coronavirus outbreak and noted the launch of initiatives to improve care for people with kidney disease, Alzheimer’s, and mental health problems.
Mr. Trump repeated his 2019 State of the Union claim that the government would help end AIDS in America by the end of the decade.
The president also announced that he was asking Congress for “an additional $50 million” to fund neonatal research. He followed that up with a plea about abortion.
“I am calling upon the members of Congress here tonight to pass legislation finally banning the late-term abortion of babies,” he said.
Insulin costs?
In the days before the speech, some news outlets had reported that Mr. Trump and the HHS were working on a plan to lower insulin prices for Medicare beneficiaries, and there were suggestions it would come up in the speech.
At least 13 members of Congress invited people advocating for lower insulin costs as their guests for the State of the Union, Stat reported. Rep. Pelosi invited twins from San Francisco with type 1 diabetes as her guests.
But Mr. Trump never mentioned insulin in his speech.
This article first appeared on Medscape.com.
President Donald J. Trump took on multiple health care issues in his State of the Union address, imploring Congress to avoid the “socialism” of Medicare-for-all, to pass legislation banning late-term abortions, and to protect insurance coverage for preexisting conditions while joining together to reduce rising drug prices.
Mr. Trump said his administration has already been “taking on the big pharmaceutical companies,” claiming that, in 2019, “for the first time in 51 years, the cost of prescription drugs actually went down.”
That statement was called “misleading” by the New York Times because such efforts have excluded some high-cost drugs, and prices had risen by the end of the year, the publication noted in a fact-check of the president’s speech.
A survey issued in December 2019 found that the United States pays the highest prices in the world for pharmaceuticals, as reported by Medscape Medical News.
But the president did throw down a gauntlet for Congress. “Working together, the Congress can reduce drug prices substantially from current levels,” he said, stating that he had been “speaking to Sen. Chuck Grassley of Iowa and others in the Congress in order to get something on drug pricing done, and done properly.
“Get a bill to my desk, and I will sign it into law without delay,” Mr. Trump said.
A group of House Democrats then stood up in the chamber and loudly chanted, “HR3, HR3,” referring to the Lower Drug Costs Now Act, which the House passed in December 2019.
The bill would give the Department of Health & Human Services the power to negotiate directly with drug companies on up to 250 drugs per year, in particular, the highest-costing and most-utilized drugs.
The Senate has not taken up the legislation, but Sen. Grassley (R) and Sen. Ron Wyden (D-Ore.) introduced a similar bill, the Prescription Drug Pricing Reduction Act. It has been approved by the Senate Finance Committee but has not been moved to the Senate floor.
“I appreciate President Trump recognizing the work we’re doing to lower prescription drug prices,” Sen. Grassley said in a statement after the State of the Union. “Iowans and Americans across the country are demanding reforms that lower sky-high drug costs. A recent poll showed 70% of Americans want Congress to make lowering drug prices its top priority.”
Rep. Greg Walden (R-Ore.), the ranking Republican on the House Energy and Commerce Committee, said he believed Trump was committed to lowering drug costs. “I’ve never seen a president lean in further than President Donald Trump on lowering health care costs,” said Rep. Walden in a statement after the speech.
Trump touted his price transparency rule, which he said would go into effect next January, as a key way to cut health care costs.
Preexisting conditions
The president said that since he’d taken office, insurance had become more affordable and that the quality of health care had improved. He also said that he was making what he called an “iron-clad pledge” to American families.
“We will always protect patients with preexisting conditions – that is a guarantee,” Mr. Trump said.
In a press conference before the speech, Speaker of the House Nancy Pelosi (D-Calif.) took issue with that pledge. “The president swears that he supports protections for people with preexisting conditions, but right now, he is fighting in federal court to eliminate these lifesaving protections and every last protection and benefit of the Affordable Care Act,” she said.
During the speech, Rep. G. K. Butterfield (D-N.C.) tweeted “#FactCheck: Claiming to protect Americans with preexisting conditions, Trump and his administration have repeatedly sought to undermine protections offered by the ACA through executive orders and the courts. He is seeking to strike down the law and its protections entirely.”
Larry Levitt, executive vice president for health policy at the Kaiser Family Foundation, pointed out in a tweet that insurance plans that Trump touted as “affordable alternatives” are in fact missing those protections.
“Ironically, the cheaper health insurance plans that President Trump has expanded are short-term plans that don’t cover preexisting conditions,” Mr. Levitt said.
Socialist takeover
Mr. Trump condemned the Medicare-for-all proposals that have been introduced in Congress and that are being backed in whole or in part by all of the Democratic candidates for president.
“As we work to improve Americans’ health care, there are those who want to take away your health care, take away your doctor, and abolish private insurance entirely,” said Mr. Trump.
He said that 132 members of Congress “have endorsed legislation to impose a socialist takeover of our health care system, wiping out the private health insurance plans of 180 million Americans.”
Added Mr. Trump: “We will never let socialism destroy American health care!”
Medicare-for-all has waxed and waned in popularity among voters, with generally more Democrats than Republicans favoring a single-payer system, with or without a public option.
Preliminary exit polls in Iowa that were conducted during Monday’s caucus found that 57% of Iowa Democratic caucus-goers supported a single-payer plan; 38% opposed such a plan, according to the Washington Post.
Opioids, the coronavirus, and abortion
In some of his final remarks on health care, Mr. Trump cited progress in the opioid crisis, noting that, in 2019, drug overdose deaths declined for the first time in 30 years.
He said that his administration was coordinating with the Chinese government regarding the coronavirus outbreak and noted the launch of initiatives to improve care for people with kidney disease, Alzheimer’s, and mental health problems.
Mr. Trump repeated his 2019 State of the Union claim that the government would help end AIDS in America by the end of the decade.
The president also announced that he was asking Congress for “an additional $50 million” to fund neonatal research. He followed that up with a plea about abortion.
“I am calling upon the members of Congress here tonight to pass legislation finally banning the late-term abortion of babies,” he said.
Insulin costs?
In the days before the speech, some news outlets had reported that Mr. Trump and the HHS were working on a plan to lower insulin prices for Medicare beneficiaries, and there were suggestions it would come up in the speech.
At least 13 members of Congress invited people advocating for lower insulin costs as their guests for the State of the Union, Stat reported. Rep. Pelosi invited twins from San Francisco with type 1 diabetes as her guests.
But Mr. Trump never mentioned insulin in his speech.
This article first appeared on Medscape.com.
President Donald J. Trump took on multiple health care issues in his State of the Union address, imploring Congress to avoid the “socialism” of Medicare-for-all, to pass legislation banning late-term abortions, and to protect insurance coverage for preexisting conditions while joining together to reduce rising drug prices.
Mr. Trump said his administration has already been “taking on the big pharmaceutical companies,” claiming that, in 2019, “for the first time in 51 years, the cost of prescription drugs actually went down.”
That statement was called “misleading” by the New York Times because such efforts have excluded some high-cost drugs, and prices had risen by the end of the year, the publication noted in a fact-check of the president’s speech.
A survey issued in December 2019 found that the United States pays the highest prices in the world for pharmaceuticals, as reported by Medscape Medical News.
But the president did throw down a gauntlet for Congress. “Working together, the Congress can reduce drug prices substantially from current levels,” he said, stating that he had been “speaking to Sen. Chuck Grassley of Iowa and others in the Congress in order to get something on drug pricing done, and done properly.
“Get a bill to my desk, and I will sign it into law without delay,” Mr. Trump said.
A group of House Democrats then stood up in the chamber and loudly chanted, “HR3, HR3,” referring to the Lower Drug Costs Now Act, which the House passed in December 2019.
The bill would give the Department of Health & Human Services the power to negotiate directly with drug companies on up to 250 drugs per year, in particular, the highest-costing and most-utilized drugs.
The Senate has not taken up the legislation, but Sen. Grassley (R) and Sen. Ron Wyden (D-Ore.) introduced a similar bill, the Prescription Drug Pricing Reduction Act. It has been approved by the Senate Finance Committee but has not been moved to the Senate floor.
“I appreciate President Trump recognizing the work we’re doing to lower prescription drug prices,” Sen. Grassley said in a statement after the State of the Union. “Iowans and Americans across the country are demanding reforms that lower sky-high drug costs. A recent poll showed 70% of Americans want Congress to make lowering drug prices its top priority.”
Rep. Greg Walden (R-Ore.), the ranking Republican on the House Energy and Commerce Committee, said he believed Trump was committed to lowering drug costs. “I’ve never seen a president lean in further than President Donald Trump on lowering health care costs,” said Rep. Walden in a statement after the speech.
Trump touted his price transparency rule, which he said would go into effect next January, as a key way to cut health care costs.
Preexisting conditions
The president said that since he’d taken office, insurance had become more affordable and that the quality of health care had improved. He also said that he was making what he called an “iron-clad pledge” to American families.
“We will always protect patients with preexisting conditions – that is a guarantee,” Mr. Trump said.
In a press conference before the speech, Speaker of the House Nancy Pelosi (D-Calif.) took issue with that pledge. “The president swears that he supports protections for people with preexisting conditions, but right now, he is fighting in federal court to eliminate these lifesaving protections and every last protection and benefit of the Affordable Care Act,” she said.
During the speech, Rep. G. K. Butterfield (D-N.C.) tweeted “#FactCheck: Claiming to protect Americans with preexisting conditions, Trump and his administration have repeatedly sought to undermine protections offered by the ACA through executive orders and the courts. He is seeking to strike down the law and its protections entirely.”
Larry Levitt, executive vice president for health policy at the Kaiser Family Foundation, pointed out in a tweet that insurance plans that Trump touted as “affordable alternatives” are in fact missing those protections.
“Ironically, the cheaper health insurance plans that President Trump has expanded are short-term plans that don’t cover preexisting conditions,” Mr. Levitt said.
Socialist takeover
Mr. Trump condemned the Medicare-for-all proposals that have been introduced in Congress and that are being backed in whole or in part by all of the Democratic candidates for president.
“As we work to improve Americans’ health care, there are those who want to take away your health care, take away your doctor, and abolish private insurance entirely,” said Mr. Trump.
He said that 132 members of Congress “have endorsed legislation to impose a socialist takeover of our health care system, wiping out the private health insurance plans of 180 million Americans.”
Added Mr. Trump: “We will never let socialism destroy American health care!”
Medicare-for-all has waxed and waned in popularity among voters, with generally more Democrats than Republicans favoring a single-payer system, with or without a public option.
Preliminary exit polls in Iowa that were conducted during Monday’s caucus found that 57% of Iowa Democratic caucus-goers supported a single-payer plan; 38% opposed such a plan, according to the Washington Post.
Opioids, the coronavirus, and abortion
In some of his final remarks on health care, Mr. Trump cited progress in the opioid crisis, noting that, in 2019, drug overdose deaths declined for the first time in 30 years.
He said that his administration was coordinating with the Chinese government regarding the coronavirus outbreak and noted the launch of initiatives to improve care for people with kidney disease, Alzheimer’s, and mental health problems.
Mr. Trump repeated his 2019 State of the Union claim that the government would help end AIDS in America by the end of the decade.
The president also announced that he was asking Congress for “an additional $50 million” to fund neonatal research. He followed that up with a plea about abortion.
“I am calling upon the members of Congress here tonight to pass legislation finally banning the late-term abortion of babies,” he said.
Insulin costs?
In the days before the speech, some news outlets had reported that Mr. Trump and the HHS were working on a plan to lower insulin prices for Medicare beneficiaries, and there were suggestions it would come up in the speech.
At least 13 members of Congress invited people advocating for lower insulin costs as their guests for the State of the Union, Stat reported. Rep. Pelosi invited twins from San Francisco with type 1 diabetes as her guests.
But Mr. Trump never mentioned insulin in his speech.
This article first appeared on Medscape.com.
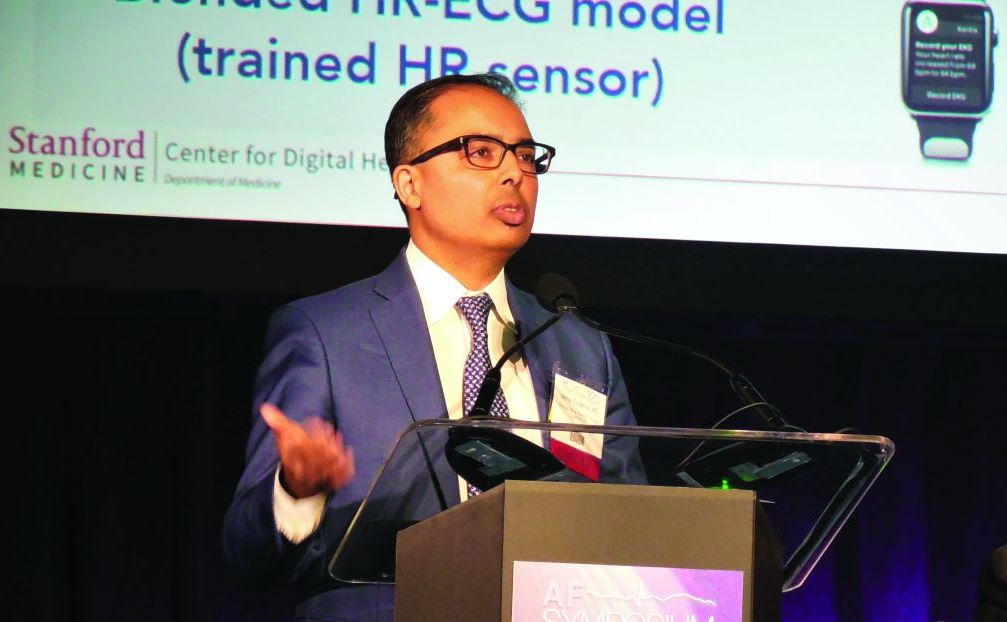
Home BP now a class Ia recommendation, with good reason
SNOWMASS, COLO. – The redefinition of hypertension as 130/80 mm Hg or higher introduced in the current American College of Cardiology/American Heart Association hypertension management guidelines has generated considerable controversy. Often overlooked, however, has been another major innovation included in the 2017 guidelines: the rise in the status of out-of-office 24-hour ambulatory blood pressure monitoring and home blood pressure self-measurement to a class I, level of evidence A recommendation, Andrew M. Kates, MD, observed at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
It’s a guideline he strongly endorses.
“We do a lot of this. It can be a challenge to get 24-hour ambulatory blood pressure monitoring covered by payers, so said Dr. Kates, professor of medicine and director of the cardiology fellowship program at Washington University, St. Louis.
He explained that one of the four key questions the guideline committee was tasked with answering at the outset of deliberations was this: What’s the evidence base for self-directed out-of-office blood pressure monitoring? Based on the panel’s systematic review of the literature, this practice wound up receiving the strongest possible class Ia recommendation, specifically for confirming the diagnosis of hypertension and for titration of antihypertensive medications. Moreover, the guidelines also endorsed home blood pressure monitoring for the detection of white-coat hypertension, this time as a Class IIa recommendation, as well as for identification of patients with masked hypertension, with class IIb status (Circulation. 2018 Oct 23;138[17]:e484-594).
The 2017 ACC/AHA guidelines include a detailed checklist for obtaining accurate measurements of office blood pressure. The suggestions include having the patient sit relaxed in a chair with both feet on the floor for at least 5 minutes before taking the measurement, no coffee or exercise for 30 minutes beforehand, empty the bladder, no talking, no clothing over the arm, and other recommendations. Many busy clinicians roll their eyes at the impracticality of doing all this on a routine basis.
“I don’t want to take an audience survey, but I’ll say that even in our office we are not successful in doing this. Patients run up the stairs to the office after dealing with traffic and the parking garage, they’re late for their appointment, in winter they’re wearing a sweater and don’t want to take it off. These are things we don’t do well, and they’re low-hanging fruit where we could do better,” Dr. Kates commented.
The challenges inherent in performing by-the-book office blood pressure measurement reinforce the importance of home self-monitoring of blood pressure in what is hopefully a more stress-free environment.
“We can give patients specific guidance about checking their blood pressure an hour after taking their medications, sitting for 5 minutes, and checking the pressures on a bare arm and not with the sleeve rolled up,” he noted.
The guidelines recommend using home blood pressure monitoring or ambulatory monitoring to detect white-coat hypertension in patients with an office blood pressure of 130/80 mm Hg or more, but less than 160/100 mm Hg, after a 3-month trial of lifestyle modification. If the home blood pressure is less than 130/80 mm Hg, that’s evidence of white-coat hypertension, for which the recommended treatment consists of continued lifestyle modification plus periodic monitoring of out-of-office blood pressures in order to promptly detect progression to hypertension. If, however, the out-of-office blood pressure is not less than 130/80 mm Hg, that’s hypertension, and the guidelines recommend starting dual-agent antihypertensive drug therapy while continuing lifestyle modification.
A confusing array of definitions of hypertension are now in use by various medical societies. While the 2017 ACC/AHA hypertension guidelines define hypertension as office blood pressure of 130/80 mm Hg or more, the 2018 European Society of Cardiology/European Society of Hypertension guidelines use a threshold of 140/90 mm Hg or more. Joint American Academy of Family Physicians/American College of Physicians guidelines recommend a treatment target of less than 150 mm Hg in hypertensive patients aged 60 years or older. And at the other end of the spectrum, the SPRINT trial showed a significant cardiovascular benefit for intensive treatment of hypertension to a target systolic blood pressure below 120 mm Hg, rather than less than 140 mm Hg (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
Dr. Kates believes the debate over the “right” treatment target misses the central point, which is that hypertension is staggeringly undertreated. Indeed, the Centers for Disease Control and Prevention estimates only one in four adults with hypertension have their disease under control. That’s a disconcerting statistic given that hypertension accounts for more cardiovascular deaths than any other modifiable cardiovascular risk factor.
“There’s been some concern raised that maybe too much weight has been put on the SPRINT trial in making the ACC/AHA recommendations, but I think it’s helpful to understand that we vastly undertreat patients with hypertension. So I think that, rather than being so concerned that we’re going to be treating people to too low a target or we’re being overly aggressive, it should give us some pause to think about the fact that we’re ordinarily not being aggressive enough with many of our patients as it is,” the cardiologist said.
Dr. Kates reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – The redefinition of hypertension as 130/80 mm Hg or higher introduced in the current American College of Cardiology/American Heart Association hypertension management guidelines has generated considerable controversy. Often overlooked, however, has been another major innovation included in the 2017 guidelines: the rise in the status of out-of-office 24-hour ambulatory blood pressure monitoring and home blood pressure self-measurement to a class I, level of evidence A recommendation, Andrew M. Kates, MD, observed at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
It’s a guideline he strongly endorses.
“We do a lot of this. It can be a challenge to get 24-hour ambulatory blood pressure monitoring covered by payers, so said Dr. Kates, professor of medicine and director of the cardiology fellowship program at Washington University, St. Louis.
He explained that one of the four key questions the guideline committee was tasked with answering at the outset of deliberations was this: What’s the evidence base for self-directed out-of-office blood pressure monitoring? Based on the panel’s systematic review of the literature, this practice wound up receiving the strongest possible class Ia recommendation, specifically for confirming the diagnosis of hypertension and for titration of antihypertensive medications. Moreover, the guidelines also endorsed home blood pressure monitoring for the detection of white-coat hypertension, this time as a Class IIa recommendation, as well as for identification of patients with masked hypertension, with class IIb status (Circulation. 2018 Oct 23;138[17]:e484-594).
The 2017 ACC/AHA guidelines include a detailed checklist for obtaining accurate measurements of office blood pressure. The suggestions include having the patient sit relaxed in a chair with both feet on the floor for at least 5 minutes before taking the measurement, no coffee or exercise for 30 minutes beforehand, empty the bladder, no talking, no clothing over the arm, and other recommendations. Many busy clinicians roll their eyes at the impracticality of doing all this on a routine basis.
“I don’t want to take an audience survey, but I’ll say that even in our office we are not successful in doing this. Patients run up the stairs to the office after dealing with traffic and the parking garage, they’re late for their appointment, in winter they’re wearing a sweater and don’t want to take it off. These are things we don’t do well, and they’re low-hanging fruit where we could do better,” Dr. Kates commented.
The challenges inherent in performing by-the-book office blood pressure measurement reinforce the importance of home self-monitoring of blood pressure in what is hopefully a more stress-free environment.
“We can give patients specific guidance about checking their blood pressure an hour after taking their medications, sitting for 5 minutes, and checking the pressures on a bare arm and not with the sleeve rolled up,” he noted.
The guidelines recommend using home blood pressure monitoring or ambulatory monitoring to detect white-coat hypertension in patients with an office blood pressure of 130/80 mm Hg or more, but less than 160/100 mm Hg, after a 3-month trial of lifestyle modification. If the home blood pressure is less than 130/80 mm Hg, that’s evidence of white-coat hypertension, for which the recommended treatment consists of continued lifestyle modification plus periodic monitoring of out-of-office blood pressures in order to promptly detect progression to hypertension. If, however, the out-of-office blood pressure is not less than 130/80 mm Hg, that’s hypertension, and the guidelines recommend starting dual-agent antihypertensive drug therapy while continuing lifestyle modification.
A confusing array of definitions of hypertension are now in use by various medical societies. While the 2017 ACC/AHA hypertension guidelines define hypertension as office blood pressure of 130/80 mm Hg or more, the 2018 European Society of Cardiology/European Society of Hypertension guidelines use a threshold of 140/90 mm Hg or more. Joint American Academy of Family Physicians/American College of Physicians guidelines recommend a treatment target of less than 150 mm Hg in hypertensive patients aged 60 years or older. And at the other end of the spectrum, the SPRINT trial showed a significant cardiovascular benefit for intensive treatment of hypertension to a target systolic blood pressure below 120 mm Hg, rather than less than 140 mm Hg (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
Dr. Kates believes the debate over the “right” treatment target misses the central point, which is that hypertension is staggeringly undertreated. Indeed, the Centers for Disease Control and Prevention estimates only one in four adults with hypertension have their disease under control. That’s a disconcerting statistic given that hypertension accounts for more cardiovascular deaths than any other modifiable cardiovascular risk factor.
“There’s been some concern raised that maybe too much weight has been put on the SPRINT trial in making the ACC/AHA recommendations, but I think it’s helpful to understand that we vastly undertreat patients with hypertension. So I think that, rather than being so concerned that we’re going to be treating people to too low a target or we’re being overly aggressive, it should give us some pause to think about the fact that we’re ordinarily not being aggressive enough with many of our patients as it is,” the cardiologist said.
Dr. Kates reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – The redefinition of hypertension as 130/80 mm Hg or higher introduced in the current American College of Cardiology/American Heart Association hypertension management guidelines has generated considerable controversy. Often overlooked, however, has been another major innovation included in the 2017 guidelines: the rise in the status of out-of-office 24-hour ambulatory blood pressure monitoring and home blood pressure self-measurement to a class I, level of evidence A recommendation, Andrew M. Kates, MD, observed at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
It’s a guideline he strongly endorses.
“We do a lot of this. It can be a challenge to get 24-hour ambulatory blood pressure monitoring covered by payers, so said Dr. Kates, professor of medicine and director of the cardiology fellowship program at Washington University, St. Louis.
He explained that one of the four key questions the guideline committee was tasked with answering at the outset of deliberations was this: What’s the evidence base for self-directed out-of-office blood pressure monitoring? Based on the panel’s systematic review of the literature, this practice wound up receiving the strongest possible class Ia recommendation, specifically for confirming the diagnosis of hypertension and for titration of antihypertensive medications. Moreover, the guidelines also endorsed home blood pressure monitoring for the detection of white-coat hypertension, this time as a Class IIa recommendation, as well as for identification of patients with masked hypertension, with class IIb status (Circulation. 2018 Oct 23;138[17]:e484-594).
The 2017 ACC/AHA guidelines include a detailed checklist for obtaining accurate measurements of office blood pressure. The suggestions include having the patient sit relaxed in a chair with both feet on the floor for at least 5 minutes before taking the measurement, no coffee or exercise for 30 minutes beforehand, empty the bladder, no talking, no clothing over the arm, and other recommendations. Many busy clinicians roll their eyes at the impracticality of doing all this on a routine basis.
“I don’t want to take an audience survey, but I’ll say that even in our office we are not successful in doing this. Patients run up the stairs to the office after dealing with traffic and the parking garage, they’re late for their appointment, in winter they’re wearing a sweater and don’t want to take it off. These are things we don’t do well, and they’re low-hanging fruit where we could do better,” Dr. Kates commented.
The challenges inherent in performing by-the-book office blood pressure measurement reinforce the importance of home self-monitoring of blood pressure in what is hopefully a more stress-free environment.
“We can give patients specific guidance about checking their blood pressure an hour after taking their medications, sitting for 5 minutes, and checking the pressures on a bare arm and not with the sleeve rolled up,” he noted.
The guidelines recommend using home blood pressure monitoring or ambulatory monitoring to detect white-coat hypertension in patients with an office blood pressure of 130/80 mm Hg or more, but less than 160/100 mm Hg, after a 3-month trial of lifestyle modification. If the home blood pressure is less than 130/80 mm Hg, that’s evidence of white-coat hypertension, for which the recommended treatment consists of continued lifestyle modification plus periodic monitoring of out-of-office blood pressures in order to promptly detect progression to hypertension. If, however, the out-of-office blood pressure is not less than 130/80 mm Hg, that’s hypertension, and the guidelines recommend starting dual-agent antihypertensive drug therapy while continuing lifestyle modification.
A confusing array of definitions of hypertension are now in use by various medical societies. While the 2017 ACC/AHA hypertension guidelines define hypertension as office blood pressure of 130/80 mm Hg or more, the 2018 European Society of Cardiology/European Society of Hypertension guidelines use a threshold of 140/90 mm Hg or more. Joint American Academy of Family Physicians/American College of Physicians guidelines recommend a treatment target of less than 150 mm Hg in hypertensive patients aged 60 years or older. And at the other end of the spectrum, the SPRINT trial showed a significant cardiovascular benefit for intensive treatment of hypertension to a target systolic blood pressure below 120 mm Hg, rather than less than 140 mm Hg (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
Dr. Kates believes the debate over the “right” treatment target misses the central point, which is that hypertension is staggeringly undertreated. Indeed, the Centers for Disease Control and Prevention estimates only one in four adults with hypertension have their disease under control. That’s a disconcerting statistic given that hypertension accounts for more cardiovascular deaths than any other modifiable cardiovascular risk factor.
“There’s been some concern raised that maybe too much weight has been put on the SPRINT trial in making the ACC/AHA recommendations, but I think it’s helpful to understand that we vastly undertreat patients with hypertension. So I think that, rather than being so concerned that we’re going to be treating people to too low a target or we’re being overly aggressive, it should give us some pause to think about the fact that we’re ordinarily not being aggressive enough with many of our patients as it is,” the cardiologist said.
Dr. Kates reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
Statin, antihypertensive treatment don’t guarantee healthier lifestyles
When people learn they have enough cardiovascular disease risk to start treatment with a statin or antihypertensive drug, the impact on their healthy-lifestyle choices seems to often be a wash, based on findings from more than 40,000 Finland residents followed for at least 4 years after starting their primary-prevention regimen.
“Patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” wrote Maarit J. Korhonen, PhD, and associates in a report published in the Journal of the American Heart Association.
“Initiation of antihypertensive or statin therapy appears to be associated with lifestyle changes, some positive and others negative,” wrote Dr. Korhonen, a pharmacoepidemiologist at the University of Turku (Finland), and associates. This was the first reported study to assess a large-scale and prospectively followed cohort to look for associations between the use of medicines that prevent cardiovascular disease (CVD) and lifestyle changes. Most previous studies of these associations “have been cross sectional and provide no information on potential lifestyle changes during the time window around the initiation of medication use,” they added.
The new study specifically found that, on average, people who began treatment with at least one CVD-prevention medication for the first time were more likely to gain weight and more likely to become less active during the years following their treatment onset. But at the same time, these patients were also more likely to either quit or cut down on their smoking and alcohol consumption, the researchers found.
Their analysis used data from 41,225 people enrolled in the Finnish Public Sector Study, which prospectively began collecting data on a large number of Finland residents in the 1990s. They specifically focused on 81,772 completed questionnaires – collected at 4-year intervals – from people who completed at least two consecutive rounds of the survey during 2000-2013, and who were also at least 40 years old and free of prevalent CVD at the time of their first survey. The participants averaged nearly 53 years of age at their first survey, and 84% were women.
The researchers subdivided the survey responses into 8,837 (11%) people who began a statin, antihypertensive drug, or both during their participation; 26,914 (33%) already on a statin or antihypertensive drug when they completed their first questionnaire; and 46,021 response sets (56%) from people who never began treatment with either drug class. People who initiated a relevant drug began a median of 1.7 years following completion of their first survey, and a median of 2.4 years before their next survey. During follow-up, about 2% of all participants became newly diagnosed with some form of CVD.
The results showed that, after full adjustment for possible confounders, the mean increase in body mass index was larger among those who initiated a CVD-prevention drug, compared with those who did not. Among participants who were obese at entry, those who started a CVD drug had a statistically significant 37% increased rate of remaining obese, compared with those not starting these drugs. Among those who were not obese at baseline, those who began a CVD prevention drug had a statistically significant 82%% higher rate of becoming obese, compared with those not on a CVD-prevention drug. In addition, average daily energy expenditure, a measure of physical activity, showed a statistically significant decline among those who started a CVD drug, compared with those who did not. In contrast, CVD drug initiators had an average 1.85 gram/week decline in alcohol intake, compared with noninitiators, and those who were current smokers at the first survey and then started a CVD drug had a 26% relative drop in their smoking prevalence, compared with those who did not start a CVD drug, both statistically significant differences.
The findings suggest that “patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” the authors concluded. “This means that expansion of pharmacologic interventions toward populations at low CVD risk may not necessarily lead to expected benefits at the population level.”
The study received no commercial funding. Dr. Korhonen had no disclosures.
SOURCE: Korhonen MJ et al. J Am Heart Assoc. 2020 Feb 5. doi: 10.1161/JAHA.119.014.168.
When people learn they have enough cardiovascular disease risk to start treatment with a statin or antihypertensive drug, the impact on their healthy-lifestyle choices seems to often be a wash, based on findings from more than 40,000 Finland residents followed for at least 4 years after starting their primary-prevention regimen.
“Patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” wrote Maarit J. Korhonen, PhD, and associates in a report published in the Journal of the American Heart Association.
“Initiation of antihypertensive or statin therapy appears to be associated with lifestyle changes, some positive and others negative,” wrote Dr. Korhonen, a pharmacoepidemiologist at the University of Turku (Finland), and associates. This was the first reported study to assess a large-scale and prospectively followed cohort to look for associations between the use of medicines that prevent cardiovascular disease (CVD) and lifestyle changes. Most previous studies of these associations “have been cross sectional and provide no information on potential lifestyle changes during the time window around the initiation of medication use,” they added.
The new study specifically found that, on average, people who began treatment with at least one CVD-prevention medication for the first time were more likely to gain weight and more likely to become less active during the years following their treatment onset. But at the same time, these patients were also more likely to either quit or cut down on their smoking and alcohol consumption, the researchers found.
Their analysis used data from 41,225 people enrolled in the Finnish Public Sector Study, which prospectively began collecting data on a large number of Finland residents in the 1990s. They specifically focused on 81,772 completed questionnaires – collected at 4-year intervals – from people who completed at least two consecutive rounds of the survey during 2000-2013, and who were also at least 40 years old and free of prevalent CVD at the time of their first survey. The participants averaged nearly 53 years of age at their first survey, and 84% were women.
The researchers subdivided the survey responses into 8,837 (11%) people who began a statin, antihypertensive drug, or both during their participation; 26,914 (33%) already on a statin or antihypertensive drug when they completed their first questionnaire; and 46,021 response sets (56%) from people who never began treatment with either drug class. People who initiated a relevant drug began a median of 1.7 years following completion of their first survey, and a median of 2.4 years before their next survey. During follow-up, about 2% of all participants became newly diagnosed with some form of CVD.
The results showed that, after full adjustment for possible confounders, the mean increase in body mass index was larger among those who initiated a CVD-prevention drug, compared with those who did not. Among participants who were obese at entry, those who started a CVD drug had a statistically significant 37% increased rate of remaining obese, compared with those not starting these drugs. Among those who were not obese at baseline, those who began a CVD prevention drug had a statistically significant 82%% higher rate of becoming obese, compared with those not on a CVD-prevention drug. In addition, average daily energy expenditure, a measure of physical activity, showed a statistically significant decline among those who started a CVD drug, compared with those who did not. In contrast, CVD drug initiators had an average 1.85 gram/week decline in alcohol intake, compared with noninitiators, and those who were current smokers at the first survey and then started a CVD drug had a 26% relative drop in their smoking prevalence, compared with those who did not start a CVD drug, both statistically significant differences.
The findings suggest that “patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” the authors concluded. “This means that expansion of pharmacologic interventions toward populations at low CVD risk may not necessarily lead to expected benefits at the population level.”
The study received no commercial funding. Dr. Korhonen had no disclosures.
SOURCE: Korhonen MJ et al. J Am Heart Assoc. 2020 Feb 5. doi: 10.1161/JAHA.119.014.168.
When people learn they have enough cardiovascular disease risk to start treatment with a statin or antihypertensive drug, the impact on their healthy-lifestyle choices seems to often be a wash, based on findings from more than 40,000 Finland residents followed for at least 4 years after starting their primary-prevention regimen.
“Patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” wrote Maarit J. Korhonen, PhD, and associates in a report published in the Journal of the American Heart Association.
“Initiation of antihypertensive or statin therapy appears to be associated with lifestyle changes, some positive and others negative,” wrote Dr. Korhonen, a pharmacoepidemiologist at the University of Turku (Finland), and associates. This was the first reported study to assess a large-scale and prospectively followed cohort to look for associations between the use of medicines that prevent cardiovascular disease (CVD) and lifestyle changes. Most previous studies of these associations “have been cross sectional and provide no information on potential lifestyle changes during the time window around the initiation of medication use,” they added.
The new study specifically found that, on average, people who began treatment with at least one CVD-prevention medication for the first time were more likely to gain weight and more likely to become less active during the years following their treatment onset. But at the same time, these patients were also more likely to either quit or cut down on their smoking and alcohol consumption, the researchers found.
Their analysis used data from 41,225 people enrolled in the Finnish Public Sector Study, which prospectively began collecting data on a large number of Finland residents in the 1990s. They specifically focused on 81,772 completed questionnaires – collected at 4-year intervals – from people who completed at least two consecutive rounds of the survey during 2000-2013, and who were also at least 40 years old and free of prevalent CVD at the time of their first survey. The participants averaged nearly 53 years of age at their first survey, and 84% were women.
The researchers subdivided the survey responses into 8,837 (11%) people who began a statin, antihypertensive drug, or both during their participation; 26,914 (33%) already on a statin or antihypertensive drug when they completed their first questionnaire; and 46,021 response sets (56%) from people who never began treatment with either drug class. People who initiated a relevant drug began a median of 1.7 years following completion of their first survey, and a median of 2.4 years before their next survey. During follow-up, about 2% of all participants became newly diagnosed with some form of CVD.
The results showed that, after full adjustment for possible confounders, the mean increase in body mass index was larger among those who initiated a CVD-prevention drug, compared with those who did not. Among participants who were obese at entry, those who started a CVD drug had a statistically significant 37% increased rate of remaining obese, compared with those not starting these drugs. Among those who were not obese at baseline, those who began a CVD prevention drug had a statistically significant 82%% higher rate of becoming obese, compared with those not on a CVD-prevention drug. In addition, average daily energy expenditure, a measure of physical activity, showed a statistically significant decline among those who started a CVD drug, compared with those who did not. In contrast, CVD drug initiators had an average 1.85 gram/week decline in alcohol intake, compared with noninitiators, and those who were current smokers at the first survey and then started a CVD drug had a 26% relative drop in their smoking prevalence, compared with those who did not start a CVD drug, both statistically significant differences.
The findings suggest that “patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” the authors concluded. “This means that expansion of pharmacologic interventions toward populations at low CVD risk may not necessarily lead to expected benefits at the population level.”
The study received no commercial funding. Dr. Korhonen had no disclosures.
SOURCE: Korhonen MJ et al. J Am Heart Assoc. 2020 Feb 5. doi: 10.1161/JAHA.119.014.168.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Hypertensive disorders of pregnancy in SLE contribute to later CV outcomes
Women with systemic lupus erythematosus (SLE) who experience hypertensive disorders of pregnancy may have a higher rate of cardiovascular outcomes after pregnancy, as well as a higher rate of hypertension later in life, than do those without maternal hypertension, according to findings from a Swedish population-based, longitudinal cohort study.
“Premature CVD [cardiovascular disease] is a well-documented complication in women with SLE, which is likely, at least in part, due to renal disease, prothrombotic [antiphospholipid antibodies], and systemic inflammation. Our data confirm that women who experience a hypertensive disorder in pregnancy [HDP] are at greater risk of developing hypertension after pregnancy, and that this association is also evident for women with SLE. Women with SLE and HDP were also at increased risk of CVD, particularly stroke, at young ages and should be monitored closely and consider treatment to attenuate risk,” wrote first author Julia F. Simard, ScD, of Stanford (Calif.) University and colleagues in Arthritis Care & Research.
To reach those conclusions, the researchers identified 3,340 women in the Swedish Medical Birth Register with their first singleton delivery during 1987-2012. They matched each of the 450 women with prevalent SLE from the Medical Birth Register to 5 women without SLE in the National Patient Register based on sex, birth year, calendar time, and county of residence.
During a median follow-up period of nearly 11 years, women with SLE had an unadjusted incidence rate of incident cardiovascular outcomes of 50 cases per 10,000 person-years versus 7.2 for women without SLE. Cardiovascular outcomes included fatal and nonfatal acute MI, fatal and nonfatal stroke, transient ischemic attacks, unstable angina, and heart failure. A history of HDP in women with SLE, including preeclampsia, was linked with about a twofold higher rate of cardiovascular outcomes regardless of multiple sensitivity analyses, both before and after adjusting for maternal age at delivery, county of birth, education, body mass index, and first-trimester smoking.
The researchers found that the hazard ratio for cardiovascular outcomes in women with SLE and HDP was about eight times higher than the hazard ratio for women without SLE but with HDP, but the relative rarity of cardiovascular events seen during the follow-up period, particularly among women without SLE, made it so that they “could not confirm established associations between HDP and CVD, possibly due to the relatively short follow-up time given that premenopausal CVD is rare among women free of SLE.”
HDP was associated with a threefold higher risk for incident hypertension later in life regardless of SLE status, even though the unadjusted incidence rate was 524 cases per 10,000 person-years among women with both SLE and HDP, compared with 177 per 10,000 person-years among women with HDP in the general population, which sensitivity analyses suggested “was not due to misclassification of antihypertensive use for renal disease in women with SLE nor antihypertensive use for possible HDP in subsequent pregnancies,” the researchers wrote.
Several authors reported research grants from the National Institutes of Health, the Karolinska Institute, the Swedish Research Council, Swedish Heart-Lung Foundation, Stockholm County Council, the King Gustaf V 80th Birthday Fund, the Swedish Rheumatism Association, and Ingegerd Johansson’s Foundation that helped to fund the study. All authors reported having no competing interests.
SOURCE: Simard JF et al. Arthritis Care Res. 2020 Jan 31. doi: 10.1002/acr.24160.
Women with systemic lupus erythematosus (SLE) who experience hypertensive disorders of pregnancy may have a higher rate of cardiovascular outcomes after pregnancy, as well as a higher rate of hypertension later in life, than do those without maternal hypertension, according to findings from a Swedish population-based, longitudinal cohort study.
“Premature CVD [cardiovascular disease] is a well-documented complication in women with SLE, which is likely, at least in part, due to renal disease, prothrombotic [antiphospholipid antibodies], and systemic inflammation. Our data confirm that women who experience a hypertensive disorder in pregnancy [HDP] are at greater risk of developing hypertension after pregnancy, and that this association is also evident for women with SLE. Women with SLE and HDP were also at increased risk of CVD, particularly stroke, at young ages and should be monitored closely and consider treatment to attenuate risk,” wrote first author Julia F. Simard, ScD, of Stanford (Calif.) University and colleagues in Arthritis Care & Research.
To reach those conclusions, the researchers identified 3,340 women in the Swedish Medical Birth Register with their first singleton delivery during 1987-2012. They matched each of the 450 women with prevalent SLE from the Medical Birth Register to 5 women without SLE in the National Patient Register based on sex, birth year, calendar time, and county of residence.
During a median follow-up period of nearly 11 years, women with SLE had an unadjusted incidence rate of incident cardiovascular outcomes of 50 cases per 10,000 person-years versus 7.2 for women without SLE. Cardiovascular outcomes included fatal and nonfatal acute MI, fatal and nonfatal stroke, transient ischemic attacks, unstable angina, and heart failure. A history of HDP in women with SLE, including preeclampsia, was linked with about a twofold higher rate of cardiovascular outcomes regardless of multiple sensitivity analyses, both before and after adjusting for maternal age at delivery, county of birth, education, body mass index, and first-trimester smoking.
The researchers found that the hazard ratio for cardiovascular outcomes in women with SLE and HDP was about eight times higher than the hazard ratio for women without SLE but with HDP, but the relative rarity of cardiovascular events seen during the follow-up period, particularly among women without SLE, made it so that they “could not confirm established associations between HDP and CVD, possibly due to the relatively short follow-up time given that premenopausal CVD is rare among women free of SLE.”
HDP was associated with a threefold higher risk for incident hypertension later in life regardless of SLE status, even though the unadjusted incidence rate was 524 cases per 10,000 person-years among women with both SLE and HDP, compared with 177 per 10,000 person-years among women with HDP in the general population, which sensitivity analyses suggested “was not due to misclassification of antihypertensive use for renal disease in women with SLE nor antihypertensive use for possible HDP in subsequent pregnancies,” the researchers wrote.
Several authors reported research grants from the National Institutes of Health, the Karolinska Institute, the Swedish Research Council, Swedish Heart-Lung Foundation, Stockholm County Council, the King Gustaf V 80th Birthday Fund, the Swedish Rheumatism Association, and Ingegerd Johansson’s Foundation that helped to fund the study. All authors reported having no competing interests.
SOURCE: Simard JF et al. Arthritis Care Res. 2020 Jan 31. doi: 10.1002/acr.24160.
Women with systemic lupus erythematosus (SLE) who experience hypertensive disorders of pregnancy may have a higher rate of cardiovascular outcomes after pregnancy, as well as a higher rate of hypertension later in life, than do those without maternal hypertension, according to findings from a Swedish population-based, longitudinal cohort study.
“Premature CVD [cardiovascular disease] is a well-documented complication in women with SLE, which is likely, at least in part, due to renal disease, prothrombotic [antiphospholipid antibodies], and systemic inflammation. Our data confirm that women who experience a hypertensive disorder in pregnancy [HDP] are at greater risk of developing hypertension after pregnancy, and that this association is also evident for women with SLE. Women with SLE and HDP were also at increased risk of CVD, particularly stroke, at young ages and should be monitored closely and consider treatment to attenuate risk,” wrote first author Julia F. Simard, ScD, of Stanford (Calif.) University and colleagues in Arthritis Care & Research.
To reach those conclusions, the researchers identified 3,340 women in the Swedish Medical Birth Register with their first singleton delivery during 1987-2012. They matched each of the 450 women with prevalent SLE from the Medical Birth Register to 5 women without SLE in the National Patient Register based on sex, birth year, calendar time, and county of residence.
During a median follow-up period of nearly 11 years, women with SLE had an unadjusted incidence rate of incident cardiovascular outcomes of 50 cases per 10,000 person-years versus 7.2 for women without SLE. Cardiovascular outcomes included fatal and nonfatal acute MI, fatal and nonfatal stroke, transient ischemic attacks, unstable angina, and heart failure. A history of HDP in women with SLE, including preeclampsia, was linked with about a twofold higher rate of cardiovascular outcomes regardless of multiple sensitivity analyses, both before and after adjusting for maternal age at delivery, county of birth, education, body mass index, and first-trimester smoking.
The researchers found that the hazard ratio for cardiovascular outcomes in women with SLE and HDP was about eight times higher than the hazard ratio for women without SLE but with HDP, but the relative rarity of cardiovascular events seen during the follow-up period, particularly among women without SLE, made it so that they “could not confirm established associations between HDP and CVD, possibly due to the relatively short follow-up time given that premenopausal CVD is rare among women free of SLE.”
HDP was associated with a threefold higher risk for incident hypertension later in life regardless of SLE status, even though the unadjusted incidence rate was 524 cases per 10,000 person-years among women with both SLE and HDP, compared with 177 per 10,000 person-years among women with HDP in the general population, which sensitivity analyses suggested “was not due to misclassification of antihypertensive use for renal disease in women with SLE nor antihypertensive use for possible HDP in subsequent pregnancies,” the researchers wrote.
Several authors reported research grants from the National Institutes of Health, the Karolinska Institute, the Swedish Research Council, Swedish Heart-Lung Foundation, Stockholm County Council, the King Gustaf V 80th Birthday Fund, the Swedish Rheumatism Association, and Ingegerd Johansson’s Foundation that helped to fund the study. All authors reported having no competing interests.
SOURCE: Simard JF et al. Arthritis Care Res. 2020 Jan 31. doi: 10.1002/acr.24160.
FROM ARTHRITIS CARE & RESEARCH
Who’ll get SAVR in 2020?
SNOWMASS, COLO. – The number of transcatheter aortic valve replacements (TAVRs) performed annually in the United States is forecast to rocket up from 75,000 in 2019 to 100,000 in 2020 in response to the procedure’s recent approval in low-surgical-risk patients with symptomatic aortic stenosis, Michael J. Mack, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“In 2020, TAVR seems like a tsunami that’s totally overwhelming SAVR [surgical aortic valve replacement]. And the question is, after the wave hits shore, is there going to be anything left in the surgical arena?” asked Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
He answered his own question with a quote from Mark Twain: “Reports of my death are greatly exaggerated.”
The trend is clear: TAVR will take over the market for isolated aortic valve replacement in much the same way that endovascular abdominal aortic aneurysm repair (EVAR) has come to dominate open surgical repair by an 80:20 margin. And By one estimate, it could include some 270,000 individuals per year in North America and the European Union (Eur Heart J. 2018 Jul 21;39[28]:2635-42).
But there’s no need to shed a tear at the prospect of SAVR surgeons standing in unemployment lines. They will continue to have their hands full performing combined SAVR plus coronary artery bypass graft (CABG) procedures, SAVR plus mitral or tricuspid valve operations, and Bentall procedures, Dr. Mack predicted.
Who should get SAVR for aortic stenosis in 2020? For starters, he said, the sorts of patients who were excluded from the major TAVR-versus-SAVR randomized trials. The low-surgical-risk trials were restricted to patients who had symptomatic aortic stenosis involving a tricuspid valve, no left ventricular outflow tract calcium, no or minimal coronary artery disease (CAD), a relatively normal left ventricular ejection fraction, and an aortic valve anatomy suitable for TAVR. And, 92% of study participants were over age 65 years.
Dr. Mack called the evidence for the safety and effectiveness of TAVR “the most robust evidence base in the history of medical devices,” backed by nine U.S. trials and 8,000 randomized patients during the last dozen years. He has played a major role in developing that evidence base, having served most recently as cochair of the landmark PARTNER 3 trial, which demonstrated superiority for TAVR over SAVR in low-surgical-risk patients. But the evidence base doesn’t apply to patients not enrolled in the trials. So for the foreseeable future, patients younger than age 65 years should probably stick with SAVR, mainly because of the still-open question of tissue valve durability and TAVR’s high rate of associated conduction system impairment and need for new pacemaker implantation. Younger patients find permanent pacemakers particularly problematic, he noted.
Others who should stick with surgery include patients with bicuspid valves, especially when aortopathy is present, individuals with low-lying coronary arteries, patients with heavy calcium deposits at the left ventricular outflow tract, those with infective endocarditis or rheumatic valve disease, and patients with structural valve deterioration after a valve-in-valve TAVR.
“Once you get beyond the first valve-in-valve, the outcomes are not going to be good. Those patients should preferentially be considered for surgery. The results for valve-in-valve have been very disappointing, with a 33% all-cause mortality at 3 years in the PARTNER Aortic Valve-in-Valve Registry,” according to the surgeon.
In patients with aortic stenosis and CAD, the clinical decision making should be based on the coronary disease. In a patient with triple-vessel disease, diabetes, and/or a high Syntax score for whom the collaborative multidisciplinary heart team would recommend surgical revascularization if aortic stenosis wasn’t present, the most appropriate option is SAVR plus CABG. On the other hand, if the CAD is amenable to percutaneous coronary intervention (PCI) and the Syntax score is low, TAVR plus PCI is a safe and solid strategy, he continued.
In addition to the unresolved issue of tissue valve durability, another unanswered question pushing against universal adoption of TAVR involves the clinical implications of bioprosthetic valve leaflet thrombosis and the optimal antithrombotic therapy, both early and late. Leaflet thrombosis post-TAVR is common – as well as post-SAVR with bioprosthetic valves, albeit less so – but the lesions often come and go. Although there is a theoretical concern that they might be a precursor to leaflet destruction, at this point, their clinical significance remains unclear. In the recent GALILEO trial, TAVR patients randomized to low-dose rivaroxaban (Xarelto) plus aspirin showed fewer leaflet motion abnormalities and less leaflet thickening than did those on dual-antiplatelet therapy, but a significantly higher all-cause mortality (N Engl J Med 2020 Jan 9;382:120-9).
“I know that nowhere else in the body is thrombus a good thing, so thrombus in the valve can’t be a good thing. The only question is, how bad is it? And right now all we know is, some of our treatments for it are worse than the disease,” the surgeon commented.
Dr. Mack indicated that, at this time, clinical decision making in aortic stenosis should begin on the basis of patient age, which influences the key decision of whether to opt for a mechanical versus tissue replacement valve. For patients aged 50-70 years, shared decision making between the heart team and patient is appropriate. The evidence suggests SAVR with a mechanical valve is the better option, but many patients in this intermediate age group loathe the ideal of lifelong oral anticoagulation and favor a tissue valve.
For patients under age 50 years, the best evidence indicates that SAVR with a mechanical valve is clearly the best option; however, most young patients are instead opting for a tissue valve, even after being cautioned about the lingering uncertainty surrounding tissue valve durability, be it SAVR or TAVR. For patients over age 70 years, a tissue valve is the best choice based on the outcomes in PARTNER 3 and other low-surgical-risk trials. If the patient is younger than 65 years and wants a tissue valve, Dr. Mack thinks the best evidence-based option is SAVR. Above age 80 years, TAVR is the clear choice. Age 65-80 years is shared–decision making territory regarding TAVR versus SAVR.
Dr. Mack reported serving as a consultant to Gore and receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
SNOWMASS, COLO. – The number of transcatheter aortic valve replacements (TAVRs) performed annually in the United States is forecast to rocket up from 75,000 in 2019 to 100,000 in 2020 in response to the procedure’s recent approval in low-surgical-risk patients with symptomatic aortic stenosis, Michael J. Mack, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“In 2020, TAVR seems like a tsunami that’s totally overwhelming SAVR [surgical aortic valve replacement]. And the question is, after the wave hits shore, is there going to be anything left in the surgical arena?” asked Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
He answered his own question with a quote from Mark Twain: “Reports of my death are greatly exaggerated.”
The trend is clear: TAVR will take over the market for isolated aortic valve replacement in much the same way that endovascular abdominal aortic aneurysm repair (EVAR) has come to dominate open surgical repair by an 80:20 margin. And By one estimate, it could include some 270,000 individuals per year in North America and the European Union (Eur Heart J. 2018 Jul 21;39[28]:2635-42).
But there’s no need to shed a tear at the prospect of SAVR surgeons standing in unemployment lines. They will continue to have their hands full performing combined SAVR plus coronary artery bypass graft (CABG) procedures, SAVR plus mitral or tricuspid valve operations, and Bentall procedures, Dr. Mack predicted.
Who should get SAVR for aortic stenosis in 2020? For starters, he said, the sorts of patients who were excluded from the major TAVR-versus-SAVR randomized trials. The low-surgical-risk trials were restricted to patients who had symptomatic aortic stenosis involving a tricuspid valve, no left ventricular outflow tract calcium, no or minimal coronary artery disease (CAD), a relatively normal left ventricular ejection fraction, and an aortic valve anatomy suitable for TAVR. And, 92% of study participants were over age 65 years.
Dr. Mack called the evidence for the safety and effectiveness of TAVR “the most robust evidence base in the history of medical devices,” backed by nine U.S. trials and 8,000 randomized patients during the last dozen years. He has played a major role in developing that evidence base, having served most recently as cochair of the landmark PARTNER 3 trial, which demonstrated superiority for TAVR over SAVR in low-surgical-risk patients. But the evidence base doesn’t apply to patients not enrolled in the trials. So for the foreseeable future, patients younger than age 65 years should probably stick with SAVR, mainly because of the still-open question of tissue valve durability and TAVR’s high rate of associated conduction system impairment and need for new pacemaker implantation. Younger patients find permanent pacemakers particularly problematic, he noted.
Others who should stick with surgery include patients with bicuspid valves, especially when aortopathy is present, individuals with low-lying coronary arteries, patients with heavy calcium deposits at the left ventricular outflow tract, those with infective endocarditis or rheumatic valve disease, and patients with structural valve deterioration after a valve-in-valve TAVR.
“Once you get beyond the first valve-in-valve, the outcomes are not going to be good. Those patients should preferentially be considered for surgery. The results for valve-in-valve have been very disappointing, with a 33% all-cause mortality at 3 years in the PARTNER Aortic Valve-in-Valve Registry,” according to the surgeon.
In patients with aortic stenosis and CAD, the clinical decision making should be based on the coronary disease. In a patient with triple-vessel disease, diabetes, and/or a high Syntax score for whom the collaborative multidisciplinary heart team would recommend surgical revascularization if aortic stenosis wasn’t present, the most appropriate option is SAVR plus CABG. On the other hand, if the CAD is amenable to percutaneous coronary intervention (PCI) and the Syntax score is low, TAVR plus PCI is a safe and solid strategy, he continued.
In addition to the unresolved issue of tissue valve durability, another unanswered question pushing against universal adoption of TAVR involves the clinical implications of bioprosthetic valve leaflet thrombosis and the optimal antithrombotic therapy, both early and late. Leaflet thrombosis post-TAVR is common – as well as post-SAVR with bioprosthetic valves, albeit less so – but the lesions often come and go. Although there is a theoretical concern that they might be a precursor to leaflet destruction, at this point, their clinical significance remains unclear. In the recent GALILEO trial, TAVR patients randomized to low-dose rivaroxaban (Xarelto) plus aspirin showed fewer leaflet motion abnormalities and less leaflet thickening than did those on dual-antiplatelet therapy, but a significantly higher all-cause mortality (N Engl J Med 2020 Jan 9;382:120-9).
“I know that nowhere else in the body is thrombus a good thing, so thrombus in the valve can’t be a good thing. The only question is, how bad is it? And right now all we know is, some of our treatments for it are worse than the disease,” the surgeon commented.
Dr. Mack indicated that, at this time, clinical decision making in aortic stenosis should begin on the basis of patient age, which influences the key decision of whether to opt for a mechanical versus tissue replacement valve. For patients aged 50-70 years, shared decision making between the heart team and patient is appropriate. The evidence suggests SAVR with a mechanical valve is the better option, but many patients in this intermediate age group loathe the ideal of lifelong oral anticoagulation and favor a tissue valve.
For patients under age 50 years, the best evidence indicates that SAVR with a mechanical valve is clearly the best option; however, most young patients are instead opting for a tissue valve, even after being cautioned about the lingering uncertainty surrounding tissue valve durability, be it SAVR or TAVR. For patients over age 70 years, a tissue valve is the best choice based on the outcomes in PARTNER 3 and other low-surgical-risk trials. If the patient is younger than 65 years and wants a tissue valve, Dr. Mack thinks the best evidence-based option is SAVR. Above age 80 years, TAVR is the clear choice. Age 65-80 years is shared–decision making territory regarding TAVR versus SAVR.
Dr. Mack reported serving as a consultant to Gore and receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
SNOWMASS, COLO. – The number of transcatheter aortic valve replacements (TAVRs) performed annually in the United States is forecast to rocket up from 75,000 in 2019 to 100,000 in 2020 in response to the procedure’s recent approval in low-surgical-risk patients with symptomatic aortic stenosis, Michael J. Mack, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“In 2020, TAVR seems like a tsunami that’s totally overwhelming SAVR [surgical aortic valve replacement]. And the question is, after the wave hits shore, is there going to be anything left in the surgical arena?” asked Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
He answered his own question with a quote from Mark Twain: “Reports of my death are greatly exaggerated.”
The trend is clear: TAVR will take over the market for isolated aortic valve replacement in much the same way that endovascular abdominal aortic aneurysm repair (EVAR) has come to dominate open surgical repair by an 80:20 margin. And By one estimate, it could include some 270,000 individuals per year in North America and the European Union (Eur Heart J. 2018 Jul 21;39[28]:2635-42).
But there’s no need to shed a tear at the prospect of SAVR surgeons standing in unemployment lines. They will continue to have their hands full performing combined SAVR plus coronary artery bypass graft (CABG) procedures, SAVR plus mitral or tricuspid valve operations, and Bentall procedures, Dr. Mack predicted.
Who should get SAVR for aortic stenosis in 2020? For starters, he said, the sorts of patients who were excluded from the major TAVR-versus-SAVR randomized trials. The low-surgical-risk trials were restricted to patients who had symptomatic aortic stenosis involving a tricuspid valve, no left ventricular outflow tract calcium, no or minimal coronary artery disease (CAD), a relatively normal left ventricular ejection fraction, and an aortic valve anatomy suitable for TAVR. And, 92% of study participants were over age 65 years.
Dr. Mack called the evidence for the safety and effectiveness of TAVR “the most robust evidence base in the history of medical devices,” backed by nine U.S. trials and 8,000 randomized patients during the last dozen years. He has played a major role in developing that evidence base, having served most recently as cochair of the landmark PARTNER 3 trial, which demonstrated superiority for TAVR over SAVR in low-surgical-risk patients. But the evidence base doesn’t apply to patients not enrolled in the trials. So for the foreseeable future, patients younger than age 65 years should probably stick with SAVR, mainly because of the still-open question of tissue valve durability and TAVR’s high rate of associated conduction system impairment and need for new pacemaker implantation. Younger patients find permanent pacemakers particularly problematic, he noted.
Others who should stick with surgery include patients with bicuspid valves, especially when aortopathy is present, individuals with low-lying coronary arteries, patients with heavy calcium deposits at the left ventricular outflow tract, those with infective endocarditis or rheumatic valve disease, and patients with structural valve deterioration after a valve-in-valve TAVR.
“Once you get beyond the first valve-in-valve, the outcomes are not going to be good. Those patients should preferentially be considered for surgery. The results for valve-in-valve have been very disappointing, with a 33% all-cause mortality at 3 years in the PARTNER Aortic Valve-in-Valve Registry,” according to the surgeon.
In patients with aortic stenosis and CAD, the clinical decision making should be based on the coronary disease. In a patient with triple-vessel disease, diabetes, and/or a high Syntax score for whom the collaborative multidisciplinary heart team would recommend surgical revascularization if aortic stenosis wasn’t present, the most appropriate option is SAVR plus CABG. On the other hand, if the CAD is amenable to percutaneous coronary intervention (PCI) and the Syntax score is low, TAVR plus PCI is a safe and solid strategy, he continued.
In addition to the unresolved issue of tissue valve durability, another unanswered question pushing against universal adoption of TAVR involves the clinical implications of bioprosthetic valve leaflet thrombosis and the optimal antithrombotic therapy, both early and late. Leaflet thrombosis post-TAVR is common – as well as post-SAVR with bioprosthetic valves, albeit less so – but the lesions often come and go. Although there is a theoretical concern that they might be a precursor to leaflet destruction, at this point, their clinical significance remains unclear. In the recent GALILEO trial, TAVR patients randomized to low-dose rivaroxaban (Xarelto) plus aspirin showed fewer leaflet motion abnormalities and less leaflet thickening than did those on dual-antiplatelet therapy, but a significantly higher all-cause mortality (N Engl J Med 2020 Jan 9;382:120-9).
“I know that nowhere else in the body is thrombus a good thing, so thrombus in the valve can’t be a good thing. The only question is, how bad is it? And right now all we know is, some of our treatments for it are worse than the disease,” the surgeon commented.
Dr. Mack indicated that, at this time, clinical decision making in aortic stenosis should begin on the basis of patient age, which influences the key decision of whether to opt for a mechanical versus tissue replacement valve. For patients aged 50-70 years, shared decision making between the heart team and patient is appropriate. The evidence suggests SAVR with a mechanical valve is the better option, but many patients in this intermediate age group loathe the ideal of lifelong oral anticoagulation and favor a tissue valve.
For patients under age 50 years, the best evidence indicates that SAVR with a mechanical valve is clearly the best option; however, most young patients are instead opting for a tissue valve, even after being cautioned about the lingering uncertainty surrounding tissue valve durability, be it SAVR or TAVR. For patients over age 70 years, a tissue valve is the best choice based on the outcomes in PARTNER 3 and other low-surgical-risk trials. If the patient is younger than 65 years and wants a tissue valve, Dr. Mack thinks the best evidence-based option is SAVR. Above age 80 years, TAVR is the clear choice. Age 65-80 years is shared–decision making territory regarding TAVR versus SAVR.
Dr. Mack reported serving as a consultant to Gore and receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
Heart rhythm data from wearables confounds EP practice
NATIONAL HARBOR, MD. – or other warnings that flagged a possible cardiac arrhythmia.
While the clinical community has yet to reach an evidence-based consensus on how to deal with this information, or even asymptomatic arrhythmias identified by more standard means, the American public is voting with their wrists. People seem to like collecting and reviewing readouts on their heart rhythm and other vital data, and then they often take their numbers to a physician, especially when their device suggests a possible problem.
“The whole paradigm of ordering a test only if you intend to act on the result has been flipped. People now get what they want directly, and our job is to guide them” after the fact. “You need to teach people what’s actionable and what’s not,” Mintu P. Turakhia, MD, said at the annual International AF Symposium.
“We’re in a situation where the ability of a sensor to detect things is separate from access to the health care system. They are no longer coupled; they are disjointed. People can create their own ICU in their house just by shopping online, but what do we do with this information, whether it’s an irregular heart rhythm or their whole genome?” asked Dr. Turakhia, executive director of the Center for Digital Health at Stanford (Calif.) University and director of cardiac electrophysiology at the VA Palo Alto (Calif.) Health Care System.
“The main challenge is people without a diagnosis who get a notification. How much monitoring should you do until you can say it was a false positive? We don’t know what to do, so we monitor them. People are trying to figure this out.” Dr. Turakhia said. Some people who seek out electrophysiologists this way “may not even have a primary care physician,” he noted.
The potential implications of widespread monitoring for heartbeat irregularities in the general public began to surface in a study that Dr. Turakhia helped run that collected wearable data from nearly 420,000 Americans. Results from the Apple Heart Study showed that, during a median 117 days of monitoring with a smart watch, 2,161 people (0.5%) received a report of an irregular pulse, which led to further investigations that eventually diagnosed atrial fibrillation (AFib) in 153 people of the 450 who underwent follow-up assessment (N Engl J Med. 2019 Nov 14;381[20]:1909-17). These results “raise questions” about the large number of people who underwent follow-up testing who did not have arrhythmia, Dr. Turakhia noted.
“The dissemination of wearables has been quite dramatic, and electrophysiologists end up owning this,” commented Jeremy N. Ruskin, MD, professor of medicine at Harvard Medical School and director emeritus of the cardiac arrhythmia service at Massachusetts General Hospital, both in Boston. “I get a ton of calls from people whom I wish never bought a smart watch, and they say ‘I have atrial fibrillation. What do I do?’ ”
To document the growth of this trend, Dr. Turakhia cited results from a survey he collaborated on, run by Stanford and Rock Health, that found a 33% ownership rate among American adults of a wearable device capable of collecting health data, and a 42% rate of people who tracked their health data with a device, app, journal, or log. Both of these rates more than doubled what a similar survey found in 2015.
The cardiac electrophysiology community took a first step toward addressing one aspect of this evolving situation. In early 2020, the Heart Rhythm Society and the Consumer Technology Association jointly issued a guidance document targeted at consumers that walks them through the kinds of information their wearable devices might collect and how to approach this information. The main message: If you have questions or concerns about your data, consult a clinician. What remains in short supply is guidance to clinicians on what to do when they see these patients.
“Until recently, device-detected AFib was the sole purview of electrophysiologists using implanted rhythm-monitoring devices. Now mobile and other devices raise issues [of asymptomatic AFib] for a much broader population,” noted Daniel E. Singer, MD, professor of medicine and epidemiology at Harvard and Massachusetts General Hospital. “The world of device-detected AFib now includes watches.”
Researchers have tried for years to better understand the stroke risk faced by patients with asymptomatic or subclinical AFib that’s detected by an implanted device, as in the ASSERT study of nearly 2,600 patients followed for a median of 2.5 years that found an increased stroke risk when the duration of individual, subclinical AFib episodes surpassed 24 hours (Eur Heart J. 2017 May 1;38[17]:1339-44). More recently, a study of AFib duration collected by implanted cardiac devices in nearly 22,000 Americans showed a relationship between stroke risk and both the duration of AFib episodes and the underlying risk of a person for stroke as measured by their CHA2DS2-VAScscore (Circulation. 2019 Nov 12;140[20]:1639-46). Just under 30% of patients in the study were diagnosed with AFib at entry.
The implications of asymptomatic episodes of AFib have so far been largely studied in people with an implanted cardiac device, which may have limited applicability to wearable users. In addition, the field has not yet fully sorted out the relationships between the duration of individual AFib episodes and overall AFib burden, and a person’s stroke risk and the window of time when the potential stroke-preventing benefits of anticoagulation outweigh its bleeding risk.
The results of trials now in progress that are examining the safety and efficacy of medical interventions designed to avert strokes in patients with asymptomatic AFib “will bear on the use of anticoagulants in a large group of patients,” including people with AFib detected by a wearable, Dr. Singer predicted.
The Apple Heart Study was sponsored Apple. Dr. Turakhia has received funding from Apple, and he has received honoraria or research funding from several other companies. Dr. Ruskin has been a consultant or adviser to several companies, is a steering committee member for Pfizer, and holds equity or options in Portola, Element Science, NewPace, Gilead, and InfoBionic. Dr. Singer has been a consultant and adviser to Boehringer Ingelheim, Bristol-Myers Squibb, Johnson & Johnson, Merck, and Pfizer, and he has received research grants from Bristol-Myers Squibb.
NATIONAL HARBOR, MD. – or other warnings that flagged a possible cardiac arrhythmia.
While the clinical community has yet to reach an evidence-based consensus on how to deal with this information, or even asymptomatic arrhythmias identified by more standard means, the American public is voting with their wrists. People seem to like collecting and reviewing readouts on their heart rhythm and other vital data, and then they often take their numbers to a physician, especially when their device suggests a possible problem.
“The whole paradigm of ordering a test only if you intend to act on the result has been flipped. People now get what they want directly, and our job is to guide them” after the fact. “You need to teach people what’s actionable and what’s not,” Mintu P. Turakhia, MD, said at the annual International AF Symposium.
“We’re in a situation where the ability of a sensor to detect things is separate from access to the health care system. They are no longer coupled; they are disjointed. People can create their own ICU in their house just by shopping online, but what do we do with this information, whether it’s an irregular heart rhythm or their whole genome?” asked Dr. Turakhia, executive director of the Center for Digital Health at Stanford (Calif.) University and director of cardiac electrophysiology at the VA Palo Alto (Calif.) Health Care System.
“The main challenge is people without a diagnosis who get a notification. How much monitoring should you do until you can say it was a false positive? We don’t know what to do, so we monitor them. People are trying to figure this out.” Dr. Turakhia said. Some people who seek out electrophysiologists this way “may not even have a primary care physician,” he noted.
The potential implications of widespread monitoring for heartbeat irregularities in the general public began to surface in a study that Dr. Turakhia helped run that collected wearable data from nearly 420,000 Americans. Results from the Apple Heart Study showed that, during a median 117 days of monitoring with a smart watch, 2,161 people (0.5%) received a report of an irregular pulse, which led to further investigations that eventually diagnosed atrial fibrillation (AFib) in 153 people of the 450 who underwent follow-up assessment (N Engl J Med. 2019 Nov 14;381[20]:1909-17). These results “raise questions” about the large number of people who underwent follow-up testing who did not have arrhythmia, Dr. Turakhia noted.
“The dissemination of wearables has been quite dramatic, and electrophysiologists end up owning this,” commented Jeremy N. Ruskin, MD, professor of medicine at Harvard Medical School and director emeritus of the cardiac arrhythmia service at Massachusetts General Hospital, both in Boston. “I get a ton of calls from people whom I wish never bought a smart watch, and they say ‘I have atrial fibrillation. What do I do?’ ”
To document the growth of this trend, Dr. Turakhia cited results from a survey he collaborated on, run by Stanford and Rock Health, that found a 33% ownership rate among American adults of a wearable device capable of collecting health data, and a 42% rate of people who tracked their health data with a device, app, journal, or log. Both of these rates more than doubled what a similar survey found in 2015.
The cardiac electrophysiology community took a first step toward addressing one aspect of this evolving situation. In early 2020, the Heart Rhythm Society and the Consumer Technology Association jointly issued a guidance document targeted at consumers that walks them through the kinds of information their wearable devices might collect and how to approach this information. The main message: If you have questions or concerns about your data, consult a clinician. What remains in short supply is guidance to clinicians on what to do when they see these patients.
“Until recently, device-detected AFib was the sole purview of electrophysiologists using implanted rhythm-monitoring devices. Now mobile and other devices raise issues [of asymptomatic AFib] for a much broader population,” noted Daniel E. Singer, MD, professor of medicine and epidemiology at Harvard and Massachusetts General Hospital. “The world of device-detected AFib now includes watches.”
Researchers have tried for years to better understand the stroke risk faced by patients with asymptomatic or subclinical AFib that’s detected by an implanted device, as in the ASSERT study of nearly 2,600 patients followed for a median of 2.5 years that found an increased stroke risk when the duration of individual, subclinical AFib episodes surpassed 24 hours (Eur Heart J. 2017 May 1;38[17]:1339-44). More recently, a study of AFib duration collected by implanted cardiac devices in nearly 22,000 Americans showed a relationship between stroke risk and both the duration of AFib episodes and the underlying risk of a person for stroke as measured by their CHA2DS2-VAScscore (Circulation. 2019 Nov 12;140[20]:1639-46). Just under 30% of patients in the study were diagnosed with AFib at entry.
The implications of asymptomatic episodes of AFib have so far been largely studied in people with an implanted cardiac device, which may have limited applicability to wearable users. In addition, the field has not yet fully sorted out the relationships between the duration of individual AFib episodes and overall AFib burden, and a person’s stroke risk and the window of time when the potential stroke-preventing benefits of anticoagulation outweigh its bleeding risk.
The results of trials now in progress that are examining the safety and efficacy of medical interventions designed to avert strokes in patients with asymptomatic AFib “will bear on the use of anticoagulants in a large group of patients,” including people with AFib detected by a wearable, Dr. Singer predicted.
The Apple Heart Study was sponsored Apple. Dr. Turakhia has received funding from Apple, and he has received honoraria or research funding from several other companies. Dr. Ruskin has been a consultant or adviser to several companies, is a steering committee member for Pfizer, and holds equity or options in Portola, Element Science, NewPace, Gilead, and InfoBionic. Dr. Singer has been a consultant and adviser to Boehringer Ingelheim, Bristol-Myers Squibb, Johnson & Johnson, Merck, and Pfizer, and he has received research grants from Bristol-Myers Squibb.
NATIONAL HARBOR, MD. – or other warnings that flagged a possible cardiac arrhythmia.
While the clinical community has yet to reach an evidence-based consensus on how to deal with this information, or even asymptomatic arrhythmias identified by more standard means, the American public is voting with their wrists. People seem to like collecting and reviewing readouts on their heart rhythm and other vital data, and then they often take their numbers to a physician, especially when their device suggests a possible problem.
“The whole paradigm of ordering a test only if you intend to act on the result has been flipped. People now get what they want directly, and our job is to guide them” after the fact. “You need to teach people what’s actionable and what’s not,” Mintu P. Turakhia, MD, said at the annual International AF Symposium.
“We’re in a situation where the ability of a sensor to detect things is separate from access to the health care system. They are no longer coupled; they are disjointed. People can create their own ICU in their house just by shopping online, but what do we do with this information, whether it’s an irregular heart rhythm or their whole genome?” asked Dr. Turakhia, executive director of the Center for Digital Health at Stanford (Calif.) University and director of cardiac electrophysiology at the VA Palo Alto (Calif.) Health Care System.
“The main challenge is people without a diagnosis who get a notification. How much monitoring should you do until you can say it was a false positive? We don’t know what to do, so we monitor them. People are trying to figure this out.” Dr. Turakhia said. Some people who seek out electrophysiologists this way “may not even have a primary care physician,” he noted.
The potential implications of widespread monitoring for heartbeat irregularities in the general public began to surface in a study that Dr. Turakhia helped run that collected wearable data from nearly 420,000 Americans. Results from the Apple Heart Study showed that, during a median 117 days of monitoring with a smart watch, 2,161 people (0.5%) received a report of an irregular pulse, which led to further investigations that eventually diagnosed atrial fibrillation (AFib) in 153 people of the 450 who underwent follow-up assessment (N Engl J Med. 2019 Nov 14;381[20]:1909-17). These results “raise questions” about the large number of people who underwent follow-up testing who did not have arrhythmia, Dr. Turakhia noted.
“The dissemination of wearables has been quite dramatic, and electrophysiologists end up owning this,” commented Jeremy N. Ruskin, MD, professor of medicine at Harvard Medical School and director emeritus of the cardiac arrhythmia service at Massachusetts General Hospital, both in Boston. “I get a ton of calls from people whom I wish never bought a smart watch, and they say ‘I have atrial fibrillation. What do I do?’ ”
To document the growth of this trend, Dr. Turakhia cited results from a survey he collaborated on, run by Stanford and Rock Health, that found a 33% ownership rate among American adults of a wearable device capable of collecting health data, and a 42% rate of people who tracked their health data with a device, app, journal, or log. Both of these rates more than doubled what a similar survey found in 2015.
The cardiac electrophysiology community took a first step toward addressing one aspect of this evolving situation. In early 2020, the Heart Rhythm Society and the Consumer Technology Association jointly issued a guidance document targeted at consumers that walks them through the kinds of information their wearable devices might collect and how to approach this information. The main message: If you have questions or concerns about your data, consult a clinician. What remains in short supply is guidance to clinicians on what to do when they see these patients.
“Until recently, device-detected AFib was the sole purview of electrophysiologists using implanted rhythm-monitoring devices. Now mobile and other devices raise issues [of asymptomatic AFib] for a much broader population,” noted Daniel E. Singer, MD, professor of medicine and epidemiology at Harvard and Massachusetts General Hospital. “The world of device-detected AFib now includes watches.”
Researchers have tried for years to better understand the stroke risk faced by patients with asymptomatic or subclinical AFib that’s detected by an implanted device, as in the ASSERT study of nearly 2,600 patients followed for a median of 2.5 years that found an increased stroke risk when the duration of individual, subclinical AFib episodes surpassed 24 hours (Eur Heart J. 2017 May 1;38[17]:1339-44). More recently, a study of AFib duration collected by implanted cardiac devices in nearly 22,000 Americans showed a relationship between stroke risk and both the duration of AFib episodes and the underlying risk of a person for stroke as measured by their CHA2DS2-VAScscore (Circulation. 2019 Nov 12;140[20]:1639-46). Just under 30% of patients in the study were diagnosed with AFib at entry.
The implications of asymptomatic episodes of AFib have so far been largely studied in people with an implanted cardiac device, which may have limited applicability to wearable users. In addition, the field has not yet fully sorted out the relationships between the duration of individual AFib episodes and overall AFib burden, and a person’s stroke risk and the window of time when the potential stroke-preventing benefits of anticoagulation outweigh its bleeding risk.
The results of trials now in progress that are examining the safety and efficacy of medical interventions designed to avert strokes in patients with asymptomatic AFib “will bear on the use of anticoagulants in a large group of patients,” including people with AFib detected by a wearable, Dr. Singer predicted.
The Apple Heart Study was sponsored Apple. Dr. Turakhia has received funding from Apple, and he has received honoraria or research funding from several other companies. Dr. Ruskin has been a consultant or adviser to several companies, is a steering committee member for Pfizer, and holds equity or options in Portola, Element Science, NewPace, Gilead, and InfoBionic. Dr. Singer has been a consultant and adviser to Boehringer Ingelheim, Bristol-Myers Squibb, Johnson & Johnson, Merck, and Pfizer, and he has received research grants from Bristol-Myers Squibb.
REPORTING FROM THE AF SYMPOSIUM 2020
Physician groups push back on Medicaid block grant plan
It took less than a day for physician groups to start pushing back at the Centers for Medicare & Medicaid Services over its new Medicaid block grant plan, which was introduced on Jan. 30.
Dubbed “Healthy Adult Opportunity,” the agency is offering all states the chance to participate in a block grant program through the 1115 waiver process.
According to a fact sheet issued by the agency, the program will focus on “adults under age 65 who are not eligible for Medicaid on the basis of disability or their need for long term care services and supports, and who are not eligible under a state plan. Other very low-income parents, children, pregnant women, elderly adults, and people eligible on the basis of a disability will not be directly affected – except from the improvement that results from states reinvesting savings into strengthening their overall programs.”
States will be operating within a defined budget when participating in the program and expenditures exceeding that defined budget will not be eligible for additional federal funding. Budgets will be based on a state’s historic costs, as well as national and regional trends, and will be tied to inflation with the potential to have adjustments made for extraordinary events. States can set their baseline using the prior year’s total spending or a per-enrollee spending model.
A Jan. 30 letter to state Medicaid directors notes that states participating in the program “will be granted extensive flexibility to test alternative approaches to implementing their Medicaid programs, including the ability to make many ongoing program adjustments without the need for demonstration or state plan amendments that require prior approval.”
Among the activities states can engage in under this plan are adjusting cost-sharing requirements, adopting a closed formulary, and applying additional conditions of eligibility. Requests, if approved, will be approved for a 5-year initial period, with a renewal option of up to 10 years.
But physician groups are not seeing a benefit with this new block grant program.
“Moving to a block grant system will likely limit the ability of Medicaid patients to receive preventive and needed medical care from their family physicians, and it will only increase the health disparities that exist in these communities, worsen overall health outcomes, and ultimately increase costs,” Gary LeRoy, MD, president of the American Academy of Family Physicians, said in a statement.
The American Medical Association concurred.
“The AMA opposes caps on federal Medicaid funding, such as block grants, because they would increase the number of uninsured and undermine Medicaid’s role as an indispensable safety net,” Patrice Harris, MD, the AMA’s president, said in a statement. “The AMA supports flexibility in Medicaid and encourages CMS to work with states to develop and test new Medicaid models that best meet the needs and priorities of low-income patients. While encouraging flexibility, the AMA is mindful that expanding Medicaid has been a literal lifesaver for low-income patients. We need to find ways to build on this success. We look forward to reviewing the proposal in detail.”
Officials at the American College of Obstetricians and Gynecologists said the changes have the potential to harm women and children’s health, as well as negatively impact physician reimbursement and ultimately access to care.
“Limits on the federal contribution to the Medicaid program would negatively impact patients by forcing states to reduce the number of people who are eligible for Medicaid coverage, eliminate covered services, and increase beneficiary cost-sharing,” ACOG President Ted Anderson, MD, said in a statement. “ACOG is also concerned that this block grant opportunity could lower physician reimbursement for certain services, forcing providers out of the program and jeopardizing patients’ ability to access health care services. Given our nation’s stark rates of maternal mortality and severe maternal morbidity, we are alarmed by the Administration’s willingness to weaken physician payment in Medicaid.”
It took less than a day for physician groups to start pushing back at the Centers for Medicare & Medicaid Services over its new Medicaid block grant plan, which was introduced on Jan. 30.
Dubbed “Healthy Adult Opportunity,” the agency is offering all states the chance to participate in a block grant program through the 1115 waiver process.
According to a fact sheet issued by the agency, the program will focus on “adults under age 65 who are not eligible for Medicaid on the basis of disability or their need for long term care services and supports, and who are not eligible under a state plan. Other very low-income parents, children, pregnant women, elderly adults, and people eligible on the basis of a disability will not be directly affected – except from the improvement that results from states reinvesting savings into strengthening their overall programs.”
States will be operating within a defined budget when participating in the program and expenditures exceeding that defined budget will not be eligible for additional federal funding. Budgets will be based on a state’s historic costs, as well as national and regional trends, and will be tied to inflation with the potential to have adjustments made for extraordinary events. States can set their baseline using the prior year’s total spending or a per-enrollee spending model.
A Jan. 30 letter to state Medicaid directors notes that states participating in the program “will be granted extensive flexibility to test alternative approaches to implementing their Medicaid programs, including the ability to make many ongoing program adjustments without the need for demonstration or state plan amendments that require prior approval.”
Among the activities states can engage in under this plan are adjusting cost-sharing requirements, adopting a closed formulary, and applying additional conditions of eligibility. Requests, if approved, will be approved for a 5-year initial period, with a renewal option of up to 10 years.
But physician groups are not seeing a benefit with this new block grant program.
“Moving to a block grant system will likely limit the ability of Medicaid patients to receive preventive and needed medical care from their family physicians, and it will only increase the health disparities that exist in these communities, worsen overall health outcomes, and ultimately increase costs,” Gary LeRoy, MD, president of the American Academy of Family Physicians, said in a statement.
The American Medical Association concurred.
“The AMA opposes caps on federal Medicaid funding, such as block grants, because they would increase the number of uninsured and undermine Medicaid’s role as an indispensable safety net,” Patrice Harris, MD, the AMA’s president, said in a statement. “The AMA supports flexibility in Medicaid and encourages CMS to work with states to develop and test new Medicaid models that best meet the needs and priorities of low-income patients. While encouraging flexibility, the AMA is mindful that expanding Medicaid has been a literal lifesaver for low-income patients. We need to find ways to build on this success. We look forward to reviewing the proposal in detail.”
Officials at the American College of Obstetricians and Gynecologists said the changes have the potential to harm women and children’s health, as well as negatively impact physician reimbursement and ultimately access to care.
“Limits on the federal contribution to the Medicaid program would negatively impact patients by forcing states to reduce the number of people who are eligible for Medicaid coverage, eliminate covered services, and increase beneficiary cost-sharing,” ACOG President Ted Anderson, MD, said in a statement. “ACOG is also concerned that this block grant opportunity could lower physician reimbursement for certain services, forcing providers out of the program and jeopardizing patients’ ability to access health care services. Given our nation’s stark rates of maternal mortality and severe maternal morbidity, we are alarmed by the Administration’s willingness to weaken physician payment in Medicaid.”
It took less than a day for physician groups to start pushing back at the Centers for Medicare & Medicaid Services over its new Medicaid block grant plan, which was introduced on Jan. 30.
Dubbed “Healthy Adult Opportunity,” the agency is offering all states the chance to participate in a block grant program through the 1115 waiver process.
According to a fact sheet issued by the agency, the program will focus on “adults under age 65 who are not eligible for Medicaid on the basis of disability or their need for long term care services and supports, and who are not eligible under a state plan. Other very low-income parents, children, pregnant women, elderly adults, and people eligible on the basis of a disability will not be directly affected – except from the improvement that results from states reinvesting savings into strengthening their overall programs.”
States will be operating within a defined budget when participating in the program and expenditures exceeding that defined budget will not be eligible for additional federal funding. Budgets will be based on a state’s historic costs, as well as national and regional trends, and will be tied to inflation with the potential to have adjustments made for extraordinary events. States can set their baseline using the prior year’s total spending or a per-enrollee spending model.
A Jan. 30 letter to state Medicaid directors notes that states participating in the program “will be granted extensive flexibility to test alternative approaches to implementing their Medicaid programs, including the ability to make many ongoing program adjustments without the need for demonstration or state plan amendments that require prior approval.”
Among the activities states can engage in under this plan are adjusting cost-sharing requirements, adopting a closed formulary, and applying additional conditions of eligibility. Requests, if approved, will be approved for a 5-year initial period, with a renewal option of up to 10 years.
But physician groups are not seeing a benefit with this new block grant program.
“Moving to a block grant system will likely limit the ability of Medicaid patients to receive preventive and needed medical care from their family physicians, and it will only increase the health disparities that exist in these communities, worsen overall health outcomes, and ultimately increase costs,” Gary LeRoy, MD, president of the American Academy of Family Physicians, said in a statement.
The American Medical Association concurred.
“The AMA opposes caps on federal Medicaid funding, such as block grants, because they would increase the number of uninsured and undermine Medicaid’s role as an indispensable safety net,” Patrice Harris, MD, the AMA’s president, said in a statement. “The AMA supports flexibility in Medicaid and encourages CMS to work with states to develop and test new Medicaid models that best meet the needs and priorities of low-income patients. While encouraging flexibility, the AMA is mindful that expanding Medicaid has been a literal lifesaver for low-income patients. We need to find ways to build on this success. We look forward to reviewing the proposal in detail.”
Officials at the American College of Obstetricians and Gynecologists said the changes have the potential to harm women and children’s health, as well as negatively impact physician reimbursement and ultimately access to care.
“Limits on the federal contribution to the Medicaid program would negatively impact patients by forcing states to reduce the number of people who are eligible for Medicaid coverage, eliminate covered services, and increase beneficiary cost-sharing,” ACOG President Ted Anderson, MD, said in a statement. “ACOG is also concerned that this block grant opportunity could lower physician reimbursement for certain services, forcing providers out of the program and jeopardizing patients’ ability to access health care services. Given our nation’s stark rates of maternal mortality and severe maternal morbidity, we are alarmed by the Administration’s willingness to weaken physician payment in Medicaid.”
Walk test may predict complications after lung cancer surgery
Risk of cardiopulmonary complications increased nearly eightfold in patients with moderate lung function decreases who failed to walk 400 m or more, according to the study, which included data on 416 patients with non–small cell lung cancer (NSCLC) who underwent lobectomy.
This is believed to be the first large study evaluating the utility of the 6-minute walk test (6MWT) to predict postoperative cardiopulmonary complications in this surgical setting, according to researchers led by Hyun Lee, MD, of Hanyang University in Seoul, South Korea.
“Our findings suggest that 6-minute walk distance would provide additional information in lung cancer patients with moderately decreased lung function who plan to undergo surgical resection,” said Dr. Lee and coauthors of the study report, which appears in CHEST.
More specifically, the option of curative resection should be considered in those lung cancer patients with moderately decreased lung function but a longer 6-minute walk distance, they added.
Exercise testing is currently recommended to further stratify risk of postoperative complications among patient with moderately decreased lung function, according to the researchers. The 6-minute walk test might be a good tool to evaluate feasibility for moderate risk patients, according to one recent review. However, studies so far have been limited by small numbers of patients, and larger studies have not specifically looked at predicted postoperative lung function status, they said.
Accordingly, the researchers evaluated data from patients expected to undergo curative lung cancer surgery who were enrolled in a prospective cohort study in Korea. They were classified as low or moderate risk based on pulmonary function tests, and further classified into short distance (less than 400 m) and long distance (400 m or more) groups based on their performance on the 6-minute walk test.
Postoperative cardiopulmonary complications were seen in 42.9% of the moderate-risk, short-distance group, versus 14.4% of patients in the moderate-risk, long-distance group. In the low-risk patients, those complications were seen in 9.5% and 8.3% of those in the long and short distance groups.
Odds for postoperative cardiopulmonary complications were significantly increased in the moderate-risk, short-distance group, compared with the low-risk, long-distance group (adjusted odds ratio, 7.84; 95% confidence interval, 2.24-27.46).
By contrast, odds for complications were not significantly increased in the moderate-risk, long-distance group, nor in the low-risk, short-distance groups, investigators said.
Dr. Lee and coauthors said they had no conflicts of interest to disclose.
SOURCE: Lee H et al. CHEST. 2020. doi: 10.1016/j.chest.2019.12.039.
Risk of cardiopulmonary complications increased nearly eightfold in patients with moderate lung function decreases who failed to walk 400 m or more, according to the study, which included data on 416 patients with non–small cell lung cancer (NSCLC) who underwent lobectomy.
This is believed to be the first large study evaluating the utility of the 6-minute walk test (6MWT) to predict postoperative cardiopulmonary complications in this surgical setting, according to researchers led by Hyun Lee, MD, of Hanyang University in Seoul, South Korea.
“Our findings suggest that 6-minute walk distance would provide additional information in lung cancer patients with moderately decreased lung function who plan to undergo surgical resection,” said Dr. Lee and coauthors of the study report, which appears in CHEST.
More specifically, the option of curative resection should be considered in those lung cancer patients with moderately decreased lung function but a longer 6-minute walk distance, they added.
Exercise testing is currently recommended to further stratify risk of postoperative complications among patient with moderately decreased lung function, according to the researchers. The 6-minute walk test might be a good tool to evaluate feasibility for moderate risk patients, according to one recent review. However, studies so far have been limited by small numbers of patients, and larger studies have not specifically looked at predicted postoperative lung function status, they said.
Accordingly, the researchers evaluated data from patients expected to undergo curative lung cancer surgery who were enrolled in a prospective cohort study in Korea. They were classified as low or moderate risk based on pulmonary function tests, and further classified into short distance (less than 400 m) and long distance (400 m or more) groups based on their performance on the 6-minute walk test.
Postoperative cardiopulmonary complications were seen in 42.9% of the moderate-risk, short-distance group, versus 14.4% of patients in the moderate-risk, long-distance group. In the low-risk patients, those complications were seen in 9.5% and 8.3% of those in the long and short distance groups.
Odds for postoperative cardiopulmonary complications were significantly increased in the moderate-risk, short-distance group, compared with the low-risk, long-distance group (adjusted odds ratio, 7.84; 95% confidence interval, 2.24-27.46).
By contrast, odds for complications were not significantly increased in the moderate-risk, long-distance group, nor in the low-risk, short-distance groups, investigators said.
Dr. Lee and coauthors said they had no conflicts of interest to disclose.
SOURCE: Lee H et al. CHEST. 2020. doi: 10.1016/j.chest.2019.12.039.
Risk of cardiopulmonary complications increased nearly eightfold in patients with moderate lung function decreases who failed to walk 400 m or more, according to the study, which included data on 416 patients with non–small cell lung cancer (NSCLC) who underwent lobectomy.
This is believed to be the first large study evaluating the utility of the 6-minute walk test (6MWT) to predict postoperative cardiopulmonary complications in this surgical setting, according to researchers led by Hyun Lee, MD, of Hanyang University in Seoul, South Korea.
“Our findings suggest that 6-minute walk distance would provide additional information in lung cancer patients with moderately decreased lung function who plan to undergo surgical resection,” said Dr. Lee and coauthors of the study report, which appears in CHEST.
More specifically, the option of curative resection should be considered in those lung cancer patients with moderately decreased lung function but a longer 6-minute walk distance, they added.
Exercise testing is currently recommended to further stratify risk of postoperative complications among patient with moderately decreased lung function, according to the researchers. The 6-minute walk test might be a good tool to evaluate feasibility for moderate risk patients, according to one recent review. However, studies so far have been limited by small numbers of patients, and larger studies have not specifically looked at predicted postoperative lung function status, they said.
Accordingly, the researchers evaluated data from patients expected to undergo curative lung cancer surgery who were enrolled in a prospective cohort study in Korea. They were classified as low or moderate risk based on pulmonary function tests, and further classified into short distance (less than 400 m) and long distance (400 m or more) groups based on their performance on the 6-minute walk test.
Postoperative cardiopulmonary complications were seen in 42.9% of the moderate-risk, short-distance group, versus 14.4% of patients in the moderate-risk, long-distance group. In the low-risk patients, those complications were seen in 9.5% and 8.3% of those in the long and short distance groups.
Odds for postoperative cardiopulmonary complications were significantly increased in the moderate-risk, short-distance group, compared with the low-risk, long-distance group (adjusted odds ratio, 7.84; 95% confidence interval, 2.24-27.46).
By contrast, odds for complications were not significantly increased in the moderate-risk, long-distance group, nor in the low-risk, short-distance groups, investigators said.
Dr. Lee and coauthors said they had no conflicts of interest to disclose.
SOURCE: Lee H et al. CHEST. 2020. doi: 10.1016/j.chest.2019.12.039.
FROM CHEST
Expanded indication for leadless pacemaker triples eligible patients
The U.S. Food and Drug Administration’s approval of an expanded indication for a leadless pacemaker for patients “who may benefit from maintenance of atrioventricular synchrony” will make this technology potentially available to nearly half of the Americans who need a pacemaker, roughly triple the number of patients who have been candidates for a leadless pacemaker up to now.
“This approval was huge. The complication rate with leadless pacemakers has been 63% less than the rate using pacemakers with transvenous leads,” said Larry A. Chinitz, MD, a cardiac electrophysiologist and a coinvestigator on some of the studies that led to the new indication. By expanding the types of patients suitable for leadless pacing “we’ll achieve AV [atrioventricular] synchrony in more patients with fewer complications,” said Dr. Chinitz, professor of medicine and director of the Cardiac Electrophysiology and Heart Rhythm Center at NYU Langone Health in New York.
Because the device is both leadless and requires no pocket owing to its small size and placement in a patient’s right ventricle, it has implications for potentially broadening the population that could benefit from the device, he said in an interview. “When we started with this pacemaker, it was limited to elderly patients with persistent atrial fibrillation who needed only ventricular pacing, a very small group,” just under 15% of the universe of patients who need pacemakers. The broadened indication, for patients with high-grade AV block who also have atrial function, makes it possible to think of using this safer and easier-to-place device in patients who need infrequent pacing, and in patients with multiple comorbidities that give them an increased complication risk, he said. The new indication means “you’re treating a much broader patient population, doing it more safely, and creating the foundation for expanding this technology.”
The Micra AV pacemaker uses the same basic design as the previously approved Micra Transcatheter Pacing System, which came onto the U.S. market in 2016 and provides single-chamber pacing. An accelerometer on the device allows it to detect atrial motion and thereby synchronize ventricular and atrial contractions, which led to the new indication. Although the Micra AV device looks similar to the original single-chamber model, it has an entirely new circuitry that prolongs battery life during dual-chamber pacing as well as new software that incorporates the accelerometer data, explained Robert Kowal, MD, a cardiac electrophysiologist, and vice president of medical affairs and chief medical officer of cardiac rhythm and heart failure at Medtronic in Minneapolis. The battery of the Micra AV is designed to last about 15 years, Dr. Chinitz noted.
Results from two studies that Dr. Chinitz helped run established the safety and efficacy of the device for dual-chamber pacing. The MARVEL (Micra Atrial Tracking Using a Ventricular Accelerometer) study included 64 patients who completed the study at 12 worldwide centers, which produced an average 80% AV synchrony in 33 patients with high-degree AV block (The other patients in the study had predominantly intrinsic AV conduction; Heart Rhythm. 2018 Sep;15[9]:1363-71). The MARVEL 2 study included 75 patients with either second- or third-degree AV block at 12 worldwide centers and showed that AV synchrony increased from an average of 27% without two-chamber pacing to 89% with the dual-chamber function turned on, and with 95% of patients achieving at least 70% AV synchrony (JACC Clin Electrophysiol. 2020 Jan;6[1]:94-106).
The 2016 indication for single-chamber pacing included patients with “high-grade” AV bloc with or without atrial fibrillation, typically patients for whom dual-chamber pacemaker was not a great option because of the risks for complication but with the downside of limited AV synchrony, a limitation now mitigated by the option of mechanical synchronization, Dr. Kowal said. The AV device remains intended for patients with high-grade AV node block, which means patients with second- or third-degree block, he added in an interview. The estimated prevalence of third-degree AV block among U.S. adults is about 0.02%, which translates into about 50,000 people; the estimated prevalence of second-degree AV block is much less, about 10% of the third-degree prevalence.
Despite the substantial cut in complications by a leadless and pocketless pacemaker, “some patients may still benefit from a traditional dual-chamber pacemaker,” specifically active patients who might sometimes get their heart rates up with exercise to levels of about 150 beats/min or higher, Dr. Kowal said. That’s because currently the programing algorithms used to synchronize the ventricle and atrium become less reliable at heart rates above 105 beats/min, he explained. However, the ability for mechanical synchronization to keep up at higher heart rates should improve as additional data are collected that can refine the algorithms. It’s also unusual for most patients who are pacemaker candidates to reach heart rates this high, he said.
The MARVEL and MARVEL 2 studies were sponsored by Medtronic, the company that markets Micra pacemakers. Dr. Chinitz has received fees and fellowship support from Medtronic, and has also received fees from Abbott, Biosense Webster, Biotronik, and Pfizer, and he has also received fellowship support from Biotronik and Boston Scientific. Dr. Kowal is a Medtronic employee.
The U.S. Food and Drug Administration’s approval of an expanded indication for a leadless pacemaker for patients “who may benefit from maintenance of atrioventricular synchrony” will make this technology potentially available to nearly half of the Americans who need a pacemaker, roughly triple the number of patients who have been candidates for a leadless pacemaker up to now.
“This approval was huge. The complication rate with leadless pacemakers has been 63% less than the rate using pacemakers with transvenous leads,” said Larry A. Chinitz, MD, a cardiac electrophysiologist and a coinvestigator on some of the studies that led to the new indication. By expanding the types of patients suitable for leadless pacing “we’ll achieve AV [atrioventricular] synchrony in more patients with fewer complications,” said Dr. Chinitz, professor of medicine and director of the Cardiac Electrophysiology and Heart Rhythm Center at NYU Langone Health in New York.
Because the device is both leadless and requires no pocket owing to its small size and placement in a patient’s right ventricle, it has implications for potentially broadening the population that could benefit from the device, he said in an interview. “When we started with this pacemaker, it was limited to elderly patients with persistent atrial fibrillation who needed only ventricular pacing, a very small group,” just under 15% of the universe of patients who need pacemakers. The broadened indication, for patients with high-grade AV block who also have atrial function, makes it possible to think of using this safer and easier-to-place device in patients who need infrequent pacing, and in patients with multiple comorbidities that give them an increased complication risk, he said. The new indication means “you’re treating a much broader patient population, doing it more safely, and creating the foundation for expanding this technology.”
The Micra AV pacemaker uses the same basic design as the previously approved Micra Transcatheter Pacing System, which came onto the U.S. market in 2016 and provides single-chamber pacing. An accelerometer on the device allows it to detect atrial motion and thereby synchronize ventricular and atrial contractions, which led to the new indication. Although the Micra AV device looks similar to the original single-chamber model, it has an entirely new circuitry that prolongs battery life during dual-chamber pacing as well as new software that incorporates the accelerometer data, explained Robert Kowal, MD, a cardiac electrophysiologist, and vice president of medical affairs and chief medical officer of cardiac rhythm and heart failure at Medtronic in Minneapolis. The battery of the Micra AV is designed to last about 15 years, Dr. Chinitz noted.
Results from two studies that Dr. Chinitz helped run established the safety and efficacy of the device for dual-chamber pacing. The MARVEL (Micra Atrial Tracking Using a Ventricular Accelerometer) study included 64 patients who completed the study at 12 worldwide centers, which produced an average 80% AV synchrony in 33 patients with high-degree AV block (The other patients in the study had predominantly intrinsic AV conduction; Heart Rhythm. 2018 Sep;15[9]:1363-71). The MARVEL 2 study included 75 patients with either second- or third-degree AV block at 12 worldwide centers and showed that AV synchrony increased from an average of 27% without two-chamber pacing to 89% with the dual-chamber function turned on, and with 95% of patients achieving at least 70% AV synchrony (JACC Clin Electrophysiol. 2020 Jan;6[1]:94-106).
The 2016 indication for single-chamber pacing included patients with “high-grade” AV bloc with or without atrial fibrillation, typically patients for whom dual-chamber pacemaker was not a great option because of the risks for complication but with the downside of limited AV synchrony, a limitation now mitigated by the option of mechanical synchronization, Dr. Kowal said. The AV device remains intended for patients with high-grade AV node block, which means patients with second- or third-degree block, he added in an interview. The estimated prevalence of third-degree AV block among U.S. adults is about 0.02%, which translates into about 50,000 people; the estimated prevalence of second-degree AV block is much less, about 10% of the third-degree prevalence.
Despite the substantial cut in complications by a leadless and pocketless pacemaker, “some patients may still benefit from a traditional dual-chamber pacemaker,” specifically active patients who might sometimes get their heart rates up with exercise to levels of about 150 beats/min or higher, Dr. Kowal said. That’s because currently the programing algorithms used to synchronize the ventricle and atrium become less reliable at heart rates above 105 beats/min, he explained. However, the ability for mechanical synchronization to keep up at higher heart rates should improve as additional data are collected that can refine the algorithms. It’s also unusual for most patients who are pacemaker candidates to reach heart rates this high, he said.
The MARVEL and MARVEL 2 studies were sponsored by Medtronic, the company that markets Micra pacemakers. Dr. Chinitz has received fees and fellowship support from Medtronic, and has also received fees from Abbott, Biosense Webster, Biotronik, and Pfizer, and he has also received fellowship support from Biotronik and Boston Scientific. Dr. Kowal is a Medtronic employee.
The U.S. Food and Drug Administration’s approval of an expanded indication for a leadless pacemaker for patients “who may benefit from maintenance of atrioventricular synchrony” will make this technology potentially available to nearly half of the Americans who need a pacemaker, roughly triple the number of patients who have been candidates for a leadless pacemaker up to now.
“This approval was huge. The complication rate with leadless pacemakers has been 63% less than the rate using pacemakers with transvenous leads,” said Larry A. Chinitz, MD, a cardiac electrophysiologist and a coinvestigator on some of the studies that led to the new indication. By expanding the types of patients suitable for leadless pacing “we’ll achieve AV [atrioventricular] synchrony in more patients with fewer complications,” said Dr. Chinitz, professor of medicine and director of the Cardiac Electrophysiology and Heart Rhythm Center at NYU Langone Health in New York.
Because the device is both leadless and requires no pocket owing to its small size and placement in a patient’s right ventricle, it has implications for potentially broadening the population that could benefit from the device, he said in an interview. “When we started with this pacemaker, it was limited to elderly patients with persistent atrial fibrillation who needed only ventricular pacing, a very small group,” just under 15% of the universe of patients who need pacemakers. The broadened indication, for patients with high-grade AV block who also have atrial function, makes it possible to think of using this safer and easier-to-place device in patients who need infrequent pacing, and in patients with multiple comorbidities that give them an increased complication risk, he said. The new indication means “you’re treating a much broader patient population, doing it more safely, and creating the foundation for expanding this technology.”
The Micra AV pacemaker uses the same basic design as the previously approved Micra Transcatheter Pacing System, which came onto the U.S. market in 2016 and provides single-chamber pacing. An accelerometer on the device allows it to detect atrial motion and thereby synchronize ventricular and atrial contractions, which led to the new indication. Although the Micra AV device looks similar to the original single-chamber model, it has an entirely new circuitry that prolongs battery life during dual-chamber pacing as well as new software that incorporates the accelerometer data, explained Robert Kowal, MD, a cardiac electrophysiologist, and vice president of medical affairs and chief medical officer of cardiac rhythm and heart failure at Medtronic in Minneapolis. The battery of the Micra AV is designed to last about 15 years, Dr. Chinitz noted.
Results from two studies that Dr. Chinitz helped run established the safety and efficacy of the device for dual-chamber pacing. The MARVEL (Micra Atrial Tracking Using a Ventricular Accelerometer) study included 64 patients who completed the study at 12 worldwide centers, which produced an average 80% AV synchrony in 33 patients with high-degree AV block (The other patients in the study had predominantly intrinsic AV conduction; Heart Rhythm. 2018 Sep;15[9]:1363-71). The MARVEL 2 study included 75 patients with either second- or third-degree AV block at 12 worldwide centers and showed that AV synchrony increased from an average of 27% without two-chamber pacing to 89% with the dual-chamber function turned on, and with 95% of patients achieving at least 70% AV synchrony (JACC Clin Electrophysiol. 2020 Jan;6[1]:94-106).
The 2016 indication for single-chamber pacing included patients with “high-grade” AV bloc with or without atrial fibrillation, typically patients for whom dual-chamber pacemaker was not a great option because of the risks for complication but with the downside of limited AV synchrony, a limitation now mitigated by the option of mechanical synchronization, Dr. Kowal said. The AV device remains intended for patients with high-grade AV node block, which means patients with second- or third-degree block, he added in an interview. The estimated prevalence of third-degree AV block among U.S. adults is about 0.02%, which translates into about 50,000 people; the estimated prevalence of second-degree AV block is much less, about 10% of the third-degree prevalence.
Despite the substantial cut in complications by a leadless and pocketless pacemaker, “some patients may still benefit from a traditional dual-chamber pacemaker,” specifically active patients who might sometimes get their heart rates up with exercise to levels of about 150 beats/min or higher, Dr. Kowal said. That’s because currently the programing algorithms used to synchronize the ventricle and atrium become less reliable at heart rates above 105 beats/min, he explained. However, the ability for mechanical synchronization to keep up at higher heart rates should improve as additional data are collected that can refine the algorithms. It’s also unusual for most patients who are pacemaker candidates to reach heart rates this high, he said.
The MARVEL and MARVEL 2 studies were sponsored by Medtronic, the company that markets Micra pacemakers. Dr. Chinitz has received fees and fellowship support from Medtronic, and has also received fees from Abbott, Biosense Webster, Biotronik, and Pfizer, and he has also received fellowship support from Biotronik and Boston Scientific. Dr. Kowal is a Medtronic employee.