User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Food insecurity drives poor glycemic control
People with diabetes who had a poor-quality diet and food insecurity were significantly more likely to have poor glycemic and cholesterol control than were those with a healthier diet and food security, based on data from a national study of more than 2,000 individuals.
The American Diabetes Association recommends a high-quality diet for people with diabetes (PWD) to achieve treatment goals; however, roughly 18% of PWD in the United States are food insecure and/or have a poor-quality diet, Sarah S. Casagrande, PhD, of DLH Corporation, Silver Spring, Md., and colleagues wrote in a poster presented at the annual scientific sessions of the ADA in New Orleans.
To examine the impact of food insecurity and diet quality on diabetes and lipid management, the researchers reviewed data from 2,075 adults with self-reported diabetes who completed the National Health and Nutrition Examination Surveys between 2013 and 2018.
Diet quality was divided into quartiles based on the 2015 Healthy Eating Index. Food insecurity was assessed using a standard 10-item questionnaire including questions about running out of food and not being able to afford more, reducing meal sizes, eating less or not at all, and going hungry because of lack of money for food.
The logistic regression analysis controlled for factors including sociodemographics, health care use, smoking, diabetes medications, blood pressure medication use, cholesterol medication use, and body mass index.
Overall, 17.6% of the participants were food insecure and had a low-quality diet, 14.2% were food insecure with a high-quality diet, 33.1% were food secure with a low-quality diet, and 35.2% were food secure with a high-quality diet.
PWD in the food insecure/low-quality diet group were significantly more likely to be younger, non-Hispanic black or Hispanic, and uninsured compared to those in the food secure/high-quality diet group (P < .001 for all).
When the researchers examined glycemic control, they found that PWD in the food insecurity/low-quality diet groups were significantly more likely than were those with food security/high-quality diets to have hemoglobin A1c of at least 7.0% (adjusted odds ratio, 1.85), A1c of at least 8.0% (aOR, 1.79), low HDL cholesterol (aOR, 1.69), and high triglycerides (aOR, 3.26).
PWD with food insecurity but a high-quality diet also were significantly more likely than were those with food security and a high quality diet to have A1c of at least 7.0% (aOR, 1.69), A1c of at least 8.0% (aOR, 1.83), and high triglycerides (aOR, 2.44). PWD with food security but a low-quality diet were significantly more likely than was the food security/high-quality diet group to have A1c of at least 7% (aOR, 1.55).
The study findings were limited by several factors including the cross-sectional design, reliance on self-reports, and inability to distinguish between type 1 and type 2 diabetes, the researchers wrote.
However, the results were strengthened by the large, nationally representative sample and the inclusion of multiple clinical outcomes in the patient assessment, they said.
The results suggest that food insecurity had a significant impact on both glycemic control and cholesterol management independent of diet quality, the researchers noted. Based on these findings, health care providers treating PWD may wish to assess their patients’ food security status, and “interventions could address disparities in food security,” they concluded.
Food insecurity a growing problem
“With more communities being pushed into state of war, drought, and famine globally, it is important to track impact of food insecurity and low quality food on common medical conditions like diabetes in our vulnerable communities,” Romesh K. Khardori, MD, professor of medicine: endocrinology, and metabolism at Eastern Virginia Medical School, Norfolk, said in an interview.
Dr. Khardori, who was not involved in the study, said he was not surprised by the current study findings.
“Type of food, amount of food, and quality of food have been stressed in diabetes management for more than 100 years,” he said. “Organizations charged with recommendations, such as the ADA and American Dietetic Association, have regularly updated their recommendations,” he noted. “It was not surprising, therefore, to find food insecurity and low quality tied to poor glycemic control.”
The take-home message for clinicians is to consider the availability and quality of food that their patients are exposed to when evaluating barriers to proper glycemic control, Dr. Khardori emphasized.
However, additional research is needed to explore whether the prescription of a sufficient amount of good quality food would alleviate the adverse impact seen in the current study, he said.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers and Dr. Khardori had no financial conflicts to disclose.
People with diabetes who had a poor-quality diet and food insecurity were significantly more likely to have poor glycemic and cholesterol control than were those with a healthier diet and food security, based on data from a national study of more than 2,000 individuals.
The American Diabetes Association recommends a high-quality diet for people with diabetes (PWD) to achieve treatment goals; however, roughly 18% of PWD in the United States are food insecure and/or have a poor-quality diet, Sarah S. Casagrande, PhD, of DLH Corporation, Silver Spring, Md., and colleagues wrote in a poster presented at the annual scientific sessions of the ADA in New Orleans.
To examine the impact of food insecurity and diet quality on diabetes and lipid management, the researchers reviewed data from 2,075 adults with self-reported diabetes who completed the National Health and Nutrition Examination Surveys between 2013 and 2018.
Diet quality was divided into quartiles based on the 2015 Healthy Eating Index. Food insecurity was assessed using a standard 10-item questionnaire including questions about running out of food and not being able to afford more, reducing meal sizes, eating less or not at all, and going hungry because of lack of money for food.
The logistic regression analysis controlled for factors including sociodemographics, health care use, smoking, diabetes medications, blood pressure medication use, cholesterol medication use, and body mass index.
Overall, 17.6% of the participants were food insecure and had a low-quality diet, 14.2% were food insecure with a high-quality diet, 33.1% were food secure with a low-quality diet, and 35.2% were food secure with a high-quality diet.
PWD in the food insecure/low-quality diet group were significantly more likely to be younger, non-Hispanic black or Hispanic, and uninsured compared to those in the food secure/high-quality diet group (P < .001 for all).
When the researchers examined glycemic control, they found that PWD in the food insecurity/low-quality diet groups were significantly more likely than were those with food security/high-quality diets to have hemoglobin A1c of at least 7.0% (adjusted odds ratio, 1.85), A1c of at least 8.0% (aOR, 1.79), low HDL cholesterol (aOR, 1.69), and high triglycerides (aOR, 3.26).
PWD with food insecurity but a high-quality diet also were significantly more likely than were those with food security and a high quality diet to have A1c of at least 7.0% (aOR, 1.69), A1c of at least 8.0% (aOR, 1.83), and high triglycerides (aOR, 2.44). PWD with food security but a low-quality diet were significantly more likely than was the food security/high-quality diet group to have A1c of at least 7% (aOR, 1.55).
The study findings were limited by several factors including the cross-sectional design, reliance on self-reports, and inability to distinguish between type 1 and type 2 diabetes, the researchers wrote.
However, the results were strengthened by the large, nationally representative sample and the inclusion of multiple clinical outcomes in the patient assessment, they said.
The results suggest that food insecurity had a significant impact on both glycemic control and cholesterol management independent of diet quality, the researchers noted. Based on these findings, health care providers treating PWD may wish to assess their patients’ food security status, and “interventions could address disparities in food security,” they concluded.
Food insecurity a growing problem
“With more communities being pushed into state of war, drought, and famine globally, it is important to track impact of food insecurity and low quality food on common medical conditions like diabetes in our vulnerable communities,” Romesh K. Khardori, MD, professor of medicine: endocrinology, and metabolism at Eastern Virginia Medical School, Norfolk, said in an interview.
Dr. Khardori, who was not involved in the study, said he was not surprised by the current study findings.
“Type of food, amount of food, and quality of food have been stressed in diabetes management for more than 100 years,” he said. “Organizations charged with recommendations, such as the ADA and American Dietetic Association, have regularly updated their recommendations,” he noted. “It was not surprising, therefore, to find food insecurity and low quality tied to poor glycemic control.”
The take-home message for clinicians is to consider the availability and quality of food that their patients are exposed to when evaluating barriers to proper glycemic control, Dr. Khardori emphasized.
However, additional research is needed to explore whether the prescription of a sufficient amount of good quality food would alleviate the adverse impact seen in the current study, he said.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers and Dr. Khardori had no financial conflicts to disclose.
People with diabetes who had a poor-quality diet and food insecurity were significantly more likely to have poor glycemic and cholesterol control than were those with a healthier diet and food security, based on data from a national study of more than 2,000 individuals.
The American Diabetes Association recommends a high-quality diet for people with diabetes (PWD) to achieve treatment goals; however, roughly 18% of PWD in the United States are food insecure and/or have a poor-quality diet, Sarah S. Casagrande, PhD, of DLH Corporation, Silver Spring, Md., and colleagues wrote in a poster presented at the annual scientific sessions of the ADA in New Orleans.
To examine the impact of food insecurity and diet quality on diabetes and lipid management, the researchers reviewed data from 2,075 adults with self-reported diabetes who completed the National Health and Nutrition Examination Surveys between 2013 and 2018.
Diet quality was divided into quartiles based on the 2015 Healthy Eating Index. Food insecurity was assessed using a standard 10-item questionnaire including questions about running out of food and not being able to afford more, reducing meal sizes, eating less or not at all, and going hungry because of lack of money for food.
The logistic regression analysis controlled for factors including sociodemographics, health care use, smoking, diabetes medications, blood pressure medication use, cholesterol medication use, and body mass index.
Overall, 17.6% of the participants were food insecure and had a low-quality diet, 14.2% were food insecure with a high-quality diet, 33.1% were food secure with a low-quality diet, and 35.2% were food secure with a high-quality diet.
PWD in the food insecure/low-quality diet group were significantly more likely to be younger, non-Hispanic black or Hispanic, and uninsured compared to those in the food secure/high-quality diet group (P < .001 for all).
When the researchers examined glycemic control, they found that PWD in the food insecurity/low-quality diet groups were significantly more likely than were those with food security/high-quality diets to have hemoglobin A1c of at least 7.0% (adjusted odds ratio, 1.85), A1c of at least 8.0% (aOR, 1.79), low HDL cholesterol (aOR, 1.69), and high triglycerides (aOR, 3.26).
PWD with food insecurity but a high-quality diet also were significantly more likely than were those with food security and a high quality diet to have A1c of at least 7.0% (aOR, 1.69), A1c of at least 8.0% (aOR, 1.83), and high triglycerides (aOR, 2.44). PWD with food security but a low-quality diet were significantly more likely than was the food security/high-quality diet group to have A1c of at least 7% (aOR, 1.55).
The study findings were limited by several factors including the cross-sectional design, reliance on self-reports, and inability to distinguish between type 1 and type 2 diabetes, the researchers wrote.
However, the results were strengthened by the large, nationally representative sample and the inclusion of multiple clinical outcomes in the patient assessment, they said.
The results suggest that food insecurity had a significant impact on both glycemic control and cholesterol management independent of diet quality, the researchers noted. Based on these findings, health care providers treating PWD may wish to assess their patients’ food security status, and “interventions could address disparities in food security,” they concluded.
Food insecurity a growing problem
“With more communities being pushed into state of war, drought, and famine globally, it is important to track impact of food insecurity and low quality food on common medical conditions like diabetes in our vulnerable communities,” Romesh K. Khardori, MD, professor of medicine: endocrinology, and metabolism at Eastern Virginia Medical School, Norfolk, said in an interview.
Dr. Khardori, who was not involved in the study, said he was not surprised by the current study findings.
“Type of food, amount of food, and quality of food have been stressed in diabetes management for more than 100 years,” he said. “Organizations charged with recommendations, such as the ADA and American Dietetic Association, have regularly updated their recommendations,” he noted. “It was not surprising, therefore, to find food insecurity and low quality tied to poor glycemic control.”
The take-home message for clinicians is to consider the availability and quality of food that their patients are exposed to when evaluating barriers to proper glycemic control, Dr. Khardori emphasized.
However, additional research is needed to explore whether the prescription of a sufficient amount of good quality food would alleviate the adverse impact seen in the current study, he said.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers and Dr. Khardori had no financial conflicts to disclose.
FROM ADA 2022
ACC/AHA issue clinical lexicon for complications of COVID-19
The American College of Cardiology and the American Heart Association have jointly issued a comprehensive set of data standards to help clarify definitions of the cardiovascular (CV) and non-CV complications of COVID-19.
It’s the work of the ACC/AHA Task Force on Clinical Data Standards and has been endorsed by the Heart Failure Society of America and Society for Cardiac Angiography and Interventions.
There is increased importance to understanding the acute and long-term impact of COVID-19 on CV health, the writing group notes. Until now, however, there has not been “clarity or consensus” on definitions of CV conditions related to COVID-19, with different diagnostic terminologies being used for overlapping conditions, such as “myocardial injury,” “myocarditis,” “type Il myocardial infarction,” “stress cardiomyopathy,” and “inflammatory cardiomyopathy,” they point out.
“We, as a research community, did some things right and some things wrong surrounding the COVID pandemic,” Sandeep Das, MD, MPH, vice chair of the writing group, noted in an interview with this news organization.
“The things that we really did right is that everybody responded with enthusiasm, kind of all hands on deck with a massive crisis response, and that was fantastic,” Dr. Das said.
“However, because of the need to hurry, we didn’t structure and organize in the way that we typically would for something that was sort of a slow burn kind of problem rather than an emergency. One of the consequences of that was fragmentation of how things are collected, reported, et cetera, and that leads to confusion,” he added.
The report was published simultaneously June 23 in the Journal of the American College of Cardiology and Circulation: Cardiovascular Quality and Outcomes.
A necessary but not glamorous project
The new data standards for COVID-19 will help standardize definitions and set the framework to capture and better understand how COVID-19 affects CV health.
“It wasn’t exactly a glamorous-type project but, at the same time, it’s super necessary to kind of get everybody on the same page and working together,” Dr. Das said.
Broad agreement on common vocabulary and definitions will help with efforts to pool or compare data from electronic health records, clinical registries, administrative datasets, and other databases, and determine whether these data apply to clinical practice and research endeavors, the writing group says.
They considered data elements relevant to the full range of care provided to COVID-19 patients in all care settings. Among the key items included in the document are:
- Case definitions for confirmed, probable, and suspected acute COVID-19, as well as postacute sequelae of COVID-19.
- Definitions for acute CV complications related to COVID-19, including acute myocardial injury, heart failure, shock, arrhythmia, thromboembolic complications, and .
- Data elements related to COVID-19 vaccination status, comorbidities, and preexisting CV conditions.
- Definitions for postacute CV sequelae of SARS-CoV-2 infection and long-term CV complications of COVID-19.
- Data elements for CV mortality during acute COVID-19.
- Data elements for non-CV complications to help document severity of illness and other competing diagnoses and complications that might affect CV outcomes.
- A list of symptoms and signs related to COVID-19 and CV complications.
- Data elements for diagnostic and therapeutic strategies for COVID-19 and CV conditions.
- A discussion of advanced therapies, including , extracorporeal membrane oxygenation, and end-of-life management strategies.
These data standards will be useful for researchers, registry developers, and clinicians, and they are proposed as a framework for ICD-10 code development of COVID-19–related CV conditions, the writing group says.
The standards are also of “great importance” to patients, clinicians, investigators, scientists, administrators, public health officials, policymakers, and payers, the group says.
Dr. Das said that, although there is no formal plan in place to update the document, he could see sections that might be refined.
“For example, there’s a nice long list of all the various variants, and unfortunately, I suspect that that is going to change and evolve over time,” Dr. Das told this news organization.
“We tried very hard not to include things like specifying specific treatments so we didn’t get proscriptive. We wanted to make it descriptive, so hopefully it will stand the test of time pretty well,” he added.
This research had no commercial funding. The writing group has no relevant disclosures.
A version of this article first appeared on Medscape.com.
The American College of Cardiology and the American Heart Association have jointly issued a comprehensive set of data standards to help clarify definitions of the cardiovascular (CV) and non-CV complications of COVID-19.
It’s the work of the ACC/AHA Task Force on Clinical Data Standards and has been endorsed by the Heart Failure Society of America and Society for Cardiac Angiography and Interventions.
There is increased importance to understanding the acute and long-term impact of COVID-19 on CV health, the writing group notes. Until now, however, there has not been “clarity or consensus” on definitions of CV conditions related to COVID-19, with different diagnostic terminologies being used for overlapping conditions, such as “myocardial injury,” “myocarditis,” “type Il myocardial infarction,” “stress cardiomyopathy,” and “inflammatory cardiomyopathy,” they point out.
“We, as a research community, did some things right and some things wrong surrounding the COVID pandemic,” Sandeep Das, MD, MPH, vice chair of the writing group, noted in an interview with this news organization.
“The things that we really did right is that everybody responded with enthusiasm, kind of all hands on deck with a massive crisis response, and that was fantastic,” Dr. Das said.
“However, because of the need to hurry, we didn’t structure and organize in the way that we typically would for something that was sort of a slow burn kind of problem rather than an emergency. One of the consequences of that was fragmentation of how things are collected, reported, et cetera, and that leads to confusion,” he added.
The report was published simultaneously June 23 in the Journal of the American College of Cardiology and Circulation: Cardiovascular Quality and Outcomes.
A necessary but not glamorous project
The new data standards for COVID-19 will help standardize definitions and set the framework to capture and better understand how COVID-19 affects CV health.
“It wasn’t exactly a glamorous-type project but, at the same time, it’s super necessary to kind of get everybody on the same page and working together,” Dr. Das said.
Broad agreement on common vocabulary and definitions will help with efforts to pool or compare data from electronic health records, clinical registries, administrative datasets, and other databases, and determine whether these data apply to clinical practice and research endeavors, the writing group says.
They considered data elements relevant to the full range of care provided to COVID-19 patients in all care settings. Among the key items included in the document are:
- Case definitions for confirmed, probable, and suspected acute COVID-19, as well as postacute sequelae of COVID-19.
- Definitions for acute CV complications related to COVID-19, including acute myocardial injury, heart failure, shock, arrhythmia, thromboembolic complications, and .
- Data elements related to COVID-19 vaccination status, comorbidities, and preexisting CV conditions.
- Definitions for postacute CV sequelae of SARS-CoV-2 infection and long-term CV complications of COVID-19.
- Data elements for CV mortality during acute COVID-19.
- Data elements for non-CV complications to help document severity of illness and other competing diagnoses and complications that might affect CV outcomes.
- A list of symptoms and signs related to COVID-19 and CV complications.
- Data elements for diagnostic and therapeutic strategies for COVID-19 and CV conditions.
- A discussion of advanced therapies, including , extracorporeal membrane oxygenation, and end-of-life management strategies.
These data standards will be useful for researchers, registry developers, and clinicians, and they are proposed as a framework for ICD-10 code development of COVID-19–related CV conditions, the writing group says.
The standards are also of “great importance” to patients, clinicians, investigators, scientists, administrators, public health officials, policymakers, and payers, the group says.
Dr. Das said that, although there is no formal plan in place to update the document, he could see sections that might be refined.
“For example, there’s a nice long list of all the various variants, and unfortunately, I suspect that that is going to change and evolve over time,” Dr. Das told this news organization.
“We tried very hard not to include things like specifying specific treatments so we didn’t get proscriptive. We wanted to make it descriptive, so hopefully it will stand the test of time pretty well,” he added.
This research had no commercial funding. The writing group has no relevant disclosures.
A version of this article first appeared on Medscape.com.
The American College of Cardiology and the American Heart Association have jointly issued a comprehensive set of data standards to help clarify definitions of the cardiovascular (CV) and non-CV complications of COVID-19.
It’s the work of the ACC/AHA Task Force on Clinical Data Standards and has been endorsed by the Heart Failure Society of America and Society for Cardiac Angiography and Interventions.
There is increased importance to understanding the acute and long-term impact of COVID-19 on CV health, the writing group notes. Until now, however, there has not been “clarity or consensus” on definitions of CV conditions related to COVID-19, with different diagnostic terminologies being used for overlapping conditions, such as “myocardial injury,” “myocarditis,” “type Il myocardial infarction,” “stress cardiomyopathy,” and “inflammatory cardiomyopathy,” they point out.
“We, as a research community, did some things right and some things wrong surrounding the COVID pandemic,” Sandeep Das, MD, MPH, vice chair of the writing group, noted in an interview with this news organization.
“The things that we really did right is that everybody responded with enthusiasm, kind of all hands on deck with a massive crisis response, and that was fantastic,” Dr. Das said.
“However, because of the need to hurry, we didn’t structure and organize in the way that we typically would for something that was sort of a slow burn kind of problem rather than an emergency. One of the consequences of that was fragmentation of how things are collected, reported, et cetera, and that leads to confusion,” he added.
The report was published simultaneously June 23 in the Journal of the American College of Cardiology and Circulation: Cardiovascular Quality and Outcomes.
A necessary but not glamorous project
The new data standards for COVID-19 will help standardize definitions and set the framework to capture and better understand how COVID-19 affects CV health.
“It wasn’t exactly a glamorous-type project but, at the same time, it’s super necessary to kind of get everybody on the same page and working together,” Dr. Das said.
Broad agreement on common vocabulary and definitions will help with efforts to pool or compare data from electronic health records, clinical registries, administrative datasets, and other databases, and determine whether these data apply to clinical practice and research endeavors, the writing group says.
They considered data elements relevant to the full range of care provided to COVID-19 patients in all care settings. Among the key items included in the document are:
- Case definitions for confirmed, probable, and suspected acute COVID-19, as well as postacute sequelae of COVID-19.
- Definitions for acute CV complications related to COVID-19, including acute myocardial injury, heart failure, shock, arrhythmia, thromboembolic complications, and .
- Data elements related to COVID-19 vaccination status, comorbidities, and preexisting CV conditions.
- Definitions for postacute CV sequelae of SARS-CoV-2 infection and long-term CV complications of COVID-19.
- Data elements for CV mortality during acute COVID-19.
- Data elements for non-CV complications to help document severity of illness and other competing diagnoses and complications that might affect CV outcomes.
- A list of symptoms and signs related to COVID-19 and CV complications.
- Data elements for diagnostic and therapeutic strategies for COVID-19 and CV conditions.
- A discussion of advanced therapies, including , extracorporeal membrane oxygenation, and end-of-life management strategies.
These data standards will be useful for researchers, registry developers, and clinicians, and they are proposed as a framework for ICD-10 code development of COVID-19–related CV conditions, the writing group says.
The standards are also of “great importance” to patients, clinicians, investigators, scientists, administrators, public health officials, policymakers, and payers, the group says.
Dr. Das said that, although there is no formal plan in place to update the document, he could see sections that might be refined.
“For example, there’s a nice long list of all the various variants, and unfortunately, I suspect that that is going to change and evolve over time,” Dr. Das told this news organization.
“We tried very hard not to include things like specifying specific treatments so we didn’t get proscriptive. We wanted to make it descriptive, so hopefully it will stand the test of time pretty well,” he added.
This research had no commercial funding. The writing group has no relevant disclosures.
A version of this article first appeared on Medscape.com.
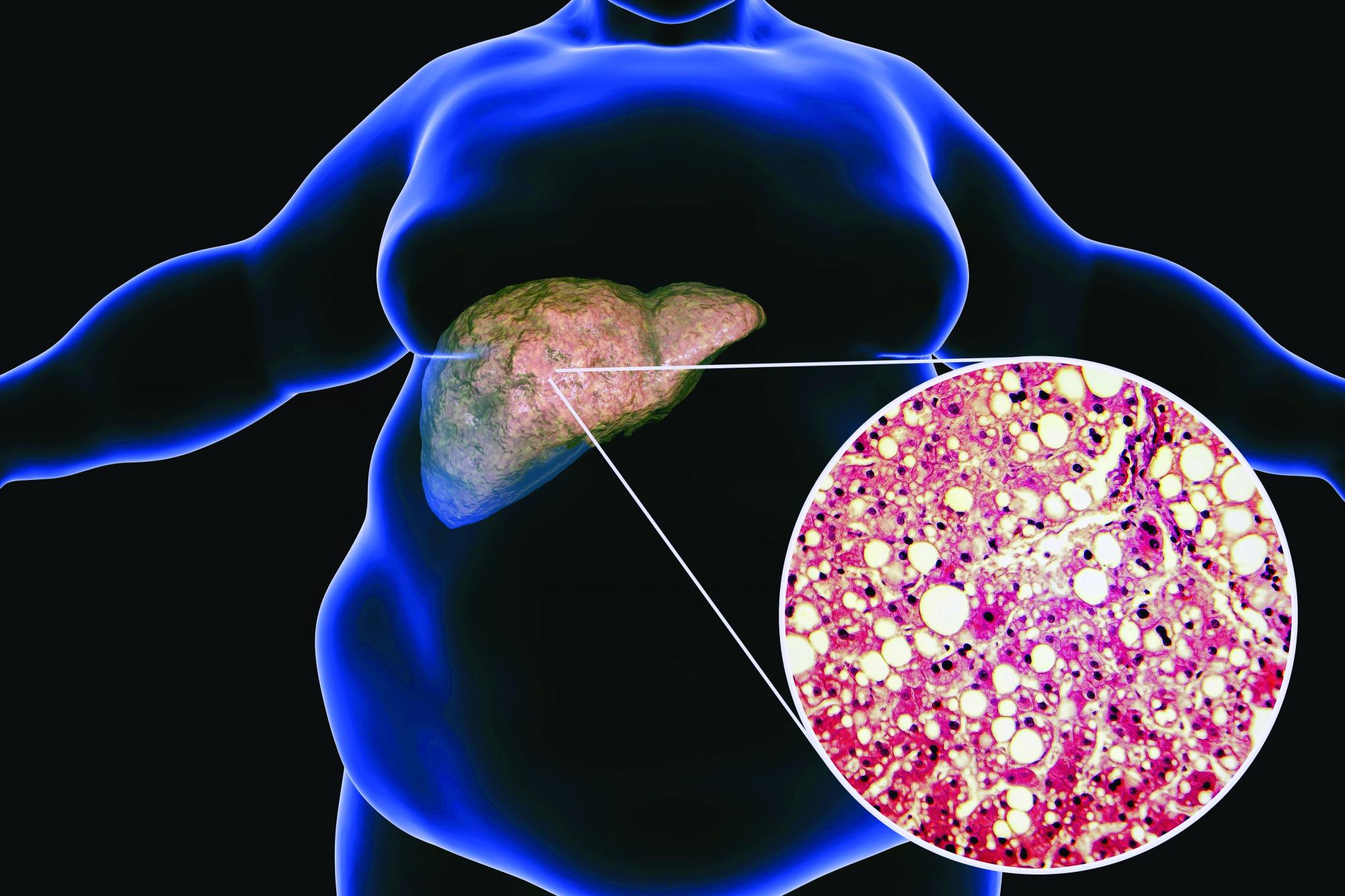
Low-carb, high-fat diet improves A1c, reduces liver fat
LONDON – A low-carbohydrate, high-fat (LCHF) diet reduced the progression of nonalcoholic fatty liver disease (NAFLD), and despite no calorie restriction, participants with both NAFLD and type 2 diabetes lost 5.8% of their body weight, according to a randomized controlled study.
“Based on these results, the LCHF diet may be recommended to people with NAFLD and type 2 diabetes,” said Camilla Dalby Hansen, MD, department of gastroenterology and hepatology, Odense University Hospital, Denmark, who presented the data at the International Liver Congress (ILC) 2022.
“Basically, if you have fat in your liver, you will benefit from eating fat,” she said.
The LCHF diet was compared with a low-fat, high-carbohydrate diet more typically followed for these conditions. The low-fat diet was also found to reduce the progression of NAFLD, but to a lesser extent than the LCHF diet.
Dr. Dalby Hansen called their study one of the most extensive investigations of the LCHF diet in patients with type 2 diabetes and fatty liver disease.
“Combining this [reduction in NAFLD score] with the huge weight loss, the lower HbA1c [blood sugar], the lowering of blood pressure in women, the rise in HDL levels, and reduction in triglycerides – all in all, this diet is very promising,” she said.
Stephen Harrison, MD, visiting professor, University of Oxford, United Kingdom, medical director of Pinnacle Clinical Research and president of Summit Clinical Research, San Antonio, commended Dr. Dalby Hansen on her methodology, which included before-and-after liver biopsies. “It’s a heinous effort to do paired liver biopsies in a lifestyle modification trial. That’s huge.”
“This study tells me that the way we manage patients doesn’t change – it is still lifestyle modification,” said Dr. Harrison, who was not involved with the study. “It’s eat less [rather] than more. It’s exercise and try to lose weight. In the long term, we give patients benefit, and we show that the disease has improved, and we offer something that means they can maintain a healthy life.”
He added that the relatively small and short trial was informative.
“They improved the NAFLD activity score [NAS],” he said. “I don’t know by how much. There was no change in fibrosis, but we wouldn’t expect this at 6 months.”
“It’s provocative work, and it gives us healthy information about how we can help manage our patients from a lifestyle perspective,” he concluded.
‘Do not lose weight. Eat until you are full’
In the study, 110 participants with type 2 diabetes and NAFLD, aged 18-78 years, were allocated to the LCHF diet, and 55 were allocated to the low-fat diet for 6 months.
The researchers performed liver biopsies at baseline and 6 months, which were blinded for scoring.
Participants had ongoing dietitian consultations, with follow-up visits at 3 and 6 months. Compliance was reported continuously through an online food diary platform.
The primary endpoint was change in glycemic control as measured by A1c level over 6 months. The secondary endpoints comprised the proportion of participants with changes in the NAS of at least 2 points over 6 months. Both these measures were compared between the two dietary groups.
The two groups were matched at baseline, with a mean age of 55-57 years, 58% were women, 89% with metabolic syndrome, and a mean BMI 34 kg/m2.
In baseline liver disease, F1 level fibrosis was the most common (58%), followed by hepatic steatosis (S1, 47%; S2, 32%), with a median NAS of 3, and 19% had nonalcoholic steatohepatitis.
The special thing about these diets was that participants were told to “not lose weight, but eat until you are full,” remarked Dr. Dalby Hansen.
Those on the LCHF diet consumed an average of 61% energy from fat, 13% from carbohydrates, and 23% from protein, compared with the low-fat diet, which comprised an average of 29% energy from fat, 46% from carbohydrates, and 21% from protein.
“It’s a lot of fat and corresponds to a quarter of a liter of olive oil per day,” said Dr. Dalby Hansen. “They really had to change their mindset a lot, because it was difficult for them to start eating all these fats, especially since we’ve all been told for decades that it isn’t good. But we supported them, and they got into it.”
The LCHF diet was primarily comprised of unsaturated fats – for example, avocado, oil, nuts, and seeds – but also included saturated fats, such as cheese, cream, and high-fat dairy products. Participants were free to eat unsaturated and saturated fats, but Dr. Dalby Hansen and her team advised participants that “good” unsaturated fats were preferable.
“Also, this diet contained vegetables but no bread, no potatoes, no rice, and no pasta. It was low in carbohydrates, below 20%,” she added.
Improved glycemic control, reduced liver fat
“We found that the LCHF diet improved diabetes control, it reduced the fat in the liver, and, even though they’re eating as many calories as they were used to until they were full, they lost 5.8% of body weight,” said Dr. Dalby Hansen in reporting the results. Participants in the low-fat group lost only 1.8% of body weight.
However, mean calorie intake dropped in both groups, by –2.2% in the LCHF group and –8.7% in the low-fat group.
“The LCHF diet improved the primary outcome of A1c by 9.5 mmol/mol, which is similar to some anti-diabetic medications, such as DPP-4 inhibitors and SGLT2 inhibitors,” she said.
The low-fat group reduced A1c by 3.4 mmol/mol, resulting in a between-group difference of 6.1 mmol/mol.
“Upon follow-up of 3 months, after stopping the diets, on average the participants in both groups returned their HbA1c levels to nearly baseline values,” she said. Results were adjusted for weight loss and baseline values.
Both diets also improved the NAS. The proportion of participants who improved their NAS score by 2 or more points was 22% in the LCHF group versus 17% in the low-fat group (P = 0.58). Additionally, in the LCHF group, 70% of participants improved their score by 1 or more points, compared with 49% in the low-fat group and fewer in the LCHF group experienced a worsening of their score (1% vs. 23%, respectively).
One participant on LCHF had high triglycerides of 12 mmol/L after 3 months. Overall, the low-density lipoprotein increased marginally by 0.2 mmol per liter in the high-fat group, said Dr. Dalby Hansen.
Dr. Dalby Hansen noted some limitations. The findings might not be applicable in more severe NAFLD, dietary assessment relied on self-reporting, no food was provided, and participants had to cook themselves. It was also an open-label study because of the nature of the intervention.
Some hope for more sustainable dieting
Many diets are difficult to adhere to, remarked Dr. Dalby Hansen. “We thought this [diet] might be easier to comply with in the longer term, and we hope that these results might provide patients with more options.”
She added that most people who started the diet adapted and complied with it. “However, it might not be for everyone, but I think we can say that if people try, and it fits into their lives, then they go for it.”
However, “it is not about going out and eating whatever fat and how much of it you want. It’s important that you cut the carbohydrates too,” she said. “With this approach, we really saw amazing results.”
Dr. Dalby Hansen added that having various diets available, including the LCHF one, meant that as clinicians they could empower patients to take control of their metabolic health.
“We can ask them directly, ‘What would fit into their life?’” she said. “We know that one size does not fit at all, and I believe that if we could engage patients more, then they can take control of their own situation.”
Asked whether these findings were enough to change guidelines, Zobair Younossi, MD, professor and chairman, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., remarked that it was the sugar at work here.
“Dietary fat – it’s not the same as fat in the liver, and this diet has more to do with the sugar levels,” he said.
“I’m always reluctant to take results from a short-term study without long-term follow-up,” Dr. Younossi said. “I want to know will patients live longer, and long-term data are needed for this. Until I have that strong evidence that outcomes are going to change, or at least some sign that the outcome is going to change, it is too early to change any guidelines.”
Dr. Dalby Hansen reports no relevant financial relationships. Dr. Harrison reported financial relationships with numerous pharmaceutical companies. Dr. Younossi reports the following financial relationships: research funds and/or consultant to Abbott, Allergan, Bristol Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
LONDON – A low-carbohydrate, high-fat (LCHF) diet reduced the progression of nonalcoholic fatty liver disease (NAFLD), and despite no calorie restriction, participants with both NAFLD and type 2 diabetes lost 5.8% of their body weight, according to a randomized controlled study.
“Based on these results, the LCHF diet may be recommended to people with NAFLD and type 2 diabetes,” said Camilla Dalby Hansen, MD, department of gastroenterology and hepatology, Odense University Hospital, Denmark, who presented the data at the International Liver Congress (ILC) 2022.
“Basically, if you have fat in your liver, you will benefit from eating fat,” she said.
The LCHF diet was compared with a low-fat, high-carbohydrate diet more typically followed for these conditions. The low-fat diet was also found to reduce the progression of NAFLD, but to a lesser extent than the LCHF diet.
Dr. Dalby Hansen called their study one of the most extensive investigations of the LCHF diet in patients with type 2 diabetes and fatty liver disease.
“Combining this [reduction in NAFLD score] with the huge weight loss, the lower HbA1c [blood sugar], the lowering of blood pressure in women, the rise in HDL levels, and reduction in triglycerides – all in all, this diet is very promising,” she said.
Stephen Harrison, MD, visiting professor, University of Oxford, United Kingdom, medical director of Pinnacle Clinical Research and president of Summit Clinical Research, San Antonio, commended Dr. Dalby Hansen on her methodology, which included before-and-after liver biopsies. “It’s a heinous effort to do paired liver biopsies in a lifestyle modification trial. That’s huge.”
“This study tells me that the way we manage patients doesn’t change – it is still lifestyle modification,” said Dr. Harrison, who was not involved with the study. “It’s eat less [rather] than more. It’s exercise and try to lose weight. In the long term, we give patients benefit, and we show that the disease has improved, and we offer something that means they can maintain a healthy life.”
He added that the relatively small and short trial was informative.
“They improved the NAFLD activity score [NAS],” he said. “I don’t know by how much. There was no change in fibrosis, but we wouldn’t expect this at 6 months.”
“It’s provocative work, and it gives us healthy information about how we can help manage our patients from a lifestyle perspective,” he concluded.
‘Do not lose weight. Eat until you are full’
In the study, 110 participants with type 2 diabetes and NAFLD, aged 18-78 years, were allocated to the LCHF diet, and 55 were allocated to the low-fat diet for 6 months.
The researchers performed liver biopsies at baseline and 6 months, which were blinded for scoring.
Participants had ongoing dietitian consultations, with follow-up visits at 3 and 6 months. Compliance was reported continuously through an online food diary platform.
The primary endpoint was change in glycemic control as measured by A1c level over 6 months. The secondary endpoints comprised the proportion of participants with changes in the NAS of at least 2 points over 6 months. Both these measures were compared between the two dietary groups.
The two groups were matched at baseline, with a mean age of 55-57 years, 58% were women, 89% with metabolic syndrome, and a mean BMI 34 kg/m2.
In baseline liver disease, F1 level fibrosis was the most common (58%), followed by hepatic steatosis (S1, 47%; S2, 32%), with a median NAS of 3, and 19% had nonalcoholic steatohepatitis.
The special thing about these diets was that participants were told to “not lose weight, but eat until you are full,” remarked Dr. Dalby Hansen.
Those on the LCHF diet consumed an average of 61% energy from fat, 13% from carbohydrates, and 23% from protein, compared with the low-fat diet, which comprised an average of 29% energy from fat, 46% from carbohydrates, and 21% from protein.
“It’s a lot of fat and corresponds to a quarter of a liter of olive oil per day,” said Dr. Dalby Hansen. “They really had to change their mindset a lot, because it was difficult for them to start eating all these fats, especially since we’ve all been told for decades that it isn’t good. But we supported them, and they got into it.”
The LCHF diet was primarily comprised of unsaturated fats – for example, avocado, oil, nuts, and seeds – but also included saturated fats, such as cheese, cream, and high-fat dairy products. Participants were free to eat unsaturated and saturated fats, but Dr. Dalby Hansen and her team advised participants that “good” unsaturated fats were preferable.
“Also, this diet contained vegetables but no bread, no potatoes, no rice, and no pasta. It was low in carbohydrates, below 20%,” she added.
Improved glycemic control, reduced liver fat
“We found that the LCHF diet improved diabetes control, it reduced the fat in the liver, and, even though they’re eating as many calories as they were used to until they were full, they lost 5.8% of body weight,” said Dr. Dalby Hansen in reporting the results. Participants in the low-fat group lost only 1.8% of body weight.
However, mean calorie intake dropped in both groups, by –2.2% in the LCHF group and –8.7% in the low-fat group.
“The LCHF diet improved the primary outcome of A1c by 9.5 mmol/mol, which is similar to some anti-diabetic medications, such as DPP-4 inhibitors and SGLT2 inhibitors,” she said.
The low-fat group reduced A1c by 3.4 mmol/mol, resulting in a between-group difference of 6.1 mmol/mol.
“Upon follow-up of 3 months, after stopping the diets, on average the participants in both groups returned their HbA1c levels to nearly baseline values,” she said. Results were adjusted for weight loss and baseline values.
Both diets also improved the NAS. The proportion of participants who improved their NAS score by 2 or more points was 22% in the LCHF group versus 17% in the low-fat group (P = 0.58). Additionally, in the LCHF group, 70% of participants improved their score by 1 or more points, compared with 49% in the low-fat group and fewer in the LCHF group experienced a worsening of their score (1% vs. 23%, respectively).
One participant on LCHF had high triglycerides of 12 mmol/L after 3 months. Overall, the low-density lipoprotein increased marginally by 0.2 mmol per liter in the high-fat group, said Dr. Dalby Hansen.
Dr. Dalby Hansen noted some limitations. The findings might not be applicable in more severe NAFLD, dietary assessment relied on self-reporting, no food was provided, and participants had to cook themselves. It was also an open-label study because of the nature of the intervention.
Some hope for more sustainable dieting
Many diets are difficult to adhere to, remarked Dr. Dalby Hansen. “We thought this [diet] might be easier to comply with in the longer term, and we hope that these results might provide patients with more options.”
She added that most people who started the diet adapted and complied with it. “However, it might not be for everyone, but I think we can say that if people try, and it fits into their lives, then they go for it.”
However, “it is not about going out and eating whatever fat and how much of it you want. It’s important that you cut the carbohydrates too,” she said. “With this approach, we really saw amazing results.”
Dr. Dalby Hansen added that having various diets available, including the LCHF one, meant that as clinicians they could empower patients to take control of their metabolic health.
“We can ask them directly, ‘What would fit into their life?’” she said. “We know that one size does not fit at all, and I believe that if we could engage patients more, then they can take control of their own situation.”
Asked whether these findings were enough to change guidelines, Zobair Younossi, MD, professor and chairman, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., remarked that it was the sugar at work here.
“Dietary fat – it’s not the same as fat in the liver, and this diet has more to do with the sugar levels,” he said.
“I’m always reluctant to take results from a short-term study without long-term follow-up,” Dr. Younossi said. “I want to know will patients live longer, and long-term data are needed for this. Until I have that strong evidence that outcomes are going to change, or at least some sign that the outcome is going to change, it is too early to change any guidelines.”
Dr. Dalby Hansen reports no relevant financial relationships. Dr. Harrison reported financial relationships with numerous pharmaceutical companies. Dr. Younossi reports the following financial relationships: research funds and/or consultant to Abbott, Allergan, Bristol Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
LONDON – A low-carbohydrate, high-fat (LCHF) diet reduced the progression of nonalcoholic fatty liver disease (NAFLD), and despite no calorie restriction, participants with both NAFLD and type 2 diabetes lost 5.8% of their body weight, according to a randomized controlled study.
“Based on these results, the LCHF diet may be recommended to people with NAFLD and type 2 diabetes,” said Camilla Dalby Hansen, MD, department of gastroenterology and hepatology, Odense University Hospital, Denmark, who presented the data at the International Liver Congress (ILC) 2022.
“Basically, if you have fat in your liver, you will benefit from eating fat,” she said.
The LCHF diet was compared with a low-fat, high-carbohydrate diet more typically followed for these conditions. The low-fat diet was also found to reduce the progression of NAFLD, but to a lesser extent than the LCHF diet.
Dr. Dalby Hansen called their study one of the most extensive investigations of the LCHF diet in patients with type 2 diabetes and fatty liver disease.
“Combining this [reduction in NAFLD score] with the huge weight loss, the lower HbA1c [blood sugar], the lowering of blood pressure in women, the rise in HDL levels, and reduction in triglycerides – all in all, this diet is very promising,” she said.
Stephen Harrison, MD, visiting professor, University of Oxford, United Kingdom, medical director of Pinnacle Clinical Research and president of Summit Clinical Research, San Antonio, commended Dr. Dalby Hansen on her methodology, which included before-and-after liver biopsies. “It’s a heinous effort to do paired liver biopsies in a lifestyle modification trial. That’s huge.”
“This study tells me that the way we manage patients doesn’t change – it is still lifestyle modification,” said Dr. Harrison, who was not involved with the study. “It’s eat less [rather] than more. It’s exercise and try to lose weight. In the long term, we give patients benefit, and we show that the disease has improved, and we offer something that means they can maintain a healthy life.”
He added that the relatively small and short trial was informative.
“They improved the NAFLD activity score [NAS],” he said. “I don’t know by how much. There was no change in fibrosis, but we wouldn’t expect this at 6 months.”
“It’s provocative work, and it gives us healthy information about how we can help manage our patients from a lifestyle perspective,” he concluded.
‘Do not lose weight. Eat until you are full’
In the study, 110 participants with type 2 diabetes and NAFLD, aged 18-78 years, were allocated to the LCHF diet, and 55 were allocated to the low-fat diet for 6 months.
The researchers performed liver biopsies at baseline and 6 months, which were blinded for scoring.
Participants had ongoing dietitian consultations, with follow-up visits at 3 and 6 months. Compliance was reported continuously through an online food diary platform.
The primary endpoint was change in glycemic control as measured by A1c level over 6 months. The secondary endpoints comprised the proportion of participants with changes in the NAS of at least 2 points over 6 months. Both these measures were compared between the two dietary groups.
The two groups were matched at baseline, with a mean age of 55-57 years, 58% were women, 89% with metabolic syndrome, and a mean BMI 34 kg/m2.
In baseline liver disease, F1 level fibrosis was the most common (58%), followed by hepatic steatosis (S1, 47%; S2, 32%), with a median NAS of 3, and 19% had nonalcoholic steatohepatitis.
The special thing about these diets was that participants were told to “not lose weight, but eat until you are full,” remarked Dr. Dalby Hansen.
Those on the LCHF diet consumed an average of 61% energy from fat, 13% from carbohydrates, and 23% from protein, compared with the low-fat diet, which comprised an average of 29% energy from fat, 46% from carbohydrates, and 21% from protein.
“It’s a lot of fat and corresponds to a quarter of a liter of olive oil per day,” said Dr. Dalby Hansen. “They really had to change their mindset a lot, because it was difficult for them to start eating all these fats, especially since we’ve all been told for decades that it isn’t good. But we supported them, and they got into it.”
The LCHF diet was primarily comprised of unsaturated fats – for example, avocado, oil, nuts, and seeds – but also included saturated fats, such as cheese, cream, and high-fat dairy products. Participants were free to eat unsaturated and saturated fats, but Dr. Dalby Hansen and her team advised participants that “good” unsaturated fats were preferable.
“Also, this diet contained vegetables but no bread, no potatoes, no rice, and no pasta. It was low in carbohydrates, below 20%,” she added.
Improved glycemic control, reduced liver fat
“We found that the LCHF diet improved diabetes control, it reduced the fat in the liver, and, even though they’re eating as many calories as they were used to until they were full, they lost 5.8% of body weight,” said Dr. Dalby Hansen in reporting the results. Participants in the low-fat group lost only 1.8% of body weight.
However, mean calorie intake dropped in both groups, by –2.2% in the LCHF group and –8.7% in the low-fat group.
“The LCHF diet improved the primary outcome of A1c by 9.5 mmol/mol, which is similar to some anti-diabetic medications, such as DPP-4 inhibitors and SGLT2 inhibitors,” she said.
The low-fat group reduced A1c by 3.4 mmol/mol, resulting in a between-group difference of 6.1 mmol/mol.
“Upon follow-up of 3 months, after stopping the diets, on average the participants in both groups returned their HbA1c levels to nearly baseline values,” she said. Results were adjusted for weight loss and baseline values.
Both diets also improved the NAS. The proportion of participants who improved their NAS score by 2 or more points was 22% in the LCHF group versus 17% in the low-fat group (P = 0.58). Additionally, in the LCHF group, 70% of participants improved their score by 1 or more points, compared with 49% in the low-fat group and fewer in the LCHF group experienced a worsening of their score (1% vs. 23%, respectively).
One participant on LCHF had high triglycerides of 12 mmol/L after 3 months. Overall, the low-density lipoprotein increased marginally by 0.2 mmol per liter in the high-fat group, said Dr. Dalby Hansen.
Dr. Dalby Hansen noted some limitations. The findings might not be applicable in more severe NAFLD, dietary assessment relied on self-reporting, no food was provided, and participants had to cook themselves. It was also an open-label study because of the nature of the intervention.
Some hope for more sustainable dieting
Many diets are difficult to adhere to, remarked Dr. Dalby Hansen. “We thought this [diet] might be easier to comply with in the longer term, and we hope that these results might provide patients with more options.”
She added that most people who started the diet adapted and complied with it. “However, it might not be for everyone, but I think we can say that if people try, and it fits into their lives, then they go for it.”
However, “it is not about going out and eating whatever fat and how much of it you want. It’s important that you cut the carbohydrates too,” she said. “With this approach, we really saw amazing results.”
Dr. Dalby Hansen added that having various diets available, including the LCHF one, meant that as clinicians they could empower patients to take control of their metabolic health.
“We can ask them directly, ‘What would fit into their life?’” she said. “We know that one size does not fit at all, and I believe that if we could engage patients more, then they can take control of their own situation.”
Asked whether these findings were enough to change guidelines, Zobair Younossi, MD, professor and chairman, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., remarked that it was the sugar at work here.
“Dietary fat – it’s not the same as fat in the liver, and this diet has more to do with the sugar levels,” he said.
“I’m always reluctant to take results from a short-term study without long-term follow-up,” Dr. Younossi said. “I want to know will patients live longer, and long-term data are needed for this. Until I have that strong evidence that outcomes are going to change, or at least some sign that the outcome is going to change, it is too early to change any guidelines.”
Dr. Dalby Hansen reports no relevant financial relationships. Dr. Harrison reported financial relationships with numerous pharmaceutical companies. Dr. Younossi reports the following financial relationships: research funds and/or consultant to Abbott, Allergan, Bristol Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
AT ILC 2022
Race drives disparities in life expectancy across states
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
FROM ANNALS OF INTERNAL MEDICINE
Cardiologists concerned for patient safety after abortion ruling
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Hydroxychloroquine risk found in some older patients with RA
Hydroxychloroquine should be initiated with caution in older patients with rheumatoid arthritis who also have heart failure or are at risk for it, say the authors of a study suggesting that the drug could increase their risk for major adverse cardiovascular events (MACE), compared with methotrexate.
A cohort study published online in the Journal of the American College of Cardiology looked at outcomes in 54,462 patients with RA aged 65 years or older and not previously treated with disease-modifying antirheumatic drugs. Half were initiated on methotrexate and half on hydroxychloroquine, making 27,231 propensity-matched pairs.
Across the entire cohort, hydroxychloroquine was not associated with a higher risk for sudden cardiac arrest, ventricular arrhythmia, or MACE, compared with methotrexate. When broken down into individual cardiovascular events, the data suggested a statistically significant 17% increase in the risk for cardiovascular mortality and 10% increase in all-cause mortality with hydroxychloroquine, although there were no differences in the risks for myocardial infarction or stroke.
However, a subgroup analysis revealed a significant 30% increase in the risk for MACE among patients starting hydroxychloroquine who also had a history of heart failure, compared with patients taking methotrexate. The researchers found no difference between the two drugs in patients without a history of heart failure. The study also suggested an overall 41% increase in the risk for hospitalization with heart failure with hydroxychloroquine, regardless of heart failure history.
Hydroxychloroquine was also associated with a 34% increase in the risk for cardiovascular mortality, a 22% increase in the risk for all-cause mortality, and a 74% increase in the risk for MI.
The lead author of the study, Elvira D’Andrea, MD, PhD, of Brigham and Women’s Hospital and Harvard Medical School in Boston, said that hydroxychloroquine is used as a first-line treatment for RA, but there was limited evidence on its cardiovascular risks. The pandemic in particular shined a spotlight on these concerns and prompted the researchers to extend their original prepandemic study to encompass additional cardiovascular outcomes.
“The emerging concerns on its cardiovascular safety in early 2020 has led the rheumatological community, and patients regularly taking hydroxychloroquine for rheumatoid arthritis, to confusion,” Dr. D’Andrea said in an interview.
She advised that clinicians be cautious when initiating hydroxychloroquine in older patients with existing heart failure or who have risk factors for it. “Although heart failure is a known concern for hydroxychloroquine use, these findings helped to clarify the relationship between the use of hydroxychloroquine or methotrexate and heart failure. Clinicians should pay careful attention to clinical manifestations of cardiomyopathy or heart failure in older patients with rheumatoid arthritis treated with hydroxychloroquine.”
Hydroxychloroquine is associated with cardiotoxicity, particularly cardiomyopathy, which may help precipitate MACE or heart failure exacerbations in patients who already have deterioration of their cardiac tissue, the authors suggested.
Short follow-up period leaves risk attribution under question
In an accompanying editorial, Elizabeth Blair Solow, MD, and Bonnie L. Bermas, MD, of the University of Texas Southwestern Medical Center, Dallas, commented that the lack of an increased risk for arrhythmic events or MACE in the overall cohort taking hydroxychloroquine was reassuring. They also suggested the subgroup analysis findings among patients with preexisting heart failure were still “exploratory and hypothesis-generating” and should be interpreted with caution.
They noted that the follow-up time of the study was relatively short – a median of 209 days – given that hydroxychloroquine does not reach a steady-state level for 6 months.
“Evidence to date suggests cardiomyopathy from HCQ [hydroxychloroquine] takes years to develop, many months beyond the exposures described here, bringing into question as to whether HCQ itself increased HF hospitalizations,” the editorialists wrote.
The editorial also raised the question of whether the association observed in the study was related to a possible cardioprotective effect of methotrexate, given that previous studies have suggested this effect in older patients with RA.
The study authors did an exploratory analysis comparing hydroxychloroquine with sulfasalazine, which appeared to support their main findings of a possible cardiovascular effect of hydroxychloroquine. However, they qualified this by pointing out that the analysis involved small numbers of patients.
Senior investigator Seoyoung C. Kim, MD, ScD, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, also noted that the study only looked at outcomes in patients aged 65 years and older.
“It would be clinically important to further examine the cardiovascular safety of hydroxychloroquine versus methotrexate in a younger population with rheumatic conditions,” she said.
The study was supported by the National Institutes of Health, Brigham and Women’s Hospital, and Harvard Medical School. Four authors declared unrelated research grants from the pharmaceutical sector, with one also declaring stock options and consulting work with the pharmaceutical sector. No other conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
Hydroxychloroquine should be initiated with caution in older patients with rheumatoid arthritis who also have heart failure or are at risk for it, say the authors of a study suggesting that the drug could increase their risk for major adverse cardiovascular events (MACE), compared with methotrexate.
A cohort study published online in the Journal of the American College of Cardiology looked at outcomes in 54,462 patients with RA aged 65 years or older and not previously treated with disease-modifying antirheumatic drugs. Half were initiated on methotrexate and half on hydroxychloroquine, making 27,231 propensity-matched pairs.
Across the entire cohort, hydroxychloroquine was not associated with a higher risk for sudden cardiac arrest, ventricular arrhythmia, or MACE, compared with methotrexate. When broken down into individual cardiovascular events, the data suggested a statistically significant 17% increase in the risk for cardiovascular mortality and 10% increase in all-cause mortality with hydroxychloroquine, although there were no differences in the risks for myocardial infarction or stroke.
However, a subgroup analysis revealed a significant 30% increase in the risk for MACE among patients starting hydroxychloroquine who also had a history of heart failure, compared with patients taking methotrexate. The researchers found no difference between the two drugs in patients without a history of heart failure. The study also suggested an overall 41% increase in the risk for hospitalization with heart failure with hydroxychloroquine, regardless of heart failure history.
Hydroxychloroquine was also associated with a 34% increase in the risk for cardiovascular mortality, a 22% increase in the risk for all-cause mortality, and a 74% increase in the risk for MI.
The lead author of the study, Elvira D’Andrea, MD, PhD, of Brigham and Women’s Hospital and Harvard Medical School in Boston, said that hydroxychloroquine is used as a first-line treatment for RA, but there was limited evidence on its cardiovascular risks. The pandemic in particular shined a spotlight on these concerns and prompted the researchers to extend their original prepandemic study to encompass additional cardiovascular outcomes.
“The emerging concerns on its cardiovascular safety in early 2020 has led the rheumatological community, and patients regularly taking hydroxychloroquine for rheumatoid arthritis, to confusion,” Dr. D’Andrea said in an interview.
She advised that clinicians be cautious when initiating hydroxychloroquine in older patients with existing heart failure or who have risk factors for it. “Although heart failure is a known concern for hydroxychloroquine use, these findings helped to clarify the relationship between the use of hydroxychloroquine or methotrexate and heart failure. Clinicians should pay careful attention to clinical manifestations of cardiomyopathy or heart failure in older patients with rheumatoid arthritis treated with hydroxychloroquine.”
Hydroxychloroquine is associated with cardiotoxicity, particularly cardiomyopathy, which may help precipitate MACE or heart failure exacerbations in patients who already have deterioration of their cardiac tissue, the authors suggested.
Short follow-up period leaves risk attribution under question
In an accompanying editorial, Elizabeth Blair Solow, MD, and Bonnie L. Bermas, MD, of the University of Texas Southwestern Medical Center, Dallas, commented that the lack of an increased risk for arrhythmic events or MACE in the overall cohort taking hydroxychloroquine was reassuring. They also suggested the subgroup analysis findings among patients with preexisting heart failure were still “exploratory and hypothesis-generating” and should be interpreted with caution.
They noted that the follow-up time of the study was relatively short – a median of 209 days – given that hydroxychloroquine does not reach a steady-state level for 6 months.
“Evidence to date suggests cardiomyopathy from HCQ [hydroxychloroquine] takes years to develop, many months beyond the exposures described here, bringing into question as to whether HCQ itself increased HF hospitalizations,” the editorialists wrote.
The editorial also raised the question of whether the association observed in the study was related to a possible cardioprotective effect of methotrexate, given that previous studies have suggested this effect in older patients with RA.
The study authors did an exploratory analysis comparing hydroxychloroquine with sulfasalazine, which appeared to support their main findings of a possible cardiovascular effect of hydroxychloroquine. However, they qualified this by pointing out that the analysis involved small numbers of patients.
Senior investigator Seoyoung C. Kim, MD, ScD, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, also noted that the study only looked at outcomes in patients aged 65 years and older.
“It would be clinically important to further examine the cardiovascular safety of hydroxychloroquine versus methotrexate in a younger population with rheumatic conditions,” she said.
The study was supported by the National Institutes of Health, Brigham and Women’s Hospital, and Harvard Medical School. Four authors declared unrelated research grants from the pharmaceutical sector, with one also declaring stock options and consulting work with the pharmaceutical sector. No other conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
Hydroxychloroquine should be initiated with caution in older patients with rheumatoid arthritis who also have heart failure or are at risk for it, say the authors of a study suggesting that the drug could increase their risk for major adverse cardiovascular events (MACE), compared with methotrexate.
A cohort study published online in the Journal of the American College of Cardiology looked at outcomes in 54,462 patients with RA aged 65 years or older and not previously treated with disease-modifying antirheumatic drugs. Half were initiated on methotrexate and half on hydroxychloroquine, making 27,231 propensity-matched pairs.
Across the entire cohort, hydroxychloroquine was not associated with a higher risk for sudden cardiac arrest, ventricular arrhythmia, or MACE, compared with methotrexate. When broken down into individual cardiovascular events, the data suggested a statistically significant 17% increase in the risk for cardiovascular mortality and 10% increase in all-cause mortality with hydroxychloroquine, although there were no differences in the risks for myocardial infarction or stroke.
However, a subgroup analysis revealed a significant 30% increase in the risk for MACE among patients starting hydroxychloroquine who also had a history of heart failure, compared with patients taking methotrexate. The researchers found no difference between the two drugs in patients without a history of heart failure. The study also suggested an overall 41% increase in the risk for hospitalization with heart failure with hydroxychloroquine, regardless of heart failure history.
Hydroxychloroquine was also associated with a 34% increase in the risk for cardiovascular mortality, a 22% increase in the risk for all-cause mortality, and a 74% increase in the risk for MI.
The lead author of the study, Elvira D’Andrea, MD, PhD, of Brigham and Women’s Hospital and Harvard Medical School in Boston, said that hydroxychloroquine is used as a first-line treatment for RA, but there was limited evidence on its cardiovascular risks. The pandemic in particular shined a spotlight on these concerns and prompted the researchers to extend their original prepandemic study to encompass additional cardiovascular outcomes.
“The emerging concerns on its cardiovascular safety in early 2020 has led the rheumatological community, and patients regularly taking hydroxychloroquine for rheumatoid arthritis, to confusion,” Dr. D’Andrea said in an interview.
She advised that clinicians be cautious when initiating hydroxychloroquine in older patients with existing heart failure or who have risk factors for it. “Although heart failure is a known concern for hydroxychloroquine use, these findings helped to clarify the relationship between the use of hydroxychloroquine or methotrexate and heart failure. Clinicians should pay careful attention to clinical manifestations of cardiomyopathy or heart failure in older patients with rheumatoid arthritis treated with hydroxychloroquine.”
Hydroxychloroquine is associated with cardiotoxicity, particularly cardiomyopathy, which may help precipitate MACE or heart failure exacerbations in patients who already have deterioration of their cardiac tissue, the authors suggested.
Short follow-up period leaves risk attribution under question
In an accompanying editorial, Elizabeth Blair Solow, MD, and Bonnie L. Bermas, MD, of the University of Texas Southwestern Medical Center, Dallas, commented that the lack of an increased risk for arrhythmic events or MACE in the overall cohort taking hydroxychloroquine was reassuring. They also suggested the subgroup analysis findings among patients with preexisting heart failure were still “exploratory and hypothesis-generating” and should be interpreted with caution.
They noted that the follow-up time of the study was relatively short – a median of 209 days – given that hydroxychloroquine does not reach a steady-state level for 6 months.
“Evidence to date suggests cardiomyopathy from HCQ [hydroxychloroquine] takes years to develop, many months beyond the exposures described here, bringing into question as to whether HCQ itself increased HF hospitalizations,” the editorialists wrote.
The editorial also raised the question of whether the association observed in the study was related to a possible cardioprotective effect of methotrexate, given that previous studies have suggested this effect in older patients with RA.
The study authors did an exploratory analysis comparing hydroxychloroquine with sulfasalazine, which appeared to support their main findings of a possible cardiovascular effect of hydroxychloroquine. However, they qualified this by pointing out that the analysis involved small numbers of patients.
Senior investigator Seoyoung C. Kim, MD, ScD, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, also noted that the study only looked at outcomes in patients aged 65 years and older.
“It would be clinically important to further examine the cardiovascular safety of hydroxychloroquine versus methotrexate in a younger population with rheumatic conditions,” she said.
The study was supported by the National Institutes of Health, Brigham and Women’s Hospital, and Harvard Medical School. Four authors declared unrelated research grants from the pharmaceutical sector, with one also declaring stock options and consulting work with the pharmaceutical sector. No other conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Women benefit but lag behind in intracoronary imaging in PCI
A real-world analysis reveals that women are consistently less likely to undergo intracoronary imaging as part of percutaneous coronary intervention (PCI), even though it benefits both sexes equally.
Results from nearly all PCIs performed in England and Wales between 2006 and 2019 showed the absolute rate of intracoronary imaging with either intravascular ultrasound (IVUS) or optical coherence tomography (OCT) was 5% lower in the later study years among women at 14.5%, compared with 19.6% in men (P < .001).
After adjustment, female sex was an independent predictor of lower intracoronary imaging use (odds ratio, 0.93; 95% confidence interval, 0.91-0.96), according to the study, published in JACC: Cardiovascular Interventions.
“One of the thoughts I had when we were running this analysis was, well, maybe the indications for that imaging, as recommended by guidelines, are less common in women,” Mamas Mamas, MD, told this news organization. “So what we did was to look at just cases where imaging is recommended by the EAPCI [European Association of Percutaneous Coronary Intervention].”
Again, the use of intracoronary imaging was consistently lower among women than among men for all of the following EAPCI-recommended indications:
- Acute coronary syndrome: 11.6% vs. 12.3% (P < .01).
- Stent thrombosis: 30.9% vs. 34.9% (P < .01).
- Long lesions: 13.1% vs. 16.3% (P < .01).
- Chronic total occlusions: 16.2% vs. 18.3% (P < .01).
- Left main stem PCI: 55.1% vs. 57.5% (P < .01).
- In-stent restenosis: 28.0% vs. 30.7%.
- Calcified lesions: 36.6% vs. 40.1% (P < .01).
- Renal disease: 17.4% vs. 19.5% (P < .01).
As to what might be driving the lower use, Dr. Mamas dismissed the argument that women undergo much simpler PCI, which wouldn’t benefit from imaging. Women do have smaller coronary arteries, however, and there is a belief that it’s easier to eyeball the size of vessels that are smaller rather than larger.
“I’m not convinced that’s entirely true,” he said. “I don’t have a good answer for you, I’m afraid. I don’t really know why we’re seeing it. I just think it’s one of those disparities that is important to highlight.”
Central to this belief is that the benefits of intracoronary imaging were found to be similar in men and women. Intracoronary imaging was associated with lower adjusted odds of in-hospital mortality (OR, 0.56; 95% CI, 0.48-0.64) and major adverse cardiac and cerebrovascular events (OR, 0.83; 95% CI, 0.76-0.91) in women and men (OR, 0.48; 95% CI, 0.44-0.53 and OR, 0.75; 95% CI, 0.71-0.80, respectively), compared with nonimaging groups.
“This really should be a call to arms, particularly given that we show this disparity persists, even in guideline-recommended cases where we should be using it,” said Dr. Mamas, from the Keele (England) Cardiovascular Research Group, Keele University, and Royal Stoke University Hospital, Stoke-on-Trent, England.
“Actually, I would argue that we should be using more imaging in women than men anyway because many of the presentations for acute coronary syndromes in women, like spontaneous coronary artery dissection or MINOCA [MI with nonobstructive coronary arteries], you often need intracoronary imaging to make that kind of diagnosis,” he observed.
Getting worse, not better
Previous studies have shown that women are less likely than men in acute coronary syndromes to receive the transradial approach and P2Y12 inhibitors, but none have specifically looked at intracoronary imaging, Dr. Mamas said.
To fill the gap, the researchers drew on data from 994,478 patients in the British Cardiovascular Intervention Society registry, of whom, 8.4% of 738,616 men and 7.9% of 255,862 women received intracoronary imaging.
Women in the imaging group were older, more likely to be an ethnic minority, and more likely to undergo PCI for non–ST-segment elevation MI than their male counterparts.
One of the more surprising findings was that rates of IVUS and OCT were superimposable between the sexes at the start of the study but quickly diverged starting in around 2012, when the technology took off, Dr. Mamas said. In the most recent data, use was about 3% lower in women overall and rising to 6% in those with stable angina.
“Whilst the disparities between men and women are significant, the bigger question is why are we using so little imaging in guideline-recommended cases where there is a benefit?” he said.
Possible actionable items, he suggested, include providing older physicians who didn’t have access to intracoronary imaging during their training with opportunities in their cath lab or with industry sponsors to increase their skills and confidence. Intracoronary imaging use could also be routinely captured in U.S. and European PCI registries and used as a quality metric.
“In left main, you see a massive difference between centers, and that’s the kind of data that drives discussion,” Dr. Mamas said. “If we start reporting quality metrics, such as radial use, intracoronary imaging, P2Y12 inhibitors by center, then you’ve got something to benchmark centers against.”
Nathaniel Smilowitz, MD, an interventional cardiologist at New York Langone Health, who was not associated with the study, said that it’s troubling to see that the utilization intravascular imaging is so low, despite randomized trials and large meta-analyses showing a mortality benefit associated with its use in PCI.
“Even among men, only 19.6% in the later years were getting intravascular imaging performed to guide their coronary intervention, so one out of five,” he said. “There are opportunities to improve.”
Dr. Smilowitz said he’s also perplexed as to why adoption would be lower in women but that the findings echo those in other domains where women receive less intensive cardiovascular therapy.
“There’s no biological, really plausible, mechanism as to why the need for intravascular imaging would be lower and, particularly, because they showed in stent thrombosis, for example, where intravascular imaging is tremendously important, there were still sex differences,” he said. “So even with clear indications for imaging, women just received the optimal therapy less often than men. It’s disappointing.”
Dr. Smilowitz agreed that there may be a need to incorporate intravascular imaging into metrics, which are reported back to physicians, potentially even for comparisons with peers or regional rates to incentivize physicians to improve uptake.
“As a society, we’ve been quite slow to integrate intravascular imaging to guide PCI and we can do better,” he said.
A version of this article first appeared on Medscape.com.
A real-world analysis reveals that women are consistently less likely to undergo intracoronary imaging as part of percutaneous coronary intervention (PCI), even though it benefits both sexes equally.
Results from nearly all PCIs performed in England and Wales between 2006 and 2019 showed the absolute rate of intracoronary imaging with either intravascular ultrasound (IVUS) or optical coherence tomography (OCT) was 5% lower in the later study years among women at 14.5%, compared with 19.6% in men (P < .001).
After adjustment, female sex was an independent predictor of lower intracoronary imaging use (odds ratio, 0.93; 95% confidence interval, 0.91-0.96), according to the study, published in JACC: Cardiovascular Interventions.
“One of the thoughts I had when we were running this analysis was, well, maybe the indications for that imaging, as recommended by guidelines, are less common in women,” Mamas Mamas, MD, told this news organization. “So what we did was to look at just cases where imaging is recommended by the EAPCI [European Association of Percutaneous Coronary Intervention].”
Again, the use of intracoronary imaging was consistently lower among women than among men for all of the following EAPCI-recommended indications:
- Acute coronary syndrome: 11.6% vs. 12.3% (P < .01).
- Stent thrombosis: 30.9% vs. 34.9% (P < .01).
- Long lesions: 13.1% vs. 16.3% (P < .01).
- Chronic total occlusions: 16.2% vs. 18.3% (P < .01).
- Left main stem PCI: 55.1% vs. 57.5% (P < .01).
- In-stent restenosis: 28.0% vs. 30.7%.
- Calcified lesions: 36.6% vs. 40.1% (P < .01).
- Renal disease: 17.4% vs. 19.5% (P < .01).
As to what might be driving the lower use, Dr. Mamas dismissed the argument that women undergo much simpler PCI, which wouldn’t benefit from imaging. Women do have smaller coronary arteries, however, and there is a belief that it’s easier to eyeball the size of vessels that are smaller rather than larger.
“I’m not convinced that’s entirely true,” he said. “I don’t have a good answer for you, I’m afraid. I don’t really know why we’re seeing it. I just think it’s one of those disparities that is important to highlight.”
Central to this belief is that the benefits of intracoronary imaging were found to be similar in men and women. Intracoronary imaging was associated with lower adjusted odds of in-hospital mortality (OR, 0.56; 95% CI, 0.48-0.64) and major adverse cardiac and cerebrovascular events (OR, 0.83; 95% CI, 0.76-0.91) in women and men (OR, 0.48; 95% CI, 0.44-0.53 and OR, 0.75; 95% CI, 0.71-0.80, respectively), compared with nonimaging groups.
“This really should be a call to arms, particularly given that we show this disparity persists, even in guideline-recommended cases where we should be using it,” said Dr. Mamas, from the Keele (England) Cardiovascular Research Group, Keele University, and Royal Stoke University Hospital, Stoke-on-Trent, England.
“Actually, I would argue that we should be using more imaging in women than men anyway because many of the presentations for acute coronary syndromes in women, like spontaneous coronary artery dissection or MINOCA [MI with nonobstructive coronary arteries], you often need intracoronary imaging to make that kind of diagnosis,” he observed.
Getting worse, not better
Previous studies have shown that women are less likely than men in acute coronary syndromes to receive the transradial approach and P2Y12 inhibitors, but none have specifically looked at intracoronary imaging, Dr. Mamas said.
To fill the gap, the researchers drew on data from 994,478 patients in the British Cardiovascular Intervention Society registry, of whom, 8.4% of 738,616 men and 7.9% of 255,862 women received intracoronary imaging.
Women in the imaging group were older, more likely to be an ethnic minority, and more likely to undergo PCI for non–ST-segment elevation MI than their male counterparts.
One of the more surprising findings was that rates of IVUS and OCT were superimposable between the sexes at the start of the study but quickly diverged starting in around 2012, when the technology took off, Dr. Mamas said. In the most recent data, use was about 3% lower in women overall and rising to 6% in those with stable angina.
“Whilst the disparities between men and women are significant, the bigger question is why are we using so little imaging in guideline-recommended cases where there is a benefit?” he said.
Possible actionable items, he suggested, include providing older physicians who didn’t have access to intracoronary imaging during their training with opportunities in their cath lab or with industry sponsors to increase their skills and confidence. Intracoronary imaging use could also be routinely captured in U.S. and European PCI registries and used as a quality metric.
“In left main, you see a massive difference between centers, and that’s the kind of data that drives discussion,” Dr. Mamas said. “If we start reporting quality metrics, such as radial use, intracoronary imaging, P2Y12 inhibitors by center, then you’ve got something to benchmark centers against.”
Nathaniel Smilowitz, MD, an interventional cardiologist at New York Langone Health, who was not associated with the study, said that it’s troubling to see that the utilization intravascular imaging is so low, despite randomized trials and large meta-analyses showing a mortality benefit associated with its use in PCI.
“Even among men, only 19.6% in the later years were getting intravascular imaging performed to guide their coronary intervention, so one out of five,” he said. “There are opportunities to improve.”
Dr. Smilowitz said he’s also perplexed as to why adoption would be lower in women but that the findings echo those in other domains where women receive less intensive cardiovascular therapy.
“There’s no biological, really plausible, mechanism as to why the need for intravascular imaging would be lower and, particularly, because they showed in stent thrombosis, for example, where intravascular imaging is tremendously important, there were still sex differences,” he said. “So even with clear indications for imaging, women just received the optimal therapy less often than men. It’s disappointing.”
Dr. Smilowitz agreed that there may be a need to incorporate intravascular imaging into metrics, which are reported back to physicians, potentially even for comparisons with peers or regional rates to incentivize physicians to improve uptake.
“As a society, we’ve been quite slow to integrate intravascular imaging to guide PCI and we can do better,” he said.
A version of this article first appeared on Medscape.com.
A real-world analysis reveals that women are consistently less likely to undergo intracoronary imaging as part of percutaneous coronary intervention (PCI), even though it benefits both sexes equally.
Results from nearly all PCIs performed in England and Wales between 2006 and 2019 showed the absolute rate of intracoronary imaging with either intravascular ultrasound (IVUS) or optical coherence tomography (OCT) was 5% lower in the later study years among women at 14.5%, compared with 19.6% in men (P < .001).
After adjustment, female sex was an independent predictor of lower intracoronary imaging use (odds ratio, 0.93; 95% confidence interval, 0.91-0.96), according to the study, published in JACC: Cardiovascular Interventions.
“One of the thoughts I had when we were running this analysis was, well, maybe the indications for that imaging, as recommended by guidelines, are less common in women,” Mamas Mamas, MD, told this news organization. “So what we did was to look at just cases where imaging is recommended by the EAPCI [European Association of Percutaneous Coronary Intervention].”
Again, the use of intracoronary imaging was consistently lower among women than among men for all of the following EAPCI-recommended indications:
- Acute coronary syndrome: 11.6% vs. 12.3% (P < .01).
- Stent thrombosis: 30.9% vs. 34.9% (P < .01).
- Long lesions: 13.1% vs. 16.3% (P < .01).
- Chronic total occlusions: 16.2% vs. 18.3% (P < .01).
- Left main stem PCI: 55.1% vs. 57.5% (P < .01).
- In-stent restenosis: 28.0% vs. 30.7%.
- Calcified lesions: 36.6% vs. 40.1% (P < .01).
- Renal disease: 17.4% vs. 19.5% (P < .01).
As to what might be driving the lower use, Dr. Mamas dismissed the argument that women undergo much simpler PCI, which wouldn’t benefit from imaging. Women do have smaller coronary arteries, however, and there is a belief that it’s easier to eyeball the size of vessels that are smaller rather than larger.
“I’m not convinced that’s entirely true,” he said. “I don’t have a good answer for you, I’m afraid. I don’t really know why we’re seeing it. I just think it’s one of those disparities that is important to highlight.”
Central to this belief is that the benefits of intracoronary imaging were found to be similar in men and women. Intracoronary imaging was associated with lower adjusted odds of in-hospital mortality (OR, 0.56; 95% CI, 0.48-0.64) and major adverse cardiac and cerebrovascular events (OR, 0.83; 95% CI, 0.76-0.91) in women and men (OR, 0.48; 95% CI, 0.44-0.53 and OR, 0.75; 95% CI, 0.71-0.80, respectively), compared with nonimaging groups.
“This really should be a call to arms, particularly given that we show this disparity persists, even in guideline-recommended cases where we should be using it,” said Dr. Mamas, from the Keele (England) Cardiovascular Research Group, Keele University, and Royal Stoke University Hospital, Stoke-on-Trent, England.
“Actually, I would argue that we should be using more imaging in women than men anyway because many of the presentations for acute coronary syndromes in women, like spontaneous coronary artery dissection or MINOCA [MI with nonobstructive coronary arteries], you often need intracoronary imaging to make that kind of diagnosis,” he observed.
Getting worse, not better
Previous studies have shown that women are less likely than men in acute coronary syndromes to receive the transradial approach and P2Y12 inhibitors, but none have specifically looked at intracoronary imaging, Dr. Mamas said.
To fill the gap, the researchers drew on data from 994,478 patients in the British Cardiovascular Intervention Society registry, of whom, 8.4% of 738,616 men and 7.9% of 255,862 women received intracoronary imaging.
Women in the imaging group were older, more likely to be an ethnic minority, and more likely to undergo PCI for non–ST-segment elevation MI than their male counterparts.
One of the more surprising findings was that rates of IVUS and OCT were superimposable between the sexes at the start of the study but quickly diverged starting in around 2012, when the technology took off, Dr. Mamas said. In the most recent data, use was about 3% lower in women overall and rising to 6% in those with stable angina.
“Whilst the disparities between men and women are significant, the bigger question is why are we using so little imaging in guideline-recommended cases where there is a benefit?” he said.
Possible actionable items, he suggested, include providing older physicians who didn’t have access to intracoronary imaging during their training with opportunities in their cath lab or with industry sponsors to increase their skills and confidence. Intracoronary imaging use could also be routinely captured in U.S. and European PCI registries and used as a quality metric.
“In left main, you see a massive difference between centers, and that’s the kind of data that drives discussion,” Dr. Mamas said. “If we start reporting quality metrics, such as radial use, intracoronary imaging, P2Y12 inhibitors by center, then you’ve got something to benchmark centers against.”
Nathaniel Smilowitz, MD, an interventional cardiologist at New York Langone Health, who was not associated with the study, said that it’s troubling to see that the utilization intravascular imaging is so low, despite randomized trials and large meta-analyses showing a mortality benefit associated with its use in PCI.
“Even among men, only 19.6% in the later years were getting intravascular imaging performed to guide their coronary intervention, so one out of five,” he said. “There are opportunities to improve.”
Dr. Smilowitz said he’s also perplexed as to why adoption would be lower in women but that the findings echo those in other domains where women receive less intensive cardiovascular therapy.
“There’s no biological, really plausible, mechanism as to why the need for intravascular imaging would be lower and, particularly, because they showed in stent thrombosis, for example, where intravascular imaging is tremendously important, there were still sex differences,” he said. “So even with clear indications for imaging, women just received the optimal therapy less often than men. It’s disappointing.”
Dr. Smilowitz agreed that there may be a need to incorporate intravascular imaging into metrics, which are reported back to physicians, potentially even for comparisons with peers or regional rates to incentivize physicians to improve uptake.
“As a society, we’ve been quite slow to integrate intravascular imaging to guide PCI and we can do better,” he said.
A version of this article first appeared on Medscape.com.
FROM JACC: CARDIOVASCULAR INTERVENTIONS
Pig-heart transplant case published with new details, insights
It’s a given that the case of David Bennett, Sr, and his transplanted, genetically modified porcine heart will have a lot to teach, and the peer-reviewed publication this week lends welcome authority to some of its earliest lessons.
Mr. Bennett lived for 2 months after receiving the heart in the pioneering surgery, and the new case report compiles the available clinical, anatomic, and histologic evidence and other potential clues to the underlying cause or causes of death.
It also describes a mystery that came to light at autopsy: a grossly enlarged heart attributable to pervasive interstitial edema, and at the cellular level, a peculiar pattern of myocardial damage that included microvascular deterioration and, potentially as a result, cellular necrosis, according to the new report.
The myocardium itself was described as “thickened and stiff,” consistent with the “diastolic heart failure” that characterized Mr. Bennett’s final 10 days and the likely convergence of several underlying processes. Missing, however, was any conventional sign of graft rejection as it is understood clinically or in animal models, the report states.
If a form of tissue rejection was the cause of graft failure, any implicating cellular evidence may simply have been unrecognizable, given the unprecedented nature of the first pig-to-human heart transplantation, the donor animal’s multiple anti-inflammatory gene deletions, and partly investigational immunosuppression regimen, speculated Bartley P. Griffith, MD, University of Maryland, College Park.
“I’m betting against it being a fulminant rejection,” he told this news organization, “because we saw nothing like the [characteristic] platelet deposition or thrombosis of the capillaries.”
Dr. Griffith, who performed the xenotransplant surgery and led Mr. Bennett’s postoperative care, is lead author on the case report published in the New England Journal of Medicine. “Additional studies are underway to characterize the pathophysiologic mechanisms that resulted in this damage,” the report states.
The report builds on recent meeting presentations on the case, which, as previously reported, gave cursory details regarding the organ damage and other clinical developments during and after the surgery, including evidence that the transplanted heart contained porcine cytomegalovirus (PCMV).
Similar details also appeared in a third-person account based in part on personal communication with Dr. Griffith. The cardiac XTx review that focused on this University of Maryland experience was published June 15 in JACC: Basic to Translational Science, with lead author Jacinthe Boulet, MD, CM, Brigham and Women’s Hospital Heart, Boston.
“The question of how to move XTx forward remains uncertain, and appropriate selection of patients for experimental XTx will be one of the most important challenges to be addressed. The first issue we must contend with is whether we are ready to move to the next XTx in a human. We strongly believe this to be the case,” the review states. “Once early experience is gained, with successive iterations of XTx, the bar for success can be raised with maturation of the technology.”
Evidence has so far not implicated several other potential mechanisms underlying the graft failure that had been the focus of early speculations. For example, the transplanted pig heart was infected with PCMV, as previously reported. Mr. Bennett showed traces of PCMV DNA in his circulation, but no actual virus in his native cells. Still, PCMV remains a suspect.
Mr. Bennett also received intravenous immunoglobulin (IVIG) on several occasions to fight rejection, and also severe infections, including a nasty episode of sepsis. A reaction to the IVIG, derived from pooled donor antibodies, could potentially have caused the unusual myocardial damage seen by the University of Maryland team, Dr. Griffith observed. Alternatively, the damage might have been partly related to the patient’s overall severely diminished condition even before the transplant surgery or his rocky postoperative clinical course.
Indeed, Mr. Bennett’s condition worsened dramatically on postoperative day 50, and echocardiography showed a striking degree of myocardial wall thickening and heart enlargement, determined to be from edema. “The heart got amazingly stiff but maintained a systolic function that wasn›t too terrible, even to the very end. But his heart seemed as though it had swollen overnight,” Dr. Griffith said. “We had never seen that type of process, the suddenness of this swelling, in our nonhuman primate studies.”
The damage to the heart muscle appeared irreversible, based on myocardial biopsy results, so the decision was made to withdraw life support 60 days after the transplant surgery, the report notes.
Among the experience’s apparent lessons for future cardiac xenotransplantation, Dr. Griffith said, would be to select patients for the surgery who are in a bit more robust condition than Mr. Bennett was, who are perhaps ambulatory, not sarcopenic, and not recently on prolonged mechanical circulatory support. “We’re going to try to pick a patient who, on the front end, is less critically ill but who is just as likely not to benefit from continued medical therapy” and who isn’t a candidate for conventional heart transplantation, he said.
Because of universal efforts to manage conditions like diabetes, hypertension, and vascular disease in the population, and “because these conditions cause many of the cases of organ failure and fuel demand for transplantation, one might wonder whether the advances reported by Dr. Griffith and colleagues presage a decreasing demand for organ transplantation,” speculates an accompanying editorialfrom Jeffrey L. Platt, MD, and Marilia Cascalho, MD, PhD, University of Michigan, Ann Arbor.
“We think the answer is no. Since aging is associated with progressive decline in the function of the heart, kidneys, and other organs, advances that extend life expectancy will ultimately increase the prevalence of organ failure and potentially the demand for transplantation.”
The donor pig was developed and provided by Revivicor, and the investigational KPL-404 antibody drug used in the experience was provided by Kiniksa. Other disclosures for the case report and editorial from Dr. Platt and Dr. Cascalho are available at NEJM.com. Dr. Boulet reports no relevant relationships; disclosures for the other authors are in their report.
A version of this article first appeared on Medscape.com.
It’s a given that the case of David Bennett, Sr, and his transplanted, genetically modified porcine heart will have a lot to teach, and the peer-reviewed publication this week lends welcome authority to some of its earliest lessons.
Mr. Bennett lived for 2 months after receiving the heart in the pioneering surgery, and the new case report compiles the available clinical, anatomic, and histologic evidence and other potential clues to the underlying cause or causes of death.
It also describes a mystery that came to light at autopsy: a grossly enlarged heart attributable to pervasive interstitial edema, and at the cellular level, a peculiar pattern of myocardial damage that included microvascular deterioration and, potentially as a result, cellular necrosis, according to the new report.
The myocardium itself was described as “thickened and stiff,” consistent with the “diastolic heart failure” that characterized Mr. Bennett’s final 10 days and the likely convergence of several underlying processes. Missing, however, was any conventional sign of graft rejection as it is understood clinically or in animal models, the report states.
If a form of tissue rejection was the cause of graft failure, any implicating cellular evidence may simply have been unrecognizable, given the unprecedented nature of the first pig-to-human heart transplantation, the donor animal’s multiple anti-inflammatory gene deletions, and partly investigational immunosuppression regimen, speculated Bartley P. Griffith, MD, University of Maryland, College Park.
“I’m betting against it being a fulminant rejection,” he told this news organization, “because we saw nothing like the [characteristic] platelet deposition or thrombosis of the capillaries.”
Dr. Griffith, who performed the xenotransplant surgery and led Mr. Bennett’s postoperative care, is lead author on the case report published in the New England Journal of Medicine. “Additional studies are underway to characterize the pathophysiologic mechanisms that resulted in this damage,” the report states.
The report builds on recent meeting presentations on the case, which, as previously reported, gave cursory details regarding the organ damage and other clinical developments during and after the surgery, including evidence that the transplanted heart contained porcine cytomegalovirus (PCMV).
Similar details also appeared in a third-person account based in part on personal communication with Dr. Griffith. The cardiac XTx review that focused on this University of Maryland experience was published June 15 in JACC: Basic to Translational Science, with lead author Jacinthe Boulet, MD, CM, Brigham and Women’s Hospital Heart, Boston.
“The question of how to move XTx forward remains uncertain, and appropriate selection of patients for experimental XTx will be one of the most important challenges to be addressed. The first issue we must contend with is whether we are ready to move to the next XTx in a human. We strongly believe this to be the case,” the review states. “Once early experience is gained, with successive iterations of XTx, the bar for success can be raised with maturation of the technology.”
Evidence has so far not implicated several other potential mechanisms underlying the graft failure that had been the focus of early speculations. For example, the transplanted pig heart was infected with PCMV, as previously reported. Mr. Bennett showed traces of PCMV DNA in his circulation, but no actual virus in his native cells. Still, PCMV remains a suspect.
Mr. Bennett also received intravenous immunoglobulin (IVIG) on several occasions to fight rejection, and also severe infections, including a nasty episode of sepsis. A reaction to the IVIG, derived from pooled donor antibodies, could potentially have caused the unusual myocardial damage seen by the University of Maryland team, Dr. Griffith observed. Alternatively, the damage might have been partly related to the patient’s overall severely diminished condition even before the transplant surgery or his rocky postoperative clinical course.
Indeed, Mr. Bennett’s condition worsened dramatically on postoperative day 50, and echocardiography showed a striking degree of myocardial wall thickening and heart enlargement, determined to be from edema. “The heart got amazingly stiff but maintained a systolic function that wasn›t too terrible, even to the very end. But his heart seemed as though it had swollen overnight,” Dr. Griffith said. “We had never seen that type of process, the suddenness of this swelling, in our nonhuman primate studies.”
The damage to the heart muscle appeared irreversible, based on myocardial biopsy results, so the decision was made to withdraw life support 60 days after the transplant surgery, the report notes.
Among the experience’s apparent lessons for future cardiac xenotransplantation, Dr. Griffith said, would be to select patients for the surgery who are in a bit more robust condition than Mr. Bennett was, who are perhaps ambulatory, not sarcopenic, and not recently on prolonged mechanical circulatory support. “We’re going to try to pick a patient who, on the front end, is less critically ill but who is just as likely not to benefit from continued medical therapy” and who isn’t a candidate for conventional heart transplantation, he said.
Because of universal efforts to manage conditions like diabetes, hypertension, and vascular disease in the population, and “because these conditions cause many of the cases of organ failure and fuel demand for transplantation, one might wonder whether the advances reported by Dr. Griffith and colleagues presage a decreasing demand for organ transplantation,” speculates an accompanying editorialfrom Jeffrey L. Platt, MD, and Marilia Cascalho, MD, PhD, University of Michigan, Ann Arbor.
“We think the answer is no. Since aging is associated with progressive decline in the function of the heart, kidneys, and other organs, advances that extend life expectancy will ultimately increase the prevalence of organ failure and potentially the demand for transplantation.”
The donor pig was developed and provided by Revivicor, and the investigational KPL-404 antibody drug used in the experience was provided by Kiniksa. Other disclosures for the case report and editorial from Dr. Platt and Dr. Cascalho are available at NEJM.com. Dr. Boulet reports no relevant relationships; disclosures for the other authors are in their report.
A version of this article first appeared on Medscape.com.
It’s a given that the case of David Bennett, Sr, and his transplanted, genetically modified porcine heart will have a lot to teach, and the peer-reviewed publication this week lends welcome authority to some of its earliest lessons.
Mr. Bennett lived for 2 months after receiving the heart in the pioneering surgery, and the new case report compiles the available clinical, anatomic, and histologic evidence and other potential clues to the underlying cause or causes of death.
It also describes a mystery that came to light at autopsy: a grossly enlarged heart attributable to pervasive interstitial edema, and at the cellular level, a peculiar pattern of myocardial damage that included microvascular deterioration and, potentially as a result, cellular necrosis, according to the new report.
The myocardium itself was described as “thickened and stiff,” consistent with the “diastolic heart failure” that characterized Mr. Bennett’s final 10 days and the likely convergence of several underlying processes. Missing, however, was any conventional sign of graft rejection as it is understood clinically or in animal models, the report states.
If a form of tissue rejection was the cause of graft failure, any implicating cellular evidence may simply have been unrecognizable, given the unprecedented nature of the first pig-to-human heart transplantation, the donor animal’s multiple anti-inflammatory gene deletions, and partly investigational immunosuppression regimen, speculated Bartley P. Griffith, MD, University of Maryland, College Park.
“I’m betting against it being a fulminant rejection,” he told this news organization, “because we saw nothing like the [characteristic] platelet deposition or thrombosis of the capillaries.”
Dr. Griffith, who performed the xenotransplant surgery and led Mr. Bennett’s postoperative care, is lead author on the case report published in the New England Journal of Medicine. “Additional studies are underway to characterize the pathophysiologic mechanisms that resulted in this damage,” the report states.
The report builds on recent meeting presentations on the case, which, as previously reported, gave cursory details regarding the organ damage and other clinical developments during and after the surgery, including evidence that the transplanted heart contained porcine cytomegalovirus (PCMV).
Similar details also appeared in a third-person account based in part on personal communication with Dr. Griffith. The cardiac XTx review that focused on this University of Maryland experience was published June 15 in JACC: Basic to Translational Science, with lead author Jacinthe Boulet, MD, CM, Brigham and Women’s Hospital Heart, Boston.
“The question of how to move XTx forward remains uncertain, and appropriate selection of patients for experimental XTx will be one of the most important challenges to be addressed. The first issue we must contend with is whether we are ready to move to the next XTx in a human. We strongly believe this to be the case,” the review states. “Once early experience is gained, with successive iterations of XTx, the bar for success can be raised with maturation of the technology.”
Evidence has so far not implicated several other potential mechanisms underlying the graft failure that had been the focus of early speculations. For example, the transplanted pig heart was infected with PCMV, as previously reported. Mr. Bennett showed traces of PCMV DNA in his circulation, but no actual virus in his native cells. Still, PCMV remains a suspect.
Mr. Bennett also received intravenous immunoglobulin (IVIG) on several occasions to fight rejection, and also severe infections, including a nasty episode of sepsis. A reaction to the IVIG, derived from pooled donor antibodies, could potentially have caused the unusual myocardial damage seen by the University of Maryland team, Dr. Griffith observed. Alternatively, the damage might have been partly related to the patient’s overall severely diminished condition even before the transplant surgery or his rocky postoperative clinical course.
Indeed, Mr. Bennett’s condition worsened dramatically on postoperative day 50, and echocardiography showed a striking degree of myocardial wall thickening and heart enlargement, determined to be from edema. “The heart got amazingly stiff but maintained a systolic function that wasn›t too terrible, even to the very end. But his heart seemed as though it had swollen overnight,” Dr. Griffith said. “We had never seen that type of process, the suddenness of this swelling, in our nonhuman primate studies.”
The damage to the heart muscle appeared irreversible, based on myocardial biopsy results, so the decision was made to withdraw life support 60 days after the transplant surgery, the report notes.
Among the experience’s apparent lessons for future cardiac xenotransplantation, Dr. Griffith said, would be to select patients for the surgery who are in a bit more robust condition than Mr. Bennett was, who are perhaps ambulatory, not sarcopenic, and not recently on prolonged mechanical circulatory support. “We’re going to try to pick a patient who, on the front end, is less critically ill but who is just as likely not to benefit from continued medical therapy” and who isn’t a candidate for conventional heart transplantation, he said.
Because of universal efforts to manage conditions like diabetes, hypertension, and vascular disease in the population, and “because these conditions cause many of the cases of organ failure and fuel demand for transplantation, one might wonder whether the advances reported by Dr. Griffith and colleagues presage a decreasing demand for organ transplantation,” speculates an accompanying editorialfrom Jeffrey L. Platt, MD, and Marilia Cascalho, MD, PhD, University of Michigan, Ann Arbor.
“We think the answer is no. Since aging is associated with progressive decline in the function of the heart, kidneys, and other organs, advances that extend life expectancy will ultimately increase the prevalence of organ failure and potentially the demand for transplantation.”
The donor pig was developed and provided by Revivicor, and the investigational KPL-404 antibody drug used in the experience was provided by Kiniksa. Other disclosures for the case report and editorial from Dr. Platt and Dr. Cascalho are available at NEJM.com. Dr. Boulet reports no relevant relationships; disclosures for the other authors are in their report.
A version of this article first appeared on Medscape.com.
Stroke risk rises for women with history of infertility, miscarriage, stillbirth
Infertility, pregnancy loss, and stillbirth increased women’s later risk of both nonfatal and fatal stroke, based on data from more than 600,000 women.
“To date, multiple studies have generated an expanding body of evidence on the association between pregnancy complications (e.g., gestational diabetes and preeclampsia) and the long-term risk of stroke, but studies on associations with infertility, miscarriage, or stillbirth have produced mixed evidence,” Chen Liang, a PhD candidate at the University of Queensland, Brisbane, Australia, and colleagues wrote.
In a study published in the BMJ, the researchers reviewed data from eight observational cohort studies across seven countries (Australia, China, Japan, the Netherlands, Sweden, the United Kingdom, and the United States). The participants were part of the InterLACE (International Collaboration for a Life Course Approach to Reproductive Health and Chronic Disease Events) consortium established in 2021. Most observational studies included in the analysis began between 1990 and 2000.
The study population included 618,851 women aged 32-73 years at baseline for whom data on infertility, miscarriage, or stillbirth, were available. The primary outcome was the association of infertility, recurrent miscarriage, and stillbirth with risk of first fatal or nonfatal stroke, and the results were further stratified by subtype. Stroke was identified through self-reports, linked hospital data, national patient registers, or death registry data. Baseline was defined as the first incidence of infertility, miscarriage, or stillbirth. The exception was the National Survey of Health and Development, a British birth cohort started in 1946, that collected data retrospectively.
The median follow-up period was 13 years for nonfatal stroke and 9.4 years for fatal stroke.
Overall, 17.2%, 16.6%, and 4.6% of the women experienced infertility, miscarriage, and stillbirth, respectively.
Women with a history of infertility had a significantly higher nonfatal stroke risk, compared with those without infertility (hazard ratio, 1.14). Further analysis by stroke subtypes showed an increased association between miscarriage and ischemic stroke (HR, 1.15).
Those with a history of miscarriage also had an increased risk of nonfatal stroke, compared with those without miscarriages (HR, 1.11). In the miscarriage group, the risk of stroke increased with the number of miscarriages, with adjusted HRs of 1.07, 1.12, and 1.35 for women with one, two, and three or more miscarriages, respectively. When stratified by stroke subtype, women with three or more miscarriages were more likely than women with no miscarriages to experience ischemic and hemorrhagic nonfatal strokes.
Associations were similar between miscarriage history and fatal stroke risk. Women with one, two, and three or more miscarriages had increased risk of fatal stroke, compared with those with no miscarriages (aHR, 1.08, 1.26, and 1.82, respectively, and women with three or more miscarriages had a higher risk of ischemic and hemorrhagic stroke (aHR, 1.83 and 1.84, respectively).
Women with a history of stillbirth had an approximately 31% increased risk of nonfatal stroke, compared with those with no history of stillbirth, with aHRs similar for single and recurrent stillbirths (1.32 and 1.29, respectively). Ischemic nonfatal stroke risk was higher in women with any stillbirth, compared with those without stillbirth (aHR, 1.77). Fatal stroke risk also was higher in women with any stillbirth, compared with those without, and this risk increased with the number of stillbirths (HR, 0.97 and HR, 1.26 for those with one stillbirth and two or more, respectively).
“The increased risk of stroke associated with infertility or recurrent stillbirths was mainly driven by a single subtype of stroke (nonfatal ischemic stroke or fatal hemorrhagic stroke, respectively), whereas the risk of stroke associated with recurrent miscarriages was driven by both subtypes,” the researchers wrote.
The researchers cited endothelial dysfunction as a potential underlying mechanism for increased stroke risk associated with pregnancy complications. “Endothelial dysfunction might lead to pregnancy loss through placentation-related defects, persist after a complicated pregnancy, and contribute to the development of stroke through reduced vasodilation, proinflammatory status, and prothrombic properties,” and that history of recurrent pregnancy loss might be a female-specific risk factor for stroke.
To mitigate this risk, they advised early monitoring of women with a history of recurrent miscarriages and stillbirths for stroke risk factors such as high blood pressure, blood sugar levels, and lipid levels.
The study findings were limited by several factors including the use of questionnaires to collect information on infertility, miscarriage, and stillbirth, and the potential variation in definitions of infertility, miscarriage, and stillbirth across the included studies, and a lack of data on the effect of different causes or treatments based on reproductive histories, the researchers noted. Other limitations include incomplete data on stroke subtypes and inability to adjust for all covariates such as thyroid disorders and endometriosis. However, the results were strengthened by the large study size and geographically and racially diverse population, extend the current knowledge on associations between infertility, miscarriage, and stillbirth with stroke, and highlight the need for more research on underlying mechanisms.
Data support gender-specific stroke risk stratification
“Studies that seek to understand gender differences and disparities in adverse outcomes, such as stroke risk, are extremely important given that women historically were excluded from research studies,” Catherine M. Albright, MD, of the University of Washington, Seattle, said in an interview. “By doing these studies, we are able to better risk stratify people in order to better predict and modify risks,” added Dr. Albright, who was not involved in the current study.
“It is well known than adverse pregnancy outcomes such as hypertension in pregnancy, fetal growth restriction, and preterm birth, lead to increased risk of cardiovascular disease and stroke later in life, so the general findings of an association between other adverse reproductive and pregnancy outcomes leads to increased stroke risk are not surprising,” she said.
“The take-home message is that outcomes for pregnancy really do provide a window to future health,” said Dr. Albright. “For clinicians, especially non-ob.gyns., knowing a complete pregnancy history for any new patient is important and can help risk-stratify patients, especially as we continue to gain knowledge like what is shown in this study.”
However, “this study did not evaluate why individual patients may have had infertility, recurrent pregnancy loss, or stillbirth, so research to look further into this association to determine if there is an underlying medical condition that could be treated and therefore possibly reduce both pregnancy complications and future stroke risks would be important,” Dr. Albright noted.
The study was supported by the Australian National Health and Medical Research Council Centres of Research Excellence; one corresponding author was supported by an Australian National Health and Medical Research Council Investigator grant. The researchers had no financial conflicts to disclose. Dr. Albright had no financial conflicts to disclose.
Infertility, pregnancy loss, and stillbirth increased women’s later risk of both nonfatal and fatal stroke, based on data from more than 600,000 women.
“To date, multiple studies have generated an expanding body of evidence on the association between pregnancy complications (e.g., gestational diabetes and preeclampsia) and the long-term risk of stroke, but studies on associations with infertility, miscarriage, or stillbirth have produced mixed evidence,” Chen Liang, a PhD candidate at the University of Queensland, Brisbane, Australia, and colleagues wrote.
In a study published in the BMJ, the researchers reviewed data from eight observational cohort studies across seven countries (Australia, China, Japan, the Netherlands, Sweden, the United Kingdom, and the United States). The participants were part of the InterLACE (International Collaboration for a Life Course Approach to Reproductive Health and Chronic Disease Events) consortium established in 2021. Most observational studies included in the analysis began between 1990 and 2000.
The study population included 618,851 women aged 32-73 years at baseline for whom data on infertility, miscarriage, or stillbirth, were available. The primary outcome was the association of infertility, recurrent miscarriage, and stillbirth with risk of first fatal or nonfatal stroke, and the results were further stratified by subtype. Stroke was identified through self-reports, linked hospital data, national patient registers, or death registry data. Baseline was defined as the first incidence of infertility, miscarriage, or stillbirth. The exception was the National Survey of Health and Development, a British birth cohort started in 1946, that collected data retrospectively.
The median follow-up period was 13 years for nonfatal stroke and 9.4 years for fatal stroke.
Overall, 17.2%, 16.6%, and 4.6% of the women experienced infertility, miscarriage, and stillbirth, respectively.
Women with a history of infertility had a significantly higher nonfatal stroke risk, compared with those without infertility (hazard ratio, 1.14). Further analysis by stroke subtypes showed an increased association between miscarriage and ischemic stroke (HR, 1.15).
Those with a history of miscarriage also had an increased risk of nonfatal stroke, compared with those without miscarriages (HR, 1.11). In the miscarriage group, the risk of stroke increased with the number of miscarriages, with adjusted HRs of 1.07, 1.12, and 1.35 for women with one, two, and three or more miscarriages, respectively. When stratified by stroke subtype, women with three or more miscarriages were more likely than women with no miscarriages to experience ischemic and hemorrhagic nonfatal strokes.
Associations were similar between miscarriage history and fatal stroke risk. Women with one, two, and three or more miscarriages had increased risk of fatal stroke, compared with those with no miscarriages (aHR, 1.08, 1.26, and 1.82, respectively, and women with three or more miscarriages had a higher risk of ischemic and hemorrhagic stroke (aHR, 1.83 and 1.84, respectively).
Women with a history of stillbirth had an approximately 31% increased risk of nonfatal stroke, compared with those with no history of stillbirth, with aHRs similar for single and recurrent stillbirths (1.32 and 1.29, respectively). Ischemic nonfatal stroke risk was higher in women with any stillbirth, compared with those without stillbirth (aHR, 1.77). Fatal stroke risk also was higher in women with any stillbirth, compared with those without, and this risk increased with the number of stillbirths (HR, 0.97 and HR, 1.26 for those with one stillbirth and two or more, respectively).
“The increased risk of stroke associated with infertility or recurrent stillbirths was mainly driven by a single subtype of stroke (nonfatal ischemic stroke or fatal hemorrhagic stroke, respectively), whereas the risk of stroke associated with recurrent miscarriages was driven by both subtypes,” the researchers wrote.
The researchers cited endothelial dysfunction as a potential underlying mechanism for increased stroke risk associated with pregnancy complications. “Endothelial dysfunction might lead to pregnancy loss through placentation-related defects, persist after a complicated pregnancy, and contribute to the development of stroke through reduced vasodilation, proinflammatory status, and prothrombic properties,” and that history of recurrent pregnancy loss might be a female-specific risk factor for stroke.
To mitigate this risk, they advised early monitoring of women with a history of recurrent miscarriages and stillbirths for stroke risk factors such as high blood pressure, blood sugar levels, and lipid levels.
The study findings were limited by several factors including the use of questionnaires to collect information on infertility, miscarriage, and stillbirth, and the potential variation in definitions of infertility, miscarriage, and stillbirth across the included studies, and a lack of data on the effect of different causes or treatments based on reproductive histories, the researchers noted. Other limitations include incomplete data on stroke subtypes and inability to adjust for all covariates such as thyroid disorders and endometriosis. However, the results were strengthened by the large study size and geographically and racially diverse population, extend the current knowledge on associations between infertility, miscarriage, and stillbirth with stroke, and highlight the need for more research on underlying mechanisms.
Data support gender-specific stroke risk stratification
“Studies that seek to understand gender differences and disparities in adverse outcomes, such as stroke risk, are extremely important given that women historically were excluded from research studies,” Catherine M. Albright, MD, of the University of Washington, Seattle, said in an interview. “By doing these studies, we are able to better risk stratify people in order to better predict and modify risks,” added Dr. Albright, who was not involved in the current study.
“It is well known than adverse pregnancy outcomes such as hypertension in pregnancy, fetal growth restriction, and preterm birth, lead to increased risk of cardiovascular disease and stroke later in life, so the general findings of an association between other adverse reproductive and pregnancy outcomes leads to increased stroke risk are not surprising,” she said.
“The take-home message is that outcomes for pregnancy really do provide a window to future health,” said Dr. Albright. “For clinicians, especially non-ob.gyns., knowing a complete pregnancy history for any new patient is important and can help risk-stratify patients, especially as we continue to gain knowledge like what is shown in this study.”
However, “this study did not evaluate why individual patients may have had infertility, recurrent pregnancy loss, or stillbirth, so research to look further into this association to determine if there is an underlying medical condition that could be treated and therefore possibly reduce both pregnancy complications and future stroke risks would be important,” Dr. Albright noted.
The study was supported by the Australian National Health and Medical Research Council Centres of Research Excellence; one corresponding author was supported by an Australian National Health and Medical Research Council Investigator grant. The researchers had no financial conflicts to disclose. Dr. Albright had no financial conflicts to disclose.
Infertility, pregnancy loss, and stillbirth increased women’s later risk of both nonfatal and fatal stroke, based on data from more than 600,000 women.
“To date, multiple studies have generated an expanding body of evidence on the association between pregnancy complications (e.g., gestational diabetes and preeclampsia) and the long-term risk of stroke, but studies on associations with infertility, miscarriage, or stillbirth have produced mixed evidence,” Chen Liang, a PhD candidate at the University of Queensland, Brisbane, Australia, and colleagues wrote.
In a study published in the BMJ, the researchers reviewed data from eight observational cohort studies across seven countries (Australia, China, Japan, the Netherlands, Sweden, the United Kingdom, and the United States). The participants were part of the InterLACE (International Collaboration for a Life Course Approach to Reproductive Health and Chronic Disease Events) consortium established in 2021. Most observational studies included in the analysis began between 1990 and 2000.
The study population included 618,851 women aged 32-73 years at baseline for whom data on infertility, miscarriage, or stillbirth, were available. The primary outcome was the association of infertility, recurrent miscarriage, and stillbirth with risk of first fatal or nonfatal stroke, and the results were further stratified by subtype. Stroke was identified through self-reports, linked hospital data, national patient registers, or death registry data. Baseline was defined as the first incidence of infertility, miscarriage, or stillbirth. The exception was the National Survey of Health and Development, a British birth cohort started in 1946, that collected data retrospectively.
The median follow-up period was 13 years for nonfatal stroke and 9.4 years for fatal stroke.
Overall, 17.2%, 16.6%, and 4.6% of the women experienced infertility, miscarriage, and stillbirth, respectively.
Women with a history of infertility had a significantly higher nonfatal stroke risk, compared with those without infertility (hazard ratio, 1.14). Further analysis by stroke subtypes showed an increased association between miscarriage and ischemic stroke (HR, 1.15).
Those with a history of miscarriage also had an increased risk of nonfatal stroke, compared with those without miscarriages (HR, 1.11). In the miscarriage group, the risk of stroke increased with the number of miscarriages, with adjusted HRs of 1.07, 1.12, and 1.35 for women with one, two, and three or more miscarriages, respectively. When stratified by stroke subtype, women with three or more miscarriages were more likely than women with no miscarriages to experience ischemic and hemorrhagic nonfatal strokes.
Associations were similar between miscarriage history and fatal stroke risk. Women with one, two, and three or more miscarriages had increased risk of fatal stroke, compared with those with no miscarriages (aHR, 1.08, 1.26, and 1.82, respectively, and women with three or more miscarriages had a higher risk of ischemic and hemorrhagic stroke (aHR, 1.83 and 1.84, respectively).
Women with a history of stillbirth had an approximately 31% increased risk of nonfatal stroke, compared with those with no history of stillbirth, with aHRs similar for single and recurrent stillbirths (1.32 and 1.29, respectively). Ischemic nonfatal stroke risk was higher in women with any stillbirth, compared with those without stillbirth (aHR, 1.77). Fatal stroke risk also was higher in women with any stillbirth, compared with those without, and this risk increased with the number of stillbirths (HR, 0.97 and HR, 1.26 for those with one stillbirth and two or more, respectively).
“The increased risk of stroke associated with infertility or recurrent stillbirths was mainly driven by a single subtype of stroke (nonfatal ischemic stroke or fatal hemorrhagic stroke, respectively), whereas the risk of stroke associated with recurrent miscarriages was driven by both subtypes,” the researchers wrote.
The researchers cited endothelial dysfunction as a potential underlying mechanism for increased stroke risk associated with pregnancy complications. “Endothelial dysfunction might lead to pregnancy loss through placentation-related defects, persist after a complicated pregnancy, and contribute to the development of stroke through reduced vasodilation, proinflammatory status, and prothrombic properties,” and that history of recurrent pregnancy loss might be a female-specific risk factor for stroke.
To mitigate this risk, they advised early monitoring of women with a history of recurrent miscarriages and stillbirths for stroke risk factors such as high blood pressure, blood sugar levels, and lipid levels.
The study findings were limited by several factors including the use of questionnaires to collect information on infertility, miscarriage, and stillbirth, and the potential variation in definitions of infertility, miscarriage, and stillbirth across the included studies, and a lack of data on the effect of different causes or treatments based on reproductive histories, the researchers noted. Other limitations include incomplete data on stroke subtypes and inability to adjust for all covariates such as thyroid disorders and endometriosis. However, the results were strengthened by the large study size and geographically and racially diverse population, extend the current knowledge on associations between infertility, miscarriage, and stillbirth with stroke, and highlight the need for more research on underlying mechanisms.
Data support gender-specific stroke risk stratification
“Studies that seek to understand gender differences and disparities in adverse outcomes, such as stroke risk, are extremely important given that women historically were excluded from research studies,” Catherine M. Albright, MD, of the University of Washington, Seattle, said in an interview. “By doing these studies, we are able to better risk stratify people in order to better predict and modify risks,” added Dr. Albright, who was not involved in the current study.
“It is well known than adverse pregnancy outcomes such as hypertension in pregnancy, fetal growth restriction, and preterm birth, lead to increased risk of cardiovascular disease and stroke later in life, so the general findings of an association between other adverse reproductive and pregnancy outcomes leads to increased stroke risk are not surprising,” she said.
“The take-home message is that outcomes for pregnancy really do provide a window to future health,” said Dr. Albright. “For clinicians, especially non-ob.gyns., knowing a complete pregnancy history for any new patient is important and can help risk-stratify patients, especially as we continue to gain knowledge like what is shown in this study.”
However, “this study did not evaluate why individual patients may have had infertility, recurrent pregnancy loss, or stillbirth, so research to look further into this association to determine if there is an underlying medical condition that could be treated and therefore possibly reduce both pregnancy complications and future stroke risks would be important,” Dr. Albright noted.
The study was supported by the Australian National Health and Medical Research Council Centres of Research Excellence; one corresponding author was supported by an Australian National Health and Medical Research Council Investigator grant. The researchers had no financial conflicts to disclose. Dr. Albright had no financial conflicts to disclose.
FROM THE BMJ
‘Can I survive without payments from insurers?’
It took Michael Golden, MD, 5 years to decide to switch to a concierge practice, in which patients pay a monthly or annual fee for more personalized care. Dr. Golden, an internist in Beverly, Mass., changed course in 2021, during the COVID-19 pandemic.
“I’m not sure why I hesitated for so long,” said Dr. Golden.
But taking the plunge is a big step that they sometimes put off for years.
“The main factors for waiting are fear, uncertainty, and doubt,” said Leigh “Jack” Forbush, DO, a family physician who runs a DPC practice in Hampden, Maine, and mentors doctors contemplating the switch.
According to Dr. Forbush, the critical questions doctors ask themselves are, “Will I be able to find enough paying patients?” and – in the case of DPC practices, which cancel insurance – “Can I live without the money I get from insurers?”
Terry Bauer, CEO of Specialdocs Consultants in Highland Park, Ill., which helps doctors move to a concierge practice, said many of his clients put off the decision for as long as 15 years.
“Clients became progressively worn out – or even burnt out – by the demands of fee-for-service medicine,” said Dr. Bauer. “For women, the tipping point can be when their kids ask, ‘Mom, do you like your job better than me?’ For men, it may be more about feeling tired and unsatisfied with their work.”
But once these doctors make the switch, it’s with all their heart. “A client recently told me that if he couldn’t open a concierge practice, he might have to quit medicine,” Dr. Bauer said. “And he’s only 51.”
Few doctors regret switching
A 2020 survey of DPC physicians for the Society of Actuaries found that 99% reported having better or much better overall personal and professional satisfaction.
Retainer-based physicians report feeling much more relaxed after they start a concierge practice. On many workdays, Dr. Golden takes a walk on a trail in the woods behind his office. “That’s something I couldn’t do before,” he said. “And I go to my kids’ soccer games. I’m able to be present in their lives now.”
Since retainer-based doctors have markedly fewer patients, they can form personal relationships with each one. When Dr. Golden switched, he “went from having a couple of thousand patients to a few hundred,” he said.
“I know each patient now,” said Dorothy Cohen Serna, MD, an internist in Cypress, Tex., who moved to concierge in 2017. “I don’t need to look at their chart to know who they are.”
Dr. Serna said patients’ close relationship with her helped them get through the worst months of the pandemic. “They were scared, depressed, and concerned, and they needed a lot of individual attention,” she said.
Because they see fewer patients, concierge doctors can lengthen appointment times to about 30 minutes – or longer, if necessary. They no longer have a problem answering patients’ “doorknob questions” – wholly new concerns brought up at the end of the visit.
“The appointment might be for a sprained ankle, and then the patient might mention they haven’t been sleeping well,” Dr. Golden said. “I have time to talk about that without worrying that my schedule is getting backed up.”
Why patients sign up
Retainer-based practices are still an exotic concept in many areas, but patients are beginning to understand the value, said Shalini Kaneriya, MD, an internist in Herndon, Va,, who switched her practice to concierge in 2018.
Several hundred patients followed her into her new practice because “people realized their care would be better if they had a concierge doctor,” she said. Two years ago, partly because of growing demand, she recruited another physician as an associate.
“People want a relationship with their doctor,” Dr. Serna added. “It’s hard to provide that in a regular practice.”
Todd Granger, MD, an internist who opened a DPC practice in Chapel Hill, N.C., in 2016, said new patients often mention feeling rushed through appointments with their previous doctors. Also, “it’s hard to get to see a doctor around here.”
Scott Bernstein, MD, an internist who runs a DPC practice in Scottsdale, Ariz., said he can arrange to have patients see specialists much faster than if they try to make appointments on their own. “I personally call specialists and then prep my patients on how to deal with the appointment,” he said.
Retainer-based practices tend to have a greater number of older and chronically ill patients, but they also attract patients who need less care. “The healthier patients find value in our proactive approach to prevention and wellness,” Dr. Serna said.
Some concierge physicians charge higher fees to patients who need more care, but many decide this is too complicated and charge everyone the same fee. Dr. Granger said he initially had a variable fee schedule, but when some lower-paying patients began to need more visits, he had to consider charging them extra. “Now I basically have just one fee,” he said.
Not a good fit for many physicians
Dr. Bauer said a lot of physicians are interested in retainer-based practice, but many of them might not make the income they had hoped for. Specialdocs interviews physicians who inquire about the model and ultimately doesn’t contract with 80% of them, Dr. Bauer said.
To be able to sign up and retain enough patients, the doctor’s attitude is important. “You have to be driven by the desire to go deep with patients -- to work hard with them and deal with their issues,” said Erika Bliss, MD, who runs a DPC practice in Seattle.
Dr. Bernstein said retainer-based physicians have to be interested in lifestyle issues, such as diet, exercise, and sleep. “I spend a lot of time dealing with issues like how to incorporate physical activity into daily routines,” he said. “Some doctors wouldn’t enjoy doing that.”
Also, concierge physicians have to be available all the time. “Patients have my cell phone number,” Dr. Granger said. “They could call in the middle of the night, but they usually don’t.”
To ensure that they get some time off, many concierge physicians have partners. Dr. Bernstein and another DPC doctor maintain separate practices but cover for each other. Each takes every other weekend off plus 6 weeks every year.
Can you attract enough patients?
A key challenge is finding enough patients to sustain a concierge practice. Planning the switch involves setting a target number of patients needed for the doctor to make a decent income after paying practice expenses. For example, a doctor charging $300 a month to 250 patients would gross $900,000 per year, and then pay practice expenses from that.
Attracting the target number of patients can take months or even years. After almost 6 years, Dr. Granger said, he has around 240 patients ― well below his target number of 440.
Partly because the practice model is not well known in North Carolina, Dr. Granger set his fee very low, at $60 a month, then raised it to $75. That means his practice has been grossing just $216,000 a year. But he is not about to give up. He plans to raise his fee in July and hopes that word of mouth will add more patients.
If physicians cannot earn enough in their concierge practice, Dr. Bauer said, they may moonlight at a local hospital or work for a telemedicine company. He hasn’t heard of physicians closing their concierge practice and returning to their previous practice model. “They didn’t like what they were doing before,” he said.
Opening up to lower-income patients
Dr. Granger’s $75 monthly fee is an example of how retainer-based medicine has transformed itself from a gold-plated service for rich people to a service that middle-class and even lower-income people can afford. DPC practices like Dr. Granger’s have dramatically lowered expenses by cutting out the need to bill insurance companies. Some DPC practices further reduce expenses by not having any staff and by renting out office space.
Dr. Forbush’s Pine Tree State patients are mostly blue-collar workers – electricians, plumbers, people who work in small businesses. He charges them $150 a month, which most patients who don’t have health insurance can afford. He said three-quarters of his patients lack health insurance, although some have back-up finances, such as health savings accounts.
Since his patients have to pay out of pocket for tests and specialists, Dr. Forbush keeps referrals in check by handling many problems himself. “Since I have more time to spend with the patient, I can often work out issues that other doctors might ask specialists to deal with,” he said.
He has learned some dermatologic procedures. “There are plenty of things I can handle on my own,” he said.
Dr. Granger adds that by examining patients during longer appointments, expensive diagnostic exams are not always necessary.
The challenges for this model
Many experts warn that retainer-based practices won’t work for doctors who want to leave employment or for doctors fresh out of residency. Not having your own patients to bring into the new practice is a big minus, because this is the best way to start the new practice.
Still, there are other ways to find patients. Dr. Bauer said physicians can advertise online, make themselves known by giving speeches in the community, or contract with small employers to treat their workers.
Dr. Bauer said some of his clients were employed physicians, and he thinks they will become a bigger factor now that fewer doctors remain in private practice. The chief barrier for employed physicians is the restrictive covenant that prevents them from setting up a practice nearby. But Dr. Bauer said some employers are willing to waive restrictive covenants for retainer-based doctors.
New physicians are also adopting the concierge model. Dr. Forbush said physicians straight out of residency have set up DPC practices in Maine. They signed up patients for their new practices even before they graduated, he said.
Retainer-based medicine is still mainly limited to primary care physicians, but according to Dr. Bauer, it can also work for specialists who have long-term relationships with patients, such as cardiologists, ob.gyns., rheumatologists, neurologists, and endocrinologists.
No going back
Most doctors who make the switch to retainer-based practice understand that there’s likely no going back. When Dr. Bernstein switched, he announced the change to patients and canceled insurance contracts. “It was make or break,” he said. “I had no parachute.”
A version of this article first appeared on Medscape.com.
It took Michael Golden, MD, 5 years to decide to switch to a concierge practice, in which patients pay a monthly or annual fee for more personalized care. Dr. Golden, an internist in Beverly, Mass., changed course in 2021, during the COVID-19 pandemic.
“I’m not sure why I hesitated for so long,” said Dr. Golden.
But taking the plunge is a big step that they sometimes put off for years.
“The main factors for waiting are fear, uncertainty, and doubt,” said Leigh “Jack” Forbush, DO, a family physician who runs a DPC practice in Hampden, Maine, and mentors doctors contemplating the switch.
According to Dr. Forbush, the critical questions doctors ask themselves are, “Will I be able to find enough paying patients?” and – in the case of DPC practices, which cancel insurance – “Can I live without the money I get from insurers?”
Terry Bauer, CEO of Specialdocs Consultants in Highland Park, Ill., which helps doctors move to a concierge practice, said many of his clients put off the decision for as long as 15 years.
“Clients became progressively worn out – or even burnt out – by the demands of fee-for-service medicine,” said Dr. Bauer. “For women, the tipping point can be when their kids ask, ‘Mom, do you like your job better than me?’ For men, it may be more about feeling tired and unsatisfied with their work.”
But once these doctors make the switch, it’s with all their heart. “A client recently told me that if he couldn’t open a concierge practice, he might have to quit medicine,” Dr. Bauer said. “And he’s only 51.”
Few doctors regret switching
A 2020 survey of DPC physicians for the Society of Actuaries found that 99% reported having better or much better overall personal and professional satisfaction.
Retainer-based physicians report feeling much more relaxed after they start a concierge practice. On many workdays, Dr. Golden takes a walk on a trail in the woods behind his office. “That’s something I couldn’t do before,” he said. “And I go to my kids’ soccer games. I’m able to be present in their lives now.”
Since retainer-based doctors have markedly fewer patients, they can form personal relationships with each one. When Dr. Golden switched, he “went from having a couple of thousand patients to a few hundred,” he said.
“I know each patient now,” said Dorothy Cohen Serna, MD, an internist in Cypress, Tex., who moved to concierge in 2017. “I don’t need to look at their chart to know who they are.”
Dr. Serna said patients’ close relationship with her helped them get through the worst months of the pandemic. “They were scared, depressed, and concerned, and they needed a lot of individual attention,” she said.
Because they see fewer patients, concierge doctors can lengthen appointment times to about 30 minutes – or longer, if necessary. They no longer have a problem answering patients’ “doorknob questions” – wholly new concerns brought up at the end of the visit.
“The appointment might be for a sprained ankle, and then the patient might mention they haven’t been sleeping well,” Dr. Golden said. “I have time to talk about that without worrying that my schedule is getting backed up.”
Why patients sign up
Retainer-based practices are still an exotic concept in many areas, but patients are beginning to understand the value, said Shalini Kaneriya, MD, an internist in Herndon, Va,, who switched her practice to concierge in 2018.
Several hundred patients followed her into her new practice because “people realized their care would be better if they had a concierge doctor,” she said. Two years ago, partly because of growing demand, she recruited another physician as an associate.
“People want a relationship with their doctor,” Dr. Serna added. “It’s hard to provide that in a regular practice.”
Todd Granger, MD, an internist who opened a DPC practice in Chapel Hill, N.C., in 2016, said new patients often mention feeling rushed through appointments with their previous doctors. Also, “it’s hard to get to see a doctor around here.”
Scott Bernstein, MD, an internist who runs a DPC practice in Scottsdale, Ariz., said he can arrange to have patients see specialists much faster than if they try to make appointments on their own. “I personally call specialists and then prep my patients on how to deal with the appointment,” he said.
Retainer-based practices tend to have a greater number of older and chronically ill patients, but they also attract patients who need less care. “The healthier patients find value in our proactive approach to prevention and wellness,” Dr. Serna said.
Some concierge physicians charge higher fees to patients who need more care, but many decide this is too complicated and charge everyone the same fee. Dr. Granger said he initially had a variable fee schedule, but when some lower-paying patients began to need more visits, he had to consider charging them extra. “Now I basically have just one fee,” he said.
Not a good fit for many physicians
Dr. Bauer said a lot of physicians are interested in retainer-based practice, but many of them might not make the income they had hoped for. Specialdocs interviews physicians who inquire about the model and ultimately doesn’t contract with 80% of them, Dr. Bauer said.
To be able to sign up and retain enough patients, the doctor’s attitude is important. “You have to be driven by the desire to go deep with patients -- to work hard with them and deal with their issues,” said Erika Bliss, MD, who runs a DPC practice in Seattle.
Dr. Bernstein said retainer-based physicians have to be interested in lifestyle issues, such as diet, exercise, and sleep. “I spend a lot of time dealing with issues like how to incorporate physical activity into daily routines,” he said. “Some doctors wouldn’t enjoy doing that.”
Also, concierge physicians have to be available all the time. “Patients have my cell phone number,” Dr. Granger said. “They could call in the middle of the night, but they usually don’t.”
To ensure that they get some time off, many concierge physicians have partners. Dr. Bernstein and another DPC doctor maintain separate practices but cover for each other. Each takes every other weekend off plus 6 weeks every year.
Can you attract enough patients?
A key challenge is finding enough patients to sustain a concierge practice. Planning the switch involves setting a target number of patients needed for the doctor to make a decent income after paying practice expenses. For example, a doctor charging $300 a month to 250 patients would gross $900,000 per year, and then pay practice expenses from that.
Attracting the target number of patients can take months or even years. After almost 6 years, Dr. Granger said, he has around 240 patients ― well below his target number of 440.
Partly because the practice model is not well known in North Carolina, Dr. Granger set his fee very low, at $60 a month, then raised it to $75. That means his practice has been grossing just $216,000 a year. But he is not about to give up. He plans to raise his fee in July and hopes that word of mouth will add more patients.
If physicians cannot earn enough in their concierge practice, Dr. Bauer said, they may moonlight at a local hospital or work for a telemedicine company. He hasn’t heard of physicians closing their concierge practice and returning to their previous practice model. “They didn’t like what they were doing before,” he said.
Opening up to lower-income patients
Dr. Granger’s $75 monthly fee is an example of how retainer-based medicine has transformed itself from a gold-plated service for rich people to a service that middle-class and even lower-income people can afford. DPC practices like Dr. Granger’s have dramatically lowered expenses by cutting out the need to bill insurance companies. Some DPC practices further reduce expenses by not having any staff and by renting out office space.
Dr. Forbush’s Pine Tree State patients are mostly blue-collar workers – electricians, plumbers, people who work in small businesses. He charges them $150 a month, which most patients who don’t have health insurance can afford. He said three-quarters of his patients lack health insurance, although some have back-up finances, such as health savings accounts.
Since his patients have to pay out of pocket for tests and specialists, Dr. Forbush keeps referrals in check by handling many problems himself. “Since I have more time to spend with the patient, I can often work out issues that other doctors might ask specialists to deal with,” he said.
He has learned some dermatologic procedures. “There are plenty of things I can handle on my own,” he said.
Dr. Granger adds that by examining patients during longer appointments, expensive diagnostic exams are not always necessary.
The challenges for this model
Many experts warn that retainer-based practices won’t work for doctors who want to leave employment or for doctors fresh out of residency. Not having your own patients to bring into the new practice is a big minus, because this is the best way to start the new practice.
Still, there are other ways to find patients. Dr. Bauer said physicians can advertise online, make themselves known by giving speeches in the community, or contract with small employers to treat their workers.
Dr. Bauer said some of his clients were employed physicians, and he thinks they will become a bigger factor now that fewer doctors remain in private practice. The chief barrier for employed physicians is the restrictive covenant that prevents them from setting up a practice nearby. But Dr. Bauer said some employers are willing to waive restrictive covenants for retainer-based doctors.
New physicians are also adopting the concierge model. Dr. Forbush said physicians straight out of residency have set up DPC practices in Maine. They signed up patients for their new practices even before they graduated, he said.
Retainer-based medicine is still mainly limited to primary care physicians, but according to Dr. Bauer, it can also work for specialists who have long-term relationships with patients, such as cardiologists, ob.gyns., rheumatologists, neurologists, and endocrinologists.
No going back
Most doctors who make the switch to retainer-based practice understand that there’s likely no going back. When Dr. Bernstein switched, he announced the change to patients and canceled insurance contracts. “It was make or break,” he said. “I had no parachute.”
A version of this article first appeared on Medscape.com.
It took Michael Golden, MD, 5 years to decide to switch to a concierge practice, in which patients pay a monthly or annual fee for more personalized care. Dr. Golden, an internist in Beverly, Mass., changed course in 2021, during the COVID-19 pandemic.
“I’m not sure why I hesitated for so long,” said Dr. Golden.
But taking the plunge is a big step that they sometimes put off for years.
“The main factors for waiting are fear, uncertainty, and doubt,” said Leigh “Jack” Forbush, DO, a family physician who runs a DPC practice in Hampden, Maine, and mentors doctors contemplating the switch.
According to Dr. Forbush, the critical questions doctors ask themselves are, “Will I be able to find enough paying patients?” and – in the case of DPC practices, which cancel insurance – “Can I live without the money I get from insurers?”
Terry Bauer, CEO of Specialdocs Consultants in Highland Park, Ill., which helps doctors move to a concierge practice, said many of his clients put off the decision for as long as 15 years.
“Clients became progressively worn out – or even burnt out – by the demands of fee-for-service medicine,” said Dr. Bauer. “For women, the tipping point can be when their kids ask, ‘Mom, do you like your job better than me?’ For men, it may be more about feeling tired and unsatisfied with their work.”
But once these doctors make the switch, it’s with all their heart. “A client recently told me that if he couldn’t open a concierge practice, he might have to quit medicine,” Dr. Bauer said. “And he’s only 51.”
Few doctors regret switching
A 2020 survey of DPC physicians for the Society of Actuaries found that 99% reported having better or much better overall personal and professional satisfaction.
Retainer-based physicians report feeling much more relaxed after they start a concierge practice. On many workdays, Dr. Golden takes a walk on a trail in the woods behind his office. “That’s something I couldn’t do before,” he said. “And I go to my kids’ soccer games. I’m able to be present in their lives now.”
Since retainer-based doctors have markedly fewer patients, they can form personal relationships with each one. When Dr. Golden switched, he “went from having a couple of thousand patients to a few hundred,” he said.
“I know each patient now,” said Dorothy Cohen Serna, MD, an internist in Cypress, Tex., who moved to concierge in 2017. “I don’t need to look at their chart to know who they are.”
Dr. Serna said patients’ close relationship with her helped them get through the worst months of the pandemic. “They were scared, depressed, and concerned, and they needed a lot of individual attention,” she said.
Because they see fewer patients, concierge doctors can lengthen appointment times to about 30 minutes – or longer, if necessary. They no longer have a problem answering patients’ “doorknob questions” – wholly new concerns brought up at the end of the visit.
“The appointment might be for a sprained ankle, and then the patient might mention they haven’t been sleeping well,” Dr. Golden said. “I have time to talk about that without worrying that my schedule is getting backed up.”
Why patients sign up
Retainer-based practices are still an exotic concept in many areas, but patients are beginning to understand the value, said Shalini Kaneriya, MD, an internist in Herndon, Va,, who switched her practice to concierge in 2018.
Several hundred patients followed her into her new practice because “people realized their care would be better if they had a concierge doctor,” she said. Two years ago, partly because of growing demand, she recruited another physician as an associate.
“People want a relationship with their doctor,” Dr. Serna added. “It’s hard to provide that in a regular practice.”
Todd Granger, MD, an internist who opened a DPC practice in Chapel Hill, N.C., in 2016, said new patients often mention feeling rushed through appointments with their previous doctors. Also, “it’s hard to get to see a doctor around here.”
Scott Bernstein, MD, an internist who runs a DPC practice in Scottsdale, Ariz., said he can arrange to have patients see specialists much faster than if they try to make appointments on their own. “I personally call specialists and then prep my patients on how to deal with the appointment,” he said.
Retainer-based practices tend to have a greater number of older and chronically ill patients, but they also attract patients who need less care. “The healthier patients find value in our proactive approach to prevention and wellness,” Dr. Serna said.
Some concierge physicians charge higher fees to patients who need more care, but many decide this is too complicated and charge everyone the same fee. Dr. Granger said he initially had a variable fee schedule, but when some lower-paying patients began to need more visits, he had to consider charging them extra. “Now I basically have just one fee,” he said.
Not a good fit for many physicians
Dr. Bauer said a lot of physicians are interested in retainer-based practice, but many of them might not make the income they had hoped for. Specialdocs interviews physicians who inquire about the model and ultimately doesn’t contract with 80% of them, Dr. Bauer said.
To be able to sign up and retain enough patients, the doctor’s attitude is important. “You have to be driven by the desire to go deep with patients -- to work hard with them and deal with their issues,” said Erika Bliss, MD, who runs a DPC practice in Seattle.
Dr. Bernstein said retainer-based physicians have to be interested in lifestyle issues, such as diet, exercise, and sleep. “I spend a lot of time dealing with issues like how to incorporate physical activity into daily routines,” he said. “Some doctors wouldn’t enjoy doing that.”
Also, concierge physicians have to be available all the time. “Patients have my cell phone number,” Dr. Granger said. “They could call in the middle of the night, but they usually don’t.”
To ensure that they get some time off, many concierge physicians have partners. Dr. Bernstein and another DPC doctor maintain separate practices but cover for each other. Each takes every other weekend off plus 6 weeks every year.
Can you attract enough patients?
A key challenge is finding enough patients to sustain a concierge practice. Planning the switch involves setting a target number of patients needed for the doctor to make a decent income after paying practice expenses. For example, a doctor charging $300 a month to 250 patients would gross $900,000 per year, and then pay practice expenses from that.
Attracting the target number of patients can take months or even years. After almost 6 years, Dr. Granger said, he has around 240 patients ― well below his target number of 440.
Partly because the practice model is not well known in North Carolina, Dr. Granger set his fee very low, at $60 a month, then raised it to $75. That means his practice has been grossing just $216,000 a year. But he is not about to give up. He plans to raise his fee in July and hopes that word of mouth will add more patients.
If physicians cannot earn enough in their concierge practice, Dr. Bauer said, they may moonlight at a local hospital or work for a telemedicine company. He hasn’t heard of physicians closing their concierge practice and returning to their previous practice model. “They didn’t like what they were doing before,” he said.
Opening up to lower-income patients
Dr. Granger’s $75 monthly fee is an example of how retainer-based medicine has transformed itself from a gold-plated service for rich people to a service that middle-class and even lower-income people can afford. DPC practices like Dr. Granger’s have dramatically lowered expenses by cutting out the need to bill insurance companies. Some DPC practices further reduce expenses by not having any staff and by renting out office space.
Dr. Forbush’s Pine Tree State patients are mostly blue-collar workers – electricians, plumbers, people who work in small businesses. He charges them $150 a month, which most patients who don’t have health insurance can afford. He said three-quarters of his patients lack health insurance, although some have back-up finances, such as health savings accounts.
Since his patients have to pay out of pocket for tests and specialists, Dr. Forbush keeps referrals in check by handling many problems himself. “Since I have more time to spend with the patient, I can often work out issues that other doctors might ask specialists to deal with,” he said.
He has learned some dermatologic procedures. “There are plenty of things I can handle on my own,” he said.
Dr. Granger adds that by examining patients during longer appointments, expensive diagnostic exams are not always necessary.
The challenges for this model
Many experts warn that retainer-based practices won’t work for doctors who want to leave employment or for doctors fresh out of residency. Not having your own patients to bring into the new practice is a big minus, because this is the best way to start the new practice.
Still, there are other ways to find patients. Dr. Bauer said physicians can advertise online, make themselves known by giving speeches in the community, or contract with small employers to treat their workers.
Dr. Bauer said some of his clients were employed physicians, and he thinks they will become a bigger factor now that fewer doctors remain in private practice. The chief barrier for employed physicians is the restrictive covenant that prevents them from setting up a practice nearby. But Dr. Bauer said some employers are willing to waive restrictive covenants for retainer-based doctors.
New physicians are also adopting the concierge model. Dr. Forbush said physicians straight out of residency have set up DPC practices in Maine. They signed up patients for their new practices even before they graduated, he said.
Retainer-based medicine is still mainly limited to primary care physicians, but according to Dr. Bauer, it can also work for specialists who have long-term relationships with patients, such as cardiologists, ob.gyns., rheumatologists, neurologists, and endocrinologists.
No going back
Most doctors who make the switch to retainer-based practice understand that there’s likely no going back. When Dr. Bernstein switched, he announced the change to patients and canceled insurance contracts. “It was make or break,” he said. “I had no parachute.”
A version of this article first appeared on Medscape.com.