User login
Diabetes Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving options for treating and preventing Type 2 Diabetes in at-risk patients. The Diabetes Hub is powered by Frontline Medical Communications.
Complications rise for young people who miss glycemic goals
VIENNA – Young people worldwide who have type 1 diabetes are not achieving their glycemic targets and, as a result, experience suboptimal outcomes.
About 70% of children and teens and 81% of young adults did not meet their hemoglobin A1c targets, in a large records review. As a result, many are experiencing significantly more complications from poorly controlled diabetes, Dr. Lori Laffel and her colleagues reported at the annual meeting of the European Association for the Study of Diabetes.
“These results highlight the need for further improvements in the management of glycemic control ... in young people with type 1 diabetes, particularly for patents aged 19-25 years,” wrote Dr. Laffel, chief of the pediatric, adolescent, and young adult section at the Joslin Diabetes Center, Boston.
The study comprised the European participants (2,943) in the TEENs study, a worldwide, observational study of 5,960 young patients with type 1 diabetes (aged 8-25 years) who were treated at 219 centers in 20 countries. The target HbA1c levels varied by age: 7.5% for patients 18 years and younger, and 7% for those 19 years and older. Younger patients were divided into two groups (8-12 and 13-18 years old), while the third group comprised those aged 19-25 years.
The overall mean HbA1c in was 8.5%, with 35% of the entire group meeting their goals. Control rates did not vary much among the younger patients (39% in those aged 8-12 years and 37% in those aged 12-18 years). A smaller percentage of the older patients stayed on target (23%).
Associated complications were significantly more common in uncontrolled patients: In the 6 months before data were collected, about 6% of both younger groups and 7% of the older group had experienced diabetic ketoacidosis. In contrast, the incidence among well-controlled patients in all three groups was about 3%.
The oldest uncontrolled patients also had the highest incidence of severe hypoglycemia resulting in loss of consciousness or seizure – 6% compared to 36% of well-controlled patients that age.
Among the youngest uncontrolled patients, the incidence was less than 3% in each group. Severe hypoglycemia incidence was similar in the middle group, at about 2% in the uncontrolled vs. 3% in the controlled patients.
The incidence of microalbuminuria soared among the oldest uncontrolled patients, reaching almost 9%, compared with just under 6% of controlled patients. For the youngest patients, the rates were similar (about 1% of each group). It was doubled in the middle group, at 5% in uncontrolled vs. 2.4% of controlled patients.
Neuropathy occurred in 10% of the oldest uncontrolled patients vs. 8% of well controlled. For the youngest, the rates doubled (3% vs. 1.5%, respectively). They more than doubled in the middle group (almost 6% vs. 2%).
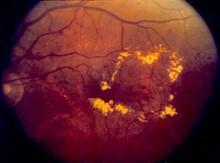
The rates of retinopathy needing treatment were also elevated in the oldest uncontrolled patients, compared with the controlled patients (4% vs. 1.5%). However, in both younger groups, they were well under 1% regardless of control.
A multivariate analysis determined that diabetic ketoacidosis and diabetic neuropathy were significantly associated with uncontrolled HbA1c (odds ratio, 0.53 and 0.47, respectively).
Dr Laffel has received research support from Sanofi-Aventis, which funded the study, as well as other pharmaceutical companies. Two coauthors were Sanofi employees.
On Twitter @alz_gal
VIENNA – Young people worldwide who have type 1 diabetes are not achieving their glycemic targets and, as a result, experience suboptimal outcomes.
About 70% of children and teens and 81% of young adults did not meet their hemoglobin A1c targets, in a large records review. As a result, many are experiencing significantly more complications from poorly controlled diabetes, Dr. Lori Laffel and her colleagues reported at the annual meeting of the European Association for the Study of Diabetes.
“These results highlight the need for further improvements in the management of glycemic control ... in young people with type 1 diabetes, particularly for patents aged 19-25 years,” wrote Dr. Laffel, chief of the pediatric, adolescent, and young adult section at the Joslin Diabetes Center, Boston.
The study comprised the European participants (2,943) in the TEENs study, a worldwide, observational study of 5,960 young patients with type 1 diabetes (aged 8-25 years) who were treated at 219 centers in 20 countries. The target HbA1c levels varied by age: 7.5% for patients 18 years and younger, and 7% for those 19 years and older. Younger patients were divided into two groups (8-12 and 13-18 years old), while the third group comprised those aged 19-25 years.
The overall mean HbA1c in was 8.5%, with 35% of the entire group meeting their goals. Control rates did not vary much among the younger patients (39% in those aged 8-12 years and 37% in those aged 12-18 years). A smaller percentage of the older patients stayed on target (23%).
Associated complications were significantly more common in uncontrolled patients: In the 6 months before data were collected, about 6% of both younger groups and 7% of the older group had experienced diabetic ketoacidosis. In contrast, the incidence among well-controlled patients in all three groups was about 3%.
The oldest uncontrolled patients also had the highest incidence of severe hypoglycemia resulting in loss of consciousness or seizure – 6% compared to 36% of well-controlled patients that age.
Among the youngest uncontrolled patients, the incidence was less than 3% in each group. Severe hypoglycemia incidence was similar in the middle group, at about 2% in the uncontrolled vs. 3% in the controlled patients.
The incidence of microalbuminuria soared among the oldest uncontrolled patients, reaching almost 9%, compared with just under 6% of controlled patients. For the youngest patients, the rates were similar (about 1% of each group). It was doubled in the middle group, at 5% in uncontrolled vs. 2.4% of controlled patients.
Neuropathy occurred in 10% of the oldest uncontrolled patients vs. 8% of well controlled. For the youngest, the rates doubled (3% vs. 1.5%, respectively). They more than doubled in the middle group (almost 6% vs. 2%).
The rates of retinopathy needing treatment were also elevated in the oldest uncontrolled patients, compared with the controlled patients (4% vs. 1.5%). However, in both younger groups, they were well under 1% regardless of control.
A multivariate analysis determined that diabetic ketoacidosis and diabetic neuropathy were significantly associated with uncontrolled HbA1c (odds ratio, 0.53 and 0.47, respectively).
Dr Laffel has received research support from Sanofi-Aventis, which funded the study, as well as other pharmaceutical companies. Two coauthors were Sanofi employees.
On Twitter @alz_gal
VIENNA – Young people worldwide who have type 1 diabetes are not achieving their glycemic targets and, as a result, experience suboptimal outcomes.
About 70% of children and teens and 81% of young adults did not meet their hemoglobin A1c targets, in a large records review. As a result, many are experiencing significantly more complications from poorly controlled diabetes, Dr. Lori Laffel and her colleagues reported at the annual meeting of the European Association for the Study of Diabetes.
“These results highlight the need for further improvements in the management of glycemic control ... in young people with type 1 diabetes, particularly for patents aged 19-25 years,” wrote Dr. Laffel, chief of the pediatric, adolescent, and young adult section at the Joslin Diabetes Center, Boston.
The study comprised the European participants (2,943) in the TEENs study, a worldwide, observational study of 5,960 young patients with type 1 diabetes (aged 8-25 years) who were treated at 219 centers in 20 countries. The target HbA1c levels varied by age: 7.5% for patients 18 years and younger, and 7% for those 19 years and older. Younger patients were divided into two groups (8-12 and 13-18 years old), while the third group comprised those aged 19-25 years.
The overall mean HbA1c in was 8.5%, with 35% of the entire group meeting their goals. Control rates did not vary much among the younger patients (39% in those aged 8-12 years and 37% in those aged 12-18 years). A smaller percentage of the older patients stayed on target (23%).
Associated complications were significantly more common in uncontrolled patients: In the 6 months before data were collected, about 6% of both younger groups and 7% of the older group had experienced diabetic ketoacidosis. In contrast, the incidence among well-controlled patients in all three groups was about 3%.
The oldest uncontrolled patients also had the highest incidence of severe hypoglycemia resulting in loss of consciousness or seizure – 6% compared to 36% of well-controlled patients that age.
Among the youngest uncontrolled patients, the incidence was less than 3% in each group. Severe hypoglycemia incidence was similar in the middle group, at about 2% in the uncontrolled vs. 3% in the controlled patients.
The incidence of microalbuminuria soared among the oldest uncontrolled patients, reaching almost 9%, compared with just under 6% of controlled patients. For the youngest patients, the rates were similar (about 1% of each group). It was doubled in the middle group, at 5% in uncontrolled vs. 2.4% of controlled patients.
Neuropathy occurred in 10% of the oldest uncontrolled patients vs. 8% of well controlled. For the youngest, the rates doubled (3% vs. 1.5%, respectively). They more than doubled in the middle group (almost 6% vs. 2%).
The rates of retinopathy needing treatment were also elevated in the oldest uncontrolled patients, compared with the controlled patients (4% vs. 1.5%). However, in both younger groups, they were well under 1% regardless of control.
A multivariate analysis determined that diabetic ketoacidosis and diabetic neuropathy were significantly associated with uncontrolled HbA1c (odds ratio, 0.53 and 0.47, respectively).
Dr Laffel has received research support from Sanofi-Aventis, which funded the study, as well as other pharmaceutical companies. Two coauthors were Sanofi employees.
On Twitter @alz_gal
AT EASD 2014
Key clinical point: About three-fourths of children and young people with type 1 diabetes did not meet their hemoglobin A1c goals.
Major finding: Complications for those with uncontrolled diabetes were especially frequent in patients aged 19-25 years, with 10% developing neuropathy and 9% microalbuminuria.
Data source: TEENs, a records review comprising 5,960 type 1 diabetes patients aged 8-25 years.
Disclosures: Dr Laffel has received research support from Sanofi-Aventis, which funded the study, as well as other pharmaceutical companies. Two coauthors were Sanofi employees.
UTIs in type 2 diabetes can be costly
VIENNA – Urinary tract infections are relatively common and can be quite expensive among patients with newly diagnosed diabetes.
In a large patient database, the infection rate was about 128/1,000 patients, Shengsheng Yu, Ph.D., said at the annual meeting of the European Association for the Study of Diabetes. While only about 4% of these patients were hospitalized, their treatment costs hovered around $3,407 in Germany, where the study was conducted.
These data were extracted from a large German patient claims database, said Dr. Yu of Merck Sharp & Dohme, Whitehouse Station, N.J. The cohort comprised 530,918 patients who had type 2 diabetes during the study years of 2010-2012. Of these, 64,332 had incident disease.
Patients with newly diagnosed diabetes were significantly younger than was the diabetes-prevalent population (70 vs. 73 years), and had a significantly lower than the Charlson comorbidity index (5.4 vs. 7.3 years). Their diabetes was also less severe when measured by the adapted Diabetes Complication Severity Index (1.5 vs. 2.4).
During the study period, roughly 20% of patients had at least 1 urinary tract infection (UTI); 6% had two or more.
UTIs were twice as common in women. Prevalence also grew with advancing age in both sexes. Among those with newly diagnosed diabetes, women developed their UTI significantly more quickly than did men. By the end of the study, 20% of those women had developed one, compared with 10% of the men.
A multivariate analysis determined the risk factors associated with UTIs. These included having had a previous UTI (odds ratio, 3.5), female gender (OR, 1.7), higher Charlson comorbidity status (OR, 1.5), and age (OR, 1.4 for those older than 79 years).
Hemoglobin A1c levels were also a significant independent predictor of UTI, with an odds ratio of 1.5 for levels of 9.5%-10%, compared with 7%-7.5%.
In an analysis of the development of a first UTI after diagnosis, all of those predictive factors remained significant.
The investigators also examined costs associated with inpatient and outpatient treatment. Total costs included antibiotics and the cost of either ambulatory, outpatient, or in-hospital care.
The majority were treated by a physicians as an outpatient, with a median cost of 86 euros (US$111). About 46,500 received a prescription only, at a median cost of 22 euros (US$25). The smallest number (3,445) required hospitalization – a very expensive experience – with a mean cost of 2,627 euros (US$3,407).
During the discussion period, the issue of infection validation was a concern. Many physicians treat on symptoms only, or on a single urinalysis that might show a small amount of blood or protein. The number of culture-proven UTIs is much less, it was suggested.
Dr. Yu admitted that this is a common occurrence and could be affecting the validity of her conclusions somewhat.
She is an employee of Merck.
On Twitter @alz_gal
VIENNA – Urinary tract infections are relatively common and can be quite expensive among patients with newly diagnosed diabetes.
In a large patient database, the infection rate was about 128/1,000 patients, Shengsheng Yu, Ph.D., said at the annual meeting of the European Association for the Study of Diabetes. While only about 4% of these patients were hospitalized, their treatment costs hovered around $3,407 in Germany, where the study was conducted.
These data were extracted from a large German patient claims database, said Dr. Yu of Merck Sharp & Dohme, Whitehouse Station, N.J. The cohort comprised 530,918 patients who had type 2 diabetes during the study years of 2010-2012. Of these, 64,332 had incident disease.
Patients with newly diagnosed diabetes were significantly younger than was the diabetes-prevalent population (70 vs. 73 years), and had a significantly lower than the Charlson comorbidity index (5.4 vs. 7.3 years). Their diabetes was also less severe when measured by the adapted Diabetes Complication Severity Index (1.5 vs. 2.4).
During the study period, roughly 20% of patients had at least 1 urinary tract infection (UTI); 6% had two or more.
UTIs were twice as common in women. Prevalence also grew with advancing age in both sexes. Among those with newly diagnosed diabetes, women developed their UTI significantly more quickly than did men. By the end of the study, 20% of those women had developed one, compared with 10% of the men.
A multivariate analysis determined the risk factors associated with UTIs. These included having had a previous UTI (odds ratio, 3.5), female gender (OR, 1.7), higher Charlson comorbidity status (OR, 1.5), and age (OR, 1.4 for those older than 79 years).
Hemoglobin A1c levels were also a significant independent predictor of UTI, with an odds ratio of 1.5 for levels of 9.5%-10%, compared with 7%-7.5%.
In an analysis of the development of a first UTI after diagnosis, all of those predictive factors remained significant.
The investigators also examined costs associated with inpatient and outpatient treatment. Total costs included antibiotics and the cost of either ambulatory, outpatient, or in-hospital care.
The majority were treated by a physicians as an outpatient, with a median cost of 86 euros (US$111). About 46,500 received a prescription only, at a median cost of 22 euros (US$25). The smallest number (3,445) required hospitalization – a very expensive experience – with a mean cost of 2,627 euros (US$3,407).
During the discussion period, the issue of infection validation was a concern. Many physicians treat on symptoms only, or on a single urinalysis that might show a small amount of blood or protein. The number of culture-proven UTIs is much less, it was suggested.
Dr. Yu admitted that this is a common occurrence and could be affecting the validity of her conclusions somewhat.
She is an employee of Merck.
On Twitter @alz_gal
VIENNA – Urinary tract infections are relatively common and can be quite expensive among patients with newly diagnosed diabetes.
In a large patient database, the infection rate was about 128/1,000 patients, Shengsheng Yu, Ph.D., said at the annual meeting of the European Association for the Study of Diabetes. While only about 4% of these patients were hospitalized, their treatment costs hovered around $3,407 in Germany, where the study was conducted.
These data were extracted from a large German patient claims database, said Dr. Yu of Merck Sharp & Dohme, Whitehouse Station, N.J. The cohort comprised 530,918 patients who had type 2 diabetes during the study years of 2010-2012. Of these, 64,332 had incident disease.
Patients with newly diagnosed diabetes were significantly younger than was the diabetes-prevalent population (70 vs. 73 years), and had a significantly lower than the Charlson comorbidity index (5.4 vs. 7.3 years). Their diabetes was also less severe when measured by the adapted Diabetes Complication Severity Index (1.5 vs. 2.4).
During the study period, roughly 20% of patients had at least 1 urinary tract infection (UTI); 6% had two or more.
UTIs were twice as common in women. Prevalence also grew with advancing age in both sexes. Among those with newly diagnosed diabetes, women developed their UTI significantly more quickly than did men. By the end of the study, 20% of those women had developed one, compared with 10% of the men.
A multivariate analysis determined the risk factors associated with UTIs. These included having had a previous UTI (odds ratio, 3.5), female gender (OR, 1.7), higher Charlson comorbidity status (OR, 1.5), and age (OR, 1.4 for those older than 79 years).
Hemoglobin A1c levels were also a significant independent predictor of UTI, with an odds ratio of 1.5 for levels of 9.5%-10%, compared with 7%-7.5%.
In an analysis of the development of a first UTI after diagnosis, all of those predictive factors remained significant.
The investigators also examined costs associated with inpatient and outpatient treatment. Total costs included antibiotics and the cost of either ambulatory, outpatient, or in-hospital care.
The majority were treated by a physicians as an outpatient, with a median cost of 86 euros (US$111). About 46,500 received a prescription only, at a median cost of 22 euros (US$25). The smallest number (3,445) required hospitalization – a very expensive experience – with a mean cost of 2,627 euros (US$3,407).
During the discussion period, the issue of infection validation was a concern. Many physicians treat on symptoms only, or on a single urinalysis that might show a small amount of blood or protein. The number of culture-proven UTIs is much less, it was suggested.
Dr. Yu admitted that this is a common occurrence and could be affecting the validity of her conclusions somewhat.
She is an employee of Merck.
On Twitter @alz_gal
AT EASD 2014
Key clinical point: Urinary tract infections are not uncommon in patients with type 2 diabetes.
Major finding: Urinary tract infections occurred in about 20% of female and 10% of male patients, with a treatment cost of about $3,400 for every hospitalization.
Disclosures: Dr. Yu is an employee of Merck.
Fitness attenuates systolic BP’s age-related rise
Systolic blood pressure begins a steady rise among men in their mid-40s, but that increase can be attenuated by physical fitness, to the extent that very fit men can stave off high systolic BP by a decade, compared with their unfit age-mates, according to a report published online Sept. 15 in the Journal of the American College of Cardiology.
Investigators performed a secondary analysis of data from the Aerobics Center Longitudinal Study to assess the trajectory of blood pressure over time and determine whether physical fitness, as measured by maximal treadmill exercise testing, influenced that trajectory. The ACLS was a large cohort study of healthy adults who underwent serial preventive medical assessments between 1970 and 2006, said Dr. Junxiu Liu of the department of epidemiology and biostatistics, University of South Carolina, Columbia, and her associates.
For their study, Dr. Liu and her colleagues focused on 13,953 men aged 20-90 years at baseline who participated in the ACLS, almost all of whom were white and 95% of whom were college-educated professionals. Overall, systolic blood pressure showed a linear increase with aging, while diastolic blood pressure did not. For each increase of 1 year in age, systolic BP increased by 0.30 mm Hg.
Systolic BP typically began to exceed 120 mm Hg at roughly age 46 years vin men with the lowest level of physical fitness but did not do so until age 54 years in those with the highest level of physical fitness. This suggests that engaging in physical activity reduces the duration of elevated systolic BP, which in turn may reduce the risk of developing cardiovascular disease, other hypertension-related chronic diseases, medical costs, major morbidity, and mortality, the investigators said (J. Am. Coll. Cardiol. 2014;64:1245-53 [doi:10.1016/j.jacc.2014.06.1184]).
In an analysis that accounted for numerous factors, age, body fat percent, waist circumference, resting heart rate, fasting glucose level, triglyceride level, cholesterol level, alcohol consumption status, and parental history of hypertension were all positively associated with systolic BP.
The major new finding from this study is that men who were in the highest fitness category demonstrated lower systolic blood pressure throughout the adult life span, compared with men who had moderate and low fitness levels. This difference could not be explained by differences in body fatness, waist circumference, lipid profiles, smoking status, alcohol intake, or other factors related to blood pressure, which were statistically controlled for. Indeed, habitual aerobic exercise/physical activity may even counteract the burden of cardiometabolic abnormalities that accelerate artery stiffening and therefore slow the onset and severity of isolated systolic hypertension. Dr. Stanley S. Franklin is in the heart disease prevention program at the University of California, Irvine. Gary L. Pierce, Ph.D., is in the department of health and human physiology at the University of Iowa, Iowa City. They made these remarks in an editorial accompanying Dr. Liu’s report (J. Am. Coll. Cardiol. 2014;1254-6 [doi:10.1016;j.jacc.2014.06.1183]). Dr. Franklin and Dr. Pierce reported no financial conflicts of interest.
The major new finding from this study is that men who were in the highest fitness category demonstrated lower systolic blood pressure throughout the adult life span, compared with men who had moderate and low fitness levels. This difference could not be explained by differences in body fatness, waist circumference, lipid profiles, smoking status, alcohol intake, or other factors related to blood pressure, which were statistically controlled for. Indeed, habitual aerobic exercise/physical activity may even counteract the burden of cardiometabolic abnormalities that accelerate artery stiffening and therefore slow the onset and severity of isolated systolic hypertension. Dr. Stanley S. Franklin is in the heart disease prevention program at the University of California, Irvine. Gary L. Pierce, Ph.D., is in the department of health and human physiology at the University of Iowa, Iowa City. They made these remarks in an editorial accompanying Dr. Liu’s report (J. Am. Coll. Cardiol. 2014;1254-6 [doi:10.1016;j.jacc.2014.06.1183]). Dr. Franklin and Dr. Pierce reported no financial conflicts of interest.
The major new finding from this study is that men who were in the highest fitness category demonstrated lower systolic blood pressure throughout the adult life span, compared with men who had moderate and low fitness levels. This difference could not be explained by differences in body fatness, waist circumference, lipid profiles, smoking status, alcohol intake, or other factors related to blood pressure, which were statistically controlled for. Indeed, habitual aerobic exercise/physical activity may even counteract the burden of cardiometabolic abnormalities that accelerate artery stiffening and therefore slow the onset and severity of isolated systolic hypertension. Dr. Stanley S. Franklin is in the heart disease prevention program at the University of California, Irvine. Gary L. Pierce, Ph.D., is in the department of health and human physiology at the University of Iowa, Iowa City. They made these remarks in an editorial accompanying Dr. Liu’s report (J. Am. Coll. Cardiol. 2014;1254-6 [doi:10.1016;j.jacc.2014.06.1183]). Dr. Franklin and Dr. Pierce reported no financial conflicts of interest.
Systolic blood pressure begins a steady rise among men in their mid-40s, but that increase can be attenuated by physical fitness, to the extent that very fit men can stave off high systolic BP by a decade, compared with their unfit age-mates, according to a report published online Sept. 15 in the Journal of the American College of Cardiology.
Investigators performed a secondary analysis of data from the Aerobics Center Longitudinal Study to assess the trajectory of blood pressure over time and determine whether physical fitness, as measured by maximal treadmill exercise testing, influenced that trajectory. The ACLS was a large cohort study of healthy adults who underwent serial preventive medical assessments between 1970 and 2006, said Dr. Junxiu Liu of the department of epidemiology and biostatistics, University of South Carolina, Columbia, and her associates.
For their study, Dr. Liu and her colleagues focused on 13,953 men aged 20-90 years at baseline who participated in the ACLS, almost all of whom were white and 95% of whom were college-educated professionals. Overall, systolic blood pressure showed a linear increase with aging, while diastolic blood pressure did not. For each increase of 1 year in age, systolic BP increased by 0.30 mm Hg.
Systolic BP typically began to exceed 120 mm Hg at roughly age 46 years vin men with the lowest level of physical fitness but did not do so until age 54 years in those with the highest level of physical fitness. This suggests that engaging in physical activity reduces the duration of elevated systolic BP, which in turn may reduce the risk of developing cardiovascular disease, other hypertension-related chronic diseases, medical costs, major morbidity, and mortality, the investigators said (J. Am. Coll. Cardiol. 2014;64:1245-53 [doi:10.1016/j.jacc.2014.06.1184]).
In an analysis that accounted for numerous factors, age, body fat percent, waist circumference, resting heart rate, fasting glucose level, triglyceride level, cholesterol level, alcohol consumption status, and parental history of hypertension were all positively associated with systolic BP.
Systolic blood pressure begins a steady rise among men in their mid-40s, but that increase can be attenuated by physical fitness, to the extent that very fit men can stave off high systolic BP by a decade, compared with their unfit age-mates, according to a report published online Sept. 15 in the Journal of the American College of Cardiology.
Investigators performed a secondary analysis of data from the Aerobics Center Longitudinal Study to assess the trajectory of blood pressure over time and determine whether physical fitness, as measured by maximal treadmill exercise testing, influenced that trajectory. The ACLS was a large cohort study of healthy adults who underwent serial preventive medical assessments between 1970 and 2006, said Dr. Junxiu Liu of the department of epidemiology and biostatistics, University of South Carolina, Columbia, and her associates.
For their study, Dr. Liu and her colleagues focused on 13,953 men aged 20-90 years at baseline who participated in the ACLS, almost all of whom were white and 95% of whom were college-educated professionals. Overall, systolic blood pressure showed a linear increase with aging, while diastolic blood pressure did not. For each increase of 1 year in age, systolic BP increased by 0.30 mm Hg.
Systolic BP typically began to exceed 120 mm Hg at roughly age 46 years vin men with the lowest level of physical fitness but did not do so until age 54 years in those with the highest level of physical fitness. This suggests that engaging in physical activity reduces the duration of elevated systolic BP, which in turn may reduce the risk of developing cardiovascular disease, other hypertension-related chronic diseases, medical costs, major morbidity, and mortality, the investigators said (J. Am. Coll. Cardiol. 2014;64:1245-53 [doi:10.1016/j.jacc.2014.06.1184]).
In an analysis that accounted for numerous factors, age, body fat percent, waist circumference, resting heart rate, fasting glucose level, triglyceride level, cholesterol level, alcohol consumption status, and parental history of hypertension were all positively associated with systolic BP.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Physically fit men may postpone the inevitable rise of systolic blood pressure by 10 years.
Major finding: Systolic BP typically began to exceed 120 mm Hg at approximately age 46 years among men with the lowest level of physical fitness but did not do so until age 54 years among men with the highest level of physical fitness.
Data source: A secondary analysis of data from a longitudinal cohort study, involving 13,953 men aged 20-90 years at baseline who underwent serial medical assessments between 1970 and 2006.
Disclosures: This study was supported by the National Institutes of Health. Dr. Liu reported no financial conflicts of interest; an associate reported ties to Technogym, Santech, Clarity, Coca-Cola, and BodyMedia.
GLP-1 and basal insulin offer improved glycemic control, weight loss in type 2 diabetes
Combination treatment with GLP-1 agonist and basal insulin helps diabetes patients achieve glycemic control without increasing their risk of hypoglycemia or weight gain, a new meta-analysis has found.
The research, published online Sept. 12 in The Lancet, suggests that glucagon-like peptide-1 (GLP-1) agonists, injectable agents currently used mainly as second- or third-line treatments after oral diabetes therapies have failed, might merit a more prominent role in the treatment pathway in combination with basal insulin.
The authors of the meta-analysis, led by Conrad Eng of Mount Sinai Hospital, Toronto, analyzed results from 15 studies enrolling 4,348 patients with type 2 diabetes. All the studies compared GLP-1 agonists, including exenatide (Byetta), liraglutide (Victoza), and albiglutide (Tanzeum), and basal insulin with other regimens, which included oral agents with or without insulin, and insulin-only regimens.
A GLP-1 agonist plus basal insulin was associated with a reduction of 0.44% in more lowering of hemoglobin A1c and a near doubling in the likelihood of achieving a target HbA1c of 7% or below (relative risk, 1.92), compared with other diabetes treatments. No increased risk of hypoglycemia was seen associated with the GLP-1 and basal insulin regimens, and a mean reduction in weight of 3.22 kg was seen for these compared to the other treatments. Compared with full basal-bolus insulin regimens, a GLP-1 agonist plus basal insulin was seen associated with minimal reduction in HbA1c (–0.1%), but with lower risk of hypoglycemia (RR 0.67) and a reduction in mean weight of 5.66 kg.
The meta-analysis yielded “robust and consistent findings that lend support to the benefits of GLP-1 agonist and basal insulin combination treatment. Indeed, this consistency is apparent despite the fact that these studies differ in several ways, including the antidiabetic treatments assessed, the background oral antidiabetic drugs, the GLP-1 preparation under study, and the sequence of its initiation in relation to that of basal insulin,” Mr. Eng and his colleagues wrote. They acknowledged as limitations of their study the open-label design, industry funding, and short duration of some of the included clinical trials.
The study had no outside funding; one coauthor, Dr. Bernard Zinman, reported financial relationships with Novo Nordisk, Boehringer Ingelheim, Merck, Eli Lilly, AstraZeneca, Jansen, Takeda, and Sanofi-Aventis. Dr. Ravi Retnakaran, corresponding author, disclosed past compensation from Novo Nordisk and Merck.
It has been a 20-year journey, but the combination of GLP-1 agonist and basal insulin has finally arrived as a more powerful and safer alternative to insulin in the management of type 2 diabetes. Perhaps the most practical and immediate issue is whether the fixed-dose combinations of a GLP-1 agonist and basal insulin in development will supersede other approaches. This is an unsettled question, but it seems likely that fixed-dose combinations will be welcomed in view of their convenience and efficacy. The major barrier to widespread adoption of these treatments is cost both GLP-1 agonists and insulin analogues are among the most expensive in diabetes care. One can hope that some incremental cost savings will come with combined products.
Dr. John Buse and Dr. Laura Young of University of North Carolina, Chapel Hill, N.C., made these remarks in an accompanying editorial. Both authors report funding from pharmaceutical manufacturers, including Boehringer Ingelheim, Eli Lilly, Johnson & Johnson, Sanofi. Dr. Buse is a consultant to PhaseBio Pharmaceuticals, and receives stock options and payments.
It has been a 20-year journey, but the combination of GLP-1 agonist and basal insulin has finally arrived as a more powerful and safer alternative to insulin in the management of type 2 diabetes. Perhaps the most practical and immediate issue is whether the fixed-dose combinations of a GLP-1 agonist and basal insulin in development will supersede other approaches. This is an unsettled question, but it seems likely that fixed-dose combinations will be welcomed in view of their convenience and efficacy. The major barrier to widespread adoption of these treatments is cost both GLP-1 agonists and insulin analogues are among the most expensive in diabetes care. One can hope that some incremental cost savings will come with combined products.
Dr. John Buse and Dr. Laura Young of University of North Carolina, Chapel Hill, N.C., made these remarks in an accompanying editorial. Both authors report funding from pharmaceutical manufacturers, including Boehringer Ingelheim, Eli Lilly, Johnson & Johnson, Sanofi. Dr. Buse is a consultant to PhaseBio Pharmaceuticals, and receives stock options and payments.
It has been a 20-year journey, but the combination of GLP-1 agonist and basal insulin has finally arrived as a more powerful and safer alternative to insulin in the management of type 2 diabetes. Perhaps the most practical and immediate issue is whether the fixed-dose combinations of a GLP-1 agonist and basal insulin in development will supersede other approaches. This is an unsettled question, but it seems likely that fixed-dose combinations will be welcomed in view of their convenience and efficacy. The major barrier to widespread adoption of these treatments is cost both GLP-1 agonists and insulin analogues are among the most expensive in diabetes care. One can hope that some incremental cost savings will come with combined products.
Dr. John Buse and Dr. Laura Young of University of North Carolina, Chapel Hill, N.C., made these remarks in an accompanying editorial. Both authors report funding from pharmaceutical manufacturers, including Boehringer Ingelheim, Eli Lilly, Johnson & Johnson, Sanofi. Dr. Buse is a consultant to PhaseBio Pharmaceuticals, and receives stock options and payments.
Combination treatment with GLP-1 agonist and basal insulin helps diabetes patients achieve glycemic control without increasing their risk of hypoglycemia or weight gain, a new meta-analysis has found.
The research, published online Sept. 12 in The Lancet, suggests that glucagon-like peptide-1 (GLP-1) agonists, injectable agents currently used mainly as second- or third-line treatments after oral diabetes therapies have failed, might merit a more prominent role in the treatment pathway in combination with basal insulin.
The authors of the meta-analysis, led by Conrad Eng of Mount Sinai Hospital, Toronto, analyzed results from 15 studies enrolling 4,348 patients with type 2 diabetes. All the studies compared GLP-1 agonists, including exenatide (Byetta), liraglutide (Victoza), and albiglutide (Tanzeum), and basal insulin with other regimens, which included oral agents with or without insulin, and insulin-only regimens.
A GLP-1 agonist plus basal insulin was associated with a reduction of 0.44% in more lowering of hemoglobin A1c and a near doubling in the likelihood of achieving a target HbA1c of 7% or below (relative risk, 1.92), compared with other diabetes treatments. No increased risk of hypoglycemia was seen associated with the GLP-1 and basal insulin regimens, and a mean reduction in weight of 3.22 kg was seen for these compared to the other treatments. Compared with full basal-bolus insulin regimens, a GLP-1 agonist plus basal insulin was seen associated with minimal reduction in HbA1c (–0.1%), but with lower risk of hypoglycemia (RR 0.67) and a reduction in mean weight of 5.66 kg.
The meta-analysis yielded “robust and consistent findings that lend support to the benefits of GLP-1 agonist and basal insulin combination treatment. Indeed, this consistency is apparent despite the fact that these studies differ in several ways, including the antidiabetic treatments assessed, the background oral antidiabetic drugs, the GLP-1 preparation under study, and the sequence of its initiation in relation to that of basal insulin,” Mr. Eng and his colleagues wrote. They acknowledged as limitations of their study the open-label design, industry funding, and short duration of some of the included clinical trials.
The study had no outside funding; one coauthor, Dr. Bernard Zinman, reported financial relationships with Novo Nordisk, Boehringer Ingelheim, Merck, Eli Lilly, AstraZeneca, Jansen, Takeda, and Sanofi-Aventis. Dr. Ravi Retnakaran, corresponding author, disclosed past compensation from Novo Nordisk and Merck.
Combination treatment with GLP-1 agonist and basal insulin helps diabetes patients achieve glycemic control without increasing their risk of hypoglycemia or weight gain, a new meta-analysis has found.
The research, published online Sept. 12 in The Lancet, suggests that glucagon-like peptide-1 (GLP-1) agonists, injectable agents currently used mainly as second- or third-line treatments after oral diabetes therapies have failed, might merit a more prominent role in the treatment pathway in combination with basal insulin.
The authors of the meta-analysis, led by Conrad Eng of Mount Sinai Hospital, Toronto, analyzed results from 15 studies enrolling 4,348 patients with type 2 diabetes. All the studies compared GLP-1 agonists, including exenatide (Byetta), liraglutide (Victoza), and albiglutide (Tanzeum), and basal insulin with other regimens, which included oral agents with or without insulin, and insulin-only regimens.
A GLP-1 agonist plus basal insulin was associated with a reduction of 0.44% in more lowering of hemoglobin A1c and a near doubling in the likelihood of achieving a target HbA1c of 7% or below (relative risk, 1.92), compared with other diabetes treatments. No increased risk of hypoglycemia was seen associated with the GLP-1 and basal insulin regimens, and a mean reduction in weight of 3.22 kg was seen for these compared to the other treatments. Compared with full basal-bolus insulin regimens, a GLP-1 agonist plus basal insulin was seen associated with minimal reduction in HbA1c (–0.1%), but with lower risk of hypoglycemia (RR 0.67) and a reduction in mean weight of 5.66 kg.
The meta-analysis yielded “robust and consistent findings that lend support to the benefits of GLP-1 agonist and basal insulin combination treatment. Indeed, this consistency is apparent despite the fact that these studies differ in several ways, including the antidiabetic treatments assessed, the background oral antidiabetic drugs, the GLP-1 preparation under study, and the sequence of its initiation in relation to that of basal insulin,” Mr. Eng and his colleagues wrote. They acknowledged as limitations of their study the open-label design, industry funding, and short duration of some of the included clinical trials.
The study had no outside funding; one coauthor, Dr. Bernard Zinman, reported financial relationships with Novo Nordisk, Boehringer Ingelheim, Merck, Eli Lilly, AstraZeneca, Jansen, Takeda, and Sanofi-Aventis. Dr. Ravi Retnakaran, corresponding author, disclosed past compensation from Novo Nordisk and Merck.
Key clinical point: Adding a GLP-1 agonist to insulin may achieve effective glycemic control with no increased hypoglycemia or weight gain.
Major finding: A GLP-1 agonist plus basal insulin was associated with a reduction of 0.44% in HbA1c and a near doubling in the likelihood of achieving a target HbA1c of 7% or below, compared with other diabetes treatments.
Data source: A meta-analysis of 15 studies in more than 4,000 patients with type 2 diabetes.
Disclosures: The study had no outside funding; one coauthor, Dr. Bernard Zinman, reported financial relationships with Novo Nordisk, Boehringer Ingelheim, Merck, Eli Lilly, AstraZeneca, Jansen, Takeda, and Sanofi-Aventis. Dr. Ravi Retnakaran, corresponding author, disclosed past compensation from Novo Nordisk and Merck.
FDA panel backs diabetes drug for weight loss indication
A diabetes drug is now poised to become a weight loss therapeutic, even in patients without the condition, after a panel of Food and Drug Administration advisers recommended approval of liraglutide for weight management.
The glucagon-like peptide-1 receptor agonist, to be marketed as Saxenda by Novo Nordisk, has been on the market since 2010 for treatment of type 2 diabetes under the brand name Victoza. The FDA’s Endocrinologic and Metabolic Drugs Advisory Committee voted 14-1 that Saxenda is safe and effective and should be approved as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults with an initial body mass index of at least 30 kg/m2, or 27 kg/m2 with at least one weight-related comorbidity.
Liraglutide is marketed at a lower dose for diabetes – a 1.8-mg, once-daily dose that’s delivered subcutaneously through a pen-like device – than that proposed for weight management, which would be a 3-mg dose delivered the same way.
The vote to approve came despite the fact that even the lower dose of liraglutide currently carries a boxed warning about the potential for medullary thyroid (C-cell) tumors, and includes warnings and precautions about the potential for pancreatitis, serious hypoglycemia, renal impairment, and hypersensitivity. There also have been significant adverse events in clinical trials and reported to the FDA since the drug has been on the market, including nausea and vomiting and increases in heart rate.
In the phase III studies of Saxenda – which included more than 3,000 patients who took the drug – there were 48 cancers detected, including 7 C-cell thyroid tumors and 14 breast neoplasms.
The panel discussed at length whether the 3-mg dose may trigger more tumors or spur a greater incidence of other side effects, especially since the anticipated wider use may expose even more patients to the drug’s downsides.
Fourteen of the committee members put aside their concerns and voted for approval, but it was not cut-and-dried for all of them.
“For me it was more of a difficult decision rendering an opinion on the risk-benefit ratio,” said Dr. Kenneth Burman, acting chairperson of the committee.
He said he was not completely convinced that the risk for medullary thyroid tumors was minimal. Dr. Burman, director of the endocrine section at the Washington Hospital Center, also said that he was concerned that there was no real guidance on how long a patient should take liraglutide for weight management, especially if the effect plateaued as it did in trials, or was reversed.
Medullary tumors are rare in the general population, and though rare in the phase III clinical trials in 3-mg liraglutide, the data still suggested the possibility of an increased risk, said FDA reviewers. There was also a small excess risk of breast cancers in those trials, which suggested a potential signal, said Christian Hampp, Ph.D., a reviewer from the epidemiology division at the FDA’s Center for Drug Evaluation and Research.
However, Dr. Julie Golden, a medical officer in the FDA’s division of metabolism and endocrinology products, noted that there’s little evidence to suggest that liraglutide has a role in promoting breast cancer.
Panelist Barbara Hansen, Ph.D., agreed that there seemed to be little biological plausibility. “I’m happy with the amount of risk that has been identified,” said Dr. Hansen, professor of internal medicine, University of South Florida College of Medicine, Tampa. “I don’t see a signal there,” she said.
The majority of the committee agreed that liraglutide was effective for weight loss and met the FDA criteria, which was a 5% difference in mean weight loss between the drug and placebo; or at least 35% of patients on therapy losing at least 5% of their baseline weight and double the number on placebo who lost that much; and, improvement in cardiometabolic parameters.
More than 5,000 patients were enrolled in the four phase III trials; over 3,000 took the 3-mg dose of liraglutide. All patients were required to have a stable body weight and to have failed previous dietary intervention. Once in the study, they were told to reduce caloric intake by 500 kcal a day and to maintain or add at least 150 minutes week of physical activity.
The mean age was 47 years, and most participants were women. The mean BMI was 38 kg/m2.
In the largest trial, 3,731 patients were studied for 56 weeks, and were stratified by the presence or absence of prediabetes. Of patients taking liraglutide, 64% lost at least 5% of their body weight and 33% lost at least 10%, compared with 27% and 10% of the placebo patients, respectively. There were no significant differences in these endpoints between patients with prediabetes and those without.
Results were similar across the three other phase III studies, though not as pronounced. In addition, Novo Nordisk said that weight loss began to plateau for many patients at 34 weeks. Although liraglutide also helped reduce hypertension, blood lipids, blood glucose, and waist circumference, there were still signs that it might have some adverse cardiovascular effects.
Many panel members said they’d like to see more specific study of cardiovascular outcomes in patients taking a 3-mg dose.
Earlier this week, the FDA approved a combination drug, Contrave (naltrexone and bupropion) for weight management. If approved, Saxenda would be the fourth weight management drug on the U.S. market, after Contrave, the phentermine/topiramate combo Qsymia, and lorcaserin (Belviq).
The FDA is not bound by its advisory panels’ advice, but usually follows their recommendations.
On Twitter @aliciaault
A diabetes drug is now poised to become a weight loss therapeutic, even in patients without the condition, after a panel of Food and Drug Administration advisers recommended approval of liraglutide for weight management.
The glucagon-like peptide-1 receptor agonist, to be marketed as Saxenda by Novo Nordisk, has been on the market since 2010 for treatment of type 2 diabetes under the brand name Victoza. The FDA’s Endocrinologic and Metabolic Drugs Advisory Committee voted 14-1 that Saxenda is safe and effective and should be approved as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults with an initial body mass index of at least 30 kg/m2, or 27 kg/m2 with at least one weight-related comorbidity.
Liraglutide is marketed at a lower dose for diabetes – a 1.8-mg, once-daily dose that’s delivered subcutaneously through a pen-like device – than that proposed for weight management, which would be a 3-mg dose delivered the same way.
The vote to approve came despite the fact that even the lower dose of liraglutide currently carries a boxed warning about the potential for medullary thyroid (C-cell) tumors, and includes warnings and precautions about the potential for pancreatitis, serious hypoglycemia, renal impairment, and hypersensitivity. There also have been significant adverse events in clinical trials and reported to the FDA since the drug has been on the market, including nausea and vomiting and increases in heart rate.
In the phase III studies of Saxenda – which included more than 3,000 patients who took the drug – there were 48 cancers detected, including 7 C-cell thyroid tumors and 14 breast neoplasms.
The panel discussed at length whether the 3-mg dose may trigger more tumors or spur a greater incidence of other side effects, especially since the anticipated wider use may expose even more patients to the drug’s downsides.
Fourteen of the committee members put aside their concerns and voted for approval, but it was not cut-and-dried for all of them.
“For me it was more of a difficult decision rendering an opinion on the risk-benefit ratio,” said Dr. Kenneth Burman, acting chairperson of the committee.
He said he was not completely convinced that the risk for medullary thyroid tumors was minimal. Dr. Burman, director of the endocrine section at the Washington Hospital Center, also said that he was concerned that there was no real guidance on how long a patient should take liraglutide for weight management, especially if the effect plateaued as it did in trials, or was reversed.
Medullary tumors are rare in the general population, and though rare in the phase III clinical trials in 3-mg liraglutide, the data still suggested the possibility of an increased risk, said FDA reviewers. There was also a small excess risk of breast cancers in those trials, which suggested a potential signal, said Christian Hampp, Ph.D., a reviewer from the epidemiology division at the FDA’s Center for Drug Evaluation and Research.
However, Dr. Julie Golden, a medical officer in the FDA’s division of metabolism and endocrinology products, noted that there’s little evidence to suggest that liraglutide has a role in promoting breast cancer.
Panelist Barbara Hansen, Ph.D., agreed that there seemed to be little biological plausibility. “I’m happy with the amount of risk that has been identified,” said Dr. Hansen, professor of internal medicine, University of South Florida College of Medicine, Tampa. “I don’t see a signal there,” she said.
The majority of the committee agreed that liraglutide was effective for weight loss and met the FDA criteria, which was a 5% difference in mean weight loss between the drug and placebo; or at least 35% of patients on therapy losing at least 5% of their baseline weight and double the number on placebo who lost that much; and, improvement in cardiometabolic parameters.
More than 5,000 patients were enrolled in the four phase III trials; over 3,000 took the 3-mg dose of liraglutide. All patients were required to have a stable body weight and to have failed previous dietary intervention. Once in the study, they were told to reduce caloric intake by 500 kcal a day and to maintain or add at least 150 minutes week of physical activity.
The mean age was 47 years, and most participants were women. The mean BMI was 38 kg/m2.
In the largest trial, 3,731 patients were studied for 56 weeks, and were stratified by the presence or absence of prediabetes. Of patients taking liraglutide, 64% lost at least 5% of their body weight and 33% lost at least 10%, compared with 27% and 10% of the placebo patients, respectively. There were no significant differences in these endpoints between patients with prediabetes and those without.
Results were similar across the three other phase III studies, though not as pronounced. In addition, Novo Nordisk said that weight loss began to plateau for many patients at 34 weeks. Although liraglutide also helped reduce hypertension, blood lipids, blood glucose, and waist circumference, there were still signs that it might have some adverse cardiovascular effects.
Many panel members said they’d like to see more specific study of cardiovascular outcomes in patients taking a 3-mg dose.
Earlier this week, the FDA approved a combination drug, Contrave (naltrexone and bupropion) for weight management. If approved, Saxenda would be the fourth weight management drug on the U.S. market, after Contrave, the phentermine/topiramate combo Qsymia, and lorcaserin (Belviq).
The FDA is not bound by its advisory panels’ advice, but usually follows their recommendations.
On Twitter @aliciaault
A diabetes drug is now poised to become a weight loss therapeutic, even in patients without the condition, after a panel of Food and Drug Administration advisers recommended approval of liraglutide for weight management.
The glucagon-like peptide-1 receptor agonist, to be marketed as Saxenda by Novo Nordisk, has been on the market since 2010 for treatment of type 2 diabetes under the brand name Victoza. The FDA’s Endocrinologic and Metabolic Drugs Advisory Committee voted 14-1 that Saxenda is safe and effective and should be approved as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults with an initial body mass index of at least 30 kg/m2, or 27 kg/m2 with at least one weight-related comorbidity.
Liraglutide is marketed at a lower dose for diabetes – a 1.8-mg, once-daily dose that’s delivered subcutaneously through a pen-like device – than that proposed for weight management, which would be a 3-mg dose delivered the same way.
The vote to approve came despite the fact that even the lower dose of liraglutide currently carries a boxed warning about the potential for medullary thyroid (C-cell) tumors, and includes warnings and precautions about the potential for pancreatitis, serious hypoglycemia, renal impairment, and hypersensitivity. There also have been significant adverse events in clinical trials and reported to the FDA since the drug has been on the market, including nausea and vomiting and increases in heart rate.
In the phase III studies of Saxenda – which included more than 3,000 patients who took the drug – there were 48 cancers detected, including 7 C-cell thyroid tumors and 14 breast neoplasms.
The panel discussed at length whether the 3-mg dose may trigger more tumors or spur a greater incidence of other side effects, especially since the anticipated wider use may expose even more patients to the drug’s downsides.
Fourteen of the committee members put aside their concerns and voted for approval, but it was not cut-and-dried for all of them.
“For me it was more of a difficult decision rendering an opinion on the risk-benefit ratio,” said Dr. Kenneth Burman, acting chairperson of the committee.
He said he was not completely convinced that the risk for medullary thyroid tumors was minimal. Dr. Burman, director of the endocrine section at the Washington Hospital Center, also said that he was concerned that there was no real guidance on how long a patient should take liraglutide for weight management, especially if the effect plateaued as it did in trials, or was reversed.
Medullary tumors are rare in the general population, and though rare in the phase III clinical trials in 3-mg liraglutide, the data still suggested the possibility of an increased risk, said FDA reviewers. There was also a small excess risk of breast cancers in those trials, which suggested a potential signal, said Christian Hampp, Ph.D., a reviewer from the epidemiology division at the FDA’s Center for Drug Evaluation and Research.
However, Dr. Julie Golden, a medical officer in the FDA’s division of metabolism and endocrinology products, noted that there’s little evidence to suggest that liraglutide has a role in promoting breast cancer.
Panelist Barbara Hansen, Ph.D., agreed that there seemed to be little biological plausibility. “I’m happy with the amount of risk that has been identified,” said Dr. Hansen, professor of internal medicine, University of South Florida College of Medicine, Tampa. “I don’t see a signal there,” she said.
The majority of the committee agreed that liraglutide was effective for weight loss and met the FDA criteria, which was a 5% difference in mean weight loss between the drug and placebo; or at least 35% of patients on therapy losing at least 5% of their baseline weight and double the number on placebo who lost that much; and, improvement in cardiometabolic parameters.
More than 5,000 patients were enrolled in the four phase III trials; over 3,000 took the 3-mg dose of liraglutide. All patients were required to have a stable body weight and to have failed previous dietary intervention. Once in the study, they were told to reduce caloric intake by 500 kcal a day and to maintain or add at least 150 minutes week of physical activity.
The mean age was 47 years, and most participants were women. The mean BMI was 38 kg/m2.
In the largest trial, 3,731 patients were studied for 56 weeks, and were stratified by the presence or absence of prediabetes. Of patients taking liraglutide, 64% lost at least 5% of their body weight and 33% lost at least 10%, compared with 27% and 10% of the placebo patients, respectively. There were no significant differences in these endpoints between patients with prediabetes and those without.
Results were similar across the three other phase III studies, though not as pronounced. In addition, Novo Nordisk said that weight loss began to plateau for many patients at 34 weeks. Although liraglutide also helped reduce hypertension, blood lipids, blood glucose, and waist circumference, there were still signs that it might have some adverse cardiovascular effects.
Many panel members said they’d like to see more specific study of cardiovascular outcomes in patients taking a 3-mg dose.
Earlier this week, the FDA approved a combination drug, Contrave (naltrexone and bupropion) for weight management. If approved, Saxenda would be the fourth weight management drug on the U.S. market, after Contrave, the phentermine/topiramate combo Qsymia, and lorcaserin (Belviq).
The FDA is not bound by its advisory panels’ advice, but usually follows their recommendations.
On Twitter @aliciaault
AT AN FDA ADVISORY COMMITTEE MEETING
After 3-year stumble, new weight-loss drug wins FDA approval
After a delay of more than 3 years, the Food and Drug Administration has approved the nation’s third weight-loss drug, a combination of naltrexone and bupropion.
The extended release tablets (Contrave; Orexigen and Takeda) are approved for use in adults who have a body mass index of at least 30 kg/m2, or those with a BMI of at least 27 kg/m2 and at least one additional weight-related condition such as hypertension, type 2 diabetes, or dyslipidemia. The agency recommended that Contrave be used in addition to caloric restriction and increased physical activity.
Dr. Timothy Garvey, chair of the American Association of Clinical Endocrinologists’ scientific committee, lauded the approval.
"We have a new tool now to treat obesity – and that is very good news," he said in an interview.
He said Contrave will be a valuable addition to the existing weight-loss medications: the phentermine/topiramate combo (Qsymia; Vivus) and lorcaserin (Belviq; Arena).
"There are no head-to-head trials with the other drugs, so we really can’t say much about relative efficacy," said Dr. Garvey. "But when you look at the placebo-subtracted weight loss in all the phase III data, it looks like Contrave is in the middle, with about a 6% loss over lifestyle interventions alone. So it’s not as effective as the topiramate combination, but more effective than lorcaserin."
In the pivotal, 56-week phase III trials, those taking Contrave lost 5%-8% of their baseline body weight, compared with a loss of 1%-2% in those on placebo. The proportion of those who lost at least 5% of their baseline body weight ranged from 45%-56% of those on the proposed dose, compared with 16%-43% of those on placebo.
The FDA guidance on weight-loss drugs suggests a 12-week efficacy evaluation – if the patient has not lost at least 5% of total body weight by then, the drug should be discontinued and another started.
It’s not possible to predict who will respond best to which drug, although there are some things to consider when choosing, said Dr. Garvey, who is chair of the department of nutrition at the University of Alabama at Birmingham.
"For example, women of childbearing age need to take precautions against becoming pregnant if they take the topiramate combination, and should stop it right away if they do become pregnant. And since lorcaserin is a serotonergic drug, it has to be used very cautiously in patients who are on other serotonergic medications. We definitely need more safety data there."
Additionally, none of the weight-loss drugs should be used in children or teens until more studies confirm their safety for those patients, "All of the companies are planning these trials, and we hope they will complete them expeditiously," Dr. Garvey said. "Childhood and adolescent obesity is a huge problem, and we really need some good treatment options there."
Because it contains bupropion, an antidepressant that has been associated with an increased risk of suicidal thoughts and actions, the drug carries a black box warning. Bupropion is also known to lower seizure threshold, so the drug should not be used in patients with seizure disorders. If a seizure occurs while taking on the medication, it should be permanently discontinued. Nor should it be used in patients with uncontrolled hypertension.
Orexigen and Takeda originally brought the drug forward in December 2011. It was not approved at that time because of concerns about its effect on blood pressure – an unexpected move, and one that Orexigen management called "a big setback."
About a quarter of those in the 56-week pivotal phase III trial experienced significant blood pressure increases of at least 10% above their baseline, compared with about 20% of those in the control arm. Increases of diastolic blood pressure of at least 5 mm Hg over baseline occurred in 37% of those on the combination, compared with 29% of those on placebo. About a quarter in the active arm also had heart rate increases of at least 10 beats per minute, compared with 19% of those taking placebo.
Because of these concerns, the FDA required the drug companies to conduct a large, double-blinded, randomized, placebo-controlled trial to investigate the risk of major cardiovascular events. Takeda and Orexigen then launched the 4-year, 8,900 patient Light study, which is still ongoing. Endpoints are major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke) in overweight and obese subjects who have concomitant diabetes and/or other cardiovascular risk factors.
In June, citing encouraging preliminary results, Takeda and Orexigen brought Contrave to the FDA once more – only to be shot down again, at least temporarily. The agency required a review extension in order to come to agreement on the final form of postmarketing surveillance, said Denise Powell, a spokeswoman for Orexigen.
"At that time, FDA said the data looked good," she said in an interview. "We just needed more time to work out the postmarketing requirements."
Those will include:
• A cardiovascular outcomes trial to assess the cardiovascular risk associated with Contrave use.
• Two efficacy, safety, and clinical pharmacology studies in pediatric patients (one in patients 12-17 years old, and one in patients 7-11 years old).
• A juvenile animal toxicity study with a particular focus on growth and development as well as behavior, learning, and memory.
• A cardiac conduction study.
• Clinical trials to evaluate dosing in patients with hepatic or renal impairment.
• A clinical trial to evaluate the potential for interactions between the medication and other drugs.
Contrave contains an extended-release formulation of 8 mg naltrexone and 90 mg bupropion. It is to be administered in an in a 4-week upward titration schedule, with a single morning tablet during week 1; a single tablet at morning and evening during week 2; two tablets in the morning and one in the evening during week 3; and two tablets both morning and evening from week 4 and onward.
Dr. Garvey is a consultant for Daiichi Sankyo, LipoScience, Takeda, Vivus, Boehringer Ingelheim, Janssen, Eisai, and Novo Nordisk. He has received research funding from Merck, AstraZeneca, Weight Watchers, Eisai, and Sanofi.
On Twitter @alz_gal
After a delay of more than 3 years, the Food and Drug Administration has approved the nation’s third weight-loss drug, a combination of naltrexone and bupropion.
The extended release tablets (Contrave; Orexigen and Takeda) are approved for use in adults who have a body mass index of at least 30 kg/m2, or those with a BMI of at least 27 kg/m2 and at least one additional weight-related condition such as hypertension, type 2 diabetes, or dyslipidemia. The agency recommended that Contrave be used in addition to caloric restriction and increased physical activity.
Dr. Timothy Garvey, chair of the American Association of Clinical Endocrinologists’ scientific committee, lauded the approval.
"We have a new tool now to treat obesity – and that is very good news," he said in an interview.
He said Contrave will be a valuable addition to the existing weight-loss medications: the phentermine/topiramate combo (Qsymia; Vivus) and lorcaserin (Belviq; Arena).
"There are no head-to-head trials with the other drugs, so we really can’t say much about relative efficacy," said Dr. Garvey. "But when you look at the placebo-subtracted weight loss in all the phase III data, it looks like Contrave is in the middle, with about a 6% loss over lifestyle interventions alone. So it’s not as effective as the topiramate combination, but more effective than lorcaserin."
In the pivotal, 56-week phase III trials, those taking Contrave lost 5%-8% of their baseline body weight, compared with a loss of 1%-2% in those on placebo. The proportion of those who lost at least 5% of their baseline body weight ranged from 45%-56% of those on the proposed dose, compared with 16%-43% of those on placebo.
The FDA guidance on weight-loss drugs suggests a 12-week efficacy evaluation – if the patient has not lost at least 5% of total body weight by then, the drug should be discontinued and another started.
It’s not possible to predict who will respond best to which drug, although there are some things to consider when choosing, said Dr. Garvey, who is chair of the department of nutrition at the University of Alabama at Birmingham.
"For example, women of childbearing age need to take precautions against becoming pregnant if they take the topiramate combination, and should stop it right away if they do become pregnant. And since lorcaserin is a serotonergic drug, it has to be used very cautiously in patients who are on other serotonergic medications. We definitely need more safety data there."
Additionally, none of the weight-loss drugs should be used in children or teens until more studies confirm their safety for those patients, "All of the companies are planning these trials, and we hope they will complete them expeditiously," Dr. Garvey said. "Childhood and adolescent obesity is a huge problem, and we really need some good treatment options there."
Because it contains bupropion, an antidepressant that has been associated with an increased risk of suicidal thoughts and actions, the drug carries a black box warning. Bupropion is also known to lower seizure threshold, so the drug should not be used in patients with seizure disorders. If a seizure occurs while taking on the medication, it should be permanently discontinued. Nor should it be used in patients with uncontrolled hypertension.
Orexigen and Takeda originally brought the drug forward in December 2011. It was not approved at that time because of concerns about its effect on blood pressure – an unexpected move, and one that Orexigen management called "a big setback."
About a quarter of those in the 56-week pivotal phase III trial experienced significant blood pressure increases of at least 10% above their baseline, compared with about 20% of those in the control arm. Increases of diastolic blood pressure of at least 5 mm Hg over baseline occurred in 37% of those on the combination, compared with 29% of those on placebo. About a quarter in the active arm also had heart rate increases of at least 10 beats per minute, compared with 19% of those taking placebo.
Because of these concerns, the FDA required the drug companies to conduct a large, double-blinded, randomized, placebo-controlled trial to investigate the risk of major cardiovascular events. Takeda and Orexigen then launched the 4-year, 8,900 patient Light study, which is still ongoing. Endpoints are major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke) in overweight and obese subjects who have concomitant diabetes and/or other cardiovascular risk factors.
In June, citing encouraging preliminary results, Takeda and Orexigen brought Contrave to the FDA once more – only to be shot down again, at least temporarily. The agency required a review extension in order to come to agreement on the final form of postmarketing surveillance, said Denise Powell, a spokeswoman for Orexigen.
"At that time, FDA said the data looked good," she said in an interview. "We just needed more time to work out the postmarketing requirements."
Those will include:
• A cardiovascular outcomes trial to assess the cardiovascular risk associated with Contrave use.
• Two efficacy, safety, and clinical pharmacology studies in pediatric patients (one in patients 12-17 years old, and one in patients 7-11 years old).
• A juvenile animal toxicity study with a particular focus on growth and development as well as behavior, learning, and memory.
• A cardiac conduction study.
• Clinical trials to evaluate dosing in patients with hepatic or renal impairment.
• A clinical trial to evaluate the potential for interactions between the medication and other drugs.
Contrave contains an extended-release formulation of 8 mg naltrexone and 90 mg bupropion. It is to be administered in an in a 4-week upward titration schedule, with a single morning tablet during week 1; a single tablet at morning and evening during week 2; two tablets in the morning and one in the evening during week 3; and two tablets both morning and evening from week 4 and onward.
Dr. Garvey is a consultant for Daiichi Sankyo, LipoScience, Takeda, Vivus, Boehringer Ingelheim, Janssen, Eisai, and Novo Nordisk. He has received research funding from Merck, AstraZeneca, Weight Watchers, Eisai, and Sanofi.
On Twitter @alz_gal
After a delay of more than 3 years, the Food and Drug Administration has approved the nation’s third weight-loss drug, a combination of naltrexone and bupropion.
The extended release tablets (Contrave; Orexigen and Takeda) are approved for use in adults who have a body mass index of at least 30 kg/m2, or those with a BMI of at least 27 kg/m2 and at least one additional weight-related condition such as hypertension, type 2 diabetes, or dyslipidemia. The agency recommended that Contrave be used in addition to caloric restriction and increased physical activity.
Dr. Timothy Garvey, chair of the American Association of Clinical Endocrinologists’ scientific committee, lauded the approval.
"We have a new tool now to treat obesity – and that is very good news," he said in an interview.
He said Contrave will be a valuable addition to the existing weight-loss medications: the phentermine/topiramate combo (Qsymia; Vivus) and lorcaserin (Belviq; Arena).
"There are no head-to-head trials with the other drugs, so we really can’t say much about relative efficacy," said Dr. Garvey. "But when you look at the placebo-subtracted weight loss in all the phase III data, it looks like Contrave is in the middle, with about a 6% loss over lifestyle interventions alone. So it’s not as effective as the topiramate combination, but more effective than lorcaserin."
In the pivotal, 56-week phase III trials, those taking Contrave lost 5%-8% of their baseline body weight, compared with a loss of 1%-2% in those on placebo. The proportion of those who lost at least 5% of their baseline body weight ranged from 45%-56% of those on the proposed dose, compared with 16%-43% of those on placebo.
The FDA guidance on weight-loss drugs suggests a 12-week efficacy evaluation – if the patient has not lost at least 5% of total body weight by then, the drug should be discontinued and another started.
It’s not possible to predict who will respond best to which drug, although there are some things to consider when choosing, said Dr. Garvey, who is chair of the department of nutrition at the University of Alabama at Birmingham.
"For example, women of childbearing age need to take precautions against becoming pregnant if they take the topiramate combination, and should stop it right away if they do become pregnant. And since lorcaserin is a serotonergic drug, it has to be used very cautiously in patients who are on other serotonergic medications. We definitely need more safety data there."
Additionally, none of the weight-loss drugs should be used in children or teens until more studies confirm their safety for those patients, "All of the companies are planning these trials, and we hope they will complete them expeditiously," Dr. Garvey said. "Childhood and adolescent obesity is a huge problem, and we really need some good treatment options there."
Because it contains bupropion, an antidepressant that has been associated with an increased risk of suicidal thoughts and actions, the drug carries a black box warning. Bupropion is also known to lower seizure threshold, so the drug should not be used in patients with seizure disorders. If a seizure occurs while taking on the medication, it should be permanently discontinued. Nor should it be used in patients with uncontrolled hypertension.
Orexigen and Takeda originally brought the drug forward in December 2011. It was not approved at that time because of concerns about its effect on blood pressure – an unexpected move, and one that Orexigen management called "a big setback."
About a quarter of those in the 56-week pivotal phase III trial experienced significant blood pressure increases of at least 10% above their baseline, compared with about 20% of those in the control arm. Increases of diastolic blood pressure of at least 5 mm Hg over baseline occurred in 37% of those on the combination, compared with 29% of those on placebo. About a quarter in the active arm also had heart rate increases of at least 10 beats per minute, compared with 19% of those taking placebo.
Because of these concerns, the FDA required the drug companies to conduct a large, double-blinded, randomized, placebo-controlled trial to investigate the risk of major cardiovascular events. Takeda and Orexigen then launched the 4-year, 8,900 patient Light study, which is still ongoing. Endpoints are major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke) in overweight and obese subjects who have concomitant diabetes and/or other cardiovascular risk factors.
In June, citing encouraging preliminary results, Takeda and Orexigen brought Contrave to the FDA once more – only to be shot down again, at least temporarily. The agency required a review extension in order to come to agreement on the final form of postmarketing surveillance, said Denise Powell, a spokeswoman for Orexigen.
"At that time, FDA said the data looked good," she said in an interview. "We just needed more time to work out the postmarketing requirements."
Those will include:
• A cardiovascular outcomes trial to assess the cardiovascular risk associated with Contrave use.
• Two efficacy, safety, and clinical pharmacology studies in pediatric patients (one in patients 12-17 years old, and one in patients 7-11 years old).
• A juvenile animal toxicity study with a particular focus on growth and development as well as behavior, learning, and memory.
• A cardiac conduction study.
• Clinical trials to evaluate dosing in patients with hepatic or renal impairment.
• A clinical trial to evaluate the potential for interactions between the medication and other drugs.
Contrave contains an extended-release formulation of 8 mg naltrexone and 90 mg bupropion. It is to be administered in an in a 4-week upward titration schedule, with a single morning tablet during week 1; a single tablet at morning and evening during week 2; two tablets in the morning and one in the evening during week 3; and two tablets both morning and evening from week 4 and onward.
Dr. Garvey is a consultant for Daiichi Sankyo, LipoScience, Takeda, Vivus, Boehringer Ingelheim, Janssen, Eisai, and Novo Nordisk. He has received research funding from Merck, AstraZeneca, Weight Watchers, Eisai, and Sanofi.
On Twitter @alz_gal
Insulin degludec noninferior to insulin detemir in pediatric diabetes
TORONTO – Insulin degludec given once daily was noninferior to insulin detemir in children and adolescents with type 1 diabetes, according to a randomized trial.
The rates of severe, confirmed and nocturnal hypoglycemia were comparable with the two insulins, but hyperglycemia with ketosis was significantly lower in those treated with insulin degludec, compared with insulin detemir.
"Obviously, I don’t need to tell this audience that achieving good glycemic control is a challenge in childhood," said Dr. Nandu Thalange from Norfolk and Norwich (England) University Hospital at the annual conference of the International Society for Pediatric and Adolescent Diabetes.
"We have the twin perils of hypo- and hyperglycemia and, particularly with hyperglycemia, the risks of diabetic ketoacidosis, which in childhood diabetes is the leading cause of death," he said.
Novo Nordisk’s insulin degludec (Tresiba) is a long-acting insulin analogue that has been approved in the European Union and some other places, but was rejected by the U.S. Food and Drug Administration in February 2013 because of cardiovascular concerns. The agent has undergone extensive trials in adults but not in children, and pediatric use is not yet licensed anywhere.
This randomized, controlled, open-label noninferiority trial was designed to generate efficacy and safety data in children and adolescents. A total of 350 children with type 1 diabetes were randomly assigned to either insulin degludec once daily in combination with bolus insulin aspart or insulin detemir once daily or twice daily in combination with insulin aspart.
Eligible participants were aged 1-17 years, were already taking insulin for at least 3 months, were not taking oral antidiabetes drugs, and had hemoglobin A1c values of up to 11%. The primary endpoint was the percentage change from baseline in HbA1c after 26 weeks of treatment.
In a 26-week extension phase designed to gather additional safety and outcomes data, 280 of the original 350 participants were followed for the key secondary outcomes of HbA1c, fasting plasma glucose (FPG), insulin dose, hypoglycemia, hyperglycemia with ketosis, and adverse events. Compliance was monitored via weekly titration of their insulin doses and numerous visits and telephone calls over the study period.
Noninferiority of insulin degludec over insulin detemir at 26 weeks was confirmed for the primary endpoint of HbA1c, with an estimated treatment difference of 0.15 percentage points (P for noninferiority less than .05). This noninferiority was maintained at 52 weeks, when HbA1c was 7.9% in the study arm and 7.8% in the control arm, Dr. Thalange and his coinvestigators reported.
As would be expected in patients on a longer-acting insulin analogue, the mean FPG was 7.8 mmol/L in those treated with insulin degludec, compared with 9.5 mmol/L in the insulin detemir arm.
The incidence and rates of severe hypoglycemia trended higher with insulin degludec than with insulin detemir, at 17.8% and 13.7%, respectively, and 0.51 vs. 0.33 events per 100 patient-years of exposure, albeit without reaching statistical significance. Similarly, rates of severe hypoglycemia (including only episodes of semiconscious/unconscious state and coma with or without convulsions) did not differ significantly between the degludec and detemir groups, at 0.09 and 0.14 events per 100 patient-years of exposure; nor did the occurrence of confirmed nocturnal hypoglycemia differ between groups.
Noting that there were more than 17,000 hypoglycemia events in 1 year among the 350 children enrolled in the study, Dr. Thalange noted, "I think my colleagues treating adults often forget how much hypoglycemia children have."
Rates of hyperglycemia with ketosis were significantly lower in the insulin degludec arm at 0.7, as compared with 0.11 events per 100 patient-years (rate ratio, 0.41).
"As you can see, there was a 59% lower rate of ketosis with hyperglycemia in those treated with insulin degludec, and I think my diabetes nurses would welcome having 60% fewer calls from worried and anxious families."
Other than the higher rate of hypoglycemia seen in the insulin degludec arm, the adverse event profiles were similar for the two agents.
Novo Nordisk sponsored the study. Dr. Thalange reported receiving research support from and being a consultant to Novo Nordisk.
TORONTO – Insulin degludec given once daily was noninferior to insulin detemir in children and adolescents with type 1 diabetes, according to a randomized trial.
The rates of severe, confirmed and nocturnal hypoglycemia were comparable with the two insulins, but hyperglycemia with ketosis was significantly lower in those treated with insulin degludec, compared with insulin detemir.
"Obviously, I don’t need to tell this audience that achieving good glycemic control is a challenge in childhood," said Dr. Nandu Thalange from Norfolk and Norwich (England) University Hospital at the annual conference of the International Society for Pediatric and Adolescent Diabetes.
"We have the twin perils of hypo- and hyperglycemia and, particularly with hyperglycemia, the risks of diabetic ketoacidosis, which in childhood diabetes is the leading cause of death," he said.
Novo Nordisk’s insulin degludec (Tresiba) is a long-acting insulin analogue that has been approved in the European Union and some other places, but was rejected by the U.S. Food and Drug Administration in February 2013 because of cardiovascular concerns. The agent has undergone extensive trials in adults but not in children, and pediatric use is not yet licensed anywhere.
This randomized, controlled, open-label noninferiority trial was designed to generate efficacy and safety data in children and adolescents. A total of 350 children with type 1 diabetes were randomly assigned to either insulin degludec once daily in combination with bolus insulin aspart or insulin detemir once daily or twice daily in combination with insulin aspart.
Eligible participants were aged 1-17 years, were already taking insulin for at least 3 months, were not taking oral antidiabetes drugs, and had hemoglobin A1c values of up to 11%. The primary endpoint was the percentage change from baseline in HbA1c after 26 weeks of treatment.
In a 26-week extension phase designed to gather additional safety and outcomes data, 280 of the original 350 participants were followed for the key secondary outcomes of HbA1c, fasting plasma glucose (FPG), insulin dose, hypoglycemia, hyperglycemia with ketosis, and adverse events. Compliance was monitored via weekly titration of their insulin doses and numerous visits and telephone calls over the study period.
Noninferiority of insulin degludec over insulin detemir at 26 weeks was confirmed for the primary endpoint of HbA1c, with an estimated treatment difference of 0.15 percentage points (P for noninferiority less than .05). This noninferiority was maintained at 52 weeks, when HbA1c was 7.9% in the study arm and 7.8% in the control arm, Dr. Thalange and his coinvestigators reported.
As would be expected in patients on a longer-acting insulin analogue, the mean FPG was 7.8 mmol/L in those treated with insulin degludec, compared with 9.5 mmol/L in the insulin detemir arm.
The incidence and rates of severe hypoglycemia trended higher with insulin degludec than with insulin detemir, at 17.8% and 13.7%, respectively, and 0.51 vs. 0.33 events per 100 patient-years of exposure, albeit without reaching statistical significance. Similarly, rates of severe hypoglycemia (including only episodes of semiconscious/unconscious state and coma with or without convulsions) did not differ significantly between the degludec and detemir groups, at 0.09 and 0.14 events per 100 patient-years of exposure; nor did the occurrence of confirmed nocturnal hypoglycemia differ between groups.
Noting that there were more than 17,000 hypoglycemia events in 1 year among the 350 children enrolled in the study, Dr. Thalange noted, "I think my colleagues treating adults often forget how much hypoglycemia children have."
Rates of hyperglycemia with ketosis were significantly lower in the insulin degludec arm at 0.7, as compared with 0.11 events per 100 patient-years (rate ratio, 0.41).
"As you can see, there was a 59% lower rate of ketosis with hyperglycemia in those treated with insulin degludec, and I think my diabetes nurses would welcome having 60% fewer calls from worried and anxious families."
Other than the higher rate of hypoglycemia seen in the insulin degludec arm, the adverse event profiles were similar for the two agents.
Novo Nordisk sponsored the study. Dr. Thalange reported receiving research support from and being a consultant to Novo Nordisk.
TORONTO – Insulin degludec given once daily was noninferior to insulin detemir in children and adolescents with type 1 diabetes, according to a randomized trial.
The rates of severe, confirmed and nocturnal hypoglycemia were comparable with the two insulins, but hyperglycemia with ketosis was significantly lower in those treated with insulin degludec, compared with insulin detemir.
"Obviously, I don’t need to tell this audience that achieving good glycemic control is a challenge in childhood," said Dr. Nandu Thalange from Norfolk and Norwich (England) University Hospital at the annual conference of the International Society for Pediatric and Adolescent Diabetes.
"We have the twin perils of hypo- and hyperglycemia and, particularly with hyperglycemia, the risks of diabetic ketoacidosis, which in childhood diabetes is the leading cause of death," he said.
Novo Nordisk’s insulin degludec (Tresiba) is a long-acting insulin analogue that has been approved in the European Union and some other places, but was rejected by the U.S. Food and Drug Administration in February 2013 because of cardiovascular concerns. The agent has undergone extensive trials in adults but not in children, and pediatric use is not yet licensed anywhere.
This randomized, controlled, open-label noninferiority trial was designed to generate efficacy and safety data in children and adolescents. A total of 350 children with type 1 diabetes were randomly assigned to either insulin degludec once daily in combination with bolus insulin aspart or insulin detemir once daily or twice daily in combination with insulin aspart.
Eligible participants were aged 1-17 years, were already taking insulin for at least 3 months, were not taking oral antidiabetes drugs, and had hemoglobin A1c values of up to 11%. The primary endpoint was the percentage change from baseline in HbA1c after 26 weeks of treatment.
In a 26-week extension phase designed to gather additional safety and outcomes data, 280 of the original 350 participants were followed for the key secondary outcomes of HbA1c, fasting plasma glucose (FPG), insulin dose, hypoglycemia, hyperglycemia with ketosis, and adverse events. Compliance was monitored via weekly titration of their insulin doses and numerous visits and telephone calls over the study period.
Noninferiority of insulin degludec over insulin detemir at 26 weeks was confirmed for the primary endpoint of HbA1c, with an estimated treatment difference of 0.15 percentage points (P for noninferiority less than .05). This noninferiority was maintained at 52 weeks, when HbA1c was 7.9% in the study arm and 7.8% in the control arm, Dr. Thalange and his coinvestigators reported.
As would be expected in patients on a longer-acting insulin analogue, the mean FPG was 7.8 mmol/L in those treated with insulin degludec, compared with 9.5 mmol/L in the insulin detemir arm.
The incidence and rates of severe hypoglycemia trended higher with insulin degludec than with insulin detemir, at 17.8% and 13.7%, respectively, and 0.51 vs. 0.33 events per 100 patient-years of exposure, albeit without reaching statistical significance. Similarly, rates of severe hypoglycemia (including only episodes of semiconscious/unconscious state and coma with or without convulsions) did not differ significantly between the degludec and detemir groups, at 0.09 and 0.14 events per 100 patient-years of exposure; nor did the occurrence of confirmed nocturnal hypoglycemia differ between groups.
Noting that there were more than 17,000 hypoglycemia events in 1 year among the 350 children enrolled in the study, Dr. Thalange noted, "I think my colleagues treating adults often forget how much hypoglycemia children have."
Rates of hyperglycemia with ketosis were significantly lower in the insulin degludec arm at 0.7, as compared with 0.11 events per 100 patient-years (rate ratio, 0.41).
"As you can see, there was a 59% lower rate of ketosis with hyperglycemia in those treated with insulin degludec, and I think my diabetes nurses would welcome having 60% fewer calls from worried and anxious families."
Other than the higher rate of hypoglycemia seen in the insulin degludec arm, the adverse event profiles were similar for the two agents.
Novo Nordisk sponsored the study. Dr. Thalange reported receiving research support from and being a consultant to Novo Nordisk.
AT ISPAD 2014
Key clinical point: Both drugs improved long-term glycemic control. Rates of severe hypoglycemia trended higher with insulin degludec than with insulin detemir (the difference was not significant), but hyperglycemia with ketosis was significantly lower in the degludec group.
Major finding: Insulin degludec was noninferior to insulin detemir for the primary endpoint of HbA1c in type 1 diabetes patients aged 1-17 years. This noninferiority was maintained at 52 weeks, when HbA1c was 7.9% in the study arm and 7.8% in the control arm.
Data source: A randomized, controlled, open-label, 26-week noninferiority trial in 350 children and adolescents with type 1 diabetes.
Disclosures: Novo Nordisk sponsored the study. Dr. Thalange reported receiving research support from and being a consultant to Novo Nordisk.
FDA committee gives thumbs-down to hypertension combo
A Food and Drug Administration advisory committee has withheld its recommendation of approval for a fixed-dose combination hypertension drug, saying that it offered no significant benefits over its individual components.
The Cardiovascular and Renal Drugs Advisory Committee voted 6-4 against recommending the drug, a combination of nebivolol 20 mg and valsartan 320 mg.
In a large, well-powered study, the combination lowered systolic blood pressure by a mean of 17 mm Hg, and diastolic BP by 12.5 mm Hg, for a mean benefit of 1.2 mm Hg diastolic and 2.9 mm Hg systolic over nebivolol 40 mg alone. But while the systolic endpoint was statistically significant, neither it nor the diastolic endpoint were clinically meaningful, the committee said.
About 5% more of those who took the combination than those who took nebivolol alone achieved the target systolic goals of 140 and 130 mm Hg – another nonsignificant finding.
In discussing their decisions, several committee members said that approving a minimally effective combination antihypertensive available could be counterproductive.
"Approving a drug with this small effect could lead to physicians choosing this over other combinations that work better," extending even further the time it takes patients to reach blood pressure goals, said Dr. James DeLemos, professor of medicine at the University of Texas Southwestern, Dallas. "We don’t need more combinations. We need fewer, which offer clear advantages over their individual components."
The pivotal 8-week, double-blind efficacy trial randomized 4,161 patients to five doses of the combination of nebivolol and valsartan or to the highest approved doses of the individual components, following a 4- to 6-week single-blind, placebo run-in phase. Forest Laboratories brought the 20/320 fixed dose forward to the FDA. The primary comparator was nebivolol 40 mg; the primary endpoint was change in diastolic blood pressure.
The comparison was a sticking point from the beginning, however, as committee members pointed out that nebivolol 40 mg is not an approved dose in the United States, and the likelihood of a clinician prescribing two 20-mg tablets is small. Forest considered using the 20-mg dose as the primary comparator, but went with 40 mg because FDA regulatory standards require using the highest available dose.
Dr. Stuart Rich said the comparison was unfortunate.
"We were asked to make a judgment on a combination compared to a monotherapy that isn’t even available. My sense is it works better than valsartan alone and better than the lower dose of nebivolol alone, but we’re left with this hypothetical comparison. If we had clear-cut data for the 20-mg nebivolol, the decision would be easier," said Dr. Rich, professor of medicine at the University of Chicago.
The combination was safe, with a very low rate of serious adverse events (0.2%). There were significantly fewer adverse events leading to discontinuation in the combination group than in the nebivolol-alone group (1.6% vs. 4%). These were driven by bradycardia, which occurred in three patients taking the combination (0.5%) and eight taking only nebivolol (1.3%).
However, all of the bradycardia cases were asymptomatic, a finding that led the committee chairman reviewer to question the events’ clinical significance.
"They have not provided any compelling evidence that these were clinically important events," said Dr. Michael Lincoff of the Cleveland Clinic. "It was an artificial measurement that didn’t demonstrate better tolerability of the combination."
Members of the committee had no financial disclosures.
A Food and Drug Administration advisory committee has withheld its recommendation of approval for a fixed-dose combination hypertension drug, saying that it offered no significant benefits over its individual components.
The Cardiovascular and Renal Drugs Advisory Committee voted 6-4 against recommending the drug, a combination of nebivolol 20 mg and valsartan 320 mg.
In a large, well-powered study, the combination lowered systolic blood pressure by a mean of 17 mm Hg, and diastolic BP by 12.5 mm Hg, for a mean benefit of 1.2 mm Hg diastolic and 2.9 mm Hg systolic over nebivolol 40 mg alone. But while the systolic endpoint was statistically significant, neither it nor the diastolic endpoint were clinically meaningful, the committee said.
About 5% more of those who took the combination than those who took nebivolol alone achieved the target systolic goals of 140 and 130 mm Hg – another nonsignificant finding.
In discussing their decisions, several committee members said that approving a minimally effective combination antihypertensive available could be counterproductive.
"Approving a drug with this small effect could lead to physicians choosing this over other combinations that work better," extending even further the time it takes patients to reach blood pressure goals, said Dr. James DeLemos, professor of medicine at the University of Texas Southwestern, Dallas. "We don’t need more combinations. We need fewer, which offer clear advantages over their individual components."
The pivotal 8-week, double-blind efficacy trial randomized 4,161 patients to five doses of the combination of nebivolol and valsartan or to the highest approved doses of the individual components, following a 4- to 6-week single-blind, placebo run-in phase. Forest Laboratories brought the 20/320 fixed dose forward to the FDA. The primary comparator was nebivolol 40 mg; the primary endpoint was change in diastolic blood pressure.
The comparison was a sticking point from the beginning, however, as committee members pointed out that nebivolol 40 mg is not an approved dose in the United States, and the likelihood of a clinician prescribing two 20-mg tablets is small. Forest considered using the 20-mg dose as the primary comparator, but went with 40 mg because FDA regulatory standards require using the highest available dose.
Dr. Stuart Rich said the comparison was unfortunate.
"We were asked to make a judgment on a combination compared to a monotherapy that isn’t even available. My sense is it works better than valsartan alone and better than the lower dose of nebivolol alone, but we’re left with this hypothetical comparison. If we had clear-cut data for the 20-mg nebivolol, the decision would be easier," said Dr. Rich, professor of medicine at the University of Chicago.
The combination was safe, with a very low rate of serious adverse events (0.2%). There were significantly fewer adverse events leading to discontinuation in the combination group than in the nebivolol-alone group (1.6% vs. 4%). These were driven by bradycardia, which occurred in three patients taking the combination (0.5%) and eight taking only nebivolol (1.3%).
However, all of the bradycardia cases were asymptomatic, a finding that led the committee chairman reviewer to question the events’ clinical significance.
"They have not provided any compelling evidence that these were clinically important events," said Dr. Michael Lincoff of the Cleveland Clinic. "It was an artificial measurement that didn’t demonstrate better tolerability of the combination."
Members of the committee had no financial disclosures.
A Food and Drug Administration advisory committee has withheld its recommendation of approval for a fixed-dose combination hypertension drug, saying that it offered no significant benefits over its individual components.
The Cardiovascular and Renal Drugs Advisory Committee voted 6-4 against recommending the drug, a combination of nebivolol 20 mg and valsartan 320 mg.
In a large, well-powered study, the combination lowered systolic blood pressure by a mean of 17 mm Hg, and diastolic BP by 12.5 mm Hg, for a mean benefit of 1.2 mm Hg diastolic and 2.9 mm Hg systolic over nebivolol 40 mg alone. But while the systolic endpoint was statistically significant, neither it nor the diastolic endpoint were clinically meaningful, the committee said.
About 5% more of those who took the combination than those who took nebivolol alone achieved the target systolic goals of 140 and 130 mm Hg – another nonsignificant finding.
In discussing their decisions, several committee members said that approving a minimally effective combination antihypertensive available could be counterproductive.
"Approving a drug with this small effect could lead to physicians choosing this over other combinations that work better," extending even further the time it takes patients to reach blood pressure goals, said Dr. James DeLemos, professor of medicine at the University of Texas Southwestern, Dallas. "We don’t need more combinations. We need fewer, which offer clear advantages over their individual components."
The pivotal 8-week, double-blind efficacy trial randomized 4,161 patients to five doses of the combination of nebivolol and valsartan or to the highest approved doses of the individual components, following a 4- to 6-week single-blind, placebo run-in phase. Forest Laboratories brought the 20/320 fixed dose forward to the FDA. The primary comparator was nebivolol 40 mg; the primary endpoint was change in diastolic blood pressure.
The comparison was a sticking point from the beginning, however, as committee members pointed out that nebivolol 40 mg is not an approved dose in the United States, and the likelihood of a clinician prescribing two 20-mg tablets is small. Forest considered using the 20-mg dose as the primary comparator, but went with 40 mg because FDA regulatory standards require using the highest available dose.
Dr. Stuart Rich said the comparison was unfortunate.
"We were asked to make a judgment on a combination compared to a monotherapy that isn’t even available. My sense is it works better than valsartan alone and better than the lower dose of nebivolol alone, but we’re left with this hypothetical comparison. If we had clear-cut data for the 20-mg nebivolol, the decision would be easier," said Dr. Rich, professor of medicine at the University of Chicago.
The combination was safe, with a very low rate of serious adverse events (0.2%). There were significantly fewer adverse events leading to discontinuation in the combination group than in the nebivolol-alone group (1.6% vs. 4%). These were driven by bradycardia, which occurred in three patients taking the combination (0.5%) and eight taking only nebivolol (1.3%).
However, all of the bradycardia cases were asymptomatic, a finding that led the committee chairman reviewer to question the events’ clinical significance.
"They have not provided any compelling evidence that these were clinically important events," said Dr. Michael Lincoff of the Cleveland Clinic. "It was an artificial measurement that didn’t demonstrate better tolerability of the combination."
Members of the committee had no financial disclosures.
AT AN FDA ADVISORY COMMITTEE MEETING
Statins do not worsen diabetes microvascular complications, may be protective
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
FROM THE LANCET DIABETES & ENDOCRINOLOGY
Key clinical point: Statins may protect against microvascular complications in diabetes patients.
Major finding: Statin users were significantly less likely to be diagnosed with diabetic neuropathy (HR, 0.66) and diabetic retinopathy (HR, 0.60) than non–statin users.
Data source: A registry study compared 62,716 patients with diabetes: 15,679 statin users and 47,037 non–statin users.
Disclosures: Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Prediabetes increases cancer risk by 15%
Prediabetes increases cancer risk in adults by 15%, with significantly increased risk for cancer of the stomach, liver, pancreas, breast, and endometrium, in a meta-analysis published Sept. 8 in Diabetologia.
Moreover, that increase in risk for all cancer types was seen in studies that used the low-threshold cutoff for impaired fasting glucose recommended by the American Diabetes Association, suggesting that international experts should adopt the ADA’s definition.
The meta-analysis included 16 eligible studies comprising 891,426 adults aged 18 and older. The study evaluated cancer risk associated with impaired fasting glucose and impaired glucose tolerance, reported Dr. Yi Huang and associates at the Clinical Medicine Research Center, First People’s Hospital of Shunde, Foshan, China.
Participants met the inclusion criteria of elevated blood glucose at baseline, duration of 3 years’ follow-up or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Prediabetes was defined as impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or both. IFG was defined as a fasting plasma glucose (FPG) range of 5.6-6.9 mmol/L if the study used American Diabetes Association guidelines (Diabetes Care 26[Suppl 1]:S5–S20), or 6.1-6.9 mmol/L if the study used international guidelines. IGT was defined as a 2-hour plasma glucose of 7.8-11.1 mmol/L during an oral glucose tolerance test.
Prediabetes was associated with a 15% increased risk of cancer overall, compared with normoglycemia. The lowered ADA threshold of 5.6 mmol/L resulted in 49% increase in risk, whereas the higher threshold was linked with an 11% increase in risk. Measured by IFG, the cancer risk was 25% higher. However, these differences in risk between prediabetes definitions did not reach statistical significance, the investigators said (Diabetologia 2014 Sept. 8 [doi:10.1007/s00125-014-3361-2]).
Additionally, a secondary analysis of site-specific cancer risk showed that prediabetes was significantly associated with an increased risk of cancer of the stomach, liver, pancreas, breast, and endometrium, but was not associated with cancer of the lung, prostate, ovary, kidney, or bladder.
Subgroup analyses showed no differences in cancer risk by sex, age, or follow-up duration, but did reveal a significantly higher relative risk for Asian (1.50) than non-Asian patients (1.12).
Dr. Huang and colleagues said the results of this study have important implications for the definition and treatment of prediabetes.
"One of the most important arguments against using the lower threshold is that it greatly increases the prevalence of IFG, but without enough data to support the clinical prognostic implications," they wrote.
These results demonstrate similar cancer risk with different definitions of prediabetes, thus providing evidence for the use of the new ADA definition, which has not yet been accepted by the World Health Organization and other international groups, they said.
"These findings support the lower threshold definition IFG proposed by the ADA, and highlight the clinical value of the early management of hyperglycemia to prevent cancer," they said.
They added that several factors – insulin resistance, genetic interferences, and chronic hyperglycemia and its related conditions, such as chronic oxidative stress – may contribute to the increased cancer risk in persons with prediabetes. Typically, lifestyle intervention is the preferred treatment in prediabetes patients, and metformin may be added to delay progression to diabetes in those who present with additional risk factors such as a body mass index of at least 35 kg/m2, dyslipidemia, hypertension, or a family history of diabetes.
Research has shown that metformin may contribute to a 30% decrease in cancer risk in diabetes patients. Future exploration should focus on the possibility of protective anticancer properties of metformin in adults with prediabetes as well, the investigators said.
The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.
Prediabetes increases cancer risk in adults by 15%, with significantly increased risk for cancer of the stomach, liver, pancreas, breast, and endometrium, in a meta-analysis published Sept. 8 in Diabetologia.
Moreover, that increase in risk for all cancer types was seen in studies that used the low-threshold cutoff for impaired fasting glucose recommended by the American Diabetes Association, suggesting that international experts should adopt the ADA’s definition.
The meta-analysis included 16 eligible studies comprising 891,426 adults aged 18 and older. The study evaluated cancer risk associated with impaired fasting glucose and impaired glucose tolerance, reported Dr. Yi Huang and associates at the Clinical Medicine Research Center, First People’s Hospital of Shunde, Foshan, China.
Participants met the inclusion criteria of elevated blood glucose at baseline, duration of 3 years’ follow-up or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Prediabetes was defined as impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or both. IFG was defined as a fasting plasma glucose (FPG) range of 5.6-6.9 mmol/L if the study used American Diabetes Association guidelines (Diabetes Care 26[Suppl 1]:S5–S20), or 6.1-6.9 mmol/L if the study used international guidelines. IGT was defined as a 2-hour plasma glucose of 7.8-11.1 mmol/L during an oral glucose tolerance test.
Prediabetes was associated with a 15% increased risk of cancer overall, compared with normoglycemia. The lowered ADA threshold of 5.6 mmol/L resulted in 49% increase in risk, whereas the higher threshold was linked with an 11% increase in risk. Measured by IFG, the cancer risk was 25% higher. However, these differences in risk between prediabetes definitions did not reach statistical significance, the investigators said (Diabetologia 2014 Sept. 8 [doi:10.1007/s00125-014-3361-2]).
Additionally, a secondary analysis of site-specific cancer risk showed that prediabetes was significantly associated with an increased risk of cancer of the stomach, liver, pancreas, breast, and endometrium, but was not associated with cancer of the lung, prostate, ovary, kidney, or bladder.
Subgroup analyses showed no differences in cancer risk by sex, age, or follow-up duration, but did reveal a significantly higher relative risk for Asian (1.50) than non-Asian patients (1.12).
Dr. Huang and colleagues said the results of this study have important implications for the definition and treatment of prediabetes.
"One of the most important arguments against using the lower threshold is that it greatly increases the prevalence of IFG, but without enough data to support the clinical prognostic implications," they wrote.
These results demonstrate similar cancer risk with different definitions of prediabetes, thus providing evidence for the use of the new ADA definition, which has not yet been accepted by the World Health Organization and other international groups, they said.
"These findings support the lower threshold definition IFG proposed by the ADA, and highlight the clinical value of the early management of hyperglycemia to prevent cancer," they said.
They added that several factors – insulin resistance, genetic interferences, and chronic hyperglycemia and its related conditions, such as chronic oxidative stress – may contribute to the increased cancer risk in persons with prediabetes. Typically, lifestyle intervention is the preferred treatment in prediabetes patients, and metformin may be added to delay progression to diabetes in those who present with additional risk factors such as a body mass index of at least 35 kg/m2, dyslipidemia, hypertension, or a family history of diabetes.
Research has shown that metformin may contribute to a 30% decrease in cancer risk in diabetes patients. Future exploration should focus on the possibility of protective anticancer properties of metformin in adults with prediabetes as well, the investigators said.
The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.
Prediabetes increases cancer risk in adults by 15%, with significantly increased risk for cancer of the stomach, liver, pancreas, breast, and endometrium, in a meta-analysis published Sept. 8 in Diabetologia.
Moreover, that increase in risk for all cancer types was seen in studies that used the low-threshold cutoff for impaired fasting glucose recommended by the American Diabetes Association, suggesting that international experts should adopt the ADA’s definition.
The meta-analysis included 16 eligible studies comprising 891,426 adults aged 18 and older. The study evaluated cancer risk associated with impaired fasting glucose and impaired glucose tolerance, reported Dr. Yi Huang and associates at the Clinical Medicine Research Center, First People’s Hospital of Shunde, Foshan, China.
Participants met the inclusion criteria of elevated blood glucose at baseline, duration of 3 years’ follow-up or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Prediabetes was defined as impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or both. IFG was defined as a fasting plasma glucose (FPG) range of 5.6-6.9 mmol/L if the study used American Diabetes Association guidelines (Diabetes Care 26[Suppl 1]:S5–S20), or 6.1-6.9 mmol/L if the study used international guidelines. IGT was defined as a 2-hour plasma glucose of 7.8-11.1 mmol/L during an oral glucose tolerance test.
Prediabetes was associated with a 15% increased risk of cancer overall, compared with normoglycemia. The lowered ADA threshold of 5.6 mmol/L resulted in 49% increase in risk, whereas the higher threshold was linked with an 11% increase in risk. Measured by IFG, the cancer risk was 25% higher. However, these differences in risk between prediabetes definitions did not reach statistical significance, the investigators said (Diabetologia 2014 Sept. 8 [doi:10.1007/s00125-014-3361-2]).
Additionally, a secondary analysis of site-specific cancer risk showed that prediabetes was significantly associated with an increased risk of cancer of the stomach, liver, pancreas, breast, and endometrium, but was not associated with cancer of the lung, prostate, ovary, kidney, or bladder.
Subgroup analyses showed no differences in cancer risk by sex, age, or follow-up duration, but did reveal a significantly higher relative risk for Asian (1.50) than non-Asian patients (1.12).
Dr. Huang and colleagues said the results of this study have important implications for the definition and treatment of prediabetes.
"One of the most important arguments against using the lower threshold is that it greatly increases the prevalence of IFG, but without enough data to support the clinical prognostic implications," they wrote.
These results demonstrate similar cancer risk with different definitions of prediabetes, thus providing evidence for the use of the new ADA definition, which has not yet been accepted by the World Health Organization and other international groups, they said.
"These findings support the lower threshold definition IFG proposed by the ADA, and highlight the clinical value of the early management of hyperglycemia to prevent cancer," they said.
They added that several factors – insulin resistance, genetic interferences, and chronic hyperglycemia and its related conditions, such as chronic oxidative stress – may contribute to the increased cancer risk in persons with prediabetes. Typically, lifestyle intervention is the preferred treatment in prediabetes patients, and metformin may be added to delay progression to diabetes in those who present with additional risk factors such as a body mass index of at least 35 kg/m2, dyslipidemia, hypertension, or a family history of diabetes.
Research has shown that metformin may contribute to a 30% decrease in cancer risk in diabetes patients. Future exploration should focus on the possibility of protective anticancer properties of metformin in adults with prediabetes as well, the investigators said.
The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.
FROM DIABETOLOGIA
Key clinical point: Prediabetes patients may have an increased risk of cancer.
Major finding: Prediabetes was associated with a 15% increased risk of cancer overall, and was significantly associated with increased risk of cancer of the stomach/colorectum, liver, pancreas, breast, and endometrium.
Data source: A meta-analysis of 16 studies comprising 891,426 adults with elevated blood glucose at baseline, follow-up of 3 years or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Disclosures: The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.