User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Managing ‘difficult’ patient encounters
“I did not like those patients… They made me angry and I found myself irritated to experience them as they seemed so distant from myself and from all that is human. This is an astonishing intolerance which brands me a poor psychiatrist.”
Sigmund Freud, Letter to István Hollós (1928)
While Freud was referring to psychotic patients,1 his evident frustration shows that difficult and challenging patients have vexed even the best of us. All physicians and other clinicians will experience patient encounters that lead to anger or frustration, or even challenge their sense of equanimity and professional identity. In short, difficult and challenging patient interactions are unavoidable, regardless of the physician’s discipline.2-5 At times, physicians might struggle with demanding, unpleasant, ungrateful, and possibly dangerous patients, while sometimes the struggle is with the patient’s family members. No physician is immune to the problem, which makes it crucial to learn to anticipate and manage difficult patient interactions, skills which are generally not taught in medical schools or residency programs.
One prospective study of clinic patients found that up to 15% of patient encounters are deemed “difficult.”6 Common scenarios include patients (or their relatives) who seek certain tests after researching symptoms online, threats of legal or social media action in response to feeling that the physician is not listening to them, demands for a second opinion after disagreeing with the physician’s diagnosis, and mistrust of doctors after presenting with symptoms and not receiving a diagnosis. It is also common to care for patients who focus on negative outcomes or fail to adhere to treatment recommendations. These encounters can make physicians feel stressed out, disrespected, abused, or even fearful if threatened. Some physicians may come to feel they are trapped in a hostile work environment with little support from their supervisors or administrators. Patients often have a complaint office or department to turn to, but there is no equivalent for physicians, who are expected to soldier on regardless.
This article highlights a model that describes poor physician-patient encounters, factors contributing to these issues, how to manage these difficult interactions, and what to do if the relationship cannot be remediated.
Describing the ‘difficult’ patient
In a landmark 1978 paper, Groves7 provided one of the first descriptions of “difficult” patients. His colorful observations continue to provide useful insights. Groves emphasized that most medical texts ignore the issue of difficult patients and provide little or no guidance—which is still true 43 years later. He observed that physicians cannot avoid occasional negative feelings toward some patients. Further, Groves suggested that countertransference is often at the root of hateful reactions, a process he defines as “conscious or unconscious unbidden and unwanted hostile or sexual feelings toward the patient.”7Table 17 outlines how Groves divided “hateful” patients into several categories, and how physicians might respond to such patients.

A model for understanding difficult patient encounters
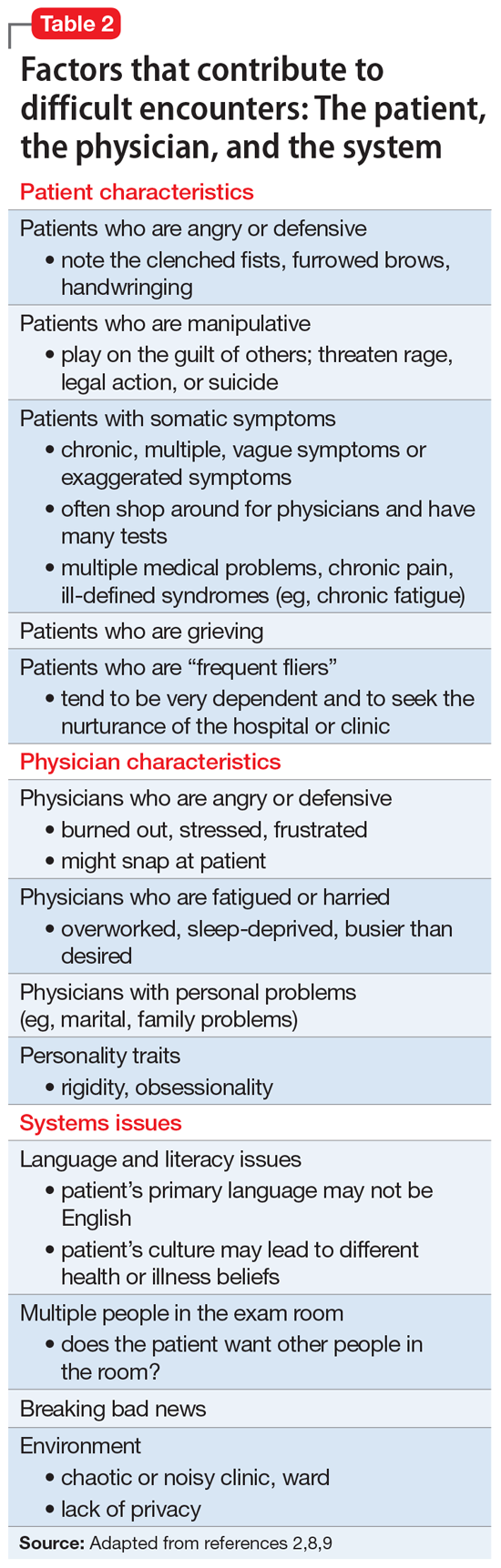
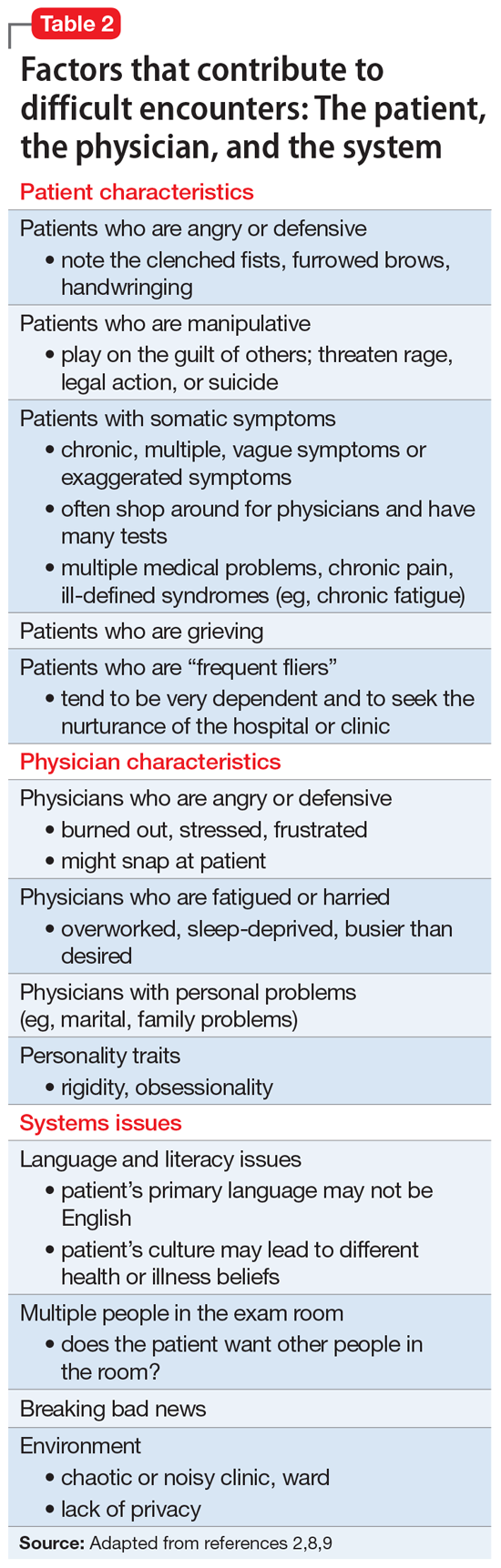
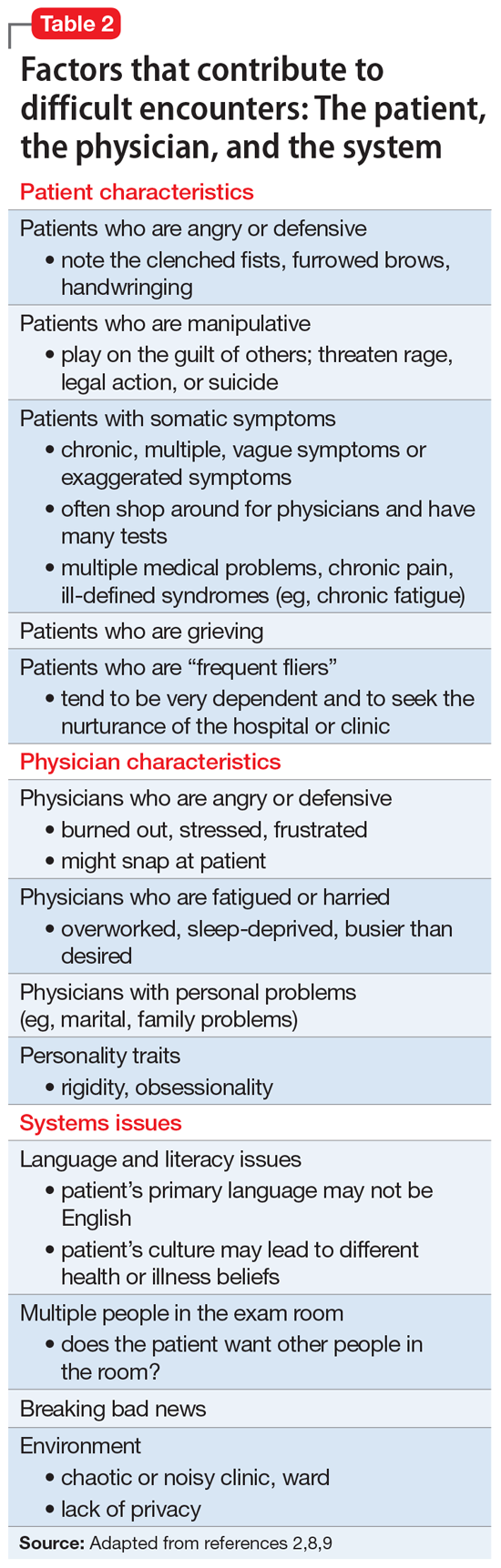
Adams and Murray2 created a model to help explain interactions with difficult or challenging patients that consists of 3 elements: the patient, the physician, and the system (ie, situation or environment). Hull and Broquet8 and Hardavella et al9 later adapted the model and described its components (Table 22,8,9).
Continue to: When considering...
When considering difficult interactions, it is important to be aware that all 3 components could interact, or merely 1 or 2 could come into play, but all should be explored as possible contributing factors.
Patient factors
The patient’s role in initiating or maintaining a problematic interaction should be explored. While some physicians are tempted to conclude that a personality disorder underlies difficult interactions, research shows a more complex picture. First, not all difficult patients have a psychiatric disorder, let alone a personality disorder. Jackson and Kroenke6 reported that among 74 difficult patients in an ambulatory clinic, 29% had a depressive disorder or anxiety disorder, with 11% experiencing 2 or more disorders. Major depressive disorder was present in 8.4% patients, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2%.6 These researchers found that difficult patient interactions were associated with the presence of a psychiatric disorder, especially depressive or anxiety disorders, and multiple physical symptoms.
Importantly, difficult patients are not unique to psychiatry, and are found in all medical disciplines and every type of practice situation. Some problematic patients have a substance use disorder, and their difficulty might stem from intoxication, withdrawal, or drug-seeking behaviors. Psychotic disorders can be the source of difficult interactions, typically resulting from the patient’s symptoms (ie, hallucinations, delusions, or bizarre behavior). Physicians tend to be forgiving toward these patients because they understand the extent of the individual’s illness. The same is true for a patient with dementia, who might be disruptive and loud, yet clearly is not in control of their behavior.
Koekkoek et al5 reviewed 94 articles that focused on difficult patients seen in mental health settings. Most patients were male (60% to 68%), and most were age 26 to 32 years. Diagnoses of psychotic disorders and personality disorders were the most frequent, while mood and other disorders were less common. In 1 of the studies reviewed, 6% of psychiatric inpatients were considered difficult. Koekkoek et al5 proposed that there are 3 groups of difficult patients:
- care avoiders: patients with psychosis who lack insight
- care seekers: patients who are chronically ill who have trouble maintaining a steady relationship with their caregivers
- care claimers: patients who do not require long-term care, but need housing, medication, or a “declaration of incompetence.”
Physician factors
Physicians are frequent contributors to bad interactions with their patients.2,7,8 They can become angry or defensive because of burnout, stress, or frustration, which might lead them to snap or otherwise respond inappropriately to their patients. Many physicians are overworked, sleep-deprived, or busier than they would prefer. Personal problems can be preoccupying and contribute to a physician being ill-tempered or distracted (eg, marital or family problems). Some physicians are simply poor communicators and might not understand the need to adapt their communication style to their patient, instead using medical jargon the patient does not understand. Ideally, physicians should modify their language to suit the patient’s level of education, degree of medical sophistication, and cultural background.
Continue to: A physician's personality traits...
A physician’s personality traits could clash with those of the patient, particularly if the physician is especially rigid or obsessional. Rather than “going with the flow,” the overly rigid physician might become impatient with patients who fail to understand diagnostic assessments or treatment recommendations. Inefficient physicians might not be able to keep up with the daily schedule, which could fuel impatience and perhaps even lead them to think that the patient is taking too much of their valuable time. Some might not know how to convey empathy, for example when giving bad news (“The tests show you have cancer…”). Others fail to make consistent eye contact with patients without understanding its importance to communication, a problem made worse by the use of electronic medical record systems (EMRs).
Systems issues
Systems issues also contribute to suboptimal physician-patient interactions, and some issues can be attributed to administrative problems. Examples of systems issues include:
- when a patient has difficulty making an appointment and is forced to listen to a confusing menu of choices
- a busy clinic that can only offer a patient an appointment 6 months away
- crowded or noisy waiting rooms
- language barriers for patients whose primary langage is not English. Not having access to an interpreter can exacerbate their frustration
- the use of EMRs is a growing threat to positive physician-patient interactions, yet their influence is often ignored. Widely disliked by physicians,10 EMRs are required in all but the smallest independent practice settings. Many busy physicians focus their attention on the computer, giving the patient the impression that the physician is not listening to them. Many patients conclude that they are less important than the process.
The consequences of difficult interactions
Following a bad interaction, dissatisfied patients are more likely to leave the clinic or hospital and ignore medical advice. These patients might then show up in crowded emergency departments, which may lead to poor use of health care resources. For physicians, challenging situations sap their emotional energy, cause demoralization, and interfere with their sense of job fulfillment. In extreme cases, such feelings might lead the physician to dislike and even avoid the patient.
How to manage challenging situations
Taking the following steps can help physicians work through challenging situations with their patients.
Diagnose the problem. First, recognize the difficult situation, analyze it, and identify how the patient, the physician, and the system are contributing to a bad physician-patient interaction. Diagnosing the interactional difficulty should precede the diagnosis and management of the patient’s disease. Physicians should acknowledge their own contribution through their attitude or actions. Finally, determine if there are system issues that are contributing to the problem, or if it is the clinic or inpatient setting itself (eg, noisy inpatient unit).
Continue to: Maintain your cool
Maintain your cool. With any difficult interaction, a physician’s first obligation is to remain calm and professional, while modeling appropriate behavior. If the patient is angry or emotionally intense, talking over them or interrupting them only makes the situation worse. Try to see the interaction from the patient’s perspective. Both parties should work together to find a common ground.
Collaborate, respect boundaries, and empathize. One study of a group of 100 family physicians found that having the following 3 skills were essential to successfully managing situations with difficult patients11,12:
- the ability to collaborate (vs opposition)
- the appropriate use of power (vs misuse of power, or violation of boundaries by either party)
- the ability to empathize, which for most physicians involves understanding and validating the patient’s subjective experiences.
Although a description of the many facets of empathy (cognitive, affective, motivational) is beyond the scope of this article, it is worth pointing out that a patient’s positive perception of their physician’s empathy improves not only patient satisfaction but health outcomes.13 The Box describes a difficult patient whose actions changed through the collaboration and empathy of his treatment team.
Box 1
Mr. L, a 60-year-old veteran, is admitted to an inpatient unit following a suicide attempt that was prompted by eviction from his apartment. Mr. L is physically disabled and has difficulty walking without assistance. His main concern is his homelessness, and he insists that the inpatient team find a suitable “Americans with Disabilities (ADA)-compliant apartment” that he can afford on his $800 monthly income. He implies that he will kill himself if the team fails in that task. He makes it clear that his problems are the team’s problems. He is prescribed an antidepressant, and both his mood and reported suicidal ideations gradually resolve.
The team’s social worker finds an opening at a well-run veterans home, but Mr. L rejects it because he doesn’t want to “give up his independence.” The social worker finds a small apartment in a nearby community that is ADA-compliant, but Mr. L complains that it is small. He asks the resident psychiatrist, “Where will I put all my things?” The next day, after insulting the attending psychiatrist for failing to find an adequate apartment, Mr. L says from under the bedsheet: “How come none of you ever help me?”
Mr. L presents a challenge to the entire team. At times, he is rude, demanding, and entitled. The team recognizes that although he had served in the military with distinction, he is now alone after having divorced many years earlier, and nearly friendless because of his increasing disability. The team surmises that Mr. L lashes out due to frustration and feelings of powerlessness.
Resolving this conflict involves treating Mr. L with respect and listening without judgment. No one ever confronts him or argues with him. The team psychologist meets with him to help him work through his many losses. Closer to discharge, he is enrolled in several post-hospitalization programs to keep him connected with other veterans. At discharge, the hospital arranges for his belongings that had been in storage to be delivered to his new home. He is pleasant and social with his peers, and although he is still concerned about the size of the apartment, he thanks the team members for their care.
Verbalize the difficulty. It is important to openly discuss the problem. For example, “We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?” This approach names the “elephant in the room” and avoids casting blame. It also creates a sense of shared ownership by externalizing the problem from both the patient and physician. Verbalizing the difficulty can help build trust and pave the way to working together toward a common solution.
Consider other explanations for the patient’s behavior. For example, anger directed at a physician could be due to anxiety about an unrelated matter, such as the patient’s recent job loss or impending divorce. Psychiatrists might understand this behavior better as displacement, which is considered a maladaptive defense mechanism. It is important to listen to the patient and offer empathy, which will help the patient feel supported and build a rapport that can help to resolve the encounter.
Continue to: When helping patients...
When helping patients with multiple issues, which is a common scenario, the physician might start by asking, “What would you like to address today?”14 Keep a list of the issues so you do not forget the patient’s concerns, and then ask: “What do you think is going on?” Give patients time to verbalize their concerns. Physicians should:
- validate concerns: “I understand where you’re coming from.”
- offer empathy: “I can see how difficult this has been for you.”
- reframe: “Let me make sure I hear you correctly.”
- refocus: “Let’s agree on what we need to do at this visit.”
Find common ground. When the patient and physician have different ideas on diagnosis or treatment, finding common ground is another way to resolve a difficult encounter. Difficulties arise when there appears to be little common ground, which often results from unrealistic expectations. Patients might be seen as “demanding” or “manipulative”’ if they push for a diagnosis or treatment the doctor is not comfortable with. As soon as there is some overlap and common ground, the difficulty rapidly subsides.
Set clear boundaries and limits. Physicians should set limits on what patient behavior might “cross the line.” A “behavioral contract” (or “treatment contract”) can help by setting explicit expectations. For example, showing up late for appointments or inappropriately seeking drugs of abuse (eg, opioids, benzodiazepines) might be identified as violations of the contract. Once the contract is set, the patient should be asked to restate key components. Clarify any confusion or barriers to compliance and define clear expectations. The patient should be informed of potential consequences of contract violations, including termination.
Staff members involved in the patient’s care should agree with the terms of any behavioral contract, and should receive a copy of it. Patients should have “buy in,” meaning that they have had an opportunity to provide input to the contract and have agreed to its elements. Both the physician and patient should sign the document.
When all else fails
When there is a breakdown in rapport that makes it difficult or impossible to continue offering treatment, consider termination. This could be due to threatening or abusive patient behavior, sexual advances, repeated no-shows, treatment noncompliance that jeopardizes patient safety, refusal to follow the treatment plan, or violating the terms of a behavioral contract. In some settings, it might be the failure to pay bills.
Continue to: If a patient is unable to...
If a patient is unable to follow the contract, the physician should explore possible extenuating circumstances. The physician should seek to remedy the problem and involve other team members if possible (eg, case manager, nurse), advising a patient about behaviors that could lead to termination.
If the problem is irremediable, notify the patient in writing, give them time to find another physician, and facilitate the transfer of care.15 Take steps to prevent the patient from running out of any medications associated with withdrawal or discontinuation syndromes (eg, selective serotonin reuptake inhibitors, benzodiazepines) during the care transition. While there is no requirement regarding the amount of time allowed, at least 30 days is typical.
Bottom Line
Difficult patient interactions are common and unavoidable. Physicians should acknowledge and recognize contributing factors in such encounters—including their own role. When handling such situations, physicians should remain calm and model appropriate behavior. Improving communication, offering empathy, and validating the patient’s concerns can help resolve factors that contribute to poor patient interactions. If efforts to remediate the physician-patient relationship fail, termination may be necessary.
Related Resources
- Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
- Pereira MR, Figueiredo AF. Challenging patient-doctor interactions in psychiatry – difficult patient syndrome. European Psychiatry. 2017;41(supplement):S719. doi. org/10.1016/j.eurpsy.2017.01.1297
1. Dupont J. Ferenczi’s madness. Contemp Psychoanal. 1988;24(2):250-261.
2. Adams J, Murray R. The difficult diagnosis: the general approach to the difficult patient. Emerg Med Clin North Am. 1998;16(4):689-700.
3. Davies M. Managing challenging interactions with patients. BMJ. 2013;347:f4673. doi: https://doi.org/10.1136/bmj.f4673
4. Chou C. Dealing with the “difficult” patient. Wisc Med J. 2004;103:35-38.
5. Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
6. Jackson JL, Kroenke K. Difficult patient encounter in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med 1999;159(10):1069-1075.
7. Groves JE. Taking care of the hateful patient. N Eng J Med. 1978;298:883-887.
8. Hull S, Broquet K. How to manage difficult encounters. Fam Prac Manag. 2007;14(6):30-34.
9. Hardavella G, Aamli-Gaagnat A, Frille A, et al. Top tips to deal with challenging situations: doctor patient interactions. Breathe. 2017;13(2):129-135.
10. Black DW, Balon R. Editorial: electronic medical records (EMRs) and the psychiatrist shortage. Ann Clin Psychiatry. 2018;30(4):257-259.
11. Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med. 2006;19(6):533-541.
12. Campbell RJ. Campbell’s Psychiatric Dictionary. 8th Edition. Oxford University Press; 2004:219-220.
13. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2014;8:457. https://doi.org/10.3389/fnbeh.2014.00457
14. Klugman B. The difficult patient. Accessed May 24, 2021. https://www.umassmed.edu/globalassets/office-of-continuing-medical-education/pdfs/cme-primary-care-days/e2-the-difficult-patient.pdf
15. Mossman D, Farrell HM, Gilday E. ‘Firing’ a patient: may psychiatrists unilaterally terminate care? Current Psychiatry. 2010;9(12):18-29.
“I did not like those patients… They made me angry and I found myself irritated to experience them as they seemed so distant from myself and from all that is human. This is an astonishing intolerance which brands me a poor psychiatrist.”
Sigmund Freud, Letter to István Hollós (1928)
While Freud was referring to psychotic patients,1 his evident frustration shows that difficult and challenging patients have vexed even the best of us. All physicians and other clinicians will experience patient encounters that lead to anger or frustration, or even challenge their sense of equanimity and professional identity. In short, difficult and challenging patient interactions are unavoidable, regardless of the physician’s discipline.2-5 At times, physicians might struggle with demanding, unpleasant, ungrateful, and possibly dangerous patients, while sometimes the struggle is with the patient’s family members. No physician is immune to the problem, which makes it crucial to learn to anticipate and manage difficult patient interactions, skills which are generally not taught in medical schools or residency programs.
One prospective study of clinic patients found that up to 15% of patient encounters are deemed “difficult.”6 Common scenarios include patients (or their relatives) who seek certain tests after researching symptoms online, threats of legal or social media action in response to feeling that the physician is not listening to them, demands for a second opinion after disagreeing with the physician’s diagnosis, and mistrust of doctors after presenting with symptoms and not receiving a diagnosis. It is also common to care for patients who focus on negative outcomes or fail to adhere to treatment recommendations. These encounters can make physicians feel stressed out, disrespected, abused, or even fearful if threatened. Some physicians may come to feel they are trapped in a hostile work environment with little support from their supervisors or administrators. Patients often have a complaint office or department to turn to, but there is no equivalent for physicians, who are expected to soldier on regardless.
This article highlights a model that describes poor physician-patient encounters, factors contributing to these issues, how to manage these difficult interactions, and what to do if the relationship cannot be remediated.
Describing the ‘difficult’ patient
In a landmark 1978 paper, Groves7 provided one of the first descriptions of “difficult” patients. His colorful observations continue to provide useful insights. Groves emphasized that most medical texts ignore the issue of difficult patients and provide little or no guidance—which is still true 43 years later. He observed that physicians cannot avoid occasional negative feelings toward some patients. Further, Groves suggested that countertransference is often at the root of hateful reactions, a process he defines as “conscious or unconscious unbidden and unwanted hostile or sexual feelings toward the patient.”7Table 17 outlines how Groves divided “hateful” patients into several categories, and how physicians might respond to such patients.

A model for understanding difficult patient encounters
Adams and Murray2 created a model to help explain interactions with difficult or challenging patients that consists of 3 elements: the patient, the physician, and the system (ie, situation or environment). Hull and Broquet8 and Hardavella et al9 later adapted the model and described its components (Table 22,8,9).
Continue to: When considering...
When considering difficult interactions, it is important to be aware that all 3 components could interact, or merely 1 or 2 could come into play, but all should be explored as possible contributing factors.
Patient factors
The patient’s role in initiating or maintaining a problematic interaction should be explored. While some physicians are tempted to conclude that a personality disorder underlies difficult interactions, research shows a more complex picture. First, not all difficult patients have a psychiatric disorder, let alone a personality disorder. Jackson and Kroenke6 reported that among 74 difficult patients in an ambulatory clinic, 29% had a depressive disorder or anxiety disorder, with 11% experiencing 2 or more disorders. Major depressive disorder was present in 8.4% patients, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2%.6 These researchers found that difficult patient interactions were associated with the presence of a psychiatric disorder, especially depressive or anxiety disorders, and multiple physical symptoms.
Importantly, difficult patients are not unique to psychiatry, and are found in all medical disciplines and every type of practice situation. Some problematic patients have a substance use disorder, and their difficulty might stem from intoxication, withdrawal, or drug-seeking behaviors. Psychotic disorders can be the source of difficult interactions, typically resulting from the patient’s symptoms (ie, hallucinations, delusions, or bizarre behavior). Physicians tend to be forgiving toward these patients because they understand the extent of the individual’s illness. The same is true for a patient with dementia, who might be disruptive and loud, yet clearly is not in control of their behavior.
Koekkoek et al5 reviewed 94 articles that focused on difficult patients seen in mental health settings. Most patients were male (60% to 68%), and most were age 26 to 32 years. Diagnoses of psychotic disorders and personality disorders were the most frequent, while mood and other disorders were less common. In 1 of the studies reviewed, 6% of psychiatric inpatients were considered difficult. Koekkoek et al5 proposed that there are 3 groups of difficult patients:
- care avoiders: patients with psychosis who lack insight
- care seekers: patients who are chronically ill who have trouble maintaining a steady relationship with their caregivers
- care claimers: patients who do not require long-term care, but need housing, medication, or a “declaration of incompetence.”
Physician factors
Physicians are frequent contributors to bad interactions with their patients.2,7,8 They can become angry or defensive because of burnout, stress, or frustration, which might lead them to snap or otherwise respond inappropriately to their patients. Many physicians are overworked, sleep-deprived, or busier than they would prefer. Personal problems can be preoccupying and contribute to a physician being ill-tempered or distracted (eg, marital or family problems). Some physicians are simply poor communicators and might not understand the need to adapt their communication style to their patient, instead using medical jargon the patient does not understand. Ideally, physicians should modify their language to suit the patient’s level of education, degree of medical sophistication, and cultural background.
Continue to: A physician's personality traits...
A physician’s personality traits could clash with those of the patient, particularly if the physician is especially rigid or obsessional. Rather than “going with the flow,” the overly rigid physician might become impatient with patients who fail to understand diagnostic assessments or treatment recommendations. Inefficient physicians might not be able to keep up with the daily schedule, which could fuel impatience and perhaps even lead them to think that the patient is taking too much of their valuable time. Some might not know how to convey empathy, for example when giving bad news (“The tests show you have cancer…”). Others fail to make consistent eye contact with patients without understanding its importance to communication, a problem made worse by the use of electronic medical record systems (EMRs).
Systems issues
Systems issues also contribute to suboptimal physician-patient interactions, and some issues can be attributed to administrative problems. Examples of systems issues include:
- when a patient has difficulty making an appointment and is forced to listen to a confusing menu of choices
- a busy clinic that can only offer a patient an appointment 6 months away
- crowded or noisy waiting rooms
- language barriers for patients whose primary langage is not English. Not having access to an interpreter can exacerbate their frustration
- the use of EMRs is a growing threat to positive physician-patient interactions, yet their influence is often ignored. Widely disliked by physicians,10 EMRs are required in all but the smallest independent practice settings. Many busy physicians focus their attention on the computer, giving the patient the impression that the physician is not listening to them. Many patients conclude that they are less important than the process.
The consequences of difficult interactions
Following a bad interaction, dissatisfied patients are more likely to leave the clinic or hospital and ignore medical advice. These patients might then show up in crowded emergency departments, which may lead to poor use of health care resources. For physicians, challenging situations sap their emotional energy, cause demoralization, and interfere with their sense of job fulfillment. In extreme cases, such feelings might lead the physician to dislike and even avoid the patient.
How to manage challenging situations
Taking the following steps can help physicians work through challenging situations with their patients.
Diagnose the problem. First, recognize the difficult situation, analyze it, and identify how the patient, the physician, and the system are contributing to a bad physician-patient interaction. Diagnosing the interactional difficulty should precede the diagnosis and management of the patient’s disease. Physicians should acknowledge their own contribution through their attitude or actions. Finally, determine if there are system issues that are contributing to the problem, or if it is the clinic or inpatient setting itself (eg, noisy inpatient unit).
Continue to: Maintain your cool
Maintain your cool. With any difficult interaction, a physician’s first obligation is to remain calm and professional, while modeling appropriate behavior. If the patient is angry or emotionally intense, talking over them or interrupting them only makes the situation worse. Try to see the interaction from the patient’s perspective. Both parties should work together to find a common ground.
Collaborate, respect boundaries, and empathize. One study of a group of 100 family physicians found that having the following 3 skills were essential to successfully managing situations with difficult patients11,12:
- the ability to collaborate (vs opposition)
- the appropriate use of power (vs misuse of power, or violation of boundaries by either party)
- the ability to empathize, which for most physicians involves understanding and validating the patient’s subjective experiences.
Although a description of the many facets of empathy (cognitive, affective, motivational) is beyond the scope of this article, it is worth pointing out that a patient’s positive perception of their physician’s empathy improves not only patient satisfaction but health outcomes.13 The Box describes a difficult patient whose actions changed through the collaboration and empathy of his treatment team.
Box 1
Mr. L, a 60-year-old veteran, is admitted to an inpatient unit following a suicide attempt that was prompted by eviction from his apartment. Mr. L is physically disabled and has difficulty walking without assistance. His main concern is his homelessness, and he insists that the inpatient team find a suitable “Americans with Disabilities (ADA)-compliant apartment” that he can afford on his $800 monthly income. He implies that he will kill himself if the team fails in that task. He makes it clear that his problems are the team’s problems. He is prescribed an antidepressant, and both his mood and reported suicidal ideations gradually resolve.
The team’s social worker finds an opening at a well-run veterans home, but Mr. L rejects it because he doesn’t want to “give up his independence.” The social worker finds a small apartment in a nearby community that is ADA-compliant, but Mr. L complains that it is small. He asks the resident psychiatrist, “Where will I put all my things?” The next day, after insulting the attending psychiatrist for failing to find an adequate apartment, Mr. L says from under the bedsheet: “How come none of you ever help me?”
Mr. L presents a challenge to the entire team. At times, he is rude, demanding, and entitled. The team recognizes that although he had served in the military with distinction, he is now alone after having divorced many years earlier, and nearly friendless because of his increasing disability. The team surmises that Mr. L lashes out due to frustration and feelings of powerlessness.
Resolving this conflict involves treating Mr. L with respect and listening without judgment. No one ever confronts him or argues with him. The team psychologist meets with him to help him work through his many losses. Closer to discharge, he is enrolled in several post-hospitalization programs to keep him connected with other veterans. At discharge, the hospital arranges for his belongings that had been in storage to be delivered to his new home. He is pleasant and social with his peers, and although he is still concerned about the size of the apartment, he thanks the team members for their care.
Verbalize the difficulty. It is important to openly discuss the problem. For example, “We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?” This approach names the “elephant in the room” and avoids casting blame. It also creates a sense of shared ownership by externalizing the problem from both the patient and physician. Verbalizing the difficulty can help build trust and pave the way to working together toward a common solution.
Consider other explanations for the patient’s behavior. For example, anger directed at a physician could be due to anxiety about an unrelated matter, such as the patient’s recent job loss or impending divorce. Psychiatrists might understand this behavior better as displacement, which is considered a maladaptive defense mechanism. It is important to listen to the patient and offer empathy, which will help the patient feel supported and build a rapport that can help to resolve the encounter.
Continue to: When helping patients...
When helping patients with multiple issues, which is a common scenario, the physician might start by asking, “What would you like to address today?”14 Keep a list of the issues so you do not forget the patient’s concerns, and then ask: “What do you think is going on?” Give patients time to verbalize their concerns. Physicians should:
- validate concerns: “I understand where you’re coming from.”
- offer empathy: “I can see how difficult this has been for you.”
- reframe: “Let me make sure I hear you correctly.”
- refocus: “Let’s agree on what we need to do at this visit.”
Find common ground. When the patient and physician have different ideas on diagnosis or treatment, finding common ground is another way to resolve a difficult encounter. Difficulties arise when there appears to be little common ground, which often results from unrealistic expectations. Patients might be seen as “demanding” or “manipulative”’ if they push for a diagnosis or treatment the doctor is not comfortable with. As soon as there is some overlap and common ground, the difficulty rapidly subsides.
Set clear boundaries and limits. Physicians should set limits on what patient behavior might “cross the line.” A “behavioral contract” (or “treatment contract”) can help by setting explicit expectations. For example, showing up late for appointments or inappropriately seeking drugs of abuse (eg, opioids, benzodiazepines) might be identified as violations of the contract. Once the contract is set, the patient should be asked to restate key components. Clarify any confusion or barriers to compliance and define clear expectations. The patient should be informed of potential consequences of contract violations, including termination.
Staff members involved in the patient’s care should agree with the terms of any behavioral contract, and should receive a copy of it. Patients should have “buy in,” meaning that they have had an opportunity to provide input to the contract and have agreed to its elements. Both the physician and patient should sign the document.
When all else fails
When there is a breakdown in rapport that makes it difficult or impossible to continue offering treatment, consider termination. This could be due to threatening or abusive patient behavior, sexual advances, repeated no-shows, treatment noncompliance that jeopardizes patient safety, refusal to follow the treatment plan, or violating the terms of a behavioral contract. In some settings, it might be the failure to pay bills.
Continue to: If a patient is unable to...
If a patient is unable to follow the contract, the physician should explore possible extenuating circumstances. The physician should seek to remedy the problem and involve other team members if possible (eg, case manager, nurse), advising a patient about behaviors that could lead to termination.
If the problem is irremediable, notify the patient in writing, give them time to find another physician, and facilitate the transfer of care.15 Take steps to prevent the patient from running out of any medications associated with withdrawal or discontinuation syndromes (eg, selective serotonin reuptake inhibitors, benzodiazepines) during the care transition. While there is no requirement regarding the amount of time allowed, at least 30 days is typical.
Bottom Line
Difficult patient interactions are common and unavoidable. Physicians should acknowledge and recognize contributing factors in such encounters—including their own role. When handling such situations, physicians should remain calm and model appropriate behavior. Improving communication, offering empathy, and validating the patient’s concerns can help resolve factors that contribute to poor patient interactions. If efforts to remediate the physician-patient relationship fail, termination may be necessary.
Related Resources
- Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
- Pereira MR, Figueiredo AF. Challenging patient-doctor interactions in psychiatry – difficult patient syndrome. European Psychiatry. 2017;41(supplement):S719. doi. org/10.1016/j.eurpsy.2017.01.1297
“I did not like those patients… They made me angry and I found myself irritated to experience them as they seemed so distant from myself and from all that is human. This is an astonishing intolerance which brands me a poor psychiatrist.”
Sigmund Freud, Letter to István Hollós (1928)
While Freud was referring to psychotic patients,1 his evident frustration shows that difficult and challenging patients have vexed even the best of us. All physicians and other clinicians will experience patient encounters that lead to anger or frustration, or even challenge their sense of equanimity and professional identity. In short, difficult and challenging patient interactions are unavoidable, regardless of the physician’s discipline.2-5 At times, physicians might struggle with demanding, unpleasant, ungrateful, and possibly dangerous patients, while sometimes the struggle is with the patient’s family members. No physician is immune to the problem, which makes it crucial to learn to anticipate and manage difficult patient interactions, skills which are generally not taught in medical schools or residency programs.
One prospective study of clinic patients found that up to 15% of patient encounters are deemed “difficult.”6 Common scenarios include patients (or their relatives) who seek certain tests after researching symptoms online, threats of legal or social media action in response to feeling that the physician is not listening to them, demands for a second opinion after disagreeing with the physician’s diagnosis, and mistrust of doctors after presenting with symptoms and not receiving a diagnosis. It is also common to care for patients who focus on negative outcomes or fail to adhere to treatment recommendations. These encounters can make physicians feel stressed out, disrespected, abused, or even fearful if threatened. Some physicians may come to feel they are trapped in a hostile work environment with little support from their supervisors or administrators. Patients often have a complaint office or department to turn to, but there is no equivalent for physicians, who are expected to soldier on regardless.
This article highlights a model that describes poor physician-patient encounters, factors contributing to these issues, how to manage these difficult interactions, and what to do if the relationship cannot be remediated.
Describing the ‘difficult’ patient
In a landmark 1978 paper, Groves7 provided one of the first descriptions of “difficult” patients. His colorful observations continue to provide useful insights. Groves emphasized that most medical texts ignore the issue of difficult patients and provide little or no guidance—which is still true 43 years later. He observed that physicians cannot avoid occasional negative feelings toward some patients. Further, Groves suggested that countertransference is often at the root of hateful reactions, a process he defines as “conscious or unconscious unbidden and unwanted hostile or sexual feelings toward the patient.”7Table 17 outlines how Groves divided “hateful” patients into several categories, and how physicians might respond to such patients.

A model for understanding difficult patient encounters
Adams and Murray2 created a model to help explain interactions with difficult or challenging patients that consists of 3 elements: the patient, the physician, and the system (ie, situation or environment). Hull and Broquet8 and Hardavella et al9 later adapted the model and described its components (Table 22,8,9).
Continue to: When considering...
When considering difficult interactions, it is important to be aware that all 3 components could interact, or merely 1 or 2 could come into play, but all should be explored as possible contributing factors.
Patient factors
The patient’s role in initiating or maintaining a problematic interaction should be explored. While some physicians are tempted to conclude that a personality disorder underlies difficult interactions, research shows a more complex picture. First, not all difficult patients have a psychiatric disorder, let alone a personality disorder. Jackson and Kroenke6 reported that among 74 difficult patients in an ambulatory clinic, 29% had a depressive disorder or anxiety disorder, with 11% experiencing 2 or more disorders. Major depressive disorder was present in 8.4% patients, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2%.6 These researchers found that difficult patient interactions were associated with the presence of a psychiatric disorder, especially depressive or anxiety disorders, and multiple physical symptoms.
Importantly, difficult patients are not unique to psychiatry, and are found in all medical disciplines and every type of practice situation. Some problematic patients have a substance use disorder, and their difficulty might stem from intoxication, withdrawal, or drug-seeking behaviors. Psychotic disorders can be the source of difficult interactions, typically resulting from the patient’s symptoms (ie, hallucinations, delusions, or bizarre behavior). Physicians tend to be forgiving toward these patients because they understand the extent of the individual’s illness. The same is true for a patient with dementia, who might be disruptive and loud, yet clearly is not in control of their behavior.
Koekkoek et al5 reviewed 94 articles that focused on difficult patients seen in mental health settings. Most patients were male (60% to 68%), and most were age 26 to 32 years. Diagnoses of psychotic disorders and personality disorders were the most frequent, while mood and other disorders were less common. In 1 of the studies reviewed, 6% of psychiatric inpatients were considered difficult. Koekkoek et al5 proposed that there are 3 groups of difficult patients:
- care avoiders: patients with psychosis who lack insight
- care seekers: patients who are chronically ill who have trouble maintaining a steady relationship with their caregivers
- care claimers: patients who do not require long-term care, but need housing, medication, or a “declaration of incompetence.”
Physician factors
Physicians are frequent contributors to bad interactions with their patients.2,7,8 They can become angry or defensive because of burnout, stress, or frustration, which might lead them to snap or otherwise respond inappropriately to their patients. Many physicians are overworked, sleep-deprived, or busier than they would prefer. Personal problems can be preoccupying and contribute to a physician being ill-tempered or distracted (eg, marital or family problems). Some physicians are simply poor communicators and might not understand the need to adapt their communication style to their patient, instead using medical jargon the patient does not understand. Ideally, physicians should modify their language to suit the patient’s level of education, degree of medical sophistication, and cultural background.
Continue to: A physician's personality traits...
A physician’s personality traits could clash with those of the patient, particularly if the physician is especially rigid or obsessional. Rather than “going with the flow,” the overly rigid physician might become impatient with patients who fail to understand diagnostic assessments or treatment recommendations. Inefficient physicians might not be able to keep up with the daily schedule, which could fuel impatience and perhaps even lead them to think that the patient is taking too much of their valuable time. Some might not know how to convey empathy, for example when giving bad news (“The tests show you have cancer…”). Others fail to make consistent eye contact with patients without understanding its importance to communication, a problem made worse by the use of electronic medical record systems (EMRs).
Systems issues
Systems issues also contribute to suboptimal physician-patient interactions, and some issues can be attributed to administrative problems. Examples of systems issues include:
- when a patient has difficulty making an appointment and is forced to listen to a confusing menu of choices
- a busy clinic that can only offer a patient an appointment 6 months away
- crowded or noisy waiting rooms
- language barriers for patients whose primary langage is not English. Not having access to an interpreter can exacerbate their frustration
- the use of EMRs is a growing threat to positive physician-patient interactions, yet their influence is often ignored. Widely disliked by physicians,10 EMRs are required in all but the smallest independent practice settings. Many busy physicians focus their attention on the computer, giving the patient the impression that the physician is not listening to them. Many patients conclude that they are less important than the process.
The consequences of difficult interactions
Following a bad interaction, dissatisfied patients are more likely to leave the clinic or hospital and ignore medical advice. These patients might then show up in crowded emergency departments, which may lead to poor use of health care resources. For physicians, challenging situations sap their emotional energy, cause demoralization, and interfere with their sense of job fulfillment. In extreme cases, such feelings might lead the physician to dislike and even avoid the patient.
How to manage challenging situations
Taking the following steps can help physicians work through challenging situations with their patients.
Diagnose the problem. First, recognize the difficult situation, analyze it, and identify how the patient, the physician, and the system are contributing to a bad physician-patient interaction. Diagnosing the interactional difficulty should precede the diagnosis and management of the patient’s disease. Physicians should acknowledge their own contribution through their attitude or actions. Finally, determine if there are system issues that are contributing to the problem, or if it is the clinic or inpatient setting itself (eg, noisy inpatient unit).
Continue to: Maintain your cool
Maintain your cool. With any difficult interaction, a physician’s first obligation is to remain calm and professional, while modeling appropriate behavior. If the patient is angry or emotionally intense, talking over them or interrupting them only makes the situation worse. Try to see the interaction from the patient’s perspective. Both parties should work together to find a common ground.
Collaborate, respect boundaries, and empathize. One study of a group of 100 family physicians found that having the following 3 skills were essential to successfully managing situations with difficult patients11,12:
- the ability to collaborate (vs opposition)
- the appropriate use of power (vs misuse of power, or violation of boundaries by either party)
- the ability to empathize, which for most physicians involves understanding and validating the patient’s subjective experiences.
Although a description of the many facets of empathy (cognitive, affective, motivational) is beyond the scope of this article, it is worth pointing out that a patient’s positive perception of their physician’s empathy improves not only patient satisfaction but health outcomes.13 The Box describes a difficult patient whose actions changed through the collaboration and empathy of his treatment team.
Box 1
Mr. L, a 60-year-old veteran, is admitted to an inpatient unit following a suicide attempt that was prompted by eviction from his apartment. Mr. L is physically disabled and has difficulty walking without assistance. His main concern is his homelessness, and he insists that the inpatient team find a suitable “Americans with Disabilities (ADA)-compliant apartment” that he can afford on his $800 monthly income. He implies that he will kill himself if the team fails in that task. He makes it clear that his problems are the team’s problems. He is prescribed an antidepressant, and both his mood and reported suicidal ideations gradually resolve.
The team’s social worker finds an opening at a well-run veterans home, but Mr. L rejects it because he doesn’t want to “give up his independence.” The social worker finds a small apartment in a nearby community that is ADA-compliant, but Mr. L complains that it is small. He asks the resident psychiatrist, “Where will I put all my things?” The next day, after insulting the attending psychiatrist for failing to find an adequate apartment, Mr. L says from under the bedsheet: “How come none of you ever help me?”
Mr. L presents a challenge to the entire team. At times, he is rude, demanding, and entitled. The team recognizes that although he had served in the military with distinction, he is now alone after having divorced many years earlier, and nearly friendless because of his increasing disability. The team surmises that Mr. L lashes out due to frustration and feelings of powerlessness.
Resolving this conflict involves treating Mr. L with respect and listening without judgment. No one ever confronts him or argues with him. The team psychologist meets with him to help him work through his many losses. Closer to discharge, he is enrolled in several post-hospitalization programs to keep him connected with other veterans. At discharge, the hospital arranges for his belongings that had been in storage to be delivered to his new home. He is pleasant and social with his peers, and although he is still concerned about the size of the apartment, he thanks the team members for their care.
Verbalize the difficulty. It is important to openly discuss the problem. For example, “We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?” This approach names the “elephant in the room” and avoids casting blame. It also creates a sense of shared ownership by externalizing the problem from both the patient and physician. Verbalizing the difficulty can help build trust and pave the way to working together toward a common solution.
Consider other explanations for the patient’s behavior. For example, anger directed at a physician could be due to anxiety about an unrelated matter, such as the patient’s recent job loss or impending divorce. Psychiatrists might understand this behavior better as displacement, which is considered a maladaptive defense mechanism. It is important to listen to the patient and offer empathy, which will help the patient feel supported and build a rapport that can help to resolve the encounter.
Continue to: When helping patients...
When helping patients with multiple issues, which is a common scenario, the physician might start by asking, “What would you like to address today?”14 Keep a list of the issues so you do not forget the patient’s concerns, and then ask: “What do you think is going on?” Give patients time to verbalize their concerns. Physicians should:
- validate concerns: “I understand where you’re coming from.”
- offer empathy: “I can see how difficult this has been for you.”
- reframe: “Let me make sure I hear you correctly.”
- refocus: “Let’s agree on what we need to do at this visit.”
Find common ground. When the patient and physician have different ideas on diagnosis or treatment, finding common ground is another way to resolve a difficult encounter. Difficulties arise when there appears to be little common ground, which often results from unrealistic expectations. Patients might be seen as “demanding” or “manipulative”’ if they push for a diagnosis or treatment the doctor is not comfortable with. As soon as there is some overlap and common ground, the difficulty rapidly subsides.
Set clear boundaries and limits. Physicians should set limits on what patient behavior might “cross the line.” A “behavioral contract” (or “treatment contract”) can help by setting explicit expectations. For example, showing up late for appointments or inappropriately seeking drugs of abuse (eg, opioids, benzodiazepines) might be identified as violations of the contract. Once the contract is set, the patient should be asked to restate key components. Clarify any confusion or barriers to compliance and define clear expectations. The patient should be informed of potential consequences of contract violations, including termination.
Staff members involved in the patient’s care should agree with the terms of any behavioral contract, and should receive a copy of it. Patients should have “buy in,” meaning that they have had an opportunity to provide input to the contract and have agreed to its elements. Both the physician and patient should sign the document.
When all else fails
When there is a breakdown in rapport that makes it difficult or impossible to continue offering treatment, consider termination. This could be due to threatening or abusive patient behavior, sexual advances, repeated no-shows, treatment noncompliance that jeopardizes patient safety, refusal to follow the treatment plan, or violating the terms of a behavioral contract. In some settings, it might be the failure to pay bills.
Continue to: If a patient is unable to...
If a patient is unable to follow the contract, the physician should explore possible extenuating circumstances. The physician should seek to remedy the problem and involve other team members if possible (eg, case manager, nurse), advising a patient about behaviors that could lead to termination.
If the problem is irremediable, notify the patient in writing, give them time to find another physician, and facilitate the transfer of care.15 Take steps to prevent the patient from running out of any medications associated with withdrawal or discontinuation syndromes (eg, selective serotonin reuptake inhibitors, benzodiazepines) during the care transition. While there is no requirement regarding the amount of time allowed, at least 30 days is typical.
Bottom Line
Difficult patient interactions are common and unavoidable. Physicians should acknowledge and recognize contributing factors in such encounters—including their own role. When handling such situations, physicians should remain calm and model appropriate behavior. Improving communication, offering empathy, and validating the patient’s concerns can help resolve factors that contribute to poor patient interactions. If efforts to remediate the physician-patient relationship fail, termination may be necessary.
Related Resources
- Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
- Pereira MR, Figueiredo AF. Challenging patient-doctor interactions in psychiatry – difficult patient syndrome. European Psychiatry. 2017;41(supplement):S719. doi. org/10.1016/j.eurpsy.2017.01.1297
1. Dupont J. Ferenczi’s madness. Contemp Psychoanal. 1988;24(2):250-261.
2. Adams J, Murray R. The difficult diagnosis: the general approach to the difficult patient. Emerg Med Clin North Am. 1998;16(4):689-700.
3. Davies M. Managing challenging interactions with patients. BMJ. 2013;347:f4673. doi: https://doi.org/10.1136/bmj.f4673
4. Chou C. Dealing with the “difficult” patient. Wisc Med J. 2004;103:35-38.
5. Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
6. Jackson JL, Kroenke K. Difficult patient encounter in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med 1999;159(10):1069-1075.
7. Groves JE. Taking care of the hateful patient. N Eng J Med. 1978;298:883-887.
8. Hull S, Broquet K. How to manage difficult encounters. Fam Prac Manag. 2007;14(6):30-34.
9. Hardavella G, Aamli-Gaagnat A, Frille A, et al. Top tips to deal with challenging situations: doctor patient interactions. Breathe. 2017;13(2):129-135.
10. Black DW, Balon R. Editorial: electronic medical records (EMRs) and the psychiatrist shortage. Ann Clin Psychiatry. 2018;30(4):257-259.
11. Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med. 2006;19(6):533-541.
12. Campbell RJ. Campbell’s Psychiatric Dictionary. 8th Edition. Oxford University Press; 2004:219-220.
13. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2014;8:457. https://doi.org/10.3389/fnbeh.2014.00457
14. Klugman B. The difficult patient. Accessed May 24, 2021. https://www.umassmed.edu/globalassets/office-of-continuing-medical-education/pdfs/cme-primary-care-days/e2-the-difficult-patient.pdf
15. Mossman D, Farrell HM, Gilday E. ‘Firing’ a patient: may psychiatrists unilaterally terminate care? Current Psychiatry. 2010;9(12):18-29.
1. Dupont J. Ferenczi’s madness. Contemp Psychoanal. 1988;24(2):250-261.
2. Adams J, Murray R. The difficult diagnosis: the general approach to the difficult patient. Emerg Med Clin North Am. 1998;16(4):689-700.
3. Davies M. Managing challenging interactions with patients. BMJ. 2013;347:f4673. doi: https://doi.org/10.1136/bmj.f4673
4. Chou C. Dealing with the “difficult” patient. Wisc Med J. 2004;103:35-38.
5. Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
6. Jackson JL, Kroenke K. Difficult patient encounter in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med 1999;159(10):1069-1075.
7. Groves JE. Taking care of the hateful patient. N Eng J Med. 1978;298:883-887.
8. Hull S, Broquet K. How to manage difficult encounters. Fam Prac Manag. 2007;14(6):30-34.
9. Hardavella G, Aamli-Gaagnat A, Frille A, et al. Top tips to deal with challenging situations: doctor patient interactions. Breathe. 2017;13(2):129-135.
10. Black DW, Balon R. Editorial: electronic medical records (EMRs) and the psychiatrist shortage. Ann Clin Psychiatry. 2018;30(4):257-259.
11. Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med. 2006;19(6):533-541.
12. Campbell RJ. Campbell’s Psychiatric Dictionary. 8th Edition. Oxford University Press; 2004:219-220.
13. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2014;8:457. https://doi.org/10.3389/fnbeh.2014.00457
14. Klugman B. The difficult patient. Accessed May 24, 2021. https://www.umassmed.edu/globalassets/office-of-continuing-medical-education/pdfs/cme-primary-care-days/e2-the-difficult-patient.pdf
15. Mossman D, Farrell HM, Gilday E. ‘Firing’ a patient: may psychiatrists unilaterally terminate care? Current Psychiatry. 2010;9(12):18-29.
Minor-attracted persons: A neglected population
Approximately 1 in 5 Americans report childhood sexual abuse.1 While 50% to 65% of child sexual abuse occurs in the absence of pedophilic interests and is thought to be driven by additional factors such as the availability of an appropriate sexual partner,2,3 a substantial portion of childhood sexual abuse is perpetrated by individuals with pedophilia.
However, many individuals with pedophilic interests never have sexual contact with a child or the penal system. This non-offending pedophile group reports a greater prevalence of psychiatric symptoms compared with the general population, but given the intense stigmatization of their preferences, they are largely psychiatrically underrecognized and underserved. This article focuses on the unique psychiatric needs of this neglected population. By understanding and addressing the treatment needs of these patients, psychiatrists and other mental health clinicians can serve a pivotal role in decreasing stigma, promoting wellness, and preventing sexual abuse.
Understanding the terminology
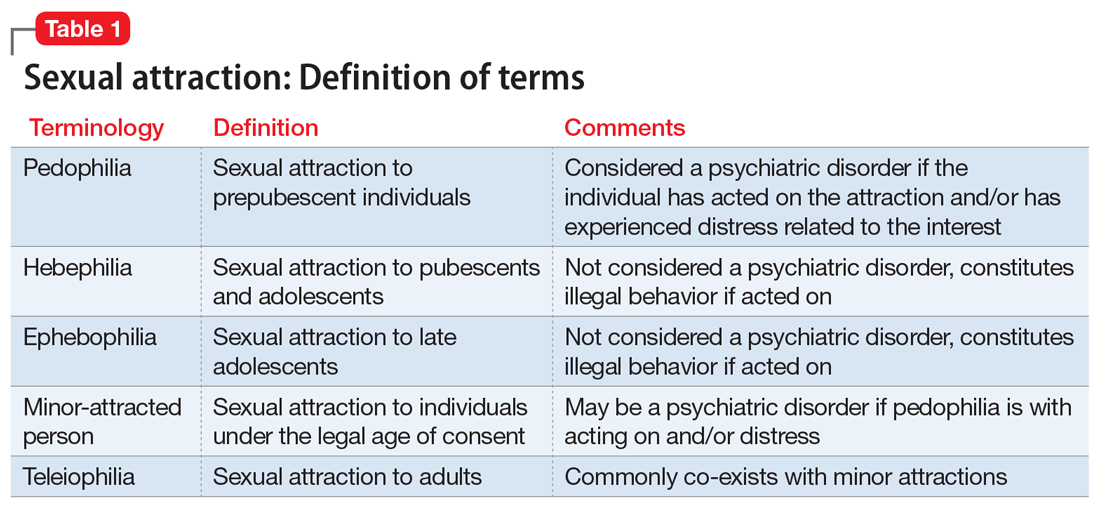
DSM-5 defines paraphilia as “any intense and persistent sexual interest other than sexual interest in genital stimulation or preparatory fondling with phenotypically normal, physiologically mature, consenting human partners.”4 The addition of the word “disorder” to the paraphilias was introduced in DSM-5 to distinguish between paraphilias that are not of clinical concern and paraphilic disorders that cause distress or impairment to the individual, or whereby satisfaction entails personal harm or risk of harm to others. As outlined in DSM-5, pedophilic disorder refers to at least 6 months of recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child.4 The individual has either acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty. Lastly, the individual must be at least age 16 years and at least 5 years older than the child. Sexual attraction to peri- or postpubescent minors is not considered a psychiatric disorder, but is illegal.
Coined by B4U-ACT (www.b4uact.org), the term minor-attracted person (MAP) refers to individuals with sexual attraction to individuals who are minors or below the legal age of consent. MAP is an umbrella term that includes sexual attraction to prepubescent individuals but also includes sexual attraction to peri- and postpubescent individuals (Table 1). A MAP may or may not meet criteria for pedophilia or pedophilic disorder, based on the age of their sexual interest and whether they have experienced distress or acted on the attraction. Although many individuals with minor attraction identify with the term MAP, not all do. The term has been critiqued for being too inclusive and conflating pedophilia with minor attractions.
It is important to keep in mind that the terms pedophilia and minor attraction are not synonymous with childhood sexual abuser or “child molester” because neither term specifies whether the individual has had sexual contact with a child or legal consequences. The terms offending/non-offending and acting/non-acting are used to specify the presence of sexual contact with a child, and do not convey any clinical information.
Prevalence data
The true prevalence of pedophilia and/or attraction to minors is unknown, and estimates vary considerably. In some studies, 1% to 4% of the general population were thought to have persistent attraction to prepubescent children.5,6 In a community sample of 8,718 German men, 4.1% reported sexual fantasies involving prepubescent children, 3.2% reported sexual offending against prepubescent children, and 0.1% reported a pedophilic sexual preference.5 In a study of 367 adult German men surveyed from the community, 15.5% reported fantasies (9.5% daydream and 6.0% masturbation fantasies) involving prepubescent children.7
Stigmatization of minor-attracted persons
Stigmatization is the process of forming negative evaluations of an individual or groups of people based on limited characteristics.8,9 MAPs are a highly stigmatized group. This stigmatization can be profound, regardless of whether the MAP has had sexual contact with a child. A public survey of nearly 1,000 individuals showed that 39% believed that non-acting MAPs should be incarcerated, and 14% believed that they would be “better off dead.”10 Societal misconceptions of minor attraction are pervasive and include10:
- MAP sexual orientation is a choice
- MAPs cannot resist their sexual urges
- all MAPs have offended, or inevitably will
- MAPs will not respond to therapy
- MAPs are fundamentally predatory and immoral.
Continue to: In addition to...
In addition to societal stigma, internalized stigma among MAPs has been documented. Lievesley et al9 found that MAPs who engaged in suppression of unwanted thought strategies had higher levels of shame and guilt, low levels of hope, and a propensity to actively avoid children. Similarly, Grady et al11 surveyed 293 MAPs and found prominent themes of viewing themselves as “bad.”
Psychiatric presentations include suicidal ideation
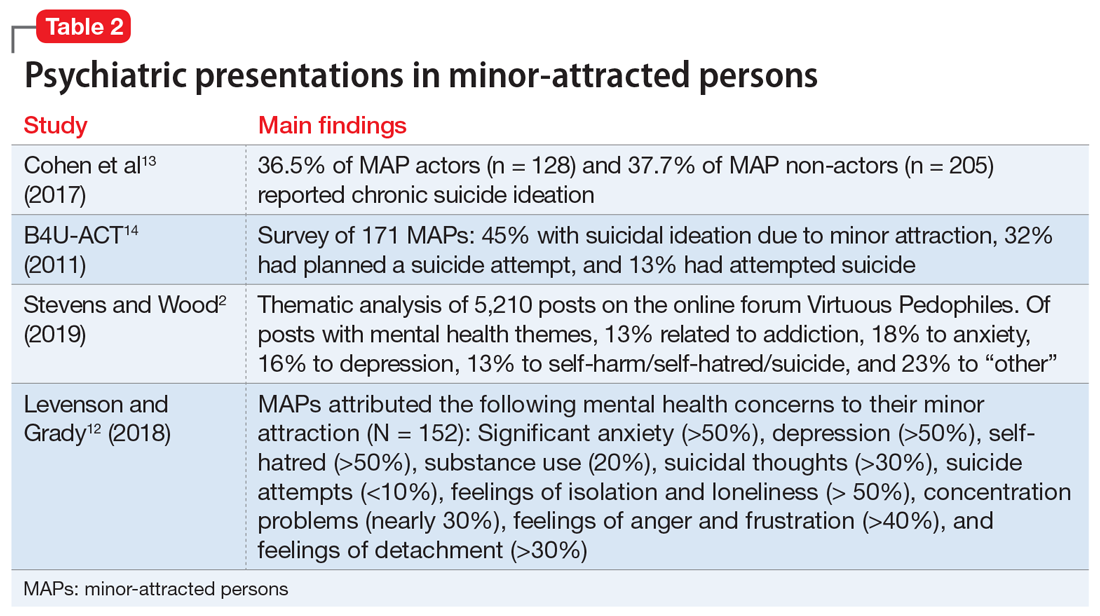
Many MAPs, including non-acting MAPs, internalize this societal stigma, which contributes to a significant mental health burden.12 A survey of 342 MAP actors and 223 MAP non-actors revealed that one-third of both groups reported chronic suicidal ideation.13 In addition, online surveys conducted by B4U-ACT and Virtuous Pedophiles (www.virped.org)—both internet-based organizations dedicated to supporting non-acting MAPs—have provided similar results. In a 2011 B4U-ACT survey, nearly one-half of participants reported suicidal ideation due to their minor attraction, 32% had planned suicide attempts, and 13% had non-fatal suicide attempts. Notably, the age group with the most prevalent suicidal ideation was age 14 to 16 years,14 which makes minor attraction a prominent risk factor for suicidal ideation among patients seen by child psychiatrists.
A 2019 thematic analysis of 5,210 posts on the Virtuous Pedophiles website showed high rates of addiction, anxiety, depression, self-harm, self-hatred, and suicidal thoughts and behaviors among MAPs.2 The majority of posts regarding substance use described such use as a means of dissociation. One post read, “…There are days I cannot bear to be sober … I … drink myself into a coma.” Anxiety themes regarding the ability to have a meaningful relationship with an age-appropriate partner and concerns about being “outed” followed by public persecution were prominent. Posts regarding self-injurious and suicidal behavior were common: “I want to kill myself so badly … I have to mutilate myself as punishment for my attractions. I wish myself dead. I don’t want to be attracted to children; I despise myself for fantasizing about them.”2
A study that analyzed a survey of 152 MAPs sampled from websites such as Virtuous Pedophiles and others showed >50% of respondents had strong feelings of isolation and loneliness, nearly 30% had extreme difficulty with concentration, >40% had significant anger and frustration, and >30% were struggling with feelings of detachment.12 Notably, the respondents attributed these difficulties to their minor attraction.12 Table 22,12-14 summarizes the findings of studies evaluating psychiatric symptoms in MAPs.
Consider OCD, hypersexuality
It is important to be aware that an attraction to minors may be a symptom of obsessive-compulsive disorder (OCD) or hypersexuality.15 Pedophilia-themed OCD (POCD) is a manifestation of OCD in which the individual experiences shame, fear, and excessive worry related to sexual attraction to children. Typically, individuals with POCD experience sexual thoughts of children as ego-dystonic, whereas MAPs experience such thoughts as ego-syntonic and arousing.15 However, much like individuals with POCD, MAPs also experience sexual thoughts of minors as distressing. Initial presentations of POCD may be confused with MAPs or pedophilia because of the overlap of symptoms such as anxiety, shame, distress, or suicidal ideation related to the idea of child sexual interests. The distinguishing feature of POCD is the absence of sexual arousal to children.
Continue to: Clinical presentations of...
Clinical presentations of hypersexuality may include sexual arousal to children. These individuals are distinguished from MAPs or those with pedophilia because they lack a preferred or sustained sexual interest in this group. On the contrary, individuals with hypersexuality present with a diversity of sexual interests explained by their high libido. Some individuals, however, may meet criteria for both hypersexuality and pedophilia. These individuals may pose a higher risk of sexual offending due to the presence of a heightened sexual drive and pedophilic interests, and thereby may require more intensive treatment, such as biologic treatment.
Focus on individualized treatment needs
Understanding the treatment needs of MAPs means understanding the goals of the individual MAP. Improving self-esteem, decreasing social isolation, and managing stigma are common treatment goals among MAPs.16 Levenson and Grady12 found that most MAPs identified treatment goals unrelated to sexual interests, such as addressing depression, anxiety, and low self-esteem. A smaller percentage identified sexual frustration related to the absence of healthy sexual outlets. Because many MAPs identify common psychiatric treatment needs, most clinicians should be equipped to foster a nonjudgmental therapeutic alliance to treat these patients. Effective treatment outcomes occur when comorbid psychiatric illnesses are treated as well as addressing the internal stigmatization that many MAPs experience.
Specialized treatment may be indicated for individuals who request treatment specific to sexual interests. This may include safety planning, including developing support systems to decrease the risk around children. For MAPs who have been unsuccessful at managing their sexual interests, pharmacotherapy may be an option. To date, research on pharmacotherapy for pedophilia is largely limited to studies of sexual offenders. Testosterone-lowering medications such as gonadotropin-releasing hormone (GnRH) analogue treatment constitutes the most effective treatment for patients who are not helped by conventional psychotherapeutic interventions.17 Other psychotropic medications, such as selective serotonin reuptake inhibitors or naltrexone, have not demonstrated efficacy outside of case reports.17
Addressing barriers to care
MAPs have a strong desire but significant hesitation when seeking mental health treatment.13,18 Nearly half (47%) of the 154 MAP respondents in the Levenson and Grady12 survey had never told anyone about their minor attraction. MAPs are understandably hesitant to disclose these thoughts and feelings due to fear of public exposure and intense stigmatization, as well as potential punitive and legal consequences.18,19 One post from the 2011 B4U-ACT online survey read, “Parents will disown you; teachers will report you; friends will abandon you … people in my situation can’t discuss this without serious risk of persecution and/or harassment.”14 In this survey, 78% of respondents feared a negative reaction by the professional, 78% feared being reported to law enforcement, and 68% feared being reported to family, an employer, or the community.14 This hesitancy due to fear of being exposed even extended to accessing self-help books, informational websites, and online forums, even though these sources are strongly desired and perceived as helpful.20
Even if MAPs were to decide to seek help, the lack of specific training and experience among psychiatrists make them unlikely to find it in the medical field.21 Furthermore, MAPs who desire help often worry it will be inadequate and they will be misunderstood by their clinicians.22 According to the Levenson and Grady survey,12 when asked what they would like most from therapy, most MAPs said they would want the treatment to focus on depression, anxiety, and low self-esteem rather than on sexual interest. In the B4U-ACT survey,14 many respondents identified the need for treatment of issues surrounding their sexual attraction, such as assistance in learning how to live in society with the attraction, dealing with society’s negative response to the attraction, and improving their self-concept in the presence of the extreme shame associated with the attraction. However, many MAPs find that clinicians tend to focus on protecting society from them, rather than on offering general psychiatric treatment or treatment focused on improving their well-being.18 This inability to locate appropriate services is known to exacerbate depression, suicidality, fear, anxiety, hopelessness, and substance abuse among MAPs.18 There is also evidence that individuals with minor attraction who are in a negative affective state are more likely to act on their attractions.23
Continue to: An ethical responsibility
An ethical responsibility. Physicians have a long-recognized responsibility to participate in activities to protect and promote the health of the public. The American Medical Association Code of Medical Ethics includes “justice,” or treating patients fairly and equitably.24 This includes patients who have pedophilic interests. Unfortunately, the stigma associated with individuals who have sexual attraction to children is pervasive in our society, including among medical professionals. The first consideration in treating MAPs is to overcome the stigmatization within our field, to remember that as physicians we took an oath to provide treatment fairly, equitably, and in accordance with the patient’s rights and entitlement.24 This includes listening to MAPs’ treatment needs. Not all MAPs want or need treatment related to their sexual interest. As is the case with all patients, listening to the individual’s chief complaint is paramount. If a patient’s treatment needs are beyond the clinician’s expertise, the patient should be referred to another clinician.
Mandated reporting. MAPs may not engage in psychiatric treatment for fear of being reported to authorities as a result of mandated reporting laws. Although the circumstances under which mandated reporting may be required vary by jurisdiction, they generally include situations in which the health care professional has reasonable cause to believe that a child is suffering from abuse or neglect. A patient’s report of sexual urges and fantasies to have sexual contact with minors is not sufficient for mandated reporting. While professionals vary in their interpretation of mandated reporting laws, sexual thoughts alone do not meet the threshold for mandated reporting. Mandated reporting duties should be discussed when first meeting a patient with minor attraction. For clinicians who are uneasy about such distinctions, either supervision or not working with such patients is the solution.
The importance of providing competent and individualized treatment to MAPs is 2-fold. First, individuals who are experiencing psychiatric symptoms deserve to have access treatment. Second, providing psychiatric treatment to individuals with minor attractions is a step toward preventing child sexual abuse. The Prevention Project Dunkelfeld in Germany used public service announcements to advertise confidential treatment for individuals who had sexual interest in children.25 Many of the participants were interested in mental health treatment unrelated to their sexual interests. Such projects may help us understand the best way to meet the treatment needs of minor-attracted individuals, as well as reduce child sexual abuse. As psychiatrists, we can stop making the problem worse by withholding psychiatric treatment from an important population.
Resources for MAPs and clinicians
Currently, resources for MAPs and clinicians are limited. MAPs can communicate and find support among other MAPs in online forums (see Related Resources). These websites provide online peer support groups and guides for seeking therapy. Information for mental health professionals, including available literature, research projects, clinicians who provide specialized treatment, and a monthly “dialog on therapy” can be found on the B4U-ACT and the Global Prevention Project websites. However, beyond the DSM-5 definitions, psychiatric education and training on this topic is almost entirely lacking.
In light of the information discussed in this article, several important issues remain, including how psychiatrists can best reach this population, and how they can work toward decreasing stigma so they can provide meaningful care. The solutions start with education. Educating psychiatrists about this important population can decrease stigma and facilitate appropriate, compassionate care to these patients, with the result of improving the mental health of people with minor attraction and decreasing the incidence of child sexual abuse.
Continue to: Bottom Line
Bottom Line
Minor-attracted persons report a high prevalence of general psychiatric symptoms that often go untreated due to a lack of willing clinicians with appropriate expertise. Providing psychiatric treatment to these patients can improve their mental health and possibly decrease the incidence of individuals who act on their attractions.
Related Resources
- B4U-ACT. www.b4uact.org • The Global Prevention Project. http://theglobalprevention project.org
- Virtuous Pedophiles. www.virped.org
Drug Brand Names
Naltrexone • ReVia
1. Briere J, Elliott D. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse Negl. 2003;27(10):1205-1222. doi: 10.1016/j.chiabu.2003.09.008
2. Stevens E, Wood J. “I despise myself for thinking about them.” A thematic analysis of the mental health implications and employed coping mechanisms of self-reported non-offending minor attracted persons. J Child Sex Abus. 2019;28(8):968-989. doi: 10.1080/10538712.2019.1657539
3. Sorrentino R. Normal human sexuality and sexual and gender identity disorders: paraphilias. In: Sadock BJ, Sadock VA, Ruis P, eds. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 9th ed. Wolters Kluwer; 2012:2093-2094.
4. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013:685-705.
5. Dombert B, Schmidt AF, Banse R, et al. How common is men’s self-reported sexual interest in prepubescent children? J Sex Res. 2016;53(2):214-23. doi: 10.1080/00224499.2015.1020108
6. Seto MC. Pedophilia and sexual offending against children: theory, assessment, and intervention. 2nd ed. American Psychological Association; 2018.
7. Ahlers CJ, Schaefer GA, Mundt IA, et al. How unusual are the contents of paraphilias? Paraphilia-associated sexual arousal patterns in a community-based sample of men. J Sex Med. 2011;8(5):1362-1370. doi: 10.1111/j.1743-6109.2009.01597.x
8. Corrigan PW, Roe D, Tsang HWH. Challenging the public stigma of mental illness: lessons for therapists and advocates. Wiley Blackwell; 2011:55-114.
9. Lievesley R, Harper CA, Elliott H. The internalization of social stigma among minor-attracted persons: implications for treatment. Arch Sex Behav. 2020;49(4):1291-1304. doi: 10.1007/s10508-019-01569-x
10. Jahnke S, Imhoff R, Hoyer J. Stigmatization of people with pedophilia: two comparative surveys. Arch Sex Behav. 2015;44(1):21-34. doi: 10.1007/s10508-014-0312-4
11. Grady MD, Levenson JS, Mesias G, et al. “‘I can’t talk about that”: Stigma and fear as barriers to preventative services for minor-attracted persons. Stigma and Health. 2019;4(4):400-410. doi: 10.1037/sah0000154
12. Levenson JS, Grady MD. Preventing sexual abuse: perspectives of minor-attracted persons about seeking help. Sex Abuse. 2019;31(8):991-1013. doi: 10.1177/1079063218797713
13. Cohen L, Ndukwe N, Yaseen Z, et al. Comparison of self-identified minor-attracted persons who have and have not successfully refrained from sexual activity with children. J Sex Marital Ther. 2018;44(3):217-230. doi: 10.1080/0092623X.2017.1377129
14. B4U-ACT. Awareness of sexuality in youth, suicidality, and seeking care. 2011. Accessed June 4, 2021. www.b4uact.org/research/survey-results/spring-2011-survey
15. Bruce SL, Ching THW, Williams MT. Pedophilia-themed obsessive-compulsive disorder: assessment, differential diagnosis, and treatment with exposure and response prevention. Arch Sex Behav. 2018;47(2):389-402. doi: 10.1007/s10508-017-1031-4
16. Levenson JS, Grady MD, Morin JW. Beyond the “ick factor”: counseling non-offending persons with pedophilia. Clinical Social Work Journal. 2020;48:380-388. doi: 10.007/s10615-019-00712-4
1 7. Thibaut F, Cosyns P, Fedoroff JP, et al; WFSBP Task Force on Paraphilias. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J Biol Psychiatry. 2020;21(6):412-490. doi: 10.1080/15622975.2020.1744723
18. B4U-ACT. Principles and perspectives of practice. 2017. Accessed June 4, 2021. www.b4uact.org/about-us/principles-and-perspectives-of-practice/
19. McPhail IV, Stephens S, Heasman A. Legal and ethical issues in treating clients with pedohebephilic interests. Canadian Psychology/Psychologie Canadienne. 2018;59(4):369-381. doi:10.1037/cap0000157
20. Levenson JS, Willis GM, Vicencio CP. Obstacles to help-seeking for sexual offenders: implications for prevention of sexual abuse. J Child Sex Abus. 2017;26(2):99-120. doi: 10.1080/10538712.2016.1276116
21. Sorrentino R. DSM-5 and paraphilias: what psychiatrists need to know. Psychiatric Times. November 28, 2016. Accessed June 4, 2021. https://www.psychiatrictimes.com/view/dsm-5-and-paraphilias-what-psychiatrists-need-know
22. Cantor JM, McPhail IV. Non-offending pedophiles. Current Sexual Health Reports. 2016;8:121-128. doi:10.1007/s11930-016-0076-z
23. Ward T, Louden K, Hudson SM, et al. A descriptive model of the offense chain for child molesters. Journal of Interpersonal Violence. 1995;10(4):452-472. doi:10.1177/088626095010004005
24. American Medical Association. AMA Code of Medical Ethics. 2016. Accessed June 4, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/principles-of-medical-ethics.pdf
25. Beier KM, Grundmann D, Kuhle LF, et al. The German Dunkelfeld project: a pilot study to prevent child sexual abuse and the use of child abusive images. J Sex Med. 2015;12(2):529-42. doi: 10.1111/jsm.12785
Approximately 1 in 5 Americans report childhood sexual abuse.1 While 50% to 65% of child sexual abuse occurs in the absence of pedophilic interests and is thought to be driven by additional factors such as the availability of an appropriate sexual partner,2,3 a substantial portion of childhood sexual abuse is perpetrated by individuals with pedophilia.
However, many individuals with pedophilic interests never have sexual contact with a child or the penal system. This non-offending pedophile group reports a greater prevalence of psychiatric symptoms compared with the general population, but given the intense stigmatization of their preferences, they are largely psychiatrically underrecognized and underserved. This article focuses on the unique psychiatric needs of this neglected population. By understanding and addressing the treatment needs of these patients, psychiatrists and other mental health clinicians can serve a pivotal role in decreasing stigma, promoting wellness, and preventing sexual abuse.
Understanding the terminology
DSM-5 defines paraphilia as “any intense and persistent sexual interest other than sexual interest in genital stimulation or preparatory fondling with phenotypically normal, physiologically mature, consenting human partners.”4 The addition of the word “disorder” to the paraphilias was introduced in DSM-5 to distinguish between paraphilias that are not of clinical concern and paraphilic disorders that cause distress or impairment to the individual, or whereby satisfaction entails personal harm or risk of harm to others. As outlined in DSM-5, pedophilic disorder refers to at least 6 months of recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child.4 The individual has either acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty. Lastly, the individual must be at least age 16 years and at least 5 years older than the child. Sexual attraction to peri- or postpubescent minors is not considered a psychiatric disorder, but is illegal.
Coined by B4U-ACT (www.b4uact.org), the term minor-attracted person (MAP) refers to individuals with sexual attraction to individuals who are minors or below the legal age of consent. MAP is an umbrella term that includes sexual attraction to prepubescent individuals but also includes sexual attraction to peri- and postpubescent individuals (Table 1). A MAP may or may not meet criteria for pedophilia or pedophilic disorder, based on the age of their sexual interest and whether they have experienced distress or acted on the attraction. Although many individuals with minor attraction identify with the term MAP, not all do. The term has been critiqued for being too inclusive and conflating pedophilia with minor attractions.
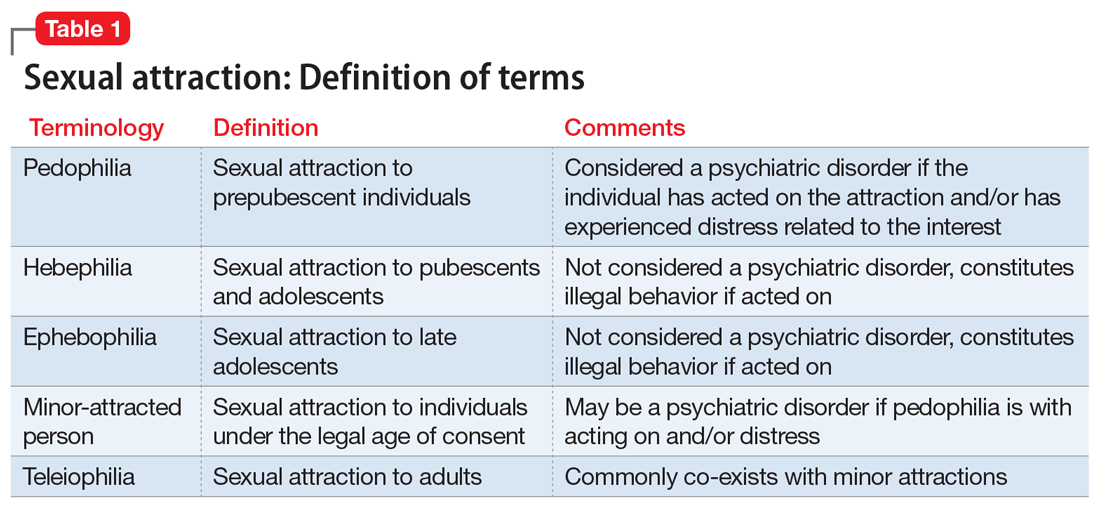
It is important to keep in mind that the terms pedophilia and minor attraction are not synonymous with childhood sexual abuser or “child molester” because neither term specifies whether the individual has had sexual contact with a child or legal consequences. The terms offending/non-offending and acting/non-acting are used to specify the presence of sexual contact with a child, and do not convey any clinical information.
Prevalence data
The true prevalence of pedophilia and/or attraction to minors is unknown, and estimates vary considerably. In some studies, 1% to 4% of the general population were thought to have persistent attraction to prepubescent children.5,6 In a community sample of 8,718 German men, 4.1% reported sexual fantasies involving prepubescent children, 3.2% reported sexual offending against prepubescent children, and 0.1% reported a pedophilic sexual preference.5 In a study of 367 adult German men surveyed from the community, 15.5% reported fantasies (9.5% daydream and 6.0% masturbation fantasies) involving prepubescent children.7
Stigmatization of minor-attracted persons
Stigmatization is the process of forming negative evaluations of an individual or groups of people based on limited characteristics.8,9 MAPs are a highly stigmatized group. This stigmatization can be profound, regardless of whether the MAP has had sexual contact with a child. A public survey of nearly 1,000 individuals showed that 39% believed that non-acting MAPs should be incarcerated, and 14% believed that they would be “better off dead.”10 Societal misconceptions of minor attraction are pervasive and include10:
- MAP sexual orientation is a choice
- MAPs cannot resist their sexual urges
- all MAPs have offended, or inevitably will
- MAPs will not respond to therapy
- MAPs are fundamentally predatory and immoral.
Continue to: In addition to...
In addition to societal stigma, internalized stigma among MAPs has been documented. Lievesley et al9 found that MAPs who engaged in suppression of unwanted thought strategies had higher levels of shame and guilt, low levels of hope, and a propensity to actively avoid children. Similarly, Grady et al11 surveyed 293 MAPs and found prominent themes of viewing themselves as “bad.”
Psychiatric presentations include suicidal ideation
Many MAPs, including non-acting MAPs, internalize this societal stigma, which contributes to a significant mental health burden.12 A survey of 342 MAP actors and 223 MAP non-actors revealed that one-third of both groups reported chronic suicidal ideation.13 In addition, online surveys conducted by B4U-ACT and Virtuous Pedophiles (www.virped.org)—both internet-based organizations dedicated to supporting non-acting MAPs—have provided similar results. In a 2011 B4U-ACT survey, nearly one-half of participants reported suicidal ideation due to their minor attraction, 32% had planned suicide attempts, and 13% had non-fatal suicide attempts. Notably, the age group with the most prevalent suicidal ideation was age 14 to 16 years,14 which makes minor attraction a prominent risk factor for suicidal ideation among patients seen by child psychiatrists.
A 2019 thematic analysis of 5,210 posts on the Virtuous Pedophiles website showed high rates of addiction, anxiety, depression, self-harm, self-hatred, and suicidal thoughts and behaviors among MAPs.2 The majority of posts regarding substance use described such use as a means of dissociation. One post read, “…There are days I cannot bear to be sober … I … drink myself into a coma.” Anxiety themes regarding the ability to have a meaningful relationship with an age-appropriate partner and concerns about being “outed” followed by public persecution were prominent. Posts regarding self-injurious and suicidal behavior were common: “I want to kill myself so badly … I have to mutilate myself as punishment for my attractions. I wish myself dead. I don’t want to be attracted to children; I despise myself for fantasizing about them.”2
A study that analyzed a survey of 152 MAPs sampled from websites such as Virtuous Pedophiles and others showed >50% of respondents had strong feelings of isolation and loneliness, nearly 30% had extreme difficulty with concentration, >40% had significant anger and frustration, and >30% were struggling with feelings of detachment.12 Notably, the respondents attributed these difficulties to their minor attraction.12 Table 22,12-14 summarizes the findings of studies evaluating psychiatric symptoms in MAPs.
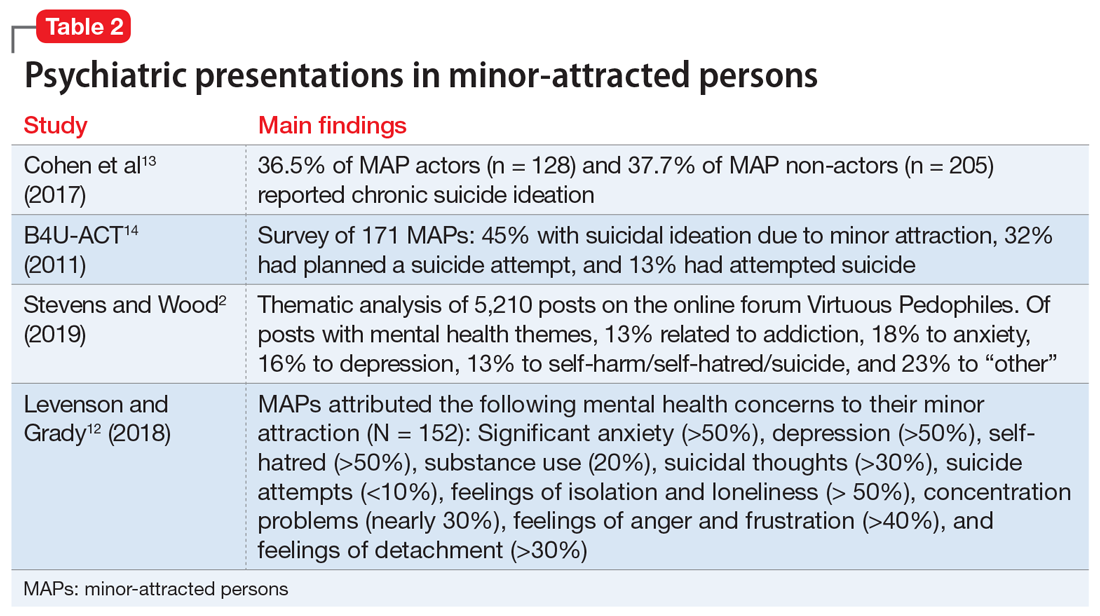
Consider OCD, hypersexuality
It is important to be aware that an attraction to minors may be a symptom of obsessive-compulsive disorder (OCD) or hypersexuality.15 Pedophilia-themed OCD (POCD) is a manifestation of OCD in which the individual experiences shame, fear, and excessive worry related to sexual attraction to children. Typically, individuals with POCD experience sexual thoughts of children as ego-dystonic, whereas MAPs experience such thoughts as ego-syntonic and arousing.15 However, much like individuals with POCD, MAPs also experience sexual thoughts of minors as distressing. Initial presentations of POCD may be confused with MAPs or pedophilia because of the overlap of symptoms such as anxiety, shame, distress, or suicidal ideation related to the idea of child sexual interests. The distinguishing feature of POCD is the absence of sexual arousal to children.
Continue to: Clinical presentations of...
Clinical presentations of hypersexuality may include sexual arousal to children. These individuals are distinguished from MAPs or those with pedophilia because they lack a preferred or sustained sexual interest in this group. On the contrary, individuals with hypersexuality present with a diversity of sexual interests explained by their high libido. Some individuals, however, may meet criteria for both hypersexuality and pedophilia. These individuals may pose a higher risk of sexual offending due to the presence of a heightened sexual drive and pedophilic interests, and thereby may require more intensive treatment, such as biologic treatment.
Focus on individualized treatment needs
Understanding the treatment needs of MAPs means understanding the goals of the individual MAP. Improving self-esteem, decreasing social isolation, and managing stigma are common treatment goals among MAPs.16 Levenson and Grady12 found that most MAPs identified treatment goals unrelated to sexual interests, such as addressing depression, anxiety, and low self-esteem. A smaller percentage identified sexual frustration related to the absence of healthy sexual outlets. Because many MAPs identify common psychiatric treatment needs, most clinicians should be equipped to foster a nonjudgmental therapeutic alliance to treat these patients. Effective treatment outcomes occur when comorbid psychiatric illnesses are treated as well as addressing the internal stigmatization that many MAPs experience.
Specialized treatment may be indicated for individuals who request treatment specific to sexual interests. This may include safety planning, including developing support systems to decrease the risk around children. For MAPs who have been unsuccessful at managing their sexual interests, pharmacotherapy may be an option. To date, research on pharmacotherapy for pedophilia is largely limited to studies of sexual offenders. Testosterone-lowering medications such as gonadotropin-releasing hormone (GnRH) analogue treatment constitutes the most effective treatment for patients who are not helped by conventional psychotherapeutic interventions.17 Other psychotropic medications, such as selective serotonin reuptake inhibitors or naltrexone, have not demonstrated efficacy outside of case reports.17
Addressing barriers to care
MAPs have a strong desire but significant hesitation when seeking mental health treatment.13,18 Nearly half (47%) of the 154 MAP respondents in the Levenson and Grady12 survey had never told anyone about their minor attraction. MAPs are understandably hesitant to disclose these thoughts and feelings due to fear of public exposure and intense stigmatization, as well as potential punitive and legal consequences.18,19 One post from the 2011 B4U-ACT online survey read, “Parents will disown you; teachers will report you; friends will abandon you … people in my situation can’t discuss this without serious risk of persecution and/or harassment.”14 In this survey, 78% of respondents feared a negative reaction by the professional, 78% feared being reported to law enforcement, and 68% feared being reported to family, an employer, or the community.14 This hesitancy due to fear of being exposed even extended to accessing self-help books, informational websites, and online forums, even though these sources are strongly desired and perceived as helpful.20
Even if MAPs were to decide to seek help, the lack of specific training and experience among psychiatrists make them unlikely to find it in the medical field.21 Furthermore, MAPs who desire help often worry it will be inadequate and they will be misunderstood by their clinicians.22 According to the Levenson and Grady survey,12 when asked what they would like most from therapy, most MAPs said they would want the treatment to focus on depression, anxiety, and low self-esteem rather than on sexual interest. In the B4U-ACT survey,14 many respondents identified the need for treatment of issues surrounding their sexual attraction, such as assistance in learning how to live in society with the attraction, dealing with society’s negative response to the attraction, and improving their self-concept in the presence of the extreme shame associated with the attraction. However, many MAPs find that clinicians tend to focus on protecting society from them, rather than on offering general psychiatric treatment or treatment focused on improving their well-being.18 This inability to locate appropriate services is known to exacerbate depression, suicidality, fear, anxiety, hopelessness, and substance abuse among MAPs.18 There is also evidence that individuals with minor attraction who are in a negative affective state are more likely to act on their attractions.23
Continue to: An ethical responsibility
An ethical responsibility. Physicians have a long-recognized responsibility to participate in activities to protect and promote the health of the public. The American Medical Association Code of Medical Ethics includes “justice,” or treating patients fairly and equitably.24 This includes patients who have pedophilic interests. Unfortunately, the stigma associated with individuals who have sexual attraction to children is pervasive in our society, including among medical professionals. The first consideration in treating MAPs is to overcome the stigmatization within our field, to remember that as physicians we took an oath to provide treatment fairly, equitably, and in accordance with the patient’s rights and entitlement.24 This includes listening to MAPs’ treatment needs. Not all MAPs want or need treatment related to their sexual interest. As is the case with all patients, listening to the individual’s chief complaint is paramount. If a patient’s treatment needs are beyond the clinician’s expertise, the patient should be referred to another clinician.
Mandated reporting. MAPs may not engage in psychiatric treatment for fear of being reported to authorities as a result of mandated reporting laws. Although the circumstances under which mandated reporting may be required vary by jurisdiction, they generally include situations in which the health care professional has reasonable cause to believe that a child is suffering from abuse or neglect. A patient’s report of sexual urges and fantasies to have sexual contact with minors is not sufficient for mandated reporting. While professionals vary in their interpretation of mandated reporting laws, sexual thoughts alone do not meet the threshold for mandated reporting. Mandated reporting duties should be discussed when first meeting a patient with minor attraction. For clinicians who are uneasy about such distinctions, either supervision or not working with such patients is the solution.
The importance of providing competent and individualized treatment to MAPs is 2-fold. First, individuals who are experiencing psychiatric symptoms deserve to have access treatment. Second, providing psychiatric treatment to individuals with minor attractions is a step toward preventing child sexual abuse. The Prevention Project Dunkelfeld in Germany used public service announcements to advertise confidential treatment for individuals who had sexual interest in children.25 Many of the participants were interested in mental health treatment unrelated to their sexual interests. Such projects may help us understand the best way to meet the treatment needs of minor-attracted individuals, as well as reduce child sexual abuse. As psychiatrists, we can stop making the problem worse by withholding psychiatric treatment from an important population.
Resources for MAPs and clinicians
Currently, resources for MAPs and clinicians are limited. MAPs can communicate and find support among other MAPs in online forums (see Related Resources). These websites provide online peer support groups and guides for seeking therapy. Information for mental health professionals, including available literature, research projects, clinicians who provide specialized treatment, and a monthly “dialog on therapy” can be found on the B4U-ACT and the Global Prevention Project websites. However, beyond the DSM-5 definitions, psychiatric education and training on this topic is almost entirely lacking.
In light of the information discussed in this article, several important issues remain, including how psychiatrists can best reach this population, and how they can work toward decreasing stigma so they can provide meaningful care. The solutions start with education. Educating psychiatrists about this important population can decrease stigma and facilitate appropriate, compassionate care to these patients, with the result of improving the mental health of people with minor attraction and decreasing the incidence of child sexual abuse.
Continue to: Bottom Line
Bottom Line
Minor-attracted persons report a high prevalence of general psychiatric symptoms that often go untreated due to a lack of willing clinicians with appropriate expertise. Providing psychiatric treatment to these patients can improve their mental health and possibly decrease the incidence of individuals who act on their attractions.
Related Resources
- B4U-ACT. www.b4uact.org • The Global Prevention Project. http://theglobalprevention project.org
- Virtuous Pedophiles. www.virped.org
Drug Brand Names
Naltrexone • ReVia
Approximately 1 in 5 Americans report childhood sexual abuse.1 While 50% to 65% of child sexual abuse occurs in the absence of pedophilic interests and is thought to be driven by additional factors such as the availability of an appropriate sexual partner,2,3 a substantial portion of childhood sexual abuse is perpetrated by individuals with pedophilia.
However, many individuals with pedophilic interests never have sexual contact with a child or the penal system. This non-offending pedophile group reports a greater prevalence of psychiatric symptoms compared with the general population, but given the intense stigmatization of their preferences, they are largely psychiatrically underrecognized and underserved. This article focuses on the unique psychiatric needs of this neglected population. By understanding and addressing the treatment needs of these patients, psychiatrists and other mental health clinicians can serve a pivotal role in decreasing stigma, promoting wellness, and preventing sexual abuse.
Understanding the terminology
DSM-5 defines paraphilia as “any intense and persistent sexual interest other than sexual interest in genital stimulation or preparatory fondling with phenotypically normal, physiologically mature, consenting human partners.”4 The addition of the word “disorder” to the paraphilias was introduced in DSM-5 to distinguish between paraphilias that are not of clinical concern and paraphilic disorders that cause distress or impairment to the individual, or whereby satisfaction entails personal harm or risk of harm to others. As outlined in DSM-5, pedophilic disorder refers to at least 6 months of recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child.4 The individual has either acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty. Lastly, the individual must be at least age 16 years and at least 5 years older than the child. Sexual attraction to peri- or postpubescent minors is not considered a psychiatric disorder, but is illegal.
Coined by B4U-ACT (www.b4uact.org), the term minor-attracted person (MAP) refers to individuals with sexual attraction to individuals who are minors or below the legal age of consent. MAP is an umbrella term that includes sexual attraction to prepubescent individuals but also includes sexual attraction to peri- and postpubescent individuals (Table 1). A MAP may or may not meet criteria for pedophilia or pedophilic disorder, based on the age of their sexual interest and whether they have experienced distress or acted on the attraction. Although many individuals with minor attraction identify with the term MAP, not all do. The term has been critiqued for being too inclusive and conflating pedophilia with minor attractions.
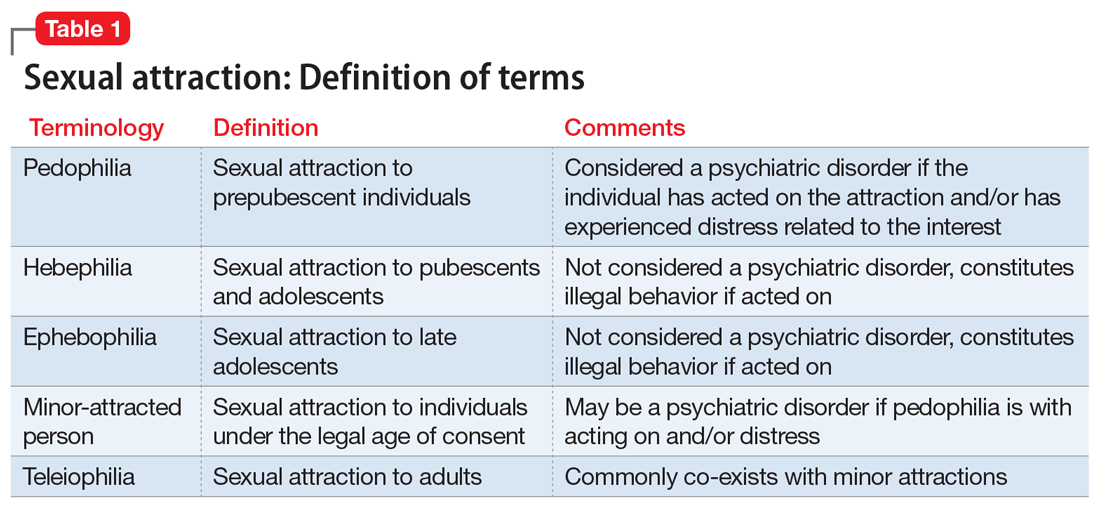
It is important to keep in mind that the terms pedophilia and minor attraction are not synonymous with childhood sexual abuser or “child molester” because neither term specifies whether the individual has had sexual contact with a child or legal consequences. The terms offending/non-offending and acting/non-acting are used to specify the presence of sexual contact with a child, and do not convey any clinical information.
Prevalence data
The true prevalence of pedophilia and/or attraction to minors is unknown, and estimates vary considerably. In some studies, 1% to 4% of the general population were thought to have persistent attraction to prepubescent children.5,6 In a community sample of 8,718 German men, 4.1% reported sexual fantasies involving prepubescent children, 3.2% reported sexual offending against prepubescent children, and 0.1% reported a pedophilic sexual preference.5 In a study of 367 adult German men surveyed from the community, 15.5% reported fantasies (9.5% daydream and 6.0% masturbation fantasies) involving prepubescent children.7
Stigmatization of minor-attracted persons
Stigmatization is the process of forming negative evaluations of an individual or groups of people based on limited characteristics.8,9 MAPs are a highly stigmatized group. This stigmatization can be profound, regardless of whether the MAP has had sexual contact with a child. A public survey of nearly 1,000 individuals showed that 39% believed that non-acting MAPs should be incarcerated, and 14% believed that they would be “better off dead.”10 Societal misconceptions of minor attraction are pervasive and include10:
- MAP sexual orientation is a choice
- MAPs cannot resist their sexual urges
- all MAPs have offended, or inevitably will
- MAPs will not respond to therapy
- MAPs are fundamentally predatory and immoral.
Continue to: In addition to...
In addition to societal stigma, internalized stigma among MAPs has been documented. Lievesley et al9 found that MAPs who engaged in suppression of unwanted thought strategies had higher levels of shame and guilt, low levels of hope, and a propensity to actively avoid children. Similarly, Grady et al11 surveyed 293 MAPs and found prominent themes of viewing themselves as “bad.”
Psychiatric presentations include suicidal ideation
Many MAPs, including non-acting MAPs, internalize this societal stigma, which contributes to a significant mental health burden.12 A survey of 342 MAP actors and 223 MAP non-actors revealed that one-third of both groups reported chronic suicidal ideation.13 In addition, online surveys conducted by B4U-ACT and Virtuous Pedophiles (www.virped.org)—both internet-based organizations dedicated to supporting non-acting MAPs—have provided similar results. In a 2011 B4U-ACT survey, nearly one-half of participants reported suicidal ideation due to their minor attraction, 32% had planned suicide attempts, and 13% had non-fatal suicide attempts. Notably, the age group with the most prevalent suicidal ideation was age 14 to 16 years,14 which makes minor attraction a prominent risk factor for suicidal ideation among patients seen by child psychiatrists.
A 2019 thematic analysis of 5,210 posts on the Virtuous Pedophiles website showed high rates of addiction, anxiety, depression, self-harm, self-hatred, and suicidal thoughts and behaviors among MAPs.2 The majority of posts regarding substance use described such use as a means of dissociation. One post read, “…There are days I cannot bear to be sober … I … drink myself into a coma.” Anxiety themes regarding the ability to have a meaningful relationship with an age-appropriate partner and concerns about being “outed” followed by public persecution were prominent. Posts regarding self-injurious and suicidal behavior were common: “I want to kill myself so badly … I have to mutilate myself as punishment for my attractions. I wish myself dead. I don’t want to be attracted to children; I despise myself for fantasizing about them.”2
A study that analyzed a survey of 152 MAPs sampled from websites such as Virtuous Pedophiles and others showed >50% of respondents had strong feelings of isolation and loneliness, nearly 30% had extreme difficulty with concentration, >40% had significant anger and frustration, and >30% were struggling with feelings of detachment.12 Notably, the respondents attributed these difficulties to their minor attraction.12 Table 22,12-14 summarizes the findings of studies evaluating psychiatric symptoms in MAPs.
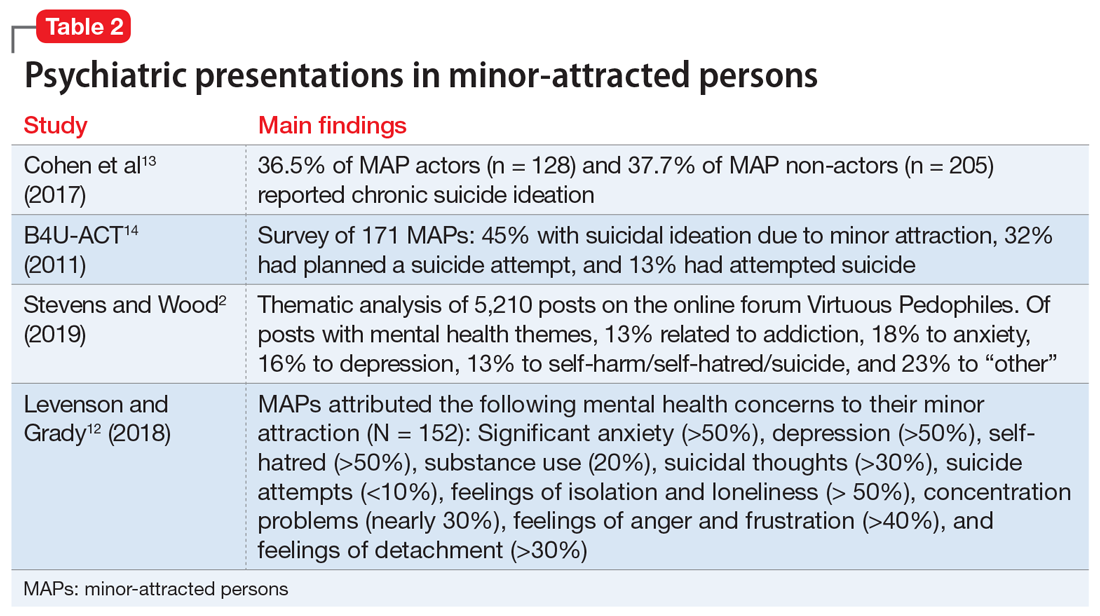
Consider OCD, hypersexuality
It is important to be aware that an attraction to minors may be a symptom of obsessive-compulsive disorder (OCD) or hypersexuality.15 Pedophilia-themed OCD (POCD) is a manifestation of OCD in which the individual experiences shame, fear, and excessive worry related to sexual attraction to children. Typically, individuals with POCD experience sexual thoughts of children as ego-dystonic, whereas MAPs experience such thoughts as ego-syntonic and arousing.15 However, much like individuals with POCD, MAPs also experience sexual thoughts of minors as distressing. Initial presentations of POCD may be confused with MAPs or pedophilia because of the overlap of symptoms such as anxiety, shame, distress, or suicidal ideation related to the idea of child sexual interests. The distinguishing feature of POCD is the absence of sexual arousal to children.
Continue to: Clinical presentations of...
Clinical presentations of hypersexuality may include sexual arousal to children. These individuals are distinguished from MAPs or those with pedophilia because they lack a preferred or sustained sexual interest in this group. On the contrary, individuals with hypersexuality present with a diversity of sexual interests explained by their high libido. Some individuals, however, may meet criteria for both hypersexuality and pedophilia. These individuals may pose a higher risk of sexual offending due to the presence of a heightened sexual drive and pedophilic interests, and thereby may require more intensive treatment, such as biologic treatment.
Focus on individualized treatment needs
Understanding the treatment needs of MAPs means understanding the goals of the individual MAP. Improving self-esteem, decreasing social isolation, and managing stigma are common treatment goals among MAPs.16 Levenson and Grady12 found that most MAPs identified treatment goals unrelated to sexual interests, such as addressing depression, anxiety, and low self-esteem. A smaller percentage identified sexual frustration related to the absence of healthy sexual outlets. Because many MAPs identify common psychiatric treatment needs, most clinicians should be equipped to foster a nonjudgmental therapeutic alliance to treat these patients. Effective treatment outcomes occur when comorbid psychiatric illnesses are treated as well as addressing the internal stigmatization that many MAPs experience.
Specialized treatment may be indicated for individuals who request treatment specific to sexual interests. This may include safety planning, including developing support systems to decrease the risk around children. For MAPs who have been unsuccessful at managing their sexual interests, pharmacotherapy may be an option. To date, research on pharmacotherapy for pedophilia is largely limited to studies of sexual offenders. Testosterone-lowering medications such as gonadotropin-releasing hormone (GnRH) analogue treatment constitutes the most effective treatment for patients who are not helped by conventional psychotherapeutic interventions.17 Other psychotropic medications, such as selective serotonin reuptake inhibitors or naltrexone, have not demonstrated efficacy outside of case reports.17
Addressing barriers to care
MAPs have a strong desire but significant hesitation when seeking mental health treatment.13,18 Nearly half (47%) of the 154 MAP respondents in the Levenson and Grady12 survey had never told anyone about their minor attraction. MAPs are understandably hesitant to disclose these thoughts and feelings due to fear of public exposure and intense stigmatization, as well as potential punitive and legal consequences.18,19 One post from the 2011 B4U-ACT online survey read, “Parents will disown you; teachers will report you; friends will abandon you … people in my situation can’t discuss this without serious risk of persecution and/or harassment.”14 In this survey, 78% of respondents feared a negative reaction by the professional, 78% feared being reported to law enforcement, and 68% feared being reported to family, an employer, or the community.14 This hesitancy due to fear of being exposed even extended to accessing self-help books, informational websites, and online forums, even though these sources are strongly desired and perceived as helpful.20
Even if MAPs were to decide to seek help, the lack of specific training and experience among psychiatrists make them unlikely to find it in the medical field.21 Furthermore, MAPs who desire help often worry it will be inadequate and they will be misunderstood by their clinicians.22 According to the Levenson and Grady survey,12 when asked what they would like most from therapy, most MAPs said they would want the treatment to focus on depression, anxiety, and low self-esteem rather than on sexual interest. In the B4U-ACT survey,14 many respondents identified the need for treatment of issues surrounding their sexual attraction, such as assistance in learning how to live in society with the attraction, dealing with society’s negative response to the attraction, and improving their self-concept in the presence of the extreme shame associated with the attraction. However, many MAPs find that clinicians tend to focus on protecting society from them, rather than on offering general psychiatric treatment or treatment focused on improving their well-being.18 This inability to locate appropriate services is known to exacerbate depression, suicidality, fear, anxiety, hopelessness, and substance abuse among MAPs.18 There is also evidence that individuals with minor attraction who are in a negative affective state are more likely to act on their attractions.23
Continue to: An ethical responsibility
An ethical responsibility. Physicians have a long-recognized responsibility to participate in activities to protect and promote the health of the public. The American Medical Association Code of Medical Ethics includes “justice,” or treating patients fairly and equitably.24 This includes patients who have pedophilic interests. Unfortunately, the stigma associated with individuals who have sexual attraction to children is pervasive in our society, including among medical professionals. The first consideration in treating MAPs is to overcome the stigmatization within our field, to remember that as physicians we took an oath to provide treatment fairly, equitably, and in accordance with the patient’s rights and entitlement.24 This includes listening to MAPs’ treatment needs. Not all MAPs want or need treatment related to their sexual interest. As is the case with all patients, listening to the individual’s chief complaint is paramount. If a patient’s treatment needs are beyond the clinician’s expertise, the patient should be referred to another clinician.
Mandated reporting. MAPs may not engage in psychiatric treatment for fear of being reported to authorities as a result of mandated reporting laws. Although the circumstances under which mandated reporting may be required vary by jurisdiction, they generally include situations in which the health care professional has reasonable cause to believe that a child is suffering from abuse or neglect. A patient’s report of sexual urges and fantasies to have sexual contact with minors is not sufficient for mandated reporting. While professionals vary in their interpretation of mandated reporting laws, sexual thoughts alone do not meet the threshold for mandated reporting. Mandated reporting duties should be discussed when first meeting a patient with minor attraction. For clinicians who are uneasy about such distinctions, either supervision or not working with such patients is the solution.
The importance of providing competent and individualized treatment to MAPs is 2-fold. First, individuals who are experiencing psychiatric symptoms deserve to have access treatment. Second, providing psychiatric treatment to individuals with minor attractions is a step toward preventing child sexual abuse. The Prevention Project Dunkelfeld in Germany used public service announcements to advertise confidential treatment for individuals who had sexual interest in children.25 Many of the participants were interested in mental health treatment unrelated to their sexual interests. Such projects may help us understand the best way to meet the treatment needs of minor-attracted individuals, as well as reduce child sexual abuse. As psychiatrists, we can stop making the problem worse by withholding psychiatric treatment from an important population.
Resources for MAPs and clinicians
Currently, resources for MAPs and clinicians are limited. MAPs can communicate and find support among other MAPs in online forums (see Related Resources). These websites provide online peer support groups and guides for seeking therapy. Information for mental health professionals, including available literature, research projects, clinicians who provide specialized treatment, and a monthly “dialog on therapy” can be found on the B4U-ACT and the Global Prevention Project websites. However, beyond the DSM-5 definitions, psychiatric education and training on this topic is almost entirely lacking.
In light of the information discussed in this article, several important issues remain, including how psychiatrists can best reach this population, and how they can work toward decreasing stigma so they can provide meaningful care. The solutions start with education. Educating psychiatrists about this important population can decrease stigma and facilitate appropriate, compassionate care to these patients, with the result of improving the mental health of people with minor attraction and decreasing the incidence of child sexual abuse.
Continue to: Bottom Line
Bottom Line
Minor-attracted persons report a high prevalence of general psychiatric symptoms that often go untreated due to a lack of willing clinicians with appropriate expertise. Providing psychiatric treatment to these patients can improve their mental health and possibly decrease the incidence of individuals who act on their attractions.
Related Resources
- B4U-ACT. www.b4uact.org • The Global Prevention Project. http://theglobalprevention project.org
- Virtuous Pedophiles. www.virped.org
Drug Brand Names
Naltrexone • ReVia
1. Briere J, Elliott D. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse Negl. 2003;27(10):1205-1222. doi: 10.1016/j.chiabu.2003.09.008
2. Stevens E, Wood J. “I despise myself for thinking about them.” A thematic analysis of the mental health implications and employed coping mechanisms of self-reported non-offending minor attracted persons. J Child Sex Abus. 2019;28(8):968-989. doi: 10.1080/10538712.2019.1657539
3. Sorrentino R. Normal human sexuality and sexual and gender identity disorders: paraphilias. In: Sadock BJ, Sadock VA, Ruis P, eds. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 9th ed. Wolters Kluwer; 2012:2093-2094.
4. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013:685-705.
5. Dombert B, Schmidt AF, Banse R, et al. How common is men’s self-reported sexual interest in prepubescent children? J Sex Res. 2016;53(2):214-23. doi: 10.1080/00224499.2015.1020108
6. Seto MC. Pedophilia and sexual offending against children: theory, assessment, and intervention. 2nd ed. American Psychological Association; 2018.
7. Ahlers CJ, Schaefer GA, Mundt IA, et al. How unusual are the contents of paraphilias? Paraphilia-associated sexual arousal patterns in a community-based sample of men. J Sex Med. 2011;8(5):1362-1370. doi: 10.1111/j.1743-6109.2009.01597.x
8. Corrigan PW, Roe D, Tsang HWH. Challenging the public stigma of mental illness: lessons for therapists and advocates. Wiley Blackwell; 2011:55-114.
9. Lievesley R, Harper CA, Elliott H. The internalization of social stigma among minor-attracted persons: implications for treatment. Arch Sex Behav. 2020;49(4):1291-1304. doi: 10.1007/s10508-019-01569-x
10. Jahnke S, Imhoff R, Hoyer J. Stigmatization of people with pedophilia: two comparative surveys. Arch Sex Behav. 2015;44(1):21-34. doi: 10.1007/s10508-014-0312-4
11. Grady MD, Levenson JS, Mesias G, et al. “‘I can’t talk about that”: Stigma and fear as barriers to preventative services for minor-attracted persons. Stigma and Health. 2019;4(4):400-410. doi: 10.1037/sah0000154
12. Levenson JS, Grady MD. Preventing sexual abuse: perspectives of minor-attracted persons about seeking help. Sex Abuse. 2019;31(8):991-1013. doi: 10.1177/1079063218797713
13. Cohen L, Ndukwe N, Yaseen Z, et al. Comparison of self-identified minor-attracted persons who have and have not successfully refrained from sexual activity with children. J Sex Marital Ther. 2018;44(3):217-230. doi: 10.1080/0092623X.2017.1377129
14. B4U-ACT. Awareness of sexuality in youth, suicidality, and seeking care. 2011. Accessed June 4, 2021. www.b4uact.org/research/survey-results/spring-2011-survey
15. Bruce SL, Ching THW, Williams MT. Pedophilia-themed obsessive-compulsive disorder: assessment, differential diagnosis, and treatment with exposure and response prevention. Arch Sex Behav. 2018;47(2):389-402. doi: 10.1007/s10508-017-1031-4
16. Levenson JS, Grady MD, Morin JW. Beyond the “ick factor”: counseling non-offending persons with pedophilia. Clinical Social Work Journal. 2020;48:380-388. doi: 10.007/s10615-019-00712-4
1 7. Thibaut F, Cosyns P, Fedoroff JP, et al; WFSBP Task Force on Paraphilias. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J Biol Psychiatry. 2020;21(6):412-490. doi: 10.1080/15622975.2020.1744723
18. B4U-ACT. Principles and perspectives of practice. 2017. Accessed June 4, 2021. www.b4uact.org/about-us/principles-and-perspectives-of-practice/
19. McPhail IV, Stephens S, Heasman A. Legal and ethical issues in treating clients with pedohebephilic interests. Canadian Psychology/Psychologie Canadienne. 2018;59(4):369-381. doi:10.1037/cap0000157
20. Levenson JS, Willis GM, Vicencio CP. Obstacles to help-seeking for sexual offenders: implications for prevention of sexual abuse. J Child Sex Abus. 2017;26(2):99-120. doi: 10.1080/10538712.2016.1276116
21. Sorrentino R. DSM-5 and paraphilias: what psychiatrists need to know. Psychiatric Times. November 28, 2016. Accessed June 4, 2021. https://www.psychiatrictimes.com/view/dsm-5-and-paraphilias-what-psychiatrists-need-know
22. Cantor JM, McPhail IV. Non-offending pedophiles. Current Sexual Health Reports. 2016;8:121-128. doi:10.1007/s11930-016-0076-z
23. Ward T, Louden K, Hudson SM, et al. A descriptive model of the offense chain for child molesters. Journal of Interpersonal Violence. 1995;10(4):452-472. doi:10.1177/088626095010004005
24. American Medical Association. AMA Code of Medical Ethics. 2016. Accessed June 4, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/principles-of-medical-ethics.pdf
25. Beier KM, Grundmann D, Kuhle LF, et al. The German Dunkelfeld project: a pilot study to prevent child sexual abuse and the use of child abusive images. J Sex Med. 2015;12(2):529-42. doi: 10.1111/jsm.12785
1. Briere J, Elliott D. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse Negl. 2003;27(10):1205-1222. doi: 10.1016/j.chiabu.2003.09.008
2. Stevens E, Wood J. “I despise myself for thinking about them.” A thematic analysis of the mental health implications and employed coping mechanisms of self-reported non-offending minor attracted persons. J Child Sex Abus. 2019;28(8):968-989. doi: 10.1080/10538712.2019.1657539
3. Sorrentino R. Normal human sexuality and sexual and gender identity disorders: paraphilias. In: Sadock BJ, Sadock VA, Ruis P, eds. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 9th ed. Wolters Kluwer; 2012:2093-2094.
4. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013:685-705.
5. Dombert B, Schmidt AF, Banse R, et al. How common is men’s self-reported sexual interest in prepubescent children? J Sex Res. 2016;53(2):214-23. doi: 10.1080/00224499.2015.1020108
6. Seto MC. Pedophilia and sexual offending against children: theory, assessment, and intervention. 2nd ed. American Psychological Association; 2018.
7. Ahlers CJ, Schaefer GA, Mundt IA, et al. How unusual are the contents of paraphilias? Paraphilia-associated sexual arousal patterns in a community-based sample of men. J Sex Med. 2011;8(5):1362-1370. doi: 10.1111/j.1743-6109.2009.01597.x
8. Corrigan PW, Roe D, Tsang HWH. Challenging the public stigma of mental illness: lessons for therapists and advocates. Wiley Blackwell; 2011:55-114.
9. Lievesley R, Harper CA, Elliott H. The internalization of social stigma among minor-attracted persons: implications for treatment. Arch Sex Behav. 2020;49(4):1291-1304. doi: 10.1007/s10508-019-01569-x
10. Jahnke S, Imhoff R, Hoyer J. Stigmatization of people with pedophilia: two comparative surveys. Arch Sex Behav. 2015;44(1):21-34. doi: 10.1007/s10508-014-0312-4
11. Grady MD, Levenson JS, Mesias G, et al. “‘I can’t talk about that”: Stigma and fear as barriers to preventative services for minor-attracted persons. Stigma and Health. 2019;4(4):400-410. doi: 10.1037/sah0000154
12. Levenson JS, Grady MD. Preventing sexual abuse: perspectives of minor-attracted persons about seeking help. Sex Abuse. 2019;31(8):991-1013. doi: 10.1177/1079063218797713
13. Cohen L, Ndukwe N, Yaseen Z, et al. Comparison of self-identified minor-attracted persons who have and have not successfully refrained from sexual activity with children. J Sex Marital Ther. 2018;44(3):217-230. doi: 10.1080/0092623X.2017.1377129
14. B4U-ACT. Awareness of sexuality in youth, suicidality, and seeking care. 2011. Accessed June 4, 2021. www.b4uact.org/research/survey-results/spring-2011-survey
15. Bruce SL, Ching THW, Williams MT. Pedophilia-themed obsessive-compulsive disorder: assessment, differential diagnosis, and treatment with exposure and response prevention. Arch Sex Behav. 2018;47(2):389-402. doi: 10.1007/s10508-017-1031-4
16. Levenson JS, Grady MD, Morin JW. Beyond the “ick factor”: counseling non-offending persons with pedophilia. Clinical Social Work Journal. 2020;48:380-388. doi: 10.007/s10615-019-00712-4
1 7. Thibaut F, Cosyns P, Fedoroff JP, et al; WFSBP Task Force on Paraphilias. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J Biol Psychiatry. 2020;21(6):412-490. doi: 10.1080/15622975.2020.1744723
18. B4U-ACT. Principles and perspectives of practice. 2017. Accessed June 4, 2021. www.b4uact.org/about-us/principles-and-perspectives-of-practice/
19. McPhail IV, Stephens S, Heasman A. Legal and ethical issues in treating clients with pedohebephilic interests. Canadian Psychology/Psychologie Canadienne. 2018;59(4):369-381. doi:10.1037/cap0000157
20. Levenson JS, Willis GM, Vicencio CP. Obstacles to help-seeking for sexual offenders: implications for prevention of sexual abuse. J Child Sex Abus. 2017;26(2):99-120. doi: 10.1080/10538712.2016.1276116
21. Sorrentino R. DSM-5 and paraphilias: what psychiatrists need to know. Psychiatric Times. November 28, 2016. Accessed June 4, 2021. https://www.psychiatrictimes.com/view/dsm-5-and-paraphilias-what-psychiatrists-need-know
22. Cantor JM, McPhail IV. Non-offending pedophiles. Current Sexual Health Reports. 2016;8:121-128. doi:10.1007/s11930-016-0076-z
23. Ward T, Louden K, Hudson SM, et al. A descriptive model of the offense chain for child molesters. Journal of Interpersonal Violence. 1995;10(4):452-472. doi:10.1177/088626095010004005
24. American Medical Association. AMA Code of Medical Ethics. 2016. Accessed June 4, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/principles-of-medical-ethics.pdf
25. Beier KM, Grundmann D, Kuhle LF, et al. The German Dunkelfeld project: a pilot study to prevent child sexual abuse and the use of child abusive images. J Sex Med. 2015;12(2):529-42. doi: 10.1111/jsm.12785
Liability protection when practicing during a disaster: How the laws work
Disasters—both natural and human-caused—can strike at any time, causing severe trauma for those impacted. Disasters may create circumstances where the need for mental health resources could exceed capacity, and hospitals and clinics would be unable to meet the needs of the affected communities. As psychiatric clinicians, we may want to provide our services in such situations; however, we are still at risk for civil, criminal, or constitutional liability claims against us if we fail to meet our legal obligations related to psychiatric practice. Ideally, whether we live and work in an area affected by a disaster or volunteer from other states, we should be able to care for patients without fear of facing unreasonable liability risks. Although an exhaustive list of all relevant federal and state laws and regulations is beyond the scope of this article, here I discuss some of the federal and state laws and regulations that could provide protection from these risks, and some limitations of liability protection.
A familiar list of liability concerns
From a liability perspective, what should we be aware of when practicing during disasters? The same liability concerns we have during our day-to-day practice also exist during disasters, especially when there are suboptimal or adverse outcomes.
Box
During disasters, changes in the usual standard of practice may be necessary to save as many lives as possible, and when resources are scarce, the focus of mental health services could shift from individualized patient care to those who are most in need. Examples of potential liability concerns clinicians may face in such situations include:
Negligence. Clinicians may have to provide emergent care for patients that may result in an adverse outcome. Examples include applying a tourniquet to a patient’s badly injured limb without their consent, and then that patient loses their limb, or administering the COVID-19 vaccine to a patient because of significant clinician shortages, and then that patient develops complications. These scenarios could possibly give rise to ordinary negligence claims of practicing outside the usual scope of practice, especially for a clinician who does not have liability protections.
Practicing without the proper state medical license. When out-of-state clinicians come to a facility that needs emergency assistance, they can face liability concerns for practicing without a properly recognized state medical license.1 Because care is deemed to have been provided where the patient was physically present when services were provided, liability can occur when providing services to patients in a state where the psychiatrist does not have a medical license. An example of this would be a psychiatrist in South Carolina who provides telehealth services to patients in a Florida community ravaged by a hurricane when the psychiatrist does not have a Florida medical license.
Abandonment. When we take a confirmatory step to provide care to an individual, it may create a clinician-patient relationship and a duty on behalf of the clinician within the applicable standard of care.2 With disasters, the customary expectations and parameters associated with clinician-patient relationships can change. We may have to cease treating some patients so that we can focus our time or resources elsewhere, which could open up liability concerns regarding claims of abandonment.1 At times, we may refuse to treat patients outright, creating conflicts with the Emergency Medical Treatment & Active Labor Act (EMTALA) and its state counterparts.
Liability protections
There are no comprehensive national liability protections for all practitioners during disasters.1 Limited immunity is often provided through a patchwork of federal and state laws and regulations, which can be complex and are often modified. This immunity depends on several factors, such as applicable regulations, the type of services that are provided, and whether the clinicians are volunteering their services (ie, they are not being paid for providing services).2 There is usually no immunity due to willful or wanton acts, gross negligence, providing care while intoxicated, or criminal acts.2
Federal laws and regulations
Most of the federal laws that provide liability protections are activated once a disaster is declared. However, some laws provide liability protections without requiring such declarations. Additional federal laws and regulations that provide additional liability protections, especially to volunteers, can be enacted after disasters occur.
Federal Tort Claims Act
The Federal Tort Claims Act (FTCA)3 protects federal government employees from tort liability by substituting the federal government as the defendant in certain types of suits brought against the federal government. These suits may involve injury, loss of personal property, personal injury, or death by the negligent or wrongful act or omission of any federal government employees while acting in the scope of their office or employment.3,4 It does not require that an emergency be declared before immunity is conferred. FTCA covers all federal government employees, including volunteers.4 In the context of an emergency response, volunteers can assert the liability protections afforded to federal employees if they are designated as unpaid employees of the federal government.4 Federal employees are immune from suit under state tort law.4
Volunteer Protection Act
The Volunteer Protection Act (VPA) of 19975 provides liability protections to uncompensated volunteer health professionals (VHPs) who perform services for nonprofit organizations or government entities against claims of ordinary negligence committed within the scope of their volunteer responsibilities.4 It does not require that an emergency be declared before immunity is conferred. Although VHPs are not liable for economic damages caused by providing medical care within the scope of their volunteer responsibilities, this exemption does not extend to non-economic damages, such as losses for suffering and mental anguish.5 VPA does not protect VHPs working in businesses (including for-profit hospitals) and organizational entities of any type (including nonprofit or governmental organizations) that use VHPs.4
VPA only protects VHPs practicing with a license as required by law in the state where the harm occurred, unless state authorities allow for licensure exceptions. VPA overrides state laws that are inconsistent with VPA, unless those state laws provide greater liability protection for VHPs.4 However, VPA protections are limited. VPA protects only volunteers, not clinicians working in their regular nonemergency roles and capacities.6 A nonprofit or government agent can still bring civil claims against VHPs.6 VPA does not override certain state laws that put conditions on volunteers, such as risk management requirements, vicarious liability, and a financially secure form of recovery for intended victims.6
Continue to: Health Insurance Portability and Accountability Act
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) of 1996,7 specifically Section 194, extends eligibility for FTCA liability protections to VHPs at qualifying free clinics, provided the clinic sponsors the VHPs by applying to the Health Resources and Services Administration.8 It does not require that an emergency be declared before immunity is conferred.
Public Readiness and Emergency Preparedness Act
The Public Readiness and Emergency Preparedness (PREP) Act of 20059 authorizes the US Department of Health and Human Services (HHS) Secretary to issue a declaration that provides immunity to VHPs from tort liability for claims of loss caused by the use of authorized countermeasures (eg, vaccines) against diseases or other threats of public health emergencies.4 A separate emergency determination under Public Health Service Act Section 319 or another statute is not required for PREP Act immunities to take effect.4 The PREP Act covers individual persons and entities involved in the manufacture, testing, distribution, administration, and use of covered countermeasures.4
PREP Act immunity is not absolute and does not protect against claims of willful misconduct, violation of the Americans with Disabilities Act (ADA), or other civil rights violations.4 Liability protection under the PREP Act is limited to a specific emergency and includes only the countermeasures and other conditions listed in the PREP Act declaration by the HHS Secretary.4
State laws and regulations
States have a variety of standing liability protections that could apply to VHPs who provide care in an emergency. Some states have crafted executive orders to be put into effect during a disaster. Most of these executive orders, which can include extending liability protections, are similar to what other states have done by adopting model acts such as Model State Emergency Health Powers Act.6 These orders are not actually laws; they only become effective when the governor signs them at the time of the disaster. These orders also are time-limited and must be reissued in subsequent disasters.
State tort claims acts and state claims acts
Similar to the federal government, some states have waived sovereign immunity in certain circumstances through state tort claims or state claims acts.
Continue to: State tort claims act
State tort claims acts either abolish state sovereign immunity generally and provide immunity only in specific circumstances, or preserve sovereign immunity generally but identify certain exceptions in which immunity is waived.4
State claims acts limit state sovereign immunity by establishing procedures for making claims against the state.4 These acts typically immunize state government employees from tort liability for acts or omissions committed within the scope of their employment.4 Some states extend these protections to volunteers, and some states declare volunteers to be unpaid state employees during an emergency, which allows volunteers to assert the liability protections afforded of state employees.4
Emergency power statutes
State emergency laws can trigger additional powers, suspend certain administrative requirements, and provide or enhance liability protections to specified groups of volunteers and other responders upon a gubernatorial declaration of emergency.4 These statutes can extend the rights and immunities provided to governmental employees to volunteers performing work that is eligible for coverage under governmental immunity and state tort claims acts.4 There is a wide range in the types and degrees of coverage provided to volunteers under emergency powers statutes, and these provisions can be broad or duplicative of other provisions in state law.4
State volunteer protection statutes
All states have some statutory provisions for volunteers. Similar to the VPA, these state volunteer protection statutes generally do not require that an emergency be declared, apply to uncompensated individual volunteers for nonprofit and government entities only, and apply only to individuals and not to organizations.4 Many states have adopted specific liability protections for VHPs in addition to or to supplement their emergency powers and general volunteer protection statutes.4 These statutes confer immunity from civil liability provided that certain conditions are met and are not dependent on the declaration of an emergency.4 Each state statute differs in regard to who receives immunity, which acts are immune from liability, and what liability protections are available.
Good Samaritan laws
All 50 states and the District of Columbia have enacted Good Samaritan laws. These laws, which do not need an official declaration of an emergency in order to be applicable, generally protect VHPs from liability when volunteering in good faith and without compensation at the scene of an emergency.2 Good Samaritan protections may also apply to care provided by VHPs in a hospital if the VHP is not on duty and does not charge a fee.2 However, the effect and scope of Good Samaritan laws vary dramatically from state to state. Some states include hospital settings as an emergency scene in their statutes, while others expressly exclude hospitals from their statutes.6 Some state statutes only include declared emergencies, while others are drawn to broadly cover all emergency situations.6
Continue to: Limitations
Limitations. Many Good Samaritan statutes apply only to volunteers, and not all states have statutes that allow clinicians to be designated as such,6 so receiving compensation would take a clinician outside the scope of the statute. Further, most states only shield action taken at the scene of an accident, and immunity would not extend to a hospital emergency department, or in the aftermath of an emergency as normal conditions slowly return.6 Therefore, Good Samaritan liability protection would apply to the common scenario of assisting at the scene of a car crash, but not necessarily to treating individuals in the emergency department after a hurricane or during a pandemic.6 State laws vary considerably on what constitutes “good faith” and “without compensation,” which would determine whether protection applies for a clinician who is otherwise salaried in a regular job.1
Mutual aid agreements
Mutual aid agreements are mechanisms through which jurisdictions can aid other jurisdictions during emergencies.4 These agreements also include provisions for reimbursing expenses, providing liability protections to governmental employees and volunteers who provide aid, and awarding compensation for injuries to personnel deployed under the agreement.4 These protections are not automatic and are limited in their applicability.
The Emergency Management Assistance Compact (EMAC), the most widely adopted mutual aid agreement in the United States, has been adopted by all 50 states, the District of Columbia, and some territories.10 It only becomes effective once an emergency has been declared. EMAC provides immunity to officers from the state that is rendering aid to the state requesting aid, in which officers are considered agents of the requesting state for tort liability and immunity purposes.8 These individuals, who must be properly dispatched in response to an EMAC request, are not to be held liable for acts or omissions rendered in good faith; however, EMAC does not provide liability protection for actions constituting willful misconduct, gross negligence, or recklessness.6 EMAC also provides reciprocity for individuals who are properly dispatched in response to an EMAC request who hold medical licenses to practice medicine in the receiving state, subject to any limitations imposed by the receiving state.4 Clinicians can familiarize themselves with a state’s medical licensing requirements by reviewing that state’s medical board website. For EMAC protections to apply, a state must make a request to another/other state(s) through EMAC, and such requests must be formally accepted by the rendering state.8 EMAC does not require participating states to actually provide aid.10
Non-volunteer health care clinicians
Non-volunteer (salaried or paid) health care clinicians are more likely to bear the brunt of providing care during a disaster, especially in the early stages before VHPs arrive; however, most legislation does not address the associated disproportionate liability risk burden of non-volunteer health care clinicians.1,11 As opposed to VHPs and government employees, non-volunteer health care clinicians performing their regular job duties during a disaster are generally not provided immunity from negligence by most legislation.1,6 One exception is the PREP Act, which provides immunity for all clinicians from claims that may arise from dispensing a specific countermeasure during a declared public health emergency.1,9 Some states have enacted the Model State Emergency Health Powers Act, which may offer immunity from negligence if the non-volunteer clinician is rendering care under contract with or at the request of a state1; however, non-volunteer clinicians who practice from their office or a local hospital will not receive protection through these laws.1 Good Samaritan laws may not apply unless care is provided at a scene of an emergency.
A few states have attempted to narrow this legislative gap by enacting laws that provide immunity more broadly for clinicians, regardless of their volunteer or compensation status.1 Elements of these states’ laws include acting in response to a declared emergency or disaster in which there is a recognized depletion of resources attributable to the disaster, at express or implied request of the state government, and consistent with emergency plans.1
Continue to: Bottom Line
Bottom Line
There are potential liability risks when treating patients during a disaster. Statutory protections that limit liability may be enacted when the US President or a state Governor declares an official state of emergency. Although some federal and state laws and regulations provide liability protections during these situations, there is a discrepancy in the protections offered to non-volunteer vs volunteer clinicians.
Related Resources
- Federal Emergency Management Agency. https://www.fema.gov/
- Federation of State Medical Boards. https://www.fsmb.org
1. Altman RL, Santucci KA, Anderson MR, et al. American Academy of Pediatrics Committee on Medical Liability and Risk Management. Understanding liability risks and protections for pediatric providers during disasters. Pediatrics. 2019;143(3):e20183893. doi.org/10.1542/peds.2018-3892
2. Lambert K, Wertheimer M. American Professional Agency: Risk management in disaster response. Published September 2017. Accessed May 25, 2021. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/disaster/resource_group/resources/orgs/RMDisasterResp.pdf
3. Federal Torts Claims Act, as amended. Codified at 28 USC. §1346 (1946).
4. Association of State and Territorial Health Officials (ASTHO). Liability, immunity, and workers’ compensation issue in public health emergencies. Published 2012. Accessed May 25, 2021. https://www.astho.org/Programs/Preparedness/Public-Health-Emergency-Law/Emergency-Authority-and-Immunity-Toolkit/Liability,-Immunity,-and-Workers%E2%80%99-Compensation-Issues-in-Public-Health-Emergencies-Issue-Brief/
5. Volunteer Protection Act of 1997. Pub. L. 105-19, 111 Stat. 221.
6. Pope TM, Palazzo MF. Legal briefing: crisis standards of care and legal protections during disasters and emergencies. J Clin Ethics. 2010;21(4):358-367.
7. Health Insurance Portability and Accountability Act of 1996. Pub. L. 104-191, 110 Stat. 1936. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf
8. American Medical Association. Liability protections for health care professionals during COVID-19. Updated April 8, 2020. Accessed May 25, 2021. https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19
9. Public Readiness and Emergency Preparedness Act of 2005. Pub. L. 109-148, 119 Stat. 2818. https://www.govinfo.gov/content/pkg/PLAW-109publ148/html/PLAW-109publ148.htm
10. Emergency Management Assistance Compact (EMAC). Accessed May 25, 2021. https://www.emacweb.org/
11. Hodge JG, Garcia AM, Anderson ED, et al. Emergency legal preparedness for hospitals and health care personnel. Disaster Med Public Health Prep. 2009;3(2 Supplement):S37-S44. doi: 10.1097/DMP.0b013e31819d977c
Disasters—both natural and human-caused—can strike at any time, causing severe trauma for those impacted. Disasters may create circumstances where the need for mental health resources could exceed capacity, and hospitals and clinics would be unable to meet the needs of the affected communities. As psychiatric clinicians, we may want to provide our services in such situations; however, we are still at risk for civil, criminal, or constitutional liability claims against us if we fail to meet our legal obligations related to psychiatric practice. Ideally, whether we live and work in an area affected by a disaster or volunteer from other states, we should be able to care for patients without fear of facing unreasonable liability risks. Although an exhaustive list of all relevant federal and state laws and regulations is beyond the scope of this article, here I discuss some of the federal and state laws and regulations that could provide protection from these risks, and some limitations of liability protection.
A familiar list of liability concerns
From a liability perspective, what should we be aware of when practicing during disasters? The same liability concerns we have during our day-to-day practice also exist during disasters, especially when there are suboptimal or adverse outcomes.
Box
During disasters, changes in the usual standard of practice may be necessary to save as many lives as possible, and when resources are scarce, the focus of mental health services could shift from individualized patient care to those who are most in need. Examples of potential liability concerns clinicians may face in such situations include:
Negligence. Clinicians may have to provide emergent care for patients that may result in an adverse outcome. Examples include applying a tourniquet to a patient’s badly injured limb without their consent, and then that patient loses their limb, or administering the COVID-19 vaccine to a patient because of significant clinician shortages, and then that patient develops complications. These scenarios could possibly give rise to ordinary negligence claims of practicing outside the usual scope of practice, especially for a clinician who does not have liability protections.
Practicing without the proper state medical license. When out-of-state clinicians come to a facility that needs emergency assistance, they can face liability concerns for practicing without a properly recognized state medical license.1 Because care is deemed to have been provided where the patient was physically present when services were provided, liability can occur when providing services to patients in a state where the psychiatrist does not have a medical license. An example of this would be a psychiatrist in South Carolina who provides telehealth services to patients in a Florida community ravaged by a hurricane when the psychiatrist does not have a Florida medical license.
Abandonment. When we take a confirmatory step to provide care to an individual, it may create a clinician-patient relationship and a duty on behalf of the clinician within the applicable standard of care.2 With disasters, the customary expectations and parameters associated with clinician-patient relationships can change. We may have to cease treating some patients so that we can focus our time or resources elsewhere, which could open up liability concerns regarding claims of abandonment.1 At times, we may refuse to treat patients outright, creating conflicts with the Emergency Medical Treatment & Active Labor Act (EMTALA) and its state counterparts.
Liability protections
There are no comprehensive national liability protections for all practitioners during disasters.1 Limited immunity is often provided through a patchwork of federal and state laws and regulations, which can be complex and are often modified. This immunity depends on several factors, such as applicable regulations, the type of services that are provided, and whether the clinicians are volunteering their services (ie, they are not being paid for providing services).2 There is usually no immunity due to willful or wanton acts, gross negligence, providing care while intoxicated, or criminal acts.2
Federal laws and regulations
Most of the federal laws that provide liability protections are activated once a disaster is declared. However, some laws provide liability protections without requiring such declarations. Additional federal laws and regulations that provide additional liability protections, especially to volunteers, can be enacted after disasters occur.
Federal Tort Claims Act
The Federal Tort Claims Act (FTCA)3 protects federal government employees from tort liability by substituting the federal government as the defendant in certain types of suits brought against the federal government. These suits may involve injury, loss of personal property, personal injury, or death by the negligent or wrongful act or omission of any federal government employees while acting in the scope of their office or employment.3,4 It does not require that an emergency be declared before immunity is conferred. FTCA covers all federal government employees, including volunteers.4 In the context of an emergency response, volunteers can assert the liability protections afforded to federal employees if they are designated as unpaid employees of the federal government.4 Federal employees are immune from suit under state tort law.4
Volunteer Protection Act
The Volunteer Protection Act (VPA) of 19975 provides liability protections to uncompensated volunteer health professionals (VHPs) who perform services for nonprofit organizations or government entities against claims of ordinary negligence committed within the scope of their volunteer responsibilities.4 It does not require that an emergency be declared before immunity is conferred. Although VHPs are not liable for economic damages caused by providing medical care within the scope of their volunteer responsibilities, this exemption does not extend to non-economic damages, such as losses for suffering and mental anguish.5 VPA does not protect VHPs working in businesses (including for-profit hospitals) and organizational entities of any type (including nonprofit or governmental organizations) that use VHPs.4
VPA only protects VHPs practicing with a license as required by law in the state where the harm occurred, unless state authorities allow for licensure exceptions. VPA overrides state laws that are inconsistent with VPA, unless those state laws provide greater liability protection for VHPs.4 However, VPA protections are limited. VPA protects only volunteers, not clinicians working in their regular nonemergency roles and capacities.6 A nonprofit or government agent can still bring civil claims against VHPs.6 VPA does not override certain state laws that put conditions on volunteers, such as risk management requirements, vicarious liability, and a financially secure form of recovery for intended victims.6
Continue to: Health Insurance Portability and Accountability Act
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) of 1996,7 specifically Section 194, extends eligibility for FTCA liability protections to VHPs at qualifying free clinics, provided the clinic sponsors the VHPs by applying to the Health Resources and Services Administration.8 It does not require that an emergency be declared before immunity is conferred.
Public Readiness and Emergency Preparedness Act
The Public Readiness and Emergency Preparedness (PREP) Act of 20059 authorizes the US Department of Health and Human Services (HHS) Secretary to issue a declaration that provides immunity to VHPs from tort liability for claims of loss caused by the use of authorized countermeasures (eg, vaccines) against diseases or other threats of public health emergencies.4 A separate emergency determination under Public Health Service Act Section 319 or another statute is not required for PREP Act immunities to take effect.4 The PREP Act covers individual persons and entities involved in the manufacture, testing, distribution, administration, and use of covered countermeasures.4
PREP Act immunity is not absolute and does not protect against claims of willful misconduct, violation of the Americans with Disabilities Act (ADA), or other civil rights violations.4 Liability protection under the PREP Act is limited to a specific emergency and includes only the countermeasures and other conditions listed in the PREP Act declaration by the HHS Secretary.4
State laws and regulations
States have a variety of standing liability protections that could apply to VHPs who provide care in an emergency. Some states have crafted executive orders to be put into effect during a disaster. Most of these executive orders, which can include extending liability protections, are similar to what other states have done by adopting model acts such as Model State Emergency Health Powers Act.6 These orders are not actually laws; they only become effective when the governor signs them at the time of the disaster. These orders also are time-limited and must be reissued in subsequent disasters.
State tort claims acts and state claims acts
Similar to the federal government, some states have waived sovereign immunity in certain circumstances through state tort claims or state claims acts.
Continue to: State tort claims act
State tort claims acts either abolish state sovereign immunity generally and provide immunity only in specific circumstances, or preserve sovereign immunity generally but identify certain exceptions in which immunity is waived.4
State claims acts limit state sovereign immunity by establishing procedures for making claims against the state.4 These acts typically immunize state government employees from tort liability for acts or omissions committed within the scope of their employment.4 Some states extend these protections to volunteers, and some states declare volunteers to be unpaid state employees during an emergency, which allows volunteers to assert the liability protections afforded of state employees.4
Emergency power statutes
State emergency laws can trigger additional powers, suspend certain administrative requirements, and provide or enhance liability protections to specified groups of volunteers and other responders upon a gubernatorial declaration of emergency.4 These statutes can extend the rights and immunities provided to governmental employees to volunteers performing work that is eligible for coverage under governmental immunity and state tort claims acts.4 There is a wide range in the types and degrees of coverage provided to volunteers under emergency powers statutes, and these provisions can be broad or duplicative of other provisions in state law.4
State volunteer protection statutes
All states have some statutory provisions for volunteers. Similar to the VPA, these state volunteer protection statutes generally do not require that an emergency be declared, apply to uncompensated individual volunteers for nonprofit and government entities only, and apply only to individuals and not to organizations.4 Many states have adopted specific liability protections for VHPs in addition to or to supplement their emergency powers and general volunteer protection statutes.4 These statutes confer immunity from civil liability provided that certain conditions are met and are not dependent on the declaration of an emergency.4 Each state statute differs in regard to who receives immunity, which acts are immune from liability, and what liability protections are available.
Good Samaritan laws
All 50 states and the District of Columbia have enacted Good Samaritan laws. These laws, which do not need an official declaration of an emergency in order to be applicable, generally protect VHPs from liability when volunteering in good faith and without compensation at the scene of an emergency.2 Good Samaritan protections may also apply to care provided by VHPs in a hospital if the VHP is not on duty and does not charge a fee.2 However, the effect and scope of Good Samaritan laws vary dramatically from state to state. Some states include hospital settings as an emergency scene in their statutes, while others expressly exclude hospitals from their statutes.6 Some state statutes only include declared emergencies, while others are drawn to broadly cover all emergency situations.6
Continue to: Limitations
Limitations. Many Good Samaritan statutes apply only to volunteers, and not all states have statutes that allow clinicians to be designated as such,6 so receiving compensation would take a clinician outside the scope of the statute. Further, most states only shield action taken at the scene of an accident, and immunity would not extend to a hospital emergency department, or in the aftermath of an emergency as normal conditions slowly return.6 Therefore, Good Samaritan liability protection would apply to the common scenario of assisting at the scene of a car crash, but not necessarily to treating individuals in the emergency department after a hurricane or during a pandemic.6 State laws vary considerably on what constitutes “good faith” and “without compensation,” which would determine whether protection applies for a clinician who is otherwise salaried in a regular job.1
Mutual aid agreements
Mutual aid agreements are mechanisms through which jurisdictions can aid other jurisdictions during emergencies.4 These agreements also include provisions for reimbursing expenses, providing liability protections to governmental employees and volunteers who provide aid, and awarding compensation for injuries to personnel deployed under the agreement.4 These protections are not automatic and are limited in their applicability.
The Emergency Management Assistance Compact (EMAC), the most widely adopted mutual aid agreement in the United States, has been adopted by all 50 states, the District of Columbia, and some territories.10 It only becomes effective once an emergency has been declared. EMAC provides immunity to officers from the state that is rendering aid to the state requesting aid, in which officers are considered agents of the requesting state for tort liability and immunity purposes.8 These individuals, who must be properly dispatched in response to an EMAC request, are not to be held liable for acts or omissions rendered in good faith; however, EMAC does not provide liability protection for actions constituting willful misconduct, gross negligence, or recklessness.6 EMAC also provides reciprocity for individuals who are properly dispatched in response to an EMAC request who hold medical licenses to practice medicine in the receiving state, subject to any limitations imposed by the receiving state.4 Clinicians can familiarize themselves with a state’s medical licensing requirements by reviewing that state’s medical board website. For EMAC protections to apply, a state must make a request to another/other state(s) through EMAC, and such requests must be formally accepted by the rendering state.8 EMAC does not require participating states to actually provide aid.10
Non-volunteer health care clinicians
Non-volunteer (salaried or paid) health care clinicians are more likely to bear the brunt of providing care during a disaster, especially in the early stages before VHPs arrive; however, most legislation does not address the associated disproportionate liability risk burden of non-volunteer health care clinicians.1,11 As opposed to VHPs and government employees, non-volunteer health care clinicians performing their regular job duties during a disaster are generally not provided immunity from negligence by most legislation.1,6 One exception is the PREP Act, which provides immunity for all clinicians from claims that may arise from dispensing a specific countermeasure during a declared public health emergency.1,9 Some states have enacted the Model State Emergency Health Powers Act, which may offer immunity from negligence if the non-volunteer clinician is rendering care under contract with or at the request of a state1; however, non-volunteer clinicians who practice from their office or a local hospital will not receive protection through these laws.1 Good Samaritan laws may not apply unless care is provided at a scene of an emergency.
A few states have attempted to narrow this legislative gap by enacting laws that provide immunity more broadly for clinicians, regardless of their volunteer or compensation status.1 Elements of these states’ laws include acting in response to a declared emergency or disaster in which there is a recognized depletion of resources attributable to the disaster, at express or implied request of the state government, and consistent with emergency plans.1
Continue to: Bottom Line
Bottom Line
There are potential liability risks when treating patients during a disaster. Statutory protections that limit liability may be enacted when the US President or a state Governor declares an official state of emergency. Although some federal and state laws and regulations provide liability protections during these situations, there is a discrepancy in the protections offered to non-volunteer vs volunteer clinicians.
Related Resources
- Federal Emergency Management Agency. https://www.fema.gov/
- Federation of State Medical Boards. https://www.fsmb.org
Disasters—both natural and human-caused—can strike at any time, causing severe trauma for those impacted. Disasters may create circumstances where the need for mental health resources could exceed capacity, and hospitals and clinics would be unable to meet the needs of the affected communities. As psychiatric clinicians, we may want to provide our services in such situations; however, we are still at risk for civil, criminal, or constitutional liability claims against us if we fail to meet our legal obligations related to psychiatric practice. Ideally, whether we live and work in an area affected by a disaster or volunteer from other states, we should be able to care for patients without fear of facing unreasonable liability risks. Although an exhaustive list of all relevant federal and state laws and regulations is beyond the scope of this article, here I discuss some of the federal and state laws and regulations that could provide protection from these risks, and some limitations of liability protection.
A familiar list of liability concerns
From a liability perspective, what should we be aware of when practicing during disasters? The same liability concerns we have during our day-to-day practice also exist during disasters, especially when there are suboptimal or adverse outcomes.
Box
During disasters, changes in the usual standard of practice may be necessary to save as many lives as possible, and when resources are scarce, the focus of mental health services could shift from individualized patient care to those who are most in need. Examples of potential liability concerns clinicians may face in such situations include:
Negligence. Clinicians may have to provide emergent care for patients that may result in an adverse outcome. Examples include applying a tourniquet to a patient’s badly injured limb without their consent, and then that patient loses their limb, or administering the COVID-19 vaccine to a patient because of significant clinician shortages, and then that patient develops complications. These scenarios could possibly give rise to ordinary negligence claims of practicing outside the usual scope of practice, especially for a clinician who does not have liability protections.
Practicing without the proper state medical license. When out-of-state clinicians come to a facility that needs emergency assistance, they can face liability concerns for practicing without a properly recognized state medical license.1 Because care is deemed to have been provided where the patient was physically present when services were provided, liability can occur when providing services to patients in a state where the psychiatrist does not have a medical license. An example of this would be a psychiatrist in South Carolina who provides telehealth services to patients in a Florida community ravaged by a hurricane when the psychiatrist does not have a Florida medical license.
Abandonment. When we take a confirmatory step to provide care to an individual, it may create a clinician-patient relationship and a duty on behalf of the clinician within the applicable standard of care.2 With disasters, the customary expectations and parameters associated with clinician-patient relationships can change. We may have to cease treating some patients so that we can focus our time or resources elsewhere, which could open up liability concerns regarding claims of abandonment.1 At times, we may refuse to treat patients outright, creating conflicts with the Emergency Medical Treatment & Active Labor Act (EMTALA) and its state counterparts.
Liability protections
There are no comprehensive national liability protections for all practitioners during disasters.1 Limited immunity is often provided through a patchwork of federal and state laws and regulations, which can be complex and are often modified. This immunity depends on several factors, such as applicable regulations, the type of services that are provided, and whether the clinicians are volunteering their services (ie, they are not being paid for providing services).2 There is usually no immunity due to willful or wanton acts, gross negligence, providing care while intoxicated, or criminal acts.2
Federal laws and regulations
Most of the federal laws that provide liability protections are activated once a disaster is declared. However, some laws provide liability protections without requiring such declarations. Additional federal laws and regulations that provide additional liability protections, especially to volunteers, can be enacted after disasters occur.
Federal Tort Claims Act
The Federal Tort Claims Act (FTCA)3 protects federal government employees from tort liability by substituting the federal government as the defendant in certain types of suits brought against the federal government. These suits may involve injury, loss of personal property, personal injury, or death by the negligent or wrongful act or omission of any federal government employees while acting in the scope of their office or employment.3,4 It does not require that an emergency be declared before immunity is conferred. FTCA covers all federal government employees, including volunteers.4 In the context of an emergency response, volunteers can assert the liability protections afforded to federal employees if they are designated as unpaid employees of the federal government.4 Federal employees are immune from suit under state tort law.4
Volunteer Protection Act
The Volunteer Protection Act (VPA) of 19975 provides liability protections to uncompensated volunteer health professionals (VHPs) who perform services for nonprofit organizations or government entities against claims of ordinary negligence committed within the scope of their volunteer responsibilities.4 It does not require that an emergency be declared before immunity is conferred. Although VHPs are not liable for economic damages caused by providing medical care within the scope of their volunteer responsibilities, this exemption does not extend to non-economic damages, such as losses for suffering and mental anguish.5 VPA does not protect VHPs working in businesses (including for-profit hospitals) and organizational entities of any type (including nonprofit or governmental organizations) that use VHPs.4
VPA only protects VHPs practicing with a license as required by law in the state where the harm occurred, unless state authorities allow for licensure exceptions. VPA overrides state laws that are inconsistent with VPA, unless those state laws provide greater liability protection for VHPs.4 However, VPA protections are limited. VPA protects only volunteers, not clinicians working in their regular nonemergency roles and capacities.6 A nonprofit or government agent can still bring civil claims against VHPs.6 VPA does not override certain state laws that put conditions on volunteers, such as risk management requirements, vicarious liability, and a financially secure form of recovery for intended victims.6
Continue to: Health Insurance Portability and Accountability Act
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) of 1996,7 specifically Section 194, extends eligibility for FTCA liability protections to VHPs at qualifying free clinics, provided the clinic sponsors the VHPs by applying to the Health Resources and Services Administration.8 It does not require that an emergency be declared before immunity is conferred.
Public Readiness and Emergency Preparedness Act
The Public Readiness and Emergency Preparedness (PREP) Act of 20059 authorizes the US Department of Health and Human Services (HHS) Secretary to issue a declaration that provides immunity to VHPs from tort liability for claims of loss caused by the use of authorized countermeasures (eg, vaccines) against diseases or other threats of public health emergencies.4 A separate emergency determination under Public Health Service Act Section 319 or another statute is not required for PREP Act immunities to take effect.4 The PREP Act covers individual persons and entities involved in the manufacture, testing, distribution, administration, and use of covered countermeasures.4
PREP Act immunity is not absolute and does not protect against claims of willful misconduct, violation of the Americans with Disabilities Act (ADA), or other civil rights violations.4 Liability protection under the PREP Act is limited to a specific emergency and includes only the countermeasures and other conditions listed in the PREP Act declaration by the HHS Secretary.4
State laws and regulations
States have a variety of standing liability protections that could apply to VHPs who provide care in an emergency. Some states have crafted executive orders to be put into effect during a disaster. Most of these executive orders, which can include extending liability protections, are similar to what other states have done by adopting model acts such as Model State Emergency Health Powers Act.6 These orders are not actually laws; they only become effective when the governor signs them at the time of the disaster. These orders also are time-limited and must be reissued in subsequent disasters.
State tort claims acts and state claims acts
Similar to the federal government, some states have waived sovereign immunity in certain circumstances through state tort claims or state claims acts.
Continue to: State tort claims act
State tort claims acts either abolish state sovereign immunity generally and provide immunity only in specific circumstances, or preserve sovereign immunity generally but identify certain exceptions in which immunity is waived.4
State claims acts limit state sovereign immunity by establishing procedures for making claims against the state.4 These acts typically immunize state government employees from tort liability for acts or omissions committed within the scope of their employment.4 Some states extend these protections to volunteers, and some states declare volunteers to be unpaid state employees during an emergency, which allows volunteers to assert the liability protections afforded of state employees.4
Emergency power statutes
State emergency laws can trigger additional powers, suspend certain administrative requirements, and provide or enhance liability protections to specified groups of volunteers and other responders upon a gubernatorial declaration of emergency.4 These statutes can extend the rights and immunities provided to governmental employees to volunteers performing work that is eligible for coverage under governmental immunity and state tort claims acts.4 There is a wide range in the types and degrees of coverage provided to volunteers under emergency powers statutes, and these provisions can be broad or duplicative of other provisions in state law.4
State volunteer protection statutes
All states have some statutory provisions for volunteers. Similar to the VPA, these state volunteer protection statutes generally do not require that an emergency be declared, apply to uncompensated individual volunteers for nonprofit and government entities only, and apply only to individuals and not to organizations.4 Many states have adopted specific liability protections for VHPs in addition to or to supplement their emergency powers and general volunteer protection statutes.4 These statutes confer immunity from civil liability provided that certain conditions are met and are not dependent on the declaration of an emergency.4 Each state statute differs in regard to who receives immunity, which acts are immune from liability, and what liability protections are available.
Good Samaritan laws
All 50 states and the District of Columbia have enacted Good Samaritan laws. These laws, which do not need an official declaration of an emergency in order to be applicable, generally protect VHPs from liability when volunteering in good faith and without compensation at the scene of an emergency.2 Good Samaritan protections may also apply to care provided by VHPs in a hospital if the VHP is not on duty and does not charge a fee.2 However, the effect and scope of Good Samaritan laws vary dramatically from state to state. Some states include hospital settings as an emergency scene in their statutes, while others expressly exclude hospitals from their statutes.6 Some state statutes only include declared emergencies, while others are drawn to broadly cover all emergency situations.6
Continue to: Limitations
Limitations. Many Good Samaritan statutes apply only to volunteers, and not all states have statutes that allow clinicians to be designated as such,6 so receiving compensation would take a clinician outside the scope of the statute. Further, most states only shield action taken at the scene of an accident, and immunity would not extend to a hospital emergency department, or in the aftermath of an emergency as normal conditions slowly return.6 Therefore, Good Samaritan liability protection would apply to the common scenario of assisting at the scene of a car crash, but not necessarily to treating individuals in the emergency department after a hurricane or during a pandemic.6 State laws vary considerably on what constitutes “good faith” and “without compensation,” which would determine whether protection applies for a clinician who is otherwise salaried in a regular job.1
Mutual aid agreements
Mutual aid agreements are mechanisms through which jurisdictions can aid other jurisdictions during emergencies.4 These agreements also include provisions for reimbursing expenses, providing liability protections to governmental employees and volunteers who provide aid, and awarding compensation for injuries to personnel deployed under the agreement.4 These protections are not automatic and are limited in their applicability.
The Emergency Management Assistance Compact (EMAC), the most widely adopted mutual aid agreement in the United States, has been adopted by all 50 states, the District of Columbia, and some territories.10 It only becomes effective once an emergency has been declared. EMAC provides immunity to officers from the state that is rendering aid to the state requesting aid, in which officers are considered agents of the requesting state for tort liability and immunity purposes.8 These individuals, who must be properly dispatched in response to an EMAC request, are not to be held liable for acts or omissions rendered in good faith; however, EMAC does not provide liability protection for actions constituting willful misconduct, gross negligence, or recklessness.6 EMAC also provides reciprocity for individuals who are properly dispatched in response to an EMAC request who hold medical licenses to practice medicine in the receiving state, subject to any limitations imposed by the receiving state.4 Clinicians can familiarize themselves with a state’s medical licensing requirements by reviewing that state’s medical board website. For EMAC protections to apply, a state must make a request to another/other state(s) through EMAC, and such requests must be formally accepted by the rendering state.8 EMAC does not require participating states to actually provide aid.10
Non-volunteer health care clinicians
Non-volunteer (salaried or paid) health care clinicians are more likely to bear the brunt of providing care during a disaster, especially in the early stages before VHPs arrive; however, most legislation does not address the associated disproportionate liability risk burden of non-volunteer health care clinicians.1,11 As opposed to VHPs and government employees, non-volunteer health care clinicians performing their regular job duties during a disaster are generally not provided immunity from negligence by most legislation.1,6 One exception is the PREP Act, which provides immunity for all clinicians from claims that may arise from dispensing a specific countermeasure during a declared public health emergency.1,9 Some states have enacted the Model State Emergency Health Powers Act, which may offer immunity from negligence if the non-volunteer clinician is rendering care under contract with or at the request of a state1; however, non-volunteer clinicians who practice from their office or a local hospital will not receive protection through these laws.1 Good Samaritan laws may not apply unless care is provided at a scene of an emergency.
A few states have attempted to narrow this legislative gap by enacting laws that provide immunity more broadly for clinicians, regardless of their volunteer or compensation status.1 Elements of these states’ laws include acting in response to a declared emergency or disaster in which there is a recognized depletion of resources attributable to the disaster, at express or implied request of the state government, and consistent with emergency plans.1
Continue to: Bottom Line
Bottom Line
There are potential liability risks when treating patients during a disaster. Statutory protections that limit liability may be enacted when the US President or a state Governor declares an official state of emergency. Although some federal and state laws and regulations provide liability protections during these situations, there is a discrepancy in the protections offered to non-volunteer vs volunteer clinicians.
Related Resources
- Federal Emergency Management Agency. https://www.fema.gov/
- Federation of State Medical Boards. https://www.fsmb.org
1. Altman RL, Santucci KA, Anderson MR, et al. American Academy of Pediatrics Committee on Medical Liability and Risk Management. Understanding liability risks and protections for pediatric providers during disasters. Pediatrics. 2019;143(3):e20183893. doi.org/10.1542/peds.2018-3892
2. Lambert K, Wertheimer M. American Professional Agency: Risk management in disaster response. Published September 2017. Accessed May 25, 2021. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/disaster/resource_group/resources/orgs/RMDisasterResp.pdf
3. Federal Torts Claims Act, as amended. Codified at 28 USC. §1346 (1946).
4. Association of State and Territorial Health Officials (ASTHO). Liability, immunity, and workers’ compensation issue in public health emergencies. Published 2012. Accessed May 25, 2021. https://www.astho.org/Programs/Preparedness/Public-Health-Emergency-Law/Emergency-Authority-and-Immunity-Toolkit/Liability,-Immunity,-and-Workers%E2%80%99-Compensation-Issues-in-Public-Health-Emergencies-Issue-Brief/
5. Volunteer Protection Act of 1997. Pub. L. 105-19, 111 Stat. 221.
6. Pope TM, Palazzo MF. Legal briefing: crisis standards of care and legal protections during disasters and emergencies. J Clin Ethics. 2010;21(4):358-367.
7. Health Insurance Portability and Accountability Act of 1996. Pub. L. 104-191, 110 Stat. 1936. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf
8. American Medical Association. Liability protections for health care professionals during COVID-19. Updated April 8, 2020. Accessed May 25, 2021. https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19
9. Public Readiness and Emergency Preparedness Act of 2005. Pub. L. 109-148, 119 Stat. 2818. https://www.govinfo.gov/content/pkg/PLAW-109publ148/html/PLAW-109publ148.htm
10. Emergency Management Assistance Compact (EMAC). Accessed May 25, 2021. https://www.emacweb.org/
11. Hodge JG, Garcia AM, Anderson ED, et al. Emergency legal preparedness for hospitals and health care personnel. Disaster Med Public Health Prep. 2009;3(2 Supplement):S37-S44. doi: 10.1097/DMP.0b013e31819d977c
1. Altman RL, Santucci KA, Anderson MR, et al. American Academy of Pediatrics Committee on Medical Liability and Risk Management. Understanding liability risks and protections for pediatric providers during disasters. Pediatrics. 2019;143(3):e20183893. doi.org/10.1542/peds.2018-3892
2. Lambert K, Wertheimer M. American Professional Agency: Risk management in disaster response. Published September 2017. Accessed May 25, 2021. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/disaster/resource_group/resources/orgs/RMDisasterResp.pdf
3. Federal Torts Claims Act, as amended. Codified at 28 USC. §1346 (1946).
4. Association of State and Territorial Health Officials (ASTHO). Liability, immunity, and workers’ compensation issue in public health emergencies. Published 2012. Accessed May 25, 2021. https://www.astho.org/Programs/Preparedness/Public-Health-Emergency-Law/Emergency-Authority-and-Immunity-Toolkit/Liability,-Immunity,-and-Workers%E2%80%99-Compensation-Issues-in-Public-Health-Emergencies-Issue-Brief/
5. Volunteer Protection Act of 1997. Pub. L. 105-19, 111 Stat. 221.
6. Pope TM, Palazzo MF. Legal briefing: crisis standards of care and legal protections during disasters and emergencies. J Clin Ethics. 2010;21(4):358-367.
7. Health Insurance Portability and Accountability Act of 1996. Pub. L. 104-191, 110 Stat. 1936. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf
8. American Medical Association. Liability protections for health care professionals during COVID-19. Updated April 8, 2020. Accessed May 25, 2021. https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19
9. Public Readiness and Emergency Preparedness Act of 2005. Pub. L. 109-148, 119 Stat. 2818. https://www.govinfo.gov/content/pkg/PLAW-109publ148/html/PLAW-109publ148.htm
10. Emergency Management Assistance Compact (EMAC). Accessed May 25, 2021. https://www.emacweb.org/
11. Hodge JG, Garcia AM, Anderson ED, et al. Emergency legal preparedness for hospitals and health care personnel. Disaster Med Public Health Prep. 2009;3(2 Supplement):S37-S44. doi: 10.1097/DMP.0b013e31819d977c
The challenge of ‘holding space’ while holding the pager
At morning shift change a few months ago on my consultation-liaison rotation, I thanked the night float resident who had been called to a case that was not at all psychiatrically acute. When I told my colleague I was sorry she had had such a “soft consult” during a busy shift, she graciously replied that the patient had been exceedingly pleasant. She said, “Sometimes we just offer our presence, and you know what? I’m glad I’m in that kind of field. The ‘being-present’ kind of field.”
As mental health professionals, we pride ourselves on being present for our patients and our colleagues alike. Winnicott1 originally coined the psychoanalytic term “holding” to denote one of the earliest stages of parental care, wherein an environment of both physical and emotional reliability allows a child to develop their sense of self. The complementary concept of “containing,” developed by Bion,2 indicates a parental figure’s receiving the child’s emotions, however difficult, and then processing them into a more tolerable form. I am frequently struck by how often our role as psychiatrists is not necessarily to offer a specific diagnosis or medication recommendation, but instead to “hold” by listening, “contain” whatever emotions emerge, and offer a sense of validation and perhaps a biopsychosocial formulation for the patient’s experience.3-5 In the consultation-liaison setting, we might assess the contribution of sleep cycle disturbance, postoperative opioids, and anticholinergic medications on a patient’s mental status. Just as important, we might help the patient and their primary team understand that the patient’s history of childhood trauma could, under stressful conditions such as a prolonged hospitalization, lead to affective dysregulation and result in projective identification through which the team felt just as frustrated and helpless as the patient.
The relentless pursuit of efficiency vs time spent with patients
In inpatient work, I may serve as short-term psychotherapist for the patient, their family members, or a consulting team, and I treasure the time spent in those roles. But I concurrently hold various other responsibilities during my shift, including the roles of triage clinician, medical ethicist, and psychopharmacology expert (or, in the case of a newly-third-year resident such as myself, a nonexpert trying to build her knowledge base). I am also literally holding a pager, which intrudes—with aggressive cacophony, vibration, or both—upon the sanctity of any space. The pager is a reminder of a myriad of tasks: calling collateral, answering questions from team members, pre-charting, note-writing, ordering labs, checking labs, updating the handoff, reconciling medication lists, filling out legal paperwork, triaging the next consult. These are unavoidable and generally necessary parts of clinical work, but sometimes they veer into sheer drudgery.
As a medical student, learning to complete tasks is a substantial part of each clinical rotation, and task completion provides plenty of dopaminergic reinforcements that could masquerade as job satisfaction. Through my first year and a half of residency, I pushed hard to build “efficiency” in my workflow, but eventually, task completion stopped providing sufficient inherent satisfaction. It has been a relief to find that amid the stream of checkboxes, the true work of psychiatric care (the interactions with patients, their clinical presentations, and considering their differential diagnoses and treatment options) feels deeply meaningful and ever more fascinating.
At times, I am angered by the reality of limited clinician bandwidth. This frustration motivates me to seek system-level improvements that can enable us to deliver quality psychiatric care while mitigating the risk of clinician burnout. What ends up shortchanged in the relentless pursuit of efficiency is the time spent with patients. This is never more apparent than during a busy inpatient shift, when I often need to compress patient interactions and focus only on the most acute clinical questions. When I have to apologize for stepping out of the interview room to answer yet another page, I marvel at seeing attending psychiatrists who—with apparent ease—make patients feel as if they have all the time in the world, and I wonder when I will be able to do the same.
And yet, there are other times when my pager stays blessedly quiet, time can slow down in the room, and I can make a patient feel heard, held, and contained. In those moments, I also hold my own need for connection with the patient, and can recall what my colleague reminded me: what a privilege it is to be in the “being-present” kind of field.
1. Winnicott DW. The theory of the parent-infant relationship. Int J Psychoanal. 1961;41:585-595.
2. Bion WR. Learning from experience. William Heinemann Medical Books; 1962.
3. Green SA. Psychotherapeutic principles and techniques: principles of medical psychotherapy. In: Fogel BS, Greenberg DB, eds. Psychiatric care of the medical patient. 3rd ed. Oxford University Press; 2015:191-204.
4. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109-116. doi:10.1176/appi.psy.46.2.109
5. Nash SS, Kent LK, Muskin PR. Psychodynamics in medically ill patients. Harv Rev Psychiatry. 2009;17(6):389-397. doi:10.3109/10673220903465726
At morning shift change a few months ago on my consultation-liaison rotation, I thanked the night float resident who had been called to a case that was not at all psychiatrically acute. When I told my colleague I was sorry she had had such a “soft consult” during a busy shift, she graciously replied that the patient had been exceedingly pleasant. She said, “Sometimes we just offer our presence, and you know what? I’m glad I’m in that kind of field. The ‘being-present’ kind of field.”
As mental health professionals, we pride ourselves on being present for our patients and our colleagues alike. Winnicott1 originally coined the psychoanalytic term “holding” to denote one of the earliest stages of parental care, wherein an environment of both physical and emotional reliability allows a child to develop their sense of self. The complementary concept of “containing,” developed by Bion,2 indicates a parental figure’s receiving the child’s emotions, however difficult, and then processing them into a more tolerable form. I am frequently struck by how often our role as psychiatrists is not necessarily to offer a specific diagnosis or medication recommendation, but instead to “hold” by listening, “contain” whatever emotions emerge, and offer a sense of validation and perhaps a biopsychosocial formulation for the patient’s experience.3-5 In the consultation-liaison setting, we might assess the contribution of sleep cycle disturbance, postoperative opioids, and anticholinergic medications on a patient’s mental status. Just as important, we might help the patient and their primary team understand that the patient’s history of childhood trauma could, under stressful conditions such as a prolonged hospitalization, lead to affective dysregulation and result in projective identification through which the team felt just as frustrated and helpless as the patient.
The relentless pursuit of efficiency vs time spent with patients
In inpatient work, I may serve as short-term psychotherapist for the patient, their family members, or a consulting team, and I treasure the time spent in those roles. But I concurrently hold various other responsibilities during my shift, including the roles of triage clinician, medical ethicist, and psychopharmacology expert (or, in the case of a newly-third-year resident such as myself, a nonexpert trying to build her knowledge base). I am also literally holding a pager, which intrudes—with aggressive cacophony, vibration, or both—upon the sanctity of any space. The pager is a reminder of a myriad of tasks: calling collateral, answering questions from team members, pre-charting, note-writing, ordering labs, checking labs, updating the handoff, reconciling medication lists, filling out legal paperwork, triaging the next consult. These are unavoidable and generally necessary parts of clinical work, but sometimes they veer into sheer drudgery.
As a medical student, learning to complete tasks is a substantial part of each clinical rotation, and task completion provides plenty of dopaminergic reinforcements that could masquerade as job satisfaction. Through my first year and a half of residency, I pushed hard to build “efficiency” in my workflow, but eventually, task completion stopped providing sufficient inherent satisfaction. It has been a relief to find that amid the stream of checkboxes, the true work of psychiatric care (the interactions with patients, their clinical presentations, and considering their differential diagnoses and treatment options) feels deeply meaningful and ever more fascinating.
At times, I am angered by the reality of limited clinician bandwidth. This frustration motivates me to seek system-level improvements that can enable us to deliver quality psychiatric care while mitigating the risk of clinician burnout. What ends up shortchanged in the relentless pursuit of efficiency is the time spent with patients. This is never more apparent than during a busy inpatient shift, when I often need to compress patient interactions and focus only on the most acute clinical questions. When I have to apologize for stepping out of the interview room to answer yet another page, I marvel at seeing attending psychiatrists who—with apparent ease—make patients feel as if they have all the time in the world, and I wonder when I will be able to do the same.
And yet, there are other times when my pager stays blessedly quiet, time can slow down in the room, and I can make a patient feel heard, held, and contained. In those moments, I also hold my own need for connection with the patient, and can recall what my colleague reminded me: what a privilege it is to be in the “being-present” kind of field.
At morning shift change a few months ago on my consultation-liaison rotation, I thanked the night float resident who had been called to a case that was not at all psychiatrically acute. When I told my colleague I was sorry she had had such a “soft consult” during a busy shift, she graciously replied that the patient had been exceedingly pleasant. She said, “Sometimes we just offer our presence, and you know what? I’m glad I’m in that kind of field. The ‘being-present’ kind of field.”
As mental health professionals, we pride ourselves on being present for our patients and our colleagues alike. Winnicott1 originally coined the psychoanalytic term “holding” to denote one of the earliest stages of parental care, wherein an environment of both physical and emotional reliability allows a child to develop their sense of self. The complementary concept of “containing,” developed by Bion,2 indicates a parental figure’s receiving the child’s emotions, however difficult, and then processing them into a more tolerable form. I am frequently struck by how often our role as psychiatrists is not necessarily to offer a specific diagnosis or medication recommendation, but instead to “hold” by listening, “contain” whatever emotions emerge, and offer a sense of validation and perhaps a biopsychosocial formulation for the patient’s experience.3-5 In the consultation-liaison setting, we might assess the contribution of sleep cycle disturbance, postoperative opioids, and anticholinergic medications on a patient’s mental status. Just as important, we might help the patient and their primary team understand that the patient’s history of childhood trauma could, under stressful conditions such as a prolonged hospitalization, lead to affective dysregulation and result in projective identification through which the team felt just as frustrated and helpless as the patient.
The relentless pursuit of efficiency vs time spent with patients
In inpatient work, I may serve as short-term psychotherapist for the patient, their family members, or a consulting team, and I treasure the time spent in those roles. But I concurrently hold various other responsibilities during my shift, including the roles of triage clinician, medical ethicist, and psychopharmacology expert (or, in the case of a newly-third-year resident such as myself, a nonexpert trying to build her knowledge base). I am also literally holding a pager, which intrudes—with aggressive cacophony, vibration, or both—upon the sanctity of any space. The pager is a reminder of a myriad of tasks: calling collateral, answering questions from team members, pre-charting, note-writing, ordering labs, checking labs, updating the handoff, reconciling medication lists, filling out legal paperwork, triaging the next consult. These are unavoidable and generally necessary parts of clinical work, but sometimes they veer into sheer drudgery.
As a medical student, learning to complete tasks is a substantial part of each clinical rotation, and task completion provides plenty of dopaminergic reinforcements that could masquerade as job satisfaction. Through my first year and a half of residency, I pushed hard to build “efficiency” in my workflow, but eventually, task completion stopped providing sufficient inherent satisfaction. It has been a relief to find that amid the stream of checkboxes, the true work of psychiatric care (the interactions with patients, their clinical presentations, and considering their differential diagnoses and treatment options) feels deeply meaningful and ever more fascinating.
At times, I am angered by the reality of limited clinician bandwidth. This frustration motivates me to seek system-level improvements that can enable us to deliver quality psychiatric care while mitigating the risk of clinician burnout. What ends up shortchanged in the relentless pursuit of efficiency is the time spent with patients. This is never more apparent than during a busy inpatient shift, when I often need to compress patient interactions and focus only on the most acute clinical questions. When I have to apologize for stepping out of the interview room to answer yet another page, I marvel at seeing attending psychiatrists who—with apparent ease—make patients feel as if they have all the time in the world, and I wonder when I will be able to do the same.
And yet, there are other times when my pager stays blessedly quiet, time can slow down in the room, and I can make a patient feel heard, held, and contained. In those moments, I also hold my own need for connection with the patient, and can recall what my colleague reminded me: what a privilege it is to be in the “being-present” kind of field.
1. Winnicott DW. The theory of the parent-infant relationship. Int J Psychoanal. 1961;41:585-595.
2. Bion WR. Learning from experience. William Heinemann Medical Books; 1962.
3. Green SA. Psychotherapeutic principles and techniques: principles of medical psychotherapy. In: Fogel BS, Greenberg DB, eds. Psychiatric care of the medical patient. 3rd ed. Oxford University Press; 2015:191-204.
4. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109-116. doi:10.1176/appi.psy.46.2.109
5. Nash SS, Kent LK, Muskin PR. Psychodynamics in medically ill patients. Harv Rev Psychiatry. 2009;17(6):389-397. doi:10.3109/10673220903465726
1. Winnicott DW. The theory of the parent-infant relationship. Int J Psychoanal. 1961;41:585-595.
2. Bion WR. Learning from experience. William Heinemann Medical Books; 1962.
3. Green SA. Psychotherapeutic principles and techniques: principles of medical psychotherapy. In: Fogel BS, Greenberg DB, eds. Psychiatric care of the medical patient. 3rd ed. Oxford University Press; 2015:191-204.
4. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109-116. doi:10.1176/appi.psy.46.2.109
5. Nash SS, Kent LK, Muskin PR. Psychodynamics in medically ill patients. Harv Rev Psychiatry. 2009;17(6):389-397. doi:10.3109/10673220903465726
From ideology to articles of faith: The ‘religification’ of political beliefs
Man is a political animal.
— Aristotle, Politics , Book 1, Section 1253a
Religion is the opium of the people.
— Karl Marx, A contribution to the critique of Hegel’s philosophy of right , introduction
Beliefs are at the core of psychiatric practice. Our patients are often shackled by their anomalous beliefs, which are not reality-based. These beliefs are often the primary targets of psychiatric treatment. Consider a day at the office of a psychiatrist who may see several patients impaired by false beliefs, such as:
- My neighbor is reading my mind remotely and is plotting to kill me
- If I ride on a plane, it will crash and I will die
- I am a failure, a worthless person, and a burden on my family
- I am hopeless and helpless; life is too painful and not worth living anymore
- I am a prophet with supernatural gifts, and I can predict the future
- Whenever I take this substance, I feel I can jump out of a window and fly
- If I do not shower 5 times in a row every night before going to bed, something terrible will happen to my family.
Patients with false beliefs obviously need psychiatric care. However, a large number of religious individuals harbor “unusual” beliefs involving angels and devils and hell and paradise after death. Those people of faith are not considered to have a DSM-5 psychiatric disorder. Billions of people around the world belong to one of the approximately 4,300 religions, which they celebrate using one of the more than 6,800 living languages. Psychiatrists encourage patients to have a faith because it can be quite comforting to its adherents, enhancing their social relations and providing them with hope and resilience during the darkest days of life. Regular attendance at a house of worship is a measure of the strong roots of one’s faith.
So why have there been so many religious wars over centuries of recorded history? Why have millions of people died during conflicts among religions? Why does one religious group adamantly believe that theirs is the real God, while the god of other religions is fake? And why have people who withdrew from or refused to adopt a certain religious belief been persecuted; labeled as “heretic,” “infidel,” “heathen,” or “apostate”; and burned at the stake or beheaded? Perhaps religion is not always a kinder, gentler belief system.
Continue to: Recent statistics...
Recent statistics show a precipitous decline in religious observance in the United States.1 So what happens to a society that gradually abandons its previously entrenched religious beliefs and becomes secular? This trend is spreading widely in Europe and North America. But widely held beliefs with powerful personal meaning don’t just fizzle away: they re-emerge in another form. The substantial energy of religious faith must be invested elsewhere and manifested in an alternative form with similar dynamics.
Enter politics!
It seems that humans’ need to uphold a strong belief is so powerful that they either incorporate political doctrines side-by-side with their religious beliefs (if the 2 are compatible) or adopt a strong political belief if they abandon their religion and become secular. This does not have to be an intellectually wrenching change because there are many similarities between hyper-religiosity and fanatic political beliefs (Table).
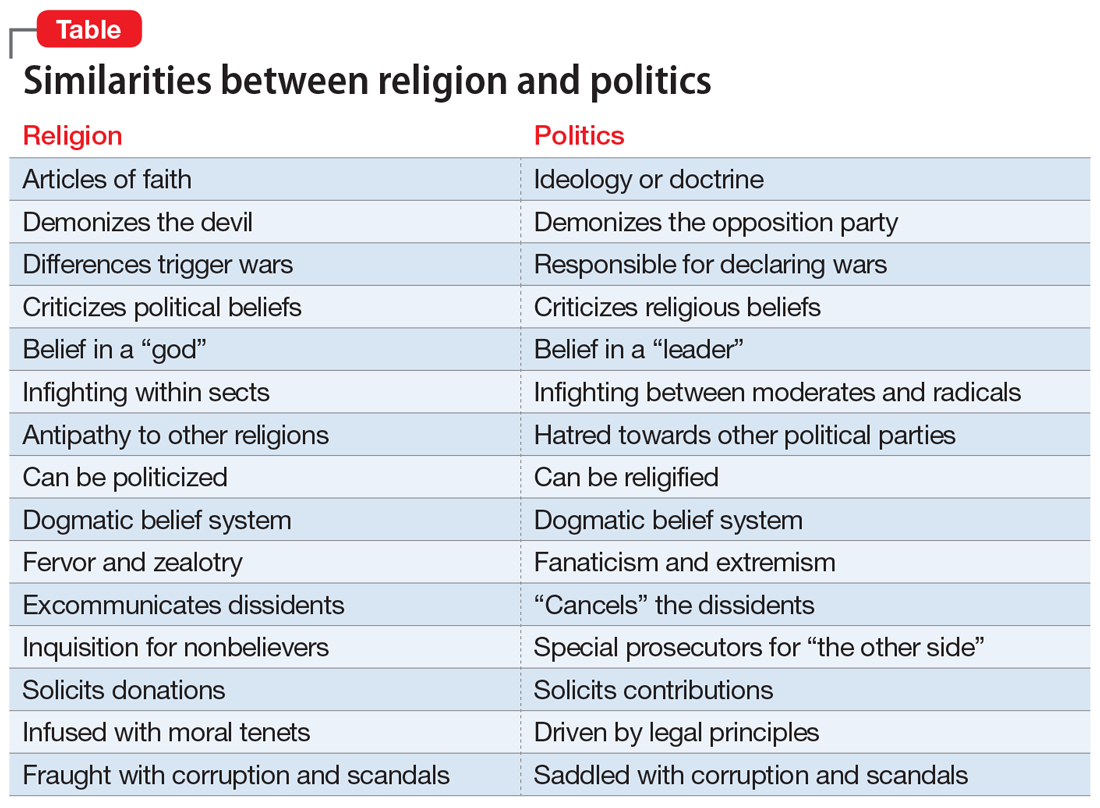
The toxic hyperpartisanship that has dominated the United States over the past several years may be the culmination of an intensified “religification” of politics. The incendiary mix of religious zealotry and political fanaticism is conducive to intensified loathing, hostility, and animus to those with an opposing political ideology.
So it all boils down to the human imperative of harboring a strong personal belief. What is the origin of beliefs, religious, political, or otherwise? Why does the human species have the overwhelming need to uphold a belief? Research suggests that it is the result of evolution and the phylogenetic enlargement of the brain, including the parietal and medial frontal cortex in humans.2 And according to many studies, abnormal and delusional beliefs encountered in psychiatric practice appear to be caused by altered perception and/or misattribution of aversive meaning.3 Lesions in the right hemisphere have been reported to play an important role in generating delusional beliefs.4 A healthy right hemisphere plays an important role in:
- pragmatic communications
- perceptual integration
- attentional surveillance and anomaly novelty detection
- belief updating.4
Right hemispheric pathology disrupts those functions and can lead to false beliefs such as delusions, or, on a milder scale, strongly held superstitions.
One wonders how the structure and function of the right hemisphere generates and perpetuates a belief in a religion or political ideology that ultimately shapes one’s life. Religiosity and politics are an inherent part of human nature, and they can replace each other or merge together. If one is to believe what Durkheim5 proposed more than a century ago, the existence of belief systems is essential for societal stability. He posited that the absence of stable belief systems can lead to what he labeled “anomie,” leading to a surge of suicide and crime. If that is true, then the coexistence of religious and political beliefs may have a significant upside, but also with a palpable downside when either or both of those belief systems become excessively antagonistic or extreme. Three cheers for religious and political moderation that allows them to peacefully coexist.
1. Jones JM. U.S. church membership falls below majority for first time. Gallup. March 29, 2021. Accessed June 7, 2021. https://news.gallup.com/poll/341963/church-membership-falls-below-majority-first-time.aspx
2. Seitz RJ, Angel HF. Belief formation—a driving force for brain evolution. Brain Cogn. 2020;140:105548. doi: 10.1016/j.bandc.2020.105548
3. Seitz RJ. Beliefs: a challenge in neuropsychological disorders. J Neuropsychol. 2021. doi: 10.1111/jnp.12249
4. Gurin L, Blum S. Delusions and the right hemisphere: a review of the case for the right hemisphere as a mediator of reality-based belief. J Neuropsychiatry Clin Neurosci. 2017;29(3):225-235. doi: 10.1176/appi.neuropsych.16060118
5. Durkheim E. Suicide: a study in sociology. The Free Press; 1951.
Man is a political animal.
— Aristotle, Politics , Book 1, Section 1253a
Religion is the opium of the people.
— Karl Marx, A contribution to the critique of Hegel’s philosophy of right , introduction
Beliefs are at the core of psychiatric practice. Our patients are often shackled by their anomalous beliefs, which are not reality-based. These beliefs are often the primary targets of psychiatric treatment. Consider a day at the office of a psychiatrist who may see several patients impaired by false beliefs, such as:
- My neighbor is reading my mind remotely and is plotting to kill me
- If I ride on a plane, it will crash and I will die
- I am a failure, a worthless person, and a burden on my family
- I am hopeless and helpless; life is too painful and not worth living anymore
- I am a prophet with supernatural gifts, and I can predict the future
- Whenever I take this substance, I feel I can jump out of a window and fly
- If I do not shower 5 times in a row every night before going to bed, something terrible will happen to my family.
Patients with false beliefs obviously need psychiatric care. However, a large number of religious individuals harbor “unusual” beliefs involving angels and devils and hell and paradise after death. Those people of faith are not considered to have a DSM-5 psychiatric disorder. Billions of people around the world belong to one of the approximately 4,300 religions, which they celebrate using one of the more than 6,800 living languages. Psychiatrists encourage patients to have a faith because it can be quite comforting to its adherents, enhancing their social relations and providing them with hope and resilience during the darkest days of life. Regular attendance at a house of worship is a measure of the strong roots of one’s faith.
So why have there been so many religious wars over centuries of recorded history? Why have millions of people died during conflicts among religions? Why does one religious group adamantly believe that theirs is the real God, while the god of other religions is fake? And why have people who withdrew from or refused to adopt a certain religious belief been persecuted; labeled as “heretic,” “infidel,” “heathen,” or “apostate”; and burned at the stake or beheaded? Perhaps religion is not always a kinder, gentler belief system.
Continue to: Recent statistics...
Recent statistics show a precipitous decline in religious observance in the United States.1 So what happens to a society that gradually abandons its previously entrenched religious beliefs and becomes secular? This trend is spreading widely in Europe and North America. But widely held beliefs with powerful personal meaning don’t just fizzle away: they re-emerge in another form. The substantial energy of religious faith must be invested elsewhere and manifested in an alternative form with similar dynamics.
Enter politics!
It seems that humans’ need to uphold a strong belief is so powerful that they either incorporate political doctrines side-by-side with their religious beliefs (if the 2 are compatible) or adopt a strong political belief if they abandon their religion and become secular. This does not have to be an intellectually wrenching change because there are many similarities between hyper-religiosity and fanatic political beliefs (Table).
The toxic hyperpartisanship that has dominated the United States over the past several years may be the culmination of an intensified “religification” of politics. The incendiary mix of religious zealotry and political fanaticism is conducive to intensified loathing, hostility, and animus to those with an opposing political ideology.
So it all boils down to the human imperative of harboring a strong personal belief. What is the origin of beliefs, religious, political, or otherwise? Why does the human species have the overwhelming need to uphold a belief? Research suggests that it is the result of evolution and the phylogenetic enlargement of the brain, including the parietal and medial frontal cortex in humans.2 And according to many studies, abnormal and delusional beliefs encountered in psychiatric practice appear to be caused by altered perception and/or misattribution of aversive meaning.3 Lesions in the right hemisphere have been reported to play an important role in generating delusional beliefs.4 A healthy right hemisphere plays an important role in:
- pragmatic communications
- perceptual integration
- attentional surveillance and anomaly novelty detection
- belief updating.4
Right hemispheric pathology disrupts those functions and can lead to false beliefs such as delusions, or, on a milder scale, strongly held superstitions.
One wonders how the structure and function of the right hemisphere generates and perpetuates a belief in a religion or political ideology that ultimately shapes one’s life. Religiosity and politics are an inherent part of human nature, and they can replace each other or merge together. If one is to believe what Durkheim5 proposed more than a century ago, the existence of belief systems is essential for societal stability. He posited that the absence of stable belief systems can lead to what he labeled “anomie,” leading to a surge of suicide and crime. If that is true, then the coexistence of religious and political beliefs may have a significant upside, but also with a palpable downside when either or both of those belief systems become excessively antagonistic or extreme. Three cheers for religious and political moderation that allows them to peacefully coexist.
Man is a political animal.
— Aristotle, Politics , Book 1, Section 1253a
Religion is the opium of the people.
— Karl Marx, A contribution to the critique of Hegel’s philosophy of right , introduction
Beliefs are at the core of psychiatric practice. Our patients are often shackled by their anomalous beliefs, which are not reality-based. These beliefs are often the primary targets of psychiatric treatment. Consider a day at the office of a psychiatrist who may see several patients impaired by false beliefs, such as:
- My neighbor is reading my mind remotely and is plotting to kill me
- If I ride on a plane, it will crash and I will die
- I am a failure, a worthless person, and a burden on my family
- I am hopeless and helpless; life is too painful and not worth living anymore
- I am a prophet with supernatural gifts, and I can predict the future
- Whenever I take this substance, I feel I can jump out of a window and fly
- If I do not shower 5 times in a row every night before going to bed, something terrible will happen to my family.
Patients with false beliefs obviously need psychiatric care. However, a large number of religious individuals harbor “unusual” beliefs involving angels and devils and hell and paradise after death. Those people of faith are not considered to have a DSM-5 psychiatric disorder. Billions of people around the world belong to one of the approximately 4,300 religions, which they celebrate using one of the more than 6,800 living languages. Psychiatrists encourage patients to have a faith because it can be quite comforting to its adherents, enhancing their social relations and providing them with hope and resilience during the darkest days of life. Regular attendance at a house of worship is a measure of the strong roots of one’s faith.
So why have there been so many religious wars over centuries of recorded history? Why have millions of people died during conflicts among religions? Why does one religious group adamantly believe that theirs is the real God, while the god of other religions is fake? And why have people who withdrew from or refused to adopt a certain religious belief been persecuted; labeled as “heretic,” “infidel,” “heathen,” or “apostate”; and burned at the stake or beheaded? Perhaps religion is not always a kinder, gentler belief system.
Continue to: Recent statistics...
Recent statistics show a precipitous decline in religious observance in the United States.1 So what happens to a society that gradually abandons its previously entrenched religious beliefs and becomes secular? This trend is spreading widely in Europe and North America. But widely held beliefs with powerful personal meaning don’t just fizzle away: they re-emerge in another form. The substantial energy of religious faith must be invested elsewhere and manifested in an alternative form with similar dynamics.
Enter politics!
It seems that humans’ need to uphold a strong belief is so powerful that they either incorporate political doctrines side-by-side with their religious beliefs (if the 2 are compatible) or adopt a strong political belief if they abandon their religion and become secular. This does not have to be an intellectually wrenching change because there are many similarities between hyper-religiosity and fanatic political beliefs (Table).
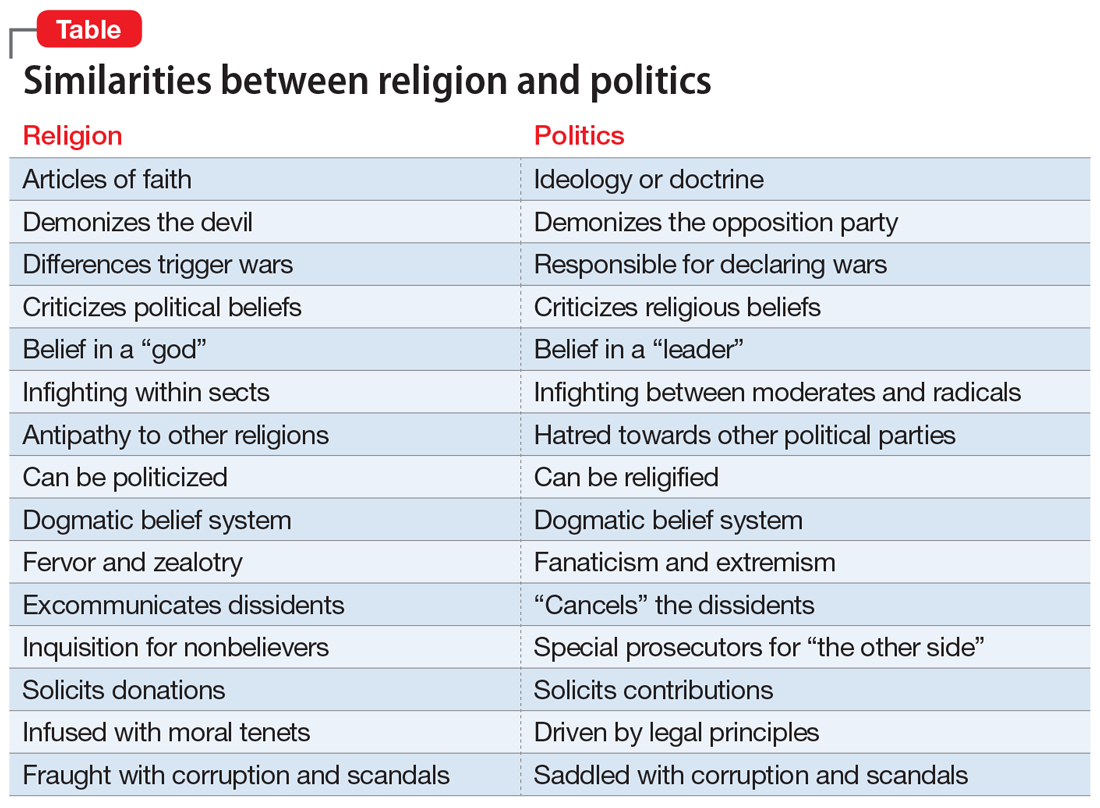
The toxic hyperpartisanship that has dominated the United States over the past several years may be the culmination of an intensified “religification” of politics. The incendiary mix of religious zealotry and political fanaticism is conducive to intensified loathing, hostility, and animus to those with an opposing political ideology.
So it all boils down to the human imperative of harboring a strong personal belief. What is the origin of beliefs, religious, political, or otherwise? Why does the human species have the overwhelming need to uphold a belief? Research suggests that it is the result of evolution and the phylogenetic enlargement of the brain, including the parietal and medial frontal cortex in humans.2 And according to many studies, abnormal and delusional beliefs encountered in psychiatric practice appear to be caused by altered perception and/or misattribution of aversive meaning.3 Lesions in the right hemisphere have been reported to play an important role in generating delusional beliefs.4 A healthy right hemisphere plays an important role in:
- pragmatic communications
- perceptual integration
- attentional surveillance and anomaly novelty detection
- belief updating.4
Right hemispheric pathology disrupts those functions and can lead to false beliefs such as delusions, or, on a milder scale, strongly held superstitions.
One wonders how the structure and function of the right hemisphere generates and perpetuates a belief in a religion or political ideology that ultimately shapes one’s life. Religiosity and politics are an inherent part of human nature, and they can replace each other or merge together. If one is to believe what Durkheim5 proposed more than a century ago, the existence of belief systems is essential for societal stability. He posited that the absence of stable belief systems can lead to what he labeled “anomie,” leading to a surge of suicide and crime. If that is true, then the coexistence of religious and political beliefs may have a significant upside, but also with a palpable downside when either or both of those belief systems become excessively antagonistic or extreme. Three cheers for religious and political moderation that allows them to peacefully coexist.
1. Jones JM. U.S. church membership falls below majority for first time. Gallup. March 29, 2021. Accessed June 7, 2021. https://news.gallup.com/poll/341963/church-membership-falls-below-majority-first-time.aspx
2. Seitz RJ, Angel HF. Belief formation—a driving force for brain evolution. Brain Cogn. 2020;140:105548. doi: 10.1016/j.bandc.2020.105548
3. Seitz RJ. Beliefs: a challenge in neuropsychological disorders. J Neuropsychol. 2021. doi: 10.1111/jnp.12249
4. Gurin L, Blum S. Delusions and the right hemisphere: a review of the case for the right hemisphere as a mediator of reality-based belief. J Neuropsychiatry Clin Neurosci. 2017;29(3):225-235. doi: 10.1176/appi.neuropsych.16060118
5. Durkheim E. Suicide: a study in sociology. The Free Press; 1951.
1. Jones JM. U.S. church membership falls below majority for first time. Gallup. March 29, 2021. Accessed June 7, 2021. https://news.gallup.com/poll/341963/church-membership-falls-below-majority-first-time.aspx
2. Seitz RJ, Angel HF. Belief formation—a driving force for brain evolution. Brain Cogn. 2020;140:105548. doi: 10.1016/j.bandc.2020.105548
3. Seitz RJ. Beliefs: a challenge in neuropsychological disorders. J Neuropsychol. 2021. doi: 10.1111/jnp.12249
4. Gurin L, Blum S. Delusions and the right hemisphere: a review of the case for the right hemisphere as a mediator of reality-based belief. J Neuropsychiatry Clin Neurosci. 2017;29(3):225-235. doi: 10.1176/appi.neuropsych.16060118
5. Durkheim E. Suicide: a study in sociology. The Free Press; 1951.
More on long-acting injectable antipsychotics
Benefits of early LAI use
I want to thank Dr. Nasrallah for his editorial calling for more frequent and earlier use of long-acting injectable antipsychotics (LAIs) in schizophrenia (From the Editor,
In addition to the neuroprotective biologic effects of early LAI usage, I’ve found that many of my FEP patients find great psychological comfort from incorporating LAIs into their treatment plan. The first psychotic break is generally when a person (and their family) feels the most afraid about the future and is in desperate need of hope that they can have a full life—with educational opportunities, sustained employment, meaningful relationships, and more. Just as society has seen the COVID-19 vaccines as a symbol of hope and the first step in overcoming the oppression of living in fear of an uncertain future, we need to help people experiencing FEP find hope in a needle.
Craig Chepke, MD, FAPA
Excel Psychiatric Associates
Huntersville, North Carolina
Reference
1. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
Dr. Nasrallah responds
Thank you, Dr. Chepke, for your letter confirming full support for using LAIs in schizophrenia. I like the phrase you coined: “hope in a needle.” The early use of LAIs in schizophrenia can provide the same type of hope that the vaccines against the life-threatening COVID-19 virus have generated in our society. Based on my direct observations, I also agree with you that the longer patients with schizophrenia remain on LAIs, the more engaged and happy they are with their progress and the quality of their lives. It is tragic that many patients never had the opportunity to return to their baseline with the early use of LAIs immediately following their first psychotic episode, instead of relapsing again and again due to their inability to adhere completely to their oral medications.
Henry A. Nasrallah, MD
Editor-In-Chief
Continue to: LAIs as the standard of care
LAIs as the standard of care
Thank you, Dr. Nasrallah, for reiterating the importance of compliance with pharmacologic management of schizophrenia after FEP (From the Editor,
As you point out in your editorial, the facts are powerful, well-known, undisputed, and yet not adopted in the United States, when in other countries LAIs are first-line care. Yes, LAIs are expensive, but not nearly as expensive as the disabilities caused by noncompliance are to society.
Why isn’t LAI use the standard of care here in the United States? In the United States, there is advocacy for treatment because there’s money in it. There is no good advocacy for preventive care because there’s no immediate money in it. We have another good example of this in the United States: private, for-profit prisons. They have a vested interest in keeping prisons full and building new ones. Patients with FEP are most often treated in the hospital, where a standard of care could easily be established that mandates LAIs as first-tier care. Why is that not so? Who is pushing for it? Who is resisting?
Your editorial inspired me to advocate more strongly. Do you have advice about how to effect policy change? I know administrators respond when we talk dollars and cents, not quality of care. What is the dollar cost of not using LAIs as the standard of care after FEP? Who cares? Who would listen to the numbers?
Edward A. Major, MD, LFAPA
Clinical Professor of Psychiatry
Upstate Medical Center
Syracuse, New York
Dr. Nasrallah responds
Dr. Major, thanks for your message. Establishing a standard of care for the use of LAIs (or any other therapy) is not that simple. It requires well-coordinated collaboration among several stakeholders (clinicians, researchers, payors, advocacy groups, and a national organization such as the American Psychiatric Association). The cost issue is certainly powerful, but the equation works in favor of LAIs because 1 psychiatric hospitalization due to a psychotic relapse costs up to 3 times the annual cost of an LAI medication that can prevent that rehospitalization. In addition, disability comprises the lion’s share of the large indirect costs of schizophrenia (disability payments, lifetime room and board, incarceration and legal costs, and loss of work and generation of taxes). LAIs can save both lives and expenditures, and a lot of suffering by patients and their families. I, too, long to see the emergence of a rational standard of care for schizophrenia using LAIs right after the initial psychotic episode. Oncology and cardiology have standards of care, so why not psychiatry?
Henry A. Nasrallah, MD
Editor-In-Chief
Continue to: Psychosis and epilepsy
Psychosis and epilepsy
I just read your editorial regarding the devastating consequences of psychotic relapses (From the Editor,
I work in the spheres of psychiatry, epileptology, and whole genome sequencing, and have experienced a psychotic episode myself (in 2013, after temporal lobe resection and overdose). I now consider myself even more lucky to be out the other side! As Governor for South London and Maudsley NHS Foundation Trust (SLaM) and Trustee for Epilepsy Action, many of our patients have psychosis. Some patients with epilepsy even experience postictal psychosis. Just yesterday, we had a call at SLaM regarding patients from a secure unit, and a psychiatric nurse spoke about patients at risk to themselves and others because of their psychotic illness, and how crucial effective long-term care was.
Torie Robinson
CEO, Epilepsy Sparks
Dr. Nasrallah responds
Ms. Robinson, thank you for sharing your story. It is important to note that the neurobiology of the psychosis that may occur with epilepsy may not be as neurodegenerative as the psychosis of schizophrenia. Many neurologic conditions can be associated with psychotic episodes, not only epilepsy. I am glad you overcame your post-temporal lobectomy psychotic episode and have had a very good outcome with high functioning.
Henry A. Nasrallah, MD
Editor-In-Chief
Disclosures
Dr. Chepke is a consultant to and speaker for Janssen Pharmaceuticals, Otsuka Pharmaceuticals, and Alkermes. The other authors report no financial relationships with any companies whose products are mentioned in their letters, or with manufacturers of competing products.
Benefits of early LAI use
I want to thank Dr. Nasrallah for his editorial calling for more frequent and earlier use of long-acting injectable antipsychotics (LAIs) in schizophrenia (From the Editor,
In addition to the neuroprotective biologic effects of early LAI usage, I’ve found that many of my FEP patients find great psychological comfort from incorporating LAIs into their treatment plan. The first psychotic break is generally when a person (and their family) feels the most afraid about the future and is in desperate need of hope that they can have a full life—with educational opportunities, sustained employment, meaningful relationships, and more. Just as society has seen the COVID-19 vaccines as a symbol of hope and the first step in overcoming the oppression of living in fear of an uncertain future, we need to help people experiencing FEP find hope in a needle.
Craig Chepke, MD, FAPA
Excel Psychiatric Associates
Huntersville, North Carolina
Reference
1. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
Dr. Nasrallah responds
Thank you, Dr. Chepke, for your letter confirming full support for using LAIs in schizophrenia. I like the phrase you coined: “hope in a needle.” The early use of LAIs in schizophrenia can provide the same type of hope that the vaccines against the life-threatening COVID-19 virus have generated in our society. Based on my direct observations, I also agree with you that the longer patients with schizophrenia remain on LAIs, the more engaged and happy they are with their progress and the quality of their lives. It is tragic that many patients never had the opportunity to return to their baseline with the early use of LAIs immediately following their first psychotic episode, instead of relapsing again and again due to their inability to adhere completely to their oral medications.
Henry A. Nasrallah, MD
Editor-In-Chief
Continue to: LAIs as the standard of care
LAIs as the standard of care
Thank you, Dr. Nasrallah, for reiterating the importance of compliance with pharmacologic management of schizophrenia after FEP (From the Editor,
As you point out in your editorial, the facts are powerful, well-known, undisputed, and yet not adopted in the United States, when in other countries LAIs are first-line care. Yes, LAIs are expensive, but not nearly as expensive as the disabilities caused by noncompliance are to society.
Why isn’t LAI use the standard of care here in the United States? In the United States, there is advocacy for treatment because there’s money in it. There is no good advocacy for preventive care because there’s no immediate money in it. We have another good example of this in the United States: private, for-profit prisons. They have a vested interest in keeping prisons full and building new ones. Patients with FEP are most often treated in the hospital, where a standard of care could easily be established that mandates LAIs as first-tier care. Why is that not so? Who is pushing for it? Who is resisting?
Your editorial inspired me to advocate more strongly. Do you have advice about how to effect policy change? I know administrators respond when we talk dollars and cents, not quality of care. What is the dollar cost of not using LAIs as the standard of care after FEP? Who cares? Who would listen to the numbers?
Edward A. Major, MD, LFAPA
Clinical Professor of Psychiatry
Upstate Medical Center
Syracuse, New York
Dr. Nasrallah responds
Dr. Major, thanks for your message. Establishing a standard of care for the use of LAIs (or any other therapy) is not that simple. It requires well-coordinated collaboration among several stakeholders (clinicians, researchers, payors, advocacy groups, and a national organization such as the American Psychiatric Association). The cost issue is certainly powerful, but the equation works in favor of LAIs because 1 psychiatric hospitalization due to a psychotic relapse costs up to 3 times the annual cost of an LAI medication that can prevent that rehospitalization. In addition, disability comprises the lion’s share of the large indirect costs of schizophrenia (disability payments, lifetime room and board, incarceration and legal costs, and loss of work and generation of taxes). LAIs can save both lives and expenditures, and a lot of suffering by patients and their families. I, too, long to see the emergence of a rational standard of care for schizophrenia using LAIs right after the initial psychotic episode. Oncology and cardiology have standards of care, so why not psychiatry?
Henry A. Nasrallah, MD
Editor-In-Chief
Continue to: Psychosis and epilepsy
Psychosis and epilepsy
I just read your editorial regarding the devastating consequences of psychotic relapses (From the Editor,
I work in the spheres of psychiatry, epileptology, and whole genome sequencing, and have experienced a psychotic episode myself (in 2013, after temporal lobe resection and overdose). I now consider myself even more lucky to be out the other side! As Governor for South London and Maudsley NHS Foundation Trust (SLaM) and Trustee for Epilepsy Action, many of our patients have psychosis. Some patients with epilepsy even experience postictal psychosis. Just yesterday, we had a call at SLaM regarding patients from a secure unit, and a psychiatric nurse spoke about patients at risk to themselves and others because of their psychotic illness, and how crucial effective long-term care was.
Torie Robinson
CEO, Epilepsy Sparks
Dr. Nasrallah responds
Ms. Robinson, thank you for sharing your story. It is important to note that the neurobiology of the psychosis that may occur with epilepsy may not be as neurodegenerative as the psychosis of schizophrenia. Many neurologic conditions can be associated with psychotic episodes, not only epilepsy. I am glad you overcame your post-temporal lobectomy psychotic episode and have had a very good outcome with high functioning.
Henry A. Nasrallah, MD
Editor-In-Chief
Disclosures
Dr. Chepke is a consultant to and speaker for Janssen Pharmaceuticals, Otsuka Pharmaceuticals, and Alkermes. The other authors report no financial relationships with any companies whose products are mentioned in their letters, or with manufacturers of competing products.
Benefits of early LAI use
I want to thank Dr. Nasrallah for his editorial calling for more frequent and earlier use of long-acting injectable antipsychotics (LAIs) in schizophrenia (From the Editor,
In addition to the neuroprotective biologic effects of early LAI usage, I’ve found that many of my FEP patients find great psychological comfort from incorporating LAIs into their treatment plan. The first psychotic break is generally when a person (and their family) feels the most afraid about the future and is in desperate need of hope that they can have a full life—with educational opportunities, sustained employment, meaningful relationships, and more. Just as society has seen the COVID-19 vaccines as a symbol of hope and the first step in overcoming the oppression of living in fear of an uncertain future, we need to help people experiencing FEP find hope in a needle.
Craig Chepke, MD, FAPA
Excel Psychiatric Associates
Huntersville, North Carolina
Reference
1. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
Dr. Nasrallah responds
Thank you, Dr. Chepke, for your letter confirming full support for using LAIs in schizophrenia. I like the phrase you coined: “hope in a needle.” The early use of LAIs in schizophrenia can provide the same type of hope that the vaccines against the life-threatening COVID-19 virus have generated in our society. Based on my direct observations, I also agree with you that the longer patients with schizophrenia remain on LAIs, the more engaged and happy they are with their progress and the quality of their lives. It is tragic that many patients never had the opportunity to return to their baseline with the early use of LAIs immediately following their first psychotic episode, instead of relapsing again and again due to their inability to adhere completely to their oral medications.
Henry A. Nasrallah, MD
Editor-In-Chief
Continue to: LAIs as the standard of care
LAIs as the standard of care
Thank you, Dr. Nasrallah, for reiterating the importance of compliance with pharmacologic management of schizophrenia after FEP (From the Editor,
As you point out in your editorial, the facts are powerful, well-known, undisputed, and yet not adopted in the United States, when in other countries LAIs are first-line care. Yes, LAIs are expensive, but not nearly as expensive as the disabilities caused by noncompliance are to society.
Why isn’t LAI use the standard of care here in the United States? In the United States, there is advocacy for treatment because there’s money in it. There is no good advocacy for preventive care because there’s no immediate money in it. We have another good example of this in the United States: private, for-profit prisons. They have a vested interest in keeping prisons full and building new ones. Patients with FEP are most often treated in the hospital, where a standard of care could easily be established that mandates LAIs as first-tier care. Why is that not so? Who is pushing for it? Who is resisting?
Your editorial inspired me to advocate more strongly. Do you have advice about how to effect policy change? I know administrators respond when we talk dollars and cents, not quality of care. What is the dollar cost of not using LAIs as the standard of care after FEP? Who cares? Who would listen to the numbers?
Edward A. Major, MD, LFAPA
Clinical Professor of Psychiatry
Upstate Medical Center
Syracuse, New York
Dr. Nasrallah responds
Dr. Major, thanks for your message. Establishing a standard of care for the use of LAIs (or any other therapy) is not that simple. It requires well-coordinated collaboration among several stakeholders (clinicians, researchers, payors, advocacy groups, and a national organization such as the American Psychiatric Association). The cost issue is certainly powerful, but the equation works in favor of LAIs because 1 psychiatric hospitalization due to a psychotic relapse costs up to 3 times the annual cost of an LAI medication that can prevent that rehospitalization. In addition, disability comprises the lion’s share of the large indirect costs of schizophrenia (disability payments, lifetime room and board, incarceration and legal costs, and loss of work and generation of taxes). LAIs can save both lives and expenditures, and a lot of suffering by patients and their families. I, too, long to see the emergence of a rational standard of care for schizophrenia using LAIs right after the initial psychotic episode. Oncology and cardiology have standards of care, so why not psychiatry?
Henry A. Nasrallah, MD
Editor-In-Chief
Continue to: Psychosis and epilepsy
Psychosis and epilepsy
I just read your editorial regarding the devastating consequences of psychotic relapses (From the Editor,
I work in the spheres of psychiatry, epileptology, and whole genome sequencing, and have experienced a psychotic episode myself (in 2013, after temporal lobe resection and overdose). I now consider myself even more lucky to be out the other side! As Governor for South London and Maudsley NHS Foundation Trust (SLaM) and Trustee for Epilepsy Action, many of our patients have psychosis. Some patients with epilepsy even experience postictal psychosis. Just yesterday, we had a call at SLaM regarding patients from a secure unit, and a psychiatric nurse spoke about patients at risk to themselves and others because of their psychotic illness, and how crucial effective long-term care was.
Torie Robinson
CEO, Epilepsy Sparks
Dr. Nasrallah responds
Ms. Robinson, thank you for sharing your story. It is important to note that the neurobiology of the psychosis that may occur with epilepsy may not be as neurodegenerative as the psychosis of schizophrenia. Many neurologic conditions can be associated with psychotic episodes, not only epilepsy. I am glad you overcame your post-temporal lobectomy psychotic episode and have had a very good outcome with high functioning.
Henry A. Nasrallah, MD
Editor-In-Chief
Disclosures
Dr. Chepke is a consultant to and speaker for Janssen Pharmaceuticals, Otsuka Pharmaceuticals, and Alkermes. The other authors report no financial relationships with any companies whose products are mentioned in their letters, or with manufacturers of competing products.
Mood stabilizers: Balancing tolerability, serum levels, and dosage
Mr. B, age 32, was diagnosed with bipolar disorder 10 years ago after experiencing a manic episode that resulted in his first psychiatric hospitalization. He was prescribed quetiapine, 400 mg/d, and remained stable for the next several years. Unfortunately, Mr. B developed significant metabolic adverse effects, including diabetes and a 30-pound weight gain, so he was switched from quetiapine to lithium. Mr. B was unable to tolerate the sedation and cognitive effects of lithium, and the dose could not be titrated to within the therapeutic window. As a result, Mr. B experienced a moderate depressive episode. His current clinician would like to initiate lamotrigine at a starting dose of 25 mg/d. Mr. B has not had a manic episode since the index hospitalization, and this is his first depressive episode.
The term “mood stabilizer” has come to refer to medications that treat a depressive and/or manic episode without inducing the other. In conventional terms, it refers to non-antipsychotic medications such as lithium, divalproex, and lamotrigine. Except for lithium, mood stabilizers are also antiepileptic drugs (AEDs). The role of AEDs for treating psychiatric conditions was discovered after they were originally FDA-approved for treating seizures. Following this discovery, the recommended doses and therapeutic ranges for these agents when applied to psychiatric treatment fell into a gray area.
Every patient is different and requires an individualized treatment plan, but this often leaves the clinician wondering, “How high is too high for this mood stabilizer?” or “My patient is responding well, but could a higher dose be even more effective?” In the case of Mr. B, who has trialed 2 medications with poor tolerability, how high can the lamotrigine dose be titrated to achieve a therapeutic response without adverse effects? The literature on this topic does not provide an exact answer, but does shed some light on key considerations for such decisions.
Which mood stabilizers are recommended?
One of the most recently updated guidelines for the treatment of bipolar disorder was released in 2018 by the Canadian Network for Mood and Anxiety Treatments (CANMAT).1 Lithium, divalproex, and lamotrigine were each recommended as a first-line option for treating bipolar disorder. For lithium and divalproex, the CANMAT guidelines recommend serum level monitoring for efficacy and tolerability; however, they do not recommend serum level monitoring for lamotrigine. Lithium and divalproex each have safety and tolerability concerns, particularly when selected for maintenance therapy, whereas lamotrigine is typically much better tolerated.1 Divalproex and lithium can cause weight gain, gastrointestinal adverse effects (nausea, vomiting, diarrhea), and tremor. Additional tolerability concerns with lithium include renal toxicity, electrocardiogram abnormalities, hypothyroidism, cognitive impairment, and dermatologic reactions. Divalproex can produce greater levels of sedation and may impact reproductive function (oligomenorrhea or hyperandrogenism). One of the most common adverse effects of lamotrigine is a non-serious rash; however, slow dose titration is necessary to decrease the risk of a serious, life-threatening rash such as Stevens-Johnson syndrome.
Lithium
Lithium continues to be regarded as a gold-standard therapy for bipolar disorder. The exact serum levels corresponding to efficacy and tolerability vary. The Lithiumeter: Version 2.0 is a schematic that incorporates the various levels recommended by different clinical guidelines.2 The recommended serum levels range from 0.6 to 1.0 mEq/L for mania and 0.4 to 0.8 mEq/L for depression.2 One of the main issues with lithium dosing is balancing a therapeutic level with tolerability and toxicity. Toxicity may begin when lithium levels exceed 1.2 mEq/L, and levels >2.0 mEq/L can be lethal. Signs of acute toxicity include tremor, headache, arrhythmia, nausea, vomiting, diarrhea, polyuria, and polydipsia. Conversely, chronic lithium use may lead to chronic toxicity as patients age and their physical health changes. Signs of chronic toxicity include ataxia, confusion, renal dysfunction, and tremor. There is no “one size fits all” when it comes to lithium dosing. Individualized dosing is necessary to balance efficacy and tolerability.
Divalproex
Divalproex was initially studied for use as an AED, and its therapeutic levels as an AED are not the same as those indicated for bipolar disorder. Generally, patients with bipolar disorder require a divalproex serum level >50 µg/mL. Ranges closer to 100 µg/mL have been found to be most effective for treating acute mania.3 A loading dose of 20 to 30 mg/kg/d can be administered to help achieve mood stabilization. Again, efficacy must be balanced against toxicity. The maximum dose of divalproex is 60 mg/kg/d, which is rarely seen in psychiatric practice. Early studies of divalproex found adverse effects greatest in individuals with plasma levels >100 µg/mL. Reported adverse effects included alopecia, weight gain, tremor, and mental status changes.4
Lamotrigine
Unlike lithium and divalproex, lamotrigine therapeutic drug monitoring is not common. The accepted therapeutic reference range (TRR) for lamotrigine as an AED is 3,000 to 14,000 ng/mL. Unholzer et al5 evaluated the dose and TRR for individuals with bipolar disorder treated with lamotrigine. No statistically significant difference in lamotrigine serum levels was found in responders vs nonresponders.5 Most patients were prescribed ≤200 mg/d; however, some were prescribed higher doses. The maximum dose recommended when lamotrigine is used as an AED is 400 mg/d; however, this study furthered the evidence that lower doses tend to be effective in bipolar disorder.
Continue to: CASE
CASE CONTINUED
It has been 3 months since Mr. B was initiated on lamotrigine, and he has since been titrated to his current, stable dose of 100 mg/d. Mr. B is no longer experiencing the sedation he had with lithium and has the energy to commit to an exercise routine. This has allowed him to lose 15 pounds so far and greatly improve control of his diabetes.
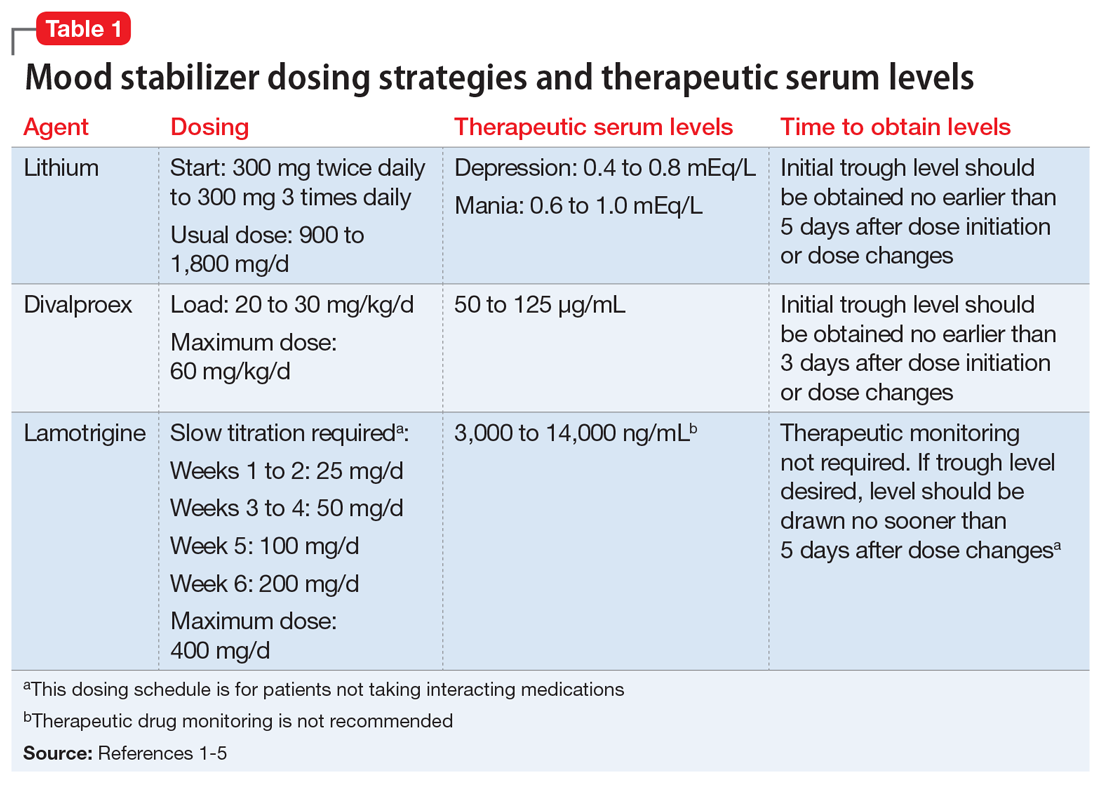
Dosage summary
Most available evidence supports dosing lithium and divalproex to effect, typically seen between 0.6 to 1.0 mEq/L and 50 to 125 µg/mL, respectively. Higher plasma levels tend to correspond to more adverse effects and toxicity. Lamotrigine does not have such a narrow therapeutic window. Lamotrigine for psychiatric treatment yields greatest efficacy at approximately 200 mg/d, but doses can be increased if warranted, which could be the case in Mr. B.
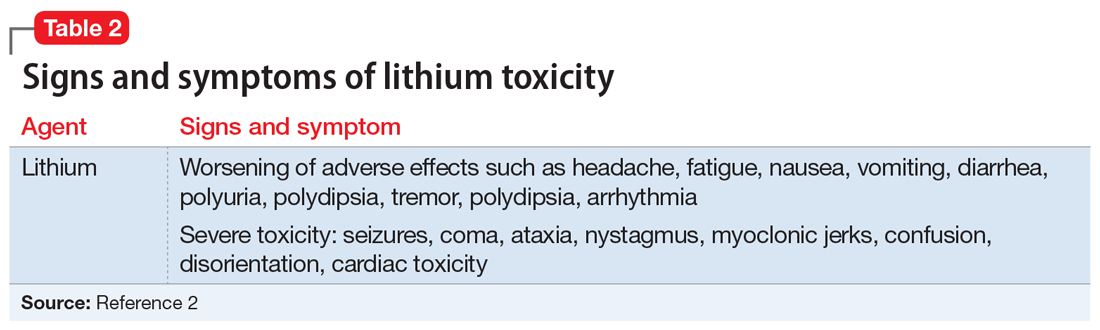
Table 11-5 outlines dosing strategies and therapeutic serum levels for lithium, divalproex, and lamotrigine. Table 22 lists signs and symptoms of lithium toxicity, and Table 31,2 describes strategies for managing adverse effects of lithium and divalproex.
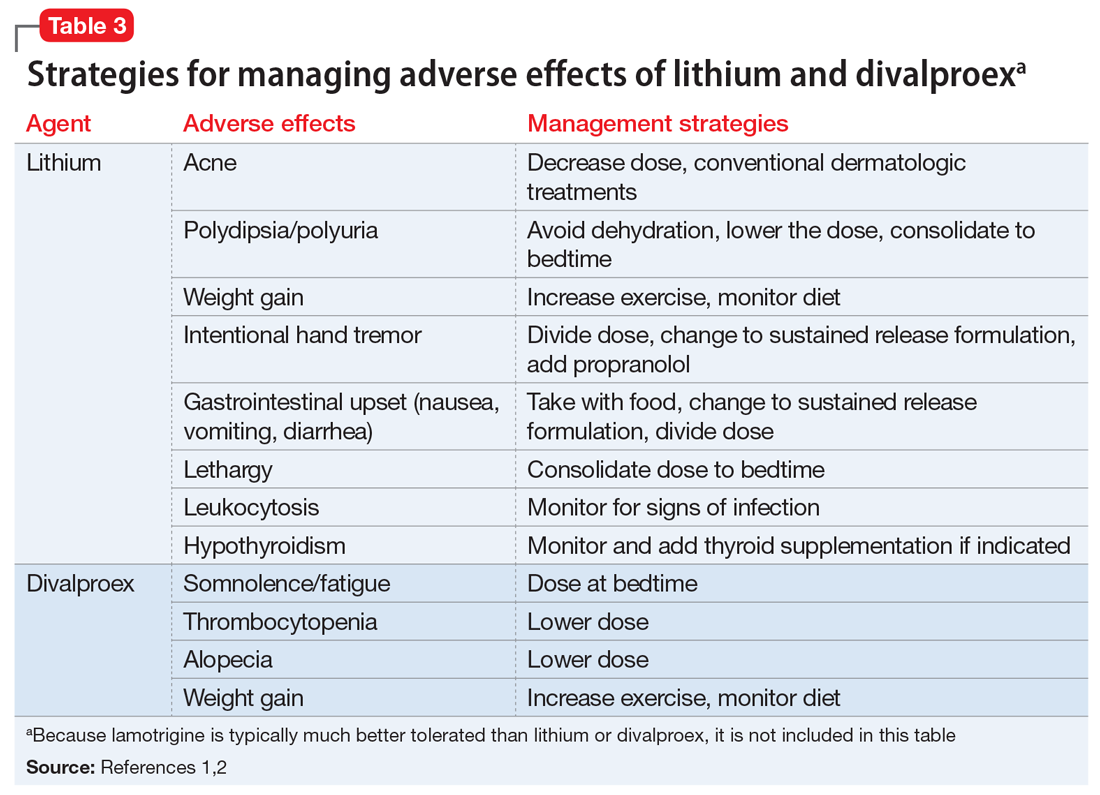
1. Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97-170.
2. Malhi GS, Gershon S, Outhred T. Lithiumeter: version 2.0. Bipolar Disord. 2016;18(8):631-641.
3. Allen MH, Hirschfeld RM, Wozniak PJ, et al. Linear relationship of valproate serum concentration to response and optimal serum levels for acute mania. Am J Psychiatry. 2006;163(2):272-275.
4. Turnbull DM, Rawlins MD, Weightman D, et al. Plasma concentrations of sodium valproate: their clinical value. Ann Neurol. 1983;14(1):38-42.
5. Unholzer S, Haen E. Retrospective analysis of therapeutic drug monitoring data for treatment of bipolar disorder with lamotrigine. Pharmacopsychiatry. 2015;48(7):296.
Mr. B, age 32, was diagnosed with bipolar disorder 10 years ago after experiencing a manic episode that resulted in his first psychiatric hospitalization. He was prescribed quetiapine, 400 mg/d, and remained stable for the next several years. Unfortunately, Mr. B developed significant metabolic adverse effects, including diabetes and a 30-pound weight gain, so he was switched from quetiapine to lithium. Mr. B was unable to tolerate the sedation and cognitive effects of lithium, and the dose could not be titrated to within the therapeutic window. As a result, Mr. B experienced a moderate depressive episode. His current clinician would like to initiate lamotrigine at a starting dose of 25 mg/d. Mr. B has not had a manic episode since the index hospitalization, and this is his first depressive episode.
The term “mood stabilizer” has come to refer to medications that treat a depressive and/or manic episode without inducing the other. In conventional terms, it refers to non-antipsychotic medications such as lithium, divalproex, and lamotrigine. Except for lithium, mood stabilizers are also antiepileptic drugs (AEDs). The role of AEDs for treating psychiatric conditions was discovered after they were originally FDA-approved for treating seizures. Following this discovery, the recommended doses and therapeutic ranges for these agents when applied to psychiatric treatment fell into a gray area.
Every patient is different and requires an individualized treatment plan, but this often leaves the clinician wondering, “How high is too high for this mood stabilizer?” or “My patient is responding well, but could a higher dose be even more effective?” In the case of Mr. B, who has trialed 2 medications with poor tolerability, how high can the lamotrigine dose be titrated to achieve a therapeutic response without adverse effects? The literature on this topic does not provide an exact answer, but does shed some light on key considerations for such decisions.
Which mood stabilizers are recommended?
One of the most recently updated guidelines for the treatment of bipolar disorder was released in 2018 by the Canadian Network for Mood and Anxiety Treatments (CANMAT).1 Lithium, divalproex, and lamotrigine were each recommended as a first-line option for treating bipolar disorder. For lithium and divalproex, the CANMAT guidelines recommend serum level monitoring for efficacy and tolerability; however, they do not recommend serum level monitoring for lamotrigine. Lithium and divalproex each have safety and tolerability concerns, particularly when selected for maintenance therapy, whereas lamotrigine is typically much better tolerated.1 Divalproex and lithium can cause weight gain, gastrointestinal adverse effects (nausea, vomiting, diarrhea), and tremor. Additional tolerability concerns with lithium include renal toxicity, electrocardiogram abnormalities, hypothyroidism, cognitive impairment, and dermatologic reactions. Divalproex can produce greater levels of sedation and may impact reproductive function (oligomenorrhea or hyperandrogenism). One of the most common adverse effects of lamotrigine is a non-serious rash; however, slow dose titration is necessary to decrease the risk of a serious, life-threatening rash such as Stevens-Johnson syndrome.
Lithium
Lithium continues to be regarded as a gold-standard therapy for bipolar disorder. The exact serum levels corresponding to efficacy and tolerability vary. The Lithiumeter: Version 2.0 is a schematic that incorporates the various levels recommended by different clinical guidelines.2 The recommended serum levels range from 0.6 to 1.0 mEq/L for mania and 0.4 to 0.8 mEq/L for depression.2 One of the main issues with lithium dosing is balancing a therapeutic level with tolerability and toxicity. Toxicity may begin when lithium levels exceed 1.2 mEq/L, and levels >2.0 mEq/L can be lethal. Signs of acute toxicity include tremor, headache, arrhythmia, nausea, vomiting, diarrhea, polyuria, and polydipsia. Conversely, chronic lithium use may lead to chronic toxicity as patients age and their physical health changes. Signs of chronic toxicity include ataxia, confusion, renal dysfunction, and tremor. There is no “one size fits all” when it comes to lithium dosing. Individualized dosing is necessary to balance efficacy and tolerability.
Divalproex
Divalproex was initially studied for use as an AED, and its therapeutic levels as an AED are not the same as those indicated for bipolar disorder. Generally, patients with bipolar disorder require a divalproex serum level >50 µg/mL. Ranges closer to 100 µg/mL have been found to be most effective for treating acute mania.3 A loading dose of 20 to 30 mg/kg/d can be administered to help achieve mood stabilization. Again, efficacy must be balanced against toxicity. The maximum dose of divalproex is 60 mg/kg/d, which is rarely seen in psychiatric practice. Early studies of divalproex found adverse effects greatest in individuals with plasma levels >100 µg/mL. Reported adverse effects included alopecia, weight gain, tremor, and mental status changes.4
Lamotrigine
Unlike lithium and divalproex, lamotrigine therapeutic drug monitoring is not common. The accepted therapeutic reference range (TRR) for lamotrigine as an AED is 3,000 to 14,000 ng/mL. Unholzer et al5 evaluated the dose and TRR for individuals with bipolar disorder treated with lamotrigine. No statistically significant difference in lamotrigine serum levels was found in responders vs nonresponders.5 Most patients were prescribed ≤200 mg/d; however, some were prescribed higher doses. The maximum dose recommended when lamotrigine is used as an AED is 400 mg/d; however, this study furthered the evidence that lower doses tend to be effective in bipolar disorder.
Continue to: CASE
CASE CONTINUED
It has been 3 months since Mr. B was initiated on lamotrigine, and he has since been titrated to his current, stable dose of 100 mg/d. Mr. B is no longer experiencing the sedation he had with lithium and has the energy to commit to an exercise routine. This has allowed him to lose 15 pounds so far and greatly improve control of his diabetes.
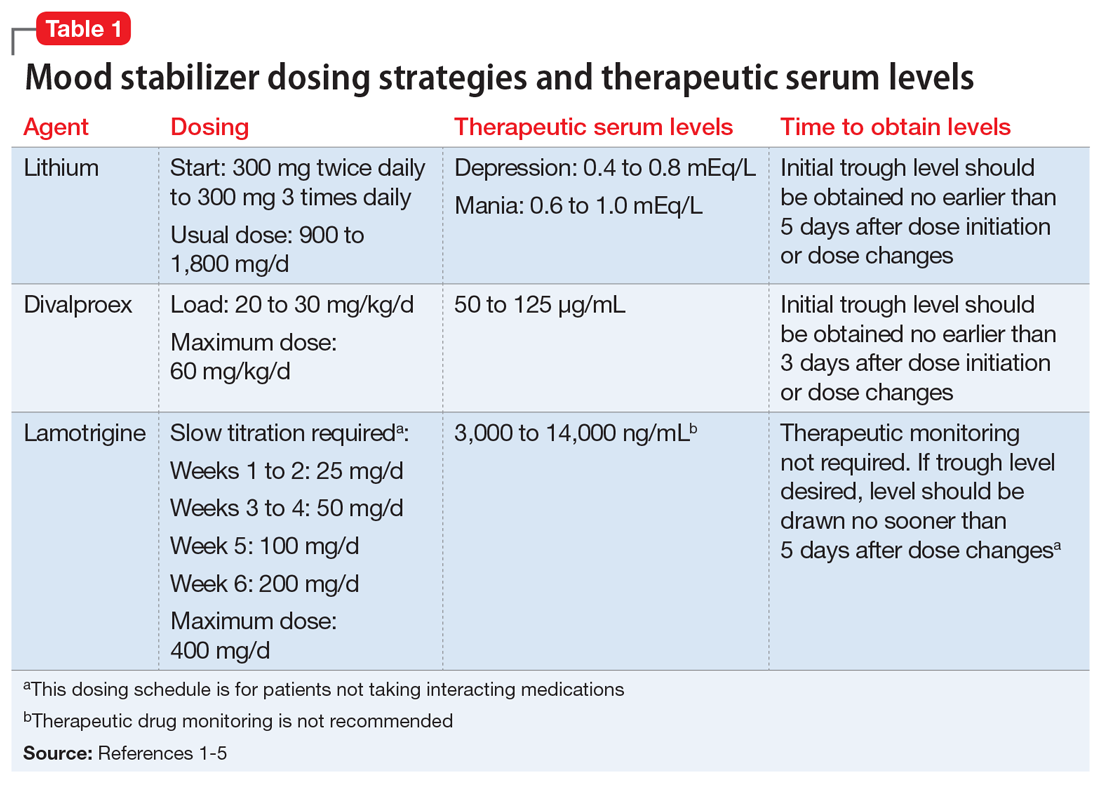
Dosage summary
Most available evidence supports dosing lithium and divalproex to effect, typically seen between 0.6 to 1.0 mEq/L and 50 to 125 µg/mL, respectively. Higher plasma levels tend to correspond to more adverse effects and toxicity. Lamotrigine does not have such a narrow therapeutic window. Lamotrigine for psychiatric treatment yields greatest efficacy at approximately 200 mg/d, but doses can be increased if warranted, which could be the case in Mr. B.
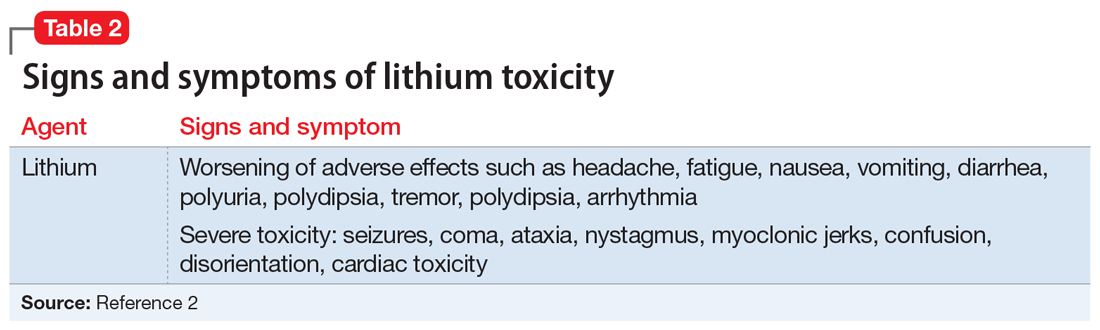
Table 11-5 outlines dosing strategies and therapeutic serum levels for lithium, divalproex, and lamotrigine. Table 22 lists signs and symptoms of lithium toxicity, and Table 31,2 describes strategies for managing adverse effects of lithium and divalproex.
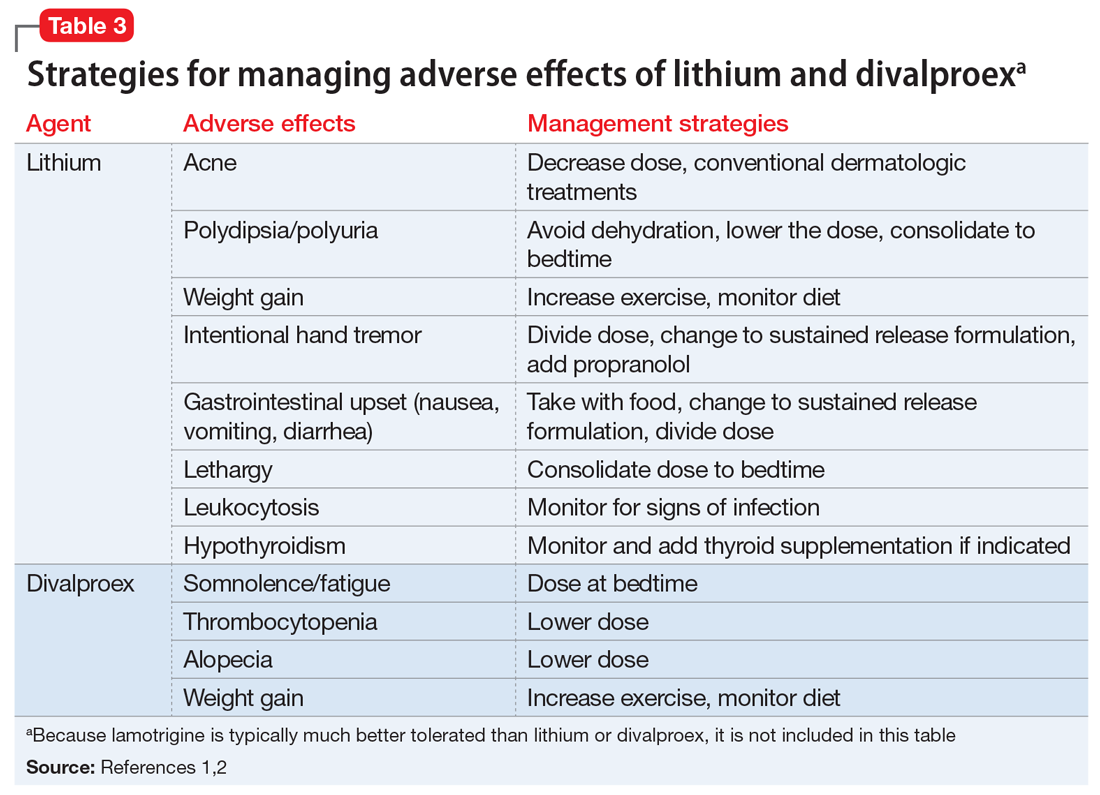
Mr. B, age 32, was diagnosed with bipolar disorder 10 years ago after experiencing a manic episode that resulted in his first psychiatric hospitalization. He was prescribed quetiapine, 400 mg/d, and remained stable for the next several years. Unfortunately, Mr. B developed significant metabolic adverse effects, including diabetes and a 30-pound weight gain, so he was switched from quetiapine to lithium. Mr. B was unable to tolerate the sedation and cognitive effects of lithium, and the dose could not be titrated to within the therapeutic window. As a result, Mr. B experienced a moderate depressive episode. His current clinician would like to initiate lamotrigine at a starting dose of 25 mg/d. Mr. B has not had a manic episode since the index hospitalization, and this is his first depressive episode.
The term “mood stabilizer” has come to refer to medications that treat a depressive and/or manic episode without inducing the other. In conventional terms, it refers to non-antipsychotic medications such as lithium, divalproex, and lamotrigine. Except for lithium, mood stabilizers are also antiepileptic drugs (AEDs). The role of AEDs for treating psychiatric conditions was discovered after they were originally FDA-approved for treating seizures. Following this discovery, the recommended doses and therapeutic ranges for these agents when applied to psychiatric treatment fell into a gray area.
Every patient is different and requires an individualized treatment plan, but this often leaves the clinician wondering, “How high is too high for this mood stabilizer?” or “My patient is responding well, but could a higher dose be even more effective?” In the case of Mr. B, who has trialed 2 medications with poor tolerability, how high can the lamotrigine dose be titrated to achieve a therapeutic response without adverse effects? The literature on this topic does not provide an exact answer, but does shed some light on key considerations for such decisions.
Which mood stabilizers are recommended?
One of the most recently updated guidelines for the treatment of bipolar disorder was released in 2018 by the Canadian Network for Mood and Anxiety Treatments (CANMAT).1 Lithium, divalproex, and lamotrigine were each recommended as a first-line option for treating bipolar disorder. For lithium and divalproex, the CANMAT guidelines recommend serum level monitoring for efficacy and tolerability; however, they do not recommend serum level monitoring for lamotrigine. Lithium and divalproex each have safety and tolerability concerns, particularly when selected for maintenance therapy, whereas lamotrigine is typically much better tolerated.1 Divalproex and lithium can cause weight gain, gastrointestinal adverse effects (nausea, vomiting, diarrhea), and tremor. Additional tolerability concerns with lithium include renal toxicity, electrocardiogram abnormalities, hypothyroidism, cognitive impairment, and dermatologic reactions. Divalproex can produce greater levels of sedation and may impact reproductive function (oligomenorrhea or hyperandrogenism). One of the most common adverse effects of lamotrigine is a non-serious rash; however, slow dose titration is necessary to decrease the risk of a serious, life-threatening rash such as Stevens-Johnson syndrome.
Lithium
Lithium continues to be regarded as a gold-standard therapy for bipolar disorder. The exact serum levels corresponding to efficacy and tolerability vary. The Lithiumeter: Version 2.0 is a schematic that incorporates the various levels recommended by different clinical guidelines.2 The recommended serum levels range from 0.6 to 1.0 mEq/L for mania and 0.4 to 0.8 mEq/L for depression.2 One of the main issues with lithium dosing is balancing a therapeutic level with tolerability and toxicity. Toxicity may begin when lithium levels exceed 1.2 mEq/L, and levels >2.0 mEq/L can be lethal. Signs of acute toxicity include tremor, headache, arrhythmia, nausea, vomiting, diarrhea, polyuria, and polydipsia. Conversely, chronic lithium use may lead to chronic toxicity as patients age and their physical health changes. Signs of chronic toxicity include ataxia, confusion, renal dysfunction, and tremor. There is no “one size fits all” when it comes to lithium dosing. Individualized dosing is necessary to balance efficacy and tolerability.
Divalproex
Divalproex was initially studied for use as an AED, and its therapeutic levels as an AED are not the same as those indicated for bipolar disorder. Generally, patients with bipolar disorder require a divalproex serum level >50 µg/mL. Ranges closer to 100 µg/mL have been found to be most effective for treating acute mania.3 A loading dose of 20 to 30 mg/kg/d can be administered to help achieve mood stabilization. Again, efficacy must be balanced against toxicity. The maximum dose of divalproex is 60 mg/kg/d, which is rarely seen in psychiatric practice. Early studies of divalproex found adverse effects greatest in individuals with plasma levels >100 µg/mL. Reported adverse effects included alopecia, weight gain, tremor, and mental status changes.4
Lamotrigine
Unlike lithium and divalproex, lamotrigine therapeutic drug monitoring is not common. The accepted therapeutic reference range (TRR) for lamotrigine as an AED is 3,000 to 14,000 ng/mL. Unholzer et al5 evaluated the dose and TRR for individuals with bipolar disorder treated with lamotrigine. No statistically significant difference in lamotrigine serum levels was found in responders vs nonresponders.5 Most patients were prescribed ≤200 mg/d; however, some were prescribed higher doses. The maximum dose recommended when lamotrigine is used as an AED is 400 mg/d; however, this study furthered the evidence that lower doses tend to be effective in bipolar disorder.
Continue to: CASE
CASE CONTINUED
It has been 3 months since Mr. B was initiated on lamotrigine, and he has since been titrated to his current, stable dose of 100 mg/d. Mr. B is no longer experiencing the sedation he had with lithium and has the energy to commit to an exercise routine. This has allowed him to lose 15 pounds so far and greatly improve control of his diabetes.
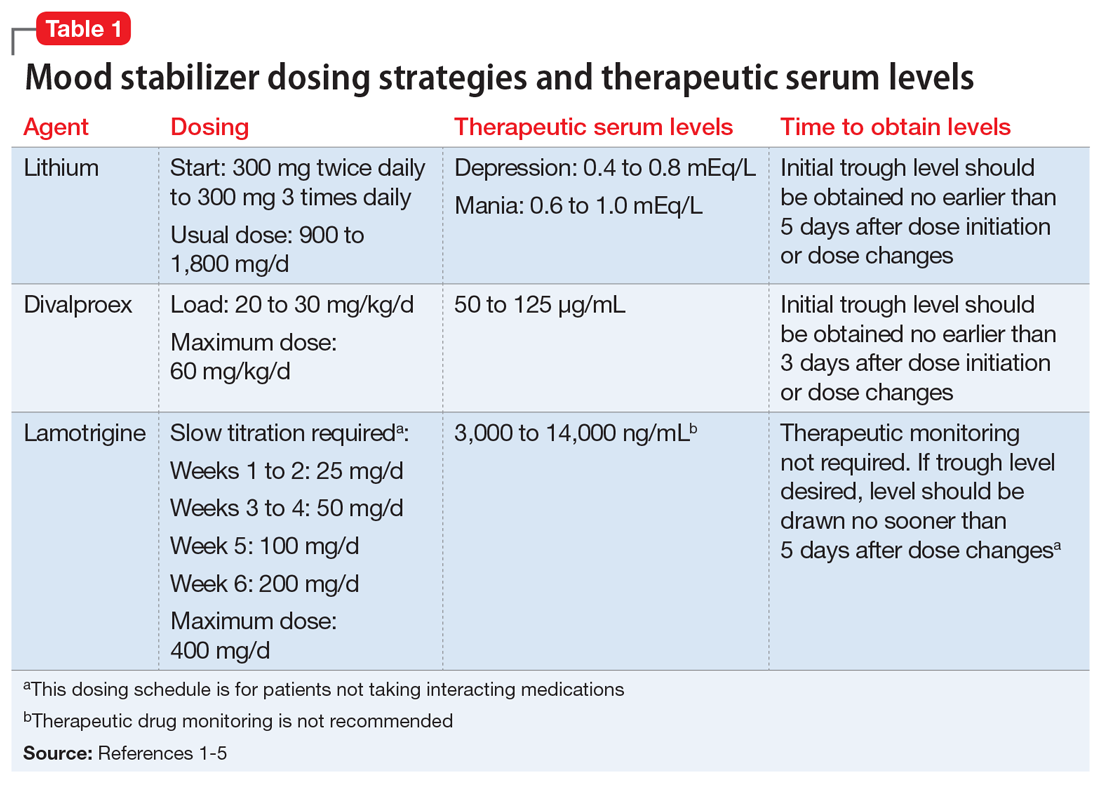
Dosage summary
Most available evidence supports dosing lithium and divalproex to effect, typically seen between 0.6 to 1.0 mEq/L and 50 to 125 µg/mL, respectively. Higher plasma levels tend to correspond to more adverse effects and toxicity. Lamotrigine does not have such a narrow therapeutic window. Lamotrigine for psychiatric treatment yields greatest efficacy at approximately 200 mg/d, but doses can be increased if warranted, which could be the case in Mr. B.
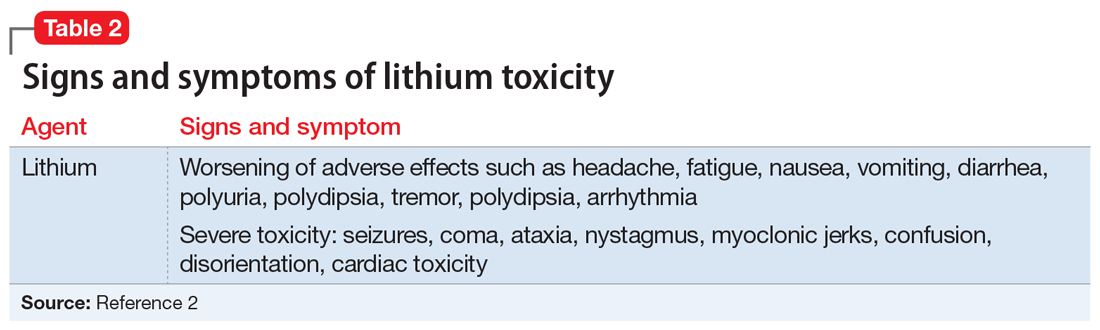
Table 11-5 outlines dosing strategies and therapeutic serum levels for lithium, divalproex, and lamotrigine. Table 22 lists signs and symptoms of lithium toxicity, and Table 31,2 describes strategies for managing adverse effects of lithium and divalproex.
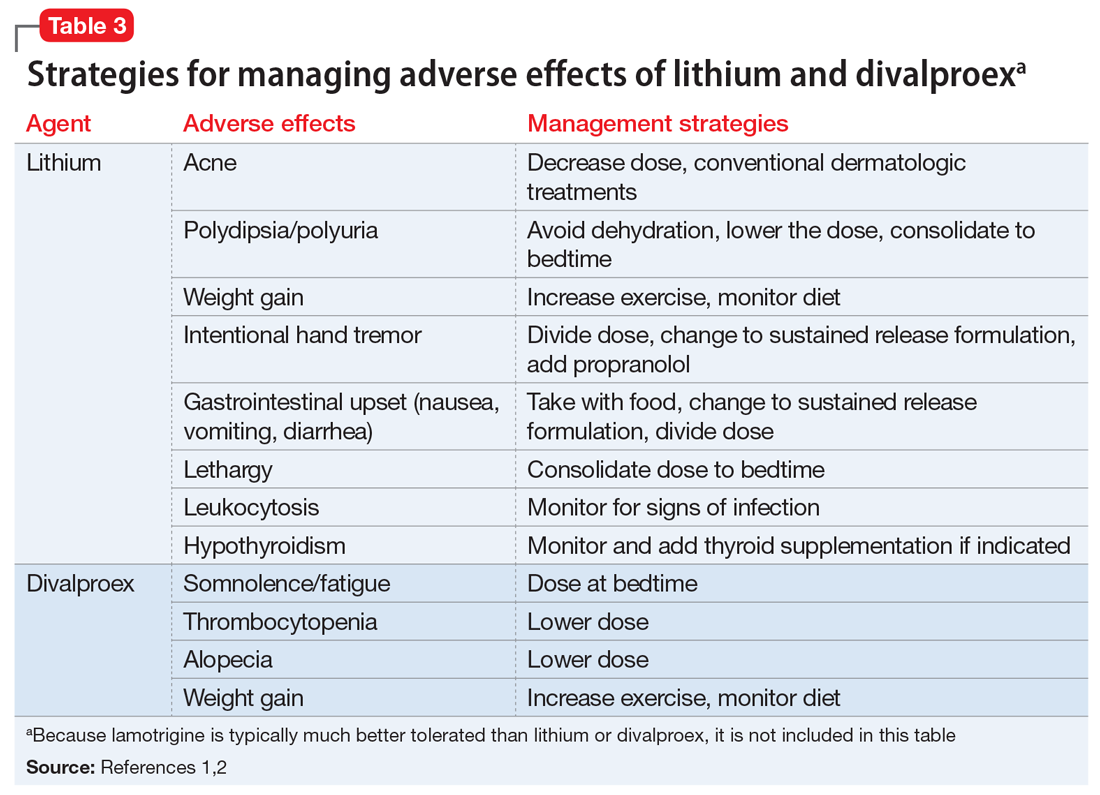
1. Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97-170.
2. Malhi GS, Gershon S, Outhred T. Lithiumeter: version 2.0. Bipolar Disord. 2016;18(8):631-641.
3. Allen MH, Hirschfeld RM, Wozniak PJ, et al. Linear relationship of valproate serum concentration to response and optimal serum levels for acute mania. Am J Psychiatry. 2006;163(2):272-275.
4. Turnbull DM, Rawlins MD, Weightman D, et al. Plasma concentrations of sodium valproate: their clinical value. Ann Neurol. 1983;14(1):38-42.
5. Unholzer S, Haen E. Retrospective analysis of therapeutic drug monitoring data for treatment of bipolar disorder with lamotrigine. Pharmacopsychiatry. 2015;48(7):296.
1. Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97-170.
2. Malhi GS, Gershon S, Outhred T. Lithiumeter: version 2.0. Bipolar Disord. 2016;18(8):631-641.
3. Allen MH, Hirschfeld RM, Wozniak PJ, et al. Linear relationship of valproate serum concentration to response and optimal serum levels for acute mania. Am J Psychiatry. 2006;163(2):272-275.
4. Turnbull DM, Rawlins MD, Weightman D, et al. Plasma concentrations of sodium valproate: their clinical value. Ann Neurol. 1983;14(1):38-42.
5. Unholzer S, Haen E. Retrospective analysis of therapeutic drug monitoring data for treatment of bipolar disorder with lamotrigine. Pharmacopsychiatry. 2015;48(7):296.
COVID-19’s impact on internet gaming disorder among children and adolescents
The impact of the COVID-19 pandemic on the well-being of youth has been significant. Its possible effects range from boredom, depression, anxiety, and suicidal ideation to potential increased rates of internet gaming disorder (IGD), which may have worsened during a nationwide shutdown and extended period of limited social interactions. Presently, there is a paucity of research on the impact of internet gaming on children and adolescents’ mental health and well-being during COVID-19. This article aims to bring awareness to the possible rising impact of the COVID-19 pandemic on IGD and mental health in youth.
Gaming offers benefits—and risks
The gaming industry has grown immensely over the past several years. While many businesses were impacted negatively during the pandemic, the gaming industry grew. It was estimated to be worth $159.3 billion in 2020, an increase of 9.3% from 2019.1
Stay-at-home orders and quarantine protocols during the COVID-19 pandemic have significantly disrupted normal activities, resulting in increased time for digital entertainment, including online gaming and related activities. Internet gaming offers some benefits for children and adolescents, including socialization and connection with peers, which was especially important for avoiding isolation during the pandemic. Empirical evidence of the positive effects of internet gaming can be seen in studies of youth undergoing chemotherapy, those receiving psychotherapy for anxiety or depression, and those having emotional and behavioral problems.2 Internet gaming also provides participants with a platform to communicate with the outside world while maintaining social distancing, and might reduce anxiety, and in some cases, depression.3
Despite these benefits, for some youth, excessive internet gaming can have adverse effects. Due to its addictive properties, internet gaming can be dangerous for vulnerable individuals and lead to unhealthy habits, such as disturbed sleep patterns and increased anxiety.4 In a cross-sectional study conducted in China, Yu et al5 examined the association between IGD and suicidal ideation. They concluded that IGD was positively associated with insomnia and then depression, which in turn contributed to suicide ideation.5 A study based on a survey conducted in Iran from May to August 2020 in individuals age 13 to 18 years found that depression, anxiety, and stress were significant mediators in the association between IGD and self-reported quality of life.2
Internet gaming disorder is included in DSM-5 as a “condition for further study” and in ICD-11.6 Before the COVID-19 pandemic, a study of 1,178 American youth age 8 to 18 years revealed that 8.5% of gamers met the criteria for IGD.7 In a meta-analysis that included 16 studies, the pooled prevalence of IGD among adolescents was 4.6%.8 Some countries, including China and South Korea, have developed treatment plans for IGD,6 but in the United States treatment guidelines have not been established due to insufficient evidence.9
The COVID-19 pandemic has likely led to an increased number of children and adolescents with IGD and its adverse effects on their mental health and well-being. It remains to be seen whether these youth will improve as the pandemic resolves and they resume normal activities, or if impairments will persist.
In conclusion, while internet gaming during the COVID-19 pandemic has provided benefits for many children and adolescents, the negative impact for those who develop IGD may be significant. We should be prepared to detect and address the needs of these youth and their families. Additional research is needed on the post-pandemic prevalence of IGD, its impact on youth mental health, and treatment strategies.
1. WePC. Video game industry statistics, trends and data in 2021. Accessed June 7, 2021. https://www.wepc.com/news/video-game-statistics/
2. Fazeli S, Mohammadi Zeidi I, Lin CY, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. 2020;12:100307. doi: 10.1016/j.abrep.2020.100307
3. Özçetin M, Gümüstas F, Çag˘ Y, et al. The relationships between video game experience and cognitive abilities in adolescents. Neuropsychiatr Dis Treat. 2019;15:1171-1180. doi: 10.2147/NDT.S206271
4. Männikkö N, Ruotsalainen H, Miettunen J, et al. Problematic gaming behaviour and health-related outcomes: a systematic review and meta-analysis. J Health Psychol. 2020;25(1):67-81. doi: 10.1177/1359105317740414
5. Yu Y, Yang X, Wang S, et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry. 2020;20(1):460. doi: 10.1186/s12888-020-02870-zz
6. American Psychiatric Association. Internet gaming. Published June 2018. Accessed June 7, 2021. www.psychiatry.org/patients-families/internet-gaming
7. Gentile D. Pathological video-game use among youth ages 8 to 18: a national study. Psychol Sci. 2009;20(5):594-602. doi: 10.1111/j.1467-9280.2009.02340.x
8. Fam JY. Prevalence of internet gaming disorder in adolescents: A meta-analysis across three decades. Scand J Psychol. 2018;59(5):524-531. doi: 10.1111/sjop.12459
9. Gentile DA, Bailey K, Bavelier D, et al. Internet gaming disorder in children and adolescents. Pediatrics. 2017;140(suppl 2):S81-S85. doi: 10.1542/peds.2016-1758H
The impact of the COVID-19 pandemic on the well-being of youth has been significant. Its possible effects range from boredom, depression, anxiety, and suicidal ideation to potential increased rates of internet gaming disorder (IGD), which may have worsened during a nationwide shutdown and extended period of limited social interactions. Presently, there is a paucity of research on the impact of internet gaming on children and adolescents’ mental health and well-being during COVID-19. This article aims to bring awareness to the possible rising impact of the COVID-19 pandemic on IGD and mental health in youth.
Gaming offers benefits—and risks
The gaming industry has grown immensely over the past several years. While many businesses were impacted negatively during the pandemic, the gaming industry grew. It was estimated to be worth $159.3 billion in 2020, an increase of 9.3% from 2019.1
Stay-at-home orders and quarantine protocols during the COVID-19 pandemic have significantly disrupted normal activities, resulting in increased time for digital entertainment, including online gaming and related activities. Internet gaming offers some benefits for children and adolescents, including socialization and connection with peers, which was especially important for avoiding isolation during the pandemic. Empirical evidence of the positive effects of internet gaming can be seen in studies of youth undergoing chemotherapy, those receiving psychotherapy for anxiety or depression, and those having emotional and behavioral problems.2 Internet gaming also provides participants with a platform to communicate with the outside world while maintaining social distancing, and might reduce anxiety, and in some cases, depression.3
Despite these benefits, for some youth, excessive internet gaming can have adverse effects. Due to its addictive properties, internet gaming can be dangerous for vulnerable individuals and lead to unhealthy habits, such as disturbed sleep patterns and increased anxiety.4 In a cross-sectional study conducted in China, Yu et al5 examined the association between IGD and suicidal ideation. They concluded that IGD was positively associated with insomnia and then depression, which in turn contributed to suicide ideation.5 A study based on a survey conducted in Iran from May to August 2020 in individuals age 13 to 18 years found that depression, anxiety, and stress were significant mediators in the association between IGD and self-reported quality of life.2
Internet gaming disorder is included in DSM-5 as a “condition for further study” and in ICD-11.6 Before the COVID-19 pandemic, a study of 1,178 American youth age 8 to 18 years revealed that 8.5% of gamers met the criteria for IGD.7 In a meta-analysis that included 16 studies, the pooled prevalence of IGD among adolescents was 4.6%.8 Some countries, including China and South Korea, have developed treatment plans for IGD,6 but in the United States treatment guidelines have not been established due to insufficient evidence.9
The COVID-19 pandemic has likely led to an increased number of children and adolescents with IGD and its adverse effects on their mental health and well-being. It remains to be seen whether these youth will improve as the pandemic resolves and they resume normal activities, or if impairments will persist.
In conclusion, while internet gaming during the COVID-19 pandemic has provided benefits for many children and adolescents, the negative impact for those who develop IGD may be significant. We should be prepared to detect and address the needs of these youth and their families. Additional research is needed on the post-pandemic prevalence of IGD, its impact on youth mental health, and treatment strategies.
The impact of the COVID-19 pandemic on the well-being of youth has been significant. Its possible effects range from boredom, depression, anxiety, and suicidal ideation to potential increased rates of internet gaming disorder (IGD), which may have worsened during a nationwide shutdown and extended period of limited social interactions. Presently, there is a paucity of research on the impact of internet gaming on children and adolescents’ mental health and well-being during COVID-19. This article aims to bring awareness to the possible rising impact of the COVID-19 pandemic on IGD and mental health in youth.
Gaming offers benefits—and risks
The gaming industry has grown immensely over the past several years. While many businesses were impacted negatively during the pandemic, the gaming industry grew. It was estimated to be worth $159.3 billion in 2020, an increase of 9.3% from 2019.1
Stay-at-home orders and quarantine protocols during the COVID-19 pandemic have significantly disrupted normal activities, resulting in increased time for digital entertainment, including online gaming and related activities. Internet gaming offers some benefits for children and adolescents, including socialization and connection with peers, which was especially important for avoiding isolation during the pandemic. Empirical evidence of the positive effects of internet gaming can be seen in studies of youth undergoing chemotherapy, those receiving psychotherapy for anxiety or depression, and those having emotional and behavioral problems.2 Internet gaming also provides participants with a platform to communicate with the outside world while maintaining social distancing, and might reduce anxiety, and in some cases, depression.3
Despite these benefits, for some youth, excessive internet gaming can have adverse effects. Due to its addictive properties, internet gaming can be dangerous for vulnerable individuals and lead to unhealthy habits, such as disturbed sleep patterns and increased anxiety.4 In a cross-sectional study conducted in China, Yu et al5 examined the association between IGD and suicidal ideation. They concluded that IGD was positively associated with insomnia and then depression, which in turn contributed to suicide ideation.5 A study based on a survey conducted in Iran from May to August 2020 in individuals age 13 to 18 years found that depression, anxiety, and stress were significant mediators in the association between IGD and self-reported quality of life.2
Internet gaming disorder is included in DSM-5 as a “condition for further study” and in ICD-11.6 Before the COVID-19 pandemic, a study of 1,178 American youth age 8 to 18 years revealed that 8.5% of gamers met the criteria for IGD.7 In a meta-analysis that included 16 studies, the pooled prevalence of IGD among adolescents was 4.6%.8 Some countries, including China and South Korea, have developed treatment plans for IGD,6 but in the United States treatment guidelines have not been established due to insufficient evidence.9
The COVID-19 pandemic has likely led to an increased number of children and adolescents with IGD and its adverse effects on their mental health and well-being. It remains to be seen whether these youth will improve as the pandemic resolves and they resume normal activities, or if impairments will persist.
In conclusion, while internet gaming during the COVID-19 pandemic has provided benefits for many children and adolescents, the negative impact for those who develop IGD may be significant. We should be prepared to detect and address the needs of these youth and their families. Additional research is needed on the post-pandemic prevalence of IGD, its impact on youth mental health, and treatment strategies.
1. WePC. Video game industry statistics, trends and data in 2021. Accessed June 7, 2021. https://www.wepc.com/news/video-game-statistics/
2. Fazeli S, Mohammadi Zeidi I, Lin CY, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. 2020;12:100307. doi: 10.1016/j.abrep.2020.100307
3. Özçetin M, Gümüstas F, Çag˘ Y, et al. The relationships between video game experience and cognitive abilities in adolescents. Neuropsychiatr Dis Treat. 2019;15:1171-1180. doi: 10.2147/NDT.S206271
4. Männikkö N, Ruotsalainen H, Miettunen J, et al. Problematic gaming behaviour and health-related outcomes: a systematic review and meta-analysis. J Health Psychol. 2020;25(1):67-81. doi: 10.1177/1359105317740414
5. Yu Y, Yang X, Wang S, et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry. 2020;20(1):460. doi: 10.1186/s12888-020-02870-zz
6. American Psychiatric Association. Internet gaming. Published June 2018. Accessed June 7, 2021. www.psychiatry.org/patients-families/internet-gaming
7. Gentile D. Pathological video-game use among youth ages 8 to 18: a national study. Psychol Sci. 2009;20(5):594-602. doi: 10.1111/j.1467-9280.2009.02340.x
8. Fam JY. Prevalence of internet gaming disorder in adolescents: A meta-analysis across three decades. Scand J Psychol. 2018;59(5):524-531. doi: 10.1111/sjop.12459
9. Gentile DA, Bailey K, Bavelier D, et al. Internet gaming disorder in children and adolescents. Pediatrics. 2017;140(suppl 2):S81-S85. doi: 10.1542/peds.2016-1758H
1. WePC. Video game industry statistics, trends and data in 2021. Accessed June 7, 2021. https://www.wepc.com/news/video-game-statistics/
2. Fazeli S, Mohammadi Zeidi I, Lin CY, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. 2020;12:100307. doi: 10.1016/j.abrep.2020.100307
3. Özçetin M, Gümüstas F, Çag˘ Y, et al. The relationships between video game experience and cognitive abilities in adolescents. Neuropsychiatr Dis Treat. 2019;15:1171-1180. doi: 10.2147/NDT.S206271
4. Männikkö N, Ruotsalainen H, Miettunen J, et al. Problematic gaming behaviour and health-related outcomes: a systematic review and meta-analysis. J Health Psychol. 2020;25(1):67-81. doi: 10.1177/1359105317740414
5. Yu Y, Yang X, Wang S, et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry. 2020;20(1):460. doi: 10.1186/s12888-020-02870-zz
6. American Psychiatric Association. Internet gaming. Published June 2018. Accessed June 7, 2021. www.psychiatry.org/patients-families/internet-gaming
7. Gentile D. Pathological video-game use among youth ages 8 to 18: a national study. Psychol Sci. 2009;20(5):594-602. doi: 10.1111/j.1467-9280.2009.02340.x
8. Fam JY. Prevalence of internet gaming disorder in adolescents: A meta-analysis across three decades. Scand J Psychol. 2018;59(5):524-531. doi: 10.1111/sjop.12459
9. Gentile DA, Bailey K, Bavelier D, et al. Internet gaming disorder in children and adolescents. Pediatrics. 2017;140(suppl 2):S81-S85. doi: 10.1542/peds.2016-1758H
Stuck in a rut with the wrong diagnosis
CASE Aggressive behaviors, psychosis
Ms. N, age 58, has a long history of bipolar disorder with psychotic features. She presents to our emergency department (ED) after an acute fall and frequent violent behaviors at her nursing home, where she had resided since being diagnosed with an unspecified neurocognitive disorder. For several weeks before her fall, she was physically aggressive, throwing objects at nursing home staff, and was unable to have her behavior redirected.
While in the ED, Ms. N rambles and appears to be responding to internal stimuli. Suddenly, she stops responding and begins to stare.
HISTORY Severe, chronic psychosis and hospitalization
Ms. N is well-known at our inpatient psychiatry and electroconvulsive therapy (ECT) services. During the last 10 years, she has had worsening manic, psychotic, and catatonic (both excited and stuporous subtype) episodes. Three years ago, she had experienced a period of severe, chronic psychosis and excited catatonia that required extended inpatient treatment. While hospitalized, Ms. N had marginal responses to clozapine and benzodiazepines, but improved dramatically with ECT. After Ms. N left the hospital, she went to live with her boyfriend. She remained stable on monthly maintenance ECT treatments (bifrontal) before she was lost to follow-up 14 months prior to the current presentation. Ms. N’s family reports that she needed a cardiac clearance before continuing ECT treatment; however, she was hospitalized at another hospital with pneumonia and subsequent complications that interrupted the maintenance ECT treatments.
Approximately 3 months after medical issues requiring hospitalization began, Ms. N received a diagnosis of neurocognitive disorder due to difficulty with activities of daily living and cognitive decline. She was transferred to a nursing home by the outside hospital. When Ms. N’s symptoms of psychosis returned and she required inpatient psychiatric care, she was transferred to a nearby facility that did not have ECT available or knowledge of her history of catatonia resistant to pharmacologic management. Ms. N had a documented history of catatonia that spanned 10 years. During the last 4 years, Ms. N often required ECT treatment. Her current medication regimen prescribed by an outpatient psychiatrist includes clozapine, 300 mg twice daily, and clonazepam, 0.5 mg twice daily, both for bipolar disorder.
EVALUATION An unusual mix of symptoms
In the ED, Ms. N undergoes a CT of the head, which is found to be nonacute. Laboratory results show that her white blood cell count is 14.3 K/µL, which is mildly elevated. Results from a urinalysis and electrocardiogram (ECG) are unremarkable.
After Ms. N punches a radiology technician, she is administered IV lorazepam, 2 mg once, for her agitation. Twenty minutes after receiving IV lorazepam, she is calm and cooperative. However, approximately 4 hours later, Ms. N is yelling, tearful, and expressing delusions of grandeur—she believes she is God.
After she is admitted to the medical floor, Ms. N is seen by our consultation and liaison psychiatry service. She exhibits several signs of catatonia, including grasp reflex, gegenhalten (oppositional paratonia), waxy flexibility, and echolalia. Ms. N also has an episode of urinary incontinence. At some parts of the day, she is alert and oriented to self and location; at other times, she is somnolent and disoriented. The treatment team continues Ms. N’s previous medication regimen of clozapine, 300 mg twice daily, and clonazepam, 0.5 mg twice daily. Unfortunately, at times Ms. N spits out and hides her administered oral medications, which leads to the decision to discontinue clozapine. Once medically cleared, Ms. N is transferred to the psychiatric floor.
[polldaddy:10869949]
Continue to: TREATMENT
TREATMENT Bifrontal ECT initiated
On hospital Day 3 Ms. N is administered a trial of IM lorazepam, titrated up to 6 mg/d (maximum tolerated dose) while the treatment team initiates the legal process to conduct ECT because she is unable to give consent. Once Ms. N begins tolerating oral medications, amantadine, 100 mg twice daily, is added to treat her catatonia. As in prior hospitalizations, Ms. N is unresponsive to pharmacotherapy alone for her catatonic symptoms. On hospital Day 8, forced ECT is granted, which is 5 days after the process of filing paperwork was started. Bifrontal ECT is utilized with the following settings: frequency 70 Hz, pulse width 1.5 ms, 100% energy dose, 504 mC. Ms. N does not experience a significant improvement until she receives 10 ECT treatments as part of a 3-times-per-week acute series protocol. The Bush-Francis Catatonia Rating Scale (BFCRS) and the KANNER scale are used to monitor her progress. Her initial BFCRS score is 17 and initial KANNER scale, part 2 score is 26.
Ms. N spends a total of 61 days in the hospital, which is significantly longer than her previous hospital admissions on our psychiatric unit; these previous admissions were for treatment of both stuporous and excited subtypes of catatonia. This increased length of stay coincides with a significantly longer duration of untreated catatonia. Knowledge of her history of both the stuporous and excited subtypes of catatonia would have allowed for faster diagnosis and treatment.1
The authors’ observations
Originally conceptualized as a separate syndrome by Karl Kahlbaum, catatonia was considered only as a specifier for neuropsychiatric conditions (primarily schizophrenia) as recently as DSM-IV-TR.2 DSM-5 describes catatonia as a marked psychomotor disturbance and acknowledges its connection to schizophrenia by keeping it in the same chapter.3 DSM-5 includes separate diagnoses for catatonia, catatonia due to a general medical condition, and unspecified catatonia (for catatonia without a known underlying disorder).3 A recent meta-analysis found the prevalence of catatonia is higher in patients with medical/neurologic illness, bipolar disorder, and autism than in those with schizophrenia.4
Table 13 highlights the DSM-5 criteria for catatonia. DSM-5 requires 3 of 12 symptoms to be present, although symptoms may fluctuate with time.3 If a clinician is not specifically looking for catatonia, it can be a difficult syndrome to diagnose. Does rigidity indicate catatonia, or excessive dopamine blockade from an antipsychotic? How can seemingly contradictory symptoms be part of the same syndrome? Many clinicians associate catatonia with the stuporous subtype (immobility, posturing, catalepsy), which is more prevalent, but the excited subtype, which may involve severe agitation, autonomic dysfunction, and impaired consciousness, can be lethal.2 The diversity in presentation of catatonia is not unlike the challenging variety of symptoms of heart attacks.
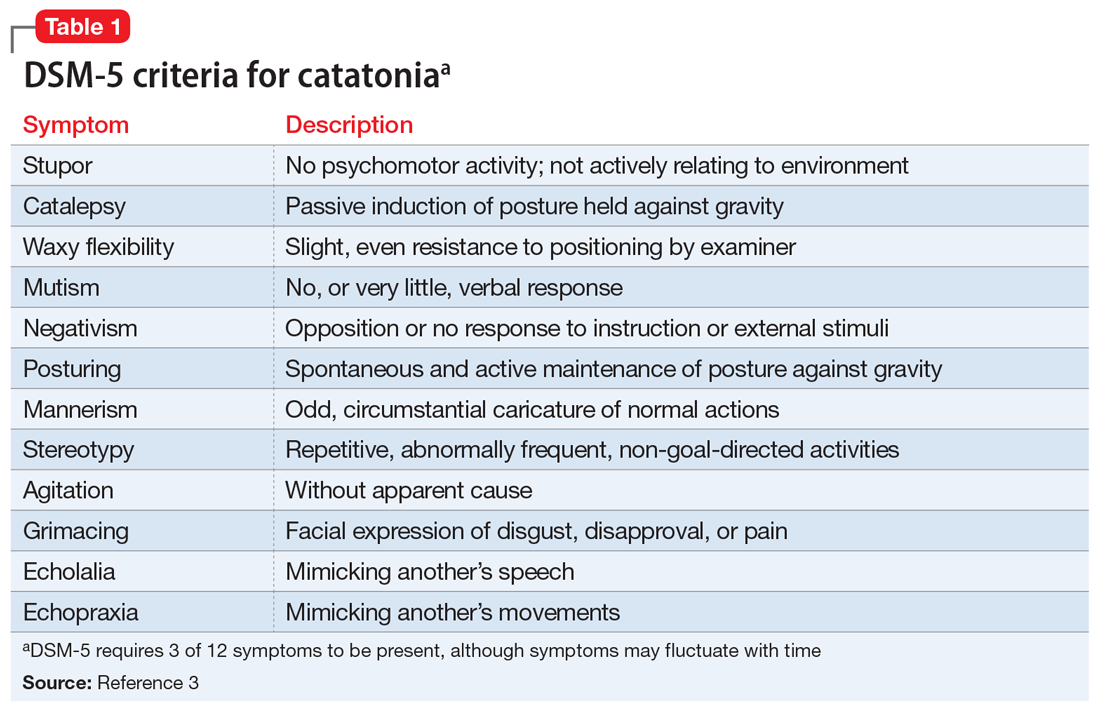
A retrospective study of all adults admitted to a hospital found that only 41% of patients who met criteria for catatonia received this diagnosis.5 Further complicating the diagnosis, delirium and catatonia can co-exist; one study found this was the case in 1 of 3 critically ill patients.6 DSM-5 criteria for catatonia due to another medical condition exclude the diagnosis if delirium is present, but this study and others suggest this needs to be reconsidered.3
Continue to: A standardized evaluation is key
A standardized evaluation is key
Just as a patient who presents with chest pain requires a standardized evaluation, including a pertinent history, laboratory workup, and ECG, psychiatrists may also use standardized diagnostic instruments to aid in the diagnosis of catatonia. One study of hospitalized patients with schizophrenia found that using a standardized diagnostic procedure for catatonia resulted in a 7-fold increase in the diagnosis.7 The BFCRS is the most common standardized instrument for catatonia, likely due to its high inter-rater reliability.8 Other scales include the KANNER scale and Northoff Catatonia Scale, which emphasize different aspects of the disease or for certain clinical populations (eg, the KANNER scale adjusts for patients who are nonverbal at baseline). One study suggested that BFCRS has lower reliability for less-severe illness.9 These differences emphasize that psychiatry does not have a thorough understanding of the intricacies of catatonia. However, using validated screening tools can lead to more consistent diagnoses and continue important research on this often-misunderstood illness.
Dangers of untreated catatonia
Rapid treatment of catatonia is necessary to prevent mortality. A study of patients in Kentucky’s state psychiatric hospitals found that untreated catatonia with resultant death from pulmonary embolism was the leading cause of preventable death.10 A 17-year retrospective study of patients with schizophrenia admitted to 1 hospital found that those with catatonia were >4 times as likely to die during hospitalization than those without catatonia.11 The significant morbidity and mortality from untreated catatonia are typically attributed to the consequences of poorly controlled movements, immobility, autonomic instability, and poor/no oral intake. Reduced oral intake can result in malnutrition, dehydration, arrhythmias, and increased risk of infections. Furthermore, chronic catatonic episodes are more difficult to treat.12 In addition to the aggressive management of neuropsychiatric symptoms, it is vital to evaluate relevant medical etiologies that may be contributing to the syndrome (Table 213). Tracking vital signs and laboratory values, such as creatine kinase, electrolytes, and complete blood count, is required to ensure the medical condition does not become life-threatening.
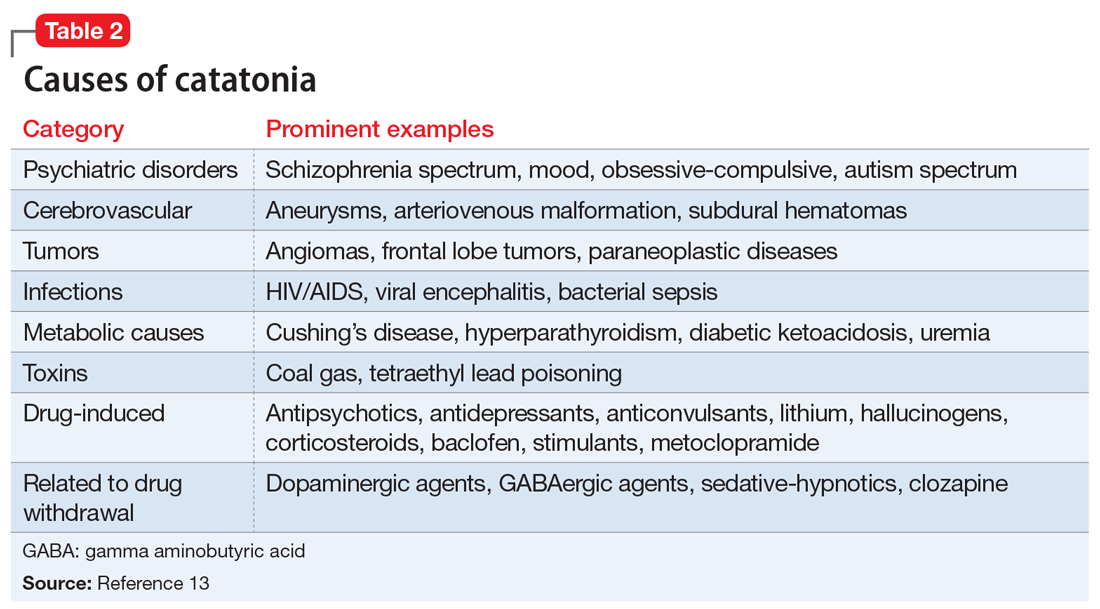
Treatment options
Studies and expert opinion suggest that benzodiazepines (specifically lorazepam, because it is the most studied agent) are the first-line treatment for catatonia. A lorazepam challenge test—providing 1 or 2 mg of IV lorazepam—is considered diagnostic and therapeutic given the high rate of response within 10 minutes.14 Patients with limited response to lorazepam or who are medically compromised should undergo ECT. Electroconvulsive therapy is considered the gold-standard treatment for catatonia; estimated response rates range from 59% to 100%, even in patients who fail to respond to pharmacotherapy.15 Although highly effective, ECT is often hindered by the time required to initiate treatment, stigma, lack of access, and other logistical challenges.
Table 314-18 highlights the advantages and disadvantages of treatment options for catatonia. Some researchers have suggested a zolpidem challenge test could augment lorazepam because some patients respond only to zolpidem.14 The efficacy of these medications along with some evidence of anti-N-methyl-
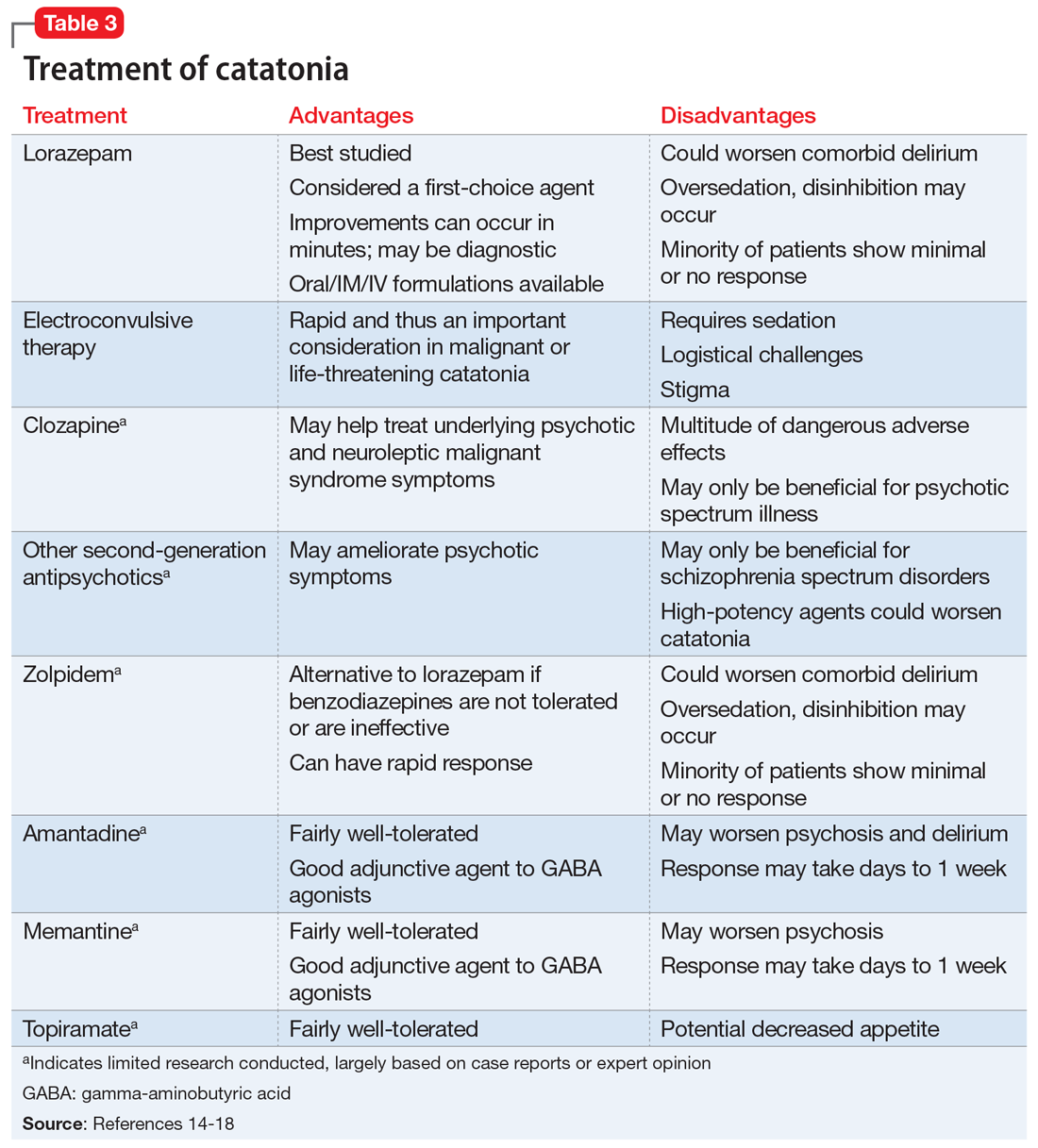
Ms. N was ultimately diagnosed with bipolar disorder, current episode mixed, with psychotic and catatonic features. Ms. N had symptoms of mania including grandiosity, periods of lack of sleep, delusions as well as depressive symptoms of tearfulness and low mood. The treatment team had considered that Ms. N had delirious mania because she had fluctuating sensorium, which included varying degrees of orientation and ability to answer questioning. However, the literature supporting the differentiation between delirious mania and excited catatonia is unclear, and both conditions may respond to ECT.18 A diagnosis of catatonia allowed the team to use rating scales to track Ms. N’s progress by monitoring for specific signs, such as grasp reflex and waxy flexibility.
Continue to: OUTCOME
OUTCOME Return to baseline
Before discharge, Ms. N’s BFCRS score decreases from the initial score of 17 to 0, and her KANNER scale score decreases from the initial score of 26 to 4, which correlates with vast improvement in clinical presentation. Once Ms. N completes the acute ECT treatment, she returns to her baseline level of functioning, and is discharged to live with her boyfriend. She is advised to continue weekly ECT for the first several months to ensure clinical stability. This regimen is later transitioned to biweekly and then monthly. Electroconvulsive therapy protocols from previous research were utilized in Ms. N’s case, but ultimately the lowest number of ECT treatments needed to maintain stability is determined clinically over many years.19 Ms. N is discharged on aripiprazole, 15 mg/d; bupropion ER, 300 mg/d (added after depressive symptoms emerge while catatonia symptoms improve midway through her lengthy hospitalization); and memantine, 10 mg/d. Ideally, clozapine would have been continued; however, due to her history of nonadherence and frequent restarting of the medication at a low dose, clozapine was discontinued and aripiprazole initiated.
More than 1 year later, Ms. N remains stable and continues to receive monthly ECT maintenance treatments.
Bottom Line
Catatonia should always be considered in a patient who presents with acute neuropsychiatric symptoms. Rapid diagnosis with standardized screening instruments and aggressive treatment are vital to prevent morbidity and mortality.
Related Resource
- Freudenreich O, Francis A, Fricchione GL. Chapter 9. Psychosis, mania, and catatonia. In: Levenson, James L, ed. The American Psychiatric Association Publishing textbook of psychosomatic medicine and consultation-liaison psychiatry. 3rd ed. American Psychiatric Association Publishing; 2019.
Drug Brand Names
Amantadine • Symmetrel
Aripiprazole • Abilify
Baclofen • Ozobax
Bupropion ER • Wellbutrin XL
Clonazepam • Klonopin
Clozapine • Clozaril
Lithium • Eskalith, Lithobid
Lorazepam • Ativan
Metoclopramide • Reglan
Memantine • Namenda
Topiramate • Topamax
Zolpidem • Ambien
1. Carroll BT. The universal field hypothesis of catatonia and neuroleptic malignant syndrome. CNS Spectrums. 2000;5(7):26-33.
2. Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: our current understanding of its diagnosis, treatment and pathophysiology. World J Psychiatry. 2016;6(4):391‐398.
3. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013. 119-121.
4. Solmi M, Pigato GG, Roiter B, et al. Prevalence of catatonia and its moderators in clinical samples: results from a meta-analysis and meta-regression analysis. Schizophrenia Bulletin. 2017;44(5):1133-1150.
5. Llesuy JR, Medina M, Jacobson KC, et al. Catatonia under-diagnosis in the general hospital. J Neuropsychiatry Clin Neurosci. 2018;30(2):145-151.
6. Wilson JE, Carlson R, Duggan MC, et al. Delirium and catatonia in critically ill patients. Crit Care Med. 2017;45(11):1837-1844.
7. Heijden FVD, Tuinier S, Arts N, et al. Catatonia: disappeared or under-diagnosed? Psychopathology. 2005;38(1):3-8.
8. Sarkar S, Sakey S, Mathan K, et al. Assessing catatonia using four different instruments: inter-rater reliability and prevalence in inpatient clinical population. Asian J Psychiatr. 2016;23:27-31.
9. Wilson JE, Niu K, Nicolson SE, et al. The diagnostic criteria and structure of catatonia. Schizophr Res. 2015;164(1-3):256-262.
10. Puentes R, Brenzel A, Leon JD. Pulmonary embolism during stuporous episodes of catatonia was found to be the most frequent cause of preventable death according to a state mortality review: 6 deaths in 15 years. Clin Schizophr Relat Psychoses. 2017; doi:10.3371/csrp.rpab.071317
11. Funayama M, Takata T, Koreki A, et al. Catatonic stupor in schizophrenic disorders and subsequent medical complications and mortality. Psychosomatic Medicine. 2018:80(4):370-376.
12. Perugi G, Medda P, Toni C, et al. The role of electroconvulsive therapy (ECT) in bipolar disorder: effectiveness in 522 patients with bipolar depression, mixed-state, mania and catatonic features. Curr Neuropharmacol. 2017;15(3):359-371.
13. Freudenreich O, Francis A, Fricchione GL. Chapter 9. Psychosis, mania, and catatonia. In: Levenson, James L, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2019.
14. Sienaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
15. Pelzer A, Heijden FVD, Boer ED. Systematic review of catatonia treatment. Neuropsychiatr Dis Treat. 2018;14:317-326.
16. Carroll BT, Goforth HW, Thomas C, et al. Review of adjunctive glutamate antagonist therapy in the treatment of catatonic syndromes. J Neuropsychiatry and Clin Neurosci. 2007;19(4):406-412.
17. Fink M. Rediscovering catatonia: the biography of a treatable syndrome. Acta Psychiatr Scand Suppl. 2013;(441):1-47.
18. Fink M, Taylor MA. Catatonia: a clinician’s guide to diagnosis and treatment. Cambridge University Press; 2006.
19. Petrides G, Tobias KG, Kellner CH, et al. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64(3):129-140.
CASE Aggressive behaviors, psychosis
Ms. N, age 58, has a long history of bipolar disorder with psychotic features. She presents to our emergency department (ED) after an acute fall and frequent violent behaviors at her nursing home, where she had resided since being diagnosed with an unspecified neurocognitive disorder. For several weeks before her fall, she was physically aggressive, throwing objects at nursing home staff, and was unable to have her behavior redirected.
While in the ED, Ms. N rambles and appears to be responding to internal stimuli. Suddenly, she stops responding and begins to stare.
HISTORY Severe, chronic psychosis and hospitalization
Ms. N is well-known at our inpatient psychiatry and electroconvulsive therapy (ECT) services. During the last 10 years, she has had worsening manic, psychotic, and catatonic (both excited and stuporous subtype) episodes. Three years ago, she had experienced a period of severe, chronic psychosis and excited catatonia that required extended inpatient treatment. While hospitalized, Ms. N had marginal responses to clozapine and benzodiazepines, but improved dramatically with ECT. After Ms. N left the hospital, she went to live with her boyfriend. She remained stable on monthly maintenance ECT treatments (bifrontal) before she was lost to follow-up 14 months prior to the current presentation. Ms. N’s family reports that she needed a cardiac clearance before continuing ECT treatment; however, she was hospitalized at another hospital with pneumonia and subsequent complications that interrupted the maintenance ECT treatments.
Approximately 3 months after medical issues requiring hospitalization began, Ms. N received a diagnosis of neurocognitive disorder due to difficulty with activities of daily living and cognitive decline. She was transferred to a nursing home by the outside hospital. When Ms. N’s symptoms of psychosis returned and she required inpatient psychiatric care, she was transferred to a nearby facility that did not have ECT available or knowledge of her history of catatonia resistant to pharmacologic management. Ms. N had a documented history of catatonia that spanned 10 years. During the last 4 years, Ms. N often required ECT treatment. Her current medication regimen prescribed by an outpatient psychiatrist includes clozapine, 300 mg twice daily, and clonazepam, 0.5 mg twice daily, both for bipolar disorder.
EVALUATION An unusual mix of symptoms
In the ED, Ms. N undergoes a CT of the head, which is found to be nonacute. Laboratory results show that her white blood cell count is 14.3 K/µL, which is mildly elevated. Results from a urinalysis and electrocardiogram (ECG) are unremarkable.
After Ms. N punches a radiology technician, she is administered IV lorazepam, 2 mg once, for her agitation. Twenty minutes after receiving IV lorazepam, she is calm and cooperative. However, approximately 4 hours later, Ms. N is yelling, tearful, and expressing delusions of grandeur—she believes she is God.
After she is admitted to the medical floor, Ms. N is seen by our consultation and liaison psychiatry service. She exhibits several signs of catatonia, including grasp reflex, gegenhalten (oppositional paratonia), waxy flexibility, and echolalia. Ms. N also has an episode of urinary incontinence. At some parts of the day, she is alert and oriented to self and location; at other times, she is somnolent and disoriented. The treatment team continues Ms. N’s previous medication regimen of clozapine, 300 mg twice daily, and clonazepam, 0.5 mg twice daily. Unfortunately, at times Ms. N spits out and hides her administered oral medications, which leads to the decision to discontinue clozapine. Once medically cleared, Ms. N is transferred to the psychiatric floor.
[polldaddy:10869949]
Continue to: TREATMENT
TREATMENT Bifrontal ECT initiated
On hospital Day 3 Ms. N is administered a trial of IM lorazepam, titrated up to 6 mg/d (maximum tolerated dose) while the treatment team initiates the legal process to conduct ECT because she is unable to give consent. Once Ms. N begins tolerating oral medications, amantadine, 100 mg twice daily, is added to treat her catatonia. As in prior hospitalizations, Ms. N is unresponsive to pharmacotherapy alone for her catatonic symptoms. On hospital Day 8, forced ECT is granted, which is 5 days after the process of filing paperwork was started. Bifrontal ECT is utilized with the following settings: frequency 70 Hz, pulse width 1.5 ms, 100% energy dose, 504 mC. Ms. N does not experience a significant improvement until she receives 10 ECT treatments as part of a 3-times-per-week acute series protocol. The Bush-Francis Catatonia Rating Scale (BFCRS) and the KANNER scale are used to monitor her progress. Her initial BFCRS score is 17 and initial KANNER scale, part 2 score is 26.
Ms. N spends a total of 61 days in the hospital, which is significantly longer than her previous hospital admissions on our psychiatric unit; these previous admissions were for treatment of both stuporous and excited subtypes of catatonia. This increased length of stay coincides with a significantly longer duration of untreated catatonia. Knowledge of her history of both the stuporous and excited subtypes of catatonia would have allowed for faster diagnosis and treatment.1
The authors’ observations
Originally conceptualized as a separate syndrome by Karl Kahlbaum, catatonia was considered only as a specifier for neuropsychiatric conditions (primarily schizophrenia) as recently as DSM-IV-TR.2 DSM-5 describes catatonia as a marked psychomotor disturbance and acknowledges its connection to schizophrenia by keeping it in the same chapter.3 DSM-5 includes separate diagnoses for catatonia, catatonia due to a general medical condition, and unspecified catatonia (for catatonia without a known underlying disorder).3 A recent meta-analysis found the prevalence of catatonia is higher in patients with medical/neurologic illness, bipolar disorder, and autism than in those with schizophrenia.4
Table 13 highlights the DSM-5 criteria for catatonia. DSM-5 requires 3 of 12 symptoms to be present, although symptoms may fluctuate with time.3 If a clinician is not specifically looking for catatonia, it can be a difficult syndrome to diagnose. Does rigidity indicate catatonia, or excessive dopamine blockade from an antipsychotic? How can seemingly contradictory symptoms be part of the same syndrome? Many clinicians associate catatonia with the stuporous subtype (immobility, posturing, catalepsy), which is more prevalent, but the excited subtype, which may involve severe agitation, autonomic dysfunction, and impaired consciousness, can be lethal.2 The diversity in presentation of catatonia is not unlike the challenging variety of symptoms of heart attacks.
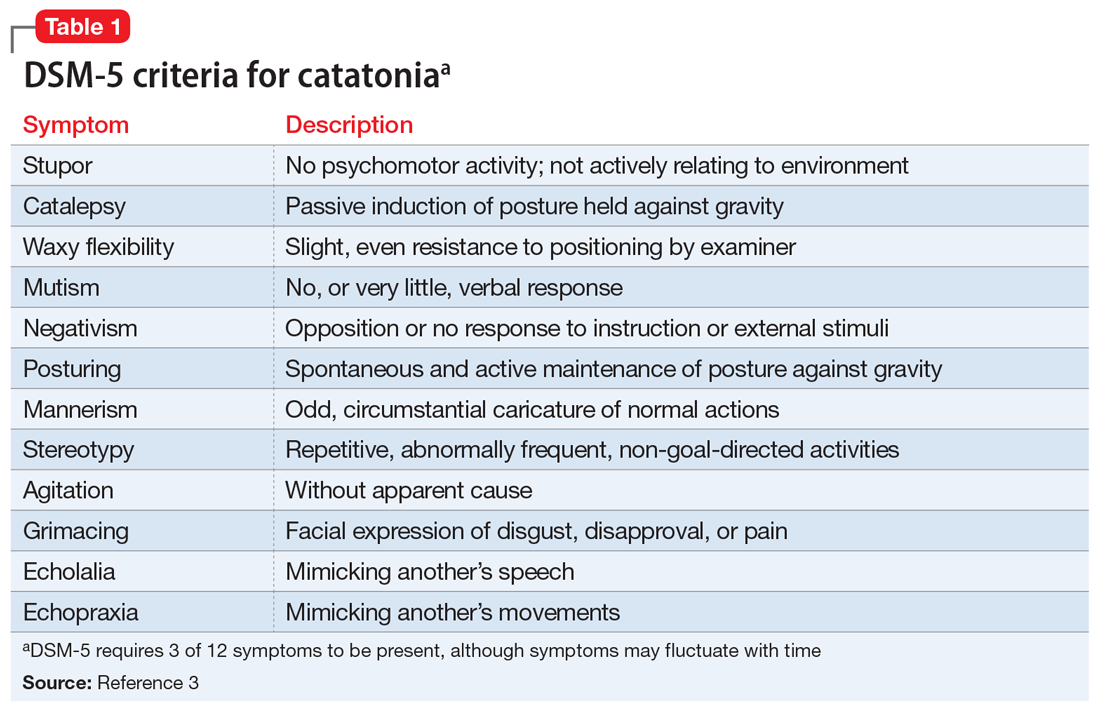
A retrospective study of all adults admitted to a hospital found that only 41% of patients who met criteria for catatonia received this diagnosis.5 Further complicating the diagnosis, delirium and catatonia can co-exist; one study found this was the case in 1 of 3 critically ill patients.6 DSM-5 criteria for catatonia due to another medical condition exclude the diagnosis if delirium is present, but this study and others suggest this needs to be reconsidered.3
Continue to: A standardized evaluation is key
A standardized evaluation is key
Just as a patient who presents with chest pain requires a standardized evaluation, including a pertinent history, laboratory workup, and ECG, psychiatrists may also use standardized diagnostic instruments to aid in the diagnosis of catatonia. One study of hospitalized patients with schizophrenia found that using a standardized diagnostic procedure for catatonia resulted in a 7-fold increase in the diagnosis.7 The BFCRS is the most common standardized instrument for catatonia, likely due to its high inter-rater reliability.8 Other scales include the KANNER scale and Northoff Catatonia Scale, which emphasize different aspects of the disease or for certain clinical populations (eg, the KANNER scale adjusts for patients who are nonverbal at baseline). One study suggested that BFCRS has lower reliability for less-severe illness.9 These differences emphasize that psychiatry does not have a thorough understanding of the intricacies of catatonia. However, using validated screening tools can lead to more consistent diagnoses and continue important research on this often-misunderstood illness.
Dangers of untreated catatonia
Rapid treatment of catatonia is necessary to prevent mortality. A study of patients in Kentucky’s state psychiatric hospitals found that untreated catatonia with resultant death from pulmonary embolism was the leading cause of preventable death.10 A 17-year retrospective study of patients with schizophrenia admitted to 1 hospital found that those with catatonia were >4 times as likely to die during hospitalization than those without catatonia.11 The significant morbidity and mortality from untreated catatonia are typically attributed to the consequences of poorly controlled movements, immobility, autonomic instability, and poor/no oral intake. Reduced oral intake can result in malnutrition, dehydration, arrhythmias, and increased risk of infections. Furthermore, chronic catatonic episodes are more difficult to treat.12 In addition to the aggressive management of neuropsychiatric symptoms, it is vital to evaluate relevant medical etiologies that may be contributing to the syndrome (Table 213). Tracking vital signs and laboratory values, such as creatine kinase, electrolytes, and complete blood count, is required to ensure the medical condition does not become life-threatening.
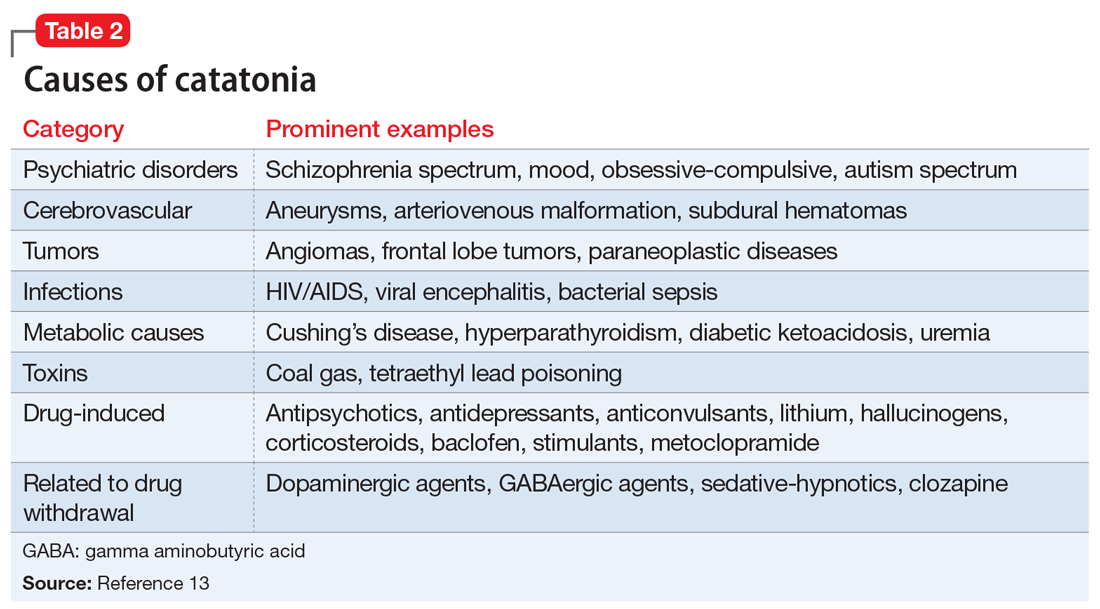
Treatment options
Studies and expert opinion suggest that benzodiazepines (specifically lorazepam, because it is the most studied agent) are the first-line treatment for catatonia. A lorazepam challenge test—providing 1 or 2 mg of IV lorazepam—is considered diagnostic and therapeutic given the high rate of response within 10 minutes.14 Patients with limited response to lorazepam or who are medically compromised should undergo ECT. Electroconvulsive therapy is considered the gold-standard treatment for catatonia; estimated response rates range from 59% to 100%, even in patients who fail to respond to pharmacotherapy.15 Although highly effective, ECT is often hindered by the time required to initiate treatment, stigma, lack of access, and other logistical challenges.
Table 314-18 highlights the advantages and disadvantages of treatment options for catatonia. Some researchers have suggested a zolpidem challenge test could augment lorazepam because some patients respond only to zolpidem.14 The efficacy of these medications along with some evidence of anti-N-methyl-
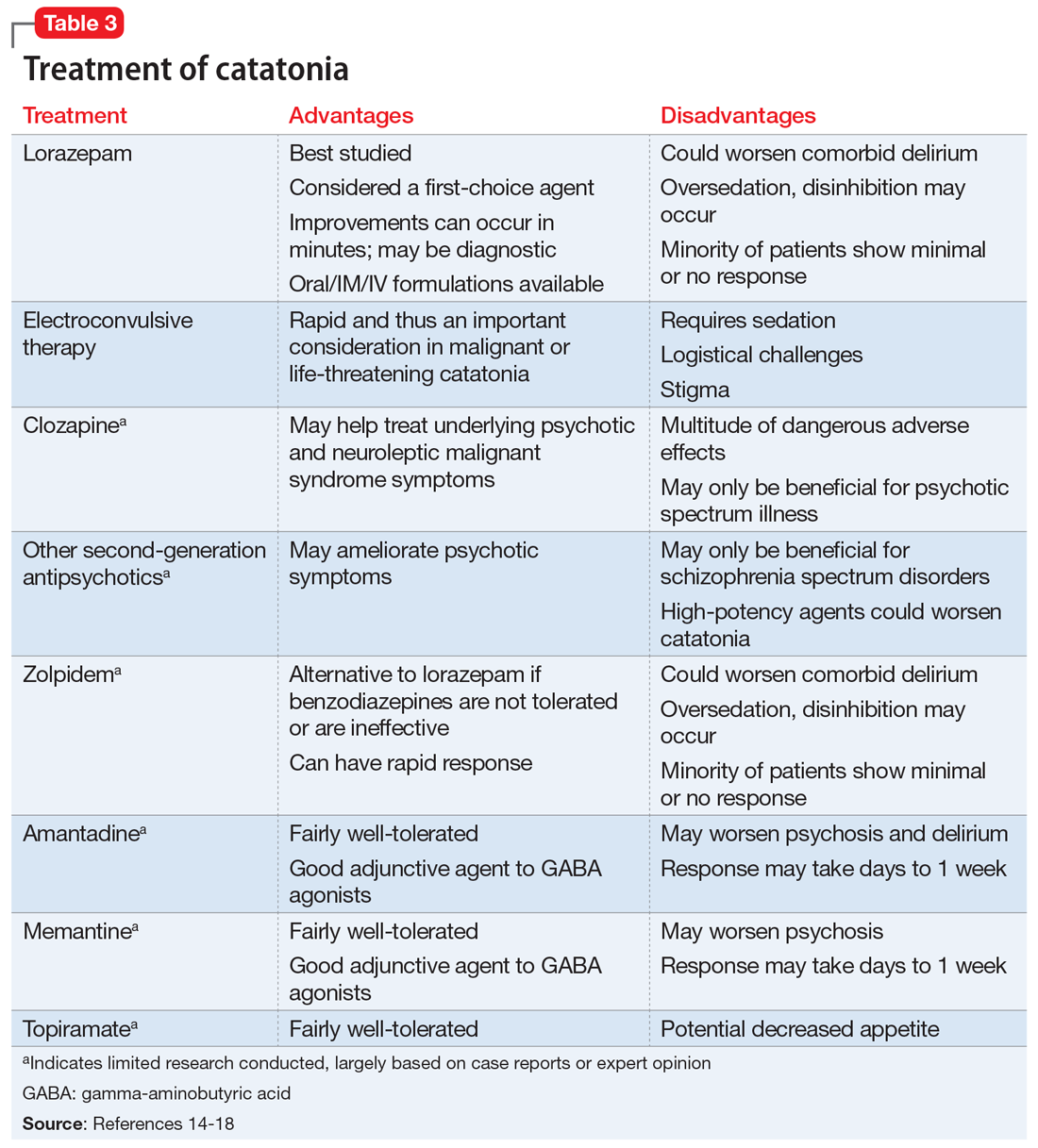
Ms. N was ultimately diagnosed with bipolar disorder, current episode mixed, with psychotic and catatonic features. Ms. N had symptoms of mania including grandiosity, periods of lack of sleep, delusions as well as depressive symptoms of tearfulness and low mood. The treatment team had considered that Ms. N had delirious mania because she had fluctuating sensorium, which included varying degrees of orientation and ability to answer questioning. However, the literature supporting the differentiation between delirious mania and excited catatonia is unclear, and both conditions may respond to ECT.18 A diagnosis of catatonia allowed the team to use rating scales to track Ms. N’s progress by monitoring for specific signs, such as grasp reflex and waxy flexibility.
Continue to: OUTCOME
OUTCOME Return to baseline
Before discharge, Ms. N’s BFCRS score decreases from the initial score of 17 to 0, and her KANNER scale score decreases from the initial score of 26 to 4, which correlates with vast improvement in clinical presentation. Once Ms. N completes the acute ECT treatment, she returns to her baseline level of functioning, and is discharged to live with her boyfriend. She is advised to continue weekly ECT for the first several months to ensure clinical stability. This regimen is later transitioned to biweekly and then monthly. Electroconvulsive therapy protocols from previous research were utilized in Ms. N’s case, but ultimately the lowest number of ECT treatments needed to maintain stability is determined clinically over many years.19 Ms. N is discharged on aripiprazole, 15 mg/d; bupropion ER, 300 mg/d (added after depressive symptoms emerge while catatonia symptoms improve midway through her lengthy hospitalization); and memantine, 10 mg/d. Ideally, clozapine would have been continued; however, due to her history of nonadherence and frequent restarting of the medication at a low dose, clozapine was discontinued and aripiprazole initiated.
More than 1 year later, Ms. N remains stable and continues to receive monthly ECT maintenance treatments.
Bottom Line
Catatonia should always be considered in a patient who presents with acute neuropsychiatric symptoms. Rapid diagnosis with standardized screening instruments and aggressive treatment are vital to prevent morbidity and mortality.
Related Resource
- Freudenreich O, Francis A, Fricchione GL. Chapter 9. Psychosis, mania, and catatonia. In: Levenson, James L, ed. The American Psychiatric Association Publishing textbook of psychosomatic medicine and consultation-liaison psychiatry. 3rd ed. American Psychiatric Association Publishing; 2019.
Drug Brand Names
Amantadine • Symmetrel
Aripiprazole • Abilify
Baclofen • Ozobax
Bupropion ER • Wellbutrin XL
Clonazepam • Klonopin
Clozapine • Clozaril
Lithium • Eskalith, Lithobid
Lorazepam • Ativan
Metoclopramide • Reglan
Memantine • Namenda
Topiramate • Topamax
Zolpidem • Ambien
CASE Aggressive behaviors, psychosis
Ms. N, age 58, has a long history of bipolar disorder with psychotic features. She presents to our emergency department (ED) after an acute fall and frequent violent behaviors at her nursing home, where she had resided since being diagnosed with an unspecified neurocognitive disorder. For several weeks before her fall, she was physically aggressive, throwing objects at nursing home staff, and was unable to have her behavior redirected.
While in the ED, Ms. N rambles and appears to be responding to internal stimuli. Suddenly, she stops responding and begins to stare.
HISTORY Severe, chronic psychosis and hospitalization
Ms. N is well-known at our inpatient psychiatry and electroconvulsive therapy (ECT) services. During the last 10 years, she has had worsening manic, psychotic, and catatonic (both excited and stuporous subtype) episodes. Three years ago, she had experienced a period of severe, chronic psychosis and excited catatonia that required extended inpatient treatment. While hospitalized, Ms. N had marginal responses to clozapine and benzodiazepines, but improved dramatically with ECT. After Ms. N left the hospital, she went to live with her boyfriend. She remained stable on monthly maintenance ECT treatments (bifrontal) before she was lost to follow-up 14 months prior to the current presentation. Ms. N’s family reports that she needed a cardiac clearance before continuing ECT treatment; however, she was hospitalized at another hospital with pneumonia and subsequent complications that interrupted the maintenance ECT treatments.
Approximately 3 months after medical issues requiring hospitalization began, Ms. N received a diagnosis of neurocognitive disorder due to difficulty with activities of daily living and cognitive decline. She was transferred to a nursing home by the outside hospital. When Ms. N’s symptoms of psychosis returned and she required inpatient psychiatric care, she was transferred to a nearby facility that did not have ECT available or knowledge of her history of catatonia resistant to pharmacologic management. Ms. N had a documented history of catatonia that spanned 10 years. During the last 4 years, Ms. N often required ECT treatment. Her current medication regimen prescribed by an outpatient psychiatrist includes clozapine, 300 mg twice daily, and clonazepam, 0.5 mg twice daily, both for bipolar disorder.
EVALUATION An unusual mix of symptoms
In the ED, Ms. N undergoes a CT of the head, which is found to be nonacute. Laboratory results show that her white blood cell count is 14.3 K/µL, which is mildly elevated. Results from a urinalysis and electrocardiogram (ECG) are unremarkable.
After Ms. N punches a radiology technician, she is administered IV lorazepam, 2 mg once, for her agitation. Twenty minutes after receiving IV lorazepam, she is calm and cooperative. However, approximately 4 hours later, Ms. N is yelling, tearful, and expressing delusions of grandeur—she believes she is God.
After she is admitted to the medical floor, Ms. N is seen by our consultation and liaison psychiatry service. She exhibits several signs of catatonia, including grasp reflex, gegenhalten (oppositional paratonia), waxy flexibility, and echolalia. Ms. N also has an episode of urinary incontinence. At some parts of the day, she is alert and oriented to self and location; at other times, she is somnolent and disoriented. The treatment team continues Ms. N’s previous medication regimen of clozapine, 300 mg twice daily, and clonazepam, 0.5 mg twice daily. Unfortunately, at times Ms. N spits out and hides her administered oral medications, which leads to the decision to discontinue clozapine. Once medically cleared, Ms. N is transferred to the psychiatric floor.
[polldaddy:10869949]
Continue to: TREATMENT
TREATMENT Bifrontal ECT initiated
On hospital Day 3 Ms. N is administered a trial of IM lorazepam, titrated up to 6 mg/d (maximum tolerated dose) while the treatment team initiates the legal process to conduct ECT because she is unable to give consent. Once Ms. N begins tolerating oral medications, amantadine, 100 mg twice daily, is added to treat her catatonia. As in prior hospitalizations, Ms. N is unresponsive to pharmacotherapy alone for her catatonic symptoms. On hospital Day 8, forced ECT is granted, which is 5 days after the process of filing paperwork was started. Bifrontal ECT is utilized with the following settings: frequency 70 Hz, pulse width 1.5 ms, 100% energy dose, 504 mC. Ms. N does not experience a significant improvement until she receives 10 ECT treatments as part of a 3-times-per-week acute series protocol. The Bush-Francis Catatonia Rating Scale (BFCRS) and the KANNER scale are used to monitor her progress. Her initial BFCRS score is 17 and initial KANNER scale, part 2 score is 26.
Ms. N spends a total of 61 days in the hospital, which is significantly longer than her previous hospital admissions on our psychiatric unit; these previous admissions were for treatment of both stuporous and excited subtypes of catatonia. This increased length of stay coincides with a significantly longer duration of untreated catatonia. Knowledge of her history of both the stuporous and excited subtypes of catatonia would have allowed for faster diagnosis and treatment.1
The authors’ observations
Originally conceptualized as a separate syndrome by Karl Kahlbaum, catatonia was considered only as a specifier for neuropsychiatric conditions (primarily schizophrenia) as recently as DSM-IV-TR.2 DSM-5 describes catatonia as a marked psychomotor disturbance and acknowledges its connection to schizophrenia by keeping it in the same chapter.3 DSM-5 includes separate diagnoses for catatonia, catatonia due to a general medical condition, and unspecified catatonia (for catatonia without a known underlying disorder).3 A recent meta-analysis found the prevalence of catatonia is higher in patients with medical/neurologic illness, bipolar disorder, and autism than in those with schizophrenia.4
Table 13 highlights the DSM-5 criteria for catatonia. DSM-5 requires 3 of 12 symptoms to be present, although symptoms may fluctuate with time.3 If a clinician is not specifically looking for catatonia, it can be a difficult syndrome to diagnose. Does rigidity indicate catatonia, or excessive dopamine blockade from an antipsychotic? How can seemingly contradictory symptoms be part of the same syndrome? Many clinicians associate catatonia with the stuporous subtype (immobility, posturing, catalepsy), which is more prevalent, but the excited subtype, which may involve severe agitation, autonomic dysfunction, and impaired consciousness, can be lethal.2 The diversity in presentation of catatonia is not unlike the challenging variety of symptoms of heart attacks.
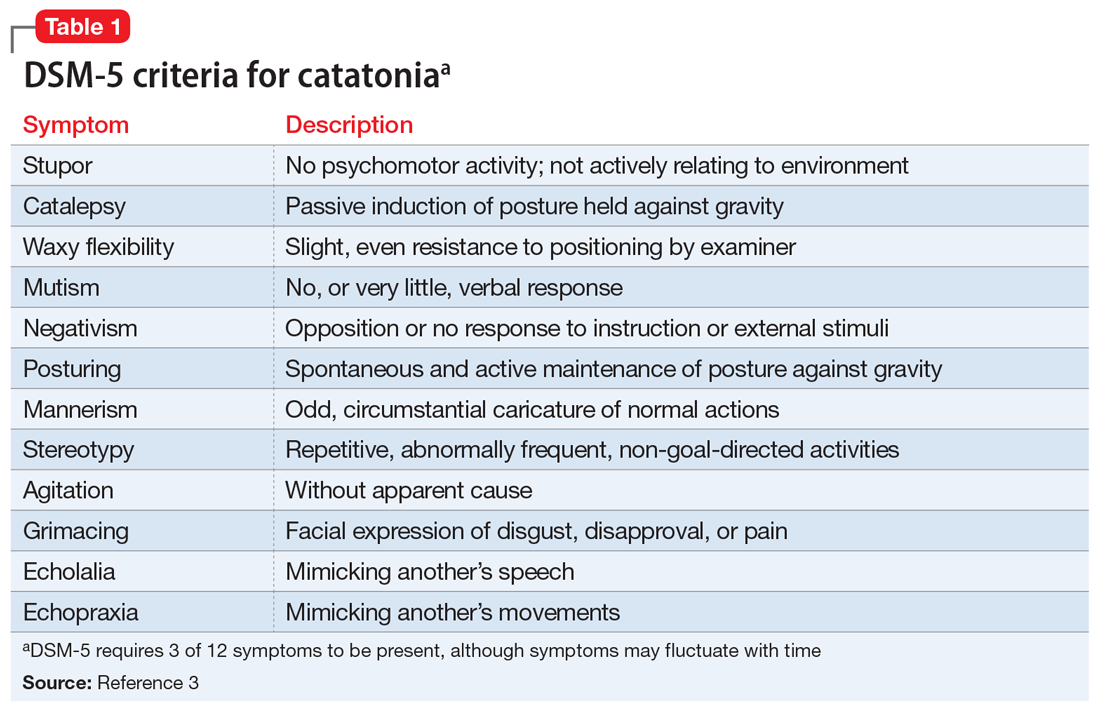
A retrospective study of all adults admitted to a hospital found that only 41% of patients who met criteria for catatonia received this diagnosis.5 Further complicating the diagnosis, delirium and catatonia can co-exist; one study found this was the case in 1 of 3 critically ill patients.6 DSM-5 criteria for catatonia due to another medical condition exclude the diagnosis if delirium is present, but this study and others suggest this needs to be reconsidered.3
Continue to: A standardized evaluation is key
A standardized evaluation is key
Just as a patient who presents with chest pain requires a standardized evaluation, including a pertinent history, laboratory workup, and ECG, psychiatrists may also use standardized diagnostic instruments to aid in the diagnosis of catatonia. One study of hospitalized patients with schizophrenia found that using a standardized diagnostic procedure for catatonia resulted in a 7-fold increase in the diagnosis.7 The BFCRS is the most common standardized instrument for catatonia, likely due to its high inter-rater reliability.8 Other scales include the KANNER scale and Northoff Catatonia Scale, which emphasize different aspects of the disease or for certain clinical populations (eg, the KANNER scale adjusts for patients who are nonverbal at baseline). One study suggested that BFCRS has lower reliability for less-severe illness.9 These differences emphasize that psychiatry does not have a thorough understanding of the intricacies of catatonia. However, using validated screening tools can lead to more consistent diagnoses and continue important research on this often-misunderstood illness.
Dangers of untreated catatonia
Rapid treatment of catatonia is necessary to prevent mortality. A study of patients in Kentucky’s state psychiatric hospitals found that untreated catatonia with resultant death from pulmonary embolism was the leading cause of preventable death.10 A 17-year retrospective study of patients with schizophrenia admitted to 1 hospital found that those with catatonia were >4 times as likely to die during hospitalization than those without catatonia.11 The significant morbidity and mortality from untreated catatonia are typically attributed to the consequences of poorly controlled movements, immobility, autonomic instability, and poor/no oral intake. Reduced oral intake can result in malnutrition, dehydration, arrhythmias, and increased risk of infections. Furthermore, chronic catatonic episodes are more difficult to treat.12 In addition to the aggressive management of neuropsychiatric symptoms, it is vital to evaluate relevant medical etiologies that may be contributing to the syndrome (Table 213). Tracking vital signs and laboratory values, such as creatine kinase, electrolytes, and complete blood count, is required to ensure the medical condition does not become life-threatening.
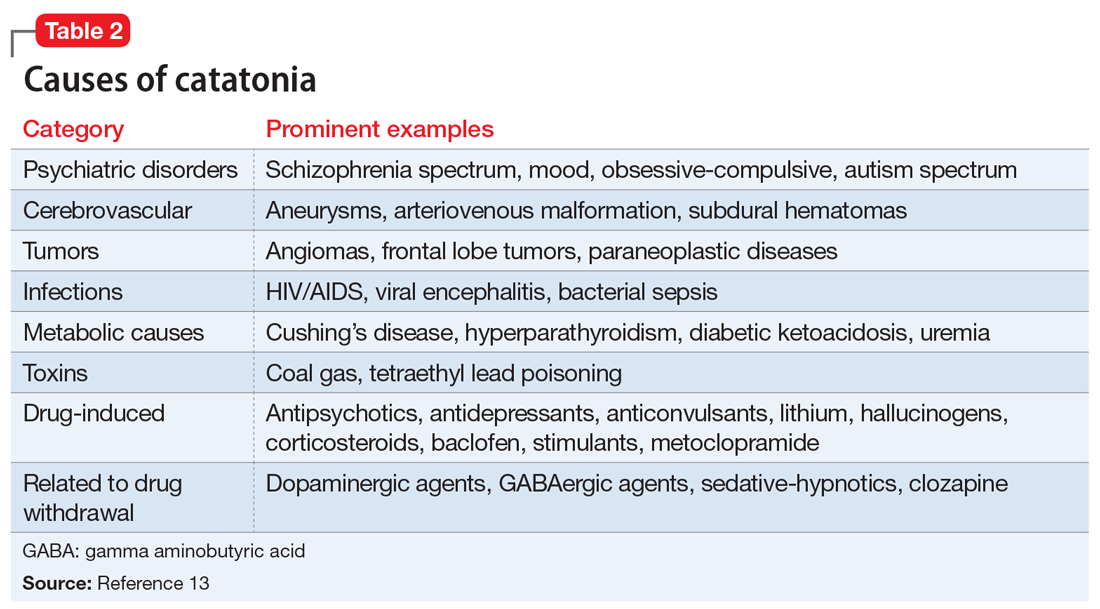
Treatment options
Studies and expert opinion suggest that benzodiazepines (specifically lorazepam, because it is the most studied agent) are the first-line treatment for catatonia. A lorazepam challenge test—providing 1 or 2 mg of IV lorazepam—is considered diagnostic and therapeutic given the high rate of response within 10 minutes.14 Patients with limited response to lorazepam or who are medically compromised should undergo ECT. Electroconvulsive therapy is considered the gold-standard treatment for catatonia; estimated response rates range from 59% to 100%, even in patients who fail to respond to pharmacotherapy.15 Although highly effective, ECT is often hindered by the time required to initiate treatment, stigma, lack of access, and other logistical challenges.
Table 314-18 highlights the advantages and disadvantages of treatment options for catatonia. Some researchers have suggested a zolpidem challenge test could augment lorazepam because some patients respond only to zolpidem.14 The efficacy of these medications along with some evidence of anti-N-methyl-
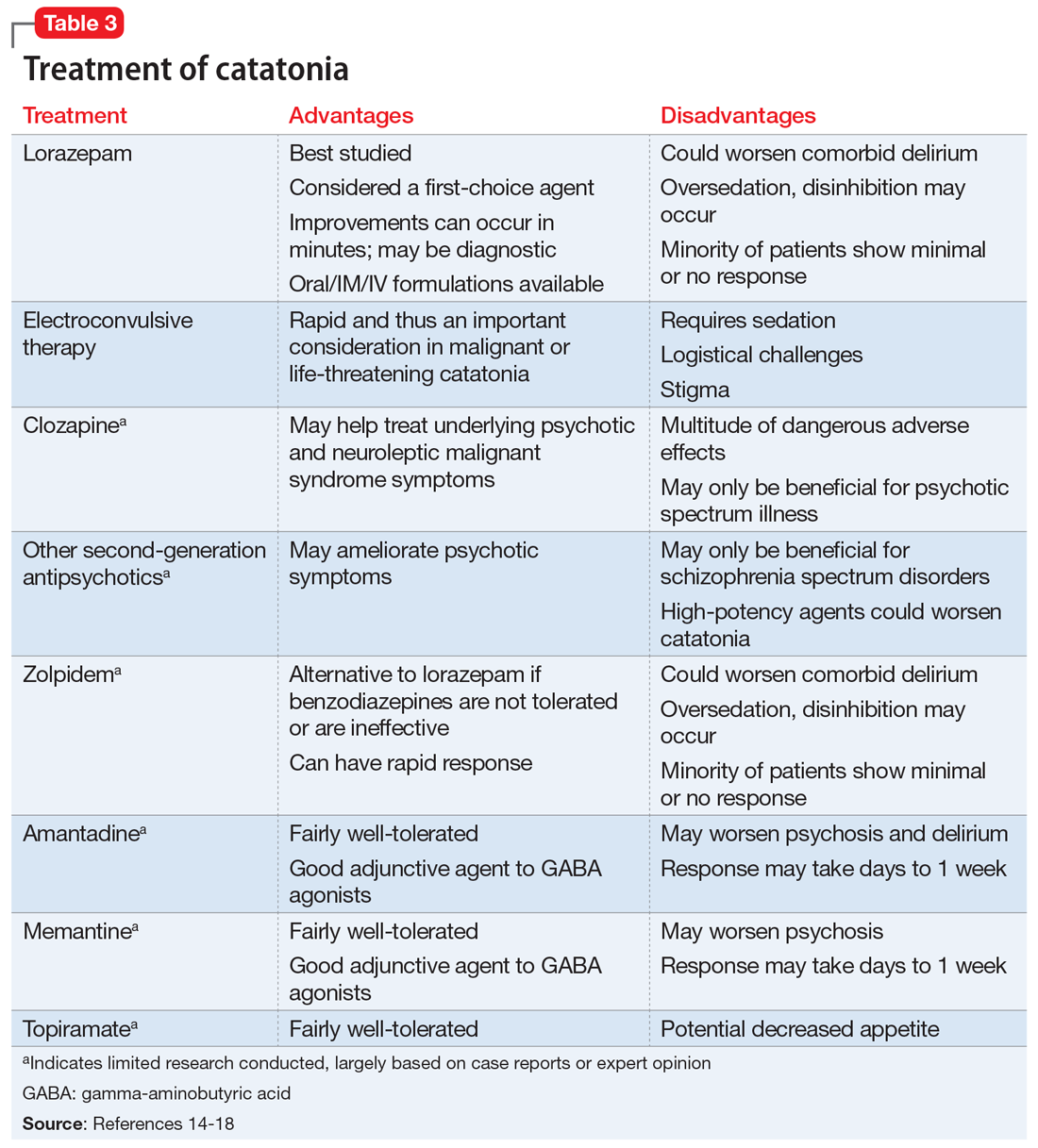
Ms. N was ultimately diagnosed with bipolar disorder, current episode mixed, with psychotic and catatonic features. Ms. N had symptoms of mania including grandiosity, periods of lack of sleep, delusions as well as depressive symptoms of tearfulness and low mood. The treatment team had considered that Ms. N had delirious mania because she had fluctuating sensorium, which included varying degrees of orientation and ability to answer questioning. However, the literature supporting the differentiation between delirious mania and excited catatonia is unclear, and both conditions may respond to ECT.18 A diagnosis of catatonia allowed the team to use rating scales to track Ms. N’s progress by monitoring for specific signs, such as grasp reflex and waxy flexibility.
Continue to: OUTCOME
OUTCOME Return to baseline
Before discharge, Ms. N’s BFCRS score decreases from the initial score of 17 to 0, and her KANNER scale score decreases from the initial score of 26 to 4, which correlates with vast improvement in clinical presentation. Once Ms. N completes the acute ECT treatment, she returns to her baseline level of functioning, and is discharged to live with her boyfriend. She is advised to continue weekly ECT for the first several months to ensure clinical stability. This regimen is later transitioned to biweekly and then monthly. Electroconvulsive therapy protocols from previous research were utilized in Ms. N’s case, but ultimately the lowest number of ECT treatments needed to maintain stability is determined clinically over many years.19 Ms. N is discharged on aripiprazole, 15 mg/d; bupropion ER, 300 mg/d (added after depressive symptoms emerge while catatonia symptoms improve midway through her lengthy hospitalization); and memantine, 10 mg/d. Ideally, clozapine would have been continued; however, due to her history of nonadherence and frequent restarting of the medication at a low dose, clozapine was discontinued and aripiprazole initiated.
More than 1 year later, Ms. N remains stable and continues to receive monthly ECT maintenance treatments.
Bottom Line
Catatonia should always be considered in a patient who presents with acute neuropsychiatric symptoms. Rapid diagnosis with standardized screening instruments and aggressive treatment are vital to prevent morbidity and mortality.
Related Resource
- Freudenreich O, Francis A, Fricchione GL. Chapter 9. Psychosis, mania, and catatonia. In: Levenson, James L, ed. The American Psychiatric Association Publishing textbook of psychosomatic medicine and consultation-liaison psychiatry. 3rd ed. American Psychiatric Association Publishing; 2019.
Drug Brand Names
Amantadine • Symmetrel
Aripiprazole • Abilify
Baclofen • Ozobax
Bupropion ER • Wellbutrin XL
Clonazepam • Klonopin
Clozapine • Clozaril
Lithium • Eskalith, Lithobid
Lorazepam • Ativan
Metoclopramide • Reglan
Memantine • Namenda
Topiramate • Topamax
Zolpidem • Ambien
1. Carroll BT. The universal field hypothesis of catatonia and neuroleptic malignant syndrome. CNS Spectrums. 2000;5(7):26-33.
2. Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: our current understanding of its diagnosis, treatment and pathophysiology. World J Psychiatry. 2016;6(4):391‐398.
3. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013. 119-121.
4. Solmi M, Pigato GG, Roiter B, et al. Prevalence of catatonia and its moderators in clinical samples: results from a meta-analysis and meta-regression analysis. Schizophrenia Bulletin. 2017;44(5):1133-1150.
5. Llesuy JR, Medina M, Jacobson KC, et al. Catatonia under-diagnosis in the general hospital. J Neuropsychiatry Clin Neurosci. 2018;30(2):145-151.
6. Wilson JE, Carlson R, Duggan MC, et al. Delirium and catatonia in critically ill patients. Crit Care Med. 2017;45(11):1837-1844.
7. Heijden FVD, Tuinier S, Arts N, et al. Catatonia: disappeared or under-diagnosed? Psychopathology. 2005;38(1):3-8.
8. Sarkar S, Sakey S, Mathan K, et al. Assessing catatonia using four different instruments: inter-rater reliability and prevalence in inpatient clinical population. Asian J Psychiatr. 2016;23:27-31.
9. Wilson JE, Niu K, Nicolson SE, et al. The diagnostic criteria and structure of catatonia. Schizophr Res. 2015;164(1-3):256-262.
10. Puentes R, Brenzel A, Leon JD. Pulmonary embolism during stuporous episodes of catatonia was found to be the most frequent cause of preventable death according to a state mortality review: 6 deaths in 15 years. Clin Schizophr Relat Psychoses. 2017; doi:10.3371/csrp.rpab.071317
11. Funayama M, Takata T, Koreki A, et al. Catatonic stupor in schizophrenic disorders and subsequent medical complications and mortality. Psychosomatic Medicine. 2018:80(4):370-376.
12. Perugi G, Medda P, Toni C, et al. The role of electroconvulsive therapy (ECT) in bipolar disorder: effectiveness in 522 patients with bipolar depression, mixed-state, mania and catatonic features. Curr Neuropharmacol. 2017;15(3):359-371.
13. Freudenreich O, Francis A, Fricchione GL. Chapter 9. Psychosis, mania, and catatonia. In: Levenson, James L, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2019.
14. Sienaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
15. Pelzer A, Heijden FVD, Boer ED. Systematic review of catatonia treatment. Neuropsychiatr Dis Treat. 2018;14:317-326.
16. Carroll BT, Goforth HW, Thomas C, et al. Review of adjunctive glutamate antagonist therapy in the treatment of catatonic syndromes. J Neuropsychiatry and Clin Neurosci. 2007;19(4):406-412.
17. Fink M. Rediscovering catatonia: the biography of a treatable syndrome. Acta Psychiatr Scand Suppl. 2013;(441):1-47.
18. Fink M, Taylor MA. Catatonia: a clinician’s guide to diagnosis and treatment. Cambridge University Press; 2006.
19. Petrides G, Tobias KG, Kellner CH, et al. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64(3):129-140.
1. Carroll BT. The universal field hypothesis of catatonia and neuroleptic malignant syndrome. CNS Spectrums. 2000;5(7):26-33.
2. Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: our current understanding of its diagnosis, treatment and pathophysiology. World J Psychiatry. 2016;6(4):391‐398.
3. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013. 119-121.
4. Solmi M, Pigato GG, Roiter B, et al. Prevalence of catatonia and its moderators in clinical samples: results from a meta-analysis and meta-regression analysis. Schizophrenia Bulletin. 2017;44(5):1133-1150.
5. Llesuy JR, Medina M, Jacobson KC, et al. Catatonia under-diagnosis in the general hospital. J Neuropsychiatry Clin Neurosci. 2018;30(2):145-151.
6. Wilson JE, Carlson R, Duggan MC, et al. Delirium and catatonia in critically ill patients. Crit Care Med. 2017;45(11):1837-1844.
7. Heijden FVD, Tuinier S, Arts N, et al. Catatonia: disappeared or under-diagnosed? Psychopathology. 2005;38(1):3-8.
8. Sarkar S, Sakey S, Mathan K, et al. Assessing catatonia using four different instruments: inter-rater reliability and prevalence in inpatient clinical population. Asian J Psychiatr. 2016;23:27-31.
9. Wilson JE, Niu K, Nicolson SE, et al. The diagnostic criteria and structure of catatonia. Schizophr Res. 2015;164(1-3):256-262.
10. Puentes R, Brenzel A, Leon JD. Pulmonary embolism during stuporous episodes of catatonia was found to be the most frequent cause of preventable death according to a state mortality review: 6 deaths in 15 years. Clin Schizophr Relat Psychoses. 2017; doi:10.3371/csrp.rpab.071317
11. Funayama M, Takata T, Koreki A, et al. Catatonic stupor in schizophrenic disorders and subsequent medical complications and mortality. Psychosomatic Medicine. 2018:80(4):370-376.
12. Perugi G, Medda P, Toni C, et al. The role of electroconvulsive therapy (ECT) in bipolar disorder: effectiveness in 522 patients with bipolar depression, mixed-state, mania and catatonic features. Curr Neuropharmacol. 2017;15(3):359-371.
13. Freudenreich O, Francis A, Fricchione GL. Chapter 9. Psychosis, mania, and catatonia. In: Levenson, James L, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2019.
14. Sienaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
15. Pelzer A, Heijden FVD, Boer ED. Systematic review of catatonia treatment. Neuropsychiatr Dis Treat. 2018;14:317-326.
16. Carroll BT, Goforth HW, Thomas C, et al. Review of adjunctive glutamate antagonist therapy in the treatment of catatonic syndromes. J Neuropsychiatry and Clin Neurosci. 2007;19(4):406-412.
17. Fink M. Rediscovering catatonia: the biography of a treatable syndrome. Acta Psychiatr Scand Suppl. 2013;(441):1-47.
18. Fink M, Taylor MA. Catatonia: a clinician’s guide to diagnosis and treatment. Cambridge University Press; 2006.
19. Petrides G, Tobias KG, Kellner CH, et al. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64(3):129-140.