User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Could semaglutide treat addiction as well as obesity?
As demand for semaglutide for weight loss grew following approval of Wegovy by the U.S. Food and Drug Administration in 2021, anecdotal reports of unexpected potential added benefits also began to surface.
Some patients taking these drugs for type 2 diabetes or weight loss also lost interest in addictive and compulsive behaviors such as drinking alcohol, smoking, shopping, nail biting, and skin picking, as reported in articles in the New York Times and The Atlantic, among others.
There is also some preliminary research to support these observations.
This news organization invited three experts to weigh in.
Recent and upcoming studies
The senior author of a recent randomized controlled trial of 127 patients with alcohol use disorder (AUD), Anders Fink-Jensen, MD, said: “I hope that GLP-1 analogs in the future can be used against AUD, but before that can happen, several GLP-1 trials [are needed to] prove an effect on alcohol intake.”
His study involved patients who received exenatide (Byetta, Bydureon, AstraZeneca), the first-generation GLP-1 agonist approved for type 2 diabetes, over 26 weeks, but treatment did not reduce the number of heavy drinking days (the primary outcome), compared with placebo.
However, in post hoc, exploratory analyses, heavy drinking days and total alcohol intake were significantly reduced in the subgroup of patients with AUD and obesity (body mass index > 30 kg/m2).
The participants were also shown pictures of alcohol or neutral subjects while they underwent functional magnetic resonance imaging. Those who had received exenatide, compared with placebo, had significantly less activation of brain reward centers when shown the pictures of alcohol.
“Something is happening in the brain and activation of the reward center is hampered by the GLP-1 compound,” Dr. Fink-Jensen, a clinical psychologist at the Psychiatric Centre Copenhagen, remarked in an email.
“If patients with AUD already fulfill the criteria for semaglutide (or other GLP-1 analogs) by having type 2 diabetes and/or a BMI over 30 kg/m2, they can of course use the compound right now,” he noted.
His team is also beginning a study in patients with AUD and a BMI ≥ 30 kg/m2 to investigate the effects on alcohol intake of semaglutide up to 2.4 mg weekly, the maximum dose currently approved for obesity in the United States.
“Based on the potency of exenatide and semaglutide,” Dr. Fink-Jensen said, “we expect that semaglutide will cause a stronger reduction in alcohol intake” than exenatide.
Animal studies have also shown that GLP-1 agonists suppress alcohol-induced reward, alcohol intake, motivation to consume alcohol, alcohol seeking, and relapse drinking of alcohol, Elisabet Jerlhag Holm, PhD, noted.
Interestingly, these agents also suppress the reward, intake, and motivation to consume other addictive drugs like cocaine, amphetamine, nicotine, and some opioids, Jerlhag Holm, professor, department of pharmacology, University of Gothenburg, Sweden, noted in an email.
In a recently published preclinical study, her group provides evidence to help explain anecdotal reports from patients with obesity treated with semaglutide who claim they also reduced their alcohol intake. In the study, semaglutide both reduced alcohol intake (and relapse-like drinking) and decreased body weight of rats of both sexes.
“Future research should explore the possibility of semaglutide decreasing alcohol intake in patients with AUD, particularly those who are overweight,” said Prof. Holm.
“AUD is a heterogenous disorder, and one medication is most likely not helpful for all AUD patients,” she added. “Therefore, an arsenal of different medications is beneficial when treating AUD.”
Janice J. Hwang, MD, MHS, echoed these thoughts: “Anecdotally, there are a lot of reports from patients (and in the news) that this class of medication [GLP-1 agonists] impacts cravings and could impact addictive behaviors.”
“I would say, overall, the jury is still out,” as to whether anecdotal reports of GLP-1 agonists curbing addictions will be borne out in randomized controlled trials.
“I think it is much too early to tell” whether these drugs might be approved for treating addictions without more solid clinical trial data, noted Dr. Hwang, who is an associate professor of medicine and chief, division of endocrinology and metabolism, at the University of North Carolina at Chapel Hill.
Meanwhile, another research group at the University of North Carolina at Chapel Hill, led by psychiatrist Christian Hendershot, PhD, is conducting a clinical trial in 48 participants with AUD who are also smokers.
They aim to determine if patients who receive semaglutide at escalating doses (0.25 mg to 1.0 mg per week via subcutaneous injection) over 9 weeks will consume less alcohol (the primary outcome) and smoke less (a secondary outcome) than those who receive a sham placebo injection. Results are expected in October 2023.
Dr. Fink-Jensen has received an unrestricted research grant from Novo Nordisk to investigate the effects of GLP-1 receptor stimulation on weight gain and metabolic disturbances in patients with schizophrenia treated with an antipsychotic.
A version of this article first appeared on Medscape.com.
As demand for semaglutide for weight loss grew following approval of Wegovy by the U.S. Food and Drug Administration in 2021, anecdotal reports of unexpected potential added benefits also began to surface.
Some patients taking these drugs for type 2 diabetes or weight loss also lost interest in addictive and compulsive behaviors such as drinking alcohol, smoking, shopping, nail biting, and skin picking, as reported in articles in the New York Times and The Atlantic, among others.
There is also some preliminary research to support these observations.
This news organization invited three experts to weigh in.
Recent and upcoming studies
The senior author of a recent randomized controlled trial of 127 patients with alcohol use disorder (AUD), Anders Fink-Jensen, MD, said: “I hope that GLP-1 analogs in the future can be used against AUD, but before that can happen, several GLP-1 trials [are needed to] prove an effect on alcohol intake.”
His study involved patients who received exenatide (Byetta, Bydureon, AstraZeneca), the first-generation GLP-1 agonist approved for type 2 diabetes, over 26 weeks, but treatment did not reduce the number of heavy drinking days (the primary outcome), compared with placebo.
However, in post hoc, exploratory analyses, heavy drinking days and total alcohol intake were significantly reduced in the subgroup of patients with AUD and obesity (body mass index > 30 kg/m2).
The participants were also shown pictures of alcohol or neutral subjects while they underwent functional magnetic resonance imaging. Those who had received exenatide, compared with placebo, had significantly less activation of brain reward centers when shown the pictures of alcohol.
“Something is happening in the brain and activation of the reward center is hampered by the GLP-1 compound,” Dr. Fink-Jensen, a clinical psychologist at the Psychiatric Centre Copenhagen, remarked in an email.
“If patients with AUD already fulfill the criteria for semaglutide (or other GLP-1 analogs) by having type 2 diabetes and/or a BMI over 30 kg/m2, they can of course use the compound right now,” he noted.
His team is also beginning a study in patients with AUD and a BMI ≥ 30 kg/m2 to investigate the effects on alcohol intake of semaglutide up to 2.4 mg weekly, the maximum dose currently approved for obesity in the United States.
“Based on the potency of exenatide and semaglutide,” Dr. Fink-Jensen said, “we expect that semaglutide will cause a stronger reduction in alcohol intake” than exenatide.
Animal studies have also shown that GLP-1 agonists suppress alcohol-induced reward, alcohol intake, motivation to consume alcohol, alcohol seeking, and relapse drinking of alcohol, Elisabet Jerlhag Holm, PhD, noted.
Interestingly, these agents also suppress the reward, intake, and motivation to consume other addictive drugs like cocaine, amphetamine, nicotine, and some opioids, Jerlhag Holm, professor, department of pharmacology, University of Gothenburg, Sweden, noted in an email.
In a recently published preclinical study, her group provides evidence to help explain anecdotal reports from patients with obesity treated with semaglutide who claim they also reduced their alcohol intake. In the study, semaglutide both reduced alcohol intake (and relapse-like drinking) and decreased body weight of rats of both sexes.
“Future research should explore the possibility of semaglutide decreasing alcohol intake in patients with AUD, particularly those who are overweight,” said Prof. Holm.
“AUD is a heterogenous disorder, and one medication is most likely not helpful for all AUD patients,” she added. “Therefore, an arsenal of different medications is beneficial when treating AUD.”
Janice J. Hwang, MD, MHS, echoed these thoughts: “Anecdotally, there are a lot of reports from patients (and in the news) that this class of medication [GLP-1 agonists] impacts cravings and could impact addictive behaviors.”
“I would say, overall, the jury is still out,” as to whether anecdotal reports of GLP-1 agonists curbing addictions will be borne out in randomized controlled trials.
“I think it is much too early to tell” whether these drugs might be approved for treating addictions without more solid clinical trial data, noted Dr. Hwang, who is an associate professor of medicine and chief, division of endocrinology and metabolism, at the University of North Carolina at Chapel Hill.
Meanwhile, another research group at the University of North Carolina at Chapel Hill, led by psychiatrist Christian Hendershot, PhD, is conducting a clinical trial in 48 participants with AUD who are also smokers.
They aim to determine if patients who receive semaglutide at escalating doses (0.25 mg to 1.0 mg per week via subcutaneous injection) over 9 weeks will consume less alcohol (the primary outcome) and smoke less (a secondary outcome) than those who receive a sham placebo injection. Results are expected in October 2023.
Dr. Fink-Jensen has received an unrestricted research grant from Novo Nordisk to investigate the effects of GLP-1 receptor stimulation on weight gain and metabolic disturbances in patients with schizophrenia treated with an antipsychotic.
A version of this article first appeared on Medscape.com.
As demand for semaglutide for weight loss grew following approval of Wegovy by the U.S. Food and Drug Administration in 2021, anecdotal reports of unexpected potential added benefits also began to surface.
Some patients taking these drugs for type 2 diabetes or weight loss also lost interest in addictive and compulsive behaviors such as drinking alcohol, smoking, shopping, nail biting, and skin picking, as reported in articles in the New York Times and The Atlantic, among others.
There is also some preliminary research to support these observations.
This news organization invited three experts to weigh in.
Recent and upcoming studies
The senior author of a recent randomized controlled trial of 127 patients with alcohol use disorder (AUD), Anders Fink-Jensen, MD, said: “I hope that GLP-1 analogs in the future can be used against AUD, but before that can happen, several GLP-1 trials [are needed to] prove an effect on alcohol intake.”
His study involved patients who received exenatide (Byetta, Bydureon, AstraZeneca), the first-generation GLP-1 agonist approved for type 2 diabetes, over 26 weeks, but treatment did not reduce the number of heavy drinking days (the primary outcome), compared with placebo.
However, in post hoc, exploratory analyses, heavy drinking days and total alcohol intake were significantly reduced in the subgroup of patients with AUD and obesity (body mass index > 30 kg/m2).
The participants were also shown pictures of alcohol or neutral subjects while they underwent functional magnetic resonance imaging. Those who had received exenatide, compared with placebo, had significantly less activation of brain reward centers when shown the pictures of alcohol.
“Something is happening in the brain and activation of the reward center is hampered by the GLP-1 compound,” Dr. Fink-Jensen, a clinical psychologist at the Psychiatric Centre Copenhagen, remarked in an email.
“If patients with AUD already fulfill the criteria for semaglutide (or other GLP-1 analogs) by having type 2 diabetes and/or a BMI over 30 kg/m2, they can of course use the compound right now,” he noted.
His team is also beginning a study in patients with AUD and a BMI ≥ 30 kg/m2 to investigate the effects on alcohol intake of semaglutide up to 2.4 mg weekly, the maximum dose currently approved for obesity in the United States.
“Based on the potency of exenatide and semaglutide,” Dr. Fink-Jensen said, “we expect that semaglutide will cause a stronger reduction in alcohol intake” than exenatide.
Animal studies have also shown that GLP-1 agonists suppress alcohol-induced reward, alcohol intake, motivation to consume alcohol, alcohol seeking, and relapse drinking of alcohol, Elisabet Jerlhag Holm, PhD, noted.
Interestingly, these agents also suppress the reward, intake, and motivation to consume other addictive drugs like cocaine, amphetamine, nicotine, and some opioids, Jerlhag Holm, professor, department of pharmacology, University of Gothenburg, Sweden, noted in an email.
In a recently published preclinical study, her group provides evidence to help explain anecdotal reports from patients with obesity treated with semaglutide who claim they also reduced their alcohol intake. In the study, semaglutide both reduced alcohol intake (and relapse-like drinking) and decreased body weight of rats of both sexes.
“Future research should explore the possibility of semaglutide decreasing alcohol intake in patients with AUD, particularly those who are overweight,” said Prof. Holm.
“AUD is a heterogenous disorder, and one medication is most likely not helpful for all AUD patients,” she added. “Therefore, an arsenal of different medications is beneficial when treating AUD.”
Janice J. Hwang, MD, MHS, echoed these thoughts: “Anecdotally, there are a lot of reports from patients (and in the news) that this class of medication [GLP-1 agonists] impacts cravings and could impact addictive behaviors.”
“I would say, overall, the jury is still out,” as to whether anecdotal reports of GLP-1 agonists curbing addictions will be borne out in randomized controlled trials.
“I think it is much too early to tell” whether these drugs might be approved for treating addictions without more solid clinical trial data, noted Dr. Hwang, who is an associate professor of medicine and chief, division of endocrinology and metabolism, at the University of North Carolina at Chapel Hill.
Meanwhile, another research group at the University of North Carolina at Chapel Hill, led by psychiatrist Christian Hendershot, PhD, is conducting a clinical trial in 48 participants with AUD who are also smokers.
They aim to determine if patients who receive semaglutide at escalating doses (0.25 mg to 1.0 mg per week via subcutaneous injection) over 9 weeks will consume less alcohol (the primary outcome) and smoke less (a secondary outcome) than those who receive a sham placebo injection. Results are expected in October 2023.
Dr. Fink-Jensen has received an unrestricted research grant from Novo Nordisk to investigate the effects of GLP-1 receptor stimulation on weight gain and metabolic disturbances in patients with schizophrenia treated with an antipsychotic.
A version of this article first appeared on Medscape.com.
Daily multivitamins boost memory in older adults: A randomized trial
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. , known as COSMOS (Cocoa Supplement and Multivitamins Outcome Study). This is the second COSMOS trial to show a benefit of multivitamins on memory and cognition. This trial involved a collaboration between Brigham and Columbia University and was published in the American Journal of Clinical Nutrition. I’d like to acknowledge that I am a coauthor of this study, together with Dr. Howard Sesso, who co-leads the main COSMOS trial with me.
Preserving memory and cognitive function is of critical importance to older adults. Nutritional interventions play an important role because we know the brain requires several nutrients for optimal health, and deficiencies in one or more of these nutrients may accelerate cognitive decline. Some of the micronutrients that are known to be important for brain health include vitamin B12, thiamin, other B vitamins, lutein, magnesium, and zinc, among others.
The current trial included 3,500 participants aged 60 or older, looking at performance on a web-based memory test. The multivitamin group did significantly better than the placebo group on memory tests and word recall, a finding that was estimated as the equivalent of slowing age-related memory loss by about 3 years. The benefit was first seen at 1 year and was sustained across the 3 years of the trial.
Intriguingly, in both COSMOS and COSMOS-Web, and the earlier COSMOS-Mind study, which was done in collaboration with Wake Forest, the participants with a history of cardiovascular disease showed the greatest benefits from multivitamins, perhaps due to lower nutrient status. But the basis for this finding needs to be explored further.
A few important caveats need to be emphasized. First, multivitamins and other dietary supplements will never be a substitute for a healthy diet and healthy lifestyle and should not distract from those goals. But multivitamins may have a role as a complementary strategy. Another caveat is that the randomized trials tested recommended dietary allowances and not megadoses of these micronutrients. In fact, randomized trials of high doses of isolated micronutrients have not clearly shown cognitive benefits, and this suggests that more is not necessarily better and may be worse. High doses also may be associated with toxicity, or they may interfere with absorption or bioavailability of other nutrients.
In COSMOS, over the average 3.6 years of follow-up and in the earlier Physicians’ Health Study II, over 1 year of supplementation, multivitamins were found to be safe without any clear risks or safety concerns. A further caveat is that although Centrum Silver was tested in this trial, we would not expect that this is a brand-specific benefit, and other high-quality multivitamin brands would be expected to confer similar benefits. Of course, it’s important to check bottles for quality-control documentation such as the seals of the U.S. Pharmacopeia, National Science Foundation, ConsumerLab.com, and other auditors.
Overall, the finding that a daily multivitamin improved memory and slowed cognitive decline in two separate COSMOS randomized trials is exciting, suggesting that multivitamin supplementation holds promise as a safe, accessible, and affordable approach to protecting cognitive health in older adults. Further research will be needed to understand who is most likely to benefit and the biological mechanisms involved. Expert committees will have to look at the research and decide whether any changes in guidelines are indicated in the future.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School and director of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston. She reported receiving funding/donations from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. , known as COSMOS (Cocoa Supplement and Multivitamins Outcome Study). This is the second COSMOS trial to show a benefit of multivitamins on memory and cognition. This trial involved a collaboration between Brigham and Columbia University and was published in the American Journal of Clinical Nutrition. I’d like to acknowledge that I am a coauthor of this study, together with Dr. Howard Sesso, who co-leads the main COSMOS trial with me.
Preserving memory and cognitive function is of critical importance to older adults. Nutritional interventions play an important role because we know the brain requires several nutrients for optimal health, and deficiencies in one or more of these nutrients may accelerate cognitive decline. Some of the micronutrients that are known to be important for brain health include vitamin B12, thiamin, other B vitamins, lutein, magnesium, and zinc, among others.
The current trial included 3,500 participants aged 60 or older, looking at performance on a web-based memory test. The multivitamin group did significantly better than the placebo group on memory tests and word recall, a finding that was estimated as the equivalent of slowing age-related memory loss by about 3 years. The benefit was first seen at 1 year and was sustained across the 3 years of the trial.
Intriguingly, in both COSMOS and COSMOS-Web, and the earlier COSMOS-Mind study, which was done in collaboration with Wake Forest, the participants with a history of cardiovascular disease showed the greatest benefits from multivitamins, perhaps due to lower nutrient status. But the basis for this finding needs to be explored further.
A few important caveats need to be emphasized. First, multivitamins and other dietary supplements will never be a substitute for a healthy diet and healthy lifestyle and should not distract from those goals. But multivitamins may have a role as a complementary strategy. Another caveat is that the randomized trials tested recommended dietary allowances and not megadoses of these micronutrients. In fact, randomized trials of high doses of isolated micronutrients have not clearly shown cognitive benefits, and this suggests that more is not necessarily better and may be worse. High doses also may be associated with toxicity, or they may interfere with absorption or bioavailability of other nutrients.
In COSMOS, over the average 3.6 years of follow-up and in the earlier Physicians’ Health Study II, over 1 year of supplementation, multivitamins were found to be safe without any clear risks or safety concerns. A further caveat is that although Centrum Silver was tested in this trial, we would not expect that this is a brand-specific benefit, and other high-quality multivitamin brands would be expected to confer similar benefits. Of course, it’s important to check bottles for quality-control documentation such as the seals of the U.S. Pharmacopeia, National Science Foundation, ConsumerLab.com, and other auditors.
Overall, the finding that a daily multivitamin improved memory and slowed cognitive decline in two separate COSMOS randomized trials is exciting, suggesting that multivitamin supplementation holds promise as a safe, accessible, and affordable approach to protecting cognitive health in older adults. Further research will be needed to understand who is most likely to benefit and the biological mechanisms involved. Expert committees will have to look at the research and decide whether any changes in guidelines are indicated in the future.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School and director of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston. She reported receiving funding/donations from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. , known as COSMOS (Cocoa Supplement and Multivitamins Outcome Study). This is the second COSMOS trial to show a benefit of multivitamins on memory and cognition. This trial involved a collaboration between Brigham and Columbia University and was published in the American Journal of Clinical Nutrition. I’d like to acknowledge that I am a coauthor of this study, together with Dr. Howard Sesso, who co-leads the main COSMOS trial with me.
Preserving memory and cognitive function is of critical importance to older adults. Nutritional interventions play an important role because we know the brain requires several nutrients for optimal health, and deficiencies in one or more of these nutrients may accelerate cognitive decline. Some of the micronutrients that are known to be important for brain health include vitamin B12, thiamin, other B vitamins, lutein, magnesium, and zinc, among others.
The current trial included 3,500 participants aged 60 or older, looking at performance on a web-based memory test. The multivitamin group did significantly better than the placebo group on memory tests and word recall, a finding that was estimated as the equivalent of slowing age-related memory loss by about 3 years. The benefit was first seen at 1 year and was sustained across the 3 years of the trial.
Intriguingly, in both COSMOS and COSMOS-Web, and the earlier COSMOS-Mind study, which was done in collaboration with Wake Forest, the participants with a history of cardiovascular disease showed the greatest benefits from multivitamins, perhaps due to lower nutrient status. But the basis for this finding needs to be explored further.
A few important caveats need to be emphasized. First, multivitamins and other dietary supplements will never be a substitute for a healthy diet and healthy lifestyle and should not distract from those goals. But multivitamins may have a role as a complementary strategy. Another caveat is that the randomized trials tested recommended dietary allowances and not megadoses of these micronutrients. In fact, randomized trials of high doses of isolated micronutrients have not clearly shown cognitive benefits, and this suggests that more is not necessarily better and may be worse. High doses also may be associated with toxicity, or they may interfere with absorption or bioavailability of other nutrients.
In COSMOS, over the average 3.6 years of follow-up and in the earlier Physicians’ Health Study II, over 1 year of supplementation, multivitamins were found to be safe without any clear risks or safety concerns. A further caveat is that although Centrum Silver was tested in this trial, we would not expect that this is a brand-specific benefit, and other high-quality multivitamin brands would be expected to confer similar benefits. Of course, it’s important to check bottles for quality-control documentation such as the seals of the U.S. Pharmacopeia, National Science Foundation, ConsumerLab.com, and other auditors.
Overall, the finding that a daily multivitamin improved memory and slowed cognitive decline in two separate COSMOS randomized trials is exciting, suggesting that multivitamin supplementation holds promise as a safe, accessible, and affordable approach to protecting cognitive health in older adults. Further research will be needed to understand who is most likely to benefit and the biological mechanisms involved. Expert committees will have to look at the research and decide whether any changes in guidelines are indicated in the future.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School and director of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston. She reported receiving funding/donations from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
No apparent drug interaction with ozanimod and antidepressants
DENVER – , according to research presented at the annual meeting of the Consortium of Multiple Sclerosis Centers.
“Depression and anxiety are prevalent comorbidities occurring in up to 54% of patients with multiple sclerosis, and selective serotonin reuptake inhibitors (SSRIs)/serotonin-norepinephrine reuptake inhibitors (SNRIs) are first-line treatments for depression and anxiety disorders,” Robert T. Naismith, MD, of Washington University in St. Louis, and his colleagues reported.
“Coadministration of ozanimod with drugs that increase serotonin could hypothetically lead to serotonin accumulation,” which can increase the likelihood of hypertension. U.S. prescribing information recommends that patients taking both ozanimod and medications that increase norepinephrine or serotonin be monitored for hypertension, an adverse reaction reported in 3.9% of patients receiving ozanimod in the phase 3 trials for relapsing MS.
Clarifying the risk
“It’s important to be aware of potential drug interactions and risks from MS disease modifying therapies,” Lauren Gluck, MD, an assistant professor and director of the division of multiple sclerosis at Montefiore Medical Center/Albert Einstein College of Medicine, New York, said in an interview. Dr. Gluck was not involved in this study but described some of the history that revealed the value of this type of research. For example, the first sphingosine-1-phosphate receptor (S1PR) modulator approved for MS, fingolimod (Gilenya), has a risk of cardiac conduction dysfunction with QTc prolongation, so people taking fingolimod with other medications that prolong QTc, such as SSRIs, need additional monitoring.
“Ozanimod is a newer, more selective S1PR modulator that initially raised concerns about interaction with serotonin-increasing drugs based on in vitro studies,” Dr. Gluck said. “This could mean that people on ozanimod and other serotonin-increasing medicine could be at risk for dangerous events like serotonin syndrome. However, in vitro studies do not always translate to how something affects the human body, so it is not clear how much risk truly exists.”
Examining open-label extension trial data
The researchers therefore evaluated the safety of taking ozanimod and SSRIs or SNRIs in a subset of patients with relapsing MS who participated in the DAYBREAK open-label extension trial. The phase 3 parent trials compared 30 mcg once weekly of intramuscular interferon beta-1a with 0.92 mg of once-daily oral ozanimod and 0.46 mg of once-daily oral ozanimod. In the DAYBREAK open-label extension, 2,256 participants underwent a dose escalation over one week until all reached 0.92 mg of ozanimod, where they remained for an average of just under 5 years of follow-up. Nearly all the participants (99.4%) were White, and two-thirds (66.5%) were female.
The researchers searched the study data for terms related to serotonin toxicity and compared the rates of adverse events related with those terms and the rates of hypertension in the 274 participants who were and the 2,032 participant who were not taking antidepressants at the same time as ozanimod.
They found that 13.9% of patients taking SSRIs or SNRIs experienced at least one treatment-emergent adverse event related to their search criteria, compared with 17.7% of patients not taking SSRIs or SNRIs. Similarly, 9.2% of trial participants not taking SSRIs or SNRIs had hypertension, compared with 4.7% of participants who were taking antidepressants. The authors further noted that “similar trends were observed when 6 weeks after the end date of concomitant SSRIs/SNRI use were included in the ‘on SSRI/SNRI’ analysis period.”
When the researchers searched specifically for three terms directly related to serotonin toxicity – “serotonin syndrome,” “neuroleptic malignant syndrome,” and “hyperthermia malignant” – they did not find any patients who had treatment-emergent adverse events related to those terms.
“SSRIs/SNRIs were freely allowed as concomitant medications in the DAYBREAK open-label extension, and among the patients from SUNBEAM or RADIANCE who were followed for up to 6 years, there have been no reported safety concerns during the concurrent administration of serotonergic antidepressants and ozanimod in patients with relapsing MS as of the data cutoff,” concluded the authors, though they also noted that the overall rate of SSRI and SNRI use was low in the extension trial.
A reassuring finding for clinicians and patients alike
“It is reassuring, if not unexpected, that there were no clinically significant rates of symptoms associated with excess serotonin in patients on ozanimod and SSRI/SNRIs,” Dr. Gluck commented. “These findings are important for both clinicians and patients – they can help [both] feel comfortable considering ozanimod if SSRI/SNRIs are already being used. There is also freedom to use SSRI/SNRIs for symptom management in patients already on ozanimod.”
The research was funded by Bristol Myers Squibb. Dr. Naismith reported consulting for Abata Therapeutics, Banner Life Sciences, BeiGene, Biogen, Bristol Myers Squibb, Celltrion, Genentech, Genzyme, GW Therapeutics, Janssen, Horizon Therapeutics, Lundbeck, NervGen, and TG Therapeutics. Six other authors reported disclosures for various pharmaceutical companies, and six other authors are employees and/or shareholders of Bristol Myers Squibb. Dr. Gluck has served on advisory boards with Genentech and EMD Serono.
DENVER – , according to research presented at the annual meeting of the Consortium of Multiple Sclerosis Centers.
“Depression and anxiety are prevalent comorbidities occurring in up to 54% of patients with multiple sclerosis, and selective serotonin reuptake inhibitors (SSRIs)/serotonin-norepinephrine reuptake inhibitors (SNRIs) are first-line treatments for depression and anxiety disorders,” Robert T. Naismith, MD, of Washington University in St. Louis, and his colleagues reported.
“Coadministration of ozanimod with drugs that increase serotonin could hypothetically lead to serotonin accumulation,” which can increase the likelihood of hypertension. U.S. prescribing information recommends that patients taking both ozanimod and medications that increase norepinephrine or serotonin be monitored for hypertension, an adverse reaction reported in 3.9% of patients receiving ozanimod in the phase 3 trials for relapsing MS.
Clarifying the risk
“It’s important to be aware of potential drug interactions and risks from MS disease modifying therapies,” Lauren Gluck, MD, an assistant professor and director of the division of multiple sclerosis at Montefiore Medical Center/Albert Einstein College of Medicine, New York, said in an interview. Dr. Gluck was not involved in this study but described some of the history that revealed the value of this type of research. For example, the first sphingosine-1-phosphate receptor (S1PR) modulator approved for MS, fingolimod (Gilenya), has a risk of cardiac conduction dysfunction with QTc prolongation, so people taking fingolimod with other medications that prolong QTc, such as SSRIs, need additional monitoring.
“Ozanimod is a newer, more selective S1PR modulator that initially raised concerns about interaction with serotonin-increasing drugs based on in vitro studies,” Dr. Gluck said. “This could mean that people on ozanimod and other serotonin-increasing medicine could be at risk for dangerous events like serotonin syndrome. However, in vitro studies do not always translate to how something affects the human body, so it is not clear how much risk truly exists.”
Examining open-label extension trial data
The researchers therefore evaluated the safety of taking ozanimod and SSRIs or SNRIs in a subset of patients with relapsing MS who participated in the DAYBREAK open-label extension trial. The phase 3 parent trials compared 30 mcg once weekly of intramuscular interferon beta-1a with 0.92 mg of once-daily oral ozanimod and 0.46 mg of once-daily oral ozanimod. In the DAYBREAK open-label extension, 2,256 participants underwent a dose escalation over one week until all reached 0.92 mg of ozanimod, where they remained for an average of just under 5 years of follow-up. Nearly all the participants (99.4%) were White, and two-thirds (66.5%) were female.
The researchers searched the study data for terms related to serotonin toxicity and compared the rates of adverse events related with those terms and the rates of hypertension in the 274 participants who were and the 2,032 participant who were not taking antidepressants at the same time as ozanimod.
They found that 13.9% of patients taking SSRIs or SNRIs experienced at least one treatment-emergent adverse event related to their search criteria, compared with 17.7% of patients not taking SSRIs or SNRIs. Similarly, 9.2% of trial participants not taking SSRIs or SNRIs had hypertension, compared with 4.7% of participants who were taking antidepressants. The authors further noted that “similar trends were observed when 6 weeks after the end date of concomitant SSRIs/SNRI use were included in the ‘on SSRI/SNRI’ analysis period.”
When the researchers searched specifically for three terms directly related to serotonin toxicity – “serotonin syndrome,” “neuroleptic malignant syndrome,” and “hyperthermia malignant” – they did not find any patients who had treatment-emergent adverse events related to those terms.
“SSRIs/SNRIs were freely allowed as concomitant medications in the DAYBREAK open-label extension, and among the patients from SUNBEAM or RADIANCE who were followed for up to 6 years, there have been no reported safety concerns during the concurrent administration of serotonergic antidepressants and ozanimod in patients with relapsing MS as of the data cutoff,” concluded the authors, though they also noted that the overall rate of SSRI and SNRI use was low in the extension trial.
A reassuring finding for clinicians and patients alike
“It is reassuring, if not unexpected, that there were no clinically significant rates of symptoms associated with excess serotonin in patients on ozanimod and SSRI/SNRIs,” Dr. Gluck commented. “These findings are important for both clinicians and patients – they can help [both] feel comfortable considering ozanimod if SSRI/SNRIs are already being used. There is also freedom to use SSRI/SNRIs for symptom management in patients already on ozanimod.”
The research was funded by Bristol Myers Squibb. Dr. Naismith reported consulting for Abata Therapeutics, Banner Life Sciences, BeiGene, Biogen, Bristol Myers Squibb, Celltrion, Genentech, Genzyme, GW Therapeutics, Janssen, Horizon Therapeutics, Lundbeck, NervGen, and TG Therapeutics. Six other authors reported disclosures for various pharmaceutical companies, and six other authors are employees and/or shareholders of Bristol Myers Squibb. Dr. Gluck has served on advisory boards with Genentech and EMD Serono.
DENVER – , according to research presented at the annual meeting of the Consortium of Multiple Sclerosis Centers.
“Depression and anxiety are prevalent comorbidities occurring in up to 54% of patients with multiple sclerosis, and selective serotonin reuptake inhibitors (SSRIs)/serotonin-norepinephrine reuptake inhibitors (SNRIs) are first-line treatments for depression and anxiety disorders,” Robert T. Naismith, MD, of Washington University in St. Louis, and his colleagues reported.
“Coadministration of ozanimod with drugs that increase serotonin could hypothetically lead to serotonin accumulation,” which can increase the likelihood of hypertension. U.S. prescribing information recommends that patients taking both ozanimod and medications that increase norepinephrine or serotonin be monitored for hypertension, an adverse reaction reported in 3.9% of patients receiving ozanimod in the phase 3 trials for relapsing MS.
Clarifying the risk
“It’s important to be aware of potential drug interactions and risks from MS disease modifying therapies,” Lauren Gluck, MD, an assistant professor and director of the division of multiple sclerosis at Montefiore Medical Center/Albert Einstein College of Medicine, New York, said in an interview. Dr. Gluck was not involved in this study but described some of the history that revealed the value of this type of research. For example, the first sphingosine-1-phosphate receptor (S1PR) modulator approved for MS, fingolimod (Gilenya), has a risk of cardiac conduction dysfunction with QTc prolongation, so people taking fingolimod with other medications that prolong QTc, such as SSRIs, need additional monitoring.
“Ozanimod is a newer, more selective S1PR modulator that initially raised concerns about interaction with serotonin-increasing drugs based on in vitro studies,” Dr. Gluck said. “This could mean that people on ozanimod and other serotonin-increasing medicine could be at risk for dangerous events like serotonin syndrome. However, in vitro studies do not always translate to how something affects the human body, so it is not clear how much risk truly exists.”
Examining open-label extension trial data
The researchers therefore evaluated the safety of taking ozanimod and SSRIs or SNRIs in a subset of patients with relapsing MS who participated in the DAYBREAK open-label extension trial. The phase 3 parent trials compared 30 mcg once weekly of intramuscular interferon beta-1a with 0.92 mg of once-daily oral ozanimod and 0.46 mg of once-daily oral ozanimod. In the DAYBREAK open-label extension, 2,256 participants underwent a dose escalation over one week until all reached 0.92 mg of ozanimod, where they remained for an average of just under 5 years of follow-up. Nearly all the participants (99.4%) were White, and two-thirds (66.5%) were female.
The researchers searched the study data for terms related to serotonin toxicity and compared the rates of adverse events related with those terms and the rates of hypertension in the 274 participants who were and the 2,032 participant who were not taking antidepressants at the same time as ozanimod.
They found that 13.9% of patients taking SSRIs or SNRIs experienced at least one treatment-emergent adverse event related to their search criteria, compared with 17.7% of patients not taking SSRIs or SNRIs. Similarly, 9.2% of trial participants not taking SSRIs or SNRIs had hypertension, compared with 4.7% of participants who were taking antidepressants. The authors further noted that “similar trends were observed when 6 weeks after the end date of concomitant SSRIs/SNRI use were included in the ‘on SSRI/SNRI’ analysis period.”
When the researchers searched specifically for three terms directly related to serotonin toxicity – “serotonin syndrome,” “neuroleptic malignant syndrome,” and “hyperthermia malignant” – they did not find any patients who had treatment-emergent adverse events related to those terms.
“SSRIs/SNRIs were freely allowed as concomitant medications in the DAYBREAK open-label extension, and among the patients from SUNBEAM or RADIANCE who were followed for up to 6 years, there have been no reported safety concerns during the concurrent administration of serotonergic antidepressants and ozanimod in patients with relapsing MS as of the data cutoff,” concluded the authors, though they also noted that the overall rate of SSRI and SNRI use was low in the extension trial.
A reassuring finding for clinicians and patients alike
“It is reassuring, if not unexpected, that there were no clinically significant rates of symptoms associated with excess serotonin in patients on ozanimod and SSRI/SNRIs,” Dr. Gluck commented. “These findings are important for both clinicians and patients – they can help [both] feel comfortable considering ozanimod if SSRI/SNRIs are already being used. There is also freedom to use SSRI/SNRIs for symptom management in patients already on ozanimod.”
The research was funded by Bristol Myers Squibb. Dr. Naismith reported consulting for Abata Therapeutics, Banner Life Sciences, BeiGene, Biogen, Bristol Myers Squibb, Celltrion, Genentech, Genzyme, GW Therapeutics, Janssen, Horizon Therapeutics, Lundbeck, NervGen, and TG Therapeutics. Six other authors reported disclosures for various pharmaceutical companies, and six other authors are employees and/or shareholders of Bristol Myers Squibb. Dr. Gluck has served on advisory boards with Genentech and EMD Serono.
AT CMSC 2023
FDA panel unanimously endorses lecanemab for Alzheimer’s
“Overall, the study demonstrated clearly that this is an effective treatment,” said acting chair Robert C. Alexander, MD, chief scientific officer, Alzheimer’s Prevention Initiative, Banner Alzheimer’s Institute, and research professor, department of psychiatry, University of Arizona, Phoenix, during the meeting.
An intravenous infusion targeting amyloid-beta, lecanemab received accelerated FDA approved earlier in 2023 for the treatment of early Alzheimer’s disease (AD). The company was required to complete a confirmatory study to verify and describe the product’s clinical benefit.
The Peripheral and Central Nervous System Drugs Advisory Committee met to discuss this phase 3 study (CLARITY-AD). The multicenter, double-blind study included 1,795 patients (mean age, 71 years) who had mild cognitive impairment caused by AD or mild AD dementia.
Delayed progression
Study participants had a broad range of comorbidities, and many were concomitantly receiving other medications. Black people were underrepresented in the study at just 3% of the total cohort.
Patients were randomly assigned to receive placebo or lecanemab 10 mg/kg biweekly. In addition to a placebo-controlled period and safety follow-up, the study has an ongoing extension phase of up to 4 years.
The study met its primary endpoint, showing a highly statistically significant 27% less decline on the Clinical Dementia Rating-Sum of Boxes at 18 months (difference in adjusted mean, –0.45; 95% CI, –0.67 to –0.23; P = .00005).
This was supported by a significant 26% difference on the AD Assessment Scale–Cognitive Subscale with 14 tasks (ADAS-Cog 14).
The drug also affected function, with a 37% decrease, compared with placebo, on the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment.
Committee members heard that the results signal delays in disease progression by about 5 months, giving patients more time to live independently and participate in hobbies and interests.
Patients who received the active drug also experienced quality of life benefits. Compared with patients who received placebo, those who took lecanemab had 49% less decline as measured with the European Quality of Life–5 Dimensions scale and 56% less decline as measured by the Quality of Life in AD scale, and caregivers reported less burden.
Lecanemab also affected biomarkers of amyloid, tau, and neurodegeneration, providing a biological basis for the treatment effects consistent with slowing of disease progression.
Unanimous support
All six committee members agreed by vote that the study provides evidence of clinical benefit. They variously descried the study and results as “robust,” “compelling,” “well conducted,” “clear and consistent,” and “clinically meaningful.”
In the active treatment group, there was a higher incidence of amyloid-related imaging abnormalities (ARIAs), which can be serious and life-threatening but are usually asymptomatic. In this study, most ARIAs had resolved by 3 months.
Deaths occurred in 0.8% of the placebo and 0.7% of the treatment group. Dean Follmann, PhD, assistant director for biostatistics, National Institute of Allergy and Infectious Diseases, Bethesda, Md., noted that the numbers of deaths and serious adverse events were “quite similar” in the two groups.
“And for serious ARIA, there was an imbalance favoring placebo, but overall, these were pretty rare,” he said.
Subgroup concerns
Committee members discussed the risk/benefit profile for three subgroups of patients – those with apolipoprotein E4 (apo E4) allele, patients taking an anticoagulant, and those with cerebral amyloid angiopathy (CAA).
In the apo E4 group, the study’s primary endpoint did not favor the drug, but secondary endpoints did.
“I think the general feeling [for apo E4 status] is that the risk/benefit still remains favorable, especially when looking across multiple endpoints,” said Dr. Alexander.
However, some members supported recommending genetic testing before initiating the drug.
The views were more diverse for the use of lecanemab in the presence of an anticoagulant, which may increase the risk for cerebral hemorrhage. Some committee members strongly recommended that these patients not receive lecanemab, while others highlighted the need for more information, owing to uncertainties about the risks.
With respect to CAA, most members supported the idea of considering use of the drug in the presence of this condition, but only after discussing the risks with patients and their families and in the presence of a robust reporting system.
An Alzheimer’s Association representative was in attendance during the public hearing portion of the meeting to express support for traditional approval of lecanemab for people with early AD.
The association strongly favors full Medicare coverage for FDA-approved AD treatments. The Centers for Medicare & Medicaid Services has determined that AD treatments receiving traditional FDA approval will be covered if clinicians register and enter data in a registry.
“While this is an important signal that CMS wants to improve access to FDA-approved treatments, registry as a condition of coverage is an unnecessary and potentially harmful barrier,” said the Alzheimer’s Association in a press release following the meeting.
A version of this article first appeared on Medscape.com.
“Overall, the study demonstrated clearly that this is an effective treatment,” said acting chair Robert C. Alexander, MD, chief scientific officer, Alzheimer’s Prevention Initiative, Banner Alzheimer’s Institute, and research professor, department of psychiatry, University of Arizona, Phoenix, during the meeting.
An intravenous infusion targeting amyloid-beta, lecanemab received accelerated FDA approved earlier in 2023 for the treatment of early Alzheimer’s disease (AD). The company was required to complete a confirmatory study to verify and describe the product’s clinical benefit.
The Peripheral and Central Nervous System Drugs Advisory Committee met to discuss this phase 3 study (CLARITY-AD). The multicenter, double-blind study included 1,795 patients (mean age, 71 years) who had mild cognitive impairment caused by AD or mild AD dementia.
Delayed progression
Study participants had a broad range of comorbidities, and many were concomitantly receiving other medications. Black people were underrepresented in the study at just 3% of the total cohort.
Patients were randomly assigned to receive placebo or lecanemab 10 mg/kg biweekly. In addition to a placebo-controlled period and safety follow-up, the study has an ongoing extension phase of up to 4 years.
The study met its primary endpoint, showing a highly statistically significant 27% less decline on the Clinical Dementia Rating-Sum of Boxes at 18 months (difference in adjusted mean, –0.45; 95% CI, –0.67 to –0.23; P = .00005).
This was supported by a significant 26% difference on the AD Assessment Scale–Cognitive Subscale with 14 tasks (ADAS-Cog 14).
The drug also affected function, with a 37% decrease, compared with placebo, on the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment.
Committee members heard that the results signal delays in disease progression by about 5 months, giving patients more time to live independently and participate in hobbies and interests.
Patients who received the active drug also experienced quality of life benefits. Compared with patients who received placebo, those who took lecanemab had 49% less decline as measured with the European Quality of Life–5 Dimensions scale and 56% less decline as measured by the Quality of Life in AD scale, and caregivers reported less burden.
Lecanemab also affected biomarkers of amyloid, tau, and neurodegeneration, providing a biological basis for the treatment effects consistent with slowing of disease progression.
Unanimous support
All six committee members agreed by vote that the study provides evidence of clinical benefit. They variously descried the study and results as “robust,” “compelling,” “well conducted,” “clear and consistent,” and “clinically meaningful.”
In the active treatment group, there was a higher incidence of amyloid-related imaging abnormalities (ARIAs), which can be serious and life-threatening but are usually asymptomatic. In this study, most ARIAs had resolved by 3 months.
Deaths occurred in 0.8% of the placebo and 0.7% of the treatment group. Dean Follmann, PhD, assistant director for biostatistics, National Institute of Allergy and Infectious Diseases, Bethesda, Md., noted that the numbers of deaths and serious adverse events were “quite similar” in the two groups.
“And for serious ARIA, there was an imbalance favoring placebo, but overall, these were pretty rare,” he said.
Subgroup concerns
Committee members discussed the risk/benefit profile for three subgroups of patients – those with apolipoprotein E4 (apo E4) allele, patients taking an anticoagulant, and those with cerebral amyloid angiopathy (CAA).
In the apo E4 group, the study’s primary endpoint did not favor the drug, but secondary endpoints did.
“I think the general feeling [for apo E4 status] is that the risk/benefit still remains favorable, especially when looking across multiple endpoints,” said Dr. Alexander.
However, some members supported recommending genetic testing before initiating the drug.
The views were more diverse for the use of lecanemab in the presence of an anticoagulant, which may increase the risk for cerebral hemorrhage. Some committee members strongly recommended that these patients not receive lecanemab, while others highlighted the need for more information, owing to uncertainties about the risks.
With respect to CAA, most members supported the idea of considering use of the drug in the presence of this condition, but only after discussing the risks with patients and their families and in the presence of a robust reporting system.
An Alzheimer’s Association representative was in attendance during the public hearing portion of the meeting to express support for traditional approval of lecanemab for people with early AD.
The association strongly favors full Medicare coverage for FDA-approved AD treatments. The Centers for Medicare & Medicaid Services has determined that AD treatments receiving traditional FDA approval will be covered if clinicians register and enter data in a registry.
“While this is an important signal that CMS wants to improve access to FDA-approved treatments, registry as a condition of coverage is an unnecessary and potentially harmful barrier,” said the Alzheimer’s Association in a press release following the meeting.
A version of this article first appeared on Medscape.com.
“Overall, the study demonstrated clearly that this is an effective treatment,” said acting chair Robert C. Alexander, MD, chief scientific officer, Alzheimer’s Prevention Initiative, Banner Alzheimer’s Institute, and research professor, department of psychiatry, University of Arizona, Phoenix, during the meeting.
An intravenous infusion targeting amyloid-beta, lecanemab received accelerated FDA approved earlier in 2023 for the treatment of early Alzheimer’s disease (AD). The company was required to complete a confirmatory study to verify and describe the product’s clinical benefit.
The Peripheral and Central Nervous System Drugs Advisory Committee met to discuss this phase 3 study (CLARITY-AD). The multicenter, double-blind study included 1,795 patients (mean age, 71 years) who had mild cognitive impairment caused by AD or mild AD dementia.
Delayed progression
Study participants had a broad range of comorbidities, and many were concomitantly receiving other medications. Black people were underrepresented in the study at just 3% of the total cohort.
Patients were randomly assigned to receive placebo or lecanemab 10 mg/kg biweekly. In addition to a placebo-controlled period and safety follow-up, the study has an ongoing extension phase of up to 4 years.
The study met its primary endpoint, showing a highly statistically significant 27% less decline on the Clinical Dementia Rating-Sum of Boxes at 18 months (difference in adjusted mean, –0.45; 95% CI, –0.67 to –0.23; P = .00005).
This was supported by a significant 26% difference on the AD Assessment Scale–Cognitive Subscale with 14 tasks (ADAS-Cog 14).
The drug also affected function, with a 37% decrease, compared with placebo, on the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment.
Committee members heard that the results signal delays in disease progression by about 5 months, giving patients more time to live independently and participate in hobbies and interests.
Patients who received the active drug also experienced quality of life benefits. Compared with patients who received placebo, those who took lecanemab had 49% less decline as measured with the European Quality of Life–5 Dimensions scale and 56% less decline as measured by the Quality of Life in AD scale, and caregivers reported less burden.
Lecanemab also affected biomarkers of amyloid, tau, and neurodegeneration, providing a biological basis for the treatment effects consistent with slowing of disease progression.
Unanimous support
All six committee members agreed by vote that the study provides evidence of clinical benefit. They variously descried the study and results as “robust,” “compelling,” “well conducted,” “clear and consistent,” and “clinically meaningful.”
In the active treatment group, there was a higher incidence of amyloid-related imaging abnormalities (ARIAs), which can be serious and life-threatening but are usually asymptomatic. In this study, most ARIAs had resolved by 3 months.
Deaths occurred in 0.8% of the placebo and 0.7% of the treatment group. Dean Follmann, PhD, assistant director for biostatistics, National Institute of Allergy and Infectious Diseases, Bethesda, Md., noted that the numbers of deaths and serious adverse events were “quite similar” in the two groups.
“And for serious ARIA, there was an imbalance favoring placebo, but overall, these were pretty rare,” he said.
Subgroup concerns
Committee members discussed the risk/benefit profile for three subgroups of patients – those with apolipoprotein E4 (apo E4) allele, patients taking an anticoagulant, and those with cerebral amyloid angiopathy (CAA).
In the apo E4 group, the study’s primary endpoint did not favor the drug, but secondary endpoints did.
“I think the general feeling [for apo E4 status] is that the risk/benefit still remains favorable, especially when looking across multiple endpoints,” said Dr. Alexander.
However, some members supported recommending genetic testing before initiating the drug.
The views were more diverse for the use of lecanemab in the presence of an anticoagulant, which may increase the risk for cerebral hemorrhage. Some committee members strongly recommended that these patients not receive lecanemab, while others highlighted the need for more information, owing to uncertainties about the risks.
With respect to CAA, most members supported the idea of considering use of the drug in the presence of this condition, but only after discussing the risks with patients and their families and in the presence of a robust reporting system.
An Alzheimer’s Association representative was in attendance during the public hearing portion of the meeting to express support for traditional approval of lecanemab for people with early AD.
The association strongly favors full Medicare coverage for FDA-approved AD treatments. The Centers for Medicare & Medicaid Services has determined that AD treatments receiving traditional FDA approval will be covered if clinicians register and enter data in a registry.
“While this is an important signal that CMS wants to improve access to FDA-approved treatments, registry as a condition of coverage is an unnecessary and potentially harmful barrier,” said the Alzheimer’s Association in a press release following the meeting.
A version of this article first appeared on Medscape.com.
What’s best for patients who are dying of anorexia?
SAN FRANCISCO – The patient at a Florida eating disorder clinic said she was eating plenty even though she acknowledged purging once a week. But her vitals told a different story: Her body mass index (BMI) was 12.2, down from 14.8 a couple of years before – a dangerously low value.
While the woman agreed that she needed to gain weight, she refused advice to pursue residential or inpatient treatment. This left her team with a big dilemma: Should they force her into care because she wouldn’t eat? Was that even possible under the law? Did she have the capacity to make decisions about her future? What other alternatives were there?
Determining the best course of action in cases like this is anything but simple, Dr. Cacodcar said. To make matters more complicated, .
“At least in my state of Florida, we know that it can be very, very hard to get patients expert care,” said Dr. Cacodcar. And, she said, it can be even tougher for certain types of patients, such as those that are LGBTQ and those who have severe illness but don’t meet the criteria.
As Dr. Cacodcar noted, the APA released new practice guidelines regarding eating disorders earlier this year, marking their first update since 2006. The guidelines highlight research that suggests nearly 1% – 0.8% – of the U.S. population will develop AN over their lifetimes. Recent studies also suggest that eating disorder numbers rose during the pandemic, with one analysis finding that patients under inpatient care doubled in 2020.
“Mortality rates are high for anorexia nervosa, up to 10 times higher than matched controls,” Dr. Cacodcar said. “It has the highest mortality rate of the psychiatric diseases with the exception of opioid use disorder.”
As for outcomes, she pointed to a 2019 study that surveyed 387 parents who had children with eating disorders, mostly AN. Only 20% made a full recovery. “The farther you get out from the onset of anorexia, the less likely you are to achieve recovery,” Dr. Cacodcar said. “A lot of the control behaviors become very automatic.”
Determining capacity
In some cases of AN, psychiatrists must determine whether they have the capacity to make decisions about treatment, said Gabriel Jerkins, MD, a chief resident of psychiatry at the University of Florida. At issue is “the ability of the individual to comprehend the information being disclosed in regard to their condition, as well as the nature and potential risks and benefits of the proposed treatment alternatives. They include of course, no treatment at all.”
“We know psychiatric conditions can limit one’s ability to appreciate consequence,” he said.
One option is to seek to institutionalize patients with severe AN because they are a danger to themselves. Clinicians opted to not do this in the case of the patient profiled by Dr. Cacodcar, the one with the BMI of 12.2 who didn’t want inpatient or residential care. (A 5-foot-8 person with a BMI of 12.2 would weigh 80 pounds.)
“The main reason we did not hospitalize her is because an appropriate level of care was not going to be readily available,” Dr. Cacodcar said, and her treatment would have been substandard.
Fortunately, the woman did return after a couple of months and accept residential care. No facility in Florida was willing to accept her because of her low BMI, but she did find one in North Carolina, where she stayed for 2 months. She’s doing well, and her BMI is now 21, Dr. Cacodcar said.
The patient’s story shows that involuntary hospitalization “is not necessarily the best course of action,” Dr. Cacodcar said. “It wasn’t necessarily going to be in the patient’s best interest.”
In another case, a 22-year-old woman had severe AN. She had been a gymnast and dancer, Dr. Jerkins said, “and I include that here only because of how commonly we see that kind of demographic information in patients with anorexia nervosa.”
Her BMI was 17.5, and clinicians discussed feeding her through a feeding tube. She still had “no insight that her symptoms were related to an underlying eating disorder,” Dr. Jerkins said, raising questions about her capacity. “Is it sufficient that the patient understand that she’s underweight?”
Ultimately, he said, she received a feeding tube at a time when her BMI had dropped to 16.3. She suffered from an infection but ultimately she improved and has stabilized at a BMI of around 19, he said.
“I do wonder if allowing her to have some control of how to pursue treatment in this case was therapeutic in a way,” he said, especially since matters of control are deeply ingrained in AN.
A former physical trainer, the patient had a BMI of 17.6. The University of Florida’s eating disorder clinic sent her to an out-of-state residential program, but she was discharged when her blood glucose dipped dangerously low as she compulsively exercised. Her BMI dipped to 16.2.
Dr. Schmidt had the patient involuntarily committed upon her return, but she went home after 12 days with no change in her weight. Ultimately, the patient was referred to an eating disorder center in Colorado for medical stabilization where she was given a feeding tube. But her medical situation was so dire that she was discharged to her home, where she went on hospice and died.
“I’m not arguing for or against the term ‘terminal anorexia.’ But this case does make me think about it,” said Dr. Schmidt. She was referring to a controversial term used by some clinicians to refer to patients who face inevitable death from AN. “Unfortunately,” wrote the authors of a recent report proposing a clinical definition, “these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa.”
SAN FRANCISCO – The patient at a Florida eating disorder clinic said she was eating plenty even though she acknowledged purging once a week. But her vitals told a different story: Her body mass index (BMI) was 12.2, down from 14.8 a couple of years before – a dangerously low value.
While the woman agreed that she needed to gain weight, she refused advice to pursue residential or inpatient treatment. This left her team with a big dilemma: Should they force her into care because she wouldn’t eat? Was that even possible under the law? Did she have the capacity to make decisions about her future? What other alternatives were there?
Determining the best course of action in cases like this is anything but simple, Dr. Cacodcar said. To make matters more complicated, .
“At least in my state of Florida, we know that it can be very, very hard to get patients expert care,” said Dr. Cacodcar. And, she said, it can be even tougher for certain types of patients, such as those that are LGBTQ and those who have severe illness but don’t meet the criteria.
As Dr. Cacodcar noted, the APA released new practice guidelines regarding eating disorders earlier this year, marking their first update since 2006. The guidelines highlight research that suggests nearly 1% – 0.8% – of the U.S. population will develop AN over their lifetimes. Recent studies also suggest that eating disorder numbers rose during the pandemic, with one analysis finding that patients under inpatient care doubled in 2020.
“Mortality rates are high for anorexia nervosa, up to 10 times higher than matched controls,” Dr. Cacodcar said. “It has the highest mortality rate of the psychiatric diseases with the exception of opioid use disorder.”
As for outcomes, she pointed to a 2019 study that surveyed 387 parents who had children with eating disorders, mostly AN. Only 20% made a full recovery. “The farther you get out from the onset of anorexia, the less likely you are to achieve recovery,” Dr. Cacodcar said. “A lot of the control behaviors become very automatic.”
Determining capacity
In some cases of AN, psychiatrists must determine whether they have the capacity to make decisions about treatment, said Gabriel Jerkins, MD, a chief resident of psychiatry at the University of Florida. At issue is “the ability of the individual to comprehend the information being disclosed in regard to their condition, as well as the nature and potential risks and benefits of the proposed treatment alternatives. They include of course, no treatment at all.”
“We know psychiatric conditions can limit one’s ability to appreciate consequence,” he said.
One option is to seek to institutionalize patients with severe AN because they are a danger to themselves. Clinicians opted to not do this in the case of the patient profiled by Dr. Cacodcar, the one with the BMI of 12.2 who didn’t want inpatient or residential care. (A 5-foot-8 person with a BMI of 12.2 would weigh 80 pounds.)
“The main reason we did not hospitalize her is because an appropriate level of care was not going to be readily available,” Dr. Cacodcar said, and her treatment would have been substandard.
Fortunately, the woman did return after a couple of months and accept residential care. No facility in Florida was willing to accept her because of her low BMI, but she did find one in North Carolina, where she stayed for 2 months. She’s doing well, and her BMI is now 21, Dr. Cacodcar said.
The patient’s story shows that involuntary hospitalization “is not necessarily the best course of action,” Dr. Cacodcar said. “It wasn’t necessarily going to be in the patient’s best interest.”
In another case, a 22-year-old woman had severe AN. She had been a gymnast and dancer, Dr. Jerkins said, “and I include that here only because of how commonly we see that kind of demographic information in patients with anorexia nervosa.”
Her BMI was 17.5, and clinicians discussed feeding her through a feeding tube. She still had “no insight that her symptoms were related to an underlying eating disorder,” Dr. Jerkins said, raising questions about her capacity. “Is it sufficient that the patient understand that she’s underweight?”
Ultimately, he said, she received a feeding tube at a time when her BMI had dropped to 16.3. She suffered from an infection but ultimately she improved and has stabilized at a BMI of around 19, he said.
“I do wonder if allowing her to have some control of how to pursue treatment in this case was therapeutic in a way,” he said, especially since matters of control are deeply ingrained in AN.
A former physical trainer, the patient had a BMI of 17.6. The University of Florida’s eating disorder clinic sent her to an out-of-state residential program, but she was discharged when her blood glucose dipped dangerously low as she compulsively exercised. Her BMI dipped to 16.2.
Dr. Schmidt had the patient involuntarily committed upon her return, but she went home after 12 days with no change in her weight. Ultimately, the patient was referred to an eating disorder center in Colorado for medical stabilization where she was given a feeding tube. But her medical situation was so dire that she was discharged to her home, where she went on hospice and died.
“I’m not arguing for or against the term ‘terminal anorexia.’ But this case does make me think about it,” said Dr. Schmidt. She was referring to a controversial term used by some clinicians to refer to patients who face inevitable death from AN. “Unfortunately,” wrote the authors of a recent report proposing a clinical definition, “these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa.”
SAN FRANCISCO – The patient at a Florida eating disorder clinic said she was eating plenty even though she acknowledged purging once a week. But her vitals told a different story: Her body mass index (BMI) was 12.2, down from 14.8 a couple of years before – a dangerously low value.
While the woman agreed that she needed to gain weight, she refused advice to pursue residential or inpatient treatment. This left her team with a big dilemma: Should they force her into care because she wouldn’t eat? Was that even possible under the law? Did she have the capacity to make decisions about her future? What other alternatives were there?
Determining the best course of action in cases like this is anything but simple, Dr. Cacodcar said. To make matters more complicated, .
“At least in my state of Florida, we know that it can be very, very hard to get patients expert care,” said Dr. Cacodcar. And, she said, it can be even tougher for certain types of patients, such as those that are LGBTQ and those who have severe illness but don’t meet the criteria.
As Dr. Cacodcar noted, the APA released new practice guidelines regarding eating disorders earlier this year, marking their first update since 2006. The guidelines highlight research that suggests nearly 1% – 0.8% – of the U.S. population will develop AN over their lifetimes. Recent studies also suggest that eating disorder numbers rose during the pandemic, with one analysis finding that patients under inpatient care doubled in 2020.
“Mortality rates are high for anorexia nervosa, up to 10 times higher than matched controls,” Dr. Cacodcar said. “It has the highest mortality rate of the psychiatric diseases with the exception of opioid use disorder.”
As for outcomes, she pointed to a 2019 study that surveyed 387 parents who had children with eating disorders, mostly AN. Only 20% made a full recovery. “The farther you get out from the onset of anorexia, the less likely you are to achieve recovery,” Dr. Cacodcar said. “A lot of the control behaviors become very automatic.”
Determining capacity
In some cases of AN, psychiatrists must determine whether they have the capacity to make decisions about treatment, said Gabriel Jerkins, MD, a chief resident of psychiatry at the University of Florida. At issue is “the ability of the individual to comprehend the information being disclosed in regard to their condition, as well as the nature and potential risks and benefits of the proposed treatment alternatives. They include of course, no treatment at all.”
“We know psychiatric conditions can limit one’s ability to appreciate consequence,” he said.
One option is to seek to institutionalize patients with severe AN because they are a danger to themselves. Clinicians opted to not do this in the case of the patient profiled by Dr. Cacodcar, the one with the BMI of 12.2 who didn’t want inpatient or residential care. (A 5-foot-8 person with a BMI of 12.2 would weigh 80 pounds.)
“The main reason we did not hospitalize her is because an appropriate level of care was not going to be readily available,” Dr. Cacodcar said, and her treatment would have been substandard.
Fortunately, the woman did return after a couple of months and accept residential care. No facility in Florida was willing to accept her because of her low BMI, but she did find one in North Carolina, where she stayed for 2 months. She’s doing well, and her BMI is now 21, Dr. Cacodcar said.
The patient’s story shows that involuntary hospitalization “is not necessarily the best course of action,” Dr. Cacodcar said. “It wasn’t necessarily going to be in the patient’s best interest.”
In another case, a 22-year-old woman had severe AN. She had been a gymnast and dancer, Dr. Jerkins said, “and I include that here only because of how commonly we see that kind of demographic information in patients with anorexia nervosa.”
Her BMI was 17.5, and clinicians discussed feeding her through a feeding tube. She still had “no insight that her symptoms were related to an underlying eating disorder,” Dr. Jerkins said, raising questions about her capacity. “Is it sufficient that the patient understand that she’s underweight?”
Ultimately, he said, she received a feeding tube at a time when her BMI had dropped to 16.3. She suffered from an infection but ultimately she improved and has stabilized at a BMI of around 19, he said.
“I do wonder if allowing her to have some control of how to pursue treatment in this case was therapeutic in a way,” he said, especially since matters of control are deeply ingrained in AN.
A former physical trainer, the patient had a BMI of 17.6. The University of Florida’s eating disorder clinic sent her to an out-of-state residential program, but she was discharged when her blood glucose dipped dangerously low as she compulsively exercised. Her BMI dipped to 16.2.
Dr. Schmidt had the patient involuntarily committed upon her return, but she went home after 12 days with no change in her weight. Ultimately, the patient was referred to an eating disorder center in Colorado for medical stabilization where she was given a feeding tube. But her medical situation was so dire that she was discharged to her home, where she went on hospice and died.
“I’m not arguing for or against the term ‘terminal anorexia.’ But this case does make me think about it,” said Dr. Schmidt. She was referring to a controversial term used by some clinicians to refer to patients who face inevitable death from AN. “Unfortunately,” wrote the authors of a recent report proposing a clinical definition, “these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa.”
AT APA 2023
Alcohol dependence in teens tied to subsequent depression
TOPLINE
Alcohol dependence, but not consumption, at age 18 years increases the risk for depression at age 24 years.
METHODOLOGY
- The study included 3,902 mostly White adolescents, about 58% female, born in England from April 1991 to December 1992, who were part of the Avon Longitudinal Study of Parents and Children (ALSPAC) that examined genetic and environmental determinants of health and development.
- Participants completed the self-report Alcohol Use Disorders Identification Test (AUDIT) between the ages of 16 and 23 years, a period when average alcohol use increases rapidly.
- The primary outcome was probability for depression at age 24 years, using the Clinical Interview Schedule Revised (CIS-R), a self-administered computerized clinical assessment of common mental disorder symptoms during the past week.
- Researchers assessed frequency and quantity of alcohol consumption as well as alcohol dependence.
- Confounders included sex, housing type, maternal education and depressive symptoms, parents’ alcohol use, conduct problems at age 4 years, being bullied, and smoking status.
TAKEAWAYS
- After adjustments, alcohol dependence at age 18 years was associated with depression at age 24 years (unstandardized probit coefficient 0.13; 95% confidence interval, 0.02-0.25; P = .019)
- The relationship appeared to persist for alcohol dependence at each age of the growth curve (17-22 years).
- There was no evidence that frequency or quantity of alcohol consumption at age 18 was significantly associated with depression at age 24, suggesting these factors may not increase the risk for later depression unless there are also features of dependency.
IN PRACTICE
“Our findings suggest that preventing alcohol dependence during adolescence, or treating it early, could reduce the risk of depression,” which could have important public health implications, the researchers write.
STUDY DETAILS
The study was carried out by researchers at the University of Bristol; University College London; Critical Thinking Unit, Public Health Directorate, NHS; University of Nottingham, all in the United Kingdom. It was published online in Lancet Psychiatry
LIMITATIONS
There was substantial attrition in the ALSPAC cohort from birth to age 24 years. The sample was recruited from one U.K. region and most participants were White. Measures of alcohol consumption and dependence excluded some features of abuse. And as this is an observational study, the possibility of residual confounding can’t be excluded.
DISCLOSURES
The investigators report no relevant disclosures. The study received support from the UK Medical Research Council and Alcohol Research UK.
A version of this article first appeared on Medscape.com.
TOPLINE
Alcohol dependence, but not consumption, at age 18 years increases the risk for depression at age 24 years.
METHODOLOGY
- The study included 3,902 mostly White adolescents, about 58% female, born in England from April 1991 to December 1992, who were part of the Avon Longitudinal Study of Parents and Children (ALSPAC) that examined genetic and environmental determinants of health and development.
- Participants completed the self-report Alcohol Use Disorders Identification Test (AUDIT) between the ages of 16 and 23 years, a period when average alcohol use increases rapidly.
- The primary outcome was probability for depression at age 24 years, using the Clinical Interview Schedule Revised (CIS-R), a self-administered computerized clinical assessment of common mental disorder symptoms during the past week.
- Researchers assessed frequency and quantity of alcohol consumption as well as alcohol dependence.
- Confounders included sex, housing type, maternal education and depressive symptoms, parents’ alcohol use, conduct problems at age 4 years, being bullied, and smoking status.
TAKEAWAYS
- After adjustments, alcohol dependence at age 18 years was associated with depression at age 24 years (unstandardized probit coefficient 0.13; 95% confidence interval, 0.02-0.25; P = .019)
- The relationship appeared to persist for alcohol dependence at each age of the growth curve (17-22 years).
- There was no evidence that frequency or quantity of alcohol consumption at age 18 was significantly associated with depression at age 24, suggesting these factors may not increase the risk for later depression unless there are also features of dependency.
IN PRACTICE
“Our findings suggest that preventing alcohol dependence during adolescence, or treating it early, could reduce the risk of depression,” which could have important public health implications, the researchers write.
STUDY DETAILS
The study was carried out by researchers at the University of Bristol; University College London; Critical Thinking Unit, Public Health Directorate, NHS; University of Nottingham, all in the United Kingdom. It was published online in Lancet Psychiatry
LIMITATIONS
There was substantial attrition in the ALSPAC cohort from birth to age 24 years. The sample was recruited from one U.K. region and most participants were White. Measures of alcohol consumption and dependence excluded some features of abuse. And as this is an observational study, the possibility of residual confounding can’t be excluded.
DISCLOSURES
The investigators report no relevant disclosures. The study received support from the UK Medical Research Council and Alcohol Research UK.
A version of this article first appeared on Medscape.com.
TOPLINE
Alcohol dependence, but not consumption, at age 18 years increases the risk for depression at age 24 years.
METHODOLOGY
- The study included 3,902 mostly White adolescents, about 58% female, born in England from April 1991 to December 1992, who were part of the Avon Longitudinal Study of Parents and Children (ALSPAC) that examined genetic and environmental determinants of health and development.
- Participants completed the self-report Alcohol Use Disorders Identification Test (AUDIT) between the ages of 16 and 23 years, a period when average alcohol use increases rapidly.
- The primary outcome was probability for depression at age 24 years, using the Clinical Interview Schedule Revised (CIS-R), a self-administered computerized clinical assessment of common mental disorder symptoms during the past week.
- Researchers assessed frequency and quantity of alcohol consumption as well as alcohol dependence.
- Confounders included sex, housing type, maternal education and depressive symptoms, parents’ alcohol use, conduct problems at age 4 years, being bullied, and smoking status.
TAKEAWAYS
- After adjustments, alcohol dependence at age 18 years was associated with depression at age 24 years (unstandardized probit coefficient 0.13; 95% confidence interval, 0.02-0.25; P = .019)
- The relationship appeared to persist for alcohol dependence at each age of the growth curve (17-22 years).
- There was no evidence that frequency or quantity of alcohol consumption at age 18 was significantly associated with depression at age 24, suggesting these factors may not increase the risk for later depression unless there are also features of dependency.
IN PRACTICE
“Our findings suggest that preventing alcohol dependence during adolescence, or treating it early, could reduce the risk of depression,” which could have important public health implications, the researchers write.
STUDY DETAILS
The study was carried out by researchers at the University of Bristol; University College London; Critical Thinking Unit, Public Health Directorate, NHS; University of Nottingham, all in the United Kingdom. It was published online in Lancet Psychiatry
LIMITATIONS
There was substantial attrition in the ALSPAC cohort from birth to age 24 years. The sample was recruited from one U.K. region and most participants were White. Measures of alcohol consumption and dependence excluded some features of abuse. And as this is an observational study, the possibility of residual confounding can’t be excluded.
DISCLOSURES
The investigators report no relevant disclosures. The study received support from the UK Medical Research Council and Alcohol Research UK.
A version of this article first appeared on Medscape.com.
After backlash, publisher to retract article that surveyed parents of children with gender dysphoria, says coauthor
The move is “due to concerns about lack of informed consent,” according to tweets by one of the paper’s authors.
The article, “Rapid Onset Gender Dysphoria: Parent Reports on 1655 Possible Cases,” was published in March in the Archives of Sexual Behavior. It has not been cited in the scientific literature, according to Clarivate’s Web of Science, but Altmetric, which tracks the online attention papers receive, ranks the article in the top 1% of all articles of a similar age.
Rapid Onset Gender Dysphoria (ROGD) is, the article stated, a “controversial theory” that “common cultural beliefs, values, and preoccupations cause some adolescents (especially female adolescents) to attribute their social problems, feelings, and mental health issues to gender dysphoria,” and that “youth with ROGD falsely believe that they are transgender,” in part due to social influences.
Michael Bailey, a psychology professor at Northwestern University in Evanston, Ill., and the paper’s corresponding author, tweeted: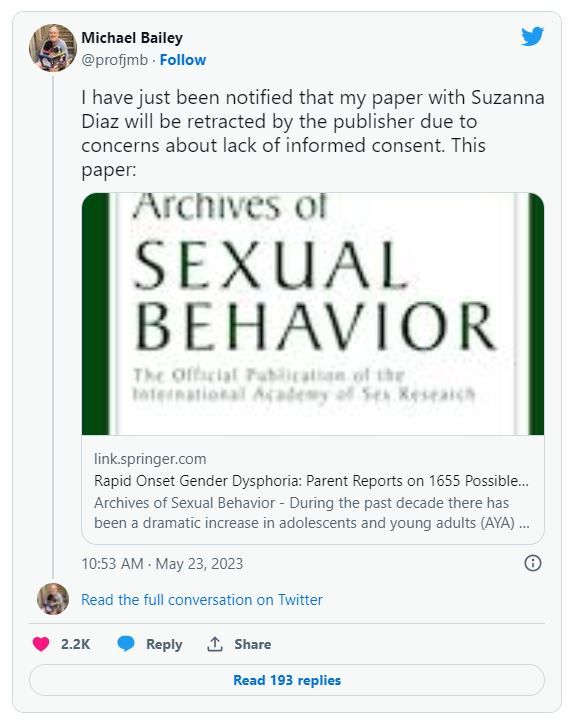
Bailey told Retraction Watch that he would “respond when [he] can” to our request for comment, following “new developments on our end.” Neither Springer Nature nor Kenneth Zucker, editor in chief of Archives of Sexual Behavior, has responded to similar requests.
The paper reported the results of a survey of parents who contacted the website ParentsofROGDKids.com, with which the first author is affiliated. According to the abstract, the authors found:
“Pre-existing mental health issues were common, and youths with these issues were more likely than those without them to have socially and medically transitioned. Parents reported that they had often felt pressured by clinicians to affirm their AYA [adolescent and young adult] child’s new gender and support their transition. According to the parents, AYA children’s mental health deteriorated considerably after social transition.”
Soon after publication, the paper attracted criticism that its method of gathering study participants was biased, and that the authors ignored information that didn’t support the theory of ROGD.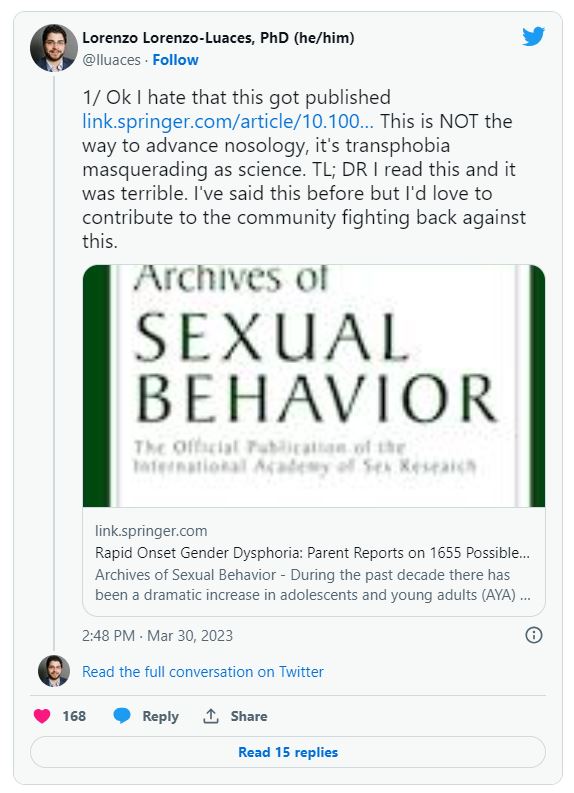
Archives of Sexual Behavior is the official publication of the International Academy of Sex Research, which tweeted on April 19:
The episode prompted a May 5 “Open Letter in Support of Dr. Kenneth Zucker and the Need to Promote Robust Scientific Debate” from the Foundation Against Intolerance and Racism that has now been signed by nearly 2000 people.
On May 10, the following publisher’s note was added to the article:
“readers are alerted that concerns have been raised regarding methodology as described in this article. The publisher is currently investigating this matter and a further response will follow the conclusion of this investigation.
Six days later, the publisher removed the article’s supplementary information “due to a lack of documented consent by study participants.”
The story may feel familiar to readers who recall what happened to another paper in 2018. In that paper, Brown University’s Lisa Littman coined the term ROGD. Following a backlash, Brown took down a press release touting the results, and the paper was eventually republished with corrections.
Bailey has been accused of mistreating transgender research participants, but an investigation by bioethicist Alice Dreger found that of the many accusations, “almost none appear to have been legitimate.”
In a post on UnHerd earlier this month, Bailey responded to the reported concerns about the study lacking approval by an Institutional Review Board (IRB), and that the way the participants were recruited biased the results.
IRB approval was not necessary, Bailey wrote, because Suzanna Diaz, the first author who collected the data, was not affiliated with an institution that required it. “Suzanna Diaz” is a pseudonym for “the mother of a gender dysphoric child she believes has ROGD” who wishes to remain anonymous for the sake of her family, Bailey wrote.
The paper included the following statement about its ethical approval:
“The first author and creator of the survey is not affiliated with any university or hospital. Thus, she did not seek approval from an IRB. After seeing a presentation of preliminary survey results by the first author, the second author suggested the data to be analyzed and submitted as an academic article (he was not involved in collecting the data). The second author consulted with his university’s IRB, who declined to certify the study because data were already collected. However, they advised that publishing the results was likely ethical provided data were deidentified. Editor’s note: After I reviewed the manuscript, I concluded that its publication is ethically appropriate, consistent with Springer policy.”
In his UnHerd post, Bailey quoted from the journal’s submission guidelines:
“If a study has not been granted ethics committee approval prior to commencing, retrospective ethics approval usually cannot be obtained and it may not be possible to consider the manuscript for peer review. The decision on whether to proceed to peer review in such cases is at the Editor’s discretion.”
“Regarding the methodological limitations of the study, these were addressed forthrightly and thoroughly in our article,” Bailey wrote.
Adam Marcus, a cofounder of Retraction Watch, is an editor at this news organization.
A version of this article first appeared on RetractionWatch.com.
The move is “due to concerns about lack of informed consent,” according to tweets by one of the paper’s authors.
The article, “Rapid Onset Gender Dysphoria: Parent Reports on 1655 Possible Cases,” was published in March in the Archives of Sexual Behavior. It has not been cited in the scientific literature, according to Clarivate’s Web of Science, but Altmetric, which tracks the online attention papers receive, ranks the article in the top 1% of all articles of a similar age.
Rapid Onset Gender Dysphoria (ROGD) is, the article stated, a “controversial theory” that “common cultural beliefs, values, and preoccupations cause some adolescents (especially female adolescents) to attribute their social problems, feelings, and mental health issues to gender dysphoria,” and that “youth with ROGD falsely believe that they are transgender,” in part due to social influences.
Michael Bailey, a psychology professor at Northwestern University in Evanston, Ill., and the paper’s corresponding author, tweeted:
Bailey told Retraction Watch that he would “respond when [he] can” to our request for comment, following “new developments on our end.” Neither Springer Nature nor Kenneth Zucker, editor in chief of Archives of Sexual Behavior, has responded to similar requests.
The paper reported the results of a survey of parents who contacted the website ParentsofROGDKids.com, with which the first author is affiliated. According to the abstract, the authors found:
“Pre-existing mental health issues were common, and youths with these issues were more likely than those without them to have socially and medically transitioned. Parents reported that they had often felt pressured by clinicians to affirm their AYA [adolescent and young adult] child’s new gender and support their transition. According to the parents, AYA children’s mental health deteriorated considerably after social transition.”
Soon after publication, the paper attracted criticism that its method of gathering study participants was biased, and that the authors ignored information that didn’t support the theory of ROGD.
Archives of Sexual Behavior is the official publication of the International Academy of Sex Research, which tweeted on April 19:
The episode prompted a May 5 “Open Letter in Support of Dr. Kenneth Zucker and the Need to Promote Robust Scientific Debate” from the Foundation Against Intolerance and Racism that has now been signed by nearly 2000 people.
On May 10, the following publisher’s note was added to the article:
“readers are alerted that concerns have been raised regarding methodology as described in this article. The publisher is currently investigating this matter and a further response will follow the conclusion of this investigation.
Six days later, the publisher removed the article’s supplementary information “due to a lack of documented consent by study participants.”
The story may feel familiar to readers who recall what happened to another paper in 2018. In that paper, Brown University’s Lisa Littman coined the term ROGD. Following a backlash, Brown took down a press release touting the results, and the paper was eventually republished with corrections.
Bailey has been accused of mistreating transgender research participants, but an investigation by bioethicist Alice Dreger found that of the many accusations, “almost none appear to have been legitimate.”
In a post on UnHerd earlier this month, Bailey responded to the reported concerns about the study lacking approval by an Institutional Review Board (IRB), and that the way the participants were recruited biased the results.
IRB approval was not necessary, Bailey wrote, because Suzanna Diaz, the first author who collected the data, was not affiliated with an institution that required it. “Suzanna Diaz” is a pseudonym for “the mother of a gender dysphoric child she believes has ROGD” who wishes to remain anonymous for the sake of her family, Bailey wrote.
The paper included the following statement about its ethical approval:
“The first author and creator of the survey is not affiliated with any university or hospital. Thus, she did not seek approval from an IRB. After seeing a presentation of preliminary survey results by the first author, the second author suggested the data to be analyzed and submitted as an academic article (he was not involved in collecting the data). The second author consulted with his university’s IRB, who declined to certify the study because data were already collected. However, they advised that publishing the results was likely ethical provided data were deidentified. Editor’s note: After I reviewed the manuscript, I concluded that its publication is ethically appropriate, consistent with Springer policy.”
In his UnHerd post, Bailey quoted from the journal’s submission guidelines:
“If a study has not been granted ethics committee approval prior to commencing, retrospective ethics approval usually cannot be obtained and it may not be possible to consider the manuscript for peer review. The decision on whether to proceed to peer review in such cases is at the Editor’s discretion.”
“Regarding the methodological limitations of the study, these were addressed forthrightly and thoroughly in our article,” Bailey wrote.
Adam Marcus, a cofounder of Retraction Watch, is an editor at this news organization.
A version of this article first appeared on RetractionWatch.com.
The move is “due to concerns about lack of informed consent,” according to tweets by one of the paper’s authors.
The article, “Rapid Onset Gender Dysphoria: Parent Reports on 1655 Possible Cases,” was published in March in the Archives of Sexual Behavior. It has not been cited in the scientific literature, according to Clarivate’s Web of Science, but Altmetric, which tracks the online attention papers receive, ranks the article in the top 1% of all articles of a similar age.
Rapid Onset Gender Dysphoria (ROGD) is, the article stated, a “controversial theory” that “common cultural beliefs, values, and preoccupations cause some adolescents (especially female adolescents) to attribute their social problems, feelings, and mental health issues to gender dysphoria,” and that “youth with ROGD falsely believe that they are transgender,” in part due to social influences.
Michael Bailey, a psychology professor at Northwestern University in Evanston, Ill., and the paper’s corresponding author, tweeted:
Bailey told Retraction Watch that he would “respond when [he] can” to our request for comment, following “new developments on our end.” Neither Springer Nature nor Kenneth Zucker, editor in chief of Archives of Sexual Behavior, has responded to similar requests.
The paper reported the results of a survey of parents who contacted the website ParentsofROGDKids.com, with which the first author is affiliated. According to the abstract, the authors found:
“Pre-existing mental health issues were common, and youths with these issues were more likely than those without them to have socially and medically transitioned. Parents reported that they had often felt pressured by clinicians to affirm their AYA [adolescent and young adult] child’s new gender and support their transition. According to the parents, AYA children’s mental health deteriorated considerably after social transition.”
Soon after publication, the paper attracted criticism that its method of gathering study participants was biased, and that the authors ignored information that didn’t support the theory of ROGD.
Archives of Sexual Behavior is the official publication of the International Academy of Sex Research, which tweeted on April 19:
The episode prompted a May 5 “Open Letter in Support of Dr. Kenneth Zucker and the Need to Promote Robust Scientific Debate” from the Foundation Against Intolerance and Racism that has now been signed by nearly 2000 people.
On May 10, the following publisher’s note was added to the article:
“readers are alerted that concerns have been raised regarding methodology as described in this article. The publisher is currently investigating this matter and a further response will follow the conclusion of this investigation.
Six days later, the publisher removed the article’s supplementary information “due to a lack of documented consent by study participants.”
The story may feel familiar to readers who recall what happened to another paper in 2018. In that paper, Brown University’s Lisa Littman coined the term ROGD. Following a backlash, Brown took down a press release touting the results, and the paper was eventually republished with corrections.
Bailey has been accused of mistreating transgender research participants, but an investigation by bioethicist Alice Dreger found that of the many accusations, “almost none appear to have been legitimate.”
In a post on UnHerd earlier this month, Bailey responded to the reported concerns about the study lacking approval by an Institutional Review Board (IRB), and that the way the participants were recruited biased the results.
IRB approval was not necessary, Bailey wrote, because Suzanna Diaz, the first author who collected the data, was not affiliated with an institution that required it. “Suzanna Diaz” is a pseudonym for “the mother of a gender dysphoric child she believes has ROGD” who wishes to remain anonymous for the sake of her family, Bailey wrote.
The paper included the following statement about its ethical approval:
“The first author and creator of the survey is not affiliated with any university or hospital. Thus, she did not seek approval from an IRB. After seeing a presentation of preliminary survey results by the first author, the second author suggested the data to be analyzed and submitted as an academic article (he was not involved in collecting the data). The second author consulted with his university’s IRB, who declined to certify the study because data were already collected. However, they advised that publishing the results was likely ethical provided data were deidentified. Editor’s note: After I reviewed the manuscript, I concluded that its publication is ethically appropriate, consistent with Springer policy.”
In his UnHerd post, Bailey quoted from the journal’s submission guidelines:
“If a study has not been granted ethics committee approval prior to commencing, retrospective ethics approval usually cannot be obtained and it may not be possible to consider the manuscript for peer review. The decision on whether to proceed to peer review in such cases is at the Editor’s discretion.”
“Regarding the methodological limitations of the study, these were addressed forthrightly and thoroughly in our article,” Bailey wrote.
Adam Marcus, a cofounder of Retraction Watch, is an editor at this news organization.
A version of this article first appeared on RetractionWatch.com.
Is ChatGPT a friend or foe of medical publishing?
. These tools should not be listed as authors, and researchers must denote how AI-assisted technologies were used, the committee said.
These new guidelines are the latest effort for medical journals to define policies for using these large-scale language models (LLMs) in scientific publication. While these AI-assisted tools can help with tasks such as writing, analyzing data, catching mistakes, and much more, they are also prone to errors, noted Casey Greene, PhD, a professor of biomedical informatics at the University of Colorado at Denver, Aurora. It is also not totally clear how information is stored and processed in these kinds of tools, and who has access to that information, he noted.
At the same time, experts argue that these AI tools could have a positive impact on the field by limiting some of the linguistic disparities in scientific publishing as well as alleviating the burden of some monotonous or mechanical tasks that come along with manuscript writing.
What experts can agree on, though, is that the use of AI tools is here to stay. “This is going to become a common tool,” Dr. Greene said. “I don’t think there’s a way out of that at this point.”
A change in medical publishing
OpenAI released ChatGPT in November 2022. In its own words, ChatGPT is “a deep learning model that has been trained on a massive amount of text data to understand and generate humanlike text.” Enter a question or a prompt, and it will respond. For example, when asked how the AI tool can be used in scientific publishing, ChatGPT responded:
“ChatGPT can aid scientific publishing by generating ideas, clarifying concepts, conducting preliminary literature reviews, providing proofreading and editing suggestions, and assisting with outlining and organizing scientific papers. However, it should be used as a supportive tool alongside domain expertise and validation from trusted scientific sources.”
Just a few months after ChatGPT became available, researchers began using this tool in their own work. One individual, Som Biswas, MD, a radiologist at the University of Tennessee Health Science Center in Memphis, reportedly used ChatGPT to author 16 scientific articles in just 4 months, according to the Daily Beast. Five of these articles have been published in four different journals. Dr. Biswas declined to be interviewed for this article.
There were also reports of papers with ChatGPT as one of the listed authors, which sparked backlash. In response, JAMA, Nature, and Science all published editorials in January outlining their policies for using ChatGPT and other large language models in the scientific authoring process. Editors from the journals of the American College of Cardiology and the American College of Rheumatology also updated their policies to reflect the influence of AI authoring tools.
The consensus is that AI has no place on the author byline.
“We think that’s not appropriate, because coauthorship means that you are taking responsibility for the analysis and the generation of data that are included in a manuscript. A machine that is dictated by AI can’t take responsibility,” said Daniel Solomon, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, and the editor in chief of the ACR journal Arthritis & Rheumatology.
Issues with AI
One of the big concerns around using AI in writing is that it can generate text that seems plausible but is untrue or not supported by data. For example, Dr. Greene and colleague Milton Pividori, PhD, also of the University of Colorado, were writing a journal article about new software they developed that uses a large language model to revise scientific manuscripts.
“We used the same software to revise that article and at one point, it added a line that noted that the large language model had been fine-tuned on a data set of manuscripts from within the same field. This makes a lot of sense, and is absolutely something you could do, but was not something that we did,” Dr. Greene said. “Without a really careful review of the content, it becomes possible to invent things that were not actually done.”
In another case, ChatGPT falsely stated that a prominent law professor had been accused of sexual assault, citing a Washington Post article that did not exist.
“We live in a society where we are extremely concerned about fake news,” Dr. Pividori added, “and [these kinds of errors] could certainly exacerbate that in the scientific community, which is very concerning because science informs public policy.”
Another issue is the lack of transparency around how large language models like ChatGPT process and store data used to make queries.
“We have no idea how they are recording all the prompts and things that we input into ChatGPT and their systems,” Dr. Pividori said.
OpenAI recently addressed some privacy concerns by allowing users to turn off their chat history with the AI chatbot, so conversations cannot be used to train or improve the company’s models. But Dr. Greene noted that the terms of service “still remain pretty nebulous.”
Dr. Solomon is also concerned with researchers using these AI tools in authoring without knowing how they work. “The thing we are really concerned about is that fact that [LLMs] are a bit of a black box – people don’t really understand the methodologies,” he said.
A positive tool?
But despite these concerns, many think that these types of AI-assisted tools could have a positive impact on medical publishing, particularly for researchers for whom English is not their first language, noted Catherine Gao, MD, a pulmonary and critical care instructor at Northwestern University, Chicago. She recently led research comparing scientific abstracts written by ChatGPT and real abstracts and discovered that reviewers found it “surprisingly difficult” to differentiate the two.
“The majority of research is published in English,” she said in an email. “Responsible use of LLMs can potentially reduce the burden of writing for busy scientists and improve equity for those who are not native English speakers.”
Dr. Pividori agreed, adding that as a non-native English speaker, he spends much more time working on the structure and grammar of sentences when authoring a manuscript, compared with people who speak English as a first language. He noted that these tools can also be used to automate some of the more monotonous tasks that come along with writing manuscripts and allow researchers to focus on the more creative aspects.
In the future, “I want to focus more on the things that only a human can do and let these tools do all the rest of it,” he said.
New rules
But despite how individual researchers feel about LLMs, they agree that these AI tools are here to stay.
“I think that we should anticipate that they will become part of the medical research establishment over time, when we figure out how to use them appropriately,” Dr. Solomon said.
While the debate of how to best use AI in medical publications will continue, journal editors agree that all authors of a manuscript are solely responsible for content in articles that used AI-assisted technology.
“Authors should carefully review and edit the result because AI can generate authoritative-sounding output that can be incorrect, incomplete, or biased,” the ICMJE guidelines state. “Authors should be able to assert that there is no plagiarism in their paper, including in text and images produced by the AI.” This includes appropriate attribution of all cited materials.
The committee also recommends that authors write in both the cover letter and submitted work how AI was used in the manuscript writing process. Recently updated guidelines from the World Association of Medical Editors recommend that all prompts used to generate new text or analytical work should be provided in submitted work. Dr. Greene also noted that if authors used an AI tool to revise their work, they can include a version of the manuscript untouched by LLMs.
It is similar to a preprint, he said, but rather than publishing a version of a paper prior to peer review, someone is showing a version of a manuscript before it was reviewed and revised by AI. “This type of practice could be a path that lets us benefit from these models,” he said, “without having the drawbacks that many are concerned about.”
Dr. Solomon has financial relationships with AbbVie, Amgen, Janssen, CorEvitas, and Moderna. Both Dr. Greene and Dr. Pividori are inventors in the U.S. Provisional Patent Application No. 63/486,706 that the University of Colorado has filed for the “Publishing Infrastructure For AI-Assisted Academic Authoring” invention with the U.S. Patent and Trademark Office. Dr. Greene and Dr. Pividori also received a grant from the Alfred P. Sloan Foundation to improve their AI-based manuscript revision tool. Dr. Gao reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
. These tools should not be listed as authors, and researchers must denote how AI-assisted technologies were used, the committee said.
These new guidelines are the latest effort for medical journals to define policies for using these large-scale language models (LLMs) in scientific publication. While these AI-assisted tools can help with tasks such as writing, analyzing data, catching mistakes, and much more, they are also prone to errors, noted Casey Greene, PhD, a professor of biomedical informatics at the University of Colorado at Denver, Aurora. It is also not totally clear how information is stored and processed in these kinds of tools, and who has access to that information, he noted.
At the same time, experts argue that these AI tools could have a positive impact on the field by limiting some of the linguistic disparities in scientific publishing as well as alleviating the burden of some monotonous or mechanical tasks that come along with manuscript writing.
What experts can agree on, though, is that the use of AI tools is here to stay. “This is going to become a common tool,” Dr. Greene said. “I don’t think there’s a way out of that at this point.”
A change in medical publishing
OpenAI released ChatGPT in November 2022. In its own words, ChatGPT is “a deep learning model that has been trained on a massive amount of text data to understand and generate humanlike text.” Enter a question or a prompt, and it will respond. For example, when asked how the AI tool can be used in scientific publishing, ChatGPT responded:
“ChatGPT can aid scientific publishing by generating ideas, clarifying concepts, conducting preliminary literature reviews, providing proofreading and editing suggestions, and assisting with outlining and organizing scientific papers. However, it should be used as a supportive tool alongside domain expertise and validation from trusted scientific sources.”
Just a few months after ChatGPT became available, researchers began using this tool in their own work. One individual, Som Biswas, MD, a radiologist at the University of Tennessee Health Science Center in Memphis, reportedly used ChatGPT to author 16 scientific articles in just 4 months, according to the Daily Beast. Five of these articles have been published in four different journals. Dr. Biswas declined to be interviewed for this article.
There were also reports of papers with ChatGPT as one of the listed authors, which sparked backlash. In response, JAMA, Nature, and Science all published editorials in January outlining their policies for using ChatGPT and other large language models in the scientific authoring process. Editors from the journals of the American College of Cardiology and the American College of Rheumatology also updated their policies to reflect the influence of AI authoring tools.
The consensus is that AI has no place on the author byline.
“We think that’s not appropriate, because coauthorship means that you are taking responsibility for the analysis and the generation of data that are included in a manuscript. A machine that is dictated by AI can’t take responsibility,” said Daniel Solomon, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, and the editor in chief of the ACR journal Arthritis & Rheumatology.
Issues with AI
One of the big concerns around using AI in writing is that it can generate text that seems plausible but is untrue or not supported by data. For example, Dr. Greene and colleague Milton Pividori, PhD, also of the University of Colorado, were writing a journal article about new software they developed that uses a large language model to revise scientific manuscripts.
“We used the same software to revise that article and at one point, it added a line that noted that the large language model had been fine-tuned on a data set of manuscripts from within the same field. This makes a lot of sense, and is absolutely something you could do, but was not something that we did,” Dr. Greene said. “Without a really careful review of the content, it becomes possible to invent things that were not actually done.”
In another case, ChatGPT falsely stated that a prominent law professor had been accused of sexual assault, citing a Washington Post article that did not exist.
“We live in a society where we are extremely concerned about fake news,” Dr. Pividori added, “and [these kinds of errors] could certainly exacerbate that in the scientific community, which is very concerning because science informs public policy.”
Another issue is the lack of transparency around how large language models like ChatGPT process and store data used to make queries.
“We have no idea how they are recording all the prompts and things that we input into ChatGPT and their systems,” Dr. Pividori said.
OpenAI recently addressed some privacy concerns by allowing users to turn off their chat history with the AI chatbot, so conversations cannot be used to train or improve the company’s models. But Dr. Greene noted that the terms of service “still remain pretty nebulous.”
Dr. Solomon is also concerned with researchers using these AI tools in authoring without knowing how they work. “The thing we are really concerned about is that fact that [LLMs] are a bit of a black box – people don’t really understand the methodologies,” he said.
A positive tool?
But despite these concerns, many think that these types of AI-assisted tools could have a positive impact on medical publishing, particularly for researchers for whom English is not their first language, noted Catherine Gao, MD, a pulmonary and critical care instructor at Northwestern University, Chicago. She recently led research comparing scientific abstracts written by ChatGPT and real abstracts and discovered that reviewers found it “surprisingly difficult” to differentiate the two.
“The majority of research is published in English,” she said in an email. “Responsible use of LLMs can potentially reduce the burden of writing for busy scientists and improve equity for those who are not native English speakers.”
Dr. Pividori agreed, adding that as a non-native English speaker, he spends much more time working on the structure and grammar of sentences when authoring a manuscript, compared with people who speak English as a first language. He noted that these tools can also be used to automate some of the more monotonous tasks that come along with writing manuscripts and allow researchers to focus on the more creative aspects.
In the future, “I want to focus more on the things that only a human can do and let these tools do all the rest of it,” he said.
New rules
But despite how individual researchers feel about LLMs, they agree that these AI tools are here to stay.
“I think that we should anticipate that they will become part of the medical research establishment over time, when we figure out how to use them appropriately,” Dr. Solomon said.
While the debate of how to best use AI in medical publications will continue, journal editors agree that all authors of a manuscript are solely responsible for content in articles that used AI-assisted technology.
“Authors should carefully review and edit the result because AI can generate authoritative-sounding output that can be incorrect, incomplete, or biased,” the ICMJE guidelines state. “Authors should be able to assert that there is no plagiarism in their paper, including in text and images produced by the AI.” This includes appropriate attribution of all cited materials.
The committee also recommends that authors write in both the cover letter and submitted work how AI was used in the manuscript writing process. Recently updated guidelines from the World Association of Medical Editors recommend that all prompts used to generate new text or analytical work should be provided in submitted work. Dr. Greene also noted that if authors used an AI tool to revise their work, they can include a version of the manuscript untouched by LLMs.
It is similar to a preprint, he said, but rather than publishing a version of a paper prior to peer review, someone is showing a version of a manuscript before it was reviewed and revised by AI. “This type of practice could be a path that lets us benefit from these models,” he said, “without having the drawbacks that many are concerned about.”
Dr. Solomon has financial relationships with AbbVie, Amgen, Janssen, CorEvitas, and Moderna. Both Dr. Greene and Dr. Pividori are inventors in the U.S. Provisional Patent Application No. 63/486,706 that the University of Colorado has filed for the “Publishing Infrastructure For AI-Assisted Academic Authoring” invention with the U.S. Patent and Trademark Office. Dr. Greene and Dr. Pividori also received a grant from the Alfred P. Sloan Foundation to improve their AI-based manuscript revision tool. Dr. Gao reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
. These tools should not be listed as authors, and researchers must denote how AI-assisted technologies were used, the committee said.
These new guidelines are the latest effort for medical journals to define policies for using these large-scale language models (LLMs) in scientific publication. While these AI-assisted tools can help with tasks such as writing, analyzing data, catching mistakes, and much more, they are also prone to errors, noted Casey Greene, PhD, a professor of biomedical informatics at the University of Colorado at Denver, Aurora. It is also not totally clear how information is stored and processed in these kinds of tools, and who has access to that information, he noted.
At the same time, experts argue that these AI tools could have a positive impact on the field by limiting some of the linguistic disparities in scientific publishing as well as alleviating the burden of some monotonous or mechanical tasks that come along with manuscript writing.
What experts can agree on, though, is that the use of AI tools is here to stay. “This is going to become a common tool,” Dr. Greene said. “I don’t think there’s a way out of that at this point.”
A change in medical publishing
OpenAI released ChatGPT in November 2022. In its own words, ChatGPT is “a deep learning model that has been trained on a massive amount of text data to understand and generate humanlike text.” Enter a question or a prompt, and it will respond. For example, when asked how the AI tool can be used in scientific publishing, ChatGPT responded:
“ChatGPT can aid scientific publishing by generating ideas, clarifying concepts, conducting preliminary literature reviews, providing proofreading and editing suggestions, and assisting with outlining and organizing scientific papers. However, it should be used as a supportive tool alongside domain expertise and validation from trusted scientific sources.”
Just a few months after ChatGPT became available, researchers began using this tool in their own work. One individual, Som Biswas, MD, a radiologist at the University of Tennessee Health Science Center in Memphis, reportedly used ChatGPT to author 16 scientific articles in just 4 months, according to the Daily Beast. Five of these articles have been published in four different journals. Dr. Biswas declined to be interviewed for this article.
There were also reports of papers with ChatGPT as one of the listed authors, which sparked backlash. In response, JAMA, Nature, and Science all published editorials in January outlining their policies for using ChatGPT and other large language models in the scientific authoring process. Editors from the journals of the American College of Cardiology and the American College of Rheumatology also updated their policies to reflect the influence of AI authoring tools.
The consensus is that AI has no place on the author byline.
“We think that’s not appropriate, because coauthorship means that you are taking responsibility for the analysis and the generation of data that are included in a manuscript. A machine that is dictated by AI can’t take responsibility,” said Daniel Solomon, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, and the editor in chief of the ACR journal Arthritis & Rheumatology.
Issues with AI
One of the big concerns around using AI in writing is that it can generate text that seems plausible but is untrue or not supported by data. For example, Dr. Greene and colleague Milton Pividori, PhD, also of the University of Colorado, were writing a journal article about new software they developed that uses a large language model to revise scientific manuscripts.
“We used the same software to revise that article and at one point, it added a line that noted that the large language model had been fine-tuned on a data set of manuscripts from within the same field. This makes a lot of sense, and is absolutely something you could do, but was not something that we did,” Dr. Greene said. “Without a really careful review of the content, it becomes possible to invent things that were not actually done.”
In another case, ChatGPT falsely stated that a prominent law professor had been accused of sexual assault, citing a Washington Post article that did not exist.
“We live in a society where we are extremely concerned about fake news,” Dr. Pividori added, “and [these kinds of errors] could certainly exacerbate that in the scientific community, which is very concerning because science informs public policy.”
Another issue is the lack of transparency around how large language models like ChatGPT process and store data used to make queries.
“We have no idea how they are recording all the prompts and things that we input into ChatGPT and their systems,” Dr. Pividori said.
OpenAI recently addressed some privacy concerns by allowing users to turn off their chat history with the AI chatbot, so conversations cannot be used to train or improve the company’s models. But Dr. Greene noted that the terms of service “still remain pretty nebulous.”
Dr. Solomon is also concerned with researchers using these AI tools in authoring without knowing how they work. “The thing we are really concerned about is that fact that [LLMs] are a bit of a black box – people don’t really understand the methodologies,” he said.
A positive tool?
But despite these concerns, many think that these types of AI-assisted tools could have a positive impact on medical publishing, particularly for researchers for whom English is not their first language, noted Catherine Gao, MD, a pulmonary and critical care instructor at Northwestern University, Chicago. She recently led research comparing scientific abstracts written by ChatGPT and real abstracts and discovered that reviewers found it “surprisingly difficult” to differentiate the two.
“The majority of research is published in English,” she said in an email. “Responsible use of LLMs can potentially reduce the burden of writing for busy scientists and improve equity for those who are not native English speakers.”
Dr. Pividori agreed, adding that as a non-native English speaker, he spends much more time working on the structure and grammar of sentences when authoring a manuscript, compared with people who speak English as a first language. He noted that these tools can also be used to automate some of the more monotonous tasks that come along with writing manuscripts and allow researchers to focus on the more creative aspects.
In the future, “I want to focus more on the things that only a human can do and let these tools do all the rest of it,” he said.
New rules
But despite how individual researchers feel about LLMs, they agree that these AI tools are here to stay.
“I think that we should anticipate that they will become part of the medical research establishment over time, when we figure out how to use them appropriately,” Dr. Solomon said.
While the debate of how to best use AI in medical publications will continue, journal editors agree that all authors of a manuscript are solely responsible for content in articles that used AI-assisted technology.
“Authors should carefully review and edit the result because AI can generate authoritative-sounding output that can be incorrect, incomplete, or biased,” the ICMJE guidelines state. “Authors should be able to assert that there is no plagiarism in their paper, including in text and images produced by the AI.” This includes appropriate attribution of all cited materials.
The committee also recommends that authors write in both the cover letter and submitted work how AI was used in the manuscript writing process. Recently updated guidelines from the World Association of Medical Editors recommend that all prompts used to generate new text or analytical work should be provided in submitted work. Dr. Greene also noted that if authors used an AI tool to revise their work, they can include a version of the manuscript untouched by LLMs.
It is similar to a preprint, he said, but rather than publishing a version of a paper prior to peer review, someone is showing a version of a manuscript before it was reviewed and revised by AI. “This type of practice could be a path that lets us benefit from these models,” he said, “without having the drawbacks that many are concerned about.”
Dr. Solomon has financial relationships with AbbVie, Amgen, Janssen, CorEvitas, and Moderna. Both Dr. Greene and Dr. Pividori are inventors in the U.S. Provisional Patent Application No. 63/486,706 that the University of Colorado has filed for the “Publishing Infrastructure For AI-Assisted Academic Authoring” invention with the U.S. Patent and Trademark Office. Dr. Greene and Dr. Pividori also received a grant from the Alfred P. Sloan Foundation to improve their AI-based manuscript revision tool. Dr. Gao reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Regular, optimal sleep tied to lower mortality risk
INDIANAPOLIS –
In a diverse group of older adults, those with regular and optimal sleep had about a 40% lower risk of dying of any cause during follow-up compared with peers who had irregular and insufficient sleep.
“If sleep were an 8-hour pill, it would be beneficial to take the full dose at regular times consistently,” lead researcher Joon Chung, PhD, of Harvard Medical School and Brigham and Women’s Hospital, Boston, said in a news release.
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Broad adverse health effects
“Evidence is mounting that irregular sleep is associated with pretty broad adverse health outcomes, most prominently cardiometabolic disease, obesity, and cardiovascular disease,” Dr. Chungsaid in an interview.
In the current study, the researchers estimated the association of regular sleep of optimal sleep duration with all-cause mortality using data from 1,759 adults the Multi-Ethnic Study of Atherosclerosis Sleep Study.
Sleep regularity and duration were classified using 7 days of data gathered by wrist actigraphy. Adults were categorized as “regular-optimal” sleepers (n = 1,015) or “irregular-insufficient” sleepers (n = 744).
During 7 years of follow-up, 176 people died. In the fully adjusted model, the regular-optimal group had a 39% lower mortality risk compared with the irregular-insufficient sleep group (hazard ratio, 0.61;95% confidence interval [CI], 0.45-0.83). The findings were robust in sensitivity analyses.
The regular and optimal duration sleep pattern maps behaviorally to regular bed and wake times, suggesting potential health benefits of adherence to recommended sleep practices, the researchers noted.
“Results suggest benefits of expanding the public conversation on getting ‘a good night’s sleep’ and broadening this goal to getting many good nights of sleep, in a row, on weekdays and weekends,” Dr. Chung said in the release.
He further said that “getting adequate, regular sleep seems to be something that is good for all. I don’t know of anyone who wouldn’t benefit.”
Fariha Abassi-Feinberg, MD, spokesperson for the American Academy of Sleep Medicine and sleep specialist with the Millennium Physician Group, Fort Myers, Fla., agreed.
“We know our bodies have an internal clock, known as the circadian rhythm, which regulates various biological processes, including sleep-wake cycles. Sticking to a consistent sleep schedule allows your body to align its natural rhythm with the external day-night cycle. This synchronization promotes better sleep quality and therefore better health,” said Dr. Abassi-Feinberg, who wasn’t involved in the study.
“The AASM recommends adults try to aim for at least 7 hours of sleep and I often tell my patients that keeping a regular routine is best for your sleep and health,” she said in an interview.
Funding for the study was provided by the American Academy of Sleep Medicine Foundation and the National Institutes of Health. Dr. Chung and Dr. Abassi-Feinberg report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
INDIANAPOLIS –
In a diverse group of older adults, those with regular and optimal sleep had about a 40% lower risk of dying of any cause during follow-up compared with peers who had irregular and insufficient sleep.
“If sleep were an 8-hour pill, it would be beneficial to take the full dose at regular times consistently,” lead researcher Joon Chung, PhD, of Harvard Medical School and Brigham and Women’s Hospital, Boston, said in a news release.
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Broad adverse health effects
“Evidence is mounting that irregular sleep is associated with pretty broad adverse health outcomes, most prominently cardiometabolic disease, obesity, and cardiovascular disease,” Dr. Chungsaid in an interview.
In the current study, the researchers estimated the association of regular sleep of optimal sleep duration with all-cause mortality using data from 1,759 adults the Multi-Ethnic Study of Atherosclerosis Sleep Study.
Sleep regularity and duration were classified using 7 days of data gathered by wrist actigraphy. Adults were categorized as “regular-optimal” sleepers (n = 1,015) or “irregular-insufficient” sleepers (n = 744).
During 7 years of follow-up, 176 people died. In the fully adjusted model, the regular-optimal group had a 39% lower mortality risk compared with the irregular-insufficient sleep group (hazard ratio, 0.61;95% confidence interval [CI], 0.45-0.83). The findings were robust in sensitivity analyses.
The regular and optimal duration sleep pattern maps behaviorally to regular bed and wake times, suggesting potential health benefits of adherence to recommended sleep practices, the researchers noted.
“Results suggest benefits of expanding the public conversation on getting ‘a good night’s sleep’ and broadening this goal to getting many good nights of sleep, in a row, on weekdays and weekends,” Dr. Chung said in the release.
He further said that “getting adequate, regular sleep seems to be something that is good for all. I don’t know of anyone who wouldn’t benefit.”
Fariha Abassi-Feinberg, MD, spokesperson for the American Academy of Sleep Medicine and sleep specialist with the Millennium Physician Group, Fort Myers, Fla., agreed.
“We know our bodies have an internal clock, known as the circadian rhythm, which regulates various biological processes, including sleep-wake cycles. Sticking to a consistent sleep schedule allows your body to align its natural rhythm with the external day-night cycle. This synchronization promotes better sleep quality and therefore better health,” said Dr. Abassi-Feinberg, who wasn’t involved in the study.
“The AASM recommends adults try to aim for at least 7 hours of sleep and I often tell my patients that keeping a regular routine is best for your sleep and health,” she said in an interview.
Funding for the study was provided by the American Academy of Sleep Medicine Foundation and the National Institutes of Health. Dr. Chung and Dr. Abassi-Feinberg report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
INDIANAPOLIS –
In a diverse group of older adults, those with regular and optimal sleep had about a 40% lower risk of dying of any cause during follow-up compared with peers who had irregular and insufficient sleep.
“If sleep were an 8-hour pill, it would be beneficial to take the full dose at regular times consistently,” lead researcher Joon Chung, PhD, of Harvard Medical School and Brigham and Women’s Hospital, Boston, said in a news release.
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Broad adverse health effects
“Evidence is mounting that irregular sleep is associated with pretty broad adverse health outcomes, most prominently cardiometabolic disease, obesity, and cardiovascular disease,” Dr. Chungsaid in an interview.
In the current study, the researchers estimated the association of regular sleep of optimal sleep duration with all-cause mortality using data from 1,759 adults the Multi-Ethnic Study of Atherosclerosis Sleep Study.
Sleep regularity and duration were classified using 7 days of data gathered by wrist actigraphy. Adults were categorized as “regular-optimal” sleepers (n = 1,015) or “irregular-insufficient” sleepers (n = 744).
During 7 years of follow-up, 176 people died. In the fully adjusted model, the regular-optimal group had a 39% lower mortality risk compared with the irregular-insufficient sleep group (hazard ratio, 0.61;95% confidence interval [CI], 0.45-0.83). The findings were robust in sensitivity analyses.
The regular and optimal duration sleep pattern maps behaviorally to regular bed and wake times, suggesting potential health benefits of adherence to recommended sleep practices, the researchers noted.
“Results suggest benefits of expanding the public conversation on getting ‘a good night’s sleep’ and broadening this goal to getting many good nights of sleep, in a row, on weekdays and weekends,” Dr. Chung said in the release.
He further said that “getting adequate, regular sleep seems to be something that is good for all. I don’t know of anyone who wouldn’t benefit.”
Fariha Abassi-Feinberg, MD, spokesperson for the American Academy of Sleep Medicine and sleep specialist with the Millennium Physician Group, Fort Myers, Fla., agreed.
“We know our bodies have an internal clock, known as the circadian rhythm, which regulates various biological processes, including sleep-wake cycles. Sticking to a consistent sleep schedule allows your body to align its natural rhythm with the external day-night cycle. This synchronization promotes better sleep quality and therefore better health,” said Dr. Abassi-Feinberg, who wasn’t involved in the study.
“The AASM recommends adults try to aim for at least 7 hours of sleep and I often tell my patients that keeping a regular routine is best for your sleep and health,” she said in an interview.
Funding for the study was provided by the American Academy of Sleep Medicine Foundation and the National Institutes of Health. Dr. Chung and Dr. Abassi-Feinberg report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT SLEEP 2023
Muscle fat: A new risk factor for cognitive decline?
Investigators assessed muscle fat in more than 1,600 adults in their 70s and evaluated their cognitive function over a 10-year period. They found that increases in muscle adiposity from year 1 to year 6 were associated with greater cognitive decline over time, independent of total weight, other fat deposits, muscle characteristics, and traditional dementia risk factors.
The findings were similar between Black and White people and between men and women.
“Increasing adiposity – or fat deposition – in skeletal muscles predicted faster cognitive decline, irrespective of demographics or other disease, and this effect was distinct from that of other types of fat or other muscle characteristics, such as strength or mass,” study investigator Caterina Rosano MD, MPH, professor of epidemiology at the University of Pittsburgh, said in an interview.
The study was published in the Journal of the American Geriatrics Society.
Biologically plausible
“There has been a growing recognition that overall adiposity and muscle measures, such as strength and mass, are individual indicators of future dementia risk and both strengthen the algorithms to predict cognitive decline,” said Dr. Rosano, associate director for clinical translation at the University of Pittsburgh’s Aging Institute. “However, adiposity in the muscle has not been examined.”
Some evidence supports a “biologically plausible link” between muscle adiposity and dementia risk. For example, muscle adiposity increases the risk for type 2 diabetes and hypertension, both of which are dementia risk factors.
Skeletal muscle adiposity increases with older age, even in older adults who lose weight, and is “highly prevalent” among older adults of African ancestry.
The researchers examined a large, biracial sample of older adults participating in the Health, Aging and Body Composition study, which enrolled men and women aged between 70 and 79 years. Participants were followed for an average of 9.0 ± 1.8 years.
During years 1 and 6, participants’ body composition was analyzed, including intermuscular adipose tissue (IMAT), visceral and subcutaneous adiposity, total fat mass, and muscle area.
In years 1, 3, 5, 8, and 10, participants’ cognition was measured using the modified Mini-Mental State (3MS) exam.
The main independent variable was 5-year change in thigh IMAT (year 6 minus year 1), and the main dependent variable was 3MS decline (from year 5 to year 10).
The researchers adjusted all the models for traditional dementia risk factors at baseline including 3MS, education, apo E4 allele, diabetes, hypertension, and physical activity and also calculated interactions between IMAT change by race or sex.
These models also accounted for change in muscle strength, muscle area, body weight, abdominal subcutaneous and visceral adiposity, and total body fat mass as well as cytokines related to adiposity.
‘Rich and engaging crosstalk’
The final sample included 1634 participants (mean age, 73.38 years at baseline; 48% female; 35% Black; mean baseline 3MS score, 91.6).
Thigh IMAT increased by 39.0% in all participants from year 1 to year 6, which corresponded to an increase of 4.85 cm2 or 0.97 cm2/year. During the same time period, muscle strength decreased by 14.0% (P < .05), although thigh muscle area remained stable, decreasing less than 0.5%.
There were decreases in both abdominal subcutaneous and visceral adiposity of 3.92% and 6.43%, respectively (P < .05). There was a decrease of 3.3% in 3MS from year 5 to year 10.
Several variables were associated with 3MS decline, independent of any change in thigh IMAT: older age, less education, and having at least one copy of the APOe4 allele. These variables were included in the model of IMAT change predicting 3MS change.
A statistically significant association of IMAT increase with 3MS decline was found. The IMAT increase of 4.85 cm2 corresponded to a 3MS decline of an additional 3.6 points (P < .0001) from year 5 to year 10, “indicating a clinically important change.”
The association between increasing thigh IMAT with declining 3MS “remained statistically significant” after adjusting for race, age, education, and apo E4 (P < .0001) and was independent of changes in thigh muscle area, muscle strength, and other adiposity measures.
In participants with increased IMAT in years 1-6, the mean 3MS score fell to approximately 87 points at year 10, compared with those without increased IMAT, with a 3MS score that dropped to approximately 89 points.
Interactions by race and sex were not statistically significant (P > .08).
“Our results suggest that adiposity in muscles can predict cognitive decline, in addition to (not instead of) other traditional dementia risk factors,” said Dr. Rosano.
There is “a rich and engaging crosstalk between muscle, adipose tissue, and the brain all throughout our lives, happening through factors released in the bloodstream that can reach the brain, however, the specific identity of the factors responsible for the crosstalk of muscle adiposity and brain in older adults has not yet been discovered,” she noted.
Although muscle adiposity is “not yet routinely measured in clinical settings, it is being measured opportunistically on clinical CT scans obtained as part of routine patient care,” she added. “These CT measurements have already been validated in many studies of older adults; thus, clinicians could have access to this novel information without additional cost, time, or radiation exposure.”
Causality not proven
In a comment, Bruce Albala, PhD, professor, department of environmental and occupational health, University of California, Irvine, noted that the 3MS assessment is scored on a 100-point scale, with a score less than 78 “generally regarded as indicating cognitive impairment or approaching a dementia condition.” In the current study, the mean 3MS score of participants with increased IMAT was still “well above the dementia cut-off.”
Moreover, “even if there is a relationship or correlation between IMAT and cognition, this does not prove or even suggest causality, especially from a biological mechanistic approach,” said Dr. Albaba, an adjunct professor of neurology, who was not involved in the study. “Clearly, more research is needed even to understand the relationship between these two factors.”
The study was supported by the National Institute on Aging. Dr. Rosano and coauthors and Dr. Albala declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators assessed muscle fat in more than 1,600 adults in their 70s and evaluated their cognitive function over a 10-year period. They found that increases in muscle adiposity from year 1 to year 6 were associated with greater cognitive decline over time, independent of total weight, other fat deposits, muscle characteristics, and traditional dementia risk factors.
The findings were similar between Black and White people and between men and women.
“Increasing adiposity – or fat deposition – in skeletal muscles predicted faster cognitive decline, irrespective of demographics or other disease, and this effect was distinct from that of other types of fat or other muscle characteristics, such as strength or mass,” study investigator Caterina Rosano MD, MPH, professor of epidemiology at the University of Pittsburgh, said in an interview.
The study was published in the Journal of the American Geriatrics Society.
Biologically plausible
“There has been a growing recognition that overall adiposity and muscle measures, such as strength and mass, are individual indicators of future dementia risk and both strengthen the algorithms to predict cognitive decline,” said Dr. Rosano, associate director for clinical translation at the University of Pittsburgh’s Aging Institute. “However, adiposity in the muscle has not been examined.”
Some evidence supports a “biologically plausible link” between muscle adiposity and dementia risk. For example, muscle adiposity increases the risk for type 2 diabetes and hypertension, both of which are dementia risk factors.
Skeletal muscle adiposity increases with older age, even in older adults who lose weight, and is “highly prevalent” among older adults of African ancestry.
The researchers examined a large, biracial sample of older adults participating in the Health, Aging and Body Composition study, which enrolled men and women aged between 70 and 79 years. Participants were followed for an average of 9.0 ± 1.8 years.
During years 1 and 6, participants’ body composition was analyzed, including intermuscular adipose tissue (IMAT), visceral and subcutaneous adiposity, total fat mass, and muscle area.
In years 1, 3, 5, 8, and 10, participants’ cognition was measured using the modified Mini-Mental State (3MS) exam.
The main independent variable was 5-year change in thigh IMAT (year 6 minus year 1), and the main dependent variable was 3MS decline (from year 5 to year 10).
The researchers adjusted all the models for traditional dementia risk factors at baseline including 3MS, education, apo E4 allele, diabetes, hypertension, and physical activity and also calculated interactions between IMAT change by race or sex.
These models also accounted for change in muscle strength, muscle area, body weight, abdominal subcutaneous and visceral adiposity, and total body fat mass as well as cytokines related to adiposity.
‘Rich and engaging crosstalk’
The final sample included 1634 participants (mean age, 73.38 years at baseline; 48% female; 35% Black; mean baseline 3MS score, 91.6).
Thigh IMAT increased by 39.0% in all participants from year 1 to year 6, which corresponded to an increase of 4.85 cm2 or 0.97 cm2/year. During the same time period, muscle strength decreased by 14.0% (P < .05), although thigh muscle area remained stable, decreasing less than 0.5%.
There were decreases in both abdominal subcutaneous and visceral adiposity of 3.92% and 6.43%, respectively (P < .05). There was a decrease of 3.3% in 3MS from year 5 to year 10.
Several variables were associated with 3MS decline, independent of any change in thigh IMAT: older age, less education, and having at least one copy of the APOe4 allele. These variables were included in the model of IMAT change predicting 3MS change.
A statistically significant association of IMAT increase with 3MS decline was found. The IMAT increase of 4.85 cm2 corresponded to a 3MS decline of an additional 3.6 points (P < .0001) from year 5 to year 10, “indicating a clinically important change.”
The association between increasing thigh IMAT with declining 3MS “remained statistically significant” after adjusting for race, age, education, and apo E4 (P < .0001) and was independent of changes in thigh muscle area, muscle strength, and other adiposity measures.
In participants with increased IMAT in years 1-6, the mean 3MS score fell to approximately 87 points at year 10, compared with those without increased IMAT, with a 3MS score that dropped to approximately 89 points.
Interactions by race and sex were not statistically significant (P > .08).
“Our results suggest that adiposity in muscles can predict cognitive decline, in addition to (not instead of) other traditional dementia risk factors,” said Dr. Rosano.
There is “a rich and engaging crosstalk between muscle, adipose tissue, and the brain all throughout our lives, happening through factors released in the bloodstream that can reach the brain, however, the specific identity of the factors responsible for the crosstalk of muscle adiposity and brain in older adults has not yet been discovered,” she noted.
Although muscle adiposity is “not yet routinely measured in clinical settings, it is being measured opportunistically on clinical CT scans obtained as part of routine patient care,” she added. “These CT measurements have already been validated in many studies of older adults; thus, clinicians could have access to this novel information without additional cost, time, or radiation exposure.”
Causality not proven
In a comment, Bruce Albala, PhD, professor, department of environmental and occupational health, University of California, Irvine, noted that the 3MS assessment is scored on a 100-point scale, with a score less than 78 “generally regarded as indicating cognitive impairment or approaching a dementia condition.” In the current study, the mean 3MS score of participants with increased IMAT was still “well above the dementia cut-off.”
Moreover, “even if there is a relationship or correlation between IMAT and cognition, this does not prove or even suggest causality, especially from a biological mechanistic approach,” said Dr. Albaba, an adjunct professor of neurology, who was not involved in the study. “Clearly, more research is needed even to understand the relationship between these two factors.”
The study was supported by the National Institute on Aging. Dr. Rosano and coauthors and Dr. Albala declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators assessed muscle fat in more than 1,600 adults in their 70s and evaluated their cognitive function over a 10-year period. They found that increases in muscle adiposity from year 1 to year 6 were associated with greater cognitive decline over time, independent of total weight, other fat deposits, muscle characteristics, and traditional dementia risk factors.
The findings were similar between Black and White people and between men and women.
“Increasing adiposity – or fat deposition – in skeletal muscles predicted faster cognitive decline, irrespective of demographics or other disease, and this effect was distinct from that of other types of fat or other muscle characteristics, such as strength or mass,” study investigator Caterina Rosano MD, MPH, professor of epidemiology at the University of Pittsburgh, said in an interview.
The study was published in the Journal of the American Geriatrics Society.
Biologically plausible
“There has been a growing recognition that overall adiposity and muscle measures, such as strength and mass, are individual indicators of future dementia risk and both strengthen the algorithms to predict cognitive decline,” said Dr. Rosano, associate director for clinical translation at the University of Pittsburgh’s Aging Institute. “However, adiposity in the muscle has not been examined.”
Some evidence supports a “biologically plausible link” between muscle adiposity and dementia risk. For example, muscle adiposity increases the risk for type 2 diabetes and hypertension, both of which are dementia risk factors.
Skeletal muscle adiposity increases with older age, even in older adults who lose weight, and is “highly prevalent” among older adults of African ancestry.
The researchers examined a large, biracial sample of older adults participating in the Health, Aging and Body Composition study, which enrolled men and women aged between 70 and 79 years. Participants were followed for an average of 9.0 ± 1.8 years.
During years 1 and 6, participants’ body composition was analyzed, including intermuscular adipose tissue (IMAT), visceral and subcutaneous adiposity, total fat mass, and muscle area.
In years 1, 3, 5, 8, and 10, participants’ cognition was measured using the modified Mini-Mental State (3MS) exam.
The main independent variable was 5-year change in thigh IMAT (year 6 minus year 1), and the main dependent variable was 3MS decline (from year 5 to year 10).
The researchers adjusted all the models for traditional dementia risk factors at baseline including 3MS, education, apo E4 allele, diabetes, hypertension, and physical activity and also calculated interactions between IMAT change by race or sex.
These models also accounted for change in muscle strength, muscle area, body weight, abdominal subcutaneous and visceral adiposity, and total body fat mass as well as cytokines related to adiposity.
‘Rich and engaging crosstalk’
The final sample included 1634 participants (mean age, 73.38 years at baseline; 48% female; 35% Black; mean baseline 3MS score, 91.6).
Thigh IMAT increased by 39.0% in all participants from year 1 to year 6, which corresponded to an increase of 4.85 cm2 or 0.97 cm2/year. During the same time period, muscle strength decreased by 14.0% (P < .05), although thigh muscle area remained stable, decreasing less than 0.5%.
There were decreases in both abdominal subcutaneous and visceral adiposity of 3.92% and 6.43%, respectively (P < .05). There was a decrease of 3.3% in 3MS from year 5 to year 10.
Several variables were associated with 3MS decline, independent of any change in thigh IMAT: older age, less education, and having at least one copy of the APOe4 allele. These variables were included in the model of IMAT change predicting 3MS change.
A statistically significant association of IMAT increase with 3MS decline was found. The IMAT increase of 4.85 cm2 corresponded to a 3MS decline of an additional 3.6 points (P < .0001) from year 5 to year 10, “indicating a clinically important change.”
The association between increasing thigh IMAT with declining 3MS “remained statistically significant” after adjusting for race, age, education, and apo E4 (P < .0001) and was independent of changes in thigh muscle area, muscle strength, and other adiposity measures.
In participants with increased IMAT in years 1-6, the mean 3MS score fell to approximately 87 points at year 10, compared with those without increased IMAT, with a 3MS score that dropped to approximately 89 points.
Interactions by race and sex were not statistically significant (P > .08).
“Our results suggest that adiposity in muscles can predict cognitive decline, in addition to (not instead of) other traditional dementia risk factors,” said Dr. Rosano.
There is “a rich and engaging crosstalk between muscle, adipose tissue, and the brain all throughout our lives, happening through factors released in the bloodstream that can reach the brain, however, the specific identity of the factors responsible for the crosstalk of muscle adiposity and brain in older adults has not yet been discovered,” she noted.
Although muscle adiposity is “not yet routinely measured in clinical settings, it is being measured opportunistically on clinical CT scans obtained as part of routine patient care,” she added. “These CT measurements have already been validated in many studies of older adults; thus, clinicians could have access to this novel information without additional cost, time, or radiation exposure.”
Causality not proven
In a comment, Bruce Albala, PhD, professor, department of environmental and occupational health, University of California, Irvine, noted that the 3MS assessment is scored on a 100-point scale, with a score less than 78 “generally regarded as indicating cognitive impairment or approaching a dementia condition.” In the current study, the mean 3MS score of participants with increased IMAT was still “well above the dementia cut-off.”
Moreover, “even if there is a relationship or correlation between IMAT and cognition, this does not prove or even suggest causality, especially from a biological mechanistic approach,” said Dr. Albaba, an adjunct professor of neurology, who was not involved in the study. “Clearly, more research is needed even to understand the relationship between these two factors.”
The study was supported by the National Institute on Aging. Dr. Rosano and coauthors and Dr. Albala declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN GERIATRICS SOCIETY