User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Top U.S. hospitals for psychiatric care ranked
McLean Hospital claimed the top spot in the 2022-2023 ranking as well.
Massachusetts General Hospital in Boston holds the No. 2 spot in the 2023-2024 U.S. News ranking for best psychiatry hospitals, up from No. 3 in 2022-2023.
New York–Presbyterian Hospital–Columbia and Cornell sits at No. 3 in 2023-2024, up from No. 4 in 2022-2023, while Johns Hopkins Hospital, Baltimore is ranked No. 4, down from No. 2.
Resnick Neuropsychiatric Hospital at the University of California, Los Angeles, is ranked No. 5 in 2023-2024 (up from No. 6 in 2022-2023), while UCSF Health–UCSF Medical Center, San Francisco, dropped to No. 6 in 2023-2024 (from No. 5 in 2022-2023).
No. 7 in 2023-2024 is Menninger Clinic, Houston, which held the No. 10 spot in 2022-2023.
According to U.S. News, the psychiatry rating is based on the expert opinion of surveyed psychiatrists. The seven ranked hospitals in psychiatry or psychiatric care were recommended by at least 5% of the psychiatric specialists responding to the magazine’s surveys in 2021, 2022, and 2023 as a facility where they would refer their patients.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News also recognized “honor roll” hospitals that have excelled across multiple areas of care. However, in 2023-2024, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the magazine’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the Honor Roll hospitals have attained the highest standard of care in the nation,” the letter reads.
With the new format, honor roll hospitals are listed in alphabetical order. In 2023-2024 there are 22.
2023-2024 Honor Roll Hospitals
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania–Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York
- New York–Presbyterian Hospital–Columbia and Cornell
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
According to U.S. News, to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles on USNews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
McLean Hospital claimed the top spot in the 2022-2023 ranking as well.
Massachusetts General Hospital in Boston holds the No. 2 spot in the 2023-2024 U.S. News ranking for best psychiatry hospitals, up from No. 3 in 2022-2023.
New York–Presbyterian Hospital–Columbia and Cornell sits at No. 3 in 2023-2024, up from No. 4 in 2022-2023, while Johns Hopkins Hospital, Baltimore is ranked No. 4, down from No. 2.
Resnick Neuropsychiatric Hospital at the University of California, Los Angeles, is ranked No. 5 in 2023-2024 (up from No. 6 in 2022-2023), while UCSF Health–UCSF Medical Center, San Francisco, dropped to No. 6 in 2023-2024 (from No. 5 in 2022-2023).
No. 7 in 2023-2024 is Menninger Clinic, Houston, which held the No. 10 spot in 2022-2023.
According to U.S. News, the psychiatry rating is based on the expert opinion of surveyed psychiatrists. The seven ranked hospitals in psychiatry or psychiatric care were recommended by at least 5% of the psychiatric specialists responding to the magazine’s surveys in 2021, 2022, and 2023 as a facility where they would refer their patients.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News also recognized “honor roll” hospitals that have excelled across multiple areas of care. However, in 2023-2024, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the magazine’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the Honor Roll hospitals have attained the highest standard of care in the nation,” the letter reads.
With the new format, honor roll hospitals are listed in alphabetical order. In 2023-2024 there are 22.
2023-2024 Honor Roll Hospitals
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania–Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York
- New York–Presbyterian Hospital–Columbia and Cornell
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
According to U.S. News, to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles on USNews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
McLean Hospital claimed the top spot in the 2022-2023 ranking as well.
Massachusetts General Hospital in Boston holds the No. 2 spot in the 2023-2024 U.S. News ranking for best psychiatry hospitals, up from No. 3 in 2022-2023.
New York–Presbyterian Hospital–Columbia and Cornell sits at No. 3 in 2023-2024, up from No. 4 in 2022-2023, while Johns Hopkins Hospital, Baltimore is ranked No. 4, down from No. 2.
Resnick Neuropsychiatric Hospital at the University of California, Los Angeles, is ranked No. 5 in 2023-2024 (up from No. 6 in 2022-2023), while UCSF Health–UCSF Medical Center, San Francisco, dropped to No. 6 in 2023-2024 (from No. 5 in 2022-2023).
No. 7 in 2023-2024 is Menninger Clinic, Houston, which held the No. 10 spot in 2022-2023.
According to U.S. News, the psychiatry rating is based on the expert opinion of surveyed psychiatrists. The seven ranked hospitals in psychiatry or psychiatric care were recommended by at least 5% of the psychiatric specialists responding to the magazine’s surveys in 2021, 2022, and 2023 as a facility where they would refer their patients.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News also recognized “honor roll” hospitals that have excelled across multiple areas of care. However, in 2023-2024, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the magazine’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the Honor Roll hospitals have attained the highest standard of care in the nation,” the letter reads.
With the new format, honor roll hospitals are listed in alphabetical order. In 2023-2024 there are 22.
2023-2024 Honor Roll Hospitals
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania–Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York
- New York–Presbyterian Hospital–Columbia and Cornell
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
According to U.S. News, to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles on USNews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
OxyContin marketing push still exacting a deadly toll, study says
The uptick in rates of infectious diseases, namely, hepatitis and infective endocarditis, occurred after 2010, when OxyContin maker Purdue Pharma reformulated OxyContin to make it harder to crush and snort. This led many people who were already addicted to the powerful pain pills to move on to injecting heroin or fentanyl, which fueled the spread of infectious disease.
“Our results suggest that the mortality and morbidity consequences of OxyContin marketing continue to be salient more than 25 years later,” write Julia Dennett, PhD, and Gregg Gonsalves, PhD, with Yale University School of Public Health, New Haven, Conn.
Their study was published online in Health Affairs.
Long-term effects revealed
Until now, the long-term effects of widespread OxyContin marketing with regard to complications of injection drug use were unknown.
Dr. Dennett and Dr. Gonsalves evaluated the effects of OxyContin marketing on the long-term trajectories of various injection drug use–related outcomes. Using a difference-in-difference analysis, they compared states with high vs. low exposure to OxyContin marketing before and after the 2010 reformulation of the drug.
Before 2010, rates of infections associated with injection drug use and overdose deaths were similar in high- and low-marketing states, they found.
Those rates diverged after the 2010 reformulation, with more infections related to injection drug use in states exposed to more marketing.
Specifically, from 2010 until 2020, high-exposure states saw, on average, an additional 0.85 acute hepatitis B cases, 0.83 hepatitis C cases, and 0.62 cases of death from infective endocarditis per 100,000 residents.
High-exposure states also had 5.3 more deaths per 100,000 residents from synthetic opioid overdose.
“Prior to 2010, among these states, there were generally no statistically significant differences in these outcomes. After 2010, you saw them diverge dramatically,” Dr. Dennett said in a news release.
Dr. Dennett and Dr. Gonsalves say their findings support the view that the opioid epidemic is creating a converging public health crisis, as it is fueling a surge in infectious diseases, particularly hepatitis, infective endocarditis, and HIV.
“This study highlights a critical need for actions to address the spread of viral and bacterial infections and overdose associated with injection drug use, both in the states that were subject to Purdue’s promotional campaign and across the U.S. more broadly,” they add.
Purdue Pharma did not provide a comment on the study.
Funding for the study was provided by the National Institute on Drug Abuse. Disclosures for Dr. Dennett and Dr. Gonsalves were not available.
A version of this article first appeared on Medscape.com.
The uptick in rates of infectious diseases, namely, hepatitis and infective endocarditis, occurred after 2010, when OxyContin maker Purdue Pharma reformulated OxyContin to make it harder to crush and snort. This led many people who were already addicted to the powerful pain pills to move on to injecting heroin or fentanyl, which fueled the spread of infectious disease.
“Our results suggest that the mortality and morbidity consequences of OxyContin marketing continue to be salient more than 25 years later,” write Julia Dennett, PhD, and Gregg Gonsalves, PhD, with Yale University School of Public Health, New Haven, Conn.
Their study was published online in Health Affairs.
Long-term effects revealed
Until now, the long-term effects of widespread OxyContin marketing with regard to complications of injection drug use were unknown.
Dr. Dennett and Dr. Gonsalves evaluated the effects of OxyContin marketing on the long-term trajectories of various injection drug use–related outcomes. Using a difference-in-difference analysis, they compared states with high vs. low exposure to OxyContin marketing before and after the 2010 reformulation of the drug.
Before 2010, rates of infections associated with injection drug use and overdose deaths were similar in high- and low-marketing states, they found.
Those rates diverged after the 2010 reformulation, with more infections related to injection drug use in states exposed to more marketing.
Specifically, from 2010 until 2020, high-exposure states saw, on average, an additional 0.85 acute hepatitis B cases, 0.83 hepatitis C cases, and 0.62 cases of death from infective endocarditis per 100,000 residents.
High-exposure states also had 5.3 more deaths per 100,000 residents from synthetic opioid overdose.
“Prior to 2010, among these states, there were generally no statistically significant differences in these outcomes. After 2010, you saw them diverge dramatically,” Dr. Dennett said in a news release.
Dr. Dennett and Dr. Gonsalves say their findings support the view that the opioid epidemic is creating a converging public health crisis, as it is fueling a surge in infectious diseases, particularly hepatitis, infective endocarditis, and HIV.
“This study highlights a critical need for actions to address the spread of viral and bacterial infections and overdose associated with injection drug use, both in the states that were subject to Purdue’s promotional campaign and across the U.S. more broadly,” they add.
Purdue Pharma did not provide a comment on the study.
Funding for the study was provided by the National Institute on Drug Abuse. Disclosures for Dr. Dennett and Dr. Gonsalves were not available.
A version of this article first appeared on Medscape.com.
The uptick in rates of infectious diseases, namely, hepatitis and infective endocarditis, occurred after 2010, when OxyContin maker Purdue Pharma reformulated OxyContin to make it harder to crush and snort. This led many people who were already addicted to the powerful pain pills to move on to injecting heroin or fentanyl, which fueled the spread of infectious disease.
“Our results suggest that the mortality and morbidity consequences of OxyContin marketing continue to be salient more than 25 years later,” write Julia Dennett, PhD, and Gregg Gonsalves, PhD, with Yale University School of Public Health, New Haven, Conn.
Their study was published online in Health Affairs.
Long-term effects revealed
Until now, the long-term effects of widespread OxyContin marketing with regard to complications of injection drug use were unknown.
Dr. Dennett and Dr. Gonsalves evaluated the effects of OxyContin marketing on the long-term trajectories of various injection drug use–related outcomes. Using a difference-in-difference analysis, they compared states with high vs. low exposure to OxyContin marketing before and after the 2010 reformulation of the drug.
Before 2010, rates of infections associated with injection drug use and overdose deaths were similar in high- and low-marketing states, they found.
Those rates diverged after the 2010 reformulation, with more infections related to injection drug use in states exposed to more marketing.
Specifically, from 2010 until 2020, high-exposure states saw, on average, an additional 0.85 acute hepatitis B cases, 0.83 hepatitis C cases, and 0.62 cases of death from infective endocarditis per 100,000 residents.
High-exposure states also had 5.3 more deaths per 100,000 residents from synthetic opioid overdose.
“Prior to 2010, among these states, there were generally no statistically significant differences in these outcomes. After 2010, you saw them diverge dramatically,” Dr. Dennett said in a news release.
Dr. Dennett and Dr. Gonsalves say their findings support the view that the opioid epidemic is creating a converging public health crisis, as it is fueling a surge in infectious diseases, particularly hepatitis, infective endocarditis, and HIV.
“This study highlights a critical need for actions to address the spread of viral and bacterial infections and overdose associated with injection drug use, both in the states that were subject to Purdue’s promotional campaign and across the U.S. more broadly,” they add.
Purdue Pharma did not provide a comment on the study.
Funding for the study was provided by the National Institute on Drug Abuse. Disclosures for Dr. Dennett and Dr. Gonsalves were not available.
A version of this article first appeared on Medscape.com.
FROM HEALTH AFFAIRS
Cigna accused of using AI, not doctors, to deny claims: Lawsuit
and forcing providers to bill patients in full.
In a complaint filed recently in California’s eastern district court, plaintiffs and Cigna health plan members Suzanne Kisting-Leung and Ayesha Smiley and their attorneys say that Cigna violates state insurance regulations by failing to conduct a “thorough, fair, and objective” review of their and other members’ claims.
The lawsuit says that, instead, Cigna relies on an algorithm, PxDx, to review and frequently deny medically necessary claims. According to court records, the system allows Cigna’s doctors to “instantly reject claims on medical grounds without ever opening patient files.” With use of the system, the average claims processing time is 1.2 seconds.
Cigna says it uses technology to verify coding on standard, low-cost procedures and to expedite physician reimbursement. In a statement to CBS News, the company called the lawsuit “highly questionable.”
The case highlights growing concerns about AI and its ability to replace humans for tasks and interactions in health care, business, and beyond. Public advocacy law firm Clarkson, which is representing the plaintiffs, has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ personal and professional data to train their AI systems.
According to the complaint, Cigna denied the plaintiffs medically necessary tests, including blood work to screen for vitamin D deficiency and ultrasounds for patients suspected of having ovarian cancer. The plaintiffs’ attempts to appeal were unfruitful, and they were forced to pay out of pocket.
The plaintiff’s attorneys argue that the claims do not undergo more detailed reviews by physicians and employees, as mandated by California insurance laws, and that Cigna benefits by saving on labor costs.
Clarkson is demanding a jury trial and has asked the court to certify the Cigna case as a federal class action, potentially allowing the insurer’s other 2 million health plan members in California to join the lawsuit.
I. Glenn Cohen, JD, deputy dean and professor at Harvard Law School, Cambridge, Mass., said in an interview that this is the first lawsuit he’s aware of in which AI was involved in denying health insurance claims and that it is probably an uphill battle for the plaintiffs.
“In the last 25 years, the U.S. Supreme Court’s decisions have made getting a class action approved more difficult. If allowed to go forward as a class action, which Cigna is likely to vigorously oppose, then the pressure on Cigna to settle the case becomes enormous,” he said.
The allegations come after a recent deep dive by the nonprofit ProPublica uncovered similar claim denial issues. One physician who worked for Cigna told the nonprofit that he and other company doctors essentially rubber-stamped the denials in batches, which took “all of 10 seconds to do 50 at a time.”
In 2022, the American Medical Association and two state physician groups joined another class action against Cigna stemming from allegations that the insurer’s intermediary, Multiplan, intentionally underpaid medical claims. And in March, Cigna’s pharmacy benefit manager, Express Scripts, was accused of conspiring with other PBMs to drive up prescription drug prices for Ohio consumers, violating state antitrust laws.
Mr. Cohen said he expects Cigna to push back in court about the California class size, which the plaintiff’s attorneys hope will encompass all Cigna health plan members in the state.
“The injury is primarily to those whose claims were denied by AI, presumably a much smaller set of individuals and harder to identify,” said Mr. Cohen.
A version of this article first appeared on Medscape.com.
and forcing providers to bill patients in full.
In a complaint filed recently in California’s eastern district court, plaintiffs and Cigna health plan members Suzanne Kisting-Leung and Ayesha Smiley and their attorneys say that Cigna violates state insurance regulations by failing to conduct a “thorough, fair, and objective” review of their and other members’ claims.
The lawsuit says that, instead, Cigna relies on an algorithm, PxDx, to review and frequently deny medically necessary claims. According to court records, the system allows Cigna’s doctors to “instantly reject claims on medical grounds without ever opening patient files.” With use of the system, the average claims processing time is 1.2 seconds.
Cigna says it uses technology to verify coding on standard, low-cost procedures and to expedite physician reimbursement. In a statement to CBS News, the company called the lawsuit “highly questionable.”
The case highlights growing concerns about AI and its ability to replace humans for tasks and interactions in health care, business, and beyond. Public advocacy law firm Clarkson, which is representing the plaintiffs, has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ personal and professional data to train their AI systems.
According to the complaint, Cigna denied the plaintiffs medically necessary tests, including blood work to screen for vitamin D deficiency and ultrasounds for patients suspected of having ovarian cancer. The plaintiffs’ attempts to appeal were unfruitful, and they were forced to pay out of pocket.
The plaintiff’s attorneys argue that the claims do not undergo more detailed reviews by physicians and employees, as mandated by California insurance laws, and that Cigna benefits by saving on labor costs.
Clarkson is demanding a jury trial and has asked the court to certify the Cigna case as a federal class action, potentially allowing the insurer’s other 2 million health plan members in California to join the lawsuit.
I. Glenn Cohen, JD, deputy dean and professor at Harvard Law School, Cambridge, Mass., said in an interview that this is the first lawsuit he’s aware of in which AI was involved in denying health insurance claims and that it is probably an uphill battle for the plaintiffs.
“In the last 25 years, the U.S. Supreme Court’s decisions have made getting a class action approved more difficult. If allowed to go forward as a class action, which Cigna is likely to vigorously oppose, then the pressure on Cigna to settle the case becomes enormous,” he said.
The allegations come after a recent deep dive by the nonprofit ProPublica uncovered similar claim denial issues. One physician who worked for Cigna told the nonprofit that he and other company doctors essentially rubber-stamped the denials in batches, which took “all of 10 seconds to do 50 at a time.”
In 2022, the American Medical Association and two state physician groups joined another class action against Cigna stemming from allegations that the insurer’s intermediary, Multiplan, intentionally underpaid medical claims. And in March, Cigna’s pharmacy benefit manager, Express Scripts, was accused of conspiring with other PBMs to drive up prescription drug prices for Ohio consumers, violating state antitrust laws.
Mr. Cohen said he expects Cigna to push back in court about the California class size, which the plaintiff’s attorneys hope will encompass all Cigna health plan members in the state.
“The injury is primarily to those whose claims were denied by AI, presumably a much smaller set of individuals and harder to identify,” said Mr. Cohen.
A version of this article first appeared on Medscape.com.
and forcing providers to bill patients in full.
In a complaint filed recently in California’s eastern district court, plaintiffs and Cigna health plan members Suzanne Kisting-Leung and Ayesha Smiley and their attorneys say that Cigna violates state insurance regulations by failing to conduct a “thorough, fair, and objective” review of their and other members’ claims.
The lawsuit says that, instead, Cigna relies on an algorithm, PxDx, to review and frequently deny medically necessary claims. According to court records, the system allows Cigna’s doctors to “instantly reject claims on medical grounds without ever opening patient files.” With use of the system, the average claims processing time is 1.2 seconds.
Cigna says it uses technology to verify coding on standard, low-cost procedures and to expedite physician reimbursement. In a statement to CBS News, the company called the lawsuit “highly questionable.”
The case highlights growing concerns about AI and its ability to replace humans for tasks and interactions in health care, business, and beyond. Public advocacy law firm Clarkson, which is representing the plaintiffs, has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ personal and professional data to train their AI systems.
According to the complaint, Cigna denied the plaintiffs medically necessary tests, including blood work to screen for vitamin D deficiency and ultrasounds for patients suspected of having ovarian cancer. The plaintiffs’ attempts to appeal were unfruitful, and they were forced to pay out of pocket.
The plaintiff’s attorneys argue that the claims do not undergo more detailed reviews by physicians and employees, as mandated by California insurance laws, and that Cigna benefits by saving on labor costs.
Clarkson is demanding a jury trial and has asked the court to certify the Cigna case as a federal class action, potentially allowing the insurer’s other 2 million health plan members in California to join the lawsuit.
I. Glenn Cohen, JD, deputy dean and professor at Harvard Law School, Cambridge, Mass., said in an interview that this is the first lawsuit he’s aware of in which AI was involved in denying health insurance claims and that it is probably an uphill battle for the plaintiffs.
“In the last 25 years, the U.S. Supreme Court’s decisions have made getting a class action approved more difficult. If allowed to go forward as a class action, which Cigna is likely to vigorously oppose, then the pressure on Cigna to settle the case becomes enormous,” he said.
The allegations come after a recent deep dive by the nonprofit ProPublica uncovered similar claim denial issues. One physician who worked for Cigna told the nonprofit that he and other company doctors essentially rubber-stamped the denials in batches, which took “all of 10 seconds to do 50 at a time.”
In 2022, the American Medical Association and two state physician groups joined another class action against Cigna stemming from allegations that the insurer’s intermediary, Multiplan, intentionally underpaid medical claims. And in March, Cigna’s pharmacy benefit manager, Express Scripts, was accused of conspiring with other PBMs to drive up prescription drug prices for Ohio consumers, violating state antitrust laws.
Mr. Cohen said he expects Cigna to push back in court about the California class size, which the plaintiff’s attorneys hope will encompass all Cigna health plan members in the state.
“The injury is primarily to those whose claims were denied by AI, presumably a much smaller set of individuals and harder to identify,” said Mr. Cohen.
A version of this article first appeared on Medscape.com.
FDA approves first pill for postpartum depression
a condition that affects an estimated one in seven mothers in the United States.
The pill, zuranolone (Zurzuvae), is a neuroactive steroid that acts on GABAA receptors in the brain responsible for regulating mood, arousal, behavior, and cognition, according to Biogen, which, along with Sage Therapeutics, developed the product. The recommended dose for Zurzuvae is 50 mg taken once daily for 14 days, in the evening with a fatty meal, according to the FDA.
Postpartum depression often goes undiagnosed and untreated. Many mothers are hesitant to reveal their symptoms to family and clinicians, fearing they’ll be judged on their parenting. A 2017 study found that suicide accounted for roughly 5% of perinatal deaths among women in Canada, with most of those deaths occurring in the first 3 months in the year after giving birth.
“Postpartum depression is a serious and potentially life-threatening condition in which women experience sadness, guilt, worthlessness – even, in severe cases, thoughts of harming themselves or their child. And, because postpartum depression can disrupt the maternal-infant bond, it can also have consequences for the child’s physical and emotional development,” Tiffany R. Farchione, MD, director of the division of psychiatry at the FDA’s Center for Drug Evaluation and Research, said in a statement about the approval. “Having access to an oral medication will be a beneficial option for many of these women coping with extreme, and sometimes life-threatening, feelings.”
The other approved therapy for postpartum depression is the intravenous agent brexanolone (Zulresso; Sage). But the product requires prolonged infusions in hospital settings and costs $34,000.
FDA approval of Zurzuvae was based in part on data reported in a 2023 study in the American Journal of Psychiatry, which showed that the drug led to significantly greater improvement in depressive symptoms at 15 days compared with the placebo group. Improvements were observed on day 3, the earliest assessment, and were sustained at all subsequent visits during the treatment and follow-up period (through day 42).
Patients with anxiety who received the active drug experienced improvement in related symptoms compared with the patients who received a placebo.
The most common adverse events reported in the trial were somnolence and headaches. Weight gain, sexual dysfunction, withdrawal symptoms, and increased suicidal ideation or behavior were not observed.
The packaging for Zurzuvae will include a boxed warning noting that the drug can affect a user’s ability to drive and perform other potentially hazardous activities, possibly without their knowledge of the impairment, the FDA said. As a result, people who use Zurzuvae should not drive or operate heavy machinery for at least 12 hours after taking the pill.
A version of this article first appeared on Medscape.com.
a condition that affects an estimated one in seven mothers in the United States.
The pill, zuranolone (Zurzuvae), is a neuroactive steroid that acts on GABAA receptors in the brain responsible for regulating mood, arousal, behavior, and cognition, according to Biogen, which, along with Sage Therapeutics, developed the product. The recommended dose for Zurzuvae is 50 mg taken once daily for 14 days, in the evening with a fatty meal, according to the FDA.
Postpartum depression often goes undiagnosed and untreated. Many mothers are hesitant to reveal their symptoms to family and clinicians, fearing they’ll be judged on their parenting. A 2017 study found that suicide accounted for roughly 5% of perinatal deaths among women in Canada, with most of those deaths occurring in the first 3 months in the year after giving birth.
“Postpartum depression is a serious and potentially life-threatening condition in which women experience sadness, guilt, worthlessness – even, in severe cases, thoughts of harming themselves or their child. And, because postpartum depression can disrupt the maternal-infant bond, it can also have consequences for the child’s physical and emotional development,” Tiffany R. Farchione, MD, director of the division of psychiatry at the FDA’s Center for Drug Evaluation and Research, said in a statement about the approval. “Having access to an oral medication will be a beneficial option for many of these women coping with extreme, and sometimes life-threatening, feelings.”
The other approved therapy for postpartum depression is the intravenous agent brexanolone (Zulresso; Sage). But the product requires prolonged infusions in hospital settings and costs $34,000.
FDA approval of Zurzuvae was based in part on data reported in a 2023 study in the American Journal of Psychiatry, which showed that the drug led to significantly greater improvement in depressive symptoms at 15 days compared with the placebo group. Improvements were observed on day 3, the earliest assessment, and were sustained at all subsequent visits during the treatment and follow-up period (through day 42).
Patients with anxiety who received the active drug experienced improvement in related symptoms compared with the patients who received a placebo.
The most common adverse events reported in the trial were somnolence and headaches. Weight gain, sexual dysfunction, withdrawal symptoms, and increased suicidal ideation or behavior were not observed.
The packaging for Zurzuvae will include a boxed warning noting that the drug can affect a user’s ability to drive and perform other potentially hazardous activities, possibly without their knowledge of the impairment, the FDA said. As a result, people who use Zurzuvae should not drive or operate heavy machinery for at least 12 hours after taking the pill.
A version of this article first appeared on Medscape.com.
a condition that affects an estimated one in seven mothers in the United States.
The pill, zuranolone (Zurzuvae), is a neuroactive steroid that acts on GABAA receptors in the brain responsible for regulating mood, arousal, behavior, and cognition, according to Biogen, which, along with Sage Therapeutics, developed the product. The recommended dose for Zurzuvae is 50 mg taken once daily for 14 days, in the evening with a fatty meal, according to the FDA.
Postpartum depression often goes undiagnosed and untreated. Many mothers are hesitant to reveal their symptoms to family and clinicians, fearing they’ll be judged on their parenting. A 2017 study found that suicide accounted for roughly 5% of perinatal deaths among women in Canada, with most of those deaths occurring in the first 3 months in the year after giving birth.
“Postpartum depression is a serious and potentially life-threatening condition in which women experience sadness, guilt, worthlessness – even, in severe cases, thoughts of harming themselves or their child. And, because postpartum depression can disrupt the maternal-infant bond, it can also have consequences for the child’s physical and emotional development,” Tiffany R. Farchione, MD, director of the division of psychiatry at the FDA’s Center for Drug Evaluation and Research, said in a statement about the approval. “Having access to an oral medication will be a beneficial option for many of these women coping with extreme, and sometimes life-threatening, feelings.”
The other approved therapy for postpartum depression is the intravenous agent brexanolone (Zulresso; Sage). But the product requires prolonged infusions in hospital settings and costs $34,000.
FDA approval of Zurzuvae was based in part on data reported in a 2023 study in the American Journal of Psychiatry, which showed that the drug led to significantly greater improvement in depressive symptoms at 15 days compared with the placebo group. Improvements were observed on day 3, the earliest assessment, and were sustained at all subsequent visits during the treatment and follow-up period (through day 42).
Patients with anxiety who received the active drug experienced improvement in related symptoms compared with the patients who received a placebo.
The most common adverse events reported in the trial were somnolence and headaches. Weight gain, sexual dysfunction, withdrawal symptoms, and increased suicidal ideation or behavior were not observed.
The packaging for Zurzuvae will include a boxed warning noting that the drug can affect a user’s ability to drive and perform other potentially hazardous activities, possibly without their knowledge of the impairment, the FDA said. As a result, people who use Zurzuvae should not drive or operate heavy machinery for at least 12 hours after taking the pill.
A version of this article first appeared on Medscape.com.
Bipolar disorder tied to a sixfold increased risk of early death
In addition, patients with BD are three times more likely to die prematurely of all causes, compared with the general population, with alcohol-related diseases contributing to more premature deaths than cardiovascular disease (CVD), diabetes, and cancer.
The study results emphasize the need for personalized approaches to risk prediction and prevention of premature cause-specific mortality over the life-course of individuals with BD, lead investigator Tapio Paljärvi, PhD, an epidemiologist at Niuvanniemi Hospital in Kuopio, Finland, told this news organization.
The findings were published online in BMJ Mental Health.
Alcohol a major contributor to early death
A number of studies have established that those with BD have twice the risk of dying prematurely, compared with those without the disorder.
To learn more about the factors contributing to early death in this patient population, the investigators analyzed data from nationwide Finnish medical and insurance registries. They identified and tracked the health of 47,000 patients, aged 15-64 years, with BD between 2004 and 2018.
The average age at the beginning of the monitoring period was 38 years, and 57% of the cohort were women.
To determine the excess deaths directly attributable to BD, the researchers compared the ratio of deaths observed over the monitoring period in those with BD to the number expected to die in the general population, also known as the standard mortality ratio.
Of the group with BD, 3,300 died during the monitoring period. The average age at death was 50, and almost two-thirds (65%, or 2,137) of those who died were men.
Investigators grouped excess deaths in BD patients into two categories – somatic and external.
Of those with BD who died from somatic or disease-related causes, alcohol caused the highest rate of death (29%). The second-leading cause was heart disease and stroke (27%), followed by cancer (22%), respiratory diseases (4%), and diabetes (2%).
Among the 595 patients with BD who died because of alcohol consumption, liver disease was the leading cause of death (48%). The second cause was accidental alcohol poisoning (28%), followed by alcohol dependence (10%).
The leading cause of death from external causes in BD patients was suicide (58%, or 740), nearly half of which (48%) were from an overdose with prescribed psychotropic medications.
Overall, 64%, or 2,104, of the deaths in BD patients from any cause were considered excess deaths, that is, the number of deaths above those expected for those without BD of comparable age and sex.
Most of the excess deaths from somatic illness were either from alcohol-related causes (40%) – a rate three times higher than that of the general population – CVD (26%), or cancer (10%).
High suicide rate
When the team examined excess deaths from external causes, they found that 61% (651) were attributable to suicide, a rate eight times higher than that of the general population.
“In terms of absolute numbers, somatic causes of death represented the majority of all deaths in BD, as also reported in previous research,” Dr. Paljärvi said.
“However, this finding reflects the fact that in many high-income countries most of the deaths are due to somatic causes; with CVD, cancers, and diseases of the nervous system as the leading causes of death in the older age groups,” he added.
Dr. Paljärvi advised that clinicians treating patients with BD balance therapeutic response with potentially serious long-term medication side effects, to prevent premature deaths.
A stronger emphasis on identifying and treating comorbid substance abuse is also warranted, he noted.
Dr. Paljärvi noted that the underlying causes of the excess somatic mortality in people with BD are not fully understood, but may result from the “complex interaction between various established risk factors, including tobacco use, alcohol abuse, physical inactivity, unhealthy diet, obesity, hypertension, etc.”
Regarding the generalizability of the findings, he said many previous studies have been based only on inpatient data and noted that the current study included individuals from various sources including inpatient and outpatient registries as well as social insurance registries.
“While the reported excess all-cause mortality rates are strikingly similar across populations globally, there is a paucity of more detailed cause-specific analyses of excess mortality in BD,” said Dr. Paljärvi, adding that these findings should be replicated in other countries, including the United States.
Chronic inflammation
Commenting on the findings, Benjamin Goldstein, MD, PhD, professor of psychiatry and pharmacology at the University of Toronto, noted that there are clear disparities in access to, and quality of care among, patients with BD and other serious mental illnesses.
“Taking heart disease as an example, disparities exist at virtually every point of contact, ranging from the point of preventive care to the time it takes to be assessed in the ER, to the likelihood of receiving cardiac catheterization, to the quality of postdischarge care,” said Dr. Goldstein.
He also noted that CVD occurs in patients with BD, on average, 10-15 years earlier than the general population. However, he added, “there is important evidence that when people with BD receive the same standard of care as those without BD their cardiovascular outcomes are similar.”
Dr. Goldstein also noted that inflammation, which is a driver of cardiovascular risk, is elevated among patients with BD, particularly during mania and depression.
“Given that the average person with BD has some degree of mood symptoms about 40% of the time, chronically elevated inflammation likely contributes in part to the excess risk of heart disease in bipolar disorder,” he said.
Dr. Goldstein’s team’s research focuses on microvessels. “We have found that microvessel function in both the heart and the brain, determined by MRI, is reduced among teens with BD,” he said.
His team has also found that endothelial function in fingertip microvessels, an indicator of future heart disease risk, varies according to mood states.
“Collectively, these findings suggest the microvascular problems may explain, in part, the extra risk of heart disease beyond traditional risk factors in BD,” he added.
The study was funded by a Wellcome Trust Senior Clinical Research Fellowship and by the Oxford Health Biomedical Research Centre. Dr. Paljärvi and Dr. Goldstein report no relevant financial relationships.
A version of this article appeared on Medscape.com.
In addition, patients with BD are three times more likely to die prematurely of all causes, compared with the general population, with alcohol-related diseases contributing to more premature deaths than cardiovascular disease (CVD), diabetes, and cancer.
The study results emphasize the need for personalized approaches to risk prediction and prevention of premature cause-specific mortality over the life-course of individuals with BD, lead investigator Tapio Paljärvi, PhD, an epidemiologist at Niuvanniemi Hospital in Kuopio, Finland, told this news organization.
The findings were published online in BMJ Mental Health.
Alcohol a major contributor to early death
A number of studies have established that those with BD have twice the risk of dying prematurely, compared with those without the disorder.
To learn more about the factors contributing to early death in this patient population, the investigators analyzed data from nationwide Finnish medical and insurance registries. They identified and tracked the health of 47,000 patients, aged 15-64 years, with BD between 2004 and 2018.
The average age at the beginning of the monitoring period was 38 years, and 57% of the cohort were women.
To determine the excess deaths directly attributable to BD, the researchers compared the ratio of deaths observed over the monitoring period in those with BD to the number expected to die in the general population, also known as the standard mortality ratio.
Of the group with BD, 3,300 died during the monitoring period. The average age at death was 50, and almost two-thirds (65%, or 2,137) of those who died were men.
Investigators grouped excess deaths in BD patients into two categories – somatic and external.
Of those with BD who died from somatic or disease-related causes, alcohol caused the highest rate of death (29%). The second-leading cause was heart disease and stroke (27%), followed by cancer (22%), respiratory diseases (4%), and diabetes (2%).
Among the 595 patients with BD who died because of alcohol consumption, liver disease was the leading cause of death (48%). The second cause was accidental alcohol poisoning (28%), followed by alcohol dependence (10%).
The leading cause of death from external causes in BD patients was suicide (58%, or 740), nearly half of which (48%) were from an overdose with prescribed psychotropic medications.
Overall, 64%, or 2,104, of the deaths in BD patients from any cause were considered excess deaths, that is, the number of deaths above those expected for those without BD of comparable age and sex.
Most of the excess deaths from somatic illness were either from alcohol-related causes (40%) – a rate three times higher than that of the general population – CVD (26%), or cancer (10%).
High suicide rate
When the team examined excess deaths from external causes, they found that 61% (651) were attributable to suicide, a rate eight times higher than that of the general population.
“In terms of absolute numbers, somatic causes of death represented the majority of all deaths in BD, as also reported in previous research,” Dr. Paljärvi said.
“However, this finding reflects the fact that in many high-income countries most of the deaths are due to somatic causes; with CVD, cancers, and diseases of the nervous system as the leading causes of death in the older age groups,” he added.
Dr. Paljärvi advised that clinicians treating patients with BD balance therapeutic response with potentially serious long-term medication side effects, to prevent premature deaths.
A stronger emphasis on identifying and treating comorbid substance abuse is also warranted, he noted.
Dr. Paljärvi noted that the underlying causes of the excess somatic mortality in people with BD are not fully understood, but may result from the “complex interaction between various established risk factors, including tobacco use, alcohol abuse, physical inactivity, unhealthy diet, obesity, hypertension, etc.”
Regarding the generalizability of the findings, he said many previous studies have been based only on inpatient data and noted that the current study included individuals from various sources including inpatient and outpatient registries as well as social insurance registries.
“While the reported excess all-cause mortality rates are strikingly similar across populations globally, there is a paucity of more detailed cause-specific analyses of excess mortality in BD,” said Dr. Paljärvi, adding that these findings should be replicated in other countries, including the United States.
Chronic inflammation
Commenting on the findings, Benjamin Goldstein, MD, PhD, professor of psychiatry and pharmacology at the University of Toronto, noted that there are clear disparities in access to, and quality of care among, patients with BD and other serious mental illnesses.
“Taking heart disease as an example, disparities exist at virtually every point of contact, ranging from the point of preventive care to the time it takes to be assessed in the ER, to the likelihood of receiving cardiac catheterization, to the quality of postdischarge care,” said Dr. Goldstein.
He also noted that CVD occurs in patients with BD, on average, 10-15 years earlier than the general population. However, he added, “there is important evidence that when people with BD receive the same standard of care as those without BD their cardiovascular outcomes are similar.”
Dr. Goldstein also noted that inflammation, which is a driver of cardiovascular risk, is elevated among patients with BD, particularly during mania and depression.
“Given that the average person with BD has some degree of mood symptoms about 40% of the time, chronically elevated inflammation likely contributes in part to the excess risk of heart disease in bipolar disorder,” he said.
Dr. Goldstein’s team’s research focuses on microvessels. “We have found that microvessel function in both the heart and the brain, determined by MRI, is reduced among teens with BD,” he said.
His team has also found that endothelial function in fingertip microvessels, an indicator of future heart disease risk, varies according to mood states.
“Collectively, these findings suggest the microvascular problems may explain, in part, the extra risk of heart disease beyond traditional risk factors in BD,” he added.
The study was funded by a Wellcome Trust Senior Clinical Research Fellowship and by the Oxford Health Biomedical Research Centre. Dr. Paljärvi and Dr. Goldstein report no relevant financial relationships.
A version of this article appeared on Medscape.com.
In addition, patients with BD are three times more likely to die prematurely of all causes, compared with the general population, with alcohol-related diseases contributing to more premature deaths than cardiovascular disease (CVD), diabetes, and cancer.
The study results emphasize the need for personalized approaches to risk prediction and prevention of premature cause-specific mortality over the life-course of individuals with BD, lead investigator Tapio Paljärvi, PhD, an epidemiologist at Niuvanniemi Hospital in Kuopio, Finland, told this news organization.
The findings were published online in BMJ Mental Health.
Alcohol a major contributor to early death
A number of studies have established that those with BD have twice the risk of dying prematurely, compared with those without the disorder.
To learn more about the factors contributing to early death in this patient population, the investigators analyzed data from nationwide Finnish medical and insurance registries. They identified and tracked the health of 47,000 patients, aged 15-64 years, with BD between 2004 and 2018.
The average age at the beginning of the monitoring period was 38 years, and 57% of the cohort were women.
To determine the excess deaths directly attributable to BD, the researchers compared the ratio of deaths observed over the monitoring period in those with BD to the number expected to die in the general population, also known as the standard mortality ratio.
Of the group with BD, 3,300 died during the monitoring period. The average age at death was 50, and almost two-thirds (65%, or 2,137) of those who died were men.
Investigators grouped excess deaths in BD patients into two categories – somatic and external.
Of those with BD who died from somatic or disease-related causes, alcohol caused the highest rate of death (29%). The second-leading cause was heart disease and stroke (27%), followed by cancer (22%), respiratory diseases (4%), and diabetes (2%).
Among the 595 patients with BD who died because of alcohol consumption, liver disease was the leading cause of death (48%). The second cause was accidental alcohol poisoning (28%), followed by alcohol dependence (10%).
The leading cause of death from external causes in BD patients was suicide (58%, or 740), nearly half of which (48%) were from an overdose with prescribed psychotropic medications.
Overall, 64%, or 2,104, of the deaths in BD patients from any cause were considered excess deaths, that is, the number of deaths above those expected for those without BD of comparable age and sex.
Most of the excess deaths from somatic illness were either from alcohol-related causes (40%) – a rate three times higher than that of the general population – CVD (26%), or cancer (10%).
High suicide rate
When the team examined excess deaths from external causes, they found that 61% (651) were attributable to suicide, a rate eight times higher than that of the general population.
“In terms of absolute numbers, somatic causes of death represented the majority of all deaths in BD, as also reported in previous research,” Dr. Paljärvi said.
“However, this finding reflects the fact that in many high-income countries most of the deaths are due to somatic causes; with CVD, cancers, and diseases of the nervous system as the leading causes of death in the older age groups,” he added.
Dr. Paljärvi advised that clinicians treating patients with BD balance therapeutic response with potentially serious long-term medication side effects, to prevent premature deaths.
A stronger emphasis on identifying and treating comorbid substance abuse is also warranted, he noted.
Dr. Paljärvi noted that the underlying causes of the excess somatic mortality in people with BD are not fully understood, but may result from the “complex interaction between various established risk factors, including tobacco use, alcohol abuse, physical inactivity, unhealthy diet, obesity, hypertension, etc.”
Regarding the generalizability of the findings, he said many previous studies have been based only on inpatient data and noted that the current study included individuals from various sources including inpatient and outpatient registries as well as social insurance registries.
“While the reported excess all-cause mortality rates are strikingly similar across populations globally, there is a paucity of more detailed cause-specific analyses of excess mortality in BD,” said Dr. Paljärvi, adding that these findings should be replicated in other countries, including the United States.
Chronic inflammation
Commenting on the findings, Benjamin Goldstein, MD, PhD, professor of psychiatry and pharmacology at the University of Toronto, noted that there are clear disparities in access to, and quality of care among, patients with BD and other serious mental illnesses.
“Taking heart disease as an example, disparities exist at virtually every point of contact, ranging from the point of preventive care to the time it takes to be assessed in the ER, to the likelihood of receiving cardiac catheterization, to the quality of postdischarge care,” said Dr. Goldstein.
He also noted that CVD occurs in patients with BD, on average, 10-15 years earlier than the general population. However, he added, “there is important evidence that when people with BD receive the same standard of care as those without BD their cardiovascular outcomes are similar.”
Dr. Goldstein also noted that inflammation, which is a driver of cardiovascular risk, is elevated among patients with BD, particularly during mania and depression.
“Given that the average person with BD has some degree of mood symptoms about 40% of the time, chronically elevated inflammation likely contributes in part to the excess risk of heart disease in bipolar disorder,” he said.
Dr. Goldstein’s team’s research focuses on microvessels. “We have found that microvessel function in both the heart and the brain, determined by MRI, is reduced among teens with BD,” he said.
His team has also found that endothelial function in fingertip microvessels, an indicator of future heart disease risk, varies according to mood states.
“Collectively, these findings suggest the microvascular problems may explain, in part, the extra risk of heart disease beyond traditional risk factors in BD,” he added.
The study was funded by a Wellcome Trust Senior Clinical Research Fellowship and by the Oxford Health Biomedical Research Centre. Dr. Paljärvi and Dr. Goldstein report no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM BMJ MENTAL HEALTH
A new and completely different pain medicine
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
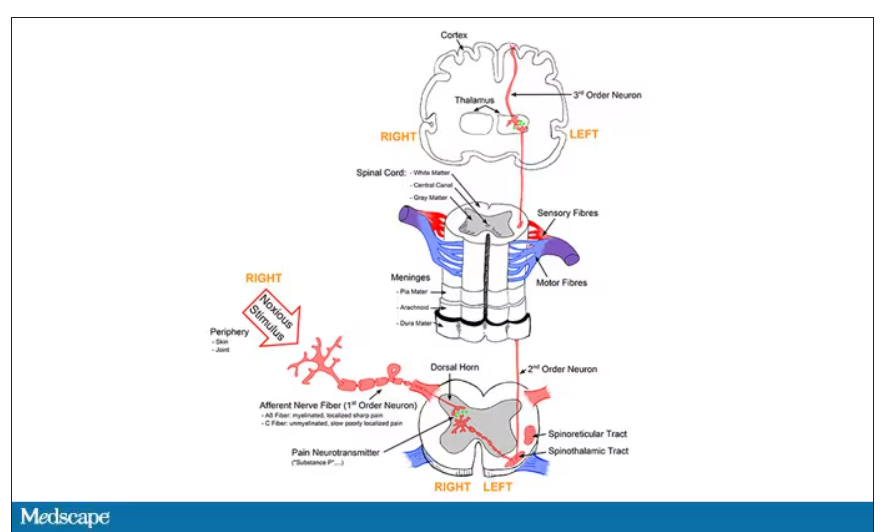
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
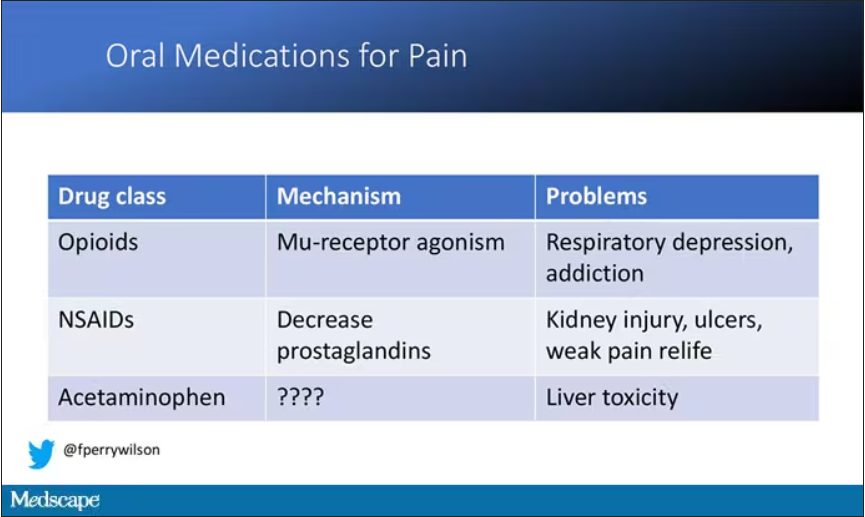
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
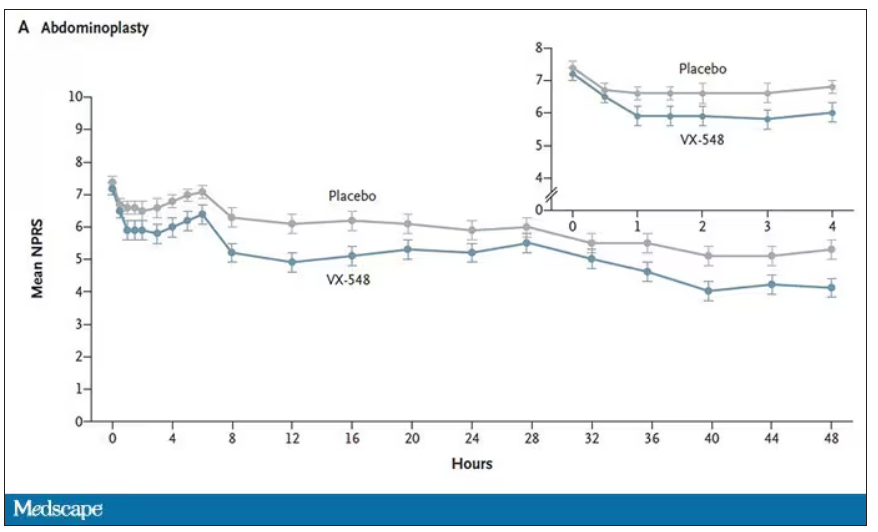
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
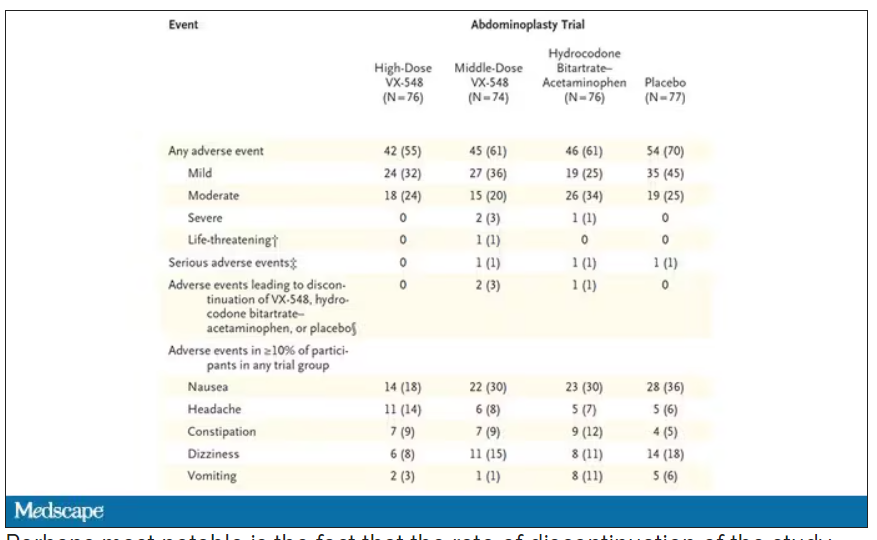
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
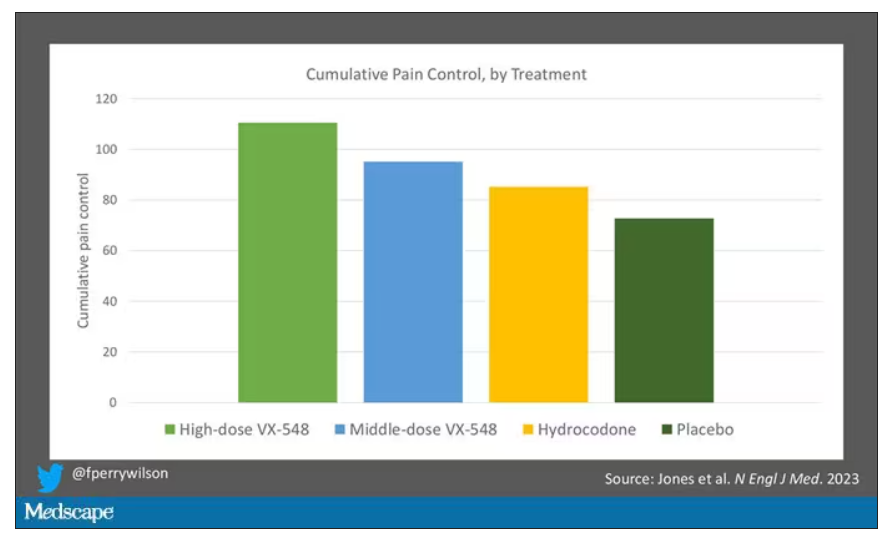
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Long COVID disability court battles just ‘tip of iceberg’
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
Depression at any stage of life tied to increased dementia risk
Adults with depression have more than double the risk of developing dementia and the risk persists regardless of when in life depression is diagnosed, a large population-based study shows.
That the association between depression and dementia persisted even among individuals first diagnosed with depression in early or mid-life provides “strong evidence that depression is not only an early symptom of dementia, but also that depression increases dementia risk,” study investigator Holly Elser, MD, PhD, epidemiologist and resident physician, University of Pennsylvania, Philadelphia, told this news organization.
The study was published online in JAMA Neurology.
Double the risk
Several prior studies that have examined the relationship between depression and dementia over the life course have consistently shown depression later in life is associated with subsequent dementia.
“Late-life depression is generally thought to be an early symptom of dementia or a reaction to subclinical cognitive decline,” said Dr. Elser.
The investigators wanted to examine whether the association between depression and dementia persists even when depression is diagnosed earlier in life, which may suggest it increases the risk of dementia.
“To my knowledge, ours is the largest study on this topic to date, leveraging routinely and prospectively collected data from more than 1.4 million Danish citizens followed from 1977 to 2018,” Dr. Elser noted.
The cohort included 246,499 individuals diagnosed with depression and 1,190,302 individuals without depression.
In both groups, the median age was 50 years and 65% were women. Roughly two-thirds (68%) of those diagnosed with depression were diagnosed before age 60 years.
In Cox proportional hazards regression models, the overall hazard of dementia was more than doubled in those diagnosed with depression (hazard ratio [HR] 2.41). The risk of dementia with depression was more pronounced for men (HR, 2.98) than in women (HR, 2.21).
This association persisted even when the time elapsed from depression diagnosis was between 20 and 39 years (HR, 1.79) and whether depression was diagnosed in early life (18-44 years: HR, 3.08), mid-life (45-59 years: HR, 2.95), or late life (≥ 60 years: HR, 2.31).
It remains unclear whether effective treatment of depression modifies the risk of dementia, as the current study explored the role of antidepressants in a “very limited fashion,” Dr. Elser said.
Specifically, the researchers considered whether an individual was treated with an antidepressant within 6 months of the initial depression diagnosis and found no evidence of a difference in dementia risk between the treated and untreated groups.
“Research that explores implications of the timing and duration of treatment with antidepressants for dementia, treatment with cognitive behavioral therapy, and is able to evaluate the effectiveness of those treatments will be extremely important,” Dr. Elser said.
‘An assault on the brain’
Reached for comment, John Showalter, MD, chief product officer at Linus Health, said one of the most “intriguing” findings of the study is that a depression diagnosis earlier in adulthood conferred a greater risk of developing vascular dementia (HR, 3.28) than did dementia due to Alzheimer’s disease (HR, 1.73).
“The difference in risk for subtypes of dementia is a meaningful addition to our understanding of depression’s connection to dementia,” said Dr. Showalter, who was not involved in the study.
Also weighing in, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the findings from this “far-reaching investigation leave little room for doubt – depression unleashes a devastating storm within the brain, wreaking havoc on the lives of those ensnared by its grip.
“This massive, multi-decade, and high-data quality registry study adds another brick to the growing edifice of evidence attesting to the profound connection between psychiatric health and the very essence of brain health,” said Dr. Lakhan, who was not involved in the study.
“In a resounding declaration, this research underscores that psychiatric health should be perceived as an integral component of overall health – a paradigm shift that challenges long-standing misconceptions and stigmas surrounding mental disorders. Depression, once marginalized, now claims its rightful place on the pedestal of health concerns that must be addressed with unwavering resolve,” said Dr. Lakhan.
He noted that depression is “not just a mental battle, it’s a profound assault on the very fabric of the brain, leaving lives in turmoil and hearts in search of hope. No longer shrouded in silence, depression demands society’s attention.”
The study had no specific funding. Dr. Elser, Dr. Showalter, and Dr. Lakhan have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Adults with depression have more than double the risk of developing dementia and the risk persists regardless of when in life depression is diagnosed, a large population-based study shows.
That the association between depression and dementia persisted even among individuals first diagnosed with depression in early or mid-life provides “strong evidence that depression is not only an early symptom of dementia, but also that depression increases dementia risk,” study investigator Holly Elser, MD, PhD, epidemiologist and resident physician, University of Pennsylvania, Philadelphia, told this news organization.
The study was published online in JAMA Neurology.
Double the risk
Several prior studies that have examined the relationship between depression and dementia over the life course have consistently shown depression later in life is associated with subsequent dementia.
“Late-life depression is generally thought to be an early symptom of dementia or a reaction to subclinical cognitive decline,” said Dr. Elser.
The investigators wanted to examine whether the association between depression and dementia persists even when depression is diagnosed earlier in life, which may suggest it increases the risk of dementia.
“To my knowledge, ours is the largest study on this topic to date, leveraging routinely and prospectively collected data from more than 1.4 million Danish citizens followed from 1977 to 2018,” Dr. Elser noted.
The cohort included 246,499 individuals diagnosed with depression and 1,190,302 individuals without depression.
In both groups, the median age was 50 years and 65% were women. Roughly two-thirds (68%) of those diagnosed with depression were diagnosed before age 60 years.
In Cox proportional hazards regression models, the overall hazard of dementia was more than doubled in those diagnosed with depression (hazard ratio [HR] 2.41). The risk of dementia with depression was more pronounced for men (HR, 2.98) than in women (HR, 2.21).
This association persisted even when the time elapsed from depression diagnosis was between 20 and 39 years (HR, 1.79) and whether depression was diagnosed in early life (18-44 years: HR, 3.08), mid-life (45-59 years: HR, 2.95), or late life (≥ 60 years: HR, 2.31).
It remains unclear whether effective treatment of depression modifies the risk of dementia, as the current study explored the role of antidepressants in a “very limited fashion,” Dr. Elser said.
Specifically, the researchers considered whether an individual was treated with an antidepressant within 6 months of the initial depression diagnosis and found no evidence of a difference in dementia risk between the treated and untreated groups.
“Research that explores implications of the timing and duration of treatment with antidepressants for dementia, treatment with cognitive behavioral therapy, and is able to evaluate the effectiveness of those treatments will be extremely important,” Dr. Elser said.
‘An assault on the brain’
Reached for comment, John Showalter, MD, chief product officer at Linus Health, said one of the most “intriguing” findings of the study is that a depression diagnosis earlier in adulthood conferred a greater risk of developing vascular dementia (HR, 3.28) than did dementia due to Alzheimer’s disease (HR, 1.73).
“The difference in risk for subtypes of dementia is a meaningful addition to our understanding of depression’s connection to dementia,” said Dr. Showalter, who was not involved in the study.
Also weighing in, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the findings from this “far-reaching investigation leave little room for doubt – depression unleashes a devastating storm within the brain, wreaking havoc on the lives of those ensnared by its grip.
“This massive, multi-decade, and high-data quality registry study adds another brick to the growing edifice of evidence attesting to the profound connection between psychiatric health and the very essence of brain health,” said Dr. Lakhan, who was not involved in the study.
“In a resounding declaration, this research underscores that psychiatric health should be perceived as an integral component of overall health – a paradigm shift that challenges long-standing misconceptions and stigmas surrounding mental disorders. Depression, once marginalized, now claims its rightful place on the pedestal of health concerns that must be addressed with unwavering resolve,” said Dr. Lakhan.
He noted that depression is “not just a mental battle, it’s a profound assault on the very fabric of the brain, leaving lives in turmoil and hearts in search of hope. No longer shrouded in silence, depression demands society’s attention.”
The study had no specific funding. Dr. Elser, Dr. Showalter, and Dr. Lakhan have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Adults with depression have more than double the risk of developing dementia and the risk persists regardless of when in life depression is diagnosed, a large population-based study shows.
That the association between depression and dementia persisted even among individuals first diagnosed with depression in early or mid-life provides “strong evidence that depression is not only an early symptom of dementia, but also that depression increases dementia risk,” study investigator Holly Elser, MD, PhD, epidemiologist and resident physician, University of Pennsylvania, Philadelphia, told this news organization.
The study was published online in JAMA Neurology.
Double the risk
Several prior studies that have examined the relationship between depression and dementia over the life course have consistently shown depression later in life is associated with subsequent dementia.
“Late-life depression is generally thought to be an early symptom of dementia or a reaction to subclinical cognitive decline,” said Dr. Elser.
The investigators wanted to examine whether the association between depression and dementia persists even when depression is diagnosed earlier in life, which may suggest it increases the risk of dementia.
“To my knowledge, ours is the largest study on this topic to date, leveraging routinely and prospectively collected data from more than 1.4 million Danish citizens followed from 1977 to 2018,” Dr. Elser noted.
The cohort included 246,499 individuals diagnosed with depression and 1,190,302 individuals without depression.
In both groups, the median age was 50 years and 65% were women. Roughly two-thirds (68%) of those diagnosed with depression were diagnosed before age 60 years.
In Cox proportional hazards regression models, the overall hazard of dementia was more than doubled in those diagnosed with depression (hazard ratio [HR] 2.41). The risk of dementia with depression was more pronounced for men (HR, 2.98) than in women (HR, 2.21).
This association persisted even when the time elapsed from depression diagnosis was between 20 and 39 years (HR, 1.79) and whether depression was diagnosed in early life (18-44 years: HR, 3.08), mid-life (45-59 years: HR, 2.95), or late life (≥ 60 years: HR, 2.31).
It remains unclear whether effective treatment of depression modifies the risk of dementia, as the current study explored the role of antidepressants in a “very limited fashion,” Dr. Elser said.
Specifically, the researchers considered whether an individual was treated with an antidepressant within 6 months of the initial depression diagnosis and found no evidence of a difference in dementia risk between the treated and untreated groups.
“Research that explores implications of the timing and duration of treatment with antidepressants for dementia, treatment with cognitive behavioral therapy, and is able to evaluate the effectiveness of those treatments will be extremely important,” Dr. Elser said.
‘An assault on the brain’
Reached for comment, John Showalter, MD, chief product officer at Linus Health, said one of the most “intriguing” findings of the study is that a depression diagnosis earlier in adulthood conferred a greater risk of developing vascular dementia (HR, 3.28) than did dementia due to Alzheimer’s disease (HR, 1.73).
“The difference in risk for subtypes of dementia is a meaningful addition to our understanding of depression’s connection to dementia,” said Dr. Showalter, who was not involved in the study.
Also weighing in, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the findings from this “far-reaching investigation leave little room for doubt – depression unleashes a devastating storm within the brain, wreaking havoc on the lives of those ensnared by its grip.
“This massive, multi-decade, and high-data quality registry study adds another brick to the growing edifice of evidence attesting to the profound connection between psychiatric health and the very essence of brain health,” said Dr. Lakhan, who was not involved in the study.
“In a resounding declaration, this research underscores that psychiatric health should be perceived as an integral component of overall health – a paradigm shift that challenges long-standing misconceptions and stigmas surrounding mental disorders. Depression, once marginalized, now claims its rightful place on the pedestal of health concerns that must be addressed with unwavering resolve,” said Dr. Lakhan.
He noted that depression is “not just a mental battle, it’s a profound assault on the very fabric of the brain, leaving lives in turmoil and hearts in search of hope. No longer shrouded in silence, depression demands society’s attention.”
The study had no specific funding. Dr. Elser, Dr. Showalter, and Dr. Lakhan have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Prescribing lifestyle changes: When medicine isn’t enough
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
Medicare to pay for at-home dementia care coordination
Under a new Medicare pilot program that will begin in 2024, the federal government will pay clinicians to coordinate at-home dementia support services, including respite care for family members.
A Department of Health & Human Services initiative, part of the aim of the Guiding an Improved Dementia Experience (GUIDE) program is to help Medicare beneficiaries with dementia stay in the community for as long as possible. It is estimated that there are 6.7 million Americans living with Alzheimer’s disease or some other form of dementia, said HHS.
The program is voluntary and will be open to Medicare-enrolled clinicians and other providers who can assemble an interdisciplinary care team and meet the program’s participation criteria.
“Our new GUIDE Model has the potential to improve the quality of life for people with dementia and alleviate the significant strain on our families,” said HHS Secretary Xavier Becerra, in a statement.
“Not only is dementia care management a proven way to improve the quality of care and quality of life for those living with Alzheimer’s and other dementia, but now we know that it would also save the federal government billions of dollars,” Robert Egge, Alzheimer’s Association chief public policy officer and Alzheimer’s Impact Movement (AIM) executive director, said in a statement.
Mr. Egge cited a recent analysis commissioned by AIM that found that dementia care management would save the federal government nearly $21 billion over 10 years.
“People living with dementia and their caregivers too often struggle to manage their health care and connect with key supports that can allow them to remain in their homes and communities,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure, in the HHS statement.
“Fragmented care contributes to the mental and physical health strain of caring for someone with dementia, as well as the substantial financial burden,” she said, adding that Black, Hispanic, Asian American, Native Hawaiian, and Pacific Islander populations have been especially disadvantaged.
The GUIDE Model will provide new resources and greater access to specialty care to those communities, said Ms. Brooks-LaSure.
Care teams that seek to participate in the GUIDE model must have a care navigator who has received required training in dementia, assessment, and care planning.
The teams also must have a clinician with dementia proficiency as recognized by experience caring for adults with cognitive impairment; experience caring for patients aged 65 years old or older; or specialty designation in neurology, psychiatry, geriatrics, geriatric psychiatry, behavioral neurology, or geriatric neurology.
Medicare beneficiaries will be eligible if they are not residing in a nursing home; are not enrolled in hospice; and have a confirmed dementia diagnosis.
Beneficiaries who receive care from GUIDE participants will be placed in one of five “tiers,” based on a combination of disease stage and caregiver status. Beneficiary needs, and care intensity and payment, increase by tier.
GUIDE teams will receive a monthly, per-beneficiary amount for providing care management and coordination and caregiver education and support services. They can also bill for respite services – up to an annual cap – for Medicare beneficiaries who have an unpaid caregiver.
Clinicians seeking to participate in GUIDE can apply beginning in the fall. The program will run for 8 years beginning July 1, 2024.
Alzheimer’s Association President and CEO Joanne Pike, DrPH, said in a statement that the organization had “advocated for this approach for years, believing it [to be] the key to addressing systemic challenges faced by those with dementia, their families and those who provide them with care and support.”
The John A. Hartford Foundation noted that it also had long pushed for a comprehensive dementia care program. “Comprehensive dementia care supports both the medical and nonmedical needs of patients and their family caregivers,” said Foundation President Terry Fulmer, PhD, RN, FAAN, in a statement.
“Notably and necessarily, the model will help improve equity in access to care for underserved communities by addressing unpaid caregiver needs, including respite services and screening for health-related social needs,” added Dr. Fulmer.
A version of this article first appeared on Medscape.com.
Under a new Medicare pilot program that will begin in 2024, the federal government will pay clinicians to coordinate at-home dementia support services, including respite care for family members.
A Department of Health & Human Services initiative, part of the aim of the Guiding an Improved Dementia Experience (GUIDE) program is to help Medicare beneficiaries with dementia stay in the community for as long as possible. It is estimated that there are 6.7 million Americans living with Alzheimer’s disease or some other form of dementia, said HHS.
The program is voluntary and will be open to Medicare-enrolled clinicians and other providers who can assemble an interdisciplinary care team and meet the program’s participation criteria.
“Our new GUIDE Model has the potential to improve the quality of life for people with dementia and alleviate the significant strain on our families,” said HHS Secretary Xavier Becerra, in a statement.
“Not only is dementia care management a proven way to improve the quality of care and quality of life for those living with Alzheimer’s and other dementia, but now we know that it would also save the federal government billions of dollars,” Robert Egge, Alzheimer’s Association chief public policy officer and Alzheimer’s Impact Movement (AIM) executive director, said in a statement.
Mr. Egge cited a recent analysis commissioned by AIM that found that dementia care management would save the federal government nearly $21 billion over 10 years.
“People living with dementia and their caregivers too often struggle to manage their health care and connect with key supports that can allow them to remain in their homes and communities,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure, in the HHS statement.
“Fragmented care contributes to the mental and physical health strain of caring for someone with dementia, as well as the substantial financial burden,” she said, adding that Black, Hispanic, Asian American, Native Hawaiian, and Pacific Islander populations have been especially disadvantaged.
The GUIDE Model will provide new resources and greater access to specialty care to those communities, said Ms. Brooks-LaSure.
Care teams that seek to participate in the GUIDE model must have a care navigator who has received required training in dementia, assessment, and care planning.
The teams also must have a clinician with dementia proficiency as recognized by experience caring for adults with cognitive impairment; experience caring for patients aged 65 years old or older; or specialty designation in neurology, psychiatry, geriatrics, geriatric psychiatry, behavioral neurology, or geriatric neurology.
Medicare beneficiaries will be eligible if they are not residing in a nursing home; are not enrolled in hospice; and have a confirmed dementia diagnosis.
Beneficiaries who receive care from GUIDE participants will be placed in one of five “tiers,” based on a combination of disease stage and caregiver status. Beneficiary needs, and care intensity and payment, increase by tier.
GUIDE teams will receive a monthly, per-beneficiary amount for providing care management and coordination and caregiver education and support services. They can also bill for respite services – up to an annual cap – for Medicare beneficiaries who have an unpaid caregiver.
Clinicians seeking to participate in GUIDE can apply beginning in the fall. The program will run for 8 years beginning July 1, 2024.
Alzheimer’s Association President and CEO Joanne Pike, DrPH, said in a statement that the organization had “advocated for this approach for years, believing it [to be] the key to addressing systemic challenges faced by those with dementia, their families and those who provide them with care and support.”
The John A. Hartford Foundation noted that it also had long pushed for a comprehensive dementia care program. “Comprehensive dementia care supports both the medical and nonmedical needs of patients and their family caregivers,” said Foundation President Terry Fulmer, PhD, RN, FAAN, in a statement.
“Notably and necessarily, the model will help improve equity in access to care for underserved communities by addressing unpaid caregiver needs, including respite services and screening for health-related social needs,” added Dr. Fulmer.
A version of this article first appeared on Medscape.com.
Under a new Medicare pilot program that will begin in 2024, the federal government will pay clinicians to coordinate at-home dementia support services, including respite care for family members.
A Department of Health & Human Services initiative, part of the aim of the Guiding an Improved Dementia Experience (GUIDE) program is to help Medicare beneficiaries with dementia stay in the community for as long as possible. It is estimated that there are 6.7 million Americans living with Alzheimer’s disease or some other form of dementia, said HHS.
The program is voluntary and will be open to Medicare-enrolled clinicians and other providers who can assemble an interdisciplinary care team and meet the program’s participation criteria.
“Our new GUIDE Model has the potential to improve the quality of life for people with dementia and alleviate the significant strain on our families,” said HHS Secretary Xavier Becerra, in a statement.
“Not only is dementia care management a proven way to improve the quality of care and quality of life for those living with Alzheimer’s and other dementia, but now we know that it would also save the federal government billions of dollars,” Robert Egge, Alzheimer’s Association chief public policy officer and Alzheimer’s Impact Movement (AIM) executive director, said in a statement.
Mr. Egge cited a recent analysis commissioned by AIM that found that dementia care management would save the federal government nearly $21 billion over 10 years.
“People living with dementia and their caregivers too often struggle to manage their health care and connect with key supports that can allow them to remain in their homes and communities,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure, in the HHS statement.
“Fragmented care contributes to the mental and physical health strain of caring for someone with dementia, as well as the substantial financial burden,” she said, adding that Black, Hispanic, Asian American, Native Hawaiian, and Pacific Islander populations have been especially disadvantaged.
The GUIDE Model will provide new resources and greater access to specialty care to those communities, said Ms. Brooks-LaSure.
Care teams that seek to participate in the GUIDE model must have a care navigator who has received required training in dementia, assessment, and care planning.
The teams also must have a clinician with dementia proficiency as recognized by experience caring for adults with cognitive impairment; experience caring for patients aged 65 years old or older; or specialty designation in neurology, psychiatry, geriatrics, geriatric psychiatry, behavioral neurology, or geriatric neurology.
Medicare beneficiaries will be eligible if they are not residing in a nursing home; are not enrolled in hospice; and have a confirmed dementia diagnosis.
Beneficiaries who receive care from GUIDE participants will be placed in one of five “tiers,” based on a combination of disease stage and caregiver status. Beneficiary needs, and care intensity and payment, increase by tier.
GUIDE teams will receive a monthly, per-beneficiary amount for providing care management and coordination and caregiver education and support services. They can also bill for respite services – up to an annual cap – for Medicare beneficiaries who have an unpaid caregiver.
Clinicians seeking to participate in GUIDE can apply beginning in the fall. The program will run for 8 years beginning July 1, 2024.
Alzheimer’s Association President and CEO Joanne Pike, DrPH, said in a statement that the organization had “advocated for this approach for years, believing it [to be] the key to addressing systemic challenges faced by those with dementia, their families and those who provide them with care and support.”
The John A. Hartford Foundation noted that it also had long pushed for a comprehensive dementia care program. “Comprehensive dementia care supports both the medical and nonmedical needs of patients and their family caregivers,” said Foundation President Terry Fulmer, PhD, RN, FAAN, in a statement.
“Notably and necessarily, the model will help improve equity in access to care for underserved communities by addressing unpaid caregiver needs, including respite services and screening for health-related social needs,” added Dr. Fulmer.
A version of this article first appeared on Medscape.com.