User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Hospitals update hydroxychloroquine protocols after FDA warning
Across the country, hospitals are incorporating Friday’s warning from the US Food and Drug Administration (FDA) about the risks of prescribing hydroxychloroquine and chloroquine for COVID-19 into their treatment protocols.
For some hospitals, the message affirmed the cautious approach they were already taking with hydroxychloroquine. “From a New York state or Northwell perspective, there is no major change,” said Onisis Stefas, PharmD, vice president of pharmacy at Northwell Health in New York. “We were not prescribing it out in the community very early on because of the concerns associated with the heart arrhythmias.”
Brigham and Women’s Hospital in Boston, Massachusetts, is currently in the process of updating its publicly available COVID-19 protocols website “to incorporate the FDA’s updated safety assessment and ongoing clinical trials,” a hospital spokesperson told Medscape Medical News. Prior to the updates, the treatment protocols indicated that hydroxychloroquine should only be considered after weighing the risks and benefits for patients who are not candidates for other clinical trials and meet a specific set of health criteria.
The warning is a timely and important synthesis of what physicians know about the drugs so far and how cautiously clinicians across the country should be using them, said Rajesh T. Gandhi, MD, infectious diseases physician at Massachusetts General Hospital (MGH), Boston, professor of medicine at Harvard Medical School, member of the Infectious Diseases Society of America (IDSA), and chair-elect of the HIV Medicine Association.
“I think to be honest it’s a really important message to the public and clinicians across the country,” said Gandhi. “Because we all know there is just a ton of discussion around this drug ... and it came out fairly and said what we know right now.”
The two antimalarial drugs have been at the center of much political debate and scientific scrutiny in recent weeks, following President Trump’s endorsement and the FDA’s emergency use authorization for the two medications in March. Hospitals across the country had incorporated hydroxychloroquine and chloroquine into their constantly evolving treatment protocols for patients with COVID-19.
But the evidence that these drugs actually help treat COVID-19 remains scant. Some small studies suggest the therapies help patients with COVID-19, while others conclude the drugs have no effect or even harm patients. In the United States, medical societies including the American Heart Association have also warned about the serious cardiac issues that can accompany these drugs for some patients.
In the new warning, the FDA said it “cautions against use of hydroxychloroquine or chloroquine for COVID-19 patients outside of the hospital setting or a clinical trial” and urged “close supervision” of patients treated with these therapies, citing cardiac side effects.
The FDA also said it is aware that the outpatient prescription of these medications has increased since its March authorization, but the drugs still have not been shown to be safe or effective in treating or preventing COVID-19.
The FDA announcement is consistent with protocols established by the National Institutes of Health and IDSA earlier this month that recommend against using hydroxychloroquine or chloroquine, except when these drugs are administered as part of a clinical trial.
“We agree wholeheartedly with the FDA and have been hoping that the FDA would in fact issue that kind of clarification,” said Samuel Brown, MD, study committee cochair of the ORCHID clinical trial, a multicenter, blinded study investigating the safety and efficacy of hydroxychloroquine. These medications need to be tested in clinical trials that are able to focus closely on safety monitoring, he said. Experts at Vanderbilt University, one of the medical centers participating in the ORCHID clinical trial, decided before Tennessee had any cases of COVID-19 that unproven therapies like hydroxychloroquine would only be available through clinical trials, said Wesley Self, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tennessee, and chair of the ORCHID study committee.
Northwell Health, like other hospitals in New York, has been following a March executive order issued by Governor Andrew Cuomo limiting the use of these drugs for COVID-19 outside of clinical trials, said Stefas. At Northwell Health, patients with COVID-19 only receive hydroxychloroquine or chloroquine when treated in hospital, where they can be closely monitored, or as part of a clinical trial. The hospital system’s protocols currently do not recommend pairing hydroxychloroquine with azithromycin, said Stefas. The new FDA announcement is “very similar” to New York’s existing executive order, he said. “Reading through this reinforces a lot of what we originally thought.”
At MGH in Boston, the FDA safety warning is in line with and “solidifies” the hospital’s evolving protocols, said Gandhi. Clinicians at MGH have been steadily moving away from prescribing hydroxychloroquine outside of clinical trials as the efficacy has remained murky, the serious side effects have become more evident, and clinical trials to assess the drug have gotten underway in recent weeks, he said. Given the conflicting evidence, Gandhi feels the use of these drugs needs to be focused in clinical trials, where scientists can truly evaluate how much they help or harm.
“We know fundamentally that’s the way to do this,” Gandhi said. “We also don’t know that it doesn’t work, so it is ethical and incumbent upon us to do a study,” Gandhi said.
Other hospitals are already heeding the FDA’s warning. At UW Medicine in Washington state, for example, hydroxychloroquine was considered a possible treatment for COVID-19 prior to the FDA’s recent announcement. “Based on FDA guidance, hydroxychloroquine is no longer recommended as therapy for COVID-19 unless done through a clinical trial,” said Tim Dellit, MD, chief medical officer for UW Medicine.
Michigan Medicine stopped using hydroxychloroquine and azithromycin (both separately and in combination) about a month ago, said Daniel Kaul, MD, a professor of infectious disease at the University of Michigan. “When we reviewed the data that was available in more detail, we realized that it was essentially uninterpretable,” he said. As of Monday, the only patients receiving this drug at Michigan Medicine are those enrolled in the ORCHID clinical trial.
But that does not seem to be the case everywhere. Most patients transferred to Michigan Medicine from other hospitals have received these drugs, indicating they are still being widely used, said Kaul. “I think this FDA guidance is appropriate and may reduce usage of this drug and make people more aware of the potential side effects both in inpatient and outpatient settings.”
Hopefully, the FDA guidance will help slow the use of these drugs outside the appropriate clinical trial setting, said Kaul. “I think that the kind of politicization of this drug, which is pretty much unprecedented in my experience, created a really harmful environment where calm decision making and assessment of the relative risks and benefits became somewhat impossible,” said Kaul.
This article first appeared on Medscape.com.
Across the country, hospitals are incorporating Friday’s warning from the US Food and Drug Administration (FDA) about the risks of prescribing hydroxychloroquine and chloroquine for COVID-19 into their treatment protocols.
For some hospitals, the message affirmed the cautious approach they were already taking with hydroxychloroquine. “From a New York state or Northwell perspective, there is no major change,” said Onisis Stefas, PharmD, vice president of pharmacy at Northwell Health in New York. “We were not prescribing it out in the community very early on because of the concerns associated with the heart arrhythmias.”
Brigham and Women’s Hospital in Boston, Massachusetts, is currently in the process of updating its publicly available COVID-19 protocols website “to incorporate the FDA’s updated safety assessment and ongoing clinical trials,” a hospital spokesperson told Medscape Medical News. Prior to the updates, the treatment protocols indicated that hydroxychloroquine should only be considered after weighing the risks and benefits for patients who are not candidates for other clinical trials and meet a specific set of health criteria.
The warning is a timely and important synthesis of what physicians know about the drugs so far and how cautiously clinicians across the country should be using them, said Rajesh T. Gandhi, MD, infectious diseases physician at Massachusetts General Hospital (MGH), Boston, professor of medicine at Harvard Medical School, member of the Infectious Diseases Society of America (IDSA), and chair-elect of the HIV Medicine Association.
“I think to be honest it’s a really important message to the public and clinicians across the country,” said Gandhi. “Because we all know there is just a ton of discussion around this drug ... and it came out fairly and said what we know right now.”
The two antimalarial drugs have been at the center of much political debate and scientific scrutiny in recent weeks, following President Trump’s endorsement and the FDA’s emergency use authorization for the two medications in March. Hospitals across the country had incorporated hydroxychloroquine and chloroquine into their constantly evolving treatment protocols for patients with COVID-19.
But the evidence that these drugs actually help treat COVID-19 remains scant. Some small studies suggest the therapies help patients with COVID-19, while others conclude the drugs have no effect or even harm patients. In the United States, medical societies including the American Heart Association have also warned about the serious cardiac issues that can accompany these drugs for some patients.
In the new warning, the FDA said it “cautions against use of hydroxychloroquine or chloroquine for COVID-19 patients outside of the hospital setting or a clinical trial” and urged “close supervision” of patients treated with these therapies, citing cardiac side effects.
The FDA also said it is aware that the outpatient prescription of these medications has increased since its March authorization, but the drugs still have not been shown to be safe or effective in treating or preventing COVID-19.
The FDA announcement is consistent with protocols established by the National Institutes of Health and IDSA earlier this month that recommend against using hydroxychloroquine or chloroquine, except when these drugs are administered as part of a clinical trial.
“We agree wholeheartedly with the FDA and have been hoping that the FDA would in fact issue that kind of clarification,” said Samuel Brown, MD, study committee cochair of the ORCHID clinical trial, a multicenter, blinded study investigating the safety and efficacy of hydroxychloroquine. These medications need to be tested in clinical trials that are able to focus closely on safety monitoring, he said. Experts at Vanderbilt University, one of the medical centers participating in the ORCHID clinical trial, decided before Tennessee had any cases of COVID-19 that unproven therapies like hydroxychloroquine would only be available through clinical trials, said Wesley Self, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tennessee, and chair of the ORCHID study committee.
Northwell Health, like other hospitals in New York, has been following a March executive order issued by Governor Andrew Cuomo limiting the use of these drugs for COVID-19 outside of clinical trials, said Stefas. At Northwell Health, patients with COVID-19 only receive hydroxychloroquine or chloroquine when treated in hospital, where they can be closely monitored, or as part of a clinical trial. The hospital system’s protocols currently do not recommend pairing hydroxychloroquine with azithromycin, said Stefas. The new FDA announcement is “very similar” to New York’s existing executive order, he said. “Reading through this reinforces a lot of what we originally thought.”
At MGH in Boston, the FDA safety warning is in line with and “solidifies” the hospital’s evolving protocols, said Gandhi. Clinicians at MGH have been steadily moving away from prescribing hydroxychloroquine outside of clinical trials as the efficacy has remained murky, the serious side effects have become more evident, and clinical trials to assess the drug have gotten underway in recent weeks, he said. Given the conflicting evidence, Gandhi feels the use of these drugs needs to be focused in clinical trials, where scientists can truly evaluate how much they help or harm.
“We know fundamentally that’s the way to do this,” Gandhi said. “We also don’t know that it doesn’t work, so it is ethical and incumbent upon us to do a study,” Gandhi said.
Other hospitals are already heeding the FDA’s warning. At UW Medicine in Washington state, for example, hydroxychloroquine was considered a possible treatment for COVID-19 prior to the FDA’s recent announcement. “Based on FDA guidance, hydroxychloroquine is no longer recommended as therapy for COVID-19 unless done through a clinical trial,” said Tim Dellit, MD, chief medical officer for UW Medicine.
Michigan Medicine stopped using hydroxychloroquine and azithromycin (both separately and in combination) about a month ago, said Daniel Kaul, MD, a professor of infectious disease at the University of Michigan. “When we reviewed the data that was available in more detail, we realized that it was essentially uninterpretable,” he said. As of Monday, the only patients receiving this drug at Michigan Medicine are those enrolled in the ORCHID clinical trial.
But that does not seem to be the case everywhere. Most patients transferred to Michigan Medicine from other hospitals have received these drugs, indicating they are still being widely used, said Kaul. “I think this FDA guidance is appropriate and may reduce usage of this drug and make people more aware of the potential side effects both in inpatient and outpatient settings.”
Hopefully, the FDA guidance will help slow the use of these drugs outside the appropriate clinical trial setting, said Kaul. “I think that the kind of politicization of this drug, which is pretty much unprecedented in my experience, created a really harmful environment where calm decision making and assessment of the relative risks and benefits became somewhat impossible,” said Kaul.
This article first appeared on Medscape.com.
Across the country, hospitals are incorporating Friday’s warning from the US Food and Drug Administration (FDA) about the risks of prescribing hydroxychloroquine and chloroquine for COVID-19 into their treatment protocols.
For some hospitals, the message affirmed the cautious approach they were already taking with hydroxychloroquine. “From a New York state or Northwell perspective, there is no major change,” said Onisis Stefas, PharmD, vice president of pharmacy at Northwell Health in New York. “We were not prescribing it out in the community very early on because of the concerns associated with the heart arrhythmias.”
Brigham and Women’s Hospital in Boston, Massachusetts, is currently in the process of updating its publicly available COVID-19 protocols website “to incorporate the FDA’s updated safety assessment and ongoing clinical trials,” a hospital spokesperson told Medscape Medical News. Prior to the updates, the treatment protocols indicated that hydroxychloroquine should only be considered after weighing the risks and benefits for patients who are not candidates for other clinical trials and meet a specific set of health criteria.
The warning is a timely and important synthesis of what physicians know about the drugs so far and how cautiously clinicians across the country should be using them, said Rajesh T. Gandhi, MD, infectious diseases physician at Massachusetts General Hospital (MGH), Boston, professor of medicine at Harvard Medical School, member of the Infectious Diseases Society of America (IDSA), and chair-elect of the HIV Medicine Association.
“I think to be honest it’s a really important message to the public and clinicians across the country,” said Gandhi. “Because we all know there is just a ton of discussion around this drug ... and it came out fairly and said what we know right now.”
The two antimalarial drugs have been at the center of much political debate and scientific scrutiny in recent weeks, following President Trump’s endorsement and the FDA’s emergency use authorization for the two medications in March. Hospitals across the country had incorporated hydroxychloroquine and chloroquine into their constantly evolving treatment protocols for patients with COVID-19.
But the evidence that these drugs actually help treat COVID-19 remains scant. Some small studies suggest the therapies help patients with COVID-19, while others conclude the drugs have no effect or even harm patients. In the United States, medical societies including the American Heart Association have also warned about the serious cardiac issues that can accompany these drugs for some patients.
In the new warning, the FDA said it “cautions against use of hydroxychloroquine or chloroquine for COVID-19 patients outside of the hospital setting or a clinical trial” and urged “close supervision” of patients treated with these therapies, citing cardiac side effects.
The FDA also said it is aware that the outpatient prescription of these medications has increased since its March authorization, but the drugs still have not been shown to be safe or effective in treating or preventing COVID-19.
The FDA announcement is consistent with protocols established by the National Institutes of Health and IDSA earlier this month that recommend against using hydroxychloroquine or chloroquine, except when these drugs are administered as part of a clinical trial.
“We agree wholeheartedly with the FDA and have been hoping that the FDA would in fact issue that kind of clarification,” said Samuel Brown, MD, study committee cochair of the ORCHID clinical trial, a multicenter, blinded study investigating the safety and efficacy of hydroxychloroquine. These medications need to be tested in clinical trials that are able to focus closely on safety monitoring, he said. Experts at Vanderbilt University, one of the medical centers participating in the ORCHID clinical trial, decided before Tennessee had any cases of COVID-19 that unproven therapies like hydroxychloroquine would only be available through clinical trials, said Wesley Self, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tennessee, and chair of the ORCHID study committee.
Northwell Health, like other hospitals in New York, has been following a March executive order issued by Governor Andrew Cuomo limiting the use of these drugs for COVID-19 outside of clinical trials, said Stefas. At Northwell Health, patients with COVID-19 only receive hydroxychloroquine or chloroquine when treated in hospital, where they can be closely monitored, or as part of a clinical trial. The hospital system’s protocols currently do not recommend pairing hydroxychloroquine with azithromycin, said Stefas. The new FDA announcement is “very similar” to New York’s existing executive order, he said. “Reading through this reinforces a lot of what we originally thought.”
At MGH in Boston, the FDA safety warning is in line with and “solidifies” the hospital’s evolving protocols, said Gandhi. Clinicians at MGH have been steadily moving away from prescribing hydroxychloroquine outside of clinical trials as the efficacy has remained murky, the serious side effects have become more evident, and clinical trials to assess the drug have gotten underway in recent weeks, he said. Given the conflicting evidence, Gandhi feels the use of these drugs needs to be focused in clinical trials, where scientists can truly evaluate how much they help or harm.
“We know fundamentally that’s the way to do this,” Gandhi said. “We also don’t know that it doesn’t work, so it is ethical and incumbent upon us to do a study,” Gandhi said.
Other hospitals are already heeding the FDA’s warning. At UW Medicine in Washington state, for example, hydroxychloroquine was considered a possible treatment for COVID-19 prior to the FDA’s recent announcement. “Based on FDA guidance, hydroxychloroquine is no longer recommended as therapy for COVID-19 unless done through a clinical trial,” said Tim Dellit, MD, chief medical officer for UW Medicine.
Michigan Medicine stopped using hydroxychloroquine and azithromycin (both separately and in combination) about a month ago, said Daniel Kaul, MD, a professor of infectious disease at the University of Michigan. “When we reviewed the data that was available in more detail, we realized that it was essentially uninterpretable,” he said. As of Monday, the only patients receiving this drug at Michigan Medicine are those enrolled in the ORCHID clinical trial.
But that does not seem to be the case everywhere. Most patients transferred to Michigan Medicine from other hospitals have received these drugs, indicating they are still being widely used, said Kaul. “I think this FDA guidance is appropriate and may reduce usage of this drug and make people more aware of the potential side effects both in inpatient and outpatient settings.”
Hopefully, the FDA guidance will help slow the use of these drugs outside the appropriate clinical trial setting, said Kaul. “I think that the kind of politicization of this drug, which is pretty much unprecedented in my experience, created a really harmful environment where calm decision making and assessment of the relative risks and benefits became somewhat impossible,” said Kaul.
This article first appeared on Medscape.com.
Reproductive psychiatry during the COVID-19 pandemic
When last I wrote this column, I was preparing for travel to professional meetings in the spring, planning a presentation for an upcoming grand rounds, and readying to host a scientific advisory board meeting as part of a large scientific project we conduct in Center for Women’s Mental Health. We were also awaiting the relocation of several junior faculty and research staff to Boston this spring and summer as we build our team.

It is now obvious that the COVID-19 pandemic is not a passing squall, but rather a persistent gale that has placed our collective sails in the water. It has not capsized the boat, however, thanks in part to the actions of courageous frontline caregivers and first responders who have mobilized in the wake of this recent public health crisis. From doctors, nurses, and hospital staff to grocery store clerks, home health aides, and neighbors checking in on the elderly – to name just a few – a whole crew of members across society have helped buoy our collective ship. Resilience also is required by all of us who are managing the array of feelings brought about by the day-in, day-out challenges of living life with restricted movement and freedom to engage in pre-COVID-19 activities we took for granted. What seemed like a temporary workaround is now becoming the “new normal” for an unknown amount of time looking forward.
For over 3 decades, my colleagues and I have worked with women who suffer from serious psychiatric disorders and whose treatment has required psychiatric medications such as antidepressants, mood stabilizers, and anxiolytics. The challenge of our work with women who are pregnant or planning pregnancy has been the configuration of the safest ways to navigate treatment on an individual basis for these women across pregnancy and post partum, with continual assessments of how to minimize the risk to fetus from in utero exposure to medications that have been instrumental in the treatment of psychiatric disorders on one hand versus the risks of untreated psychiatric disorder on the other. This work has been the essence of the clinical mission and the cornerstone of the research conducted at the Center for Women’s Mental Health since its inception.
While I have worked shoulder to shoulder with obstetricians for years, my respect for these colleagues during these past weeks has only grown as they have instituted the swiftest protocols to mitigate risk associated with COVID-19 for our pregnant patients, some of whom have tested positive for COVID-19, all in an effort to keep both mother, fetus, and newborn as safe as possible.
For those of us providing mental health services to pregnant women during this time, certain clinical situations have arisen in the context of the COVID-19 pandemic which require particular attention and discussion.
Planned pregnancy and contraception during the COVID-19 pandemic
Half of the pregnancies in this country are unplanned. Now more than ever, it is critical that decisions about moving forward with a plan to conceive be deliberate. These considerations range from the existential to the most concrete. For example, during these last weeks, we have consulted on cases where couples on the cusp of attempts to conceive face concerns about COVID-19, hence making more complicated their timeline with respect to actual plans to get pregnant. These are complicated decisions, particularly for women who may be slightly older and at the reproductive age where delaying pregnancy may have an adverse effect on fertility.
A concrete example of how the pandemic has affected fertility is evident as we encounter situations where women may defer starting a prescription oral contraceptive or lapse in its use because they have had difficulty coordinating visits with health care providers and may fear picking up prescriptions from pharmacies. We also have seen that procedures such as IUD placements have been deferred or canceled, or that some patients decline trips to the hospital or clinic to receive this type of service. These new barriers to access of contraception may require more planning at this time so that decisions about family planning are by design and not default during a time as complicated as the current public health crisis.
Telemedicine: telepsychiatry and obstetrics virtual visits
While wide-scale use of telemedicine platforms was not the standard day-to-day practice in either obstetrics or psychiatry prior to the pandemic, telepsychiatry has come up to speed within a short number of weeks. At our institution, 85% of outpatient visits are being conducted remotely, with in-person visits being reserved for only urgent or emergent visits. Our inpatient psychiatry service remains a setting where psychiatric patients, regardless of their COVID-19 status, can receive necessary care.
The use of telemedicine and specifically telepsychiatry is critical to mitigate the likelihood of exposure to SARS-CoV-2. On our reproductive psychiatry service, it has actually been an opportunity to engage with patients for comprehensive initial consults about reproductive safety of psychiatric medications currently being taken, or for ongoing consultation and direct patient care during follow-up visits during pregnancy to see that patients are sustaining emotional well-being or have changes for treatment implemented if they are not well. An increased frequency of visits allows us more opportunity to capture any signs of early clinical worsening of symptoms that might have been missed previously using the more traditional in-person setting.
Telepsychiatry and “virtual visits” have allowed us to do real-time, nimble modifications of treatment regimens with both pharmacologic and nonpharmacologic interventions to keep women well and to keep them out of the hospital for psychiatric care as often as possible. It also has facilitated a closer collaboration with our colleagues in obstetrics. In a way, the team of providers, including psychiatrists, obstetrical providers, social workers, and therapists can more easily communicate virtually than has sometimes been the case previously, when day-to-day use of telemedicine and virtual team meetings was less common.
Recognition and treatment of anxiety in perinatal patients
Even pregnant women without preexisting anxiety disorders may have heightened anxiety during usual times, and women and their partners cope with this typically in numerous ways including participation in peer-support opportunities, wellness and self-care activities, leveraging support from care providers, and engaging with family. But the previously “typical pregnancy experience” has shifted in the context of COVID-19. Specifically, added concerns of pregnant women about becoming infected, of potential separation from family if they do become ill, or of separation from partners or support systems during labor and delivery (an issue that has been largely resolved in many hospitals), as well as the possibility that a neonate might become ill with exposure to the coronavirus are obviously understandable and real. Such contingencies are unsettling, even for the most settled of our patients. Labor and delivery plans, and plans for outside help from family or others with the baby and older children in the postpartum period, have been upended for many patients.
These are anxious times. The number of nonpharmacologic virtual interventions available to mitigate anxiety are filling email inboxes daily. Curating these options can be a challenge, although several resources are worth noting, such as our department’s page on mental health resources.
During these past weeks, we have seen growing numbers of women for whom the normative anxiety of pregnancy is increasing to the point of causing distress to the level of functional impairment. Many patients for the first time meet criteria for frank anxiety disorders. These patients deserve prompt evaluation by mental health professionals and treatment with evidence-based therapies for anxiety disorders whether nonpharmacologic or pharmacologic so as to mitigate the risk of untreated anxiety on maternal and fetal well-being and also to limit risk for postpartum depression and postpartum anxiety disorders.
Miscarriage and infertility
A 36-year-old patient came to see me in clinic in late January following a miscarriage. She had a history of a previous miscarriage a year before and had an episode of major depression to follow for which she received treatment with an antidepressant and cognitive-behavioral therapy; she also attended a perinatal loss support group. She saw me in early March, anxious to try to conceive but extremely concerned about the risks associated with becoming pregnant at this point in time. Following a lengthy discussion with me and her obstetrician, the patient decided to wait until “the curve flattened” in Boston in terms of new cases of COVID-19, and then start trying to conceive. The case of another patient with a very similar history was presented at our rounds a few weeks ago; she also elected to defer attempts to conceive until life is more settled.
Perhaps one of the most dramatic examples of the impact of COVID-19 on fertility has been for those women with plans to pursue treatment with one of the assisted reproductive technologies. They have been told that professional societies have made recommendations regarding use of assisted reproductive technologies that are not entirely consistent across the country, but where in many places such interventions have been suspended during the COVID-19 pandemic. For many women near the end of their reproductive years, delays in trying to conceive either with or without the aid of fertility treatments may indelibly shape their plans to have children.
Sustaining emotional well-being across pregnancy
Because most psychiatric disorders are chronic in course, it is often the situation where women are treated to wellness for serious psychiatric disorders, with the goal of maintaining wellness across pregnancy and the post partum. One of the most critical takeaway points from 30 years of working with psychiatrically ill pregnant women is the maxim that keeping women well during pregnancy is simply imperative. Maternal psychiatric well-being during pregnancy is a strong predictor of obstetrical and neonatal outcomes, postpartum mental health, and longer-term neurobehavioral outcomes in children. Critically, in the context of the pandemic, keeping women out of psychiatric crises mitigates the necessity of visits to urgent clinical settings such as EDs and psychiatric inpatient units, which can increase the likelihood of exposure to the coronavirus.
Preservation of sleep
Disruption in sleep (duration and quality) can be seen in well over half of women during pregnancy with and without psychiatric disorders, and our experience has been that this has been exacerbated for many women during the COVID-19 crisis. Yet there are very rich data showing that sleep deprivation or sleep dysregulation in women, for example, who suffer from bipolar disorder or major depression can be a strong trigger for psychiatric relapse of underlying illness during pregnancy and the postpartum period.
During a time when normal rhythms of day-to-day life have been shifted – if not frankly disrupted – by swift transitions to remote work, cancellation of school and associated school activities across the country, complaints of insomnia and non-restorative sleep have been exceedingly common. Relevant to all but particularly for pregnant women with histories of psychiatric disorder, attention to sleep hygiene, moderation of caffeine use (if any), and use of any number of biobehavioral interventions to enhance relaxation and modulate stress may be of great value.
Cognitive-behavioral therapy for insomnia (CBT-I) has been demonstrated to be effective in pregnant women. Fortunately, there are user-friendly options on digital platforms that can be used during the pandemic that may play an important role in sustaining emotional well-being for pregnant women who have frank symptoms of insomnia.
Maintenance of ongoing antidepressant treatment during pregnancy among women with histories of mood disorder
Over a decade ago, my colleagues and I wrote about the comparison of outcomes for women with histories of recurrent major depression, demonstrating the value of maintenance treatment with antidepressants, compared with discontinuation of these medications during pregnancy (JAMA. 2006 Feb 1;295[5]:499-507). Recently, I was asked if maintenance antidepressant use in women with histories of recurrent depression was still our clinical recommendation. Over the last decade, we have noted that nearly half of women treated with antidepressants, regardless of illness severity, will discontinue their use of these medications prior to or early on in pregnancy given concerns about potential unknown effects of fetal exposure to medications, even medications for which there are robust data supporting reproductive safety regarding risk of congenital malformations. Routine discontinuation of antidepressants prior to or during pregnancy continues, despite the fact that we showed nearly 70% of those women with past histories of depression on maintenance antidepressant treatment relapsed shortly after discontinuing medication.
While we do not dictate the decisions women make about antidepressant use before, during, or after pregnancy, women with the same severity of illness will frequently make different decisions (a good thing) but we are now having very frank discussions about the particular need during a pandemic to avoid the relapse of serious psychiatric disorders. We typically endorse maintenance medication use with all but a very few number of psychotropic medications for which benefit may not outweigh risk to the fetus. However, for women who have decided nonetheless to discontinue antidepressants or other psychotropics during pregnancy despite the known risk of relapse, we strongly advise that they initiate treatment with evidence-based nonpharmacologic intervention such as CBT or mindfulness-based cognitive therapy (MBCT).
As in other areas of medicine, the pandemic is prompting we professionals in psychiatry, and specifically in perinatal psychiatry, to use all of our tools to keep pregnant and postpartum women well. The availability of digital tools to deliver MBCT and CBT has made the use of such interventions particularly viable at a time of social distancing. That being said, for patients with highly recurrent affective disorder with histories of previous recurrence when they stop their antidepressants, we are more strongly recommending serious consideration of maintenance medication treatment.
Virtual rounds in reproductive psychiatry and women’s mental health
The use of virtual platforms to connect with both patients and colleagues also has provided new opportunities for interaction with the reproductive psychiatry community as a whole. Peer teaching and peer support has been a critical part of our mission, and we decided 1 month ago to establish Virtual Rounds at the Center for Women’s Mental Health. This is a free digital platform, held on a weekly basis with our colleagues from across the country, where we discuss cases that come up in our own clinical rounds and also questions that get put forth by our colleagues in the area of reproductive psychiatry as they manage patients during the pandemic.
Changes in the postpartum experience
The last decade has brought a growing appreciation of postpartum depression and the need to screen and treat postpartum psychiatric disorders, such as postpartum mood and anxiety disorders. Yet in the era of this pandemic, the postpartum experience is itself is changing. Changes in carefully configured plans for the postpartum period – from family coming and going to mobilizing extra support at home and to now having new moms having to manage families and their other children at home – has been an enormous stressor for many women. Plans to have more elderly parents visit during the acute postpartum period, and the increased concerns about people traveling to and from a home where there is a newborn and the need to quarantine, has made the transition to motherhood much more complicated for all postpartum women, let alone for those postpartum women who have histories of psychiatric disorder.
There is a risk of social isolation for postpartum women even under normal circumstances, and this is profoundly more likely during this pandemic. We are actively working with our postpartum patients and optimizing treatment, brainstorming options in terms of using both virtual and real-time support to the extent that it is safe in order to keep women healthy during such a stressful and critical time.
I am heartened by the efforts on the part of organizations such as Postpartum Support International to make available virtually their resources with respect to community-based support and education for women who feel increasingly isolated during the postpartum period, a time where connectedness is so critical.
Summarily, these have been challenging times, but also times of opportunity. The COVID-19 pandemic has prompted us to get even more creative as we configure ways to optimize the emotional well-being of our patients who are planning to get pregnant, who are pregnant, or who are post partum.
The current time, while challenging in so many ways and a time of great pain, loss, and grief for far too many, has also provided an opportunity to work even more collaboratively with our colleagues, coming up with new paradigms of treatments as we weather this historic challenge.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
When last I wrote this column, I was preparing for travel to professional meetings in the spring, planning a presentation for an upcoming grand rounds, and readying to host a scientific advisory board meeting as part of a large scientific project we conduct in Center for Women’s Mental Health. We were also awaiting the relocation of several junior faculty and research staff to Boston this spring and summer as we build our team.

It is now obvious that the COVID-19 pandemic is not a passing squall, but rather a persistent gale that has placed our collective sails in the water. It has not capsized the boat, however, thanks in part to the actions of courageous frontline caregivers and first responders who have mobilized in the wake of this recent public health crisis. From doctors, nurses, and hospital staff to grocery store clerks, home health aides, and neighbors checking in on the elderly – to name just a few – a whole crew of members across society have helped buoy our collective ship. Resilience also is required by all of us who are managing the array of feelings brought about by the day-in, day-out challenges of living life with restricted movement and freedom to engage in pre-COVID-19 activities we took for granted. What seemed like a temporary workaround is now becoming the “new normal” for an unknown amount of time looking forward.
For over 3 decades, my colleagues and I have worked with women who suffer from serious psychiatric disorders and whose treatment has required psychiatric medications such as antidepressants, mood stabilizers, and anxiolytics. The challenge of our work with women who are pregnant or planning pregnancy has been the configuration of the safest ways to navigate treatment on an individual basis for these women across pregnancy and post partum, with continual assessments of how to minimize the risk to fetus from in utero exposure to medications that have been instrumental in the treatment of psychiatric disorders on one hand versus the risks of untreated psychiatric disorder on the other. This work has been the essence of the clinical mission and the cornerstone of the research conducted at the Center for Women’s Mental Health since its inception.
While I have worked shoulder to shoulder with obstetricians for years, my respect for these colleagues during these past weeks has only grown as they have instituted the swiftest protocols to mitigate risk associated with COVID-19 for our pregnant patients, some of whom have tested positive for COVID-19, all in an effort to keep both mother, fetus, and newborn as safe as possible.
For those of us providing mental health services to pregnant women during this time, certain clinical situations have arisen in the context of the COVID-19 pandemic which require particular attention and discussion.
Planned pregnancy and contraception during the COVID-19 pandemic
Half of the pregnancies in this country are unplanned. Now more than ever, it is critical that decisions about moving forward with a plan to conceive be deliberate. These considerations range from the existential to the most concrete. For example, during these last weeks, we have consulted on cases where couples on the cusp of attempts to conceive face concerns about COVID-19, hence making more complicated their timeline with respect to actual plans to get pregnant. These are complicated decisions, particularly for women who may be slightly older and at the reproductive age where delaying pregnancy may have an adverse effect on fertility.
A concrete example of how the pandemic has affected fertility is evident as we encounter situations where women may defer starting a prescription oral contraceptive or lapse in its use because they have had difficulty coordinating visits with health care providers and may fear picking up prescriptions from pharmacies. We also have seen that procedures such as IUD placements have been deferred or canceled, or that some patients decline trips to the hospital or clinic to receive this type of service. These new barriers to access of contraception may require more planning at this time so that decisions about family planning are by design and not default during a time as complicated as the current public health crisis.
Telemedicine: telepsychiatry and obstetrics virtual visits
While wide-scale use of telemedicine platforms was not the standard day-to-day practice in either obstetrics or psychiatry prior to the pandemic, telepsychiatry has come up to speed within a short number of weeks. At our institution, 85% of outpatient visits are being conducted remotely, with in-person visits being reserved for only urgent or emergent visits. Our inpatient psychiatry service remains a setting where psychiatric patients, regardless of their COVID-19 status, can receive necessary care.
The use of telemedicine and specifically telepsychiatry is critical to mitigate the likelihood of exposure to SARS-CoV-2. On our reproductive psychiatry service, it has actually been an opportunity to engage with patients for comprehensive initial consults about reproductive safety of psychiatric medications currently being taken, or for ongoing consultation and direct patient care during follow-up visits during pregnancy to see that patients are sustaining emotional well-being or have changes for treatment implemented if they are not well. An increased frequency of visits allows us more opportunity to capture any signs of early clinical worsening of symptoms that might have been missed previously using the more traditional in-person setting.
Telepsychiatry and “virtual visits” have allowed us to do real-time, nimble modifications of treatment regimens with both pharmacologic and nonpharmacologic interventions to keep women well and to keep them out of the hospital for psychiatric care as often as possible. It also has facilitated a closer collaboration with our colleagues in obstetrics. In a way, the team of providers, including psychiatrists, obstetrical providers, social workers, and therapists can more easily communicate virtually than has sometimes been the case previously, when day-to-day use of telemedicine and virtual team meetings was less common.
Recognition and treatment of anxiety in perinatal patients
Even pregnant women without preexisting anxiety disorders may have heightened anxiety during usual times, and women and their partners cope with this typically in numerous ways including participation in peer-support opportunities, wellness and self-care activities, leveraging support from care providers, and engaging with family. But the previously “typical pregnancy experience” has shifted in the context of COVID-19. Specifically, added concerns of pregnant women about becoming infected, of potential separation from family if they do become ill, or of separation from partners or support systems during labor and delivery (an issue that has been largely resolved in many hospitals), as well as the possibility that a neonate might become ill with exposure to the coronavirus are obviously understandable and real. Such contingencies are unsettling, even for the most settled of our patients. Labor and delivery plans, and plans for outside help from family or others with the baby and older children in the postpartum period, have been upended for many patients.
These are anxious times. The number of nonpharmacologic virtual interventions available to mitigate anxiety are filling email inboxes daily. Curating these options can be a challenge, although several resources are worth noting, such as our department’s page on mental health resources.
During these past weeks, we have seen growing numbers of women for whom the normative anxiety of pregnancy is increasing to the point of causing distress to the level of functional impairment. Many patients for the first time meet criteria for frank anxiety disorders. These patients deserve prompt evaluation by mental health professionals and treatment with evidence-based therapies for anxiety disorders whether nonpharmacologic or pharmacologic so as to mitigate the risk of untreated anxiety on maternal and fetal well-being and also to limit risk for postpartum depression and postpartum anxiety disorders.
Miscarriage and infertility
A 36-year-old patient came to see me in clinic in late January following a miscarriage. She had a history of a previous miscarriage a year before and had an episode of major depression to follow for which she received treatment with an antidepressant and cognitive-behavioral therapy; she also attended a perinatal loss support group. She saw me in early March, anxious to try to conceive but extremely concerned about the risks associated with becoming pregnant at this point in time. Following a lengthy discussion with me and her obstetrician, the patient decided to wait until “the curve flattened” in Boston in terms of new cases of COVID-19, and then start trying to conceive. The case of another patient with a very similar history was presented at our rounds a few weeks ago; she also elected to defer attempts to conceive until life is more settled.
Perhaps one of the most dramatic examples of the impact of COVID-19 on fertility has been for those women with plans to pursue treatment with one of the assisted reproductive technologies. They have been told that professional societies have made recommendations regarding use of assisted reproductive technologies that are not entirely consistent across the country, but where in many places such interventions have been suspended during the COVID-19 pandemic. For many women near the end of their reproductive years, delays in trying to conceive either with or without the aid of fertility treatments may indelibly shape their plans to have children.
Sustaining emotional well-being across pregnancy
Because most psychiatric disorders are chronic in course, it is often the situation where women are treated to wellness for serious psychiatric disorders, with the goal of maintaining wellness across pregnancy and the post partum. One of the most critical takeaway points from 30 years of working with psychiatrically ill pregnant women is the maxim that keeping women well during pregnancy is simply imperative. Maternal psychiatric well-being during pregnancy is a strong predictor of obstetrical and neonatal outcomes, postpartum mental health, and longer-term neurobehavioral outcomes in children. Critically, in the context of the pandemic, keeping women out of psychiatric crises mitigates the necessity of visits to urgent clinical settings such as EDs and psychiatric inpatient units, which can increase the likelihood of exposure to the coronavirus.
Preservation of sleep
Disruption in sleep (duration and quality) can be seen in well over half of women during pregnancy with and without psychiatric disorders, and our experience has been that this has been exacerbated for many women during the COVID-19 crisis. Yet there are very rich data showing that sleep deprivation or sleep dysregulation in women, for example, who suffer from bipolar disorder or major depression can be a strong trigger for psychiatric relapse of underlying illness during pregnancy and the postpartum period.
During a time when normal rhythms of day-to-day life have been shifted – if not frankly disrupted – by swift transitions to remote work, cancellation of school and associated school activities across the country, complaints of insomnia and non-restorative sleep have been exceedingly common. Relevant to all but particularly for pregnant women with histories of psychiatric disorder, attention to sleep hygiene, moderation of caffeine use (if any), and use of any number of biobehavioral interventions to enhance relaxation and modulate stress may be of great value.
Cognitive-behavioral therapy for insomnia (CBT-I) has been demonstrated to be effective in pregnant women. Fortunately, there are user-friendly options on digital platforms that can be used during the pandemic that may play an important role in sustaining emotional well-being for pregnant women who have frank symptoms of insomnia.
Maintenance of ongoing antidepressant treatment during pregnancy among women with histories of mood disorder
Over a decade ago, my colleagues and I wrote about the comparison of outcomes for women with histories of recurrent major depression, demonstrating the value of maintenance treatment with antidepressants, compared with discontinuation of these medications during pregnancy (JAMA. 2006 Feb 1;295[5]:499-507). Recently, I was asked if maintenance antidepressant use in women with histories of recurrent depression was still our clinical recommendation. Over the last decade, we have noted that nearly half of women treated with antidepressants, regardless of illness severity, will discontinue their use of these medications prior to or early on in pregnancy given concerns about potential unknown effects of fetal exposure to medications, even medications for which there are robust data supporting reproductive safety regarding risk of congenital malformations. Routine discontinuation of antidepressants prior to or during pregnancy continues, despite the fact that we showed nearly 70% of those women with past histories of depression on maintenance antidepressant treatment relapsed shortly after discontinuing medication.
While we do not dictate the decisions women make about antidepressant use before, during, or after pregnancy, women with the same severity of illness will frequently make different decisions (a good thing) but we are now having very frank discussions about the particular need during a pandemic to avoid the relapse of serious psychiatric disorders. We typically endorse maintenance medication use with all but a very few number of psychotropic medications for which benefit may not outweigh risk to the fetus. However, for women who have decided nonetheless to discontinue antidepressants or other psychotropics during pregnancy despite the known risk of relapse, we strongly advise that they initiate treatment with evidence-based nonpharmacologic intervention such as CBT or mindfulness-based cognitive therapy (MBCT).
As in other areas of medicine, the pandemic is prompting we professionals in psychiatry, and specifically in perinatal psychiatry, to use all of our tools to keep pregnant and postpartum women well. The availability of digital tools to deliver MBCT and CBT has made the use of such interventions particularly viable at a time of social distancing. That being said, for patients with highly recurrent affective disorder with histories of previous recurrence when they stop their antidepressants, we are more strongly recommending serious consideration of maintenance medication treatment.
Virtual rounds in reproductive psychiatry and women’s mental health
The use of virtual platforms to connect with both patients and colleagues also has provided new opportunities for interaction with the reproductive psychiatry community as a whole. Peer teaching and peer support has been a critical part of our mission, and we decided 1 month ago to establish Virtual Rounds at the Center for Women’s Mental Health. This is a free digital platform, held on a weekly basis with our colleagues from across the country, where we discuss cases that come up in our own clinical rounds and also questions that get put forth by our colleagues in the area of reproductive psychiatry as they manage patients during the pandemic.
Changes in the postpartum experience
The last decade has brought a growing appreciation of postpartum depression and the need to screen and treat postpartum psychiatric disorders, such as postpartum mood and anxiety disorders. Yet in the era of this pandemic, the postpartum experience is itself is changing. Changes in carefully configured plans for the postpartum period – from family coming and going to mobilizing extra support at home and to now having new moms having to manage families and their other children at home – has been an enormous stressor for many women. Plans to have more elderly parents visit during the acute postpartum period, and the increased concerns about people traveling to and from a home where there is a newborn and the need to quarantine, has made the transition to motherhood much more complicated for all postpartum women, let alone for those postpartum women who have histories of psychiatric disorder.
There is a risk of social isolation for postpartum women even under normal circumstances, and this is profoundly more likely during this pandemic. We are actively working with our postpartum patients and optimizing treatment, brainstorming options in terms of using both virtual and real-time support to the extent that it is safe in order to keep women healthy during such a stressful and critical time.
I am heartened by the efforts on the part of organizations such as Postpartum Support International to make available virtually their resources with respect to community-based support and education for women who feel increasingly isolated during the postpartum period, a time where connectedness is so critical.
Summarily, these have been challenging times, but also times of opportunity. The COVID-19 pandemic has prompted us to get even more creative as we configure ways to optimize the emotional well-being of our patients who are planning to get pregnant, who are pregnant, or who are post partum.
The current time, while challenging in so many ways and a time of great pain, loss, and grief for far too many, has also provided an opportunity to work even more collaboratively with our colleagues, coming up with new paradigms of treatments as we weather this historic challenge.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
When last I wrote this column, I was preparing for travel to professional meetings in the spring, planning a presentation for an upcoming grand rounds, and readying to host a scientific advisory board meeting as part of a large scientific project we conduct in Center for Women’s Mental Health. We were also awaiting the relocation of several junior faculty and research staff to Boston this spring and summer as we build our team.

It is now obvious that the COVID-19 pandemic is not a passing squall, but rather a persistent gale that has placed our collective sails in the water. It has not capsized the boat, however, thanks in part to the actions of courageous frontline caregivers and first responders who have mobilized in the wake of this recent public health crisis. From doctors, nurses, and hospital staff to grocery store clerks, home health aides, and neighbors checking in on the elderly – to name just a few – a whole crew of members across society have helped buoy our collective ship. Resilience also is required by all of us who are managing the array of feelings brought about by the day-in, day-out challenges of living life with restricted movement and freedom to engage in pre-COVID-19 activities we took for granted. What seemed like a temporary workaround is now becoming the “new normal” for an unknown amount of time looking forward.
For over 3 decades, my colleagues and I have worked with women who suffer from serious psychiatric disorders and whose treatment has required psychiatric medications such as antidepressants, mood stabilizers, and anxiolytics. The challenge of our work with women who are pregnant or planning pregnancy has been the configuration of the safest ways to navigate treatment on an individual basis for these women across pregnancy and post partum, with continual assessments of how to minimize the risk to fetus from in utero exposure to medications that have been instrumental in the treatment of psychiatric disorders on one hand versus the risks of untreated psychiatric disorder on the other. This work has been the essence of the clinical mission and the cornerstone of the research conducted at the Center for Women’s Mental Health since its inception.
While I have worked shoulder to shoulder with obstetricians for years, my respect for these colleagues during these past weeks has only grown as they have instituted the swiftest protocols to mitigate risk associated with COVID-19 for our pregnant patients, some of whom have tested positive for COVID-19, all in an effort to keep both mother, fetus, and newborn as safe as possible.
For those of us providing mental health services to pregnant women during this time, certain clinical situations have arisen in the context of the COVID-19 pandemic which require particular attention and discussion.
Planned pregnancy and contraception during the COVID-19 pandemic
Half of the pregnancies in this country are unplanned. Now more than ever, it is critical that decisions about moving forward with a plan to conceive be deliberate. These considerations range from the existential to the most concrete. For example, during these last weeks, we have consulted on cases where couples on the cusp of attempts to conceive face concerns about COVID-19, hence making more complicated their timeline with respect to actual plans to get pregnant. These are complicated decisions, particularly for women who may be slightly older and at the reproductive age where delaying pregnancy may have an adverse effect on fertility.
A concrete example of how the pandemic has affected fertility is evident as we encounter situations where women may defer starting a prescription oral contraceptive or lapse in its use because they have had difficulty coordinating visits with health care providers and may fear picking up prescriptions from pharmacies. We also have seen that procedures such as IUD placements have been deferred or canceled, or that some patients decline trips to the hospital or clinic to receive this type of service. These new barriers to access of contraception may require more planning at this time so that decisions about family planning are by design and not default during a time as complicated as the current public health crisis.
Telemedicine: telepsychiatry and obstetrics virtual visits
While wide-scale use of telemedicine platforms was not the standard day-to-day practice in either obstetrics or psychiatry prior to the pandemic, telepsychiatry has come up to speed within a short number of weeks. At our institution, 85% of outpatient visits are being conducted remotely, with in-person visits being reserved for only urgent or emergent visits. Our inpatient psychiatry service remains a setting where psychiatric patients, regardless of their COVID-19 status, can receive necessary care.
The use of telemedicine and specifically telepsychiatry is critical to mitigate the likelihood of exposure to SARS-CoV-2. On our reproductive psychiatry service, it has actually been an opportunity to engage with patients for comprehensive initial consults about reproductive safety of psychiatric medications currently being taken, or for ongoing consultation and direct patient care during follow-up visits during pregnancy to see that patients are sustaining emotional well-being or have changes for treatment implemented if they are not well. An increased frequency of visits allows us more opportunity to capture any signs of early clinical worsening of symptoms that might have been missed previously using the more traditional in-person setting.
Telepsychiatry and “virtual visits” have allowed us to do real-time, nimble modifications of treatment regimens with both pharmacologic and nonpharmacologic interventions to keep women well and to keep them out of the hospital for psychiatric care as often as possible. It also has facilitated a closer collaboration with our colleagues in obstetrics. In a way, the team of providers, including psychiatrists, obstetrical providers, social workers, and therapists can more easily communicate virtually than has sometimes been the case previously, when day-to-day use of telemedicine and virtual team meetings was less common.
Recognition and treatment of anxiety in perinatal patients
Even pregnant women without preexisting anxiety disorders may have heightened anxiety during usual times, and women and their partners cope with this typically in numerous ways including participation in peer-support opportunities, wellness and self-care activities, leveraging support from care providers, and engaging with family. But the previously “typical pregnancy experience” has shifted in the context of COVID-19. Specifically, added concerns of pregnant women about becoming infected, of potential separation from family if they do become ill, or of separation from partners or support systems during labor and delivery (an issue that has been largely resolved in many hospitals), as well as the possibility that a neonate might become ill with exposure to the coronavirus are obviously understandable and real. Such contingencies are unsettling, even for the most settled of our patients. Labor and delivery plans, and plans for outside help from family or others with the baby and older children in the postpartum period, have been upended for many patients.
These are anxious times. The number of nonpharmacologic virtual interventions available to mitigate anxiety are filling email inboxes daily. Curating these options can be a challenge, although several resources are worth noting, such as our department’s page on mental health resources.
During these past weeks, we have seen growing numbers of women for whom the normative anxiety of pregnancy is increasing to the point of causing distress to the level of functional impairment. Many patients for the first time meet criteria for frank anxiety disorders. These patients deserve prompt evaluation by mental health professionals and treatment with evidence-based therapies for anxiety disorders whether nonpharmacologic or pharmacologic so as to mitigate the risk of untreated anxiety on maternal and fetal well-being and also to limit risk for postpartum depression and postpartum anxiety disorders.
Miscarriage and infertility
A 36-year-old patient came to see me in clinic in late January following a miscarriage. She had a history of a previous miscarriage a year before and had an episode of major depression to follow for which she received treatment with an antidepressant and cognitive-behavioral therapy; she also attended a perinatal loss support group. She saw me in early March, anxious to try to conceive but extremely concerned about the risks associated with becoming pregnant at this point in time. Following a lengthy discussion with me and her obstetrician, the patient decided to wait until “the curve flattened” in Boston in terms of new cases of COVID-19, and then start trying to conceive. The case of another patient with a very similar history was presented at our rounds a few weeks ago; she also elected to defer attempts to conceive until life is more settled.
Perhaps one of the most dramatic examples of the impact of COVID-19 on fertility has been for those women with plans to pursue treatment with one of the assisted reproductive technologies. They have been told that professional societies have made recommendations regarding use of assisted reproductive technologies that are not entirely consistent across the country, but where in many places such interventions have been suspended during the COVID-19 pandemic. For many women near the end of their reproductive years, delays in trying to conceive either with or without the aid of fertility treatments may indelibly shape their plans to have children.
Sustaining emotional well-being across pregnancy
Because most psychiatric disorders are chronic in course, it is often the situation where women are treated to wellness for serious psychiatric disorders, with the goal of maintaining wellness across pregnancy and the post partum. One of the most critical takeaway points from 30 years of working with psychiatrically ill pregnant women is the maxim that keeping women well during pregnancy is simply imperative. Maternal psychiatric well-being during pregnancy is a strong predictor of obstetrical and neonatal outcomes, postpartum mental health, and longer-term neurobehavioral outcomes in children. Critically, in the context of the pandemic, keeping women out of psychiatric crises mitigates the necessity of visits to urgent clinical settings such as EDs and psychiatric inpatient units, which can increase the likelihood of exposure to the coronavirus.
Preservation of sleep
Disruption in sleep (duration and quality) can be seen in well over half of women during pregnancy with and without psychiatric disorders, and our experience has been that this has been exacerbated for many women during the COVID-19 crisis. Yet there are very rich data showing that sleep deprivation or sleep dysregulation in women, for example, who suffer from bipolar disorder or major depression can be a strong trigger for psychiatric relapse of underlying illness during pregnancy and the postpartum period.
During a time when normal rhythms of day-to-day life have been shifted – if not frankly disrupted – by swift transitions to remote work, cancellation of school and associated school activities across the country, complaints of insomnia and non-restorative sleep have been exceedingly common. Relevant to all but particularly for pregnant women with histories of psychiatric disorder, attention to sleep hygiene, moderation of caffeine use (if any), and use of any number of biobehavioral interventions to enhance relaxation and modulate stress may be of great value.
Cognitive-behavioral therapy for insomnia (CBT-I) has been demonstrated to be effective in pregnant women. Fortunately, there are user-friendly options on digital platforms that can be used during the pandemic that may play an important role in sustaining emotional well-being for pregnant women who have frank symptoms of insomnia.
Maintenance of ongoing antidepressant treatment during pregnancy among women with histories of mood disorder
Over a decade ago, my colleagues and I wrote about the comparison of outcomes for women with histories of recurrent major depression, demonstrating the value of maintenance treatment with antidepressants, compared with discontinuation of these medications during pregnancy (JAMA. 2006 Feb 1;295[5]:499-507). Recently, I was asked if maintenance antidepressant use in women with histories of recurrent depression was still our clinical recommendation. Over the last decade, we have noted that nearly half of women treated with antidepressants, regardless of illness severity, will discontinue their use of these medications prior to or early on in pregnancy given concerns about potential unknown effects of fetal exposure to medications, even medications for which there are robust data supporting reproductive safety regarding risk of congenital malformations. Routine discontinuation of antidepressants prior to or during pregnancy continues, despite the fact that we showed nearly 70% of those women with past histories of depression on maintenance antidepressant treatment relapsed shortly after discontinuing medication.
While we do not dictate the decisions women make about antidepressant use before, during, or after pregnancy, women with the same severity of illness will frequently make different decisions (a good thing) but we are now having very frank discussions about the particular need during a pandemic to avoid the relapse of serious psychiatric disorders. We typically endorse maintenance medication use with all but a very few number of psychotropic medications for which benefit may not outweigh risk to the fetus. However, for women who have decided nonetheless to discontinue antidepressants or other psychotropics during pregnancy despite the known risk of relapse, we strongly advise that they initiate treatment with evidence-based nonpharmacologic intervention such as CBT or mindfulness-based cognitive therapy (MBCT).
As in other areas of medicine, the pandemic is prompting we professionals in psychiatry, and specifically in perinatal psychiatry, to use all of our tools to keep pregnant and postpartum women well. The availability of digital tools to deliver MBCT and CBT has made the use of such interventions particularly viable at a time of social distancing. That being said, for patients with highly recurrent affective disorder with histories of previous recurrence when they stop their antidepressants, we are more strongly recommending serious consideration of maintenance medication treatment.
Virtual rounds in reproductive psychiatry and women’s mental health
The use of virtual platforms to connect with both patients and colleagues also has provided new opportunities for interaction with the reproductive psychiatry community as a whole. Peer teaching and peer support has been a critical part of our mission, and we decided 1 month ago to establish Virtual Rounds at the Center for Women’s Mental Health. This is a free digital platform, held on a weekly basis with our colleagues from across the country, where we discuss cases that come up in our own clinical rounds and also questions that get put forth by our colleagues in the area of reproductive psychiatry as they manage patients during the pandemic.
Changes in the postpartum experience
The last decade has brought a growing appreciation of postpartum depression and the need to screen and treat postpartum psychiatric disorders, such as postpartum mood and anxiety disorders. Yet in the era of this pandemic, the postpartum experience is itself is changing. Changes in carefully configured plans for the postpartum period – from family coming and going to mobilizing extra support at home and to now having new moms having to manage families and their other children at home – has been an enormous stressor for many women. Plans to have more elderly parents visit during the acute postpartum period, and the increased concerns about people traveling to and from a home where there is a newborn and the need to quarantine, has made the transition to motherhood much more complicated for all postpartum women, let alone for those postpartum women who have histories of psychiatric disorder.
There is a risk of social isolation for postpartum women even under normal circumstances, and this is profoundly more likely during this pandemic. We are actively working with our postpartum patients and optimizing treatment, brainstorming options in terms of using both virtual and real-time support to the extent that it is safe in order to keep women healthy during such a stressful and critical time.
I am heartened by the efforts on the part of organizations such as Postpartum Support International to make available virtually their resources with respect to community-based support and education for women who feel increasingly isolated during the postpartum period, a time where connectedness is so critical.
Summarily, these have been challenging times, but also times of opportunity. The COVID-19 pandemic has prompted us to get even more creative as we configure ways to optimize the emotional well-being of our patients who are planning to get pregnant, who are pregnant, or who are post partum.
The current time, while challenging in so many ways and a time of great pain, loss, and grief for far too many, has also provided an opportunity to work even more collaboratively with our colleagues, coming up with new paradigms of treatments as we weather this historic challenge.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
Contact tracing, isolation have impact, study shows
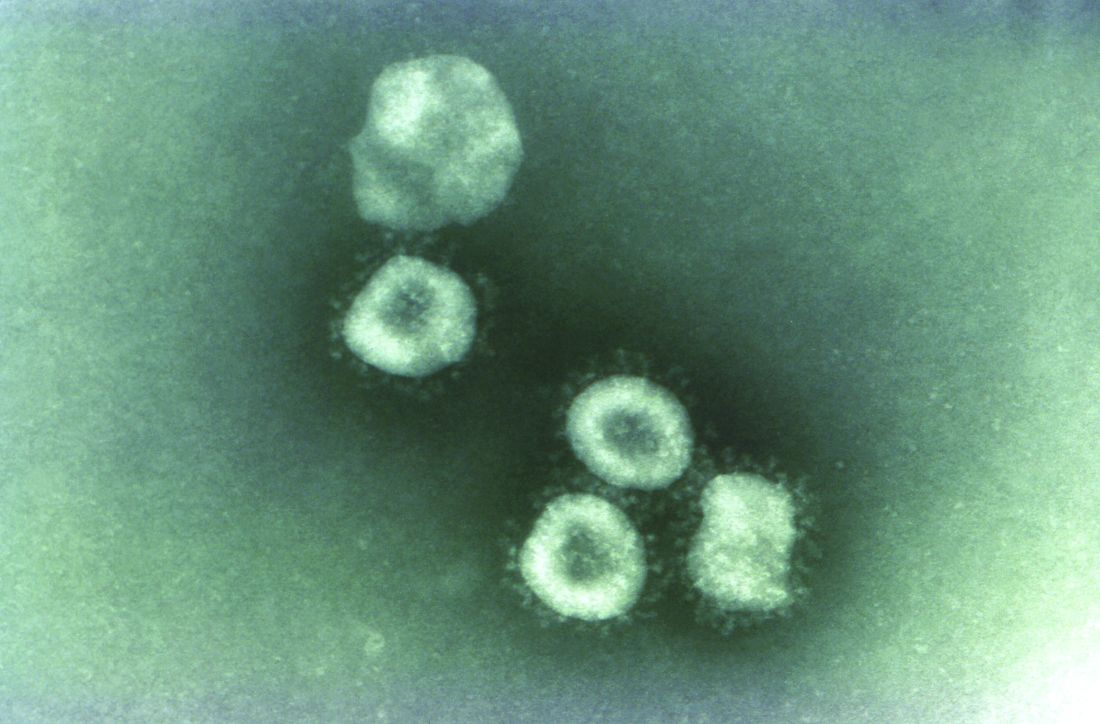
A far-reaching surveillance initiative was implemented in Shenzhen, China, to isolate and contact trace people suspected of having the COVID-19 coronavirus. This initiative led to faster confirmation of new cases and reduced the window of time during which people were infectious in the community. This potentially reduced the number of new infections that arose from each case, according to a study of patients and contacts over 4 weeks (Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099[20]30287-5).
“The experience of COVID-19 in the city of Shenzhen may demonstrate the huge scale of testing and contact tracing that’s needed to reduce the virus spreading,” said study coauthor Ting Ma, PhD, of Harbin Institute of Technology at Shenzhen.
Dr. Ma acknowledged that some of the measures the program used, such as isolating people outside their homes, may be difficult to impose in other countries, “but we urge governments to consider our findings in the global response to COVID-19.”
The study followed 391 coronavirus cases and 1,286 close contacts identified by the Shenzhen Center for Disease Control and Prevention from Jan. 14 to Feb. 12 this year. The study showed that contact tracing led to confirming new diagnoses within 3.2 days on average vs. 5.5 for symptom-based surveillance, and reduced the time it took to isolate newly infected people by 2 days, from an average of 4.6 to 2.7 days. Eighty-seven people were diagnosed with COVID-19 after they were contact traced and tested. Twenty percent of them had no symptoms, and 29% had no fever. Three deaths occurred in the group during the study period.
The surveillance program was comprehensive and intense. On Jan. 8, the Shenzhen CDC started monitoring travelers from Hubei province, of which Wuhan is the capital, for symptoms of COVID-19. Shenzhen is a city of about 12.5 million people in southeastern China, near Hong Kong, and is about 560 miles south of Wuhan. Over the next 2 weeks, the Shenzhen CDC expanded that surveillance program to all travelers from Hubei regardless of symptoms, along with local hospital patients and people detected by fever screenings at area clinics.
Suspected cases and close contacts underwent nasal-swab testing at 40 different locations in the city. The program identified close contacts through contact tracing, and included anyone who lived in the same dwelling, shared a meal, traveled, or had a social interaction with an index 2 days before symptoms appeared. Casual contacts and some close contacts, such as clinic nurses, who wore masks during the encounters were excluded.
“To achieve similar results, other countries might be able to combine near-universal testing and intensive contact tracing with social distancing and partial lockdowns,” said Dr. Ma. “Although no lockdown measures were introduced in Shenzhen until the end of our study period, Wuhan’s lockdown could have significantly restricted the spread of coronavirus to Shenzhen.”
The researchers noted that children are as susceptible to the virus as are adults, even though their symptoms are not as severe as those of adults. The rate of infection in children 10 and younger was similar to the overall infection rate, 7.4% vs. 6.6%, so the researchers noted that surveillance measures should target them as well.
“This study to me confirms a lot of what we’ve already known,” Aaron E. Glatt, MD, chairman of medicine and an epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “It’s an elegant study, but at the same time it sends us a message that we’re at a critical point of time for us to intervene and prevent cases at the very beginning.”
He acknowledged that the Shenzhen effort was intense. “It’s always a resource-intense requirement to do such extensive contact tracing, but that doesn’t mean it shouldn’t be done to the best of your ability to do so,” he said. He was struck by the low relative rate of infection among contacts in the study – around 7%. “There are differences obviously in infection rates in every outbreak,” he said. “Every individual has their own particular infection rate. While we can take ranges and statistical guesses for every individual patient, it could be very high or very low, and that’s most critical to nip it in the bud.”
Lead author Qifang Bi and study coauthors had no financial relationships to disclose.
SOURCE: Bi Q et al. Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099(20)30287-5.
A far-reaching surveillance initiative was implemented in Shenzhen, China, to isolate and contact trace people suspected of having the COVID-19 coronavirus. This initiative led to faster confirmation of new cases and reduced the window of time during which people were infectious in the community. This potentially reduced the number of new infections that arose from each case, according to a study of patients and contacts over 4 weeks (Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099[20]30287-5).
“The experience of COVID-19 in the city of Shenzhen may demonstrate the huge scale of testing and contact tracing that’s needed to reduce the virus spreading,” said study coauthor Ting Ma, PhD, of Harbin Institute of Technology at Shenzhen.
Dr. Ma acknowledged that some of the measures the program used, such as isolating people outside their homes, may be difficult to impose in other countries, “but we urge governments to consider our findings in the global response to COVID-19.”
The study followed 391 coronavirus cases and 1,286 close contacts identified by the Shenzhen Center for Disease Control and Prevention from Jan. 14 to Feb. 12 this year. The study showed that contact tracing led to confirming new diagnoses within 3.2 days on average vs. 5.5 for symptom-based surveillance, and reduced the time it took to isolate newly infected people by 2 days, from an average of 4.6 to 2.7 days. Eighty-seven people were diagnosed with COVID-19 after they were contact traced and tested. Twenty percent of them had no symptoms, and 29% had no fever. Three deaths occurred in the group during the study period.
The surveillance program was comprehensive and intense. On Jan. 8, the Shenzhen CDC started monitoring travelers from Hubei province, of which Wuhan is the capital, for symptoms of COVID-19. Shenzhen is a city of about 12.5 million people in southeastern China, near Hong Kong, and is about 560 miles south of Wuhan. Over the next 2 weeks, the Shenzhen CDC expanded that surveillance program to all travelers from Hubei regardless of symptoms, along with local hospital patients and people detected by fever screenings at area clinics.
Suspected cases and close contacts underwent nasal-swab testing at 40 different locations in the city. The program identified close contacts through contact tracing, and included anyone who lived in the same dwelling, shared a meal, traveled, or had a social interaction with an index 2 days before symptoms appeared. Casual contacts and some close contacts, such as clinic nurses, who wore masks during the encounters were excluded.
“To achieve similar results, other countries might be able to combine near-universal testing and intensive contact tracing with social distancing and partial lockdowns,” said Dr. Ma. “Although no lockdown measures were introduced in Shenzhen until the end of our study period, Wuhan’s lockdown could have significantly restricted the spread of coronavirus to Shenzhen.”
The researchers noted that children are as susceptible to the virus as are adults, even though their symptoms are not as severe as those of adults. The rate of infection in children 10 and younger was similar to the overall infection rate, 7.4% vs. 6.6%, so the researchers noted that surveillance measures should target them as well.
“This study to me confirms a lot of what we’ve already known,” Aaron E. Glatt, MD, chairman of medicine and an epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “It’s an elegant study, but at the same time it sends us a message that we’re at a critical point of time for us to intervene and prevent cases at the very beginning.”
He acknowledged that the Shenzhen effort was intense. “It’s always a resource-intense requirement to do such extensive contact tracing, but that doesn’t mean it shouldn’t be done to the best of your ability to do so,” he said. He was struck by the low relative rate of infection among contacts in the study – around 7%. “There are differences obviously in infection rates in every outbreak,” he said. “Every individual has their own particular infection rate. While we can take ranges and statistical guesses for every individual patient, it could be very high or very low, and that’s most critical to nip it in the bud.”
Lead author Qifang Bi and study coauthors had no financial relationships to disclose.
SOURCE: Bi Q et al. Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099(20)30287-5.
A far-reaching surveillance initiative was implemented in Shenzhen, China, to isolate and contact trace people suspected of having the COVID-19 coronavirus. This initiative led to faster confirmation of new cases and reduced the window of time during which people were infectious in the community. This potentially reduced the number of new infections that arose from each case, according to a study of patients and contacts over 4 weeks (Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099[20]30287-5).
“The experience of COVID-19 in the city of Shenzhen may demonstrate the huge scale of testing and contact tracing that’s needed to reduce the virus spreading,” said study coauthor Ting Ma, PhD, of Harbin Institute of Technology at Shenzhen.
Dr. Ma acknowledged that some of the measures the program used, such as isolating people outside their homes, may be difficult to impose in other countries, “but we urge governments to consider our findings in the global response to COVID-19.”
The study followed 391 coronavirus cases and 1,286 close contacts identified by the Shenzhen Center for Disease Control and Prevention from Jan. 14 to Feb. 12 this year. The study showed that contact tracing led to confirming new diagnoses within 3.2 days on average vs. 5.5 for symptom-based surveillance, and reduced the time it took to isolate newly infected people by 2 days, from an average of 4.6 to 2.7 days. Eighty-seven people were diagnosed with COVID-19 after they were contact traced and tested. Twenty percent of them had no symptoms, and 29% had no fever. Three deaths occurred in the group during the study period.
The surveillance program was comprehensive and intense. On Jan. 8, the Shenzhen CDC started monitoring travelers from Hubei province, of which Wuhan is the capital, for symptoms of COVID-19. Shenzhen is a city of about 12.5 million people in southeastern China, near Hong Kong, and is about 560 miles south of Wuhan. Over the next 2 weeks, the Shenzhen CDC expanded that surveillance program to all travelers from Hubei regardless of symptoms, along with local hospital patients and people detected by fever screenings at area clinics.
Suspected cases and close contacts underwent nasal-swab testing at 40 different locations in the city. The program identified close contacts through contact tracing, and included anyone who lived in the same dwelling, shared a meal, traveled, or had a social interaction with an index 2 days before symptoms appeared. Casual contacts and some close contacts, such as clinic nurses, who wore masks during the encounters were excluded.
“To achieve similar results, other countries might be able to combine near-universal testing and intensive contact tracing with social distancing and partial lockdowns,” said Dr. Ma. “Although no lockdown measures were introduced in Shenzhen until the end of our study period, Wuhan’s lockdown could have significantly restricted the spread of coronavirus to Shenzhen.”
The researchers noted that children are as susceptible to the virus as are adults, even though their symptoms are not as severe as those of adults. The rate of infection in children 10 and younger was similar to the overall infection rate, 7.4% vs. 6.6%, so the researchers noted that surveillance measures should target them as well.
“This study to me confirms a lot of what we’ve already known,” Aaron E. Glatt, MD, chairman of medicine and an epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “It’s an elegant study, but at the same time it sends us a message that we’re at a critical point of time for us to intervene and prevent cases at the very beginning.”
He acknowledged that the Shenzhen effort was intense. “It’s always a resource-intense requirement to do such extensive contact tracing, but that doesn’t mean it shouldn’t be done to the best of your ability to do so,” he said. He was struck by the low relative rate of infection among contacts in the study – around 7%. “There are differences obviously in infection rates in every outbreak,” he said. “Every individual has their own particular infection rate. While we can take ranges and statistical guesses for every individual patient, it could be very high or very low, and that’s most critical to nip it in the bud.”
Lead author Qifang Bi and study coauthors had no financial relationships to disclose.
SOURCE: Bi Q et al. Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099(20)30287-5.
FROM LANCET INFECTIOUS DISEASE
Supreme Court: Government owes more than $12 billion to health plans
The federal government owes billions of dollars to health insurers under an Affordable Care Act provision intended to help insurers mitigate risk, the U.S. Supreme Court has ruled.
In an 8-to-1 vote announced April 27, justices sided with the plaintiff health plans in Maine Community Health Options v. United States, ruling that the risk corridors statute created a government obligation to pay insurers the full amount originally calculated and that appropriation measures later passed by Congress did not repeal this obligation.
“In establishing the temporary risk corridors program, Congress created a rare money-mandating obligation requiring the federal government to make payments under [Section 1342 of the Affordable Care Act’s] formula,” Associate Justice Sonia Sotomayor wrote in the majority opinion. “Lacking other statutory paths to relief ... petitioners may seek to collect payment through a damages action in the Court of Federal Claims.”
Maine Community Health Options v. United States, which consolidates several lawsuits against the government, centers on the ACA’s risk corridor program, which required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged by more than $12 billion all together.
The U.S. Department of Justice countered that the government is not required to pay the plans because of measures passed by Congress in 2014 and later years that limited the funding available to compensate insurers for their losses.
The U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
The U.S. Supreme Court disagreed. Justices noted that even after Congress enacted the first rider, HHS and the Centers for Medicare & Medicaid Services reiterated that the ACA requires the Secretary to make full payments to issuers and that “HHS [would] record risk corridors payments due as an obligation of the United States government for which full payment is required,” according to the Supreme Court opinion.
“They understood that profitable insurers’ payments to the government would not dispel the Secretary’s obligation to pay unprofitable insurers, even ‘in the event of a shortfall,’ ” Justice Sotomayor wrote in the majority opinion.
Associate Justice Samuel Alito Jr. however, took issue with his fellow justices’ decision. In his dissenting opinion, Justice Alito wrote that under the ruling, billions of taxpayer dollars will be turned over to insurance companies that bet unsuccessfully on the success of the program in question.
“This money will have to be paid even though Congress has pointedly declined to appropriate money for that purpose,” he wrote. “Not only will today’s decision have a massive immediate impact, its potential consequences go much further.”
The high court remanded the consolidated cases to the lower court for further proceedings on details of the disbursement.
The federal government owes billions of dollars to health insurers under an Affordable Care Act provision intended to help insurers mitigate risk, the U.S. Supreme Court has ruled.
In an 8-to-1 vote announced April 27, justices sided with the plaintiff health plans in Maine Community Health Options v. United States, ruling that the risk corridors statute created a government obligation to pay insurers the full amount originally calculated and that appropriation measures later passed by Congress did not repeal this obligation.
“In establishing the temporary risk corridors program, Congress created a rare money-mandating obligation requiring the federal government to make payments under [Section 1342 of the Affordable Care Act’s] formula,” Associate Justice Sonia Sotomayor wrote in the majority opinion. “Lacking other statutory paths to relief ... petitioners may seek to collect payment through a damages action in the Court of Federal Claims.”
Maine Community Health Options v. United States, which consolidates several lawsuits against the government, centers on the ACA’s risk corridor program, which required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged by more than $12 billion all together.
The U.S. Department of Justice countered that the government is not required to pay the plans because of measures passed by Congress in 2014 and later years that limited the funding available to compensate insurers for their losses.
The U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
The U.S. Supreme Court disagreed. Justices noted that even after Congress enacted the first rider, HHS and the Centers for Medicare & Medicaid Services reiterated that the ACA requires the Secretary to make full payments to issuers and that “HHS [would] record risk corridors payments due as an obligation of the United States government for which full payment is required,” according to the Supreme Court opinion.
“They understood that profitable insurers’ payments to the government would not dispel the Secretary’s obligation to pay unprofitable insurers, even ‘in the event of a shortfall,’ ” Justice Sotomayor wrote in the majority opinion.
Associate Justice Samuel Alito Jr. however, took issue with his fellow justices’ decision. In his dissenting opinion, Justice Alito wrote that under the ruling, billions of taxpayer dollars will be turned over to insurance companies that bet unsuccessfully on the success of the program in question.
“This money will have to be paid even though Congress has pointedly declined to appropriate money for that purpose,” he wrote. “Not only will today’s decision have a massive immediate impact, its potential consequences go much further.”
The high court remanded the consolidated cases to the lower court for further proceedings on details of the disbursement.
The federal government owes billions of dollars to health insurers under an Affordable Care Act provision intended to help insurers mitigate risk, the U.S. Supreme Court has ruled.
In an 8-to-1 vote announced April 27, justices sided with the plaintiff health plans in Maine Community Health Options v. United States, ruling that the risk corridors statute created a government obligation to pay insurers the full amount originally calculated and that appropriation measures later passed by Congress did not repeal this obligation.
“In establishing the temporary risk corridors program, Congress created a rare money-mandating obligation requiring the federal government to make payments under [Section 1342 of the Affordable Care Act’s] formula,” Associate Justice Sonia Sotomayor wrote in the majority opinion. “Lacking other statutory paths to relief ... petitioners may seek to collect payment through a damages action in the Court of Federal Claims.”
Maine Community Health Options v. United States, which consolidates several lawsuits against the government, centers on the ACA’s risk corridor program, which required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged by more than $12 billion all together.
The U.S. Department of Justice countered that the government is not required to pay the plans because of measures passed by Congress in 2014 and later years that limited the funding available to compensate insurers for their losses.
The U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
The U.S. Supreme Court disagreed. Justices noted that even after Congress enacted the first rider, HHS and the Centers for Medicare & Medicaid Services reiterated that the ACA requires the Secretary to make full payments to issuers and that “HHS [would] record risk corridors payments due as an obligation of the United States government for which full payment is required,” according to the Supreme Court opinion.
“They understood that profitable insurers’ payments to the government would not dispel the Secretary’s obligation to pay unprofitable insurers, even ‘in the event of a shortfall,’ ” Justice Sotomayor wrote in the majority opinion.
Associate Justice Samuel Alito Jr. however, took issue with his fellow justices’ decision. In his dissenting opinion, Justice Alito wrote that under the ruling, billions of taxpayer dollars will be turned over to insurance companies that bet unsuccessfully on the success of the program in question.
“This money will have to be paid even though Congress has pointedly declined to appropriate money for that purpose,” he wrote. “Not only will today’s decision have a massive immediate impact, its potential consequences go much further.”
The high court remanded the consolidated cases to the lower court for further proceedings on details of the disbursement.
More doctors used digital tools in 2019
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
COVID-19 spurs telemedicine, furloughs, retirement
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
Will COVID-19 finally trigger action on health disparities?
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Consensus recommendations on AMI management during COVID-19
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
New advocacy group aims to give ‘every physician’ a voice
A new advocacy organization is launching on April 28 to give “every physician” a voice in decisions that affect their professional lives. But this group doesn’t intend to use the top-down approach to decision making seen in many medical societies.
Paul Teirstein, MD, chief of cardiology for Scripps Clinic in La Jolla, Calif., and founder of the new organization United Physicians, said in an interviewit is a nonprofit group that will operate through online participation.
He said
Projects would need the support of a two-thirds majority of United Physicians’ members to proceed with any proposals. Meetings will be held publicly online, Dr. Teirstein explained.
There is a need for a broad-based organization that will respond to the voice of practicing physicians rather than dictate legislative priorities from management ranks, he said.
Dr. Teirstein said he learned how challenging it is to bring physicians together on issues in 2014 in his battles against changes in maintenance of certification rules. The result of his efforts was the National Board of Physicians and Surgeons (NBPAS), set up to provide a means of certification different from the one offered by the American Board of Internal Medicine.
Dr. Teirstein has argued that the approach of ABIM unfairly burdened physicians with a stepped-up schedule of testing and relied on an outdated approach to the practice of medicine.
Physicians busy with their practices feel they lack a unified voice in contesting the growing administrative burden and unproductive federal and state policies, Dr. Teirstein said.
He cited the limited enrollment in the largest physician groups as evidence of how disenfranchised many clinicians feel. There are about 1 million professional active physicians in the United States, according to the nonprofit Kaiser Family Foundation. Yet, even the largest physician group, the American Medical Association, has about 250,000 members, according to its 2018 annual report
“Clearly, most physicians believe they have little voice when it comes to health care decisions,” Dr. Teirstein said. “Our physician associations are governed from the top down. The leaders set the agenda. There may be delegates, but does leadership really listen to the delegates? Do the delegates really listen to the physician community?”
On its website, AMA describes itself as “physicians’ powerful ally in patient care” that works with more than 190 state and specialty medical societies. In recent months, James L. Madara, MD, the group’s chief executive officer, has urged governors to remove obstacles for physicians who want to fill workforce gaps in COVID-19 hot spots, among other actions.
In its annual report, the AMA, which declined to comment for this article, said its membership rose by 3.4% in 2018, double the growth rate of the previous year, thanks to a membership drive.
“The campaign celebrates the powerful work of our physician members and showcases how their individual efforts – along with the AMA – are moving medicine forward,” wrote Dr. Madara and other organization leaders in the report.
What Dr. Teirstein proposes is an inversion of the structure used by other medical societies, in which he says leaders and delegates dictate priorities.
United Physicians will use meetings and votes held by members online to decide which projects to pursue. Fees would be kept nominal, likely about $10 a year, depending on the number of members. Fees would be subject to change on the basis of expenses. The AMA has a sliding fee schedule that tops out with annual dues for physicians in regular practice of $420.
“There are no delegates, no representatives, and no board of directors. We want every physician to join and every physician to vote on every issue,” Dr. Teirstein said.
He stressed that he sees United Physicians as being complementary to the AMA.
“We do not compete with other organizations. Ideally, other organizations will use the platform,” Dr. Teirstein said. “If the AMA is considering a new policy, it can use the United Physicians platform to measure physician support. For example, through online discussions, petitions, and voting, it might learn a proposed policy needs a few tweaks to be accepted by most physicians.”
No compensation
Dr. Teirstein is among physician leaders who in recent years have sought to rally their colleagues to fight back against growing administrative burdens.
In a 2015 article in JAMA that was written with Medscape’s editor in chief, Eric Topol, MD, Dr. Teirstein criticized the ABIM’s drive to have physicians complete tests every 2 years and participate in continuous certification instead of recertifying once a decade, as had been the practice.
Dr. Teirstein formed the NBPAS as an alternative path for certification, with Dr. Topol serving on the board for that organization. Dr. Topol also will serve as a member of the advisory board for Teirstein’s United Physicians.
Dr. Topol wrote an article that appeared in the New Yorker last August that argued for physicians to move beyond the confines of medical societies and seek a path for broad-based activism. He said he intended to challenge medical societies, which, for all the good they do, can sometimes lose focus on that core relationship in favor of the bottom line.
Dr. Topol said in an interview that his colleague’s new project is a “good idea for a democratized platform at a time when physician solidarity is needed more than ever.”
Dr. Teirstein plans to run United Physicians on a volunteer basis. This builds on the approach he has used for NBPAS. He and the directors of the NBPAS will receive no compensation, he said, as was confirmed by the NBPAS.
In contrast, Dr. Madara made about $2.5 million in total compensation for 2018, according to the organization’s Internal Revenue Service filing. Physicians who served as trustees and officials for the AMA that year received annual compensation that ranged from around $60,000 to $291,980, depending on their duties.
“Having volunteer leadership mitigates conflict of interest. It also ensures leadership has a ‘day job’ that keeps them in touch with issues impacting practicing physicians,” Dr. Teirstein said
Start-up costs for United Physicians will be supported by NBPAS, but it will function as a completely independent organization, he added.
In introducing the group, Dr. Teirstein outlined suggestions for proposals it might pursue. These include making hospitals secure adequate supplies of personal protective equipment ahead of health crises such as the COVID-19 pandemic.
His outline also includes suggestions for issues that likely will persist beyond the response to the pandemic.
Dr. Teirstein proposed a project for persuading insurance companies to provide online calendar appointments for peer-to-peer patient preauthorization. Failure of the insurer’s representative to attend would trigger approval of authorization under this proposal. He also suggested a lobbying effort for specific reimbursement for peer-to-peer, patient preauthorization phone calls.
Dr. Teirstein said he hopes most of the proposals will come from physicians who join United Physicians. Still, it is unclear whether United Physicians will succeed. An initial challenge could be in sorting through a barrage of competing ideas submitted to United Physicians.
But Dr. Teirstein appears hopeful about the changes for this experiment in online advocacy. He intends for United Physicians to be a pathway for clinicians to translate their complaints about policies into calls for action, with only a short investment of their time.
“Most of us have wonderful, engrossing jobs. It’s hard to beat helping a patient, and most of us get to do it every day,” Dr. .Teirstein said. “Will we take the 30 seconds required to sign up and become a United Physicians member? Will we spend a little time each week reviewing the issues and voting? I think it’s an experiment worth watching.”
A version of this article originally appeared on Medscape.com.
A new advocacy organization is launching on April 28 to give “every physician” a voice in decisions that affect their professional lives. But this group doesn’t intend to use the top-down approach to decision making seen in many medical societies.
Paul Teirstein, MD, chief of cardiology for Scripps Clinic in La Jolla, Calif., and founder of the new organization United Physicians, said in an interviewit is a nonprofit group that will operate through online participation.
He said
Projects would need the support of a two-thirds majority of United Physicians’ members to proceed with any proposals. Meetings will be held publicly online, Dr. Teirstein explained.
There is a need for a broad-based organization that will respond to the voice of practicing physicians rather than dictate legislative priorities from management ranks, he said.
Dr. Teirstein said he learned how challenging it is to bring physicians together on issues in 2014 in his battles against changes in maintenance of certification rules. The result of his efforts was the National Board of Physicians and Surgeons (NBPAS), set up to provide a means of certification different from the one offered by the American Board of Internal Medicine.
Dr. Teirstein has argued that the approach of ABIM unfairly burdened physicians with a stepped-up schedule of testing and relied on an outdated approach to the practice of medicine.
Physicians busy with their practices feel they lack a unified voice in contesting the growing administrative burden and unproductive federal and state policies, Dr. Teirstein said.
He cited the limited enrollment in the largest physician groups as evidence of how disenfranchised many clinicians feel. There are about 1 million professional active physicians in the United States, according to the nonprofit Kaiser Family Foundation. Yet, even the largest physician group, the American Medical Association, has about 250,000 members, according to its 2018 annual report
“Clearly, most physicians believe they have little voice when it comes to health care decisions,” Dr. Teirstein said. “Our physician associations are governed from the top down. The leaders set the agenda. There may be delegates, but does leadership really listen to the delegates? Do the delegates really listen to the physician community?”
On its website, AMA describes itself as “physicians’ powerful ally in patient care” that works with more than 190 state and specialty medical societies. In recent months, James L. Madara, MD, the group’s chief executive officer, has urged governors to remove obstacles for physicians who want to fill workforce gaps in COVID-19 hot spots, among other actions.
In its annual report, the AMA, which declined to comment for this article, said its membership rose by 3.4% in 2018, double the growth rate of the previous year, thanks to a membership drive.
“The campaign celebrates the powerful work of our physician members and showcases how their individual efforts – along with the AMA – are moving medicine forward,” wrote Dr. Madara and other organization leaders in the report.
What Dr. Teirstein proposes is an inversion of the structure used by other medical societies, in which he says leaders and delegates dictate priorities.
United Physicians will use meetings and votes held by members online to decide which projects to pursue. Fees would be kept nominal, likely about $10 a year, depending on the number of members. Fees would be subject to change on the basis of expenses. The AMA has a sliding fee schedule that tops out with annual dues for physicians in regular practice of $420.
“There are no delegates, no representatives, and no board of directors. We want every physician to join and every physician to vote on every issue,” Dr. Teirstein said.
He stressed that he sees United Physicians as being complementary to the AMA.
“We do not compete with other organizations. Ideally, other organizations will use the platform,” Dr. Teirstein said. “If the AMA is considering a new policy, it can use the United Physicians platform to measure physician support. For example, through online discussions, petitions, and voting, it might learn a proposed policy needs a few tweaks to be accepted by most physicians.”
No compensation
Dr. Teirstein is among physician leaders who in recent years have sought to rally their colleagues to fight back against growing administrative burdens.
In a 2015 article in JAMA that was written with Medscape’s editor in chief, Eric Topol, MD, Dr. Teirstein criticized the ABIM’s drive to have physicians complete tests every 2 years and participate in continuous certification instead of recertifying once a decade, as had been the practice.
Dr. Teirstein formed the NBPAS as an alternative path for certification, with Dr. Topol serving on the board for that organization. Dr. Topol also will serve as a member of the advisory board for Teirstein’s United Physicians.
Dr. Topol wrote an article that appeared in the New Yorker last August that argued for physicians to move beyond the confines of medical societies and seek a path for broad-based activism. He said he intended to challenge medical societies, which, for all the good they do, can sometimes lose focus on that core relationship in favor of the bottom line.
Dr. Topol said in an interview that his colleague’s new project is a “good idea for a democratized platform at a time when physician solidarity is needed more than ever.”
Dr. Teirstein plans to run United Physicians on a volunteer basis. This builds on the approach he has used for NBPAS. He and the directors of the NBPAS will receive no compensation, he said, as was confirmed by the NBPAS.
In contrast, Dr. Madara made about $2.5 million in total compensation for 2018, according to the organization’s Internal Revenue Service filing. Physicians who served as trustees and officials for the AMA that year received annual compensation that ranged from around $60,000 to $291,980, depending on their duties.
“Having volunteer leadership mitigates conflict of interest. It also ensures leadership has a ‘day job’ that keeps them in touch with issues impacting practicing physicians,” Dr. Teirstein said
Start-up costs for United Physicians will be supported by NBPAS, but it will function as a completely independent organization, he added.
In introducing the group, Dr. Teirstein outlined suggestions for proposals it might pursue. These include making hospitals secure adequate supplies of personal protective equipment ahead of health crises such as the COVID-19 pandemic.
His outline also includes suggestions for issues that likely will persist beyond the response to the pandemic.
Dr. Teirstein proposed a project for persuading insurance companies to provide online calendar appointments for peer-to-peer patient preauthorization. Failure of the insurer’s representative to attend would trigger approval of authorization under this proposal. He also suggested a lobbying effort for specific reimbursement for peer-to-peer, patient preauthorization phone calls.
Dr. Teirstein said he hopes most of the proposals will come from physicians who join United Physicians. Still, it is unclear whether United Physicians will succeed. An initial challenge could be in sorting through a barrage of competing ideas submitted to United Physicians.
But Dr. Teirstein appears hopeful about the changes for this experiment in online advocacy. He intends for United Physicians to be a pathway for clinicians to translate their complaints about policies into calls for action, with only a short investment of their time.
“Most of us have wonderful, engrossing jobs. It’s hard to beat helping a patient, and most of us get to do it every day,” Dr. .Teirstein said. “Will we take the 30 seconds required to sign up and become a United Physicians member? Will we spend a little time each week reviewing the issues and voting? I think it’s an experiment worth watching.”
A version of this article originally appeared on Medscape.com.
A new advocacy organization is launching on April 28 to give “every physician” a voice in decisions that affect their professional lives. But this group doesn’t intend to use the top-down approach to decision making seen in many medical societies.
Paul Teirstein, MD, chief of cardiology for Scripps Clinic in La Jolla, Calif., and founder of the new organization United Physicians, said in an interviewit is a nonprofit group that will operate through online participation.
He said
Projects would need the support of a two-thirds majority of United Physicians’ members to proceed with any proposals. Meetings will be held publicly online, Dr. Teirstein explained.
There is a need for a broad-based organization that will respond to the voice of practicing physicians rather than dictate legislative priorities from management ranks, he said.
Dr. Teirstein said he learned how challenging it is to bring physicians together on issues in 2014 in his battles against changes in maintenance of certification rules. The result of his efforts was the National Board of Physicians and Surgeons (NBPAS), set up to provide a means of certification different from the one offered by the American Board of Internal Medicine.
Dr. Teirstein has argued that the approach of ABIM unfairly burdened physicians with a stepped-up schedule of testing and relied on an outdated approach to the practice of medicine.
Physicians busy with their practices feel they lack a unified voice in contesting the growing administrative burden and unproductive federal and state policies, Dr. Teirstein said.
He cited the limited enrollment in the largest physician groups as evidence of how disenfranchised many clinicians feel. There are about 1 million professional active physicians in the United States, according to the nonprofit Kaiser Family Foundation. Yet, even the largest physician group, the American Medical Association, has about 250,000 members, according to its 2018 annual report
“Clearly, most physicians believe they have little voice when it comes to health care decisions,” Dr. Teirstein said. “Our physician associations are governed from the top down. The leaders set the agenda. There may be delegates, but does leadership really listen to the delegates? Do the delegates really listen to the physician community?”
On its website, AMA describes itself as “physicians’ powerful ally in patient care” that works with more than 190 state and specialty medical societies. In recent months, James L. Madara, MD, the group’s chief executive officer, has urged governors to remove obstacles for physicians who want to fill workforce gaps in COVID-19 hot spots, among other actions.
In its annual report, the AMA, which declined to comment for this article, said its membership rose by 3.4% in 2018, double the growth rate of the previous year, thanks to a membership drive.
“The campaign celebrates the powerful work of our physician members and showcases how their individual efforts – along with the AMA – are moving medicine forward,” wrote Dr. Madara and other organization leaders in the report.
What Dr. Teirstein proposes is an inversion of the structure used by other medical societies, in which he says leaders and delegates dictate priorities.
United Physicians will use meetings and votes held by members online to decide which projects to pursue. Fees would be kept nominal, likely about $10 a year, depending on the number of members. Fees would be subject to change on the basis of expenses. The AMA has a sliding fee schedule that tops out with annual dues for physicians in regular practice of $420.
“There are no delegates, no representatives, and no board of directors. We want every physician to join and every physician to vote on every issue,” Dr. Teirstein said.
He stressed that he sees United Physicians as being complementary to the AMA.
“We do not compete with other organizations. Ideally, other organizations will use the platform,” Dr. Teirstein said. “If the AMA is considering a new policy, it can use the United Physicians platform to measure physician support. For example, through online discussions, petitions, and voting, it might learn a proposed policy needs a few tweaks to be accepted by most physicians.”
No compensation
Dr. Teirstein is among physician leaders who in recent years have sought to rally their colleagues to fight back against growing administrative burdens.
In a 2015 article in JAMA that was written with Medscape’s editor in chief, Eric Topol, MD, Dr. Teirstein criticized the ABIM’s drive to have physicians complete tests every 2 years and participate in continuous certification instead of recertifying once a decade, as had been the practice.
Dr. Teirstein formed the NBPAS as an alternative path for certification, with Dr. Topol serving on the board for that organization. Dr. Topol also will serve as a member of the advisory board for Teirstein’s United Physicians.
Dr. Topol wrote an article that appeared in the New Yorker last August that argued for physicians to move beyond the confines of medical societies and seek a path for broad-based activism. He said he intended to challenge medical societies, which, for all the good they do, can sometimes lose focus on that core relationship in favor of the bottom line.
Dr. Topol said in an interview that his colleague’s new project is a “good idea for a democratized platform at a time when physician solidarity is needed more than ever.”
Dr. Teirstein plans to run United Physicians on a volunteer basis. This builds on the approach he has used for NBPAS. He and the directors of the NBPAS will receive no compensation, he said, as was confirmed by the NBPAS.
In contrast, Dr. Madara made about $2.5 million in total compensation for 2018, according to the organization’s Internal Revenue Service filing. Physicians who served as trustees and officials for the AMA that year received annual compensation that ranged from around $60,000 to $291,980, depending on their duties.
“Having volunteer leadership mitigates conflict of interest. It also ensures leadership has a ‘day job’ that keeps them in touch with issues impacting practicing physicians,” Dr. Teirstein said
Start-up costs for United Physicians will be supported by NBPAS, but it will function as a completely independent organization, he added.
In introducing the group, Dr. Teirstein outlined suggestions for proposals it might pursue. These include making hospitals secure adequate supplies of personal protective equipment ahead of health crises such as the COVID-19 pandemic.
His outline also includes suggestions for issues that likely will persist beyond the response to the pandemic.
Dr. Teirstein proposed a project for persuading insurance companies to provide online calendar appointments for peer-to-peer patient preauthorization. Failure of the insurer’s representative to attend would trigger approval of authorization under this proposal. He also suggested a lobbying effort for specific reimbursement for peer-to-peer, patient preauthorization phone calls.
Dr. Teirstein said he hopes most of the proposals will come from physicians who join United Physicians. Still, it is unclear whether United Physicians will succeed. An initial challenge could be in sorting through a barrage of competing ideas submitted to United Physicians.
But Dr. Teirstein appears hopeful about the changes for this experiment in online advocacy. He intends for United Physicians to be a pathway for clinicians to translate their complaints about policies into calls for action, with only a short investment of their time.
“Most of us have wonderful, engrossing jobs. It’s hard to beat helping a patient, and most of us get to do it every day,” Dr. .Teirstein said. “Will we take the 30 seconds required to sign up and become a United Physicians member? Will we spend a little time each week reviewing the issues and voting? I think it’s an experiment worth watching.”
A version of this article originally appeared on Medscape.com.
CMS suspends advance payment program to clinicians for COVID-19 relief
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.