User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
COVID-19: A primary care perspective
With the COVID-19 pandemic, we are experiencing a once-in-a-100-year event. Dr. Steven A. Schulz, who is serving children on the front line in upstate New York, and I outline some of the challenges primary care pediatricians have been facing and solutions that have succeeded.
Reduction in direct patient care and its consequences
Because of the unknowns of COVID-19, many parents have not wanted to bring their children to a medical office because of fear of contracting SARS-CoV-2. At the same time, pediatricians have restricted in-person visits to prevent spread of SARS-CoV-2 and to help flatten the curve of infection. Use of pediatric medical professional services, compared with last year, dropped by 52% in March 2020 and by 58% in April, according to FAIR Health, a nonprofit organization that manages a database of 31 million claims. This is resulting in decreased immunization rates, which increases concern for secondary spikes of other preventable illnesses; for example, data from the Centers for Disease Control and Prevention showed that, from mid-March to mid-April 2020, physicians in the Vaccines for Children program ordered 2.5 million fewer doses of vaccines and 250,000 fewer doses of measles-containing vaccines, compared with the same period in 2019. Fewer children are being seen for well visits, which means opportunities are lost for adequate monitoring of growth, development, physical wellness, and social determinants of health.
This is occurring at a time when families have been experiencing increased stress in terms of finances, social isolation, finding adequate child care, and serving as parent, teacher, and breadwinner. An increase in injuries is occurring because of inadequate parental supervision because many parents have been distracted while working from home. An increase in cases of severe abuse is occurring because schools, child care providers, physicians, and other mandated reporters in the community have decreased interaction with children. Children’s Hospital Colorado in Colorado Springs saw a 118% increase in the number of trauma cases in its ED between January and April 2020. Some of these were accidental injuries caused by falls or bicycle accidents, but there was a 200% increase in nonaccidental trauma, which was associated with a steep fall in calls to the state’s child abuse hotline. Academic gains are being lost, and there has been worry for a prolonged “summer slide” risk, especially for children living in poverty and children with developmental disabilities.
The COVID-19 pandemic also is affecting physicians and staff. As frontline personnel, we are at risk to contract the virus, and news media reminds us of severe illness and deaths among health care workers. The pandemic is affecting financial viability; estimated revenue of pediatric offices fell by 45% in March 2020 and 48% in April, compared with the previous year, according to FAIR Health. Nurses and staff have been furloughed. Practices have had to apply for grants and Paycheck Protection Program funds while extending credit lines.
Limited testing capability for SARS-CoV-2
Testing for SARS-CoV-2 has been variably available. There have been problems with false positive and especially false negative results (BMJ. 2020 May 12. doi: 10.1136/bmj.m1808).The best specimen collection method has yet to be determined. Blood testing for antibody has been touted, but it remains unclear if there is clinical benefit because a positive result offers no guarantee of immunity, and immunity may quickly wane. Perhaps widespread primary care office–based testing will be in place by the fall, with hope for future reliable point of care results.
Evolving knowledge regarding SARS-CoV-2 and MIS-C
It initially was thought that children were relatively spared from serious illness caused by COVID-19. Then reports of cases of newly identified multisystem inflammatory syndrome of children occurred. It has been unclear how children contribute to the spread of COVID-19 illness, although emerging evidence indicates it is lower than adult transmission. What will happen when children return to school and daycare in the fall?
The challenges have led to creative solutions for how to deliver care.
Adapting to telehealth to provide care
At least for the short term, HIPAA regulations have been relaxed to allow for video visits using platforms such as FaceTime, Skype, Zoom, Doximity, and Doxy.me. Some of these platforms are HIPAA compliant and will be long-term solutions; however, electronic medical record portals allowing for video visits are the more secure option, according to HIPAA.
It has been a learning experience to see what can be accomplished with a video visit. Taking a history and visual examination of injuries and rashes has been possible. Addressing mental health concerns through the video exchange generally has been effective.
However, video visits change the provider-patient interpersonal dynamic and offer only visual exam capabilities, compared with an in-person visit. We cannot look in ears, palpate a liver and spleen, touch and examine a joint or bone, or feel a rash. Video visits also are dependent on the quality of patient Internet access, sufficient data plans, and mutual capabilities to address the inevitable technological glitches on the provider’s end as well. Expanding information technology infrastructure ability and added licensure costs have occurred. Practices and health systems have been working with insurance companies to ensure telephone and video visits are reimbursed on a comparable level to in-office visits.
A new type of office visit and developing appropriate safety plans
Patients must be universally screened prior to arrival during appointment scheduling for well and illness visits. Patients aged older than 2 years and caregivers must wear masks on entering the facility. In many practices, patients are scheduled during specific sick or well visit time slots throughout the day. Waiting rooms chairs need to be spaced for 6-foot social distancing, and cars in the parking lot often serve as waiting rooms until staff can meet patients at the door and take them to the exam room. Alternate entrances, car-side exams, and drive-by and/or tent testing facilities often have become part of the new normal everyday practice. Creating virtual visit time blocks in provider’s schedules has allowed for decreased office congestion. Patients often are checked out from their room, as opposed to waiting in a line at a check out desk. Nurse triage protocols also have been adapted and enhanced to meet needs and concerns.
With the need for summer physicals and many regions opening up, a gradual return toward baseline has been evolving, although some of the twists of a “new normal” will stay in place. The new normal has been for providers and staff to wear surgical masks and face shields; sometimes N95 masks, gloves, and gowns have been needed. Cleaning rooms and equipment between patient visits has become a major, new time-consuming task. Acquiring and maintaining adequate supplies has been a challenge.
Summary
The American Academy of Pediatrics, CDC, and state and local health departments have been providing informative and regular updates, webinars, and best practices guidelines. Pediatricians, community organizations, schools, and mental health professionals have been collaborating, overcoming hurdles, and working together to help mitigate the effects of the pandemic on children, their families, and our communities. Continued education, cooperation, and adaptation will be needed in the months ahead. If there is a silver lining to this pandemic experience, it may be that families have grown closer together as they sheltered in place (and we have grown closer to our own families as well). One day perhaps a child who lived through this pandemic might be asked what it was like, and their recollection might be that it was a wonderful time because their parents stayed home all the time, took care of them, taught them their school work, and took lots of long family walks.
Dr. Schulz is pediatric medical director, Rochester (N.Y.) Regional Health. Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. Dr. Schulz and Dr. Pichichero said they have no relevant financial disclosures. Email them at [email protected].
This article was updated 7/16/2020.
With the COVID-19 pandemic, we are experiencing a once-in-a-100-year event. Dr. Steven A. Schulz, who is serving children on the front line in upstate New York, and I outline some of the challenges primary care pediatricians have been facing and solutions that have succeeded.
Reduction in direct patient care and its consequences
Because of the unknowns of COVID-19, many parents have not wanted to bring their children to a medical office because of fear of contracting SARS-CoV-2. At the same time, pediatricians have restricted in-person visits to prevent spread of SARS-CoV-2 and to help flatten the curve of infection. Use of pediatric medical professional services, compared with last year, dropped by 52% in March 2020 and by 58% in April, according to FAIR Health, a nonprofit organization that manages a database of 31 million claims. This is resulting in decreased immunization rates, which increases concern for secondary spikes of other preventable illnesses; for example, data from the Centers for Disease Control and Prevention showed that, from mid-March to mid-April 2020, physicians in the Vaccines for Children program ordered 2.5 million fewer doses of vaccines and 250,000 fewer doses of measles-containing vaccines, compared with the same period in 2019. Fewer children are being seen for well visits, which means opportunities are lost for adequate monitoring of growth, development, physical wellness, and social determinants of health.
This is occurring at a time when families have been experiencing increased stress in terms of finances, social isolation, finding adequate child care, and serving as parent, teacher, and breadwinner. An increase in injuries is occurring because of inadequate parental supervision because many parents have been distracted while working from home. An increase in cases of severe abuse is occurring because schools, child care providers, physicians, and other mandated reporters in the community have decreased interaction with children. Children’s Hospital Colorado in Colorado Springs saw a 118% increase in the number of trauma cases in its ED between January and April 2020. Some of these were accidental injuries caused by falls or bicycle accidents, but there was a 200% increase in nonaccidental trauma, which was associated with a steep fall in calls to the state’s child abuse hotline. Academic gains are being lost, and there has been worry for a prolonged “summer slide” risk, especially for children living in poverty and children with developmental disabilities.
The COVID-19 pandemic also is affecting physicians and staff. As frontline personnel, we are at risk to contract the virus, and news media reminds us of severe illness and deaths among health care workers. The pandemic is affecting financial viability; estimated revenue of pediatric offices fell by 45% in March 2020 and 48% in April, compared with the previous year, according to FAIR Health. Nurses and staff have been furloughed. Practices have had to apply for grants and Paycheck Protection Program funds while extending credit lines.
Limited testing capability for SARS-CoV-2
Testing for SARS-CoV-2 has been variably available. There have been problems with false positive and especially false negative results (BMJ. 2020 May 12. doi: 10.1136/bmj.m1808).The best specimen collection method has yet to be determined. Blood testing for antibody has been touted, but it remains unclear if there is clinical benefit because a positive result offers no guarantee of immunity, and immunity may quickly wane. Perhaps widespread primary care office–based testing will be in place by the fall, with hope for future reliable point of care results.
Evolving knowledge regarding SARS-CoV-2 and MIS-C
It initially was thought that children were relatively spared from serious illness caused by COVID-19. Then reports of cases of newly identified multisystem inflammatory syndrome of children occurred. It has been unclear how children contribute to the spread of COVID-19 illness, although emerging evidence indicates it is lower than adult transmission. What will happen when children return to school and daycare in the fall?
The challenges have led to creative solutions for how to deliver care.
Adapting to telehealth to provide care
At least for the short term, HIPAA regulations have been relaxed to allow for video visits using platforms such as FaceTime, Skype, Zoom, Doximity, and Doxy.me. Some of these platforms are HIPAA compliant and will be long-term solutions; however, electronic medical record portals allowing for video visits are the more secure option, according to HIPAA.
It has been a learning experience to see what can be accomplished with a video visit. Taking a history and visual examination of injuries and rashes has been possible. Addressing mental health concerns through the video exchange generally has been effective.
However, video visits change the provider-patient interpersonal dynamic and offer only visual exam capabilities, compared with an in-person visit. We cannot look in ears, palpate a liver and spleen, touch and examine a joint or bone, or feel a rash. Video visits also are dependent on the quality of patient Internet access, sufficient data plans, and mutual capabilities to address the inevitable technological glitches on the provider’s end as well. Expanding information technology infrastructure ability and added licensure costs have occurred. Practices and health systems have been working with insurance companies to ensure telephone and video visits are reimbursed on a comparable level to in-office visits.
A new type of office visit and developing appropriate safety plans
Patients must be universally screened prior to arrival during appointment scheduling for well and illness visits. Patients aged older than 2 years and caregivers must wear masks on entering the facility. In many practices, patients are scheduled during specific sick or well visit time slots throughout the day. Waiting rooms chairs need to be spaced for 6-foot social distancing, and cars in the parking lot often serve as waiting rooms until staff can meet patients at the door and take them to the exam room. Alternate entrances, car-side exams, and drive-by and/or tent testing facilities often have become part of the new normal everyday practice. Creating virtual visit time blocks in provider’s schedules has allowed for decreased office congestion. Patients often are checked out from their room, as opposed to waiting in a line at a check out desk. Nurse triage protocols also have been adapted and enhanced to meet needs and concerns.
With the need for summer physicals and many regions opening up, a gradual return toward baseline has been evolving, although some of the twists of a “new normal” will stay in place. The new normal has been for providers and staff to wear surgical masks and face shields; sometimes N95 masks, gloves, and gowns have been needed. Cleaning rooms and equipment between patient visits has become a major, new time-consuming task. Acquiring and maintaining adequate supplies has been a challenge.
Summary
The American Academy of Pediatrics, CDC, and state and local health departments have been providing informative and regular updates, webinars, and best practices guidelines. Pediatricians, community organizations, schools, and mental health professionals have been collaborating, overcoming hurdles, and working together to help mitigate the effects of the pandemic on children, their families, and our communities. Continued education, cooperation, and adaptation will be needed in the months ahead. If there is a silver lining to this pandemic experience, it may be that families have grown closer together as they sheltered in place (and we have grown closer to our own families as well). One day perhaps a child who lived through this pandemic might be asked what it was like, and their recollection might be that it was a wonderful time because their parents stayed home all the time, took care of them, taught them their school work, and took lots of long family walks.
Dr. Schulz is pediatric medical director, Rochester (N.Y.) Regional Health. Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. Dr. Schulz and Dr. Pichichero said they have no relevant financial disclosures. Email them at [email protected].
This article was updated 7/16/2020.
With the COVID-19 pandemic, we are experiencing a once-in-a-100-year event. Dr. Steven A. Schulz, who is serving children on the front line in upstate New York, and I outline some of the challenges primary care pediatricians have been facing and solutions that have succeeded.
Reduction in direct patient care and its consequences
Because of the unknowns of COVID-19, many parents have not wanted to bring their children to a medical office because of fear of contracting SARS-CoV-2. At the same time, pediatricians have restricted in-person visits to prevent spread of SARS-CoV-2 and to help flatten the curve of infection. Use of pediatric medical professional services, compared with last year, dropped by 52% in March 2020 and by 58% in April, according to FAIR Health, a nonprofit organization that manages a database of 31 million claims. This is resulting in decreased immunization rates, which increases concern for secondary spikes of other preventable illnesses; for example, data from the Centers for Disease Control and Prevention showed that, from mid-March to mid-April 2020, physicians in the Vaccines for Children program ordered 2.5 million fewer doses of vaccines and 250,000 fewer doses of measles-containing vaccines, compared with the same period in 2019. Fewer children are being seen for well visits, which means opportunities are lost for adequate monitoring of growth, development, physical wellness, and social determinants of health.
This is occurring at a time when families have been experiencing increased stress in terms of finances, social isolation, finding adequate child care, and serving as parent, teacher, and breadwinner. An increase in injuries is occurring because of inadequate parental supervision because many parents have been distracted while working from home. An increase in cases of severe abuse is occurring because schools, child care providers, physicians, and other mandated reporters in the community have decreased interaction with children. Children’s Hospital Colorado in Colorado Springs saw a 118% increase in the number of trauma cases in its ED between January and April 2020. Some of these were accidental injuries caused by falls or bicycle accidents, but there was a 200% increase in nonaccidental trauma, which was associated with a steep fall in calls to the state’s child abuse hotline. Academic gains are being lost, and there has been worry for a prolonged “summer slide” risk, especially for children living in poverty and children with developmental disabilities.
The COVID-19 pandemic also is affecting physicians and staff. As frontline personnel, we are at risk to contract the virus, and news media reminds us of severe illness and deaths among health care workers. The pandemic is affecting financial viability; estimated revenue of pediatric offices fell by 45% in March 2020 and 48% in April, compared with the previous year, according to FAIR Health. Nurses and staff have been furloughed. Practices have had to apply for grants and Paycheck Protection Program funds while extending credit lines.
Limited testing capability for SARS-CoV-2
Testing for SARS-CoV-2 has been variably available. There have been problems with false positive and especially false negative results (BMJ. 2020 May 12. doi: 10.1136/bmj.m1808).The best specimen collection method has yet to be determined. Blood testing for antibody has been touted, but it remains unclear if there is clinical benefit because a positive result offers no guarantee of immunity, and immunity may quickly wane. Perhaps widespread primary care office–based testing will be in place by the fall, with hope for future reliable point of care results.
Evolving knowledge regarding SARS-CoV-2 and MIS-C
It initially was thought that children were relatively spared from serious illness caused by COVID-19. Then reports of cases of newly identified multisystem inflammatory syndrome of children occurred. It has been unclear how children contribute to the spread of COVID-19 illness, although emerging evidence indicates it is lower than adult transmission. What will happen when children return to school and daycare in the fall?
The challenges have led to creative solutions for how to deliver care.
Adapting to telehealth to provide care
At least for the short term, HIPAA regulations have been relaxed to allow for video visits using platforms such as FaceTime, Skype, Zoom, Doximity, and Doxy.me. Some of these platforms are HIPAA compliant and will be long-term solutions; however, electronic medical record portals allowing for video visits are the more secure option, according to HIPAA.
It has been a learning experience to see what can be accomplished with a video visit. Taking a history and visual examination of injuries and rashes has been possible. Addressing mental health concerns through the video exchange generally has been effective.
However, video visits change the provider-patient interpersonal dynamic and offer only visual exam capabilities, compared with an in-person visit. We cannot look in ears, palpate a liver and spleen, touch and examine a joint or bone, or feel a rash. Video visits also are dependent on the quality of patient Internet access, sufficient data plans, and mutual capabilities to address the inevitable technological glitches on the provider’s end as well. Expanding information technology infrastructure ability and added licensure costs have occurred. Practices and health systems have been working with insurance companies to ensure telephone and video visits are reimbursed on a comparable level to in-office visits.
A new type of office visit and developing appropriate safety plans
Patients must be universally screened prior to arrival during appointment scheduling for well and illness visits. Patients aged older than 2 years and caregivers must wear masks on entering the facility. In many practices, patients are scheduled during specific sick or well visit time slots throughout the day. Waiting rooms chairs need to be spaced for 6-foot social distancing, and cars in the parking lot often serve as waiting rooms until staff can meet patients at the door and take them to the exam room. Alternate entrances, car-side exams, and drive-by and/or tent testing facilities often have become part of the new normal everyday practice. Creating virtual visit time blocks in provider’s schedules has allowed for decreased office congestion. Patients often are checked out from their room, as opposed to waiting in a line at a check out desk. Nurse triage protocols also have been adapted and enhanced to meet needs and concerns.
With the need for summer physicals and many regions opening up, a gradual return toward baseline has been evolving, although some of the twists of a “new normal” will stay in place. The new normal has been for providers and staff to wear surgical masks and face shields; sometimes N95 masks, gloves, and gowns have been needed. Cleaning rooms and equipment between patient visits has become a major, new time-consuming task. Acquiring and maintaining adequate supplies has been a challenge.
Summary
The American Academy of Pediatrics, CDC, and state and local health departments have been providing informative and regular updates, webinars, and best practices guidelines. Pediatricians, community organizations, schools, and mental health professionals have been collaborating, overcoming hurdles, and working together to help mitigate the effects of the pandemic on children, their families, and our communities. Continued education, cooperation, and adaptation will be needed in the months ahead. If there is a silver lining to this pandemic experience, it may be that families have grown closer together as they sheltered in place (and we have grown closer to our own families as well). One day perhaps a child who lived through this pandemic might be asked what it was like, and their recollection might be that it was a wonderful time because their parents stayed home all the time, took care of them, taught them their school work, and took lots of long family walks.
Dr. Schulz is pediatric medical director, Rochester (N.Y.) Regional Health. Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. Dr. Schulz and Dr. Pichichero said they have no relevant financial disclosures. Email them at [email protected].
This article was updated 7/16/2020.
Psychiatry trainees subjected to high levels of physical, sexual, verbal abuse from patients
More than 80% of psychiatric trainees have experienced some kind of verbal, physical, or sexual assault from patients, and approximately one-third have been physically attacked multiple times, new survey results show.
Such incidents, said study investigator Victor Pereira-Sanchez, MD, from the department of child and adolescent psychiatry at New York University take a toll on the trainees’ well-being and may ultimately affect the quality of patient care.
“The extent of violence against psychiatric trainees is alarming and calls for the implementation of effective training, prevention, and intervention measures,” Dr. Pereira-Sanchez said in an interview.
The findings were presented at the European Psychiatric Association (EPA) 2020 Congress, which was virtual this year because of the COVID-19 pandemic.
Widespread problem
Violence against health care professionals is widespread among clinicians in EDs with psychiatry trainees “more exposed and vulnerable,” Dr. Pereira-Sanchez said during his presentation.
In 2017, the European Federation of Psychiatric Trainees established a group of researchers to describe “the extent and consequences of violence against psychiatric trainees in Europe and beyond,” he said. The group developed a 15-item questionnaire asking young clinicians about experiences of physical, sexual, and verbal assault at work. The survey was posted online by partner institutions via social media.
A total of 827 psychiatric trainees, the majority of whom were from France and the United Kingdom, completed the survey. Respondents had an average age of 31 years, and 68% were women. On average, respondents had completed 51.3% of their psychiatric training.
with 92.0% reporting verbal assaults, 44.1% physical assaults, and 9.3% sexual assaults. In addition, 14.2% had been assaulted once, 51.9% had been assaulted two to five times, and 33.9% had been assaulted more than five times during their training. Results also showed that assaults were more likely to occur on an inpatient ward (63.4%) or the ED (56.9%), although 37.2% occurred in an outpatient setting and 4.2% in community settings. The majority of respondents (69.0%) did not report their assaults, and 67.3% did not call police or security personnel.
The most common emotions experienced by trainees following an assault were fear, rage, and anxiety. Guilt, sadness, feeling unsupported, and self-doubt were also reported.
Dr. Pereira-Sanchez noted the low rate of reported assaults is likely because trainees view it as “part of the job to get insulted, it’s part of the job to suffer minor physical violence.”
Individuals who did report assaults tended to be those who had been assaulted more than five times and those who felt more anxiety, rage, and fear.
“Basically, those who experience more emotional consequences and physical consequences tend to report more,” he said.
In addition, trainees tended to report assaults if they worked in an institution that provided protocols and training in prevention and management of patient aggression.
However, he added, most respondents reported they were not aware of their center’s protocols with respect to assaults and were not trained in the management or prevention of patient violence.
Management tools key
Commenting on the study in an interview, Renee Binder, MD, professor of psychiatry at University of California, San Francisco, said the findings show that, “when patients are out of control, they may act inappropriately, including verbal, physical, and sexual assaults.”
Consequently, “clinicians should be prepared and have management tools,” said Dr. Binder, who was not involved in the research.
She noted that derogatory statements and racial slurs were included among the verbal assaults, which is particularly common in inpatient units and EDs where “patients may be acutely psychotic or manic and out of control,” she said.
However, Dr. Binder pointed out that the investigators did not separate mild and more severe forms of physical and sexual assault.
“If the authors had more finely separated out the types of physical and sexual assaults, they probably would have found that mild types of assaults are much more common than more severe assaults,” she said.
Dr. Pereira-Sanchez’s fellowship program is funded by Fundacion Alicia Koplowitz. He and Dr. Binder have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
More than 80% of psychiatric trainees have experienced some kind of verbal, physical, or sexual assault from patients, and approximately one-third have been physically attacked multiple times, new survey results show.
Such incidents, said study investigator Victor Pereira-Sanchez, MD, from the department of child and adolescent psychiatry at New York University take a toll on the trainees’ well-being and may ultimately affect the quality of patient care.
“The extent of violence against psychiatric trainees is alarming and calls for the implementation of effective training, prevention, and intervention measures,” Dr. Pereira-Sanchez said in an interview.
The findings were presented at the European Psychiatric Association (EPA) 2020 Congress, which was virtual this year because of the COVID-19 pandemic.
Widespread problem
Violence against health care professionals is widespread among clinicians in EDs with psychiatry trainees “more exposed and vulnerable,” Dr. Pereira-Sanchez said during his presentation.
In 2017, the European Federation of Psychiatric Trainees established a group of researchers to describe “the extent and consequences of violence against psychiatric trainees in Europe and beyond,” he said. The group developed a 15-item questionnaire asking young clinicians about experiences of physical, sexual, and verbal assault at work. The survey was posted online by partner institutions via social media.
A total of 827 psychiatric trainees, the majority of whom were from France and the United Kingdom, completed the survey. Respondents had an average age of 31 years, and 68% were women. On average, respondents had completed 51.3% of their psychiatric training.
with 92.0% reporting verbal assaults, 44.1% physical assaults, and 9.3% sexual assaults. In addition, 14.2% had been assaulted once, 51.9% had been assaulted two to five times, and 33.9% had been assaulted more than five times during their training. Results also showed that assaults were more likely to occur on an inpatient ward (63.4%) or the ED (56.9%), although 37.2% occurred in an outpatient setting and 4.2% in community settings. The majority of respondents (69.0%) did not report their assaults, and 67.3% did not call police or security personnel.
The most common emotions experienced by trainees following an assault were fear, rage, and anxiety. Guilt, sadness, feeling unsupported, and self-doubt were also reported.
Dr. Pereira-Sanchez noted the low rate of reported assaults is likely because trainees view it as “part of the job to get insulted, it’s part of the job to suffer minor physical violence.”
Individuals who did report assaults tended to be those who had been assaulted more than five times and those who felt more anxiety, rage, and fear.
“Basically, those who experience more emotional consequences and physical consequences tend to report more,” he said.
In addition, trainees tended to report assaults if they worked in an institution that provided protocols and training in prevention and management of patient aggression.
However, he added, most respondents reported they were not aware of their center’s protocols with respect to assaults and were not trained in the management or prevention of patient violence.
Management tools key
Commenting on the study in an interview, Renee Binder, MD, professor of psychiatry at University of California, San Francisco, said the findings show that, “when patients are out of control, they may act inappropriately, including verbal, physical, and sexual assaults.”
Consequently, “clinicians should be prepared and have management tools,” said Dr. Binder, who was not involved in the research.
She noted that derogatory statements and racial slurs were included among the verbal assaults, which is particularly common in inpatient units and EDs where “patients may be acutely psychotic or manic and out of control,” she said.
However, Dr. Binder pointed out that the investigators did not separate mild and more severe forms of physical and sexual assault.
“If the authors had more finely separated out the types of physical and sexual assaults, they probably would have found that mild types of assaults are much more common than more severe assaults,” she said.
Dr. Pereira-Sanchez’s fellowship program is funded by Fundacion Alicia Koplowitz. He and Dr. Binder have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
More than 80% of psychiatric trainees have experienced some kind of verbal, physical, or sexual assault from patients, and approximately one-third have been physically attacked multiple times, new survey results show.
Such incidents, said study investigator Victor Pereira-Sanchez, MD, from the department of child and adolescent psychiatry at New York University take a toll on the trainees’ well-being and may ultimately affect the quality of patient care.
“The extent of violence against psychiatric trainees is alarming and calls for the implementation of effective training, prevention, and intervention measures,” Dr. Pereira-Sanchez said in an interview.
The findings were presented at the European Psychiatric Association (EPA) 2020 Congress, which was virtual this year because of the COVID-19 pandemic.
Widespread problem
Violence against health care professionals is widespread among clinicians in EDs with psychiatry trainees “more exposed and vulnerable,” Dr. Pereira-Sanchez said during his presentation.
In 2017, the European Federation of Psychiatric Trainees established a group of researchers to describe “the extent and consequences of violence against psychiatric trainees in Europe and beyond,” he said. The group developed a 15-item questionnaire asking young clinicians about experiences of physical, sexual, and verbal assault at work. The survey was posted online by partner institutions via social media.
A total of 827 psychiatric trainees, the majority of whom were from France and the United Kingdom, completed the survey. Respondents had an average age of 31 years, and 68% were women. On average, respondents had completed 51.3% of their psychiatric training.
with 92.0% reporting verbal assaults, 44.1% physical assaults, and 9.3% sexual assaults. In addition, 14.2% had been assaulted once, 51.9% had been assaulted two to five times, and 33.9% had been assaulted more than five times during their training. Results also showed that assaults were more likely to occur on an inpatient ward (63.4%) or the ED (56.9%), although 37.2% occurred in an outpatient setting and 4.2% in community settings. The majority of respondents (69.0%) did not report their assaults, and 67.3% did not call police or security personnel.
The most common emotions experienced by trainees following an assault were fear, rage, and anxiety. Guilt, sadness, feeling unsupported, and self-doubt were also reported.
Dr. Pereira-Sanchez noted the low rate of reported assaults is likely because trainees view it as “part of the job to get insulted, it’s part of the job to suffer minor physical violence.”
Individuals who did report assaults tended to be those who had been assaulted more than five times and those who felt more anxiety, rage, and fear.
“Basically, those who experience more emotional consequences and physical consequences tend to report more,” he said.
In addition, trainees tended to report assaults if they worked in an institution that provided protocols and training in prevention and management of patient aggression.
However, he added, most respondents reported they were not aware of their center’s protocols with respect to assaults and were not trained in the management or prevention of patient violence.
Management tools key
Commenting on the study in an interview, Renee Binder, MD, professor of psychiatry at University of California, San Francisco, said the findings show that, “when patients are out of control, they may act inappropriately, including verbal, physical, and sexual assaults.”
Consequently, “clinicians should be prepared and have management tools,” said Dr. Binder, who was not involved in the research.
She noted that derogatory statements and racial slurs were included among the verbal assaults, which is particularly common in inpatient units and EDs where “patients may be acutely psychotic or manic and out of control,” she said.
However, Dr. Binder pointed out that the investigators did not separate mild and more severe forms of physical and sexual assault.
“If the authors had more finely separated out the types of physical and sexual assaults, they probably would have found that mild types of assaults are much more common than more severe assaults,” she said.
Dr. Pereira-Sanchez’s fellowship program is funded by Fundacion Alicia Koplowitz. He and Dr. Binder have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Move over supplements, here come medical foods
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.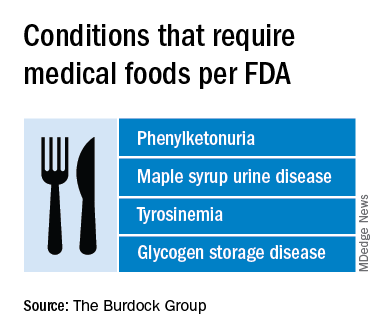
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
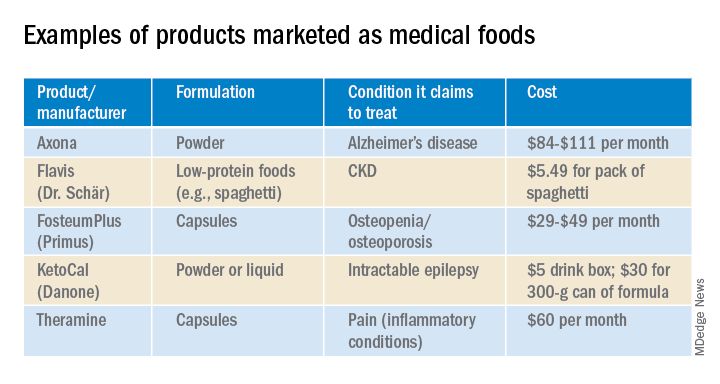
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.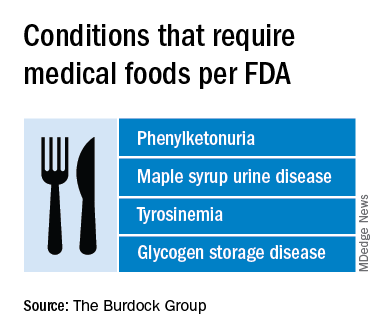
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
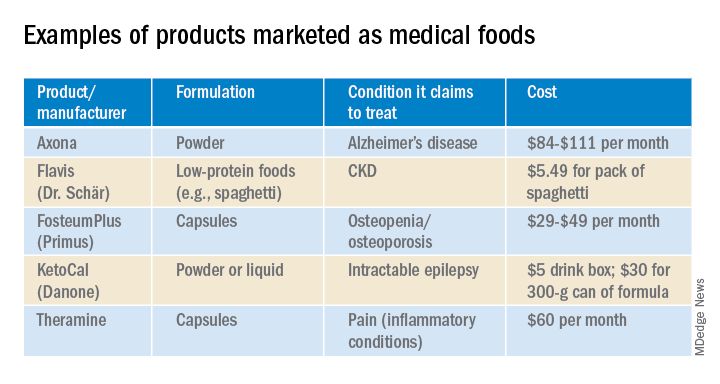
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.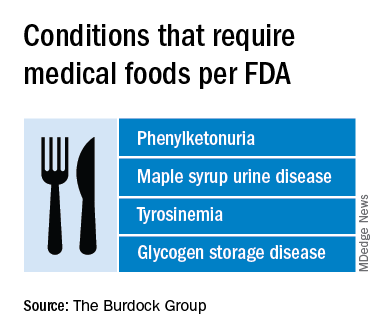
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
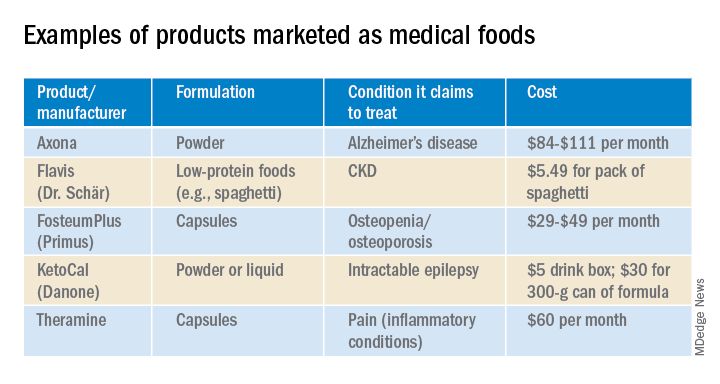
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
How to not miss something
It’s a mad, mad, mad world. In California, we seem bent on swelling our curve. We’d just begun bringing our patients back into the office. We felt safe, back to business. Then air raid sirens again. Retreat to the Underground. Minimize waiting room waiting, convert to telephone and video. Do what we can to protect our patients and people.
As doctors, we’ve gotten proficient at being triage nurses, examining each appointment request, and sorting who should be seen in person and who could be cared for virtually. We do it for every clinic now.
My 11 a.m. patient last Thursday was an 83-year-old Filipino man with at least a 13-year history of hand dermatitis (based on his long electronic medical record). He had plenty of betamethasone refills. There were even photos of his large, brown hands in his chart. Grandpa hands, calloused by tending his garden and scarred from fixing bikes, building sheds, and doing oil changes for any nephew or niece who asked. The most recent uploads showed a bit of fingertip fissuring, some lichenified plaques. Not much different than they looked after planting persimmon trees a decade ago. I called him early that morning to offer a phone appointment. Perhaps I could save him from venturing out.
“I see that you have an appointment with me in a few hours. If you’d like, I might be able to help you by phone instead.” “Oh, thank you, doc,” he replied. “It’s so kind of you to call. But doc, I think maybe it is better if I come in to see you.” “Are you sure?” “Oh, yes. I will be careful.”
He checked in at 10:45. When I walked into the room he was wearing a face mask and a face shield – good job! He also had a cane and U.S. Navy Destroyer hat. And on the bottom left of his plastic shield was a sticker decal of a U.S. Navy Chief Petty Officer, dress blue insignia. His hands looked just like the photos: no purpura, plenty of lentigines. Fissures, calluses, lichenified plaques. I touched them. In the unaffected areas, his skin was remarkably soft. What stories these hands told. “I was 20 years in the Navy, doc,” he said. “I would have stayed longer but my wife, who’s younger, wanted me back home.” He talked about his nine grandchildren, some of whom went on to join the navy too – but as officers, he noted with pride. Now he spends his days caring for his wife; she has dementia. He can’t stay long because she’s in the waiting room and is likely to get confused if alone for too long.
We quickly reviewed good hand care. I ordered clobetasol ointment. He was pleased; that seemed to work years ago and he was glad to have it again.
So, why did he need to come in? Clearly I could have done this remotely. “Thank you so much for seeing me, doc,” as he stood to walk out. “Proper inspections have to be done in person, right?” Yes, I thought. Otherwise, you might miss something.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
It’s a mad, mad, mad world. In California, we seem bent on swelling our curve. We’d just begun bringing our patients back into the office. We felt safe, back to business. Then air raid sirens again. Retreat to the Underground. Minimize waiting room waiting, convert to telephone and video. Do what we can to protect our patients and people.
As doctors, we’ve gotten proficient at being triage nurses, examining each appointment request, and sorting who should be seen in person and who could be cared for virtually. We do it for every clinic now.
My 11 a.m. patient last Thursday was an 83-year-old Filipino man with at least a 13-year history of hand dermatitis (based on his long electronic medical record). He had plenty of betamethasone refills. There were even photos of his large, brown hands in his chart. Grandpa hands, calloused by tending his garden and scarred from fixing bikes, building sheds, and doing oil changes for any nephew or niece who asked. The most recent uploads showed a bit of fingertip fissuring, some lichenified plaques. Not much different than they looked after planting persimmon trees a decade ago. I called him early that morning to offer a phone appointment. Perhaps I could save him from venturing out.
“I see that you have an appointment with me in a few hours. If you’d like, I might be able to help you by phone instead.” “Oh, thank you, doc,” he replied. “It’s so kind of you to call. But doc, I think maybe it is better if I come in to see you.” “Are you sure?” “Oh, yes. I will be careful.”
He checked in at 10:45. When I walked into the room he was wearing a face mask and a face shield – good job! He also had a cane and U.S. Navy Destroyer hat. And on the bottom left of his plastic shield was a sticker decal of a U.S. Navy Chief Petty Officer, dress blue insignia. His hands looked just like the photos: no purpura, plenty of lentigines. Fissures, calluses, lichenified plaques. I touched them. In the unaffected areas, his skin was remarkably soft. What stories these hands told. “I was 20 years in the Navy, doc,” he said. “I would have stayed longer but my wife, who’s younger, wanted me back home.” He talked about his nine grandchildren, some of whom went on to join the navy too – but as officers, he noted with pride. Now he spends his days caring for his wife; she has dementia. He can’t stay long because she’s in the waiting room and is likely to get confused if alone for too long.
We quickly reviewed good hand care. I ordered clobetasol ointment. He was pleased; that seemed to work years ago and he was glad to have it again.
So, why did he need to come in? Clearly I could have done this remotely. “Thank you so much for seeing me, doc,” as he stood to walk out. “Proper inspections have to be done in person, right?” Yes, I thought. Otherwise, you might miss something.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
It’s a mad, mad, mad world. In California, we seem bent on swelling our curve. We’d just begun bringing our patients back into the office. We felt safe, back to business. Then air raid sirens again. Retreat to the Underground. Minimize waiting room waiting, convert to telephone and video. Do what we can to protect our patients and people.
As doctors, we’ve gotten proficient at being triage nurses, examining each appointment request, and sorting who should be seen in person and who could be cared for virtually. We do it for every clinic now.
My 11 a.m. patient last Thursday was an 83-year-old Filipino man with at least a 13-year history of hand dermatitis (based on his long electronic medical record). He had plenty of betamethasone refills. There were even photos of his large, brown hands in his chart. Grandpa hands, calloused by tending his garden and scarred from fixing bikes, building sheds, and doing oil changes for any nephew or niece who asked. The most recent uploads showed a bit of fingertip fissuring, some lichenified plaques. Not much different than they looked after planting persimmon trees a decade ago. I called him early that morning to offer a phone appointment. Perhaps I could save him from venturing out.
“I see that you have an appointment with me in a few hours. If you’d like, I might be able to help you by phone instead.” “Oh, thank you, doc,” he replied. “It’s so kind of you to call. But doc, I think maybe it is better if I come in to see you.” “Are you sure?” “Oh, yes. I will be careful.”
He checked in at 10:45. When I walked into the room he was wearing a face mask and a face shield – good job! He also had a cane and U.S. Navy Destroyer hat. And on the bottom left of his plastic shield was a sticker decal of a U.S. Navy Chief Petty Officer, dress blue insignia. His hands looked just like the photos: no purpura, plenty of lentigines. Fissures, calluses, lichenified plaques. I touched them. In the unaffected areas, his skin was remarkably soft. What stories these hands told. “I was 20 years in the Navy, doc,” he said. “I would have stayed longer but my wife, who’s younger, wanted me back home.” He talked about his nine grandchildren, some of whom went on to join the navy too – but as officers, he noted with pride. Now he spends his days caring for his wife; she has dementia. He can’t stay long because she’s in the waiting room and is likely to get confused if alone for too long.
We quickly reviewed good hand care. I ordered clobetasol ointment. He was pleased; that seemed to work years ago and he was glad to have it again.
So, why did he need to come in? Clearly I could have done this remotely. “Thank you so much for seeing me, doc,” as he stood to walk out. “Proper inspections have to be done in person, right?” Yes, I thought. Otherwise, you might miss something.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Revisiting Xanax amid the coronavirus crisis
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
Less REM sleep tied to higher mortality
Less rapid eye movement (REM) sleep is associated with an increased risk for death in middle-aged and older adults, new research suggests.
Investigators at the University of California, San Diego, found that, over a 12-year period, each 5% reduction in REM sleep was associated with a 13% increase in mortality rate. However, the investigators noted that this is only an association and does not indicate cause and effect.
“Determining causality can be difficult,” study investigator Sonia Ancoli-Israel, PhD, professor emeritus of psychiatry at the University of California, San Diego, said in an interview.
“It is therefore important that physicians and the public understand that our findings suggest an increased risk, but that does not mean that reduced REM will always result in shorter survival. With all the self-monitoring sleep gadgets available to the public, I would caution against any panic if one notices reduced REM. But mentioning it to a physician may be a clue to examine what else might be going on with that patient that could more easily be targeted,” Dr. Ancoli-Israel added.
The research was published online July 6 in JAMA Neurology.
Negative consequences
Approximately 50-70 million Americans have problems with sleep. Such problems have a multitude of consequences for health, including cardiovascular disease; metabolic, psychiatric, and cognitive disorders; lower quality of life; and increased mortality.
The investigators noted that the aspects of sleep that may be driving this association remain unclear. Because decreased REM sleep has been associated with poor mental and physical health outcomes, the researchers hypothesized that decreased REM sleep may be associated with an increased risk for death.
To test this hypothesis, they conducted a multicenter, population-based, cross-sectional investigation using data from independent cohorts – the Outcomes of Sleep Disorders in Older Men (MrOS) Sleep Study and the Wisconsin Sleep Cohort (WSC). The MrOS cohort included 2,675 men (mean age, 76.3 years) who were recruited from December 2003 to March 2005 at six U.S. centers and were followed for a median of 12.1 years. The WSC cohort included 1,386 individuals (54.3% men; mean age, 51.5 years) and had a median follow-up of 20.8 years. Data from this study were used to replicate the findings from the MrOS study.
Primary outcome measures included all-cause and cause-specific mortality, which were confirmed using death certificates.
Participants in both cohorts underwent polysomnography and evaluation with the Epworth Sleepiness Scale. For MrOS participants, investigators calculated the total number of minutes per night spent in REM sleep and the corresponding percentage of total sleep time.
Less sleep, more death
Self-report sleep measures in MrOS participants were collected using the Pittsburgh Sleep Quality Index and the Functional Outcomes of Sleep Questionnaire
The investigators contacted participants in MrOS every 4 months to determine vital status. Cause of death was categorized by the ICD-9 as cardiovascular, cancer, and other. In WSC, the researchers identified deaths by matching participants’ social security numbers with national and state registries. The cause of death was categorized in the same manner as in the MrOS cohort.
Approximately half (53%) of the MrOS cohort died during follow-up. For each mortality category, the highest percentage of deaths occurred among those in the lowest quartile percentage of REM sleep. Adjusted analyses revealed that the MrOS participants had a 13% higher mortality rate for every 5% reduction in REM sleep (hazard ratio, 1.13; 95% confidence interval, 1.08-1.19). These findings were similar for cardiovascular and other causes of death but were not significant for cancer-related mortality. For all mortality categories, the mortality rate was higher for participants who had less than 15% REM sleep per night in comparison with individuals who had 15% or more.
The findings were similar in the WSC cohort despite its younger age, the inclusion of women, and longer follow-up (HR, 1.13; 95% CI, 1.08-1.19). Compared with MrOS participants, WSC participants were more likely to be obese and to use more antidepressants or sedatives. Overall, the mean percentage of REM sleep was 19.2%. Participants in the lowest quartile of REM sleep generally were older, had higher rates of antidepressant use, hypertension, heart attack, and transient ischemic attack, as well as engaging in less physical activity.
Ask about sleep
When the data were stratified by sex, the association between decreased REM sleep and mortality was significant for women but not for men.
“Obtaining a sleep study, representative of the patient’s usual sleep, that shows reduced REM time should alert the neurologist to look for reasons for low REM,” the study’s coinvestigator, Susan Redline, MD, MPH, Peter C. Farrell Professor of Sleep Medicine at Harvard Medical School in Boston, said in an interview.
Dr. Redline added that measures to promote sleep health, such as encouraging regular, sufficient nightly sleep; offering guidance on avoiding alcohol before bedtime and on other healthy sleep practices; and treating sleep disorders may be beneficial.
Low REM time, especially interpreted with other relevant clinical information, may alert the neurologist that a patient may have risk factors for poorer health, she added.
Sleep studies are expensive and are in high demand, so “the most realistic approach is for the neurologist to be asking each and every patient about their sleep,” said Ancoli-Israel.
“By asking a few more questions in every intake, the neurologist is more likely to determine if there are any occult sleep disorders that need to be addressed. By improving sleep in general, one is more likely to also improve any REM abnormalities,” she said.
Disease indicator?
In an accompanying editorial, Michael S. Jaffee, MD, vice chair of neurology at the University of Florida in Gainesville, and colleagues noted that the study raises the question of whether REM sleep “could serve as a biomarker for general health.”
“Since the known roles of REM sleep do not easily suggest a causal link with mortality ... it seems more likely that REM sleep reduction is either a crude marker of health or specific disease states that decrease REM sleep may play an important role in contributing to mortality,” they wrote.
Neurologists should remember that certain medications affect sleep architecture, the editorialists advised. They note that serotonin reuptake inhibitors, selective serotonin and norepinephrine reuptake inhibitors, and tricyclic antidepressants reduce REM sleep, and that gabapentin, prazosin, and bupropion, on the other hand, increase REM sleep. However, data regarding whether these medications have an effect on mortality are insufficient.
The editorialists wrote that the study findings are a “welcome addition to the literature and demonstrate definitively that the association between sleep and mortality extends beyond the simple measure of total sleep time.”
Funding for the MrOS and WSC studies was provided by the National Institutes of Health and the National Institute on Aging. Dr. Ancoli-Israel consults for Eisai and Merck on matters unrelated to the study. Dr. Redline has received grants and personal fees from Jazz Pharmaceuticals, consulting fees from Respicardia, and personal fees from Eisai unrelated to the study. Dr. Jaffee served on a data and safety monitoring board for Helius Medical Technologies and consulted for the National Collegiate Athletic Association and the Department of Defense.
A version of this article originally appeared on Medscape.com.
Less rapid eye movement (REM) sleep is associated with an increased risk for death in middle-aged and older adults, new research suggests.
Investigators at the University of California, San Diego, found that, over a 12-year period, each 5% reduction in REM sleep was associated with a 13% increase in mortality rate. However, the investigators noted that this is only an association and does not indicate cause and effect.
“Determining causality can be difficult,” study investigator Sonia Ancoli-Israel, PhD, professor emeritus of psychiatry at the University of California, San Diego, said in an interview.
“It is therefore important that physicians and the public understand that our findings suggest an increased risk, but that does not mean that reduced REM will always result in shorter survival. With all the self-monitoring sleep gadgets available to the public, I would caution against any panic if one notices reduced REM. But mentioning it to a physician may be a clue to examine what else might be going on with that patient that could more easily be targeted,” Dr. Ancoli-Israel added.
The research was published online July 6 in JAMA Neurology.
Negative consequences
Approximately 50-70 million Americans have problems with sleep. Such problems have a multitude of consequences for health, including cardiovascular disease; metabolic, psychiatric, and cognitive disorders; lower quality of life; and increased mortality.
The investigators noted that the aspects of sleep that may be driving this association remain unclear. Because decreased REM sleep has been associated with poor mental and physical health outcomes, the researchers hypothesized that decreased REM sleep may be associated with an increased risk for death.
To test this hypothesis, they conducted a multicenter, population-based, cross-sectional investigation using data from independent cohorts – the Outcomes of Sleep Disorders in Older Men (MrOS) Sleep Study and the Wisconsin Sleep Cohort (WSC). The MrOS cohort included 2,675 men (mean age, 76.3 years) who were recruited from December 2003 to March 2005 at six U.S. centers and were followed for a median of 12.1 years. The WSC cohort included 1,386 individuals (54.3% men; mean age, 51.5 years) and had a median follow-up of 20.8 years. Data from this study were used to replicate the findings from the MrOS study.
Primary outcome measures included all-cause and cause-specific mortality, which were confirmed using death certificates.
Participants in both cohorts underwent polysomnography and evaluation with the Epworth Sleepiness Scale. For MrOS participants, investigators calculated the total number of minutes per night spent in REM sleep and the corresponding percentage of total sleep time.
Less sleep, more death
Self-report sleep measures in MrOS participants were collected using the Pittsburgh Sleep Quality Index and the Functional Outcomes of Sleep Questionnaire
The investigators contacted participants in MrOS every 4 months to determine vital status. Cause of death was categorized by the ICD-9 as cardiovascular, cancer, and other. In WSC, the researchers identified deaths by matching participants’ social security numbers with national and state registries. The cause of death was categorized in the same manner as in the MrOS cohort.
Approximately half (53%) of the MrOS cohort died during follow-up. For each mortality category, the highest percentage of deaths occurred among those in the lowest quartile percentage of REM sleep. Adjusted analyses revealed that the MrOS participants had a 13% higher mortality rate for every 5% reduction in REM sleep (hazard ratio, 1.13; 95% confidence interval, 1.08-1.19). These findings were similar for cardiovascular and other causes of death but were not significant for cancer-related mortality. For all mortality categories, the mortality rate was higher for participants who had less than 15% REM sleep per night in comparison with individuals who had 15% or more.
The findings were similar in the WSC cohort despite its younger age, the inclusion of women, and longer follow-up (HR, 1.13; 95% CI, 1.08-1.19). Compared with MrOS participants, WSC participants were more likely to be obese and to use more antidepressants or sedatives. Overall, the mean percentage of REM sleep was 19.2%. Participants in the lowest quartile of REM sleep generally were older, had higher rates of antidepressant use, hypertension, heart attack, and transient ischemic attack, as well as engaging in less physical activity.
Ask about sleep
When the data were stratified by sex, the association between decreased REM sleep and mortality was significant for women but not for men.
“Obtaining a sleep study, representative of the patient’s usual sleep, that shows reduced REM time should alert the neurologist to look for reasons for low REM,” the study’s coinvestigator, Susan Redline, MD, MPH, Peter C. Farrell Professor of Sleep Medicine at Harvard Medical School in Boston, said in an interview.
Dr. Redline added that measures to promote sleep health, such as encouraging regular, sufficient nightly sleep; offering guidance on avoiding alcohol before bedtime and on other healthy sleep practices; and treating sleep disorders may be beneficial.
Low REM time, especially interpreted with other relevant clinical information, may alert the neurologist that a patient may have risk factors for poorer health, she added.
Sleep studies are expensive and are in high demand, so “the most realistic approach is for the neurologist to be asking each and every patient about their sleep,” said Ancoli-Israel.
“By asking a few more questions in every intake, the neurologist is more likely to determine if there are any occult sleep disorders that need to be addressed. By improving sleep in general, one is more likely to also improve any REM abnormalities,” she said.
Disease indicator?
In an accompanying editorial, Michael S. Jaffee, MD, vice chair of neurology at the University of Florida in Gainesville, and colleagues noted that the study raises the question of whether REM sleep “could serve as a biomarker for general health.”
“Since the known roles of REM sleep do not easily suggest a causal link with mortality ... it seems more likely that REM sleep reduction is either a crude marker of health or specific disease states that decrease REM sleep may play an important role in contributing to mortality,” they wrote.
Neurologists should remember that certain medications affect sleep architecture, the editorialists advised. They note that serotonin reuptake inhibitors, selective serotonin and norepinephrine reuptake inhibitors, and tricyclic antidepressants reduce REM sleep, and that gabapentin, prazosin, and bupropion, on the other hand, increase REM sleep. However, data regarding whether these medications have an effect on mortality are insufficient.
The editorialists wrote that the study findings are a “welcome addition to the literature and demonstrate definitively that the association between sleep and mortality extends beyond the simple measure of total sleep time.”
Funding for the MrOS and WSC studies was provided by the National Institutes of Health and the National Institute on Aging. Dr. Ancoli-Israel consults for Eisai and Merck on matters unrelated to the study. Dr. Redline has received grants and personal fees from Jazz Pharmaceuticals, consulting fees from Respicardia, and personal fees from Eisai unrelated to the study. Dr. Jaffee served on a data and safety monitoring board for Helius Medical Technologies and consulted for the National Collegiate Athletic Association and the Department of Defense.
A version of this article originally appeared on Medscape.com.
Less rapid eye movement (REM) sleep is associated with an increased risk for death in middle-aged and older adults, new research suggests.
Investigators at the University of California, San Diego, found that, over a 12-year period, each 5% reduction in REM sleep was associated with a 13% increase in mortality rate. However, the investigators noted that this is only an association and does not indicate cause and effect.
“Determining causality can be difficult,” study investigator Sonia Ancoli-Israel, PhD, professor emeritus of psychiatry at the University of California, San Diego, said in an interview.
“It is therefore important that physicians and the public understand that our findings suggest an increased risk, but that does not mean that reduced REM will always result in shorter survival. With all the self-monitoring sleep gadgets available to the public, I would caution against any panic if one notices reduced REM. But mentioning it to a physician may be a clue to examine what else might be going on with that patient that could more easily be targeted,” Dr. Ancoli-Israel added.
The research was published online July 6 in JAMA Neurology.
Negative consequences
Approximately 50-70 million Americans have problems with sleep. Such problems have a multitude of consequences for health, including cardiovascular disease; metabolic, psychiatric, and cognitive disorders; lower quality of life; and increased mortality.
The investigators noted that the aspects of sleep that may be driving this association remain unclear. Because decreased REM sleep has been associated with poor mental and physical health outcomes, the researchers hypothesized that decreased REM sleep may be associated with an increased risk for death.
To test this hypothesis, they conducted a multicenter, population-based, cross-sectional investigation using data from independent cohorts – the Outcomes of Sleep Disorders in Older Men (MrOS) Sleep Study and the Wisconsin Sleep Cohort (WSC). The MrOS cohort included 2,675 men (mean age, 76.3 years) who were recruited from December 2003 to March 2005 at six U.S. centers and were followed for a median of 12.1 years. The WSC cohort included 1,386 individuals (54.3% men; mean age, 51.5 years) and had a median follow-up of 20.8 years. Data from this study were used to replicate the findings from the MrOS study.
Primary outcome measures included all-cause and cause-specific mortality, which were confirmed using death certificates.
Participants in both cohorts underwent polysomnography and evaluation with the Epworth Sleepiness Scale. For MrOS participants, investigators calculated the total number of minutes per night spent in REM sleep and the corresponding percentage of total sleep time.
Less sleep, more death
Self-report sleep measures in MrOS participants were collected using the Pittsburgh Sleep Quality Index and the Functional Outcomes of Sleep Questionnaire
The investigators contacted participants in MrOS every 4 months to determine vital status. Cause of death was categorized by the ICD-9 as cardiovascular, cancer, and other. In WSC, the researchers identified deaths by matching participants’ social security numbers with national and state registries. The cause of death was categorized in the same manner as in the MrOS cohort.
Approximately half (53%) of the MrOS cohort died during follow-up. For each mortality category, the highest percentage of deaths occurred among those in the lowest quartile percentage of REM sleep. Adjusted analyses revealed that the MrOS participants had a 13% higher mortality rate for every 5% reduction in REM sleep (hazard ratio, 1.13; 95% confidence interval, 1.08-1.19). These findings were similar for cardiovascular and other causes of death but were not significant for cancer-related mortality. For all mortality categories, the mortality rate was higher for participants who had less than 15% REM sleep per night in comparison with individuals who had 15% or more.
The findings were similar in the WSC cohort despite its younger age, the inclusion of women, and longer follow-up (HR, 1.13; 95% CI, 1.08-1.19). Compared with MrOS participants, WSC participants were more likely to be obese and to use more antidepressants or sedatives. Overall, the mean percentage of REM sleep was 19.2%. Participants in the lowest quartile of REM sleep generally were older, had higher rates of antidepressant use, hypertension, heart attack, and transient ischemic attack, as well as engaging in less physical activity.
Ask about sleep
When the data were stratified by sex, the association between decreased REM sleep and mortality was significant for women but not for men.
“Obtaining a sleep study, representative of the patient’s usual sleep, that shows reduced REM time should alert the neurologist to look for reasons for low REM,” the study’s coinvestigator, Susan Redline, MD, MPH, Peter C. Farrell Professor of Sleep Medicine at Harvard Medical School in Boston, said in an interview.
Dr. Redline added that measures to promote sleep health, such as encouraging regular, sufficient nightly sleep; offering guidance on avoiding alcohol before bedtime and on other healthy sleep practices; and treating sleep disorders may be beneficial.
Low REM time, especially interpreted with other relevant clinical information, may alert the neurologist that a patient may have risk factors for poorer health, she added.
Sleep studies are expensive and are in high demand, so “the most realistic approach is for the neurologist to be asking each and every patient about their sleep,” said Ancoli-Israel.
“By asking a few more questions in every intake, the neurologist is more likely to determine if there are any occult sleep disorders that need to be addressed. By improving sleep in general, one is more likely to also improve any REM abnormalities,” she said.
Disease indicator?
In an accompanying editorial, Michael S. Jaffee, MD, vice chair of neurology at the University of Florida in Gainesville, and colleagues noted that the study raises the question of whether REM sleep “could serve as a biomarker for general health.”
“Since the known roles of REM sleep do not easily suggest a causal link with mortality ... it seems more likely that REM sleep reduction is either a crude marker of health or specific disease states that decrease REM sleep may play an important role in contributing to mortality,” they wrote.
Neurologists should remember that certain medications affect sleep architecture, the editorialists advised. They note that serotonin reuptake inhibitors, selective serotonin and norepinephrine reuptake inhibitors, and tricyclic antidepressants reduce REM sleep, and that gabapentin, prazosin, and bupropion, on the other hand, increase REM sleep. However, data regarding whether these medications have an effect on mortality are insufficient.
The editorialists wrote that the study findings are a “welcome addition to the literature and demonstrate definitively that the association between sleep and mortality extends beyond the simple measure of total sleep time.”
Funding for the MrOS and WSC studies was provided by the National Institutes of Health and the National Institute on Aging. Dr. Ancoli-Israel consults for Eisai and Merck on matters unrelated to the study. Dr. Redline has received grants and personal fees from Jazz Pharmaceuticals, consulting fees from Respicardia, and personal fees from Eisai unrelated to the study. Dr. Jaffee served on a data and safety monitoring board for Helius Medical Technologies and consulted for the National Collegiate Athletic Association and the Department of Defense.
A version of this article originally appeared on Medscape.com.
The public’s trust in science
Having been a bench research scientist 30 years ago, I am flabbergasted at what is and is not currently possible. In a few weeks, scientists sequenced a novel coronavirus and used the genetic sequence to select candidate molecules for a vaccine. But we still can’t reliably say how much protection a cloth mask provides. Worse yet, even if/when we could reliably quantify contagion, it isn’t clear that the public will believe us anyhow.
The good news is that the public worldwide did believe scientists about the threat of a pandemic and the need to flatten the curve. Saving lives has not been about the strength of an antibiotic or the skill in managing a ventilator, but the credibility of medical scientists. The degree of acceptance was variable and subject to a variety of delays caused by regional politicians, but The bad news is that the public’s trust in that scientific advice has waned, the willingness to accept onerous restrictions has fatigued, and the cooperation for maintaining these social changes is evaporating.
I will leave pontificating about the spread of COVID-19 to other experts in other forums. My focus is on the public’s trust in the professionalism of physicians, nurses, medical scientists, and the health care industry as a whole. That trust has been our most valuable tool in fighting the pandemic so far. There have been situations in which weaknesses in modern science have let society down during the pandemic of the century. In my February 2020 column, at the beginning of the outbreak, a month before it was declared a pandemic, when its magnitude was still unclear, I emphasized the importance of having a trusted scientific spokesperson providing timely, accurate information to the public. That, obviously, did not happen in the United States and the degree of the ensuing disaster is still to be revealed.
Scientists have made some wrong decisions about this novel threat. The advice on masks is an illustrative example. For many years, infection control nurses have insisted that medical students wear a mask to protect themselves, even if they were observing rounds from just inside the doorway of a room of a baby with bronchiolitis. The landfills are full of briefly worn surgical masks. Now the story goes: Surgical masks don’t protect staff; they protect others. Changes like that contribute to a credibility gap.
For 3 months, there was conflicting advice about the appropriateness of masks. In early March 2020, some health care workers were disciplined for wearing personal masks. Now, most scientists recommend the public use masks to reduce contagion. Significant subgroups in the U.S. population have refused, mostly to signal their contrarian politics. In June there was an anecdote of a success story from the Show Me state of Missouri, where a mask is credited for preventing an outbreak from a sick hair stylist.
It is hard to find something more reliable than an anecdote. On June 1, a meta-analysis funded by the World Health Organization was published online by Lancet. It supports the idea that masks are beneficial. It is mostly forest plots, so you can try to interpret it yourself. There were 172 observational studies in the systematic review, and the meta-analysis contains 44 relevant comparative studies and 0 randomized controlled trials. Most of those forest plots have an I2 of 75% or worse, which to me indicates that they are not much more reliable than a good anecdote. My primary conclusion was that modern academic science, in an era with a shortage of toilet paper, should convert to printing on soft tissue paper.
It is important to note that the guesstimated overall benefit of cloth masks was a relative risk of 0.30. That benefit is easily nullified if the false security of a mask causes people to congregate together in groups three times larger or for three times more minutes. N95 masks were more effective.
A different article was published in PNAS on June 11. Its senior author was awarded the Nobel Prize in Chemistry in 1995. That article touted the benefits of masks. The article is facing heavy criticism for flaws in methodology and flaws in the peer review process. A long list of signatories have joined a letter asking for the article’s retraction.
This article, when combined with the two instances of prominent articles being retracted in the prior month by the New England Journal of Medicine and The Lancet, is accumulating evidence the peer review system is not working as intended.
There are many heroes in this pandemic, from the frontline health care workers in hotspots to the grocery workers and cleaning staff. There is hope, indeed some faith, that medical scientists in the foreseeable future will provide treatments and a vaccine for this viral plague. This month, the credibility of scientists again plays a major role as communities respond to outbreaks related to reopening the economy. Let’s celebrate the victories, resolve to fix the impure system, and restore a high level of public trust in science. Lives depend on it.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no relevant financial disclosures. Email him at [email protected].
Having been a bench research scientist 30 years ago, I am flabbergasted at what is and is not currently possible. In a few weeks, scientists sequenced a novel coronavirus and used the genetic sequence to select candidate molecules for a vaccine. But we still can’t reliably say how much protection a cloth mask provides. Worse yet, even if/when we could reliably quantify contagion, it isn’t clear that the public will believe us anyhow.
The good news is that the public worldwide did believe scientists about the threat of a pandemic and the need to flatten the curve. Saving lives has not been about the strength of an antibiotic or the skill in managing a ventilator, but the credibility of medical scientists. The degree of acceptance was variable and subject to a variety of delays caused by regional politicians, but The bad news is that the public’s trust in that scientific advice has waned, the willingness to accept onerous restrictions has fatigued, and the cooperation for maintaining these social changes is evaporating.
I will leave pontificating about the spread of COVID-19 to other experts in other forums. My focus is on the public’s trust in the professionalism of physicians, nurses, medical scientists, and the health care industry as a whole. That trust has been our most valuable tool in fighting the pandemic so far. There have been situations in which weaknesses in modern science have let society down during the pandemic of the century. In my February 2020 column, at the beginning of the outbreak, a month before it was declared a pandemic, when its magnitude was still unclear, I emphasized the importance of having a trusted scientific spokesperson providing timely, accurate information to the public. That, obviously, did not happen in the United States and the degree of the ensuing disaster is still to be revealed.
Scientists have made some wrong decisions about this novel threat. The advice on masks is an illustrative example. For many years, infection control nurses have insisted that medical students wear a mask to protect themselves, even if they were observing rounds from just inside the doorway of a room of a baby with bronchiolitis. The landfills are full of briefly worn surgical masks. Now the story goes: Surgical masks don’t protect staff; they protect others. Changes like that contribute to a credibility gap.
For 3 months, there was conflicting advice about the appropriateness of masks. In early March 2020, some health care workers were disciplined for wearing personal masks. Now, most scientists recommend the public use masks to reduce contagion. Significant subgroups in the U.S. population have refused, mostly to signal their contrarian politics. In June there was an anecdote of a success story from the Show Me state of Missouri, where a mask is credited for preventing an outbreak from a sick hair stylist.
It is hard to find something more reliable than an anecdote. On June 1, a meta-analysis funded by the World Health Organization was published online by Lancet. It supports the idea that masks are beneficial. It is mostly forest plots, so you can try to interpret it yourself. There were 172 observational studies in the systematic review, and the meta-analysis contains 44 relevant comparative studies and 0 randomized controlled trials. Most of those forest plots have an I2 of 75% or worse, which to me indicates that they are not much more reliable than a good anecdote. My primary conclusion was that modern academic science, in an era with a shortage of toilet paper, should convert to printing on soft tissue paper.
It is important to note that the guesstimated overall benefit of cloth masks was a relative risk of 0.30. That benefit is easily nullified if the false security of a mask causes people to congregate together in groups three times larger or for three times more minutes. N95 masks were more effective.
A different article was published in PNAS on June 11. Its senior author was awarded the Nobel Prize in Chemistry in 1995. That article touted the benefits of masks. The article is facing heavy criticism for flaws in methodology and flaws in the peer review process. A long list of signatories have joined a letter asking for the article’s retraction.
This article, when combined with the two instances of prominent articles being retracted in the prior month by the New England Journal of Medicine and The Lancet, is accumulating evidence the peer review system is not working as intended.
There are many heroes in this pandemic, from the frontline health care workers in hotspots to the grocery workers and cleaning staff. There is hope, indeed some faith, that medical scientists in the foreseeable future will provide treatments and a vaccine for this viral plague. This month, the credibility of scientists again plays a major role as communities respond to outbreaks related to reopening the economy. Let’s celebrate the victories, resolve to fix the impure system, and restore a high level of public trust in science. Lives depend on it.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no relevant financial disclosures. Email him at [email protected].
Having been a bench research scientist 30 years ago, I am flabbergasted at what is and is not currently possible. In a few weeks, scientists sequenced a novel coronavirus and used the genetic sequence to select candidate molecules for a vaccine. But we still can’t reliably say how much protection a cloth mask provides. Worse yet, even if/when we could reliably quantify contagion, it isn’t clear that the public will believe us anyhow.
The good news is that the public worldwide did believe scientists about the threat of a pandemic and the need to flatten the curve. Saving lives has not been about the strength of an antibiotic or the skill in managing a ventilator, but the credibility of medical scientists. The degree of acceptance was variable and subject to a variety of delays caused by regional politicians, but The bad news is that the public’s trust in that scientific advice has waned, the willingness to accept onerous restrictions has fatigued, and the cooperation for maintaining these social changes is evaporating.
I will leave pontificating about the spread of COVID-19 to other experts in other forums. My focus is on the public’s trust in the professionalism of physicians, nurses, medical scientists, and the health care industry as a whole. That trust has been our most valuable tool in fighting the pandemic so far. There have been situations in which weaknesses in modern science have let society down during the pandemic of the century. In my February 2020 column, at the beginning of the outbreak, a month before it was declared a pandemic, when its magnitude was still unclear, I emphasized the importance of having a trusted scientific spokesperson providing timely, accurate information to the public. That, obviously, did not happen in the United States and the degree of the ensuing disaster is still to be revealed.
Scientists have made some wrong decisions about this novel threat. The advice on masks is an illustrative example. For many years, infection control nurses have insisted that medical students wear a mask to protect themselves, even if they were observing rounds from just inside the doorway of a room of a baby with bronchiolitis. The landfills are full of briefly worn surgical masks. Now the story goes: Surgical masks don’t protect staff; they protect others. Changes like that contribute to a credibility gap.
For 3 months, there was conflicting advice about the appropriateness of masks. In early March 2020, some health care workers were disciplined for wearing personal masks. Now, most scientists recommend the public use masks to reduce contagion. Significant subgroups in the U.S. population have refused, mostly to signal their contrarian politics. In June there was an anecdote of a success story from the Show Me state of Missouri, where a mask is credited for preventing an outbreak from a sick hair stylist.
It is hard to find something more reliable than an anecdote. On June 1, a meta-analysis funded by the World Health Organization was published online by Lancet. It supports the idea that masks are beneficial. It is mostly forest plots, so you can try to interpret it yourself. There were 172 observational studies in the systematic review, and the meta-analysis contains 44 relevant comparative studies and 0 randomized controlled trials. Most of those forest plots have an I2 of 75% or worse, which to me indicates that they are not much more reliable than a good anecdote. My primary conclusion was that modern academic science, in an era with a shortage of toilet paper, should convert to printing on soft tissue paper.
It is important to note that the guesstimated overall benefit of cloth masks was a relative risk of 0.30. That benefit is easily nullified if the false security of a mask causes people to congregate together in groups three times larger or for three times more minutes. N95 masks were more effective.
A different article was published in PNAS on June 11. Its senior author was awarded the Nobel Prize in Chemistry in 1995. That article touted the benefits of masks. The article is facing heavy criticism for flaws in methodology and flaws in the peer review process. A long list of signatories have joined a letter asking for the article’s retraction.
This article, when combined with the two instances of prominent articles being retracted in the prior month by the New England Journal of Medicine and The Lancet, is accumulating evidence the peer review system is not working as intended.
There are many heroes in this pandemic, from the frontline health care workers in hotspots to the grocery workers and cleaning staff. There is hope, indeed some faith, that medical scientists in the foreseeable future will provide treatments and a vaccine for this viral plague. This month, the credibility of scientists again plays a major role as communities respond to outbreaks related to reopening the economy. Let’s celebrate the victories, resolve to fix the impure system, and restore a high level of public trust in science. Lives depend on it.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no relevant financial disclosures. Email him at [email protected].
Good for profits, good for patients: A new form of medical visits
Ten patients smiled and waved out on the computer monitor, as Jacob Mirsky, MD, greeted each one, asked them to introduce themselves, and inquired as to how each was doing with their stress reduction tactics.
The attendees of the online session had been patients at in-person group visits at the Massachusetts General Hospital Revere HealthCare Center. But those in-person group sessions, known as shared medical appointments (SMAs), were shut down when COVID-19 arrived.
“Our group patients have been missing the sessions,” said Dr. Mirsky, a general internist who codirects the center’s group visit program. The online sessions, called virtual SMAs (V-SMAs), work well with COVID-19 social distancing.
In the group sessions, Dr. Mirsky reads a standardized message that addresses privacy concerns during the session. For the next 60-90 minutes, “we ask them to talk about what has gone well for them and what they are struggling with,” he said. “Then I answer their questions using materials in a PowerPoint to address key points, such as reducing salt for high blood pressure or interpreting blood sugar levels for diabetes.
“I try to end group sessions with one area of focus,” Dr. Mirsky said. “In the stress reduction group, this could be meditation. In the diabetes group, it could be a discussion on weight loss.” Then the program’s health coach goes over some key concepts on behavior change and invites participants to contact her after the session.
“The nice thing is that these virtual sessions are fully reimbursable by all of our insurers in Massachusetts,” Dr. Mirsky said. Through evaluation and management (E/M) codes, each patient in a group visit is paid the same as a patient in an individual visit with the same level of complexity.
Dr. Mirsky writes a note in the chart about each patient who was in the group session. “This includes information about the specific patient, such as the history and physical, and information about the group meeting,” he said. In the next few months, the center plans to put its other group sessions online – on blood pressure, obesity, diabetes, and insomnia.
Attracting doctors who hadn’t done groups before
said Marianne Sumego, MD, director of the Cleveland Clinic’s SMA program, which began 21 years ago.
In this era of COVID-19, group visits have either switched to V-SMAs or halted. However, the COVID-19 crisis has given group visits a second wind. Some doctors who never used SMAs before are now trying out this new mode of patient engagement,
Many of the 100 doctors using SMAs at the Cleveland Clinic have switched over to V-SMAs for now, and the new mode is also attracting colleagues who are new to SMAs, she said.
“When doctors started using telemedicine, virtual group visits started making sense to them,” Dr. Sumego said. “This is a time of a great deal of experimentation in practice design.”
Indeed, V-SMAs have eliminated some problems that had discouraged doctors from trying SMAs, said Amy Wheeler, MD, a general internist who founded the Revere SMA program and codirects it with Dr. Mirsky.
V-SMAs eliminate the need for a large space to hold sessions and reduce the number of staff needed to run sessions, Dr. Wheeler said. “Virtual group visits can actually be easier to use than in-person group visits.”
Dr. Sumego believes small practices in particular will take up V-SMAs because they are easier to run than regular SMAs. “Necessity drives change,” she said. “Across the country everyone is looking at the virtual group model.”
Group visits can help your bottom line
Medicare and many private payers cover group visits. In most cases, they tend to pay the same rate as for an individual office visit. As with telehealth, Medicare and many other payers are temporarily reimbursing for virtual visits at the same rate as for real visits.
Not all payers have a stated policy about covering SMAs, and physicians have to ask. The Centers for Medicare & Medicaid Services, for example, has not published any coding rules on SMAs. But in response to a query by the American Academy of Family Physicians, CMS said it would allow use of CPT codes for E/M services for individual patients.
Blue Cross Blue Shield of North Carolina is one of the few payers with a clearly stated policy on its website. Like Medicare, the insurer accepts E/M codes, and it requires that patients’ attendance must be voluntary; they must be established patients; and the visit must be specific to a disease or condition, although several conditions are allowed.
Dr. Mirsky said his group uses the same E/M level – 99213 – for all of his SMA patients. “Since a regular primary care visit is usually billed at a level 3 or 4, depending on how many topics are covered, we chose level 3 for groups, because the group session deals with just one topic.”
One challenge for billing for SMAs is that most health insurers require patients to provide a copay for each visit, which can discourage patients in groups that meet frequently, says Wayne Dysinger, MD, founder of Lifestyle Medical Solutions, a two-physician primary care practice in Riverside, Calif.
But Dr. Dysinger, who has been using SMAs for 5 years, usually doesn’t have to worry about copays because much of his work is capitated and doesn’t require a copay.
Also, some of Dr. Dysinger’s SMA patients are in direct primary care, in which the patients pay an $18 monthly membership fee. Other practices may charge a flat out-of-pocket fee.
How group visits operate
SMAs are based on the observation that patients with the same condition generally ask their doctor the same questions, and rather than repeat the answers each time, why not provide them to a group?
Dr. Wheeler said trying to be more efficient with her time was the primary reason she became interested in SMAs a dozen years ago. “I was trying to squeeze the advice patients needed into a normal patient visit, and it wasn’t working. When I tried to tell them everything they needed to know, I’d run behind for the rest of my day’s visits.”
She found she was continually repeating the same conversation with patients, but these talks weren’t detailed enough to be effective. “When my weight loss patients came back for the next appointment, they had not made the recommended changes in lifestyle. I started to realize how complicated weight loss was.” So Dr. Wheeler founded the SMA program at the Revere Center.
Doctors enjoy the patient interaction
Some doctors who use SMAs talk about how connected they feel with their patients. “For me, the group sessions are the most gratifying part of the week,” Dr. Dysinger says. “I like to see the patients interacting with me and with each other, and watch their health behavior change over time.”
“These groups have a great deal of energy,” he said. “They have a kind of vulnerability that is very raw, very human. People make commitments to meet goals. Will they meet them or not?”
Dr. Dysinger’s enthusiasm has been echoed by other doctors. In a study of older patients, physicians who used SMAs were more satisfied with care than physicians who relied on standard one-to-one interactions. In another study, the researchers surmised that, in SMAs, doctors learn from their patients how they can better meet their needs.
Dr. Dysinger thinks SMAs are widely applicable in primary care. He estimates that 80%-85% of appointments at a primary care practice involve chronic diseases, and this type of patient is a good fit for group visits. SMAs typically treat patients with diabetes, asthma, arthritis, and obesity.
Dr. Sumego said SMAs are used for specialty care at Cleveland Clinic, such as to help patients before and after bariatric surgery. SMAs have also been used to treat patients with ulcerative colitis, multiple sclerosis, cancer, HIV, menopause, insomnia, and stress, according to one report.
Dr. Dysinger, who runs a small practice, organizes his group sessions somewhat differently. He doesn’t organize his groups around conditions like diabetes, but instead his groups focus on four “pillars” of lifestyle medicine: nourishment, movement, resilience (involving sleep and stress), and connectedness.
Why patients like group visits
Feeling part of a whole is a major draw for many patients. “Patients seem to like committing to something bigger than just themselves,” Dr. Wheeler said. “They enjoy the sense of community that groups have, the joy of supporting one another.”
“It’s feeling that you’re not alone,” Dr. Mirsky said. “When a patient struggling with diabetes hears how hard it is for another patient, it validates their experience and gives them someone to connect with. There is a positive peer pressure.”
Many programs, including Dr. Wheeler’s and Dr. Mirsky’s in Boston, allow patients to drop in and out of sessions, rather than attending one course all the way through. But even under this format, Dr. Wheeler said that patients often tend to stick together. “At the end of a session, one patient asks another: ‘Which session do you want to go to next?’ ” she said.
Patients also learn from each other in SMAs. Patients exchange experiences and share advice they may not have had the chance to get during an individual visit.
The group dynamic can make it easier for some patients to reveal sensitive information, said Dr. Dysinger. “In these groups, people feel free to talk about their bowel movements, or about having to deal with the influence of a parent on their lives,” Dr. Dysinger said. “The sessions can have the feel of an [Alcoholics Anonymous] meeting, but they’re firmly grounded in medicine.”
Potential downsides of virtual group visits
SMAs and VSMAs may not work for every practice. Some small practices may not have enough patients to organize a group visit around a particular condition – even a common one like diabetes. In a presentation before the Society of General Internal Medicine, a physician from the Medical University of South Carolina, Charleston, warned that it may be difficult for a practice to fill diabetes group visits every year.
Additionally, some patients don’t want to talk about personal matters in a group. “They may not want to reveal certain things about themselves,” Dr. Mirsky said. “So I tell the group that if there is anything that anyone wants to talk about in private, I’m available.”
Another drawback of SMAs is that more experienced patients may have to slog through information they already know, which is a particular problem when patients can drop in and out of sessions. Dr. Mirsky noted that “what often ends up happening is that the experienced participant helps the newcomer.”
Finally, confidentially is a big concern in a group session. “In a one-on-one visit, you can go into details about the patient’s health, and even bring up an entry in the chart,” Dr. Wheeler said. “But in a group visit, you can’t raise any personal details about a patient unless the patient brings it up first.”
SMA patients sign confidentiality agreements in which they agree not to talk about other patients outside the session. Ensuring confidentiality becomes more complicated in virtual group visits, because someone located in the room near a participant could overhear the conversation. For this reason, patients in V-SMAs are advised to use headphones or, at a minimum, close the door to the room they are in.
To address privacy concerns, Zoom encrypts its data, but some privacy breeches have been reported, and a U.S. senator has been looking into Zoom’s privacy vulnerabilities.
Transferring groups to virtual groups
It took the COVID-19 crisis for most doctors to take up virtual SMAs. Dr. Sumego said that the Cleveland Clinic started virtual SMAs more than a year ago, but most other groups operating SMAs were apparently not providing them virtually before COVID-19 started.
Dr. Dysinger said he tried virtual SMAs in 2017 but dropped them because the technology – using Zoom – was challenging at the time, and his staff and most patients were resistant. “Only three to five people were attending the virtual sessions, and the meetings took place in the evening, which was hard on the staff.”
“When COVID-19 first appeared, our initial response was to try to keep the in-person group and add social distancing to it, but that wasn’t workable, so very quickly we shifted to Zoom meetings,” Dr. Dysinger said. “We had experience with Zoom already, and the Zoom technology had improved and was easier to use. COVID-19 forced it all forward.”
Are V-SMAs effective? While there have been many studies showing the effectiveness of in-person SMAs, there have been very few on V-SMAs. One 2018 study of obesity patients found that those attending in-person SMAs lost somewhat more weight than those in V-SMAs.
As with telemedicine, some patients have trouble with the technology of V-SMAs. Dr. Dysinger said 5%-10% of his SMA patients don’t make the switch over to V-SMAs – mainly because of problems in adapting to the technology – but the rest are happy. “We’re averaging 10 people per meeting, and as many as 20.”
Getting comfortable with group visits
Dealing with group visits takes a very different mindset than what doctors normally have, Dr. Wheeler said. “It took me 6-8 months to feel comfortable enough with group sessions to do them myself,” she recalled. “This was a very different way to practice, compared to the one-on-one care I was trained to give patients. Others may find the transition easier, though.
“Doctors are used to being in control of the patient visit, but the exchange in a group visit is more fluid,” Dr. Wheeler said. “Patients offer their own opinions, and this sends the discussion off on a tangent that is often quite useful. As doctors, we have to learn when to let these tangents continue, and know when the discussion might have to be brought back to the theme at hand. Often it’s better not to intercede.”
Do doctors need training to conduct SMAs? Patients in group visits reported worse communication with physicians than those in individual visits, according to a 2014 study. The authors surmised that the doctors needed to learn how to talk to groups and suggested that they get some training.
The potential staying power of V-SMAs post COVID?
Once the COVID-19 crisis is over, Medicare is scheduled to no longer provide the same level of reimbursement for virtual sessions as for real sessions. Dr. Mirsky anticipates a great deal of resistance to this change from thousands of physicians and patients who have become comfortable with telehealth, including virtual SMAs.
Dr. Dysinger thinks V-SMAs will continue. “When COVID-19 clears and we can go back to in-person groups, we expect to keep some virtual groups. People have already come to accept and value virtual groups.”
Dr. Wheeler sees virtual groups playing an essential role post COVID-19, when practices have to get back up to speed. “Virtual group visits could make it easier to deal with a large backlog of patients who couldn’t be seen up until now,” she said. “And virtual groups will be the only way to see patients who are still reluctant to meet in a group.”
A version of this article originally appeared on Medscape.com.
Ten patients smiled and waved out on the computer monitor, as Jacob Mirsky, MD, greeted each one, asked them to introduce themselves, and inquired as to how each was doing with their stress reduction tactics.
The attendees of the online session had been patients at in-person group visits at the Massachusetts General Hospital Revere HealthCare Center. But those in-person group sessions, known as shared medical appointments (SMAs), were shut down when COVID-19 arrived.
“Our group patients have been missing the sessions,” said Dr. Mirsky, a general internist who codirects the center’s group visit program. The online sessions, called virtual SMAs (V-SMAs), work well with COVID-19 social distancing.
In the group sessions, Dr. Mirsky reads a standardized message that addresses privacy concerns during the session. For the next 60-90 minutes, “we ask them to talk about what has gone well for them and what they are struggling with,” he said. “Then I answer their questions using materials in a PowerPoint to address key points, such as reducing salt for high blood pressure or interpreting blood sugar levels for diabetes.
“I try to end group sessions with one area of focus,” Dr. Mirsky said. “In the stress reduction group, this could be meditation. In the diabetes group, it could be a discussion on weight loss.” Then the program’s health coach goes over some key concepts on behavior change and invites participants to contact her after the session.
“The nice thing is that these virtual sessions are fully reimbursable by all of our insurers in Massachusetts,” Dr. Mirsky said. Through evaluation and management (E/M) codes, each patient in a group visit is paid the same as a patient in an individual visit with the same level of complexity.
Dr. Mirsky writes a note in the chart about each patient who was in the group session. “This includes information about the specific patient, such as the history and physical, and information about the group meeting,” he said. In the next few months, the center plans to put its other group sessions online – on blood pressure, obesity, diabetes, and insomnia.
Attracting doctors who hadn’t done groups before
said Marianne Sumego, MD, director of the Cleveland Clinic’s SMA program, which began 21 years ago.
In this era of COVID-19, group visits have either switched to V-SMAs or halted. However, the COVID-19 crisis has given group visits a second wind. Some doctors who never used SMAs before are now trying out this new mode of patient engagement,
Many of the 100 doctors using SMAs at the Cleveland Clinic have switched over to V-SMAs for now, and the new mode is also attracting colleagues who are new to SMAs, she said.
“When doctors started using telemedicine, virtual group visits started making sense to them,” Dr. Sumego said. “This is a time of a great deal of experimentation in practice design.”
Indeed, V-SMAs have eliminated some problems that had discouraged doctors from trying SMAs, said Amy Wheeler, MD, a general internist who founded the Revere SMA program and codirects it with Dr. Mirsky.
V-SMAs eliminate the need for a large space to hold sessions and reduce the number of staff needed to run sessions, Dr. Wheeler said. “Virtual group visits can actually be easier to use than in-person group visits.”
Dr. Sumego believes small practices in particular will take up V-SMAs because they are easier to run than regular SMAs. “Necessity drives change,” she said. “Across the country everyone is looking at the virtual group model.”
Group visits can help your bottom line
Medicare and many private payers cover group visits. In most cases, they tend to pay the same rate as for an individual office visit. As with telehealth, Medicare and many other payers are temporarily reimbursing for virtual visits at the same rate as for real visits.
Not all payers have a stated policy about covering SMAs, and physicians have to ask. The Centers for Medicare & Medicaid Services, for example, has not published any coding rules on SMAs. But in response to a query by the American Academy of Family Physicians, CMS said it would allow use of CPT codes for E/M services for individual patients.
Blue Cross Blue Shield of North Carolina is one of the few payers with a clearly stated policy on its website. Like Medicare, the insurer accepts E/M codes, and it requires that patients’ attendance must be voluntary; they must be established patients; and the visit must be specific to a disease or condition, although several conditions are allowed.
Dr. Mirsky said his group uses the same E/M level – 99213 – for all of his SMA patients. “Since a regular primary care visit is usually billed at a level 3 or 4, depending on how many topics are covered, we chose level 3 for groups, because the group session deals with just one topic.”
One challenge for billing for SMAs is that most health insurers require patients to provide a copay for each visit, which can discourage patients in groups that meet frequently, says Wayne Dysinger, MD, founder of Lifestyle Medical Solutions, a two-physician primary care practice in Riverside, Calif.
But Dr. Dysinger, who has been using SMAs for 5 years, usually doesn’t have to worry about copays because much of his work is capitated and doesn’t require a copay.
Also, some of Dr. Dysinger’s SMA patients are in direct primary care, in which the patients pay an $18 monthly membership fee. Other practices may charge a flat out-of-pocket fee.
How group visits operate
SMAs are based on the observation that patients with the same condition generally ask their doctor the same questions, and rather than repeat the answers each time, why not provide them to a group?
Dr. Wheeler said trying to be more efficient with her time was the primary reason she became interested in SMAs a dozen years ago. “I was trying to squeeze the advice patients needed into a normal patient visit, and it wasn’t working. When I tried to tell them everything they needed to know, I’d run behind for the rest of my day’s visits.”
She found she was continually repeating the same conversation with patients, but these talks weren’t detailed enough to be effective. “When my weight loss patients came back for the next appointment, they had not made the recommended changes in lifestyle. I started to realize how complicated weight loss was.” So Dr. Wheeler founded the SMA program at the Revere Center.
Doctors enjoy the patient interaction
Some doctors who use SMAs talk about how connected they feel with their patients. “For me, the group sessions are the most gratifying part of the week,” Dr. Dysinger says. “I like to see the patients interacting with me and with each other, and watch their health behavior change over time.”
“These groups have a great deal of energy,” he said. “They have a kind of vulnerability that is very raw, very human. People make commitments to meet goals. Will they meet them or not?”
Dr. Dysinger’s enthusiasm has been echoed by other doctors. In a study of older patients, physicians who used SMAs were more satisfied with care than physicians who relied on standard one-to-one interactions. In another study, the researchers surmised that, in SMAs, doctors learn from their patients how they can better meet their needs.
Dr. Dysinger thinks SMAs are widely applicable in primary care. He estimates that 80%-85% of appointments at a primary care practice involve chronic diseases, and this type of patient is a good fit for group visits. SMAs typically treat patients with diabetes, asthma, arthritis, and obesity.
Dr. Sumego said SMAs are used for specialty care at Cleveland Clinic, such as to help patients before and after bariatric surgery. SMAs have also been used to treat patients with ulcerative colitis, multiple sclerosis, cancer, HIV, menopause, insomnia, and stress, according to one report.
Dr. Dysinger, who runs a small practice, organizes his group sessions somewhat differently. He doesn’t organize his groups around conditions like diabetes, but instead his groups focus on four “pillars” of lifestyle medicine: nourishment, movement, resilience (involving sleep and stress), and connectedness.
Why patients like group visits
Feeling part of a whole is a major draw for many patients. “Patients seem to like committing to something bigger than just themselves,” Dr. Wheeler said. “They enjoy the sense of community that groups have, the joy of supporting one another.”
“It’s feeling that you’re not alone,” Dr. Mirsky said. “When a patient struggling with diabetes hears how hard it is for another patient, it validates their experience and gives them someone to connect with. There is a positive peer pressure.”
Many programs, including Dr. Wheeler’s and Dr. Mirsky’s in Boston, allow patients to drop in and out of sessions, rather than attending one course all the way through. But even under this format, Dr. Wheeler said that patients often tend to stick together. “At the end of a session, one patient asks another: ‘Which session do you want to go to next?’ ” she said.
Patients also learn from each other in SMAs. Patients exchange experiences and share advice they may not have had the chance to get during an individual visit.
The group dynamic can make it easier for some patients to reveal sensitive information, said Dr. Dysinger. “In these groups, people feel free to talk about their bowel movements, or about having to deal with the influence of a parent on their lives,” Dr. Dysinger said. “The sessions can have the feel of an [Alcoholics Anonymous] meeting, but they’re firmly grounded in medicine.”
Potential downsides of virtual group visits
SMAs and VSMAs may not work for every practice. Some small practices may not have enough patients to organize a group visit around a particular condition – even a common one like diabetes. In a presentation before the Society of General Internal Medicine, a physician from the Medical University of South Carolina, Charleston, warned that it may be difficult for a practice to fill diabetes group visits every year.
Additionally, some patients don’t want to talk about personal matters in a group. “They may not want to reveal certain things about themselves,” Dr. Mirsky said. “So I tell the group that if there is anything that anyone wants to talk about in private, I’m available.”
Another drawback of SMAs is that more experienced patients may have to slog through information they already know, which is a particular problem when patients can drop in and out of sessions. Dr. Mirsky noted that “what often ends up happening is that the experienced participant helps the newcomer.”
Finally, confidentially is a big concern in a group session. “In a one-on-one visit, you can go into details about the patient’s health, and even bring up an entry in the chart,” Dr. Wheeler said. “But in a group visit, you can’t raise any personal details about a patient unless the patient brings it up first.”
SMA patients sign confidentiality agreements in which they agree not to talk about other patients outside the session. Ensuring confidentiality becomes more complicated in virtual group visits, because someone located in the room near a participant could overhear the conversation. For this reason, patients in V-SMAs are advised to use headphones or, at a minimum, close the door to the room they are in.
To address privacy concerns, Zoom encrypts its data, but some privacy breeches have been reported, and a U.S. senator has been looking into Zoom’s privacy vulnerabilities.
Transferring groups to virtual groups
It took the COVID-19 crisis for most doctors to take up virtual SMAs. Dr. Sumego said that the Cleveland Clinic started virtual SMAs more than a year ago, but most other groups operating SMAs were apparently not providing them virtually before COVID-19 started.
Dr. Dysinger said he tried virtual SMAs in 2017 but dropped them because the technology – using Zoom – was challenging at the time, and his staff and most patients were resistant. “Only three to five people were attending the virtual sessions, and the meetings took place in the evening, which was hard on the staff.”
“When COVID-19 first appeared, our initial response was to try to keep the in-person group and add social distancing to it, but that wasn’t workable, so very quickly we shifted to Zoom meetings,” Dr. Dysinger said. “We had experience with Zoom already, and the Zoom technology had improved and was easier to use. COVID-19 forced it all forward.”
Are V-SMAs effective? While there have been many studies showing the effectiveness of in-person SMAs, there have been very few on V-SMAs. One 2018 study of obesity patients found that those attending in-person SMAs lost somewhat more weight than those in V-SMAs.
As with telemedicine, some patients have trouble with the technology of V-SMAs. Dr. Dysinger said 5%-10% of his SMA patients don’t make the switch over to V-SMAs – mainly because of problems in adapting to the technology – but the rest are happy. “We’re averaging 10 people per meeting, and as many as 20.”
Getting comfortable with group visits
Dealing with group visits takes a very different mindset than what doctors normally have, Dr. Wheeler said. “It took me 6-8 months to feel comfortable enough with group sessions to do them myself,” she recalled. “This was a very different way to practice, compared to the one-on-one care I was trained to give patients. Others may find the transition easier, though.
“Doctors are used to being in control of the patient visit, but the exchange in a group visit is more fluid,” Dr. Wheeler said. “Patients offer their own opinions, and this sends the discussion off on a tangent that is often quite useful. As doctors, we have to learn when to let these tangents continue, and know when the discussion might have to be brought back to the theme at hand. Often it’s better not to intercede.”
Do doctors need training to conduct SMAs? Patients in group visits reported worse communication with physicians than those in individual visits, according to a 2014 study. The authors surmised that the doctors needed to learn how to talk to groups and suggested that they get some training.
The potential staying power of V-SMAs post COVID?
Once the COVID-19 crisis is over, Medicare is scheduled to no longer provide the same level of reimbursement for virtual sessions as for real sessions. Dr. Mirsky anticipates a great deal of resistance to this change from thousands of physicians and patients who have become comfortable with telehealth, including virtual SMAs.
Dr. Dysinger thinks V-SMAs will continue. “When COVID-19 clears and we can go back to in-person groups, we expect to keep some virtual groups. People have already come to accept and value virtual groups.”
Dr. Wheeler sees virtual groups playing an essential role post COVID-19, when practices have to get back up to speed. “Virtual group visits could make it easier to deal with a large backlog of patients who couldn’t be seen up until now,” she said. “And virtual groups will be the only way to see patients who are still reluctant to meet in a group.”
A version of this article originally appeared on Medscape.com.
Ten patients smiled and waved out on the computer monitor, as Jacob Mirsky, MD, greeted each one, asked them to introduce themselves, and inquired as to how each was doing with their stress reduction tactics.
The attendees of the online session had been patients at in-person group visits at the Massachusetts General Hospital Revere HealthCare Center. But those in-person group sessions, known as shared medical appointments (SMAs), were shut down when COVID-19 arrived.
“Our group patients have been missing the sessions,” said Dr. Mirsky, a general internist who codirects the center’s group visit program. The online sessions, called virtual SMAs (V-SMAs), work well with COVID-19 social distancing.
In the group sessions, Dr. Mirsky reads a standardized message that addresses privacy concerns during the session. For the next 60-90 minutes, “we ask them to talk about what has gone well for them and what they are struggling with,” he said. “Then I answer their questions using materials in a PowerPoint to address key points, such as reducing salt for high blood pressure or interpreting blood sugar levels for diabetes.
“I try to end group sessions with one area of focus,” Dr. Mirsky said. “In the stress reduction group, this could be meditation. In the diabetes group, it could be a discussion on weight loss.” Then the program’s health coach goes over some key concepts on behavior change and invites participants to contact her after the session.
“The nice thing is that these virtual sessions are fully reimbursable by all of our insurers in Massachusetts,” Dr. Mirsky said. Through evaluation and management (E/M) codes, each patient in a group visit is paid the same as a patient in an individual visit with the same level of complexity.
Dr. Mirsky writes a note in the chart about each patient who was in the group session. “This includes information about the specific patient, such as the history and physical, and information about the group meeting,” he said. In the next few months, the center plans to put its other group sessions online – on blood pressure, obesity, diabetes, and insomnia.
Attracting doctors who hadn’t done groups before
said Marianne Sumego, MD, director of the Cleveland Clinic’s SMA program, which began 21 years ago.
In this era of COVID-19, group visits have either switched to V-SMAs or halted. However, the COVID-19 crisis has given group visits a second wind. Some doctors who never used SMAs before are now trying out this new mode of patient engagement,
Many of the 100 doctors using SMAs at the Cleveland Clinic have switched over to V-SMAs for now, and the new mode is also attracting colleagues who are new to SMAs, she said.
“When doctors started using telemedicine, virtual group visits started making sense to them,” Dr. Sumego said. “This is a time of a great deal of experimentation in practice design.”
Indeed, V-SMAs have eliminated some problems that had discouraged doctors from trying SMAs, said Amy Wheeler, MD, a general internist who founded the Revere SMA program and codirects it with Dr. Mirsky.
V-SMAs eliminate the need for a large space to hold sessions and reduce the number of staff needed to run sessions, Dr. Wheeler said. “Virtual group visits can actually be easier to use than in-person group visits.”
Dr. Sumego believes small practices in particular will take up V-SMAs because they are easier to run than regular SMAs. “Necessity drives change,” she said. “Across the country everyone is looking at the virtual group model.”
Group visits can help your bottom line
Medicare and many private payers cover group visits. In most cases, they tend to pay the same rate as for an individual office visit. As with telehealth, Medicare and many other payers are temporarily reimbursing for virtual visits at the same rate as for real visits.
Not all payers have a stated policy about covering SMAs, and physicians have to ask. The Centers for Medicare & Medicaid Services, for example, has not published any coding rules on SMAs. But in response to a query by the American Academy of Family Physicians, CMS said it would allow use of CPT codes for E/M services for individual patients.
Blue Cross Blue Shield of North Carolina is one of the few payers with a clearly stated policy on its website. Like Medicare, the insurer accepts E/M codes, and it requires that patients’ attendance must be voluntary; they must be established patients; and the visit must be specific to a disease or condition, although several conditions are allowed.
Dr. Mirsky said his group uses the same E/M level – 99213 – for all of his SMA patients. “Since a regular primary care visit is usually billed at a level 3 or 4, depending on how many topics are covered, we chose level 3 for groups, because the group session deals with just one topic.”
One challenge for billing for SMAs is that most health insurers require patients to provide a copay for each visit, which can discourage patients in groups that meet frequently, says Wayne Dysinger, MD, founder of Lifestyle Medical Solutions, a two-physician primary care practice in Riverside, Calif.
But Dr. Dysinger, who has been using SMAs for 5 years, usually doesn’t have to worry about copays because much of his work is capitated and doesn’t require a copay.
Also, some of Dr. Dysinger’s SMA patients are in direct primary care, in which the patients pay an $18 monthly membership fee. Other practices may charge a flat out-of-pocket fee.
How group visits operate
SMAs are based on the observation that patients with the same condition generally ask their doctor the same questions, and rather than repeat the answers each time, why not provide them to a group?
Dr. Wheeler said trying to be more efficient with her time was the primary reason she became interested in SMAs a dozen years ago. “I was trying to squeeze the advice patients needed into a normal patient visit, and it wasn’t working. When I tried to tell them everything they needed to know, I’d run behind for the rest of my day’s visits.”
She found she was continually repeating the same conversation with patients, but these talks weren’t detailed enough to be effective. “When my weight loss patients came back for the next appointment, they had not made the recommended changes in lifestyle. I started to realize how complicated weight loss was.” So Dr. Wheeler founded the SMA program at the Revere Center.
Doctors enjoy the patient interaction
Some doctors who use SMAs talk about how connected they feel with their patients. “For me, the group sessions are the most gratifying part of the week,” Dr. Dysinger says. “I like to see the patients interacting with me and with each other, and watch their health behavior change over time.”
“These groups have a great deal of energy,” he said. “They have a kind of vulnerability that is very raw, very human. People make commitments to meet goals. Will they meet them or not?”
Dr. Dysinger’s enthusiasm has been echoed by other doctors. In a study of older patients, physicians who used SMAs were more satisfied with care than physicians who relied on standard one-to-one interactions. In another study, the researchers surmised that, in SMAs, doctors learn from their patients how they can better meet their needs.
Dr. Dysinger thinks SMAs are widely applicable in primary care. He estimates that 80%-85% of appointments at a primary care practice involve chronic diseases, and this type of patient is a good fit for group visits. SMAs typically treat patients with diabetes, asthma, arthritis, and obesity.
Dr. Sumego said SMAs are used for specialty care at Cleveland Clinic, such as to help patients before and after bariatric surgery. SMAs have also been used to treat patients with ulcerative colitis, multiple sclerosis, cancer, HIV, menopause, insomnia, and stress, according to one report.
Dr. Dysinger, who runs a small practice, organizes his group sessions somewhat differently. He doesn’t organize his groups around conditions like diabetes, but instead his groups focus on four “pillars” of lifestyle medicine: nourishment, movement, resilience (involving sleep and stress), and connectedness.
Why patients like group visits
Feeling part of a whole is a major draw for many patients. “Patients seem to like committing to something bigger than just themselves,” Dr. Wheeler said. “They enjoy the sense of community that groups have, the joy of supporting one another.”
“It’s feeling that you’re not alone,” Dr. Mirsky said. “When a patient struggling with diabetes hears how hard it is for another patient, it validates their experience and gives them someone to connect with. There is a positive peer pressure.”
Many programs, including Dr. Wheeler’s and Dr. Mirsky’s in Boston, allow patients to drop in and out of sessions, rather than attending one course all the way through. But even under this format, Dr. Wheeler said that patients often tend to stick together. “At the end of a session, one patient asks another: ‘Which session do you want to go to next?’ ” she said.
Patients also learn from each other in SMAs. Patients exchange experiences and share advice they may not have had the chance to get during an individual visit.
The group dynamic can make it easier for some patients to reveal sensitive information, said Dr. Dysinger. “In these groups, people feel free to talk about their bowel movements, or about having to deal with the influence of a parent on their lives,” Dr. Dysinger said. “The sessions can have the feel of an [Alcoholics Anonymous] meeting, but they’re firmly grounded in medicine.”
Potential downsides of virtual group visits
SMAs and VSMAs may not work for every practice. Some small practices may not have enough patients to organize a group visit around a particular condition – even a common one like diabetes. In a presentation before the Society of General Internal Medicine, a physician from the Medical University of South Carolina, Charleston, warned that it may be difficult for a practice to fill diabetes group visits every year.
Additionally, some patients don’t want to talk about personal matters in a group. “They may not want to reveal certain things about themselves,” Dr. Mirsky said. “So I tell the group that if there is anything that anyone wants to talk about in private, I’m available.”
Another drawback of SMAs is that more experienced patients may have to slog through information they already know, which is a particular problem when patients can drop in and out of sessions. Dr. Mirsky noted that “what often ends up happening is that the experienced participant helps the newcomer.”
Finally, confidentially is a big concern in a group session. “In a one-on-one visit, you can go into details about the patient’s health, and even bring up an entry in the chart,” Dr. Wheeler said. “But in a group visit, you can’t raise any personal details about a patient unless the patient brings it up first.”
SMA patients sign confidentiality agreements in which they agree not to talk about other patients outside the session. Ensuring confidentiality becomes more complicated in virtual group visits, because someone located in the room near a participant could overhear the conversation. For this reason, patients in V-SMAs are advised to use headphones or, at a minimum, close the door to the room they are in.
To address privacy concerns, Zoom encrypts its data, but some privacy breeches have been reported, and a U.S. senator has been looking into Zoom’s privacy vulnerabilities.
Transferring groups to virtual groups
It took the COVID-19 crisis for most doctors to take up virtual SMAs. Dr. Sumego said that the Cleveland Clinic started virtual SMAs more than a year ago, but most other groups operating SMAs were apparently not providing them virtually before COVID-19 started.
Dr. Dysinger said he tried virtual SMAs in 2017 but dropped them because the technology – using Zoom – was challenging at the time, and his staff and most patients were resistant. “Only three to five people were attending the virtual sessions, and the meetings took place in the evening, which was hard on the staff.”
“When COVID-19 first appeared, our initial response was to try to keep the in-person group and add social distancing to it, but that wasn’t workable, so very quickly we shifted to Zoom meetings,” Dr. Dysinger said. “We had experience with Zoom already, and the Zoom technology had improved and was easier to use. COVID-19 forced it all forward.”
Are V-SMAs effective? While there have been many studies showing the effectiveness of in-person SMAs, there have been very few on V-SMAs. One 2018 study of obesity patients found that those attending in-person SMAs lost somewhat more weight than those in V-SMAs.
As with telemedicine, some patients have trouble with the technology of V-SMAs. Dr. Dysinger said 5%-10% of his SMA patients don’t make the switch over to V-SMAs – mainly because of problems in adapting to the technology – but the rest are happy. “We’re averaging 10 people per meeting, and as many as 20.”
Getting comfortable with group visits
Dealing with group visits takes a very different mindset than what doctors normally have, Dr. Wheeler said. “It took me 6-8 months to feel comfortable enough with group sessions to do them myself,” she recalled. “This was a very different way to practice, compared to the one-on-one care I was trained to give patients. Others may find the transition easier, though.
“Doctors are used to being in control of the patient visit, but the exchange in a group visit is more fluid,” Dr. Wheeler said. “Patients offer their own opinions, and this sends the discussion off on a tangent that is often quite useful. As doctors, we have to learn when to let these tangents continue, and know when the discussion might have to be brought back to the theme at hand. Often it’s better not to intercede.”
Do doctors need training to conduct SMAs? Patients in group visits reported worse communication with physicians than those in individual visits, according to a 2014 study. The authors surmised that the doctors needed to learn how to talk to groups and suggested that they get some training.
The potential staying power of V-SMAs post COVID?
Once the COVID-19 crisis is over, Medicare is scheduled to no longer provide the same level of reimbursement for virtual sessions as for real sessions. Dr. Mirsky anticipates a great deal of resistance to this change from thousands of physicians and patients who have become comfortable with telehealth, including virtual SMAs.
Dr. Dysinger thinks V-SMAs will continue. “When COVID-19 clears and we can go back to in-person groups, we expect to keep some virtual groups. People have already come to accept and value virtual groups.”
Dr. Wheeler sees virtual groups playing an essential role post COVID-19, when practices have to get back up to speed. “Virtual group visits could make it easier to deal with a large backlog of patients who couldn’t be seen up until now,” she said. “And virtual groups will be the only way to see patients who are still reluctant to meet in a group.”
A version of this article originally appeared on Medscape.com.
Caution urged for antidepressant use in bipolar depression
Although patients with bipolar disorder commonly experience depressive symptoms, clinicians should be very cautious about treating them with antidepressants, especially as monotherapy, experts asserted in a recent debate on the topic as part of the European Psychiatric Association (EPA) 2020 Congress.
At the Congress, which was virtual this year because of the COVID-19 pandemic, psychiatric experts said that clinicians should also screen patients for mixed symptoms that are better treated with mood stabilizers. These same experts also raised concerns over long-term antidepressant use, recommending continued use only in patients who relapse after stopping antidepressants.
Isabella Pacchiarotti, MD, PhD, Centro de Investigación Biomédica en Red de Salud Mental, Barcelona, Spain, argued against the use of antidepressants in treating bipolar disorder; Guy Goodwin, PhD, however, took the “pro” stance.
Goodwin, a professor of psychiatry at the University of Oxford in the UK, admitted that there is a “paucity of data” on the role of antidepressants in bipolar disorder.
Nevertheless, there are “circumstances that one really has to treat with antidepressants simply because other things have been tried and have not worked,” he told conference attendees.
Challenging, Controversial Topic
The debate was chaired by Eduard Vieta, MD, PhD, chair of the Department of Psychiatry and Psychology at the University of Barcelona Hospital Clinic, Spain.
Vieta said the question over whether antidepressants should be used in the depressive phase of bipolar illness is “perhaps the most challenging ... especially in the area of bipolar disorder.”
At the beginning of the presentation, Vieta asked the audience for their opinion in order to have a “baseline” for the debate: among 164 respondents, 73% were in favor of using antidepressants in bipolar depression.
“Clearly there is a majority, so Isabella [Dr Pacchiarotti] is going to have a hard time improving these numbers,” Vieta noted.
Up first, Pacchiarotti began by noting that this topic remains “an area of big controversy.” However, the real question “should not be the pros and cons of antidepressants but more when and how to use them.»
Of the three phases of bipolar disorder, acute depression «poses the greatest difficulties,» she added.
This is because of the relative paucity of studies in the area, the often heated debates on the specific role of antidepressants, the discrepancy in conclusions between meta-analyses, and the currently approved therapeutic options being associated with “not very high response rates,” Pacchiarotti said.
The diagnostic criteria for unipolar and bipolar depression are “basically the same,” she noted. However, it’s important to be able to distinguish between the two conditions, as up to one fifth of patients with unipolar depression suffer from undiagnosed bipolar disorder, she explained.
Moreover, several studies have identified key symptoms in bipolar depression, such as hyperphagia and hypersomnia, increased anxiety, and psychotic and psychomotor symptoms.
As previously reported by Medscape Medical News, a task force report was released in 2013 by the International Society for Bipolar Disorder (ISBD) on antidepressant use in bipolar disorders. Pacchiarotti and Goodwin were among the report’s authors, which concluded that available evidence on this issue is methodologically weak.
This is largely because of a lack of placebo-controlled studies in this patient population (bipolar depression, alongside suicidal ideation, is often an exclusion criteria in clinical antidepressant trials).
Many guidelines consequently do not consider antidepressants to be a first-line option as monotherapy in bipolar depression, although some name the drugs as second- or third-line options.
In 2013, the ISBD recommended that antidepressant monotherapy should be “avoided” in bipolar I disorder; and in bipolar I and II depression, the treatment should be accompanied by at least two concomitant core manic symptoms.
“What Has Changed?”
Antidepressants should be used “only if there is a history of a positive response,” whereas maintenance therapy should be considered if a patient relapses into a depressive episode after stopping the drugs, the report notes.
Pacchiarotti noted that since the recommendations were published nothing has changed, noting that antidepressant efficacy in bipolar depression “remains unproven.”
The issue is not whether antidepressants are effective in bipolar depression but rather are there subpopulations where these medications are helpful or harmful, she added.
The key to understanding the heterogeneity of responses to antidepressants, she said, is the concept of a bipolar spectrum and a dimensional approach to distinguishing between bipolar disorder and unipolar depression.
In addition, the definition of a mixed episode in the DSM-IV-TR differs from that of an episode with mixed characteristics in the DSM-5, which Pacchiarotti said offers a better understanding of the phenomenon while seemingly disposing with the idea of mixed depression.
Based on previous research, there is some suggestion that a depressive state exists between major depressive disorder and bipolar I disorder with mixed features, and hypomania state between bipolar II and I disorder, also with mixed features.
Pacchiarotti said the role of antidepressants in the treatment of bipolar depression remains “controversial” and there is a need for both short- and long-term studies of their use in both bipolar I and bipolar II disorder with real-world inclusion criteria.
The concept of a bipolar spectrum needs to be considered a more “dimensional approach” to depression, with mixed features seen as a “transversal” contraindication for antidepressant use, she concluded.
In Favor — With Caveats
Taking the opposite position and arguing in favor of antidepressant use, albeit cautiously, Goodwin said previous work has shown that stable patients with bipolar disorder experience depression of variable severity about 50% of the time.
The truth is that patients do not have a depressive episode for extended periods but instead have depressive symptoms, he said. “So how we manage and treat depression really matters.”
In an analysis, Goodwin and his colleagues estimated that the cost of bipolar disorder is approximately £12,600 ($16,000) per patient per year, of which only 30.6% is attributable to healthcare costs and 68.1% to indirect costs. This means the impact on the patient is also felt by society.
He agreed with Pacchiarotti’s assertion of a bipolar spectrum and the need for a dimensional approach.
“All the patients along the spectrum have the symptoms of depression and they differ in the extent to which they show symptoms of mania, which will include irritability,” he added.
Goodwin argued that there is no evidence to suggest that the depression experienced at one end of the scale is any different from that at the other. However, safety issues around antidepressant use “really relate to the additional symptoms you see with increasing evidence of bipolarity.”
In addition, the whole discussion is confounded by comorbidity, “with symptoms that sometimes coalesce into our concept of borderline personality disorder” or attention deficit hyperactivity disorder, he said.
Goodwin said there is “very little doubt” that antidepressants have an effect vs placebo. “The argument is over whether the effect is large and whether we should regard it as clinically significant.”
He noted that previous studies have shown a range of effect sizes with antidepressants, but the “massive” confidence intervals mean that “one is free to believe pretty much what one likes.”
The only antidepressant medication that is statistically significantly different from placebo is fluoxetine combined with olanzapine. However, that conclusion is based on “little data,” said Goodwin.
In terms of long-term management, there is “extremely little” randomized data for maintenance treatment with antidepressants in bipolar disorder. “So this does not support” long-term use, he added.
Still, although choice of antidepressant remains a guess, there is “just about support” for using them, Goodwin noted.
He urged clinicians not to dismiss antidepressant use, but to use them only where there is a clinical need and for as little time as possible. Patients with bipolar disorder should continue to take antidepressants if they relapse after they come off these medications.
However, all of that sits “in contrast” to how they’re currently used in clinical practice, Goodwin said.
Caution Urged
After the debate, the audience was asked to vote again. This time, The remaining 12% voted against the practice.
Summarizing the discussion, Vieta said that “we should be cautious” when using antidepressants in bipolar depression. However, “we should be able to use them when necessary,” he added.
Although their use as monotherapy is not best practice, especially in bipolar I disorder, there may be a subset of bipolar II patients in whom monotherapy “might still be acceptable; but I don’t think it’s a good idea,” Vieta said.
He added that clinicians should very carefully screen for mixed symptoms, which call for the prescription of other drugs, such as olanzapine and fluoxetine.
“The other important message is that we have to be even more cautious in the long term with the use of antidepressants, and we should be able to use them when there is a comorbidity” that calls for their use, Vieta concluded.
Pacchiarotti reported having received speaker fees and educational grants from Adamed, AstraZeneca, Janssen-Cilag, and Lundbeck. Goodwin reported having received honoraria from Angellini, Medscape, Pfizer, Servier, Shire, and Sun; having shares in P1vital Products; past employment as medical director of P1vital Products; and advisory board membership for Compass Pathways, Minerva, MSD, Novartis, Lundbeck, Sage, Servier, and Shire. Vieta has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Although patients with bipolar disorder commonly experience depressive symptoms, clinicians should be very cautious about treating them with antidepressants, especially as monotherapy, experts asserted in a recent debate on the topic as part of the European Psychiatric Association (EPA) 2020 Congress.
At the Congress, which was virtual this year because of the COVID-19 pandemic, psychiatric experts said that clinicians should also screen patients for mixed symptoms that are better treated with mood stabilizers. These same experts also raised concerns over long-term antidepressant use, recommending continued use only in patients who relapse after stopping antidepressants.
Isabella Pacchiarotti, MD, PhD, Centro de Investigación Biomédica en Red de Salud Mental, Barcelona, Spain, argued against the use of antidepressants in treating bipolar disorder; Guy Goodwin, PhD, however, took the “pro” stance.
Goodwin, a professor of psychiatry at the University of Oxford in the UK, admitted that there is a “paucity of data” on the role of antidepressants in bipolar disorder.
Nevertheless, there are “circumstances that one really has to treat with antidepressants simply because other things have been tried and have not worked,” he told conference attendees.
Challenging, Controversial Topic
The debate was chaired by Eduard Vieta, MD, PhD, chair of the Department of Psychiatry and Psychology at the University of Barcelona Hospital Clinic, Spain.
Vieta said the question over whether antidepressants should be used in the depressive phase of bipolar illness is “perhaps the most challenging ... especially in the area of bipolar disorder.”
At the beginning of the presentation, Vieta asked the audience for their opinion in order to have a “baseline” for the debate: among 164 respondents, 73% were in favor of using antidepressants in bipolar depression.
“Clearly there is a majority, so Isabella [Dr Pacchiarotti] is going to have a hard time improving these numbers,” Vieta noted.
Up first, Pacchiarotti began by noting that this topic remains “an area of big controversy.” However, the real question “should not be the pros and cons of antidepressants but more when and how to use them.»
Of the three phases of bipolar disorder, acute depression «poses the greatest difficulties,» she added.
This is because of the relative paucity of studies in the area, the often heated debates on the specific role of antidepressants, the discrepancy in conclusions between meta-analyses, and the currently approved therapeutic options being associated with “not very high response rates,” Pacchiarotti said.
The diagnostic criteria for unipolar and bipolar depression are “basically the same,” she noted. However, it’s important to be able to distinguish between the two conditions, as up to one fifth of patients with unipolar depression suffer from undiagnosed bipolar disorder, she explained.
Moreover, several studies have identified key symptoms in bipolar depression, such as hyperphagia and hypersomnia, increased anxiety, and psychotic and psychomotor symptoms.
As previously reported by Medscape Medical News, a task force report was released in 2013 by the International Society for Bipolar Disorder (ISBD) on antidepressant use in bipolar disorders. Pacchiarotti and Goodwin were among the report’s authors, which concluded that available evidence on this issue is methodologically weak.
This is largely because of a lack of placebo-controlled studies in this patient population (bipolar depression, alongside suicidal ideation, is often an exclusion criteria in clinical antidepressant trials).
Many guidelines consequently do not consider antidepressants to be a first-line option as monotherapy in bipolar depression, although some name the drugs as second- or third-line options.
In 2013, the ISBD recommended that antidepressant monotherapy should be “avoided” in bipolar I disorder; and in bipolar I and II depression, the treatment should be accompanied by at least two concomitant core manic symptoms.
“What Has Changed?”
Antidepressants should be used “only if there is a history of a positive response,” whereas maintenance therapy should be considered if a patient relapses into a depressive episode after stopping the drugs, the report notes.
Pacchiarotti noted that since the recommendations were published nothing has changed, noting that antidepressant efficacy in bipolar depression “remains unproven.”
The issue is not whether antidepressants are effective in bipolar depression but rather are there subpopulations where these medications are helpful or harmful, she added.
The key to understanding the heterogeneity of responses to antidepressants, she said, is the concept of a bipolar spectrum and a dimensional approach to distinguishing between bipolar disorder and unipolar depression.
In addition, the definition of a mixed episode in the DSM-IV-TR differs from that of an episode with mixed characteristics in the DSM-5, which Pacchiarotti said offers a better understanding of the phenomenon while seemingly disposing with the idea of mixed depression.
Based on previous research, there is some suggestion that a depressive state exists between major depressive disorder and bipolar I disorder with mixed features, and hypomania state between bipolar II and I disorder, also with mixed features.
Pacchiarotti said the role of antidepressants in the treatment of bipolar depression remains “controversial” and there is a need for both short- and long-term studies of their use in both bipolar I and bipolar II disorder with real-world inclusion criteria.
The concept of a bipolar spectrum needs to be considered a more “dimensional approach” to depression, with mixed features seen as a “transversal” contraindication for antidepressant use, she concluded.
In Favor — With Caveats
Taking the opposite position and arguing in favor of antidepressant use, albeit cautiously, Goodwin said previous work has shown that stable patients with bipolar disorder experience depression of variable severity about 50% of the time.
The truth is that patients do not have a depressive episode for extended periods but instead have depressive symptoms, he said. “So how we manage and treat depression really matters.”
In an analysis, Goodwin and his colleagues estimated that the cost of bipolar disorder is approximately £12,600 ($16,000) per patient per year, of which only 30.6% is attributable to healthcare costs and 68.1% to indirect costs. This means the impact on the patient is also felt by society.
He agreed with Pacchiarotti’s assertion of a bipolar spectrum and the need for a dimensional approach.
“All the patients along the spectrum have the symptoms of depression and they differ in the extent to which they show symptoms of mania, which will include irritability,” he added.
Goodwin argued that there is no evidence to suggest that the depression experienced at one end of the scale is any different from that at the other. However, safety issues around antidepressant use “really relate to the additional symptoms you see with increasing evidence of bipolarity.”
In addition, the whole discussion is confounded by comorbidity, “with symptoms that sometimes coalesce into our concept of borderline personality disorder” or attention deficit hyperactivity disorder, he said.
Goodwin said there is “very little doubt” that antidepressants have an effect vs placebo. “The argument is over whether the effect is large and whether we should regard it as clinically significant.”
He noted that previous studies have shown a range of effect sizes with antidepressants, but the “massive” confidence intervals mean that “one is free to believe pretty much what one likes.”
The only antidepressant medication that is statistically significantly different from placebo is fluoxetine combined with olanzapine. However, that conclusion is based on “little data,” said Goodwin.
In terms of long-term management, there is “extremely little” randomized data for maintenance treatment with antidepressants in bipolar disorder. “So this does not support” long-term use, he added.
Still, although choice of antidepressant remains a guess, there is “just about support” for using them, Goodwin noted.
He urged clinicians not to dismiss antidepressant use, but to use them only where there is a clinical need and for as little time as possible. Patients with bipolar disorder should continue to take antidepressants if they relapse after they come off these medications.
However, all of that sits “in contrast” to how they’re currently used in clinical practice, Goodwin said.
Caution Urged
After the debate, the audience was asked to vote again. This time, The remaining 12% voted against the practice.
Summarizing the discussion, Vieta said that “we should be cautious” when using antidepressants in bipolar depression. However, “we should be able to use them when necessary,” he added.
Although their use as monotherapy is not best practice, especially in bipolar I disorder, there may be a subset of bipolar II patients in whom monotherapy “might still be acceptable; but I don’t think it’s a good idea,” Vieta said.
He added that clinicians should very carefully screen for mixed symptoms, which call for the prescription of other drugs, such as olanzapine and fluoxetine.
“The other important message is that we have to be even more cautious in the long term with the use of antidepressants, and we should be able to use them when there is a comorbidity” that calls for their use, Vieta concluded.
Pacchiarotti reported having received speaker fees and educational grants from Adamed, AstraZeneca, Janssen-Cilag, and Lundbeck. Goodwin reported having received honoraria from Angellini, Medscape, Pfizer, Servier, Shire, and Sun; having shares in P1vital Products; past employment as medical director of P1vital Products; and advisory board membership for Compass Pathways, Minerva, MSD, Novartis, Lundbeck, Sage, Servier, and Shire. Vieta has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Although patients with bipolar disorder commonly experience depressive symptoms, clinicians should be very cautious about treating them with antidepressants, especially as monotherapy, experts asserted in a recent debate on the topic as part of the European Psychiatric Association (EPA) 2020 Congress.
At the Congress, which was virtual this year because of the COVID-19 pandemic, psychiatric experts said that clinicians should also screen patients for mixed symptoms that are better treated with mood stabilizers. These same experts also raised concerns over long-term antidepressant use, recommending continued use only in patients who relapse after stopping antidepressants.
Isabella Pacchiarotti, MD, PhD, Centro de Investigación Biomédica en Red de Salud Mental, Barcelona, Spain, argued against the use of antidepressants in treating bipolar disorder; Guy Goodwin, PhD, however, took the “pro” stance.
Goodwin, a professor of psychiatry at the University of Oxford in the UK, admitted that there is a “paucity of data” on the role of antidepressants in bipolar disorder.
Nevertheless, there are “circumstances that one really has to treat with antidepressants simply because other things have been tried and have not worked,” he told conference attendees.
Challenging, Controversial Topic
The debate was chaired by Eduard Vieta, MD, PhD, chair of the Department of Psychiatry and Psychology at the University of Barcelona Hospital Clinic, Spain.
Vieta said the question over whether antidepressants should be used in the depressive phase of bipolar illness is “perhaps the most challenging ... especially in the area of bipolar disorder.”
At the beginning of the presentation, Vieta asked the audience for their opinion in order to have a “baseline” for the debate: among 164 respondents, 73% were in favor of using antidepressants in bipolar depression.
“Clearly there is a majority, so Isabella [Dr Pacchiarotti] is going to have a hard time improving these numbers,” Vieta noted.
Up first, Pacchiarotti began by noting that this topic remains “an area of big controversy.” However, the real question “should not be the pros and cons of antidepressants but more when and how to use them.»
Of the three phases of bipolar disorder, acute depression «poses the greatest difficulties,» she added.
This is because of the relative paucity of studies in the area, the often heated debates on the specific role of antidepressants, the discrepancy in conclusions between meta-analyses, and the currently approved therapeutic options being associated with “not very high response rates,” Pacchiarotti said.
The diagnostic criteria for unipolar and bipolar depression are “basically the same,” she noted. However, it’s important to be able to distinguish between the two conditions, as up to one fifth of patients with unipolar depression suffer from undiagnosed bipolar disorder, she explained.
Moreover, several studies have identified key symptoms in bipolar depression, such as hyperphagia and hypersomnia, increased anxiety, and psychotic and psychomotor symptoms.
As previously reported by Medscape Medical News, a task force report was released in 2013 by the International Society for Bipolar Disorder (ISBD) on antidepressant use in bipolar disorders. Pacchiarotti and Goodwin were among the report’s authors, which concluded that available evidence on this issue is methodologically weak.
This is largely because of a lack of placebo-controlled studies in this patient population (bipolar depression, alongside suicidal ideation, is often an exclusion criteria in clinical antidepressant trials).
Many guidelines consequently do not consider antidepressants to be a first-line option as monotherapy in bipolar depression, although some name the drugs as second- or third-line options.
In 2013, the ISBD recommended that antidepressant monotherapy should be “avoided” in bipolar I disorder; and in bipolar I and II depression, the treatment should be accompanied by at least two concomitant core manic symptoms.
“What Has Changed?”
Antidepressants should be used “only if there is a history of a positive response,” whereas maintenance therapy should be considered if a patient relapses into a depressive episode after stopping the drugs, the report notes.
Pacchiarotti noted that since the recommendations were published nothing has changed, noting that antidepressant efficacy in bipolar depression “remains unproven.”
The issue is not whether antidepressants are effective in bipolar depression but rather are there subpopulations where these medications are helpful or harmful, she added.
The key to understanding the heterogeneity of responses to antidepressants, she said, is the concept of a bipolar spectrum and a dimensional approach to distinguishing between bipolar disorder and unipolar depression.
In addition, the definition of a mixed episode in the DSM-IV-TR differs from that of an episode with mixed characteristics in the DSM-5, which Pacchiarotti said offers a better understanding of the phenomenon while seemingly disposing with the idea of mixed depression.
Based on previous research, there is some suggestion that a depressive state exists between major depressive disorder and bipolar I disorder with mixed features, and hypomania state between bipolar II and I disorder, also with mixed features.
Pacchiarotti said the role of antidepressants in the treatment of bipolar depression remains “controversial” and there is a need for both short- and long-term studies of their use in both bipolar I and bipolar II disorder with real-world inclusion criteria.
The concept of a bipolar spectrum needs to be considered a more “dimensional approach” to depression, with mixed features seen as a “transversal” contraindication for antidepressant use, she concluded.
In Favor — With Caveats
Taking the opposite position and arguing in favor of antidepressant use, albeit cautiously, Goodwin said previous work has shown that stable patients with bipolar disorder experience depression of variable severity about 50% of the time.
The truth is that patients do not have a depressive episode for extended periods but instead have depressive symptoms, he said. “So how we manage and treat depression really matters.”
In an analysis, Goodwin and his colleagues estimated that the cost of bipolar disorder is approximately £12,600 ($16,000) per patient per year, of which only 30.6% is attributable to healthcare costs and 68.1% to indirect costs. This means the impact on the patient is also felt by society.
He agreed with Pacchiarotti’s assertion of a bipolar spectrum and the need for a dimensional approach.
“All the patients along the spectrum have the symptoms of depression and they differ in the extent to which they show symptoms of mania, which will include irritability,” he added.
Goodwin argued that there is no evidence to suggest that the depression experienced at one end of the scale is any different from that at the other. However, safety issues around antidepressant use “really relate to the additional symptoms you see with increasing evidence of bipolarity.”
In addition, the whole discussion is confounded by comorbidity, “with symptoms that sometimes coalesce into our concept of borderline personality disorder” or attention deficit hyperactivity disorder, he said.
Goodwin said there is “very little doubt” that antidepressants have an effect vs placebo. “The argument is over whether the effect is large and whether we should regard it as clinically significant.”
He noted that previous studies have shown a range of effect sizes with antidepressants, but the “massive” confidence intervals mean that “one is free to believe pretty much what one likes.”
The only antidepressant medication that is statistically significantly different from placebo is fluoxetine combined with olanzapine. However, that conclusion is based on “little data,” said Goodwin.
In terms of long-term management, there is “extremely little” randomized data for maintenance treatment with antidepressants in bipolar disorder. “So this does not support” long-term use, he added.
Still, although choice of antidepressant remains a guess, there is “just about support” for using them, Goodwin noted.
He urged clinicians not to dismiss antidepressant use, but to use them only where there is a clinical need and for as little time as possible. Patients with bipolar disorder should continue to take antidepressants if they relapse after they come off these medications.
However, all of that sits “in contrast” to how they’re currently used in clinical practice, Goodwin said.
Caution Urged
After the debate, the audience was asked to vote again. This time, The remaining 12% voted against the practice.
Summarizing the discussion, Vieta said that “we should be cautious” when using antidepressants in bipolar depression. However, “we should be able to use them when necessary,” he added.
Although their use as monotherapy is not best practice, especially in bipolar I disorder, there may be a subset of bipolar II patients in whom monotherapy “might still be acceptable; but I don’t think it’s a good idea,” Vieta said.
He added that clinicians should very carefully screen for mixed symptoms, which call for the prescription of other drugs, such as olanzapine and fluoxetine.
“The other important message is that we have to be even more cautious in the long term with the use of antidepressants, and we should be able to use them when there is a comorbidity” that calls for their use, Vieta concluded.
Pacchiarotti reported having received speaker fees and educational grants from Adamed, AstraZeneca, Janssen-Cilag, and Lundbeck. Goodwin reported having received honoraria from Angellini, Medscape, Pfizer, Servier, Shire, and Sun; having shares in P1vital Products; past employment as medical director of P1vital Products; and advisory board membership for Compass Pathways, Minerva, MSD, Novartis, Lundbeck, Sage, Servier, and Shire. Vieta has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Six snags docs hit when seeing patients again
Sachin Dave, MD, an internist in Greenwood, Ind., never thought he’d tell his patients to avoid coming into the office. But these days, he must balance the need for face-to-face visits with the risk for COVID-19 transmission. Although he connects with most patients by telehealth, some patients still demand in-office care.
“My older patients actually insist on coming to see me in person,” said Dr. Dave, who is part of Indiana Internal Medicine Consultants, a large group practice near Indianapolis. “I have to tell them it’s not safe.”
It’s a minor hitch as his practice ramps up again – but one of those things you can’t overlook, he said. “We need to educate our patients and communicate the risk to them.”
senior vice president of patient safety and risk management for the Doctors Company, a physician-owned malpractice insurer. “It’s about minimizing risk.”
As practices increase patient volume, physicians are juggling a desire for a return to patient care and increased revenue with a need to maximize patient and staff safety. Avoiding some of these common snags may help make the transition smoother.
1. Unclear or nonexistent polices and protocols
Some physicians know what general rules they want to follow, but they haven’t conveyed them in a readily available document. Although you and your staff may have a sense of what they are, patients may be less aware of how mandatory you consider them. It’s important to develop a formal framework that you will follow and to make sure patients and staff know it.
Dr. Dave and colleagues have stringent safety protocols in place for the small percentage of patients he does feel a need to be seen in person. Masks are mandatory for staff and patients. The waiting room is set up for social distancing. If it begins getting crowded, patients are asked to wait in their cars until an exam room is ready.
“I’m not going to see a patient who refuses to put a mask on, because when I put a mask on, I’m trying to protect my patients,” said Dr. Dave. He makes it clear that he expects the same from his patients; they must wear a mask to protect his staff and himself.
“I am going to let them in with the caveat that they don’t have qualms about wearing a mask. If they have qualms about wearing a mask, then I have qualms about seeing them in person,” he said.
Be sure that all patients understand and will adhere to your protocols before they come to the office. Patients should be triaged over the phone before arriving, according to Centers for Disease Control and Prevention recommendations. (Remember that refusing assessment or care could lead to issues of patient abandonment.)
When you don’t really have a framework to follow, you don’t really know what the structure is going to be and how your practice is going to provide care. The question is, how do you build a framework for right now? said Ron Holder, chief operations officer of the Medical Group Management Association. “The first step is do no harm.”
2. Trying to see too many patients too soon
On average, practices have reported a 55% decrease in revenue and a 60% decrease in patient volume since the beginning of the COVID-19 crisis, according to the MGMA. It’s natural that many want to ramp up immediately and go back to their prior patient volume. But they need to take it slow and ensure that the correct safety protocols are in place, Mr. Holder said.
For example, telehealth is still reimbursable at parity, so physicians should keep taking advantage of that. MGMA’s practice reopening checklist has links to additional resources and considerations.
Some doctors want to see an overload of patients and want to get back to how they practiced before the pandemic, says orthopedic surgeon Charles Ruotolo, MD, president of Total Orthopedics and Sports Medicine in Massapequa, N.Y., and chairman of the department of orthopedics, Nassau University Medical Center, East Meadow, N.Y., “but at the same time, you know we still have to limit how many people are coming into the office.”
It’s not fair if some doctors in your practice are seeing 45 patients daily as they did previously whereas others are seeing half that many, he explained. “We must remain cognizant and constantly review schedules and remember we have to still keep the numbers down.”
“COVID is not going to be completely over in our lifetime,” says Evan Levine, MD, a cardiologist in Ridgefield, Conn. Taking advantage of technologies is one way to reduce risk.
He predicts that the demand will continue to increase as patients become more comfortable with virtual visits. Using Bluetooth and WiFi devices to assess patients is no longer futuristic and can help reduce the number of people in the waiting room, according to Dr. Levine, a solo practitioner and author of “What Your Doctor Won’t (or Can’t) Tell You.” “That’s a very good thing, especially as we look to fall and to flu season.”
3. Undercommunicating with patients and staff
Don’t assume patients know that you’ve opened back up and are seeing people in the office, Mr. Holder said. Update your practice website, send letters or newsletters to patients’ homes, maintain telephone and email contact, and post signs at the facility explaining your reopening process. The CDC has an excellent phone script that practices can adapt. Everyone should know what to expect and what’s expected of them.
He advised overcommunicating – more than you think is necessary – to your staff and patients. Tell them about the extra steps you’re taking. Let them know that their safety and health are the most important thing and that you are taking all these extra measures to make sure that they feel comfortable.
Keep staff appraised of policy changes. Stress what you’re doing to ensure the safety of your team members. “Even though you could be doing all those things, if you’re not communicating, then no one knows it,” said Mr. Holder.
He predicted the practices that emerge stronger from this crisis will be those with great patient education that have built up a lot of goodwill. Patients should know they can go to this practice’s patient portal as a trusted resource about COVID-19 and safety-related measures. This approach will pay dividends over the long term.
4. Giving inadequate staff training and holding too-high expectations
Staff members are scared, really scared, Ms. Bashaw said. Some may not return because they’re unsure what to expect; others may have to stay home to care for children or older relatives. Clear guidance on what is being done to ensure everyone’s safety, what is expected from staff, and flexibility with scheduling can help address these issues.
Most practices’ staff are not used to donning and removing personal protective equipment, and they’re not used to wearing masks when working with patients. Expect some mistakes.
“We had a scenario where a provider was in a room with an older patient, and the provider pulled his mask down so the patient could hear him better. He then kept the mask down while giving the patient an injection. When the family found out, they were very upset,” Ms. Bashaw related. “It was done with good intentions, to improve communication, but it’s a slip-up that could have found him liable if she became ill.”
Dr. Ruotolo had to implement new policies throughout his practice’s multiple locations in the New York metro area. They encompassed everything from staggering appointments and staff to establishing designated employee eating areas so front desk staff weren’t taking their masks off to snack.
Having specific guidelines for staff helps reassure patients that safety protocols are being adhered to. “Patients want to see we’re all doing the right thing,” he said.
Have those policies clearly written so everyone’s on the same page, Dr. Ruotolo advised. Also make sure staff knows what the rules are for patients.
Dr. Ruotolo’s reception staff hand every patient a disinfectant wipe when they arrive. They are asked to wipe down the check-in kiosk before and after using it. Assistants know not to cut corners when disinfecting exam rooms, equipment, or tables. “It’s the little things you have to think about, and make sure it’s reiterated with your staff so they’re doing it.”
If your practice isn’t back up to full staffing volume, it’s a good idea to cross train staff members so some jobs overlap, suggests Mr. Holder. Although smaller practices may already do this, at larger practices, staff members’ roles may be more specific. “You may be able to pull employees from other positions in the practice, but it’s a good idea to have some redundancy.”
5. Neglecting to document everything – even more so than before
The standard of care is changing every day, and so are the regulations, says Ms. Bashaw. Many physicians who work in larger practices or for health systems don’t take advantage of internal risk management departments, which can help them keep tabs on all of these changes.
Writing down simple protocols and having a consistent work flow are extremely important right now. What have you told staff and patients? Are they comfortable with how you’re minimizing their risk? Physicians can find a seven-page checklist that helps practitioners organize and methodically go through reopening process at the Doctors Company website.
Implementing state and local statutes or public health requirements and keeping track of when things stop and start can be complex, says Ms. Bashaw. Take a look at your pre–COVID-19 policies and procedures, and make sure you’re on top of the current standards for your office, including staff education. The most important step is connecting with your local public health authority and taking direction from them.
Ms. Bashaw strongly encouraged physicians to conduct huddles with their staff; it’s an evidence-based leadership practice that’s important from a medical malpractice perspective. Review the day’s game plan, then conduct a debriefing at the end of the day.
Discuss what worked well, what didn’t, and what tomorrow looks like. And be sure to document it all. “A standard routine and debrief gets everyone on the same page and shows due diligence,” she said.
Keep an administrative file so 2 years down the road, you remember what you did and when. That way, if there’s a problem or a breach or the standard isn’t adhered to, it’s documented in the file. Note what happened and when and what was done to mitigate it or what corrective action was taken.
All practices need to stay on top of regulatory changes. Smaller practices don’t have full-time staff dedicated to monitoring what’s happening in Washington. Associations such as the MGMA can help target what’s important and actionable.
6. Forgetting about your own and your staff’s physical and mental health
Physicians need to be worried about burnout and mental health problems from their team members, their colleagues, their patients, and themselves, according to Mr. Holder.
“There’s a mental exhaustion that is just pervasive in the world and the United States right now about all this COVID stuff and stress, not to mention all the other things that are going on,” he said.
That’s going to carry over, so physicians must make sure there’s a positive culture at the practice, where everyone’s taking care of and watching out for each other.
A version of this article originally appeared on Medscape.com.
Sachin Dave, MD, an internist in Greenwood, Ind., never thought he’d tell his patients to avoid coming into the office. But these days, he must balance the need for face-to-face visits with the risk for COVID-19 transmission. Although he connects with most patients by telehealth, some patients still demand in-office care.
“My older patients actually insist on coming to see me in person,” said Dr. Dave, who is part of Indiana Internal Medicine Consultants, a large group practice near Indianapolis. “I have to tell them it’s not safe.”
It’s a minor hitch as his practice ramps up again – but one of those things you can’t overlook, he said. “We need to educate our patients and communicate the risk to them.”
senior vice president of patient safety and risk management for the Doctors Company, a physician-owned malpractice insurer. “It’s about minimizing risk.”
As practices increase patient volume, physicians are juggling a desire for a return to patient care and increased revenue with a need to maximize patient and staff safety. Avoiding some of these common snags may help make the transition smoother.
1. Unclear or nonexistent polices and protocols
Some physicians know what general rules they want to follow, but they haven’t conveyed them in a readily available document. Although you and your staff may have a sense of what they are, patients may be less aware of how mandatory you consider them. It’s important to develop a formal framework that you will follow and to make sure patients and staff know it.
Dr. Dave and colleagues have stringent safety protocols in place for the small percentage of patients he does feel a need to be seen in person. Masks are mandatory for staff and patients. The waiting room is set up for social distancing. If it begins getting crowded, patients are asked to wait in their cars until an exam room is ready.
“I’m not going to see a patient who refuses to put a mask on, because when I put a mask on, I’m trying to protect my patients,” said Dr. Dave. He makes it clear that he expects the same from his patients; they must wear a mask to protect his staff and himself.
“I am going to let them in with the caveat that they don’t have qualms about wearing a mask. If they have qualms about wearing a mask, then I have qualms about seeing them in person,” he said.
Be sure that all patients understand and will adhere to your protocols before they come to the office. Patients should be triaged over the phone before arriving, according to Centers for Disease Control and Prevention recommendations. (Remember that refusing assessment or care could lead to issues of patient abandonment.)
When you don’t really have a framework to follow, you don’t really know what the structure is going to be and how your practice is going to provide care. The question is, how do you build a framework for right now? said Ron Holder, chief operations officer of the Medical Group Management Association. “The first step is do no harm.”
2. Trying to see too many patients too soon
On average, practices have reported a 55% decrease in revenue and a 60% decrease in patient volume since the beginning of the COVID-19 crisis, according to the MGMA. It’s natural that many want to ramp up immediately and go back to their prior patient volume. But they need to take it slow and ensure that the correct safety protocols are in place, Mr. Holder said.
For example, telehealth is still reimbursable at parity, so physicians should keep taking advantage of that. MGMA’s practice reopening checklist has links to additional resources and considerations.
Some doctors want to see an overload of patients and want to get back to how they practiced before the pandemic, says orthopedic surgeon Charles Ruotolo, MD, president of Total Orthopedics and Sports Medicine in Massapequa, N.Y., and chairman of the department of orthopedics, Nassau University Medical Center, East Meadow, N.Y., “but at the same time, you know we still have to limit how many people are coming into the office.”
It’s not fair if some doctors in your practice are seeing 45 patients daily as they did previously whereas others are seeing half that many, he explained. “We must remain cognizant and constantly review schedules and remember we have to still keep the numbers down.”
“COVID is not going to be completely over in our lifetime,” says Evan Levine, MD, a cardiologist in Ridgefield, Conn. Taking advantage of technologies is one way to reduce risk.
He predicts that the demand will continue to increase as patients become more comfortable with virtual visits. Using Bluetooth and WiFi devices to assess patients is no longer futuristic and can help reduce the number of people in the waiting room, according to Dr. Levine, a solo practitioner and author of “What Your Doctor Won’t (or Can’t) Tell You.” “That’s a very good thing, especially as we look to fall and to flu season.”
3. Undercommunicating with patients and staff
Don’t assume patients know that you’ve opened back up and are seeing people in the office, Mr. Holder said. Update your practice website, send letters or newsletters to patients’ homes, maintain telephone and email contact, and post signs at the facility explaining your reopening process. The CDC has an excellent phone script that practices can adapt. Everyone should know what to expect and what’s expected of them.
He advised overcommunicating – more than you think is necessary – to your staff and patients. Tell them about the extra steps you’re taking. Let them know that their safety and health are the most important thing and that you are taking all these extra measures to make sure that they feel comfortable.
Keep staff appraised of policy changes. Stress what you’re doing to ensure the safety of your team members. “Even though you could be doing all those things, if you’re not communicating, then no one knows it,” said Mr. Holder.
He predicted the practices that emerge stronger from this crisis will be those with great patient education that have built up a lot of goodwill. Patients should know they can go to this practice’s patient portal as a trusted resource about COVID-19 and safety-related measures. This approach will pay dividends over the long term.
4. Giving inadequate staff training and holding too-high expectations
Staff members are scared, really scared, Ms. Bashaw said. Some may not return because they’re unsure what to expect; others may have to stay home to care for children or older relatives. Clear guidance on what is being done to ensure everyone’s safety, what is expected from staff, and flexibility with scheduling can help address these issues.
Most practices’ staff are not used to donning and removing personal protective equipment, and they’re not used to wearing masks when working with patients. Expect some mistakes.
“We had a scenario where a provider was in a room with an older patient, and the provider pulled his mask down so the patient could hear him better. He then kept the mask down while giving the patient an injection. When the family found out, they were very upset,” Ms. Bashaw related. “It was done with good intentions, to improve communication, but it’s a slip-up that could have found him liable if she became ill.”
Dr. Ruotolo had to implement new policies throughout his practice’s multiple locations in the New York metro area. They encompassed everything from staggering appointments and staff to establishing designated employee eating areas so front desk staff weren’t taking their masks off to snack.
Having specific guidelines for staff helps reassure patients that safety protocols are being adhered to. “Patients want to see we’re all doing the right thing,” he said.
Have those policies clearly written so everyone’s on the same page, Dr. Ruotolo advised. Also make sure staff knows what the rules are for patients.
Dr. Ruotolo’s reception staff hand every patient a disinfectant wipe when they arrive. They are asked to wipe down the check-in kiosk before and after using it. Assistants know not to cut corners when disinfecting exam rooms, equipment, or tables. “It’s the little things you have to think about, and make sure it’s reiterated with your staff so they’re doing it.”
If your practice isn’t back up to full staffing volume, it’s a good idea to cross train staff members so some jobs overlap, suggests Mr. Holder. Although smaller practices may already do this, at larger practices, staff members’ roles may be more specific. “You may be able to pull employees from other positions in the practice, but it’s a good idea to have some redundancy.”
5. Neglecting to document everything – even more so than before
The standard of care is changing every day, and so are the regulations, says Ms. Bashaw. Many physicians who work in larger practices or for health systems don’t take advantage of internal risk management departments, which can help them keep tabs on all of these changes.
Writing down simple protocols and having a consistent work flow are extremely important right now. What have you told staff and patients? Are they comfortable with how you’re minimizing their risk? Physicians can find a seven-page checklist that helps practitioners organize and methodically go through reopening process at the Doctors Company website.
Implementing state and local statutes or public health requirements and keeping track of when things stop and start can be complex, says Ms. Bashaw. Take a look at your pre–COVID-19 policies and procedures, and make sure you’re on top of the current standards for your office, including staff education. The most important step is connecting with your local public health authority and taking direction from them.
Ms. Bashaw strongly encouraged physicians to conduct huddles with their staff; it’s an evidence-based leadership practice that’s important from a medical malpractice perspective. Review the day’s game plan, then conduct a debriefing at the end of the day.
Discuss what worked well, what didn’t, and what tomorrow looks like. And be sure to document it all. “A standard routine and debrief gets everyone on the same page and shows due diligence,” she said.
Keep an administrative file so 2 years down the road, you remember what you did and when. That way, if there’s a problem or a breach or the standard isn’t adhered to, it’s documented in the file. Note what happened and when and what was done to mitigate it or what corrective action was taken.
All practices need to stay on top of regulatory changes. Smaller practices don’t have full-time staff dedicated to monitoring what’s happening in Washington. Associations such as the MGMA can help target what’s important and actionable.
6. Forgetting about your own and your staff’s physical and mental health
Physicians need to be worried about burnout and mental health problems from their team members, their colleagues, their patients, and themselves, according to Mr. Holder.
“There’s a mental exhaustion that is just pervasive in the world and the United States right now about all this COVID stuff and stress, not to mention all the other things that are going on,” he said.
That’s going to carry over, so physicians must make sure there’s a positive culture at the practice, where everyone’s taking care of and watching out for each other.
A version of this article originally appeared on Medscape.com.
Sachin Dave, MD, an internist in Greenwood, Ind., never thought he’d tell his patients to avoid coming into the office. But these days, he must balance the need for face-to-face visits with the risk for COVID-19 transmission. Although he connects with most patients by telehealth, some patients still demand in-office care.
“My older patients actually insist on coming to see me in person,” said Dr. Dave, who is part of Indiana Internal Medicine Consultants, a large group practice near Indianapolis. “I have to tell them it’s not safe.”
It’s a minor hitch as his practice ramps up again – but one of those things you can’t overlook, he said. “We need to educate our patients and communicate the risk to them.”
senior vice president of patient safety and risk management for the Doctors Company, a physician-owned malpractice insurer. “It’s about minimizing risk.”
As practices increase patient volume, physicians are juggling a desire for a return to patient care and increased revenue with a need to maximize patient and staff safety. Avoiding some of these common snags may help make the transition smoother.
1. Unclear or nonexistent polices and protocols
Some physicians know what general rules they want to follow, but they haven’t conveyed them in a readily available document. Although you and your staff may have a sense of what they are, patients may be less aware of how mandatory you consider them. It’s important to develop a formal framework that you will follow and to make sure patients and staff know it.
Dr. Dave and colleagues have stringent safety protocols in place for the small percentage of patients he does feel a need to be seen in person. Masks are mandatory for staff and patients. The waiting room is set up for social distancing. If it begins getting crowded, patients are asked to wait in their cars until an exam room is ready.
“I’m not going to see a patient who refuses to put a mask on, because when I put a mask on, I’m trying to protect my patients,” said Dr. Dave. He makes it clear that he expects the same from his patients; they must wear a mask to protect his staff and himself.
“I am going to let them in with the caveat that they don’t have qualms about wearing a mask. If they have qualms about wearing a mask, then I have qualms about seeing them in person,” he said.
Be sure that all patients understand and will adhere to your protocols before they come to the office. Patients should be triaged over the phone before arriving, according to Centers for Disease Control and Prevention recommendations. (Remember that refusing assessment or care could lead to issues of patient abandonment.)
When you don’t really have a framework to follow, you don’t really know what the structure is going to be and how your practice is going to provide care. The question is, how do you build a framework for right now? said Ron Holder, chief operations officer of the Medical Group Management Association. “The first step is do no harm.”
2. Trying to see too many patients too soon
On average, practices have reported a 55% decrease in revenue and a 60% decrease in patient volume since the beginning of the COVID-19 crisis, according to the MGMA. It’s natural that many want to ramp up immediately and go back to their prior patient volume. But they need to take it slow and ensure that the correct safety protocols are in place, Mr. Holder said.
For example, telehealth is still reimbursable at parity, so physicians should keep taking advantage of that. MGMA’s practice reopening checklist has links to additional resources and considerations.
Some doctors want to see an overload of patients and want to get back to how they practiced before the pandemic, says orthopedic surgeon Charles Ruotolo, MD, president of Total Orthopedics and Sports Medicine in Massapequa, N.Y., and chairman of the department of orthopedics, Nassau University Medical Center, East Meadow, N.Y., “but at the same time, you know we still have to limit how many people are coming into the office.”
It’s not fair if some doctors in your practice are seeing 45 patients daily as they did previously whereas others are seeing half that many, he explained. “We must remain cognizant and constantly review schedules and remember we have to still keep the numbers down.”
“COVID is not going to be completely over in our lifetime,” says Evan Levine, MD, a cardiologist in Ridgefield, Conn. Taking advantage of technologies is one way to reduce risk.
He predicts that the demand will continue to increase as patients become more comfortable with virtual visits. Using Bluetooth and WiFi devices to assess patients is no longer futuristic and can help reduce the number of people in the waiting room, according to Dr. Levine, a solo practitioner and author of “What Your Doctor Won’t (or Can’t) Tell You.” “That’s a very good thing, especially as we look to fall and to flu season.”
3. Undercommunicating with patients and staff
Don’t assume patients know that you’ve opened back up and are seeing people in the office, Mr. Holder said. Update your practice website, send letters or newsletters to patients’ homes, maintain telephone and email contact, and post signs at the facility explaining your reopening process. The CDC has an excellent phone script that practices can adapt. Everyone should know what to expect and what’s expected of them.
He advised overcommunicating – more than you think is necessary – to your staff and patients. Tell them about the extra steps you’re taking. Let them know that their safety and health are the most important thing and that you are taking all these extra measures to make sure that they feel comfortable.
Keep staff appraised of policy changes. Stress what you’re doing to ensure the safety of your team members. “Even though you could be doing all those things, if you’re not communicating, then no one knows it,” said Mr. Holder.
He predicted the practices that emerge stronger from this crisis will be those with great patient education that have built up a lot of goodwill. Patients should know they can go to this practice’s patient portal as a trusted resource about COVID-19 and safety-related measures. This approach will pay dividends over the long term.
4. Giving inadequate staff training and holding too-high expectations
Staff members are scared, really scared, Ms. Bashaw said. Some may not return because they’re unsure what to expect; others may have to stay home to care for children or older relatives. Clear guidance on what is being done to ensure everyone’s safety, what is expected from staff, and flexibility with scheduling can help address these issues.
Most practices’ staff are not used to donning and removing personal protective equipment, and they’re not used to wearing masks when working with patients. Expect some mistakes.
“We had a scenario where a provider was in a room with an older patient, and the provider pulled his mask down so the patient could hear him better. He then kept the mask down while giving the patient an injection. When the family found out, they were very upset,” Ms. Bashaw related. “It was done with good intentions, to improve communication, but it’s a slip-up that could have found him liable if she became ill.”
Dr. Ruotolo had to implement new policies throughout his practice’s multiple locations in the New York metro area. They encompassed everything from staggering appointments and staff to establishing designated employee eating areas so front desk staff weren’t taking their masks off to snack.
Having specific guidelines for staff helps reassure patients that safety protocols are being adhered to. “Patients want to see we’re all doing the right thing,” he said.
Have those policies clearly written so everyone’s on the same page, Dr. Ruotolo advised. Also make sure staff knows what the rules are for patients.
Dr. Ruotolo’s reception staff hand every patient a disinfectant wipe when they arrive. They are asked to wipe down the check-in kiosk before and after using it. Assistants know not to cut corners when disinfecting exam rooms, equipment, or tables. “It’s the little things you have to think about, and make sure it’s reiterated with your staff so they’re doing it.”
If your practice isn’t back up to full staffing volume, it’s a good idea to cross train staff members so some jobs overlap, suggests Mr. Holder. Although smaller practices may already do this, at larger practices, staff members’ roles may be more specific. “You may be able to pull employees from other positions in the practice, but it’s a good idea to have some redundancy.”
5. Neglecting to document everything – even more so than before
The standard of care is changing every day, and so are the regulations, says Ms. Bashaw. Many physicians who work in larger practices or for health systems don’t take advantage of internal risk management departments, which can help them keep tabs on all of these changes.
Writing down simple protocols and having a consistent work flow are extremely important right now. What have you told staff and patients? Are they comfortable with how you’re minimizing their risk? Physicians can find a seven-page checklist that helps practitioners organize and methodically go through reopening process at the Doctors Company website.
Implementing state and local statutes or public health requirements and keeping track of when things stop and start can be complex, says Ms. Bashaw. Take a look at your pre–COVID-19 policies and procedures, and make sure you’re on top of the current standards for your office, including staff education. The most important step is connecting with your local public health authority and taking direction from them.
Ms. Bashaw strongly encouraged physicians to conduct huddles with their staff; it’s an evidence-based leadership practice that’s important from a medical malpractice perspective. Review the day’s game plan, then conduct a debriefing at the end of the day.
Discuss what worked well, what didn’t, and what tomorrow looks like. And be sure to document it all. “A standard routine and debrief gets everyone on the same page and shows due diligence,” she said.
Keep an administrative file so 2 years down the road, you remember what you did and when. That way, if there’s a problem or a breach or the standard isn’t adhered to, it’s documented in the file. Note what happened and when and what was done to mitigate it or what corrective action was taken.
All practices need to stay on top of regulatory changes. Smaller practices don’t have full-time staff dedicated to monitoring what’s happening in Washington. Associations such as the MGMA can help target what’s important and actionable.
6. Forgetting about your own and your staff’s physical and mental health
Physicians need to be worried about burnout and mental health problems from their team members, their colleagues, their patients, and themselves, according to Mr. Holder.
“There’s a mental exhaustion that is just pervasive in the world and the United States right now about all this COVID stuff and stress, not to mention all the other things that are going on,” he said.
That’s going to carry over, so physicians must make sure there’s a positive culture at the practice, where everyone’s taking care of and watching out for each other.
A version of this article originally appeared on Medscape.com.














