User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
‘Celebration’ will be ‘short-lived’ if COVID vaccine rushed: Experts
on Wednesday.
The career staff of the Food and Drug Administration can be counted on to appropriately weigh whether a vaccine should be cleared for use in preventing COVID-19, witnesses, including Paul A. Offit, MD, of Children’s Hospital of Philadelphia, told the House Energy and Commerce Committee’s oversight and investigations panel.
FDA staffers would object to attempts by the Trump administration to rush a vaccine to the public without proper vetting, as would veteran federal researchers, including National Institutes of Health Director Francis S. Collins, MD, PhD, and Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, Offit said.
“If COVID-19 vaccines are released before they’re ready to be released, you will hear from these people, and you will also hear from people like Dr. Francis Collins and Tony Fauci, both of whom are trusted by the American public, as well as many other academicians and researchers who wouldn’t stand for this,” he said.
“The public is already nervous about these vaccines,” said Offit, who serves on key FDA and Centers for Disease Control and Prevention committees overseeing vaccine policy. “If trusted health officials stand up and decry a premature release, the celebration by the administration will be short-lived.”
Overly optimistic estimates about a potential approval can only serve to erode the public’s trust in these crucial vaccines, said another witness, Ashish K. Jha, MD, MPH, the dean of Brown University’s School of Public Health, in Providence, Rhode Island.
“All political leaders need to stop talking about things like time lines,” Jha told the lawmakers.
President Donald Trump has several times suggested that a COVID vaccine might be approved ahead of the November 3 election, where he faces a significant challenge from his Democratic rival, former Vice President Joe Biden.
In a Tuesday night debate with Biden, Trump again raised the idea of a quick approval. “Now we’re weeks away from a vaccine,” Trump said during the debate.
Trump’s estimates, though, are not in line with those offered by most firms involved with making vaccines. The most optimistic projections have come from Pfizer Inc. The drugmaker’s chief executive, Albert Bourla, has spoken about his company possibly having data to present to the FDA as early as late October about the safety and effectiveness of a vaccine.
In a September 8 interview with the Today show, Bourla said there was a 60% chance his company would meet that goal. In response to a question, he made it clear his comments applied to a potential Pfizer application, not an approval or release of a vaccine by that time.
In response to concerns about political pressures, the FDA in June issued guidance outlining what its staff would require for approval of a COVID-19 vaccine.
Pushback on politics
Another witness at the Wednesday hearing, Mark McClellan, MD, PhD, a former FDA commissioner (2002 – 2004), pushed back on objections to a potential release of further guidance from the agency.
“Some recent statements from the White House have implied that FDA’s plan to release additional written guidance on its expectations for emergency use authorization of a vaccine is unnecessarily raising the bar on regulatory standards for authorization,” said McClellan in his testimony for the House panel. “That is not the case.”
Instead, further FDA guidance would be a welcome form of feedback for the firms trying to develop COVID-19 vaccines, according to McClellan, who also serves on the board of directors for Johnson & Johnson. Johnson & Johnson is among the firms that have advanced a COVID-19 vaccine candidate to phase 3 testing. In his role as a director, he serves on the board’s regulatory compliance committee.
Along with politics, recent stumbles at FDA with emergency use authorizations (EUAs) of treatments for COVID-19 have eroded the public’s confidence in the agency, Jha told the House panel. The FDA approved hydroxychloroquine, a medicine promoted by Trump for use in COVID, under an EUA in March and then revoked this clearance in June.
Jha said the FDA’s most serious misstep was its handling of convalescent plasma, which was approved through an EUA on August 23 “in a highly advertised and widely televised announcement including the president.
“The announcement solidified in the public conversation the impression that, increasingly with this administration, politics are taking over trusted, nonpartisan scientific institutions,” he said in his testimony.
Approving a COVID-19 vaccine on the limited evidence through an EUA would mark a serious departure from FDA policy, according to Jha.
“While we sometimes accept a certain level of potential harm in experimental treatments for those who are severely ill, vaccines are given to healthy people and therefore need to have a substantially higher measure of safety and effectiveness,” he explained.
Jha said the FDA has only once before used this EUA approach for a vaccine. That was for a vaccine against inhaled anthrax and was mostly distributed to high-risk soldiers and civilians in war zones.
COVID-19, in contrast, is an infection that has changed lives around the world. The virus has contributed to more than 1 million deaths, including more than 200,000 in the United States, according to the World Health Organization.
Scientists are hoping vaccines will help curb this infection, although much of the future success of vaccines depends on how widely they are used, witnesses told the House panel.
Debate on approaches for vaccine effectiveness
In his testimony, Jha also noted concerns about COVID-19 vaccine trials. He included a reference to a Sept. 22 opinion article titled, “These Coronavirus Trials Don›t Answer the One Question We Need to Know,” which was written by Peter Doshi, PhD, of the University of Maryland School of Pharmacy, in Baltimore, and Eric Topol, MD, a professor of molecular medicine at Scripps Research in La Jolla, Calif. Topol is also editor in chief of Medscape.
Topol and Doshi questioned why the firms Moderna, Pfizer, and AstraZeneca structured their competing trials such that “a vaccine could meet the companies’ benchmark for success if it lowered the risk of mild Covid-19, but was never shown to reduce moderate or severe forms of the disease, or the risk of hospitalization, admissions to the intensive care unit or death.”
“To say a vaccine works should mean that most people no longer run the risk of getting seriously sick,” Topol and Doshi wrote. “That’s not what these trials will determine.”
There was disagreement about this point at the hearing. U.S. Representative Morgan Griffith (R-Va.) read the section of the Doshi-Topol article quoted above and asked one witness, Offit, to weigh in.
“Do you agree with those concerns? And either way, tell me why,” Griffith asked.
“I don’t agree,” Offit responded.
“I think it’s actually much harder to prevent asymptomatic infection or mildly symptomatic infection,” he said. “If you can prevent that, you are much more likely to prevent moderate to severe disease. So I think they have it backwards.”
But other researchers also question the approaches used with the current crop of COVID-19 vaccines.
“With the current protocols, it is conceivable that a vaccine might be considered effective – and eventually approved – based primarily on its ability to prevent mild cases alone,” wrote William Haseltine, PhD, president of the nonprofit ACCESS Health International, in a September 22 opinion article in the Washington Post titled: “Beware of COVID-19 Vaccine Trials Designed to Succeed From the Start.”
In an interview with Medscape Medical News on Wednesday, Haseltine said he maintains these concerns about the tests. Earlier in his career, he was a leader in HIV research through his lab at Harvard University in Cambridge, Massachusetts, and he subsequently led a biotech company, Human Genome Sciences.
He fears consumers will not get what they might expect from the vaccines being tested.
“What people care about is if this is going to keep them out of the hospital and will it keep them alive. And that’s not even part of this protocol,” Haseltine said.
This article first appeared on Medscape.com.
on Wednesday.
The career staff of the Food and Drug Administration can be counted on to appropriately weigh whether a vaccine should be cleared for use in preventing COVID-19, witnesses, including Paul A. Offit, MD, of Children’s Hospital of Philadelphia, told the House Energy and Commerce Committee’s oversight and investigations panel.
FDA staffers would object to attempts by the Trump administration to rush a vaccine to the public without proper vetting, as would veteran federal researchers, including National Institutes of Health Director Francis S. Collins, MD, PhD, and Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, Offit said.
“If COVID-19 vaccines are released before they’re ready to be released, you will hear from these people, and you will also hear from people like Dr. Francis Collins and Tony Fauci, both of whom are trusted by the American public, as well as many other academicians and researchers who wouldn’t stand for this,” he said.
“The public is already nervous about these vaccines,” said Offit, who serves on key FDA and Centers for Disease Control and Prevention committees overseeing vaccine policy. “If trusted health officials stand up and decry a premature release, the celebration by the administration will be short-lived.”
Overly optimistic estimates about a potential approval can only serve to erode the public’s trust in these crucial vaccines, said another witness, Ashish K. Jha, MD, MPH, the dean of Brown University’s School of Public Health, in Providence, Rhode Island.
“All political leaders need to stop talking about things like time lines,” Jha told the lawmakers.
President Donald Trump has several times suggested that a COVID vaccine might be approved ahead of the November 3 election, where he faces a significant challenge from his Democratic rival, former Vice President Joe Biden.
In a Tuesday night debate with Biden, Trump again raised the idea of a quick approval. “Now we’re weeks away from a vaccine,” Trump said during the debate.
Trump’s estimates, though, are not in line with those offered by most firms involved with making vaccines. The most optimistic projections have come from Pfizer Inc. The drugmaker’s chief executive, Albert Bourla, has spoken about his company possibly having data to present to the FDA as early as late October about the safety and effectiveness of a vaccine.
In a September 8 interview with the Today show, Bourla said there was a 60% chance his company would meet that goal. In response to a question, he made it clear his comments applied to a potential Pfizer application, not an approval or release of a vaccine by that time.
In response to concerns about political pressures, the FDA in June issued guidance outlining what its staff would require for approval of a COVID-19 vaccine.
Pushback on politics
Another witness at the Wednesday hearing, Mark McClellan, MD, PhD, a former FDA commissioner (2002 – 2004), pushed back on objections to a potential release of further guidance from the agency.
“Some recent statements from the White House have implied that FDA’s plan to release additional written guidance on its expectations for emergency use authorization of a vaccine is unnecessarily raising the bar on regulatory standards for authorization,” said McClellan in his testimony for the House panel. “That is not the case.”
Instead, further FDA guidance would be a welcome form of feedback for the firms trying to develop COVID-19 vaccines, according to McClellan, who also serves on the board of directors for Johnson & Johnson. Johnson & Johnson is among the firms that have advanced a COVID-19 vaccine candidate to phase 3 testing. In his role as a director, he serves on the board’s regulatory compliance committee.
Along with politics, recent stumbles at FDA with emergency use authorizations (EUAs) of treatments for COVID-19 have eroded the public’s confidence in the agency, Jha told the House panel. The FDA approved hydroxychloroquine, a medicine promoted by Trump for use in COVID, under an EUA in March and then revoked this clearance in June.
Jha said the FDA’s most serious misstep was its handling of convalescent plasma, which was approved through an EUA on August 23 “in a highly advertised and widely televised announcement including the president.
“The announcement solidified in the public conversation the impression that, increasingly with this administration, politics are taking over trusted, nonpartisan scientific institutions,” he said in his testimony.
Approving a COVID-19 vaccine on the limited evidence through an EUA would mark a serious departure from FDA policy, according to Jha.
“While we sometimes accept a certain level of potential harm in experimental treatments for those who are severely ill, vaccines are given to healthy people and therefore need to have a substantially higher measure of safety and effectiveness,” he explained.
Jha said the FDA has only once before used this EUA approach for a vaccine. That was for a vaccine against inhaled anthrax and was mostly distributed to high-risk soldiers and civilians in war zones.
COVID-19, in contrast, is an infection that has changed lives around the world. The virus has contributed to more than 1 million deaths, including more than 200,000 in the United States, according to the World Health Organization.
Scientists are hoping vaccines will help curb this infection, although much of the future success of vaccines depends on how widely they are used, witnesses told the House panel.
Debate on approaches for vaccine effectiveness
In his testimony, Jha also noted concerns about COVID-19 vaccine trials. He included a reference to a Sept. 22 opinion article titled, “These Coronavirus Trials Don›t Answer the One Question We Need to Know,” which was written by Peter Doshi, PhD, of the University of Maryland School of Pharmacy, in Baltimore, and Eric Topol, MD, a professor of molecular medicine at Scripps Research in La Jolla, Calif. Topol is also editor in chief of Medscape.
Topol and Doshi questioned why the firms Moderna, Pfizer, and AstraZeneca structured their competing trials such that “a vaccine could meet the companies’ benchmark for success if it lowered the risk of mild Covid-19, but was never shown to reduce moderate or severe forms of the disease, or the risk of hospitalization, admissions to the intensive care unit or death.”
“To say a vaccine works should mean that most people no longer run the risk of getting seriously sick,” Topol and Doshi wrote. “That’s not what these trials will determine.”
There was disagreement about this point at the hearing. U.S. Representative Morgan Griffith (R-Va.) read the section of the Doshi-Topol article quoted above and asked one witness, Offit, to weigh in.
“Do you agree with those concerns? And either way, tell me why,” Griffith asked.
“I don’t agree,” Offit responded.
“I think it’s actually much harder to prevent asymptomatic infection or mildly symptomatic infection,” he said. “If you can prevent that, you are much more likely to prevent moderate to severe disease. So I think they have it backwards.”
But other researchers also question the approaches used with the current crop of COVID-19 vaccines.
“With the current protocols, it is conceivable that a vaccine might be considered effective – and eventually approved – based primarily on its ability to prevent mild cases alone,” wrote William Haseltine, PhD, president of the nonprofit ACCESS Health International, in a September 22 opinion article in the Washington Post titled: “Beware of COVID-19 Vaccine Trials Designed to Succeed From the Start.”
In an interview with Medscape Medical News on Wednesday, Haseltine said he maintains these concerns about the tests. Earlier in his career, he was a leader in HIV research through his lab at Harvard University in Cambridge, Massachusetts, and he subsequently led a biotech company, Human Genome Sciences.
He fears consumers will not get what they might expect from the vaccines being tested.
“What people care about is if this is going to keep them out of the hospital and will it keep them alive. And that’s not even part of this protocol,” Haseltine said.
This article first appeared on Medscape.com.
on Wednesday.
The career staff of the Food and Drug Administration can be counted on to appropriately weigh whether a vaccine should be cleared for use in preventing COVID-19, witnesses, including Paul A. Offit, MD, of Children’s Hospital of Philadelphia, told the House Energy and Commerce Committee’s oversight and investigations panel.
FDA staffers would object to attempts by the Trump administration to rush a vaccine to the public without proper vetting, as would veteran federal researchers, including National Institutes of Health Director Francis S. Collins, MD, PhD, and Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, Offit said.
“If COVID-19 vaccines are released before they’re ready to be released, you will hear from these people, and you will also hear from people like Dr. Francis Collins and Tony Fauci, both of whom are trusted by the American public, as well as many other academicians and researchers who wouldn’t stand for this,” he said.
“The public is already nervous about these vaccines,” said Offit, who serves on key FDA and Centers for Disease Control and Prevention committees overseeing vaccine policy. “If trusted health officials stand up and decry a premature release, the celebration by the administration will be short-lived.”
Overly optimistic estimates about a potential approval can only serve to erode the public’s trust in these crucial vaccines, said another witness, Ashish K. Jha, MD, MPH, the dean of Brown University’s School of Public Health, in Providence, Rhode Island.
“All political leaders need to stop talking about things like time lines,” Jha told the lawmakers.
President Donald Trump has several times suggested that a COVID vaccine might be approved ahead of the November 3 election, where he faces a significant challenge from his Democratic rival, former Vice President Joe Biden.
In a Tuesday night debate with Biden, Trump again raised the idea of a quick approval. “Now we’re weeks away from a vaccine,” Trump said during the debate.
Trump’s estimates, though, are not in line with those offered by most firms involved with making vaccines. The most optimistic projections have come from Pfizer Inc. The drugmaker’s chief executive, Albert Bourla, has spoken about his company possibly having data to present to the FDA as early as late October about the safety and effectiveness of a vaccine.
In a September 8 interview with the Today show, Bourla said there was a 60% chance his company would meet that goal. In response to a question, he made it clear his comments applied to a potential Pfizer application, not an approval or release of a vaccine by that time.
In response to concerns about political pressures, the FDA in June issued guidance outlining what its staff would require for approval of a COVID-19 vaccine.
Pushback on politics
Another witness at the Wednesday hearing, Mark McClellan, MD, PhD, a former FDA commissioner (2002 – 2004), pushed back on objections to a potential release of further guidance from the agency.
“Some recent statements from the White House have implied that FDA’s plan to release additional written guidance on its expectations for emergency use authorization of a vaccine is unnecessarily raising the bar on regulatory standards for authorization,” said McClellan in his testimony for the House panel. “That is not the case.”
Instead, further FDA guidance would be a welcome form of feedback for the firms trying to develop COVID-19 vaccines, according to McClellan, who also serves on the board of directors for Johnson & Johnson. Johnson & Johnson is among the firms that have advanced a COVID-19 vaccine candidate to phase 3 testing. In his role as a director, he serves on the board’s regulatory compliance committee.
Along with politics, recent stumbles at FDA with emergency use authorizations (EUAs) of treatments for COVID-19 have eroded the public’s confidence in the agency, Jha told the House panel. The FDA approved hydroxychloroquine, a medicine promoted by Trump for use in COVID, under an EUA in March and then revoked this clearance in June.
Jha said the FDA’s most serious misstep was its handling of convalescent plasma, which was approved through an EUA on August 23 “in a highly advertised and widely televised announcement including the president.
“The announcement solidified in the public conversation the impression that, increasingly with this administration, politics are taking over trusted, nonpartisan scientific institutions,” he said in his testimony.
Approving a COVID-19 vaccine on the limited evidence through an EUA would mark a serious departure from FDA policy, according to Jha.
“While we sometimes accept a certain level of potential harm in experimental treatments for those who are severely ill, vaccines are given to healthy people and therefore need to have a substantially higher measure of safety and effectiveness,” he explained.
Jha said the FDA has only once before used this EUA approach for a vaccine. That was for a vaccine against inhaled anthrax and was mostly distributed to high-risk soldiers and civilians in war zones.
COVID-19, in contrast, is an infection that has changed lives around the world. The virus has contributed to more than 1 million deaths, including more than 200,000 in the United States, according to the World Health Organization.
Scientists are hoping vaccines will help curb this infection, although much of the future success of vaccines depends on how widely they are used, witnesses told the House panel.
Debate on approaches for vaccine effectiveness
In his testimony, Jha also noted concerns about COVID-19 vaccine trials. He included a reference to a Sept. 22 opinion article titled, “These Coronavirus Trials Don›t Answer the One Question We Need to Know,” which was written by Peter Doshi, PhD, of the University of Maryland School of Pharmacy, in Baltimore, and Eric Topol, MD, a professor of molecular medicine at Scripps Research in La Jolla, Calif. Topol is also editor in chief of Medscape.
Topol and Doshi questioned why the firms Moderna, Pfizer, and AstraZeneca structured their competing trials such that “a vaccine could meet the companies’ benchmark for success if it lowered the risk of mild Covid-19, but was never shown to reduce moderate or severe forms of the disease, or the risk of hospitalization, admissions to the intensive care unit or death.”
“To say a vaccine works should mean that most people no longer run the risk of getting seriously sick,” Topol and Doshi wrote. “That’s not what these trials will determine.”
There was disagreement about this point at the hearing. U.S. Representative Morgan Griffith (R-Va.) read the section of the Doshi-Topol article quoted above and asked one witness, Offit, to weigh in.
“Do you agree with those concerns? And either way, tell me why,” Griffith asked.
“I don’t agree,” Offit responded.
“I think it’s actually much harder to prevent asymptomatic infection or mildly symptomatic infection,” he said. “If you can prevent that, you are much more likely to prevent moderate to severe disease. So I think they have it backwards.”
But other researchers also question the approaches used with the current crop of COVID-19 vaccines.
“With the current protocols, it is conceivable that a vaccine might be considered effective – and eventually approved – based primarily on its ability to prevent mild cases alone,” wrote William Haseltine, PhD, president of the nonprofit ACCESS Health International, in a September 22 opinion article in the Washington Post titled: “Beware of COVID-19 Vaccine Trials Designed to Succeed From the Start.”
In an interview with Medscape Medical News on Wednesday, Haseltine said he maintains these concerns about the tests. Earlier in his career, he was a leader in HIV research through his lab at Harvard University in Cambridge, Massachusetts, and he subsequently led a biotech company, Human Genome Sciences.
He fears consumers will not get what they might expect from the vaccines being tested.
“What people care about is if this is going to keep them out of the hospital and will it keep them alive. And that’s not even part of this protocol,” Haseltine said.
This article first appeared on Medscape.com.
Nerve damage linked to prone positioning in COVID-19
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
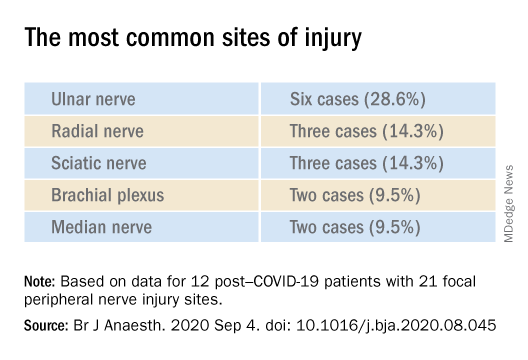
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
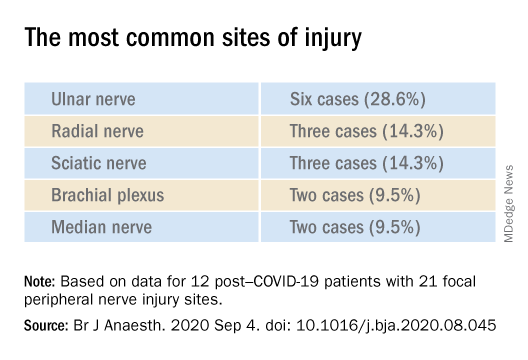
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
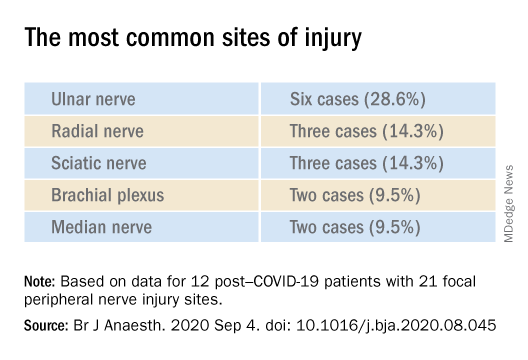
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF ANAESTHESIOLOGY
Trump signs Medicare loan relief bill delaying repayments
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
‘Overwhelming evidence’ FDA’s opioid approval process is shoddy
Despite the ongoing epidemic of misuse, overuse, and diversion of opioids, the Food and Drug Administration has set a low bar for approval of these medications over the past 20 years, new research suggests.
The study results also show that the FDA did not require manufacturers to collect safety data on tolerance, withdrawal, overdose, misuse, and diversion in any rigorous fashion.
In addition, during the study period, 17 of the 39 new drug applications (NDAs) (only one was an innovator product, known as a new molecular entity) for chronic pain were approved with an “enriched enrollment randomized withdrawal” (EERW) trial design. Such a design, in this case, allowed manufacturers to exclude 32%-43% of the initially enrolled patients from the double-blind treatment phase.
“The question for regulators, policy makers, and others is: How did we get to a point where these approvals took place based on trials that were by design unlikely to yield some of the most important information about safety and efficacy that patients and clinicians would care about?” study investigator G. Caleb Alexander, MD, Johns Hopkins University, Baltimore, said in an interview.
The study was published online Sept. 29 in the Annals of Internal Medicine.
‘Cooking the books’
Little is known about the evidence required by the FDA for new approvals of opioid analgesics.
To characterize the quality of safety and efficacy data in NDAs for opioid analgesics approved by the FDA between 1997 and 2018, the investigators conducted the cross-sectional analysis using data from ClinicalTrials.gov, FDA reviews, and peer-reviewed publications regarding phase 3 pivotal trials.
The investigators examined the key characteristics of each NDA, including the number, size, and duration of pivotal trials, trial control groups, use of EERW, and systematically measured safety outcomes.
Results showed that most of the 48 NDAs evaluated were for new dosage forms (52.1%) or new formulations (18.8%). Only one (2.1%) was for a new molecular entity.
Of 39 NDAs approved for the treatment of chronic pain, only 21 products were supported by at least one pivotal trial. The mean duration of these 28 trials was 84 days, and they enrolled a median of 299 patients.
Results showed that, for 17 of the 39 opioids approved for chronic pain, pivotal trials had an EERW design. For the latest period – 2012-2018 – trials of all eight of the approved opioids used the EERW method.
This EERW design allows the manufacturer to assess efficacy “among a subset of patients most likely to respond and least likely to have adverse effects, reducing generalizability to real-world settings,” the investigators noted.
They called on the FDA to stop relying on this type of trial to assess opioid efficacy.
In an August 2020 article, Andrew Kolodny, MD, pointed out the pitfalls of the EERW approach. In such a study, all participants are made physiologically dependent on the opioid in a 4- to 6-week open-label phase. Only those who tolerate the drug and find it helpful are included in the randomized study. Dr. Kolodny is codirector of opioid policy research at Brandeis University, Waltham, Mass.
“Critics of EERW have correctly described this methodology as ‘cooking the books,’ ” Dr. Kolodny writes.
He noted that the agency’s decision to rely on EERW trials for opioids was “based on discussions at private meetings between FDA officials and pharmaceutical company executives hosted by an organization called Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials.” The 2013 meetings were reported in an article published in the Washington Post.
Little sign of change
Among NDAs for chronic pain, the investigators found that eight (20.5%) included pooled safety reviews that reported systematic assessment of diversion. Seven (17.9%) reported systematic measurement of nonmedical use, and 15 (38.5%) assessed incident tolerance.
The study revealed that eight of nine products that were approved for acute pain were supported by at least one pivotal trial. The median duration of these 19 trials was 1 day, and they enrolled a median of 329 patients.
The investigators noted that the findings “underscore the evidence gaps that have limited clinicians’ and patients’ understanding and appreciation of the inherent risks of prescription opioid analgesics.”
Dr. Alexander, who has been an FDA advisory committee chairman and currently serves as a consultant to plaintiffs who are suing opioid manufacturers in federal multidistrict litigation, said the study “is a story about missed opportunities to improve the safety and to improve the regulatory review of these products.”
Coinvestigator Peter Lurie, MD, who was an official at the FDA from 2009 to 2017, said that “there’s not a lot of signs that things are changing” at the agency.
The study shows that the FDA has “accepted what the companies have been presenting,” said Dr. Lurie, who is president of the Center for Science in the Public Interest.
The FDA “absolutely has the authority” to require manufacturers to undertake more rigorous trials, but agency culture keeps it from making such demands, especially if doing so means a new applicant might have to conduct trials that weren’t previously required, Dr. Lurie said in an interview.
“FDA is pretty rigorous about trying to establish a level playing field. That’s a virtuous thing, but it becomes problematic when that prevents change,” said Dr. Lurie.
The most recent FDA guidance to manufacturers, issued in 2019, does not provide advice on criteria for endpoints, study duration, or which populations are most likely to benefit from opioid treatment. The agency also does not require drug manufacturers to formally collect data on safety, tolerance, overdose symptoms, or constipation.
The guidance does suggest that the agency would likely take into account public health considerations when evaluating opioids, such as the risk to the overall population for overdose and diversion.
‘Overwhelming evidence’
Dr. Kolodny said that, as far as he is aware, “this is the first scientific publication in a peer-reviewed journal demonstrating clearly the problems with FDA’s opioid approval process.”
The article offers “overwhelming evidence that they are improperly approving the most dangerous medications – medications that killed more people than any other medication on the market,” added Dr. Kolodny, who is also president of Physicians for Responsible Opioid Prescribing.
Asked to respond to the study findings, FDA spokesperson Charles Kohler said the agency “does not comment on specific studies but evaluates them as part of the body of evidence to further our understanding about a particular issue and assist in our mission to protect public health.”
A version of this article originally appeared on Medscape.com.
Despite the ongoing epidemic of misuse, overuse, and diversion of opioids, the Food and Drug Administration has set a low bar for approval of these medications over the past 20 years, new research suggests.
The study results also show that the FDA did not require manufacturers to collect safety data on tolerance, withdrawal, overdose, misuse, and diversion in any rigorous fashion.
In addition, during the study period, 17 of the 39 new drug applications (NDAs) (only one was an innovator product, known as a new molecular entity) for chronic pain were approved with an “enriched enrollment randomized withdrawal” (EERW) trial design. Such a design, in this case, allowed manufacturers to exclude 32%-43% of the initially enrolled patients from the double-blind treatment phase.
“The question for regulators, policy makers, and others is: How did we get to a point where these approvals took place based on trials that were by design unlikely to yield some of the most important information about safety and efficacy that patients and clinicians would care about?” study investigator G. Caleb Alexander, MD, Johns Hopkins University, Baltimore, said in an interview.
The study was published online Sept. 29 in the Annals of Internal Medicine.
‘Cooking the books’
Little is known about the evidence required by the FDA for new approvals of opioid analgesics.
To characterize the quality of safety and efficacy data in NDAs for opioid analgesics approved by the FDA between 1997 and 2018, the investigators conducted the cross-sectional analysis using data from ClinicalTrials.gov, FDA reviews, and peer-reviewed publications regarding phase 3 pivotal trials.
The investigators examined the key characteristics of each NDA, including the number, size, and duration of pivotal trials, trial control groups, use of EERW, and systematically measured safety outcomes.
Results showed that most of the 48 NDAs evaluated were for new dosage forms (52.1%) or new formulations (18.8%). Only one (2.1%) was for a new molecular entity.
Of 39 NDAs approved for the treatment of chronic pain, only 21 products were supported by at least one pivotal trial. The mean duration of these 28 trials was 84 days, and they enrolled a median of 299 patients.
Results showed that, for 17 of the 39 opioids approved for chronic pain, pivotal trials had an EERW design. For the latest period – 2012-2018 – trials of all eight of the approved opioids used the EERW method.
This EERW design allows the manufacturer to assess efficacy “among a subset of patients most likely to respond and least likely to have adverse effects, reducing generalizability to real-world settings,” the investigators noted.
They called on the FDA to stop relying on this type of trial to assess opioid efficacy.
In an August 2020 article, Andrew Kolodny, MD, pointed out the pitfalls of the EERW approach. In such a study, all participants are made physiologically dependent on the opioid in a 4- to 6-week open-label phase. Only those who tolerate the drug and find it helpful are included in the randomized study. Dr. Kolodny is codirector of opioid policy research at Brandeis University, Waltham, Mass.
“Critics of EERW have correctly described this methodology as ‘cooking the books,’ ” Dr. Kolodny writes.
He noted that the agency’s decision to rely on EERW trials for opioids was “based on discussions at private meetings between FDA officials and pharmaceutical company executives hosted by an organization called Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials.” The 2013 meetings were reported in an article published in the Washington Post.
Little sign of change
Among NDAs for chronic pain, the investigators found that eight (20.5%) included pooled safety reviews that reported systematic assessment of diversion. Seven (17.9%) reported systematic measurement of nonmedical use, and 15 (38.5%) assessed incident tolerance.
The study revealed that eight of nine products that were approved for acute pain were supported by at least one pivotal trial. The median duration of these 19 trials was 1 day, and they enrolled a median of 329 patients.
The investigators noted that the findings “underscore the evidence gaps that have limited clinicians’ and patients’ understanding and appreciation of the inherent risks of prescription opioid analgesics.”
Dr. Alexander, who has been an FDA advisory committee chairman and currently serves as a consultant to plaintiffs who are suing opioid manufacturers in federal multidistrict litigation, said the study “is a story about missed opportunities to improve the safety and to improve the regulatory review of these products.”
Coinvestigator Peter Lurie, MD, who was an official at the FDA from 2009 to 2017, said that “there’s not a lot of signs that things are changing” at the agency.
The study shows that the FDA has “accepted what the companies have been presenting,” said Dr. Lurie, who is president of the Center for Science in the Public Interest.
The FDA “absolutely has the authority” to require manufacturers to undertake more rigorous trials, but agency culture keeps it from making such demands, especially if doing so means a new applicant might have to conduct trials that weren’t previously required, Dr. Lurie said in an interview.
“FDA is pretty rigorous about trying to establish a level playing field. That’s a virtuous thing, but it becomes problematic when that prevents change,” said Dr. Lurie.
The most recent FDA guidance to manufacturers, issued in 2019, does not provide advice on criteria for endpoints, study duration, or which populations are most likely to benefit from opioid treatment. The agency also does not require drug manufacturers to formally collect data on safety, tolerance, overdose symptoms, or constipation.
The guidance does suggest that the agency would likely take into account public health considerations when evaluating opioids, such as the risk to the overall population for overdose and diversion.
‘Overwhelming evidence’
Dr. Kolodny said that, as far as he is aware, “this is the first scientific publication in a peer-reviewed journal demonstrating clearly the problems with FDA’s opioid approval process.”
The article offers “overwhelming evidence that they are improperly approving the most dangerous medications – medications that killed more people than any other medication on the market,” added Dr. Kolodny, who is also president of Physicians for Responsible Opioid Prescribing.
Asked to respond to the study findings, FDA spokesperson Charles Kohler said the agency “does not comment on specific studies but evaluates them as part of the body of evidence to further our understanding about a particular issue and assist in our mission to protect public health.”
A version of this article originally appeared on Medscape.com.
Despite the ongoing epidemic of misuse, overuse, and diversion of opioids, the Food and Drug Administration has set a low bar for approval of these medications over the past 20 years, new research suggests.
The study results also show that the FDA did not require manufacturers to collect safety data on tolerance, withdrawal, overdose, misuse, and diversion in any rigorous fashion.
In addition, during the study period, 17 of the 39 new drug applications (NDAs) (only one was an innovator product, known as a new molecular entity) for chronic pain were approved with an “enriched enrollment randomized withdrawal” (EERW) trial design. Such a design, in this case, allowed manufacturers to exclude 32%-43% of the initially enrolled patients from the double-blind treatment phase.
“The question for regulators, policy makers, and others is: How did we get to a point where these approvals took place based on trials that were by design unlikely to yield some of the most important information about safety and efficacy that patients and clinicians would care about?” study investigator G. Caleb Alexander, MD, Johns Hopkins University, Baltimore, said in an interview.
The study was published online Sept. 29 in the Annals of Internal Medicine.
‘Cooking the books’
Little is known about the evidence required by the FDA for new approvals of opioid analgesics.
To characterize the quality of safety and efficacy data in NDAs for opioid analgesics approved by the FDA between 1997 and 2018, the investigators conducted the cross-sectional analysis using data from ClinicalTrials.gov, FDA reviews, and peer-reviewed publications regarding phase 3 pivotal trials.
The investigators examined the key characteristics of each NDA, including the number, size, and duration of pivotal trials, trial control groups, use of EERW, and systematically measured safety outcomes.
Results showed that most of the 48 NDAs evaluated were for new dosage forms (52.1%) or new formulations (18.8%). Only one (2.1%) was for a new molecular entity.
Of 39 NDAs approved for the treatment of chronic pain, only 21 products were supported by at least one pivotal trial. The mean duration of these 28 trials was 84 days, and they enrolled a median of 299 patients.
Results showed that, for 17 of the 39 opioids approved for chronic pain, pivotal trials had an EERW design. For the latest period – 2012-2018 – trials of all eight of the approved opioids used the EERW method.
This EERW design allows the manufacturer to assess efficacy “among a subset of patients most likely to respond and least likely to have adverse effects, reducing generalizability to real-world settings,” the investigators noted.
They called on the FDA to stop relying on this type of trial to assess opioid efficacy.
In an August 2020 article, Andrew Kolodny, MD, pointed out the pitfalls of the EERW approach. In such a study, all participants are made physiologically dependent on the opioid in a 4- to 6-week open-label phase. Only those who tolerate the drug and find it helpful are included in the randomized study. Dr. Kolodny is codirector of opioid policy research at Brandeis University, Waltham, Mass.
“Critics of EERW have correctly described this methodology as ‘cooking the books,’ ” Dr. Kolodny writes.
He noted that the agency’s decision to rely on EERW trials for opioids was “based on discussions at private meetings between FDA officials and pharmaceutical company executives hosted by an organization called Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials.” The 2013 meetings were reported in an article published in the Washington Post.
Little sign of change
Among NDAs for chronic pain, the investigators found that eight (20.5%) included pooled safety reviews that reported systematic assessment of diversion. Seven (17.9%) reported systematic measurement of nonmedical use, and 15 (38.5%) assessed incident tolerance.
The study revealed that eight of nine products that were approved for acute pain were supported by at least one pivotal trial. The median duration of these 19 trials was 1 day, and they enrolled a median of 329 patients.
The investigators noted that the findings “underscore the evidence gaps that have limited clinicians’ and patients’ understanding and appreciation of the inherent risks of prescription opioid analgesics.”
Dr. Alexander, who has been an FDA advisory committee chairman and currently serves as a consultant to plaintiffs who are suing opioid manufacturers in federal multidistrict litigation, said the study “is a story about missed opportunities to improve the safety and to improve the regulatory review of these products.”
Coinvestigator Peter Lurie, MD, who was an official at the FDA from 2009 to 2017, said that “there’s not a lot of signs that things are changing” at the agency.
The study shows that the FDA has “accepted what the companies have been presenting,” said Dr. Lurie, who is president of the Center for Science in the Public Interest.
The FDA “absolutely has the authority” to require manufacturers to undertake more rigorous trials, but agency culture keeps it from making such demands, especially if doing so means a new applicant might have to conduct trials that weren’t previously required, Dr. Lurie said in an interview.
“FDA is pretty rigorous about trying to establish a level playing field. That’s a virtuous thing, but it becomes problematic when that prevents change,” said Dr. Lurie.
The most recent FDA guidance to manufacturers, issued in 2019, does not provide advice on criteria for endpoints, study duration, or which populations are most likely to benefit from opioid treatment. The agency also does not require drug manufacturers to formally collect data on safety, tolerance, overdose symptoms, or constipation.
The guidance does suggest that the agency would likely take into account public health considerations when evaluating opioids, such as the risk to the overall population for overdose and diversion.
‘Overwhelming evidence’
Dr. Kolodny said that, as far as he is aware, “this is the first scientific publication in a peer-reviewed journal demonstrating clearly the problems with FDA’s opioid approval process.”
The article offers “overwhelming evidence that they are improperly approving the most dangerous medications – medications that killed more people than any other medication on the market,” added Dr. Kolodny, who is also president of Physicians for Responsible Opioid Prescribing.
Asked to respond to the study findings, FDA spokesperson Charles Kohler said the agency “does not comment on specific studies but evaluates them as part of the body of evidence to further our understanding about a particular issue and assist in our mission to protect public health.”
A version of this article originally appeared on Medscape.com.
COVID-19’s psychological impact gets a name
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
Listening to Mozart helps tame epilepsy
Listening to Mozart’s piano music improves epilepsy, according to a meta-analysis presented at the virtual congress of the European College of Neuropsychopharmacology.
The results of the meta-analysis of 12 published studies of the so-called Mozart Effect that met rigorous Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines demonstrate that listening to Mozart results in significant reductions in both epileptic seizure frequency and interictal epileptiform discharges (IED), compared with baseline.
The benefits were apparent during and after even a single listening session, although the effect was greater with regular daily listening sessions, according to Gianluca Sesso, MD, a resident in child and adolescent psychiatry at the University of Pisa (Italy.)
“Obviously other music may have similar effects, but it may be that Mozart’s sonatas have distinctive rhythmic structures which are particularly suited to working on epilepsy,” he speculated, adding that the mechanism involved in the Mozart Effect on brain systems remains unclear.
“The highly consistent results of our meta-analysis strongly suggest that music-based neurostimulation may improve the clinical outcome in epilepsy by reducing seizures and IED, and thus deserves to be included in the set of nonpharmacologic complementary approaches for treating epilepsy,” Dr. Sesso added.
Four studies examined the effects of listening to Mozart’s Sonata for Two Pianos in D, K.448, the most-studied piece of music as a treatment for epilepsy. The data documented a 31% reduction in seizure frequency and 28% decrease in IED during a single listen, and a 79% reduction in IED after long-term Mozart music therapy. Similarly, studies demonstrated that listening to a set of Mozart’s compositions resulted in a 36% reduction in IED during and 38% decrease after a single listen, while regular listening in a prolonged treatment period resulted in a 66% reduction in seizure frequency from baseline.
Several studies compared the benefits of listening to K. 488 with those accrued through listening to Piano Sonata No. 16 in C major, K. 545. There was no significant difference between the two, according to Dr. Sesso.
He reported having no financial conflicts regarding his meta-analysis, carried out free of commercial support.
The full details of the meta-analysis were recently published in Clinical Neurophysiology.
Listening to Mozart’s piano music improves epilepsy, according to a meta-analysis presented at the virtual congress of the European College of Neuropsychopharmacology.
The results of the meta-analysis of 12 published studies of the so-called Mozart Effect that met rigorous Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines demonstrate that listening to Mozart results in significant reductions in both epileptic seizure frequency and interictal epileptiform discharges (IED), compared with baseline.
The benefits were apparent during and after even a single listening session, although the effect was greater with regular daily listening sessions, according to Gianluca Sesso, MD, a resident in child and adolescent psychiatry at the University of Pisa (Italy.)
“Obviously other music may have similar effects, but it may be that Mozart’s sonatas have distinctive rhythmic structures which are particularly suited to working on epilepsy,” he speculated, adding that the mechanism involved in the Mozart Effect on brain systems remains unclear.
“The highly consistent results of our meta-analysis strongly suggest that music-based neurostimulation may improve the clinical outcome in epilepsy by reducing seizures and IED, and thus deserves to be included in the set of nonpharmacologic complementary approaches for treating epilepsy,” Dr. Sesso added.
Four studies examined the effects of listening to Mozart’s Sonata for Two Pianos in D, K.448, the most-studied piece of music as a treatment for epilepsy. The data documented a 31% reduction in seizure frequency and 28% decrease in IED during a single listen, and a 79% reduction in IED after long-term Mozart music therapy. Similarly, studies demonstrated that listening to a set of Mozart’s compositions resulted in a 36% reduction in IED during and 38% decrease after a single listen, while regular listening in a prolonged treatment period resulted in a 66% reduction in seizure frequency from baseline.
Several studies compared the benefits of listening to K. 488 with those accrued through listening to Piano Sonata No. 16 in C major, K. 545. There was no significant difference between the two, according to Dr. Sesso.
He reported having no financial conflicts regarding his meta-analysis, carried out free of commercial support.
The full details of the meta-analysis were recently published in Clinical Neurophysiology.
Listening to Mozart’s piano music improves epilepsy, according to a meta-analysis presented at the virtual congress of the European College of Neuropsychopharmacology.
The results of the meta-analysis of 12 published studies of the so-called Mozart Effect that met rigorous Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines demonstrate that listening to Mozart results in significant reductions in both epileptic seizure frequency and interictal epileptiform discharges (IED), compared with baseline.
The benefits were apparent during and after even a single listening session, although the effect was greater with regular daily listening sessions, according to Gianluca Sesso, MD, a resident in child and adolescent psychiatry at the University of Pisa (Italy.)
“Obviously other music may have similar effects, but it may be that Mozart’s sonatas have distinctive rhythmic structures which are particularly suited to working on epilepsy,” he speculated, adding that the mechanism involved in the Mozart Effect on brain systems remains unclear.
“The highly consistent results of our meta-analysis strongly suggest that music-based neurostimulation may improve the clinical outcome in epilepsy by reducing seizures and IED, and thus deserves to be included in the set of nonpharmacologic complementary approaches for treating epilepsy,” Dr. Sesso added.
Four studies examined the effects of listening to Mozart’s Sonata for Two Pianos in D, K.448, the most-studied piece of music as a treatment for epilepsy. The data documented a 31% reduction in seizure frequency and 28% decrease in IED during a single listen, and a 79% reduction in IED after long-term Mozart music therapy. Similarly, studies demonstrated that listening to a set of Mozart’s compositions resulted in a 36% reduction in IED during and 38% decrease after a single listen, while regular listening in a prolonged treatment period resulted in a 66% reduction in seizure frequency from baseline.
Several studies compared the benefits of listening to K. 488 with those accrued through listening to Piano Sonata No. 16 in C major, K. 545. There was no significant difference between the two, according to Dr. Sesso.
He reported having no financial conflicts regarding his meta-analysis, carried out free of commercial support.
The full details of the meta-analysis were recently published in Clinical Neurophysiology.
FROM ECNP 2020
Suicide in America: The urban-rural divide
The gap in suicide rates between rural and urban areas has widened since 2000 for both males and females, according to a recent report from the National Center for Health Statistics.

After remaining stable from 2000 to 2007, the suicide rate for rural males rose 34% from 2007 to 2018, versus 17% among urban males over the same period. Suicide rates for females were significantly lower than those of men, but the changes were larger. For rural females, the rate increased 91% from 2000 to 2018, compared with 51% for urban females, Kristen Pettrone, MD, MPH, and Sally C. Curtin, MA, said in an NCHS Data Brief.
For 2018, the last year with available data, the age-adjusted rates look like this: 21.5 per 100,000 population for urban males, 30.7 for rural males, 5.9 per 100,000 for urban females, and 8.0 for rural females. The overall rate for the United States was 14.2 per 100,000, with combined male/female rates of 13.4 in urban areas and 19.4 in rural areas, the researchers said.
Methods of suicide also varied by sex and urban-rural status. Firearms were the leading method for males in both rural and urban areas, but females split between firearms in rural areas and suffocation (including hangings) in urban areas, said Dr. Pettrone of the Centers for Disease Control and Prevention and Ms. Curtin of the NCHS.
Suffocation, however, was the fastest-growing method from 2000 to 2018, regardless of sex or location. Suffocation-related suicide rates more than quadrupled for rural females, and more than doubled for urban females and rural males, while rates rose 85% among males in urban areas, based on data from the National Vital Statistics System.
“Suicide has remained the 10th leading cause of death in the United States since 2008,” they wrote, and
SOURCE: Pettrone K, Curtin SC. 2020 Aug. NCHS Data Brief, No 373.
The gap in suicide rates between rural and urban areas has widened since 2000 for both males and females, according to a recent report from the National Center for Health Statistics.

After remaining stable from 2000 to 2007, the suicide rate for rural males rose 34% from 2007 to 2018, versus 17% among urban males over the same period. Suicide rates for females were significantly lower than those of men, but the changes were larger. For rural females, the rate increased 91% from 2000 to 2018, compared with 51% for urban females, Kristen Pettrone, MD, MPH, and Sally C. Curtin, MA, said in an NCHS Data Brief.
For 2018, the last year with available data, the age-adjusted rates look like this: 21.5 per 100,000 population for urban males, 30.7 for rural males, 5.9 per 100,000 for urban females, and 8.0 for rural females. The overall rate for the United States was 14.2 per 100,000, with combined male/female rates of 13.4 in urban areas and 19.4 in rural areas, the researchers said.
Methods of suicide also varied by sex and urban-rural status. Firearms were the leading method for males in both rural and urban areas, but females split between firearms in rural areas and suffocation (including hangings) in urban areas, said Dr. Pettrone of the Centers for Disease Control and Prevention and Ms. Curtin of the NCHS.
Suffocation, however, was the fastest-growing method from 2000 to 2018, regardless of sex or location. Suffocation-related suicide rates more than quadrupled for rural females, and more than doubled for urban females and rural males, while rates rose 85% among males in urban areas, based on data from the National Vital Statistics System.
“Suicide has remained the 10th leading cause of death in the United States since 2008,” they wrote, and
SOURCE: Pettrone K, Curtin SC. 2020 Aug. NCHS Data Brief, No 373.
The gap in suicide rates between rural and urban areas has widened since 2000 for both males and females, according to a recent report from the National Center for Health Statistics.

After remaining stable from 2000 to 2007, the suicide rate for rural males rose 34% from 2007 to 2018, versus 17% among urban males over the same period. Suicide rates for females were significantly lower than those of men, but the changes were larger. For rural females, the rate increased 91% from 2000 to 2018, compared with 51% for urban females, Kristen Pettrone, MD, MPH, and Sally C. Curtin, MA, said in an NCHS Data Brief.
For 2018, the last year with available data, the age-adjusted rates look like this: 21.5 per 100,000 population for urban males, 30.7 for rural males, 5.9 per 100,000 for urban females, and 8.0 for rural females. The overall rate for the United States was 14.2 per 100,000, with combined male/female rates of 13.4 in urban areas and 19.4 in rural areas, the researchers said.
Methods of suicide also varied by sex and urban-rural status. Firearms were the leading method for males in both rural and urban areas, but females split between firearms in rural areas and suffocation (including hangings) in urban areas, said Dr. Pettrone of the Centers for Disease Control and Prevention and Ms. Curtin of the NCHS.
Suffocation, however, was the fastest-growing method from 2000 to 2018, regardless of sex or location. Suffocation-related suicide rates more than quadrupled for rural females, and more than doubled for urban females and rural males, while rates rose 85% among males in urban areas, based on data from the National Vital Statistics System.
“Suicide has remained the 10th leading cause of death in the United States since 2008,” they wrote, and
SOURCE: Pettrone K, Curtin SC. 2020 Aug. NCHS Data Brief, No 373.
OTC ‘brain boosters’ may pose serious risks, experts say
, new research shows.
“Americans spend more than $600 million on over-the-counter smart pills every year, but we know very little about what is actually in these products,” said Pieter A. Cohen, MD, of the department of medicine at Harvard Medical School, Boston.
“Finding new combinations of drugs [that have] never been tested in humans in over-the-counter brain-boosting supplements is alarming,” said Dr. Cohen.
The study was published online Sept. 23 in Neurology Clinical Practice, a journal of the American Academy of Neurology.
Buyer beware
In a search of the National Institutes of Health Dietary Supplement Label Database and the Natural Medicines Database, Dr. Cohen and colleagues identified 10 supplements labeled as containing omberacetam, aniracetam, phenylpiracetam, or oxiracetam – four analogues of piracetam that are not approved for human use in the United States. Piracetam is also not approved in the United States.
In these 10 products, five unapproved drugs were discovered – omberacetam and aniracetam along with three others (phenibut, vinpocetine and picamilon).
By consuming the recommended serving size of these products, consumers could be exposed to pharmaceutical-level dosages of drugs including a maximum of 40.6 mg omberacetam (typical pharmacologic dose 10 mg), 502 mg of aniracetam (typical pharmacologic dose 200-750 mg), 15.4 mg of phenibut (typical dose 250-500 mg), 4.3 mg of vinpocetine (typical dose 5-40 mg), and 90.1 mg of picamilon (typical dose 50-200 mg), the study team reported.
Several drugs detected in these “smart” pills were not declared on the label, and several declared drugs were not detected in the products. For those products with drug quantities provided on the labels, three-quarters of declared quantities were inaccurate.
Consumers who use these cognitive enhancers could be exposed to amounts of these unapproved drugs that are fourfold greater than pharmaceutical dosages and combinations never tested in humans, the study team says. One product combined three different unapproved drugs and another product contained four different drugs.
“We have previously shown that these products may contain individual foreign drugs, but in our new study we found complex combinations of foreign drugs, up to four different drugs in a single product,” Dr. Cohen said.
The presence of these unapproved drugs in supplements, including at supratherapeutic dosages, suggests “serious risks to consumers and weaknesses in the regulatory framework under which supplements are permitted to be introduced in the U.S.,” Dr. Cohen and colleagues wrote.
“We should counsel our patients to avoid over-the-counter ‘smart pills’ until we can be assured as to the safety and efficacy of these products,” said Dr. Cohen.
Concerning findings
Glen R. Finney, MD, director of the Geisinger Memory and Cognition Program at the Neuroscience Institute, Geisinger Health System, Wilkes-Barre, Penn., said in an interview that two findings are very concerning: the lack of listed ingredients and especially the presence of unlisted drugs at active levels. “What if a person has a sensitivity or allergy to one of the unlisted drugs? This is a safety issue and a consumer issue,” Dr. Finney said.
Despite being widely promoted on television, “over-the-counter supplements are not regulated, so there is no guarantee that they contain what they claim, and there is very little evidence that they help memory and thinking even when they do have the ingredients they claim in the supplement,” said Dr. Finney,
“The best way to stay safe and help memory and thinking is to speak with your health providers about proven treatments that have good safety regulation, so you know what you’re getting, and what you’re getting from it,” Dr. Finney advised.
The study had no targeted funding. Dr. Cohen has collaborated in research with NSF International, received compensation from UptoDate, and received research support from Consumers Union and PEW Charitable Trusts. Dr. Finney has no relevant disclosures.
A version of this article originally appeared on Medscape.com.
, new research shows.
“Americans spend more than $600 million on over-the-counter smart pills every year, but we know very little about what is actually in these products,” said Pieter A. Cohen, MD, of the department of medicine at Harvard Medical School, Boston.
“Finding new combinations of drugs [that have] never been tested in humans in over-the-counter brain-boosting supplements is alarming,” said Dr. Cohen.
The study was published online Sept. 23 in Neurology Clinical Practice, a journal of the American Academy of Neurology.
Buyer beware
In a search of the National Institutes of Health Dietary Supplement Label Database and the Natural Medicines Database, Dr. Cohen and colleagues identified 10 supplements labeled as containing omberacetam, aniracetam, phenylpiracetam, or oxiracetam – four analogues of piracetam that are not approved for human use in the United States. Piracetam is also not approved in the United States.
In these 10 products, five unapproved drugs were discovered – omberacetam and aniracetam along with three others (phenibut, vinpocetine and picamilon).
By consuming the recommended serving size of these products, consumers could be exposed to pharmaceutical-level dosages of drugs including a maximum of 40.6 mg omberacetam (typical pharmacologic dose 10 mg), 502 mg of aniracetam (typical pharmacologic dose 200-750 mg), 15.4 mg of phenibut (typical dose 250-500 mg), 4.3 mg of vinpocetine (typical dose 5-40 mg), and 90.1 mg of picamilon (typical dose 50-200 mg), the study team reported.
Several drugs detected in these “smart” pills were not declared on the label, and several declared drugs were not detected in the products. For those products with drug quantities provided on the labels, three-quarters of declared quantities were inaccurate.
Consumers who use these cognitive enhancers could be exposed to amounts of these unapproved drugs that are fourfold greater than pharmaceutical dosages and combinations never tested in humans, the study team says. One product combined three different unapproved drugs and another product contained four different drugs.
“We have previously shown that these products may contain individual foreign drugs, but in our new study we found complex combinations of foreign drugs, up to four different drugs in a single product,” Dr. Cohen said.
The presence of these unapproved drugs in supplements, including at supratherapeutic dosages, suggests “serious risks to consumers and weaknesses in the regulatory framework under which supplements are permitted to be introduced in the U.S.,” Dr. Cohen and colleagues wrote.
“We should counsel our patients to avoid over-the-counter ‘smart pills’ until we can be assured as to the safety and efficacy of these products,” said Dr. Cohen.
Concerning findings
Glen R. Finney, MD, director of the Geisinger Memory and Cognition Program at the Neuroscience Institute, Geisinger Health System, Wilkes-Barre, Penn., said in an interview that two findings are very concerning: the lack of listed ingredients and especially the presence of unlisted drugs at active levels. “What if a person has a sensitivity or allergy to one of the unlisted drugs? This is a safety issue and a consumer issue,” Dr. Finney said.
Despite being widely promoted on television, “over-the-counter supplements are not regulated, so there is no guarantee that they contain what they claim, and there is very little evidence that they help memory and thinking even when they do have the ingredients they claim in the supplement,” said Dr. Finney,
“The best way to stay safe and help memory and thinking is to speak with your health providers about proven treatments that have good safety regulation, so you know what you’re getting, and what you’re getting from it,” Dr. Finney advised.
The study had no targeted funding. Dr. Cohen has collaborated in research with NSF International, received compensation from UptoDate, and received research support from Consumers Union and PEW Charitable Trusts. Dr. Finney has no relevant disclosures.
A version of this article originally appeared on Medscape.com.
, new research shows.
“Americans spend more than $600 million on over-the-counter smart pills every year, but we know very little about what is actually in these products,” said Pieter A. Cohen, MD, of the department of medicine at Harvard Medical School, Boston.
“Finding new combinations of drugs [that have] never been tested in humans in over-the-counter brain-boosting supplements is alarming,” said Dr. Cohen.
The study was published online Sept. 23 in Neurology Clinical Practice, a journal of the American Academy of Neurology.
Buyer beware
In a search of the National Institutes of Health Dietary Supplement Label Database and the Natural Medicines Database, Dr. Cohen and colleagues identified 10 supplements labeled as containing omberacetam, aniracetam, phenylpiracetam, or oxiracetam – four analogues of piracetam that are not approved for human use in the United States. Piracetam is also not approved in the United States.
In these 10 products, five unapproved drugs were discovered – omberacetam and aniracetam along with three others (phenibut, vinpocetine and picamilon).
By consuming the recommended serving size of these products, consumers could be exposed to pharmaceutical-level dosages of drugs including a maximum of 40.6 mg omberacetam (typical pharmacologic dose 10 mg), 502 mg of aniracetam (typical pharmacologic dose 200-750 mg), 15.4 mg of phenibut (typical dose 250-500 mg), 4.3 mg of vinpocetine (typical dose 5-40 mg), and 90.1 mg of picamilon (typical dose 50-200 mg), the study team reported.
Several drugs detected in these “smart” pills were not declared on the label, and several declared drugs were not detected in the products. For those products with drug quantities provided on the labels, three-quarters of declared quantities were inaccurate.
Consumers who use these cognitive enhancers could be exposed to amounts of these unapproved drugs that are fourfold greater than pharmaceutical dosages and combinations never tested in humans, the study team says. One product combined three different unapproved drugs and another product contained four different drugs.
“We have previously shown that these products may contain individual foreign drugs, but in our new study we found complex combinations of foreign drugs, up to four different drugs in a single product,” Dr. Cohen said.
The presence of these unapproved drugs in supplements, including at supratherapeutic dosages, suggests “serious risks to consumers and weaknesses in the regulatory framework under which supplements are permitted to be introduced in the U.S.,” Dr. Cohen and colleagues wrote.
“We should counsel our patients to avoid over-the-counter ‘smart pills’ until we can be assured as to the safety and efficacy of these products,” said Dr. Cohen.
Concerning findings
Glen R. Finney, MD, director of the Geisinger Memory and Cognition Program at the Neuroscience Institute, Geisinger Health System, Wilkes-Barre, Penn., said in an interview that two findings are very concerning: the lack of listed ingredients and especially the presence of unlisted drugs at active levels. “What if a person has a sensitivity or allergy to one of the unlisted drugs? This is a safety issue and a consumer issue,” Dr. Finney said.
Despite being widely promoted on television, “over-the-counter supplements are not regulated, so there is no guarantee that they contain what they claim, and there is very little evidence that they help memory and thinking even when they do have the ingredients they claim in the supplement,” said Dr. Finney,
“The best way to stay safe and help memory and thinking is to speak with your health providers about proven treatments that have good safety regulation, so you know what you’re getting, and what you’re getting from it,” Dr. Finney advised.
The study had no targeted funding. Dr. Cohen has collaborated in research with NSF International, received compensation from UptoDate, and received research support from Consumers Union and PEW Charitable Trusts. Dr. Finney has no relevant disclosures.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY CLINICAL PRACTICE
Cognitive impairments in major depression cluster in three patterns
Objective neuropsychological tests can be used to subclassify the cognitive symptoms present in patients with major depression into three patterns having implications for treatment responsiveness, Gitte Moos Knudsen, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Our data highlight the importance of assessing and targeting cognitive symptoms,” said Dr. Knudsen, the ECNP president and professor of neurology at the University of Copenhagen.
She was a coauthor of the Danish NeuroPharm study, in which 92 antidepressant-free patients with moderate or severe major depressive disorder and 103 healthy controls completed a comprehensive neuropsychological test battery. The testing included a validation study of the EMOTICOM test battery, a novel neuropsychological test battery developed specifically to assess what has been called “hot” cognition, such as emotion processing, social cognition, and affective verbal memory.
Overall, the depressed patients collectively showed moderate increases in measures of guilt and shame, moderate deficits in working and verbal memory, moderately slowed reaction time, and mild to moderate negative affective bias, compared with controls. No correlation was found between performance on any of the individual cognitive domains and depression severity as measured using the Hamilton Depression Rating Scale, underscoring the concept that cognitive impairment is a distinct component of depressive pathology rather than an extension of the classic mood and somatic symptoms of major depression.
Cluster analysis revealed three distinct patterns of cognitive impairment in the study population. Unlike the individual cognitive domains, these cognitive clusters did correlate with depression severity. The implication is that as they become available.
Investigators classified 38 of the 92 patients with major depressive disorder as falling within Cluster A. That is, they exhibited marked deficits in hot cognition expressed in a greatly impaired ability to accurately identify facial emotions on photographs, with resultant high scores for emotion recognition bias and emotion misattribution bias. This impairment in hot cognition was accompanied by minimal guilt and shame and little or no deficits in the cold cognitive domains of verbal and working memory.
Cluster B, composed of 28 patients, was characterized by generally good cognitive function, with positive biases in emotion processing, near-normal guilt and shame ratings, but moderate deficits across the cold cognition domains, making for a mirror image of Cluster A.
The 26 patients in Cluster C demonstrated large deficits in both the hot and cold cognition domains, with particularly pronounced guilt and shame scores.
The three clusters didn’t differ in terms of age or sex. However, patients in Cluster C had significantly more severe core depressive symptoms as measured by Hamilton scores than in Clusters A and B.
This analysis from the NeuroPharm study was cross-sectional. Dr. Knudsen cited a recent large Chinese longitudinal study to underscore how the prevalence of patient-reported cognitive deficits in major depressive disorder is high. And while those deficits decrease over time, they nonetheless remain substantial after 6 months on antidepressant therapy.
That study included 598 Chinese outpatients with major depressive disorder. At baseline, 77% had cognitive symptoms as evidenced by a total score of 21 or more on the self-rated Perceived Deficits Questionnaire–Depression (PDQ-D). One month after going on antidepressant monotherapy, the prevalence of cognitive symptoms had dropped to 59%. At 2 months, the rate was 45%. And at month 6, a PDQ-D score of 21 or greater was still present in 32.4% of patients. High baseline PDQ-D scores were associated with worse clinical outcomes, including a lower treatment response rate at 1 month and a lower remission rate at 2 months. Moreover, high PDQ-D scores at 2 months were associated with lower remission and higher relapse rates at 6 months.
Dr. Knudsen reported having no financial conflicts regarding the NeuroPharm study, which was conducted free of commercial support. She serves as an adviser to Sage Therapeutics and Sanos.
Objective neuropsychological tests can be used to subclassify the cognitive symptoms present in patients with major depression into three patterns having implications for treatment responsiveness, Gitte Moos Knudsen, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Our data highlight the importance of assessing and targeting cognitive symptoms,” said Dr. Knudsen, the ECNP president and professor of neurology at the University of Copenhagen.
She was a coauthor of the Danish NeuroPharm study, in which 92 antidepressant-free patients with moderate or severe major depressive disorder and 103 healthy controls completed a comprehensive neuropsychological test battery. The testing included a validation study of the EMOTICOM test battery, a novel neuropsychological test battery developed specifically to assess what has been called “hot” cognition, such as emotion processing, social cognition, and affective verbal memory.
Overall, the depressed patients collectively showed moderate increases in measures of guilt and shame, moderate deficits in working and verbal memory, moderately slowed reaction time, and mild to moderate negative affective bias, compared with controls. No correlation was found between performance on any of the individual cognitive domains and depression severity as measured using the Hamilton Depression Rating Scale, underscoring the concept that cognitive impairment is a distinct component of depressive pathology rather than an extension of the classic mood and somatic symptoms of major depression.
Cluster analysis revealed three distinct patterns of cognitive impairment in the study population. Unlike the individual cognitive domains, these cognitive clusters did correlate with depression severity. The implication is that as they become available.
Investigators classified 38 of the 92 patients with major depressive disorder as falling within Cluster A. That is, they exhibited marked deficits in hot cognition expressed in a greatly impaired ability to accurately identify facial emotions on photographs, with resultant high scores for emotion recognition bias and emotion misattribution bias. This impairment in hot cognition was accompanied by minimal guilt and shame and little or no deficits in the cold cognitive domains of verbal and working memory.
Cluster B, composed of 28 patients, was characterized by generally good cognitive function, with positive biases in emotion processing, near-normal guilt and shame ratings, but moderate deficits across the cold cognition domains, making for a mirror image of Cluster A.
The 26 patients in Cluster C demonstrated large deficits in both the hot and cold cognition domains, with particularly pronounced guilt and shame scores.
The three clusters didn’t differ in terms of age or sex. However, patients in Cluster C had significantly more severe core depressive symptoms as measured by Hamilton scores than in Clusters A and B.
This analysis from the NeuroPharm study was cross-sectional. Dr. Knudsen cited a recent large Chinese longitudinal study to underscore how the prevalence of patient-reported cognitive deficits in major depressive disorder is high. And while those deficits decrease over time, they nonetheless remain substantial after 6 months on antidepressant therapy.
That study included 598 Chinese outpatients with major depressive disorder. At baseline, 77% had cognitive symptoms as evidenced by a total score of 21 or more on the self-rated Perceived Deficits Questionnaire–Depression (PDQ-D). One month after going on antidepressant monotherapy, the prevalence of cognitive symptoms had dropped to 59%. At 2 months, the rate was 45%. And at month 6, a PDQ-D score of 21 or greater was still present in 32.4% of patients. High baseline PDQ-D scores were associated with worse clinical outcomes, including a lower treatment response rate at 1 month and a lower remission rate at 2 months. Moreover, high PDQ-D scores at 2 months were associated with lower remission and higher relapse rates at 6 months.
Dr. Knudsen reported having no financial conflicts regarding the NeuroPharm study, which was conducted free of commercial support. She serves as an adviser to Sage Therapeutics and Sanos.
Objective neuropsychological tests can be used to subclassify the cognitive symptoms present in patients with major depression into three patterns having implications for treatment responsiveness, Gitte Moos Knudsen, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Our data highlight the importance of assessing and targeting cognitive symptoms,” said Dr. Knudsen, the ECNP president and professor of neurology at the University of Copenhagen.
She was a coauthor of the Danish NeuroPharm study, in which 92 antidepressant-free patients with moderate or severe major depressive disorder and 103 healthy controls completed a comprehensive neuropsychological test battery. The testing included a validation study of the EMOTICOM test battery, a novel neuropsychological test battery developed specifically to assess what has been called “hot” cognition, such as emotion processing, social cognition, and affective verbal memory.
Overall, the depressed patients collectively showed moderate increases in measures of guilt and shame, moderate deficits in working and verbal memory, moderately slowed reaction time, and mild to moderate negative affective bias, compared with controls. No correlation was found between performance on any of the individual cognitive domains and depression severity as measured using the Hamilton Depression Rating Scale, underscoring the concept that cognitive impairment is a distinct component of depressive pathology rather than an extension of the classic mood and somatic symptoms of major depression.
Cluster analysis revealed three distinct patterns of cognitive impairment in the study population. Unlike the individual cognitive domains, these cognitive clusters did correlate with depression severity. The implication is that as they become available.
Investigators classified 38 of the 92 patients with major depressive disorder as falling within Cluster A. That is, they exhibited marked deficits in hot cognition expressed in a greatly impaired ability to accurately identify facial emotions on photographs, with resultant high scores for emotion recognition bias and emotion misattribution bias. This impairment in hot cognition was accompanied by minimal guilt and shame and little or no deficits in the cold cognitive domains of verbal and working memory.
Cluster B, composed of 28 patients, was characterized by generally good cognitive function, with positive biases in emotion processing, near-normal guilt and shame ratings, but moderate deficits across the cold cognition domains, making for a mirror image of Cluster A.
The 26 patients in Cluster C demonstrated large deficits in both the hot and cold cognition domains, with particularly pronounced guilt and shame scores.
The three clusters didn’t differ in terms of age or sex. However, patients in Cluster C had significantly more severe core depressive symptoms as measured by Hamilton scores than in Clusters A and B.
This analysis from the NeuroPharm study was cross-sectional. Dr. Knudsen cited a recent large Chinese longitudinal study to underscore how the prevalence of patient-reported cognitive deficits in major depressive disorder is high. And while those deficits decrease over time, they nonetheless remain substantial after 6 months on antidepressant therapy.
That study included 598 Chinese outpatients with major depressive disorder. At baseline, 77% had cognitive symptoms as evidenced by a total score of 21 or more on the self-rated Perceived Deficits Questionnaire–Depression (PDQ-D). One month after going on antidepressant monotherapy, the prevalence of cognitive symptoms had dropped to 59%. At 2 months, the rate was 45%. And at month 6, a PDQ-D score of 21 or greater was still present in 32.4% of patients. High baseline PDQ-D scores were associated with worse clinical outcomes, including a lower treatment response rate at 1 month and a lower remission rate at 2 months. Moreover, high PDQ-D scores at 2 months were associated with lower remission and higher relapse rates at 6 months.
Dr. Knudsen reported having no financial conflicts regarding the NeuroPharm study, which was conducted free of commercial support. She serves as an adviser to Sage Therapeutics and Sanos.
FROM ECNP 2020
COVID-19 shutdown fuels sharp rise in alcohol use
Americans sharply increased their alcohol intake last spring as many areas of the country shutdown because of the coronavirus pandemic, results of a national survey show.
The overall frequency of alcohol consumption increased by 14% among adults over age 30 in the spring of 2020 versus the same period a year earlier.
The increase was most evident in adults aged 30-59, women, and non-Hispanic Whites.
“Alcohol consumption can have significant negative health consequences, so this information suggests another way that the pandemic may be affecting the physical and mental health of Americans,” Michael Pollard, PhD, lead investigator and sociologist at Rand, said in a news release.
The results were published online as a research letter Sept. 29 in JAMA Network Open.
Booming business
After some U.S. states issued stay-at-home orders to fight the spread of SARS-CoV-2, one study noted a 54% increase in national sales of alcohol for the week ending March 21, 2020, relative to 1 year earlier and a 262% increase in online alcohol sales.
“We’ve had anecdotal information about people buying and consuming more alcohol,” Dr. Pollard said, but the Rand study provides the first survey-based information that shows how much alcohol consumption has increased during the pandemic.
The findings are based on 1,540 adults (mean age, 56.6 years; 57% women) from the Rand American Life Panel, a nationally representative sample of Americans who were surveyed about their alcohol consumption before the pandemic in the spring of 2019, and again in the spring of 2020 during the early months of the shutdown.
Overall, in spring 2020, respondents reported drinking alcohol 6.22 days in the prior month on average, a 14% increase from the monthly average of 5.48 days reported in spring 2019.
Among adults aged 30 to 59 years, the frequency of alcohol consumption increased from 4.98 days prepandemic to 5.91 days during the pandemic, a 19% increase.
Women reported drinking an average of 5.36 days in the prior month in the early pandemic period, a 17% increase from 4.58 monthly drinking days before the pandemic.
In addition, compared with spring 2019, in spring 2020 women reported a 41% increase in heavy drinking days – four or more drinks in a couple of hours.
Independent of consumption level, nearly 1 in 10 women had an increase in alcohol-related problems in the pandemic period, based on responses to the Short Inventory of Problems scale.
For non-Hispanic White individuals, the overall frequency of alcohol intake rose 10% during the early pandemic period.
“The population level changes for women, younger, and non-Hispanic White individuals highlight that health systems may need to educate consumers through print or online media about increased alcohol use during the pandemic and identify factors associated with susceptibility and resilience to the impacts of COVID-19,” write Dr. Pollard and colleagues.
The authors note , and whether psychological and physical well-being are subsequently affected.
The study was supported by the National Institute of Alcohol Abuse and Alcoholism. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Americans sharply increased their alcohol intake last spring as many areas of the country shutdown because of the coronavirus pandemic, results of a national survey show.
The overall frequency of alcohol consumption increased by 14% among adults over age 30 in the spring of 2020 versus the same period a year earlier.
The increase was most evident in adults aged 30-59, women, and non-Hispanic Whites.
“Alcohol consumption can have significant negative health consequences, so this information suggests another way that the pandemic may be affecting the physical and mental health of Americans,” Michael Pollard, PhD, lead investigator and sociologist at Rand, said in a news release.
The results were published online as a research letter Sept. 29 in JAMA Network Open.
Booming business
After some U.S. states issued stay-at-home orders to fight the spread of SARS-CoV-2, one study noted a 54% increase in national sales of alcohol for the week ending March 21, 2020, relative to 1 year earlier and a 262% increase in online alcohol sales.
“We’ve had anecdotal information about people buying and consuming more alcohol,” Dr. Pollard said, but the Rand study provides the first survey-based information that shows how much alcohol consumption has increased during the pandemic.
The findings are based on 1,540 adults (mean age, 56.6 years; 57% women) from the Rand American Life Panel, a nationally representative sample of Americans who were surveyed about their alcohol consumption before the pandemic in the spring of 2019, and again in the spring of 2020 during the early months of the shutdown.
Overall, in spring 2020, respondents reported drinking alcohol 6.22 days in the prior month on average, a 14% increase from the monthly average of 5.48 days reported in spring 2019.
Among adults aged 30 to 59 years, the frequency of alcohol consumption increased from 4.98 days prepandemic to 5.91 days during the pandemic, a 19% increase.
Women reported drinking an average of 5.36 days in the prior month in the early pandemic period, a 17% increase from 4.58 monthly drinking days before the pandemic.
In addition, compared with spring 2019, in spring 2020 women reported a 41% increase in heavy drinking days – four or more drinks in a couple of hours.
Independent of consumption level, nearly 1 in 10 women had an increase in alcohol-related problems in the pandemic period, based on responses to the Short Inventory of Problems scale.
For non-Hispanic White individuals, the overall frequency of alcohol intake rose 10% during the early pandemic period.
“The population level changes for women, younger, and non-Hispanic White individuals highlight that health systems may need to educate consumers through print or online media about increased alcohol use during the pandemic and identify factors associated with susceptibility and resilience to the impacts of COVID-19,” write Dr. Pollard and colleagues.
The authors note , and whether psychological and physical well-being are subsequently affected.
The study was supported by the National Institute of Alcohol Abuse and Alcoholism. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Americans sharply increased their alcohol intake last spring as many areas of the country shutdown because of the coronavirus pandemic, results of a national survey show.
The overall frequency of alcohol consumption increased by 14% among adults over age 30 in the spring of 2020 versus the same period a year earlier.
The increase was most evident in adults aged 30-59, women, and non-Hispanic Whites.
“Alcohol consumption can have significant negative health consequences, so this information suggests another way that the pandemic may be affecting the physical and mental health of Americans,” Michael Pollard, PhD, lead investigator and sociologist at Rand, said in a news release.
The results were published online as a research letter Sept. 29 in JAMA Network Open.
Booming business
After some U.S. states issued stay-at-home orders to fight the spread of SARS-CoV-2, one study noted a 54% increase in national sales of alcohol for the week ending March 21, 2020, relative to 1 year earlier and a 262% increase in online alcohol sales.
“We’ve had anecdotal information about people buying and consuming more alcohol,” Dr. Pollard said, but the Rand study provides the first survey-based information that shows how much alcohol consumption has increased during the pandemic.
The findings are based on 1,540 adults (mean age, 56.6 years; 57% women) from the Rand American Life Panel, a nationally representative sample of Americans who were surveyed about their alcohol consumption before the pandemic in the spring of 2019, and again in the spring of 2020 during the early months of the shutdown.
Overall, in spring 2020, respondents reported drinking alcohol 6.22 days in the prior month on average, a 14% increase from the monthly average of 5.48 days reported in spring 2019.
Among adults aged 30 to 59 years, the frequency of alcohol consumption increased from 4.98 days prepandemic to 5.91 days during the pandemic, a 19% increase.
Women reported drinking an average of 5.36 days in the prior month in the early pandemic period, a 17% increase from 4.58 monthly drinking days before the pandemic.
In addition, compared with spring 2019, in spring 2020 women reported a 41% increase in heavy drinking days – four or more drinks in a couple of hours.
Independent of consumption level, nearly 1 in 10 women had an increase in alcohol-related problems in the pandemic period, based on responses to the Short Inventory of Problems scale.
For non-Hispanic White individuals, the overall frequency of alcohol intake rose 10% during the early pandemic period.
“The population level changes for women, younger, and non-Hispanic White individuals highlight that health systems may need to educate consumers through print or online media about increased alcohol use during the pandemic and identify factors associated with susceptibility and resilience to the impacts of COVID-19,” write Dr. Pollard and colleagues.
The authors note , and whether psychological and physical well-being are subsequently affected.
The study was supported by the National Institute of Alcohol Abuse and Alcoholism. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.

