User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
National Practitioner Data Bank should go public, group says
arguing that extra public scrutiny could pressure state medical boards to be more aggressive watchdogs.
Public Citizen’s report includes an analysis of how frequently medical boards sanctioned physicians in 2019, 2020, and 2021. These sanctions include license revocations, suspensions, voluntary surrenders of licenses, and limitations on practice while under investigation.
The report used data from the National Practitioner Data Bank (NPDB), a federal repository of reports about state licensure, discipline, and certification actions as well as medical malpractice payments. The database is closed to the public, but hospitals, malpractice insurers, and investigators can query it.
According to Public Citizen’s calculations, states most likely to take serious disciplinary action against physicians were:
- Michigan: 1.74 serious disciplinary actions per 1,000 physicians per year
- Ohio: 1.61
- North Dakota: 1.60
- Colorado: 1.55
- Arizona: 1.53
- The states least likely to do so were:
- Nevada: 0.24 serious disciplinary actions per 1,000 physicians per year
- New Hampshire: 0.25
- Georgia: 0.27
- Indiana: 0.28
- Nebraska: 0.32
- California, the largest U.S. state by both population and number of physicians, landed near the middle, ranking 27th with a rate of 0.83 serious actions per 1,000 physicians, Public Citizen said.
“There is no evidence that physicians in any state are, overall, more or less likely to be incompetent or miscreant than the physicians in any other state,” said Robert Oshel, PhD, a former NPDB associate director for research and an author of the report.
The differences instead reflect variations in boards’ enforcement of medical practice laws, domination of licensing boards by physicians, and inadequate budgets, he noted.
Public Citizen said Congress should change federal law to let members of the public get information from the NPDB to do a background check on physicians whom they are considering seeing or are already seeing. This would not only help individuals but also would spur state licensing boards to do their own checks with the NPDB, the group said.
“If licensing boards routinely queried the NPDB, they would not be faulted by the public and state legislators for not knowing about malpractice payments or disciplinary actions affecting their licensees and therefore not taking reasonable actions concerning their licensees found to have poor records,” the report said.
Questioning NPDB access for consumers
Michelle Mello, JD, PhD, a professor of law and health policy at Stanford (Calif.) University, has studied the current applications of the NPDB. In 2019, she published an article in The New England Journal of Medicine examining changes in practice patterns for clinicians who faced multiple malpractice claims.
Dr. Mello questioned what benefit consumers would get from direct access to the NPDB’s information.
“It provides almost no context for the information it reports, making it even harder for patients to make sense of what they see there,” Dr. Mello said in an interview.
Hospitals are already required to routinely query the NPDB. This legal requirement should be expanded to include licensing boards, which the report called “the last line of defense for the public from incompetent and miscreant physicians,” Public Citizen said.
“Ideally, this amendment should include free continuous query access by medical boards for all their licensees,” the report said. “In the absence of any action by Congress, individual state legislatures should require their licensing boards to query all their licensees or enroll in continuous query, as a few states already do.”
The Federation of State Medical Boards agreed with some of the other suggestions Public Citizen offered in the report. The two concur on the need for increased funding to state medical boards to ensure that they have adequate resources and staffing to fulfill their duties, FSMB said in a statement.
But FSMB disagreed with Public Citizens’ approach to ranking boards, saying it could mislead. The report lacks context about how boards’ funding and authority vary, Humayun Chaudhry, DO, FSMB’s chief executive officer, said. He also questioned the decision to focus only on serious disciplinary actions.
“The Public Citizen report does not take into account the wide range of disciplinary steps boards can take such as letters of reprimand or fines, which are often enough to stop problem behaviors – preempting further problems in the future,” Dr. Chaudhry said.
D.C. gets worst rating
The District of Columbia earned the worst mark in the Public Citizen ranking, holding the 51st spot, the same place it held in the group’s similar ranking on actions taken in the 2017-2019 period. There were 0.19 serious disciplinary actions per 1,000 physicians a year in Washington, Public Citizen said.
In an email to this news organization, Dr. Oshel said that the Public Citizen analysis focused on the number of licensed physicians in each state and D.C. that can be obtained and compared reliably. It avoided using the term “practicing physicians” owing in part to doubts about the reliability of these counts, he said.
As many as 20% of physicians nationwide are focused primarily on work outside of clinical care, Dr. Oshel estimated. In D.C., perhaps 40% of physicians may fall into this category. Of the more than 13,700 physicians licensed in D.C., there may be only about 8,126 actively practicing, according to Dr. Oshel.
But even using that lower estimate of practicing physicians would only raise D.C.’s ranking to 46, signaling a need for stepped-up enforcement, Dr. Oshel said.
“[Whether it’s] 46th or 51st, both are bad,” Dr. Oshel said.
A version of this article first appeared on Medscape.com.
arguing that extra public scrutiny could pressure state medical boards to be more aggressive watchdogs.
Public Citizen’s report includes an analysis of how frequently medical boards sanctioned physicians in 2019, 2020, and 2021. These sanctions include license revocations, suspensions, voluntary surrenders of licenses, and limitations on practice while under investigation.
The report used data from the National Practitioner Data Bank (NPDB), a federal repository of reports about state licensure, discipline, and certification actions as well as medical malpractice payments. The database is closed to the public, but hospitals, malpractice insurers, and investigators can query it.
According to Public Citizen’s calculations, states most likely to take serious disciplinary action against physicians were:
- Michigan: 1.74 serious disciplinary actions per 1,000 physicians per year
- Ohio: 1.61
- North Dakota: 1.60
- Colorado: 1.55
- Arizona: 1.53
- The states least likely to do so were:
- Nevada: 0.24 serious disciplinary actions per 1,000 physicians per year
- New Hampshire: 0.25
- Georgia: 0.27
- Indiana: 0.28
- Nebraska: 0.32
- California, the largest U.S. state by both population and number of physicians, landed near the middle, ranking 27th with a rate of 0.83 serious actions per 1,000 physicians, Public Citizen said.
“There is no evidence that physicians in any state are, overall, more or less likely to be incompetent or miscreant than the physicians in any other state,” said Robert Oshel, PhD, a former NPDB associate director for research and an author of the report.
The differences instead reflect variations in boards’ enforcement of medical practice laws, domination of licensing boards by physicians, and inadequate budgets, he noted.
Public Citizen said Congress should change federal law to let members of the public get information from the NPDB to do a background check on physicians whom they are considering seeing or are already seeing. This would not only help individuals but also would spur state licensing boards to do their own checks with the NPDB, the group said.
“If licensing boards routinely queried the NPDB, they would not be faulted by the public and state legislators for not knowing about malpractice payments or disciplinary actions affecting their licensees and therefore not taking reasonable actions concerning their licensees found to have poor records,” the report said.
Questioning NPDB access for consumers
Michelle Mello, JD, PhD, a professor of law and health policy at Stanford (Calif.) University, has studied the current applications of the NPDB. In 2019, she published an article in The New England Journal of Medicine examining changes in practice patterns for clinicians who faced multiple malpractice claims.
Dr. Mello questioned what benefit consumers would get from direct access to the NPDB’s information.
“It provides almost no context for the information it reports, making it even harder for patients to make sense of what they see there,” Dr. Mello said in an interview.
Hospitals are already required to routinely query the NPDB. This legal requirement should be expanded to include licensing boards, which the report called “the last line of defense for the public from incompetent and miscreant physicians,” Public Citizen said.
“Ideally, this amendment should include free continuous query access by medical boards for all their licensees,” the report said. “In the absence of any action by Congress, individual state legislatures should require their licensing boards to query all their licensees or enroll in continuous query, as a few states already do.”
The Federation of State Medical Boards agreed with some of the other suggestions Public Citizen offered in the report. The two concur on the need for increased funding to state medical boards to ensure that they have adequate resources and staffing to fulfill their duties, FSMB said in a statement.
But FSMB disagreed with Public Citizens’ approach to ranking boards, saying it could mislead. The report lacks context about how boards’ funding and authority vary, Humayun Chaudhry, DO, FSMB’s chief executive officer, said. He also questioned the decision to focus only on serious disciplinary actions.
“The Public Citizen report does not take into account the wide range of disciplinary steps boards can take such as letters of reprimand or fines, which are often enough to stop problem behaviors – preempting further problems in the future,” Dr. Chaudhry said.
D.C. gets worst rating
The District of Columbia earned the worst mark in the Public Citizen ranking, holding the 51st spot, the same place it held in the group’s similar ranking on actions taken in the 2017-2019 period. There were 0.19 serious disciplinary actions per 1,000 physicians a year in Washington, Public Citizen said.
In an email to this news organization, Dr. Oshel said that the Public Citizen analysis focused on the number of licensed physicians in each state and D.C. that can be obtained and compared reliably. It avoided using the term “practicing physicians” owing in part to doubts about the reliability of these counts, he said.
As many as 20% of physicians nationwide are focused primarily on work outside of clinical care, Dr. Oshel estimated. In D.C., perhaps 40% of physicians may fall into this category. Of the more than 13,700 physicians licensed in D.C., there may be only about 8,126 actively practicing, according to Dr. Oshel.
But even using that lower estimate of practicing physicians would only raise D.C.’s ranking to 46, signaling a need for stepped-up enforcement, Dr. Oshel said.
“[Whether it’s] 46th or 51st, both are bad,” Dr. Oshel said.
A version of this article first appeared on Medscape.com.
arguing that extra public scrutiny could pressure state medical boards to be more aggressive watchdogs.
Public Citizen’s report includes an analysis of how frequently medical boards sanctioned physicians in 2019, 2020, and 2021. These sanctions include license revocations, suspensions, voluntary surrenders of licenses, and limitations on practice while under investigation.
The report used data from the National Practitioner Data Bank (NPDB), a federal repository of reports about state licensure, discipline, and certification actions as well as medical malpractice payments. The database is closed to the public, but hospitals, malpractice insurers, and investigators can query it.
According to Public Citizen’s calculations, states most likely to take serious disciplinary action against physicians were:
- Michigan: 1.74 serious disciplinary actions per 1,000 physicians per year
- Ohio: 1.61
- North Dakota: 1.60
- Colorado: 1.55
- Arizona: 1.53
- The states least likely to do so were:
- Nevada: 0.24 serious disciplinary actions per 1,000 physicians per year
- New Hampshire: 0.25
- Georgia: 0.27
- Indiana: 0.28
- Nebraska: 0.32
- California, the largest U.S. state by both population and number of physicians, landed near the middle, ranking 27th with a rate of 0.83 serious actions per 1,000 physicians, Public Citizen said.
“There is no evidence that physicians in any state are, overall, more or less likely to be incompetent or miscreant than the physicians in any other state,” said Robert Oshel, PhD, a former NPDB associate director for research and an author of the report.
The differences instead reflect variations in boards’ enforcement of medical practice laws, domination of licensing boards by physicians, and inadequate budgets, he noted.
Public Citizen said Congress should change federal law to let members of the public get information from the NPDB to do a background check on physicians whom they are considering seeing or are already seeing. This would not only help individuals but also would spur state licensing boards to do their own checks with the NPDB, the group said.
“If licensing boards routinely queried the NPDB, they would not be faulted by the public and state legislators for not knowing about malpractice payments or disciplinary actions affecting their licensees and therefore not taking reasonable actions concerning their licensees found to have poor records,” the report said.
Questioning NPDB access for consumers
Michelle Mello, JD, PhD, a professor of law and health policy at Stanford (Calif.) University, has studied the current applications of the NPDB. In 2019, she published an article in The New England Journal of Medicine examining changes in practice patterns for clinicians who faced multiple malpractice claims.
Dr. Mello questioned what benefit consumers would get from direct access to the NPDB’s information.
“It provides almost no context for the information it reports, making it even harder for patients to make sense of what they see there,” Dr. Mello said in an interview.
Hospitals are already required to routinely query the NPDB. This legal requirement should be expanded to include licensing boards, which the report called “the last line of defense for the public from incompetent and miscreant physicians,” Public Citizen said.
“Ideally, this amendment should include free continuous query access by medical boards for all their licensees,” the report said. “In the absence of any action by Congress, individual state legislatures should require their licensing boards to query all their licensees or enroll in continuous query, as a few states already do.”
The Federation of State Medical Boards agreed with some of the other suggestions Public Citizen offered in the report. The two concur on the need for increased funding to state medical boards to ensure that they have adequate resources and staffing to fulfill their duties, FSMB said in a statement.
But FSMB disagreed with Public Citizens’ approach to ranking boards, saying it could mislead. The report lacks context about how boards’ funding and authority vary, Humayun Chaudhry, DO, FSMB’s chief executive officer, said. He also questioned the decision to focus only on serious disciplinary actions.
“The Public Citizen report does not take into account the wide range of disciplinary steps boards can take such as letters of reprimand or fines, which are often enough to stop problem behaviors – preempting further problems in the future,” Dr. Chaudhry said.
D.C. gets worst rating
The District of Columbia earned the worst mark in the Public Citizen ranking, holding the 51st spot, the same place it held in the group’s similar ranking on actions taken in the 2017-2019 period. There were 0.19 serious disciplinary actions per 1,000 physicians a year in Washington, Public Citizen said.
In an email to this news organization, Dr. Oshel said that the Public Citizen analysis focused on the number of licensed physicians in each state and D.C. that can be obtained and compared reliably. It avoided using the term “practicing physicians” owing in part to doubts about the reliability of these counts, he said.
As many as 20% of physicians nationwide are focused primarily on work outside of clinical care, Dr. Oshel estimated. In D.C., perhaps 40% of physicians may fall into this category. Of the more than 13,700 physicians licensed in D.C., there may be only about 8,126 actively practicing, according to Dr. Oshel.
But even using that lower estimate of practicing physicians would only raise D.C.’s ranking to 46, signaling a need for stepped-up enforcement, Dr. Oshel said.
“[Whether it’s] 46th or 51st, both are bad,” Dr. Oshel said.
A version of this article first appeared on Medscape.com.
‘Patients fail’ despite benefits of sustained weight loss
Don’t look for the publication of a study detailing the probability of blood pressure reduction to normotensive among adults with hypertension who aren’t offered pharmacotherapy in a JAMA journal. It’s not because hypertension doesn’t respond to intentional behavior change. On the contrary, it absolutely does, but when it comes to hypertension, physicians don’t require patients to fail to manage their hypertension through personal responsibility before medications are discussed and involved.
Not so, of course, with obesity.
A few weeks ago a paper was published in JAMA Network Open entitled “Probability of 5% or greater weight loss or BMI reduction to healthy weight among adults with overweight or obesity,” which authors, peer reviewers, and editors deemed worthy of publication. Now, to be fair, it might be worthy of publication if the call to action and thrust of the paper was to chastise physicians for not offering patients effective treatments; the medical education system for failing to teach physicians how to effectively manage obesity; or, if medication is being offered, addressing the barriers to its use. Instead, the main thrust was that patients are failing to help themselves despite the known health benefits of sustained weight loss.
It’s not at all surprising that, despite known benefits, sustained weight loss without pharmacotherapy or surgery is elusive. Just as with virtually every other chronic noncommunicable disease with lifestyle levers, intentional behavior change as treatment – which, by definition for chronic diseases, needs to be employed in perpetuity – requires wide-ranging degrees of privilege and is not a reasonable expectation. And if outcomes from the FREEE trial are applicable broadly, this may be true even if the behavior change required is minimal, the cost is free, and the motivation is large.
The FREEE trial studied whether cost had a role to play in why so many people, even after a myocardial infarction, don’t follow through with the simplest of intentional behavior changes – taking prescribed medications – by providing free medications known to reduce the risk of having a second MI to study participants who had just suffered an MI.
Results showed that, although the group receiving free medications were taking more of them than the group that had a copay for them, at 1.5 years post-MI, only 41% of those receiving all their medications for free were taking them.
And what of those who have a copay? This study found that fewer than 30% of Medicare beneficiaries 65-74 years of age who were hospitalized for heart attacks filled their new statin prescriptions within 90 days of discharge. That the vast majority of patients who’d had actual heart attacks didn’t even take on the behavior change of simply filling their prescription for, let alone taking, a medication shown to reduce their risk of having another heart attack, speaks to the folly of believing that knowledge drives behavior change.
The message is that And yet here we have a paper that concludes with the inference of surprise that few people, without treatment, lost clinically meaningful amounts of weight “despite the known benefits of clinically meaningful weight loss.”
While this paper does suggest in passing that yes, maybe we should offer effective treatments to patients with obesity, medicine needs to stop framing obesity as some surprising personal-responsibility knowledge gap and instead focus on the real problems at hand: the barriers to physicians treating obesity as they do every other chronic noncommunicable disease; why, unlike hypertension, for example, primary care providers are generally not well trained in its effective management; and why those who aren’t, despite obesity’s prevalence and impact, don’t see it as worthwhile to go out of their way to learn.
Dr. Freedhoff is an associate professor in the department of family medicine at the University of Ottawa (Ont.) and medical director of the Bariatric Medical Institute, also in Ottawa. He reported conflicts of interest with Constant Health, Novo Nordisk, and Weighty Matters.
A version of this article first appeared on Medscape.com.
Don’t look for the publication of a study detailing the probability of blood pressure reduction to normotensive among adults with hypertension who aren’t offered pharmacotherapy in a JAMA journal. It’s not because hypertension doesn’t respond to intentional behavior change. On the contrary, it absolutely does, but when it comes to hypertension, physicians don’t require patients to fail to manage their hypertension through personal responsibility before medications are discussed and involved.
Not so, of course, with obesity.
A few weeks ago a paper was published in JAMA Network Open entitled “Probability of 5% or greater weight loss or BMI reduction to healthy weight among adults with overweight or obesity,” which authors, peer reviewers, and editors deemed worthy of publication. Now, to be fair, it might be worthy of publication if the call to action and thrust of the paper was to chastise physicians for not offering patients effective treatments; the medical education system for failing to teach physicians how to effectively manage obesity; or, if medication is being offered, addressing the barriers to its use. Instead, the main thrust was that patients are failing to help themselves despite the known health benefits of sustained weight loss.
It’s not at all surprising that, despite known benefits, sustained weight loss without pharmacotherapy or surgery is elusive. Just as with virtually every other chronic noncommunicable disease with lifestyle levers, intentional behavior change as treatment – which, by definition for chronic diseases, needs to be employed in perpetuity – requires wide-ranging degrees of privilege and is not a reasonable expectation. And if outcomes from the FREEE trial are applicable broadly, this may be true even if the behavior change required is minimal, the cost is free, and the motivation is large.
The FREEE trial studied whether cost had a role to play in why so many people, even after a myocardial infarction, don’t follow through with the simplest of intentional behavior changes – taking prescribed medications – by providing free medications known to reduce the risk of having a second MI to study participants who had just suffered an MI.
Results showed that, although the group receiving free medications were taking more of them than the group that had a copay for them, at 1.5 years post-MI, only 41% of those receiving all their medications for free were taking them.
And what of those who have a copay? This study found that fewer than 30% of Medicare beneficiaries 65-74 years of age who were hospitalized for heart attacks filled their new statin prescriptions within 90 days of discharge. That the vast majority of patients who’d had actual heart attacks didn’t even take on the behavior change of simply filling their prescription for, let alone taking, a medication shown to reduce their risk of having another heart attack, speaks to the folly of believing that knowledge drives behavior change.
The message is that And yet here we have a paper that concludes with the inference of surprise that few people, without treatment, lost clinically meaningful amounts of weight “despite the known benefits of clinically meaningful weight loss.”
While this paper does suggest in passing that yes, maybe we should offer effective treatments to patients with obesity, medicine needs to stop framing obesity as some surprising personal-responsibility knowledge gap and instead focus on the real problems at hand: the barriers to physicians treating obesity as they do every other chronic noncommunicable disease; why, unlike hypertension, for example, primary care providers are generally not well trained in its effective management; and why those who aren’t, despite obesity’s prevalence and impact, don’t see it as worthwhile to go out of their way to learn.
Dr. Freedhoff is an associate professor in the department of family medicine at the University of Ottawa (Ont.) and medical director of the Bariatric Medical Institute, also in Ottawa. He reported conflicts of interest with Constant Health, Novo Nordisk, and Weighty Matters.
A version of this article first appeared on Medscape.com.
Don’t look for the publication of a study detailing the probability of blood pressure reduction to normotensive among adults with hypertension who aren’t offered pharmacotherapy in a JAMA journal. It’s not because hypertension doesn’t respond to intentional behavior change. On the contrary, it absolutely does, but when it comes to hypertension, physicians don’t require patients to fail to manage their hypertension through personal responsibility before medications are discussed and involved.
Not so, of course, with obesity.
A few weeks ago a paper was published in JAMA Network Open entitled “Probability of 5% or greater weight loss or BMI reduction to healthy weight among adults with overweight or obesity,” which authors, peer reviewers, and editors deemed worthy of publication. Now, to be fair, it might be worthy of publication if the call to action and thrust of the paper was to chastise physicians for not offering patients effective treatments; the medical education system for failing to teach physicians how to effectively manage obesity; or, if medication is being offered, addressing the barriers to its use. Instead, the main thrust was that patients are failing to help themselves despite the known health benefits of sustained weight loss.
It’s not at all surprising that, despite known benefits, sustained weight loss without pharmacotherapy or surgery is elusive. Just as with virtually every other chronic noncommunicable disease with lifestyle levers, intentional behavior change as treatment – which, by definition for chronic diseases, needs to be employed in perpetuity – requires wide-ranging degrees of privilege and is not a reasonable expectation. And if outcomes from the FREEE trial are applicable broadly, this may be true even if the behavior change required is minimal, the cost is free, and the motivation is large.
The FREEE trial studied whether cost had a role to play in why so many people, even after a myocardial infarction, don’t follow through with the simplest of intentional behavior changes – taking prescribed medications – by providing free medications known to reduce the risk of having a second MI to study participants who had just suffered an MI.
Results showed that, although the group receiving free medications were taking more of them than the group that had a copay for them, at 1.5 years post-MI, only 41% of those receiving all their medications for free were taking them.
And what of those who have a copay? This study found that fewer than 30% of Medicare beneficiaries 65-74 years of age who were hospitalized for heart attacks filled their new statin prescriptions within 90 days of discharge. That the vast majority of patients who’d had actual heart attacks didn’t even take on the behavior change of simply filling their prescription for, let alone taking, a medication shown to reduce their risk of having another heart attack, speaks to the folly of believing that knowledge drives behavior change.
The message is that And yet here we have a paper that concludes with the inference of surprise that few people, without treatment, lost clinically meaningful amounts of weight “despite the known benefits of clinically meaningful weight loss.”
While this paper does suggest in passing that yes, maybe we should offer effective treatments to patients with obesity, medicine needs to stop framing obesity as some surprising personal-responsibility knowledge gap and instead focus on the real problems at hand: the barriers to physicians treating obesity as they do every other chronic noncommunicable disease; why, unlike hypertension, for example, primary care providers are generally not well trained in its effective management; and why those who aren’t, despite obesity’s prevalence and impact, don’t see it as worthwhile to go out of their way to learn.
Dr. Freedhoff is an associate professor in the department of family medicine at the University of Ottawa (Ont.) and medical director of the Bariatric Medical Institute, also in Ottawa. He reported conflicts of interest with Constant Health, Novo Nordisk, and Weighty Matters.
A version of this article first appeared on Medscape.com.
Liraglutide fixes learning limit tied to insulin resistance
A single injection of the GLP-1 receptor agonist liraglutide led to short-term normalization of associative learning in people with obesity and insulin resistance, a finding that suggests say the authors of a recent report in Nature Metabolism.
“We demonstrated that dopamine-driven associative learning about external sensory cues crucially depends on metabolic signaling,” said Marc Tittgemeyer, PhD, professor at the Max Planck Institute for Metabolism Research in Cologne, Germany, and senior author of the study. Study participants with impaired insulin sensitivity “exhibited a reduced amplitude of behavioral updating that was normalized” by a single subcutaneous injection of 0.6 mg of liraglutide (the starting daily dose for liraglutide for weight loss, available as Saxenda, Novo Nordisk) given the evening before testing.
The findings, from 30 adults with normal insulin sensitivity and normal weight and 24 adults with impaired insulin sensitivity and obesity, suggest that metabolic signals, particularly ones that promote energy restoration in a setting of energy deprivation caused by insulin or a glucagon-like peptide-1 (GLP-1) receptor agonist, “profoundly influence neuronal processing,” said Dr. Tittgemeyer. The findings suggest that impaired metabolic signaling such as occurs with insulin resistance in people with obesity can cause deficiencies in associative learning.
‘Liraglutide can normalize learning of associations’
“We show that in people with obesity, disrupted circuit mechanisms lead to impaired learning about sensory associations,” Dr. Tittgemeyer said in an interview. “The information provided by sensory systems that the brain must interpret to select a behavioral response are ‘off tune’ ” in these individuals.
“This is rather consequential for understanding food-intake behaviors. Modern obesity treatments, such as liraglutide, can normalize learning of associations and thereby render people susceptible again for sensory signals and make them more prone to react to subliminal interactions, such as weight-normalizing diets and conscious eating,” he added.
The normalization in associative learning that one dose of liraglutide produced in people with obesity “fits with studies showing that these drugs restore a normal feeling of satiety, causing people to eat less and therefore lose weight,” he explained.
Dr. Tittgemeyer noted that this effect is likely shared by other agents in the GLP-1 receptor agonist class, such as semaglutide (Ozempic, Wegovy, Novo Nordisk) but is likely not an effect when agents agonize receptors to other nutrient-stimulated hormones such as glucagon and the glucose-dependent insulinotropic polypeptide.
The findings “show that liraglutide restores associative learning in participants with greater insulin resistance,” a “highly relevant” discovery, commented Nils B. Kroemer, PhD, head of the section of medical psychology at the University of Bonn, Germany, who was not involved with this research, in a written statement.
The study run by Dr. Tittgemeyer and his associates included 54 healthy adult volunteers whom they assessed for insulin sensitivity with their homeostasis model assessment of insulin resistance. The researchers divided the cohort into groups; one group included 24 people with impaired insulin sensitivity, and one included 30 with normal insulin sensitivity. The average body mass index (BMI) of the normal sensitivity group was about 24 kg/m2; in the insulin-resistant subgroup, BMI averaged about 33 kg/m2.
The associative learning task tested the ability of participants to learn associations between auditory cues (a high or low tone) and a subsequent visual outcome (a picture of a face or a house). During each associative learning session, participants also underwent functional MRI of the brain.
Liraglutide treatment leveled learning
The results showed that the learning rate was significantly lower in the subgroup with impaired insulin sensitivity, compared with those with normal insulin sensitivity following treatment with a placebo injection. This indicates a decreased adaptation of learning to predictability variations in individuals with impaired insulin sensitivity.
In contrast, treatment with a single dose of liraglutide significantly enhanced the learning rate in the group with impaired insulin sensitivity but significantly reduced the learning rate in the group with normal insulin sensitivity. Liraglutide’s effect was twice as large in the group with impaired insulin sensitivity than in the group with normal insulin sensitivity, and these opposing effects of liraglutide resulted in a convergence of the two groups’ adaptive learning rates so that there wasn’t any significant between-group difference following liraglutide treatment.
After analyzing the functional MRI data along with the learning results, the researchers concluded that liraglutide normalized learning in individuals with impaired insulin sensitivity by enhancing adaptive prediction error encoding in the brain’s ventral striatum and mesocortical projection sites.
This apparent ability of GLP-1 analogues to correct this learning deficit in people with impaired insulin sensitivity and obesity has implications regarding potential benefit for people with other pathologies characterized by impaired dopaminergic function and associated with metabolic impairments, such as psychosis, Parkinson’s disease, and depression, the researchers say.
“The fascinating thing about GLP-1 receptor agonists is that they have an additional mechanism that relates to anti-inflammatory effects, especially for alleviating cell stress,” said Dr. Tittgemeyer. “Many ongoing clinical trials are assessing their effects in neuropsychiatric diseases,” he noted.
The study received no commercial funding. Dr. Tittgemyer and most of his coauthors had no disclosures. One coauthor had several disclosures, which are detailed in the report. Dr. Kroemer had no disclosures.
A version of this article first appeared on Medscape.com.
A single injection of the GLP-1 receptor agonist liraglutide led to short-term normalization of associative learning in people with obesity and insulin resistance, a finding that suggests say the authors of a recent report in Nature Metabolism.
“We demonstrated that dopamine-driven associative learning about external sensory cues crucially depends on metabolic signaling,” said Marc Tittgemeyer, PhD, professor at the Max Planck Institute for Metabolism Research in Cologne, Germany, and senior author of the study. Study participants with impaired insulin sensitivity “exhibited a reduced amplitude of behavioral updating that was normalized” by a single subcutaneous injection of 0.6 mg of liraglutide (the starting daily dose for liraglutide for weight loss, available as Saxenda, Novo Nordisk) given the evening before testing.
The findings, from 30 adults with normal insulin sensitivity and normal weight and 24 adults with impaired insulin sensitivity and obesity, suggest that metabolic signals, particularly ones that promote energy restoration in a setting of energy deprivation caused by insulin or a glucagon-like peptide-1 (GLP-1) receptor agonist, “profoundly influence neuronal processing,” said Dr. Tittgemeyer. The findings suggest that impaired metabolic signaling such as occurs with insulin resistance in people with obesity can cause deficiencies in associative learning.
‘Liraglutide can normalize learning of associations’
“We show that in people with obesity, disrupted circuit mechanisms lead to impaired learning about sensory associations,” Dr. Tittgemeyer said in an interview. “The information provided by sensory systems that the brain must interpret to select a behavioral response are ‘off tune’ ” in these individuals.
“This is rather consequential for understanding food-intake behaviors. Modern obesity treatments, such as liraglutide, can normalize learning of associations and thereby render people susceptible again for sensory signals and make them more prone to react to subliminal interactions, such as weight-normalizing diets and conscious eating,” he added.
The normalization in associative learning that one dose of liraglutide produced in people with obesity “fits with studies showing that these drugs restore a normal feeling of satiety, causing people to eat less and therefore lose weight,” he explained.
Dr. Tittgemeyer noted that this effect is likely shared by other agents in the GLP-1 receptor agonist class, such as semaglutide (Ozempic, Wegovy, Novo Nordisk) but is likely not an effect when agents agonize receptors to other nutrient-stimulated hormones such as glucagon and the glucose-dependent insulinotropic polypeptide.
The findings “show that liraglutide restores associative learning in participants with greater insulin resistance,” a “highly relevant” discovery, commented Nils B. Kroemer, PhD, head of the section of medical psychology at the University of Bonn, Germany, who was not involved with this research, in a written statement.
The study run by Dr. Tittgemeyer and his associates included 54 healthy adult volunteers whom they assessed for insulin sensitivity with their homeostasis model assessment of insulin resistance. The researchers divided the cohort into groups; one group included 24 people with impaired insulin sensitivity, and one included 30 with normal insulin sensitivity. The average body mass index (BMI) of the normal sensitivity group was about 24 kg/m2; in the insulin-resistant subgroup, BMI averaged about 33 kg/m2.
The associative learning task tested the ability of participants to learn associations between auditory cues (a high or low tone) and a subsequent visual outcome (a picture of a face or a house). During each associative learning session, participants also underwent functional MRI of the brain.
Liraglutide treatment leveled learning
The results showed that the learning rate was significantly lower in the subgroup with impaired insulin sensitivity, compared with those with normal insulin sensitivity following treatment with a placebo injection. This indicates a decreased adaptation of learning to predictability variations in individuals with impaired insulin sensitivity.
In contrast, treatment with a single dose of liraglutide significantly enhanced the learning rate in the group with impaired insulin sensitivity but significantly reduced the learning rate in the group with normal insulin sensitivity. Liraglutide’s effect was twice as large in the group with impaired insulin sensitivity than in the group with normal insulin sensitivity, and these opposing effects of liraglutide resulted in a convergence of the two groups’ adaptive learning rates so that there wasn’t any significant between-group difference following liraglutide treatment.
After analyzing the functional MRI data along with the learning results, the researchers concluded that liraglutide normalized learning in individuals with impaired insulin sensitivity by enhancing adaptive prediction error encoding in the brain’s ventral striatum and mesocortical projection sites.
This apparent ability of GLP-1 analogues to correct this learning deficit in people with impaired insulin sensitivity and obesity has implications regarding potential benefit for people with other pathologies characterized by impaired dopaminergic function and associated with metabolic impairments, such as psychosis, Parkinson’s disease, and depression, the researchers say.
“The fascinating thing about GLP-1 receptor agonists is that they have an additional mechanism that relates to anti-inflammatory effects, especially for alleviating cell stress,” said Dr. Tittgemeyer. “Many ongoing clinical trials are assessing their effects in neuropsychiatric diseases,” he noted.
The study received no commercial funding. Dr. Tittgemyer and most of his coauthors had no disclosures. One coauthor had several disclosures, which are detailed in the report. Dr. Kroemer had no disclosures.
A version of this article first appeared on Medscape.com.
A single injection of the GLP-1 receptor agonist liraglutide led to short-term normalization of associative learning in people with obesity and insulin resistance, a finding that suggests say the authors of a recent report in Nature Metabolism.
“We demonstrated that dopamine-driven associative learning about external sensory cues crucially depends on metabolic signaling,” said Marc Tittgemeyer, PhD, professor at the Max Planck Institute for Metabolism Research in Cologne, Germany, and senior author of the study. Study participants with impaired insulin sensitivity “exhibited a reduced amplitude of behavioral updating that was normalized” by a single subcutaneous injection of 0.6 mg of liraglutide (the starting daily dose for liraglutide for weight loss, available as Saxenda, Novo Nordisk) given the evening before testing.
The findings, from 30 adults with normal insulin sensitivity and normal weight and 24 adults with impaired insulin sensitivity and obesity, suggest that metabolic signals, particularly ones that promote energy restoration in a setting of energy deprivation caused by insulin or a glucagon-like peptide-1 (GLP-1) receptor agonist, “profoundly influence neuronal processing,” said Dr. Tittgemeyer. The findings suggest that impaired metabolic signaling such as occurs with insulin resistance in people with obesity can cause deficiencies in associative learning.
‘Liraglutide can normalize learning of associations’
“We show that in people with obesity, disrupted circuit mechanisms lead to impaired learning about sensory associations,” Dr. Tittgemeyer said in an interview. “The information provided by sensory systems that the brain must interpret to select a behavioral response are ‘off tune’ ” in these individuals.
“This is rather consequential for understanding food-intake behaviors. Modern obesity treatments, such as liraglutide, can normalize learning of associations and thereby render people susceptible again for sensory signals and make them more prone to react to subliminal interactions, such as weight-normalizing diets and conscious eating,” he added.
The normalization in associative learning that one dose of liraglutide produced in people with obesity “fits with studies showing that these drugs restore a normal feeling of satiety, causing people to eat less and therefore lose weight,” he explained.
Dr. Tittgemeyer noted that this effect is likely shared by other agents in the GLP-1 receptor agonist class, such as semaglutide (Ozempic, Wegovy, Novo Nordisk) but is likely not an effect when agents agonize receptors to other nutrient-stimulated hormones such as glucagon and the glucose-dependent insulinotropic polypeptide.
The findings “show that liraglutide restores associative learning in participants with greater insulin resistance,” a “highly relevant” discovery, commented Nils B. Kroemer, PhD, head of the section of medical psychology at the University of Bonn, Germany, who was not involved with this research, in a written statement.
The study run by Dr. Tittgemeyer and his associates included 54 healthy adult volunteers whom they assessed for insulin sensitivity with their homeostasis model assessment of insulin resistance. The researchers divided the cohort into groups; one group included 24 people with impaired insulin sensitivity, and one included 30 with normal insulin sensitivity. The average body mass index (BMI) of the normal sensitivity group was about 24 kg/m2; in the insulin-resistant subgroup, BMI averaged about 33 kg/m2.
The associative learning task tested the ability of participants to learn associations between auditory cues (a high or low tone) and a subsequent visual outcome (a picture of a face or a house). During each associative learning session, participants also underwent functional MRI of the brain.
Liraglutide treatment leveled learning
The results showed that the learning rate was significantly lower in the subgroup with impaired insulin sensitivity, compared with those with normal insulin sensitivity following treatment with a placebo injection. This indicates a decreased adaptation of learning to predictability variations in individuals with impaired insulin sensitivity.
In contrast, treatment with a single dose of liraglutide significantly enhanced the learning rate in the group with impaired insulin sensitivity but significantly reduced the learning rate in the group with normal insulin sensitivity. Liraglutide’s effect was twice as large in the group with impaired insulin sensitivity than in the group with normal insulin sensitivity, and these opposing effects of liraglutide resulted in a convergence of the two groups’ adaptive learning rates so that there wasn’t any significant between-group difference following liraglutide treatment.
After analyzing the functional MRI data along with the learning results, the researchers concluded that liraglutide normalized learning in individuals with impaired insulin sensitivity by enhancing adaptive prediction error encoding in the brain’s ventral striatum and mesocortical projection sites.
This apparent ability of GLP-1 analogues to correct this learning deficit in people with impaired insulin sensitivity and obesity has implications regarding potential benefit for people with other pathologies characterized by impaired dopaminergic function and associated with metabolic impairments, such as psychosis, Parkinson’s disease, and depression, the researchers say.
“The fascinating thing about GLP-1 receptor agonists is that they have an additional mechanism that relates to anti-inflammatory effects, especially for alleviating cell stress,” said Dr. Tittgemeyer. “Many ongoing clinical trials are assessing their effects in neuropsychiatric diseases,” he noted.
The study received no commercial funding. Dr. Tittgemyer and most of his coauthors had no disclosures. One coauthor had several disclosures, which are detailed in the report. Dr. Kroemer had no disclosures.
A version of this article first appeared on Medscape.com.
FROM NATURE METABOLISM
Apple cider vinegar, fenugreek best herbal remedies for T2D: Review
The review included 44 randomized clinical trials with more than 3,000 participants using six herbal remedies: apple cider vinegar, cinnamon, curcumin, fenugreek seeds, ginger, and saffron.
Apple cider vinegar, fenugreek seeds, curcumin (turmeric), and cinnamon resulted in statistically significant reductions in fasting blood glucose, compared with the control groups in the clinical trials. Out of all the remedies, the authors found apple cider vinegar to be the most effective for lowering fasting blood glucose levels.
The review also found that apple cider vinegar and fenugreek seeds had a statistically significant effect on reducing A1c, compared with the control groups. The authors found the herbal remedies made no difference to insulin level or homeostatic model assessment for insulin resistance (HOMA-IR).
The results are published online in Diabetes & Metabolic Syndrome: Clinical Research & Reviews. The authors said they hoped the review would help medical professionals and people with type 2 diabetes understand the effectiveness of different herbal remedies and consider incorporating these remedies into standard care.
“Some people use curcumin, some use ginger, some use apple cider [vinegar], but it’s not clear which is better,” said Shiv Mudgal, PhD, corresponding author of the paper and an associate professor in nursing at the All India Institute of Medical Sciences in Deoghar, India.
“We thought it would be nice to get some idea about how they work and how they compete with each other,” said Subodh Kumar, MD, the first author and an associate professor in pharmacology at the All India Institute of Medical Sciences in Deoghar, India.
They wanted to understand how the herbal remedies worked by including insulin level and HOMA-IR as measurable outcomes but found nothing conclusive. Instead, they speculated that the effect of apple cider vinegar and fenugreek seeds on blood glucose and A1c could be related to delayed gastric emptying, among other mechanisms.
However, the results should be interpreted with caution, said Dr. Kumar.
Apple cider vinegar had three clinical trials to back the finding, and fenugreek seeds had four studies supporting the results – fewer than the other included remedies. The authors also identified risks of bias from the randomization process and the allocation concealment process in several of the included trials.
Most of the studies included only short follow-up periods, meaning that the long-term effects of using these herbal remedies to help manage type 2 diabetes remain unclear.
The six herbal remedies included in the study were chosen out of dozens of popular complementary medicines for the strength and number of clinical trials backing their use.
The limited number included in the review is a drawback, according to Merlin Willcox, DPhil, a clinical lecturer in general practice at the University of Southampton, England, who was not involved in the research.
“It means they’ve left out stuff that’s potentially effective,” Dr. Willcox said in an interview.
Dr. Willcox, who has coauthored a review of herbal remedies for glycemic control in type 2 diabetes, said he was surprised that apple cider vinegar came out on top in this analysis.
His review concluded that aloe vera leaf gel, psyllium fiber, and fenugreek seeds appeared to be the most effective at reducing A1c, compared with the control groups of the included trials, out of 18 plant-based remedies.
There were no adverse effects associated with the herbal remedies, according to Dr. Mudgal. However, the evidence for the herbal remedies included in their review also lacked substantial follow-up periods assessing their long-term effects.
“You need to look at the evidence for each individual remedy; it’s not just about what plant it is, but it’s about what preparation, what dose. All of that comes into play,” Dr. Willcox said.
Up to 3.6 million people use herbal remedies to manage type 2 diabetes in the United States, according to a 2014 study cited by the review authors. The number is much higher elsewhere: As many as two-thirds of patients with diabetes in India and Saudi Arabia incorporate herbal remedies to help manage symptoms, whereas about half of patients with diabetes in the United Kingdom use herbal medicines.
Experts warn of the risks associated with using herbal medicines to complement traditional therapies.
“I caution my patients about dietary supplements and herbals because of the lack of high-quality data demonstrating efficacy and safety,” Katherine H. Saunders, MD, DABOM, cofounder of Intellihealth and clinical assistant professor of medicine at Weill Cornell Medicine, New York, said in an interview.
For Dr. Willcox, the risks relate to where patients get their information from. Many patients with type 2 diabetes are too scared to talk to their doctor about herbal medicines.
“They think their doctor is going to be negative or dismissive,” Dr. Willcox said. “So patients are getting their information from family and friends or from the Internet, which is not necessarily the most reliable, evidence-based source of information.”
The authors have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
The review included 44 randomized clinical trials with more than 3,000 participants using six herbal remedies: apple cider vinegar, cinnamon, curcumin, fenugreek seeds, ginger, and saffron.
Apple cider vinegar, fenugreek seeds, curcumin (turmeric), and cinnamon resulted in statistically significant reductions in fasting blood glucose, compared with the control groups in the clinical trials. Out of all the remedies, the authors found apple cider vinegar to be the most effective for lowering fasting blood glucose levels.
The review also found that apple cider vinegar and fenugreek seeds had a statistically significant effect on reducing A1c, compared with the control groups. The authors found the herbal remedies made no difference to insulin level or homeostatic model assessment for insulin resistance (HOMA-IR).
The results are published online in Diabetes & Metabolic Syndrome: Clinical Research & Reviews. The authors said they hoped the review would help medical professionals and people with type 2 diabetes understand the effectiveness of different herbal remedies and consider incorporating these remedies into standard care.
“Some people use curcumin, some use ginger, some use apple cider [vinegar], but it’s not clear which is better,” said Shiv Mudgal, PhD, corresponding author of the paper and an associate professor in nursing at the All India Institute of Medical Sciences in Deoghar, India.
“We thought it would be nice to get some idea about how they work and how they compete with each other,” said Subodh Kumar, MD, the first author and an associate professor in pharmacology at the All India Institute of Medical Sciences in Deoghar, India.
They wanted to understand how the herbal remedies worked by including insulin level and HOMA-IR as measurable outcomes but found nothing conclusive. Instead, they speculated that the effect of apple cider vinegar and fenugreek seeds on blood glucose and A1c could be related to delayed gastric emptying, among other mechanisms.
However, the results should be interpreted with caution, said Dr. Kumar.
Apple cider vinegar had three clinical trials to back the finding, and fenugreek seeds had four studies supporting the results – fewer than the other included remedies. The authors also identified risks of bias from the randomization process and the allocation concealment process in several of the included trials.
Most of the studies included only short follow-up periods, meaning that the long-term effects of using these herbal remedies to help manage type 2 diabetes remain unclear.
The six herbal remedies included in the study were chosen out of dozens of popular complementary medicines for the strength and number of clinical trials backing their use.
The limited number included in the review is a drawback, according to Merlin Willcox, DPhil, a clinical lecturer in general practice at the University of Southampton, England, who was not involved in the research.
“It means they’ve left out stuff that’s potentially effective,” Dr. Willcox said in an interview.
Dr. Willcox, who has coauthored a review of herbal remedies for glycemic control in type 2 diabetes, said he was surprised that apple cider vinegar came out on top in this analysis.
His review concluded that aloe vera leaf gel, psyllium fiber, and fenugreek seeds appeared to be the most effective at reducing A1c, compared with the control groups of the included trials, out of 18 plant-based remedies.
There were no adverse effects associated with the herbal remedies, according to Dr. Mudgal. However, the evidence for the herbal remedies included in their review also lacked substantial follow-up periods assessing their long-term effects.
“You need to look at the evidence for each individual remedy; it’s not just about what plant it is, but it’s about what preparation, what dose. All of that comes into play,” Dr. Willcox said.
Up to 3.6 million people use herbal remedies to manage type 2 diabetes in the United States, according to a 2014 study cited by the review authors. The number is much higher elsewhere: As many as two-thirds of patients with diabetes in India and Saudi Arabia incorporate herbal remedies to help manage symptoms, whereas about half of patients with diabetes in the United Kingdom use herbal medicines.
Experts warn of the risks associated with using herbal medicines to complement traditional therapies.
“I caution my patients about dietary supplements and herbals because of the lack of high-quality data demonstrating efficacy and safety,” Katherine H. Saunders, MD, DABOM, cofounder of Intellihealth and clinical assistant professor of medicine at Weill Cornell Medicine, New York, said in an interview.
For Dr. Willcox, the risks relate to where patients get their information from. Many patients with type 2 diabetes are too scared to talk to their doctor about herbal medicines.
“They think their doctor is going to be negative or dismissive,” Dr. Willcox said. “So patients are getting their information from family and friends or from the Internet, which is not necessarily the most reliable, evidence-based source of information.”
The authors have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
The review included 44 randomized clinical trials with more than 3,000 participants using six herbal remedies: apple cider vinegar, cinnamon, curcumin, fenugreek seeds, ginger, and saffron.
Apple cider vinegar, fenugreek seeds, curcumin (turmeric), and cinnamon resulted in statistically significant reductions in fasting blood glucose, compared with the control groups in the clinical trials. Out of all the remedies, the authors found apple cider vinegar to be the most effective for lowering fasting blood glucose levels.
The review also found that apple cider vinegar and fenugreek seeds had a statistically significant effect on reducing A1c, compared with the control groups. The authors found the herbal remedies made no difference to insulin level or homeostatic model assessment for insulin resistance (HOMA-IR).
The results are published online in Diabetes & Metabolic Syndrome: Clinical Research & Reviews. The authors said they hoped the review would help medical professionals and people with type 2 diabetes understand the effectiveness of different herbal remedies and consider incorporating these remedies into standard care.
“Some people use curcumin, some use ginger, some use apple cider [vinegar], but it’s not clear which is better,” said Shiv Mudgal, PhD, corresponding author of the paper and an associate professor in nursing at the All India Institute of Medical Sciences in Deoghar, India.
“We thought it would be nice to get some idea about how they work and how they compete with each other,” said Subodh Kumar, MD, the first author and an associate professor in pharmacology at the All India Institute of Medical Sciences in Deoghar, India.
They wanted to understand how the herbal remedies worked by including insulin level and HOMA-IR as measurable outcomes but found nothing conclusive. Instead, they speculated that the effect of apple cider vinegar and fenugreek seeds on blood glucose and A1c could be related to delayed gastric emptying, among other mechanisms.
However, the results should be interpreted with caution, said Dr. Kumar.
Apple cider vinegar had three clinical trials to back the finding, and fenugreek seeds had four studies supporting the results – fewer than the other included remedies. The authors also identified risks of bias from the randomization process and the allocation concealment process in several of the included trials.
Most of the studies included only short follow-up periods, meaning that the long-term effects of using these herbal remedies to help manage type 2 diabetes remain unclear.
The six herbal remedies included in the study were chosen out of dozens of popular complementary medicines for the strength and number of clinical trials backing their use.
The limited number included in the review is a drawback, according to Merlin Willcox, DPhil, a clinical lecturer in general practice at the University of Southampton, England, who was not involved in the research.
“It means they’ve left out stuff that’s potentially effective,” Dr. Willcox said in an interview.
Dr. Willcox, who has coauthored a review of herbal remedies for glycemic control in type 2 diabetes, said he was surprised that apple cider vinegar came out on top in this analysis.
His review concluded that aloe vera leaf gel, psyllium fiber, and fenugreek seeds appeared to be the most effective at reducing A1c, compared with the control groups of the included trials, out of 18 plant-based remedies.
There were no adverse effects associated with the herbal remedies, according to Dr. Mudgal. However, the evidence for the herbal remedies included in their review also lacked substantial follow-up periods assessing their long-term effects.
“You need to look at the evidence for each individual remedy; it’s not just about what plant it is, but it’s about what preparation, what dose. All of that comes into play,” Dr. Willcox said.
Up to 3.6 million people use herbal remedies to manage type 2 diabetes in the United States, according to a 2014 study cited by the review authors. The number is much higher elsewhere: As many as two-thirds of patients with diabetes in India and Saudi Arabia incorporate herbal remedies to help manage symptoms, whereas about half of patients with diabetes in the United Kingdom use herbal medicines.
Experts warn of the risks associated with using herbal medicines to complement traditional therapies.
“I caution my patients about dietary supplements and herbals because of the lack of high-quality data demonstrating efficacy and safety,” Katherine H. Saunders, MD, DABOM, cofounder of Intellihealth and clinical assistant professor of medicine at Weill Cornell Medicine, New York, said in an interview.
For Dr. Willcox, the risks relate to where patients get their information from. Many patients with type 2 diabetes are too scared to talk to their doctor about herbal medicines.
“They think their doctor is going to be negative or dismissive,” Dr. Willcox said. “So patients are getting their information from family and friends or from the Internet, which is not necessarily the most reliable, evidence-based source of information.”
The authors have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM DIABETES & METABOLIC SYNDROME: CLINICAL RESEARCH & REVIEWS
Continuous glucose monitors for pregnant patients?
Patients with pregestational diabetes may benefit from use of a continuous subcutaneous insulin infusion pump paired with a continuous glucose monitor. Use of the tools has been associated with a reduction in maternal and neonatal morbidity, a recent study found.
“We were seeing an unacceptable burden of both maternal and fetal disease in our diabetic population,” said Neil Hamill, MD, a maternal-fetal medicine specialist at Methodist Women’s Hospital, Omaha, Neb., and an author of the study. “We thought the success with this technology in the nonpregnant population would and should translate into the pregnant population.”
Dr. Hamill and his colleagues analyzed data from 55 pregnant patients who received care at the Women’s Hospital Perinatal Center at the Nebraska Methodist Health System between October 2019 and October 2022. Everyone in the cohort had pregestational diabetes and required insulin prior to week 20 of pregnancy. They used CGMs for more than 2 weeks. The study set blood glucose levels of less than 140 mg/dL as a healthy benchmark.
Participants who had severe preeclampsia, who had delivered preterm, who had delivered a neonate with respiratory distress syndrome, and/or who had given birth to a larger-than-expected infant spent less time in the safe zone – having a blood glucose level below 140 mg/dL – than women who did not have those risk factors.
“When blood sugar control is better, maternal and fetal outcomes are improved,” Dr. Hamill said.
Neetu Sodhi, MD, an ob.gyn. at Providence Cedars-Sinai Tarzana Medical Center, Los Angeles, expressed optimism that use of blood glucose monitors and insulin pumps can improve outcomes for pregnant patients with pregestational diabetes.
“This is just another case for why it’s so important for patients to have access to these types of devices that really, really improve their outcomes and their health, and now it’s proven in the case of pregnancy outcomes too – or at least suggested strongly with this data,” Dr. Sodhi said.
Mark Ebell, MD, a professor of epidemiology at the University of Georgia, Athens, was more skeptical, pointing out that study participants might have used other methods in addition to the technology to lower their blood sugar levels.
The findings suggest that insulin pumps are more manageable than multiple, daily self-injections. About 1 in 9 women have diabetes in the United States, and 35% of people newly diagnosed with the condition are women of reproductive age.
Dr. Hamill said that in future research, use of a stricter criterion for baseline blood sugar levels (< 140 mg/dL) would be helpful, as would exploring how much time patients need to spend below that level for optimal outcomes.
“Those questions are really absent in the literature,” Dr. Hamill said. “Most of our obstetrical literature is comparing treatment types. All those things are secondary. It’s the blood sugar that confers the risk, and if we get the blood sugar better, risk is reduced.”
Dr. Hamill added that the benefits of these technologies for patients with gestational diabetes are unclear in consideration of the limited duration of the disease and the time required to implant or install a monitor and pump, as well as associated risks and the cost of the devices.
Dr. Sodhi said clinicians who see patients during family planning visits should review morbidities and medical problems related to diabetes.
“I think this is a study that’s maybe too early,” Dr. Sodhi said. “They did ‘guesstimates’ on what target blood glucose ranges to be looking at, but I think over time, we might, with more studies like this, be building a case to try to put these types of monitors in for patients who are young for the purpose of optimizing pregnancy outcomes.”
The authors have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Patients with pregestational diabetes may benefit from use of a continuous subcutaneous insulin infusion pump paired with a continuous glucose monitor. Use of the tools has been associated with a reduction in maternal and neonatal morbidity, a recent study found.
“We were seeing an unacceptable burden of both maternal and fetal disease in our diabetic population,” said Neil Hamill, MD, a maternal-fetal medicine specialist at Methodist Women’s Hospital, Omaha, Neb., and an author of the study. “We thought the success with this technology in the nonpregnant population would and should translate into the pregnant population.”
Dr. Hamill and his colleagues analyzed data from 55 pregnant patients who received care at the Women’s Hospital Perinatal Center at the Nebraska Methodist Health System between October 2019 and October 2022. Everyone in the cohort had pregestational diabetes and required insulin prior to week 20 of pregnancy. They used CGMs for more than 2 weeks. The study set blood glucose levels of less than 140 mg/dL as a healthy benchmark.
Participants who had severe preeclampsia, who had delivered preterm, who had delivered a neonate with respiratory distress syndrome, and/or who had given birth to a larger-than-expected infant spent less time in the safe zone – having a blood glucose level below 140 mg/dL – than women who did not have those risk factors.
“When blood sugar control is better, maternal and fetal outcomes are improved,” Dr. Hamill said.
Neetu Sodhi, MD, an ob.gyn. at Providence Cedars-Sinai Tarzana Medical Center, Los Angeles, expressed optimism that use of blood glucose monitors and insulin pumps can improve outcomes for pregnant patients with pregestational diabetes.
“This is just another case for why it’s so important for patients to have access to these types of devices that really, really improve their outcomes and their health, and now it’s proven in the case of pregnancy outcomes too – or at least suggested strongly with this data,” Dr. Sodhi said.
Mark Ebell, MD, a professor of epidemiology at the University of Georgia, Athens, was more skeptical, pointing out that study participants might have used other methods in addition to the technology to lower their blood sugar levels.
The findings suggest that insulin pumps are more manageable than multiple, daily self-injections. About 1 in 9 women have diabetes in the United States, and 35% of people newly diagnosed with the condition are women of reproductive age.
Dr. Hamill said that in future research, use of a stricter criterion for baseline blood sugar levels (< 140 mg/dL) would be helpful, as would exploring how much time patients need to spend below that level for optimal outcomes.
“Those questions are really absent in the literature,” Dr. Hamill said. “Most of our obstetrical literature is comparing treatment types. All those things are secondary. It’s the blood sugar that confers the risk, and if we get the blood sugar better, risk is reduced.”
Dr. Hamill added that the benefits of these technologies for patients with gestational diabetes are unclear in consideration of the limited duration of the disease and the time required to implant or install a monitor and pump, as well as associated risks and the cost of the devices.
Dr. Sodhi said clinicians who see patients during family planning visits should review morbidities and medical problems related to diabetes.
“I think this is a study that’s maybe too early,” Dr. Sodhi said. “They did ‘guesstimates’ on what target blood glucose ranges to be looking at, but I think over time, we might, with more studies like this, be building a case to try to put these types of monitors in for patients who are young for the purpose of optimizing pregnancy outcomes.”
The authors have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Patients with pregestational diabetes may benefit from use of a continuous subcutaneous insulin infusion pump paired with a continuous glucose monitor. Use of the tools has been associated with a reduction in maternal and neonatal morbidity, a recent study found.
“We were seeing an unacceptable burden of both maternal and fetal disease in our diabetic population,” said Neil Hamill, MD, a maternal-fetal medicine specialist at Methodist Women’s Hospital, Omaha, Neb., and an author of the study. “We thought the success with this technology in the nonpregnant population would and should translate into the pregnant population.”
Dr. Hamill and his colleagues analyzed data from 55 pregnant patients who received care at the Women’s Hospital Perinatal Center at the Nebraska Methodist Health System between October 2019 and October 2022. Everyone in the cohort had pregestational diabetes and required insulin prior to week 20 of pregnancy. They used CGMs for more than 2 weeks. The study set blood glucose levels of less than 140 mg/dL as a healthy benchmark.
Participants who had severe preeclampsia, who had delivered preterm, who had delivered a neonate with respiratory distress syndrome, and/or who had given birth to a larger-than-expected infant spent less time in the safe zone – having a blood glucose level below 140 mg/dL – than women who did not have those risk factors.
“When blood sugar control is better, maternal and fetal outcomes are improved,” Dr. Hamill said.
Neetu Sodhi, MD, an ob.gyn. at Providence Cedars-Sinai Tarzana Medical Center, Los Angeles, expressed optimism that use of blood glucose monitors and insulin pumps can improve outcomes for pregnant patients with pregestational diabetes.
“This is just another case for why it’s so important for patients to have access to these types of devices that really, really improve their outcomes and their health, and now it’s proven in the case of pregnancy outcomes too – or at least suggested strongly with this data,” Dr. Sodhi said.
Mark Ebell, MD, a professor of epidemiology at the University of Georgia, Athens, was more skeptical, pointing out that study participants might have used other methods in addition to the technology to lower their blood sugar levels.
The findings suggest that insulin pumps are more manageable than multiple, daily self-injections. About 1 in 9 women have diabetes in the United States, and 35% of people newly diagnosed with the condition are women of reproductive age.
Dr. Hamill said that in future research, use of a stricter criterion for baseline blood sugar levels (< 140 mg/dL) would be helpful, as would exploring how much time patients need to spend below that level for optimal outcomes.
“Those questions are really absent in the literature,” Dr. Hamill said. “Most of our obstetrical literature is comparing treatment types. All those things are secondary. It’s the blood sugar that confers the risk, and if we get the blood sugar better, risk is reduced.”
Dr. Hamill added that the benefits of these technologies for patients with gestational diabetes are unclear in consideration of the limited duration of the disease and the time required to implant or install a monitor and pump, as well as associated risks and the cost of the devices.
Dr. Sodhi said clinicians who see patients during family planning visits should review morbidities and medical problems related to diabetes.
“I think this is a study that’s maybe too early,” Dr. Sodhi said. “They did ‘guesstimates’ on what target blood glucose ranges to be looking at, but I think over time, we might, with more studies like this, be building a case to try to put these types of monitors in for patients who are young for the purpose of optimizing pregnancy outcomes.”
The authors have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Answering the protein question when prescribing plant-based diets
Science supports the use of a whole food, predominantly plant-based dietary pattern for optimal health, including reduced risk for chronic disease, and best practice in treatment of leading chronic disease.
We’ve all heard it, and it’s understandable. Patients know that protein is essential for their health and strength, and animal foods have developed a reputation for being the premier protein sources that humans should prioritize through diet. But widespread misconceptions about human needs for protein have inaccurately equated animal food as the best and only sources of protein, augmented by fad diets and modern food marketing. All of this leads to confusion about how much protein people should actually consume and the quality of protein found in plant foods, making many patients reluctant to fully embrace a whole food, predominately plant-based diet.
To ensure that patients have all the facts when making dietary decisions, clinicians need to be prepared to respond to concerns about protein adequacy and quality with evidence-based information. A good starting point for these conversations is to assess how much protein patients are already consuming. A review of the 2015-2016 National Health and Nutrition Examination Survey found that women normally consume an average of 69 g and men an average of 97 g of protein daily.
As a general point of reference, the recommended dietary allowance for protein is about 0.8 g/kg of bodyweight (or 0.36 g/lb), which equates to about 52 g of protein per day for a 145-lb woman and 65 g for a 180-lb man. But for many patients, it may be best to get a more precise recommendation based upon age, gender and physical activity level by using a handy Department of Agriculture tool for health care professionals to calculate daily protein and other nutrient needs. Patients can also use one of countless apps to track their protein and other nutrient intake. By using the tool and a tracking app, both clinician and patients can be fully informed whether protein needs are being met.
The recommended daily allowances for protein are easily met by consuming a variety of whole plant foods, including a variety of minimally processed vegetables, fruits, whole grains, legumes, nuts, and seeds. One cup of cooked red lentils or black beans, for example, contains between 15 g and 18 g of protein. A quarter cup of almonds contains about 7 g of protein and one cup of cooked oats has 5 g.
What about those amino acids?
An area of contention around plant food protein is “complete versus incomplete protein,” terms used to describe whether a protein contains all nine essential amino acids that our bodies require from a single source. Animal food sources usually contain all the essential amino acids, whereas plant sources of protein may contain varying amounts of these amino acids or may even be missing some.
This leads to a misconception that someone adopting a diet of predominately plant food may have to stack or combine specific plant foods in a meal to ensure their protein intake includes an appropriate proportion of amino acids. But the process of protein breakdown turnover solves this problem. The body continuously breaks down protein and recombines it with amino acids stored in tissue for use when needed. Once absorbed by the small intestine, it doesn’t matter whether the protein or amino acids came from the same meal. As long as a person is eating a variety of plant-based protein sources, they will consume adequate amounts of all essential amino acids.
This is true even for athletes, older adults and pregnant women. It is also the position of the Academy of Nutrition and Dietetics that a whole-food, predominately plant-based eating pattern is appropriate for athletes and “all stages of the life cycle, including pregnancy, lactation, infancy, childhood, adolescence, older adulthood.”
The plant-based diet
For examples of healthy plant-based eating plans, The American College of Lifestyle Medicine offers a complimentary guide for a whole food, predominantly plant-based diet that demonstrates how easily the recommended dietary allowance of protein is satisfied. A breakfast of rolled oats, a lunch of bean burritos, and a dinner of mashed potatoes, with chickpeas with a couple snacks throughout the day, adds up to 71 g of protein. Other plant-based meal plans top 100 g or 90 g, with all meal plans meeting or surpassing recommended allowances.
Along with the protein, plant food delivers other beneficial nutrients and dietary components like fiber, antioxidants, anti-inflammatory properties, various vitamins and nutrients, and phytochemicals and vitamin D, without the saturated fats and sodium in meat. But U.S. adults get approximately two-thirds of their protein from animal sources, which lack fiber and have higher levels of saturated fats or sodium that can raise cholesterol and increase the risks for heart disease and stroke.
For clinicians, ACLM published a 10-part series of research white papers on the benefits of a whole food, plant-predominant dietary lifestyle and offers a catalogue of food as medicine continuing medical education and continuing education courses.
Patients hunger for knowledge about health-promoting nutrition but may have difficulty sorting myths from evidence-based facts. Each healthcare professional has an important and powerful opportunity to steer patients in a healthier direction through their diet.
Dr. Collings is director of lifestyle medicine, Silicon Valley Medical Development; President, American College of Lifestyle Medicine, Mountain View, Calif. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Science supports the use of a whole food, predominantly plant-based dietary pattern for optimal health, including reduced risk for chronic disease, and best practice in treatment of leading chronic disease.
We’ve all heard it, and it’s understandable. Patients know that protein is essential for their health and strength, and animal foods have developed a reputation for being the premier protein sources that humans should prioritize through diet. But widespread misconceptions about human needs for protein have inaccurately equated animal food as the best and only sources of protein, augmented by fad diets and modern food marketing. All of this leads to confusion about how much protein people should actually consume and the quality of protein found in plant foods, making many patients reluctant to fully embrace a whole food, predominately plant-based diet.
To ensure that patients have all the facts when making dietary decisions, clinicians need to be prepared to respond to concerns about protein adequacy and quality with evidence-based information. A good starting point for these conversations is to assess how much protein patients are already consuming. A review of the 2015-2016 National Health and Nutrition Examination Survey found that women normally consume an average of 69 g and men an average of 97 g of protein daily.
As a general point of reference, the recommended dietary allowance for protein is about 0.8 g/kg of bodyweight (or 0.36 g/lb), which equates to about 52 g of protein per day for a 145-lb woman and 65 g for a 180-lb man. But for many patients, it may be best to get a more precise recommendation based upon age, gender and physical activity level by using a handy Department of Agriculture tool for health care professionals to calculate daily protein and other nutrient needs. Patients can also use one of countless apps to track their protein and other nutrient intake. By using the tool and a tracking app, both clinician and patients can be fully informed whether protein needs are being met.
The recommended daily allowances for protein are easily met by consuming a variety of whole plant foods, including a variety of minimally processed vegetables, fruits, whole grains, legumes, nuts, and seeds. One cup of cooked red lentils or black beans, for example, contains between 15 g and 18 g of protein. A quarter cup of almonds contains about 7 g of protein and one cup of cooked oats has 5 g.
What about those amino acids?
An area of contention around plant food protein is “complete versus incomplete protein,” terms used to describe whether a protein contains all nine essential amino acids that our bodies require from a single source. Animal food sources usually contain all the essential amino acids, whereas plant sources of protein may contain varying amounts of these amino acids or may even be missing some.
This leads to a misconception that someone adopting a diet of predominately plant food may have to stack or combine specific plant foods in a meal to ensure their protein intake includes an appropriate proportion of amino acids. But the process of protein breakdown turnover solves this problem. The body continuously breaks down protein and recombines it with amino acids stored in tissue for use when needed. Once absorbed by the small intestine, it doesn’t matter whether the protein or amino acids came from the same meal. As long as a person is eating a variety of plant-based protein sources, they will consume adequate amounts of all essential amino acids.
This is true even for athletes, older adults and pregnant women. It is also the position of the Academy of Nutrition and Dietetics that a whole-food, predominately plant-based eating pattern is appropriate for athletes and “all stages of the life cycle, including pregnancy, lactation, infancy, childhood, adolescence, older adulthood.”
The plant-based diet
For examples of healthy plant-based eating plans, The American College of Lifestyle Medicine offers a complimentary guide for a whole food, predominantly plant-based diet that demonstrates how easily the recommended dietary allowance of protein is satisfied. A breakfast of rolled oats, a lunch of bean burritos, and a dinner of mashed potatoes, with chickpeas with a couple snacks throughout the day, adds up to 71 g of protein. Other plant-based meal plans top 100 g or 90 g, with all meal plans meeting or surpassing recommended allowances.
Along with the protein, plant food delivers other beneficial nutrients and dietary components like fiber, antioxidants, anti-inflammatory properties, various vitamins and nutrients, and phytochemicals and vitamin D, without the saturated fats and sodium in meat. But U.S. adults get approximately two-thirds of their protein from animal sources, which lack fiber and have higher levels of saturated fats or sodium that can raise cholesterol and increase the risks for heart disease and stroke.
For clinicians, ACLM published a 10-part series of research white papers on the benefits of a whole food, plant-predominant dietary lifestyle and offers a catalogue of food as medicine continuing medical education and continuing education courses.
Patients hunger for knowledge about health-promoting nutrition but may have difficulty sorting myths from evidence-based facts. Each healthcare professional has an important and powerful opportunity to steer patients in a healthier direction through their diet.
Dr. Collings is director of lifestyle medicine, Silicon Valley Medical Development; President, American College of Lifestyle Medicine, Mountain View, Calif. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Science supports the use of a whole food, predominantly plant-based dietary pattern for optimal health, including reduced risk for chronic disease, and best practice in treatment of leading chronic disease.
We’ve all heard it, and it’s understandable. Patients know that protein is essential for their health and strength, and animal foods have developed a reputation for being the premier protein sources that humans should prioritize through diet. But widespread misconceptions about human needs for protein have inaccurately equated animal food as the best and only sources of protein, augmented by fad diets and modern food marketing. All of this leads to confusion about how much protein people should actually consume and the quality of protein found in plant foods, making many patients reluctant to fully embrace a whole food, predominately plant-based diet.
To ensure that patients have all the facts when making dietary decisions, clinicians need to be prepared to respond to concerns about protein adequacy and quality with evidence-based information. A good starting point for these conversations is to assess how much protein patients are already consuming. A review of the 2015-2016 National Health and Nutrition Examination Survey found that women normally consume an average of 69 g and men an average of 97 g of protein daily.
As a general point of reference, the recommended dietary allowance for protein is about 0.8 g/kg of bodyweight (or 0.36 g/lb), which equates to about 52 g of protein per day for a 145-lb woman and 65 g for a 180-lb man. But for many patients, it may be best to get a more precise recommendation based upon age, gender and physical activity level by using a handy Department of Agriculture tool for health care professionals to calculate daily protein and other nutrient needs. Patients can also use one of countless apps to track their protein and other nutrient intake. By using the tool and a tracking app, both clinician and patients can be fully informed whether protein needs are being met.
The recommended daily allowances for protein are easily met by consuming a variety of whole plant foods, including a variety of minimally processed vegetables, fruits, whole grains, legumes, nuts, and seeds. One cup of cooked red lentils or black beans, for example, contains between 15 g and 18 g of protein. A quarter cup of almonds contains about 7 g of protein and one cup of cooked oats has 5 g.
What about those amino acids?
An area of contention around plant food protein is “complete versus incomplete protein,” terms used to describe whether a protein contains all nine essential amino acids that our bodies require from a single source. Animal food sources usually contain all the essential amino acids, whereas plant sources of protein may contain varying amounts of these amino acids or may even be missing some.
This leads to a misconception that someone adopting a diet of predominately plant food may have to stack or combine specific plant foods in a meal to ensure their protein intake includes an appropriate proportion of amino acids. But the process of protein breakdown turnover solves this problem. The body continuously breaks down protein and recombines it with amino acids stored in tissue for use when needed. Once absorbed by the small intestine, it doesn’t matter whether the protein or amino acids came from the same meal. As long as a person is eating a variety of plant-based protein sources, they will consume adequate amounts of all essential amino acids.
This is true even for athletes, older adults and pregnant women. It is also the position of the Academy of Nutrition and Dietetics that a whole-food, predominately plant-based eating pattern is appropriate for athletes and “all stages of the life cycle, including pregnancy, lactation, infancy, childhood, adolescence, older adulthood.”
The plant-based diet
For examples of healthy plant-based eating plans, The American College of Lifestyle Medicine offers a complimentary guide for a whole food, predominantly plant-based diet that demonstrates how easily the recommended dietary allowance of protein is satisfied. A breakfast of rolled oats, a lunch of bean burritos, and a dinner of mashed potatoes, with chickpeas with a couple snacks throughout the day, adds up to 71 g of protein. Other plant-based meal plans top 100 g or 90 g, with all meal plans meeting or surpassing recommended allowances.
Along with the protein, plant food delivers other beneficial nutrients and dietary components like fiber, antioxidants, anti-inflammatory properties, various vitamins and nutrients, and phytochemicals and vitamin D, without the saturated fats and sodium in meat. But U.S. adults get approximately two-thirds of their protein from animal sources, which lack fiber and have higher levels of saturated fats or sodium that can raise cholesterol and increase the risks for heart disease and stroke.
For clinicians, ACLM published a 10-part series of research white papers on the benefits of a whole food, plant-predominant dietary lifestyle and offers a catalogue of food as medicine continuing medical education and continuing education courses.
Patients hunger for knowledge about health-promoting nutrition but may have difficulty sorting myths from evidence-based facts. Each healthcare professional has an important and powerful opportunity to steer patients in a healthier direction through their diet.
Dr. Collings is director of lifestyle medicine, Silicon Valley Medical Development; President, American College of Lifestyle Medicine, Mountain View, Calif. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Wegovy scores HFpEF benefits in people with obesity
AMSTERDAM – Adults with heart failure with preserved ejection fraction (HFpEF) but without diabetes showed significant improvements in their heart failure-related symptoms and physical limitations, exercise function, and weight loss when treated with a weight-reducing dose of semaglutide for 52 weeks, compared with placebo, in the randomized STEP-HFpEF trial.
The results, which also showed the treatment’s safety in these patients, “indicate that treatment with semaglutide is a valuable therapeutic approach in the management of patients with HFpEF and obesity,” Mikhail Kosiborod, MD, said at the annual congress of the European Society of Cardiology.
The findings establish semaglutide, a glucagonlike peptide–1 (GLP-1) receptor agonist, as a second class of medication with proven efficacy and safety for people with HFpEF, joining two agents also proven beneficial for people with HFpEF, dapagliflozin (Farxiga) and empagliflozin (Jardiance), both from the class of sodium-glucose cotransporter 2 (SGLT2) inhibitors.
When administered at the approved dose for weight loss of 2.4 mg, injected subcutaneously weekly for 52 weeks, semaglutide (Wegovy) produced an average 7.8-point incremental improvement in patients’ scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated measure of symptoms and functional limitations, compared with controls who received placebo injections, as well as an average incremental weight loss from baseline, compared with placebo, of 10.7%. Both were significant effects, compared with placebo, and clinically meaningful benefits for the study’s two primary endpoints.
Simultaneously with Kosiborod’s report the results also appeared in a report posted online in the New England Journal of Medicine.
A ‘paradigm shift’ for medical weight loss in cardiology
The findings from this study with 529 randomized patients immediately propelled the weight loss formulation of semaglutide into the ranks of agents used to treat and prevent cardiovascular disease events. This evolution in the indications for semaglutide will be driven not only by the STEP-HFpEF results but also by findings from the SELECT trial, which tested the same semaglutide weight-loss dose in people with obesity, established cardiovascular disease, and had positive top-line results for prevention of major cardiovascular adverse events, according to a press release from Novo Nordisk on Aug. 8.
The STEP-HFpEF and SELECT results will trigger “a paradigm shift” for cardiologists, who will now need to consider prescribing a weight-loss medication to many of their patients, agents that until now were not part of the usual pharmacologic toolbox for cardiologists, said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. This shift will require education to bring the clinical cardiology community on board, he added in an interview.
Given that semaglutide administered at this dose already has a Food and Drug Administration–approved indication for weight loss in people with obesity or overweight plus at least one comorbidity, clinicians could immediately start using the treatment in people with obesity and HFpEF, said Dr. Kosiborod and other cardiologists.
Weekly semaglutide injections “could be considered a treatment option right now” for people with obesity and HFpEF, Dr. Kosiborod said during a press briefing.
Other experts agreed, especially because the STEP-HFpEF results confirmed that weight loss treatment with semaglutide was safe in this population.
‘A terrific win for patients’
The new findings are “a terrific win and game changer for patients with HFpEF,” commented Gregg C. Fonarow, MD, professor and cochief of cardiology at the University of California, Los Angeles, who was not involved with the study.
“The magnitude of improvement in the patient-reported health status scores are large and impressive. These data support clinical use of this agent for individuals with HFpEF with a body mass index of 30 kg/m2, patients who already fall within existing indications,” Dr. Fonarow said in an interview.
“Given the improvements in clinical outcomes in the STEP-HFpEF and SELECT trials, cardiologists should be prescribing these medications to eligible patients without conditions,” he added. “The perception of [semaglutide] needs to shift and be viewed as a component of the comprehensive medical therapies provided to individuals with established cardiovascular disease or HFpEF who also have elevated body mass index to improve their clinical outcomes.”
Historically, cardiologists have had a concern that weight loss was potentially harmful in people with heart failure and that obesity was protective, a phenomenon known as the “obesity paradox,” but the STEP-HFpEF data help disprove that notion, commented Nancy K. Sweitzer, MD, PhD, a heart failure specialist and vice chair of clinical research in the department of medicine at Washington University in St. Louis, who also was not involved in the study.
No signal of an obesity paradox
“There’s been a concern in the heart failure community to use weight-loss strategies in people with heart failure because of this, but this evidence provides a lot of confidence that it’s safe to use this weight loss treatment. The results show that patients feel better and lose weight with no signal of harm,” Dr. Sweitzer said in an interview.
The “encouraging findings” for semaglutide in patients with HFpEF “potentially add a much needed extra option for these patients and provide another upstream treatment for patients with signs of this condition plus a high body mass index,” commented Yigal M. Pinto, MD, PhD, in an editorial that accompanied the published report.
“How these findings translate to hard end points remains to be established and will be important in determining the role of GLP-1 agonism,” wrote Dr. Pinto, a professor and heart failure specialist at Amsterdam University Medical Center.
But Dr. Kosiborod said that the improvement seen in the KCCQ score was itself an important benefit for patients. “Heart failure is defined clinically based on symptoms,” he noted, and results in prior studies documented that patients value improvements in symptoms and physical limitations even more than they value “hard endpoints” such as survival.
The new findings, which indicate that two different and expensive classes of medications are now standard of care for many people with HFpEF and obesity – the SGLT2 inhibitors and the GLP-1 receptor agonist semaglutide – also raise concerns over patient access and affordability, as many U.S. insurers have a history of requiring prior authorization, high copays, or coverage denials for these two medical classes.
But Dr. Sweitzer and Dr. Kosiborod both said that the insurance-coverage climate seems, in just the past couple of years or so, to have dramatically improved, although it’s still not ideal.
Prior authorization hoops have decreased
“We still have prior-authorization hoops to jump through, but I expect these will continue to decrease over time as evidence for clinical benefits [from weight loss] continues to accumulate,” said Dr. Sweitzer.
And “the SELECT data mean that cardiologists will need to become comfortable prescribing GLP-1 receptor agonists,” she added.
“It’s not okay for insurers to say we are not going to cover weight loss medications because it’s a cosmetic indication,” said Dr. Kosiborod. “Obesity appears to be very important in the pathogenesis and progression of heart failure, and if patients derive substantial benefit, they should have access to this treatment.”
The improvements in KCCQ score, as well as in several secondary and exploratory endpoints including a significant reduction in C-reactive protein (an indication of a potent anti-inflammatory effect), an average 20 m increase in 6-minute walk distance, a significant average drop in N-terminal pro-brain natriuretic peptide, and a drop in heart failure hospitalizations or urgent heart failure visits (although the trial was not powered to show differences in clinical events), “were the largest benefits in these outcomes we’ve seen,” compared with any other medical intervention in people with HFpEF, he noted.
“About 80% of U.S. patients with HFpEF have obesity or overweight,” Dr. Kosiborod noted. Using semaglutide on these patients “is an issue of access and insurance coverage. My hope is that these and other data will favorably change this.”
A related trial with a similar design, STEP-HFpEF DM, is still in progress and testing the same semaglutide treatment in adults with HFpEF, obesity, and type 2 diabetes, noted Dr. Kosiborod, who is also lead investigator for that study. He said those results will likely become available before the end of 2023.
The study was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to and has received honoraria from Novo Nordisk. He has also been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Fonarow has been a consultant to Abbott, Amgen, AstraZeneca, CHF Solutions, Cytokinetics, Edwards, Janssen, Medtronic, Merck, Novartis, and Regeneron. Dr. Sweitzer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AMSTERDAM – Adults with heart failure with preserved ejection fraction (HFpEF) but without diabetes showed significant improvements in their heart failure-related symptoms and physical limitations, exercise function, and weight loss when treated with a weight-reducing dose of semaglutide for 52 weeks, compared with placebo, in the randomized STEP-HFpEF trial.
The results, which also showed the treatment’s safety in these patients, “indicate that treatment with semaglutide is a valuable therapeutic approach in the management of patients with HFpEF and obesity,” Mikhail Kosiborod, MD, said at the annual congress of the European Society of Cardiology.
The findings establish semaglutide, a glucagonlike peptide–1 (GLP-1) receptor agonist, as a second class of medication with proven efficacy and safety for people with HFpEF, joining two agents also proven beneficial for people with HFpEF, dapagliflozin (Farxiga) and empagliflozin (Jardiance), both from the class of sodium-glucose cotransporter 2 (SGLT2) inhibitors.
When administered at the approved dose for weight loss of 2.4 mg, injected subcutaneously weekly for 52 weeks, semaglutide (Wegovy) produced an average 7.8-point incremental improvement in patients’ scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated measure of symptoms and functional limitations, compared with controls who received placebo injections, as well as an average incremental weight loss from baseline, compared with placebo, of 10.7%. Both were significant effects, compared with placebo, and clinically meaningful benefits for the study’s two primary endpoints.
Simultaneously with Kosiborod’s report the results also appeared in a report posted online in the New England Journal of Medicine.
A ‘paradigm shift’ for medical weight loss in cardiology
The findings from this study with 529 randomized patients immediately propelled the weight loss formulation of semaglutide into the ranks of agents used to treat and prevent cardiovascular disease events. This evolution in the indications for semaglutide will be driven not only by the STEP-HFpEF results but also by findings from the SELECT trial, which tested the same semaglutide weight-loss dose in people with obesity, established cardiovascular disease, and had positive top-line results for prevention of major cardiovascular adverse events, according to a press release from Novo Nordisk on Aug. 8.
The STEP-HFpEF and SELECT results will trigger “a paradigm shift” for cardiologists, who will now need to consider prescribing a weight-loss medication to many of their patients, agents that until now were not part of the usual pharmacologic toolbox for cardiologists, said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. This shift will require education to bring the clinical cardiology community on board, he added in an interview.
Given that semaglutide administered at this dose already has a Food and Drug Administration–approved indication for weight loss in people with obesity or overweight plus at least one comorbidity, clinicians could immediately start using the treatment in people with obesity and HFpEF, said Dr. Kosiborod and other cardiologists.
Weekly semaglutide injections “could be considered a treatment option right now” for people with obesity and HFpEF, Dr. Kosiborod said during a press briefing.
Other experts agreed, especially because the STEP-HFpEF results confirmed that weight loss treatment with semaglutide was safe in this population.
‘A terrific win for patients’
The new findings are “a terrific win and game changer for patients with HFpEF,” commented Gregg C. Fonarow, MD, professor and cochief of cardiology at the University of California, Los Angeles, who was not involved with the study.
“The magnitude of improvement in the patient-reported health status scores are large and impressive. These data support clinical use of this agent for individuals with HFpEF with a body mass index of 30 kg/m2, patients who already fall within existing indications,” Dr. Fonarow said in an interview.
“Given the improvements in clinical outcomes in the STEP-HFpEF and SELECT trials, cardiologists should be prescribing these medications to eligible patients without conditions,” he added. “The perception of [semaglutide] needs to shift and be viewed as a component of the comprehensive medical therapies provided to individuals with established cardiovascular disease or HFpEF who also have elevated body mass index to improve their clinical outcomes.”
Historically, cardiologists have had a concern that weight loss was potentially harmful in people with heart failure and that obesity was protective, a phenomenon known as the “obesity paradox,” but the STEP-HFpEF data help disprove that notion, commented Nancy K. Sweitzer, MD, PhD, a heart failure specialist and vice chair of clinical research in the department of medicine at Washington University in St. Louis, who also was not involved in the study.
No signal of an obesity paradox
“There’s been a concern in the heart failure community to use weight-loss strategies in people with heart failure because of this, but this evidence provides a lot of confidence that it’s safe to use this weight loss treatment. The results show that patients feel better and lose weight with no signal of harm,” Dr. Sweitzer said in an interview.
The “encouraging findings” for semaglutide in patients with HFpEF “potentially add a much needed extra option for these patients and provide another upstream treatment for patients with signs of this condition plus a high body mass index,” commented Yigal M. Pinto, MD, PhD, in an editorial that accompanied the published report.
“How these findings translate to hard end points remains to be established and will be important in determining the role of GLP-1 agonism,” wrote Dr. Pinto, a professor and heart failure specialist at Amsterdam University Medical Center.
But Dr. Kosiborod said that the improvement seen in the KCCQ score was itself an important benefit for patients. “Heart failure is defined clinically based on symptoms,” he noted, and results in prior studies documented that patients value improvements in symptoms and physical limitations even more than they value “hard endpoints” such as survival.
The new findings, which indicate that two different and expensive classes of medications are now standard of care for many people with HFpEF and obesity – the SGLT2 inhibitors and the GLP-1 receptor agonist semaglutide – also raise concerns over patient access and affordability, as many U.S. insurers have a history of requiring prior authorization, high copays, or coverage denials for these two medical classes.
But Dr. Sweitzer and Dr. Kosiborod both said that the insurance-coverage climate seems, in just the past couple of years or so, to have dramatically improved, although it’s still not ideal.
Prior authorization hoops have decreased
“We still have prior-authorization hoops to jump through, but I expect these will continue to decrease over time as evidence for clinical benefits [from weight loss] continues to accumulate,” said Dr. Sweitzer.
And “the SELECT data mean that cardiologists will need to become comfortable prescribing GLP-1 receptor agonists,” she added.
“It’s not okay for insurers to say we are not going to cover weight loss medications because it’s a cosmetic indication,” said Dr. Kosiborod. “Obesity appears to be very important in the pathogenesis and progression of heart failure, and if patients derive substantial benefit, they should have access to this treatment.”
The improvements in KCCQ score, as well as in several secondary and exploratory endpoints including a significant reduction in C-reactive protein (an indication of a potent anti-inflammatory effect), an average 20 m increase in 6-minute walk distance, a significant average drop in N-terminal pro-brain natriuretic peptide, and a drop in heart failure hospitalizations or urgent heart failure visits (although the trial was not powered to show differences in clinical events), “were the largest benefits in these outcomes we’ve seen,” compared with any other medical intervention in people with HFpEF, he noted.
“About 80% of U.S. patients with HFpEF have obesity or overweight,” Dr. Kosiborod noted. Using semaglutide on these patients “is an issue of access and insurance coverage. My hope is that these and other data will favorably change this.”
A related trial with a similar design, STEP-HFpEF DM, is still in progress and testing the same semaglutide treatment in adults with HFpEF, obesity, and type 2 diabetes, noted Dr. Kosiborod, who is also lead investigator for that study. He said those results will likely become available before the end of 2023.
The study was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to and has received honoraria from Novo Nordisk. He has also been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Fonarow has been a consultant to Abbott, Amgen, AstraZeneca, CHF Solutions, Cytokinetics, Edwards, Janssen, Medtronic, Merck, Novartis, and Regeneron. Dr. Sweitzer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AMSTERDAM – Adults with heart failure with preserved ejection fraction (HFpEF) but without diabetes showed significant improvements in their heart failure-related symptoms and physical limitations, exercise function, and weight loss when treated with a weight-reducing dose of semaglutide for 52 weeks, compared with placebo, in the randomized STEP-HFpEF trial.
The results, which also showed the treatment’s safety in these patients, “indicate that treatment with semaglutide is a valuable therapeutic approach in the management of patients with HFpEF and obesity,” Mikhail Kosiborod, MD, said at the annual congress of the European Society of Cardiology.
The findings establish semaglutide, a glucagonlike peptide–1 (GLP-1) receptor agonist, as a second class of medication with proven efficacy and safety for people with HFpEF, joining two agents also proven beneficial for people with HFpEF, dapagliflozin (Farxiga) and empagliflozin (Jardiance), both from the class of sodium-glucose cotransporter 2 (SGLT2) inhibitors.
When administered at the approved dose for weight loss of 2.4 mg, injected subcutaneously weekly for 52 weeks, semaglutide (Wegovy) produced an average 7.8-point incremental improvement in patients’ scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated measure of symptoms and functional limitations, compared with controls who received placebo injections, as well as an average incremental weight loss from baseline, compared with placebo, of 10.7%. Both were significant effects, compared with placebo, and clinically meaningful benefits for the study’s two primary endpoints.
Simultaneously with Kosiborod’s report the results also appeared in a report posted online in the New England Journal of Medicine.
A ‘paradigm shift’ for medical weight loss in cardiology
The findings from this study with 529 randomized patients immediately propelled the weight loss formulation of semaglutide into the ranks of agents used to treat and prevent cardiovascular disease events. This evolution in the indications for semaglutide will be driven not only by the STEP-HFpEF results but also by findings from the SELECT trial, which tested the same semaglutide weight-loss dose in people with obesity, established cardiovascular disease, and had positive top-line results for prevention of major cardiovascular adverse events, according to a press release from Novo Nordisk on Aug. 8.
The STEP-HFpEF and SELECT results will trigger “a paradigm shift” for cardiologists, who will now need to consider prescribing a weight-loss medication to many of their patients, agents that until now were not part of the usual pharmacologic toolbox for cardiologists, said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. This shift will require education to bring the clinical cardiology community on board, he added in an interview.
Given that semaglutide administered at this dose already has a Food and Drug Administration–approved indication for weight loss in people with obesity or overweight plus at least one comorbidity, clinicians could immediately start using the treatment in people with obesity and HFpEF, said Dr. Kosiborod and other cardiologists.
Weekly semaglutide injections “could be considered a treatment option right now” for people with obesity and HFpEF, Dr. Kosiborod said during a press briefing.
Other experts agreed, especially because the STEP-HFpEF results confirmed that weight loss treatment with semaglutide was safe in this population.
‘A terrific win for patients’
The new findings are “a terrific win and game changer for patients with HFpEF,” commented Gregg C. Fonarow, MD, professor and cochief of cardiology at the University of California, Los Angeles, who was not involved with the study.
“The magnitude of improvement in the patient-reported health status scores are large and impressive. These data support clinical use of this agent for individuals with HFpEF with a body mass index of 30 kg/m2, patients who already fall within existing indications,” Dr. Fonarow said in an interview.
“Given the improvements in clinical outcomes in the STEP-HFpEF and SELECT trials, cardiologists should be prescribing these medications to eligible patients without conditions,” he added. “The perception of [semaglutide] needs to shift and be viewed as a component of the comprehensive medical therapies provided to individuals with established cardiovascular disease or HFpEF who also have elevated body mass index to improve their clinical outcomes.”
Historically, cardiologists have had a concern that weight loss was potentially harmful in people with heart failure and that obesity was protective, a phenomenon known as the “obesity paradox,” but the STEP-HFpEF data help disprove that notion, commented Nancy K. Sweitzer, MD, PhD, a heart failure specialist and vice chair of clinical research in the department of medicine at Washington University in St. Louis, who also was not involved in the study.
No signal of an obesity paradox
“There’s been a concern in the heart failure community to use weight-loss strategies in people with heart failure because of this, but this evidence provides a lot of confidence that it’s safe to use this weight loss treatment. The results show that patients feel better and lose weight with no signal of harm,” Dr. Sweitzer said in an interview.
The “encouraging findings” for semaglutide in patients with HFpEF “potentially add a much needed extra option for these patients and provide another upstream treatment for patients with signs of this condition plus a high body mass index,” commented Yigal M. Pinto, MD, PhD, in an editorial that accompanied the published report.
“How these findings translate to hard end points remains to be established and will be important in determining the role of GLP-1 agonism,” wrote Dr. Pinto, a professor and heart failure specialist at Amsterdam University Medical Center.
But Dr. Kosiborod said that the improvement seen in the KCCQ score was itself an important benefit for patients. “Heart failure is defined clinically based on symptoms,” he noted, and results in prior studies documented that patients value improvements in symptoms and physical limitations even more than they value “hard endpoints” such as survival.
The new findings, which indicate that two different and expensive classes of medications are now standard of care for many people with HFpEF and obesity – the SGLT2 inhibitors and the GLP-1 receptor agonist semaglutide – also raise concerns over patient access and affordability, as many U.S. insurers have a history of requiring prior authorization, high copays, or coverage denials for these two medical classes.
But Dr. Sweitzer and Dr. Kosiborod both said that the insurance-coverage climate seems, in just the past couple of years or so, to have dramatically improved, although it’s still not ideal.
Prior authorization hoops have decreased
“We still have prior-authorization hoops to jump through, but I expect these will continue to decrease over time as evidence for clinical benefits [from weight loss] continues to accumulate,” said Dr. Sweitzer.
And “the SELECT data mean that cardiologists will need to become comfortable prescribing GLP-1 receptor agonists,” she added.
“It’s not okay for insurers to say we are not going to cover weight loss medications because it’s a cosmetic indication,” said Dr. Kosiborod. “Obesity appears to be very important in the pathogenesis and progression of heart failure, and if patients derive substantial benefit, they should have access to this treatment.”
The improvements in KCCQ score, as well as in several secondary and exploratory endpoints including a significant reduction in C-reactive protein (an indication of a potent anti-inflammatory effect), an average 20 m increase in 6-minute walk distance, a significant average drop in N-terminal pro-brain natriuretic peptide, and a drop in heart failure hospitalizations or urgent heart failure visits (although the trial was not powered to show differences in clinical events), “were the largest benefits in these outcomes we’ve seen,” compared with any other medical intervention in people with HFpEF, he noted.
“About 80% of U.S. patients with HFpEF have obesity or overweight,” Dr. Kosiborod noted. Using semaglutide on these patients “is an issue of access and insurance coverage. My hope is that these and other data will favorably change this.”
A related trial with a similar design, STEP-HFpEF DM, is still in progress and testing the same semaglutide treatment in adults with HFpEF, obesity, and type 2 diabetes, noted Dr. Kosiborod, who is also lead investigator for that study. He said those results will likely become available before the end of 2023.
The study was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to and has received honoraria from Novo Nordisk. He has also been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Fonarow has been a consultant to Abbott, Amgen, AstraZeneca, CHF Solutions, Cytokinetics, Edwards, Janssen, Medtronic, Merck, Novartis, and Regeneron. Dr. Sweitzer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT THE ESC CONGRESS 2023
It’s not ‘reckless’ to consider Ozempic
A stylish 40-something-year-old walks into my office looking mildly sheepish. She is a well-known actress who was recently panned by the paparazzi for having “too much cellulite” after they illegally photographed her playing with her child on a private beach.
Without a doubt, she will request semaglutide (Ozempic) before long, but first we will need to wade through the morass of social condemnation out there about Ozempic to assure her that she is being neither immoral nor reckless for considering it.
Ozempic is nothing new, people! Endocrinologists have been using this class of medication since Byetta hit the market in 2005. We have had 18 years to make informed risk-benefit analyses.
People are obsessed with the risk for pancreatitis. Any type of weight loss can cause gallstones, and this is what can trigger pancreatitis. Unless you’re the type of person who worries that your balanced Weight Watchers diet is going to cause pancreatitis, you should probably remove this risk from your calculations.
Glucagonlike peptide–1 (GLP-1) receptor agonists are naturally occurring gut hormones that reduce inflammatory cascades and clotting risk. We are not giving a dangerous treatment (e.g., fen-phen) that increases cardiovascular risk – quite the contrary, in fact.
Just because influencers are promoting a product doesn’t mean the product is inherently worthless. One of my patients accused me of prescribing a medication that is the “laughingstock of America.” Try telling that to the scores of cardiologists who send patients to my colleagues and me to start Ozempic to help lower their patients’ risk for stroke and heart attack. Or tell this to my patient who survived an episode of rapid atrial fibrillation and was told by his cardiologist that he definitely would have died if he had not lost 30 pounds from Ozempic in the preceding year.
Sometimes it seems like society has become more judgmental about Ozempic than about plastic surgery for weight loss. If we have to choose between liposuction (which doesn’t reduce visceral fat – the dangerous type of fat) or Ozempic, the latter clearly wins because of its real health benefits.
How does it make any sense to say that this medication should be reserved for patients who already have obesity and type 2 diabetes? Why should we penalize patients who have not yet reached those thresholds by denying access to preventive care? Don’t we constantly hear about how our health care system would be much more efficient if we focused on preventive care and not just treatment?
Some people claim that we have to limit access to this medication because of drug shortages. Thankfully, the United States responds to supply and demand economics and will quickly adjust.
I’ve had more patients than I can possibly number with severe binge eating disorders (resistant to years of therapy and medication) who finally developed healthy relationships with food while taking these types of medications. Mounjaro, I’m talking about you…
I always hear the argument that it is immoral to give these medications to patients with a history of restrictive eating patterns. Although every patient needs to be carefully evaluated, often these medications remove food as both the enemy and primary focus of every waking thought. They allow patients to refocus on other aspects of their lives – such as family, friends, hobbies, work – and regain a sense of purpose. If anyone wants to run a trial on this little hypothesis of mine, please reach out to me.
Okay, I agree you might get a little constipated (most often described by patients as the “rabbit pellet phenomenon”), but it’s a small price to pay, no? I’ll throw in a few prunes with the prescription.
Suffice it to say, I did give my 40-something-year-old patient the medication she desired, and she has a new lease on life (as well as better blood pressure and cholesterol).
A version of this article first appeared on Medscape.com.
A stylish 40-something-year-old walks into my office looking mildly sheepish. She is a well-known actress who was recently panned by the paparazzi for having “too much cellulite” after they illegally photographed her playing with her child on a private beach.
Without a doubt, she will request semaglutide (Ozempic) before long, but first we will need to wade through the morass of social condemnation out there about Ozempic to assure her that she is being neither immoral nor reckless for considering it.
Ozempic is nothing new, people! Endocrinologists have been using this class of medication since Byetta hit the market in 2005. We have had 18 years to make informed risk-benefit analyses.
People are obsessed with the risk for pancreatitis. Any type of weight loss can cause gallstones, and this is what can trigger pancreatitis. Unless you’re the type of person who worries that your balanced Weight Watchers diet is going to cause pancreatitis, you should probably remove this risk from your calculations.
Glucagonlike peptide–1 (GLP-1) receptor agonists are naturally occurring gut hormones that reduce inflammatory cascades and clotting risk. We are not giving a dangerous treatment (e.g., fen-phen) that increases cardiovascular risk – quite the contrary, in fact.
Just because influencers are promoting a product doesn’t mean the product is inherently worthless. One of my patients accused me of prescribing a medication that is the “laughingstock of America.” Try telling that to the scores of cardiologists who send patients to my colleagues and me to start Ozempic to help lower their patients’ risk for stroke and heart attack. Or tell this to my patient who survived an episode of rapid atrial fibrillation and was told by his cardiologist that he definitely would have died if he had not lost 30 pounds from Ozempic in the preceding year.
Sometimes it seems like society has become more judgmental about Ozempic than about plastic surgery for weight loss. If we have to choose between liposuction (which doesn’t reduce visceral fat – the dangerous type of fat) or Ozempic, the latter clearly wins because of its real health benefits.
How does it make any sense to say that this medication should be reserved for patients who already have obesity and type 2 diabetes? Why should we penalize patients who have not yet reached those thresholds by denying access to preventive care? Don’t we constantly hear about how our health care system would be much more efficient if we focused on preventive care and not just treatment?
Some people claim that we have to limit access to this medication because of drug shortages. Thankfully, the United States responds to supply and demand economics and will quickly adjust.
I’ve had more patients than I can possibly number with severe binge eating disorders (resistant to years of therapy and medication) who finally developed healthy relationships with food while taking these types of medications. Mounjaro, I’m talking about you…
I always hear the argument that it is immoral to give these medications to patients with a history of restrictive eating patterns. Although every patient needs to be carefully evaluated, often these medications remove food as both the enemy and primary focus of every waking thought. They allow patients to refocus on other aspects of their lives – such as family, friends, hobbies, work – and regain a sense of purpose. If anyone wants to run a trial on this little hypothesis of mine, please reach out to me.
Okay, I agree you might get a little constipated (most often described by patients as the “rabbit pellet phenomenon”), but it’s a small price to pay, no? I’ll throw in a few prunes with the prescription.
Suffice it to say, I did give my 40-something-year-old patient the medication she desired, and she has a new lease on life (as well as better blood pressure and cholesterol).
A version of this article first appeared on Medscape.com.
A stylish 40-something-year-old walks into my office looking mildly sheepish. She is a well-known actress who was recently panned by the paparazzi for having “too much cellulite” after they illegally photographed her playing with her child on a private beach.
Without a doubt, she will request semaglutide (Ozempic) before long, but first we will need to wade through the morass of social condemnation out there about Ozempic to assure her that she is being neither immoral nor reckless for considering it.
Ozempic is nothing new, people! Endocrinologists have been using this class of medication since Byetta hit the market in 2005. We have had 18 years to make informed risk-benefit analyses.
People are obsessed with the risk for pancreatitis. Any type of weight loss can cause gallstones, and this is what can trigger pancreatitis. Unless you’re the type of person who worries that your balanced Weight Watchers diet is going to cause pancreatitis, you should probably remove this risk from your calculations.
Glucagonlike peptide–1 (GLP-1) receptor agonists are naturally occurring gut hormones that reduce inflammatory cascades and clotting risk. We are not giving a dangerous treatment (e.g., fen-phen) that increases cardiovascular risk – quite the contrary, in fact.
Just because influencers are promoting a product doesn’t mean the product is inherently worthless. One of my patients accused me of prescribing a medication that is the “laughingstock of America.” Try telling that to the scores of cardiologists who send patients to my colleagues and me to start Ozempic to help lower their patients’ risk for stroke and heart attack. Or tell this to my patient who survived an episode of rapid atrial fibrillation and was told by his cardiologist that he definitely would have died if he had not lost 30 pounds from Ozempic in the preceding year.
Sometimes it seems like society has become more judgmental about Ozempic than about plastic surgery for weight loss. If we have to choose between liposuction (which doesn’t reduce visceral fat – the dangerous type of fat) or Ozempic, the latter clearly wins because of its real health benefits.
How does it make any sense to say that this medication should be reserved for patients who already have obesity and type 2 diabetes? Why should we penalize patients who have not yet reached those thresholds by denying access to preventive care? Don’t we constantly hear about how our health care system would be much more efficient if we focused on preventive care and not just treatment?
Some people claim that we have to limit access to this medication because of drug shortages. Thankfully, the United States responds to supply and demand economics and will quickly adjust.
I’ve had more patients than I can possibly number with severe binge eating disorders (resistant to years of therapy and medication) who finally developed healthy relationships with food while taking these types of medications. Mounjaro, I’m talking about you…
I always hear the argument that it is immoral to give these medications to patients with a history of restrictive eating patterns. Although every patient needs to be carefully evaluated, often these medications remove food as both the enemy and primary focus of every waking thought. They allow patients to refocus on other aspects of their lives – such as family, friends, hobbies, work – and regain a sense of purpose. If anyone wants to run a trial on this little hypothesis of mine, please reach out to me.
Okay, I agree you might get a little constipated (most often described by patients as the “rabbit pellet phenomenon”), but it’s a small price to pay, no? I’ll throw in a few prunes with the prescription.
Suffice it to say, I did give my 40-something-year-old patient the medication she desired, and she has a new lease on life (as well as better blood pressure and cholesterol).
A version of this article first appeared on Medscape.com.
Human frailty is a cash cow
Doctor, if you are caring for patients with diabetes, I sure hope you know more about it than I do. The longer I live, it seems, the less I understand.
In a free society, people can do what they want, and that’s great except when it isn’t. That’s why societies develop ethics and even public laws if ethics are not strong enough to protect us from ourselves and others.
Sugar, sugar
When I was growing up in small-town Alabama during the Depression and World War II, we called it sugar diabetes. Eat too much sugar, you got fat; your blood sugar went up, and you spilled sugar into your urine. Diabetes was fairly rare, and so was obesity. Doctors treated it by limiting the intake of sugar (and various sweet foods), along with attempting weight loss. If that didn’t do the trick, insulin injections.
From then until now, note these trends.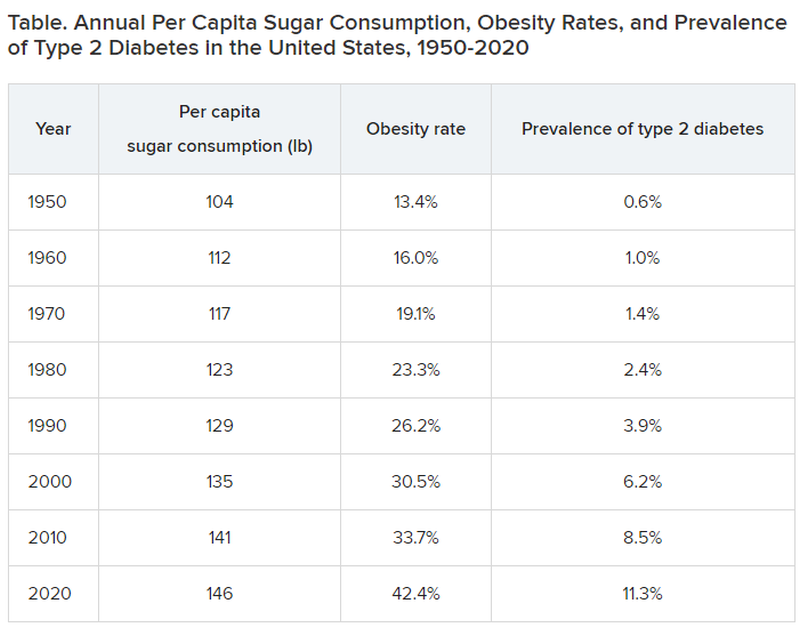
Type 2 diabetes was diagnosed even more infrequently before 1950:
- 1920: 0.2% of the population
- 1930: 0.3% of the population
- 1940: 0.4% of the population
In 2020, although 11.3% of the population was diagnosed with type 2 diabetes, the unknown undiagnosed proportion could be much higher.
Notice a correlation between sugar consumption and prevalence of diabetes? Of course, correlation is not causation, but at the same time, it sure as hell is not negation. Such concordance can be considered hypothesis generating. It may not be true causation, but it’s a good bet when 89% of people with diabetes have overweight or obesity.
What did the entire medical, public health, government, agriculture, nursing, food manufacturing, marketing, advertising, restaurant, and education constituencies do about this as it was happening? They observed, documented, gave lip service, and wrung their hands in public a bit. I do not believe that this is an organized active conspiracy; it would take too many players cooperating over too long a period of time. But it certainly may be a passive conspiracy, and primary care physicians and their patients are trapped.
The proper daily practice of medicine consists of one patient, one physician, one moment, and one decision. Let it be a shared decision, informed by the best evidence and taking cost into consideration. That encounter represents an opportunity, a responsibility, and a conundrum.
Individual health is subsumed under the collective health of the public. As such, a patient’s health is out of the control of both physician and patient; instead, patients are the beneficiaries or victims of the “marketplace.” Humans are frail and easily taken advantage of by the brilliant and highly motivated strategic planning and execution of Big Agriculture, Big Food, Big Pharma, Big Marketing, and Big Money-Driven Medicine and generally failed by Big Government, Big Public Health, Big Education, Big Psychology, and Big Religion.
Rethinking diabetes
Consider diabetes as one of many examples. What a terrific deal for capitalism. then it discovers (invents) long-term, very expensive, compelling treatments to slim us down, with no end in sight, and still without ever understanding the true nature of diabetes.
Gary Taubes’s great new book, “Rethinking Diabetes: What Science Reveals About Diet, Insulin, and Successful Treatments,” is being published by Alfred A. Knopf in early 2024.
It is 404 pages of (dense) text, with 401 numbered references and footnotes, a bibliography of 790 references, alphabetically arranged for easy cross-checking, and a 25-page index.
Remember Mr. Taubes’s earlier definitive historical treatises: “Good Calories, Bad Calories” (2007), “Why We Get Fat” (2010), “The Case Against Sugar” (2016), and “The Case for Keto” (2020)?
This new book is more like “Good Calories, Bad Calories”: long, dense, detailed, definitive, and of great historical reference value, including original research information from other countries in other languages. The author told me that the many early research reference sources were available only in German and that his use of generative artificial intelligence as an assistant researcher was of great value.
Nonphysician author Mr. Taubes uses his deep understanding of science and history to inform his long-honed talents of impartial investigative journalism as he attempts to understand and then explain why after all these years, the medical scientific community still does not have a sound consensus about the essence of diabetes, diet, insulin, and proper prevention and treatment at a level that is actually effective – amazing and so sad.
To signal these evolved and evolving conflicts, the book includes the following chapters:
- “Rise of the Carbohydrate-Rich and Very-Low-Carbohydrate Diets”
- “The Fear of Fat and High-Fat Diets”
- “Insulin and The End of Carbohydrate Restriction and Low Blood Sugar”
Yes, it is difficult. Imagine the bookend segments: “The Nature of Medical Knowledge” and “The Conflicts of Evidence-Based Medicine.” There is also a detailed discussion of good versus bad science spanning three long chapters.
If all that reads like a greatly confused mess to you then you’re beginning to understand. If you are a fan of an unbiased explication of the evolution of understanding the ins and outs of scientific history in richly documented detail, this is a book for you. It’s not a quick nor easy read. And don’t expect to discover whether the newest wonder drugs for weight loss and control of diabetes will be the long-term solution for people with obesity and diabetes worldwide.
Obesity and overweight are major risk factors for type 2 diabetes. About 90% of patients with diabetes have either overweight or obesity. Thus, the complications of these two conditions, which largely overlap, include atherosclerotic cardiovascular disease; myocardial infarction; stroke; hypertension; metabolic syndrome; lower-extremity gangrene; chronic kidney disease; retinopathy; glaucoma; cataracts; disabling osteoarthritis; breast, endometrial, colon, and other cancers; fatty liver; sleep apnea; and peripheral neuropathy. These diseases create a major lucrative business for a wide swathe of medical and surgical specialties, plus hospital, clinic, device, pharmaceutical, and food industries.
In summary, we’ve just been through 40 years of failure to recognize the sugar-elephant in the room and intervene with serious preventive efforts. Forty years of fleshing out both the populace and the American medical-industrial complex (AMIC). Talk about a sweet spot. The only successful long-term treatment of obesity (and with it, diabetes) is prevention. Don’t emphasize losing weight. Focus on preventing excessive weight gain, right now, for the population, beginning with yourselves. Otherwise, we continue openly to perpetuate a terrific deal for the AMIC, a travesty for everyone else. Time for some industrial grade penance and a course correction.
Meanwhile, here we are living out Big Pharma’s dream of a big populace, produced by the agriculture and food industries, enjoyed by capitalism after failures of education, medicine, and public health: a seemingly endless supply of people living with big complications who are ready for big (expensive, new) medications to fix the world’s big health problems.
Dr. Lundberg is editor in chief, Cancer Commons. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Doctor, if you are caring for patients with diabetes, I sure hope you know more about it than I do. The longer I live, it seems, the less I understand.
In a free society, people can do what they want, and that’s great except when it isn’t. That’s why societies develop ethics and even public laws if ethics are not strong enough to protect us from ourselves and others.
Sugar, sugar
When I was growing up in small-town Alabama during the Depression and World War II, we called it sugar diabetes. Eat too much sugar, you got fat; your blood sugar went up, and you spilled sugar into your urine. Diabetes was fairly rare, and so was obesity. Doctors treated it by limiting the intake of sugar (and various sweet foods), along with attempting weight loss. If that didn’t do the trick, insulin injections.
From then until now, note these trends.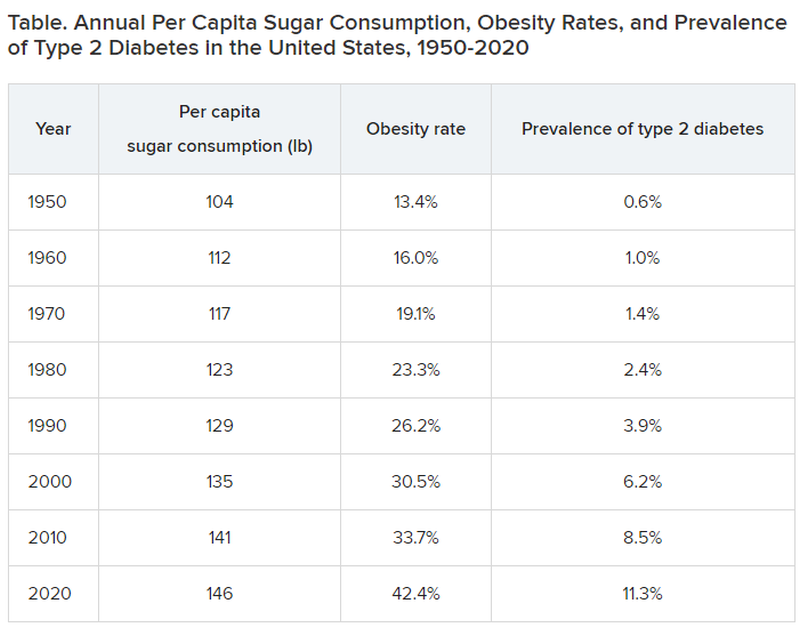
Type 2 diabetes was diagnosed even more infrequently before 1950:
- 1920: 0.2% of the population
- 1930: 0.3% of the population
- 1940: 0.4% of the population
In 2020, although 11.3% of the population was diagnosed with type 2 diabetes, the unknown undiagnosed proportion could be much higher.
Notice a correlation between sugar consumption and prevalence of diabetes? Of course, correlation is not causation, but at the same time, it sure as hell is not negation. Such concordance can be considered hypothesis generating. It may not be true causation, but it’s a good bet when 89% of people with diabetes have overweight or obesity.
What did the entire medical, public health, government, agriculture, nursing, food manufacturing, marketing, advertising, restaurant, and education constituencies do about this as it was happening? They observed, documented, gave lip service, and wrung their hands in public a bit. I do not believe that this is an organized active conspiracy; it would take too many players cooperating over too long a period of time. But it certainly may be a passive conspiracy, and primary care physicians and their patients are trapped.
The proper daily practice of medicine consists of one patient, one physician, one moment, and one decision. Let it be a shared decision, informed by the best evidence and taking cost into consideration. That encounter represents an opportunity, a responsibility, and a conundrum.
Individual health is subsumed under the collective health of the public. As such, a patient’s health is out of the control of both physician and patient; instead, patients are the beneficiaries or victims of the “marketplace.” Humans are frail and easily taken advantage of by the brilliant and highly motivated strategic planning and execution of Big Agriculture, Big Food, Big Pharma, Big Marketing, and Big Money-Driven Medicine and generally failed by Big Government, Big Public Health, Big Education, Big Psychology, and Big Religion.
Rethinking diabetes
Consider diabetes as one of many examples. What a terrific deal for capitalism. then it discovers (invents) long-term, very expensive, compelling treatments to slim us down, with no end in sight, and still without ever understanding the true nature of diabetes.
Gary Taubes’s great new book, “Rethinking Diabetes: What Science Reveals About Diet, Insulin, and Successful Treatments,” is being published by Alfred A. Knopf in early 2024.
It is 404 pages of (dense) text, with 401 numbered references and footnotes, a bibliography of 790 references, alphabetically arranged for easy cross-checking, and a 25-page index.
Remember Mr. Taubes’s earlier definitive historical treatises: “Good Calories, Bad Calories” (2007), “Why We Get Fat” (2010), “The Case Against Sugar” (2016), and “The Case for Keto” (2020)?
This new book is more like “Good Calories, Bad Calories”: long, dense, detailed, definitive, and of great historical reference value, including original research information from other countries in other languages. The author told me that the many early research reference sources were available only in German and that his use of generative artificial intelligence as an assistant researcher was of great value.
Nonphysician author Mr. Taubes uses his deep understanding of science and history to inform his long-honed talents of impartial investigative journalism as he attempts to understand and then explain why after all these years, the medical scientific community still does not have a sound consensus about the essence of diabetes, diet, insulin, and proper prevention and treatment at a level that is actually effective – amazing and so sad.
To signal these evolved and evolving conflicts, the book includes the following chapters:
- “Rise of the Carbohydrate-Rich and Very-Low-Carbohydrate Diets”
- “The Fear of Fat and High-Fat Diets”
- “Insulin and The End of Carbohydrate Restriction and Low Blood Sugar”
Yes, it is difficult. Imagine the bookend segments: “The Nature of Medical Knowledge” and “The Conflicts of Evidence-Based Medicine.” There is also a detailed discussion of good versus bad science spanning three long chapters.
If all that reads like a greatly confused mess to you then you’re beginning to understand. If you are a fan of an unbiased explication of the evolution of understanding the ins and outs of scientific history in richly documented detail, this is a book for you. It’s not a quick nor easy read. And don’t expect to discover whether the newest wonder drugs for weight loss and control of diabetes will be the long-term solution for people with obesity and diabetes worldwide.
Obesity and overweight are major risk factors for type 2 diabetes. About 90% of patients with diabetes have either overweight or obesity. Thus, the complications of these two conditions, which largely overlap, include atherosclerotic cardiovascular disease; myocardial infarction; stroke; hypertension; metabolic syndrome; lower-extremity gangrene; chronic kidney disease; retinopathy; glaucoma; cataracts; disabling osteoarthritis; breast, endometrial, colon, and other cancers; fatty liver; sleep apnea; and peripheral neuropathy. These diseases create a major lucrative business for a wide swathe of medical and surgical specialties, plus hospital, clinic, device, pharmaceutical, and food industries.
In summary, we’ve just been through 40 years of failure to recognize the sugar-elephant in the room and intervene with serious preventive efforts. Forty years of fleshing out both the populace and the American medical-industrial complex (AMIC). Talk about a sweet spot. The only successful long-term treatment of obesity (and with it, diabetes) is prevention. Don’t emphasize losing weight. Focus on preventing excessive weight gain, right now, for the population, beginning with yourselves. Otherwise, we continue openly to perpetuate a terrific deal for the AMIC, a travesty for everyone else. Time for some industrial grade penance and a course correction.
Meanwhile, here we are living out Big Pharma’s dream of a big populace, produced by the agriculture and food industries, enjoyed by capitalism after failures of education, medicine, and public health: a seemingly endless supply of people living with big complications who are ready for big (expensive, new) medications to fix the world’s big health problems.
Dr. Lundberg is editor in chief, Cancer Commons. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Doctor, if you are caring for patients with diabetes, I sure hope you know more about it than I do. The longer I live, it seems, the less I understand.
In a free society, people can do what they want, and that’s great except when it isn’t. That’s why societies develop ethics and even public laws if ethics are not strong enough to protect us from ourselves and others.
Sugar, sugar
When I was growing up in small-town Alabama during the Depression and World War II, we called it sugar diabetes. Eat too much sugar, you got fat; your blood sugar went up, and you spilled sugar into your urine. Diabetes was fairly rare, and so was obesity. Doctors treated it by limiting the intake of sugar (and various sweet foods), along with attempting weight loss. If that didn’t do the trick, insulin injections.
From then until now, note these trends.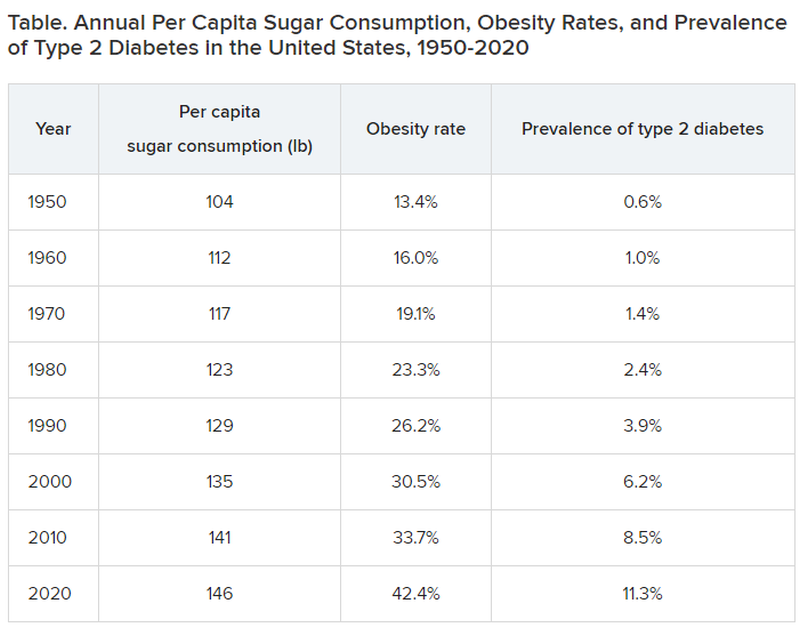
Type 2 diabetes was diagnosed even more infrequently before 1950:
- 1920: 0.2% of the population
- 1930: 0.3% of the population
- 1940: 0.4% of the population
In 2020, although 11.3% of the population was diagnosed with type 2 diabetes, the unknown undiagnosed proportion could be much higher.
Notice a correlation between sugar consumption and prevalence of diabetes? Of course, correlation is not causation, but at the same time, it sure as hell is not negation. Such concordance can be considered hypothesis generating. It may not be true causation, but it’s a good bet when 89% of people with diabetes have overweight or obesity.
What did the entire medical, public health, government, agriculture, nursing, food manufacturing, marketing, advertising, restaurant, and education constituencies do about this as it was happening? They observed, documented, gave lip service, and wrung their hands in public a bit. I do not believe that this is an organized active conspiracy; it would take too many players cooperating over too long a period of time. But it certainly may be a passive conspiracy, and primary care physicians and their patients are trapped.
The proper daily practice of medicine consists of one patient, one physician, one moment, and one decision. Let it be a shared decision, informed by the best evidence and taking cost into consideration. That encounter represents an opportunity, a responsibility, and a conundrum.
Individual health is subsumed under the collective health of the public. As such, a patient’s health is out of the control of both physician and patient; instead, patients are the beneficiaries or victims of the “marketplace.” Humans are frail and easily taken advantage of by the brilliant and highly motivated strategic planning and execution of Big Agriculture, Big Food, Big Pharma, Big Marketing, and Big Money-Driven Medicine and generally failed by Big Government, Big Public Health, Big Education, Big Psychology, and Big Religion.
Rethinking diabetes
Consider diabetes as one of many examples. What a terrific deal for capitalism. then it discovers (invents) long-term, very expensive, compelling treatments to slim us down, with no end in sight, and still without ever understanding the true nature of diabetes.
Gary Taubes’s great new book, “Rethinking Diabetes: What Science Reveals About Diet, Insulin, and Successful Treatments,” is being published by Alfred A. Knopf in early 2024.
It is 404 pages of (dense) text, with 401 numbered references and footnotes, a bibliography of 790 references, alphabetically arranged for easy cross-checking, and a 25-page index.
Remember Mr. Taubes’s earlier definitive historical treatises: “Good Calories, Bad Calories” (2007), “Why We Get Fat” (2010), “The Case Against Sugar” (2016), and “The Case for Keto” (2020)?
This new book is more like “Good Calories, Bad Calories”: long, dense, detailed, definitive, and of great historical reference value, including original research information from other countries in other languages. The author told me that the many early research reference sources were available only in German and that his use of generative artificial intelligence as an assistant researcher was of great value.
Nonphysician author Mr. Taubes uses his deep understanding of science and history to inform his long-honed talents of impartial investigative journalism as he attempts to understand and then explain why after all these years, the medical scientific community still does not have a sound consensus about the essence of diabetes, diet, insulin, and proper prevention and treatment at a level that is actually effective – amazing and so sad.
To signal these evolved and evolving conflicts, the book includes the following chapters:
- “Rise of the Carbohydrate-Rich and Very-Low-Carbohydrate Diets”
- “The Fear of Fat and High-Fat Diets”
- “Insulin and The End of Carbohydrate Restriction and Low Blood Sugar”
Yes, it is difficult. Imagine the bookend segments: “The Nature of Medical Knowledge” and “The Conflicts of Evidence-Based Medicine.” There is also a detailed discussion of good versus bad science spanning three long chapters.
If all that reads like a greatly confused mess to you then you’re beginning to understand. If you are a fan of an unbiased explication of the evolution of understanding the ins and outs of scientific history in richly documented detail, this is a book for you. It’s not a quick nor easy read. And don’t expect to discover whether the newest wonder drugs for weight loss and control of diabetes will be the long-term solution for people with obesity and diabetes worldwide.
Obesity and overweight are major risk factors for type 2 diabetes. About 90% of patients with diabetes have either overweight or obesity. Thus, the complications of these two conditions, which largely overlap, include atherosclerotic cardiovascular disease; myocardial infarction; stroke; hypertension; metabolic syndrome; lower-extremity gangrene; chronic kidney disease; retinopathy; glaucoma; cataracts; disabling osteoarthritis; breast, endometrial, colon, and other cancers; fatty liver; sleep apnea; and peripheral neuropathy. These diseases create a major lucrative business for a wide swathe of medical and surgical specialties, plus hospital, clinic, device, pharmaceutical, and food industries.
In summary, we’ve just been through 40 years of failure to recognize the sugar-elephant in the room and intervene with serious preventive efforts. Forty years of fleshing out both the populace and the American medical-industrial complex (AMIC). Talk about a sweet spot. The only successful long-term treatment of obesity (and with it, diabetes) is prevention. Don’t emphasize losing weight. Focus on preventing excessive weight gain, right now, for the population, beginning with yourselves. Otherwise, we continue openly to perpetuate a terrific deal for the AMIC, a travesty for everyone else. Time for some industrial grade penance and a course correction.
Meanwhile, here we are living out Big Pharma’s dream of a big populace, produced by the agriculture and food industries, enjoyed by capitalism after failures of education, medicine, and public health: a seemingly endless supply of people living with big complications who are ready for big (expensive, new) medications to fix the world’s big health problems.
Dr. Lundberg is editor in chief, Cancer Commons. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Long COVID leads to greater health risks, research finds
That is the finding of a new study from Washington University in St. Louis. The school distributed a press release about the study, which was published in the journal Nature Medicine.
“Some estimates show more than 90% of the U.S. population has been infected with COVID-19,” Ziyad Al-Aly, chief of research and development at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University, told the St. Louis Post–Dispatch. “Doctors need to realize that their patients could be at risk of these conditions, be it heart disease or lung problems or brain problems – they’re at risk.”
The researchers compared the health records for 138,000 patients who had been infected with those of 6 million who had not. They followed 80 health conditions associated with long COVID for 2 years. They used unnamed records from the VA.
“There was really nothing at all looking at what happens to people at two years after the infection,” Dr. Al-Aly said. “So we decided to take a look.”
Patients who hadn’t been hospitalized within 30 days of infection had a higher risk of death 6 months after recovery, and a higher risk of hospitalization within 18 months. They had higher risk of diabetes, fatigue, joint pain, and other problems compared with people who had not been infected.
“In the nonhospitalized group, risks remained elevated for several problems, for several organ systems,” Dr. Al-Aly said. “For the people who were hospitalized, the risk was ubiquitous across all organ systems. It really spans the gamut with respect to the organ systems that are affected.”
People who had been hospitalized had a 65% greater risk of illnesses after 2 years. Nonhospitalized patients had just a 35% greater risk.
A version of this article first appeared on WebMD.com.
That is the finding of a new study from Washington University in St. Louis. The school distributed a press release about the study, which was published in the journal Nature Medicine.
“Some estimates show more than 90% of the U.S. population has been infected with COVID-19,” Ziyad Al-Aly, chief of research and development at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University, told the St. Louis Post–Dispatch. “Doctors need to realize that their patients could be at risk of these conditions, be it heart disease or lung problems or brain problems – they’re at risk.”
The researchers compared the health records for 138,000 patients who had been infected with those of 6 million who had not. They followed 80 health conditions associated with long COVID for 2 years. They used unnamed records from the VA.
“There was really nothing at all looking at what happens to people at two years after the infection,” Dr. Al-Aly said. “So we decided to take a look.”
Patients who hadn’t been hospitalized within 30 days of infection had a higher risk of death 6 months after recovery, and a higher risk of hospitalization within 18 months. They had higher risk of diabetes, fatigue, joint pain, and other problems compared with people who had not been infected.
“In the nonhospitalized group, risks remained elevated for several problems, for several organ systems,” Dr. Al-Aly said. “For the people who were hospitalized, the risk was ubiquitous across all organ systems. It really spans the gamut with respect to the organ systems that are affected.”
People who had been hospitalized had a 65% greater risk of illnesses after 2 years. Nonhospitalized patients had just a 35% greater risk.
A version of this article first appeared on WebMD.com.
That is the finding of a new study from Washington University in St. Louis. The school distributed a press release about the study, which was published in the journal Nature Medicine.
“Some estimates show more than 90% of the U.S. population has been infected with COVID-19,” Ziyad Al-Aly, chief of research and development at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University, told the St. Louis Post–Dispatch. “Doctors need to realize that their patients could be at risk of these conditions, be it heart disease or lung problems or brain problems – they’re at risk.”
The researchers compared the health records for 138,000 patients who had been infected with those of 6 million who had not. They followed 80 health conditions associated with long COVID for 2 years. They used unnamed records from the VA.
“There was really nothing at all looking at what happens to people at two years after the infection,” Dr. Al-Aly said. “So we decided to take a look.”
Patients who hadn’t been hospitalized within 30 days of infection had a higher risk of death 6 months after recovery, and a higher risk of hospitalization within 18 months. They had higher risk of diabetes, fatigue, joint pain, and other problems compared with people who had not been infected.
“In the nonhospitalized group, risks remained elevated for several problems, for several organ systems,” Dr. Al-Aly said. “For the people who were hospitalized, the risk was ubiquitous across all organ systems. It really spans the gamut with respect to the organ systems that are affected.”
People who had been hospitalized had a 65% greater risk of illnesses after 2 years. Nonhospitalized patients had just a 35% greater risk.
A version of this article first appeared on WebMD.com.
FROM NATURE MEDICINE




