User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Underprescribed menopause relief: Women suffer needlessly
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
Five ways to avert a malpractice lawsuit with better EHR techniques
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Low-dose aspirin cuts type 2 diabetes risk in over-65s
The data come from a secondary analysis of ASPREE, a double-blind, placebo-controlled trial of healthy adults aged 65 years or older, showing that 100 mg of aspirin taken daily for about 5 years did not provide a cardiovascular benefit but did significantly raise the risk for bleeding.
This new analysis shows that individuals taking aspirin had a 15% lower risk for developing type 2 diabetes and that the medication slowed the rate of increase in fasting plasma glucose, compared with placebo, during follow-up.
However, lead author Sophia Zoungas, MBBS, PhD, head of the School of Public Health and Preventive Medicine, Monash University, Melbourne, said: “Major prescribing guidelines now recommend older adults take daily aspirin only when there is a medical reason to do so, such as after a heart attack. ... Although these new findings are of interest, they do not change the clinical advice about aspirin use in older people at this time.”
Nonetheless, she said in an interview, “at this time, our findings are exploratory but ignite the debate of the important role that anti-inflammatory approaches may play in preventing diabetes. Further work is currently underway to understand which subpopulations may be better targeted and to understand the balance of risk versus benefit.”
The results are scheduled to be presented at the upcoming meeting of the European Association for the Study of Diabetes, taking place Oct. 2-6 in Hamburg, Germany.
New findings not robust enough to change current practice
Asked to comment, Debabrata Mukherjee, MD, said: “Given the post hoc secondary nature of the analysis, the findings should be considered hypothesis generating and not definitive… At this time, based on prospective randomized studies, the risks of aspirin outweigh the benefits for aspirin in older adults.”
Among those studies was an ASPREE substudy showing failure of low-dose aspirin to reduce fracture risk while increasing the risk for serious falls, and two other trials, ARRIVE and ASCEND, also showing that harms of aspirin outweigh the benefits in people with cardiovascular risk but not diabetes, and in those with diabetes, respectively, said Dr. Mukherjee, professor and chair of the department of internal medicine at Texas Tech University Health Sciences Center at El Paso.
And, Mukherjee noted, in 2019 the American College of Cardiology updated its practice guidelines to say that low-dose aspirin should not be administered on a routine basis for the primary prevention of atherosclerotic cardiovascular disease in adults over age 70. In 2021, the American Diabetes Association seconded that recommendation.
Asked whether these newest findings might change current practice for any higher-risk subgroup, such as people with prediabetes, Dr. Mukherjee replied: “Unless there is a prospective randomized trial that validates these findings in those with prediabetes, the findings should not change practice. There are also no data [showing] that another antiplatelet agent would be indicated or would be beneficial. Instead, I would recommend lifestyle changes including regular exercise and a healthy diet to minimize risk of diabetes.”
The 16,209 ASPREE participants were community dwelling and did not have diabetes, cardiovascular disease, or dementia at baseline. They were randomized in a 1:1 ratio to receive 100 mg/d of enteric-coated aspirin or placebo. Over a median follow-up of 4.7 years, the proportions developing type 2 diabetes were 5.7% with aspirin versus 6.6% with placebo (hazard ratio, 0.85; P = .01).
The annual rate of increase in fasting plasma glucose over the follow-up period was slowed by 0.006 mmol/L with aspirin, compared with placebo, also a significant difference (P = .004).
According to Dr. Zoungas, “the potential for anti-inflammatory agents like aspirin to prevent type 2 diabetes or improve glucose levels needs further study.”
The ASPREE trial was supported by the U.S. National Institutes of Health, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Dr. Zoungas and Dr. Mukherjee have no disclosures.
A version of this article first appeared on Medscape.com.
The data come from a secondary analysis of ASPREE, a double-blind, placebo-controlled trial of healthy adults aged 65 years or older, showing that 100 mg of aspirin taken daily for about 5 years did not provide a cardiovascular benefit but did significantly raise the risk for bleeding.
This new analysis shows that individuals taking aspirin had a 15% lower risk for developing type 2 diabetes and that the medication slowed the rate of increase in fasting plasma glucose, compared with placebo, during follow-up.
However, lead author Sophia Zoungas, MBBS, PhD, head of the School of Public Health and Preventive Medicine, Monash University, Melbourne, said: “Major prescribing guidelines now recommend older adults take daily aspirin only when there is a medical reason to do so, such as after a heart attack. ... Although these new findings are of interest, they do not change the clinical advice about aspirin use in older people at this time.”
Nonetheless, she said in an interview, “at this time, our findings are exploratory but ignite the debate of the important role that anti-inflammatory approaches may play in preventing diabetes. Further work is currently underway to understand which subpopulations may be better targeted and to understand the balance of risk versus benefit.”
The results are scheduled to be presented at the upcoming meeting of the European Association for the Study of Diabetes, taking place Oct. 2-6 in Hamburg, Germany.
New findings not robust enough to change current practice
Asked to comment, Debabrata Mukherjee, MD, said: “Given the post hoc secondary nature of the analysis, the findings should be considered hypothesis generating and not definitive… At this time, based on prospective randomized studies, the risks of aspirin outweigh the benefits for aspirin in older adults.”
Among those studies was an ASPREE substudy showing failure of low-dose aspirin to reduce fracture risk while increasing the risk for serious falls, and two other trials, ARRIVE and ASCEND, also showing that harms of aspirin outweigh the benefits in people with cardiovascular risk but not diabetes, and in those with diabetes, respectively, said Dr. Mukherjee, professor and chair of the department of internal medicine at Texas Tech University Health Sciences Center at El Paso.
And, Mukherjee noted, in 2019 the American College of Cardiology updated its practice guidelines to say that low-dose aspirin should not be administered on a routine basis for the primary prevention of atherosclerotic cardiovascular disease in adults over age 70. In 2021, the American Diabetes Association seconded that recommendation.
Asked whether these newest findings might change current practice for any higher-risk subgroup, such as people with prediabetes, Dr. Mukherjee replied: “Unless there is a prospective randomized trial that validates these findings in those with prediabetes, the findings should not change practice. There are also no data [showing] that another antiplatelet agent would be indicated or would be beneficial. Instead, I would recommend lifestyle changes including regular exercise and a healthy diet to minimize risk of diabetes.”
The 16,209 ASPREE participants were community dwelling and did not have diabetes, cardiovascular disease, or dementia at baseline. They were randomized in a 1:1 ratio to receive 100 mg/d of enteric-coated aspirin or placebo. Over a median follow-up of 4.7 years, the proportions developing type 2 diabetes were 5.7% with aspirin versus 6.6% with placebo (hazard ratio, 0.85; P = .01).
The annual rate of increase in fasting plasma glucose over the follow-up period was slowed by 0.006 mmol/L with aspirin, compared with placebo, also a significant difference (P = .004).
According to Dr. Zoungas, “the potential for anti-inflammatory agents like aspirin to prevent type 2 diabetes or improve glucose levels needs further study.”
The ASPREE trial was supported by the U.S. National Institutes of Health, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Dr. Zoungas and Dr. Mukherjee have no disclosures.
A version of this article first appeared on Medscape.com.
The data come from a secondary analysis of ASPREE, a double-blind, placebo-controlled trial of healthy adults aged 65 years or older, showing that 100 mg of aspirin taken daily for about 5 years did not provide a cardiovascular benefit but did significantly raise the risk for bleeding.
This new analysis shows that individuals taking aspirin had a 15% lower risk for developing type 2 diabetes and that the medication slowed the rate of increase in fasting plasma glucose, compared with placebo, during follow-up.
However, lead author Sophia Zoungas, MBBS, PhD, head of the School of Public Health and Preventive Medicine, Monash University, Melbourne, said: “Major prescribing guidelines now recommend older adults take daily aspirin only when there is a medical reason to do so, such as after a heart attack. ... Although these new findings are of interest, they do not change the clinical advice about aspirin use in older people at this time.”
Nonetheless, she said in an interview, “at this time, our findings are exploratory but ignite the debate of the important role that anti-inflammatory approaches may play in preventing diabetes. Further work is currently underway to understand which subpopulations may be better targeted and to understand the balance of risk versus benefit.”
The results are scheduled to be presented at the upcoming meeting of the European Association for the Study of Diabetes, taking place Oct. 2-6 in Hamburg, Germany.
New findings not robust enough to change current practice
Asked to comment, Debabrata Mukherjee, MD, said: “Given the post hoc secondary nature of the analysis, the findings should be considered hypothesis generating and not definitive… At this time, based on prospective randomized studies, the risks of aspirin outweigh the benefits for aspirin in older adults.”
Among those studies was an ASPREE substudy showing failure of low-dose aspirin to reduce fracture risk while increasing the risk for serious falls, and two other trials, ARRIVE and ASCEND, also showing that harms of aspirin outweigh the benefits in people with cardiovascular risk but not diabetes, and in those with diabetes, respectively, said Dr. Mukherjee, professor and chair of the department of internal medicine at Texas Tech University Health Sciences Center at El Paso.
And, Mukherjee noted, in 2019 the American College of Cardiology updated its practice guidelines to say that low-dose aspirin should not be administered on a routine basis for the primary prevention of atherosclerotic cardiovascular disease in adults over age 70. In 2021, the American Diabetes Association seconded that recommendation.
Asked whether these newest findings might change current practice for any higher-risk subgroup, such as people with prediabetes, Dr. Mukherjee replied: “Unless there is a prospective randomized trial that validates these findings in those with prediabetes, the findings should not change practice. There are also no data [showing] that another antiplatelet agent would be indicated or would be beneficial. Instead, I would recommend lifestyle changes including regular exercise and a healthy diet to minimize risk of diabetes.”
The 16,209 ASPREE participants were community dwelling and did not have diabetes, cardiovascular disease, or dementia at baseline. They were randomized in a 1:1 ratio to receive 100 mg/d of enteric-coated aspirin or placebo. Over a median follow-up of 4.7 years, the proportions developing type 2 diabetes were 5.7% with aspirin versus 6.6% with placebo (hazard ratio, 0.85; P = .01).
The annual rate of increase in fasting plasma glucose over the follow-up period was slowed by 0.006 mmol/L with aspirin, compared with placebo, also a significant difference (P = .004).
According to Dr. Zoungas, “the potential for anti-inflammatory agents like aspirin to prevent type 2 diabetes or improve glucose levels needs further study.”
The ASPREE trial was supported by the U.S. National Institutes of Health, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Dr. Zoungas and Dr. Mukherjee have no disclosures.
A version of this article first appeared on Medscape.com.
FROM EASD 2023
Domestic violence in health care is real and underreported
To protect survivors’ identities, some names have been changed or shortened.
Natasha Abadilla, MD, met the man who would become her abuser while working abroad for a public health nonprofit. When he began emotionally and physically abusing her, she did everything she could to hide it.
“My coworkers knew nothing of the abuse. I became an expert in applying makeup to hide the bruises,” recalls Dr. Abadilla, now a second-year resident and pediatric neurologist at Lucile Packard Children’s Hospital at Stanford.
Dr. Abadilla says she strongly identifies as a hard worker and – to this day – hopes her work did not falter despite her partner’s constant drain on her. But the impact of the abuse continued to affect her for years. Like many survivors of domestic violence, she struggled with PTSD and depression.
Health care workers are often the first point of contact for survivors of domestic violence. Experts and advocates continue to push for more training for clinicians to identify and respond to signs among their patients. Often missing from this conversation is the reality that those tasked with screening can also be victims of intimate partner violence themselves.
What’s more: The very strengths that medical professionals often pride themselves on – perfectionism, empathy, grit – can make it harder for them to identify abuse in their own relationships and push through humiliation and shame to seek help.
Dr. Abadilla is exceptional among survivors in the medical field. Rather than keep her experience quiet, she has shared it publicly.
Awareness, she believes, can save lives.
An understudied problem in an underserved group
The majority of research on health care workers in this area has focused on workplace violence, which 62% experience worldwide. But intimate partner violence remains understudied and underdiscussed. Some medical professionals are even saddled with a “double burden,” facing trauma at work and at home, note the authors of a 2022 meta-analysis published in the journal Trauma, Violence, & Abuse.
The problem has had dire consequences. In recent years, many health care workers have been killed by their abusers:
- In 2016, Casey M. Drawert, MD, a Texas-based critical care anesthesiologist, was fatally shot by her husband in a murder-suicide.
- In 2018, Tamara O’Neal, MD, an ER physician, and Dayna Less, a first-year pharmacy resident, were killed by Dr. O’Neal’s ex-fiancé at Mercy Hospital in Chicago.
- In 2019, Sarah Hawley, MD, a first-year University of Utah resident, was fatally shot by her boyfriend in a murder-suicide.
- In 2021, Moria Kinsey, a nurse practitioner in Tahlequah, Okla., was murdered by a physician.
- In July of 2023, Gwendolyn Lavonne Riddick, DO, an ob.gyn. in North Carolina, was fatally shot by the father of her 3-year-old son.
There are others.
In the wake of these tragedies, calls for health care workers to screen each other as well as patients have grown. But for an untold number of survivors, breaking the silence is still not possible due to concerns about their reputation, professional consequences, the threat of harassment from abusers who are often in the same field, a medical culture of selfless endurance, and a lack of appropriate resources.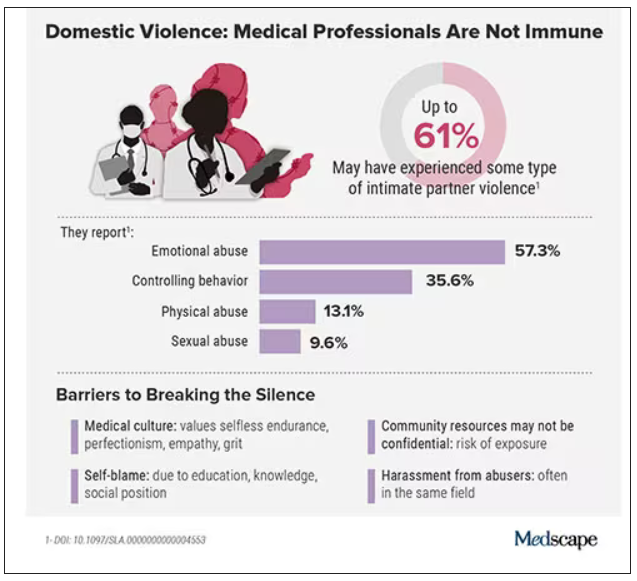
While the vast majority have stayed silent, those who have spoken out say there’s a need for targeted interventions to educate medical professionals as well as more supportive policies throughout the health care system.
Are health care workers more at risk?
Although more studies are needed, research indicates health care workers experience domestic violence at rates comparable to those of other populations, whereas some data suggest rates may be higher.
In the United States, more than one in three women and one in four men experience some form of intimate partner violence in their lifetime. Similarly, a 2020 study found that 24% of 400 physicians responding to a survey reported a history of domestic violence, with 15% reporting verbal abuse, 8% reporting physical violence, 4% reporting sexual abuse, and 4% reporting stalking.
Meanwhile, in an anonymous survey completed by 882 practicing surgeons and trainees in the United States from late 2018 to early 2019, more than 60% reported experiencing some type of intimate partner violence, most commonly emotional abuse.
Recent studies in the United Kingdom, Australia, and elsewhere show that significant numbers of medical professionals are fighting this battle. A 2019 study of more than 2,000 nurses, midwives, and health care assistants in the United Kingdom found that nurses were three times more likely to experience domestic violence than the average person.
What would help solve this problem: More study of health care worker-survivors as a unique group with unique risk factors. In general, domestic violence is most prevalent among women and people in marginalized groups. But young adults, such as medical students and trainees, can face an increased risk due to economic strain. Major life changes, such as relocating for residency, can also drive up stress and fray social connections, further isolating victims.
Why it’s so much harder for medical professionals to reveal abuse
For medical professionals accustomed to being strong and forging on, identifying as a victim of abuse can seem like a personal contradiction. It can feel easier to separate their personal and professional lives rather than face a complex reality.
In a personal essay on KevinMD.com, medical student Chloe N. L. Lee describes this emotional turmoil. “As an aspiring psychiatrist, I questioned my character judgment (how did I end up with a misogynistic abuser?) and wondered if I ought to have known better. I worried that my colleagues would deem me unfit to care for patients. And I thought that this was not supposed to happen to women like me,” Ms. Lee writes.
Kimberly, a licensed therapist, experienced a similar pattern of self-blame when her partner began exhibiting violent behavior. “For a long time, I felt guilty because I said to myself, You’re a therapist. You’re supposed to know this,” she recalls. At the same time, she felt driven to help him and sought couples therapy as his violence escalated.
Whitney, a pharmacist, recognized the “hallmarks” of abuse in her relationship, but she coped by compartmentalizing. Whitney says she was vulnerable to her abuser as a young college student who struggled financially. As he showered her with gifts, she found herself waving away red flags like aggressiveness or overprotectiveness.
After Whitney graduated, her partner’s emotional manipulation escalated into frequent physical assaults. When he gave her a black eye, she could not bring herself to go into work. She quit her job without notice. Despite a spotless record, none of her coworkers ever reached out to investigate her sudden departure.
It would take 8 years for Whitney to acknowledge the abuse and seize a moment to escape. She fled with just her purse and started over in a new city, rebuilding her life in the midst of harassment and threats from her ex. She says she’s grateful to be alive.
An imperfect system doesn’t help
Health care workers rarely ask for support or disclose abuse at work. Some have cited stigma, a lack of confidentiality (especially when the abuser is also in health care), fears about colleagues’ judgment, and a culture that doesn’t prioritize self-care.
Sometimes policies get in the way: In a 2021 qualitative study of interviews with 21 female physician-survivors in the United Kingdom, many said that despite the intense stress of abuse and recovery, they were unable to take any time off.
Of 180 UK-based midwife-survivors interviewed in a 2018 study, only 60 sought support at work and 30 received it. Many said their supervisors pressured them to report the abuse and get back to work, called social services behind their back, or reported them to their professional regulator. “I was treated like the perpetrator,” one said. Barbara Hernandez, PhD, a researcher who studies physician-survivors and director of physician vitality at Loma Linda University in southern California, says workplace violence and mistreatment from patients or colleagues – and a poor institutional response – can make those in health care feel like they have to “shut up and put up,” priming them to also tolerate abuse at home.
When survivors do reach out, there can be a disconnect between the resources they need and those they’re offered, Dr. Hernandez adds. In a recent survey of 400 physicians she conducted, respondents typically said they would advise a physician-survivor to “get to a shelter quickly.” But when roles were reversed, they admitted going to a shelter was the least feasible option. Support groups can also be problematic in smaller communities where physicians might be recognized or see their own patients.
Complicating matters further, the violence often comes from within the medical community. This can lead to particularly malicious abuse tactics like sending false accusations to a victim’s regulatory college or board; prolonged court and custody battles to drain them of all resources and their ability to hold a job; or even sabotage, harassment, or violence at work. The sheen of the abuser’s public persona, on the other hand, can guard them from any accountability.
For example, one physician-survivor said her ex-partner, a psychiatrist, coerced her into believing she was mentally ill, claimed she was “psychotic” in order to take back their children after she left, and had numerous colleagues serve as character witnesses in court for him, “saying he couldn’t have done any of these things, how great he is, and what a wonderful father he is.”
Slow progress is still progress
After Sherilyn M. Gordon-Burroughs, MD, a Texas-based transplant surgeon, mother, and educator, was killed by her husband in a murder-suicide in 2017, her friends Barbara Lee Bass, MD, president of the American College of Surgeons, and Patricia L. Turner, MD, were spurred into action. Together, they founded the ACS Intimate Partner Violence Task Force. Their mission is to educate surgeons to identify the signs of intimate partner violence (IPV) in themselves and their colleagues and connect them with resources.
“There is a concerted effort to close that gap,” says D’Andrea K. Joseph, MD, cochair of the task force and chief of trauma and acute care surgery at NYU Langone in New York. In the future, Dr. Joseph predicts, “making this a part of the curriculum, that it’s standardized for residents and trainees, that there is a safe place for victims ... and that we can band together and really recognize and assist our colleagues who are in trouble.”
Resources created by the ACS IPV task force, such as the toolkit and curriculum, provide a model for other health care leaders. But there have been few similar initiatives aimed at increasing IPV intervention within the medical system.
What you can do in your workplace
In her essay, Ms. Lee explains that a major turning point came when a physician friend explicitly asked if she was experiencing abuse. He then gently confirmed she was, and asked without judgment how he could support her, an approach that mirrors advice from the National Domestic Violence Hotline.
“Having a physician validate that this was, indeed, an abusive situation helped enormously ... I believe it may have saved my life,” she writes.
That validation can be crucial, and Dr. Abadilla urges other physicians to regularly check in with colleagues, especially those who seem particularly positive with a go-getter attitude and yet may not seem themselves. That was how she presented when she was struggling the most.
Supporting systemic changes within your organization and beyond is also important. The authors of the 2022 meta-analysis stress the need for domestic violence training, legislative changes, paid leave, and union support.
Finding strength in recovery
Over a decade after escaping her abuser, Whitney says she’s only just begun to share her experience, but what she’s learned has made her a better pharmacist. She says she’s more attuned to subtle signs something could be off with patients and coworkers. When someone makes comments about feeling anxious or that they can’t do anything right, it’s important to ask why, she says.
Recently, Kimberly has opened up to her mentor and other therapists, many of whom have shared that they’re also survivors.
“The last thing I said to [my abuser] is you think you’ve won and you’re hurting me, but what you’ve done to me – I’m going to utilize this and I’m going to help other people,” Kimberly says. “This pain that I have will go away, and I’m going to save the lives of others.”
A version of this article first appeared on Medscape.com.
To protect survivors’ identities, some names have been changed or shortened.
Natasha Abadilla, MD, met the man who would become her abuser while working abroad for a public health nonprofit. When he began emotionally and physically abusing her, she did everything she could to hide it.
“My coworkers knew nothing of the abuse. I became an expert in applying makeup to hide the bruises,” recalls Dr. Abadilla, now a second-year resident and pediatric neurologist at Lucile Packard Children’s Hospital at Stanford.
Dr. Abadilla says she strongly identifies as a hard worker and – to this day – hopes her work did not falter despite her partner’s constant drain on her. But the impact of the abuse continued to affect her for years. Like many survivors of domestic violence, she struggled with PTSD and depression.
Health care workers are often the first point of contact for survivors of domestic violence. Experts and advocates continue to push for more training for clinicians to identify and respond to signs among their patients. Often missing from this conversation is the reality that those tasked with screening can also be victims of intimate partner violence themselves.
What’s more: The very strengths that medical professionals often pride themselves on – perfectionism, empathy, grit – can make it harder for them to identify abuse in their own relationships and push through humiliation and shame to seek help.
Dr. Abadilla is exceptional among survivors in the medical field. Rather than keep her experience quiet, she has shared it publicly.
Awareness, she believes, can save lives.
An understudied problem in an underserved group
The majority of research on health care workers in this area has focused on workplace violence, which 62% experience worldwide. But intimate partner violence remains understudied and underdiscussed. Some medical professionals are even saddled with a “double burden,” facing trauma at work and at home, note the authors of a 2022 meta-analysis published in the journal Trauma, Violence, & Abuse.
The problem has had dire consequences. In recent years, many health care workers have been killed by their abusers:
- In 2016, Casey M. Drawert, MD, a Texas-based critical care anesthesiologist, was fatally shot by her husband in a murder-suicide.
- In 2018, Tamara O’Neal, MD, an ER physician, and Dayna Less, a first-year pharmacy resident, were killed by Dr. O’Neal’s ex-fiancé at Mercy Hospital in Chicago.
- In 2019, Sarah Hawley, MD, a first-year University of Utah resident, was fatally shot by her boyfriend in a murder-suicide.
- In 2021, Moria Kinsey, a nurse practitioner in Tahlequah, Okla., was murdered by a physician.
- In July of 2023, Gwendolyn Lavonne Riddick, DO, an ob.gyn. in North Carolina, was fatally shot by the father of her 3-year-old son.
There are others.
In the wake of these tragedies, calls for health care workers to screen each other as well as patients have grown. But for an untold number of survivors, breaking the silence is still not possible due to concerns about their reputation, professional consequences, the threat of harassment from abusers who are often in the same field, a medical culture of selfless endurance, and a lack of appropriate resources.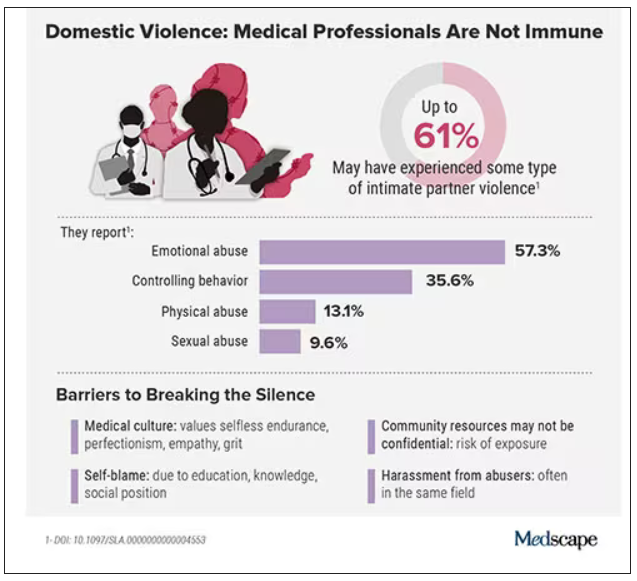
While the vast majority have stayed silent, those who have spoken out say there’s a need for targeted interventions to educate medical professionals as well as more supportive policies throughout the health care system.
Are health care workers more at risk?
Although more studies are needed, research indicates health care workers experience domestic violence at rates comparable to those of other populations, whereas some data suggest rates may be higher.
In the United States, more than one in three women and one in four men experience some form of intimate partner violence in their lifetime. Similarly, a 2020 study found that 24% of 400 physicians responding to a survey reported a history of domestic violence, with 15% reporting verbal abuse, 8% reporting physical violence, 4% reporting sexual abuse, and 4% reporting stalking.
Meanwhile, in an anonymous survey completed by 882 practicing surgeons and trainees in the United States from late 2018 to early 2019, more than 60% reported experiencing some type of intimate partner violence, most commonly emotional abuse.
Recent studies in the United Kingdom, Australia, and elsewhere show that significant numbers of medical professionals are fighting this battle. A 2019 study of more than 2,000 nurses, midwives, and health care assistants in the United Kingdom found that nurses were three times more likely to experience domestic violence than the average person.
What would help solve this problem: More study of health care worker-survivors as a unique group with unique risk factors. In general, domestic violence is most prevalent among women and people in marginalized groups. But young adults, such as medical students and trainees, can face an increased risk due to economic strain. Major life changes, such as relocating for residency, can also drive up stress and fray social connections, further isolating victims.
Why it’s so much harder for medical professionals to reveal abuse
For medical professionals accustomed to being strong and forging on, identifying as a victim of abuse can seem like a personal contradiction. It can feel easier to separate their personal and professional lives rather than face a complex reality.
In a personal essay on KevinMD.com, medical student Chloe N. L. Lee describes this emotional turmoil. “As an aspiring psychiatrist, I questioned my character judgment (how did I end up with a misogynistic abuser?) and wondered if I ought to have known better. I worried that my colleagues would deem me unfit to care for patients. And I thought that this was not supposed to happen to women like me,” Ms. Lee writes.
Kimberly, a licensed therapist, experienced a similar pattern of self-blame when her partner began exhibiting violent behavior. “For a long time, I felt guilty because I said to myself, You’re a therapist. You’re supposed to know this,” she recalls. At the same time, she felt driven to help him and sought couples therapy as his violence escalated.
Whitney, a pharmacist, recognized the “hallmarks” of abuse in her relationship, but she coped by compartmentalizing. Whitney says she was vulnerable to her abuser as a young college student who struggled financially. As he showered her with gifts, she found herself waving away red flags like aggressiveness or overprotectiveness.
After Whitney graduated, her partner’s emotional manipulation escalated into frequent physical assaults. When he gave her a black eye, she could not bring herself to go into work. She quit her job without notice. Despite a spotless record, none of her coworkers ever reached out to investigate her sudden departure.
It would take 8 years for Whitney to acknowledge the abuse and seize a moment to escape. She fled with just her purse and started over in a new city, rebuilding her life in the midst of harassment and threats from her ex. She says she’s grateful to be alive.
An imperfect system doesn’t help
Health care workers rarely ask for support or disclose abuse at work. Some have cited stigma, a lack of confidentiality (especially when the abuser is also in health care), fears about colleagues’ judgment, and a culture that doesn’t prioritize self-care.
Sometimes policies get in the way: In a 2021 qualitative study of interviews with 21 female physician-survivors in the United Kingdom, many said that despite the intense stress of abuse and recovery, they were unable to take any time off.
Of 180 UK-based midwife-survivors interviewed in a 2018 study, only 60 sought support at work and 30 received it. Many said their supervisors pressured them to report the abuse and get back to work, called social services behind their back, or reported them to their professional regulator. “I was treated like the perpetrator,” one said. Barbara Hernandez, PhD, a researcher who studies physician-survivors and director of physician vitality at Loma Linda University in southern California, says workplace violence and mistreatment from patients or colleagues – and a poor institutional response – can make those in health care feel like they have to “shut up and put up,” priming them to also tolerate abuse at home.
When survivors do reach out, there can be a disconnect between the resources they need and those they’re offered, Dr. Hernandez adds. In a recent survey of 400 physicians she conducted, respondents typically said they would advise a physician-survivor to “get to a shelter quickly.” But when roles were reversed, they admitted going to a shelter was the least feasible option. Support groups can also be problematic in smaller communities where physicians might be recognized or see their own patients.
Complicating matters further, the violence often comes from within the medical community. This can lead to particularly malicious abuse tactics like sending false accusations to a victim’s regulatory college or board; prolonged court and custody battles to drain them of all resources and their ability to hold a job; or even sabotage, harassment, or violence at work. The sheen of the abuser’s public persona, on the other hand, can guard them from any accountability.
For example, one physician-survivor said her ex-partner, a psychiatrist, coerced her into believing she was mentally ill, claimed she was “psychotic” in order to take back their children after she left, and had numerous colleagues serve as character witnesses in court for him, “saying he couldn’t have done any of these things, how great he is, and what a wonderful father he is.”
Slow progress is still progress
After Sherilyn M. Gordon-Burroughs, MD, a Texas-based transplant surgeon, mother, and educator, was killed by her husband in a murder-suicide in 2017, her friends Barbara Lee Bass, MD, president of the American College of Surgeons, and Patricia L. Turner, MD, were spurred into action. Together, they founded the ACS Intimate Partner Violence Task Force. Their mission is to educate surgeons to identify the signs of intimate partner violence (IPV) in themselves and their colleagues and connect them with resources.
“There is a concerted effort to close that gap,” says D’Andrea K. Joseph, MD, cochair of the task force and chief of trauma and acute care surgery at NYU Langone in New York. In the future, Dr. Joseph predicts, “making this a part of the curriculum, that it’s standardized for residents and trainees, that there is a safe place for victims ... and that we can band together and really recognize and assist our colleagues who are in trouble.”
Resources created by the ACS IPV task force, such as the toolkit and curriculum, provide a model for other health care leaders. But there have been few similar initiatives aimed at increasing IPV intervention within the medical system.
What you can do in your workplace
In her essay, Ms. Lee explains that a major turning point came when a physician friend explicitly asked if she was experiencing abuse. He then gently confirmed she was, and asked without judgment how he could support her, an approach that mirrors advice from the National Domestic Violence Hotline.
“Having a physician validate that this was, indeed, an abusive situation helped enormously ... I believe it may have saved my life,” she writes.
That validation can be crucial, and Dr. Abadilla urges other physicians to regularly check in with colleagues, especially those who seem particularly positive with a go-getter attitude and yet may not seem themselves. That was how she presented when she was struggling the most.
Supporting systemic changes within your organization and beyond is also important. The authors of the 2022 meta-analysis stress the need for domestic violence training, legislative changes, paid leave, and union support.
Finding strength in recovery
Over a decade after escaping her abuser, Whitney says she’s only just begun to share her experience, but what she’s learned has made her a better pharmacist. She says she’s more attuned to subtle signs something could be off with patients and coworkers. When someone makes comments about feeling anxious or that they can’t do anything right, it’s important to ask why, she says.
Recently, Kimberly has opened up to her mentor and other therapists, many of whom have shared that they’re also survivors.
“The last thing I said to [my abuser] is you think you’ve won and you’re hurting me, but what you’ve done to me – I’m going to utilize this and I’m going to help other people,” Kimberly says. “This pain that I have will go away, and I’m going to save the lives of others.”
A version of this article first appeared on Medscape.com.
To protect survivors’ identities, some names have been changed or shortened.
Natasha Abadilla, MD, met the man who would become her abuser while working abroad for a public health nonprofit. When he began emotionally and physically abusing her, she did everything she could to hide it.
“My coworkers knew nothing of the abuse. I became an expert in applying makeup to hide the bruises,” recalls Dr. Abadilla, now a second-year resident and pediatric neurologist at Lucile Packard Children’s Hospital at Stanford.
Dr. Abadilla says she strongly identifies as a hard worker and – to this day – hopes her work did not falter despite her partner’s constant drain on her. But the impact of the abuse continued to affect her for years. Like many survivors of domestic violence, she struggled with PTSD and depression.
Health care workers are often the first point of contact for survivors of domestic violence. Experts and advocates continue to push for more training for clinicians to identify and respond to signs among their patients. Often missing from this conversation is the reality that those tasked with screening can also be victims of intimate partner violence themselves.
What’s more: The very strengths that medical professionals often pride themselves on – perfectionism, empathy, grit – can make it harder for them to identify abuse in their own relationships and push through humiliation and shame to seek help.
Dr. Abadilla is exceptional among survivors in the medical field. Rather than keep her experience quiet, she has shared it publicly.
Awareness, she believes, can save lives.
An understudied problem in an underserved group
The majority of research on health care workers in this area has focused on workplace violence, which 62% experience worldwide. But intimate partner violence remains understudied and underdiscussed. Some medical professionals are even saddled with a “double burden,” facing trauma at work and at home, note the authors of a 2022 meta-analysis published in the journal Trauma, Violence, & Abuse.
The problem has had dire consequences. In recent years, many health care workers have been killed by their abusers:
- In 2016, Casey M. Drawert, MD, a Texas-based critical care anesthesiologist, was fatally shot by her husband in a murder-suicide.
- In 2018, Tamara O’Neal, MD, an ER physician, and Dayna Less, a first-year pharmacy resident, were killed by Dr. O’Neal’s ex-fiancé at Mercy Hospital in Chicago.
- In 2019, Sarah Hawley, MD, a first-year University of Utah resident, was fatally shot by her boyfriend in a murder-suicide.
- In 2021, Moria Kinsey, a nurse practitioner in Tahlequah, Okla., was murdered by a physician.
- In July of 2023, Gwendolyn Lavonne Riddick, DO, an ob.gyn. in North Carolina, was fatally shot by the father of her 3-year-old son.
There are others.
In the wake of these tragedies, calls for health care workers to screen each other as well as patients have grown. But for an untold number of survivors, breaking the silence is still not possible due to concerns about their reputation, professional consequences, the threat of harassment from abusers who are often in the same field, a medical culture of selfless endurance, and a lack of appropriate resources.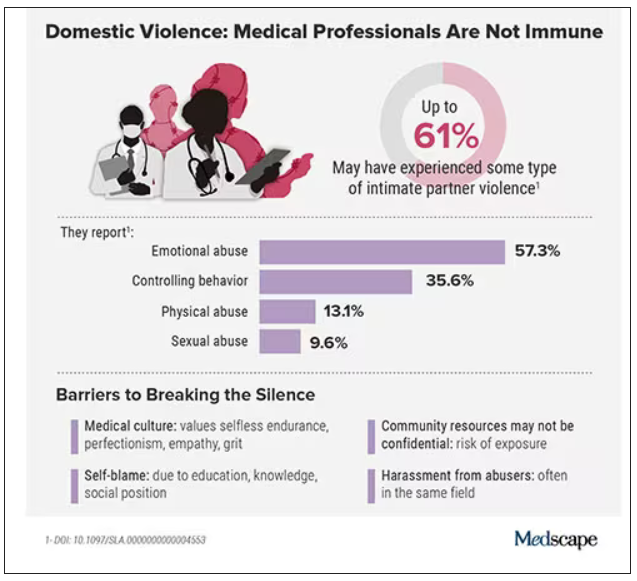
While the vast majority have stayed silent, those who have spoken out say there’s a need for targeted interventions to educate medical professionals as well as more supportive policies throughout the health care system.
Are health care workers more at risk?
Although more studies are needed, research indicates health care workers experience domestic violence at rates comparable to those of other populations, whereas some data suggest rates may be higher.
In the United States, more than one in three women and one in four men experience some form of intimate partner violence in their lifetime. Similarly, a 2020 study found that 24% of 400 physicians responding to a survey reported a history of domestic violence, with 15% reporting verbal abuse, 8% reporting physical violence, 4% reporting sexual abuse, and 4% reporting stalking.
Meanwhile, in an anonymous survey completed by 882 practicing surgeons and trainees in the United States from late 2018 to early 2019, more than 60% reported experiencing some type of intimate partner violence, most commonly emotional abuse.
Recent studies in the United Kingdom, Australia, and elsewhere show that significant numbers of medical professionals are fighting this battle. A 2019 study of more than 2,000 nurses, midwives, and health care assistants in the United Kingdom found that nurses were three times more likely to experience domestic violence than the average person.
What would help solve this problem: More study of health care worker-survivors as a unique group with unique risk factors. In general, domestic violence is most prevalent among women and people in marginalized groups. But young adults, such as medical students and trainees, can face an increased risk due to economic strain. Major life changes, such as relocating for residency, can also drive up stress and fray social connections, further isolating victims.
Why it’s so much harder for medical professionals to reveal abuse
For medical professionals accustomed to being strong and forging on, identifying as a victim of abuse can seem like a personal contradiction. It can feel easier to separate their personal and professional lives rather than face a complex reality.
In a personal essay on KevinMD.com, medical student Chloe N. L. Lee describes this emotional turmoil. “As an aspiring psychiatrist, I questioned my character judgment (how did I end up with a misogynistic abuser?) and wondered if I ought to have known better. I worried that my colleagues would deem me unfit to care for patients. And I thought that this was not supposed to happen to women like me,” Ms. Lee writes.
Kimberly, a licensed therapist, experienced a similar pattern of self-blame when her partner began exhibiting violent behavior. “For a long time, I felt guilty because I said to myself, You’re a therapist. You’re supposed to know this,” she recalls. At the same time, she felt driven to help him and sought couples therapy as his violence escalated.
Whitney, a pharmacist, recognized the “hallmarks” of abuse in her relationship, but she coped by compartmentalizing. Whitney says she was vulnerable to her abuser as a young college student who struggled financially. As he showered her with gifts, she found herself waving away red flags like aggressiveness or overprotectiveness.
After Whitney graduated, her partner’s emotional manipulation escalated into frequent physical assaults. When he gave her a black eye, she could not bring herself to go into work. She quit her job without notice. Despite a spotless record, none of her coworkers ever reached out to investigate her sudden departure.
It would take 8 years for Whitney to acknowledge the abuse and seize a moment to escape. She fled with just her purse and started over in a new city, rebuilding her life in the midst of harassment and threats from her ex. She says she’s grateful to be alive.
An imperfect system doesn’t help
Health care workers rarely ask for support or disclose abuse at work. Some have cited stigma, a lack of confidentiality (especially when the abuser is also in health care), fears about colleagues’ judgment, and a culture that doesn’t prioritize self-care.
Sometimes policies get in the way: In a 2021 qualitative study of interviews with 21 female physician-survivors in the United Kingdom, many said that despite the intense stress of abuse and recovery, they were unable to take any time off.
Of 180 UK-based midwife-survivors interviewed in a 2018 study, only 60 sought support at work and 30 received it. Many said their supervisors pressured them to report the abuse and get back to work, called social services behind their back, or reported them to their professional regulator. “I was treated like the perpetrator,” one said. Barbara Hernandez, PhD, a researcher who studies physician-survivors and director of physician vitality at Loma Linda University in southern California, says workplace violence and mistreatment from patients or colleagues – and a poor institutional response – can make those in health care feel like they have to “shut up and put up,” priming them to also tolerate abuse at home.
When survivors do reach out, there can be a disconnect between the resources they need and those they’re offered, Dr. Hernandez adds. In a recent survey of 400 physicians she conducted, respondents typically said they would advise a physician-survivor to “get to a shelter quickly.” But when roles were reversed, they admitted going to a shelter was the least feasible option. Support groups can also be problematic in smaller communities where physicians might be recognized or see their own patients.
Complicating matters further, the violence often comes from within the medical community. This can lead to particularly malicious abuse tactics like sending false accusations to a victim’s regulatory college or board; prolonged court and custody battles to drain them of all resources and their ability to hold a job; or even sabotage, harassment, or violence at work. The sheen of the abuser’s public persona, on the other hand, can guard them from any accountability.
For example, one physician-survivor said her ex-partner, a psychiatrist, coerced her into believing she was mentally ill, claimed she was “psychotic” in order to take back their children after she left, and had numerous colleagues serve as character witnesses in court for him, “saying he couldn’t have done any of these things, how great he is, and what a wonderful father he is.”
Slow progress is still progress
After Sherilyn M. Gordon-Burroughs, MD, a Texas-based transplant surgeon, mother, and educator, was killed by her husband in a murder-suicide in 2017, her friends Barbara Lee Bass, MD, president of the American College of Surgeons, and Patricia L. Turner, MD, were spurred into action. Together, they founded the ACS Intimate Partner Violence Task Force. Their mission is to educate surgeons to identify the signs of intimate partner violence (IPV) in themselves and their colleagues and connect them with resources.
“There is a concerted effort to close that gap,” says D’Andrea K. Joseph, MD, cochair of the task force and chief of trauma and acute care surgery at NYU Langone in New York. In the future, Dr. Joseph predicts, “making this a part of the curriculum, that it’s standardized for residents and trainees, that there is a safe place for victims ... and that we can band together and really recognize and assist our colleagues who are in trouble.”
Resources created by the ACS IPV task force, such as the toolkit and curriculum, provide a model for other health care leaders. But there have been few similar initiatives aimed at increasing IPV intervention within the medical system.
What you can do in your workplace
In her essay, Ms. Lee explains that a major turning point came when a physician friend explicitly asked if she was experiencing abuse. He then gently confirmed she was, and asked without judgment how he could support her, an approach that mirrors advice from the National Domestic Violence Hotline.
“Having a physician validate that this was, indeed, an abusive situation helped enormously ... I believe it may have saved my life,” she writes.
That validation can be crucial, and Dr. Abadilla urges other physicians to regularly check in with colleagues, especially those who seem particularly positive with a go-getter attitude and yet may not seem themselves. That was how she presented when she was struggling the most.
Supporting systemic changes within your organization and beyond is also important. The authors of the 2022 meta-analysis stress the need for domestic violence training, legislative changes, paid leave, and union support.
Finding strength in recovery
Over a decade after escaping her abuser, Whitney says she’s only just begun to share her experience, but what she’s learned has made her a better pharmacist. She says she’s more attuned to subtle signs something could be off with patients and coworkers. When someone makes comments about feeling anxious or that they can’t do anything right, it’s important to ask why, she says.
Recently, Kimberly has opened up to her mentor and other therapists, many of whom have shared that they’re also survivors.
“The last thing I said to [my abuser] is you think you’ve won and you’re hurting me, but what you’ve done to me – I’m going to utilize this and I’m going to help other people,” Kimberly says. “This pain that I have will go away, and I’m going to save the lives of others.”
A version of this article first appeared on Medscape.com.
One in five doctors with long COVID can no longer work: Survey
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Resident creates AI alternative to U.S. News med school ranking
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Q&A: What to know about the new BA 2.86 COVID variant
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
Unlocking the secrets of brown fat
Brown fat, or thermogenic adipose tissue, appears to act as a “nutrient sink,” consuming glucose and lactate, among other metabolites, say U.S. researchers in a mouse study that supports its potential role in tackling obesity and even cancer.
The research, published recently in Nature Metabolism, was led by David A. Guertin, PhD, of the program in molecular medicine, University of Massachusetts, Worcester.
What is adaptive thermogenesis, and why is it important in temperature regulation?
Adaptive thermogenesis is a physiologic process that occurs in a special type of fat cell, called a brown adipocyte, in which intracellular stored lipids and nutrients taken up from the blood are catabolized to generate heat.
The heat generated by these thermogenic adipocytes is critical for warming the blood and maintaining body temperature in cold environments, and is especially critical in human infants and small mammals, which are more sensitive to low temperatures.
The process is stimulated by the sympathetic nervous system, especially in response to feeling cold, but it can be activated by other stresses as well.
While adaptative thermogenesis is also called nonshivering thermogenesis to distinguish it from muscle shivering, both means of generating heat can work together to maintain body temperature.
Why is it considered a potential target for obesity?
Adult humans have brown adipocytes in specific locations in the body called brown adipose tissues (BAT) or, more simply, “brown fat.”
Intriguingly, clinical data show that the more BAT you have, the more likely you are to be protected against cardiometabolic disorders associated with obesity.
Since obesity results from an imbalance between energy intake and energy expenditure, one model proposes that brown adipocytes rebalance this formula by expending the excess energy (calories) as heat rather than storing it.
This has been referred to as the “nutrient sink” model, and the ability to activate this process therapeutically is a very attractive antiobesity strategy.
Why was it important to understand which circulating metabolites BAT uses for thermogenesis?
It is still not clear why brown fat is so beneficial for human health, and thus there is strong rationale for understanding its metabolism and how it cooperates with other tissues in the body.
For example, prior to our work, the field lacked a broad quantitative picture of how much any individual nutrient from the blood was used by brown fat, or which specific nutrients brown fat prefers to use to make heat – such as lipids, glucose, amino acids, etc. Knowing this information helps us identify more precise strategies to activate brown fat.
In addition, circulating metabolites sometimes also have messenger functions, similar to those of hormones, that stimulate physiologic processes such as adaptative thermogenesis. Highly metabolic tissues also put metabolites back into the blood, which can send messages to the brain and other tissues.
We don’t have a lot of information yet on how brown fat might engage in these processes, and so our study also aimed at finding these special metabolite messengers.
You found that glucose and lactate predominate as BAT fuel sources. What does that tell us?
The major fuels used by brown fat have been debated for a long time.
Our study suggests that BAT in mice mainly prefers glucose and lactate, which is generated from glucose. On one hand, this shows us that thermogenic adipocytes may be especially useful in treating hyperglycemia, or even tumors, by reducing the amount of circulating glucose.
It also tells us that we need to focus more on why brown fat needs so much glucose. Other studies suggest that glucose is not just used as a fuel to generate heat but also may have other important functions in keeping brown adipocytes active and healthy.
We need to know that information so that therapeutic strategies targeting brown adipocytes can be optimized to have the best chance of success.
It’s worth noting that we did our study in mice that had free access to food. If the mice were fasting, they would use more lipids from the blood to supplement for the lack of available glucose, but we think that a baseline amount of glucose is still necessary.
What could be the clinical implications of your results if replicated in humans?
They suggest that glucose is an important resource that thermogenic adipocytes cannot do without, and moreover, that glucose is more than just a carbon source.
Resolving those other functions of glucose may provide insight into mechanisms to stimulate these cells or help explain why overweight or obese people who are insulin resistant have less brown fat activity, as insulin stimulates glucose uptake.
Beyond glucose, if any of these other metabolites made or released by brown fat have beneficial messenger functions, there may be ways to pharmacologically mimic them.
How easily do you think your findings could be applied to humans?
On a fundamental level, the basic cellular mechanisms that drive adaptative thermogenesis are likely the same between mice and humans, but the wiring to the sympathetic nervous system is a bit different.
This is why it’s important to look deeply at brown fat metabolism in mouse models to find pathways fundamental to the basic mechanisms of adaptative thermogenesis in both mice and humans, which could reveal unique therapeutic opportunities.
Another big challenge with comparing humans and mice is that humans typically keep their environment warm, so their brown fat is not that active.
In contrast, mice are often raised their entire lives in a facility kept at room temperature, around 22° C (72° F). While comfortable for the humans working with them, it’s cold for a small mouse, and so mice live with constantly active brown fat.
We can change the mouse environment to alter mouse brown fat activity, but that can’t be done with people. This makes comparative studies difficult.
Nevertheless, studies have shown that people who live in cold climates often have more brown fat, and, conversely, mice raised in warmer environments have brown fat that looks a lot more like human brown fat.
What further research do you have planned, or are looking forward to, in this area?
This is the most fun part of what we do, and I’ve been fortunate to have an amazing team passionately working on these questions.
One is to figure out why glucose is so important for these fascinating cells, which will keep us busy for years. We also need to modify the dietary conditions to determine whether the body prioritizes the use of glucose for adaptive thermogenesis even when there isn’t much available.
Another goal is to test whether any of the other metabolites we identified have bioactive functions. We also discovered a unique role for glutamine metabolism in brown fat, through the consumption of amino acids, that we haven’t yet resolved.
Finally, we want to understand how and why brown fat protects other organs from metabolic diseases, and we are just at the tip of the iceberg here.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases; the National Institute on Alcohol Abuse and Alcoholism; the National Heart, Lung, & Blood Institute; the National Institutes of Health; the AASLD Foundation Pinnacle Research Award in Liver Disease; the Edward Mallinckrodt Jr. Foundation Award; and the Basic Science Research Program of the Ministry of Education (South Korea). No relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
Brown fat, or thermogenic adipose tissue, appears to act as a “nutrient sink,” consuming glucose and lactate, among other metabolites, say U.S. researchers in a mouse study that supports its potential role in tackling obesity and even cancer.
The research, published recently in Nature Metabolism, was led by David A. Guertin, PhD, of the program in molecular medicine, University of Massachusetts, Worcester.
What is adaptive thermogenesis, and why is it important in temperature regulation?
Adaptive thermogenesis is a physiologic process that occurs in a special type of fat cell, called a brown adipocyte, in which intracellular stored lipids and nutrients taken up from the blood are catabolized to generate heat.
The heat generated by these thermogenic adipocytes is critical for warming the blood and maintaining body temperature in cold environments, and is especially critical in human infants and small mammals, which are more sensitive to low temperatures.
The process is stimulated by the sympathetic nervous system, especially in response to feeling cold, but it can be activated by other stresses as well.
While adaptative thermogenesis is also called nonshivering thermogenesis to distinguish it from muscle shivering, both means of generating heat can work together to maintain body temperature.
Why is it considered a potential target for obesity?
Adult humans have brown adipocytes in specific locations in the body called brown adipose tissues (BAT) or, more simply, “brown fat.”
Intriguingly, clinical data show that the more BAT you have, the more likely you are to be protected against cardiometabolic disorders associated with obesity.
Since obesity results from an imbalance between energy intake and energy expenditure, one model proposes that brown adipocytes rebalance this formula by expending the excess energy (calories) as heat rather than storing it.
This has been referred to as the “nutrient sink” model, and the ability to activate this process therapeutically is a very attractive antiobesity strategy.
Why was it important to understand which circulating metabolites BAT uses for thermogenesis?
It is still not clear why brown fat is so beneficial for human health, and thus there is strong rationale for understanding its metabolism and how it cooperates with other tissues in the body.
For example, prior to our work, the field lacked a broad quantitative picture of how much any individual nutrient from the blood was used by brown fat, or which specific nutrients brown fat prefers to use to make heat – such as lipids, glucose, amino acids, etc. Knowing this information helps us identify more precise strategies to activate brown fat.
In addition, circulating metabolites sometimes also have messenger functions, similar to those of hormones, that stimulate physiologic processes such as adaptative thermogenesis. Highly metabolic tissues also put metabolites back into the blood, which can send messages to the brain and other tissues.
We don’t have a lot of information yet on how brown fat might engage in these processes, and so our study also aimed at finding these special metabolite messengers.
You found that glucose and lactate predominate as BAT fuel sources. What does that tell us?
The major fuels used by brown fat have been debated for a long time.
Our study suggests that BAT in mice mainly prefers glucose and lactate, which is generated from glucose. On one hand, this shows us that thermogenic adipocytes may be especially useful in treating hyperglycemia, or even tumors, by reducing the amount of circulating glucose.
It also tells us that we need to focus more on why brown fat needs so much glucose. Other studies suggest that glucose is not just used as a fuel to generate heat but also may have other important functions in keeping brown adipocytes active and healthy.
We need to know that information so that therapeutic strategies targeting brown adipocytes can be optimized to have the best chance of success.
It’s worth noting that we did our study in mice that had free access to food. If the mice were fasting, they would use more lipids from the blood to supplement for the lack of available glucose, but we think that a baseline amount of glucose is still necessary.
What could be the clinical implications of your results if replicated in humans?
They suggest that glucose is an important resource that thermogenic adipocytes cannot do without, and moreover, that glucose is more than just a carbon source.
Resolving those other functions of glucose may provide insight into mechanisms to stimulate these cells or help explain why overweight or obese people who are insulin resistant have less brown fat activity, as insulin stimulates glucose uptake.
Beyond glucose, if any of these other metabolites made or released by brown fat have beneficial messenger functions, there may be ways to pharmacologically mimic them.
How easily do you think your findings could be applied to humans?
On a fundamental level, the basic cellular mechanisms that drive adaptative thermogenesis are likely the same between mice and humans, but the wiring to the sympathetic nervous system is a bit different.
This is why it’s important to look deeply at brown fat metabolism in mouse models to find pathways fundamental to the basic mechanisms of adaptative thermogenesis in both mice and humans, which could reveal unique therapeutic opportunities.
Another big challenge with comparing humans and mice is that humans typically keep their environment warm, so their brown fat is not that active.
In contrast, mice are often raised their entire lives in a facility kept at room temperature, around 22° C (72° F). While comfortable for the humans working with them, it’s cold for a small mouse, and so mice live with constantly active brown fat.
We can change the mouse environment to alter mouse brown fat activity, but that can’t be done with people. This makes comparative studies difficult.
Nevertheless, studies have shown that people who live in cold climates often have more brown fat, and, conversely, mice raised in warmer environments have brown fat that looks a lot more like human brown fat.
What further research do you have planned, or are looking forward to, in this area?
This is the most fun part of what we do, and I’ve been fortunate to have an amazing team passionately working on these questions.
One is to figure out why glucose is so important for these fascinating cells, which will keep us busy for years. We also need to modify the dietary conditions to determine whether the body prioritizes the use of glucose for adaptive thermogenesis even when there isn’t much available.
Another goal is to test whether any of the other metabolites we identified have bioactive functions. We also discovered a unique role for glutamine metabolism in brown fat, through the consumption of amino acids, that we haven’t yet resolved.
Finally, we want to understand how and why brown fat protects other organs from metabolic diseases, and we are just at the tip of the iceberg here.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases; the National Institute on Alcohol Abuse and Alcoholism; the National Heart, Lung, & Blood Institute; the National Institutes of Health; the AASLD Foundation Pinnacle Research Award in Liver Disease; the Edward Mallinckrodt Jr. Foundation Award; and the Basic Science Research Program of the Ministry of Education (South Korea). No relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
Brown fat, or thermogenic adipose tissue, appears to act as a “nutrient sink,” consuming glucose and lactate, among other metabolites, say U.S. researchers in a mouse study that supports its potential role in tackling obesity and even cancer.
The research, published recently in Nature Metabolism, was led by David A. Guertin, PhD, of the program in molecular medicine, University of Massachusetts, Worcester.
What is adaptive thermogenesis, and why is it important in temperature regulation?
Adaptive thermogenesis is a physiologic process that occurs in a special type of fat cell, called a brown adipocyte, in which intracellular stored lipids and nutrients taken up from the blood are catabolized to generate heat.
The heat generated by these thermogenic adipocytes is critical for warming the blood and maintaining body temperature in cold environments, and is especially critical in human infants and small mammals, which are more sensitive to low temperatures.
The process is stimulated by the sympathetic nervous system, especially in response to feeling cold, but it can be activated by other stresses as well.
While adaptative thermogenesis is also called nonshivering thermogenesis to distinguish it from muscle shivering, both means of generating heat can work together to maintain body temperature.
Why is it considered a potential target for obesity?
Adult humans have brown adipocytes in specific locations in the body called brown adipose tissues (BAT) or, more simply, “brown fat.”
Intriguingly, clinical data show that the more BAT you have, the more likely you are to be protected against cardiometabolic disorders associated with obesity.
Since obesity results from an imbalance between energy intake and energy expenditure, one model proposes that brown adipocytes rebalance this formula by expending the excess energy (calories) as heat rather than storing it.
This has been referred to as the “nutrient sink” model, and the ability to activate this process therapeutically is a very attractive antiobesity strategy.
Why was it important to understand which circulating metabolites BAT uses for thermogenesis?
It is still not clear why brown fat is so beneficial for human health, and thus there is strong rationale for understanding its metabolism and how it cooperates with other tissues in the body.
For example, prior to our work, the field lacked a broad quantitative picture of how much any individual nutrient from the blood was used by brown fat, or which specific nutrients brown fat prefers to use to make heat – such as lipids, glucose, amino acids, etc. Knowing this information helps us identify more precise strategies to activate brown fat.
In addition, circulating metabolites sometimes also have messenger functions, similar to those of hormones, that stimulate physiologic processes such as adaptative thermogenesis. Highly metabolic tissues also put metabolites back into the blood, which can send messages to the brain and other tissues.
We don’t have a lot of information yet on how brown fat might engage in these processes, and so our study also aimed at finding these special metabolite messengers.
You found that glucose and lactate predominate as BAT fuel sources. What does that tell us?
The major fuels used by brown fat have been debated for a long time.
Our study suggests that BAT in mice mainly prefers glucose and lactate, which is generated from glucose. On one hand, this shows us that thermogenic adipocytes may be especially useful in treating hyperglycemia, or even tumors, by reducing the amount of circulating glucose.
It also tells us that we need to focus more on why brown fat needs so much glucose. Other studies suggest that glucose is not just used as a fuel to generate heat but also may have other important functions in keeping brown adipocytes active and healthy.
We need to know that information so that therapeutic strategies targeting brown adipocytes can be optimized to have the best chance of success.
It’s worth noting that we did our study in mice that had free access to food. If the mice were fasting, they would use more lipids from the blood to supplement for the lack of available glucose, but we think that a baseline amount of glucose is still necessary.
What could be the clinical implications of your results if replicated in humans?
They suggest that glucose is an important resource that thermogenic adipocytes cannot do without, and moreover, that glucose is more than just a carbon source.
Resolving those other functions of glucose may provide insight into mechanisms to stimulate these cells or help explain why overweight or obese people who are insulin resistant have less brown fat activity, as insulin stimulates glucose uptake.
Beyond glucose, if any of these other metabolites made or released by brown fat have beneficial messenger functions, there may be ways to pharmacologically mimic them.
How easily do you think your findings could be applied to humans?
On a fundamental level, the basic cellular mechanisms that drive adaptative thermogenesis are likely the same between mice and humans, but the wiring to the sympathetic nervous system is a bit different.
This is why it’s important to look deeply at brown fat metabolism in mouse models to find pathways fundamental to the basic mechanisms of adaptative thermogenesis in both mice and humans, which could reveal unique therapeutic opportunities.
Another big challenge with comparing humans and mice is that humans typically keep their environment warm, so their brown fat is not that active.
In contrast, mice are often raised their entire lives in a facility kept at room temperature, around 22° C (72° F). While comfortable for the humans working with them, it’s cold for a small mouse, and so mice live with constantly active brown fat.
We can change the mouse environment to alter mouse brown fat activity, but that can’t be done with people. This makes comparative studies difficult.
Nevertheless, studies have shown that people who live in cold climates often have more brown fat, and, conversely, mice raised in warmer environments have brown fat that looks a lot more like human brown fat.
What further research do you have planned, or are looking forward to, in this area?
This is the most fun part of what we do, and I’ve been fortunate to have an amazing team passionately working on these questions.
One is to figure out why glucose is so important for these fascinating cells, which will keep us busy for years. We also need to modify the dietary conditions to determine whether the body prioritizes the use of glucose for adaptive thermogenesis even when there isn’t much available.
Another goal is to test whether any of the other metabolites we identified have bioactive functions. We also discovered a unique role for glutamine metabolism in brown fat, through the consumption of amino acids, that we haven’t yet resolved.
Finally, we want to understand how and why brown fat protects other organs from metabolic diseases, and we are just at the tip of the iceberg here.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases; the National Institute on Alcohol Abuse and Alcoholism; the National Heart, Lung, & Blood Institute; the National Institutes of Health; the AASLD Foundation Pinnacle Research Award in Liver Disease; the Edward Mallinckrodt Jr. Foundation Award; and the Basic Science Research Program of the Ministry of Education (South Korea). No relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
FROM NATURE METABOLISM
Experts debate low-carb diets for people with diabetes
It’s an ongoing debate in the diabetes world: Is it ideal to consume a very-low-carbohydrate diet, or is it better to go with moderate amounts of healthful carbs?
At the annual scientific sessions of the American Diabetes Association, Carol F. Kirkpatrick, PhD, RDN, spoke first, arguing in favor of diets consisting of moderate, high-quality carbohydrates.
Dina Hafez Griauzde, MD, countered that very-low-carbohydrate diets are more beneficial for people with diabetes, primarily type 2 diabetes.
Both speakers based their arguments on published evidence but agreed in the end that discussion with patients about individual dietary preferences should play a major role in the ultimate decision.
Moderate-carbohydrate eating is best
Dr. Kirkpatrick began by explaining that definitions of “low carb” vary in the literature, which makes comparisons between studies difficult. On the basis of a 2019 review that she coauthored, “moderate” carbohydrate consumption was defined as a diet in which 26%-44% of total daily calories are from carbohydrates. “Low” carbohydrate consumption was defined as a diet in which 10%-25% of calories were from carbohydrates. Consuming less than 10% was defined as a very-low-carbohydrate diet (i.e., a ketogenic diet).
Across studies, she noted, the literature shows that within the first 6 months weight loss is typically greater with carbohydrate-restricted diets than with higher-carbohydrate diets, but that by 1 year and beyond weight loss is similar.
“That can be partly due to the difficulty in people maintaining that very severe dietary restriction, although ... we can all acknowledge that it’s difficult for patients to adhere to any dietary pattern, so for sure by 12 months, the difference in the weight loss is gone between the two,” said Dr. Kirkpatrick, of Midwest Biomedical Research, Pocatello, Idaho.
In a recent meta-analysis of 35 trials that examined the dose-dependent effects of carbohydrate restriction for patients with type 2 diabetes, there was a significant decrease in weight as carbohydrates were reduced. But by 12 months (17 trials), the greatest weight reduction was seen at 35% carbohydrate intake.
“It may just be that people were able to adhere to that moderate intake better,” she explained.
Regarding lipids, in her 2019 review and in several meta-analyses since, the effects on low-density lipoprotein cholesterol (LDL-C) varied. For some patients, adhering to a low-carb diet led to reductions in LDL-C, especially if the participants also lost weight, whereas in other patients, a low-carb diet led to an increase in LDL-C.
Either way, a high intake of saturated fatty acids is key to an increase in LDL-C, Dr. Kirkpatrick noted. “So, it’s important that, if a patient chooses to follow a very low carbohydrate diet or any kind of dietary pattern that restricts carbohydrate, that they replace the carbohydrate with unsaturated fat and not saturated fatty acid foods to avoid that increase in LDL-C.”
Generally, the evidence also shows that carbohydrate restriction typically leads to lower triglyceride levels and higher high-density lipoprotein (HDL) cholesterol levels. However, the same meta-analysis showed that the greatest reduction in LDL-C occurred at about 40% carbohydrate consumption.
Another recent meta-analysis showed that LDL-C rose significantly by an average 12.4 mg/dL with very-low-carb (3%-30%) diets, but only slightly, by 0.4 mg/dL, with moderate carb (40%-45%) intake.
Consuming very-low-carb diets did lead to greater reductions in triglycerides, compared with consuming moderate carb diets (23.9 mg/dL vs. 8.9 mg/dL).
“However, in terms of cardiovascular health, we are not entirely sure what that means. ... We have to look at the overall results in the presence of both triglyceride lowering as well as LDL cholesterol,” Dr. Kirkpatrick noted.
Carbohydrate restriction did consistently lead to lower hemoglobin A1c levels by an average of 0.4, 0.6, and 1.0 percentage points at 6 months for diets of 40%, 30%, and 15% carbohydrate, respectively. However, by 12 months, the effect had waned to 0.15, 0.2, and 0.4 A1c percentage points.
“Again, carbohydrate restriction, especially severe, is difficult for people to adhere to, and moderate carbohydrate intake would allow our patients to consume an appropriate amount of carbohydrate and still achieve improved glycemic control,” Dr. Kirkpatrick said.
Two large randomized controlled trials – PREDIMED and CORDIOPREV – examined the effects of the Mediterranean diet on cardiovascular disease prevention. Both showed a decrease in cardiovascular events with the Mediterranean diet, which involves consuming moderate amounts of carbohydrates.
“The Mediterranean dietary pattern has the strongest evidence for benefit, and it’s moderate in carbohydrates,” she concluded.
Very-low-carbohydrate eating is best
Dr. Griauzde was a last-minute replacement speaker for William S. Yancy Jr, MD, of Duke University, Durham, N.C., and presented his slides. She argued that consuming a very low carb diet improves glycemia and that it does not increase but possibly lowers cardiovascular risk.
She began by noting that prior to the discovery of insulin very-low-carb diets had been consumed for over a century to prolong life for people with type 1 diabetes.
“We have long recognized the deleterious role of carbohydrate in type 1 diabetes management, and we have increasingly recognized that role in the management of type 2 diabetes,” said Dr. Griauzde of the University of Michigan in Ann Arbor.
In a small study that compared maintaining a very-low-carb diet for 2 weeks with maintaining a high-carb diet for 2 weeks, total glucose areas under the curve were substantially lower (P < .05) during the low-carb phase, while A1c levels dropped from 7.3% to 6.8% (P = .006).
“We don’t see those outcomes with meds,” Dr. Griauzde noted, adding, “A diet very low in carbohydrates is one of the most potent tools we have to help our patients achieve glycemic control.”
Dr. Griauzde said that the carbohydrate-insulin model provides an explanation for why dietary carbohydrates are particularly obesogenic and metabolically harmful. That model contrasts with the energy balance model, which suggests that all calories are equal.
The rationale of the carbohydrate-insulin model is that dietary carbohydrate – either sugar or starch – raises serum glucose and insulin levels. A carbohydrate-restricted diet therefore reduces the dietary contribution to serum glucose, which then results in lower insulin levels. Insulin is a potent stimulator of lipogenesis (fat storage), and it is a potent inhibitor of lipolysis (the burning of fat). By lowering insulin levels, stored body fat is burned, serum ketone levels increase, and body weight is lowered.
This model suggests that, when insulin levels are chronically high because of excess carbohydrate consumption, circulating fuels are lowered, which leads to an increase in hunger and to overeating. This was demonstrated in a study that compared different levels of isocaloric glycemic index diets in 12 teenage boys with overweight or obesity. The higher-carbohydrate meals led to higher glucose and insulin levels and more food consumption.
In a systematic review of 13 trials of restricted-carbohydrate diets (< 45% carbohydrates) for adults with diabetes, the degree of improvement in A1c level correlated with the degree of carbohydrate restriction over 2-26 weeks (P = .013).
And in a network meta-analysis of 56 trials that compared nine diets among a total of 4,937 participants with type 2 diabetes, one conclusion was that “for reducing A1c, the low-carbohydrate diet was ranked as the best dietary approach (SUCRA: 84%), followed by the Mediterranean diet (80%), and Paleolithic diet (76%), compared with a control diet.”
Regarding the criticism that very-low-carbohydrate diets are high in saturated fat and therefore raise the risk of cardiovascular disease, Dr. Griauzde pointed to another meta-analysis of 21 prospective studies with more than 300,000 participants with 5-25 years of follow-up. In that analysis, the intake of saturated fat was not associated with an increased risk of cardiovascular disease or stroke.
Furthermore, a 12-week randomized controlled trial that involved 40 adults with overweight also suggested that a very-low-carb diet may be superior to a low-fat diet in improving aspects of the metabolic syndrome, including body mass index, lipid levels, and insulin sensitivity. Small LDL particles, which are more atherogenic than larger LDL particles, also decreased despite a threefold increase in saturated fat intake.
Rebuttals: Overall diet, patient preference matter
During the rebuttals, Dr. Kirkpatrick pointed out that large LDL particles are also atherogenic. In addition, she noted that the studies that showed that saturated fat isn’t associated with cardiovascular disease didn’t consider the macronutrients that replaced the saturated fat.
“It really is about increasing consumption of foods that we know are associated with cardiovascular benefit, including plant-based foods that are high quality and not refined carbohydrates ... and healthy protein sources. ... Hopefully we can step away from just looking at macronutrients and look at the total amount of food that people are choosing to eat.”
Importantly, Dr. Kirkpatrick said, patients need to be asked about their current dietary patterns and preferences. “Interventions should be patient centered and sensitive to cultural differences. Personalized lifestyle interventions increase the likelihood of success.”
Dr. Griauzde pointed out that newer antiobesity drugs can be added to any diet to decrease appetite and enhance adherence.
Dr. Griauzde also observed, “We can label a very-low-carbohydrate diet ‘extreme,’ but maybe, from the patient’s perspective, it’s extreme to take 200 units of insulin a day. If you can give them the opportunity to discontinue use of the insulin by following a very-low-carbohydrate dietary pattern, that is the opportunity that our patients deserve to have.”
But overall, she agreed with Dr. Kirkpatrick about individualizing any dietary approach: “We will never know from any of the trials that have been done or that will be done in the future what diet is best for an individual patient. ... Our job is to help our patients find the dietary approach that works best for them.”
Dr. Kirkpatrick is a clinical scientist with Midwest Biomedical Research, which has received funding from various food and pharmaceutical companies. She has not received any direct funding. Dr. Yancy is a consultant for The Simply Good Foods Co. Dr. Griauzde has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s an ongoing debate in the diabetes world: Is it ideal to consume a very-low-carbohydrate diet, or is it better to go with moderate amounts of healthful carbs?
At the annual scientific sessions of the American Diabetes Association, Carol F. Kirkpatrick, PhD, RDN, spoke first, arguing in favor of diets consisting of moderate, high-quality carbohydrates.
Dina Hafez Griauzde, MD, countered that very-low-carbohydrate diets are more beneficial for people with diabetes, primarily type 2 diabetes.
Both speakers based their arguments on published evidence but agreed in the end that discussion with patients about individual dietary preferences should play a major role in the ultimate decision.
Moderate-carbohydrate eating is best
Dr. Kirkpatrick began by explaining that definitions of “low carb” vary in the literature, which makes comparisons between studies difficult. On the basis of a 2019 review that she coauthored, “moderate” carbohydrate consumption was defined as a diet in which 26%-44% of total daily calories are from carbohydrates. “Low” carbohydrate consumption was defined as a diet in which 10%-25% of calories were from carbohydrates. Consuming less than 10% was defined as a very-low-carbohydrate diet (i.e., a ketogenic diet).
Across studies, she noted, the literature shows that within the first 6 months weight loss is typically greater with carbohydrate-restricted diets than with higher-carbohydrate diets, but that by 1 year and beyond weight loss is similar.
“That can be partly due to the difficulty in people maintaining that very severe dietary restriction, although ... we can all acknowledge that it’s difficult for patients to adhere to any dietary pattern, so for sure by 12 months, the difference in the weight loss is gone between the two,” said Dr. Kirkpatrick, of Midwest Biomedical Research, Pocatello, Idaho.
In a recent meta-analysis of 35 trials that examined the dose-dependent effects of carbohydrate restriction for patients with type 2 diabetes, there was a significant decrease in weight as carbohydrates were reduced. But by 12 months (17 trials), the greatest weight reduction was seen at 35% carbohydrate intake.
“It may just be that people were able to adhere to that moderate intake better,” she explained.
Regarding lipids, in her 2019 review and in several meta-analyses since, the effects on low-density lipoprotein cholesterol (LDL-C) varied. For some patients, adhering to a low-carb diet led to reductions in LDL-C, especially if the participants also lost weight, whereas in other patients, a low-carb diet led to an increase in LDL-C.
Either way, a high intake of saturated fatty acids is key to an increase in LDL-C, Dr. Kirkpatrick noted. “So, it’s important that, if a patient chooses to follow a very low carbohydrate diet or any kind of dietary pattern that restricts carbohydrate, that they replace the carbohydrate with unsaturated fat and not saturated fatty acid foods to avoid that increase in LDL-C.”
Generally, the evidence also shows that carbohydrate restriction typically leads to lower triglyceride levels and higher high-density lipoprotein (HDL) cholesterol levels. However, the same meta-analysis showed that the greatest reduction in LDL-C occurred at about 40% carbohydrate consumption.
Another recent meta-analysis showed that LDL-C rose significantly by an average 12.4 mg/dL with very-low-carb (3%-30%) diets, but only slightly, by 0.4 mg/dL, with moderate carb (40%-45%) intake.
Consuming very-low-carb diets did lead to greater reductions in triglycerides, compared with consuming moderate carb diets (23.9 mg/dL vs. 8.9 mg/dL).
“However, in terms of cardiovascular health, we are not entirely sure what that means. ... We have to look at the overall results in the presence of both triglyceride lowering as well as LDL cholesterol,” Dr. Kirkpatrick noted.
Carbohydrate restriction did consistently lead to lower hemoglobin A1c levels by an average of 0.4, 0.6, and 1.0 percentage points at 6 months for diets of 40%, 30%, and 15% carbohydrate, respectively. However, by 12 months, the effect had waned to 0.15, 0.2, and 0.4 A1c percentage points.
“Again, carbohydrate restriction, especially severe, is difficult for people to adhere to, and moderate carbohydrate intake would allow our patients to consume an appropriate amount of carbohydrate and still achieve improved glycemic control,” Dr. Kirkpatrick said.
Two large randomized controlled trials – PREDIMED and CORDIOPREV – examined the effects of the Mediterranean diet on cardiovascular disease prevention. Both showed a decrease in cardiovascular events with the Mediterranean diet, which involves consuming moderate amounts of carbohydrates.
“The Mediterranean dietary pattern has the strongest evidence for benefit, and it’s moderate in carbohydrates,” she concluded.
Very-low-carbohydrate eating is best
Dr. Griauzde was a last-minute replacement speaker for William S. Yancy Jr, MD, of Duke University, Durham, N.C., and presented his slides. She argued that consuming a very low carb diet improves glycemia and that it does not increase but possibly lowers cardiovascular risk.
She began by noting that prior to the discovery of insulin very-low-carb diets had been consumed for over a century to prolong life for people with type 1 diabetes.
“We have long recognized the deleterious role of carbohydrate in type 1 diabetes management, and we have increasingly recognized that role in the management of type 2 diabetes,” said Dr. Griauzde of the University of Michigan in Ann Arbor.
In a small study that compared maintaining a very-low-carb diet for 2 weeks with maintaining a high-carb diet for 2 weeks, total glucose areas under the curve were substantially lower (P < .05) during the low-carb phase, while A1c levels dropped from 7.3% to 6.8% (P = .006).
“We don’t see those outcomes with meds,” Dr. Griauzde noted, adding, “A diet very low in carbohydrates is one of the most potent tools we have to help our patients achieve glycemic control.”
Dr. Griauzde said that the carbohydrate-insulin model provides an explanation for why dietary carbohydrates are particularly obesogenic and metabolically harmful. That model contrasts with the energy balance model, which suggests that all calories are equal.
The rationale of the carbohydrate-insulin model is that dietary carbohydrate – either sugar or starch – raises serum glucose and insulin levels. A carbohydrate-restricted diet therefore reduces the dietary contribution to serum glucose, which then results in lower insulin levels. Insulin is a potent stimulator of lipogenesis (fat storage), and it is a potent inhibitor of lipolysis (the burning of fat). By lowering insulin levels, stored body fat is burned, serum ketone levels increase, and body weight is lowered.
This model suggests that, when insulin levels are chronically high because of excess carbohydrate consumption, circulating fuels are lowered, which leads to an increase in hunger and to overeating. This was demonstrated in a study that compared different levels of isocaloric glycemic index diets in 12 teenage boys with overweight or obesity. The higher-carbohydrate meals led to higher glucose and insulin levels and more food consumption.
In a systematic review of 13 trials of restricted-carbohydrate diets (< 45% carbohydrates) for adults with diabetes, the degree of improvement in A1c level correlated with the degree of carbohydrate restriction over 2-26 weeks (P = .013).
And in a network meta-analysis of 56 trials that compared nine diets among a total of 4,937 participants with type 2 diabetes, one conclusion was that “for reducing A1c, the low-carbohydrate diet was ranked as the best dietary approach (SUCRA: 84%), followed by the Mediterranean diet (80%), and Paleolithic diet (76%), compared with a control diet.”
Regarding the criticism that very-low-carbohydrate diets are high in saturated fat and therefore raise the risk of cardiovascular disease, Dr. Griauzde pointed to another meta-analysis of 21 prospective studies with more than 300,000 participants with 5-25 years of follow-up. In that analysis, the intake of saturated fat was not associated with an increased risk of cardiovascular disease or stroke.
Furthermore, a 12-week randomized controlled trial that involved 40 adults with overweight also suggested that a very-low-carb diet may be superior to a low-fat diet in improving aspects of the metabolic syndrome, including body mass index, lipid levels, and insulin sensitivity. Small LDL particles, which are more atherogenic than larger LDL particles, also decreased despite a threefold increase in saturated fat intake.
Rebuttals: Overall diet, patient preference matter
During the rebuttals, Dr. Kirkpatrick pointed out that large LDL particles are also atherogenic. In addition, she noted that the studies that showed that saturated fat isn’t associated with cardiovascular disease didn’t consider the macronutrients that replaced the saturated fat.
“It really is about increasing consumption of foods that we know are associated with cardiovascular benefit, including plant-based foods that are high quality and not refined carbohydrates ... and healthy protein sources. ... Hopefully we can step away from just looking at macronutrients and look at the total amount of food that people are choosing to eat.”
Importantly, Dr. Kirkpatrick said, patients need to be asked about their current dietary patterns and preferences. “Interventions should be patient centered and sensitive to cultural differences. Personalized lifestyle interventions increase the likelihood of success.”
Dr. Griauzde pointed out that newer antiobesity drugs can be added to any diet to decrease appetite and enhance adherence.
Dr. Griauzde also observed, “We can label a very-low-carbohydrate diet ‘extreme,’ but maybe, from the patient’s perspective, it’s extreme to take 200 units of insulin a day. If you can give them the opportunity to discontinue use of the insulin by following a very-low-carbohydrate dietary pattern, that is the opportunity that our patients deserve to have.”
But overall, she agreed with Dr. Kirkpatrick about individualizing any dietary approach: “We will never know from any of the trials that have been done or that will be done in the future what diet is best for an individual patient. ... Our job is to help our patients find the dietary approach that works best for them.”
Dr. Kirkpatrick is a clinical scientist with Midwest Biomedical Research, which has received funding from various food and pharmaceutical companies. She has not received any direct funding. Dr. Yancy is a consultant for The Simply Good Foods Co. Dr. Griauzde has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s an ongoing debate in the diabetes world: Is it ideal to consume a very-low-carbohydrate diet, or is it better to go with moderate amounts of healthful carbs?
At the annual scientific sessions of the American Diabetes Association, Carol F. Kirkpatrick, PhD, RDN, spoke first, arguing in favor of diets consisting of moderate, high-quality carbohydrates.
Dina Hafez Griauzde, MD, countered that very-low-carbohydrate diets are more beneficial for people with diabetes, primarily type 2 diabetes.
Both speakers based their arguments on published evidence but agreed in the end that discussion with patients about individual dietary preferences should play a major role in the ultimate decision.
Moderate-carbohydrate eating is best
Dr. Kirkpatrick began by explaining that definitions of “low carb” vary in the literature, which makes comparisons between studies difficult. On the basis of a 2019 review that she coauthored, “moderate” carbohydrate consumption was defined as a diet in which 26%-44% of total daily calories are from carbohydrates. “Low” carbohydrate consumption was defined as a diet in which 10%-25% of calories were from carbohydrates. Consuming less than 10% was defined as a very-low-carbohydrate diet (i.e., a ketogenic diet).
Across studies, she noted, the literature shows that within the first 6 months weight loss is typically greater with carbohydrate-restricted diets than with higher-carbohydrate diets, but that by 1 year and beyond weight loss is similar.
“That can be partly due to the difficulty in people maintaining that very severe dietary restriction, although ... we can all acknowledge that it’s difficult for patients to adhere to any dietary pattern, so for sure by 12 months, the difference in the weight loss is gone between the two,” said Dr. Kirkpatrick, of Midwest Biomedical Research, Pocatello, Idaho.
In a recent meta-analysis of 35 trials that examined the dose-dependent effects of carbohydrate restriction for patients with type 2 diabetes, there was a significant decrease in weight as carbohydrates were reduced. But by 12 months (17 trials), the greatest weight reduction was seen at 35% carbohydrate intake.
“It may just be that people were able to adhere to that moderate intake better,” she explained.
Regarding lipids, in her 2019 review and in several meta-analyses since, the effects on low-density lipoprotein cholesterol (LDL-C) varied. For some patients, adhering to a low-carb diet led to reductions in LDL-C, especially if the participants also lost weight, whereas in other patients, a low-carb diet led to an increase in LDL-C.
Either way, a high intake of saturated fatty acids is key to an increase in LDL-C, Dr. Kirkpatrick noted. “So, it’s important that, if a patient chooses to follow a very low carbohydrate diet or any kind of dietary pattern that restricts carbohydrate, that they replace the carbohydrate with unsaturated fat and not saturated fatty acid foods to avoid that increase in LDL-C.”
Generally, the evidence also shows that carbohydrate restriction typically leads to lower triglyceride levels and higher high-density lipoprotein (HDL) cholesterol levels. However, the same meta-analysis showed that the greatest reduction in LDL-C occurred at about 40% carbohydrate consumption.
Another recent meta-analysis showed that LDL-C rose significantly by an average 12.4 mg/dL with very-low-carb (3%-30%) diets, but only slightly, by 0.4 mg/dL, with moderate carb (40%-45%) intake.
Consuming very-low-carb diets did lead to greater reductions in triglycerides, compared with consuming moderate carb diets (23.9 mg/dL vs. 8.9 mg/dL).
“However, in terms of cardiovascular health, we are not entirely sure what that means. ... We have to look at the overall results in the presence of both triglyceride lowering as well as LDL cholesterol,” Dr. Kirkpatrick noted.
Carbohydrate restriction did consistently lead to lower hemoglobin A1c levels by an average of 0.4, 0.6, and 1.0 percentage points at 6 months for diets of 40%, 30%, and 15% carbohydrate, respectively. However, by 12 months, the effect had waned to 0.15, 0.2, and 0.4 A1c percentage points.
“Again, carbohydrate restriction, especially severe, is difficult for people to adhere to, and moderate carbohydrate intake would allow our patients to consume an appropriate amount of carbohydrate and still achieve improved glycemic control,” Dr. Kirkpatrick said.
Two large randomized controlled trials – PREDIMED and CORDIOPREV – examined the effects of the Mediterranean diet on cardiovascular disease prevention. Both showed a decrease in cardiovascular events with the Mediterranean diet, which involves consuming moderate amounts of carbohydrates.
“The Mediterranean dietary pattern has the strongest evidence for benefit, and it’s moderate in carbohydrates,” she concluded.
Very-low-carbohydrate eating is best
Dr. Griauzde was a last-minute replacement speaker for William S. Yancy Jr, MD, of Duke University, Durham, N.C., and presented his slides. She argued that consuming a very low carb diet improves glycemia and that it does not increase but possibly lowers cardiovascular risk.
She began by noting that prior to the discovery of insulin very-low-carb diets had been consumed for over a century to prolong life for people with type 1 diabetes.
“We have long recognized the deleterious role of carbohydrate in type 1 diabetes management, and we have increasingly recognized that role in the management of type 2 diabetes,” said Dr. Griauzde of the University of Michigan in Ann Arbor.
In a small study that compared maintaining a very-low-carb diet for 2 weeks with maintaining a high-carb diet for 2 weeks, total glucose areas under the curve were substantially lower (P < .05) during the low-carb phase, while A1c levels dropped from 7.3% to 6.8% (P = .006).
“We don’t see those outcomes with meds,” Dr. Griauzde noted, adding, “A diet very low in carbohydrates is one of the most potent tools we have to help our patients achieve glycemic control.”
Dr. Griauzde said that the carbohydrate-insulin model provides an explanation for why dietary carbohydrates are particularly obesogenic and metabolically harmful. That model contrasts with the energy balance model, which suggests that all calories are equal.
The rationale of the carbohydrate-insulin model is that dietary carbohydrate – either sugar or starch – raises serum glucose and insulin levels. A carbohydrate-restricted diet therefore reduces the dietary contribution to serum glucose, which then results in lower insulin levels. Insulin is a potent stimulator of lipogenesis (fat storage), and it is a potent inhibitor of lipolysis (the burning of fat). By lowering insulin levels, stored body fat is burned, serum ketone levels increase, and body weight is lowered.
This model suggests that, when insulin levels are chronically high because of excess carbohydrate consumption, circulating fuels are lowered, which leads to an increase in hunger and to overeating. This was demonstrated in a study that compared different levels of isocaloric glycemic index diets in 12 teenage boys with overweight or obesity. The higher-carbohydrate meals led to higher glucose and insulin levels and more food consumption.
In a systematic review of 13 trials of restricted-carbohydrate diets (< 45% carbohydrates) for adults with diabetes, the degree of improvement in A1c level correlated with the degree of carbohydrate restriction over 2-26 weeks (P = .013).
And in a network meta-analysis of 56 trials that compared nine diets among a total of 4,937 participants with type 2 diabetes, one conclusion was that “for reducing A1c, the low-carbohydrate diet was ranked as the best dietary approach (SUCRA: 84%), followed by the Mediterranean diet (80%), and Paleolithic diet (76%), compared with a control diet.”
Regarding the criticism that very-low-carbohydrate diets are high in saturated fat and therefore raise the risk of cardiovascular disease, Dr. Griauzde pointed to another meta-analysis of 21 prospective studies with more than 300,000 participants with 5-25 years of follow-up. In that analysis, the intake of saturated fat was not associated with an increased risk of cardiovascular disease or stroke.
Furthermore, a 12-week randomized controlled trial that involved 40 adults with overweight also suggested that a very-low-carb diet may be superior to a low-fat diet in improving aspects of the metabolic syndrome, including body mass index, lipid levels, and insulin sensitivity. Small LDL particles, which are more atherogenic than larger LDL particles, also decreased despite a threefold increase in saturated fat intake.
Rebuttals: Overall diet, patient preference matter
During the rebuttals, Dr. Kirkpatrick pointed out that large LDL particles are also atherogenic. In addition, she noted that the studies that showed that saturated fat isn’t associated with cardiovascular disease didn’t consider the macronutrients that replaced the saturated fat.
“It really is about increasing consumption of foods that we know are associated with cardiovascular benefit, including plant-based foods that are high quality and not refined carbohydrates ... and healthy protein sources. ... Hopefully we can step away from just looking at macronutrients and look at the total amount of food that people are choosing to eat.”
Importantly, Dr. Kirkpatrick said, patients need to be asked about their current dietary patterns and preferences. “Interventions should be patient centered and sensitive to cultural differences. Personalized lifestyle interventions increase the likelihood of success.”
Dr. Griauzde pointed out that newer antiobesity drugs can be added to any diet to decrease appetite and enhance adherence.
Dr. Griauzde also observed, “We can label a very-low-carbohydrate diet ‘extreme,’ but maybe, from the patient’s perspective, it’s extreme to take 200 units of insulin a day. If you can give them the opportunity to discontinue use of the insulin by following a very-low-carbohydrate dietary pattern, that is the opportunity that our patients deserve to have.”
But overall, she agreed with Dr. Kirkpatrick about individualizing any dietary approach: “We will never know from any of the trials that have been done or that will be done in the future what diet is best for an individual patient. ... Our job is to help our patients find the dietary approach that works best for them.”
Dr. Kirkpatrick is a clinical scientist with Midwest Biomedical Research, which has received funding from various food and pharmaceutical companies. She has not received any direct funding. Dr. Yancy is a consultant for The Simply Good Foods Co. Dr. Griauzde has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADA 2023
Weight loss linked to mortality risk in older women
Weight loss of at least 5% over a 3-year period was associated with significantly increased mortality in women at age 90, 95, and 100 years compared with those whose weight remained stable, based on data from more than 50,000 individuals.
Previous studies of later-life weight changes and mortality have yielded inconsistent results driven by considerations of weight loss intentionality, and data on older adults in particular are limited, wrote Aladdin H. Shadyab, PhD, of the University of California, San Diego, and colleagues.
In a study published in the Journals of Gerontology: Medical Sciences, the researchers reviewed data from the Women’s Health Initiative, a prospective study of factors affecting chronic disease development in postmenopausal women. The study population included 54,437 women who entered the WHI between 1993 and 1998 at ages 50-79 years. The mean baseline age was 69.8 years; 89.5% of the participants were White, 5.7% were Black, 2.7% were Asian, 2.5% were Hispanic/Latino, and the remaining 1.0% were multiracial, American Indian/Alaskan Native, Native Hawaiian/Other Pacific Islander, or unknown.
The primary outcomes were the associations of short-term (3-year) and long-term (10-year) weight changes with survival to ages 90, 95, and 100 years.
A total of 30,647 women survived to at least 90 years (56.3%).
Overall, women with a short-term weight loss of 5% or more of body weight were 33% less likely to survive to age 90 years, 35% less likely to survive to age 95 years, and 38% less likely to survive to age 100 years than were those whose weight remained stable (odds ratios, 0.67, 0.65, and 0.62, respectively).
The associations were stronger in cases of unintentional short-term weight loss. Intentional weight loss from baseline to year 3 was associated with 17% lower odds of survival to age 90 compared to stable weight (OR, 0.83), but unintentional weight loss was associated with 51% lower odds of survival to age 90 (OR, 0.49).
Similarly, women with 10-year weight loss of at least 5% were 40% less likely to survive to 90 years and 49% less likely to survive to 95 years (OR, 0.60 and OR, 0.51, respectively). The sample size was too small to assess the relation of 10-year weight loss with survival to 100 years, and intentionality was not assessed for 10-year weight changes.
By contrast, weight gain of at least 5% had no significant effect on survival to ages 90, 95, or 100 years, but stable weight over time increased the odds of living to ages 90 to 100 years by 1.2-fold to 2-fold compared to either intentional or unintentional weight loss of at least 5%.
The trends in results were similar across body weight categories (normal weight, overweight, and obese as defined by body mass index). Baseline age and smoking status had no significant effect on the results.
Some of the proportion of self-reported intentional weight loss in the study population may have been unintentional, the researchers wrote in their discussion.
“It is important to note that perceived intentionality of weight loss may be influenced by the many societal pressures to lose weight, especially among women, and therefore overestimate the behavioral changes underlying experienced weight loss in older adults,” they said.
The findings were limited by several factors including the potential for inaccurate self-reported weight loss intention, and the likelihood that the mean older age of the population at baseline (older than 60 years) meant that they were more likely to live longer regardless of weight changes, the researchers noted. Other limitations included the primarily White study population, and other residual confounding factors such as ill health that might drive weight loss, the researchers noted.
However, the results were strengthened by the large sample size and long follow-up period, and suggest that “blanket recommendations for weight loss in older women are unlikely to lead to better survival at advanced ages,” they concluded.
Data support weight monitoring
The investigators acknowledged that their data do not affect clinical recommendations for moderate weight loss in older women to improve health outcomes, especially in those with overweight or obesity, but instead “support close monitoring of the amount and speed of weight loss, particularly when unintentional, as an indicator of underlying poor health and predictor of decreased lifespan in older women.”
Neil Skolnik, MD, professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, agreed with this conclusion. The current study suggests that when older women lose a significant amount of weight unintentionally, it could be a sign of failing health, he said.
Weight gain or loss in old age is very different from weight issues in younger people, where clinicians may be encouraging weight loss to improve health outcomes, Dr. Skolnik said in an interview.
A key take-home message for clinicians, in addition to monitoring weight in older patients, is to emphasize nutrition for individuals in their 80s, 90s, and beyond, he said.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Shadyab had no financial conflicts to disclose. Dr. Skolnik had no financial conflicts to disclose and serves on the editorial advisory board of Family Practice News.
Weight loss of at least 5% over a 3-year period was associated with significantly increased mortality in women at age 90, 95, and 100 years compared with those whose weight remained stable, based on data from more than 50,000 individuals.
Previous studies of later-life weight changes and mortality have yielded inconsistent results driven by considerations of weight loss intentionality, and data on older adults in particular are limited, wrote Aladdin H. Shadyab, PhD, of the University of California, San Diego, and colleagues.
In a study published in the Journals of Gerontology: Medical Sciences, the researchers reviewed data from the Women’s Health Initiative, a prospective study of factors affecting chronic disease development in postmenopausal women. The study population included 54,437 women who entered the WHI between 1993 and 1998 at ages 50-79 years. The mean baseline age was 69.8 years; 89.5% of the participants were White, 5.7% were Black, 2.7% were Asian, 2.5% were Hispanic/Latino, and the remaining 1.0% were multiracial, American Indian/Alaskan Native, Native Hawaiian/Other Pacific Islander, or unknown.
The primary outcomes were the associations of short-term (3-year) and long-term (10-year) weight changes with survival to ages 90, 95, and 100 years.
A total of 30,647 women survived to at least 90 years (56.3%).
Overall, women with a short-term weight loss of 5% or more of body weight were 33% less likely to survive to age 90 years, 35% less likely to survive to age 95 years, and 38% less likely to survive to age 100 years than were those whose weight remained stable (odds ratios, 0.67, 0.65, and 0.62, respectively).
The associations were stronger in cases of unintentional short-term weight loss. Intentional weight loss from baseline to year 3 was associated with 17% lower odds of survival to age 90 compared to stable weight (OR, 0.83), but unintentional weight loss was associated with 51% lower odds of survival to age 90 (OR, 0.49).
Similarly, women with 10-year weight loss of at least 5% were 40% less likely to survive to 90 years and 49% less likely to survive to 95 years (OR, 0.60 and OR, 0.51, respectively). The sample size was too small to assess the relation of 10-year weight loss with survival to 100 years, and intentionality was not assessed for 10-year weight changes.
By contrast, weight gain of at least 5% had no significant effect on survival to ages 90, 95, or 100 years, but stable weight over time increased the odds of living to ages 90 to 100 years by 1.2-fold to 2-fold compared to either intentional or unintentional weight loss of at least 5%.
The trends in results were similar across body weight categories (normal weight, overweight, and obese as defined by body mass index). Baseline age and smoking status had no significant effect on the results.
Some of the proportion of self-reported intentional weight loss in the study population may have been unintentional, the researchers wrote in their discussion.
“It is important to note that perceived intentionality of weight loss may be influenced by the many societal pressures to lose weight, especially among women, and therefore overestimate the behavioral changes underlying experienced weight loss in older adults,” they said.
The findings were limited by several factors including the potential for inaccurate self-reported weight loss intention, and the likelihood that the mean older age of the population at baseline (older than 60 years) meant that they were more likely to live longer regardless of weight changes, the researchers noted. Other limitations included the primarily White study population, and other residual confounding factors such as ill health that might drive weight loss, the researchers noted.
However, the results were strengthened by the large sample size and long follow-up period, and suggest that “blanket recommendations for weight loss in older women are unlikely to lead to better survival at advanced ages,” they concluded.
Data support weight monitoring
The investigators acknowledged that their data do not affect clinical recommendations for moderate weight loss in older women to improve health outcomes, especially in those with overweight or obesity, but instead “support close monitoring of the amount and speed of weight loss, particularly when unintentional, as an indicator of underlying poor health and predictor of decreased lifespan in older women.”
Neil Skolnik, MD, professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, agreed with this conclusion. The current study suggests that when older women lose a significant amount of weight unintentionally, it could be a sign of failing health, he said.
Weight gain or loss in old age is very different from weight issues in younger people, where clinicians may be encouraging weight loss to improve health outcomes, Dr. Skolnik said in an interview.
A key take-home message for clinicians, in addition to monitoring weight in older patients, is to emphasize nutrition for individuals in their 80s, 90s, and beyond, he said.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Shadyab had no financial conflicts to disclose. Dr. Skolnik had no financial conflicts to disclose and serves on the editorial advisory board of Family Practice News.
Weight loss of at least 5% over a 3-year period was associated with significantly increased mortality in women at age 90, 95, and 100 years compared with those whose weight remained stable, based on data from more than 50,000 individuals.
Previous studies of later-life weight changes and mortality have yielded inconsistent results driven by considerations of weight loss intentionality, and data on older adults in particular are limited, wrote Aladdin H. Shadyab, PhD, of the University of California, San Diego, and colleagues.
In a study published in the Journals of Gerontology: Medical Sciences, the researchers reviewed data from the Women’s Health Initiative, a prospective study of factors affecting chronic disease development in postmenopausal women. The study population included 54,437 women who entered the WHI between 1993 and 1998 at ages 50-79 years. The mean baseline age was 69.8 years; 89.5% of the participants were White, 5.7% were Black, 2.7% were Asian, 2.5% were Hispanic/Latino, and the remaining 1.0% were multiracial, American Indian/Alaskan Native, Native Hawaiian/Other Pacific Islander, or unknown.
The primary outcomes were the associations of short-term (3-year) and long-term (10-year) weight changes with survival to ages 90, 95, and 100 years.
A total of 30,647 women survived to at least 90 years (56.3%).
Overall, women with a short-term weight loss of 5% or more of body weight were 33% less likely to survive to age 90 years, 35% less likely to survive to age 95 years, and 38% less likely to survive to age 100 years than were those whose weight remained stable (odds ratios, 0.67, 0.65, and 0.62, respectively).
The associations were stronger in cases of unintentional short-term weight loss. Intentional weight loss from baseline to year 3 was associated with 17% lower odds of survival to age 90 compared to stable weight (OR, 0.83), but unintentional weight loss was associated with 51% lower odds of survival to age 90 (OR, 0.49).
Similarly, women with 10-year weight loss of at least 5% were 40% less likely to survive to 90 years and 49% less likely to survive to 95 years (OR, 0.60 and OR, 0.51, respectively). The sample size was too small to assess the relation of 10-year weight loss with survival to 100 years, and intentionality was not assessed for 10-year weight changes.
By contrast, weight gain of at least 5% had no significant effect on survival to ages 90, 95, or 100 years, but stable weight over time increased the odds of living to ages 90 to 100 years by 1.2-fold to 2-fold compared to either intentional or unintentional weight loss of at least 5%.
The trends in results were similar across body weight categories (normal weight, overweight, and obese as defined by body mass index). Baseline age and smoking status had no significant effect on the results.
Some of the proportion of self-reported intentional weight loss in the study population may have been unintentional, the researchers wrote in their discussion.
“It is important to note that perceived intentionality of weight loss may be influenced by the many societal pressures to lose weight, especially among women, and therefore overestimate the behavioral changes underlying experienced weight loss in older adults,” they said.
The findings were limited by several factors including the potential for inaccurate self-reported weight loss intention, and the likelihood that the mean older age of the population at baseline (older than 60 years) meant that they were more likely to live longer regardless of weight changes, the researchers noted. Other limitations included the primarily White study population, and other residual confounding factors such as ill health that might drive weight loss, the researchers noted.
However, the results were strengthened by the large sample size and long follow-up period, and suggest that “blanket recommendations for weight loss in older women are unlikely to lead to better survival at advanced ages,” they concluded.
Data support weight monitoring
The investigators acknowledged that their data do not affect clinical recommendations for moderate weight loss in older women to improve health outcomes, especially in those with overweight or obesity, but instead “support close monitoring of the amount and speed of weight loss, particularly when unintentional, as an indicator of underlying poor health and predictor of decreased lifespan in older women.”
Neil Skolnik, MD, professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, agreed with this conclusion. The current study suggests that when older women lose a significant amount of weight unintentionally, it could be a sign of failing health, he said.
Weight gain or loss in old age is very different from weight issues in younger people, where clinicians may be encouraging weight loss to improve health outcomes, Dr. Skolnik said in an interview.
A key take-home message for clinicians, in addition to monitoring weight in older patients, is to emphasize nutrition for individuals in their 80s, 90s, and beyond, he said.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Shadyab had no financial conflicts to disclose. Dr. Skolnik had no financial conflicts to disclose and serves on the editorial advisory board of Family Practice News.
FROM THE JOURNALS OF GERONTOLOGY: MEDICAL SCIENCES



