User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Early menopause linked with increased risk of heart problems
SEOUL, South Korea – Menopause before age 40 is associated with elevated risk of heart failure and atrial fibrillation, according to a study published in European Heart Journal, from the European Society of Cardiology (ESC). The study of more than 1.4 million women revealed that the younger the age at menopause, the higher the risk of heart failure and atrial fibrillation.
“Women with premature menopause should be aware that they may be more likely to develop heart failure or atrial fibrillation than their peers,” said study author Ga Eun Nam, MD, PhD, of Korea University College of Medicine, Seoul. “This may be good motivation to improve lifestyle habits known to be linked with heart disease, such as quitting smoking and exercising.”
Cardiovascular disease typically occurs up to 10 years later in women than men. Premenopausal women are thought to benefit from estrogen’s protective effect on the cardiovascular system. The cessation of menstruation and subsequent decline of estrogen levels may make women more vulnerable to cardiovascular disease.
A national population
Premature menopause affects 1% of women younger than 40 years, the ESC press release stated. Prior studies have found a link between premature (before age 40 years) and early (before age 45 years) menopause and cardiovascular disease overall, but the evidence for heart failure or atrial fibrillation alone is limited. This study examined the associations between premature menopause, age at menopause, and incident heart failure and atrial fibrillation. Data were obtained from the Korean National Health Insurance System (NHIS), which provides health screening at least every 2 years and includes 97% of the population.
The study included 1,401,175 postmenopausal women aged 30 years and older who completed the NHIS health checkup in 2009. Participants were monitored until the end of 2018 for new-onset heart failure and atrial fibrillation. Information was collected on demographics, health behaviors, and reproductive factors, including age at menopause and use of hormone replacement therapy (HRT). Age at menopause was split into four categories: younger than 40 years, 40-44 years, 45-49 years, and 50 years or older. Premature menopause was defined as having the final menstrual period before age 40 years.
Some 28,111 (2%) participants had a history of premature menopause. For these women, the average age at menopause was 36.7 years. The average age at study enrollment for women with and for those without a history of premature menopause was 60 and 61.5 years, respectively. During an average follow-up of 9.1 years, 42,699 (3.0%) developed heart failure, and 44,834 (3.2%) developed atrial fibrillation.
The researchers analyzed the association between history of premature menopause and incident heart failure and atrial fibrillation after adjusting for age, smoking, alcohol use, physical activity, income, body mass index, hypertension, type 2 diabetes, dyslipidemia, chronic kidney disease, coronary heart disease, HRT, and age at menarche. Women who experienced premature menopause had a 33% higher risk for heart failure and 9% higher risk for atrial fibrillation, compared with those who did not.
Reproductive history
The researchers then analyzed the associations between age at menopause and incidence of heart failure and atrial fibrillation after adjusting for the same factors as in the previous analyses. The risk for incident heart failure increased as the age at menopause decreased. Compared with women aged 50 years and older at menopause, those aged 45-49 years, 40-44 years, and younger than 40 years at menopause had 11%, 23%, and 39% greater risk for incident heart failure, respectively. Similarly, the risk for incident atrial fibrillation increased as the age at menopause decreased; the risk was 4%, 10%, and 11% higher for those aged 45-49 years, 40-44 years, and younger than 40 years at menopause, respectively, compared with women aged 50 years and older at menopause.
The authors said that several factors may explain the associations between menopausal age, heart failure, and atrial fibrillation, such as the drop in estrogen levels and changes in body fat distribution.
Dr. Nam concluded, “The misconception that heart disease primarily affects men has meant that sex-specific risk factors have been largely ignored. Evidence is growing that undergoing menopause before the age of 40 years may increase the likelihood of heart disease later in life. Our study indicates that reproductive history should be routinely considered in addition to traditional risk factors such as smoking when evaluating the future likelihood of heart failure and atrial fibrillation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
SEOUL, South Korea – Menopause before age 40 is associated with elevated risk of heart failure and atrial fibrillation, according to a study published in European Heart Journal, from the European Society of Cardiology (ESC). The study of more than 1.4 million women revealed that the younger the age at menopause, the higher the risk of heart failure and atrial fibrillation.
“Women with premature menopause should be aware that they may be more likely to develop heart failure or atrial fibrillation than their peers,” said study author Ga Eun Nam, MD, PhD, of Korea University College of Medicine, Seoul. “This may be good motivation to improve lifestyle habits known to be linked with heart disease, such as quitting smoking and exercising.”
Cardiovascular disease typically occurs up to 10 years later in women than men. Premenopausal women are thought to benefit from estrogen’s protective effect on the cardiovascular system. The cessation of menstruation and subsequent decline of estrogen levels may make women more vulnerable to cardiovascular disease.
A national population
Premature menopause affects 1% of women younger than 40 years, the ESC press release stated. Prior studies have found a link between premature (before age 40 years) and early (before age 45 years) menopause and cardiovascular disease overall, but the evidence for heart failure or atrial fibrillation alone is limited. This study examined the associations between premature menopause, age at menopause, and incident heart failure and atrial fibrillation. Data were obtained from the Korean National Health Insurance System (NHIS), which provides health screening at least every 2 years and includes 97% of the population.
The study included 1,401,175 postmenopausal women aged 30 years and older who completed the NHIS health checkup in 2009. Participants were monitored until the end of 2018 for new-onset heart failure and atrial fibrillation. Information was collected on demographics, health behaviors, and reproductive factors, including age at menopause and use of hormone replacement therapy (HRT). Age at menopause was split into four categories: younger than 40 years, 40-44 years, 45-49 years, and 50 years or older. Premature menopause was defined as having the final menstrual period before age 40 years.
Some 28,111 (2%) participants had a history of premature menopause. For these women, the average age at menopause was 36.7 years. The average age at study enrollment for women with and for those without a history of premature menopause was 60 and 61.5 years, respectively. During an average follow-up of 9.1 years, 42,699 (3.0%) developed heart failure, and 44,834 (3.2%) developed atrial fibrillation.
The researchers analyzed the association between history of premature menopause and incident heart failure and atrial fibrillation after adjusting for age, smoking, alcohol use, physical activity, income, body mass index, hypertension, type 2 diabetes, dyslipidemia, chronic kidney disease, coronary heart disease, HRT, and age at menarche. Women who experienced premature menopause had a 33% higher risk for heart failure and 9% higher risk for atrial fibrillation, compared with those who did not.
Reproductive history
The researchers then analyzed the associations between age at menopause and incidence of heart failure and atrial fibrillation after adjusting for the same factors as in the previous analyses. The risk for incident heart failure increased as the age at menopause decreased. Compared with women aged 50 years and older at menopause, those aged 45-49 years, 40-44 years, and younger than 40 years at menopause had 11%, 23%, and 39% greater risk for incident heart failure, respectively. Similarly, the risk for incident atrial fibrillation increased as the age at menopause decreased; the risk was 4%, 10%, and 11% higher for those aged 45-49 years, 40-44 years, and younger than 40 years at menopause, respectively, compared with women aged 50 years and older at menopause.
The authors said that several factors may explain the associations between menopausal age, heart failure, and atrial fibrillation, such as the drop in estrogen levels and changes in body fat distribution.
Dr. Nam concluded, “The misconception that heart disease primarily affects men has meant that sex-specific risk factors have been largely ignored. Evidence is growing that undergoing menopause before the age of 40 years may increase the likelihood of heart disease later in life. Our study indicates that reproductive history should be routinely considered in addition to traditional risk factors such as smoking when evaluating the future likelihood of heart failure and atrial fibrillation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
SEOUL, South Korea – Menopause before age 40 is associated with elevated risk of heart failure and atrial fibrillation, according to a study published in European Heart Journal, from the European Society of Cardiology (ESC). The study of more than 1.4 million women revealed that the younger the age at menopause, the higher the risk of heart failure and atrial fibrillation.
“Women with premature menopause should be aware that they may be more likely to develop heart failure or atrial fibrillation than their peers,” said study author Ga Eun Nam, MD, PhD, of Korea University College of Medicine, Seoul. “This may be good motivation to improve lifestyle habits known to be linked with heart disease, such as quitting smoking and exercising.”
Cardiovascular disease typically occurs up to 10 years later in women than men. Premenopausal women are thought to benefit from estrogen’s protective effect on the cardiovascular system. The cessation of menstruation and subsequent decline of estrogen levels may make women more vulnerable to cardiovascular disease.
A national population
Premature menopause affects 1% of women younger than 40 years, the ESC press release stated. Prior studies have found a link between premature (before age 40 years) and early (before age 45 years) menopause and cardiovascular disease overall, but the evidence for heart failure or atrial fibrillation alone is limited. This study examined the associations between premature menopause, age at menopause, and incident heart failure and atrial fibrillation. Data were obtained from the Korean National Health Insurance System (NHIS), which provides health screening at least every 2 years and includes 97% of the population.
The study included 1,401,175 postmenopausal women aged 30 years and older who completed the NHIS health checkup in 2009. Participants were monitored until the end of 2018 for new-onset heart failure and atrial fibrillation. Information was collected on demographics, health behaviors, and reproductive factors, including age at menopause and use of hormone replacement therapy (HRT). Age at menopause was split into four categories: younger than 40 years, 40-44 years, 45-49 years, and 50 years or older. Premature menopause was defined as having the final menstrual period before age 40 years.
Some 28,111 (2%) participants had a history of premature menopause. For these women, the average age at menopause was 36.7 years. The average age at study enrollment for women with and for those without a history of premature menopause was 60 and 61.5 years, respectively. During an average follow-up of 9.1 years, 42,699 (3.0%) developed heart failure, and 44,834 (3.2%) developed atrial fibrillation.
The researchers analyzed the association between history of premature menopause and incident heart failure and atrial fibrillation after adjusting for age, smoking, alcohol use, physical activity, income, body mass index, hypertension, type 2 diabetes, dyslipidemia, chronic kidney disease, coronary heart disease, HRT, and age at menarche. Women who experienced premature menopause had a 33% higher risk for heart failure and 9% higher risk for atrial fibrillation, compared with those who did not.
Reproductive history
The researchers then analyzed the associations between age at menopause and incidence of heart failure and atrial fibrillation after adjusting for the same factors as in the previous analyses. The risk for incident heart failure increased as the age at menopause decreased. Compared with women aged 50 years and older at menopause, those aged 45-49 years, 40-44 years, and younger than 40 years at menopause had 11%, 23%, and 39% greater risk for incident heart failure, respectively. Similarly, the risk for incident atrial fibrillation increased as the age at menopause decreased; the risk was 4%, 10%, and 11% higher for those aged 45-49 years, 40-44 years, and younger than 40 years at menopause, respectively, compared with women aged 50 years and older at menopause.
The authors said that several factors may explain the associations between menopausal age, heart failure, and atrial fibrillation, such as the drop in estrogen levels and changes in body fat distribution.
Dr. Nam concluded, “The misconception that heart disease primarily affects men has meant that sex-specific risk factors have been largely ignored. Evidence is growing that undergoing menopause before the age of 40 years may increase the likelihood of heart disease later in life. Our study indicates that reproductive history should be routinely considered in addition to traditional risk factors such as smoking when evaluating the future likelihood of heart failure and atrial fibrillation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
NSAIDs linked to heart failure risk in diabetes
People with diabetes who take nonsteroidal anti-inflammatory drugs even on a short-term basis may have about a 50% greater risk of developing heart failure, according to results from a national registry study of more than 330,000 patients to be presented at the annual congress of the European Society of Cardiology.
“According to data from this study, even short-term NSAID use – within 28 days – in patients with type 2 diabetes mellitus are associated with an increased risk of first-time heart failure hospitalization,” lead author Anders Holt, MD, said in an interview.
“Further, it seems that patients above 79 years of age or with elevated hemoglobin A1c levels, along with new users of NSAIDs, are particularly susceptible.” He added that no such association was found in patients below age 65 years with normal A1c levels.
Dr. Holt has a dual appointment as a cardiologist at Copenhagen University and Herlev-Gentofte Hospital in Hellerup, Denmark, and the department of epidemiology and biostatistics at the University of Auckland (New Zealand). Jarl Emmanuel Strange, MD, PhD, a fellow at Copenhagen University, is to present the abstract on Aug. 26.
“This is quite an important observation given that, unfortunately, NSAIDs continue to be prescribed rather easily to people with diabetes and these agents do have risk,” said Rodica Busui, MD, PhD, codirector of the JDRF Center of Excellence at the University of Michigan, Ann Arbor, and president-elect for medicine and science of the American Diabetes Association. Dr. Busui is also lead author of an ADA/American College of Cardiology consensus report on heart failure in diabetes.
The study hypothesized that fluid retention “is a known but underappreciated side effect” of NSAID use and that short-term NSAID use could lead to heart failure in patients with type 2 diabetes, which has been linked to subclinical cardiomyopathy and kidney dysfunction.
“According to this study and particularly the subgroups analyses, it seems that incident heart failure associated with short-term NSAID use could be more than ‘just fluid overload,’ ” Dr. Holt said. “Further investigations into the specific mechanisms causing these associations are warranted.”
The study identified 331,189 patients with type 2 diabetes in nationwide Danish registries from 1998 to 2018. Median age was 62 years, and 23,308 (7%) were hospitalized with heart failure during follow-up, Dr. Holt said. Of them, 16% claimed at least one NSAID prescription within 2 years and 3% claimed they had at least three prescriptions.
Study follow-up started 120 days after the first-time type 2 diabetes diagnosis and focused on patients who had no previous diagnosis of heart failure or rheumatologic disease. The investigators reported on patients who had one, two, three or four prescriptions for NSAID within a year of starting follow-up.
The study used a case-crossover design, which, the abstract stated, “uses each individual as his or her own control making it suitable to study the effect of short-term exposure on immediate events while mitigating unmeasured confounding.”
Dr. Holt noted that short-term NSAID use was linked to increased risk of heart failure hospitalization (odds ratio, 1.43; 95% confidence interval, 1.27-1.63). The investigators identified even greater risks in three subgroups: age of at least 80 years (OR, 1.78; 95% CI, 1.39-2.28), elevated A1c levels treated with one or less antidiabetic medication (OR 1.68; 95% CI, 1-2.88), and patients without previous NSAID use (OR, 2.71; 95% CI, 1.78-4.23).
In the cohort, celecoxib and naproxen were rarely used (0.4 and 0.9%, respectively), while 3.3% of patients took diclofenac or 12.2% ibuprofen. The latter two NSAIDs had ORs of 1.48 and 1.46, respectively, for hospitalization for new-onset heart failure using 28-day exposure windows (95% CI for both, 1.1-2 and 1.26-1.69). No increased risk emerged for celecoxib or naproxen.
“High age and A1c levels and being a new user were tied to the strongest associations, along with known use of RASi [renin-angiotensin system inhibitors] and diuretics,” Dr. Holt said. “On the contrary, it seemed safe – from our data – to prescribe short-term NSAIDs for patients below 65 years of age and patients with normal A1c levels.
“Interestingly,” he added, “subclinical structural heart disease among patients with type 2 diabetes could play an important role.”
The findings are noteworthy, Dr. Busui said. “Although there are some limitations with the study design in general when one looks at data extracted from registers, the very large sample size and the fact that the Danish national register captures data in a standardized fashion does make the findings very relevant, especially now that we have confirmed that heart failure is the most prevalent cardiovascular complication in people with diabetes, as we have highlighted in the most recent ADA/ACC consensus on heart failure in diabetes.”
The study received funding from the Danish Heart Foundation and a number of private foundations. Dr. Holt and colleagues have no disclosures. Dr. Busui disclosed relationships with AstraZeneca, Boehringer Ingelheim–Lilly Alliance, Novo Nordisk, Averitas Pharma, Nevro, Regenacy Pharmaceuticals and Roche Diagnostics.
People with diabetes who take nonsteroidal anti-inflammatory drugs even on a short-term basis may have about a 50% greater risk of developing heart failure, according to results from a national registry study of more than 330,000 patients to be presented at the annual congress of the European Society of Cardiology.
“According to data from this study, even short-term NSAID use – within 28 days – in patients with type 2 diabetes mellitus are associated with an increased risk of first-time heart failure hospitalization,” lead author Anders Holt, MD, said in an interview.
“Further, it seems that patients above 79 years of age or with elevated hemoglobin A1c levels, along with new users of NSAIDs, are particularly susceptible.” He added that no such association was found in patients below age 65 years with normal A1c levels.
Dr. Holt has a dual appointment as a cardiologist at Copenhagen University and Herlev-Gentofte Hospital in Hellerup, Denmark, and the department of epidemiology and biostatistics at the University of Auckland (New Zealand). Jarl Emmanuel Strange, MD, PhD, a fellow at Copenhagen University, is to present the abstract on Aug. 26.
“This is quite an important observation given that, unfortunately, NSAIDs continue to be prescribed rather easily to people with diabetes and these agents do have risk,” said Rodica Busui, MD, PhD, codirector of the JDRF Center of Excellence at the University of Michigan, Ann Arbor, and president-elect for medicine and science of the American Diabetes Association. Dr. Busui is also lead author of an ADA/American College of Cardiology consensus report on heart failure in diabetes.
The study hypothesized that fluid retention “is a known but underappreciated side effect” of NSAID use and that short-term NSAID use could lead to heart failure in patients with type 2 diabetes, which has been linked to subclinical cardiomyopathy and kidney dysfunction.
“According to this study and particularly the subgroups analyses, it seems that incident heart failure associated with short-term NSAID use could be more than ‘just fluid overload,’ ” Dr. Holt said. “Further investigations into the specific mechanisms causing these associations are warranted.”
The study identified 331,189 patients with type 2 diabetes in nationwide Danish registries from 1998 to 2018. Median age was 62 years, and 23,308 (7%) were hospitalized with heart failure during follow-up, Dr. Holt said. Of them, 16% claimed at least one NSAID prescription within 2 years and 3% claimed they had at least three prescriptions.
Study follow-up started 120 days after the first-time type 2 diabetes diagnosis and focused on patients who had no previous diagnosis of heart failure or rheumatologic disease. The investigators reported on patients who had one, two, three or four prescriptions for NSAID within a year of starting follow-up.
The study used a case-crossover design, which, the abstract stated, “uses each individual as his or her own control making it suitable to study the effect of short-term exposure on immediate events while mitigating unmeasured confounding.”
Dr. Holt noted that short-term NSAID use was linked to increased risk of heart failure hospitalization (odds ratio, 1.43; 95% confidence interval, 1.27-1.63). The investigators identified even greater risks in three subgroups: age of at least 80 years (OR, 1.78; 95% CI, 1.39-2.28), elevated A1c levels treated with one or less antidiabetic medication (OR 1.68; 95% CI, 1-2.88), and patients without previous NSAID use (OR, 2.71; 95% CI, 1.78-4.23).
In the cohort, celecoxib and naproxen were rarely used (0.4 and 0.9%, respectively), while 3.3% of patients took diclofenac or 12.2% ibuprofen. The latter two NSAIDs had ORs of 1.48 and 1.46, respectively, for hospitalization for new-onset heart failure using 28-day exposure windows (95% CI for both, 1.1-2 and 1.26-1.69). No increased risk emerged for celecoxib or naproxen.
“High age and A1c levels and being a new user were tied to the strongest associations, along with known use of RASi [renin-angiotensin system inhibitors] and diuretics,” Dr. Holt said. “On the contrary, it seemed safe – from our data – to prescribe short-term NSAIDs for patients below 65 years of age and patients with normal A1c levels.
“Interestingly,” he added, “subclinical structural heart disease among patients with type 2 diabetes could play an important role.”
The findings are noteworthy, Dr. Busui said. “Although there are some limitations with the study design in general when one looks at data extracted from registers, the very large sample size and the fact that the Danish national register captures data in a standardized fashion does make the findings very relevant, especially now that we have confirmed that heart failure is the most prevalent cardiovascular complication in people with diabetes, as we have highlighted in the most recent ADA/ACC consensus on heart failure in diabetes.”
The study received funding from the Danish Heart Foundation and a number of private foundations. Dr. Holt and colleagues have no disclosures. Dr. Busui disclosed relationships with AstraZeneca, Boehringer Ingelheim–Lilly Alliance, Novo Nordisk, Averitas Pharma, Nevro, Regenacy Pharmaceuticals and Roche Diagnostics.
People with diabetes who take nonsteroidal anti-inflammatory drugs even on a short-term basis may have about a 50% greater risk of developing heart failure, according to results from a national registry study of more than 330,000 patients to be presented at the annual congress of the European Society of Cardiology.
“According to data from this study, even short-term NSAID use – within 28 days – in patients with type 2 diabetes mellitus are associated with an increased risk of first-time heart failure hospitalization,” lead author Anders Holt, MD, said in an interview.
“Further, it seems that patients above 79 years of age or with elevated hemoglobin A1c levels, along with new users of NSAIDs, are particularly susceptible.” He added that no such association was found in patients below age 65 years with normal A1c levels.
Dr. Holt has a dual appointment as a cardiologist at Copenhagen University and Herlev-Gentofte Hospital in Hellerup, Denmark, and the department of epidemiology and biostatistics at the University of Auckland (New Zealand). Jarl Emmanuel Strange, MD, PhD, a fellow at Copenhagen University, is to present the abstract on Aug. 26.
“This is quite an important observation given that, unfortunately, NSAIDs continue to be prescribed rather easily to people with diabetes and these agents do have risk,” said Rodica Busui, MD, PhD, codirector of the JDRF Center of Excellence at the University of Michigan, Ann Arbor, and president-elect for medicine and science of the American Diabetes Association. Dr. Busui is also lead author of an ADA/American College of Cardiology consensus report on heart failure in diabetes.
The study hypothesized that fluid retention “is a known but underappreciated side effect” of NSAID use and that short-term NSAID use could lead to heart failure in patients with type 2 diabetes, which has been linked to subclinical cardiomyopathy and kidney dysfunction.
“According to this study and particularly the subgroups analyses, it seems that incident heart failure associated with short-term NSAID use could be more than ‘just fluid overload,’ ” Dr. Holt said. “Further investigations into the specific mechanisms causing these associations are warranted.”
The study identified 331,189 patients with type 2 diabetes in nationwide Danish registries from 1998 to 2018. Median age was 62 years, and 23,308 (7%) were hospitalized with heart failure during follow-up, Dr. Holt said. Of them, 16% claimed at least one NSAID prescription within 2 years and 3% claimed they had at least three prescriptions.
Study follow-up started 120 days after the first-time type 2 diabetes diagnosis and focused on patients who had no previous diagnosis of heart failure or rheumatologic disease. The investigators reported on patients who had one, two, three or four prescriptions for NSAID within a year of starting follow-up.
The study used a case-crossover design, which, the abstract stated, “uses each individual as his or her own control making it suitable to study the effect of short-term exposure on immediate events while mitigating unmeasured confounding.”
Dr. Holt noted that short-term NSAID use was linked to increased risk of heart failure hospitalization (odds ratio, 1.43; 95% confidence interval, 1.27-1.63). The investigators identified even greater risks in three subgroups: age of at least 80 years (OR, 1.78; 95% CI, 1.39-2.28), elevated A1c levels treated with one or less antidiabetic medication (OR 1.68; 95% CI, 1-2.88), and patients without previous NSAID use (OR, 2.71; 95% CI, 1.78-4.23).
In the cohort, celecoxib and naproxen were rarely used (0.4 and 0.9%, respectively), while 3.3% of patients took diclofenac or 12.2% ibuprofen. The latter two NSAIDs had ORs of 1.48 and 1.46, respectively, for hospitalization for new-onset heart failure using 28-day exposure windows (95% CI for both, 1.1-2 and 1.26-1.69). No increased risk emerged for celecoxib or naproxen.
“High age and A1c levels and being a new user were tied to the strongest associations, along with known use of RASi [renin-angiotensin system inhibitors] and diuretics,” Dr. Holt said. “On the contrary, it seemed safe – from our data – to prescribe short-term NSAIDs for patients below 65 years of age and patients with normal A1c levels.
“Interestingly,” he added, “subclinical structural heart disease among patients with type 2 diabetes could play an important role.”
The findings are noteworthy, Dr. Busui said. “Although there are some limitations with the study design in general when one looks at data extracted from registers, the very large sample size and the fact that the Danish national register captures data in a standardized fashion does make the findings very relevant, especially now that we have confirmed that heart failure is the most prevalent cardiovascular complication in people with diabetes, as we have highlighted in the most recent ADA/ACC consensus on heart failure in diabetes.”
The study received funding from the Danish Heart Foundation and a number of private foundations. Dr. Holt and colleagues have no disclosures. Dr. Busui disclosed relationships with AstraZeneca, Boehringer Ingelheim–Lilly Alliance, Novo Nordisk, Averitas Pharma, Nevro, Regenacy Pharmaceuticals and Roche Diagnostics.
FROM ESC CONGRESS 2022
COVID to blame as U.S. life expectancy falls
All 50 states and the District of Columbia saw drops in life expectancy, according to the report from the Centers for Disease Control and Prevention’s National Center for Health Statistics.
The declines were mostly because of COVID-19 and “unintentional injuries,” such as drug overdoses.
The overall drop took national life expectancy from 78.8 years in 2019 to 77 years in 2020, the first year of the pandemic, ABC News reported.
States in the West and Northwest generally had higher life expectancy, with states in the South having the lowest.
Hawaii had the highest life expectancy at 80.7 years. It was followed by Washington, Minnesota, California, and Massachusetts. Mississippi had the lowest at 71.9 years, the figures show. The others in the bottom five were West Virginia, Louisiana, Alabama, and Kentucky.
In 2020, COVID-19 was the third-highest cause of death, leading to more than 350,000, the CDC reported earlier this year. At the same time, more people are dying annually from drug overdoses. A record 83,500 fatal overdoses were reported in 2020.
A version of this article first appeared on WebMD.com.
All 50 states and the District of Columbia saw drops in life expectancy, according to the report from the Centers for Disease Control and Prevention’s National Center for Health Statistics.
The declines were mostly because of COVID-19 and “unintentional injuries,” such as drug overdoses.
The overall drop took national life expectancy from 78.8 years in 2019 to 77 years in 2020, the first year of the pandemic, ABC News reported.
States in the West and Northwest generally had higher life expectancy, with states in the South having the lowest.
Hawaii had the highest life expectancy at 80.7 years. It was followed by Washington, Minnesota, California, and Massachusetts. Mississippi had the lowest at 71.9 years, the figures show. The others in the bottom five were West Virginia, Louisiana, Alabama, and Kentucky.
In 2020, COVID-19 was the third-highest cause of death, leading to more than 350,000, the CDC reported earlier this year. At the same time, more people are dying annually from drug overdoses. A record 83,500 fatal overdoses were reported in 2020.
A version of this article first appeared on WebMD.com.
All 50 states and the District of Columbia saw drops in life expectancy, according to the report from the Centers for Disease Control and Prevention’s National Center for Health Statistics.
The declines were mostly because of COVID-19 and “unintentional injuries,” such as drug overdoses.
The overall drop took national life expectancy from 78.8 years in 2019 to 77 years in 2020, the first year of the pandemic, ABC News reported.
States in the West and Northwest generally had higher life expectancy, with states in the South having the lowest.
Hawaii had the highest life expectancy at 80.7 years. It was followed by Washington, Minnesota, California, and Massachusetts. Mississippi had the lowest at 71.9 years, the figures show. The others in the bottom five were West Virginia, Louisiana, Alabama, and Kentucky.
In 2020, COVID-19 was the third-highest cause of death, leading to more than 350,000, the CDC reported earlier this year. At the same time, more people are dying annually from drug overdoses. A record 83,500 fatal overdoses were reported in 2020.
A version of this article first appeared on WebMD.com.
FDA clears tubeless, automated insulin system for children age 2 and older
The Food and Drug Administration has approved use of the Omnipod 5 automated insulin delivery system (Insulet Corp) for children aged 2 years and older with type 1 diabetes, the company announced on Aug. 22.
Omnipod 5 was originally cleared for use in individuals age 6 and older in Jan. 2022, as previously reported by this news organization. It is the third semi-automated closed-loop system approved in the United States but the first that is tubing-free. It integrates with the Dexcom G6 continuous glucose monitor system and a compatible smartphone to automatically adjust insulin and protect against high and low glucose levels.
“We received tremendous first-hand reports of how Omnipod 5 made diabetes management easier for our pivotal trial participants, and the clinical data demonstrated impressive glycemic improvements as well,” Trang Ly, MBBS, PhD, senior vice president and medical director at Insulet, said in a news release. “This expanded indication for younger children gives us great pride, knowing we can further ease the burden of glucose management for these children and their caregivers with our simple to use, elegant, automated insulin delivery system.”
In a recent clinical trial in very young children (age 2-5.9 years) with type 1 diabetes, Jennifer L. Sherr, MD, PhD, and colleagues found that the Omnipod 5 lowered A1c by 0.55 percentage points and reduced time in hypoglycemia (< 70 mg/dL) by 0.27%. According to their findings, published in Diabetes Care, time spent in target glucose range (70-180 mg/dL) increased by 11%, or by 2.6 hours more per day, in children in the study.
According to the release, the Omnipod 5 can now be prescribed to patients with insurance coverage. Patients can access their prescription through the pharmacy.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved use of the Omnipod 5 automated insulin delivery system (Insulet Corp) for children aged 2 years and older with type 1 diabetes, the company announced on Aug. 22.
Omnipod 5 was originally cleared for use in individuals age 6 and older in Jan. 2022, as previously reported by this news organization. It is the third semi-automated closed-loop system approved in the United States but the first that is tubing-free. It integrates with the Dexcom G6 continuous glucose monitor system and a compatible smartphone to automatically adjust insulin and protect against high and low glucose levels.
“We received tremendous first-hand reports of how Omnipod 5 made diabetes management easier for our pivotal trial participants, and the clinical data demonstrated impressive glycemic improvements as well,” Trang Ly, MBBS, PhD, senior vice president and medical director at Insulet, said in a news release. “This expanded indication for younger children gives us great pride, knowing we can further ease the burden of glucose management for these children and their caregivers with our simple to use, elegant, automated insulin delivery system.”
In a recent clinical trial in very young children (age 2-5.9 years) with type 1 diabetes, Jennifer L. Sherr, MD, PhD, and colleagues found that the Omnipod 5 lowered A1c by 0.55 percentage points and reduced time in hypoglycemia (< 70 mg/dL) by 0.27%. According to their findings, published in Diabetes Care, time spent in target glucose range (70-180 mg/dL) increased by 11%, or by 2.6 hours more per day, in children in the study.
According to the release, the Omnipod 5 can now be prescribed to patients with insurance coverage. Patients can access their prescription through the pharmacy.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved use of the Omnipod 5 automated insulin delivery system (Insulet Corp) for children aged 2 years and older with type 1 diabetes, the company announced on Aug. 22.
Omnipod 5 was originally cleared for use in individuals age 6 and older in Jan. 2022, as previously reported by this news organization. It is the third semi-automated closed-loop system approved in the United States but the first that is tubing-free. It integrates with the Dexcom G6 continuous glucose monitor system and a compatible smartphone to automatically adjust insulin and protect against high and low glucose levels.
“We received tremendous first-hand reports of how Omnipod 5 made diabetes management easier for our pivotal trial participants, and the clinical data demonstrated impressive glycemic improvements as well,” Trang Ly, MBBS, PhD, senior vice president and medical director at Insulet, said in a news release. “This expanded indication for younger children gives us great pride, knowing we can further ease the burden of glucose management for these children and their caregivers with our simple to use, elegant, automated insulin delivery system.”
In a recent clinical trial in very young children (age 2-5.9 years) with type 1 diabetes, Jennifer L. Sherr, MD, PhD, and colleagues found that the Omnipod 5 lowered A1c by 0.55 percentage points and reduced time in hypoglycemia (< 70 mg/dL) by 0.27%. According to their findings, published in Diabetes Care, time spent in target glucose range (70-180 mg/dL) increased by 11%, or by 2.6 hours more per day, in children in the study.
According to the release, the Omnipod 5 can now be prescribed to patients with insurance coverage. Patients can access their prescription through the pharmacy.
A version of this article first appeared on Medscape.com.
Metformin fails as early COVID-19 treatment but shows potential
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
No fish can escape this net ... of COVID testing
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
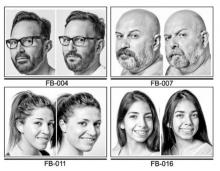
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
‘Conservative’ USPSTF primary prevention statin guidance finalized
Questions about how to prescribe statins for primary prevention abound more than 3 decades after the drugs swept into clinical practice to become a first-line medical approach to cutting cardiovascular (CV) risk. Statin usage recommendations from different bodies can vary in ways both limited and fundamental, spurring the kind of debate that accompanies such a document newly issued by the United States Preventive Services Task Force.
The document, little changed from the draft guidance released for public comment in February, was published online Aug. 23 in JAMA and the USPSTF website. It replaces a similar document issued by the task force in 2016.
The guidance has much in common with, but also sharp differences from, the influential 2018 guidelines on blood cholesterol management developed by the American College of Cardiology, American Heart Association, and 10 other medical societies.
And it is provocative enough to elicit at least four editorials issued the same day across the JAMA family of journals. They highlight key differences between the two documents, among them the USPSTF guidance’s consistent, narrow reliance on 7.5% and 10% cut points for 10-year risk levels as estimated from the ACC/AHA pooled cohort equations (PCE).
The guidance pairs the 10-year risk metric with at least one of only four prescribed CV risk factors to arrive at a limited choice of statin therapy recommendations. But its decision process isn’t bolstered by coronary artery calcium (CAC) scores or the prespecified “risk enhancers” that allowed the ACC/AHA-multisociety guidelines to be applied broadly and still be closely personalized. Those guidelines provide more PCE-based risk tiers for greater discrimination of risk and allow statins to be considered across a broader age group.
The USPSTF guidance’s evidence base consists of 23 clinical trials and three observational studies that directly compared a statin to either placebo or no statin, task force member John B. Wong, MD, Tufts University School of Medicine, Boston, told this news organization.
“In either kind of study, we found that the vast majority of patients had one or more of four risk factors – dyslipidemia, hypertension, diabetes, or smoking. So, when we categorized high risk or increased risk, we included the presence of one or more of those risk factors,” said Dr. Wong, who is director of comparative effectiveness research at Tufts Clinical Translational Science Institute.
‘Sensible and practical’
The USPSTF guidance applies only to adults aged 40-75 without CV signs or symptoms and recommends a statin prescription for persons at “high risk,” that is with an estimated 10-year PCE-based risk for death or CV events of 10% or higher plus at least one of the four risk factors, a level B recommendation.
It recommends that “clinicians selectively offer a statin” to such persons at “increased risk,” who have at least one of the risk factors and an estimated 10-year risk for death or CV events of 7.5% to less than 10%, a level C recommendation. “The likelihood of benefit is smaller in this group” than in persons at high risk, the document states.
“These recommendations from the USPSTF are sensible and practical,” states Salim S. Virani, MD, PhD, DeBakey Veterans Affairs Medical Center, Houston, in a related editorial published the same day in JAMA Network Open. He calls the former B-level recommendation “a conservative approach” and the latter C-level recommendation a “nuanced approach.”
Both are “understandable” given that some studies suggest that the PCE may overestimate the CV risk, Dr. Virani observes. “On the other hand, statin therapy has been shown to be efficacious” at 10-year CV-risk levels down to about 5%.
The USPSTF document “I think is going to perpetuate a problem that we have in this country, which is vast undertreatment of lipids,” Eric D. Peterson, MD, MPH, University of Texas Southwestern Medical Center, Dallas, said in an interview.
“We have a ton of good drugs that can lower cholesterol like crazy. If you lower cholesterol a lot, you improve outcomes,” he said. Dyslipidemia needs to be more widely and consistently treated, but “right now we have a pool of people in primary prevention who undertreat lipids and wait until disease happens – and then cardiologists get engaged. That’s an avoidable miss,” Dr. Peterson adds. He and JAMA Cardiology associate editor Ann Marie Navar, MD, PhD, provided JAMA with an editorial that accompanies the USPSTF guidance.
“My own personal bias would be that the [ACC/AHA-multisociety guidelines] are closer to being right,” Dr. Peterson said. They – unlike the USPSTF guidance – cover people with risk levels below 7.5%, down to at least 5%. They allow risk enhancers like metabolic syndrome, inflammatory diseases, or family history into the decision process. “And they’re more aggressive in diabetes and more aggressive in older people,” he said.
Higher threshold for therapy
The USPSTF guidance also explicitly omits some high-risk groups and makes little accommodation for others who might especially benefit from statins, several of the editorials contend. For example, states a related JAMA Cardiology editorial published the same day, “The USPSTF does not comment on familial hypercholesterolemia or an LDL-C level of 190 mg/dL or higher,” yet they are covered by the ACC/AHA-multispecialty guidelines.
In addition, write the editorialists, led by Neil J. Stone, MD, Northwestern University, Chicago, “the USPSTF uses a slightly higher threshold for initiation of statin therapy” than was used in the ACC/AHA-multisociety guidelines. USPSTF, for example, calls for 10-year risk to reach 10% before recommending a statin prescription.
“One concern about the USPSTF setting the bar higher for statin initiation is that it reduces the number of young patients (age 40-50 years) at risk for premature myocardial infarction considered for treatment,” write Dr. Stone and colleagues.
That may be related to a weakness of the PCE-based decision process. “Because the PCE estimates of 10-year CV disease risk rely so heavily on age, sex, and race, use of these estimates to identify candidates for statins results in significant skewing of the population recommended for statins,” write Dr. Navar and Dr. Peterson in their JAMA editorial.
The risk enhancers in the ACC/AHA-multispecialty guidelines, about a dozen of them, compensate for that limitation to some extent. But the PCE-dominated USPSTF risk estimates will likely miss some groups that could potentially benefit from statin therapy, Dr. Peterson agreed in an interview.
For example, younger adults facing years of high LDL-cholesterol levels could easily have PCE-based 10-year risk below 10%. “Having a high LDL over a lifetime puts you at really high risk,” he said. “Young people are missed even though their longitudinal risk is high.” So, by waiting for the lofty 10% level of risk over 10 years, “we limit the use of medicine that’s pretty cheap and highly effective.”
Dose intensity, adverse events
Also at variance from the ACC/AHA-multispecialty guidelines, the USPSTF states that, “Based on available evidence, use of moderate-intensity statin therapy seems reasonable for the primary prevention of CV disease in most persons.”
The task force specifically explored whether evidence supports some use of high-intensity vs. moderate-intensity statins, Tufts University’s Dr. Wong said. “We found only one study that looked at that particular question, and it didn’t give us a strong answer.” An elevated rosuvastatin-related diabetes risk was apparent in the JUPITER trial, “but for the other studies, we did not find that association.”
Most of the studies that explored statins for reducing risk for a first stroke or myocardial infarction used a moderate-dose statin, Dr. Wong said. “So that’s what we would usually recommend.”
But, Dr. Virani writes, consistent with the ACC/AHA-multispecialty guidelines, “clinicians should consider titrating the intensity of therapy to the risk of the individual.” Persons in certain high-risk primary prevention groups, such as those with end-organ injury from diabetes or LDL cholesterol at least 190 mg/dL, “may derive further benefit from the use of high-intensity statin therapy.”
Low-intensity statins are another potential option, but “in contrast with its 2016 recommendations, the USPSTF no longer recommends use of low-intensity statins in certain situations,” observes a fourth editorial published the same day in JAMA Internal Medicine, with lead author Anand R. Habib, MD, MPhil, and senior author Rita F. Redberg, MD, MSc, both of the University of California, San Francisco. Dr. Redberg is the journal’s editor and has long expressed cautions about statin safety.
“While it is understandable that the Task Force was limited by lack of data on dosing, this change is unfortunate for patients because the frequency of adverse effects increases as the statin dose increases,” the editorial states. Although USPSTF did not find statistically significant harm from the drugs, “in clinical practice, adverse events are commonly reported with use of statins.”
It continues: “At present, there are further reasons to curb our enthusiasm about the use of statins for primary prevention of CV disease.” To illustrate, the editorial questioned primary-prevention statins’ balance of risk vs. clinically meaningful benefit, not benefit that is merely statistically significant.
“The purported benefits of statins in terms of relative risk reduction are fairly constant across baseline lipid levels and cardiovascular risk score categories for primary prevention,” the editorial states.
“Therefore, the absolute benefit for those in lower-risk categories is likely small given that their baseline absolute risk is low, while the chance of adverse effects is constant across risk categories.”
However, USPSTF states, “In pooled analyses of trial data, statin therapy was not associated with increased risk of study withdrawal due to adverse events or serious adverse events.” Nor did it find significant associations with cancers, liver enzyme abnormalities, or diabetes, including new-onset diabetes.
And, the USPSTF adds, “Evidence on the association between statins and renal or cognitive harms is very limited but does not indicate increased risk.”
USPSTF is supported by the U.S. Agency for Healthcare Research and Quality. Dr. Virani discloses receiving grants from the Department of Veterans Affairs, National Institutes of Health, and the World Heart Federation; and personal fees from the American College of Cardiology. Dr. Peterson discloses serving on the JAMA editorial board and receiving research support to his institution from Amgen, Bristol-Myers Squibb, Esperion, and Janssen; and consulting fees from Novo Nordisk, Bayer, and Novartis. Dr. Navar discloses receiving research support to her institution from Amgen, Bristol-Myers Squibb, Esperion, and Janssen; and receiving honoraria and consulting fees from AstraZeneca, Boehringer Ingelheim, Bayer, Janssen, Lilly, Novo Nordisk, Novartis, New Amsterdam, and Pfizer. Dr. Stone discloses receiving an honorarium from Knowledge to Practice, an educational company not associated with the pharmaceutical industry; disclosures for the other authors are in the report. Dr. Redberg discloses receiving research funding from the Arnold Ventures Foundation and the Greenwall Foundation.
A version of this article first appeared on Medscape.com.
Questions about how to prescribe statins for primary prevention abound more than 3 decades after the drugs swept into clinical practice to become a first-line medical approach to cutting cardiovascular (CV) risk. Statin usage recommendations from different bodies can vary in ways both limited and fundamental, spurring the kind of debate that accompanies such a document newly issued by the United States Preventive Services Task Force.
The document, little changed from the draft guidance released for public comment in February, was published online Aug. 23 in JAMA and the USPSTF website. It replaces a similar document issued by the task force in 2016.
The guidance has much in common with, but also sharp differences from, the influential 2018 guidelines on blood cholesterol management developed by the American College of Cardiology, American Heart Association, and 10 other medical societies.
And it is provocative enough to elicit at least four editorials issued the same day across the JAMA family of journals. They highlight key differences between the two documents, among them the USPSTF guidance’s consistent, narrow reliance on 7.5% and 10% cut points for 10-year risk levels as estimated from the ACC/AHA pooled cohort equations (PCE).
The guidance pairs the 10-year risk metric with at least one of only four prescribed CV risk factors to arrive at a limited choice of statin therapy recommendations. But its decision process isn’t bolstered by coronary artery calcium (CAC) scores or the prespecified “risk enhancers” that allowed the ACC/AHA-multisociety guidelines to be applied broadly and still be closely personalized. Those guidelines provide more PCE-based risk tiers for greater discrimination of risk and allow statins to be considered across a broader age group.
The USPSTF guidance’s evidence base consists of 23 clinical trials and three observational studies that directly compared a statin to either placebo or no statin, task force member John B. Wong, MD, Tufts University School of Medicine, Boston, told this news organization.
“In either kind of study, we found that the vast majority of patients had one or more of four risk factors – dyslipidemia, hypertension, diabetes, or smoking. So, when we categorized high risk or increased risk, we included the presence of one or more of those risk factors,” said Dr. Wong, who is director of comparative effectiveness research at Tufts Clinical Translational Science Institute.
‘Sensible and practical’
The USPSTF guidance applies only to adults aged 40-75 without CV signs or symptoms and recommends a statin prescription for persons at “high risk,” that is with an estimated 10-year PCE-based risk for death or CV events of 10% or higher plus at least one of the four risk factors, a level B recommendation.
It recommends that “clinicians selectively offer a statin” to such persons at “increased risk,” who have at least one of the risk factors and an estimated 10-year risk for death or CV events of 7.5% to less than 10%, a level C recommendation. “The likelihood of benefit is smaller in this group” than in persons at high risk, the document states.
“These recommendations from the USPSTF are sensible and practical,” states Salim S. Virani, MD, PhD, DeBakey Veterans Affairs Medical Center, Houston, in a related editorial published the same day in JAMA Network Open. He calls the former B-level recommendation “a conservative approach” and the latter C-level recommendation a “nuanced approach.”
Both are “understandable” given that some studies suggest that the PCE may overestimate the CV risk, Dr. Virani observes. “On the other hand, statin therapy has been shown to be efficacious” at 10-year CV-risk levels down to about 5%.
The USPSTF document “I think is going to perpetuate a problem that we have in this country, which is vast undertreatment of lipids,” Eric D. Peterson, MD, MPH, University of Texas Southwestern Medical Center, Dallas, said in an interview.
“We have a ton of good drugs that can lower cholesterol like crazy. If you lower cholesterol a lot, you improve outcomes,” he said. Dyslipidemia needs to be more widely and consistently treated, but “right now we have a pool of people in primary prevention who undertreat lipids and wait until disease happens – and then cardiologists get engaged. That’s an avoidable miss,” Dr. Peterson adds. He and JAMA Cardiology associate editor Ann Marie Navar, MD, PhD, provided JAMA with an editorial that accompanies the USPSTF guidance.
“My own personal bias would be that the [ACC/AHA-multisociety guidelines] are closer to being right,” Dr. Peterson said. They – unlike the USPSTF guidance – cover people with risk levels below 7.5%, down to at least 5%. They allow risk enhancers like metabolic syndrome, inflammatory diseases, or family history into the decision process. “And they’re more aggressive in diabetes and more aggressive in older people,” he said.
Higher threshold for therapy
The USPSTF guidance also explicitly omits some high-risk groups and makes little accommodation for others who might especially benefit from statins, several of the editorials contend. For example, states a related JAMA Cardiology editorial published the same day, “The USPSTF does not comment on familial hypercholesterolemia or an LDL-C level of 190 mg/dL or higher,” yet they are covered by the ACC/AHA-multispecialty guidelines.
In addition, write the editorialists, led by Neil J. Stone, MD, Northwestern University, Chicago, “the USPSTF uses a slightly higher threshold for initiation of statin therapy” than was used in the ACC/AHA-multisociety guidelines. USPSTF, for example, calls for 10-year risk to reach 10% before recommending a statin prescription.
“One concern about the USPSTF setting the bar higher for statin initiation is that it reduces the number of young patients (age 40-50 years) at risk for premature myocardial infarction considered for treatment,” write Dr. Stone and colleagues.
That may be related to a weakness of the PCE-based decision process. “Because the PCE estimates of 10-year CV disease risk rely so heavily on age, sex, and race, use of these estimates to identify candidates for statins results in significant skewing of the population recommended for statins,” write Dr. Navar and Dr. Peterson in their JAMA editorial.
The risk enhancers in the ACC/AHA-multispecialty guidelines, about a dozen of them, compensate for that limitation to some extent. But the PCE-dominated USPSTF risk estimates will likely miss some groups that could potentially benefit from statin therapy, Dr. Peterson agreed in an interview.
For example, younger adults facing years of high LDL-cholesterol levels could easily have PCE-based 10-year risk below 10%. “Having a high LDL over a lifetime puts you at really high risk,” he said. “Young people are missed even though their longitudinal risk is high.” So, by waiting for the lofty 10% level of risk over 10 years, “we limit the use of medicine that’s pretty cheap and highly effective.”
Dose intensity, adverse events
Also at variance from the ACC/AHA-multispecialty guidelines, the USPSTF states that, “Based on available evidence, use of moderate-intensity statin therapy seems reasonable for the primary prevention of CV disease in most persons.”
The task force specifically explored whether evidence supports some use of high-intensity vs. moderate-intensity statins, Tufts University’s Dr. Wong said. “We found only one study that looked at that particular question, and it didn’t give us a strong answer.” An elevated rosuvastatin-related diabetes risk was apparent in the JUPITER trial, “but for the other studies, we did not find that association.”
Most of the studies that explored statins for reducing risk for a first stroke or myocardial infarction used a moderate-dose statin, Dr. Wong said. “So that’s what we would usually recommend.”
But, Dr. Virani writes, consistent with the ACC/AHA-multispecialty guidelines, “clinicians should consider titrating the intensity of therapy to the risk of the individual.” Persons in certain high-risk primary prevention groups, such as those with end-organ injury from diabetes or LDL cholesterol at least 190 mg/dL, “may derive further benefit from the use of high-intensity statin therapy.”
Low-intensity statins are another potential option, but “in contrast with its 2016 recommendations, the USPSTF no longer recommends use of low-intensity statins in certain situations,” observes a fourth editorial published the same day in JAMA Internal Medicine, with lead author Anand R. Habib, MD, MPhil, and senior author Rita F. Redberg, MD, MSc, both of the University of California, San Francisco. Dr. Redberg is the journal’s editor and has long expressed cautions about statin safety.
“While it is understandable that the Task Force was limited by lack of data on dosing, this change is unfortunate for patients because the frequency of adverse effects increases as the statin dose increases,” the editorial states. Although USPSTF did not find statistically significant harm from the drugs, “in clinical practice, adverse events are commonly reported with use of statins.”
It continues: “At present, there are further reasons to curb our enthusiasm about the use of statins for primary prevention of CV disease.” To illustrate, the editorial questioned primary-prevention statins’ balance of risk vs. clinically meaningful benefit, not benefit that is merely statistically significant.
“The purported benefits of statins in terms of relative risk reduction are fairly constant across baseline lipid levels and cardiovascular risk score categories for primary prevention,” the editorial states.
“Therefore, the absolute benefit for those in lower-risk categories is likely small given that their baseline absolute risk is low, while the chance of adverse effects is constant across risk categories.”
However, USPSTF states, “In pooled analyses of trial data, statin therapy was not associated with increased risk of study withdrawal due to adverse events or serious adverse events.” Nor did it find significant associations with cancers, liver enzyme abnormalities, or diabetes, including new-onset diabetes.
And, the USPSTF adds, “Evidence on the association between statins and renal or cognitive harms is very limited but does not indicate increased risk.”
USPSTF is supported by the U.S. Agency for Healthcare Research and Quality. Dr. Virani discloses receiving grants from the Department of Veterans Affairs, National Institutes of Health, and the World Heart Federation; and personal fees from the American College of Cardiology. Dr. Peterson discloses serving on the JAMA editorial board and receiving research support to his institution from Amgen, Bristol-Myers Squibb, Esperion, and Janssen; and consulting fees from Novo Nordisk, Bayer, and Novartis. Dr. Navar discloses receiving research support to her institution from Amgen, Bristol-Myers Squibb, Esperion, and Janssen; and receiving honoraria and consulting fees from AstraZeneca, Boehringer Ingelheim, Bayer, Janssen, Lilly, Novo Nordisk, Novartis, New Amsterdam, and Pfizer. Dr. Stone discloses receiving an honorarium from Knowledge to Practice, an educational company not associated with the pharmaceutical industry; disclosures for the other authors are in the report. Dr. Redberg discloses receiving research funding from the Arnold Ventures Foundation and the Greenwall Foundation.
A version of this article first appeared on Medscape.com.
Questions about how to prescribe statins for primary prevention abound more than 3 decades after the drugs swept into clinical practice to become a first-line medical approach to cutting cardiovascular (CV) risk. Statin usage recommendations from different bodies can vary in ways both limited and fundamental, spurring the kind of debate that accompanies such a document newly issued by the United States Preventive Services Task Force.
The document, little changed from the draft guidance released for public comment in February, was published online Aug. 23 in JAMA and the USPSTF website. It replaces a similar document issued by the task force in 2016.
The guidance has much in common with, but also sharp differences from, the influential 2018 guidelines on blood cholesterol management developed by the American College of Cardiology, American Heart Association, and 10 other medical societies.
And it is provocative enough to elicit at least four editorials issued the same day across the JAMA family of journals. They highlight key differences between the two documents, among them the USPSTF guidance’s consistent, narrow reliance on 7.5% and 10% cut points for 10-year risk levels as estimated from the ACC/AHA pooled cohort equations (PCE).
The guidance pairs the 10-year risk metric with at least one of only four prescribed CV risk factors to arrive at a limited choice of statin therapy recommendations. But its decision process isn’t bolstered by coronary artery calcium (CAC) scores or the prespecified “risk enhancers” that allowed the ACC/AHA-multisociety guidelines to be applied broadly and still be closely personalized. Those guidelines provide more PCE-based risk tiers for greater discrimination of risk and allow statins to be considered across a broader age group.
The USPSTF guidance’s evidence base consists of 23 clinical trials and three observational studies that directly compared a statin to either placebo or no statin, task force member John B. Wong, MD, Tufts University School of Medicine, Boston, told this news organization.
“In either kind of study, we found that the vast majority of patients had one or more of four risk factors – dyslipidemia, hypertension, diabetes, or smoking. So, when we categorized high risk or increased risk, we included the presence of one or more of those risk factors,” said Dr. Wong, who is director of comparative effectiveness research at Tufts Clinical Translational Science Institute.
‘Sensible and practical’
The USPSTF guidance applies only to adults aged 40-75 without CV signs or symptoms and recommends a statin prescription for persons at “high risk,” that is with an estimated 10-year PCE-based risk for death or CV events of 10% or higher plus at least one of the four risk factors, a level B recommendation.
It recommends that “clinicians selectively offer a statin” to such persons at “increased risk,” who have at least one of the risk factors and an estimated 10-year risk for death or CV events of 7.5% to less than 10%, a level C recommendation. “The likelihood of benefit is smaller in this group” than in persons at high risk, the document states.
“These recommendations from the USPSTF are sensible and practical,” states Salim S. Virani, MD, PhD, DeBakey Veterans Affairs Medical Center, Houston, in a related editorial published the same day in JAMA Network Open. He calls the former B-level recommendation “a conservative approach” and the latter C-level recommendation a “nuanced approach.”
Both are “understandable” given that some studies suggest that the PCE may overestimate the CV risk, Dr. Virani observes. “On the other hand, statin therapy has been shown to be efficacious” at 10-year CV-risk levels down to about 5%.
The USPSTF document “I think is going to perpetuate a problem that we have in this country, which is vast undertreatment of lipids,” Eric D. Peterson, MD, MPH, University of Texas Southwestern Medical Center, Dallas, said in an interview.
“We have a ton of good drugs that can lower cholesterol like crazy. If you lower cholesterol a lot, you improve outcomes,” he said. Dyslipidemia needs to be more widely and consistently treated, but “right now we have a pool of people in primary prevention who undertreat lipids and wait until disease happens – and then cardiologists get engaged. That’s an avoidable miss,” Dr. Peterson adds. He and JAMA Cardiology associate editor Ann Marie Navar, MD, PhD, provided JAMA with an editorial that accompanies the USPSTF guidance.
“My own personal bias would be that the [ACC/AHA-multisociety guidelines] are closer to being right,” Dr. Peterson said. They – unlike the USPSTF guidance – cover people with risk levels below 7.5%, down to at least 5%. They allow risk enhancers like metabolic syndrome, inflammatory diseases, or family history into the decision process. “And they’re more aggressive in diabetes and more aggressive in older people,” he said.
Higher threshold for therapy
The USPSTF guidance also explicitly omits some high-risk groups and makes little accommodation for others who might especially benefit from statins, several of the editorials contend. For example, states a related JAMA Cardiology editorial published the same day, “The USPSTF does not comment on familial hypercholesterolemia or an LDL-C level of 190 mg/dL or higher,” yet they are covered by the ACC/AHA-multispecialty guidelines.
In addition, write the editorialists, led by Neil J. Stone, MD, Northwestern University, Chicago, “the USPSTF uses a slightly higher threshold for initiation of statin therapy” than was used in the ACC/AHA-multisociety guidelines. USPSTF, for example, calls for 10-year risk to reach 10% before recommending a statin prescription.
“One concern about the USPSTF setting the bar higher for statin initiation is that it reduces the number of young patients (age 40-50 years) at risk for premature myocardial infarction considered for treatment,” write Dr. Stone and colleagues.
That may be related to a weakness of the PCE-based decision process. “Because the PCE estimates of 10-year CV disease risk rely so heavily on age, sex, and race, use of these estimates to identify candidates for statins results in significant skewing of the population recommended for statins,” write Dr. Navar and Dr. Peterson in their JAMA editorial.
The risk enhancers in the ACC/AHA-multispecialty guidelines, about a dozen of them, compensate for that limitation to some extent. But the PCE-dominated USPSTF risk estimates will likely miss some groups that could potentially benefit from statin therapy, Dr. Peterson agreed in an interview.
For example, younger adults facing years of high LDL-cholesterol levels could easily have PCE-based 10-year risk below 10%. “Having a high LDL over a lifetime puts you at really high risk,” he said. “Young people are missed even though their longitudinal risk is high.” So, by waiting for the lofty 10% level of risk over 10 years, “we limit the use of medicine that’s pretty cheap and highly effective.”
Dose intensity, adverse events
Also at variance from the ACC/AHA-multispecialty guidelines, the USPSTF states that, “Based on available evidence, use of moderate-intensity statin therapy seems reasonable for the primary prevention of CV disease in most persons.”
The task force specifically explored whether evidence supports some use of high-intensity vs. moderate-intensity statins, Tufts University’s Dr. Wong said. “We found only one study that looked at that particular question, and it didn’t give us a strong answer.” An elevated rosuvastatin-related diabetes risk was apparent in the JUPITER trial, “but for the other studies, we did not find that association.”
Most of the studies that explored statins for reducing risk for a first stroke or myocardial infarction used a moderate-dose statin, Dr. Wong said. “So that’s what we would usually recommend.”
But, Dr. Virani writes, consistent with the ACC/AHA-multispecialty guidelines, “clinicians should consider titrating the intensity of therapy to the risk of the individual.” Persons in certain high-risk primary prevention groups, such as those with end-organ injury from diabetes or LDL cholesterol at least 190 mg/dL, “may derive further benefit from the use of high-intensity statin therapy.”
Low-intensity statins are another potential option, but “in contrast with its 2016 recommendations, the USPSTF no longer recommends use of low-intensity statins in certain situations,” observes a fourth editorial published the same day in JAMA Internal Medicine, with lead author Anand R. Habib, MD, MPhil, and senior author Rita F. Redberg, MD, MSc, both of the University of California, San Francisco. Dr. Redberg is the journal’s editor and has long expressed cautions about statin safety.
“While it is understandable that the Task Force was limited by lack of data on dosing, this change is unfortunate for patients because the frequency of adverse effects increases as the statin dose increases,” the editorial states. Although USPSTF did not find statistically significant harm from the drugs, “in clinical practice, adverse events are commonly reported with use of statins.”
It continues: “At present, there are further reasons to curb our enthusiasm about the use of statins for primary prevention of CV disease.” To illustrate, the editorial questioned primary-prevention statins’ balance of risk vs. clinically meaningful benefit, not benefit that is merely statistically significant.
“The purported benefits of statins in terms of relative risk reduction are fairly constant across baseline lipid levels and cardiovascular risk score categories for primary prevention,” the editorial states.
“Therefore, the absolute benefit for those in lower-risk categories is likely small given that their baseline absolute risk is low, while the chance of adverse effects is constant across risk categories.”
However, USPSTF states, “In pooled analyses of trial data, statin therapy was not associated with increased risk of study withdrawal due to adverse events or serious adverse events.” Nor did it find significant associations with cancers, liver enzyme abnormalities, or diabetes, including new-onset diabetes.
And, the USPSTF adds, “Evidence on the association between statins and renal or cognitive harms is very limited but does not indicate increased risk.”
USPSTF is supported by the U.S. Agency for Healthcare Research and Quality. Dr. Virani discloses receiving grants from the Department of Veterans Affairs, National Institutes of Health, and the World Heart Federation; and personal fees from the American College of Cardiology. Dr. Peterson discloses serving on the JAMA editorial board and receiving research support to his institution from Amgen, Bristol-Myers Squibb, Esperion, and Janssen; and consulting fees from Novo Nordisk, Bayer, and Novartis. Dr. Navar discloses receiving research support to her institution from Amgen, Bristol-Myers Squibb, Esperion, and Janssen; and receiving honoraria and consulting fees from AstraZeneca, Boehringer Ingelheim, Bayer, Janssen, Lilly, Novo Nordisk, Novartis, New Amsterdam, and Pfizer. Dr. Stone discloses receiving an honorarium from Knowledge to Practice, an educational company not associated with the pharmaceutical industry; disclosures for the other authors are in the report. Dr. Redberg discloses receiving research funding from the Arnold Ventures Foundation and the Greenwall Foundation.
A version of this article first appeared on Medscape.com.
FROM JAMA
Barcelona beckons for first hybrid ESC Congress
After 2 years of virtual gatherings, the annual European Society of Cardiology Congress 2022 is back and celebrating its 70th birthday live in the raucously beautiful city of Barcelona.
Much of the upcoming event, scheduled for Aug. 26 to 29, however, will also be broadcast online, and the full program will be available on-demand after the meeting.
The hybrid format is intentional, leveraging the social interaction that only live meetings can provide and the global reach of online access, Program Committee Chair Stephan Windecker, MD, Bern University Hospital, Switzerland, told this news organization.
“It enables a lot of people who, for some reason, cannot travel to still connect, and it also provides what we’ve done in the past, but I think in a more natural way of doing it,” he said. “You can connect later on again, read, digest, look at sessions that you may have missed, and that’s a nice experience to take advantage of.”
Thus far, early registrations are favoring the sunny climes, with about 14,000 onsite and 4,200 online attendees.
This year’s spotlight theme is cardiac imaging, with programming throughout the Congress devoted to its role in diagnosis, treatment, follow-up, and, increasingly, guidance of interventions.
“Particularly as it relates to the transcatheter heart valves, it’s really a new discipline, and I think you can’t overemphasize that enough, because the interventional result directly depends on the quality of imaging,” Dr. Windecker said. “This will certainly logarithmically increase during the next few years.”
The always highly anticipated Hot Line sessions mushroomed this year to 10, featuring 36 studies, up from just 4 sessions and 20 studies last year.
“Especially during the COVID pandemic, many investigators and trialists experienced difficulties in recruitment, difficulties in terms of also personnel shortages, and so on. So really, we feel very privileged at the large number of submissions,” he said. “I think there are really very interesting ones, which we tried to spread throughout the 4 days.”
Hot Line sessions 1-5
Among the studies Dr. Windecker highlighted is TIME, which kicks off Hot Line 1 on Friday, Aug. 26, and aimed to establish whether antihypertensive medications taken at night are truly more cardioprotective than those taken in the morning.
The topic has been hotly debated, with proponents pointing to a near halving of mortality and cardiovascular events with bedtime dosing in the Hygia Chronotherapy trial. Skeptics question the validity and conduct of the trial, however, prompting an investigation by the European Heart Journal, which found no evidence of misconduct but has many looking for more definitive data.
Also in this session is SECURE, pitting a cardiovascular polypill that contains aspirin, ramipril, and atorvastatin against usual care in secondary prevention, and PERSPECTIVE, comparing the effects of sacubitril/valsartan with valsartan on cognitive function in patients with chronic heart failure and preserved ejection fraction (HFpEF).
Hot Line 2, the first of three Hot Lines taking place on Saturday, Aug. 27, features the Danish cardiovascular screening trial DANCAVAS, the phase 4 ADVOR trial of acetazolamide (Diamox) in acute decompensated heart failure (HF), and the DANFLU-1 trial of high- versus standard-dose influenza vaccine in the elderly.
Also on tap is the BOX trial, comparing two blood pressure and two oxygenation targets in comatose out-of-hospital cardiac arrest patients.
“It addresses an understudied patient population, and the second element is that sometimes things you do out of ordinary application – so, the application of oxygen – may have beneficial but also adverse impact,” Dr. Windecker said. “So, to study this in a randomized clinical trial is really important.”
Additionally, he highlighted REVIVED, which will be presented in Hot Line 3 and is the first trial to examine percutaneous coronary intervention (PCI) with optimal medical therapy (OMT) versus OMT alone in the setting of severe ischemic cardiomyopathy.
“We have data from the STICH trial, where surgical revascularization was investigated in ischemic cardiomyopathy, but the open question is: What about PCI as revascularization?” Dr. Windecker said. “The other reason it’s interesting is that we have these evidence-based drugs that have dramatically improved outcomes in patients with heart failure, and REVIVED certainly has been conducted now in an era where at least some of these drugs are more systematically implemented.”
Rounding out this session are the Scottish ALL-HEART study of allopurinol in ischemic heart disease and EchoNet-RCT, looking at whether artificial intelligence (AI) can improve the accuracy of echocardiograms.
Hot Line 4 features DELIVER, a phase 3 trial of the SGLT2 inhibitor dapagliflozin (Farxiga) in HF with preserved or mildly reduced ejection fraction. Topline results, released in May, showed that the study has met its primary endpoint of cardiovascular death or worsening HF.
Dr. Windecker said DELIVER will be a “highlight” of the meeting, particularly because EMPEROR-Preserved, presented at ESC 2021, showed a benefit for another SGLT2 inhibitor, empagliflozin, in this very specific setting. Two prespecified analyses will also be presented, pooling data from EMPEROR-Preserved and from the DAPA-HF study of dapagliflozin in patients with reduced EF. “This will be a session very rich in terms of information.”
Another not-to-be-missed session is Hot Line 5, which will focus on antithrombotic therapy, according to Dr. Windecker, who will cochair the Sunday, Aug. 28 session.
First up is the investigator-initiated INVICTUS-VKA, testing rivaroxaban noninferiority versus standard vitamin K antagonists in patients with atrial fibrillation (AFib) and rheumatic heart disease, a setting in which non–vitamin K antagonists have not been sufficiently tested.
This is followed by three phase 2 trials – PACIFIC-AMI, PACIFIC-STROKE, and AXIOMATIC-SSP – investigating the novel factor XIa inhibitors BAY 2433334 and BMS-986177 in patients with myocardial infarction or stroke.
Hot Line sessions 6-10
Sunday’s Hot Line 6 takes another look at smartphone-based AFib screening in eBRAVE-HF, use of causal AI to improve the validity of cardiovascular risk prediction, and AI-enhanced detection of aortic stenosis.
Hot Line 7 rounds out the day, putting coronary imaging center stage. It includes perfusion scanning with MR or PET after a positive angiogram in DanNICAD-2, the PET tracer 18F-sodium fluoride as a marker of high-risk coronary plaques in patients with recent MIs in PREFFIR, and fractional flow reserve- versus angiography-guided PCI in acute MI with multivessel disease in FRAME-AMI.
After a weekend of top-notch science and, no doubt, a spot of revelry, the focus returns on Monday, Aug. 29 to three Hot Line sessions. The first of these, Hot Line 8, updates five clinical trials, including 5-year outcomes from ISCHEMIA-CKD EXTEND, 15-month results from MASTER DAPT, and primary results from FOURIER-OLE, the open-label extension study of evolocumab out to 5 years in approximately 1,600 study participants.
The session closes out with causes of mortality in the FIDELITY trial of finerenone and a win-ratio analysis of PARADISE-MI.
Hot Line 9, billed as an “evidence synthesis on clinically important questions,” includes a Cholesterol Treatment Trialists’ (CTT) Collaboration meta-analysis on the effects of statins on muscle symptoms and a meta-analysis of angiotensin-receptor blockers and beta-blockers in Marfan syndrome from the Marfan Treatment Trialists’ Collaboration.
Also featured is evidence on radial versus femoral access for coronary procedures, and PANTHER, a patient-level meta-analysis of aspirin or P2Y12 inhibitor monotherapy as secondary prevention in patients with established coronary artery disease.
COVID-19, deeply rooted in the minds of attendees and considered in 52 separate sessions, takes over the final Hot Line session of the Congress. Hot Line 10 will report on antithrombotic therapy in critically ill patients in COVID-PACT and on anti-inflammatory therapy with colchicine and antithrombotic therapy with aspirin alone or in combination with rivaroxaban in the ACT inpatient and outpatient trials. Although such early trials have been largely negative, the latest details will be interesting to see, Dr. Windecker suggested.
In terms of COVID-19 protocols, ESC will recommend but not mandate masks and will have test kits available should attendees wish to have a test or if they become symptomatic, he noted.
New guidelines released
Four new ESC guidelines will be released during the congress on cardio-oncology, ventricular arrhythmias and sudden cardiac death, pulmonary hypertension, and cardiovascular assessment and management of patients undergoing noncardiac surgery.
In addition to a guideline overview on Friday, one guideline will be featured each day in a 1-hour session, with additional time for discussions with guideline task force members, and six sessions devoted to the implementation of existing guidelines in clinical practice.
The ESC already has a position paper on cardio-oncology, but now, for the first time, has a full guideline with formal laws and level-of-evidence recommendations, Dr. Windecker pointed out.
“I think what will be the great asset, not only of the guideline but out of this emerging field, is that people in the future will probably not only be treated when it’s too late or suffer from toxicity but that there will be screening, and people will be aware before the implementation of therapy,” he added.
A version of this article first appeared on Medscape.com.
After 2 years of virtual gatherings, the annual European Society of Cardiology Congress 2022 is back and celebrating its 70th birthday live in the raucously beautiful city of Barcelona.
Much of the upcoming event, scheduled for Aug. 26 to 29, however, will also be broadcast online, and the full program will be available on-demand after the meeting.
The hybrid format is intentional, leveraging the social interaction that only live meetings can provide and the global reach of online access, Program Committee Chair Stephan Windecker, MD, Bern University Hospital, Switzerland, told this news organization.
“It enables a lot of people who, for some reason, cannot travel to still connect, and it also provides what we’ve done in the past, but I think in a more natural way of doing it,” he said. “You can connect later on again, read, digest, look at sessions that you may have missed, and that’s a nice experience to take advantage of.”
Thus far, early registrations are favoring the sunny climes, with about 14,000 onsite and 4,200 online attendees.
This year’s spotlight theme is cardiac imaging, with programming throughout the Congress devoted to its role in diagnosis, treatment, follow-up, and, increasingly, guidance of interventions.
“Particularly as it relates to the transcatheter heart valves, it’s really a new discipline, and I think you can’t overemphasize that enough, because the interventional result directly depends on the quality of imaging,” Dr. Windecker said. “This will certainly logarithmically increase during the next few years.”
The always highly anticipated Hot Line sessions mushroomed this year to 10, featuring 36 studies, up from just 4 sessions and 20 studies last year.
“Especially during the COVID pandemic, many investigators and trialists experienced difficulties in recruitment, difficulties in terms of also personnel shortages, and so on. So really, we feel very privileged at the large number of submissions,” he said. “I think there are really very interesting ones, which we tried to spread throughout the 4 days.”
Hot Line sessions 1-5
Among the studies Dr. Windecker highlighted is TIME, which kicks off Hot Line 1 on Friday, Aug. 26, and aimed to establish whether antihypertensive medications taken at night are truly more cardioprotective than those taken in the morning.
The topic has been hotly debated, with proponents pointing to a near halving of mortality and cardiovascular events with bedtime dosing in the Hygia Chronotherapy trial. Skeptics question the validity and conduct of the trial, however, prompting an investigation by the European Heart Journal, which found no evidence of misconduct but has many looking for more definitive data.
Also in this session is SECURE, pitting a cardiovascular polypill that contains aspirin, ramipril, and atorvastatin against usual care in secondary prevention, and PERSPECTIVE, comparing the effects of sacubitril/valsartan with valsartan on cognitive function in patients with chronic heart failure and preserved ejection fraction (HFpEF).
Hot Line 2, the first of three Hot Lines taking place on Saturday, Aug. 27, features the Danish cardiovascular screening trial DANCAVAS, the phase 4 ADVOR trial of acetazolamide (Diamox) in acute decompensated heart failure (HF), and the DANFLU-1 trial of high- versus standard-dose influenza vaccine in the elderly.
Also on tap is the BOX trial, comparing two blood pressure and two oxygenation targets in comatose out-of-hospital cardiac arrest patients.
“It addresses an understudied patient population, and the second element is that sometimes things you do out of ordinary application – so, the application of oxygen – may have beneficial but also adverse impact,” Dr. Windecker said. “So, to study this in a randomized clinical trial is really important.”
Additionally, he highlighted REVIVED, which will be presented in Hot Line 3 and is the first trial to examine percutaneous coronary intervention (PCI) with optimal medical therapy (OMT) versus OMT alone in the setting of severe ischemic cardiomyopathy.
“We have data from the STICH trial, where surgical revascularization was investigated in ischemic cardiomyopathy, but the open question is: What about PCI as revascularization?” Dr. Windecker said. “The other reason it’s interesting is that we have these evidence-based drugs that have dramatically improved outcomes in patients with heart failure, and REVIVED certainly has been conducted now in an era where at least some of these drugs are more systematically implemented.”
Rounding out this session are the Scottish ALL-HEART study of allopurinol in ischemic heart disease and EchoNet-RCT, looking at whether artificial intelligence (AI) can improve the accuracy of echocardiograms.
Hot Line 4 features DELIVER, a phase 3 trial of the SGLT2 inhibitor dapagliflozin (Farxiga) in HF with preserved or mildly reduced ejection fraction. Topline results, released in May, showed that the study has met its primary endpoint of cardiovascular death or worsening HF.
Dr. Windecker said DELIVER will be a “highlight” of the meeting, particularly because EMPEROR-Preserved, presented at ESC 2021, showed a benefit for another SGLT2 inhibitor, empagliflozin, in this very specific setting. Two prespecified analyses will also be presented, pooling data from EMPEROR-Preserved and from the DAPA-HF study of dapagliflozin in patients with reduced EF. “This will be a session very rich in terms of information.”
Another not-to-be-missed session is Hot Line 5, which will focus on antithrombotic therapy, according to Dr. Windecker, who will cochair the Sunday, Aug. 28 session.
First up is the investigator-initiated INVICTUS-VKA, testing rivaroxaban noninferiority versus standard vitamin K antagonists in patients with atrial fibrillation (AFib) and rheumatic heart disease, a setting in which non–vitamin K antagonists have not been sufficiently tested.
This is followed by three phase 2 trials – PACIFIC-AMI, PACIFIC-STROKE, and AXIOMATIC-SSP – investigating the novel factor XIa inhibitors BAY 2433334 and BMS-986177 in patients with myocardial infarction or stroke.
Hot Line sessions 6-10
Sunday’s Hot Line 6 takes another look at smartphone-based AFib screening in eBRAVE-HF, use of causal AI to improve the validity of cardiovascular risk prediction, and AI-enhanced detection of aortic stenosis.
Hot Line 7 rounds out the day, putting coronary imaging center stage. It includes perfusion scanning with MR or PET after a positive angiogram in DanNICAD-2, the PET tracer 18F-sodium fluoride as a marker of high-risk coronary plaques in patients with recent MIs in PREFFIR, and fractional flow reserve- versus angiography-guided PCI in acute MI with multivessel disease in FRAME-AMI.
After a weekend of top-notch science and, no doubt, a spot of revelry, the focus returns on Monday, Aug. 29 to three Hot Line sessions. The first of these, Hot Line 8, updates five clinical trials, including 5-year outcomes from ISCHEMIA-CKD EXTEND, 15-month results from MASTER DAPT, and primary results from FOURIER-OLE, the open-label extension study of evolocumab out to 5 years in approximately 1,600 study participants.
The session closes out with causes of mortality in the FIDELITY trial of finerenone and a win-ratio analysis of PARADISE-MI.
Hot Line 9, billed as an “evidence synthesis on clinically important questions,” includes a Cholesterol Treatment Trialists’ (CTT) Collaboration meta-analysis on the effects of statins on muscle symptoms and a meta-analysis of angiotensin-receptor blockers and beta-blockers in Marfan syndrome from the Marfan Treatment Trialists’ Collaboration.
Also featured is evidence on radial versus femoral access for coronary procedures, and PANTHER, a patient-level meta-analysis of aspirin or P2Y12 inhibitor monotherapy as secondary prevention in patients with established coronary artery disease.
COVID-19, deeply rooted in the minds of attendees and considered in 52 separate sessions, takes over the final Hot Line session of the Congress. Hot Line 10 will report on antithrombotic therapy in critically ill patients in COVID-PACT and on anti-inflammatory therapy with colchicine and antithrombotic therapy with aspirin alone or in combination with rivaroxaban in the ACT inpatient and outpatient trials. Although such early trials have been largely negative, the latest details will be interesting to see, Dr. Windecker suggested.
In terms of COVID-19 protocols, ESC will recommend but not mandate masks and will have test kits available should attendees wish to have a test or if they become symptomatic, he noted.
New guidelines released
Four new ESC guidelines will be released during the congress on cardio-oncology, ventricular arrhythmias and sudden cardiac death, pulmonary hypertension, and cardiovascular assessment and management of patients undergoing noncardiac surgery.
In addition to a guideline overview on Friday, one guideline will be featured each day in a 1-hour session, with additional time for discussions with guideline task force members, and six sessions devoted to the implementation of existing guidelines in clinical practice.
The ESC already has a position paper on cardio-oncology, but now, for the first time, has a full guideline with formal laws and level-of-evidence recommendations, Dr. Windecker pointed out.
“I think what will be the great asset, not only of the guideline but out of this emerging field, is that people in the future will probably not only be treated when it’s too late or suffer from toxicity but that there will be screening, and people will be aware before the implementation of therapy,” he added.
A version of this article first appeared on Medscape.com.
After 2 years of virtual gatherings, the annual European Society of Cardiology Congress 2022 is back and celebrating its 70th birthday live in the raucously beautiful city of Barcelona.
Much of the upcoming event, scheduled for Aug. 26 to 29, however, will also be broadcast online, and the full program will be available on-demand after the meeting.
The hybrid format is intentional, leveraging the social interaction that only live meetings can provide and the global reach of online access, Program Committee Chair Stephan Windecker, MD, Bern University Hospital, Switzerland, told this news organization.
“It enables a lot of people who, for some reason, cannot travel to still connect, and it also provides what we’ve done in the past, but I think in a more natural way of doing it,” he said. “You can connect later on again, read, digest, look at sessions that you may have missed, and that’s a nice experience to take advantage of.”
Thus far, early registrations are favoring the sunny climes, with about 14,000 onsite and 4,200 online attendees.
This year’s spotlight theme is cardiac imaging, with programming throughout the Congress devoted to its role in diagnosis, treatment, follow-up, and, increasingly, guidance of interventions.
“Particularly as it relates to the transcatheter heart valves, it’s really a new discipline, and I think you can’t overemphasize that enough, because the interventional result directly depends on the quality of imaging,” Dr. Windecker said. “This will certainly logarithmically increase during the next few years.”
The always highly anticipated Hot Line sessions mushroomed this year to 10, featuring 36 studies, up from just 4 sessions and 20 studies last year.
“Especially during the COVID pandemic, many investigators and trialists experienced difficulties in recruitment, difficulties in terms of also personnel shortages, and so on. So really, we feel very privileged at the large number of submissions,” he said. “I think there are really very interesting ones, which we tried to spread throughout the 4 days.”
Hot Line sessions 1-5
Among the studies Dr. Windecker highlighted is TIME, which kicks off Hot Line 1 on Friday, Aug. 26, and aimed to establish whether antihypertensive medications taken at night are truly more cardioprotective than those taken in the morning.
The topic has been hotly debated, with proponents pointing to a near halving of mortality and cardiovascular events with bedtime dosing in the Hygia Chronotherapy trial. Skeptics question the validity and conduct of the trial, however, prompting an investigation by the European Heart Journal, which found no evidence of misconduct but has many looking for more definitive data.
Also in this session is SECURE, pitting a cardiovascular polypill that contains aspirin, ramipril, and atorvastatin against usual care in secondary prevention, and PERSPECTIVE, comparing the effects of sacubitril/valsartan with valsartan on cognitive function in patients with chronic heart failure and preserved ejection fraction (HFpEF).
Hot Line 2, the first of three Hot Lines taking place on Saturday, Aug. 27, features the Danish cardiovascular screening trial DANCAVAS, the phase 4 ADVOR trial of acetazolamide (Diamox) in acute decompensated heart failure (HF), and the DANFLU-1 trial of high- versus standard-dose influenza vaccine in the elderly.
Also on tap is the BOX trial, comparing two blood pressure and two oxygenation targets in comatose out-of-hospital cardiac arrest patients.
“It addresses an understudied patient population, and the second element is that sometimes things you do out of ordinary application – so, the application of oxygen – may have beneficial but also adverse impact,” Dr. Windecker said. “So, to study this in a randomized clinical trial is really important.”
Additionally, he highlighted REVIVED, which will be presented in Hot Line 3 and is the first trial to examine percutaneous coronary intervention (PCI) with optimal medical therapy (OMT) versus OMT alone in the setting of severe ischemic cardiomyopathy.
“We have data from the STICH trial, where surgical revascularization was investigated in ischemic cardiomyopathy, but the open question is: What about PCI as revascularization?” Dr. Windecker said. “The other reason it’s interesting is that we have these evidence-based drugs that have dramatically improved outcomes in patients with heart failure, and REVIVED certainly has been conducted now in an era where at least some of these drugs are more systematically implemented.”
Rounding out this session are the Scottish ALL-HEART study of allopurinol in ischemic heart disease and EchoNet-RCT, looking at whether artificial intelligence (AI) can improve the accuracy of echocardiograms.
Hot Line 4 features DELIVER, a phase 3 trial of the SGLT2 inhibitor dapagliflozin (Farxiga) in HF with preserved or mildly reduced ejection fraction. Topline results, released in May, showed that the study has met its primary endpoint of cardiovascular death or worsening HF.
Dr. Windecker said DELIVER will be a “highlight” of the meeting, particularly because EMPEROR-Preserved, presented at ESC 2021, showed a benefit for another SGLT2 inhibitor, empagliflozin, in this very specific setting. Two prespecified analyses will also be presented, pooling data from EMPEROR-Preserved and from the DAPA-HF study of dapagliflozin in patients with reduced EF. “This will be a session very rich in terms of information.”
Another not-to-be-missed session is Hot Line 5, which will focus on antithrombotic therapy, according to Dr. Windecker, who will cochair the Sunday, Aug. 28 session.
First up is the investigator-initiated INVICTUS-VKA, testing rivaroxaban noninferiority versus standard vitamin K antagonists in patients with atrial fibrillation (AFib) and rheumatic heart disease, a setting in which non–vitamin K antagonists have not been sufficiently tested.
This is followed by three phase 2 trials – PACIFIC-AMI, PACIFIC-STROKE, and AXIOMATIC-SSP – investigating the novel factor XIa inhibitors BAY 2433334 and BMS-986177 in patients with myocardial infarction or stroke.
Hot Line sessions 6-10
Sunday’s Hot Line 6 takes another look at smartphone-based AFib screening in eBRAVE-HF, use of causal AI to improve the validity of cardiovascular risk prediction, and AI-enhanced detection of aortic stenosis.
Hot Line 7 rounds out the day, putting coronary imaging center stage. It includes perfusion scanning with MR or PET after a positive angiogram in DanNICAD-2, the PET tracer 18F-sodium fluoride as a marker of high-risk coronary plaques in patients with recent MIs in PREFFIR, and fractional flow reserve- versus angiography-guided PCI in acute MI with multivessel disease in FRAME-AMI.
After a weekend of top-notch science and, no doubt, a spot of revelry, the focus returns on Monday, Aug. 29 to three Hot Line sessions. The first of these, Hot Line 8, updates five clinical trials, including 5-year outcomes from ISCHEMIA-CKD EXTEND, 15-month results from MASTER DAPT, and primary results from FOURIER-OLE, the open-label extension study of evolocumab out to 5 years in approximately 1,600 study participants.
The session closes out with causes of mortality in the FIDELITY trial of finerenone and a win-ratio analysis of PARADISE-MI.
Hot Line 9, billed as an “evidence synthesis on clinically important questions,” includes a Cholesterol Treatment Trialists’ (CTT) Collaboration meta-analysis on the effects of statins on muscle symptoms and a meta-analysis of angiotensin-receptor blockers and beta-blockers in Marfan syndrome from the Marfan Treatment Trialists’ Collaboration.
Also featured is evidence on radial versus femoral access for coronary procedures, and PANTHER, a patient-level meta-analysis of aspirin or P2Y12 inhibitor monotherapy as secondary prevention in patients with established coronary artery disease.
COVID-19, deeply rooted in the minds of attendees and considered in 52 separate sessions, takes over the final Hot Line session of the Congress. Hot Line 10 will report on antithrombotic therapy in critically ill patients in COVID-PACT and on anti-inflammatory therapy with colchicine and antithrombotic therapy with aspirin alone or in combination with rivaroxaban in the ACT inpatient and outpatient trials. Although such early trials have been largely negative, the latest details will be interesting to see, Dr. Windecker suggested.
In terms of COVID-19 protocols, ESC will recommend but not mandate masks and will have test kits available should attendees wish to have a test or if they become symptomatic, he noted.
New guidelines released
Four new ESC guidelines will be released during the congress on cardio-oncology, ventricular arrhythmias and sudden cardiac death, pulmonary hypertension, and cardiovascular assessment and management of patients undergoing noncardiac surgery.
In addition to a guideline overview on Friday, one guideline will be featured each day in a 1-hour session, with additional time for discussions with guideline task force members, and six sessions devoted to the implementation of existing guidelines in clinical practice.
The ESC already has a position paper on cardio-oncology, but now, for the first time, has a full guideline with formal laws and level-of-evidence recommendations, Dr. Windecker pointed out.
“I think what will be the great asset, not only of the guideline but out of this emerging field, is that people in the future will probably not only be treated when it’s too late or suffer from toxicity but that there will be screening, and people will be aware before the implementation of therapy,” he added.
A version of this article first appeared on Medscape.com.
How much weight does my patient need to lose?
What is the real goal of weight loss? In health care, reducing excess body fat is known to improve many complications faced by patients with obesity. Even modest to moderate weight loss contributes to improvements in health. Normalizing body weight is not required.
While our culture promotes an ideal body size, in the health care setting, our attention must focus on achieving health improvement. We need to be more tolerant of variations in body size if patients are healthy. Of note, varying amounts of weight loss produce improvement in the different complications of obesity, so the amount of weight loss required for improving one condition differs from that required to improve another condition.
When we prescribe weight loss for health improvement, we are trying to reduce both the mechanical burden of fat and the excess ectopic and visceral body fat that is driving disease. The good news about the physiology of weight loss is that we do not need to attain a body mass index (BMI) of 25 or even 30 to have health improvement. The excess abnormal body fat is the first to go!
Losing weight causes a disproportional reduction in ectopic and visceral fat depots. With a 5% weight loss, visceral fat is reduced by 9%. With 16% weight loss, visceral fat is reduced by 30%. Clearing of liver fat is even more dramatic. With 16% weight loss, 65% of liver fat is cleared.
Because ectopic abnormal fat is cleared preferentially with weight loss, it affects different tissues with varying amounts of weight loss.
Weight loss and diabetes
A close relationship exists between weight loss and insulin sensitivity. With just 5% weight loss, insulin sensitivity in the liver and adipose tissue is greatly improved, but while muscle insulin sensitivity is improved at just 5% weight loss, it continues to improve with further weight loss. Indeed, weight loss has enormous benefits in improving glycemia in prediabetes and diabetes.
In patients with impaired glucose tolerance, weight loss of 10% can eliminate progression to type 2 diabetes. In patients with type 2 diabetes who still have beta-cell reserve, 15% weight loss can produce diabetes remission – normoglycemia without diabetes medications.
Weight loss and cardiovascular risk factors
Even very small amounts of weight loss – 3% – can improve triglycerides and glycemia. It takes 5% weight loss to show benefits in systolic and diastolic blood pressure, as well as in HDL and LDL cholesterol levels. For all of these, additional weight loss brings more improvement. Inflammatory markers are more difficult. It takes 10%-15% weight loss to improve most of these – for example, C-reactive protein.
Weight loss and other complications
It takes 10% or more weight loss to demonstrate improvements in symptoms in obstructive sleep apnea and gastroesophageal reflux disease. For knee pain, the relationship to improvement is not based on achieving a percentage loss. Each pound of weight lost can result in a fourfold reduction in the load exerted on the knee per step during daily activities, but it is important to reduce weight before there is structural damage, because weight loss can’t repair damaged knee joints. Moderate weight loss (5%-10%) produces improvements in quality-of-life measures, in urinary stress incontinence symptoms, and in measures of sexual function. It probably takes 15% or more weight loss to demonstrate improvement in cardiovascular events.
Must heavier patients lose more weight?
To answer this question, it is important to think in terms of percent weight loss rather than pounds or kilograms. In large studies of lifestyle intervention, of course individuals with higher BMI lost more weight. But the percentage weight loss was the same across BMI categories: class 1 (BMI 30-35), class 2 (BMI 35-40), class 3 (BMI > 40). Furthermore, the improvement in risk factors was the same across BMI categories. Those with class 3 obesity had the same improvements as those with class 1. This provides further rationale for thinking about weight loss as a percentage from baseline weight rather than as simply a weight-loss goal in pounds.
Goal setting is an important part of any behavioral intervention
At the start of a weight-loss intervention, the health care provider should raise the issue of the goal and the time course for achieving it. Patients often have unrealistic expectations, wanting to achieve large amounts of weight loss rapidly. Unfortunately, popular culture has reinforced this idea with advertisements using “lose 10 pounds the first week” and promoting before-and-after pictures of weight-loss results. The job of the health care provider is to coach and guide the patient in terms of achievable weight loss that can bring health improvement safely. Managing patient expectations is critical to long-term success.
Think in terms of percentage weight loss, not pounds, and set goals at achievable time points
Help patients translate a percent weight-loss goal to a pounds goal at 3, 6, and 12 months. With the emergence of medications approved for chronic weight management with robust weight-loss efficacy, it now is possible to achieve a weight-loss goal of 10% or 15% with regularity, and some patients will be able to achieve 20% or 25% weight loss with newer medications.
We should help our patients set a goal by calculating a goal for certain time points. A good goal for 3 months would be 5% weight loss. For our 200-lb patient, we would translate that to 10 lb in 3 months. For 6 months, the goal should be 10% (20 lb for our 200-lb patient). The usual trajectory of weight loss with lifestyle intervention alone is for a “plateau” at 6 months, although with newer medications, weight loss will continue for more than a year. That 1-year goal might be 15% (30 lb for our 200-lb patient) or even more, based on the patient’s baseline weight and body composition.
Weight-loss calculators can be useful tools for patients and health care providers. They can be found online and include the National Institutes of Health Body Weight Planner and the Pennington Biomedical Weight Loss Predictor Calculator. These tools give patients a realistic expectation of how fast weight loss can occur and provide guidelines to measure success.
Can patients lose too much weight?
In this patient population, losing too much weight is not typically a concern. However, newer medications are achieving average weight losses of 17% and 22% at 62 weeks, as reported by this news organization. There is a wide variation in response to these newer agents which target appetite, and many patients are losing more than the average percentages.
Remembering that the goal of weight loss is the reduction of excess abnormal body fat, we want patients to preserve as much lean mass as possible. Weight-bearing exercise can help during the weight-loss phase, but large or rapid weight loss can be concerning, especially in older individuals. When the BMI drops below 25, we want to watch patients carefully. Measurement of body composition, including bone mineral density, with dual-energy x-ray absorptiometry (DEXA) can help. This is a scenario where dose reduction of antiobesity medication can be indicated, and good clinical judgment is required to keep weight loss at healthy levels.
The future of weight loss
In the past, our strategy has been to promote as much weight loss as possible. With more effective medications, our strategy will have to change to a treat-to-target approach, such as we already use in hypertension and diabetes.
With the ability to produce powerful effects on appetite will come the need to not only target weight loss but to target preservation of lean mass and even to target different approaches for weight-loss maintenance. At present, we have no evidence that stopping medications results in anything other than weight regain. The study of different approaches to weight-loss maintenance will require our full attention.
Dr. Ryan has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, consultant, or trustee for: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand. Received income in an amount equal to or greater than $250 from: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand.
Donna Ryan, MD, is Professor Emerita, Pennington Biomedical Research Center, Louisiana State University, New Orleans.
A version of this article first appeared on Medscape.com.
What is the real goal of weight loss? In health care, reducing excess body fat is known to improve many complications faced by patients with obesity. Even modest to moderate weight loss contributes to improvements in health. Normalizing body weight is not required.
While our culture promotes an ideal body size, in the health care setting, our attention must focus on achieving health improvement. We need to be more tolerant of variations in body size if patients are healthy. Of note, varying amounts of weight loss produce improvement in the different complications of obesity, so the amount of weight loss required for improving one condition differs from that required to improve another condition.
When we prescribe weight loss for health improvement, we are trying to reduce both the mechanical burden of fat and the excess ectopic and visceral body fat that is driving disease. The good news about the physiology of weight loss is that we do not need to attain a body mass index (BMI) of 25 or even 30 to have health improvement. The excess abnormal body fat is the first to go!
Losing weight causes a disproportional reduction in ectopic and visceral fat depots. With a 5% weight loss, visceral fat is reduced by 9%. With 16% weight loss, visceral fat is reduced by 30%. Clearing of liver fat is even more dramatic. With 16% weight loss, 65% of liver fat is cleared.
Because ectopic abnormal fat is cleared preferentially with weight loss, it affects different tissues with varying amounts of weight loss.
Weight loss and diabetes
A close relationship exists between weight loss and insulin sensitivity. With just 5% weight loss, insulin sensitivity in the liver and adipose tissue is greatly improved, but while muscle insulin sensitivity is improved at just 5% weight loss, it continues to improve with further weight loss. Indeed, weight loss has enormous benefits in improving glycemia in prediabetes and diabetes.
In patients with impaired glucose tolerance, weight loss of 10% can eliminate progression to type 2 diabetes. In patients with type 2 diabetes who still have beta-cell reserve, 15% weight loss can produce diabetes remission – normoglycemia without diabetes medications.
Weight loss and cardiovascular risk factors
Even very small amounts of weight loss – 3% – can improve triglycerides and glycemia. It takes 5% weight loss to show benefits in systolic and diastolic blood pressure, as well as in HDL and LDL cholesterol levels. For all of these, additional weight loss brings more improvement. Inflammatory markers are more difficult. It takes 10%-15% weight loss to improve most of these – for example, C-reactive protein.
Weight loss and other complications
It takes 10% or more weight loss to demonstrate improvements in symptoms in obstructive sleep apnea and gastroesophageal reflux disease. For knee pain, the relationship to improvement is not based on achieving a percentage loss. Each pound of weight lost can result in a fourfold reduction in the load exerted on the knee per step during daily activities, but it is important to reduce weight before there is structural damage, because weight loss can’t repair damaged knee joints. Moderate weight loss (5%-10%) produces improvements in quality-of-life measures, in urinary stress incontinence symptoms, and in measures of sexual function. It probably takes 15% or more weight loss to demonstrate improvement in cardiovascular events.
Must heavier patients lose more weight?
To answer this question, it is important to think in terms of percent weight loss rather than pounds or kilograms. In large studies of lifestyle intervention, of course individuals with higher BMI lost more weight. But the percentage weight loss was the same across BMI categories: class 1 (BMI 30-35), class 2 (BMI 35-40), class 3 (BMI > 40). Furthermore, the improvement in risk factors was the same across BMI categories. Those with class 3 obesity had the same improvements as those with class 1. This provides further rationale for thinking about weight loss as a percentage from baseline weight rather than as simply a weight-loss goal in pounds.
Goal setting is an important part of any behavioral intervention
At the start of a weight-loss intervention, the health care provider should raise the issue of the goal and the time course for achieving it. Patients often have unrealistic expectations, wanting to achieve large amounts of weight loss rapidly. Unfortunately, popular culture has reinforced this idea with advertisements using “lose 10 pounds the first week” and promoting before-and-after pictures of weight-loss results. The job of the health care provider is to coach and guide the patient in terms of achievable weight loss that can bring health improvement safely. Managing patient expectations is critical to long-term success.
Think in terms of percentage weight loss, not pounds, and set goals at achievable time points
Help patients translate a percent weight-loss goal to a pounds goal at 3, 6, and 12 months. With the emergence of medications approved for chronic weight management with robust weight-loss efficacy, it now is possible to achieve a weight-loss goal of 10% or 15% with regularity, and some patients will be able to achieve 20% or 25% weight loss with newer medications.
We should help our patients set a goal by calculating a goal for certain time points. A good goal for 3 months would be 5% weight loss. For our 200-lb patient, we would translate that to 10 lb in 3 months. For 6 months, the goal should be 10% (20 lb for our 200-lb patient). The usual trajectory of weight loss with lifestyle intervention alone is for a “plateau” at 6 months, although with newer medications, weight loss will continue for more than a year. That 1-year goal might be 15% (30 lb for our 200-lb patient) or even more, based on the patient’s baseline weight and body composition.
Weight-loss calculators can be useful tools for patients and health care providers. They can be found online and include the National Institutes of Health Body Weight Planner and the Pennington Biomedical Weight Loss Predictor Calculator. These tools give patients a realistic expectation of how fast weight loss can occur and provide guidelines to measure success.
Can patients lose too much weight?
In this patient population, losing too much weight is not typically a concern. However, newer medications are achieving average weight losses of 17% and 22% at 62 weeks, as reported by this news organization. There is a wide variation in response to these newer agents which target appetite, and many patients are losing more than the average percentages.
Remembering that the goal of weight loss is the reduction of excess abnormal body fat, we want patients to preserve as much lean mass as possible. Weight-bearing exercise can help during the weight-loss phase, but large or rapid weight loss can be concerning, especially in older individuals. When the BMI drops below 25, we want to watch patients carefully. Measurement of body composition, including bone mineral density, with dual-energy x-ray absorptiometry (DEXA) can help. This is a scenario where dose reduction of antiobesity medication can be indicated, and good clinical judgment is required to keep weight loss at healthy levels.
The future of weight loss
In the past, our strategy has been to promote as much weight loss as possible. With more effective medications, our strategy will have to change to a treat-to-target approach, such as we already use in hypertension and diabetes.
With the ability to produce powerful effects on appetite will come the need to not only target weight loss but to target preservation of lean mass and even to target different approaches for weight-loss maintenance. At present, we have no evidence that stopping medications results in anything other than weight regain. The study of different approaches to weight-loss maintenance will require our full attention.
Dr. Ryan has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, consultant, or trustee for: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand. Received income in an amount equal to or greater than $250 from: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand.
Donna Ryan, MD, is Professor Emerita, Pennington Biomedical Research Center, Louisiana State University, New Orleans.
A version of this article first appeared on Medscape.com.
What is the real goal of weight loss? In health care, reducing excess body fat is known to improve many complications faced by patients with obesity. Even modest to moderate weight loss contributes to improvements in health. Normalizing body weight is not required.
While our culture promotes an ideal body size, in the health care setting, our attention must focus on achieving health improvement. We need to be more tolerant of variations in body size if patients are healthy. Of note, varying amounts of weight loss produce improvement in the different complications of obesity, so the amount of weight loss required for improving one condition differs from that required to improve another condition.
When we prescribe weight loss for health improvement, we are trying to reduce both the mechanical burden of fat and the excess ectopic and visceral body fat that is driving disease. The good news about the physiology of weight loss is that we do not need to attain a body mass index (BMI) of 25 or even 30 to have health improvement. The excess abnormal body fat is the first to go!
Losing weight causes a disproportional reduction in ectopic and visceral fat depots. With a 5% weight loss, visceral fat is reduced by 9%. With 16% weight loss, visceral fat is reduced by 30%. Clearing of liver fat is even more dramatic. With 16% weight loss, 65% of liver fat is cleared.
Because ectopic abnormal fat is cleared preferentially with weight loss, it affects different tissues with varying amounts of weight loss.
Weight loss and diabetes
A close relationship exists between weight loss and insulin sensitivity. With just 5% weight loss, insulin sensitivity in the liver and adipose tissue is greatly improved, but while muscle insulin sensitivity is improved at just 5% weight loss, it continues to improve with further weight loss. Indeed, weight loss has enormous benefits in improving glycemia in prediabetes and diabetes.
In patients with impaired glucose tolerance, weight loss of 10% can eliminate progression to type 2 diabetes. In patients with type 2 diabetes who still have beta-cell reserve, 15% weight loss can produce diabetes remission – normoglycemia without diabetes medications.
Weight loss and cardiovascular risk factors
Even very small amounts of weight loss – 3% – can improve triglycerides and glycemia. It takes 5% weight loss to show benefits in systolic and diastolic blood pressure, as well as in HDL and LDL cholesterol levels. For all of these, additional weight loss brings more improvement. Inflammatory markers are more difficult. It takes 10%-15% weight loss to improve most of these – for example, C-reactive protein.
Weight loss and other complications
It takes 10% or more weight loss to demonstrate improvements in symptoms in obstructive sleep apnea and gastroesophageal reflux disease. For knee pain, the relationship to improvement is not based on achieving a percentage loss. Each pound of weight lost can result in a fourfold reduction in the load exerted on the knee per step during daily activities, but it is important to reduce weight before there is structural damage, because weight loss can’t repair damaged knee joints. Moderate weight loss (5%-10%) produces improvements in quality-of-life measures, in urinary stress incontinence symptoms, and in measures of sexual function. It probably takes 15% or more weight loss to demonstrate improvement in cardiovascular events.
Must heavier patients lose more weight?
To answer this question, it is important to think in terms of percent weight loss rather than pounds or kilograms. In large studies of lifestyle intervention, of course individuals with higher BMI lost more weight. But the percentage weight loss was the same across BMI categories: class 1 (BMI 30-35), class 2 (BMI 35-40), class 3 (BMI > 40). Furthermore, the improvement in risk factors was the same across BMI categories. Those with class 3 obesity had the same improvements as those with class 1. This provides further rationale for thinking about weight loss as a percentage from baseline weight rather than as simply a weight-loss goal in pounds.
Goal setting is an important part of any behavioral intervention
At the start of a weight-loss intervention, the health care provider should raise the issue of the goal and the time course for achieving it. Patients often have unrealistic expectations, wanting to achieve large amounts of weight loss rapidly. Unfortunately, popular culture has reinforced this idea with advertisements using “lose 10 pounds the first week” and promoting before-and-after pictures of weight-loss results. The job of the health care provider is to coach and guide the patient in terms of achievable weight loss that can bring health improvement safely. Managing patient expectations is critical to long-term success.
Think in terms of percentage weight loss, not pounds, and set goals at achievable time points
Help patients translate a percent weight-loss goal to a pounds goal at 3, 6, and 12 months. With the emergence of medications approved for chronic weight management with robust weight-loss efficacy, it now is possible to achieve a weight-loss goal of 10% or 15% with regularity, and some patients will be able to achieve 20% or 25% weight loss with newer medications.
We should help our patients set a goal by calculating a goal for certain time points. A good goal for 3 months would be 5% weight loss. For our 200-lb patient, we would translate that to 10 lb in 3 months. For 6 months, the goal should be 10% (20 lb for our 200-lb patient). The usual trajectory of weight loss with lifestyle intervention alone is for a “plateau” at 6 months, although with newer medications, weight loss will continue for more than a year. That 1-year goal might be 15% (30 lb for our 200-lb patient) or even more, based on the patient’s baseline weight and body composition.
Weight-loss calculators can be useful tools for patients and health care providers. They can be found online and include the National Institutes of Health Body Weight Planner and the Pennington Biomedical Weight Loss Predictor Calculator. These tools give patients a realistic expectation of how fast weight loss can occur and provide guidelines to measure success.
Can patients lose too much weight?
In this patient population, losing too much weight is not typically a concern. However, newer medications are achieving average weight losses of 17% and 22% at 62 weeks, as reported by this news organization. There is a wide variation in response to these newer agents which target appetite, and many patients are losing more than the average percentages.
Remembering that the goal of weight loss is the reduction of excess abnormal body fat, we want patients to preserve as much lean mass as possible. Weight-bearing exercise can help during the weight-loss phase, but large or rapid weight loss can be concerning, especially in older individuals. When the BMI drops below 25, we want to watch patients carefully. Measurement of body composition, including bone mineral density, with dual-energy x-ray absorptiometry (DEXA) can help. This is a scenario where dose reduction of antiobesity medication can be indicated, and good clinical judgment is required to keep weight loss at healthy levels.
The future of weight loss
In the past, our strategy has been to promote as much weight loss as possible. With more effective medications, our strategy will have to change to a treat-to-target approach, such as we already use in hypertension and diabetes.
With the ability to produce powerful effects on appetite will come the need to not only target weight loss but to target preservation of lean mass and even to target different approaches for weight-loss maintenance. At present, we have no evidence that stopping medications results in anything other than weight regain. The study of different approaches to weight-loss maintenance will require our full attention.
Dr. Ryan has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, consultant, or trustee for: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand. Received income in an amount equal to or greater than $250 from: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand.
Donna Ryan, MD, is Professor Emerita, Pennington Biomedical Research Center, Louisiana State University, New Orleans.
A version of this article first appeared on Medscape.com.
One hour of walking per week may boost longevity for octogenarians
Adults aged 85 years and older who logged an hour or more of walking each week had a 40% reduced risk of all-cause mortality compared with less active peers, according to data from more than 7,000 individuals.
“Aging is accompanied by reduced physical activity and increased sedentary behavior, and reduced physical activity is associated with decreased life expectancy,” Moo-Nyun Jin, MD, of Inje University Sanggye Paik Hospital, Seoul, South Korea, said in an interview.
Reduced physical activity was especially likely in the elderly during the COVID-19 pandemic, he added.
“Promoting walking may be a simple way to help older adults avoid inactivity and encourage an active lifestyle for all-cause and cardiovascular mortality risk reduction,” Dr. Jin said.
Although walking is generally an easy form of exercise for the older adult population, the specific benefit of walking on reducing mortality has not been well studied, according to Dr. Jin and colleagues.
For adults of any age, current guidelines recommend at least 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity, but the amount of physical activity tends to decline with age, and activity recommendations are more difficult to meet, the authors wrote in a press release accompanying their study.
In the study, to be presented at the European Society of Cardiology Congress on Aug. 28 (Abstract 85643), the researchers reviewed data from 7,047 adults aged 85 years and older who participated in the Korean National Health Screening Program. The average age of the study population was 87 years, and 68% were women. Participants completed questionnaires about the amount of time spent in leisure time activities each week, including walking at a slow pace, moderate activity (such as cycling or brisk walking), and vigorous activity (such as running).
Those who walked at a slow pace for at least 1 hour per week had a 40% reduced risk of all-cause mortality and a 39% reduced risk of cardiovascular mortality, compared with inactive participants.
The proportions of participants who reported walking, moderate activity, and vigorous intensity physical activity were 42.5%, 14.7%, and 11.0%, respectively. Roughly one-third (33%) of those who reported slow walking each week also reported moderate or vigorous physical activity.
However, walking for 1 hour per week significantly reduced the risk for all-cause mortality and cardiovascular mortality among individuals who reported walking only, without other moderate or vigorous physical activity (hazard ratio, 0.50 and 0.46, respectively).
“Walking was linked with a lower likelihood of dying in older adults, regardless of whether or not they did any moderate to vigorous intensity physical activity,” Dr. Jin told this news organization. “Our study indicates that walking even just 1 hour every week is advantageous to those aged 85 years and older compared to being inactive.”
The hour of walking need not be in long bouts, 10 minutes each day will do, Dr. Jin added.
The participants were divided into five groups based on reported amount of weekly walking. More than half (57.5%) reported no slow walking, 8.5% walked less than 1 hour per week, 12.0% walked 1-2 hours, 8.7% walked 2-3 hours, and 13.3% walked more than 3 hours.
Although the study was limited by the reliance on self-reports, the results were strengthened by the large sample size and support the value of easy walking for adults aged 85 years and older compared to being inactive.
“Walking may present an opportunity for promoting physical activity among the elderly population, offering a simple way to avoid inactivity and increase physical activity,” said Dr. Jin. However, more research is needed to evaluate the association between mortality and walking by objective measurement of walking levels, using a device such as a smart watch, he noted.
Results are preliminary
“This is an observational study, not an experiment, so it means causality cannot be presumed,” said Maria Fiatarone Singh, MD, a geriatrician with a focus on exercise physiology at the University of Sydney, in an interview. “In other words, it is possible that diseases resulting in mortality prevented people from walking rather than the other way around,” she noted. The only published experimental study on exercise and mortality in older adults was conducted by Dr. Fiatarone Singh and colleagues in Norway. In that study, published in the British Medical Journal in 2020, high-intensity training programs were associated with reduced all-cause mortality compared with inactive controls and individuals who engaged in moderate intensity exercise.
The current study “would have needed to control for many factors related to mortality, such as cardiovascular disease, hypertension, diabetes, malnutrition, and dementia to see what residual benefit might be related to walking,” Dr. Fiatarone Singh said.
“Although walking seems easy and safe, in fact people who are frail, sarcopenic, osteoporotic, or have fallen are recommended to do resistance and balance training rather than walking, and add walking later when they are able to do it safely,” she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Fiatarone Singh had no financial conflicts to disclose.
Adults aged 85 years and older who logged an hour or more of walking each week had a 40% reduced risk of all-cause mortality compared with less active peers, according to data from more than 7,000 individuals.
“Aging is accompanied by reduced physical activity and increased sedentary behavior, and reduced physical activity is associated with decreased life expectancy,” Moo-Nyun Jin, MD, of Inje University Sanggye Paik Hospital, Seoul, South Korea, said in an interview.
Reduced physical activity was especially likely in the elderly during the COVID-19 pandemic, he added.
“Promoting walking may be a simple way to help older adults avoid inactivity and encourage an active lifestyle for all-cause and cardiovascular mortality risk reduction,” Dr. Jin said.
Although walking is generally an easy form of exercise for the older adult population, the specific benefit of walking on reducing mortality has not been well studied, according to Dr. Jin and colleagues.
For adults of any age, current guidelines recommend at least 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity, but the amount of physical activity tends to decline with age, and activity recommendations are more difficult to meet, the authors wrote in a press release accompanying their study.
In the study, to be presented at the European Society of Cardiology Congress on Aug. 28 (Abstract 85643), the researchers reviewed data from 7,047 adults aged 85 years and older who participated in the Korean National Health Screening Program. The average age of the study population was 87 years, and 68% were women. Participants completed questionnaires about the amount of time spent in leisure time activities each week, including walking at a slow pace, moderate activity (such as cycling or brisk walking), and vigorous activity (such as running).
Those who walked at a slow pace for at least 1 hour per week had a 40% reduced risk of all-cause mortality and a 39% reduced risk of cardiovascular mortality, compared with inactive participants.
The proportions of participants who reported walking, moderate activity, and vigorous intensity physical activity were 42.5%, 14.7%, and 11.0%, respectively. Roughly one-third (33%) of those who reported slow walking each week also reported moderate or vigorous physical activity.
However, walking for 1 hour per week significantly reduced the risk for all-cause mortality and cardiovascular mortality among individuals who reported walking only, without other moderate or vigorous physical activity (hazard ratio, 0.50 and 0.46, respectively).
“Walking was linked with a lower likelihood of dying in older adults, regardless of whether or not they did any moderate to vigorous intensity physical activity,” Dr. Jin told this news organization. “Our study indicates that walking even just 1 hour every week is advantageous to those aged 85 years and older compared to being inactive.”
The hour of walking need not be in long bouts, 10 minutes each day will do, Dr. Jin added.
The participants were divided into five groups based on reported amount of weekly walking. More than half (57.5%) reported no slow walking, 8.5% walked less than 1 hour per week, 12.0% walked 1-2 hours, 8.7% walked 2-3 hours, and 13.3% walked more than 3 hours.
Although the study was limited by the reliance on self-reports, the results were strengthened by the large sample size and support the value of easy walking for adults aged 85 years and older compared to being inactive.
“Walking may present an opportunity for promoting physical activity among the elderly population, offering a simple way to avoid inactivity and increase physical activity,” said Dr. Jin. However, more research is needed to evaluate the association between mortality and walking by objective measurement of walking levels, using a device such as a smart watch, he noted.
Results are preliminary
“This is an observational study, not an experiment, so it means causality cannot be presumed,” said Maria Fiatarone Singh, MD, a geriatrician with a focus on exercise physiology at the University of Sydney, in an interview. “In other words, it is possible that diseases resulting in mortality prevented people from walking rather than the other way around,” she noted. The only published experimental study on exercise and mortality in older adults was conducted by Dr. Fiatarone Singh and colleagues in Norway. In that study, published in the British Medical Journal in 2020, high-intensity training programs were associated with reduced all-cause mortality compared with inactive controls and individuals who engaged in moderate intensity exercise.
The current study “would have needed to control for many factors related to mortality, such as cardiovascular disease, hypertension, diabetes, malnutrition, and dementia to see what residual benefit might be related to walking,” Dr. Fiatarone Singh said.
“Although walking seems easy and safe, in fact people who are frail, sarcopenic, osteoporotic, or have fallen are recommended to do resistance and balance training rather than walking, and add walking later when they are able to do it safely,” she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Fiatarone Singh had no financial conflicts to disclose.
Adults aged 85 years and older who logged an hour or more of walking each week had a 40% reduced risk of all-cause mortality compared with less active peers, according to data from more than 7,000 individuals.
“Aging is accompanied by reduced physical activity and increased sedentary behavior, and reduced physical activity is associated with decreased life expectancy,” Moo-Nyun Jin, MD, of Inje University Sanggye Paik Hospital, Seoul, South Korea, said in an interview.
Reduced physical activity was especially likely in the elderly during the COVID-19 pandemic, he added.
“Promoting walking may be a simple way to help older adults avoid inactivity and encourage an active lifestyle for all-cause and cardiovascular mortality risk reduction,” Dr. Jin said.
Although walking is generally an easy form of exercise for the older adult population, the specific benefit of walking on reducing mortality has not been well studied, according to Dr. Jin and colleagues.
For adults of any age, current guidelines recommend at least 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity, but the amount of physical activity tends to decline with age, and activity recommendations are more difficult to meet, the authors wrote in a press release accompanying their study.
In the study, to be presented at the European Society of Cardiology Congress on Aug. 28 (Abstract 85643), the researchers reviewed data from 7,047 adults aged 85 years and older who participated in the Korean National Health Screening Program. The average age of the study population was 87 years, and 68% were women. Participants completed questionnaires about the amount of time spent in leisure time activities each week, including walking at a slow pace, moderate activity (such as cycling or brisk walking), and vigorous activity (such as running).
Those who walked at a slow pace for at least 1 hour per week had a 40% reduced risk of all-cause mortality and a 39% reduced risk of cardiovascular mortality, compared with inactive participants.
The proportions of participants who reported walking, moderate activity, and vigorous intensity physical activity were 42.5%, 14.7%, and 11.0%, respectively. Roughly one-third (33%) of those who reported slow walking each week also reported moderate or vigorous physical activity.
However, walking for 1 hour per week significantly reduced the risk for all-cause mortality and cardiovascular mortality among individuals who reported walking only, without other moderate or vigorous physical activity (hazard ratio, 0.50 and 0.46, respectively).
“Walking was linked with a lower likelihood of dying in older adults, regardless of whether or not they did any moderate to vigorous intensity physical activity,” Dr. Jin told this news organization. “Our study indicates that walking even just 1 hour every week is advantageous to those aged 85 years and older compared to being inactive.”
The hour of walking need not be in long bouts, 10 minutes each day will do, Dr. Jin added.
The participants were divided into five groups based on reported amount of weekly walking. More than half (57.5%) reported no slow walking, 8.5% walked less than 1 hour per week, 12.0% walked 1-2 hours, 8.7% walked 2-3 hours, and 13.3% walked more than 3 hours.
Although the study was limited by the reliance on self-reports, the results were strengthened by the large sample size and support the value of easy walking for adults aged 85 years and older compared to being inactive.
“Walking may present an opportunity for promoting physical activity among the elderly population, offering a simple way to avoid inactivity and increase physical activity,” said Dr. Jin. However, more research is needed to evaluate the association between mortality and walking by objective measurement of walking levels, using a device such as a smart watch, he noted.
Results are preliminary
“This is an observational study, not an experiment, so it means causality cannot be presumed,” said Maria Fiatarone Singh, MD, a geriatrician with a focus on exercise physiology at the University of Sydney, in an interview. “In other words, it is possible that diseases resulting in mortality prevented people from walking rather than the other way around,” she noted. The only published experimental study on exercise and mortality in older adults was conducted by Dr. Fiatarone Singh and colleagues in Norway. In that study, published in the British Medical Journal in 2020, high-intensity training programs were associated with reduced all-cause mortality compared with inactive controls and individuals who engaged in moderate intensity exercise.
The current study “would have needed to control for many factors related to mortality, such as cardiovascular disease, hypertension, diabetes, malnutrition, and dementia to see what residual benefit might be related to walking,” Dr. Fiatarone Singh said.
“Although walking seems easy and safe, in fact people who are frail, sarcopenic, osteoporotic, or have fallen are recommended to do resistance and balance training rather than walking, and add walking later when they are able to do it safely,” she emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Fiatarone Singh had no financial conflicts to disclose.
FROM ESC CONGRESS 2022