User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
How much do we really know about gender dysphoria?
At the risk of losing a digit or two I am going to dip my toes into the murky waters of gender-affirming care, sometimes referred to as trans care. Recently, Moira Szilagyi, MD, PhD, president of the American Academy of Pediatrics, released two statements, one in the Aug. 22, 2022, Wall Street Journal, the other summarized in the Aug. 25, 2022, AAP Daily Briefing, in which she attempts to clarify the academy’s position on gender-affirming care. They were well-worded and heroic attempts to clear the air. I fear these explanations will do little to encourage informed and courteous discussions between those entrenched on either side of a disagreement that is unfortunately being played out on media outlets and state legislatures instead of the offices of primary care physicians and specialists where it belongs.
The current mess is an example of what can happen when there is a paucity of reliable data, a superabundance of emotion, and a system that feeds on instant news and sound bites with little understanding of how science should work.
Some of the turmoil is a response to the notion that in certain situations gender dysphoria may be a condition that can be learned or mimicked from exposure to other gender-dysphoric individuals. Two papers anchor either side of the debate. The first paper was published in 2018 by a then–Brown University health expert who hypothesized the existence of a condition which she labeled “rapid-onset gender dysphoria [ROGD]”. One can imagine that “social contagion” might be considered as one of the potential contributors to this hypothesized condition. Unfortunately, the publication of the paper ignited a firestorm of criticism from a segment of the population that advocates for the transgender community, prompting the university and the online publisher to backpedal and reevaluate the quality of the research on which the paper was based.
One of the concerns voiced at the time of publication was that the research could be used to support the transphobic agenda by some state legislatures hoping to ban gender-affirming care. How large a role the paper played in the current spate of legislation in is unclear. I suspect it has been small. But, one can’t deny the potential exists.
Leaping forward to 2022, the second paper was published in the August issue of Pediatrics, in which the authors attempted to test the ROGD hypothesis and question the inference of social contagion.
The investigators found that in 2017 and 2019 the birth ratios of transgender-diverse (TGD) individuals did not favor assigned female-sex-at-birth (AFAB) individuals. They also discovered that in their sample overall there was a decrease in the percentage of adolescents who self-identified as TGD. Not surprisingly, “bullying victimization and suicidality were higher among TGD youth when compared with their cisgender peers.” The authors concluded that their findings were “incongruent with an ROGD hypothesis that posits social contagion” nor should it be used to restrict access to gender-affirming care.
There you have it. Are we any closer to understanding gender dysphoria and its origins? I don’t think so. The media is somewhat less confused. The NBC News online presence headline on Aug. 3, 2022, reads “‘Social contagion’ isn’t causing more youths to be transgender, study finds.”
My sense is that the general population perceives an increase in the prevalence of gender dysphoria. It is very likely that this perception is primarily a reflection of a more compassionate and educated attitude in a significant portion of the population making it less challenging for gender-dysphoric youth to surface. However, it should not surprise us that some parents and observers are concerned that a percentage of this increased prevalence is the result of social contagion. Nor should it surprise us that some advocates for the trans population feel threatened by this hypothesis.
Neither of these studies really answers the question of whether some cases of gender dysphoria are the result of social contagion. Both were small samples using methodology that has been called into question. The bottom line is that we need more studies and must remain open to considering their results. That’s how science should work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
At the risk of losing a digit or two I am going to dip my toes into the murky waters of gender-affirming care, sometimes referred to as trans care. Recently, Moira Szilagyi, MD, PhD, president of the American Academy of Pediatrics, released two statements, one in the Aug. 22, 2022, Wall Street Journal, the other summarized in the Aug. 25, 2022, AAP Daily Briefing, in which she attempts to clarify the academy’s position on gender-affirming care. They were well-worded and heroic attempts to clear the air. I fear these explanations will do little to encourage informed and courteous discussions between those entrenched on either side of a disagreement that is unfortunately being played out on media outlets and state legislatures instead of the offices of primary care physicians and specialists where it belongs.
The current mess is an example of what can happen when there is a paucity of reliable data, a superabundance of emotion, and a system that feeds on instant news and sound bites with little understanding of how science should work.
Some of the turmoil is a response to the notion that in certain situations gender dysphoria may be a condition that can be learned or mimicked from exposure to other gender-dysphoric individuals. Two papers anchor either side of the debate. The first paper was published in 2018 by a then–Brown University health expert who hypothesized the existence of a condition which she labeled “rapid-onset gender dysphoria [ROGD]”. One can imagine that “social contagion” might be considered as one of the potential contributors to this hypothesized condition. Unfortunately, the publication of the paper ignited a firestorm of criticism from a segment of the population that advocates for the transgender community, prompting the university and the online publisher to backpedal and reevaluate the quality of the research on which the paper was based.
One of the concerns voiced at the time of publication was that the research could be used to support the transphobic agenda by some state legislatures hoping to ban gender-affirming care. How large a role the paper played in the current spate of legislation in is unclear. I suspect it has been small. But, one can’t deny the potential exists.
Leaping forward to 2022, the second paper was published in the August issue of Pediatrics, in which the authors attempted to test the ROGD hypothesis and question the inference of social contagion.
The investigators found that in 2017 and 2019 the birth ratios of transgender-diverse (TGD) individuals did not favor assigned female-sex-at-birth (AFAB) individuals. They also discovered that in their sample overall there was a decrease in the percentage of adolescents who self-identified as TGD. Not surprisingly, “bullying victimization and suicidality were higher among TGD youth when compared with their cisgender peers.” The authors concluded that their findings were “incongruent with an ROGD hypothesis that posits social contagion” nor should it be used to restrict access to gender-affirming care.
There you have it. Are we any closer to understanding gender dysphoria and its origins? I don’t think so. The media is somewhat less confused. The NBC News online presence headline on Aug. 3, 2022, reads “‘Social contagion’ isn’t causing more youths to be transgender, study finds.”
My sense is that the general population perceives an increase in the prevalence of gender dysphoria. It is very likely that this perception is primarily a reflection of a more compassionate and educated attitude in a significant portion of the population making it less challenging for gender-dysphoric youth to surface. However, it should not surprise us that some parents and observers are concerned that a percentage of this increased prevalence is the result of social contagion. Nor should it surprise us that some advocates for the trans population feel threatened by this hypothesis.
Neither of these studies really answers the question of whether some cases of gender dysphoria are the result of social contagion. Both were small samples using methodology that has been called into question. The bottom line is that we need more studies and must remain open to considering their results. That’s how science should work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
At the risk of losing a digit or two I am going to dip my toes into the murky waters of gender-affirming care, sometimes referred to as trans care. Recently, Moira Szilagyi, MD, PhD, president of the American Academy of Pediatrics, released two statements, one in the Aug. 22, 2022, Wall Street Journal, the other summarized in the Aug. 25, 2022, AAP Daily Briefing, in which she attempts to clarify the academy’s position on gender-affirming care. They were well-worded and heroic attempts to clear the air. I fear these explanations will do little to encourage informed and courteous discussions between those entrenched on either side of a disagreement that is unfortunately being played out on media outlets and state legislatures instead of the offices of primary care physicians and specialists where it belongs.
The current mess is an example of what can happen when there is a paucity of reliable data, a superabundance of emotion, and a system that feeds on instant news and sound bites with little understanding of how science should work.
Some of the turmoil is a response to the notion that in certain situations gender dysphoria may be a condition that can be learned or mimicked from exposure to other gender-dysphoric individuals. Two papers anchor either side of the debate. The first paper was published in 2018 by a then–Brown University health expert who hypothesized the existence of a condition which she labeled “rapid-onset gender dysphoria [ROGD]”. One can imagine that “social contagion” might be considered as one of the potential contributors to this hypothesized condition. Unfortunately, the publication of the paper ignited a firestorm of criticism from a segment of the population that advocates for the transgender community, prompting the university and the online publisher to backpedal and reevaluate the quality of the research on which the paper was based.
One of the concerns voiced at the time of publication was that the research could be used to support the transphobic agenda by some state legislatures hoping to ban gender-affirming care. How large a role the paper played in the current spate of legislation in is unclear. I suspect it has been small. But, one can’t deny the potential exists.
Leaping forward to 2022, the second paper was published in the August issue of Pediatrics, in which the authors attempted to test the ROGD hypothesis and question the inference of social contagion.
The investigators found that in 2017 and 2019 the birth ratios of transgender-diverse (TGD) individuals did not favor assigned female-sex-at-birth (AFAB) individuals. They also discovered that in their sample overall there was a decrease in the percentage of adolescents who self-identified as TGD. Not surprisingly, “bullying victimization and suicidality were higher among TGD youth when compared with their cisgender peers.” The authors concluded that their findings were “incongruent with an ROGD hypothesis that posits social contagion” nor should it be used to restrict access to gender-affirming care.
There you have it. Are we any closer to understanding gender dysphoria and its origins? I don’t think so. The media is somewhat less confused. The NBC News online presence headline on Aug. 3, 2022, reads “‘Social contagion’ isn’t causing more youths to be transgender, study finds.”
My sense is that the general population perceives an increase in the prevalence of gender dysphoria. It is very likely that this perception is primarily a reflection of a more compassionate and educated attitude in a significant portion of the population making it less challenging for gender-dysphoric youth to surface. However, it should not surprise us that some parents and observers are concerned that a percentage of this increased prevalence is the result of social contagion. Nor should it surprise us that some advocates for the trans population feel threatened by this hypothesis.
Neither of these studies really answers the question of whether some cases of gender dysphoria are the result of social contagion. Both were small samples using methodology that has been called into question. The bottom line is that we need more studies and must remain open to considering their results. That’s how science should work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Omega-3 fatty acids and depression: Are they protective?
New research is suggesting that there are “meaningful” associations between higher dietary intake of omega-3 fatty acids and lower risk for depressive episodes.
In addition, consumption of total fatty acids and alpha-linolenic acid was associated with a reduced risk for incident depressive episodes (9% and 29%, respectively).
“Our results showed an important protective effect from the consumption of omega-3,” Maria de Jesus Mendes da Fonseca, University of the State of Rio de Janeiro, and colleagues write.
The findings were published online in Nutrients.
Mixed bag of studies
Epidemiologic evidence suggests that deficient dietary omega-3 intake is a modifiable risk factor for depression and that individuals with low consumption of omega-3 food sources have more depressive symptoms.
However, the results are inconsistent, and few longitudinal studies have addressed this association, the investigators note.
The new analysis included 13,879 adults (aged 39-65 years or older) participating in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) from 2008 to 2014.
Data on depressive episodes were obtained with the Clinical Interview Schedule Revised (CIS-R), and food consumption was measured with the Food Frequency Questionnaire (FFQ).
The target dietary components were total polyunsaturated fatty acids (PUFA) and the omega-3 fatty acids: alpha-linolenic acid, eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and docosapentaenoic acid (DPA).
The majority of participants had adequate dietary intake of omega-3 fatty acids, and none was taking omega-3 supplements.
In the fully adjusted model, consumption of fatty acids from the omega-3 family had a protective effect against maintenance of depressive episodes, showing “important associations, although the significance levels are borderline, possibly due to the sample size,” the researchers report.
In regard to onset of depressive episodes, estimates from the fully adjusted model suggest that a higher consumption of omega-3 acids (total and subtypes) is associated with lower risk for depressive episodes – with significant associations for omega-3 and alpha-linolenic acid.
The investigators note that strengths of the study include “its originality, as it is the first to assess associations between maintenance and incidence of depressive episodes and consumption of omega-3, besides the use of data from the ELSA-Brasil Study, with rigorous data collection protocols and reliable and validated instruments, thus guaranteeing the quality of the sample and the data.”
A study limitation, however, was that the ELSA-Brasil sample consists only of public employees, with the potential for a selection bias such as healthy worker phenomenon, the researchers note. Another was the use of the FFQ, which may underestimate daily intake of foods and depends on individual participant recall – all of which could possibly lead to a differential classification bias.
Interpret cautiously
Commenting on the study, David Mischoulon, MD, PhD, professor of psychiatry, Harvard Medical School, and director of the depression clinical and research program at Massachusetts General Hospital, both in Boston, said that data on omega-3s in depression are “very mixed.”
“A lot of the studies don’t necessarily agree with each other. Certainly, in studies that try to seek an association between omega-3 use and depression, it’s always complicated because it can be difficult to control for all variables that could be contributing to the result that you get,” said Dr. Mischoulon, who is also a member of the Anxiety and Depression Association of America and was not involved in the research.
A caveat to the current study was that diet was assessed only at baseline, “so we don’t really know whether there were any substantial dietary changes over time, he noted.
He also cautioned that it is hard to draw any firm conclusions from this type of study.
“In general, in studies with a large sample, which this study has, it’s easier to find statistically significant differences. But you need to ask yourself: Does it really matter? Is it enough to have a clinical impact and make a difference?” Dr. Mischoulon said.
The ELSA-Brasil study was funded by the Brazilian Ministry of Science, Technology, and Innovation and by the Ministry of Health. The investigators have reported no relevant financial relationships. Dr. Mischoulon has received research support from Nordic Naturals and heckel medizintechnik GmbH and honoraria for speaking from the Massachusetts General Hospital Psychiatry Academy. He also works with the MGH Clinical Trials Network and Institute, which has received research funding from multiple pharmaceutical companies and the National Institute of Mental Health.
A version of this article first appeared on Medscape.com.
New research is suggesting that there are “meaningful” associations between higher dietary intake of omega-3 fatty acids and lower risk for depressive episodes.
In addition, consumption of total fatty acids and alpha-linolenic acid was associated with a reduced risk for incident depressive episodes (9% and 29%, respectively).
“Our results showed an important protective effect from the consumption of omega-3,” Maria de Jesus Mendes da Fonseca, University of the State of Rio de Janeiro, and colleagues write.
The findings were published online in Nutrients.
Mixed bag of studies
Epidemiologic evidence suggests that deficient dietary omega-3 intake is a modifiable risk factor for depression and that individuals with low consumption of omega-3 food sources have more depressive symptoms.
However, the results are inconsistent, and few longitudinal studies have addressed this association, the investigators note.
The new analysis included 13,879 adults (aged 39-65 years or older) participating in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) from 2008 to 2014.
Data on depressive episodes were obtained with the Clinical Interview Schedule Revised (CIS-R), and food consumption was measured with the Food Frequency Questionnaire (FFQ).
The target dietary components were total polyunsaturated fatty acids (PUFA) and the omega-3 fatty acids: alpha-linolenic acid, eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and docosapentaenoic acid (DPA).
The majority of participants had adequate dietary intake of omega-3 fatty acids, and none was taking omega-3 supplements.
In the fully adjusted model, consumption of fatty acids from the omega-3 family had a protective effect against maintenance of depressive episodes, showing “important associations, although the significance levels are borderline, possibly due to the sample size,” the researchers report.
In regard to onset of depressive episodes, estimates from the fully adjusted model suggest that a higher consumption of omega-3 acids (total and subtypes) is associated with lower risk for depressive episodes – with significant associations for omega-3 and alpha-linolenic acid.
The investigators note that strengths of the study include “its originality, as it is the first to assess associations between maintenance and incidence of depressive episodes and consumption of omega-3, besides the use of data from the ELSA-Brasil Study, with rigorous data collection protocols and reliable and validated instruments, thus guaranteeing the quality of the sample and the data.”
A study limitation, however, was that the ELSA-Brasil sample consists only of public employees, with the potential for a selection bias such as healthy worker phenomenon, the researchers note. Another was the use of the FFQ, which may underestimate daily intake of foods and depends on individual participant recall – all of which could possibly lead to a differential classification bias.
Interpret cautiously
Commenting on the study, David Mischoulon, MD, PhD, professor of psychiatry, Harvard Medical School, and director of the depression clinical and research program at Massachusetts General Hospital, both in Boston, said that data on omega-3s in depression are “very mixed.”
“A lot of the studies don’t necessarily agree with each other. Certainly, in studies that try to seek an association between omega-3 use and depression, it’s always complicated because it can be difficult to control for all variables that could be contributing to the result that you get,” said Dr. Mischoulon, who is also a member of the Anxiety and Depression Association of America and was not involved in the research.
A caveat to the current study was that diet was assessed only at baseline, “so we don’t really know whether there were any substantial dietary changes over time, he noted.
He also cautioned that it is hard to draw any firm conclusions from this type of study.
“In general, in studies with a large sample, which this study has, it’s easier to find statistically significant differences. But you need to ask yourself: Does it really matter? Is it enough to have a clinical impact and make a difference?” Dr. Mischoulon said.
The ELSA-Brasil study was funded by the Brazilian Ministry of Science, Technology, and Innovation and by the Ministry of Health. The investigators have reported no relevant financial relationships. Dr. Mischoulon has received research support from Nordic Naturals and heckel medizintechnik GmbH and honoraria for speaking from the Massachusetts General Hospital Psychiatry Academy. He also works with the MGH Clinical Trials Network and Institute, which has received research funding from multiple pharmaceutical companies and the National Institute of Mental Health.
A version of this article first appeared on Medscape.com.
New research is suggesting that there are “meaningful” associations between higher dietary intake of omega-3 fatty acids and lower risk for depressive episodes.
In addition, consumption of total fatty acids and alpha-linolenic acid was associated with a reduced risk for incident depressive episodes (9% and 29%, respectively).
“Our results showed an important protective effect from the consumption of omega-3,” Maria de Jesus Mendes da Fonseca, University of the State of Rio de Janeiro, and colleagues write.
The findings were published online in Nutrients.
Mixed bag of studies
Epidemiologic evidence suggests that deficient dietary omega-3 intake is a modifiable risk factor for depression and that individuals with low consumption of omega-3 food sources have more depressive symptoms.
However, the results are inconsistent, and few longitudinal studies have addressed this association, the investigators note.
The new analysis included 13,879 adults (aged 39-65 years or older) participating in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) from 2008 to 2014.
Data on depressive episodes were obtained with the Clinical Interview Schedule Revised (CIS-R), and food consumption was measured with the Food Frequency Questionnaire (FFQ).
The target dietary components were total polyunsaturated fatty acids (PUFA) and the omega-3 fatty acids: alpha-linolenic acid, eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and docosapentaenoic acid (DPA).
The majority of participants had adequate dietary intake of omega-3 fatty acids, and none was taking omega-3 supplements.
In the fully adjusted model, consumption of fatty acids from the omega-3 family had a protective effect against maintenance of depressive episodes, showing “important associations, although the significance levels are borderline, possibly due to the sample size,” the researchers report.
In regard to onset of depressive episodes, estimates from the fully adjusted model suggest that a higher consumption of omega-3 acids (total and subtypes) is associated with lower risk for depressive episodes – with significant associations for omega-3 and alpha-linolenic acid.
The investigators note that strengths of the study include “its originality, as it is the first to assess associations between maintenance and incidence of depressive episodes and consumption of omega-3, besides the use of data from the ELSA-Brasil Study, with rigorous data collection protocols and reliable and validated instruments, thus guaranteeing the quality of the sample and the data.”
A study limitation, however, was that the ELSA-Brasil sample consists only of public employees, with the potential for a selection bias such as healthy worker phenomenon, the researchers note. Another was the use of the FFQ, which may underestimate daily intake of foods and depends on individual participant recall – all of which could possibly lead to a differential classification bias.
Interpret cautiously
Commenting on the study, David Mischoulon, MD, PhD, professor of psychiatry, Harvard Medical School, and director of the depression clinical and research program at Massachusetts General Hospital, both in Boston, said that data on omega-3s in depression are “very mixed.”
“A lot of the studies don’t necessarily agree with each other. Certainly, in studies that try to seek an association between omega-3 use and depression, it’s always complicated because it can be difficult to control for all variables that could be contributing to the result that you get,” said Dr. Mischoulon, who is also a member of the Anxiety and Depression Association of America and was not involved in the research.
A caveat to the current study was that diet was assessed only at baseline, “so we don’t really know whether there were any substantial dietary changes over time, he noted.
He also cautioned that it is hard to draw any firm conclusions from this type of study.
“In general, in studies with a large sample, which this study has, it’s easier to find statistically significant differences. But you need to ask yourself: Does it really matter? Is it enough to have a clinical impact and make a difference?” Dr. Mischoulon said.
The ELSA-Brasil study was funded by the Brazilian Ministry of Science, Technology, and Innovation and by the Ministry of Health. The investigators have reported no relevant financial relationships. Dr. Mischoulon has received research support from Nordic Naturals and heckel medizintechnik GmbH and honoraria for speaking from the Massachusetts General Hospital Psychiatry Academy. He also works with the MGH Clinical Trials Network and Institute, which has received research funding from multiple pharmaceutical companies and the National Institute of Mental Health.
A version of this article first appeared on Medscape.com.
FROM NUTRIENTS
New ovulatory disorder classifications from FIGO replace 50-year-old system
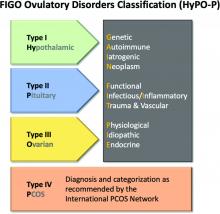
The first major revision in the systematic description of ovulatory disorders in nearly 50 years has been proposed by a consensus of experts organized by the International Federation of Gynecology and Obstetrics.
“The FIGO HyPO-P system for the classification of ovulatory disorders is submitted for consideration as a worldwide standard,” according to the writing committee, who published their methodology and their proposed applications in the International Journal of Gynecology and Obstetrics.
The classification system was created to replace the much-modified World Health Organization system first described in 1973. Since that time, many modifications have been proposed to accommodate advances in imaging and new information about underlying pathologies, but there has been no subsequent authoritative reference with these modifications or any other newer organizing system.
The new consensus was developed under the aegis of FIGO, but the development group consisted of representatives from national organizations and the major subspecialty societies. Recognized experts in ovulatory disorders and representatives from lay advocacy organizations also participated.
The HyPO-P system is based largely on anatomy. The acronym refers to ovulatory disorders related to the hypothalamus (type I), the pituitary (type II), and the ovary (type III).
Polycystic ovary syndrome (PCOS), one of the most common ovulatory disorders, was given a separate category (type IV) because of its complexity as well as the fact that PCOS is a heterogeneous systemic disorder with manifestations not limited to an impact on ovarian function.
As the first level of classification, three of the four primary categories (I-III) focus attention on the dominant anatomic source of the change in ovulatory function. The original WHO classification system identified as many as seven major groups, but they were based primarily on assays for gonadotropins and estradiol.
The new system “provides a different structure for determining the diagnosis. Blood tests are not a necessary first step,” explained Malcolm G. Munro, MD, clinical professor, department of obstetrics and gynecology, University of California, Los Angeles. Dr. Munro was the first author of the publication.
The classification system “is not as focused on the specific steps for investigation of ovulatory dysfunction as much as it explains how to structure an investigation of the girl or woman with an ovulatory disorder and then how to characterize the underlying cause,” Dr. Munro said in an interview. “It is designed to allow everyone, whether clinicians, researchers, or patients, to speak the same language.”
New system employs four categories
The four primary categories provide just the first level of classification. The next step is encapsulated in the GAIN-FIT-PIE acronym, which frames the presumed or documented categories of etiologies for the primary categories. GAIN stands for genetic, autoimmune, iatrogenic, or neoplasm etiologies. FIT stands for functional, infectious/inflammatory, or trauma and vascular etiologies. PIE stands for physiological, idiopathic, and endocrine etiologies.
By this methodology, a patient with irregular menses, galactorrhea, and elevated prolactin and an MRI showing a pituitary tumor would be identified a type 2-N, signifying pituitary (type 2) involvement with a neoplasm (N).
A third level of classification permits specific diagnostic entities to be named, allowing the patient in the example above to receive a diagnosis of a prolactin-secreting adenoma.
Not all etiologies can be identified with current diagnostic studies, even assuming clinicians have access to the resources, such as advanced imaging, that will increase diagnostic yield. As a result, the authors acknowledged that the classification system will be “aspirational” in at least some patients, but the structure of this system is expected to lead to greater precision in understanding the causes and defining features of ovulatory disorders, which, in turn, might facilitate new research initiatives.
In the published report, diagnostic protocols based on symptoms were described as being “beyond the spectrum” of this initial description. Rather, Dr. Munro explained that the most important contribution of this new classification system are standardization and communication. The system will be amenable for educating trainees and patients, for communicating between clinicians, and as a framework for research where investigators focus on more homogeneous populations of patients.
“There are many causes of ovulatory disorders that are not related to ovarian function. This is one message. Another is that ovulatory disorders are not binary. They occur on a spectrum. These range from transient instances of delayed or failed ovulation to chronic anovulation,” he said.
The new system is “ a welcome update,” according to Mark P. Trolice, MD, director of the IVF Center and professor of obstetrics and gynecology at the University of Central Florida, both in Orlando.
Dr. Trolice pointed to the clinical value of placing PCOS in a separate category. He noted that it affects 8%-13% of women, making it the most common single cause of ovulatory dysfunction.
“Another area that required clarification from prior WHO classifications was hyperprolactinemia, which is now placed in the type II category,” Dr. Trolice said in an interview.
Better terminology can help address a complex set of disorders with multiple causes and variable manifestations.
“In the evaluation of ovulation dysfunction, it is important to remember that regular menstrual intervals do not ensure ovulation,” Dr. Trolice pointed out. Even though a serum progesterone level of higher than 3 ng/mL is one of the simplest laboratory markers for ovulation, this level, he noted, “can vary through the luteal phase and even throughout the day.”
The proposed classification system, while providing a framework for describing ovulatory disorders, is designed to be adaptable, permitting advances in the understanding of the causes of ovulatory dysfunction, in the diagnosis of the causes, and in the treatments to be incorporated.
“No system should be considered permanent,” according to Dr. Munro and his coauthors. “Review and careful modification and revision should be carried out regularly.”
Dr. Munro reports financial relationships with AbbVie, American Regent, Daiichi Sankyo, Hologic, Myovant, and Pharmacosmos. Dr. Trolice reports no potential conflicts of interest.
The first major revision in the systematic description of ovulatory disorders in nearly 50 years has been proposed by a consensus of experts organized by the International Federation of Gynecology and Obstetrics.
“The FIGO HyPO-P system for the classification of ovulatory disorders is submitted for consideration as a worldwide standard,” according to the writing committee, who published their methodology and their proposed applications in the International Journal of Gynecology and Obstetrics.
The classification system was created to replace the much-modified World Health Organization system first described in 1973. Since that time, many modifications have been proposed to accommodate advances in imaging and new information about underlying pathologies, but there has been no subsequent authoritative reference with these modifications or any other newer organizing system.
The new consensus was developed under the aegis of FIGO, but the development group consisted of representatives from national organizations and the major subspecialty societies. Recognized experts in ovulatory disorders and representatives from lay advocacy organizations also participated.
The HyPO-P system is based largely on anatomy. The acronym refers to ovulatory disorders related to the hypothalamus (type I), the pituitary (type II), and the ovary (type III).
Polycystic ovary syndrome (PCOS), one of the most common ovulatory disorders, was given a separate category (type IV) because of its complexity as well as the fact that PCOS is a heterogeneous systemic disorder with manifestations not limited to an impact on ovarian function.
As the first level of classification, three of the four primary categories (I-III) focus attention on the dominant anatomic source of the change in ovulatory function. The original WHO classification system identified as many as seven major groups, but they were based primarily on assays for gonadotropins and estradiol.
The new system “provides a different structure for determining the diagnosis. Blood tests are not a necessary first step,” explained Malcolm G. Munro, MD, clinical professor, department of obstetrics and gynecology, University of California, Los Angeles. Dr. Munro was the first author of the publication.
The classification system “is not as focused on the specific steps for investigation of ovulatory dysfunction as much as it explains how to structure an investigation of the girl or woman with an ovulatory disorder and then how to characterize the underlying cause,” Dr. Munro said in an interview. “It is designed to allow everyone, whether clinicians, researchers, or patients, to speak the same language.”
New system employs four categories
The four primary categories provide just the first level of classification. The next step is encapsulated in the GAIN-FIT-PIE acronym, which frames the presumed or documented categories of etiologies for the primary categories. GAIN stands for genetic, autoimmune, iatrogenic, or neoplasm etiologies. FIT stands for functional, infectious/inflammatory, or trauma and vascular etiologies. PIE stands for physiological, idiopathic, and endocrine etiologies.
By this methodology, a patient with irregular menses, galactorrhea, and elevated prolactin and an MRI showing a pituitary tumor would be identified a type 2-N, signifying pituitary (type 2) involvement with a neoplasm (N).
A third level of classification permits specific diagnostic entities to be named, allowing the patient in the example above to receive a diagnosis of a prolactin-secreting adenoma.
Not all etiologies can be identified with current diagnostic studies, even assuming clinicians have access to the resources, such as advanced imaging, that will increase diagnostic yield. As a result, the authors acknowledged that the classification system will be “aspirational” in at least some patients, but the structure of this system is expected to lead to greater precision in understanding the causes and defining features of ovulatory disorders, which, in turn, might facilitate new research initiatives.
In the published report, diagnostic protocols based on symptoms were described as being “beyond the spectrum” of this initial description. Rather, Dr. Munro explained that the most important contribution of this new classification system are standardization and communication. The system will be amenable for educating trainees and patients, for communicating between clinicians, and as a framework for research where investigators focus on more homogeneous populations of patients.
“There are many causes of ovulatory disorders that are not related to ovarian function. This is one message. Another is that ovulatory disorders are not binary. They occur on a spectrum. These range from transient instances of delayed or failed ovulation to chronic anovulation,” he said.
The new system is “ a welcome update,” according to Mark P. Trolice, MD, director of the IVF Center and professor of obstetrics and gynecology at the University of Central Florida, both in Orlando.
Dr. Trolice pointed to the clinical value of placing PCOS in a separate category. He noted that it affects 8%-13% of women, making it the most common single cause of ovulatory dysfunction.
“Another area that required clarification from prior WHO classifications was hyperprolactinemia, which is now placed in the type II category,” Dr. Trolice said in an interview.
Better terminology can help address a complex set of disorders with multiple causes and variable manifestations.
“In the evaluation of ovulation dysfunction, it is important to remember that regular menstrual intervals do not ensure ovulation,” Dr. Trolice pointed out. Even though a serum progesterone level of higher than 3 ng/mL is one of the simplest laboratory markers for ovulation, this level, he noted, “can vary through the luteal phase and even throughout the day.”
The proposed classification system, while providing a framework for describing ovulatory disorders, is designed to be adaptable, permitting advances in the understanding of the causes of ovulatory dysfunction, in the diagnosis of the causes, and in the treatments to be incorporated.
“No system should be considered permanent,” according to Dr. Munro and his coauthors. “Review and careful modification and revision should be carried out regularly.”
Dr. Munro reports financial relationships with AbbVie, American Regent, Daiichi Sankyo, Hologic, Myovant, and Pharmacosmos. Dr. Trolice reports no potential conflicts of interest.
The first major revision in the systematic description of ovulatory disorders in nearly 50 years has been proposed by a consensus of experts organized by the International Federation of Gynecology and Obstetrics.
“The FIGO HyPO-P system for the classification of ovulatory disorders is submitted for consideration as a worldwide standard,” according to the writing committee, who published their methodology and their proposed applications in the International Journal of Gynecology and Obstetrics.
The classification system was created to replace the much-modified World Health Organization system first described in 1973. Since that time, many modifications have been proposed to accommodate advances in imaging and new information about underlying pathologies, but there has been no subsequent authoritative reference with these modifications or any other newer organizing system.
The new consensus was developed under the aegis of FIGO, but the development group consisted of representatives from national organizations and the major subspecialty societies. Recognized experts in ovulatory disorders and representatives from lay advocacy organizations also participated.
The HyPO-P system is based largely on anatomy. The acronym refers to ovulatory disorders related to the hypothalamus (type I), the pituitary (type II), and the ovary (type III).
Polycystic ovary syndrome (PCOS), one of the most common ovulatory disorders, was given a separate category (type IV) because of its complexity as well as the fact that PCOS is a heterogeneous systemic disorder with manifestations not limited to an impact on ovarian function.
As the first level of classification, three of the four primary categories (I-III) focus attention on the dominant anatomic source of the change in ovulatory function. The original WHO classification system identified as many as seven major groups, but they were based primarily on assays for gonadotropins and estradiol.
The new system “provides a different structure for determining the diagnosis. Blood tests are not a necessary first step,” explained Malcolm G. Munro, MD, clinical professor, department of obstetrics and gynecology, University of California, Los Angeles. Dr. Munro was the first author of the publication.
The classification system “is not as focused on the specific steps for investigation of ovulatory dysfunction as much as it explains how to structure an investigation of the girl or woman with an ovulatory disorder and then how to characterize the underlying cause,” Dr. Munro said in an interview. “It is designed to allow everyone, whether clinicians, researchers, or patients, to speak the same language.”
New system employs four categories
The four primary categories provide just the first level of classification. The next step is encapsulated in the GAIN-FIT-PIE acronym, which frames the presumed or documented categories of etiologies for the primary categories. GAIN stands for genetic, autoimmune, iatrogenic, or neoplasm etiologies. FIT stands for functional, infectious/inflammatory, or trauma and vascular etiologies. PIE stands for physiological, idiopathic, and endocrine etiologies.
By this methodology, a patient with irregular menses, galactorrhea, and elevated prolactin and an MRI showing a pituitary tumor would be identified a type 2-N, signifying pituitary (type 2) involvement with a neoplasm (N).
A third level of classification permits specific diagnostic entities to be named, allowing the patient in the example above to receive a diagnosis of a prolactin-secreting adenoma.
Not all etiologies can be identified with current diagnostic studies, even assuming clinicians have access to the resources, such as advanced imaging, that will increase diagnostic yield. As a result, the authors acknowledged that the classification system will be “aspirational” in at least some patients, but the structure of this system is expected to lead to greater precision in understanding the causes and defining features of ovulatory disorders, which, in turn, might facilitate new research initiatives.
In the published report, diagnostic protocols based on symptoms were described as being “beyond the spectrum” of this initial description. Rather, Dr. Munro explained that the most important contribution of this new classification system are standardization and communication. The system will be amenable for educating trainees and patients, for communicating between clinicians, and as a framework for research where investigators focus on more homogeneous populations of patients.
“There are many causes of ovulatory disorders that are not related to ovarian function. This is one message. Another is that ovulatory disorders are not binary. They occur on a spectrum. These range from transient instances of delayed or failed ovulation to chronic anovulation,” he said.
The new system is “ a welcome update,” according to Mark P. Trolice, MD, director of the IVF Center and professor of obstetrics and gynecology at the University of Central Florida, both in Orlando.
Dr. Trolice pointed to the clinical value of placing PCOS in a separate category. He noted that it affects 8%-13% of women, making it the most common single cause of ovulatory dysfunction.
“Another area that required clarification from prior WHO classifications was hyperprolactinemia, which is now placed in the type II category,” Dr. Trolice said in an interview.
Better terminology can help address a complex set of disorders with multiple causes and variable manifestations.
“In the evaluation of ovulation dysfunction, it is important to remember that regular menstrual intervals do not ensure ovulation,” Dr. Trolice pointed out. Even though a serum progesterone level of higher than 3 ng/mL is one of the simplest laboratory markers for ovulation, this level, he noted, “can vary through the luteal phase and even throughout the day.”
The proposed classification system, while providing a framework for describing ovulatory disorders, is designed to be adaptable, permitting advances in the understanding of the causes of ovulatory dysfunction, in the diagnosis of the causes, and in the treatments to be incorporated.
“No system should be considered permanent,” according to Dr. Munro and his coauthors. “Review and careful modification and revision should be carried out regularly.”
Dr. Munro reports financial relationships with AbbVie, American Regent, Daiichi Sankyo, Hologic, Myovant, and Pharmacosmos. Dr. Trolice reports no potential conflicts of interest.
FROM INTERNATIONAL JOURNAL OF GYNECOLOGY AND OBSTETRICS
How do you live with COVID? One doctor’s personal experience
Early in 2020, Anne Peters, MD, caught COVID-19. The author of Medscape’s “Peters on Diabetes” column was sick in March 2020 before state-mandated lockdowns, and well before there were any vaccines.
She remembers sitting in a small exam room with two patients who had flown to her Los Angeles office from New York. The elderly couple had hearing difficulties, so Dr. Peters sat close to them, putting on a continuous glucose monitor. “At that time, we didn’t think of COVID-19 as being in L.A.,” Dr. Peters recalled, “so I think we were not terribly consistent at mask-wearing due to the need to educate.”
“Several days later, I got COVID, but I didn’t know I had COVID per se. I felt crappy, had a terrible sore throat, lost my sense of taste and smell [which was not yet described as a COVID symptom], was completely exhausted, but had no fever or cough, which were the only criteria for getting COVID tested at the time. I didn’t know I had been exposed until 2 weeks later, when the patient’s assistant returned the sensor warning us to ‘be careful’ with it because the patient and his wife were recovering from COVID.”
That early battle with COVID-19 was just the beginning of what would become a 2-year struggle, including familial loss amid her own health problems and concerns about the under-resourced patients she cares for. Here, she shares her journey through the pandemic with this news organization.
Question: Thanks for talking to us. Let’s discuss your journey over these past 2.5 years.
Answer: Everybody has their own COVID story because we all went through this together. Some of us have worse COVID stories, and some of us have better ones, but all have been impacted.
I’m not a sick person. I’m a very healthy person but COVID made me so unwell for 2 years. The brain fog and fatigue were nothing compared to the autonomic neuropathy that affected my heart. It was really limiting for me. And I still don’t know the long-term implications, looking 20-30 years from now.
Q: When you initially had COVID, what were your symptoms? What was the impact?
A: I had all the symptoms of COVID, except for a cough and fever. I lost my sense of taste and smell. I had a horrible headache, a sore throat, and I was exhausted. I couldn’t get tested because I didn’t have the right symptoms.
Despite being sick, I never stopped working but just switched to telemedicine. I also took my regular monthly trip to our cabin in Montana. I unknowingly flew on a plane with COVID. I wore a well-fitted N95 mask, so I don’t think I gave anybody COVID. I didn’t give COVID to my partner, Eric, which is hard to believe as – at 77 – he’s older than me. He has diabetes, heart disease, and every other high-risk characteristic. If he’d gotten COVID back then, it would have been terrible, as there were no treatments, but luckily he didn’t get it.
Q: When were you officially diagnosed?
A: Two or 3 months after I thought I might have had COVID, I checked my antibodies, which tested strongly positive for a prior COVID infection. That was when I knew all the symptoms I’d had were due to the disease.
Q: Not only were you dealing with your own illness, but also that of those close to you. Can you talk about that?
A: In April 2020, my mother who was in her 90s and otherwise healthy except for dementia, got COVID. She could have gotten it from me. I visited often but wore a mask. She had all the horrible pulmonary symptoms. In her advance directive, she didn’t want to be hospitalized so I kept her in her home. She died from COVID in her own bed. It was fairly brutal, but at least I kept her where she felt comforted.
My 91-year-old dad was living in a different residential facility. Throughout COVID he had become very depressed because his social patterns had changed. Prior to COVID, they all ate together, but during the pandemic they were unable to. He missed his social connections, disliked being isolated in his room, hated everyone in masks.
He was a bit demented, but not so much that he couldn’t communicate with me or remember where his grandson was going to law school. I wasn’t allowed inside the facility, which was hard on him. I hadn’t told him his wife died because the hospice social workers advised me that I shouldn’t give him news that he couldn’t process readily until I could spend time with him. Unfortunately, that time never came. In December 2020, he got COVID. One of the people in that facility had gone to the hospital, came back, and tested negative, but actually had COVID and gave it to my dad. The guy who gave it to my dad didn’t die but my dad was terribly ill. He died 2 weeks short of getting his vaccine. He was coherent enough to have a conversation. I asked him: ‘Do you want to go to the hospital?’ And he said: ‘No, because it would be too scary,’ since he couldn’t be with me. I put him on hospice and held his hand as he died from pulmonary COVID, which was awful. I couldn’t give him enough morphine or valium to ease his breathing. But his last words to me were “I love you,” and at the very end he seemed peaceful, which was a blessing.
I got an autopsy, because he wanted one. Nothing else was wrong with him other than COVID. It destroyed his lungs. The rest of him was fine – no heart disease, cancer, or anything else. He died of COVID-19, the same as my mother.
That same week, my aunt, my only surviving older relative, who was in Des Moines, Iowa, died of COVID-19. All three family members died before the vaccine came out.
It was hard to lose my parents. I’m the only surviving child because my sister died in her 20s. It’s not been an easy pandemic. But what pandemic is easy? I just happened to have lost more people than most. Ironically, my grandfather was one of the legionnaires at the Bellevue-Stratford Hotel in Philadelphia in 1976 and died of Legionnaire’s disease before we knew what was causing the outbreak.
Q: Were you still struggling with COVID?
A: COVID impacted my whole body. I lost a lot of weight. I didn’t want to eat, and my gastrointestinal system was not happy. It took a while for my sense of taste and smell to come back. Nothing tasted good. I’m not a foodie; I don’t really care about food. We could get takeout or whatever, but none of it appealed to me. I’m not so sure it was a taste thing, I just didn’t feel like eating.
I didn’t realize I had “brain fog” per se, because I felt stressed and overwhelmed by the pandemic and my patients’ concerns. But one day, about 3 months after I had developed COVID, I woke up without the fog. Which made me aware that I hadn’t been feeling right up until that point.
The worst symptoms, however, were cardiac. I noticed also immediately that my heart rate went up very quickly with minimal exertion. My pulse has always been in the 55-60 bpm range, and suddenly just walking across a room made it go up to over 140 bpm. If I did any aerobic activity, it went up over 160 and would be associated with dyspnea and chest pain. I believed these were all post-COVID symptoms and felt validated when reports of others having similar issues were published in the literature.
Q: Did you continue seeing patients?
A: Yes, of course. Patients never needed their doctors more. In East L.A., where patients don’t have easy access to telemedicine, I kept going into clinic throughout the pandemic. In the more affluent Westside of Los Angeles, we switched to telemedicine, which was quite effective for most. However, because diabetes was associated with an increased risk of hospitalization and death from COVID, my patients were understandably afraid. I’ve never been busier, but (like all health care providers), I became more of a COVID provider than a diabetologist.
Q: Do you feel your battle with COVID impacted your work?
A: It didn’t affect me at work. If I was sitting still, I was fine. Sitting at home at a desk, I didn’t notice any symptoms. But as a habitual stair-user, I would be gasping for breath in the stairwell because I couldn’t go up the stairs to my office as I once could.
I think you empathize more with people who had COVID (when you’ve had it yourself). There was such a huge patient burden. And I think that’s been the thing that’s affected health care providers the most – no matter what specialty we’re in – that nobody has answers.
Q: What happened after you had your vaccine?
A: The vaccine itself was fine. I didn’t have any reaction to the first two doses. But the first booster made my cardiac issues worse.
By this point, my cardiac problems stopped me from exercising. I even went to the ER with chest pain once because I was having palpitations and chest pressure caused by simply taking my morning shower. Fortunately, I wasn’t having an MI, but I certainly wasn’t “normal.”
My measure of my fitness is the cross-country skiing trail I use in Montana. I know exactly how far I can ski. Usually I can do the loop in 35 minutes. After COVID, I lasted 10 minutes. I would be tachycardic, short of breath with chest pain radiating down my left arm. I would rest and try to keep going. But with each rest period, I only got worse. I would be laying in the snow and strangers would ask if I needed help.
Q: What helped you?
A: I’ve read a lot about long COVID and have tried to learn from the experts. Of course, I never went to a doctor directly, although I did ask colleagues for advice. What I learned was to never push myself. I forced myself to create an exercise schedule where I only exercised three times a week with rest days in between. When exercising, the second my heart rate went above 140 bpm, I stopped until I could get it back down. I would push against this new limit, even though my limit was low.
Additionally, I worked on my breathing patterns and did meditative breathing for 10 minutes twice daily using a commercially available app.
Although progress was slow, I did improve, and by June 2022, I seemed back to normal. I was not as fit as I was prior to COVID and needed to improve, but the tachycardic response to exercise and cardiac symptoms were gone. I felt like my normal self. Normal enough to go on a spot packing trip in the Sierras in August. (Horses carried us and a mule carried the gear over the 12,000-foot pass into the mountains, and then left my friend and me high in the Sierras for a week.) We were camped above 10,000 feet and every day hiked up to another high mountain lake where we fly-fished for trout that we ate for dinner. The hikes were a challenge, but not abnormally so. Not as they would have been while I had long COVID.
Q: What is the current atmosphere in your clinic?
A: COVID is much milder now in my vaccinated patients, but I feel most health care providers are exhausted. Many of my staff left when COVID hit because they didn’t want to keep working. It made practicing medicine exhausting. There’s been a shortage of nurses, a shortage of everything. We’ve been required to do a whole lot more than we ever did before. It’s much harder to be a doctor. This pandemic is the first time I’ve ever thought of quitting. Granted, I lost my whole family, or at least the older generation, but it’s just been almost overwhelming.
On the plus side, almost every one of my patients has been vaccinated, because early on, people would ask: “Do you trust this vaccine?” I would reply: “I saw my parents die from COVID when they weren’t vaccinated, so you’re getting vaccinated. This is real and the vaccines help.” It made me very good at convincing people to get vaccines because I knew what it was like to see someone dying from COVID up close.
Q: What advice do you have for those struggling with the COVID pandemic?
A: People need to decide what their own risk is for getting sick and how many times they want to get COVID. At this point, I want people to go out, but safely. In the beginning, when my patients said, “can I go visit my granddaughter?” I said, “no,” but that was before we had the vaccine. Now I feel it is safe to go out using common sense. I still have my patients wear masks on planes. I still have patients try to eat outside as much as possible. And I tell people to take the precautions that make sense, but I tell them to go out and do things because life is short.
I had a patient in his 70s who has many risk factors like heart disease and diabetes. His granddaughter’s Bat Mitzvah in Florida was coming up. He asked: “Can I go?” I told him “Yes,” but to be safe – to wear an N95 mask on the plane and at the event, and stay in his own hotel room, rather than with the whole family. I said, “You need to do this.” Earlier in the pandemic, I saw people who literally died from loneliness and isolation.
He and his wife flew there. He sent me a picture of himself with his granddaughter. When he returned, he showed me a handwritten note from her that said, “I love you so much. Everyone else canceled, which made me cry. You’re the only one who came. You have no idea how much this meant to me.”
He’s back in L.A., and he didn’t get COVID. He said, “It was the best thing I’ve done in years.” That’s what I need to help people with, navigating this world with COVID and assessing risks and benefits. As with all of medicine, my advice is individualized. My advice changes based on the major circulating variant and the rates of the virus in the population, as well as the risk factors of the individual.
Q: What are you doing now?
A: I’m trying to avoid getting COVID again, or another booster. I could get pre-exposure monoclonal antibodies but am waiting to do anything further until I see what happens over the fall and winter. I still wear a mask inside but now do a mix of in-person and telemedicine visits. I still try to go to outdoor restaurants, which is easy in California. But I’m flying to see my son in New York and plan to go to Europe this fall for a meeting. I also go to my cabin in Montana every month to get my “dose” of the wilderness. Overall, I travel for conferences and speaking engagements much less because I have learned the joy of staying home.
Thinking back on my life as a doctor, my career began as an intern at Stanford rotating through Ward 5B, the AIDS unit at San Francisco General Hospital, and will likely end with COVID. In spite of all our medical advances, my generation of physicians, much as many generations before us, has a front-row seat to the vulnerability of humans to infectious diseases and how far we still need to go to protect our patients from communicable illness.
A version of this article first appeared on Medscape.com.
Anne L. Peters, MD, is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts; three books on diabetes; and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations.
Early in 2020, Anne Peters, MD, caught COVID-19. The author of Medscape’s “Peters on Diabetes” column was sick in March 2020 before state-mandated lockdowns, and well before there were any vaccines.
She remembers sitting in a small exam room with two patients who had flown to her Los Angeles office from New York. The elderly couple had hearing difficulties, so Dr. Peters sat close to them, putting on a continuous glucose monitor. “At that time, we didn’t think of COVID-19 as being in L.A.,” Dr. Peters recalled, “so I think we were not terribly consistent at mask-wearing due to the need to educate.”
“Several days later, I got COVID, but I didn’t know I had COVID per se. I felt crappy, had a terrible sore throat, lost my sense of taste and smell [which was not yet described as a COVID symptom], was completely exhausted, but had no fever or cough, which were the only criteria for getting COVID tested at the time. I didn’t know I had been exposed until 2 weeks later, when the patient’s assistant returned the sensor warning us to ‘be careful’ with it because the patient and his wife were recovering from COVID.”
That early battle with COVID-19 was just the beginning of what would become a 2-year struggle, including familial loss amid her own health problems and concerns about the under-resourced patients she cares for. Here, she shares her journey through the pandemic with this news organization.
Question: Thanks for talking to us. Let’s discuss your journey over these past 2.5 years.
Answer: Everybody has their own COVID story because we all went through this together. Some of us have worse COVID stories, and some of us have better ones, but all have been impacted.
I’m not a sick person. I’m a very healthy person but COVID made me so unwell for 2 years. The brain fog and fatigue were nothing compared to the autonomic neuropathy that affected my heart. It was really limiting for me. And I still don’t know the long-term implications, looking 20-30 years from now.
Q: When you initially had COVID, what were your symptoms? What was the impact?
A: I had all the symptoms of COVID, except for a cough and fever. I lost my sense of taste and smell. I had a horrible headache, a sore throat, and I was exhausted. I couldn’t get tested because I didn’t have the right symptoms.
Despite being sick, I never stopped working but just switched to telemedicine. I also took my regular monthly trip to our cabin in Montana. I unknowingly flew on a plane with COVID. I wore a well-fitted N95 mask, so I don’t think I gave anybody COVID. I didn’t give COVID to my partner, Eric, which is hard to believe as – at 77 – he’s older than me. He has diabetes, heart disease, and every other high-risk characteristic. If he’d gotten COVID back then, it would have been terrible, as there were no treatments, but luckily he didn’t get it.
Q: When were you officially diagnosed?
A: Two or 3 months after I thought I might have had COVID, I checked my antibodies, which tested strongly positive for a prior COVID infection. That was when I knew all the symptoms I’d had were due to the disease.
Q: Not only were you dealing with your own illness, but also that of those close to you. Can you talk about that?
A: In April 2020, my mother who was in her 90s and otherwise healthy except for dementia, got COVID. She could have gotten it from me. I visited often but wore a mask. She had all the horrible pulmonary symptoms. In her advance directive, she didn’t want to be hospitalized so I kept her in her home. She died from COVID in her own bed. It was fairly brutal, but at least I kept her where she felt comforted.
My 91-year-old dad was living in a different residential facility. Throughout COVID he had become very depressed because his social patterns had changed. Prior to COVID, they all ate together, but during the pandemic they were unable to. He missed his social connections, disliked being isolated in his room, hated everyone in masks.
He was a bit demented, but not so much that he couldn’t communicate with me or remember where his grandson was going to law school. I wasn’t allowed inside the facility, which was hard on him. I hadn’t told him his wife died because the hospice social workers advised me that I shouldn’t give him news that he couldn’t process readily until I could spend time with him. Unfortunately, that time never came. In December 2020, he got COVID. One of the people in that facility had gone to the hospital, came back, and tested negative, but actually had COVID and gave it to my dad. The guy who gave it to my dad didn’t die but my dad was terribly ill. He died 2 weeks short of getting his vaccine. He was coherent enough to have a conversation. I asked him: ‘Do you want to go to the hospital?’ And he said: ‘No, because it would be too scary,’ since he couldn’t be with me. I put him on hospice and held his hand as he died from pulmonary COVID, which was awful. I couldn’t give him enough morphine or valium to ease his breathing. But his last words to me were “I love you,” and at the very end he seemed peaceful, which was a blessing.
I got an autopsy, because he wanted one. Nothing else was wrong with him other than COVID. It destroyed his lungs. The rest of him was fine – no heart disease, cancer, or anything else. He died of COVID-19, the same as my mother.
That same week, my aunt, my only surviving older relative, who was in Des Moines, Iowa, died of COVID-19. All three family members died before the vaccine came out.
It was hard to lose my parents. I’m the only surviving child because my sister died in her 20s. It’s not been an easy pandemic. But what pandemic is easy? I just happened to have lost more people than most. Ironically, my grandfather was one of the legionnaires at the Bellevue-Stratford Hotel in Philadelphia in 1976 and died of Legionnaire’s disease before we knew what was causing the outbreak.
Q: Were you still struggling with COVID?
A: COVID impacted my whole body. I lost a lot of weight. I didn’t want to eat, and my gastrointestinal system was not happy. It took a while for my sense of taste and smell to come back. Nothing tasted good. I’m not a foodie; I don’t really care about food. We could get takeout or whatever, but none of it appealed to me. I’m not so sure it was a taste thing, I just didn’t feel like eating.
I didn’t realize I had “brain fog” per se, because I felt stressed and overwhelmed by the pandemic and my patients’ concerns. But one day, about 3 months after I had developed COVID, I woke up without the fog. Which made me aware that I hadn’t been feeling right up until that point.
The worst symptoms, however, were cardiac. I noticed also immediately that my heart rate went up very quickly with minimal exertion. My pulse has always been in the 55-60 bpm range, and suddenly just walking across a room made it go up to over 140 bpm. If I did any aerobic activity, it went up over 160 and would be associated with dyspnea and chest pain. I believed these were all post-COVID symptoms and felt validated when reports of others having similar issues were published in the literature.
Q: Did you continue seeing patients?
A: Yes, of course. Patients never needed their doctors more. In East L.A., where patients don’t have easy access to telemedicine, I kept going into clinic throughout the pandemic. In the more affluent Westside of Los Angeles, we switched to telemedicine, which was quite effective for most. However, because diabetes was associated with an increased risk of hospitalization and death from COVID, my patients were understandably afraid. I’ve never been busier, but (like all health care providers), I became more of a COVID provider than a diabetologist.
Q: Do you feel your battle with COVID impacted your work?
A: It didn’t affect me at work. If I was sitting still, I was fine. Sitting at home at a desk, I didn’t notice any symptoms. But as a habitual stair-user, I would be gasping for breath in the stairwell because I couldn’t go up the stairs to my office as I once could.
I think you empathize more with people who had COVID (when you’ve had it yourself). There was such a huge patient burden. And I think that’s been the thing that’s affected health care providers the most – no matter what specialty we’re in – that nobody has answers.
Q: What happened after you had your vaccine?
A: The vaccine itself was fine. I didn’t have any reaction to the first two doses. But the first booster made my cardiac issues worse.
By this point, my cardiac problems stopped me from exercising. I even went to the ER with chest pain once because I was having palpitations and chest pressure caused by simply taking my morning shower. Fortunately, I wasn’t having an MI, but I certainly wasn’t “normal.”
My measure of my fitness is the cross-country skiing trail I use in Montana. I know exactly how far I can ski. Usually I can do the loop in 35 minutes. After COVID, I lasted 10 minutes. I would be tachycardic, short of breath with chest pain radiating down my left arm. I would rest and try to keep going. But with each rest period, I only got worse. I would be laying in the snow and strangers would ask if I needed help.
Q: What helped you?
A: I’ve read a lot about long COVID and have tried to learn from the experts. Of course, I never went to a doctor directly, although I did ask colleagues for advice. What I learned was to never push myself. I forced myself to create an exercise schedule where I only exercised three times a week with rest days in between. When exercising, the second my heart rate went above 140 bpm, I stopped until I could get it back down. I would push against this new limit, even though my limit was low.
Additionally, I worked on my breathing patterns and did meditative breathing for 10 minutes twice daily using a commercially available app.
Although progress was slow, I did improve, and by June 2022, I seemed back to normal. I was not as fit as I was prior to COVID and needed to improve, but the tachycardic response to exercise and cardiac symptoms were gone. I felt like my normal self. Normal enough to go on a spot packing trip in the Sierras in August. (Horses carried us and a mule carried the gear over the 12,000-foot pass into the mountains, and then left my friend and me high in the Sierras for a week.) We were camped above 10,000 feet and every day hiked up to another high mountain lake where we fly-fished for trout that we ate for dinner. The hikes were a challenge, but not abnormally so. Not as they would have been while I had long COVID.
Q: What is the current atmosphere in your clinic?
A: COVID is much milder now in my vaccinated patients, but I feel most health care providers are exhausted. Many of my staff left when COVID hit because they didn’t want to keep working. It made practicing medicine exhausting. There’s been a shortage of nurses, a shortage of everything. We’ve been required to do a whole lot more than we ever did before. It’s much harder to be a doctor. This pandemic is the first time I’ve ever thought of quitting. Granted, I lost my whole family, or at least the older generation, but it’s just been almost overwhelming.
On the plus side, almost every one of my patients has been vaccinated, because early on, people would ask: “Do you trust this vaccine?” I would reply: “I saw my parents die from COVID when they weren’t vaccinated, so you’re getting vaccinated. This is real and the vaccines help.” It made me very good at convincing people to get vaccines because I knew what it was like to see someone dying from COVID up close.
Q: What advice do you have for those struggling with the COVID pandemic?
A: People need to decide what their own risk is for getting sick and how many times they want to get COVID. At this point, I want people to go out, but safely. In the beginning, when my patients said, “can I go visit my granddaughter?” I said, “no,” but that was before we had the vaccine. Now I feel it is safe to go out using common sense. I still have my patients wear masks on planes. I still have patients try to eat outside as much as possible. And I tell people to take the precautions that make sense, but I tell them to go out and do things because life is short.
I had a patient in his 70s who has many risk factors like heart disease and diabetes. His granddaughter’s Bat Mitzvah in Florida was coming up. He asked: “Can I go?” I told him “Yes,” but to be safe – to wear an N95 mask on the plane and at the event, and stay in his own hotel room, rather than with the whole family. I said, “You need to do this.” Earlier in the pandemic, I saw people who literally died from loneliness and isolation.
He and his wife flew there. He sent me a picture of himself with his granddaughter. When he returned, he showed me a handwritten note from her that said, “I love you so much. Everyone else canceled, which made me cry. You’re the only one who came. You have no idea how much this meant to me.”
He’s back in L.A., and he didn’t get COVID. He said, “It was the best thing I’ve done in years.” That’s what I need to help people with, navigating this world with COVID and assessing risks and benefits. As with all of medicine, my advice is individualized. My advice changes based on the major circulating variant and the rates of the virus in the population, as well as the risk factors of the individual.
Q: What are you doing now?
A: I’m trying to avoid getting COVID again, or another booster. I could get pre-exposure monoclonal antibodies but am waiting to do anything further until I see what happens over the fall and winter. I still wear a mask inside but now do a mix of in-person and telemedicine visits. I still try to go to outdoor restaurants, which is easy in California. But I’m flying to see my son in New York and plan to go to Europe this fall for a meeting. I also go to my cabin in Montana every month to get my “dose” of the wilderness. Overall, I travel for conferences and speaking engagements much less because I have learned the joy of staying home.
Thinking back on my life as a doctor, my career began as an intern at Stanford rotating through Ward 5B, the AIDS unit at San Francisco General Hospital, and will likely end with COVID. In spite of all our medical advances, my generation of physicians, much as many generations before us, has a front-row seat to the vulnerability of humans to infectious diseases and how far we still need to go to protect our patients from communicable illness.
A version of this article first appeared on Medscape.com.
Anne L. Peters, MD, is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts; three books on diabetes; and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations.
Early in 2020, Anne Peters, MD, caught COVID-19. The author of Medscape’s “Peters on Diabetes” column was sick in March 2020 before state-mandated lockdowns, and well before there were any vaccines.
She remembers sitting in a small exam room with two patients who had flown to her Los Angeles office from New York. The elderly couple had hearing difficulties, so Dr. Peters sat close to them, putting on a continuous glucose monitor. “At that time, we didn’t think of COVID-19 as being in L.A.,” Dr. Peters recalled, “so I think we were not terribly consistent at mask-wearing due to the need to educate.”
“Several days later, I got COVID, but I didn’t know I had COVID per se. I felt crappy, had a terrible sore throat, lost my sense of taste and smell [which was not yet described as a COVID symptom], was completely exhausted, but had no fever or cough, which were the only criteria for getting COVID tested at the time. I didn’t know I had been exposed until 2 weeks later, when the patient’s assistant returned the sensor warning us to ‘be careful’ with it because the patient and his wife were recovering from COVID.”
That early battle with COVID-19 was just the beginning of what would become a 2-year struggle, including familial loss amid her own health problems and concerns about the under-resourced patients she cares for. Here, she shares her journey through the pandemic with this news organization.
Question: Thanks for talking to us. Let’s discuss your journey over these past 2.5 years.
Answer: Everybody has their own COVID story because we all went through this together. Some of us have worse COVID stories, and some of us have better ones, but all have been impacted.
I’m not a sick person. I’m a very healthy person but COVID made me so unwell for 2 years. The brain fog and fatigue were nothing compared to the autonomic neuropathy that affected my heart. It was really limiting for me. And I still don’t know the long-term implications, looking 20-30 years from now.
Q: When you initially had COVID, what were your symptoms? What was the impact?
A: I had all the symptoms of COVID, except for a cough and fever. I lost my sense of taste and smell. I had a horrible headache, a sore throat, and I was exhausted. I couldn’t get tested because I didn’t have the right symptoms.
Despite being sick, I never stopped working but just switched to telemedicine. I also took my regular monthly trip to our cabin in Montana. I unknowingly flew on a plane with COVID. I wore a well-fitted N95 mask, so I don’t think I gave anybody COVID. I didn’t give COVID to my partner, Eric, which is hard to believe as – at 77 – he’s older than me. He has diabetes, heart disease, and every other high-risk characteristic. If he’d gotten COVID back then, it would have been terrible, as there were no treatments, but luckily he didn’t get it.
Q: When were you officially diagnosed?
A: Two or 3 months after I thought I might have had COVID, I checked my antibodies, which tested strongly positive for a prior COVID infection. That was when I knew all the symptoms I’d had were due to the disease.
Q: Not only were you dealing with your own illness, but also that of those close to you. Can you talk about that?
A: In April 2020, my mother who was in her 90s and otherwise healthy except for dementia, got COVID. She could have gotten it from me. I visited often but wore a mask. She had all the horrible pulmonary symptoms. In her advance directive, she didn’t want to be hospitalized so I kept her in her home. She died from COVID in her own bed. It was fairly brutal, but at least I kept her where she felt comforted.
My 91-year-old dad was living in a different residential facility. Throughout COVID he had become very depressed because his social patterns had changed. Prior to COVID, they all ate together, but during the pandemic they were unable to. He missed his social connections, disliked being isolated in his room, hated everyone in masks.
He was a bit demented, but not so much that he couldn’t communicate with me or remember where his grandson was going to law school. I wasn’t allowed inside the facility, which was hard on him. I hadn’t told him his wife died because the hospice social workers advised me that I shouldn’t give him news that he couldn’t process readily until I could spend time with him. Unfortunately, that time never came. In December 2020, he got COVID. One of the people in that facility had gone to the hospital, came back, and tested negative, but actually had COVID and gave it to my dad. The guy who gave it to my dad didn’t die but my dad was terribly ill. He died 2 weeks short of getting his vaccine. He was coherent enough to have a conversation. I asked him: ‘Do you want to go to the hospital?’ And he said: ‘No, because it would be too scary,’ since he couldn’t be with me. I put him on hospice and held his hand as he died from pulmonary COVID, which was awful. I couldn’t give him enough morphine or valium to ease his breathing. But his last words to me were “I love you,” and at the very end he seemed peaceful, which was a blessing.
I got an autopsy, because he wanted one. Nothing else was wrong with him other than COVID. It destroyed his lungs. The rest of him was fine – no heart disease, cancer, or anything else. He died of COVID-19, the same as my mother.
That same week, my aunt, my only surviving older relative, who was in Des Moines, Iowa, died of COVID-19. All three family members died before the vaccine came out.
It was hard to lose my parents. I’m the only surviving child because my sister died in her 20s. It’s not been an easy pandemic. But what pandemic is easy? I just happened to have lost more people than most. Ironically, my grandfather was one of the legionnaires at the Bellevue-Stratford Hotel in Philadelphia in 1976 and died of Legionnaire’s disease before we knew what was causing the outbreak.
Q: Were you still struggling with COVID?
A: COVID impacted my whole body. I lost a lot of weight. I didn’t want to eat, and my gastrointestinal system was not happy. It took a while for my sense of taste and smell to come back. Nothing tasted good. I’m not a foodie; I don’t really care about food. We could get takeout or whatever, but none of it appealed to me. I’m not so sure it was a taste thing, I just didn’t feel like eating.
I didn’t realize I had “brain fog” per se, because I felt stressed and overwhelmed by the pandemic and my patients’ concerns. But one day, about 3 months after I had developed COVID, I woke up without the fog. Which made me aware that I hadn’t been feeling right up until that point.
The worst symptoms, however, were cardiac. I noticed also immediately that my heart rate went up very quickly with minimal exertion. My pulse has always been in the 55-60 bpm range, and suddenly just walking across a room made it go up to over 140 bpm. If I did any aerobic activity, it went up over 160 and would be associated with dyspnea and chest pain. I believed these were all post-COVID symptoms and felt validated when reports of others having similar issues were published in the literature.
Q: Did you continue seeing patients?
A: Yes, of course. Patients never needed their doctors more. In East L.A., where patients don’t have easy access to telemedicine, I kept going into clinic throughout the pandemic. In the more affluent Westside of Los Angeles, we switched to telemedicine, which was quite effective for most. However, because diabetes was associated with an increased risk of hospitalization and death from COVID, my patients were understandably afraid. I’ve never been busier, but (like all health care providers), I became more of a COVID provider than a diabetologist.
Q: Do you feel your battle with COVID impacted your work?
A: It didn’t affect me at work. If I was sitting still, I was fine. Sitting at home at a desk, I didn’t notice any symptoms. But as a habitual stair-user, I would be gasping for breath in the stairwell because I couldn’t go up the stairs to my office as I once could.
I think you empathize more with people who had COVID (when you’ve had it yourself). There was such a huge patient burden. And I think that’s been the thing that’s affected health care providers the most – no matter what specialty we’re in – that nobody has answers.
Q: What happened after you had your vaccine?
A: The vaccine itself was fine. I didn’t have any reaction to the first two doses. But the first booster made my cardiac issues worse.
By this point, my cardiac problems stopped me from exercising. I even went to the ER with chest pain once because I was having palpitations and chest pressure caused by simply taking my morning shower. Fortunately, I wasn’t having an MI, but I certainly wasn’t “normal.”
My measure of my fitness is the cross-country skiing trail I use in Montana. I know exactly how far I can ski. Usually I can do the loop in 35 minutes. After COVID, I lasted 10 minutes. I would be tachycardic, short of breath with chest pain radiating down my left arm. I would rest and try to keep going. But with each rest period, I only got worse. I would be laying in the snow and strangers would ask if I needed help.
Q: What helped you?
A: I’ve read a lot about long COVID and have tried to learn from the experts. Of course, I never went to a doctor directly, although I did ask colleagues for advice. What I learned was to never push myself. I forced myself to create an exercise schedule where I only exercised three times a week with rest days in between. When exercising, the second my heart rate went above 140 bpm, I stopped until I could get it back down. I would push against this new limit, even though my limit was low.
Additionally, I worked on my breathing patterns and did meditative breathing for 10 minutes twice daily using a commercially available app.
Although progress was slow, I did improve, and by June 2022, I seemed back to normal. I was not as fit as I was prior to COVID and needed to improve, but the tachycardic response to exercise and cardiac symptoms were gone. I felt like my normal self. Normal enough to go on a spot packing trip in the Sierras in August. (Horses carried us and a mule carried the gear over the 12,000-foot pass into the mountains, and then left my friend and me high in the Sierras for a week.) We were camped above 10,000 feet and every day hiked up to another high mountain lake where we fly-fished for trout that we ate for dinner. The hikes were a challenge, but not abnormally so. Not as they would have been while I had long COVID.
Q: What is the current atmosphere in your clinic?
A: COVID is much milder now in my vaccinated patients, but I feel most health care providers are exhausted. Many of my staff left when COVID hit because they didn’t want to keep working. It made practicing medicine exhausting. There’s been a shortage of nurses, a shortage of everything. We’ve been required to do a whole lot more than we ever did before. It’s much harder to be a doctor. This pandemic is the first time I’ve ever thought of quitting. Granted, I lost my whole family, or at least the older generation, but it’s just been almost overwhelming.
On the plus side, almost every one of my patients has been vaccinated, because early on, people would ask: “Do you trust this vaccine?” I would reply: “I saw my parents die from COVID when they weren’t vaccinated, so you’re getting vaccinated. This is real and the vaccines help.” It made me very good at convincing people to get vaccines because I knew what it was like to see someone dying from COVID up close.
Q: What advice do you have for those struggling with the COVID pandemic?
A: People need to decide what their own risk is for getting sick and how many times they want to get COVID. At this point, I want people to go out, but safely. In the beginning, when my patients said, “can I go visit my granddaughter?” I said, “no,” but that was before we had the vaccine. Now I feel it is safe to go out using common sense. I still have my patients wear masks on planes. I still have patients try to eat outside as much as possible. And I tell people to take the precautions that make sense, but I tell them to go out and do things because life is short.
I had a patient in his 70s who has many risk factors like heart disease and diabetes. His granddaughter’s Bat Mitzvah in Florida was coming up. He asked: “Can I go?” I told him “Yes,” but to be safe – to wear an N95 mask on the plane and at the event, and stay in his own hotel room, rather than with the whole family. I said, “You need to do this.” Earlier in the pandemic, I saw people who literally died from loneliness and isolation.
He and his wife flew there. He sent me a picture of himself with his granddaughter. When he returned, he showed me a handwritten note from her that said, “I love you so much. Everyone else canceled, which made me cry. You’re the only one who came. You have no idea how much this meant to me.”
He’s back in L.A., and he didn’t get COVID. He said, “It was the best thing I’ve done in years.” That’s what I need to help people with, navigating this world with COVID and assessing risks and benefits. As with all of medicine, my advice is individualized. My advice changes based on the major circulating variant and the rates of the virus in the population, as well as the risk factors of the individual.
Q: What are you doing now?
A: I’m trying to avoid getting COVID again, or another booster. I could get pre-exposure monoclonal antibodies but am waiting to do anything further until I see what happens over the fall and winter. I still wear a mask inside but now do a mix of in-person and telemedicine visits. I still try to go to outdoor restaurants, which is easy in California. But I’m flying to see my son in New York and plan to go to Europe this fall for a meeting. I also go to my cabin in Montana every month to get my “dose” of the wilderness. Overall, I travel for conferences and speaking engagements much less because I have learned the joy of staying home.
Thinking back on my life as a doctor, my career began as an intern at Stanford rotating through Ward 5B, the AIDS unit at San Francisco General Hospital, and will likely end with COVID. In spite of all our medical advances, my generation of physicians, much as many generations before us, has a front-row seat to the vulnerability of humans to infectious diseases and how far we still need to go to protect our patients from communicable illness.
A version of this article first appeared on Medscape.com.
Anne L. Peters, MD, is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts; three books on diabetes; and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations.
Infographic: Is physician behavior on social media really so bad?
The medical profession is held to a high standard of personal conduct, so physicians keep a sharp eye out for how fellow doctors behave. That goes for social media as well as in-person conduct.
(and it’s not as egregious as you might think). If you’re interested in delving deeper into the data, check out the Medscape Physicians Behaving Badly Report 2022.
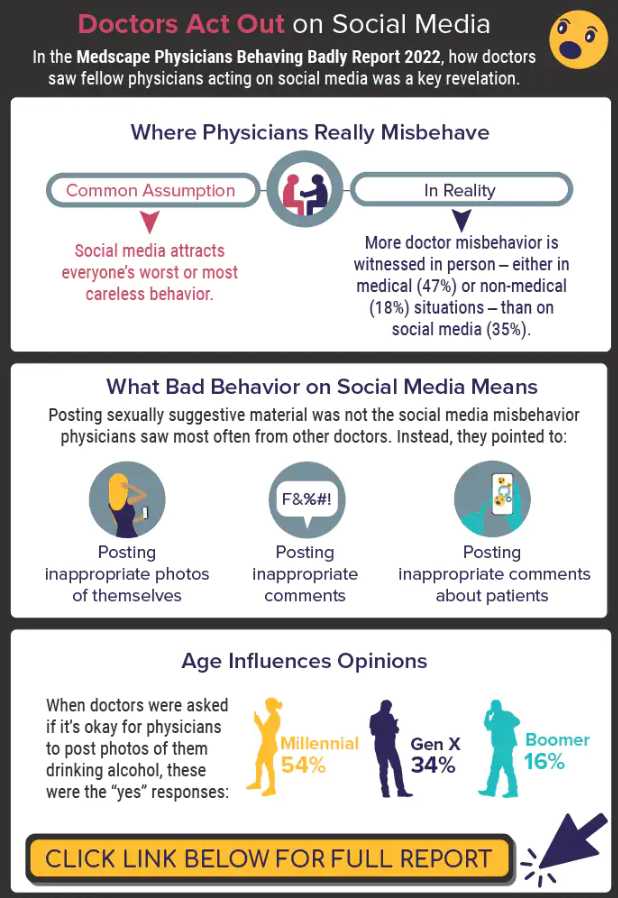
A version of this article first appeared on Medscape.com.
The medical profession is held to a high standard of personal conduct, so physicians keep a sharp eye out for how fellow doctors behave. That goes for social media as well as in-person conduct.
(and it’s not as egregious as you might think). If you’re interested in delving deeper into the data, check out the Medscape Physicians Behaving Badly Report 2022.
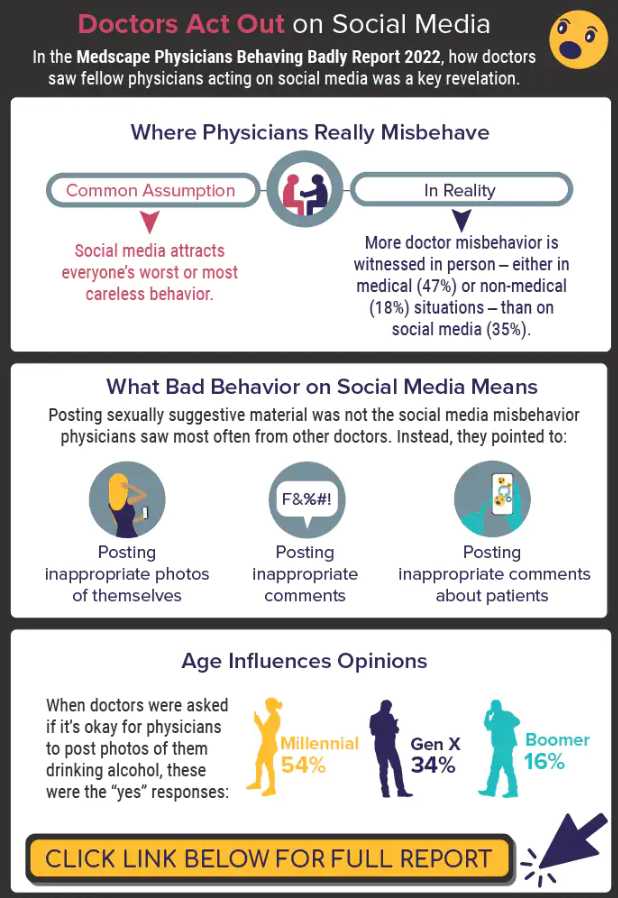
A version of this article first appeared on Medscape.com.
The medical profession is held to a high standard of personal conduct, so physicians keep a sharp eye out for how fellow doctors behave. That goes for social media as well as in-person conduct.
(and it’s not as egregious as you might think). If you’re interested in delving deeper into the data, check out the Medscape Physicians Behaving Badly Report 2022.
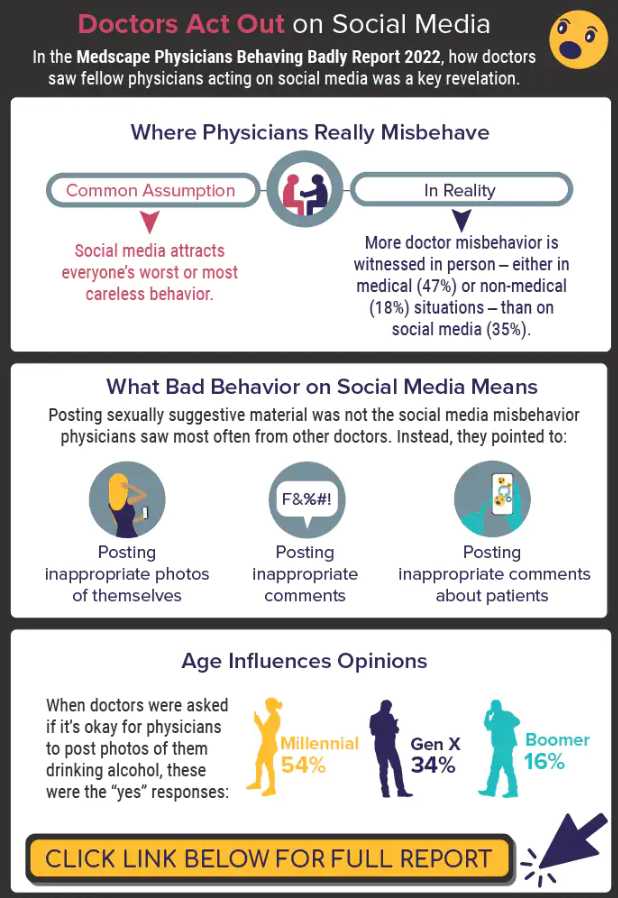
A version of this article first appeared on Medscape.com.
Paxlovid reduces risk of COVID death by 79% in older adults
The antiviral drug Paxlovid appears to reduce the risk of dying from COVID-19 by 79% and decrease hospitalizations by 73% in at-risk patients who are ages 65 and older, according to a new study published in The New England Journal of Medicine.
The pill, which is a combination of the drugs nirmatrelvir and ritonavir, received FDA emergency use authorization in December 2021 to treat mild to moderate disease in ages 12 and older who face high risks for having severe COVID-19, hospitalization, and death.
“The results of the study show unequivocally that treatment with Paxlovid significantly reduces the risk of hospitalization and death from COVID-19,” Doron Netzer, MD, the senior study author and a researcher with Clalit Health Services, Tel Aviv, told The Jerusalem Post.
“We are the country’s leader in the provision of giving Paxlovid to relevant patients,” he said. “It was given to patients all over the country, with medical teams monitoring the patients who took the pills.”
, the news outlet reported. The research team analyzed information from Clalit’s electronic medical records. The health care organization covers about 52% of the Israeli population and almost two-thirds of older adults. More than 30,000 COVID-19 patients in Israel have been treated with the drug so far.
Dr. Netzer and colleagues looked at hospitalization and death data for at-risk COVID-19 patients ages 40 and older between Jan. 9 and March 31, when the original Omicron variant was the dominant strain in Israel. During that time, more than 1.1 million Clalit patients were infected with COVID-19, 109,000 patients were considered at-risk, and 3,900 patients received the drug.
The average age of the patients was 60, and 39% of the patients were 65 and older. Overall, 78% of the patients had previous COVID-19 immunity due to vaccination, prior infection, or both.
Among ages 65 and older, the rate of COVID-19 hospitalization was 14.7 cases per 100,000 person-days among treated patients, compared with 58.9 cases per 100,000 person-days among untreated patients. This represented a 73% lower chance of being hospitalized.
Among ages 40-64, the rate of hospitalization due to COVID-19 was 15.2 cases per 100,000 person-days among treated patients, compared with 15.8 cases per 100,000 person-days among untreated patients. The risk of hospitalization wasn’t significantly lower for this age group.
Among ages 65 and older, there were two deaths from COVID-19 in 2,484 treated patients, compared with 158 in the 40,337 untreated patients. This represented a 79% lower chance of dying from COVID-19.
Among ages 40-64, there was one death from COVID-19 in 1,418 treated patients, compared with 16 in the 65,015 untreated patients. The risk of death wasn’t significantly lower for this age group.
For both age groups, a lack of previous COVID-19 immunity and a previous hospitalization were most strongly linked to high rates of hospitalization during the Omicron wave.
The researchers noted that they didn’t break down the data on ages 40-64 who had cancer and other severe conditions that weaken the immune system. These patients may be more likely to benefit from Paxlovid, they said, though future studies will need to analyze the data.
The study didn’t receive any financial or in-kind support, the authors said.
A version of this article first appeared on WebMD.com.
The antiviral drug Paxlovid appears to reduce the risk of dying from COVID-19 by 79% and decrease hospitalizations by 73% in at-risk patients who are ages 65 and older, according to a new study published in The New England Journal of Medicine.
The pill, which is a combination of the drugs nirmatrelvir and ritonavir, received FDA emergency use authorization in December 2021 to treat mild to moderate disease in ages 12 and older who face high risks for having severe COVID-19, hospitalization, and death.
“The results of the study show unequivocally that treatment with Paxlovid significantly reduces the risk of hospitalization and death from COVID-19,” Doron Netzer, MD, the senior study author and a researcher with Clalit Health Services, Tel Aviv, told The Jerusalem Post.
“We are the country’s leader in the provision of giving Paxlovid to relevant patients,” he said. “It was given to patients all over the country, with medical teams monitoring the patients who took the pills.”
, the news outlet reported. The research team analyzed information from Clalit’s electronic medical records. The health care organization covers about 52% of the Israeli population and almost two-thirds of older adults. More than 30,000 COVID-19 patients in Israel have been treated with the drug so far.
Dr. Netzer and colleagues looked at hospitalization and death data for at-risk COVID-19 patients ages 40 and older between Jan. 9 and March 31, when the original Omicron variant was the dominant strain in Israel. During that time, more than 1.1 million Clalit patients were infected with COVID-19, 109,000 patients were considered at-risk, and 3,900 patients received the drug.
The average age of the patients was 60, and 39% of the patients were 65 and older. Overall, 78% of the patients had previous COVID-19 immunity due to vaccination, prior infection, or both.
Among ages 65 and older, the rate of COVID-19 hospitalization was 14.7 cases per 100,000 person-days among treated patients, compared with 58.9 cases per 100,000 person-days among untreated patients. This represented a 73% lower chance of being hospitalized.
Among ages 40-64, the rate of hospitalization due to COVID-19 was 15.2 cases per 100,000 person-days among treated patients, compared with 15.8 cases per 100,000 person-days among untreated patients. The risk of hospitalization wasn’t significantly lower for this age group.
Among ages 65 and older, there were two deaths from COVID-19 in 2,484 treated patients, compared with 158 in the 40,337 untreated patients. This represented a 79% lower chance of dying from COVID-19.
Among ages 40-64, there was one death from COVID-19 in 1,418 treated patients, compared with 16 in the 65,015 untreated patients. The risk of death wasn’t significantly lower for this age group.
For both age groups, a lack of previous COVID-19 immunity and a previous hospitalization were most strongly linked to high rates of hospitalization during the Omicron wave.
The researchers noted that they didn’t break down the data on ages 40-64 who had cancer and other severe conditions that weaken the immune system. These patients may be more likely to benefit from Paxlovid, they said, though future studies will need to analyze the data.
The study didn’t receive any financial or in-kind support, the authors said.
A version of this article first appeared on WebMD.com.
The antiviral drug Paxlovid appears to reduce the risk of dying from COVID-19 by 79% and decrease hospitalizations by 73% in at-risk patients who are ages 65 and older, according to a new study published in The New England Journal of Medicine.
The pill, which is a combination of the drugs nirmatrelvir and ritonavir, received FDA emergency use authorization in December 2021 to treat mild to moderate disease in ages 12 and older who face high risks for having severe COVID-19, hospitalization, and death.
“The results of the study show unequivocally that treatment with Paxlovid significantly reduces the risk of hospitalization and death from COVID-19,” Doron Netzer, MD, the senior study author and a researcher with Clalit Health Services, Tel Aviv, told The Jerusalem Post.
“We are the country’s leader in the provision of giving Paxlovid to relevant patients,” he said. “It was given to patients all over the country, with medical teams monitoring the patients who took the pills.”
, the news outlet reported. The research team analyzed information from Clalit’s electronic medical records. The health care organization covers about 52% of the Israeli population and almost two-thirds of older adults. More than 30,000 COVID-19 patients in Israel have been treated with the drug so far.
Dr. Netzer and colleagues looked at hospitalization and death data for at-risk COVID-19 patients ages 40 and older between Jan. 9 and March 31, when the original Omicron variant was the dominant strain in Israel. During that time, more than 1.1 million Clalit patients were infected with COVID-19, 109,000 patients were considered at-risk, and 3,900 patients received the drug.
The average age of the patients was 60, and 39% of the patients were 65 and older. Overall, 78% of the patients had previous COVID-19 immunity due to vaccination, prior infection, or both.
Among ages 65 and older, the rate of COVID-19 hospitalization was 14.7 cases per 100,000 person-days among treated patients, compared with 58.9 cases per 100,000 person-days among untreated patients. This represented a 73% lower chance of being hospitalized.
Among ages 40-64, the rate of hospitalization due to COVID-19 was 15.2 cases per 100,000 person-days among treated patients, compared with 15.8 cases per 100,000 person-days among untreated patients. The risk of hospitalization wasn’t significantly lower for this age group.
Among ages 65 and older, there were two deaths from COVID-19 in 2,484 treated patients, compared with 158 in the 40,337 untreated patients. This represented a 79% lower chance of dying from COVID-19.
Among ages 40-64, there was one death from COVID-19 in 1,418 treated patients, compared with 16 in the 65,015 untreated patients. The risk of death wasn’t significantly lower for this age group.
For both age groups, a lack of previous COVID-19 immunity and a previous hospitalization were most strongly linked to high rates of hospitalization during the Omicron wave.
The researchers noted that they didn’t break down the data on ages 40-64 who had cancer and other severe conditions that weaken the immune system. These patients may be more likely to benefit from Paxlovid, they said, though future studies will need to analyze the data.
The study didn’t receive any financial or in-kind support, the authors said.
A version of this article first appeared on WebMD.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
ACC fills gaps on guidance for nonstatin therapies for LDL-C lowering
To address current gaps in expert guidance on newer nonstatin agents, the American College of Cardiology has issued an expert consensus decision pathway on the role of nonstatin therapies in LDL cholesterol lowering for risk reduction in atherosclerotic cardiovascular disease (ASCVD).
Since the publication of the most recent AHA/ACC cholesterol guidelines in 2018, a number of newer nonstatin medications have become available for management of lipid-associated risk, including bempedoic acid, inclisiran, evinacumab, and icosapent ethyl.
These medications were not addressed in the 2018 AHA/ACC Guideline on the Management of Blood Cholesterol.
The 53-page document – 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk – was published online in the Journal of the American College of Cardiology.
The new expert consensus document provides guidance for clinicians until the next formal guidelines are produced, Donald Lloyd-Jones, MD, chair of the writing committee, told this news organization.
The writing group focused on three key areas regarding the use of nonstatin therapies where recent scientific evidence is still under review and clinical trials are still underway:
- In what patient populations should newer nonstatin therapies be considered?
- In what situations should newer nonstatin therapies be considered?
- If newer nonstatin therapies are to be added, which therapies should be considered and in what order to maximize patient benefit and preference?
The document provides algorithms that endorse the four evidence-based patient groups identified in the 2018 guidelines and assumes that the patient is currently taking or has attempted to take a statin, given that that is the most effective initial therapy, the writing group says.
“The algorithms have been streamlined for ease of use by clinicians to help them identify who may need adjunctive nonstatin medications, to provide thresholds for consideration of those medications, and to provide a prioritization of those medications based on the strength of available evidence of efficacy,” said Dr. Lloyd-Jones, chair of the department of preventive medicine at Northwestern University’s Feinberg School of Medicine, Chicago.
“We hope that these pathways will assist the decision-making process for clinicians and patients,” he added.
He also noted that statins remain the “most important first-line therapy for reducing ASCVD risk, because of their efficacy, safety, and low cost. However, for some patients, there are now options if statins do not fully achieve the goals for reducing ASCVD risk or if statins are not tolerated at effective doses.”
“The new expert consensus document highlights that higher-risk patients should be considered more often for adjunctive therapy and provides user-friendly decision pathways to assist in considering the reasonable choices available under different clinical scenarios,” Dr. Lloyd-Jones said.
The document has been endorsed by the National Lipid Association.
This research had no commercial funding. Dr. Lloyd-Jones has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
To address current gaps in expert guidance on newer nonstatin agents, the American College of Cardiology has issued an expert consensus decision pathway on the role of nonstatin therapies in LDL cholesterol lowering for risk reduction in atherosclerotic cardiovascular disease (ASCVD).
Since the publication of the most recent AHA/ACC cholesterol guidelines in 2018, a number of newer nonstatin medications have become available for management of lipid-associated risk, including bempedoic acid, inclisiran, evinacumab, and icosapent ethyl.
These medications were not addressed in the 2018 AHA/ACC Guideline on the Management of Blood Cholesterol.
The 53-page document – 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk – was published online in the Journal of the American College of Cardiology.
The new expert consensus document provides guidance for clinicians until the next formal guidelines are produced, Donald Lloyd-Jones, MD, chair of the writing committee, told this news organization.
The writing group focused on three key areas regarding the use of nonstatin therapies where recent scientific evidence is still under review and clinical trials are still underway:
- In what patient populations should newer nonstatin therapies be considered?
- In what situations should newer nonstatin therapies be considered?
- If newer nonstatin therapies are to be added, which therapies should be considered and in what order to maximize patient benefit and preference?
The document provides algorithms that endorse the four evidence-based patient groups identified in the 2018 guidelines and assumes that the patient is currently taking or has attempted to take a statin, given that that is the most effective initial therapy, the writing group says.
“The algorithms have been streamlined for ease of use by clinicians to help them identify who may need adjunctive nonstatin medications, to provide thresholds for consideration of those medications, and to provide a prioritization of those medications based on the strength of available evidence of efficacy,” said Dr. Lloyd-Jones, chair of the department of preventive medicine at Northwestern University’s Feinberg School of Medicine, Chicago.
“We hope that these pathways will assist the decision-making process for clinicians and patients,” he added.
He also noted that statins remain the “most important first-line therapy for reducing ASCVD risk, because of their efficacy, safety, and low cost. However, for some patients, there are now options if statins do not fully achieve the goals for reducing ASCVD risk or if statins are not tolerated at effective doses.”
“The new expert consensus document highlights that higher-risk patients should be considered more often for adjunctive therapy and provides user-friendly decision pathways to assist in considering the reasonable choices available under different clinical scenarios,” Dr. Lloyd-Jones said.
The document has been endorsed by the National Lipid Association.
This research had no commercial funding. Dr. Lloyd-Jones has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
To address current gaps in expert guidance on newer nonstatin agents, the American College of Cardiology has issued an expert consensus decision pathway on the role of nonstatin therapies in LDL cholesterol lowering for risk reduction in atherosclerotic cardiovascular disease (ASCVD).
Since the publication of the most recent AHA/ACC cholesterol guidelines in 2018, a number of newer nonstatin medications have become available for management of lipid-associated risk, including bempedoic acid, inclisiran, evinacumab, and icosapent ethyl.
These medications were not addressed in the 2018 AHA/ACC Guideline on the Management of Blood Cholesterol.
The 53-page document – 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk – was published online in the Journal of the American College of Cardiology.
The new expert consensus document provides guidance for clinicians until the next formal guidelines are produced, Donald Lloyd-Jones, MD, chair of the writing committee, told this news organization.
The writing group focused on three key areas regarding the use of nonstatin therapies where recent scientific evidence is still under review and clinical trials are still underway:
- In what patient populations should newer nonstatin therapies be considered?
- In what situations should newer nonstatin therapies be considered?
- If newer nonstatin therapies are to be added, which therapies should be considered and in what order to maximize patient benefit and preference?
The document provides algorithms that endorse the four evidence-based patient groups identified in the 2018 guidelines and assumes that the patient is currently taking or has attempted to take a statin, given that that is the most effective initial therapy, the writing group says.
“The algorithms have been streamlined for ease of use by clinicians to help them identify who may need adjunctive nonstatin medications, to provide thresholds for consideration of those medications, and to provide a prioritization of those medications based on the strength of available evidence of efficacy,” said Dr. Lloyd-Jones, chair of the department of preventive medicine at Northwestern University’s Feinberg School of Medicine, Chicago.
“We hope that these pathways will assist the decision-making process for clinicians and patients,” he added.
He also noted that statins remain the “most important first-line therapy for reducing ASCVD risk, because of their efficacy, safety, and low cost. However, for some patients, there are now options if statins do not fully achieve the goals for reducing ASCVD risk or if statins are not tolerated at effective doses.”
“The new expert consensus document highlights that higher-risk patients should be considered more often for adjunctive therapy and provides user-friendly decision pathways to assist in considering the reasonable choices available under different clinical scenarios,” Dr. Lloyd-Jones said.
The document has been endorsed by the National Lipid Association.
This research had no commercial funding. Dr. Lloyd-Jones has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 vaccine safe in patients with heart failure
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
AXIOMATIC-SSP: Cautious optimism on factor XI inhibitor in stroke
The new factor XI inhibitor antithrombotic, milvexian (Bristol-Myers Squibb/Janssen), has shown promising results in a dose-finding phase 2 trial in patients with acute ischemic stroke or transient ischemic attack (TIA), when given in addition to dual antiplatelet therapy.
Although there was no significant reduction in the primary composite endpoint of ischemic stroke or incident infarct on brain MRI at 90 days with milvexian versus placebo in the AXIOMATIC-SSP study, with no apparent dose response, the drug numerically reduced the risk for symptomatic ischemic stroke at most doses. And doses from 25 mg to 100 mg twice daily showed an approximately 30% relative risk reduction in symptomatic ischemic stroke versus placebo.
Milvexian at 25 mg once and twice daily was associated with a low incidence of major bleeding; a moderate increase in bleeding was seen with higher doses.
There was no increase in severe bleeding, compared with placebo, and no fatal bleeding occurred any study group.
“Based on the observed efficacy signal for ischemic stroke, the bleeding profile, and the overall safety and tolerability, milvexian will be further studied in a phase 3 trial in a similar stroke population,” concluded lead investigator, Mukul Sharma, MD, associate professor of medicine at McMaster University, Hamilton, Ont.
Dr. Sharma presented the AXIOMATIC-SSP study results at the annual congress of the European Society of Cardiology.
New generation
Dr. Sharma explained that factor XI inhibitors represent the latest hope for a new generation of antithrombotic drugs with a low bleeding risk.
This has come about after observations that individuals born with factor XI deficiency have lower rates of ischemic stroke and thromboembolism than matched controls, without an offsetting increase in cerebral hemorrhage. In addition, spontaneous bleeding in these individuals is uncommon, and it is thought that factor XI is a strong driver of thrombus growth but plays a less important role in hemostasis, he noted.
“I think there is a tremendous niche for these drugs in stroke prevention,” Dr. Sharma said in an interview. “There is a huge unmet need in stroke patients for something other than aspirin over the long term which is effective but doesn’t cause hemorrhage.”
Dr. Sharma reported that antithrombotic efficacy of milvexian has already been demonstrated in a study of patients undergoing knee replacement in which the drug showed similar or increased efficacy in reducing thromboembolism, compared with enoxaparin, 40 mg, without an increase in major bleeding.
The aim of the current AXIOMATIC-SSP study was to find a dose suitable for use in the treatment of patients with acute stroke or TIA.
Patients with an acute ischemic stroke or TIA are at a high risk for another stroke in the first few months. Although antiplatelet drugs have reduced this event rate, there is still a significant residual risk for ischemic stroke, and the potential for major bleeding with additional antithrombotic therapies has limited the effectiveness of these options, Dr. Sharma explained. Currently, no anticoagulants are approved for noncardioembolic ischemic stroke prevention in the early phase.
The AXIOMATIC-SSP study included 2,366 patients within 48 hours of onset of a mild to moderate acute nonlacunar ischemic stroke. All patients had visible atherosclerotic plaque in a vessel supplying the affected brain region, and they all received background treatment with open-label aspirin and clopidogrel for 21 days, followed by open-label aspirin alone from days 22 to 90.
They were randomly assigned to one of five doses of milvexian (25, 50, 100, or 200 mg twice daily or 25 mg once daily) or placebo daily for 90 days.
The primary efficacy endpoint (symptomatic ischemic stroke or incident infarct on brain MRI) was numerically lower at the 50-mg and 100-mg twice-daily doses, and there was no apparent dose response (placebo, 16.6%; 25 mg once daily, 16.2%; 25 mg twice daily, 18.5%; 50 mg twice daily, 14.1%; 100 mg twice daily, 14.7%; 200 mg twice daily, 16.4%).
However, milvexian was associated with a numerically lower risk for clinical ischemic stroke at all doses except 200 mg twice daily, with doses from 25 to 100 mg twice daily showing an approximately 30% relative risk reduction versus placebo (placebo, 5.5%; 25 mg once daily, 4.6%; 25 mg twice daily, 3.8%; 50 mg twice daily, 4.0%; 100 mg twice daily, 3.5%; 200 mg twice daily, 7.7%).
The main safety endpoint was major bleeding, defined as Bleeding Academic Research Consortium type 3 or 5 bleeding. This was similar to placebo for milvexian 25 mg once daily and twice daily (all 0.6%) but was moderately increased in the 50 mg twice daily (1.5%), 100 mg twice daily (1.6%), and 200 mg twice daily (1.5%) groups.
Most major bleeding episodes were gastrointestinal. There was no increase in severe bleeding or symptomatic intracranial hemorrhage versus placebo, and no fatal bleeding occurred in any arm of the study.
Incremental improvement
On the hope for a class of drugs that reduce ischemic events without increasing bleeding, Dr. Sharma said, “we keep hoping for a home run where there is no increase in bleeding with a new generation of antithrombotic, but what we seem to get is an incremental improvement with each new class.
“Factor Xa inhibitors have a lower rate of bleeding, compared to warfarin. I think we will see another incremental improvement in bleeding with these new factor XI inhibitors and hopefully less of the more serious bleeding,” he said in an interview.
He pointed out that, in this study, milvexian was given on top of dual antiplatelet therapy. “In stroke neurology that sounds very risky as we know that going from a single antiplatelet to two antiplatelet agents increases the risk of bleeding and now we are adding in a third antithrombotic, but we feel comfortable doing it because of what has been observed in patients who have a genetic deficiency of factor XI – very low rates of spontaneous bleeding and they don’t bleed intracranially largely,” he added.
In addition to milvexian, another oral factor XI inhibitor, asundexian (Bayer), is also in development, and similar results were reported in a phase 2 stroke trial (PACIFIC-STROKE) at the same ESC session.
Both drugs are now believed to be going forward into phase 3 trials.
Discussant of the study at the ESC Hotline session, Giovanna Liuzzo, MD, Catholic University of Rome, highlighted the large unmet need for stroke therapies, noting that patients with acute stroke or TIA have a stroke recurrence rate of 5% at 30 days and 17% at 2 years. Although antiplatelet agents are recommended, the use of anticoagulants has been limited by concerns over bleeding risk, and the factor XI inhibitors are promising in that they have the potential for a lower bleeding risk.
She suggested that results from the AXIOMATIC-SSP could point to a dose of milvexian of 25 mg twice daily as a balance between efficacy and bleeding to be taken into larger phase 3 trials
“The jury is still out on the safety and efficacy of milvexian as an adjunct to dual antiplatelet therapy for the prevention of recurrent noncardioembolic stroke,” Dr. Liuzzo concluded. “Only large-scale phase 3 trials will establish the safety and efficacy of factor XI inhibitors in the prevention of venous and arterial thrombosis.”
The AXIOMATIC-SSP study was funded by the Bristol-Myers Squibb/Janssen alliance. Dr. Sharma reported research contracts with Bristol-Myers Squibb, Bayer, and AstraZeneca, and consulting fees from Janssen, Bayer, HLS Therapeutics, and Alexion.
A version of this article first appeared on Medscape.com.
The new factor XI inhibitor antithrombotic, milvexian (Bristol-Myers Squibb/Janssen), has shown promising results in a dose-finding phase 2 trial in patients with acute ischemic stroke or transient ischemic attack (TIA), when given in addition to dual antiplatelet therapy.
Although there was no significant reduction in the primary composite endpoint of ischemic stroke or incident infarct on brain MRI at 90 days with milvexian versus placebo in the AXIOMATIC-SSP study, with no apparent dose response, the drug numerically reduced the risk for symptomatic ischemic stroke at most doses. And doses from 25 mg to 100 mg twice daily showed an approximately 30% relative risk reduction in symptomatic ischemic stroke versus placebo.
Milvexian at 25 mg once and twice daily was associated with a low incidence of major bleeding; a moderate increase in bleeding was seen with higher doses.
There was no increase in severe bleeding, compared with placebo, and no fatal bleeding occurred any study group.
“Based on the observed efficacy signal for ischemic stroke, the bleeding profile, and the overall safety and tolerability, milvexian will be further studied in a phase 3 trial in a similar stroke population,” concluded lead investigator, Mukul Sharma, MD, associate professor of medicine at McMaster University, Hamilton, Ont.
Dr. Sharma presented the AXIOMATIC-SSP study results at the annual congress of the European Society of Cardiology.
New generation
Dr. Sharma explained that factor XI inhibitors represent the latest hope for a new generation of antithrombotic drugs with a low bleeding risk.
This has come about after observations that individuals born with factor XI deficiency have lower rates of ischemic stroke and thromboembolism than matched controls, without an offsetting increase in cerebral hemorrhage. In addition, spontaneous bleeding in these individuals is uncommon, and it is thought that factor XI is a strong driver of thrombus growth but plays a less important role in hemostasis, he noted.
“I think there is a tremendous niche for these drugs in stroke prevention,” Dr. Sharma said in an interview. “There is a huge unmet need in stroke patients for something other than aspirin over the long term which is effective but doesn’t cause hemorrhage.”
Dr. Sharma reported that antithrombotic efficacy of milvexian has already been demonstrated in a study of patients undergoing knee replacement in which the drug showed similar or increased efficacy in reducing thromboembolism, compared with enoxaparin, 40 mg, without an increase in major bleeding.
The aim of the current AXIOMATIC-SSP study was to find a dose suitable for use in the treatment of patients with acute stroke or TIA.
Patients with an acute ischemic stroke or TIA are at a high risk for another stroke in the first few months. Although antiplatelet drugs have reduced this event rate, there is still a significant residual risk for ischemic stroke, and the potential for major bleeding with additional antithrombotic therapies has limited the effectiveness of these options, Dr. Sharma explained. Currently, no anticoagulants are approved for noncardioembolic ischemic stroke prevention in the early phase.
The AXIOMATIC-SSP study included 2,366 patients within 48 hours of onset of a mild to moderate acute nonlacunar ischemic stroke. All patients had visible atherosclerotic plaque in a vessel supplying the affected brain region, and they all received background treatment with open-label aspirin and clopidogrel for 21 days, followed by open-label aspirin alone from days 22 to 90.
They were randomly assigned to one of five doses of milvexian (25, 50, 100, or 200 mg twice daily or 25 mg once daily) or placebo daily for 90 days.
The primary efficacy endpoint (symptomatic ischemic stroke or incident infarct on brain MRI) was numerically lower at the 50-mg and 100-mg twice-daily doses, and there was no apparent dose response (placebo, 16.6%; 25 mg once daily, 16.2%; 25 mg twice daily, 18.5%; 50 mg twice daily, 14.1%; 100 mg twice daily, 14.7%; 200 mg twice daily, 16.4%).
However, milvexian was associated with a numerically lower risk for clinical ischemic stroke at all doses except 200 mg twice daily, with doses from 25 to 100 mg twice daily showing an approximately 30% relative risk reduction versus placebo (placebo, 5.5%; 25 mg once daily, 4.6%; 25 mg twice daily, 3.8%; 50 mg twice daily, 4.0%; 100 mg twice daily, 3.5%; 200 mg twice daily, 7.7%).
The main safety endpoint was major bleeding, defined as Bleeding Academic Research Consortium type 3 or 5 bleeding. This was similar to placebo for milvexian 25 mg once daily and twice daily (all 0.6%) but was moderately increased in the 50 mg twice daily (1.5%), 100 mg twice daily (1.6%), and 200 mg twice daily (1.5%) groups.
Most major bleeding episodes were gastrointestinal. There was no increase in severe bleeding or symptomatic intracranial hemorrhage versus placebo, and no fatal bleeding occurred in any arm of the study.
Incremental improvement
On the hope for a class of drugs that reduce ischemic events without increasing bleeding, Dr. Sharma said, “we keep hoping for a home run where there is no increase in bleeding with a new generation of antithrombotic, but what we seem to get is an incremental improvement with each new class.
“Factor Xa inhibitors have a lower rate of bleeding, compared to warfarin. I think we will see another incremental improvement in bleeding with these new factor XI inhibitors and hopefully less of the more serious bleeding,” he said in an interview.
He pointed out that, in this study, milvexian was given on top of dual antiplatelet therapy. “In stroke neurology that sounds very risky as we know that going from a single antiplatelet to two antiplatelet agents increases the risk of bleeding and now we are adding in a third antithrombotic, but we feel comfortable doing it because of what has been observed in patients who have a genetic deficiency of factor XI – very low rates of spontaneous bleeding and they don’t bleed intracranially largely,” he added.
In addition to milvexian, another oral factor XI inhibitor, asundexian (Bayer), is also in development, and similar results were reported in a phase 2 stroke trial (PACIFIC-STROKE) at the same ESC session.
Both drugs are now believed to be going forward into phase 3 trials.
Discussant of the study at the ESC Hotline session, Giovanna Liuzzo, MD, Catholic University of Rome, highlighted the large unmet need for stroke therapies, noting that patients with acute stroke or TIA have a stroke recurrence rate of 5% at 30 days and 17% at 2 years. Although antiplatelet agents are recommended, the use of anticoagulants has been limited by concerns over bleeding risk, and the factor XI inhibitors are promising in that they have the potential for a lower bleeding risk.
She suggested that results from the AXIOMATIC-SSP could point to a dose of milvexian of 25 mg twice daily as a balance between efficacy and bleeding to be taken into larger phase 3 trials
“The jury is still out on the safety and efficacy of milvexian as an adjunct to dual antiplatelet therapy for the prevention of recurrent noncardioembolic stroke,” Dr. Liuzzo concluded. “Only large-scale phase 3 trials will establish the safety and efficacy of factor XI inhibitors in the prevention of venous and arterial thrombosis.”
The AXIOMATIC-SSP study was funded by the Bristol-Myers Squibb/Janssen alliance. Dr. Sharma reported research contracts with Bristol-Myers Squibb, Bayer, and AstraZeneca, and consulting fees from Janssen, Bayer, HLS Therapeutics, and Alexion.
A version of this article first appeared on Medscape.com.
The new factor XI inhibitor antithrombotic, milvexian (Bristol-Myers Squibb/Janssen), has shown promising results in a dose-finding phase 2 trial in patients with acute ischemic stroke or transient ischemic attack (TIA), when given in addition to dual antiplatelet therapy.
Although there was no significant reduction in the primary composite endpoint of ischemic stroke or incident infarct on brain MRI at 90 days with milvexian versus placebo in the AXIOMATIC-SSP study, with no apparent dose response, the drug numerically reduced the risk for symptomatic ischemic stroke at most doses. And doses from 25 mg to 100 mg twice daily showed an approximately 30% relative risk reduction in symptomatic ischemic stroke versus placebo.
Milvexian at 25 mg once and twice daily was associated with a low incidence of major bleeding; a moderate increase in bleeding was seen with higher doses.
There was no increase in severe bleeding, compared with placebo, and no fatal bleeding occurred any study group.
“Based on the observed efficacy signal for ischemic stroke, the bleeding profile, and the overall safety and tolerability, milvexian will be further studied in a phase 3 trial in a similar stroke population,” concluded lead investigator, Mukul Sharma, MD, associate professor of medicine at McMaster University, Hamilton, Ont.
Dr. Sharma presented the AXIOMATIC-SSP study results at the annual congress of the European Society of Cardiology.
New generation
Dr. Sharma explained that factor XI inhibitors represent the latest hope for a new generation of antithrombotic drugs with a low bleeding risk.
This has come about after observations that individuals born with factor XI deficiency have lower rates of ischemic stroke and thromboembolism than matched controls, without an offsetting increase in cerebral hemorrhage. In addition, spontaneous bleeding in these individuals is uncommon, and it is thought that factor XI is a strong driver of thrombus growth but plays a less important role in hemostasis, he noted.
“I think there is a tremendous niche for these drugs in stroke prevention,” Dr. Sharma said in an interview. “There is a huge unmet need in stroke patients for something other than aspirin over the long term which is effective but doesn’t cause hemorrhage.”
Dr. Sharma reported that antithrombotic efficacy of milvexian has already been demonstrated in a study of patients undergoing knee replacement in which the drug showed similar or increased efficacy in reducing thromboembolism, compared with enoxaparin, 40 mg, without an increase in major bleeding.
The aim of the current AXIOMATIC-SSP study was to find a dose suitable for use in the treatment of patients with acute stroke or TIA.
Patients with an acute ischemic stroke or TIA are at a high risk for another stroke in the first few months. Although antiplatelet drugs have reduced this event rate, there is still a significant residual risk for ischemic stroke, and the potential for major bleeding with additional antithrombotic therapies has limited the effectiveness of these options, Dr. Sharma explained. Currently, no anticoagulants are approved for noncardioembolic ischemic stroke prevention in the early phase.
The AXIOMATIC-SSP study included 2,366 patients within 48 hours of onset of a mild to moderate acute nonlacunar ischemic stroke. All patients had visible atherosclerotic plaque in a vessel supplying the affected brain region, and they all received background treatment with open-label aspirin and clopidogrel for 21 days, followed by open-label aspirin alone from days 22 to 90.
They were randomly assigned to one of five doses of milvexian (25, 50, 100, or 200 mg twice daily or 25 mg once daily) or placebo daily for 90 days.
The primary efficacy endpoint (symptomatic ischemic stroke or incident infarct on brain MRI) was numerically lower at the 50-mg and 100-mg twice-daily doses, and there was no apparent dose response (placebo, 16.6%; 25 mg once daily, 16.2%; 25 mg twice daily, 18.5%; 50 mg twice daily, 14.1%; 100 mg twice daily, 14.7%; 200 mg twice daily, 16.4%).
However, milvexian was associated with a numerically lower risk for clinical ischemic stroke at all doses except 200 mg twice daily, with doses from 25 to 100 mg twice daily showing an approximately 30% relative risk reduction versus placebo (placebo, 5.5%; 25 mg once daily, 4.6%; 25 mg twice daily, 3.8%; 50 mg twice daily, 4.0%; 100 mg twice daily, 3.5%; 200 mg twice daily, 7.7%).
The main safety endpoint was major bleeding, defined as Bleeding Academic Research Consortium type 3 or 5 bleeding. This was similar to placebo for milvexian 25 mg once daily and twice daily (all 0.6%) but was moderately increased in the 50 mg twice daily (1.5%), 100 mg twice daily (1.6%), and 200 mg twice daily (1.5%) groups.
Most major bleeding episodes were gastrointestinal. There was no increase in severe bleeding or symptomatic intracranial hemorrhage versus placebo, and no fatal bleeding occurred in any arm of the study.
Incremental improvement
On the hope for a class of drugs that reduce ischemic events without increasing bleeding, Dr. Sharma said, “we keep hoping for a home run where there is no increase in bleeding with a new generation of antithrombotic, but what we seem to get is an incremental improvement with each new class.
“Factor Xa inhibitors have a lower rate of bleeding, compared to warfarin. I think we will see another incremental improvement in bleeding with these new factor XI inhibitors and hopefully less of the more serious bleeding,” he said in an interview.
He pointed out that, in this study, milvexian was given on top of dual antiplatelet therapy. “In stroke neurology that sounds very risky as we know that going from a single antiplatelet to two antiplatelet agents increases the risk of bleeding and now we are adding in a third antithrombotic, but we feel comfortable doing it because of what has been observed in patients who have a genetic deficiency of factor XI – very low rates of spontaneous bleeding and they don’t bleed intracranially largely,” he added.
In addition to milvexian, another oral factor XI inhibitor, asundexian (Bayer), is also in development, and similar results were reported in a phase 2 stroke trial (PACIFIC-STROKE) at the same ESC session.
Both drugs are now believed to be going forward into phase 3 trials.
Discussant of the study at the ESC Hotline session, Giovanna Liuzzo, MD, Catholic University of Rome, highlighted the large unmet need for stroke therapies, noting that patients with acute stroke or TIA have a stroke recurrence rate of 5% at 30 days and 17% at 2 years. Although antiplatelet agents are recommended, the use of anticoagulants has been limited by concerns over bleeding risk, and the factor XI inhibitors are promising in that they have the potential for a lower bleeding risk.
She suggested that results from the AXIOMATIC-SSP could point to a dose of milvexian of 25 mg twice daily as a balance between efficacy and bleeding to be taken into larger phase 3 trials
“The jury is still out on the safety and efficacy of milvexian as an adjunct to dual antiplatelet therapy for the prevention of recurrent noncardioembolic stroke,” Dr. Liuzzo concluded. “Only large-scale phase 3 trials will establish the safety and efficacy of factor XI inhibitors in the prevention of venous and arterial thrombosis.”
The AXIOMATIC-SSP study was funded by the Bristol-Myers Squibb/Janssen alliance. Dr. Sharma reported research contracts with Bristol-Myers Squibb, Bayer, and AstraZeneca, and consulting fees from Janssen, Bayer, HLS Therapeutics, and Alexion.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
ALL-HEART: No benefit of allopurinol in ischemic heart disease
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022