User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Patients who refuse to wear masks: Responses that won’t get you sued
What do you do now?
Your waiting room is filled with mask-wearing individuals, except for one person. Your staff offers a mask to this person, citing your office policy of requiring masks for all persons in order to prevent asymptomatic COVID-19 spread, and the patient refuses to put it on.
What can you/should you/must you do? Are you required to see a patient who refuses to wear a mask? If you ask the patient to leave without being seen, can you be accused of patient abandonment? If you allow the patient to stay, could you be liable for negligence for exposing others to a deadly illness?
The rules on mask-wearing, while initially downright confusing, have inexorably come to a rough consensus. By governors’ orders, masks are now mandatory in most states, though when and where they are required varies. For example, effective July 7, the governor of Washington has ordered that a business not allow a customer to enter without a face covering.
Nor do we have case law to help us determine whether patient abandonment would apply if a patient is sent home without being seen.
We can apply the legal principles and cases from other situations to this one, however, to tell us what constitutes negligence or patient abandonment. The practical questions, legally, are who might sue and on what basis?
Who might sue?
Someone who is injured in a public place may sue the owner for negligence if the owner knew or should have known of a danger and didn’t do anything about it. For example, individuals have sued grocery stores successfully after they slipped on a banana peel and fell. If, say, the banana peel was black, that indicates that it had been there for a while, and judges have found that the store management should have known about it and removed it.
Compare the banana peel scenario with the scenario where most news outlets and health departments are telling people, every day, to wear masks while in indoor public spaces, yet owners of a medical practice or facility allow individuals who are not wearing masks to sit in their waiting room. If an individual who was also in the waiting room with the unmasked individual develops COVID-19 2 days later, the ill individual may sue the medical practice for negligence for not removing the unmasked individual.
What about the individual’s responsibility to move away from the person not wearing a mask? That is the aspect of this scenario that attorneys and experts could argue about, for days, in a court case. But to go back to the banana peel case, one could argue that a customer in a grocery store should be looking out for banana peels on the floor and avoid them, yet courts have assigned liability to grocery stores when customers slip and fall.
Let’s review the four elements of negligence which a plaintiff would need to prove:
- Duty: Obligation of one person to another
- Breach: Improper act or omission, in the context of proper behavior to avoid imposing undue risks of harm to other persons and their property
- Damage
- Causation: That the act or omission caused the harm
Those who run medical offices and facilities have a duty to provide reasonably safe public spaces. Unmasked individuals are a risk to others nearby, so the “breach” element is satisfied if a practice fails to impose safety measures. Causation could be proven, or at least inferred, if contact tracing of an individual with COVID-19 showed that the only contact likely to have exposed the ill individual to the virus was an unmasked individual in a medical practice’s waiting room, especially if the unmasked individual was COVID-19 positive before, during, or shortly after the visit to the practice.
What about patient abandonment?
“Patient abandonment” is the legal term for terminating the physician-patient relationship in such a manner that the patient is denied necessary medical care. It is a form of negligence.
Refusing to see a patient unless the patient wears a mask is not denying care, in this attorney’s view, but rather establishing reasonable conditions for getting care. The patient simply needs to put on a mask.
What about the patient who refuses to wear a mask for medical reasons? There are exceptions in most of the governors’ orders for individuals with medical conditions that preclude covering nose and mouth with a mask. A medical office is the perfect place to test an individual’s ability or inability to breathe well while wearing a mask. “Put the mask on and we’ll see how you do” is a reasonable response. Monitor the patient visually and apply a pulse oximeter with mask off and mask on.
One physician recently wrote about measuring her own oxygen levels while wearing four different masks for 5 minutes each, with no change in breathing.
Editor’s note: Read more about mask exemptions in a Medscape interview with pulmonologist Albert Rizzo, MD, chief medical officer of the American Lung Association.
What are some practical tips?
Assuming that a patient is not in acute distress, options in this scenario include:
- Send the patient home and offer a return visit if masked or when the pandemic is over.
- Offer a telehealth visit, with the patient at home.
What if the unmasked person is not a patient but the companion of a patient? What if the individual refusing to wear a mask is an employee? In neither of these two hypotheticals is there a basis for legal action against a practice whose policy requires that everyone wear masks on the premises.
A companion who arrives without a mask should leave the office. An employee who refuses to mask up could be sent home. If the employee has a disability covered by the Americans with Disabilities Act, then the practice may need to make reasonable accommodations so that the employee works in a room alone if unable to work from home.
Those who manage medical practices should check the websites of the state health department and medical societies at least weekly, to see whether the agencies have issued guidance. For example, the Texas Medical Association has issued limited guidance.
A version of this article originally appeared on Medscape.com.
What do you do now?
Your waiting room is filled with mask-wearing individuals, except for one person. Your staff offers a mask to this person, citing your office policy of requiring masks for all persons in order to prevent asymptomatic COVID-19 spread, and the patient refuses to put it on.
What can you/should you/must you do? Are you required to see a patient who refuses to wear a mask? If you ask the patient to leave without being seen, can you be accused of patient abandonment? If you allow the patient to stay, could you be liable for negligence for exposing others to a deadly illness?
The rules on mask-wearing, while initially downright confusing, have inexorably come to a rough consensus. By governors’ orders, masks are now mandatory in most states, though when and where they are required varies. For example, effective July 7, the governor of Washington has ordered that a business not allow a customer to enter without a face covering.
Nor do we have case law to help us determine whether patient abandonment would apply if a patient is sent home without being seen.
We can apply the legal principles and cases from other situations to this one, however, to tell us what constitutes negligence or patient abandonment. The practical questions, legally, are who might sue and on what basis?
Who might sue?
Someone who is injured in a public place may sue the owner for negligence if the owner knew or should have known of a danger and didn’t do anything about it. For example, individuals have sued grocery stores successfully after they slipped on a banana peel and fell. If, say, the banana peel was black, that indicates that it had been there for a while, and judges have found that the store management should have known about it and removed it.
Compare the banana peel scenario with the scenario where most news outlets and health departments are telling people, every day, to wear masks while in indoor public spaces, yet owners of a medical practice or facility allow individuals who are not wearing masks to sit in their waiting room. If an individual who was also in the waiting room with the unmasked individual develops COVID-19 2 days later, the ill individual may sue the medical practice for negligence for not removing the unmasked individual.
What about the individual’s responsibility to move away from the person not wearing a mask? That is the aspect of this scenario that attorneys and experts could argue about, for days, in a court case. But to go back to the banana peel case, one could argue that a customer in a grocery store should be looking out for banana peels on the floor and avoid them, yet courts have assigned liability to grocery stores when customers slip and fall.
Let’s review the four elements of negligence which a plaintiff would need to prove:
- Duty: Obligation of one person to another
- Breach: Improper act or omission, in the context of proper behavior to avoid imposing undue risks of harm to other persons and their property
- Damage
- Causation: That the act or omission caused the harm
Those who run medical offices and facilities have a duty to provide reasonably safe public spaces. Unmasked individuals are a risk to others nearby, so the “breach” element is satisfied if a practice fails to impose safety measures. Causation could be proven, or at least inferred, if contact tracing of an individual with COVID-19 showed that the only contact likely to have exposed the ill individual to the virus was an unmasked individual in a medical practice’s waiting room, especially if the unmasked individual was COVID-19 positive before, during, or shortly after the visit to the practice.
What about patient abandonment?
“Patient abandonment” is the legal term for terminating the physician-patient relationship in such a manner that the patient is denied necessary medical care. It is a form of negligence.
Refusing to see a patient unless the patient wears a mask is not denying care, in this attorney’s view, but rather establishing reasonable conditions for getting care. The patient simply needs to put on a mask.
What about the patient who refuses to wear a mask for medical reasons? There are exceptions in most of the governors’ orders for individuals with medical conditions that preclude covering nose and mouth with a mask. A medical office is the perfect place to test an individual’s ability or inability to breathe well while wearing a mask. “Put the mask on and we’ll see how you do” is a reasonable response. Monitor the patient visually and apply a pulse oximeter with mask off and mask on.
One physician recently wrote about measuring her own oxygen levels while wearing four different masks for 5 minutes each, with no change in breathing.
Editor’s note: Read more about mask exemptions in a Medscape interview with pulmonologist Albert Rizzo, MD, chief medical officer of the American Lung Association.
What are some practical tips?
Assuming that a patient is not in acute distress, options in this scenario include:
- Send the patient home and offer a return visit if masked or when the pandemic is over.
- Offer a telehealth visit, with the patient at home.
What if the unmasked person is not a patient but the companion of a patient? What if the individual refusing to wear a mask is an employee? In neither of these two hypotheticals is there a basis for legal action against a practice whose policy requires that everyone wear masks on the premises.
A companion who arrives without a mask should leave the office. An employee who refuses to mask up could be sent home. If the employee has a disability covered by the Americans with Disabilities Act, then the practice may need to make reasonable accommodations so that the employee works in a room alone if unable to work from home.
Those who manage medical practices should check the websites of the state health department and medical societies at least weekly, to see whether the agencies have issued guidance. For example, the Texas Medical Association has issued limited guidance.
A version of this article originally appeared on Medscape.com.
What do you do now?
Your waiting room is filled with mask-wearing individuals, except for one person. Your staff offers a mask to this person, citing your office policy of requiring masks for all persons in order to prevent asymptomatic COVID-19 spread, and the patient refuses to put it on.
What can you/should you/must you do? Are you required to see a patient who refuses to wear a mask? If you ask the patient to leave without being seen, can you be accused of patient abandonment? If you allow the patient to stay, could you be liable for negligence for exposing others to a deadly illness?
The rules on mask-wearing, while initially downright confusing, have inexorably come to a rough consensus. By governors’ orders, masks are now mandatory in most states, though when and where they are required varies. For example, effective July 7, the governor of Washington has ordered that a business not allow a customer to enter without a face covering.
Nor do we have case law to help us determine whether patient abandonment would apply if a patient is sent home without being seen.
We can apply the legal principles and cases from other situations to this one, however, to tell us what constitutes negligence or patient abandonment. The practical questions, legally, are who might sue and on what basis?
Who might sue?
Someone who is injured in a public place may sue the owner for negligence if the owner knew or should have known of a danger and didn’t do anything about it. For example, individuals have sued grocery stores successfully after they slipped on a banana peel and fell. If, say, the banana peel was black, that indicates that it had been there for a while, and judges have found that the store management should have known about it and removed it.
Compare the banana peel scenario with the scenario where most news outlets and health departments are telling people, every day, to wear masks while in indoor public spaces, yet owners of a medical practice or facility allow individuals who are not wearing masks to sit in their waiting room. If an individual who was also in the waiting room with the unmasked individual develops COVID-19 2 days later, the ill individual may sue the medical practice for negligence for not removing the unmasked individual.
What about the individual’s responsibility to move away from the person not wearing a mask? That is the aspect of this scenario that attorneys and experts could argue about, for days, in a court case. But to go back to the banana peel case, one could argue that a customer in a grocery store should be looking out for banana peels on the floor and avoid them, yet courts have assigned liability to grocery stores when customers slip and fall.
Let’s review the four elements of negligence which a plaintiff would need to prove:
- Duty: Obligation of one person to another
- Breach: Improper act or omission, in the context of proper behavior to avoid imposing undue risks of harm to other persons and their property
- Damage
- Causation: That the act or omission caused the harm
Those who run medical offices and facilities have a duty to provide reasonably safe public spaces. Unmasked individuals are a risk to others nearby, so the “breach” element is satisfied if a practice fails to impose safety measures. Causation could be proven, or at least inferred, if contact tracing of an individual with COVID-19 showed that the only contact likely to have exposed the ill individual to the virus was an unmasked individual in a medical practice’s waiting room, especially if the unmasked individual was COVID-19 positive before, during, or shortly after the visit to the practice.
What about patient abandonment?
“Patient abandonment” is the legal term for terminating the physician-patient relationship in such a manner that the patient is denied necessary medical care. It is a form of negligence.
Refusing to see a patient unless the patient wears a mask is not denying care, in this attorney’s view, but rather establishing reasonable conditions for getting care. The patient simply needs to put on a mask.
What about the patient who refuses to wear a mask for medical reasons? There are exceptions in most of the governors’ orders for individuals with medical conditions that preclude covering nose and mouth with a mask. A medical office is the perfect place to test an individual’s ability or inability to breathe well while wearing a mask. “Put the mask on and we’ll see how you do” is a reasonable response. Monitor the patient visually and apply a pulse oximeter with mask off and mask on.
One physician recently wrote about measuring her own oxygen levels while wearing four different masks for 5 minutes each, with no change in breathing.
Editor’s note: Read more about mask exemptions in a Medscape interview with pulmonologist Albert Rizzo, MD, chief medical officer of the American Lung Association.
What are some practical tips?
Assuming that a patient is not in acute distress, options in this scenario include:
- Send the patient home and offer a return visit if masked or when the pandemic is over.
- Offer a telehealth visit, with the patient at home.
What if the unmasked person is not a patient but the companion of a patient? What if the individual refusing to wear a mask is an employee? In neither of these two hypotheticals is there a basis for legal action against a practice whose policy requires that everyone wear masks on the premises.
A companion who arrives without a mask should leave the office. An employee who refuses to mask up could be sent home. If the employee has a disability covered by the Americans with Disabilities Act, then the practice may need to make reasonable accommodations so that the employee works in a room alone if unable to work from home.
Those who manage medical practices should check the websites of the state health department and medical societies at least weekly, to see whether the agencies have issued guidance. For example, the Texas Medical Association has issued limited guidance.
A version of this article originally appeared on Medscape.com.
Children rarely transmit SARS-CoV-2 within households
“Unlike with other viral respiratory infections, children do not seem to be a major vector of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission, with most pediatric cases described inside familial clusters and no documentation of child-to-child or child-to-adult transmission,” said Klara M. Posfay-Barbe, MD, of the University of Geneva, Switzerland, and colleagues.
In a study published in Pediatrics, the researchers analyzed data from all COVID-19 patients younger than 16 years who were identified between March 10, 2020, and April 10, 2020, through a hospital surveillance network. Parents and household contacts were called for contact tracing.
In 31 of 39 (79%) households, at least one adult family member had a suspected or confirmed SARS-CoV-2 infection before onset of symptoms in the child. These findings support data from previous studies suggesting that children mainly become infected from adult family members rather than transmitting the virus to them, the researchers said
In only 3 of 39 (8%) households was the study child the first to develop symptoms. “Surprisingly, in 33% of households, symptomatic HHCs [household contacts] tested negative despite belonging to a familial cluster with confirmed SARS-CoV-2 cases, suggesting an underreporting of cases,” Dr. Posfay-Barbe and associates noted.
The findings were limited by several factors including potential underreporting of cases because those with mild or atypical presentations may not have sought medical care, and the inability to confirm child-to-adult transmission. The results were strengthened by the extensive contact tracing and very few individuals lost to follow-up, they said; however, more diagnostic screening and contact tracing are needed to improve understanding of household transmission of SARS-CoV-2, they concluded.
Resolving the issue of how much children contribute to transmission of SARS-CoV-2 is essential to making informed decisions about public health, including how to structure schools and child-care facility reopening, Benjamin Lee, MD, and William V. Raszka Jr., MD, both of the University of Vermont, Burlington, said in an accompanying editorial (Pediatrics. 2020 Jul 10. doi: 10.1542/peds/2020-004879).
The data in the current study support other studies of transmission among household contacts in China suggesting that, in most cases of childhood infections, “the child was not the source of infection and that children most frequently acquire COVID-19 from adults, rather than transmitting it to them,” they wrote.
In addition, the limited data on transmission of SARS-CoV-2 by children outside of the household show few cases of secondary infection from children identified with SARS-CoV-2 in school settings in studies from France and Australia, Dr. Lee and Dr. Raszka noted.
the editorialists wrote. “This would be another manner by which SARS-CoV2 differs drastically from influenza, for which school-based transmission is well recognized as a significant driver of epidemic disease and forms the basis for most evidence regarding school closures as public health strategy.”
“Therefore, serious consideration should be paid toward strategies that allow schools to remain open, even during periods of COVID-19 spread,” the editorialists concluded. “In doing so, we could minimize the potentially profound adverse social, developmental, and health costs that our children will continue to suffer until an effective treatment or vaccine can be developed and distributed or, failing that, until we reach herd immunity,” Dr. Lee and Dr. Raszka emphasized.
The study received no outside funding. The researchers and editorialists had no financial conflicts to disclose.
SOURCE: Posfay-Barbe KM et al. Pediatrics. 2020 Jul 10. doi: 10.1542/peds.2020-1576.
“Unlike with other viral respiratory infections, children do not seem to be a major vector of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission, with most pediatric cases described inside familial clusters and no documentation of child-to-child or child-to-adult transmission,” said Klara M. Posfay-Barbe, MD, of the University of Geneva, Switzerland, and colleagues.
In a study published in Pediatrics, the researchers analyzed data from all COVID-19 patients younger than 16 years who were identified between March 10, 2020, and April 10, 2020, through a hospital surveillance network. Parents and household contacts were called for contact tracing.
In 31 of 39 (79%) households, at least one adult family member had a suspected or confirmed SARS-CoV-2 infection before onset of symptoms in the child. These findings support data from previous studies suggesting that children mainly become infected from adult family members rather than transmitting the virus to them, the researchers said
In only 3 of 39 (8%) households was the study child the first to develop symptoms. “Surprisingly, in 33% of households, symptomatic HHCs [household contacts] tested negative despite belonging to a familial cluster with confirmed SARS-CoV-2 cases, suggesting an underreporting of cases,” Dr. Posfay-Barbe and associates noted.
The findings were limited by several factors including potential underreporting of cases because those with mild or atypical presentations may not have sought medical care, and the inability to confirm child-to-adult transmission. The results were strengthened by the extensive contact tracing and very few individuals lost to follow-up, they said; however, more diagnostic screening and contact tracing are needed to improve understanding of household transmission of SARS-CoV-2, they concluded.
Resolving the issue of how much children contribute to transmission of SARS-CoV-2 is essential to making informed decisions about public health, including how to structure schools and child-care facility reopening, Benjamin Lee, MD, and William V. Raszka Jr., MD, both of the University of Vermont, Burlington, said in an accompanying editorial (Pediatrics. 2020 Jul 10. doi: 10.1542/peds/2020-004879).
The data in the current study support other studies of transmission among household contacts in China suggesting that, in most cases of childhood infections, “the child was not the source of infection and that children most frequently acquire COVID-19 from adults, rather than transmitting it to them,” they wrote.
In addition, the limited data on transmission of SARS-CoV-2 by children outside of the household show few cases of secondary infection from children identified with SARS-CoV-2 in school settings in studies from France and Australia, Dr. Lee and Dr. Raszka noted.
the editorialists wrote. “This would be another manner by which SARS-CoV2 differs drastically from influenza, for which school-based transmission is well recognized as a significant driver of epidemic disease and forms the basis for most evidence regarding school closures as public health strategy.”
“Therefore, serious consideration should be paid toward strategies that allow schools to remain open, even during periods of COVID-19 spread,” the editorialists concluded. “In doing so, we could minimize the potentially profound adverse social, developmental, and health costs that our children will continue to suffer until an effective treatment or vaccine can be developed and distributed or, failing that, until we reach herd immunity,” Dr. Lee and Dr. Raszka emphasized.
The study received no outside funding. The researchers and editorialists had no financial conflicts to disclose.
SOURCE: Posfay-Barbe KM et al. Pediatrics. 2020 Jul 10. doi: 10.1542/peds.2020-1576.
“Unlike with other viral respiratory infections, children do not seem to be a major vector of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission, with most pediatric cases described inside familial clusters and no documentation of child-to-child or child-to-adult transmission,” said Klara M. Posfay-Barbe, MD, of the University of Geneva, Switzerland, and colleagues.
In a study published in Pediatrics, the researchers analyzed data from all COVID-19 patients younger than 16 years who were identified between March 10, 2020, and April 10, 2020, through a hospital surveillance network. Parents and household contacts were called for contact tracing.
In 31 of 39 (79%) households, at least one adult family member had a suspected or confirmed SARS-CoV-2 infection before onset of symptoms in the child. These findings support data from previous studies suggesting that children mainly become infected from adult family members rather than transmitting the virus to them, the researchers said
In only 3 of 39 (8%) households was the study child the first to develop symptoms. “Surprisingly, in 33% of households, symptomatic HHCs [household contacts] tested negative despite belonging to a familial cluster with confirmed SARS-CoV-2 cases, suggesting an underreporting of cases,” Dr. Posfay-Barbe and associates noted.
The findings were limited by several factors including potential underreporting of cases because those with mild or atypical presentations may not have sought medical care, and the inability to confirm child-to-adult transmission. The results were strengthened by the extensive contact tracing and very few individuals lost to follow-up, they said; however, more diagnostic screening and contact tracing are needed to improve understanding of household transmission of SARS-CoV-2, they concluded.
Resolving the issue of how much children contribute to transmission of SARS-CoV-2 is essential to making informed decisions about public health, including how to structure schools and child-care facility reopening, Benjamin Lee, MD, and William V. Raszka Jr., MD, both of the University of Vermont, Burlington, said in an accompanying editorial (Pediatrics. 2020 Jul 10. doi: 10.1542/peds/2020-004879).
The data in the current study support other studies of transmission among household contacts in China suggesting that, in most cases of childhood infections, “the child was not the source of infection and that children most frequently acquire COVID-19 from adults, rather than transmitting it to them,” they wrote.
In addition, the limited data on transmission of SARS-CoV-2 by children outside of the household show few cases of secondary infection from children identified with SARS-CoV-2 in school settings in studies from France and Australia, Dr. Lee and Dr. Raszka noted.
the editorialists wrote. “This would be another manner by which SARS-CoV2 differs drastically from influenza, for which school-based transmission is well recognized as a significant driver of epidemic disease and forms the basis for most evidence regarding school closures as public health strategy.”
“Therefore, serious consideration should be paid toward strategies that allow schools to remain open, even during periods of COVID-19 spread,” the editorialists concluded. “In doing so, we could minimize the potentially profound adverse social, developmental, and health costs that our children will continue to suffer until an effective treatment or vaccine can be developed and distributed or, failing that, until we reach herd immunity,” Dr. Lee and Dr. Raszka emphasized.
The study received no outside funding. The researchers and editorialists had no financial conflicts to disclose.
SOURCE: Posfay-Barbe KM et al. Pediatrics. 2020 Jul 10. doi: 10.1542/peds.2020-1576.
FROM PEDIATRICS
Perioperative sleep medicine: The Society of Anesthesia and Sleep Medicine
Obstructive sleep apnea (OSA) has been recognized to increase the risk of adverse cardiopulmonary perioperative outcomes for some time now.1 An ever growing body of literature supports this finding,2 including a large prospective study published in 2019 highlighting the significant risk of poor cardiac-related postoperative outcomes in patients with unrecognized OSA.3 As the majority of patients presenting for elective surgery with OSA will not be diagnosed at the time of presentation,3,4 many centers have developed preoperative screening programs to identify these patients, though the practice is not universal and a desire for better guidance is needed.5 In addition, best practices for patients with suspected or known OSA undergoing surgery have been a matter of debate. Out of these concerns, the Society of Anesthesia and Sleep Medicine (SASM) was formed over 10 years ago to promote interdisciplinary communication, education, and research into matters common to anesthesia and sleep.
Pulmonary and sleep medicine providers are often asked to provide preoperative clearance and recommendations for patients with suspected or known OSA. Recognizing the need for guidance in this area, a task force assembled by SASM obtained input from experts in anesthesiology, sleep medicine, and perioperative medicine to develop and publish an evidence-based / expert consensus guideline on the preoperative assessment and best practices for patients with suspected or known OSA.6 While specifics regarding logistics of preoperative screening and optimization of patients will vary based on each medical center’s infrastructure and organization, the recommendations presented should be able to be adapted by most, if not all, institutions. Preoperative evaluation and management is only part of the overall perioperative journey however, and SASM thus followed this document with guidelines for the intraoperative management of patients with OSA.7 To complete this set of recommendations, guidelines for the postoperative care of these patients are being planned. Guidelines for pediatric and obstetric perioperative OSA management are also currently being developed by SASM task forces to address these unique areas.
OSA is not the only sleep disorder where the perioperative environment may pose problems for our patients. Sleep disorders such as the hypersomnias and sleep-related movement disorders (including restless legs syndrome) may both impact and be impacted by the perioperative environment and may create safety concerns for some patients.8,9 These issues are also under active investigation by SASM. In addition, understanding the basic mechanisms determining unconsciousness in both anesthesia and sleep, as well as examination of the interrelationships between sleep disturbance, sedation and their effects on clinical outcomes, are areas of interest that have implications beyond the perioperative arena.
SASM is currently planning to host its 10th anniversary conference in Washington DC on October 1-2, public health issues permitting. The meeting has consistently enlisted expert speakers from anesthesia, sleep medicine, and other relevant fields, and this year will be no different. Given the host city, discussions on important healthcare policy issues will be included, as well. Registration for the meeting, as well as meeting updates, are on the SASM website (sasmhq.org).
Dr. Auckley is with the Division of Pulmonary, Critical Care and Sleep Medicine, MetroHealth Medical Center, Professor of Medicine, Case Western Reserve University, Cleveland, OH. He is the current president of the Society of Anesthesia and Sleep Medicine.
References
1. Gupta RM, et al. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc. 2001;76(9):897.
2. Opperer M, et al. Does obstructive sleep apnea influence perioperative outcome? A qualitative systematic review for the Society of Anesthesia and Sleep Medicine Task Force on Preoperative Preparation of Patients with Sleep-Disordered Breathing. Anesth Analg. 2016;122(5):1321.
3. Chan MTV, et al. Association of unrecognized obstructive sleep apnea with postoperative cardiovascular events in patients undergoing major noncardiac surgery. JAMA. 2019;321(18):1788.
4. Finkel KJ, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic center. Sleep Med. 2009;10(7):753.
5. Auckley D, et al. Attitudes regarding perioperative care of patients with OSA: a survey study of four specialties in the United States. Sleep Breath. 2015;19(1):315.
6. Chung F, et al. Society of Anesthesia and Sleep Medicine Guidelines (SASM) on Preoperative Screening and Assessment of Adult Patients with Obstructive Sleep Apnea. Anesth Analg. 2016;123(2):452.
7. Memtsoudis SG, et al. Society of Anesthesia and Sleep Medicine Guideline (SASM) on Intraoperative Management of Adult Patients with Obstructive Sleep Apnea. Anesth Analg. 2018;127(4):967.
8. Hershner S, et al. Knowledge gaps in the perioperative management of adults with narcolepsy: A call for further research. Anesth Analg. 2019 Jul;129(1):204.
9. Goldstein C. Management of restless legs syndrome / Willis-Ekbom disease in hospitalized and perioperative patients. Sleep Med Clin. 2015;10(3):303.
Obstructive sleep apnea (OSA) has been recognized to increase the risk of adverse cardiopulmonary perioperative outcomes for some time now.1 An ever growing body of literature supports this finding,2 including a large prospective study published in 2019 highlighting the significant risk of poor cardiac-related postoperative outcomes in patients with unrecognized OSA.3 As the majority of patients presenting for elective surgery with OSA will not be diagnosed at the time of presentation,3,4 many centers have developed preoperative screening programs to identify these patients, though the practice is not universal and a desire for better guidance is needed.5 In addition, best practices for patients with suspected or known OSA undergoing surgery have been a matter of debate. Out of these concerns, the Society of Anesthesia and Sleep Medicine (SASM) was formed over 10 years ago to promote interdisciplinary communication, education, and research into matters common to anesthesia and sleep.
Pulmonary and sleep medicine providers are often asked to provide preoperative clearance and recommendations for patients with suspected or known OSA. Recognizing the need for guidance in this area, a task force assembled by SASM obtained input from experts in anesthesiology, sleep medicine, and perioperative medicine to develop and publish an evidence-based / expert consensus guideline on the preoperative assessment and best practices for patients with suspected or known OSA.6 While specifics regarding logistics of preoperative screening and optimization of patients will vary based on each medical center’s infrastructure and organization, the recommendations presented should be able to be adapted by most, if not all, institutions. Preoperative evaluation and management is only part of the overall perioperative journey however, and SASM thus followed this document with guidelines for the intraoperative management of patients with OSA.7 To complete this set of recommendations, guidelines for the postoperative care of these patients are being planned. Guidelines for pediatric and obstetric perioperative OSA management are also currently being developed by SASM task forces to address these unique areas.
OSA is not the only sleep disorder where the perioperative environment may pose problems for our patients. Sleep disorders such as the hypersomnias and sleep-related movement disorders (including restless legs syndrome) may both impact and be impacted by the perioperative environment and may create safety concerns for some patients.8,9 These issues are also under active investigation by SASM. In addition, understanding the basic mechanisms determining unconsciousness in both anesthesia and sleep, as well as examination of the interrelationships between sleep disturbance, sedation and their effects on clinical outcomes, are areas of interest that have implications beyond the perioperative arena.
SASM is currently planning to host its 10th anniversary conference in Washington DC on October 1-2, public health issues permitting. The meeting has consistently enlisted expert speakers from anesthesia, sleep medicine, and other relevant fields, and this year will be no different. Given the host city, discussions on important healthcare policy issues will be included, as well. Registration for the meeting, as well as meeting updates, are on the SASM website (sasmhq.org).
Dr. Auckley is with the Division of Pulmonary, Critical Care and Sleep Medicine, MetroHealth Medical Center, Professor of Medicine, Case Western Reserve University, Cleveland, OH. He is the current president of the Society of Anesthesia and Sleep Medicine.
References
1. Gupta RM, et al. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc. 2001;76(9):897.
2. Opperer M, et al. Does obstructive sleep apnea influence perioperative outcome? A qualitative systematic review for the Society of Anesthesia and Sleep Medicine Task Force on Preoperative Preparation of Patients with Sleep-Disordered Breathing. Anesth Analg. 2016;122(5):1321.
3. Chan MTV, et al. Association of unrecognized obstructive sleep apnea with postoperative cardiovascular events in patients undergoing major noncardiac surgery. JAMA. 2019;321(18):1788.
4. Finkel KJ, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic center. Sleep Med. 2009;10(7):753.
5. Auckley D, et al. Attitudes regarding perioperative care of patients with OSA: a survey study of four specialties in the United States. Sleep Breath. 2015;19(1):315.
6. Chung F, et al. Society of Anesthesia and Sleep Medicine Guidelines (SASM) on Preoperative Screening and Assessment of Adult Patients with Obstructive Sleep Apnea. Anesth Analg. 2016;123(2):452.
7. Memtsoudis SG, et al. Society of Anesthesia and Sleep Medicine Guideline (SASM) on Intraoperative Management of Adult Patients with Obstructive Sleep Apnea. Anesth Analg. 2018;127(4):967.
8. Hershner S, et al. Knowledge gaps in the perioperative management of adults with narcolepsy: A call for further research. Anesth Analg. 2019 Jul;129(1):204.
9. Goldstein C. Management of restless legs syndrome / Willis-Ekbom disease in hospitalized and perioperative patients. Sleep Med Clin. 2015;10(3):303.
Obstructive sleep apnea (OSA) has been recognized to increase the risk of adverse cardiopulmonary perioperative outcomes for some time now.1 An ever growing body of literature supports this finding,2 including a large prospective study published in 2019 highlighting the significant risk of poor cardiac-related postoperative outcomes in patients with unrecognized OSA.3 As the majority of patients presenting for elective surgery with OSA will not be diagnosed at the time of presentation,3,4 many centers have developed preoperative screening programs to identify these patients, though the practice is not universal and a desire for better guidance is needed.5 In addition, best practices for patients with suspected or known OSA undergoing surgery have been a matter of debate. Out of these concerns, the Society of Anesthesia and Sleep Medicine (SASM) was formed over 10 years ago to promote interdisciplinary communication, education, and research into matters common to anesthesia and sleep.
Pulmonary and sleep medicine providers are often asked to provide preoperative clearance and recommendations for patients with suspected or known OSA. Recognizing the need for guidance in this area, a task force assembled by SASM obtained input from experts in anesthesiology, sleep medicine, and perioperative medicine to develop and publish an evidence-based / expert consensus guideline on the preoperative assessment and best practices for patients with suspected or known OSA.6 While specifics regarding logistics of preoperative screening and optimization of patients will vary based on each medical center’s infrastructure and organization, the recommendations presented should be able to be adapted by most, if not all, institutions. Preoperative evaluation and management is only part of the overall perioperative journey however, and SASM thus followed this document with guidelines for the intraoperative management of patients with OSA.7 To complete this set of recommendations, guidelines for the postoperative care of these patients are being planned. Guidelines for pediatric and obstetric perioperative OSA management are also currently being developed by SASM task forces to address these unique areas.
OSA is not the only sleep disorder where the perioperative environment may pose problems for our patients. Sleep disorders such as the hypersomnias and sleep-related movement disorders (including restless legs syndrome) may both impact and be impacted by the perioperative environment and may create safety concerns for some patients.8,9 These issues are also under active investigation by SASM. In addition, understanding the basic mechanisms determining unconsciousness in both anesthesia and sleep, as well as examination of the interrelationships between sleep disturbance, sedation and their effects on clinical outcomes, are areas of interest that have implications beyond the perioperative arena.
SASM is currently planning to host its 10th anniversary conference in Washington DC on October 1-2, public health issues permitting. The meeting has consistently enlisted expert speakers from anesthesia, sleep medicine, and other relevant fields, and this year will be no different. Given the host city, discussions on important healthcare policy issues will be included, as well. Registration for the meeting, as well as meeting updates, are on the SASM website (sasmhq.org).
Dr. Auckley is with the Division of Pulmonary, Critical Care and Sleep Medicine, MetroHealth Medical Center, Professor of Medicine, Case Western Reserve University, Cleveland, OH. He is the current president of the Society of Anesthesia and Sleep Medicine.
References
1. Gupta RM, et al. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc. 2001;76(9):897.
2. Opperer M, et al. Does obstructive sleep apnea influence perioperative outcome? A qualitative systematic review for the Society of Anesthesia and Sleep Medicine Task Force on Preoperative Preparation of Patients with Sleep-Disordered Breathing. Anesth Analg. 2016;122(5):1321.
3. Chan MTV, et al. Association of unrecognized obstructive sleep apnea with postoperative cardiovascular events in patients undergoing major noncardiac surgery. JAMA. 2019;321(18):1788.
4. Finkel KJ, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic center. Sleep Med. 2009;10(7):753.
5. Auckley D, et al. Attitudes regarding perioperative care of patients with OSA: a survey study of four specialties in the United States. Sleep Breath. 2015;19(1):315.
6. Chung F, et al. Society of Anesthesia and Sleep Medicine Guidelines (SASM) on Preoperative Screening and Assessment of Adult Patients with Obstructive Sleep Apnea. Anesth Analg. 2016;123(2):452.
7. Memtsoudis SG, et al. Society of Anesthesia and Sleep Medicine Guideline (SASM) on Intraoperative Management of Adult Patients with Obstructive Sleep Apnea. Anesth Analg. 2018;127(4):967.
8. Hershner S, et al. Knowledge gaps in the perioperative management of adults with narcolepsy: A call for further research. Anesth Analg. 2019 Jul;129(1):204.
9. Goldstein C. Management of restless legs syndrome / Willis-Ekbom disease in hospitalized and perioperative patients. Sleep Med Clin. 2015;10(3):303.
COVID-19 and the future of telehealth for sleep medicine
On March 18, 2020, the doors to our sleep center were physically closed. Two potential exposures to COVID-19 within a few hours, the palpable anxiety of our team, and a poor grasp of the virus and the growing pandemic moved us to make this decision. Up to that point, we could not help but feel we were playing “catch up” with our evolving set of safety measures to the escalating risk. Like so many other sleep centers around the country, a complete transition to virtual care was needed to ensure the safety of our patients and our team. It was perhaps that moment that we felt the emotional impact that our world had changed, altering both our personal lives and sleep medicine practice as we knew it. This event, while unfortunate, also provided a transformative opportunity to reimagine our identity, accelerating the efforts to bring the future of sleep medicine into the present.
Our team’s clinical evolution and innovation efforts have been guided by efforts to reconsider sleep medicine paradigms. Innovation progress was deliberate with incremental implementations that typically required repeat business cases with multiple approving parties and budgetary access. Those barriers largely dissolved once COVID-19 intensified, and a large portion of the strategies on our roadmap were put into production. In a matter of a couple weeks, our services completely transitioned to remote and virtual care, while most of the team of 55 persons were moved to “work-from-home.” A suite of technologies (automated questionnaires, automated and two-way text messaging templates, consumer wearable technologies, and population management dashboards) were put on the table (Somnoware, Inc.), and each of our longitudinal care teams (eg, adult obstructive sleep apnea, pediatrics, chronic respiratory failure, commercial driver, insomnia programs, etc) worked to embed them into new care pathways. This effort further consolidated technology as the backbone of our work and the enabler of remote virtual collaboration between sleep center personnel (respiratory case managers, medical assistants and nursing team, and physician and leadership personnel) to enhance our team-based approach. Moreover, we felt this point in time was ripe to swallow the proverbial “red pill” and approach patient care with shifted paradigms. We discuss three areas of active effort to leverage technology in this COVID-19 environment to accelerate a transition toward how we envision the future of sleep medicine.
Reimagined sleep diagnostics
Our virtual obstructive sleep apnea (OSA) diagnostic process includes utilizing a disposable home sleep apnea test (HSAT) device with wireless data transfer (WatchPAT ONE, Itamar Medical) while HSAT and PAP (positive airway pressure) setups are supported by information sheets, online videos (YouTube), automated interactive platforms (Emmi Solutions; Hwang D. Am J Respir Crit Care Med. 2018 Jan 1;197[1]:117), and synchronous provider video visits. Our more radical shift, however, is in approaching OSA diagnosis based principally on symptoms and secondarily supported by physiologic measurements and response to therapy. This “clinical diagnosis” approach reduces our reliance on traditional sleep testing and allows patient wearables to provide supportive physiologic data (eg, oximetry) to help determine OSA severity and phenotype. Its immediate impact is in limiting the need to send and retrieve potentially contaminated equipment. Broader clinical advantages include overcoming the imprecise nature of the apnea-hypopnea index (which often has dramatic night-to-night variability) through data collection over extended durations, improving disease assessment due to availability of complementary sleep/activity data in the person’s usual setting, and tracking changes after therapy initiation.
Our post-COVID-19 re-opening of polysomnography (PSG) services, after a temporary shutdown, introduces home PSG (Type II) for approximately half our patients without suspected complex breathing conditions while reserving attended PSG (Type I) for those who may require noninvasive ventilation. The immediate incentive is in reducing viral exposure by limiting patient traffic and risk of PAP trial aerosolization while also improving access to accommodate the backlog of patients requiring PSG. This approach furthers the paradigm shift to emphasizing care in the home setting. Testing in the patient’s usual environment and enabling multiple night/day testing may be clinically advantageous.
Shift in emphasis to care management
The emphasis of sleep medicine has traditionally focused on diagnostics through performing PSG and HSAT. Our field has invested tremendous effort in developing guidelines for processing sleep studies, but the scoring and interpretation of those studies is extremely labor intensive. Reimagining the diagnostic approach reduces the need to manually process studies—wearable data are produced automatically, HSAT can be auto-scored, and artificial intelligence platforms can score PSGs (Goldstein CA. J Clin Sleep Med. 2020 Apr 15;16[4]:609), which allows a shift in resources and emphasis to follow-up care. A comprehensive discussion of technology-based tools to enhance care management is beyond the purview of this editorial. However, an overview of our current efforts includes: (1) utilizing population management dashboards to automatically risk stratify different cohorts of patients (eg, adult OSA, pediatrics, commercial drivers, chronic respiratory failure, etc) to identify patients “at-risk” (eg, based on OSA severity, symptoms, co-morbidities, and PAP adherence); (2) applying enhanced patient-provider interchange tools that include automated and “intelligent” electronic questionnaires, automated personalized text messaging/emails, and two-way messaging to deliver care; (3) utilizing remote patient monitoring to enhance holistic, personalized management, such as with remote activity/sleep trackers, blood pressure monitors, glucometers, and weight scales. We are engaged with efforts to validate the impact of these data to provide more personalized feedback, directly impact clinical outcomes, facilitate interdisciplinary collaboration, and identify acutely ill patients. Furthermore, a holistic approach beyond a narrow focus on PAP may create a positive collateral effect on adherence by targeting engagement with broader areas of health; and (4) implementing machine learning tools to directly support providers and patients (examples discussed in the next section.) Each of our teams has created workflows embedding these strategies throughout new care pathways. 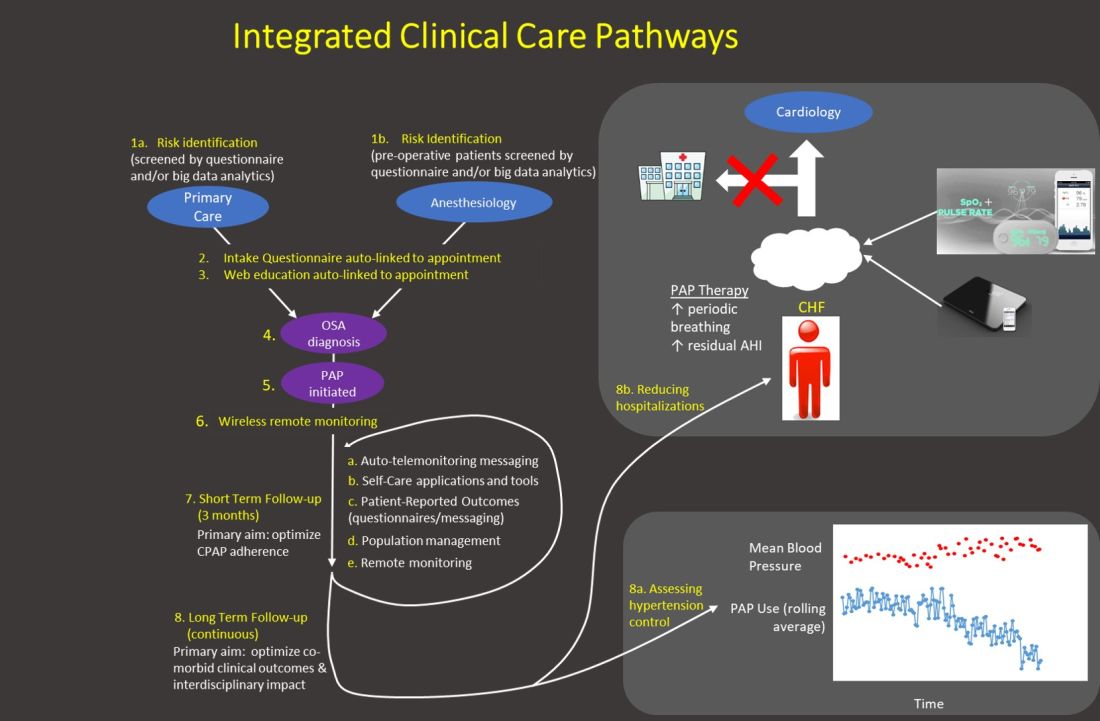
Generally, our emphasis during the first 3 months after PAP initiation focuses on achieving therapy adherence, and the post-3-month period broadens the efforts to target clinical outcomes. Recent trials with low PAP usage that failed to confirm the benefit of PAP on cardiovascular outcomes (McEvoy DR, et al. N Engl J Med. 2016;375:919) strongly suggest greater investment in cost-effective long-term strategies is imperative to increase our field’s relevance.
Application of artificial intelligence
We describe current efforts to apply artificial intelligence (AI) into clinical care: (1) We are implementing machine learning (ML) PSG scoring, which can potentially improve both the consistency and efficiency of scoring, further enabling greater investment in follow-up care. The future of sleep study processing, however, will likely depend on computer vision to “view” details inaccessible to the human eye and produce novel metrics that better inform clinical phenotypes (eg, cardiovascular risk, response to alternative therapies, etc). For example, “brain age” has been derived from EEG tracings that could reflect the degree of impact of sleep disorders on neurocognitive function (Fernandez C, unpublished data); (2) Machine learning clinical decision tools are in development to predict PAP adherence and timing of discontinuation, predict timing of cardiovascular disease onset and hospitalization, personalizing adherence targets, automating triaging of patients to home or PSG testing, and innumerable other predictions at clinical decision inflection points. Prediction outputs may be presented as risk profiles embedded in each patient’s “chart,” as personalized alerts, and in gamification strategies. For example, machine learning personalized cardiovascular risk scores can be regularly updated based on degree of PAP use to incentivize adherence; (3) Artificial providers may provide consistent, personalized, and holistic supplementary care. Many people rely on AI-bots for social support and cognitive-behavioral therapy (CBT) for depression. A sleep wellness bot, currently in planning stages, is intended to be the primary interface for many of the strategies described above that enhance engagement with PAP and therapies for comorbid conditions, provide CBT and lifestyle accountability, and collect patient reported data. This artificial provider would be a constant companion providing interactive, personalized, and continuous management to complement traditional intermittent live-person care.
The current health-care environment embodies the principle to “never let a serious crisis go to waste.” COVID-19 has accelerated the progression into the future by fostering an opening to embrace novel application of technologies to support changes in paradigms. Furthermore, health-care infrastructures that typically progress deliberately changed seemingly in a single moment. The Center for Medicare Services issued broad authorization to reimburse for telemedicine in response to COVID-19. Continued evolution in infrastructures will dictate progress with innovation, and a greater transition to outcomes-based incentives may be necessary to accommodate many of the strategies described above that rely on nonsynchronous care. But, we may be experiencing the moment when health care starts to catch up with the world in its embrace of technology. Sleep and pulmonary medicine can be a leader by providing a successful template for other specialties in optimizing chronic disease management.
Dr. Hwang is Medical Director, Kaiser Permanente SBC Sleep Center, and co-chair, Sleep Medicine, Kaiser Permanente Southern California.
On March 18, 2020, the doors to our sleep center were physically closed. Two potential exposures to COVID-19 within a few hours, the palpable anxiety of our team, and a poor grasp of the virus and the growing pandemic moved us to make this decision. Up to that point, we could not help but feel we were playing “catch up” with our evolving set of safety measures to the escalating risk. Like so many other sleep centers around the country, a complete transition to virtual care was needed to ensure the safety of our patients and our team. It was perhaps that moment that we felt the emotional impact that our world had changed, altering both our personal lives and sleep medicine practice as we knew it. This event, while unfortunate, also provided a transformative opportunity to reimagine our identity, accelerating the efforts to bring the future of sleep medicine into the present.
Our team’s clinical evolution and innovation efforts have been guided by efforts to reconsider sleep medicine paradigms. Innovation progress was deliberate with incremental implementations that typically required repeat business cases with multiple approving parties and budgetary access. Those barriers largely dissolved once COVID-19 intensified, and a large portion of the strategies on our roadmap were put into production. In a matter of a couple weeks, our services completely transitioned to remote and virtual care, while most of the team of 55 persons were moved to “work-from-home.” A suite of technologies (automated questionnaires, automated and two-way text messaging templates, consumer wearable technologies, and population management dashboards) were put on the table (Somnoware, Inc.), and each of our longitudinal care teams (eg, adult obstructive sleep apnea, pediatrics, chronic respiratory failure, commercial driver, insomnia programs, etc) worked to embed them into new care pathways. This effort further consolidated technology as the backbone of our work and the enabler of remote virtual collaboration between sleep center personnel (respiratory case managers, medical assistants and nursing team, and physician and leadership personnel) to enhance our team-based approach. Moreover, we felt this point in time was ripe to swallow the proverbial “red pill” and approach patient care with shifted paradigms. We discuss three areas of active effort to leverage technology in this COVID-19 environment to accelerate a transition toward how we envision the future of sleep medicine.
Reimagined sleep diagnostics
Our virtual obstructive sleep apnea (OSA) diagnostic process includes utilizing a disposable home sleep apnea test (HSAT) device with wireless data transfer (WatchPAT ONE, Itamar Medical) while HSAT and PAP (positive airway pressure) setups are supported by information sheets, online videos (YouTube), automated interactive platforms (Emmi Solutions; Hwang D. Am J Respir Crit Care Med. 2018 Jan 1;197[1]:117), and synchronous provider video visits. Our more radical shift, however, is in approaching OSA diagnosis based principally on symptoms and secondarily supported by physiologic measurements and response to therapy. This “clinical diagnosis” approach reduces our reliance on traditional sleep testing and allows patient wearables to provide supportive physiologic data (eg, oximetry) to help determine OSA severity and phenotype. Its immediate impact is in limiting the need to send and retrieve potentially contaminated equipment. Broader clinical advantages include overcoming the imprecise nature of the apnea-hypopnea index (which often has dramatic night-to-night variability) through data collection over extended durations, improving disease assessment due to availability of complementary sleep/activity data in the person’s usual setting, and tracking changes after therapy initiation.
Our post-COVID-19 re-opening of polysomnography (PSG) services, after a temporary shutdown, introduces home PSG (Type II) for approximately half our patients without suspected complex breathing conditions while reserving attended PSG (Type I) for those who may require noninvasive ventilation. The immediate incentive is in reducing viral exposure by limiting patient traffic and risk of PAP trial aerosolization while also improving access to accommodate the backlog of patients requiring PSG. This approach furthers the paradigm shift to emphasizing care in the home setting. Testing in the patient’s usual environment and enabling multiple night/day testing may be clinically advantageous.
Shift in emphasis to care management
The emphasis of sleep medicine has traditionally focused on diagnostics through performing PSG and HSAT. Our field has invested tremendous effort in developing guidelines for processing sleep studies, but the scoring and interpretation of those studies is extremely labor intensive. Reimagining the diagnostic approach reduces the need to manually process studies—wearable data are produced automatically, HSAT can be auto-scored, and artificial intelligence platforms can score PSGs (Goldstein CA. J Clin Sleep Med. 2020 Apr 15;16[4]:609), which allows a shift in resources and emphasis to follow-up care. A comprehensive discussion of technology-based tools to enhance care management is beyond the purview of this editorial. However, an overview of our current efforts includes: (1) utilizing population management dashboards to automatically risk stratify different cohorts of patients (eg, adult OSA, pediatrics, commercial drivers, chronic respiratory failure, etc) to identify patients “at-risk” (eg, based on OSA severity, symptoms, co-morbidities, and PAP adherence); (2) applying enhanced patient-provider interchange tools that include automated and “intelligent” electronic questionnaires, automated personalized text messaging/emails, and two-way messaging to deliver care; (3) utilizing remote patient monitoring to enhance holistic, personalized management, such as with remote activity/sleep trackers, blood pressure monitors, glucometers, and weight scales. We are engaged with efforts to validate the impact of these data to provide more personalized feedback, directly impact clinical outcomes, facilitate interdisciplinary collaboration, and identify acutely ill patients. Furthermore, a holistic approach beyond a narrow focus on PAP may create a positive collateral effect on adherence by targeting engagement with broader areas of health; and (4) implementing machine learning tools to directly support providers and patients (examples discussed in the next section.) Each of our teams has created workflows embedding these strategies throughout new care pathways. 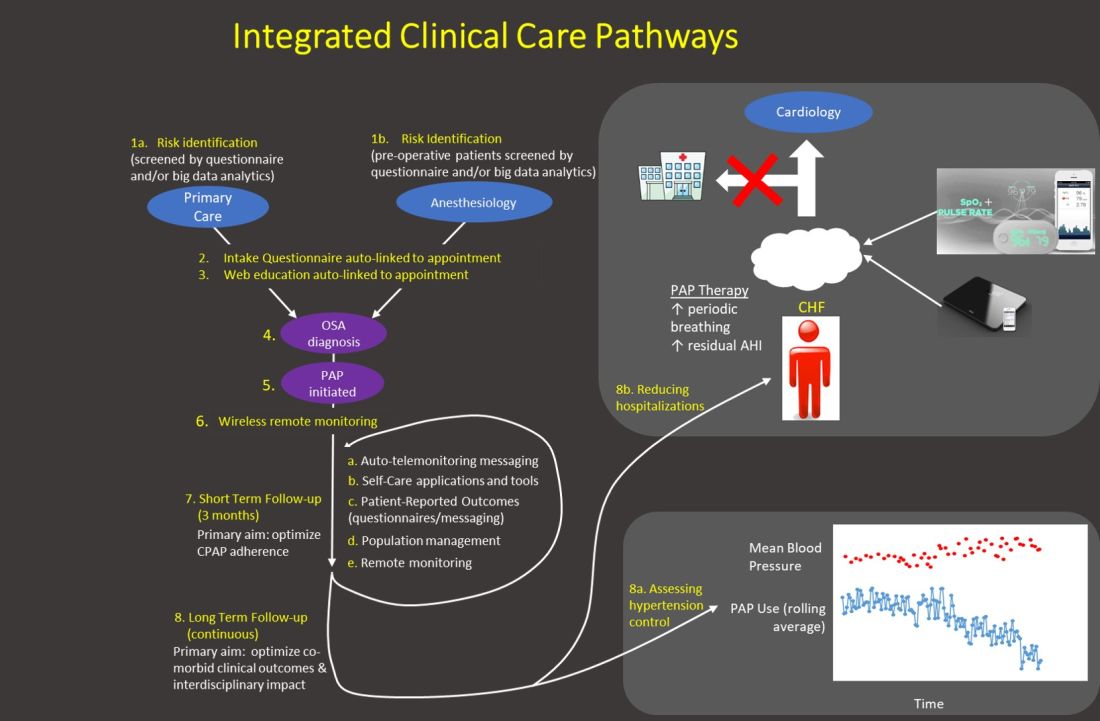
Generally, our emphasis during the first 3 months after PAP initiation focuses on achieving therapy adherence, and the post-3-month period broadens the efforts to target clinical outcomes. Recent trials with low PAP usage that failed to confirm the benefit of PAP on cardiovascular outcomes (McEvoy DR, et al. N Engl J Med. 2016;375:919) strongly suggest greater investment in cost-effective long-term strategies is imperative to increase our field’s relevance.
Application of artificial intelligence
We describe current efforts to apply artificial intelligence (AI) into clinical care: (1) We are implementing machine learning (ML) PSG scoring, which can potentially improve both the consistency and efficiency of scoring, further enabling greater investment in follow-up care. The future of sleep study processing, however, will likely depend on computer vision to “view” details inaccessible to the human eye and produce novel metrics that better inform clinical phenotypes (eg, cardiovascular risk, response to alternative therapies, etc). For example, “brain age” has been derived from EEG tracings that could reflect the degree of impact of sleep disorders on neurocognitive function (Fernandez C, unpublished data); (2) Machine learning clinical decision tools are in development to predict PAP adherence and timing of discontinuation, predict timing of cardiovascular disease onset and hospitalization, personalizing adherence targets, automating triaging of patients to home or PSG testing, and innumerable other predictions at clinical decision inflection points. Prediction outputs may be presented as risk profiles embedded in each patient’s “chart,” as personalized alerts, and in gamification strategies. For example, machine learning personalized cardiovascular risk scores can be regularly updated based on degree of PAP use to incentivize adherence; (3) Artificial providers may provide consistent, personalized, and holistic supplementary care. Many people rely on AI-bots for social support and cognitive-behavioral therapy (CBT) for depression. A sleep wellness bot, currently in planning stages, is intended to be the primary interface for many of the strategies described above that enhance engagement with PAP and therapies for comorbid conditions, provide CBT and lifestyle accountability, and collect patient reported data. This artificial provider would be a constant companion providing interactive, personalized, and continuous management to complement traditional intermittent live-person care.
The current health-care environment embodies the principle to “never let a serious crisis go to waste.” COVID-19 has accelerated the progression into the future by fostering an opening to embrace novel application of technologies to support changes in paradigms. Furthermore, health-care infrastructures that typically progress deliberately changed seemingly in a single moment. The Center for Medicare Services issued broad authorization to reimburse for telemedicine in response to COVID-19. Continued evolution in infrastructures will dictate progress with innovation, and a greater transition to outcomes-based incentives may be necessary to accommodate many of the strategies described above that rely on nonsynchronous care. But, we may be experiencing the moment when health care starts to catch up with the world in its embrace of technology. Sleep and pulmonary medicine can be a leader by providing a successful template for other specialties in optimizing chronic disease management.
Dr. Hwang is Medical Director, Kaiser Permanente SBC Sleep Center, and co-chair, Sleep Medicine, Kaiser Permanente Southern California.
On March 18, 2020, the doors to our sleep center were physically closed. Two potential exposures to COVID-19 within a few hours, the palpable anxiety of our team, and a poor grasp of the virus and the growing pandemic moved us to make this decision. Up to that point, we could not help but feel we were playing “catch up” with our evolving set of safety measures to the escalating risk. Like so many other sleep centers around the country, a complete transition to virtual care was needed to ensure the safety of our patients and our team. It was perhaps that moment that we felt the emotional impact that our world had changed, altering both our personal lives and sleep medicine practice as we knew it. This event, while unfortunate, also provided a transformative opportunity to reimagine our identity, accelerating the efforts to bring the future of sleep medicine into the present.
Our team’s clinical evolution and innovation efforts have been guided by efforts to reconsider sleep medicine paradigms. Innovation progress was deliberate with incremental implementations that typically required repeat business cases with multiple approving parties and budgetary access. Those barriers largely dissolved once COVID-19 intensified, and a large portion of the strategies on our roadmap were put into production. In a matter of a couple weeks, our services completely transitioned to remote and virtual care, while most of the team of 55 persons were moved to “work-from-home.” A suite of technologies (automated questionnaires, automated and two-way text messaging templates, consumer wearable technologies, and population management dashboards) were put on the table (Somnoware, Inc.), and each of our longitudinal care teams (eg, adult obstructive sleep apnea, pediatrics, chronic respiratory failure, commercial driver, insomnia programs, etc) worked to embed them into new care pathways. This effort further consolidated technology as the backbone of our work and the enabler of remote virtual collaboration between sleep center personnel (respiratory case managers, medical assistants and nursing team, and physician and leadership personnel) to enhance our team-based approach. Moreover, we felt this point in time was ripe to swallow the proverbial “red pill” and approach patient care with shifted paradigms. We discuss three areas of active effort to leverage technology in this COVID-19 environment to accelerate a transition toward how we envision the future of sleep medicine.
Reimagined sleep diagnostics
Our virtual obstructive sleep apnea (OSA) diagnostic process includes utilizing a disposable home sleep apnea test (HSAT) device with wireless data transfer (WatchPAT ONE, Itamar Medical) while HSAT and PAP (positive airway pressure) setups are supported by information sheets, online videos (YouTube), automated interactive platforms (Emmi Solutions; Hwang D. Am J Respir Crit Care Med. 2018 Jan 1;197[1]:117), and synchronous provider video visits. Our more radical shift, however, is in approaching OSA diagnosis based principally on symptoms and secondarily supported by physiologic measurements and response to therapy. This “clinical diagnosis” approach reduces our reliance on traditional sleep testing and allows patient wearables to provide supportive physiologic data (eg, oximetry) to help determine OSA severity and phenotype. Its immediate impact is in limiting the need to send and retrieve potentially contaminated equipment. Broader clinical advantages include overcoming the imprecise nature of the apnea-hypopnea index (which often has dramatic night-to-night variability) through data collection over extended durations, improving disease assessment due to availability of complementary sleep/activity data in the person’s usual setting, and tracking changes after therapy initiation.
Our post-COVID-19 re-opening of polysomnography (PSG) services, after a temporary shutdown, introduces home PSG (Type II) for approximately half our patients without suspected complex breathing conditions while reserving attended PSG (Type I) for those who may require noninvasive ventilation. The immediate incentive is in reducing viral exposure by limiting patient traffic and risk of PAP trial aerosolization while also improving access to accommodate the backlog of patients requiring PSG. This approach furthers the paradigm shift to emphasizing care in the home setting. Testing in the patient’s usual environment and enabling multiple night/day testing may be clinically advantageous.
Shift in emphasis to care management
The emphasis of sleep medicine has traditionally focused on diagnostics through performing PSG and HSAT. Our field has invested tremendous effort in developing guidelines for processing sleep studies, but the scoring and interpretation of those studies is extremely labor intensive. Reimagining the diagnostic approach reduces the need to manually process studies—wearable data are produced automatically, HSAT can be auto-scored, and artificial intelligence platforms can score PSGs (Goldstein CA. J Clin Sleep Med. 2020 Apr 15;16[4]:609), which allows a shift in resources and emphasis to follow-up care. A comprehensive discussion of technology-based tools to enhance care management is beyond the purview of this editorial. However, an overview of our current efforts includes: (1) utilizing population management dashboards to automatically risk stratify different cohorts of patients (eg, adult OSA, pediatrics, commercial drivers, chronic respiratory failure, etc) to identify patients “at-risk” (eg, based on OSA severity, symptoms, co-morbidities, and PAP adherence); (2) applying enhanced patient-provider interchange tools that include automated and “intelligent” electronic questionnaires, automated personalized text messaging/emails, and two-way messaging to deliver care; (3) utilizing remote patient monitoring to enhance holistic, personalized management, such as with remote activity/sleep trackers, blood pressure monitors, glucometers, and weight scales. We are engaged with efforts to validate the impact of these data to provide more personalized feedback, directly impact clinical outcomes, facilitate interdisciplinary collaboration, and identify acutely ill patients. Furthermore, a holistic approach beyond a narrow focus on PAP may create a positive collateral effect on adherence by targeting engagement with broader areas of health; and (4) implementing machine learning tools to directly support providers and patients (examples discussed in the next section.) Each of our teams has created workflows embedding these strategies throughout new care pathways. 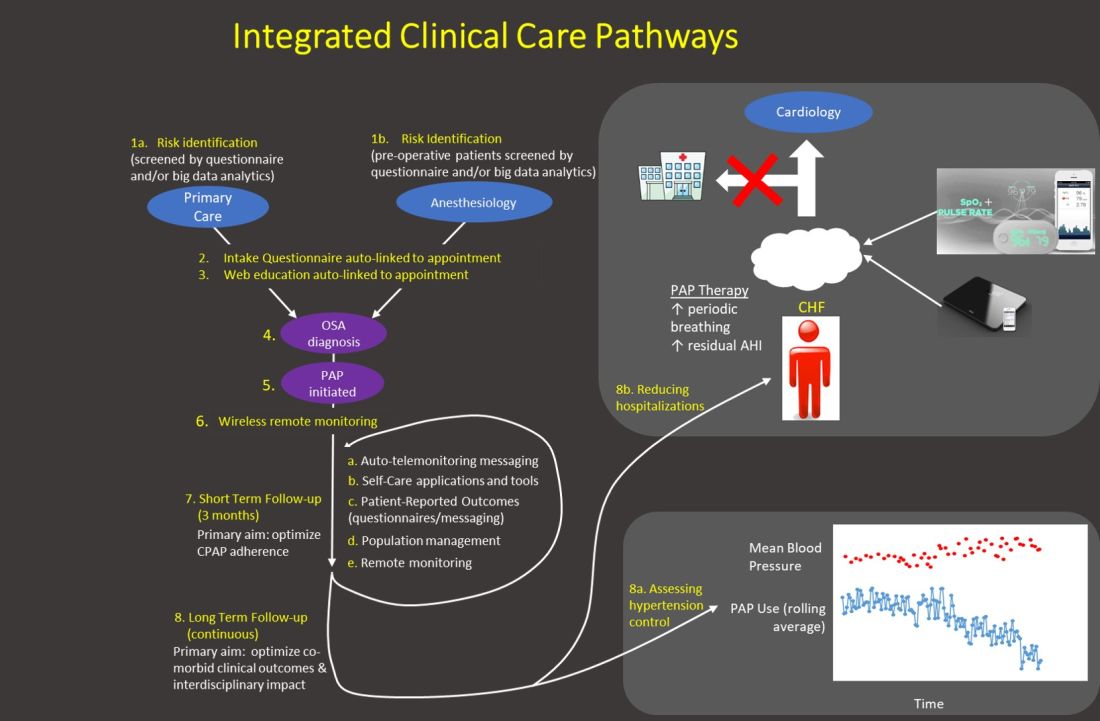
Generally, our emphasis during the first 3 months after PAP initiation focuses on achieving therapy adherence, and the post-3-month period broadens the efforts to target clinical outcomes. Recent trials with low PAP usage that failed to confirm the benefit of PAP on cardiovascular outcomes (McEvoy DR, et al. N Engl J Med. 2016;375:919) strongly suggest greater investment in cost-effective long-term strategies is imperative to increase our field’s relevance.
Application of artificial intelligence
We describe current efforts to apply artificial intelligence (AI) into clinical care: (1) We are implementing machine learning (ML) PSG scoring, which can potentially improve both the consistency and efficiency of scoring, further enabling greater investment in follow-up care. The future of sleep study processing, however, will likely depend on computer vision to “view” details inaccessible to the human eye and produce novel metrics that better inform clinical phenotypes (eg, cardiovascular risk, response to alternative therapies, etc). For example, “brain age” has been derived from EEG tracings that could reflect the degree of impact of sleep disorders on neurocognitive function (Fernandez C, unpublished data); (2) Machine learning clinical decision tools are in development to predict PAP adherence and timing of discontinuation, predict timing of cardiovascular disease onset and hospitalization, personalizing adherence targets, automating triaging of patients to home or PSG testing, and innumerable other predictions at clinical decision inflection points. Prediction outputs may be presented as risk profiles embedded in each patient’s “chart,” as personalized alerts, and in gamification strategies. For example, machine learning personalized cardiovascular risk scores can be regularly updated based on degree of PAP use to incentivize adherence; (3) Artificial providers may provide consistent, personalized, and holistic supplementary care. Many people rely on AI-bots for social support and cognitive-behavioral therapy (CBT) for depression. A sleep wellness bot, currently in planning stages, is intended to be the primary interface for many of the strategies described above that enhance engagement with PAP and therapies for comorbid conditions, provide CBT and lifestyle accountability, and collect patient reported data. This artificial provider would be a constant companion providing interactive, personalized, and continuous management to complement traditional intermittent live-person care.
The current health-care environment embodies the principle to “never let a serious crisis go to waste.” COVID-19 has accelerated the progression into the future by fostering an opening to embrace novel application of technologies to support changes in paradigms. Furthermore, health-care infrastructures that typically progress deliberately changed seemingly in a single moment. The Center for Medicare Services issued broad authorization to reimburse for telemedicine in response to COVID-19. Continued evolution in infrastructures will dictate progress with innovation, and a greater transition to outcomes-based incentives may be necessary to accommodate many of the strategies described above that rely on nonsynchronous care. But, we may be experiencing the moment when health care starts to catch up with the world in its embrace of technology. Sleep and pulmonary medicine can be a leader by providing a successful template for other specialties in optimizing chronic disease management.
Dr. Hwang is Medical Director, Kaiser Permanente SBC Sleep Center, and co-chair, Sleep Medicine, Kaiser Permanente Southern California.
This month in the journal CHEST®: Editor’s picks
Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China.By Dr. L. Shiyue, et al.
Effect of intermittent or continuous feed on muscle wasting in critical illness a phase II clinical trial. By Dr. A. McNelly, et al.
Triage of scarce critical care resources in COVID-19: An implementation guide for regional allocation: A CHEST and Task Force for Mass Critical Care Expert Panel Report.By Dr. J. Dichter, et al.
Managing Chronic Cough as a Symptom in Children and Management Algorithms: CHEST Guideline and Expert Panel Report. By Dr. A. Chang, et al.
Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China.By Dr. L. Shiyue, et al.
Effect of intermittent or continuous feed on muscle wasting in critical illness a phase II clinical trial. By Dr. A. McNelly, et al.
Triage of scarce critical care resources in COVID-19: An implementation guide for regional allocation: A CHEST and Task Force for Mass Critical Care Expert Panel Report.By Dr. J. Dichter, et al.
Managing Chronic Cough as a Symptom in Children and Management Algorithms: CHEST Guideline and Expert Panel Report. By Dr. A. Chang, et al.
Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China.By Dr. L. Shiyue, et al.
Effect of intermittent or continuous feed on muscle wasting in critical illness a phase II clinical trial. By Dr. A. McNelly, et al.
Triage of scarce critical care resources in COVID-19: An implementation guide for regional allocation: A CHEST and Task Force for Mass Critical Care Expert Panel Report.By Dr. J. Dichter, et al.
Managing Chronic Cough as a Symptom in Children and Management Algorithms: CHEST Guideline and Expert Panel Report. By Dr. A. Chang, et al.
Reflections on a virtual happy hour
On a Wednesday night in April, CHEST Women and Pulmonary Advisory Board hosted a virtual happy hour that was not just a webinar but also on Facebook Live, entitled Wellness Wednesday. During the 2-hour event, the hosts of the happy hour exchanged experiences during the pandemic, thoughts, hopes, and some very practical ideas on how to stay well in the midst of the pandemic. I was thrilled to co-host this event with Drs. Aneesa Das, Doreen Addrizzo-Harris, Margaret Pisani, Michele Cao, and Rachel Quaney.
We started off toasting with whatever drink people chose to have and each member shared what she was doing during the pandemic. There were many amazing stories of how these women adapted to the changing environment. Dr. Addrizzo-Harris told us how she and her husband literally split their apartment in half since they work in different hospitals and did not want to risk infecting not just one another but also their respective patients. Both she and her husband were working long shifts and most days of the week in the hospital and had not really seen each other since the lockdown started in New York. She also gave us an update on the pandemic and response in New York and reiterated her appreciation for health-care providers who came from elsewhere to help. Drs. Das and Quaney made a point to say that Ohio had done a great job planning for and preventing an onslaught of infected patients and that they were quite thankful to be able to do virtual visits and keep up with their patients.
With regards to work, a few panelists described not only the change in the hospital census and environment but also the impact on education for everyone. We shared ideas for keeping up with pulmonary and critical care that were not related to COVID-19 and ways to not feel overwhelmed by it. I mentioned that we kept our weekly clinical case conference for non-COVID cases and that our fellows and faculty found it refreshing and reinvigorating. Dr. Quaney, who is still in training, mentioned the impact the pandemic had on her education but was also thankful for all that was being done to mitigate that.
While several of us were going into the hospitals and working with COVID-19 patients, others were working from home. It may seem like that would be low stress but think about the challenges of doing virtual visits from home while young children are running around! Dr. Cao gave us a few stories about this and made us all laugh.
So much has changed in our lives and what we must do to care for ourselves, our families, and our patients. On this topic, many of the panelists mentioned that self-care is imperative, as well as all the other things we do. Many shared what they do to remain calm and to relieve stress, such as yoga, hiking, calls with friends and family, etc. Dr. Pisani in particular mentioned the importance of self-care while also lamenting that we have gone backwards with regard to delirium prevention in the ICU due to the isolation needed for COVID 19 patients.
The laughter and camaraderie amongst the panelist extended to the online participants. We had over 2,400 viewers either on Facebook live or via the webinar link! Many people who joined us asked questions or shared stories of how they were coping and what they miss about the pre-pandemic life. Most agreed that the lack of interpersonal interaction, especially with friends and family, has been difficult and that something as simple as this virtual happy hour was a welcome addition to all the other online meetings and patient visits. After the event, many online participants reached out personally and via social media to express how much they enjoyed it and hopes that we continue something like this going forward. I believe we all agreed at least a quarterly Wednesday Wellness event would be great, so I hope you will join us next time!
On a Wednesday night in April, CHEST Women and Pulmonary Advisory Board hosted a virtual happy hour that was not just a webinar but also on Facebook Live, entitled Wellness Wednesday. During the 2-hour event, the hosts of the happy hour exchanged experiences during the pandemic, thoughts, hopes, and some very practical ideas on how to stay well in the midst of the pandemic. I was thrilled to co-host this event with Drs. Aneesa Das, Doreen Addrizzo-Harris, Margaret Pisani, Michele Cao, and Rachel Quaney.
We started off toasting with whatever drink people chose to have and each member shared what she was doing during the pandemic. There were many amazing stories of how these women adapted to the changing environment. Dr. Addrizzo-Harris told us how she and her husband literally split their apartment in half since they work in different hospitals and did not want to risk infecting not just one another but also their respective patients. Both she and her husband were working long shifts and most days of the week in the hospital and had not really seen each other since the lockdown started in New York. She also gave us an update on the pandemic and response in New York and reiterated her appreciation for health-care providers who came from elsewhere to help. Drs. Das and Quaney made a point to say that Ohio had done a great job planning for and preventing an onslaught of infected patients and that they were quite thankful to be able to do virtual visits and keep up with their patients.
With regards to work, a few panelists described not only the change in the hospital census and environment but also the impact on education for everyone. We shared ideas for keeping up with pulmonary and critical care that were not related to COVID-19 and ways to not feel overwhelmed by it. I mentioned that we kept our weekly clinical case conference for non-COVID cases and that our fellows and faculty found it refreshing and reinvigorating. Dr. Quaney, who is still in training, mentioned the impact the pandemic had on her education but was also thankful for all that was being done to mitigate that.
While several of us were going into the hospitals and working with COVID-19 patients, others were working from home. It may seem like that would be low stress but think about the challenges of doing virtual visits from home while young children are running around! Dr. Cao gave us a few stories about this and made us all laugh.
So much has changed in our lives and what we must do to care for ourselves, our families, and our patients. On this topic, many of the panelists mentioned that self-care is imperative, as well as all the other things we do. Many shared what they do to remain calm and to relieve stress, such as yoga, hiking, calls with friends and family, etc. Dr. Pisani in particular mentioned the importance of self-care while also lamenting that we have gone backwards with regard to delirium prevention in the ICU due to the isolation needed for COVID 19 patients.
The laughter and camaraderie amongst the panelist extended to the online participants. We had over 2,400 viewers either on Facebook live or via the webinar link! Many people who joined us asked questions or shared stories of how they were coping and what they miss about the pre-pandemic life. Most agreed that the lack of interpersonal interaction, especially with friends and family, has been difficult and that something as simple as this virtual happy hour was a welcome addition to all the other online meetings and patient visits. After the event, many online participants reached out personally and via social media to express how much they enjoyed it and hopes that we continue something like this going forward. I believe we all agreed at least a quarterly Wednesday Wellness event would be great, so I hope you will join us next time!
On a Wednesday night in April, CHEST Women and Pulmonary Advisory Board hosted a virtual happy hour that was not just a webinar but also on Facebook Live, entitled Wellness Wednesday. During the 2-hour event, the hosts of the happy hour exchanged experiences during the pandemic, thoughts, hopes, and some very practical ideas on how to stay well in the midst of the pandemic. I was thrilled to co-host this event with Drs. Aneesa Das, Doreen Addrizzo-Harris, Margaret Pisani, Michele Cao, and Rachel Quaney.
We started off toasting with whatever drink people chose to have and each member shared what she was doing during the pandemic. There were many amazing stories of how these women adapted to the changing environment. Dr. Addrizzo-Harris told us how she and her husband literally split their apartment in half since they work in different hospitals and did not want to risk infecting not just one another but also their respective patients. Both she and her husband were working long shifts and most days of the week in the hospital and had not really seen each other since the lockdown started in New York. She also gave us an update on the pandemic and response in New York and reiterated her appreciation for health-care providers who came from elsewhere to help. Drs. Das and Quaney made a point to say that Ohio had done a great job planning for and preventing an onslaught of infected patients and that they were quite thankful to be able to do virtual visits and keep up with their patients.
With regards to work, a few panelists described not only the change in the hospital census and environment but also the impact on education for everyone. We shared ideas for keeping up with pulmonary and critical care that were not related to COVID-19 and ways to not feel overwhelmed by it. I mentioned that we kept our weekly clinical case conference for non-COVID cases and that our fellows and faculty found it refreshing and reinvigorating. Dr. Quaney, who is still in training, mentioned the impact the pandemic had on her education but was also thankful for all that was being done to mitigate that.
While several of us were going into the hospitals and working with COVID-19 patients, others were working from home. It may seem like that would be low stress but think about the challenges of doing virtual visits from home while young children are running around! Dr. Cao gave us a few stories about this and made us all laugh.
So much has changed in our lives and what we must do to care for ourselves, our families, and our patients. On this topic, many of the panelists mentioned that self-care is imperative, as well as all the other things we do. Many shared what they do to remain calm and to relieve stress, such as yoga, hiking, calls with friends and family, etc. Dr. Pisani in particular mentioned the importance of self-care while also lamenting that we have gone backwards with regard to delirium prevention in the ICU due to the isolation needed for COVID 19 patients.
The laughter and camaraderie amongst the panelist extended to the online participants. We had over 2,400 viewers either on Facebook live or via the webinar link! Many people who joined us asked questions or shared stories of how they were coping and what they miss about the pre-pandemic life. Most agreed that the lack of interpersonal interaction, especially with friends and family, has been difficult and that something as simple as this virtual happy hour was a welcome addition to all the other online meetings and patient visits. After the event, many online participants reached out personally and via social media to express how much they enjoyed it and hopes that we continue something like this going forward. I believe we all agreed at least a quarterly Wednesday Wellness event would be great, so I hope you will join us next time!
COVID-19 and asthma. Remdesivir for COVID-19. Burnout in unprecedented times. Advances in molecular imaging in pulmonary fibrosis.
Airways
COVID-19 and asthma: Much remains unknown
Viral-induced asthma exacerbations are common, but there has yet to be a published data set showing worse outcomes among asthmatics with COVID-19.
It is possible that inhaled corticosteroids (ICS) may provide some protection from viral infection. A 2014 study showed that ICS may reduce exacerbations by modulating inflammation and reducing airway viral receptors (Yamaya, et al. Respir Investig. 2014;52[4]:251). Analysis from the SARP-3 database showed ICS use associated with reduced expression of both ACE2 and transmembrane protease serine 2 (TMPRSS2), two receptors used by SARS-CoV-2 (Peters, et al. Am J Respir Crit Care Med. 2020. Online ahead of print). Another study showed a similar effect of ICS on the seasonal coronavirus strain HCoV-229E (Yamaya M, et al. Respir Investig. 2020;58[3]:155), and one study reported decreased ACE2 expression in allergic asthma (Jackson, et al. J Allergy Clin Immunol. Article in press, 2020). While these findings could support a hypothesis of reduced risk for COVID-19 infection among asthmatics using ICS, one would generally expect those with underlying lung disease, such as asthma, to be at higher risk for more severe infection.
Despite physiologic hypotheses of protective mechanisms, clinical outcomes may suffer as clinical operations and the American economy are impacted by this pandemic. Reduced access to or utilization of outpatient care, loss of employment, loss of health insurance, or a new difficulty in affording or accessing medications may all result in worsening asthma control for patients. Poorly controlled asthmatics are at higher risk for a more severe exacerbation of disease triggered by viral infection. Current recommendations are for patients to continue all controller medications; the use of systemic corticosteroids in treatment of COVID pneumonia is controversial, but their use in treating a COVID-associated asthma exacerbation should be based on individual assessment. As we care for asthma patients through this pandemic, much remains unknown but may be elucidated by further study.
Megan Conroy, MD
Fellow-in-Training Member
Steering Committee Member
Clinical Research and Quality Improvement
Remdesivir for COVID-19: A ray of hope?
The year 2020 witnessed a pandemic of unprecedented proportions, caused by a novel corona virus strain (SARS-CoV2). Across the globe, there have been more than 6.5 million positive cases of COVID-19 and more than 380,000 deaths. (WHO COVID-19 Dashboard [https://covid19.who.int]). Multiple therapeutic agents are currently being studied as potential treatment options for this novel disease. With negative trials so far on lopinavir-ritonavir and hydroxychloroquine, the only candidate drug showing benefit is remdesivir.
Results of the randomized double-blind placebo controlled Adaptive COVID-19 Treatment Trial (ACTT-1) trial (Beigel, J et al. N Engl J Med. 2020; e-pub ahead of print) shows remdesivir improved recovery time in COVID -19 patients as compared with control subjects. Remdesivir is an inhibitor of viral RNA polymerase that has been shown to inhibit coronaviruses in animal models and SARS-CoV2 in-vitro. The ACTT-1 trial enrolled 1,063 patients with 541 assigned to the remdesivir arm and 522 to the placebo group. Primary outcome measure was time to recovery. Mortality at 14 and 28 days and incidence of adverse events were also evaluated.
As interim analysis showed positive results, the data safety and monitoring board recommended early termination of the trial. Patients in the remdesivir group had a shorter time to recovery, with median recovery time of 11 days as compared with 15 days in placebo group (95% CI:1.12-1.55; P < .001). Hospitalized patients requiring supplemental oxygen (but not high-flow, mechanical ventilation or ECMO) derived the maximum benefit with a rate ratio of recovery being 1.47(95% CI:1.17-1.84). Thus, early drug administration may be beneficial. The difference in mortality at 14 days was not statistically significant and data on mortality difference at 28 days were not available at the time of publication.
In summary, this trial along with previous publications shows that remdesivir is a potential therapeutic option for COVID -19. The Food and Drug Administration (FDA) approved remdesivir under Emergency Use Authorization (EUA) for COVID-19 and larger trials are currently underway to study the full effect of this agent.
Aravind Menon, MD
Fellow-in-Training Member
Critical Care
Burnout in unprecedented times
Even in typical times, intensivists have a significantly higher rate of burnout compared with other medical specialties. We fight for lives, dealing with death, dying, and tragedy on a daily basis. Regrettably, we are no longer in ‘typical’ times. This is a prodigious and uncharted era.
The COVID-19 pandemic has created all new hardships. Added to the complex world of critical care, we undertake lack of appropriate medical equipment and PPE, the possibility of becoming ill or infecting our families, potential financial struggles, and the unpredictability of the future. Additionally, in our efforts to care for patients, we face increasing moral distress when placed in situations in which we cannot do what we feel is right. And we carry the burdens and guilt of patients’ families who cannot be with loved ones during this process, even during death.
What does burnout look like in this new era? Burnout is a continuum and can manifest differently depending on the individual. Even a typical day in the ICU may be cause for the symptoms of burnout including frustration, anger, anxiety, or sadness which can progress to feelings of powerlessness, self-doubt or depersonalization.
This crisis is a test of endurance. But we don’t have to face it alone. The ICU is a team environment, and we can help each other make it to the end. Consider beginning the shift with a group morale boosting activity. Perhaps debrief after the end of each shift to discuss ways of combatting these stressful times. Have a virtual happy hour with colleagues after work. Call on leadership for support. Watch each other’s back. Together we will get through these unprecedented times.
John P. Gaillard, MD
Steering Committee Member
Resources for confronting burnout:
http://ccsconline.org/optimizing-the-workforce/burnout
https://www.ama-assn.org/topics/physician-burnout
https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
Home-Based Mechanical Ventilation and Neuromuscular Disease
Use of modified RADs
Investigators have begun exploring ways to convert devices typically used to treat sleep-disordered breathing (respiratory assist device, RAD), with modifications to minimize risk of aerosolization of pathogen in the COVID-19 pandemic. These devices are presently not considered an effective means of treating acute respiratory distress syndrome (ARDS). In an emergency, however, it is reasonable to consider all the options available with a healthy respect for inherent device limitations.
A RAD could be converted from an open ventilation single-limb respiratory circuit to a closed ventilation circuit with a passive exhalation valve. This circuit could provide adequate minute ventilation and allow for adequate exhalation of CO2 to prevent rebreathing. Strategic placement of the passive exhalation valve proximal to a viricidal filter would allow the device to be used with either an endotracheal tube or a nonvented oronasal mask (Figure). These devices by design are pressure-regulated, and a backup rate would be necessary to control minute ventilation. Close monitoring would be necessary given lack of alarm capability for a critically ill patient and the need to ensure adequate oxygen bleed-in.
The primary limitation to these devices is the inability to achieve adequate mean airway pressure for ARDS. While such a converted device is not ready for prime time, it could be considered for patients who are close to weaning from conventional mechanical ventilation (i.e., freeing up a ventilator for a sicker patient) or temporizing a patient early in disease to stave off invasive ventilation.
MAJ Brian E. Foster, DO, USA
Fellow Member
Steering Committee Member
Interstitial and Diffuse Lung Disease NetWork
Advances in molecular imaging in pulmonary fibrosis
Fibrotic interstitial lung diseases (ILD), including idiopathic pulmonary fibrosis (IPF), have poor prognosis with marked heterogeneity in the clinical course. Treatment options, including antfibrotic drugs and immunosuppressants, are fairly limited for either conditions, and there is wide variability in drug responsiveness. Biomarkers that predict disease course and enable patient stratification to assess responsiveness to specific therapies play a crucial role in management of this fatal disease.
Molecular imaging has the ability to noninvasively provide both structural details, as well as functional/molecular information at the cellular level; it has thus developed into a powerful tool for several inflammatory and malignant disease processes. Probes that specifically target fibrosis-specific pathways utilizing positron emission tomography (PET) or magnetic resonance (MR) imaging have gained traction recently.
The most commonly used radiopharmaceutical for PET, 18F-FDG, is significantly increased in areas of established fibrosis in patients with IPF and autoimmune ILDs (Win, et al. Eur J Nucl Med Mol Imaging. 2018 May;45[5]:806; Uehara, et al. Mod Rheumatol. 2016;26[1]:121-7), as well as areas with seemingly normal morphologic appearance on HRCT scan (Win, et al. Eur J Nucl Med Mol Imaging. 2014 Feb;41[2]:337). While this probe was shown to have some potential for prognostication, there has been concern regarding the specificity of FDG uptake in fibrotic lung diseases. Hence, other probes that target specific fibrosis-related cellular mechanisms such as macrophages (Withana, et al. Nature Scientific Reports. 2016;6 [Jan 22):19755], and John, et al. J Nucl Med. 2013;54[12]:2146) and matrix proteins (Montesi, et al. Am J Respir Crit Care Med. 2019 Jul 15;200[2]:258) have been developed in preclinical fibrosis/lung injury models and are being translated to human subjects.
With the ability to capture early fibrogenesis and target engagement, molecular imaging has the potential to prognosticate patients, provide earlier evaluation of treatment responsiveness and have a promising application in clinical trial design for fibrotic lung diseases.
Tejaswini Kulkarni, MD
Steering Committee Member
Airways
COVID-19 and asthma: Much remains unknown
Viral-induced asthma exacerbations are common, but there has yet to be a published data set showing worse outcomes among asthmatics with COVID-19.
It is possible that inhaled corticosteroids (ICS) may provide some protection from viral infection. A 2014 study showed that ICS may reduce exacerbations by modulating inflammation and reducing airway viral receptors (Yamaya, et al. Respir Investig. 2014;52[4]:251). Analysis from the SARP-3 database showed ICS use associated with reduced expression of both ACE2 and transmembrane protease serine 2 (TMPRSS2), two receptors used by SARS-CoV-2 (Peters, et al. Am J Respir Crit Care Med. 2020. Online ahead of print). Another study showed a similar effect of ICS on the seasonal coronavirus strain HCoV-229E (Yamaya M, et al. Respir Investig. 2020;58[3]:155), and one study reported decreased ACE2 expression in allergic asthma (Jackson, et al. J Allergy Clin Immunol. Article in press, 2020). While these findings could support a hypothesis of reduced risk for COVID-19 infection among asthmatics using ICS, one would generally expect those with underlying lung disease, such as asthma, to be at higher risk for more severe infection.
Despite physiologic hypotheses of protective mechanisms, clinical outcomes may suffer as clinical operations and the American economy are impacted by this pandemic. Reduced access to or utilization of outpatient care, loss of employment, loss of health insurance, or a new difficulty in affording or accessing medications may all result in worsening asthma control for patients. Poorly controlled asthmatics are at higher risk for a more severe exacerbation of disease triggered by viral infection. Current recommendations are for patients to continue all controller medications; the use of systemic corticosteroids in treatment of COVID pneumonia is controversial, but their use in treating a COVID-associated asthma exacerbation should be based on individual assessment. As we care for asthma patients through this pandemic, much remains unknown but may be elucidated by further study.
Megan Conroy, MD
Fellow-in-Training Member
Steering Committee Member
Clinical Research and Quality Improvement
Remdesivir for COVID-19: A ray of hope?
The year 2020 witnessed a pandemic of unprecedented proportions, caused by a novel corona virus strain (SARS-CoV2). Across the globe, there have been more than 6.5 million positive cases of COVID-19 and more than 380,000 deaths. (WHO COVID-19 Dashboard [https://covid19.who.int]). Multiple therapeutic agents are currently being studied as potential treatment options for this novel disease. With negative trials so far on lopinavir-ritonavir and hydroxychloroquine, the only candidate drug showing benefit is remdesivir.
Results of the randomized double-blind placebo controlled Adaptive COVID-19 Treatment Trial (ACTT-1) trial (Beigel, J et al. N Engl J Med. 2020; e-pub ahead of print) shows remdesivir improved recovery time in COVID -19 patients as compared with control subjects. Remdesivir is an inhibitor of viral RNA polymerase that has been shown to inhibit coronaviruses in animal models and SARS-CoV2 in-vitro. The ACTT-1 trial enrolled 1,063 patients with 541 assigned to the remdesivir arm and 522 to the placebo group. Primary outcome measure was time to recovery. Mortality at 14 and 28 days and incidence of adverse events were also evaluated.
As interim analysis showed positive results, the data safety and monitoring board recommended early termination of the trial. Patients in the remdesivir group had a shorter time to recovery, with median recovery time of 11 days as compared with 15 days in placebo group (95% CI:1.12-1.55; P < .001). Hospitalized patients requiring supplemental oxygen (but not high-flow, mechanical ventilation or ECMO) derived the maximum benefit with a rate ratio of recovery being 1.47(95% CI:1.17-1.84). Thus, early drug administration may be beneficial. The difference in mortality at 14 days was not statistically significant and data on mortality difference at 28 days were not available at the time of publication.
In summary, this trial along with previous publications shows that remdesivir is a potential therapeutic option for COVID -19. The Food and Drug Administration (FDA) approved remdesivir under Emergency Use Authorization (EUA) for COVID-19 and larger trials are currently underway to study the full effect of this agent.
Aravind Menon, MD
Fellow-in-Training Member
Critical Care
Burnout in unprecedented times
Even in typical times, intensivists have a significantly higher rate of burnout compared with other medical specialties. We fight for lives, dealing with death, dying, and tragedy on a daily basis. Regrettably, we are no longer in ‘typical’ times. This is a prodigious and uncharted era.
The COVID-19 pandemic has created all new hardships. Added to the complex world of critical care, we undertake lack of appropriate medical equipment and PPE, the possibility of becoming ill or infecting our families, potential financial struggles, and the unpredictability of the future. Additionally, in our efforts to care for patients, we face increasing moral distress when placed in situations in which we cannot do what we feel is right. And we carry the burdens and guilt of patients’ families who cannot be with loved ones during this process, even during death.
What does burnout look like in this new era? Burnout is a continuum and can manifest differently depending on the individual. Even a typical day in the ICU may be cause for the symptoms of burnout including frustration, anger, anxiety, or sadness which can progress to feelings of powerlessness, self-doubt or depersonalization.
This crisis is a test of endurance. But we don’t have to face it alone. The ICU is a team environment, and we can help each other make it to the end. Consider beginning the shift with a group morale boosting activity. Perhaps debrief after the end of each shift to discuss ways of combatting these stressful times. Have a virtual happy hour with colleagues after work. Call on leadership for support. Watch each other’s back. Together we will get through these unprecedented times.
John P. Gaillard, MD
Steering Committee Member
Resources for confronting burnout:
http://ccsconline.org/optimizing-the-workforce/burnout
https://www.ama-assn.org/topics/physician-burnout
https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
Home-Based Mechanical Ventilation and Neuromuscular Disease
Use of modified RADs
Investigators have begun exploring ways to convert devices typically used to treat sleep-disordered breathing (respiratory assist device, RAD), with modifications to minimize risk of aerosolization of pathogen in the COVID-19 pandemic. These devices are presently not considered an effective means of treating acute respiratory distress syndrome (ARDS). In an emergency, however, it is reasonable to consider all the options available with a healthy respect for inherent device limitations.
A RAD could be converted from an open ventilation single-limb respiratory circuit to a closed ventilation circuit with a passive exhalation valve. This circuit could provide adequate minute ventilation and allow for adequate exhalation of CO2 to prevent rebreathing. Strategic placement of the passive exhalation valve proximal to a viricidal filter would allow the device to be used with either an endotracheal tube or a nonvented oronasal mask (Figure). These devices by design are pressure-regulated, and a backup rate would be necessary to control minute ventilation. Close monitoring would be necessary given lack of alarm capability for a critically ill patient and the need to ensure adequate oxygen bleed-in.
The primary limitation to these devices is the inability to achieve adequate mean airway pressure for ARDS. While such a converted device is not ready for prime time, it could be considered for patients who are close to weaning from conventional mechanical ventilation (i.e., freeing up a ventilator for a sicker patient) or temporizing a patient early in disease to stave off invasive ventilation.
MAJ Brian E. Foster, DO, USA
Fellow Member
Steering Committee Member
Interstitial and Diffuse Lung Disease NetWork
Advances in molecular imaging in pulmonary fibrosis
Fibrotic interstitial lung diseases (ILD), including idiopathic pulmonary fibrosis (IPF), have poor prognosis with marked heterogeneity in the clinical course. Treatment options, including antfibrotic drugs and immunosuppressants, are fairly limited for either conditions, and there is wide variability in drug responsiveness. Biomarkers that predict disease course and enable patient stratification to assess responsiveness to specific therapies play a crucial role in management of this fatal disease.
Molecular imaging has the ability to noninvasively provide both structural details, as well as functional/molecular information at the cellular level; it has thus developed into a powerful tool for several inflammatory and malignant disease processes. Probes that specifically target fibrosis-specific pathways utilizing positron emission tomography (PET) or magnetic resonance (MR) imaging have gained traction recently.
The most commonly used radiopharmaceutical for PET, 18F-FDG, is significantly increased in areas of established fibrosis in patients with IPF and autoimmune ILDs (Win, et al. Eur J Nucl Med Mol Imaging. 2018 May;45[5]:806; Uehara, et al. Mod Rheumatol. 2016;26[1]:121-7), as well as areas with seemingly normal morphologic appearance on HRCT scan (Win, et al. Eur J Nucl Med Mol Imaging. 2014 Feb;41[2]:337). While this probe was shown to have some potential for prognostication, there has been concern regarding the specificity of FDG uptake in fibrotic lung diseases. Hence, other probes that target specific fibrosis-related cellular mechanisms such as macrophages (Withana, et al. Nature Scientific Reports. 2016;6 [Jan 22):19755], and John, et al. J Nucl Med. 2013;54[12]:2146) and matrix proteins (Montesi, et al. Am J Respir Crit Care Med. 2019 Jul 15;200[2]:258) have been developed in preclinical fibrosis/lung injury models and are being translated to human subjects.
With the ability to capture early fibrogenesis and target engagement, molecular imaging has the potential to prognosticate patients, provide earlier evaluation of treatment responsiveness and have a promising application in clinical trial design for fibrotic lung diseases.
Tejaswini Kulkarni, MD
Steering Committee Member
Airways
COVID-19 and asthma: Much remains unknown
Viral-induced asthma exacerbations are common, but there has yet to be a published data set showing worse outcomes among asthmatics with COVID-19.
It is possible that inhaled corticosteroids (ICS) may provide some protection from viral infection. A 2014 study showed that ICS may reduce exacerbations by modulating inflammation and reducing airway viral receptors (Yamaya, et al. Respir Investig. 2014;52[4]:251). Analysis from the SARP-3 database showed ICS use associated with reduced expression of both ACE2 and transmembrane protease serine 2 (TMPRSS2), two receptors used by SARS-CoV-2 (Peters, et al. Am J Respir Crit Care Med. 2020. Online ahead of print). Another study showed a similar effect of ICS on the seasonal coronavirus strain HCoV-229E (Yamaya M, et al. Respir Investig. 2020;58[3]:155), and one study reported decreased ACE2 expression in allergic asthma (Jackson, et al. J Allergy Clin Immunol. Article in press, 2020). While these findings could support a hypothesis of reduced risk for COVID-19 infection among asthmatics using ICS, one would generally expect those with underlying lung disease, such as asthma, to be at higher risk for more severe infection.
Despite physiologic hypotheses of protective mechanisms, clinical outcomes may suffer as clinical operations and the American economy are impacted by this pandemic. Reduced access to or utilization of outpatient care, loss of employment, loss of health insurance, or a new difficulty in affording or accessing medications may all result in worsening asthma control for patients. Poorly controlled asthmatics are at higher risk for a more severe exacerbation of disease triggered by viral infection. Current recommendations are for patients to continue all controller medications; the use of systemic corticosteroids in treatment of COVID pneumonia is controversial, but their use in treating a COVID-associated asthma exacerbation should be based on individual assessment. As we care for asthma patients through this pandemic, much remains unknown but may be elucidated by further study.
Megan Conroy, MD
Fellow-in-Training Member
Steering Committee Member
Clinical Research and Quality Improvement
Remdesivir for COVID-19: A ray of hope?
The year 2020 witnessed a pandemic of unprecedented proportions, caused by a novel corona virus strain (SARS-CoV2). Across the globe, there have been more than 6.5 million positive cases of COVID-19 and more than 380,000 deaths. (WHO COVID-19 Dashboard [https://covid19.who.int]). Multiple therapeutic agents are currently being studied as potential treatment options for this novel disease. With negative trials so far on lopinavir-ritonavir and hydroxychloroquine, the only candidate drug showing benefit is remdesivir.
Results of the randomized double-blind placebo controlled Adaptive COVID-19 Treatment Trial (ACTT-1) trial (Beigel, J et al. N Engl J Med. 2020; e-pub ahead of print) shows remdesivir improved recovery time in COVID -19 patients as compared with control subjects. Remdesivir is an inhibitor of viral RNA polymerase that has been shown to inhibit coronaviruses in animal models and SARS-CoV2 in-vitro. The ACTT-1 trial enrolled 1,063 patients with 541 assigned to the remdesivir arm and 522 to the placebo group. Primary outcome measure was time to recovery. Mortality at 14 and 28 days and incidence of adverse events were also evaluated.
As interim analysis showed positive results, the data safety and monitoring board recommended early termination of the trial. Patients in the remdesivir group had a shorter time to recovery, with median recovery time of 11 days as compared with 15 days in placebo group (95% CI:1.12-1.55; P < .001). Hospitalized patients requiring supplemental oxygen (but not high-flow, mechanical ventilation or ECMO) derived the maximum benefit with a rate ratio of recovery being 1.47(95% CI:1.17-1.84). Thus, early drug administration may be beneficial. The difference in mortality at 14 days was not statistically significant and data on mortality difference at 28 days were not available at the time of publication.
In summary, this trial along with previous publications shows that remdesivir is a potential therapeutic option for COVID -19. The Food and Drug Administration (FDA) approved remdesivir under Emergency Use Authorization (EUA) for COVID-19 and larger trials are currently underway to study the full effect of this agent.
Aravind Menon, MD
Fellow-in-Training Member
Critical Care
Burnout in unprecedented times
Even in typical times, intensivists have a significantly higher rate of burnout compared with other medical specialties. We fight for lives, dealing with death, dying, and tragedy on a daily basis. Regrettably, we are no longer in ‘typical’ times. This is a prodigious and uncharted era.
The COVID-19 pandemic has created all new hardships. Added to the complex world of critical care, we undertake lack of appropriate medical equipment and PPE, the possibility of becoming ill or infecting our families, potential financial struggles, and the unpredictability of the future. Additionally, in our efforts to care for patients, we face increasing moral distress when placed in situations in which we cannot do what we feel is right. And we carry the burdens and guilt of patients’ families who cannot be with loved ones during this process, even during death.
What does burnout look like in this new era? Burnout is a continuum and can manifest differently depending on the individual. Even a typical day in the ICU may be cause for the symptoms of burnout including frustration, anger, anxiety, or sadness which can progress to feelings of powerlessness, self-doubt or depersonalization.
This crisis is a test of endurance. But we don’t have to face it alone. The ICU is a team environment, and we can help each other make it to the end. Consider beginning the shift with a group morale boosting activity. Perhaps debrief after the end of each shift to discuss ways of combatting these stressful times. Have a virtual happy hour with colleagues after work. Call on leadership for support. Watch each other’s back. Together we will get through these unprecedented times.
John P. Gaillard, MD
Steering Committee Member
Resources for confronting burnout:
http://ccsconline.org/optimizing-the-workforce/burnout
https://www.ama-assn.org/topics/physician-burnout
https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
Home-Based Mechanical Ventilation and Neuromuscular Disease
Use of modified RADs
Investigators have begun exploring ways to convert devices typically used to treat sleep-disordered breathing (respiratory assist device, RAD), with modifications to minimize risk of aerosolization of pathogen in the COVID-19 pandemic. These devices are presently not considered an effective means of treating acute respiratory distress syndrome (ARDS). In an emergency, however, it is reasonable to consider all the options available with a healthy respect for inherent device limitations.
A RAD could be converted from an open ventilation single-limb respiratory circuit to a closed ventilation circuit with a passive exhalation valve. This circuit could provide adequate minute ventilation and allow for adequate exhalation of CO2 to prevent rebreathing. Strategic placement of the passive exhalation valve proximal to a viricidal filter would allow the device to be used with either an endotracheal tube or a nonvented oronasal mask (Figure). These devices by design are pressure-regulated, and a backup rate would be necessary to control minute ventilation. Close monitoring would be necessary given lack of alarm capability for a critically ill patient and the need to ensure adequate oxygen bleed-in.
The primary limitation to these devices is the inability to achieve adequate mean airway pressure for ARDS. While such a converted device is not ready for prime time, it could be considered for patients who are close to weaning from conventional mechanical ventilation (i.e., freeing up a ventilator for a sicker patient) or temporizing a patient early in disease to stave off invasive ventilation.
MAJ Brian E. Foster, DO, USA
Fellow Member
Steering Committee Member
Interstitial and Diffuse Lung Disease NetWork
Advances in molecular imaging in pulmonary fibrosis
Fibrotic interstitial lung diseases (ILD), including idiopathic pulmonary fibrosis (IPF), have poor prognosis with marked heterogeneity in the clinical course. Treatment options, including antfibrotic drugs and immunosuppressants, are fairly limited for either conditions, and there is wide variability in drug responsiveness. Biomarkers that predict disease course and enable patient stratification to assess responsiveness to specific therapies play a crucial role in management of this fatal disease.
Molecular imaging has the ability to noninvasively provide both structural details, as well as functional/molecular information at the cellular level; it has thus developed into a powerful tool for several inflammatory and malignant disease processes. Probes that specifically target fibrosis-specific pathways utilizing positron emission tomography (PET) or magnetic resonance (MR) imaging have gained traction recently.
The most commonly used radiopharmaceutical for PET, 18F-FDG, is significantly increased in areas of established fibrosis in patients with IPF and autoimmune ILDs (Win, et al. Eur J Nucl Med Mol Imaging. 2018 May;45[5]:806; Uehara, et al. Mod Rheumatol. 2016;26[1]:121-7), as well as areas with seemingly normal morphologic appearance on HRCT scan (Win, et al. Eur J Nucl Med Mol Imaging. 2014 Feb;41[2]:337). While this probe was shown to have some potential for prognostication, there has been concern regarding the specificity of FDG uptake in fibrotic lung diseases. Hence, other probes that target specific fibrosis-related cellular mechanisms such as macrophages (Withana, et al. Nature Scientific Reports. 2016;6 [Jan 22):19755], and John, et al. J Nucl Med. 2013;54[12]:2146) and matrix proteins (Montesi, et al. Am J Respir Crit Care Med. 2019 Jul 15;200[2]:258) have been developed in preclinical fibrosis/lung injury models and are being translated to human subjects.
With the ability to capture early fibrogenesis and target engagement, molecular imaging has the potential to prognosticate patients, provide earlier evaluation of treatment responsiveness and have a promising application in clinical trial design for fibrotic lung diseases.
Tejaswini Kulkarni, MD
Steering Committee Member
CHEST Foundation
These last few months have been something that none of us has ever experienced. As many of you have witnessed firsthand, life is full of uncertainty and, as many of us try to get back to the “new normal,” we know that much of this uncertainty will persist. We are now not only dealing with a pandemic and caring for our patients but also addressing civil unrest and taking the time to grow and understand the importance of human life, no matter what race, ethnicity, or gender. In response, the CHEST Foundation has made efforts to further research in COVID-19 and increase our efforts in diversity and inclusion.
While we all race for solutions, we cannot overlook the immediate need in our local communities. The CHEST Foundation, along with partners across the nation, is taking a stand to deliver new resources and support now.
I proudly support the CHEST Foundation and am asking for your support, as well. Give a gift today, and together we can effect change for the better in our communities.
Warmest regards,
Doreen J. Addrizzo-Harris, MD, FCCP
Immediate Past President & Trustee
These last few months have been something that none of us has ever experienced. As many of you have witnessed firsthand, life is full of uncertainty and, as many of us try to get back to the “new normal,” we know that much of this uncertainty will persist. We are now not only dealing with a pandemic and caring for our patients but also addressing civil unrest and taking the time to grow and understand the importance of human life, no matter what race, ethnicity, or gender. In response, the CHEST Foundation has made efforts to further research in COVID-19 and increase our efforts in diversity and inclusion.
While we all race for solutions, we cannot overlook the immediate need in our local communities. The CHEST Foundation, along with partners across the nation, is taking a stand to deliver new resources and support now.
I proudly support the CHEST Foundation and am asking for your support, as well. Give a gift today, and together we can effect change for the better in our communities.
Warmest regards,
Doreen J. Addrizzo-Harris, MD, FCCP
Immediate Past President & Trustee
These last few months have been something that none of us has ever experienced. As many of you have witnessed firsthand, life is full of uncertainty and, as many of us try to get back to the “new normal,” we know that much of this uncertainty will persist. We are now not only dealing with a pandemic and caring for our patients but also addressing civil unrest and taking the time to grow and understand the importance of human life, no matter what race, ethnicity, or gender. In response, the CHEST Foundation has made efforts to further research in COVID-19 and increase our efforts in diversity and inclusion.
While we all race for solutions, we cannot overlook the immediate need in our local communities. The CHEST Foundation, along with partners across the nation, is taking a stand to deliver new resources and support now.
I proudly support the CHEST Foundation and am asking for your support, as well. Give a gift today, and together we can effect change for the better in our communities.
Warmest regards,
Doreen J. Addrizzo-Harris, MD, FCCP
Immediate Past President & Trustee
Primary prevention statins cut mortality even in the very elderly: VHA study
Patients in the Veterans Health Administration (VHA) system 75 years or older, free of cardiovascular (CV) disease and prescribed statins for the first time, had a one-fourth lower risk for death and a 20% lower risk for CV death over an average 7 years than that of comparable patients not prescribed the drugs in an observational study.
Ariela R. Orkaby, MD, MPH, lead author on the study, published in the July 7 issue of JAMA, said in an interview.
The very elderly are frequently undertreated, particularly in primary prevention, as many physicians consider it unnecessary for them to initiate or continue preventive measures, said Dr. Orkaby, of VA Boston Healthcare System and Harvard Medical School, Boston.
“From available data, we don’t really expect statins to start providing benefit in primary prevention until they’ve been taken for about 2 to 5 years. So for people who have very limited life expectancy, it may not be a great idea to add to their pill burden or increase the possibility that they might decline functionally,” Dr. Orkaby said.
“But what we saw in this study is that there is benefit to prescribing statins even in elderly patients, even within 2 years” of follow-up.
Despite being among the most studied drugs in the world, statins are understudied in older people. Fewer than 2% of the 186,854 participants in 28 statin trials were aged 75 years or older, wrote Dr. Orkaby and associates.
Most of what is known about initiating statin therapy in the 75-and-older age group comes from underpowered subgroup analyses and a few observational studies, Steven J. Nicholls, MBBS, PhD, Monash University, Melbourne, and Adam J. Nelson, MBBS, PhD, Duke Clinical Research Institute, Durham, N.C., wrote in an accompanying editorial. As a result, the evidence is conflicting, with some reports suggesting marked benefit and others possible harm.
The current findings, they wrote, “provide additional support for treatment guidelines that have increasingly advocated for more widespread use of statin therapy for ASCVD prevention in older individuals.”
Of the 326,981 people in the analysis, 57,178 (17.5%) were new statin users or initiated a statin during the study period, usually simvastatin. Their mean age was about 81 years, and 97.3% of the patients were men, 90% were white, and 72% were former smokers.
Using propensity scoring, the authors compared statin users with the other remaining patients who had the same likelihood of being prescribed a statin based on clinical characteristics but did not receive a prescription for a statin.
Michael W. Rich, MD, Washington University, St. Louis, who was not involved in the study but has previously worked with Dr. Orkaby, praised the analysis.
“It’s one of the best studies I’ve seen addressing this particular issue. It’s a large sample size, the analysis was very well done, and I think that it comes to a pretty unequivocal conclusion that, at least in this population, those individuals who were started on statins for the first time, and having no known prior ASCVD, clearly had a lower all-cause mortality and cardiovascular mortality, as well as a lower risk of composite cardiovascular events,” he said in an interview.
But the data have limitations, he added. The findings are still observational and could be confounded by unknown variables, and the select population – mostly white, male veterans – is known to be at somewhat higher risk for events than the general population.
Perhaps even more impressive than the risk reductions seen at a mean 6.8 years of follow-up, Dr. Rich said, are the sensitivity analyses at 2, 4, and 6 years that showed the benefit manifesting early.
The researchers saw a 32% reduction in all-cause mortality risk (P < .05) at 2 years, 21% at 4 years, and 13% at 6 years (P < .05 for all). Risk reductions for CV death followed a similar pattern, they wrote.
Dr. Rich said that the trial, although not a “slam dunk,” has persuaded him to shift from being very conservative about prescribing statins to elderly patients to being much more willing to consider it.
“This doesn’t mean that I will be running to routinely prescribe my 90-plus patients a statin, nor should we should be starting statins in everyone over 75, not even in all male former smokers over 75 – the type of people in this study – but I do think that it provides a stronger basis for talking to these patients about the possibility of starting a statin.”
There are two ongoing trials that may provide greater clarity, the authors observed. The STAREE trial has enrolled adults 70 years and older in Australia and includes serial evaluation of cognitive scores. Also, PREVENTABLE will examine the role of statins for prevention of dementia and disability-free survival in adults 75 years and older.
However, neither trial may fully resolve the question of primary prevention statin use in the elderly, they wrote. “While these trials are necessary to broaden the evidence base for older adults, it is unlikely that any trial will enroll large numbers of individuals at very advanced ages, black individuals, and those with dementia, as were included in this study.”
Dr. Orkaby had no disclosures; potential conflicts for the other authors are in the report. Dr. Rich reported having no conflicts of interest. Dr. Nicholls disclosed receiving research support from AstraZeneca, Amgen, Anthera, Eli Lilly, Novartis, Cerenis, The Medicines Company, Resverlogix, InfraReDx, Roche, Sanofi-Regeneron, and LipoScience; and receiving consulting fees or honoraria from AstraZeneca, Eli Lilly, Anthera, Omthera, Merck, Takeda, Resverlogix, Sanofi-Regeneron, CSL Behring, Esperion, and Boehringer Ingelheim. Dr. Nelson had no disclosures.
A version of this article originally appeared on Medscape.com.
Patients in the Veterans Health Administration (VHA) system 75 years or older, free of cardiovascular (CV) disease and prescribed statins for the first time, had a one-fourth lower risk for death and a 20% lower risk for CV death over an average 7 years than that of comparable patients not prescribed the drugs in an observational study.
Ariela R. Orkaby, MD, MPH, lead author on the study, published in the July 7 issue of JAMA, said in an interview.
The very elderly are frequently undertreated, particularly in primary prevention, as many physicians consider it unnecessary for them to initiate or continue preventive measures, said Dr. Orkaby, of VA Boston Healthcare System and Harvard Medical School, Boston.
“From available data, we don’t really expect statins to start providing benefit in primary prevention until they’ve been taken for about 2 to 5 years. So for people who have very limited life expectancy, it may not be a great idea to add to their pill burden or increase the possibility that they might decline functionally,” Dr. Orkaby said.
“But what we saw in this study is that there is benefit to prescribing statins even in elderly patients, even within 2 years” of follow-up.
Despite being among the most studied drugs in the world, statins are understudied in older people. Fewer than 2% of the 186,854 participants in 28 statin trials were aged 75 years or older, wrote Dr. Orkaby and associates.
Most of what is known about initiating statin therapy in the 75-and-older age group comes from underpowered subgroup analyses and a few observational studies, Steven J. Nicholls, MBBS, PhD, Monash University, Melbourne, and Adam J. Nelson, MBBS, PhD, Duke Clinical Research Institute, Durham, N.C., wrote in an accompanying editorial. As a result, the evidence is conflicting, with some reports suggesting marked benefit and others possible harm.
The current findings, they wrote, “provide additional support for treatment guidelines that have increasingly advocated for more widespread use of statin therapy for ASCVD prevention in older individuals.”
Of the 326,981 people in the analysis, 57,178 (17.5%) were new statin users or initiated a statin during the study period, usually simvastatin. Their mean age was about 81 years, and 97.3% of the patients were men, 90% were white, and 72% were former smokers.
Using propensity scoring, the authors compared statin users with the other remaining patients who had the same likelihood of being prescribed a statin based on clinical characteristics but did not receive a prescription for a statin.
Michael W. Rich, MD, Washington University, St. Louis, who was not involved in the study but has previously worked with Dr. Orkaby, praised the analysis.
“It’s one of the best studies I’ve seen addressing this particular issue. It’s a large sample size, the analysis was very well done, and I think that it comes to a pretty unequivocal conclusion that, at least in this population, those individuals who were started on statins for the first time, and having no known prior ASCVD, clearly had a lower all-cause mortality and cardiovascular mortality, as well as a lower risk of composite cardiovascular events,” he said in an interview.
But the data have limitations, he added. The findings are still observational and could be confounded by unknown variables, and the select population – mostly white, male veterans – is known to be at somewhat higher risk for events than the general population.
Perhaps even more impressive than the risk reductions seen at a mean 6.8 years of follow-up, Dr. Rich said, are the sensitivity analyses at 2, 4, and 6 years that showed the benefit manifesting early.
The researchers saw a 32% reduction in all-cause mortality risk (P < .05) at 2 years, 21% at 4 years, and 13% at 6 years (P < .05 for all). Risk reductions for CV death followed a similar pattern, they wrote.
Dr. Rich said that the trial, although not a “slam dunk,” has persuaded him to shift from being very conservative about prescribing statins to elderly patients to being much more willing to consider it.
“This doesn’t mean that I will be running to routinely prescribe my 90-plus patients a statin, nor should we should be starting statins in everyone over 75, not even in all male former smokers over 75 – the type of people in this study – but I do think that it provides a stronger basis for talking to these patients about the possibility of starting a statin.”
There are two ongoing trials that may provide greater clarity, the authors observed. The STAREE trial has enrolled adults 70 years and older in Australia and includes serial evaluation of cognitive scores. Also, PREVENTABLE will examine the role of statins for prevention of dementia and disability-free survival in adults 75 years and older.
However, neither trial may fully resolve the question of primary prevention statin use in the elderly, they wrote. “While these trials are necessary to broaden the evidence base for older adults, it is unlikely that any trial will enroll large numbers of individuals at very advanced ages, black individuals, and those with dementia, as were included in this study.”
Dr. Orkaby had no disclosures; potential conflicts for the other authors are in the report. Dr. Rich reported having no conflicts of interest. Dr. Nicholls disclosed receiving research support from AstraZeneca, Amgen, Anthera, Eli Lilly, Novartis, Cerenis, The Medicines Company, Resverlogix, InfraReDx, Roche, Sanofi-Regeneron, and LipoScience; and receiving consulting fees or honoraria from AstraZeneca, Eli Lilly, Anthera, Omthera, Merck, Takeda, Resverlogix, Sanofi-Regeneron, CSL Behring, Esperion, and Boehringer Ingelheim. Dr. Nelson had no disclosures.
A version of this article originally appeared on Medscape.com.
Patients in the Veterans Health Administration (VHA) system 75 years or older, free of cardiovascular (CV) disease and prescribed statins for the first time, had a one-fourth lower risk for death and a 20% lower risk for CV death over an average 7 years than that of comparable patients not prescribed the drugs in an observational study.
Ariela R. Orkaby, MD, MPH, lead author on the study, published in the July 7 issue of JAMA, said in an interview.
The very elderly are frequently undertreated, particularly in primary prevention, as many physicians consider it unnecessary for them to initiate or continue preventive measures, said Dr. Orkaby, of VA Boston Healthcare System and Harvard Medical School, Boston.
“From available data, we don’t really expect statins to start providing benefit in primary prevention until they’ve been taken for about 2 to 5 years. So for people who have very limited life expectancy, it may not be a great idea to add to their pill burden or increase the possibility that they might decline functionally,” Dr. Orkaby said.
“But what we saw in this study is that there is benefit to prescribing statins even in elderly patients, even within 2 years” of follow-up.
Despite being among the most studied drugs in the world, statins are understudied in older people. Fewer than 2% of the 186,854 participants in 28 statin trials were aged 75 years or older, wrote Dr. Orkaby and associates.
Most of what is known about initiating statin therapy in the 75-and-older age group comes from underpowered subgroup analyses and a few observational studies, Steven J. Nicholls, MBBS, PhD, Monash University, Melbourne, and Adam J. Nelson, MBBS, PhD, Duke Clinical Research Institute, Durham, N.C., wrote in an accompanying editorial. As a result, the evidence is conflicting, with some reports suggesting marked benefit and others possible harm.
The current findings, they wrote, “provide additional support for treatment guidelines that have increasingly advocated for more widespread use of statin therapy for ASCVD prevention in older individuals.”
Of the 326,981 people in the analysis, 57,178 (17.5%) were new statin users or initiated a statin during the study period, usually simvastatin. Their mean age was about 81 years, and 97.3% of the patients were men, 90% were white, and 72% were former smokers.
Using propensity scoring, the authors compared statin users with the other remaining patients who had the same likelihood of being prescribed a statin based on clinical characteristics but did not receive a prescription for a statin.
Michael W. Rich, MD, Washington University, St. Louis, who was not involved in the study but has previously worked with Dr. Orkaby, praised the analysis.
“It’s one of the best studies I’ve seen addressing this particular issue. It’s a large sample size, the analysis was very well done, and I think that it comes to a pretty unequivocal conclusion that, at least in this population, those individuals who were started on statins for the first time, and having no known prior ASCVD, clearly had a lower all-cause mortality and cardiovascular mortality, as well as a lower risk of composite cardiovascular events,” he said in an interview.
But the data have limitations, he added. The findings are still observational and could be confounded by unknown variables, and the select population – mostly white, male veterans – is known to be at somewhat higher risk for events than the general population.
Perhaps even more impressive than the risk reductions seen at a mean 6.8 years of follow-up, Dr. Rich said, are the sensitivity analyses at 2, 4, and 6 years that showed the benefit manifesting early.
The researchers saw a 32% reduction in all-cause mortality risk (P < .05) at 2 years, 21% at 4 years, and 13% at 6 years (P < .05 for all). Risk reductions for CV death followed a similar pattern, they wrote.
Dr. Rich said that the trial, although not a “slam dunk,” has persuaded him to shift from being very conservative about prescribing statins to elderly patients to being much more willing to consider it.
“This doesn’t mean that I will be running to routinely prescribe my 90-plus patients a statin, nor should we should be starting statins in everyone over 75, not even in all male former smokers over 75 – the type of people in this study – but I do think that it provides a stronger basis for talking to these patients about the possibility of starting a statin.”
There are two ongoing trials that may provide greater clarity, the authors observed. The STAREE trial has enrolled adults 70 years and older in Australia and includes serial evaluation of cognitive scores. Also, PREVENTABLE will examine the role of statins for prevention of dementia and disability-free survival in adults 75 years and older.
However, neither trial may fully resolve the question of primary prevention statin use in the elderly, they wrote. “While these trials are necessary to broaden the evidence base for older adults, it is unlikely that any trial will enroll large numbers of individuals at very advanced ages, black individuals, and those with dementia, as were included in this study.”
Dr. Orkaby had no disclosures; potential conflicts for the other authors are in the report. Dr. Rich reported having no conflicts of interest. Dr. Nicholls disclosed receiving research support from AstraZeneca, Amgen, Anthera, Eli Lilly, Novartis, Cerenis, The Medicines Company, Resverlogix, InfraReDx, Roche, Sanofi-Regeneron, and LipoScience; and receiving consulting fees or honoraria from AstraZeneca, Eli Lilly, Anthera, Omthera, Merck, Takeda, Resverlogix, Sanofi-Regeneron, CSL Behring, Esperion, and Boehringer Ingelheim. Dr. Nelson had no disclosures.
A version of this article originally appeared on Medscape.com.
USPSTF: Earlier lung cancer screening can double eligibility
The new proposals include lowering the age at which screening starts from 55 to 50 years, and to reduce the smoking history from 30 to 20 pack-years.
The draft recommendation from the United States Preventive Service Task Force (USPSTF) is available for public comment until August 3.
The task force recommends that adults age 50 to 80 who have a 20 pack-year or greater smoking history and currently smoke or have quit within the last 15 years undergo annual screening for lung cancer with low-dose CT,
“In my opinion, the proposed criteria by USPSTF represent a huge step in the right direction,” Lecia Sequist, MD, director of innovation at the Mass General Cancer Center in Boston, told Medscape Medical News.
“If these are adopted and implemented, we could see the benefit of screening (measured as reduction in lung cancer mortality) go from 9.8% with current parameters up to 13% with the broader parameters,” she said. “In addition, the new criteria should reduce racial disparities in screening eligibility.”
The recommendation also earned high marks from the American Lung Association.
The USPSTF has continued its ‘B’ recommendation – allowing for coverage of the screening with no cost for many under the Affordable Care Act – and is now proposing to expand the eligibility criteria “so that even more Americans at higher risk for lung cancer can be screened,” the ALA commented.
Start screening at 50
Lowering the minimum age of screening to 50 would likely mean that more Black individuals and women would be eligible for screening, the recommendation authors contend. The current screening age of 55 is currently recommended under guidelines issued by the American Association for Thoracic Surgery, American Cancer Society, American College of Chest Physicians, and National Comprehensive Cancer Network.
“African Americans have a higher risk of lung cancer, compared with whites, and this risk difference is more apparent at lower levels of smoking intensity,” they write.
As previously reported by Medscape Medical News, lung cancer screening in an urban, largely black cohort yielded roughly double the rates of positive screens and detected lung cancers compared with results from the National Lung Screening Trial, which enrolled mostly White individuals.
In addition, although lung cancer risk is greater for men than women who smoke, and women generally accumulate fewer pack-years than men, there is evidence to suggest that women who smoke may develop lung cancer earlier and with lower levels of exposure.
Therefore, “a strategy of screening persons ages 50 to 80 years who have at least a 20 pack-year smoking history and currently smoke or have quit within the past 15 years (A-50-80-20-15) would lead to a relative increase in the percentage of persons eligible for screening by 81% in men and by 96% in women,” the proposed recommendation states.
What’s the harm?
One of the major concerns about low-dose CT screening for lung cancer is the relatively high rate of false-positive results reported in two large scale clinical trials, the recommendation authors acknowledged.
For example, in the NLST, which was the basis for an earlier USPSTF recommendation (for annual screening of adults 55 to 80 years of age who have a 30 pack-year smoking history and currently smoke or have quit in the previous 15 years), the false-positive rates were 26.3% at baseline, 27.2% at year 1, and 15.9% at year 2.
Similarly, in the NELSON trial, results of which were published earlier this year, false-positive rates for men were 19.8% at baseline, 7.1% at year 1, 9% at year 3, and 3.9% at year 5.5 of screening, they noted.
“Yes, false-positive results are one of the things we need to think carefully about when embarking on lung screening,” Dr. Sequist told Medscape Medical News. “The potential harm of a false-positive (unnecessary scans, biopsies or even surgery) can be minimized by having a multidisciplinary team with experience working up lung nodules see patients who have a positive screening test. In fact, the American College of Radiology recommends that all lung screening programs be paired with such a team.”
Mass General has a pulmonary nodule clinic to evaluate screen-detected lung nodules, with the goal of minimizing unnecessary procedures, she noted.
Asked about the potential harm from radiation exposure, Sequist said that exposure from low-dose CT screening is fairly minimal, comparable to that from solar radiation at sea level over a 6-month period, or about the level from three cross-country airplane trips.
“While it is not zero radiation, there is very little concern that this low level of radiation would cause a cancer or damage one’s lungs,” she said.
Albert Rizzo, MD, chief medical officer of the ALA, said that the potential harms of unnecessary interventions are outweighed by the benefits of detecting lung cancer at an early stage.
“I think what has been learned over the last 5 years is that the original recommendations that were put out really allowed the overall rate of positivity well within what’s seen with mammography, for example, and the number of patients who have needlessly gone on to procedures remains very low, and the morbidity of those procedures remains low as well,” Dr. Rizzo told Medscape Medical News.
Not enough takers
Despite the clear benefits of low-dose CT screening, however, US screening rates for high-risk individuals are still very low, ranging from 12.3% in Massachusetts to a low of 0.5% in Nevada, according to a 2019 research report on the state of lung cancer from the ALA.
“For screening to be most effective, more of the high-risk population should be screened. Currently, screening rates are very low among those at high risk. This may be because of a lack of access or low awareness and knowledge among patients and providers. As rates vary tremendously between states, it is clear that more can be done to increase screening rates,” the report stated.
“I think that there are some mixed messages sent out into the population as to whether or not an individual patient should be screened,” Dr. Rizzo said.
He noted that some physicians may be reluctant to take on the nuanced risk–benefit discussion required, or may not have the time during a brief patient visit.
“It really boils down to that discussion between the physician and the patient who falls under these risk categories, to say, ‘Look, this is what these studies have found, and you fall under a category where if we find a cancer early, it’s very likely you’re going to be saved,’ as compared for waiting for it to present by itself,” he said.
Dr. Sequist and Dr. Rizzo have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The new proposals include lowering the age at which screening starts from 55 to 50 years, and to reduce the smoking history from 30 to 20 pack-years.
The draft recommendation from the United States Preventive Service Task Force (USPSTF) is available for public comment until August 3.
The task force recommends that adults age 50 to 80 who have a 20 pack-year or greater smoking history and currently smoke or have quit within the last 15 years undergo annual screening for lung cancer with low-dose CT,
“In my opinion, the proposed criteria by USPSTF represent a huge step in the right direction,” Lecia Sequist, MD, director of innovation at the Mass General Cancer Center in Boston, told Medscape Medical News.
“If these are adopted and implemented, we could see the benefit of screening (measured as reduction in lung cancer mortality) go from 9.8% with current parameters up to 13% with the broader parameters,” she said. “In addition, the new criteria should reduce racial disparities in screening eligibility.”
The recommendation also earned high marks from the American Lung Association.
The USPSTF has continued its ‘B’ recommendation – allowing for coverage of the screening with no cost for many under the Affordable Care Act – and is now proposing to expand the eligibility criteria “so that even more Americans at higher risk for lung cancer can be screened,” the ALA commented.
Start screening at 50
Lowering the minimum age of screening to 50 would likely mean that more Black individuals and women would be eligible for screening, the recommendation authors contend. The current screening age of 55 is currently recommended under guidelines issued by the American Association for Thoracic Surgery, American Cancer Society, American College of Chest Physicians, and National Comprehensive Cancer Network.
“African Americans have a higher risk of lung cancer, compared with whites, and this risk difference is more apparent at lower levels of smoking intensity,” they write.
As previously reported by Medscape Medical News, lung cancer screening in an urban, largely black cohort yielded roughly double the rates of positive screens and detected lung cancers compared with results from the National Lung Screening Trial, which enrolled mostly White individuals.
In addition, although lung cancer risk is greater for men than women who smoke, and women generally accumulate fewer pack-years than men, there is evidence to suggest that women who smoke may develop lung cancer earlier and with lower levels of exposure.
Therefore, “a strategy of screening persons ages 50 to 80 years who have at least a 20 pack-year smoking history and currently smoke or have quit within the past 15 years (A-50-80-20-15) would lead to a relative increase in the percentage of persons eligible for screening by 81% in men and by 96% in women,” the proposed recommendation states.
What’s the harm?
One of the major concerns about low-dose CT screening for lung cancer is the relatively high rate of false-positive results reported in two large scale clinical trials, the recommendation authors acknowledged.
For example, in the NLST, which was the basis for an earlier USPSTF recommendation (for annual screening of adults 55 to 80 years of age who have a 30 pack-year smoking history and currently smoke or have quit in the previous 15 years), the false-positive rates were 26.3% at baseline, 27.2% at year 1, and 15.9% at year 2.
Similarly, in the NELSON trial, results of which were published earlier this year, false-positive rates for men were 19.8% at baseline, 7.1% at year 1, 9% at year 3, and 3.9% at year 5.5 of screening, they noted.
“Yes, false-positive results are one of the things we need to think carefully about when embarking on lung screening,” Dr. Sequist told Medscape Medical News. “The potential harm of a false-positive (unnecessary scans, biopsies or even surgery) can be minimized by having a multidisciplinary team with experience working up lung nodules see patients who have a positive screening test. In fact, the American College of Radiology recommends that all lung screening programs be paired with such a team.”
Mass General has a pulmonary nodule clinic to evaluate screen-detected lung nodules, with the goal of minimizing unnecessary procedures, she noted.
Asked about the potential harm from radiation exposure, Sequist said that exposure from low-dose CT screening is fairly minimal, comparable to that from solar radiation at sea level over a 6-month period, or about the level from three cross-country airplane trips.
“While it is not zero radiation, there is very little concern that this low level of radiation would cause a cancer or damage one’s lungs,” she said.
Albert Rizzo, MD, chief medical officer of the ALA, said that the potential harms of unnecessary interventions are outweighed by the benefits of detecting lung cancer at an early stage.
“I think what has been learned over the last 5 years is that the original recommendations that were put out really allowed the overall rate of positivity well within what’s seen with mammography, for example, and the number of patients who have needlessly gone on to procedures remains very low, and the morbidity of those procedures remains low as well,” Dr. Rizzo told Medscape Medical News.
Not enough takers
Despite the clear benefits of low-dose CT screening, however, US screening rates for high-risk individuals are still very low, ranging from 12.3% in Massachusetts to a low of 0.5% in Nevada, according to a 2019 research report on the state of lung cancer from the ALA.
“For screening to be most effective, more of the high-risk population should be screened. Currently, screening rates are very low among those at high risk. This may be because of a lack of access or low awareness and knowledge among patients and providers. As rates vary tremendously between states, it is clear that more can be done to increase screening rates,” the report stated.
“I think that there are some mixed messages sent out into the population as to whether or not an individual patient should be screened,” Dr. Rizzo said.
He noted that some physicians may be reluctant to take on the nuanced risk–benefit discussion required, or may not have the time during a brief patient visit.
“It really boils down to that discussion between the physician and the patient who falls under these risk categories, to say, ‘Look, this is what these studies have found, and you fall under a category where if we find a cancer early, it’s very likely you’re going to be saved,’ as compared for waiting for it to present by itself,” he said.
Dr. Sequist and Dr. Rizzo have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The new proposals include lowering the age at which screening starts from 55 to 50 years, and to reduce the smoking history from 30 to 20 pack-years.
The draft recommendation from the United States Preventive Service Task Force (USPSTF) is available for public comment until August 3.
The task force recommends that adults age 50 to 80 who have a 20 pack-year or greater smoking history and currently smoke or have quit within the last 15 years undergo annual screening for lung cancer with low-dose CT,
“In my opinion, the proposed criteria by USPSTF represent a huge step in the right direction,” Lecia Sequist, MD, director of innovation at the Mass General Cancer Center in Boston, told Medscape Medical News.
“If these are adopted and implemented, we could see the benefit of screening (measured as reduction in lung cancer mortality) go from 9.8% with current parameters up to 13% with the broader parameters,” she said. “In addition, the new criteria should reduce racial disparities in screening eligibility.”
The recommendation also earned high marks from the American Lung Association.
The USPSTF has continued its ‘B’ recommendation – allowing for coverage of the screening with no cost for many under the Affordable Care Act – and is now proposing to expand the eligibility criteria “so that even more Americans at higher risk for lung cancer can be screened,” the ALA commented.
Start screening at 50
Lowering the minimum age of screening to 50 would likely mean that more Black individuals and women would be eligible for screening, the recommendation authors contend. The current screening age of 55 is currently recommended under guidelines issued by the American Association for Thoracic Surgery, American Cancer Society, American College of Chest Physicians, and National Comprehensive Cancer Network.
“African Americans have a higher risk of lung cancer, compared with whites, and this risk difference is more apparent at lower levels of smoking intensity,” they write.
As previously reported by Medscape Medical News, lung cancer screening in an urban, largely black cohort yielded roughly double the rates of positive screens and detected lung cancers compared with results from the National Lung Screening Trial, which enrolled mostly White individuals.
In addition, although lung cancer risk is greater for men than women who smoke, and women generally accumulate fewer pack-years than men, there is evidence to suggest that women who smoke may develop lung cancer earlier and with lower levels of exposure.
Therefore, “a strategy of screening persons ages 50 to 80 years who have at least a 20 pack-year smoking history and currently smoke or have quit within the past 15 years (A-50-80-20-15) would lead to a relative increase in the percentage of persons eligible for screening by 81% in men and by 96% in women,” the proposed recommendation states.
What’s the harm?
One of the major concerns about low-dose CT screening for lung cancer is the relatively high rate of false-positive results reported in two large scale clinical trials, the recommendation authors acknowledged.
For example, in the NLST, which was the basis for an earlier USPSTF recommendation (for annual screening of adults 55 to 80 years of age who have a 30 pack-year smoking history and currently smoke or have quit in the previous 15 years), the false-positive rates were 26.3% at baseline, 27.2% at year 1, and 15.9% at year 2.
Similarly, in the NELSON trial, results of which were published earlier this year, false-positive rates for men were 19.8% at baseline, 7.1% at year 1, 9% at year 3, and 3.9% at year 5.5 of screening, they noted.
“Yes, false-positive results are one of the things we need to think carefully about when embarking on lung screening,” Dr. Sequist told Medscape Medical News. “The potential harm of a false-positive (unnecessary scans, biopsies or even surgery) can be minimized by having a multidisciplinary team with experience working up lung nodules see patients who have a positive screening test. In fact, the American College of Radiology recommends that all lung screening programs be paired with such a team.”
Mass General has a pulmonary nodule clinic to evaluate screen-detected lung nodules, with the goal of minimizing unnecessary procedures, she noted.
Asked about the potential harm from radiation exposure, Sequist said that exposure from low-dose CT screening is fairly minimal, comparable to that from solar radiation at sea level over a 6-month period, or about the level from three cross-country airplane trips.
“While it is not zero radiation, there is very little concern that this low level of radiation would cause a cancer or damage one’s lungs,” she said.
Albert Rizzo, MD, chief medical officer of the ALA, said that the potential harms of unnecessary interventions are outweighed by the benefits of detecting lung cancer at an early stage.
“I think what has been learned over the last 5 years is that the original recommendations that were put out really allowed the overall rate of positivity well within what’s seen with mammography, for example, and the number of patients who have needlessly gone on to procedures remains very low, and the morbidity of those procedures remains low as well,” Dr. Rizzo told Medscape Medical News.
Not enough takers
Despite the clear benefits of low-dose CT screening, however, US screening rates for high-risk individuals are still very low, ranging from 12.3% in Massachusetts to a low of 0.5% in Nevada, according to a 2019 research report on the state of lung cancer from the ALA.
“For screening to be most effective, more of the high-risk population should be screened. Currently, screening rates are very low among those at high risk. This may be because of a lack of access or low awareness and knowledge among patients and providers. As rates vary tremendously between states, it is clear that more can be done to increase screening rates,” the report stated.
“I think that there are some mixed messages sent out into the population as to whether or not an individual patient should be screened,” Dr. Rizzo said.
He noted that some physicians may be reluctant to take on the nuanced risk–benefit discussion required, or may not have the time during a brief patient visit.
“It really boils down to that discussion between the physician and the patient who falls under these risk categories, to say, ‘Look, this is what these studies have found, and you fall under a category where if we find a cancer early, it’s very likely you’re going to be saved,’ as compared for waiting for it to present by itself,” he said.
Dr. Sequist and Dr. Rizzo have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.