User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Urine metabolites could predict end of life in lung cancer
Lung cancer patients could soon have their risk of dying over the following 3 months accurately predicted by analyzing their urine samples, allowing them to better prepare for their end of life, say U.K. researchers.
Dr. Seamus Coyle, consultant in palliative medicine, the Clatterbridge Cancer Centre, Liverpool, and colleagues studied urine samples from more than 100 lung cancer patients, deriving a model based on their metabolite profile.
This allowed patients to be divided into high- and low-risk groups for dying over the following 3 months, with an accuracy of 88%.
The model “predicts dying … for every single day for the last 3 months of life,” Dr. Coyle said.
“That’s an outstanding prediction,” Dr. Coyle added, “based on the fact that people actively die over 2 to 3 days on average,” while “some die over a day.”
He continued: “It’s the only test that predicts dying within the last 2 weeks of life, and that’s what I’m passionate about: The earlier recognition of dying.”
The research was presented at the 2021 American Society of Clinical Oncology Annual Meeting on June 4.
‘Promising and important pilot study’
Dr. Nathan Pennell, an ASCO expert, told this news organization that “predicting the actual ‘time’ someone has left is more of an art than a science.”
“For people who may be closer to death, this would potentially allow more focus on supportive care and allow families and patients to plan more accurately for supporting their loved one through the dying process.”
He continued that “while this is a promising and important pilot study, there is more work to be done before this could be used in practice.”
For example, the treatment status of the patients was not clear.
“Were these patients all in hospice, or were some undergoing treatment which, if effective, could ‘rescue’ them from their poor prognostic state?”
Dr. Pennell continued: “Would measuring kidney function be just as good? Is this something that could be intervened upon?
“For example, if someone has a high-risk score for dying, could medical intervention to treat an infection or some other modifiable action change that ‘fate’?”
Death ‘difficult to predict’
Dr. Coyle began by saying that, while for him recognizing that a patient is dying is the start of good end of life care, “recognizing dying accurately, when someone is in the last days of life, is difficult.”
He noted that the 2019 National Audit of Care at the End of Life found that people were recognized to be dying at median of 34 hours before death, with 20% recognized in the last 8 hours.
Moreover, 50% of people who are dying “are unconscious and unable to be involved in any conversation that [is] pertinent to them.”
In an attempt to better predict the onset of dying, the researchers conducted a prospective, longitudinal study in which 424 urine samples were collected from 162 lung cancer patients from six centers.
Of those, 63 patients gave a sample within the last 28 days of life, and 29 within the last week of life.
Urine samples were analyzed using a liquid chromatography quadrupole time-of-flight mass spectrometer for 112 patients, who had a median age of 71 years and a range of 47-89 years, and 40.2% were female. The most common diagnosis was non–small cell lung cancer, in 55.4%, while 19.6% had small cell lung cancer.
Performing Cox Lasso regression analysis on the “hundreds of metabolites” identified in the urine samples, the team developed an End of Life Metabolome (ELM) that predicted an individual’s risk of dying over the following 3 months.
Kaplan-Meier analysis allowed the patients to be divided into five risk groups based on their ELM (P < .001 for trend), which showed that all patients in the lowest-risk group were still alive after more than 2 months following the urine sample.
In contrast, more than 50% of patients in the highest-risk group died within 1 week of their urine sample being taken, and 100% had died within 3 weeks.
Calculating the area under the receiver operating characteristic curve revealed that the ELM was able to predict the risk of dying for every day for the last 3 months of life with an accuracy of 88%.
ELM is being validated in a new cohort of lung cancer patients and it is being assessed in multiple cancers.
The study was funded by the Wellcome Trust UK and North West Cancer Research UK.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
Lung cancer patients could soon have their risk of dying over the following 3 months accurately predicted by analyzing their urine samples, allowing them to better prepare for their end of life, say U.K. researchers.
Dr. Seamus Coyle, consultant in palliative medicine, the Clatterbridge Cancer Centre, Liverpool, and colleagues studied urine samples from more than 100 lung cancer patients, deriving a model based on their metabolite profile.
This allowed patients to be divided into high- and low-risk groups for dying over the following 3 months, with an accuracy of 88%.
The model “predicts dying … for every single day for the last 3 months of life,” Dr. Coyle said.
“That’s an outstanding prediction,” Dr. Coyle added, “based on the fact that people actively die over 2 to 3 days on average,” while “some die over a day.”
He continued: “It’s the only test that predicts dying within the last 2 weeks of life, and that’s what I’m passionate about: The earlier recognition of dying.”
The research was presented at the 2021 American Society of Clinical Oncology Annual Meeting on June 4.
‘Promising and important pilot study’
Dr. Nathan Pennell, an ASCO expert, told this news organization that “predicting the actual ‘time’ someone has left is more of an art than a science.”
“For people who may be closer to death, this would potentially allow more focus on supportive care and allow families and patients to plan more accurately for supporting their loved one through the dying process.”
He continued that “while this is a promising and important pilot study, there is more work to be done before this could be used in practice.”
For example, the treatment status of the patients was not clear.
“Were these patients all in hospice, or were some undergoing treatment which, if effective, could ‘rescue’ them from their poor prognostic state?”
Dr. Pennell continued: “Would measuring kidney function be just as good? Is this something that could be intervened upon?
“For example, if someone has a high-risk score for dying, could medical intervention to treat an infection or some other modifiable action change that ‘fate’?”
Death ‘difficult to predict’
Dr. Coyle began by saying that, while for him recognizing that a patient is dying is the start of good end of life care, “recognizing dying accurately, when someone is in the last days of life, is difficult.”
He noted that the 2019 National Audit of Care at the End of Life found that people were recognized to be dying at median of 34 hours before death, with 20% recognized in the last 8 hours.
Moreover, 50% of people who are dying “are unconscious and unable to be involved in any conversation that [is] pertinent to them.”
In an attempt to better predict the onset of dying, the researchers conducted a prospective, longitudinal study in which 424 urine samples were collected from 162 lung cancer patients from six centers.
Of those, 63 patients gave a sample within the last 28 days of life, and 29 within the last week of life.
Urine samples were analyzed using a liquid chromatography quadrupole time-of-flight mass spectrometer for 112 patients, who had a median age of 71 years and a range of 47-89 years, and 40.2% were female. The most common diagnosis was non–small cell lung cancer, in 55.4%, while 19.6% had small cell lung cancer.
Performing Cox Lasso regression analysis on the “hundreds of metabolites” identified in the urine samples, the team developed an End of Life Metabolome (ELM) that predicted an individual’s risk of dying over the following 3 months.
Kaplan-Meier analysis allowed the patients to be divided into five risk groups based on their ELM (P < .001 for trend), which showed that all patients in the lowest-risk group were still alive after more than 2 months following the urine sample.
In contrast, more than 50% of patients in the highest-risk group died within 1 week of their urine sample being taken, and 100% had died within 3 weeks.
Calculating the area under the receiver operating characteristic curve revealed that the ELM was able to predict the risk of dying for every day for the last 3 months of life with an accuracy of 88%.
ELM is being validated in a new cohort of lung cancer patients and it is being assessed in multiple cancers.
The study was funded by the Wellcome Trust UK and North West Cancer Research UK.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
Lung cancer patients could soon have their risk of dying over the following 3 months accurately predicted by analyzing their urine samples, allowing them to better prepare for their end of life, say U.K. researchers.
Dr. Seamus Coyle, consultant in palliative medicine, the Clatterbridge Cancer Centre, Liverpool, and colleagues studied urine samples from more than 100 lung cancer patients, deriving a model based on their metabolite profile.
This allowed patients to be divided into high- and low-risk groups for dying over the following 3 months, with an accuracy of 88%.
The model “predicts dying … for every single day for the last 3 months of life,” Dr. Coyle said.
“That’s an outstanding prediction,” Dr. Coyle added, “based on the fact that people actively die over 2 to 3 days on average,” while “some die over a day.”
He continued: “It’s the only test that predicts dying within the last 2 weeks of life, and that’s what I’m passionate about: The earlier recognition of dying.”
The research was presented at the 2021 American Society of Clinical Oncology Annual Meeting on June 4.
‘Promising and important pilot study’
Dr. Nathan Pennell, an ASCO expert, told this news organization that “predicting the actual ‘time’ someone has left is more of an art than a science.”
“For people who may be closer to death, this would potentially allow more focus on supportive care and allow families and patients to plan more accurately for supporting their loved one through the dying process.”
He continued that “while this is a promising and important pilot study, there is more work to be done before this could be used in practice.”
For example, the treatment status of the patients was not clear.
“Were these patients all in hospice, or were some undergoing treatment which, if effective, could ‘rescue’ them from their poor prognostic state?”
Dr. Pennell continued: “Would measuring kidney function be just as good? Is this something that could be intervened upon?
“For example, if someone has a high-risk score for dying, could medical intervention to treat an infection or some other modifiable action change that ‘fate’?”
Death ‘difficult to predict’
Dr. Coyle began by saying that, while for him recognizing that a patient is dying is the start of good end of life care, “recognizing dying accurately, when someone is in the last days of life, is difficult.”
He noted that the 2019 National Audit of Care at the End of Life found that people were recognized to be dying at median of 34 hours before death, with 20% recognized in the last 8 hours.
Moreover, 50% of people who are dying “are unconscious and unable to be involved in any conversation that [is] pertinent to them.”
In an attempt to better predict the onset of dying, the researchers conducted a prospective, longitudinal study in which 424 urine samples were collected from 162 lung cancer patients from six centers.
Of those, 63 patients gave a sample within the last 28 days of life, and 29 within the last week of life.
Urine samples were analyzed using a liquid chromatography quadrupole time-of-flight mass spectrometer for 112 patients, who had a median age of 71 years and a range of 47-89 years, and 40.2% were female. The most common diagnosis was non–small cell lung cancer, in 55.4%, while 19.6% had small cell lung cancer.
Performing Cox Lasso regression analysis on the “hundreds of metabolites” identified in the urine samples, the team developed an End of Life Metabolome (ELM) that predicted an individual’s risk of dying over the following 3 months.
Kaplan-Meier analysis allowed the patients to be divided into five risk groups based on their ELM (P < .001 for trend), which showed that all patients in the lowest-risk group were still alive after more than 2 months following the urine sample.
In contrast, more than 50% of patients in the highest-risk group died within 1 week of their urine sample being taken, and 100% had died within 3 weeks.
Calculating the area under the receiver operating characteristic curve revealed that the ELM was able to predict the risk of dying for every day for the last 3 months of life with an accuracy of 88%.
ELM is being validated in a new cohort of lung cancer patients and it is being assessed in multiple cancers.
The study was funded by the Wellcome Trust UK and North West Cancer Research UK.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
Looking to the future of physiologically informed sepsis resuscitation: The role of dynamic fluid-responsive measurement
Current guideline recommendations for fluid resuscitation in sepsis patients calls for an initial crystalloid fluid bolus of at least 30 mL/kg (Rhodes, et al. Intensive Care Med. 2017;43[3]:304-77) For fluid management beyond this initial bolus, recommendations had previously called for using early goal-directed therapy (EGDT) with central venous pressure (CVP) and central venous oxygen saturation to guide the use of IV fluids, vasopressors, transfusions, and dobutamine, based on the results of one single-center study that found an improvement in mortality using EGDT as compared with standard therapy.
The triad of sepsis studies
In the following years, multiple concerns were raised regarding the generalizability of this study. Three large multicenter trials were conducted in multiple countries to test the recommendations for EGDT.
PROMISE: ProMISe was a 1,260-patient randomized trial comparing the impact of EGDT vs usual care on 90-day all-cause mortality in patients with early septic shock at 56 hospitals in England. There was no significant difference in the primary study endpoint with 90-day mortality rates of 29.5% and 29.2% (RR: 1.01, 95% CI: 0.85-1.20, P =.90) (Mouncey, et al. N Engl J Med. 2015;372[14]:1301-11).
PROCESS: ProCESS was a 1,351-patient randomized trial comparing the impact of protocol-based EGDT, protocol-based standard of care, and usual care on 60 day in-hospital mortality in patients with early septic shock at 31 hospitals in the United States. There was no significant difference in the primary study endpoint with 60-day mortality rates of 21.0%, 18.2%, and 18.9% (P = .83) or in the secondary outcome of 90-day mortality with rates of 31.9%, 30.8%, and 33.7% (P = .66) (ProCESS Investigators, et al. N Engl J Med. 2014;370[18]:1683-93).
ARISE: ARISE was a 1,600-patient randomized trial comparing the impact of EGDT vs usual care on 90-day all-cause mortality in patients with early septic shock at 51 hospitals in New Zealand and Australia. There was no significant difference in the primary study end point with 90-day mortality rates of 18.6% and 18.8% (RR: 0.98, 95% CI: 0.80-1.21, P = .90). There were also no significant differences in 28-day or in-hospital mortality, duration of organ support, or length of hospital stay (ARISE Investigators, et al. N Engl J Med. 2014;371[16]:1496-506).
In summary, all three “triad” trials found no improvement with EGDT over usual care (Rowan, et al. N Engl J Med. 2017;376[23]:2223-34) calling into question the recommended methods of universally protocolized approaches to fluid and pressor resuscitation. Probable reasons for why structured EGDT was ineffective at improving outcomes over usual care in the “triad” trials was that (a) liberal fluid volume administration was the “usual care” in most enrolled patients and (b) that macrocirculatory hemodynamics, such as BP, and static intravascular pressures such as CVP and pulmonary arterial wedge pressure are poor correlates and predictors of effective circulatory volumes and the presence of fluid responsiveness.
Counterintuitively, in situations of central hypovolemia, peripheral sympathetic activity remains high in many patients while stroke volume decreases. This provides insight into why some patients appear not to benefit from fluid administration as peripheral arterial pressure may be maintained despite low central filling pressure (Convertino VA, et al. Auton Neurosci. 2004;111[2]:127-34). Many patients with sepsis and septic shock initially present in an undifferentiated state and empiric treatment decisions regarding fluid and pressor treatments are then misaligned to functional physiological status.
Novel methods and approaches are needed to differentiate these patients and provide appropriate, physiologically guided fluid resuscitation. Dynamic measurement of stroke volume (SV) after a passive leg raise (PLR) or a small IV fluid challenge is an emerging method for determining fluid responsiveness. Evidence suggests that the use of SV-guided resuscitation can reduce net fluid balance, ICU length of stay, risk of mechanical ventilation, time on vasopressors, and risk of renal replacement therapy.(Latham HE, et al. J Crit Care. 2017;42:42-6).
In addition to the lack of efficacy from administering fluid to nonfluid responsive patients, there remains a risk of over-resuscitation from excessive fluid administration. Excessive fluid administration causes hypervolemia and is associated with a variety of negative patient outcomes including tissue edema, organ dysfunction, increased ICU length of stay, prolonged ventilator dependence, and higher mortality rates (Tigabu BM, et al. J Crit Care. 2018;48:153-9). Further, unnecessary initial fluid administration necessitates a “de-resuscitative” phase that can prolong hospital stay and is associated with amplification of sepsis-associated organ failures. Specifically, a 2017 analysis of hospital discharge data found that large volume fluid resuscitation in sepsis patients during the first 24 hours of care was associated with higher rates of hospital mortality than was predicted for patients’ disease severity (Mansoori JN, et al. Crit Care. 2020;24[1]:25).
The FRESH trial
The Fluid Response Evaluation in Sepsis Hypotension and Shock (FRESH) trial was a prospective, randomized clinical trial in adults with septic shock comparing PLR-guided SV responsiveness (intervention) as a guide for fluid management with usual care. Patients presented to the ER with sepsis-associated hypotension and anticipated ICU admission. In the intervention arm, patients were assessed for fluid responsiveness (FR) before any clinically driven fluid bolus or increase in vasopressors. If a patient’s stroke volume increased by ≥10% in response to a PLR, they were considered fluid responsive and fluid was recommended as the first therapy. If a patient’s stroke volume increased by <10% then the patient was considered not to be FR and vasopressors were recommended as first-line therapy. The control arm received usual care. The primary end point was the difference in positive fluid balance at the first of either 72 hours or ICU discharge. Patients had received ~2.3 L of crystalloid fluid prior to randomization (~3.5 h from initial presentation), in keeping with 30 mL/kg recommendations. Patients treated with the PLR-guided fluid and pressor protocol had a significant lower net fluid balance (1.37 L (95% CI: 2.53-0.21, P = .021) at 72 hours or ICU discharge. In addition, the intervention group experienced significantly less frequent requirement for renal replacement therapy with a difference of 12.4% (95% CI: 27%-1%, P = .042) as well as a decreased requirement for ventilator use with a difference of 16.42% (95% CI: 33%-0%, P = .044) (Douglas IS, et al. Chest. 2020;158[4]:1431-45).
FRESH demonstrated that PLR-guided FR drove lower fluid balance in patients with septic shock who present to the ER with sepsis and creates a paradigm for future management of fluid and pressor resuscitation beyond the initial 30 mL/kg bolus. Functional evaluation for lack of FR adequately identifies a group of patients with sepsis-associated hypotension who are unlikely to benefit from additional IV fluids to establish hemodynamically stability. It facilitated physiologically informed treatment decisions for the individual patient at a specific moment in their course of treatment as opposed to relying on static measurements and goals that may ultimately not be indicative of fluid responsiveness and circulatory effectiveness. This could reduce the likelihood of fluid overload and associated organ failure and, thus, improve patient outcomes.
Microcirculatory function is significantly impacted by sepsis with a decline in capillary density and inappropriate vasodilation/constriction resulting in insufficient tissue and organ perfusion and increased oxidative stress. Such dysfunction has been found to be associated with worsened patient outcomes, including mortality. However, microcirculatory function does not correlate well with traditionally used macrohemodynamic assessments and treating to improve macrohemodynamic values does not ensure that microcirculation will improve (Charlton M, et al. J Intensive Care Soc. 2017;18(3):221-7).
Ongoing studies are exploring if dynamic fluid-guided resuscitation has the potential to improve survival in sepsis by providing insight into whether the administration of fluid will impact the microcirculation and subsequent organ perfusion of the patient.
Future directions include expanding the dynamic treatment algorithm into other settings, such as rapid response calls, or other patient populations, including those initially presenting with undifferentiated hypotension. While FRESH was not sufficiently powered to detect differences in mortality, there are currently multiple large studies being conducted aimed at determining the impact of a restricted fluid and early vasopressor strategy as compared with a large initial IV fluid bolus on mortality. The results of these studies could be used to determine if the results of FRESH will translate into patient survival outcomes.
Current guideline recommendations for fluid resuscitation in sepsis patients calls for an initial crystalloid fluid bolus of at least 30 mL/kg (Rhodes, et al. Intensive Care Med. 2017;43[3]:304-77) For fluid management beyond this initial bolus, recommendations had previously called for using early goal-directed therapy (EGDT) with central venous pressure (CVP) and central venous oxygen saturation to guide the use of IV fluids, vasopressors, transfusions, and dobutamine, based on the results of one single-center study that found an improvement in mortality using EGDT as compared with standard therapy.
The triad of sepsis studies
In the following years, multiple concerns were raised regarding the generalizability of this study. Three large multicenter trials were conducted in multiple countries to test the recommendations for EGDT.
PROMISE: ProMISe was a 1,260-patient randomized trial comparing the impact of EGDT vs usual care on 90-day all-cause mortality in patients with early septic shock at 56 hospitals in England. There was no significant difference in the primary study endpoint with 90-day mortality rates of 29.5% and 29.2% (RR: 1.01, 95% CI: 0.85-1.20, P =.90) (Mouncey, et al. N Engl J Med. 2015;372[14]:1301-11).
PROCESS: ProCESS was a 1,351-patient randomized trial comparing the impact of protocol-based EGDT, protocol-based standard of care, and usual care on 60 day in-hospital mortality in patients with early septic shock at 31 hospitals in the United States. There was no significant difference in the primary study endpoint with 60-day mortality rates of 21.0%, 18.2%, and 18.9% (P = .83) or in the secondary outcome of 90-day mortality with rates of 31.9%, 30.8%, and 33.7% (P = .66) (ProCESS Investigators, et al. N Engl J Med. 2014;370[18]:1683-93).
ARISE: ARISE was a 1,600-patient randomized trial comparing the impact of EGDT vs usual care on 90-day all-cause mortality in patients with early septic shock at 51 hospitals in New Zealand and Australia. There was no significant difference in the primary study end point with 90-day mortality rates of 18.6% and 18.8% (RR: 0.98, 95% CI: 0.80-1.21, P = .90). There were also no significant differences in 28-day or in-hospital mortality, duration of organ support, or length of hospital stay (ARISE Investigators, et al. N Engl J Med. 2014;371[16]:1496-506).
In summary, all three “triad” trials found no improvement with EGDT over usual care (Rowan, et al. N Engl J Med. 2017;376[23]:2223-34) calling into question the recommended methods of universally protocolized approaches to fluid and pressor resuscitation. Probable reasons for why structured EGDT was ineffective at improving outcomes over usual care in the “triad” trials was that (a) liberal fluid volume administration was the “usual care” in most enrolled patients and (b) that macrocirculatory hemodynamics, such as BP, and static intravascular pressures such as CVP and pulmonary arterial wedge pressure are poor correlates and predictors of effective circulatory volumes and the presence of fluid responsiveness.
Counterintuitively, in situations of central hypovolemia, peripheral sympathetic activity remains high in many patients while stroke volume decreases. This provides insight into why some patients appear not to benefit from fluid administration as peripheral arterial pressure may be maintained despite low central filling pressure (Convertino VA, et al. Auton Neurosci. 2004;111[2]:127-34). Many patients with sepsis and septic shock initially present in an undifferentiated state and empiric treatment decisions regarding fluid and pressor treatments are then misaligned to functional physiological status.
Novel methods and approaches are needed to differentiate these patients and provide appropriate, physiologically guided fluid resuscitation. Dynamic measurement of stroke volume (SV) after a passive leg raise (PLR) or a small IV fluid challenge is an emerging method for determining fluid responsiveness. Evidence suggests that the use of SV-guided resuscitation can reduce net fluid balance, ICU length of stay, risk of mechanical ventilation, time on vasopressors, and risk of renal replacement therapy.(Latham HE, et al. J Crit Care. 2017;42:42-6).
In addition to the lack of efficacy from administering fluid to nonfluid responsive patients, there remains a risk of over-resuscitation from excessive fluid administration. Excessive fluid administration causes hypervolemia and is associated with a variety of negative patient outcomes including tissue edema, organ dysfunction, increased ICU length of stay, prolonged ventilator dependence, and higher mortality rates (Tigabu BM, et al. J Crit Care. 2018;48:153-9). Further, unnecessary initial fluid administration necessitates a “de-resuscitative” phase that can prolong hospital stay and is associated with amplification of sepsis-associated organ failures. Specifically, a 2017 analysis of hospital discharge data found that large volume fluid resuscitation in sepsis patients during the first 24 hours of care was associated with higher rates of hospital mortality than was predicted for patients’ disease severity (Mansoori JN, et al. Crit Care. 2020;24[1]:25).
The FRESH trial
The Fluid Response Evaluation in Sepsis Hypotension and Shock (FRESH) trial was a prospective, randomized clinical trial in adults with septic shock comparing PLR-guided SV responsiveness (intervention) as a guide for fluid management with usual care. Patients presented to the ER with sepsis-associated hypotension and anticipated ICU admission. In the intervention arm, patients were assessed for fluid responsiveness (FR) before any clinically driven fluid bolus or increase in vasopressors. If a patient’s stroke volume increased by ≥10% in response to a PLR, they were considered fluid responsive and fluid was recommended as the first therapy. If a patient’s stroke volume increased by <10% then the patient was considered not to be FR and vasopressors were recommended as first-line therapy. The control arm received usual care. The primary end point was the difference in positive fluid balance at the first of either 72 hours or ICU discharge. Patients had received ~2.3 L of crystalloid fluid prior to randomization (~3.5 h from initial presentation), in keeping with 30 mL/kg recommendations. Patients treated with the PLR-guided fluid and pressor protocol had a significant lower net fluid balance (1.37 L (95% CI: 2.53-0.21, P = .021) at 72 hours or ICU discharge. In addition, the intervention group experienced significantly less frequent requirement for renal replacement therapy with a difference of 12.4% (95% CI: 27%-1%, P = .042) as well as a decreased requirement for ventilator use with a difference of 16.42% (95% CI: 33%-0%, P = .044) (Douglas IS, et al. Chest. 2020;158[4]:1431-45).
FRESH demonstrated that PLR-guided FR drove lower fluid balance in patients with septic shock who present to the ER with sepsis and creates a paradigm for future management of fluid and pressor resuscitation beyond the initial 30 mL/kg bolus. Functional evaluation for lack of FR adequately identifies a group of patients with sepsis-associated hypotension who are unlikely to benefit from additional IV fluids to establish hemodynamically stability. It facilitated physiologically informed treatment decisions for the individual patient at a specific moment in their course of treatment as opposed to relying on static measurements and goals that may ultimately not be indicative of fluid responsiveness and circulatory effectiveness. This could reduce the likelihood of fluid overload and associated organ failure and, thus, improve patient outcomes.
Microcirculatory function is significantly impacted by sepsis with a decline in capillary density and inappropriate vasodilation/constriction resulting in insufficient tissue and organ perfusion and increased oxidative stress. Such dysfunction has been found to be associated with worsened patient outcomes, including mortality. However, microcirculatory function does not correlate well with traditionally used macrohemodynamic assessments and treating to improve macrohemodynamic values does not ensure that microcirculation will improve (Charlton M, et al. J Intensive Care Soc. 2017;18(3):221-7).
Ongoing studies are exploring if dynamic fluid-guided resuscitation has the potential to improve survival in sepsis by providing insight into whether the administration of fluid will impact the microcirculation and subsequent organ perfusion of the patient.
Future directions include expanding the dynamic treatment algorithm into other settings, such as rapid response calls, or other patient populations, including those initially presenting with undifferentiated hypotension. While FRESH was not sufficiently powered to detect differences in mortality, there are currently multiple large studies being conducted aimed at determining the impact of a restricted fluid and early vasopressor strategy as compared with a large initial IV fluid bolus on mortality. The results of these studies could be used to determine if the results of FRESH will translate into patient survival outcomes.
Current guideline recommendations for fluid resuscitation in sepsis patients calls for an initial crystalloid fluid bolus of at least 30 mL/kg (Rhodes, et al. Intensive Care Med. 2017;43[3]:304-77) For fluid management beyond this initial bolus, recommendations had previously called for using early goal-directed therapy (EGDT) with central venous pressure (CVP) and central venous oxygen saturation to guide the use of IV fluids, vasopressors, transfusions, and dobutamine, based on the results of one single-center study that found an improvement in mortality using EGDT as compared with standard therapy.
The triad of sepsis studies
In the following years, multiple concerns were raised regarding the generalizability of this study. Three large multicenter trials were conducted in multiple countries to test the recommendations for EGDT.
PROMISE: ProMISe was a 1,260-patient randomized trial comparing the impact of EGDT vs usual care on 90-day all-cause mortality in patients with early septic shock at 56 hospitals in England. There was no significant difference in the primary study endpoint with 90-day mortality rates of 29.5% and 29.2% (RR: 1.01, 95% CI: 0.85-1.20, P =.90) (Mouncey, et al. N Engl J Med. 2015;372[14]:1301-11).
PROCESS: ProCESS was a 1,351-patient randomized trial comparing the impact of protocol-based EGDT, protocol-based standard of care, and usual care on 60 day in-hospital mortality in patients with early septic shock at 31 hospitals in the United States. There was no significant difference in the primary study endpoint with 60-day mortality rates of 21.0%, 18.2%, and 18.9% (P = .83) or in the secondary outcome of 90-day mortality with rates of 31.9%, 30.8%, and 33.7% (P = .66) (ProCESS Investigators, et al. N Engl J Med. 2014;370[18]:1683-93).
ARISE: ARISE was a 1,600-patient randomized trial comparing the impact of EGDT vs usual care on 90-day all-cause mortality in patients with early septic shock at 51 hospitals in New Zealand and Australia. There was no significant difference in the primary study end point with 90-day mortality rates of 18.6% and 18.8% (RR: 0.98, 95% CI: 0.80-1.21, P = .90). There were also no significant differences in 28-day or in-hospital mortality, duration of organ support, or length of hospital stay (ARISE Investigators, et al. N Engl J Med. 2014;371[16]:1496-506).
In summary, all three “triad” trials found no improvement with EGDT over usual care (Rowan, et al. N Engl J Med. 2017;376[23]:2223-34) calling into question the recommended methods of universally protocolized approaches to fluid and pressor resuscitation. Probable reasons for why structured EGDT was ineffective at improving outcomes over usual care in the “triad” trials was that (a) liberal fluid volume administration was the “usual care” in most enrolled patients and (b) that macrocirculatory hemodynamics, such as BP, and static intravascular pressures such as CVP and pulmonary arterial wedge pressure are poor correlates and predictors of effective circulatory volumes and the presence of fluid responsiveness.
Counterintuitively, in situations of central hypovolemia, peripheral sympathetic activity remains high in many patients while stroke volume decreases. This provides insight into why some patients appear not to benefit from fluid administration as peripheral arterial pressure may be maintained despite low central filling pressure (Convertino VA, et al. Auton Neurosci. 2004;111[2]:127-34). Many patients with sepsis and septic shock initially present in an undifferentiated state and empiric treatment decisions regarding fluid and pressor treatments are then misaligned to functional physiological status.
Novel methods and approaches are needed to differentiate these patients and provide appropriate, physiologically guided fluid resuscitation. Dynamic measurement of stroke volume (SV) after a passive leg raise (PLR) or a small IV fluid challenge is an emerging method for determining fluid responsiveness. Evidence suggests that the use of SV-guided resuscitation can reduce net fluid balance, ICU length of stay, risk of mechanical ventilation, time on vasopressors, and risk of renal replacement therapy.(Latham HE, et al. J Crit Care. 2017;42:42-6).
In addition to the lack of efficacy from administering fluid to nonfluid responsive patients, there remains a risk of over-resuscitation from excessive fluid administration. Excessive fluid administration causes hypervolemia and is associated with a variety of negative patient outcomes including tissue edema, organ dysfunction, increased ICU length of stay, prolonged ventilator dependence, and higher mortality rates (Tigabu BM, et al. J Crit Care. 2018;48:153-9). Further, unnecessary initial fluid administration necessitates a “de-resuscitative” phase that can prolong hospital stay and is associated with amplification of sepsis-associated organ failures. Specifically, a 2017 analysis of hospital discharge data found that large volume fluid resuscitation in sepsis patients during the first 24 hours of care was associated with higher rates of hospital mortality than was predicted for patients’ disease severity (Mansoori JN, et al. Crit Care. 2020;24[1]:25).
The FRESH trial
The Fluid Response Evaluation in Sepsis Hypotension and Shock (FRESH) trial was a prospective, randomized clinical trial in adults with septic shock comparing PLR-guided SV responsiveness (intervention) as a guide for fluid management with usual care. Patients presented to the ER with sepsis-associated hypotension and anticipated ICU admission. In the intervention arm, patients were assessed for fluid responsiveness (FR) before any clinically driven fluid bolus or increase in vasopressors. If a patient’s stroke volume increased by ≥10% in response to a PLR, they were considered fluid responsive and fluid was recommended as the first therapy. If a patient’s stroke volume increased by <10% then the patient was considered not to be FR and vasopressors were recommended as first-line therapy. The control arm received usual care. The primary end point was the difference in positive fluid balance at the first of either 72 hours or ICU discharge. Patients had received ~2.3 L of crystalloid fluid prior to randomization (~3.5 h from initial presentation), in keeping with 30 mL/kg recommendations. Patients treated with the PLR-guided fluid and pressor protocol had a significant lower net fluid balance (1.37 L (95% CI: 2.53-0.21, P = .021) at 72 hours or ICU discharge. In addition, the intervention group experienced significantly less frequent requirement for renal replacement therapy with a difference of 12.4% (95% CI: 27%-1%, P = .042) as well as a decreased requirement for ventilator use with a difference of 16.42% (95% CI: 33%-0%, P = .044) (Douglas IS, et al. Chest. 2020;158[4]:1431-45).
FRESH demonstrated that PLR-guided FR drove lower fluid balance in patients with septic shock who present to the ER with sepsis and creates a paradigm for future management of fluid and pressor resuscitation beyond the initial 30 mL/kg bolus. Functional evaluation for lack of FR adequately identifies a group of patients with sepsis-associated hypotension who are unlikely to benefit from additional IV fluids to establish hemodynamically stability. It facilitated physiologically informed treatment decisions for the individual patient at a specific moment in their course of treatment as opposed to relying on static measurements and goals that may ultimately not be indicative of fluid responsiveness and circulatory effectiveness. This could reduce the likelihood of fluid overload and associated organ failure and, thus, improve patient outcomes.
Microcirculatory function is significantly impacted by sepsis with a decline in capillary density and inappropriate vasodilation/constriction resulting in insufficient tissue and organ perfusion and increased oxidative stress. Such dysfunction has been found to be associated with worsened patient outcomes, including mortality. However, microcirculatory function does not correlate well with traditionally used macrohemodynamic assessments and treating to improve macrohemodynamic values does not ensure that microcirculation will improve (Charlton M, et al. J Intensive Care Soc. 2017;18(3):221-7).
Ongoing studies are exploring if dynamic fluid-guided resuscitation has the potential to improve survival in sepsis by providing insight into whether the administration of fluid will impact the microcirculation and subsequent organ perfusion of the patient.
Future directions include expanding the dynamic treatment algorithm into other settings, such as rapid response calls, or other patient populations, including those initially presenting with undifferentiated hypotension. While FRESH was not sufficiently powered to detect differences in mortality, there are currently multiple large studies being conducted aimed at determining the impact of a restricted fluid and early vasopressor strategy as compared with a large initial IV fluid bolus on mortality. The results of these studies could be used to determine if the results of FRESH will translate into patient survival outcomes.
Evolution of ECMO. COVID-19 and pulmonary aspergillus. Lung cancer screening. Food as medicine. Air pollution.
Cardiovascular medicine and surgery
Evolution of ECMO as a result of COVID
A year and a half ago, the enormity of this pandemic was only beginning to be realized. Likewise, we have never before been so well-equipped to communicate, investigate, and collaborate through modern innovations. Despite our monumental progress with diagnostics and expedited vaccine production, there remain significant challenges with management of infected individuals suffering from severe sequelae after infection such as respiratory failure. Pharmacologic therapies with steroids, antivirals, and targeted immune modulators have demonstrated modest results at best thus far.
Early intubation unsurprisingly resulted in poor outcomes and a return to other established methods using high-flow nasal cannula and noninvasive positive-pressure ventilation (NIPPV) with a goal of avoiding mechanical ventilation are again the standard of care (Rola P, et al. Clin Exp Emerg Med. 2020 Jun 10. doi: 10.15441/ceem.20.043). Furthermore, limited resources encouraged utilization of established and probably previously underutilized techniques, such as proning with expected improvements in outcomes.
When conventional lung protective mechanical ventilation strategies have been unsuccessful, we have seen improved survival with the incorporation of extracorporeal membrane oxygenation (ECMO), especially when cannulated earlier (Giraud R, et al. 2021. Phys Rep). Many centers now offer ECMO support with considerable expertise and trends toward earlier ECMO cannulation, which permit ultraprotective lung ventilation (Schmidt M, et al. Am J Respir Crit Care Med. 2019 Oct 15;200[8]:1002-12). With benefits that parallel early tracheostomy, early ECMO may permit decreased sedation and earlier mobilization, which contribute to improved outcomes (Levin NM, et al. J Clin Med. 2021 Jan 12;10[2]:25). We may be approaching a paradigm shift where ECMO is performed in lieu of mechanical ventilation (Kurihara C, et al. 2018. Crit Care Med. 2018 Nov;46[11]:e1070-e1073). Future randomized clinical trials will need to be designed to answer this question.
Robert Baeten, II, DSc, PA-C, FCCP
NetWork Steering Committee Member
Chest infections
COVID-19-associated pulmonary aspergillosis: A cause for concern?
Since the global spread of SARS-CoV-2 more than a year ago, reports of secondary infections with Aspergillus spp. have emerged. Like influenza, there has been speculation that severe COVID-19 pneumonia is a unique risk factor for invasive pulmonary aspergillosis (IPA). This entity has been dubbed CAPA, or COVID-associated pulmonary aspergillosis. While the reported incidence of CAPA has ranged from around 5% to 35% in critically ill patients, it has been difficult to distinguish reports of colonization from true infection as histopathologic evidence of disease has been limited. Using stringent diagnostic criteria, a retrospective review of 145 mechanically ventilated patients with COVID-19 found the incidence of CAPA to be 4.8% (Fekkar A, et al. Am J Respir Crit Care Med. 2021 Feb 1;203[3]:307-17) which is similar to other non-COVID ARDS series. The authors found solid organ transplant and prolonged steroid treatment to be risk factors. Like other studies, no comparator group was utilized, limiting the conclusions regarding COVID-19 as an independent risk factor for IPA. Diagnostic criteria have been adapted to assist clinicians and allow for future research: Proven infection requires temporal relation with COVID-19 ICU admission and histopathologic evidence of Aspergillus spp. invasion or positive culture from sterile sites (Koehler P, et al. Lancet Infect Dis. 2020 Dec 14;S1473-3099[20]30847-1).
Aspergillus conidia are ubiquitous in the environment, and the respiratory epithelium and associated cilia act as the first defense against IPA. Distinct from influenza pneumonia, severe COVID-19 causes diffuse alveolar damage and does not appear to cause significant damage to the respiratory epithelium (Borczuk AC, et al. Mod Pathol. 2020;33[11]:2156-68). This coupled with the lack of histopathologic evidence of invasion in most reports of CAPA raises question regarding the extent of the association between COVID-19 and IPA. Nonetheless, immune perturbation caused by COVID-19 immunomodulating therapies, such as corticosteroids and IL-6 inhibitors, may ultimately leave patients susceptible to IPA and other opportunistic infections.
Kelly M. Pennington, MD
Charles S. Dela Cruz, MD
Sebastion Kurz, MD
NetWork Steering Committee Members
Clinical pulmonary medicine
New USPSTF guidelines for lung cancer screening: A step forward
Despite lung cancer being the number one cause of cancer-related death in America, screening for lung cancer remains low, with only 2-16% eligible patients being offered screening since the US Preventive Services Task Force (USPSTF) recommendation in 2013. New guidelines published in JAMA (Krist AH, et al. JAMA. 2021;325[10]:962-970; Meza R, et al. JAMA. 2021;325[10]:988-97; Jonas DE, at al. JAMA. 2021;325[10]:971-87) have suggested broadening eligibility to those 50-80 years old, who are smokers or previously quit in the past 15 years and have a minimum 20 pack-year smoking history (Grade B recommendation). The change lowers the starting age to 50 and the smoking requirement from 30 to 20 pack-years. Based on Cancer Intervention and Surveillance Modeling Network (CISNET) modeling, utilized by the UPSTF, this change can result in 503 (vs. 381 in the prior guideline) cancer deaths averted for every 100,000 adults and an estimated 13% reduction in lung cancer mortality and 6,918 life-years gained.
This recommendation will dramatically increase the number of eligible adults for screening by 6.4 million people, an increase of 86% compared with the 2013 guidelines. Most importantly, the decrease in pack-year requirement to 20 is expected to increase eligibility for women and minimize racial disparities. African American men have a higher incidence of lung cancer with less smoke exposure compared with white men. Non-Hispanic Black, Hispanics, American Indian/Alaska Native persons are hoped to have significant benefit from these new recommendations. Original recommendations in the 2013 guideline mirrored the National Lung Screening Trial, in which 91% participants were White. Regardless of these updated recommendations, serious socioeconomic barriers may continue to limit racial/ethnic minorities from accessing high-quality lung cancer screening programs. Besides changing the screening criteria, barriers to access will need to be addressed to achieve maximal benefits of the lung cancer screening program.
Munish Luthra, MD, FCCP
Samantha D’Annunzio, MD
Steering Committee Members
Interprofessional team
Let food be thy medicine and medicine be thy food – Hippocrates
Recently an article published in The Lancet discussed malnutrition in the patient with COVID-19 infection requiring non-invasive ventilation (NIV) (Turner P, et al. Lancet. 2021 Apr 3;397[10281]:126). It is known that COVID-19 infection causes hyperinflammation and hypercatabolism, resulting in disruption of metabolic pathways leading to muscle wasting, including cardiac muscle dysfunction, muscle weakness, and prolonged fatigue (Singer PJ, et al. 2021. Intensive Med. In press).
Lipids, specifically DHA and EPA, are known to inhibit cyclooxygenase enzyme and may suppress prostaglandin production and block platelet-activating factor. Consumption of carbohydrates with high glycemic indexes can result in free radical synthesis (increasing inflammatory cytokines C reactive protein, tumor necrosis alpha and interleukin-6). Other nutrients known to have an anti-inflammatory role include vitamins A & D, selenium, and copper. Vitamin A is known to enhance an antigen-specific immune response. Probiotics may also play a role in enhancing the immune response (Turner P, et al. 2021. Lancet. 2021 Apr 3;397[10281]:1261).
Patients requiring NIV encounter impaired tolerance to oral nutrition, and enteral nutrition (EN) is prescribed (Singer PJ, et al. 2021. Intensive Med. In press). Advantages of EN are maintenance of gut integrity and intestinal permeability as well as down regulation of the inflammatory response and insulin resistance. Furthermore, negative energy balance is associated with poor outcomes. Better focus on nutrition assessment practices is needed to overcome energy deficits during treatment of COVID-19 pneumonia. An interprofessional team approach increases use of nutritional scores and optimizes nutritional interventions.
If oral nutrition is feasible, prescribing small, frequent meals and high‐protein, calorically dense foods can ensure adequate caloric intake. (Behrens S, et al. Nutr Clin Pract. 2021 Feb;36[1]:105-9). When EN is indicated, the Intensive Care Society endorses the use of fine bore feeding tubes and NIV masks with special nasogastric tube adapters to reduce mask leak. Head-of-bed elevation and avoidance of bolus feeding improve EN tolerance (Pardo T, et al. 2021. Anaesth Crit Care Pain Med. 2020 Dec;39[6]:738-9).
*Due to the novelty of this disease information is limited and further study is warranted.
David W. Unkle, MSN, APN, FCCP
Robert Baeten, DMSc, PA-C, FCCP
Nikky Keer, DO
NetWork Steering Committee Members
Occupational and environmental health
Not just COVID in the air
Particulate matter (PM) is a specific type of air pollution referred to by its size in micrometers. A direct correlation has been shown between non-accidental death and PM2.5 concentration with a 1.5% increase in daily mortality (Schwartz J, et al. J Air Waste Manag Assoc. 1996 Oct;46[10]:927-39). From 2000-2019, PM2.5 concentrations have steadily decreased over 43% (Environmental Protection Agency). Significant decline in air pollution has occurred early in the COVID-19 pandemic. PM2.5 declined in counties from states instituting early non-essential business closures in the U.S. Additionally, NASA models revealed a nearly 20% drop in global nitrogen dioxide concentrations using a COVID-19-free 2020 model to compare with actual space and ground-based observations since February 2020 (NASA Model Reveals How Much COVID-related Pollution Levels Deviated from the Norm. 2020 Nov 17. The pandemic has shown that there is a significant human behavior-driven contribution to air pollution. The historic fire season of 2020 in the western states contributed to record high air pollution with attributable mortality (Liu X, et al. medRxiv 2020.09.20197921). Additionally, the COVID-19 pandemic impeded firefighting response (Burke M, et al. PNAS. 2021;11[2]:e2011048118).
Despite the pandemic related reduction, racial-ethnic disparities continue to exist in consumption of PM2.5. In a model looking at production of PM2.5, defined as consumption by the consumer and exposure as where the product or service originated, African American and Hispanic individuals have up to 12-21% greater pollution exposure within the United States (Tessum CW, et al. Proc Natl Acad Sci USA. 2019 Mar 26;116[13]:6001-6). PM pollution increased the risk of asthma attacks corresponding to zip codes with higher poverty levels and eligibility to Medicaid (O’Lenick CR, et al. Epidemiol Community Health. 2017 Feb;71[2]:129-36). Other studies have shown people with a lower socioeconomic position, have less education, live nearer to major sources of pollution, greater reliance on public transportation and unemployment are at higher risk from effects of PM pollution (American Lung Association. Disparities in the impact of air pollution.
Disclaimer: The views expressed in this article are those of the author(s) and do not reflect the official policy of the Department of Army/Navy/Air Force, Department of Defense, or US government.
Tyler Church, DO
Fellow-in-Training Member
Bathmapriya Balakrishnan, MD
Dixie Harris, MD
NetWork Steering Committee Members
Cardiovascular medicine and surgery
Evolution of ECMO as a result of COVID
A year and a half ago, the enormity of this pandemic was only beginning to be realized. Likewise, we have never before been so well-equipped to communicate, investigate, and collaborate through modern innovations. Despite our monumental progress with diagnostics and expedited vaccine production, there remain significant challenges with management of infected individuals suffering from severe sequelae after infection such as respiratory failure. Pharmacologic therapies with steroids, antivirals, and targeted immune modulators have demonstrated modest results at best thus far.
Early intubation unsurprisingly resulted in poor outcomes and a return to other established methods using high-flow nasal cannula and noninvasive positive-pressure ventilation (NIPPV) with a goal of avoiding mechanical ventilation are again the standard of care (Rola P, et al. Clin Exp Emerg Med. 2020 Jun 10. doi: 10.15441/ceem.20.043). Furthermore, limited resources encouraged utilization of established and probably previously underutilized techniques, such as proning with expected improvements in outcomes.
When conventional lung protective mechanical ventilation strategies have been unsuccessful, we have seen improved survival with the incorporation of extracorporeal membrane oxygenation (ECMO), especially when cannulated earlier (Giraud R, et al. 2021. Phys Rep). Many centers now offer ECMO support with considerable expertise and trends toward earlier ECMO cannulation, which permit ultraprotective lung ventilation (Schmidt M, et al. Am J Respir Crit Care Med. 2019 Oct 15;200[8]:1002-12). With benefits that parallel early tracheostomy, early ECMO may permit decreased sedation and earlier mobilization, which contribute to improved outcomes (Levin NM, et al. J Clin Med. 2021 Jan 12;10[2]:25). We may be approaching a paradigm shift where ECMO is performed in lieu of mechanical ventilation (Kurihara C, et al. 2018. Crit Care Med. 2018 Nov;46[11]:e1070-e1073). Future randomized clinical trials will need to be designed to answer this question.
Robert Baeten, II, DSc, PA-C, FCCP
NetWork Steering Committee Member
Chest infections
COVID-19-associated pulmonary aspergillosis: A cause for concern?
Since the global spread of SARS-CoV-2 more than a year ago, reports of secondary infections with Aspergillus spp. have emerged. Like influenza, there has been speculation that severe COVID-19 pneumonia is a unique risk factor for invasive pulmonary aspergillosis (IPA). This entity has been dubbed CAPA, or COVID-associated pulmonary aspergillosis. While the reported incidence of CAPA has ranged from around 5% to 35% in critically ill patients, it has been difficult to distinguish reports of colonization from true infection as histopathologic evidence of disease has been limited. Using stringent diagnostic criteria, a retrospective review of 145 mechanically ventilated patients with COVID-19 found the incidence of CAPA to be 4.8% (Fekkar A, et al. Am J Respir Crit Care Med. 2021 Feb 1;203[3]:307-17) which is similar to other non-COVID ARDS series. The authors found solid organ transplant and prolonged steroid treatment to be risk factors. Like other studies, no comparator group was utilized, limiting the conclusions regarding COVID-19 as an independent risk factor for IPA. Diagnostic criteria have been adapted to assist clinicians and allow for future research: Proven infection requires temporal relation with COVID-19 ICU admission and histopathologic evidence of Aspergillus spp. invasion or positive culture from sterile sites (Koehler P, et al. Lancet Infect Dis. 2020 Dec 14;S1473-3099[20]30847-1).
Aspergillus conidia are ubiquitous in the environment, and the respiratory epithelium and associated cilia act as the first defense against IPA. Distinct from influenza pneumonia, severe COVID-19 causes diffuse alveolar damage and does not appear to cause significant damage to the respiratory epithelium (Borczuk AC, et al. Mod Pathol. 2020;33[11]:2156-68). This coupled with the lack of histopathologic evidence of invasion in most reports of CAPA raises question regarding the extent of the association between COVID-19 and IPA. Nonetheless, immune perturbation caused by COVID-19 immunomodulating therapies, such as corticosteroids and IL-6 inhibitors, may ultimately leave patients susceptible to IPA and other opportunistic infections.
Kelly M. Pennington, MD
Charles S. Dela Cruz, MD
Sebastion Kurz, MD
NetWork Steering Committee Members
Clinical pulmonary medicine
New USPSTF guidelines for lung cancer screening: A step forward
Despite lung cancer being the number one cause of cancer-related death in America, screening for lung cancer remains low, with only 2-16% eligible patients being offered screening since the US Preventive Services Task Force (USPSTF) recommendation in 2013. New guidelines published in JAMA (Krist AH, et al. JAMA. 2021;325[10]:962-970; Meza R, et al. JAMA. 2021;325[10]:988-97; Jonas DE, at al. JAMA. 2021;325[10]:971-87) have suggested broadening eligibility to those 50-80 years old, who are smokers or previously quit in the past 15 years and have a minimum 20 pack-year smoking history (Grade B recommendation). The change lowers the starting age to 50 and the smoking requirement from 30 to 20 pack-years. Based on Cancer Intervention and Surveillance Modeling Network (CISNET) modeling, utilized by the UPSTF, this change can result in 503 (vs. 381 in the prior guideline) cancer deaths averted for every 100,000 adults and an estimated 13% reduction in lung cancer mortality and 6,918 life-years gained.
This recommendation will dramatically increase the number of eligible adults for screening by 6.4 million people, an increase of 86% compared with the 2013 guidelines. Most importantly, the decrease in pack-year requirement to 20 is expected to increase eligibility for women and minimize racial disparities. African American men have a higher incidence of lung cancer with less smoke exposure compared with white men. Non-Hispanic Black, Hispanics, American Indian/Alaska Native persons are hoped to have significant benefit from these new recommendations. Original recommendations in the 2013 guideline mirrored the National Lung Screening Trial, in which 91% participants were White. Regardless of these updated recommendations, serious socioeconomic barriers may continue to limit racial/ethnic minorities from accessing high-quality lung cancer screening programs. Besides changing the screening criteria, barriers to access will need to be addressed to achieve maximal benefits of the lung cancer screening program.
Munish Luthra, MD, FCCP
Samantha D’Annunzio, MD
Steering Committee Members
Interprofessional team
Let food be thy medicine and medicine be thy food – Hippocrates
Recently an article published in The Lancet discussed malnutrition in the patient with COVID-19 infection requiring non-invasive ventilation (NIV) (Turner P, et al. Lancet. 2021 Apr 3;397[10281]:126). It is known that COVID-19 infection causes hyperinflammation and hypercatabolism, resulting in disruption of metabolic pathways leading to muscle wasting, including cardiac muscle dysfunction, muscle weakness, and prolonged fatigue (Singer PJ, et al. 2021. Intensive Med. In press).
Lipids, specifically DHA and EPA, are known to inhibit cyclooxygenase enzyme and may suppress prostaglandin production and block platelet-activating factor. Consumption of carbohydrates with high glycemic indexes can result in free radical synthesis (increasing inflammatory cytokines C reactive protein, tumor necrosis alpha and interleukin-6). Other nutrients known to have an anti-inflammatory role include vitamins A & D, selenium, and copper. Vitamin A is known to enhance an antigen-specific immune response. Probiotics may also play a role in enhancing the immune response (Turner P, et al. 2021. Lancet. 2021 Apr 3;397[10281]:1261).
Patients requiring NIV encounter impaired tolerance to oral nutrition, and enteral nutrition (EN) is prescribed (Singer PJ, et al. 2021. Intensive Med. In press). Advantages of EN are maintenance of gut integrity and intestinal permeability as well as down regulation of the inflammatory response and insulin resistance. Furthermore, negative energy balance is associated with poor outcomes. Better focus on nutrition assessment practices is needed to overcome energy deficits during treatment of COVID-19 pneumonia. An interprofessional team approach increases use of nutritional scores and optimizes nutritional interventions.
If oral nutrition is feasible, prescribing small, frequent meals and high‐protein, calorically dense foods can ensure adequate caloric intake. (Behrens S, et al. Nutr Clin Pract. 2021 Feb;36[1]:105-9). When EN is indicated, the Intensive Care Society endorses the use of fine bore feeding tubes and NIV masks with special nasogastric tube adapters to reduce mask leak. Head-of-bed elevation and avoidance of bolus feeding improve EN tolerance (Pardo T, et al. 2021. Anaesth Crit Care Pain Med. 2020 Dec;39[6]:738-9).
*Due to the novelty of this disease information is limited and further study is warranted.
David W. Unkle, MSN, APN, FCCP
Robert Baeten, DMSc, PA-C, FCCP
Nikky Keer, DO
NetWork Steering Committee Members
Occupational and environmental health
Not just COVID in the air
Particulate matter (PM) is a specific type of air pollution referred to by its size in micrometers. A direct correlation has been shown between non-accidental death and PM2.5 concentration with a 1.5% increase in daily mortality (Schwartz J, et al. J Air Waste Manag Assoc. 1996 Oct;46[10]:927-39). From 2000-2019, PM2.5 concentrations have steadily decreased over 43% (Environmental Protection Agency). Significant decline in air pollution has occurred early in the COVID-19 pandemic. PM2.5 declined in counties from states instituting early non-essential business closures in the U.S. Additionally, NASA models revealed a nearly 20% drop in global nitrogen dioxide concentrations using a COVID-19-free 2020 model to compare with actual space and ground-based observations since February 2020 (NASA Model Reveals How Much COVID-related Pollution Levels Deviated from the Norm. 2020 Nov 17. The pandemic has shown that there is a significant human behavior-driven contribution to air pollution. The historic fire season of 2020 in the western states contributed to record high air pollution with attributable mortality (Liu X, et al. medRxiv 2020.09.20197921). Additionally, the COVID-19 pandemic impeded firefighting response (Burke M, et al. PNAS. 2021;11[2]:e2011048118).
Despite the pandemic related reduction, racial-ethnic disparities continue to exist in consumption of PM2.5. In a model looking at production of PM2.5, defined as consumption by the consumer and exposure as where the product or service originated, African American and Hispanic individuals have up to 12-21% greater pollution exposure within the United States (Tessum CW, et al. Proc Natl Acad Sci USA. 2019 Mar 26;116[13]:6001-6). PM pollution increased the risk of asthma attacks corresponding to zip codes with higher poverty levels and eligibility to Medicaid (O’Lenick CR, et al. Epidemiol Community Health. 2017 Feb;71[2]:129-36). Other studies have shown people with a lower socioeconomic position, have less education, live nearer to major sources of pollution, greater reliance on public transportation and unemployment are at higher risk from effects of PM pollution (American Lung Association. Disparities in the impact of air pollution.
Disclaimer: The views expressed in this article are those of the author(s) and do not reflect the official policy of the Department of Army/Navy/Air Force, Department of Defense, or US government.
Tyler Church, DO
Fellow-in-Training Member
Bathmapriya Balakrishnan, MD
Dixie Harris, MD
NetWork Steering Committee Members
Cardiovascular medicine and surgery
Evolution of ECMO as a result of COVID
A year and a half ago, the enormity of this pandemic was only beginning to be realized. Likewise, we have never before been so well-equipped to communicate, investigate, and collaborate through modern innovations. Despite our monumental progress with diagnostics and expedited vaccine production, there remain significant challenges with management of infected individuals suffering from severe sequelae after infection such as respiratory failure. Pharmacologic therapies with steroids, antivirals, and targeted immune modulators have demonstrated modest results at best thus far.
Early intubation unsurprisingly resulted in poor outcomes and a return to other established methods using high-flow nasal cannula and noninvasive positive-pressure ventilation (NIPPV) with a goal of avoiding mechanical ventilation are again the standard of care (Rola P, et al. Clin Exp Emerg Med. 2020 Jun 10. doi: 10.15441/ceem.20.043). Furthermore, limited resources encouraged utilization of established and probably previously underutilized techniques, such as proning with expected improvements in outcomes.
When conventional lung protective mechanical ventilation strategies have been unsuccessful, we have seen improved survival with the incorporation of extracorporeal membrane oxygenation (ECMO), especially when cannulated earlier (Giraud R, et al. 2021. Phys Rep). Many centers now offer ECMO support with considerable expertise and trends toward earlier ECMO cannulation, which permit ultraprotective lung ventilation (Schmidt M, et al. Am J Respir Crit Care Med. 2019 Oct 15;200[8]:1002-12). With benefits that parallel early tracheostomy, early ECMO may permit decreased sedation and earlier mobilization, which contribute to improved outcomes (Levin NM, et al. J Clin Med. 2021 Jan 12;10[2]:25). We may be approaching a paradigm shift where ECMO is performed in lieu of mechanical ventilation (Kurihara C, et al. 2018. Crit Care Med. 2018 Nov;46[11]:e1070-e1073). Future randomized clinical trials will need to be designed to answer this question.
Robert Baeten, II, DSc, PA-C, FCCP
NetWork Steering Committee Member
Chest infections
COVID-19-associated pulmonary aspergillosis: A cause for concern?
Since the global spread of SARS-CoV-2 more than a year ago, reports of secondary infections with Aspergillus spp. have emerged. Like influenza, there has been speculation that severe COVID-19 pneumonia is a unique risk factor for invasive pulmonary aspergillosis (IPA). This entity has been dubbed CAPA, or COVID-associated pulmonary aspergillosis. While the reported incidence of CAPA has ranged from around 5% to 35% in critically ill patients, it has been difficult to distinguish reports of colonization from true infection as histopathologic evidence of disease has been limited. Using stringent diagnostic criteria, a retrospective review of 145 mechanically ventilated patients with COVID-19 found the incidence of CAPA to be 4.8% (Fekkar A, et al. Am J Respir Crit Care Med. 2021 Feb 1;203[3]:307-17) which is similar to other non-COVID ARDS series. The authors found solid organ transplant and prolonged steroid treatment to be risk factors. Like other studies, no comparator group was utilized, limiting the conclusions regarding COVID-19 as an independent risk factor for IPA. Diagnostic criteria have been adapted to assist clinicians and allow for future research: Proven infection requires temporal relation with COVID-19 ICU admission and histopathologic evidence of Aspergillus spp. invasion or positive culture from sterile sites (Koehler P, et al. Lancet Infect Dis. 2020 Dec 14;S1473-3099[20]30847-1).
Aspergillus conidia are ubiquitous in the environment, and the respiratory epithelium and associated cilia act as the first defense against IPA. Distinct from influenza pneumonia, severe COVID-19 causes diffuse alveolar damage and does not appear to cause significant damage to the respiratory epithelium (Borczuk AC, et al. Mod Pathol. 2020;33[11]:2156-68). This coupled with the lack of histopathologic evidence of invasion in most reports of CAPA raises question regarding the extent of the association between COVID-19 and IPA. Nonetheless, immune perturbation caused by COVID-19 immunomodulating therapies, such as corticosteroids and IL-6 inhibitors, may ultimately leave patients susceptible to IPA and other opportunistic infections.
Kelly M. Pennington, MD
Charles S. Dela Cruz, MD
Sebastion Kurz, MD
NetWork Steering Committee Members
Clinical pulmonary medicine
New USPSTF guidelines for lung cancer screening: A step forward
Despite lung cancer being the number one cause of cancer-related death in America, screening for lung cancer remains low, with only 2-16% eligible patients being offered screening since the US Preventive Services Task Force (USPSTF) recommendation in 2013. New guidelines published in JAMA (Krist AH, et al. JAMA. 2021;325[10]:962-970; Meza R, et al. JAMA. 2021;325[10]:988-97; Jonas DE, at al. JAMA. 2021;325[10]:971-87) have suggested broadening eligibility to those 50-80 years old, who are smokers or previously quit in the past 15 years and have a minimum 20 pack-year smoking history (Grade B recommendation). The change lowers the starting age to 50 and the smoking requirement from 30 to 20 pack-years. Based on Cancer Intervention and Surveillance Modeling Network (CISNET) modeling, utilized by the UPSTF, this change can result in 503 (vs. 381 in the prior guideline) cancer deaths averted for every 100,000 adults and an estimated 13% reduction in lung cancer mortality and 6,918 life-years gained.
This recommendation will dramatically increase the number of eligible adults for screening by 6.4 million people, an increase of 86% compared with the 2013 guidelines. Most importantly, the decrease in pack-year requirement to 20 is expected to increase eligibility for women and minimize racial disparities. African American men have a higher incidence of lung cancer with less smoke exposure compared with white men. Non-Hispanic Black, Hispanics, American Indian/Alaska Native persons are hoped to have significant benefit from these new recommendations. Original recommendations in the 2013 guideline mirrored the National Lung Screening Trial, in which 91% participants were White. Regardless of these updated recommendations, serious socioeconomic barriers may continue to limit racial/ethnic minorities from accessing high-quality lung cancer screening programs. Besides changing the screening criteria, barriers to access will need to be addressed to achieve maximal benefits of the lung cancer screening program.
Munish Luthra, MD, FCCP
Samantha D’Annunzio, MD
Steering Committee Members
Interprofessional team
Let food be thy medicine and medicine be thy food – Hippocrates
Recently an article published in The Lancet discussed malnutrition in the patient with COVID-19 infection requiring non-invasive ventilation (NIV) (Turner P, et al. Lancet. 2021 Apr 3;397[10281]:126). It is known that COVID-19 infection causes hyperinflammation and hypercatabolism, resulting in disruption of metabolic pathways leading to muscle wasting, including cardiac muscle dysfunction, muscle weakness, and prolonged fatigue (Singer PJ, et al. 2021. Intensive Med. In press).
Lipids, specifically DHA and EPA, are known to inhibit cyclooxygenase enzyme and may suppress prostaglandin production and block platelet-activating factor. Consumption of carbohydrates with high glycemic indexes can result in free radical synthesis (increasing inflammatory cytokines C reactive protein, tumor necrosis alpha and interleukin-6). Other nutrients known to have an anti-inflammatory role include vitamins A & D, selenium, and copper. Vitamin A is known to enhance an antigen-specific immune response. Probiotics may also play a role in enhancing the immune response (Turner P, et al. 2021. Lancet. 2021 Apr 3;397[10281]:1261).
Patients requiring NIV encounter impaired tolerance to oral nutrition, and enteral nutrition (EN) is prescribed (Singer PJ, et al. 2021. Intensive Med. In press). Advantages of EN are maintenance of gut integrity and intestinal permeability as well as down regulation of the inflammatory response and insulin resistance. Furthermore, negative energy balance is associated with poor outcomes. Better focus on nutrition assessment practices is needed to overcome energy deficits during treatment of COVID-19 pneumonia. An interprofessional team approach increases use of nutritional scores and optimizes nutritional interventions.
If oral nutrition is feasible, prescribing small, frequent meals and high‐protein, calorically dense foods can ensure adequate caloric intake. (Behrens S, et al. Nutr Clin Pract. 2021 Feb;36[1]:105-9). When EN is indicated, the Intensive Care Society endorses the use of fine bore feeding tubes and NIV masks with special nasogastric tube adapters to reduce mask leak. Head-of-bed elevation and avoidance of bolus feeding improve EN tolerance (Pardo T, et al. 2021. Anaesth Crit Care Pain Med. 2020 Dec;39[6]:738-9).
*Due to the novelty of this disease information is limited and further study is warranted.
David W. Unkle, MSN, APN, FCCP
Robert Baeten, DMSc, PA-C, FCCP
Nikky Keer, DO
NetWork Steering Committee Members
Occupational and environmental health
Not just COVID in the air
Particulate matter (PM) is a specific type of air pollution referred to by its size in micrometers. A direct correlation has been shown between non-accidental death and PM2.5 concentration with a 1.5% increase in daily mortality (Schwartz J, et al. J Air Waste Manag Assoc. 1996 Oct;46[10]:927-39). From 2000-2019, PM2.5 concentrations have steadily decreased over 43% (Environmental Protection Agency). Significant decline in air pollution has occurred early in the COVID-19 pandemic. PM2.5 declined in counties from states instituting early non-essential business closures in the U.S. Additionally, NASA models revealed a nearly 20% drop in global nitrogen dioxide concentrations using a COVID-19-free 2020 model to compare with actual space and ground-based observations since February 2020 (NASA Model Reveals How Much COVID-related Pollution Levels Deviated from the Norm. 2020 Nov 17. The pandemic has shown that there is a significant human behavior-driven contribution to air pollution. The historic fire season of 2020 in the western states contributed to record high air pollution with attributable mortality (Liu X, et al. medRxiv 2020.09.20197921). Additionally, the COVID-19 pandemic impeded firefighting response (Burke M, et al. PNAS. 2021;11[2]:e2011048118).
Despite the pandemic related reduction, racial-ethnic disparities continue to exist in consumption of PM2.5. In a model looking at production of PM2.5, defined as consumption by the consumer and exposure as where the product or service originated, African American and Hispanic individuals have up to 12-21% greater pollution exposure within the United States (Tessum CW, et al. Proc Natl Acad Sci USA. 2019 Mar 26;116[13]:6001-6). PM pollution increased the risk of asthma attacks corresponding to zip codes with higher poverty levels and eligibility to Medicaid (O’Lenick CR, et al. Epidemiol Community Health. 2017 Feb;71[2]:129-36). Other studies have shown people with a lower socioeconomic position, have less education, live nearer to major sources of pollution, greater reliance on public transportation and unemployment are at higher risk from effects of PM pollution (American Lung Association. Disparities in the impact of air pollution.
Disclaimer: The views expressed in this article are those of the author(s) and do not reflect the official policy of the Department of Army/Navy/Air Force, Department of Defense, or US government.
Tyler Church, DO
Fellow-in-Training Member
Bathmapriya Balakrishnan, MD
Dixie Harris, MD
NetWork Steering Committee Members
Are we there yet? Lung cancer screening – current landscape
Lung cancer is the second-most common cancer and one of the leading causes of mortality in the United States among both men and women. It accounts for almost 25% of all cancer deaths, and every year more people die of lung cancer than colon, breast, and prostate cancers combined. The American Cancer Society estimates about 235,760 new lung cancer cases and about 131,880 deaths from lung cancer in 2021.
Smoking and increasing age are the two most important risk factors for lung cancer. Lung cancer has a higher incidence among Black men than White men, and among White women compared with Black women. These differences are likely related to smoking exposure. Early diagnosis of lung cancer can improve survival, and hence screening for lung cancer in high-risk populations is desired. Among the available cancer screening tests, radiology is primarily involved in breast and lung cancer screening (LCS). In 2011, the National Lung Screening Trial (NLST) showed a benefit of annual low- dose chest CT for LCS, with about 20% reduction in lung cancer-related mortality in high-risk participants compared with chest radiographs (Aberle DR, et al. N Engl J Med. 2011 Aug 4;365[5]:395-409).
In 2013, the United States Preventative Services Task Force (USPSTF) issued a grade B recommendation in support of annual LCS by CT scan for individuals between the ages of 55-80 years with smoking history of 30 or more pack-years who are current smokers or had quit smoking in the last 15 years. Many other professional societies followed with their own recommendations with minor differences. In 2015, after the Centers for Medicare and Medicaid (CMS) decision of coverage, millions of Americans at high risk became eligible for CT LCS with no copayment or cost sharing by the patient.
The results from the European NELSON trial in 2020 augmented the NLST data showing a 24% decrease in lung cancer mortality. Nodules were measured using volume and volume doubling time rather than bidimensional axial measurements, reducing the false-positive results to 56% compared with 96% in NLST. With growing evidence of the benefits from LCS, recently USPSTF summarized with moderate certainty that annual LCS CT has moderate net benefit in people at high risk for lung cancer based on age, cumulative smoking exposure, and years since quitting smoking.
In March 2021, USPSTF has issued new recommendations with a decrease in the screening age to 50 years, and the smoking history that triggers screening to 20 pack-years (Screening for Lung Cancer: USPSTF Statement. JAMA. 2021 Mar 9;325[10]:962-70. doi: 10.1001/jama.2021.1117). These expanded eligibility criteria are projected to double the number of eligible candidates of LCS in the United States, reduce annual deaths by up to 50%, and benefit minorities and women. By widening the screening criteria to include younger individuals and who have smoked less tobacco, more lives will be saved by early detection of lung cancer. Since the NLST and NELSON trials enrolled relatively healthy people, USPSTF recommends discontinuation of screening once the person has not smoked for 15 years and in persons with any health problem that severely limits the life expectancy or the ability or willingness to undergo surgery. All screening programs must incorporate smoking cessation counseling and interventions for all the enrolled individuals who are current smokers. The USPSTF has also made recommendations on interventions to prevent the initiation of tobacco use in children and adolescents, including counseling and pharmacotherapy.
The decision to undergo LCS is inherently complex, and primary care and pulmonary physicians play a pivotal role by identifying the eligible patients, participating in shared decision-making (SDM), offering smoking cessation, ordering the CT, and managing follow-up. SDM between the patient and clinician includes a discussion of the benefits, risks, limitations, and potential harms of screening. The potential harms of screening include overdiagnosis, false-positive results, incidental findings, and the anxiety leading to further testing or follow-up. The risk of radiation exposure is markedly reduced using low-dose CT protocols compared with conventional chest CT. SDM visit also emphasizes the importance of adherence to annual screening and patient willingness and ability to undergo treatment if required. In 2015, CMS approved the addition of LCS counseling and SDM visits that are performed by physicians or qualified nonphysician practitioners (physician assistant, nurse practitioner, or clinical nurse specialist). Studies have shown that these visits improve the screening uptake rate.
To minimize the variations in the evaluation and management of screen-detected lung nodules, the American College of Radiology (ACR) developed the Lung Imaging Reporting and Data System (Lung-RADS) to be used in LCS CT reports. The latest revised version 1.1 of Lung-RADS was released in 2019. The Lung-RADS defines a positive screen and provides accepted nodule care pathways depending on their size, characteristics, and additional findings, and has been shown to decrease the rate of false-positive results in LCS. To be a designated LCS center, the department of radiology must comply with stringent requirements of technical and facility specification, with radiologist qualification, and with reporting and communication as outlined by the ACR. In addition, participation in the National LCS Registry to meet CMS quality reporting requirements is mandatory for facilities to be reimbursed by CMS.
After more than 10 years since its inception, the participation in LCS has been low. Out of 8 million eligible Americans, less than 4% have been screened (American Cancer Society, NSCLC statistics 2020) compared with breast cancer (up to 75%) (Breast Cancer: Facts and Figures 2019-2020). Adherence to annual LCS between 1-3 years in the US is only about 55%. Non-White patients, current smokers, those aged 65-73 years, and those who lack a college education are most likely to be less adherent to follow-up screening. There are hurdles at multiple levels including but not limited to patient and physician awareness, patient enrollment, adherence, follow-up, and insurance coverage. Expanding the reach of LCS in socially and economically disadvantaged, racial and ethnic minorities, and women has been even more challenging.
Significant differences exist in opinions and practices between primary care physicians (PCPs) and pulmonologists regarding referral for LCS and its benefits. Educational intervention at the PCP level aimed at awareness of USPSTF guidelines may improve utilization and adherence to screening. Increasing lung cancer awareness by community outreach programs, promoting related discussions, and providing information about available screening services to eligible population is crucial to derive the maximum benefits of LCS. Presenting decision aid tools on smartphones and online has shown to improve the participants’ knowledge of LCS, to reduce the decisional conflict, and to be acceptable among patients and providers. Implementation strategies such as involving a nonphysician provider, keeping the training on these tools brief and simple, and providing it to participants prior to the clinical encounter might be effective. Electronic medical record systems can be optimized to simplify the ordering procedure to ensure the eligibility criteria are met, to provide results to the physicians, and to direct further management of positive screen results. Most LCS programs have a nonphysician program coordinator to convey the results to the patients and physician, to send out reminders for scheduled follow up appointment, and to maintain the registry data.
In the future, newer imaging technology, and molecular biomarkers or other technologies to differentiate lung cancer more accurately from a benign nodule, and to determine its aggressiveness, will supplement the LCS to decrease false positive results. Better risk prediction models will influence screening eligibility and prognostication in a screen-detected cancer. Robust data collection from ongoing clinical programs will determine if the benefits of LCS seen in clinical trials are comparable when applied to diverse community settings.
Dr. Stowell and Dr. Sonavane are with the Mayo Clinic in Jacksonville, Fla.
Lung cancer is the second-most common cancer and one of the leading causes of mortality in the United States among both men and women. It accounts for almost 25% of all cancer deaths, and every year more people die of lung cancer than colon, breast, and prostate cancers combined. The American Cancer Society estimates about 235,760 new lung cancer cases and about 131,880 deaths from lung cancer in 2021.
Smoking and increasing age are the two most important risk factors for lung cancer. Lung cancer has a higher incidence among Black men than White men, and among White women compared with Black women. These differences are likely related to smoking exposure. Early diagnosis of lung cancer can improve survival, and hence screening for lung cancer in high-risk populations is desired. Among the available cancer screening tests, radiology is primarily involved in breast and lung cancer screening (LCS). In 2011, the National Lung Screening Trial (NLST) showed a benefit of annual low- dose chest CT for LCS, with about 20% reduction in lung cancer-related mortality in high-risk participants compared with chest radiographs (Aberle DR, et al. N Engl J Med. 2011 Aug 4;365[5]:395-409).
In 2013, the United States Preventative Services Task Force (USPSTF) issued a grade B recommendation in support of annual LCS by CT scan for individuals between the ages of 55-80 years with smoking history of 30 or more pack-years who are current smokers or had quit smoking in the last 15 years. Many other professional societies followed with their own recommendations with minor differences. In 2015, after the Centers for Medicare and Medicaid (CMS) decision of coverage, millions of Americans at high risk became eligible for CT LCS with no copayment or cost sharing by the patient.
The results from the European NELSON trial in 2020 augmented the NLST data showing a 24% decrease in lung cancer mortality. Nodules were measured using volume and volume doubling time rather than bidimensional axial measurements, reducing the false-positive results to 56% compared with 96% in NLST. With growing evidence of the benefits from LCS, recently USPSTF summarized with moderate certainty that annual LCS CT has moderate net benefit in people at high risk for lung cancer based on age, cumulative smoking exposure, and years since quitting smoking.
In March 2021, USPSTF has issued new recommendations with a decrease in the screening age to 50 years, and the smoking history that triggers screening to 20 pack-years (Screening for Lung Cancer: USPSTF Statement. JAMA. 2021 Mar 9;325[10]:962-70. doi: 10.1001/jama.2021.1117). These expanded eligibility criteria are projected to double the number of eligible candidates of LCS in the United States, reduce annual deaths by up to 50%, and benefit minorities and women. By widening the screening criteria to include younger individuals and who have smoked less tobacco, more lives will be saved by early detection of lung cancer. Since the NLST and NELSON trials enrolled relatively healthy people, USPSTF recommends discontinuation of screening once the person has not smoked for 15 years and in persons with any health problem that severely limits the life expectancy or the ability or willingness to undergo surgery. All screening programs must incorporate smoking cessation counseling and interventions for all the enrolled individuals who are current smokers. The USPSTF has also made recommendations on interventions to prevent the initiation of tobacco use in children and adolescents, including counseling and pharmacotherapy.
The decision to undergo LCS is inherently complex, and primary care and pulmonary physicians play a pivotal role by identifying the eligible patients, participating in shared decision-making (SDM), offering smoking cessation, ordering the CT, and managing follow-up. SDM between the patient and clinician includes a discussion of the benefits, risks, limitations, and potential harms of screening. The potential harms of screening include overdiagnosis, false-positive results, incidental findings, and the anxiety leading to further testing or follow-up. The risk of radiation exposure is markedly reduced using low-dose CT protocols compared with conventional chest CT. SDM visit also emphasizes the importance of adherence to annual screening and patient willingness and ability to undergo treatment if required. In 2015, CMS approved the addition of LCS counseling and SDM visits that are performed by physicians or qualified nonphysician practitioners (physician assistant, nurse practitioner, or clinical nurse specialist). Studies have shown that these visits improve the screening uptake rate.
To minimize the variations in the evaluation and management of screen-detected lung nodules, the American College of Radiology (ACR) developed the Lung Imaging Reporting and Data System (Lung-RADS) to be used in LCS CT reports. The latest revised version 1.1 of Lung-RADS was released in 2019. The Lung-RADS defines a positive screen and provides accepted nodule care pathways depending on their size, characteristics, and additional findings, and has been shown to decrease the rate of false-positive results in LCS. To be a designated LCS center, the department of radiology must comply with stringent requirements of technical and facility specification, with radiologist qualification, and with reporting and communication as outlined by the ACR. In addition, participation in the National LCS Registry to meet CMS quality reporting requirements is mandatory for facilities to be reimbursed by CMS.
After more than 10 years since its inception, the participation in LCS has been low. Out of 8 million eligible Americans, less than 4% have been screened (American Cancer Society, NSCLC statistics 2020) compared with breast cancer (up to 75%) (Breast Cancer: Facts and Figures 2019-2020). Adherence to annual LCS between 1-3 years in the US is only about 55%. Non-White patients, current smokers, those aged 65-73 years, and those who lack a college education are most likely to be less adherent to follow-up screening. There are hurdles at multiple levels including but not limited to patient and physician awareness, patient enrollment, adherence, follow-up, and insurance coverage. Expanding the reach of LCS in socially and economically disadvantaged, racial and ethnic minorities, and women has been even more challenging.
Significant differences exist in opinions and practices between primary care physicians (PCPs) and pulmonologists regarding referral for LCS and its benefits. Educational intervention at the PCP level aimed at awareness of USPSTF guidelines may improve utilization and adherence to screening. Increasing lung cancer awareness by community outreach programs, promoting related discussions, and providing information about available screening services to eligible population is crucial to derive the maximum benefits of LCS. Presenting decision aid tools on smartphones and online has shown to improve the participants’ knowledge of LCS, to reduce the decisional conflict, and to be acceptable among patients and providers. Implementation strategies such as involving a nonphysician provider, keeping the training on these tools brief and simple, and providing it to participants prior to the clinical encounter might be effective. Electronic medical record systems can be optimized to simplify the ordering procedure to ensure the eligibility criteria are met, to provide results to the physicians, and to direct further management of positive screen results. Most LCS programs have a nonphysician program coordinator to convey the results to the patients and physician, to send out reminders for scheduled follow up appointment, and to maintain the registry data.
In the future, newer imaging technology, and molecular biomarkers or other technologies to differentiate lung cancer more accurately from a benign nodule, and to determine its aggressiveness, will supplement the LCS to decrease false positive results. Better risk prediction models will influence screening eligibility and prognostication in a screen-detected cancer. Robust data collection from ongoing clinical programs will determine if the benefits of LCS seen in clinical trials are comparable when applied to diverse community settings.
Dr. Stowell and Dr. Sonavane are with the Mayo Clinic in Jacksonville, Fla.
Lung cancer is the second-most common cancer and one of the leading causes of mortality in the United States among both men and women. It accounts for almost 25% of all cancer deaths, and every year more people die of lung cancer than colon, breast, and prostate cancers combined. The American Cancer Society estimates about 235,760 new lung cancer cases and about 131,880 deaths from lung cancer in 2021.
Smoking and increasing age are the two most important risk factors for lung cancer. Lung cancer has a higher incidence among Black men than White men, and among White women compared with Black women. These differences are likely related to smoking exposure. Early diagnosis of lung cancer can improve survival, and hence screening for lung cancer in high-risk populations is desired. Among the available cancer screening tests, radiology is primarily involved in breast and lung cancer screening (LCS). In 2011, the National Lung Screening Trial (NLST) showed a benefit of annual low- dose chest CT for LCS, with about 20% reduction in lung cancer-related mortality in high-risk participants compared with chest radiographs (Aberle DR, et al. N Engl J Med. 2011 Aug 4;365[5]:395-409).
In 2013, the United States Preventative Services Task Force (USPSTF) issued a grade B recommendation in support of annual LCS by CT scan for individuals between the ages of 55-80 years with smoking history of 30 or more pack-years who are current smokers or had quit smoking in the last 15 years. Many other professional societies followed with their own recommendations with minor differences. In 2015, after the Centers for Medicare and Medicaid (CMS) decision of coverage, millions of Americans at high risk became eligible for CT LCS with no copayment or cost sharing by the patient.
The results from the European NELSON trial in 2020 augmented the NLST data showing a 24% decrease in lung cancer mortality. Nodules were measured using volume and volume doubling time rather than bidimensional axial measurements, reducing the false-positive results to 56% compared with 96% in NLST. With growing evidence of the benefits from LCS, recently USPSTF summarized with moderate certainty that annual LCS CT has moderate net benefit in people at high risk for lung cancer based on age, cumulative smoking exposure, and years since quitting smoking.
In March 2021, USPSTF has issued new recommendations with a decrease in the screening age to 50 years, and the smoking history that triggers screening to 20 pack-years (Screening for Lung Cancer: USPSTF Statement. JAMA. 2021 Mar 9;325[10]:962-70. doi: 10.1001/jama.2021.1117). These expanded eligibility criteria are projected to double the number of eligible candidates of LCS in the United States, reduce annual deaths by up to 50%, and benefit minorities and women. By widening the screening criteria to include younger individuals and who have smoked less tobacco, more lives will be saved by early detection of lung cancer. Since the NLST and NELSON trials enrolled relatively healthy people, USPSTF recommends discontinuation of screening once the person has not smoked for 15 years and in persons with any health problem that severely limits the life expectancy or the ability or willingness to undergo surgery. All screening programs must incorporate smoking cessation counseling and interventions for all the enrolled individuals who are current smokers. The USPSTF has also made recommendations on interventions to prevent the initiation of tobacco use in children and adolescents, including counseling and pharmacotherapy.
The decision to undergo LCS is inherently complex, and primary care and pulmonary physicians play a pivotal role by identifying the eligible patients, participating in shared decision-making (SDM), offering smoking cessation, ordering the CT, and managing follow-up. SDM between the patient and clinician includes a discussion of the benefits, risks, limitations, and potential harms of screening. The potential harms of screening include overdiagnosis, false-positive results, incidental findings, and the anxiety leading to further testing or follow-up. The risk of radiation exposure is markedly reduced using low-dose CT protocols compared with conventional chest CT. SDM visit also emphasizes the importance of adherence to annual screening and patient willingness and ability to undergo treatment if required. In 2015, CMS approved the addition of LCS counseling and SDM visits that are performed by physicians or qualified nonphysician practitioners (physician assistant, nurse practitioner, or clinical nurse specialist). Studies have shown that these visits improve the screening uptake rate.
To minimize the variations in the evaluation and management of screen-detected lung nodules, the American College of Radiology (ACR) developed the Lung Imaging Reporting and Data System (Lung-RADS) to be used in LCS CT reports. The latest revised version 1.1 of Lung-RADS was released in 2019. The Lung-RADS defines a positive screen and provides accepted nodule care pathways depending on their size, characteristics, and additional findings, and has been shown to decrease the rate of false-positive results in LCS. To be a designated LCS center, the department of radiology must comply with stringent requirements of technical and facility specification, with radiologist qualification, and with reporting and communication as outlined by the ACR. In addition, participation in the National LCS Registry to meet CMS quality reporting requirements is mandatory for facilities to be reimbursed by CMS.
After more than 10 years since its inception, the participation in LCS has been low. Out of 8 million eligible Americans, less than 4% have been screened (American Cancer Society, NSCLC statistics 2020) compared with breast cancer (up to 75%) (Breast Cancer: Facts and Figures 2019-2020). Adherence to annual LCS between 1-3 years in the US is only about 55%. Non-White patients, current smokers, those aged 65-73 years, and those who lack a college education are most likely to be less adherent to follow-up screening. There are hurdles at multiple levels including but not limited to patient and physician awareness, patient enrollment, adherence, follow-up, and insurance coverage. Expanding the reach of LCS in socially and economically disadvantaged, racial and ethnic minorities, and women has been even more challenging.
Significant differences exist in opinions and practices between primary care physicians (PCPs) and pulmonologists regarding referral for LCS and its benefits. Educational intervention at the PCP level aimed at awareness of USPSTF guidelines may improve utilization and adherence to screening. Increasing lung cancer awareness by community outreach programs, promoting related discussions, and providing information about available screening services to eligible population is crucial to derive the maximum benefits of LCS. Presenting decision aid tools on smartphones and online has shown to improve the participants’ knowledge of LCS, to reduce the decisional conflict, and to be acceptable among patients and providers. Implementation strategies such as involving a nonphysician provider, keeping the training on these tools brief and simple, and providing it to participants prior to the clinical encounter might be effective. Electronic medical record systems can be optimized to simplify the ordering procedure to ensure the eligibility criteria are met, to provide results to the physicians, and to direct further management of positive screen results. Most LCS programs have a nonphysician program coordinator to convey the results to the patients and physician, to send out reminders for scheduled follow up appointment, and to maintain the registry data.
In the future, newer imaging technology, and molecular biomarkers or other technologies to differentiate lung cancer more accurately from a benign nodule, and to determine its aggressiveness, will supplement the LCS to decrease false positive results. Better risk prediction models will influence screening eligibility and prognostication in a screen-detected cancer. Robust data collection from ongoing clinical programs will determine if the benefits of LCS seen in clinical trials are comparable when applied to diverse community settings.
Dr. Stowell and Dr. Sonavane are with the Mayo Clinic in Jacksonville, Fla.
CHEST 2021 safety efforts – everyone has a role
Over the past year, you’ve had to adapt to Zoom calls and socially distanced learning. It’s time to come back together, face-to-face, for our top-tier learning event in sunny Orlando, Florida.
Grab your sunscreen and book your flights – we’re ready to welcome you back to CHEST 2021 with team-focused learning sessions, immersive gaming opportunities, expert-led faculty presentations, and more. We are making the meeting as safe as possible so you can attend in person.
After careful planning, we are excited to be able at the Orange County Convention Center (OCCC) for CHEST 2021. Health and safety are our biggest concerns for the meeting, which is why we chose this location. The convention center features the extra square footage we needed to design a meeting space with ample room for social distancing.
We are committed to create a meeting experience where you can safely and effectively conduct business, network with colleagues, and experience high-quality education. With your feedback, we have implemented COVID-19 safety measures similar to what is used in your hospitals and facilities. To ensure your health and safety, there will be a few requirements asked of in-person attendees.
Preparing for CHEST 2021
As the pandemic continues and vaccines are more readily available, we are requiring all attendees – participants, vendors, and staff – to be vaccinated to attend in person in Orlando, Florida. Your second vaccination shot should take place at least 2 weeks prior to the conference start. When you complete your registration information, you will be asked to attest that you have or will have completed an FDA-approved vaccination for COVID-19 by October 17, 2021.
We also suggest scheduling extra time at your arrival to the conference site. Realize that registration, lunch lines, hotel check-in, etc, may take longer as we navigate a new way to meet in person. This year, registration will be contactless. Have your digital or print confirmation ready when you arrive – the more prepared you are, the faster registration will be.
While the venue will regularly sanitize all high touch points in the public space throughout the day, remember to pack any personal supplies you may need for individual use, especially masks. Attendees will be required to wear a mask covering the mouth and nose at all times during the meeting. There will be masks on-site in case you forget or misplace your own.
Before making your way to Orlando, complete one last health self-assessment. Are you symptom free? Consider what advice you would give your patient if they felt the way you do in that moment. When in doubt, stay home and join us online. That’s one of the benefits of CHEST 2021.
Keeping safe while experiencing CHEST 2021
Any time you are in the conference center and the Hilton Hotel, the no-contact policy is applicable. Greet your colleagues and new friends using elbow bumps, waves, and any other form of contactless gestures. We will save our handshakes and hugs for CHEST 2022!
By attending in person, you are also agreeing to perform a health status self-check every day for any onset of COVID symptoms as defined by the CDC. If you are feeling ill, immediately notify the first aid office at the meeting.
Help us deliver a high-quality experience with the lowest reasonable risk in a manner that protects us all by complying to these health and safety measures. In addition, the layout and schedule of the conference is being designed to allow time for cleaning spaces between sessions. This means more time to get to your next location, visit the exhibit hall, or spend with your colleagues.
Our commitment to your safety
CHEST is taking extra precautions to keep you safe too – it’s not just on you! Daily temperature screenings will be conducted upon entry to the convention center and Hilton Orlando for everyone.
During the meeting, floor graphics will be used to outline 6-ft social distancing. In the concession areas, seating will be properly distanced and transparent shields will be in place. The exhibit hall will have extra wide aisles, which are not only safe, but easier to move through.
Public space and public restrooms are monitored by OCCC Environmental Services. They conduct sanitizing tasks within the restroom banks throughout the day and a thorough cleaning overnight. They also regularly sanitize all high touch points in the public space throughout the day as well; ie, door handles, ATMs, escalator handrails, elevator buttons, etc.
Staff and security have been increased to provide the best customer service and information accessibility to all in-person attendees. Medical personnel will also be present on site and available to help individuals who are feeling unwell.
It’s been a long year apart from our CHEST community. We can’t wait to see you in Orlando, Florida, October 17-20, for the high-quality education you expect.
Over the past year, you’ve had to adapt to Zoom calls and socially distanced learning. It’s time to come back together, face-to-face, for our top-tier learning event in sunny Orlando, Florida.
Grab your sunscreen and book your flights – we’re ready to welcome you back to CHEST 2021 with team-focused learning sessions, immersive gaming opportunities, expert-led faculty presentations, and more. We are making the meeting as safe as possible so you can attend in person.
After careful planning, we are excited to be able at the Orange County Convention Center (OCCC) for CHEST 2021. Health and safety are our biggest concerns for the meeting, which is why we chose this location. The convention center features the extra square footage we needed to design a meeting space with ample room for social distancing.
We are committed to create a meeting experience where you can safely and effectively conduct business, network with colleagues, and experience high-quality education. With your feedback, we have implemented COVID-19 safety measures similar to what is used in your hospitals and facilities. To ensure your health and safety, there will be a few requirements asked of in-person attendees.
Preparing for CHEST 2021
As the pandemic continues and vaccines are more readily available, we are requiring all attendees – participants, vendors, and staff – to be vaccinated to attend in person in Orlando, Florida. Your second vaccination shot should take place at least 2 weeks prior to the conference start. When you complete your registration information, you will be asked to attest that you have or will have completed an FDA-approved vaccination for COVID-19 by October 17, 2021.
We also suggest scheduling extra time at your arrival to the conference site. Realize that registration, lunch lines, hotel check-in, etc, may take longer as we navigate a new way to meet in person. This year, registration will be contactless. Have your digital or print confirmation ready when you arrive – the more prepared you are, the faster registration will be.
While the venue will regularly sanitize all high touch points in the public space throughout the day, remember to pack any personal supplies you may need for individual use, especially masks. Attendees will be required to wear a mask covering the mouth and nose at all times during the meeting. There will be masks on-site in case you forget or misplace your own.
Before making your way to Orlando, complete one last health self-assessment. Are you symptom free? Consider what advice you would give your patient if they felt the way you do in that moment. When in doubt, stay home and join us online. That’s one of the benefits of CHEST 2021.
Keeping safe while experiencing CHEST 2021
Any time you are in the conference center and the Hilton Hotel, the no-contact policy is applicable. Greet your colleagues and new friends using elbow bumps, waves, and any other form of contactless gestures. We will save our handshakes and hugs for CHEST 2022!
By attending in person, you are also agreeing to perform a health status self-check every day for any onset of COVID symptoms as defined by the CDC. If you are feeling ill, immediately notify the first aid office at the meeting.
Help us deliver a high-quality experience with the lowest reasonable risk in a manner that protects us all by complying to these health and safety measures. In addition, the layout and schedule of the conference is being designed to allow time for cleaning spaces between sessions. This means more time to get to your next location, visit the exhibit hall, or spend with your colleagues.
Our commitment to your safety
CHEST is taking extra precautions to keep you safe too – it’s not just on you! Daily temperature screenings will be conducted upon entry to the convention center and Hilton Orlando for everyone.
During the meeting, floor graphics will be used to outline 6-ft social distancing. In the concession areas, seating will be properly distanced and transparent shields will be in place. The exhibit hall will have extra wide aisles, which are not only safe, but easier to move through.
Public space and public restrooms are monitored by OCCC Environmental Services. They conduct sanitizing tasks within the restroom banks throughout the day and a thorough cleaning overnight. They also regularly sanitize all high touch points in the public space throughout the day as well; ie, door handles, ATMs, escalator handrails, elevator buttons, etc.
Staff and security have been increased to provide the best customer service and information accessibility to all in-person attendees. Medical personnel will also be present on site and available to help individuals who are feeling unwell.
It’s been a long year apart from our CHEST community. We can’t wait to see you in Orlando, Florida, October 17-20, for the high-quality education you expect.
Over the past year, you’ve had to adapt to Zoom calls and socially distanced learning. It’s time to come back together, face-to-face, for our top-tier learning event in sunny Orlando, Florida.
Grab your sunscreen and book your flights – we’re ready to welcome you back to CHEST 2021 with team-focused learning sessions, immersive gaming opportunities, expert-led faculty presentations, and more. We are making the meeting as safe as possible so you can attend in person.
After careful planning, we are excited to be able at the Orange County Convention Center (OCCC) for CHEST 2021. Health and safety are our biggest concerns for the meeting, which is why we chose this location. The convention center features the extra square footage we needed to design a meeting space with ample room for social distancing.
We are committed to create a meeting experience where you can safely and effectively conduct business, network with colleagues, and experience high-quality education. With your feedback, we have implemented COVID-19 safety measures similar to what is used in your hospitals and facilities. To ensure your health and safety, there will be a few requirements asked of in-person attendees.
Preparing for CHEST 2021
As the pandemic continues and vaccines are more readily available, we are requiring all attendees – participants, vendors, and staff – to be vaccinated to attend in person in Orlando, Florida. Your second vaccination shot should take place at least 2 weeks prior to the conference start. When you complete your registration information, you will be asked to attest that you have or will have completed an FDA-approved vaccination for COVID-19 by October 17, 2021.
We also suggest scheduling extra time at your arrival to the conference site. Realize that registration, lunch lines, hotel check-in, etc, may take longer as we navigate a new way to meet in person. This year, registration will be contactless. Have your digital or print confirmation ready when you arrive – the more prepared you are, the faster registration will be.
While the venue will regularly sanitize all high touch points in the public space throughout the day, remember to pack any personal supplies you may need for individual use, especially masks. Attendees will be required to wear a mask covering the mouth and nose at all times during the meeting. There will be masks on-site in case you forget or misplace your own.
Before making your way to Orlando, complete one last health self-assessment. Are you symptom free? Consider what advice you would give your patient if they felt the way you do in that moment. When in doubt, stay home and join us online. That’s one of the benefits of CHEST 2021.
Keeping safe while experiencing CHEST 2021
Any time you are in the conference center and the Hilton Hotel, the no-contact policy is applicable. Greet your colleagues and new friends using elbow bumps, waves, and any other form of contactless gestures. We will save our handshakes and hugs for CHEST 2022!
By attending in person, you are also agreeing to perform a health status self-check every day for any onset of COVID symptoms as defined by the CDC. If you are feeling ill, immediately notify the first aid office at the meeting.
Help us deliver a high-quality experience with the lowest reasonable risk in a manner that protects us all by complying to these health and safety measures. In addition, the layout and schedule of the conference is being designed to allow time for cleaning spaces between sessions. This means more time to get to your next location, visit the exhibit hall, or spend with your colleagues.
Our commitment to your safety
CHEST is taking extra precautions to keep you safe too – it’s not just on you! Daily temperature screenings will be conducted upon entry to the convention center and Hilton Orlando for everyone.
During the meeting, floor graphics will be used to outline 6-ft social distancing. In the concession areas, seating will be properly distanced and transparent shields will be in place. The exhibit hall will have extra wide aisles, which are not only safe, but easier to move through.
Public space and public restrooms are monitored by OCCC Environmental Services. They conduct sanitizing tasks within the restroom banks throughout the day and a thorough cleaning overnight. They also regularly sanitize all high touch points in the public space throughout the day as well; ie, door handles, ATMs, escalator handrails, elevator buttons, etc.
Staff and security have been increased to provide the best customer service and information accessibility to all in-person attendees. Medical personnel will also be present on site and available to help individuals who are feeling unwell.
It’s been a long year apart from our CHEST community. We can’t wait to see you in Orlando, Florida, October 17-20, for the high-quality education you expect.
CHEST Health Policy and Advocacy Committee perspective on the FDA’s announcement of prohibiting menthol cigarettes and flavored cigars
The recently announced ruling by the FDA to ban menthol in tobacco products is a large step forward toward abolishing tobacco-related disease and death. It is also a big step forward to abolishing the institutional racism of the tobacco industry, which has targeted Black communities with menthol cigarettes for decades, and a step toward improving health equity. Although tobacco use across the United States has decreased from 45% of adults smoking in the 1950s to only 14% smoking today, tobacco continues to be the leading cause of preventable disease and death. Critically, some populations have not seen reductions in tobacco use that benefited others, namely communities of color, low-income populations and LGBTQ+ individuals. A key to this health disparity is the preference for menthol-flavored tobacco products by these groups. Menthol within cigarettes and cigars masks the unpleasant smell of tobacco and numbs the airways to irritation caused by tobacco smoke, while amplifying the effects of nicotine. Eighteen million people smoke menthol cigarettes, with 85% of Black smokers using menthol cigarettes – tobacco ends 45,000 Black lives every year, and menthol is the primary driver of over 38,000 of these Black deaths.
The data supporting a menthol ban has been strong for years. It is well known that flavors, like menthol, increase the appeal of tobacco and increase initiation of tobacco use by women, children, young adults, people of color, low-income, and LGBTQ+ communities. Menthol in particular increases the addictive potential of tobacco and makes it harder for menthol smokers to quit. The evidence behind banning menthol across tobacco products and flavored cigars to protect our children and young adults is also strong. Half of adolescents who try tobacco choose menthol-flavored products; 74% of teenagers aged 14-17 who smoke cigars say they do so because they enjoy the flavors.
There are many reasons why we as pulmonary and critical care medicine physicians are excited about this recent FDA ruling. The most important of which is that this rule is an important step toward advancing health equity in our country. Banning menthol-flavored tobacco products will save lives, including those of thousands of Black Americans. Banning menthol will reduce tobacco addiction, diminish youth experimentation and youth initiation of tobacco use, and increase the ability of tobacco smokers to successfully quit.
While celebrating this incredible win against the racist institution that is Big Tobacco, we must acknowledge the hard work of those who made it happen: the African American Tobacco Control Leadership Council, Center for Black Health & Equity, Campaign for Tobacco-Free Kids, American Medical Association, and many others. It is extremely exciting that menthol cigarettes, which are responsible for 10,000 deaths per year and >265,000 new smokers per year since 1980 (Le TT and Mendez D, Tob Control. 2021 Feb 25. doi: 10.1136/tobaccocontrol-2020-056256).
will soon be a thing of the past. Next on the CHEST Health Policy and Advocacy Committee (HPAC) to-do list? Ensuring that the menthol ban is extended to e-cigarettes, another tobacco product that targets Americans of all kinds. Finally, we must continue the fight to end tobacco-related disease and death across the country and across the world by helping our patients with smoking cessation efforts and by working to prevent initiation of tobacco use (including e-cigarettes and other vaping devices) by children, at-risk individuals, and communities of all kinds.
Laura E. Crotty Alexander, MD, is with UC San Diego and the VA San Diego Healthcare System.
The recently announced ruling by the FDA to ban menthol in tobacco products is a large step forward toward abolishing tobacco-related disease and death. It is also a big step forward to abolishing the institutional racism of the tobacco industry, which has targeted Black communities with menthol cigarettes for decades, and a step toward improving health equity. Although tobacco use across the United States has decreased from 45% of adults smoking in the 1950s to only 14% smoking today, tobacco continues to be the leading cause of preventable disease and death. Critically, some populations have not seen reductions in tobacco use that benefited others, namely communities of color, low-income populations and LGBTQ+ individuals. A key to this health disparity is the preference for menthol-flavored tobacco products by these groups. Menthol within cigarettes and cigars masks the unpleasant smell of tobacco and numbs the airways to irritation caused by tobacco smoke, while amplifying the effects of nicotine. Eighteen million people smoke menthol cigarettes, with 85% of Black smokers using menthol cigarettes – tobacco ends 45,000 Black lives every year, and menthol is the primary driver of over 38,000 of these Black deaths.
The data supporting a menthol ban has been strong for years. It is well known that flavors, like menthol, increase the appeal of tobacco and increase initiation of tobacco use by women, children, young adults, people of color, low-income, and LGBTQ+ communities. Menthol in particular increases the addictive potential of tobacco and makes it harder for menthol smokers to quit. The evidence behind banning menthol across tobacco products and flavored cigars to protect our children and young adults is also strong. Half of adolescents who try tobacco choose menthol-flavored products; 74% of teenagers aged 14-17 who smoke cigars say they do so because they enjoy the flavors.
There are many reasons why we as pulmonary and critical care medicine physicians are excited about this recent FDA ruling. The most important of which is that this rule is an important step toward advancing health equity in our country. Banning menthol-flavored tobacco products will save lives, including those of thousands of Black Americans. Banning menthol will reduce tobacco addiction, diminish youth experimentation and youth initiation of tobacco use, and increase the ability of tobacco smokers to successfully quit.
While celebrating this incredible win against the racist institution that is Big Tobacco, we must acknowledge the hard work of those who made it happen: the African American Tobacco Control Leadership Council, Center for Black Health & Equity, Campaign for Tobacco-Free Kids, American Medical Association, and many others. It is extremely exciting that menthol cigarettes, which are responsible for 10,000 deaths per year and >265,000 new smokers per year since 1980 (Le TT and Mendez D, Tob Control. 2021 Feb 25. doi: 10.1136/tobaccocontrol-2020-056256).
will soon be a thing of the past. Next on the CHEST Health Policy and Advocacy Committee (HPAC) to-do list? Ensuring that the menthol ban is extended to e-cigarettes, another tobacco product that targets Americans of all kinds. Finally, we must continue the fight to end tobacco-related disease and death across the country and across the world by helping our patients with smoking cessation efforts and by working to prevent initiation of tobacco use (including e-cigarettes and other vaping devices) by children, at-risk individuals, and communities of all kinds.
Laura E. Crotty Alexander, MD, is with UC San Diego and the VA San Diego Healthcare System.
The recently announced ruling by the FDA to ban menthol in tobacco products is a large step forward toward abolishing tobacco-related disease and death. It is also a big step forward to abolishing the institutional racism of the tobacco industry, which has targeted Black communities with menthol cigarettes for decades, and a step toward improving health equity. Although tobacco use across the United States has decreased from 45% of adults smoking in the 1950s to only 14% smoking today, tobacco continues to be the leading cause of preventable disease and death. Critically, some populations have not seen reductions in tobacco use that benefited others, namely communities of color, low-income populations and LGBTQ+ individuals. A key to this health disparity is the preference for menthol-flavored tobacco products by these groups. Menthol within cigarettes and cigars masks the unpleasant smell of tobacco and numbs the airways to irritation caused by tobacco smoke, while amplifying the effects of nicotine. Eighteen million people smoke menthol cigarettes, with 85% of Black smokers using menthol cigarettes – tobacco ends 45,000 Black lives every year, and menthol is the primary driver of over 38,000 of these Black deaths.
The data supporting a menthol ban has been strong for years. It is well known that flavors, like menthol, increase the appeal of tobacco and increase initiation of tobacco use by women, children, young adults, people of color, low-income, and LGBTQ+ communities. Menthol in particular increases the addictive potential of tobacco and makes it harder for menthol smokers to quit. The evidence behind banning menthol across tobacco products and flavored cigars to protect our children and young adults is also strong. Half of adolescents who try tobacco choose menthol-flavored products; 74% of teenagers aged 14-17 who smoke cigars say they do so because they enjoy the flavors.
There are many reasons why we as pulmonary and critical care medicine physicians are excited about this recent FDA ruling. The most important of which is that this rule is an important step toward advancing health equity in our country. Banning menthol-flavored tobacco products will save lives, including those of thousands of Black Americans. Banning menthol will reduce tobacco addiction, diminish youth experimentation and youth initiation of tobacco use, and increase the ability of tobacco smokers to successfully quit.
While celebrating this incredible win against the racist institution that is Big Tobacco, we must acknowledge the hard work of those who made it happen: the African American Tobacco Control Leadership Council, Center for Black Health & Equity, Campaign for Tobacco-Free Kids, American Medical Association, and many others. It is extremely exciting that menthol cigarettes, which are responsible for 10,000 deaths per year and >265,000 new smokers per year since 1980 (Le TT and Mendez D, Tob Control. 2021 Feb 25. doi: 10.1136/tobaccocontrol-2020-056256).
will soon be a thing of the past. Next on the CHEST Health Policy and Advocacy Committee (HPAC) to-do list? Ensuring that the menthol ban is extended to e-cigarettes, another tobacco product that targets Americans of all kinds. Finally, we must continue the fight to end tobacco-related disease and death across the country and across the world by helping our patients with smoking cessation efforts and by working to prevent initiation of tobacco use (including e-cigarettes and other vaping devices) by children, at-risk individuals, and communities of all kinds.
Laura E. Crotty Alexander, MD, is with UC San Diego and the VA San Diego Healthcare System.
This month in the journal CHEST®
Editor’s picks
1. POINT: Is It Ethically Permissible to Unilaterally Withdraw Life-Sustaining Treatments During Crisis Standards of Care? YesBy Dr. J. Bishop and Dr. J. Eberl
2. COUNTERPOINT: Is It Ethically Permissible to Unilaterally Withdraw Life-Sustaining Treatments for Reallocation During Crisis Standards of Care? NoBy Dr. D. Sulmasy and Dr. F. Maldonado
3. National Trends and Disparities in Health-Care Access and Coverage Among Adults With Asthma and COPD: 1997-2018By Dr. A. Gaffney, et al.
4. Geographic Variation in Racial Disparities in Mortality From Influenza and Pneumonia in the United States in the Pre-Coronavirus Disease 2019 EraBy Dr. S. Donaldson, et al.
5. Palliative Care Needs and Integration of Palliative Care Support in COPD: A Qualitative StudyBy Dr. F. Yu, et al.
6. How I Do It: Building Teams in Health CareBy. Dr. J. Stoller
Editor’s picks
Editor’s picks
1. POINT: Is It Ethically Permissible to Unilaterally Withdraw Life-Sustaining Treatments During Crisis Standards of Care? YesBy Dr. J. Bishop and Dr. J. Eberl
2. COUNTERPOINT: Is It Ethically Permissible to Unilaterally Withdraw Life-Sustaining Treatments for Reallocation During Crisis Standards of Care? NoBy Dr. D. Sulmasy and Dr. F. Maldonado
3. National Trends and Disparities in Health-Care Access and Coverage Among Adults With Asthma and COPD: 1997-2018By Dr. A. Gaffney, et al.
4. Geographic Variation in Racial Disparities in Mortality From Influenza and Pneumonia in the United States in the Pre-Coronavirus Disease 2019 EraBy Dr. S. Donaldson, et al.
5. Palliative Care Needs and Integration of Palliative Care Support in COPD: A Qualitative StudyBy Dr. F. Yu, et al.
6. How I Do It: Building Teams in Health CareBy. Dr. J. Stoller
1. POINT: Is It Ethically Permissible to Unilaterally Withdraw Life-Sustaining Treatments During Crisis Standards of Care? YesBy Dr. J. Bishop and Dr. J. Eberl
2. COUNTERPOINT: Is It Ethically Permissible to Unilaterally Withdraw Life-Sustaining Treatments for Reallocation During Crisis Standards of Care? NoBy Dr. D. Sulmasy and Dr. F. Maldonado
3. National Trends and Disparities in Health-Care Access and Coverage Among Adults With Asthma and COPD: 1997-2018By Dr. A. Gaffney, et al.
4. Geographic Variation in Racial Disparities in Mortality From Influenza and Pneumonia in the United States in the Pre-Coronavirus Disease 2019 EraBy Dr. S. Donaldson, et al.
5. Palliative Care Needs and Integration of Palliative Care Support in COPD: A Qualitative StudyBy Dr. F. Yu, et al.
6. How I Do It: Building Teams in Health CareBy. Dr. J. Stoller
Under new administration, best time to lobby for health care may be now
The ambitious infrastructure bill now being debated in the US Congress might be one of the best immediate opportunities to lobby for legislative or policy changes in delivery of health care during the current Biden administration, according to an analysis delivered at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
The infrastructure bill is likely to be pushed forward in the filibuster-proof reconciliation process, which means “that some things might get passed that otherwise would not,” explained Keith S. Studdard, Vice President, Jeffrey J. Kimbell & Associates, Washington, DC.
With few exceptions, the key players in the health care team of President Joe Biden’s new administration are in place, according to Mr. Studdard, who is a lobbyist and health care expert. By moving quickly to fill key positions, the new administration “got off to a good start” for a health care agenda that Mr. Studdard believes will be a focus of the Biden presidency. There is some degree of urgency.
“The amount of time [the Biden administration has] to get their agenda through is fairly limited,” Mr. Studdard reported. The problems include a slim majority of fellow Democrats in the House of Representatives (222 vs 213), no majority of Democrats over Republicans in the Senate (50 vs 50), and mid-term elections that are already looming.
“Midterms historically favor the opposition party,” Mr. Studdard said. He expects party lines to harden as the midterms approach, dissipating the already limited appetite for bipartisan cooperation.
The midterms provide the basis for trying to affect change in advance of legislative gridlock, but the recently announced $2 trillion infrastructure bill is an even more compelling impetus. Infrastructure in this case is not limited to the construction of bridges and roads. Rather, this bill “is a massive package that will almost certainly touch on health care policy,” according to Mr. Studdard.
As the infrastructure bill winds its way through the legislative process, Mr. Studdard expects there will be efforts to include language that favors expansion of services and funding for health care. This includes those related to the Affordable Care Act (ACA) and the temporary modifications permitted under the CARES Act, which was passed during the early months of the COVID-19 pandemic.
For those who think that waivers and exceptions introduced in the CARES Act, such as the expansion of telehealth, should be made permanent, “this will be your main shot on goal,” Mr. Studdard said.
The debates around the ambitious infrastructure bill are “all that we will be hearing about from the legislative standpoint for the next few months,” Mr. Studdard said. He expects major lobbying efforts in regard to this legislation from a vast array of interest groups, not just those with a stake in health care.
If the bill passes, it will likely to be greatly helped by a vote under the reconciliation process. Created in 1974 to allow expedited consideration of spending legislation, the reconciliation process allows bills to be enacted with a simple majority, which is 51 votes in the Senate and 218 votes in the House. Filibustering is not permitted.
This means that the infrastructure bill, like the CARES Act, which was also passed through the reconciliation process, can be made into law even if all 50 Republican senators vote against it. As she has already done three times since taking office—most recently for COVID19 relief bill in early March—Vice President Kamala Harris can break a 50-50 tie with her vote for the administration’s agenda.
Legislation is one of two paths for altering funding and rules regarding health care in the United States. Policy is the other. For reaching decision makers with influence on policy, Mr. Studdard provided a long list of agencies, political appointees, and elected representatives that could be targeted. Many, such as the director of the Centers for Medicare & Medicaid Services (CMS), are well known, but others might be overlooked without a detailed list of the players.
As one example, he pointed to the Center for Medicare and Medicaid Innovation (CMMI), which is a relatively new organization within CMS. Led by Liz Fowler, a former Senate aide involved in writing the ACA, the CMMI has broad authority over several aspects of health policy, such as value-based care.
“The CCMI is something you should put on your radar. It moves with more flexibility than the HHS [Department of Health and Human Services],” Mr. Studdard said.
Mr. Studdard’s detailed overview of the intricacies of how to affect change in health policy and the likely trajectory under the Biden Administration included frequent comments about the traits, background, and goals of the specific decision makers he identified. The implication is that personal relations matter. Mr. Studdard indicated that knowing who to contact is just the first step.
For the Health Policy and Advocacy Committee, this information is critical. In his outline of the numerous paths for influencing health care policy, Mr. Studdard’s comments lead directly to strategies to lobbying goals for CHEST.
“CHEST and its Health Policy and Advocacy Committee are keeping a focus on health care policy to improve access and to improve care for our patients and reduce the burden on our providers,” according to the Chair of the Committee, Neil Freedman, MD, FCCP. Dr, Freedman is the Division Head Pulmonary, Critical Care, Allergy, and Immunology, Northshore University HeatlhSystem, Evanston, Illinois.
“We would hope that, in addition to the proposed infrastructure bill subsidizing some additional costs for the ACA and COBRA [Consolidated Omnibus Budget Reconciliation Act] and enhancing Medicaid eligibility, the bill would also provide some additional funding for the provider relief fund,” he said.
Mr. Studdard or his lobbying firm represent 62 clients with interests in health care policy.
The ambitious infrastructure bill now being debated in the US Congress might be one of the best immediate opportunities to lobby for legislative or policy changes in delivery of health care during the current Biden administration, according to an analysis delivered at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
The infrastructure bill is likely to be pushed forward in the filibuster-proof reconciliation process, which means “that some things might get passed that otherwise would not,” explained Keith S. Studdard, Vice President, Jeffrey J. Kimbell & Associates, Washington, DC.
With few exceptions, the key players in the health care team of President Joe Biden’s new administration are in place, according to Mr. Studdard, who is a lobbyist and health care expert. By moving quickly to fill key positions, the new administration “got off to a good start” for a health care agenda that Mr. Studdard believes will be a focus of the Biden presidency. There is some degree of urgency.
“The amount of time [the Biden administration has] to get their agenda through is fairly limited,” Mr. Studdard reported. The problems include a slim majority of fellow Democrats in the House of Representatives (222 vs 213), no majority of Democrats over Republicans in the Senate (50 vs 50), and mid-term elections that are already looming.
“Midterms historically favor the opposition party,” Mr. Studdard said. He expects party lines to harden as the midterms approach, dissipating the already limited appetite for bipartisan cooperation.
The midterms provide the basis for trying to affect change in advance of legislative gridlock, but the recently announced $2 trillion infrastructure bill is an even more compelling impetus. Infrastructure in this case is not limited to the construction of bridges and roads. Rather, this bill “is a massive package that will almost certainly touch on health care policy,” according to Mr. Studdard.
As the infrastructure bill winds its way through the legislative process, Mr. Studdard expects there will be efforts to include language that favors expansion of services and funding for health care. This includes those related to the Affordable Care Act (ACA) and the temporary modifications permitted under the CARES Act, which was passed during the early months of the COVID-19 pandemic.
For those who think that waivers and exceptions introduced in the CARES Act, such as the expansion of telehealth, should be made permanent, “this will be your main shot on goal,” Mr. Studdard said.
The debates around the ambitious infrastructure bill are “all that we will be hearing about from the legislative standpoint for the next few months,” Mr. Studdard said. He expects major lobbying efforts in regard to this legislation from a vast array of interest groups, not just those with a stake in health care.
If the bill passes, it will likely to be greatly helped by a vote under the reconciliation process. Created in 1974 to allow expedited consideration of spending legislation, the reconciliation process allows bills to be enacted with a simple majority, which is 51 votes in the Senate and 218 votes in the House. Filibustering is not permitted.
This means that the infrastructure bill, like the CARES Act, which was also passed through the reconciliation process, can be made into law even if all 50 Republican senators vote against it. As she has already done three times since taking office—most recently for COVID19 relief bill in early March—Vice President Kamala Harris can break a 50-50 tie with her vote for the administration’s agenda.
Legislation is one of two paths for altering funding and rules regarding health care in the United States. Policy is the other. For reaching decision makers with influence on policy, Mr. Studdard provided a long list of agencies, political appointees, and elected representatives that could be targeted. Many, such as the director of the Centers for Medicare & Medicaid Services (CMS), are well known, but others might be overlooked without a detailed list of the players.
As one example, he pointed to the Center for Medicare and Medicaid Innovation (CMMI), which is a relatively new organization within CMS. Led by Liz Fowler, a former Senate aide involved in writing the ACA, the CMMI has broad authority over several aspects of health policy, such as value-based care.
“The CCMI is something you should put on your radar. It moves with more flexibility than the HHS [Department of Health and Human Services],” Mr. Studdard said.
Mr. Studdard’s detailed overview of the intricacies of how to affect change in health policy and the likely trajectory under the Biden Administration included frequent comments about the traits, background, and goals of the specific decision makers he identified. The implication is that personal relations matter. Mr. Studdard indicated that knowing who to contact is just the first step.
For the Health Policy and Advocacy Committee, this information is critical. In his outline of the numerous paths for influencing health care policy, Mr. Studdard’s comments lead directly to strategies to lobbying goals for CHEST.
“CHEST and its Health Policy and Advocacy Committee are keeping a focus on health care policy to improve access and to improve care for our patients and reduce the burden on our providers,” according to the Chair of the Committee, Neil Freedman, MD, FCCP. Dr, Freedman is the Division Head Pulmonary, Critical Care, Allergy, and Immunology, Northshore University HeatlhSystem, Evanston, Illinois.
“We would hope that, in addition to the proposed infrastructure bill subsidizing some additional costs for the ACA and COBRA [Consolidated Omnibus Budget Reconciliation Act] and enhancing Medicaid eligibility, the bill would also provide some additional funding for the provider relief fund,” he said.
Mr. Studdard or his lobbying firm represent 62 clients with interests in health care policy.
The ambitious infrastructure bill now being debated in the US Congress might be one of the best immediate opportunities to lobby for legislative or policy changes in delivery of health care during the current Biden administration, according to an analysis delivered at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
The infrastructure bill is likely to be pushed forward in the filibuster-proof reconciliation process, which means “that some things might get passed that otherwise would not,” explained Keith S. Studdard, Vice President, Jeffrey J. Kimbell & Associates, Washington, DC.
With few exceptions, the key players in the health care team of President Joe Biden’s new administration are in place, according to Mr. Studdard, who is a lobbyist and health care expert. By moving quickly to fill key positions, the new administration “got off to a good start” for a health care agenda that Mr. Studdard believes will be a focus of the Biden presidency. There is some degree of urgency.
“The amount of time [the Biden administration has] to get their agenda through is fairly limited,” Mr. Studdard reported. The problems include a slim majority of fellow Democrats in the House of Representatives (222 vs 213), no majority of Democrats over Republicans in the Senate (50 vs 50), and mid-term elections that are already looming.
“Midterms historically favor the opposition party,” Mr. Studdard said. He expects party lines to harden as the midterms approach, dissipating the already limited appetite for bipartisan cooperation.
The midterms provide the basis for trying to affect change in advance of legislative gridlock, but the recently announced $2 trillion infrastructure bill is an even more compelling impetus. Infrastructure in this case is not limited to the construction of bridges and roads. Rather, this bill “is a massive package that will almost certainly touch on health care policy,” according to Mr. Studdard.
As the infrastructure bill winds its way through the legislative process, Mr. Studdard expects there will be efforts to include language that favors expansion of services and funding for health care. This includes those related to the Affordable Care Act (ACA) and the temporary modifications permitted under the CARES Act, which was passed during the early months of the COVID-19 pandemic.
For those who think that waivers and exceptions introduced in the CARES Act, such as the expansion of telehealth, should be made permanent, “this will be your main shot on goal,” Mr. Studdard said.
The debates around the ambitious infrastructure bill are “all that we will be hearing about from the legislative standpoint for the next few months,” Mr. Studdard said. He expects major lobbying efforts in regard to this legislation from a vast array of interest groups, not just those with a stake in health care.
If the bill passes, it will likely to be greatly helped by a vote under the reconciliation process. Created in 1974 to allow expedited consideration of spending legislation, the reconciliation process allows bills to be enacted with a simple majority, which is 51 votes in the Senate and 218 votes in the House. Filibustering is not permitted.
This means that the infrastructure bill, like the CARES Act, which was also passed through the reconciliation process, can be made into law even if all 50 Republican senators vote against it. As she has already done three times since taking office—most recently for COVID19 relief bill in early March—Vice President Kamala Harris can break a 50-50 tie with her vote for the administration’s agenda.
Legislation is one of two paths for altering funding and rules regarding health care in the United States. Policy is the other. For reaching decision makers with influence on policy, Mr. Studdard provided a long list of agencies, political appointees, and elected representatives that could be targeted. Many, such as the director of the Centers for Medicare & Medicaid Services (CMS), are well known, but others might be overlooked without a detailed list of the players.
As one example, he pointed to the Center for Medicare and Medicaid Innovation (CMMI), which is a relatively new organization within CMS. Led by Liz Fowler, a former Senate aide involved in writing the ACA, the CMMI has broad authority over several aspects of health policy, such as value-based care.
“The CCMI is something you should put on your radar. It moves with more flexibility than the HHS [Department of Health and Human Services],” Mr. Studdard said.
Mr. Studdard’s detailed overview of the intricacies of how to affect change in health policy and the likely trajectory under the Biden Administration included frequent comments about the traits, background, and goals of the specific decision makers he identified. The implication is that personal relations matter. Mr. Studdard indicated that knowing who to contact is just the first step.
For the Health Policy and Advocacy Committee, this information is critical. In his outline of the numerous paths for influencing health care policy, Mr. Studdard’s comments lead directly to strategies to lobbying goals for CHEST.
“CHEST and its Health Policy and Advocacy Committee are keeping a focus on health care policy to improve access and to improve care for our patients and reduce the burden on our providers,” according to the Chair of the Committee, Neil Freedman, MD, FCCP. Dr, Freedman is the Division Head Pulmonary, Critical Care, Allergy, and Immunology, Northshore University HeatlhSystem, Evanston, Illinois.
“We would hope that, in addition to the proposed infrastructure bill subsidizing some additional costs for the ACA and COBRA [Consolidated Omnibus Budget Reconciliation Act] and enhancing Medicaid eligibility, the bill would also provide some additional funding for the provider relief fund,” he said.
Mr. Studdard or his lobbying firm represent 62 clients with interests in health care policy.
REPORTING FROM THE CHEST HEALTH POLICY AND ADVOCACY CONFERENCE
By the numbers: Children and COVID-19 prevention
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
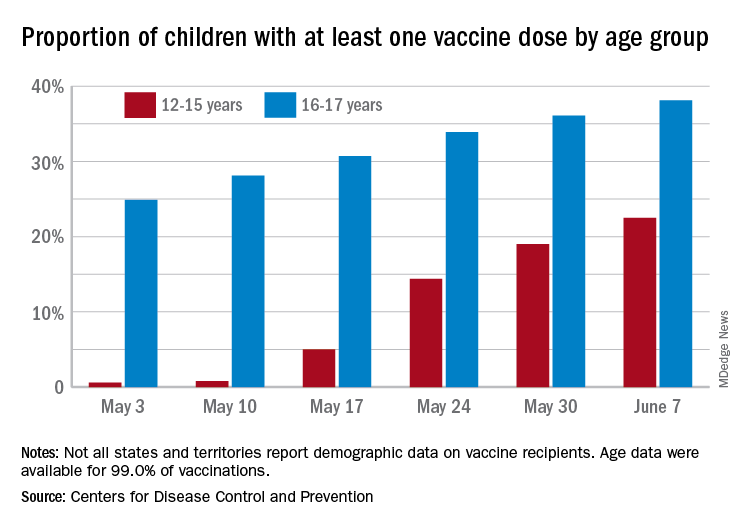
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
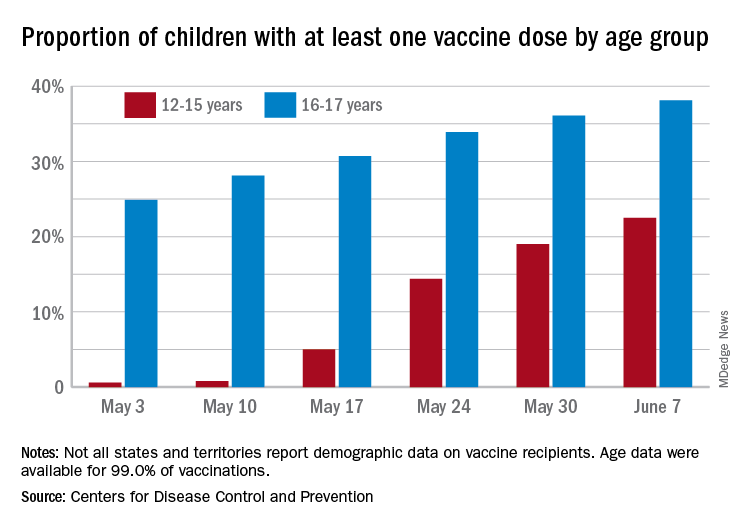
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
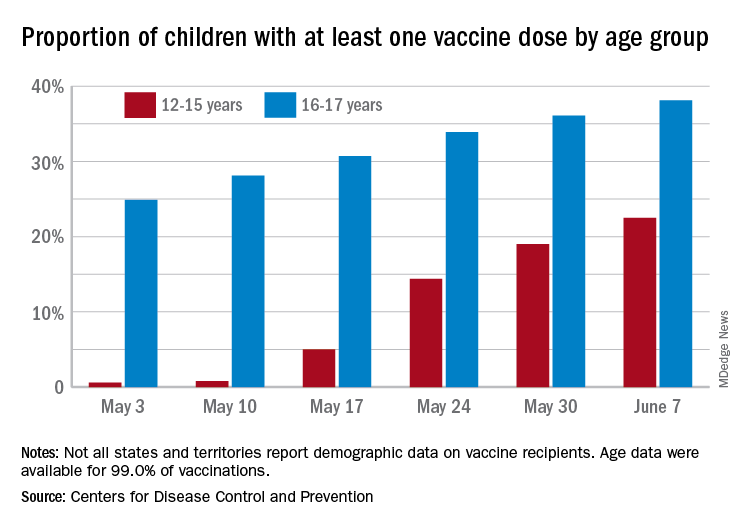
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
NIAID advances universal flu vaccine candidate into phase 1 trial
Last month, U.S. government researchers began a test of an experimental influenza vaccine that they hope will provide long-lasting immunity against multiple strains of the virus. Their project adds to the many approaches that have been tried in the decades-long quest for a universal flu shot.
For the first time, the National Institute of Allergy and Infectious Diseases (NIAID) is testing an investigational flu vaccine, known as FluMos-v1, on people. Researchers in recent years have targeted the stalk or stem of an influenza surface protein called hemagglutinin (HA) in trying to develop better flu vaccines. NIAID said FluMos-v1 is designed to spark production of antibodies against the HA protein from different virus strains, which could make it superior to vaccines now available, NIAID said.
“It could be longer lasting than the traditional flu vaccine and give us what we call super seasonal protection that might go beyond just one flu season to next year’s or the year after, or offer additional protection in a pandemic setting,” Alicia T. Widge, MD, of NIAID’s Vaccine Research Center, who is the principal investigator of the trial, said in an interview.
The phase 1 study (NCT04896086) aims to enroll 35 participants, 15 of whom will receive a single intramuscular injection of a comparator treatment, Flucelvax, which has already been approved by the U.S. Food and Drug Administration. The FluMos-v1 group will start with five participants who will receive one 20-μg dose. If no safety problems emerge at that dosage, another 15 volunteers will receive one 60-μg dose of the investigational vaccine.
The incorporation of a comparator group in the phase 1 study may help investigators get an early idea of how well FluMos-v1 compares to a marketed product, Dr. Widge said. The test will be carried out through the National Institutes of Health Clinical Center.
‘Renaissance’ of flu-vaccine research?
Currently, flu vaccines are reformulated each year in an attempt to match the dominant strain for the upcoming season, an effort that often falls notably short. The estimated vaccine effectiveness rate in the United States has ranged from a low of 19% to a high of 60% in recent years, according to the Centers for Disease Control and Prevention.
Scientists have been working for decades on a universal flu vaccine that would offer better results but haven’t yet identified the right strategy to outwit mutations in the virus. Recent setbacks include BiondVax Pharmaceuticals’ October 2020 announcement of a failed phase 3 trial of its experimental M-001 universal flu vaccine candidate.
But advances in understanding the immune system may set the stage for a “renaissance” in efforts to develop a universal flu vaccine, Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said in an interview.
The COVID-19 pandemic has spurred greater interest in the need to develop a universal flu vaccine, he said. Dr. Osterholm said he is “more optimistic now than ever” about the chances for developing vaccines that can fend off multiple strains over longer periods, although the goal of a shot that can ward off influenza in all cases may remain elusive.
“How good can we make them? Will they ever be really universal? Will they have long periods of protection? I don’t think any of us know that yet,” Dr. Osterholm said. “But this is not the influenza vaccine world of 5 or 7 years ago.”
The mRNA technology used to develop the world’s first approved COVID-19 vaccines, for example, may be applied against influenza, Dr. Osterholm said.
In January 2021, Moderna announced plans to test three development candidates for a seasonal influenza vaccine and aims to start a phase 1 study this year. In an April interview on CNBC’s Squawk Box program, Moderna’s chief executive, Stephané Bancel, spoke about the company’s plans to eventually create a combination vaccine for SARS-Cov-2 and flu viruses.
SARS-CoV-2 “is not going away.” Like flu, this virus will persist and change forms, Ms. Bancel said. Creating a flu shot that outperforms the existing ones would boost confidence in influenza vaccines, which many people now skip, Ms. Bancel said. People might someday be able to get a combination of this more effective flu shot with a COVID-19 vaccine booster in their local pharmacies.
“You can take one dose and then have a nice winter,” Ms. Bancel said of Moderna’s goal for a combination vaccine.
A version of this article first appeared on Medscape.com.
Last month, U.S. government researchers began a test of an experimental influenza vaccine that they hope will provide long-lasting immunity against multiple strains of the virus. Their project adds to the many approaches that have been tried in the decades-long quest for a universal flu shot.
For the first time, the National Institute of Allergy and Infectious Diseases (NIAID) is testing an investigational flu vaccine, known as FluMos-v1, on people. Researchers in recent years have targeted the stalk or stem of an influenza surface protein called hemagglutinin (HA) in trying to develop better flu vaccines. NIAID said FluMos-v1 is designed to spark production of antibodies against the HA protein from different virus strains, which could make it superior to vaccines now available, NIAID said.
“It could be longer lasting than the traditional flu vaccine and give us what we call super seasonal protection that might go beyond just one flu season to next year’s or the year after, or offer additional protection in a pandemic setting,” Alicia T. Widge, MD, of NIAID’s Vaccine Research Center, who is the principal investigator of the trial, said in an interview.
The phase 1 study (NCT04896086) aims to enroll 35 participants, 15 of whom will receive a single intramuscular injection of a comparator treatment, Flucelvax, which has already been approved by the U.S. Food and Drug Administration. The FluMos-v1 group will start with five participants who will receive one 20-μg dose. If no safety problems emerge at that dosage, another 15 volunteers will receive one 60-μg dose of the investigational vaccine.
The incorporation of a comparator group in the phase 1 study may help investigators get an early idea of how well FluMos-v1 compares to a marketed product, Dr. Widge said. The test will be carried out through the National Institutes of Health Clinical Center.
‘Renaissance’ of flu-vaccine research?
Currently, flu vaccines are reformulated each year in an attempt to match the dominant strain for the upcoming season, an effort that often falls notably short. The estimated vaccine effectiveness rate in the United States has ranged from a low of 19% to a high of 60% in recent years, according to the Centers for Disease Control and Prevention.
Scientists have been working for decades on a universal flu vaccine that would offer better results but haven’t yet identified the right strategy to outwit mutations in the virus. Recent setbacks include BiondVax Pharmaceuticals’ October 2020 announcement of a failed phase 3 trial of its experimental M-001 universal flu vaccine candidate.
But advances in understanding the immune system may set the stage for a “renaissance” in efforts to develop a universal flu vaccine, Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said in an interview.
The COVID-19 pandemic has spurred greater interest in the need to develop a universal flu vaccine, he said. Dr. Osterholm said he is “more optimistic now than ever” about the chances for developing vaccines that can fend off multiple strains over longer periods, although the goal of a shot that can ward off influenza in all cases may remain elusive.
“How good can we make them? Will they ever be really universal? Will they have long periods of protection? I don’t think any of us know that yet,” Dr. Osterholm said. “But this is not the influenza vaccine world of 5 or 7 years ago.”
The mRNA technology used to develop the world’s first approved COVID-19 vaccines, for example, may be applied against influenza, Dr. Osterholm said.
In January 2021, Moderna announced plans to test three development candidates for a seasonal influenza vaccine and aims to start a phase 1 study this year. In an April interview on CNBC’s Squawk Box program, Moderna’s chief executive, Stephané Bancel, spoke about the company’s plans to eventually create a combination vaccine for SARS-Cov-2 and flu viruses.
SARS-CoV-2 “is not going away.” Like flu, this virus will persist and change forms, Ms. Bancel said. Creating a flu shot that outperforms the existing ones would boost confidence in influenza vaccines, which many people now skip, Ms. Bancel said. People might someday be able to get a combination of this more effective flu shot with a COVID-19 vaccine booster in their local pharmacies.
“You can take one dose and then have a nice winter,” Ms. Bancel said of Moderna’s goal for a combination vaccine.
A version of this article first appeared on Medscape.com.
Last month, U.S. government researchers began a test of an experimental influenza vaccine that they hope will provide long-lasting immunity against multiple strains of the virus. Their project adds to the many approaches that have been tried in the decades-long quest for a universal flu shot.
For the first time, the National Institute of Allergy and Infectious Diseases (NIAID) is testing an investigational flu vaccine, known as FluMos-v1, on people. Researchers in recent years have targeted the stalk or stem of an influenza surface protein called hemagglutinin (HA) in trying to develop better flu vaccines. NIAID said FluMos-v1 is designed to spark production of antibodies against the HA protein from different virus strains, which could make it superior to vaccines now available, NIAID said.
“It could be longer lasting than the traditional flu vaccine and give us what we call super seasonal protection that might go beyond just one flu season to next year’s or the year after, or offer additional protection in a pandemic setting,” Alicia T. Widge, MD, of NIAID’s Vaccine Research Center, who is the principal investigator of the trial, said in an interview.
The phase 1 study (NCT04896086) aims to enroll 35 participants, 15 of whom will receive a single intramuscular injection of a comparator treatment, Flucelvax, which has already been approved by the U.S. Food and Drug Administration. The FluMos-v1 group will start with five participants who will receive one 20-μg dose. If no safety problems emerge at that dosage, another 15 volunteers will receive one 60-μg dose of the investigational vaccine.
The incorporation of a comparator group in the phase 1 study may help investigators get an early idea of how well FluMos-v1 compares to a marketed product, Dr. Widge said. The test will be carried out through the National Institutes of Health Clinical Center.
‘Renaissance’ of flu-vaccine research?
Currently, flu vaccines are reformulated each year in an attempt to match the dominant strain for the upcoming season, an effort that often falls notably short. The estimated vaccine effectiveness rate in the United States has ranged from a low of 19% to a high of 60% in recent years, according to the Centers for Disease Control and Prevention.
Scientists have been working for decades on a universal flu vaccine that would offer better results but haven’t yet identified the right strategy to outwit mutations in the virus. Recent setbacks include BiondVax Pharmaceuticals’ October 2020 announcement of a failed phase 3 trial of its experimental M-001 universal flu vaccine candidate.
But advances in understanding the immune system may set the stage for a “renaissance” in efforts to develop a universal flu vaccine, Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said in an interview.
The COVID-19 pandemic has spurred greater interest in the need to develop a universal flu vaccine, he said. Dr. Osterholm said he is “more optimistic now than ever” about the chances for developing vaccines that can fend off multiple strains over longer periods, although the goal of a shot that can ward off influenza in all cases may remain elusive.
“How good can we make them? Will they ever be really universal? Will they have long periods of protection? I don’t think any of us know that yet,” Dr. Osterholm said. “But this is not the influenza vaccine world of 5 or 7 years ago.”
The mRNA technology used to develop the world’s first approved COVID-19 vaccines, for example, may be applied against influenza, Dr. Osterholm said.
In January 2021, Moderna announced plans to test three development candidates for a seasonal influenza vaccine and aims to start a phase 1 study this year. In an April interview on CNBC’s Squawk Box program, Moderna’s chief executive, Stephané Bancel, spoke about the company’s plans to eventually create a combination vaccine for SARS-Cov-2 and flu viruses.
SARS-CoV-2 “is not going away.” Like flu, this virus will persist and change forms, Ms. Bancel said. Creating a flu shot that outperforms the existing ones would boost confidence in influenza vaccines, which many people now skip, Ms. Bancel said. People might someday be able to get a combination of this more effective flu shot with a COVID-19 vaccine booster in their local pharmacies.
“You can take one dose and then have a nice winter,” Ms. Bancel said of Moderna’s goal for a combination vaccine.
A version of this article first appeared on Medscape.com.





