User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Staying up to date with consumer sleep technology
With Siri and Alexa sitting at our kitchen tables and listening to our conversations, we have all but forgotten about the before times – when we had to use the Yellow Pages to look up a number or address and when we had no idea how many steps we took in a given day. Wearable technology has become ubiquitous and has us watching not only our step count but also our sleep. Did I get enough deep sleep? What does my sleep score of 82 mean? Should I be worried?
As clinicians, we must also navigate how this information impacts our clinical decision-making and consider how our patients are interpreting these data on a daily basis. There is an inherent assumption that we, as sleep clinicians, will understand the nuances of each consumer-facing sleep technology (CST) whether it is a wearable, a nearable (a device that sits near the body but not on the body), or an app. Very little validation data exist, as most of these technologies are marketed as wellness devices and are not intended to render a diagnosis. It therefore falls to us to determine how to utilize this information in an already busy clinic.
One strategy is to use these technologies as patient engagement tools – a way to increase public awareness of the importance of sleep. While this certainly should be beneficial, oftentimes, the data are confusing and can lead to misunderstandings about what normal sleep should look like. Approaching these data as partners to our patients allows us to set expectations around normal sleep cycles and sleep duration. It also allows us to discuss appropriate sleep timing and sleep hygiene.
Many wearable devices have incorporated oximetry into their metrics, and some claim to have accuracy that is better than hospital-grade oximeters. Many of these companies are no longer in business. Others specify higher accuracy in dark-skinned individuals (“CIRCUL Ring Pulse Oximeter in Dark-Pigmented Individuals: Clinical Study Validates Efficacy and Reliability,” Medical Device News Magazine, Feb. 26, 2021).
Despite these claims, they are registered as wellness devices with the FDA and are not diagnostic devices. Logically, if one of these devices demonstrates worrisome data, then it can prompt further clinical queries and, potentially, objective testing for obstructive sleep apnea (OSA). The reverse, however, cannot be claimed. A normal reading by CST does not obviate the need for objective testing if the clinical symptoms warrant it.
There are CSTs that have been created around very specific needs - such as jet lag- and provide guidance for how to quickly acclimate to the destination time zone by providing nudges for light exposure and timed melatonin or dark glasses (https://www.timeshifter.com/).
Others analyze the sleep space for extrinsic sounds (https://www.sleepcycle.com/), while a plethora of apps provides advice for how to optimize your sleep environment and wind-down routine. There is even a sleep robot designed to facilitate sleep onset (https://somnox.com/). This bean-shaped device is designed to “breathe” as you hold it, and the user is meant to emulate those same breathing patterns. It is a take on the 4-7-8 breathing pattern long endorsed by yogis.
Although validation data are lacking for the vast majority of CST, a recent study (www.ncbi.nlm.nih.gov/pmc/articles/PMC8120339/pdf/zsaa291.pdf).demonstrated that CST had high performance when compared with actigraphy in assessing sleep and wakefulness and, as such, may improve the evaluation of sleep and wake opportunities prior to MSLT or improve identification of circadian sleep-wake disorders. Many practices do not currently utilize actigraphy due to its expense and very limited potential for reimbursement. Using a patient’s sleep-tracking device may allow access to these data without financial outlay. While these data demonstrate the ability of CST to potentially differentiate sleep from wakefulness, it is notable that this study also found that the determination of individual sleep stages is less robust. In general, CST cannot identify an underlying sleep disorder, however, may raise awareness that a disorder might be present.
This leads to more reflection on the role of CST in a typical sleep clinic. Many years ago, discussion around this technology was primarily patient-initiated and often times met with skepticism on the part of the clinician. As technology has improved and has become more accessible, there appears to be more acceptance among our colleagues – not, perhaps, in terms of absolute actionable data, but rather as an opportunity to discuss sleep with our patients and to support their own efforts at improving their sleep. Trends in the data in response to CBT-I or medications can be observed. Abnormalities identified via CST often serve as the initial prompt for a clinical visit and, as such, should not be eschewed. Rather, reframing the use of this information while also addressing other sleep issues is likely to be the more appropriate path forward.
Assessing this information can be time-consuming, and best practice suggests establishing expectations around this process (J Clin Sleep Med 2018 May 15. doi: 10.5664/jcsm.7128).
Agreements can be made with patients that the data are reviewed in the context of a clinical visit rather than longitudinally as data are uploaded and then sent via messaging unless such an understanding has already been agreed upon. RPM billing codes may ultimately allow for reimbursement and recognition of this workload. At the present time, RPM billing is limited to FDA-cleared, prescription devices, and CST does not yet qualify.
There also needs to be recognition of potential harm from CST. Inevitably, some patients will develop orthosomnia, a term coined by Dr. Kelly Baron, where patients become so fixated on achieving perfect sleep scores that it contributes to insomnia. In this case, identification of orthosomnia is made via the clinical visit and patients are advised to stop tracking their sleep for a set period of time. This allows the anxiety around achieving “perfect sleep” to dissipate.
Google and the AASM recently announced a partnership. Essentially, the Google Nest Hub will serve to detect sleep concerns (such as timing of sleep, snoring, insufficient sleep, etc.) and will direct the user to educational resources such as www.sleepeducation.org. The idea behind this is that people are often unaware of an underlying sleep disorder such as OSA and don’t know what to search for. The Nest Hub uses information it collects and directs users to appropriate resources, thus obviating the need to know what to Google.
Clearly, big tech has invested heavily in our field. Between the copious wearables, nearables, and apps that are sleep-focused, these industry giants obviously believe that sleep is worthy of such a significant allocation of resources. This has improved the overall awareness of the importance of sleep and of identifying and treating sleep disorders. While these technologies are no replacement for a clinical evaluation, they can serve as patient engagement tools, as well as potentially large-scale OSA screening tools and may help us improve the percentage of patients with undiagnosed OSA, estimated to be 80% (Frost and Sullivan, “Hidden Health Crisis Costing America Billions,” American Academy of Sleep Medicine, 2016).
CST may allow us to better identify circadian sleep-wake disorders and evaluate sleep satiation prior to MLST that no longer requires investment in expensive actigraphy devices. They also allow us to partner with our patients by meeting them where they are and recognizing the efforts they have already made to improve their sleep before we even meet them.
Dr. Khosla is Medical Director, North Dakota Center for Sleep, Fargo, North Dakota.
With Siri and Alexa sitting at our kitchen tables and listening to our conversations, we have all but forgotten about the before times – when we had to use the Yellow Pages to look up a number or address and when we had no idea how many steps we took in a given day. Wearable technology has become ubiquitous and has us watching not only our step count but also our sleep. Did I get enough deep sleep? What does my sleep score of 82 mean? Should I be worried?
As clinicians, we must also navigate how this information impacts our clinical decision-making and consider how our patients are interpreting these data on a daily basis. There is an inherent assumption that we, as sleep clinicians, will understand the nuances of each consumer-facing sleep technology (CST) whether it is a wearable, a nearable (a device that sits near the body but not on the body), or an app. Very little validation data exist, as most of these technologies are marketed as wellness devices and are not intended to render a diagnosis. It therefore falls to us to determine how to utilize this information in an already busy clinic.
One strategy is to use these technologies as patient engagement tools – a way to increase public awareness of the importance of sleep. While this certainly should be beneficial, oftentimes, the data are confusing and can lead to misunderstandings about what normal sleep should look like. Approaching these data as partners to our patients allows us to set expectations around normal sleep cycles and sleep duration. It also allows us to discuss appropriate sleep timing and sleep hygiene.
Many wearable devices have incorporated oximetry into their metrics, and some claim to have accuracy that is better than hospital-grade oximeters. Many of these companies are no longer in business. Others specify higher accuracy in dark-skinned individuals (“CIRCUL Ring Pulse Oximeter in Dark-Pigmented Individuals: Clinical Study Validates Efficacy and Reliability,” Medical Device News Magazine, Feb. 26, 2021).
Despite these claims, they are registered as wellness devices with the FDA and are not diagnostic devices. Logically, if one of these devices demonstrates worrisome data, then it can prompt further clinical queries and, potentially, objective testing for obstructive sleep apnea (OSA). The reverse, however, cannot be claimed. A normal reading by CST does not obviate the need for objective testing if the clinical symptoms warrant it.
There are CSTs that have been created around very specific needs - such as jet lag- and provide guidance for how to quickly acclimate to the destination time zone by providing nudges for light exposure and timed melatonin or dark glasses (https://www.timeshifter.com/).
Others analyze the sleep space for extrinsic sounds (https://www.sleepcycle.com/), while a plethora of apps provides advice for how to optimize your sleep environment and wind-down routine. There is even a sleep robot designed to facilitate sleep onset (https://somnox.com/). This bean-shaped device is designed to “breathe” as you hold it, and the user is meant to emulate those same breathing patterns. It is a take on the 4-7-8 breathing pattern long endorsed by yogis.
Although validation data are lacking for the vast majority of CST, a recent study (www.ncbi.nlm.nih.gov/pmc/articles/PMC8120339/pdf/zsaa291.pdf).demonstrated that CST had high performance when compared with actigraphy in assessing sleep and wakefulness and, as such, may improve the evaluation of sleep and wake opportunities prior to MSLT or improve identification of circadian sleep-wake disorders. Many practices do not currently utilize actigraphy due to its expense and very limited potential for reimbursement. Using a patient’s sleep-tracking device may allow access to these data without financial outlay. While these data demonstrate the ability of CST to potentially differentiate sleep from wakefulness, it is notable that this study also found that the determination of individual sleep stages is less robust. In general, CST cannot identify an underlying sleep disorder, however, may raise awareness that a disorder might be present.
This leads to more reflection on the role of CST in a typical sleep clinic. Many years ago, discussion around this technology was primarily patient-initiated and often times met with skepticism on the part of the clinician. As technology has improved and has become more accessible, there appears to be more acceptance among our colleagues – not, perhaps, in terms of absolute actionable data, but rather as an opportunity to discuss sleep with our patients and to support their own efforts at improving their sleep. Trends in the data in response to CBT-I or medications can be observed. Abnormalities identified via CST often serve as the initial prompt for a clinical visit and, as such, should not be eschewed. Rather, reframing the use of this information while also addressing other sleep issues is likely to be the more appropriate path forward.
Assessing this information can be time-consuming, and best practice suggests establishing expectations around this process (J Clin Sleep Med 2018 May 15. doi: 10.5664/jcsm.7128).
Agreements can be made with patients that the data are reviewed in the context of a clinical visit rather than longitudinally as data are uploaded and then sent via messaging unless such an understanding has already been agreed upon. RPM billing codes may ultimately allow for reimbursement and recognition of this workload. At the present time, RPM billing is limited to FDA-cleared, prescription devices, and CST does not yet qualify.
There also needs to be recognition of potential harm from CST. Inevitably, some patients will develop orthosomnia, a term coined by Dr. Kelly Baron, where patients become so fixated on achieving perfect sleep scores that it contributes to insomnia. In this case, identification of orthosomnia is made via the clinical visit and patients are advised to stop tracking their sleep for a set period of time. This allows the anxiety around achieving “perfect sleep” to dissipate.
Google and the AASM recently announced a partnership. Essentially, the Google Nest Hub will serve to detect sleep concerns (such as timing of sleep, snoring, insufficient sleep, etc.) and will direct the user to educational resources such as www.sleepeducation.org. The idea behind this is that people are often unaware of an underlying sleep disorder such as OSA and don’t know what to search for. The Nest Hub uses information it collects and directs users to appropriate resources, thus obviating the need to know what to Google.
Clearly, big tech has invested heavily in our field. Between the copious wearables, nearables, and apps that are sleep-focused, these industry giants obviously believe that sleep is worthy of such a significant allocation of resources. This has improved the overall awareness of the importance of sleep and of identifying and treating sleep disorders. While these technologies are no replacement for a clinical evaluation, they can serve as patient engagement tools, as well as potentially large-scale OSA screening tools and may help us improve the percentage of patients with undiagnosed OSA, estimated to be 80% (Frost and Sullivan, “Hidden Health Crisis Costing America Billions,” American Academy of Sleep Medicine, 2016).
CST may allow us to better identify circadian sleep-wake disorders and evaluate sleep satiation prior to MLST that no longer requires investment in expensive actigraphy devices. They also allow us to partner with our patients by meeting them where they are and recognizing the efforts they have already made to improve their sleep before we even meet them.
Dr. Khosla is Medical Director, North Dakota Center for Sleep, Fargo, North Dakota.
With Siri and Alexa sitting at our kitchen tables and listening to our conversations, we have all but forgotten about the before times – when we had to use the Yellow Pages to look up a number or address and when we had no idea how many steps we took in a given day. Wearable technology has become ubiquitous and has us watching not only our step count but also our sleep. Did I get enough deep sleep? What does my sleep score of 82 mean? Should I be worried?
As clinicians, we must also navigate how this information impacts our clinical decision-making and consider how our patients are interpreting these data on a daily basis. There is an inherent assumption that we, as sleep clinicians, will understand the nuances of each consumer-facing sleep technology (CST) whether it is a wearable, a nearable (a device that sits near the body but not on the body), or an app. Very little validation data exist, as most of these technologies are marketed as wellness devices and are not intended to render a diagnosis. It therefore falls to us to determine how to utilize this information in an already busy clinic.
One strategy is to use these technologies as patient engagement tools – a way to increase public awareness of the importance of sleep. While this certainly should be beneficial, oftentimes, the data are confusing and can lead to misunderstandings about what normal sleep should look like. Approaching these data as partners to our patients allows us to set expectations around normal sleep cycles and sleep duration. It also allows us to discuss appropriate sleep timing and sleep hygiene.
Many wearable devices have incorporated oximetry into their metrics, and some claim to have accuracy that is better than hospital-grade oximeters. Many of these companies are no longer in business. Others specify higher accuracy in dark-skinned individuals (“CIRCUL Ring Pulse Oximeter in Dark-Pigmented Individuals: Clinical Study Validates Efficacy and Reliability,” Medical Device News Magazine, Feb. 26, 2021).
Despite these claims, they are registered as wellness devices with the FDA and are not diagnostic devices. Logically, if one of these devices demonstrates worrisome data, then it can prompt further clinical queries and, potentially, objective testing for obstructive sleep apnea (OSA). The reverse, however, cannot be claimed. A normal reading by CST does not obviate the need for objective testing if the clinical symptoms warrant it.
There are CSTs that have been created around very specific needs - such as jet lag- and provide guidance for how to quickly acclimate to the destination time zone by providing nudges for light exposure and timed melatonin or dark glasses (https://www.timeshifter.com/).
Others analyze the sleep space for extrinsic sounds (https://www.sleepcycle.com/), while a plethora of apps provides advice for how to optimize your sleep environment and wind-down routine. There is even a sleep robot designed to facilitate sleep onset (https://somnox.com/). This bean-shaped device is designed to “breathe” as you hold it, and the user is meant to emulate those same breathing patterns. It is a take on the 4-7-8 breathing pattern long endorsed by yogis.
Although validation data are lacking for the vast majority of CST, a recent study (www.ncbi.nlm.nih.gov/pmc/articles/PMC8120339/pdf/zsaa291.pdf).demonstrated that CST had high performance when compared with actigraphy in assessing sleep and wakefulness and, as such, may improve the evaluation of sleep and wake opportunities prior to MSLT or improve identification of circadian sleep-wake disorders. Many practices do not currently utilize actigraphy due to its expense and very limited potential for reimbursement. Using a patient’s sleep-tracking device may allow access to these data without financial outlay. While these data demonstrate the ability of CST to potentially differentiate sleep from wakefulness, it is notable that this study also found that the determination of individual sleep stages is less robust. In general, CST cannot identify an underlying sleep disorder, however, may raise awareness that a disorder might be present.
This leads to more reflection on the role of CST in a typical sleep clinic. Many years ago, discussion around this technology was primarily patient-initiated and often times met with skepticism on the part of the clinician. As technology has improved and has become more accessible, there appears to be more acceptance among our colleagues – not, perhaps, in terms of absolute actionable data, but rather as an opportunity to discuss sleep with our patients and to support their own efforts at improving their sleep. Trends in the data in response to CBT-I or medications can be observed. Abnormalities identified via CST often serve as the initial prompt for a clinical visit and, as such, should not be eschewed. Rather, reframing the use of this information while also addressing other sleep issues is likely to be the more appropriate path forward.
Assessing this information can be time-consuming, and best practice suggests establishing expectations around this process (J Clin Sleep Med 2018 May 15. doi: 10.5664/jcsm.7128).
Agreements can be made with patients that the data are reviewed in the context of a clinical visit rather than longitudinally as data are uploaded and then sent via messaging unless such an understanding has already been agreed upon. RPM billing codes may ultimately allow for reimbursement and recognition of this workload. At the present time, RPM billing is limited to FDA-cleared, prescription devices, and CST does not yet qualify.
There also needs to be recognition of potential harm from CST. Inevitably, some patients will develop orthosomnia, a term coined by Dr. Kelly Baron, where patients become so fixated on achieving perfect sleep scores that it contributes to insomnia. In this case, identification of orthosomnia is made via the clinical visit and patients are advised to stop tracking their sleep for a set period of time. This allows the anxiety around achieving “perfect sleep” to dissipate.
Google and the AASM recently announced a partnership. Essentially, the Google Nest Hub will serve to detect sleep concerns (such as timing of sleep, snoring, insufficient sleep, etc.) and will direct the user to educational resources such as www.sleepeducation.org. The idea behind this is that people are often unaware of an underlying sleep disorder such as OSA and don’t know what to search for. The Nest Hub uses information it collects and directs users to appropriate resources, thus obviating the need to know what to Google.
Clearly, big tech has invested heavily in our field. Between the copious wearables, nearables, and apps that are sleep-focused, these industry giants obviously believe that sleep is worthy of such a significant allocation of resources. This has improved the overall awareness of the importance of sleep and of identifying and treating sleep disorders. While these technologies are no replacement for a clinical evaluation, they can serve as patient engagement tools, as well as potentially large-scale OSA screening tools and may help us improve the percentage of patients with undiagnosed OSA, estimated to be 80% (Frost and Sullivan, “Hidden Health Crisis Costing America Billions,” American Academy of Sleep Medicine, 2016).
CST may allow us to better identify circadian sleep-wake disorders and evaluate sleep satiation prior to MLST that no longer requires investment in expensive actigraphy devices. They also allow us to partner with our patients by meeting them where they are and recognizing the efforts they have already made to improve their sleep before we even meet them.
Dr. Khosla is Medical Director, North Dakota Center for Sleep, Fargo, North Dakota.
CHEST 2021: The beginning of the rest of your career
Is this your first CHEST Annual Meeting? Co-Chair David Zielinski, MD, FCCP, shares some words of wisdom recounting his first experience at CHEST and what first-time attendees can expect from the annual meeting.
My very first CHEST meeting was 10 years ago at CHEST 2011 in Honolulu, Hawaii. I clearly remember my first session being a postgraduate course on Respiratory Management of Neuromuscular Disease and having the opportunity for hands-on teaching with devices and techniques.
Simulation was unique at medical conferences at that time and has continued to evolve at subsequent CHEST meetings.
Looking back, what really sticks out about this experience is what it started for me in terms of my career and learning. I was in a session with some of the biggest names in the field—people who I always looked up to as a relatively junior faculty. I was encouraged to get more involved at CHEST and with the committees. It put the bug in my ear.
A few years later, I started to get involved in the NetWorks. Eventually, I became a faculty member myself alongside these individuals at subsequent CHEST meetings. Meeting these chest medicine professionals also led to more collaborations with them outside of CHEST.
I never imagined this during my first meeting ten years ago. I have now been back to every meeting but one since that first one.
The CHEST Annual Meeting has always stood out for its focus on quality clinical teaching, being ahead of the curve on interactivity and adjusting to the audience’s learning needs.
For me personally, though, the three things that I have always enjoyed are as follows:
Simulation opportunities
One thing that sets apart CHEST 2021 from other conferences is the simulation sessions being offered online.
These sessions are an opportunity to practice your skills and techniques with some of the best educators anywhere in the world. I have always come out of these sessions impressed. I encourage you to try it at least once.
The fun
From the receptions, the meet-ups, pop-up events, CHEST Challenge, the games… the list goes on: the fun element of CHEST makes it a more immersive atmosphere. When the meeting was solely virtual last year, CHEST still aimed to provide fun and will continue to do the same this year. Challenge your colleagues and new friends to games at the CHEST Player Hub online to see which one of you rises to the top of the leaderboard.
The community
CHEST 2021 (and CHEST the organization) helps you make connections and provides opportunities for leadership involvement. CHEST committees are always looking for leaders at all stages of their careers. Attending satellite meetings, like the NetWork open forums that are occurring online before the meeting starts this year, will allow you to begin networking with those with similar interests to your own and hopefully will spark your interest in getting more involved in the future.
For many of us at CHEST, the NetWorks were a great place to start, and you can join one in the area that interests you most. Through my involvement in CHEST, I have become a part of the community, meeting so many other clinicians and educators in my field. I have made great friendships, which keep me coming back every year.
Moving forward
From the beginning, we have been planning CHEST 2021 so that if we needed to go entirely online, we could do so as seamlessly as possible. With the recent decision to cancel the in-person meeting and go fully online, plans are already underway to make CHEST 2021 just as successful as last year’s meeting.
We can give you our commitment that your CHEST 2021 experience will live up to being a world-class event that separates itself from other current online offerings. I will be in attendance and hope to see you online.
Start planning your days with the CHEST 2021 Schedule at A Glance at chestmeeting.chestnet.org.
Is this your first CHEST Annual Meeting? Co-Chair David Zielinski, MD, FCCP, shares some words of wisdom recounting his first experience at CHEST and what first-time attendees can expect from the annual meeting.
My very first CHEST meeting was 10 years ago at CHEST 2011 in Honolulu, Hawaii. I clearly remember my first session being a postgraduate course on Respiratory Management of Neuromuscular Disease and having the opportunity for hands-on teaching with devices and techniques.
Simulation was unique at medical conferences at that time and has continued to evolve at subsequent CHEST meetings.
Looking back, what really sticks out about this experience is what it started for me in terms of my career and learning. I was in a session with some of the biggest names in the field—people who I always looked up to as a relatively junior faculty. I was encouraged to get more involved at CHEST and with the committees. It put the bug in my ear.
A few years later, I started to get involved in the NetWorks. Eventually, I became a faculty member myself alongside these individuals at subsequent CHEST meetings. Meeting these chest medicine professionals also led to more collaborations with them outside of CHEST.
I never imagined this during my first meeting ten years ago. I have now been back to every meeting but one since that first one.
The CHEST Annual Meeting has always stood out for its focus on quality clinical teaching, being ahead of the curve on interactivity and adjusting to the audience’s learning needs.
For me personally, though, the three things that I have always enjoyed are as follows:
Simulation opportunities
One thing that sets apart CHEST 2021 from other conferences is the simulation sessions being offered online.
These sessions are an opportunity to practice your skills and techniques with some of the best educators anywhere in the world. I have always come out of these sessions impressed. I encourage you to try it at least once.
The fun
From the receptions, the meet-ups, pop-up events, CHEST Challenge, the games… the list goes on: the fun element of CHEST makes it a more immersive atmosphere. When the meeting was solely virtual last year, CHEST still aimed to provide fun and will continue to do the same this year. Challenge your colleagues and new friends to games at the CHEST Player Hub online to see which one of you rises to the top of the leaderboard.
The community
CHEST 2021 (and CHEST the organization) helps you make connections and provides opportunities for leadership involvement. CHEST committees are always looking for leaders at all stages of their careers. Attending satellite meetings, like the NetWork open forums that are occurring online before the meeting starts this year, will allow you to begin networking with those with similar interests to your own and hopefully will spark your interest in getting more involved in the future.
For many of us at CHEST, the NetWorks were a great place to start, and you can join one in the area that interests you most. Through my involvement in CHEST, I have become a part of the community, meeting so many other clinicians and educators in my field. I have made great friendships, which keep me coming back every year.
Moving forward
From the beginning, we have been planning CHEST 2021 so that if we needed to go entirely online, we could do so as seamlessly as possible. With the recent decision to cancel the in-person meeting and go fully online, plans are already underway to make CHEST 2021 just as successful as last year’s meeting.
We can give you our commitment that your CHEST 2021 experience will live up to being a world-class event that separates itself from other current online offerings. I will be in attendance and hope to see you online.
Start planning your days with the CHEST 2021 Schedule at A Glance at chestmeeting.chestnet.org.
Is this your first CHEST Annual Meeting? Co-Chair David Zielinski, MD, FCCP, shares some words of wisdom recounting his first experience at CHEST and what first-time attendees can expect from the annual meeting.
My very first CHEST meeting was 10 years ago at CHEST 2011 in Honolulu, Hawaii. I clearly remember my first session being a postgraduate course on Respiratory Management of Neuromuscular Disease and having the opportunity for hands-on teaching with devices and techniques.
Simulation was unique at medical conferences at that time and has continued to evolve at subsequent CHEST meetings.
Looking back, what really sticks out about this experience is what it started for me in terms of my career and learning. I was in a session with some of the biggest names in the field—people who I always looked up to as a relatively junior faculty. I was encouraged to get more involved at CHEST and with the committees. It put the bug in my ear.
A few years later, I started to get involved in the NetWorks. Eventually, I became a faculty member myself alongside these individuals at subsequent CHEST meetings. Meeting these chest medicine professionals also led to more collaborations with them outside of CHEST.
I never imagined this during my first meeting ten years ago. I have now been back to every meeting but one since that first one.
The CHEST Annual Meeting has always stood out for its focus on quality clinical teaching, being ahead of the curve on interactivity and adjusting to the audience’s learning needs.
For me personally, though, the three things that I have always enjoyed are as follows:
Simulation opportunities
One thing that sets apart CHEST 2021 from other conferences is the simulation sessions being offered online.
These sessions are an opportunity to practice your skills and techniques with some of the best educators anywhere in the world. I have always come out of these sessions impressed. I encourage you to try it at least once.
The fun
From the receptions, the meet-ups, pop-up events, CHEST Challenge, the games… the list goes on: the fun element of CHEST makes it a more immersive atmosphere. When the meeting was solely virtual last year, CHEST still aimed to provide fun and will continue to do the same this year. Challenge your colleagues and new friends to games at the CHEST Player Hub online to see which one of you rises to the top of the leaderboard.
The community
CHEST 2021 (and CHEST the organization) helps you make connections and provides opportunities for leadership involvement. CHEST committees are always looking for leaders at all stages of their careers. Attending satellite meetings, like the NetWork open forums that are occurring online before the meeting starts this year, will allow you to begin networking with those with similar interests to your own and hopefully will spark your interest in getting more involved in the future.
For many of us at CHEST, the NetWorks were a great place to start, and you can join one in the area that interests you most. Through my involvement in CHEST, I have become a part of the community, meeting so many other clinicians and educators in my field. I have made great friendships, which keep me coming back every year.
Moving forward
From the beginning, we have been planning CHEST 2021 so that if we needed to go entirely online, we could do so as seamlessly as possible. With the recent decision to cancel the in-person meeting and go fully online, plans are already underway to make CHEST 2021 just as successful as last year’s meeting.
We can give you our commitment that your CHEST 2021 experience will live up to being a world-class event that separates itself from other current online offerings. I will be in attendance and hope to see you online.
Start planning your days with the CHEST 2021 Schedule at A Glance at chestmeeting.chestnet.org.
Community service grants bedrock of support for communities in need
Community service grants are one way the Foundation strives to make a tangible, lasting impact on the lives of the patients we serve – they’re not just one-off projects with limited effects. But how do we really know that we’re making a difference?
For Dr. Roberta Kato, it’s when she gets to witness an “Aha!” moment – a time when everything clicks and a parent finally understands how to better care for their child. For Marina Lima, MD, MSc, it’s knowing that one more teen isn’t gasping for air. And for Dr. Joseph Huang, it’s seeing a country of 100 million people gain access to 14 pulmonologists when there was previously only one.
Whether it’s hosting family workshops in children’s museums across Los Angeles, developing a gaming app to help children in Brazil control their asthma symptoms, or establishing a pulmonary and critical care training program in Uganda, the Foundation community service grants all focus on the same goal: to enable our underserved patients gain access to the resources and care they need when they need it most.
Why community service grants?
The Foundation began giving community service grants in 1997 under the leadership of CHEST President D. Robert McCaffree, MD, Master FCCP. He believed the program would be the best way to support his colleagues in achieving their community service endeavors .To date, over $2 million has been given specifically to community service projects. “
Our physicians experience the limitations of our health care system first-hand – a system that isn’t built to assist the people who need help the most. Finding solutions requires a willingness to think and operate creatively. The funding the Foundation provides through our community service grants supplies the resources to do just that – implement real-world solutions that will help patients gain better access to care.
Cases in point
Marina Lima, MD, MSc, was seeing an inordinate number of children and teens with uncontrolled asthma symptoms in Brazil. She applied for and was awarded a grant to make Asthmaland, the first gamified pediatric asthma educational program in Portuguese.
Besides her “Aha!” moments, Dr. Roberta Kato revealed a way she knows her work is making a difference: the funding is helping to shift the nonprofit landscape in her community.
“Sometimes there is a rift between different organizations. When I ask them to collaborate or advertise together, I get resistance. However, when I’ve reached out and said that I’ve received funding for an initiative, all of a sudden, there is forward movement. That is how I am hoping to make the biggest difference,” explained Dr. Kato.
Dr. Joseph Huang, who received a grant to fund the East Africa Training Initiative (EATI), is faced with a different obstacle. “We’ve been awarded the grant many times, and I know the Foundation is focused on supporting new, up-and-coming programs. Therefore, I’m committed to ensuring that my program can continue even after we stop receiving funding.”
How is Dr. Huang going to do that? Besides procuring ICU equipment, EATI focuses on training pulmonology fellows in east Africa. The fellows who graduate will train other physicians and care team members across the continent, both in hospitals and rural clinics, safeguarding the future of his program.
A clear vision for the future
While the Foundation is ready to tackle new problems, community service grants will remain the constant thread woven throughout the work, and it’s obvious why. As Dr. Huang emphasized, his grant “will ensure that the people living in Africa have a better chance at getting access to the care they need.”
When you strip away everything else, community service grants boil down to one thing: helping people live healthier, more fulfilled lives. What can be more worthwhile?
Help us continue this important work
While we are privileged to award numerous grants over the past 2 decades, our community service grants have always held a special place in the hearts and minds of everyone involved with the CHEST Foundation. We hope they hold a special place in your heart too.
Please consider donating so that we can continue this work together.
Community service grants are one way the Foundation strives to make a tangible, lasting impact on the lives of the patients we serve – they’re not just one-off projects with limited effects. But how do we really know that we’re making a difference?
For Dr. Roberta Kato, it’s when she gets to witness an “Aha!” moment – a time when everything clicks and a parent finally understands how to better care for their child. For Marina Lima, MD, MSc, it’s knowing that one more teen isn’t gasping for air. And for Dr. Joseph Huang, it’s seeing a country of 100 million people gain access to 14 pulmonologists when there was previously only one.
Whether it’s hosting family workshops in children’s museums across Los Angeles, developing a gaming app to help children in Brazil control their asthma symptoms, or establishing a pulmonary and critical care training program in Uganda, the Foundation community service grants all focus on the same goal: to enable our underserved patients gain access to the resources and care they need when they need it most.
Why community service grants?
The Foundation began giving community service grants in 1997 under the leadership of CHEST President D. Robert McCaffree, MD, Master FCCP. He believed the program would be the best way to support his colleagues in achieving their community service endeavors .To date, over $2 million has been given specifically to community service projects. “
Our physicians experience the limitations of our health care system first-hand – a system that isn’t built to assist the people who need help the most. Finding solutions requires a willingness to think and operate creatively. The funding the Foundation provides through our community service grants supplies the resources to do just that – implement real-world solutions that will help patients gain better access to care.
Cases in point
Marina Lima, MD, MSc, was seeing an inordinate number of children and teens with uncontrolled asthma symptoms in Brazil. She applied for and was awarded a grant to make Asthmaland, the first gamified pediatric asthma educational program in Portuguese.
Besides her “Aha!” moments, Dr. Roberta Kato revealed a way she knows her work is making a difference: the funding is helping to shift the nonprofit landscape in her community.
“Sometimes there is a rift between different organizations. When I ask them to collaborate or advertise together, I get resistance. However, when I’ve reached out and said that I’ve received funding for an initiative, all of a sudden, there is forward movement. That is how I am hoping to make the biggest difference,” explained Dr. Kato.
Dr. Joseph Huang, who received a grant to fund the East Africa Training Initiative (EATI), is faced with a different obstacle. “We’ve been awarded the grant many times, and I know the Foundation is focused on supporting new, up-and-coming programs. Therefore, I’m committed to ensuring that my program can continue even after we stop receiving funding.”
How is Dr. Huang going to do that? Besides procuring ICU equipment, EATI focuses on training pulmonology fellows in east Africa. The fellows who graduate will train other physicians and care team members across the continent, both in hospitals and rural clinics, safeguarding the future of his program.
A clear vision for the future
While the Foundation is ready to tackle new problems, community service grants will remain the constant thread woven throughout the work, and it’s obvious why. As Dr. Huang emphasized, his grant “will ensure that the people living in Africa have a better chance at getting access to the care they need.”
When you strip away everything else, community service grants boil down to one thing: helping people live healthier, more fulfilled lives. What can be more worthwhile?
Help us continue this important work
While we are privileged to award numerous grants over the past 2 decades, our community service grants have always held a special place in the hearts and minds of everyone involved with the CHEST Foundation. We hope they hold a special place in your heart too.
Please consider donating so that we can continue this work together.
Community service grants are one way the Foundation strives to make a tangible, lasting impact on the lives of the patients we serve – they’re not just one-off projects with limited effects. But how do we really know that we’re making a difference?
For Dr. Roberta Kato, it’s when she gets to witness an “Aha!” moment – a time when everything clicks and a parent finally understands how to better care for their child. For Marina Lima, MD, MSc, it’s knowing that one more teen isn’t gasping for air. And for Dr. Joseph Huang, it’s seeing a country of 100 million people gain access to 14 pulmonologists when there was previously only one.
Whether it’s hosting family workshops in children’s museums across Los Angeles, developing a gaming app to help children in Brazil control their asthma symptoms, or establishing a pulmonary and critical care training program in Uganda, the Foundation community service grants all focus on the same goal: to enable our underserved patients gain access to the resources and care they need when they need it most.
Why community service grants?
The Foundation began giving community service grants in 1997 under the leadership of CHEST President D. Robert McCaffree, MD, Master FCCP. He believed the program would be the best way to support his colleagues in achieving their community service endeavors .To date, over $2 million has been given specifically to community service projects. “
Our physicians experience the limitations of our health care system first-hand – a system that isn’t built to assist the people who need help the most. Finding solutions requires a willingness to think and operate creatively. The funding the Foundation provides through our community service grants supplies the resources to do just that – implement real-world solutions that will help patients gain better access to care.
Cases in point
Marina Lima, MD, MSc, was seeing an inordinate number of children and teens with uncontrolled asthma symptoms in Brazil. She applied for and was awarded a grant to make Asthmaland, the first gamified pediatric asthma educational program in Portuguese.
Besides her “Aha!” moments, Dr. Roberta Kato revealed a way she knows her work is making a difference: the funding is helping to shift the nonprofit landscape in her community.
“Sometimes there is a rift between different organizations. When I ask them to collaborate or advertise together, I get resistance. However, when I’ve reached out and said that I’ve received funding for an initiative, all of a sudden, there is forward movement. That is how I am hoping to make the biggest difference,” explained Dr. Kato.
Dr. Joseph Huang, who received a grant to fund the East Africa Training Initiative (EATI), is faced with a different obstacle. “We’ve been awarded the grant many times, and I know the Foundation is focused on supporting new, up-and-coming programs. Therefore, I’m committed to ensuring that my program can continue even after we stop receiving funding.”
How is Dr. Huang going to do that? Besides procuring ICU equipment, EATI focuses on training pulmonology fellows in east Africa. The fellows who graduate will train other physicians and care team members across the continent, both in hospitals and rural clinics, safeguarding the future of his program.
A clear vision for the future
While the Foundation is ready to tackle new problems, community service grants will remain the constant thread woven throughout the work, and it’s obvious why. As Dr. Huang emphasized, his grant “will ensure that the people living in Africa have a better chance at getting access to the care they need.”
When you strip away everything else, community service grants boil down to one thing: helping people live healthier, more fulfilled lives. What can be more worthwhile?
Help us continue this important work
While we are privileged to award numerous grants over the past 2 decades, our community service grants have always held a special place in the hearts and minds of everyone involved with the CHEST Foundation. We hope they hold a special place in your heart too.
Please consider donating so that we can continue this work together.
Update – CHEST clinical practice guidelines
CHEST has a long history of developing high quality clinical practice guidelines based on rigorous methodology, particularly in Thoracic Oncology, Pulmonary Vascular/Venous Thromboembolic Disease, and Clinical Pulmonary Medicine/Cough. Using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, CHEST guidelines aim to optimize patient care by providing evidence-based recommendations that are transparent and free from bias.
Recently, CHEST invested in reassessing how we could further enhance the relevance, timeliness, and impact of guidelines on patient care and outcomes. We re-evaluated how we prioritize guideline topics to ensure we identify conditions in which patient care might be significantly improved by the application of evidence-based recommendations. In addition to re-committing to the rigorous GRADE approach, we also committed to timelier guideline development that would cover a broader scope of clinical topics, better mirroring the needs of our membership.
Since resuming our guideline process last year, we completed four Expert Panel Reports covering COVID-19–related topics, as well as several CHEST clinical practice guidelines. This includes publications on the management of cough in various conditions and populations – chronic bronchitis, acute bronchitis in the immunocompromised adult, asthma and nonasthmatic eosinophilic bronchitis, and in children. We also published Diagnosis and Evaluation of Hypersensitivity Pneumonitis earlier this year. This guideline outlines a patient-centered and interdisciplinary diagnostic approach to aid clinicians and patients in navigating many of the uncertainties in the evaluation of this condition.
Updates from two of our guidelines following our ‘living guideline’ model were also recently published – Screening for Lung Cancer and Antithrombic Therapy for VTE Disease. The Screening for Lung Cancer update provides guidance on patient selection for lung cancer screening, updating the age and smoking history criteria based on new evidence published since the original CHEST guideline. The updated guideline also provides recommendations for implementing high-quality lung cancer screening programs to optimize the overall benefits of screening.
In Antithrombotic Therapy for VTE, the structure of recommendations follows the chronology of VTE management: ‘Whether to treat,’ ‘Interventional and adjunctive treatments,’ ‘Initiation phase,’ ‘Treatment phase,’ ‘Extended phase,’ and ‘Complications of VTE.’ This guideline was designed to provide a comprehensive reference for VTE management in patients at any stage of the disease. Several recommendations are new from prior versions of the guideline, including whether patients with cerebral venous sinus thrombosis should be treated with anticoagulation and the choice of anticoagulant therapy for patients with antiphospholipid syndrome and thrombosis.
As we look toward the future of guideline development at CHEST, we are excited by the opportunity to expand the CHEST guideline portfolio. Starting in 2022, we will be broadening the scope of CHEST guidelines to include topics in nine clinical domains: Airway Disorders, Chest Infections, Clinical Pulmonary Medicine, Critical Care, Interstitial Lung Disease, Interventional Pulmonology, Pulmonary Vascular Disease (including venous thromboembolic disease), Thoracic Oncology, and Sleep. We anticipate issuing a Request for Proposals in select areas from these domains in the Spring of 2022, allowing CHEST members the opportunity to propose topics for which clinical guidance is needed.
As we recommit to the rigorous guideline methodology for which CHEST is known and broaden our impact across the spectrum of chest disease, we seek to ensure CHEST remains the leading resource for evidence-based guidelines in the field of chest medicine.
CHEST has a long history of developing high quality clinical practice guidelines based on rigorous methodology, particularly in Thoracic Oncology, Pulmonary Vascular/Venous Thromboembolic Disease, and Clinical Pulmonary Medicine/Cough. Using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, CHEST guidelines aim to optimize patient care by providing evidence-based recommendations that are transparent and free from bias.
Recently, CHEST invested in reassessing how we could further enhance the relevance, timeliness, and impact of guidelines on patient care and outcomes. We re-evaluated how we prioritize guideline topics to ensure we identify conditions in which patient care might be significantly improved by the application of evidence-based recommendations. In addition to re-committing to the rigorous GRADE approach, we also committed to timelier guideline development that would cover a broader scope of clinical topics, better mirroring the needs of our membership.
Since resuming our guideline process last year, we completed four Expert Panel Reports covering COVID-19–related topics, as well as several CHEST clinical practice guidelines. This includes publications on the management of cough in various conditions and populations – chronic bronchitis, acute bronchitis in the immunocompromised adult, asthma and nonasthmatic eosinophilic bronchitis, and in children. We also published Diagnosis and Evaluation of Hypersensitivity Pneumonitis earlier this year. This guideline outlines a patient-centered and interdisciplinary diagnostic approach to aid clinicians and patients in navigating many of the uncertainties in the evaluation of this condition.
Updates from two of our guidelines following our ‘living guideline’ model were also recently published – Screening for Lung Cancer and Antithrombic Therapy for VTE Disease. The Screening for Lung Cancer update provides guidance on patient selection for lung cancer screening, updating the age and smoking history criteria based on new evidence published since the original CHEST guideline. The updated guideline also provides recommendations for implementing high-quality lung cancer screening programs to optimize the overall benefits of screening.
In Antithrombotic Therapy for VTE, the structure of recommendations follows the chronology of VTE management: ‘Whether to treat,’ ‘Interventional and adjunctive treatments,’ ‘Initiation phase,’ ‘Treatment phase,’ ‘Extended phase,’ and ‘Complications of VTE.’ This guideline was designed to provide a comprehensive reference for VTE management in patients at any stage of the disease. Several recommendations are new from prior versions of the guideline, including whether patients with cerebral venous sinus thrombosis should be treated with anticoagulation and the choice of anticoagulant therapy for patients with antiphospholipid syndrome and thrombosis.
As we look toward the future of guideline development at CHEST, we are excited by the opportunity to expand the CHEST guideline portfolio. Starting in 2022, we will be broadening the scope of CHEST guidelines to include topics in nine clinical domains: Airway Disorders, Chest Infections, Clinical Pulmonary Medicine, Critical Care, Interstitial Lung Disease, Interventional Pulmonology, Pulmonary Vascular Disease (including venous thromboembolic disease), Thoracic Oncology, and Sleep. We anticipate issuing a Request for Proposals in select areas from these domains in the Spring of 2022, allowing CHEST members the opportunity to propose topics for which clinical guidance is needed.
As we recommit to the rigorous guideline methodology for which CHEST is known and broaden our impact across the spectrum of chest disease, we seek to ensure CHEST remains the leading resource for evidence-based guidelines in the field of chest medicine.
CHEST has a long history of developing high quality clinical practice guidelines based on rigorous methodology, particularly in Thoracic Oncology, Pulmonary Vascular/Venous Thromboembolic Disease, and Clinical Pulmonary Medicine/Cough. Using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, CHEST guidelines aim to optimize patient care by providing evidence-based recommendations that are transparent and free from bias.
Recently, CHEST invested in reassessing how we could further enhance the relevance, timeliness, and impact of guidelines on patient care and outcomes. We re-evaluated how we prioritize guideline topics to ensure we identify conditions in which patient care might be significantly improved by the application of evidence-based recommendations. In addition to re-committing to the rigorous GRADE approach, we also committed to timelier guideline development that would cover a broader scope of clinical topics, better mirroring the needs of our membership.
Since resuming our guideline process last year, we completed four Expert Panel Reports covering COVID-19–related topics, as well as several CHEST clinical practice guidelines. This includes publications on the management of cough in various conditions and populations – chronic bronchitis, acute bronchitis in the immunocompromised adult, asthma and nonasthmatic eosinophilic bronchitis, and in children. We also published Diagnosis and Evaluation of Hypersensitivity Pneumonitis earlier this year. This guideline outlines a patient-centered and interdisciplinary diagnostic approach to aid clinicians and patients in navigating many of the uncertainties in the evaluation of this condition.
Updates from two of our guidelines following our ‘living guideline’ model were also recently published – Screening for Lung Cancer and Antithrombic Therapy for VTE Disease. The Screening for Lung Cancer update provides guidance on patient selection for lung cancer screening, updating the age and smoking history criteria based on new evidence published since the original CHEST guideline. The updated guideline also provides recommendations for implementing high-quality lung cancer screening programs to optimize the overall benefits of screening.
In Antithrombotic Therapy for VTE, the structure of recommendations follows the chronology of VTE management: ‘Whether to treat,’ ‘Interventional and adjunctive treatments,’ ‘Initiation phase,’ ‘Treatment phase,’ ‘Extended phase,’ and ‘Complications of VTE.’ This guideline was designed to provide a comprehensive reference for VTE management in patients at any stage of the disease. Several recommendations are new from prior versions of the guideline, including whether patients with cerebral venous sinus thrombosis should be treated with anticoagulation and the choice of anticoagulant therapy for patients with antiphospholipid syndrome and thrombosis.
As we look toward the future of guideline development at CHEST, we are excited by the opportunity to expand the CHEST guideline portfolio. Starting in 2022, we will be broadening the scope of CHEST guidelines to include topics in nine clinical domains: Airway Disorders, Chest Infections, Clinical Pulmonary Medicine, Critical Care, Interstitial Lung Disease, Interventional Pulmonology, Pulmonary Vascular Disease (including venous thromboembolic disease), Thoracic Oncology, and Sleep. We anticipate issuing a Request for Proposals in select areas from these domains in the Spring of 2022, allowing CHEST members the opportunity to propose topics for which clinical guidance is needed.
As we recommit to the rigorous guideline methodology for which CHEST is known and broaden our impact across the spectrum of chest disease, we seek to ensure CHEST remains the leading resource for evidence-based guidelines in the field of chest medicine.
New guidance on preventing cutaneous SCC in solid organ transplant patients
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.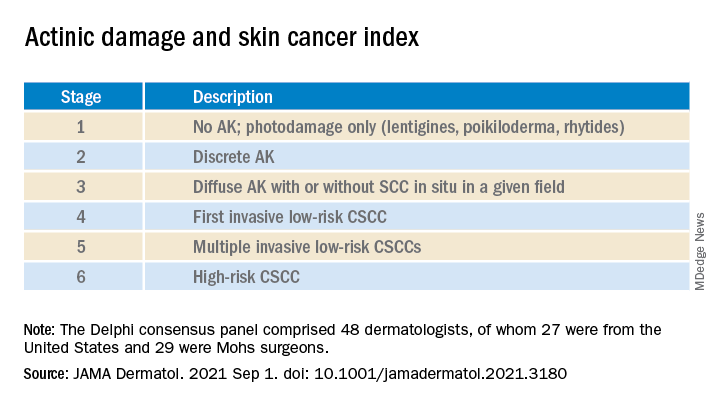
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.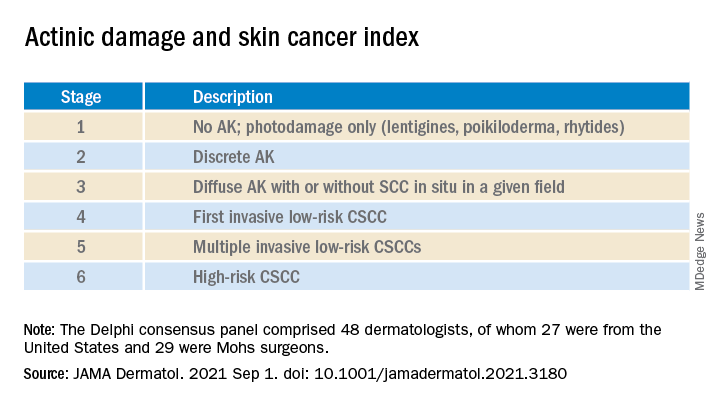
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.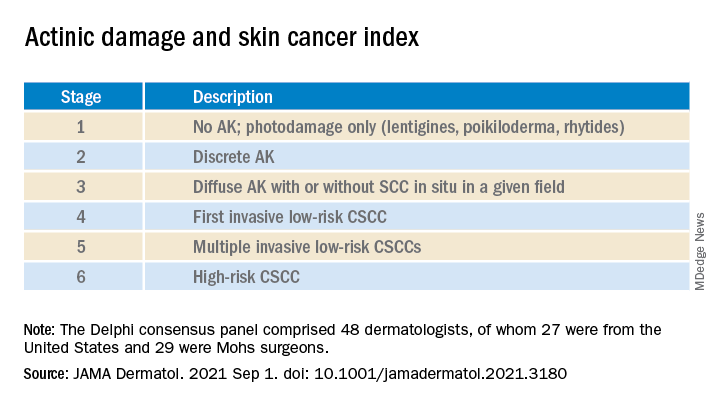
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
Even those who just test positive at more risk for long COVID: CDC
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Seizure a first sign of COVID in kids?
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Microwave ablation an alternative therapy in lung malignancy
Lung cancer patients with relatively small nodules who cannot or will not undergo surgery or radiotherapy can be successfully treated with targeted transbronchial microwave ablation, indicate results from a U.K.-led preliminary trial.
The NAVABLATE study included 30 patients from the U.K. and Hong Kong who had malignant lung nodules no more than 30 mm in diameter, who underwent transbronchial microwave ablation and were followed up one month later.
On the day, the technique was performed successfully in all 30 patients, while follow-up imaging at one month suggested that the ablation had been satisfactory in every case, with no repeat procedures necessary.
It was also associated with a “low rate of device-related adverse events and no serious adverse events,” said lead author Kevin Lau, Barts Thorax Centre, St. Bartholomew’s Hospital, Barts Health NHS Trust, London.
Consequently, transbronchial microwave ablation can be considered “an alternative treatment modality for patients with primary and metastatic malignant lung nodules … who decline or are ineligible” for surgery and radiotherapy.
The research was presented at the European Respiratory Society International Congress (ERS) 2021 on September 5.
‘Encouraging’ results
Professor Stefano Elia, head of the European Respiratory Society’s Assembly on Thoracic Surgery and Transplantation, told this news organization that the results “are encouraging.”
However, the patient numbers are “very low, so it is difficult to draw value conclusions,” and he would like to have seen more detailed characterization of the patients’ tumors.
Prof. Elia, from the University of Rome Tor Vergata, added that transbronchial microwave ablation should, in line with the study’s inclusion criteria, “probably be reserved” for lung cancer patients “who are unfit for or refuse surgery or alternative treatment strategies.”
He added that “prospective, randomized trials are warranted to see if the technique is feasible, safe and indicated” in these patients, and the potential cost of performing it needs to be specified.
Study details
Presenting the study, Mr. Lau explained that NAVABLATE was a prospective, multicenter study that enrolled patients with a confirmed malignant lung nodule ≤30 mm that did not abut the pleura, fissure, or critical structures.
In addition, the patients had declined or were not eligible for both surgery and stereotactic body radiotherapy.
They underwent transbronchial microwave ablation with the Emprint ablation catheter (Medtronic) in a hybrid theatre while undergoing cone-beam computed tomography. Only one nodule was ablated if the patients had more than one.
The team recruited 30 patients at two centres in the U.K. and Hong Kong, who had a mean age of 68.4 years and of whom 40% were female. The majority (66.7%) were prior or current tobacco users.
Primary lung cancer was the diagnosis in 20 patients, while 10 had oligometastatic disease, and the median nodule size was 12.5 mm. Thirty percent of patients had previously undergone lobectomy and 16.7% wedge resection.
Thirty-nine ablations were performed in the 30 patients, with 22 having a single ablation. Two ablations were performed in seven patients, while one had three ablations.
The most common ablation times were 10 minutes, in 21 procedures, and 7 minutes, in eight procedures, and the average total bronchoscopy time was 127 minutes.
Technical success
The procedure was deemed a technical success, defined as the nodule being reached and ablated according to the study protocol, in all patients.
The average ablation margin was 9.9 mm, and 1-month follow-up imaging was performed in all patients. This revealed a satisfactory ablation in 100% of cases. No patients required retreatment.
One patient had an adverse event relating to the ablation itself over the one-month follow-up, consisting of grade 1 mild haemoptysis on day 5, which self-resolved.
Adverse events relating to any aspect of the bronchoscopy were seen in 70% of patients, while 13.3% had grade ≥3 events, These included post-procedure pleuritic chest pain in two patients, pleural effusion in two patients, post-ablation syndrome in one patient, and ablation site infection in one patient, all grade 3.
The researchers found that the patients reported only mild pain immediately post-procedure, at an average score of 1.5 on a 10-point scale, falling to 1.4 one week later. At one month, the average pain score was 0.5.
Quality of life, as measured on the EQ-5D-3L was unaffected by the procedure, with scores rising slightly from 74.6 at baseline to 77.4 at the one-month follow-up.
The study was sponsored and funded by Medtronic.
Mr. Lau declares relationships with Medtronic, Philips, and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
Lung cancer patients with relatively small nodules who cannot or will not undergo surgery or radiotherapy can be successfully treated with targeted transbronchial microwave ablation, indicate results from a U.K.-led preliminary trial.
The NAVABLATE study included 30 patients from the U.K. and Hong Kong who had malignant lung nodules no more than 30 mm in diameter, who underwent transbronchial microwave ablation and were followed up one month later.
On the day, the technique was performed successfully in all 30 patients, while follow-up imaging at one month suggested that the ablation had been satisfactory in every case, with no repeat procedures necessary.
It was also associated with a “low rate of device-related adverse events and no serious adverse events,” said lead author Kevin Lau, Barts Thorax Centre, St. Bartholomew’s Hospital, Barts Health NHS Trust, London.
Consequently, transbronchial microwave ablation can be considered “an alternative treatment modality for patients with primary and metastatic malignant lung nodules … who decline or are ineligible” for surgery and radiotherapy.
The research was presented at the European Respiratory Society International Congress (ERS) 2021 on September 5.
‘Encouraging’ results
Professor Stefano Elia, head of the European Respiratory Society’s Assembly on Thoracic Surgery and Transplantation, told this news organization that the results “are encouraging.”
However, the patient numbers are “very low, so it is difficult to draw value conclusions,” and he would like to have seen more detailed characterization of the patients’ tumors.
Prof. Elia, from the University of Rome Tor Vergata, added that transbronchial microwave ablation should, in line with the study’s inclusion criteria, “probably be reserved” for lung cancer patients “who are unfit for or refuse surgery or alternative treatment strategies.”
He added that “prospective, randomized trials are warranted to see if the technique is feasible, safe and indicated” in these patients, and the potential cost of performing it needs to be specified.
Study details
Presenting the study, Mr. Lau explained that NAVABLATE was a prospective, multicenter study that enrolled patients with a confirmed malignant lung nodule ≤30 mm that did not abut the pleura, fissure, or critical structures.
In addition, the patients had declined or were not eligible for both surgery and stereotactic body radiotherapy.
They underwent transbronchial microwave ablation with the Emprint ablation catheter (Medtronic) in a hybrid theatre while undergoing cone-beam computed tomography. Only one nodule was ablated if the patients had more than one.
The team recruited 30 patients at two centres in the U.K. and Hong Kong, who had a mean age of 68.4 years and of whom 40% were female. The majority (66.7%) were prior or current tobacco users.
Primary lung cancer was the diagnosis in 20 patients, while 10 had oligometastatic disease, and the median nodule size was 12.5 mm. Thirty percent of patients had previously undergone lobectomy and 16.7% wedge resection.
Thirty-nine ablations were performed in the 30 patients, with 22 having a single ablation. Two ablations were performed in seven patients, while one had three ablations.
The most common ablation times were 10 minutes, in 21 procedures, and 7 minutes, in eight procedures, and the average total bronchoscopy time was 127 minutes.
Technical success
The procedure was deemed a technical success, defined as the nodule being reached and ablated according to the study protocol, in all patients.
The average ablation margin was 9.9 mm, and 1-month follow-up imaging was performed in all patients. This revealed a satisfactory ablation in 100% of cases. No patients required retreatment.
One patient had an adverse event relating to the ablation itself over the one-month follow-up, consisting of grade 1 mild haemoptysis on day 5, which self-resolved.
Adverse events relating to any aspect of the bronchoscopy were seen in 70% of patients, while 13.3% had grade ≥3 events, These included post-procedure pleuritic chest pain in two patients, pleural effusion in two patients, post-ablation syndrome in one patient, and ablation site infection in one patient, all grade 3.
The researchers found that the patients reported only mild pain immediately post-procedure, at an average score of 1.5 on a 10-point scale, falling to 1.4 one week later. At one month, the average pain score was 0.5.
Quality of life, as measured on the EQ-5D-3L was unaffected by the procedure, with scores rising slightly from 74.6 at baseline to 77.4 at the one-month follow-up.
The study was sponsored and funded by Medtronic.
Mr. Lau declares relationships with Medtronic, Philips, and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
Lung cancer patients with relatively small nodules who cannot or will not undergo surgery or radiotherapy can be successfully treated with targeted transbronchial microwave ablation, indicate results from a U.K.-led preliminary trial.
The NAVABLATE study included 30 patients from the U.K. and Hong Kong who had malignant lung nodules no more than 30 mm in diameter, who underwent transbronchial microwave ablation and were followed up one month later.
On the day, the technique was performed successfully in all 30 patients, while follow-up imaging at one month suggested that the ablation had been satisfactory in every case, with no repeat procedures necessary.
It was also associated with a “low rate of device-related adverse events and no serious adverse events,” said lead author Kevin Lau, Barts Thorax Centre, St. Bartholomew’s Hospital, Barts Health NHS Trust, London.
Consequently, transbronchial microwave ablation can be considered “an alternative treatment modality for patients with primary and metastatic malignant lung nodules … who decline or are ineligible” for surgery and radiotherapy.
The research was presented at the European Respiratory Society International Congress (ERS) 2021 on September 5.
‘Encouraging’ results
Professor Stefano Elia, head of the European Respiratory Society’s Assembly on Thoracic Surgery and Transplantation, told this news organization that the results “are encouraging.”
However, the patient numbers are “very low, so it is difficult to draw value conclusions,” and he would like to have seen more detailed characterization of the patients’ tumors.
Prof. Elia, from the University of Rome Tor Vergata, added that transbronchial microwave ablation should, in line with the study’s inclusion criteria, “probably be reserved” for lung cancer patients “who are unfit for or refuse surgery or alternative treatment strategies.”
He added that “prospective, randomized trials are warranted to see if the technique is feasible, safe and indicated” in these patients, and the potential cost of performing it needs to be specified.
Study details
Presenting the study, Mr. Lau explained that NAVABLATE was a prospective, multicenter study that enrolled patients with a confirmed malignant lung nodule ≤30 mm that did not abut the pleura, fissure, or critical structures.
In addition, the patients had declined or were not eligible for both surgery and stereotactic body radiotherapy.
They underwent transbronchial microwave ablation with the Emprint ablation catheter (Medtronic) in a hybrid theatre while undergoing cone-beam computed tomography. Only one nodule was ablated if the patients had more than one.
The team recruited 30 patients at two centres in the U.K. and Hong Kong, who had a mean age of 68.4 years and of whom 40% were female. The majority (66.7%) were prior or current tobacco users.
Primary lung cancer was the diagnosis in 20 patients, while 10 had oligometastatic disease, and the median nodule size was 12.5 mm. Thirty percent of patients had previously undergone lobectomy and 16.7% wedge resection.
Thirty-nine ablations were performed in the 30 patients, with 22 having a single ablation. Two ablations were performed in seven patients, while one had three ablations.
The most common ablation times were 10 minutes, in 21 procedures, and 7 minutes, in eight procedures, and the average total bronchoscopy time was 127 minutes.
Technical success
The procedure was deemed a technical success, defined as the nodule being reached and ablated according to the study protocol, in all patients.
The average ablation margin was 9.9 mm, and 1-month follow-up imaging was performed in all patients. This revealed a satisfactory ablation in 100% of cases. No patients required retreatment.
One patient had an adverse event relating to the ablation itself over the one-month follow-up, consisting of grade 1 mild haemoptysis on day 5, which self-resolved.
Adverse events relating to any aspect of the bronchoscopy were seen in 70% of patients, while 13.3% had grade ≥3 events, These included post-procedure pleuritic chest pain in two patients, pleural effusion in two patients, post-ablation syndrome in one patient, and ablation site infection in one patient, all grade 3.
The researchers found that the patients reported only mild pain immediately post-procedure, at an average score of 1.5 on a 10-point scale, falling to 1.4 one week later. At one month, the average pain score was 0.5.
Quality of life, as measured on the EQ-5D-3L was unaffected by the procedure, with scores rising slightly from 74.6 at baseline to 77.4 at the one-month follow-up.
The study was sponsored and funded by Medtronic.
Mr. Lau declares relationships with Medtronic, Philips, and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
FDA moves to block some vape products, delays action on Juul
The agency had a court-ordered deadline of Sept. 9 to review more than 6.5 million applications for approval of what are considered new tobacco products – the vast majority of which are e-cigarettes and liquids, none of which have gone through FDA review before.
The FDA reviewed 93% of those applications in the past year, acting FDA Commissioner Janet Woodcock, MD, and Mitch Zeller, director of the FDA’s Center for Tobacco Products, said in a statement.
Of those reviewed, the agency rejected more than 946,000 flavored vape products, “because their applications lacked sufficient evidence that they have a benefit to adult smokers sufficient to overcome the public health threat posed by the well-documented, alarming levels of youth use of such products,” Dr. Woodcock and Mr. Zeller said.
The pair said more work is needed to finish the reviews to “ensure that we continue taking appropriate action to protect our nation’s youth from the dangers of all tobacco products, including e-cigarettes, which remain the most commonly used tobacco product by youth in the United States.”
No e-cigarette product has been given official FDA approval to be sold, meaning all e-cigarette products technically are on the market illegally, the agency said in 2020, but federal officials decided only to begin enforcing rules against flavored products, which surveys show are more often used by children. Tobacco-flavored and menthol e-cigarette products – which some adults use to quit smoking cigarettes – were exempted.
The American Cancer Society and other advocacy groups slammed the FDA’s decision to withhold action on major e-cigarette manufacturers, including Juul.
“The FDA’s failure today to act on applications by Juul, the manufacturer with the single biggest e-cigarette market share, is extremely disappointing and will allow the industry to further endanger public health and hook more kids on their highly addictive products,” Lisa Lacasse, president of ACS CAN, said in a statement, according to CNN.
“The FDA has had ample time to review the applications and allowing additional delays is unconscionable. There is overwhelming data to demonstrate the negative impact these kinds of flavored products have had on public health and their role in the youth e-cigarette epidemic. The time to act is now,” Ms. Lacasse added.
E-cigarette use among high school students rose from 11.7% in 2017 to 19.6% in 2020, the American Cancer Society said. Nearly 5% of middle schoolers reported using them in 2020.
A version of this article first appeared on WebMD.com.
The agency had a court-ordered deadline of Sept. 9 to review more than 6.5 million applications for approval of what are considered new tobacco products – the vast majority of which are e-cigarettes and liquids, none of which have gone through FDA review before.
The FDA reviewed 93% of those applications in the past year, acting FDA Commissioner Janet Woodcock, MD, and Mitch Zeller, director of the FDA’s Center for Tobacco Products, said in a statement.
Of those reviewed, the agency rejected more than 946,000 flavored vape products, “because their applications lacked sufficient evidence that they have a benefit to adult smokers sufficient to overcome the public health threat posed by the well-documented, alarming levels of youth use of such products,” Dr. Woodcock and Mr. Zeller said.
The pair said more work is needed to finish the reviews to “ensure that we continue taking appropriate action to protect our nation’s youth from the dangers of all tobacco products, including e-cigarettes, which remain the most commonly used tobacco product by youth in the United States.”
No e-cigarette product has been given official FDA approval to be sold, meaning all e-cigarette products technically are on the market illegally, the agency said in 2020, but federal officials decided only to begin enforcing rules against flavored products, which surveys show are more often used by children. Tobacco-flavored and menthol e-cigarette products – which some adults use to quit smoking cigarettes – were exempted.
The American Cancer Society and other advocacy groups slammed the FDA’s decision to withhold action on major e-cigarette manufacturers, including Juul.
“The FDA’s failure today to act on applications by Juul, the manufacturer with the single biggest e-cigarette market share, is extremely disappointing and will allow the industry to further endanger public health and hook more kids on their highly addictive products,” Lisa Lacasse, president of ACS CAN, said in a statement, according to CNN.
“The FDA has had ample time to review the applications and allowing additional delays is unconscionable. There is overwhelming data to demonstrate the negative impact these kinds of flavored products have had on public health and their role in the youth e-cigarette epidemic. The time to act is now,” Ms. Lacasse added.
E-cigarette use among high school students rose from 11.7% in 2017 to 19.6% in 2020, the American Cancer Society said. Nearly 5% of middle schoolers reported using them in 2020.
A version of this article first appeared on WebMD.com.
The agency had a court-ordered deadline of Sept. 9 to review more than 6.5 million applications for approval of what are considered new tobacco products – the vast majority of which are e-cigarettes and liquids, none of which have gone through FDA review before.
The FDA reviewed 93% of those applications in the past year, acting FDA Commissioner Janet Woodcock, MD, and Mitch Zeller, director of the FDA’s Center for Tobacco Products, said in a statement.
Of those reviewed, the agency rejected more than 946,000 flavored vape products, “because their applications lacked sufficient evidence that they have a benefit to adult smokers sufficient to overcome the public health threat posed by the well-documented, alarming levels of youth use of such products,” Dr. Woodcock and Mr. Zeller said.
The pair said more work is needed to finish the reviews to “ensure that we continue taking appropriate action to protect our nation’s youth from the dangers of all tobacco products, including e-cigarettes, which remain the most commonly used tobacco product by youth in the United States.”
No e-cigarette product has been given official FDA approval to be sold, meaning all e-cigarette products technically are on the market illegally, the agency said in 2020, but federal officials decided only to begin enforcing rules against flavored products, which surveys show are more often used by children. Tobacco-flavored and menthol e-cigarette products – which some adults use to quit smoking cigarettes – were exempted.
The American Cancer Society and other advocacy groups slammed the FDA’s decision to withhold action on major e-cigarette manufacturers, including Juul.
“The FDA’s failure today to act on applications by Juul, the manufacturer with the single biggest e-cigarette market share, is extremely disappointing and will allow the industry to further endanger public health and hook more kids on their highly addictive products,” Lisa Lacasse, president of ACS CAN, said in a statement, according to CNN.
“The FDA has had ample time to review the applications and allowing additional delays is unconscionable. There is overwhelming data to demonstrate the negative impact these kinds of flavored products have had on public health and their role in the youth e-cigarette epidemic. The time to act is now,” Ms. Lacasse added.
E-cigarette use among high school students rose from 11.7% in 2017 to 19.6% in 2020, the American Cancer Society said. Nearly 5% of middle schoolers reported using them in 2020.
A version of this article first appeared on WebMD.com.
COVID-19 spares lung function in young adults
Here’s some encouraging news for once regarding SARS-CoV-2 infections: A study of young adults for whom prepandemic spirometry data were available showed that COVID-19 did not have a significant impact on lung function, even among patients with asthma.
Among 853 Swedish men and women (mean age, 22 years) who were part of a birth cohort study, there were no significant differences in either forced expiratory volume in 1 second (FEV1) or in the ratio of FEV1 to forced vital capacity, reported Ida Mogensen, MD, PhD, a postdoctoral fellow at the Karolinska Institute in Stockholm.
“We found no effect of COVID-19 on spirometric lung function in generally healthy adults,” she said in an oral abstract presented at the European Respiratory Society 2021 International Congress.
The findings echo those of a small study that involved 73 children and adolescents with COVID-19 and 45 uninfected control persons. The investigators in that study, which was also presented at ERS 2021, found that there were no significant differences in the frequency of abnormal pulmonary function measures between case patients and control patients (abstract OA1303).
“The findings from these two studies provide important reassurance about the impact of COVID infection on lung function in children and young adults,” commented Anita Simonds, MD, an honorary consultant in respiratory and sleep medicine at the Royal Brompton Hospital, London.
“We know already that this group is less likely to suffer severe illness if they contract the virus, and these studies, which importantly include comparator groups without COVID-19, show that they are also less likely to suffer long-term consequences with respect to lung function,” she said. Dr. Simonds was not involved in either study.
Young adult study
Dr. Mogenson and colleagues assessed data on 853 participants in the BAMSE Project, a prospective birth cohort study that included 4,089 children born in Stockholm from 1994 to 1996. Of the participants, 147 had asthma. They have been regularly followed with questionnaires on respiratory symptoms and medications. In addition, at 8 and 16 years’ follow-up, spirometry measures and fractional exhaled nitric oxide (FeNO) levels were assessed, allergic sensitization tests were administered, and blood eosinophil levels were measured.
In 2020 and 2021, during the pandemic, the participants underwent spirometry testing and were assessed for antibodies against SARS-CoV-2, and they self-reported use of inhaled corticosteroids.
The investigators defined asthma as any physician diagnosis and asthma symptoms and/or asthma medication use within the previous year. Participants were determined to be COVID-19 seropositive if they had IgG antibodies to the SARS-CoV-2 spike greater than 25.09 AU/mL, IgM antibodies greater than 14.42 AU/mL, or IgA antibodies greater than 2.61 AU/mL, as measured with enzyme-linked immunosorbent assay.
Participants who had been vaccinated against COVID-19 were excluded.
No significant decreases
A total of 243 participants, including 38 with asthma, were seropositive for SARS-CoV-2 antibodies. The mean change in lung function from before the pandemic to the study end date during the pandemic were not significantly different between seropositive participants and seronegative participants or IgM-positive participants and seronegative participants.
Similarly, there were no significant differences in lung function between seropositive and seronegative participants in an analysis that was adjusted for sex, body mass index, smoking status, or prepandemic lung function.
Although there was a trend toward slightly lower function among seropositive participants with asthma in comparison with seronegative patients with asthma, it was not statistically significant, Dr. Mogenson said.
There were also no significant decreases in lung function from the prepandemic measure to the present in any of the inflammatory parameters, including blood eosinophil levels, FeNO, allergic sensitization, or inhaled corticosteroid use.
Potential misclassification
In the question-and-answer period that followed the presentation, session comoderator Sam Bayat, MD, PhD, from the University of Grenoble (France), who was not involved in the study, noted that “some subjects can have positive serology without any symptoms, while others can have symptomatic disease and a couple of months later they have negative serology.”
He asked Dr. Mogenson whether they had included in their study participants with symptomatic COVID-19 and whether that would change the findings.
“We did not have access to RNA testing, so we only had serology, and of course some participants could be wrongly classified to have disease – probably around 15%,” she acknowledged.
She noted that there were no significant changes in lung function among patients who reported having respiratory symptoms.
The study was funded by the Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Research Council for Health, Working Life and Welfare, the Karolinska Institutet, Formas, the European Research Council, and Region Stockholm. Dr. Mogenson, Dr. Simonds, and Dr. Bayat disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Here’s some encouraging news for once regarding SARS-CoV-2 infections: A study of young adults for whom prepandemic spirometry data were available showed that COVID-19 did not have a significant impact on lung function, even among patients with asthma.
Among 853 Swedish men and women (mean age, 22 years) who were part of a birth cohort study, there were no significant differences in either forced expiratory volume in 1 second (FEV1) or in the ratio of FEV1 to forced vital capacity, reported Ida Mogensen, MD, PhD, a postdoctoral fellow at the Karolinska Institute in Stockholm.
“We found no effect of COVID-19 on spirometric lung function in generally healthy adults,” she said in an oral abstract presented at the European Respiratory Society 2021 International Congress.
The findings echo those of a small study that involved 73 children and adolescents with COVID-19 and 45 uninfected control persons. The investigators in that study, which was also presented at ERS 2021, found that there were no significant differences in the frequency of abnormal pulmonary function measures between case patients and control patients (abstract OA1303).
“The findings from these two studies provide important reassurance about the impact of COVID infection on lung function in children and young adults,” commented Anita Simonds, MD, an honorary consultant in respiratory and sleep medicine at the Royal Brompton Hospital, London.
“We know already that this group is less likely to suffer severe illness if they contract the virus, and these studies, which importantly include comparator groups without COVID-19, show that they are also less likely to suffer long-term consequences with respect to lung function,” she said. Dr. Simonds was not involved in either study.
Young adult study
Dr. Mogenson and colleagues assessed data on 853 participants in the BAMSE Project, a prospective birth cohort study that included 4,089 children born in Stockholm from 1994 to 1996. Of the participants, 147 had asthma. They have been regularly followed with questionnaires on respiratory symptoms and medications. In addition, at 8 and 16 years’ follow-up, spirometry measures and fractional exhaled nitric oxide (FeNO) levels were assessed, allergic sensitization tests were administered, and blood eosinophil levels were measured.
In 2020 and 2021, during the pandemic, the participants underwent spirometry testing and were assessed for antibodies against SARS-CoV-2, and they self-reported use of inhaled corticosteroids.
The investigators defined asthma as any physician diagnosis and asthma symptoms and/or asthma medication use within the previous year. Participants were determined to be COVID-19 seropositive if they had IgG antibodies to the SARS-CoV-2 spike greater than 25.09 AU/mL, IgM antibodies greater than 14.42 AU/mL, or IgA antibodies greater than 2.61 AU/mL, as measured with enzyme-linked immunosorbent assay.
Participants who had been vaccinated against COVID-19 were excluded.
No significant decreases
A total of 243 participants, including 38 with asthma, were seropositive for SARS-CoV-2 antibodies. The mean change in lung function from before the pandemic to the study end date during the pandemic were not significantly different between seropositive participants and seronegative participants or IgM-positive participants and seronegative participants.
Similarly, there were no significant differences in lung function between seropositive and seronegative participants in an analysis that was adjusted for sex, body mass index, smoking status, or prepandemic lung function.
Although there was a trend toward slightly lower function among seropositive participants with asthma in comparison with seronegative patients with asthma, it was not statistically significant, Dr. Mogenson said.
There were also no significant decreases in lung function from the prepandemic measure to the present in any of the inflammatory parameters, including blood eosinophil levels, FeNO, allergic sensitization, or inhaled corticosteroid use.
Potential misclassification
In the question-and-answer period that followed the presentation, session comoderator Sam Bayat, MD, PhD, from the University of Grenoble (France), who was not involved in the study, noted that “some subjects can have positive serology without any symptoms, while others can have symptomatic disease and a couple of months later they have negative serology.”
He asked Dr. Mogenson whether they had included in their study participants with symptomatic COVID-19 and whether that would change the findings.
“We did not have access to RNA testing, so we only had serology, and of course some participants could be wrongly classified to have disease – probably around 15%,” she acknowledged.
She noted that there were no significant changes in lung function among patients who reported having respiratory symptoms.
The study was funded by the Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Research Council for Health, Working Life and Welfare, the Karolinska Institutet, Formas, the European Research Council, and Region Stockholm. Dr. Mogenson, Dr. Simonds, and Dr. Bayat disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Here’s some encouraging news for once regarding SARS-CoV-2 infections: A study of young adults for whom prepandemic spirometry data were available showed that COVID-19 did not have a significant impact on lung function, even among patients with asthma.
Among 853 Swedish men and women (mean age, 22 years) who were part of a birth cohort study, there were no significant differences in either forced expiratory volume in 1 second (FEV1) or in the ratio of FEV1 to forced vital capacity, reported Ida Mogensen, MD, PhD, a postdoctoral fellow at the Karolinska Institute in Stockholm.
“We found no effect of COVID-19 on spirometric lung function in generally healthy adults,” she said in an oral abstract presented at the European Respiratory Society 2021 International Congress.
The findings echo those of a small study that involved 73 children and adolescents with COVID-19 and 45 uninfected control persons. The investigators in that study, which was also presented at ERS 2021, found that there were no significant differences in the frequency of abnormal pulmonary function measures between case patients and control patients (abstract OA1303).
“The findings from these two studies provide important reassurance about the impact of COVID infection on lung function in children and young adults,” commented Anita Simonds, MD, an honorary consultant in respiratory and sleep medicine at the Royal Brompton Hospital, London.
“We know already that this group is less likely to suffer severe illness if they contract the virus, and these studies, which importantly include comparator groups without COVID-19, show that they are also less likely to suffer long-term consequences with respect to lung function,” she said. Dr. Simonds was not involved in either study.
Young adult study
Dr. Mogenson and colleagues assessed data on 853 participants in the BAMSE Project, a prospective birth cohort study that included 4,089 children born in Stockholm from 1994 to 1996. Of the participants, 147 had asthma. They have been regularly followed with questionnaires on respiratory symptoms and medications. In addition, at 8 and 16 years’ follow-up, spirometry measures and fractional exhaled nitric oxide (FeNO) levels were assessed, allergic sensitization tests were administered, and blood eosinophil levels were measured.
In 2020 and 2021, during the pandemic, the participants underwent spirometry testing and were assessed for antibodies against SARS-CoV-2, and they self-reported use of inhaled corticosteroids.
The investigators defined asthma as any physician diagnosis and asthma symptoms and/or asthma medication use within the previous year. Participants were determined to be COVID-19 seropositive if they had IgG antibodies to the SARS-CoV-2 spike greater than 25.09 AU/mL, IgM antibodies greater than 14.42 AU/mL, or IgA antibodies greater than 2.61 AU/mL, as measured with enzyme-linked immunosorbent assay.
Participants who had been vaccinated against COVID-19 were excluded.
No significant decreases
A total of 243 participants, including 38 with asthma, were seropositive for SARS-CoV-2 antibodies. The mean change in lung function from before the pandemic to the study end date during the pandemic were not significantly different between seropositive participants and seronegative participants or IgM-positive participants and seronegative participants.
Similarly, there were no significant differences in lung function between seropositive and seronegative participants in an analysis that was adjusted for sex, body mass index, smoking status, or prepandemic lung function.
Although there was a trend toward slightly lower function among seropositive participants with asthma in comparison with seronegative patients with asthma, it was not statistically significant, Dr. Mogenson said.
There were also no significant decreases in lung function from the prepandemic measure to the present in any of the inflammatory parameters, including blood eosinophil levels, FeNO, allergic sensitization, or inhaled corticosteroid use.
Potential misclassification
In the question-and-answer period that followed the presentation, session comoderator Sam Bayat, MD, PhD, from the University of Grenoble (France), who was not involved in the study, noted that “some subjects can have positive serology without any symptoms, while others can have symptomatic disease and a couple of months later they have negative serology.”
He asked Dr. Mogenson whether they had included in their study participants with symptomatic COVID-19 and whether that would change the findings.
“We did not have access to RNA testing, so we only had serology, and of course some participants could be wrongly classified to have disease – probably around 15%,” she acknowledged.
She noted that there were no significant changes in lung function among patients who reported having respiratory symptoms.
The study was funded by the Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Research Council for Health, Working Life and Welfare, the Karolinska Institutet, Formas, the European Research Council, and Region Stockholm. Dr. Mogenson, Dr. Simonds, and Dr. Bayat disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.